Aug 18, 2020 | Volume 10 - Issue 3
Melissa Sitton, Tina Du Rocher Schudlich, Christina Byrne, Chase M. Ochrach, Seneca E. A. Erwin
A family systems framework guided our investigation of self-injurious behavior (SIB) in adolescents. As part of a larger study, we collected data examining SIB and family functioning from 29 adolescents (Mage = 15.66) and their caregivers. These adolescents with traits of borderline personality disorder were seeking counseling from community-based practitioners specializing in dialectical behavior therapy. Our primary aim was to better understand the family environment of these adolescents. A second aim was to elucidate interrelations among family communication, roles, problem-solving, affective involvement, affective responsiveness, behavioral control, and conflict and SIB. We found a high rate of SIB among adolescent participants. There was significant congruence between adolescent and caregiver reports of the family environment, with families demonstrating unhealthy levels of functioning in several indicators of family environment. The latent variable of family functioning significantly predicted nonsuicidal and ambivalent SIB. Counselors working with adolescents should consider family functioning when assessing risk for SIB.
Keywords: self-injurious behavior, adolescents, family systems, borderline personality disorder, family functioning
Although emotion dysregulation and unstable personal relationships are common for adolescents, those with symptoms of borderline personality disorder (BPD) often report more extreme experiences (A. L. Miller et al., 2008). BPD is characterized by impaired or unstable emotional and social functioning (American Psychiatric Association, 2013). Individuals with BPD—especially adolescents—may experience impairments in daily functioning as well as within interpersonal relationships (Chanen et al., 2007).
Linehan’s (1993) biosocial theory proposed that BPD can result from an individual’s biological predisposition toward emotion dysregulation and a social environment that amplifies this vulnerability. Given that adolescents spend a substantial amount of time with their family, it is important to examine an adolescent’s familial environment to understand the etiology of BPD symptoms; such examination requires a framework like family systems theory, which emphasizes the relationships between family members rather than focusing on the individual members themselves (Goldenberg & Goldenberg, 2013); this includes family communication, roles, problem-solving, affective involvement, affective responsiveness, and behavioral control (I. W. Miller et al., 2000).
Self-Injurious Behavior (SIB)
Regrettably, it is common for adolescents with BPD to engage in SIB (Kaess et al., 2014). SIB is an umbrella term for all purposeful, self-inflicted acts of bodily harm, whether the intent is suicidal, nonsuicidal (i.e., nonsuicidal self-injury), or ambivalent (i.e., neither strictly suicidal nor nonsuicidal). In fact, SIB is one diagnostic criteria for BPD in adolescents and adults.
Although originally developed to explain the etiology of BPD, the biosocial theory has been applied to the development of SIB as well (Crowell et al., 2009). Countless studies have examined the role of emotion dysregulation and affective reinforcement in SIB, but it is important to also consider the influence of social variables. Indeed, in their four-function model, Nock and Prinstein (2004, 2005) suggested that both affective and social variables can positively and negatively reinforce nonsuicidal SIB. Similarly, Joiner’s (2005) interpersonal theory of suicidal SIB posited that social variables (particularly thwarted belongingness and perceived burdensomeness) drive the desire for suicide. Thus, although there are clear links between affective variables and SIB, social variables are also relevant. For adolescents, an important social variable related to SIB is family environment. From the family systems approach, adolescent SIB is best understood when rooted in the context of family environment. As Levenkron (1998) suggested, “the ways in which all the family members relate to each other… [is] the fuel that drives [SIB]” (pp. 125–126).
Although limited in number, some previous studies have examined family environment and SIB in adolescents. For example, Halstead et al. (2014) found that SIB was related to dysfunctional family environments. Studies have also found relationships between adolescent SIB and familial communication (Halstead et al., 2014; Latina et al., 2015) and conflict (Huang et al., 2017). Additionally, Adrian et al. (2011) demonstrated a link between stress and failure to meet expectations of familial roles. To our knowledge, no studies to date have examined SIB and familial problem-solving, affective involvement, affective responsiveness, and behavioral control. However, studies have linked SIB to an individual’s lack of problem-solving skills (Walker et al., 2017), ability to regulate affective responses (Adrian et al., 2011), and behavioral control related to impulsivity and compulsivity (Hamza et al., 2015).
Current Study
Despite the clear influence of family members on SIB (Halstead et al., 2014) and the significant amount of time adolescents tend to spend with family members, more research is needed to evaluate family environment in relation to SIB. Specifically, we investigated the families of treatment-seeking adolescents with traits of BPD who engage in SIB. Our objectives were to: (a) assess family environment using multiple indicators of family functioning, (b) assess SIB in these treatment-seeking adolescents, including SIB done with suicidal intent, nonsuicidal intent, and ambivalence toward life, and (c) evaluate family functioning as a statistical predictor of lifetime SIB.
Method
Participants and Procedure
We used data from a larger ongoing, unpublished study on dialectical behavior therapy. In the larger study, participants were adolescents and young adults who sought counseling from community-based clinicians specializing in dialectical behavior therapy. Participants sought counseling for symptoms of BPD, particularly SIB. The counselors recruited participants for the research study by explaining voluntary research participation during their standard intake process for new clients at the clinic. The counselors also obtained informed consent for research from the participants. The counselors collaborated with researchers at a local university for this larger study, and the university’s IRB approved the study.
For the current study, we used the existing pretest data from the adolescents only (N = 29; Mage = 15.66, SDage = 1.34, age range = 13–18). A majority of the adolescent sample (82.8%; n = 24) reported no previous experience with counseling. This sample was predominately Caucasian (82.8%; n = 24) and most adolescents identified as female (89.7%; n = 26).
Caregiver participants (N = 29) were involved in the adolescents’ treatment and the accompanying research study. Most caregiver participants were the biological mother (81.5%; n = 22) or adoptive mother (7.4%; n = 2). However, a few adolescents were accompanied by an extended family member (7.4%; n = 2) or their biological father (3.7%; n = 1). A majority of adolescents reported that at least one of their caregivers had attended some (22.2%; n = 6) or all (29.6%; n = 8) of college, or some (3.7%; n = 1) or all (29.6%; n = 8) of graduate school.
Most adolescents reported they currently lived with both biological parents (58.6%; n = 17) or at least one biological parent (31.0%; n = 9), though some lived with non-biological parents or caregivers (10.3%; n = 3). Most adolescents (86.2%; n = 25) also reported having at least one sibling; 58.6% of adolescents (n = 17) reported having at least one biological brother, 37.9% had at least one biological sister (n = 11), and 24.1% had a half- or step-sibling (n = 7). One-way analysis of variance (ANOVA) tests demonstrated that adolescents did not differ in total SIB based on family characteristics (e.g., number of siblings, number of employed caregivers; all values of p > .05).
Measures
Family Functioning
The Family Assessment Device (FAD; Epstein et al., 1983) is a 53-item measure with a 4-point Likert scale used to rate agreement with statements about how the adolescents’ family members interact and relate to each other (e.g., “After our family tries to solve a problem, we usually discuss whether it worked or not”). Both adolescents and caregivers completed the FAD. Subscales of the FAD assess six dimensions of family functioning, including family problem-solving, roles, communication, affective responsiveness, affective involvement, and behavioral control. The scores for each subscale are averaged, with higher scores indicating worse functioning and more problems within families. The FAD has good test-retest reliability and construct validity (I. W. Miller et al., 1985). In this study, the reliability of the FAD was excellent for both samples (Cronbach’s alpha = .95 for adolescents and .96 for caregivers).
The Conflict Behavior Questionnaire (CBQ; Prinz et al., 1979) assesses self-reported familial interactions within the past two weeks. The CBQ has both an adolescent and a caregiver version; both versions consist of 20 true/false items. Scores can range from 0 to 20, with higher scores indicating more conflict between caregiver and adolescent. Studies have shown that CBQ scores delineated between distressed and non-distressed families (Robin & Foster, 1989). The CBQ has good internal consistency and test-retest reliability (Rallis et al., 2015; Robin & Foster, 1989), as well as construct validity (Prinz et al., 1979). In the current study, the reliability of the CBQ was excellent for both samples (Cronbach’s alpha = .88 for adolescents and .92 for caregivers).
Self-Injurious Behavior (SIB)
We used the Lifetime Suicide Attempt Self-Injury Interview (LSASI; Linehan & Comtois, 1996) to assess participants’ history of SIB, including frequency, method, and intent. Using 20 items, the LSASI asks participants to report the dates of the most recent and most severe SIB, as well as their lifetime frequency of 11 different methods of SIB with suicidal intent, without suicidal intent, and with ambivalence. Participants also report the total frequency of each SIB method (combining suicidal, nonsuicidal, and ambivalent), and the number of times medical treatment was received for the SIB method. Higher scores indicate more SIB in the past. In the current study, reliability across all SIB intent types (four variables: suicidal SIB, nonsuicidal SIB, ambivalent SIB, and total SIB) was .65. Because the LSASI was designed for clinical use rather than research, to our knowledge there are no existing studies demonstrating the reliability or validity of the LSASI. Notably, this measure was already in use at the counseling clinic, and the decision to use it for this research study was counselor-driven.
Data Analysis
As part of our preliminary analyses, we first tested all variables for the assumptions of analysis. Specifically, when examining the skew and kurtosis of the composite variables, we used ± 2 as our acceptable range of values. Following advice from Tabachnick and Fidell (2019), we transformed variables that did not meet our criteria for normality.
To better understand family functioning, we conducted descriptive analyses for all seven predictive variables (problem-solving, communication, roles, affective responsiveness, affective involvement, behavioral control, and conflict) separately for adolescent and caregiver scores. We assessed the degree of healthy family functioning using I. W. Miller et al.’s (1985) suggested cut-off scores, which can be used to distinguish between healthy and unhealthy family environments. We also conducted paired sample t-tests to compare the adolescent and caregiver reports of family functioning.
Next, we tested the fit of our theoretical model of family functioning using structural equation modeling (SEM) with maximum likelihood as the method of estimation. We used multiple fit indices to assess the model fit. Specifically, the chi-square statistic assesses absolute model fit, demonstrating good fit when not statistically significant. The chi-square test can also be used to compare the relative fit of two models. Additionally, comparative fit index (CFI), root mean square error of approximation (RMSEA), and standardized root-mean-square residual (SRMR) are all indicators of model fit, with 0.95 or higher, 0.05 or lower, and 0.08 or lower indicating good fit, respectively (for more information on SEM fit indices, see Hooper et al., 2008). Notably, Iacobucci (2010) suggested that researchers can use SEM and establish good model fit even with small samples.
We also conducted descriptive analyses of the participants’ self-reported SIB. We left these variables raw (untransformed) to evaluate how participants viewed their own SIB. We examined the specific SIB methods that participants reported using (e.g., cutting, burning) as well as three outcome variables (suicidal SIB, nonsuicidal SIB, and ambivalent SIB; all transformed because of issues with skew and kurtosis).
Lastly, we used SEM to predict SIB with the proposed model of family functioning. Given our small sample size, we conducted this analysis separately for suicidal SIB, nonsuicidal SIB, and ambivalent SIB. We set alpha at .05 for each model; given the small sample size, we did not apply corrections to the alpha for the multiple analyses.
Results
We used SPSS 24.0 and Amos 24 to analyze our data. Because this study was primarily descriptive, we conducted multiple analyses to better understand the family environment of treatment-seeking adolescents, experiences of SIB for adolescents, and the role of family environment in adolescent engagement in SIB.
Family Characteristics and Functioning
Means, standard deviations, and range of scores for the family functioning variables are shown in Table 1. With the exception of the caregiver reports on affective responsiveness and behavioral control, both adolescent and caregiver reports on every subscale of the FAD fell above the McMaster clinical cut-off (see Table 1) described by I. W. Miller et al.’s (1985) cut-off scores, indicating on average all of the families demonstrated unhealthy functioning. It is worth noting that adolescents and their caregivers reported similar levels in five of the seven indicators of family functioning from the FAD and CBQ (e.g., there was no statistical difference between the two reports, all values of p > .05). As shown in Table 1, adolescent and caregiver reports only statistically differed for behavioral control (t[28] = 4.23, p < .001) and communication (t[28] = 2.96, p = .006). Specifically, adolescents reported higher levels of both behavioral control and communication; these high levels are considered indicative of unhealthy or distressed families (I. W. Miller et al., 1985).
Table 1
Descriptive Statistics and Group Comparisons of Family Functioning Variables as Reported by Adolescents and Caregivers
| Variable |
|
Adolescent |
Caregiver |
|
|
|
Cut-Off |
M |
SD |
Range |
M |
SD |
Range |
t(28) |
p |
| Problem-solving |
2.2 |
2.58 |
0.65 |
1.00–3.80 |
2.29 |
0.57 |
1.40–3.80 |
1.88 |
.071 |
| Communication |
2.2 |
2.56 |
0.37 |
1.83–3.17 |
2.30 |
0.37 |
1.50–3.00 |
2.96 |
.006 |
| Roles |
2.3 |
2.58 |
0.37 |
1.75–3.38 |
2.45 |
0.37 |
1.75–3.38 |
1.57 |
.128 |
| Affective Resp. |
2.2 |
2.34 |
0.68 |
1.00–4.00 |
2.12 |
0.62 |
1.00–3.67 |
1.48 |
.151 |
| Affective Inv. |
2.1 |
2.37 |
0.28 |
1.71–3.00 |
2.44 |
0.23 |
1.86–3.00 |
– 1.61 |
.118 |
| Behav. Control |
1.9 |
2.12 |
0.44 |
1.00–3.11 |
1.77 |
0.41 |
1.00–2.78 |
4.23 |
< .001 |
| Conflict |
— |
9.60 |
4.83 |
0.00–18.00 |
10.05 |
5.67 |
1.00–20.00 |
– 0.46 |
.649 |
Note. Cut-Off = McMaster Cut-Off score; Affective Resp. = Affective responsiveness; Affective Inv. = Affective involvement; Behav. Control = Behavioral control.
We used SEM to test the fit of our theory-driven, congeneric model of family functioning using seven subscales from each source (14 variables; seven for adolescents and seven for caregivers, with the error terms of each subscale correlated between the two sources) to predict family functioning as reported by each source (two latent variables; one for adolescents and one for caregivers). The absolute fit of the model was marginal: χ2(69) = 104.39, p = .004, CFI = 0.79, RMSEA = 0.14, SRMR = 0.14.
In order to reduce variables in our theoretical model, we averaged adolescent and caregiver reports for problem-solving, roles, affective responsiveness, affective involvement, and conflict because these did not statistically differ (all values of p > .05). However, we kept the two reports as separate predictors for communication and behavioral control. This left us with nine predictor variables for subsequent analysis (five averaged predictors and four single-source predictors).
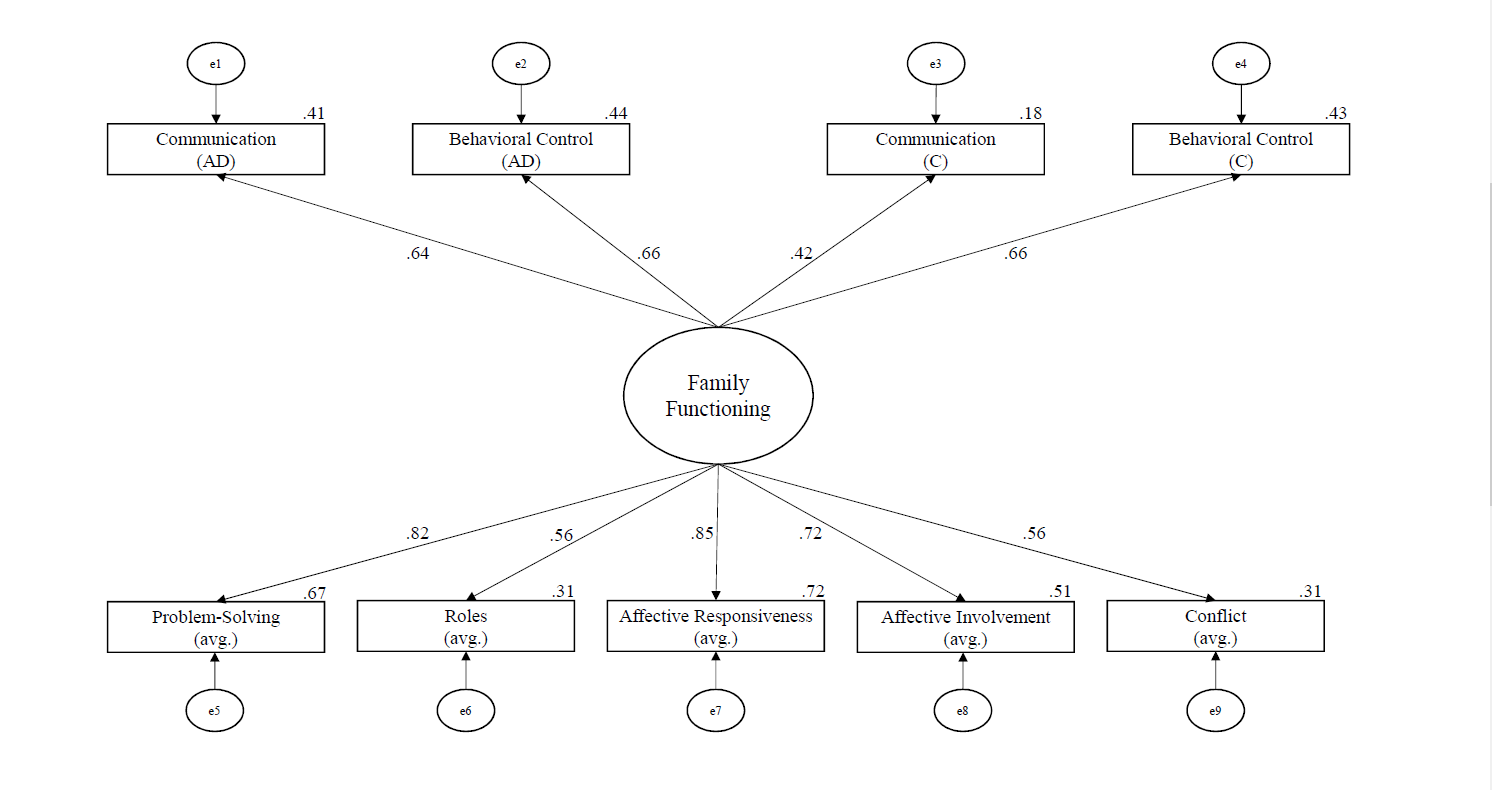
Next, we used SEM to test the fit of the simplified model with the nine observed variables and one latent variable of family functioning. We found that the absolute model fit of this simplified model was acceptable overall. Specifically, the fit indices mostly indicated good fit (χ2[27] = 33.11, p = .194, CFI = 0.93, SRMR = 0.08), though one fit index suggested poor fit (RMSEA = 0.09). Differences in the chi-squares of our two models showed the simplified model was statistically better than the initial model: χ2(42) = 71.28, p = .003. Thus, we selected the simplified model as the final model of family functioning (see Figure 1). See Table 2 for descriptive analyses of the nine predictors in the final model. All variables were positively related to family functioning. The strongest predictors of family functioning in this model were affective responsiveness (average of adolescent and caregiver report; β = .85, B = 1.04, SE B = 0.21, p < .001, R2 = .72), affective involvement (averaged; β = .72, B = 0.88, SE B = 0.22, p < .001, R2 = .51), and problem-solving (averaged; β = .82, R2 = .67; this was the constrained parameter used to identify the regression model).
Figure 1
The Output Structural Regression Model of Family Functioning Developed Using SEM
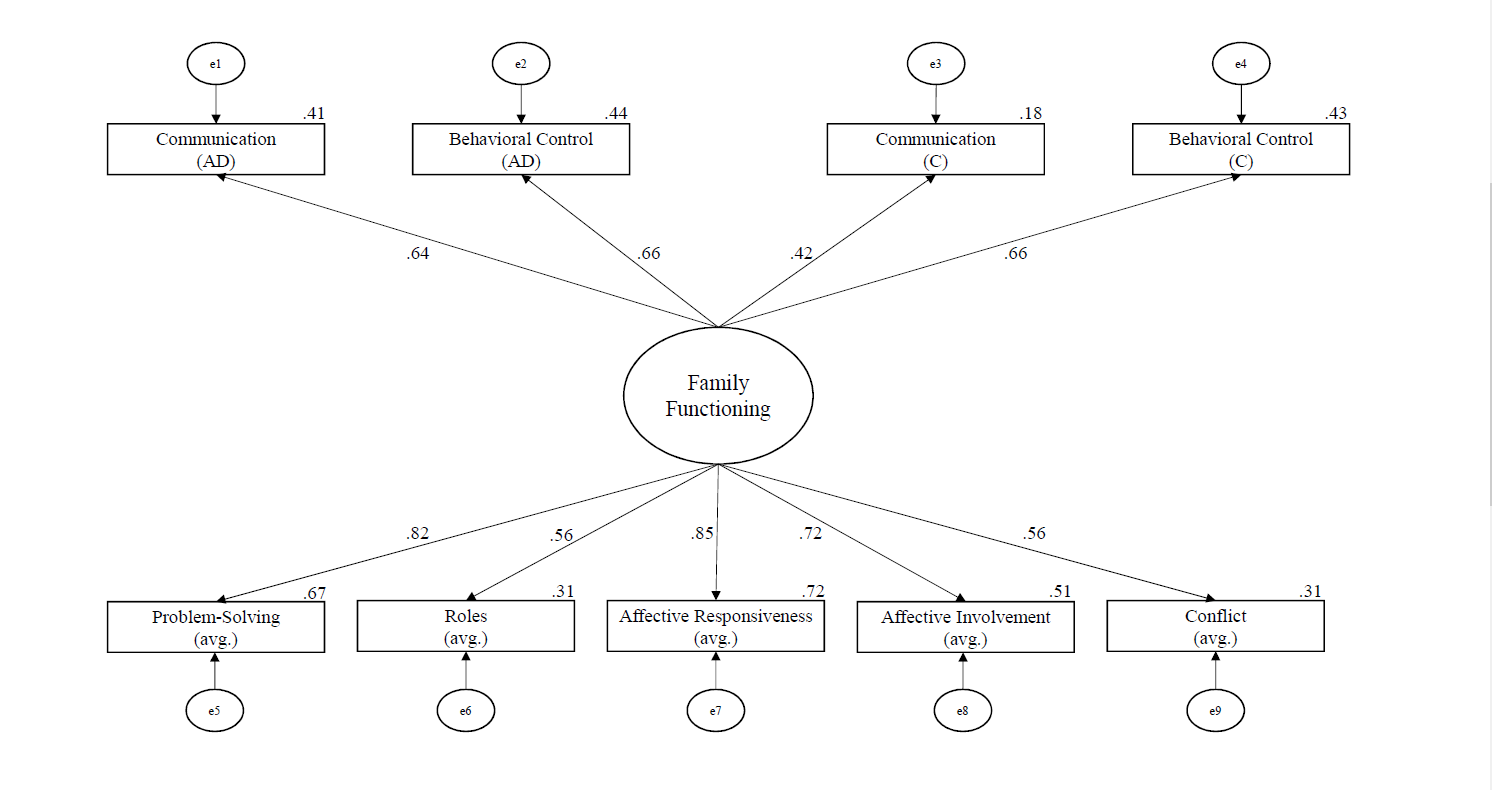
Note. The large circle represents a latent variable, boxes are measured variables, small circles (with “e”) are error terms, and solid lines show regression paths. The numbers on paths are the standardized path coefficients, and the offset values on endogenous variables are the R² effect sizes. (AD) = adolescent report; (C) = caregiver report; (avg.) = averaged score of adolescent and caregiver report.
Table 2
Descriptive Analyses of Predictors of Family Functioning
| Variable |
M |
SD |
| Problem-Solving |
2.43 |
0.44 |
| Roles |
2.51 |
0.29 |
| Affective Responsiveness |
2.23 |
0.51 |
| Affective Involvement |
2.40 |
0.23 |
| Conflict |
9.82 |
4.56 |
| Communication (AD) |
2.56 |
0.37 |
| Communication (C) |
2.30 |
0.37 |
| Behavioral Control (AD) |
2.12 |
0.44 |
| Behavioral Control (C) |
1.77 |
0.41 |
Note. (AD) = adolescent report; (C) = caregiver report.
Adolescent Engagement in SIB
All adolescents reported engaging in SIB in their lifetime, and the average lifetime frequency of SIB was 438.72 (SD = 1,216.65, range = 1–6,079; transformed to address normality: M = 4.41, SD = 1.80). Specifically, most participants reported engaging in nonsuicidal SIB (n = 26) and using it with higher frequency than SIB with other intent (i.e., suicidal or ambivalent SIB), with a lifetime average of 340.16 (SD = 975.22, range = 0–4,565; transformed: M = 3.49, SD = 2.25). Many adolescents also reported engaging in ambivalent SIB (n = 18), with moderate average frequency rates (M = 22.28, SD = 52.02, range = 0–248; transformed: M = 1.62, SD = 1.69). Lastly, fewer adolescents reported engaging in suicidal SIB (n = 18), with the lowest average lifetime frequency (M = 7.34, SD = 25.03, range = 0–136; transformed: M = 0.97, SD = 0.95). See Table 3 for descriptive information on SIB methods (e.g., cutting) used by adolescents in our sample. On average, participants used 3.78 (SD = 2.15) methods of SIB in their lifetime.
Table 3
Descriptive Statistics for All Self-Injurious Behavior Completed in One’s Lifetime (N = 29)
| Variable |
n |
Ma |
SDa |
Rangea |
n of Severe Cases |
| Cutting |
27 |
179.55 |
330.42 |
0–1,500 |
7 |
| Hitting head/body |
16 |
240.90 |
730.59 |
0–3,000 |
0 |
| Overdosing |
13 |
1.88 |
3.59 |
0–15 |
7 |
| Burning |
13 |
6.12 |
14.99 |
0–60 |
1 |
| Strangling/hanging |
8 |
2.18 |
6.42 |
0–30 |
0 |
| Stabbing/puncturing |
8 |
0.80 |
1.64 |
0–7 |
2 |
| Asphyxiating |
7 |
1.66 |
3.90 |
0–15.62 |
0 |
| Other |
6 |
272.92 |
602.33 |
0–1,500 |
2 |
| Jumping |
4 |
1.27 |
5.31 |
0–25 |
1 |
| Drowning |
4 |
0.40 |
.99 |
0–4 |
0 |
| Poisoning |
3 |
0.14 |
.36 |
0–1 |
1 |
Note. The descriptive statistics are based on the total self-injurious behavior, combining acts completed with suicidal intent, nonsuicidal intent, and ambivalence. Other = adolescent-reported participating in a type of self-injury that was not listed; Jumping = jumping from a high place to cause injury; Severe Cases = requiring medical treatment.
a The frequency that adolescents reported engaging in the various methods of self-injury.
Predicting SIB With Family Functioning
To understand the relationships between family functioning and SIB, we conducted correlational analyses of the three outcome variables and nine predictors. As shown in Table 4, problem-solving was moderately associated with ambivalent SIB (r = .44 , p = .018), conflict was moderately associated with nonsuicidal SIB (r = .38 , p = .049), and adolescent-reported communication was moderately to strongly associated with all three SIB variables (suicidal r = .61, p < .001; nonsuicidal r = .47, p = .011; ambivalent r = .56, p = .002). All associations were positive (see Table 4), meaning that worse family functioning scores were associated with more SIB.
Table 4
Bivariate Correlations Between Predictor Variables
|
1. |
2. |
3. |
4. |
5. |
6. |
7. |
8. |
9. |
10. |
11. |
| 1. Nonsuicidal SIB |
– |
|
|
|
|
|
|
|
|
|
|
| 2. Ambivalent SIB |
.35 |
– |
|
|
|
|
|
|
|
|
|
| 3. Suicidal SIB |
.16 |
.46* |
– |
|
|
|
|
|
|
|
|
| 4. Problem-Solving |
.35 |
.44* |
.19 |
– |
|
|
|
|
|
|
|
| 5. Roles |
.21 |
-.01 |
.27 |
.39* |
– |
|
|
|
|
|
|
| 6. Affect. Resp. |
.25 |
.36 |
.28 |
.68*** |
.42* |
– |
|
|
|
|
|
| 7. Affect. Involv. |
.22 |
.13 |
.27 |
.52** |
.43* |
.72*** |
– |
|
|
|
|
| 8. Conflict |
.38* |
.35 |
.26 |
.66*** |
.14 |
.45* |
.15 |
– |
|
|
|
| 9. Comm. (AD) |
.47* |
.56** |
.61*** |
.57** |
.44* |
.51** |
.50** |
.43* |
– |
|
|
| 10. Comm. (C) |
.09 |
.11 |
.04 |
.42* |
.28 |
.29 |
.29 |
.27 |
.17 |
– |
|
| 11. Beh. Cont. (AD) |
.27 |
.06 |
-.21 |
.54** |
.48** |
.51** |
.56** |
.34 |
.41* |
.25 |
– |
| 12. Beh. Cont. (C) |
.27 |
.26 |
.13 |
.49** |
.53** |
.61*** |
.36 |
.38* |
.33 |
.40* |
.47* |
Note. SIB = self-injurious behavior; Affect. Resp. = Affective Responsiveness; Affect. Involv. = Affective Involvement; Comm. = Communication; (AD) = adolescent report; (C) = caregiver report; Beh. Cont. = Behavioral Control.
* p < .05. ** p < .01. *** p < .001.
Next, we used SEM to predict SIB with our simplified model of family functioning. We tested three SIB outcomes separately because of concerns with sample size. For all models predicting SIB, we freed all FAD factors (problem-solving, roles, affective responsiveness, affective involvement, adolescent-reported communication and behavioral control, and caregiver-reported communication and behavioral control) to correlate because variables from the same measure are likely to be related.
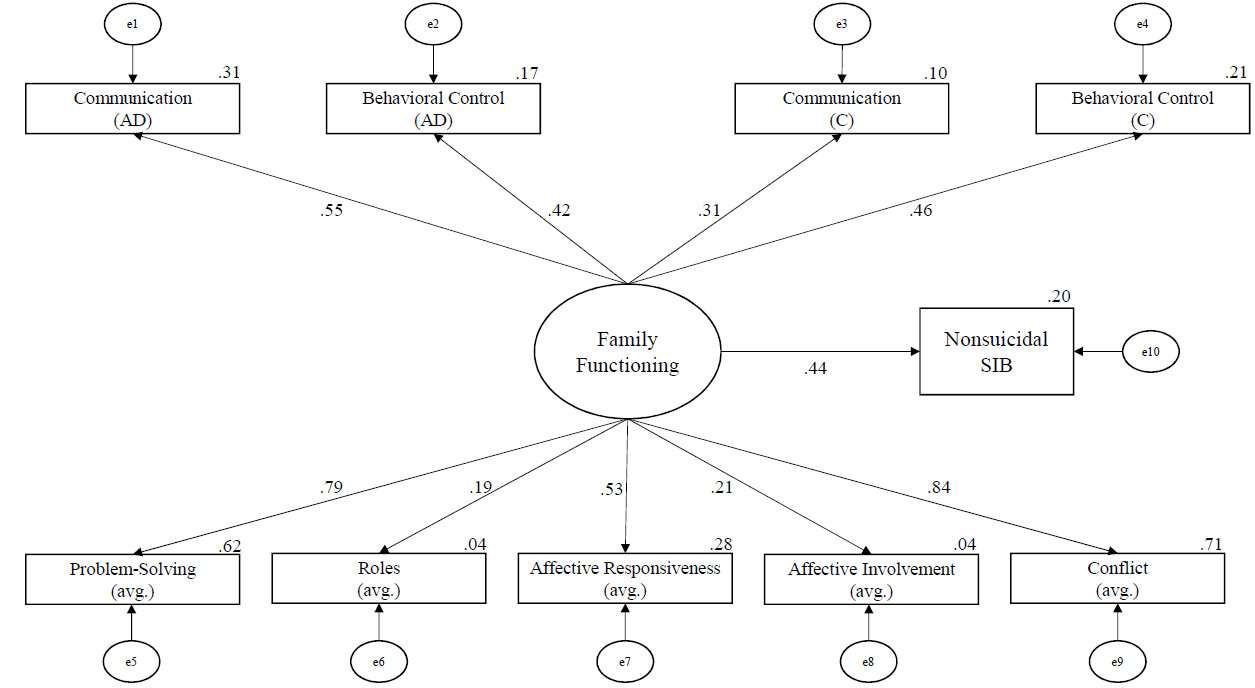
The model predicting nonsuicidal SIB had good absolute fit: χ2(7) = 4.28, p = .747, CFI = 1.00, RMSEA = 0.00, SRMR = 0.04. In all, family functioning explains 20% of the variance in nonsuicidal SIB. See Figure 2 for the standardized path coefficients between family functioning variables, the latent variable of family functioning, and nonsuicidal SIB. Notably, family functioning predicted nonsuicidal SIB:
β = .44, B = 1.27, SE B = 0.62, p = .039. Based on effect sizes (see Figure 2), the strongest predictors were problem-solving (averaged; β = .79, B = 0.90, SE B = 0.03, p = .008, R² = .62), communication (adolescent-reported; β = .55, B = 0.05, SE B = 0.03, p = .034, R² = .31), and conflict (averaged; β = .84, R² = .71; this was the constrained parameter used to identify the regression model).
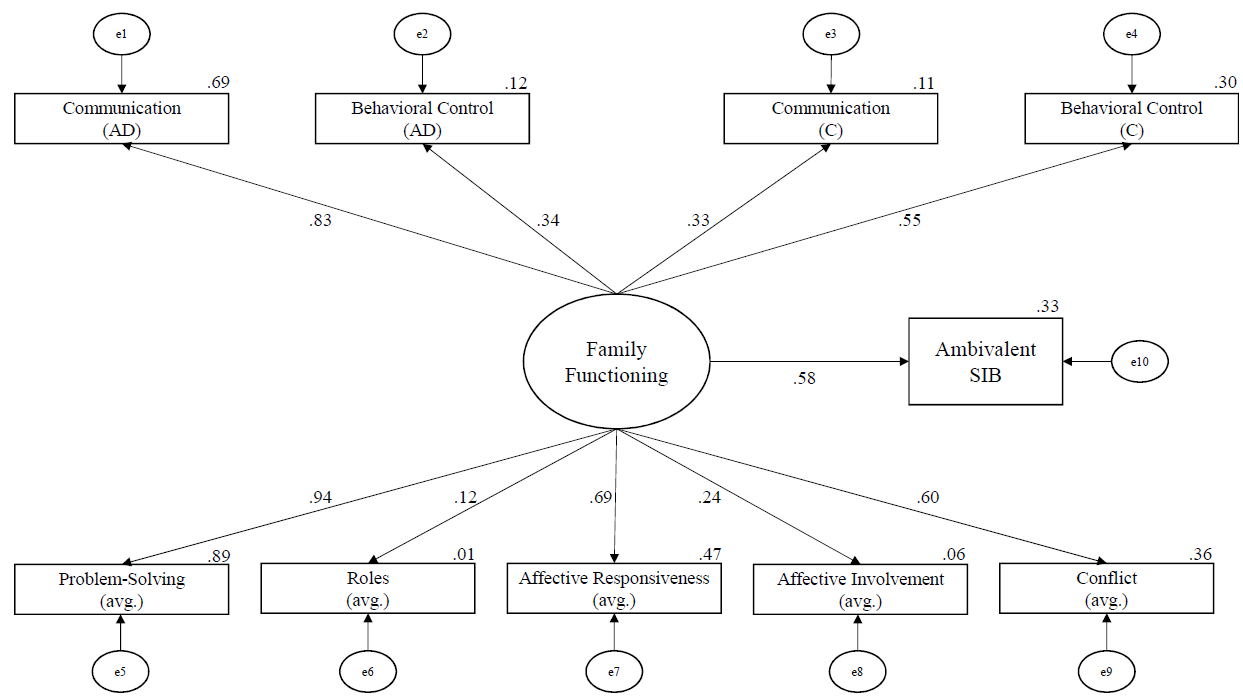
The model predicting ambivalent SIB had good absolute fit: χ²(7) = 5.69, p = .577, CFI = 1.00, RMSEA = 0.00, SRMR = 0.04. In all, family functioning explains 33% of the variance in ambivalent SIB. See Figure 3 for the standardized path coefficients between family functioning variables, the latent variable of family functioning, and ambivalent SIB. Notably, family functioning predicted ambivalent SIB: β = .58, B = 1.04, SE B = 0.46, p = .025. Based on effect sizes (see Figure 3), the strongest predictors were problem-solving (averaged; β = .94, B = 0.15, SE B = 0.07, p = .022, R² = .89), communication (adolescent-reported; β = .83, B = 0.11, SE B = 0.05, p = .030, R² = .69), and affective responsiveness (averaged; β = .69, B = 0.13, SE B = 0.07, p = .049, R² = .47).
Figure 2
The Output Structural Regression Model of Nonsuicidal SIB Developed Using SEM
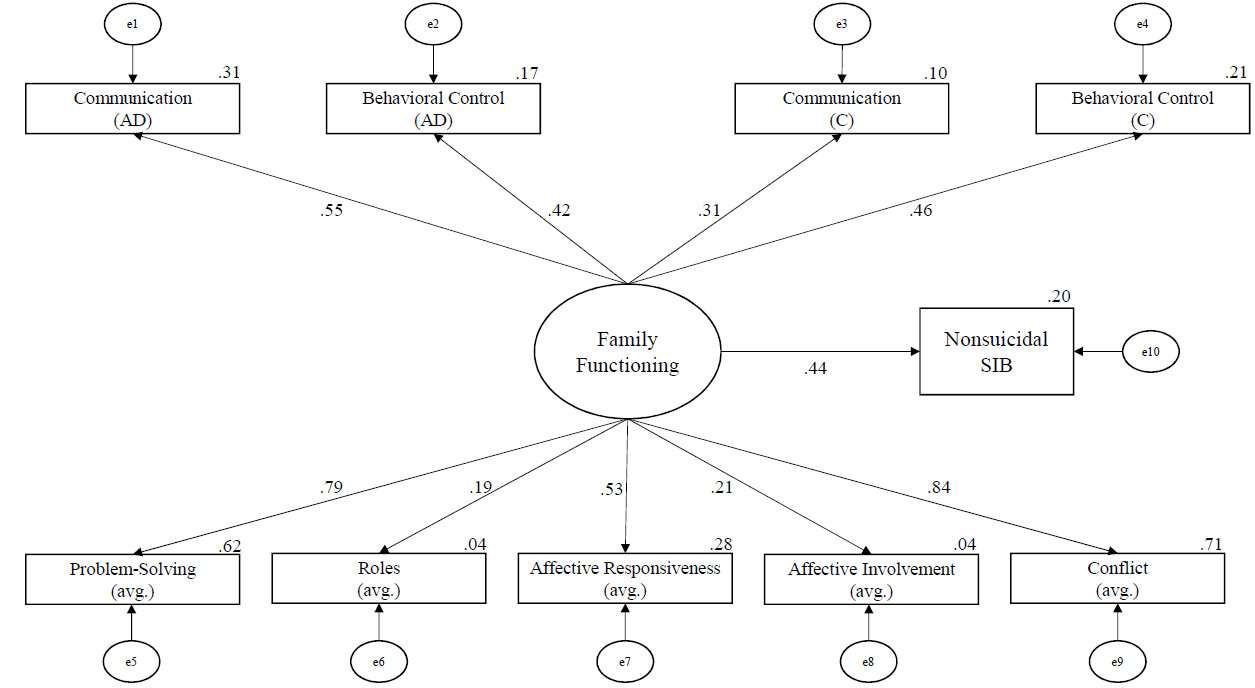
Note. The numbers on paths are the standardized path coefficients, and the offset values on endogenous variables are the R2 effect sizes. (AD) = adolescent report; (C) = caregiver report; (avg.) = averaged score of adolescent and caregiver report.
Figure 3
The Output Structural Regression Model of Ambivalent SIB Developed Using SEM
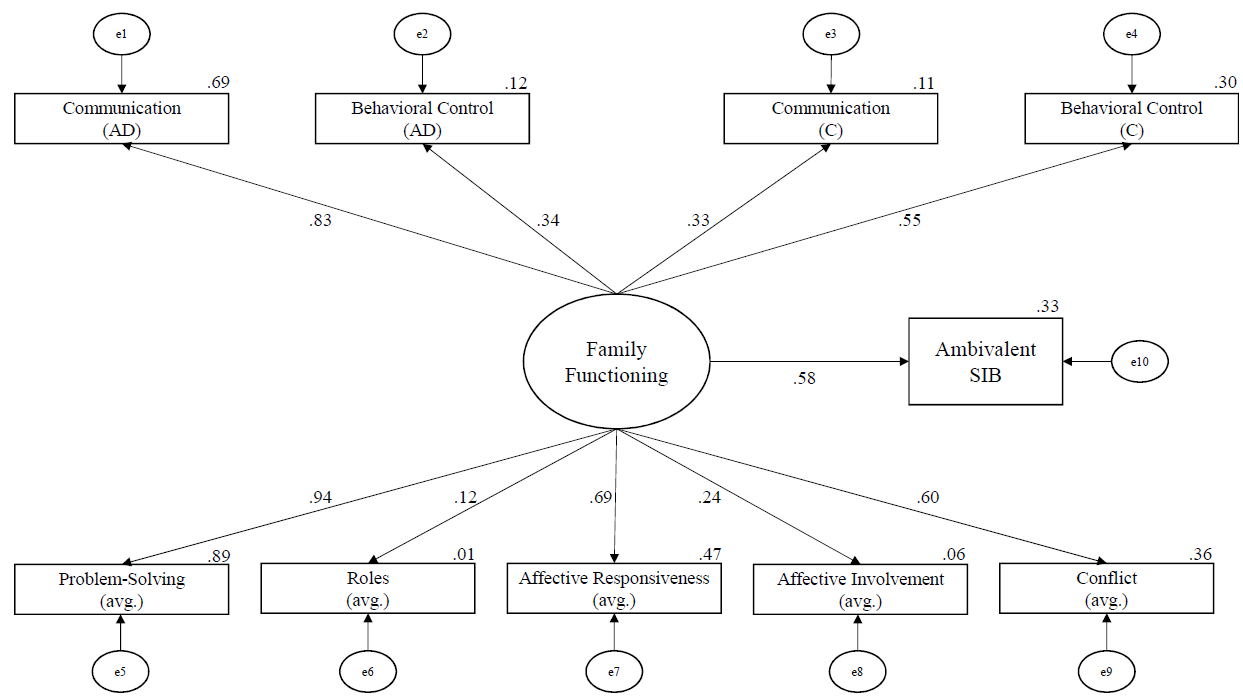
Note. The numbers on paths are the standardized path coefficients, and the offset values on endogenous variables are the R² effect sizes. (AD) = adolescent report; (C) = caregiver report; (avg.) = averaged score of adolescent and caregiver report.
Lastly, the model using family functioning to predict suicidal SIB was not able to successfully converge because of reaching the iteration limit, possibly because of the small sample size. After examining the suggested modification indices, the model was still not able to converge. Thus, we concluded that the suicidal SIB model was a poor model, meaning that family functioning alone was not predictive of suicidal SIB in our sample.
Discussion
The goals of the current study were to examine the family environment of adolescents seeking treatment for symptoms of BPD, as well as their experiences of SIB, and to better understand what aspects of family functioning relate to SIB. Unique strengths of this study include the emphasis on assessing models of family functioning as it relates to SIB and exploring differences between SIB intent types (suicidal SIB, nonsuicidal SIB, and SIB with ambivalence toward life). Further, because participants were clients seeking counseling from community-based master’s-level clinicians and no clients were excluded from participating in this study, results may generalize to other community samples.
We found that adolescents and caregivers often reported family functioning scores that met criteria for distressed families. Interestingly, adolescents and caregivers agreed on a majority of the subscales of family functioning, suggesting that the distress is mutually experienced. Adolescents and their caregivers only differed on reports of behavioral control (e.g., “[my family does not] hold any rules or standards”) and communication (e.g., “when someone [in my family] is upset the others know why”). This self-reported familial distress supports the social component of the biosocial theory (Linehan, 1993) in that the adolescents with traits of BPD engaged in SIB and experienced unhealthy family environments. Additionally, we found high lifetime rates of SIB in our sample of adolescents. As in previous studies (e.g., Anestis et al., 2015), adolescents in the current study engaged in nonsuicidal SIB more frequently than suicidal or ambivalent SIB, and cutting was the most common method.
Notably, our model of family functioning successfully predicted higher levels of both nonsuicidal SIB and ambivalent SIB. In particular, problem-solving, conflict, and adolescent-reported communication had consistently large effect sizes, suggesting that these subscales contributed more to SIB than other subscales. Although no previous studies have examined adolescent SIB and familial problem-solving to our knowledge, the findings that SIB was related to familial conflict (Huang et al., 2017) and communication (Halstead et al., 2014) corroborate the results of previous studies.
The success of the family functioning model in predicting SIB aligns with family systems theory. Specifically, adolescents in our sample may engage in SIB as a coping skill because their family lacks healthy problem-solving skills and thus models poor coping (which aligns with a description by Halstead et al., 2014). Additionally, adolescent SIB may function to temporarily end conflict in the family because it diverts the family’s attention away from the immediate problems. For example, Oldershaw et al. (2008) found that parents avoided conflict and felt like they were “walking on eggshells” (p. 142) after learning of their adolescents’ SIB. Another possible explanation is that the adolescents in our sample may serve as scapegoats within their family, acting as a focal point of a disturbed family system. From a structural family systems perspective, when there are problems within family subsystem relationships, oftentimes the child—typically the most vulnerable one—becomes the focus of the family’s problems (Wetchler, 2003); this trend is consistent with our findings.
It is worth noting that family functioning alone did not sufficiently predict suicidal SIB. One possible explanation is that our family functioning variables did not encompass the factors of thwarted belongingness and perceived burdensomeness, both of which Joiner (2005) suggested may lead to suicide.
Limitations and Future Directions
A strength of this study is that the results may generalize to other real-world settings in which adolescent clients seek counseling services from community-based master’s-level clinicians who specialize in dialectical behavior therapy. However, this ecological validity comes with some relative limitations.
One notable limitation of this study is that we examined family functioning at one point in time, when the adolescent was beginning treatment. Given this single timepoint, we are unable to fully describe the relationship between family functioning and SIB. Considering the biosocial theory, it seems likely that the distressed family environment preceded the SIB; however, it is possible that the SIB caused greater familial distress. Therefore, it would be useful to assess changes in family functioning and SIB across time.
Another limitation is our SIB measure; as Crowell et al. (2013) explained, the LSASI is commonly used in clinical practice but not often in research. In addition to issues with reliability, the LSASI is a lifetime measure as opposed to one focusing on recent behavior. Although all participants reported engaging in SIB in the past year, it is unclear how recently they engaged in SIB relative to the time of the study. Despite the benefit of creating more variability in the data by allowing participants to report their specific frequency of SIB, the alternative of a dichotomous variable of current SIB might be more compatible with our measures of current family functioning.
Additionally, the small sample size limits the power of our analyses as well as the generalizability of our results. A small sample increases the likelihood of a Type II error, meaning an increased likelihood of not finding significant results. However, it is notable that we found statistically significant results (e.g., good model fit of family functioning) despite our low power. Nevertheless, replication studies with much larger samples are needed.
Implications for Practice
Our findings suggest that family functioning is related to SIB in adolescents, particularly nonsuicidal and ambivalent SIB. Although counselors often include families when working with young children, it is common for counselors to work with adolescents individually. This practice is consistent with state laws allowing adolescents to consent to their own mental health treatment, and there are many presenting concerns and situations in which individual counseling may be the most effective modality. However, the connection between family functioning and SIB in adolescents in our sample indicates that it may be important to include family members in treating adolescent SIB; in fact, dialectical behavior therapy for adolescents (originally adapted by A. L. Miller et al., 1997) encourages family involvement in treatment. Counselors therefore need to educate parents and caregivers who may be reluctant to engage in the counseling process with their teen that SIB is an issue for which their participation in counseling could make a positive difference in treatment outcome. Further, from a family systems perspective, it can be challenging for teens to successfully use the coping skills and strategies they learn in counseling if the rest of the family system remains unchanged. Including at least some family members may therefore help adolescents maintain changes gained through the counseling process.
When including family members in counseling with adolescents who have engaged in nonsuicidal and ambivalent SIB, findings from our study suggest that three important targets for assessment and intervention include the domains of familial problem-solving, familial conflict, and adolescent-reported communication. Two of these, conflict and communication, were previously identified in the literature, and our study supports those findings. Our study newly identified familial problem-solving as an additional important predictor of SIB in adolescents. Counselors must keep in mind, however, that these variables were not sufficient in predicting suicidal SIB in adolescents. For these teens, we encourage the use of a broader assessment that includes elements of Joiner et al.’s (2009) interpersonal theory of suicide, especially the crucial interpersonal constructs of thwarted belongingness and perceived burdensomeness.
Conclusion
Based on our findings, it appears there is a relationship between engagement in SIB (especially nonsuicidal and ambivalent SIB) and familial environment for community-based treatment-seeking adolescents with traits of BPD. Additionally, both adolescents and their caregivers in our sample reported distressed levels of multiple indicators of family functioning, suggesting the need for family-based intervention. Counselors and service providers should consider multiple markers of family environment (particularly problem-solving, conflict, and adolescent-reported communication) when assessing risk for and treatment of adolescent SIB.
Conflict of Interest and Funding Disclosure
This study was partially funded by a grant from
Western Washington University awarded to
Dr. Christina Byrne. The authors reported no
conflict of interest for the development of this manuscript.
References
Adrian, M., Zeman, J., Erdley, C., Lisa, L., & Sim, L. (2011). Emotional dysregulation and interpersonal
difficulties as risk factors for nonsuicidal self-injury in adolescent girls. Journal of Abnormal Child
Psychology, 39(3), 389–400. https://doi.org/10.1007/s10802-010-9465-3
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
https://doi.org/10.1176/appi.books.9780890425596
Anestis, M. D., Khazem, L. R., & Law, K. C. (2015). How many times and how many ways: The impact of number of nonsuicidal self-injury methods on the relationship between nonsuicidal self-injury frequency and suicidal behavior. Suicide and Life-Threatening Behavior, 45(2), 164–177. https://doi.org/10.1111/sltb.12120
Chanen, A. M., Jovev, M., & Jackson, H. J. (2007). Adaptive functioning and psychiatric symptoms in adolescents with borderline personality disorder. The Journal of Clinical Psychiatry, 68(2), 297–306.
http://doi.org/10.4088/JCP.v68n0217
Crowell, S. E., Baucom, B. R., McCauley, E., Potapova, N. V., Fitelson, M., Barth, H., Smith, C. J., & Beauchaine, T. P. (2013). Mechanisms of contextual risk for adolescent self-injury: Invalidation and conflict escalation in mother–child interactions. Journal of Clinical Child & Adolescent Psychology, 42(4), 467–480. https://doi.org/10.1080/15374416.2013.785360
Crowell, S. E., Beauchaine, T. P., & Linehan, M. M. (2009). A biosocial developmental model of borderline personality: Elaborating and extending Linehan’s theory. Psychological Bulletin, 135(3), 495–510. https://doi.org/10.1037/a0015616
Epstein, N. B., Baldwin, L. M., & Bishop, D. S. (1983). The McMaster Family Assessment Device. Journal of Marital and Family Therapy, 9(2), 171–180. https://doi.org/10.1111/j.1752-0606.1983.tb01497.x
Goldenberg, H., & Goldenberg, I. (2013). Family therapy: An overview (8th ed.). Brooks/Cole.
Halstead, R. O., Pavkov, T. W., Hecker, L. L., & Seliner, M. M. (2014). Family dynamics and self-injury behaviors: A correlation analysis. Journal of Marital and Family Therapy, 40(2), 246–259.
https://doi.org/10.1111/j.1752-0606.2012.00336.x
Hamza, C. A., Willoughby, T., & Heffer, T. (2015). Impulsivity and nonsuicidal self-injury: A review and meta-analysis. Clinical Psychology Review, 38, 13–24. https://doi.org/10.1016/j.cpr.2015.02.010
Hooper, D., Coughlan, J., & Mullen, M. R. (2008). Structural equation modelling: Guidelines for determining model fit. Electronic Journal of Business Research Methods, 6(1), 53–60. https://doi.org/10.21427/D7CF7R
Huang, Y.-H., Liu, H.-C., Sun, F.-J., Tsai, F.-J., Huang, K.-Y., Chen, T.-C., Huang, Y.-P., & Liu, S.-I. (2017). Relationship between predictors of incident deliberate self-harm and suicide attempts among adolescents. Journal of Adolescent Health, 60(5), 612–618. https://doi.org/10.1016/j.jadohealth.2016.12.005
Iacobucci, D. (2010). Structural equations modeling: Fit indices, sample size, and advanced topics. Journal of Consumer Psychology, 20(1), 90–98. https://doi.org/10.1016/j.jcps.2009.09.003
Joiner, T. E. (2005). Why people die by suicide. Harvard University Press.
Joiner, T. E., Jr., Van Orden, K. A., Witte, T. K., & Rudd, M. D. (2009). The interpersonal theory of suicide: Guidance for working with suicidal clients. American Psychological Association. https://doi.org/10.1037/11869-000
Kaess, M., Brunner, R., & Chanen, A. (2014). Borderline personality disorder in adolescence. Pediatrics, 134(4), 782–793. https://doi.org/10.1542/peds.2013-3677
Latina, D., Giannotta, F., & Rabaglietti, E. (2015). Do friends’ co-rumination and communication with parents prevent depressed adolescents from self-harm? Journal of Applied Developmental Psychology, 41, 120–128. https://doi.org/10.1016/j.appdev.2015.10.001
Levenkron, S. (1998). Cutting: Understanding and overcoming self-mutilation. W. W. Norton.
Linehan, M. M. (1993). Cognitive-behavioral treatment of borderline personality disorder. Guilford.
Linehan, M. M., & Comtois, K. A. (1996). Lifetime parasuicide count. Unpublished manuscript, Department of Psychology, University of Washington, Seattle, Washington.
Miller, A. L., Muehlenkamp, J. J., & Jacobson, C. M. (2008). Fact or fiction: Diagnosing borderline personality disorder in adolescents. Clinical Psychology Review, 28(6), 969–981. https://doi.org/10.1016/j.cpr.2008.02.004
Miller, A. L., Rathus, J. H., Linehan, M. M., Wetzler, S., & Leigh, E. (1997). Dialectical behavior therapy adapted for suicidal adolescents. Journal of Practical Psychiatry and Behavioral Health, 3(2), 78–86.
Miller, I. W., Epstein, N. B., Bishop, D. S., & Keitner, G. I. (1985). The McMaster Family Assessment Device: Reliability and validity. Journal of Marital and Family Therapy, 11(4), 345–356.
https://doi.org/10.1111/j.1752-0606.1985.tb00028.x
Miller, I. W., Ryan, C. E., Keitner, G. I., Bishop, D. S., & Epstein, N. B. (2000). The McMaster approach to families: Theory, assessment, treatment and research. Journal of Family Therapy, 22(2), 168–189.
https://doi.org/10.1111/1467-6427.00145
Nock, M. K., & Prinstein, M. J. (2004). A functional approach to the assessment of self-mutilative behavior. Journal of Consulting and Clinical Psychology, 72(5), 885–890. https://doi.org/10.1037/0022-006X.72.5.885
Nock, M. K., & Prinstein, M. J. (2005). Contextual features and behavioral functions of self-mutilation among adolescents. Journal of Abnormal Psychology, 114(1), 140–146. https://doi.org/10.1037/0021-843X.114.1.140
Oldershaw, A., Richards, C., Simic, M., & Schmidt, U. (2008). Parents’ perspectives on adolescent self-harm: Qualitative study. The British Journal of Psychiatry, 193(2), 140–144. https://doi.org/10.1192/bjp.bp.107.045930
Prinz, R. J., Foster, S. L., Kent, R. N., & O’Leary, K. D. (1979). Multivariate assessment of conflict in distressed and nondistressed mother–adolescent dyads. Journal of Applied Behavior Analysis, 12(4), 691–700.
https://doi.org/10.1901/jaba.1979.12-691
Rallis, B. A., Esposito-Smythers, C., & Mehlenbeck, R. (2015). Family environment as a moderator of the association between conduct disorder and suicidality. Journal of Aggression, Maltreatment & Trauma, 24(2), 150–168. https://doi.org/10.1080/10926771.2015.997909
Robin, A. L., & Foster, S. L. (1989). Negotiating parent–adolescent conflict: A behavioral–family systems approach. Guilford.
Tabachnick, B. G., & Fidell, L. S. (2019). Using multivariate statistics (7th ed.). Pearson Education.
Walker, K. L., Hirsch, J. K., Chang, E. C., & Jeglic, E. L. (2017). Non-suicidal self-injury and suicidal behavior in a diverse sample: The moderating role of social problem-solving ability. International Journal of Mental Health and Addiction, 15(3), 471–484. https://doi.org./10.1007/s11469-017-9755-x
Wetchler, J. L. (2003). Structural family therapy. In L. L. Hecker & J. L. Wetchler (Eds.), An introduction to marriage
and family therapy (pp. 63–93). Haworth Clinical Practice Press.
Melissa Sitton, MS, is a doctoral student at Southern Methodist University. Tina Du Rocher Schudlich, PhD, MHP, is a professor at Western Washington University. Christina Byrne, PhD, is an associate professor at Western Washington University. Chase M. Ochrach, MS, is a doctoral student at the University of Wisconsin–Madison. Seneca E. A. Erwin, BS, is a doctoral student at the University of Northern Colorado. Correspondence may be addressed to Tina Du Rocher Schudlich, 516 High St., MS 9172, Bellingham, WA 98225, tina.schudlich@wwu.edu.
Aug 18, 2020 | Volume 10 - Issue 3
S Anandavalli, John J. S. Harrichand, Stacey Diane Arañez Litam
Amidst the global health crisis of COVID-19, international students’ safety and well-being is threatened by community- and policy-level animus. In addition to adjusting to a foreign culture, a series of draconian policies and communal hate crimes during the pandemic have placed international students in an especially vulnerable position. In this context, professional counselors must be well prepared to support this community. The authors describe the current sociopolitical events that have adversely impacted international students in the United States. Next, challenges to international students’ mental health are identified to aid counselors’ understanding of this community’s needs. Finally, recommendations grounded in critical feminist and bioecological approaches are offered to facilitate counselors’ clinical and advocacy work with international students.
Keywords: COVID-19, international students, critical feminist, bioecological, advocacy
COVID-19–related fears have resulted in social and political responses characterized by racial discrimination and xenophobia toward marginalized groups (Devakumar et al., 2020; Litam, 2020; Litam & Hipolito-Delgado, in press), including international students (Anandavalli, 2020; Zhai & Du, 2020). Rates of misleading media portrayals and xenophobic rhetoric substantially increased after President Trump referred to COVID-19 as the “Chinese virus” on March 16, 2020, and have steadily risen across social media platforms (Lyu et al., 2020). Exposure to COVID-19–related racial discrimination has deleterious effects on the mental health and life satisfaction of racial minorities (Litam, 2020; Litam & Oh, in press; Wen et al., 2020), including international students residing in the United States (Zhai & Du, 2020). The extant body of literature has clearly established lower levels of help seeking, barriers to counseling, and increased rates of mental health distress among international students compared to their domestic counterparts (Auerbach et al., 2018; Clough et al., 2018; Sawir et al., 2008; Zhai & Du, 2020). These existing challenges and psychosocial stressors may uniquely combine with current sociopolitical messages and policies to further exacerbate the unique developmental and cultural stressors encountered by international students. Thus, counselors working in various roles (e.g., college counselors, private practitioners) are called to develop a deeper understanding of the ways in which international students are negatively affected by xenophobic policies following COVID-19 and to employ culturally sensitive strategies grounded in systems approaches.
Although all counselors working with international students must consider the impact of larger systemic issues on international students’ mental health, college counselors might be in a unique position to support this population because of their close proximity. Counselors must consider how the combined effects of sociopolitical influences, systemic inequity, intersectionality, and COVID-19–related experiences of xenophobia uniquely contribute to the mental health disparities of international students in a post-pandemic reality. It is vital that counselors consider the impact of social and political structures, as Anandavalli (2020) found that contextual and systemic influences (e.g., elections, travel bans, anti-immigrant sentiment) have a profound impact on international students’ mental health. Unfortunately, despite repeated calls to action, counselors may be unprepared to support international students in the United States (e.g., Kim et al., 2019). Even years after Yoon and Portman’s (2004) critique, accredited counseling programs continue to offer little to no training to students to work effectively with international students. Perhaps as a result of years of limited training and research on international students’ mental health experiences, counselors continue to have inadequate cultural competence when working with international students. In a recent study, Liu et al. (2020) noted that although Korean and Chinese international students in their study had a cautiously optimistic attitude toward their college counselors, a third of them felt hurt and disappointed by their college counselors’ cultural incompetence and reported incidents of counselors’ cultural ignorance and stereotyping. With limited attention to social justice and equity issues, counselors can further traumatize and alienate some international students (Jones et al., 2017).
Within the counseling literature, even the few studies that explored the mental health of international students from a relational and systemic perspective (e.g., Lértora & Croffie, 2020; Page et al., 2019) have failed to adopt a critical lens and examine the impact and accountability of larger social institutions on the community’s well-being. At present, a review on PsycINFO, Google Scholar, and SocINDEX using the search terms international student mental health, international students counseling bioecological model, and international students multicultural critical race theory yielded no counseling literature that addressed strategies to support the mental health of international students in the United States from a critical perspective. Thus, the following article contributes to the extant body of literature on the topic by (a) describing the ways in which current sociopolitical events and policies send denigrating messages that devalue international students, (b) outlining the mental health challenges of international students, and (c) offering specific suggestions for counselors working with this vulnerable population through a critical feminist and bioecological lens.
Sociopolitical Policies Affecting International Students
According to the Institute of International Education (IIE; 2019), as the most popular study abroad destination, the United States hosts more than 1 million international (foreign-born) students. However, in the context of the racialized COVID-19 pandemic, Chirikov and Soria (2020) found that as many as 17% of the surveyed international students have experienced xenophobic actions that threaten their safety and presence. Further, they found these rates were higher among students from East Asian and Southeast Asian countries such as Japan, China, and Vietnam (22%–30%), given increasing Sinophobia (anti-Chinese sentiment) in the country. In addition to pursuing higher education, each year thousands of international students seek post-education professional experiences to receive practical training through an H-1B visa. An H-1B visa authorizes international students and professionals to work in the United States because of their experience in specialty occupations of distinguished merit and ability (U.S. Department of Labor, n.d.). On June 22, 2020, H-1B visa holders were notified that effective June 24, 2020, the U.S. embassy would not be issuing new H-1B visa stamps; additionally, the ruling dictated that without a valid H-1B visa stamp, individuals could not enter the United States until December 31, 2020 (The White House, 2020). This xenophobic proclamation left thousands of international professionals stranded and placed them at risk of losing their employment. The announcement to ban H-1B visa holders devalued international students and professionals in the United States and reminded international students of their fragile futures and conditional status.
The most recent incident in the upsurge of xenophobic sociopolitical messages negatively affecting international students was introduced by the U.S. Immigration and Customs Enforcement (ICE) on July 6, 2020. A few weeks prior to the fall 2020 semester, international students were informed that they would be deported to their home countries if they were enrolled in fully online programs (ICE, 2020). International students became tasked with an impossible decision to either prioritize their health or their education. Unlike domestic students, who could safely attend programs online, the proclamation required international students to attend in-person classes to remain in the country (ICE, 2020). Although the proclamation was later amended to allow international students to attend online courses without deportation (ICE, 2020), the disparaging messages toward international students could not be overlooked. The presence of a discriminatory order that forced international students to choose between their safety and educational training is reflective of larger anti-immigration sentiments that push many students toward an emotional breakdown (Garcini et al., 2020).
Mental Health Challenges for International Students
Although international students contributed about $45 billion to the U.S. economy and to the development of 450,000 new jobs in the United States in 2018–19 (National Association of Foreign Student Advisers [NAFSA], 2020), worldviews that position international students as harbingers of innovation, intellectual diversity, economic success, and a necessity for sustaining higher education institutions are uncommon within American society (Williams & Johnson, 2011). Sadly, experiences of hate crimes are so frequent that many international students perceive them as normal consequences of being an international person in the United States (Lee & Rice, 2007; Pottie-Sherman, 2018). According to George Mwangi et al. (2019), for many international students, universities are far from being spaces of inclusivity and openness. Often, they were described as sites of oppression and “Americanization.” Interviews with international students from Africa indicated that due to their intersecting identities as racial and cultural minorities, participants in the study endured constant messages and actions undermining their culture and knowledge. In fact, persistent incidents of prejudice and discrimination made the participants feel “crazy” (George Mwangi et al., 2019). Chronic exposure to xenophobia, discrimination, and anti-immigrant sentiments has been documented to have profound impacts on international students’ psychological well-being (Houshmand et al., 2014; Ong et al., 2013). As a result of multiple factors, including xenophobia, international students suffer from severe psychological symptoms. One example is a recent study by Dovchin (2020), who found that parochial attitudes toward non-native English speakers and embedded linguistic racism had “serious ‘psychological damages’” (p. 815) on the international students’ mental health. Notably, the impact of “ethnic accent bullying” (p. 815) on her international student participants included development of social anxiety symptoms and suicidal ideation. Given that many of the instances of linguistic racism were found within classrooms, it is imperative that college counselors consider the pervasive influence of systemic inequities on international students’ mental health.
Critical Feminist Perspectives
Critical feminist paradigms acknowledge the powerful role of systemic influences and focus on change at structural levels. These paradigms challenge larger social structures (e.g., national and institutional policies) and promote the pursuit of social justice through clinical practice and inquiry (Moradi & Grzanka, 2017; Mosley et al., 2020). Thus, critical feminist paradigms are grounded in the philosophy that current social landscapes are inequitable and therefore unjust (Bonilla-Silva, 2013). Specifically, the critical feminist theory of intersectionality describes how systems of oppression and the social constructions of race, socioeconomic class, gender, and other identities interact in ways that influence one’s social positioning (Crenshaw, 1989). Given many international students’ intersecting identities as linguistic, racial, and ethnic minorities, counselors must consider how their unique combination of marginalized and privileged identities contribute to their social position and worldview as outlined in the Multicultural and Social Justice Counseling Competencies (MSJCC; Ratts et al., 2015). Consistent with the focus on addressing the pervasive role of sociopolitical systemic influences, the analysis and recommendations offered in this article are grounded in the critical feminist paradigm.
Bioecological Systems Theory
Oppression and change occur across multiple levels of human interactions, and each level may require varied strategies for advocacy on the part of the counselor (Ratts et al., 2015). These interactions range from everyday occurrences in one’s immediate surroundings (e.g., classrooms) to international policies (e.g., travel bans). To address the powerful influence of multiple systems on the mental health of international students, a critical feminist paradigm was applied to Bronfenbrenner’s (1979) bioecological systems theory. The bioecological systems theory outlines how systems and environment interact with an individual in ways that impact their overall well-being. According to the model (Bronfenbrenner, 1994), individuals experience a bidirectional relationship (directly and indirectly) as a result of interacting with environmental systems where the impact of the relationship is dependent on the amount of interaction taking place. The bioecological theory is represented by five concentric circles that expand to represent multiple levels of permeable systems that affect one’s development (Bronfenbrenner, 1994). The systems within Bronfenbrenner’s model include: (a) microsystem, the immediate environment (e.g., family, school, peer group, neighborhood); (b), mesosytem, connections within the immediate environment, such as college campus and roommates; (c) exosystem, external environmental settings that only indirectly affect development, such as religious institutions outside of one’s faith; (d) macrosystem, which refers to one’s larger cultural context; and (e) chronosystem, encompassing patterns and transitions over the course of time and development (Bronfenbrenner, 1994).
Although the bioecological model represents a relatively robust theory, the model is not without its limitations. Christensen (2016) noted that the theory fails to account for the effects of globalization and technological developments that affect various parts of the world differently. These disparities can be addressed by combining the bioecological model with the critical feminist paradigm, which challenges institutions and structures that cut across national boundaries. Both models combine to create a unique framework that may guide concrete recommendations for counselors actively seeking to support and advocate for international students.
Implications for Counseling International Students
As the extant counseling literature on international students suffers from a limited emphasis on a critical feminist and bioecological lens, the current manuscript offers a systemic framework for counseling international students. We invite college counselors to adopt a critical feminist and systems perspective to hold larger systems accountable for their harmful role in international students’ mental health concerns (e.g., a university’s unwillingness to engage in culturally responsive and linguistically inclusive teaching strategies; Archer, 2007). The following counseling recommendations were developed from the authors’ direct experiences through counseling international students, and through a review of relevant literature. Although these recommendations may apply to all counselors irrespective of their settings, some may be specific to a particular role (e.g., college counselor).
Microsystem
The microsystem level includes the bidirectional relationships between the international student and the people with whom they regularly interact (Bronfenbrenner, 1979). College counselors and community counselors working with this population can support international students at the microsystem level by asking them to identify and deeply explore “safe” and “unsafe” relationships that exist within their college/university campus, neighborhood, and relevant religious group. Next, counselors can empower international students by framing their concerns as part of a larger systemic issue to minimize self-blame (i.e., seeing themselves as the cause of their challenges; Sue & Sue, 1990). Here, the focus is placed on empowering international students to engage in self-advocacy within the systems they occupy (Haskins & Singh, 2015). The reframe may also aid in enhancing the international student’s critical consciousness (Ratts, 2017; Ratts & Greenleaf, 2017) and help them shift their perspectives from self-blame to acknowledging the role(s) of external oppressive forces (e.g., racism, xenophobia, Sinophobia; Manzano et al., 2017). Indeed, engaging in the internalization of problems in response to stressors is prevalent among many international cultures (Wong et al., 2013).
Interventions at this level might involve the use of microinterventions (Sue et al., 2019) to empower international students. Sue et al. (2019) defined microinterventions as deeds and interactions that communicate affirmation and validation to targets of microaggressions. These interventions have the potential to enhance the psychological well-being and self-efficacy of the target and disarm the effects of microaggressions by challenging the perpetrator. Counselors can provide psychoeducation on microinterventions, using caution and clinical judgment to avoid further harm to the student. It is imperative that counselors recognize and educate the international student that it could be dangerous to employ microinterventions without understanding the specificities of the context. Sue et al. noted that the minoritized individual (target) employing microinterventions must be intentional about picking their battles, as endless responses to each encountered incident of microaggression can be damaging to the target’s well-being. The target should be aware of the context of the microaggression and modify their response as the situation requires. Given that racism and oppression permeate classroom spaces, college counselors can also provide opportunities for practicing microinterventions through role plays (Litam, 2020). One microintervention is making the “invisible” visible by responding to instances of racial discrimination on campus, making the offending party (e.g., domestic students, staff) aware of their offensive actions or words, and/or compelling them to consider their impact (Sue et al., 2019). Counselors may further guide international students in educating the offender (Sue et al., 2019). Litam (2020) noted that although it is of critical importance to avoid placing the onus of responsibility on minoritized individuals (e.g., international students) to educate and/or confront their offenders, when they do engage in thoughtful responses the opportunity to educate can result in positive changes and healthier relationships.
Finally, counselors can support international students to incorporate mindfulness and self-compassion as culturally sensitive tools to address the xenophobic experiences of COVID-19–related racial discrimination (Litam, 2020). Compassion meditation may help international students release their feelings of anger and intentionally cultivate experiences of self-compassion and positive regard toward self and others. Self-compassion may be cultivated by encouraging international students to attend to their immediate needs by remaining present and non-judgmental (Germer & Neff, 2015). Grounded in the Buddhist concept of loving-kindness, international students may be trained to pay attention to their somatic experiences with a non-judgmental curiosity. For instance, as these students confront chronic racism, they may benefit from opportunities to be kind to themselves. Counselors may also guide them to engage in mindful breathing to ground themselves in the face of chronic stress (Germer & Neff, 2015).
Additionally, empowering international students to cultivate a strong sense of ethnic identity may also represent an important strategy at this level. Extant research continues to identify the role of ethnic identity as a protective factor for experiences of racial discrimination (Carter et al., 2019; Chae & Foley, 2010; Choi et al., 2016; Tran & Sangalang, 2016), including experiences of COVID-19–related racial discrimination (Litam & Oh, in press).
Mesosystem
Counselors working with international students at the mesosystem level may continue to strengthen the interventions at the microsystem level while exploring mental health stressors that may arise through interactions between the student and their peers and/or members of the college/university campus community. Counselors who interact with various social groups uniquely position themselves in ways that establish new relationships, building support with spiritual and religious leaders (Sue et al., 2019) and mid- and senior-level administrators who are then able to directly or indirectly support international students on and off campus (Mac et al., 2019).
Leveraging their network within the university system, college counselors can explore how faculty members, administrators, and staff may improve their cultural humility and competence by collaborating with them in efforts to support international students within the campus (Hook et al., 2013). For instance, faculty members and staff could be invited to on-campus ethnic interest groups, cultural festivals, or language clubs on a regular basis to immerse themselves in their students’ cultural practices. Additionally, many international students on campus occupy shared housing. College counselors can teach international students’ roommates, peers, and resident advisors to detect signs of distress and isolation. This can potentially help student leaders and other residents better support international students and promote wellness in the student body more broadly. Engaging the community in culturally relevant strategies for promoting the mental health of international students and recognizing their distress may help college counselors in early detection of distress for this community.
Exosystem
The exosystem level examines social settings that indirectly impact the student but in which the student has no direct impacts (e.g., local politics, medical and social services; Bronfenbrenner, 1979). Interventions at the exosystem level might examine how educational training grounded in Eurocentrism may further marginalize international students and negatively impact their academic standing and their overall mental health and well-being (George Mwangi et al., 2019; Ploner & Nada, 2020). Counselors working with international students at the exosystem level must shift their perspectives from interpersonal interventions toward a greater examination of systemic influences. Counselors may utilize the MSJCC (Ratts et al., 2015) to consider the intersecting ways in which the privileged and oppressed identities of international students uniquely influence their mental health experiences. A detailed description of how counselors can apply the MSJCC to counseling international students can be found in Kim et al. (2019).
College counselors working at the exosystem level must play an active role in advocating on behalf of international students by working to dismantle White supremacy in college/university counseling settings (Ratts, 2017) and academic settings (Haskins & Singh, 2015). Furthermore, counselors working at the exosystem level are called to advocate for inclusive spaces and educational curricula that incorporate diversity of thought and pedagogical practices that cater to all student groups. Other examples of exosystem-level advocacy include involvement with academic units, institutions, organizations such as NAFSA and the American College Personnel Association, and communities that indirectly impact international students (Manzano et al., 2017). Trainings for educators and staff at colleges/universities about the importance of dismantling systemic racism and facilitating anti-oppressive pedagogy may also be provided (Berlak, 2004).
Furthermore, community counselors working with this population may collaborate with various social groups (e.g., host families) to develop antiracist approaches that address internalized racism and White supremacy (Kendi, 2019; Singh, 2019). These collaborations may also aid in facilitating the help-seeking behavior of international students and countering the embedded stigma against seeking mental health support (Liu et al., 2020).
Macrosystem
The macrosystem-level focus is on cultural norms, values, and laws that influence the international student without being directly influenced by the student (Bronfenbrenner, 1979). At this level, college counselors may collaborate with other health specialists (e.g., community mental health counselors, social workers, medical doctors) and explore how current U.S. political structures impact the mental health and well-being of international students. These alliances can help students as counselors engage in advocacy initiatives and tackle public policy on behalf of the student (Chan et al., 2019). For example, college counselors can engage in advocacy efforts similar to those that encouraged college and university administrators to oppose the ICE policy by President Trump that targeted international students.
In addition to seeking change to public policies that discriminate against international students, college counselors working at the macrosystem level can also advocate for equitable practices within college and university systems and promote an educational climate that celebrates international students on campuses. Forming alliances with stakeholders (e.g., administrators, legislators, legislative staff) who directly and indirectly impact cultural norms and values in society could also be a helpful strategy for counselors supporting international students at the macrosystem level (Mac et al., 2019). Similarly, community counselors can offer cultural sensitivity training programs to members of local government agencies (e.g., credit unions, DMV). Knowledge of how visa regulations and cultural norms operate can help state and national organizations better serve this population. Finally, platforms such as the National Association for College Admission Counseling and The Chronicle of Higher Education may offer unique spaces for collaboration among counselors, educators, and allies to advocate for this community.
Chronosystem
The chronosystem encompasses all other societal systems that directly and indirectly impact the international student over time (e.g., federal employment policies; Bronfenbrenner, 1979). Interventions at the chronosystem level could address how the transition from an international student to worker in the United States (e.g., H-1B visa–holding professional) impacts how they are perceived by American society. For example, counselors can design programs that identify and address the needs of international students based on past and current sociopolitical events (e.g., 9/11 attacks, COVID-19 pandemic). Furthermore, college counselors may consider how these sociopolitical events might lead to disparaging attitudes toward international students and actively work to facilitate workshops, webinars, or trainings that identify and dispel harmful notions. Both college and community counselors must critically consider how systems continue to evolve over time (Chan et al., 2019). Therefore, they need to be actively attuned to the needs of international students, stay abreast of the current events that affect them, and actively participate in professional advocacy efforts across various systemic levels (e.g., institutional, state, national) to continue supporting this vulnerable community.
Future Directions
Using the search terms listed earlier, we completed an extensive review of the counseling literature. A paucity of empirical research exists in the counseling profession on international students’ mental health needs and experiences from a critical and systemic perspective. Empirical data can help counselors discern which types of interventions are most effective for international students within the counseling setting across various systems. In this article, we highlight that because of racial, linguistic, gender, and other differences within the international student community, an intersectional approach to inquiry is necessary. For instance, the experiences of a White, German, male international student will be vastly different from the experiences of a Black, Ghanaian, female student. Thus, inquiry on the experiences of this community must be positioned in the intersectionality framework (Crenshaw, 1989). Limited access to critical scholarship on the mental health experiences of international students within the counseling setting puts counselors at risk for retraumatizing their minoritized clients (Jones et al., 2017) through potential use of microaggressions and stereotypes, as shared by participants in the study by Liu et al. (2020). Thus, a tutorial stance grounded in cultural humility (Hook et al., 2013) and openness may be needed to build a safe and meaningful therapeutic relationship (Gonzalez et al., 2020). Future inquiries may help practitioners develop training modules and culturally responsive resources to improve their counseling skills and advocacy work with international students.
Conclusion
This article outlines a critical feminist and bioecological systems approach to supporting international students who are at higher risk for mental health distress because of xenophobic policies, racial discrimination, and systemic barriers. Discriminatory attitudes and behaviors toward international students have heightened during the current COVID-19 pandemic. Amidst this burgeoning crisis, counselors practicing in all settings are called to consider how each of these factors uniquely contribute to the mental health and overall well-being of this vulnerable population. Future research is needed to establish specific interventions that are most effective in mitigating the effects of pandemic-related stressors on the mental health of international students. Counselors are called to engage in advocacy efforts that dismantle systems of oppression at various levels, including within the community, in university/college settings, and in state and federal policies.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Archer, L. (2007). Diversity, equality and higher education: A critical reflection on the ab/uses of equity
discourse within widening participation. Teaching in Higher Education, 12(5–6), 635–653.
https://doi.org/10.1080/13562510701595325
Anandavalli, S. (2020). Lived experiences of international graduate students of color and their cultural capital: A critical
perspective [Doctoral dissertation, The University of North Carolina at Greensboro]. Dissertation
Abstracts International Section A: Humanities and Social Sciences. https://libres.uncg.edu/ir/uncg/f/
Anandavalli_uncg_0154D_12696.pdf
Auerbach, R. P., Mortier, P., Bruffaerts, R., Alonso, J., Benjet, C., Cuijpers, P., Demyttenaere, K., Ebert, D. D., Green, J. G., Hasking, P., Lee, S., Lochner, C., McLafferty, M., Nock, M. K., Petukhova, M. V., Pinder-Amaker, S., Rosellini, A. J., Sampson, N. A., Vilagut, G., Zaslavsky, A. M., & Kessler, R. C. (2018). Mental disorder comorbidity and suicidal thoughts and behaviors in the World Health Organization World Mental Health Surveys International College Student Initiative. International Journal of Methods in Psychiatric Research, 28(2), 1–16. https://doi.org/10.1002/mpr.1752
Berlak, A. C. (2004). Confrontation and pedagogy: Cultural secrets, trauma, and emotion in antioppressive pedagogies. Counterpoints, 240, 123–144. www.jstor.org/stable/42978384
Bonilla-Silva, E. (2013). Racism without racists: Color-blind racism and the persistence of racial inequality in America (4th ed.). Rowman & Littlefield.
Bronfenbrenner, U. (1979). The ecology of human development: Experiments by nature and design. Harvard University Press.
Bronfenbrenner, U. (1994). Ecological models of human development. In International Encyclopedia of Education (Vol. 3, 2nd ed., pp. 37–43). Elsevier.
Carter, R. T., Johnson, V. E., Kirkinis, K., Roberson, K., Muchow, C., & Galgay, C. (2019). A meta-analytic review of racial discrimination: Relationships to health and culture. Race and Social Problems, 11, 15–32. https://doi.org/10.1007/s12552-018-9256-y
Chae, M. H., & Foley, P. F. (2010). Relationship of ethnic identity, acculturation, and psychological well-being among Chinese, Japanese, and Korean Americans. Journal of Counseling & Development, 88(4), 466–476. https://doi.org/10.1002/j.1556-6678.2010.tb00047.x
Chan, C. D., DeDiego, A. C., & Band, M. P. (2019). Moving counselor educators to influential roles as advocates: An ecological systems approach to student-focused advocacy. Journal of Counselor Leadership and Advocacy, 6(1), 30–41. https://doi.org/10.1080/2326716X.2018.1545614
Chirikov, I., & Soria, K. M. (2020). International students’ experiences and concerns during the pandemic. SERU Consortium, University of California – Berkeley and University of Minnesota. https://docs.google.com/document/d/1lZdc4dWiX9C_8o1vH-4H7XokIHoJ4yjjVNRv0vS3tBE/edit#headin
g=h.ivkygr983tef
Choi, S., Lewis, J. A., Harwood, S., Mendenhall, R., & Huntt, M. B. (2016). Is ethnic identity a buffer? Exploring the relations between racial microaggressions and depressive symptoms among Asian-American individuals. Journal of Ethnic & Cultural Diversity in Social Work, 26(1–2), 18–29. http://doi.org/10.1080/15313204.2016.1263815
Christensen, J. (2016). A critical reflection of Bronfenbrenner’s development ecology model. Problems of Education in the 21st Century, 69, 22–28. https://doi.org/10.13140/RG.2.1.2959.7681
Clough, B. A., Nazareth, S. M., Day, J. J., & Casey, L. M. (2018). A comparison of mental health literacy, attitudes, and help-seeking intentions among domestic and international tertiary students. British Journal of Guidance & Counselling, 47(1), 123–135. https://doi.org/10.1080/03069885.2018.1459473
Crenshaw, K. W. (1989). Demarginalizing the intersection of race and sex: A Black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. University of Chicago Legal Forum, 1989(1), 139–167.
Devakumar, D., Shannon, G., Bhopal, S. S., & Abubakar, I. (2020). Racism and discrimination in COVID-19 responses. The Lancet, 395(10231), 1194. https://doi.org/10.1016/S0140-6736(20)30792-3
Dovchin, S. (2020). The psychological damages of linguistic racism and international students in Australia. International Journal of Bilingual Education and Bilingualism, 23(7), 804–818. https://doi.org/10.1080/13670050.2020.1759504
Garcini, L. M., Domenech Rodríguez, M. M., Mercado, A., & Paris, M. (2020). A tale of two crises: The compounded effect of COVID-19 and anti-immigration policy in the United States. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S230–S232. https://doi.org/10.1037/tra0000775
George Mwangi, C. A., Changamire, N., & Mosselson, J. (2019). An intersectional understanding of African international graduate students’ experiences in U.S. higher education. Journal of Diversity in Higher Education, 12(1), 52–64. https://doi.org/10.1037/dhe0000076
Germer, C. K., & Neff, K. D. (2015). Cultivating self-compassion in trauma survivors. In V. M. Follette, J. Briere, D. Rozelle, J. W. Hopper, & D. I. Rome (Eds.), Mindfulness-oriented interventions for trauma: Integrating contemplative practices (pp. 43–58). Guilford.
Gonzalez, E., Sperandio, K. R., Mullen, P. R., & Tuazon, V. E. (2020). Development and initial testing of the Multidimensional Cultural Humility Scale. Measurement and Evaluation in Counseling and Development, 1–16. https://doi.org/10.1080/07481756.2020.1745648
Haskins, N. H., & Singh, A. (2015). Critical race theory and counselor education pedagogy: Creating equitable training. Counselor Education and Supervision, 54(4), 288–301. https://doi.org/10.1002/ceas.12027
Hook, J. N., Davis, D. E., Owen, J., Worthington, E. L., Jr., & Utsey, S. O. (2013). Cultural humility: Measuring openness to culturally diverse clients. Journal of Counseling Psychology, 60(3), 353–366. https://doi.org/10.1037/a0032595
Houshmand, S., Spanierman, L. B., & Tafarodi, R. W. (2014). Excluded and avoided: Racial microaggressions targeting Asian international students in Canada. Cultural Diversity and Ethnic Minority Psychology, 20(3), 377–388. https://doi.org/10.1037/a0035404
Institute of International Education. (2019). Fast facts Open Doors 2019. https://opendoorsdata.org/fast_facts/fast-facts-2019
Jones, L. K., Rybak, C., & Russell-Chapin, L. A. (2017). Neurophysiology of traumatic stress. In T. A. Field, L. K. Jones, & L. A. Russell-Chapin (Eds.), Neurocounseling: Brain-based clinical approaches (pp. 61–80). American Counseling Association. https://doi.org/10.1002/9781119375487.ch4
Kendi, I. X. (2019). How to be an antiracist. One World.
Kim, N., Oh, S., & Mumbauer, J. (2019). Supporting international students: Enhancing college counselors’ multicultural counseling competence. Journal of College Counseling, 22(2), 179–192. https://doi.org/10.1002/jocc.12129
Lee, J. J., & Rice, C. (2007). Welcome to America? International student perceptions of discrimination. Higher Education, 53(3), 381–409. https://doi.org/10.1007/s10734-005-4508-3
Lértora, I. M., & Croffie, A. L. (2020). Using relational-cultural theory to conceptualize international student transitions. Journal of Creativity in Mental Health, 15(1), 30–42. https://doi.org/10.1080/15401383.2019.1638862
Litam, S. D. A. (2020). “Take your Kung Flu back to Wuhan”: Counseling Asians, Asian Americans, and Pacific Islanders with race-based trauma related to COVID-19. The Professional Counselor, 10(2), 144–156. https://doi.org/10.15241/sdal.10.2.144
Litam, S. D. A., & Hipolito-Delgado, C. P. (in press). When being “essential” illuminates disparities: Counseling clients affected by COVID-19. Journal of Counseling & Development, 99(1).
Litam, S. D. A., & Oh, S. (in press). Ethnic identity and coping strategies as moderators of COVID-19 racial discrimination experiences among Chinese Americans. Counseling Outcome Research and Evaluation.
Liu, H., Wong, Y. J., Mitts, N. G., Li, P. F. J., & Cheng, J. (2020). A phenomenological study of East Asian international students’ experience of counseling. International Journal for the Advancement of Counselling, 42(3), 269–291. https://doi.org/10.1007/s10447-020-09399-6
Lyu, H., Chen, L., Luo, J., & Wang, Y. (2020). Sense and sensibility: Characterizing social media users regarding the use of controversial terms for COVID-19. https://covid-19.conacyt.mx/jspui/bitstream/1000/1890/1/1100781.pdf
Mac, J., Sarreal, A. D., Wang, A. C., & Museus, S. D. (2019). Conditions that catalyze the emergence of Asian American and Native American Pacific Islander serving institutions. New Directions for Higher Education, 2019(186), 67–77. https://doi.org/10.1002/he.20324
Manzano, L. J., Poon, O. A., & Na, V. S. (2017). Asian American student engagement in student leadership and activism. New Directions for Student Services, 2017(160), 65–79. https://doi.org/10.1002/ss.20244
Moradi, B., & Grzanka, P. R. (2017). Using intersectionality responsibly: Toward critical epistemology, structural analysis, and social justice activism. Journal of Counseling Psychology, 64(5), 500–513.
https://doi.org/10.1037/cou0000203
Mosley, D. V., Hargons, C. N., Meiller, C., Angyal, B., Wheeler, P., Davis, C., & Stevens-Watkins, D. (2020). Critical consciousness of anti-Black racism: A practical model to prevent and resist racial trauma. Journal of Counseling Psychology. https://doi.org/10.1037/cou0000430
National Association of Foreign Student Advisers: Association of International Educators. (2020). Losing talent 2020: An economic and foreign policy risk America can’t ignore. https://www.nafsa.org/sites/default/files/media/document/nafsa-losing-talent.pdf
Ong, A. D., Burrow, A. L., Fuller-Rowell, T. E., Ja, N. M., & Sue, D. W. (2013). Racial microaggressions and daily well-being among Asian Americans. Journal of Counseling Psychology, 60(2), 188–199.
https://doi.org/10.1037/a0031736
Page, N., Beecher, M. E., Griner, D., Smith, T. B., Jackson, A. P., Hobbs, K., & Kirchhoefer, J. (2019). International student support groups: Learning from experienced group members and leaders. Journal of College Student Psychotherapy, 33(3), 180–198. https://doi.org/10.1080/87568225.2018.1450106
Ploner, J., & Nada, C. (2020). International student migration and the postcolonial heritage of European higher education: Perspectives from Portugal and the UK. Higher Education, 80(2), 373–389.
https://doi.org/10.1007/s10734-019-00485-2
Pottie-Sherman, Y. (2018). Retaining international students in northeast Ohio: Opportunities and challenges in the ‘age of Trump.’ Geoforum, 96, 32–40. https://doi.org/10.1016/j.geoforum.2018.07.015
Ratts, M. J. (2017). Charting the center and the margins: Addressing identity, marginalization, and privilege in counseling. Journal of Mental Health Counseling, 39(2), 87–103. https://doi.org/10.17744/mehc.39.2.01
Ratts, M. J., & Greenleaf, A. T. (2017). Multicultural and social justice counseling competencies: A leadership framework for professional school counselors. Professional School Counseling, 21(1b), 1–9.
https://doi.org/10.1177/2156759X18773582
Ratts, M. J., Singh, A. A., Nassar-McMillan, S., Butler, S. K., & McCullough, J. R. (2015). Multicultural and social justice counseling competencies. https://www.counseling.org/docs/default-source/competencies/multicultural-and-social-justice-counseling-competencies.pdf?sfvrsn=8573422c_20
Sawir, E., Marginson, S., Deumert, A., Nyland, C., & Ramia, G. (2008). Loneliness and international students: An Australian study. Journal of Studies in International Education, 12(2), 148–180.
https://doi.org/10.1177/1028315307299699
Singh, A. A. (2019). The racial healing handbook: Practical activities to help you challenge privilege, confront systemic racism & engage in collective healing. New Harbinger.
Sue, D. W., Alsaidi, S., Awad, M. N., Glaeser, E., Calle, C. Z., & Mendez, N. (2019). Disarming racial microaggressions: Microintervention strategies for targets, White allies, and bystanders. American Psychologist, 74(1), 128–142. https://doi.org/10.1037/amp0000296
Sue, D. W., & Sue, D. (1990). Counseling the culturally different: Theory and practice (2nd ed.). Wiley.
Tran, A. G. T. T., & Sangalang, C. C. (2016). Personal discrimination and satisfaction with life: Exploring
perceived functional effects of Asian American race/ethnicity as a moderator. Cultural Diversity and
Ethnic Minority Psychology, 22(1), 83–92. https://doi.org/10.1037/cdp0000052
U.S. Department of Labor. (n.d.). H-1B Program. https://www.dol.gov/agencies/whd/immigration/h1b
U.S. Immigration and Customs Enforcement. (2020, July 6). SEVP modifies temporary exemptions for nonimmigrant students taking online courses during fall 2020 semester. https://www.ice.gov/news/releases/sevp-modifies-temporary-exemptions-nonimmigrant-students-taking-online-courses-during
Wen, J., Aston, J., Liu, X., & Ying, T. (2020). Effects of misleading media coverage on public health crisis: A case of the 2019 novel coronavirus outbreak in China. Anatolia: An International Journal of Tourism and Hospitality Research, 31(2), 331–336. https://doi.org/10.1080/13032917.2020.1730621
The White House. (2020, June 22). Proclamation suspending entry of aliens who present a risk to the U.S. labor market following the Coronavirus outbreak. https://www.whitehouse.gov/presidential-actions/proclamation-suspending-entry-aliens-present-risk-u-s-labor-market-following-coronavirus-outbreak
Williams, C. T., & Johnson, L. R. (2011). Why can’t we be friends?: Multicultural attitudes and friendships with international students. International Journal of Intercultural Relations, 35(1), 41–48.
https://doi.org/10.1016/j.ijintrel.2010.11.001
Wong, Y. J., Wang, K. T., & Maffini, C. S. (2013). Asian international students’ mental health-related outcomes: A person × context cultural framework. The Counseling Psychologist, 42(2), 278–305.
https://doi.org/10.1177/0011000013482592
Yoon, E., & Portman, T. A. A. (2004). Critical issues of literature on counseling international students. Journal of Multicultural Counseling and Development, 32(1), 33–44. https://doi.org/10.1002/j.2161-1912.2004.tb00359.x
Zhai, Y., & Du, X. (2020). Mental health care for international Chinese students affected by the COVID-19
outbreak. The Lancet Psychiatry, 7(4), E22. https://doi.org/10.1016/S2215-0366(20)30089-4
S Anandavalli, PhD, NCC, LPC-I, is an assistant professor at Southern Oregon University. John J. S. Harrichand, PhD, NCC, CCMHC, ACS, LPC, LMHC, is an assistant professor at State University of New York at Brockport. Stacey Diane Arañez Litam, PhD, NCC, CCMHC, LPCC, is an assistant professor at Cleveland State University. Correspondence may be addressed to S Anandavalli, Clinical Mental Health Counseling, Southern Oregon University, 1250 Siskiyou Blvd, Ashland, OR 97520, anandavas@sou.edu.
Aug 18, 2020 | Volume 10 - Issue 3
Jacob Olsen, Sejal Parikh Foxx, Claudia Flowers
Researchers analyzed data from a national sample of American School Counselor Association (ASCA) members practicing in elementary, middle, secondary, or K–12 school settings (N = 4,066) to test the underlying structure of the School Counselor Knowledge and Skills Survey for Multi-Tiered Systems of Support (SCKSS). Using both exploratory and confirmatory factor analyses, results suggested that a second-order four-factor model had the best fit for the data. The SCKSS provides counselor educators, state and district leaders, and practicing school counselors with a psychometrically sound measure of school counselors’ knowledge and skills related to MTSS, which is aligned with the ASCA National Model and best practices related to MTSS. The SCKSS can be used to assess pre-service and in-service school counselors’ knowledge and skills for MTSS, identify strengths and areas in need of improvement, and support targeted school counselor training and professional development focused on school counseling program and MTSS alignment.
Keywords: school counselor knowledge and skills, survey, multi-tiered systems of support, factor analysis, school counseling
The role of the school counselor has evolved significantly since the days of “vocational guidance” in the early 1900s (Gysbers, 2010, p. 1). School counselors are now called to base their programs on the American School Counselor Association (ASCA) National Model for school counseling programs (ASCA, 2019a). The ASCA National Model consists of four components: Define (i.e., professional and student standards), Manage (i.e., program focus and planning), Deliver (i.e., direct and indirect services), and Assess (i.e., program assessment and school counselor assessment and appraisal; ASCA, 2019a). Within the ASCA National Model framework, school counselors lead and contribute to schoolwide efforts aimed at supporting the academic, career, and social/emotional development and success of all students (ASCA, 2019b). In addition, school counselors are uniquely trained to provide small-group counseling and psychoeducational groups, and to collect and analyze data to show the impact of these services (ASCA, 2014; Gruman & Hoelzen, 2011; Martens & Andreen, 2013; Olsen, 2019; Rose & Steen, 2015; Sink et al., 2012; Smith et al., 2015). School counselors also support students with the most intensive needs by providing referrals to community resources, collaborating with intervention teams, and consulting with key stakeholders involved in student support plans (Grothaus, 2013; Pearce, 2009; Ziomek-Daigle et al., 2019).
This model for meeting the needs of all students aligns with a multi-tiered systems of support (MTSS) framework, one of the most widely implemented and researched approaches to “providing high-quality instruction and interventions matched to student need across domains and monitoring progress frequently to make decisions about changes in instruction or goals” (McIntosh & Goodman, 2016, p. 6). In an MTSS framework, there are typically three progressive tiers with increasing intensity of supports based on student responses to core instruction and interventions (J. Freeman et al., 2017). Schoolwide universal systems (i.e., Tier 1), including high-quality research-based instruction, are put in place to support all students academically, socially, and behaviorally; targeted interventions (i.e., Tier 2) are put in place for students not responding positively to schoolwide universal supports; and intensive team-based systems (i.e., Tier 3) are put in place for individual students needing function-based intensive interventions beyond what is received at Tier 1 and Tier 2 (Sugai et al., 2000).
Strategies for aligning school counseling programs and MTSS have been thoroughly documented in the literature (Belser et al., 2016; Goodman-Scott et al., 2015; Goodman-Scott & Grothaus, 2017a; Ockerman et al., 2012). There is also a growing body of research documenting the impact of this alignment on important student outcomes (Betters-Bubon & Donohue, 2016; Campbell et al., 2013; Goodman-Scott et al., 2014) and the role of school counselors (Betters-Bubon et al., 2016; Goodman-Scott, 2013). In addition, ASCA recognizes the significance of school counselors’ roles in MTSS implementation, highlighting that “school counselors are stakeholders in the development and implementation of a Multi-Tiered System of Supports (MTSS)” and “align their work with MTSS through the implementation of a comprehensive school counseling program” (ASCA, 2018, p. 47).
The benefits of school counseling program and MTSS alignment are clear; however, effective alignment depends on school counselors having knowledge and skills for MTSS (Sink & Ockerman, 2016). Despite consensus in the literature about the knowledge and skills for MTSS that school counselors need to align their programs, there is a lack of psychometrically sound surveys that measure school counselors’ knowledge and skills for MTSS. Therefore, the validation of such a survey is a critical component to advancing the process of school counselors developing the knowledge and skills needed to contribute to MTSS implementation and align their programs with existing MTSS frameworks.
Knowledge and Skills for MTSS
The core features of MTSS include (a) universal screening, (b) data-based decision-making, (c) a continuum of evidence-based practices, (d) a focus on fidelity of implementation, and (e) staff training on evidence-based practices (Berkeley et al., 2009; Center on Positive Behavioral Interventions and Supports, 2015; Chard et al., 2008; Hughes & Dexter, 2011; Michigan’s Integrated Behavior & Learning Support Initiative, 2015; Sugai & Simonsen, 2012). For effective MTSS implementation, school staff need the knowledge and skills to plan for and assess the systems and practices embedded in each of the core features (Eagle et al., 2015; Leko et al., 2015). Despite this need, researchers have found that school staff, including school counselors, often lack knowledge and skills of key components for MTSS (Bambara et al., 2009; Patrikakou et al., 2016; Prasse et al., 2012). For example, Patrikakou et al. (2016) conducted a national survey and found that school counselors understood the MTSS framework and felt prepared to deliver Tier 1 counseling supports. However, school counselors felt least prepared to use data management systems for decision-making and assessing the impact of MTSS interventions (Patrikakou et al., 2016).
As a result of the gap in knowledge and skills for MTSS, the need to more effectively prepare pre-service educators to implement MTSS has become an increasingly urgent issue across many disciplines within education (Briere et al., 2015; Harvey et al., 2015; Kuo, 2014; Leko et al., 2015; Prasse et al., 2012; Sullivan et al., 2011). This urgency is the result of the widespread use of MTSS and the measurable impact MTSS has on student behavior (Barrett et al., 2008; Bradshaw et al., 2010), academic engagement (Benner et al., 2013; Lassen et al., 2006), attendance (J. Freeman et al., 2016; Pas & Bradshaw, 2012), school safety (Horner et al., 2009), and school climate (Bradshaw et al., 2009). This urgency has been especially emphasized in recent calls for MTSS knowledge and skills to be included in school counselor preparation programs (Goodman-Scott & Grothaus, 2017b; Olsen, Parikh-Foxx, et al., 2016; Sink, 2016).
Given that many pre-service preparation programs have only recently begun integrating MTSS into their training, the opportunity for school staff to gain the knowledge and skills for MTSS continues to be through in-service professional development opportunities at the state, district, or school level (Brendle, 2015; R. Freeman et al., 2015; Hollenbeck & Patrikakou, 2014; Swindlehurst et al., 2015). For in-service school counselors, research shows that MTSS-focused professional development is related to increased knowledge and skills for MTSS (Olsen, Parikh-Foxx, et al., 2016). Further, when school counselors participate in professional development focused on MTSS, the knowledge and skills gained contribute to increased participation in MTSS leadership roles (Betters-Bubon & Donohue, 2016), increased data-based decision-making (Harrington et al., 2016), and decreases in student problem behaviors (Cressey et al., 2014; Curtis et al., 2010).
The knowledge and skills required to implement MTSS effectively have been established in the literature (Bambara et al., 2009; Bastable et al., 2020; Handler et al., 2007; Harlacher & Siler, 2011; Prasse et al., 2012; Scheuermann et al., 2013). In addition, it is evident that school counselors and school counselor educators have begun to address the need to increase knowledge and skills for MTSS so school counselors can better align their programs with MTSS and ultimately provide multiple tiers of support for all students (Belser et al., 2016; Ockerman et al., 2015; Patrikakou et al., 2016). Despite this encouraging movement in the profession, little attention has been given to the measurement of school counselors’ knowledge and skills for MTSS. Thus, the development of a survey that yields valid and reliable inferences about pre-service and in-service efforts to increase school counselors’ knowledge and skills for MTSS will be critical to assessing the development of knowledge and skills over time (e.g., before, during, and after MTSS-focused professional development).
Measuring Knowledge and Skills for MTSS
A critical aspect of effective MTSS implementation is evaluation (Algozzine et al., 2010; Elfner-Childs et al., 2010). Along with student outcome data, MTSS evaluation typically includes measuring the extent to which school staff use knowledge and skills to apply core components of MTSS (i.e., fidelity of implementation), and there are multiple measurement tools that have been developed and validated to aid external evaluators and school teams in this process (Algozzine et al., 2019; Kittelman et al., 2018; McIntosh & Lane, 2019). Despite agreement that school staff need knowledge and skills for MTSS to effectively apply core components (Eagle et al., 2015; Leko et al., 2015; McIntosh et al., 2013), little attention has been given to measuring individual school staff members’ knowledge and skills for MTSS, particularly those of school counselors. Therefore, efficient and reliable ways to measure inferences about school counselor knowledge and skills for MTSS are needed to provide a baseline of understanding and determine gaps that need to be addressed in pre-service and in-service training (Olsen, Parikh-Foxx, et al., 2016; Patrikakou et al., 2016). In addition, the validation of an instrument that measures school counselors’ knowledge and skills for MTSS is timely given that school counselors have been identified as potential key leaders in MTSS implementation given their unique skill set (Ryan et al., 2011; Ziomek-Daigle et al., 2016).
The purpose of this study was to examine the latent structure of the School Counselor Knowledge and Skills Survey for Multi-Tiered Systems of Support (SCKSS). Using confirmatory factor analysis, the number of underlying factors of the survey and the pattern of item–factor relationships were examined to address the research question: What is the factor structure of the SCKSS? Results of this study provide information on possible uses and scoring procedures of the SCKSS for examining MTSS knowledge and skills.
Method
Participants
The potential participants in this study were a sample of the 15,106 ASCA members who were practicing in K–12 settings at the time of this study. In all, 4,598 school counselors responded to the survey (30% response rate). In addition, 532 only responded to a few survey items (i.e., one or two) and were therefore excluded from the analyses. The final sample size for the analyses was 4,066. The sample used for this study mirrors school counselor demographics nationwide (ASCA, 2020; Bruce & Bridgeland, 2012). Overall, 87% of participants identified as female, 84% as Caucasian, and 74% as being between the ages of 31 and 60. Most of the school counselors in the sample reported being certified for 1–8 years (59%), working in schools with 500–1,000 students (40%) in various regions across the nation, and having student caseloads ranging from 251–500 students (54%). In addition, 25%–50% of their students were eligible for free and reduced lunch, and 54% reported that their students were racially or ethnically diverse. Lastly, most participants worked in suburban (45%) high school (37%) settings.
Sampling Procedures
Prior to conducting the research, a pilot study was conducted to assess 1) the clarity and conciseness of the directions and items on the demographic questionnaire and SCKSS, and 2) the amount of time it takes to complete the demographic questionnaire and survey (Andrews et al., 2003; Dillman et al., 2014). Four school counselors completed the demographic questionnaire and survey. Following completion, the school counselors were asked to provide feedback on the clarity and conciseness of the directions and items on the demographic questionnaire and survey as well as how much time it took to complete both measures. All pilot study participants reported that the directions were clear and easy to follow. Based on the feedback from the pilot study, the demographic questionnaire and survey were expected to take participants approximately 10–15 minutes to complete.
After obtaining approval from the IRB, SurveyShare was used to distribute an introductory email and survey link to ASCA members practicing in K–12 settings. After following the link, potential participants were given an informed consent form on the SurveyShare website. Participants who completed the survey were given the opportunity to participate in a random drawing using disassociated email addresses to increase participation (Dillman et al., 2014). Following informed consent, participants were directed to the demographic questionnaire and SCKSS. A follow-up email was sent to potential participants who did not complete the survey 7 days after the original email was sent. After 3 weeks, the link was closed.
Survey and Data Analyses
School Counselor Knowledge and Skills Survey for Multi-Tiered Systems of Support
The SCKSS was developed based on the work of Blum and Cheney (2009; 2012). The Teacher Knowledge and Skills Survey for Positive Behavior Support (TKSS) has 33 self-report items using a 5-point Likert scale to measure teachers’ knowledge and skills for Positive Behavior Supports (PBS; Blum & Cheney, 2012). Items incorporate evidence-based knowledge and skills consistent with PBS. Conceptually, items of the TKSS were developed based on five factors: (a) Specialized Behavior Supports and Practices, (b) Targeted Intervention Supports and Practices, (c) Schoolwide Positive Behavior Support Practices, (d) Individualized Curriculum Supports and Practices, and (e) Positive Classroom Supports and Practices. A confirmatory factor analysis (CFA) conducted by Blum and Cheney (2009) indicated reliability coefficients for the five factors as follows: 0.86 for Specialized Behavior Supports and Practices, 0.87 for Targeted Intervention Supports and Practices, 0.86 for Schoolwide Positive Behavior Support Practices, 0.84 for Individualized Curriculum Supports and Practices, and 0.82 for Positive Classroom Supports and Practices.
Table 1
Items, Means, and Standard Deviation for the SCKSS
| Rate the following regarding your knowledge on the item: |
M |
SD |
| 1. I know our school’s policies and programs regarding the prevention of behavior problems. |
3.66 |
0.95 |
| 2. I understand the role and function of our schoolwide behavior team. |
3.58 |
1.12 |
| 3. I know our annual goals and objectives for the schoolwide behavior program. |
3.33 |
1.19 |
| 4. I know our school’s system for screening with students with behavior problems. |
3.35 |
1.20 |
| 5. I know how to access and use our school’s pre-referral teacher assistance team. |
3.23 |
1.43 |
| 6. I know how to provide access and implement our school’s counseling programs. |
4.20 |
0.84 |
| 7. I know the influence of cultural/ethnic variables on student’s school behavior. |
3.83 |
0.87 |
8. I know the programs our school uses to help students with their social and emotional development
(schoolwide expectations, conflict resolution, etc.). |
3.92 |
0.95 |
| 9. I know a range of community services to assist students with emotional/behavioral problems. |
3.72 |
0.93 |
10. I know our school’s discipline process—the criteria for referring students to the office, the methods
used to address the problem behavior, and how and when students are returned to the classroom. |
3.72 |
1.03 |
11. I know what functional behavioral assessments are and how they are used to develop behavior
intervention plans for students. |
3.35 |
1.12 |
12. I know how our schoolwide behavior team collects and uses data to evaluate our schoolwide
behavior program. |
3.12 |
1.29 |
13. I know how to provide accommodations and modifications for students with emotional and
behavioral disabilities (EBD) to support their successful participation in the general education setting. |
3.34 |
1.09 |
| 14. I know our school’s crisis intervention plan for emergency situations. |
3.74 |
1.06 |
| Rate how effectively you use the following skills/strategies: |
|
|
| 15. Approaches for helping students to solve social/interpersonal problems. |
4.04 |
0.71 |
| 16. Methods for teaching the schoolwide behavioral expectations/social skills. |
3.62 |
0.96 |
| 17. Methods for encouraging and reinforcing the use of expectations/social skills. |
3.80 |
0.84 |
| 18. Strategies for improving family–school partnerships. |
3.35 |
0.92 |
| 19. Collaborating with the school’s student assistance team to implement student’s behavior intervention plans. |
3.50 |
1.11 |
| 20. Collaborating with the school’s IEP team to implement student’s individualized education programs. |
3.53 |
1.09 |
| 21. Evaluating the effectiveness of student’s intervention plans and programs. |
3.38 |
1.01 |
| 22. Modifying curriculum to meet individual performance levels. |
3.10 |
1.09 |
| 23. Selecting and using materials that respond to cultural, gender, or developmental differences. |
3.26 |
1.02 |
| 24. Establishing and maintaining a positive and consistent classroom environment. |
3.71 |
0.98 |
| 25. Identifying the function of student’s behavior problems. |
3.52 |
0.92 |
| 26. Using data in my decision-making process for student’s behavioral programs. |
3.39 |
1.01 |
| 27. Using prompts and cues to remind students of behavioral expectations. |
3.67 |
0.95 |
| 28. Using self-monitoring approaches to help students demonstrate behavioral expectations. |
3.48 |
0.96 |
| 29. Communicating regularly with parents/guardians about student’s behavioral progress. |
3.64 |
0.97 |
30. Using alternative settings or methods to resolve student’s social/emotional problems (problem-
solving, think time, or buddy room, etc. not a timeout room). |
3.45 |
1.06 |
| 31. Methods for diffusing or deescalating student’s social/emotional problems. |
3.76 |
0.87 |
| 32. Methods for enhancing interpersonal relationships of students (e.g., circle of friends, buddy system, peer mentors). |
3.62 |
0.92 |
| 33. Linking family members to needed services and resources in the school. |
3.72 |
0.91 |
The TKSS was adapted in collaboration with the authors to develop the SCKSS (Olsen, Blum, et al., 2016) to specifically target school counselors and to reflect the updated terminology recommended in the literature (Sugai & Horner, 2009). To update terminology, multi-tiered systems of support (MTSS) replaced Positive Behavior Supports (PBS) throughout the survey. In addition, school counselor replaced teacher to reflect the role of intended participants. Finally, item 6 was updated from “I know how to access and use our school’s counseling programs” to “I know how to provide access and implement our school’s counseling programs” because of school counselors’ roles and interactions with their own programs. Further, item 6 was adjusted to be an internally oriented question about the delivery of the school counseling program rather than the school counselor’s knowledge of another school service or system in order to assess participants’ perceived mastery of school counseling program implementation rather than their perception of another service not already measured in the SCKSS. A description of the 33 SCKSS items and the means and standard deviations of each item for the current study are located in Table 1.
Data Analyses
A cross-validation holdout method was used to examine the data–model fit of the SCKSS. Prior to statistical analyses, data were screened for missing data, multivariate outliers, and the assumptions for multivariate regression. Less than 5% of the data for any variable was missing and Little’s MCAR test (χ2 = 108.47, df = 101, p = .29) indicated missing values could be considered as missing completely at random. Multiple imputation was used to estimate missing values. Although there were some outliers, results of a sensitivity analysis indicated that none of the outliers were overly influential. The assumptions of linearity, normality, multicollinearity, and homoscedasticity suggested that all the assumptions were tenable. The original sample (N = 4,066) was randomly divided into two sub-samples (N = 2,033). The first subset was used to conduct exploratory analyses and develop a model that fit the data. The second subset of participants was used to conduct confirmatory analyses without modifications.
Exploratory Factor Analysis (EFA). Using the first subset from the sample, an EFA was conducted, using SPSS, to explore the number of factors and the alignment of items to factors. The number of factors extracted was estimated based on eigenvalues greater than 1.0 and a visual inspection of the scree plot. Several rotation methods were used, including varimax and direct oblimin with changing the delta value (from 0 to 0.2). The goal of the EFA was to find a factor solution that was theoretically sound.
Confirmatory Factor Analysis (CFA). The estimation method employed for the CFA was maximum likelihood robust estimation, which is a more accurate estimate for non-normal data (Savalei, 2010). Although the data were ordinal (i.e., Likert-type scale), Mplus uses a different maximum likelihood fitting function for categorical variables. The Satorra-Bentler scaled chi-square difference test was used to determine the best model. The pattern coefficient for the first indicator of each latent variable was fixed to 1.00. Indices of model–data fit considered were chi-square test, root-mean-square error of approximation (RMSEA), standardized root-mean-square residual (SRMR), comparative fit index (CFI), and Akaike information criterion (AIC). Browne and Cudeck (1993) suggested that values greater than .10 might indicate a lack of fit. In this study, an upper 90% confidence interval value lower than .08 was used to suggest an acceptable fit. CFI values greater than .90, which indicate that the proposed model is greater than 90% of the baseline model, served as an indicator of adequate fit (Kline, 2016). Perfect model fit is indicated by SRMR = 0, and values greater than .10 may indicate poor fit (Kline, 2016). Reliability was assessed using Cronbach’s alpha (α). CFAs were used in both the exploratory and confirmatory phases of this study. In the exploratory phase (i.e., using the first subset from the sample), the researchers used the residual estimates and modification indices to identify local misfit. Respecification of correlated error variances was expected because of the data collection method (i.e., counselors responding to a single
survey) and similar wording of the items.
Results
Exploratory Phase
Exploratory Factor Analysis
An EFA was used to evaluate the structure of the 33 items on the SCKSS. Principal axis factoring was used as the extraction method. The Kaiser-Meyer-Olkin test value was .97, which suggests the sample was acceptable for conducting an EFA. The decrease in eigenvalues leveled off at five factors, with four factors having eigenvalues greater than 1.0. Parallel analysis confirmed that four factors should be retained in the solution. An oblique rotation, which was selected to allow correlation among the factors, was performed and used to determine the number of factors and item pattern.
The total variance accounted for by four factors was 64%. The item communalities were all above 0.5. Item pattern (i.e., > 0.4) and structure (i.e., > 0.5) coefficients were examined to determine the relationship of the items to the factors. Twenty-nine items clearly aligned to one factor and three items loaded in multiple factors. In a review of the item patterns, it was determined by the researchers that the three items theoretically fit in specific factors. The fourth factor only aligned with three items. In an expert review, it was determined that the three items differentiated enough from the other factors to warrant a separate factor. The alignment of items and factors are reported in Table 2.
Table 2
Alignment of Items and Factors based on EFA
| Factor |
Items |
| Individualized Supports and Practices |
11, 13, 16, 17, 22, 23, 25, 26, 27, 28, 29, 30, 31, 32 |
| Schoolwide Supports and Practices |
1, 2, 3, 4, 5, 8, 10, 12, 14, 24 |
| Targeted Supports and Practices |
6, 7, 9, 15, 18, 33 |
| Collaborative Supports and Practices |
19, 20, 21 |
The first factor was named Individualized Supports and Practices. This factor contained 14 items focused on school counselors’ knowledge and skills for supporting students individually based on need. Examples of items on the Individualized Supports and Practices factor included: “Selecting and using materials that respond to cultural, gender, or developmental differences” and “Methods for diffusing or deescalating student’s social/emotional problems.” The second factor was Schoolwide Supports and Practices, with 10 items focused on school counselors’ knowledge and skills of schoolwide and team-based efforts aimed at supporting all students and preventing student problem behavior and academic decline. Examples of items on the Schoolwide Supports and Practices factor included: “I know our annual goals and objectives for the schoolwide behavior program” and “I know our school’s crisis intervention plan for emergency situations.” Factor 3 was named Targeted Supports and Practices and contained six items. These items focused on school counselors’ knowledge and skills related to providing targeted supports for small groups of students not responding positively to schoolwide prevention efforts. Examples of items on the Targeted Supports and Practices factor included: “I know the influence of cultural/ethnic variables on student’s school behavior” and “Strategies for improving family–partnerships.” The fourth and final factor was Collaborative Supports and Practices, which contained three items focused on school counselors’ knowledge and skills related to collaborating with school personnel to implement student interventions. An example item of the Collaborative Supports and Practices factor was: “Collaborating with the school’s IEP team to implement student’s individualized education programs.” This four-factor model served as our preferred model, but competing models were explored using CFA on the first subset from the sample.
CFA Using First Subset Sample
The competing models were examined to determine the best data–model fit by conducting a CFA using MPlus. The following models were tested: (a) one-factor model, (b) four-factor model, and
(c) second-order four-factor model. Model modifications were allowed during the exploratory phases. The results of the CFA are reported in Table 3.
Table 3
Results of the Confirmatory Factor Analyses for the Exploratory Phase
|
Competing Models |
Chi-square |
df |
SRMR |
RMSEA |
90% CI, RMSEA |
TLI |
CFI |
AIC |
|
|
|
|
|
|
|
|
|
|
|
Exploratory Analyses |
|
|
|
|
|
|
|
|
| 1 |
One-Factor (initial) |
8,518.75 |
495 |
.057 |
.084 |
[.083, .086] |
0.79 |
.80 |
168,279.20 |
|
One-Factor (modification) a |
4,465.60 |
478 |
.048 |
.060 |
[.059, .062] |
0.89 |
.90 |
162,654.94 |
|
|
|
|
|
|
|
|
|
|
| 2 |
Four-Factor (initial) |
5,619.01 |
489 |
.058 |
.068 |
[.066, .069] |
0.86 |
.87 |
164,253.62 |
|
Four-Factor (modification) b |
3,866.27 |
481 |
.048 |
.055 |
[.054, .057] |
0.91 |
.92 |
161,407.48 |
|
|
|
|
|
|
|
|
|
|
| 3 |
Four-Factor second order |
5,632.53 |
491 |
.058 |
.068 |
[.066, .069] |
0.86 |
.87 |
164,270.54 |
|
Four-Factor second order (modified) b |
3,866.27 |
483 |
.048 |
.055 |
[.054, .057] |
0.91 |
.91 |
161,432.63 |
|
|
|
|
|
|
|
|
|
|
|
Confirmatory Analysis |
|
|
|
|
|
|
|
|
|
Four-Factor second order |
5,424.82 |
490 |
0.058 |
0.066 |
[.065, .068] |
0.87 |
.88 |
164,999.81 |
|
Four-Factor second order (modified) b |
4,468.62 |
483 |
0.051 |
0.060 |
[.058, .062] |
0.89 |
.90 |
163,723.53 |
Note. All chi-square tests were statistically significant at < .001.
a Seventeen correlated error variances were estimated. b Eight correlated error variances were estimated.
The initial one-factor model did not fit the data (chi-square = 8,518.75, df = 495, p < .001; RMSEA = .084, 90% CI [.083, .086]; CFI = .80; SRMR = .057), but after modification (i.e., 17 correlated error variances between observed variables), the one-factor model had an adequate fit (chi-square = 4,465.60, df = 478, p < .001; RMSEA = .060, 90% CI [.059, .062]; CFI = .90; SRMR = .048). Reasonable data–model fit was obtained for the modified models in both the four-factor and four-factor second-order models (see Table 3). Modifications included freeing eight correlated error variances between observed variables. A content expert reviewed the suggested modification to determine the appropriateness of allowing the error variances to correlate. In all but one case, the suggested correlated item error variances were adjacent to each other on the survey (i.e., item 2 with 3, 6 with 7, 11 with 12, 17 with 18, 20 with 21, 22 with 23, and 27 with 28). Given the proximity of the items, it was plausible that some systematic error variance between items would correlate. The only pair of items that were not adjacent were item 5 and item 19. Both of these items referred to the school’s teacher assistance team. For all the models, the path coefficients were statistically significant (p < .001).
Results of the Satorra-Bentler scaled chi-square difference test suggested that the four-factor model was a better model than the one-factor model (p < .001), and there was no statistically significant difference between the four-factor model and the second-order four-factor model. Because of the high intercorrelations among the factors (ranging from .81 to .92), the second-order four-factor model was tested using the second subset from the sample.
Confirmatory Phase
The holdout sample of 2,033 participants was used to verify the second-order four-factor model. The initial model (see bottom of Table 3) with no modifications suggested the model marginally fit the data (chi-square = 5,424.82, RMSEA = .066, CFI = .88, SRMR = .058). After modifying the model by allowing for the eight correlated error variances, which were the same eight correlated error variances identified in the exploratory stage, as expected there was an improvement in the model fit (chi-square = 4,468.62, RMSEA = .060, CFI = .90, SRMR = .051). The observed item loading coefficients and standard errors are reported in Table 4. All coefficients are statistically significant and all above 0.50, suggesting stable item alignment to the factor being measured. Coefficient alpha values were 0.95 for total score with all items, 0.88 for Factor 1 (Individualized Supports and Practices), 0.86 for Factor 2 (Schoolwide Supports and Practices), 0.78 for Factor 3 (Targeted Supports and Practices), and 0.65 for Factor 4 (Collaborative Supports and Practices). The results provide evidence that the SCKSS has potential to provide inferences about counselors’ knowledge and skills for MTSS.
Discussion and Implications
The SCKSS was based on the TKSS, which measured teachers’ knowledge and skills related to PBS. After adapting the survey to align to MTSS and the role of school counselors, this study aimed to examine the latent structure of the SCKSS for examining MTSS knowledge and skills. Using both exploratory and confirmatory factor analyses, results suggest that a second-order four-factor model had the best fit. The findings indicate that the SCKSS has high internal consistency with Cronbach’s alpha for the total score at 0.95, and a range between 0.65 and 0.88 for each of the four factors. The first factor, Individualized Supports and Practices, contains 14 items; the second factor, Schoolwide Supports and Practices, contains 10 items; the third factor, Targeted Supports and Practices, contains six items; and the fourth factor, Collaborative Supports and Practices, is composed of three items. These findings confirm that the SCKSS yields valid and reliable inferences about school counselors’ knowledge and skills for MTSS. Previous measures that were specific to school counselors focused on confidence and beliefs in implementing response to intervention (RtI; Ockerman et al., 2015; Patrikakou et al., 2016). Although these studies contribute to the literature by aligning RtI with the ASCA National Model, they did not focus on the specific knowledge and skills related to MTSS.
Table 4
Loading Coefficients and Standard Errors for Best Fitting Model
| Factor 1 |
Individualized Supports and Practices |
Item |
Loading |
SE |
|
|
11 |
.652 |
.014 |
|
|
13 |
.735 |
.011 |
|
|
16 |
.712 |
.013 |
|
|
17 |
.762 |
.011 |
|
|
22 |
.645 |
.014 |
|
|
23 |
.674 |
.013 |
|
|
25 |
.801 |
.009 |
|
|
26 |
.736 |
.012 |
|
|
27 |
.779 |
.010 |
|
|
28 |
.799 |
.009 |
|
|
29 |
.709 |
.012 |
|
|
30 |
.753 |
.012 |
|
|
31 |
.774 |
.010 |
|
|
32 |
.772 |
.010 |
| Factor 2 |
Schoolwide Supports and Practices |
|
|
|
|
|
1 |
.816 |
.009 |
|
|
2 |
.817 |
.010 |
|
|
3 |
.813 |
.010 |
|
|
4 |
.805 |
.010 |
|
|
5 |
.612 |
.016 |
|
|
8 |
.731 |
.012 |
|
|
10 |
.755 |
.011 |
|
|
12 |
.773 |
.011 |
|
|
14 |
.659 |
.014 |
|
|
24 |
.567 |
.017 |
| Factor 3 |
Targeted Supports and Practices |
|
|
|
|
|
6 |
.685 |
.015 |
|
|
7 |
.664 |
.014 |
|
|
9 |
.729 |
.012 |
|
|
15 |
.766 |
.011 |
|
|
18 |
.729 |
.012 |
|
|
33 |
.764 |
.012 |
| Factor 4 |
Collaborative Supports and Practices |
|
|
|
|
|
19 |
.760 |
.013 |
|
|
20 |
.618 |
.017 |
|
|
21 |
.806 |
.012 |
|
|
|
|
|
|
Higher order coefficients |
F1 |
.968 |
.006 |
|
|
F2 |
.872 |
.009 |
|
|
F3 |
.911 |
.008 |
|
|
F4 |
.944 |
.010 |
The four factors of the SCKSS can be used to support improvement practices through the use of targeted professional development. This extends previous research that found when school counselors received MTSS-focused training, there was an increase in knowledge and skills (Olsen, Parikh-Foxx, et al., 2016). Accordingly, the four factors of the SCKSS may provide a baseline of school counselors’ knowledge and skills related to MTSS and help determine gaps that need to be addressed in pre-service and in-service training. Through targeted professional development and pre-service training activities, school districts and counselor educators can identify areas in which practitioners need additional training to increase knowledge and skills related to MTSS.
The four factors of the SCKSS align with MTSS tiers and school counselor roles recommended in the ASCA National Model (2019a). The first factor, Individualized Supports and Practices, aligns with the role of school counselors providing individualized indirect services (e.g., data-based decision-making, referrals) for students who need Tier 3 supports (Ziomek-Daigle et al., 2019). The second factor, Schoolwide Supports and Practices, aligns with the role of school counselors providing Tier 1 universal supports (e.g., school counseling lessons, schoolwide initiatives, family workshops) for all students (Sink, 2019). The third factor, Targeted Supports and Practices, aligns with Tier 2 supports provided by school counselors, including small group counseling and psychoeducational group instruction for students who do not successfully respond to schoolwide support services (Olsen, 2019). Finally, the fourth factor, Collaborative Supports and Practices, aligns with the school counselor’s role across multiple tiers of support, providing access to community resources through appropriate referrals and collaborating and consulting with intervention teams (Cholewa & Laundy, 2019).
The SCKSS survey can also be used to improve current school counseling practices. This is an important consideration given Patrikakou et al. (2016) found that although school counselors reported feeling prepared to deliver Tier 1 counseling support services, they felt least prepared to collect and analyze data to determine the effectiveness of interventions. Given that the ASCA National Model (2019a) has a theme entitled Assess, school counselors should be trained to engage in program improvements that move toward positively impacting students. As such, using the SCKSS to improve MTSS practices has the potential to improve ASCA National Model–related activities.
Limitations
There are several limitations in the current study. First, respondents were from a national school counseling association. Their responses could have been influenced by having access to professional development and literature related to MTSS. Second, this was a self-report survey, so the respondents could have answered in a manner that was socially desirable. Third, given the 30% survey return rate, generalizing these results to the population of counselors is not recommended. Fourth, rewording item 6 to an internally oriented question about delivery of the school counseling program rather than school counselors’ knowledge of another school service or system may have impacted the best fit model. Finally, because this was an online survey, only those with access to email and internet at the time of the survey had the opportunity to participate.
Future Research
Although participants in this study included a large national sample of school counselors, they were all members of a national association. Therefore, researchers could replicate this study with school counselors who are non-members and conduct further testing of the psychometric properties of the survey. Second, research could examine how professional development impacts specific aspects of knowledge and skills in relation to student outcomes. That is, if school counselors have targeted professional development around each of the four factors, does that affect student outcomes in areas such as discipline, social/emotional well-being, school climate, or even academic performance? Finally, future studies could explore other variables that impact the development and application of school counselors’ knowledge and skills for MTSS.
Conclusion
There is growing evidence supporting the impact of school counseling program and MTSS alignment (Betters-Bubon et al., 2016; Betters-Bubon & Donohue, 2016; Campbell et al., 2013; Goodman-Scott, 2013; Goodman-Scott et al., 2014). In order for school counselors to align their programs with MTSS and contribute to MTSS implementation, foundational knowledge and skills are essential. Given that research has shown that key factors such as school level (i.e., elementary, middle, high) and MTSS training impact school counselors’ knowledge and skills for MTSS (Olsen, Parikh-Foxx, et al., 2016), the development and validation of an MTSS knowledge and skills survey to measure school counselors’ knowledge and skills over time is an important next step to advancing school counseling program and MTSS alignment. The four factors of the SCKSS (i.e., Individualized Supports and Practices, Schoolwide Supports and Practices, Targeted Supports and Practices, Collaborative Supports and Practices) provide school counselors with an opportunity to reflect on their strengths and areas in need of improvement related to the tiers of the MTSS framework. Further application research and validation of the SCKSS is needed; however, this study indicates the SCKSS provides counselor educators, pre-service school counselors, and in-service school counselors with a tool to measure the development of MTSS knowledge and skills.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Algozzine, B., Barrett, S., Eber, L., George, H., Horner, R., Lewis, T., Putnam, B., Swain-Bradway, J., McIntosh, K., & Sugai, G. (2019). School-wide PBIS Tiered Fidelity Inventory version 2.1. OSEP Technical Assistance Center on Positive Behavioral Interventions and Supports. https://www.pbisapps.org/Resources/SWIS%20Publications/SWPBIS%20Tiered%20Fidelity%20Inventory%20(TFI).pdf
Algozzine, B., Horner, R. H., Sugai, G., Barrett, S., Dickey, C. R., Eber, L., Kincaid, D., Lewis, T., & Tobin, T. (2010). Evaluation blueprint for school-wide positive behavior support. National Technical Assistance Center on Positive Behavioral Interventions and Support. https://www.pbisapps.org/Resources/SWIS%20Publications/Evaluation%20Blueprint%20for%20School-Wide%20Positive%20Behavior%20Support.pdf
American School Counselor Association. (2014). The school counselor and group counseling. ASCA Position Statements, pp. 35–36. https://www.schoolcounselor.org/asca/media/asca/PositionStatements/PositionStatements.pdf
American School Counselor Association. (2018). The school counselor and multitiered system of supports. ASCA Position Statements, pp. 47–48. https://www.schoolcounselor.org/asca/media/asca/PositionStatements/PositionStatements.pdf
American School Counselor Association. (2019a). The ASCA national model: A framework for school counseling programs (4th ed.).
American School Counselor Association. (2019b). Role of the school counselor. https://www.schoolcounselor.org/administrators/role-of-the-school-counselor
American School Counselor Association. (2020). ASCA membership demographics. https://www.schoolcounselor.org/asca/media/asca/home/MemberDemographics.pdf
Andrews, D., Nonnecke, B., & Preece, J. (2003). Electronic survey methodology: A case study in reaching hard-to-involve internet users. International Journal of Human–Computer Interaction, 16(2), 185–210.
https://doi.org/10.1207/S15327590IJHC1602_04
Bambara, L. M., Nonnemacher, S., & Kern, L. (2009). Sustaining school-based individualized positive behavior support: Perceived barriers and enablers. Journal of Positive Behavior Interventions, 11(3), 161–176.
https://doi.org/10.1177/1098300708330878
Barrett, S. B., Bradshaw, C. P., & Lewis-Palmer, T. (2008). Maryland statewide PBIS initiative: Systems, evaluation, and next steps. Journal of Positive Behavior Interventions, 10(2), 105–114.
https://doi.org/10.1177/1098300707312541
Bastable, E., Massar, M. M., & McIntosh, K. (2020). A survey of team members’ perceptions of coaching activities related to Tier 1 SWPBIS implementation. Journal of Positive Behavior Interventions, 22(1), 51–61. https://doi.org/10.1177/1098300719861566
Belser, C. T., Shillingford, M. A., & Joe, J. R. (2016). The ASCA model and a multi-tiered system of supports: A framework to support students of color with problem behavior. The Professional Counselor, 6(3), 251–262. https://doi.org/10.15241/cb.6.3.251
Benner, G. J., Kutash, K., Nelson, J. R., & Fisher, M. B. (2013). Closing the achievement gap of youth with emotional and behavioral disorders through multi-tiered systems of support. Education and Treatment of Children, 36(3), 15–29. https://doi.org/10.1353/etc.2013.0018
Berkeley, S., Bender, W. N., Peaster, L. G., & Saunders, L. (2009). Implementation of response to intervention: A snapshot of progress. Journal of Learning Disabilities, 42(1), 85–95. https://doi.org/10.1177/0022219408326214
Betters-Bubon, J., Brunner, T., & Kansteiner, A. (2016). Success for all? The role of the school counselor in creating and sustaining culturally responsive positive behavior interventions and supports programs. The Professional Counselor, 6(3), 263–277. https://doi.org/10.15241/jbb.6.3.263
Betters-Bubon, J., & Donohue, P. (2016). Professional capacity building for school counselors through school-wide positive behavior interventions and supports implementation. Journal of School Counseling, 14(3). http://jsc.montana.edu/articles/v14n3.pdf
Blum, C., & Cheney, D. (2009). The validity and reliability of the Teacher Knowledge and Skills Survey for Positive Behavior Support. Teacher Education and Special Education, 32(3), 239–256.
https://doi.org/10.1177/0888406409340013
Blum, C., & Cheney, D. (2012). Teacher Knowledge and Skills Survey for Positive Behavior Support. Illinois State University.
Bradshaw, C. P., Koth, C. W., Thornton, L. A., & Leaf, P. J. (2009). Altering school climate through school-wide positive behavioral interventions and supports: Findings from a group-randomized effectiveness trial. Prevention Science, 10(2), 100–115. https://doi.org/10.1007/s11121-008-0114-9
Bradshaw, C. P., Mitchell, M. M., & Leaf, P. J. (2010). Examining the effects of schoolwide positive behavioral interventions and supports on student outcomes: Results from a randomized controlled effectiveness trial in elementary schools. Journal of Positive Behavioral Interventions, 12(3), 133–148.
https://doi.org/10.1177/1098300709334798
Brendle, J. (2015). A survey of response to intervention team members’ effective practices in rural elementary schools. Rural Special Education Quarterly, 34(2), 3–8. https://doi.org/10.1177/875687051503400202
Briere, D. E., Simonsen, B., Sugai, G., & Myers, D. (2015). Increasing new teachers’ specific praise using a within-school consultation intervention. Journal of Positive Behavior Interventions, 17(1), 50–60.
https://doi.org/10.1177/1098300713497098
Browne, M. W., & Cudeck, R. (1993). Alternative ways of assessing model fit. In K. A. Bollen and J. S. Long (Eds.), Testing structural equation models (pp. 136–162). SAGE.
Bruce, M., & Bridgeland, J. (2012). 2012 national survey of school counselors—True north: Charting the course to college and career readiness.https://secure-media.collegeboard.org/digitalServices/pdf/nosca/true-north.pdf
Campbell, A., Rodriguez, B. J., Anderson, C., & Barnes, A. (2013). Effects of a Tier 2 intervention on classroom disruptive behavior and academic engagement. Journal of Curriculum & Instruction, 7(1), 32–54.
https://doi.org/10.3776/joci.2013.v7n1p32-54
Center on Positive Behavioral Interventions and Supports. (2015). Positive behavioral interventions and supports (PBIS) implementation blueprint. University of Oregon. https://www.pbis.org/resource/pbis-implementation-blueprint
Chard, D. J., Harn, B. A., Sugai, G., Horner, R. H., Simmons, D. C., & Kame’enui, E. J. (2008). Core features of multi-tiered systems of reading and behavioral support. In C. G. Greenwood, T. R. Kratochwill, & M. Clements (Eds.), Schoolwide prevention models: Lessons learned in elementary schools (pp. 31–60). Guilford.
Cholewa, B., & Laundy, K. C. (2019). School counselors consulting and collaborating within MTSS. In E. Goodman-Scott, J. Betters-Bubon, & P. Donohue (Eds.), The school counselor’s guide to multi-tiered systems of support (pp. 222–245). Routledge.
Cressey, J. M., Whitcomb, S. A., McGilvray-Rivet, S. J., Morrison, R. J., & Shander-Reynolds, K. J. (2014). Handling PBIS with care: Scaling up to school-wide implementation. Professional School Counseling, 18(1), 90–99. https://doi.org/10.1177/2156759X0001800104
Curtis, R., Van Horne, J. W., Robertson, P., & Karvonen, M. (2010). Outcomes of a school-wide positive behavioral support program. Professional School Counseling, 13(3), 159–164.
Dillman, D. A., Smyth, J. D., & Christian, L. M. (2014). Internet, phone, mail, and mixed-mode surveys: The tailored design method. Wiley.
Eagle, J. W., Dowd-Eagle, S. E., Snyder, A., & Holtzman, E. G. (2015). Implementing a multi-tiered system of support (MTSS): Collaboration between school psychologists and administrators to promote systems-level change. Journal of Educational and Psychological Consultation, 25(2–3), 160–177.
https://doi.org/10.1080/10474412.2014.929960
Elfner Childs, K., Kincaid, D., & George, H. P. (2010). A model for statewide evaluation of a universal positive behavior support initiative. Journal of Positive Behavior Interventions, 12(4), 198–210.
https://doi.org/10.1177/1098300709340699
Freeman, R., Miller, D., & Newcomer, L. (2015). Integration of academic and behavioral MTSS at the district level using implementation science. Learning Disabilities: A Contemporary Journal, 13(1), 59–72.
Freeman, J., Simonsen, B., McCoach, D. B., Sugai, G., Lombardi, A., & Horner, R. (2016). Relationship between school-wide positive behavior interventions and supports and academic, attendance, and behavior outcomes in high schools. Journal of Positive Behavior Interventions, 18(1), 41–51.
https://doi.org/10.1177/1098300715580992
Freeman, J., Sugai, G., Simonsen, B., & Everett, S. (2017). MTSS coaching: Bridging knowing to doing. Theory Into Practice, 56(1), 29–37. https://doi.org/10.1080/00405841.2016.1241946
Goodman-Scott, E. (2013). Maximizing school counselors’ efforts by implementing school-wide positive behavioral interventions and supports: A case study from the field. Professional School Counseling, 17(1), 111–119. https://doi.org/10.1177/2156759X0001700106
Goodman-Scott, E., Betters-Bubon, J., & Donohue, P. (2015). Aligning comprehensive school counseling programs and positive behavioral interventions and supports to maximize school counselors’ efforts. Professional School Counseling, 19(1), 57–67. https://doi.org/10.5330/1096-2409-19.1.57
Goodman-Scott, E., Doyle, B., & Brott, P. (2014). An action research project to determine the utility of bully prevention in positive behavior support for elementary school bullying prevention. Professional School Counseling, 17(1), 120–129. https://doi.org/10.5330/prsc.17.1.53346473u5052044
Goodman-Scott, E., & Grothaus, T. (2017a). RAMP and PBIS: “They definitely support one another”: The results of a phenomenological study. Professional School Counseling, 21(1), 119–129.
https://doi.org/10.5330/1096-2409-21.1.119
Goodman-Scott, E., & Grothaus, T. (2017b). School counselors’ roles in RAMP and PBIS: A phenomenological investigation. Professional School Counseling, 21(1), 130–141. https://doi.org/10.5330/1096-2409-21.1.130
Grothaus, T. (2013). School counselors serving students with disruptive behavior disorders. Professional School Counseling, 16(2), 245–255. https://doi.org/10.1177/2156759X12016002S04
Gruman, D. H., & Hoelzen, B. (2011). Determining responsiveness to school counseling interventions using behavioral observations. Professional School Counseling, 14(3), 183–190.
Gysbers, N. C. (2010). School counseling principles: Remembering the past, shaping the future: A history of school counseling. American School Counselor Association.
Handler, M. W., Rey, J., Connell, J., Thier, K., Feinberg, A., & Putnam, R. (2007). Practical considerations in creating school-wide positive behavior support in public schools. Psychology in the Schools, 44(1), 29–39. https://doi.org/10.1002/pits.20203
Harlacher, J. E., & Siler, C. E. (2011). Factors related to successful RtI implementation. Communique, 39(6), 20–22.
Harrington, K., Griffith, C., Gray, K., & Greenspan, S. (2016). A grant project to initiate school counselors’ development of a multi-tiered system of supports based on social-emotional data. The Professional Counselor, 6(3), 278–294. https://doi.org/10.15241/kh.6.3.278
Harvey, M. W., Yssel, N., & Jones, R. E. (2015). Response to intervention preparation for preservice teachers: What is the status for Midwest institutions of higher education. Teacher Education and Special Education, 38(2), 105–120. https://doi.org/10.1177/0888406414548598
Hollenbeck, A. F., & Patrikakou, E. (2014). Response to intervention in Illinois: An exploration of school professionals’ attitudes and beliefs. Mid-Western Educational Researcher, 26(2), 58–82.
Horner, R. H., Sugai, G., Smolkowski, K., Eber, L., Nakasato, J., Todd, A. W., & Esperanza, J., (2009). A randomized, wait-list controlled effectiveness trial assessing school-wide positive behavior support in elementary schools. Journal of Positive Behavior Interventions, 11(3), 133–144. https://doi.org/10.1177/1098300709332067
Hughes, C. A., & Dexter, D. D. (2011). Response to intervention: A research-based summary. Theory Into Practice, 50(1), 4–11. https://doi.org/10.1080/00405841.2011.534909
Kittelman, A., Eliason, B. M., Dickey, C. R., & McIntosh, K. (2018). How are schools using the SWPBIS Tiered Fidelity Inventory (TFI)? OSEP Technical Assistance Center on Positive Behavioral Interventions and Supports. https://www.pbis.org/resource/how-are-schools-using-the-swpbis-tiered-fidelity-inventory-tfi
Kline, R. B. (2016). Principles and practice of structural equation modeling (4th ed.). Guilford.
Kuo, N.-C. (2014). Why is response to intervention (RTI) so important that we should incorporate it into teacher education programs and how can online learning help? Journal of Online Learning & Teaching, 10(4), 610–624.
Lassen, S. R., Steele, M. M., & Sailor, W. (2006). The relationship of school-wide positive behavior support to academic achievement in an urban middle school. Psychology in the Schools, 43(6), 701–712.
https://doi.org/10.1002/pits.20177
Leko, M. M., Brownell, M. T., Sindelar, P. T., & Kiely, M. T. (2015). Envisioning the future of special education personnel preparation in a standards-based era. Exceptional Children, 82(1), 25–43.
https://doi.org/10.1177/0014402915598782
Martens, K., & Andreen, K. (2013). School counselors’ involvement with a school-wide positive behavior support intervention: Addressing student behavior issues in a proactive and positive manner. Professional School Counseling, 16(5), 313–322. https://doi.org/10.1177/2156759X1201600504
McIntosh, K., & Goodman, S. (2016). Integrated multi-tiered systems of support: Blending RTI and PBIS. Guilford.
McIntosh, K., & Lane, K. L. (2019). Advances in measurement in school-wide positive behavioral interventions and supports. Remedial and Special Education, 40(1), 3–5. https://doi.org/10.1177/0741932518800388
McIntosh, K., Mercer, S. H., Hume, A. E., Frank, J. L., Turri, M. G., & Mathews, S. (2013). Factors related to sustained implementation of schoolwide positive behavior support. Exceptional Children, 79(3), 293–311.
Michigan’s Integrated Behavior & Learning Support Initiative. (2015). An abstract regarding multi-tier system of supports (MTSS) and Michigan’s integrated behavior and learning support initiative (MiBLSi). https://mimtsstac.org/sites/default/files/Documents/MIBLSI_Model/MTSS/MiBLSi%20MTSS%20Abstract%20May%202015.pdf
Ockerman, M. S., Mason, E. C. M., & Hollenbeck, A. F. (2012). Integrating RTI with school counseling programs: Being a proactive professional school counselor. Journal of School Counseling, 10(15). https://files.eric.ed.gov/fulltext/EJ978870.pdf
Ockerman, M. S., Patrikakou, E., & Hollenbeck, A. F. (2015). Preparation of school counselors and response to intervention: A profession at the crossroads. Journal of Counselor Preparation & Supervision, 7(3), 161–184. https://doi.org/10.7729/73.1106
Olsen, J. (2019). Tier 2: Providing supports for students with elevated needs. In E. Goodman-Scott, J. Betters-Bubon, & P. Donohue (Eds.), The school counselor’s guide to multi-tiered systems of support (pp. 133–162). Routledge.
Olsen, J. A., Blum, C., & Cheney, D. (2016). School counselor knowledge and skills survey for multi-tiered systems of support. Unpublished survey, Department of Counseling, University of North Carolina at Charlotte.
Olsen, J., Parikh-Foxx, S., Flowers, C., & Algozzine, B. (2016). An examination of factors that relate to school counselors’ knowledge and skills in multi-tiered systems of support. Professional School Counseling, 20(1), 159–171. https://doi.org/10.5330/1096-2409-20.1.159
Pas, E. T., & Bradshaw, C. P. (2012). Examining the association between implementation and outcomes: State-wide scale-up of school-wide positive behavior intervention and supports. The Journal of Behavioral Health Services & Research, 39(4), 417–433. https://doi.org/10.1007/s11414-012-9290-2
Patrikakou, E., Ockerman, M. S., & Hollenbeck, A. F. (2016). Needs and contradictions of a changing field: Evidence from a national response to intervention implementation study. The Professional Counselor, 6(3), 233–250. https://doi.org/10.15241/ep.6.3.233
Pearce, L. R. (2009). Helping children with emotional difficulties: A response to intervention investigation. The Rural Educator, 30(2), 34–46.
Prasse, D. P., Breunlin, R. J., Giroux, D., Hunt, J., Morrison, D., & Thier, K. (2012). Embedding multi-tiered
system of supports/response to intervention into teacher preparation. Learning Disabilities: A Contemporary Journal, 10(2), 75–93.
Rose, J., & Steen, S. (2015). The Achieving Success Everyday group counseling model: Fostering resiliency in middle school students. Professional School Counseling, 18(1), 28–37. https://doi.org/10.1177/2156759X0001800116
Ryan, T., Kaffenberger, C. J., & Carroll, A. G. (2011). Response to intervention: An opportunity for school
counselor leadership. Professional School Counseling, 14(3), 211–221.
https://doi.org/10.1177/2156759X1101400305
Savalei, V. (2010). Expected versus observed information in SEM with incomplete normal and nonnormal data. Psychological Methods, 15(4), 352–367. https://doi.org/10.1037/a0020143
Scheuermann, B. K., Duchaine, E. L., Bruntmyer, D. T., Wang, E. W., Nelson, C. M., & Lopez, A. (2013). An exploratory survey of the perceived value of coaching activities to support PBIS implementation in secure juvenile education settings. Education and Treatment of Children, 36(3), 147–160.
https://doi.org/10.1353/etc.2013.0021
Sink, C. A. (2016). Incorporating a multi-tiered system of supports into school counselor preparation. The Professional Counselor, 6(3), 203–219. https://doi.org/10.15241/cs.6.3.203
Sink, C. (2019). Tier 1: Creating strong universal systems of support and facilitating systemic change. In E. Goodman-Scott, J. Betters-Bubon, & P. Donohue (Eds.), The school counselor’s guide to multi-tiered systems of support (pp. 62–98). Routledge.
Sink, C. A., Edwards, C., & Eppler, C. (2012). School based group counseling. Brooks/Cole.
Sink, C. A., & Ockerman, M. S. (2016). Introduction to the special issue: School counselors and a multi-tiered system of supports: Cultivating systemic change and equitable outcomes. The Professional Counselor, 6(3), v–ix. https://doi.org/csmo.6.3.v
Smith, H. M., Evans-McCleon, T. N., Urbanski, B., & Justice, C. (2015). Check in/check out intervention with peer monitoring for a student with emotional-behavioral difficulties. Journal of Counseling & Development, 93(4), 451–459. https://doi.org/10.1002/jcad.12043
Sugai, G., & Horner, R. H. (2009). Responsiveness-to-intervention and school-wide positive behavior supports: Integration of multi-tiered system approaches. Exceptionality, 17(4), 223–237.
https://doi.org/10.1080/09362830903235375
Sugai, G. M., Horner, R. H., Dunlap, G., Hieneman, M., Lewis, T. J., Nelson, C. M., Scott, T. M., Liaupsin, C.,
Sailor, W., Turnbull, A. P., Turnbull, H. R., Wickham, D., Wilcox, B., & Ruef, M. (2000). Applying positive behavior support and functional behavioral assessment in schools. Journal of Positive Behavior Interventions, 2(3), 131–143. https://doi.org/10.1177/109830070000200302
Sugai, G., & Simonsen, B. (2012). Positive behavioral interventions and supports: History, defining features, and misconceptions (2012, June 19). University of Connecticut: Center for PBIS & Center for Positive Behavioral Interventions and Supports. http://www.pbis.org/common/cms/files/pbisresources/PBIS_revisited_June19r_2012
.pdf
Sullivan, A. L., Long, L., & Kucera, M. (2011). A survey of school psychologists’ preparation, participation, and perceptions related to positive behavior interventions and supports. Psychology in the Schools, 48(10), 971–985. https://doi.org/10.1002/pits.20605
Swindlehurst, K., Shepherd, K., Salembier, G., & Hurley, S. (2015). Implementing response to intervention: Results of a survey of school principals. Rural Special Education Quarterly, 34(2), 9–16.
https://doi.org/10.1177/875687051503400203
Ziomek-Daigle, J., Cavin, J., Diaz, J., Henderson, B., & Huguelet, A. (2019). Tier 3: Specialized services for students with intensive needs. In E. Goodman-Scott, J. Betters-Bubon, & P. Donohue (Eds.), The school counselor’s guide to multi-tiered systems of support (pp. 163–188). Routledge.
Ziomek-Daigle, J., Goodman-Scott, E., Cavin, J., & Donohue, P. (2016). Integrating a multi-tiered system of support with comprehensive school counseling programs. The Professional Counselor, 6(3), 220–232. https://doi.org/10.15241/jzd.6.3.220
Jacob Olsen, PhD, is an assistant professor at California State University Long Beach. Sejal Parikh Foxx, PhD, is a professor and Chair of the Department of Counseling at the University of North Carolina at Charlotte. Claudia Flowers, PhD, is a professor at the University of North Carolina at Charlotte. Correspondence may be addressed to Jacob Olsen, College of Education, 1250 Bellflower Boulevard, Long Beach, CA 90840-2201, jacob.olsen@csulb.edu.
Aug 18, 2020 | Volume 10 - Issue 3
Atsuko Seto, Nancy L. A. Forth
Results from a systematic review of the empirical literature on bilingual counseling published between 2000 and 2019 are presented. The findings from 15 articles are divided into three areas: counselor perspectives, client perspectives, and training and supervision. The review revealed that the studies published within the past two decades have focused on examining counselors’ perspectives on bilingual counseling. Studies that seek to understand clients’ perspectives as well as training and supervision of bilingual counselors seemed to be scarce. Recommendations drawn from the existing literature are provided for future research, counselor preparation, and the practice of counseling with linguistically diverse clients.
Keywords: bilingual counseling, counselor perspectives, client perspectives, training and supervision, linguistically diverse
The bilingual population in the United States is diverse (Pérez Rojas et al., 2014). According to the American Community Survey from the U.S. Census Bureau (2015), over 350 languages, including 150 native North American languages, are spoken in the United States. This data, collected from 2009 to 2013, reflects the total U.S. population older than five years of age. In 2018, over 41 million people in the United States spoke Spanish at home, followed by approximately 3.47 million Chinese-speaking and 1.76 million Tagalog-speaking individuals (U.S. Census Bureau, 2018). Furthermore, the total number of bilingual populations in the country has nearly doubled since 1980, with one in five individuals speaking a language other than English at home (Grosjean, 2018). In considering this staggering data, counselors in both community and school settings are encouraged to increase competencies necessary for work with linguistically diverse clients.
Several scholars in the mental health professions have discussed the significance of bilingualism within counseling practices, specifically with the Latinx population. First, both the English and Spanish language are essential to a Latinx person’s day-to-day living and interactions with the mainstream society and the ethnic community (Cofresi & Gorman, 2004). Second, an individual’s language proficiency is instrumental in gaining access to mental health services and is a critical component of counseling (Delgado-Romero et al., 2018). When clients have considerably limited English proficiency, they are less likely to seek counseling services that require comprehension of the language. Third, to develop appropriate treatment plans, counselors are encouraged to consider clients’ language background (Santiago-Rivera & Altarriba, 2002). Finally, because of potential language barriers and cultural mismatch, a shortage of Spanish–English-speaking mental health providers may discourage individuals of Latinx descent from seeking professional help (Delgado-Romero et al., 2018). It is also important to acknowledge the considerable diversity that exists within the Latinx population, and other terms, such as Hispanic/Latino (Santiago-Rivera & Altarriba, 2002; Smith-Adcock et al., 2006), Latino (Cofresi & Gorman, 2004), and Latino/a that (Pérez Rojas et al., 2014) appear in the existing literature on counseling with Spanish–English-speaking clients. Although these aforementioned points specifically refer to the Latinx client population, they speak to the need for increased efforts to understand counseling services for linguistically diverse clients.
Despite the growing number of individuals who speak more than one language, the use of bilingual counseling and its effectiveness are underrepresented in the current literature (Ali, 2004; Ivers & Villalba, 2015; Santiago-Rivera & Altarriba, 2002; Softas-Nall et al., 2015). Gallardo-Cooper (2008) defined bilingual counseling as “therapeutic discourse that accommodates the client’s linguistic characteristics and incorporates bilingual or multilingual factors as vital components of psychological and contextual functioning” (p. 1022). In 2004, Fuertes published a review of the existing literature on this topic and conceptualized bilingual counseling as “a special form of counseling” (p. 85). Fuertes’ review underscored the need for more studies in this area, stating that “there has been a dearth of conceptual and empirical literature on the topic of bilingual counseling and virtually no conceptual or empirical research on the topic of bilingual supervision” (p. 84). Moreover, coming to a consensus on what is bilingual can be difficult because different dimensions (e.g., reading, writing, speaking) need to be assessed to determine a person’s language proficiency (Santiago-Rivera & Altarriba, 2002). To gain a more accurate understanding of the current practice of bilingual counseling, its effectiveness, and related training and supervision, a systematic review of the literature published in the past two decades was conducted in this study.
Method
Two counselor educators formed a research team for this study. The team used the work of Edwards and Pedrotti (2008) as a guide for developing the steps to conduct a comprehensive search of relevant articles. First, several keywords were identified with the intent to identify journal articles that paid particular attention to bilingual counseling. The keywords included counseling, counselling, therapy, and psychotherapy combined with the words bilingual, multilingual, bi-lingual, and multi-lingual (e.g., bilingual counseling, multilingual counselling, bilingual therapy, multilingual psychotherapy). Additionally, the keywords bilingual client, bi-lingual client, multilingual client, and multi-lingual client were included to conduct searches as thoroughly as possible. Each team member independently ran multiple searches on major online databases (e.g., PsycINFO, ERIC, PsycARTICLES) by using the keywords to locate as many peer-reviewed journal articles published between 2000 and 2019 as possible. Collectively, the searches generated over 750 hits. Second, the abstracts of the articles from our respective searches were reviewed to determine whether they specifically focused on bilingual counseling. Third, the results from the two independent reviews were compiled into a list of potential articles for a final review. Forty articles were selected for this final review process. Upon the review of all 40 abstracts and discussion on the applicability of each article for this study, it was determined that 22 articles addressed the practice of bilingual counseling as the primary content. Of these articles, seven of them were removed from the list because they did not offer findings from an original study. Hence, the remaining 15 articles were included in this systematic review (see Table 1).
Results
The selected articles provided insights into the experiences of clients and/or counselors in bilingual counseling settings, including interpreter-mediated sessions. Additionally, a few articles (Ivers & Villalba, 2015; Mirza et al., 2017; Trepal et al., 2014) discussed experiences of graduate counseling and psychology students and their perceived cultural competency. The present review is organized into three areas: client perspectives, counselor perspectives, and training and supervision. Some of the articles are included in two sections (e.g., counselor perspectives and training and supervision) because the study findings covered more than one aspect of bilingual counseling.
Table 1
Articles About Bilingual Counseling (N = 15)
| Study |
Design |
Sample |
Focus |
| Costa & Dewaele, 2014 |
Mixed |
101 counselors (84 women and 17 men;
18 monolingual and 83 bilingual) |
Co |
| Ivers & Villalba, 2015 |
Quantitative |
178 master’s-level students (142 women, 33 men, 1 transgender, and 2 didn’t identify; 71 bilingual) |
T/S |
| Johal, 2017 |
Qualitative |
11 bilingual counselors (10 women and 1 man) |
Co, T/S |
| Kokaliari, 2013 |
Qualitative |
10 bilingual counselors (7 women and 3 men) |
Co |
| Mirza et al., 2017 |
Qualitative |
6 clients with limited English proficiency (6 men)
5 interpreters (1 woman and 4 men)
1 doctoral-level psychology student |
Co |
| Nguyen, 2014 |
Qualitative |
9 bilingual counselors |
Co |
| Pérez Rojas et al., 2014 |
Quantitative |
63 bilingual Latinx university students
(51 women and 12 men) |
Cl |
| Ramos-Sánchez, 2007 |
Quantitative |
65 Mexican American college students
(40 women and 25 men)
4 master’s-level psychology students (4 women) |
Cl |
| Ramos-Sánchez, 2009 |
Quantitative |
65 Mexican American college students
(40 women and 25 men) |
Cl |
| Rolland et al., 2017 |
Mixed |
109 bilingual clients (92 women and 17 men) |
Cl |
| Santiago-Rivera et al., 2009 |
Qualitative |
9 English–Spanish-speaking bilingual counselors
(6 women and 3 men) |
Co |
| Smith-Adcock et al., 2006 |
Mixed |
55 student services administrators |
T/S |
| Trepal et al., 2014 |
Qualitative |
6 bilingual practicum/internship students
(5 women and 1 man) |
Co, T/S |
| Vaquero & Williams, 2017 |
Qualitative |
8 English–Spanish-speaking bilingual counselors
(7 women and 1 man) |
Co, T/S |
| Verdinelli & Biever, 2009 |
Qualitative |
13 English–Spanish-speaking bilingual counselors
(9 women and 4 men) |
Co |
Note. Cl = Client; Co = Counselor; T/S = Training and Supervision
Client Perspectives
Four of the 15 studies (Pérez Rojas et al., 2014; Ramos-Sánchez, 2007, 2009; Rolland et al., 2017) addressed the perspectives of clients as part of the investigation. Of those studies, the participants in only one (Rolland et al., 2017) consisted of actual clients. In this study, Rolland et al. (2017) conducted an online survey with over 100 participants. Collectively, these participants represented 42 nationalities and had experienced counseling as a client in 19 different countries. The participants reported that they switched languages or used words in another language (code-switching) to express certain emotions, recall particular memories, or translate words and phrases into another language. For expression of emotions or recalling specific memories, some participants used a second language to distance themselves from painful experiences, whereas others used their primary language to express their feelings more accurately. Participants reported that they were more likely to engage in code-switching or language switching when they knew that their counselor was also bilingual. Although the participants generally appreciated their counselors’ efforts to switch languages and felt connected with their counselors in doing so, a few stated that they felt disconnected from their counselor when they were asked to switch languages. Rolland et al. offered insight into the intricacy of bilingualism in counseling and noted that
language has the power to transport the speaker to a different place, and depending on how this is handled the client may be able to share a different part of themselves with the therapist, or may find themselves disconnected, alone with the memories and inner self. (p. 81)
Another noteworthy point from this study was that the client’s language background was often unaddressed in sessions. Over half of the study participants stated that they never discussed their linguistic background with their counselors, and roughly 89% did not recall discussing with their counselors which language(s) could be utilized in sessions.
Three articles (Pérez Rojas et al., 2014; Ramos-Sánchez, 2007, 2009) discussed the effects of the language-switching technique on counseling relationships and clients’ perceptions of counselors, particularly in Spanish–English simulated counseling settings. Participants in these studies were college students as opposed to actual clients. In the study by Pérez Rojas et al. (2014), 51 Latina and 12 Latino students were asked to review one of two 15-minute recorded counseling sessions. In one session, a bilingual counselor invited a client to switch from English to Spanish in order to express the client’s feelings and thoughts, whereas in another session, a bilingual counselor did not invite a client to switch languages. Results in this study did not support the authors’ main hypothesis that a counselor’s invitation to switch to Spanish would foster a therapeutic bond with a client. Furthermore, the participants did not perceive the bilingual counselor as more culturally competent and credible than the counselor who only spoke English with the client. The authors speculated that bilingual clients may have varying reactions to counselors when being prompted to switch languages in sessions and that evaluation criteria for bilingual counselors may differ from that of non–mental health bilingual individuals.
In the area of perceived counselor credibility, past studies have typically focused on counselor ethnicity (Atkinson et al., 1989; Coleman et al., 1995). In 1999, Ramos-Sánchez et al. explored perceived counselor credibility by Mexican Americans regarding language. Because of the lack of findings, Ramos-Sánchez suggested further exploration in language switching and conducted another study. The findings from this subsequent study, using the same sample of 65 Mexican American college students, were presented in two articles (Ramos-Sánchez, 2007, 2009). Each participant played the role of a client in one of four experimental groups: a session led by a Mexican American counselor who only spoke English, a European American counselor who only spoke English, a Mexican American bilingual counselor, or a European American bilingual counselor. In addition to exploring the participants’ perspectives as a client in an interview, four observers rated clients’ emotional expressions in these four different conditions (Ramos-Sánchez, 2007). Results revealed that participants were more likely to engage in emotional disclosures in the language-switching conditions than the participants in the English-only settings (Ramos-Sánchez, 2007). The findings also suggested that ethnic and language differences or similarities between clients and counselors did not have a significant impact on the participants’ perceptions of counselor credibility and multicultural competency (Ramos-Sánchez, 2009). It is notable to mention that the Mexican American English-only speaking counselors were rated the highest among all counselors. Moreover, the European American bilingual counselors were rated higher than the Mexican American bilingual counselors. The findings support the idea that strong counseling relationships can be established despite ethnic differences between counselors and clients. Additionally, the findings may speak to the importance of training both Latinx and non-Latinx counselors on bilingual counseling in order to support Spanish–English-speaking clients (Ramos-Sánchez, 2007, 2009).
The primary limitations among the aforementioned studies (Pérez Rojas et al., 2014; Ramos-Sánchez, 2007, 2009) include having a small sample size and using volunteer college students in a controlled laboratory setting as opposed to actual clients. Although the participant group in Rolland et al.’s (2017) study consisted of actual clients, the study relied on the participants’ recollections of their counseling experiences and did not include the perspectives of counselors.
Counselor Perspectives
Nine articles (Costa & Dewaele, 2014; Johal, 2017; Kokaliari et al., 2013; Mirza et al., 2017; Nguyen, 2014; Santiago-Rivera et al., 2009; Trepal et al., 2014; Vaquero & Williams, 2019; Verdinelli & Biever, 2009) offered counselors’ perspectives on bilingualism in the counseling process and its impact on therapeutic relationships. Of those articles, six studies (Kokaliari et al., 2013; Mirza et al., 2017; Santiago-Rivera et al., 2009; Trepal et al., 2014; Vaquero & Williams, 2019; Verdinelli & Biever, 2009) were conducted in the United States. In terms of counselor theoretical orientations, this present review found two articles (Kokaliari et al., 2013; Nguyen, 2014) with psychoanalytic/psychodynamic framework, whereas some studies included counselors from a wide range of theoretical orientations. For example, the participants in Costa and Dewaele’s study (2014) employed integrative approaches, cognitive behavior therapy, systemic approaches, and psychodynamic therapy. A qualitative study (Santiago-Rivera et al., 2009) with nine Spanish–English-speaking counselors reported using cognitive behavior, person-centered, family systems, psychodynamic, and/or psychoanalytic theory in their practice.
Of these nine articles, six articles (Kokaliari et al., 2013; Mirza et al., 2017; Santiago-Rivera et al., 2009; Trepal et al., 2014; Vaquero & Williams, 2019; Verdinelli & Biever, 2009) explored bilingual counselors’ insights into working with linguistically diverse clients. Three articles in particular (Santiago-Rivera et al., 2009; Vaquero & Williams, 2019; Verdinelli & Biever, 2009) involved Spanish–English-speaking bilingual counselors, and four articles included bilingual and multilingual counselors with various language combinations. One article (Costa & Dewaele, 2014) included both monolingual and bilingual counselors, and one article (Mirza et al., 2017) focused on a monolingual counselor’s experience working with bilingual mediators to support clients whose primary language was not English.
Perceived Challenges
The existing studies suggested that utilization of more than one language within therapeutic relationships could become a source of anxiety for some counselors. The factors associated with their anxiety included speaking a different dominant language than clients, counseling clients in languages other than English despite receiving their training only in English, having an accent that is not familiar to clients, and being an entry-level counselor. Verdinelli and Biever (2009) indicated that some of the native Spanish-speaking bilingual counselors in their study perceived potential difficulty communicating with native English-speaking clients and were concerned about how their clients perceived their accents. Non-Latinx bilingual counselors in Vaquero and Williams’ (2019) study shared their concerns about their limited vocabulary in Spanish and their ability to facilitate clients’ emotional expressions effectively. Similarly, bilingual counselors in Johal’s (2017) study expressed their discomfort in using languages other than English in their practice and did not believe bilingual counseling strengthened a counseling relationship. Johal further explained that these participants received their formal training in English only, which may partially explain the findings. Master’s-level interns who participated in the study by Trepal et al. (2014) also stated that anxiety related to providing counseling services in languages other than English was exacerbated by their novice status as a counselor and a lack of training they received in bilingual counseling.
Participants in Verdinelli and Biever’s (2009) study spoke about the complexity of the bilingual counseling process. Specifically, some of the heritage Spanish speakers, who acquired a second language later on in their lives, discussed the challenges of conducting counseling sessions in Spanish because of language variations that exist within Spanish-speaking communities. Although the participants in Vaquero and Williams (2019) were seasoned professionals who had worked with bilingual families for an average of 15 years, they recognized the challenge of switching languages without excluding a particular family member. Specifically, speaking Spanish to connect with a parent or an adult caregiver whose primary language is Spanish might have excluded a child client whose primary language is English.
Contexts within which clients live may also influence therapeutic relationships. Nguyen (2014) interviewed bilingual counselors from seven different countries. Together, the participants spoke 14 languages in addition to English. Some of the participants believed that the shared identity of being bilingual fostered therapeutic relationships with clients. However, a few participants recounted situations in which a client became concerned about a possible breach of confidentiality because the counselor not only spoke the client’s language but also shared the same cultural background with the client, resulting in being a member of the same local ethnic community. Kokaliari et al. (2013) had similar findings in their study, in which a few participants described how the sameness between clients and counselors could blur therapeutic boundaries when counselors are unaware of potential transference or countertransference in sessions. Although having the same language background may foster counseling relationships, it could also present concerns for clients depending on the social contexts in which this similarity occurs.
Time was another challenging factor in findings by Trepal et al. (2014) and Johal (2017). In Johal’s study, some of the participants who provided bilingual counseling (in their second language) were often challenged by the amount of time it took to translate what they would say in their primary language to the language spoken by their clients. Similarly, participants in the study by Trepal et al. found that they often rehearsed speaking their second language (e.g., role-playing with a bilingual family member) as a means to feel better prepared for their sessions.
Perceived Benefits
These challenges notwithstanding, participants from five studies (Costa & Dewaele, 2014; Kokaliari et al., 2013; Trepal et al., 2014; Vaquero & Williams, 2019; Verdinelli & Biever, 2009) stated that the shared language and ethnic background with clients nurtured therapeutic bonds. For example, Latinx bilingual counselors reported switching languages—in this case, English to Spanish or vice versa—effortlessly to build rapport with clients (Vaquero & Williams, 2019). Participants in three studies (Costa & Dewaele, 2014; Kokaliari et al., 2013; Nguyen, 2014) reported that they became more mindful of the danger of overidentifying with clients who shared the same linguistic and cultural background. Both monolingual and bilingual counselors in Costa and Dewaele’s study (2014) agreed that they were more attentive to the client’s statements and nonverbal communication in bilingual counseling settings than in working with native English-speaking clients.
Several scholars explored counselors’ understanding of clients’ intention behind switching languages in counseling sessions. These included clients’ attempts and desires to: (a) express emotions more accurately and comprehensively (Kokaliari et al., 2013; Verdinelli & Biever, 2009); (b) enhance communication with a counselor (Kokaliari et al., 2013; Verdinelli & Biever, 2009); (c) recall specific memories such as traumatic events and dreams (Kokaliari et al., 2013); or (d) emphasize their point of view to a counselor (Kokaliari et al., 2013). As discussed earlier, these findings significantly overlapped with the clients’ perceptions of the roles of language in counseling (Rolland et al., 2017). In the study by Vaquero and Williams (2019), the counselors worked with bilingual families—young children and their parents/caregivers. These counselors noted that caregivers spoke with their children in Spanish to communicate their affection, whereas English was often used to discipline children.
The participants in Verdinelli and Biever’s study (2009) noticed that clients tended to discuss particular events in the language in which those experiences occurred. According to Kokaliari et al. (2013), the participants explained how some clients used their non-native language to discuss topics that are considered culturally taboo (e.g., sexual abuse, sexual orientation) or not consistent with their cultural framework. According to Verdinelli and Biever (2009), some participants believed that clients switched languages to avoid engaging in a deeper level of self-exploration. A similar observation was made by the participants in Kokaliari et al.’s (2013) study, in that clients seemed to use a second language when they needed to process highly emotional events such as trauma. In this case, participants perceived the client’s decision to switch languages as a form of self-protection.
With regard to a counselor’s intention to switch languages, Santiago-Rivera et al. (2009) indicated that Spanish–English-speaking bilingual counselors in their study switched from English to Spanish in order to establish a strong rapport with clients, engage or redirect clients in session, facilitate a client’s self-reflection and emotional expression, or foster self-awareness. According to Vaquero and Williams (2019), the Spanish–English bilingual counselors stated that they often deliberately switched to Spanish to connect with parents/caregivers in a counseling session, whereas they switched to English to build rapport with child clients. These counselors also switched languages to strengthen caregiver–child relationships.
Collaboration With Interpreters
To meet the needs of linguistically diverse clients, counselors, when possible and appropriate, may work with an interpreter. Mirza et al. (2017) examined potential challenges and benefits of collaboration with interpreters in counseling sessions. In this study, a doctoral-level psychology student served as the counselor and conducted interpreter-mediated counseling sessions with six clients whose primary language was not English. This counselor encountered a few challenges, including feeling excluded from side talks between the interpreter and the client, difficulty ensuring the accuracy and thoroughness of interpretations, and redirecting the interpreter to facilitate a session. The counselor perceived that using simple words and concise statements, checking in with clients periodically for clarification, and consecutive interpretations (translation following a statement by a counselor or a client) as opposed to simultaneous interpretations were helpful to a therapeutic relationship. To make an interpreter-mediated session beneficial to clients, the counselor in this study found it critical that both the interpreter and the counselor make the necessary adjustments to the counseling or interpretation approach as well as clearly defining each other’s roles in a session. In other words, when there is a synergy between a counselor and an interpreter, the interpreter’s involvement is likely to foster a counselor–client relationship and offer additional support to a client.
Several scholars (Johal, 2017; Kokaliari et al., 2013; Mirza et al., 2017; Nguyen, 2014; Vaquero & Williams, 2019) mentioned a small sample size as a common limitation of their studies. Focusing only on one set of a bilingual combination (Santiago-Rivera et al., 2009) or a particular ethnic group (Verdinelli & Biever, 2009) also made it challenging to generalize study findings to larger populations. Nguyen (2014) and Santiago-Rivera et al. (2009) cautioned that study findings were based only on counselors’ perceptions, which may differ from that of clients. In addition to Nguyen and Santiago-Rivera et al., Johal (2017) and Trepal et al. (2014) also noted the importance of acknowledging the potential effects of researcher bias on data collection and analysis of qualitative research studies.
Training and Supervision
In reviewing the 15 selected articles for this present study, five of them (Ivers & Villalba, 2015; Johal, 2017; Smith-Adcock et al., 2006; Trepal et al., 2014; Vaquero & Williams, 2019) focused on implications and recommendations for training and supervision in counseling practice. Two groups of scholars (Ivers & Villalba, 2015; Trepal et al., 2014) conducted their studies examining the effects of bilingualism with counseling students at a university in the southwest region of the United States. One common theme regarding the connection between counselors-in-training and their clients emerged in the two studies—when counselors-in-training shared the same language as the client during sessions, they felt more connected with their clients and more confident, as they perceived a higher level of multicultural counseling skills and awareness.
Supervision was specifically addressed in three of the 15 selected articles. Both Trepal et al. (2014) and Johal (2017) shared challenges experienced by supervisees who provided bilingual counseling with clients. Vaquero and Williams (2019) explored counselors’ perceptions of bilingual supervision as part of their study. The participants in Johal’s study stated that the practice of bilingual counseling was minimally addressed in their training, and they received little support from their employers and supervisors in this area. Several participants in the study by Trepal et al. (2014) stated that they needed to translate client session tapes for their supervisors—who were not bilingual—before receiving supervision, which added more involved time on their part. Participants in all three studies (Johal, 2017; Trepal et al., 2014; Vaquero & Williams, 2019) believed supervision was more effective when their supervisors spoke the same language that they used with their clients. For example, some bilingual supervisors were able to help the participants learn different terms and provide a clear example of a counseling process in Spanish (Vaquero & Williams, 2019).
Smith-Adcock et al. (2006) conducted a survey study with district-level directors of student services in Florida. They sent questionnaires to assess the needs of bilingual school counselors of Hispanic/Latinx children and families in their school districts. Specifically, the majority of the participants in this study reported that their school district needed more bilingual counselors, and 82% stated that students and families would benefit from receiving educational materials in Spanish. In addition, the participants believed that school counselors should be equipped to educate school communities on Hispanic/Latinx cultures, be aware of community resources, and engage in outreach efforts to involve parents in their children’s school experiences. These results suggest that bilingual counselors may be expected to fulfill various needs of linguistically diverse students and clients in addition to providing counseling services. Although this study did not specifically address training and supervision in bilingual counseling, the findings underscore the importance of developing training programs that are responsive to the specific needs of bilingual and multilingual communities.
Of the five articles that addressed training and supervision, four of them (Ivers & Villalba, 2015; Johal, 2017; Trepal et al., 2014; Vaquero & Williams, 2019) shared a common limitation to their studies that is typically found in research. These authors believed their results might not be generalized to all populations and settings because a small number of participants were used in their respective studies. As mentioned previously, Trepal et al. (2014) and Johal (2017) suggested that personal bias might have occurred, affecting their results. Finally, Ivers and Villalba (2015) cautioned that their use of a self-report instrument might have resulted in skewed findings.
Discussion
The purpose of this study was to gain a greater understanding of the topics that have been addressed in the existing literature regarding bilingual counseling, training, and supervision. Fifteen empirical articles were included in this study. Results reveal that more studies have explored perspectives of counselors on bilingual counseling than that of clients. Only one study involved current or former clients of counseling services. This may be due to the fact that recruitment of actual clients is more difficult than relying on convenience samples.
The results also suggest that more studies are needed for reaching consensus among scholars on what makes bilingual counseling therapeutic and effective. For example, participants in several qualitative studies (e.g., Kokaliari et al., 2013; Trepal et al., 2014; Vaquero & Williams, 2019; Verdinelli & Biever, 2009) perceived that speaking in the client’s primary language positively contributed to counseling relationships. Rolland et al. (2017) postulated that language switching, when used appropriately, is beneficial to clients because it can facilitate a deeper level of self-reflection and exploration. On the contrary, no statistical significance was found on the effects of the language switch on therapeutic bonds in two quantitative studies (Pérez Rojas et al., 2014; Ramos-Sánchez, 2007, 2009). These quantitative studies were conducted in a lab setting with college students, which the authors mention as a potential limitation of their studies. These findings may suggest that switching languages is an art of counseling; it is multifaceted, and its effectiveness may be contextually based. Additionally, more studies that explore the perspectives of both clients and counselors as well as examine variables that impact bilingual counseling relationships are needed. Pérez Rojas et al. (2014) helps to explain these inconclusive findings by stating that “the role that language switching plays in psychotherapy may be more complex than what has been theorized so far” (p. 71).
In terms of the specific language combinations that have been included in the previous studies, the Spanish–English-speaking population seems to be the group that has been most represented in the literature. This finding may not be surprising given the fact that Spanish is the second most spoken language in addition to English in the United States. Strong advocacy to support Spanish-speaking populations may also explain why this specific language combination has received the most attention in the profession. It is important to acknowledge that some scholars (e.g., Kakaliari et al., 2013; Rolland et al., 2017) in more recent years have conducted studies that involved multiple languages. Equally encouraging is an increased attention to the training and supervision of bilingual counselors. Although the existing literature in this area is considerably limited, several scholars (e.g., Ivers & Villalba, 2015; Johal, 2017; Trepal et al., 2014) have shed some light on the experiences of bilingual counselors and graduate counseling students and have offered some helpful recommendations for the training and supervision of counselors.
Implications
Counseling Practice
Findings from the present study suggest that switching languages, when done appropriately, may bolster therapeutic relationships with clients and facilitate clients’ self-exploration and expression. However, a few studies included in the present analysis also revealed that in some cases, the language match between the counselor and client may not strengthen therapeutic relationships. Determining when to switch languages may depend on a client’s preference, presenting concerns, history of language acquisition (e.g., growing up bilingual or acquiring another language as an adult), and level of language proficiency with each language spoken. Consequently, meeting the needs of bilingual clients requires counselors to know how to assess a client’s language background accurately. Only one study (Rolland et al., 2017) in the present analysis addressed clients’ perceptions of the assessment of their language background by counselors. As discussed previously, many participants reported counselors neither asked about their language backgrounds nor discussed which language(s) could be used in session. Cofresi and Gorman (2004) recommend that counselors assess the client’s language background (e.g., how they acquired a second language) and proficiency, dominant language, preferred language, and level of acculturation. They also suggest that, where possible and feasible, assessments should be conducted in the language “most compatible with the bilingual client’s language proficiency and dominance” (p. 104).
Bilingual clients have the ability to choose which language better offers a vehicle for the expression of ideas. Therefore, framing bilingualism as a client’s strength rather than deficiency or barrier (Santiago-Rivera & Altarriba, 2002) is crucial in fostering a genuine rapport with the client. The acquisition of an additional language has been associated with advanced cognitive abilities, including in the areas of problem-solving, reading, spelling, and memory recall (Ivers et al., 2013). Instead of assuming language barriers with a bilingual client, counselors are highly encouraged to communicate their genuine curiosity to learn about the client’s experience as a bilingual individual, explore benefits of bilingualism, and work to create a therapeutic environment that appreciates linguistic diversity.
Findings from the present study suggest that clients may switch languages for several different reasons. These include but may not be limited to expressing emotions more fully, recalling and discussing particular memories or events, and improving communication with others. In some cases, clients preferred to use a second language to process traumatic events and intense emotions or discuss topics that are considered culturally taboo or sensitive (Kokaliari et al., 2013; Verdinelli & Biever, 2009). In addition to asking clients about their preferences for using a particular language in session, discussing potential benefits and limitations of bilingual counseling may be helpful during the initial phase of counseling. Doing so may encourage clients and counselors to engage in ongoing and open discussions about the impact of languages on the client’s progress and counseling relationships.
Counselor Preparation
There is a significant shortage of training programs that equip counselors-in-training to provide bilingual counseling. Delgado-Romero et al. (2018) explained: “While professional mental health organizations recognize the need to provide linguistically and culturally appropriate services, there are limited opportunities to learn or use a second language in graduate mental health counseling programs” (pp. 341–342). This point was reflected in Trepal et al.’s (2014) study, in which the counseling interns expressed their concerns about engaging in bilingual counseling because they had not received any training on bilingual counseling. Trepal et al. also noted that some counseling interns in their study might have experienced increased anxiety for not only practicing counseling for the first time but having to do so in a bilingual setting. As counselor programs work to prepare more students for working with linguistically diverse clients, it seems imperative to provide appropriate supervision and additional support to those who are expected to provide bilingual counseling services during their clinical experiences. For example, the participants in Trepal et al.’s study recommended that programs assist bilingual students in forming a peer support group that allows exchange of information on bilingual counseling and promotes bilingualism.
The participants in Johal’s study (2017) made an essential point; that is, it should not be assumed that bilingual counselors know how to provide counseling in more than one language simply because they speak the language. Developing training programs that prepare students to work with bilingual clients (Costa & Dewaele, 2014; Santiago-Rivera & Altarriba, 2002) as well as increasing the number of bilingual counselors (Ivers & Villalba, 2015) are therefore critical steps to serving linguistically diverse client populations. Four of the 15 articles reviewed for this study (Ivers & Villalba, 2015; Johal, 2017; Trepal et al., 2014; Vaquero & Williams, 2019) offered one common suggestion for counseling training programs. All spoke of the importance of providing additional training that increases awareness in culture and language. Several scholars whose studies focused on supporting the Latinx population offered helpful recommendations for graduate counselor education and training programs, including: (a) integrating a community-engagement and collaboration component into the training curriculum (Smith-Adcock et al., 2006); (b) creating opportunities for cultural immersion experiences (Ivers & Villalba, 2015); (c) offering courses in both English and Spanish (Ramos-Sánchez, 2007); (d) delivering some content (e.g., diagnostic terms) in Spanish (Vaquero & Williams, 2019); and (e) developing standards for evaluating counselor competency in providing bilingual counseling (Verdinelli & Biever, 2009). Additionally, training programs should emphasize the significance of understanding history, nationality, culture, community, and geographic settings (e.g., living in an urban vs. rural community) of linguistically diverse clients (Vaquero & Williams, 2019). These recommendations may be applicable and helpful to counselor education programs that are committed to preparing students for providing bilingual counseling services to meet the needs of their local communities. Furthermore, some counselors may have an opportunity to offer counseling services to clients in collaboration with an interpreter. It is essential that specialized training is available to counselors and interpreters who are interested in joining forces to serve clients within the context of mental health service delivery. Such training curricula should address the effectiveness of evidence-based approaches to providing interpreter-mediated counseling services (Mirza et al., 2017).
Conclusion and Future Research
Scholars who have written about the current practice of bilingual counseling encourage researchers to explore the following areas in future studies: (a) associations between counselor language proficiency and clients’ perceptions of counselors and counseling relationships (Ramos-Sánchez, 2009; Trepal et al., 2014; Verdinelli & Biever, 2009); (b) actual clients’ experiences of mental health services (Johal, 2017; Ramos-Sánchez, 2009); (c) effectiveness, roles, and use of language switching in counseling (Costa & Dewaele, 2014; Pérez Rojas et al., 2014; Ramos-Sánchez, 2007, 2009; Santiago-Rivera & Altarriba, 2002; Vaquero & Williams, 2019); (d) relationships between counselors’ bilingualism and their multicultural counseling competency by combining self-reports and external observations (Ivers & Villalba, 2015); and (e) efficacy of bilingual supervision and training models on bilingual counseling (Trepal et al., 2014).
The purpose of this study was to gain a more accurate understanding of the practice of bilingual counseling, its effectiveness, and related training and supervision by conducting a systematic review of the literature published over the past two decades. It is important to note that the search results for this present review were limited by the selected keywords and available databases. In addition, some of the dissertation studies might have not been included unless they were published in peer-reviewed journals. With this in mind, this systematic analysis of existing literature on bilingual counseling suggests that very few studies have examined the experiences of linguistically diverse clients in counseling settings.
Similarly, there is a lack of literature that discusses how graduate-level counseling programs are addressing bilingual counseling and supervision as part of their curriculum. However, it is encouraging to see that more recently conducted studies have collectively begun to examine the complexity of bilingual counseling in both clinical settings and training programs. Given the Latinx population being by far the largest bilingual group within the United States, this group seems to have received the most attention among linguistically diverse groups. While continuing to undertake studies with this particular population, conducting more studies that involve clients, counselors, and graduate students of other bilingual backgrounds may contribute to the existing body of the literature.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Ali, R. K. (2004). Bilingualism and systemic psychotherapy: Some formulations and explorations. Journal of Family Therapy, 26(4), 340–357. https://doi.org/10.1111/j.1467-6427.2004.00288.x
Atkinson, D. R., Poston, W. C., Furlong, M. J., & Mercado, P. (1989). Ethnic group preferences for counselor characteristics. Journal of Counseling Psychology, 36(1), 68–72. https://doi.org/10.1037/0022-0167.36.1.68
Cofresi, N. I., & Gorman, A. A. (2004). Testing and assessment issues with Spanish-English bilingual Latinos. Journal of Counseling & Development, 82(1), 99–106. https://doi.org/10.1002/j.1556-6678.2004.tb00290.x
Coleman, H. L. K., Wampold, B. E., & Casali, S. L. (1995). Ethnic minorities’ ratings of ethnically similar and European American counselors: A meta-analysis. Journal of Counseling Psychology, 42(1), 55–64.
https://doi.org/10.1037/0022-0167.42.1.55
Costa, B., & Dewaele, J.-M. (2014). Psychotherapy across languages: Beliefs, attitudes and practices of monolingual and multilingual therapists with their multilingual patients. Counselling and Psychotherapy Research, 14(3), 235–244. https://doi.org/10.1080/14733145.2013.838338
Delgado-Romero, E. A., De Los Santos, J., Raman, V. S., Merrifield, J. N., Vazquez, M. S., Monroig, M. M., Bautista, E. C., & Durán, M. Y. (2018). Caught in the middle: Spanish-speaking bilingual mental health counselors as language brokers. Journal of Mental Health Counseling, 40(4), 341–352. https://doi.org/10.17744/mehc.40.4.06
Edwards, L. M., & Pedrotti, J. T. (2008). A content and methodological review of articles concerning multiracial issues in six major counseling journals. Journal of Counseling Psychology, 55(3), 411–418.
https://doi.org/10.1037/0022-0167.55.3.411
Fuertes, J. N. (2004). Supervision in bilingual counseling: Service delivery, training, and research considerations. Journal of Multicultural Counseling and Development, 32(2), 84–94. https://doi.org/10.1002/j.2161-1912.2004.tb00363.x
Gallardo-Cooper, M. (2008). Bilingual counseling. In F. T. L. Leong (Ed.), Encyclopedia of counseling: Vol 3. Cross-cultural counseling (pp. 1022–1024). SAGE.
Grosjean, F. (2018, September 11). The amazing rise of bilingualism in the United States. https://www.psycholo
gytoday.com/intl/blog/life-bilingual/201809/the-amazing-rise-bilingualism-in-the-united-states
Ivers, N. N., Ivers, J. J., Sr., & Duffey, T. (2013). Second language acquisition: Cultural, cognitive, and clinical considerations for counseling practice. Journal of Creativity in Mental Health, 8(3), 219–234.
https://doi.org/10.1080/15401383.2013.821920
Ivers, N. N., & Villalba, J. A. (2015). The effect of bilingualism on self-perceived multicultural counseling competence. The Professional Counselor, 5(3), 419–430. https://doi.org/10.15241/nni.5.3.419
Johal, J. (2017). ‘No one ever speaks about it’: A qualitative investigation exploring the experiences of multilingual counsellors in practice. Counselling and Psychotherapy Research, 17(4), 291–300.
https://doi.org/10.1002/capr.12134
Kokaliari, E., Catanzarite, G., & Berzoff, J. (2013). It is called a mother tongue for a reason: A qualitative study of therapists’ perspectives on bilingual psychotherapy—Treatment implications. Smith College Studies in Social Work, 83(1), 97–118. https://doi.org/10.1080/00377317.2013.747396
Mirza, M., Harrison, E. A., Chang, H.-C., Salo, C. D., & Birman, D. (2017). Making sense of three-way conversations: A qualitative study of cross-cultural counseling with refugee men. International Journal of Intercultural Relations, 56, 52–64. http://doi.org/10.1016/j.ijintrel.2016.12.002
Nguyen, B. P. (2014). Identification: A qualitative study of the experiences of bilingual therapists with their monolinguals and bilingual clients. Psychodynamic Practice, 20(4), 340–355. http://doi.org/10.1080/14753634.2014.947168
Pérez Rojas, A. E., Gelso, C. J., & Bhatia, A. (2014). To switch or not to switch: Inviting bilingual clients to switch languages in psychotherapy. Counselling Psychology Quarterly, 27(1), 55–74.
http://doi.org/10.1080/09515070.2013.870124
Ramos-Sánchez, L. (2007). Language switching and Mexican Americans’ emotional expression. Journal of Multicultural Counseling and Development, 35(3), 154–168. https://doi.org/10.1002/j.2161-1912.2007.tb00057.x
Ramos-Sánchez, L. (2009). Counselor bilingual ability, counselor ethnicity, acculturation, and Mexican Americans’ perceived counselor credibility. Journal of Counseling & Development, 87(3), 311–318.
https://doi.org/10.1002/j.1556-6678.2009.tb00112.x
Ramos-Sánchez, L., Atkinson, D. R., & Fraga, E. D. (1999). Mexican Americans’ bilingual ability, counselor bilingualism cues, counselor ethnicity, and perceived counselor credibility. Journal of Counseling Psychology, 46(1), 125–131. https://doi.org/10.1037/0022-0167.46.1.125
Rolland, L., Dewaele, J.-M., & Costa, B. (2017). Multilingualism and psychotherapy: Exploring multilingual clients’ experiences of language practices in psychotherapy. International Journal of Multilingualism, 14(1), 69–85. https://doi.org/10.1080/14790718.2017.1259009
Santiago-Rivera, A. L., & Altarriba, J. (2002). The role of language in therapy with the Spanish-English bilingual client. Professional Psychology: Research and Practice, 33(1), 30–38. https://doi.org/10.1037/0735-7028.33.1.30
Santiago-Rivera, A. L., Altarriba, J., Poll, N., Gonzalez-Miller, N., & Cragun, C. (2009). Therapists’ views on working with bilingual Spanish–English speaking clients: A qualitative investigation. Professional Psychology: Research and Practice, 40(5), 436–443. https://doi.org/10.1037/a0015933
Smith-Adcock, S., Daniels, M. H., Lee, S. M., Villalba, J. A., & Indelicato, N. A. (2006). Culturally responsive school counseling for Hispanic/Latino students and families: The need for bilingual school counselors. Professional School Counseling, 10(1), 92–101. https://doi.org/10.1177/2156759X0601000104
Softas-Nall, L., Cardona, B., & Barritt, J. (2015). Challenges and diversity issues working with multilingual and bilingual couples and families: Implications for counseling. The Family Journal, 23(1), 13–17.
https://doi.org/10.1177/1066480714548402
Trepal, H. C., Ivers, N. N., & Lopez, A. (2014). Students’ experiences with bilingual counseling. The Journal of Counselor Preparation and Supervision, 6(2). http://doi.org/10.7729/62.1096
U.S. Census Bureau. (2015, November 3). Census Bureau reports at least 350 languages spoken in U.S. homes. https://www.census.gov/newsroom/press-releases/2015/cb15-185.html
U.S. Census Bureau. (2018). Language spoken at home by ability to speak English for the population 5 years and over. https://data.census.gov/cedsci/table?q=B16&d=ACS%201-Year%20Estimates%20Detailed%20Table
s&tid=ACSDT1Y2018.B16001
Vaquero, J., & Williams, M. E. (2019). Experiences of Spanish–English bilingual early childhood psychotherapists providing services to bilingual caregiver–child dyads: An exploratory qualitative study. Journal of Latinx Psychology, 7(3), 195–211. https://doi.org/10.1037/lat0000115
Verdinelli, S., & Biever, J. L. (2009). Spanish–English bilingual psychotherapists: Personal and professional language development use. Cultural Diversity and Ethnic Minority Psychology, 15(3), 230–242.
https://doi.org/10.1037/a0015111
Atsuko Seto, PhD, NCC, ACS, LPC, is an associate professor at The College of New Jersey. Nancy L. A. Forth, PhD, NCC, LPC, is a professor and program coordinator at the University of Central Missouri. Correspondence may be addressed to Atsuko Seto, 2000 Pennington Road, Ewing, NJ 08628, seto@tcnj.edu.
May 13, 2020 | Book Reviews
by Shauna Frisbie
Working with the adolescent population can be difficult. These are the years when people develop their sense of self and identity, and with the world at their fingertips through social media, that sense of self can be skewed. Today’s young individuals are bombarded by images that are not realistic and many times see themselves as flawed in comparison. This is when an eating disorder can develop. A Therapist’s Guide to Treating Eating Disorders in a Social Media Age presents an innovative therapeutic approach to eating disorders that highlights the influence of social media.
The author, Dr. Shauna Frisbie, has spent over 25 years treating clients with eating disorders. This experience has given her a firsthand understanding of how social media has changed the playing field when treating adolescents. She begins the book by describing eating disorders and how they can be affected by social media as well as the world we live in. She discusses the COVID-19 pandemic and the quarantine-related effects that have led to higher use of social media. As this pandemic continues, adolescents are becoming more and more secluded and reliant on social media for their social interactions. Screen time has replaced social gatherings and activities with others as they navigate this new existence.
Dr. Frisbie explores how cultural influences and our human need for social belonging can be skewed by the use of social media. This is very evident in the most recent generations, Gen Z and Millennials. She then takes the reader on a journey into the visual culture that each of us interacts with daily, developing the reader’s understanding of phototherapy techniques and treatment. From this base the reader moves to an understanding of what identity formation is, how it is developed, and how it can be affected by the use of social media. Dr. Frisbie explores family and identity through client narratives of childhood experiences. With the use of case studies throughout the book, the reader is given a look inside the therapy room.
The technique of using images for narrative creation with the client allows the therapist to understand the client’s perspective. By using this technique, the client discovers the underlying messages that are impacting the relationship they have with their bodies. Social media is full of images—good, bad, and ugly. By using images to help the adolescent discover their narrative of self, the therapist can make the client comfortable.
Dr. Frisbie has given the reader a great deal of information that is quite easy to absorb and put into practice. The depth of the information when discussing the science behind our identities and how social media may play a role in that development is enough to give the reader an understanding without the weight of being overwhelmed by it. The reader will walk away with a better grasp on how social media may play a role in their clients’ lives. With this understanding, a therapist can navigate the possible troubled waters of the adolescent client and their body image.
Frisbie, S. (2020). A Therapist’s Guide to Treating Eating Disorders in a Social Media Age. W. W. Norton.
Reviewed by: Amy Perschbacher, MA, NCC, LPC, Ronan Psychological Associates
The Professional Counselor
https://tpcwordpress.azurewebsites.net