Jul 1, 2014 | Article, Volume 4 - Issue 3
Let us start with two important disclaimers. First, I will be identifying the many ways that the Diagnostic and Statistical Manual of Mental Disorders (DSM) system has been detrimental to psychotherapy and how the fifth edition (DSM-5; American Psychiatric Association [APA], 2013) will make the current situation even worse. However, this does not mean that I consider DSM diagnosis irrelevant to psychotherapy and counseling, nor do I believe that psychotherapists and counselors should neglect learning about diagnosis. I do not trust therapists who focus their contact with the client exclusively around the DSM diagnosis. Hippocrates believed that it is more important to know the person who has the disease than the disease the person has. Nevertheless, I also do not trust therapists who are completely free-form, impressionistic and idiosyncratic in their approach to clients. DSM diagnosis is only a small part of what goes into therapy, but it is often a crucial part. We need to know what makes each person different and unique; on the other hand, we also need to group clients with similar problems as a way of choosing interventions and predicting the treatment course.
The second disclaimer relates to the proper roles of medication, psychotherapy and counseling. The DSM has promoted a reductionistic medicalization of mental illness that, in combination with misleading drug company marketing strategies, has created a strong bias toward treatment with medication and against treatment with psychotherapy and counseling. I am greatly disturbed by the resulting enormous overuse of psychotropic drugs among both adults and children, many of whom do not need psychotropic drugs and would do much better without them. However, we must be equally alert to the fact that many people who need medication do not receive it. Psychotherapists and counselors are important gatekeepers who should recognize when medication is needed and when it is not. It makes no sense to be for or against medicating clients. It is crucial that medication not be used carelessly, but also essential to realize that it is sometimes absolutely necessary.
I will offer a brief history. Before the publication of the DSM-III (APA) in 1980, psychiatric diagnosis was a subject of little interest or importance because it was unreliable and not particularly useful for treatment planning. The DSM-III marked a sudden and dramatic change—it made diagnosis a major focus of clinical attention and the starting point of all treatment guidelines. Its provision of clearly defined criteria allowed for reasonably reliable diagnosis and for targeting specific symptoms that became the focus of treatment. The DSM-III’s influence exceeded all expectations, in some ways useful, but also with a significant defect. The prevailing mental health approach before the DSM-III was the well-rounded biopsychosocial model. At that time, clinicians conceptualized symptoms as arising from the complex interplay of brain functioning, psychological factors, and familial and social contexts. Perhaps without intention, the DSM-III downgraded the psychological and social factors and promoted undue emphasis on the biological factors. The DSM-III was advertised as “atheoretical” and neutral, usable by practitioners of all professional orientations. To some small degree, this was true; yet the DSM-III’s emphasis on purely descriptive psychiatry strongly favored biological treatments over cognitive-behavioral treatments. This bias proved to be irrelevant and eventually destructive to family and psychodynamic therapies. The descriptive DSM-III method focused attention on surface symptoms in the individual and ignored both deeper psychological understanding and the social and familial contexts. Clinicians often adopted a symptom checklist approach to evaluation and forgot that a complete evaluation must account for psychological factors, social supports and stressors.
In addition to its considerable impact on the mental health profession, the DSM-III also significantly affected the pharmaceutical industry. Drug companies benefited greatly from the DSM-III approach, particularly since 1987 when Prozac established the template for promoting blockbuster psychiatric drugs. Pharma realized that the best way to sell pills is to promote disease-mongering. Their marketing campaign offers the misleading idea that mental disorders are underdiagnosed, easy to diagnose due to chemical imbalances in the brain and best treated with a pill. The marketing targeted psychiatrists first, then primary care physicians and, since 1997, the general public. In the United States and New Zealand, drug companies have successfully bullied the government into allowing direct advertising to consumers on television, in print and on the Internet. Use of medication has skyrocketed as a result of these billion-dollar marketing budgets, turning us into a pill-popping society. This increase in drug use is great for Pharma shareholders and executives, but often inappropriate for clients and terribly costly to the economy. More than $40 billion a year are spent on psychiatric drugs. Most of these (80%) are prescribed by primary care doctors with little training or interest in psychiatric diagnosis or treatment, while under strong pressure from patients and drug company representatives, and after only seven minutes of evaluation on average. During the last decade, many drug companies have received enormous fines (e.g., one fine was $3.3 billion) for illegal marketing practices, but they continue because the rewards are so great.
For mild to moderate psychiatric problems, psychotherapy and counseling are just as effective as medication, and their effects are much more enduring. Most people taking medication would probably have been better off had they received psychotherapy or counseling. Unfortunately, psychotherapy and counseling suffer from two great disadvantages in their competition with drug treatment. Drug companies are enormously profitable industrial giants with billion-dollar budgets to push their products. In contrast, the mental health field is more of a nickel-and-dime, mom-and-pop operation with absolutely no marketing punch. Insurance companies further tilt the playing field by consistently favoring medication management over psychotherapy and counseling based on the mistaken assumption that it will be cheaper. In fact, brief treatments are often much more cost-effective because their effects are lasting, whereas medication may be necessary for years or a lifetime.
The medicalization of mental illness has had a dire impact on our clients and our society. Twenty percent of the population regularly takes a psychiatric drug, many for problems of everyday life more amenable to watchful waiting or psychotherapy and counseling than to drug treatment. It is astounding that there are now more overdoses and deaths from prescription drugs than street drugs. The tremendous societal investment in psychiatric drugs also misallocates resources much better spent on terribly underfunded social investments. Would it not be better for children to have smaller classes and more gym periods than for so many of them to be on pills for ADHD?
In preparing the DSM-IV (APA, 1994), we attempted to hold the line against diagnostic inflation and the medicalization of normality; however, we failed. During the past 20 years, the United States has experienced fad epidemics of ADHD, autism and bipolar disorder. We were conservative in writing the DSM-IV, but failed to anticipate or prevent its careless misuse under external pressure, particularly drug company marketing and the requirement of a psychiatric diagnosis for clients to qualify for school services and disability benefits. The quick fix is to give a diagnosis, but often this does more harm than good in the long run. Inaccurate diagnoses are easy to give but hard to remove. Often they haunt the client for life with stigma, unnecessary treatments and reduced expectations. Making an accurate diagnosis requires really knowing one’s client, which may take weeks or even months. In uncertain situations, it is better to underdiagnose than overdiagnose a symptom pattern, and better to be safe than sorry.
The DSM-5 will considerably increase medicalization and may turn our current diagnostic inflation into hyperinflation. Overdiagnosis transforms normal grief into major depressive disorder, normal temper tantrums into disruptive mood dysregulation disorder, normal forgetfulness of old age into minor neurocognitive disorder, poor eating habits into binge eating disorder, and expectable worry about physical symptoms into somatic symptom disorder. It also further loosens the already far too slack criteria for attention deficit disorder and contains a completely confusing definition of autism. Experience teaches that whenever the diagnostic spigot is unrestricted, drug company revenues increase, and less funding is available to support psychotherapy and counseling visits.
The DSM is only one guide to diagnosis—it is not a bible or official manual of diagnosis. The DSM codes that clinicians routinely use for reimbursement are in fact all International Classification of Diseases, Clinical Modification (ICD-CM) codes that are available for free on the Internet. DSM-5 is one suggested way to arrive at an ICD-CM diagnosis, but it is not the only or best way. Other more reliable guides to psychiatric diagnosis are available. Therapists do not have to buy or use the DSM-5 unless they work for an institution that requires it.
Receiving a psychiatric diagnosis can be a turning point in a client’s life. An accurate diagnosis can lead to an effective treatment plan; an inaccurate diagnosis can lead to side effects, stigma, high costs, reduced opportunities and needless suffering. Severe and classic presentations require quick diagnosis and immediate intervention, usually including medication. Milder, equivocal presentations allow for and require a more cautious approach. Therefore, watchful waiting or brief counseling is usually best.
Conflict of Interest and Funding Disclosure
The author published two books that critically
review the DSM-5, titled Saving Normal and
Essentials of Psychiatric Diagnosis.
References
American Psychiatric Association. (1980). Diagnostic and statistical manual of mental disorders (3rd ed.). Washington, DC: Author.
American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
Apr 7, 2014 | Article, Volume 4 - Issue 2
Elizabeth A. Prosek, Jessica M. Holm
The U.S. Department of Veterans Affairs (VA) and TRICARE have approved professional counselors to work within the military system. Counselors need to be aware of potential ethical conflicts between counselor ethical guidelines and military protocol. This article examines confidentiality, multiple relationships and cultural competency, as well as ethical models to navigate potential dilemmas with veterans. The first model describes three approaches for navigating the ethical quandaries: military manual approach, stealth approach, and best interest approach. The second model describes 10-stages to follow when navigating ethical dilemmas. A case study is used for analysis.
Keywords: military, ethics, veterans, counselors, competency, confidentiality
The American Community Survey (ACS; U.S. Census Bureau, 2011) estimated that 21.5 million veterans live in the United States. A reported 1.6 million veterans served in the Gulf War operations that began post-9/11 in 2001 (U.S. Census Bureau, 2011). Gulf War post-9/11 veterans served mainly in Iraq and Afghanistan, in operations including but not limited to Operations Enduring Freedom (OEF), Iraqi Freedom (OIF), and New Dawn (OND) (M. E. Otey, personal communication, October 23, 2012). Holder (2007) estimated that veterans represent 10% of the total U.S. population ages 17 years and older. Pre-9/11 data suggested that 11% of military service members utilized mental health services in the year 2000 (Garvey Wilson, Messer, & Hoge, 2009). In 2003, post-9/11 comparative data reported that 19% of veterans deployed to Iraq accessed mental health services within one year of return (Hoge, Auchterlonie, & Milliken, 2006). Recognizing the increased need for mental health assessment, the U.S. Department of Defense (DOD) mandated the Post-Deployment Health Assessment (PDHA) for all returning service members (Hoge et al., 2006). The PDHA is a brief three-page self-report screening of symptoms to include post-traumatic stress, depression, suicidal ideation and aggression (U.S. DOD, n.d.). The assessment also indicates service member self-report interest in accessing mental health services.
Military service members access mental health services for a variety of reasons. In a qualitative study of veterans who accessed services at a Veterans Affairs (VA) mental health clinic, 48% of participants reported seeking treatment because of relational problems, and 44% sought treatment because of anger and/or irritable mood (Snell & Tusaie, 2008). Veterans may also present with mental health symptoms related to post-traumatic stress disorder (PTSD), depression, and suicidal ideation (Hoge et al., 2006). Depression is considered a common risk factor of suicide among the general population, and veterans are additionally at risk due to combat exposure (Martin, Ghahramanlou-Holloway, Lou, & Tucciarone, 2009). The DOD (2012) confirmed that 165 active-duty Army service members committed suicide in 2011. Furthermore, researchers asserted that suicide caused service member deaths more often than combat (O’Gorman, 2012). Hoge et al. (2004) reported that veterans were most likely to access mental health services 3–4 months post-deployment. Unfortunately, researchers suggested that service members were hesitant to access mental health treatment, citing the stigma of labels (Kim, Britt, Klocko, Riviere, & Adler, 2011). Studies indicated that mental health service needs are underestimated among the military population and are therefore a potential burden to an understaffed helping profession (Garvey Wilson et al., 2009; Hoge et al., 2006). In May of 2013, the DOD and VA created 1,400 new positions for mental health providers to serve military personnel (DOD, 2013). Moreover, as of March 2013, the DOD-sponsored veterans crisis line reported more than 800,000 calls (DOD, 2013). It is evident that the veteran population remains at risk for problems related to optimal mental health functioning and therefore requires assistance from trained helping professionals.
Historically, the DOD employed social workers and psychologists almost exclusively to provide mental health services in the military setting. Recently, the DOD and VA expanded services and created more positions for mental health clinicians (U.S. VA, 2012). Because licensed professional counselors (LPCs) are now employable by VA service providers (e.g., VA hospitals) and approved TRICARE providers (Barstow & Terrazas, 2012), it is imperative to develop an understanding of the military system, especially of the potential conflict that may exist between military protocol and counselor ethical guidelines. The military health system requires mental health professionals to be appropriately credentialed (e.g., licensed), and credentialing results in the mandatory adherence to a set of professional ethical standards (Johnson, Grasso, & Maslowski, 2010). However, there may be times when professional ethical standards do not align with military regulations. Thus, an analysis of the counselor ethical codes relevant to the military population is presented. At times, discrepancies between military protocol and counselor ethical codes may emerge; therefore, recommendations for navigating such ethical dilemmas are provided. A case study and analysis from the perspective of two ethical decision-making models are presented.
Ethical Considerations for Counselors
The mission of the American Counseling Association (ACA) Code of Ethics (2005) is to establish a set of standards for professional counselors, which ensure that the counseling profession continues to enhance the profession and quality of care with regard to diversity. As professional counselors become employed by various VA mental health agencies or apply for TRICARE provider status, it is important to identify specific ethical codes relevant to the military population. Therefore, three categories of ethical considerations pertinent to working with military service members are presented: confidentiality, multiple relationships, and cultural competence.
Confidentiality
The ACA Code of Ethics (2005) suggests that informed consent (A.2.a., p. 4) be a written and verbal discussion of rights and responsibilities in the counseling relationship. This document includes the client right for confidentiality (B.1.c., p. 7) with explanation of limitations (B.1.d., p. 7). The limitations, or exceptions, to confidentiality include harm to self, harm to others and illegal substance use. In the military setting, counselors may need to consider other exceptions to confidentiality including domestic violence (Reger, Etherage, Reger, & Gahm, 2008), harassment, criminal activity and areas associated with fitness for duty (Kennedy & Johnson, 2009). Also, military administrators may require mandated reporting when service members are referred for substance abuse treatment (Reger et al., 2008). When these conditions arise in counseling, the military may require reporting beyond the standard ethical protocol to which counselors are accustomed.
Counselors working in the VA mental health system or within TRICARE may need to be flexible with informed consent documents, depending on the purpose of services sought. Historically, veterans represented those who returned from deployment and stayed home. Currently, military members may serve multiple tours of combat duty; therefore, the definition of veterans now includes active-duty personnel. This modern definition of veteran speaks to issues of fitness for duty, where the goal is to return service members ready for combat. Informed consent documents may need to outline disclosures to commanding officers. For example, if a service member is in need of a Command-Directed Evaluation (CDE), then the commander is authorized to see the results of the assessment (Reger et al., 2008). Fitness for duty is also relevant when service members are mandated to the Soldier Readiness Program (SRP) to determine their readiness for deployment. In these situations, counselors need to clearly explain the exception to confidentiality before conducting the assessment. Depending on the type of agency and its connection to the DOD, active-duty veterans’ health records may be considered government property, not the property of the service provider (McCauley, Hacker Hughes, & Liebling-Kalifani, 2008). It is imperative that counselors are educated on the protocols of the setting or assessments, because “providing feedback to a commander in the wrong situation can be an ethical violation that is reviewable by a state licensing authority” (Reger et al., 2008, p. 30). Thus, in order to protect the client and the counselor, limitations to confidentiality within the military setting must be accurately observed at all times. Knowledge of appropriate communication between the counselor and military system also speaks to the issue of multiple relationships.
Multiple Relationships
Kennedy and Johnson (2009) suggested creating collaborative relationships with interdisciplinary teams in a military setting in order to create a network of consultants (e.g., lawyers, psychologists, psychiatrists), which is consistent with ACA ethical code D.1.b to develop interdisciplinary relationships (2005, p. 11). However, when interdisciplinary teams are formed, there are ACA (2005) ethical guidelines that must be considered. These guidelines state that interdisciplinary teams must focus on collaboratively helping the client by utilizing the knowledge of each professional on the team (D.1.c., p. 11). Counselors also must make the other members of the team aware of the constraints of confidentiality that may arise (D.1.d., p. 11). In addition, counselors should adhere to employer policies (D.1.g., p. 11), openly communicating with VA superiors to navigate potential discrepancies between employers’ expectations and counselors’ roles in best helping the client.
In the military environment, case transfers are common because of the high incidence of client relocation, which increases the need for the interdisciplinary teams to develop time-sensitive treatment plans (Reger et al., 2008). Therefore, treatment plans not only need to follow the guidelines of A.1.c., in which counseling plans “offer reasonable promise of success and are consistent with abilities and circumstances of clients” (ACA, 2005, p. 4), but they also need to reflect brief interventions or treatment modalities that can be easily transferred to a new professional. Mental health professionals may work together to best utilize their specialized services in order to meet the needs of military service members in a minimal time allowance.
For those working with military service members, consideration of multiple relationships in terms of client caseload also is important. Service members who work together within the same unit may seek mental health services at the same agency. Members of a military unit may be considered a support network which, according to ethical code A.1.d., may be used as a resource for the client and/or counselor (ACA, 2005, p. 4). However, learning about a military unit as a network from multiple member perspectives may also create a dilemma. Service members within a unit may be tempted to probe the counselor for information about other service members, or tempt the counselor to become involved in the unit dynamic. McCauley et al. (2008) recommended that mental health professionals avoid mediating conflicts between service members in order to remain neutral in the agency setting.
However, there are times when the unit cohesion may be used to support the therapeutic relationship. Basic military training for service members emphasizes the value of teamwork and the collective mind as essential to success (Strom et al., 2012). It is important for counselors to approach military service member clients from this perspective, not from a traditional Western individualistic lens. Mental health professionals also are warned not to be discouraged if rapport is more challenging to build than expected. Hall (2011) suggested that the importance of secrecy in the military setting might make it more difficult for service members to readily share in the therapeutic relationship. Researchers noted that military service members easily built rapport with each other in a group therapy session, often leaving out the civilian group leader (Strom et al., 2012). It might behoove counselors to build upon the framework of collectivism in order to earn the trust of members of the military population. Navigating the dynamic of a unit or the population of service members accessing care at the agency may be a challenge; however, counselors are able to alleviate this challenge with increased knowledge of the military culture in general.
Cultural Competence
The military population represents a group of people with a unique “language, a code of manners, norms of behavior, belief systems, dress, and rituals” and therefore can be considered a cultural group (Reger et al., 2008, p. 22). Reger et al. (2008) suggested that many clinical psychologists learned about military culture as active service members themselves. While there may be many veterans currently working as professional counselors, civilian counselors also serve the mental health needs of the military population; and as civilians, they require further training. The ACA Code of Ethics (2005) suggests that counselors communicate with their clients in ways that are culturally appropriate to ensure understanding (A.2.c., p. 4). This can be achieved by prolonged exposure to military culture or by seeking supervision from a professional involved with the military mental health system (Reger et al., 2008). Strom et al. (2012) outlined examples of military-specific cultural components for professionals to learn: importance of rank, unique terminology and value of teamwork. It behooves counselors intending to work with the military population to learn terminology in order to understand service members. For example, R&R refers to vacation leave and MOS or rate refers to a job category (Strom et al., 2012).
Personal values may cause dilemmas for a mental health professional working within the VA system. This can be especially true during times of war. Stone (2008) suggested that treating veterans of past wars may be easier than working with military service members during current combat because politics may be intensified. A counselor who does not support the current wartime mission may be conflicted when clients are mandated to return to active-duty assignments (Stone, 2008). The ACA Code of Ethics (2005) addresses the impact of counselors’ personal values (A.4.b., pp. 4–5) on the therapeutic relationship. It is recommended that counselors be aware of their own values and beliefs and respect the diversity of their clients. Counselors need to find a way to value the contributions of their client when personal or political opinion conflicts with the DOD’s plans or efforts overseas. If one wants to be successful with this population, Johnson (2008) suggested the foundational importance of accepting the military mission. If this is in direct conflict with the counselor’s values, it may be recommended for the counselor to consider the client’s value of the mission.
The ACA ethical code stresses the importance of mental health professionals practicing within the boundaries of their competence and continuing to broaden their knowledge to work with diverse clients (ACA, 2005, C.2.a., p. 9). Counselors should only develop new specialty areas after appropriate training and supervised experience (ACA, 2005, C.2.b., p. 9). Working within the VA mental health system, mental health professionals may be asked to provide a service in which they are not competent (Kennedy & Johnson, 2009). Such a request may occur more frequently here than in other settings, due to the high demand of mental health services and low availability of trained professionals (Garvey Wilson et al., 2009; Hoge et al., 2006). Counselors must determine if their experience and training can be generalized to working with military service members (Kennedy & Johnson, 2009), and may be their own best advocate for receiving appropriate training.
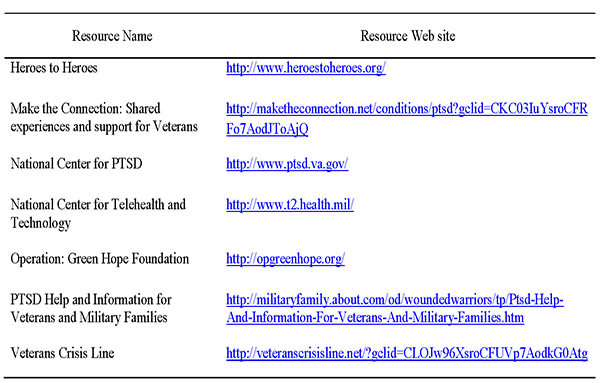
Awareness of when and how military service members access mental health services also might be important to consider. Reger et al. (2008) reported that military personnel were more likely to access services before and after a deployment. Researchers specified a higher prevalence rate of access 3–4 months after a deployment (Hoge et al., 2004). The relationship of time between deployment and help-seeking behaviors suggests that counselors should be prepared for issues related to trauma. For women, combat-related trauma is compounded with increased rates of reported military sexual trauma (Kelly et al., 2008). Counselors would benefit from additional trainings in trauma intervention strategies. The VA and related military organizations offer many resources online to educate professionals working with military members with identified trauma symptoms (U.S. VA., n.d.).
Advocating for appropriate training in areas of incompetence is the responsibility of the professional, who should pursue such training in order to best meet the needs of the military population. It is best practice for mental health professionals to be engaged in ongoing trainings to ensure utilization of the latest protocols and treatment modalities (McCauley et al., 2008). Trainings may need to extend beyond general military culture, because each branch of service (e.g., Army, Marines, Navy) could be considered a cultural subgroup with unique language and standards. For example, service members in the Army are soldiers, whereas members of the Navy are sailors (Strom et al., 2012).
This article has outlined many ACA (2005) ethical guidelines pertinent to working with the military population. However, as presented, there are times when counselor ethical codes conflict with military regulations. Counselors interested in working in the military setting or with military personnel may consider decision-making models to address ethical dilemmas.
Recommendations for Counselors
The military mental health system has almost exclusively employed psychologists and social workers. Counselors interested in employment within VA agencies or as TRICARE providers may utilize the resources created by these practitioners to better serve the military population. Two ethical decision-making models are presented, and a case study is provided to demonstrate how to implement the models.
Ethical Models
The ACA Code of Ethics (2005) advises counselors to adhere to the code of ethics whenever possible, working towards a resolution of the conflict (H.1.b., p. 19). If a favorable resolution cannot be formed, counselors have the choice to act in accordance with the law or regulation. Psychology researchers have suggested ethical models for professionals to use during times of dilemma within the military setting. The first model presented considers three overarching approaches to address ethical dilemmas; and the second model presented is a more specific stage model with which to approach dilemmas. These models may serve to assist counselors as the counseling profession gains more experience in the VA system and eventually develops counselor-specific decision-making models.
Approach model. Johnson and Wilson (1993) identified three approaches for psychologists to consider when navigating the ethical quandaries of the military mental health system. The first, the military manual approach, occurs when professionals adhere strictly to military regulations without consideration for the specific client’s needs. The second, the stealth approach, occurs when there is strict adherence to the mental health professionals’ code of ethics, regardless of the legalities surrounding the circumstances. While the client’s best interests may be at the forefront in this approach, the counselor must also take into account the possibility of being the subject of legal action for not adhering to the standards set by the military. For example, the counselor may use ambiguous wording within the client file or leave some information out altogether, so that if the files were requested, the client’s information would be protected (Johnson & Wilson, 1993). The third, the best interest approach, occurs when the counselor maintains focus on the client’s best interest while also adhering to the standards of the military. This may require professionals to adhere to the minimum professional standards in order to accommodate the client’s best interest. Although most professionals have deemed this approach the best option, it also leads to the most ambiguity. Under certain circumstances, the counselor also must take into account what is in the best interest for society as a whole, while also navigating a responsibility to the client and the military mental health system. Researchers in psychology responded to the ambiguity of this model by developing a more specific stage model to assist professionals with ethical dilemmas.
Stage model. Barnett and Johnson (2008) proposed a 10-stage model to follow when navigating an ethical dilemma. They advise that professionals must do the following:
1. Clearly define the situation.
2. Determine what parties could be affected.
3. Reference the pertinent ethical codes.
4. Reference the pertinent laws and regulations.
5. Reflect on personal thoughts and competencies on the issue.
6. Select knowledgeable colleagues with whom to consult.
7. Develop alternate courses of action.
8. Evaluate the impact on all parties involved.
9. Consult with professional organizations, ethics committees and colleagues.
10. Decide on a course of action.
Barnett and Johnson (2008) also noted that once a decision is made, the process does not end. It is best practice to monitor the implications and, if necessary, modify the plan. Documentation throughout this entire process is necessary for the protection of the counselor, the client and other involved stakeholders. Counselors working in the military mental health system may find this 10-stage model helpful when navigating ethical dilemmas.
To better understand the implementation of the two presented ethical decision-making models, a case study was developed. The case is then conceptualized from both the approach model and stage model, and the ethical dilemmas associated with the case are discussed.
Case Study
Megan is a licensed professional counselor employed at a clinic that serves military service members. She provides individual outpatient counseling to veterans and family members, as well as facilitates veteran support groups. Megan’s client, Robert, is a Petty Officer First Class in the Navy. Robert is married with two children. In recent sessions, Megan became concerned with Robert’s increased alcohol use. Recently, Robert described a weekend of heavy drinking at the local bar. Although Robert drove after leaving the bar both nights, Megan suspected that he was not sober enough to drive. In a follow-up session, Robert reported that his binge-drinking weekend caused friction at home with his wife, and that he missed his children’s soccer games. During his most recent session, Robert was visibly distressed as he disclosed to Megan that he received orders for a deployment in 3 months. Robert is anxious about informing his wife and children of the pending 6-month deployment, as he knows it will only increase conflict at home. Robert reported that his family could use the increase in pay associated with family separation and tax-free wages during deployment. However, he also knows that deployments cause tension with his wife, which has already increased due to Robert’s recent drinking binges. While leaving the session, he mentioned with a laugh that he would rather go to the bar than go home.
Analysis from approach model. Megan may consider using Johnson and Wilson’s (1993) ethical approach model as she conceptualizes the potential ethical dilemma presented in Robert’s case. From a military manual approach, Megan may need to report Robert’s recent alcohol abuse behavior to his superior, as it may impact his fitness for duty on his next deployment. And although Robert has not been caught drinking and driving or charged with a crime, his behavior also puts him at risk of military conduct violations. However, when Robert originally came to the clinic, he did so of his own accord, not under orders, which could mean that notifying a commanding officer is an ethical violation. In consideration of the stealth approach, Megan may review the ACA (2005) ethical guidelines and conclude that there are no violations at risk if she chooses not to report Robert’s drinking habits. However, Megan contemplates whether addressing Robert’s drinking binges is in his best interest overall. She understands that the money associated with deployment is important to Robert’s family at this time; however, his drinking may put him at increased risk during deployment. Finally, Megan applies the best-interest approach to Robert’s situation. Megan may refer Robert to the center’s substance use support group. This referral will be reflected in Robert’s records, but if he begins receiving treatment for his alcohol abuse now (3 months before deployment), there may be time for Robert to demonstrate significant progress before his fitness for duty assessment.
Analysis from stage model. Megan may consider her ethical dilemma from Barnett and Johnson’s (2008) 10-stage model. In stage 1, she clearly defines the situation as Robert’s alcohol abuse and pending deployment. In stage 2, Megan considers who may be affected in this situation. She understands that Robert’s family would benefit from the extra money associated with the deployment, and therefore the family may be impacted if Robert is not deployed. Megan also notes that the family is already negatively impacted by his recent drinking binge (e.g., conflict with his wife, missed soccer games). If Robert’s problematic drinking continues, he is at risk for evaluation and promotion issues. In stage 3, Megan reflects upon the ACA (2005) ethical codes in order to better understand her dilemma from a counselor’s view. Robert has a right to confidentiality (B.1.c., p. 7) with limitations including illegal substance use (B.1.d., p. 7). However, Robert’s current substance is alcohol, which is a legal substance. Megan considers the importance of his support network (A.1.d., p. 4) including his family and unit, but she does not have the ethical right to disclose her concerns about his substance abuse. In stage 4, Megan considers the pertinent laws and regulations of the dilemma. As per the clinic regulations, she is aware that if she makes a substance use program referral, it will be reflected in Robert’s record, which is the property of the military. Megan also is aware that Robert has not committed a documented crime of driving under the influence.
In stage 5 of the 10-stage ethical decision-making model, Megan must reflect on her personal thoughts and competencies. She is very concerned about Robert’s increased use of alcohol and is worried for his safety if deployed. Megan feels less confident in her ability to accurately assess for substance use problems. She facilitates the PTSD support group for the clinic, which is her specialty area. Megan recognizes that she is fond of Robert as a client and is disappointed that he could be jeopardizing his family and career with his alcohol abuse. She considers whether she is overreacting to his binge-drinking incident because of her higher expectations of him. In stage 6, Megan consults with her colleague who leads the substance use support groups at the clinic. She describes Robert’s recent abuse of alcohol and inquires as to whether he is a good candidate for the substance use group, needs more intense treatment, or needs no treatment at all. The colleague suggests that the group would be a very appropriate fit for someone with Robert’s symptoms.
In stage 7, Megan develops her course of action to refer Robert to the substance use group. Then, in stage 8, she evaluates the plan for potential impact on parties involved. Megan conceptualizes that Robert may be at risk for losing his deployment orders if he is accessing substance use treatment. Megan believes she has reduced this potential impact by referring to the substance support group, rather than an inpatient treatment facility, which may be more appropriate for a dependence issue. Megan recognizes that attending a 90-minute group each week will take Robert away from his family, but she also realizes that the 90-minute commitment is less than his current time spent away from the family when binge drinking. Megan reflects upon how her therapeutic relationship with Robert may be strained at the time of referral, and is prepared for a potential negative response from her client. She trusts in their therapeutic relationship and moves forward. In stage 9, Megan presents her planned course of action to her supervisor at the clinic. The supervisor approves the referral for the support group, but also suggests that Megan consider a referral to couples counseling for Robert and his wife, which may assist with resolving conflicts before the deployment.
In the final stage, Megan proposes the treatment plan of action to Robert in their next session. Megan explains that she feels ethically obligated to refer Robert to the substance use support group, and that as of now, Robert may make this choice for himself. Megan and Robert discuss the potential that substance use treatment may no longer be a choice in the future if his current drinking behavior continues. There is more discussion of fitness for duty and how participation in the support group will positively reflect upon the assessment in the future. Megan also presents Robert with the recommendation of couples counseling to help mediate relationship conflicts before deployment. She reports that if Robert and his wife decide to receive couples counseling, she can provide a referral for them at that time.
With the ethical decision-making models presented, the counselor is able to successfully navigate the military mental health system, while still maintaining the professional standards of the counseling profession. In each model, the situation is resolved with considerable attention to the client’s best interest, while maintaining the expectations of the military clinic. Psychologists developed the two ethical models presented, and counselors may choose to utilize these approaches until more counselor-specific ethical processes are created. As counselors become more permanent fixtures in the VA mental health system and as TRICARE providers, opportunities to develop an ethical decision-making model will likely arise.
Conclusion
The recent inclusion of counselors as mental health professionals within the VA system and as TRICARE providers allows for new employment opportunities with the military population. However, these new opportunities are not without potential dilemmas. Counselors interested in working with service members need to be educated on the potential conflict between counselor professional ethical guidelines and military protocols. Future research in the counseling field may develop a counselor-specific ethical decision-making model. In the meantime, counselors may utilize or adapt the ethical decision-making models created by other mental health professionals, who have a longer history working with the military population.
References
American Counseling Association. (2005). ACA code of ethics. Retrieved from http://www.counseling.org/Resources/aca-code-of-ethics.pdf
Barnett, J. E., & Johnson, W. B. (2008). The ethics desk reference for psychologists. Washington DC: American Psychological Association.
Barstow, S., & Terrazas, A. (2012, February). DoD releases TRICARE rule on independent practice for counselors. Counseling Today, 54(8), 10. Retrieved from
http://ct.counseling.org/2012/02/dod-releases-tricare-rule-on-independent-practice-for-counselors/
Garvey Wilson, A. L., Messer, S. C., & Hoge, C. W. (2009). U.S. military mental health care utilization and attrition prior to the wars in Iraq and Afghanistan. Social Psychiatry and Psychiatric Epidemiology, 44, 473–481. doi:10.1007/s00127-008-0461-7
Hall, L. (2011). The importance of understanding military culture. Social Work in Health Care, 50, 4–18. doi:10.1080/00981389.2010.513914
Hoge, C. W., Auchterlonie, J. L., & Milliken, C. S. (2006). Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. The Journal of the American Medical Association, 295(9), 1023–1032. doi:10.1001/jama.295.9.1023
Hoge, C. W., Castro, C. A., Messer, S. C., McGurk, D., Cotting, D. I., & Koffman, R. L. (2004). Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. The New England Journal of Medicine, 351(1), 13–22. doi:10.1056/NEJMoa040603
Holder, K. A. (2007). Comparison of ACS and ASEC data on veteran status and period of military service: 2007. U.S. Census Bureau: Housing and Household Economics Statistics Division. Retrieved from http://www.census.gov/hhes/veterans/files/comparison_report.pdf
Johnson, W. B. (2008). Top ethical challenges for military clinical psychologists. Military Psychology, 20, 49–62. doi:10.1080/08995600701753185
Johnson, W. B., Grasso, I., & Maslowski, K. (2010). Conflicts between ethics and law for military mental health providers. Military Medicine, 175, 548–553.
Johnson, W., & Wilson, K. (1993). The military internship: A retrospective analysis. Professional Psychology: Research and Practice, 24(3), 312–318. doi:10.1037/0735-7028.24.3.312
Kelly, M. M., Vogt, D. S., Scheiderer, E. M., Ouimette, P., Daley, J., & Wolfe, J. (2008). Effects of military trauma exposure on women veterans’ use and perceptions of Veterans Health Administration care. Journal of General Internal Medicine, 23, 741–747. doi:10.1007/s11606-008-0589-x
Kennedy, C. H., & Johnson, W. B. (2009). Mixed agency in military psychology: Applying the American Psychological Association ethics code. Psychological Services, 6(1), 22–31. doi:10.1037/a0014602
Kim, P. Y., Britt, T. W., Klocko, R. P., Riviere, L. A., & Adler, A. B. (2011). Stigma, negative attitudes about treatment, and utilization of mental health care among soldiers. Military Psychology, 23, 65–81. doi:10.1080/08995605.2011.534415
Martin, J., Ghahramanlou-Holloway, M., Lou, K., & Tucciarone, P. (2009). A comparative review of U.S. military and civilian suicide behavior: Implications for OEF/OIF suicide prevention efforts. Journal of Mental Health Counseling, 31(2), 101–118.
McCauley, M., Hacker Hughes, J., & Liebling-Kalifani, H. (2008). Ethical considerations for military clinical psychologists: A review of selected literature. Military Psychology, 20, 7–20. doi:10.1080/08995600701753128
O’Gorman, K. (2012, August 16). Army reports record suicides in July [Blog post]. Retrieved from http://iava.org/blog/army-reports-record-high-suicides-july
Reger, M. A., Etherage, J. R., Reger, G. M., & Gahm, G. A. (2008). Civilian psychologists in an army culture: The ethical challenge of cultural competence. Military Psychology, 20, 21–35. doi:10.1080/08995600701753144
Snell, F., & Tusaie, K. R. (2008). Veterans reported reasons for seeking mental health treatment. Archives of Psychiatric Nursing, 22(5), 313–314. doi:10.1016/j.apnu.2008.06.003
Stone, A. M. (2008). Dual agency for VA clinicians: Defining an evolving ethical question. Military Psychology, 20, 37–48. doi:10.1080/08995600701753177
Strom, T. Q., Gavian, M. E., Possis, E., Loughlin, J., Bui, T., Linardatos, E.,…Siegel, W. (2012). Cultural and ethical considerations when working with military personnel and veterans: A primer for VA training programs. Training and Education in Professional Psychology, 6(2), 67–75. doi:10.1037/a0028275
U.S. Census Bureau, American Community Survey. (2011). B21002: Period of military service for civilian veterans 18 years and over (2011 American Community Survey 1-year estimates). Retrieved from http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_11_1YR_B21002&prodType=table
U.S. Department of Defense. (n.d.). Enhanced post-deployment health assessment (PDHA) process (DD Form 2796). Retrieved from http://www.pdhealth.mil/dcs/dd_form_2796.asp
U.S. Department of Defense. (2012). Army releases July suicide data, No. 683-12. Retrieved from http://www.defense.gov/releases/release.aspx?releaseid=15517
U.S. Department of Defense. (2013). DOD, VA and HHS partner to expand access to mental health services for veterans, service members, and families, No. 353-13. Retrieved from http://www.defense.gov/releases/release.aspx?releaseid=16024
U.S. Department of Veterans Affairs. (n.d.). PTSD: National center for PTSD. Retrieved from http://www.ptsd.va.gov/professional/index.asp
U.S. Department of Veterans Affairs (2012, April). VA adding family therapists and mental health counselors to workforce. Retrieved from http://www.va.gov/opa/pressrel/pressrelease.cfm?id=2303
Elizabeth A. Prosek, NCC, is an Assistant Professor at the University of North Texas. Jessica M. Holm is a doctoral student at the University of North Texas. Correspondence can be addressed to Elizabeth A. Prosek, University of North Texas, 1155 Union Circle #310829, Denton, TX 76203-5017, elizabeth.prosek@unt.edu.
Apr 6, 2014 | Article, Volume 4 - Issue 2
S. Beth Ruff, Michael A. Keim
There are 1.2 million school-age children with military parents in the United States, and approximately 90% attend public schools. On average, military children move three times more often than their civilian peers. Tensions at home, enrollment issues, adapting to new schools, and a lack of familiarity with military culture by public school professionals may adversely impact the academic, social and emotional growth of these students. Public school faculty and staff need to understand the challenges that multiple school transitions impose on military children in order to effectively meet the needs of this student population. In this article, the authors review the literature concerning obstacles and challenges mobile military children face, and discuss positive interventions that professional school counselors can employ to ease these transitions.
Keywords: school counselors, school transitions, military children, military culture
The Department of Defense (DOD) Demographics Report (2010) revealed that approximately 1.85 million children have one or both parents serving in the U.S. military. The report further explained that 1.2 million of these children have active-duty parents, and approximately 660,000 children have parents that serve in reserve positions in the military. Out of the 1.85 million military children, 1.2 million of them fall into the K–12 education range of 6–18 years of age (DOD, 2010). The Department of Defense Dependents Education (DODDE, 2012) budget for fiscal year 2013 estimated that 90% of these school-age military children attend public schools that are not sponsored by the DOD.
On average, military children move and change schools 6–9 times from the start of kindergarten to high school graduation (Astor, 2011; Berg, 2008; Kitmitto et al., 2011; Sherman & Glenn, 2011). Additionally, these military children move three times more often than their civilian peers, relocating every 1–4 years (Berg, 2008; Bradshaw, Sudhinaraset, Mmari, & Blum, 2010; Hipps, 2011). With military children comprising nearly 4% of the nation’s entire school-age population, public school administrators, teachers and school counselors should expect military students to transition in and out of their school populations (Rossen & Carter, 2011). Public school faculty and staff need to understand the challenges that multiple school transitions impose on military children in order to effectively meet the needs of this student population. In this article, the authors review the literature concerning the obstacles and challenges mobile military children face, and discuss positive interventions that professional school counselors can employ to ease transition.
Stressors for Military Families and Children
Military families face a unique set of life stressors specific to their culture. Hall (2008) describes the challenges faced by military families by stating that “the defining word for the military family is change; change is what their lives are about” (p. 193). As such, military families experience change and transition so frequently they often do not have time to grieve over the last transition before planning and preparing for the next. Relocation becomes a consistent stressor in the lives of military families, as the average military move occurs every 3 years, and some families, particularly families of high-ranking officers, move more frequently (Hall, 2008).
As noted in Weber and Weber (2005), previous studies (Pribesh & Downey, 1999; Simpson & Fowler, 1994; Wood, Halfon, Scarlatta, Newacheck, & Nessim, 1993) found relocation stress to have a detrimental effect on civilian child populations. School-age military children are especially vulnerable to the stress related to frequent transitions, as they must simultaneously cope with normal developmental stressors such as establishing peer relationships (Kelley, Finkel, & Ashby, 2003), conflict in parent/child relationships (Gibbs, Martin, Kupper, & Johnson, 2007; Lowe, Adams, Browne, & Hinkel, 2012), and increased academic demands (Engel, Gallagher, & Lyle, 2010). These additional stressors in conjunction with multiple school transitions could negatively affect the children’s adaption to new school environments. In addition to normative developmental stressors and frequent relocations, military children’s parents are often deployed, which can exacerbate stress in the children and may result in more barriers and maladjustment (Mmari, Bradshaw, Sudhinaraset, & Blum, 2010).
Transitional Barriers for Military Adolescent Students
Recognizing that these significant stressors for military children may be further complicated by multiple school transitions, the U.S. Army began to explore the lives of these children in order to identify ways to minimize the negative impacts of frequent relocation (Berg, 2008). In conjunction with the Military Child Education Coalition (MCEC), the Secondary Education Transition Study (SETS) was completed, which revealed specific educational challenges associated with multiple transitions (MCEC, 2001). The SETS study exposed several obstacles to transition between schools that impacted military children socially, emotionally and academically. Specific transition challenges identified by SETS for military adolescents include the following: slow transfer of school records and differences in curricula between schools, adapting to new school environments and making friends, limited access to extracurricular activities, a lack of understanding of military culture by public school teachers and staff, and tension at home and parental deployment (MCEC, 2001). The authors reviewed the literature for relevant information on each stressor.
Slow transfer of records and differences in curricula between schools. With each move to another state and school, military children encounter the challenges of slow transfer of records and differences in school curricula, which increase frustration with the transition process for parents and students (Sherman & Glenn, 2011). Kitmitto et al. (2011) found that enrollment into a new school could take up to 3 weeks, as the new school awaits the arrival of official records from the previous school. The lack of communication between the previous and receiving schools regarding history of schools attended, curricula, achievements, and stresses and traumas can lead to academic weaknesses (Berg, 2008). As military parents fulfill their duties to serve and protect the United States, the nation’s schools may hinder student progress by requiring them to take classes over again or denying them placement into gifted or special needs education due to slow school record exchange (Astor, 2011).
Military children face several academic challenges as a result of frequent school transition. The differences in curricula and school requirements result in educational gaps for military children, which might entail repeating classes and lessons, and missing crucial topics such as multiplication and fractions (Bradshaw et al., 2010). Mmari et al. (2010) noted that parents expressed their concern for their children’s education quality; because of the differences in grade levels between schools, children had to learn the same material or read the same books repeatedly. A recent study by the MCEC reported that the differences in curricula continue to vary from school to school; and parents’ most commonly discussed concerns were the differences in scope and sequence in mathematics, specifically as it leads up to algebra and higher-level coursework (MCEC, 2012). Military parents work hard to fill the gaps in their child’s education due to transition, but many feel that if they do not advocate for their children, they will fall significantly behind their peers academically (Mmari et al., 2010).
Adapting to new school environments and making friends. With each move, military children must cope with the stress of making new friends and leaving others behind, adapting to a new school environment at awkward times, and figuring out how to fit in (Kitmitto et al., 2011). In a study conducted by Bradshaw et al. (2010), military students reported that some significant stressors in school transition were adjusting to the physical campus and to the culture of the school, including being aware of the school’s procedures and policies. Military students often transition at random times throughout the school year and experience added stressors such as learning the layout of the school and assimilating into already-established social groups (Bradshaw et al., 2010). Lack of information from the new school, such as not providing a campus map or an explanation of the course schedule, may lead the child to believe that the school is not supportive, which in turn can negatively impact the child’s adjustment to transition to the new school environment (Bradshaw et al., 2010).
Military children are frequently forced to end relationships with friends at a previous school and begin new peer relationships at the new school. In a qualitative study of military children, the most commonly mentioned stressor related to school transitions was the challenge of making and maintaining close friendships (Bradshaw et al., 2010). Many students described that the inevitable ending of close relationships led them to avoid making close connections with peers at new schools. With each move, letting go and saying goodbye to friendships becomes harder for the military students; and to avoid the inevitable grief, many students will choose to have superficial relationships instead of close friendships. It is more difficult with such relationships to gain acceptance from established cliques and social networks. This leads to military students often lacking a feeling of connectedness with others in their new schools, which in turn may lead to maladjustment in the transition (Bradshaw et al., 2010).
Limited access to extracurricular activities. With each school transition, military students encounter further challenges to retaining or gaining eligibility to participate in athletics and extracurricular activities at their new school (Sherman & Glenn, 2011). Students involved in sports who move late into the school year may miss tryouts for teams. Additionally, transferring to another state may mean that the new school does not offer the same athletic programs (Bradshaw et al., 2010). Even when students are eligible to participate in sports, military students can have difficulty breaking into established athletic programs and teams. Mmari and colleagues (2010) found that military children often experience discrimination when they participate in athletics at the new school. Athletic coaches were reluctant to put military students on teams or in starting positions, as doing so could disrupt the team dynamics. Military students also struggled to bond with their new teammates, especially if a military student’s new position on the team resulted in an established teammate losing a starting position (Mmari et al., 2010).
Students taking part in other extracurricular activities, like student government, face similar challenges that limit their involvement. New military students may find that student government elections either happened before they entered the school or rely heavily on established popularity and previous school involvement, which would be difficult or impossible for a new student to demonstrate (Bradshaw et al., 2010). These challenges can negatively affect the military student’s adjustment to a new school, as they may hinder connectedness to the new school environment or create a sense of loss if the student was involved in high-status positions at a former school (Bradshaw et al, 2010). Limited access to these activities can lead to additional mental health concerns for the military student, as a decline in participation in such activities can cause further withdrawal and depressive symptoms (Rossen & Carter, 2011). The transition to a new school includes challenges both in the classroom and beyond.
Lack of understanding of military culture by public school teachers and staff. The way in which school teachers and staff interact with military students who transfer to their school can either increase or reduce the students’ stress. Unfortunately, administrators, educators and counselors in public schools tend to be unfamiliar with the specific issues and stressors that mobile military students encounter (Harrison & Vannest, 2008). Horton (2005) noted that because of their limited experience with the military, civilian school staff have a knowledge gap that affects their competence and effectiveness in working with military students and families. The school staff’s lack of understanding about the military students’ culture results in varying degrees of interactions ranging from overly sensitive to completely insensitive to their needs. Bradshaw et al. (2010) found that teachers’ expectations differ because they struggle with the right thing to do. Some teachers have high expectations for new military students and expect them to assimilate rather than acknowledging their unique issues. Other teachers recognize some of the issues military students face because of deployment, but choose to avoid the topic of war in the classroom or discourage the students from talking about their experiences as to not upset the students (Bradshaw et al., 2010).
In addition to the issue of sensitivity, teachers who are not familiar with military culture may maintain negative stereotypes or political ideologies that influence the way they interact with military students (Fenell, 2008). Horton (2005) explained that it is also possible for public school staff members to harbor strong negative feelings about the military, which may impact their treatment of the military students. Fear of discrimination may also be a factor that impedes school staff from identifying military students in their schools, as parents and students may not reveal their military connection (Bradshaw et al. 2010; Mmari et al., 2010). Additionally, Mmari and colleagues (2010) found that many teachers and counselors had not received information that would help them identify students connected to the military. While part of the school staff felt that properly identifying military students could aid in assisting and connecting with these students, others felt that labeling this population could result in prejudice toward the students by anti-military staff. A majority of the parents in the study reported that school staff did not know how to deal with and support military children and issues such as deployment, and that more training is needed (Mmari et al., 2010).
Tension at home and parental deployment. Relocation increases stress for all military family members. In preparing to move, parents are swamped with concerns and to-do lists, and may not have the patience or time to consider a child who is resistant to the transition (Hall, 2008). The numerous moves can leave parents feeling physically and emotionally exhausted, and less emotionally able to help their children cope with stress related to relocation (Bradshaw et al., 2010). Several studies reported that parental stress directly impacts the child’s ability to cope during stressful situations (Hall, 2008; Mmari et al., 2010; Waliski, Bokony, Edlund, & Kirchner, 2012). Further, parental stress increases the likelihood of conflicts between the parent and child and could lead to child maltreatment (Rentz et al., 2007; Waliski et al., 2012). Parents’ stress can exacerbate the emotional stress and frustration already felt by the military child due to transition.
In a qualitative research study by Bradshaw et al. (2010), the majority of military students reported that moving increased tension in the home. Some students reported feeling anger and resentment toward their parents and the military because of the constant uprooting and disruption due to change of duty stations. Many students reported telling parents that they refused to move or would run away to avoid moving again (Bradshaw et al., 2010). This negative and resistant behavior from a child can be an additional source of stress for the family. Parents may in turn view the behavior as a problem and punish or avoid the child instead of acknowledging the emotional strain the student is facing with transition (Harrison & Vannest, 2008).
The emotional stress of relocation can be further complicated if the military parent is deployed or at risk of being deployed. The constant fear for a parent’s safety can negatively affect a child academically, emotionally and behaviorally (Chawla & Solinas-Saunders, 2011; Harrison & Vannest, 2008; Mmari et al., 2010). Having a parent deployed in conjunction with a transition can lead to increased feelings of depression and anxiety. In a qualitative study of military students, many participants reported increased fear and anxiety for deployed parent’s safety. These military students also reported difficulty coping with the absence of the deployed parent at special occasions such as birthdays, school programs and sporting events (Mmari et al., 2010). Absence of the deployed parent from these significant life events can cause stress, depression, feelings of loss, and anxiety for the military child. These feelings are often externalized in the form of declining grades and behavior problems at home and school (Harrison & Vannest, 2008). Adolescents also may experience increased stress with role ambiguity during a parent’s deployment—as the family instantly becomes a single-parent home, the adolescent may take on additional responsibilities to support the remaining parent (Chawla & Solinas-Saunders, 2011; Harrison & Vannest, 2008).
Research following Operations Desert Shield and Desert Storm during the Gulf War in 1991 confirmed that stresses do occur within families during and after deployment (Jensen & Shaw, 1996; Kelley, 1994; Norwood, Fullerton, & Hagen, 1996; Pierce, Vinokur, & Buck, 1998; Rosen, Teitelbaum, & Westhuis, 1993). In their study of absent Navy mothers due to deployment during the Gulf War, Kelley, Herzog-Simmer, and Harris (1994) found that maternal depression, decreased self-esteem, and dysphoria were significantly correlated with children’s internalizing behavior (e.g., anxiety, depression).
Likewise, nondeployed parents also experience stress during times of deployment (Mmari et al., 2010), which in turn may be felt by children in the home (Chawla & Solinas-Saunders, 2011). Harrison and Vannest (2008) report that in addition to feelings of worry and fear for their spouse’s safety, the remaining parent also grapples with the stress of increased role expectation and responsibilities as a single parent. Without support, the remaining parent may cope with role strain and anxiety by withdrawing emotionally from their children or responding with severe punishment to misbehavior (Harrison & Vannest, 2008). These children may face an increased risk of maltreatment or neglect as the remaining parent may become abusive to the children when a spouse is deployed (Chawla & Solinas-Saunders, 2011; Gibbs et al., 2007; Rentz et al., 2007). Deployment can have significant detrimental effects on an entire military family’s well-being and coping skills.
Support Systems and Military Children
While researchers have found many negative outcomes associated with school transitions for military children, supportive relationships appear to have a positive influence on outcomes for this group. Although the majority of the literature discusses the damaging consequences that multiple school transitions have on children from military families, some studies found that multiple school transitions fostered strength and resiliency. Lyle (2006) reported that there are mixed results in the literature regarding the effects of multiple school transitions. Multiple transitions have been shown to equip military children with more adaptability, accelerated maturity, deeper appreciation for cultural differences, and strong social skills in comparison to their civilian peers (Bradshaw et al., 2010; Mmari et al., 2010; Sherman & Glenn, 2011; Strobino & Salvaterra, 2000). Weber and Weber (2005) actually reported a lower rate of problems experienced by military adolescents exposed to increased frequency and number of relocations. Strobino and Salvaterra (2000) stated that whether transition affects military children positively or negatively depends largely upon their support systems. Students’ preoccupation with feelings of isolation and loneliness during school transition could result in poor grades and a decline in academic achievement. In contrast, military students who welcome change and find a new sense of responsibility during school transition may experience improved academic performance and achievement. It also was found that despite five or more school transitions, military children reported average to above-average grades, active involvement in extracurricular activities, and support of teachers and parents. This study attributed the positive adjustment of military students during multiple school transitions to supportive school cultures and strong parental involvement. The positive and negative results reveal that the level of school and parent support may be indicators of how well military students adjust during multiple school transitions (Strobino & Salvaterra, 2000).
Implications for School Counselors
Given the extensive influence that the school environment has on military students’ adjustment during school transitions, the importance of developing a supportive and understanding relationship with this student population is paramount. Rush and Akos (2007) note that school counselors are uniquely qualified to assist students with social, emotional and academic concerns. School counselors are specifically trained in child development, and they work closely with numerous sources of student support including parents, teachers and peers. Waliski et al. (2012) confirm that counselors possess the education and skills needed to help military students and are readily accessible within their community. Professional school counselors also have access to academic data that can be used to identify the specific needs of an enrolling military student, such as standardized test scores, attendance records, discipline referrals and report cards. Moreover, school counselors serve students directly by developing and implementing preventive programs and interventions that facilitate support and social belonging such as classroom guidance, intentional guidance groups and peer mentoring (Rush & Akos, 2007). The role of school counselors within the school environment places them in a unique position to serve and advocate for enrolling military students and consequently transform school transition into a positive experience. The following sections will provide an overview of ways that school counselors can support military students in their own schools.
Becoming Informed About Military Life
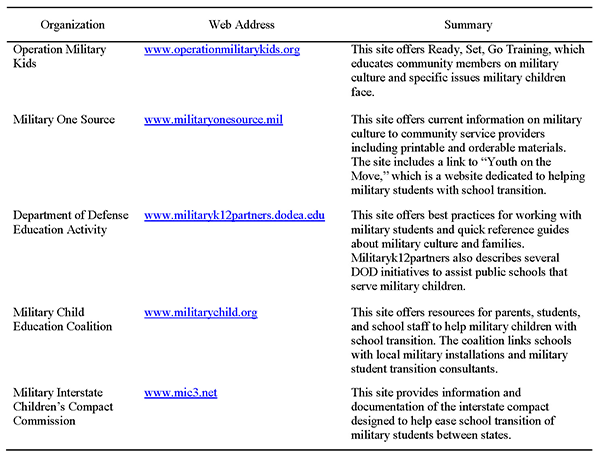
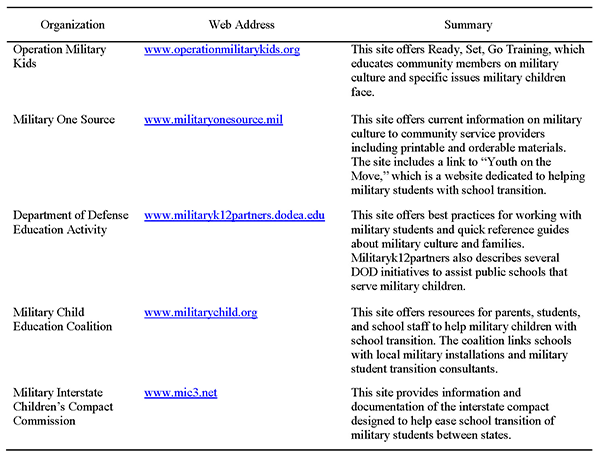
To initiate change, school counselors must first be informed about military life and become knowledgeable about resources and culturally sensitive interventions suited for military students (Waliski et al., 2012). Understanding the challenges and the unique needs of military students will help school counselors support military students and families during times of crisis (Harrison & Vannest, 2008). Several resources are available to assist school counselors in becoming advocates for and providing resources and interventions to military students. Organizations such as Operation Military Kids (OMK) and Military One Source provide specific tools and trainings on assisting military children and parents for school staff and community stakeholders (Eason, 2012). These resources could be used in staff development, classroom guidance, parent/teacher conferences, and small group and individual counseling (see Table 1).
Student-to-Student Interactions
With regard to strategies and programs that acclimatize new students to schools and ease the transition process, student-to-student programs were noted repeatedly in the literature (Berg, 2008; Bradshaw et al., 2010; Harrison & Vannest, 2008; Mmari et al., 2010; Strobino & Salvaterra, 2000). These programs connect new students with current students, who act as guides to the school grounds and reduce anxiety by initiating the friend-making process. One such program is noted by Rush and Akos (2007) in working with middle school students. The authors developed a 10-session, combination psychoeducational-counseling group created by school counselors to increase student knowledge concerning the deployment process. In addition to information sharing by the group leaders and group members early in the process and at the beginning of each session, the “later sessions, and the latter part of each session, are purposefully structured to be less directive and more process oriented to allow group members to pursue individual goals and provide more intrapersonal focus to help with particular issues that emerge” (Rush & Akos, p. 116). Students are further supported through the development of coping skills in a safe, encouraging environment.
Table 1
Web Resources to Support Military Students with Transition
Community Resources
Another avenue to help students adjust and adapt is connecting parents and caregivers to community resources. Mmari et al. (2010) found that some military parents did not utilize resources simply because they did not know they were available. Waliski et al. (2012) explained that counselors can serve as gatekeepers through whom military families can gain access to appropriate programs and services. Additionally, school counselors are in an advantageous position to develop partnerships between families and communities, to identify challenges such as transitions, to address these issues, and to advance student progress (Epstein & Van Voorhis, 2010). As military families transition, they may be unfamiliar with their new community and struggle to locate health care providers, childcare, tutoring, and mental health and counseling resources. School counselors are often equipped with lists for local providers and resources that could ease the transition for mobile military families. In addition to local resources, school counselors can proactively assist military children and their families by maintaining a record of resources specific to military families. For example, Tutor.com provides free tutoring and resources for military students (“Tutor.com for U.S. military families,” 2014). Also, a new Web site sponsored by the Department of Veterans Affairs, “Parenting for Service Members and Veterans,” has been launched just for military families (Department of Veterans Affairs, 2013). This resource addresses the unique challenges of parenting in military families through an online anonymous parenting course, interactive activities, and stories of real military and veteran families that provide valuable skills for the everyday challenges of raising military children. The course and content were developed by experts from the DOD. By connecting parents to resources, the school counselor can assist in reducing tension at home and increasing parental support and school involvement.
Staff Trainings
An important strategy for school counselors to implement in their schools is facilitating school staff trainings specific to military culture and needs of military students. Harrison and Vannest (2008) suggest that teachers receive professional development focused on military culture and the skills necessary to assist their military students. Strobino and Salvaterra (2000) explain that it is important for all stakeholders to be aware of the relationship between the student’s experiences and school success. School counselors and other school professionals are encouraged to focus on identifying the strengths of military students. Staff training can facilitate cultural sensitivity and supportive student/teacher relationships that contribute to positive school experiences.
A number of organizations—from the community to the national level—can provide training to assist educational professionals in working with the military community. Veterans’ organizations, such as Veterans of Foreign Wars (VFW) or the American Legion, have posts in local communities with representatives appointed to serve schools and other civic institutions. National Guard or reserve posts and active-duty military installations have a public affairs officer (PAO) who is available to discuss military-related issues such as deployment with the educational community as well. Additionally, the MCEC (2012), a federally recognized nonprofit organization, is specifically “focused on ensuring quality educational opportunities for all military children affected by mobility, family separation, and transition.” They provide ongoing training for school counselors and other education professionals both online and in face-to-face settings. Two MCEC programs in particular relate directly to school transitions. The Supporting Military Children through School Transitions: Foundations focuses on the military-connected child’s experience with transitions by addressing “military lifestyle and culture, school transition perspectives, and identifying local transition challenges.” The second program—Supporting Military Children through School Transitions: Social/Emotional Institute—focuses on the social and emotional effects of student transitions, including “deployment and separation, building confidence and resiliency, and supporting children through trauma and loss” (MCEC, 2012).
Advocating for Military Students
In addition to interventions used at the individual school level, school counselors can advocate for military students at the local, district and state levels. A valuable resource for school counselors is the Military Children Interstate Compact Commission. The Council of State Governments and the DOD worked collaboratively to develop an Interstate Compact that would address the challenges military families face with each school transition (Kitmitto et al., 2011). The Compact addresses transition issues such as slow transfer of records, course and curriculum differences and equivalents, attendance, accessibility to extracurricular activities, and graduation requirements. Through the guidelines and detailed governance structure, the Compact allows for the uniform treatment of these challenges at the state and local district level. Currently, 43 states have signed the Interstate Compact (Matthews, 2012). It is important for school counselors to be aware of their state’s standing on the Compact. School counselors can advocate for compliance with the guidelines set by their adoption and for implementation of the guidelines if their state has not become a signatory.
Conclusion
Military families experience unique stressors related to the military culture, such as parental deployment and multiple relocations. The literature attributes the negative effects of multiple school transitions to factors such as tension at home and parental absence, slow transfer of school records and differences in curricula between schools, adapting to new school environments and making friends, limited access to extracurricular activities, and a lack of understanding by school teachers and staff of military culture. The majority of the reviewed literature found that the challenges of mobile military students can lead to a decline in academic achievement and social/emotional problems.
Research seems to suggest that supportive relationships and an encouraging school environment can help military students adjust to the struggles that they are likely to face. The literature points to the professional school counselor as being the most appropriate staff member to foster these positive experiences and advocate for new enrolling military students. School counselors can create a positive experience for new enrolling military students by connecting parents and caregivers to community resources, advocating for quick transfer of school records, creating programs that acclimate new students to school grounds and culture, encouraging accessibility to extracurricular activities, and facilitating school staff trainings specific to military culture and the particular needs of military students.
References
Astor, R. A. (2011, June 8). The need to support students from military families. Education Week, 30(33), 27, 32. Retrieved from http://www.edweek.org/ew/articles/2011/06/08/33astor_ep.h30.html
Berg, K. F. (2008). Easing transitions of military dependents into Hawaii public schools: An invitational educational link. Journal of Invitational Theory and Practice, 14, 41–55.
Bradshaw, C. P., Sudhinaraset, M., Mmari, K., & Blum, R. W. (2010). School transitions among military adolescents: A qualitative study of stress and coping. School Psychology Review, 39, 84–105.
Chawla, N., & Solinas-Saunders, M. (2011). Supporting military parent and child adjustment to deployment separations with filial therapy. The American Journal of Family Therapy, 39, 179–192. doi:10.1080/01926187.2010.531647
Department of Defense. (2010). Demographics, 2010: Profile of the military community [Annual report]. Retrieved from http://www.militaryonesource.mil/12038/MOS/Reports/2010_Demographics_Report.pdf
Department of Defense Dependents Education. (2012). Fiscal year 2013 budget estimates: Department of Defense Dependents Education (DODDE) [Annual report]. Retrieved from http://comptroller.defense.gov/Portals/45/Documents/defbudget/fy2013/budget_justification/pdfs/
01_Operation_and_Maintenance/O_M_VOL_1_PARTS/O_M_VOL_1_BASE_PARTS/DoDDE_OP-5.pdf
Department of Veterans Affairs. (2013). Parenting for service members and veterans. Retrieved from http://militaryparenting.t2.health.mil
Eason, M. (2012, November). Operation military kids. Program session presented at the annual conference of the Georgia School Counselors Association, Athens, GA.
Engel, R. C., Gallagher, L. B., & Lyle, D. S. (2010). Military deployments and children’s academic achievement: Evidence from Department of Defense Education Activity schools. Economics of Education Review, 29, 73–82. doi:10.1016/j.econedurev.2008.12.003
Epstein, J. L., & Van Voorhis, F. L. (2010). School counselors’ roles in developing partnerships with families and communities for student success. Professional School Counseling, 14, 1–14.
Fenell, D. L. (2008, June 14). A distinct culture. Counseling Today, 50(12), 8–9, 35. Retrieved from http://ct.counseling.org/2008/06/a-distinct-culture/
Gibbs, D. A., Martin, S. L., Kupper, L. L., & Johnson, R. E. (2007). Child maltreatment in enlisted soldiers’ families during combat-related deployments. Journal of the American Medical Association, 298, 528–535. doi:10.1001/jama.298.5.528
Hall, L. K. (2008). Counseling military families: What mental health professionals need to know. New York, NY: Routledge.
Harrison, J., & Vannest, K. J. (2008). Educators supporting families in times of crisis: Military reserve deployments. Preventing School Failure, 52(4), 17–24. doi:10.3200/PSFL.52.4.17-24
Hipps, T. (2011, June). Removing educational obstacles for military kids. Soldiers, 66(6), 16–19.
Horton, D. (2005). Consultation with military children and schools: A proposed model. Consulting Psychology Journal: Practice and Research, 57(4), 259–265. doi:10.1037/1065-9293.57.4.259
Jensen, P. S., & Shaw, J. A. (1996). The effects of war and parental deployment upon children and adolescents. In R. J. Ursano & A. E. Norwood (Eds.), Emotional aftermath of the Persian Gulf War: Veterans, families, communities, and nations (pp. 83–109). Washington, DC: American Psychiatric.
Kelley, M. L. (1994). The effects of military-induced separation on family factors and child behavior. American Journal of Orthopsychiatry, 64, 103–111. doi:10.1037/h0079499
Kelley, M. L., Finkel, L. B., & Ashby, J. (2003). Geographic mobility, family, and maternal variables as related to the psychosocial adjustment of military children. Military Medicine, 168, 1019–1024.
Kelley, M. L., Herzog-Simmer, P. A., & Harris, M. A. (1994). Effects of military-induced separation on the parenting stress and family functioning of deploying mothers. Military Psychology, 6, 125–138.
Kitmitto, S., Huberman, M., Blankenship, C., Hannan, S., Norris, D., & Christenson, B. (2011). Educational options and performance of military-connected school districts research study – final report. San Mateo, CA: American Institutes for Research. Retrieved from http://www.militaryk12partners.dodea.edu/docs/2011-air-report.pdf
Lowe, K. N., Adams, K. S., Browne, B. L., & Hinkle, K. T. (2012). Impact of military deployment on family relationships. Journal of Family Studies, 18, 17–27.
Lyle, D. S. (2006). Using military deployments and job assignments to estimate the effect of parental absences and household relocations on children’s academic achievement. Journal of Labor Economics, 24(2), 319–350. doi:10.1086/499975
Matthews, W. J., III. (2012, June). Commission picks up member states 42 and 43. MIC3…News, Views, and Transitions: Newsletter for the Interstate Commission on Educational Opportunity for Military Children, 3, 5. Retrieved from http://www.mic3.net/documents/MIC3June2012InteractiveNewsletter2.pdf
Military Child Education Coalition. (2001). U.S. Army secondary education transition study: Executive summary. Arlington, VA: Military Resource Center.
Military Child Education Coalition. (2012). Programs. Retrieved from http://www.militarychild.org/professionals/programs
Mmari, K. N., Bradshaw, C. P., Sudhinaraset, M., & Blum, R. (2010). Exploring the role of social connectedness among military youth: Perceptions from youth, parents, and school personnel. Child and Youth Care Forum, 39, 351–366. doi:10.1007/s10566-010-9109-3
Norwood, A. E., Fullerton, C. S., & Hagen, K. P. (1996). Those left behind: Military families. In R. J. Ursano & A. E. Norwood (Eds.), Emotional aftermath of the Persian Gulf War: Veterans, families, communities, and nations (pp. 163–196). Washington, DC: American Psychiatric.
Pierce, P. F., Vinokur, A. D., & Buck, C. L. (1998). Effects of war-induced maternal separation on children’s adjustment during the Gulf War and two years later. Journal of Applied Social Psychology, 28(14), 1286–1311. doi:10.1111/j.1559-1816.1998.tb01677.x
Pribesh, S., & Downey, D. B. (1999). Why are residential and school moves associated with poor school performance? Demography, 36, 521–534.
Rentz, E. D., Marshall, S. W., Loomis, D., Casteel, C., Martin, S. L., & Gibbs, D. A. (2007). Effect of deployment on the occurrence of child maltreatment in military and nonmilitary families. American Journal of Epidemiology, 165, 1199–1206. doi:10.1093/aje/kwm008
Rosen, L. N., Teitelbaum, J. M., & Westhuis, D. J. (1993). Children’s reactions to the Desert Storm deployment: Initial findings from a survey of Army families. Military Medicine, 158, 465–469.
Rossen, E., & Carter, C. D. (2011, February). Supporting students from military families. Principal Leadership, 11(6), 14–18.
Rush, C. M., & Akos, P. (2007). Supporting children and adolescents with deployed caregivers: A structured group approach for school counselors. The Journal for Specialists in Group Work, 32(2), 113–125. doi:10.1080/01933920701227034
Sherman, M. D., & Glenn, M. A. (2011, January/February). Opportunities for school psychologists working with children of military families. Communiqué: The Newspaper of the National Association of School Psychologists, 39(5), 17–19.
Simpson, G. A., & Fowler, M. G. (1994). Geographic mobility and children’s emotional/behavioral adjustment and school functioning. Pediatrics, 93, 303–309.
Strobino, J., & Salvaterra, M. (2000). School transitions among adolescent children of military personnel: A strengths perspective. Social Work in Education, 22, 95–107.
Tutor.com. (2014). Tutor.com for U.S. military families. Retrieved from http://www.tutor.com/military
Waliski, A., Bokony, P., Edlund, C. N., & Kirchner, J. (2012). Counselors called for service: Impact of parental deployment on preschool children. The Family Journal: Counseling and Therapy for Couples and Families, 20(2), 157–163. doi:10.1177/1066480712438531
Weber, E. G., & Weber, D. K. (2005). Geographic relocation frequency, resilience, and military adolescent behavior. Military Medicine, 170, 638–642.
Wood, D., Halfon, N., Scarlata, D., Newacheck, P., & Nessim, S. (1993). Impact of family relocation on children’s growth, development, school function, and behavior. Journal of the American Medical Association, 270, 1334–1338. doi:10.1001/jama.1993.03510110074035
S. Beth Ruff is a school counselor at Bright Star Elementary School in Douglasville, GA, and a doctoral student at the University of West Georgia. Michael A. Keim, NCC, is an Assistant Professor of Professional Counseling at the University of West Georgia. Correspondence can be addressed to S. Beth Ruff, Bright Star Elementary School, 6300 John West Road, Douglasville, GA 30134, Beth.ruff@douglas.k12.ga.us.
Apr 5, 2014 | Article, Volume 4 - Issue 1
Melodie H. Frick, Harriet L. Glosoff
Counselor education doctoral students are influenced by many factors as they train to become supervisors. One of these factors, self-efficacy beliefs, plays an important role in supervisor development. In this phenomenological, qualitative research, 16 counselor education doctoral students participated in focus groups and discussed their experiences and perceptions of self-efficacy as supervisors. Data analyses revealed four themes associated with self-efficacy beliefs: ambivalence in the middle tier of supervision, influential people, receiving performance feedback, and conducting evaluations. Recommendations for counselor education and supervision, as well as future research, are provided.
Keywords: supervision, doctoral students, counselor education, self-efficacy, phenomenological, focus groups
Counselor education programs accredited by the Council for Accreditation and Related Educational Programs (CACREP) require doctoral students to learn supervision theories and practices (CACREP, 2009). Professional literature highlights information on supervision theories (e.g., Bernard & Goodyear, 2009), supervising counselors-in-training (e.g., Woodside, Oberman, Cole, & Carruth, 2007), and effective supervision interventions and styles (e.g., Fernando & Hulse-Killacky, 2005) that assist with supervisor training and development. Until recently, however, few researchers have studied the experiences of counselor education doctoral students as they prepare to become supervisors (Hughes & Kleist, 2005; Limberg et al., 2013; Protivnak & Foss, 2011) or “the transition from supervisee to supervisor” (Rapisarda, Desmond, & Nelson, 2011, p. 121). Specifically, an exploration of factors associated with the self-efficacy beliefs of counselor education doctoral student supervisors is warranted to expand this topic and enhance counselor education training of supervisor development.
Bernard and Goodyear (2009) described supervisor development as a process shaped by changes in self-perceptions and roles, much like counselors-in-training experience in their developmental stages. Researchers have examined factors that may influence supervisors’ development (e.g., experiential learning and the influence of feedback). For example, Nelson, Oliver, and Capps (2006) explored the training experiences of 21 doctoral students in two cohorts of the same counseling program and reported that experiential learning, the use of role-plays, and receiving feedback from both professors and peers were equally as helpful in learning supervision skills as the actual practice of supervising counselors-in-training. Conversely, a supervisor’s development may be negatively influenced by unclear expectations of the supervision process or dual relationships with supervisees, which may lead to role ambiguity (Bernard & Goodyear, 2009). For example, Nilsson and Duan (2007) examined the relationship between role ambiguity and self-efficacy with 69 psychology doctoral student supervisors and found that when participants received clear supervision expectations, they reported higher rates of self-efficacy.
Self-efficacy is one of the self-regulation functions in Bandura’s social cognitive theory (Bandura, 1986) and is a factor in Larson’s (1998) social cognitive model of counselor training (SCMCT). Self-efficacy, the differentiated beliefs held by individuals about their capabilities to perform (Bandura, 2006), plays an important role in counselor and supervisor development (Barnes, 2004; Cashwell & Dooley, 2001) and is influenced by many factors (Schunk, 2004). Along with the counselor’s training environment, self-efficacy beliefs may influence a counselor’s learning process and resulting counseling performance (Larson, 1998). Daniels and Larson (2001) conducted a quantitative study with 45 counseling graduate students and found that performance feedback influenced counselors’ self-efficacy beliefs; self-efficacy increased with positive feedback and decreased with negative feedback. Steward (1998), however, identified missing components in the SCMCT, such as the role and level of self-efficacy of the supervisor, the possible influence of a faculty supervisor, and doctoral students giving and receiving feedback to supervisees and members of their cohort. For example, results of both quantitative studies (e.g., Hollingsworth & Fassinger, 2002) and qualitative studies (e.g., Majcher & Daniluk, 2009; Nelson et al., 2006) indicate the importance of mentoring experiences and relationships with faculty supervisors to the development of doctoral students and self-efficacy in their supervisory skills.
During their supervision training, doctoral students are in a unique position of supervising counselors-in-training while also being supervised by faculty. For the purpose of this study, the term middle tier will be used to describe this position. This term is not often used in the counseling literature, but may be compared to the position of middle managers in the business field—people who are subordinate to upper managers while having the responsibility of managing subordinates (Agnes, 2003). Similar to middle managers, doctoral student supervisors tend to have increased responsibility for supervising future counselors, albeit with limited authority in supervisory decisions, and may have experiences similar to middle managers in other disciplines. For example, performance-related feedback as perceived by middle managers appears to influence their role satisfaction and self-efficacy (Reynolds, 2006). In Reynolds’s (2006) study, 353 participants who represented four levels of management in a company in the United States reported that receiving positive feedback from supervisors had an affirming or encouraging effect on their self-efficacy, and that their self-efficacy was reduced after they received negative supervisory feedback. Translated to the field of counselor supervision, these findings suggest that doctoral students who participate in tiered supervision and receive positive performance feedback may have higher self-efficacy.
Findings to date illuminate factors that influence self-efficacy beliefs, such as performance feedback, clear supervisor expectations and mentoring relations. There is a need, however, to examine what other factors enhance or detract from the self-efficacy beliefs of counselor education doctoral student supervisors to ensure effective supervisor development and training. The purpose of this study, therefore, was to build on previous research and further examine the experiences of doctoral students as they train to become supervisors in a tiered supervision model. The overarching research questions that guided this study included: (a) What are the experiences of counselor education doctoral students who work within a tiered supervision training model as they train to become supervisors? and (b) What experiences influenced their sense of self-efficacy as supervisors?
Method
Design
A phenomenological research approach was selected to explore how counselor education doctoral students experience and make meaning of their reality (Merriam, 2009), and to provide richer descriptions of the experiences of doctoral student supervisors-in-training, which a quantitative study may not afford. A qualitative design using a constructivist-interpretivist method provided the opportunity to interact with doctoral students via focus groups and follow-up questionnaires to explore their self-constructed realities as counselor supervisors-in-training, and the meaning they placed on their experiences as they supervised master’s-level students while being supervised by faculty supervisors. Focus groups were chosen as part of the design, as they are often used in qualitative research (Kress & Shoffner, 2007; Limberg et al., 2013), and multiple-case sampling increases confidence and robustness in findings (Miles & Huberman, 1994).
Participants
Sixteen doctoral students from three CACREP-accredited counselor education programs in the southeastern United States volunteered to participate in this study. These programs were selected due to similarity in supervision training among participants (e.g., all were CACREP-accredited, required students to take at least one supervision course, utilized a full-time cohort design), and were in close proximity to the principal investigator. None of the participants attended the first author’s university or had any relationships with the authors. Criterion sampling was used to select participants that met the criteria of providing supervision to master’s-level counselors-in-training and receiving supervision by faculty supervisors at the time of their participation. The ages of the participants ranged from 27–61 years with a mean age of 36 years (SD = 1.56). Fourteen of the participants were women and two were men; two participants described their race as African-American (12.5%), one participant as Asian-American (6.25%), 12 participants as Caucasian (75%), and one participant as “more than one ethnicity” (6.25%). Seven of the 16 participants reported having 4 months to 12 years of work experience as counselor supervisors (M = 2.5 years, SD = 3.9 years) before beginning their doctoral studies. At the time of this study, all participants had completed a supervision course as part of their doctoral program, were supervising two to six master’s students in the same program (M = 4, SD = 1.2), and received weekly supervision with faculty supervisors in their respective programs.
Researcher Positionality
In presenting results of phenomenological research, it is critical to discuss the authors’ characteristics as researchers, as such characteristics influence data collection and analysis. The authors have experience as counselors, counselor educators, and clinical supervisors. Both authors share an interest in understanding how doctoral students move from the role of student to the role of supervisor, especially when providing supervision to master’s students who may experience critical incidents (with their clients or in their own development). The first author became engaged when she saw the different emotional reactions of her cohort when faced with the gatekeeping process, whether the reactions were based on personality, prior supervision experience, or stressors from inside and outside of the counselor education program. She wondered how doctoral students in other programs experienced the aforementioned situations, what kind of structure other programs used to work with critical incidents that involve remediation plans, and if there were ways to improve supervision training. It was critical to account for personal and professional biases throughout the research process to minimize biases in the collection or interpretation of data. Bracketing, therefore, was an important step during analysis (Moustakas, 1994) to reduce researcher biases. The first author accomplished this by meeting with her dissertation committee and with the second author throughout the study, as well as using peer reviewers to assess researcher bias in the design of the study, research questions, and theme development.
Quality and Trustworthiness
To strengthen the rigor of this study, the authors addressed credibility, dependability, transferability and confirmability (Merriam, 2009). One way to reinforce credibility is to have prolonged and persistent contact with participants (Hunt, 2011). The first author contacted participants before each focus group to convey the nature, scope and reasons for the study. She facilitated 90-minute focus group discussions and allowed participants to add or change the summary provided at the end of each focus group. Further, information was gathered from each participant through a follow-up questionnaire and afforded the opportunity for participants to contact her through e-mail with additional questions or thoughts.
By keeping an ongoing reflexive journal and analytical memos, the first author addressed dependability by keeping a detailed account throughout the research study, indicating how data were collected and analyzed and how decisions were made (Merriam, 2009). The first author included information on how data were reduced and themes and displays were constructed, and the second author conducted an audit trail on items such as transcripts, analytic memos, reflection notes, and process notes connecting findings to existing literature.
Through the use of rich, thick description of the information provided by participants, the authors made efforts to increase transferability. In addition, they offered a clear account of each stage of the process as well as the demographics of the participants (Hunt, 2011) to promote transferability.
Finally, the first author strengthened confirmability by examining her role as a research instrument. Selected colleagues chosen as peer reviewers (Kline, 2008), along with the first author’s dissertation committee members, had access to the audit trail and discussed and questioned the authors’ decisions, further increasing the integrity of the design. Two doctoral students who had provided supervision and had completed courses in qualitative research, but who had no connection to the research study, volunteered to serve as peer reviewers. They reviewed the focus group protocol for researcher bias, read the focus group transcripts (with pseudonyms inserted) and questionnaires, and the emergent themes, to confirm or contest the interpretation of the data. Further, they reviewed the quotes chosen to support themes for richness of description and provided feedback regarding the textural-structural descriptions as they were being developed. Their recommendations, such as not having emotional reactions to participants’ comments, guided the authors in data collection and analysis.
Data Collection
Upon receiving approval from the university’s Institutional Review Board, the first author contacted the directors of three CACREP-accredited counselor education programs and discussed the purpose of the study, participants’ rights, and logistical needs. Program directors disseminated an e-mail about this study to their doctoral students, instructing volunteer participants to contact the first author about participating in the focus groups.
Within a two-week period, she conducted three focus groups—one at each counselor education program site. Each focus group included five to six participants and lasted approximately 90 minutes. She employed a semi-structured interview protocol consisting of 17 questions (see Appendix). The questions were based on an extensive literature review on counselor and supervisor self-efficacy studies (e.g., Bandura, 2006; Cashwell & Dooley, 2001; Corrigan & Schmidt, 1983; Fernando & Hulse-Killacky, 2005; Gore, 2006; Israelashvili & Socher, 2007; Steward, 1998; Tang et al., 2004). The initial questions were open and general at first, so as to not lead or bias the participants in their responses. As the focus groups continued, the first author explored more specific information about participants’ experiences as doctoral student supervisors, focusing questions around their responses (Kline, 2008). Conducting a semi-structured interview with participants ensured that she asked specific questions and addressed predetermined topics related to the focus of the study, while also allowing for freedom to follow up on relevant information provided by participants during the focus groups.
Approximately six to eight weeks after each focus group, participants received a follow-up questionnaire consisting of four questions: (a) What factors (inside and outside of the program) influence your perceptions of your abilities as a supervisor? (b) How do you feel about working in the middle tier of supervision (i.e., working between a faculty supervisor and the counselors-in-training that you supervise)? (c) What, if anything, could help you feel more competent as a supervisor? (d) How can your supervision training be improved? The purpose of the follow-up questions was to explore participants’ responses after they gained more experiences as supervisors and to provide a means for them to respond to questions about their supervisory experiences privately, without concern of peer judgment.
Data Analysis
Data analysis began during the transcription process, with analysis occurring simultaneously with the collection of the data. The first author transcribed, verbatim, the recording of each focus group and changed participant names to protect their anonymity. Data analysis was then conducted in three stages: first, data were analyzed to identify significant issues within each focus group; second, data were cross-analyzed to identify common themes across all three focus groups; and third, follow-up questionnaires were analyzed to corroborate established themes and to identify additional, or different themes.
During data analysis, a Miles and Huberman (1994) approach was employed by using initial codes from focus-group question themes. Inductive analysis occurred with immersion in the data by reading and rereading focus group transcripts. It was during this immersion process that the first author began to identify core ideas and differentiate meanings and emergent themes for each focus group. She accomplished data reduction by identifying themes in participants’ answers to the interview protocol and focus group discussions until saturation was reached, and displayed narrative data in a figure to organize and compare developed themes. Finally, she used deductive verification of findings with previous research literature. During within-group analysis, she identified themes if more than half (i.e., more than three participants) of a focus group reported similar experiences, feelings or beliefs. Likewise, in across-group analyses, she confirmed themes if statements made by more than half (more than eight) of the participants matched. There were three cases in which the peer reviewers and the first author had differences of opinion on theme development. In those cases, she made changes guided by the suggestions of the peer reviewers. In addition, she sent the final list of themes related to the research questions to the second author and other members of the dissertation committee for purposes of confirmability.
Results
Results of this phenomenological study revealed several themes associated with doctoral students’ perceptions of self-efficacy as supervisors (see Figure 1). Cross-group analyses are provided with participant quotes that are most relevant to each theme being discussed. Considerable overlap of four themes emerged across groups: ambivalence in the middle tier of supervision, influential people, receiving feedback, and conducting evaluations.
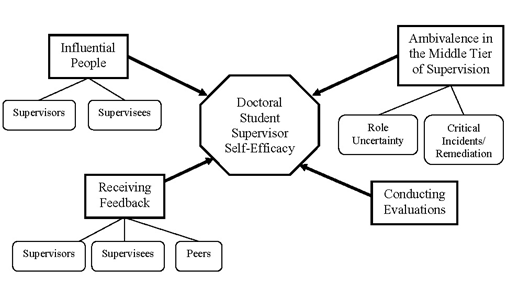
Figure 1. Emergent themes of doctoral student supervisors’ self-efficacy beliefs. Factors identified by doctoral student as affecting their self-efficacy as supervisors are represented with directional, bold-case arrows from each theme toward supervisor self-efficacy; below themes are sub-themes in each group connected with non-directional lines.
Ambivalence in the Middle Tier of Supervision
All participants noted how working in the middle tier of supervision brought up issues about their roles and perceptions about their capabilities as supervisors. All 16 participants reported feeling ambivalent about working in the middle tier, especially in relation to their role as supervisors and about dealing with critical incidents with supervisees involving the need for remediation. What follows is a presentation of representative quotations from one or two participants in the emergent sub-themes of role uncertainty and critical incidents/remediation.
Role Uncertainty. Participants raised the issue of role uncertainty in all three focus groups. For example, one participant described how it felt to be in the middle tier by stating the following:
I think that’s exactly how it feels [to be in the middle] sometimes….not really knowing how much you know, what does my voice really mean? How much of a say do we have if we have big concerns? And is what I recognize really a big concern? So I think kind of knowing that we have this piece of responsibility but then not really knowing how much authority or how much say-so we have in things, or even do I have the knowledge and experience to have much say-so?
Further, another participant expressed uncertainty regarding her middle-tier supervisory role as follows:
[I feel a] lack of power, not having real and true authority over what is happening or if something does happen, being able to make those concrete decisions…Where do I really fit in here? What am I really able to do with this supervisee?…kind of a little middle child, you know really not knowing where your identity really and truly is. You’re trying to figure out who you really are.
Participants also indicated difficulty discerning their role when supervising counselors-in-training who were from different specialty areas such as college counseling, mental health counseling, and school counseling. All participants stated that they had not had any specific counseling or supervision training in different tracks, which was bothersome for nine participants who supervised students in specialties other than their own. For example, one participant stated the following:
I’m a mental health counselor and worked in the community and I have two school counselor interns, and so it was one of my very first questions was like, what do I do with these people? ’Cause I’m not aware of the differences and what I should be guiding them on anything.
Another participant noted how having more information on the different counseling tracks (e.g., mental health, school, college) would be helpful:
We’re going to be counselor educators. We may find ourselves having to supervise people in various tracks and I could see how it would be helpful for us to all have a little bit more information on a variety of tracks so that we could know what to offer, or how things are a little bit different.
Working in the middle tier of supervision appeared to be vexing for focus group participants. They expressed feelings of uncertainty, especially in dealing with critical incidents or remediation of supervisees. In addition to defining their roles as supervisors in the middle tier, another sub-theme emerged in which participants identified how they wanted to have a better understanding of how remediation plans work and have the opportunity to collaborate with faculty supervisors in addressing critical incidents with supervisees.
Critical Incidents/Remediation. Part of the focus group discussion centered on what critical incidents participants had with their supervisees and how comfortable they were, or would be, in implementing remediation plans with their supervisees. All participants expressed concerns about their roles as supervisors when remediation plans were required for master’s students in their respective programs and were uncertain of how the remediation process worked in their programs. Thirteen of the 16 participants expressed a desire to be a part of the remediation process of their supervisees in collaboration with faculty supervisors. They discussed seeing this as an important way to learn from the process, assuming that as future supervisors and counselor educators they will need to be the ones to implement such remediation plans. For example, one participant explained the following:
If we are in the position to provide supervision and we’re doing this to enhance our professional development so in the hopes that one day we’re going to be in the position of counselor educators, let’s say faculty supervisors, my concern with that is how are we going to know what to do unless we are involved [in the remediation process] now? And so I feel like that should be something that we’re provided that opportunity to do it.
Another participant indicated that she felt not being part of the remediation process took away the doctoral student supervisors’ credibility:
I don’t have my license yet, and I’m not sure how that plays into when there is an issue with a supervisee, but I know when there is an issue, there is something we have to do if you have a supervisee who is not performing as well, then that’s kind of taken out of your hands and given to a faculty. So they’re like, ‘Yeah you are capable of providing supervision,’ but when there’s an issue it seems like you’re no longer capable.
Another participant noted wanting “to see us do more of the cases where we need to do remediation” in order to be better prepared in identifying critical incidents, thus feeling more capable in the role as supervisor. Discussion on the middle tier proved to be a topic participants both related to and had concerns about. In addition to talking about critical incidents and the remediation process, another emergent theme included people within the participants’ training programs who were influential to their self-efficacy beliefs as supervisors.
Influential People
When asked about influences they had from inside and outside of their training programs, all participants identified people and things (e.g., previous work experience, support of significant others, conferences, spiritual meditation, supervision literature) as factors that affected their perceived abilities as supervisors. The specific factors most often identified by more than half of the participants, however, were the influence of supervisors and supervisees in their training programs.
Supervisors. All participants indicated that interactions with current and previous supervisors influenced their self-efficacy as supervisors. Ten participants reported supervisors modeling their supervision style and techniques as influential. For example, in regard to watching supervision tapes of the faculty supervisors, one participant stated that it has “been helpful for me to see the stance that they [faculty supervisors] take and the model that they use” when developing her own supervision skills. Seven participants also indicated having the space to grow as supervisors as a positive influence on their self-efficacy. One participant explained as follows:
I know people at other universities and it’s like boot camp, they [faculty supervisors] break them down and build them up in their own image like they’re gods. And I don’t feel that here. I feel like I’m able to be who I am and they’re supportive and helping me develop who I am.
In addition to the information provided during the focus groups, 11 focus group participants reiterated on their follow-up questionnaires that faculty supervisors had a positive influence on the development of their self-efficacy. For example, for one participant, “a lot of support from faculty supervisors in terms of their accessibility and willingness to answer questions” was a factor in strengthening her perception of her abilities as a counselor supervisor. Participants also noted the importance of working with their supervisees as beneficial and influential to their perceptions of self-efficacy as supervisors.
Supervisees. All participants in the focus groups discussed supervising counselors-in-training as having both direct and vicarious influences on their self-efficacy. One participant stated that having the direct experience of supervising counselors-in-training at different levels of training (e.g., pre-practicum, practicum, internship) was something that “really helped me to develop my ability as a supervisor.” In addition, one participant described a supervision session that influenced him as a supervisor: “When there are those ‘aha’ moments that either you both experience or they experience. That usually feels pretty good. So that’s when I feel the most competent, I think as a supervisor.” Further, another participant described a time when she felt competent as a supervisor: “When [the supervisees] reflect that they have taken what we’ve talked about and actually tried to implement it or it’s influenced their work, that’s when I have felt closest to competence.” In addition to working relations with supervisors and supervisees, receiving feedback was noted as an emergent theme and influential to the growth of the doctoral student supervisors.
Receiving Feedback
Of all of the emergent themes, performance feedback appeared to have the most overlap across focus groups. The authors asked participants how they felt about receiving feedback on their supervisory skills. Sub-themes emerged when participants identified receiving feedback from their supervisors, supervisees and peers as shaping to their self-efficacy beliefs as supervisors.
Supervisors. Fifteen participants discussed the process of receiving performance feedback from faculty as an important factor in their self-efficacy. Overall, participants reported receiving constructive feedback as critical to their learning, albeit with mixed reactions. One participant noted that “at the time it feels kind of crappy, but you learn something from it and you’re a better supervisor.” Some participants indicated how they valued their supervisors’ feedback and they preferred specific feedback over vague feedback. For example, as one participant explained, “I kind of just hang on her every word….it is important. I anticipate and look forward to that and am even somewhat disappointed if she kind of dances around an issue.” Constructive feedback was most preferred across all participants. In addition to the impact of receiving feedback from supervisors, participants commented on being influenced by the feedback they received from their supervisees.
Supervisees. Thirteen focus group participants reported that receiving performance evaluations from supervisees affected their sense of self-efficacy as supervisors and appeared to be beneficial to all participants. Participants indicated that they were more influenced by specific rather than general feedback, and they preferred receiving written feedback from their supervisees rather than having supervisees subjectively rate their performance with a number. One participant commented that “it’s more helpful for me when [supervisees] include written feedback versus just doing the number [rating]…something that’s more constructive.” Further, a participant described how receiving constructive feedback from supervisees influenced his self-efficacy as a supervisor:
I’d say it affects me a little bit. I’m thinking of some evaluations that I have received and some of them make me feel like I have that self-efficacy that I can do this. And then the other side, there have been some constructive comments as well, and some of those I think do influence me and help me develop.
Similar to feedback received from supervisors and supervisees, participants reiterated their preference in receiving clear and constructive feedback. Focus group participants also described receiving feedback from their peers as being influential in the development of their supervision skills.
Peers. Eleven participants shared that feedback received from peers was influential in shaping the perception of their skills and how they conducted supervision sessions. Participants described viewing videotapes of supervision sessions in group supervision and receiving feedback from peers on their taped supervision sessions as positive influences. For example, one participant stated that “there was one point in one of our classes when I’d shown a tape and I got some very… specific positive feedback [from peers] that made me feel really good, like made me feel more competent.” Another participant noted how much peers had helped her increase her comfort level in evaluating her supervisees: “I had a huge problem with evaluation when we started out….in supervision, my group really worked on that issue with me and I feel like I’m in a much better place.”
Performance feedback from faculty supervisors, supervisees, and peers was a common theme in all three focus groups and instrumental in the development of supervisory style and self-efficacy as supervisors. Constructive and specific feedback appeared to more positively influence participants’ self-efficacy than vague or unclear subjective rating scales. In addition to receiving performance feedback, another theme emerged when participants identified issues with providing supervisees’ performance evaluations.
Conducting Evaluations
Participants viewed evaluating supervisees with mixed emotions and believed that this process affected their self-efficacy beliefs as supervisors. Thirteen participants reported having difficulty providing supervisees with evaluative feedback. For example, one participant stated the following:
I had a huge problem with evaluation when we started out. It’s something I don’t like. I feel like I’m judging someone….And after, I guess, my fifth semester….I don’t feel like I’m judging them so much as it is a necessity of what we have to do, and as a gatekeeper we have to do this. And I see it more as a way of helping them grow now.
Conversely, one participant, who had experience as a supervisor before starting the doctoral counselor education program stated, “I didn’t really have too much discomfort with evaluating supervisees because of the fact that I was a previous supervisor before I got into this program.” Other participants, who either had previous experience with supervisory positions or who had been in the program for a longer period of time, confirmed this sentiment—that with more experience the anxiety-provoking feelings subsided.
All focus group participants, however, reported a lack of adequate instruction on how to conduct evaluations of supervisee performance. For example, participants indicated a lack of training on evaluating supervisees’ tapes of counseling sessions and in providing formal summative evaluations. One participant addressed how receiving more specific training in evaluating supervisees would have helped her feel more competent as a supervisor:
I felt like I had different experiences with different supervisors of how supervision was given, but I still felt like I didn’t know how to give the feedback or what all my options were, it would have just helped my confidence… to get that sort of encouragement that I’m on the right track or, so maybe more modeling specifically of how to do an evaluation and how to do a tape review.
All focus group participants raised the issue of using Likert-type questions as part of the evaluation process, specifically the subjectivity of interpretation of the scales in relation to supervisee performance and how supervisors used them differently. For example, a participant stated, “I wish there had been a little bit more concrete training in how to do an evaluation.” A second participant expanded this notion:
I would say about that scale it’s not only subjective but then our students, I think, talk to each other and then we’ve all evaluated them sometimes using the same form and given them a different number ’cause we interpret it differently…. It seems like another thing that sets us up for this weird ‘in the middle’ relationship because we’re not faculty.
Discussions about providing performance evaluations seemed to be one of the most vibrant parts of focus group discussions. Thus, it appears that having the support of influential people (e.g., supervisors and supervisees) and feedback from supervisors, supervisees and peers was helpful. Having more instruction on conducting evaluations and clarifying their role identity and expectations, however, would increase their sense of self as supervisors in the middle tier of supervision.
Discussion
The purpose of this study was to explore what counselor education doctoral students experienced working in the middle tier of supervision and how their experiences related to their sense of self-efficacy as beginning supervisors. Data analysis revealed alignment with previous research that self-efficacy of an individual or group is influenced by extrinsic and intrinsic factors, direct and vicarious experiences, incentives, performance achievements, and verbal persuasion (Bandura, 1986), and that a person’s self-efficacy may increase from four experiential sources: mastery, modeling, social persuasion, and affective arousal (Larson, 1998). For example, participants identified factors that influence their self-efficacy as supervisors such as the direct experience of supervising counselors-in-training (mastery) as “shaping,” and how they learned vicariously from others in supervision classes. Participants also noted the positive influence of observing faculty supervision sessions (modeling) and receiving constructive feedback by supervisors, supervisees, and peers (verbal persuasion). In addition, participants described competent moments with their supervisees as empowering performance achievements, especially when they observed growth of their supervisees resulting from exchanges in their supervision sessions. Further, participants indicated social persuasion via support from their peers and future careers as counselor supervisors and counselor educators were incentives that influenced their learning experiences. Finally, participants discussed how feelings of anxiety and self-doubt (affective arousal) when giving performance evaluations to supervisees influenced their self-efficacy as supervisors.
Results from this study also support previous research on receiving constructive feedback, structural support, role ambiguity, and clear supervision goals from supervisors as influential factors on self-efficacy beliefs (Bernard & Goodyear, 2009; Nilsson & Duan, 2007; Reynolds, 2006). In addition, participants’ difficulty in conducting evaluations due to feeling judgmental and having a lack of clear instructions on evaluation methods are congruent with supervision literature (e.g., Corey, Haynes, Moulton, & Muratori, 2010; Falender & Shafranske, 2004). Finally, participants’ responses bolster previous research findings that receiving support from mentoring relationships and having trusting relationships with peers positively influence self-efficacy (Hollingsworth & Fassinger, 2002; Wong-Wylie, 2007).
Implications for Practice
The comments from participants across the three focus groups underscore the importance of receiving constructive and specific feedback from their faculty supervisors. Providing specific feedback requires that faculty supervisors employ methods of direct observation of the doctoral student’s work with supervisees (e.g., live observation, recorded sessions) rather than relying solely on self-report. Participants also wanted more information on how to effectively and consistently evaluate supervisee performance, especially those involving Likert-type questions, and how to effectively supervise master’s students who are studying in different areas of concentration (e.g., mental health, school counseling, and college counseling). Counselor educators could include modules addressing these topics before or during the time that doctoral supervisors work with master’s students, providing both information and opportunities to practice or role-play specific scenarios.
In response to questions about dealing with critical incidents in supervision, participants across groups discussed the importance of being prepared in handling remediation issues and wanting specific examples of remediation cases as well as clarity regarding their role in remediation processes. Previous research findings indicate teaching about critical incidents prior to engaging in job requirements as effective (Collins & Pieterse, 2007; Halpern, Gurevich, Schwartz, & Brazeau, 2009). As such, faculty supervisors may consider providing opportunities to role-play and share tapes of supervision sessions with master’s students in which faculty (or other doctoral students) effectively address critical incidents. In addition, faculty could share strategies with doctoral student supervisors on the design and implementation of remediation plans, responsibilities of faculty and school administrators, the extent to which doctoral student supervisors may be involved in the remediation process (e.g., no involvement, co-supervise with faculty, or full responsibility), and the ethical and legal factors that may impact the supervisors’ involvement. Participants viewed being included in the development and implementation of remediation plans for master’s supervisees as important for their development even though some participants experienced initial discomfort in evaluating supervisees. This further indicates the importance of fostering supportive working relationships that promote students’ growth and satisfaction in supervision training.
Limitations
Findings from this study are beneficial to counselor doctoral students, counselor supervisors, and supervisors in various fields. Limitations, however, exist in this study. The first is researcher perspective. The authors’ collective experiences influenced the inclusion of questions related to critical incidents and working in the middle tier of supervision. However, the first author made efforts to discern researcher bias by first examining her role as a research instrument before and throughout conducting this study, by triangulating sources, and by processing the interview protocol and analysis with peer reviewers and dissertation committee members. A second limitation is participant bias. Participants’ responses were based on their perceptions of events and recall. Situations participants experienced could have been colored or exaggerated and participants may have chosen safe responses in order to save face in front of their peers or in fear that faculty would be privy to their responses—an occurrence that may happen when using focus groups. The first author addressed this limitation by using follow-up questionnaires to provide participants an opportunity to express their views without their peers’ knowledge, and she reinforced confidentiality at the beginning of each focus group.
Recommendations for Future Research
Findings from this study suggest possible directions for future research. The first recommendation is to expand to a more diverse sample. The participants in this study were predominantly White (75%) and female (87.5%) from one region in the United States. As with all qualitative research, the findings from this study are not meant to be generalized to a wider group, and increasing the number of focus groups may offer a greater understanding as to the applicability of the current findings to doctoral student supervisors not represented in the current study. A second recommendation is to conduct a longitudinal study by following one or more cohorts of doctoral student supervisors throughout their supervision training to identify stages of growth and transition as supervisors, focusing on those factors that influence participants’ self-efficacy and supervisor development.
Conclusion
The purpose of this phenomenological study was to expand previous research on counselor supervision and to provide a view of doctoral student supervisors’ experiences as they train in a tiered supervision model. Findings revealed factors that may be associated with self-efficacy beliefs of doctoral students as they prepare to become counseling supervisors. Recommendations may assist faculty supervisors when considering training protocols and doctoral students as they develop their identities as supervisors.
References
Agnes, M. (Ed.). (2003). Webster’s new world dictionary (4th ed.). New York, NY: Wiley.
Bandura, A. (1986). Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice Hall.
Bandura, A. (2006). Guide for creating self-efficacy scales. In F. Pajares & T. C. Urdan (Eds.), Self-efficacy beliefs of adolescents (pp. 307–337). Greenwich, CT: Information Age.
Barnes, K. L. (2004). Applying self-efficacy theory to counselor training and supervision: A comparison of two approaches. Counselor Education and Supervision, 44, 56–69. doi:10.1002/j.1556-6978.2004.tb01860.x
Bernard, J. M., & Goodyear, R. K. (2009). Fundamentals of clinical supervision (4th ed.). Upper Saddle River, NJ: Merrill/Pearson.
Cashwell, T. H., & Dooley, K. (2001). The impact of supervision on counselor self-efficacy. The Clinical Supervisor, 20(1), 39–47. doi:10.1300/J001v20n01_03
Collins, N. M., & Pieterse, A. L. (2007). Critical incident analysis based training: An approach for developing active racial/cultural awareness. Journal of Counseling & Development, 85, 14–23. doi:10.1002/j.1556-6678.2007.tb00439.x
Corey, G., Haynes, R., Moulton, P., & Muratori, M. (2010). Clinical supervision in the helping professions: A practical guide (2nd ed.). Alexandria, VA: American Counseling Association.
Corrigan, J. D., & Schmidt, L. D. (1983). Development and validation of revisions in the
counselor rating form. Journal of Counseling Psychology, 30, 64–75. doi:10.1037/0022-0167.30.1.64
Council for Accreditation of Counseling and Related Educational Programs. (2009). 2009 CACREP accreditation manual. Alexandria, VA: Author.
Daniels, J. A., & Larson, L. M. (2001). The impact of performance feedback on counseling self-efficacy and counseling anxiety. Counselor Education and Supervision, 41, 120–130. doi:10.1002/j.1556-6978.2001.tb01276.x
Falender, C. A., & Shafranske, E. P. (2004). Clinical supervision: A competency-based approach. Washington, DC: American Psychological Association.
Fernando, D. M., & Hulse-Killacky, D. (2005). The relationship of supervisory styles to satisfaction with supervision and the perceived self-efficacy of master’s-level counseling students. Counselor Education and Supervision, 44, 293–304. doi:10.1002/j.1556-6978.2005.tb01757.x
Gore, P. A., Jr. (2006). Academic self-efficacy as a predictor of college outcomes: Two incremental validity studies. Journal of Career Assessment, 14(1), 92–115. doi:10.1177/ 1069072705281367
Halpern, J., Gurevich, M., Schwartz, B., & Brazeau, P. (2009). What makes an incident critical for ambulance workers? Emotional outcomes and implications for intervention. Work & Stress, 23(2), 173–189. doi:10.1080/02678370903057317
Hollingsworth, M. A., & Fassinger, R. E. (2002). The role of faculty mentors in the research
training of counseling psychology doctoral students. Journal of Counseling Psychology, 49, 324–330. doi:10.1037/0022-0167.49.3.324
Hughes, F. R., & Kleist, D. M. (2005). First-semester experiences of counselor education
doctoral students. Counselor Education and Supervision, 45, 97–108. doi:10.1002/ j.1556-6978.2005.tb00133.x
Hunt, B. (2011). Publishing qualitative research in counseling journals. Journal of Counseling & Development, 89, 296–300. doi:10.1002/j.1556-6678.2011.tb00092.x
Israelashvili, M., & Socher, P. (2007). An examination of a counselor self-efficacy scale (COSE) using an Israeli sample. International Journal for the Advancement of Counselling, 29, 1–9. doi:10.1007/s10447-006-9019-0
Kline, W. B. (2008). Developing and submitting credible qualitative manuscripts. Counselor Education and Supervision, 47, 210–217. doi:10.1002/j.1556 6978.2008.tb00052.x
Kress, V. E., & Shoffner, M. F. (2007). Focus groups: A practical and applied research approach for counselors. Journal of Counseling & Development, 85(2), 189–195. doi:10.1002/j.1556-6678.2007.tb00462.x
Larson, L. M. (1998). The social cognitive model of counselor training. The Counseling Psychologist, 26(2), 219–273. doi:10.1177/0011000098262002
Limberg, D., Bell, H., Super, J. T., Jacobson, L., Fox, J., DePue, M. K, . . . Lambie, G. W. (2013). Professional identity development of counselor education doctoral students: A qualitative investigation. The Professional Counselor, 3(1), 40–53.
Majcher, J., & Daniluk, J. C. (2009). The process of becoming a supervisor for students in a doctoral supervision training course. Training and Education in Professional Psychology, 3, 63–71. doi:10.1037/a0014470
Merriam, S. B. (Ed.). (2002). Qualitative research in practice: Examples for discussion and analysis. San Francisco, CA: Jossey-Bass.
Miles, M. B., & Huberman, A. M. (1994). Qualitative data analysis: An expanded sourcebook (2nd ed.). Thousand Oaks, CA: Sage.
Moustakas, C. E. (1994). Phenomenological research methods. Thousand Oaks, CA: Sage.
Nilsson, J. E., & Duan, C. (2007). Experiences of prejudice, role difficulties, and counseling self-efficacy among U.S. racial and ethnic minority supervisees working with white supervisors. Journal of Multicultural Counseling and Development, 35(4), 219–229. doi:10.1002/j.2161-1912.2007.tb00062.x
Nelson, K. W., Oliver, M., & Capps, F. (2006). Becoming a supervisor: Doctoral student perceptions of the training experience. Counselor Education and Supervision, 46, 17–31. doi:10.1002/j.1556-6978.2006.tb00009.x
Protivnak, J. J., & Foss, L. L. (2009). An exploration of themes that influence the counselor education doctoral student experience. Counselor Education and Supervision, 48(4), 239–256. doi:10.1002/j.1556-6978.2009.tb00078.x
Rapisarda, C. A., Desmond, K. J., & Nelson, J. R. (2011). Student reflections on the journey to being a supervisor. The Clinical Supervisor, 30, 109–113. doi:10.1080/07325223.2011.564958
Reynolds, D. (2006). To what extent does performance-related feedback affect managers’ self-efficacy? International Journal of Hospitality Management, 25, 54–68. doi:10.1016/j.ijhm.2004.12.007
Schunk, D. H. (2004). Learning theories: An educational perspective (4th ed.). Upper Saddle River, NJ: Pearson/Merrill/Prentice Hall.
Steward, R. J. (1998). Connecting counselor self-efficacy and supervisor self-efficacy: The continued search for counseling competence. The Counseling Psychologist, 26, 285–294. doi:10.1177/0011000098262004
Tang, M., Addison, K. D., LaSure-Bryant, D., Norman, R., O’Connell, W., & Stewart-Sicking, J. A. (2004). Factors that influence self-efficacy of counseling students: An exploratory study. Counselor Education and Supervision, 44, 70–80. doi:10.1002/j.1556-6978.2004.tb01861.x
Wong-Wylie, G. (2007). Barriers and facilitators of reflective practice in counsellor education: Critical incidents from doctoral graduates. Canadian Journal of Counselling, 41(2), 59–76.
Woodside, M., Oberman, A. H., Cole, K. G., & Carruth, E. K. (2007). Learning to be a
counselor: A prepracticum point of view. Counselor Education and Supervision, 47, 14–28. doi:10.1002/j.1556-6978.2007.tb00035.x
Appendix
Focus Group Protocol
-
- How is your program designed to provide supervision training?
- What factors influence your perceptions of your abilities as supervisors?
Prompt: colleagues, professors, equipment, schedules, age, cultural factors such as gender, ethnicity, social class, whether you have had prior or no prior experience as supervisors.
-
- How does it feel to evaluate the supervisees’ performance?
- How, if at all, do your supervisees provide you with feedback about your performance?
- How do you feel about evaluations from your supervisees?
Prompt: How, if at all, do you think or feel supervisees’ evaluations influence how you perceive your skills as a supervisor?
-
- How, if at all, do your supervisors provide you with feedback about your performance?
- How do you feel about evaluations from your faculty supervisor?
Prompt: In what ways, if any, do evaluations from your faculty supervisor influence how you perceive your skills as a supervisor?
-
- What strengths or supports do you have in your program that guide you as a supervisor?
- What barriers or obstacles do you experience as a supervisor?
- What influences do you have from outside of the program that affect how you feel in your role as a supervisor?
- How does it feel to be in the middle tier of supervision: working between a faculty supervisor and master’s-level supervisee?
Prompt: Empowered, stuck in the middle, neutral, powerless.
-
- What, if any, critical incidents have you encountered in supervision?
Prompt: Supervisee that has a client who was suicidal or it becomes clear to you that a supervisee has not developed basic skills needed to work with current clients.
- If a critical incident occurred, or would occur in the future, what procedures did you or would you follow? How comfortable do you feel in having the responsibility of dealing with critical incidents?
- If not already mentioned by participants, ask if they have been faced with a situation in which their supervisee was not performing adequately/up to program expectations. If yes, ask them to describe their role in any remediation plan that was developed. If no, ask what concerns come to mind when they think about the possibility of dealing with such a situation.
- Describe a time when you felt least competent as a supervisor.
- Describe a time when you felt the most competent as a supervisor.
- How could supervision training be improved, especially in terms of anything that could help you feel more competent as a supervisor?
Melodie H. Frick, NCC, is an Assistant Professor at Western Carolina University. Harriett L. Glosoff, NCC, is a Professor at Montclair State University. Correspondence can be addressed to Melodie H. Frick, 91 Killian Building Lane, Room 204, Cullowhee, NC, 28723, mhfrick@email.wcu.edu.
Apr 5, 2014 | Article, Volume 4 - Issue 2
Mary Alice Fernandez, Melissa Short
This article offers mental health counselors a compilation of best practices and technology in the treatment of combat veterans suffering from post-traumatic stress disorder (PTSD). The goal is to increase counselors’ awareness of the resources available to enhance their repertoire of tools and techniques to assess, diagnose, case-conceptualize and treat the growing population of combat veterans with PTSD. The National Center for PTSD provides guidelines for diagnosing PTSD using the DSM-5. PTSD is now recognized as a trauma disorder related to an external event rather than an anxiety disorder associated with mental illness. The authors describe assessment tools and treatment strategies for PTSD validated on veteran populations. The paper also highlights new technology and mobile apps designed to assist in the treatment of combat PTSD.
Keywords: combat PTSD, trauma disorder, treatment of combat veterans, National Center for PTSD, mobile apps
Volunteering to serve one’s country during wartime is an act of heroism, and counselors working with combat veterans are in a unique position to honor these heroes. Combat veterans have offered the supreme sacrifice and some are paying a price by suffering from combat post-traumatic stress disorder (PTSD). The task of providing mental health services to a growing veteran population and their immediate family members is complicated by the lack of accessible services and the complexities of the disorder. To begin to address this challenge, Senator Jon Tester (D-MT) recently introduced legislation focused on improving access to mental health counselors by tasking the Department of Veterans Affairs (VA) with recruiting more licensed professional mental health counselors (Tester, 2013).
This article offers an overview of resources available to mental health counselors to assess, case-conceptualize, diagnose and treat a growing population of combat veterans with PTSD. The goal is to increase the awareness of both beginning counselors and more experienced counselors of new therapies as well as best practices in treating combat PTSD. The compilation of resources begins with diagnostic criteria, assessment tools, and evidence-based practices, including new technologies for treating PTSD, and culminates with a list of resources available to counselors and veterans.
Diagnosing PTSD
Changes in the Diagnostic and Statistical Manual for Mental Disorders, Fifth Edition (DSM-5) place PTSD under a new heading, Trauma and Stressor-Related Disorders, and remove it from the DSM-4 anxiety category. This new DSM-5 categorization de-stigmatizes PTSD because it recognizes PTSD as a trauma disorder related to an external event rather than an anxiety related to mental illness (Staggs, 2014). The DSM-5 provides eight clear criteria for diagnosing PTSD, beginning with identifying a traumatic event (criterion A) and then noting behavioral symptoms related to PTSD. It organizes symptoms into four clusters: intrusions (criterion B), avoidance (criterion C), negative symptoms (criterion D), and arousal (criterion E) (American Psychological Association, 2013). In order for a client to meet the full criteria for a PTSD diagnosis, his or her symptoms must last longer than a month (criterion F), must prevent him or her from functioning well in significant area(s) of life (criterion G), and cannot be due to physical factors such as a medical condition or substance use (criterion H).
The National Center for PTSD (2014a) provides guidelines for diagnosing PTSD using the DSM-5. Criterion A (stressor) indicates that the person was exposed to at least one of the following: death, threatened death, actual or threatened serious injury, or actual or threatened sexual violence. The person must persistently re-experience at least one of the intrusion symptoms (criterion B) of the traumatic event and one of the avoidance efforts (criterion C) of distressing trauma-related stimuli. Two negative symptoms or alterations in cognition or mood (criterion D) and two alterations in arousal and reactivity (criterion E) that began or worsened after the traumatic event must be present for a diagnosis of PTSD. Although symptoms may occur soon after the event, a person does not qualify for a PTSD diagnosis until at least six months after the traumatic event. An individual with PTSD will experience high levels of either depersonalization or derealization (National Center for PTSD, 2014a).
Nussbaum’s (2013) brief version for diagnosing PTSD begins by asking the following:
What is the worst thing that has ever happened to you? Have you ever experienced or witnessed an event in which you were seriously injured or your life was in danger, or you thought you were going to be seriously injured or endangered? (p. 90)
If the client answers in the affirmative, the counselor is to ask these questions: “Do you think about or re-experience these events? Does thinking about these experiences ever cause significant trouble with your friends or family, at work, or in another setting?” (Nussbaum, 2013, p. 90). Nussbaum (2013) provides a set of questions for each cluster and its associated symptoms to guide the process of diagnosis.
Assessment Tools
Ottati and Ferraro (2009) describe three assessment tools, validated on veteran populations, to screen for combat-related PTSD: the 17-item self-report PTSD Checklist (PCL), the 35-item self-report Mississippi Scale for Combat-Related PTSD (M-PTSD), and the Clinician-Administered PTSD Scale (CAPS). The PCL was recently updated to 20 items to reflect the changes in DSM-5. PCL-5 is a self-report measure that takes 5–10 minutes to complete and may be used to screen, diagnose and monitor changes during and after treatment of PTSD (Weathers et al., 2013). The M-PTSD uses a 5-point Likert scale to rate PTSD symptoms and related symptoms of substance abuse, suicidal ideation, and depression. It provides a PTSD symptom severity index with scores ranging from 35–175. The M-PTSD has not been revised since DSM-3, but may still be useful since it was normed with veteran populations (National Center for PTSD, 2014b). CAPS is a diagnostic structured interview that also measures the severity of symptoms and was recently revised to assess the DSM-5 PTSD symptoms. CAPS-5 is a 30-item questionnaire that takes 45–60 minutes to administer and yields a single score of PTSD severity (Weathers et al., 2013).
Other instruments are available to counselors for consideration. The PTSD Symptom Scale, Interview Version (PSS-I) with 17 items is a shorter clinical interview comparable to CAPS (Peterson, Luethcke, Borah, Borah, & Young-McCaughan, 2011). The PSS-I can be administered in about 20 minutes by a trained lay interviewer, and each item consists of a brief question so that an initial assessment can be made in shorter time (Peterson et al., 2011).The Emotion Regulation Questionnaire (ERQ) assesses differences between expressive suppression and cognitive reappraisal during treatment intake and discharge (Boden et al., 2013). The ERQ assessment assists the counselor in targeting and reducing maladaptive regulation strategies within the context of PTSD treatment in order to help the veteran develop alternative coping skills (Boden et al., 2013). The Quick Test for PTSD (Q-PTSD) is useful for identifying individuals with a true disability (Morel, 2008). Q-PTSD is a time-efficient method of detecting malingering in veterans applying for disability; it may be used by the counselor as an initial assessment of the disorder (Morel, 2008).
Other useful instruments can be incorporated into a treatment plan, such as a strengths-based assessment, depression inventory, substance abuse assessment, and insomnia inventory. Seligman (2011) also recommends the Post-Traumatic Growth Inventory (PTGI) for use with veterans. The 21-item PTGI “measures the extent to which survivors of traumatic events perceive personal benefits, including changes in perceptions of self, relationships with others, and philosophy of life accruing with their attempt to cope with trauma and its aftermath” (Tedeschi & Calhoun, 1996, p. 458). Seligman (2011) suggests that trauma often sets the stage for growth; a counselor may use the PTGI to facilitate veterans’ understanding of the conditions under which growth can happen.
Making a diagnosis of PTSD requires assessing symptoms and also gathering data from multiple assessments, a structured interview, and other knowledge of the client in order to make an evaluative judgment that leads to the development of a sound treatment plan (Ottati & Ferraro, 2009).
PTSD Treatment
Cognitive behavioral therapy (CBT) is unanimously endorsed as the best-practice treatment for PTSD by the VA and the Department of Defense (DOD; U.S. VA & U.S. DOD, 2010), the International Society for Traumatic Stress Studies (Foa, Keane, & Friedman, 2000), and the American Psychiatric Association (Ursano et al., 2010). Tramontin (2010) specifically states that the VA supports Prolonged Exposure (PE) therapy and Cognitive Processing Therapy (CPT).
In CPT and CBT, counselors challenge clients’ automatic thoughts connected with trauma. Through the use of written narratives in CPT, counselors target issues of safety, trust, power, control and self-esteem. Counselors also work with veterans to identify and label feelings as they work through impasses in their stories (Moran, Schmidt, & Burker, 2013). Exposure therapy is an evidence-based practice for many types of trauma including PTSD. According to Rauch, Eftekhari, and Ruzek (2012), PE therapy reduces PTSD symptoms and aids in treating comorbid issues. Rauch et al. (2012) explain that PE therapy consists of four components: psychoeducation, in vivo exposure, imaginal exposure, and emotional processing. Psychoeducation can help those suffering from trauma to understand their PTSD (Rauch et al., 2012). In vivo exposure consists of literally confronting the variables associated with the trauma (i.e., people, places and things; Rauch et al., 2012). Imaginal exposure involves reliving the memories associated with the trauma and engaging the accompanying emotions (Rauch et al., 2012). Emotional processing involves the counselor posing open-ended questions to the client in order to elicit both the emotions the client felt associated with the trauma and present emotions (Rauch et al., 2012).
Virtual reality exposure. In recent years, a new development of a virtual reality exposure therapy has surfaced. Albert “Skip” Rizzo developed a program titled “Virtual Iraq,” a virtual reality simulation designed to assist in the treatment of PTSD (Virtually Better, Inc., 2013). Rizzo developed the program after stumbling upon a video game called “Full Spectrum Warrior” that was originally created to train military service men and women. According to Rothbaum, Rizzo and Difede (2010), the current generation of military service members may be more comfortable participating in virtual reality treatment than conventional talk therapy, due to its similarity to gaming. After viewing several videos that demonstrate the Virtual Iraq system, the authors understand the connection between the exposure to trauma variables in PE and the exposure to trauma variables in virtual reality programs. Sharpless and Barber (2011) found several studies demonstrating the efficacy of virtual reality in treating veterans.
The protocol for virtual reality treatment involves veterans selecting a traumatic combat experience that relates closely to their most severe PTSD symptoms (McLay et al., 2012). Counselors create a realistic experience for the veteran by utilizing various sensory components of the virtual reality environment. Clients then use their senses and are immersed into the virtual reality world where they relive their trauma. Following the treatment, the counselor and the veteran process the material that surfaced in the exposure (McLay et al., 2012). In a study using virtual reality exposure therapy, McLay et al. (2012) found that “75% of participants experienced at least a 50% reduction in PTSD symptoms” (p. 635).
In addition to Virtual Iraq, Virtually Better, Inc. (2013) has developed other programs, including Virtual Vietnam, Afghanistan, Airports, and the World Trade Center. During a phone interview with Emilio Coirini, Director and Business Developer at Virtually Better, Inc., the interviewee stated that a soldier who suffers PTSD costs the government about $50,000 a year to treat, with the average treatment lasting 20 years. In contrast, the virtual reality system costs only about $30,000 with clinical training (E. Coirini, personal communication, November 16, 2012). At the time of the interview, there were about 70 systems installed throughout the United States, and Coirini explained that it is possible to receive grants for the cost of the system.
Animal-assisted treatment. In contrast to the relatively new use of virtual reality technology, animals have been assisting persons with disabilities for many years; there are a growing number of organizations that provide trained animals, specifically canines, to veterans who suffer from PTSD. According to Thompson (2010), in order to qualify as a service animal, the animal must undergo training to do work or perform helpful tasks. McConnell (2011) conducted a study that found that having a pet can provide meaningful social support that improves lives. One organization, Pets for Vets, provides animal companions to veterans with PTSD who are capable of caring for a pet. Pets for Vets states the following (2014):
Our goal is to help heal the emotional wounds of military veterans by pairing them with a shelter animal that is specially selected to match his or her personality. Professional animal trainers rehabilitate the animals and teach them good manners to fit into the veteran’s lifestyle. Training can also include desensitization to wheel chairs or crutches as well as recognizing panic or anxiety disorder behaviors. (para. 2)
Animals have been therapeutic partners to persons with disabilities for generations, and they are now serving wounded warriors.
Utilization of mobile phone applications. While researching other tools to help in treating PTSD, the authors discovered a few mobile applications available for both the iPhone and the Android that are well-developed, user-friendly and comprehensive. The first application, PTSD Coach (U.S. VA, 2014b), is elaborate in design, taking into account potential areas of concern for those who suffer from PTSD. The four main divisions of the application include Learn, Self-Assessment, Manage Symptoms and Find Support. The learning division of the application provides a comprehensive base and answers questions such as What is PTSD? and Who develops PTSD? In addition, the learning division includes answers regarding who should seek professional assistance and possible treatment protocols. The questions in the professional care subsection include Will it really work? and What if I am embarrassed about seeking help? The self-assessment section gives a person insight into the possibility of having PTSD. An example of an evaluative question is, “In the past month how often have you been bothered by disturbing memories, thoughts or images of the traumatic experience?” Users can track the history of their symptoms and schedule assessments to take periodically to provide a comparison of improvement or decline. When utilizing the manage symptoms option, users can select a mental state such as sadness or hopelessness, and the application will provide a suggestion to improve mood, depending on mood severity. Finally, users can set up their own support network, get support immediately or find professional care by choosing the finding support option. (The Apple phone app version may be found at https://itunes.apple.com/us/app/ptsd-coach/id430646302?mt=8, and the Android version may be found at https://play.google.com/store/apps/details?id=gov.va.ptsd.ptsdcoach.)
Another application, T2 Mood Tracker (The National Center for Telehealth and Technology, 2014), aids individuals in keeping track of their moods, which they can then report to their medical or mental health professional(s). The application can be used as a daily tool to track a client’s mood, keep notes regarding stressors, and chart a graph of the information provided. The initial screen asks whether the user would like to rate anxiety, depression, general well-being, head injury, post-traumatic stress, or general stress. The user selects one of the previously stated fields and is then required to rate several factors associated with the chosen field. The user can then graph results, create reports, save reports, or view notes. The application is user-friendly and simple in design, yet intricate enough to help the user and counselor in developing treatment protocols. (The Apple phone app version may be found at https://itunes.apple.com/us/app/t2-mood-tracker/id428373825?mt=8, and the Android version may be found at https://play.google.com/store/apps/details?id=com.t2.vas.)
A third application worthy of acknowledgement is the PE Coach, developed by the VA (2014a). The PE Coach requires a counselor trained in PE therapy. According to the National Center for PTSD (2014c), the PE Coach is a treatment companion that helps the client and counselor work through the PE treatment manual. The features of this application include the following: learning about PE therapy and the most common reactions to trauma, recording therapy sessions for personal use, setting reminders for homework and future therapy appointments, tracking tasks between sessions, practicing breathing exercises, and tracking PTSD symptoms. Currently, anecdotal accounts from veterans indicate that the mobile applications are helpful (U.S. DOD, American Forces Press Service, 2012). (The Apple phone app version may be found at https://itunes.apple.com/us/app/pe-coach/id507357193?mt=8, and the Android version may be found at https://play.google.com/store/apps/details?id=org.t2health.pe.)
Conclusion
Wendling (2008) reported results from an online survey administered to mental health practitioners after they had attended a conference called “Healing the Scars of War.” She found that most counselors did not understand military culture or appear to follow best-practice guidelines. The authors hope this paper serves to increase understanding of this critical area.
Technology makes it possible to access information about military families and resources to serve this special population. The VA has PTSD videos, training courses, and other materials available to inform counselors of the needs and unique cultural experiences of a diverse veteran population experiencing PTSD.
The resources identified (see Table 1) can be readily accessed by counselors and veterans to begin the therapeutic journey. We, the authors, salute the wounded warriors and continue to fight for their healing as they have fought for freedom.
Table 1
Informative Resources about Veterans and PTSD
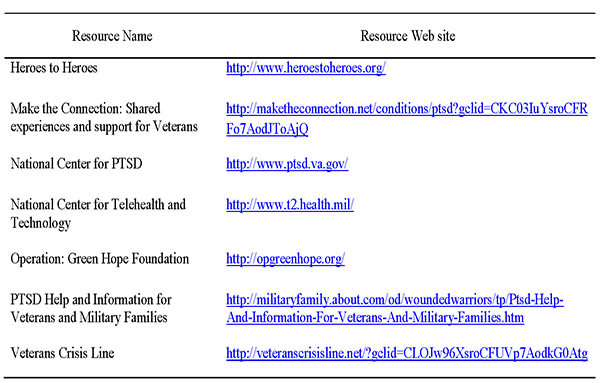
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5 (5th ed.). Washington, DC: American Psychiatric Publishing.
Boden, M. T., Westermann, S., McRae, K., Kuo, J., Alvarez, J., Kulkarni, M. R., … Bonn-Miller, M. O. (2013). Emotion regulation and posttraumatic stress disorder: A prospective investigation. Journal of Social & Clinical Psychology, 32(3), 296–314. doi:10.1521/jscp.2013.32.3.296
Foa, E. B., Keane, T. M., & Friedman, M. J. (Eds.). (2000). Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies. New York, NY: The Guilford Press.
McConnell, A. R. (2011, July 11). Friends with benefits: Pets make us happier, healthier. Psychology Today. Retrieved from http://www.psychologytoday.com/blog/the-social-self/201107/friends-benefits-pets-make-us-happier-healthier
McLay, R. N., Graap, K., Spira, J., Perlman, K., Johnston, S., Rothbaum, B. O., … Rizzo, A. (2012). Development and testing of virtual reality exposure therapy for post-traumatic stress disorder in active duty service members who served in Iraq and Afghanistan. Military Medicine, 177(6), 635–642.
Moran, S., Schmidt, J., & Burker, E. J. (2013). Posttraumatic growth and posttraumatic stress disorder in veterans. Journal of Rehabilitation, 79(2), 34–43.
Morel, K. R. (2008). Development of a validity scale for combat-related posttraumatic stress disorder: Evidence from simulated malingerers and actual disability claimants. Journal of Forensic Psychiatry & Psychology, 19(1), 52–63. doi:10.1080/14789940701594645
National Center for PTSD. (2014a, January 3). DSM-5 criteria for PTSD. Retrieved from http://www.ptsd.va.gov/professional/PTSD-overview/dsm5_criteria_ptsd.asp
National Center for PTSD. (2014b, January 3). Mississippi Scale for Combat-Related PTSD (M-PTSD). Retrieved from http://www.ptsd.va.gov/professional/assessment/adult-sr/mississippi-scale-m-ptsd.asp
National Center for PTSD. (2014c, January 28). Mobile app: PE coach. Retrieved from http://www.ptsd.va.gov/public/materials/apps/pecoach_mobileapp-public.asp
The National Center for Telehealth and Technology. (2014). T2 Mood Tracker [Mobile application software]. Available from https://itunes.apple.com/us/app/t2-mood-tracker/id428373825?mt=8 or https://play.google.com/store/apps/details?id=com.t2.vas
Nussbaum, A.M. (2013). The Pocket Guide to the DSM-5 Diagnostic Exam. Washington, DC: American Psychiatric Publishing.
Ottati, A., & Ferraro, F. R. (2009). Combat-related PTSD treatment: Indications for exercise therapy. Psychology Journal, 6(4), 184–196.
Peterson, A. L., Luethcke, C. A., Borah, E. V., Borah, A. M., & Young-McCaughan, S. (2011). Assessment and treatment of combat-related PTSD in returning war veterans. Journal of Clinical Psychology in Medical Settings, 18(2), 164–175. doi:10.1007/s10880-011-9238-3
Pets for Vets. (2014). Healing vets and saving pets. Retrieved from http://pets-for-vets.com
Rauch, S. A. M., Eftekhari, A., & Ruzek, J. I. (2012). Review of exposure therapy: A gold standard for PTSD treatment. Journal of Rehabilitation Research & Development, 49(6), 679–687.
Rothbaum, B. O., Rizzo, A., & Difede, J. (2010). Virtual reality exposure therapy for combat-related posttraumatic stress disorder. Annals of the New York Academy of Sciences, 1208, 126–132. doi:10.1111/j.1749-6632.2010.05691.x
Seligman, M. E. P. (2011). Flourish: A visionary new understanding of happiness and well-being. New York, NY: Free Press.
Sharpless, B. A., & Barber, J. P. (2011). A clinician’s guide to PTSD treatment for returning veterans. Professional Psychology: Research and Practice, 42(1), 8–15. doi:10.1037/a0022351
Staggs, S. (2014). Symptoms & diagnosis of PTSD. Retrieved from http://psychcentral.com/lib/symptoms-and-diagnosis-of-ptsd/000158
Tedeschi, R. G., & Calhoun, L. G. (1996). The posttraumatic growth inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress, 9(3), 455–471. doi:10.1002/jts.2490090305
Tester, J. (2013, June 13). Tester introduces comprehensive veterans’ health care legislation [Press release]. Retrieved from http://www.tester.senate.gov/?p=press_release&id=2965
Thompson, M. (2010, November 22). Bringing dogs to heal. Time, 176(21), 54–57. Retrieved from http://p2v.org/wp-content/uploads/2010/11/p2v-time-web.pdf
Tramontin, M. (2010). Exit wounds: current issues pertaining to combat-related PTSD of relevance to the legal system. Developments in Mental Health Law, 29, 23–47.
U.S. Department of Defense, American Forces Press Service. (2012, July 31). DOD, VA release mobile app targeting post-traumatic stress [News release]. Retrieved from http://www.defense.gov/news/newsarticle.aspx?id=117339
U.S. Department of Veterans Affairs. (2014a). PE coach [Mobile application software]. Available from https://itunes.apple.com/us/app/pe-coach/id507357193?mt=8 or https://play.google.com/store/apps/details?id=org.t2health.pe
U.S. Department of Veterans Affairs. (2014b). PTSD coach [Mobile application software]. Available from https://itunes.apple.com/us/app/ptsd-coach/id430646302?mt=8 or https://play.google.com/store/apps/details?id=gov.va.ptsd.ptsdcoach
U.S. Department of Veterans Affairs, & U.S. Department of Defense. (2010). VA/DoD clinical practice guideline for management of post-traumatic stress. Washington, DC: Management of Post-Traumatic Stress Working Group. Retrieved from http://www.healthquality.va.gov/ptsd/cpg_PTSD-FULL-201011612.pdf
Ursano, R. J., Bell, C., Eth, S., Friedman, M., Norwood, A., Pfefferbaum, B., … Benedek, D. M. (2010). Practice guideline for the treatment of patients with acute stress disorder and posttraumatic stress disorder. Arlington, VA: American Psychiatric Association. Retrieved from http://psychiatryonline.org/pdfaccess.ashx?ResourceID=243186&PDFSource=6
Virtually Better, Inc. (2013). Virtual Iraq. Retrieved from http://www.virtuallybetter.com/virtual-iraq/
Weathers, F. W., Blake, D. D., Schnurr, P. P., Kaloupek, D. G., Marx, B. P. & Keane, T. M. (2013). The clinician-administered PTSD scale for DSM-5 (CAP-5). Retrieved from http://www.ptsd.va.gov/professional/assessment/adult-int/caps.asp
Wendling, P. (2008). Knowledge gap exists on best practices for PTSD. Retrieved from http://www.thefreelibrary.com/Knowledge gap exists on best practices for PTSD.-a0199814983
Mary Alice Fernandez, NCC, is an assistant professor at Texas A&M University – Corpus Christi. Melissa Short is a doctoral student at Walden University Online. Correspondence can be addressed to Mary Alice Fernandez, 6300 Ocean Drive, Unit 5834, Corpus Christi, TX 78412-5834, mary.fernandez@tamucc.edu.
Apr 4, 2014 | Article, Volume 4 - Issue 2
Kristin A. Vincenzes, Laura Haddock, Gregory Hickman
Past research has indicated the negative and positive impacts of deployment on military wives. Furthermore, research has indicated the need to further understand the different deployment stages, specifically the post-deployment period. The authors examined Bowlby’s and Ainsworth’s attachment theories, specifically separation anxiety occurrence as experienced by stay-behind wives during their husbands’ post-deployment period. Purposive/volunteer sampling was used to survey 57 military wives currently experiencing the post-deployment period. A linear regression analysis produced a significant positive relationship between duration of deployment and the wife’s psychological distress during the post-deployment period. As deployments increased in duration, specifically to longer than 6 months, the levels of psychological distress significantly increased. Implications for counselors and researchers are addressed.
Keywords: post-deployment, attachment, military wives, separation anxiety, deployment
Between 2001 and 2012, the U.S. government sent 2.4 million soldiers to Iraq and Afghanistan (U.S. Department of Veteran Affairs, 2012). According to Demers (2008), deployments affected both the soldier and the stay-behind wife (over 56% of the soldiers reported being married according to the Department of Defense, 2012). The couple’s relationship may play an intricate role in identifying effects that a deployment could have on a stay-behind wife. Specifically, stay-behind wives may have both positive and negative experiences in response to prolonged separation from their husbands (Barker & Berry, 2009; Demers, 2008; Morse, 2006).
This study focuses specifically on wives of male soldiers, and applies Bowlby’s and Ainsworth’s attachment theories (Ainsworth & Bell, 1970; Bowlby, 1969) to military wives’ post-deployment experiences. Bowlby (1969) asserted that an accumulation of early attachment experiences create expectations for future relationships. Over 40 years ago, Ainsworth and Bell (1970) identified three primary types of attachment: secure, avoidant and ambivalent. More specifically, the researchers found that children with an ambivalent attachment style exhibited anxiety following separation when the mother returned, going near the mother, but also exhibiting signs of anger by pushing her away (Ainsworth & Bell, 1970). In comparison, children with a secure attachment welcomed their mother’s return, and children with an avoidant attachment showed little interest in their returning mother (Ainsworth & Bell, 1970). Robertson and Bowlby (1952) also examined the idea of separation anxiety, identifying specific infant stages of attachment. The three phases an infant goes through when separated from their mother include protest, despair, and denial or detachment (Robertson & Bowlby, 1952).
The three separation anxiety phases may be applied to attachment issues that military wives experience during and after their husbands’ out-of-country deployment (Basham, 2008; Riggs & Riggs, 2011). The first phase, protest, occurs when a child is separated from his or her mother, with sadness and anxiety presenting as the most common initial emotional reactions. The protest phase is linked to pre-deployment and deployment time periods, as wives often feel numb, angry and abandoned due to an upcoming or current separation from their husbands (Pincus, House, Christenson, & Adler, 2001). Furthermore, wives also may experience sadness, loneliness and anxiety during this phase (SteelFisher, Zaslavsky, & Blendon, 2008).
The second phase of separation anxiety is despair, characterized by feelings of extreme sadness (Riggs & Riggs, 2011; Robertson & Bowlby, 1952). A wife may often go through similar stages of grief and mourning when her husband is deployed (Pincus et al., 2001). Initially a wife may be in denial that her husband is gone, believing that she will be fine and that he is only away for a few days’ training (Pincus et al., 2001). As time passes, she may experience depression and withdrawal as she realizes that her husband will not return for a long time, if at all (Vormbrock, 1993).
The nature of the military deployments to Iraq and Afghanistan are characterized by continual life-threatening experiences, coupled with the absence of any “safe” place (Demers, 2008). Constant media coverage spotlights the dangers of deployment to active combat zones and undoubtedly impacts a wife’s ability to trust that her husband will safely return (Demers, 2008). Wives have reported being in constant fear for their soldiers’ safety, which may result in feeling helpless throughout the deployment (Demers, 2008; Spera, 2009). Eventually, a wife may begin to accept that her husband is gone, and transfer her love to someone else, such as a child or different partner (Morse, 2006).
The final phase of separation anxiety, denial or detachment, can occur during both the deployment period and the post-deployment period (Morse, 2006). Robertson and Bowlby (1952) postulated that this last phase serves as a defense mechanism, which wives utilize when their husbands abruptly rejoin their families (Pincus et al., 2001; Riggs & Riggs, 2011). Anxiety combined with excitement has been found to impact the restabilization of the couple (Morse, 2006; Pincus et al., 2001). Attempting to regain a physical and emotional connection with one another after a long, seemingly permanent separation has been found to be extremely stressful, resulting in struggles with communication, coparenting, returning to pre-deployment routines, and marital intimacy (Orthner & Rose, 2005).
Additional challenges during the post-deployment period may entail negotiating new roles and boundaries within the family system, household management, financial status, parental rejection and new social supports (Drummet, Coleman, & Cable, 2003). If the husband returns and attempts to resume roles that existed prior to his deployment, it may diminish the stay-behind wife’s feelings of worth and accomplishment, since she successfully managed the various facets of daily life in her husband’s absence (Drummet et al., 2003), further straining the attachment between the couple. Although each endured the deployment simultaneously, the experiences were likely uniquely and vastly different from one another (Pincus et al., 2001).
Purpose
This quantitative study examined how stay-behind wives experience separation anxiety, through examining the relationship between duration of deployment and psychological distress during post-deployment. The theoretical framework for this study focused on attachment between a husband and wife and how a couple cope with separation. Surveys of wives were conducted during the post-deployment period in an effort to capture data from the time that couples were reattaching. For the purposes of this study, post-deployment is defined as the 12-month period after the husband has returned from deployment.
Research Design
A nonexperimental, correlational design was chosen for this study. In order to gain access to a multitude of military wives, there was no specific inclusion criteria with regard to the soldier’s branch in the military, rank, or if the husband was active duty, Reserves, or National Guard. In order to attempt to control for the potential confounding variable of gender, this study included only stay-behind wives. Stay-behind wives may or may not have children. Finally, stay-behind wives must currently be in the post-deployment stage; therefore, the husbands must have returned from their deployment within the past 12 months (Vincenzes, 2013).
Data Collection
The sampling method used for this research was volunteer purposive sampling. Inclusion criteria included the following: female, currently married and experiencing the post-deployment period (within the 12 months since her husband returned from the deployment), and a deployment that had lasted 6 or more months. Approximately 30 original e-mails were sent out to military advocacy groups, current military wives, the Army Wives Network, and a military advocacy group called Pennsylvania Americans showing Compassion, Assistance, and Reaching out with Empathy for Service members (PA C.A.R.E.S.). These individuals were asked to forward the initial e-mail soliciting military wives for the current study (Vincenzes, 2013).
If individuals agreed to volunteer for the study, they immediately received a background questionnaire, which assessed the duration of deployment (independent variable). Duration of deployment was operationalized as the total number of months that the soldier was deployed, from the day he left until the day he returned (Vincenzes, 2013). Furthermore, the participants took the Depression Anxiety Stress Scales (DASS-21; Lovibond & Lovibond, 1995), which was used to operationally define the dependent variable of psychological distress. The DASS-21 is a 21-item Likert scale survey and consists of three subscales (Depression, Anxiety, and Stress). In addition to individual scores on the subscales, the assessment provides an overall global psychological distress level, which was the score this particular study used. The reliability for this measure was high with a .93 internal consistency on the overall global scale (Henry & Crawford, 2005). In addition, the DASS-21 illustrated good convergent and discriminant validity as compared to the Hospital Anxiety and Depression Scale and Personal Disturbance Scale (Henry & Crawford, 2005).
Results
Of the 145 participants who responded to the survey, 48.9% (n = 68) met the criteria, but 14.7% (n = 10) had missing data. Thus, the final data sample contained 40% (n = 58) of the participants who volunteered. The inclusive sample accurately depicted the dispersion of active duty military (56.9% Army, 22.4% Air Force, 12.1% Navy, and 1.4% Marine Corps); however, fewer participants were associated with the National Guard (5.2%) and Reserves (1.7%) than expected.
The age of the wives ranged from 21–47 (M = 31.2, SD = 6.7), and 50% were 29 years old or younger. The majority of the participants (93.1 %) had some years of college (only 6.9% had a high school diploma/GED or less). Furthermore, 29.3% had some college, but no degree; 20.7% had an associate degree, 31% had a bachelor’s degree, and 12.1% had a graduate degree. With regard to employment status, 53.4% of the participants were not employed and 46.6% were employed. The number of years couples were married ranged from 1–20 (M = 7.2, SD = 5) and 48.3% of the participants had been married 5 years or less. The number of children under 17 who lived in the household ranged from 0–4 (M = 1.5, SD = 1.3) and 51.7% had either no children or one child. The length of deployments ranged from 6–16 months (M = 9.5, SD = 2.8). Finally, the length of time since the husband returned from deployment ranged from 0–12 months (M = 6.0, SD = 4.2).
The study’s null hypothesis stated that in the population under investigation, the proportion of variance in post-deployment psychological distress level explained by the duration of deployment (as measured by the DASS-21) was zero. Linear regression analysis predicted psychological distress from the duration of husband’s deployment. Results from the analysis indicated that duration of deployment significantly predicted psychological distress: F(1, 57) = 5.384, p = .024, R=.296, Adj. R2 = .071. Duration of deployment accounted for 8.8% of the variance in psychological distress and was positively related to psychological distress ( = .296, sr 2 =.088). Based on these results, the null hypothesis, which stated that distress levels would be zero or not change following longer deployments, was rejected. Thus, as the duration of deployment increases, the psychological distress levels for stay-behind wives also increases.
Discussion
This study confirmed prior research and extended existing literature regarding attachment theory as it relates to stay-behind military wives. For example, researchers have found that when husbands are deployed or away on military duties for several months, the wives not only demonstrate feelings of anger during the deployments, but that their feelings of anger persist even after their husbands return from deployment and military duties (Pincus et al., 2001; Riggs & Riggs, 2011; Zeff, Lewis, & Hirsch, 1997). Indeed, the findings from this current study supported prior research, as the author found a positive relationship between deployments of increasing length and an increase in distress levels among stay-behind military wives. Although this study did not specifically evaluate wives’ anger, other researchers have found that high distress levels are correlated with the development of anger among military wives (Drummet et al., 2003).
The results of this study illustrate that post-deployment is indeed very stressful for the wife, particularly when the husband was deployed for 6 months or more. Since deployments lasting 6 or more months significantly predicted psychological distress for the wives, it may be that as deployment length increases, stress levels also may increase, resulting in a wife emotionally withdrawing from her husband. The findings from this study support prior research that has identified the coping strategy of emotional withdrawal, which results from psychological distress and may enable the wife to continue her daily life, while also creating a new support system and sense of emotional equilibrium (Pincus et al., 2001).
Some stay-behind wives function well on a daily basis while their husbands are deployed; however, other stay-behind wives appear to struggle with their husbands’ deployment (Riggs & Riggs, 2011). Such research supports the notion that wives who made secure attachments while growing up may be better able to cope with military separations (Riggs & Riggs, 2011). It should be noted, however, that only in the past several years have some deployments lasted up to 15 or 16 months (Sheppard, Malatras, & Israel, 2010). The length of deployments, especially 6 or more months, may significantly alter the ability of stay-behind wives to successfully cope, regardless of their attachment styles. Further research should examine the impact of lengthy deployments (e.g., 6 or more months) on stay-behind wives’ ability to cope as it relates to attachment style, as there may be a point of diminishing returns at which, regardless of one’s attachment to her parents growing up, the ability to cope disappears.
Vormbrock (1993) predicted that as the duration of deployment increased, so too would distress levels during the couple’s reunion. This was hypothesized to be due to the continual unavailability of the attachment figure. The current study supports Vormbrock’s theory in that participants’ reported distress levels during post-deployment were significantly higher (p = .023) as deployment duration increased. Perhaps when the husband is gone for 6 months or more, the potential for the marriage to grow apart or detach may increase. Vormbrock (1993) found that wives can successfully focus on the brevity of their separation as a means of coping; however, as the deployments increase in length, it may affect wives’ ability to maintain the mentality that this separation is only temporary. Deployments that require the couple to be apart for 6 or more months may result in the wife feeling that the separation is more permanent. The longer the husband is away, the more independent the wife may become by creating new schedules and ways of doing things (Morse, 2006; Pincus et al., 2001).
Although this research elaborated on the relationship of the post-deployment period and distress among stay-behind military wives, there are some limitations to the study. The first limitation may be a self-selection bias, which may have impacted the internal validity. More specifically, since participants were volunteers, some individuals may have extremely negative feelings toward the military and may have opted not to participate. This could have inadvertently skewed the population sample, thus impacting the results. Indeed, researchers have discussed that volunteer samples may have biased tendencies as a motivation for their participation in a specific study (Frankfort-Nachmias & Nachmias, 2008). In addition to self-selection bias, an instrumentation threat could be present, as this survey relied on participants’ honesty. Another possible limitation is that this study was a regression study, which relies on the correlational nature of two variables. Perhaps there are extraneous variables that could be moderating or mediating the relationship of deployment length and distress level among stay-behind military wives.
Conclusions and Implications
Despite existing limitations, this study supported research regarding military deployment as a significant concern for military families, as well as for military leaders who rely on the husbands of these stay-behind wives to provide national security. As surveys within the last decade indicate that nearly 60% of American military members are married (Sierra & Kemp, n.d.), the results of this study also offer further insight into the contextual factors that are part of a therapeutic treatment intervention. Military couples are unique and a counselor’s awareness of needs particular to this group is imperative for therapeutic success.
The current research found a positive correlation between the duration of deployment and stay-behind wives’ psychological distress levels during post-deployment. This finding corroborates the research on separation anxiety for children, particularly when children illustrate signs of detachment from their mother following a separation. Attachment figures may include other vital individuals in one’s life, especially for military couples. Since many military couples do not live close to immediate biological family members, the wife may solely depend on the husband to meet her emotional, physical and social needs, just as an infant child often relies on their mother to meet these same basic needs. With this in mind, the notion of separation anxiety may not be just applicable to young children but also adults, particularly military wives.
Counselors may want to educate stay-behind wives on separation anxiety and assist them in processing their experiences, as well as recognize wives’ desire for a stable, secure relationship and assist them to this end. Furthermore, since deployments are unpredictable and out of the wives’ control, it may be helpful for counselors to assist the wives in gaining a greater sense of control throughout their daily lives. Just as counselors often recommend that children with separation anxiety have a consistent routine, as well as partake in positive social activities, it also may be helpful to encourage stay-behind wives to create predictable routines that include engaging in various social events with friends and/or other military wives.
This study also has implications for further research regarding the human services industry (e.g., clergy, educators) who directly work with such military families. One might assume that not all soldiers or their wives experience deployment the same way, and thus counselors must be prepared to individualize interventions and compose treatment plans according to the needs of the individual as well as needs as a couple. For example, the post-deployment period may entail negotiating new roles and boundaries within the family system. Wives frequently experience the emotion of celebration for the return of their husbands, while also feeling confusion over what it will mean to share a home again after becoming more independent. This experience of boundary ambiguity can be very confusing for wives who recognize that their husbands are physically present, but who are still transitioning toward psychological acceptance that he is present.
Role ambiguity may increase if the couple is not comfortable communicating with each other regarding roles, responsibilities and needs. Simultaneously, a soldier may feel disconnected and unaware of how to reengage without interfering with the family’s new roles. Thus, helping professionals must be prepared to work with the couple on strengthening basic communication skills and nurturing a climate that facilitates safe and transparent information exchange.
Future research could evaluate the experiences of deployed husbands in terms of understanding how the distress level of their stay-behind wives impacts their duties while deployed. Such research might have national security implications. In addition, future research could examine deployments of 6 months or more regarding the struggles, challenges, resiliency, social and psychological effects, educational outcomes, parenting styles, and attachment of the deployed husbands, the stay-behind wives, and their children.
One particular variable that may moderate the relationship between duration of deployment and psychological distress is the stay-behind wife’s social support system. Larsen and Kia-Keating (2010) found that a social support system significantly aided resiliency for stay-behind wives who experienced a military deployment. Furthermore, a wife’s well-being was positively impacted by having a mentor who had previously experienced a deployment herself (Larsen & Kia-Keating, 2010). This brings up an interesting perception of what social support may be necessary for a military wife. Whereas some social support indices examine tangible support (i.e., someone to help around the house), the stay-behind wife may need a social support that relies more on reducing emotional stress.
Future research could qualitatively explore the social support construct further by interviewing stay-behind wives and identifying the indices of social support that they deem important in terms of reducing stress during the post-deployment period. Such a qualitative process could then lead to the quantitative development of a more valid measure of social support necessary to reduce stress for stay-behind military wives, and therefore indirectly for their deployed husbands. Perhaps such a study could examine whether social support serves as a moderating or mediating influence on the relationship between deployment length and psychological distress of stay-behind wives. Such research could have both positive and negative implications for their families, the military, and society at large, as American society depends greatly on its military for national security.
References
Ainsworth, M. D. S., & Bell, S. M. (1970). Attachment, exploration, and separation: Illustrated by the behavior of one-year-olds in a strange situation. Child Development, 41, 49–67.
Barker, L. H., & Berry, K. D. (2009). Developmental issues impacting military families with young children during single and multiple deployments. Military Medicine, 174, 1033–1040.
Basham, K. (2008). Homecoming as safe haven or the new front: Attachment and detachment in military couples. Clinical Social Work Journal, 36, 83–96. doi:10.1007/s10615-007-0138-9
Bowlby, J. (1969). Attachment and loss: Volume 1: Attachment. New York, NY: Basic Books.
Demers, A. (2008). The war at home: Consequences of loving a veteran of the Iraq and Afghanistan wars. Internet Journal of Mental Health, 6, 1–12. doi:10.5580/5ac
Drummet, A. R., Coleman, M., & Cable, S. (2003). Military families under stress: Implications for family life education. Family Relations, 52, 279–287.
Frankfort-Nachmias, C., & Nachmias, D. (2008). Research methods in the social sciences (7th ed.). New York, NY: Worth.
Henry, J. D., & Crawford, J. R. (2005). The short-form version of the Depression Anxiety Stress Scales (DASS-21): Construct validity and normative data in a large non-clinical sample. British Journal of Clinical Psychology, 44, 227–239. doi:10.1348/014466505X29657
Larsen, J., & Kia-Keating, M. (2010, August). Resilience based ecological model of military family coping during deployment. Poster session presented at the annual conference of the American Psychological Association, San Diego, CA.
Lovibond, P. F., & Lovibond, S. H. (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy, 33(3), 335–343. doi:10.1016/0005-7967(94)00075-U
Morse, J. (2006). New emotional cycles of deployment for service members and their families. U.S. Department of Defense: Deployment Health and Family Readiness Library. San Diego, CA. Retrieved from http://deploymenthealthlibrary.fhp.osd.mil/Product/RetrieveFile?prodId=241
Orthner, D. K., & Rose, R. (2005). SAF V survey report: Reunion adjustment among Army civilian spouses with returned soldiers. Retrieved from www.army.mil/fmwrc/docs/saf5reunionreport.pdf
Pincus, S. H., House, R., Christenson, J., & Adler, L. E. (2001, April/June). The emotional cycle of deployment: A military family perspective. U.S. Army Medical Department Journal, 15–23. Retrieved from http://cdm15290.contentdm.oclc.org/cdm/ref/collection/p15290coll3/id/898
Renshaw, K. D., Rodrigues, C. S. & Jones, D. H. (2008). Psychological symptoms and marital satisfaction in spouses of operation Iraqi freedom veterans: Relationships with spouses’ perceptions of veterans’ experiences and symptoms. Journal of Family Psychology, 22, 586–594.
Riggs, S. A., & Riggs, D. S. (2011). Risk and resilience in military families experiencing deployment: The role of the family attachment network. Journal of Family Psychology, 25, 675–687. doi:10.1037/a0025286
Robertson, J., & Bowlby, J. (1952). Responses of young children to separation from their mothers. Courrier of the International Children’s Centre, Paris, II, 131–140.
Sheppard, S. C., Malatras, J. W., & Israel, A. C. (2010). The impact of deployment on U.S. military families. American Psychologist, 65, 599–609. doi:10.1037/a0020332
Sierra, T. A. & Kemp, H. (n.d.). Strategies for working with military couples in hope focused couples approach. Retrieved from
http://j.b5z.net/i/u/2043019/i/Strategies_for_Working_with_Military_Couples_in_Hope_Focused_Couples_Approach.pdf
Spera, C. (2009). Spouses’ ability to cope with deployment and adjust to Air Force family demands: Identification of risk and protective factors. Armed Forces & Society, 35, 286–306. doi:10.1177/0095327X08316150
SteelFisher, G. K., Zaslavsky, A. M., & Blendon, R. J. (2008). Health-related impact of deployment extensions on spouses of active duty Army personnel. Military Medicine, 173, 221–229.
U.S. Department of Defense. (2012). 2012 demographics profile of the military community. Retrieved from http://www.militaryonesource.mil/12038/MOS/Reports/2012_Demographics_Report.pdf
U.S. Department of Veteran Affairs. (2012). Analysis of VA health care utilization among Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF) and Operation New Dawn (OND) veterans. Retrieved from www.publichealth.va.gov/docs/epidemiology/healthcare-utilization-report-fy2012-qtr1.pdf
Vincenzes, K. A. (2013). The impact of social support on the relationship between length of deployment and psychological distress for military wives during post-deployment. (Doctoral dissertation). Retrieved from ProQuest/UMI. (13775).
Vormbrock, J. K. (1993). Attachment theory as applied to wartime and job-related marital separation. Psychological Bulletin, 114, 122–144. doi:10.1037/0033-2909.114.1.122
Zeff, K. N., Lewis, S. J., & Hirsch, K. A. (1997). Military family adaptation to United Nations operations in Somalia. Military Medicine, 162, 384–387.
Kristin A. Vincenzes, NCC, is an Assistant Professor and Director of the Clinical Mental Health Counseling program at Lock Haven University. Laura Haddock, NCC, is a Core Faculty member and CES Program Coordinator at Walden University. Gregory Hickman is a Core Faculty member at Walden University. Correspondence can be addressed to Kristin A. Vincenzes, 401 N. Fairview Street, Courthouse Annex Room 301, Lock Haven, PA, 17745, KAV813@lhup.edu.