Sep 1, 2014 | Article, Volume 2 - Issue 1
Jonathan H. Ohrt, Laura K. Cunningham
Burnout and impairment among professional counselors are serious concerns. Additionally, counselors’ work environments may influence their levels of wellness, impairment and burnout. This phenomenological study included the perspectives of 10 professional counselors who responded to questions about how their work environments influence their sense of wellness. Five themes emerged: (a) agency resources, (b) time management, (c) occupational hazards, (d) agency culture, and (e) individual differences. Implications for professional counselors and future research are discussed.
Keywords: professional counselors, agencies, wellness, burnout, impairment
Wellness promotion focuses on individual strengths and emphasizes holistic growth and development. For example, Myers, Sweeney and Witmer (2000) defined wellness as:
A way of life oriented towards optimal health and well-being in which body, mind, and spirit are integrated by the individual to live life more fully within the human and natural community. Ideally, it is the optimum state of health and well-being that each individual is capable of achieving. (p. 252)
The authors’ definition of wellness alludes to one’s overall well-being. Counselors often advocate holism, exploration of self and self-actualization for their clients (Cain, 2001). Such aspirations may be achieved through a holistic wellness approach (i.e., attending to intellectual, emotional, physical, occupational and spiritual well-being; Witmer & Young, 1996). Therefore, counselors view wellness as an important aspect of overall human functioning. Although this fundamental view has historically been applied to clients, professional counselors themselves now recognize that they also may benefit from a wellness focus (Maslach, 2003).
Professional counseling organizations (e.g., American Counseling Association [ACA]; American Mental Health Counselors Association [AMHCA]; National Board for Certified Counselors [NBCC]) specifically emphasize the importance of counselor wellness and impairment prevention. For example, counselors are ethically required to recognize when they are impaired. The ACA (2005) ethical standards state that “Counselors are alert to the signs of impairment from their own physical, mental, or emotional problems and refrain from offering or providing professional services when such impairment is likely to harm a client or others” (Standard C.2.g). The AMHCA (2010) ethical standards further state that counselors:
recognize that their effectiveness is dependent on their own mental and physical health. Should their involvement in any activity, or any mental, emotional, or physical health problem, compromise sound professional judgment and competency, they seek capable professional assistance to determine whether to limit, suspend, or terminate services to their clients. (Standard C.1.h)
Furthermore, the NBCC (2005) ethical standards indicate that certified counselors discontinue providing services “if the mental or physical condition of the certified counselor renders it unlikely that a professional relationship will be maintained” (Standard A.15).
The Governing Council of the ACA states that “Therapeutic impairment occurs when there is a significant negative impact on a counselor’s professional functioning which compromises client care or poses the potential for harm to the client” (Lawson & Venart, 2005, p. 3). In 2003, this council became proactive in addressing the issue of counselor wellness by creating a task force on counselor wellness and impairment. The task force seeks to educate counselors about impairment prevention, promote resources for prevention and treatment of impaired counselors and to advocate within ACA and its division to address the broader issue of counselor impairment. As a result, they have distributed information on risk factors, assessment, resources and wellness strategies. Thus, a wellness focus is essential for professional counselors to prevent impairment and provide effective counseling services to clients (Witmer & Young, 1996).
Unfortunately, professional counselors encounter multiple factors that threaten their wellness (Lawson, 2007). For instance, counselors are at a particularly high risk for burnout due to the intense and psychologically close work they do with clients (Skovholt, 2001). Although there are many definitions of burnout, Pines and Maslach (1978) described it as “a condition of physical and emotional exhaustion, involving the development of a negative self-concept, negative job attitude, and loss of concern and feelings for clients” (p. 233). Additional consequences of burnout may include low energy and fatigue, cynicism towards clients, feelings of hopelessness and being late or absent from work (Lambie, 2006). When counselors fail to address burnout it can lead to impairment. Counselors also may experience occupational hazards such as compassion or empathy fatigue and vicarious traumatization (Figley, 2002; Lawson, 2007; Stebniki, 2007). Stebniki (2007) defined empathy fatigue as a state wherein counselors are exhausted by their duties because of their constant exposure to the suffering of others, which induces feelings of hopelessness and despair. Similarly, vicarious traumatization occurs when a counselor becomes emotionally impaired due to being exposed to an accumulation of traumatic stories from multiple therapy sessions (McCann & Perlman, 1990). Therefore, the actual nature of counselors’ work is a potential threat to their ability to be well.
In addition, environmental factors in counselors’ work settings also may be detrimental to their wellness (Ducharme, Knudsen, & Roman, 2008; Knudsen, Ducharme, & Roman, 2006; Vredenburgh, Carlozzi, & Stein, 1999). In a survey that included 501 professional counselors, Lawson (2007) found that those working in community agencies experienced higher levels of burnout and compassion fatigue and vicarious traumatization than those working in private practice. Agency variables that are associated with burnout include: work overload, low remuneration, lack of control over services, unsupportive or unhealthy work peers and ineffective or punitive supervisors (Lloyd, King, & Chenoweth, 2002). For example, low remuneration is a specific concern in many Southeastern states. Lambie and Young (2007) offered the following example of a work environment in a specific agency: “an employee assistance program in this area requires its counselors to conduct sessions for 35 clients a week…the counselor in such an organization faces stresses and work hours similar to a first year lawyer in a large firm, without the mitigating effects of financial compensation” (p.101). Additional stressors stem from nonprofit agencies’ dependence on government and state funding sources to operate. Agency compliance with government and state policies to maintain funding often require administrations to focus on the “bottom line,” sometimes to the detriment of client services and employee wellness (Rupert & Morgan, 2005). Counselors who experience such stressors are at serious risk for burnout. Nevertheless, counselors are ethically expected to avoid burnout because it ultimately reduces the quality of services provided to clients, compromises client care and creates potential for harm to the clients (Lawson & Venart, 2005).
Leaders in the counseling profession strongly encourage counselors to be proactive in maintaining their own wellness and self-care. Counselors need to “fill the well” of their own sense of well-being continually, so they can “pour it out” for their clients (Shapiro, Brown, & Biegel, 2007). For example, Lawson (2007) reported that counselors who endorsed 15 highly valued career sustaining behaviors scored higher on compassion satisfaction and lower on burnout. However, despite individuals’ efforts to maintain a wellness lifestyle, the work environment may have a significant role in impeding or supporting wellness efforts. If the work environment does not allow for rejuvenation, or if wellness is not valued, employees (counselors) may become distressed and impaired (Maslach, Leiter, & Schaufeli, 2008). Witmer and Young (1996) suggested that counselor education programs promote and model wellness for their students so they can prepare themselves to make lasting changes in their life to reduce the risk of impairment. Further, if counselors create an individual sense of wellness, they can advocate for their personal well-being in the agency and redirect energies towards organization wellness (Lambie & Young, 2007).
Previous authors suggested that the agencies in which counselors work can help to create wellness environments that contribute to counselors’ overall functioning. For example, Witmer and Young (1996) posited that counselor education programs, employing organizations and regulatory boards should develop systemic preventative wellness protocols to prevent counselor impairment. Their recommendations to agencies included equally distributing the most difficult cases, providing employee assistance programs that include family counseling, adequate peer support, and supervision and team building exercises. Stokes, Henley, and Herget (2006) offered some concrete suggestions to increase wellness including healthy food options, on-site exercise facilities, smoke-free environments, break stations away from the work areas, wellness challenges, support groups, social activities, health risk assessments, self-care information, employee counseling, financial incentives for long term employees and conflict resolution training for supervisors. Further, Lambie and Young (2007) recommended that mental health agencies reduce stress and promote wellness among their employees (counselors) by reducing paperwork and cutting “red tape,” adopting a collaborative management style, improving interpersonal relationships and teamwork, developing ways to reduce role stress, helping counselors grow on the job (e.g., professional development) and improving environmental conditions.
Although the potential hazards related to counselor’s work have received some attention (Gaal, 2009), there is limited research about how counselors conceptualize their wellness in relation to the influence of their work environment. Thus, the purpose of this exploratory study was to gain a greater understanding of how counselors experience wellness and how their work environment influences their sense of wellness. A qualitative phenomenological approach was the most appropriate method to implement because we were seeking to understand the participants’ lived experience of the phenomena (Creswell, 2007). Following the phenomenological tradition, we sought to uncover the central underlying meaning of their experience by reducing data, analyzing specific statements, searching for all possible meanings and creating meaning units (Creswell, 2009). Thus, we developed two research questions. The first question was, “How do you relate to the concept of wellness as a professional counselor?” and the second question was, “How do you perceive your agency influences your sense of wellness?” The first open-ended question was designed to gain information on each of the counselors’ thoughts about wellness and how they interpret the concept. The second question was designed to obtain information about how they believe their work environment affects their sense of wellness.
Method
Research Team
The research team consisted of two counselor educators who at the time of the study were doctoral students at a university in the southeastern U.S. The first author is a Caucasian male and the second author is a Caucasian female. The first author has previous work experience in a residential treatment setting and in a secondary school setting where he experienced a high level of turnover and burnout among the staff. The second author has previous work experience in a variety of agency settings and experienced different levels of emphasis on wellness in each agency. She became interested in researching in this area to assist counselors in the field. Both authors believe a wellness focus is important for professionals in the helping professions. Furthermore, the authors believe that one’s work environment affects each counselor’s ability to be well.
Procedure
Prior to facilitating the interviews and focus groups, we obtained approval from the Institutional Review Board (IRB) to conduct the study. Next, we recruited the 10 participants through a mixture of criterion-based and snowball-sampling strategies (Teddlie & Yu, 2007). The criterion included contacting counselors or agency directors who were currently or very recently employed at mental health agencies in a southeastern state. The snowball strategy included contacting individuals from the first and second authors’ previous employers, e-mailing invites on group servers for counselors who are alumni from a university that educates counselors and through following up recommendations from other counselors. After we secured participants for the study, we obtained informed consent and confirmed dates for the interviews and focus group.
Participants
The sample included seven female and three male professional counselors whose ages ranged from 25 to 53. Seven of the counselors were Caucasian, one counselor was of Indian descent, one was Latino, and one was of Middle Eastern descent. Two participants were employed by an agency that provides palliative care by way of in-home visits. One participant was a clinical director of an adolescent residential unit. One was previously a clinical director of a domestic violence shelter and a community counseling clinic. One participant worked in a behavioral hospital while another participant worked in an inpatient facility and previously in a residential setting. Three of the participants worked in a university-based clinic. Three counselors were present in the focus group interview and seven counselors were interviewed individually on separate occasions. See Appendix for pseudonyms and demographics.
Data Collection
Demographic questionnaire. Participants completed a demographic questionnaire consisting of questions about their age, race/ethnicity, socioeconomic status, gender, years in the field and work setting prior to participating in the interviews.
Individual interviews. The second author facilitated individual, semi-structured interviews with seven of the participants. Each interview lasted between 60 and 90 minutes. The interview started with the interviewer explaining the purpose of the study and then posing the first question: “How do you relate to the concept of wellness as a professional counselor?” Once this area was completely explored between the researcher and the interviewee, the researcher posed the second question: “How do you perceive your agency impacts your sense of wellness?” The researchers used follow-up, open-ended questions to elicit significant depth for each of the questions.
Focus group. The focus group included three counselors at a university-based counseling clinic and was facilitated by the second author. Prior to the group, the researcher reminded the interviewees about confidentiality and its limitations. The group lasted approximately 90 minutes and followed the same protocol as the individual interviews.
Data Analysis
After completing the interviews, we transcribed the audio-recorded sessions. All identifying information of the participants and location of employment were altered to maintain confidentiality. Next, the first and second authors read through transcripts to find initial categories. We employed inductive coding to devise categories that represented the overall essential message that was being conveyed in each interview and the focus group. The coding categories that emerged were recorded as well as thoughts about possible relationships between the categories (Glesne, 2006). Next, using the qualitative research software ATLAS.ti (Muhr, 2004), we loaded the documents and reduced the data using a chunking method, which requires the researcher to highlight sections of the transcription and assign codes or categories. Finally, we numbered the code list and noted connections among the interviewees’ coded chunks. This procedure consists of the researcher reviewing the codes to determine if a pattern, theme or relationship occurs (Glesne, 2006).
Verification Procedures
We implemented multiple verification procedures in order to ensure the trustworthiness of the study (Creswell, 2008). First, we performed member checks with participants to verify that the themes developed captured the essence of their experience. We addressed the threat of subjectivity through revealing our positionality and attempting to view information as objectively as possible. Additionally, we employed a peer-debriefer who continuously asked the primary author questions about the study, reviewed the relationship between the data and the research questions and reviewed the accuracy of the data analysis in comparison to the transcriptions.
Findings
In this study, we conducted seven individual interviews and a focus group to explore wellness for professional counselors in various mental health agencies. From the two research questions, “How do you relate to the concept of wellness as a professional counselor?” and, “How do you perceive your agency influences your sense of wellness?” five themes emerged: (a) resources, (b) time management, (c) occupational hazards, (d) agency culture, and (e) individual differences. We discuss each theme with thick, rich descriptions.
Agency Resources
Resources within the agency appeared to be a common theme that influenced participants’ sense of wellness. Participants consistently discussed areas such as salary, staff coverage and workloads as barriers to wellness. For example, participants discussed how financial compensation affected their feelings of being valued as well as their means to do things to maintain wellness. One participant, Anne, explained, “I am a 37-year-old woman who has to live with a roommate… I’m paid half of what nurses [at the same facility] are paid for the same amount of time.” When asked how she handled being paid less than other helping professionals, Anne responded, “I commiserate with other people in the field about being underpaid and undervalued. I can’t beat my head against a wall.” Another participant, Brian, discussed how his salary often impeded his ability to engage in wellness activities:
One of the struggles I had at the beginning was pay. Because it didn’t afford me, literally, the chance to do things to take care of myself, that I wanted to do to take care of myself. So if I had a weekend I couldn’t take a trip to the beach for the weekend. It had to be a quick jaunt and back because I couldn’t afford a hotel.
Resources also included counselor workloads, specifically in terms of how many clients each counselor had to see a day to maintain reimbursement policies. Brian discussed the lack of funding and explained that agencies must work “bare bones…skeleton crew basically.” One participant, Helen, commented on her caseload:
Money can drive a lot of things. Like the choices that you could make [before reimbursement] were more about the clients and what was needed, or what you wanted to try, and then you know Medicaid or other external forces enter, and then decisions have to be made on a different basis. The number of people you would even take would change. [before Medicaid]… There was a lot of flexibility, there was no external pressure to take a certain amount of clients and then there were great conversations and the ability to envision what you should do, and there was the time do it, and there was opportunity to review what you have done, and build the relationships and get feedback on your work, and whereas now, you have put in the time and you have to make the numbers and you lose the time to create relationships or talk about what you are doing.
Similarly, Brian discussed how large caseloads and working with clients back-to-back affected his performance when stating:
Basically, it took away from the services I was able to offer. But most of all it took away from me. You know my energy level, and just across the board I wasn’t able to do all of the things you would like to do as a quality counselor like planning…often it was sort of on the cusp.
Participants described the various resources within their agencies that influenced their sense of wellness. They identified the lack of resources as a barrier to their wellness, which also affected the quality of client care and enthusiasm for their work.
Time Management
Participants discussed time constraints as barriers to their wellness and their ability to maintain optimal performance with clients. They mentioned heavy caseloads as well as administrative duties and paperwork requirements as obstacles to their wellness that also reduced the quality of client services. Additionally, they believed that there was not adequate time for other important aspects of their development, such as supervision. One participant, David, discussed his frustration with not being able to sufficiently prepare for sessions, stating, “there was kind of this disconnect with how long it took to prepare for a session to do it right, or how long it would take to do a group, and to do it right.” He further proposed that the problem may be lessened even without reducing the caseload; “maybe it’s not about the number of clients as much as, maybe it’s just about a scheduling thing too, if you could just spread these clients out, thin enough.”
Participants also discussed administrative duties such as paperwork as wellness barriers that take away from the true meaning of their work. For instance, David stated that, “what was most stressful wasn’t working one-on-one with clients, it was just the amount of paperwork and catch up. You literally feel like you’re running a marathon when you walk in the room.” Brian described the draining effects of paperwork by stating, “I found myself very disenchanted because the work that I wanted to do was with people and often I found I was just doing documentation.”
Finally, participants discussed the importance of making time for appropriate supervision and consultation in maintaining their wellness. For example, when comparing an agency where she felt greater wellness to her previous agency, Fatin stated that the difference is:
The support and the peer consultation, and the time to do that. The level of respect is much higher. There is respect for the administrator; you can approach her with feedback. [There are] high ethical standards and consulting, and the open-door policy. Just makes it so you never feel worried that you will make a mistake, because a lot of people are holding you up.
When talking about the need to differentiate client staffing from clinical supervision, Brian explained that supervisors often, “don’t do supervision with their employees…or supervision is staffing. It’s the same.” He further explained, “Ideally, you have a sit-down with a person and do supervision. So they have a chance to talk about how they’re feeling, the problems they are having, in a safe place to do that.” He conceded that time constraints often hinder this process because, “there’s a lot of crisis and things come up at any given moment. So, you have a schedule, but something trumps it very quickly.” David discussed the benefits of having a positive supervisor who made time for clinical supervision with him, stating:
It was a really important part of me so when I was getting close to burnout or when I was stressed out or in a funk or whatever, I could talk to him and that kind of supervision process which was more than just once a week for an hour. It was more of an as needed kind of a thing and was very, very helpful. It was more than just clients, so it was very helpful for personal growth and so I was totally happy to have that.
Participants described time constraints as significant barriers to their wellness and consequently their ability to provide the best care to clients. However, they also discussed how access to human resources (e.g., supervisors) can positively influence their sense of wellness and development.
Occupational Hazards
A second theme that emerged was occupational hazards. This theme involved the psychologically intense characteristics of the work itself that threaten wellness and included concepts such as empathy fatigue, vicarious traumatization, depersonalization, lack of meaning and wounded healing. Participants discussed the challenges of helping difficult clients while attempting to maintain their own wellness.
One participant, Peter, discussed his struggle to not personally take on too much of the clients’ concerns. He stated that:
I think the biggest challenge that I’ve faced, and I can’t say this challenge is gone to this day, is that I took on a lot of my clients’ stuff. You know, you hear as a counselor you develop empathy for your clients with their challenges and their stories and experiences can be very traumatic and you know can be very impactful. So I think the biggest thing that I had that was impactful is I feel I would take on a lot and I would feel a lot more of what others struggled to face, as opposed to be there in the moment and then walk away from it… That was something, if you think about wellness as this bubble around me and that bubble keeps me from taking on too much of people’s stuff and keeps me mentally and personally safe, then my wellness was gone, the bubble was gone.
Another participant, Anne, discussed the burden that builds when occupational hazards are ignored by the agency and/or supervisors:
A lot of vicarious trauma, grief trauma left unprocessed. When a patient dies it is like—okay next. My administrator actually said that we assume you are coming in with the clinical skills and you will take care of yourself with that. There is no facilitative process or it is not acknowledged in our agency—that it could be happening to us as counselors. We are not given a moment to have that time. [The administrators say] be sure your taking care of yourselves out there—it is sort of you take care of yourself out there.
Yet another participant, David, discussed how the quick client turnaround in the inpatient facility led him to question the value and meaning in his work when he stated:
It was a lot of treat and street, so in other words they come in, you’re basically working on discharge paperwork from the first day you meet them, so you are already thinking about where they need to go…I mean they had lost everyone else in their lives and they felt isolated and alone, so the relationship was incredibly crucial and I think most people would agree that the relationship is the most important part of the counseling process, and you can’t build a relationship if basically when they are coming in you are looking at the chart trying to get the form filled out and trying to get them out the door because either insurance won’t pay or it’s a bed that needs to be emptied out so it can be filled with someone who can maybe last longer.
David went on to discuss his resulting emotions:
There is almost like this shame/guilt you are kind of feeling or struggling with where you feel like you can’t seem to get anywhere, or I am not doing anything, or what am I doing…Am I helping?…Does this matter? And I think that once you have lost that meaning in your work, that passion for what you are doing then it just kind of all, it’s a sinking ship at that point and wellness is just kind of out the window, you just get frustrated.
Participants also discussed the potential setbacks that can occur when professional counselors over-identify with their clients (e.g., wounded healer). Helen comments on how unfinished business unfolds in an agency:
It isn’t quite a straight line. In other words, it is whatever the underlying energy of the agency that draws people in. If people come and then they go, they may not relate to it, but those people who stay for a while, for [more than] three years, that is an issue. You have to constantly reflect back ‘why am I here?’ What is it about this job that has pulled me here and what is it that I need to learn. I think you could stay in the field and never reflect or heal from anything.
One participant, Romie, who also does clinical supervision, discussed the importance of processing empathy fatigue and often spends her time processing the “heaviness of the work.” She responded that “managing the occupational hazards is a matter of keeping the counselors happy…if they are happy and they feel good, and if they feel rewarded in their work they are going to produce and stay.”
Participants discussed that intense and emotionally close work they do with clients is a potential barrier to their wellness. They alluded to the need to set personal boundaries while still finding meaning in their work. Additionally, participants discussed needing time to process the emotions that may arise.
Agency Culture
The next theme that emerged was agency culture. The participants expressed that the messages the administration convey as well as the morale of the agency often influence their sense of wellness. Participants discussed wanting to feel valued and respected by their agency. Sarita stated that she felt valued by her agency. When she was asked how that message was conveyed to her, she replied:
I have been made to feel okay about my developmental level, just…you know…. normalizing my learning level. Everyone can speak up about what their opinion is, even if they are new, you feel part of the team. You know you have been selected for a reason to work here. They have confidence in you and they remind you of that.
Romie paralleled Sarita’s statement:
I happen to believe that wellness comes from the agency itself through feeling valued as an employee, [when] someone hears you in the company and that you have a voice. Having a sense that you say things and that they are respected. Feeling like that if there is anything that the company could do to help, they would. People feel happier, more rewarded and better. What that is in an agency I think is different for each one. It is more of a relationship and personal style.
Brian discussed the value when agencies respect the employees’ need to take care of their family:
Most of the programs that I’ve been in—they are more than willing to let you take care of your family as long as you are doing your job. That’s been the biggest piece I think from a wellness standpoint is the understanding of that from the top.
Participants also discussed how the overall morale of the agency and coworker relationships influence their sense of wellness. For example, Helen commented on how one of her previous places of employment communicated messages of wellness through promoting coworker relationships:
A lot that has to do with the attitude with the people running the place, what they valued, that fact they were invested in relationships. They realized we have to have connection with each other in order to give support to do the work here.
Similarly, Peter discussed how he believed staff cohesion plays a role in wellness:
My experience is that when there is a sense of cohesion, a sense of togetherness and teamwork, I think that people get along better and there’s a natural well, not well, but a natural happiness that goes along with it. My experience, where I’ve had the most stable or happy wellness have been places that encourage staff meals or having staff getaways, or doing events that brought the staff together to enjoy one another…not to work, but just to be around one another and enjoy one another and support one another.
Participants also discussed how agency directors and supervisors directly advocate for self-care. Catherine commented about self-care and wellness:
There is an encouragement for self-care. It is double-binded, you have to get your stuff done, but you know it is like it is Friday, let’s go home. They encourage each other to work less and have fun. Other places (agencies) had more pressure to get it done. There is a consciousness of balance.
Peter also discussed positive feelings when his supervisor supported his self-care efforts, “There was one day there was an accumulation of things, a combination of feeling sick, but also in the middle of a stressful time…he said go home, have a great day. So he was in support of wellness.” Peter continued, “he understood the job is not always easy and can bring on a lot of stress and he was willing to let us take care of ourselves if we needed to.”
Overall, when the agency promoted the respect and value of professional counselors and encouraged counselors to have a voice and affect change, it promoted the counselors’ own sense of wellness. Furthermore, sensing an investment in work relationships and promoting a work-life balance influenced the wellness of these counselors.
Individual Differences
The final theme that emerged involved the different perspectives of the participants and how that influenced their feelings of wellness. Two participants from the same agency held very different feelings about how their agencies influenced their sense of wellness. Jill felt very positive about her agency and spoke of the many financial incentives and freedoms allotted and that the agency’s independent scheduling fit her. Anne also mentioned the same financial incentives, but believed that she received negative mixed messages and that her wellness was being negatively affected by the same agency. Conversely, Jill, who felt positive towards her agency, noted, “No one had to tell me to take care of myself.” David also expressed that wellness is often left up to the individual; when speaking about one of his agencies he stated, “it wasn’t really like it was a place of wellness. Wellness is something that happened, or self-care happened long after you left.” Romie responded about her intentionality with wellness:
Personally, what I do is many things. I exercise; I make sure I get plenty of sleep. I take time for myself when I need to. I will do yoga and meditate and do a lot of reading and I am highly spiritual. I have a wonderful home-life, a very supportive love-mate in my life. I am really in a good place.
Throughout the interviews, the participants discussed very different values in terms of their wellness. Some of the participants mentioned spiritual practice and journaling as being important in maintaining wellness. Others expressed time with family as being most important, whereas others discussed setting clear boundaries or finding meaning in their work.
Other participants discussed how wellness initiatives within their agencies often seemed inconvenient to them. When talking about a discounted gym membership that was offered, Brian viewed the offer as superficial, saying “in my experience, most of what they offer in terms of wellness is, in my experience, is somewhat superficial.” He further stated, “Very few people are able to utilize the gym membership because of the hours they work and where it’s located and the cost is still too high for the employees.” Peter discussed the positives and negatives of a wellness initiative:
The book was a 40 week-by-week event where you learned about wellness…physical, mental, spiritual; all these different components. The problem was they had these events that took place scattered all over the district and so for anyone to attend them, they would have to drive half an hour to 45 minutes to attend them and which if you’re trying to have a good basis for wellness, then having people drive 45 minutes after a long day of work is not a good place to start for that.
However, Peter acknowledged that this may be only his view, stating:
The planning of the events I felt could have been better. And of course, not to say other people didn’t go to them and find them successful, but it was just my experience of do I go home or drive 45 minutes then attend a 2-hour meeting on nutrition. I felt like going home was more beneficial for me at that time.
These statements reveal that professional counselors may value different things related to wellness. Other counselors in Brian or Peter’s agency may have appreciated the wellness initiatives.
The participants responded differently in terms of wellness values. One cannot overlook how different individuals will react to the stress of being a counselor. Knowing what type of atmosphere is the best fit for the counselor’s personality and interests can factor in overall well-being. Romie commented, “It is good to know what kind of atmosphere is the best fit for you, if you love it, then that is your wellness, if you don’t, then nothing you do will ever click.”
Discussion
The findings in this study suggest that the environment in which the participants work may play an important role in their overall wellness. This finding is consistent with previous research that suggested agencies directly affect well-being and satisfaction of counselors (Knudsen, Ducharme, & Roman, 2006; Lloyd, King, & Chenowith, 2002; Maslach, 1982, 1986). Participants in this study discussed lack of resources as potential barriers to wellness including unsatisfactory salaries, large caseloads, heavy paperwork and lack of supervision. This finding is consistent with previous research that maintaining caseloads above 15 per week increases chances of occupational hazards (Trippany, Kress, & Wilcoxon, 2004). Additionally, counselors have reported increased salaries as directly relating to their wellness (Bell et al., 2003), and comprised a major setback for counselors in this study. Further, our findings support previous research that poor supervision, little to no peer-to-peer conversations, low salaries, heavy paperwork, lack of control over services and managed care influences are all correlated with decreased wellness and increased likelihood of burnout (Ackerly, Burnell, Holder, & Kurdek, 1998; Gaal, 2009). Clients deserve to receive the best care possible in agencies; therefore, funding sources should be aware of what counselors specifically need to function at their best. However, it is the responsibility of all counseling professionals to organize and advocate for gains such as salary increases, caseload limits, qualified supervisors, and funding for wellness activities. Advocating through joining local, state and national organizations is one way to work toward these goals, as organizations stay abreast of current legislative changes and locate opportunities to improve the counseling profession.
The finding in this study that occupational hazards influenced counselors’ wellness is consistent with previous literature (Skovholt, 2001; Stebnicki, 2007). Additionally, participants in this study discussed the importance of supervision and processing time in order to work through such hazards. This finding reinforces the importance of supportive environments where counselors can obtain peer support and adequate supervision. Consequently, counselors’ wellness may be increased when agencies have consistent treatment-team meetings and supervision sessions, where counselors have an opportunity to process their work with others and obtain consultation. Additionally, supervisors should have appropriate training in supervision to ensure that a quality supervision experience occurs.
Participants in this study expressed that the culture of the agency influenced their sense of wellness. Factors that positively influenced them included feeling valued by administrators, feeling that they had a voice, being respected and feeling cohesion with coworkers. Agencies may assist in counselor wellness by developing employee committees that provide a forum for counselors to express concerns and provide recommendations to the agency. This may help to foster a sense of value among the counselors when their perspectives are heard. Additionally, employee committees may serve to organize wellness activities and professional development opportunities for the staff, encourage peer support and cohesion, and organize advocacy efforts.
Implications for Professional Counselors
The findings in this study suggest that one’s wellness is very personal and is heavily influenced by personally salient values. In this study, the participants mentioned different wellness values. Individually, counselors can develop holistic wellness plans and gain self-knowledge concerning what aids them in performing at their best, while considering the realities of their work environment and resources that are available to them. Counselor educators can model wellness activities and highlight the resilience that stems from a comprehensive wellness plan so new professionals are prepared to attend to wellness when they enter the field. Counselor educators also should educate counselor trainees as to the realities of agency work (e.g., caseloads, paperwork, difficult clients) so they can prepare themselves mentally to enter the system. Counselors and clinical directors can vocalize ways to enhance the well-being of the atmosphere in the agencies by advocating for reasonable caseloads and encouraging wellness days for the staff (e.g., days where the entire staff rejuvenates together through team building or other enjoyable workshops or activities). Given that funding is often mentioned as a factor that influences wellness, agencies and individual counselors may benefit from learning how to secure various types of grants to assist with resources (e.g., additional staff, technology, wellness initiatives). Additionally, agencies may benefit from developing ad-hoc committees that will evaluate processes and procedures (e.g., paperwork, documentation) to potentially reduce workloads and ensure that counselors’ time is used efficiently. Finally, counselors should be proactive in seeking out further training in wellness, self-care and burnout prevention through conferences (e.g., ACA, AMHCA) or other professional development opportunities, and should advocate that their agencies provide these types of trainings.
Limitations and Future Research
Despite the depth and richness of information obtained in this exploratory study, there are multiple limitations. First, we did not spend prolonged time in the field in order to gather further data about wellness practices through observation or document analysis. Future researchers may benefit from direct observations of wellness practices in the natural setting. Additionally, we only utilized one source of data for interpretation (i.e., interview/focus group) which may have affected the depth of information obtained. Finally, although generalizability is not a major goal of qualitative research, readers should be mindful that the findings may not be representative of other counselors in different settings.
Future researchers could explore wellness experiences of more diverse racial/ethnic groups and those at various income levels. Additional studies may include more prolonged engagement in the field by the researcher in order to make observations about wellness practices as well as multiple data sources (e.g., observations, questionnaires, reflective journals). Other studies may include agencies that are currently implementing specific wellness practices in order to evaluate their effect on counselor wellness. Finally, future researchers may benefit from identifying particular agencies that maintain effective wellness practices and exploring them through in-depth analysis.
Conclusion
Counselor wellness is an important aspect of ensuring effective and ethical services to clients (ACA, 2010; NBCC, 2005). The findings in this study provide some initial information about the various aspects of wellness that may be influenced by professional counselors’ work environment. Although agencies may not be able to immediately change all aspects of the work environment (e.g., salary, caseloads, work hours), other aspects such as agency culture and adequate supervision are easier to address. Counselors and clinical directors may benefit from evaluating their current wellness practices through staff questionnaires, focus groups, or needs’ assessments. Attending to professional counselors’ wellness needs may help to improve the morale in the agency, help counselors avoid burnout, and ensure more quality care for clients.
References
Ackerly, G. D., Burnell, J., Holder, D. C., & Kurdek, L.A. (1988). Burnout among licensed psychologists. Professional Psychology: Research and Practice, 19, 624–631.
American Counseling Association. (2005). ACA code of ethics. Alexandria, VA: Author. American Mental Health Counselors Association. (2010). AMHCA code of ethics. Author.
Bell, H., Kulkarni, S., & Dalton, L. (2003). Organizational prevention of vicarious trauma. Families in Society: The Journal of Contemporary Services, 84, 463–470.
Cain, D. J. (2001). Defining characteristics, history, and evolution of humanistic psychotherapies. In D. J. Cain & J. Seeman (Eds.), Humanistic psychotherapies: Handbook of research and practice (pp. 3–54). Washington, DC: American Psychological Association.
Creswell, J. W. (2007). Qualitative inquiry and research design: Choosing among five traditions (2nd ed.). Thousand Oaks, CA: Sage.
Creswell, J. W. (2009). Research design: Qualitative, quantitative, and mixed methods approaches (3rd ed.). Thousand Oaks, CA: Sage.
Ducharme, L. J., Knudsen, H. K., & Roman, P. M. (2008). Emotional exhaustion and turnover intention in human
service occupations: The protective role of coworker support. Sociological Spectrum, 28, 81–104. doi:10.1016/j.jsat.2006.04.003
Figley, C. R. (2002). Treating compassion fatigue. New York, NY: Routledge.
Gaal, N. (2009). Comparing burnout levels experienced by therapists working in a mental health organization versus therapists working in private practice. (Doctoral dissertation). Retrieved from ProQuest. (3360424)
Glesne, C. (2006). Becoming qualitative researchers (3rd ed.). Boston, MA: Pearson Education.
Knudsen, H. K., Ducharme, L. J., & Roman, P. M. (2006). Counselor emotional exhaustion and turnover intention in therapeutic communities. Journal of Substance Abuse Treatment, 31(2), 173–180. doi:10.1016/j.jsat.2006.04.003
Lambie, G., & Young, M. E. (2007). Wellness in school and mental health systems: Organizational influences. Journal of Humanistic Counseling, Education and Development, 46, 98–113.
Lawson, G. (2007). Counselor wellness and impairment: A national survey. Journal of Humanistic Counseling, Education and Development, 46, 21–34.
Lawson, G., & Venart, B. (2005). Preventing counselor impairment: Vulnerability, wellness, and resilience. In G. R. Walz & R. K. Yep (Eds.), VISTAS: Compelling perspectives on counseling 2005 (pp. 243–246). Alexandria, VA: American Counseling Association.
Lloyd, C., King, R., & Chenoweth, L. (2002). Social work, stress and burnout: A review. Journal of Mental Health, 11, 255–265. doi; 10.1080/09638230020023642
Maslach, C. (1982/2003). Burnout: The cost of caring. Cambridge, MA: Malor Books.
Maslach, C. (1986). Burnout research in the social services: A critique. Journal of Social Service Research, 10, 95–105.
Maslach, C., Leiter, M.P., & Schaufeli, W.B. (2008). Measuring burnout. In Cooper, C.L., Cartwright, S. (Eds), The Oxford handbook of organizational wellbeing (pp. 86–108). Oxford: Oxford University Press.
McCann, I. L., & Pearlman, L. A. (1990). Vicarious traumatization: A framework for understanding the psychological effects of working with victims. Journal of Traumatic Stress, 3, 131–149. doi: 10.1007/BF00975140
Muhr, T. (2004). ATLAS.ti 5.0 (Version 5:). Berlin, Germany: ATLAS.ti Scientific Software Development GmbH. Available from http://www. Atlasti.com/
Myers, J. E., Sweeney, T. J., & Witmer, J. M. (2000). The wheel of wellness counseling for wellness: A holistic model for treatment planning. Journal of Counseling & Development, 78, 251–266. Retrieved from http://aca.metapress.com/link.asp?id=pxpkullf5qnetnax.
National Board for Certified Counselors (2005). NBCC code of ethics. Greensboro, NC: Author.
Pines, A., & Maslach, P. (1978) Characteristics of staff burnout in mental health settings. Hospital and Community Psychiatry, 29, 233–237.
Rupert, P., & Morgan, D. (2005). Work setting and burnout among professional psychologists. Professional Psychology: Research and Practice, 36, 544–550. doi: 10.1037/0735-7028.36.5.544
Shapiro, S., Brown, K., & Biegel, G. (2007). Teaching self-care to caregivers: Effects of mindfulness-based stress reduction on the mental health of therapists in training, Training and Education in Professional Psychology, 1, 105–115. doi: 10.1037/1931-3918.1.2.105
Skovholt, T. M. (2001). The resilient practitioner: Burnout prevention and self-care strategies for counselors, therapists, teachers, and health professionals. Boston, MA: Allyn & Bacon.
Stebnicki, M. (2007). Empathy fatigue: Healing the mind, body, and spirit of professional counselors. American Journal of Psychiatric Rehabilitation, 10, 317–338. doi:10.1080/15487760701680570
Stokes, G., Henley, N. & Herget, C. (2006), Creating a culture of wellness in workplaces. North Carolina Medical Journal, 67, 446–448.
Teddlie, C., & Fen, Yu (2007). Mixed methods sampling: A typology of examples. Journal of Mixed Methods Research, 1, 77–100. doi: 10.1177/2345678906292430
Trippany, R. Kress, V., & Wilcoxon, S. (2004). Preventing vicarious trauma: What counselors should know when working with trauma survivors. Journal of Counseling & Development, 82, 31–37.
Vredenburgh, L., Dale , C., Alfred, F., & Stein, L. B.(1999). Burnout in counseling psychologists: Type of practice setting and pertinent demographics. Counselling Psychology Quarterly, 12, 293–302. doi: 10.1080/09515079908254099
Witmer, M., & Young, M. E. (1996). Preventing counselor impairment: A wellness approach. Journal of Humanistic Counseling, Education, & Development, 34, 141–156.
Jonathan H. Ohrt is an Assistant Professor at the University of North Texas. Laura K. Cunningham, NCC, is an Assistant
Professor at Argosy University. Correspondence can be addressed to Jonathan H. Ohrt, University of North Texas, 1155 Union Circle #310829, Denton, TX 76203, jonathan.ohrt@unt.edu.
Appendix
Participant Demographics
Name (pseudonyms were assigned) Type of Facility Gender Age Race Experience in Field Interview Method
Anne
Palliative Care Facility
Female
37
Caucasian
11 Years
Individual
Jill
Palliative Care Facility Female 40 Caucasian 2 Years Individual
Helen
Clinical Director for Domestic Violence Shelter and Community Counseling Center Female 45 Caucasian 13 Years Individual
Romie
Clinical Director of an Adolescent Residential unit
Female 53 Caucasian 20 Years Individual
Fatin
University Counselor
Female 27 Caucasian/Middle Eastern 1 Year Focus Group
Catherine
University Counselor
Female 28 Caucasian 9 Months Focus Group
Sarita
University Counselor
Female 33 East Indian 1 Year Focus Group
David Behavioral Hospital Male 29 Latino 3 Years Individual
Peter Inpatient & Residential Male 28 Caucasian 3 Years Individual
Brian Adolescent Residential Male 38 Caucasian 13 Years Individual
Sep 1, 2014 | Article, Volume 1 - Issue 3
Danica G. Hays, Rebecca E. Michel, Rebekah F. Cole, Kelly Emelianchik, Julia Forman, Sonya Lorelle, Rebecca McBride, April Sikes
Despite the prevalence of dating violence, incidences often go unreported due to a lack of awareness among students as to appropriate dating behaviors. This phenomenology investigated how adolescents conceptualize and experience dating relationships. We explored adolescent females’ definitions of healthy and abusive relationships, experiences with unhealthy relationships, and responses to dating violence in order to develop effective strategies to intervene with this population. Implications for school counseling and mental health counseling practice, training, interventions and future research are discussed.
Keywords: dating violence, adolescent, female, school counseling, mental health counseling, interventions
Dating violence, which involves actual or threatened emotional, physical, and/or sexual abuse within a dating relationship, has become an increasing concern among counselors working with adolescent populations (Craigen, Sikes, Healey, & Hays, 2009; Hays, Green, Orr, & Flowers, 2007). There are significant mental, physical and behavioral consequences of adolescent dating violence, including depression, anxiety, PTSD, suicidal ideation, poor self-concept, disordered eating, substance use/abuse, risky sexual behavior, and school disengagement (Ackard & Neumark-Sztainer, 2002; Banyard & Cross, 2008; Howard, Beck, Kerr, & Shattuck, 2005; Howard, Wang, & Yan, 2007; Masho & Ahmed, 2007; O’Keefe, 2005; Silverman, Raj, Mucci, & Hathaway, 2001). Due to the severity of negative health outcomes, it is imperative for counselors to understand the experiences of adolescents to facilitate early intervention with this at risk population (Hays et al., 2007). Few studies have given voice to the individuals themselves.
Dating serves as an important developmental milestone as individuals come to understand social and relational goals. For many, dating begins in adolescence, with an estimated 72% of 11- to 14-year-olds dating before age 14 (Teen Research Unlimited, 2008). Unfortunately, young adolescents may be unaware how to behave in a dating relationship, so they are vulnerable to inaccurate messages from their family of origin, peers and the media (Connolly, Friedlander, Pepler, Craig, & Laporte, 2010). With respect to family influences, many individuals are socialized that violence is a normal and appropriate response to conflict in intimate family relationships (Hays et al., 2007). Adolescents living in urban communities or experiencing socioeconomic disadvantages may be exposed to increased levels of family and community violence (Banyard, Cross, & Modecki, 2006; Vézina & Hébert 2007). Compared with their peers, female and male adolescents with a history of family violence are at a greater risk of dating violence victimization and perpetration, respectively (Laporte, Jiang, Pepler, & Chamberland, 2011).
Peers and media also influence behaviors and attitudes. Research suggests between 50 to 80% of adolescents report knowing friends who were involved in dating violence (Ashley & Foshee, 2005; Halpern, Oslak, Young, Martin & Kupper, 2001; Teen Research Unlimited, 2008). Adolescents with friends who experience dating violence are more likely to perpetrate violence against their dating partner (Foshee, McNaughton, Reyes, & Ennett, 2010). Further, media exposure may impact adolescent attitudes surrounding dating violence, specifically the belief that violence is a way to resolve relationship problems (Manganello, 2008; Rivadeneyra & Lebo, 2008). Adolescents who prefer aggressive media such as physical or verbal violence in television, movies, music and video games are likely to exhibit violent relationship patterns (Connolly et al., 2010). When faced with fictional dating situations, the majority of young adolescents resorted to aggressive conflict resolution techniques, such as fighting (Prospero, 2006).
Adolescent perceptions of social dating norms (Sears & Byers, 2010) as well as mental health issues may also impact students’ exposure to dating violence. There is a direct relationship between tolerant attitudes toward violence and becoming a physically violent dating partner (Josephson & Proulx, 2008). Female aggression against peers and depression have also significantly predicted dating violence perpetration (Foshee et al., 2010). Clearly, there are many environmental and personal factors that contribute to relationship violence.
Dating violence is often under reported because students lack awareness about appropriate dating behaviors (Hays et al., 2007; Lewis & Fremouw, 2001). Adolescents may be reluctant to disclose dating violence to adults for fear of a possible confidentiality breach, personal denial of the situation, labeling harmful behaviors as “love” and fear of repercussion from the violent partner (Close, 2005). Others may believe disclosure would impact their academic performance or lead to disciplinary issues (Moyer & Sullivan, 2008). Survey data indicate that dating violence prevalence rates range from 21 to 80%, depending on type of violence (Cyr, McDuff, & Wright, 2006; Harned, 2002; Holt & Espelage, 2005; Sears & Byers, 2010; Wolitzky-Taylor, Ruggiero, Danielson, Resnick, Hanson, & Smith, 2008).
A majority of research indicates that female and male adolescents are equally likely to experience dating violence (Ackard & Neumark-Sztainer, 2002; Sears, Byers, & Price, 2007; Schnurr & Lohman, 2008). While both males and females experience dating violence, research suggests violence has a greater impact on females than on males (Cleveland, Herrera, & Stuewig, 2003). Sears and Byers (2010) found adolescent females report a stronger emotional reaction to dating violence than their male peers. Thus, it is important to assess female adolescent reactions to dating violence.
There is limited research that explores dating violence perceptions and experiences of young adolescents. Previous qualitative studies have either been retrospective or involved adolescents 14 and older. One retrospective study (Draucker, et al., 2010) sought to classify typical violent events within adolescent relationships by interviewing young adults about dating violence experienced between 13 and 18. Draucker and colleagues (2010) also found that jealousy and relationship threats often led to threatening and controlling events in the future. Communication problems, such as an inability to express feelings, often led to additional disagreements among dating partners. Livingston, Hequembourg, Testa, and VanZile-Tamsen (2007) found women who had been sexually victimized as adolescents reported the following areas of vulnerability may have contributed to their victimization: lack of guardianship, inexperience with dating, substance use, social and relationship concerns and powerlessness.
In addition to retrospective studies, other researchers have explored older adolescents’ experiences with dating violence. Lavoie, Robitaille, and Heberts (2000) interviewed individuals between ages 14 and 19 about their dating relationships. Participants provided examples and reasons for teen intimate partner violence. The young adults explained that physical abuse was usually aimed at provoking fear in the victim. Psychological abuse often included gossip and was meant to be damaging to adolescents’ reputations. While participants generally viewed perpetrators negatively, some viewed their own violent behavior as acceptable. For example, females believed using violence in self-defense was preferred over being hurt without reciprocation. Aside from self-defense, other reasons given for abuse included: jealousy, need for power, substance use, previous violent relationships, communication problems, and need for affiliation.
Other researchers explored perceptions of dating violence among females ages 15 to 17 living in Thailand (Thongpriwan & McElmurry, 2009). Major themes that emerged included (a) descriptions of adolescent relationships, (b) influences on relationships, (c) perceptions of dating violence, (d) cycle of dating-violence experiences, and (e) influences on adolescent perceptions of dating violence. The majority of participants were 17, and the authors indicated that younger students may have different views and experiences (Thongpriwan & McElmurry, 2009).
Information gathered from qualitative studies provides researchers with information about perceived risk factors and perceptions of violence, which can aid in the development of age and culturally appropriate interventions to reduce dating violence. Adolescence is an optimal time to intervene with education and skills to promote healthy dating relationships (Collins & Sroufe, 1999) and school and community counselors are well-positioned to help adolescents navigate these relationships (Davis & Benshoff, 1999; Hays, Craigen, Knight, Healey, & Sikes, 2009). To develop effective interventions, researchers must further understand the context of adolescent dating violence. In addition, counselors must be knowledgeable about dating violence indicators, peer influence, and adolescent opinions about healthy and abusive dating relationships in order to appropriately intervene in potentially harmful dating situations (Craigen et al., 2009).
While many adolescents begin dating before age 14, no previous studies to date have explored how adolescents perceive and experience dating relationships. The purpose of this phenomenological study was to capture the essence of young adolescent female conceptualizations and experiences of intimate partner relationships and potentially identify counseling interventions. The following research questions were explored: (a) How do young adolescent females conceptualize healthy and abusive dating relationships? (b) What experiences do young adolescent females identify related to unhealthy relationships? and (c) What methods do young adolescent females identify as helpful in preventing and intervening in dating violence?
Method
Participants
Seven adolescent females ages 11 to 14 who had witnessed intimate violence participated in the study. Participants were recruited from a community group, and the primary researcher (first author) had a rapport with the group facilitator. The primary researcher secured parental consent and child assent for each participant. The females lived in the Mid-Atlantic region of the United States and had been acquainted with each other at least 1 year prior to the research study. Participants were from varying racial backgrounds: four identified as White/European American, two as Asian/Pacific Islanders, and one as Native American. Participant living arrangements were mixed: two lived with a mother and father, two with divorced mothers, one with a divorced father, one with a single-never-married mother, and one with a guardian after being removed from the home due to severe child neglect. Regarding current dating relationships, two participants reported dating and all identified as “liking boys.”
Measures and Procedures
IRB approval, parental consent and child assent were obtained prior to data collection. Data were collected through four independent focus group interviews averaging 45–60 minutes. The researchers utilized semi-structured open-ended questions to focus the interviews. Sample interview questions across the focus group interviews included the following: What do you think makes a good dating relationship? What do you think makes a bad dating relationship? How do you define abuse? How would you respond to abuse in a relationship? Subsequent focus group interviews were used to elaborate or clarify on responses from previous focus groups. All participants attended all focus groups. Research team members transcribed each audio-recorded focus group interview data verbatim. Focus group interviewers developed memos for each session. Participants also completed a demographic sheet that consisted of questions regarding age, race/ethnicity, gender, grade level, sexual orientation, dating behaviors and family status.
Data Analysis
Researchers bracketed their assumptions prior to beginning the study to ensure credibility of the results (Hays & Singh, 2011). Researchers assumed participants would: (a) report minimal knowledge of dating violence prevalence and characteristics; (b) describe instances when female peers were victims of dating violence; and (c) state uncertainty for intervening in dating violence. Each research team member independently analyzed the sentence transcript data using horizontalization. The research team then consensus coded to describe textures (meaning and depths) related to their experiences (textural descriptions) (Hays & Singh, 2012). A final codebook outlining four primary themes and several subthemes was developed from the recursive coding process.
The research team used several practices to establish trustworthiness throughout the study. The research team members maintained prolonged engagement with participants over the course of one year. During meetings, field notes were kept to capture data and self-reflective thoughts and feelings. Simultaneous data collection and analysis occurred in order to further explore themes in each subsequent interview. Each interview was transcribed verbatim and checked by another member for accuracy. During this time, memos were created to organize thoughts and connections emerging from each interview. Researchers provided thick description by incorporating verbatim quotes throughout the data analysis and results, providing interpretive depth and detail.
Results
The following four themes were identified: conceptualization of healthy dating relationships; conceptualization of unhealthy dating relationships; exposure to relationship violence; and dating violence interventions.
Conceptualization of Healthy Dating Relationships
Participants identified several components of healthy relationships, including honesty, trustworthiness, openness, compassion toward animals, fun, holding opposite views and attractiveness. The first component, honesty, was best described by one participant: “If you don’t know everything about that person … you are not going to be happy because you wanted to find it out from them and not someone else.” Trustworthiness was important to participants, as one stated, “you cannot really trust them if [they] are lying behind your back… I am going through that right now.” A third identified component was openness: “he has to be able to be open to what is said… like when you’re talking they’re not judging.” Compassion toward animals and nature was described by a participant: “I am a fan of people who like the earth and animals… people that abuse animals. I hate those kind.” Several participants indicated they enjoyed having fun: “I like people who can make me laugh… can take a joke.” Overall, they valued holding opposite views from their partner: “if you have a person that is different from you, then you can experience different things.” Finally, participants agreed that they looked for attractiveness in relationships: “I want someone that’s good to look at [laughs].”
Participants also identified several components of healthy relationships that related to interpersonal dynamics, including independence, security, and lack of abuse, sexual pressure and conflict. When describing healthy relationships, adolescents mentioned the importance of independence. For example, participants explained, “I need my personal time.” “[Not] always around you, always calling you, always trying to get a hold of you.” Security was also noted as a component of healthy relationships: “Don’t we date for security? Isn’t that kind of why you date? You date because you want to feel safe with someone.” Participants believed physical abuse and sexual pressure should be absent from healthy relationships. A participant explained, “I have learned that the more you get beat in the head, the more brain cells you lose and you can’t get brain cells back.” Another participant noted, “If I didn’t want to have sex then the other person wouldn’t pressure me.”
Participants supported varying views on the role of conflict in healthy relationships. Some participants believed less conflict was indicative of healthier dating relationships. One participant stated: “If you agree with someone there is less confrontation of any kind and it makes things a little bit easier.” However, approximately half of participants viewed conflict as a normal and fun aspect of relationships: “disagreeing is kind of fun because you get to debate… no one agrees on everything, so you have arguments.”
Overall, participants described characteristics of healthy dating relationships similarly to those of healthy peer and family relationships. One participant noted, “I want someone who would be nice and kind, like in any kind of relationship.” Additionally, participants noted healthy dating relationships can be fragile. For example, one participant stated, “if you don’t start it off with truthfulness, then if you are not honest the entire time then you may never actually see that person again if they find out who you really are.” Another participant noted, “like in the movies they are in a marriage and then they get divorced.” While many participants provided examples and descriptions of healthy relationships, initially 2 of the 7 participants could not clearly articulate their opinion: “I don’t know the exact definition. I can see pictures in my head but I can’t put it into words.” As the groups progressed, participants provided additional descriptions and components of healthy relationships.
Conceptualization of Unhealthy Dating Relationships
The second major theme refers to components of unhealthy romantic relationships, conceptualization of dating violence, and dating violence consequences. Participants believed certain components perpetuated unhealthy relationships, including addictions and abuse. Participants reported a connection between unhealthy relationships and addictions. For instance, one participant suggested “you shouldn’t sell her wedding ring for drugs, and don’t get addicted to drugs or cigarettes or anything.” Another participant stated “one time he told her that if he had to choose he said he would choose drugs over his own children.” In addition to addiction, participants indicated abuse served to facilitate unhealthy relationships. One participant discussed how one of her friends was recently a victim of dating violence and as a result ended the relationship. She indicated, “Unhealthy would definitely be abuse, one of them cheating on the other, and unfortunately one of our girls actually had to experience that recently and she broke up with him.”
The young adolescents spent significant time conceptualizing dating violence, notably emotional, physical and sexual abuse. Emotional abuse was described as “when you’re being told that you’re worth nothing.” Another participant conceptualized physical dating violence as a male beating a female just because he can. She stated, “They can just like hurt you, they can beat you up just because…like dating, if the girl doesn’t agree with the guy if he wants to he can just, like, beat her up.” Participants also displayed knowledge of types, signs, and prevalence of dating violence. One participant suggested, “If you are going to be a victim of sexual abuse then look for signs like trying to get you to do things that you don’t want to do or touching you in a certain manner.” Another adolescent reported, “I think it is like 50 or 60% of people like experience or have couples around them that experience dating violence.”
The girls identified numerous perpetrator factors which perpetuated dating violence. Techniques to gain control over a victim included manipulation, peer pressure, and jealousy. Participants indicated perpetrators might make threats or use manipulation to force them to stay in a relationship. One participant suggested a perpetrator might say, “‘I will hurt you if you break up with me…and she says she will be forced to stay because she doesn’t want to get hurt.” Another girl stated, “he said nobody’s going to love you like I do,” displaying the incidence of manipulation and control. Participants also discussed how perpetrators might use peer pressure or isolation to stay in control. One participant said, “Sometimes they try to push you into doing things that [you don’t want to].” When asked by the facilitator why perpetrators may want to keep victims in isolation one participant suggested, “So they can get closer to you…and do more damage.” Further, participants discussed how perpetrators might try to use jealousy to control victims. One participant discussed how she experienced jealousy in a previous relationship. She shared, “He was trying to make me jealous by going out with [name] but it didn’t work.”
The young females brainstormed various consequences of dating violence. Specifically, they described what could happen to them physically, emotionally and behaviorally as a dating violence victim. One participant discussed physical consequences victims may face. She stated, “[one] could, um, get diseases, AIDS, you could get hurt.” Another participant explained, “you could, you could, die” demonstrating the perceived severity of victim consequences. Another participant reported the danger of abuse, “those that are exposed to emotional abuse, they could possibly have, like if they are being told they’re too fat, they could possibly become anorexic.”
When referring to the types of emotions victims may experience, one participant stated, “mixed emotions that you have like sometimes you’ll be sad, and sometimes you’ll be mad, sometimes you’re actually hurt.” Participants indicated victims may turn to substance use to relieve their pain. One participant stated: “they drink because they have a lot of stress. Sometimes people smoke and do drugs because they have too much stress on them and they do it to relieve the stress.” Participants also recognized the consequence of victim self-blame. One participant stated, “I think I know why they would blame themselves because they let themselves be attacked and they could have gone and tried to get help any chance they got.” Another participant stated, “They could have prevented it.” These statements suggest participants perceive dating violence to be the victim’s fault. Participant conceptualizations of perpetrator factors included jealousy, threats and manipulation, isolation, peer pressure, and exposure to violence within the family of origin. Victim consequences associated with dating violence were identified as physical consequence (e.g., disease, AIDS), emotional consequences (e.g., depression, suicide), body image issues, substance use, self-blame, and fear of others.
Exposure to Relationship Violence
Exposure to relationship violence refers to the experiences one has with violence, including witnessing physical, sexual, or emotional violence within the family of origin, media, within the community, and in one’s peer groups. Participants reported violent acts between parents, siblings, and/or relatives. One participant indicated,
Something that happened recently between my brother and my dad, um, my dad
actually threatened to hurt my brother, and, and, so my brother kind of took a hammer
just in case, just in case, cause he wouldn’t hit my dad unless he really needed to and then he left for 2 days but we knew where he was so, or I knew where he was.
Many participants noted exposure to violence in the media, including the witnessing of violence via the television, magazines, the internet, and pop culture. One participant provided an example within pop culture, “what about [two pop stars], she was mad about what he did but…..I think it’s her fault.” Another example of media exposure to violence came from television, “the thing where someone is growing up in an abusive house dating someone from a less hostile home, like it’s um, kind of sounds like [two characters] from Secret Life [television show].”
In addition to pop culture and media exposure to violence, participants reported exposure within the larger community. This includes violence that takes place within neighborhoods and the larger community. For example, one participant shared:
I’ve actually witnessed, like on the corner [near my house] … [The] guy in the relationship keeps grabbing her and taking her back into the car… and I got close enough to be able to see and hear… she looked at me and said help me… I felt good that I helped with the situation but I felt really bad for her.
Participants also noted exposure to violence within their own peer groups, which includes the witnessing or sharing of violence that takes place among friends and peers. Participants made a number of statements, including:
And I’m not going to say names but one of our current girls actually experienced being with one of our girls’ brother. Or almost. But, I don’t know…I guess he had her pinned up against the wall or something.
In addition to peer exposure to dating violence, participants reported direct personal experience with physical, emotional, and sexual relationship violence. Participants discussed violence in dating, familial, and casual relationships. Personal experience within dating relationships includes violence perpetrated or experienced during a dating relationship. One participant shared, “One of my ex-boyfriends one time pulled a knife on me because I wouldn’t do some sexual things with him… he said nobody’s going to love you like I do.” Personal experience of violence in family of origin occurs within families where the adolescent is directly involved in the violent act. For example, one participant reported, “In my family there is a lot of yelling. It was hard because if I did one thing, he would yell at me and I was on restriction like every single day for just doing the littlest thing.” Other areas of personal experience of violence include friends and peer groups. One participant explained, “I am very fun…. I’m pretty kind but I do hit my friends. It is a joke. I don’t hurt them.”
Dating Violence Responses
The research team identified three primary themes regarding how participants recommended responding to dating violence: prevention strategies, factors influencing responses, and dating violence interventions. Participants proposed several methods to prevent dating violence. They suggested to “check your partner’s background” by doing “criminal background” checks or asking friends about their ex-partner’s behavior. It was assumed an individual’s past relationship history is indicative of future behavior. One girl suggested avoiding, “a guy who has had many ex-girlfriends.” They also discussed trusting their instincts about people and stated, “I know he’s just not the right guy. I know that something’s wrong with him, something’s going to happen.”
The participants discussed influences on responding to dating violence. Participants made statements suggesting they view reporting as dangerous. One female explained, “I know people who wouldn’t want to tell because if you go back to that person…they can hurt you even more.” Another girl stated, “What if you’re like scared to see somebody about it? Like you’re just like scared you’re going to get into trouble about it or the person who did what was wrong will come back.” Participants noted gender differences in reporting choices. For example, one participant explained, “[Girls] give in to telling people because they actually want to be safe. But boys … they probably think they’re tough.” Participants also imagined scenarios where someone may choose to not report the violence due to what their friends might think. “People might actually try to cover it up because they don’t want them to see that they are in a bad relationship.” Another participant suggested someone’s own ambivalence about the relationship could cause them to hide the violence, and stated, “They don’t want their friends to know because they might like their partner at certain times.”
While participants noted the challenge others may face when reporting relationship violence, the participants suggested they would actually tell an adult or friend about violence they experience. Several participants identified a particular adult such as a parent, aunt, uncle, teacher or police as someone they would report to. One participant indicated, “I live with someone who talks to me about it all the time. My mom…she is always talking about it.” One participant would tell a friend in order to be able to talk through the problem and stated, “She’s a good listener and that’s sometimes really all you need.”
The girls had a sense if they were not treated well the best option was to end the relationship. One adolescent stated, “If he is going to tease you, he is not right for you because your partner is supposed to be nice and loving.” Several girls suggested there would be warning signs they could respond to. One remarked, “If you sense it coming you can say I want to end it.” Participants also noted that staying may be an option, but suggested different reasons for choosing that alternative. Some participants saw hope in resolving the conflict and suggested to “talk it out” and “ask why he is mad or sad.” Another participant stated she would “try to make them happier.” Other participants suggested they would stay because they would see no other options, “So you don’t know what you’re going to do and they think you’re crazy, so you don’t know what you’re going to do, so you might just stay a little bit longer.”
The most prevalent response to intervening in dating violence included using violence themselves. They reported imagined behaviors in a violent relationship. Participants made statements including, “I always say you abuse me, I abuse you back,” and “If someone tries to, I’m just going to have to cut them.” They also discussed incidents in which they or their friends have used violence in the past to resolve conflict. One girl stated, “My friend…says she kicks guys in the ankles.” Two other participants recollected, “[I] remember almost having to kick this guy’s butt one time.”
Discussion
Findings related to participant conceptualizations of healthy and unhealthy relationships, experienced relationship violence, and potential responses to dating violence. Components of a healthy relationship included openness, trustworthiness, honesty, lack of pressure to become intimate, and humor. Participants cited attractiveness, lack of physical abuse, independence, and kindness to the environment and to animals as being important. Interestingly, participants also identified conflict as a normal component of a healthy relationship. However, participants did specify healthy relationships would have less conflict than unhealthy relationships.
Participants distinguished between healthy and unhealthy dating relationships. Adolescents believed addiction and abuse perpetuated unhealthy relationships, which is similar to previous research findings (Foshee et al., 2010; Livingston et al., 2007). As with other qualitative research, adolescents exhibited awareness of verbal abuse, emotional abuse, physical abuse and sexual abuse (Lavoie et al., 2000; Thongpriwan & McElmurry, 2009). Furthermore, participants displayed knowledge regarding the consequences of various forms of abuse, which have been well documented in the literature (Ackard & Neumark-Sztainer, 2002; Banyard & Cross, 2008). Participants noted physical, mental and behavioral consequences, such as the contraction of AIDS or death, depression, anger, body image issues potentially leading to anorexia, substance abuse and addiction, and self-blame in regards to not being able to prevent or stop an attack.
The young adolescents clearly noted the dynamics of power and control in unhealthy relationships. Participants discussed how a perpetrator could manipulate victims to stay in unhealthy relationships. Others cited that a perpetrator could threaten violence if the victim attempted to disengage. Also noted was how a perpetrator may isolate the victim, therefore reducing the chances of the victim leaving the relationship. Participant conceptualizations of unhealthy relationships mainly focused upon male to female violence and were consistent with forms of abuse and consequences cited in previous literature (Craigen et al., 2009; Cyr et al., 2006; Hays et al., 2007; Holt & Espelage, 2005; Wolitzky-Taylor et al., 2008).
Exposure to relationship violence was also a salient theme throughout the focus group interviews. Participants discussed the following personal exposures to violence: displays of violence in the media, witnessing violence in their communities, peer groups and family of origin, and personal experience with violence. Such exposure has been previously noted in the literature (Ashley & Foshee, 2005; Banyard et al., 2006; Laporte et al., 2011; Manganello, 2008). All participants in the study report exposure to violence in some situation. It is critical to note many of the participants, although aware of the consequences of violent behavior, had themselves resorted to violence. This was especially evident with the perpetration of violence against the opposite sex, which supports findings by Lavoie and colleagues (2000). Female adolescents cited examples of hitting their peers and digging their fingernails into another’s skin to gain attention or to solve a conflict. This type of violent behavior by adolescent girls is alarming, as female aggression against peers has significantly predicted dating violence perpetration (Foshee et al., 2010).
In addition to violence, participants suggested a number of strategies to intervene with dating violence, including prevention strategies, factors influencing reporting, and dating violence interventions. Prevention strategies included knowing your partner’s background, being aware of one’s own safety, and trusting one’s instincts. Consistent with previous research, participants indicated fear and reluctance to report dating violence due to either the potential for incarceration or further harm from the perpetrator (Close, 2005). The participants’ conceptualized personal interventions ranged from hitting or abusing the perpetrator back, leaving the relationship, telling someone, or hiding the violence.
Counseling Implications
This study fills a gap in the research on young adolescent conceptualizations of dating relationships. Adolescents exposed to dating violence are more likely to experience future relationship violence (Close, 2005). Thus, adolescence is an optimal time for school and community counselors to intervene to promote healthy dating relationships (Collins & Sroufe, 1999; Davis & Benshoff, 1999; Hays et al., 2009). Many adolescents are striving to form their identities within relationships. Without intervention, females experiencing dating violence might conceptualize themselves victims and seek future relationships to support this role (Klem, Owens, Ross, Edwards, & Cobia, 2009). However, supportive therapeutic interventions could assist adolescent females to learn healthy ways of relating to others (Klem et al., 2009). Counselors are in a position to recognize and respond to adolescent dating violence (Hays et al., 2009). Carlson (2003) asserted counselors working with youth must not only recognize violent actions, but also seek to understand the underlying issues causing such behavior. As counselors gain access to adolescent conceptualizations of dating violence, they can more appropriately and effectively intervene in harmful situations.
In order to screen, intervene and measure dating violence interventions, counselors must partner with school and community leaders. Standardized dating violence screening could be administered at school, in the community or with a health care provider (Close, 2005). Counselors could modify their language to encourage student disclosure of violence by asking if students have experienced specific events (e.g., disparaging events, violating events, controlling events), rather than broadly asking about abuse (Draucker et al., 2010). Counselors can monitor middle school student behaviors for warning signs of possible dating violence, including physical or emotional complaints without explanation of the problem, depression, and academic decline (Close, 2005). Students experiencing dating violence often have difficulty concentrating and learning in school, as dating violence is most prevalent among adolescents earning low grades (Eaton, Davis, Barrios, Brener, & Noonan, 2007; Howard, Wang & Yan, 2007). When behavioral and emotional changes are witnessed, individuals can be assessed to determine if they are experiencing relationship violence and counselors can intervene accordingly (Draucker et al., 2010).
There is no widely accepted intervention strategy to combat young adolescent dating violence in the schools. However, school counselors can rely on empirically tested prevention and intervention programs to target populations based on dating violence risk. School counselors could develop a three-tier model of support which includes (a) universal prevention programming offered to all students, (b) peer education and classroom guidance for individuals at moderate risk, and (c) support groups, individual response services and referrals for adolescents at the highest risk for dating violence (O’Leary, Woodin, & Fritz, 2006). Since adolescent dating violence is a problem with significant mental and physical health consequences, many prevention programs have been developed to target this vulnerable population (Draucker et al., 2010). Most dating violence prevention programs universally target middle or high school students in a brief, school-based venue (Whitaker et al., 2006). Empirically tested programs strive to increase participant knowledge about dating violence, levels of abuse, warning signs, and community resources using didactic and process-based learning (O’Leary, Woodin, & Fritz, 2006). Such programs alert participants to the deleterious impact dating violence has on both perpetrators and survivors, such as increased mental health issues, substance use and school disengagement (Ackard & Neumark-Sztainer, 2002; Banyard & Cross, 2008; Howard et al., 2007; O’Keefe, 2005). Several programs also incorporate communication and conflict management strategies. Student perceptions of dating violence can be discussed through such school-wide initiatives. Adolescents place a high value on peer and dating relationships; thus, they may be more motivated to develop skills to improve their relationships (Davis & Benshoff, 1999). While many prevention programs demonstrate increases in participant knowledge about dating violence, most do not measure or report significant behavioral change or target at-risk populations (O’Leary, Woodin, & Fritz, 2006). Thus, at-risk students would benefit from additional school counseling interventions.
At the next level of support, counselors could offer peer-support programs and classroom guidance lessons to teach students healthy strategies to interact with peers and partners without resorting to relationship violence (Weisz & Black, 2010). Peer education programs might include didactic presentations, skits, art, creative writing, and public service announcements. Benefits to this modality include peer role-modeling and personal knowledge of effective ways to target peers. However, coordinating peer education programs may be time consuming and require close monitoring in order to be effective (Weisz & Black, 2010).
Classroom guidance interventions for middle school students should be age-appropriate and culturally sensitive, utilizing multiple learning modalities including role-plays, art projects, and interactive games (Close, 2005). The young females in this study affirmed that media outlets impact adolescent attitudes around violence, and research has shown a relationship between tolerant attitudes and perpetrating violence (Connolly et al., 2010; Josephson & Proulx, 2008; Manganello, 2008). Thus, counselors could initiate a dialogue to assess adolescent attitudes about violence by listening to clips from movies, television shows and popular music. Students could brainstorm dating violence prevention and intervention strategies through participation in interactive games. The young females in this study suggested knowing your partner’s background, being aware of one’s own safety, and trusting one’s instincts. The school counselor could discuss the pros and cons of each strategy in order to correct less effective strategies offered, such as resorting to violence or hiding the abuse.
As the interviews suggested, adolescents lack effective communication skills and are likely to resort to aggressive or avoidant strategies to handle conflict (Draucker et al., 2010; Prospero, 2006). These young females could benefit from communication and conflict resolution skill training. Additionally, many young adolescents have friends experiencing dating violence and report relying on peers for support rather than disclosing dating violence to adults (Ashley & Foshee, 2005; Close, 2005). Thus, young adolescents must be prepared with how to appropriately respond when a friend is in trouble. Adolescents may not know how to support their friends, as individuals in this study discussed self-blame as an acceptable response to dating violence. Females often report a stronger emotional reaction to dating violence than males, so it would be important to assess their reactions to possible abuse (Sears & Byers, 2010). Counselors could encourage students to participate in interactive skits with fictional dating scenarios to explore healthy conflict resolution, strategies to intervene when friends are experiencing abuse, benefits of adult disclosure and reactions to abuse.
At the most intensive level of support, school counselors would target individuals at serious risk for relationship violence. These might include individuals experiencing multiple forms of aggression, demonstrating aggression toward their peers, experiencing depression, using substances, or those with a family history of violence (Foshee et al., 2010; Laporte et al., 2011; Sears & Byers, 2010). Group and individual interventions targeted at females can address depression, self-esteem, substance use, aggression against peers, and anxiety, since these concerns are both risk factors and consequences of dating violence (Foshee et al., 2010). Counselors may offer support groups to adolescents experiencing dating violence. Rosen and Bezold (1996) implemented a school-based didactic support group to help young women (a) identify type and levels of abuse, (b) believe they are entitled to relationships without abuse, (c) discuss the personal consequences of dating violence, (d) enhance interpersonal skills, and (e) conceptualize themselves as able to make effective choices.
Individual responsive services may include motivational interviewing, social skills development, anger management and relationship therapy (O’Leary et al., 2006). Counselors could educate students about dating violence risk factors, including peer aggression and family violence. Female adolescents view peer violence as an acceptable self-defense technique (Lavoie et al., 2000). Counselors could teach adolescents about the cycle of violence and healthier techniques to resolve relationship conflict. Counselors working with those witnessing relationship violence might identify areas of strength, enhance self-esteem, and explore problem-solving strategies (Fontes, 2000). Counselors should assess students for known consequences of dating violence, including depression, anxiety, poor self-concept, suicidal ideation, PTSD, disordered eating, and substance use (Ackard & Neumark-Sztainer, 2002; Banyard & Cross, 2008; Mashow & Ahmed, 2007).
One approach counselors might utilize is existential counseling. Using this framework, adolescents could explore meaning, family of origin issues, resistance to change and other existential issues in order to ultimately create new meaning outside of the violent relationship (Klem et al., 2009). However, there are limitations to this approach, notably that adolescents must be cognitively able to discuss existential concerns and must also be committed to accept responsibility for personal choices (Klem et al., 2009). Regardless of the approach, when counselors are welcoming and willing to discuss relationship issues, they can have a lasting impact on students’ current and future relationships (Davis & Benshoff, 1999).
Limitations and Future Directions
While this research provides important information about young adolescent female perceptions of dating violence, the results must be taken into context within the limitations. An expansion of this study to explore adolescent conceptualizations of healthy relationships is warranted. This study focused on views of adolescent females and did not include the voice of males. Future studies could explore the dating perceptions and experiences of young adolescent males. Also, the sample only included seven individuals representing three ethnic groups from the same geographic region. Future research could include a more diverse sample. Study findings may not readily apply to other adolescent females, and thus additional research with various sample types and sizes is needed. Clinicians and researchers are encouraged to examine how young adolescent males and females of various demographics—as victims and perpetrators—describe and experience healthy and abusive relationships in order to effectively intervene and reduce adolescent victimization in our schools and communities.
References
Ackard, D.M., & Neumark-Sztainer, D. (2002). Date violence and date rape among adolescents: Associations with disordered eating behaviors and psychological health. Child Abuse and Neglect, 26, 455–473.
Ashley, O. S., & Foshee, V. A. (2005). Adolescent help-seeking for dating violence:prevalence, sociodemographic correlates, and sources of help. Journal of Adolescent Health, 36, 25–31.
Banyard, V. L., & Cross, C. (2008). Consequences of teen dating violence: Understanding intervening variables in ecological context. Violence Against Women, 14, 998–1013.
Banyard, V. L., Cross, C., & Modecki, K. (2006). Interpersonal violence in adolescence: Ecological correlates of self-reported perpetration. Journal of Interpersonal Violence, 21, 1314–1332.
Carlson, L. A. (2003). Existential theory: Helping school counselors attend to youth at risk for violence. Professional School Counseling, 6, 310–315.
Cleveland, H. H., Herrera, V. M., & Stuewig, J. (2003). Abusive males and abused females in adolescent relationships: Risk factor similarity and dissimilarity and the role of relationship seriousness. Journal of Family Violence, 18, 325–339.
Close, S. M. (2005). Dating violence prevention in middle school and high school youth. Journal of Child and Adolescent Psychiatric Nursing, 18, 2–9.
Collins, W. A., & Sroufe, L. A. (1999). Capacity for intimate relationships: A developmental construction. In W. Furman, B. Brown, & B. Bradford (Eds.), The development of romantic relationships in adolescence. Cambridge studies in social and emotional development (pp. 125–147). New York, NY: Cambridge University Press.
Connolly J., Friedlander, L., Pepler, D., Craig, W., & Laporte, L. (2010). The ecology of adolescent dating aggression: Attitudes, relationships, media use and socio-demographic risk factors. Journal of Aggression, Maltreatment & Trauma, 19, 469–491.
Craigen, L. M., Sikes, A., Healey, A., & Hays, D. G. (2009). School counselors’ role in dating violence intervention. Journal of School Counseling, 7(18). Retrieved from http://www.jsc.montana.edu/articles/v7n18.pdf
Cyr, M., McDuff, P., & Wright, J. (2006). Prevalence and predictors of dating violence among adolescent female victims of child sexual abuse. Journal of Interpersonal Violence, 21, 1000–1017.
Davis, K. M., & Benshoff, J. M. (1999). A proactive approach to couples counseling with adolescents. Professional School Counseling, 2, 391–394.
Draucker, C. B., Martsolf, D., Stephenson, P., Risko, J., Heckman, R., Sheehan, D., Perkins, S., Washington, K., Cook, C., & Ferguson, C. (2010). Aggressive events in adolescent dating violence. Issues in Mental Health Nursing, 31, 599–610.
Eaton, D., Davis, K., Barrios, L., Brener, N., & Noonan, R. (2007). Associations of dating violence victimization with lifetime participation, co-occurrence, and early initiation of risk behaviors among U.S. high school students. Journal of Interpersonal Violence, 22, 585–602.
Fontes, L. A. (2000). Children exposed to marital violence: How school counselors can help. Professional School Counseling, 3(4), 231–237.
Foshee, V.A., McNaughton Reyes, H. L., & Ennett, S. T. (2010). Examination of sex and race differences in longitudinal predictors of the initiation of adolescent dating violence perpetration. Journal of Aggression, Maltreatment & Trauma, 19, 492–516.
Halpern, C. T., Oslak, S. G., Young, M. L., Martin, S. L., & Kupper, L. L. (2001). Partner violence among adolescents in opposite-sex romantic relationships: Findings from the national longitudinal study of adolescent health. American Journal of Public Health, 91,1679–1685.
Harned, M. S. (2002). A multivariate analysis of risk markers for dating violence victimization. Journal of Interpersonal Violence, 17, 1179–1197.
Hays, D. G., Craigen, L. M., Knight, J. Healey, A. & Sikes, A. (2009). Duty to warn and protect against self-destructive behaviors and interpersonal violence. Journal of School Counseling, 7(11).
Hays, D. G., Green, E., Orr, J. J., & Flowers, L. (2007). Advocacy counseling for female survivors of partner abuse: Implications for counselor education. Counselor Education and Supervision, 46(3), 184–198.
Hays, D. G., & Singh, A. A. (2012). Qualitative inquiry in clinical and educational settings. New York, NY : Guilford Publications.
Holt, M. K., & Espelage, D. L. (2005). Social support as a moderator between dating violence victimization and depression/anxiety among African American and Caucasian adolescents. School Psychology Review, 34(3), 309–328.
Howard, D. E., Beck, K., Kerr, M., & Shattuck, T. (2005). Psychosocial correlates of dating violence victimization among Latino youth. Adolescence, 40, 320–331.
Howard, D. E., Wang, M., & Yan, F. (2007). Psychosocial factors associated with reports of physical dating violence among U.S. adolescent females. Adolescence, 42, 311–324.
Josephson, W. L., & Proulx, J. B. (2008). Violence in young adolescents’ relationships: A path model. Journal of Interpersonal Violence, 23(2), 189–208.
Klem, J., Owens, A., Ross, A., Edwards, L., & Cobia, D. C. (2009). Dating violence: Counseling adolescent females from an existential perspective. Journal of Humanistic Counseling, Education and Development, 48, 48–64.
Laporte, L., Jiang, D., Pepler, D. J., & Chamberland, C. (2011). The relationship between adolescents’ experience of family violence and dating violence. Youth & Society, 43, 3–27. doi:10.1177/0044118X09336631
Lavoie, F., Robitaille, L., & Hebert, M. (2000). Teen dating relationships and aggression: An exploratory study. Violence Against Women, 6, 6–36. doi:10.1177/10778010022181688
Lewis, S., & Fremouw, W. (2001). Dating Violence: A critical review of the literature. Clinical Psychology Review, 21, 105–127.
Livingston, J. A., Hequembourg, A., Testa, M., & VanZile-Tamsen, C. (2007). Unique aspects of adolescent sexual victimization experiences. Psychology of Women Quarterly, 31, 331–343.
Masho, S. W., & Ahmed, G. A. (2007). Age at sexual assault and post-traumatic stress disorder among women: Prevalence, correlates, and implications for prevention. Journal of Women’s Health, 16, 262–271.
Manganello, J. A. (2008). Teens, dating violence, and media use: A review of the literature and conceptual model for future research. Trauma, Violence, & Abuse, 9, 3–18.
Moyer, M., & Sullivan, J. (2008). Student-risk taking behaviors: When do school counselors break confidentiality? Professional School Counseling, 11(4), 236–245.
O’Keefe, M. (2005). Teen dating violence: A review of risk factors and prevention efforts. Applied Research Forum, April, 1–13.
O’Leary, K. D., Woodin, E. M., & Fritz, P. A. T. (2006). Can we prevent the hitting? Recommendations for preventing intimate partner violence between young adults. Journal of Aggression, Maltreatment & Trauma, 13, 121–178.
Prospero, M. (2006). The role of perceptions in dating violence among young adolescents. Journal of Interpersonal Violence, 21(4), 470–484. doi:10.1177/0886260505285725
Rivadeneyra, R., & Lebo, M. J. (2008). The association between television-viewing behaviors and adolescent dating role attitudes and behaviors. Journal of Adolescence, 31(3), 291–305.
Rosen, K. H., & Bezold, A. (1996). Dating violence prevention: A didactic support group for young women. Journal of Counseling & Development, 74(5), 521–25.
Schnurr, M., & Lohman, B. (2008). How much does school matter? An examination of adolescent dating violence perpetration. Journal of Youth Adolescence, 37, 266–283.
Sears, H. A., & Byers, E. S. (2010). Adolescent girls’ and boys’ experiences of psychologically, physically and sexually aggressive behaviors in their dating relationships: Co-occurrence and emotional reaction. Journal of Aggression, Maltreatment & Trauma, 19, 517–539. doi:10.1080/10926771.2010.495035
Sears, H. A., Byers, E. S., & Price, E. L. (2007). The co-occurrence of adolescents boys’ and girls’ use of psychologically, physically, and sexually abusive behaviours in their dating relationships. Journal of Adolescence, 30, 487–504.
Silverman, J. G., Raj, A., Mucci, L. A., & Hathaway, J. E. (2001). Dating violence against adolescent girls and associated substance use, unhealthy weight control, sexual risk behavior, pregnancy, and suicidality. The Journal of the American Medical Association, 286, 572–579.
Teen Research Unlimited. (2008) Study on teen dating abuse. Retrieved from: www.loveisnot abuse.com=statistics.htm
Thongpriwan, V., & McElmurry, B. J. (2009). Thai female adolescent perceptions of dating violence. Health Care for Women International, 30, 871–891. doi:10.1080/07399330903066392
Vézina, J., & Hébert, M. (2007). Risk factors for victimization in romantic relationships of young women: A review of empirical studies and implications for prevention. Trauma, Violence, & Abuse, 8, 33–66.
Weisz, A. N., & Black, B. M. (2010). Peer education and leadership in dating violence prevention: Strengths and challenges. Journal of Aggression, Maltreatment & Trauma, 19(6), 641–660.
Whitaker, D. J., Morrison, S., Lindquist, C., Hawkins, S. R., O’Neil, J. A., Nesius, A. M., Mathew, A., & Reese, L. (2006). A critical review of interventions for the primary prevention of perpetration of partner violence. Aggression and Violent Behavior, 11, 151–166.
Wolitzky-Taylor, K. B., Ruggiero, K. J., Danielson, C. K., Resnick, H. S., Hanson, R. F., Smith, D. W., et al. (2008). Prevalence and correlates of dating violence in a national sample of adolescents. Journal of American Academy of Child and Adolescent Psychiatry, 47(7), 755–762.
Danica G. Hays, NCC, is an Associate Professor and Department Chair at Old Dominion University. Rebecca E. Michel, NCC, is a doctoral candidate and Rebekah F. Cole, NCC, is an Adjunct Professor, both at Old Dominion University. Kelly Emelianchik, NCC is an Assistant Professor at Argosy University-Atlanta. Julia Forman, NCC, is an Instructor at Walden University. Sonya Lorelle, NCC, is an Adjunct Professor at the University of North Carolina–Charlotte. Rebecca McBride, NCC, is an Adjunct Professor at Old Dominion University. April Sikes, NCC, is an assistant Professor at Georgia State University. Correspondence can be addressed to Danica G. Hays Old Dominion University, 110 Education Building, Norfolk, VA, 23529, dhays@odu.edu.
Sep 1, 2014 | Article, Volume 1 - Issue 2
Brandon Hunt, Genevieve Weber Gilmore
In an effort to ensure the efficacy of preparing emerging counselors in the field, CACREP standards require that by 2013 all core faculty at accredited universities have a doctorate in Counselor Education and Supervision. However, literature suggests that a disparity may exist in the preparation of counselor educators and the actual responsibilities of faculty members. As such, the present study investigated CACREP-accredited doctoral programs’ preparation of students to teach from the perspective of both students and program coordinators. Results support a didactic course in teaching and a co-teaching internship to help doctoral students learn to develop course materials, manage classroom behavior, and develop a teaching style and philosophy. Recommendations for effective counselor education training practices are provided.
Keywords: counselor education, faculty, CACREP, doctoral students, teaching
The field of counselor education continues to grow and with the rise in counseling programs there is an increased need for doctoral level counselor educators. In support of this need, the 2009 Council on Accreditation of Counseling and Related Educational Programs (CACREP) standards require that by 2013 all new core faculty have a doctorate in Counselor Education and Supervision (CES), since they are trained to teach, conduct research, and contribute service to the counseling profession (Sears & Davis, 2003). The training mission of CACREP-accredited CES doctoral programs meets the growing interest in reform for graduate education and the needs of a changing academy (Austin & Wulff, 2004).
An examination of the literature raises curiosity about the consistency between graduate preparation and the roles and responsibilities of faculty members. For example, faculty members spend more than half their time on teaching (Davis, Levitt, McGlothlin, & Hill, 2006; Golde & Dore, 2001), yet research is often the dominant focus of doctoral-level training. This leaves graduates better prepared for the role of researcher and less prepared for the role of teacher (Golde & Dore, 2001; Heppner & Johnston, 1994; Orr, Hall, & Hulse-Killacky, 2008). For example, Rogers, Gill-Wigal, Harrigan, and Abbey-Hines (1998) found that counseling faculty ranked experience in the area of teaching higher than publication experience in the faculty selection process. The focus on research in doctoral preparation appears contrary to what programs want in faculty—that is, well-rounded faculty who are prepared to teach, conduct research, and provide service to their institution, profession, and community.
According to Burke (2001), doctoral programs typically prepare students for careers at research institutions, and in doing so offer graduate fellowships, assistantships, and other training opportunities in research. This traditional model emphasizes research preparation while paying little attention to other faculty responsibilities like teaching (Rogers et al., 1998; Wulff, Austin, Nyquist, & Sprague, 2004). Consequently, many new faculty members lack didactic and hands-on training in teaching. Heppner (1994) supports this notion and found few graduate programs had systematic curricular experiences designed to prepare graduate students to teach, and those that did typically involved two to three days of seminar-based instruction that emphasized topics like grading and academic dishonesty. Without formal curricular experiences designed to train teachers, doctoral students who plan to enter a career in academia are too often not receiving training in the basic aspects of how to teach. As a result, new faculty are learning to teach during their first year while simultaneously adapting to a new professional environment, and in some cases developing a research agenda (Berberet, 2008; Burke, 2001).
A few studies that examined early experiences of new assistant professors have been identified in the literature. In a qualitative study by Magnuson, Black, and Lahman (2006), new assistant professors in counselor education were interviewed about their first three years as academicians. One participant described feeling “competent clinically,” but “completely ill prepared” for the role of counselor educator (p. 176). Wulff et al. (2004) investigated how graduate students’ experiences contributed to their development as educators and the types of training that most effectively prepared them for the professoriate. Their findings underscored a lack of “systematic feedback and mentoring” (Wulff et al., p. 62) in graduate students’ development as educators. Students reported their departments did not prepare them for the role of educator or provide feedback on their teaching skills. For students who did receive feedback, it was not “thorough or carefully designed to help them grow as teachers” (Wulff et al., p. 62). Consequently, participants relied on formal and informal feedback from students as well as their students’ grades to identify their most effective teaching strategies (Wulff et al.).
Doctoral students sometimes gain experience as teaching assistants (TA), yet these experiences may not adequately prepare them for the activities necessary for successful faculty careers. Although TA opportunities can help graduate students learn how to deliver a lecture and evaluate student work, these assistantships often serve as “mechanisms for financial aid and provide a labor pool of junior instructors for the university” (Golde & Dore, 2001, p. 25). According to Fagen and Suedkamp Wells (2004), “Teaching assistants are thrown into teaching environments in a sink-or-swim manner. No advice, preparation, or supervision is given” (p. 84). Therefore, one cannot assume that teaching assistantships are the answer to preparing doctoral students for the professoriate.
Without formal curriculum designed to train teachers, students who plan to enter a career in academia lack training in important aspects of teaching such as developing a teaching philosophy, incorporating information technology into the classroom, and creating inclusive classroom environments (Golde & Dore, 2001). This lack of training prevents aspiring faculty from truly understanding the art of teaching; that is, guiding students to new levels of understanding rather than standing in front of the room and lecturing (Wulff et al., 2004).
Researchers suggest that graduate students who experience progressively challenging teaching roles with faculty supervision benefit most from their graduate teaching experiences (Wulff et al., 2004), yet less than 50% of graduate students receive appropriate training before they enter the academy and they lack appropriate supervision to help enhance their teaching skills (Fagen & Suedkamp Wells, 2004). Accordingly, recommendations to graduate programs to provide greater opportunities for students to develop teaching skills have been proposed. One such opportunity is the teaching internship, which can help broaden the program emphasis beyond that of research to better prepare students for jobs in academia (Nerad, Aanerud, & Cerny, 2004).
According to Burke (2001), requiring a teaching internship for doctoral students can lead to a powerful climate change in academe that benefits graduate students, their doctoral programs, their institutions, and higher education as a whole. Burke contends that adding an elective or a required course in teaching is not enough. Rather, doctoral programs should provide students with varied teaching opportunities that become increasingly more demanding, require more responsibility, and allow for activities including but not limited to advisement and the development of a teaching philosophy (Wulff & Austin, 2004). It is important to note that adding a teaching internship is not intended to deemphasize the importance of research; rather, doctoral training for the professoriate should be strengthened to include emphasis on the most time-consuming activity of a professor—teaching.
Rationale for the Study
CACREP-accredited doctoral programs have responded to the growing interest in reform in graduate education by increasing their emphasis on training the next generation of faculty to teach. Zimpfer et al. (1997) reported that counselor education doctoral programs rated instructional and co-teaching activities as highly important student activities, yet a description of such teaching activities and an investigation of their effectiveness was not provided. According to CACREP Doctoral Standard III.B,
Doctoral students are required to complete doctoral-level counseling internships that total a minimum of 600 clock hours. The 600 hours include supervised experiences in counselor education and supervision (e.g., clinical practice, research, teaching). The internship includes most of the activities of a regularly employed professional in the setting. The 600 hours may be allocated at the discretion of the doctoral advisor and the student on the basis of experience and training. (CACREP, 2009, p. 54; emphasis added)
This standard, however, does not specifically describe or offer suggestions on how doctoral programs should train their students to teach or how a teaching internship should be developed and implemented. CACREP Standard II.B.2 also mandates students should be provided with opportunities to “develop collaborative relationships with program faculty in teaching, supervision, research, professional writing, and service to the profession and the public” (CACREP, 2009, p. 53l; emphasis added). Finally, as stated in the “Doctoral Learning Outcomes” section of the 2009 CACREP Standards, graduates should be knowledgeable about theory and methods related to teaching and they should have developed their own philosophy of teaching.
Our interest in this topic grew out of our experiences learning to teach at the graduate level. The first author learned to teach by co-teaching with a faculty member when she was a doctoral student, even though her program did not have a formal teaching internship. The faculty member then required doctoral advisees to complete a formal teaching internship until the time her program made the decision that all counselor education doctoral students were required to complete a didactic course on teaching as well as complete a teaching internship. The second author completed a didactic course as part of her doctoral program, and did her teaching internship with the first author. Our basic assumption going into the study was that completing a teaching internship is important in helping doctoral students become competent teachers. We discussed our assumptions and thoughts about the teaching experiences of CES students before and during the current study.
A review of the counseling literature uncovered no research related to how doctoral students in counselor education are being trained to teach in accordance with CACREP standards. Thus, CES students who plan to spend a significant portion of their academic careers teaching are not able to access information that describes how CES graduates are best prepared to teach, specifically what works and what does not work from the perspectives of faculty and other students. To address this gap in the literature, we conducted a preliminary study to answer the following research questions: (a) How are doctoral programs in counselor education training their CES students to teach? And, (b) What are the experiences of CES students who have completed a teaching internship?
Methodology
We used both quantitative and qualitative questions to answer the research questions. We collected descriptive data to investigate how counselor education programs are training CES students to teach and used general qualitative inquiry to learn about the teaching internship experiences of CES students. Our study was conducted in two phases. In Phase 1, we surveyed CES professors who were doctoral coordinators about the training their programs provide to doctoral students with regard to teaching. In Phase 2 we surveyed CES students who were completing or had recently completed their teaching internship. We could not find an appropriate survey for our study, so we developed questions for both phases of the study based on our review of the literature on teaching at the collegiate level.
For Phase 1 of the study, we sent email surveys to the doctoral coordinators for all CACREP-accredited CES programs. The survey, which included the language from CACREP (2009) Doctoral Standard III.B, consisted of the following questions: (a) How many doctoral students are accepted into your program each year? (b) What is the main focus of your program (i.e., train faculty, train researchers, train supervisors and practitioners)? (c) How does your program meet CACREP Doctoral Standard II.B? (d) Does your program offer or require a didactic teaching course? (e) Does your program offer or require a teaching internship? And, (f) What other opportunities does your program offer that allow doctoral students to gain teaching experience? At the time we collected data there were 44 CACREP accredited doctoral programs, and despite repeated contacts with program coordinators encouraging their participation, we received responses from only 16 doctoral coordinators (36% response rate).
For Phase 2, we sent email surveys containing open-ended questions to the ten doctoral coordinators who responded that their programs offered a teaching internship—not all programs offered a teaching internship—asking them to forward the survey to students currently completing or who had completed their teaching internship. Fourteen students responded and all questions were answered. The student survey noted we were looking specifically at the teaching internship experience, not teaching assistant experiences, and asked questions about (a) teaching experiences prior to the doctoral teaching internship, (b) what students appreciated most about the teaching internship, (c) what they found most and least helpful about the teaching internship, (d) if they had a separate didactic course related to teaching, what was most and least helpful about the course, (e) what would they have liked to have known before they started the teaching internship/co-teaching experience, and (f) how prepared they felt to teach independently after completing the teaching internship?
Results
CES program coordinators provided commentary on the status of the teaching internship at their institution (Phase 1), and doctoral students on their experiences with the teaching internship (Phase 2).
Phase 1: Program Coordinator Responses
Coordinators for the 16 programs noted they typically accepted six CES students a year. With regard to the main focus of the program (i.e., train faculty, train supervisors and practitioners, train researchers), 10 coordinators noted their program focused on training counselor education faculty, one program emphasized training of counselor education faculty as well as training of supervisors and practitioners, one program focused exclusively on training supervisors and practitioners, and four programs had an equal balance between all three areas.
With regard to how programs met the CACREP standard regarding teaching, the responses were varied with 15 of 16 participants responding to this question. Three coordinators noted their programs required no teaching experience as part of doctoral training. Of these, two noted that while their programs did not require a teaching experience most CES students co-taught a course with a faculty member. Nine coordinators said their students must complete a formal teaching internship, which typically entailed teaching a master’s level lecture course with a program faculty member. Of the programs that required a teaching internship, eight also required that students complete a didactic course on college teaching. Four coordinators noted they offered the course on teaching in their department, and four participants noted the required teaching course was offered outside of their department. When asked what other opportunities their programs offered for CES students to gain additional teaching experience, eight coordinators responded that their students had the opportunity to teach an undergraduate course independently, three programs provided opportunities for students to lead workshops, and two programs provided opportunities for CES students to teach master’s level courses independently.
Phase 2: Experiences of CES Student Respondents Who Completed the Teaching Internship
As noted, 14 doctoral students responded to Phase 2 of the study. They were asked to answer questions about their experiences prior to, during, and following their teaching internship. Eight respondents reported they had some level of teaching experience prior to their doctoral programs, which included teaching at the K–12, undergraduate, and master’s level. Following the principles of the constant comparative method of analysis (Lincoln & Guba, 1985), we reviewed and coded the responses to the remaining eight questions independently and placed them in categories. Then we met to discuss our independent categories until we came to consensus about the categories’ titles and meanings.
We took several steps to verify our findings. First, we used multiple participants as a form of data triangulation (Creswell, 2007; Patton 2002). Second, we analyzed the data independently and then together, which is a form of investigator triangulation (Lincoln & Guba, 1985; Patton, 2002). We also revisited participant responses when necessary throughout the analysis process, which provided us with opportunities to remain aware of potential research biases as well as to support or refute our categories. Finally, we used “thick description” (i.e., quotes) from the participants to add detail to their experiences (Lincoln & Guba, 1985).
Based on our analysis, responses emerged in the following four categories: (a) most and least helpful aspects of the teaching internship, (b) most and least helpful aspects of the didactic course on teaching, (c) what students should know before starting their teaching internship, and (d) how prepared students felt to teach independently. Responses will be described in detail, including exemplary quotes from the participants.
Most and least helpful aspects of the teaching internship. According to one respondent, the teaching internship is an opportunity for doctoral students to observe, model, and collaborate with “trusted and experienced” professors in preparation for their careers as counselor educators. Of the 14 doctoral students who responded, only one person wrote that the teaching experience was not helpful. The remaining respondents appreciated the support and guidance provided by the professors with whom they taught, which according to one respondent helped guide the student through “the rough spots” and improved his/her teaching skills. One respondent wrote, “I appreciated working closely with my supervisor to ensure that I had the support necessary to do the job right.” Another respondent shared that support and guidance were received through “bouncing ideas and feelings off” professors and collaboration on curriculum development and leading class discussions.
Respondents also appreciated the autonomy fostered by co-instruction opportunities, which allowed them to “have control over what assignments were being given.” One respondent underscored the importance of co-creating course syllabi and being involved with “in-class demonstrations and mini-lectures.” The flexibility and freedom to generate course curriculum and relevant materials encouraged the development of teaching philosophies and styles, both of which are essential to effective pedagogy. Another respondent stated, “My professor allowed me to choose half of the lectures and create my own materials for the class. I felt a sense of independence and empowerment as a co-instructor.”
Weekly teaching internship meetings where doctoral students and a professor met either individually or in a group to discuss ideas and concerns related to the teaching internship were described as beneficial. Respondents appreciated sharing ideas and hearing “strengths and areas of improvement” with regard to their teaching competencies. One respondent noted “meeting with the instructor of record to co-plan for [class]… helped me to deal with different problems that arose…[as well as] having trust and confidence placed in my abilities and me.”
Having a sense of being supervised too closely by the faculty co-instructor, however, was described by a few respondents as unhelpful, as the presence of the professor “made it hard to establish rapport and authority with students.” Feelings of frustration arose for one respondent when students would bypass the doctoral student and go directly to the faculty member of record “when it came to issues of grades, or syllabus-dictated course requirements.”
Additionally, although the majority of respondents viewed professors as experienced and excellent role models, several observed faculty who “did not model successful teaching strategies” or did not have a mastery of the material. One respondent stated, “Having to meet in a tiered supervision group with a professor who did not understand the unique aspects of the school counseling setting was not helpful.”
The “hands-on” training approach of the teaching internship was described as a valuable component of the experience as it promoted doctoral students’ observation and participation in realistic roles and responsibilities of professors. One respondent indicated, “I really got to experience how much prep work goes into teaching.” Others noted the opportunity “to teach a variety of courses” and “interact with different students” helped strengthen their abilities to reach and teach “all types of thinkers.” Some participants reported, however, that they felt unprepared for the “hands-on” approach, and found a number of characteristics of the teaching internship unhelpful. For example, one respondent noted, “prior knowledge of the level of preparation needed to teach a subject would have been helpful.” Another respondent struggled with “not knowing the level of competence of the students ahead of time,” and a third respondent found it “challenging to teach some students who were very unengaged in the course.”
Most and least helpful aspects of the didactic teaching course. Most graduate student respondents found their didactic course on teaching helpful in preparing them to teach. In particular, the didactic course provided opportunities for doctoral students to develop syllabi, exams, and grading rubrics, as well as receive feedback from professors and classmates. One respondent wrote,
Every assignment and class meeting was valuable. Assignments included writing a syllabus from start to finish and revising it after receiving feedback, keeping a journal on relevant topics (philosophy of teaching and learning, dealing with problems from students or other situations, our own biases), writing a sample test utilizing different types of test items, sharing and critiquing a video of us teaching, and creating a teaching portfolio that includes our philosophy of teaching, the things we created, and how we would evaluate students and ourselves.
Another respondent stated that the course on teaching required that respondents read the text they would be teaching the semester prior to teaching. This assignment, as described by the respondent, was “helpful in developing and receiving feedback on a tentative syllabus and lesson plans.” Respondents also indicated they enjoyed the opportunity to interact with other doctoral students, allowing for the comparison of “experiences” and acquisition of “new ideas.” Overall, these didactic experiences increased respondents’ knowledge of the course content, and furthered the development of their basic teaching skills and overall teaching philosophies.
Although many respondents found the didactic component of the teaching internship helpful, a few respondents shared that the course overemphasized the development of lesson plans. One respondent noted, “it was least helpful to develop individual lesson plans when we would be co-teaching.” The respondent continued with this recommendation: “it would have been more useful to develop lesson plans with our co-instructor, instead of having to merge and blend them together the first day of class.” One respondent shared his dislike for the course’s lack of emphasis on actual teaching. Two other respondents described the quality of course materials and the course curriculum as not beneficial. One respondent noted, “…a lot of the course was review, and for the parts that were new, I think I could have just written a paper based on the book,” and a second respondent identified her readings for the course as unhelpful.
What students should know before starting their teaching internship. Respondents provided various suggestions to future students with regard to what they should know before beginning the teaching internship. Mentorship was described as an important area of support for graduate students in counselor education. For those students who can choose the professor with whom they will teach, one respondent underscored the importance of “choosing a professor whose style you value” rather than choosing a particular course only based on interest. Furthermore, it is beneficial to consider “which ‘profs’ were the best teachers” and to “try to incorporate the successful strategies employed by your favorite teachers.” This comment speaks to the importance of faculty modeling effective teaching strategies to teaching interns. Another respondent provided a suggestion that emphasized the value of supervision:
Use your mentor as a sounding board, especially if you have never taught before. Rarely will you be presented with an issue in your class with which your supervisor has not had prior experience. Pay attention to the way effective professors do business.
Structured supervision also was indicated as an important area of interest. For graduate students who might not have a formal teaching supervision experience in place, one respondent advised, “Find out with whom they can consult formally or informally. Do not try to teach in a vacuum, especially if they are new to teaching…form an informal peer supervision group or seek outside supervision from another knowledgeable source.”
In addition, classroom management also was identified as a practical area that graduate students should know before beginning their teaching internship. Responses included dealing with “student issues,” “classroom dynamics,” and engaging “the difficult-to-engage student.” A few respondents commented on the importance of understanding and using effective ways to interact with students. For example, one respondent stated, “make sure you pay attention to how people react to being challenged…or how people go about disagreeing…[since] not everyone responds to criticism or being challenged in the same way.” Another respondent underscored the value of having structure in the classroom, noting: “It is easier to be ruthlessly rigid and demanding at first and then loosen the reigns toward the end of the semester than it is to be lax in enforcing grading or class rules and then try to put the hammer down at the end of the semester.” This respondent also recommended that teaching interns “set the tone from the start” of the course.
Finally, a few respondents recommended doctoral students understand the time, dedication, and competence required to develop course materials and integrate technology into the curriculum. For example, one respondent suggested doctoral students should know the “most professional issues relevant to the course; how to develop a syllabus; and how to create assignments that truly measure knowledge gained by students.” One respondent proposed that doctoral students plan “to double their estimated time of preparation and to try to gain competence in the use of technology like ANGEL and WEBCT,” which are computerized course management systems.
How prepared students felt to teach independently. Overall, respondents described the teaching internship as an essential component in preparing them to teach independently. Emphasis was placed on the importance of didactic training and the co-teaching experience in addition to teaching assistantship opportunities. One respondent noted, “The teaching internship is so essential for counselor educators…and this means a structured course or practicum beyond just being a teaching assistant!” Co-teaching experiences allowed students to gain knowledge of course material as well as skills to manage the classroom, both of which were invaluable to their training. One respondent noted the value of having a didactic course and teaching internship as part of his training: “I believe that my internship alone did not 100% prepare me to teach independently. I think that internship, the class on college teaching and other co-teaching experiences TOGETHER have helped me feel prepared to teach.” After completing the teaching internship, one person indicated she was hired by her department as an instructor for a master’s level course, which helped her gain additional experience and earn extra income during her doctoral studies.
Discussion
Findings from Phase 1 of the study show the majority of faculty respondents, all from CACREP-accredited CES programs, focused on training doctoral students to become faculty with particular emphasis on teaching, research, and service. Given that the master’s degree is the professional-level degree in counselor education, it seems appropriate that doctoral programs focus on training future faculty to teach. The majority of participants noted they were providing some level of teaching opportunities to CES students even if it was not offered in a formalized and systematic way. Doctoral coordinators for three programs did not respond to this question, and three noted they did not require students to complete any kind of teaching experience despite teaching being noted as an important element of doctoral training in the CACREP standards. Nine programs required students to complete a formal teaching internship, typically co-teaching a master’s-level counseling course with a counselor education faculty member, and of those programs eight required students to complete a didactic course on teaching. Additional training experiences offered to CES students included teaching undergraduate or graduate courses independently and leading workshops.
As noted earlier, results from our analysis of the student responses (Phase 2 of the study) provided information on the most and least helpful aspects of the teaching internship and the didactic teaching course, as well as what students should know before starting their teaching internship. Mentorship, support and guidance from faculty and peers, and weekly supervision were helpful aspects of the teaching internship. Teaching supervision that was too intensive and working with weak role models of quality teaching were unhelpful aspects of the teaching internship. Although most respondents found the didactic teaching course to be helpful, a few respondents expressed concern over the heavy focus on developing lesson plans (when they were not teaching a course yet) and the lack of actual teaching experience in the course. As a result, respondents recommended that other students be selective about with whom students complete their teaching internship, focusing on the instructor rather than the course content; make full use of the supervision provided by the faculty mentor as well as peer support; learn good classroom management skills; and be aware of the amount of time and energy required to develop and teach a course. All these recommendations are made possible through a didactic teaching course coupled with hands-on teaching experience.
Students respondents also described how prepared they felt to teach independently. Overall, the teaching internship, beyond being a teaching assistant, was very important in helping them feel prepared to teach independently since respondents learned both how to present content and manage the classroom elements of teaching.
Findings from our study are contrary to Wulff et al. (2004) and Fagan and Suedkamp Wells (2004), who found that doctoral students who wanted to become faculty reported they did not receive adequate orientation, preparation, or training to enter the classroom as teachers. Although the comparative research examined experiences across many disciplines and was not primarily focused on counselors, it is the only literature that could be located relevant to the current topic. It appears that students enrolled in CES programs that include a teaching internship requirement, if not requiring both a didactic course and the internship, felt supported as they learned to teach and believed they were well prepared to teach independently. Wulff et al. also suggested that students engage in teaching experiences that are progressively more challenging, moving from some level of teaching observation or a didactic course to then co-teaching with faculty, and then teaching independently, which happened for a number of the doctoral participants in our CES study.
Our findings support Heppner’s (1994) assertion that providing graduate students (five psychology students in this case) with the opportunity to engage in a teaching practicum or internship experience significantly increased their knowledge about teaching as well as teaching self-efficacy. Participants in Heppner’s study stated that receiving feedback from faculty co-instructors and peers as well as sharing ideas with their peers was particularly helpful, which is similar to our findings.
Limitations and Implications
As with all research, this study has limitations. Because of the preliminary nature of the study and the relatively low response rate for Phase 1, it is not possible to generalize the findings to all CACREP-accredited CES programs or to all counselor education doctoral programs. In addition, our findings reflect research institutions that train counselor education doctoral students. Therefore, caution should be used in interpreting our findings. Limitations for Phase 2 could include some degree of researcher bias since the authors initially had a student-professor relationship and worked together in a teaching internship, but we took the steps described above to ensure trustworthiness and attend to potential biases.
Despite these limitations, there are several implications that arise from our findings. First, CES programs would benefit from developing a systematic process for training doctoral students to teach. Having a required process is not only important in terms of meeting the CACREP standards, but also has an important influence on how we train future generations of master’s-level counselors. This process could include having students complete a didactic course on teaching, preferably offered within the department, and either simultaneously and sequentially completing a co-teaching internship with a faculty member.
Based on the research and our findings, it seems most effective to have doctoral students select the faculty member with whom they want to co-teach and that they receive consistent supervision. Burke (2001) takes the process even further, recommending that doctoral students complete a year long teaching internship that would include teaching two courses a semester and being involved in departmental meetings where curricular issues are discussed, as well as advising students. For specifics on a model designed to meet the CACREP standards for training counselor education doctoral students on how to teach, see Orr et al. (2008), who developed the collaborative teaching teams (CTT) model to help CES students gain experience and increase their sense of competence in teaching.
During the teaching internship students should be provided with formal opportunities to interact with other doctoral students completing their teaching internship, preferably in a weekly group setting. Again, our findings and existing research support the idea that peer support and critique is as important, if not more important, to doctoral students as they learn to become effective and confident teachers. Respondents benefitted from seeing what their colleagues did in similar teaching situations and imagining how they might handle a challenge that a doctoral peer was facing.
Lastly, counselor education programs can help doctoral students broaden their definition of teaching to include community and conference presentations, workshops, and other public speaking opportunities where CES students can use their counseling and teaching skills to educate others. Teacher training also should include specific content about how to assess and handle classroom situations where students may have committed academic misconduct or may be impaired in some way and what campus resources exist to help faculty and students navigate these challenging situations, including how codes of ethics and university policies and procedures apply in the classroom.
As Heppner and Johnston (1994) stated, “the development of excellent teaching skills involves continuous learning, a lifelong process…Given the complexity of the skills required for outstanding teaching, it is surprising that most faculty members have not had formal training in teaching” (p. 492). By providing the same level of focus and attention to teaching in CES programs that we do to research, we can help future CES faculty increase their level of competence and self-efficacy as counselor educators, thus effecting positive change in the classrooms of counselor education master’s programs across the country where our graduates are hired to teach. Our provision of quality and comprehensive doctoral-level education also responds to the call for reform for graduate education, particularly in preparing future faculty members to meet the needs of a changing academy.
References
Berberet, J. (2008). Perceptions of early career faculty: Managing the transition from graduate school to the professorial career. New York: TIAA-CREF Institute. Retrieved from http://www.tiaa-crefinstitute.org/articles/92.html
Burke, J. C. (2001, October 5). Graduate schools should require internships for teaching. The Chronicle of Higher Education. Retrieved from http://chronicle.com/weekly/v48/i06/06b01601.htm
Council for Accreditation of Counseling and Related Educational Programs. (2000). CACREP accreditation manual. Alexandria, VA: Author.
Council for Accreditation of Counseling and Related Educational Programs. (2009). CACREP accreditation manual. Alexandria, VA: Author.
Creswell, J. W. (2007). Qualitative inquiry and research design: Choosing among five traditions (2nd ed.). Thousand Oaks, CA: Sage.
Davis, T. E., Levitt, D. H., McGlothlin, J. M., & Hill, N. R. (2006). Perceived expectations related to promotion and tenure: A national survey of CACREP program liaisons. Counselor Education & Supervision, 46, 146–156.
Fagen, A. P., & Suedkamp Wells, K. M. (2004). The 2000 National Doctoral Program Survey. In D. H. Wulff & A. E. Austin, Paths to the professoriate: Strategies for enriching the preparation of future faculty (pp. 74–136). San Francisco, CA: Jossey-Bass.
Golde, C. M., & Dore, T. M. (2001). At cross purposes: What the experiences of doctoral students reveal about doctoral education. Philadelphia: A Report for The Pew Charitable Trusts. Retrieved from http://www.phd-survey.org
Heppner, M. J. (1994). An empirical investigation of the effects of a teaching practicum on prospective faculty. Journal of Counseling & Development, 72, 500–507.
Heppner, P. P., & Johnston, J. A. (1994). Peer consultation: Faculty and students working together to improve teaching. Journal of Counseling & Development, 72, 492–499.
Lincoln, Y. S., & Guba, E. G. (1985). Naturalistic inquiry. Newbury Park, CA: Sage.
Magnuson, S. Black, L., & Lahman, M. (2006). The 2000 cohort of new assistant professors of counselor education: Year 3. Counselor Education and Supervision, 45, 162–179.
Nerad, M., Aanerud, R., & Cerny, J. (2004). So you want to be a professor! Lessons from the PhDs–ten years later study. In D. H. Wulff, & A. E. Austin, Paths to the professoriate: Strategies for enriching the preparation of future faculty (pp. 137–158). San Francisco, CA: Jossey-Bass.
Orr, J. J., Hall, S. F., & Hulse-Killacky, D. (2008). A model for collaborative teaching teams in counseling education. Counselor Education & Supervision, 47, 146–163.
Patton, M. Q. (2002). Qualitative research and evaluation methods (3rd ed.). Thousand Oaks, CA: Sage.
Rogers, J. R., Gill-Wigal, J. A., Harrigan, M., & Abbey-Hines, L. (1998). Academic hiring policies and projections: A survey of CACREP- and APA-accredited counseling programs. Counselor Education & Supervision, 37, 166–177.
Wulff, D. H., & Austin, A. E. (2004). Paths to the professoriate: Strategies for enriching the preparation of future faculty. San Francisco, CA: Jossey-Bass.
Wulff, D. H., Austin, A. E., Nyquist, J. D., & Sprague, J. (2004). The development of graduate students as teaching scholars: A four year longitudinal study. In D. H. Wulff, & A. E. Austin, Paths to the professoriate: Strategies for enriching the preparation of future faculty (pp. 46–73). San Francisco, CA: Jossey-Bass.
Zimpfer, D. G., Cox, J. A., West, J. D. Bubenzer, D. L., & Brooks, D. K. (1997). An examination of counselor preparation doctoral programs. Counselor Education and Supervision, 36, 318–331.
Brandon Hunt, NCC, is a Professor at Counselor Education, Counseling Psychology, and Rehabilitation Services at Penn State University. Genevieve Weber Gilmore is an Assistant Professor of Counseling at Hofstra University. Correspondence can be addressed to Brandon Hunt, Penn State University, University Park, PA, 16802, bbh2@psu.edu.
Sep 1, 2014 | Article, Volume 1 - Issue 1
Joel F. Diambra, Melinda M. Gibbons, Jeff L. Cochran, Shawn Spurgeon, Whitney L. Jarnagin, Porche’ Wynn
To inform and guide their practices, counselor educators would benefit from having a clearer picture of how the research literature and professional standards of the field correspond and contrast. To elucidate this relationship, researchers analyzed 538 Journal of Counseling and Development articles published from 1997–2006 for fit with the 2001 and 2009 eight core areas of Council for Accreditation of Counseling and Related Educational Programs (CACREP). The articles fell into three tiers delineated by year and based on the number of articles assigned to each core area. Human Growth and Development and Helping Relationships are the two core areas most frequently represented across the 10 year time span examined.
Keywords: professional standards, research literature, CACREP, NBCC, ACA, Human growth and development, helping relationships
There is an inherent symbiotic relationship that exists among related professional organizations. Within the counseling profession, there are a number of organizations or entities that coexist, support one another, encourage and challenge one another, disseminate information, and act as gatekeepers. These major counseling entities include the American Counseling Association (ACA), the National Board of Certified Counselors (NBCC), the Council for Accreditation of Counseling and Related Educational Programs (CACREP) and the Journal of Counseling and Development (JCD). These entities mutually influence each other by acting and reacting to needs, changes and research findings within the counseling profession.
Given the new CACREP 2009 standards, it is now time for counselor educators to review and possibly revamp their training programs to better reflect the current issues faced by those in the counseling field. Counselor educators will benefit from having a clearer picture of how our research literature and professional standards correspond and contrast to inform and guide our practices.
As the respective flagship journal and primary accrediting standards of the counseling field, the JCD and the CACREP standards are predominant guiding resources that reflect, communicate, and shape the values, interests, and work of counselor educators. As JCD is the journal for ACA, and as the National Counselor Examination is based on CACREP requirements, an obvious extension to include these entities occurs as well. These entities also influence each other. JCD and CACREP can be seen as leaders of an input loop in the counseling profession. JCD, as the flagship journal for the American Counseling Association (ACA), shapes counselors’, stakeholders’ and counselor educators’ views of the counseling field. Continuing the loop, every seven years CACREP engages in a review of its standards for counseling programs. This review includes invitations for input from all counselors and stakeholders (Bobby & Kandor, 1995). As the revised standards are enacted in CACREP and CACREP-modeled programs, the standards influence the education and licensing of counselors, which then influences the work, research, writing, and submissions to JCD from the counseling field over time; JCD article topics, content, and methodology loop again to inform counseling practitioners, students, and educators.
While the 2009 CACREP standards revisions are implemented into counseling programs, it seems an important time for counselor educators to reflect on and explore the profession’s flagship journal articles in relation to future CACREP standards and to discuss future counseling literature that will shape and inform directions for counselor educators and the counseling field. Calls for a strong professional counselor identity (CACREP, 2009; Gale & Austin, 2003; Goodyear, 1984; Hansen, 2003) and professional unity from a recent ACA President (Canfield, 2007) would also seem to indicate the need to reflect on and gain perspective from the trends and foci of our professional literature. The current study provides an analysis and discussion of the fit of JCD articles from 1997–2006 with the eight core areas in both the 2001 and adopted 2009 CACREP standards. We selected this 10-year span because the research project began in late 2007 and 2006 represented the last complete year of JCD articles at that time. We hope such an analysis will help illuminate areas for potential change in counselor education programs.
Professional Organizations and Publications in Counseling
American Counseling Association
With its roots as far back as 1952, ACA is the world’s largest association focused exclusively on representing professional counselors. As reflected on their website, “The ACA is dedicated to the growth and development of the counseling profession and those who are served” (ACA, 2010). Its mission is to enhance the quality of life in society and promote the development of professional counselors, advance the counseling profession, and use the profession and practice of counseling to promote respect for human dignity and diversity (ACA). ACA has 56 chartered branches in the U.S., Latin America and Europe and currently boasts 42,594 members. To communicate to its membership and inform the profession of contemporary issues and treatment modalities, ACA publishes an online website, numerous textbooks, Counseling Today (its monthly magazine) and JCD (its official journal).
Journal of Counseling and Development
In addition to being ACA’s primary journal, JCD appears to have grown to a significant readership, and this is particularly interesting considering that at least two-thirds of ACA members receive JCD as their only ACA journal. According to ACA (personal communication, Rae Ann Sites, December 20, 2007), the JCD Winter 2008 issue had a total print run circulation of 43,500 journals. Approximately 1,000 of these subscribers are institutional subscribers (i.e., college/university libraries). Therefore, it seems logical to assume the majority of subscribers are individual ACA members.
Members also have the option to join one or more of 17 divisions within ACA and many of these divisions publish their own journals. As of December 20, 2007, the cumulative membership in these 17 divisions was 16,279. At most, division membership could represent 37% of ACA members, but it is important to note that some ACA members join multiple divisions, thus exaggerating the 37% figure. Following ACA’s 1997 decision to allow ACA membership exclusive of a division membership and the 2004 decision to permit division separation from ACA, the American Mental Health Counseling Association (AMHCA) and American School Counseling Association (ASCA) announced independence from ACA and are no longer included in these 17 divisions. ACA data available from June 30, 2007, indicate 2,182 (approximately 5%) of ACA members who also were AMHCA members and 2,648 (approximately 6%) who also were ASCA members (personal communication, Jennifer Bauk, December 3, 2007). When compared to the total membership figures of these two professional counseling organizations (AMHCA, 5,860 [personal communication, Mark Hamilton, November 27, 2007]; ASCA, 23,021 [personal communication, Jennifer Bauk, December 3, 2007]), the percentage of AMHCA members who joined ACA was 37% and ASCA members 16%. From these data, it is apparent that JCD is circulated to a wide and diverse counselor audience. Therefore, we can assume that many graduates of our training programs will read only JCD as their professional journal to inform them of current issues and important research.
Council for Accreditation of Counseling and Related Educational Programs
CACREP has evolved to be a significant influence on the counseling field. A brief recap highlights CACREP’s growing influence. Bobby and Kandor (1992) reported that 44 programs housed within 16 institutions were granted approval by CACREP’s Board of Directors at the Council’s first meeting in 1981. In 1992, 195 programs had gained accreditation (Bobby & Kandor); and in 2004, that number had risen to 434 (McGlothlin & Davis, 2004). Currently, CACREP has accredited 505 programs housed within 210 institutions across 48 states, the District of Columbia, and Canada. In addition, 117 programs are currently being considered for CACREP accreditation. This is evidence of CACREP becoming more wide spread and ingrained within the counseling profession (CACREP, 2007).
National Board for Certified Counselors
Developed in 1982, NBCC conducts a national certification program for professional counselors; it is one of two leading certification organizations for the counseling profession, the other being the Commission on Rehabilitation Counselor Certification (CRCC). Although initially created by ACA, NBCC operates as an independent body without direct connection to ACA. Currently, over 46,000 counselors hold the National Certified Counselor (NCC) credential (NBCC, n. d.). In 41 states (82%), NBCC’s National Counselor Examination (NCE) is used as part of the licensure process.
The NCE contains eight content and five work behavior areas. The eight content areas mirror those in CACREP’s core curriculum and include human growth and development, social and cultural foundations, helping relationships, group work, career and lifestyle development, appraisal, research and program evaluation, and professional orientation and ethics. The five work behavior areas include fundamentals of counseling, assessment and career, group, programmatic and clinical intervention, and professional practice (NBCC, n. d.). Given this consistent overlap in core components and the growing use of the NCE for state licensure requirements, it is apparent that NBCC, ACA, JCD, and CACREP are linked in their view of what effective counselors need to know.
Support for Professional Organizations in Counseling
CACREP, JCD and NBCC have been the focus of several empirical studies. Over the past 10 years, researchers have examined issues pertaining to CACREP standards including supervision (LaFountain & Baer, 1999), spirituality and religion (Burke, Hackney, Hudson, Maranti, Watts, & Epp, 1999), community counseling (Hershenson & Berger, 1999), and school counseling (Holcomb-McCoy, Bryan, & Rahill, 2002). Haight (1992) investigated the CACREP standards, focusing on the quality of the standards. In addition, researchers have explored CACREP standards’ relevance to counselor preparation (Vacc, 1992) and their perceived benefit for practitioners (McGlothlin & Davis, 2004). Although some researchers have challenged the standards, most reviews and discussions related to CACREP have been favorable (Schmidt, 1999).
Vacc (1992) investigated counselor educator perceptions of the 1988 standards relevance to the preparation of counselors. He found that respondents judged each of the eight CACREP core areas as crucial or important to counselor preparation. Percentages of perceived importance ranged from 91% to 100%, with Social and Cultural Competence perceived as least relevant and Group Development, Dynamics, and Counseling Theories perceived as most relevant. Based on these findings, Vacc concluded that the data provided evidence to support the validity of the standards.
McGlothlin and Davis (2004) investigated perceived benefits of the CACREP standards. They surveyed counselors to determine perceptions of the benefits of the 2001 core curriculum standards. The core curriculum standards were perceived as being beneficial overall. Ranked in order of perceived benefit (highest to lowest) were: Helping Relationships, Human Growth and Development, Social and Cultural Diversity, Group Work, Professional Identity, Assessment, Career Development, and Research and Program Evaluation. Both studies established credibility for CACREP’s eight core standards.
As noted earlier, NBCC provides the examination used for professional licensure in the U.S. (NBCC, n. d.). Support exists for NBCC due to its oversight of the NCE. Adams (2006) compared NBCC National Counselor Exam scores across CACREP and non-accredited programs. She found that graduates of CACREP-accredited programs scored significantly higher than those from non-accredited programs. Pistole and Roberts (2002) encourage licensure as a primary way to secure professional identity. Similarly, Calley and Hawley (2008) identified professional certification and licensure, along with membership in professional organizations such as ACA, as ways counselor educators help promote a professional counseling identity. Support for both NBCC and the NCE is evident and furthers counselor professional identity.
JCD publications can be seen as shaped by a number of forces and as evolving over time. For example, Weinrach (1987) argued that JCD had been fashioned by contributors’ articles and editors’ aims. Twelve years later Williams and Buboltz (1999) asserted that JCD publications were influenced by changes within society, evolving counselor and student needs, the teaching aims of professors, and most importantly by the research and practical topics that are popular during a historical period.
The content analysis by Williams and Buboltz (1999) of volumes 67–74 most closely resembles the aims of the current study. Their article analysis covered a nine-year span and cross-classified articles into 11 categories (e.g., Counselor Selection, Training and Evaluation, Personal Development and Adjustment, Technology and Media, and Special Groups) and sub-grouped articles by editorship. The purpose of their study was to identify possible topic changes and trends over time and JCD editors. Overall ranking of topics pertinent to the 8 core areas identified by CACREP included Individual, Group Counseling, and Consultation ranked first, Special Groups third, Vocational Development and Adjustment/ Career Counseling seventh, and Technology and Media tenth.
In this study, ACA is assumed to be represented by its flagship journal, JCD, while NBCC is represented by CACREP, as the NCE is based on CACREP accreditation standards. To date, no study has analyzed JCD article content by CACREP core areas. In addition, no study could be found that focused on the similarities and differences between what is required for appropriate training and licensure of counselors and what is represented in the flagship journal of the counseling profession. Therefore, the purpose of the current study is to provide that analysis and discussion for the consideration of counselor educators and the counseling field.
Method
Procedure
Using first the 2001 standards and later the 2009 revisions, two researchers used a qualitative content analysis method to sort articles into the eight CACREP core areas. The eight CACREP core areas included Professional Orientation and Ethical Practice; Social and Cultural Diversity; Human Growth and Development; Career Development; Helping Relationships; Group Work; Assessment; and Research and Program Evaluation. Researchers independently analyzed content by sorting articles by CACREP core area. As per classic content analysis procedures described by Ryan and Bernard (2000), researchers assumed that the eight 2001 CACREP core curricular experience areas were the pre-defined codes of interest. Because of the time span from which articles were analyzed (i.e., 1997–2006), the researchers determined that both an analysis of the 2001 and 2009 standards was appropriate given that the 2001 standards were adopted during this time period and analysis of the 2009 standards would provide insight as to how previous articles would fit into the future standards.
First, researchers independently analyzed the JCD articles using the 2001 standards. After independent analysis, the two researchers compared findings, identified matching results and noted findings on which they differed. A list was established identifying the articles on which the two researchers disagreed. The same two researchers independently reanalyzed these articles and then met to compare findings again. No comparisons were made between the first and second attempts in order to maintain the independence of the second analysis. After this second attempt, the researchers obtained a cross-rater reliability of .93 for the 2001 data. Of the remaining articles for which coding differed, 20 differed in coding for CACREP core area. These articles were equally distributed throughout the 10 years of JCD being analyzed and were not representative of a single time period or editor. These remaining articles were coded by a third researcher, once again independent of the first two analyses. The three coders then reviewed each article together and, through consensus, determined the best placement for each.
After completing analysis using the 2001 CACREP standards, the two researchers addressed the data using the 2009 CACREP standards. The researchers noted that the eight core CACREP area titles remained constant between 2001 and 2009. However, differences between the 2001 and 2009 standards included changes within the eight core areas. Changes typically included additions of specific counseling related practices into core areas. Within the Professional Orientation and Ethical Practice core, additions were made related to crisis management and counselor self-care. Under Social Cultural Diversity, counselor self-awareness, social justice, and cultural skill development were added. In the Human Growth and Development core, additions included the effects of crises on individuals and theories of resiliency. The Career Development core remained relatively unchanged. Helping Relationships added crisis response and wellness orientation. Group Work and Assessment core areas remained substantively unchanged while Research and Program Evaluation incorporated evaluative measures and ethics related to research (CACREP, 2009). One overall change appeared to be that culturally inclusive language was more represented across most of the core areas. With these changes in mind, the two researchers independently re-reviewed titles and abstracts of all articles for 2009 CACREP core area best fit.
Analysis
The total number of articles in the JCD 1997–2006 issues was 538, excluding minutes from ethics committees and calls for editorial board members. Researchers examined 479 out of the 538 possible articles. Fifty-nine articles (11%) were eliminated from coding including interviews of well-known counselors and reviews of other articles (typically found in the Trends section). These articles did not fit into the predetermined coding categories. In all cases, an attempt was made to select only one option per area. Coding was based on the core area which was most representative of describing the article. For the 2001 Standards, approximately 7% of the cases (35 of 479 articles), were impossible to fit into only one area, so two areas were selected for coding. Three additional articles needed two areas after being reanalyzed with the 2009 Standards. For example, some articles were equally about a client issue and how counselors could effectively address the issue. These articles were coded as representative of both the Human Growth and Development and Helping Relationships core areas. In the two cases that no CACREP core area was found to match the article, an ‘Other’ category was selected. This category was used only when both researchers found it impossible to connect the article to a CACREP area.
When analyzing JCD articles using the 2009 CACREP core areas, researchers identified 97 articles that required reanalysis. These 97 articles were fully analyzed again. Fifty-nine of the 97 articles remained unchanged from the original assigned coding. Three articles were changed from representing two core areas to just one core area. Six articles were changed from representing one core area to two core areas (included originally coded CACREP core area plus one additional CACREP core area). Twenty-nine articles were recoded to a new core area.
Results
Due to the fact that only 29 (6%) of the 479 articles differed across core areas coding from the 2001 to 2009 CACREP standards, and because the proportional ranks remain the same, researchers are providing the 2009 CACREP Standards results, as 2009 is the current standard. CACREP core area results are presented in Table 1. The core area with the most articles was Human Growth and Development, followed by Helping Relationships and Social and Cultural Diversity. Group Work, Research and Program Evaluation, and Career Development were the least represented core areas. Thirty-eight of the articles were coded in two core areas, and all of the core areas were represented at least twice in a two-coded article. Seventeen of the two-coded articles involved Social and Cultural Diversity, 15 involved Helping Relationships, and 14 involved Human Growth and Development.
Table 1
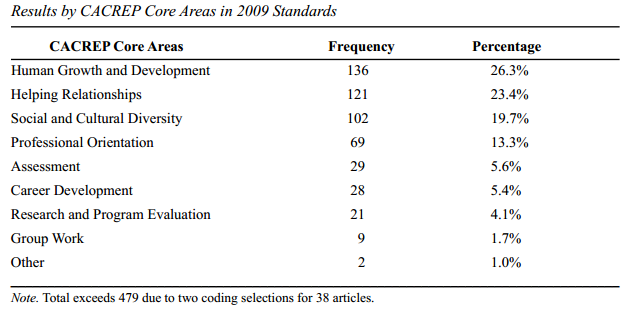
Rankings of core areas by percentage of articles tended to be stable throughout the 10-year focus period of this study. Human Growth and Development and Helping Relationships had the top two highest percentages of articles in the 10-year average and maintained consistently high percentages across the years, having been the first or second largest article category each year, except one. Within our analysis, these core areas formed the highest tier. Social and Cultural Diversity and Professional Orientation had the third and fourth highest percentages of articles and were ranked third or fourth each year (except one year for Professional Orientation and two years for Social and Cultural Diversity, affected by a special issue focused on that topic in 1999). Within our analysis, these core areas formed the middle tier. Assessment, Career Development, Research and Program Evaluation, and Group Work consistently varied from fourth to eighth in article percentages and formed the lowest tier of the rankings. These core areas not only occupied the lowest tier, but the percentages of articles representing them were noticeably lower than those representing the four leading core areas.
Table 2
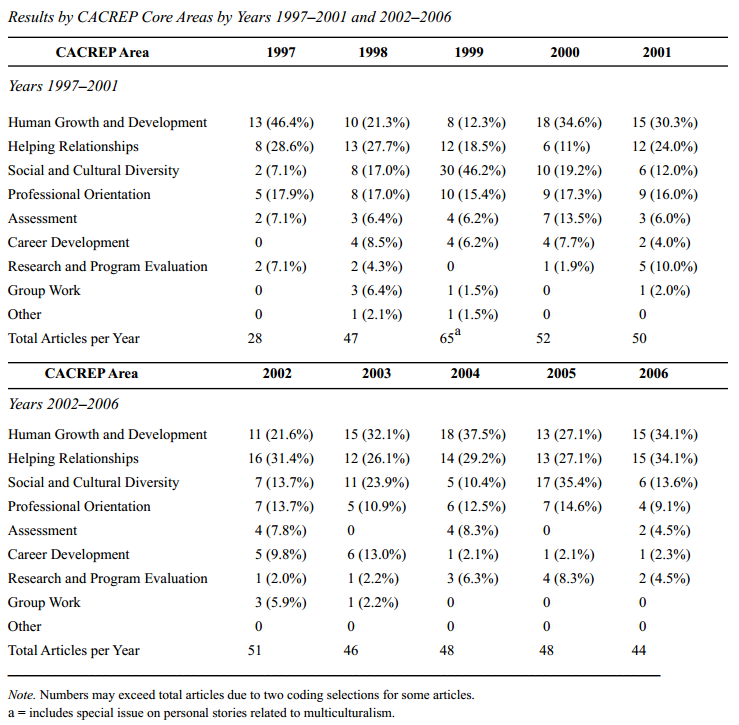
Results by CACREP Core Areas across the ten year span are presented in Table 2. Over the 10-year period, most CACREP core areas are equivalently represented with minor fluctuations between years. Human Growth and Development and Helping Relationships are the two core areas most frequently represented and are reasonably consistent in percentage of articles representation from year to year across the 10 years. Human Growth and Development core area articles ranged in frequency from 8 to 19 across the years with a mean of 13.6 articles per year. Helping Relationships articles ranged from 6 to 16 with a mean of 12.1 articles published per year. Professional Orientation is the most consistent core area from year to year (range of 4 to 9 articles) with a moderate number (mean = 6.7) of articles published per year. Social and Cultural Diversity fluctuates substantially from year to year with a low of 2 articles published in 1997, a high of 30 articles in 1999 and a mean of 10.2 for all ten years. Assessment articles are relatively steady from year to year, yet low in number with a range from 0 to 7 articles each year and a mean of 2.9 articles per year. Research and Program Evaluation is similar to Assessment in low but steady frequency across the years with a range from 0 to 5 articles and a mean of 2.1 per year. Notably, Research and Program Evaluation articles increased slightly in the latter five years. Career Development is low in frequency, but less steady across the years with a range from 0 to 6 and mean of 2.8 articles per year. Notably, only 3 articles were published in this core area in the last three years of this study (i.e., 2004–2006), one article each year. Lastly, Group Work article frequency ranged from 0 to 3 and the lowest average frequency at .9 per year. In the last three years no articles were published in the Group Work core area.
Discussion
Having established the symbiotic relationship between four central counselor entities (i.e., CACREP, ACA, NBCC and JCD), the researchers focused their review on the overlap between the required CACREP training core and the topics represented in the counseling profession’s flagship journal, JCD. We were primarily interested in relating the content of articles from 1997–2006 to the eight CACREP core areas. When we began our study, we made the assumption that JCD and CACREP served as informative tools for its members and that CACREP standards were an appropriate measure of adequate counselor training. JCD purports “to publish articles that inform practicing professional counselors with diverse populations in a variety of settings and that address issues related to counselor education and supervision, as represented by the membership of the American Counseling Association” (JCD, n.d.). Whereas many specialty journals highlight one specific aspect or one core area, JCD attempts to provide relevant information that cuts across all CACREP core areas. Additionally, CACREP reports being “dedicated to (1) encouraging and promoting the continuing development and improvement of preparation programs, and (2) preparing counseling and related professionals to provide service consistent with the ideal of optimal human development” (CACREP, n.d.). In the counseling flagship journal and accrediting body, a goal exists to prepare, train, and provide counselors with information necessary to good clinical practice. As stated earlier, JCD is the journal representing ACA, and NBCC bases the NCE on current CACREP standards.
The results highlight an overlap between the missions and goals of JCD and CACREP with a weighted emphasis in key CACREP core areas. Results in Table 1 indicate that almost 70% of the articles published during this time period fall under three CACREP areas: Human Growth and Development, Helping Relationships, and Social and Cultural Diversity. It seems sensible and fitting to us that JCD articles would emphasize these areas. Remley and Herlihy (2007) stated that one of the essential beliefs in the counseling profession is that problems individuals face in life are developmental in nature. JCD’s emphasis on Human Growth and Development aligns with CACREP’s view that counseling helps clients work toward optimal human development. Additionally, the focus on Helping Relationships in JCD seems appropriate given the preponderance of research and literature across time that support relationship variables as most important in predicting outcome in counseling (e.g., Bergin & Lambert, 1978; Cochran & Cochran, 2006, Krumboltz, Becker-Haver, & Burnett, 1979; Lambert & Okiishi; 1997; Lubersky et al.,1986; Norcross, 2002; & Wampold, 2001). Finally, the 2009 CACREP standards support both a broad definition of Social and Cultural Diversity as a core area and the more specific recommendation of incorporating this concept into every course. This change relates to the current belief that cultural issues are not separate from other aspects of counseling, but rather integrated into all counseling activities.
Results indicated subtle yet notable shifts in the literature focus from those in previous research studies. For example, when Vacc (1992) investigated counselor educator perceptions of the CACREP standards relevance to the preparation of counselors, he found Social and Cultural Competence perceived as least relevant while results of the current study indicate Social and Cultural Diversity as in the middle tier of topic occurrence in JCD from 1996–2007. This seems to reflect the increased emphasis given to Social and Cultural Diversity within the counseling field in the last 20 years. Additionally, Vacc found Group Development and Dynamics was perceived as one of the core areas considered most relevant by counselor educators. The current study indicates that JCD articles focused on Group Work ranked in the lowest tier of frequency of occurrence. This could indicate a shift in importance over time or incongruence between counselor educator perceived importance and the number of JCD articles published in core areas. Finally, whereas group counseling and vocational development were covered extensively in JCD in the mid-1980s and early 1990s (William & Buboltz, 1999), our findings demonstrated considerably less focus on these areas over the last 10 years. Clearly, some important shifts in the literature have occurred over the past 25 years.
We find it important to also note the match between the ranked frequencies of JCD articles within the CACREP core areas and the results of McGlothlin and Davis’ (2004) study of the core areas perceived benefits. McGlothlin and Davis’ survey results ranked counselors’ perceptions of the importance of the core areas in nearly the exact rank of article frequency in JCD by core area. This suggests an overall match between publication patterns of JCD and the valuing of CACREP core areas among counselors.
Implications for Counselor Educators and Practitioners
It is clear that the articles published in JCD follow many of the trends suggested by CACREP as training requirements for counselors. If, however, as the earlier statistics suggest, JCD is the only professional journal received by the majority of ACA members, it is important for practitioners to recognize that they may not regularly be receiving as much ongoing information in these core areas compared to others, especially if they are only receiving JCD. Career development is viewed as a central factor in the lives of most people (Betz & Corning, 1993). For counselors working with children and adolescents, career development is influenced by a multitude of factors, including perceived barriers and supports (Kenny, Blustein, Chaves, Grossman, & Gallagher, 2003), family background (Eccles, Vida, & Barber, 2004), and self-efficacy beliefs (Pinquart, Juang, & Silbereisan, 2003). In adults, career-related concerns are linked with traumatic experiences (Strauser, Lustig, Cogdal, & Uruk, 2006), relationship problems (Risch, Riley, & Lawler, 2003), and overall stress (Pinquart et al.). Clearly, most counselors will encounter a need to discuss career-related issues with their clients, yet findings suggest that counselors may not receive a robust and ongoing supply of contemporary theoretical or research-based treatment approaches on this topic in JCD.
In addition, many counselors have the opportunity to facilitate groups as a part of their work. Vacc’s (1992) finding that counselor educators perceived Group Development and Dynamics as one of the most relevant core areas to the preparation of counselors and McGlothlin and Davis’ (2004) finding that Group Work ranked fourth in perceived benefit of the CACREP standards suggests that Group Work may be of importance to current working counselors, even though it is not well represented in JCD. Continuing education through professional journals can be a way to keep counselors-in-training, practicing counselors, supervisors and counselor educators abreast of new research and ideas regarding career and groups. Counselor educators, as well as clinical supervisors and counseling practitioners, would benefit by realizing that supplemental journals are needed to ensure adequate information on group dynamics is reaching their students and supervisee’s or informing their counseling practice.
Research and Program Evaluation and Assessment also received less representation in JCD. Counselors-in-training often struggle with these subjects or report disliking the bland content of these courses (Stockton & Toth, 1997). In fact, Bauman (2004) surveyed school counselors and found only 49% agreed or strongly agreed that they felt prepared to critique research, and only 43% agreed or strongly agreed that they had the skills needed to complete a research project on their own. Currently, a call in the profession exists promoting practitioners to conduct research in the field (Kaffenberger, 2009; Niles, 2003; Whiston, 1996), but with these feelings about research and assessment, it is unlikely that many will do so. Practitioners need to look beyond JCD for professional development on becoming competent and self-assured researchers. Knowing that a single journal is not the best option for gaining research self-efficacy might push practitioners to seek help elsewhere, rather than simply continuing on without furthering their knowledge.
Counselor educators and students can benefit in general from the findings of this study. For example, when conducting literature reviews or submitting research manuscripts for review, results provide guidance as to which counseling-related topics are more frequently or less frequently addressed in JCD. Results help to inform counselor educators when to best use and recommend JCD as an initial resource or different journal when they or their students are investigating specific topics within CACREP core areas. Additionally, one could argue that results suggest a reason to join multiple professional counseling organizations such as ASCA or AMHCA, or join the smaller sub-interest groups (e.g., National Career Development Association and Association of Specialists in Group Work) when first joining ACA or renewing their ACA membership. Overall, having more information available on major sources of training and continuing education can only assist practitioners and educators in their roles.
Implications for Future Research
Although this study provides an analysis of JCD articles over a 10-year period, with CACREP guidelines, additional research in this area is needed. Several ideas for future research foci are provided as preliminary courses of action. Researchers could help to identify students’, counselor educators’ and working counselors’ perceptions as to the importance of some of the lesser represented areas, such as Career and Group. Additionally, perceptions from these same constituents on how JCD, ACA, NBCC, and/or CACREP shape their views of the counseling field seems to be worthy of investigation. More research focused on specific CACREP areas and articles from other journals (e.g., the types of articles that represent each CACREP area and the impact on continuing education and training of future counselors) would further illuminate the relationship between the accrediting body and the counseling journals in general. Regardless of the exact focus of future research, it is clear that there is a link between the counseling accrediting body and the flagship journal. Further research is needed into how JCD and other counseling journals, along with CACREP and NBCC, may have or will influence each other over time.
Conclusion
It is our hope that the findings of the present study will be included in the perpetual input loop linking ACA, NBCC, JCD, CACREP and the counseling profession. With CACREP’s 2009 accreditation standards being implemented, we believe now is a good time for the counseling profession to re-examine the roles of the major counseling entities’ relationships to each other. Continuing this discussion, especially focusing on CACREP and ACA, may help strengthen the unity of our profession and further cement our identity as professional counselors.
References
Adams, S. (2006). Does CACREP accreditation make a difference? A look at NCE results and answers. Journal of Professional Counseling, Practice, Theory, & Research, 33, 60–76.
Bauman, S. (2004). School counselors and research revisited. Professional School Counseling, 7, 141–151.
Bergin, A. E., & Lambert, M. J. (1978).The evaluation of therapeutic outcomes. In S.L. Garfield and A.E. Bergin (Eds.), Handbook of psychotherapy and behavior change (2nd ed.; pp. 139–189). New York, NY: John Wiley.
Betz, N. E., & Corning, A. F. (1993). The inseparability of ‘career’ and ‘personal’ counseling. Career Development Quarterly, 42, 137–142.
Bobby, C. L., & Kandor, J. R. (1992). Assessment of selected CACREP standards by accredited and non accredited programs. Journal of Counseling & Development, 70, 677–684.
Bobby, C. L., & Kandor, J. R. (1995). CACREP accreditation: Assessment and evaluation in the standards and process. ERIC digest. (ERIC Document Reproduction Service No. ED388884).
Burke, M. T., Hackney, H., Hudson, P., Maranti, J., Watts, G. A., & Epp, L. (1999). Spirituality, religion, and CACREP curriculum standards. Journal of Counseling & Development, 77, 251–257.
Calley, N. G., & Hawley, L. D. (2008). Professional identity of counselor educators. Clinical Supervisor, 27, 3–16. doi: 10.1080/07325220802221454
Canfield, B. S. (2007, October). Many uniting into one [President’s message]. Counseling Today, 6.
Cochran, J. L., & Cochran, N. H. (2006). The heart of counseling: A guide to developing therapeutic relationships. Belmont, CA: Thomson Brooks/Cole.
Council for Accreditation of Counseling and Related Educational Programs (2007). Directory of accredited programs. Retrieved from http://www.cacrep.org/directory-current.html
Council for Accreditation of Counseling and Related Educational Programs (2009). 2009 CACREP Standards. Retrieved from http://67.199.126.156/doc/2009%20Standards.pdf
Eccles, J. S., Vida, M. N., & Barber, B. (2004). The relation of early adolescents’ college plans and both academic ability and task-value beliefs to subsequent college enrollment. Journal of Early Adolescence, 24, 63–77. doi:10.1177/0272431603260919
Gale, A. U., & Austin, B. D. (2003). Professionalisms challenges to professional counselors collective identity. Journal of Counseling & Development, 81, 3–10.
Goodyear, R. K. (1984). On our journal’s evolution: Historical developments, transitions, and future directions. Journal of Counseling & Development, 63, 3–8.
Haight, D. A. (1992). The pursuit of quality: A look into the future of CACREP. Journal of Counseling and Development, 70, 1992.
Hansen, J. T. (2003). Including diagnostic training in counseling curricula: Implications for professional identity development. Counselor Education and Supervision, 43, 96–107.
Hershenson, D. B., & Berger, G. P. (1999). The state of community counseling: A survey of directors of CACREP- accredited programs. Journal of Counseling & Development, 79, 188–193.
Holcomb-McCoy, C., Byan, J., & Rahill, S. (2002). Importance of the CACREP school counseling standards: School counselors’ perceptions. Professional School Counseling, 6, 112–119.
Kenny, M. E., Blustein, D. L., Chaves, A., Grossman, J. M., & Gallagher, L. A. (2003). The role of perceived barriers and relational support in the educational and vocational lives of urban high school students. Journal of Counseling Psychology 50, 142–155. doi: 10.1037/0022 0167.50.2.142
Krumboltz, J. D., Becker-Haven, J. F., & Burnett, K. F. (1979). Counseling psychology. Annual Review of Psychology, 30, 555–602.
LaFountain, R. M., & Baer, E. C. (1999). Increasing CACREP’s name recognition: The effect of written correspondence on site supervisor’s awareness level. Journal of Counseling & Development, 79, 194–199.
Lambert, M. J., & Okiishi, J. C. (1997). The effects of the individual psychotherapist and implications for future research. Clinical Psychology: Science and Practice, 4, 66–75. doi: 10.1111/j.1468-2850.1997.tb00100.x
Lubersky, L., Crits-Christoph, P., McClellan, T., Woody, G., Piper, W., Liberman, B., Imber, S., & Pilkenis, P. (1986). Do therapists vary much in success? Findings from four outcome studies. American Journal of Orthopsychiatry, 56, 501–512.
McGlothlin, J. M., & Davis, T. (2004). Perceived benefits of CACREP (2001) core curriculum standards. Counselor Education and Supervision, 43, 274–285.
Norcross, J. C. (2002). Empirically supported therapy relationships. In J. C. Norcross (Ed.), Psychotherapy relationships that work: Therapist contributions and responsiveness to patients (pp. 3–16). Oxford, England: Oxford University Press.
Pinquart, M., Juang, L. P., & Silbereisen, R. K. (2003). Self-efficacy and successful school-to-work transition: A longitudinal study. Journal of Vocational Behavior, 63, 329–346. doi:10.1016/S0001-8791(02)00031-3
Pistole, M. C., & Roberts, A. (2002). Mental health counseling: Toward resolving identity confusions. Journal of Mental Health Counseling, 24, 1–19.
Remley, T. P., Jr., & Herlihy, B. (2007). Ethical, legal, and professional issues in counseling (Updated 2nd ed.). Upper Saddle River, NJ: Prentice Hall.
Risch, G. S., Riley, L. A., & Lawler, M. G. (2003). Problematic issues in the early years of marriage: Content for premarital education. Journal of Psychology and Theology, 31, 253–269.
Ryan, G. W., & Bernard, H. R. (2000). Data management and analysis methods. In N. K. Denzin & Y. S. Lincoln (Eds.), Handbook of qualitative research (pp. 769–802). London, England: Sage.
Schmidt, J. J. (1999). Two decades of CACREP and what do we know? Counselor Education and Supervision, 39, 34-45.
Stockton, R., & Toth, P. L. (1997). Applying a general research training model to group work. Journal of Specialists in Group Work, 22, 241–252. doi:10.1080/01933929708415528
Strauser, D. R., Lustig, D. C., Cogdal, P. A, & Uruk, A. C. (2006). Trauma symptoms: Relationship with career thoughts, vocational identity, and developmental work personality. Career Development Quarterly, 54, 346–360.
Vacc, N. A. (1992). An assessment of the perceived relevance of the CACREP standards. Journal of Counseling & Development, 70, 685–687.
Wampold, B. E. (2001). The great psychotherapy debate: Models, methods, and findings. Mahwah, NJ: Erlbaum.
Weinrach, S. G. (1987). Some serious and some not so serious reactions to AACD and its journals. Journal of Counseling & Development, 65, 395–399.
Williams, M. E., & Buboltz, W. C. Jr. (1999). Content analysis of the Journal of Counseling & Development: Volumes 67-74. Journal of Counseling & Development, 77, 344–349.
Yep, R. (2010). American Counseling Association Year-in-Review 2009, 1–9. Retrieved from http://www.counseling.org/Sub/BlastEmails/YIR_2009.pdf
Joel F. Diambra, NCC, Melinda M. Gibbons, NCC, Jeff L. Cochran, NCC, and Shawn Spurgeon, ACS, teach Counselor Education at the University of Tennessee at Knoxville. Whitney L. Jarnagin, NCC, teaches at Walters State Community College. Porche’ Wynn is a counselor education doctoral candidate at the University of Tennessee. Correspondence can be addressed to Joel F. Diambra, University of Tennessee at Knoxville, 449 Claxton Complex, 1122 Volunteer Blvd. Knoxville, TN, 37996-3452, jdiambra@utk.edu.
Jul 23, 2014 | TPC Outstanding Scholar
Jeffrey M. Warren and Edwin R. Gerler, Jr.

Jeffrey M. Warren and Edwin R. Gerler Jr. received the 2013 Outstanding Scholar Award for Quantitative or Qualitative Research for their article “Effects of School Counselors’ Cognitive Behavioral Consultation on Irrational and Efficacy Beliefs of Elementary School Teachers.” Dr. Warren is an assistant professor of counselor education at the University of North Carolina at Pembroke. He cochairs the Research Quality Task Force for the Transforming School Counseling and College Access Interest Network (TSCCAIN) of the Association for Counselor Education. He is a National Certified Counselor (NCC) and a National Certified School Counselor (NCSC). Dr. Gerler is a professor of counselor education at North Carolina State University. He has served as editor-in-chief of two national counseling journals and was the founding editor of the Journal of School Violence and the founding coeditor of the online publication Meridian, a school computer technologies journal.