May 22, 2024 | Volume 14 - Issue 1
Jennifer M. Cook, Melissa D. Deroche, Lee Za Ong
The phenomenon of microaggressions is well established within the counseling literature, particularly as it relates to race, ethnicity, gender, and affectual orientation. However, research related to disability or ableist microaggressions is still in its infancy, so counseling professionals have limited information about experiences of disability and ableist microaggressions. The purpose of this qualitative content analysis was to describe participants’ self-reported experiences with ableist microaggressions. Participants (N = 90) had a diagnosed disability and the majority (91.11%) identified as having two or more nondominant identities beyond their disability. We report two categories and 10 themes. While participants were part of the general population, we position our discussion and implications within the context of professional counseling to increase counseling professionals’ awareness and knowledge so counselors can avoid ableist microaggressions and provide affirmative counseling services to persons with disabilities.
Keywords: disability, ableist microaggressions, professional counseling, nondominant identities, affirmative counseling
Day by day, what you choose, what you think, and what you do is who you become.
—Heraclitus, pre-Socratic philosopher
Each person is a complex makeup of dominant and nondominant sociocultural identities. Individuals with dominant cultural identities (e.g., able-bodied, White, middle social class) experience societal privilege, have more sociocultural influence, and have unencumbered access to resources. People with nondominant identities, including people with disabilities (PWD), people of color, and people in lower social class, frequently have less influence and experience structural and interpersonal inequities, limitations, and discrimination (Sue & Spanierman, 2020). As such, people with nondominant identities often experience microaggressions. Microaggressions are unintentional or deliberate verbal, nonverbal, and/or environmental messages that convey disapproval, distaste, and condemnation of an individual based on their nondominant identity (Sue et al., 2007).
Professional counselors are aware and knowledgeable that their identity constellation and their
experiences with microaggressions, as well as those of their clients, impact their worldviews, experiences, and—importantly—the counseling relationship (Ratts et al., 2016). While microaggressions associated with several cultural identities have been well-researched within counseling (e.g., race, ethnicity, gender, affectual orientation), others, like ableist microaggressions, have been examined far less frequently (Deroche et al., 2024). The purpose of this article is to describe the microaggression experiences that PWD (N = 90) encounter. Our intention is to increase counseling professionals’ awareness and knowledge about ableist microaggressions so they can examine their beliefs about disability, identify how they may have participated in ableist microaggressions and, ultimately, provide affirmative counseling services to PWD.
Literature Review
Although the term microaggressions was coined by Pierce in the 1970s, it was not until 2007 that it took hold within the allied helping professions (Sue et al., 2007). Initially, the term was used to describe experiences based on race, yet the term has been applied more broadly to the dismissive experiences people with other nondominant identities (e.g., gender, affectual/sexual orientation) encounter (Sue & Spanierman, 2020). In 2010, Keller and Galgay initiated foundational research about the microaggressions that PWD experience. Through their qualitative study, they identified eight microaggression domains experienced by PWD and described their harmful effects on the psychological and emotional well-being of PWD. Those eight domains are: (a) denial of identity, (b) denial of privacy, (c) helplessness, (d) secondary gain, (e) spread effect, (f) patronization, (g) second-class citizenship, and (h) desexualization (i.e., ignoring or avoiding the sexual needs, wants, or desires of PWD). This study marked the beginning of ableist microaggressions research that led scholars not only to naming (e.g., Dávila, 2015) and measuring (e.g., Conover et al., 2017a) specific microaggressions toward PWD, but also describing experiences with ableist microaggressions within specific disability groups (e.g., Coalson et al., 2022; Eisenman et al., 2020) and exploring the impact for specific cultural groups of PWD (e.g., Miller & Smith, 2021).
Before continuing further, it is important for us to explain our use of the term ableist microaggressions, rather than the term disability microaggressions, because it deviates from the typical convention used to name microaggressions (e.g., racial microaggressions, gender microaggressions). While some authors have used the term disability microaggressions (e.g., Dávila, 2015), we believe that this term undercuts and minimizes PWD’s microaggression experiences, as it fails to explicitly communicate that these microaggressions are forms of ableism. Therefore, to validate PWD’s experiences and to align with the disability movement’s philosophy of diversity and social justice, we use the term ableist microaggressions (Perrin, 2019).
The qualitative ableist microaggression studies we reviewed all utilized and endorsed the themes Keller and Galgay (2010) found in their qualitative study, while adding nuance and new information about ableist microaggressions. For instance, Olkin et al.’s (2019) focus group research with women who had both hidden and apparent disabilities (N = 30) supported Keller and Galgay’s eight themes while identifying two others: medical professionals not believing PWD’s symptoms and experiences of having their disability discounted based on appearing young and/or healthy. Similarly, Coalson et al. (2022), who utilized focus groups with adults who stutter (N = 7), endorsed six of Keller and Galgay’s themes and identified participants’ perceptions of microaggressive behaviors (i.e., Exonerated the Listener, Benefit of the Doubt, Focusing on Benefits, and Aggression Viewed as Microaggression) while noting that some participants had minimal or no microaggression experiences.
Although Eisenman et al. (2020) endorsed five of Keller and Galgay’s (2010) themes, they took a different approach to how they analyzed and organized their findings by using Sue et al.’s (2007) microaggression taxonomy. Of note, these researchers were the first to identify and establish microaffirmations within disability microaggressions research. According to Rolón-Dow and Davison (2018) microaffirmations are:
behaviors, verbal remarks or environmental cues experienced by individuals from minoritized racial groups in the course of their everyday lives that affirm their racial identities, acknowledge their racialized realities, resist racism or advance cultural and ideological norms of racial justice. (p. 1)
Like microaggressions, microaffirmations may be intentional or unintentional, but they have a positive rather than a negative impact on people with nondominant racial identities. Eisenman et al. (2020) found all four race-related microaffirmation types identified by Rolón-Dow and Davison (2021)—Microrecognitions, Microvalidations, Microtransformations, and Microprotections—with their sample of people with intellectual disabilities.
Finally, Miller and Smith (2021) conducted individual interviews (N = 25) with undergraduate and graduate students who identified as members of the LGBTQ community with a disability. They, too, found Keller and Galgay’s (2010) domains present in their study and identified eight additional categories. Five categories captured cultural components in addition to disability (i.e., Biphobia, Intersectionality Microaggression, Queer Passing/Disclosure, Racism, and Sexism), while the remaining three were specific to ableist microaggression–focused data: Ableism Avoidance, Faculty Accommodations, and Structural Ableism/Inaccessibility.
The purpose of our study is to add to the burgeoning disability and microaggressions discourse by analyzing participants’ responses to a qualitative prompt offered to them after they completed the Ableist Microaggression Scale (AMS; Conover et al., 2017b). We corroborate prior research findings while adding novel findings that increase professional knowledge about ableist microaggressions and their impact.
Methodology
To ensure compliance with Section 508 of the Rehabilitation Act, the federal law that requires PWD to have access to electronic information equivalent to that available to nondisabled individuals, we utilized digital accessibility tools on the internet platform used for this study (Qualtrics) and recruited PWD to test the accessibility of the study survey and questions. The data analyzed and reported in this article were part of a larger, IRB-approved study (N = 201) in which we investigated participants’ ableist microaggression experiences quantitatively using the AMS (Conover et al., 2017b) to uncover whether participants’ AMS scores were impacted by visibility of disability, type of disability, and their other nondominant identities (Deroche et al., 2024). After participants completed the survey, they were invited to provide a written response to the open-ended question: “What, if any, information do you think would be helpful for us to know about your personal experiences regarding ableist microaggressions?” Ninety participants (44.77% of the overall sample) responded with rich data that warranted analysis and reporting in an independent article. Because the open-ended question occurred after participants completed the AMS, we agreed that the survey likely influenced their responses, so we chose to conduct a content analysis using an a priori codebook grounded in the AMS subscales (Minimization, Denial of Personhood, Otherization, and Helplessness; Conover et al., 2017b), with additional coding categories for data that did not fit the a priori codes (i.e., Fortitude/Resilience/Coping, Contextual Factors, Impact of Microaggressions/Ableism on Mental Health/Wellness, Microaggression Experiences Are Different Depending on Visibility of Disability, Internalized Ableism, and Microaggressions Include Identities Other Than Disability).
Procedure
Using online data collection via Qualtrics survey, we recruited participants nationally by contacting disability organizations, listservs, social media, and professional contacts who work with organizations that serve PWD. The recruitment included a description of the research; inclusion criteria; and a confidential, anonymized survey link. The survey was Section 508–compliant and optimized to be taken on a computer or mobile device. Data were collected over a 3-month period.
Inclusion Criteria and Participants
To participate in the study, individuals (a) were at least 18 years of age, (b) had earned a high school diploma or GED, and (c) had a diagnosed disability. Under the Americans with Disabilities Act (ADA), the term disability is defined within the context of a person’s significant limitations to engage in major life activities. Different agencies and organizations such as the World Health Organization and the U.S. Social Security Administration define disability differently (Patel & Brown, 2017). For this study, we categorized disability as (a) physical disability (i.e., mobility-related disability), (b) sensory disability (i.e., seeing- or hearing-related disability), (c) psychiatric/mental disability (e.g., bipolar disorder, depression, post-traumatic stress disorder), or (d) neurodevelopmental disability (e.g., autism spectrum disorder, learning disability, or ADHD). Participants’ disabilities were apparent/visible (i.e., recognizable by others without the person disclosing they have a disability) or hidden (i.e., others are unlikely to know the individual has a disability, so the person must disclose they have a disability for it to be known), and they could identify with one or more disability categories listed above. Ninety individuals provided usable responses. Table 1 details participant demographics. The bulk of the sample, 84.43%, identified as having two (36.66%), three (26.66%), or four (21.11%) nondominant cultural identities out of the six identities the study targeted, while the rest of the sample comprised individuals who noted six (n = 2; 2.22%), five (n = 4; 4.4%), one (n = 7; 7.77%), or no (n = 1; 1.11%) nondominant identities.
Of note, a higher percentage of participants with hidden or both apparent and hidden disabilities participated in the qualitative portion of the study compared to those who completed only the quantitative portion (45.5% compared to 41.8% and 33.3% compared to 27.4%, respectively). Similarly, there was a lower response rate from participants who earned a high school diploma or GED (5.6%), completed an associate degree or trade school (7.8%), completed some college (7.8%), or earned a doctoral degree (10%). There was an increase in responses from participants who earned a bachelor’s degree (26.7% compared to 21.9% in the quantitative portion) or a master’s degree (42.2% compared to 35.8%, respectively).
Data Analysis
We analyzed data for this study using MacQueen et al.’s (1998) framework to create a codebook to promote coder consistency. We established six codes, four of which were definitionally congruent with the AMS subscales (i.e., Helplessness, Minimization, Denial of Personhood, and Otherization; Conover et al., 2017a). While we used Conover et al.’s definitions as the foundation, we utilized Keller and Galgay’s (2010) definitions to add additional nuance. The next code, Other Data, was an a priori code reserved for data that did not fit the AMS subscale codes. After completing the pilot, we added a sixth code, Fortitude/Resilience/Coping, to capture data that demonstrated ways in which participants developed strengths, dealt with adversity and microaggressions, and persevered despite their microaggressive experiences. Identifying PWD’s fortitude/resilience/coping abilities is indicative of a strengths-based framework that promotes inclusion, equity, and higher quality of life. Research has shown that resilience in PWD such as improved well-being, higher social role satisfaction, and lower mental health symptoms are correlated with positive psychological and employment outcomes (Ordway et al., 2020; Norwood et al., 2022). Once this code was established, the Other Data code was used for any data that did not fit the five a priori codes. After the pilot, we added to the codebook definitions for clarity—though no codes were changed. All codes we established had substantial representation in the data and are reported as themes in the results section. The auditor (second author Melissa D. Deroche) gave feedback on the codebook and confirmed the codebook was sound prior to analysis.
Table 1
Demographic Characteristics of Participants (N = 90)
| Variable |
n |
% |
| Disability Type |
|
|
|
Single Type: Physical |
21 |
23.33 |
|
Single Type: Sensory |
17 |
18.88 |
|
Single Type: Neurodevelopmental |
6 |
6.66 |
|
Single Type: Psychiatric/Mental Health |
6 |
6.66 |
|
Combination (2): Physical and Psychiatric/Mental Health |
8 |
8.88 |
|
Combination (2): Neurodevelopmental and Psychiatric/Mental Health |
6 |
6.66 |
|
Combination (2): Sensory and Psychiatric/Mental Health |
5 |
5.55 |
|
Combination (2): Sensory and Physical |
4 |
4.44 |
|
Combination (2): Neurodevelopmental and Physical |
2 |
2.22 |
|
Combination (2): Sensory and Neurodevelopmental |
2 |
2.22 |
|
Combination (3): Physical, Psychiatric/Mental Health, Neurodevelopmental |
4 |
4.44 |
|
Combination (3): Physical, Sensory, Neurodevelopmental |
4 |
4.44 |
|
Combination (3): Sensory, Psychiatric/Mental Health, Neurodevelopmental |
2 |
2.22 |
|
Combination (3): Physical, Sensory, Psychiatric/Mental Health |
1 |
1.11 |
|
Combination (4): Physical, Sensory, Psychiatric/Mental Health,
Neurodevelopmental |
2 |
2.22 |
| Visibility of Disability |
|
|
|
Visible/Apparent |
19 |
21.11 |
|
Hidden/Concealed |
41 |
45.55 |
|
Both |
30 |
33.33 |
| Biological Sex/Sex Assigned at Birth |
|
|
|
Female |
74 |
82.22 |
|
Male |
16 |
17.77 |
| Gender Identity |
|
|
|
Gender Fluid/Gender Queer |
6 |
6.66 |
|
Man |
16 |
17.77 |
|
Woman |
68 |
75.55 |
| Affectual/Sexual Orientation |
|
|
|
Asexual |
2 |
2.22 |
|
Bisexual |
9 |
10.00 |
|
Gay |
2 |
2.22 |
|
Heterosexual |
68 |
75.55 |
|
Lesbian |
3 |
3.33 |
|
Pansexual |
4 |
4.44 |
|
Queer |
1 |
1.11 |
|
Questioning |
1 |
1.11 |
| Racial/Ethnic Identity |
|
|
|
African American/Black |
4 |
4.44 |
|
Asian or Pacific Islander |
3 |
3.33 |
|
Biracial |
2 |
2.22 |
|
Euro-American/White |
69 |
76.66 |
|
Indigenous |
1 |
1.11 |
|
Jewish |
5 |
5.55 |
|
Latino/a or Hispanic |
3 |
3.33 |
|
Middle Eastern |
1 |
1.11 |
|
Multiracial |
2 |
2.22 |
| Religious/Spiritual Identity |
|
|
|
Atheist |
8 |
8.88 |
|
Catholic |
12 |
13.3 |
|
Jewish |
4 |
4.44 |
|
Not Religious |
1 |
1.11 |
|
Pagan |
1 |
1.11 |
|
Protestant |
36 |
40.00 |
|
Questioning |
2 |
2.22 |
|
Spiritual Not Religious |
5 |
5.55 |
|
Unitarian Universalist |
2 |
2.22 |
|
Self-Identify in Another Way |
19 |
21.11 |
| Highest Level of Education |
|
|
|
High School Diploma or GED |
5 |
5.55 |
|
Associate or Trade School Degree |
7 |
7.77 |
|
Some College, No Degree |
7 |
7.77 |
|
Bachelor’s Degree |
24 |
26.66 |
|
Master’s Degree |
38 |
42.22 |
|
PhD, EdD, JD, MD, etc. |
9 |
10.00 |
|
No Response |
1 |
1.11 |
| Employment Status |
|
|
|
Full-Time |
40 |
44.44 |
|
Part-Time |
16 |
17.77 |
|
Retired |
9 |
10.00 |
|
Student |
11 |
12.22 |
|
Unemployed |
14 |
15.55 |
| Employment Compared to Training and Skills |
|
|
|
Training/Education/Skills are lower than job responsibilities/position |
2 |
2.22 |
|
Training/Education/Skills are on par with job responsibilities/position |
42 |
46.66 |
|
Training/Education/Skills exceed job responsibilities/position |
24 |
26.66 |
|
Not applicable |
22 |
24.44 |
|
|
|
|
|
We began analysis by piloting 10% of the data (n = 9) using the initial codebook (Boyatzis, 1998). Two researchers (first and third authors Jennifer M. Cook and Lee Za Ong) coded data independently and then worked together to reach consensus. Once the pilot analysis was complete, we coded the remaining data and recoded pilot data to ensure they fit the revised coding frame. After all data were coded, we further coded the data that were assigned to Other Data using in vivo codes to establish codes that best captured the data. We identified five codes within Other Data: Contextual Factors, Impact of Microaggressions/Ableism on Mental Health/Wellness, Microaggression Experiences Are Different Depending on Visibility of Disability, Internalized Ableism, and Microaggressions Include Identities Other Than Disability.
Trustworthiness
Cook and Ong coded all data independently and then met to reach consensus. Prior to coding commencement, we identified our beliefs and potential biases about the data and discussed how they might impact coding; we continued these conversations throughout analysis. For the pilot coding phase, independent coder agreement prior to consensus was 40%. Independent coder agreement prior to consensus during regular coding was 56%, and 69% for Other Data independent coding. We reached consensus for all coded data through a team meetings consensus process (Boyatzis, 1998). Finally, we utilized an auditor (Deroche). Deroche reviewed all consensus findings during all analysis stages. The coding team met with the auditor to resolve questions and discrepancies, such as a few instances in which data were misassigned to a code.
Research Team
The research team comprised three cisgender women between the ages of 45 and 55 who are all licensed professional counselors and work as counselor educators. Cook and Deroche identify as White and hold PhDs in counselor education, while Ong holds a PhD in rehabilitation psychology and is Asian American of Chinese descent and an immigrant from Malaysia. Deroche identifies as a person with a disability, Deroche and Ong have worked extensively with PWD, and all three authors have conducted research about PWD. Cook has abundant publications in qualitative research designs related to multicultural counseling. Finally, all three authors have extensive research training and experience in qualitative and quantitative research designs.
Findings
The findings described below are organized into two categories: findings that align with the AMS subscales and unique findings that are independent of the AMS subscales. Themes are listed in their appropriate category with participants’ quotes to illustrate and substantiate each theme (see Table 2). When we provide participant quotes, we refer to them by their randomly assigned participant numbers (e.g., P105, P109).
Table 2
Categories and Themes
| Category/Theme |
n |
% of Sample |
| Category 1: Findings That Align With the AMS Subscales |
|
|
|
Minimization |
35 |
38.88 |
|
Denial of Personhood |
26 |
28.88 |
|
Otherization |
17 |
18.88 |
|
Helplessness |
16 |
17.77 |
| Category 2: Unique Findings Independent of the AMS Subscales |
|
|
|
Fortitude/Resilience/Coping |
27 |
30.00 |
|
Contextual Factors |
17 |
18.88 |
|
Impact of Microaggressions/Ableism on Mental Health/Wellness |
10 |
9.00 |
|
Microaggression Experiences Are Different Depending on Visibility of Disability |
6 |
6.66 |
|
Internalized Ableism |
4 |
4.44 |
|
Microaggressions Include Identities Other Than Disability |
4 |
4.44 |
Note. N = 90.
Category 1: Findings That Align With the AMS Subscales
Our analysis revealed that the AMS a priori codes fit the study data. As such, the codes were transitioned to themes: Minimization (n = 35), Denial of Personhood (n = 26), Otherization (n = 17), and Helplessness (n = 16). The quotes selected for each theme illustrate the lived experiences of the theme definitions and add context and nuance about the impact of ableist microaggressions.
Minimization
Conover et al. (2017a) defined Minimization as microaggression experiences demonstrating the belief that PWD are “overstating their impairment or needs” and that “individuals with a disability could be able-bodied if they wanted to be or that they are actually able-bodied” (p. 581). Thirty-five of the 90 participants’ responses (33.33%) indicated instances of Minimization.
For example, P105 described incidents from their formative years that highlight the belief that PWD are, in fact, able-bodied and overstating their impairment:
As a child, children and adults alike would test the limits of my blindness. My piers [sic] would ask me how many fingers they were holding up. And in one instance, teachers lined a hallway with chairs to see if I’d run into them. Spoiler alert, I did.
P109 spoke to their interactions with family that highlight how disbelief about a person’s disability can result in Minimization:
Family is really bad. They still don’t believe me. I was asked (when I couldn’t climb stairs into a restaurant) are you trying to make a point? My visible disability has gotten worse over 40 years. I think because they saw me before I started using a cane, they just won’t believe me.
P158 illuminated a fallacy that can result in Minimization: “Because my disability is invisible people assume I need no help, [and] when I do, they discount my disability. I hear, ‘you don’t look like you have a disability‚’ ‘don’t sell yourself short.’”
Finally, P137 spoke to the blame that underlies Minimization:
On[e] of the most frequent microaggressions encountered living with my particular invisible disability (type 1 diabetes) is the ableist idea that health is entirely a personal responsibility. There is this assumption that whatever problems we face with our health are a direct result of poor choices (dietary, financial) completely ignoring the systematic problems with for-profit health care in this country.
Denial of Personhood
Denial of Personhood is characterized by PWD being “treated with the assumption that a physical disability indicates decreased mental capacity and therefore, being reduced to one’s physicality” (Conover et al., 2017a, p. 581); such microaggressions can occur “when any aspect of a person’s identity other than disability is ignored or denied” (Keller & Galgay, 2010, p. 249). Twenty-six participants (28.88%) endorsed this theme. For example, P142 described their experiences in the workplace that illustrate the erroneous belief that PWD have diminished mental capacity: “All my life I was pushed out of jobs for not hearing. People would actually tell me, ‘if you can’t hear—how can you do anything’ even though all my performance reviews exceeded expectations.” P123 spoke to a similar sentiment: “[I] am often asked ‘what’s wrong with you?’ ‘how did you get through college?’” Finally, P173 summarized the belief that seemingly underlies Denial of Personhood microaggressions and issued a corrective action:
Disabled doesn’t mean stupid. We can figure out most things for ourselves and if we can’t we know to ask for help. Don’t tell us how to live our lives or say we don’t deserve love, happiness and children. If you don’t know the level of someone’s disability you shouldn’t have the right to judge them about such things.
Otherization
Seventeen participants (18.88%) described Otherization as part of their narrative responses. Otherization microaggressions are those in which PWD are “treated as abnormal, an oddity, or nonhuman, and imply people with disabilities are or should be outside the natural order” (Conover et al., 2017a, p. 581) and that their “rights to equality are denied” (Keller & Galgay, 2010, p. 249). Participants shared several examples of these types of microaggressions. For instance, P140 shared:
When we (PWD) ask for simple things (e.g., can you turn on the captioning) and people grumble, say they can’t, etc. it just reinforces that we’re not on equal footing and at least for me it eats away a little bit every time.
P185 indicated another manifestation of Otherization: “As a deaf person, I get frustrated when whoever I’m talking to stops listening when someone else (non-deaf person) speaks verbally, leaving me mid-sentence.” P108 shared that they have been “prayed for in public without asking,” while P106 expressed, “I hate when people compliment me on how well I push my chair or say I must have super strong arms. I just have normal arms not athletic looking or anything.”
Helplessness
Helplessness microaggressions are those in which PWD are “treated as if they are incapable, useless, dependent, or broken, and imply they are unable to perform any activity without assistance” (Conover et al., 2017a, p. 581). Sixteen participants (17.77%) described Helplessness microaggressions. For P174, the most common Helplessness microaggression they experience is when “people speak to the person I am with instead of to me. Drives me crazy! Worse is when the person I’m with answers for me.” P126 corroborated the “devastating” nature of when “people make decisions for you.” P129 shared that, “As a person with an invisible disability, I most often encounter microaggressions in the form of unsolicited advice when I disclose my disability.” Similarly, P134 noted:
Although my disability is not apparent, if people know about it, they often just act on my behalf without asking me for input or feedback. That is very frustrating and often does not change even if I bring it up to the individual who does it.
This final quote from P134 is powerful because it, like P174’s experience, demonstrates how people without disabilities participate in perpetuating ableism even when they were not the ones who initiated it.
Category 2: Unique Findings Independent of the AMS Subscales
As we indicated earlier, we separated data that did not fit into AMS codes and coded them using in vivo codes. This analysis resulted in six novel themes (i.e., Fortitude/Resilience/Coping, Contextual Factors, Impact of Microaggressions/Ableism on Mental Health/Wellness, Microaggression Experiences Are Different Depending on Visibility of Disability, Internalized Ableism, and Microaggressions Include Identities Other Than Disability) that are independent from the AMS-driven themes discussed in the prior section, yet are interrelated because they add unique insights and helpful context for understanding ableist microaggressions within the lived experiences of PWD.
Fortitude/Resilience/Coping
We defined Fortitude/Resilience/Coping as ways in which participants have developed strength, dealt with adversity/microaggressions, and persevered despite their microaggressive experiences. Thirty percent (n = 27) of participants disclosed a wide range of attitudinal and experiential tactics related to this theme. P103 shared, “I maintain what I call a healthy sense of humor about my own body and being disabled,” while P145 demonstrated a sense of humor as they shared how they cope:
I just have to remind them and myself that my brain works differently and that I am just as competent as anyone else. I have learned not to beat myself up when I forget something or can’t get my paperwork done correctly for the tenth time. (I really hate paperwork.)
Participants 138 and 127 both spoke directly to the role knowledge plays. P138 shared:
I want to put out there that knowledge & understanding are power. Knowing & understanding your rights as a person with a disability as well as knowing & understanding your unique experience with your own disability (to the best of your ability) is key to making forward strides in environments that can often times feel ableist.
P127 spoke to knowledge, too, with their belief that “most microaggressions stem from a lack of education. I am often the first person they have met with a disability and the experience makes them uncomfortable.”
Finally, P187 spoke to the power of their resilience and its impact on their life, experiences which they draw from to help others:
I’ve been physically and emotionally abused my entire life, until I took control and stopped it. I’m middle aged and it took me 40 years to forgive everything that I’ve . . . had to endure. Never from my family, or close friends, but it’s been a difficult life, and now I’m all ok with it and try to help others with disabilities that are having a hard time.
Contextual Factors
Seventeen participants (18.88%) described Contextual Factors, which are data that depict relational, situational, or environmental elements that impact participants’ experiences of ableist microaggressions.
P110 shared that “microaggressions can be hard to label because they can vary based on the relationship you have with the person.” P175 added: “Most times the microaggression I receive are by people when they don’t know me, or first meet me, as opposed to get to know me better.” P162 spoke to additional situational/relational nuances: “I have very different experiences depending on what assistive technology I’m using in a given space (basically to what degree I pass as able-bodied) and how people know me.”
P163 spoke to relational roles as well as environmental context: “The attitudes about me are distinctly divided between the power structures. A case manager, medical doctor, neighbor or family member will certainly show their attitude differently. The same goes for academic settings [versus] job placement.” For P152, “The worst comments have come from mental health therapists [who] are medical professionals who should be the most compassionate towards their patients.”
P117 and P131 both identified situational differences they have noticed. P117 shared, “I find that people have treated me differently at different ages and stages in my life, particularly when I was raising three children as a divorced mom.” P131 identified their work environment as positive: “I work in the field of vocational rehabilitation so [I] interact with more people who have a more nuanced understanding of disability than the general population.” However, P165 offered an alternate view, noting that “many microaggressions are more insidious or come from within the disabled community.”
Impact of Microaggressions/Ableism on Mental Health/Wellness
Ten participants (9%) expressed how microaggressions and ableism experiences have impacted their mental health and wellness. P172 stated, “I struggle with my mental wellness and I have been hospitalized for severe depression that manifests from a combination of my disability and situations that are overwhelming.” P157 expressed a similar combination effect of having a disability and being “ostracized” by others: “The combination is very heavy on my heart and leaves me feeling incredibly alone.”
P159 expressed feeling “pathetic and weak. Sometimes I feel useless and disgraced. Most of the time I feel dumb and stupid.” P103 added additional impacts while acknowledging the differences between their experiences and those of their colleagues of color: “None of these [microaggressions] were overt, but all contributed to stress and frustration and generalized anxiety. I have seen much worse with coworkers of color and disabled Black and Brown folks in my community.”
P126 admitted that completing the study survey “evoked difficult memories.” Additionally, this participant described the turmoil and cognitive dissonance they experience:
I’m reminded taking this survey of the inner conflict with identifying as disabled. Is my disability qualifying enough, will I be rejected? I felt hints of defensiveness emerge, like imposter syndrome. I also recognize that I desire to be abled and that keeps the conflict churning.
Microaggression Experiences Are Different Depending on Visibility of Disability
Six participants (6.6%) spoke to how individuals with hidden disabilities experience microaggressions differently than individuals with visible/apparent disabilities. P141 asserted that “because my disabilities are hidden, I don’t hear many microaggressions regarding me,” and P183 corroborated that microaggressions are “different the more severe and obvious the disabilities are.”
P146 suggested that “invisible disabilities offer up a whole different category of microaggressions than those with visible disabilities,” and P151 added that “hidden disabilities is [sic] a double edged sword,” highlighting both the privilege and the dismissiveness hidden disabilities can bring. P150 emphasized the privilege of others not knowing about their disability: “In some ways, this benefits me because I’m not associated with the stigma of a disability.”
Internalized Ableism
A small number of participants (n = 4) expressed comments that were consistent with Internalized Ableism. Internalized Ableism includes believing the stereotypes, myths, and misconceptions about PWD, such as the notion that all disabilities are visible and that PWD cannot live independently, and it can manifest as beliefs about their own disability or others’ disabilities. One manifestation of Internalized Ableism is when a PWD expresses that another’s disability is not real or true compared to their own disability. For example, P112 stated: “Every time I go out I have great difficulty finding available accessible parking. I watch & people using the spots are walking/functioning just fine. Sick of hearing about ‘hidden disability.’ I think the majority are inconsiderate lazy people.”
Another manifestation of Internalized Ableism can be when PWD deny the existence of ableist microaggressions. P183 shared:
I don’t think that most people have microaggressions toward PWD. Maybe that’s different the more severe and obvious the disabilities are. It tends to be older people like 60s or 70s that treat me differently period it seems like the younger generation just sees most of us as people not disabled people. And I also think the term ableist separates PWD and people without. If we don’t want to be labeled, we shouldn’t label them.
Microaggressions Include Identities Other Than Disability
For this final theme, four participants (4.44%) spoke to the complexity related to microaggressions when a PWD has additional nondominant cultural identities. P167 expressed the compounding effect: “I have multiple minoritized identities—the intersection leads to more biases.” P161 articulated the inherent confusion when one has multiple nondominant identities: “I do not know whether I am treated in the ways I indicated because of my disabilities or because I am a person of color.” These quotes highlight the inherent increase and subsequent impact on PWD who have more than one nondominant cultural identity.
Discussion
The purpose of our analysis was to illuminate participants’ lived experiences with ableist microaggressions that were important to them. We revealed contextual information about participants’ experiences that aligned with the AMS subscales (i.e., Minimization, Denial of Personhood, Otherization, and Helplessness). Although prior qualitative ableist microaggression studies (e.g., Coalson et al., 2022; Eisenman et al., 2020; Olkin et al., 2019) grounded their research in Keller and Galgay’s (2010) eight categories rather than in Conover et al.’s (2017a) four subscales, it is fair to say that our findings substantiate other researchers’ findings because Conover et al.’s four subscales were devised based on Keller and Galgay’s findings.
While the corroboration of prior research findings based on the AMS subscales is illustrative and essential, the crucial findings from this study lie in the unique themes that arose from the in vivo coding process (i.e., Fortitude/Resilience/Coping, Contextual Factors, Impact of Microaggressions/Ableism on Mental Health/Wellness, Microaggression Experiences Are Different Depending on Visibility of Disability, Internalized Ableism, and Microaggressions Include Identities Other Than Disability). These themes introduce both novel and less-explored aspects of disability and of ableist microaggressions.
Fortitude/Resilience/Coping is a unique theme. Participants described how they became stronger and persevered despite microaggressive experiences. Eisenman et al. (2020) were the first to identify microaffirmations within ableist microaggressions research and Coalson et al. (2022) found that their participants perceived benefits that came from microaggressive experiences; both are important contributions. However, both instances of seeming positives related to ableist microaggressions in these studies are framed within the context of how others acted toward PWD rather than the autonomous choices and personal development of the person with the disability in the face of adversity. Our findings demonstrate PWD’s abilities—both innate qualities and learned skills—that rendered life-giving fortitude, resilience, and coping in which they are personally empowered and persevere despite external stimuli; they are not dependent upon whether others act appropriately. This is a key finding for counselors because they have the ability to create a therapeutic environment in which PWD can process, develop, and refine their fortitude, resilience, and coping further, acknowledging that PWD have these skills already.
Unsurprisingly, some participants spoke to the impact of ableist microaggressions and ableism on their mental health and wellness; these impacts included depression, loneliness, stress, frustration, and feeling “pathetic and weak.” What was surprising is that only 9% of the sample spoke to this impact directly, given how well-documented the harmful mental health effects of microaggressions are (Sue & Spanierman, 2020). This seeming underrepresentation of mental health ramifications amongst participants led us to wonder, based on the high percentage of participants (30%) who endorsed Fortitude/Resilience/Coping, whether this specific sample had a uniquely high ability to cope with adversity as compared to the overall disability population or if it is possible that ableist microaggression experiences have begun to decrease. While we are unable to answer these questions directly as part of this study, we posit three considerations: (a) microaggressions continue to have a negative effect on some PWD and need to be screened for and attended to within the counseling process; (b) screening for and helping clients with disabilities name, develop, or refine coping, fortitude, and resilience can prove beneficial; and (c) it is worthwhile to continue to work to reduce microaggressive behaviors in every way possible.
Although we had an independent theme in which participants indicated the differences between apparent and hidden disabilities, the participant quotes within every theme illustrate these differences as well. For instance, within the Minimization theme, P137 highlighted that those with hidden disabilities may be told that “personal responsibility” is the cause of their disability, while P105 and P109 spoke to having to “prove” their apparent disability to others, including family. Having to prove one’s disability or not being believed tracks with several other researchers’ findings including Olkin et al. (2019), who found that medical professionals did not believe PWD’s symptoms and experiences. The Helplessness theme revealed differences such as P129 receiving unsolicited advice once people learn of their hidden disability; however, this theme revealed similarities, too. Participants with both apparent and hidden disabilities experienced others acting on their behalf without their consent.
The Microaggression Experiences Are Different Depending on Visibility of Disability theme may explain why a higher percentage of participants with hidden disabilities or those who have both hidden and apparent disabilities participated in the qualitative portion of the study than those with apparent disabilities, which was the higher percentage in the quantitative part of the study. By definition, microaggressions can leave those who experience them questioning whether what they experienced was real, and this could be compounded when PWD have hidden disabilities; these participants may have needed to express their experiences more than those with apparent disabilities. While our data demonstrate that having a hidden disability may be a protective factor from experiencing ableist microaggressions, their disability experience often can be overlooked or ignored, resulting in a form of minimization that is both congruent with and distinct from the Minimization subscale definition.
Participants made a case for how Contextual Factors, defined as relational, situational, and/or environmental components, impact microaggression experiences. Implicitly, several authors spoke to what we have named as Contextual Factors (e.g., Coalson et al., 2022; Eisenman et al., 2020; Miller & Smith, 2021), yet the specificity and nuance participants provided in this study warranted a distinct theme. Relationally, participants noted that whether the perpetrator knew them and if there was a relational power differential between them and the perpetrator (e.g., doctors or counselors vs. family member or neighbor) makes a difference. Damningly, P152 stated that “the worst comments” they have received “have come from mental health therapists.” Participants noted, too, that work environments, life stage, the type of assistive technology they are using at the time, and being part of the disability community can all be impactful in both affirming and deleterious ways. It is imperative that counselors assess and understand thoroughly each client’s specific contextual factors so they can identify ways in which clients have internal and external resources and support, as well as areas in which they may want strategies, support, resources, and, potentially, advocacy intervention.
A small number of participants (n = 4) spoke to Internalized Ableism. Although this was a less robust theme, it was important to report because it adds to professional knowledge about what some clients with disabilities might believe and express during counseling sessions. We defined Internalized Ableism as participants expressing stereotypes, myths, and misconceptions about PWD that can manifest as beliefs about their own disability or the disabilities of others. One participant expressed disdain for hidden disabilities and expressed disbelief about others’ needs to use parking for disabled persons, while another participant questioned whether most PWD experience ableist microaggressions. While our study findings are not congruent with these statements, counselors must take clients’ expressions seriously, work to understand how clients have developed these beliefs, and seek to understand their impact on the client who is stating them.
Finally, four participants indicated that Microaggressions Include Identities Other Than Disability. Given the high percentage of the sample that had multiple nondominant identities, it is curious that so few participants spoke to this phenomenon. However, we theorize that this may have to do with identity salience (Hunt et al., 2006) and the fact that this was a study about ableist microaggressions. For the participants who spoke to this theme, the important features they reported were the compounding effect of microaggressions when one has multiple nondominant identities and the inherent confusion that results from microaggressive experiences, particularly when one has multiple nondominant identities. Again, counselors must screen for and be prepared to address the complexity and the impact of ableist microaggressions based on each client’s unique identities and experiences.
Implications for Practice
The study findings illustrate the ubiquitous, troubling, and impactful nature of ableist microaggressions. These findings expose many counselors, supervisors, and educators to a world they may not know well or at all, while for others, these findings validate experiences they know all too well personally and professionally. We began this article with a quote from the pre-Socratic philosopher Heraclitus: “Day by day, what you choose, what you think, and what you do is who you become.” This quote captures the charge we are issuing to counseling professionals: It is time to take action to become counseling professionals who think as, act as, and are disability-affirming professionals. The task at hand is for each counseling professional to decide what steps to take next to strengthen their disability-affirming identity based on their current awareness, knowledge, and skill level, as well as how they can enact their disability-affirming identity based on their professional roles.
Fundamentally, disability-affirming professionals validate, support, encourage, and advocate for and with PWD consistently throughout their professional activities. For many, this begins with developing their awareness and knowledge, followed later by their skills. Based on the findings presented in this article, we suggest counseling professionals engage in self-reflexivity by examining the ways in which they have unwittingly adopted the dominant discourses about disability, what they believe about the abilities and lives of PWD, how they understand disability within the context of other nondominant identities, and the ways in which they have participated in perpetuating ableist microaggressions. Without engaging in disability self-awareness development, professionals risk conveying ableist microaggressions to clients that can result in early termination, impede the therapeutic relationship, and/or inflict additional psychological harm (Sue & Spanierman, 2020). For example, counselors may assume that clients with disabilities have diminished social–emotional learning skills compared to clients without disabilities and initiate formalized assessment based on this assumption. While counselors should be attuned to all clients’ social–emotional skills, it can be damaging to PWD’s sense of self and the counseling relationship to assume their social–emotional learning skills are deficient rather than assessing how environments are not conducive to PWD’s social–emotional needs (Lindsay et al., 2023).
Counselors’ self-reflexive process is meant to foster self-awareness; to better equip counselors to recognize ableist microaggressions in clients’ stories when they occur in personal, training, and professional environments; and for them to avoid unintentionally communicating ableist microaggressions in their practice. To start this process, we encourage counselors to question whether any of the study findings rang true, whether as someone who has experienced ableist microaggressions or as one who has perpetrated them, and to ascertain whether their attitudes and beliefs about PWD differ based on the visibility of disability. Additionally, we proffer that counselors who engage in self-reflective activities, such as the ones mentioned above, and those who learn more about PWD’s lives and experiences are more apt to create a plan to work through any negative attitudes or biases they have and, in turn, refine their skills so they are more disability-affirming in their practice. Counselors who engage in these processes will benefit those they serve, whether clients, students, or supervisees.
This study represents only a slice of the microaggression experiences of PWD. We concur with Rivas and Hill (2023) that counselors must adopt an evolving commitment to develop disability counseling effectiveness. Ways that counselors can take steps toward developing their disability-affirmative counselor identity and effectiveness include familiarizing themselves with and applying the American Rehabilitation Counseling Association (ARCA) disability competencies (Chapin et al., 2018); reading additional studies (e.g., Olkin et al., 2019; Peters et al., 2017); listening to podcasts (e.g., Swenor & Reed, n.d.); reading blogs and books (e.g., Heumann & Joiner, 2020); and watching shows and movies that highlight PWD’s experiences, microaggressive and otherwise—PWD are telling their stories and want others to learn from them.
Within the relational context, no matter one’s professional roles, it is important to be prepared to attend to the interaction of identity constellations within professional relationships and the power dynamics that are present (Ratts et al., 2016). Broaching these topics initially, including ability status and similarities and differences with our experiences, is a helpful start; however, this is the beginning of the process, not the entire process. Accordingly, clinicians must continually assess PWD’s contextual factors and their impact, lived experiences of their multiple identities, resilience, fortitude, and coping skills. To do so, clinicians must first create space for clients to process their microaggression experiences through actively listening to their stories; allowing PWD to openly express their frustrations, anger, or other emotions; and validating their experiences using advanced empathy. In other words, it is critical not to dismiss such topics nor unilaterally make them the presenting problem—balance is needed to attend to microaggression experiences appropriately. Essentially, counselors need to guide clients to discern the impact and to identify what they need rather than doing it for them, and to be ready, willing, and able to advocate with and on behalf of clients. All advocacy actions must be discussed with clients so as to center their autonomy.
Clients’ resiliencies and strengths must be fostered unceasingly. It is not uncommon for clients who have experienced ableist microaggressions to feel diminished and worthless and to question their purpose. Counselors must prioritize assisting clients in naming their strengths and telling stories about how they have developed resiliencies, and they must encourage clients to draw on both when facing adversity—particularly ableist microaggressions. While the goal is to eradicate ableist microaggressions, we must reinforce with clients that they are armed with tools to safeguard against ableist microaggressions’ impact and that they can seek trusted support when they need it.
As we move forward into the future as disability-affirming counseling professionals, counselor educators and supervisors have a specific charge to include disability status and disability/ableist microaggressions as part of their professional endeavors when working with students and supervisees. For many, the aforementioned recommendations likely apply because they, too, did not receive education about disability and disability microaggressions (Deroche et al., 2020). This is a setback, but not a limitation. Counselor educators and supervisors are continual learners who seek additional awareness, knowledge, skills, and advocacy actions to positively impact their work with counselors-in-training. Webinars, disability-specific conference sessions, and engaging with community disability organizations are helpful ways to start, and we recommend counselor educators and supervisors engage in the same self-examination strategies mentioned above to begin combating any biases they may hold about PWD. More specifically, counselor educators and supervisors can introduce and teach the ARCA disability competencies to trainees and supervisees, deliberately integrate self-exploration activities regarding disability into coursework, direct trainees and supervisees to inquire about ability status in intake and assessment procedures, and use cultural broaching behaviors to model appropriate use with clients (Deroche et al., 2020).
Limitations and Future Research
There are important limitations to consider to contextualize the study findings. The data used in this analysis were the result of one open-ended prompt as part of a larger quantitative study. Although participants offered robust and illustrative responses, it is a significant limitation that no follow-up questions were asked. Additionally, because the study utilized the AMS (Conover et al., 2017b), we analyzed data using the AMS subscales. While this was an appropriate choice given the context, it limited our ability to compare our findings with other qualitative studies that used Keller and Galgay (2010) to explain their findings.
We recommend that future research investigates the unique themes from this study in more detail to ascertain whether they are applicable to the larger PWD population. We suggest that focus groups combined with individual interviews may help to tease out nuances and could potentially lead to developing theory related to ableist microaggressions and best practices that will support PWD. Finally, we propose that more in-depth intersectionality research would benefit PWD and the professionals who serve them. The confounding nature of microaggressions combined with individuals’ unique identity compositions that often include both nondominant and dominant identities can make this type of research challenging, yet both are the reality for many PWD and this research is therefore needed.
Conclusion
Ableist microaggressions are ubiquitous and damaging to PWD. Through our analysis, we found that participants’ experiences corroborated prior researchers’ findings related to established ableist microaggression categories and added new knowledge by introducing six novel themes. We envision a disability-affirmative counseling profession and offered concrete recommendations for clinicians, supervisors, and counselor educators. Together, we can create a reality in which all PWD who seek counseling services will experience relief, validation, and empowerment as we work to create a society that provides access to all.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Boyatzis, R. E. (1998). Transforming qualitative information. SAGE.
Chapin, M., McCarthy, H., Shaw, L., Bradham-Cousar, M., Chapman, R., Nosek, M., Peterson, S., Yilmaz, Z., & Ysasi, N. (2018). Disability-related counseling competencies. American Rehabilitation Counseling Association (ARCA) Task Force on Competencies for Counseling Persons with Disabilities. https://arcaweb.org/wp-content/uploads/2023/12/ARCA-Disability-Related-Counseling-Competencies.pdf
Coalson, G. A., Crawford, A., Treleaven, S. B., Byrd, C. T., Davis, L., Dang, L., Edgerly, J., & Turk, A. (2022). Microaggression and the adult stuttering experience. Journal of Communication Disorders, 95, 106180. https://doi.org/10.1016/j.jcomdis.2021.106180
Conover, K. J., Israel, T., & Nylund-Gibson, K. (2017a). Development and validation of the Ableist Microaggressions Scale. The Counseling Psychologist, 45(4), 570–599. https://doi.org/10.1177/0011000017715317
Conover, K. J., Israel, T., & Nylund-Gibson, K. (2017b). Ableist Microaggressions Scale (AMS) [Database record]. APA PsycTESTS. https://doi.org/10.1037/t64519-000
Dávila, B. (2015). Critical race theory, disability microaggressions, and Latina/o student experiences in special education. Race, Ethnicity, and Education, 18(4), 443–468. https://doi.org/10.1080/13613324.2014.885422
Deroche, M. D., Herlihy, B., & Lyons, M. L. (2020). Counselor trainee self-perceived disability competence: Implications for training. Counselor Education and Supervision, 59(3), 187–199. https://doi.org/10.1002/ceas.12183
Deroche, M. D., Ong, L. Z., & Cook, J. M. (2024). Ableist microaggressions, disability characteristics, and nondominant identities. The Professional Counselor, 13(4), 404–417. https://doi.org/10.15241/mdd.13.4.404
Eisenman, L. T., Rolón-Dow, R., Freedman, B., Davison, A., & Yates, N. (2020). “Disabled or not, people just want to feel welcome”: Stories of microaggressions and microaffirmations from college students with intellectual disability. Critical Education, 11(17), 1–21.
Heumann, J., & Joiner, K. (2020). Being Heumann: An unrepentant memoir of a disability rights activist. Beacon Press.
Hunt, B., Matthews, C., Milsom, A., & Lammel, J. A. (2006). Lesbians with physical disabilities: A qualitative study of their experiences with counseling. Journal of Counseling & Development, 84(2), 163–173. https://doi.org/10.1002/j.1556-6678.2006.tb00392.x
Keller, R. M., & Galgay, C. E. (2010). Microaggressive experiences of people with disabilities. In D. W. Sue (Ed.), Microaggressions and marginality: Manifestation, dynamics, and impact (pp. 241–268). Wiley.
Lindsay, S., Fuentes, K., Ragunathan, S., Lamaj, L., & Dyson, J. (2023). Ableism within health care professions: A systematic review of the experiences and impact of discrimination against health care providers with disabilities. Disability and Rehabilitation, 45(17), 2715–2731. https://doi.org/10.1080/09638288.2022.2107086
MacQueen, K. M., McLellan, E., Kay, K., & Milstein, B. (1998). Codebook development for team-based qualitative analysis. Cultural Anthropology Methods, 10(2), 31–36. https://doi.org/10.1177/1525822X980100020301
Miller, R. A., & Smith, A. C. (2021). Microaggressions experienced by LGBTQ students with disabilities. Journal of Student Affairs Research and Practice, 58(5), 491–506. https://doi.org/10.1080/19496591.2020.1835669
Norwood, M. F., Lakhani, A., Hedderman, B., & Kendall, E. (2022). Does being psychologically resilient assist in optimising physical outcomes from a spinal cord injury? Findings from a systematic scoping review. Disability and Rehabilitation, 44(20), 6082–6093. https://doi.org/10.1080/09638288.2021.1952320
Olkin, R., Hayward, H., Abbene, M. S., & VanHeel, G. (2019). The experiences of microaggressions against women with visible and invisible disabilities. Journal of Social Issues, 75(3), 757–785. https://doi.org/10.1111/josi.12342
Ordway, A. R., Johnson, K. L., Amtmann, D., Bocell, F. D., Jensen, M. P., & Molton, I. R. (2020). The relationship between resilience, self-efficacy, and employment in people with physical disabilities. Rehabilitation Counseling Bulletin, 63(4), 195–205. https://doi.org/10.1177/0034355219886660
Patel, D. R., & Brown, K. A. (2017). An overview of the conceptual framework and definitions of disability. International Journal of Child Health and Human Development, 10(3), 247–252.
Perrin, P. B. (2019). Diversity and social justice in disability: The heart and soul of rehabilitation psychology. Rehabilitation Psychology, 64(2), 105–110. https://doi.org/10.1037/rep0000278
Peters, H. J., Schwenk, H. N., Ahlstrom, Z. R., & Mclalwain, L. N. (2017). Microaggressions: The experience of individuals with mental illness. Counselling Psychology Quarterly, 30(1), 86–112. https://doi.org/10.1080/09515070.2016.1164666
Ratts, M. J., Singh, A. A., Nassar-McMillan, S., Butler, S. K., & McCullough, J. R. (2016). Multicultural and social justice counseling competencies: Guidelines for the counseling profession. Journal of Multicultural Counseling and Development, 44(1), 28–48. https://doi.org/10.1002/jmcd.12035
Rivas, M., & Hill, N. R. (2023). A grounded theory of counselors’ post-graduation development of disability counseling effectiveness. Journal of Counselor Preparation and Supervision, 17(1). https://digitalcommons.sacredheart.edu/jcps/vol17/iss1/7
Rolón-Dow, R., & Davison, A. (2018). Racial microaffirmations: Learning from student stories of moments that matter. Diversity Discourse, 1(4), 1–9. https://udspace.udel.edu/server/api/core/bitstreams/4230ddcd-b196-4ee2-a5bf-18120b2b1f24/content
Rolón-Dow, R., & Davison, A. (2021). Theorizing racial microaffirmations: A critical race/LatCrit approach. Race Ethnicity and Education, 24(2), 245–261. https://doi.org/10.1080/13613324.2020.1798381
Sue, D. W., Capodilupo, C. M., Torino, G. C., Bucceri, J. M., Holder, A. M. B., Nadal, K. L., & Esquilin, M. (2007). Racial microaggressions in everyday life: Implications for clinical practice. American Psychologist, 62(4), 271–286. https://doi.org/10.1037/0003-066X.62.4.271
Sue, D. W., & Spanierman, L. (2020). Microaggressions in everyday life (2nd ed.). Wiley.
Swenor, B., & Reed, N. (Hosts). (n.d.). Included: The disability equity podcast [Audio podcast]. Johns Hopkins University Disability Health Research Center. https://disabilityhealth.jhu.edu/included
Jennifer M. Cook, PhD, NCC, ACS, LPC, is an associate professor at the University of Texas at San Antonio. Melissa D. Deroche, PhD, NCC, ACS, LPC-S, is an assistant professor at Tarleton State University. Lee Za Ong, PhD, LPC, CRC, is an assistant professor at Marquette University. Correspondence may be addressed to Jennifer M. Cook, University of Texas at San Antonio, Department of Counseling, 501 W. Cesar E. Chavez Blvd, San Antonio, TX 78207, jennifer.cook@utsa.edu.
May 22, 2024 | Volume 14 - Issue 1
Rebekah Cole, Christine Ward, Taqueena Quintana, Elizabeth Burgin
Military spouses face many challenges as a result of the military lifestyle. Much focus has been placed on enhancing the resilience of military spouses by both the military and civilian communities. However, no research currently exists regarding spouses’ perceptions of their resilience or how they define resilience for themselves and their community. This qualitative study explored the perceptions of eight military spouses regarding their resilience through individual semi-structured interviews. The following themes emerged: 1) shaped by service member and mission priority; 2) challenges within the military lifestyle; 3) outside expectations of spouse resilience; 4) sense of responsibility for family’s resilience; 5) individual resilience; and 6) collective resilience. We discuss ways military leadership and the counseling profession can best understand and enhance the resilience of military spouses.
Keywords: military spouses, resilience, military lifestyle, perceptions, counseling
Because of the unique stressors associated with the military lifestyle, military spouses are at an increased risk for poor mental health (Donoho et al., 2018; Mailey et al., 2018; Numbers & Bruneau, 2017). They may experience mental health concerns, such as anxiety and depression, due to a number of reasons, including separation from their deployed service member, loss of support networks after a relocation, or issues with adjusting to the uncertain and frequent changes of the military (Cole et al., 2021). Additional concerns that arise, such as employment, marital, and financial issues, can also negatively affect the military spouse’s mental health (Cole et al., 2021; Mailey et al., 2018). Dorvil (2017) reported that 51% of active-duty spouses experience more stress than normal. Furthermore, 25% of military spouses meet the criteria for generalized anxiety disorder (Blue Star Families [BSF], 2021). Depression in military spouses is also higher than the rate found within the general population (Verdeli et al., 2011). As a military spouse casts aside their own personal needs to support their service member, stressors may continue to increase, which can contribute to the rise of mental health needs of military spouses (Moustafa et al., 2020).
Resilience and Military Spouses
Nature of Resilience
Given the challenges inherent in the military lifestyle and the associated mental health risks, military spouse resilience is essential. Resilience is a complex and multifaceted construct, significant to researchers, practitioners, and policymakers across numerous disciplines, including mental health and military science. The American Psychological Association (2020) defined resilience as “the process of adapting well in the face of adversity, trauma, tragedy, threats, or even significant sources of stress” (para. 4). Within the military community, resilience has been defined as the ability to withstand, recover, and grow in the face of stressors and changing demands (Meadows et al., 2015). Importantly, determinants of resilience include the interaction of biological, psychological, social, and cultural factors in response to stressors (Southwick et al., 2014). In addition to these salient variables embedded in resilience science, resilience may be operationalized as a trait (e.g., optimism), process (e.g., adaptability in changing conditions), or outcome (e.g., mental health diagnosis, post-traumatic growth; Southwick et al., 2014).
Resilience may also vary on a continuum across domains of functioning (Pietrzak & Southwick, 2011) and change as a function of development and the interaction of systems (Masten, 2014). Accordingly, a definition and operationalization of resilience may vary by population and context (Panter-Brick, 2014). During the post-9/11 era, the resilience of service members and their families received significant attention from stakeholders, including the Department of Defense (DoD) and National Academies of Sciences, Engineering, and Medicine (NASEM), both of which expressed a commitment to conducting research and establishing programming to enhance service member and military family resilience, resulting in increased awareness of the importance of service member and family resilience throughout the military community (NASEM, 2019).
Military Family Resilience
Though military families share the characteristics and challenges of their civilian counterparts, they additionally experience the demanding, high-risk nature of military duties; frequent separation and relocation; and caregiving for injured, ill, and wounded service members and veterans (Joining Forces Interagency Policy Committee, 2021). In recognition of the constellation of military-connected experiences military families face, the Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury (DCoE) commissioned a review of family resilience research and relevant DoD policies to inform a definition of resilience for appropriate application to military spouses and children (Meadows et al., 2015). Meadows and colleagues (2015) proposed family resilience may be best defined as “the ability of a family to respond positively to an adverse situation and emerge from that situation feeling strengthened, more resourceful, and more confident than its prior state” (see Simon et al., 2005, for a further exploration of family resilience). Further, Meadows and colleagues identified two groups of policies delineated at the Joint Chiefs of Staff or DoD levels, or within individual branches of the military: 1) existing programs modified to augment resilience or family readiness, and 2) new programs developed to target family resilience. Programs established by these policies support access to mental health services (e.g., DoD Instruction [DoDI] 6490.06); parenting education (e.g., New Parent Support Program, DoDI 6400.05); child welfare (e.g., Family Advocacy Program, DoD Directive 6400.1); and myriad physical, psychological, social, and spiritual resources. The well-being of military families represents a critical mission for the DoD, extending beyond provision and access for families to meet their basic needs to individual service member and unit readiness, and the performance, recruitment, and retention of military personnel (NASEM, 2019).
Military Spouse Resilience
Though service member and family resilience are critical for accomplishing the DoD’s mission, focusing on the unique nature of military spouse resilience is key for understanding and supporting this population’s resilience. Counseling, psychology, sociology, and military medical professional research related to military spouse resilience has focused primarily on characteristics associated with resilience. In a study by Sinclair et al. (2019), 333 spouse participants completed a survey regarding their resilience, mental health, and well-being. The results revealed that spouses who had children, were a non-minority, had social support, had less work–family conflict, and had a partner with better mental health were more resilient. Another survey study examined the characteristics associated with resilience in Special Operations Forces military spouses, determining that community support and support from the service member was essential for spouse resilience (Richer et al., 2022). A study conducted within the communication field also explored spouses’ communicative construction of resilience during deployments. Qualitative data analysis of interviews with 24 spouses indicated how spouses use communication to reconcile their contradictory realities, which increases their resilience (Villagran et al., 2013). This resilience has also been found to be a protective factor against depression and substance abuse during military deployments (Erbes et al., 2017). Finally, a survey study of Army spouses (N = 3,036) determined that spouses who were less resilient were at higher risk for mental health diagnoses (Sullivan et al., 2021). While these studies explored the nature of resilience demonstrated by military spouses, our searches in JSTOR, PubMed, ERIC, PsycINFO, and Google Scholar did not reveal any studies regarding spouses’ perceptions of their own resilience or how they define this resilience for themselves and their community. Our study fills that research gap by exploring active-duty spouses’ perceptions and definitions of resilience.
Methods
The purpose of this qualitative study was to explore the perceptions of active-duty spouses regarding their resilience. This study was guided by the following research questions: 1) What are military spouses’ perceptions of their own resilience? and 2) How do military spouses define “resilience?” Phenomenology seeks to present a certain phenomenon in its most authentic form (Moustakas, 1994). In order to most authentically and openly describe our participants’ experiences, we chose a qualitative transcendental phenomenological approach to frame our study. This tradition of qualitative research focuses on portraying a genuine representation of the participants’ perceptions and experiences. However, the distinct feature of transcendental phenomenology is its first step, which involves the researchers recognizing and bracketing their biases so they can analyze the data without any interference (Moerer-Urdahl & Creswell, 2004). We selected this design because each of our research team members were military spouses. We therefore recognized the need to mitigate our biases in order to give a true representation of the participants’ perceptions, free from our own preconceived notions.
Participants
The participants in this study were selected based on their status as active-duty military spouses and their willingness to participate in the study. There were no other inclusion or exclusion criteria for the participants in this study. After gaining IRB approval, we used convenience sampling to recruit eight participants. In qualitative research, convenience sampling is used to recruit participants who are closely accessible to the researchers (Andrade, 2021). Our research team emailed participants that we knew through living, working, and volunteering on military bases throughout the United States and at overseas duty stations who fit the active-duty military spouse criteria for this study and asked them if they were willing to participate in the study. Once the participants expressed interest, they were provided with an information sheet regarding the study’s purpose and the nature of their involvement in the study. Participant demographics are included in Table 1. All of the participants were female and all were between the ages of 30–40. Four branches of the U.S. military, including Army, Navy, Air Force, and Marine Corps, were represented in the sample. No reservist, Coast Guard, or Space Force military spouses participated in our study. Five of our participants were White and three were Black. Their tenure as military spouses ranged from 4 years to 17 years. Five of the spouses were married to a military officer, while three of the participants were married to an enlisted service member. After interviewing these eight participants, our research team met and determined that because of the distinct common patterns we found across each of the participants’ transcripts, we had reached saturation and did not need to recruit any additional participants for our study (Saunders et al., 2018).
Table 1
Participant Demographics
| Participant |
Age |
Ethnicity |
Gender |
Branch |
Spouse’s Rank |
Years as a Spouse |
| 1 |
33 |
Black |
Female |
Air Force |
Enlisted |
4 |
| 2 |
36 |
Black |
Female |
Navy |
Enlisted |
17 |
| 3 |
31 |
White |
Female |
Army |
Officer |
7 |
| 4 |
34 |
Black |
Female |
Navy |
Enlisted |
14 |
| 5 |
36 |
White |
Female |
Marine Corps |
Officer |
12 |
| 6 |
35 |
White |
Female |
Marine Corps |
Officer |
14 |
| 7 |
40 |
White |
Female |
Navy |
Officer |
16 |
| 8 |
34 |
White |
Female |
Navy |
Officer |
10 |
Data Collection
Our research team first developed the interview protocol for the study based on a thorough review of the literature regarding resiliency within military culture as well as the challenges of the military lifestyle for military spouses. Our research team members interviewed each of the participants for 1–2 hours. These semi-structured interviews were audio recorded and transcribed verbatim by an automated transcription service. The interview questions were open-ended and focused on the spouses’ definitions of resilience and their perceptions of their resilience within the military lifestyle and culture (see Appendix for interview protocol). In addition, probing questions such as “Can you explain that a bit more?” or “Can you give any examples of what you mean by that?” were used to gather more in-depth data throughout the interviews.
Data Analysis
We followed the steps of the transcendental phenomenological data analysis process to analyze our study’s results (Moerer-Urdahl, 2004). First, each member of our research team engaged in epoche, in which we bracketed our biases as military spouses so that our own thoughts, feelings, perceptions, and experiences did not influence our interpretation of our participants’ experiences. The next step in the process was horizontalization. During this step, each member of our research team read through the interview transcripts and noted significant statements throughout so we could better understand how the participants perceived, understood, and experienced resilience. Next, we met as a research team to discuss these significant statements and organize them into themes (Moustakas, 1994). Our research team then developed textual and structural descriptions of the themes, describing not only a list of the participants’ perceptions, but also an in-depth analysis of what their perceptions of resilience entailed and how they have experienced it throughout their tenure as military spouses (Moerer-Urdal, 2004; Moustakas, 1994). We then constructed a comprehensive description of the participants’ perceptions of resilience, encapsulating the “essence of the experience” (Moerer-Urdal, 2004, p. 31).
Research Team and Strategies to Increase Trustworthiness
Our research team consisted of four university faculty members, all of whom possessed extensive experience in conducting qualitative research. Three of our research team members possess PhDs in counseling and one research team member possesses an EdD in counseling. All team members had extensive experience conducting research with military-connected communities. In addition, all of our research team members were active-duty military spouses, with years of experience as a military spouse ranging from 1–23 years.
We used several strategies to increase the credibility of our results. First, the use of an experienced research team to collectively analyze the data resulted in diverse perspectives on the emerging themes of the study. However, because each member of our research team was a military spouse, we recognized the need to bracket our own experiences and biases so that they did not interfere with our interpretation of the data. Each team member took notes on their individual biases, and our research team discussed these biases when interpreting themes. Biases held by research team members included a predisposition to believe that spouses of special warfare service members endured greater stressors and were better supported by their military communities; a belief that spouses of higher-ranking service members possessed greater knowledge of and access to resources to support social, behavioral, and mental health needs; and personal experience within the military spouse community. These biases were challenged throughout the research process by each member of the team. As each theme was identified, the team referenced individual transcripts to ensure that the interpretation was justified. We found that our biases were rightfully challenged.
Additionally, to avoid leading questions, our research team made the conscious decision not to define resilience as part of the interview and follow-up process. The team wanted to derive an organic definition of spouse resilience that was not clouded by a formal definition. In addition, we used member checking, in which we emailed the interview transcripts to the participants and asked them to verify the data. The participants responded to our request with minimal change requests related to grammatical errors in the transcriptions and validated our data. Several offered additional insight related to their definition of resilience, which was included in our data analysis.
Results
The following themes emerged from our data: 1) shaped by service member and mission priority; 2) challenges within the military lifestyle; 3) outside expectations of spouse resilience; 4) sense of responsibility for family’s resilience; 5) individual resilience; and 6) collective resilience.
Theme 1: Shaped by Service Member and Mission Priority
Military/Service Member Definition
When discussing their definition of resiliency, the spouses first considered what resiliency meant for their active-duty spouse. The participants varied in their perceptions of what resilience meant for their active-duty service member, though all defined resilience as an active process of adapting or persevering when faced with adversity, rather than a personal trait or characteristic the service member possesses. Participant 3 noted that, for their spouse, resilience was “the ability to adapt to changes that are beyond your control . . . adapting to situations in an optimistic and positive way.” Participant 6 stated that resilience for their spouse meant an “ability to bounce back from a hardship.” One participant asked their spouse to comment specifically about their definition and provided the following definition in a follow-up with the interviewer: “Resilience is how you persevere in difficult circumstances. It’s not about how hard you fall, but how quick you can get back up from being knocked down” (Participant 2 [P2]).
Some participants cited specific notions of resilience that are embedded in the service members’ military community. One Navy spouse remarked that resilience, to their spouse, meant “Don’t give up the ship” (P8). Another Navy spouse mentioned that for their spouse, resilience was “knowing how to weather the storm” (P7). Yet another spouse noted that resilience “the Marine Corps way” meant their service member must “do their job” (P4). Other participants noted that the root of resilience for the military service member stems from a place of selfless service. Participant 8 commented that the resiliency of their spouse was “more about the man standing next to me, the family I’m fighting for at home, the country I’m fighting for at home, than about their own personal needs.”
Adapting, Overcoming, and Persevering
Like their active-duty members, spouses indicated that resilience was about adapting, overcoming, and persevering in the face of obstacles. Resilience to one spouse was “being able to rebound or to overcome an obstacle” (P1); to another, resilience meant they must “be flexible, adapt with whatever, overcome whatever it is that you’re going through” (P2). Spouses noted that resilience was not a one-time event. Instead, spouses suggested that their own resilience stemmed from continually persevering. Participant 6 stated that for them, resilience meant not just “going through something difficult and making it out on the other side,” but that they then had to “keep pushing forward.” One participant indicated that their personal definition of resilience and the notion to persevere stemmed directly from their spouse: “I’ve almost kind of adopted a bit of my husband’s thought process, I guess. You just keep going to get things done” (P8).
Mindset
Our participants indicated that resilience was a mindset that one must choose and that when faced with difficulties, they chose to focus on gratitude, positivity, and growth. For example, Participant 8 stated that, although they had faced and would continue to face challenging and stressful experiences as a result of being a military spouse, they believed that “whatever may come, we’ve been very blessed in our life and we should always be thankful for the life that we have.” Another participant noted that for them, overcoming and persevering meant adopting an optimistic attitude. Specifically, the spouse stated, “sometimes you just have to kinda look at the bright side of things, and you have to find the things that work for you at each place” (P5). One participant drew resilience from a growth mindset:
I think it [resilience] is really a mindset switch. I think it’s changing from “oh this is happening to me, how horrid” to like “how can I take this horrid situation and turn it into something good?” And I think that is a big mindset switch. (P7)
Resilience Variations
Walsh (2012) described risk and resilience as a process of balancing risk and protective factors over the life span. Participants in our study expanded on that idea by suggesting that they reacted to situational challenges along a continuum:
I think what I’m saying is there’s different levels of resilience, like sometimes you have to tap into that different part of yourself. Sometimes you have to let it go and just accept the things that come, and sometimes you just gotta pick yourself up and keep on trucking. (P8)
Likewise, Participant 3 suggested that resilience takes different forms depending on the situation:
Sometimes resiliency just means like surviving day to day and other times, it means figuring out how to continue with your passions to the best of your ability while also supporting your family and your [service member spouse]. I think it’s just super unique to every situation. (P3)
Our participants also recognized that their understanding of resilience was often focused on the here and now of their situation but that their reactions to stressors had long-term effects. One participant indicated that resilience is a learning process and recognized that the stressors they overcome now prepare them to address stressors they will face in the future: “I think being able to come out of extremely, extremely stressful situations, be able to come out on the other side and [know] I’m okay and I survived this, and now I’m kind of better prepared for next time” (P6). Participant 3 wondered about the long-term ramifications of resilience in the face of prolonged adversity, stating “I may be resilient right now in the moment, but in the long term, like, how will this affect me?”
Individualized
Finally, participants defined resilience as an individualized process, stating things such as “everybody has their own unique ways of being resilient, and I think that they do what works best for their families” (P7) and “my resiliency may look different than someone else’s resiliency” (P2). One participant elaborated on this individualized approach to resilience by recognizing that each person has different risk factors that affect their response to stressors, thus affecting the way each person demonstrates resilience. This participant stated that, when viewing resilience among military spouses as a whole, it is important to
take into consideration somebody’s upbringing and the baggage that they bring into this life. We don’t know what people have gone through as kids, and that I think would have a big impact on whether or not someone can be resilient, so I don’t think it’s a one-size-fits-all. (P6)
Theme 2: Challenges Within the Military Lifestyle
Lack of Control
The spouses described the common challenges of the military lifestyle to their resilience. First, they discussed the stress of the feeling of a lack of control in their lives. One participant described how she
just found out yesterday that my husband was getting deployed and he’s leaving Sunday. And I keep hearing people say, “You have to be resilient. You’re gonna be okay!” You’re resilient, but right now, what it feels like is how much can you endure for the sake of the mission? (P1)
Another echoed this sentiment: “I have no control if the Navy says they’re going to deploy my husband. There’s nothing I can do to change that” (P8).
Constant Changes
Another common challenge mentioned among all of the participants was the constant changes they experience in their lives, including moving, career changes, and changes within their family dynamics. Because they move every few years, the spouses described how they are constantly separated from their support systems: “Even though you meet these great people, you don’t get to stay with them . . . and you’re generally not near your family, which is very hard” (P5). Another described how “Once I have started on something and I’m like, ‘This is it, we gon’ be here for a while,’ then my husband is like ‘nope. Military said we got to shift and move again’”(P2).
These constant changes resulted in career struggles for the spouses. One asked, “How can I get this [job] if I’m never at one place for long? . . . How do I uproot everything that I know or everything that I am doing to follow my service member?” (P2). Another described how “moving, changing jobs, not being able to have a secure profession, you do it because you have to . . . but that doesn’t mean that there’s not a whole lot of emotional and mental load that goes with it” (P3).
Another challenge for military spouses was constantly changing family dynamics. One described the difficulty in constantly changing work schedules: “We have to kind of get into this routine without him and then when he comes back, because it’s different while he’s away. We gotta kind of try to fit him back into our routine when he gets back” (P4). Another discussed the challenge of transitioning to being the sole caregiver during a deployment: “If I go down with COVID, what am I going to do? Because, like, I was literally IT. No one is going to want to take my kids. . . . That was the first time I ever felt, like, fearful” (P7).
Mission Priority
In addition to constant change, the spouses also mentioned the challenges of the military’s clear prioritization of the mission above military members and their families: “If something is going on at home, we’re going to take care of our active person first and worry about your family later” (P2). The participants described how this focus on the mission is so intense that it affects service members physically, which increases the burden on military spouses to care for them: “My husband’s health suffers because the mission is most important to him” (P1).
Theme 3: Outside Expectations of Spouse Resilience
Expectation to “Suck It Up”
The spouses described others’ expectations for their resilience. First, they described the military’s expectation that they “suck it up.” One described how “you have a lot of the ‘suck-it-up’ mentality, and I would say when you have the leaders who kind of fall under that, whether it’s seeking the mental health treatment or having stigmas with that” (P6). Another explained that “there’s so much focus and emphasis on just being resilient and sucking it up” so there is often a mindset of “‘Oh well, military spouses are resilient so they signed up for this, they know what it takes and they just have to get over it’” (P3). Another spouse described how “they put so much pressure on you to be like, just make it work, that you’ve gotta figure out the way to make yourself happy, and that’s hard to do” (P5). Participant 7 summed up the military spouse mentality as a whole: “You toughen up and you make it work. You know?”
The participants felt their overall resilience would be enhanced if individuals outside the military community better understood the challenges faced by military families. One participant felt the “suck it up” mentality stemmed less from the military community itself and more from outside communities who might not understand the struggles of military family life: “So when . . . you’re going through another stress of a PCS [permanent change of station], you can’t find a house, they say, well, at least you get a house allowance, at least you get free health care” (P6). Participant 3 expanded on this idea by stating, “I just honestly think that a greater understanding of what sacrifices that military spouses make . . . would increase resiliency, because there’s just so much lack of understanding what it actually entails.” Lastly, one participant mentioned a sentiment they frequently hear from others in a civilian community, expressing that it was frustrating when friends outside the military told her, “I don’t know how you do it,” to which the participant responded, “I don’t know, you just do it!”
Pressure to Be Resilient
The spouses also expressed frustration at others’ misperceptions of the expectation that they and their families demonstrate resilience: “When we call military spouses or children resilient, it just seems like a cop out and relinquishes any type of burden . . . or feeling of guilt about a situation that may cause emotional or mental damage” (P3). Another participant echoed this frustration: “Sometimes I don’t feel like I’m being resilient. Sometimes I feel like I’m just doing what needs to be done because that’s what needs to be done” (P8). Another participant described how her friends
call me Superwoman because I have all these different things going on and I always seem like I got it together. . . . It’s like saying to me that I have to keep going, no matter what, and I think people should be able to just feel defeated sometimes. Or be able to say “that was just too much for me” or “I don’t really feel like being resilient today, I kind of want to lay in bed and just be upset or sad.” (P4)
Given these expectations, one spouse pointed out the danger of expecting military children to consistently demonstrate resilience:
It’s so easy for everyone to say that military kids are always so resilient and sometimes they’re not. Sometimes they are stressed out. They are feeling the crushing weight. They feel sad but everyone keeps telling them that they’re resilient. So it almost makes it seem like . . . they aren’t allowed to feel those hard things or talk about those things or act on those feelings and emotions. (P8)
One spouse proposed a solution to these misperceptions, emphasizing that resilience is unique for military spouses and should be defined to accurately reflect the way they uniquely overcome challenges:
I think it’s important for military spouses to reappropriate that term [resilience] so that it is not weaponized, and I would like to see some sort of guidance as to how we can be resilient but in a way that positively impacts our mental health and physical health and not having to endure all of the things and all of the frustration and uncertainty that comes with the onset of having to be resilient. (P1)
Theme 4: Sense of Responsibility for Family’s Resilience
With their partners focused on the mission, the spouses described their sense of responsibility to maintain their resilience so they can care for their children in the absence of their active-duty spouse: “We have our husband or our spouses gone so much, we need to be a solid parent at home for our kiddos or our family” (P7). Participant 4 likewise described how “I kind of see myself as holding down the fort, you know, because when my husband is not home it is just me and the kids.” Another explained how “I have three little ones that’s looking up to me and I can’t slip away, depressed, because daddy’s not home” (P2). In the end, the spouses defined resilience as an obligation to their families. Participant 3 described that “I have to be that way for my children.” Participant 4 added that “I think that’s what resilience is like, knowing that you kind of have to carry the load, you know, for your whole family to try to keep us afloat.”
The participants described how this resilience is especially obligatory when the active-duty spouse is unable to be resilient:
I’m kind of taking the lead with our kids . . . but I’ve also kind of had to pour into my husband, you know, because he has those times you know where things are really, really hard for him. I’ve also been like his counselor and his doctor sometimes. (P4)
Theme 5: Individual Resilience
In response to being unable to control many aspects of the military lifestyle, most of the spouses described how they have become independent in order to withstand the constantly changing variables within the military lifestyle. One described being “pretty independent, and I think that helps a lot because I don’t rely on my spouse to do all these things I do” (P5). Another described how being independent resulted in self-confidence and resilience:
You gotta figure out how to do all of it just because you can’t ever rely on the spouse being able to help. But I think being able to come out of extremely, extremely stressful situations, be able to come out on the other side and say “I’m okay, and I survived this, and now I’m kind of better prepared for next time.” (P6)
Another spouse described how maintaining an independent identity was key to separating herself from the stressors of the military lifestyle: “That’s a really important part of being a military spouse. It doesn’t have to be a job specifically, but just something that you can be your own person separate from your husband or your spouse’s job” (P8).
The spouses also described the importance of taking care of themselves physically and mentally in order to maintain their resilience. Many described exercise as key to their mental health and wellness: “My biggest coping mechanism is exercise. I’ve found that no matter where I go, I can exercise” (P5). Another spouse described how she “tried to find a kickball team every place we’ve been to since Okinawa because I figured out it’s a stress relief” (P6). Participant 7 echoed that “working out . . . just helps me. It lowers my stress.” One spouse explained how she defaults to exercise when facing the challenges of the military lifestyle because she knows her “ability to recover quickly is directly tied to the way in which I care for myself” (P1).
Theme 6: Collective Resilience
The participants described their reliance on the collective military spouse community for their survival. One spouse, for example, described a connection with other military spouses as the difference between “doing well and barely surviving” (P6). Another spouse described her reliance on the military spouse community: “Community is what it’s all about. I can’t get through anything without community” (P7). Another spouse echoed this survival mechanism: “This is a beautiful community. It’s an amazing place . . . we all get each other. So I think there are times where it’s really hard . . . but we survive, we get through it. We’re resilient. We got the grit” (P7). Participant 1 explained exactly how the military spouse community offers this support to help spouses survive the challenges of the military lifestyle: “When time calls for it, I think, collectively, we bring our resources together to help pull other military spouses up and try to just forewarn them about what the obstacles are and what may have worked for our family” (P1).
The military spouses also described the comfort they found in other military spouses’ understanding of the challenges they face: “I think the most important part and coping is finding your community, so making sure you’re surrounding yourself with women who are going through similar experiences, or who have gone through similar experiences and similar life stages” (P3).
In the midst of this supportive community, the spouses discussed how they actively seek to comfort each other: “You’re not the only one who’s in it who’s having this issue, I understand that you’ll get through this, that we know we’ve been there, we understand how it goes” (P5). This outreach seemed to be especially helpful from spouses who were more experienced with the military lifestyle: “Having that senior spouse example has been so good. . . . She’s always been somebody who said, ‘Hey, I’ve been through a lot. If you ever have any questions, I’m always here for you’” (P8).
In addition to relying on other spouses for their own wellness and resilience, the spouses expressed pride in their ability to contribute to the military spouse community. One described how “I feel like I am a better team player. I feel like I’m more committed to helping others than I have in the past because I know that others will do the same for me” (P7). The participants also described increased self-growth as a result of being a part of a community: “I really don’t think I would have allowed myself to receive help if I hadn’t been part of this phenomenal community that is constantly supporting each other” (P7). Participant 5 echoed this sentiment: “Learning to get that help from other people is something that I feel like you have to kind of get when you are a military spouse because, otherwise, you’re going to have to do everything and you don’t have to.”
Finally, our participants frequently indicated that they felt a “sense of pride” (P7), “connection” (P4), or “camaraderie” (P8) from belonging to a group of military spouses who understood their unique situation. When asked how the military could enhance resilience for military spouses, participants commonly indicated that peer support and fostering connections with senior spouses should be a priority for military commands. One participant noted that their ability to be resilient in difficult times was related to the “opportunities” they had “to connect with other people who are going through similar stuff and who are a part of the same small community” and recommended that the military facilitate more opportunities to connect (P7). Another participant suggested that military commands should “have someone that [the spouse] can talk to” that would “help them to understand the military life whether you are a new spouse or a seasoned spouse” (P2).
Discussion
The purpose of this study was to explore military spouses’ perceptions of their resilience and the ways in which they define resilience for their community. Our study’s results indicate that spouses’ definitions of resilience are currently shaped by service member and mission priority. Our participants also described how they often felt burdened by outside expectations of their resilience as well as by a sense of responsibility for their family’s resilience. Overall, the spouses relied on themselves and the military spouse community to overcome the challenges they faced. Participants expressed a desire for resources aimed specifically at enhancing spouse resilience and more awareness about resilience resources already in place throughout the military.
While past research has examined resilience factors in spouses such as communication skills, social support, and spousal support (Erbes et al., 2017; Richer et al., 2022; Sinclair et al., 2019; Villagran et al., 2013), our study provided new insight into military spouses’ perspectives of their resiliency. This revelation of the spouses’ worldview aids our understanding of ways to best support spouses and areas to focus on to support their resilience. Our participants’ definitions of their resilience were shaped by their relationship with their service member and the influence of the military’s mission. In addition, while past research has indicated that the military lifestyle and culture is challenging for spouses to navigate (Cole et al., 2021; DaLomba et al., 2021; Donoho et al., 2018; Mailey et al. 2018), our participants’ description of their feelings of responsibility for their family’s well-being reveals the added burden that military spouses face as they help their families navigate the military lifestyle. Finally, our participants confirmed that resiliency should be viewed as a variation and is unique to each individual (Pietrzak & Southwick, 2011). As outlined in the professional literature (Masten, 2014; Southwick et al., 2014), the participants confirmed the dynamic nature of resiliency, recognizing that sometimes they felt more resilient than at other times.
In the midst of these challenges, our participants emphasized that the military spouse community serves as a protective factor and a source of their resilience against mental health challenges. This perception of the military spouse community aligns with previous research highlighting the supportive role that spouses play for each other, so much so that it is a protective factor against suicide (Cole et al., 2021). Therefore, military leadership and the counseling community might focus on enhancing this community and connecting spouses with one another—especially more seasoned spouses with newer spouses. In addition, because military-sponsored resilience programs are often targeted to better support service member outcomes, community providers might find ways to focus on supporting the spouses and helping them to overcome the challenges they face in their daily lives.
Finally, the participants discussed how they overcame the challenges of the military lifestyle, including constant moving, deployments, and overall uncertainty, through their own individual and collective resilience. These lifestyle challenges that the participants described correspond to career struggles and shifting family dynamics that cause ongoing stress to the military spouse, both of which have been previously documented in the professional literature (Borah & Fina, 2017; Cole et al., 2021; DaLomba et al., 2021; Donoho et al., 2018; Mailey et al., 2018; Numbers & Bruneau, 2017). Currently, since the withdrawal of troops from Afghanistan, the United States is experiencing peacetime, whereas the nature of future conflicts is uncertain (Marsh & Hampton, 2022). Enhancing the resiliency of military spouses and finding solutions to ongoing stressors is key during this time of peace so that spouses are ready and able to face the stressors of future, potentially large-scale wars (Sefidan et al., 2021).
Implications for Counselors
Professional counselors are called to be trained and ready to meet the unique needs of military spouses, especially in understanding the nature of military culture and its impact on spouse mental health and well-being and enhancing spouse resilience in times of adversity (Cole, 2014). Our study echoes the continued struggles of military spouses described in the professional literature (Cole et al., 2021; Lewy et al., 2014; Runge et al., 2014), suggesting that new and innovative ways of understanding and approaching military spouse resilience is needed within the counseling community. For example, counselors might encourage spouses to explore how their resilience is shaped by the military community in order to increase self-awareness and understanding. They might also help spouses develop their independence and sense of self-efficacy while simultaneously seeking collective support within the military community. Counselors can help spouses examine their social support and help them develop their social skills so they can connect with others around them. Counselors should also help military spouses unpack their perceptions of outsiders’ expectations of their resiliency. Encouraging spouses to reflect on others’ expectations, and the ways in which these expectations impact their sense of well-being, may help define resilience for themselves and capitalize on their unique resiliencies during challenging times. Ultimately, because the military culture is so unique, counselors should seek out professional development so they can better understand how to help military spouses navigate this culture and enhance their resilience. When working with military spouses, professional counselors might explore spouses’ feelings of responsibility for their family members’ health and well-being that were described in our results. In addition, counselors can equip spouses with supportive mental health resources for their family members so they do not feel as if they need to care for them on their own. School counselors, in particular, can provide support for military-connected students at school and can connect military families with resources within both the civilian and military communities to support their mental health and resilience (Cole, 2017; Quintana & Cole, 2021).
Our participants revealed that often the expectation of resilience is burdensome for spouses, which serves as a contradiction to its purposes. Counselors are called to acknowledge the challenges of the military lifestyle and provide support for navigating these challenges, rather than expecting spouses to face these hurdles alone. In addition, counselors might focus on more holistic manifestations of resilience, recognizing that some spouses can be resilient, yet still struggle. Approaching spouses from a strengths-based perspective, rather than from a deficit perspective, can be empowering within the counseling relationship (Smith, 2006).
Limitations
Our recruitment strategy limited our sample size as we only sought participants that we knew through our military spouse networks. In addition, our sample lacked gender diversity, with all of the participants being female. Approximately 91% of active-duty service member spouses are female (DoD, 2022). However, the lack of male participants in the present study is a limitation, and the experience of male spouses is undoubtedly unique and worth exploring in greater depth. Research suggests that stressors and characteristics of resilience transcend gender categories (NASEM, 2019).
Finally, in qualitative research, the researcher’s biases may impact their interpretation of the data. As military spouses, our own experiences may have impacted the way in which we described our participants’ experiences. We took several steps to mitigate these biases, including intentionally bracketing them and engaging in peer debriefing throughout the research process.
Implications for Future Research
The participants in our study described a need for resources and programs geared specifically toward military spouses. Future research might determine how to best develop and implement these programs that will help to enhance spouse resilience. Key areas of focus may be ways to leverage the military spouse community and enhance spouse sense of self, which were two protective factors that emerged from our data. In addition, existing resilience programs within the military that are currently aimed at the active-duty population should undergo a program evaluation to determine their effectiveness with military spouses.
As a follow-up to our qualitative research, future quantitative research studies should address limitations noted previously. Specifically, future research should target a larger sample size and broader demographic of military spouses to further explore their understanding and definition of resilience. This larger and more diverse sample size would allow for greater generalizability and would assist with advocacy within the military. Finally, future qualitative research might explore the perceptions of male spouses, in particular, in order to determine their perception of resiliency and any unique areas of needed support.
Conclusion
Military spouses face a wide range of challenges as a result of the military lifestyle. They are expected to be resilient so as to overcome these challenges. However, our study reveals the often burdensome impact of these expectations on military spouses. Our results also illuminate how spouses uniquely conceptualize their own resilience, recognizing the resilience continuum and focusing on the positive impact of their protective community. Overall, the spouses took pride in themselves and their communities for their ability to overcome obstacles. These revelations are key for both the military and the counseling profession in their work to support military spouses wherever they are on this continuum and enhance their community, which is key to their well-being.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript. The opinions and assertions
expressed herein are those of the authors and
do not reflect the official policy or position of
the Uniformed Services University of the Health
Sciences or the Department of Defense.
References
American Psychological Association. (2020). Building your resilience. https://www.apa.org/topics/resilience/building-your-resilience
Andrade, C. (2021). The inconvenient truth about convenience and purposive samples. Indian Journal of Psychological Medicine, 43(1), 86–88. https://doi.org/10.1177/0253717620977000
Blue Star Families. (2021). Military Family Lifestyle Survey: 2020 comprehensive report. https://bluestarfam.org/wp-content/uploads/2021/03/BSF_MFLS_CompReport_FULL.pdf
Blue Star Families. (2023). Military Family Lifestyle Survey: 2022 comprehensive report. https://bluestarfam.org/wp-content/uploads/2023/03/BSF_MFLS_Spring23_Full_Report_Digital.pdf
Borah, E., & Fina, B. (2017). Military spouses speak up: A qualitative study of military and veteran spouses’ perspectives. Journal of Family Social Work, 20(2), 144–161. https://doi.org/10.1080/10522158.2017.1284702
Cole, R. F. (2014). Understanding military culture: A guide for professional school counselors. The Professional Counselor, 4(5), 497–504. https://doi.org/10.15241/rfc.4.5.497
Cole, R. F. (2017). Supporting students in military families during times of transition: A call for awareness and action. Professional School Counseling, 20(1), 36–43. https://doi.org/10.5330/1096-2409-20.1.36
Cole, R. F., Cowan, R. G., Dunn, H., & Lincoln, T. (2021). Military spouses’ perceptions of suicide in the military spouse community. The Professional Counselor, 11(2), 203–217.
https://doi.org/10.15241/rfc.11.2.203
DaLomba, E., Greer, M. J., Cruz, E., Harris, A., King, C., Laurel, L., McCuaig, T., & Wilder, R. (2021). The experiences of active duty military spouses with advanced degrees in maintaining and advancing their careers. Work, 68(2), 387–398. https://doi.org/10.3233/WOR-203380
Donoho, C. J., LeardMann, C., O’Malley, C. A., Walter, K. H., Riviere, L. A., Curry, J. F., & Adler, A. B. (2018). Depression among military spouses: Demographic, military, and service member psychological health risk factors. Depression and Anxiety, 35(12), 1137–1144. https://doi.org/10.1002/da.22820
Dorvil, M. (2017). 2017 survey of active-duty spouses. Office of People Analytics, U.S. Department of Defense. https://download.militaryones ource.mil/12038/MOS/Surveys/2017-Survey-of-Active-Duty-Spouses-Overview-Briefing.pdf
Erbes, C. R., Kramer, M., Arbisi, P. A., DeGarmo, D., & Polusny, M. A. (2017). Characterizing spouse/partner depression and alcohol problems over the course of military deployment. Journal of Consulting and Clinical Psychology, 85(4), 297–308. https://doi.org/10.1037/ccp0000190
Joining Forces Interagency Policy Committee. (2021). Strengthening America’s military families: Matching their devotion: Deepening our commitment to the families, caregivers, and survivors of service members and veterans. https://www.whitehouse.gov/wp-content/uploads/2021/09/Strengthening_Americas_Military_Families.pdf
Lewy, C. S., Oliver, C. M., & McFarland, B. H. (2014). Barriers to mental health treatment for military wives. Psychiatric Services, 65(9), 1170–1173. https://doi.org/10.1176/appi.ps.201300325
Mailey, E. L., Mershon, C., Joyce, J., & Irwin, B. C. (2018). “Everything else comes first”: A mixed-methods analysis of barriers to health behaviors among military spouses. BMC Public Health, 18(1013), 1–11. https://doi.org/10.1186/s12889-018-5938-z
Marsh, M. K., & Hampton, R. L. (2022). Army medicine’s critical role in large-scale combat operations: Enable the force. Military Review, 102(4), 106–113.
Masten, A. S. (2014). Global perspectives on resilience in children and youth. Child Development, 85(1), 6–20. https://doi.org/10.1111/cdev.12205
Meadows, S. O., Beckett, M. K., Bowling, K., Golinelli, D., Fisher, M. P., Martin, L. T., Meredith, L. S., & Osilla, K. C. (2015). Family resilience in the military: Definitions, models, and policies. RAND Health Quarterly, 5(3).
Moerer-Urdahl, T. & Creswell, J. W. (2004). Using transcendental phenomenology to explore the “ripple effect” in a leadership mentoring program. International Journal of Qualitative Methods, 3(2), 19–35. https://doi.org/10.1177/160940690400300202
Moustafa, A. A., Crouse, J. J., Herzallah, M. M., Salama, M., Mohamed, W., Misiak, B., Frydecka, D., Al-Dosari, N. F., Megreya, A. M., & Mattock, K. (2020). Depression following major life transitions in women: A review and theory. Psychological Reports, 123(5), 1501–1517. https://doi.org/10.1177/0033294119872209
Moustakas, C. (1994). Phenomenological research methods. SAGE.
National Academies of Sciences, Engineering, and Medicine. (2019). Strengthening the military family readiness system for a changing American society. The National Academies Press. https://doi.org/10.17226/25380
Numbers, M., & Bruneau, L. (2017). Creating connections and fostering self-growth: Gestalt group counseling for military spouses. In Ideas and Research You Can Use: VISTAS 2017.
Panter-Brick, C. (2014). Health, risk, and resilience: Interdisciplinary concepts and applications. Annual Review of Anthropology, 43, 431–448. https://doi.org/10.1146/annurev-anthro-102313-025944
Pietrzak, R. H., & Southwick, S. M. (2011). Psychological resilience in OEF-OIF veterans: Application of a novel classification approach and examination of demographic and psychosocial correlates. Journal of Affective Disorders, 133(3), 560–568.
Quintana, T. S., & Cole, R. F. (2021). Forward march: Implementing the ASCA National Model to support military-connected students. Journal of School Counseling, 19(7). http://www.jsc.montana.edu/articles/v19n7.pdf
Richer, I., Frank, C., & Guérin, E. (2022). Understanding Special Operations Forces spouses challenges and resilience: A mixed-method study. Military Behavioral Health, 10(2), 100–111.
https://doi.org/10.1080/21635781.2022.2067921
Runge, C. E., Waller, M., MacKenzie, A., & McGuire, A. C. L. (2014). Spouses of military members’ experiences and insights: Qualitative analysis of responses to an open-ended question in a survey of health and wellbeing. PloS ONE, 9(12), e114755. https://doi.org/10.1371/journal.pone.0114755
Saunders, B., Sim, J., Kingstone, T., Baker, S., Waterfield, J., Bartlam, B., Burroughs, H., & Jinks, C. (2018). Saturation in qualitative research: Exploring its conceptualization and operationalization. Quality & Quantity, 52(4), 1893–1907. https://doi.org/10.1007/s11135-017-0574-8
Sefidan, S., Pramstaller, M., La Marca, R., Wyss, T., Sadeghi-Bahmani, D., Annen, H., & Brand, S. (2021). Resilience as a protective factor in basic military training, a longitudinal study of the Swiss Armed Forces. International Journal of Environmental Research and Public Health, 18(11), 6077. https://doi.org/10.3390/ijerph18116077
Simon, J. B., Murphy, J. J., & Smith, S. M. (2005). Understanding and fostering family resilience. The Family Journal, 13(4), 427–436. https://doi.org/10.1177/1066480705278724
Sinclair, R. R., Paulson, A. L., & Riviere, L. A. (2019). The resilient spouse: Understanding factors associated with dispositional resilience among military spouses. Military Behavioral Health, 7(4), 376–390. https://doi.org/10.1080/21635781.2019.1608876
Smith, E. J. (2006). The strength-based counseling model. The Counseling Psychologist, 34(1), 13–79.
https://doi.org/10.1177/0011000005277018
Southwick, S. M., Bonanno, G. A., Masten, A. S., Panter-Brick, C., & Yehuda, R. (2014). Resilience definitions, theory, and challenges: Interdisciplinary perspectives. European Journal of Psychotraumatology, 5(1), 25338. https://doi.org/10.3402/ejpt.v5.25338
Sullivan, K. S., Hawkins, S. A., Gilreath, T. D., & Castro, C. A. (2021). Mental health outcomes associated with profiles of risk and resilience among U.S. Army spouses. Journal of Family Psychology, 35(1), 33–43. https://doi.org/10.1037/fam0000702
U.S. Department of Defense, Office of the Deputy Assistant Secretary of Defense for Military Community and Family Policy. (2022). 2021 demographics profile: Profile of the military community. https://download.militaryonesource.mil/12038/MOS/Reports/2021-demographics-report.pdf
Verdeli, H., Baily, C., Vousoura, E., Belser, A., Singla, D., & Manos, G. (2011). The case for treating depression in military spouses. Journal of Family Psychology, 25(4), 488–496. https://doi.org/10.1037/a0024525
Villagran, M., Canzona, M. R., & Ledford, C. J. W. (2013). The milspouse battle rhythm: Communicating resilience throughout the deployment cycle. Health Communication, 28(8), 778–788. https://doi.org/10.1080/10410236.2013.800441
Walsh, F. (2012). Family resilience: Strengths forged through adversity. In F. Walsh (Ed.), Normal family processes: Growing diversity and complexity (4th ed.; pp. 399–423). Guilford.
Rebekah Cole, PhD, MEd, NCC, LPC, is a research associate professor at the Uniformed Services University. Christine Ward, PhD, is an associate professor at Walsh University. Taqueena Quintana, EdD, NCC, ACS, BC-TMH, LPC, is an associate professor at Antioch University. Elizabeth Burgin, PhD, NCC, LPC, RPT, CCCPTS, is an assistant professor and program coordinator of the Military and Veterans Counseling program at William & Mary. Correspondence may be addressed to Rebekah Cole, rebekah.cole@usuhs.edu.
Appendix
Interview Protocol
- Tell me a little about your identity as a military spouse?
- What have been some of your rewarding experiences as a military spouse?
- What have been some of your stressful experiences as a military spouse?
- How have you coped with the more stressful experiences as a military spouse?
- How would you describe the military’s definition of “resilience?”
- What does the term “resilience” mean to you?
- What does the term “resilience” mean for your military partner/family?
- How would you describe the resilience of military spouses?
- In what ways have you, personally, been resilient as a military spouse?
- What would enhance the resilience of military spouses and their families, from your perspective?
- How, if at all, has your military experience enhanced your resilience?
- How, if at all, has the military’s focus on resilience presented you with challenges during your military spouse experiences?
- How, if at all, can resilience be a negative way to describe military spouses/families?
- Is there anything else about military resilience that is important to you that I did not ask about?
May 22, 2024 | Volume 14 - Issue 1
Ashley Ascherl Pechek, Kristin A. Vincenzes, Kellie Forziat-Pytel, Stephen Nowakowski, Leandrea Romero-Lucero
In counselor education programs, students acquire clinical experience through both practicum and internship; this time frequently marks students’ first counseling experiences working with suicide in a clinical context. Often, students in practicum or internship working with clients who may be experiencing suicidal ideations do not feel properly equipped to deal with suicide. This study aimed to develop a practice model for online counselor education programs that increases counseling students’ self-efficacy to work with clients who may present with suicidal ideations. Sixty online graduate-level clinical mental health counseling students completed a pre- and posttest self-efficacy assessment. Findings showed that students’ self-efficacy increased due to taking the online basic counseling skills class that included teaching activities related to suicide screening, assessment, and intervention.
Keywords: self-efficacy, suicide, assessment and intervention, online counselor education, practice model
Despite a growing body of research and evidence-based interventions, suicide remains the 11th leading cause of death in the United States (Centers for Disease Control and Prevention [CDC], 2021). A 2014 World Health Organization report (WHO; 2014) estimated that more lives were lost to suicide than to war, conflict, and natural disasters combined. More recently, the American Foundation for Suicide Prevention (AFSP; 2023) estimated that in 2021 there were 1.7 million suicide attempts; more than 48,000 Americans died by suicide. In 2023, trends showed about 130 suicides per day (AFSP, 2023).
To address the ongoing concern of suicide risk, counselor education programs are expected to prepare students for work with diverse clients who experience suicidal ideations (Wachter Morris & Barrio Minton, 2012). Specifically, the Council for the Accreditation of Counseling and Related Educational Programs (CACREP; 2023) requires counseling programs to provide counselors-in-training (CITs) with skills in crisis intervention, suicide prevention, and response models and strategies, as well as proper assessment and management of suicidal ideations. There are no consistent suicide prevention or intervention training standards or models among counselor education programs. Organizations such as the American Association of Suicidology have recommended that suicide knowledge and assessment be at the forefront of health care by having (a) graduate programs require suicide knowledge and skills acquisition in their curriculum, (b) state licensure boards require suicide-specific education for renewal of licenses, (c) government-funded health care systems and hospitals require staff training in suicide assessment and management, and (d) staff appropriately trained to assess, manage, or treat patients who experience suicidal thoughts (Schmitz et al., 2012).
The current study aimed to determine if a practice model used in an online basic counseling skills course was effective at increasing counseling students’ self-efficacy when working with clients who present with suicidal ideations. Results from the study were used to determine if the skills-based online course effectively taught suicide assessment and intervention skills to graduate students. Discussion and implications regarding the need to establish best practices in prevention and intervention training for CITs are included. Additional considerations are given for both online and brick-and-mortar counseling programs.
Competencies and Principles
To assist counselor educators with how to best address the ongoing concern of suicide risk in clients, the Suicide Prevention Resource Center (2006) identified several core competencies and skills needed to assess and manage individuals at risk for suicide. These competencies can be used as a framework for extensive suicide training (Granello, 2010). Other models, such as a core competency–based training workshop in suicide screening, assessment, and management, have been developed to assess the effectiveness of suicide training, including pre- and post-workshop self-assessments, evidence-based instruction, role-playing, expert demonstration, group discussions, and video-recorded risk assessments of trainees intended to provide feedback (Cramer et al., 2017). Together, these competencies and principles can be used to develop a practice model in graduate counselor education programs and to better assist CITs in preparing to work with a client experiencing suicidal thoughts.
Despite the Suicide Prevention Resource Center (2006) identifying core competencies and skills needed to properly assess and manage individuals for risk of suicide, the research from counseling graduate programs on the implementation of suicide training remains sparse (Wasylko & Stickley, 2007). Therefore, we looked at other graduate programs of similar disciplines (e.g., social work, school psychology, and school counseling) to gain a better idea of best practices in related fields. Unfortunately, literature related to best practices within graduate programs of similar disciplines also demonstrates a lack of training in suicide risk assessment and intervention (Becnel et al., 2021; LeCloux, 2021; Liebling-Boccio & Jennings, 2013). This expanded look into other mental health professions further supports the notion that limited research exists regarding training in suicide screening, assessment, and intervention at the graduate level; thus, more attention is needed in these areas.
Suicide Training in Graduate Programs
Graduates of other counseling programs have indicated that there were limitations in the suicide prevention training that they received (Wakai et al., 2020). In a national sample of American School Counselor Association members, Becnel et al. (2021) found that 38% of school counselors (N = 226) did not receive suicide prevention training during their graduate programs and 37% received no training in crisis intervention. Similar results were found in a study of 193 professional counselors; over a third reported no classroom training in crisis preparation, and 30% reported no or minimal preparation in suicide assessment (Wachter Morris & Barrio Minton, 2012).
Schmidt (2016) evaluated the confidence and preparedness of 339 mental health practitioners (i.e., professional counselors, school counselors, social workers, psychologists). Results indicated that 52% of participants had graduate course work in suicide intervention and assessment, but 19% reported feeling not very confident in working with clients who had suicidal ideations. Conversely, Binkley and Leibert (2015) found that students who received training before their practicum working with clients who experience suicidal thoughts had lower anxiety and a greater level of confidence in addressing those issues compared to those who did not receive training.
The results of these studies look at counselor training and confidence or preparedness, to support the need for additional training in this area and research on best practices in preparing CITs to work with clients who present with suicidal ideation. Studies report training levels associated with practice outcomes (e.g., confidence), but there is a lack of literature explaining how suicide assessment and intervention training occurs in counselor education programs. Although there is literature that demonstrates that self-efficacy directly influences a counselor’s development (Barbee et al., 2003; Barnes, 2004; Kozina et al., 2010; Lent et al., 2003; Pechek, 2018; Vincenzes et al., 2023), literature that specifically addresses self-efficacy as it relates to working with a client who experiences suicidal ideation is sparse. However, the literature supports that additional training is needed on this topic and that self-efficacy is an important concept to consider when developing training protocols for CITs.
Self-Efficacy
Self-efficacy is dynamic and plays a significant role in counselor training and skill development. Bandura (1986) first introduced self-efficacy as an individual’s judgment on their capabilities to execute an action to achieve a certain performance or goal. Later the term was linked to behavioral motivation in the academic setting and was defined as a student’s belief in their ability to accomplish and succeed on an academic-related task (Bandura, 1989). Bandura (1997) also found that self-efficacy beliefs can be altered through four primary sources: (a) personal performance accomplishments, (b) vicarious learning, (c) social persuasion, and (d) physiological and affective states. While self-efficacy is dynamic (Lent, 2020) and can be impacted by personal interpretation of these primary sources (Lent & Brown, 2006), research has found that self-efficacy is an important factor in counselor competency (Barbee et al., 2003; Barnes, 2004; Kozina et al., 2010; Pechek, 2018; Vincenzes et al., 2023). More specifically, Lent et al. (2003) found that CITs’ initial clinical work and experience with more difficult skills (e.g., managing a session, handling the role of the counselor) increased counselor self-efficacy (Kozina et al., 2010).
Self-Efficacy in Suicide Training
Counselors who lack self-efficacy in their ability to work with a client who is experiencing suicidal thoughts may conduct suicide screening, assessments, and interventions ineffectively (Douglas & Wachter Morris, 2015; Jahn et al., 2016). In addition, counselors with low self-efficacy are more likely to subconsciously choose not to see suicide warning signs (Douglas & Wachter Morris, 2015) or avoid the topic of suicide altogether (Jahn et al., 2016). It is important that CITs are exposed to the topic of suicide and that they gain more counseling experience involving this issue during their training so that they will feel more confident working with a client experiencing suicidal thoughts. More exposure to this topic leaves CITs feeling better equipped to address suicide in sessions and is also likely to increase their self-efficacy (Elliott & Henninger, 2020; Pechek, 2018; Sawyer et al., 2013; Shea & Barney, 2015).
Clear evidence of the positive effects of including training on suicide within counselor education programs has been documented, demonstrating a reduction of fear and more success in helping clients manage suicide-related issues (Jahn et al., 2016). CITs who had prior training in suicide experienced lower levels of anxiety and higher levels of confidence in working with a client with suicidal thoughts (Binkley & Leibert, 2015). Similarly, professional counselors who expressed confidence in their academic training on suicide experienced lower levels of fear related to negative client outcomes and had higher levels of confidence in their skills and abilities (Jahn et al., 2016).
Self-Efficacy in Suicide Training for Online Learning. Although the topic of self-efficacy in counselor education has been studied (Barbee et al., 2003; Barnes, 2004; Conteh et al., 2018; Fakhro et al., 2023; Kozina et al., 2010; Pechek, 2018; Suh et al., 2018; Vincenzes et al., 2023), the literature does not focus on how best to teach for improved self-efficacy related to suicide assessment and intervention in the online setting. Specifically, it is not clear how counselor educators can best teach suicide screening, assessment, or intervention skills online. Two recent studies in counselor education programs have tried to better explain self-efficacy in suicide training during online learning (Elliott & Henninger, 2020; Gallo et al., 2019).
Elliott and Henninger (2020) showed that different online teaching strategies (e.g., a combination of a written module, role-plays/observations, and a facilitated discussion) in an online counselor education program showed no between-group differences, while all teaching strategies showed significant improvements in self-efficacy of CITs. Another study found that a 15-hour youth suicide prevention course that included didactic and experiential activities in a master’s counseling program increased participants’ knowledge and perceived ability to help clients who experienced suicidal ideations, as well as increased their self-efficacy in screening, assessment, and intervention (Gallo et al., 2019).
Purpose of the Study
With the influx of online counselor education programs, it is essential to determine how to improve suicide training and intervention skills (Allen & Seaman, 2014) so that CITs are better prepared to address the topic of suicide. The current quantitative study examined the influence of an online counseling practice model on CITs’ self-efficacy when it came to the utilization of suicide assessment and intervention with clients. The research question was: Do CITs’ perceived levels of self-efficacy in suicide assessment and intervention change because of practicing these skills through role-plays in an online counseling course? By better understanding these findings, implications can be made for how counselor educators can teach suicide screening, assessment, and intervention skills online.
Method
Procedures
Prior to beginning this study, our research team received full approval from the IRB. Participants were then recruited from an online clinical mental health counseling program. Only students enrolled in the online basic counseling skills course were recruited to ensure that all participants were at the same place in the program regarding knowledge and skills learned. An electronic announcement was posted in the 10 online basic skill course shells. The announcement included a hyperlink directing participants to an informed consent document, which detailed their requirements and rights and allowed them to indicate their consent to participate. Before completing any survey questions, the participants created a username for data comparison in the pre- and posttests, which was also an avenue for dropping participants if they requested to leave the study. After providing their username, participants completed a brief demographic questionnaire and the Counselor Suicide Assessment Efficacy Survey (CSAES; Douglas & Wachter Morris, 2015). To protect participant anonymity, no additional identifying information was collected.
Structure of the Basic Skills Class
Once students completed the pretest consent form, demographic questionnaire, and assessment, the counselor educators (i.e., faculty) started the class by providing participants with a variety of technology-assisted counseling experiences and activities (e.g., role-play demonstrations, best practices in telemental health counseling, lecture videos on specific counseling skills, guidelines for a preferred topic for the role-plays). To ensure consistency of content across courses, the faculty made sure to include the same teaching resources in each section of the class and continuously consulted each other to make sure that the classes were taught as similarly as possible. In addition, they decided that all students should receive the same training and teaching activities, ensuring that they were equally prepared to address the topic of suicide during their clinical courses and after graduation.
The topic of self-care was addressed with participants, as this was the first opportunity students had to practice counseling skills within the program. This focus on self-care was an important step toward decreasing the potential of significant deep-rooted issues surfacing without sufficient time or training to properly address them. Students would learn about a new basic counseling skill each week and were instructed to incorporate that skill into the week’s role-play. In addition to reading about the skill in the course textbook, students were required to view weekly lecture videos and role-plays that specifically explained and demonstrated the skill that the students would be practicing that week during their role-play. For role-plays, participants were randomly paired with other participants within the same basic counseling skills course to practice basic foundational counseling skills. Each pair of students participated in five weekly role-plays as both the counselor and the client. Two of these role-plays occurred during class and three occurred outside of class. Each role-play occurred via Zoom and lasted approximately 10–15 minutes during class or 30 minutes when completed outside of class. For in-class role-plays, participants utilized breakout rooms in Zoom. Faculty provided each participant in the counselor role with feedback at the end of each role-play. Role-plays outside of the class required participants to send their partner a Zoom link and password. The role-plays were recorded in Zoom. Participants identified one role-play to submit to the instructor for formal assessment of their basic counseling skills and to provide formative feedback to each participant when acting in the counselor role.
Preparation for Suicidal Ideation Role-Plays
After the initial five role-plays were completed, participants prepared for role-plays that focused on crisis counseling. They read a chapter from their textbook on crisis counseling and various supplemental articles on working with a client with suicidal ideations. In addition, they viewed pre-recorded role-plays on suicide assessment created by faculty in the program. Participants remained in the same randomly assigned pairs from earlier in the semester and then completed an additional five role-plays (one weekly), which allowed for them to gain experience working with a client with suicidal ideations.
Suicidal Ideation Role-Plays
Prior to beginning the role-plays, participants were provided with a brief synopsis for the topic of suicide and were also given the instructor’s phone number in case they needed immediate support or guidance. Like the previous role-plays, each of these lasted approximately 10–15 minutes during online classes or 30 minutes outside of class. Again, role-plays completed outside of class were recorded so that faculty could provide detailed feedback to students. The first in-class role-play was completed in a fishbowl format, allowing students in the class to observe. Instead of utilizing multiple breakout rooms, students remained in one room and observed one role-play at a time. This allowed students to learn vicariously from one another and to observe the ways that suicide screening, assessment, and intervention skills were demonstrated. The initial role-play also served as a way for participants in the counselor role to gain experience completing a suicide assessment while practicing other basic counseling skills. Four additional role-plays occurred and offered an opportunity for participants to continually reassess the risk of suicide of their partners, develop a safety plan, establish treatment goals, and practice other basic counseling skills. During the last role-play, participants in the counselor role conducted a termination session in which the counselor reviewed the client’s safety and treatment plans. Additionally, they reviewed the client’s goals and objectives and provided time for the client to reflect on the counseling experience.
Faculty Supervision and Learning Activities
During the semester, faculty supervision was an essential component of the process. If additional support or guidance was needed for participants, faculty were available via phone between 8 am–8 pm, Monday through Friday. Faculty were available to all role-play participants regardless of their role (i.e., counselor, client, or observer). While supervision can look different for each instructor, the counselor educators in this study regularly consulted with one another to ensure that they were conveying the same expectations to the students enrolled in the courses. This extended to making sure they discussed similar topics at the same time during the course; included the same teaching activities, readings, and assignments; and consulted with one another when a concern arose that may have changed course plans.
In addition to completing the virtual role-plays during the semester, participants completed a variety of activities and assignments that were intended to prepare them for realistic experiences needed upon graduation. For example, participants completed components of a treatment plan after each counseling session which were submitted to the instructor immediately following the role-play. Additionally, they submitted video tapes of role-plays for faculty feedback. Finally, participants transcribed one 30-minute role-play. This assignment allowed them to identify and reflect on specific foundational skills that they used when working with a client reporting suicidal ideations. At the conclusion of the semester, participants were asked to complete the posttest using the same username they created at the beginning of the semester. The posttest included the same assessment as the pretest (CSAES).
Participants
A convenience sample was used for this study. Master’s-level counseling students enrolled in the spring 2021 and spring 2022 counseling skills courses (10 sections total) in an online clinical mental health counseling graduate program were recruited via news announcements and emails to participate in this study. A total of 120 students were invited to participate in the study; however, only 60 were included because they completed both the pretest and posttest self-efficacy assessment. Included students’ ages ranged from 21–61 years old. The average age of participants was 29.03 (SD = 8.49). The sample consisted of the following racial identities: 80.0% White or Caucasian (n = 48), 10.0% Black or African American (n = 6), 6.7% Hispanic or Latino (n = 4), 1.7% Asian or Asian American (n = 1), and 1.7% did not indicate their racial identities (n = 1). Most participants identified as female (90%, n = 54) and were enrolled in the mental health counseling program full-time (51.7%, n = 31). When asked about prior experience in the mental health field, 60% (n = 36) had this experience; however, only 45% (n = 27) had prior professional experience or training in suicide risk assessment. Table 1 contains all participant demographics.
Measure
The study participants completed the CSAES (Douglas & Wachter Morris, 2015). The CSAES measures self-efficacy in suicide assessment and intervention. According to the developers (Douglas & Wachter Morris, 2015), the CSAES is comprised of 25 items that may make suicide assessment or intervention difficult for a counselor. These items are rated on a confidence scale that ranges from 1 (not confident) to 5 (highly confident). The confidence items are organized into four subscales:
- General Suicide Assessment, which has seven items and a maximum score of 35
- Assessment of Personal Characteristics, which has 10 items and a maximum score of 50
- Assessment of Suicide History, which has three items and a maximum score of 15
- Suicide Intervention, which has five items and a maximum score of 25
Sample items include the following: Q1 “I can effectively inquire if a student has had thoughts of killing oneself” (General Suicide Assessment); Q11 “I can effectively ask a student about his or her history of mental illness” (Assessment of Personal Characteristics); Q18 “I can effectively ask a student about his or her previous suicide attempts” (Assessment of Suicide History); and Q25 “I can appropriately intervene if a student is at imminent risk for suicide” (Suicide Intervention).
Table 1
Participant Demographics
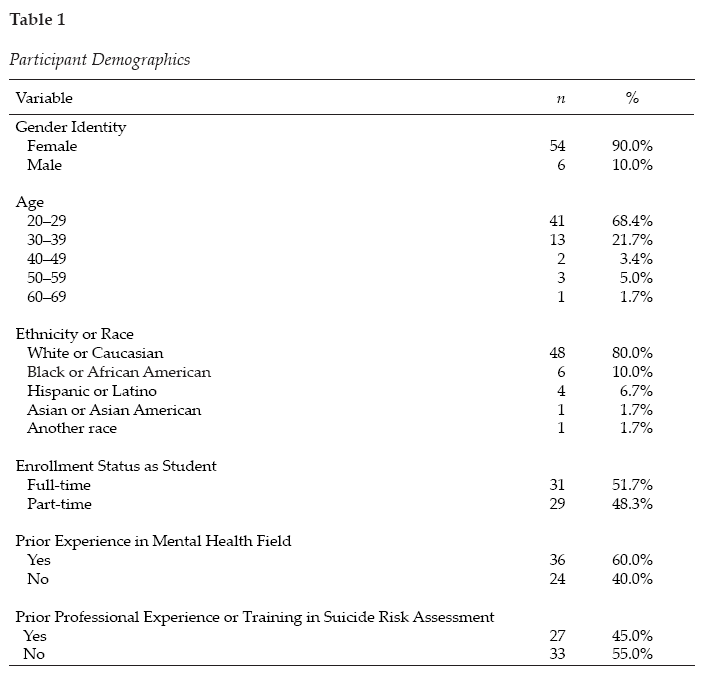
The total score for the scale is 125, with higher scores representing higher levels of self-efficacy associated with suicide assessment and intervention (Douglas & Wachter Morris, 2015). The CSAES can be scored two ways. First, the assessment can be scored individually for a more detailed understanding of what differences, if any, in self-efficacy exist between differing aspects of suicide assessment. The second way is to calculate the total sum of the assessment-related subscales and the intervention subscale. In doing so, each subscale would have a mean for the individual scale (Douglas & Wachter Morris, 2015).
The assessment developers have reported internal reliability for the CSAES as a calculation for each of the four subscales and the second-order factor of Suicide Assessment using Cronbach’s α: General Suicide Assessment α = .882, Assessment of Personal Characteristics α = .88, Assessment of Suicide History α = .81, Suicide Intervention α = .83, and Suicide Assessment α = .93 (Douglas & Wachter Morris, 2015).
The CSAES was noted for showing “structural aspects of validity and sensitivity to detect differing levels of self-efficacy” (Douglas & Wachter Morris, 2015) based on the utilization of a four-factor model that was cross-validated. The scale was validated with a total of 324 participants. Of the participants, 258 (79.63%) were female. Unfortunately, a limitation of the instrument is that the diversity of participants was unknown due to ethnicity inadvertently being left off the demographic questionnaire while it was being developed (Douglas & Wachter Morris, 2015).
The current study assessed the internal reliability of the CSAES using Cronbach’s α and omega (ω) using test-retest reliability because the measure of consistency was between two measurements of the same construct to the same group at two different times. The overall CSAES has strong reliability (α = .978; ω = .978), and each subscale had the following reliability scores: General Suicide Assessment (α = .943; ω = .946); Assessment of Personal Characteristics (α = .947; ω = .947); Assessment of Suicide History (α = .896; ω = .890); and Suicide Intervention (α = .920; ω = .915). All subscale reliability coefficients were high when looking at both α and ω, meaning that good internal consistency was found among items of the scale (Green & Salkind, 2014).
Data Analysis
Before running any analyses, we screened the data using SPSS version 26.0.0.1 software to check for (a) missing data, (b) average expected scores per the outcome variables, (c) standard deviations within range, and (d) normality of data (Green & Salkind, 2014). The initial sample included 108 surveys; however, only 60 of these could be paired with posttest data, using the username data point. Therefore, individuals with their missing pair were deleted along with any others that included missing data (i.e., listwise deletion). The final sample included 60 respondents. A power analysis using a statistical power analysis program (G*Power 3.1) for paired t-test showed an N of 54 was needed for 95% power with an alpha level of .05 and a moderate effect size of .5. Next, scales were computed, and univariate testing occurred. Data met all assumptions for conducting a paired t-test (i.e., dependent variable was continuous, normally distributed, and without outliers and the observations were independent of one another). The paired t-test was used to test the effectiveness of training for suicide assessment and intervention in a basic skills class using a single-group (pretest/posttest) design, including demographics and the CSAES. To ensure that all students received the same teaching activities and assignments, we decided not to utilize a control group. We wanted to ensure that all students were equally prepared and trained to address the topic of suicide upon entering their clinical courses and upon graduation.
Results
The purpose of the study was to compare counseling students’ pretest and posttest self-efficacy assessments when taking a basic skills course that highly emphasized skills related to suicide training and assessment. The results of a paired-samples t-test on the General Suicide Assessment subscale indicate that on average, students scored significantly higher (Mpost = 28.57, SD = 4.80) after taking the basic skills class (Mpre = 21.20, SD = 7.80), t(59) = −9.15, p < .001. A large effect was found (d = 1.182, 95% CI [−1.51, −.85]). The results of a paired-samples t-test on the Assessment of Personal Characteristics subscale indicate that on average, students scored significantly higher (Mpost = 41.17, SD = 6.59) after taking the basic skills class (Mpre = 33.80, SD = 8.75), t(59) = −8.77, p < .001. A large effect was found (d = 1.133, 95% CI [−1.46, −.81]). The results of a paired-samples t-test on the Suicide History Assessment subscale indicate that on average, students scored significantly higher (Mpost = 13.07, SD = 2.22) after taking the basic skills class (Mpre = 9.95, SD = 3.33), t(59) = −8.38, p < .001. A large effect was found (d = 1.081, 95% CI [−1.40, −.76]). The results of a paired-samples t-test on the Suicide Intervention subscale indicate that on average, students scored significantly higher (Mpost = 19.00, SD = 4.32) after taking the basic skills class (Mpre = 14.63, SD = 5.46), t(59) = −7.21, p < .001. A large effect was found (d = .931, 95% CI [−1.23, −.63]). In summary, students’ level of self-efficacy related to suicide assessment and intervention increased in all areas as a result of taking the basic counseling skills class.
Because this study had a small sample size, the risk increases that at least one test is statistically significant just by chance. Therefore, a Bonferroni correction was applied to adjust the significance levels: Bonferroni correction = .05/4 = .0125 (.05 = acceptable significance level; 4 = number of subscales of CSAES). Therefore, the familywise error value is .0125. Because the above results are looking at significance at the p <.001 value, all results remain significant.
Discussion
The initial research question was: Do CITs’ perceived levels of self-efficacy in suicide assessment and intervention change because of practicing these skills through role-plays in an online counseling course? According to the results of the current study, on average, students felt significantly more prepared and confident in their ability to counsel someone experiencing suicidal ideations after practicing the skills in their basic counseling skills online course. Prior research indicated that many students were either not taught these skills (Becnel et al., 2021) or did not feel prepared to address these issues in counseling (Schmidt, 2016). The current study points to the vitality of both teaching students about suicide screening and assessment, as well as providing them with a safe space to practice the skills. By offering students opportunities to practice suicide screening, assessment, and intervention skills, instructors could help reduce their students’ anxiety in addressing the topic during their clinical courses, which Binkley and Leibert (2015) found to be a significant student concern.
Furthermore, it is important for counselor educators to observe and provide students with feedback regarding these essential skills. Past research points to the concern that students are not adequately conducting suicide screening, assessments, and interventions (Jahn et al., 2016); therefore, it would behoove counselor educators to infuse various opportunities throughout the curriculum to strengthen these skills. In turn, feedback and practice opportunities combined may help to enhance students’ levels of self-efficacy (Elliott & Henninger, 2020; Gallo et al., 2019), thus helping them to address the issues with clients in a timely and direct manner.
Implications for Training
While CACREP (2023) requires counselor educators to prepare students to work with clients who present with suicidal ideations, there is no clear criteria as to the best way of preparing students to work with these clients. Research on the topic is limited; however, the results of this study can provide a framework for helping to inform key training areas in counselor education and future research.
As counselor educators continue to expand on the didactic knowledge of suicide screening, assessment, and intervention, more intentional efforts need to be embedded throughout the curriculum to continuously expose students to experiential opportunities for practicing these skills. This idea coincides with the recommendation from the American Association of Suicidology that proposes suicide knowledge and assessment be at the forefront of graduate program curricula (Schmitz et al., 2012). First, in foundational courses, students could become more comfortable with the topic of suicide. These courses could help break down barriers and possibly calm nerves that tend to surround the topic of suicide. In assessment courses, students could role-play giving a partner various suicide screenings and assessments and gain experience interpreting the results. These role-plays could occur during class or be recorded for faculty feedback. In skills courses, students could practice suicide intervention by broaching the topic with their classmate-clients to help them feel more comfortable with directly asking clients if they are experiencing suicidal ideations. In addition, it may be helpful if a trauma and crisis counseling course was required within the core curriculum. This course could have content devoted to suicide screening, assessment, and intervention, including both didactic and experiential opportunities. By offering these opportunities throughout the curriculum, similar to ethical and cultural considerations, students may feel more comfortable and confident as they enter their clinicals (Binkley & Leibert, 2015; Guillot Miller et al., 2013). This intentional, consistent exposure to practicing these skills could help more students gain foundational knowledge and experience with this topic. In turn, as their self-efficacy and comfort levels increase, they may be more confident addressing this topic with clients. Ultimately, this may increase client welfare by ensuring effective assessment and treatment of client needs.
Implications for Counselor Education Training Research
The topic of suicide screening, assessment, and intervention in counselor education and supervision could benefit significantly from continued outcome-based research. For example, longitudinal studies could track students’ perceived levels of self-efficacy on suicide screening, assessment, and intervention as they go through a counseling program. This may help educators become more intentional about when and how the topic is infused within the curriculum. In addition, research could compare different types of teaching methods (e.g., role-play versus lecture) that expose students to the topic and assess which methods are more influential in building students’ skills and self-efficacy. Finally, researchers could interview current mental health therapists to identify knowledge and skill gaps to help educators teach students about crisis counseling more intentionally.
Limitations
There are a few limitations to the current study that are important to discuss. First is the variability in teaching and supervision styles across different instructors, which may impact the students’ overall feelings of self-efficacy. Although the same procedures were followed, educators inevitably have different styles of giving feedback. How the feedback is perceived by the student may impact their confidence in using the acquired skills.
Another limitation involves the notion of social desirability bias. The participants in the current study were students in the program; therefore, they may have felt pressured to identify increases in their self-efficacy around suicide assessment and intervention. This pressure may have been experienced because some of their current professors also served as researchers in the study and the students may have wanted to gain favor with them.
With regard to external validity, there are a few limitations. First, our research team did not account for prior experience in suicide screening, assessment, or intervention; thus, the results could have been impacted by external experiences versus the sole experience of the course activities. Additionally, there was a large portion of the data that could not be used because the pre- and post- surveys could not be aligned. Although the current study had 60 viable pre- and post- surveys, the data could have been more reliable and generalizable with a larger dataset. Furthermore, there was a lack of diversity in the research sample. Because the participants were primarily White females, the results may be limited in its generalizability to other cultures and genders.
Future studies should attempt to better isolate these variables (i.e., teaching styles, feedback, participant recruitment, prior experience in suicide training, cultural background) and find ways to improve response rates. In addition, it would be beneficial to have a comparison course or data from other counseling programs’ basic skills classes to further determine if this practice-based model was effective. Results could be linked to more general self-efficacy increases because of growing more comfortable with learning and using interviewing skills (Holladay & Quiñones, 2003).
One final limitation worth noting is the effect size estimates of the pre- and posttest scores. All effect sizes are large. Some reasons why the effect sizes may be large in the paired-samples t-tests include: (a) large differences between paired observations (the mean scores between the pre- and posttest scores were extremely different), and (b) small within-group variability (if the within-group variability is small, then even small differences between the paired observations could result in a large effect size).
Conclusion
As counselor educators prepare students for the profession, intentional inclusion of suicide screening, assessment, and intervention skills is vital to increasing students’ confidence and preparation to address this topic with their future clients. But it is not enough for students to learn about screening, assessment, and interventions; they need experiential opportunities to practice and develop these skills. In turn, feedback and practice will increase their comfort levels to directly and adequately support their clients’ needs.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Allen, I. E., & Seaman, J. (2014). Grade change: Tracking online education in the United States. The Sloan Consortium. Sloan-C. http://www.onlinelearningsurvey.com/reports/gradechange.pdf
American Foundation for Suicide Prevention. (2023). Suicide statistics. https://afsp.org/suicide-statistics
Bandura, A. (1986). Social foundations of thought and action: A social cognitive theory. Prentice-Hall.
Bandura, A. (1989). Human agency in social cognitive theory. American Psychologist, 44(9), 1175–1184. https://doi.org/10.1037/0003-066X.44.9.1175
Bandura, A. (1997). Self-efficacy: The exercise of control. W. H. Freeman.
Barbee, P. W., Scherer, D., & Combs, D. C. (2003). Prepracticum service-learning: Examining the relationship with counselor self-efficacy and anxiety. Counselor Education and Supervision, 43(2), 108–119. https://doi.org/10.1002/j.1556-6978.2003.tb01835.x
Barnes, K. L. (2004). Applying self-efficacy theory to counselor training and supervision: A comparison of two approaches. Counselor Education and Supervision, 44(1), 56–69. https://doi.org/10.1002/j.1556-6978.2004.tb01860.x
Becnel, A. T., Range, L., & Remley, T. P., Jr. (2021). School counselors’ exposure to student suicide, suicide assessment self-efficacy, and workplace anxiety: Implications for training, practice, and research. The Professional Counselor, 11(3), 327–339. https://doi.org/10.15241/atb.11.3.327
Binkley, E. E., & Leibert, T. W. (2015). Prepracticum counseling students’ perceived preparedness for suicide response. Counselor Education and Supervision, 54(2), 98–108. https://doi.org/10.1002/ceas.12007
Centers for Disease Control and Prevention. (2021, February 20). Web-based injury statistics query and reporting system (WISQARS) fatal injury reports. https://wisqars.cdc.gov/fatal-leading
Conteh, J. A., Mariska, M. A., & Huber, M. J. (2018). An examination and validation of personal counseling and its impact on self-efficacy for counselors-in-training. Journal of Counselor Practice, 9(2), 109–138.
https://www.journalofcounselorpractice.com/uploads/6/8/9/4/68949193/jac902111_jcp_vol_9_issue_2.pdf
Council for the Accreditation of Counseling and Related Educational Programs. (2023). 2024 CACREP standards. https://www.cacrep.org/wp-content/uploads/2023/06/2024-Standards-Combined-Version-6.27.23.pdf
Cramer, R. J., Bryson, C. N., Eichorst, M. K., Keyes, L. N., & Ridge, B. E. (2017). Conceptualization and pilot testing of a core competency-based training workshop in suicide risk assessment and management: Notes from the field. Journal of Clinical Psychology, 73(3), 233–238. https://doi.org/10.1002/jclp.22329
Douglas, K. A., & Wachter Morris, C. A. (2015). Assessing counselors’ self-efficacy in suicide assessment and intervention. Counseling Outcome Research and Evaluation, 6(1), 58–69.
https://doi.org/10.1177/2150137814567471
Elliott, G. M., & Henninger, J. (2020). Online teaching and self-efficacy to work with suicidal clients. Counselor Education and Supervision, 59(4), 283–296. https://doi.org/10.1002/ceas.12189
Fakhro, D., Rujimora, J., Zeligman, M., & Mendoza, S. (2023). Counselor self-efficacy, multicultural competency, and perceived wellness among counselors in training during COVID-19: A pre- and peri-analysis. Journal of Counselor Leadership and Advocacy, 10(2), 99–111. https://doi.org/10.1080/2326716X.2023.2229323
Gallo, L. L., Doumas, D. M., Moro, R., Midgett, A., & Porchia, S. (2019). Evaluation of a youth suicide prevention course: Increasing counseling students’ knowledge, skills, and self-efficacy. Journal of Counselor Preparation and Supervision, 12(3), 1–23. https://digitalcommons.sacredheart.edu/jcps/vol12/iss3/9
Granello, D. H. (2010). The process of suicide risk assessment: Twelve core principles. Journal of Counseling & Development, 88(3), 363–370. https://doi.org/10.1002/j.1556-6678.2010.tb00034.x
Green, S. B., & Salkind, N. J. (2014). Using SPSS for Windows and Macintosh: Analyzing and understanding data (7th ed.). Pearson.
Guillot Miller, L., McGlothlin, J. M., & West, J. D. (2013). Taking the fear out of suicide assessment and intervention: A pedagogical and humanistic practice. The Journal of Humanistic Counseling, 52(1), 106–121. https://doi.org/10.1002/j.2161-1939.2013.00036.x
Holladay, C. L., & Quiñones, M. A. (2003). Practice variability and transfer of training: The role of self-efficacy generality. Journal of Applied Psychology, 88(6), 1094–1103. https://doi.org/10.1037/0021-9010.88.6.1094
Jahn, D. R., Quinnett, P., & Ries, R. (2016). The influence of training and experience on mental health practitioners’ comfort working with suicidal individuals. Professional Psychology: Research and Practice, 47(2), 130–138. https://doi.org/10.1037/pro0000070
Kozina, K., Grabovari, N., De Stefano, J., & Drapeau, M. (2010). Measuring changes in counselor self-efficacy: Further validation and implications for training and supervision. The Clinical Supervisor, 29(2), 117–127. https://doi.org/10.1080/07325223.2010.517483
LeCloux, M. (2021). Efficient, yet effective: Improvements in suicide-related knowledge, confidence, and preparedness after the deployment of a brief online module on suicide in a required MSW course. Journal of Teaching in Social Work, 41(4), 389–407. https://doi.org/10.1080/08841233.2021.1954577
Lent, R. W. (2020). Career development and counseling: A social cognitive framework. In S. D. Brown & R. W. Lent (Eds.), Career development and counseling: Putting theory and research to work (3rd ed., pp. 129–164). Wiley.
Lent, R. W., & Brown, S. D. (2006). Integrating person and situation perspectives on work satisfaction: A social-cognitive view. Journal of Vocational Behavior, 69(2), 236–247. https://doi.org/10.1016/j.jvb.2006.02.006
Lent, R. W., Hill, C. E., & Hoffman, M. A. (2003). Development and validation of the Counselor Activity Self-Efficacy Scales. Journal of Counseling Psychology, 50(1), 97–108. https://doi.org/10.1037/0022-0167.50.1.97
Liebling-Boccio, D. E., & Jennings, H. R. (2013). The current status of graduate training in suicide risk assessment. Psychology in the Schools, 50(1), 72–86. https://doi.org/10.1002/pits.21661
Pechek, A. A. (2018). Counselor education learning modalities: Do they predict counseling self-efficacy in students? (Publication No. 10785997) [Doctoral dissertation, Adams State University]. ProQuest Dissertations Publishing.
Sawyer, C., Peters, M. L., & Willis, J. (2013). Self-efficacy of beginning counselors to counsel clients in crisis. Journal of Counselor Preparation and Supervision, 5(2), 30–43. https://digitalcommons.sacredheart.edu/jcps/vol5/iss2/3/
Schmidt, R. C. (2016). Mental health practitioners’ perceived levels of preparedness, levels of confidence and methods used in the assessment of youth suicide risk. The Professional Counselor, 6(1), 76–88.
https://doi.org/10.15241/rs.6.1.76
Schmitz, W. M., Jr., Allen, M. H., Feldman, B. N., Gutin, N. J., Jahn, D. R., Kleespies, P. M., Quinnett, P., & Simpson, S. (2012). Preventing suicide through improved training in suicide risk assessment and care: An American Association of Suicidology Task Force report addressing serious gaps in U.S. mental health training. Suicide and Life-Threatening Behavior, 42(3), 292–304. https://doi.org/10.1111/j.1943-278X.2012.00090.x
Shea, S. C., & Barney, C. (2015). Teaching clinical interviewing skills using role-playing: Conveying empathy to performing a suicide assessment: A primer for individual role-playing and scripted group role-playing. Psychiatric Clinics of North America, 38(1), 147–183. https://doi.org/10.1016/j.psc.2014.10.001
Suicide Prevention Resource Center. (2006). Core competencies in the assessment and management of suicide risk.
Suh, S., Crawford, C. V., Hansing, K. K., Fox, S., Cho, M., Chang, E., Lee, S., & Lee, S. M. (2018). A cross-cultural study of the self-confidence of counselors-in-training. International Journal for the Advancement of Counselling, 40(3), 255–266. https://doi.org/10.1007/s10447-018-9324-4
Vincenzes, K., Pechek, A., & Sprong, M. (2023). Counselor trainees’ development of self-efficacy in an online skills course. Journal of Counselor Preparation and Supervision, 17(1). https://digitalcommons.sacredheart.edu/jcps/vol17/iss1/1
Wachter Morris, C. A., & Barrio Minton, C. A. (2012). Crisis in the curriculum? New counselors’ crisis preparation, experiences, and self-efficacy. Counselor Education and Supervision, 51(4), 256–269.
https://doi.org/10.1002/j.1556-6978.2012.00019.x
Wakai, S., Schilling, E. A., Aseltine, R. H., Blair, E. W., Bourbeau, J., Duarte, A., Durst, L. S., Graham, P., Hubbard, N., Hughey, K., Weidner, D., & Welsh, A. (2020). Suicide prevention skills, confidence, and training: Results from the Zero Suicide Workforce Survey of behavioral health care professionals. SAGE Open Medicine, 8, 1–12. https://doi.org/10.1177/2050312120933152
Wasylko, Y., & Stickley, T. (2007). Promoting emotional development through using drama in mental health education. In T. Stickley & T. Basset (Eds.), Teaching mental health (pp. 297–309). Wiley.
https://doi.org/10.1002/97804470713617.ch25
World Health Organization. (2014). Preventing suicide: A global imperative. https://www.who.int/publications/i/item/9789241564779
Ashley Ascherl Pechek, PhD, NCC, ACS, LPC, is an associate professor at Commonwealth University of Pennsylvania. Kristin A. Vincenzes, PhD, NCC, ACS, BC-TMH, LPC, is a professor at Commonwealth University of Pennsylvania. Kellie Forziat-Pytel, PhD, NCC, ACS, LPC, is an assistant professor at Commonwealth University of Pennsylvania. Stephen Nowakowski is a graduate student at Commonwealth University of Pennsylvania. Leandrea Romero-Lucero, PhD, ACS, LPCC, CSOTS, is an associate professor and Clinical Mental Health Counseling Program Director at Commonwealth University of Pennsylvania. Correspondence may be addressed to Ashley Ascherl Pechek, 401 N. Fairview Street, Lock Haven, PA 17745, aap402@commonwealthu.edu.
May 22, 2024 | Volume 14 - Issue 1
Joshua D. Smith, Neal D. Gray
Each year TPC presents an interview with an influential veteran in counseling as part of its Lifetime Achievement in Counseling series. This year I am honored to introduce Dr. Kathleen Brown Rice, a clinician, supervisor, and counselor educator with expertise in substance use disorders and historical trauma. In this interview, she discusses the personal and professional motivations for her work and her perspective on the future of counseling and counselor education. I am grateful to Dr. Joshua Smith and Dr. Neal Gray for highlighting the ongoing contributions of leaders in the profession for the TPC readership. —Richelle Joe, Editor
 Kathleen Brown Rice, PhD, NCC, ACS, LPC-S (TX), LPC (SD), LCMHC (NC), is a professor of counselor education in the College of Education at Sam Houston State University. She obtained her CACREP-accredited PhD in counselor education and supervision from the University of North Carolina at Charlotte and her CACREP-accredited Master of Science in counseling from South Dakota State University. Dr. Rice is a Licensed Professional Counselor-Supervisor in Texas, a Licensed Professional Counselor in South Dakota, and a Licensed Clinical Mental Health Counselor in North Carolina. Additionally, she holds the National Certified Counselor and Approved Clinical Supervisor credentials. She has worked as a professional counselor in various clinical settings and currently operates a private practice assisting clients with mental health, trauma, and substance abuse issues. Dr. Rice’s scholarly research activity focuses on counselor supervision and training with an emphasis in ethical considerations; the implications of historical and generational trauma; and the impact of substance abuse on individuals, families, and the community. She also incorporates the use of biomarkers in her research to understand emotional regulation, risky behaviors, and resiliency. As part of her extensive scholarship, she serves as an expert peer reviewer on the TPC Editorial Review Board.
Kathleen Brown Rice, PhD, NCC, ACS, LPC-S (TX), LPC (SD), LCMHC (NC), is a professor of counselor education in the College of Education at Sam Houston State University. She obtained her CACREP-accredited PhD in counselor education and supervision from the University of North Carolina at Charlotte and her CACREP-accredited Master of Science in counseling from South Dakota State University. Dr. Rice is a Licensed Professional Counselor-Supervisor in Texas, a Licensed Professional Counselor in South Dakota, and a Licensed Clinical Mental Health Counselor in North Carolina. Additionally, she holds the National Certified Counselor and Approved Clinical Supervisor credentials. She has worked as a professional counselor in various clinical settings and currently operates a private practice assisting clients with mental health, trauma, and substance abuse issues. Dr. Rice’s scholarly research activity focuses on counselor supervision and training with an emphasis in ethical considerations; the implications of historical and generational trauma; and the impact of substance abuse on individuals, families, and the community. She also incorporates the use of biomarkers in her research to understand emotional regulation, risky behaviors, and resiliency. As part of her extensive scholarship, she serves as an expert peer reviewer on the TPC Editorial Review Board.
In this interview, Dr. Rice provides her analysis of the current state of the counseling profession and the possibilities for its future, in addition to discussing the importance of social justice, access to online education, and service.
- As a counselor educator with experience in both traditional (face-to-face) and online delivery, what do you see as the benefits and challenges of both? Additionally, in your opinion, how can online delivery for skills courses ensure counselor competency?
During my master’s and doctoral studies, not one online class was offered. Things have changed immensely. According to the Council for the Accreditation of Counseling and Related Educational Programs website (CACREP; 2024), there are 12 CACREP-accredited online doctoral programs and 118 CACREP-accredited online master’s programs. I believe as telecounseling in the field increases, the number of online programs and online course offerings in face-to-face programs will also continue to grow. A 2021 Ruffalo Noel Levitz Graduate Student Recruitment Report surveyed prospective students who planned to enroll in graduate school and found that 48% preferred hybrid programs, 32% preferred fully online programs, and 20% wanted a traditional classroom program. When looking at within-group differences, doctoral students preferred traditional classroom instruction and master’s students preferred hybrid or online programs (Ruffalo Noel Levitz, 2022).
Courses and programs being offered online provide greater flexibility for our students to schedule around work and personal commitments. This can provide students with a better school–life balance. Online counseling programs can provide access to learners who would not otherwise be able to pursue their graduate education and search out specialty tracks that may not be available in their own geographical area. Online programming diversifies the learning environment by providing the opportunity for students from different backgrounds, worldviews, and cultures to engage and collaborate. While these virtual learning environments increase opportunities, there are also struggles we need to consider with this learning modality. Students in online programs may feel isolated and have fewer or qualitatively different opportunities to engage. This can result in a loss of community and feelings of being unsupported, and even have implications on their professional identity development. Given the differences in jurisdictional requirements for licensure, every program might not lead to the educational requirements for licensure where the student lives or wants to practice. There are also legal considerations related to mandatory reporting and limits of confidentiality that vary across jurisdictions. Lastly, online instruction can restrict assessment related to professional comportment issues. This can lead to students’ gate-slipping to the detriment of clients and the counseling profession.
When looking at how to best support skills courses to ensure we are training competent and ethical counselors, it is important to consider the traits of the student, faculty, and program. Vineyard (2019) recommended that a successful virtual student is one who has good time management skills, has the ability to self-regulate, and is self-motivated. Thus, we must be honest with ourselves as educators and administrators that online programming is not the right fit for every student. Additionally, to best support virtual students, educators need to think about different types of support such as providing regular live supervision of sessions and consistently reviewing recordings. Further, faculty should seek out training and continuing education to enhance their online instruction and understand gatekeeping strategies. For programs, they should be committed to providing the required online platforms and training for both students and faculty to support an online counseling training program. Also, there should be a residency component built into the program. My personal experience and the results of my research on problems of professional competency prove that having face-to-face personal contact is how most disposition problems are discovered. I believe observing how our students interact with us and each other is a crucial part of the gatekeeping process.
- Having an extensive research and publication record aimed toward understanding racial and generational trauma, particularly with Indigenous, tribal, and Native American populations, could you speak about the importance of advocacy and social justice in the counseling profession?
We have great privilege being counselors and counselor educators. Those initials behind our names have inherent power. Thus, advocacy should be embedded in everything we do from our practice, teaching, research, and mentorship. Our training and education provide us a seat at the table to promote equity and inclusion and advocate with others—and we should take full advantage. Advocacy also relates to us being engaged with the population that we are advocating for. In that, to advocate for any population, you have to know them, understand them, and ask them if and how they want your support—this is how we advocate with. Many groups that have been historically marginalized in the United States were done so under the guise of helping. One example of this relates to the Indian boarding schools.
From the beginning of the formation of the United States into the 19th century, a central agenda for many government officials was to acquire Indigenous lands (e.g., Indian Removal Act of 1830). By 1876, the majority of lands had been seized, and native people were forced to either relocate or live on reservations. Captain Richard H. Pratt believed that this segregation was wrong and supported better treatment for the native people. He delivered a speech at the Nineteenth Annual Conference of Charities and Correction regarding how to reeducate Native Americans/American Indians, where he proclaimed the only course was to “Kill the Indian, and Save the Man.” In that, to save the Indian, full assimilation into White European culture was required. Thereafter, the government and religious organizations established boarding schools (for more information, see this article). General Platt would have seen himself as an advocate. However, his actions led to the abuse of many children under the care of these schools, loss of cultural identity, and disruption of the parental relationship, and are seen as the prominent predecessor to many of the existing problems for some American Indians/Native Americans. Advocacy is crucial in the counseling profession. However, it needs to be done in a culturally competent and collaborative manner. I have been approached by researchers to ask for my assistance working in the Indigenous populations. However, when I ask them if they reached out to the community they want to research in, they most often say “no.” I believe it is crucial to be part of the community before you engage in research with the community. Learn what would be beneficial to the community, not just what will get the researcher published and/or grant funding.
- As a follow-up to the previous questions, where did this passion and pursuit originate for you?
For me, it has a both personal and professional origination and intersection. I am a linear descendent of the Chickasaw tribe. I grew up not knowing a lot about my heritage because my father was trying to protect our family. His lived experience was that it was not safe to let people know. So, our heritage remained closeted the majority of my life. For almost 20 years I worked as a paralegal. The majority of my work supported lawyers focusing on criminal and family law, which included federal law related to reservation crimes. I saw so many judicial problems occurring with many American Indian/Native American individuals, which made me curious about the reasons. I was repeatedly told “that is just how those people are.” Now, I knew that was not true because I was one of those people. I got frustrated with the pattern of what I was seeing and felt I was more part of the problem than the solution. At the age of 39, I decided to go back to school to pursue a different career.
During my undergraduate studies, I chose to take an American Indian/Native American history class to understand more. My father supported my quest for knowledge and started to share our heritage with me. This class helped me understand more about the historical components of the why. During my master’s studies, I first heard the term historical trauma. I began to research this concept and more parts of the why were answered for me. For my doctoral studies, I sought a program that specialized in multicultural competency to assist me in gaining more knowledge. However, I was still struggling with truly embracing my biracial identity—then fate interceded. I was the director of clinical experiences at the university where I was working. I received an email from a local reservation that they lost funding and had to let some counselors go and they wondered if we had any interns. No interns were available, so I said I would go. I was assigned a supervisor and during our first supervision session she said to me, “So, when are you going to tell me you’re Indian?” I started stumbling over excuses about how I was only part, and that I was not really raised a part of the culture. And she said two pivotal things to me: “You are not part, your Indian blood flows through all of you” and “Do you know how powerful it would be for the adolescents that you are going to work with to see someone from their people that is a counselor and doctor? How much you can encourage them?” She was right. I do this work to advocate for my people. That is my passion.
- Having a background in mental health and substance use counseling, what has been your experience navigating comorbidity? What changes have you seen socially and culturally as a result of the ever-changing landscape in our current society?
When I co-led my first substance abuse group as a practicum student 17 years ago, the focus was on the substance of abuse (i.e., consequences of use, identifying triggers, and changing behavior to not use). There was little discussion regarding trauma or other comorbid mental health disorders. All therapy work was done in group format. This did not leave space for individual counseling to assist clients with working through their own personal mental health struggles. When I was working at a large urban treatment facility, we were not allowed to engage in individual therapy. To meet the needs of my clients, I requested to conduct individual counseling with my group members who met the criteria for comorbidity. I was told that I could, but I would not be paid for the individual sessions and offered to clients pro bono. I agreed. Once I started working with my clients in both individual and group sessions, I saw so much improvement.
I have slowly been seeing a change in this perspective and clients getting counseling for both their substance use and other mental health concerns with the inclusion of holistic interventions. However, lately I have seen a focus more on mental health counseling only. In fact, through survey research by the Substance Abuse and Mental Health Services Administration (2022), it was found that of the 5.8 million adults aged 18 or older who reported a co-occurring mental health and illicit drug or alcohol use disorder in the past year, most (81.5%) received only mental health services. I think it is important that if a counselor is going to work with individuals who meet the criteria for comorbidity, they should be trained in both specialties. I know my educational training and clinical supervised experiences in both have been crucial to successful client outcomes.
The emergence of reality shows (e.g., Addicted, Intervention, Celebrity Rehab) and scripted shows (e.g., Euphoria, Mom, Nurse Jackie, Painkiller) related to addiction have changed how our society views addiction. These shows have allowed the general public to understand more about drug use, how people become addicted, and the consequences of addiction. I believe this has resulted in our society understanding that addiction is a disease and the person with the addiction needs treatment and support, not punishment and disdain. While media has brought some insight to substance use, words such as addict, alcoholic, drunk, and junkie are still being regularly utilized. Rather than these labeling words that are shame producing, person-first language (e.g., person with a substance use disorder) is critical to creating a therapeutic environment.
- It appears service is also an integral part of your counseling identity. What does service mean to you at the local, community, national, and international level?
Service for me encompasses two main concepts: 1) leaving things better than how I found them and 2) working for a cause not for applause. Active involvement in the department, college, university, profession, and community is an important component of service for me as a faculty member. However, I believe all service should first start on the local level. The analogy of putting your oxygen mask on first applies here. First give oxygen to your local stakeholders. I actively volunteer where gaps have been identified in my microsystem and work to fill these breaches to better serve clients and students. I then move onto service in the macrosystem. I strive to be strategic with the opportunities. We cannot be everything to everyone. Throughout my career, I have said no to roles because I knew that I did not have the bandwidth to do them competently. Service, to me, means making sure that I am only taking on those roles for which I have the time and energy to do well.
I have been honored to be appointed and elected to leadership roles in state and national organizations, serve on several editorial boards, and be selected to present at numerous national and international conferences. I value these opportunities and appreciate these roles and opportunities to provide service to the profession. However, I believe the most impactful service I have done relates to service that has no recognition by a title or line of my curriculum vitae (e.g., pro bono counseling, supervision for licensure, and workshops; consultation; mentorship). This also connects back to advocacy and leaving people with more than what they had, which are core values for me and how I hope to always operate as a counselor educator.
- What three challenges to the counseling profession as it exists today concern you most?
Counselors-in-training, professional counselors, and counselor educators not doing their own counseling work. I see the concept of the wounded healer being manifested more and more in our profession. In my opinion, this is strongly related to the aftermath of the COVID-19 pandemic. The pressure counselors, clinical supervisors, and educators had on them to immediately adjust to the new norm of telecounseling, online education, and the increase in individuals seeking service caused a perfect storm. In connection with the above is the predatory use of pre-licensed counselors. Given the jurisdictional differences related to the scope of practice and insurance companies’ view of pre-licensed counselors, the ability to bill or bill under a supervisor varies widely. This can lead to some agencies and practices over-scheduling pre-licensed counselors or bringing in too many supervisees to be supervised and, thus, supervision quality is compromised. The financial costs of a graduate education and the need to get those required hours results in many students and those working on their hours toward licensure being in a vulnerable position with little recourse to do anything regarding these situations. Lastly, there seems to be a lack of focus on evidence-based practices and research being conducted with clients. In the academic world, we have access to the latest peer-reviewed articles, and there is a research culture that motivates and encourages us to research and add to the literature. However, in the practice world, there may not be as much encouragement of counselor research engagement, consumption, and production. Therefore, there is a need to continue to find ways to bridge the research-to-practice gap and promote more counselors conducting research and gathering data with clients.
- What needs to change in the counseling profession for these three concerns to be successfully resolved or addressed?
As educators and supervisors, we need to do better with talking about going to counseling. I still do tune-ups with my counselor. We need to acknowledge what we do is difficult and that it is important that we continue our own self-care and our own work. I think we talk the talk about self-care; however, how often do we walk the walk? Are we providing space for our students and supervisees? Are we providing space for ourselves? Professional counselors, whether in training or practicing, need to remember counselor heal thyself first and to do their own work to avoid burnout and unethical practice. As our profession continues to grow, the need for good training sites and competent supervisors will continue to be a concern. I believe the responsibility for developing support for supervisors in the field is with counselor educators. We have resources and time allotted to us to work on strategies to better train and guide supervisors in the field and to advocate for more financial support for counselors-in-training. Lastly, in order for more practitioners in the field to gain access to the new developments in evidence-based practices, more counseling-related journals need to be open-access. We also need to find more ways to disseminate counseling research where counselors may tend to access information such as at scholarly conferences, in Counseling Today, and on social media platforms like the Mental Health Research Facebook page. Additionally, to get counselors more involved with conducting research and gathering data with their clients, more educators need to include practitioners as co-researchers on their studies. Ultimately, research to develop evidence-based practices should be seen as part of our service to our profession and advocacy for the clients we serve.
This concludes the ninth interview for the annual Lifetime Achievement in Counseling Series. TPC is grateful to Joshua D. Smith, PhD, NCC, LCMHC, and Neal D. Gray, PhD, LCMHC-S, for providing this interview. Joshua D. Smith is an assistant professor at the University of Mount Olive. Neal D. Gray is a professor at Lenoir-Rhyne University. Correspondence can be emailed to Joshua Smith at jsmith@umo.edu.
References
Council for Accreditation of Counseling and Related Educational Programs. (2024). Find a program. https://www.cacrep.org/directory
Ruffalo Noel Levitz. (2022). 2021 graduate student recruitment report. https://www.ruffalonl.com/papers-research-higher-education-fundraising/graduate-student-recruitment-report-2
Substance Abuse and Mental Health Services Administration. (2022). Key substance use and mental health indicators in the United States: Results from the 2021 National Survey on Drug Use and Health (HHS Publication No. PEP22-07-01-005, NSDUH Series H-57). Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/data/report/2021-nsduh-annual-national-report
Vineyard, T. E. (2019). The use of an online readiness assessment to determine necessary skills, aptitude, and propensities for successful completion in a secondary online credit course [ProQuest Information & Learning]. In Dissertation Abstracts International Section A: Humanities and Social Sciences (Vol. 80, Issue 2–A(E)).
May 15, 2024 | Book Reviews
edited by James P. Sampson, Jr., Janet G. Lenz, Emily Bullock-Yowell, Debra S. Osborn, and Seth C. W. Hayden
 I don’t know how to make this choice. While working in a university career center, I have heard these words of distress countless times from students who were feeling the unbearable weight of making a decision that they saw as having the power to shape their future, their lives, and their identities in significant and lasting ways. Fortunately, during a vocational psychology course, I studied cognitive information processing (CIP) theory, the pyramid of information processing, and the CASVE cycle, which gave me the confidence and competence to navigate the complicated decision-making process with students who felt emotionally and mentally overwhelmed by academic and career choices.
I don’t know how to make this choice. While working in a university career center, I have heard these words of distress countless times from students who were feeling the unbearable weight of making a decision that they saw as having the power to shape their future, their lives, and their identities in significant and lasting ways. Fortunately, during a vocational psychology course, I studied cognitive information processing (CIP) theory, the pyramid of information processing, and the CASVE cycle, which gave me the confidence and competence to navigate the complicated decision-making process with students who felt emotionally and mentally overwhelmed by academic and career choices.
The need to make occupational decisions is universal. Cognitive Information Processing: Career Theory, Research, and Practice provides a comprehensive exploration of CIP theory, which serves as the theoretical framework for understanding the cognitive processes that affect how individuals interpret and utilize career-related information to guide their career choices.
Drawn from both cognitive and counseling psychology, CIP theory underscores the various mental processes involved in career decision making, including information gathering, self-awareness, and goal setting. As a career intervention, CIP theory is intended to assist individuals with career-related problems by enhancing their understanding of both problem solving and decision making. One tool used to accomplish this goal is the CASVE cycle. With each letter representing a step in the decision-making model, readers are guided through a structured process that helps them make informed choices. By following this model, individuals can be supported in avoiding impulsive decisions, minimizing risks, and increasing the likelihood of achieving their desired outcomes.
Published in 2023, this book focuses on integrating theory, research, and practical applications, making it an invaluable resource with applicability across a multitude of domains. Educators and researchers studying vocational behavior and aspiring to understand the future direction(s) of CIP theory would benefit from consulting Chapter 21. Likewise, practitioners seeking evidence-based career interventions and individuals navigating the complexities of career decision-making will discover instrumental guidance in the chapters dedicated to understanding occupational, educational, and training choices, as well as those exploring the psychological and developmental factors influencing an individual’s readiness to make career decisions. For employment agencies and government policymakers aiming to establish career-focused initiatives, Chapter 16 offers both a comprehensive blueprint and essential resources for developing and executing successful career services programs.
One of the book’s strengths, as stated above, is its integration of theory with practical applications. Each chapter provides insights into how CIP theory can be translated into effective career counseling interventions. The authors lay out the discussion of complex factors that affect career decisions in a straightforward and digestible manner. Practitioners and individuals will find a set of easily understandable concepts that will equip them with the knowledge and skills needed to inform effective and satisfying academic and career decision making. Through case studies, reflective exercises, practical guidelines, and summaries offered at the end of each chapter, readers will find that these skills can also be applied to a myriad of decision-making opportunities.
In addition to its theoretical and practical contributions, this book’s attention to the impact of systemic inequalities and cultural factors on career opportunities and outcomes is also notable. The authors expertly promote a culturally sensitive approach to career counseling that recognizes, respects, and affirms the diversity of individuals’ identities, values, and beliefs. They further emphasize the significance of an inclusive and empowering counseling atmosphere that fosters clients’ self-awareness and agency while making career choices. Case examples and reflective activities are presented to encourage readers to examine their own biases and assumptions that may hinder a culturally competent approach to career counseling.
Cognitive Information Processing: Career Theory, Research, and Practice is published through Florida State Open Publishing as an open-access resource. By making the book available for free, the authors have eliminated the financial barrier to accessing this invaluable asset aimed at equipping readers with theory-based knowledge of vocational behavior and career interventions. This accessibility benefits students, educators, researchers, practitioners, and anyone wanting to establish cost-effective and evidence-based career development intervention programming that helps individuals to make informed career decisions across their life span.
Sampson, J. P., Jr., Lenz, J. G., Bullock-Yowell, E., Osborn, D. S., & Hayden, S. C. W. (Eds.). (2023). Cognitive information processing: Career theory, research, and practice. Florida State Open Publishing. https://manifold.lib.fsu.edu/projects/cognitive-information-processing-career-theory-research-and-practice
Reviewed by: Nikkie Bailey, MS, LCSW
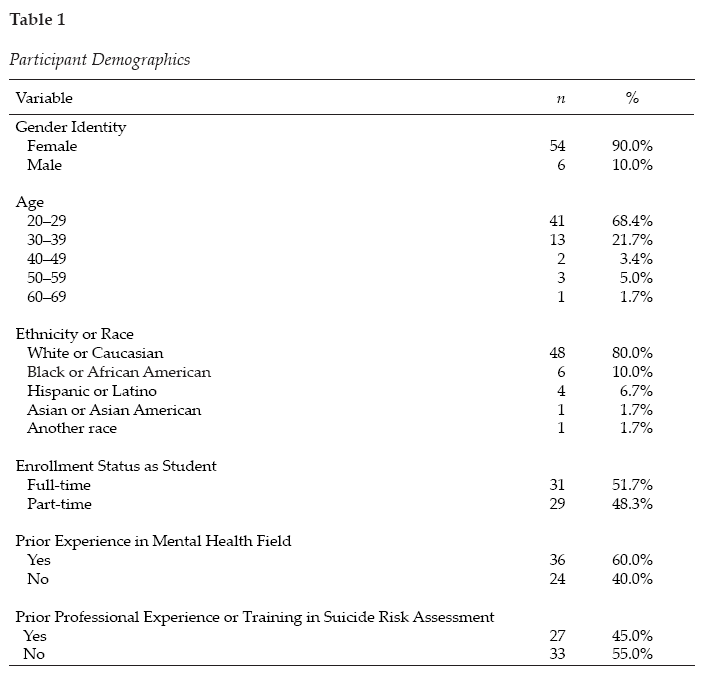
 Kathleen Brown Rice, PhD, NCC, ACS, LPC-S (TX), LPC (SD), LCMHC (NC), is a professor of counselor education in the College of Education at Sam Houston State University. She obtained her CACREP-accredited PhD in counselor education and supervision from the University of North Carolina at Charlotte and her CACREP-accredited Master of Science in counseling from South Dakota State University. Dr. Rice is a Licensed Professional Counselor-Supervisor in Texas, a Licensed Professional Counselor in South Dakota, and a Licensed Clinical Mental Health Counselor in North Carolina. Additionally, she holds the National Certified Counselor and Approved Clinical Supervisor credentials. She has worked as a professional counselor in various clinical settings and currently operates a private practice assisting clients with mental health, trauma, and substance abuse issues. Dr. Rice’s scholarly research activity focuses on counselor supervision and training with an emphasis in ethical considerations; the implications of historical and generational trauma; and the impact of substance abuse on individuals, families, and the community. She also incorporates the use of biomarkers in her research to understand emotional regulation, risky behaviors, and resiliency. As part of her extensive scholarship, she serves as an expert peer reviewer on the TPC Editorial Review Board.
Kathleen Brown Rice, PhD, NCC, ACS, LPC-S (TX), LPC (SD), LCMHC (NC), is a professor of counselor education in the College of Education at Sam Houston State University. She obtained her CACREP-accredited PhD in counselor education and supervision from the University of North Carolina at Charlotte and her CACREP-accredited Master of Science in counseling from South Dakota State University. Dr. Rice is a Licensed Professional Counselor-Supervisor in Texas, a Licensed Professional Counselor in South Dakota, and a Licensed Clinical Mental Health Counselor in North Carolina. Additionally, she holds the National Certified Counselor and Approved Clinical Supervisor credentials. She has worked as a professional counselor in various clinical settings and currently operates a private practice assisting clients with mental health, trauma, and substance abuse issues. Dr. Rice’s scholarly research activity focuses on counselor supervision and training with an emphasis in ethical considerations; the implications of historical and generational trauma; and the impact of substance abuse on individuals, families, and the community. She also incorporates the use of biomarkers in her research to understand emotional regulation, risky behaviors, and resiliency. As part of her extensive scholarship, she serves as an expert peer reviewer on the TPC Editorial Review Board. I don’t know how to make this choice. While working in a university career center, I have heard these words of distress countless times from students who were feeling the unbearable weight of making a decision that they saw as having the power to shape their future, their lives, and their identities in significant and lasting ways. Fortunately, during a vocational psychology course, I studied cognitive information processing (CIP) theory, the pyramid of information processing, and the CASVE cycle, which gave me the confidence and competence to navigate the complicated decision-making process with students who felt emotionally and mentally overwhelmed by academic and career choices.
I don’t know how to make this choice. While working in a university career center, I have heard these words of distress countless times from students who were feeling the unbearable weight of making a decision that they saw as having the power to shape their future, their lives, and their identities in significant and lasting ways. Fortunately, during a vocational psychology course, I studied cognitive information processing (CIP) theory, the pyramid of information processing, and the CASVE cycle, which gave me the confidence and competence to navigate the complicated decision-making process with students who felt emotionally and mentally overwhelmed by academic and career choices.