Oct 31, 2023 | Volume 13 - Issue 3
Wesley B. Webber, W. Leigh Atherton, Kelli S. Russell, Hilary J. Flint, Stephen J. Leierer
The COVID-19 pandemic and efforts to manage it have affected mental health around the world. Although early research on the COVID-19 pandemic showed a general decline in mental health after the pandemic began, mental health in later stages of the pandemic might be improving alongside other changes (e.g., availability of vaccines, return to in-person activities). The present study utilized data from a mental health service intervention for individuals at a southeastern university who were exposed to COVID-19 following the university’s return to in-person operations. This study tested whether time period (August–September 2021 vs. January–February 2022) predicted individuals’ likelihood of being mild or above in depression and anxiety ratings. Results showed that individuals were more likely to be mild or above in both depression and anxiety ratings during August–September of 2021 than January–February of 2022. Suggestions for future research and implications for professional counselors are discussed.
Keywords: COVID-19, mental health, depression, anxiety, university
The novel coronavirus (COVID-19), first detected in 2019, spread globally at a rapid pace, with the first confirmed case in the United States occurring on January 20, 2020, in the state of Washington (Centers for Disease Control and Prevention [CDC], 2023). By April 2020, the United States had the most reported deaths in the world due to COVID-19. It was not until December of 2020 that the first round of vaccines, authorized under emergency use authorization, was made available (Food and Drug Administration [FDA], 2021). As of October 2022 in the United States, a total of 97,063,357 cases of COVID-19 had been reported, from which there were 1,065,152 COVID-19–related deaths (CDC, 2023). A reported 111,367,843 individuals aged 5 and above in the United States had received their first booster dose of a COVID-19 vaccine as of October 2022 (CDC, 2023). Previous research has shown that the COVID-19 pandemic and efforts to manage it (e.g., lockdowns, quarantine, isolation) had negative effects on mental health in the United States and internationally (Huckins et al., 2020; Pierce et al., 2020; Son et al., 2020). Based on the extended duration of the pandemic and changes that have occurred during it (e.g., vaccine availability, lessening of initial social restrictions), more recent research has investigated possible changes in mental health in later stages of the COVID-19 pandemic (Fioravanti et al., 2022; McLeish et al., 2022; Tang et al., 2022). The present study adds to this literature by exploring whether psychosocial symptomatology (i.e., depression and anxiety) at a university in the Southeastern United States differed in individuals exposed to COVID-19 during August–September 2021 as compared to individuals exposed to COVID-19 during January–February 2022 (following the university’s return to on-campus operations in August 2021).
Challenges to Mental Health During the COVID-19 Pandemic
Since the beginning of the COVID-19 pandemic, conceptual and empirical research has focused on ways in which the pandemic and associated stressors might impact mental health (Bzdok & Dunbar, 2020; Marroquín et al., 2020; Şimşir et al., 2022). Implementation of lockdowns to deter spread of the virus led to concerns that social isolation might have severe impacts on mental health (Bzdok & Dunbar, 2020). This hypothesis was empirically supported, as stay-at-home orders and individuals’ reported levels of social distancing were positively associated with depression and anxiety (Marroquín et al., 2020). Individuals’ views on the COVID-19 pandemic evolved quickly at the outset of the pandemic, and perceptions of risk were shown to increase during the pandemic’s first week in the United States (Wise et al., 2020). Growing awareness of the dangers of the virus likely had deleterious effects on mental health; Şimşir et al. (2022) found through a meta-analysis that fear of COVID-19 was associated with a variety of mental health problems. Mental health was also negatively affected by stigmatization associated with the COVID-19 pandemic, as was the case for those exposed to COVID-19 while at their place of work (Schubert et al., 2021). Such stigmatization associated with COVID-19 exposure was found to increase risk for depression and anxiety (Schubert et al., 2021).
The lockdowns and social distancing measures that accompanied early stages of the COVID-19 pandemic also resulted in changes to routines that likely impacted mental health. For some individuals facing lockdowns or other disruptions to typical routines, reductions in physical activity occurred. Individuals who reported greater impact of COVID-19 on their level of physical activity showed greater symptoms of depression and anxiety (Silva et al., 2022). Early in the COVID-19 pandemic, based on people’s increased time spent at home and their concerns about COVID-19 developments, some people increased their media usage (e.g., news outlets, social media). Such increases in media usage were associated with decreases in mental health (Meyer et al., 2020; Riehm et al., 2020). The COVID-19 pandemic had less significant impact on mental health for those with greater tolerance of uncertainty (Rettie & Daniels, 2021) and psychological flexibility (Dawson & Golijani-Moghaddam, 2020). Thus, some individuals were uniquely suited to face the many changes and stressors brought about by the COVID-19 pandemic.
One population that previous research has identified as being especially at risk for negative mental health outcomes during the COVID-19 pandemic is college students (Xiong et al., 2020). For college students, the COVID-19 pandemic occurred alongside other stressors known to be typical for this population such as adjusting to leaving home, navigating new peer groups, and making career decisions (Beiter et al., 2015; Liu et al., 2019). Thus, for many college students, the COVID-19 pandemic disrupted a period of life already filled with many transitions. For example, shortly after the COVID-19 pandemic began, many college students were forced to leave their dormitories and peers as universities transitioned to online delivery of classes (Copeland et al., 2021). Xiong et al. (2020) found through a systematic review that college students were especially vulnerable to negative mental health outcomes at the outset of the COVID-19 pandemic as compared to others in the general population. In the United States, college students’ reported degree of life disruption due to the COVID-19 pandemic was positively associated with depression at the conclusion of the spring 2020 semester (Stamatis et al., 2022). During fall 2020, COVID-19 concerns and previous COVID-19 infection were each found to be associated with higher levels of depression and anxiety among U.S. college students (Oh et al., 2021). Overall, previous research has supported the notion that changes associated with the COVID-19 pandemic had general negative effects on mental health in the general population and in college students specifically.
Changes in Psychosocial Symptomatology Across the COVID-19 Pandemic
Although research has shown that the COVID-19 pandemic introduced unprecedented challenges and stressors that were associated with mental health problems, another important direction for research has been to characterize overall changes in psychosocial symptomatology as the COVID-19 pandemic progressed. Such research is important given that individuals might psychologically adapt to constant COVID-19 stressors or might benefit from changes that have occurred as the COVID-19 pandemic has progressed (e.g., vaccine availability, lessening of societal restrictions). Initial longitudinal studies comparing individuals’ symptomatology before the COVID-19 pandemic and after its beginning showed that mental health deteriorated after the COVID-19 pandemic began (Elmer et al., 2020; Huckins et al., 2020; Pierce et al., 2020). Prati and Mancini (2021) conducted a meta-analysis of 28 studies that used longitudinal or natural experimental designs and found that depression and anxiety showed small but statistically significant increases after implementation of the initial lockdowns in response to COVID-19. The various changes to ways of life associated with the COVID-19 pandemic appeared to result in a general deterioration in mental health.
Previous research has also explored possible changes in mental health beyond those that were observed in the initial phase of the COVID-19 pandemic. In support of the notion that individuals adapted to changes associated with the COVID-19 pandemic, Fancourt et al. (2021) found that anxiety and depression decreased across the initial lockdown period in the United Kingdom. In contrast, Ozamiz-Etxebarria et al. (2020) found that levels of depression and anxiety were higher 3 weeks into the initial lockdown period in Spain as compared to the beginning of the lockdown. Fioravanti et al. (2022) assessed psychological symptoms longitudinally in an Italian sample at three time points—the beginning of the COVID-19 pandemic and first lockdown (March 2020), the end of the first lockdown phase (May 2020), and during a second wave of COVID-19 with increased societal restrictions (November 2020). Their findings pointed to possible influences of COVID-19 waves and societal restrictions on specific psychosocial symptoms. Specifically, depression, anxiety, obsessive-compulsive disorder, and post-traumatic stress disorder all decreased at the end of the first lockdown phase (Fioravanti et al., 2022). However, all symptoms besides obsessive-compulsive disorder significantly increased from the end of the first lockdown phase to the second wave of COVID-19 (Fioravanti et al., 2022).
Recent research on mental health among college students in later stages of the COVID-19 pandemic has also focused on possible mental health changes over time (McLeish et al., 2022; Tang et al., 2022). Tang et al. (2022) reported reductions in anxiety and depression in a longitudinal study of university students in the United Kingdom between a first time point (July–September 2020, after the end of lockdown) and a second time point (January–March 2021, when vaccinations were becoming available). In contrast, McLeish et al. (2022) found through a repeated cross-sectional study that depression and anxiety among students at a specific university increased from spring 2020 to fall 2020, with the increases being maintained in spring 2021. The authors noted that vaccines were not widely available at the university until the end of spring 2021 (McLeish et al., 2022). Thus, recent studies have found mixed results as to whether psychosocial symptomatology improved over time during the COVID-19 pandemic. These discrepancies may be due to contextual differences between studies (e.g., differences in data collection time periods, availability of vaccines, or levels of COVID-19 restrictions being implemented during data collection).
The Present Study
The present study was conducted based on the need for continued research on mental health across the evolving COVID-19 pandemic and based on previous conflicting findings on possible mental health changes in later stages of the COVID-19 pandemic. Given previous research showing detrimental effects of the COVID-19 pandemic on mental health in the general population and in college students, the present study utilized data from a university population. Specifically, an archival dataset was used in the present study to examine data collected during 2021–2022 at a university in the Southeastern United States and to test whether time period would predict severity of depression and anxiety symptoms. Individuals in the study had been exposed to COVID-19 between August–September 2021 or between January–February 2022 and had requested a mental health contact during university-conducted contact tracing. These two time periods corresponded to surges in COVID-19 cases at the university due to the delta and omicron COVID-19 variants, respectively. August–September 2021 also coincided with a return to on-campus operations at the university and therefore captured psychosocial symptomatology at the beginning of a significant transition in the COVID-19 pandemic (i.e., a return to organized in-person activities on a college campus during the evolving pandemic). This study was designed to answer the following research questions:
- Among those requesting mental health contact after COVID-19 exposure, was the likelihood of having at least mild depression symptoms different for those whose contact occurred between August–September 2021 as compared to those whose contact occurred between January–February 2022?
- Among those requesting mental health contact after COVID-19 exposure, was the likelihood of having at least mild anxiety symptoms different for those whose contact occurred between August–September 2021 as compared to those whose contact occurred between January–February 2022?
Method
Design
A retrospective research design was used to analyze the possible effect of time period on severity of depression and anxiety symptoms among members of a university population who had been exposed to COVID-19 and requested a mental health check-in. The study used a de-identified dataset obtained from the service providers who completed the mental health check-in. We confirmed through consultation with the IRB that the use of archival, de-identified data does not necessitate IRB review.
COVID-19 Mental Health Check-In Dataset
The archival, de-identified dataset used in the present study was compiled as part of a mental health service occurring between February 2021 and February 2022. Participants in the dataset had tested positive for COVID-19 or been exposed to COVID-19 without a positive test. During university-conducted contact tracing, they were offered and elected to receive a subsequent mental health check-in. Individuals who were contact traced and thereby offered a mental health check-in had become known to contact tracers through one of two routes: (a) they reported their own COVID-19 diagnosis or exposure through a self-reporting mechanism as instructed by the university, or (b) they were reported by another individual as having been diagnosed with or exposed to COVID-19. The dataset used in this study included data collected during the mental health check-ins for those who elected to receive them. This data was collected over the phone and documented in RedCap (a secure web browser–based survey protocol designed for clinical research) at the time of the phone call or within 24 hours. The dataset consisted of data for 211 individuals’ check-ins. For each check-in, the dataset included participants’ demographic information, screening data (for depression, anxiety, and trauma), identified needs of the participant, resources shared with the participant, and the date of data entry.
The present study focused on check-in data for all individuals from the COVID-19 Mental Health Check-in Dataset whose check-in had occurred during one of the two time periods of focus—August–September 2021 or January–February 2022. These two time periods corresponded to surges in COVID-19 cases at the university associated with the delta and omicron COVID-19 variants, respectively. The 149 individuals who checked in during these 4 months represented 70.62% of the total number of check-ins over the 12-month dataset (N = 211), reflecting the surges in COVID-19 cases during these two periods. Of the 149 individuals in the present study, 96 (64.43%) received their check-in during August–September 2021, and 53 (35.57%) received their check-in during January–February 2022. The selection of these two time periods from the larger dataset allowed for comparison of psychosocial symptomatology during comparable levels of COVID-19 infection (i.e., surges associated with two subsequent COVID-19 variants) at comparable points in subsequent academic semesters (i.e., the first 2 months of the fall 2021 and spring 2022 semesters). The present study used only the screening data for depression and anxiety, as the scales for each of these constructs showed good internal consistency (Cronbach’s alpha > .80).
Participants
The sample in the present study consisted of 149 individuals. The selected individuals’ ages ranged from 17 to 52 (M = 22.21, SD = 7.43). With regard to gender, 67.11% identified as female, 32.21% as male, and 0.67% as non-binary. The reported races of individuals in the study were as follows: 60.4% White, 20.13% African American, 6.71% Hispanic, 3.36% Other, 2.68% Two or more races, 1.34% Middle Eastern, 1.34% Native American, and 0.67% Asian. Some participants preferred not to indicate their race (3.36%). In responding to a question about their ethnicity, 87.25% of individuals identified as not Latinx, 9.40% identified as Latinx, and 3.36% preferred not to answer. With regard to academic level/job title, 32.89% were freshmen, 20.13% were sophomores, 14.09% were juniors, 15.44% were seniors, 7.38% were graduate students, 8.05% were faculty/staff, and 2.01% preferred not to answer. Regarding employment, 53.69% were not employed (including students), 30.20% were employed part-time, 12.75% were employed full-time, and 3.36% preferred not to answer. The relationship statuses of individuals were reported as the following: 87.92% single (never married), 4.7% married, 2.01% single but cohabitating with a significant other, 1.34% in a domestic partnership or civil union, 1.34% separated, 0.67% divorced, and 2.01% preferred not to answer. Table 1 summarizes demographic responses within each of the two time periods and for the full sample.
Measures
Demographic Questionnaire
Participants responded to seven demographic questions (age, gender, race, ethnicity, academic year/job title, current employment status, and relationship status). They were informed that this information was optional and that they could choose not to answer particular questions.
Table 1
Demographic Characteristics of the Sample
|
Demographic
Characteristic |
|
| August–September 2021 |
January–February 2022 |
Full Sample |
|
n |
% |
n |
% |
n |
% |
| Gender |
|
|
|
|
|
|
| Female |
69 |
71.88 |
31 |
58.49 |
100 |
67.11 |
| Male |
27 |
28.13 |
21 |
39.62 |
48 |
32.21 |
| Non-binary |
0 |
0 |
1 |
1.89 |
1 |
0.67 |
| Race |
|
|
|
|
|
|
| White |
56 |
58.33 |
34 |
64.15 |
90 |
60.40 |
| African American |
23 |
23.96 |
7 |
13.21 |
30 |
20.13 |
| Hispanic |
8 |
8.33 |
2 |
3.77 |
10 |
6.71 |
| Other race |
1 |
1.04 |
4 |
7.55 |
5 |
3.36 |
| Two or more races |
4 |
4.17 |
0 |
0 |
4 |
2.68 |
| Middle Eastern |
2 |
2.08 |
0 |
0 |
2 |
1.34 |
| Native American |
1 |
1.04 |
1 |
1.89 |
2 |
1.34 |
| Asian |
1 |
1.04 |
0 |
0 |
1 |
0.67 |
| Prefer not to answer |
0 |
0 |
5 |
9.43 |
5 |
3.36 |
| Ethnicity |
|
|
|
|
|
|
| Not Latinx |
82 |
85.42 |
48 |
90.57 |
130 |
87.25 |
| Latinx |
12 |
12.50 |
2 |
3.77 |
14 |
9.40 |
| Prefer not to answer |
2 |
2.08 |
3 |
5.66 |
5 |
3.36 |
| Academic Year / Job Title |
|
|
|
|
|
|
| Freshman |
38 |
39.58 |
11 |
20.75 |
49 |
32.89 |
| Sophomore |
18 |
18.75 |
12 |
22.64 |
30 |
20.13 |
| Junior |
15 |
15.63 |
6 |
11.32 |
21 |
14.09 |
| Senior |
15 |
15.63 |
8 |
15.09 |
23 |
15.44 |
| Graduate Student |
6 |
6.25 |
5 |
9.43 |
11 |
7.38 |
| Faculty/Staff |
4 |
4.17 |
8 |
15.09 |
12 |
8.05 |
| Prefer not to answer |
0 |
0 |
3 |
5.66 |
3 |
2.01 |
| Employment |
|
|
|
|
|
|
| Not Employed (including student) |
62 |
64.58 |
18 |
33.96 |
80 |
53.69 |
| Employed Part-Time |
26 |
27.08 |
19 |
35.85 |
45 |
30.20 |
| Employed Full-Time |
8 |
8.33 |
11 |
20.75 |
19 |
12.75 |
| Prefer not to answer |
0 |
0 |
5 |
9.43 |
5 |
3.36 |
| Relationship Status |
|
|
|
|
|
|
| Single, never married |
87 |
90.63 |
44 |
83.02 |
131 |
87.92 |
| Married |
3 |
3.13 |
4 |
7.55 |
7 |
4.70 |
| Single, but cohabitating with a
significant other |
2 |
2.08 |
1 |
1.89 |
3 |
2.01 |
| In a domestic partnership or civil union |
2 |
2.08 |
0 |
0 |
2 |
1.34 |
| Separated |
2 |
2.08 |
0 |
0 |
2 |
1.34 |
| Divorced |
0 |
0 |
1 |
1.89 |
1 |
0.67 |
| Prefer not to answer |
0 |
0 |
3 |
5.66 |
3 |
2.01 |
| Note. Average age was 21.51 (SD = 6.98) in August–September 2021 group, 23.49 (SD = 8.11) in January–February 2022 group, and 22.21 (SD = 7.43) in the full sample. |
Patient Health Questionnaire-9 (PHQ-9)
The Patient Health Questionnaire-9 (PHQ-9; Kroenke et al., 2001) is a 9-item self-report questionnaire that measures the frequency and severity of depression symptoms over the past 2 weeks. The PHQ-9 has been validated for screening for depression in the general population (Kroenke et al., 2001; Martin et al., 2006). The questionnaire measures frequency of symptoms such as “feeling down, depressed, or hopeless,” and “little interest or pleasure in doing things.” The PHQ-9 uses a 4-point Likert scale to measure frequency of symptoms over the past 2 weeks with the response options of not at all, several days, more than half the days, and nearly every day. Scores of 0, 1, 2, and 3 are assigned to each of the four response categories, and a PHQ-9 total score is derived by adding the scores for each of the nine PHQ-9 items. Minimal depression is indicated by PHQ-9 total scores of 0–4, mild depression by scores of 5–9, moderate depression by scores of 10–14, moderately severe depression by scores of 15–19, and severe depression by scores of 20–27. Question 9 on the PHQ-9 is a single screening question assessing suicide risk. Interviewers were trained in appropriate protocol in the event of a positive screen for this question. Cronbach’s alpha for the PHQ-9 in the present study was .86.
Generalized Anxiety Disorder 7-Item Scale (GAD-7)
The Generalized Anxiety Disorder 7-Item Scale (GAD-7; Spitzer et al., 2006) is a 7-item self-report anxiety questionnaire that measures the frequency and severity of anxiety symptoms over the past 2 weeks. The GAD-7 has demonstrated reliability and validity as a measure of anxiety in the general population (Löwe et al., 2008). The questionnaire measures symptoms such as “feeling nervous, anxious, or on edge,” and “not being able to stop or control worrying.” The format of the GAD-7 is similar to the PHQ-9, using a 4-point Likert scale to measure frequency of symptoms over the past 2 weeks with response options of not at all, several days, more than half the days, and nearly every day. GAD-7 scores are calculated by assigning scores of 0, 1, 2, and 3 for response categories and then adding the scores from the 7 items to derive a total score ranging from 0 to 21. Minimal anxiety is indicated by total scores of 0–4, mild anxiety by scores of 5–9, moderate anxiety by scores of 10–14, and severe anxiety by scores of 15– 21. Cronbach’s alpha for the GAD-7 in the present study was .86.
Analytic Strategy
Total scores for the PHQ-9 and GAD-7 were found to be positively skewed for both groups of participants. Binary logistic regression was therefore an appropriate method of analysis for this dataset, as binary logistic regression does not require normality of dependent variables (Tabachnick & Fidell, 2019). For two separate binary logistic regression models, individuals were classified as being either minimal or mild or above in depression (PHQ-9) and anxiety (GAD-7) to create binary outcome variables. This choice of cutoff allowed each model (with time period as predictor) to satisfy the recommendation of Peduzzi et al. (1996) that there be at least 10 cases per outcome per predictor in binary logistic regression.
Prior to performing these intended primary analyses to answer the research questions, preliminary analyses were conducted to determine whether adding control variables to the logistic regression models was warranted. Chi-square tests of independence, Fisher-Freeman-Halton Exact tests, Fisher’s Exact tests, and an independent samples t-test were used to test for possible differences between the two time periods in individuals’ responses to demographic questions. In cases in which responses to demographic questions were shown to be significantly different across the two groups, appropriate tests were used to determine whether the demographic responses in question were associated with either of the two intended dependent variables.
Following the preliminary analyses, the intended two binary logistic regressions were conducted to answer the research questions. In the first binary logistic regression, time period was the predictor
(1 = August–September 2021, 0 = January–February 2022) and PHQ-9 depression category was the outcome (1 = mild or above, 0 = minimal). In the second logistic regression, time period was the predictor (1 = August–September 2021, 0 = January–February 2022) and GAD-7 anxiety category was the outcome (1 = mild or above, 0 = minimal). All analyses were conducted using SPSS Version 28.
Results
Preliminary Demographic Analyses
Prior to the primary analyses, preliminary analyses were conducted to determine whether the two groups differed in their responses to demographic questions. Fisher-Freeman-Halton Exact tests and an independent samples t-test were used to test for differences between groups in their responses to the seven demographic questions. Two of the seven tests were statistically significant at Bonferroni-corrected alpha level. Specifically, Fisher-Freeman-Halton Exact tests found significant differences between time periods on the race (p = .004) and employment (p < .001) demographic variables.
Based on the above significant results for the race and employment variables across the time periods, 2 x 2 tests were conducted to test for differences between specific race responses and specific employment responses across the two time periods. For these 2 x 2 tests, a chi-square test of independence was used when all expected cell counts were 5 or greater and Fisher’s Exact test was used when any expected cell counts were less than 5. To follow up the significant result for race, 2 x 2 tests were conducted for all pairs of race responses in which 2 x 2 tests were possible (i.e., in which there was at least one observation for each of the two race responses at both time periods). These follow-up 2 x 2 tests of responses to the race question across time periods found no statistically significant differences between pairs of race responses across time periods using Bonferroni-corrected alpha level. Follow-up 2 x 2 tests comparing all pairs of responses to the employment question across time periods found two statistically significant differences using Bonferroni-corrected alpha level. A chi-square test of independence showed that individuals were more likely to be employed full-time during January–February 2022 than August–September 2021 as compared to those not employed (including students), X2 (1, N = 99) = 9.29, p = .002. Fisher’s Exact test showed that individuals were more likely to indicate “prefer not to answer” during January–February 2022 than during August–September 2021 as compared to those indicating “not employed (including students),” p = .001.
The statistically significant tests for race and employment across time periods were followed up with additional tests to determine if depression or anxiety category (minimal vs. mild or above for each) was associated with individuals’ responses to the relevant race and employment questions. A Fisher-Freeman-Halton Exact test showed that depression category was not associated with individuals’ responses to the race question, p = .099. A Fisher-Freeman-Halton Exact test also showed that individuals’ anxiety category was not associated with individuals’ responses to the race question,
p = .386. With regard to employment, tests of association were conducted between the intended dependent variables and the specific employment responses that were found to differ between the two groups. A chi-square test of independence showed that individuals’ status as “not employed” vs. “employed full-time” was not associated with depression category, X2 (1, N = 99) = .63, p = .429. A chi-square test of independence also showed that these employment statuses were not associated with anxiety category, X2 (1, N = 99) = .27, p = .601. Similarly, Fisher’s Exact tests showed that individuals’ employment responses of “prefer not to answer” vs. “not employed (including students)” were not associated with depression category (p = .156) or anxiety category (p = .317). These results were interpreted as indicating that the ways in which individuals in the two time periods differed demographically did not have significant impact on the study’s dependent variables of interest. Therefore, binary logistic regressions were conducted with only time period as a predictor of each dependent variable.
Relationship Between Time Period and Severity of Depression Symptoms
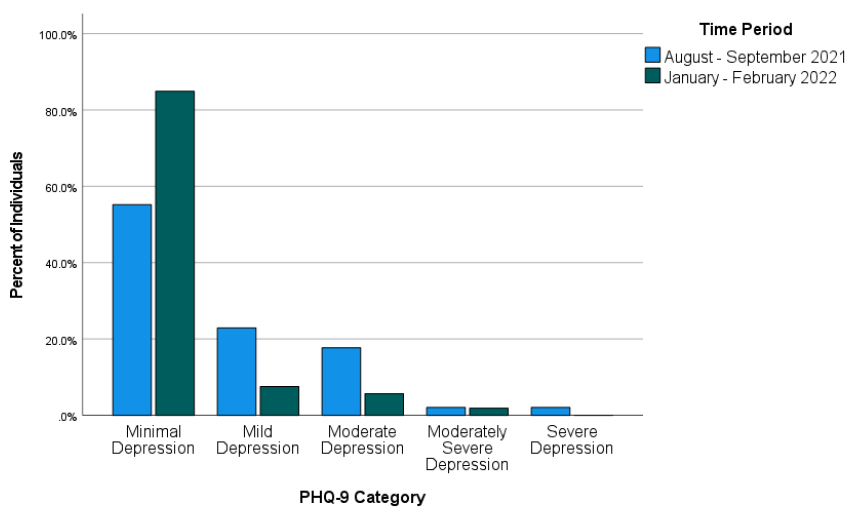
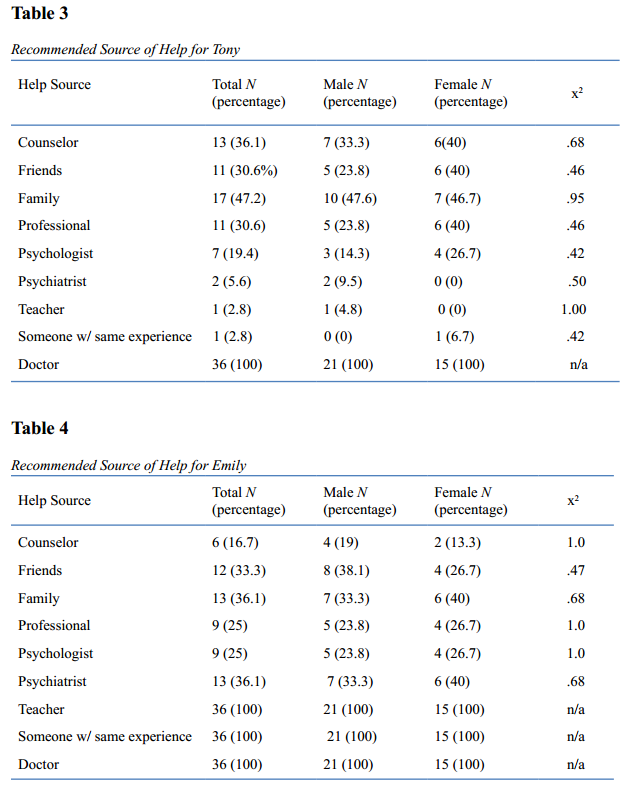
Most individuals in the study were in the minimal depression range on the PHQ-9 as compared to the other four categories. Figure 1 shows the percentage of individuals falling into each of the five PHQ-9 categories during each of the two time periods.
Figure 1
Percentages of Individuals Falling Into Each of the PHQ-9 Categories for Each of the Two Time Periods
Across both time periods combined (August–September 2021 and January–February 2022), 51 individuals (34.23%) were mild or above in depression while 98 (65.77%) were in the minimal range. Binary logistic regression was used to test whether time period predicted severity of depression symptoms. Time period was entered as a predictor (1 = August–September 2021, 0 = January–February 2022) of depression (1 = mild or above, 0 = minimal depression). The overall binary logistic regression model was found to be statistically significant, χ2(1) = 14.46, p < .001, Cox & Snell R2 = .092, Nagelkerke R2 = .128. In the model, time period was found to be a significant predictor of depression, Wald χ2(1) = 12.17, B = 1.52, SE = .44, p < .001. The model estimated that the odds of being mild or above in depression were 4.56 times higher during August–September 2021 than during January–February 2022 for individuals requesting a mental health check-in following COVID-19 exposure. Specifically, the predicted odds of being mild or above in depression were .81 during August–September 2021 and .18 during January–February 2022.
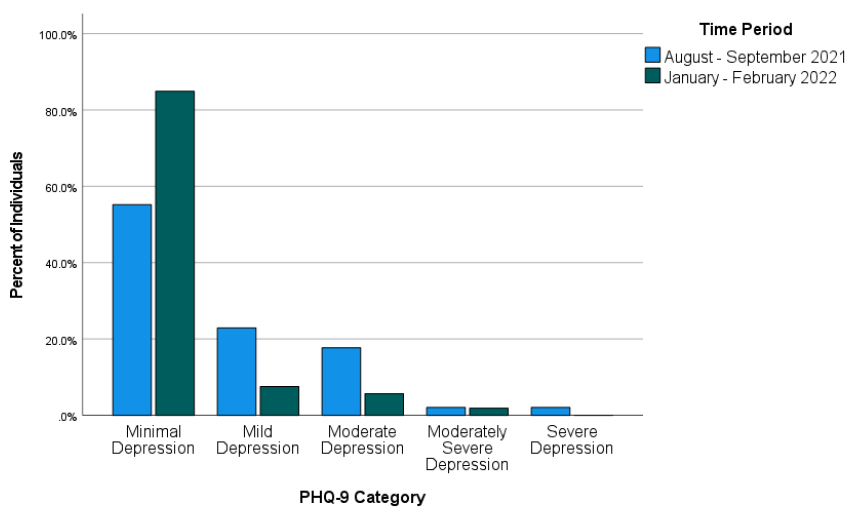
Relationship Between Time Period and Severity of Anxiety Symptoms
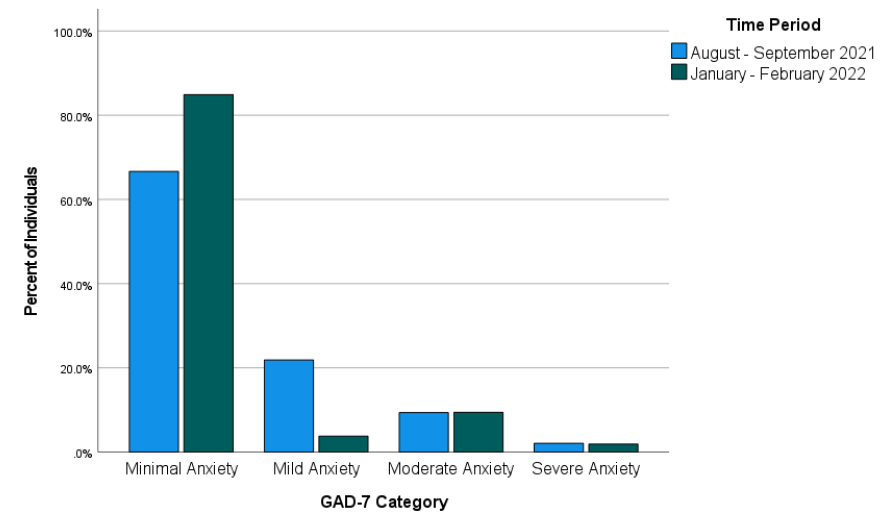
Most individuals in the study were in the minimal anxiety range on the GAD-7 as compared to the other three categories. Figure 2 shows the percentage of individuals falling into each of the four GAD-7 categories during each of the two time periods.
Figure 2
Percentages of Individuals Falling Into Each of the GAD-7 Categories for Each of the Two Time Periods
Across both time periods combined, 40 individuals (26.85%) reported anxiety at levels of mild or above and 109 individuals (73.15%) reported minimal anxiety. Binary logistic regression was used to test whether time period predicted severity of anxiety symptoms. Time period was entered as a predictor (1 = August–September 2021, 0 = January–February 2022) of anxiety (1 = mild or above, 0 = minimal anxiety). The overall binary logistic regression model was statistically significant, χ2(1) = 6.16, p = .013, Cox & Snell R2 = .041, Nagelkerke R2 = .059. In the model, time period was a significant predictor of anxiety, Wald χ2(1) = 5.51, B = 1.03, SE = .44, p = .019. Odds of being mild or above in anxiety were estimated by the model to be 2.81 times higher during August–September 2021 than during January–February 2022 for individuals requesting a mental health check-in after exposure to COVID-19. Specifically, the predicted odds of being mild or above in anxiety were .50 during August–September 2021 and .18 during January–February 2022.
Discussion
This study examined whether time period would predict severity of depression and anxiety symptoms in a sample of individuals exposed to COVID-19 at a university in the Southeastern United States. More specifically, the study addressed the possibility that the likelihood of being mild or above in depression and anxiety would differ between two time periods following the university’s return to in-person operations in August 2021. The results of the study showed that the likelihood of being mild or above in depression and the likelihood of being mild or above in anxiety after exposure to COVID-19 were both higher during August–September 2021 than during January–February 2022. This finding is in line with previous research that found improvements in psychosocial symptomatology in later stages of the COVID-19 pandemic (Tang et al., 2022) and in contrast to research that did not find such improvements (McLeish et al., 2022). Based on the results of the present study, it appears likely that factors that differed between the two assessed time periods (first two months of fall 2021 vs. first two months of spring 2022) contributed to the observed difference in likelihood of depression and anxiety symptoms. McLeish et al. (2022) noted that vaccines were not widely available in their study that did not find such differences, while Tang et al. (2022), who did find significant differences, noted that vaccines were available at their second data collection point (January–March 2021). For individuals in the present study, COVID-19 vaccinations were available. Vaccination was strongly encouraged by university administrators following the return to campus, and more individuals on campus were vaccinated in spring 2022 than in fall 2021. Vaccinations might have lessened individuals’ COVID-19 concerns and contributed to more positive psychosocial outcomes during spring 2022 than fall 2021.
Besides vaccinations possibly lessening depression and anxiety symptoms, other environmental circumstances might also have played a role. The two time periods on which this study focused also differed in their proximity to a significant environmental event—a return to in-person operations on the campus where the individuals studied and/or worked. Early research on the mental health impact of COVID-19 highlighted the negative mental health effects of factors such as reduced physical activity (Silva et al., 2022), life disruptions due to the COVID-19 pandemic (Stamatis et al., 2022), and social distancing (Marroquín et al., 2020). Therefore, it is possible that symptoms of depression and anxiety in spring 2022 were affected by changes in specific circumstances known to have negatively impacted mental health earlier in the COVID-19 pandemic. For example, individuals’ physical activity likely increased because of a return to campus, and they might have perceived less disruption to their lives through being able to resume in-person activities. Although individuals in the present study who were exposed to COVID-19 during the first 2 months after the return to campus might have reaped some benefits from the return to more normal environmental circumstances, they might also have faced a period of adjustment. In contrast, individuals exposed to COVID-19 between January and February 2022 might have been more readjusted and reaped greater benefits from the return to campus, thereby reducing depression and anxiety symptoms.
Implications
This study’s findings on psychosocial symptomatology across time during the COVID-19 pandemic have important implications for the work of counselors. Based on the results of the present study, counselors planning outreach efforts to individuals exposed to COVID-19 should consider that as time passes, these individuals might be more stable with regard to symptoms of depression and anxiety. However, some individuals directly affected by COVID-19 might still be interested in receiving mental health information despite low levels of depression and anxiety. Many individuals in the present study scored as minimal in depression and anxiety but were still interested in receiving a mental health check-in. Thus, counselors should advocate for mental health information and resources to be made available to individuals who are known to be facing stressors related to COVID-19. Counselors should be prepared to have conversations to determine the contextual needs of individuals exposed to COVID-19 rather than relying only on standardized measures of psychosocial symptomatology. For example, counselors working with employees (such as university employees in the present study) should be attentive to the possibility that employees exposed to COVID-19 may be concerned about facing stigma in their workplace due to their exposure (Schubert et al., 2021).
Given that the present study focused on individuals from a university population, the study’s results also have specific implications for college counselors. College counselors should develop approaches to reach students during circumstances that might make traditional outreach challenging. For example, the present study used data from a mental health intervention in which service providers collaborated with university contact tracers to safely provide mental health resources by telephone to individuals exposed to COVID-19. College counselors should be prepared to connect clients with services at a distance. Previous research during the COVID-19 pandemic found that college students were interested in using teletherapy and online self-help resources, particularly if such services were made available for free (Ahuvia et al., 2022).
Besides preparing for flexible modes of service delivery, college counselors should be prepared to deliver interventions most likely to be useful to college students during the COVID-19 pandemic or similar pandemics. Those recently exposed to COVID-19 might benefit from discussing possible fears associated with COVID-19, experiences of stigmatization they might have experienced due to their exposure, and ways to maintain mental health during any period of quarantine or isolation that might be required. Those not recently exposed to COVID-19 might instead benefit from interventions that address other issues that might have resulted from the COVID-19 pandemic or societal responses to it. For example, if circumstances associated with the COVID-19 pandemic led to reductions in a client’s amount of exercise, a counselor can help the client identify ways they might increase their physical activity. Interventions promoting physical activity were found to reduce anxiety and depression in college students during the COVID-19 pandemic (Luo et al., 2022).
Limitations
This study had limitations that should be considered. First, with the study being retrospective and using secondary data from a clinical intervention, it was not possible to include measures that might have better clarified mechanisms of the changes that were observed in psychosocial symptoms. Thus, the possible explanations above of what might have driven these changes are tentative and future research should test them more directly. Second, individuals in the present study were likely to have been in greater distress than the general university population based on their exposure to COVID-19, which might limit the generalizability of the study’s findings. Third, individuals in the present study were from a single university in the Southeastern United States. Thus, our findings might not generalize to other regions where university-related COVID-19 policies might have differed. Fourth, the decision to create a binary independent variable to reflect time periods (August–September 2021 and January–February 2022) in the present study also entails a limitation. This decision was justifiable on the basis that it allowed for comparisons of individuals at similar points in academic semesters and during comparable periods of COVID-19 infection. However, this analysis decision means that inferences from the study’s results are limited to the two specific time periods that were analyzed. Fifth, individuals in the present study responded to items on the GAD-7 and PHQ-9 through a phone conversation with interviewers. Interviewer-administered surveys have been previously associated with greater tendencies toward socially desirable responses than self-administered surveys (Bowling, 2005). This might limit the present study’s generalizability in contexts where self-administrations of the GAD-7 and PHQ-9 are used.
Future Research
The results of this study provide important directions for future research. Future researchers who can conduct prospective studies or who have access to larger retrospective datasets should aim to determine specific factors that might lead to improvement in mental health outcomes over time during the COVID-19 pandemic. Knowledge produced by such studies could contribute to clinical applications in the future regarding COVID-19 or other pandemics that might occur. Relatedly, future research with larger samples of demographically diverse participants should explore possible demographic differences in specific mental health trajectories in later stages of the COVID-19 pandemic.
Future research should continue to focus specifically on those who are interested in mental health information and interventions during the COVID-19 pandemic. To follow up this study’s findings, future quantitative and qualitative studies should aim to identify which individuals are interested in receiving mental health services and determine the best ways to deliver services to them. As a globally experienced stressor, the COVID-19 pandemic might have changed some individuals’ views of mental health and/or their receptiveness to mental health outreach. More specifically, some might be more receptive to available mental health information even at lower thresholds of anxiety, depression, or other psychosocial symptoms. Such clients might be interested in preventive services or their interest in mental health information might be driven by other factors. Future studies should address these possibilities more directly than was possible in the present retrospective study.
Conclusion
Overall, the present study provided a positive picture regarding psychosocial symptomatology in later stages of the COVID-19 pandemic. Results from this study of students and employees at a university in the Southeastern Unites States following their return to campus found that many individuals requesting mental health information after exposure to COVID-19 showed minimal levels of depression and anxiety. Individuals in the study were more likely to be in these minimal ranges during January–February 2022 than August–September 2021. COVID-19 will continue to have effects in individuals’ lives through future infections and potentially through lasting effects of previous stages of the COVID-19 pandemic. As organized in-person activities resume and COVID-19 infections continue, counseling researchers and practitioners should continue efforts to best characterize and address individuals’ mental health needs associated with the COVID-19 pandemic.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Ahuvia, I. L., Sung, J. Y., Dobias, M. L., Nelson, B. D., Richmond, L. L., London, B., & Schleider, J. L. (2022). College student interest in teletherapy and self-guided mental health supports during the COVID-19 pandemic. Journal of American College Health. Advance online publication.
https://doi.org/10.1080/07448481.2022.2062245
Beiter, R., Nash, R., McCrady, M., Rhoades, D., Linscomb, M., Clarahan, M., & Sammut, S. (2015). The prevalence and correlates of depression, anxiety, and stress in a sample of college students. Journal of Affective Disorders, 173, 90–96. https://doi.org/10.1016/j.jad.2014.10.054
Bowling, A. (2005). Mode of questionnaire administration can have serious effects on data quality. Journal of Public Health, 27(3), 281–291. https://doi.org/10.1093/pubmed/fdi031
Bzdok, D., & Dunbar, R. I. M. (2020). The neurobiology of social distance. Trends in Cognitive Sciences, 24(9), 717–733. https://doi.org/10.1016/j.tics.2020.05.016
Centers for Disease Control and Prevention. (2023, March 15). COVID-19 timeline. https://www.cdc.gov/museum/timeline/covid19.html
Copeland, W. E., McGinnis, E., Bai, Y., Adams, Z., Nardone, H., Devadanam, V., Rettew, J., & Hudziak, J. J. (2021). Impact of COVID-19 pandemic on college student mental health and wellness. Journal of the American Academy of Child & Adolescent Psychiatry, 60(1), 134–141.e2. https://doi.org/10.1016/j.jaac.2020.08.466
Dawson, D. L., & Golijani-Moghaddam, N. (2020). COVID-19: Psychological flexibility, coping, mental health, and wellbeing in the UK during the pandemic. Journal of Contextual Behavioral Science, 17, 126–134.
https://doi.org/10.1016/j.jcbs.2020.07.010
Elmer, T., Mepham, K., & Stadtfeld, C. (2020). Students under lockdown: Comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS ONE, 15(7), Article e0236337. https://doi.org/10.1371/journal.pone.0236337
Fancourt, D., Steptoe, A., & Bu, F. (2021). Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: A longitudinal observational study. The Lancet Psychiatry, 8(2), 141–149. https://doi.org/10.1016/S2215-0366(20)30482-X
Fioravanti, G., Benucci, S. B., Prostamo, A., Banchi, V., & Casale, S. (2022). Effects of the COVID-19 pandemic on psychological health in a sample of Italian adults: A three-wave longitudinal study. Psychiatry Research, 315, Article 114705. https://doi.org/10.1016/j.psychres.2022.114705
Food and Drug Administration. (2021, August 23). FDA approves first COVID-19 vaccine. https://www.fda.gov/news-events/press-announcements/fda-approves-first-covid-19-vaccine
Huckins, J. F., daSilva, A. W., Wang, W., Hedlund, E., Rogers, C., Nepal, S. K., Wu, J., Obuchi, M., Murphy, E. I., Meyer, M. L., Wagner, D. D., Holtzheimer, P. E., & Campbell, A. T. (2020). Mental health and behavior of college students during the early phases of the COVID-19 pandemic: Longitudinal smartphone and ecological momentary assessment study. Journal of Medical Internet Research, 22(6), Article e20185.
https://doi.org/10.2196/20185
Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Liu, C. H., Stevens, C., Wong, S. H. M., Yasui, M., & Chen, J. A. (2019). The prevalence and predictors of mental health diagnoses and suicide among U.S. college students: Implications for addressing disparities in service use. Depression and Anxiety, 36(1), 8–17. https://doi.org/10.1002/da.22830
Löwe, B., Decker, O., Müller, S., Brähler, E., Schellberg, D., Herzog, W., & Herzberg, P. Y. (2008). Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Medical Care, 46(3), 266–274. https://doi.org/10.1097/MLR.0b013e318160d093
Luo, Q., Zhang, P., Liu, Y., Ma, X., & Jennings, G. (2022). Intervention of physical activity for university students with anxiety and depression during the COVID-19 pandemic prevention and control period: A systematic review and meta-analysis. International Journal of Environmental Research and Public Health, 19(22), 15338. https://doi.org/10.3390/ijerph192215338
Marroquín, B., Vine, V., & Morgan, R. (2020). Mental health during the COVID-19 pandemic: Effects of stay-at-home policies, social distancing behavior, and social resources. Psychiatry Research, 293, Article 113419. https://doi.org/10.1016/j.psychres.2020.113419
Martin, A., Rief, W., Klaiberg, A., & Braehler, E. (2006). Validity of the Brief Patient Health Questionnaire Mood Scale (PHQ-9) in the general population. General Hospital Psychiatry, 28(1), 71–77.
https://doi.org/10.1016/j.genhosppsych.2005.07.003
McLeish, A. C., Walker, K. L., & Hart, J. L. (2022). Changes in internalizing symptoms and anxiety sensitivity among college students during the COVID-19 pandemic. Journal of Psychopathology and Behavioral Assessment, 44, 1021–1028. https://doi.org/10.1007/s10862-022-09990-8
Meyer, J., McDowell, C., Lansing, J., Brower, C., Smith, L., Tully, M., & Herring, M. (2020). Changes in physical activity and sedentary behavior in response to COVID-19 and their associations with mental health in 3052 US adults. International Journal of Environmental Research and Public Health, 17(18), Article 6469.
https://doi.org/10.3390/ijerph17186469
Oh, H., Marinovich, C., Rajkumar, R., Besecker, M., Zhou, S., Jacob, L., Koyanagi, A., & Smith, L. (2021). COVID-19 dimensions are related to depression and anxiety among US college students: Findings from the Healthy Minds Survey 2020. Journal of Affective Disorders, 292, 270–275. https://doi.org/10.1016/j.jad.2021.05.121
Ozamiz-Etxebarria, N., Idoiaga Mondragon, N., Dosil Santamaría, M., & Picaza Gorrotxategi, M. (2020). Psychological symptoms during the two stages of lockdown in response to the COVID-19 outbreak: An investigation in a sample of citizens in Northern Spain. Frontiers in Psychology, 11, Article 1491.
https://doi.org/10.3389/fpsyg.2020.01491
Peduzzi, P., Concato, J., Kemper, E., Holford, T. R., & Feinstein, A. R. (1996). A simulation study of the number of events per variable in logistic regression analysis. Journal of Clinical Epidemiology, 49(12), 1373–1379. https://doi.org/10.1016/S0895-4356(96)00236-3
Pierce, M., Hope, H., Ford, T., Hatch, S., Hotopf, M., John, A., Kontopantelis, E., Webb, R., Wessely, S., McManus, S., & Abel, K. M. (2020). Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population. The Lancet Psychiatry, 7(10), 883–892.
https://doi.org/10.1016/S2215-0366(20)30308-4
Prati, G., & Mancini, A. D. (2021). The psychological impact of COVID-19 pandemic lockdowns: A review and meta-analysis of longitudinal studies and natural experiments. Psychological Medicine, 51(2), 201–211. https://doi.org/10.1017/S0033291721000015
Rettie, H., & Daniels, J. (2021). Coping and tolerance of uncertainty: Predictors and mediators of mental health during the COVID-19 pandemic. American Psychologist, 76(3), 427–437. https://doi.org/10.1037/amp0000710
Riehm, K. E., Holingue, C., Kalb, L. G., Bennett, D., Kapteyn, A., Jiang, Q., Veldhuis, C. B., Johnson, R. M., Fallin, M. D., Kreuter, F., Stuart, E. A., & Thrul, J. (2020). Associations between media exposure and mental distress among U.S. adults at the beginning of the COVID-19 pandemic. American Journal of Preventive Medicine, 59(5), 630–638. https://doi.org/10.1016/j.amepre.2020.06.008
Schubert, M., Ludwig, J., Freiberg, A., Hahne, T. M., Romero Starke, K., Girbig, M., Faller, G., Apfelbacher, C., von dem Knesebeck, O., & Seidler, A. (2021). Stigmatization from work-related COVID-19 exposure: A systematic review with meta-analysis. International Journal of Environmental Research and Public Health, 18(12), 6183. https://doi.org/10.3390/ijerph18126183
Silva, D. T. C., Prado, W. L., Cucato, G. G., Correia, M. A., Ritti-Dias, R. M., Lofrano-Prado, M. C., Tebar, W. R., & Christofaro, D. G. D. (2022). Impact of COVID-19 pandemic on physical activity level and screen time is associated with decreased mental health in Brazillian adults: A cross-sectional epidemiological study. Psychiatry Research, 314, Article 114657. https://doi.org/10.1016/j.psychres.2022.114657
Şimşir, Z., Koç, H., Seki, T., & Griffiths, M. D. (2022). The relationship between fear of COVID-19 and mental health problems: A meta-analysis. Death Studies, 46(3), 515–523. https://doi.org/10.1080/07481187.2021.1889097
Son, C., Hegde, S., Smith, A., Wang, X., & Sasangohar, F. (2020). Effects of COVID-19 on college students’ mental health in the United States: Interview survey study. Journal of Medical Internet Research, 22(9), Article e21279. https://doi.org/10.2196/21279
Spitzer, R. L., Kroenke, K., Williams, J. B. W., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097.
https://doi.org/10.1001/archinte.166.10.1092
Stamatis, C. A., Broos, H. C., Hudiburgh, S. E., Dale, S. K., & Timpano, K. R. (2022). A longitudinal investigation of COVID-19 pandemic experiences and mental health among university students. British Journal of Clinical Psychology, 61(2), 385–404. https://doi.org/10.1111/bjc.12351
Tabachnick, B. G., & Fidell, L. S. (2019). Using multivariate statistics (7th ed.). Pearson.
Tang, N. K. Y., McEnery, K. A. M., Chandler, L., Toro, C., Walasek, L., Friend, H., Gu, S., Singh, S. P., & Meyer, C. (2022). Pandemic and student mental health: Mental health symptoms amongst university students and young adults after the first cycle of lockdown in the UK. BJPsych Open, 8(4), Article e138.
https://doi.org/10.1192/bjo.2022.523
Wise, T., Zbozinek, T. D., Michelini, G., Hagan, C. C., & Mobbs, D. (2020). Changes in risk perception and self-reported protective behaviour during the first week of the COVID-19 pandemic in the United States.
Royal Society Open Science, 7(9), Article 200742. https://doi.org/10.1098/rsos.200742
Xiong, J., Lipsitz, O., Nasri, F., Lui, L. M. W., Gill, H., Phan, L., Chen-Li, D., Iacobucci, M., Ho, R., Majeed, A., & McIntyre, R. S. (2020). Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders, 277, 55–64. https://doi.org/10.1016/j.jad.2020.08.001
Wesley B. Webber, PhD, NCC, is a postdoctoral scholar at East Carolina University. W. Leigh Atherton, PhD, LCMHCS, LCAS, CCS, CRC, is an associate professor and program director at East Carolina University. Kelli S. Russell, MPH, RHEd, is a teaching assistant professor at East Carolina University. Hilary J. Flint, NCC, LCMHCA, is a clinical counselor at C&C Betterworks. Stephen J. Leierer, PhD, is a research associate at the Florida State University Career Center. Correspondence may be addressed to Wesley B. Webber, Department of Addictions and Rehabilitation Studies, Mail Stop 677, East Carolina University, 1000 East 5th Street, Greenville, NC 27858-4353, webberw21@ecu.edu.
Apr 29, 2020 | Volume 10 - Issue 2
TeShaunda Hannor-Walker, Lynn Bohecker, Lacey Ricks, Sarah Kitchens
Literature does little to explore the perceptions of Black adolescents with depression or their perspective of treatment effectiveness. Studies are usually from urban areas and there is a dearth of research with Black adolescents from rural areas. This study explored the unique personal experiences of Black adolescents located in the rural southeastern United States, with the purpose of gaining a clearer understanding when working with this population. An interpretative qualitative method was used to explore 10 participants’ interpretation of their experiences to gain insight in how they make meaning of those experiences. Five significant categories were found to capture participant themes: (a) definition of depression, (b) seeking treatment, (c) coping and problem solving strategies, (d) types of emotional support, and (e) contributing factors to depression. Specific recommendations and interventions are suggested for mental health clinicians to become more educated and aware when working with Black adolescents.
Keywords: Black adolescents, depression, treatment effectiveness, rural, contributing factors
Depression is a leading cause of disability worldwide (World Health Organization, 2020). The World Federation for Mental Health (2012) estimated that by 2030, more people will be impacted by depression than any other health problem. In the United States, approximately 13.3% of adolescents, or 3.2 million, had at least one major depressive episode and 9.5% were Black (National Institute of Mental Health [NIMH], 2013). Black people have experienced more severe forms of mental health conditions than individuals of other races because of unmet needs and other barriers (NIMH, 2013). In fact, Black people were reported to be 10% more likely to experience serious mental health problems than the general population (Shushansky, 2017), and Black children have a suicide rate that is almost two times higher than that of their White counterparts (Bridge et al., 2018).
Weaver et al. (2015) noted that although 90% of rural Black people live in the southeastern part of the United States, there are only two studies that specifically examined depression among rural Black people using national data (i.e., Probst et al., 2006; Willis et al., 2003). Most studies of depression that include Black youth are based on data from urban communities (Al-Khattab et al., 2016; Conner & Yeh, 2018; Ofonedu et al., 2013; Robinson et al., 2015). This suggests there is a dearth of research exploring Black adolescent experiences of depression in rural communities, and there is even less research focusing on Black youth who live in the rural southeastern United States (Smokowski et al., 2015: Weaver et al., 2015). The goal of this study was to explore the unique experiences of Black adolescents living in the rural southeastern United States who had been diagnosed with depression.
Contributing Factors to Depression in Black Adolescents
Adolescents who suffer from depression may experience substantial negative health and social consequences in late adolescence and adulthood (Lu, 2019). Black adolescents are particularly vulnerable to these consequences because they are more likely to live in low-resource neighborhoods and because they contend with the negative psychological impacts of racial discrimination (Robinson et al., 2015). Choi et al. (2006) found that ethnic minorities have higher scores on social stress and mental distress and lower scores on coping, self-esteem, and family cohesion. The depressive symptoms experienced by Black adolescents are often socially and culturally based (Lu et al., 2017). Therefore, it is essential for counselors, school personnel, and related professionals to remain abreast of the current research on depressive signs and symptoms, beliefs about treatment, and specific needs of Black adolescents.
Choi et al. (2006) discovered that Black, Hispanic, and Asian adolescents in the United States have consistently higher levels of social stress beginning in childhood compared to their White counterparts. Breland-Noble et al. (2010) found that relationship problems, academic problems, bereavement, and stress were primary triggers for depressive symptoms among Black adolescents. Ofonedu et al. (2013) determined in their study of Black adolescents that life events in the home, school, and community contributed to depressive symptoms. These factors included (a) a stressful home life, (b) stressful life circumstances and unique life experiences at school, and (c) the experience of high levels of violent crimes in neighborhoods. Stress is clearly a contributing factor to the depressive symptoms of Black adolescents.
Symptoms of Depression in Black Adolescents
Although understanding national trends and contributing factors can help practitioners identify adolescents suffering from depression, it is also important to understand potential racial and ethnic differences in the expression of adolescent depression (Lu, 2019). The manifestations of depressive symptoms vary in Black youth and affect all dimensions of physical, psychological, interpersonal, and social being (Ofonedu et al., 2013). In the Black community, mental health conditions have often been unacknowledged, misunderstood, and misdiagnosed (Shushansky, 2017; Vontress et al., 2007). According to Vontress et al. (2007), Black people often experience cultural dysthymia and mental health symptoms such as low-grade depression; feelings of sadness, hopelessness, and anger; aggression; and self-destructive behaviors. Vontress et al. (2007) characterized these symptoms as a “psychosocial condition” grounded in external societal experiences of discrimination and oppression that often go unrecognized (p. 131). Additional studies are needed to show how to better identify individuals suffering from depression and thereby increase the effectiveness of treatment for Black adolescents (Ofonedu et al., 2013).
As in adults, unrecognized or undiagnosed dysthymia or symptoms of low-grade depression in adolescents can contribute to poor health and problematic behaviors (Saluja et al., 2004). Researchers discovered that untreated dysthymia elevates the risk of disruptive behaviors, anxiety, substance abuse, unsafe sexual practices, involvement in fights, lower achievement on tests, lower teacher-rated grades, and poorer peer relationships (Saluja et al., 2004). Auger (2005) discovered that the many signs and symptoms of adolescent depression were overlooked not only by parents but also by school systems, administrators, counselors, and teachers who daily were in a very unique position to identify those at risk of depression. Many cases of adolescent depression, particularly among minorities, have gone undiagnosed, misdiagnosed, and untreated (Cook et al., 2017; Shushansky, 2017). A better understanding of the unique experiences of Black adolescents diagnosed with depression would help improve symptom recognition, which may in turn reduce misdiagnosis and increase treatment effectiveness.
An understanding of the cultural implications and influence that oppression, prejudice, and various forms of discrimination have on Black people’s mental health in the United States is helpful in contextualizing and normalizing symptoms of depression and reducing instances of misdiagnosis. Hope et al. (2017) posited that discrimination remains a common experience for Black adolescents that can impact not only the onset of depression but also the quality of and access to mental health services. Furthermore, according to Liang et al. (2016), racial disparities exist, as Black youth are more likely to be misdiagnosed as having psychotic and disruptive behavior problems compared to mood (i.e., depression) and substance abuse disorders.
Lu et al. (2017) echoed these sentiments, stating that depression presents differently for Black adolescents. It is essential for Black adolescents to use their own language when describing their depressive symptoms. Additionally, it is important for clinical and school counseling professionals to be aware of gender differences in Black adolescents’ expression of depression, specifically in terms of internalizing and externalizing symptoms. The findings of Breland-Noble et al. (2010) indicated that female Black adolescents seem to internalize behaviors (e.g., becoming withdrawn, exhibiting visible sadness), while male Black adolescents seem to externalize behaviors (e.g., becoming angry or acting out). Lu et al. (2017) further highlighted that “adolescents develop [symptoms] as a means of coping in response to environmental factors” (p. 614). More research is needed to understand how depressed Black adolescents describe their symptoms and assign meaning to their experiences of depression.
Coping Strategies of Black Adolescents
In addition to presenting different symptoms than individuals of other racial groups, Black adolescents have the lowest coping skills scores compared to their peers (Conner & Yeh, 2018). Recent studies suggest that adolescents who live in low-resourced neighborhoods feel like they have limited options in how to respond to stressful and anxiety-provoking situations because of limited or ineffective coping skills (Robinson et al., 2017; Robinson et al., 2015). There are indications that Black adolescents cope with depression in a variety of contexts. Some Black adolescents describe depression as a way of life, noting that everybody becomes depressed one way or another (Ofonedu et al., 2013). Researchers have shown that some Black adolescents conceal their feelings of depression because they are uncertain of how others would perceive them (Al-Khattab et al., 2016; Ofonedu et al., 2013). For instance, some Black adolescents reported trying to manage their depression independently and only going to an adult as a last resort (Breland-Noble et al., 2010). Black adolescents have been shown to manage their depression by strong will and spiritual beliefs (Ofonedu et al., 2013). Conner and Yeh (2018) highlighted how Black adolescents cope with depression in spiritual and creative ways such as listening to music, dancing, and writing.
In 2016, Al-Khattab et al. discovered that Black adolescents controlled their depression through their interactions with other people. Al-Khattab et al. identified five typology interaction models, which include hiding feelings of depression, lashing out verbally or physically toward others, seeking help from others to address emotional feelings, joining with others in social activities, and having others approach them about behavioral and mood changes. Therefore, it is critical for Black adolescents to better understand their experiences with depression and how interactions with others may influence their symptoms.
Treatment of Depression in Black Adolescents
Cook et al. (2017) noted that there are barriers to accessing mental health services and quality of care, which include stigma associated with mental illness, distrust of the health care system, lack of providers from diverse racial/ethnic backgrounds, lack of culturally competent providers, and lack of insurance or underinsurance. Often these barriers cause Black people to be unable or reluctant to seek help (Shushansky, 2017). Although Black adolescents may feel that treatment can be effective, many are reluctant to attend therapy because of the stigma and possible misdiagnosis of their symptoms, much of which has been influenced by their culture (Al-Khattab et al., 2016; Lindsey et al., 2010; Ofonedu et al., 2013). Positive results have been seen when using family-centered prevention programs to address depressive symptoms in Black adolescents (Brody et al., 2012). Jacob et al. (2013) determined that behavioral activation was effective for decreasing depressive symptoms and impairments for the Black adolescents who participated in their study.
As highlighted by a study of Black adults from a rural faith community, Black people living in rural communities suffering from depression face additional barriers to treatment such as (a) a lack of medical resources, (b) insufficient education about depression, and (c) stigma (Bryant et al., 2013). Sullivan et al. (2017) learned that terminology was crucial when discussing treatment with rural Black adults on a stigmatized topic such as mental illness. Parental concerns about marginalization because of having a child with a mental health diagnosis and some primary care providers’ characterization of mental health symptoms as a “phase” have been found to be barriers to treatment for Black children living in rural communities (Murry et al., 2011). Working with Black children who live in poverty, Graves (2017) identified cultural and macro-level barriers that influence the process of seeking treatment.
Treatment of mental health disorders extends from diagnoses. Considering the differences in symptoms and frequency of misdiagnosis, it is not surprising that treatment options for Black adolescents have shown varied outcomes across the literature. Additionally, some researchers suggested that new measures need to be developed for accurately identifying depression in diverse populations, which would then inform modifications in treatment (Ofonedu et al., 2013). Having a better understanding of the unique and complex experiences of Black adolescents may help parents, therapists, schools, and counseling professionals understand and identify those most at risk for depression. Planey et al. (2019) discovered that Black youth viewed seeking mental health treatment as a contextual and relational process rather than an event. What is clear is that more culturally diverse training for therapists, schools, and counseling professionals is needed to prevent, detect, and implement interventions for minorities experiencing depression during the disease’s earlier stages. Likewise, research exploring Black adolescents’ unique experiences of symptoms, environmental factors, and coping strategies remains necessary in order to inform effective treatment.
Purpose of the Present Study
The review of the literature captured symptoms and coping strategies unique to Black adolescents. Studies highlight that environmental factors contribute to depressive symptoms in this population. Furthermore, disparities exist in mental health care for adolescents, specifically for minorities (Alegria et al., 2010; Brenner, 2019; Lake & Turner, 2017). This clear gap in the literature indicates insufficient knowledge regarding the personal experiences of Black adolescents with depression. Most of the studies in the extant literature took place in urban areas; little is known about rural experiences and even less is known about experiences in the southeastern United States. This qualitative study was designed to help fill that gap. It posed an overarching research question to Black adolescents living in the rural southeastern United States: “What is your experience with depression?” This study was designed to offer human services professionals a clearer understanding of the unique experiences of Black adolescents in this geographical region who had been diagnosed with depression, with the hope of informing clinical practices.
Method
The goal of this study was to explore the unique experiences of Black adolescents living in the rural southeastern United States who had been diagnosed with depression. The research design for the study was a basic interpretive qualitative method, as described by Merriam (2009). The purpose of this method is to understand the perspectives of the participants involved by uncovering and interpreting their meanings (Everall et al., 2006). This purpose was well-suited to the overall objective of this study, which was to gain a clearer understanding of the unique personal experiences of Black adolescents living with depression in the rural southeastern United States.
According to Merriam (2009), interpretive qualitative research is founded on the idea that people and their interactions with their world, or reality, socially construct meaning. Researchers using this method are interested in how individuals “interpret” their experiences, “construct their worlds,” and assign “meanings” to their experiences (Merriam, 2009, p. 38). Moreover, Merriam asserted that interpretive qualitative research has multiple meanings and is a complex phenomenon ideal for attempting to understand and treat Black adolescents with depression. Using Merriam’s (2009) model, researchers “strive to understand the meanings individuals construct regarding their world and their experiences” in a natural setting (p. 4). Another characteristic is that the researcher serves as the primary instrument for both collecting and analyzing data. The research process is inductive rather than deductive, which means that the researcher gathers data in an effort to “build concepts, hypotheses, or theories” in the forms of themes and categories (Merriam, 2009, p. 5). A final characteristic of this model is that interpretive qualitative research is richly descriptive and includes details about the context, the participants involved, and quotations and interview excerpts (Merriam, 2009).
Merriam (2009) noted that certain elements of the basic interpretive qualitative design may overlap with other designs, particularly when concepts of cultural values are discussed and explored. Merriam’s design does not require researchers to give a full sociocultural interpretation of the data, as is done in ethnography. Indeed, this study does not provide a full sociocultural interpretation. However, the data were analyzed using Patton’s (1987) content analysis model because the model provides a rigorous, systemic, and ethical procedure for analyzing data. Merriam’s model for collecting data and Patton’s model for analyzing data form a rich methodological combination that enhances the trustworthiness of the research study and improves the transferability of its findings.
Participants and Procedure
The university IRB granted approval for this study. Purposive sampling was used to identify 10 Black adolescents living in the rural southeastern United States who were being treated for depression. The southeastern part of the United States was selected because it contains fewer metropolitan areas that have been studied specifically. Each of the participants met the following criteria: (a) self-identified as Black, (b) was between the ages of 13 and 17, (c) was willing to participate, (d) had secured a signed informed consent form from their parents, (e) had signed a participant assent form, and (f) was currently under the care of a counselor either in or out of school for depression. The participants ranged in age from 13 to 17 years old and were in grades seven through 12. Six participants were female and four were male.
Approval was obtained in advance from a public school system located in the rural southeastern United States. The public school system administrator agreed to send the letter of invitation along with the consent and assent forms to the parents and potential participants. In addition, the first author sent a packet of information to a counseling agency; school professionals, including professional school counselors and school psychologists; and social workers. The packet contained an invitation letter requesting that the packet be shared with potential participants and their parents; it also contained consent and assent forms. The informed consent form described the study and the efforts that would be taken to protect the confidentiality of the participants’ information. The informed consent form stated that the risk of participating was the normal discomfort of sharing one’s experiences with depression and that if a participant felt uncomfortable, they could withdraw from the study at any time.
Parents and participants signed the consent and assent forms, respectively, and returned them to either the local counseling agency or school professionals, who forwarded the forms to the first author. The first author then contacted the parents, with the participants present, to schedule a 45- to 90-minute, face-to-face interview with the participant. The informed consent form was verbally reviewed, ensuring that the parents and participants understood that a second interview to review and correct the interpretation would be optional. Interviews took place either during the day in a private room at the school or outside of school hours in the first author’s office. Because adolescent depression is considered a sensitive topic, participants were instructed to follow up with their counselor if they experienced adverse feelings as a result of participating in the study.
Data Collection and Analysis
The first author met with each of the 10 participants for a single semi-structured interview that lasted between 45 and 90 minutes. In phenomenological research, the researcher follows the essence of participants’ responses (van Manen, 1997). The first author spent time establishing rapport with the participants. Once the first author believed a participant was comfortable, she asked the participant the overarching question, “What is your experience with depression?” Follow-up questions specific to each participant were used to probe the participants’ responses regarding their experience as Black adolescents living with depression in the rural southeastern United States. Several participants expressed a reluctance to fully disclose or discuss their experiences with depression; however, no participants withdrew from the study, and all participants completed the first interview. At the end of the first interview, the participants were notified that they would be contacted for a second interview to review the transcript of the first interview and verify its accuracy and trustworthiness.
Interviews were recorded and transcribed verbatim by both the first author and a professional transcriber. The transcripts were coded and analyzed for themes related to the research question of this study. The first author utilized Patton’s (1987) content analysis model as a process of bringing order to the data by organizing the data into major themes, categories, and case examples. The first author consulted with two experts in qualitative research in the human services field and used three levels of coding: open, axial, and selective. Open coding included reading the transcribed interviews several times and coding phrases, from one word to portions of paragraphs. Based on input from the consultants, the first author enhanced the coding process by entering the data into the NVivo QSR software program, which facilitated organization and analysis. The first author then condensed the data into five categories. Axial coding enabled the first author to organize, link, and cluster codes, while selective coding allowed the first author to analyze the words, sentences, and themes from the interviews. Data analysis via coding was a back and forth process, and staying close to the transcripts was essential. The labeling and coding allowed the first author to interpret and classify the data and themes into five categories that were supported with direct quotations from the participants.
Trustworthiness
Trustworthiness is an important aspect of qualitative research (Hays & Singh, 2012). The generally candid nature of each participant in relating even the most difficult experiences, such as rape, would suggest a high degree of trustworthiness in their responses. Member checking was offered to all participants in the form of a follow-up interview. When contacted by the first author to schedule this interview, however, none of the participants felt that it was necessary. Rather, all of the participants stated they were satisfied with their responses in the first interview. In addition to offering member checking, the first author used rich data, prolonged engagement, respondent validation, a search for discrepant data, and peer review to ensure trustworthiness. A peer review of the method was conducted by doctoral-level professors in human services who specialized in qualitative research in order to enhance internal validity (Lincoln & Guba, 1985; Merriam, 2009). The first author used an audit trail by engaging in memo-writing to express thoughts, perspectives, observations, and reactions to interviews, transcriptions, and coding. An audit trail is a strategy in which a researcher explains as best as possible how they arrived at the results of the study by documenting how the data were collected, how categories were developed, and how findings were interpreted throughout the study (Lincoln & Guba, 1985). An audit trail thus improves the quality of a study. The information and details from this study may be generalizable to other groups and may contribute to the knowledge base of best practices when working with this population in counseling.
Results
Through data analysis, the researcher identified five significant thematic categories: (a) definitions of depression, (b) seeking treatment, (c) coping and problem-solving strategies, (d) types of emotional support, and (e) contributing factors to depression. These five thematic categories were broken down into their constituent contents. Each thematic category was addressed with the invariant constituents that make up that category, including elaboration on any significant constituent patterns (such as high and low frequency of occurrence). Quotations from the participants are included in the text as examples to elucidate the invariant constituents and thematic categories. For reasons of confidentiality, some identifying information was excluded. All participants identified as Black and lived in the rural southeastern United States.
At the time of the study, the participants were living in a southeastern U.S. community in one of the lowest socioeconomic brackets of the country. In the participants’ community, the majority of the population was Black and participated in the school’s free or reduced-fee lunch program. Because of the homogeneous nature of the community, the participants did not speak of any adverse social or political circumstances, and the researcher avoided broaching the topic in an effort to do no harm. The researcher believed that overlooking the social and political climate of the community increased the trustworthiness of the participants’ responses, as the participants were not influenced by the discussion of the climate nor did they voluntarily express its relevance to their experience. As a Black adult, the researcher, who is first author, was aware of how the social and political climate played into their experience. However, because the participants were adolescents experiencing emotional pain, the first researcher attempted to instill hope in them as part of their experiences of this study. To maintain confidentiality, specific details about the contextual factors in the participants’ community have been omitted.
Definitions of Depression
Data analysis identified 18 codes that were relevant to the category regarding how participants defined depression. Of these codes, three emerged with significantly higher prevalence than the others: (a) sadness; (b) isolation, social withdrawal, or loneliness; and (c) permanent or persistent. Nine out of the 10 participants (90%) indicated that they experienced the feelings associated with these three codes. For example, in response to how he defined depression, Participant 5 noted that he became “sad, mad, and very frustrated.” Participant 1 defined depression in terms of social withdrawal, saying, “Usually I stay in my room and I don’t talk to anybody, I just stay in there, and that is about it.” Participant 4 provided an example of the theme of permanent or persistent experiences by stating, “I don’t think it could just go away, especially when it’s very serious.” Participant 3 provided an example that captured the overall essence of this category when he stated:
I have been sad a whole lot, without reason; and so, I think that is why I was depressed . . . when I am around people for too long, I get sad; but when I am alone, I am happier. I feel safe when I am by myself. When it [depression] comes on, it comes on strong. It is really bad. Because I feel really, really sad, and my thoughts aren’t, you know, normal. Sometimes they are violent . . . like I don’t have any hope at all. I don’t think like I normally would. Sometimes I don’t think at all. Sometimes when I get really sad or angry, I think about hurting people. So, I have to withdraw further. I have to push it further down into my mind so that I won’t act on it.
It is interesting to note that the next most frequently found codes were stress-related and frustration, each with a prevalence of 60%, and more common in young Black girls, which had a prevalence of 50%. Alternatively, only one participant mentioned each of the following codes with regard to defining depression: suicidal thoughts or attempts, more common in young Black boys, and feeling sick.
Seeking Treatment
The category of seeking treatment contained 10 codes. Participants expressed contradictory feelings about the effectiveness of treatment and the barriers to seeking treatment. For example, 90% of participants expressed that they felt that therapeutic treatment was effective in mitigating or curing depression, including Participant 7: “To me, to talk to my therapist was like a relief to me, because he was the only person that I can be able to tell my thoughts, get my thoughts together why I was in there.” Simultaneously, 30% of participants noted that they felt that therapy was not effective as a treatment. This overlap and apparent incompatibility in the data helped reveal the full breadth of Black adolescents’ opinions and feelings about depression and seeking treatment, as participants expressed both positive and negative experiences.
This overlapping trend was seen elsewhere in this thematic category. For example, there were codes of medication is effective (50%) and medication is not effective (30%). This apparent contradiction was highlighted not only between participants but also within a single participant. Participant 10 directly stated she believed medication to be effective; she then revealed that she had been given medication that sent her into a coma. She reported taking her medication as prescribed but “after that I passed out, and I didn’t remember nothing, all I knew I woke up in the hospital.” Three codes were identified as directly related to seeking treatment. Significant barriers to therapeutic treatment were negative connotation of mental illness (80%), uncomfortable issues brought up in treatment (80%), and lack of trust (70%). The code negative connotation of mental illness was grounded in external perceptions, as many participants indicated that they did not want other people to know that they were in treatment.
For example, Participant 2 stated, “I don’t tell them. I don’t want them to know,” when referring to his friends. Participant 3 provided an example of the code of uncomfortable issues, noting, “I don’t like to talk about it much. You know, it is kind of aggravating. It makes me feel weak when I talk to people about my problems.” Regarding the code lack of trust, Participant 6 noted, “I have very weak trust issues. Sometimes they can be strong but mostly weak.”
Three minor codes emerged relating to seeking treatment. Two were trouble expressing self in therapy (40%) and treatment was not necessary (40%). Participant 3 stated, “I have a lot of trouble expressing myself. You know, when I get into the office, I just forget what to say.” Three of the 10 participants openly discussed lack of Black people’s knowledge or education about depression as a specific barrier to treatment. They shared their perceptions of the lack of education and discussion about depression within their own community, which they felt presented a specific barrier to treatment for them. Participant 6 stated, “I can’t overly generalize it, but some people need to know more, ’cause they don’t understand, because sometimes you just need that time and people they don’t understand that you need it.” However, taking these and the other barriers in this thematic category into account, the prevalence of participants who reported that treatment was effective was three times greater than the prevalence of participants who thought that treatment was ineffective.
Coping and Problem-Solving Strategies
The third thematic category contained 29 different codes related to problem-solving strategies and behaviors or activities the participants used to cope with depressive symptoms. The participants described various strategies to cope with depression, but the most prevalent was suppressing/hiding thoughts/feelings. There were seven strategies that more than half of the participants reported using as problem-solving strategies and strategies to cope with depression. The positive problem-solving strategies were listening to music, turning to religion/going to church/praying, and talking/spending time with family. The problematic coping strategies reported were using illegal drugs, engaging in self-harm, having sex, and isolating. See Table 1 for codes and results.
It is encouraging that 18 out of the 29 codes could be characterized as neutral or positive coping strategies. The other 11 are areas of concern, even if only one participant reported engaging in the behavior. Participant responses overlapped and participants reported coping and problem-solving strategies that might be characterized as both positive and negative. In addition to contrasts in the specific codes and types of behaviors, contrasts in the percentages of participants who reported negative behaviors compared to positive behaviors were noted. For example, participants reporting the negative problem-solving strategy of engaging in self-harm as a way to cope often went into detailed narrative descriptions. This strategy was more frequently reported than any of the positive or neutral coping and problem-solving strategies.
Types of Emotional Support
This thematic category addressed the types of emotional support that the participants received during their experiences with depression. Four distinct subthemes of codes were identified: peers; family; school (teachers); and helping professionals such as hospitals, managed care facilities, and therapists. Each of the four subthemes contained codes that were sorted as either positive or negative. A lack of support or refusal of support was considered a negative, and similar to other categories, participants shared multiple overlapping experiences. Negative support from peers was the only theme to have 100% prevalence; every participant mentioned that peers had negatively affected them through a lack of emotional support during their experience with depression, including Participant 2: “They didn’t believe me at first, but later they just seem like they don’t care.” Half of the participants expressed that they had also received positive emotional support from their peers during their experience with depression. In the family group, equal percentages of participants (60%) reported receiving positive support from family and experiencing a lack of support from family. The participants were similarly split regarding their perceptions of receiving positive (50%) and negative (50%) emotional support from teachers at school. The greatest proportional difference in negative and positive emotional support was within the category of helping professionals. In this subtheme, four times as many participants (40%) reported that they had had positive emotional support from mental health care providers in a hospital, halfway house, or therapeutic community than participants reporting negative emotional support from mental health care providers (10%).
Table 1
Coping and Problem-Solving Strategies
| Strategy |
Percent of Respondents
(N = 10) |
| Positive or Neutral
Coping Strategies |
Listening to music |
70% |
| Turning to religion / going to church / praying |
70% |
| Talking / spending time with family |
60% |
| Attending therapy |
40% |
| Writing |
40% |
| Creating art |
30% |
| Playing video games |
30% |
| Watching TV |
30% |
| Crying |
30% |
| Taking prescription drugs |
20% |
| Eating food |
20% |
| Reading |
20% |
| Talking / spending time with friends |
20% |
| Distracting self |
20% |
| Laughing |
20% |
| Joining clubs |
10% |
| Working out |
10% |
| Researching |
10% |
| Problematic
Coping Strategies |
Suppressing / hiding thoughts / feelings |
90% |
| Using illegal drugs |
70% |
| Engaging in self-harm |
60% |
| Having sex |
60% |
| Isolating |
60% |
| Attempting suicide |
40% |
| Engaging in violence |
40% |
| Running away |
30% |
| Yelling / shouting |
10% |
| Having violent thoughts |
10% |
| Avoiding responsibilities / rebelling |
10% |
Contributing Factors to Depression
This theme of contributing factors to depression appeared to be the most salient to the central research question of how Black adolescents living in the rural southeastern United States described their experiences with depression. The previous themes captured definitions of depression, seeking treatment, coping and problem-solving strategies, and types of emotional support. This theme provided a description of the participants’ lives in terms of their context and environment, which the participants identified as contributing factors to their experiences of depression. When asked about contributing factors to their depression, the three most noted by the participants were verbal abuse (70%), differences from other people and being bullied (70%), and parental or family problems (70%). Participants also reported sexual abuse (40%) and physical abuse (30%) as contributing factors. Participant 6 made the following statement, which captures the essence of this theme:
My depression started really kicking in when I was around 13 . . . it runs in my family. My mom has it and when I was little, I was sexually abused . . . and I’ve been made fun of all my life . . . my weight . . . a scalp infection. People make fun of stuff like that. And that’s been going on since I was little.
The least prevalent factors mentioned by participants were foster care (20%), stress of schoolwork (20%), and a scary book (10%). Verbal abuse was reported 30% more frequently than sexual abuse and 40% more frequently than physical abuse. However, it is interesting to note that Participant 2 considered foster care to be a cause of depression and not a solution. Most participants identified a combination of these factors as contributing to the onset of their depressive symptoms.
Discussion and Implications
This study sought to examine the unique experiences of Black adolescents diagnosed with depression living in a rural community located in the southeastern part of the United States. Five themes emerged when examining the participants’ narratives with depression. These themes included definitions of depression, seeking treatment, coping and problem-solving strategies, types of emotional support, and contributing factors to depression. In defining depression, 90% of the participants in this study cited sadness, isolation, and depression’s ongoing nature. This is not surprising, as these codes fit within the diagnostic criteria for depression. It was surprising, however, that participants defined depression as stress-related, as stress is not one of the diagnostic criteria. At the same time, the idea of depression as stress-related is supported in other studies (Breland-Noble et al., 2010; Bryant et al., 2013; Choi et al., 2006; Ofonedu et al., 2013; Robinson et al., 2015). The mental health community would do well to acknowledge the differences in how Black adolescents from rural U.S. communities may define depression. When working with Black adolescent clients, practitioners may wish to inquire about stressors and consider their relation to depression in order to inform treatment plans and interventions.
Most participants who sought treatment for depression indicated that treatment was effective; however, 30% of participants expressed that therapy was ineffective. Additionally, only 50% of participants indicated that medication was an effective form of treatment. Participants also identified barriers to seeking treatment, which included negative connotations associated with mental illness and discomfort discussing issues in treatment. Barriers identified included a lack of trust, problems with self-expression, the belief that therapy was not needed, and a lack of knowledge about depression in the Black culture. These results are consistent with prior research (Al-Khattab et al., 2016; Bryant et al., 2013; Lindsey et al., 2010; Ofonedu et al., 2013; Sullivan et al., 2017), indicating that mental health conditions are often misunderstood, misdiagnosed, or unacknowledged within the Black community (Graves, 2017; Murry et al., 2011; Shushansky, 2017).
Prior research has also highlighted the stigma of mental illness in the Black community (Cook et al., 2017). This stigma helps to explain previous research showing that Black people often seek help as a last resort (Al-Khattab et al., 2016; Breland-Noble et al., 2010; Ofonedu et al., 2013; Vontress et al., 2007). It is essential that counselors acknowledge the stigma associated with mental illness and reluctance to seek treatment within the Black community. More practitioners who are aware of and sensitive to the mental health needs of Black communities are needed. It is imperative that clinicians take it upon themselves to become competent when working with this population. To address the stigma, practitioners might offer training in evidence-based practices related to Black adolescents’ mental health at churches, schools, and various community organizations in the Black community. These types of trainings could be particularly effective in rural communities where participants are likely to communicate to others about the trainings, thereby validating the information and possibly reducing the stigma. One of the codes from this study was related to the effectiveness of medication for reducing depressive symptoms. More research is needed to explore factors that may contribute to this experience. Additionally, more research is needed to understand the unique traits of Black adolescents seeking treatment in other regions of the United States.
There were a few positive strategies for coping with depression that the participants identified, including listening to music, engaging in spiritual practices, and spending time with family. These positive coping strategies supported the constructs of spiritual beliefs and relationships with others, which were established in prior studies (Al-Khattab et al., 2016; Conner & Yeh, 2018; Ofonedu et al., 2013). The theme of coping and problem-solving strategies was dominated by the most common strategy: participants hiding their thoughts and feelings as a way of managing their depressive symptoms. This result corroborates the findings of prior studies that show Black adolescents conceal their feelings and symptoms of depression (Al-Khattab et al., 2016; Breland-Noble et al., 2010; Ofonedu et al., 2013; Vontress et al., 2007). As previous studies have suggested, hiding thoughts and feelings may be due to the stigma associated with mental illness and limited options in how to respond to stressful and anxiety-provoking situations (Robinson et al., 2017; Robinson et al., 2015). The finding that the participants hide thoughts and feelings also supports previous research that Black adolescents may be fearful of how others will react to them and isolate themselves as a result (Al-Khattab et al., 2016; Breland-Noble et al., 2010; Ofonedu et al., 2013). Participants also reported engaging in unhealthy coping behaviors such as self-harm, sexual intercourse, and isolation. These harmful strategies may be due to the limited coping skills of Black adolescents that have been identified in prior research studies (Robinson et al., 2017; Robinson et al., 2015). Again, these findings highlight the need for culturally specific training regarding mental health in Black communities.
The theme of emotional support resonated with all participants in this study, suggesting the significance of relationships (Breland-Noble et al., 2010). When examining emotional support, positive and negative experiences emerged. Positive emotional supports were found in family members (60%), teachers (50%), and mental health professionals (40%). Yet all participants indicated being negatively impacted by a lack of support among their peers. Participants reported feeling invalidated or not believed by their peers. They also reported that their peers did not seem to show concern. These experiences may have exacerbated the participants’ symptoms. Only half of the participants indicated receiving positive peer support when seeking help for depressive symptoms. These findings are concerning because of the heavy emphasis placed on relationships within Black communities (Breland-Noble et al., 2010).
Relationships were identified as significant to all participants in this study, indicating that healthy relationships may be a protective factor and may increase emotional and mental health. Counseling professionals in private practice and in schools are thus encouraged to inquire about a wide range of relationships when working with their Black adolescent clients. For example, a counseling professional might ask a client to complete a detailed relationship profile for each significant person in their life. This would help to uncover significant relationships that could support the client’s current challenges and to identify those individuals who might not be providing support. Counseling professionals might also conceptualize client symptoms as connected to these relationships. Family or systemic interventions may be incorporated into treatment planning to decrease depressive symptoms.
The theme of contributing factors encompassed a surprisingly high number of significant adverse and traumatic experiences. When examining the factors contributing to the development of depression in Black adolescents, most participants in this study cited verbal abuse, differences from others/bullying, and family-related issues as salient factors. Other contributing factors included sexual and physical abuse. Participants reported verbal abuse (70%), sexual abuse (40%), and physical abuse (30%) as contributing factors of depression. However, participants did not identify one single factor but rather described multiple and overlapping factors that contributed to their depressive symptoms. The connection between adverse and traumatic experiences and depressive symptoms specifically within the Black adolescent population appears to be underreported in the literature.
It is important to note the high prevalence of abuse indicated within the study. The lack of existing studies exploring the relationship among Black adolescents, depression, and adverse childhood experiences indicates that additional research is needed. An implication of this study is that when working with Black adolescent clients who are presenting with symptoms of depression, counseling professionals might incorporate an adverse childhood experience screening tool. Assessing clients for adverse childhood experiences as a matter of regular practice may better inform preventative measures and treatment. As this study highlights, it is essential for clinical and school professionals working with Black adolescents to understand that abuse can contribute to depressive symptoms.
Overall, many of the symptoms described by participants could be associated with a diagnosis of
dysthymia as a result of oppression, supporting the work of Vontress et al. (2007). However, the participants did not use the word “oppression” and may not have recognized the systemic aspects of their experiences (Vontress et al., 2007). It may be that the participants’ adverse experiences of abuse overshadowed any cultural or historical factors that may also have been present. The current study highlighted the overlooked and undertreated experiences of Black adolescents with depression. Counseling professionals may choose to gain a preliminary understanding of Black adolescent depression and dysthymia symptoms “within the context of their legacy of discrimination and oppression” (Vontress et al., 2007, p. 132).
Limitations
Overall, these findings need to be considered in light of some specific limitations. First, the interview questions were semi-structured. This means that the researcher used open-ended questions followed by discussion. As a result, the interviewer may not have covered the exact same content with each participant. Furthermore, because of the nature of the study, some participants may have been more forthcoming about their personal experiences. Thirdly, although the participants were asked about past events, the memories of those events may have been compromised because of the passage of time or because of received or ongoing treatment. Lastly, given the limited number of participants interviewed, more research is needed to understand the mental health needs and experiences of Black adolescents who are experiencing depression.
Conclusion
In this qualitative study of 10 Black adolescents living in a rural community, the authors provided space for the participants to use their own terms and language to define depression. It is clear through this and other research that contextual factors are often involved in the onset of depression in Black adolescents, and there is not enough active therapeutic and medical treatment for Black adolescents living with depression. There is a stigma associated with mental illness and reluctance to seek treatment within the Black community, particularly in rural areas. As a result, counselors and mental health providers need to become more educated and aware when working with Black adolescents who live in rural communities.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Alegria, M., Vallas, M., & Pumariega, A. J. (2010). Racial and ethnic disparities in pediatric mental health. Child and Adolescent Psychiatric Clinics of North America, 19(4), 759–774. https://doi.org/10.1016/j.chc.2010.07.001
Al-Khattab, H., Oruche, U., Perkins, D., & Draucker, C. (2016). How African American adolescents manage depression: Being with others. Journal of the American Psychiatric Nurses Association, 22(5), 387–400. https://doi.org/10.1177/1078390316657391
Auger, R. W. (2005). School-based interventions for students with depressive disorders. Professional School Counseling, 8(4), 344–352.
Breland-Noble, A. M., Burriss, A., & Poole, H. K. (2010). Engaging depressed African American adolescents in treatment: Lessons from the AAKOMA PROJECT. Journal of Clinical Psychology, 66(8), 868–879. https://doi.org/10.1002/jclp.20708
Brenner, E. (2019). The crisis of youth mental health. Stanford Social Innovation Review. https://ssir.org/articles/entry/the_crisis_of_youth_mental_health#
Bridge, J. A., Horowitz, L. M., Fontanella, C. A., Sheftall, A. H., Greenhouse, J., Kelleher, K. J., & Campo, J. V. (2018). Age-related racial disparity in suicide rates among US youths from 2001 through 2015. JAMA Pediatrics, 172(7), 697–699. https://doi.org/10.1001/jamapediatrics.2018.0399
Brody, G. H., Chen, Y.-F., Kogan, S. M., Yu, T., Molgaard, V. K., DiClemente, R. J., & Wingood, G. M. (2012). Family-centered program deters substance use, conduct problems, and depressive symptoms in Black adolescents. Pediatrics, 129(1), 108–115. https://doi.org/10.1542/peds.2011-0623
Bryant, K., Greer-Williams, N., Willis, N., & Hartwig, M. (2013). Barriers to diagnosis and treatment of depression: Voices from a rural African-American faith community. Journal of National Black Nurses’ Association: JNBNA, 24(1), 31–38.
Choi, H., Meininger, J. C., & Roberts, R. E. (2006). Ethnic differences in adolescents’ mental distress, social stress, and resources. Adolescence, 41(162), 263–283.
Conner, L. C., & Yeh, C. J. (2018). Stress, coping, and depression among Black urban adolescents: Implications for school counseling. Journal of School Counseling, 16(15), 1–31.
Cook, B. L., Trinh, N.-H., Li, Z., Hou, S. S.-Y., & Progovac, A. M. (2017). Trends in racial–ethnic disparities in access to mental health care, 2004–2012. Psychiatric Services, 68(1), 9–16. https://doi.org/10.1176/appi.ps.201500453
Everall, R. D., Altrows, J., & Paulson, B. L. (2006). Creating a future: A study of resilience in suicidal female adolescents. Journal of Counseling & Development, 84(4), 461–471. https://doi.org/10.1002/j.1556-6678.2006.tb00430.x
Graves, L. (2017). Filters of influence: The help-seeking process of African American single mothers living in poverty seeking mental health services for their children. Child & Youth Services, 38(1), 69–90. https://doi.org/10.1080/0145935X.2016.1251836.
Hays, D. G., & Singh, A. A. (2012). Qualitative inquiry in clinical and educational settings. Guilford.
Hope, M. O., Assari, S., Cole-Lewis, Y. C., & Caldwell, C. H. (2017). Religious social support, discrimination, and psychiatric disorders among Black adolescents. Race and Social Problems, 9(2), 102–114. https://doi.org/10.1007/s12552-016-9192-7
Jacob, M., Keeley, M. L., Ritschel, L., & Craighead, W. E. (2013). Behavioural activation for the treatment of low-income, African American adolescents with major depressive disorder: A case series. Clinical Psychology & Psychotherapy, 20(1), 87–96. https://doi.org/10.1002/cpp.774
Lake, J., & Turner, M. S. (2017). Urgent need for improved mental health care and a more collaborative model of care. Permanente Journal, 21, 17–24. https://doi.org/10.7812/TPP/17-024
Liang, J., Matheson, B. E., & Douglas, J. M. (2016). Mental health diagnostic considerations in racial/ethnic minority youth. Journal of Child and Family Studies, 25(6), 1926–1940. https://doi.org/10.1007/s10826-015-0351-z
Lindsey, M. A., Joe, S., & Nebbitt, V. (2010). Family matters: The role of mental health stigma and social support on depressive symptoms and subsequent help seeking among African American boys. Journal of Black Psychology, 36(4), 458–482. https://doi.org/10.1177/0095798409355796
Lincoln, Y. S., & Guba, E. G. (1985). Naturalistic inquiry. SAGE.
Lu, W. (2019). Adolescent depression: National trends, risk factors, and healthcare disparities. American Journal of Health Behavior, 43(1), 181–194. https://doi.org/10.5993/AJHB.43.1.15
Lu, W., Lindsey, M. A., Irsheid, S., & Nebbitt, V. E. (2017). Psychometric properties of the CES-D among Black adolescents in public housing. Journal for the Society for Social Work and Research, 8(4), 595–619. https://doi.org/10.1086/694791
Merriam, S. B. (2009). Qualitative research: A guide to design and implementation (3rd ed.). Jossey-Bass.
Murry, V. M., Heflinger, C. A., Suiter, S. V., & Brody, G. H. (2011). Examining perceptions about mental health care and help-seeking among rural African American families of adolescents. Journal of Youth and Adolescence, 40(9), 1118–1131.
https://doi.org/ 10.1007/s10964-010-9627-1
National Institute of Mental Health. (2013). Major depression. https://www.nimh.nih.gov/health/statistics/major-depression.shtml
Ofonedu, M. E., Percy, W. H., Harris-Britt, A., & Belcher, H. M. E. (2013). Depression in inner city African American youth: A phenomenological study. Journal of Child and Family Studies, 22(1), 96–106. https://doi.org/10.1007/s10826-012-9583-3
Patton, M. Q. (1987). How to use qualitative methods in evaluation (2nd ed.). SAGE.
Planey, A. M., Smith, S. M., Moore, S., & Walker, T. D. (2019). Barriers and facilitators to mental health help-seeking among African American youth and their families: A systematic review study. Children and Youth Services Review, 101, 190–200. https://doi.org/10.1016/j.childyouth.2019.04.001
Probst, J. C., Laditka, S. B., Moore, C. G., Harun, N., Powell, M. P., & Baxley, E. G. (2006). Rural-urban differences in depression prevalence: implications for family medicine. Family Medicine Kansas City, 38(9), 653–660.
Robinson, W. L., Brown, M., Beasley, C. R., & Jason, L. A. (2017). Advancing prevention intervention from theory to application: Challenges and contributions of community psychology. In M. A. Bond, I. Serrano-García, C. B. Keys, & M. Shinn (Eds.), APA handbook in psychology. APA handbook of community psychology: Methods for community research and action for diverse groups and issues (pp. 193–213). American Psychological Association.
Robinson, W. L., Droege, J. R., Case, M. H., & Jason, L. A. (2015). Reducing stress and preventing anxiety in African American adolescents: A culturally-grounded approach. Global Journal of Community Psychology Practice, 6(2). https://doi.org/10.7728/0602201503
Saluja, G., Iachan, R., Scheidt, P. C., Overpeck, M. D., Sun, W., & Giedd, J. N. (2004). Prevalence of and risk factors for depressive symptoms among young adolescents. Archives of Pediatrics and Adolescent Medicine, 158(8), 760–765. https://doi.org/10.1001/archpedi.158.8.760
Shushansky, L. (2017, July 31). Disparities within minority mental health care [Blog post]. National Alliance on Mental Illness. https://www.nami.org/Blogs/NAMI-Blog/July-2017/Disparities-Within-Minority-Mental-Health-Care
Smokowski, P. R., Bacallao, M. L., Cotter, K. L., & Evans, C. B. R. (2015). The effects of positive and negative parenting practices on adolescent mental health outcomes in a multicultural sample of rural youth. Child Psychiatry & Human Development, 46(3), 333–345. https://doi.org/10.1007/s10578-014-0474-2
Sullivan, G., Cheney, A., Olson, M., Haynes, T., Bryant, K., Cottoms, N., Reaves, C., & Curran, G. (2017). Rural African Americans’ perspectives on mental health: Comparing focus groups and deliberative democracy forums. Journal of Health Care for the Poor and Underserved, 28(1), 548–565. https://doi.org/10.1353/hpu.2017.0039
van Manen, M. (1997). Researching lived experience: Human science for an action sensitive pedagogy. (2nd ed.). Althouse.
Vontress, C. E., Woodland, C. E., & Epp, L. (2007). Cultural dysthymia: An unrecognized disorder among African Americans? Journal of Multicultural Counseling and Development, 35(3), 130–141. https://doi.org/10.1002/j.2161-1912.2007.tb00055.x
Weaver, A., Himle, J. A., Taylor, R. J., Matusko, N. N., & Abelson, J. M. (2015). Urban vs. rural residence and the prevalence of depression and mood disorder among African American women and non-Hispanic white women. JAMA Psychiatry, 72(6), 576–583. https://doi.org/10.1001/jamapsychiatry.2015.10
Willis, L. A., Coombs, D. W., Drentea, P., & Cockerham, W. C. (2003). Uncovering the mystery: Factors of African American suicide. Suicide and Life-Threatening Behavior, 33(4), 412–429. https://doi.org/10.1521/suli.33.4.412.25230
World Federation for Mental Health. (2012). Depression: A global crisis. https://www.who.int/mental_health/management/depression/wfmh_paper_depression_wmhd_2012.pdf
World Health Organization. (2020). Depression. https://www.who.int/news-room/fact-sheets/detail/depression
TeShaunda Hannor-Walker, PhD, NCC, LPC, CPCS, is an assistant professor at Liberty University. Lynn Bohecker, PhD, LMFT, is an associate professor at Liberty University. Lacey Ricks, PhD, NCC, is an assistant professor at Liberty University. Sarah Kitchens, PhD, NCC, is an assistant professor at Liberty University. Correspondence may be addressed to TeShaunda Hannor-Walker, 1971 University Blvd., Lynchburg, VA 24515, thannorwalker@liberty.edu.
Dec 2, 2014 | Article, Volume 4 - Issue 5
Bryn E. Schiele, Mark D. Weist, Eric A. Youngstrom, Sharon H. Stephan, Nancy A. Lever
Counseling self-efficacy (CSE), defined as one’s beliefs about his or her ability to effectively counsel a client, is an important precursor of effective clinical practice. While research has explored the association of CSE with variables such as counselor training, aptitude and level of experience, little attention has been paid to CSE among school mental health (SMH) practitioners. This study examined the influence of quality training (involving quality assessment and improvement, modular evidence-based practices, and family engagement/empowerment) versus peer support and supervision on CSE in SMH practitioners, and the relationship between CSE and practice-related variables. ANCOVA indicated similar mean CSE changes for counselors receiving the quality training versus peer support. Regression analyses indicated that regardless of condition, postintervention CSE scores significantly predicted quality of practice, knowledge of evidence-based practices (EBP) and use of EBP specific to treating depression. Results emphasize the importance of CSE in effective practice and the need to consider mechanisms to enhance CSE among SMH clinicians.
Keywords: self-efficacy, school mental health, evidence-based practices, counselor training, depression
There are major gaps between the mental health needs of children and adolescents and the availability of effective services to meet such needs (Burns et al., 1995; Kataoka, Zhang, & Wells, 2002). This recognition is fueling efforts to improve mental health services for youth in schools (Mellin, 2009; Stephan, Weist, Kataoka, Adelsheim, & Mills, 2007). At least 20% of all youth have significant mental health needs, with roughly 5% experiencing substantial functional impairment (Leaf, Schultz, Kiser, & Pruitt, 2003). Further, less than one third of children with such mental health needs receive any services at all.
The President’s New Freedom Commission on Mental Health (2003) documented the position of schools as a point of contact and universal natural setting for youth and families, recognizing schools as a key factor in the transformation of child and adolescent mental health services (Stephan et al., 2007). In the past 2 decades, there has been a significant push for full-service schools that expand beyond a sole focus on education, and employ community mental health practitioners to respond to the emotional and behavioral needs of students (Conwill, 2003; Dryfoos, 1993; Kronick, 2000). The education sector is the most common provider of mental health services for children and adolescents (Farmer, Burns, Phillips, Angold, & Costello, 2003), with 70%–80% of youth who receive any mental health services obtaining them at school (Burns et al., 1995; Rones & Hoagwood, 2000). Therefore, attention must be paid to the quantity, quality and effectiveness of school mental health (SMH) services.
School Mental Health
In recent years, SMH programs, supported by both school staff (e.g., school psychologists, social workers, counselors) and school-based community mental health clinicians, have emerged as a promising approach to the provision of mental health services for students and families (Weist, Evans, & Lever, 2003). The growth of these programs has facilitated investigation of what constitutes high-quality SMH service provision (Nabors, Reynolds, & Weist, 2000; Weist et al., 2005). This work has been supported and furthered by the Center for School Mental Health, a federally funded technical assistance and training program to advance SMH programs within the United States. In collaboration with other SMH centers (e.g., UCLA Center for Mental Health in Schools) and interdisciplinary networks focused on school health, consensus was reached to develop a guiding framework defining best practices in SMH (Weist et al., 2005). These principles call for appropriate service provision for children and families, implementation of interventions to meet school and student needs, and coordination of mental health programs in the school with related community resources, among other things. For further explication of the framework and its development, see Weist et al. (2005).
Simultaneously, research developments through the Center for School Mental Health facilitated implementation of modular evidence-based practices (EBP; see Chorpita, Becker & Daleiden, 2007; Chorpita & Daleiden, 2009). A modular approach for intervention involves training clinicians in core, effective strategies for disorders frequently encountered in children (e.g., attention-deficit/hyperactivity disorder [ADHD], anxiety, depression, disruptive behavior disorders [DBD]). This approach enables individualized, flexible implementation of evidence-based strategies without the constraints of a manualized approach (Curry & Reinecke, 2003). The third guiding component to enhance quality in SMH practices is development of strategies to effectively engage and empower families (see Hoagwood, 2005).
Despite the development of such a framework, SMH clinicians often struggle to implement high-quality, evidence-based services (Evans et al., 2003; Evans & Weist, 2004). These clinicians are constrained by a lack of sufficient time, training in EBP, appropriate supervision, and internal and external resources (Shernoff, Kratchowill & Stoiber, 2003). For instance, a survey by Walrath et al. (2004) of Baltimore SMH clinicians suggested that the ratio of clinicians to students was 1:250, and in order to meet the mental health needs of students, clinicians would have to increase clinical hours by 79 per week to remediate student difficulties. Additionally, the school environment is often characterized as chaotic, hectic and crisis-driven (Langley, Nadeem, Kataoka, Stein, & Jaycox, 2010), with SMH clinicians citing difficulties implementing EBP given the schedules of students. As a result of the challenges limiting use of EBP in daily SMH practice, researchers are now evaluating the influences on successful delivery of EBP in schools, including the personal qualities of SMH professionals (e.g., attitudes, beliefs, skills, training; Berger, 2013), as well as environmental factors (e.g., school administrative support, access to community resources, sufficient space for practice; Powers, Edwards, Blackman & Wegmann, 2013) that may predict high-quality services (see Weist et al., 2014).
Previous work examining factors related to the provision of evidence-based SMH services by SMH clinicians suggested that the highest-rated facilitators of effective SMH practice were personal characteristics (e.g., desire to deliver mental health services), attitudes and openness toward use of EBP, and adequate training (Beidas et al., 2012; Langley et al., 2010). Alternatively, SMH clinicians reported a number of administrative, school site and personal barriers as significant obstacles to appropriate service delivery; such barriers include lack of sufficient training, overwhelming caseload, job burnout and personal mental health difficulties (Langley et al., 2010; Suldo, Friedrich, & Michalowski, 2010).
While researchers have evaluated the influence of SMH provider personal characteristics in relation to the delivery of high-quality SMH services, little attention has been paid to the importance of counseling self-efficacy (CSE). CSE is widely accepted as an important precursor to competent clinical practice (Kozina, Grabovari, De Stefano, & Drapeau, 2010). Further, building CSE is considered an important strategy in active learning when providing training in evidence-based therapies (Beidas & Kendall, 2010), and CSE in EBP is believed to be essential to implementation (Aarons, 2005). However, researchers have yet to systematically include measures of CSE in studies of EBP utilization by SMH providers.
Self-Efficacy
Social-cognitive theory and its central construct, self-efficacy, have received much attention in the psychological literature, with more than 10,000 studies including these as central variables in the past 25 years (Judge, Jackson, Shaw, Scott, & Rich, 2007). Self-efficacy is defined as an individual’s beliefs about his or her ability to achieve desired levels of performance (Bandura, 1994), and it plays a key role in the initiation and maintenance of human behavior (Iannelli, 2000). Given the influence of self-efficacy expectancies on performance, researchers have evaluated how self-efficacy impacts a variety of action-related domains, including career selection (e.g., Branch & Lichtenberg, 1987; Zeldin, Britner, & Pajares, 2008), health-behavior change (e.g., Ramo, Prochaska, & Myers, 2010; Sharpe et al., 2008) and work-related performance (e.g., Judge et al., 2007; Stajkovic & Luthans, 1998). Specific to the mental health field, previous investigations have focused on how self-efficacy is related to counseling performance.
Counseling Self-Efficacy
The construct of CSE is defined as an individual’s beliefs about his or her ability to effectively counsel a client in the near future (Larson & Daniels, 1998). Studies of the structure and influence of CSE among a variety of mental health professionals, including counseling trainees, master’s-level counselors, psychologists, school counselors and students from related professions (e.g., clergy, medicine) have yielded mixed findings. Social desirability, counselor personality, aptitude, achievement (Larson et al., 1992) and counselor age (Watson, 2012) have shown small to moderate associations with CSE. CSE also is related to external factors, including the perceived and objective work environment, supervisor characteristics, and level or quality of supervision (Larson & Daniels, 1998).
However, the relationship of CSE with level of training is unclear. For the most part, CSE is stronger for individuals with at least some counseling experience than for those with none (Melchert, Hays, Wiljanen, & Kolocek, 1996; Tang et al., 2004). While the amount of training and education obtained have been reported as statistically significant predictors of degree of CSE (Larson & Daniels, 1998; Melchert et al., 1996), more recent work has not supported the existence of such predictive relationships (Tang et al., 2004). It also has been suggested that once a counselor has obtained advanced graduate training beyond the master’s level, the influence of experience on CSE becomes rather minimal (Larson, Cardwell, & Majors, 1996; Melchert et al., 1996; Sutton & Fall, 1995).
Some work has been done to evaluate interventions aimed at enhancing CSE by utilizing the four primary sources of self-efficacy, as defined by Bandura (1977; i.e., mastery, modeling, social persuasion, affective arousal). In two studies involving undergraduate recreation students, Munson, Zoerink & Stadulis (1986) found that modeling with role-play and visual imagery served to enhance CSE greater than a wait-list control group. Larson et al. (1999) attempted to extend these findings utilizing a sample of practicum counseling trainees, and found that self-evaluation of success in the session moderated the level of CSE postintervention (Larson et al., 1999), with perception of success significantly impacting the potency of the role-play scenarios. The same effect was not found for individuals in the videotape condition.
In addition to impacting clinician performance, CSE has been reported to indirectly impact positive client outcome (Urbani et al., 2002); for example, CSE has been associated with more positive outcomes for clients, more positive self-evaluations and fewer anxieties regarding counseling performance (Larson & Daniels, 1998). Thus, increasing CSE, which decreases clinicians’ anxiety, is important for client outcomes, as anxiety is reported to decrease level of clinical judgment and performance (Urbani et al., 2002). While there is some evidence that CSE is influential for client outcomes, minimal work has been done to evaluate this relationship.
CSE has been evaluated in a variety of samples; however, little work has been done to evaluate CSE of SMH practitioners and the factors that play into its development. Additionally, although some investigation has been conducted on factors that impact SMH practitioners’ abilities and performance, CSE is an element that seldom has been studied.
The current study aimed to examine the influence of a quality assessment and improvement (QAI) intervention on CSE in SMH practitioners, as well as the importance of CSE in regard to practice-related domains. The primary question of interest was, Does an intervention focused on QAI (target) result in higher levels of CSE than a comparison condition involving a focus on professional wellness (W) and supervision (control)? We investigated the influence of differential quality training and supervision on one’s level of CSE by comparing postintervention CSE scores between each condition after evaluating preintervention equivalency of CSE levels. Thus, we hypothesized that long-term exposure to the QAI intervention, family engagement/empowerment and modular EBP would result in significantly higher reports of CSE from those exposed to the QAI intervention than those exposed to the comparison intervention. Based on previous research, it is possible that specific counselor characteristics (e.g., age, experience) would predict CSE, such that individuals who are older and have more experience counseling children and adolescents would have higher CSE (Melchert et al., 1996; Tang et al., 2004; Watson, 2012). Thus, when evaluating training effects, these variables were included as covariates in the analysis of the relation between CSE and training.
Secondarily, this study aimed to evaluate the relation of professional experiences to CSE following exposure to the intervention. For this aim, the research question was, Does postintervention level of CSE predict quality of self-reported SMH practice, as well as knowledge and use of EBP? We hypothesized that level of CSE would predict quality of SMH practice, as well as attitude toward, knowledge and use of EBP regardless of intervention condition.
Method
This article stems from a larger previous evaluation of a framework to enhance the quality of SMH (Weist et al., 2009), funded by the National Institute of Mental Health (#1R01MH71015; 2003-2007; M. Weist, PI). As a part of a 12-year research program on quality and EBP in SMH, researchers conducted a two-year, multisite (from community agencies in Delaware, Maryland, Texas) randomized controlled trial of a framework for high-quality and effective practice in SMH (EBP, family engagement/empowerment and systematic QAI) as compared to an enhanced treatment as usual condition (focused on personal and school staff wellness). Only the methods pertaining to the aims of the current study have been included here (see Stephan et al., 2012; Weist et al., 2009 for more comprehensive descriptions).
Participants
A sample of 72 SMH clinicians (i.e., clinicians employed by community mental health centers to provide clinical services within the school system) from the three SMH sites participated for the duration of the study (2004–2006), and provided complete data for all study measures via self-report. All clinicians were employed by community-based agencies with an established history of providing SMH prevention and intervention services to elementary, middle and high school students in both general and special education programs.
A total of 91 clinicians participated over the course of the study, with a sample size of 64 in Year 1 and 66 in Year 2, with 27 clinicians involved only in Year 2. Out of the Year 1 sample (35 QAI and 29 W), 24 participants did not continue into Year 2 (13 QAI and 11 W). Dropout showed no association with nonparticipation and did not differ between conditions (37% QAI versus 38% comparison dropout rate). Investigations in this particular study focused on individuals who had completed at least one year of the study and had submitted pre- and postintervention measures. The 72 participants were predominantly female (61 women, 11 men) and were 36 years old on average (SD = 11.03). In terms of race and ethnicity, participants identified as Caucasian (55%), African American (26%), Hispanic (18%) and Other (1%). Participants reported the following educational levels: graduate degree (83%), some graduate coursework (13%), bachelor’s degree (3%), and some college (1%). In terms of experience, clinicians had roughly 6 years of prior experience and had worked for their current agency for 3 years on average. The obtained sample is reflective of SMH practitioners throughout the United States (Lewis, Truscott, & Volker, 2008).
Measures
Counseling self-efficacy. Participants’ CSE was measured using the Counselor Self-Efficacy Scale (Sutton & Fall, 1995). The measure was designed to be used with school counselors, and was created using a sample of public school counselors in Maine. Sutton and Fall modified a teacher efficacy scale (Gibson & Dembo, 1984), resulting in a 33-item measure that reflected CSE and outcome expectancies. Results of a principal-component factor analysis demonstrated initial construct validity, indicating a three-factor structure, with the internal consistency of these three factors reported as adequate (.67–.75). However, the structure of the measure has received criticism, with some researchers arguing that the third factor does not measure outcome expectancies as defined by social-cognitive theory (Larson & Daniels, 1998). Thus, we made a decision to use the entire 33-item scale as a measure of overall CSE. Respondents were asked to rate each item using a 6-point Likert scale (1 = strongly disagree, 6 = strongly agree). We made slight language modifications to make the scale more applicable to the work of this sample (Weist et al., 2009); for instance, guidance program became counseling program. CSE was measured in both conditions at the beginning and end of Years 1 and 2 of the intervention program.
Quality of school mental health services. The School Mental Health Quality Assessment Questionnaire (SMHQAQ) is a 40-item research-based measure developed by the investigators of the larger study to assess 10 principles for best practice in SMH (Weist et al., 2005; Weist et al., 2006), including the following: “Programs are implemented to address needs and strengthen assets for students, families, schools, and communities” and “Students, families, teachers and other important groups are actively involved in the program’s development, oversight, evaluation, and continuous improvement.”
At the end of Year 2, clinicians rated the degree to which each principle was present in their own practice on a 6-point Likert scale, ranging from not at all in place to fully in place. Given that results from a principle components analysis indicated that all 10 principles weighed heavily on a single strong component, analyses focused primarily on total scores of the SMHQAQ. Aside from factor analytic results, validity estimates are unavailable. Internal consistency as measured by coefficient alpha was very strong (.95).
Knowledge and use of evidence-based practices. The Practice Elements Checklist (PEC) is based on the Hawaii Department of Health’s comprehensive summary of top modular EBP elements (Chorpita & Daleiden, 2007). Principal investigators of the larger study created the PEC in consultation with Bruce Chorpita of the University of California, Los Angeles, an expert in mental health technologies for children and adolescents. The PEC asks clinicians to provide ratings of the eight skills found most commonly across effective treatments for four disorder areas (ADHD, DBD, depression and anxiety). Respondents used a 6-point Likert scale to rate both current knowledge of the practice element (1= none and 6 = significant), as well as frequency of use of the element in their own practice, and frequency with which the clinician treats children whose primary presenting issue falls within one of the four disorder areas (1 = never, 6 = frequently).
In addition to total knowledge and total frequency subscales (scores ranging from 4–24), research staff calculated four knowledge and four frequency subscale scores (one for each disorder area) by averaging responses across practice elements for each disorder area (scores ranging from 1–6). Clinicians also obtained total PEC score by adding all subscale scores, resulting in a total score ranging from 16–92. Although this approach resulted in each item being counted twice, it also determined how total knowledge and skill usage are related to CSE, as well as skills in specific disorder areas. While internal consistencies were found to be excellent for each of the subscales, ranging from .84–.92, validity of the measure has yet to be evaluated. Clinicians completed the PEC at end of Year 2.
Study Design
SMH clinicians were recruited from their community agencies approximately 1 month prior to the initial staff training. After providing informed consent, clinicians completed a set of questionnaires, which included demographic information, level of current training and CSE, and were randomly assigned to the QAI intervention or the W intervention. Four training events were provided for participants in both conditions (at the beginning and end of both Years 1 and 2). During the four training events, individuals in the QAI condition received training in the three elements reviewed previously. For individuals involved in the W (i.e., comparison) condition, training events focused on general staff wellness, including stress management, coping strategies, relaxation techniques, exercise, nutrition and burnout prevention.
At each site, senior clinicians (i.e., licensed mental health professionals with a minimum of a master’s degree and 3 years experience in SMH) were chosen to serve as project supervisors for the condition to which they were assigned. These clinicians were not considered participants, and maintained their positions for the duration of the study. Over the course of the project, each research supervisor dedicated one day per week to the study, and was assigned a group of roughly 10 clinicians to supervise. Within the QAI condition, supervisors held weekly group meetings with small groups of five clinicians to review QAI processes and activities in their schools, as well as strategies for using the evidence base; in contrast, there was no study-related school support for staff in the W condition.
Results
Preliminary Analyses and Scaling
Analyses were conducted using SPSS, version 20; tests of statistical significance were conducted with a Bonferroni correction (Cohen, Cohen, West, & Aiken, 2003), resulting in the use of an alpha of .0045, two-tailed. To facilitate comparisons between variables, staff utilized a scaling method known as Percentage of Maximum Possible (POMP) scores, developed by Cohen, Cohen, Aiken, & West (1999). Using this method, raw scores are transformed so that they range from zero to 100%. This type of scoring makes no assumptions about the shape of the distributions, in contrast to z scores, for which a normal distribution is assumed. POMP scores are an easily understood and interpreted metric and cumulatively lead to a basis for agreement on the size of material effects in the domain of interest (i.e., interventions to enhance quality of services and use of EBP; Cohen et al., 1999).
Primary Aim
Initial analyses confirmed retreatment equivalence for the two conditions, t (72) = –.383, p = .703. For individuals in the QAI condition, preintervention CSE scores averaged at 71.9% of maximum possible (SD = .09), while those in the comparison condition averaged at 71.3% of maximum possible (SD = .08). These scores were comparable to level of CSE observed in counseling psychologists with similar amounts of prior experience (Melchert et al., 1996).
Correlation analyses suggested that pretreatment CSE was significantly associated with age (r = .312, p = .008), race (r = –.245, p = .029), years of counseling experience (r = .313, p = .007) and years with the agency (r = .232, p = .048). Thus, these variables were included as covariates in an analysis of covariance (ANCOVA) evaluating changes in CSE between the QAI and comparison conditions. Results suggested a nonsignificant difference in change in CSE from pre- to postintervention between conditions, F (72) = .013, p = .910. For individuals in the QAI condition, postintervention CSE scores averaged at 73.1% of maximum possible (SD = .07), and for individuals in the comparison condition, CSE scores averaged at 72.8% of maximum possible (SD = .08). Additionally, when looking across conditions, results indicated a nonsignificant difference in change in level of CSE from pre- to postintervention, F (72) = .001, p = .971. Across conditions, clinicians reported roughly similar levels of CSE at pre- and postintervention time points (72% vs. 73% of maximum possible); see Table 1.
Table 1
Analysis of Covariance (ANCOVA) Summary of Change in CSE
|
Source
|
df
|
F
|
p
|
Partial η2
|
|
|
|
|
|
| CSE |
1
|
.001
|
.971
|
.000
|
| CSE*Condition |
1
|
.013
|
.910
|
.000
|
| CSE*Age |
1
|
.281
|
.598
|
.004
|
| CSE*Race |
1
|
1.190
|
.279
|
.018
|
| CSE*Years of Experience |
1
|
.032
|
.859
|
.000
|
| CSE*Years with Agency |
1
|
.003
|
.955
|
.000
|
| Error |
66
|
|
|
|
Note. N = 72.
Secondary Aim
To investigate the influence of level of CSE on quality and practice elements in counseling, a series of individual regressions were conducted with level of postintervention CSE as the predictor variable, and indicators of attitudes toward EBP, knowledge and use of EBP, and use of quality mental health services as the outcome variables in separate analyses.
Table 2 shows that level of postintervention CSE significantly predicted the following postintervention variables: SMHQAQ quality of services (R2 = .328, F [60] = 29.34, p < .001); knowledge of EBP for ADHD (R2 = .205, F [46] = 11.54, p = .001), depression (R2 = .288, F [46]= 18.17, p < .001), DBD (R2 = .236, F [46]= 13.92, p = .001) and anxiety (R2 = .201, F [46]= 10.81, p = .002); usage of EBP specific to treating depression (R2 = .301, F [46]= 19.34, p < .001); and total knowledge of EBP (R2 = .297, F [44] = 18.20, p < .001). Results further indicated that postintervention CSE was not a significant predictor of usage of EBP for ADHD (R2 = .010, F [45] = .457, p = .502), DBD (R2 = .024, F [45] = 1.100, p = .300) and anxiety (R2 = .075, F [43] = 3.487, p = .069); and total usage of EBP (R2 = .090, F [43] = 4.244, p = .045).
Table 2
Results of Linear Regressions Between Level of Postintervention CSE and Outcome Variables
|
Variables
|
Beta
|
R2
|
Adjusted R2
|
F
|
p
|
|
|
|
|
|
|
| SMH Quality |
0.573
|
0.328
|
0.317
|
29.337
|
0.000
|
| EBP ADHD – Knowledge |
0.452
|
0.205
|
0.187
|
11.583
|
0.001
|
| EBP ADHD – Usage |
0.100
|
0.010
|
–0.012
|
0.457
|
0.502
|
| EBP Depression – Knowledge |
0.536
|
0.288
|
0.272
|
18.168
|
0.000
|
| EBP Depression – Usage |
0.548
|
0.301
|
0.285
|
19.337
|
0.000
|
| EBP DBD – Knowledge |
0.486
|
0.236
|
0.219
|
13.922
|
0.001
|
| EBP DBD – Usage |
0.154
|
0.024
|
0.002
|
1.100
|
0.300
|
| EBP Anxiety – Knowledge |
0.448
|
0.201
|
0.182
|
10.811
|
0.002
|
| EBP Anxiety – Usage |
0.274
|
0.075
|
0.053
|
3.487
|
0.069
|
| EBP Total Knowledge |
0.545
|
0.297
|
0.281
|
18.197
|
0.000
|
| EBP Total Usage |
0.300
|
0.900
|
0.069
|
4.244
|
0.045
|
Note. To control for experiment-wise error, a Bonferroni correction was used and significance was evaluated at the 0.0045 level.
Discussion
While there has been some previous examination of the association between training and CSE, results have been mixed (see Larson & Daniels, 1998), and no such evaluations have been conducted within the context of SMH services. The current study stemmed from a larger evaluation of a framework to enhance the quality of SMH, targeting quality service provision, EBP, and enhancement of family engagement and empowerment (see Weist et al., 2009).
The present study had two primary aims. The first goal was to evaluate differences in level of CSE from pre- to postintervention between two groups of SMH clinicians. We expected that those who received information, training and supervision on QAI and best practice in SMH would report higher levels of CSE postintervention than those in the W condition. The secondary aim was to evaluate whether clinician reports of postintervention CSE would serve as predictors of quality of SMH practice, as well as knowledge and use of EBP. Given the influence that clinician CSE has been found to have on practice-related variables in previous studies (see Larson & Daniels, 1998), we hypothesized that higher level of CSE would significantly predict higher quality of SMH practice, and knowledge and usage of EBP.
Controlling for age, race, years of experience and years with the agency, findings did not confirm the primary hypothesis. No statistically significant differences in clinician reports of CSE from pre- to postintervention were observed between the QAI and W conditions. Regarding the secondary aim, however, clinician postintervention level of CSE was found to serve as a significant predictor of quality of practice; total knowledge of EBP specific to treating ADHD, DBD, anxiety and depression; and usage of EBP specific to treating depression. Findings are consistent with previous literature suggesting that CSE levels influence performance in a number of practice-related domains (Larson & Daniels, 1998).
Results did not support a significant predictive relation between CSE level and usage of EBP specific to treating ADHD, DBD and anxiety. The failure to find an association may be due to evaluating level of usage of EBP across conditions due to limited power to run the analyses by condition. Results from the original study suggested that individuals in the QAI condition were more likely to use established EBP in treatment (see Weist et al., 2009). Thus, as provider characteristics including CSE (Aarons, 2005) are known to be associated with adoption of EBP, it may be that examining these associations across conditions resulted in null findings.
While current results did support the importance of high CSE regarding practice-related domains, there was no significant difference in level of CSE between those who received information, training and supervision in QAI; use of EBP; and family engagement and empowerment compared to those in the W condition. Findings from the current study contrast with other research that has documented improvements in CSE following targeted interventions. Previous targeted interventions to increase CSE have resulted in positive outcomes when using micro-skills training and mental practice (Munson, Stadulis, & Munson, 1986; Munson, Zoerink, & Stadulis, 1986), role-play and visual imagery (Larson et al., 1999), a prepracticum training course (Johnson, Baker, Kopala, Kiselica, & Thompson, 1989) and practicum experiences (Larson et al., 1993).
As a curvilinear relation is reported to exist between CSE and level of training (Larson et al., 1996; Sutton & Fall, 1995), it may be that the amount of previous training and experience of this sample of clinicians, being postlicensure, was such that the unique experiences gained through the QAI and W conditions in the current study had a minimal impact on overall CSE. Many prior studies utilized students untrained in counseling and interpersonal skills (Munson, Zoerink & Stadulis, 1986) and beginning practicum students and trainees (Easton, Martin, & Wilson, 2008; Johnson et al., 1989; Larson et al., 1992, 1993, 1999). Regarding the usefulness of a prepracticum course and practicum experiences for level of CSE, significant increases were only observed in the beginning practicum students with no significant changes seen in advanced students. Additionally, no previous studies have evaluated the success of CSE interventions with clinicians postlicensure.
It also is plausible that failure to detect an effect was due to the high preintervention levels of CSE observed across clinicians. At baseline, clinicians in the QAI condition reported CSE levels of roughly 71.9% of maximum potential, whereas those in the W condition reported CSE levels of 71.3% of maximum potential. Previous research has found high levels of CSE among practitioners with comparable amounts of previous experience, with those having 5–10 years of experience reporting mean CSE levels of 4.35 out of five points possible (Melchert et al., 1996). Thus, the average level of CSE may be accounted for by the amount of previous education and training reported by clinicians, and the observed increase of 1.5% at postintervention may be a reflection of the sample composition.
Limitations
Due to a small sample size, the power to detect changes in CSE was modest. Because of efforts to increase power by increasing the sample size, the time between reports of pre- and postintervention levels of CSE varied within the sample. Some participants completed only a year or a year and a half instead of the full 2 years.
A further limitation was reliance on self-reported information from the participating clinicians regarding their level of CSE, quality of practice, and knowledge and usage of EBP. Thus, a presentation bias may have been present in that clinicians may have reported stronger confidence in their own abilities than they felt in reality, or may have inflated responses on their knowledge and usage of EBP.
An additional limitation concerns the fact that CSE was not included as an explicit factor in training. Increasing CSE was not an explicit goal, and training and supervision were not tailored so that increases in CSE were more likely. The relation between supervisory feedback and CSE also may depend on the developmental level and pretraining CSE level of the clinicians (Larson et al., 1999; Munson, Zoerink & Stadulis, 1986), with untrained individuals reporting large increases. Thus, increased performance feedback may or may not have enhanced CSE within this sample.
Future Directions
Based on these findings, future work is suggested to evaluate ways in which CSE can be increased among clinicians. As the training procedures utilized in this study failed to change CSE, it is important to determine what facets of CSE, if any, are conducive to change. Although the current study evaluated broad CSE, Bandura (1977) theorized that overall self-efficacy is determined by the efficacy and outcome expectancies an individual has regarding a particular behavior. Efficacy expectancies are individuals’ beliefs regarding their capabilities to successfully perform the requisite behavior. Efficacy expectancies serve mediational functions between individuals and their behavior, such that if efficacy expectancies are high, individuals will engage in the behavior because they believe that they will be able to successfully complete it. Outcome expectancies, on the other hand, involve individuals’ beliefs that a certain behavior will lead to a specific outcome, and mediate the relation between behaviors and outcomes. Therefore, when outcome expectancies are low, individuals will not execute that behavior because they do not believe it will lead to a specified outcome.
As with the current study, the majority of the existing studies investigating change in CSE have evaluated broad CSE without breaking the construct down into the two types of expectancies (i.e., efficacy expectancies and outcome expectancies). Larson and Daniels (1998) found that fewer than 15% of studies on CSE examined outcome expectancies, and of the studies that did, only 60% operationalized outcome expectancies appropriately. While clinicians may believe that they can effectively perform a counseling strategy, they may not implement said strategy if they do not believe that it will produce client change. Ways in which these concepts can be evaluated may include asking, for example, for level of confidence in one’s ability to effectively deliver relaxation training, as well as for level of confidence that relaxation training produces client change. Based on the dearth of work in this area, future efforts should involve breaking down CSE and correctly operationalizing efficacy expectancies and outcome expectancies to examine what sorts of influences these expectancies have on overall CSE.
Additionally, future efforts to investigate the enhancement of CSE may evaluate the pliability of this construct depending on level of training. Is CSE more stable among experienced clinicians compared to counseling trainees? Should CSE enhancement be emphasized among new clinicians? Or are different methods needed to increase one’s CSE depending on previous experience? This goal may be accomplished by obtaining sizeable, representative samples with beginning, moderate and advanced levels of training, and examining the long-term stability of CSE.
Future work should incorporate strategies of mastery, modeling, social persuasion and affective arousal to enhance the CSE of SMH clinicians. Although role-play was utilized in the current study, future interventions could include visual imagery or mental practice of performing counseling skills, discussions of CSE, and more explicit positive supervisory feedback. Furthermore, mastery experiences (i.e., engaging in a counseling session that the counselor interprets as successful) in actual or role-play counseling settings have been found to increase CSE (Barnes, 2004); however, this result is contingent on the trainee’s perception of session success (Daniels & Larson, 2001). Future efforts to enhance CSE could strategically test how to structure practice counseling sessions and format feedback in ways that result in mastery experiences for clinicians. Future investigations also may incorporate modeling strategies into counselor training, possibly within a group setting. Structuring modeling practices in a group rather than an individual format may facilitate a fluid group session, moving from viewing a skill set to practicing with other group members and receiving feedback. This scenario could provide counselors with both vicarious and mastery experiences.
The use of verbal persuasion—the third source of efficacy—to enhance CSE also has been evaluated in counseling trainees. Verbal persuasion involves communication of progress in counseling skills, as well as overall strengths and weaknesses (Barnes, 2004). While strength-identifying feedback has been found to increase CSE, identifying skills that need improvement has resulted in a decrease in CSE. Lastly, emotional arousal, otherwise conceptualized as anxiety, is theorized to contribute to level of CSE. As opposed to the aforementioned enhancement mechanisms, increases in counselor anxiety negatively predict counselor CSE (Hiebert, Uhlemann, Marshall, & Lee, 1998). Thus, it is not recommended that identification of skills that need improvement be utilized as a tactic to develop CSE. Finally, in addition to clinician self-ratings, future research should investigate CSE’s impact on performance as measured by supervisors, as well as clients. With growing momentum for SMH across the nation, it is imperative that all factors influencing client outcomes and satisfaction with services be evaluated, including CSE.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of
interest or funding contributions for
the development of this manuscript.
References
Aarons, G. A. (2005). Measuring provider attitudes toward evidence-based practice: Consideration of organizational context and individual differences. Child and Adolescent Psychiatric Clinics of North America, 14, 255–271. doi:10.1016/j.chc.2004.04.008
Bandura, A. (1977). Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review, 84, 191–215. doi:10.1037/0033-295X.84.2.191
Bandura, A. (1994). Self-efficacy. In V. S. Ramachandran (Ed.), Encyclopedia of human behavior (Vol. 4, pp. 71–81). New York, NY: Academic Press.
Barnes, K. L. (2004). Applying self-efficacy theory to counselor training and supervision: A comparison of two approaches. Counselor Education and Supervision, 44, 56–69. doi:10.1002/j.1556-6978.2004.tb01860.x
Beidas, R. S., & Kendall, P. C. (2010). Training therapists in evidence-based practice: A critical review of studies from a systems-contextual perspective. Clinical Psychology: Science and Practice, 17, 1–30. doi:10.1111/j.1468-2850.2009.01187.x
Beidas, R. S., Mychailyszyn, M. P., Edmunds, J. M., Khanna, M. S., Downey, M. M., & Kendall, P. C. (2012). Training school mental health providers to deliver cognitive-behavioral therapy. School Mental Health, 4, 197–206. doi:10.1007/s12310-012-9047-0
Berger, T. K. (2013). School counselors’ perceptions practices and preparedness related to issues in mental health (Doctoral dissertation). Retrieved from http://hdl.handle.net/1802/26892
Branch, L. E., & Lichtenberg, J. W. (1987, August). Self-efficacy and career choice. Paper presented at the convention of the American Psychological Association, New York, NY.
Burns, B. J., Costello, E. J., Angold, A., Tweed, D., Stangl, D., Farmer, E. M., & Erkanli, A. (1995). Children’s mental health service use across service sectors. Health Affairs, 14, 147–159. doi:10.1377/hlthaff.14.3.147
Chorpita, B. F., Becker, K. D., & Daleiden, E. L. (2007). Understanding the common elements of evidence-based practice: Misconceptions and clinical examples. Journal of the American Academy of Child and Adolescent Psychiatry, 46, 647–652. doi:10.1097/chi.0b013e318033ff71
Chorpita, B. F., & Daleiden, E. L. (2009). CAMHD biennial report: Effective psychosocial interventions for youth with behavioral and emotional needs. Honolulu, HI: Child and Adolescent Mental Health Division, Hawaii Department of Health.
Cohen, P., Cohen, J., Aiken, L. S., & West, S. G. (1999). The problem of units and the circumstances for POMP. Multivariate Behavioral Research, 34, 315–346. doi:10.1207/S15327906MBR3403_2
Cohen, J., Cohen, P., West, S. G., & Aiken, L. S. (2003). Applied multiple regression/correlation analysis for the behavioral sciences (3rd ed.). Mahwah, NJ: Erlbaum.
Conwill, W. L. (2003). Consultation and collaboration: An action research model for the full-service school. Consulting Psychology Journal: Practice and Research, 55, 239–248. doi:10.1037/1061-4087.55.4.239
Curry, J. F., & Reinecke, M. A. (2003). Modular therapy for adolescents with major depression. In M. A. Reinecke, F. M. Dattilio, & A. Freeman (Eds.), Cognitive therapy with children and adolescents (2nd ed., pp. 95–127). New York, NY: Guilford.
Daniels, J. A., & Larson, L. M. (2001). The impact of performance feedback on counseling self-efficacy and counselor anxiety. Counselor Education and Supervision, 41, 120–130. doi:10.1002/j.1556-6978.2001.tb01276.x
Dryfoos, J. G. (1993). Schools as places for health, mental health, and social services. Teachers College Record, 94, 540–567.
Easton, C., Martin, W. E., Jr., & Wilson, S. (2008). Emotional intelligence and implications for counseling self-efficacy: Phase II. Counselor Education and Supervision, 47, 218–232. doi:10.1002/j.1556-6978.2008.tb00053.x
Evans, S. W., Glass-Siegel, M., Frank, A., Van Treuren, R., Lever, N. A., & Weist, M. D. (2003). Overcoming the challenges of funding school mental health programs. In M. D. Weist, S. W. Evans, & N. A. Lever (Eds.), Handbook of school mental health: Advancing practice and research (pp. 73–86). New York, NY: Kluwer Academic/Plenum.
Evans, S. W., & Weist, M. D. (2004). Implementing empirically supported treatments in the schools: What are we asking? Clinical Child and Family Psychology Review, 7, 263–267. doi:10.1007/s10567-004-6090-0
Farmer, E. M., Burns, B. J., Phillips, S. D., Angold, A., & Costello, E. J. (2003). Pathways into and through mental health services for children and adolescents. Psychiatric Services, 54, 60–66. doi:10.1176/appi.ps.54.1.60
Gibson, S., & Dembo, M. H. (1984). Teacher efficacy: A construct validation. Journal of Educational Psychology, 76, 569–582. doi:10.1037/0022-0663.76.4.569
Hiebert, B., Uhlemann, M. R., Marshall, A., & Lee, D. Y. (1998). The relationship between self-talk, anxiety, and counselling skill. Canadian Journal of Counselling and Psychotherapy, 32, 163–171.
Hoagwood, K. E. (2005). Family-based services in children’s mental health: A research review and synthesis. Journal of Child Psychology and Psychiatry, 46, 690–713. doi:10.1111/j.1469-7610.2005.01451.x
Iannelli, R. J. (2000). A structural equation modeling examination of the relationship between counseling self-efficacy, counseling outcome expectations, and counselor performance. (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database (9988728).
Johnson, E., Baker, S. B., Kopala, M., Kiselica, M. S., & Thompson, E. C., III (1989). Counseling self-efficacy and counseling competence in prepracticum training. Counselor Education and Supervision, 28, 205–218. doi:10.1002/j.1556-6978.1989.tb01109.x
Judge, T. A., Jackson, C. L., Shaw, J. C., Scott, B. A., & Rich, B. L. (2007). Self-efficacy and work-related performance: The integral role of individual differences. Journal of Applied Psychology, 92, 107–127. doi:10.1037/0021-9010.92.1.107
Kataoka, S. H., Zhang, L., & Wells, K. B. (2002). Unmet need for mental health care among U.S. children: Variation by ethnicity and insurance status. American Journal of Psychiatry, 159, 1548–1555. doi:10.1176/appi.ajp.159.9.1548
Kozina, K., Grabovari, N., De Stefano, J., & Drapeau, M. (2010). Measuring changes in counselor self-efficacy: Further validation and implications for training and supervision. The Clinical Supervisor, 29, 117–127. doi:10.1080/07325223.2010.517483
Kronick, R. F. (Ed.). (2000). Human services and the full service school: The need for collaboration. Springfield, IL: Thomas.
Langley, A. K., Nadeem, E., Kataoka, S. H., Stein, B. D., & Jaycox, L. H. (2010). Evidence-based mental health programs in schools: Barriers and facilitators of successful implementation. School Mental Health, 2, 105–113. doi:10.1007/s12310-010-9038-1
Larson, L. M., Cardwell, T. R., & Majors, M. S. (1996, August). Counselor burnout investigated in the context of social cognitive theory. Paper presented at the meeting of the American Psychological Association, Toronto, Canada.
Larson, L. M., Clark, M. P., Wesley, L. H., Koraleski, S. F., Daniels, J. A., & Smith, P. L. (1999). Video versus role plays to increase counseling self-efficacy in prepractica trainees. Counselor Education and Supervision, 38, 237–248. doi:10.1002/j.1556-6978.1999.tb00574.x
Larson, L. M., & Daniels, J. A. (1998). Review of the counseling self-efficacy literature. The Counseling Psychologist, 26, 179–218. doi:10.1177/0011000098262001
Larson, L. M., Daniels, J. A., Koraleski, S. F., Peterson, M. M., Henderson, L. A., Kwan, K. L., & Wennstedt, L. W. (1993, June). Describing changes in counseling self-efficacy during practicum. Poster presented at the meeting of the American Association of Applied and Preventive Psychology, Chicago, IL.
Larson, L. M., Suzuki, L. A., Gillespie, K. N., Potenza, M. T., Bechtel, M. A., & Toulouse, A. L. (1992). Development and validation of the counseling self-estimate inventory. Journal of Counseling Psychology, 39, 105–120. doi:10.1037/0022-0167.39.1.105
Leaf, P. J., Schultz, D., Kiser, L. J., & Pruitt, D. B. (2003). School mental health in systems of care. In M. D. Weist, S. W. Evans, & N. A. Lever (Eds.), Handbook of school mental health programs: Advancing practice and research (pp. 239–256). New York, NY: Kluwer Academic/Plenum.
Lewis, M. F., Truscott, S. D., & Volker, M. A. (2008). Demographics and professional practices of school psychologists: A comparison of NASP members and non-NASP school psychologists by telephone survey. Psychology in the Schools, 45, 467–482. doi:10.1002/pits.20317
Melchert, T. P., Hays, V. L., Wiljanen, L. M., & Kolocek, A. K. (1996). Testing models of counselor development with a measure of counseling self-efficacy. Journal of Counseling & Development, 74, 640–644. doi:10.1002/j.1556-6676.1996.tb02304.x
Mellin, E. A. (2009). Responding to the crisis in children’s mental health: Potential roles for the counseling profession. Journal of Counseling & Development, 87, 501–506. doi:10.1002/j.1556-6678.2009.tb00136.x
Munson, W. W., Stadulis, R. E., & Munson, D. G. (1986). Enhancing competence and self-efficacy of potential therapeutic recreators in decision-making counseling. Therapeutic Recreation Journal, 20(4), 85–93.
Munson, W. W., Zoerink, D. A., & Stadulis, R. E. (1986). Training potential therapeutic recreators for self-efficacy and competence in interpersonal skills. Therapeutic Recreation Journal, 20, 53–62.
Nabors, L. A., Reynolds, M. W., & Weist, M. D. (2000). Qualitative evaluation of a high school mental health program. Journal of Youth and Adolescence, 29, 1–13.
Powers, J. D., Edwards, J. D., Blackman, K. F., & Wegmann, K.M. (2013). Key elements of a successful multi-system collaboration for school-based mental health: In-depth interviews with district and agency administrators. The Urban Review, 45, 651–670. doi:10.1007/s11256-013-0239-4
President’s New Freedom Commission on Mental Health. (2003). Achieving the Promise: Transforming Mental Health Care in America. Final Report for the President’s New Freedom Commission on Mental Health (SMA Publication No. 03-3832). Rockville, MD: President’s New Freedom Commission on Mental Health.
Ramo, D. E., Prochaska, J. J., & Myers, M. G. (2010). Intentions to quit smoking among youth in substance abuse treatment. Drug and Alcohol Dependence, 106, 48–51. doi:10.1016/j.drugalcdep.2009.07.004.
Rones, M., & Hoagwood, K. (2000). School-based mental health services: A research review. Clinical Child and Family Psychology Review, 3, 223–241. doi:10.1023/A:1026425104386
Sharpe, P. A., Granner, M. L., Hutto, B. E., Wilcox, S., Peck, L., & Addy, C. L. (2008). Correlates of physical activity among African American and white women. American Journal of Health Behavior, 32, 701–713. doi:10.5555/ajhb.2008.32.6.701.
Shernoff, E. S., Kratochwill, T. R., & Stoiber, K. C. (2003). Training in evidence-based interventions (EBIs): What are school psychology programs teaching? Journal of School Psychology, 41, 467–483. doi:10.1016/j.jsp.2003.07.002
Stajkovic, A. D., & Luthans, F. (1998). Self-efficacy and work-related performance: A meta-analysis. Psychological Bulletin, 124, 240–261. doi:10.1037/0033-2909.124.2.240
Stephan, S. H., Weist, M., Kataoka, S., Adelsheim, S., & Mills, C. (2007). Transformation of children’s mental health services: The role of school mental health. Psychiatric Services, 58, 1330–1338. doi:10.1176/appi.ps.58.10.1330
Stephan, S., Westin, A., Lever, N., Medoff, D., Youngstrom, E., & Weist, M. (2012). Do school-based clinicians’ knowledge and use of common elements correlate with better treatment quality? School Mental Health, 4, 170–180. doi:10.1007/s12310-012-9079-8
Suldo, S. M., Friedrich, A., & Michalowski, J. (2010). Personal and systems-level factors that limit and facilitate school psychologists’ involvement in school-based mental health services. Psychology in the Schools, 47, 354–373. doi:10.1002/pits.20475
Sutton, J. M., Jr., & Fall, M. (1995). The relationship of school climate factors to counselor self-efficacy. Journal of Counseling & Development, 73, 331–336. doi:10.1002/j.1tb01759.x
Tang, M., Addison, K. D., LaSure-Bryant, D., Norman, R., O’Connell, W., & Stewart-Sicking, J. A. (2004). Factors that influence self-efficacy of counseling students: An exploratory study. Counselor Education and Supervision, 44, 70–80. doi:10.1002/j.1556-6978.2004.tb01861.x
Urbani, S., Smith, M. R., Maddux, C. D., Smaby, M. H., Torres-Rivera, E., & Crews, J. (2002). Skills-based training and counseling self-efficacy. Counselor Education and Supervision, 42, 92–106. doi:10.1002/j.1556-6978.2002.tb01802.x
Walrath, C. M., Bruns, E. J., Anderson, K. L., Glass-Siegal, M., & Weist, M. D. (2004). Understanding expanded school mental health services in Baltimore city. Behavior Modification, 28, 472–490. doi:10.1177/0145445503259501
Watson, J. C. (2012). Online learning and the development of counseling self-efficacy beliefs. The Professional Counselor, 2, 143–151.
Weist, M. D., Ambrose, M. G., & Lewis, C. P. (2006). Expanded school mental health: A collaborative community-school example. Children & Schools, 28, 45–50. doi:10.1093/cs/28.1.45
Weist, M. D., Evans, S. W., & Lever, N. A. (2003). Handbook of school mental health: Advancing practice and research. New York, NY: Kluwer Academic/Plenum.
Weist, M. D., Lever, N. A., Stephan, S. H., Anthony, L. G., Moore, E. A., & Harrison, B. R. (2006, February). School mental health quality assessment and improvement: Preliminary findings from an experimental study. Paper presented at the meeting of A System of Care for Children’s Mental Health: Expanding the Research Base, Tampa, FL.
Weist, M. D., Sander, M. A., Walrath, C., Link, B., Nabors, L., Adelsheim, S., . . . & Carrillo, K. (2005). Developing principles for best practice in expanded school mental health. Journal of Youth and Adolescence, 34, 7–13. doi:10.1007/s10964-005-1331-1
Weist, M., Lever, N., Stephan, S., Youngstrom, E., Moore, E., Harrison, B., . . . & Stiegler, K. (2009). Formative evaluation of a framework for high quality, evidence-based services in school mental health. School Mental Health, 1, 196–211. doi:10.1007/s12310-09-9018-5
Weist, M. D., Youngstrom, E. A., Stephan, S., Lever, N., Fowler, J., Taylor, L., . . . Hoagwood, K. (2014). Challenges and ideas from a research program on high-quality, evidence-based practice in school mental health. Journal of Clinical Child & Adolescent Psychology, 43, 244–255. doi:10.1080/15374416.2013.833097
Zeldin, A. L., Britner, S. L., & Pajares, F. (2008). A comparative study of the self-efficacy beliefs of successful men and women in mathematics, science, and technology careers. Journal of Research in Science Teaching, 45, 1036–1058. doi:10.1002/tea.20195
Bryn E. Schiele is a doctoral student at the University of South Carolina. Mark D. Weist is a professor at the University of South Carolina. Eric A. Youngstrom is a professor at the University of North Carolina at Chapel Hill. Sharon H. Stephan and Nancy A. Lever are associate professors at the University of Maryland. Correspondence can be addressed to Bryn E. Schiele, the Department of Psychology, Barnwell College, Columbia, SC 29208, schiele@email.sc.edu.
Sep 2, 2014 | Article, Volume 1 - Issue 2
John McCarthy, Michelle Bruno, Teresa E. Fernandes
The prevalence of depression increases markedly during adolescence, yet many youth are not receiving the support that they need. One factor that has been speculated as contributing to low rates of care is a lack of mental health literacy about depression and viable sources of support. This pilot study focused on mental health literacy as it relates to adolescent depression and suicidality and represented a pseudo-replication of Burns and Rapee (2006). Overall, participants (N=36) in this study were able to differentiate depressed vignettes from non-depressed vignettes and identify common symptoms of depression in their assessments. Also, sources of optimal help identified by participants varied upon the perceived degree of seriousness of the difficulties. Such results offer implications regarding the potential benefit of including adolescents in a more direct way when providing outreach or offering services.
Keywords: adolescents, mental health literacy, depression, suicidality, support
Depression in adolescence is of particular relevance, as it can continue into adulthood yet often goes undiagnosed and untreated (Wagner, Emslie, Kowatch, & Weller, 2008). According to the Diagnostic and Statistical Manual of Mental Disorders-Text Revision (DSM-IV-TR) (APA, 2000), the diagnostic criteria and duration mirror adult depression in many respects. As in adult depression, adolescent depression can include a variety of symptoms, at least one of which must be either depressed mood or loss of pleasure/interest. Furthermore, the DSM-IV-TR stipulates that, if depressed mood is chosen, it may be substituted by irritable mood in adolescents.
The rate of depression increases six-fold between the ages of 15–18 (Hankin, 2006). Approximately eight percent of teenagers—an estimated two million youth from 12–17 years of age—suffered at least one major depressive episode in 2007. Only 39% received some form of treatment for depression in the preceding 12 months. The rate of receiving professional help was much lower among those youth without health insurance (17%). Among all teenagers who obtained treatment, over half (59%) saw a counselor for assistance with their depression. Nearly 37% and 27% of youths saw a psychologist or general practitioner/family doctor, respectively (Substance Abuse and Mental Health Services Administration, 2009).
Given the prevalence of mental illness and its impact on society, it is no surprise that there is a growing interest in mental health literacy, a term first used by Jorm et al. (1997). Defined as the “knowledge and beliefs about mental disorders which aid their recognition, management or prevention” (p. 182), mental health literacy also includes knowledge about treatment and from whom to seek help. It has been found, for instance, that family and friends can be vital in the recognition of depressive symptoms (Langlands, Jorm, Kelly, & Kitchener, 2008a). However, Highet, Thompson, and McNair (2005) saw that family members usually recognized symptoms of the individual in hindsight. The general public often does not possess the knowledge base to help someone who is developing a psychotic illness (Langlands, Jorm, Kelly, & Kitchener, 2008b). Kitchener and Jorm (2002) found that individuals who took part in their Mental Health First Aid course showed improvement in recognizing disorders, and their views about treatment of disorders became more in line with those of professionals in the mental health field. In addition, the course reduced their stigma attached to mental disorders, increased their feelings of confidence in providing help, and increased the help provided to others.
Few studies have been conducted on younger populations and mental health literacy. Burns and Rapee (2006) noted, “While there is growing literature on the mental health literacy of adults, to date there has not been a parallel interest in the mental health literacy of young people” (p. 227). Wright et al. (2005) looked at young adults’ (ages 12 to 25) ability to pinpoint depression and psychosis and their recommendations for help to be sought. Nearly half of the participants were able to label the depressed vignette as depressed, but only a quarter of participants were able to label psychosis. People who were given the depressed vignette were less likely to choose a correct form of treatment than those given the psychosis vignette. Psychologists and psychiatrists were recommended more frequently for the psychosis vignette than for the depressed vignette, and a family doctor or general practitioner was chosen more often for the depressed vignette than for the psychosis vignette.
Adolescents have been found more likely to consider themselves “very confident” (Jorm, Wright, & Morgan, 2007a, p. 67) to help a peer in need with girls rating themselves as more confident than boys. In addition, across vignettes, confidence in providing help to a peer with a problem was higher for depression (without alcohol misuse) and social phobia than for psychosis and depression with alcohol misuse (Jorm et al, 2007a).
Jorm, Wright, & Morgan (2007b) found differences among Australian youth in the type of help sought for mental disorders. Participants were read vignettes describing youth of similar ages who were experiencing various disorders, then were asked a series of questions that included where they would turn with similar problems. For the vignette describing a teen suffering from depression, adolescents aged 12–17 chose family (54%) most often as a source of help and opted for mental health professional or service most infrequently (2%). Nearly one-third of young adults ages 18–25 selected family (31%) or a general practitioner/medical doctor (31%) on a similar vignette regarding depression. Overall the perceived barriers to help-seeking were personal in nature and did not relate to systemic characteristics, as they noted, “For young people, it is embarrassment or concern about what others think…” (p. 559).
Burns and Rapee (2006) used a vignette-based approach to measure mental health literacy among high school students in Australia. In their study, they utilized the Friend In Need questionnaire, created by the authors for that specific study. This instrument offers five short vignettes of teenage students, two of whom (“Tony” and “Emily”) represented youth meant to be clinically depressed. One of the two vignettes (“Emily”) offered a reference to suicidal ideation. The remaining three vignettes were of students facing difficulties, though were not intended to reflect depression.
They found that over two-thirds of participants (68%) accurately labeled “Emily” as depressed, while about one-third (34%) recognized “Tony” as depressed. Female participants were more likely to make a depressed diagnosis in both the “Tony” and “Emily” vignettes than the male participants. Female participants also showed more worry for the depressed vignettes than male participants. Among help-seeking sources, counselors were chosen most often for the helpers of the depressed teens, and this category was followed by friends and family/relatives.
To our knowledge, no study has been conducted on the mental health literacy of U.S. teens as it pertains to adolescent depression. With this point in mind, the current study represents a replication of Burns and Rapee (2006) and offers an initial sample involving older adolescents’ perspectives in the assessment, recovery time, and help-seeking recommendations regarding depression. Our central study questions were consistent with Burns and Rapee and the questions posed by the Friend in Need Questionnaire.
Procedures
Both prior to and after receiving approval by the university’s institutional review board, two of the authors met with the principal of the school where the data was collected. It was determined that eight sections of the school’s psychology and anthropology classes would be appropriate to the topic of study and ages of interest, and the primary author contacted the teachers and shared the following information with them: the parental/guardian consent form, the student consent form, details concerning the data collection process, and pertinent dates of the consent form deadlines and actual administration of the instrument used in this study. Teachers distributed the consent forms to students, who, if interested in possibly participating in the study, took them to their parents/guardians. Signed parental/guardian consent must have been completed and returned to the teachers in a four-day time period, which occurred prior to the date of the administration of the instrument. In both the parental/guardian and participant consent forms, it was made clear that the questionnaire was not a formal test and would take an estimated 25–40 minutes to complete.
On the day of the data collection, one of the two primary authors (JM and MB) went to the classroom, collected the completed parental/guardian consent form, read an abbreviated student consent form to the potential participants after giving a hard copy to them, and asked for questions at the conclusion. Students with unsigned parental/guardian consent forms were given an alternate class assignment, while those students who consented to be in the study completed the Friend in Need Questionnaire. No extra credit was granted for participation in the study. Participants completed the questionnaire in their classrooms. In a few instances, participants and the author/administrator were asked to move to a nearby vacant room for the data collection.
Approximately five classes were visited for data collection, and a total of 36 students, 21 of whom were young men, participated in the study. Most participants completed the questionnaire in approximately 20 minutes. The questionnaires were completed in an anonymous manner. In the coding process, a number was given to each questionnaire for tracking purposes only. Finally, the two authors also offered to return to the class after the data administration to further discuss the study; however, no teachers chose this option.
Instrument
Adolescents’ mental health literacy was assessed using the Friend in Need Questionnaire (Burns & Rapee, 2006). As previously described, the questionnaire presents five vignettes of young people experiencing various difficulties and solicits both close-ended and open-ended responses from participants. Specifically, participants are instructed to read each vignette and respond to the following general questions: (a) How worried would you be about the person’s overall emotional well-being? (b) What do you think is the problem of the person? (c) What aspects of the vignette provided the strongest hints that the person was having difficulties? (d) How long will it take this adolescent to feel better? and (e) Does this person need help from others to cope with his/her problems? The final question also has a supplemental, open-ended question regarding who the helper would be. The respondents are posed with all of these questions for each of the five vignettes. The complete Friend in Need Questionnaire can be found in Burns and Rapee (2006).
A coding system was devised for the open-ended responses, specifically on the responses asking about the youth’s problem, aspects of the vignette that provided hints, and the appropriate helper. For the question concerning the youth’s problem, the responses were filtered into two categories: “depressed” or “not depressed.” To qualify as “depressed,” the respondents needed to write the words “depressed/depression” or “suicide/suicidal.” Any other problems listed were considered to be “not depressed.” On the question regarding hints of the problem in the vignette, the coder was looking for responses that fit into diagnostic criteria for depression. The two depressed vignettes each had five diagnostic criteria imbedded in them, and this question tried to tease out whether respondents could identify these key criteria. Hence, the responses were categorized into the five diagnostic criteria of each vignette, with other responses not qualifying. The question that asked about the appropriate helper was split into nine possible categories of helpers. A few respondents, whose answers occurred rarely, were not included in the analyses.
Results
The findings are described in order of the items presented in the Friend in Need Questionnaire. The first question assessed whether adolescents could label a cluster of depressive symptoms in a case vignette as depressed. Respondents were asked, “What do you think is the matter with [name]?” This open-ended question elicited a variety of responses from respondents. Only responses that included “depressed,” “depression,” “suicide,” or “suicidal” were coded as a label of depression. In reviewing the responses to the two vignettes concerning students (Tony and Emily) depicted as depressed, it was evident that the majority of participants accurately labeled the vignettes, as 75% accurately identified Emily as depressed and 58% accurately labeled Tony as depressed.
The majority of respondents also accurately identified the non-depressed vignettes as such. Specifically, over 94% of respondents accurately identified Mandy as not being depressed. All participants (100%) accurately identified Jade as non-depressed, and over 97% accurately identified Nick as not being depressed. Frequencies of depressive codes for all vignettes are included in Table 1. Separate chi-square analyses were conducted to examine any differences in ratings of each vignette between male and female participants. Results indicated that no such differences exist on any of the five vignettes.
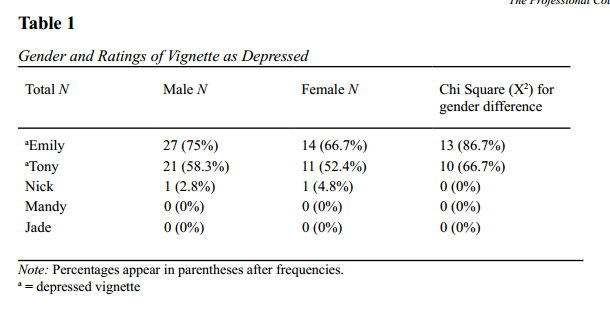
Second, in regard to respondents expressing greater worry for youth in the depressed vignettes versus the non-depressed vignettes, the Friend in Need Questionnaire instructed participants to rate their concern on a five-point scale with higher scores indicating more worry. The scores for the depressed vignettes (Emily and Tony) and non-depressed vignettes (Mandy, Jade, and Nick) were collapsed to produce mean scores of level of worry. A general linear model was used to compare sex differences (participant) in the intensity of worry scores for depressed and non-depressed vignettes. Results indicate that no significant differences existed between male (M = 3.40, SD = .38) and female participants (M = 3.45, SD = .33) regarding ratings of worry for the depressed (p < .58). No significant differences were found regarding male (M = 1.80, SD = .41) and female participants’ (M = 1.81, SD = .39) ratings of worry of the non-depressed vignettes either (p < .82).
The third question pertained to the length of recovery in the depressed and non-depressed vignettes. The respondents rated each vignette on the perceived length of time it would take the character to feel better on a four-point Likert scale from 1 (one or two days) to 4 (longer than a few months). Higher scores indicate a perception that more time is needed to feel better. Despite the use of a Likert scale, some respondents chose two answers or marked in between two options. When this occurred, the score was adjusted to reflect an average. For example, if someone circled, both “3” and “4,” a score of “3.5” was entered. This decision was made to maintain as many respondents as possible, given the small number of the sample. Overall, the respondents rated the depressed vignettes with a mean score of 3.67 (SD = .37), which indicates a recovery period of between “one or two months” and “longer than a few months.” This finding compared to a lower mean score of 1.97 (one or two days, SD = .45) for the non-depressed vignettes. Scores on the two depressed vignettes and scores on the three non-depressed vignettes were collapsed to create a composite mean score of recovery time for depressed (dependent variable) versus non-depressed vignettes (dependent variable).
A two-way MANOVA was conducted to determine if sex differences (of respondents) made a difference in the length of the recovery for both scenarios (depressed versus non-depressed). The overall model was statistically significant for the recovery time between the depressed and non-depressed vignettes F (1, 34) = 651.31; p = .01. The MANOVA did not reveal a significant interaction between participant gender and recovery time of vignettes (p < .27). Female respondents rated both the depressed vignettes (M = 3.82, SD = 24) and non-depressed vignettes (M = 2.03, SD = .43) higher than male respondents who rated the vignettes as 3.57 (SD = .53) and 1.93 (SD = .47) respectively, but this difference was not statistically significant.
Fourth, participants were asked to identify the elements of the vignette that demonstrated whether the fictitious teens were having emotional troubles. The two depressed vignettes (Emily and Tony) contained criteria of a Major Depressive Episode as described in the DSM-IV-TR (APA, 2000). In the case of Emily, respondents readily identified indicators of suicide (91%) and self-worth (72%). Respondents were less likely to identify symptoms of loss of interest (19%), fatigue (22%), and mood (19%) in this case. (See Table 2 for more complete results.) In the case of Tony, a majority of respondents identified loss of interest (75%) and weight loss (58%). Respondents were less likely to identify Tony’s fatigue (44%), insomnia (39%), and diminished ability to think or concentrate (39%).
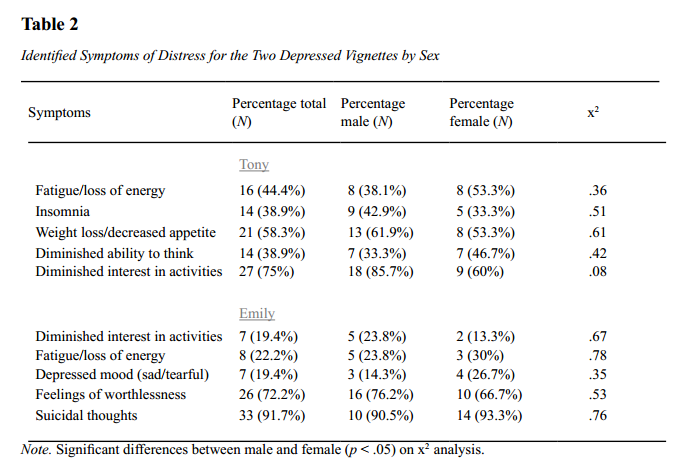
Finally, after noting which symptoms were strong indicators of problems, respondents answered an open-ended question about sources of help to aid the person in the vignette. For all five vignettes, participants answered whether they thought the person in the vignette needed help from another person. The options included “no,” “yes,” or “don’t know.” If the respondents endorsed that the person did need help, they were asked to answer a follow-up question indicating who they think should help the person. For the depressed vignettes, 58% of respondents indicated that Tony needed help, and 75% indicated the same for Emily.
In regard to the type of helpers, participants’ responses were broken down into nine categories of helpers, including counselor; friends; family; professional; psychologist; psychiatrist; doctor; teacher; and someone who has had the same difficulty. Some coding decisions included how to categorize responses not explicitly in the list. Some of these included counseling, school counselor, and guidance counselor, which were included in the category of counselor. For the friend category, other responses included “peers” and “someone who knows him/her well.” For family, “parents,” “relatives,” “siblings/brother/sister” also were included. Non-specific terms were included in the professional category, including specialist, shrink, therapist, psychotherapist, and family therapist. Other responses included in the psychiatrist category were “doctor for depression/depressed kids” and “doctor who prescribes antidepressants.” Some responses that were not coded included third party, new people, anyone, role model, someone he/she doesn’t know, and everyone.
Nearly half of the participants (47%) identified the family as the suggested primary helper for Tony, while over one-third (36%) of participants suggested a counselor. The same percentage (36%) identified the family and a psychiatrist, respectively, for Emily, as the best sources of help (see Tables 3-4 for more complete results).
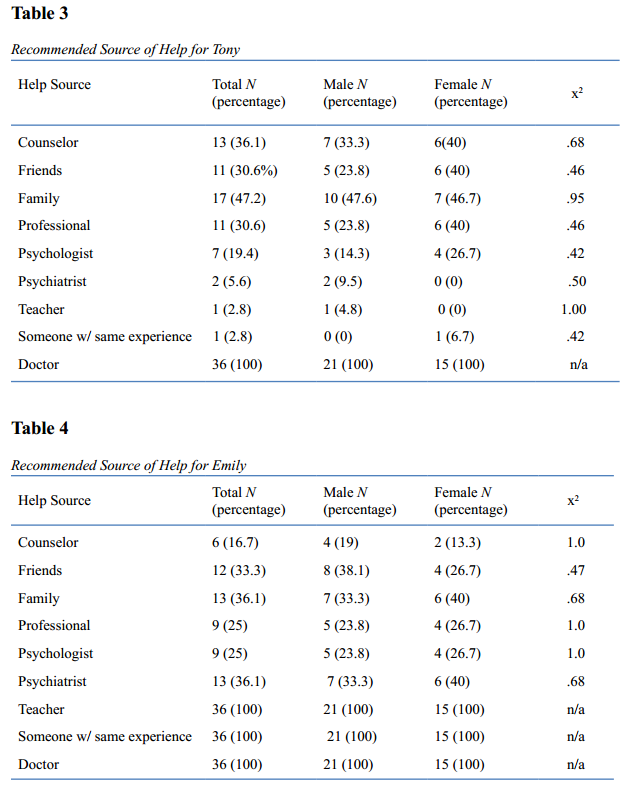
Discussion
The primary purpose of this study was to examine the level of teenagers’ mental health literacy specific to adolescent depression. Because it was a pilot study that involved a relatively small sample size, the findings are admittedly limited in generalizability. However, even with the small sample size, the results offer initial points of comparison to Burns and Rapee’s (2006) larger scale study. First and perhaps foremost, the level of detection of adolescent depression was relatively high in the present study, yet no significant differences were found as they related to gender. Over half of the participants correctly labeled both depressed-based vignettes (Emily and Tony) as being depressed, and three in four participants indicated that Emily was depressed. To their credit, participants rated both depressed vignettes as highest in terms of depression.
This finding is noteworthy. In Burns and Rapee (2006), the corresponding findings of correctly identifying depression in Emily and Tony were 68% and 34%, respectively. The higher rating of Emily as depressed was similar in both settings, yet the rating of Tony as depressed was sizably different with American participants being more inclined to have viewed the fictitious student as depressed.
A closer investigation of this finding points to critical symptoms chosen in the participants’ assessment. The vignette of Emily featured pointed comments of suicidality, and, to no surprise, it was this characteristic that was almost uniformly (92%) expressed by participants when asked about the “strongest hints that something was wrong.” The element of suicidality also was foremost in Burns and Rapee (2006) in reference to Emily, but its expression was lower (77%) among the Australian sample. At least two possibilities are present. First, it is conceivable that the Australian teenagers were not as concerned about the suicidal ideation as the U.S. participants in the present study. A second possibility is that the awareness of suicidality among adolescents has increased in more recent years in the U.S., prompting a higher rate among the U.S. teenagers.
Suicidality was absent in the vignette of Tony. However, other signs of depression were present, and these symptoms included anhedonia, fatigue, weight loss, insomnia, and diminished ability to think/concentrate. Both U.S. participants in the present study and Australian participants in Burns and Rapee (2006) placed “diminished loss of interest” as the primary symptom of an emotional difficulty at nearly identical rates (73% and 75%, respectively). The same held true for the second-rated symptom (weight loss) in both samples, again expressed by nearly the same percentage (58% in the present study and 61% in Burns and Rapee). The consistency in the ranking and percentages of both samples reflects the teenagers’ recognition of lowered interest levels and appetite difficulties leading to weight loss when an adolescent is experiencing depression. In actuality, both behaviors do indeed tend to be two of the six most frequent symptoms among teenagers who are depressed (Roberts, Lewinsohn, & Seeley, 1995).
To their credit, participants in the present study also were able to differentiate the depressed vignettes from the non-depressed vignettes. Mandy was feeling upset over a relationship termination initiated by her former boyfriend that occurred three days prior. Jade expressed family disruption and had become intoxicated at a recent party. Meanwhile, Nick was coping with the loss of a grandparent. None of these vignettes offered significant amounts in the way of genuine depression, and by and large, the majority of participants detected that their respective problems were not severe. A mere 6% of participants indicated that Mandy was depressed. Similarly, none of the participants indicated that Jade was depressed, and only 3% of them assessed Nick to be depressed. This finding offers support for the overall level of mental health literacy of the sample as it pertains to adolescent depression. Moreover, in comparison to the Australian participants in Burns and Rapee (2006), the American sample fared somewhat better: They found that, though none of their participants found Jade to be depressed, 11% and 9% of teenagers in their study did relate Nick and Mandy, respectively, to be depressed.
The participants in the present study demonstrated significantly more concern and anticipated a longer recovery period for the students in the depressive vignettes than in the non-depressed vignettes. In our study, a significant difference was accurately found in estimated recovery time.
The average duration of an initial depressive episode is eight months when no treatment is received (Brent & Birmaher, 2002). These findings add support to the conclusion that the sample possessed a considerable level of literacy. Given the fact that, to our knowledge, this pilot study is the first to assess mental health literacy for adolescent depression among American teenagers, no point of comparison exists. With this point in mind, the finding was relatively surprising. The adolescents in the present study were astute in their detection, concern, and estimated time of recovery, which could be related to a knowledge set based on their classroom education or acquired in other ways (i.e., having a friend who was depressed). Regardless of the mode of acquisition, the adolescents in this study offered greater concern for the fictitious students in the midst of a depressive episode and estimated their recovery more accurately than those students in the non-depressed vignettes.
It was mildly surprising that, unlike Burns and Rapee (2006) and Gifford-May (2002), no significant difference was found in regard to gender and mental health literacy. Burns and Rapee found that girls “clearly demonstrated” higher literacy in their abilities to not only correctly label the depressed vignettes, but also in their expression of greater concern over the students in those same vignettes (p. 232). One point of speculation on their part dealt with the higher levels of depression experienced by young women in later adolescence (Lewinsohn, Rohde, & Seeley, 1998). However, given the absence of significant differences in gender within the sample in the present study, it raises the possibility that young men in the U.S. are more insightful regarding adolescent depression than anticipated.
Burns and Rapee (2006) indicated that the primary reason for raising the mental health literacy of adolescents “is to increase the likelihood that young people can access the most appropriate help when needed” (p. 233). Taken from combined data from 2005 and 2006, an estimated 12% of American youth aged 12–17 obtained professional help for emotional or behavioral problems, and females were more likely than males to receive professional help (Office of Applied Statistics, 2008). However, the literature points to the fact that many other teenagers in need of mental health assistance for various disorders do not receive it. In fact, a mere 39% of those adolescents suffering a depressive episode receive treatment (Office of Applied Statistics, 2009).
The recommended sources for help in our sample were family and counselor, respectively, for Tony, and family and psychiatrist, both at equal percentages, for Emily. For the vignette of Emily, counselor ranked sixth of the nine helping sources. This finding is in contrast to the real-world conditions where nearly 60% of those teenagers with depression in 2007 saw or talked to a counselor in their treatment (Office of Applied Statistics, 2009).
Though the reasoning behind the choices of the helping sources was not sought, the selections lead to intriguing possibilities. First, in the case of Tony, the primary helping source was family, despite information in the vignette that the family system was deteriorating over a parental separation. Even if that played no role in the participants’ responses, the choice of family in soliciting help is striking in that parent-adolescent conflicts increase during early adolescent years (Laursen, Coy, & Collins, 1998). Suicidal adolescents reported difficulty in communicating with parents, tremendous stress in their home life, and a distressed relationship with one or both parents (Bostik & Everall, 2006). However, this finding is consistent with a qualitative study (McCarthy, Downes, & Sherman, 2008) pointing to beneficial parental partnerships that developed during depressive episodes and were instrumental in the teenager getting professional help. Counselor, the second recommended helper choice in the vignette of Tony, may not be as surprising. The school from which the data were collected does have a staff of professional school counselors, and this finding may speak to the participants’ level of comfort with counselors.
The topic of recommended helper was much different in the vignette of Emily, as the choices were much more equal in terms of the percentages. The selection of psychiatrist as the second recommended helper may point to the participants’ perception of the potential for harm and their connotation that a physician with mental health expertise and prescription privileges was needed. In a similar vein, the designations of psychologist and professional were closely behind psychiatrist in recommended helpers, again suggesting the participants’ notion that highly trained professionals who likely have a doctoral degree were needed to aid Emily. This finding mirrors recent research, as 27% of those adolescents having a depressive episode saw their family physician or a general practitioner. Roughly the same number sought help from a psychiatrist or psychologist (Office of Applied Statistics, 2009).
Surprisingly, friends were the third most common choice of helper in a case of a student marked by suicidal ideation. With the potential for harm in this student, friends may not be the best source for initial help. However, participants in the present study may have thought that friends would be supportive during an emotionally difficult period. Finally, the lower ranking of the counselor designation may be connected with a perception that a counselor is sought for less complex difficulties.
Burns and Rapee (2006) found that counselor and friend were the two primary overall recommended sources of help. In regard to counselors, they noted that this finding may be reflective of the “access and familiarity” that adolescents in many Australian schools possess with this type of professional (p. 233). Overall, however, the participants in their study offered far lower rankings of a psychologist, professional, or psychiatrist as a source of help in the depressed vignettes. This finding could point to a familiarity by American teenagers with medical professionals, particularly with the prevalence rate of medication prescribed to this population in the U.S. compared to European countries (Levin, 2008).
Limitations
Limitations are clearly evident in this study. As previously noted, the small sample size that is consistent with pilot studies restricts generalizability. The sample size also may have been composed of more sophisticated students in mental health, as many students in the sample were enrolled in a psychology class. Burns and Rapee (2006) pointed out that the vignette-based instrument of the Friend in Need Questionnaire is consistent with the manner in which other mental health literacy studies have been conducted. However, they added, “The extent to which such data can be translated into what actually is likely to happen in the real world is unclear” (p. 234). They also noted that a subsequent challenge for research in this area includes the development of research modalities that examine literacy in a naturalistic setting, such as interviews with adolescents. This suggestion connects to Dundon’s (2006) call to bring forth the “voice of the adolescent” that has been lacking in the research on adolescent depression (p. 384).
Implications
This pilot study represents a point of entry in studying American teenagers’ mental health literacy in regard to teen depression. Participants in this study showed the ability to correctly differentiate depressed vignettes from non-depressed vignettes and, in their assessment, indicated relevant symptoms of depressive symptoms faced by adolescents. Overall they also expressed sources of help that varied upon the perceived degree of seriousness of the difficulties. The outcomes offer implications regarding the potential benefit of including adolescents in a more direct way when providing outreach or offering services. They demonstrated an accurate understanding of when more intense levels of care could be beneficial.
The study produced results that also warrant further exploration of the relationships between youth and parents during adolescence. Although this developmental period can be marked by tumultuous relationships between them, there may be wisdom in providing communication skills to strengthen such relationships. Such efforts could result in more disclosure of depressive symptoms to parents, which may expedite the process of getting help as opposed to sharing such struggles only with peers. In addition to implications for teens and parents, this research can help shape additional studies in expanding the understanding of literacy.
Future research calls for additional mental health literacy investigations marked not only by larger sample sizes, but also by an in-depth investigation of adolescents of various racial/ethnic differences within the sample. Higher rates of adolescent depression have been found in youth of Latino descent (Guiao & Thompson, 2004; Twenge & Nolen-Hoeksema, 2002), for instance, and it would be important to evaluate the mental health literacy levels among respective backgrounds. With teenage depression being a pressing matter in adolescent mental health, the domain of mental health literacy in regard to this disorder is a vital one that merits additional research.
References
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author.
Bostik, K. E., & Everall, R. D. (2006). In my mind I was alone: Suicidal adolescents’ perceptions of attachment relationships. International Journal for the Advancement of Counselling, 28(3), 269–287. doi: 10.1007/s10447-006-9013-6
Brent, A., & Birmaher, B. (2002). Adolescent depression. The New England Journal of Medicine, 347(9), 667–671. doi:10.1056/NEJMcp012249
Burns, J. R., & Rapee, R. M. (2006). Adolescent mental health literacy: Young people’s knowledge of depression and help seeking. Journal of Adolescence, 29, 225–239. doi:10.1016/j.adolescence.2005.05.004
Dundon, E. E. (2006). Adolescent depression: A metasynthesis. Journal of Pediatric Health Care, 20, 384–392. doi: 10.1016/j.pedhc.2006.02.010
Gifford-May, D. (2002). Adolescents’ knowledge and beliefs about depression, coping strategies and barriers to help-seeking: Gender and ethnic difference (Unpublished master’s thesis). Macquarie University, Australia.
Guiao, I., & Thompson, E. A. (2004). Ethnicity and problem behaviors among adolescent females in the United States. Health Care for Women International, 25(4), 296–310. doi:10.1080/07399330490278330
Hankin, B. L. (2006). Adolescent depression: Description, causes, and interventions. Epilepsy & Behavior, 8, 102–114. doi:10.1016/j.yebeh.2005.10.012
Highet, N., Thompson, M., & McNair, B. (2005). Identifying depression in a family member: The carers’ experience. Journal of Affective Disorders, 87, 25–33. doi:10.1016/j.jad.2005.02.- 016
Jorm, A. F., Korten, A. E., Jacomb, P. A., Christensen, H., Rodgers, B., & Pollitt, P. (1997). “Mental health literacy”: A survey of the public’s ability to recognise mental disorders and their beliefs about the effectiveness of treatment. Medical Journal of Australia, 166, 182–186.
Jorm, A. F., Wright, A., & Morgan, A. J. (2007a). Beliefs about appropriate first aid for young people with mental disorders: Findings from an Australian national survey of youth and parents. Early Intervention in Psychiatry, 1, 61–70. doi:10.1111/j.1751-7893.2007.00012.x
Jorm, A. F., Wright, A., & Morgan, A. J. (2007b). Where to seek help for a mental disorder? National survey of the beliefs of Australian youth and their parents. The Medical Journal of Australia, 187, 556–560.
Kitchener, B. A., & Jorm, A. F. (2002). Mental health first aid training for the public: Evaluation of effects on knowledge, attitudes and helping behaviour. BioMed Central Psychiatry, 2, 10. doi:10.1186/1471-244X-2-10
Langlands, R. L., Jorm, A. F., Kelly, C. M., & Kitchener, B. A. (2008a). First aid for depression: A Delphi consensus study with consumers, carers and clinicians. Journal of Affective Disorders, 105, 157–165. doi:10.1016/j.jad.2007.05.004
Langlands, R. L., Jorm, A. F., Kelly, C. M., & Kitchener, B. A. (2008b). First aid recommendations for psychosis: Using the Delphi method to gain consensus between mental health consumers, carers, and clinicians. Schizophrenia Bulletin, 34(3), 435–443. doi:10.1093/schbul/sbm099.
Laursen, B., Coy, K. C., & Collins, W. A. (1998). Reconsidering changes in parent-child conflict across adolescence: A meta-analysis. Child Development, 69, 817–832. doi:10.1111/j.14678624.1998.00817.x
Levin, A. (2008, November 21). U.S. youth more apt than Europeans to be prescribed psychotropics. Psychiatric News, p. 18.
Lewinsohn, P. M., Rohde, P., & Seely, J. R. (1998). Major depressive disorder in older adolescents: Prevalence, risk factors, and clinical implications. Clinical Psychology Review, 18(7), 765–794. doi:10.1016/S0272-7358(98)00010-5
McCarthy, J., Downes, E. J., & Sherman, C. A. (2008). Looking back at adolescent depression: A qualitative study. Journal of Mental Health Counseling, 30(1), 49–68.
Office of Applied Statistics. (2009, May 11). Major depressive episode and treatment among adolescents. The NSDUH Report, pp. 1–4.
Roberts, R. E., Lewinsohn, P. M., & Seeley, J. R. (1995). Symptoms of DSM-III-R major depression in adolescence: Evidence from an epidemiological survey. Journal of the American Academy of Child and Adolescent Psychiatry, 34, 1608–1617. doi:10.1097/00004583-199512000-00011
Substance Abuse and Mental Health Services Administration, Office of Applied Studies. (May 11, 2009). The NSDUH Report: Major Depressive Episode and Treatment among Adolescents. Rockville, MD.
Substance Abuse and Mental Health Services Administration, Office of Applied Studies. (September 28, 2008). Mental health service use among youths aged 12 to 17: 2005 and 2006. Rockville, MD.
Twenge, J. M., & Nolen-Hoeksema, S. (2002). Age, gender, race, socioeconomic status, and birth cohort differences on the Children’s Depression Inventory: A meta-analysis. Journal of Abnormal Psychology, 111, 578–588. doi:10.1037/0021-843X.111.4.578
Wagner, K. D., Emslie, G. J., Kowatch, R. A., & Weller, E. B. (2008). An update on depression in children and adolescents. Journal of Clinical Psychiatry, 69(11), 1818–1828. doi:10.4088/JCP.v69n1118
Wright, A., Harris, M. G., Wiggers, J. H., Jorm, A. F., Cotton, S. M., Harrigan, S. M., & McGorry, P. D. (2005). Recognition of depression and psychosis by young Australians and their beliefs about treatment. The Medical Journal of Australia, 183, 18–23.
John McCarthy, NCC, is a Professor in the Department of Counseling at the Indiana University of Pennsylvania (IUP). Michelle Bruno is an Assistant Professor in the same department at IUP. Teresa E. Fernandes, NCC, is a counselor at the Meadows Psychiatric Center, Centre Hall, PA. Correspondence can be addressed to John McCarthy, Indiana University of Pennsylvania, Department of Counseling, 206 Stouffer Hall, Indiana, PA, 15705, john.mccarthy@iup.edu.