Jane E. Atieno Okech, Anne M. Geroski
This article utilizes one counselor education program’s experience as a framework for exploring how to prepare counselors to work in interdisciplinary teams. Based on an interdisciplinary training program that involves faculty and graduate students from counseling, social work, nursing, internal medicine and family medicine, the article explores the role discipline-specific orientations play in the outcome of interdisciplinary training programs. Using practical examples grounded by the program’s experiences and literature on interdisciplinary training, understanding of the dynamics of interdisciplinary training programs is explored. Implications for preparing counselors for interdisciplinary work and future research are provided.
Keywords: counselor education, interdisciplinary training, interdisciplinary teams, collaborative practice, medicine
Counselors typically work in interdisciplinary settings, requiring them to navigate the complex dynamics of collaboration while maintaining a clear focus on the best interests of their clients. Interdisciplinary settings can be described as contexts that require collaboration and consultation between professionals and non-professionals from multiple disciplines in the process of providing service (Nancarrow et al., 2013). Collin (2009) clarified that interdisciplinary collaboration differs from multidisciplinary and transdisciplinary collaboration as it refers to the work of professionals grounded in their own separate disciplines coming together to work on a project that represents a “coordinated and coherent whole” (p. 103). Collin pointed out that this is different from professionals working independently on separate aspects of a project (multidisciplinary) or the coming together of multiple and varied professionals to conceptualize a problem or work on a project that transcends any of the various disciplines (transdisciplinary).
Counselor educators have argued that interdisciplinary collaboration is “a best practice strategy for addressing some of the nation’s critical social problems” (Mellin, Hunt, & Nichols, 2011, p. 140). In fact, collaboration between disciplines has been described as being key to the effective delivery of services (McNair, 2005; Morphet et al., 2014) across a broad-spectrum of community mental health services, hospitals, institutions of higher learning and school contexts. In the field of counseling, the ACA Code of Ethics (American Counseling Association [ACA], 2014) and the standards established by the Council for Accreditation of Counseling and Related Educational Programs (CACREP, 2009) reflect this emphasis on the importance of counselors being able to work with interdisciplinary teams. The ACA Code of Ethics (ACA, 2014), for example, encourages counselors to recognize the value of interdisciplinary teamwork in meeting clients’ best interests, even when certain professional values are not shared:
Counselors who are members of interdisciplinary teams delivering multifaceted services to clients remain focused on how to best serve clients. They participate in and contribute to decisions that affect the well-being of clients by drawing on the perspectives, values, and experiences of the counseling profession and those of colleagues from other disciplines (ACA, 2014, D. 1. C., p. 10).
The ACA Code of Ethics also compels counselors to respect client rights, including those regarding confidentiality, in interdisciplinary treatment contexts (ACA, 2014, A. 2. b., p. 4; B. 3. b., p. 7). The CACREP (2009) training standards emphasize the importance of teaching counselors to understand the functions of other human service agencies and to learn strategies for inter-agency collaboration. In these standards, addictions, marriage, couples, family and career counselors are required to be familiar with the roles of other mental health professionals, and in the clinical mental health counselor standards, the importance of learning how to develop relationships across helping professions and interdisciplinary treatment teams is highlighted. Additionally, school counselors-in-training under CACREP standards also must learn models of consultation and collaboration as a part of their training programs.
Despite these standards, counselors appear to navigate the challenges of interdisciplinary collaboration with limited understanding and experience. Little has been written about interdisciplinary training or the development of interdisciplinary competencies by counseling professionals (Bemak, 1998). Counseling literature and training standards appear to operate from the premise that the process of professional development is automatically accompanied with the acquisition of skills to work in interdisciplinary teams. In contrast, the medical field and associated disciplines have actively documented interdisciplinary training initiatives as a means for facilitating interdisciplinary competencies among their professionals (Pollard & Miers, 2008). For example, in the United Kingdom, the integration of Interprofessional Education (IPE) is now mandatory in the fields of health and social care, with students being required to complete specific modules that have practical interdisciplinary components (Pollard & Miers, 2008). Medicine in the United States also is actively pursuing interdisciplinary training models with the support of the Institute of Medicine, which recognizes interdisciplinary teamwork as key to effective service delivery (Institute of Medicine, 2003; McNair, 2005). Therefore, while counselors continue to make a case for the value of interdisciplinary work, what remains unclear in the literature is how counselors can attain competence in facilitating and participating in interdisciplinary collaborative practices. It is particularly critical to examine how these competencies can be developed while neophyte counselors are also in the foundational stages of their professional development.
The purpose of this article is to use the experiences of one counselor education program currently engaged in an interdisciplinary training project as a framework for exploring some critical benefits and challenges of interdisciplinary training processes. This article provides a detailed description of the counselor education program’s training module and also describes steps the program has taken to prepare students for interdisciplinary training contextual dynamics, measures the program has taken to advocate for the counseling profession, and efforts to enhance students’ understandings of their professional roles in an interdisciplinary context. Using practical examples grounded by interdisciplinary literature, we expand understanding of shared interdisciplinary values and provide recommendations for more effective practices and future research.
Interdisciplinary Training Program Development
This training collaborative began with an interdisciplinary response to a grant call by the Substance Abuse and Mental Health Services Administration (SAMHSA) to submit a proposal on providing training in Screening, Brief Intervention, and Referral to Treatment (SBIRT). SBIRT is a comprehensive, integrated, public health approach to the delivery of early intervention and treatment services for adolescents and adults dealing with substance misuse issues (Agerwala & McCance-Katz, 2012; Davoudi & Rawson, 2010; Mitchell et al., 2012). This particular university’s SBIRT Training Collaborative brings together master’s students from the counseling program, the Department of Social Work, the College of Nursing, and family medicine and internal medicine residents in an interdisciplinary training program using a team-based care model of evidence-supported SBIRT interventions. These programs were chosen because they all are disciplines that deal with issues related to substance misuse. Additionally, these were the only disciplines at our university that responded to the call to participate in this particular project. The objective of the project is to offer brief intervention and referral training to medical residents and master’s level graduate students in the area of substance use disorders over a 3-year period. An average of 20 students from each of the participating disciplines were expected to participate in the project annually. This training program began its third year of implementation this year. The SAMHSA grant enabled the interdisciplinary training collaborative to hire SBIRT consultants, a project manager, a project training director and qualified support staff to help administer the project. The funding is a critical part of the success of this project, allowing for faculty course buyouts across the participating disciplines.
The interdisciplinary collaborative aspect of this project began during the initial meeting of educators from the various disciplines, which was organized to discuss submitting a grant proposal in support of an interdisciplinary training program. Each program’s director was required to submit a statement indicating how their program would benefit from an interdisciplinary training project. Two initial meetings and multiple e-mail exchanges later led to the formation of an interdisciplinary collaborative team and an agreement by the team on (a) the core foci of the grant, (b) the level of participation by each program and the roles of faculty representatives on the grant writing, (c) budget allocation parameters, and (d) the establishment of a project advisory council made up of the directors of each of the disciplines represented in the project. The purpose of the project’s advisory council was to develop the curriculum for the program, which included assessing and ultimately agreeing on the online modules to use on the project, and to establish clear guidelines for the clinical training protocol. Secondly, the advisory council also was charged with ensuring that each discipline provided input on the curriculum development and project evaluation processes. This aspect of the dialogue was critical as one of the objectives of the grant was for programs to incorporate interdisciplinary training foci in their individual discipline’s curriculum. Third, the council was charged with the responsibility of implementing and assessing the clinical training aspect of the interdisciplinary training project. Advisory council members committed to serve on interdisciplinary presentation panels and also to provide supervision during the interdisciplinary clinical training sessions. Finally, the council members were expected to be available to address student conduct issues as well as to meet with external grant reviewers during their visits to campus.
The SBIRT Interdisciplinary Training Model
This university’s SBIRT interdisciplinary training format is multifaceted, including online and real-time instruction and practice experiences. All family practice and internal medicine residents and master’s-level graduate students in the participating disciplines are expected to sign a contract that they will participate in all required aspects of the training experience. SBIRT training is offered in four main areas: (1) screening for substance use disorders, (2) motivational interviewing skills, (3) brief intervention, and (4) referral to treatment. Training includes providing conceptual information (e.g., substance use and motivational interviewing), teaching the use of assessment tools to establish risk or levels of substance misuse, and promoting skill development. Modeling and skill practice with feedback from faculty are important components of this training.
The first SBIRT training cohort started with first-year master’s-level graduate students and medical residents. The counseling students involved in the project were in their second semester in the program and concurrently enrolled in a practicum course. For counseling students, the training began with an orientation (counseling program pre-module orientation) to the SBIRT training experience. In the orientation, counseling faculty offered students an overview of the various components of the training project, outlining specific expectations and completion dates. Beginning in the project’s second year, the orientation included the film, The Hungry Heart (O’Brien, 2013), which explores the depth of prescription drug and opiate addiction in our home state. This film was followed by a discussion regarding the need for SBIRT screening and referral skills. While counseling students are required to participate in this orientation, the option to attend the session also is open to participants from other disciplines.
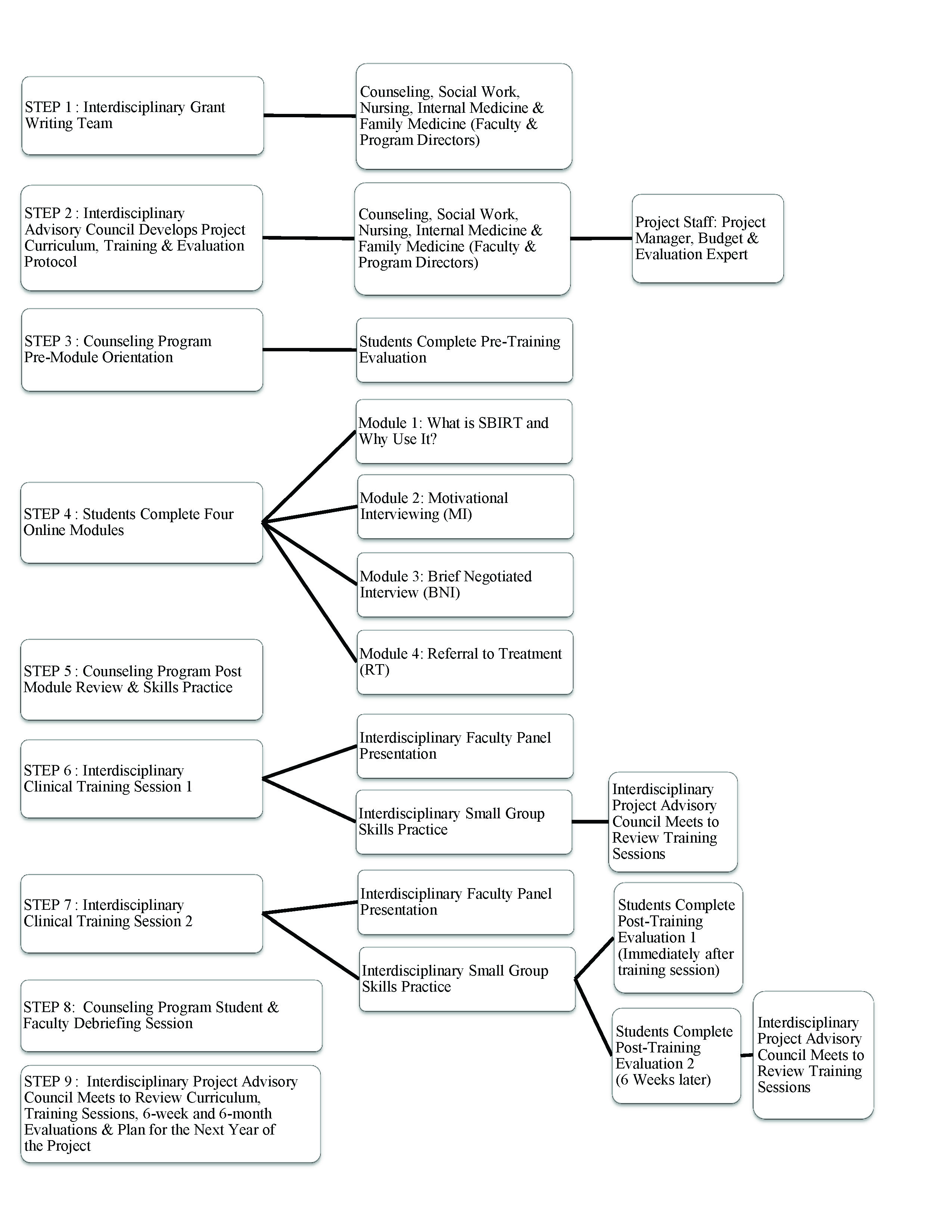
The next component of the training, conducted online, is required for all participants (faculty and students), regardless of discipline. The online training includes four instructional modules (see Figure 1) and requires a commitment of approximately four to six hours. The first of these online training modules offers an introduction to the SBIRT process and includes data regarding alcohol and substance use. This information builds a case for the need for SBIRT screening and referral practices. The other modules provide instruction in the areas of conducting a brief screening intervention, motivational interviewing, and making appropriate referrals. Each module begins with instruction in a particular area and requires completion of a test before the participant is issued a completion certificate. The certification process was included as a means of ensuring that all participating students complete the required didactic training and tests prior to participating in the interdisciplinary clinical training portions of the program.
At the end of the online training period, counseling students are required to attend a 2-hour practice review (counseling program post-module review and skills practice) session (see Figure 1). A similar post-module review and practice session is offered by other SBIRT project faculty for medical residents and to promote interdisciplinary training; each discipline-specific post-module review is open to participants from other disciplines. In this training, counseling faculty offer a brief review of the information provided in the modules, focusing primarily on the steps of the brief negotiated interview (alcohol and substance use screening) and the motivational interview. Participants engage in role-plays to practice these skills and are provided with instruction and feedback by the counseling faculty.
Figure 1 – Interdisciplinary Training Protocol
The intent of this training session is to reinforce counseling students’ sense of competence prior to engaging in interdisciplinary training sessions. This session helps students frame the online training information into counseling-specific terms, steps and experiences while providing them the opportunity to ask questions and clarify their understandings. Importantly, this session requires students to practice the SBIRT skills and to receive feedback and instruction on their use of the skills from familiar faculty in the comfortable environment of counseling peers. Ultimately, this preparation is designed to fortify the confidence that the counseling students bring into the larger, unfamiliar, interdisciplinary practice setting.
Next, all participants in the SBIRT training, regardless of specific discipline, are expected to attend two clinical interdisciplinary training sessions. The first of these focuses on screening and motivational interviewing; the second is on referrals. These sessions begin with an introduction to the concepts that will be covered in that training followed by a panel discussion about the particular application of skills in the various disciplines and the modeling of skills (a role play by two of the program directors). The participants are then required to practice the skills with “live” practice clients (i.e., professional actors from the local community that were already employed by the medical school for medical student training) playing patients/clients with substance use or misuse issues. In this part of the training, participants are randomly assigned to small practice groups, providing an interdisciplinary practice milieu, with a faculty instructor. Each interdisciplinary practice group meets with four professional clients over the course of 2 hours. The participants in each group take turns using screening, motivational interviewing and referral skills. In each group, participants receive feedback and instruction from the faculty instructor who has observed their practice. At the end of the session, the training directors engage participants in a large group discussion about their experiences and observations of being part of an interdisciplinary training group. The intent of this approach is to provide participants with the opportunity to practice with students who have different professional orientations and to receive supervision from faculty who may also have diverse experiences and perspectives; thus, the interdisciplinary focus of this project.
The final component of the training is follow-up. For counseling students, this begins with a follow-up discussion about the training experience with the counseling faculty at the end of the first year of training (after the second interdisciplinary training session). In this meeting, students are asked to reflect on their experiences in SBIRT training and also to discuss their ideas regarding the implementation of this training into their upcoming internship experiences. The purpose of this discipline-specific follow-up is to assess and solidify the integration of the interdisciplinary experiences into their development as professional counselors.
A comprehensive formal evaluation protocol also is in place for the interdisciplinary training program. Students from each of the participating disciplines complete pre- and post-training evaluation forms. During the first year of the project, formal follow-up evaluations were completed in four stages: (1) immediately after students completed the counseling program’s pre-module orientation session; (2) immediately after students completed each of the two interdisciplinary clinical training sessions; (3) six weeks after students completed the final interdisciplinary training session, and (4) six months following completion of the final interdisciplinary clinical training session. These evaluations solicit student self-perceptions of their own competence during the various training experiences and also ask for general feedback about the training process. The six-month follow-up evaluation process is meant to coincide with the students’ internship and residency experiences. The core objective of the final evaluation will be to assess the impact of interdisciplinary training on the students’ current interdisciplinary teamwork experiences.
Interdisciplinary Training Challenges
Interdisciplinary training and practice is complicated; sound logic and good intentions can easily be derailed by any number of intra- and interprofessional challenges. Here we will discuss challenges related to training in silos, and professional orientation, values and attitudes.
Training in Silos
The literature suggests that understanding the skills, knowledge and values of the various disciplines involved in an interdisciplinary collaboration is key to success (Wellmon, Gilin, Knauss, & Linn, 2012). Yet, this may be a challenge when professionals require specialized training that sometimes has the effect of narrowing their views and approaches to service delivery (Forrest, 2004). That is, it can be difficult for professionals to acquire the skills needed for communicating and collaborating across disciplines (Miller & Katz, 2014) when training in silos orients professionals to become strongly acculturated in their own language and practice styles.
We found in the interdisciplinary SBIRT project that these silo effects of discipline-specific training were apparent. It became clear immediately that most of the participants had strong discipline-specific skills and orientation allegiance, and many had little information about conditions and situations beyond their specific training area. This dynamic was evident at both faculty and trainee levels. Faculty had to navigate this dynamic during the process of planning and writing the grant proposal and negotiating the development of the training curriculum in the project’s advisory council (made up of program directors of participating disciplines). For example, the counseling director had to educate her medical practice peers on counselor education curriculum, counseling professional practice, and contexts of counseling practice. Further, the directors of counseling and social work had to educate peers on the similarities and differences between the two professions. At the same time, the directors of the family medicine and internal medicine disciplines had to educate their counseling and social work peers on the difference between the two specializations in medicine. Nursing faculty also addressed the distinct role of nurse practitioners in the field of medicine and the intersections between their roles and that of medical doctors.
At the trainee level, the discipline-specific skills and orientation allegiance was evident, particularly in both the brief intervention and the referral to treatment components of the interdisciplinary training sessions. For example, while many of the medical residents were articulate when explaining the physical effects of potential substance use to their professional clients, they were slow to pick up on sociocultural variables that may have been key to the etiology of the substance misuse (and for later referral) in these same cases. An example of this was a professional client who hinted at challenges with a transgender social location that appeared relevant to his substance misuse. This was not addressed by many of the medical residents and faculty, even when those variables were noted in the training module to be risk factors for substance misuse. This variable appeared to be more readily explored by the counseling and social work participants. Conversely, many of the counseling and social work participants struggled to articulate the medical symptoms, risk factors and ramifications of substance misuse that were so easily identified and explored by their peers in nursing and medicine.
A second example of the silo effects of discipline-specific training arose when participants were engaged in the referral to treatment training. After a few practice sessions, it became clear that many of the counseling and social work participants did not understand the difference between family and internal medicine practices, or when to refer to a nurse as opposed to a doctor. Conversely, many of the medical practitioners did not have a clear understanding of the role of social workers and counselors. Once noted, the program directors were able to address this gap in knowledge about participating professionals. For example, counseling and social work directors were able to educate the medical professionals about counseling and social work professional practice. This facilitated productive conversation about referral sources at the start of the subsequent training session; counseling and social work trainers were able to offer a more clear articulation of the professional training and role of their students. Anecdotes from a few of the medical residents and other trainers afterwards indicated that such information was useful for them in discussing referral to treatment in their practice groups. Clearly, knowing the practice parameters of colleagues is central to effective interdisciplinary practice (Wellmon et al., 2012). This knowledge should include some awareness of discipline-specific orientations, terminology and information regarding conceptual framework (McLean, 2012).
Professional Orientation, Attitudes and Values
Issues related to practicing in silos are further complicated by professional indoctrination, or professional identity orientation and development. Within each of the various helping professions, new practitioners are oriented to acquire their profession’s unique and specialized identity. For example, in the profession of counseling, the establishment of a unique professional identity is considered a foundational training practice, as demonstrated in the 20/20: A Vision for the Future of Counseling initiative (Kaplan & Gladding, 2011) and CACREP standards (CACREP, 2009). This intentional emphasis on professional identity in the counseling profession was promoted in order to emphasize the important philosophical beliefs that are the foundation of the profession (Mellin et al., 2011), to distinguish counselors from other helping professionals, to strengthen the profession, to assure licensure portability, and to establish a sense of pride (Mascari & Webber, 2013). According to Gibson, Dollarhide, and Moss (2010), new professionals are socialized into the language of their profession so as to learn what is expected of them, as well as what they can expect in practice—to behave as “native speakers” (p. 22) in their particular discipline. The challenge for counselor educators, as well as profession-specific educators in other related disciplines, is to teach students to navigate the complex dynamics of collaboration while maintaining a clear understanding of their own professional identity.
When professional identities are established in the context of practicing in silos, as well as competing for resources and job opportunities, interdisciplinary tensions may flourish. The results often are distance, barriers, mistrust and a lack of collegiality between disciplines (Arredondo, Shealy, Neale, & Winfrey, 2004; Miller & Katz, 2014). All of this is further complicated by “hierarchical schemas” (Delunas & Rouse, 2014, p. 101) in health care practice that award some individuals and professions more social capital than others (Bemak, 1998; Meyers, Hales, Young, Nesbitt, & Pomeroy, 2013). Clearly, interdisciplinary practice is hampered when some practitioners undervalue the perspectives of others (McLean, 2012).
In our training sessions, it was difficult to determine the extent to which differences in approach and conceptualization reflected different professional training orientations and professional identities or participants’ (and their professional mentors’) value orientations. That is, while it was clear that the different professions approached the practice components of SBIRT from a different lens, it also seemed that some of the participants valued their own training and knowledge over others. For example, in some of the discussion groups regarding the professional actor who played the role of a client who identified as transgender, some of the medical participants assertively questioned the utility of exploring gender orientation during the screening process. Most of the counseling and social work participants who actively explored the client’s gender orientation in their practice sessions sat in silence as their medical peers challenged faculty trainers on this point. Later, some of the counseling and social work participants described a sense of incompetence regarding knowledge about the medical aspects of substance misuse, as well as difficulties in countering the arguments raised by the medical residents, particularly those against exploring the client’s gender orientation during the screening process, an area in which they had competence.
The confident expression of dissenting opinions by some participants juxtaposed with the relative silence of others during disagreements regarding practice orientation may have been an artifact of how practitioners-in-training are exposed to and experience supervision, particularly when delivered by a professional outside of their own discipline. It also may have mirrored the dynamics of many interdisciplinary treatment teams, which tend to be shaped by professional social hierarchy discourses. Given the strong component of professional identity in the training of the counselors and social workers who participated in our SBIRT training, we wonder if the assertiveness and self-silencing that we witnessed reflects social factors at work that go beyond professional identity orientation. As mentioned by Delunas and Rouse (2014), professional hierarchies in the field and in the lay public put physicians “at the top” (p. 101) and until hierarchical profession-centered structures (Meyers et al., 2013) and power sharing (Bemak, 1998) are realized, interdisciplinary collaboration will be stymied.
Interdisciplinary Training Recommendations
Understanding the challenges that arise from practicing in silos brings up complex issues and political nuances that sit between providing specialized, discipline-specific training, and preparing practitioners to work across disciplines. Wellmon et al. (2012) reminded us that “the skills necessary to work effectively as a member of a healthcare team are not intuitive and cannot be learned exclusively ‘on the job’” (p. 26). Meyers et al. (2013) echoed this sentiment, pointing out that health care professionals simply are not taught teamwork skills. Bemak (1998) called for the deconstruction and redefinition of the counseling profession’s central paradigms so that interdisciplinary collaboration can be a core component of counseling. He also asserted that professional counselors must be provided important skills for engaging in interdisciplinary collaboration. A similar request is made of professionals from other disciplines. Ultimately, if we expect health care practitioners to engage in interdisciplinary practice, they must be trained to engage in such practice.
The literature on interdisciplinary work consistently articulates the difficulty in identifying specific factors that can contribute to effective interdisciplinary work, and it calls for more writing and research by participants in interdisciplinary training programs (Arredondo et al., 2004; Bemak, 1998; Forrest, 2004; Nancarrow et al., 2013; Reubling et al., 2014). Based on our experience in the SBIRT interdisciplinary training and extant research in the field, we offer recommendations for how to promote effective engagement in interdisciplinary work among counselors-in-training. Our recommendations are summarized below in the categories of promoting professional identity and boundaries and teaching skills for collaboration.
Professional Identity and Boundaries
Professional identity. Due to the silo effects of discipline-specific training, negotiating curriculum and training processes can be challenging in interdisciplinary collaborations. The needs of constituent groups within the training can easily be lost to the louder voices or privileged perspectives. Yet, Mascari and Webber (2006, 2013) and Mellin et al. (2011) pointed out that having a clear sense of one’s own professional identity and one’s scope of practice and also recognizing differences between counseling and other mental health disciplines enhances cross-discipline practice. These authors highlighted the importance of enlisting faculty representatives who are grounded in counselor and counselor educator identities, who also understand the value of interdisciplinary training and who have the interpersonal skills and expertise necessary for negotiating challenging interdisciplinary conversations. An understanding and appreciation of the interdisciplinary training protocol as a tool for enhancing professional interdisciplinary teamwork should be a core-guiding objective for counseling and all participating faculty members (Bemak, 1998), of course, but a solid grounding in one’s own professional identity also is critical.
We learned that counseling faculty must invest in preparing students for participation in interdisciplinary training. The preparation process should be progressive in nature with scheduled periodic check-in sessions, particularly during interdisciplinary clinical training. In our experience, the challenge of navigating professional roles and functions during the interdisciplinary clinical training sessions was most difficult for our students. Counseling students appeared to need multiple opportunities to process their interdisciplinary practice experiences. It was most beneficial to students when the participating faculty had a clear understanding of all the training protocols and processes.
Secondly, positive outcomes came from pre-coaching for skills and knowledge with students during the counseling program post-module review and skills practice review session, and encouraging them to have the confidence to speak up about their concerns, professional differences, identities, and even to volunteer to demonstrate their skills when in the interdisciplinary training sessions. This is consistent with the Reubling et al. (2014) findings in a study comparing students’ attitudes and perceptions in pre- and post-training experiences. Our experience highlighted the value of openly discussing the differences in professional and social capital in society and the impact that those differences have on students’ approaches to the interdisciplinary training experience. Such discussions helped boost students’ confidence to acknowledge issues that they avoided addressing in the initial phases of the training. Having a clear feedback loop from students to faculty, so that faculty can provide feedback to fellow collaborators at subsequent interdisciplinary training sessions, was particularly beneficial.
Finally, having a clear protocol for interventions with non-cooperative and challenging students was beneficial. For example, counseling students were required to sign a behavior and participation contract that was submitted prior to engagement in the interdisciplinary clinical training portions of the program. The foresight by the counseling program to request this contract may have been why no counseling student was cited for behavioral concerns during the interdisciplinary clinical training sessions. There were a handful of participants in other disciplines who required intervention from their own program directors regarding behavioral concerns emerging during interactions with training faculty who were not in their discipline area.
Professional boundaries. For this counselor education program’s faculty, it was necessary to have a good sense of the boundaries of engagement during the project’s initiation phases. Interdisciplinary training collaborations require much compromise in the curriculum development and training implementation phase; we wanted to be sure that the interdisciplinary training program would enhance rather than compromise the training experience of counseling students. We were consistently willing to compromise and accommodate other disciplines’ perspectives, so long as training processes that are essential to the training of counselors were incorporated in the interdisciplinary training protocol. This is consistent with the recommendations of Nancarrow et al. (2013) regarding interdisciplinary training participants needing to understand and respect the professional roles, functions and boundaries of collaborators.
An example of this negotiated process happened after the first year of collaboration, when counseling faculty suggested changes in the scenarios presented to professional actors playing the roles of clients in the clinical component of the training. During the first year, the preparation of the professional actors was handled solely by a staff member employed by the medical school. As a result, the bulk of their presenting concerns were medical in nature. The majority of the professional actors appeared unprepared to discuss their psychological and sociocultural concerns. This was a major factor that affected collaboration because it made the initial practice session challenging for counseling and social work students who understandably felt that discussing medical presenting concerns was out of the scope of their competence and practice. During the second year of the training cycle, counseling faculty submitted case scenarios for the professional actors that started with an initial contact at a school or clinical mental health setting and that represented varied sociocultural and emotional concerns that coexist with physical medical concerns. This approach was intended to ensure that counseling students would be able to experience clinical training with case scenarios that were within their scope of study and practice and also allow them to practice making referrals to social workers and medical professionals.
Additionally, counseling and social work faculty, the two disciplines outside the medical field, actively advocated for all case scenarios used in the training to be truly interdisciplinary in nature. This meant that all the presenting concerns presented by the professional actors needed to provide an opportunity for an interdisciplinary intervention during the referral process. Negotiating these changes in the second year was easier given the professional relationships, trust and mutual respect that had evolved over the year among faculty from the different participating disciplines. Our challenges in negotiating the professional weighting of the training processes are not unusual and are consistent with what Mascari and Webber (2006, 2013) and Mellin et al. (2011) discussed regarding the challenges inherent to cross-discipline practice among professionals who have received specialized training and who have unique professional identities. We should have never assumed that the coordinator of the professional actors, who is based in the medical school, would understand how to prepare the actors to engage with students in a manner that would allow for an interdisciplinary intervention.
During the second year, faculty from the counseling program were more actively involved in the development of scenarios and instructions that would be shared with the professional actors playing the role of clients/patients in the project. In hindsight, the university SBIRT advisory council should have spent more time in deliberations about the potential obstacles that would emerge from interdisciplinary collaboration. We were excited about this new initiative and spent more time discussing the benefits and potential challenges for students rather than for the faculty and staff involved in the project. Thus, some identified challenges persisted in the second year.
Interdisciplinary focus as a goal. We realized the importance of all key participants (faculty and program directors) having a clear understanding of the interdisciplinary training goal of this project. For example and as mentioned, counseling faculty had to advocate multiple times for an interdisciplinary outlook as the curriculum and training protocol was planned and developed. In hindsight, we realize that while the core focus of the project was interdisciplinary training, participants and trainers seemed to return to familiar patterns of silo training as the project was carried out. We are reminded that an interdisciplinary focus requires constant reminders and intentionality to keep the focus interdisciplinary.
Another artifact of the challenges inherent to interdisciplinary initiatives that emerged was that it appeared participants (students) were not fully prepared to receive feedback during the training from faculty who were not in their own discipline. After the first year of implementation, the program directors placed more emphasis and deliberated at length on how to assist trainees with navigating the dynamics of interdisciplinary training, and a protocol was discussed for addressing student-related training challenges. However, as mentioned above, a similar process was not identified for participating faculty and program directors. That is, at the director level, a process was not articulated for how to assure a truly interdisciplinary focus would be honored during the planning and implementation stages of the project, nor was a protocol developed to articulate how professional disagreements would be managed. While a process for navigating professional differences emerged organically, the absence of such a conversation in the early stages caused tense deliberations as participating faculty and program directors tried to communicate their professional boundaries, roles and functions. Therefore, we recommend that interdisciplinary teams develop protocols for addressing differences in perspectives for both students and training faculty. There is value in investing in leadership that understands the practice of the various disciplines involved in a project and has a commitment to infusing interdisciplinary and collaborative practices in every aspect of a training program (Nancarrow et al., 2013).
Skills for Collaboration
As previously mentioned, some authors have suggested that interdisciplinary collaboration requires particular skills or competencies (e.g., Arredondo et al., 2004; Bemak, 1998; Delunas & Rouse, 2014; Meyers et al., 2013) that are not regularly taught to health care professionals. These authors suggested that working in interdisciplinary teams also requires particular attitudes and special knowledge that are communicated through interpersonal skills.
Collaboration attitudes. Working with others across disciplines requires a certain spirit or willingness to share, collaborate and respect others (Nancarrow et al., 2013). This includes avoiding judgment, working in the spirit of “joining” (Miller & Katz, 2014, p. 7), and overcoming professional hostilities, prejudices or phobias (Bemak, 1998). It also requires openness to collective decision making, an ability to redefine one’s role in an interpersonal context (Bemak, 1998) and demonstrating a sentiment of appreciation and accommodation to multiple perspectives (Arredondo et al., 2004). Included here is an ability to be flexible—to “share your street corner” as Miller and Katz (2014, p. 10) put it, or “playing well” with others (Arredondo et al., 2004, p. 791).
Being flexible also means remembering that one professional orientation/approach is not the only valid approach (Bemak, 1998); it requires an ability to be uncomfortable—“leaning into discomfort” (Miller & Katz, 2014, p. 8). An attitude of collaboration also requires being open to feedback (Nancarrow et al., 2013) and a willingness to negotiate power (Bemak, 1998; McLean, 2012). In our SBIRT training project, it appeared that a true spirit of collaboration developed over time among trainers. Its development appeared to emerge, as the examples from earlier discussions in this article illustrate, from the assertiveness and confidence as much as from the flexibility of faculty who may have otherwise been marginalized from decision making. Thus, it is possible that collaborative attitudes are more likely to develop when everyone in the group has had an opportunity to contribute, whether by invitation or self-assertiveness. It is essential to highlight the fact that even counseling and social work faculty, who have been trained to be open to multiple perspectives, engaged from time to time in their familiar silo foundation to professional orientation.
Collaboration knowledge. Interdisciplinary practice requires that individuals have professional competence in their own areas of expertise (Nancarrow et al., 2013) as well as an ability to effectively communicate this discipline-specific information effectively to others (Wellmon et al., 2012). It also requires an ability to learn about the language and roles that define other disciplines (Miller & Katz, 2014; Nancarrow et al., 2013). Knowledge about organizations or systems theory, as well as models of consultation, also is extremely helpful to professionals working across disciplines (Arredondo et al., 2004). Arredondo et al. (2004) and McLean (2012) point to a need to have an intuitive understanding of interpersonal and group dynamics. Finally, Arredondo et al. suggested that awareness of one’s own beliefs, values and personal history—all of which are at play when interacting with others—and having “emotional intelligence” (p. 794) are necessary for effective interdisciplinary participation. It appears that as the various members of the interdisciplinary training team in our project asserted their voices at the decision-making table in our project, other trainers were able to learn more about discipline-specific practices and training needs. In order for this process to happen in a way that did not alienate others, we found it necessary to make careful decisions about what to say where and when. Knowledge of how to work in groups and teams was critical, especially for the professionals who were at risk of marginalization in the “collaborative” process.
Collaboration skills. The display of collaboration skills is predicated upon a firm grounding in collaborative attitudes and requisite knowledge, including those mentioned above. Putting these ideas into practice requires strong interpersonal skills such as listening, empathy, humor, facilitation, assessment (Arredondo et al., 2004), ability to participate in power sharing (McLean, 2012), and being able to use feedback to make subsequent changes (Nancarrow et al., 2013). Collaboration also requires problem-solving and decision-making skills (Nancarrow et al., 2013; Wellmon et al., 2012) as well as assertiveness, confidence and ability to communicate one’s ideas appropriately (Miller & Katz, 2014; Nancarrow et al., 2013). Finally, most agree that skills for collaboration include being flexible (Arredondo et al., 2004; Miller & Katz, 2014). Power sharing is possible when participants demonstrate competence in their area of expertise as well as interest in learning about collaborators’ fields of specialization. As already noted in our training project, the demonstration of professional competence, confidence and the ability to engage interpersonally in the spirit of collaboration and collegiality created an opportunity for power sharing. We also noticed in the SBIRT project that when we were flexible and willing to accommodate other’s beliefs and values, they in turn made efforts to accommodate ours.
Conclusion
Counselor educators need to examine pedagogical means of providing counseling students with the knowledge, values and skills to work effectively in interdisciplinary teams. For one counselor education program, the experience of interdisciplinary training provoked passionate dialogue among students and faculty regarding their professional roles, functions, professional advocacy and positioning among other behavioral health professionals. Multiple opportunities for exploring interdisciplinary training and professional identity development processes were evident in the training project described in this article.
Of course, learning about interdisciplinary collaboration does not need to happen solely within a project such as this. Counseling internships typically offer an abundance of opportunities for interdisciplinary collaboration, and the points raised in this article are relevant to all training venues available for counseling students. As mentioned, providing counselors-in-training with a firm foundation in professional orientation both in terms of philosophical underpinnings as well as a clear understanding of their future scope of practice are critical. Additionally, instruction on the scope of practice and roles of other professionals with whom they may be working in practice settings is important. Assuring that counselors enter into internship settings with adequate competence is, of course, critical. But additionally, providing students with positive appropriate feedback so they develop a clear sense of confidence is equally as important for work in collaborative settings. Finally, offering counseling students “pre-training” in collaborative practice, including the requisite skills and attitudes mentioned in this article, is an important component of preparing counselors for interdisciplinary practice. In training sessions such as these, counseling students should be coached to talk about the work they are trained to do, required to assert their perspective in treatment team decision making and offered feedback on the ways in which their voices are heard by others.
In terms of future directions, an exploration of counseling students’ perceptions of the impact of interdisciplinary training on their professional identity development and their ability to work with interdisciplinary teams would be valuable for the field. The outcome of such a study might increase the understanding of the pedagogical experiences that enhance interdisciplinary work competencies for counselors.
STATEMENT OF FUNDING
The interdisciplinary training initiative reported in this publication is part of the Vermont SBIRT Training Collaborative funded by the Substance Abuse and Mental Health Services Administration (SAMHSA), Grant #TI025395-01. The content is solely the responsibility of the authors and does not necessarily represent the official views of SAMHSA.
References
Agerwala, S. M., & McCance-Katz, E. F. (2012). Integrating screening, brief intervention, and referral to treatment (SBIRT) into clinical practice settings: A brief review. Journal of Psychoactive Drugs, 44, 307–317. doi:10.1080/02791072.2012.720169
American Counseling Association. (2014). ACA code of ethics. Alexandria, VA: Author.
Arredondo, P., Shealy, C., Neale, M., & Winfrey, L. L. (2004). Consultation and interprofessional collaboration: Modeling for the future. Journal of Clinical Psychology, 60, 787–800. doi:10.1002/jclp.20015
Bemak, F. (1998). Interdisciplinary collaboration for social change: Redefining the counseling profession. In C. C. Lee & G. R. Walz (Eds.), Social action: A mandate for counselors (pp. 279–292). Greensboro, NC: ERIC/CASS.
Collin, A. (2009). Multidisciplinary, interdisciplinary, and transdisciplinary collaboration: Implications for vocational psychology. International Journal for Education and Vocational Guidance, 9, 101–110. doi:10.1007/s10775-009-9155-2
Council for the Accreditation of Counseling and Related Programs (CACREP). (2009). CACREP accreditation standards and procedures manual. Alexandria, VA: Author.
Davoudi, M., & Rawson, R. A. (2010). Screening, brief intervention, and referral to treatment (SBIRT) initiatives in California: Notable trends, challenges, and recommendations. Journal of Psychoactive Drugs, 42, 239–248. doi:10.1080/02791072.2010.10400547
Delunas, L. R., & Rouse, S. (2014). Nursing and medical student attitudes about communication and collaboration before and after an interprofessional education experience. Nursing Education Perspectives, 35, 100–105. doi:10.548Q/11-716.1
Forrest, L. (2004). Moving out of our comfort zones: School counseling/counseling psychology partnerships. The Counseling Psychologist, 32, 225–234. doi:10.1177/0011000003261368
Gibson, D. M., Dollarhide, C. T., & Moss, J. M. (2010). Professional identity development: A grounded theory of transformational tasks of new counselors. Counselor Education and Supervision, 50, 21–38.
Institute of Medicine (U.S.), Greiner, A., & Knebel, E. (2003). Health professions education: A bridge to quality. Washington, DC: National Academies Press.
Kaplan, D. M., & Gladding, S. T. (2011). A vision for the future of counseling: The 20/20 “Principles for Unifying and Strengthening the Profession.” Journal of Counseling & Development, 89, 367–372. doi:10.1002/j.1556-6678.2011.tb00101.x
Mascari, J. B., & Webber, J. M. (2006). Salting the slippery slope: What licensing violations tell us about preventing dangerous ethical situations. In G. Walz, J. Bleuer, & R. Yep (Eds.), VISTAS: Compelling perspectives on counseling 2006 (pp. 165–168). Alexandria, VA: American Counseling Association.
Mascari, J. B., & Webber, J. (2013) CACREP accreditation: A solution to license portability and counselor identity problems. Journal of Counseling & Development, 91, 15–25. doi:10.1002/j.1556-6676.2013.00066.x
McLean, S. (2012), Barriers to collaboration on behalf of children with challenging behaviours: A large qualitative study of five constituent groups. Child & Family Social Work, 17, 478–486. doi:10.1111/j.1365-2206.2011.00805.x
McNair, R. P. (2005). The case for educating health care students in professionalism as the core content of interprofessional education. Medical Education, 39, 456–464. doi:10.1111/j.1365-2929.2005.02116.x
Mellin, E. A., Hunt, B., & Nichols, L. M. (2011). Counselor professional identity: Findings and implications for counseling and interprofessional collaboration. Journal of Counseling & Development, 89, 140–147. doi:10.1002/j.1556-6678.2011.tb00071.x
Meyers, F. J., Hales, R. E., Young, H. M., Nesbitt, T. S., & Pomeroy, C. (2013). Restructuring academic health centers to advance interdisciplinary collaborations: Opportunities for psychiatry departments. Academic Psychiatry, 37, 72–75. doi:10.1176/appi.ap.11120209
Miller, F. A., & Katz, J. H. (2014). 4 keys to accelerating collaboration. OD Practitioner, 46, 6–11. Retrieved from: https://c.ymcdn.com/sites/odnetwork.site-ym.com/resource/resmgr/2015_Awards/ODP-V46,No1-Miller_and_Katz.pdf
Mitchell, S. G., Gryczynski, J., Gonzales, A., Moseley, A., Peterson, T., O’Grady, K. E., & Schwartz, R. P. (2012). Screening, brief intervention, and referral to treatment (SBIRT) for substance use in a school-based program: Services and outcomes. The American Journal on Addictions, 21, S5–S13. doi:10.1111/j.1521-0391.2012.00299.x
Morphet, J., Hood, K., Cant, R., Baulch, J., Gilbee, A., & Sandry, K. (2014). Teaching teamwork: An evaluation of an interprofessional training ward placement for health care students. Advances in Medical Education and Practice, 5, 197–204. doi:10.2147/AMEP.S61189
Nancarrow, S. A., Booth, A., Ariss, S., Smith, T., Enderby, P., & Roots, A. (2013). Ten principles of good interdisciplinary team work. Human Resources for Health, 11(19), 1–11. doi:10.1186/1478-4491-11-19
O’Brien, B. (Producer & Director). (2013). The hungry heart [Motion picture]. United States: Kingdom County Productions.
Pollard, K. C., & Miers, M. E. (2008). From students to professionals: Results of a longitudinal study of attitudes to pre-qualifying collaborative learning and working in health and social care in the United Kingdom. Journal of Interprofessional Care, 22, 399–416. doi:10.1080/13561820802190483
Reubling, I., Pole, D., Breitbach, A. P., Frager, A., Kettenbach, G., Westhus, N., Kienstra, K., & Carlson, J. (2014). A comparison of student attitudes and perceptions before and after an introductory interprofessional education experience. Journal of Interprofessional Care, 28, 23–27. doi:10.3109/13561820.2013.829421
Wellmon, R., Gilin, B., Knauss, L., & Linn, M. I. (2012). Changes in student attitudes toward interprofessional learning and collaboration arising from a case-based educational experience. Journal of Allied Health, 41, 26–34.
Jane E. Atieno Okech, NCC, and Anne M. Geroski are Associate Professors at the University of Vermont. Correspondence can be addressed to Jane Okech, Mann Hall 101B, 208 Colchester Avenue, Burlington, VT 05405, jokech@uvm.edu.
