Mar 23, 2016 | Article, Volume 6 - Issue 1
Robert C. Schmidt
Youth suicide is a significant public health concern and efforts to reduce youth suicide remain a national priority (Kung, Hoyert, Xu, & Murphy, 2008; National Action Alliance for Suicide Prevention: Research Prioritization Task Force, 2014). In the United States, there were 40,600 suicides in 2012, averaging 111 suicides per day (Centers for Disease Control and Prevention [CDC], 2014a). Of the total number of suicides, 5,183 were youth suicides, averaging 14 youth suicides daily, or one youth suicide every 1 hour and 42 minutes (Drapeau & McIntosh, 2014). Youth suicide is the third leading cause of death between the ages of 10 and 14 and has become the second leading cause of death between the ages of 15 and 24 (CDC, 2014a). The results from the 2013 Youth Risk Behavior Surveillance (YRBS) reported 29.9% of high school students felt sad or hopeless almost every day for 2 weeks or more; 17% of high school students seriously considered attempting suicide; 13.6% of high school students made a suicide plan about how they would attempt suicide; and 8% of students attempted suicide one or more times (CDC, 2014b).
Efforts to address the increasing rate of youth suicide call for the identification of existing training and preparation gaps currently faced by practitioners (National Action Alliance for Suicide Prevention: Research Prioritization Task Force, 2014). These gaps pose many challenges for practitioners to effectively provide appropriate interventions. Although previous studies have investigated training gaps among specific professional disciplines (Debski, Spadafore, Jacob, Poole, & Hixson, 2007; Dexter-Mazza, & Freeman, 2003; O’Connor, Warby, Raphael, & Vassallo, 2004), the current study investigated a broader representation of disciplines including social workers, school counselors, professional counselors, school psychologists and psychologists. This study examined practitioner self-perceived levels of preparedness, levels of confidence and methods used in the assessment of youth suicide.
Practitioner readiness in suicide assessment. In approximately eight of ten suicides, youth give advance clues or warning signs of their intentions that can be detected by others (McEvoy & McEvoy, 2000; Poland & Lieberman, 2002). In a study spanning four years of youth in a rural school district (N = 5,949) screened for suicidal thoughts, 670 (11%) reported having suicidal thoughts within the past year or past few days (Schmidt, Iachini, George, Koller, & Weist, 2015). Practitioners working within school or community mental health settings have an opportunity to play a critical role in the identification, assessment and prevention of youth suicide (Singer & Slovak, 2011). Within either setting, practitioners will encounter clients having suicidal thoughts or behaviors (Rudd, 2006). The practitioner’s responsibility in the assessment of suicide is to estimate risk based on identifying warning signs and associated behaviors and to respond appropriately (Bryan & Rudd, 2006).
In a national sampling of social workers, 93% of the respondents reported having worked with a suicidal patient (Feldman & Freedenthal, 2006), and 55% of clinical social workers reported having a patient attempt suicide (Sanders, Jacobson, & Ting, 2008). In a study of psychology doctoral interns (N = 238) completed by Dexter-Mazza and Freeman (2003), 99% reported providing services to suicidal patients and 5% reported experiencing a patient death by suicide. Across professional disciplines, 22% to 30% of social workers, counselors and psychologists reported having a patient die by suicide (Jacobson, Ting, Sanders, & Harrington, 2004).
Irrespective of the level of suicide training, comfort level or experience (i.e., even those with limited training and preparedness), the circumstances for which practitioners meet with a suicidal client are not only stressful, but also have legal and ethical ramifications (Cramer, Johnson, McLaughlin, Rausch, & Conroy 2013; Poland & Lieberman, 2002). Research suggests significant gaps exist related to the practitioner’s training and readiness to perform suicide risk assessments, highlighting training deficits in the level of preparedness, level of confidence and methods used to determine suicide risk level (Smith, Silva, Covington, & Joiner, 2014).
Although youth suicide remains a national concern and priority, gaps appear most prominent in translating research into practice in developing and providing appropriate levels of training and supervision for practitioners (Smith et al., 2014). Research to support this concern offers valuable recommendations (Osteen, Frey, & Ko 2014; Schmitz, Allen, Feldman, et al., 2012); however, despite these recommendations, training and preparation continue to lag (Rudd, Cukrowicz, & Bryan, 2008). Practitioner competency skills in suicide assessment continue to be neglected by colleges, universities, licensing bodies, clinical supervisors and training sites that can have the greatest impact in reducing youth and adult suicide (Schmitz et al., 2012).
Practitioner preparedness. In the past several decades, researchers began identifying gaps in suicide risk knowledge, finding that practitioners were inadequately prepared to assess suicide risk. In master’s and doctoral clinical and counseling psychology training programs, 40–50% were found to offer formalized training in suicide assessment and management of suicide risk (Kleespies, Penk, & Forsyth, 1993). Suicide-specific training was only included in 2% of accredited professional counseling programs and 6% of accredited marriage and family therapist training programs (Wozny, 2005).
Training also has been identified as limited among social work graduate programs,
averaging 4 hours or fewer specific to suicide education (Ruth et al., 2009). In a study by Feldman and Freedenthal (2006) randomly surveying social workers through the National Association of Social Workers (N = 598), almost all of the social work participants (92.3%) reported working with a suicidal client; however, only 21.1% received any formal suicide-related training in their master’s program. Of the 21.1% of social workers receiving formal training, 46% specified their suicide-devoted training was less than 2 hours.
This pattern continued as additional studies found psychology doctoral interns did not receive adequate training in suicide assessment and/or managing suicide risk in clients. Neither did they receive the necessary levels of clinical supervision in suicide assessment (Mackelprang, Karle, Reihl, & Cash, 2014). In a study of psychology graduate school programs, 76% of the program directors indicated a need for more suicide-specific training and education within their programs but discovered barriers to implement this training (Jahn et al., 2012). The chief barrier reported by the directors was the absence of guidance and curriculum requirements to provide training and, secondly, the inability of colleges to create space in the existing curriculum schedule for added classes (Jahn et al., 2012).
In a survey that included members of the National Association of School Psychologists (N = 162), less than half (40%) of the respondents reported receiving graduate-level training in suicide risk assessment (Debski et al., 2007). Most school psychologists in this study reported feeling at least somewhat prepared to work with suicidal students while doctoral trained practitioners reported feeling well prepared.
School counselors share similar gaps in their preparation to provide suicide intervention and assessment to youth. Research conducted by Wachter (2006) indicated that 30% of school counselors had no suicide prevention training. In a study conducted by Wozny (2005), findings indicated that just 52.3% of the school counselors, averaging 5.6 years of experience, were able to identify critical suicide risk factors. This study exposed competency gaps in suicide assessment, training and intervention consistent with practitioner disciplines that were identified within this study. This is consistent with previous study findings (National Action Alliance for Suicide Prevention, 2014; Schmitz et al., 2012) that identified insufficient training and preparation of practitioners in the assessment and prevention of youth suicide and suicide in general.
Practitioner confidence. Although most practitioners will encounter youth with suicidal thoughts and behaviors, many lack the self-confidence to effectively work with suicidal youth. The lack of confidence appears related to competency levels and limited training (National Action Alliance for Suicide Prevention, 2014; Oordt, Jobes, Fonseca, & Schmidt, 2009).
In contrast, researchers found that as practitioner risk assessment skills increased through suicide-specific training, noticeable increases were measured in practitioner self-confidence (McNiel et al., 2008). Oordt and colleagues (2009) studied mental health practitioner levels of confidence after receiving empirically-based suicide assessment and treatment training. The results indicated that self-reported levels of practitioner confidence increased by 44% and measured a 54% increase specific to self-confidence levels related to the management of suicidal patients. In addition, studies of school counselors identified correlations between self-efficacy, confidence and the ability to improve clinical judgment in providing suicide interventions and assessment (Al-Damarki, 2004).
Adequate training and experience in suicide prevention and assessment has been found to increase practitioner levels of confidence in conducting risk assessments and management planning (Singer & Slovak, 2011). Research suggests that confidence increases the practitioner’s ability to estimate suicide risk level, make effective treatment decisions and base recommendations when conducting a quality assessment. However, when the assessor is not confident, the assessment is more prone to errors or missed information, decreasing the accuracy of their assessment (Douglas & Ogloff, 2003). Paradoxically, overconfidence produces similar results as practitioners lacking confidence. Tetlock (2005) reported that overconfident practitioners are more prone to making errors during a suicide risk assessment unless their clinical judgment is further supported by objective evidence such as using a formal, validated and reliable method of assessment.
Methods Used in Suicide Assessment
There are several categories of suicide assessment instruments developed for youth (Goldston, 2003; National Action Alliance for Suicide Prevention, 2014). These include detection instruments like structured and semi-structured interviews; survey screenings that include self-report inventories and behavior checklists; and risk assessment instruments that include screenings, self-report questionnaires and multi-tier screening assessments.
Across settings including schools, emergency departments, primary care offices and community mental health offices, studies indicate that inconsistent methods are used to assess suicide risk (Horowitz, Ballard, & Paoa, 2009). In most instances, the use of published and validated suicide screening tools are not being properly used as intended or designed, which impacts their reliability and validity (Boudreaux & Horowitz, 2014). This may represent and reflect the practitioner’s limited training, confidence and experience in these areas.
In addition, the documentation of the suicide assessment also can reflect the level of the practitioner’s training and knowledge of suicide assessment. O’Connor and colleagues (2004) noted that practitioner skill deficiencies in youth suicide assessment are likely to appear in clinic notes as a brief statement, “patient currently denies suicidal thoughts,” based on the practitioner’s impressionistic and subjective perception after completing a brief unstructured interview. This is commonly the only form of documentation obtained by the practitioner (O’Connor et al., 2004). Research consistently provides evidence across disciplines that some practitioners are not prepared to make clinical judgments (Debski et al., 2007; Jahn et al., 2012; Mackelprang, et al., 2014; Ruth et al., 2009; Smith et al., 2014). This study offered an opportunity to contribute to the understanding of practitioners’ self-perceived competencies in the assessment of youth suicide while identifying existing gaps in training.
The Current Study
In previous studies, research has focused on confidence and preparedness levels only in specific disciplines related to the identification and assessment of suicidal youth (Al-Damarki, 2004; Debski et al., 2007; Wozny, 2005). This study encompassed a much broader representative sample of practitioner disciplines including psychologists, social workers, school counselors, professional counselors and school psychologists.
The purpose of this study was to determine relationships among practitioners’ self-perceived levels of preparedness, levels of confidence and methods used to perform suicide risk assessments in youth. These efforts were guided by the following research question: What are the relationships among the self-perceived levels of preparedness, levels of confidence, and methods used in the assessment of suicide risk for practitioners whose responsibilities require suicide risk assessment and management? In order to address this, survey questions were designed to obtain participant responses related to skill development, preparation, confidence and methods used in the process of conducting suicide risk assessments.
Method
Procedures and Instrumentation
Since this study sought to collect data using human subjects, the proposal was reviewed and approved by the Wilmington University Human Subjects Review Committee prior to beginning this study. An exploratory descriptive survey design examined practitioner self-perceived levels of preparedness, levels of confidence and methods used to assess suicide risk in youth. Using a quantitative method to guide this study, the researcher attempted to recruit practitioners positioned and responsible for suicide risk assessment. This included working in cooperation with and posting the survey on the Maryland School Psychologists’ Association Web site and the University of Maryland Center for School Mental Health Web site. The survey was forwarded to school districts in Maryland and Virginia and directed to school counselors, school psychologists, and school-based mental health professionals, including social workers and professional counselors. In addition, the survey was forwarded to multiple outpatient mental health clinics in the mid-Atlantic region of the United States. Practitioners were provided with information about the survey, study purposes and ethical standards, and it was noted that participation was voluntary and confidential. Practitioners submitted their responses online, allowing the researcher to evaluate self-reported levels related to suicide assessment. Participants were provided with an access link to anonymously complete the survey using SurveyGizmo. The completed data were then entered into an Excel spreadsheet database.
The Child and Adolescent Suicide Intervention Preparedness Survey was the instrument developed for this study. This researcher received prior approval from the authors of two previously published surveys (Debski, et al., 2007; Stein-Erichsen, 2010) while adding specific queries for the purposes of this study. The survey by Debski and colleagues (2007) included a 42-item questionnaire with vignettes that measured the training, roles and knowledge of school psychologists. These questions targeted participant confidence and perceived levels of preparedness that also were sought in this current study, but from a broader discipline base.
The survey by Stein-Erichsen (2010) included a 55-item measure designed to identify confidence levels of school psychologists providing suicide intervention and prevention within schools. The survey questionnaires designed by Stein-Erichsen (2010) and Debski and colleagues (2007) offered questions adapted for this study specifically focusing on preparedness levels, confidence, roles, methods used to assess suicide levels, and omitted survey questions not relevant to this study. This resulted in a 23-item survey targeting practitioner levels of training, preparedness, confidence and the identification of additional training needs.
Participants
The study had 339 participants representing school counselors (N = 107/32%); social workers (N = 90/27%); school psychologists (N = 37/11%); professional counselors (N = 35/11%); psychologists (N = 5/1%); other (N = 62/18%); and three participants with unknown professional identification.
The final sampling of participants included 43 males, 292 females and four participants with unknown gender identification. Participants averaged in age ranges 22–29 (N = 33/10%), 30–39 (N = 105/31%), 40–49 (N = 94/28%), 50–59 (N = 61/18%) and ages 60 and above (N = 45/13%). The participants responded to the item querying level of education as having a bachelor’s degree (N = 18/6%), doctoral degree (N = 14/4%), master’s degree (N = 275/81%), and other (N = 28/8%) including associate levels of education, as well as four (1%) participants with unknown educational levels.
The participants represented a broad but targeted sampling from a variety of employers, including school settings (N = 166/49%); outpatient mental health settings (N = 108/32%); mental health agencies (N = 31/9%); and other settings (N = 33/10%); as well as one participant with an unknown employment setting. The participants also identified their employment environment as urban (N = 56/60%), rural (N = 174/52%), and suburban (N = 105/31%).
Participants identified the practitioner responsible to assess suicide risk within their work setting having multiple response options (see Table 1). These included a psychiatrist (N = 85/25%), nurse (N = 57/17%), school counselor (N = 179/53%), social worker (N = 168/50%), teacher (N = 7/2%), school psychologist (N = 154/46%), school mental health professional (N = 125/37%), psychologist (N = 64/19%), professional counselor (N = 101/30%), and other (N = 29/9%) including paraprofessionals, while 19 participants (6%) reported they do not complete suicide risk assessments.

Prior exposure with suicidal students/clients. In the survey, 288 (86%) of the participants reported having a student or client referred to them for being potentially suicidal; 45 (14%) did not receive a similar referral; and six participants did not respond. A majority of participants (N = 287/86%) reported having worked with a student or client initially found to be presenting with active suicidal thoughts and 48 (14%) reported not yet having worked with a suicidal student or client.
Analysis
Using descriptive data, participant responses were further examined to determine frequency and percentages of the total responses. In addition, inferential statistics were used to compute possible relationships among variables using SPSS. Data from the primary survey questions provided guidance toward establishing possible relationships between practitioner preparedness, confidence and the methods used in determining suicide risk level.
Results
Self-perceived preparedness in suicide assessment. The majority of the respondents reported some type of exposure or training in suicide intervention and assessment. The participants had an opportunity to select multiple answers: graduate course work (N = 174/52%), attending professional development workshops (N = 233/69%), in-service trainings at work (N = 213/63%), and having not received any training (N = 21/6%). In addition, participants had multiple answer options that represented self-perceived preparedness levels: not feeling at all prepared (N = 15/4%), feeling somewhat prepared (N = 120/36%), feeling well prepared (N = 202/60%), and requesting that someone more prepared meet or assess a suicidal student/client (N = 32/9%).
Self-reported confidence in suicide assessment. The confidence levels reported by the participants reflect professional skill development to conduct suicide risk assessments. The responses included feeling very confident (N = 49/15%), confident (N = 212/63%), and not very confident (N = 63/19%). A similar survey item asked about confidence levels working with a suicidal student or client. The responses included feeling very confident (N = 42/12%), confident (N = 231/69%), and not very confident (N = 63/19%). An additional survey item sought information regarding participant feelings when assessing for suicidal thoughts. Results indicated feeling not prepared (N = 39/12%), anxious (N = 116/34%), calm (N = 145/43%), and confident (N = 185/55%).
Methods Used to Determine Suicide Risk Level During Assessment. Several survey items queried participant levels of training and methods used to assess a suicidal student or client. A survey item asked participants if they had received formal training to conduct suicide risk assessments. The respondents indicated Yes (N = 201/60%) or No (N = 133/40%). In addition, a survey question asked participants if they felt qualified to complete a suicide risk assessment: Yes (N = 241/73%) or No (N = 91/27%). A follow-up survey item asked participants how they determined if the student or client was at imminent risk, high to moderate risk or low risk. The participant responses indicated they would conduct an informal, non-structured interview (N = 213/64%) or use a formal, valid suicide assessment instrument (N = 90/27%); the remaining respondents indicated other (N = 31/9%).
Participants were asked what would limit their ability to provide a suicide intervention. Using a “check all that apply” format, responses included practitioners not receiving formal training to work with suicidal students or clients (N = 55/17%), the role of suicide interventions and response is the job of others (N = 19/6%), not feeling adequately prepared to provide a suicide intervention or assessment (N = 65/20%), workplace policy does not allow formal suicide assessments (N = 12/4%), and feeling prepared (N = 225/68%). The discipline most frequently reported to encounter and assess a youth presenting with suicidal thoughts or behaviors in this study was the school counselor (53%). This supported previous research by Poland (1989) who identified that “the task of suicide assessment was likely to fall on the school counselor” (p. 74).
To determine whether relationships existed among self-perceived levels of preparedness, levels of confidence, and methods used in youth suicide assessment, the researcher completed a chi-square statistical analysis to measure numerical and categorical differences. In order to compare differences among several groups, variables were collapsed to include confident/not confident and prepared/not prepared. The first group compared practitioners’ responses of reporting confident/not confident to prepared/not prepared in the process of providing an informal versus formal suicide risk assessment in youth. The analysis indicated that there were significant differences in preparedness levels according to the method used. Seventy-three percent of those reporting use of formal assessments versus approximately 50% of those using informal assessments indicated confidence in their preparedness abilities (X2 = 12.79; df = 1. Cramer’s V = .206, p = .000). A further analysis indicated there were similar significant differences in practitioner confidence levels conducting informal, non-structured suicide risk assessments and formal assessments (X2 = 23.54, DF = 1. Cramer’s V=.280, p = .000). The results showed that 95.6% of the practitioners using formal suicide risk assessments reported higher levels of confidence versus 70.1% of the practitioners using informal, non-structured suicide risk assessments.
To identify existing gaps, participants were asked to rank by priority the trainings they needed to increase competency levels. The highest priority was (1) to receive a comprehensive training on warning signs, symptoms and suicidal behaviors, and (2) to attend several suicide assessment workshops.
Discussion
The purpose of this study was to determine if relationships existed among practitioners’ self-perceived levels of preparedness, levels of confidence and methods used when assessing for suicide risk in youth. A survey was designed to query participants representing a broad sampling of disciplines related to their perceptions, experience and involvement in youth suicide risk assessment. The results of the survey were analyzed using chi-square to determine if relationships existed among variables, including participant perceptions of feeling prepared and confident, and if this contributed to the methods used to determine suicide risk in youth.
Results of the survey indicated that a majority of the participants (86%) reported having worked with suicidal youth; however, inconsistencies in participant responses emerged related to the constructs of feeling prepared and confident in the assessment of suicide. The results suggested preparedness and training in suicide assessment is linked to practitioner confidence levels when assessing for suicide risk among youth. This finding is supported by earlier research by Oordt and colleagues (2009), who reported that practitioner confidence in suicide assessment is primarily related to competency and training levels. The interrelationship between preparedness and confidence is often reflected in the practitioner’s ability to accurately estimate risk level. This may potentially increase the likelihood of omitting critical information, which may affect the estimate of suicide risk (Douglas & Ogloff, 2003; Singer & Slovak, 2011). The results represent an important finding and highlight existing gaps in practitioner preparation. These gaps may reflect a struggle for most university and college graduate school degree programs to offer a more diversified curriculum (Allen, Burt, Bryan, Carter, Orsi, & Durkan, 2002) that includes courses specific to identifying, intervening in and assessing for suicide risk in youth (Schmitz et al., 2012).
The inconsistencies in participant responses related to feeling prepared and confident became apparent when participants rated themselves in working with a suicidal youth. Although over half of the respondents reported feeling well prepared and qualified in their ability, a much smaller percentage reported feeling confident in themselves (12%) and their skill preparation (15%) to assess for suicide. This finding may reflect a self-evaluation dilemma in wanting to self-report feeling prepared to work with a suicidal youth, but in actuality not feeling prepared or confident to provide a suicide intervention or complete an assessment.
As this study broadened its review of practitioner responses related to preparedness and confidence, findings indicated additional inconsistencies in participant responses related to self-reported feelings of preparedness and confidence when conducting a suicide intervention or suicide assessment. Despite predominantly higher levels of reported confidence, skill development and preparedness to determine if a student or client was at imminent risk, high to moderate risk, or low risk, few participants (27%/N = 90) reported using a formal suicide assessment instrument. Most respondents (64%/N = 213) reported basing their clinical judgment solely on using an informal, non-structured interview. Although practitioners reported feeling prepared and having a sense of confidence assessing for suicide risk, basing clinical judgment on this method alone raises concerns. O’Connor and colleagues (2004) described that practitioner skill deficiencies in suicide assessment are commonly reflected in clinic notes such as “patient currently denies suicidal thoughts,” based on the practitioner’s impressionistic and subjective perceptions. Consistent with identifying training deficiencies in preparation, 52% (N = 174) of the participants reported receiving limited suicide intervention or assessment training in graduate coursework.
The participants in this study who reported using a formal suicide assessment, however, indicated feeling better prepared to conduct a suicide assessment versus practitioners using an informal, non-structured interview. In addition, practitioners using a formal assessment also had greater confidence levels versus practitioners using an informal, non-structured interview. When participants were asked to rank their own levels of needed training to provide a more thorough suicide intervention, participants identified skill deficiencies and training gaps in identifying warning signs and behaviors and assessing for suicide using a suicide risk assessment. These deficiencies pose great concern and competency challenges for practitioners charged with assessing for suicide risk. The combination of skill attributes, guided interview and diagnostic assessment synthesizes the information and allows practitioners to determine risk level and base clinical judgment on a variety of sources (Rudd, 2006; Sullivan & Bongar, 2009). The skill deficiencies reflected across all disciplines represented significant training gaps. This study suggests the need for increased commitment by colleges and universities to prepare future practitioners to more effectively address the growing national youth suicide crisis.
Implications
Despite suicide being identified as a national public health priority, no significant reduction in suicide has been recorded in the past 50 years (Kung et al., 2008; National Action Alliance for Suicide Prevention, 2014). “With the majority of youth suicide deaths being preventable,” (O’Connor, Platt, & Gordon, 2011, p. 581), continued and more urgent calls for increasing practitioner preparedness, confidence and competency skills continue to be neglected.
Each of the disciplines represented in this study is faced with the challenge to address and estimate suicide risk. This study highlighted the critical role of school counselors as being identified by participants (53%) to be the most likely practitioner to respond and provide a suicide assessment. Representing a variety of disciplines and settings, participant responses suggest training deficiencies in the levels of preparedness, confidence and exposure to formal assessment measures. Previous research has made strong recommendations to increase the provisions and training in suicide assessment. Despite heeding previous calls and recommendations to prepare practitioners, more attention is needed to address previous and current identified training deficiencies among practitioners.
Transitioning research into practice includes revisiting several identified recommendations by Schmitz et al. (2012). This includes providing consistent core standards and competencies across disciplines by educational accrediting institutions. This may call for increased suicide-specific educational and training requirements beyond the baccalaureate degree level and include dissecting vignettes, role-playing, exposing practitioners to several suicide assessment instruments and interpreting the results (Fenwick, Vassilas, Carter, & Haque, 2004). This would include increased emphasis on recognizing the signs and symptoms of depression, suicidal thoughts and behaviors and increasing an understanding of potential next steps once a suicide risk level has been determined. In addition, to sustain these skills, state licensing boards can require continuing education specific to suicide identification, assessment and management. Rudd and colleagues (2008) placed emphasis on practitioners receiving increased suicide assessment strategies through supervision. The prevailing need practitioners identified as a chief priority in this study was to become more familiar with the warning signs, symptoms and behaviors associated with suicide and suicide assessment. The findings included within this study offer future research opportunities to monitor suicide training, preparation and continuing educational requirements of colleges, universities and licensing boards that govern and are responsible for the production of competent practitioners.
Although attention has focused on practitioner training deficits in the identification and assessment of youth suicide, future studies also are warranted in the measurement and impact of existing suicide prevention training programs that may provide opportunities for practitioners to increase skill sets in these areas. Another area meriting future study might include a national sampling of school counselor preparation in the identification, assessment and exposure to assessment tools. In this study, school counselors were identified to be the most likely practitioner called upon to provide an initial suicide intervention or assessment given their access to a large number of youth. This serves as a valuable finding, highlighting the call for increased and expanded counselor education, training and preparation in suicide risk identification and assessment in graduate school.
Limitations
Providing a suicide intervention or assessment involves many complex issues, and addressing the many variables paralleling these efforts could not be entirely assessed in this study. This study was intended to explore current levels of practitioner preparedness, confidence and the methods used to assess youth suicide. There are some notable limitations regarding the current study; therefore, caution is warranted regarding the generalizability of the findings.
Although the Internet provided a greater opportunity for the researcher to create survey access to targeted participants and disciplines, this method did not provide a sample size completion rate. In addition, previous Internet survey research (W. Schmidt, 1997) reported that participants have access to multiple submissions, although ethical practice instructions and consent to complete this survey was provided. In order to access participants from multiple disciplines, the survey used in this study was available online as a self-report method of completion. In this process, self-report instruments, including surveys, inherently contain participant response bias. This may be reflected in responding to questions in a socially desirable or expected manner (Heppner, Wampold, & Kivlighan 2007). In addition, online surveys can be submitted containing omitted and blank responses (Sue & Ritter, 2012).
As previously noted, The Child and Adolescent Suicide Intervention Preparedness Survey used in this study was adapted from two previous research surveys (Debski et al., 2007; Stein-Erichsen, 2010). In this study design, survey questions were created and adapted to measure participant constructs in the assessment of youth suicide. The use of a psychometrically sound survey instrument would be an ideal application to implement and duplicate for future research.
Conclusion
The findings from this study identify significant interrelationships between the practitioner’s self-perceived feelings of preparedness, confidence levels and methods used to assess for suicide risk among youth. The self-reported feelings of being prepared and confident seem to contradict the method used to obtain a suicide risk level. This finding suggests many practitioners are well intended, but lack the necessary skills to conduct a thorough suicide risk assessment. The majority of practitioners participating in this study reported conducting a suicide risk intervention using an informal, non-structured interview to formulate a suicide risk level versus using a formalized suicide risk assessment instrument. Prior experience and exposure to suicide risk assessment instruments and increased emphasis in suicide-specific training curriculum in graduate school can offer the opportunity for a practitioner to feel better prepared, feel more confident and utilize a more effective method to determine a youth’s suicide risk level. Practitioner gaps in training are typically augmented by the practitioner seeking personal training and workshops to fill these gaps. Efforts must be made by colleges and universities to increase the competency skills in this area if we are to ever reduce the growing number of youth suicides. The findings from this study supported limited previous research sounding urgent calls to better prepare practitioners, especially school counselors, in the identification of youth presenting with suicidal thoughts or behaviors.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Al-Damarki, F. R. (2004). Counselor training, anxiety, and counseling self-efficacy: Implications for training psychology students from the United Arab Emirates University. Social Behavior and Personality, 32, 429–439. doi:10.2224/sbp.2004.32.5.429
Allen, M., Burt, K., Bryan, E., Carter, D., Orsi, R., & Durkan, L. (2002). School counselor’s preparation for and participation in crisis intervention. Professional School Counseling, 6, 96–102.
Boudreaux, E. D., & Horowitz, L. M. (2014). Suicide risk screening and assessment: Designing instruments with dissemination in mind. American Journal of Preventative Medicine, 47(32), 163–169.
doi:10.1016/j.amepre.2014.06.005
Bryan, C. J., & Rudd, D. M. (2006). Advances in the assessment of suicide risk. Journal of Clinical Psychology, 62, 185–200.
Centers for Disease Control and Prevention. (2014a). Fatal injury data. Web-based injury statistics query and reporting system (WISQARS). Retrieved from http://www.cdc.gov/injury/wisqars/index.html
Centers for Disease Control and Prevention. (2014b). Youth risk behavior surveillance, United States, 2003. Morbidity and Mortality Weekly Report, 63(SS-4), 1–168.
Cramer, R. J., Johnson, S. M., McLaughlin, J., Rausch, E. M., & Conroy, M. A. (2013). Suicide risk assessment training for psychology doctoral programs. Training and Education in Professional Psychology, 7, 1–11.
Debski, J., Spadafore, C. D., Jacob, S., Poole, D. A., & Hixson, M. D. (2007). Suicide intervention: Training, roles and knowledge of school psychologists. Psychology in the Schools, 44, 157–170. doi:10.1002/pits.20213
Dexter-Mazza, E. T., & Freeman, K. A. (2003). Graduate training and the treatment of suicidal clients: The students’ perspective. Suicide and Life-Threatening Behavior, 33, 211–218.
Douglas, K. S., & Ogloff, J. R. P. (2003). The impact of confidence on the accuracy of structured professional and actuarial violence risk judgments in a sample of forensic psychiatric patients. Law and Human Behavior, 27, 573–587.
Drapeau, C. W., & McIntosh, J. L. (2014). U.S.A suicide 2012: Official final data. Washington, DC: American Association of Suicidology.
Feldman, B. N., & Freedenthal, S. (2006). Social work education in suicide intervention and prevention: An unmet need? Suicide and Life-Threatening Behavior, 36, 467–480.
Fenwick, C. D., Vassilas, C. A., Carter, H., & Haque, M. S. (2004). Training health professionals in the recognition, assessment and management of suicide risk. International Journal of Psychiatry in Clinical Practice, 8, 117–121. doi:10.1080/13651500410005658
Goldston, D. B. (2003). Measuring suicidal behavior and risk in children and adolescents. Washington, DC: American Psychological Association.
Heppner, P. P., Wampold, B. E., & Kivlighan, Jr. D. M. (2007). Research design in counseling: Research, statistics, and program evaluation (3rd ed.). Belmont, CA: Brooks/Cole.
Horowitz, L., Ballard, E., & Paoa, M. (2009). Suicide screening in schools, primary care and emergency departments. Current Opinion in Pediatrics, 21, 620–627.
Jacobson, J. M., Ting, L., Sanders, S., & Harrington, D. (2004). Prevalence of and reactions to fatal and nonfatal client suicidal behavior: A national study of mental health social workers. Omega, 49, 237–248.
Jahn, D. R., Wacha-Montes, A., Dra-Peau, C. W., Grant, B., Nadorff, M. R., Pusateri, M. J., Jr., . . . & Cukrowicz, K. C. (2012). Suicide-specific courses and training: Prevalence, beliefs, and barriers. Part I: Graduate psychology programs and professionals schools of psychology. Manuscript in preparation.
Kleespies, P., Penk, W., & Forsyth, J. (1993). The stress of patient suicidal behavior during clinical training: Incidence, impact, and recovery. Professional Psychology: Research and Practice, 24, 293–303.
Kung, H. S., Hoyert, D. L., Xu, J., & Murphy, S. L. (2008). Deaths: Final data for 2005. National Vital Statistics Reports, 56, 1–66.
Mackelprang, J. L., Karle, J., Reihl, K. M., & Cash, R. E. (2014). Suicide intervention skills: Graduate training and exposure to suicide among psychology trainees. Training and Education in Professional Psychology, 8, 136–142.
McEvoy, M. L., & McEvoy, A. W. (2000). Preventing youth suicide: A handbook for educators and human service professionals. Holmes Beach, FL: Learning Publications.
McNiel, D. E., Fordwood, S. R., Weaver, C. M., Chamberlain, J. R., Hall, S. E., & Binder, R. L. (2008). Effects of training on suicide risk assessment. Psychiatric Services, 59, 1462–1465. doi:10.1176/appi.ps.59.12.1462
National Action Alliance for Suicide Prevention: Research Prioritization Task Force. (2014). A prioritized research agenda for suicide prevention: An action plan to save lives. Rockville, MD: National Institute of Mental Health.
O’Connor, R. C., Platt, S., & Gordon, J. (2011). International Handbook of Suicide Prevention: Research, Policy and Practice. United Kingdom: John Wiley & Sons, Ltd.
O’Connor, N., Warby, M., Raphael, B., & Vassallo, T. (2004). Changeability, confidence, common sense and corroboration: Comprehensive suicide risk assessment. Australasian Psychiatry, 12, 352–360.
Oordt, M. S., Jobes, D. A., Fonseca, V. P., & Schmidt, S. M. (2009). Training mental health professionals to assess and manage suicidal behavior: Can provider confidence and practice behaviors be altered? Suicide and Life-Threatening Behavior, 39, 21–32. doi:10.1521/suli.2009.39.1.21
Osteen, P. J., Frey, J. J., & Ko, J. (2014). Advancing training to identify, intervene, and follow up with individuals at risk for suicide through research. American Journal of Preventative Medicine, 47, 216–221. doi:10.1016/j.amepre.2014.05.033
Poland, S. (1989). Suicide intervention in the schools. New York, NY: The Guilford Press.
Poland, S., & Lieberman, S. (2002). Best practices in suicide intervention. In A. Thomas & J. Grimes (Eds.), Best practices in school psychology IV – Volume II (pp. 1151–1165). Bethesda, MD: National Association of School Psychologists.
Rudd, M. D. (2006). The assessment and management of suicidality. Sarasota, FL: Professional Resource Press.
Rudd, M. D., Cukrowicz, K. C., & Bryan, C. J. (2008). Core competencies in suicide risk assessment and management: Implications for supervision. Training and Education in Professional Psychology, 2, 219–228.
Ruth, B. J., Muroff, J., Gianino, M., Feldman, B. N., McLaughlin, D., Ross, A., & Hill, E. (2009). Suicide prevention education in social work education: What do MSW deans, directors and faculty have to say? Paper session presented at the meeting of the American Public Health Association, Philadelphia, PA.
Sanders, S., Jacobson, J. M., & Ting, L. (2008). Preparing for the inevitable: Training social workers to cope with client suicide. Journal of Teaching in Social Work, 28, 1–18.
Schmidt, W. C. (1997). World-wide web survey research: Benefits, potential problems, and solutions. Behavior Research Methods, Instruments, & Computers, 29, 274–279.
Schmidt, R. C., Iachini, A. L., George, M., Koller, J., & Weist, M. (2015). Integrating a suicide prevention program into a school mental health system: A case example from a rural school district. Children & Schools, 37, 18–27.
Schmitz, W. M., Allen, M. H., Feldman, B. N., Gutin, N, J., Jahn, D. R., Kleespies, P. M., . . . & Simpson, J. D. (2012). Preventing suicide through improved training in suicide risk assessment and care: An American Association of Suicidology task force report addressing serious gaps in U.S. mental health training. Suicide and Life-Threatening Behavior, 42, 292–304. doi:10.1111/j.1943-278X.2012.00090.x
Singer, J. B., & Slovak, K. (2011). School social workers’ experiences with youth suicidal behavior: An exploratory study. Children & Schools, 33, 215–228.
Smith, A. R., Silva, C., Covington, D. W., & Joiner, T. E. (2014). An assessment of suicide related knowledge and skills among health professionals. Health Psychology, 33, 110–119.
Stein-Erichsen, J. L. (2010). School psychologists’ confidence level with suicide intervention and prevention in the schools. Retrieved from: http://digitalcommons.pcom.edu/psychology_dissertations/132.
Sue, V. M., & Ritter, L. A. (2012). Conducting online surveys (2nd ed.). Thousand Oaks, CA: Sage.
Sullivan, G. R., & Bongar, B. (2009). Assessing suicide risk in the adult patient. In P. M. Kleespies (Ed.), Behavioral emergencies: An evidenced –based resource for evaluating and managing risk of suicide, violence, and victimization (pp. 59–78). Washington, DC: American Psychological Association.
Tetlock, P. E. (2005). Expert political judgment: How good is it? How can we know? Princeton, NJ: Princeton University Press.
Wachter, C. A. (2006). Crisis in the schools: Crisis, crisis intervention training and school counselor burnout. ACES Research Grant. Association for Counselor Education and Supervision. Retrieved from http://libres.uncg.edu/ir/uncg/f/umi-uncg-1190.pdf
Wozny, D. A. (2005). Suicide risk assessment: Counselor competency. In J. R. Rodgers (Ed.), Suicide 2006: Proceedings of the 39th Annual Conference of the American Suicidology Association (pp. 224–227). Washington, DC: American Association of Suicidology.
Robert C. Schmidt, NCC, is a Behavioral Specialist at Talbot County Public Schools in Easton, MD. Correspondence can be addressed to Robert C. Schmidt, Talbot County Public Schools, 12 Magnolia Street, Easton, MD 21601, rschmidt@tcps.k12.md.us.
Mar 23, 2016 | Article, Volume 6 - Issue 1
Jeffrey M. Warren, Robyn W. Hale
Non-cognitive factors (NCFs) include strategies, skills, attitudes and behaviors upon which individual success is often dependent (Farrington et al., 2012). While knowledge and ability are important, NCFs are mediating factors that can either assist or hinder individual achievement in educational and career settings. These factors often determine college and career readiness as well as lifelong success. For example, positive self-concept (Brown & Marenco, 1980), grit (Duckworth, Peterson, Matthews, & Kelly, 2007), growth mindset (Dweck, 2006) and social belonging (Walton & Cohen, 2011) are linked to positive outcomes for students and employees and typically lead to a better quality of life.
Sedlacek (2004) noted that NCFs are predictive of the success of students with non-traditional experiences. These students generally include students of historically underrepresented populations such as African Americans, American Indians, and Hispanic and Latino Americans. Students from these groups face higher rates of suspension (Losen, Hodson, Keith, Morrison, & Belway, 2015) and are more likely to have lower GPAs and poorer attendance (Burke, 2015) as compared to their Caucasian counterparts. In the United States, 7% of African American students and 12% of Hispanic students fail to complete high school (Kena et al., 2015). American Indian students are three times more likely to drop out of school than Caucasian students (Burke, 2015). These disparities widen the achievement gap and serve as barriers to postsecondary credentials for students from these groups.
In an effort to close the achievement gap, increase college and career readiness, and promote postsecondary success, many educational organizations and institutions have invested in initiatives that promote NCFs. The American School Counselor Association (ASCA; 2014) endorsed the value of non-cognitive development in a set of standards titled “Mindsets and Behaviors for Student Success.” Professional school counselors use these standards as guides to develop competencies that promote NCFs among students across academic, career and social-emotional domains. Squier, Nailor, and Carey (2015) recently developed a construct-based approach to developing, implementing and assessing school counseling programs based on several NCFs. Initiatives to develop non-cognitive skills continue to emerge in higher education as well (Sedlacek & Sheu, 2013). Through a series of conference calls, the College Access Affinity Group organized by the United States Department of Education (2015) also acknowledged the impact of NCFs on career and college readiness.
An assortment of interventions demonstrates the potential impact of NCFs on academic and career outcomes. Mentoring programs, service learning and social-emotional learning programs show positive effects, although the magnitude of these effects is relatively small (Gutman & Schoon, 2013). Gaps exist in the research when considering long-term outcomes and the transferability of NCFs across contexts (Farrington et al., 2012). Additionally, researchers often identify, describe and measure NCFs in different ways (Duckworth & Quinn, 2009; Dweck, 2006; Farrington et al., 2012; Goldberg, 2001; Tracey & Sedlacek, 1984; Walton & Cohen, 2011). Many of these factors are interrelated; some appear fixed, yet others are malleable (Gutman & Schoon, 2013). Concepts and terms that describe NCFs continue to emerge; however, those identified by Brown and Marenco (1980) and promoted by Sedlacek (2004) are of the most widely researched and linked to college and career success.
Ellis and Bernard (1986) outlined several core values of rational emotive behavior therapy (REBT), a cognitive behavioral framework developed by Ellis (1962). When practicing the principles of REBT, individuals subscribe to a philosophy of life and an accompanying set of sub-goals. This set of sub-goals, based on a philosophy of life rooted in responsible hedonism and preferential, logical thinking, serves as a guide for individuals striving to maintain happiness and life success (Ellis, 1962). These sub-goals parallel the NCFs endorsed by Brown and Marenco (1980), Sedlacek (2004), Duckworth and Quinn (2009), and Dweck (2006). Dryden (2011) described how the REBT philosophy is broadly applied to increase motivation, tolerance and self-control, as well as other NCFs.
This paper highlights the core values of REBT and explains how they align with the NCFs endorsed by Sedlacek (2004). An overview of the philosophical tenets and the theory of REBT is provided. Theoretical and empirical evidence is explored which suggests that REBT can directly and indirectly promote non-cognitive development. Recommendations for school counselors supporting underrepresented students are presented and directions for future research are discussed.
Rational Emotive Behavior Therapy
Developed by Albert Ellis in the mid-1950s, REBT encourages self-actualization and seeks to minimize distress, lengthen life and maximize happiness during all aspects of human development (Ellis, 1962). These core values are woven throughout the philosophical tenets of REBT and serve as guides for rational thought, healthy emotions and functional behavioral outcomes. Several sub-goals, as described by Ellis and Bernard (1986), help facilitate these values: (a) self-interest, (b) social interest, (c) self-direction, (d) tolerance, (e) flexibility, (f) acceptance of uncertainty, (g) commitment, (h) self-acceptance, (i) risk-taking, (j) realistic expectations, (k) high frustration tolerance, and (l) self-responsibility.
Ellis (1962) proposed that humans are genetically predisposed to think in a rigid, irrational manner. Irrational beliefs (IBs) are the root of emotional disturbances according to REBT. While demanding is the core or primary IB, three secondary IBs exist: awfulizing, low frustration tolerance (LFT), and global evaluation (David, 2014; David, Lynn, & Ellis, 2010; Dryden, 2011).
REBT hypothesizes that extreme emotions such as anxiety, anger and depression stem from primary and secondary IBs. These unhealthy negative emotions (UNEs) lead to dysfunctional behaviors (Dryden, 2014). In turn, individuals often behave in ways that prohibit the achievement of desired goals and success.
In accordance with its values and goals, REBT promotes rational beliefs (RBs), or preferential thoughts, which are logical and realistic in nature (David, 2014). RBs are non-awfulizing, demonstrate a tolerance for frustration, and do not indicate global evaluations of self, others or life. Healthy negative emotions such as bother, concern or annoyance stem from these RBs. These emotions lead to functional behaviors and outcomes related to success.
The philosophy and values of REBT encourage lifelong happiness and responsible hedonism. It is at this place where the sub-goals of REBT and the NCFs promoted by Sedlacek (2004) appear to converge. Table 1 provides an overview of the conceptual relationships between these NCFs, the sub-goals of REBT and the IBs (evaluative schema) that impede success. Below, theoretical nuances and empirical evidence supporting the utility of REBT in promoting non-cognitive development are presented. It is important that school counselors are aware of the impact of REBT on NCFs as they strive to ensure that all students, especially those from underrepresented groups, are college and career ready.
REBT and Non-Cognitive Factors
Many factors are critical to K–12 student achievement and postsecondary success. This section presents the NCFs Sedlacek (2004) identified as most valuable in predicting educational outcomes, especially for underrepresented students. These factors include: (a) positive self-concept, (b) realistic self-appraisal, (c) leadership experience, (d) preference for long-term goals, (e) successfully handling the system, (f) availability of strong support person, (g) community involvement, and (h) knowledge in an acquired field. Theoretical and empirical evidence demonstrates how REBT directly and indirectly promotes these factors (see Table 2). Given the role school counselors play in fostering college and career readiness for all students, this evidence may serve as a catalyst for delivering services rooted in REBT.
Positive Self-Concept
Self-concept includes self-confidence and self-esteem (Sedlacek, 2004). Independence and determination also are aspects of self-concept. Positive self-concept is a determinant of success, especially among students with non-traditional experiences (Sedlacek & Sheu, 2013).
REBT promotes positive self-concept through unconditional self-acceptance (USA). Ellis (1962) emphasized self-worth and the importance of accepting the self regardless of faults or flaws. Self-worth is not contingent upon success or failure, as is often the case with self-esteem. London (1997) suggested self-esteem is problematic since the self is conditionally defined by attributes or behaviors. Attempting to constantly hold one’s self in high esteem leads to perpetual damnation and anxiety. However, Kim and Sedlacek (1996) asserted that a relationship exists between the self-concept of students of color and their level of adjustment. This presents a conundrum for students experiencing difficulty adjusting. By practicing USA, students can develop an understanding that they have worth independent of external stimuli or variables. This shift in personal philosophy leads to a stable self-concept and likelihood for greater success (Dryden, 2014).
Studies exploring the direct impact of REBT are vast and stretch over the life span. For example, Donegan and Rust (1998) noted that self-concept among second graders improved as a result of an intervention based on REBT. Additionally, Sapp (1996) and Sapp, Farrell, and Durhand (1995) found that self-concept was a mediating factor between REBT and the success of African American students. Findings from other studies also have suggested that self-concept and self-esteem are associated with IBs (Burnett, 1994; Heppner, Reeder, & Larson, 1983). Sava, Maricutoiu, Rusu, Macsinga, and Virga (2011) described a negative relationship between explicit self-esteem and self-downing IBs of undergraduate students. REBT promotes self-worth and thwarts IBs associated with low self-esteem.
Sedlacek (2004) suggested a strong sense of self is a prerequisite for student success. REBT emphasizes a healthy sense of self by disputing self-downing IBs and promoting preferential, rational thinking. By addressing IBs that impact self-concept, REBT can promote student success.
Realistic Self-Appraisal
Students who accurately evaluate personal weaknesses and strengths demonstrate realistic self-appraisal (Sedlacek, 2004). Self-appraisal is often based on one’s perceived ability to complete tasks, also known as self-efficacy beliefs (Bandura, 1986). Sedlacek and Sheu (2008) suggested that accurate assessment of strengths lead students, especially those from underrepresented groups, toward academic success.
REBT endorses the appraisal of strengths and weaknesses, but it discourages evaluating the self as a whole based on these attributes. As such, realistic expectations serve to ground individuals and promote happiness and success. When realistic expectations are maintained, IBs about the self are minimized.
Warren and Dowden (2012) explored the relationships between IBs, efficacy beliefs and UNEs. IBs were negatively related to efficacy beliefs as well as depression, stress and anxiety (Warren, 2010; Warren & Dowden, 2012). More recently, Warren and Hale (in press) elaborated on the implications that efficacy beliefs and the sources from which they are conceived (e.g., past performance, verbal encouragement) have on performance. Efficacy beliefs, whether accurate or not, can lead to IBs when expected outcomes fail to materialize (Warren & Hale, in press). These cognitive processes produce a host of emotional and behavioral consequences.
Several studies demonstrated how REBT directly promoted a realistic, functional philosophy of self and life. For example, Chamberlain and Haaga (2001) found that non-clinical university students who scored high on a measure of USA could more objectively evaluate their performance on tasks. Alternatively, McCown, Blake, & Keiser (2012) indicated that college students who procrastinated engaged more readily in global evaluations of self, others and life. Negative mood, stemming from irrational thought processes, was associated with procrastination. Similarly, a study conducted by Davies (2006) of a non-clinical sample of adults yielded findings that suggested IBs and USA are negatively related. Davies (2008) later found a causal link between these concepts. Participants exposed to IBs scored lower on a measure of USA, yet scored higher when exposed to RBs. These studies support the premise that promoting a preferential philosophy of life can enhance realistic self-appraisal. Through realistic self-appraisal, students are positioned for success and equipped to respond effectively to adversity and failure.
Leadership Experience
Students can develop abilities to lead through traditional and non-traditional experiences (Sedlacek, 2004). These experiences are often directly related to cultural and community affiliation.
A degree of assertiveness is required to accept leadership roles and achieve related tasks. Assertiveness is a predictor of success (Sedlacek, 2003), while passivity and aggressiveness often hinder success.
REBT encourages self-direction by promoting rational thoughts and minimizing the need for support or approval from others. As such, the importance of assertiveness in leadership endeavors is emphasized in REBT. Rational thoughts lead to assertiveness; IBs tend to result in either passivity or aggression. When assertive, individuals are poised to promote self-interests and social interests in a functional and effective manner. Additionally, individuals often are happier when committed to a cause or invested in a social interest. By responding to challenges or adversity in rational ways, individuals will position themselves as leaders while developing cumulative skill sets adaptable to a variety of settings.
REBT is employed in a variety of settings to directly and indirectly promote leadership skills including assertiveness. In a model of leadership presented by Grieger and Fralick (2007), REBT principles were embedded to enhance training procedures. Murthy (2014) and Nottingham (2013) also described how REBT is used to develop effective leadership practices. Coaches and consultants frequently employ concepts rooted in REBT to establish effective leadership attributes among clients. For example, Woods (1987) found that basic REBT strategies and techniques taught during a series of workshops led to reductions in discomfort and increased assertiveness among participants. REBT also can address perfectionist tendencies, which are often seen as barriers to effective leadership (Ellam-Dyson & Palmer, 2010).
When effective leaders are emotional, they often garner the support of others through the development of interpersonal relationships (George, 2000). However, Filippello, Harrington, Buzzai, Sorrenti, and Costa (2014) found that emotionally intolerant individuals often become distressed when practicing assertiveness. When the principles of REBT are practiced, leaders are viewed as flexible, realistic and authentic in their aim and scope (Fusco, Palmer, & O’Riordan, 2011). Students, especially those from underrepresented groups, can benefit from learning strategies that enhance their ability to serve effectively in leadership roles.
Preference for Long-Term Goals
The establishment of long-range goals often precedes achievement and attainment of those goals. A preference for long-term goals requires that students have the ability to plan and delay gratification. Sedlacek (2003) and Duckworth et al. (2007) suggested that perseverance and determination when striving toward long-range goals are prerequisites of academic achievement.
REBT encourages responsible hedonism, or enjoyment of life. This concept implies a delay of gratification while individuals behave in ways that lead to the attainment of goals. Self-responsibility and high frustration tolerance (HFT) are required to overcome obstacles that impede progress toward goals. Rather than giving up or blaming the self, others or life for these challenges, REBT recommends individuals take responsibility for their thoughts, feelings and behaviors (Dryden, 2014). HFT is promoted by REBT and lies in opposition to LFT, or the inability to persevere during difficult or challenging situations. Preferential thoughts related to challenges or discomforts are realistic and lead toward healthy emotions and functional behaviors. When ownership of thoughts and feelings are accepted and frustrations are tolerated, individuals are better positioned to work toward distal goals that lead to success.
Rodman, Daughters, and Lejuez (2009) described the positive relationships between HFT and distress tolerance (i.e., persistence) and the pursuit of goals despite potential discomfort. HFT is associated with optimism, preferences, non-awfulizing and acceptance—factors that support goal attainment and enhance the quality of life (Morley, 2014). Alternatively, Harrington (2005a, 2005b) found that frustration intolerance was a predictor of procrastination behaviors, including issues of self-control, among students. When working toward goals, especially ones that create discomfort, self-responsibility and HFT help move individuals forward and toward success. Responsible hedonism, a core value of REBT, appears to directly promote a preference for long-term goals rather than simple, rudimentary accomplishments. School counselors can assist students in developing and working toward distal goals such as completion of postsecondary credentials.
Successfully Handling the System
Students from underrepresented groups are not afforded the same benefits as those from privileged backgrounds. The educational system maintains barriers (e.g., racism) that impede the efforts of students from underrepresented groups. The manner in which individuals handle challenging circumstances within the system offers insight into their ability and potential for success (Sedlacek, 2004). Persistence and perseverance are crucial qualities for students who attempt to navigate or handle the system.
REBT can provide direct support to students navigating the educational system. Rather than placing demands on the system, which can lead to UNEs and unproductive responses, REBT encourages acceptance of system inequities through ULA. Additionally, HFT is fundamental to ULA when attempting to navigate the system. REBT promotes tolerance and an understanding that individuals experience difficult situations as a function of life. Tolerance is a key to self-advocacy efforts and helps students move forward productively without condemning others or life.
Responding to or interacting with the system can leave students, especially those from underrepresented groups, emotionally charged or drained and prone to respond in irrational ways. Harrington (2013) described how IBs play a central role for individuals who believe in a just or utopian world. When beliefs are rigid, individuals have difficulty adapting to adverse situations and may retaliate, thus prohibiting success (Veale, 2002). Dryden and Hurton (2013), however, acknowledged that individuals may not always act on their beliefs. When navigating the system, individuals who maintain rigid beliefs tend to be aware of their action tendencies yet refrain from responding in detrimental ways.
The tenets and practices of REBT provide a platform for restructuring students’ cognitions related to systemic prejudice, racism and stereotyping. Gregas (2006) suggested that REBT-based skills are useful for students who face discrimination. Earlier, Sapp (1996) found that African American males who learned the principles of REBT were more successful in school. REBT guided students from beliefs associated with chance or luck (i.e., external locus of control; Rotter, 1966) toward beliefs of personal control over outcomes, which promotes empowerment (i.e., internal locus of control). Regardless of where an individual places responsibility (i.e., locus of responsibility; Jones, 1997), USA, UOA and ULA offer guidance when attempting to hold the self, others, or society accountable. REBT provides psychological resources for handling the system and demonstrating personal influence over outcomes. Students from underrepresented groups who acquire these tools and strategies will respond more effectively when faced with systemic barriers. Evidence also suggested that REBT can propel individuals to reap the benefits of other NCFs such as the availability of a strong support person.
Availability of Strong Support Person
Success is often contingent upon a support network and the use of personal resources. Underrepresented students with a history of supportive relationships perform better in college (Sedlacek, 2004). Individuals should engage with support persons in emotionally healthy ways and ensure that the relationship is mutually understood.
USA and UOA are critical for students seeking support or mentorship in achieving their goals. USA allows individuals to confidently seek support without feeling worthless. With UOA, individuals are accepting of others regardless of faults or failings. Acceptance of uncertainty propels students to take the necessary steps to reach out to others and attempt to form support networks.
Individuals who are self-directed readily seek healthy relationships and support networks. They engage in these relationships to complement their efforts rather than developing a dependency for the support. Reducing anxiety and achieving goals through the incorporation of REBT can lead individuals toward independence rather than maintaining unhealthy, dependent relationships (Wood, 2004). Chamberlain and Haaga (2001) found that USA is negatively related to anxiety, which can stifle autonomy and the confidence to reach out to others for support. Similarly, a study conducted by Davies (2006) revealed that IBs were negatively related to openness, a Big 5 personality dimension promoted by McCrae and Costa (1987). Students considered to possess openness typically have a wide range of interests, creativity and insight, which have implications for establishing a diverse system of support. As such, their relationships are likely to extend well beyond and across cultural boundaries and communities.
Maintaining a strong support system can benefit students navigating difficult tasks or tackling daily life obligations. REBT appears to directly provide the tools and resources necessary for establishing, maintaining and appropriately utilizing support persons. By fostering self-direction and unconditional acceptance, REBT promotes the development of strong systems of support as described by Sedlacek (2004). The availability of a strong support person is critical for students from underrepresented groups; community involvement also plays a key role in the educational success of these students.
Community Involvement
Community involvement encompasses a student’s level of activity or interaction in groups within the larger society (Sedlacek, 2004). Students engaged in their community, or a subset of their community, are more successful than those who are disconnected or isolated. Through involvement in the community, students from underrepresented groups can hone their self-concept, leadership skills and ability to navigate the system.
Ellis and Bernard (1986) suggested that individuals who are actively engaged in something other than themselves are happier. REBT directly promotes community involvement through UOA and ULA. When students are accepting of others and life and remain assertive, they become self-directed and often take interests in the welfare of others and their community. As noted by Sedlacek (2004), a commitment to community initiatives invokes the development and attainment of other goals and skills, which all foster happiness and success.
Warren and Dowden (2012) noted the negative relationships between IBs and depression, anxiety and stress. These psychological disturbances can often impede or debilitate individuals and prevent meaningful interactions within the community. For example, university students were found to moderate their anxiety levels by removing themselves from an activity common in communities of learning (Nicastro, Luskin, Raps, & Benisovich, 1999). Imperative or irrational thinking was related to the speed of the departure, thus demonstrating the influence of thought processes on community engagement.
REBT is effective in promoting social skills, which leads students to engage with society and build a sense of community. For example, Safdari and Hadadi (2013) utilized REBT-based group counseling to reduce symptoms among individuals with mild to moderate depression. The group experience led to a reduction in ruminations about consequences, which often paralyze and prevent a satisfying life. In a study of students enrolled in secondary schools in Nigeria, Ayodele (2011) found that two interventions based on REBT were effective in promoting interpersonal behavior. Students can develop social-emotional competence, a commitment to the community, and other interpersonal skills as a result of participating in REBT interventions. REBT also can position students to more readily acquire knowledge in a field.
Knowledge Acquired in a Field
Knowledge obtained from traditional and non-traditional experiences affords students the opportunity to gain valuable insights into their “place” or “degree of fit” within a particular industry or field (Sedlacek, 2004). While operating in a field, individuals should take full advantage of the opportunities to absorb knowledge and obtain as many skills as possible. These experiences are invaluable for underrepresented students attempting to navigate their chosen field of study or work.
REBT indirectly supports the acquisition of knowledge in a field or career path. For example, individuals must maintain self-direction in order to have varied experiences in a desired field. Drive and determination are required as well as self-interest. REBT suggests that happiness stems from one’s willingness to place personal interests before others (Ellis & Bernard, 1986). Although any experience may lead to benefits, knowledge obtained from a field of interest is gratifying and rewarding. Individuals also must take risks when seeking knowledge. Students who maintain positive emotional health will take appropriate risks when attempting to acquire field experience.
Using the REBT framework, Dryden (2000) described the manner in which procrastination related to work experience, interests, opportunities and advancement hinders self-development and knowledge acquired in a field. Procrastination is related to factors that impact the acquisition of knowledge, such as motivation (Klassen & Kuzucu, 2009) and stress (Stead, Shanahan, & Neufeld, 2010). Harrington (2005b) found that discomfort intolerance, a variation of LFT, was a predictor of procrastination. Students who experience discomfort intolerance will delay experiences that would otherwise lead to knowledge acquisition.
Researchers have established that REBT can help individuals overcome barriers to taking risks and obtaining knowledge in a field. For example, during a demonstration session, Dryden (2012) explained how REBT can assist individuals in overcoming procrastination. More recently, Balkis (2013) found that RBs about studying were a mediating factor in the degree of academic procrastination and level of achievement among college students. It is important that school counselors consider the vast ways in which REBT promotes NCFs and prepares students for college and the world of work.
Recommendations for Developing NCFs Through School Counseling
The values of REBT align with many NCFs, including those endorsed by Sedlacek (2004). A variety of research studies demonstrate the impact REBT can have on NCFs. Through cognitive, emotional and behavioral support, REBT promotes NCFs in direct and indirect ways. When these factors or skills are developed and strengthened, students in elementary, secondary and postsecondary settings are more likely to experience positive educational outcomes.
Students from underrepresented groups are especially susceptible to barriers that impede their educational efforts and goal attainment. As such, disparities in graduation rates, disciplinary referrals and teacher expectations remain prevalent (Holcomb-McCoy, 2007). In order to close the achievement gap, it is imperative for school leaders, specifically school counselors, to establish evidence-based strategies that support non-cognitive development and college and career readiness.
Through comprehensive programs, school counselors can deliver a variety of direct and indirect student services that enhance educational experiences and prepare students for postsecondary success. School counselors can use REBT-based student support services to help students, parents and teachers develop strategies that foster NCFs and lead to college and career readiness. It is important that these services are innovative, extend beyond modifications to the classroom and school environments, and offer all students, especially those from underrepresented groups, skills for lifelong empowerment.
Direct Student Services
School counselors deliver direct student services through the core curriculum, student planning and responsive services (ASCA, 2012). Direct interactions that target academic achievement, personal/social growth and career development occur between school counselors and students during the delivery of these services. Professional school counselors can promote non-cognitive development by incorporating the tenets of REBT into many aspects of direct student services.
Core curriculum. The core curriculum is delivered through instruction and group activities that advance the mission and goals of the school counseling program. School counselors advance knowledge, attitudes and skills that align with standards and competencies based on Mindsets and Behaviors for Student Success (ASCA, 2014). Because these standards are based on non-cognitive research (Farrington et al., 2012), REBT appears to be a viable framework for delivering the core curriculum.
Rational Emotive Education (REE; Knaus, 1974) can promote NCFs while serving as a central component of the school counseling core curriculum. This social-emotional curriculum is based on the philosophy of REBT and aims to foster rational thought, emotional awareness and functional behaviors among children and adolescents. REE lessons can empower students from underrepresented groups who are often subjected to beliefs and emotions related to their perceived inability to succeed (Holcomb-McCoy, 2007).
More recently, Vernon (2006a, 2006b) developed an REBT-based curriculum geared to promote emotional education across K–12 settings. This curriculum fosters non-cognitive development by helping students establish a positive self-concept, engage in realistic self-evaluation, and navigate difficult and challenging situations. REBT has failed to take root in educational settings and is often overlooked when considering evidence-based social-emotional curriculums. However, schools in Australia are beginning to demonstrate the effects of rational emotive behavior education (REBE) on the social-emotional development of children and adolescents (personal communication, G. Bortolozzo, April 15, 2015).
School counselors who utilize these or similar REBT-based curriculums have the opportunity to foster the non-cognitive development of all students. Opportunities for students to apply, practice and test the strategies they learn must accompany these curriculums. For example, school counselors can coordinate and encourage experiences that allow students to become involved in the community (e.g., food drive), acquire knowledge in a field (e.g., job shadowing), and gain leadership experience (e.g., class representative). These experiences, coupled with REBT-based instruction, are especially beneficial for students from underrepresented groups. Students in K–12 settings who develop knowledge, attitudes and skills based on the REBT framework and have guided opportunities for practice will position themselves for postsecondary success.
Individual student planning and advisement. This direct service affords school counselors the opportunity to help students develop, monitor and manage long-range goals and plans (ASCA, 2012). Student advisement is especially important for students from underrepresented groups who may require additional guidance and support (Holcomb-McCoy, 2007). Through planning and advising, school counselors assess and evaluate students’ attitudes, knowledge and skills related to academic, personal and social, and career development.
Using an REBT framework, school counselors can assist students in uncovering IBs that may impede their goals of attaining a postsecondary credential (e.g., certification, degree). In some cases, students may not aspire to pursue postsecondary education due to IBs associated with unrealistic self-appraisal. School counselors can teach students REBT-based strategies that help establish healthy beliefs and emotions related to academic, personal and career planning. In turn, students are more likely to seek and acquire knowledge in a field or strengthen their support network, both keys to postsecondary success. By realizing the influence of thought, students from underrepresented groups become empowered as active participants of their educational pursuits and are positioned to “reach higher.”
Responsive services. School counselors can promote non-cognitive development through counseling and crisis response. Individual and small group counseling are often short-term and designed to address concerns that impact student success (ASCA, 2012). School counselors also assist students in overcoming crisis situations. It is important that interventions utilized during responsive services are evidence-based and promote academic achievement, personal and social growth, and career development.
REBT offers school counselors a framework for providing responsive services that are evidence-based, targeted, brief and solution-focused. School counselors can utilize cognitive, emotional and behavioral strategies to help students overcome irrational thoughts and extreme emotions that are often detrimental to student success. Non-cognitive development is promoted as students learn strategies to effectively navigate classroom, school and community experiences.
Most school counselors lack training in REBT and therefore do not fully understand its theoretical principles. However, resources are available that school counselors can use to promote the principles and philosophy of REBT during the delivery of responsive services. For example, Vernon (2002) developed a resource that offers a variety of individual activities based on the principles of REBT. This set of activities includes strategies and techniques that address issues related to self-acceptance, problem-solving, underachievement, relationships and transitions. More recently, Warren (2011) provided a variety of rational rhymes school counselors can use to promote the tenets of REBT. School counselors can help students memorize and rehearse these short songs in an effort to develop more preferential philosophies of life. These resources help school counselors equip students with tools and strategies that promote rational thought, foster NCFs and lead to empowerment. In addition to direct student services, school counselors also can provide a variety of REBT-based indirect student services. These services are complementary and aim to support non-cognitive growth in all aspects of student life.
Indirect Student Services
Indirect student services include referrals, consultation and collaboration. While often viewed as ancillary in nature, these services are an integral component of school counseling programs. School counselors should consider integrating the philosophy and principles of REBT throughout the delivery of these services. For systemic change to occur, school counselors must remain vigilant and not waiver in their efforts to close the achievement gap and promote student success. Indirect student services can advance this mission by promoting the development of NCFs.
Referrals. School counselors refer students and families to a variety of community based services. Prior to making a referral, it is important that school counselors have a clear understanding of the concerns and presenting issues. As such, school counselors who operate from an REBT perspective assess students for non-cognitive strengths and deficiencies that impact academic, personal and social, and career development. Using this framework, school counselors can more readily identify the root or underlying issues of concern and make appropriate referrals.
School counselors should consider making referrals to community agencies and organizations that understand the framework and philosophical principles used to determine the need for referral. For example, school counselors can refer students and families to mental health agencies that specialize in cognitive behavioral therapies since these frameworks promote NCFs. Local organizations that foster community involvement and establish supportive relationships with their clients also can serve as referral options. Community agencies and organizations that understand the mission of the school counseling program and the benefits of non-cognitive development are key partners in promoting the success of students from underrepresented groups.
Consultation. Consultation is a triadic interaction in which school counselors support teachers’ efforts to promote student success (Warren & Baker, 2013). School counselors also provide consultation to parents, administrators and other educational stakeholders. Consultation is a highly effective means of evoking systemic change and positively impacting the educational experiences of students. Rather than relying on eclectic approaches, school counselors are strongly encouraged to invest in the delivery of evidence-based consultation that promotes NCFs.
Rational Emotive-Social Behavioral (RE-SB) consultation, developed for K–12 teachers, fosters student-teacher relationships and quality instruction by promoting flexibility, acceptance and realistic expectations (Warren, 2013; Warren & Gerler, 2013). School counselors use this model of consultation to address IBs and UNEs commonly associated with teaching. RE-SB consultation also can address the biases and stereotypes that lead teachers to hold low expectations of students from underrepresented groups (Holcomb-McCoy, 2007).
Through RE-SB consultation, school counselors can promote the NCFs of teachers that directly impact the non-cognitive development of students. For example, students vicariously learn strategies that promote non-cognitive development from teachers who have positive self-concepts, demonstrate preferences for long-term goals and maintain strong support systems. Additionally, students are positioned to engage in realistic self-appraisal when teachers maintain high expectations.
School counselors also can utilize this model of consultation when working with parents. RE-SB consultation can promote NCFs that enhance the ways caregivers interact with and support their children. RE-SB consultation can assist parents in overcoming psychosocial barriers that hinder their child’s growth and development. For example, consultation can target a parent’s thoughts, emotions and behaviors that influence their child’s decision regarding postsecondary education.
School counselors can deliver RE-SB consultation in large group, small group and individual sessions. Ideally, school counselors utilize large group consultation in an effort to advance the principles of REBT throughout the systems of the school. For example, school counselors can encourage teachers and parents to develop a common language that promotes rational thoughts and promotes NCFs. Establishing a common set of REBT-based classroom rules and parental guidelines can ensure that students are immersed in environments conducive to promoting NCFs. Small group and individual RE-SB consultation is typically implemented to address specific concerns expressed by individual teachers or parents. Students from underrepresented groups can benefit greatly from interacting with parents and teachers who model NCFs.
Collaboration. School counselors can collaborate with parents, as well as educators and community members, in many ways. These collaborative efforts are aimed at establishing equity and access for all students (ASCA, 2012). As a result of the relationships established through collaboration, members of the school community (e.g., parents) may reach out to the school counselor for consultation and other services more readily.
Through collaborative efforts such as parent trainings, school counselors can inform parents about the value of non-cognitive development and its role in determining postsecondary success. Efforts to engage the school community in initiatives that directly support student success can strengthen the relationships between the school counselor and parents. Collaboration establishes the school counselor as a leader, student advocate and partner in advancing NCFs and college and career readiness.
School counselors also can partner with local universities to promote a college-going culture and set high expectations for postsecondary success for all students. For example, university and school partnerships can establish mentoring programs that couple K–12 students with local college students from similar underrepresented groups. These relationships would reciprocate non-cognitive development for both the mentor and mentee. This experience can empower and create opportunities for K–12 students from underrepresented groups.
It is equally important that university and college initiatives, with involvement from offices such as those responsible for enrollment, retention and diversity, engage school counselors in conversations that explore opportunities to streamline students’ experiences from high school to postsecondary education. These partnerships can lead to collaborative efforts to develop and provide REBT-based transition programs that promote non-cognitive development. These programs can offer students, especially those from underrepresented groups, additional support as they navigate the nuances of postsecondary education. Universities are advised to build on the efforts of professional school counselors and promote non-cognitive development through evidence-based practices rooted in REBT.
Conclusion
The principles and tenets of REBT align and overlap with many NCFs, especially those promoted by Sedlacek (2004). The proposed recommendations for school counselor practice appear to support the aims of ASCA (2012) and the ASCA (2014) Mindsets and Behaviors for Student Success standards and competencies. It is critical that researchers and educational leaders continue to explore ways to embed the principles of REBT throughout the educational experiences of all students in an effort to close the achievement gap, foster college and career readiness, and promote postsecondary success.
School counselors must evaluate the direct and indirect student services they provide. A variety of methods are available to help determine the outcomes of REBT-based services. Both formal and informal methods of data collection are useful in determining the impact of services such as core curriculum, small group counseling, consultation and collaboration. School counselors can attempt to directly measure non-cognitive development, including changes in students’ patterns of thoughts, emotions and behaviors. However, it is critical for school counselors to track changes in achievement-related data including attendance, discipline referrals and homework completion. From a distal perspective, understanding the influence these services have on high school graduation rates and persistence in postsecondary education, especially for students from underrepresented groups, is imperative.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
American School Counselor Association. (2012). The ASCA national model: A framework for school counseling programs (3rd ed.). Alexandria, VA: Author.
American School Counselor Association. (2014). Mindsets and behaviors for student success: K–12 college-and career-readiness standards for every student. Alexandria, VA: Author.
Ayodele, K. O. (2011). Fostering adolescents’ interpersonal behaviour: An empirical assessment of enhanced thinking skills and social skills training. Edo Journal of Counselling, 4, 62–74.
Balkis, M. (2013). Academic procrastination, academic life satisfaction and academic achievement: The mediation role of rational beliefs about studying. Journal of Cognitive and Behavioral Psychotherapies, 13, 57–74.
Bandura, A. (1986). Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall.
Brown, S. E., & Marenco, E., Jr. (1980). Law school admissions study. San Francisco, CA: Mexican American Legal Defense and Educational Fund.
Burke, A. (2015). Early identification of high school graduation outcomes in Oregon Leadership Network schools (REL 2015–079). Washington, DC: U.S. Department of Education, Institute of Education Sciences, National Center for Education Evaluation and Regional Assistance, Regional Educational Laboratory Northwest. Retrieved from http://ies.ed.gov/ncee/edlabs/regions/northwest/pdf/REL_2015079.pdf
Burnett, P. C. (1994). Self-talk in upper elementary school children: Its relationship with irrational beliefs, self- esteem, and depression. Journal of Rational-Emotive and Cognitive-Behavior Therapy, 12, 181–188.
Chamberlain, J. M., & Haaga, D. A. F. (2001). Unconditional self-acceptance and responses to negative feedback. Journal of Rational-Emotive and Cognitive-Behavior Therapy, 19, 177–189.
David, D. (2014). Rational emotive behavior therapy. In D. S. Dunn (Ed.), Oxford bibliographies in psychology. New York, NY: Oxford University Press.
David, D., Lynn, S. J., & Ellis, A. (2010). Rational and irrational beliefs. Implications for research, theory, and practice. New York, NY: Oxford University Press.
Davies, M. F. (2006). Irrational beliefs and unconditional self-acceptance. I. Correlational evidence linking two key features of REBT. Journal of Rational-Emotive and Cognitive-Behavior Therapy, 24, 113–124.
doi:10.1007/s10942-006-0027-0
Davies, M. F. (2008). Irrational beliefs and unconditional self-acceptance. III. The relative importance of different types of irrational belief. Journal of Rational-Emotive & Cognitive-Behavior Therapy, 26, 102–118. doi:10.1007/s10942-007-0061-6
Donegan, A. L., & Rust, J. O. (1998). Rational emotive education for improving self-concept in second-grade students. The Journal of Humanistic Education and Development, 36, 248–256.
doi:10.1002/j.2164-4683.1998.tb00396.x
Dryden, W. (2000) Overcoming procrastination. London, UK: Sheldon Press.
Dryden, W. (2011). Understanding psychological health: The REBT perspective. London, UK: Routledge.
Dryden, W. (2012). Dealing with procrastination: The REBT approach and a demonstration session. Journal of Rational-Emotive & Cognitive-Behavior Therapy, 30, 264–281.
Dryden, W. (2014). Rational emotive behaviour therapy: Distinctive features. London, UK: Routledge.
Dryden, W., & Hurton, N. R. (2013). What I felt like doing, but did not do when I felt hurt: An REBT-based investigation of action tendencies that are not acted on. Journal of Rational-Emotive & Cognitive-Behavior Therapy, 31, 179–198. doi:10.1007/s10942-013-0169-9
Duckworth, A. L., Peterson, C., Matthews, M. D., & Kelly, D. R. (2007). Grit: Perseverance and passion for
long-term goals. Journal of Personality and Social Psychology, 92, 1087–1101.
doi:10.1037/0022-3514.92.6.1087
Duckworth, A. L., & Quinn, P. D. (2009). Development and validation of the short grit scale (grit-s). Journal of Personality Assessment, 91, 166–174. doi:10.1080/00223890802634290
Dweck, C. S. (2006). Mindset: The new psychology of success. New York, NY: Random House.
Ellam-Dyson, V., & Palmer, S. (2010). Rational coaching with perfectionistic leaders to overcome avoidance of leadership responsibilities. The coaching psychologist, 6(2), 5–11.
Ellis, A. (1962). Reason and emotion in psychotherapy. Secaucus, NJ: Citadel.
Ellis, A., & Bernard, M. E. (1986). What is rational emotive therapy (RET)? In A. Ellis & R. Griege (Eds.), Handbook of rational emotive therapy (pp. 3–30). New York, NY: Springer.
Farrington, C. A., Roderick, M., Allensworth, E., Nagaoka, J., Keyes, T. S., Johnson, D. W., & Beechum, N. O.
(2012). Teaching adolescents to become learners. The role of noncognitive factors in shaping school performance:
A critical literature review. Chicago, IL: University of Chicago Consortium on Chicago School Research.
Retrieved from https://consortium.uchicago.edu/sites/default/files/publications/Noncognitive Report.pdf
Filippello, P., Harrington, N., Buzzai, C., Sorrenti, L., & Costa, S. (2014). The relationship between frustration
intolerance, unhealthy emotions, and assertive behaviour in Italian students. Journal of Rational-Emotive
& Cognitive-Behavior Therapy, 32, 257–278. doi:10.1007/s10942-014-0193-4
Fusco, T., Palmer, S., & O’Riordan, S. (2011). Can coaching psychology help develop authentic leaders: Part
two. The Coaching Psychologist, 7, 127–131.
George, J. M. (2000). Emotions and leadership: The role of emotional intelligence. Human Relations Journal, 53,
1027–1055. doi:10.1177/0018726700538001
Goldberg, L. R. (2001). Analyses of Digman’s child-personality data: Derivation of Big-Five factor scores from
each of six samples. Journal of Personality, 69, 709–743. doi:10.1111/1467-6494.695161
Gregas, A. J. (2006). Applying rational emotive behavior therapy to multicultural classrooms. Multicultural
Learning and Teaching, 1, 24–34. doi:10.2202/2161-2412.1008
Grieger, R., & Fralick, F. (2007). The use of REBT principles and practices in leadership training and
development. Journal of Rational-Emotive & Cognitive-Behavior Therapy, 25, 143–154.
doi:10.1007/s10942-006-0038-x
Gutman, L. M., & Schoon, I. (2013). The impact of non-cognitive skills on the outcomes of young people. Literature
review. London, UK: Education Endowment Foundation. Retrieved from https://educationendowment
foundation.org.uk/uploads/pdf/Non-cognitive_skills_literature_review_1.pdf
Harrington, N. (2005a). Dimensions of frustration intolerance and their relationship to self-control problems. Journal of Rational-Emotive and Cognitive-Behavior Therapy, 23, 1–20. doi:10.1007/s10942-005-0001-2
Harrington, N. (2005b). It’s too difficult! Frustration intolerance beliefs and procrastination. Personality and Individual Differences, 39, 873–883. doi:10.1016/j.paid.2004.12.018
Harrington, N. (2013). Irrational beliefs and socio-political extremism. Journal of Rational-Emotive & Cognitive- Behavior Therapy, 31(3), 167–178. doi:10.1007/s10942-013-0168-x
Heppner, P. P., Reeder, B. L., & Larson, L. M. (1983). Cognitive variables associated with personal problem- solving appraisal: Implications for counseling. Journal of Counseling Psychology, 30, 537–545.
Holcomb-McCoy, C. (2007). School counseling to close the achievement gap: A social justice framework for success. Thousand Oaks, CA: Corwin.
Jones, J. M. (1997). Prejudice and racism (2nd ed.). New York, NY: McGraw-Hill.
Kena, G., Musu-Gillette, L., Robinson, J., Wang, X., Rathbun, A., Zhang, J., Wilkinson-Flicker, S., Barmer, A., &
Dunlop Velez, E. (2015). The Condition of Education 2015 (NCES 2015-144). Washington, DC: U.S.
Department of Education, National Center for Education Statistics. Retrieved from http://nces.ed.gov/
pubs2015/2015144.pdf
Kim, S. H., & Sedlacek, W. E. (1996). Gender differences among incoming African-American freshmen on
academic and social expectations. Journal of the First-Year Experience & Students in Transition, 8, 25–37.
Klassen, R., & Kuzucu, E. (2009). Academic procrastination and motivation of adolescents in Turkey.
Educational Psychology, 29, 69–81. doi:10.1080/01443410802478622
Knaus, W. J. (1974). Rational emotive education: A manual for elementary school teachers. New York, NY: Institute
for Rational Living.
London, T. P. (1997). The case against self-esteem: Alternative philosophies toward self that would raise the
probability of pleasurable and productive living. Journal of Rational-Emotive & Cognitive-Behavior
Therapy, 15, 19–29.
Losen, D., Hodson, C., Keith, M. A., Morrison, K., & Belway, S. (2015). Are we closing the school discipline gap?
Los Angeles, CA: The Center for Civil Rights Remedies.
McCown, B., Blake, I. K., & Keiser, R. (2012). Content analyses of the beliefs of academic procrastinators.
Journal of Rational-Emotive & Cognitive-Behavior Therapy, 30, 213–222. doi:10.1007/s10942-012-0148-6
McCrae, R. R., & Costa, P. T. (1987) Validation of the five-factor model of personality across instruments and
observers. Journal of Personality and Social Psychology, 52, 81–90. doi:10.1037/0022-3514.52.1.81
Morley, K. (2014). The role of rational and irrational beliefs in positive and negative mental health outcomes. Retrieved
from http://esource.dbs.ie/bitstream/handle/10788/2148/ ba_morley_k_2014.pdf?sequence=1
Murthy, V. (2014). Interdisciplinary lessons for contemporary challenges: The zeitgeist leadership practice of
excelling at work. World Journal of Entrepreneurship, Management and Sustainable Development, 10, 262–
284. doi:10.1108/WJEMSD-07-2013-0035
Nicastro, R., Luskin, F., Raps, C., & Benisovich, S. (1999). The relationship of imperatives and self-efficacy to
indices of social anxiety. Journal of Rational-Emotive & Cognitive-Behavior Therapy, 17, 249–265.
Nottingham, E. (2013). Becoming an emotionally intelligent leader: Attitude and leadership. Retrieved from http://
www.themasterbusinesscoach.com/wp-content/uploads/2013/03/Attitude-and-Leadership-Revised-
2-27-13.pdf
Rodman, S. A., Daughters, S. B., & Lejuez, C. W. (2009). Distress tolerance and rational-emotive behavior
therapy: A new role for behavioral analogue tasks. Journal of Rational-Emotive & Cognitive-Behavior
Therapy, 27, 97–120. doi:10.1007/s10942-009-0090-4
Rotter, J. B. (1966). Generalized expectancies of internal versus external control of reinforcements. Psychological
Monographs, 80(1, Whole No. 609), 1–28.
Safdari, S., & Hadadi, H. (2013). The effectiveness of group therapy through rational emotive behavior therapy
(REBT) on ruminations of depressed patients. Journal of Social Issues and Humanities, 1(3), 51–55.
Sapp, M. (1996). Irrational beliefs that can lead to academic failure for African American middle school
students who are academically at-risk. Journal of Rational-Emotive & Cognitive-Behavior Therapy, 14,
123–134.
Sapp, M., & Farrell, W., & Durhand, H. (1995). Cognitive-behavioral therapy: Applications for African-
American middle school at-risk students. Journal of Instructional Psychology, 22, 169–177.
Sava, F. A., Maricuţoiu, L. P., Rusu, S., Macsinga, I., & Vîrgă, D. (2011). Implicit and explicit self-esteem and
irrational beliefs. Journal of Cognitve and Behaviorial Psychotherapies, 11, 97–111.
Sedlacek, W. E. (2003). Alternative measures in admissions and scholarship selection. Measurement and
Evaluation in Counseling and Development, 35, 263–272.
Sedlacek, W. E. (2004). Beyond the big test: Noncognitive assessment in higher education. Indianapolis, IN: Jossey-
Bass.
Sedlacek, W. E., & Sheu, H. B. (2008). The academic progress of undergraduate and graduate Gates
Millennium Scholars and non-scholars by race and gender. Readings on Equal Education, 23, 143–177.
Sedlacek, W. E., & Sheu, H. B. (2013). Selecting and supporting Asian American and Pacific Islander students
in higher education. In S. D. Museus, D. C. Maramba, & R. T. Teranishi (Eds.), The minority within the
minority: Asian Americans in higher education. (pp. 327–339). Sterling, VA: Stylus.
Stead, R., Shanahan, M. J., & Neufeld, R. W. J. (2010). “I’ll go to therapy, eventually”: Procrastination, stress and mental health. Personality and Individual Differences, 49, 175–180. doi:10.1016/j.paid.2010.03.028
Squier, K. L., Nailor, P., & Carey, J. C. (2015). Construct-based approach (CBA) toolkit on a flash drive. Thousand
Oaks, CA: Corwin.
Tracey, T. J., & Sedlacek, W. E. (1984). Noncognitive variables in predicting academic success by race.
Measurement & Evaluation in Guidance, 16, 171–178.
United States Department of Education. (2015). College access affinity group. Retrieved from http://www2.ed.gov/news/av/audio/college-access/index.html
Veale, D. (2002). Over-valued ideas: A conceptual analysis. Behaviour Research and Therapy, 40, 383–400.
doi:10.1016/S0005-7967(01)00016-X
Vernon, A. (2002). What works when with children and adolescents: A handbook of individual counseling techniques.
Champaign, IL: Research Press.
Vernon, A. (2006a). Thinking, feeling, behaving: An emotional education curriculum for adolescents, grades 1–6 (Rev.
ed.). Champaign, IL: Research Press.
Vernon, A. (2006b). Thinking, feeling, behaving: An emotional education curriculum for adolescents, grades 7–12 (Rev.
ed.). Champaign, IL: Research Press.
Walton, G. M., & Cohen, G. L. (2011) A brief social-belonging intervention improves academic and health
outcomes among minority students. Science, 331, 1447–1451. doi:10.1126/science.1198364
Warren, J. M. (2010). School counselor system support using mental health interventions. The New York State
School Counseling Association Journal, 7, 30–39.
Warren, J. M. (2011). Rational rhymes for addressing common childhood issues. Journal of Creativity in Mental
Health, 6, 329–339.
Warren, J. M. (2013). School counselor consultation: Teachers’ experiences with rational emotive behavior
therapy. Journal of Rational-Emotive & Cognitive-Behavior Therapy, 1–15. doi:10.1007/s10942-011-0139-z
Warren, J. M., & Baker, S. B. (2013). School counselor consultation: Enhancing teacher performance through
rational emotive-social behavioral consultation. In G. R. Walz, J. C. Bleuer, & R. K. Yep (Eds.), Ideas and
research you can use: VISTAS 2013. Retrieved from http://www.counseling.org
Warren, J. M., & Dowden, A. R. (2012). Elementary school teachers’ beliefs and emotions: Implications for
school counselors and counselor educators. Journal of School Counseling, 10(19), n19.
Warren, J. M., & Gerler, E. R. (2013). Effects of cognitive behavioral consultation on irrational and efficacy
beliefs of elementary school teachers. The Professional Counselor, 3, 6–15. doi:10.15241/jmw.3.1.6
Warren, J. M., & Hale, R. (in press). The influence of efficacy beliefs on teacher performance and student
success: Implications for student support services. Journal of Rational-Emotive & Cognitive-Behavior
Therapy.
Wood, J. (2004). A question of dependency: A study of a client suffering from panic disorder with
agoraphobia. Counselling Psychology Review-British Psychological Society, 19, 13–21.
Woods, P. J. (1987). Reductions in Type A behavior, anxiety, anger, and physical illness as related to changes in
irrational beliefs: Results of a demonstration project in industry. Journal of Rational Emotive Therapy, 5,
213–237.
Jeffrey M. Warren, NCC, is an Assistant Professor at the University of North Carolina at Pembroke. Robyn W. Hale is a School Counselor at Scurlock Elementary School, Hoke County Schools, NC. Correspondence can be addressed to Jeffrey Warren, 1 University Drive, Pembroke, NC 28372, jeffrey.warren@uncp.edu.
Mar 11, 2016 | Book Reviews
Depression 101 by Emily Durbin is a thorough resource for counselors of all skill levels interested in learning or refreshing themselves on the diagnostic and syntonic features of depression. This text covers Major Depressive Disorder (MDD), Dysthymic Disorder (DD), and Bipolar Disorder (BD) in such depth that it could be utilized as a reference text. The author indicates that the aim of the book is to emphasize and bring clarity to the different ways scientific disciplines have approached depression. Dr. Durbin explores how this has affected our understanding of depression spectrum disorders and in turn has resulted in how the field of counseling identifies individuals with depressive mood and structures treatment models.
The text begins by operationalizing and describing the characteristics used to diagnose MDD, DD and BD. Dr. Durbin then explains how these symptoms manifest, who is likely to be diagnosed, and how mood disturbance effects functioning. She concludes with treatment models and recommendations on how to integrate the presented information into practice. The text presents information about depression in a concise manner and consistently includes a variety of references for the topics discussed. It is evident that Dr. Durbin synthesized information from an assortment of sources to give the reader a comprehensive view of the described disorders.
The most applicable section of the text for counselors is the section on integrating the information into practice. Academic books often present a plethora of new information, but it is difficult to figure out how to incorporate it into already established therapeutic practice. This text not only presents an extensive amount of information and research, but summarizes a plan for integration at the end of the book. My only suggestion would be to lengthen this section to further examine the practical implications for the research presented in the subsequent chapters.
Overall, this text is a phenomenal resource for counselors, counselor educators and graduate students alike. I would not consider Dr. Durbin’s book a light read, but she does an excellent job of presenting a vast amount of information in a relatively short text. I have no doubt that I will be referencing this book in the future and utilizing its wide-ranging reference list. After all, depression is considered the “common cold” of psychological disorders. It would be a great disservice to many of our clients to not have a thorough understanding of the disorder that is most frequently reported. Dr. Durbin’s text is an excellent desk reference to serve that purpose.
Durbin, C. E. (2015). Depression 101. New York, NY: Springer.
Reviewed by: Charmayne R. Adams, Wake Forest University
The Professional Counselor
https://tpcwordpress.azurewebsites.net
Mar 11, 2016 | Book Reviews
Psychological Testing That Matters: Creating a Road Map for Effective Treatment is grounded in the Menninger-Topeka psychodynamic approach to testing. It fills a space between diagnostic work and clinical intervention and advances a philosophy of close alliance between those who provide test results and those who use them.
Psychological Testing That Matters lays a foundation for looking at four (and in a few cases, more than four) commonly used diagnostic tests that generate different kinds of data useful for counseling. These tests are discussed in detail, with examples of ways in which the standard administration of these tests can be augmented to discover additional information that deepens one’s ability to interpret client responses. These examples are particularly helpful to the practitioner who is reasonably new to clinical work or who may not have a deep understanding of the various tests.
Technical and specific information on the appropriate applications of the tests is especially interesting and useful. The treatment implications that are explained are good examples of the way in which the authors bring a multitude of testing data together to inform the therapeutic approach. The convergence of data is an important concept that runs through this text and illustrates for the counselor the importance of not relying on a single tool from which to draw conclusions. With precision and nuance, the authors discuss the untangling of story lines and how reserving conclusions is a way of ensuring an accurate depiction of what the data mean: “We are not rushing to conclusions,” but rather “letting connections arrange and rearrange . . . using repetition and convergence to steer the stream of ideas as they flow toward conclusions.”
Especially interesting are the ways in which the authors describe the diagnostic benefits of the test, not only for understanding the client’s ability to function in daily life, but perhaps just as importantly for understanding how the information revealed by the test administration is used to guide therapeutic strategies for engaging with the client in the therapeutic relationship by focusing on identifying circumstances that could interfere and cause a client to shut down. This is where the test results create the road map for treatment.
The organization of the material is one of the strengths of this book. It allows the reader to settle into the material comfortably and deeply, knowing the architecture of the narrative road. It also challenges the reader who may find the level of technicality, particularly in test scoring explanations, repetitive and uninspiring.
The technical diagnostic expertise and clinical prowess of the authors is remarkable and make this book a resource that many clinicians could use. However, as they insightfully acknowledge, the tools available today to simplify diagnosing and reporting also give rise to the concern that the “synthesis from a large quantity of highly complex data[,] . . . wide array of theoretically and empirically based interpretive sources[, and] . . . emotional experiences of the patient’s interior world” make this approach unmanageable in environments where counselors practice now. However, the authors do build a compelling case for the efficacy of their approach, which speaks to the art of their diagnostic and clinical work. It is clear that we may be losing an important piece of clinical competence if we lose appreciation for the knowledge the authors have mastered and share in this book.
Psychological Testing That Matters presents a multi-layered approach to effective treatment with rich case examples of many test applications. This book is important because it reinforces the appropriate uses of certain tests as one element of solid clinical diagnosis and treatment. Further, the book is accessible to a graduate-level practitioner audience in counseling and, with the elegant use of metaphors, is an engaging read.
Bram, A. D., & Peebles, M. J. (2014). Psychological testing that matters: Creating a road map for effective treatment. Washington, DC: American Psychological Association.
Reviewed by: Christine Z. Somervill, University of Phoenix, Tempe, AZ.
The Professional Counselor
https://tpcwordpress.azurewebsites.net/
Mar 11, 2016 | Book Reviews
Career counseling is often overly associated with “test-and-tell” (Preble, 2015) psychometrics such as interest inventories and personality assessments. Many leading scholars and practitioners have advocated for the addition of alternative approaches and methods, especially in this postmodern, post-recession world of work. Pyle and Hayden have afforded counselors and those in related helping professions insights for the use of groups in career development through group career counseling (GCC).
Group Career Counseling: Practices and Principles provides ample information to practitioners in a straightforward, inviting, logically sequenced and useful fashion. Pyle and Hayden organized the text in a manner that allows material to flow. First, the authors provided readers with background information that includes the aims of GCC. Then specific examples of practice, the discussion of probable settings and strategies and different applications follow. The incorporation of a spectrum of GCC foci, ranging from cognitive to affective, allows counselors to identify the appropriate type of group counseling topic for each assemblage. Finally, Pyle and Hayden demonstrated how group career counseling applies to multiple orientations and theoretical foundations through a discussion of a multitude of counseling theories—which include the full traditional gamut from Freudian Psychoanalytic to Glasser’s Reality Therapy—and career development theories—RIASEC to SCCT—with applications for each, respectively.
Pyle and Hayden aimed to promote group career counseling with goals of developing understanding, facilitating use, and catering to the needs of professional counselors. The authors differentiated group counseling from group guidance, and produced a rationale and clear definition for the former. The text espoused the benefits of GCC through a focus on basic principles. Pyle and Hayden equipped readers with a highly-detailed, scripted example comprised of multiple group sessions, and thought-out activities which could be adjusted and marketed for use in various settings. In addition, the format allows for ease of reproduction, so an individual may copy a section of the text for use in practice. Finally, references act as a database for individuals wanting more information on group counseling.
Strengths abound. Pyle and Hayden not only added to the literature regarding career development, group counseling and counseling methods, but furnished counselors with just the right amount of useful information to increase knowledge and support practice. Well organized and thought-out, with careful attention to support both practitioner and counselees, Group Career Counseling allows for the adoption, expansion and ease of facilitation. To add, the work serves as an easy-to-use reference for both scholar and practitioner, both a manual to review while preparing for a session and a resource guiding individuals toward further source materials.
Some may argue that limitations exist. For example, Pyle and Hayden did not address feminist and multicultural counseling theories. However, discussions regarding intake considerations, group settings and strategies for implementation suggest awareness of said approaches. Moreover, others may maintain that the authors fell short by not including data demonstrating the statistical significance of this approach. That said practitioners could quite easily employ their own metrics to determine the impact of GCC on their respective populations.
In the final analysis, I strongly recommend Group Career Counseling for both licensed professional counselors, school counselors at multiple levels, and various other helping professionals who focus on career development interests. Concise, efficient, informative and useful, Group Career Counseling: Practices and Principles could foster the implementation of group counseling, diversify current practices, and allow for greater employability within multiple populations.
Pyle, K. R., & Hayden, S. C. W. (2015). Group career counseling: Practices and principles (2nd edition). Broken Arrow, OK: National Career Development Association.
Reviewed by: Brian C. Preble, Old Dominion University
The Professional Counselor
https://tpcwordpress.azurewebsites.net
Jan 3, 2016 | Volume 7 - Issue 2
Stephanie Burns, Daniel R. Cruikshanks
Inconsistent counselor professional identity contributes to issues with licensure portability, parity in hiring practices, marketplace recognition in U.S. society and third-party payments for independently licensed counselors. Counselors could benefit from enhancing the counseling profession’s identity as well as individual professional identities within the counseling profession. A random sample of 472 independently licensed counselors self-rated and then documented their individual professional identity via their occupational role discussions with others. Results demonstrate that independently licensed counselors rarely accurately self-evaluate their occupational role communications. Further, counselors rarely establish the counseling profession’s identity when discussing their occupational role. Participants’ responses guided the creation of a model that can guide counselors in evaluating and improving the communication of their professional identity to clients, other professionals and the general public.
Keywords: counselor professional identity, licensed counselors, occupational role, parity, structural coding
Authors have expressed concerns about counselor professional identity for over 10 years (Gale & Austin, 2003; Gibson, Dollarhide, & Moss, 2010; Kaplan & Gladding, 2011; Mellin, Hunt, & Nichols, 2011; Myers, Sweeney, & White, 2002). An inconsistent counselor professional identity contributes to issues with licensure portability, parity in hiring practices, marketplace recognition in U.S. society and third-party payments for independently licensed counselors (Calley & Hawley, 2008; Myers et al., 2002; Reiner, Dobmeier, & Hernández, 2013). Additionally, the lack of counselor professional identity has been a factor related to students with master’s degrees in psychology becoming licensed as counselors in many states (Lincicome, 2015). If the profession of counseling appears the same as all the other mental health professions, legislators struggle to understand how specific licenses tie to specific professions that have specific graduate education programs. Licensure boards protect the public from harm by ensuring that counselors have appropriate graduate degrees based on relevant curricula and direct application experiences under supervision (Simon, 2011). Licensing boards require uniform standards to measure minimum training criteria for a profession to assist in expeditious reviews of licensure applications (Mascari & Webber, 2013). A strong counselor professional identity increases counselors’ ability to work with their client populations of interest, receive third-party reimbursement, offer all of the appropriately trained services afforded in their scope of practice and make a greater impact when advocating for clients (Calley & Hawley, 2008; Myers et al., 2002; Reiner et al., 2013).
Apprehensions exist about counselors articulating their profession in generic, non-counseling terms such as therapists or psychotherapists as a method for establishing their ability to diagnose and treat mental and emotional disorders. Confusion increases because other health providers, such as physical therapists, respiratory therapists, speech therapists, occupational therapists, massage therapists, psychologists, social workers and psychiatrists, also utilize the same generic descriptors (Lincicome, 2015). The profession of counseling lacks a consistent identity in U.S. society (Myers et al., 2002); thus, counselors must establish the counseling profession’s identity as well as counselors’ unique role within the counseling profession. This requires clearly articulating the counselor’s client population of interest and specific counseling techniques utilized and articulating the unique identity of the profession of counseling when discussing their occupational role with others (Simpson, 2016). Counselors who are strong in their professional identity understand how counselors differ from other mental health professions (Remley & Herlihy, 2014) and are able to clearly articulate how the profession of counseling is distinguished from other professions when communicating their occupational role.
The Profession’s Mandate for Counselor Professional Identity
In order to achieve parity with other mental health professions, the American Association of State Counseling Boards (AASCB), the American Counseling Association (ACA), the Council for Accreditation of Counseling and Related Education Programs (CACREP), and the National Board for Certified Counselors (NBCC) have taken up the call to promote counselor identity and the profession of counseling (Mascari & Webber, 2013). Additionally, Chi Sigma Iota (CSI; 1998), the counseling profession’s honor society, has taken steps to promote the profession of counseling and counselor identity. The following sections outline how these various organizations document counselor professional identity.
Section C of the ACA Code of Ethics (2014) articulates that counselors are to join local, state and national counseling associations and appropriately communicate their roles and scope of practice. In addition, ACA has endorsed principles directly tied to counselor professional identity through the 20/20: A Vision for the Future of Counseling workgroup. Part of that vision declares that “sharing a common professional identity is critical for counselors” and “presenting ourselves as a unified profession has multiple benefits” (Kaplan & Gladding, 2011, p. 372).
The 2016 CACREP Standards (2015) stipulate student training in the history, ethical standards, professional roles and responsibilities, professional associations, credentialing and licensure processes, professional advocacy, wellness and public policy issues relevant to the counseling profession. The CACREP Standards also require core faculty members be graduates of counselor education programs and hold counseling profession-specific memberships, certifications and licenses to strengthen counselor professional identity and the profession of counseling. These standards exist because counselor educators with dual or non-counseling identities can confuse master’s students’ professional identity in counselor education programs (Emerson, 2010; Mascari & Webber, 2006; Mellin et al., 2011).
Lastly, ACA, AASCB, CSI, and NBCC have identified CACREP accreditation as a foundation for solidifying counselor professional identity and achieving parity for counselors. CSI (2016) requires CACREP accreditation to establish a new CSI chapter. Further, starting January 2022, NBCC will allow only graduates of CACREP-accredited programs to apply for the National Certified Counselor credential (NBCC, 2014a). Additionally, securing a state counseling license often requires understanding and articulating the history and values of the profession of counseling (Emerson, 2010). The National Counselor Examination for Licensure and Examination (NCE; Loesch & Whittinghill, 2010), used in most states as the examination to obtain a counseling license, includes knowledge of the counseling profession in the professional orientation section.
The Counselor’s Development of a Professional Identity
Sweeney (2001) stated that counselor professional identity concerns how the counseling profession’s values and philosophy impact the counselor’s behaviors with clients. He noted that counselor professional identity is not based on the profession of counseling owning specific techniques. For example, cognitive behavioral therapy (CBT) is used in the professions of counseling, psychology and social work. CBT is not owned by any one profession but is used differently by the professions because of differences in each profession’s values and philosophy. Similarly, human development is not owned by any of the three professions. However, the emphasis and application of human development in each profession is different. This is like MRIs being used by oncologists, physical therapists and neurosurgeons. Although all three professions use MRIs, each profession is using that assessment differently to gather information pertinent to their specific occupational role. As such, counselor professional identity is based on the counselor embracing the distinct philosophy and values of the counseling profession.
Components of Counselor Professional Identity
Counselor professional identity first centers on distinguishing the counseling profession’s unique philosophy and values from those of other mental health professions (Calley & Hawley, 2008; Choate, Smith, & Spruill, 2005; Puglia, 2008; Remley & Herlihy, 2014; Weinrach, Thomas, & Chan, 2001; Woo, 2013). Normal development, prevention, advocacy, wellness and empowerment are hallmarks of the unique philosophy and values of the counseling profession (Healey & Hays, 2012). A summary of the five distinct hallmarks and the differentiation from other mental health professions follows.
First, counselors consider that the client’s human growth and development is ultimately positive and often expected when conceptualizing changes and challenges in clients’ lives (Remley & Herlihy, 2014). This hallmark can be found in the Preamble, Purpose, and Section A of the ACA Code of Ethics (2014). The Preamble of the ACA Code of Ethics lists “enhancing human development throughout the life span” as the first core professional value for the counseling profession (p. 3). Additionally, this hallmark is found in several 2016 CACREP Standards: five standards under Human Growth and Development, six standards under Career Development, two standards under Counseling and Helping Relationships and two standards under Assessment and Testing. Lastly, this hallmark is tested in the NCE under Counseling Process (assessing the course of development), Diagnostic and Assessment Services (assessing client’s educational preparation, conducting functional behavioral analysis, observing non-verbal behaviors, and performing a mental status exam), and Professional Practice (applying multicultural counseling models; NBCC, 2014b). In comparison, the National Association of Social Workers (NASW) Code of Ethics (2008) indicates that “Social workers should promote the general welfare of society, from local to global levels, and the development of people, their communities, and their environments” (Section 6.01, Social Welfare). Although both professions talk about development, counselors are applying development in the context of the client (individual, couple or family) while social workers focus on development in the context of local to global societies. Lastly, the American Psychological Association’s (APA’s) Ethical Principles of Psychologists and Code of Conduct (2010, p. 3) states: “Psychologists are committed to increasing scientific and professional knowledge of behavior and people’s understanding of themselves and others and to the use of such knowledge to improve the condition of individuals, organizations, and society.” In psychology, development is researched to provide information to ultimately improve conditions for individuals, organizations, and society.
Prevention services occur when counselors provide psychoeducation, help clients increase resilience and encourage healthy client development throughout the lifespan to prevent, delay or reduce the severity of client symptoms (Granello & Young, 2011). This hallmark can be found in the Preamble and Section A of the ACA Code of Ethics (2014). Section A states: “Counselors facilitate client growth and development in ways that foster the interest and welfare of clients and promote formation of healthy relationships” (p. 3). Additionally, this hallmark is found in two 2016 CACREP Counseling and Human Relationship standards. Lastly, this hallmark is tested in the NCE under Counseling Process (conducting school/community outreach, consulting with client’s support system, directing community initiatives/programs, facilitating client access to community resources, helping clients develop support systems, identifying client support systems and providing psychoeducation) and Professional Practice (conducting school/community outreach and directing community initiatives/programs; NBCC, 2014b). In comparison, the NASW Code of Ethics (2008) states that “Social workers strive to ensure access to needed information, services, and resources; equality of opportunity; and meaningful participation in decision making for all people” (Ethical Principles Section). Differences exist in how the two professions talk about prevention. Counselors apply prevention in the context of the client (individual, couple or family) while social workers focus on prevention in the context of local to global societies. Lastly, APA’s Ethical Principles of Psychologists and Code of Conduct (2010) states: “They strive to help the public in developing informed judgments and choices concerning human behavior” (p. 3). In psychology, prevention occurs when psychologists offer the public accurate information, which leads to better choices and judgments about aspects of human behavior in specific contexts.
Advocacy occurs when counselors defend both clients and the profession of counseling in the face of oppressive systems (Erford, 2013). This hallmark can be found in A.7.a and the Section C Introduction of the ACA Code of Ethics (2014): “When appropriate, counselors advocate at individual, group, institutional, and societal levels to address potential barriers and obstacles that inhibit access and/or the growth and development of clients” (p. 5). Additionally, this hallmark is found in several 2016 CACREP Standards (2015): one standard in the Faculty and Staff section, two standards in the Professional Counseling Orientation and Ethical Practice section, one standard in the Social and Cultural Diversity section, one standard in the Career Development section and one standard in the Clinical Mental Health Counseling Practice section. Lastly, this hallmark is tested in the NCE under Counseling Process (facilitating client access to community resources, identifying barriers affecting client goal attainment, identifying dynamics, obtaining pre-authorization from third-party payors, and providing adequate accommodations for clients with disabilities) and Professional Practice (advocating for client needs, advocating for the professional of counseling, participating in media interviews, providing expert testimony, consult with justice system, consult with providers about medication, consult with school staff, and participate in multidisciplinary team meetings; NBCC, 2014b). In comparison, the NASW Code of Ethics (2008) states: “Social workers pursue social change, particularly with and on behalf of vulnerable and oppressed individuals and groups of people. Social workers’ social change efforts are focused primarily on issues of poverty, unemployment, discrimination, and other forms of social injustice” (Ethical Principles Section). Counselors advocate for the client (individual, couple or family) and the profession of counseling. Social workers advocate for local to global societies. Lastly, APA’s Ethical Principles of Psychologists and Code of Conduct (2010) indicates: “Psychologists recognize that fairness and justice entitle all persons to access to and benefit from the contributions of psychology and to equal quality in the processes, procedures, and services being conducted by psychologists” (p. 3). In psychology, advocacy occurs when the research created by and the services provided by psychologists are available to all members of society.
Fourth, counselors promote wellness when helping clients establish affirmative attitudes, create self-care plans and design life balance strategies (Granello & Young, 2011). This hallmark can be found in the Preamble, Section A Introduction, A.1.a, A.1.c, A.2.c, Section C Introduction, C.2.g, Section E Introduction, F.1.a., F.5.b, F.6.b, F.8 and Section I Introduction of the ACA Code of Ethics (2014). In the Preamble, it states: “Counseling is a professional relationship that empowers diverse individuals, families, and groups to accomplish mental health, wellness, education, and career goals” (p. 3). Additionally, this hallmark is found in one standard each in the Professional Counseling Orientation and Ethical Practice, Social and Cultural Diversity, Human Growth and Development, and Career Development sections of the 2016 CACREP Standards. Lastly, this hallmark is tested in the NCE under Counseling Process (assessing one’s appropriateness for working with a specific client, consulting with client’s support system, consult with school staff, determining need for referral for other services, facilitating client access to community resources, helping client develop support systems, identifying client concerns, identifying client’s support system, providing adequate accommodations for clients with disabilities, providing client follow-up, and triage clients for service), Diagnostic and Assessment Services (assessing potential for harm to self and others, conducting functional behavioral analysis, and using test results to facilitate client decision making), Professional Practice (applying multicultural counseling models, reporting abuse to the proper authorities, and supervising contact/visitation between family members), and Professional Development, Supervision, and Consultation (consult with justice system, consult with prescribers about medication, maintain appropriate boundaries, monitor and address personal compassion fatigue, monitor personal strengths and limitations, and monitor self-reflective versus self-absorbed states of mind; NBCC, 2014b).
In comparison, the NASW Code of Ethics (2008) states that “Social workers seek to strengthen relationships among people in a purposeful effort to promote, restore, maintain, and enhance the well-being of individuals, families, social groups, organizations, and communities” (Ethical Principles Section). Counselors promote wellness in both the client (individual, couple or family) and the counselor while social workers focus on wellness with the client and local to global societies. Lastly, APA’s Ethical Principles of Psychologists and Code of Conduct (2010) indicates: “In their professional actions, psychologists seek to safeguard the welfare and rights of those with whom they interact professionally and other affected persons, and the welfare of animal subjects of research” (p. 3). In psychology, the wellness of the client is safeguarded by the psychologist.
Lastly, empowerment occurs when counselors encourage client autonomy, self-advocacy, self-validation and self-determination (Erford, 2013). This hallmark can be found in the Preamble and A.1.d of the ACA Code of Ethics (2014). The Preamble states the following as a core professional value: “honoring diversity and embracing a multicultural approach in support of the worth, dignity, potential, and uniqueness of people within their social and cultural contexts; promoting social justice” (p. 3). Additionally, this hallmark is found in several 2016 CACREP Standards: five standards in the Social and Cultural Diversity section, three standards in the Human Growth and Development section, seven standards in the Career Development section, four standards in the Counseling and Helping Relationships section, and one standard in the Assessment and Testing section. Lastly, this hallmark is tested in the NCE under Counseling Process (exploring cultural values and mores, facilitating client access to community resource, facilitating conflict resolution, facilitating interpersonal feedback, helping the client develop support systems, identifying barriers affecting client goal attainment, identifying client concerns, identifying the client’s support system, obtaining informed consent, providing adequate accommodations for clients with disabilities, and providing counseling services in the client’s preferred language), Diagnostic and Assessment Services (implementing tests for client decision making and using test results to facilitate client decision making), Professional Practice (advocating for client needs, applying multicultural counseling models, developing referral sources, empowering clients, collaborative goal setting, and decision-making skills), and Professional Development, Supervision, and Consultation (consult with justice system, consult with prescribers about medication, consult with school staff, and maintain appropriate boundaries; NBCC, 2014b).
In comparison, the NASW Code of Ethics (2008) states that:
Social workers promote clients’ socially responsible self-determination. Social workers seek to enhance clients’ capacity and opportunity to change and to address their own needs. Social workers are cognizant of their dual responsibility to clients and to the broader society. They seek to resolve conflicts between clients’ interests and the broader society’s interests in a socially responsible manner consistent with the values, ethical principles, and ethical standards of the profession (Ethical Principles Section).
Although both professions empower clients, counselors focus on empowering the client (individual, couple or family) while social workers additionally consider how an individual’s empowerment impacts society. Lastly, the APA’s Ethical Principles of Psychologists and Code of Conduct (2010) states: “Psychologists respect the dignity and worth of all people, and the rights of individuals to privacy, confidentiality, and self-determination” (p. 3). In psychology, empowerment of clients includes the right to make their own decisions, respecting cultural differences and safeguarding their welfare.
This section has demonstrated that no mental health profession exclusively owns the rights to the words human development, prevention, advocacy, wellness and empowerment. At the same time, this section has clearly outlined how the profession of counseling views these five values differently from psychologists and social workers. It becomes imperative that counselors understand how the profession of counseling views these five values in order to create a counselor professional identity.
Creating a Counselor Professional Identity
A strong counselor professional identity reportedly increases ethical behavior, counselor wellness and an accurate understanding of the counselor’s scope of practice (Brott & Myers, 1999; Grimmit & Paisley, 2008; Ponton & Duba, 2009). Many authors have discussed ways counselors can establish their professional identity. Puglia (2008) suggested behaving in harmony with the philosophy of counseling, becoming licensed and or certified as a counselor, and engaging in professional counseling associations. Calley and Hawley (2008) recommended counselors identify with the distinct values of the counseling profession, engage in professional counseling associations, disseminate scholarship for and about the profession of counseling, utilize theoretical orientations that align with the values of the counseling profession, understand the history of the counseling profession and obtain training, licensure and certifications in the profession of counseling. Remley and Herlihy (2014) identified familiarity with current and historical contexts of the profession of counseling, knowledge of the unique philosophy of counseling, understanding counselors’ roles and functions, utilizing counselor ethical codes, and obtaining memberships in professional counseling associations as six ways counselors could establish their professional identity.
Even with these recommendations, membership in ACA and being licensed as a counselor do not guarantee the ability to articulate a strong counselor professional identity (Cashwell, Kleist, & Scofield, 2009; Mascari & Webber, 2006). Several other factors also could impact counselor professional identity development. Contact with other professional counselors who have a strong counselor professional identity (such as supervisors, contemporaries and counselor educators) increases the development of an appropriate counselor professional identity (Luke & Goodrich, 2010; Puglia, 2008). Additionally, a mixture of self-reflection and connection to the unique philosophies and values of the profession of counseling drives counselor professional identity (Brott & Myers, 1999). Further, holding the counseling profession in high regard combined with a connection between the self and the profession of counseling contributes to a strong counselor professional identity (Brott & Myers, 1999; Gale & Austin, 2003; Sweeney, 2001). CSI supports this premise and states that counselor education students should graduate with pride in the profession of counseling and a strong counselor professional identity as outlined in one of the six key themes from the Counselor Advocacy Leadership Conferences in 1998 (CSI, 1998). This theme stands today as a call to action for CSI members and chapters. This combination purportedly leads to counselors who passionately defend the counseling profession against inaccuracies (Remley & Herlihy, 2014).
Purpose of the Research
Master’s counselor education students have been the focus of prior studies on counselor professional identity (Coll, Doumas, Trotter, & Freeman, 2013; Gibson et al., 2010; Healey & Hays, 2012; Luke & Goodrich, 2010; Moss, Gibson, & Dollarhide, 2014; Nelson & Jackson, 2003; Prosek & Hurt, 2014). Over half (55%) of 203 master’s-level counseling students found it of considerable importance and 28% found it of great importance to better understand the counseling profession and how to identify as a professional counselor (Busacca & Wester, 2006).
Fewer studies have focused on the articulation of professional counselor identity with independently licensed counselors. Rønnestad and Skovholt (2003) found that expressing a strong counselor professional identity required postgraduate counselors to assimilate the personal self and the professional self. Moss and colleagues (2014) stated that client contact was essential to counselor identity development along with an integration of the personal and professional self over the course of a counselor’s career. Mellin and colleagues (2011) found that independently licensed counselors developed a strong counselor professional identity when they aligned with the counseling profession’s unique philosophy and values.
Although each of these studies touches on some aspect of counselor professional identity with independently licensed counselors, none of these studies offers a concrete understanding of how independently licensed counselors articulate their professional identity to others. Further, ACA, AASCB, CACREP, CSI, NBCC have taken steps to attempt to secure a strong counselor professional identity. However, there is no understanding as to whether these efforts impact how independently licensed counselors articulate their professional identity with others. Although there is much discussion about clearly establishing a strong counselor professional identity, there is no systematic way for independently licensed counselors to determine if they articulate a counselor professional identity to others and, if not, what adjustments might be made to improve their communications.
The purpose of this study was to answer the following research questions: (a) what are the different ways (formulas) independently licensed counselors use to articulate their professional role to others, (b) would we assign more advanced professional identity formulas to independently licensed counselors who have recently graduated, (c) would we assign more advanced professional identity formulas to independently licensed counselors licensed in a specific state or region, and (d) would an independently licensed counselor’s self-ranking as consistently identifying professionally as a counselor to others agree with our classification of that counselor with an advanced counselor professional identity formula? To answer these questions, we surveyed independently licensed counselors from across the United States.
Method
Participants
We defined independently licensed counselors as counselors who have graduated with at least a master’s degree, obtained postgraduate clinical supervision and have a license to practice as a counselor without supervision in their state. Participants were 472 independently licensed counselors with a mean age of 41 (range = 25–69, SD = 10.5) who completed all sections of the survey. A majority identified as female (n = 392, 83%) and European American (n = 396, 84%). Other races represented included: African American (n = 24, 5%); Hispanic (n = 19, 4%); Biracial (n = 14, 3%); No Response (n = 9, 2%); Asian American (n = 5, 1%); and Native American (n = 5, 1%). All participants were currently independently licensed as a counselor by a state counseling licensure board; however, 14 (3%) also were licensed marriage and family therapists, nine (2%) also were licensed psychologists, and five (1%) also were licensed social workers. Thankfully these individuals comprised only 6% of the total sample. We included these 28 dually licensed participants as they are independently licensed counselors in their state and represent independently licensed counselors in the United States. These individuals are tied to counselor professional identity in the United States as well as represent independently licensed counselors to other mental health professionals, legislators, clients and society. Participants worked in various settings: counseling agency (n = 170, 36%), private practice (n = 118, 25%), state and federal governments (n = 47, 10%), hospitals and clinics (n = 42, 9%), college settings (n = 33, 7%), not currently working as a counselor (n = 28, 6%), K–12 settings (n = 24, 5%), managed care (n = 5, 1%) and unemployed (n = 5, 1%). The mean year of master’s graduation for participants was 2005 (SD = 6.08).
Data Collection Procedures
SurveyMonkey’s (2016) power analysis calculator for survey designs identified a need for at least 384 survey respondents given a 95% confidence level, 135,000 population size (United States Bureau of Labor Statistics, 2016) and confidence interval of +/- 5%. Two state counseling licensure board lists in each of the four ACA regions (eight states total) were randomly selected. The combined lists from the eight state counseling licensure boards generated a total list of 72,436 independently licensed counselors. A total stratified random sample of 2,144 participants was randomly selected with 268 participants selected from each state to ensure that the same number of participants were randomly selected from each of the four ACA regions. Because many counselors had moved from one of the eight states and were now practicing in another state, independently licensed counselors from 49 states and the District of Columbia were part of the final sample; North Dakota was not represented. Four hundred seventy-two participants completed the study, resulting in a 22% response rate.
Each participant received a postcard of explanation that included a link to a webpage. Participants received one of eight URLs to participate in the study corresponding to the state issuing the independent counseling license to participants. On the webpage, participants responded to five sections when participating in the study. They (a) consented to the informed consent form, (b) answered questions about their demography, (c) rated one Likert scale question, (d) completed the open text box prompt and (e) had the option of providing their name and e-mail address to receive a $5 e-gift card to Amazon.com, Starbucks, or Target on a separate website.
Measure
A search of the literature failed to yield examples of existing measures relevant to the topic. We established content validity before the use of this new and untested instrument. Ten experts from the counseling field completed the instrument and rated items for clarity, representativeness and appropriateness. They rated the one Likert scale question asking about the participant’s clarity in consistently identifying professionally as a counselor as well as the open text box asking participants to write how they describe their occupational role as a professional counselor to others. These 10 experts had published on counselor professional identity or served on state or national counseling professional identity committees.
Three sections comprised the survey: (a) questions about participants’ demography, (b) one Likert scale question asking about the participant’s clarity in consistently identifying professionally as a counselor, and (c) an open text box asking participants to respond to the prompt: “Please write below how you describe your occupational role as a professional counselor to others (clients, other professionals, and the public).” The demographic variables included the following: gender identity, age, all licenses held with a state licensure board, year of graduation from master’s counseling program, current employment setting, and ethnicity and race.
One Likert scale question asked about the participant’s professional identity: “I am consistently clear in my language with clients, other professionals, and the public that I am a counselor (as opposed to saying I am a psychotherapist, therapist, etc.).” Participants responding “Never Clear” scored a 0 and those responding “Always Clear” scored a 5.
Data Analysis Procedures
We performed several data analysis procedures. First, structural coding allowed for the creation of categories that summarize the different formulas used by independently licensed counselors to talk about their profession with others (Saldaña, 2013). Additionally, it allowed for the detection of the number of individual participants who endorsed each formula. We first analyzed the data using structural coding separately, and then we reevaluated the data simultaneously to check for agreement. In the separate analyses, we each found that all 472 responses naturally categorized into six different formulas. We then re-reviewed our separate analyses jointly and found complete agreement.
After utilizing structural coding, we re-analyzed the data using magnitude coding (Miles & Huberman, 1994). Magnitude coding adds a symbol (such as a number or character) to existing code to indicate the code’s intensity, direction or valuation (Saldaña, 2013). We used magnitude coding to add a numeric value to the six formulas with 0 denoting the formula with the least amount of counselor professional identity to 5 denoting the formula with the greatest amount of counselor professional identity.
Further, we performed structural coding again within each of the six main formulas to create sub-formulas that would further explain nuances found within each of the six main formulas. We separately analyzed sub-formulas for each of the six formulas. Later, we reevaluated the results simultaneously to check for agreement. We found that there were four sub-formulas within each of the six main formulas. Magnitude coding was performed by adding a numeric value to the four sub-formulas generated in this study, with a value of “a” denoting the formula with the least amount of counselor professional identity to a value of “d” denoting the formula with the greatest amount of counselor professional identity. Hence, a participant rated as a 5d demonstrated the greatest amount of counselor professional identity, and a participant rated as a 0a demonstrated the least amount of counselor professional identity (Table 1). Further, a participant rated as a 1d demonstrated more counselor professional identity than a participant rated as a 1c.
Next, we used descriptive statistics to explore survey responses from independently licensed counselors using a mail survey design (Fink & Kosecoff, 1998; Heppner, Kivlighan, & Wampold, 1992) to understand our study subjects better. Additionally, we used descriptive statistics to see how closely participants’ ratings of their expressions of professional identity matched our ratings of their professional identity statements. To determine if ratings improved with more recent graduates, we ran a Mann-Whitney U test to see if our ratings varied by participant date of graduation from their master’s counseling program. To determine if different ACA regions obtained better ratings, we performed a Kruskal-Wallis test to see if our ratings varied based upon the state that issued the independently licensed counselor’s license. Finally, we calculated Cohen’s kappa to determine the interrater agreement between participants’ self-rating about identifying consistently as a counselor to others and our ratings of their description of their occupational role as a professional counselor to others.
Results
We identified six different ways (formulas) that independently licensed counselors communicate their professional role to others; a narrative description of each of the six formulas and their four corresponding sub-formulas follows. Table 1 outlines direct quote examples, including the number and percentage of participants using the six formulas and four corresponding sub-formulas. Additionally, Figure 1 displays graphically the total number of participants in each of the six formulas as well as the number of participants in each sub-formula a–d. As noted in the literature review, the counseling profession does not own specific techniques and tools, such as CBT, the Minnesota Multiphasic Personality Inventory or the Diagnostic and Statistical Manual of Mental Disorders (DSM–5). However, counselors articulating their counselor professional identity will likely refer to their connection to specific counseling tools and techniques to help others understand their services.
Table 1
Direct Quote Participant Examples for Each of the Six Formulas With Corresponding Sub-Formulas
n, % Formula Quotes
256, 54% Formula 0 No mention of the word counselor or counseling
164, 64% Formula 0a No title, ambiguous clients and/or techniques
“A person who walks with a client to help achieve the specified goals of a client.”
“I assess, diagnose and treat clients presenting mental health issues.”
51, 20% Formula 0b No title, specific clients and/or techniques
“I am a psychotherapist for children 5–12 living in a psychiatric community residence.”
“I assist people with disabilities with obtaining and maintaining employment.”
10, 4% Formula 0c Title, ambiguous clients and/or techniques
“I am a mental health therapist working with children, adults, couples, and families.”
“I am a program director and clinical supervisor at a mental health agency.”
31, 12% Formula 0d Title, specific clients and/or techniques
“I am an In-Home Intensive Multisystemic Therapist working with willfully defiant adolescents and their families.”
“I am a Unit Manager in a treatment center for adult male inmates.”
19, 4% Formula 1 Generic mention of the word counselor or counseling along with other terms such as therapist, psychotherapist, etc.
7, 37% Formula 1a Ambiguous title, ambiguous clients and/or techniques
“I am a private practice clinician, counselor and therapist. I work in my community serving adults.”
“I provide individual, group, couples, and family therapy to those seeking counseling.”
3, 16% Formula 1b Ambiguous title, specific clients and/or techniques
“I am an independent clinician who works with people 15 and up doing individual and group counseling. I specialize in substance abuse, eating disorders, BPD, co-occurring diagnosis, and trauma.”
“I work in a school setting as a mental health therapist. The school invites our agency in the building and we provide outpatient counseling to children.”
5, 26% Formula 1c Title, ambiguous clients and/or techniques
“You can call me a Licensed Professional Counselor, Behavioral Therapist, Mental Health Therapist, or Psychotherapist. I am a helping professional in the health care field.”
“I am a therapist and counselor at a community hospital and cancer center.”
4, 21% Formula 1d Title, specific clients and/or techniques
“I am a Trauma Specialist. I provide counseling in grief and loss, couples counseling and assistance with gay and lesbian issues.”
“I am a dual-role counselor. I work as an Infant Mental Health Therapist with children ages 0–6 and their families. I also work as a Maternal and Infant Health Therapist working with mothers of all ages and providing them with therapeutic services and case management.”
52, 11% Formula 2 Identifies generically as a counselor or someone doing counseling
14, 27% Formula 2a No title, ambiguous clients and/or techniques
“I provide professional counseling skills for individuals, couples, and groups.”
“My role is to skillfully help clients meet their goals regarding the issues that brought them to counseling.”
19, 36% Formula 2b No title, specific clients and/or techniques
“I provide crisis intervention counseling to children and families.”
“I offer strength-based, solution-focused cognitive behavioral therapy but draw from a variety of theories and foundations to provide individualized counseling and assessment services.”
15, 29% Formula 2c “Counselor” title, ambiguous clients and/or techniques
“As a counselor I diagnose and treat mental and emotional disorders as well as give people empathy, feedback, advice, and guidance in dealing with life issues. In addition, I provide a safe place for people to process thoughts and emotions in an effort to come to a deeper understanding of themselves, others, and the world.”
“I am a counselor providing counseling in a safe environment to people struggling with mental health issues.”
4, 8% Formula 2d “Counselor” title, specific clients and/or techniques
“I am a counselor for a hospice agency, providing emotional support to patients and their families as the patient faces end of life.”
“I am a full-time counselor on a small, private college campus working only with students.”
9, 2% Formula 3 Identifies generically as a counselor or someone doing counseling along with discussing at least one or more distinct hallmarks of the profession of counseling
4, 45% Formula 3a No title, ambiguous clients and/or techniques, identifies one or more hallmarks of the profession of counseling
“I provide counseling services (diagnostic and biopsychosocial assessments, treatment planning, individual, group, couples counseling) and practice from a wellness model and advocate for clients as needed.”
“I provide counseling as well as advocacy for those individuals who are seeking help for a variety of issues in their lives.”
1, 11% Formula 3b No title, specific clients and/or techniques, identifies one or more hallmarks of the profession of counseling
“I provide counseling to children, adolescents and families contracted through the juvenile justice system. I also advocate for clients with community resources.”
3, 33% Formula 3c “Counselor” title, generic clients and/or techniques, identifies one or more hallmarks of the profession of counseling
“As a counselor, I help people learn more about themselves and the things which promote their well-being. I educate people about mental illness and mental well-being.”
“As a counselor, I provide various services in the field of mental or emotional health. At times this means being a source of support, other times it’s a source of information and empowerment. Ultimately I believe I’m there to serve the client, not to force them into my plan.”
1, 11% Formula 3d “Counselor” title, specific clients and/or techniques, identifies one or more hallmarks of the profession of counseling
“I am a counselor for individuals who have committed domestic violence offenses and sex offenses. I provide mental health therapy to these individuals as well as psychoeducational groups about tools to help make healthier choices.”
94, 20% Formula 4 Identifies specifically as a counselor
27, 29% Formula 4a “Professional counselor” or “mental health counselor” title, ambiguous clients and/or techniques
“As a professional counselor I assist people in navigating their complex worlds in order to live a healthier, happier life.”
“As a professional counselor, I diagnose and treat mental and emotional disorders and addictive disorders.”
20, 21% Formula 4b “Professional counselor” or “mental health counselor” title, specific clients and/or techniques
“I am a professional counselor at an incarceration facility and I work primarily with federal inmates and U.S. probation clients.”
“As a professional counselor, I primarily offer career counseling with employees in transition.”
24, 26% Formula 4c Identifies as their state counseling license title, ambiguous clients and/or techniques
“I am a Licensed Mental Health Counselor in private practice.”
“I am a Licensed Professional Counselor. I see my role as coming alongside people and helping them cope with difficulties in life, or helping them manage emotions.”
23, 24% Formula 4d Identifies as their state counseling license title, specific clients and/or techniques
“I am a Licensed Mental Health Counselor (LMHC) who works in the correctional setting by working to rehabilitate inmates.”
“I am a Licensed Mental Health Counselor working with adolescents on a U.S. military base conducting individual, group, and family therapy.”
42, 9% Formula 5 Identifies specifically as a counselor as well as identifies one or more hallmarks of the profession of counseling
33, 79% Formula 5a “Professional counselor” or “mental health counselor” title, ambiguous clients and/or techniques, identifies one or more hallmarks of the profession of counseling
“As a professional counselor, I help clients reach their personal goals with a focus on wellness, client empowerment, developmental awareness, and prevention.”
“As a professional counselor, I offer counseling, psychoeducation, and empowerment in addition to advocating for my clients in areas where they may need assistance.”
1, 2% Formula 5b “Professional counselor” or “mental health counselor” title, specific clients and/or techniques, identifies one or more hallmarks of the profession of counseling
“I am a professional counselor working with children and their parents to help them improve their relationships and reduce habits that get in the way of positive healthy lives as a means of increasing client wellness.”
2, 5% Formula 5c Identifies as their state counseling license title, ambiguous clients and/or techniques, identifies one or more hallmarks of the profession of counseling
“My role as a Licensed Mental Health Counselor is to provide guidance, increase empowerment, and promote wellness for clients.”
“My goal as a Licensed Professional Counselor is to help people maximize their full potential and wellness through advocacy, empowerment, and self-determination.”
6, 14% Formula 5d Identifies as their state counseling license title, specific clients and/or techniques, identifies one or more hallmarks of the profession of counseling
“I am a Licensed Professional Counselor specializing in working with women healing from abuse and trauma. I focus on empowerment and wellness with my clients.”
“I’m a bilingual Licensed Mental Health Counselor who works with Latino families in an outpatient setting. My role is to provide counseling services as well as to advocate on behalf of my clients so that they can maximize their well-being.”
Figure 1. Total number of participants in each of the six formulas as well as the number of participants in each sub-formula a–d.
Formula 0 participants, the lowest rated on the scale, never used the term “counselor” or “counseling” when talking about their role in the counseling profession with others. The majority of participants categorized into this formula. There were four main ways participants expressed themselves in Formula 0 when talking about their role in the counseling profession with others. Formula 0a did not offer a title and was ambiguous about clients and techniques. Formula 0b did not offer a title and was specific about clients and techniques. Formula 0c offered a title, but ambiguously discussed clients and techniques. Formula 0d offered a title and was specific about clients and techniques.
Formula 1 participants generically used the term “counselor” or “counseling” somewhere in their formulations, along with the titles clinician, specialist, social worker, educator, coordinator, administrator, coach, therapist or psychotherapist, when talking about their role in the counseling profession with others. Few participants categorized into this formula. There were four main ways participants expressed themselves in Formula 1 when talking about their role in the counseling profession with others. Formula 1a offered an ambiguous title and was ambiguous about clients and techniques. Formula 1b offered an ambiguous title but discussed specific clients and techniques. Formula 1c offered a title but ambiguously discussed clients and techniques. Formula 1d offered a title and was specific about clients and techniques.
Formula 2 participants generically used the term “counselor” or “counseling” in their formulations. This was the third largest category. There were four main ways participants expressed themselves in Formula 2 when talking about their role in the counseling profession with others. Formula 2a offered an ambiguous title and was ambiguous about clients and techniques. Formula 2b offered an ambiguous title but discussed specific clients and techniques. Formula 2c offered the generic title “counselor” but ambiguously discussed clients and techniques. Formula 2d offered the generic title “counselor” and discussed specific clients and techniques.
Formula 3 participants generically used the term “counselor” or “counseling” in their formulations along with discussing at least one distinct hallmark of the profession of counseling (normal development, prevention, wellness, advocacy or empowerment). This was the smallest category. Among the nine participants, there were at least five mentions of the concepts of wellness and empowerment along with four mentions of the concept of advocacy. There were four main ways participants expressed themselves in Formula 3 when talking about their role in the counseling profession with others. Formula 3a offered an ambiguous title and was ambiguous about clients and techniques but did mention at least one or more hallmarks of the profession of counseling. Formula 3b offered an ambiguous title, discussed specific clients and techniques and stated at least one or more hallmarks of the profession of counseling. Formula 3c offered the generic title “counselor,” ambiguously discussed clients and techniques and stated at least one or more hallmarks of the profession of counseling. Formula 3d offered the generic title “counselor,” discussed specific clients and techniques and stated at least one hallmark of the counseling profession.
Formula 4 participants identified specifically as counselors. This was the second largest category. There were four main ways participants expressed themselves in Formula 4 when talking about their role in the counseling profession with others. Formula 4a offered “professional counselor” or “mental health counselor” as a title but was ambiguous about clients and techniques. Formula 4b offered “professional counselor” or “mental health counselor” as a title and discussed specific clients and techniques. This formula offered a state counseling license title but used ambiguous descriptions of clients and techniques. Formula 4d offered a state counseling license title and used specific descriptions of clients and techniques.
Formula 5 participants identified specifically as counselors along with discussing at least one distinct hallmark of the profession of counseling (normal development, prevention, wellness, advocacy or empowerment). This was the fourth largest category. Among the 42 participants, there were at least 18 mentions of empowerment, 13 mentions of advocacy, 10 mentions of wellness, nine mentions of prevention and seven mentions of normal development. There were four main ways participants expressed themselves in Formula 5 when talking about their role in the counseling profession with others. Formula 5a offered “professional counselor” or “mental health counselor” as a title, was ambiguous about clients and techniques and discussed at least one distinct hallmark of the profession of counseling. Formula 5b offered “professional counselor” or “mental health counselor” as a title, discussed specific clients and techniques and stated at least one distinct hallmark of the profession of counseling. Formula 5c offered a state counseling license as a title, used ambiguous descriptions of clients and techniques and discussed at least one distinct hallmark of the profession of counseling. Formula 5d offered a state counseling license as a title, used specific descriptions of clients and techniques and discussed at least one distinct hallmark of the profession of counseling.
We further wanted to investigate differences between participant self-ratings about identifying consistently as a counselor to others and our ratings of their professional identity statements to determine the level of counselor professional identity actually expressed by the participant. Overall, participant scores fell in the range between “Mostly to Frequently Clear” when asked about identifying consistently as a counselor to others (N = 472, M = 3.40, SD = 1.51). We next grouped all self-ratings together from “Never Clear” (0) to “Always Clear” (5). We separated these five groups and then calculated the means and standard deviations of our ratings of the statements for each of the six self-rated groups. We rated the statements of the 38 participants who self-rated a 0 as having formulations with a mean of 1.20 (at the level of Formula 1) and a standard deviation of 1.79. We rated the statements of the 33 participants who self-rated a 1 as having formulations with a mean of 1.02 (at the level of Formula 1) and a standard deviation of 1.64. We rated the statements of the 47 participants who self-rated a 2 as having formulations with a mean of 1.57 (between Formula 1 and Formula 2) and a standard deviation of 1.93. We rated the statements of the 90 participants who self-rated a 3 as having formulations with a mean of 1.54 (between Formula 1 and Formula 2) and a standard deviation of 1.89. We rated the statements of the 108 participants who self-rated a 4 as having formulations with a mean of 1.58 (between Formula 1 and Formula 2) and a standard deviation of 1.95. We rated the statements of the 156 participants who self-rated a 5 as having formulations with a mean of 1.74 (between Formula 1 and Formula 2) and a standard deviation of 1.95. Figure 2 is a bar chart showing in black the total number of participants for the six levels of clarity in consistently communicating a professional identity to others by formula rating each participant’s statement.
Figure 2. Total number of participants’ clarity in consistently communicating a professional counselor identity to others by formula rating of each participant’s statement.
We conducted a Mann-Whitney U test to see if our rating of participants’ statements changed based upon the participant’s date of graduation: 1969–1999 (n = 57, M = 1.97, SD = 2.03) and 2000–2012 (n = 415, M = 1.50, SD = 1.90). The year 2000 saw the release of the 2001 CACREP Standards (CACREP, 2001), which emphasized student and faculty professional identity and professional orientation. Individuals graduating up to 1999 rated at Formula 2 and individuals graduating 2000 and after rated between Formula 1 and Formula 2. Median researcher ratings for participants graduating with their master’s degree from 1969–1999 (272.91) and participants graduating with their master’s degree from 2000–2012 (244.12) were not statistically different: U = 11170.5, z = -1.585, p = .11. We did not assign more advanced professional identity formulas to independently licensed counselors who had graduated more recently.
We conducted a Kruskal-Wallis test to see if our rating of participants’ statements changed based upon the state issuing the independent counseling license to participants: North Atlantic state 1 (n = 54, M = 1.96, SD = 2.07), North Atlantic state 2 (n = 68, M = 1.10, SD = 1.71), Southern state 1 (n = 47, M = 2.00, SD = 2.02), Southern state 2 (n = 64, M = 1.58, SD = 1.93), Midwestern state 1 (n = 65, M = 1.66, SD = 1.91), Midwestern state 2 (n = 71, M = 1.63, SD = 1.89), Western state 1 (n = 53, M = 1.52, SD = 1.94) and Western state 2 (n = 50, M = 1.10, SD = 1.83). Participants from one North Atlantic state rated highest with Formula 2 while participants from one Western state and one North Atlantic state rated lowest with Formula 1. When the mean was computed by region, the two Southern states rated highest with a 1.79, and the two Western states rated lowest with a 1.31. However, both ratings fell between a Formula 1 and Formula 2. Median researcher ratings for participants by state were not statistically different: χ2(7) = 11.88, p = .11. We did not assign more advanced professional identity formulas to independently licensed counselors licensed in a specific state or region.
We calculated Cohen’s kappa to determine the interrater agreement between the participants’ Likert scale self-rating about identifying consistently as a counselor to others and our rating of that participant’s discussion of their occupational role as a professional counselor to others. A kappa value of less than .20 represents poor agreement; between .21 and .40 represents fair agreement; between .41 and .60 represents moderate agreement; between .61 and .80 represents good agreement; and between .81 and 1.0 represents very good agreement beyond chance (Landis & Koch, 1977). The interrater reliability indicated k = 0.003 (95% CI, .000 to .034, p = .84). Participants’ self-rating of “Always Clear” identifying to others as a professional counselor did not agree with our ratings of these participants’ formulas. Participants’ self-rating of “Never Clear” identifying to others as a professional counselor did not agree with our ratings of these participants’ formulas. An independently licensed counselor’s self-ranking as consistently identifying professionally as a counselor to others did not agree with classification as an advanced counselor professional identity formula.
Discussion
Participants’ scores fell in the “Mostly to Frequently Clear” range when self-rating as clearly articulating to others as a professional counselor. As 56% of the participants rated themselves with the two highest ratings on the scale, it would seem that counselor professional identity is not a serious issue. However, when we evaluated participants’ narratives about their occupational role, we placed only 29% of counselors in the two highest formulas, 4 and 5. As 54% of participants never used the term “counselor” or “counseling” when discussing their occupational role with others, the continued concerns about counselor professional identity are warranted (Gale & Austin, 2003; Gibson et al., 2010; Kaplan & Gladding, 2011; Mellin et al., 2011; Myers et al., 2002). As counselors rated themselves high and the articulations shared rated low, it is not surprising that there was little agreement between a high or low self-rating of articulation and our assigning a high or low formula level to descriptions of their occupational role to others. Results also demonstrated that counselor professional identity articulations have not improved over time. We rated counselors who graduated before 2000 at a Formula 2 and those graduating 2000 and after between Formula 1 and Formula 2. There was no statistical difference between the two groups. Additionally, this study identified that all ACA regions performed on average between a Formula 1 and Formula 2.
Researchers and the major professional counseling organizations agree that counselor professional identity centers on distinguishing the counseling profession’s unique philosophy and values from other mental health professions (Calley & Hawley, 2008; Choate et al., 2005; Puglia, 2008; Remley & Herlihy, 2014; Weinrach et al., 2001; Woo, 2013). Mellin and colleagues (2011) reported that counselors naturally distinguish the counseling profession from other mental health professions by being grounded in a developmental, preventive and wellness orientation despite practicing in different counseling subspecialties. It would appear that the profession and its members have agreement on the counseling profession’s distinct hallmarks of prevention, advocacy, wellness, empowerment and normal human development. However, results from our study indicated that only 11% of participants alluded to one or more of the counseling profession’s distinct hallmarks when articulating their occupational role to others. It does not appear that independently licensed counselors are communicating how the counseling profession’s unique values and philosophy shape their professional practice (Sweeney, 2001). Clearly the ACA Code of Ethics, the NCE and the 2016 CACREP Standards are all guided by these five hallmarks of the profession of counseling. However, independently licensed counselors are not connecting consciously to the philosophy and values of the counseling profession. Once they evolve into clinical practice, independently licensed counselors severely struggle to articulate not only a counselor professional identity, but also to clearly articulate their services. Although this is a problem for the profession of counseling, this is a greater potential problem for the counselor who cannot clearly articulate why they should be hired, why a client should choose their services, why a legislator should listen to their point of view or why an individual from another health profession should make a referral.
The majority of participants (65%) used ambiguous terms to describe clients or techniques used in their counseling practice. Further, over half of the participants (54%) did not offer any title when discussing their occupational role to others. A few participants (5%) used a title that did not mention the word “counselor.” Roughly 8% of participants used their job title, which did not include the word “counselor.” Approximately 5% titled themselves only as a “counselor” while 17% titled themselves a “professional counselor” or a “mental health counselor.” About 11% identified themselves by their state counseling license. This study supports the premise that being licensed as a counselor does not guarantee a strong counselor professional identity (Cashwell et al., 2009; Mascari & Webber, 2006).
Within each of the six distinct formulations independently licensed counselors used to discuss their occupational role with others, there was a pattern of progression from the ambiguous to the specific. This progression happened in two ways; titling as well as describing clients and techniques. First, the profession of counseling in many respects “owns” the words counselor and counseling. In the ACA Code of Ethics, the word counselor or counseling occurs over 600 times. It should, as counselors are licensed at the state level as counselors and receive specialized training in providing counseling. This is a major reason that there is a license at the state level for counselors as opposed to being licensed at the state level as a psychologist or social worker. The word counseling appears in the NASW Code of Ethics four times and the APA Code of Conduct five times. It is extraordinarily problematic that 54% of participants never even used the generic terms counselor or counseling. Further, it is troubling that only 29% of participants gave themselves at least the generic “title” of professional counselor. Additionally, it is troubling how often counselors did not describe the typical types of clients they see or their expertise in working with specific counseling techniques. The inability to articulate their expertise negatively impacts their occupational role. Namely, the progression moved from (a) a weak or nonexistent title with an ambiguous discussion of clients and techniques to (b) a weak or nonexistent title with a specific discussion of clients and techniques to (c) a stronger title with an ambiguous discussion of clients and techniques to, finally, (d) a stronger title with a specific discussion of clients and techniques. Over half (52%) of participants offered some form of a weak or nonexistent title with an ambiguous discussion of clients and techniques. One fifth of the participants communicated some form of a weak or nonexistent title with a specific discussion of clients and techniques. Around 13% of participants used a stronger title with an ambiguous discussion of clients and techniques, and 15% of participants used a stronger title with a specific discussion of clients and techniques.
Implications
A poor counselor professional identity in the United States has been blamed for issues with licensure portability, parity in hiring practices, marketplace recognition in U.S. society, psychologists being licensed as counselors, and third-party payments (Calley & Hawley, 2008; Myers et al., 2002; Reiner et al., 2013). A strong counselor professional identity reportedly remedies these issues and allows counselors to take full advantage of securing their ability to work with a wide range of client populations, receive third-party reimbursement, offer all of the services afforded in their scope of practice and make a greater impact when advocating for clients (Calley & Hawley, 2008; Myers et al., 2002; Reiner et al., 2013). There is clearly much room for improvement in counselor professional identity when independently licensed counselors discuss their occupational role with others.
ACA, AASCB, CACREP, CSI and NBCC have all taken steps to attempt to secure a stronger counselor professional identity. With only 11% of participants mentioning even one of the hallmarks of the profession of counseling, it is imperative that counselors learn one unified message about the hallmarks of the profession of counseling. Healey and Hays (2012) have identified these hallmarks as normal development, prevention, wellness, advocacy and empowerment. These hallmarks are commonly found in the ACA Code of Ethics, CACREP Standards, the NCE, counselor professional identity research, and counselor professional issues and ethics textbooks. The question arises whether counselor educators are teaching counselor professional identity in ways that impact how counselors articulate their occupational role with others. Although the CACREP Standards require documentation that counselor professional identity is taught to students as well as requiring that those same standards be measured, the quality of the measurement of those standards is not under CACREP’s purview. The results of this study suggest that all of the counselor professional identity efforts of ACA, CACREP, NBCC and counselor educators have made little impact on independently licensed counselors when 54% of them do not use the generic terms counselor or counseling and only 29% assign themselves the title professional counselor. There has been much talk about counselor professional identity, but the outcomes suggest that most independently licensed counselors have no connection to counselor professional identity.
A systemic problem exists in the counseling profession’s training of counselors to adopt and articulate a counselor professional identity. It seems as if the organizations of the profession of counseling (ACA, CACREP, NBCC and CSI) know counselor professional identity is the foundation of the profession and have integrated these concepts into the ACA Code of Ethics, 2016 CACREP Standards, the NCE, and CSI’s Six Advocacy Themes. What is not known is what they mean when counselor educators state that they adopt a counselor professional identity. Do counselor educators who say they adopt a counselor professional identity actually understand how the five hallmarks of the profession of counseling are foundationally tied to the ACA Code of Ethics, the 2016 CACREP Standards, and the NCE? If counselor educators fail to tie counselor professional identity to the foundational blocks, and teaching students counselor professional identity amounts to encouraging membership in ACA and state counseling associations, it is little wonder that students graduate not tied to the foundations of the profession of counseling. As discussed in the literature review, many authors have discussed methods to support counselors in establishing their professional identity: behaving in harmony with the philosophy of counseling, becoming licensed and/or certified as a counselor, engaging in professional counseling associations, disseminating scholarship for and about the profession of counseling, understanding the history of the counseling profession, understanding counselors’ roles and functions and utilizing counselor ethical codes. The profession of counseling clearly lacks a concrete understanding of what is truly required to create a counselor professional identity with independently licensed counselors. What is apparent is that the status quo in developing counselor professional identity is not working.
The biggest threat to counselor professional identity is that over 54% of participants did not use the words counselor or counseling when discussing their occupational role. The word counselor can be used by attorneys, camp counselors, debt counselors and others. It is possible that independently licensed counselors are avoiding using the term because they do not know how to distinguish those words from other, unrelated professional roles. This is certainly an issue for independently licensed counselors which does not occur for psychologists or social workers. The reality is that independently licensed counselors are licensed at the state level as counselors and have specialized training to provide counseling. The words counselor and counseling cannot effectively be abandoned by independently licensed counselors.
More resources need to be made widely available to make an impact on how independently licensed counselors articulate their occupational role with others. They need tools to help them effectively discuss their occupational role as a counselor doing counseling. In the past, there has been no systematic way for independently licensed counselors to evaluate their counselor professional identity when communicating their role to others. Further, if the counselor is off track, there has been no resource to help them understand what adjustments could be made to improve their communication. Independently licensed counselors could use guidance to evaluate their ability to articulate a strong counselor professional identity to others.
The coding strategies identified through this research may help independently licensed counselors to evaluate their current narratives and make improvements when communicating their occupational role with others. Counselor educators may use the six formulations with their corresponding four sub-formulas in classes to help students develop their counselor professional identity statements. Lastly, professional counseling associations may use the six formulations and corresponding four sub-formulas to help professional members develop their counselor professional identity statements.
Further, Burns (2017) created a 7-step format to craft a One-Minute Counselor Professional Identity Statement. The tool helps counselors articulate a succinct and powerful counselor professional identity statement that showcases the unique contributions of the counselor as well as the field of counseling. Here is an example of a One-Minute Counselor Professional Identity Statement for an independently licensed counselor introducing themselves to a psychiatrist for referrals:
I’m Susan Jones, a Licensed Professional Counselor. I’d appreciate your consideration of my counseling services for your patients experiencing eating disorders in Detroit. My counseling practice helps clients achieve their optimal level of development and wellness through a focus on client empowerment, prevention and advocacy. I have used evidence-based treatment approaches over the last 7 years such as the Maudsley approach, a family-based therapy, and cognitive behavioral approaches. I also assist clients negotiating the use of antidepressant medications with their prescriber. I am trained to use a variety of assessment, diagnostic and counseling techniques specific to individuals experiencing eating disorders in individual, family and group settings. I promote a healthy relationship with food and others as well as help to overcome barriers to goal attainment. I am a member of the American Counseling Association, as well as the American Mental Health Counselors Association, and am bound by their codes of ethics.
This 7-step format can be used by counselors at all developmental levels and adjusted for various audiences. The 7-step format can help define counselor professional identity to ensure global audiences hear a unified voice of the hallmarks of the counseling profession.
Future Research and Limitations
Future research could examine how independently licensed counselors use the six formulations presented in this study to evaluate their professional identity statements, if they use them at all. Additionally, research could discern how independently licensed counselors view the importance of moving from lower to higher formula levels. Finally, research could determine how independently licensed counselors connect with the distinct hallmarks of counseling.
Limitations of this research include: Likert scale-based surveys suffer from self-report and social desirability bias, recruiting participants from the state counseling boards lists of only eight states across the United States, the $5 incentive could have influenced participant responses or attracted a certain type of participant, and a certain type of participant may have been drawn to respond to the survey topic. Additional limitations include the use of non-parametric data, which may lack power as compared with more traditional approaches. There is a potential bias of interpretation and research embeddedness in the topic with qualitative coding. Lastly, we do not know if any study participants hold doctorates in counselor education.
Conclusion
As inequities exist for independently licensed counselors, there has been much discussion for five decades about counselor professional identity, along with many attempts by various counseling constituencies to address this critical issue. We investigated how independently licensed counselors expressed their role as a professional counselor to others and evaluated their consistency in expressing a counselor professional identity. This study provides a concrete description of how independently licensed counselors are expressing their professional identity when describing their role as a counselor to others. Counselors may wish to review the various formulations outlined to evaluate their own communications to see if and how counselor professional identity can be strengthened.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
American Counseling Association. (2014). 2014 ACA code of ethics. Alexandria, VA: Author.
American Psychological Association. (2010). Ethical principles of psychologists and code of conduct. Washington, DC: Author.
Brott, P. E., & Myers, J. E. (1999). Development of professional school counselor identity: A grounded theory. Professional School Counseling, 2, 339–348. doi:10.1002/j.1556-6676.2014.00124.x
Burns, S. T. (2017). Crafting a one-minute counselor professional identity statement. Journal of Counselor Leadership and Advocacy, 4, 66–76. doi:10.1080/2326716X.2017.1284623
Busacca, L. A., & Wester, K. L. (2006). Career concerns of master’s-level community and school counselor trainees. The Career Development Quarterly, 55(2), 179–190. doi:10.1002/j.2161-0045.2006.tb00012.x
Calley, N. G., & Hawley, L. D. (2008). The professional identity of counselor educators. The Clinical Supervisor, 27, 3–16. doi:10.1080/07325220802221454
Cashwell, C. S., Kleist, D. M., & Scofield, T. (2009). A call for professional unity. Counseling Today, 52, 60–61.
Chi Sigma Iota. (1998). Counselor advocacy leadership conferences: May 27–29, 1998 and December 11–12, 1998. Retrieved from https://www.csi-net.org/?CPALC
Chi Sigma Iota. (2016). Establishing and maintaining an active CSI chapter. Retrieved from https://www.csi-net.org/?page=Chapter_Activate#new
Choate, L. H., Smith, S. L., & Spruill, D. A. (2005). Professional development of counselor education students: An exploratory study of professional performance indicators for assessment. International Journal for the Advancement of Counselling, 27, 383–397. doi:10.1007/s10447-005-8201-0
Coll, K. M., Doumas, D. M., Trotter, A., & Freeman, B. J. (2013). Developing the counselor as a person and as a professional: Attitudinal changes in core counseling courses. The Journal of Humanistic Counseling, 52, 54–66. doi:10.1002/j.2161-1939.2013.00032.x
Council for Accreditation of Counseling and Related Educational Programs. (2001). 2001 CACREP standards. Alexandria, VA: Author.
Council for Accreditation of Counseling and Related Educational Programs. (2015). 2016 CACREP standards. Alexandria, VA: Author.
Emerson, C. (2010). Counselor professional identity: Construction and validation of the counselor professional identity measure (Doctoral dissertation, The University of North Carolina at Greensboro). Retrieved from http://libres.uncg.edu/ir/uncg/f/emerson_uncg_0154d_10396.pdf
Erford, B. T. (2013). Orientation to the counseling profession: Advocacy, ethics, and essential professional foundations (2nd ed.). Boston, MA: Pearson.
Fink, A., & Kosecoff, J. B. (1998). How to conduct surveys: A step by step guide (2nd ed.). Thousand Oaks, CA: Sage.
Gale, A. U., & Austin, D. B. (2003). Professionalism’s challenges to professional counselors’ collective identity. Journal of Counseling & Development, 81, 3–10. doi:10.1002/j.1556-6678.2003.tb00219.x
Gibson, D. M., Dollarhide, C. T., & Moss, J. M. (2010). Professional identity development: A grounded theory of transformational tasks of new counselors. Counselor Education and Supervision, 50, 21–38.
doi:10.1002/(ISSN)1556-6978
Granello, D. H., & Young, M. E. (2011). Counseling today: Foundations of professional identity. Boston, MA: Pearson.
Grimmit, M. A., & Paisley, P. O. (2008). A preliminary investigation of school counselor beliefs regarding
important educational issues. The Journal of Humanistic Counseling, 47, 99–110.
doi:10.1002/j.2161-1939.2008.tb00050.x
Healey, A. C., & Hays, D. G. (2012). A discriminant analysis of gender and counselor professional identity development. Journal of Counseling & Development, 90, 55–62. doi:10.1111/j.1556-6676.2012.00008.x
Heppner, P. P., Kivlighan, D. M., & Wampold, B. E. (1992). Research design in counseling (1st ed.). Belmont, CA: Brooks Cole.
Kaplan, D. M., & Gladding, S. T. (2011). A vision for the future of counseling: The 20/20 principles for
unifying and strengthening the profession. Journal of Counseling & Development, 89, 367–372. doi:10.1002/j.1556-6678.2011.tb00101.x
Landis, J. R., & Koch, G. G. (1977). The measurement of observer agreement for categorical data. Biometrics, 33, 159–174.
Lincicome, M. (2015). Opening the doors: Professional identity in counselor educators (Doctoral dissertation). Retrieved from ProQuest. (UMI No. 3731246).
Loesch, L., & Whittinghill, D. (2012). NCE technical manual for the national counselor exam (rev. ed.). Greensboro, NC: National Board for Certified Counselors.
Luke, M., & Goodrich, K. M. (2010). Chi sigma iota chapter leadership and professional identity development in early career counselors. Counselor Education and Supervision, 50, 56–78.
doi:10.1002/j.1556-6978.2010.tb00108.x
Mascari, J. B., & Webber, J. (2006). Salting the slippery slope: What licensing violations tell us about preventing dangerous ethical situations. In G. Walz, J. Bleuer, & R. Yep (Eds.), VISTAS: Compelling perspectives on counseling 2006 (pp. 165–172). Alexandria, VA: American Counseling Association.
Mascari, J. B., & Webber, J. (2013). CACREP accreditation: A solution to license portability and counselor identity problems. Journal of Counseling & Development, 91, 15–25. doi:10.1002/j.1556-6676.2013.00066.x
Mellin, E. A., Hunt, B., & Nichols, L. M. (2011). Counselor professional identity: Findings and implications for counseling and interprofessional collaboration. Journal of Counseling & Development, 89, 140–147. doi:10.1002/j.1556-6678.2011.tb00071.x
Miles, M. B., & Huberman, A. M. (1994). Qualitative data analysis (2nd ed.). Thousand Oaks, CA: Sage.
Moss, J. M., Gibson, D. M., & Dollarhide, C. T. (2014). Professional identity development: A grounded theory of transformational tasks of counselors. Journal of Counseling & Development, 92, 3–12.
doi:10.1002/j.1556-6676.2014.00124.x
Myers, J. E., Sweeney, T. J., & White, V. E. (2002). Advocacy for counseling and counselors: A professional imperative. Journal of Counseling & Development, 80, 394–402. doi:10.1002/j.1556-6678.2002.tb00205.x
National Association of Social Workers. (2008). Code of ethics of the National Association of Social Workers.
Washington, DC: Author.
National Board for Certified Counselors. (2014a). Important announcement. Greensboro, NC: Author. Retrieved from http://nbcc.org/assets/Change-announcement-flyer_2014.pdf
National Board for Certified Counselors. (2014b). National counselor examination for licensure and certification preparation guide. Greensboro, NC: Author.
Nelson, K., & Jackson, S. (2003). Professional counselor identity development: A qualitative study of Hispanic student interns. Counselor Education and Supervision, 43, 2–14. doi:10.1002/j.1556-6978.2003.tb01825.x
Ponton, R. F., & Duba, J. D. (2009). The ACA code of ethics: Articulating counseling’s professional covenant. Journal of Counseling & Development, 87, 117–121. doi:10.1002/j.1556-6678.2009.tb00557.x
Prosek, E. A., & Hurt, K. M. (2014). Measuring professional identity development among counselor trainees. Counselor Education and Supervision, 53(4), 284–293. doi:10.1002/j.1556-6978.2014.00063.x
Puglia, B. (2008). The professional identity of counseling students in master’s level CACREP accredited programs (Doctoral dissertation). Retrieved from ProQuest. (UMI No. 3324071).
Reiner, S. M., Dobmeier, R. A., & Hernández, T. J. (2013). Perceived impact of professional counselor identity: An exploratory study. Journal of Counseling & Development, 91, 174–183.
doi:10.1002/j.1556-6678.2009.tb00557.x
Remley, T. P., Jr., & Herlihy, B. P. (2014). Ethical, legal, and professional issues in counseling (4th ed.). Boston, MA: Pearson.
Rønnestad, M. H., & Skovholt, T. M. (2003). The journey of the counselor and therapist: Research findings
and perspectives on professional development. Journal of Career Development, 30, 5–43. doi:10.1177/089484530303000102
Saldaña, J. (2013). The coding manual for qualitative researchers (2nd ed.). Thousand Oaks, CA: Sage.
Simon, S. (2011). A license to shampoo: Jobs needing state approval rise. Wall Street Journal. Retrieved from https://www.wsj.com/articles/SB10001424052748703445904576118030935929752
Simpson, D. (2016). “Going up?” A sport psychology consultant’s guide to the elevator speech. Journal of Sport Psychology in Action, 7(2), 109–120. doi:10.1080/21520704.2016.1182091
SurveyMonkey. (2016). Sample size calculator. Retrieved from https://www.surveymonkey.com/mp/sample-size-calculator
Sweeney, T. J. (2001). Counseling: Historical origins and philosophical roots. In D. C. Locke, J. Myers & E. L. Herr (Eds.), The handbook of counseling (pp. 3–26). Thousand Oaks, CA: Sage.
United States Bureau of Labor Statistics. (2016). Occupational employment and wages, May 2016, 21-1014 mental health counselors. Retrieved from https://www.bls.gov/oes/current/oes211014.htm
Weinrach, S. G., Thomas, K. R., & Chan, F. (2001). The professional identity of contributors to the Journal of Counseling & Development: Does it matter? Journal of Counseling & Development, 79, 166–170. doi:10.1002/j.1556-6676.2001.tb01956.x
Woo, H. (2013). Instrument construction and initial validation: Professional identity scale in counseling (PISC) (Doctoral dissertation). Retrieved from ProQuest. (UMI No. 3566722).
Stephanie Burns, NCC, is an Assistant Professor at Western Michigan University. Daniel R. Cruikshanks is a Professor at Aquinas College. Correspondence can be addressed to Stephanie Burns, 1903 W. Michigan Avenue, Kalamazoo, MI 49008-5226, stephanie.burns@wmich.edu.
Dec 10, 2015 | Article, Volume 5 - Issue 4
Theodore P. Remley, Jr.
TPC Editor Note: Earlier this year I was in the wonderful city of New Orleans and realized it was the 10th anniversary of Hurricane Katrina. In 2005 I was involved with operations at the National Board for Certified Counselors that sent 240 National Certified Counselors to New Orleans and the surrounding area to provide direct crisis counseling and disaster relief. Having done similar work in New York City following the attacks in 2011, I found myself reflecting on what it might be like 10 years later in the Crescent City from a counseling perspective.
Of course I immediately thought to contact Dr. Ted Remley, who was living in New Orleans and teaching in counselor education at the time of the storm. I knew that his personal perspective would be invaluable, leading me to ask him to write this commentary about his reflections on mental health services in New Orleans today. Dr. Remley returned to the city last year to teach in a doctoral program in counselor education and supervision. His many years of experience and astute vision of the global process of counseling have resulted in the following personal analysis. It is my hope that this article is commemorative of the challenges that all mental health workers experienced during and after Hurricane Katrina, and the heroic services they provided during a time of extreme stress and loss. — J. Scott Hinkle, NCC
Ten years after Hurricane Katrina, the counseling profession in New Orleans has changed. The author, along with a group of counseling and other mental health professionals who were providing services at the time of the hurricane and still working in the city 10 years later, provided their impressions of counseling in New Orleans a decade after the storm. The population of New Orleans and the presenting problems of clients shifted after Hurricane Katrina. The residents have required help from counselors, supervisors, counselor educators and agency administrators in order to adapt to new challenges. The need for counselors to possess skills in trauma counseling was one of the lessons learned from the disaster. Agency administrators also advised using caution after a disaster when considering funding offers and research study proposals. While it may be impossible to prepare thoroughly for each unique disaster, Hurricane Katrina taught counseling professionals in New Orleans that after a disaster, flexibility and creativity are required to survive.
Keywords: Hurricane Katrina, mental health, trauma, disaster, counselor educator
Pausing to assess counseling and other mental health services in New Orleans 10 years after Hurricane Katrina has been a worthwhile endeavor. Many people are curious about what has happened to New Orleans since the hurricane, and counselors are particularly interested in how counseling and other mental health services have changed. The unique challenges due to Hurricane Katrina faced by New Orleans counselors who live and work in the city have not been forgotten or put aside since the storm.
The state of counseling and other mental health services in New Orleans a decade after the hurricane are presented in this article along with some of my own observations. This article does not report a qualitative study, but instead offers a summary of the impressions of counseling and other mental health services from a select group of professionals who were providing services at the time of Hurricane Katrina and still working in mental health agencies in New Orleans 10 years later. Rather than presenting only my observations of the state of counseling in New Orleans today, I asked several others to share their impressions and I have attempted to summarize their experiences.
Scholars have examined the aftermath of Hurricane Katrina and studied numerous aspects of the results of the devastating storm (Chan, Lowe, Weber, & Rhodes, 2015; Wang et al., 2007; Weisler, Barbee, & Townsend, 2006). Specific areas of investigation have included a school-based disaster recovery program for children (Walker, 2008), the precipitation of suicide (Kessler, Galea, Jones, & Parker, 2006), the disruption of mental health treatment (Wang et al., 2008), and the differences between people who were displaced and those who returned to New Orleans (Priebe, 2014). Analyses have been completed of leadership in the city (Gohl, Barclay, Vidaurri, Newby, & Arquette, 2015), the restructured education system (Lazarchik, 2015), the social capital and repopulation of New Orleans (Rackin & Weil, 2015), and tourism (Thomas, 2014; Vernet, 2015). Similarly, to obtain an up-close and personal perspective of the changes in counseling and other mental health services, I contacted professionals who were working in mental health agencies in the New Orleans area before or at the time of Hurricane Katrina and were still at a local agency today. These individuals also had a perspective and analysis regarding the effects of the hurricane, having had a major role in the continuation of counseling services at their agencies after the storm. And, like all residents of New Orleans, they also had to rebuild their personal lives following the hurricane.
The Changed City
New Orleans 10 years after Hurricane Katrina is different from the New Orleans that existed in August 2005. While the French Quarter, Uptown and other affluent neighborhoods appear hardly changed, at a deeper level the city is not the same as it was before the hurricane. The most obvious change, aside from the areas where houses are still boarded up and abandoned, is the population. New Orleans now holds 93% of the number of people it had prior to Hurricane Katrina (Shrinath, Mack, & Plyer, 2014). However, it is important to note that for several months after Hurricane Katrina, the city was still covered in floodwaters and had almost no people. Although the population has been reduced by 7%, a number of people living in New Orleans are new to the city. Many residents who lived in New Orleans before Hurricane Katrina did not return. The population loss affected the day-to-day lives of both the people who relocated to other areas of the United States and those who stayed behind and lost contact with relatives, friends and neighbors. Shrinath et al. (2014) provided a review of the changes in the New Orleans population that have occurred since Hurricane Katrina based on data provided by the U.S. Census Bureau. Overall, the population has become smaller, older, more educated and a bit poorer. In addition, New Orleans is now more Hispanic and Caucasian, and less African American.
New Orleans public schools have largely been replaced since Hurricane Katrina with charter schools, which nine out of 10 students now attend (Khadaroo, 2014). Many schools now contract with agencies that provide mental health counseling at school, significantly altering the role of traditional school counselors, and in some cases, replacing them. Today, counselors working as mental health counselors in schools in New Orleans are called upon to diagnose and treat emotional and mental disorders and to be much more involved in family counseling than school counselors were in the past. Consequently, traditional school counselors have been forced to interface with contracted mental health counselors and redefine their roles and responsibilities.
Implications for Counselors and Counselor Educators in New Orleans
One of the facts that counselors learned from Hurricane Katrina is that the demographics of a population will likely change after a disaster (Arendt & Alesch, 2014). Counselors will need to shift from serving one population to another, and will be required to learn new skills. Following a disaster, administrators will need to provide continuing education for counselors so that they can learn new skills, and counselor educators will need to prepare graduate students for work in disaster environments.
Changes in the median age of New Orleans citizens after the hurricane have resulted in an older population, fewer children and more people living alone, which have had a significant impact on counselors providing services in the city today. Counselors with little to no expertise in providing services for elderly, isolated clients have had to be educated on new skills. In fact, many counselors who previously worked with children are now counseling older adults with different needs.
Prior to Hurricane Katrina, few schoolchildren had access to mental health counseling to the extent that they do in today’s charter schools. Counselor educators in New Orleans now prepare counselors who wish to work in schools for both the traditional role of school counselors in parochial or public schools and for the new role of school mental health counselors for those positions in agencies that contract to provide services in charter schools.
Counselors in New Orleans served a population challenged by poverty prior to Hurricane Katrina and continue to provide services to people who are impoverished at a much higher rate than people living in many other areas of the United States. Counseling individuals living in poverty requires special skills in order to serve their needs (Ratts & Pedersen, 2014). As a result, universities in New Orleans are required to prepare their graduates to understand and serve clients of poverty. Moreover, a report issued in the fall of 2012 by The Data Center, an independent research organization in New Orleans, indicated that 37% of the people in New Orleans live in asset poverty, defined as not having enough funds to support a household for 3 months if the main source of income was lost (Shrinath et al., 2014). Asset poverty has particularly severe implications in New Orleans because evacuations from hurricanes are necessary every few years and require funds or credit. Counselors in New Orleans who provide services to poor clients must help their clients prepare for hurricane evacuation despite not having needed financial resources. This narrative is told countless times during each evacuation maneuver.
My Story in Brief
I am a counselor educator and was one of the counseling professionals in New Orleans who chose to relocate after Hurricane Katrina. While such decisions are complicated and are motivated by multiple factors, the primary concerns that led to my departure were that the university where I was working, like all entities in New Orleans, was unstable and experiencing severe financial stress, and I was caring for my elderly mother who needed regular medical attention that was not readily available in the city after the hurricane. I resigned from the university in New Orleans in May 2006, almost a year after the hurricane, and relocated to another state to teach in a counselor education program. I had the opportunity to return to New Orleans eight years later and assumed my current position as a counselor education professor in 2014. When I left New Orleans in 2006, I was sad to be leaving my colleagues and friends, quite apprehensive about my professional future, financially vulnerable, and concerned about health care for my family members as well as myself. When I returned eight years later, I was happy to be returning to my circle of friends, delighted to be welcomed by colleagues, comfortable with my professional future, financially secure, and confident that health care was readily available in New Orleans. When I returned, I found a city that was different in many ways since the hurricane, and a city that also was much the same.
The differences in New Orleans 10 years after Hurricane Katrina, from a personal perspective, were both subtle and striking. After living with my family temporarily in the mountains of Georgia, my return to New Orleans for a visit about two months after the storm was astonishing. Public services were limited. On the other hand, the city was functioning. People were going to work, utilities had been restored, and residents who had returned were doing their best to resume the lives they had known prior to the storm. I experienced many personal challenges, which included repairing my hurricane-damaged home, finding daily care for my elderly mother, and hosting friends for a year who had lost their home in the flood that followed the hurricane. During these challenges, I remained aware and thankful that my burdens were far fewer than those of many of my neighbors, friends and fellow residents.
New Orleans 10 Years Later: My Perspective
My personal impressions of New Orleans 10 years after the storm are generally positive, but there are many scars for those living in the aftermath of the storm. When I returned in 2014, one of my friends who had not left and was still living in the city said, “After Hurricane Katrina, everything changed” (Anonymous, personal communication, August 1, 2014). He said his friends were gone, he no longer had his job, his children and their families had relocated out of state, and everything seemed a mess. His reaction was not unique. Much has been written about the hardships faced by people after Hurricane Katrina, particularly by the poor and uneducated, but many of the stories of professional mental health workers living in the city at the time of the storm have not been told. For the past decade, counselors in New Orleans have been serving the citizens, including counselors who lost their homes in the flood after the storm.
For me, day-to-day life in New Orleans 10 years after Hurricane Katrina appears to be much what it was before the disaster. There is still too much poverty and crime. Although in the French Quarter one can hardly see any differences a decade later, a drive through the Ninth Ward or the community of Lakeview near Lake Pontchartrain shows the devastating aftermath of the hurricane.
Changes in Mental Health Services in New Orleans Since Hurricane Katrina
In an effort to encourage the mental health professionals I contacted to be forthright and free from inhibition in their responses, no individuals or agencies are identified; and because of this degree of privacy, only general information is provided. Mental health professionals who were still working at agencies in New Orleans and responded to my questions included counselors, psychologists and social workers in public and private nonprofit agencies that provide a wide array of counseling and other mental health services to all levels of the population. I was able to obtain informal, personal responses to a series of questions from eight mental health professionals who were working in counseling and other mental health agencies before Hurricane Katrina and are still working in agencies a decade later. The information, perspectives and comments they provided helped paint a picture of mental health services in New Orleans today.
It is telling in itself that I was able to locate only a few mental health professionals who were still working in the same agencies in New Orleans 10 years after Hurricane Katrina. The agencies themselves have changed substantially. Although some have flourished, many have decreased in size and a number have ceased to exist. Staff turnover in New Orleans mental health agencies has been significant. Almost all top-level administration positions are held by different people, mental health practitioners have come and gone, and the number of staff members has generally decreased. I contacted the largest governmental mental health agency in the city in an effort to find a person who had been working there at the time of Hurricane Katrina and was still there. Not one administrator or mental health professional fit the criteria; there had been a 100% staff turnover in the past 10 years.
Agency differences 10 years after the hurricane. When asked to compare and contrast the current circumstances at the agencies with the situation 10 years before, the mental health professionals provided a variety of responses. Most agencies are operating 10 years after the disaster in a fashion similar to what they were doing prior to the hurricane. For an agency to have survived after Hurricane Katrina is, in itself, notable. All agencies were closed for several months during the evacuation of the city and some did not reopen for a significant period of time. In several agencies, as might be expected, the services shifted to dealing with trauma, with two agencies now specializing in trauma recovery. Several professionals reported that counseling and other mental health services after the storm were less often provided by licensed mental health professionals. For example, mental health interns who were completing their degree programs, as well as individuals who had completed their degrees and were working toward licensure, were often providing services. These changes might suggest that the quality of counseling services had been compromised in New Orleans. Certainly counselor educators and counselor supervisors have experienced an added burden of preparing new counselors to hit the road running (i.e., be better prepared to deliver professional counseling services earlier in their careers than what might normally be expected). Counseling supervisors have had to closely monitor the work of neophyte professionals to ensure that counseling services are of high quality.
One counseling agency experienced tremendous growth, morphing from a small agency with three part-time mental health professionals to an agency with over 50 mental health providers who are either licensed or working toward licensure. Such significant growth can test an organization’s capacity to function effectively. Administrators at this agency have been challenged to find and hire competent counselors with the needed expertise to serve the population.
Three agency professionals indicated that they have been more focused on evidence-based mental health practices since Hurricane Katrina. They did not indicate why this change had occurred, but it is notable that such a change did become part of the agencies’ practices. It is likely that governmental and private funding agencies required grant recipients to demonstrate engagement in mental health practices that were evidence-based.
Client needs after the hurricane. Mental health professionals reported significant shifts in the populations that they served prior to Hurricane Katrina and afterward. Several reported that the number of services for individuals suffering from trauma had significantly increased, not only from the hurricane, but also from other types of crises, including sexual trauma and other forms of violence.
One agency professional who served primarily indigent clients indicated a significant rise in the demand for free or reduced-cost services from families in households with incomes below $20,000 per year. At this particular agency, 25% of the clients came from families with incomes between zero and $8,000 per year. At the other extreme, an agency that served a more affluent population had an increase in the number of young adult clients who moved to New Orleans to take jobs assisting in the city’s recovery. Consequently, counselors at agencies have had to adjust to serving clientele they may not have worked with in the past. Agency administrators have had to provide significant in-service training to help counselors adjust to changing client needs.
Mental health professionals reported serving more Hispanic clients and indicated that attention-deficit/hyperactivity disorder and depression and anxiety issues have become more prevalent. Several agency professionals indicated that since Hurricane Katrina, they have served more clients in general, and specifically more children. In addition, some counselors who had never counseled children received in-service education in counseling children and adolescents. Currently, there is a need in the city for counselors who are bilingual and can provide counseling services in Spanish.
Changes in professional-to-client ratios since Hurricane Katrina. Five mental health professionals indicated that their agencies had established a maximum number of clients that each professional could serve in order to ensure that those who were served would receive high quality services. Some agencies established waiting lists and began offering more group services in order to avoid overburdening their professional staff.
Those agencies that had found it financially necessary to decrease their staff had correspondingly decreased the number of clients served. One mental health professional commented that challenges with Medicaid and health insurance reimbursement had made it difficult to afford the number of licensed mental health professionals needed. Agency administrators have had to protect their counselors from stress and burnout as client demand has increased and the number of staff has decreased. Administrators have met this challenge by reducing the number of clients on counselors’ caseloads, establishing waiting lists and offering more group services. The shift to more group services implies that competent group counseling skills and experiences are needed in New Orleans.
Government funding since the hurricane. When asked whether their agencies had received state or federal funding to support them since Hurricane Katrina, most professionals indicated that their agencies had received such funds. Agency administrators reported receiving funds from a local parish government agency that distributes funds from the federal government (specifically, from the U.S. Department of Housing and Urban Development and the Substance Abuse and Mental Health Services Administration). Some agency administrators also reported receiving funding from the American Red Cross, United Way, and local foundations and charities. Three agencies reported receiving Federal Emergency Management Agency funds for operating costs and reconstruction after the hurricane.
How Would Agencies Be Different if Hurricane Katrina Had Not Happened?
Mental health professionals were asked how they believed their agencies would be different today if Hurricane Katrina had not happened. Responses varied. Two mental health professionals said that if the hurricane had not occurred, their agencies would have continued to struggle financially, indicating that the hurricane had brought at least a degree of relief from financial problems. Perhaps the outside funding that flows into an area after a natural disaster can infuse funds into financially struggling counseling agencies, allowing them to continue to operate when they might not have been able to do so if the disaster had not occurred.
Several mental health professionals reported that because of Hurricane Katrina, agency personnel had learned a great deal and certainly would be able to handle any similar type of natural disaster in a better fashion if one should occur in the future. Today’s counseling graduate students are being taught disaster, crisis and emergency response counseling procedures, as required by the Council for Accreditation of Counseling and Related Educational Programs (2009) in their counselor preparation curriculum. However, most counselors completed their graduate training prior to the time that these standards were implemented, requiring in-service training in post-disaster operations.
Most agency personnel reported that their agencies had benefitted from having experienced Hurricane Katrina. One mental health professional indicated that if not for the hurricane, the agency would not have a close relationship with area schools, would lack evidence-based practices devoted to psychological trauma, and would be wanting in innovation and creativity. Another said that the agency would not have grown as much. Two mental health professionals suggested that Hurricane Katrina had provided their agencies with national attention that allowed the agencies to become leaders in their areas of specialization, which included juvenile justice and trauma. One mental health professional said that without the hurricane, the agency would not have been tested or trained in the following areas: crisis management, grief and loss due to a natural disaster, management of post-traumatic stress disorder, and how to counsel when the counselor is experiencing similar stressors. Lastly, another counseling professional indicated that staff would not have received trauma recovery training if Hurricane Katrina had not occurred.
Recommendations for Mental Health Agencies
Mental health professionals who provided information for my personal analysis offered recommendations for counselors who must contend with a disaster. They also gave recommendations to agency personnel for preparing for a disaster.
Recommendations on Contending With a Disaster
Three mental health professionals suggested that perhaps preparing for specific disasters is impossible, while there was agreement that agencies should be prepared to deal with emotional trauma in the event of a natural disaster. Two mental health professionals suggested that planning for the possibility of a disaster would most likely not be productive. One mental health professional said that “preparing for the next disaster based on experiences from Hurricane Katrina would be like preparing for the next war based on experiences from the last one.” This mental health professional added that all disasters are unique and that it would do no good to base disaster recovery plans on what New Orleans experienced as a result of Hurricane Katrina. Another mental health professional emphasized that being flexible is essential, so that programs can be developed to meet the needs of the community.
Although no amount of disaster preparation can help counseling agencies prepare for all possible challenges, perhaps the best response to disasters is to be flexible, creative and practical, taking on each problem as it is encountered. One mental health professional cautioned that agencies should be prepared not only to treat clients with post-traumatic stress disorder resulting from the disaster, but also to treat trauma symptoms that stem from unresolved trauma from childhood or past life experiences that surface after the newer trauma caused by a recent disaster. The concept that mental health agencies should always be prepared to deal with the trauma that follows a natural disaster was universally voiced by mental health professionals. In addition, self-care for counselors has become a popular topic in the professional literature (Alvarez, 2015; Ohrt & Cunningham, 2012; Thompson, Frick, & Trice-Black, 2011; Witt & McNichols, 2014), and mental health workers in New Orleans emphasized assessment of trauma among counselors for up to two years after a disaster.
The most significant disagreement among mental health professionals concerned whether it is advisable to join in collaborative efforts or partnerships with other agencies after a disaster. While one mental health professional said that collaboration is a key to recovery, and two counselors supported this idea, another mental health professional said that collaborative partnerships have the potential to support incompetence and ruin inter-organizational relationships. A third mental health professional warned that mental health agencies should not chase or accept time-limited funding after a disaster, and should not expand services based on funding that will soon disappear.
One mental health professional indicated that collaboration was touted as the best recovery tool by many after Hurricane Katrina and acknowledged that the concept of collaboration after a disaster could be a win-win for organizations leveraging their collective expertise into post-disaster response and recovery. This mental health professional said that organizations outside the community often want to create a collaborative partnership after a disaster by providing trauma intervention or counselors for a local agency at no cost. However, such offers could possibly be exploitive. Often the intervention offered is not evidence-based, and the outside organization wants to use the agency as a way to increase its own credibility or perhaps raise funds because its employees are responding to the needs of the community after a disaster. Furthermore, this mental health professional warned that university professors who want to conduct research are often more interested in increasing their scholarship productivity than helping a mental health agency recover from a disaster. Counselor educators should of course avoid exploiting disaster situations for the sole purpose of increasing their research publications. Counseling agency administrators need to be cautious after a disaster when they are approached about participating in proposed research or service projects.
One mental health professional gave the following advice regarding response to outside organizations or individuals who want to help after a disaster:
I would create collaboratives that are measured in three or six month intervals when every party can check in and decide if the partnership is still working for them. The more difficult questions can come when one of the collaborative partners is not working to their potential, or is undermining the project unintentionally or intentionally. These are often ugly and very difficult situations to solve, and I don’t have much advice on these situations other than to be transparent and honest and to communicate your concerns with leadership when you see these situations on the horizon. (Anonymous, personal communication, May 28, 2015)
This mental health professional suggested asking hard questions of potential collaborative partners, including, “What’s in it for you? What’s in it for us? How long will you be around? What’s your long-term plan after one or two years? How do we continue this after you are gone? How will your success be measured? Who do you report to and what’s their expectation of this collaborative?”
Recommendations on Preparing for a Disaster
Mental health professionals offered a host of general and specific recommendations regarding how agencies should prepare to face a disaster like Hurricane Katrina in the event that such a disaster should occur. General recommendations included ensuring that an agency is well-managed before a disaster if it is to survive the aftermath. Mental health agencies need to develop strong collaborative relationships with other agencies prior to an emergency. Putting into place evidence-based mental health practices provides a strong foundation for moving forward after a disaster. Staff members need to be flexible in their problem-solving because a culture of flexibility, in contrast to rigidity, helps agencies survive disasters.
Specific advice regarding preparing to survive a disaster such as Hurricane Katrina included the following: create an inventory of equipment to help report losses; operate within financial limitations; create a disaster plan that includes specific actions for before, during and after the disaster; create electronic records and have a server outside the area of operation; cross-train office staff; create and test a disaster communication plan; employ a staff grant writer; and create emergency plans for clients. This advice should be beneficial to counselor educators who teach classes in which disaster counseling topics are addressed.
Conclusions
After reviewing the demographics of New Orleans 10 years after the hurricane and communicating with eight mental health professionals who were working in the city prior to the hurricane, I offer the following observations. Overall, most mental health agencies have maintained the level of services they were providing before Hurricane Katrina, although some have actually expanded. Before Hurricane Katrina, there were not enough counseling and other mental health services for poor and middle-class families in New Orleans, and the same situation continues to exist 10 years after the storm.
A focus and specialty has emerged in most mental health agencies in New Orleans since Hurricane Katrina around issues of trauma. Consequently, the study of trauma has become quite popular in the professional literature (see Alvarez, 2009; Brown-Rice, 2013; Buss, Warren, & Horton, 2015; Cohen et al., 2009; Fernandez & Short, 2014; Hudspeth, 2015; Jones & Cureton, 2014; Jaycox et al., 2010; Langley et al., 2013; Parker & Henfield, 2012; Tosone, Bauwens, & Glassman, 2014). As one mental health professional pointed out, a natural disaster not only precipitates the distress resulting from the crisis experiences, but also brings unresolved prior trauma to the surface for many clients. Since trauma is likely to be a significant focus of mental health agencies after a disaster, disaster preparedness plans should include the education of all staff members on counseling trauma victims.
It appears that mental health agency personnel in other locations who want to learn from the experiences of practitioners who dealt with the aftermath of Hurricane Katrina in New Orleans should consider the advice given by several mental health professionals with whom I communicated—prepare to be flexible in case disaster occurs. Perhaps counselors and administrators who have leadership skills that include creativity and flexibility would be ideal for agencies after disasters have occurred, as opposed to those who have a high need for structure or who have trouble operating without clear procedural guidelines. \
While partnerships and collaborative arrangements have the potential for helping mental health agencies survive and even prosper after a disaster, such arrangements should be evaluated carefully prior to agreement. Leaders in one of the New Orleans agencies attributed their growth and expansion to collaborative relationships and partnerships. However, several other mental health professionals appeared to have had negative experiences with collaborative arrangements and recommended that such offers be viewed with caution. Accepting time-limited financial support also can lead to problems if agencies expand their services based on temporary support and must then scale back after financial resources disappear.
The most important lesson I learned from interviewing agency administrators in New Orleans who have been at their agencies for the 10 years since Hurricane Katrina was that it would have been impossible to prepare for the aftermath of the storm. As a result, it is important after a disaster for counselors and administrators to assess their unique situation, determine what counseling services are needed, provide in-service training when necessary, avoid relying on short-term funding to plan for the future, and pay attention to the self-care of counselors. New Orleans is unique and Hurricane Katrina’s flooding of the city was a unique event. Several mental health professionals indicated that assessing the needs of the community after the storm and responding to those needs, as well as caring for the well-being of their employees, were critical aspects of their successful survival.
Conflict of Interest and Funding Disclosure
The author reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Alvarez, C. M. (2015). Experiences of career counselors in group supervision integrating work-life balance (Doctoral dissertation). Available from ProQuest Dissertations and Theses database. (UMI No. 3689702)
Alvarez, D. M. (2009). Trauma pedagogy for teachers: Another lesson from Katrina. In A. W. Bedford & J. Kieff (Eds.), Surviving the storm: Creating opportunities for learning in response to Hurricane Katrina (pp. 75–87). Olney, MD: Association for Childhood Education International.
Arendt, L., & Alesch, D. J. (2014). Long-term community recovery from natural disasters. Boca Raton, FL: CRC Press.
Brown-Rice, K. (2013). Examining the theory of historical trauma among Native Americans. The Professional Counselor, 3, 117–130. doi:10.15241/kbr.3.3.117
Buss, K. E., Warren, J. M., & Horton, E. (2015). Trauma and treatment in early childhood: A review of the historical and emerging literature for counselors. The Professional Counselor, 5, 225–237. doi:10.15241/keb.5.2.225
Chan, C. S., Lowe, S. R., Weber, E., & Rhodes, J. E. (2015). The contribution of pre- and postdisaster social support to short- and long-term mental health after Hurricanes [sic] Katrina: A longitudinal study of low-income survivors. Social Science & Medicine, 138, 38–43. doi:10.1016/j.socscimed.2015.05.037
Cohen, J. A., Jaycox, L. H., Walker, D. W., Mannarino, A. P., Langley, A. K., & DuClos, J. L. (2009). Treating traumatized children after Hurricane Katrina: Project Fleur-de Lis [sic]. Clinical Child and Family Psychology Review, 12, 55–64. doi:10.1007/s10567-009-0039-2
Council for Accreditation of Counseling and Related Educational Programs. (2009). 2009 standards. Retrieved from www.cacrep.org/wp-content/uploads/2013/12/2009-Standards.pdf
The Data Center. (2012, August 14). Assets & opportunity profile: New Orleans. Retrieved from http://www.datacenterresearch.org/reports_analysis/assets-opportunity/
Fernandez, M. A., & Short, M. (2014). Wounded warriors with PTSD: A compilation of best practices and technology in treatment. The Professional Counselor, 4, 114–121. doi:10.15241/maf.4.2.114
Gohl, P., Barclay, H., Vidaurri, E., Newby, R., & Arquette, J. (2015, May). Leadership before and after Hurricane Katrina. Paper presented at the Symposium of University Research and Creative Expression (SOURCE), Ellensburg, WA.
Hudspeth, E. F. (2015). Children with special needs and circumstances: Conceptualization through a complex trauma lens. The Professional Counselor, 5, 195–199. doi:10.15241/efh.5.2.195
Jaycox, L. H., Cohen, J. A., Mannarino, A. P., Walker, D. W., Langley, A. K., Gegenheimer, K. L., . . . Schonlau, M. (2010). Children’s mental health care following Hurricane Katrina: A field trial of trauma-focused psychotherapies. Journal of Traumatic Stress, 23, 223–231. doi:10.1002/jts.20518
Jones, L. K., & Cureton, J. L. (2014). Trauma redefined in the DSM-5: Rationale and implications for counseling practice. The Professional Counselor, 4, 257–271. doi:10.15241/lkj.4.3.257
Kessler, R. C., Galea, S., Jones, R. T., & Parker, H. A. (2006). Mental illness and suicidality after Hurricane Katrina. Bulletin of the World Health Organization, 84, 930–939. Retrieved from http://www.scielosp.org/pdf/bwho/v84n12/v84n12a08.pdf
Khadaroo, S. T. (2014, March 1). New Orleans goes all in on charter schools. Is it showing the way? Christian Science Monitor, March 1, 2014. Retrieved from http://www.csmonitor.com/USA/2014/0301/New-Orleans-goes-all-in-on-charter-schools.-Is-it-showing-the-way
Langley, A. K., Cohen, J. A., Mannarino, A. P., Jaycox, L. H., Schonlau, M., Scott, M., . . . Gegenheimer, K. L. (2013). Trauma exposure and mental health problems among school children 15 months post-Hurricane Katrina. Journal of Child & Adolescent Trauma, 6, 143–156. doi:10.1080/19361521.2013.812171
Lazarchik, B. (2015). “Build a school, rebuild a city” An economic examination of the re-structured education system in New Orleans, 10 years after Hurricane Katrina. Retrieved from http://collected.jcu.edu/honorspapers/64/
Ohrt, J. H., & Cunningham, L. K. (2012). Wellness in mental health agencies. The Professional Counselor, 2, 90–101. doi:10.15241/jho.2.1.90
Parker, M., & Henfield, M. S. (2012). Exploring school counselors’ perceptions of vicarious trauma: A qualitative study. The Professional Counselor, 2, 134–142. doi:10.15241/mpp.2.2.134
Priebe, A. (2014, November). Examining the health and wellbeing of returnees versus out-migrants from New Orleans post-Katrina: Findings from the displaced New Orleans residents qualitative study. Paper presented at the meeting of the American Public Health Association, New Orleans, LA.
Rackin, H. M., & Weil, F. (2015, April–May). Social capital and the repopulation of New Orleans after Hurricane Katrina. Paper presented at the meeting of the Population Association of America, San Diego, CA.
Ratts, M. J., & Pedersen, P. B. (2014). Counseling for multiculturalism and social justice: Integration, theory, and application (4th ed.). Alexandria, VA: American Counseling Association.
Shrinath, N., Mack, V., & Plyer, A. (2014, October 16). Who lives in New Orleans and metro parishes now? Retrieved from http://www.datacenterresearch.org/data-resources/who-lives-in-new-orleans-now/
Thomas, L. L. (2014). Desire and disaster in New Orleans: Tourism, race, and historical memory. Durham, NC: Duke University Press.
Thompson, E. H., Frick, M. H., & Trice-Black, S. (2011). Counselor-in-Training perceptions of supervision practices related to self-care and burnout. The Professional Counselor, 1, 152–162. doi:10.15241/eht.1.3.152
Tosone, C., Bauwens, J., & Glassman, M. (2014). The shared traumatic and professional posttraumatic growth inventory. Research on Social Work Practice. Advance online publication. doi:10.1177/1049731514549814
Vernet, J. (2015). Desire and disaster in New Orleans: Tourism, race, and historical memory [Review of the book by L. L. Thomas]. Canadian Journal of History, 50, 186–187. doi:10.3138/CJH.ACH.50.1.008
Walker, D. W. (2008). A school-based mental health service model for youth exposed to disasters: Project Fleur-de-lis. The Prevention Researcher, 15(3), 11–13.
Wang, P. S., Gruber, M. J., Powers, R. E., Schoenbaum, M., Speier, A. H., Wells, K. B., & Kessler, R. C. (2007). Mental health service use among Hurricane Katrina survivors in the eight months after the disaster. Psychiatric Services, 58, 1403–1411.
Wang, P. S., Gruber, M. J., Powers, R. E., Schoenbaum, M., Speier, A. H., Wells, K. B., & Kessler, R. C. (2008). Disruption of existing mental health treatments and failure to initiate new treatment after Hurricane Katrina. American Journal of Psychiatry, 165, 34–41.
Weisler, R. H., Barbee, J. G., IV, & Townsend, M. H. (2006). Mental health and recovery in the Gulf Coast after Hurricanes Katrina and Rita. Journal of the American Medical Association, 296, 585–588. doi:10.1001/jama.296.5.585
Witt, K. J., & McNichols, C. (2014). Assessing the needs of rural counselor supervisors in Texas. Journal of Professional Counseling: Practice, Theory, and Research, 41(2), 15–29.
Theodore P. Remley, Jr. is a Professor at Our Lady of Holy Cross College. Correspondence may be addressed to Theodore P. Remley, Jr., 4123 Woodland Drive, New Orleans, LA 70131, tremley@olhcc.edu.
Dec 9, 2015 | Article, Volume 5 - Issue 4
Lindsey Mitchell
The purpose of this study was to explore the relationship of five variables—primary appraisal, secondary appraisal, coping skills, social support and stigma—to bereavement among women whose military spouses had completed suicide. Four correlations to bereavement (primary appraisal, secondary appraisal, coping skills and stigma) were significant. Hierarchical multiple regression analysis assessed the overall relationship of bereavement (the criterion variable) to the five predictor variables, along with the unique contribution of each predictor variable. In the regression, five of six models (all except Model 4) showed significance. The dissertation on which this manuscript is based has the following practical implications: statistically significant correlations between bereavement and constructs of Lazarus’ Cognitive Model of Stress (LCMS), as well as the significance of Lazarus’ construct of primary appraisal within Model 6, indicate that LCMS holds promise for understanding symptoms of bereavement in women whose military spouses have completed suicide.
Keywords: suicide, bereavement, military, spouse, Lazarus
Reports indicate that suicides in the U.S. military surged to a record number of 349 in 2013. This figure far exceeds the 295 American combat deaths in Afghanistan in 2012 and compares with the 201 military suicides in 2011 (National Institute of Mental Health [NIMH], 2013). Some private experts predict that the trend will worsen this year (Miles, 2010).
From 2008–2010, the Army reported the highest number of suicides (n = 182) among active duty troops; whereas the Navy and Air Force reported 60 and 59 respectively (National Institute of Mental Health [NIMH], 2013). The Marine Corps had the largest percentage increase in suicides in a period of 2 years (Lamorie, 2011). U.S. veterans accounted for 20% of the more than 30,000 suicide deaths in the United States in 2009. Between 2003 and 2009, approximately 6,000 veterans committed suicide annually, an average of 18 suicides each day (Congressional Quarterly, 2010; Miles, 2010). During the 2009 fiscal year, 707 members of the veteran population committed suicide, and another 10,665 made unsuccessful suicide attempts (Miles, 2010). Certain experiences of military service members (e.g., exposure to violence, act of killing the enemy, risk of injury, exposure to trauma) increase suicidal tendencies (Zamorski, 2011).
For every person who completes suicide, an estimated 20 people experience trauma related to the death (NIMH, 2010). This suggests that from the 349 military suicides in 2013, approximately 7,000 people have experienced related trauma. Suicide survivors are family members and friends whose lives significantly change because of the suicide of a loved one (Andriessen, 2009; Jordan & McIntosh, 2011; McIntosh, 1993). Survivors of suicide may have higher risk for a variety of psychological complications, including elevated rates of complicated grief and even reactive suicide (Agerbo, 2005).
It is also important to note that suicide survivors might not differ significantly from other bereaved groups regarding general mental health, depression, post-traumatic stress disorder symptoms and anxiety (Sveen & Walby, 2008). Examining the impact of suicide on surviving military family members may provide important information on minimizing negative consequences, including possible survivor suicide.
Military deaths are often sudden, unexpected, traumatic and/or violent in nature, and the family is conditioned to anticipate these types of deaths. In contrast, death by suicide is not anticipated and might not be handled well among military families (Martin, Ghahramanlou-Holloway, Lou, & Tucciarone, 2009). Suicide within the military culture is a traumatic as well as a unique experience. Service members and their families struggle with the visible and invisible wounds of war and the aftermath that combat deaths leave for the survivors. When a service member’s trauma leads to suicide, the military community is less trained and conditioned to process the grief than when death occurs as a direct result of military service (Zhang & Jia, 2009).
Stress plays a role in the grief process within the military culture when it relates to suicide. The chief identifying feature of military culture is warfare, which in turn leads to the claiming of human lives (Siebrecht, 2011). Siebrecht argued that bereavement can only be overcome if people adopt a more rational attitude and grant death its natural place in life. Association with the military ensures that most families will have to experience some form of bereavement and many forms of loss during times of war (Audoin-Rouzeau & Becker, 2002). Military men and woman are less equipped than the general population when it comes to their culture’s acceptance of outward demonstration or sharing of the emotional experience of grief (Doka, 2005).
Stigma
Historically, the stigma of suicide has been present in society (Cvinar, 2005). The biggest obstacles that families with members who have completed suicide confront are acts of informal social disapproval. The surviving family may be suspected of being partly blameworthy in a suicide death and consequently may be subjected to informal isolation and shunning (Bleed, 2007). The stigma of suicide can be subtle. It can be manifested in overt actions taken against the survivors (i.e., placing blame on the family), as well as by omitted actions (i.e., not receiving life insurance), which are probably far more common. When people experience the untimely loss of a family member, there can be feelings of being offended, wounded or abandoned (Neimeyer & Jordan, 2002). The stigmatization experienced by survivors may complicate their bereavement process (Cvinar, 2005; Jordan, 2001; McIntosh, 1993). This complexity results in communication issues, social isolation, projection of guilt, blaming of others and scapegoating (Harwood, Hawton, Hope, & Jacoby, 2002; Lindemann & Greer, 1953). There is a lack of research in the professional literature addressing the grief of surviving military family members impacted by the death, including suicide, of a loved one (Lamorie, 2011).
Suicide and Bereavement
Jordan (2001) researched suicide bereavement and concluded that there are several underlying reasons that it differs from other types of mourning. Jordan summarized that “there is considerable evidence that suicide survivors are viewed more negatively by others and by themselves” (p. 93) and that suicide “is distinct in three significant ways: the thematic content of grief, the social processes surrounding the survivor, and the impact suicide has on family systems” (p. 91). In reviewing the social processes surrounding suicide, Jordan’s analysis supports those of Worden (1991) and Ness and Pfeffer (1990), saying that “there is considerable evidence that survivors feel more isolated and stigmatized than other mourners, and may be viewed more negatively by others in their social network” (p. 93). Most traumatic death survivors will face questions regarding their own culpability in their loved one’s decision to take his or her own life. Survivors may find themselves repeatedly pondering missed warning signs and risk factors (Parrish & Tunkle, 2005). Four primary factors that distinguish the complexities of suicide bereavement for families include stigma, questions about reasons, issues of remorse and guilt, and various logistical and legal factors unique to suicide that necessarily influence the events and processes following death (Minois,1999). The question of why often comes up given the pervasive sense that suicide is a preventable event. This line of thought can often define the grief process. Combined with factors of shock from the sudden, often violent nature of the death, these questions are virtually unavoidable. In some cases, answers to questions of why may never be forthcoming or satisfactory (Steel, Dunlavy, Stillman, & Pape, 2011). Among military families, bereavement is complex. A military death often has circumstances not normally found in the civilian world. It is most likely unexpected, potentially traumatic, occurring in another country, publicized by the media, and enveloped in the commitment to duty and country. Surviving family members of military personnel are often parents, siblings, grandparents and spouses. Military widows are young, often with young families, and are living at a duty station, far away from family and longtime friends (Katzenell, Ash, Tapia, Campino, & Glassberg, 2012).
Bereavement in the Military Culture
Bereavement is a part of the military culture but is often misinterpreted as a weakness that will elicit limited outside support. Military men and women in general are uninformed about the cultural acceptability of outwardly demonstrating their grief or sharing the emotional experience of the loss (Doka, 2005). Although traditional mental health treatments predominantly encourage emotional vulnerability, the military culture values emotional toughness (Kang, Natelson, Mahan, Lee, & Murphy, 2003) and stigmatizes mental illness (Doka, 2005). These attitudes can often deter service members from seeking assistance that could help them to overcome physical and mental health issues. Military culture affects the impact of suicide on families. Each spouse and family has a different bereavement process, and this process is influenced by stigma, social support and ability to cope. In the U.S. military, these issues can be a hindrance to seeking services and can lead to feelings of isolation, which in turn are a risk factor for suicide (Christensen & Yaffe, 2012).
Conceptual Framework
The conceptual framework of Lazarus’ Cognitive Model of Stress (LCMS) was used to frame this study. The underlying construct of this model states that times of uncertainty and difficulty may assist in understanding a person’s ability and capacity to cope with the suicide of a loved one. In general, when people encounter a difficult situation, they employ strategies for dealing with and lessening perceived stress (Groomes & Leahy, 2002).
LCMS (Lazarus & Folkman, 1984) has served as a useful lens for examining the interaction between a person and situational demands. Burton, Farley, and Rhea (2009) used LCMS to frame a study of the relationship between level of perceived stress and extent of physical symptoms of stress, or somatization, among spouses of deployed versus non-deployed servicemen. Eberhardt and associates (2006) examined Lazarus and Folkman’s 1984 stress theory regarding the ways that stress mediators and perceived social support may affect anxiety (as a stress response). The above studies show the usefulness of LCMS in depicting the impact of stress and coping on perceived anxiety, acceptance, ability to lead mentally and physically satisfactory lives, and perception of social support.
LCMS includes primary appraisal, secondary appraisal, coping and perceived social support. Stress is defined as a person’s relationship to his or her environment, specifically a relationship that the person perceives as exceeding his or her resources and endangering well-being. This model supports that the person and the environment are in a dynamic, reciprocal and multidimensional relationship. This conceptualization suggests that people’s perception of stress is related to the way they evaluate, appraise and cope with difficulties.
Stress can be measured by the way an individual appraises a specific encounter. Lazarus and Folkman (1984) presented two types of appraisal. The first is primary appraisal, defined as an individual’s expressed concern in terms of harm, loss, threat or challenge. Harm and loss appraisals refer to loss or damage that has already taken place; threat appraisal refers to harm or loss that has not yet occurred (i.e., anticipatory loss); and challenge appraisal refers to the opportunity for mastery or growth (Lazarus & Folkman, 1984). The second type is secondary appraisal, defined as the focus on what the individual can do to overcome or prevent harm. Lazarus and Folkman suggested that an appraisal of threat is associated with coping resources that can mediate the relationship between stressful events (e.g., loss of spouse to suicide) and outcomes (e.g., ability to seek mental health services).
Coping resources are the personal factors that people use to help them manage situations that are appraised as stressful (Lazarus & Folkman, 1984). Coping resources can be available to the person during the grief process or can be obtained as needed. This fact suggests that the grief process following a suicide is stressful and imposes demands on coping as the bereavement process evolves. Lazarus and Folkman (1984) defined coping as “constantly changing cognitive and behavioral efforts to manage specific external or internal demands that are appraised as exceeding the resources of the person” (p. 141). Coping is a dynamic process that is called into action whenever people are faced with a situation that requires them to engage in some special effort to manage that situation (Lazarus & Folkman, 1984). The ability to cope impacts a person’s bereavement process, and the ways and ability to cope vary with each individual. Stigma and the amount of perceived social support also influence the ability to cope (Bandura, 1997). These variables impact the bereavement process, especially with the added variable of death by suicide.
Social support can strengthen an individual’s position against the stressor and reduce the level of threat (Lazarus, 1996). Research suggests there are specific reasons why survivors do not seek out social support. McMenamy, Jordan, and Mitchell (2008) identified depression and a lack of energy as substantial barriers to obtaining social support.
People who experience a traumatic event are more likely to perceive barriers and not request medical and mental health services due to this lack of energy, lack of trust in professionals and depression (Amaya-Jackson et al., 1999). Provini, Everett, and Pfeffer (2000) stated that the stigma and social isolation that survivors experience can interfere with seeking social support and the willingness of social support networks to come to the aid of the survivor. A lack of social support can increase depression, a lack of energy to complete daily tasks and isolation. Limited social support is especially common for suicide survivors. Shame and guilt surrounding a suicide can impact survivors’ ability to seek social support; however, high social support can be linked to positive mental health.
Barriers to Bereavement
Many suicide survivors struggle with questions about the meaning of life and death, report feeling more isolated and stigmatized, and have greater feelings of abandonment and anger compared with other sudden death survivors (Callahan, 2000). Moreover, the feeling of relief from no longer having to worry about the deceased may distinguish survivors of suicide from survivors of other types of sudden death (Jordan, 2001). Experiencing suicide in one’s family increases risks for family members’ mental health and family relationships (Jordan, 2001). Despite the frequency of suicide, there is limited research focusing on the needs of surviving spouses (Miers, Abbott, & Springer, 2012).
The family system in which the spouses existed as a couple is destabilized by suicide, but the survivor must continue to function. Tasks that were carried out in the relationship must now be carried out by the survivor (Murray, Terry, Vance, Battistutta, & Connolly, 2000). Cerel, Jordan, and Duberstein (2008) stated that because suicide occurs within families, the focus on the aftermath of suicide within families and the impact on the spouse are important areas to investigate in order to determine exactly how to help survivors. Helping survivors to address practical, economic and legal issues, in addition to providing information and therapeutic intervention, is important (Dyregrov, 2002; Provini et al., 2000).
Purpose of the Study
Because of the frequency of suicide in the United States, the increased number of suicides within the U.S. military, and the impact of suicide on the family, the bereavement process among female spousal survivors of military suicides deserves further exploration. The purpose of this study was to explore bereavement in female spousal survivors of military suicides. Using LCMS, the study explored the relationship of bereavement and stigma, social support, primary appraisal, secondary appraisal, and coping skills among women whose military spouse had completed suicide.
Summary of the Study and Methodology
This study investigated the linear relationship between the dependent variable of bereavement and each of five independent variables—primary appraisal, secondary appraisal, coping skills, perceived social support and stigma—among women whose military spouses had completed suicide. The following hypotheses guided the study. Hypothesis 1 stated that there would be a relationship between bereavement and stigma; this positive relationship was significant. Hypothesis 2 stated that there would be a relationship between bereavement and social support; the relationship was not statistically significant. Hypothesis 3 stated that there would be a relationship between bereavement and primary appraisal; this positive relationship was significant. Hypothesis 4 stated that there would be a relationship between bereavement and secondary appraisal; this negative relationship was significant. Hypothesis 5 stated that there would be a relationship between bereavement and coping skills; this negative relationship was significant.
Using hierarchical regression analysis, the researcher examined the relationship of five independent variables—primary appraisal, secondary appraisal, coping skills, social support and stigma—to bereavement. The relationship was statistically significant. The model was a good fit and controlled for time since death (i.e., number of years since the person completed suicide). Therefore, for this sample, the five independent variables are components of a statistically significant model.
Participants and Recruitment
The participants in this study were women aged 18 and older who had lost a military spouse to suicide. Criteria for inclusion were that (a) the service member who had completed suicide had been either on active duty or of veteran status, (b) the survivor was female and 18 years of age or older, and (c) the survivor was considered a spouse. A spouse was defined as legally married to another person or living and cohabiting with another person in a marriage-like relationship, including a marriage-like relationship between persons of the same gender. Participants were chosen from seven national organizations serving veterans. The researcher recruited participants from these organizations by explaining the study and asking for volunteers. The director or assistant director of each organization distributed study information and materials through listservs and posted them on their Web sites. Once prospective participants received an e-mail, they decided whether they wanted to participate and whether they met the eligibility requirements. If the spouses decided to participate in the study, they would complete the survey through Survey Monkey.
Variables
Demographic variables included age, race/ethnicity, length of relationship with the deceased partner, the decedent’s military status (active or retired), the decedent’s length of service, and time elapsed since death. The survey also asked about the deceased’s rank, education level, surviving children and prior suicide attempts.
A self-report online survey was constructed using the following five instruments: the Core Bereavement Items (CBI; Holland, Futterman, Thompson, Moran, & Gallagher-Thompson, 2013), the Stigma of Suicide and Suicide Survivor Scale (STOSASS; Scocco, Castriotta, Toffol, & Preti, 2012), the Coping Self-Efficacy Scale (CSES; Chesney, Neilands, Chambers, Taylor, & Folkman, 2006), the Multidimensional Scale of Perceived Social Support (MSPSS; Zimet, 1988), and the Stress Appraisal Measure (SAM; Peacock & Wong, 1990). The SAM is one measure. However, the variables of primary stress appraisal and secondary stress appraisal within it were separated, and the questions within the SAM regarding primary stress appraisal were referred to as the primary stress appraisal measure (PSAM), and the remaining questions of the SAM were referred to as the secondary stress appraisal measure (SSAM). In addition to these assessments, participants would also answer 11 demographic questions and three open-ended questions. The survey was split into seven sections.
The first section had 11 demographic questions. The second section, comprised of the MSPSS, had 12 questions regarding social support of the participant and used a 7-point Likert scale. The third section, comprised of the CBI, had 26 questions regarding the participant’s ability to cope and used a 10-point Likert scale. The fourth section, comprised of the SAM, had 19 questions regarding participant’s stress appraisal measures and used a 4-point Likert scale. The fifth section, comprised of the STOSASS, had 17 questions regarding the participant’s perceived stigma and used a 4-point Likert scale. The sixth section, comprised of the CBI, had 17 questions regarding the participant’s bereavement process and used a 4-point Likert scale. The survey included the three following open-ended questions that were derived from the Grief Evaluation Measure (GEM) and reviewed by three licensed professional counselors working in the field of suicide bereavement: (1) What do you recall about how you responded to the death of your spouse at the time?; (2) What was the most painful part of the experience to you?; and (3) How has this experience affected your view of yourself or your view of your world? To analyze the qualitative responses, the researcher identified the most commonly recurring words or phrases used by participants for each question. Three experts in the field of grief and loss were consulted and confirmed the content and face validity of the survey.
Data Analysis
The Statistical Package for the Social Sciences (SPSS), a statistical software package, generated all of the statistics for this research investigation. A Pearson correlation analysis was conducted to determine whether there was a linear relationship between primary appraisal, secondary appraisal, social support, coping skills, stigma and bereavement for women whose military spouse had completed suicide. Following this analysis, a multiple regression was used to describe the relationships of the independent or predictor variables to the dependent or criterion variable (Lussier & Sonfield, 2004). Because LCMS states that it is possible to discern the order in which a person experiences each variable with regard to a particular event, the variables were entered into the regression using the following equation: Bereavement = {time since death} + {primary appraisal} + {secondary appraisal} + {coping skills} + {perceived social support} + {perceived stigma}.
Results
Descriptive Statistics
Descriptive statistics provided simple summaries of the demographic characteristics of the sample, as well as descriptors such as means and standard deviations for these characteristics. The sample was a well-educated, racially diverse group of women who had lost their military spouses to suicide. The majority of participants were non-Hispanic White females who had attended at least some college. Most were affiliated with the Army and had been married to the military member who had completed suicide. The majority of the partners had committed suicide while on active duty. The mean age of respondents was 33.48 years (SD = 5.20; SE = .373); their ages ranged from 23–50 years. The mean number of children aged 17 or under that were a product of the relationship with the service member was 1.12 (SD = .79; SE = .064); the range was 0–4 children. The mean number of prior suicide attempts by the service member (known/confirmed by the surviving female spouse) was 1.31 (SD = 1.06; SE = .096); the range was 0–4 prior suicide attempts.
Correlation Results
Using SPSS Student Version 22.0 software, a Pearson correlation coefficient was used to measure the relationship of bereavement, primary appraisals, secondary appraisals, coping skills, social support, and stigma among women whose military spouses had completed suicide. The correlation coefficient measures the strength and direction of the relationship among variables. When conducting a correlational analysis of two co-occurring variables, the researcher can indicate whether change in one is accompanied by systematic change in the other. Examination of intercorrelations among study variables indicated statistically significant correlations between bereavement and each of four independent variables: primary appraisal, secondary appraisal, coping skill, and stigma. The results for each correlation are presented separately and summarized below as well as in Table 1.
Control variable. There was a statistically significant relationship between time since death and bereavement for women whose military spouse had completed suicide, r(194) = .277, p < .01. The shorter the amount of time elapsed, the higher the bereavement scores.
Independent variables. Primary stress appraisal, r(193) = -.309, p < .01: There is a weak negative linear relationship between bereavement and primary stress appraisal. Secondary stress appraisal, r(193) = -.309, p < .01: There is a weak negative linear relationship between secondary stress appraisal and bereavement. Coping skills, r(193) = -.174, p = .015: There is a weak negative linear relationship between coping skills and bereavement. Social support, r(193) = -.039, p = .594: There is no linear relationship between perceived social support and bereavement. Stigma, r(193) = .252, p < .01: There is a weak positive linear relationship between perceived stigma and bereavement.
Table 1
Correlations for Independent, Dependent and Control Variables
CBI TSD PSAM SSAM MSPSS CSES
1. TSD .277*
2. PSAM -.309* -.167
3. SSAM -.309* -.151 .602*
4. MSPSS -.039 .032 .379* .172*
5. CSES -.174* -.167* .494* .473* .585*
6. STOSASS .252* .095 -.196* -.221* .022 -.253
Note: N = 194; CBI = Core Bereavement Items; TSD = Time Since Death (in months);
PSAM = Primary Stress Appraisal Measure; SSAM = Secondary Stress Appraisal Measure;
CSES = Coping Self-Efficacy Scale; MSPSS = Multidimensional Scale of Perceived Social Support; STOSASS = Stigma of Suicide and Suicide Survivor Scale.
*Significant at p < .05.
Multiple Regression
Following the correlational analysis, a multiple regression was utilized. This analysis was appropriate to describe the relationships between the independent or predictor and dependent or criterion variables in an objective manner (Lussier & Sonfield, 2004). The design was appropriate because the purpose of the study was to explain the relationships between variables.
Model 1 (TSD onto bereavement) yielded R = .277, R2 = .077, F(1, 125), p < .001. The portion of the variance explained was 7%. Model 2 (TSD and primary appraisal) yielded R = .431, R2 = .186, F(2, 124), p < .001. The portion of variance explained was 18.6%. Model 3 (TSD, primary appraisal and secondary appraisal) yielded R = .454, R2 = .206, F(3, 123), p < .001. The portion of variance explained was 20.6%. Model 4 (time since death, primary appraisal, secondary appraisal and coping skills) yielded R = .455, R2 = .207, F(4, 122), p < .001. The portion of variance explained was 20.7%. Model 5 (time since death, primary appraisal, secondary appraisal, coping skills and social support) yielded R = .471, R2 = .221, F(5, 121), p < .001. The portion of variance explained was 22.1%. Model 6 (time since death, primary appraisal, secondary appraisal, coping skills, social support, and stigma) yielded R = .482, R2 = .232, F(6, 120), p < .001. The portion of variance explained was 23.2% (see Table 2).
Table 2
Hierarchical Multiple Regression
| Model |
R |
R2 |
t |
p |
B |
β |
R2 Change |
| Model 1TSD |
.277
|
.077
|
61.600
3.228
|
.000
.002
|
.049
|
.277
|
0
|
| Model 2TSDPSAM |
.431
|
.186
|
19.482
2.696
-4.074
|
.000
.008
.000
|
.039
-.406
|
.222
-.335
|
.109
|
| Model 3TSDPSAMSSAM |
.454
|
.206
|
19.646
2.618
-1.947
-1.782
|
.000
.010
.054
.077
|
.038
-.254
-.192
|
.214
-.209
-.191
|
.02
|
| Model 4TSDPSAMSSAMCSES |
.455
|
.207
|
16.971
2.622
-1.952
-1.788
.266
|
.000
.010
.053
.076
.791
|
.038
-.262
-.199
.004
|
.216
-.216
-.198
.025
|
.001
|
| Model 5TSDPSAMSSAMCSESMSPSS |
.471
|
.221
|
12.989
2.307
-2.359
-1.111
-0.710
1.505
|
.000
.023
.020
.269
.479
.135
|
.034
-.335
-.132
-.012
.091
|
.192
-.276
-.132
-.083
.167
|
.015
|
| Model 6 TSDPSAMSSAMCSESMSPSSSTOSASS |
.482
|
.232
|
9.026
2.329
-2.187
-1.105
-0.320
1.107
1.280
|
.000
.022
.031
.271
.750
.271
.203
|
.034
-.312
-.131
-.006
.069
.086
|
.194
-.257
-.131
-.039
.128
.112
|
.010
|
Note: TSD = Time Since Death (in months); PSAM = Primary Stress Appraisal Measure; SSAM = Secondary Stress Appraisal Measure; CSES = Coping Self-Efficacy Scale; MSPSS = Multidimensional Scale of Perceived Social Support; STOSASS = Stigma of Suicide and Suicide Survivor Scale.
Qualitative Component
There is a growing interest in integrating qualitative data across quantitative studies to discover patterns and common threads within a specific topic or issue (Erwin, Brotherson, & Summers, 2011). The main aim of the qualitative questions within the survey is to gain insight into the participants’ world and capture their unique experiences (e.g., naturally occurring events and/or social or human problems) and their interpretations of these experiences (Jones, 1995; Sarantakos, 1993).
A total of 55 (28.4%) participants responded to the question, “What do you recall about how you responded to the death of your spouse at the time?” Of these, 24 stated recalling “sadness” as most frequent. Fifteen participants indicated disbelief, shock, feelings of helplessness or feelings of fear. Other participants’ responses included “trying not to think about what had happened,” crying, sobbing, physical symptoms, physical pain, collapsing, fainting, being unable to forget what happened, and being unable to recall or process the event. A total of 68 (35.1%) participants responded to the question, “What was the most painful part of the experience to you?” Of these, 50 reported physical and emotional numbness and only partial recollection of learning about the death (e.g., who told them, where they were when notified, immediate responses). These participants indicated that they could recall parts of the experience but struggled with identifying feelings or emotions directly following the event. Other responses included being hospitalized, contemplating suicide, refraining from eating, and feeling that their future had been lost. Although four reported contemplating suicide following the death of their spouse, no participants reported attempting suicide at any point. A total of 36 (18.6%) participants responded to the question, “How has this experience affected your view of yourself or your view of your world?” Of these, 15 participants indicated that they no longer feared death, while seven reported having a negative reaction to relationships. Eleven participants reported that they perceived stress as more threatening than before the suicide of their spouse and were unaware of the triggers that brought on stress during the bereavement process. Ten participants indicated that their view of love had changed since the loss of their spouse. Nine participants wrote about making an effort to enjoy life after the suicide of their spouse.
Discussion
This study investigated the relationships between bereavement and primary appraisal, secondary appraisal, coping skills, perceived social support and stigma among women whose military spouses had completed suicide. There are several study findings that deserve further exploration.
First, there was a statistically significant positive relationship between stigma and bereavement, suggesting that as female survivors perceive increased stigma regarding the suicide of their spouse, they present more symptoms of bereavement. Knieper (1999) suggested that bereavement following suicide is not the same as that following natural death. He reported that stigma and avoidance continue to be central issues for suicide survivors. Psychological projection of feelings of rejection and the actual social response to the survivor interact in a complicated manner. Worden (2009) also noted a difference between suicide bereavement and other forms of bereavement, suggesting that suicide is often associated with stigma and a sense of shame. Such shame can result in the complete isolation of the bereaved during the period immediately following the suicide event. Eaton and associates (2008) examined survivors’ barriers to seeking mental health treatment after the suicide of their partners and found that spouses were 70% less likely to seek treatment following a suicide, as compared to a natural death, and that stigma was a recurrent theme in the qualitative analysis. However, Eaton et al.’s study did not directly examine the impact of stigma on bereavement. It did show that stigma is an important variable that needs to be investigated further. The present study showed similar results to Eaton et al.’s (2008) research.
The qualitative comments recorded in the open-ended question section of the survey supported the study findings. For example, one participant responded, “I blamed myself for not doing more, not being there enough, or not being there when the death happened.” Another participant noted, “Suicide is one of the most difficult and painful ways to lose someone we love, because we are left with so many unanswerable questions.” One participant expressed the following:
[I felt] anger at family members for not assisting me with my husband and anger at physicians that treated my husband and were not able to see the warning signs or provide assistance in caring for them properly. I was then left with the scars after the death and had to explain to people what happened. I felt I got blamed and it was not my fault.
Several participants expressed “numbness and isolation.” Responding to stigma, people with mental health problems often internalize public attitudes and become embarrassed or ashamed. These feelings can lead them to conceal symptoms and fail to seek treatment (President’s New Freedom Commission on Mental Health, 2003). These survey responses assist in understanding the impact of stigma upon the military spouse survivors and imply that unanswered questions, as well as guilt, are important factors to explore in the grief process following a suicide.
Second, a statistically significant relationship between primary appraisal and bereavement was reported, suggesting that survivors who perceive the death of a spouse to be stressful are more likely to experience bereavement. This result is supported by the bereavement literature (Cvinar, 2005; Jordan, 2001; McIntosh, 1993). Lazarus (2005) argued that primary appraisal shows that it is not the situation, but the way a person interprets the situation, that affects the person’s experience. The way a person appraises a situation can impact the way the person reacts to it. Primary appraisal is an important step in processing the stress of bereavement, since grieving is such an individualized experience.
The qualitative comments recorded in the open-ended question portion of the survey supported the statistical relationship between primary appraisal and bereavement. For example, one participant indicated that her worldview had changed when she responded, “My world has become gray; I have made myself closed. I live in a rain cloud and now know that good people do bad things that change lives.” The participant had changed her worldview such that her world became a smaller, more restricted place. Another stated, “This death, this loss, makes small things seem insignificant. Material things are insignificant. Relationships with people are more important. I don’t have a fear of dying and in fact, feel like I will die at a young age.” This concept of primary appraisal is based on the idea that emotional processes are dependent on a person’s expectancies about the significance and outcome of a specific event. The same event within the same community (in this case, suicide within the military) can elicit responses of different quality, intensity and duration due to individuality in experiences and personality (Krohne, Pieper, Knoll, & Breimer, 2002). The different kinds of stress identified by the primary appraisal may be embedded in specific types of emotional reactions, thus illustrating the close conjunction of the fields of stress and emotion (Lazarus & Folkman, 1984).
Third, a statistically significant negative relationship was reported between secondary appraisal and bereavement, suggesting that survivors who make a negative appraisal of their ability to control the outcomes of their spouse’s death are more likely to experience bereavement. In the future, when examining outcomes of interventions that impact coping, beliefs about a person’s ability to perform specific behaviors related to coping would need to be highlighted. This concept is known as specific coping behaviors and is also pertinent to stress, coping theory and secondary appraisal (Chesney et al., 2006). Part of secondary appraisal is the judgment that an outcome is controllable through coping; another part addresses the question of whether or not the individual believes he or she can carry out the requisite coping strategy (Chesney et al., 2006; DiClemente, 1986; Hofstetter, Sallis, & Hovell, 1990).
The qualitative comments recorded in the open-ended section of the survey supported this finding. For example, one participant indicated her appraisal of the situation by stating, “Everyone must learn to face the misfortune, because life on the road will not be smooth.” Another stated that “time can dilute all and I must face life and accept my reality;” yet another wrote, “I want to work on longer range goals to give myself some structure and direction to my life and not focus on my loss. I am only interested in rebuilding my life.” However, other participants stated that it was harder to assess the loss and to move forward after the suicide. One participant stated the following:
I often find myself complaining to God about what seems senseless or unjust and unfair. I find myself bogged down in fear and even anger at myself or the person who died and “left” me. I do not accept what happen[ed] to me and my children.
Some participants reported not knowing what to do. An example of this feeling is the statement, “I perceive stress as threatening. I feel totally helpless.” Perceived self-efficacy, defined as a belief about one’s ability to perform a specific behavior, is a salient component of this theory. It highlights the importance of personal efficacy in determining the acquisition of knowledge on which skills are founded (Bandura, 1997; Chesney et al., 2006).
Fourth, a statistically significant negative relationship between coping skills and bereavement was reported, suggesting that survivors who believe they have a low ability to cope with their spouses’ death are more likely to experience bereavement. Although it is important for survivors to become familiar with the stress appraisal process, the way they assign meaning to their spouse’s death and their past experience with death also are important in their primary appraisal to the overall coping effort. One model of this process is the transactional model of coping (Lazarus & Folkman, 1984). This model of coping implies that a person’s appraisal of his or her interaction with a difficult event naturally evokes a coping response for dealing with the situation. Experiencing a suicide or living in a social environment that hinders, stigmatizes or isolates a person who has experienced a suicidal death may cause demands to exceed his or her resources for dealing with certain situations. Few studies have examined the natural coping efforts used by suicide survivors, or have identified specific problems and needs that survivors experience following the suicide of a significant other (McMenamy et al., 2008). Interventions with suicide survivors have limited effectiveness (Jordan & McMenamy, 2004). Provini et al. (2000) presented four categories of concerns for suicide survivors: concerns related to (a) family relationships, (b) psychiatric symptoms, (c) bereavement and (d) stress. Family-related problems were the most frequently mentioned type of concerns (Provini et al., 2000). Examples of family relationship concerns included inability to maintain parenting roles, inability to maintain family routines, existence of different coping styles within the family, and inability to provide appropriate emotional support to family members.
Qualitative comments recorded in the open-ended section of the survey supported this study finding. For example, one participant stated, “I often feel distracted, forgetful, irritable, disoriented, or confused. I try to remember how I got over a death in the past, sometimes it helps and sometimes it does not.” Another participant stated, “I know I need to start to form new relationships or attachments in my life but my mind [is] telling me ‘there must be some mistake,’ or ‘this can’t be true.’ ” Regarding bereavement, one participant wrote, “Grief is perhaps the most painful companion to death.” Addressing coping, one participant stated, “I must also adjust to working or returning to work after the death. I know things can’t go back to the way they were before, very difficult and painful to deal with and I better adjust to life.” These statements support the need to further explore the relationship between one’s ability to cope with the suicide of a spouse and one’s ability to experience and acknowledge feelings and move forward with everyday life activities (e.g., employment, childcare, financial obligations). Ability to cope impacts a person’s bereavement process; the ways and ability to cope vary with the individual. Stigma and amount of perceived social support have been correlated with ability to cope (Bandura, 1997). It is important to understand the individual impacts that stigma, social support, primary appraisal, secondary appraisal and coping have on bereavement. However, it is equally important to examine the relationships of these variables within the context of a model in order to establish future interventions for bereavement within the context of a suicide.
Fifth, results indicated that the model is statistically significant in predicting bereavement outcomes and provides considerable support for using the Lazarus model as a means of understanding the relationship between stress and bereavement when placed into the equation in a particular order: CBI = TSD + PSAM + SSAM + CSES + MSPSS + STOSASS.
This study suggests that the proposed model, using LCMS and assessment of stress, identifies the constructs associated with bereavement among women whose military spouses completed suicide. Future research could further explore the assessment of primary and secondary appraisal processes, coping, stigma, and social support enhancement programs and interventions to improve the bereavement process for military spouses. When survivors can identify and address their needs, the bereavement process following a suicide can begin (Christensen & Yaffe, 2012).
Limitations
First, the majority of the sample (54.1%) were non-Hispanic White, or Euro-American. Second, there is limited representation across military branches. Third, the study collected data from a self-administered electronic survey. Fourth, although the social support measure (i.e., MSPSS) has good reliability and measures social support as a general feeling of belonging to a social network that one can turn to for advice and assistance in times of need (Uchino, 2006), it does not delineate various types of social support. Finally, most of the sample consisted of women whose spouses had completed suicide while on active duty. Active duty members typically live on base and are well connected to the military community. When the military spouse dies, these supports are often no longer available, and the stigma of a suicide could strongly affect these women.
Recommendations for Future Studies
There are several practice implications from this study. The statistically significant correlations between bereavement and four other variables (primary appraisal, secondary appraisal, coping skills and stigma), as well as the significance of the LCMS construct of primary appraisal within Model 6, indicate that LCMS holds promise for understanding symptoms of bereavement in females following the suicide of a military spouse. Primary appraisal, the most significant variable within this study, could be highlighted within bereavement research on women whose military spouses have completed suicide. When conceptualizing the responses of these women, counselors and clinicians could use LCMS, examining the three components of primary appraisal (goal relevance, goal congruence and ego involvement) and exploring the ways these components present during the client’s bereavement process. The approach would focus on the role of maladaptive cognitions during times of stress (Sudak, 2009).
The reluctance of the military community to seek mental health support contributes to an inability to move through the bereavement process in a healthy way. Within the military community, it can be quite difficult to deal with the ambiguity of bereavement that is typically associated with emotional vulnerability (Lamorie, 2011). However, the current study suggests that four constructs—primary appraisal, secondary appraisal, coping and stigma—are significant when addressing the issues of bereavement in females who have lost a military spouse to suicide. Using LCMS to address cognitions, counselors might be able to assist a population whose members have been reluctant to seek mental health services in the past. Because the components of LCMS are correlated with bereavement, clinicians could use LCMS and cognitive stress research, which together seem to be a promising direction, when assisting women who have lost a military spouse to suicide.
Conflict of Interest and Funding Disclosure
The author reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Agerbo, E. (2005). Midlife suicide risk, partner’s psychiatric illness, spouse and child bereavement by suicide or other modes of death: A gender specific study. Journal of Epidemiology and Community Health, 59, 407–412. doi:10.1136/jech.2004.024950
Amaya-Jackson, L., Davidson, J. R., Hughes, D. C., Swartz, M., Reynolds, V., George, L. K., & Blazer, D. G. (1999). Functional impairment and utilization of services associated with posttraumatic stress in the community. Journal of Traumatic Stress, 12, 709–724. doi:10.1023/A:1024781504756
Andriessen, K. (2009). Can postvention be prevention? Crisis: The Journal of Crisis Intervention and Suicide Prevention, 30, 43–47. doi:10.1027/0227-5910.30.1.43
Audoin-Rouzeau, A., & Becker, S. (2002). 14–18: Understanding the great war. New York, NY: Hill and Wang.
Bandura, A. (1997). Self-efficacy: The exercise of control. New York, NY: Worth.
Bleed, J. (2007, February 19). Howell’s life insurance payout not a sure bet. Arkansas Democrat-Gazette.
Retrieved from http://www.arkansasonline.com/
Burton, T., Farley, D., & Rhea, A. (2009). Stress-induced somatization in spouses of deployed and nondeployed servicemen. Journal of the American Academy of Nurse Practitioners, 21, 332–339. doi:10.1111/j.1745-7599.2009.00411.x
Callahan, J. (2000). Predictors and correlates of bereavement in suicide support group participants. Suicide & Life-Threatening Behavior, 30, 104–124. doi:10.1111/j.1943-278X.2000.tb01070.x
Cerel, J., Jordan, J. R., & Duberstein, P. R. (2008). The impact of suicide on the family. Crisis: The Journal of Crisis Intervention and Suicide Prevention, 29, 38–44. doi:10.1027/0227-5910.29.1.38
Chesney, M. A., Neilands, T. B., Chambers, D. B., Taylor, J. M., & Folkman, S. (2006). A validity and reliability study of the coping self-efficacy scale. British Journal of Health Psychology, 11, 421–337. doi:10.1348/135910705X53155
Christensen, B. N., & Yaffe, J. (2012). Factors affecting mental health service utilization among deployed military personnel. Military Medicine, 177, 278–283.
Congressional Quarterly. (2010). Rising military suicide: The pace is faster than combat death in Iraq and Afghanistan. Retrieved from http://www.infiniteunknown.net/2010/01/01/rising-us-military-suicides-the-pace-is-faster-than-combat-deaths-in-iraq-or-afghanistan/
Cvinar, J. C. (2005). Do suicide survivors suffer social stigma: a review of the literature. Perspectives in Psychiatric Care, 41, 14–21. doi:10.1111/j.0031-5990.2005.00004.x
DiClemente, C. C. (1986). Self-efficacy and the addictive behaviors. Journal of Social and Clinical Psychology, 4, 302–315. doi:10.1521/jscp.1986.4.3.302
Doka, K. J. (2005). Ethics, end-of-life decisions and grief. Mortality, 10, 83–90. doi:10.1080/13576270500031105
Dyregrov, K. (2002). Assistance from local authorities versus survivors’ needs for support after suicide. Death Studies, 26, 647–668. doi:10.1080/07481180290088356
Eaton, K. M., Hoge, C. W., Messer, S. C., Whitt, A. A., Cabrera, O. A., McGurk, D., . . . Castro, C. A. (2008). Prevalence of mental health problems, treatment need, and barriers to care among primary care-seeking spouses of military service members involved in Iraq and Afghanistan deployments. Military Medicine, 173, 1051–1056.
Eberhardt, B., Dilger, S., Musial, F., Wedding, U., Weiss, T., & Miltner, W. H. (2006). Short-term monitoring of cognitive functions before and during the first course of treatment. Journal of Cancer Research & Clinical Oncology, 132, 234–240. doi:10.1007/s00432-005-0070-8
Erwin, E. J., Brotherson, M. J., & Summers, J. A. (2011). Understanding qualitative metasynthesis: Issues and opportunities in early childhood intervention research. Journal of Early Intervention, 33, 186–200. doi:10.1177/1053815111425493
Groomes, D. A. G., & Leahy, M. J. (2002). The relationships among the stress appraisal process, coping disposition, and level of acceptance of disability. Rehabilitation Counseling Bulletin, 46, 15–24.
Harwood, D., Hawton, K., Hope, T., & Jacoby, R. (2002). The grief experiences and needs of bereaved relatives and friends of older people dying through suicide: A descriptive and case-control study. Journal of Affective Disorders, 72, 185–194. doi:10.1016/S0165-0327(01)00462-1
Hofstetter, C. R., Sallis, J. F., & Hovell, M. F. (1990). Some health dimensions of self-efficacy: Analysis of theoretical specificity. Social Science & Medicine, 31, 1051–1056.
Holland, J. M., Futterman, A., Thompson, L. W., Moran, C., & Gallagher-Thompson, D. (2013). Difficulties accepting the loss of a spouse: A precursor for intensified grieving among widowed older adults. Death Studies, 37, 126–144. doi:10.1080/07481187.2011.617489
Jones, R. (1995). Why do qualitative research? British Medical Journal, 311(6996), 2–3. doi:10.1136/bmj.311.6996.2
Jordan, J. R. (2001). Is suicide bereavement different? A reassessment of the literature. Suicide and Life-Threatening Behavior, 31, 91–102. doi:10.1521/suli.31.1.91.21310
Jordan, J. R., & McIntosh, J. L. (2011). Grief after suicide: Understanding the consequences and caring for the survivors. New York, NY: Routledge.
Jordan, J. R., & McMenamy, J. (2004). Interventions for suicide survivors: A review of the literature. Suicide and Life-Threatening Behavior, 34, 337–349. doi:10.1521/suli.34.4.337.53742
Kang, H. K., Natelson, B. H., Mahan, C. M., Lee, K. Y., & Murphy, F. M. (2003). Post-Traumatic stress disorder and chronic fatigue syndrome-like illness among Gulf War veterans: A population-based survey of 30,000 veterans. American Journal of Epidemiology, 157, 141–148. doi:10.1093/aje/kwf187
Katzenell, U., Ash, N., Tapia, A. L., Campino, G. A., & Glassberg, E. (2012). Analysis of the causes of death of casualties in field military setting. Military Medical Journal, 177, 1065–1068.
Knieper, A. J. (1999). The suicide survivor’s grief and recovery. Suicide and Life-Threatening Behavior, 29, 353–364. doi: 10.1111/j.1943-278X.1999.tb00530.x
Krohne, H. W., Pieper, M., Knoll, N., & Breimer, N. (2002). The cognitive regulation of emotions: The role of success versus failure experience and coping dispositions. Cognition & Emotion, 16, 217–243. doi:10.1080/02699930143000301
Lamorie, J. (2011). Operation Iraqi Freedom/Operation Enduring Freedom: Exploring wartime death and bereavement. Social Work in Health Care, 50, 543–563. doi:10.1080/00981389.2010.532050
Lazarus, A. A. (2005). Is there still a need for psychotherapy integration? Current Psychology, 24, 149–152. doi:10.1007/s12144-005-1018-5
Lazarus, A. A. (1996). Behavior therapy & beyond. New York, NY: McGraw-Hill.
Lazarus, R. S., & Folkman, S. (1984). Stress, appraisal, and coping. New York, NY: Springer.
Lindemann, E., & Greer, I. M. (1953). A study of grief: Emotional responses to suicide. Pastoral Psychology, 4, 9–13.
Lussier, R. N., & Sonfield, M. C. (2004). Family business management activities, styles and characteristics: A correlational study. Mid-American Journal of Business, 19, 47–53.
Martin, J., Ghahramanlou-Holloway, M., Lou, K., & Tucciarone, P. (2009). A comparative review of U.S. military and civilian suicide behavior: Implications for OEF/OIF suicide prevention efforts. Journal of Mental Health Counseling, 31, 101–118.
McIntosh, J. L. (1993). Control group studies of suicide survivors: A review and critique. Suicide and Life-Threatening Behavior, 23,146–161. doi:10.1111/j.1943-278X.1993.tb00379.x
McMenamy, J. M., Jordan, J. R., & Mitchell, A. M. (2008). What do suicide survivors tell us they need? Results of a pilot study. Suicide and Life-Threatening Behavior, 38, 375–389. doi:10.1521/suli.2008.38.4.375
Miers, D., Abbott, D., & Springer, P. R. (2012). A phenomenological study of family needs following the suicide of a teenager. Death Studies, 36, 118–133. doi:10.1080/07481187.2011.553341
Miles, D. (2010). VA strives to prevent veteran suicides. Retrieved from http://www.defense.gov/news/newsarticle.aspx?id=58879
Minois, G. (1999). History of suicide: Voluntary death in western culture (L. G. Cochrane, Trans.). Baltimore, MD: Johns Hopkins University Press.
Murray, J. A., Terry, D. J., Vance, J. C., Battistutta, D., & Connolly, Y. (2000). Effects of a program of intervention on parental distress following infant death. Death Studies, 24, 275–305. doi:10.1080/074811800200469
National Institute of Mental Health. (2010). Statistics. http://www.nimh.nih.gov/health/statistics/index.shtml
National Institute of Mental Health. (2013). Suicide prevention. http://www.nimh.nih.gov/health/topics/suicide-prevention/index.shtml
Neimeyer, R. A., & Jordan, J. R. (2002). Disenfranchisement as empathic failure: Grief therapy and the co-construction of meaning. In K. J. Doka (Ed.), Disenfranchised grief: New directions, challenges, and strategies for practice (pp. 95–117). Champaign, IL: Research Press.
Ness, D. E., & Pfeffer, C. R. (1990). Sequelae of bereavement resulting from suicide. American Journal of Psychiatry, 147, 279–285.
Parrish, M., & Tunkle, J. (2005). Clinical challenges following an adolescent’s death by suicide: Bereavement issues faced by family, friends, schools, and clinicians. Clinical Social Work Journal, 33, 81–102. doi:10.1007/s10615-005-2621-5
Peacock, E. J., & Wong, P. T. P. (1990). The stress appraisal measure (SAM): A multidimensional approach to cognitive appraisal. Stress Medicine, 6, 227–236. doi:10.1002/smi.2460060308
President’s New Freedom Commission on Mental Health. (2003). New freedom commission on mental health report. Retrieved from http://govinfo.library.unt.edu/mentalhealthcommission/reports/FinalReport/downloads/FinalReport.pdf
Provini, C., Everett, J. R., & Pfeffer, C. R. (2000). Adults mourning suicide: Self-Reported concerns about bereavement, needs for assistance, and help-seeking behavior. Death Studies, 24, 1–19. doi:10.1080/074811800200667
Sarantakos, S. (1993). Social research. Basingstoke, England: Macmillan.
Scocco, P., Castriotta, C., Toffol, E., & Preti, A. (2012). Stigma of Suicide Attempt (STOSA) scale and Stigma of Suicide and Suicide Survivor (STOSASS) scale: Two new assessment tools. Psychiatry Research, 200, 872–878. doi:10.1016/j.psychres.2012.06.033
Siebrecht, C. (2011). Imagining the absent dead: Rituals of bereavement and the place of the war dead in German women’s art during the First World War. German History, 29, 202–223.
Steel, J. L., Dunlavy, A. C., Stillman, J., & Pape, H. C. (2011). Measuring depression and PTSD after trauma: Common scales and checklists. Injury, 42, 288–300. doi:10.1016/j.injury.2010.11.045
Sudak, D. (2009). Training in cognitive behavioral therapy in psychiatry residency: An overview for educators. Behavior Modification, 33, 124–137. doi:10.1177/1059601108322626
Sveen, C.-A., & Walby, F. A. (2008). Suicide survivors’ mental health and grief reactions: A systematic review of controlled studies. Suicide and Life-Threatening Behavior, 38, 13–29. doi:10.1521/suli.2008.38.1.13
Uchino, B. N. (2006). Social support and health: A review of physiological processes potentially underlying links to disease outcomes. Journal of Behavior Medicine, 29, 377–387. doi:10.1007/s10865-006-9056-5
Worden, J. W. (1991). Grief counseling & grief therapy: A handbook for the mental health practitioner (2nd ed.). New York, NY: Springer.
Worden, J. W. (2009). Grief counseling and grief therapy: A handbook for the mental health practitioner (4th ed.) New York, NY: Springer.
Zamorski, M. A. (2011). Suicide prevention in military organizations. International Review of Psychiatry, 23, 173–180. doi:10.3109/09540261.2011.562186
Zhang, J., & Jia, C.-X. (2009). Attitudes toward suicide: The effect of suicide death in the family. Omega, 60, 365–382. doi:10.2190/OM.60.4.d307.
Zimet, G. D., Dahlem, N. W., Zimet, S. G., Farley, G. K. (1988). The multidimensional scale of perceived social support. Journal of Personality Assessment, 52, 30–41. doi:10.1207/s15327752jpa5201_2
Lindsey Mitchell, NCC, is the recipient of the 2015 Outstanding Dissertation Award for The Professional Counselor and a licensed counselor in both Texas and Washington, D.C. Correspondence may be addressed to Lindsey Mitchell at lmitch26@gwmail.gwu.edu.
Dec 8, 2015 | Article, Volume 5 - Issue 4
Jane E. Atieno Okech, Anne M. Geroski
This article utilizes one counselor education program’s experience as a framework for exploring how to prepare counselors to work in interdisciplinary teams. Based on an interdisciplinary training program that involves faculty and graduate students from counseling, social work, nursing, internal medicine and family medicine, the article explores the role discipline-specific orientations play in the outcome of interdisciplinary training programs. Using practical examples grounded by the program’s experiences and literature on interdisciplinary training, understanding of the dynamics of interdisciplinary training programs is explored. Implications for preparing counselors for interdisciplinary work and future research are provided.
Keywords: counselor education, interdisciplinary training, interdisciplinary teams, collaborative practice, medicine
Counselors typically work in interdisciplinary settings, requiring them to navigate the complex dynamics of collaboration while maintaining a clear focus on the best interests of their clients. Interdisciplinary settings can be described as contexts that require collaboration and consultation between professionals and non-professionals from multiple disciplines in the process of providing service (Nancarrow et al., 2013). Collin (2009) clarified that interdisciplinary collaboration differs from multidisciplinary and transdisciplinary collaboration as it refers to the work of professionals grounded in their own separate disciplines coming together to work on a project that represents a “coordinated and coherent whole” (p. 103). Collin pointed out that this is different from professionals working independently on separate aspects of a project (multidisciplinary) or the coming together of multiple and varied professionals to conceptualize a problem or work on a project that transcends any of the various disciplines (transdisciplinary).
Counselor educators have argued that interdisciplinary collaboration is “a best practice strategy for addressing some of the nation’s critical social problems” (Mellin, Hunt, & Nichols, 2011, p. 140). In fact, collaboration between disciplines has been described as being key to the effective delivery of services (McNair, 2005; Morphet et al., 2014) across a broad-spectrum of community mental health services, hospitals, institutions of higher learning and school contexts. In the field of counseling, the ACA Code of Ethics (American Counseling Association [ACA], 2014) and the standards established by the Council for Accreditation of Counseling and Related Educational Programs (CACREP, 2009) reflect this emphasis on the importance of counselors being able to work with interdisciplinary teams. The ACA Code of Ethics (ACA, 2014), for example, encourages counselors to recognize the value of interdisciplinary teamwork in meeting clients’ best interests, even when certain professional values are not shared:
Counselors who are members of interdisciplinary teams delivering multifaceted services to clients remain focused on how to best serve clients. They participate in and contribute to decisions that affect the well-being of clients by drawing on the perspectives, values, and experiences of the counseling profession and those of colleagues from other disciplines (ACA, 2014, D. 1. C., p. 10).
The ACA Code of Ethics also compels counselors to respect client rights, including those regarding confidentiality, in interdisciplinary treatment contexts (ACA, 2014, A. 2. b., p. 4; B. 3. b., p. 7). The CACREP (2009) training standards emphasize the importance of teaching counselors to understand the functions of other human service agencies and to learn strategies for inter-agency collaboration. In these standards, addictions, marriage, couples, family and career counselors are required to be familiar with the roles of other mental health professionals, and in the clinical mental health counselor standards, the importance of learning how to develop relationships across helping professions and interdisciplinary treatment teams is highlighted. Additionally, school counselors-in-training under CACREP standards also must learn models of consultation and collaboration as a part of their training programs.
Despite these standards, counselors appear to navigate the challenges of interdisciplinary collaboration with limited understanding and experience. Little has been written about interdisciplinary training or the development of interdisciplinary competencies by counseling professionals (Bemak, 1998). Counseling literature and training standards appear to operate from the premise that the process of professional development is automatically accompanied with the acquisition of skills to work in interdisciplinary teams. In contrast, the medical field and associated disciplines have actively documented interdisciplinary training initiatives as a means for facilitating interdisciplinary competencies among their professionals (Pollard & Miers, 2008). For example, in the United Kingdom, the integration of Interprofessional Education (IPE) is now mandatory in the fields of health and social care, with students being required to complete specific modules that have practical interdisciplinary components (Pollard & Miers, 2008). Medicine in the United States also is actively pursuing interdisciplinary training models with the support of the Institute of Medicine, which recognizes interdisciplinary teamwork as key to effective service delivery (Institute of Medicine, 2003; McNair, 2005). Therefore, while counselors continue to make a case for the value of interdisciplinary work, what remains unclear in the literature is how counselors can attain competence in facilitating and participating in interdisciplinary collaborative practices. It is particularly critical to examine how these competencies can be developed while neophyte counselors are also in the foundational stages of their professional development.
The purpose of this article is to use the experiences of one counselor education program currently engaged in an interdisciplinary training project as a framework for exploring some critical benefits and challenges of interdisciplinary training processes. This article provides a detailed description of the counselor education program’s training module and also describes steps the program has taken to prepare students for interdisciplinary training contextual dynamics, measures the program has taken to advocate for the counseling profession, and efforts to enhance students’ understandings of their professional roles in an interdisciplinary context. Using practical examples grounded by interdisciplinary literature, we expand understanding of shared interdisciplinary values and provide recommendations for more effective practices and future research.
Interdisciplinary Training Program Development
This training collaborative began with an interdisciplinary response to a grant call by the Substance Abuse and Mental Health Services Administration (SAMHSA) to submit a proposal on providing training in Screening, Brief Intervention, and Referral to Treatment (SBIRT). SBIRT is a comprehensive, integrated, public health approach to the delivery of early intervention and treatment services for adolescents and adults dealing with substance misuse issues (Agerwala & McCance-Katz, 2012; Davoudi & Rawson, 2010; Mitchell et al., 2012). This particular university’s SBIRT Training Collaborative brings together master’s students from the counseling program, the Department of Social Work, the College of Nursing, and family medicine and internal medicine residents in an interdisciplinary training program using a team-based care model of evidence-supported SBIRT interventions. These programs were chosen because they all are disciplines that deal with issues related to substance misuse. Additionally, these were the only disciplines at our university that responded to the call to participate in this particular project. The objective of the project is to offer brief intervention and referral training to medical residents and master’s level graduate students in the area of substance use disorders over a 3-year period. An average of 20 students from each of the participating disciplines were expected to participate in the project annually. This training program began its third year of implementation this year. The SAMHSA grant enabled the interdisciplinary training collaborative to hire SBIRT consultants, a project manager, a project training director and qualified support staff to help administer the project. The funding is a critical part of the success of this project, allowing for faculty course buyouts across the participating disciplines.
The interdisciplinary collaborative aspect of this project began during the initial meeting of educators from the various disciplines, which was organized to discuss submitting a grant proposal in support of an interdisciplinary training program. Each program’s director was required to submit a statement indicating how their program would benefit from an interdisciplinary training project. Two initial meetings and multiple e-mail exchanges later led to the formation of an interdisciplinary collaborative team and an agreement by the team on (a) the core foci of the grant, (b) the level of participation by each program and the roles of faculty representatives on the grant writing, (c) budget allocation parameters, and (d) the establishment of a project advisory council made up of the directors of each of the disciplines represented in the project. The purpose of the project’s advisory council was to develop the curriculum for the program, which included assessing and ultimately agreeing on the online modules to use on the project, and to establish clear guidelines for the clinical training protocol. Secondly, the advisory council also was charged with ensuring that each discipline provided input on the curriculum development and project evaluation processes. This aspect of the dialogue was critical as one of the objectives of the grant was for programs to incorporate interdisciplinary training foci in their individual discipline’s curriculum. Third, the council was charged with the responsibility of implementing and assessing the clinical training aspect of the interdisciplinary training project. Advisory council members committed to serve on interdisciplinary presentation panels and also to provide supervision during the interdisciplinary clinical training sessions. Finally, the council members were expected to be available to address student conduct issues as well as to meet with external grant reviewers during their visits to campus.
The SBIRT Interdisciplinary Training Model
This university’s SBIRT interdisciplinary training format is multifaceted, including online and real-time instruction and practice experiences. All family practice and internal medicine residents and master’s-level graduate students in the participating disciplines are expected to sign a contract that they will participate in all required aspects of the training experience. SBIRT training is offered in four main areas: (1) screening for substance use disorders, (2) motivational interviewing skills, (3) brief intervention, and (4) referral to treatment. Training includes providing conceptual information (e.g., substance use and motivational interviewing), teaching the use of assessment tools to establish risk or levels of substance misuse, and promoting skill development. Modeling and skill practice with feedback from faculty are important components of this training.
The first SBIRT training cohort started with first-year master’s-level graduate students and medical residents. The counseling students involved in the project were in their second semester in the program and concurrently enrolled in a practicum course. For counseling students, the training began with an orientation (counseling program pre-module orientation) to the SBIRT training experience. In the orientation, counseling faculty offered students an overview of the various components of the training project, outlining specific expectations and completion dates. Beginning in the project’s second year, the orientation included the film, The Hungry Heart (O’Brien, 2013), which explores the depth of prescription drug and opiate addiction in our home state. This film was followed by a discussion regarding the need for SBIRT screening and referral skills. While counseling students are required to participate in this orientation, the option to attend the session also is open to participants from other disciplines.
The next component of the training, conducted online, is required for all participants (faculty and students), regardless of discipline. The online training includes four instructional modules (see Figure 1) and requires a commitment of approximately four to six hours. The first of these online training modules offers an introduction to the SBIRT process and includes data regarding alcohol and substance use. This information builds a case for the need for SBIRT screening and referral practices. The other modules provide instruction in the areas of conducting a brief screening intervention, motivational interviewing, and making appropriate referrals. Each module begins with instruction in a particular area and requires completion of a test before the participant is issued a completion certificate. The certification process was included as a means of ensuring that all participating students complete the required didactic training and tests prior to participating in the interdisciplinary clinical training portions of the program.
At the end of the online training period, counseling students are required to attend a 2-hour practice review (counseling program post-module review and skills practice) session (see Figure 1). A similar post-module review and practice session is offered by other SBIRT project faculty for medical residents and to promote interdisciplinary training; each discipline-specific post-module review is open to participants from other disciplines. In this training, counseling faculty offer a brief review of the information provided in the modules, focusing primarily on the steps of the brief negotiated interview (alcohol and substance use screening) and the motivational interview. Participants engage in role-plays to practice these skills and are provided with instruction and feedback by the counseling faculty.
Figure 1 – Interdisciplinary Training Protocol
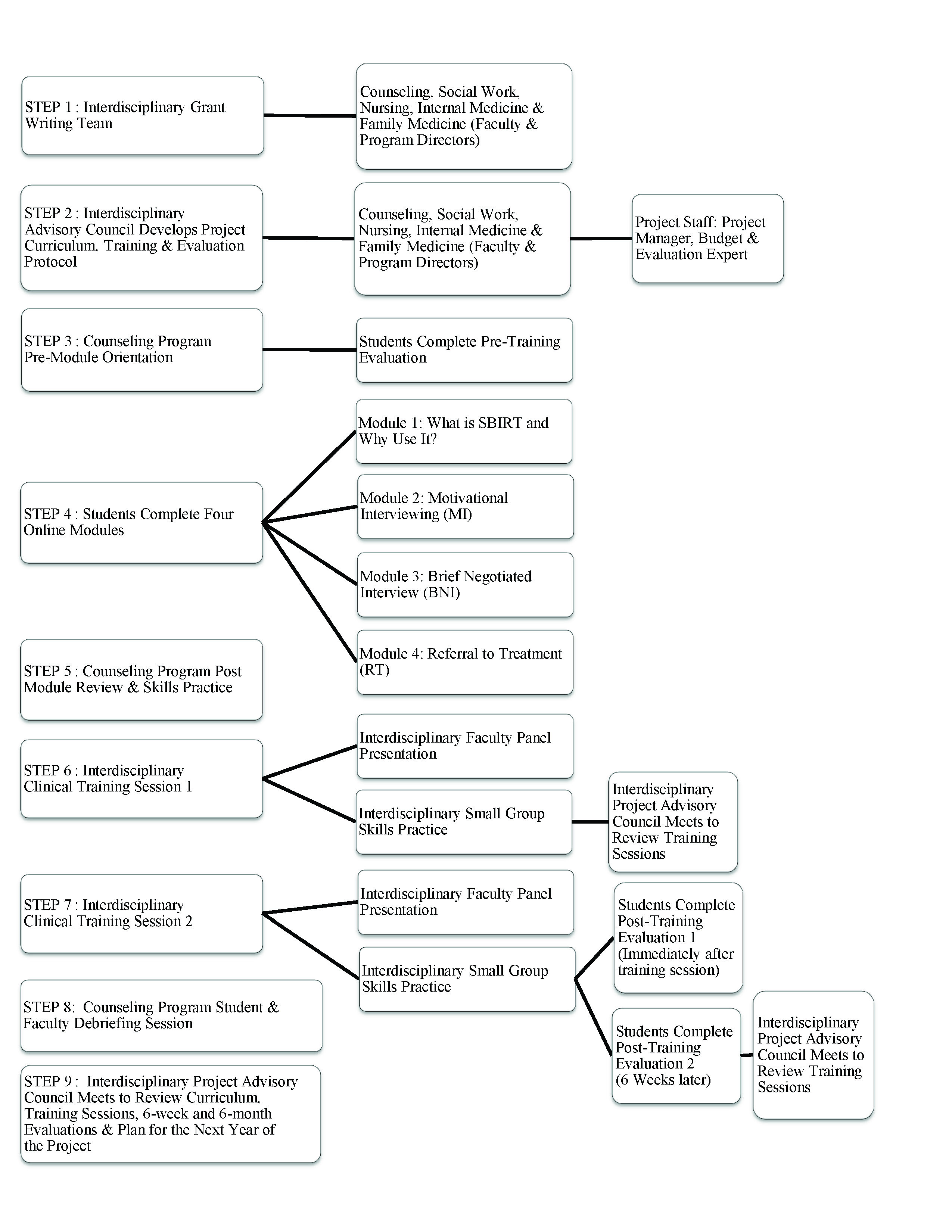
The intent of this training session is to reinforce counseling students’ sense of competence prior to engaging in interdisciplinary training sessions. This session helps students frame the online training information into counseling-specific terms, steps and experiences while providing them the opportunity to ask questions and clarify their understandings. Importantly, this session requires students to practice the SBIRT skills and to receive feedback and instruction on their use of the skills from familiar faculty in the comfortable environment of counseling peers. Ultimately, this preparation is designed to fortify the confidence that the counseling students bring into the larger, unfamiliar, interdisciplinary practice setting.
Next, all participants in the SBIRT training, regardless of specific discipline, are expected to attend two clinical interdisciplinary training sessions. The first of these focuses on screening and motivational interviewing; the second is on referrals. These sessions begin with an introduction to the concepts that will be covered in that training followed by a panel discussion about the particular application of skills in the various disciplines and the modeling of skills (a role play by two of the program directors). The participants are then required to practice the skills with “live” practice clients (i.e., professional actors from the local community that were already employed by the medical school for medical student training) playing patients/clients with substance use or misuse issues. In this part of the training, participants are randomly assigned to small practice groups, providing an interdisciplinary practice milieu, with a faculty instructor. Each interdisciplinary practice group meets with four professional clients over the course of 2 hours. The participants in each group take turns using screening, motivational interviewing and referral skills. In each group, participants receive feedback and instruction from the faculty instructor who has observed their practice. At the end of the session, the training directors engage participants in a large group discussion about their experiences and observations of being part of an interdisciplinary training group. The intent of this approach is to provide participants with the opportunity to practice with students who have different professional orientations and to receive supervision from faculty who may also have diverse experiences and perspectives; thus, the interdisciplinary focus of this project.
The final component of the training is follow-up. For counseling students, this begins with a follow-up discussion about the training experience with the counseling faculty at the end of the first year of training (after the second interdisciplinary training session). In this meeting, students are asked to reflect on their experiences in SBIRT training and also to discuss their ideas regarding the implementation of this training into their upcoming internship experiences. The purpose of this discipline-specific follow-up is to assess and solidify the integration of the interdisciplinary experiences into their development as professional counselors.
A comprehensive formal evaluation protocol also is in place for the interdisciplinary training program. Students from each of the participating disciplines complete pre- and post-training evaluation forms. During the first year of the project, formal follow-up evaluations were completed in four stages: (1) immediately after students completed the counseling program’s pre-module orientation session; (2) immediately after students completed each of the two interdisciplinary clinical training sessions; (3) six weeks after students completed the final interdisciplinary training session, and (4) six months following completion of the final interdisciplinary clinical training session. These evaluations solicit student self-perceptions of their own competence during the various training experiences and also ask for general feedback about the training process. The six-month follow-up evaluation process is meant to coincide with the students’ internship and residency experiences. The core objective of the final evaluation will be to assess the impact of interdisciplinary training on the students’ current interdisciplinary teamwork experiences.
Interdisciplinary Training Challenges
Interdisciplinary training and practice is complicated; sound logic and good intentions can easily be derailed by any number of intra- and interprofessional challenges. Here we will discuss challenges related to training in silos, and professional orientation, values and attitudes.
Training in Silos
The literature suggests that understanding the skills, knowledge and values of the various disciplines involved in an interdisciplinary collaboration is key to success (Wellmon, Gilin, Knauss, & Linn, 2012). Yet, this may be a challenge when professionals require specialized training that sometimes has the effect of narrowing their views and approaches to service delivery (Forrest, 2004). That is, it can be difficult for professionals to acquire the skills needed for communicating and collaborating across disciplines (Miller & Katz, 2014) when training in silos orients professionals to become strongly acculturated in their own language and practice styles.
We found in the interdisciplinary SBIRT project that these silo effects of discipline-specific training were apparent. It became clear immediately that most of the participants had strong discipline-specific skills and orientation allegiance, and many had little information about conditions and situations beyond their specific training area. This dynamic was evident at both faculty and trainee levels. Faculty had to navigate this dynamic during the process of planning and writing the grant proposal and negotiating the development of the training curriculum in the project’s advisory council (made up of program directors of participating disciplines). For example, the counseling director had to educate her medical practice peers on counselor education curriculum, counseling professional practice, and contexts of counseling practice. Further, the directors of counseling and social work had to educate peers on the similarities and differences between the two professions. At the same time, the directors of the family medicine and internal medicine disciplines had to educate their counseling and social work peers on the difference between the two specializations in medicine. Nursing faculty also addressed the distinct role of nurse practitioners in the field of medicine and the intersections between their roles and that of medical doctors.
At the trainee level, the discipline-specific skills and orientation allegiance was evident, particularly in both the brief intervention and the referral to treatment components of the interdisciplinary training sessions. For example, while many of the medical residents were articulate when explaining the physical effects of potential substance use to their professional clients, they were slow to pick up on sociocultural variables that may have been key to the etiology of the substance misuse (and for later referral) in these same cases. An example of this was a professional client who hinted at challenges with a transgender social location that appeared relevant to his substance misuse. This was not addressed by many of the medical residents and faculty, even when those variables were noted in the training module to be risk factors for substance misuse. This variable appeared to be more readily explored by the counseling and social work participants. Conversely, many of the counseling and social work participants struggled to articulate the medical symptoms, risk factors and ramifications of substance misuse that were so easily identified and explored by their peers in nursing and medicine.
A second example of the silo effects of discipline-specific training arose when participants were engaged in the referral to treatment training. After a few practice sessions, it became clear that many of the counseling and social work participants did not understand the difference between family and internal medicine practices, or when to refer to a nurse as opposed to a doctor. Conversely, many of the medical practitioners did not have a clear understanding of the role of social workers and counselors. Once noted, the program directors were able to address this gap in knowledge about participating professionals. For example, counseling and social work directors were able to educate the medical professionals about counseling and social work professional practice. This facilitated productive conversation about referral sources at the start of the subsequent training session; counseling and social work trainers were able to offer a more clear articulation of the professional training and role of their students. Anecdotes from a few of the medical residents and other trainers afterwards indicated that such information was useful for them in discussing referral to treatment in their practice groups. Clearly, knowing the practice parameters of colleagues is central to effective interdisciplinary practice (Wellmon et al., 2012). This knowledge should include some awareness of discipline-specific orientations, terminology and information regarding conceptual framework (McLean, 2012).
Professional Orientation, Attitudes and Values
Issues related to practicing in silos are further complicated by professional indoctrination, or professional identity orientation and development. Within each of the various helping professions, new practitioners are oriented to acquire their profession’s unique and specialized identity. For example, in the profession of counseling, the establishment of a unique professional identity is considered a foundational training practice, as demonstrated in the 20/20: A Vision for the Future of Counseling initiative (Kaplan & Gladding, 2011) and CACREP standards (CACREP, 2009). This intentional emphasis on professional identity in the counseling profession was promoted in order to emphasize the important philosophical beliefs that are the foundation of the profession (Mellin et al., 2011), to distinguish counselors from other helping professionals, to strengthen the profession, to assure licensure portability, and to establish a sense of pride (Mascari & Webber, 2013). According to Gibson, Dollarhide, and Moss (2010), new professionals are socialized into the language of their profession so as to learn what is expected of them, as well as what they can expect in practice—to behave as “native speakers” (p. 22) in their particular discipline. The challenge for counselor educators, as well as profession-specific educators in other related disciplines, is to teach students to navigate the complex dynamics of collaboration while maintaining a clear understanding of their own professional identity.
When professional identities are established in the context of practicing in silos, as well as competing for resources and job opportunities, interdisciplinary tensions may flourish. The results often are distance, barriers, mistrust and a lack of collegiality between disciplines (Arredondo, Shealy, Neale, & Winfrey, 2004; Miller & Katz, 2014). All of this is further complicated by “hierarchical schemas” (Delunas & Rouse, 2014, p. 101) in health care practice that award some individuals and professions more social capital than others (Bemak, 1998; Meyers, Hales, Young, Nesbitt, & Pomeroy, 2013). Clearly, interdisciplinary practice is hampered when some practitioners undervalue the perspectives of others (McLean, 2012).
In our training sessions, it was difficult to determine the extent to which differences in approach and conceptualization reflected different professional training orientations and professional identities or participants’ (and their professional mentors’) value orientations. That is, while it was clear that the different professions approached the practice components of SBIRT from a different lens, it also seemed that some of the participants valued their own training and knowledge over others. For example, in some of the discussion groups regarding the professional actor who played the role of a client who identified as transgender, some of the medical participants assertively questioned the utility of exploring gender orientation during the screening process. Most of the counseling and social work participants who actively explored the client’s gender orientation in their practice sessions sat in silence as their medical peers challenged faculty trainers on this point. Later, some of the counseling and social work participants described a sense of incompetence regarding knowledge about the medical aspects of substance misuse, as well as difficulties in countering the arguments raised by the medical residents, particularly those against exploring the client’s gender orientation during the screening process, an area in which they had competence.
The confident expression of dissenting opinions by some participants juxtaposed with the relative silence of others during disagreements regarding practice orientation may have been an artifact of how practitioners-in-training are exposed to and experience supervision, particularly when delivered by a professional outside of their own discipline. It also may have mirrored the dynamics of many interdisciplinary treatment teams, which tend to be shaped by professional social hierarchy discourses. Given the strong component of professional identity in the training of the counselors and social workers who participated in our SBIRT training, we wonder if the assertiveness and self-silencing that we witnessed reflects social factors at work that go beyond professional identity orientation. As mentioned by Delunas and Rouse (2014), professional hierarchies in the field and in the lay public put physicians “at the top” (p. 101) and until hierarchical profession-centered structures (Meyers et al., 2013) and power sharing (Bemak, 1998) are realized, interdisciplinary collaboration will be stymied.
Interdisciplinary Training Recommendations
Understanding the challenges that arise from practicing in silos brings up complex issues and political nuances that sit between providing specialized, discipline-specific training, and preparing practitioners to work across disciplines. Wellmon et al. (2012) reminded us that “the skills necessary to work effectively as a member of a healthcare team are not intuitive and cannot be learned exclusively ‘on the job’” (p. 26). Meyers et al. (2013) echoed this sentiment, pointing out that health care professionals simply are not taught teamwork skills. Bemak (1998) called for the deconstruction and redefinition of the counseling profession’s central paradigms so that interdisciplinary collaboration can be a core component of counseling. He also asserted that professional counselors must be provided important skills for engaging in interdisciplinary collaboration. A similar request is made of professionals from other disciplines. Ultimately, if we expect health care practitioners to engage in interdisciplinary practice, they must be trained to engage in such practice.
The literature on interdisciplinary work consistently articulates the difficulty in identifying specific factors that can contribute to effective interdisciplinary work, and it calls for more writing and research by participants in interdisciplinary training programs (Arredondo et al., 2004; Bemak, 1998; Forrest, 2004; Nancarrow et al., 2013; Reubling et al., 2014). Based on our experience in the SBIRT interdisciplinary training and extant research in the field, we offer recommendations for how to promote effective engagement in interdisciplinary work among counselors-in-training. Our recommendations are summarized below in the categories of promoting professional identity and boundaries and teaching skills for collaboration.
Professional Identity and Boundaries
Professional identity. Due to the silo effects of discipline-specific training, negotiating curriculum and training processes can be challenging in interdisciplinary collaborations. The needs of constituent groups within the training can easily be lost to the louder voices or privileged perspectives. Yet, Mascari and Webber (2006, 2013) and Mellin et al. (2011) pointed out that having a clear sense of one’s own professional identity and one’s scope of practice and also recognizing differences between counseling and other mental health disciplines enhances cross-discipline practice. These authors highlighted the importance of enlisting faculty representatives who are grounded in counselor and counselor educator identities, who also understand the value of interdisciplinary training and who have the interpersonal skills and expertise necessary for negotiating challenging interdisciplinary conversations. An understanding and appreciation of the interdisciplinary training protocol as a tool for enhancing professional interdisciplinary teamwork should be a core-guiding objective for counseling and all participating faculty members (Bemak, 1998), of course, but a solid grounding in one’s own professional identity also is critical.
We learned that counseling faculty must invest in preparing students for participation in interdisciplinary training. The preparation process should be progressive in nature with scheduled periodic check-in sessions, particularly during interdisciplinary clinical training. In our experience, the challenge of navigating professional roles and functions during the interdisciplinary clinical training sessions was most difficult for our students. Counseling students appeared to need multiple opportunities to process their interdisciplinary practice experiences. It was most beneficial to students when the participating faculty had a clear understanding of all the training protocols and processes.
Secondly, positive outcomes came from pre-coaching for skills and knowledge with students during the counseling program post-module review and skills practice review session, and encouraging them to have the confidence to speak up about their concerns, professional differences, identities, and even to volunteer to demonstrate their skills when in the interdisciplinary training sessions. This is consistent with the Reubling et al. (2014) findings in a study comparing students’ attitudes and perceptions in pre- and post-training experiences. Our experience highlighted the value of openly discussing the differences in professional and social capital in society and the impact that those differences have on students’ approaches to the interdisciplinary training experience. Such discussions helped boost students’ confidence to acknowledge issues that they avoided addressing in the initial phases of the training. Having a clear feedback loop from students to faculty, so that faculty can provide feedback to fellow collaborators at subsequent interdisciplinary training sessions, was particularly beneficial.
Finally, having a clear protocol for interventions with non-cooperative and challenging students was beneficial. For example, counseling students were required to sign a behavior and participation contract that was submitted prior to engagement in the interdisciplinary clinical training portions of the program. The foresight by the counseling program to request this contract may have been why no counseling student was cited for behavioral concerns during the interdisciplinary clinical training sessions. There were a handful of participants in other disciplines who required intervention from their own program directors regarding behavioral concerns emerging during interactions with training faculty who were not in their discipline area.
Professional boundaries. For this counselor education program’s faculty, it was necessary to have a good sense of the boundaries of engagement during the project’s initiation phases. Interdisciplinary training collaborations require much compromise in the curriculum development and training implementation phase; we wanted to be sure that the interdisciplinary training program would enhance rather than compromise the training experience of counseling students. We were consistently willing to compromise and accommodate other disciplines’ perspectives, so long as training processes that are essential to the training of counselors were incorporated in the interdisciplinary training protocol. This is consistent with the recommendations of Nancarrow et al. (2013) regarding interdisciplinary training participants needing to understand and respect the professional roles, functions and boundaries of collaborators.
An example of this negotiated process happened after the first year of collaboration, when counseling faculty suggested changes in the scenarios presented to professional actors playing the roles of clients in the clinical component of the training. During the first year, the preparation of the professional actors was handled solely by a staff member employed by the medical school. As a result, the bulk of their presenting concerns were medical in nature. The majority of the professional actors appeared unprepared to discuss their psychological and sociocultural concerns. This was a major factor that affected collaboration because it made the initial practice session challenging for counseling and social work students who understandably felt that discussing medical presenting concerns was out of the scope of their competence and practice. During the second year of the training cycle, counseling faculty submitted case scenarios for the professional actors that started with an initial contact at a school or clinical mental health setting and that represented varied sociocultural and emotional concerns that coexist with physical medical concerns. This approach was intended to ensure that counseling students would be able to experience clinical training with case scenarios that were within their scope of study and practice and also allow them to practice making referrals to social workers and medical professionals.
Additionally, counseling and social work faculty, the two disciplines outside the medical field, actively advocated for all case scenarios used in the training to be truly interdisciplinary in nature. This meant that all the presenting concerns presented by the professional actors needed to provide an opportunity for an interdisciplinary intervention during the referral process. Negotiating these changes in the second year was easier given the professional relationships, trust and mutual respect that had evolved over the year among faculty from the different participating disciplines. Our challenges in negotiating the professional weighting of the training processes are not unusual and are consistent with what Mascari and Webber (2006, 2013) and Mellin et al. (2011) discussed regarding the challenges inherent to cross-discipline practice among professionals who have received specialized training and who have unique professional identities. We should have never assumed that the coordinator of the professional actors, who is based in the medical school, would understand how to prepare the actors to engage with students in a manner that would allow for an interdisciplinary intervention.
During the second year, faculty from the counseling program were more actively involved in the development of scenarios and instructions that would be shared with the professional actors playing the role of clients/patients in the project. In hindsight, the university SBIRT advisory council should have spent more time in deliberations about the potential obstacles that would emerge from interdisciplinary collaboration. We were excited about this new initiative and spent more time discussing the benefits and potential challenges for students rather than for the faculty and staff involved in the project. Thus, some identified challenges persisted in the second year.
Interdisciplinary focus as a goal. We realized the importance of all key participants (faculty and program directors) having a clear understanding of the interdisciplinary training goal of this project. For example and as mentioned, counseling faculty had to advocate multiple times for an interdisciplinary outlook as the curriculum and training protocol was planned and developed. In hindsight, we realize that while the core focus of the project was interdisciplinary training, participants and trainers seemed to return to familiar patterns of silo training as the project was carried out. We are reminded that an interdisciplinary focus requires constant reminders and intentionality to keep the focus interdisciplinary.
Another artifact of the challenges inherent to interdisciplinary initiatives that emerged was that it appeared participants (students) were not fully prepared to receive feedback during the training from faculty who were not in their own discipline. After the first year of implementation, the program directors placed more emphasis and deliberated at length on how to assist trainees with navigating the dynamics of interdisciplinary training, and a protocol was discussed for addressing student-related training challenges. However, as mentioned above, a similar process was not identified for participating faculty and program directors. That is, at the director level, a process was not articulated for how to assure a truly interdisciplinary focus would be honored during the planning and implementation stages of the project, nor was a protocol developed to articulate how professional disagreements would be managed. While a process for navigating professional differences emerged organically, the absence of such a conversation in the early stages caused tense deliberations as participating faculty and program directors tried to communicate their professional boundaries, roles and functions. Therefore, we recommend that interdisciplinary teams develop protocols for addressing differences in perspectives for both students and training faculty. There is value in investing in leadership that understands the practice of the various disciplines involved in a project and has a commitment to infusing interdisciplinary and collaborative practices in every aspect of a training program (Nancarrow et al., 2013).
Skills for Collaboration
As previously mentioned, some authors have suggested that interdisciplinary collaboration requires particular skills or competencies (e.g., Arredondo et al., 2004; Bemak, 1998; Delunas & Rouse, 2014; Meyers et al., 2013) that are not regularly taught to health care professionals. These authors suggested that working in interdisciplinary teams also requires particular attitudes and special knowledge that are communicated through interpersonal skills.
Collaboration attitudes. Working with others across disciplines requires a certain spirit or willingness to share, collaborate and respect others (Nancarrow et al., 2013). This includes avoiding judgment, working in the spirit of “joining” (Miller & Katz, 2014, p. 7), and overcoming professional hostilities, prejudices or phobias (Bemak, 1998). It also requires openness to collective decision making, an ability to redefine one’s role in an interpersonal context (Bemak, 1998) and demonstrating a sentiment of appreciation and accommodation to multiple perspectives (Arredondo et al., 2004). Included here is an ability to be flexible—to “share your street corner” as Miller and Katz (2014, p. 10) put it, or “playing well” with others (Arredondo et al., 2004, p. 791).
Being flexible also means remembering that one professional orientation/approach is not the only valid approach (Bemak, 1998); it requires an ability to be uncomfortable—“leaning into discomfort” (Miller & Katz, 2014, p. 8). An attitude of collaboration also requires being open to feedback (Nancarrow et al., 2013) and a willingness to negotiate power (Bemak, 1998; McLean, 2012). In our SBIRT training project, it appeared that a true spirit of collaboration developed over time among trainers. Its development appeared to emerge, as the examples from earlier discussions in this article illustrate, from the assertiveness and confidence as much as from the flexibility of faculty who may have otherwise been marginalized from decision making. Thus, it is possible that collaborative attitudes are more likely to develop when everyone in the group has had an opportunity to contribute, whether by invitation or self-assertiveness. It is essential to highlight the fact that even counseling and social work faculty, who have been trained to be open to multiple perspectives, engaged from time to time in their familiar silo foundation to professional orientation.
Collaboration knowledge. Interdisciplinary practice requires that individuals have professional competence in their own areas of expertise (Nancarrow et al., 2013) as well as an ability to effectively communicate this discipline-specific information effectively to others (Wellmon et al., 2012). It also requires an ability to learn about the language and roles that define other disciplines (Miller & Katz, 2014; Nancarrow et al., 2013). Knowledge about organizations or systems theory, as well as models of consultation, also is extremely helpful to professionals working across disciplines (Arredondo et al., 2004). Arredondo et al. (2004) and McLean (2012) point to a need to have an intuitive understanding of interpersonal and group dynamics. Finally, Arredondo et al. suggested that awareness of one’s own beliefs, values and personal history—all of which are at play when interacting with others—and having “emotional intelligence” (p. 794) are necessary for effective interdisciplinary participation. It appears that as the various members of the interdisciplinary training team in our project asserted their voices at the decision-making table in our project, other trainers were able to learn more about discipline-specific practices and training needs. In order for this process to happen in a way that did not alienate others, we found it necessary to make careful decisions about what to say where and when. Knowledge of how to work in groups and teams was critical, especially for the professionals who were at risk of marginalization in the “collaborative” process.
Collaboration skills. The display of collaboration skills is predicated upon a firm grounding in collaborative attitudes and requisite knowledge, including those mentioned above. Putting these ideas into practice requires strong interpersonal skills such as listening, empathy, humor, facilitation, assessment (Arredondo et al., 2004), ability to participate in power sharing (McLean, 2012), and being able to use feedback to make subsequent changes (Nancarrow et al., 2013). Collaboration also requires problem-solving and decision-making skills (Nancarrow et al., 2013; Wellmon et al., 2012) as well as assertiveness, confidence and ability to communicate one’s ideas appropriately (Miller & Katz, 2014; Nancarrow et al., 2013). Finally, most agree that skills for collaboration include being flexible (Arredondo et al., 2004; Miller & Katz, 2014). Power sharing is possible when participants demonstrate competence in their area of expertise as well as interest in learning about collaborators’ fields of specialization. As already noted in our training project, the demonstration of professional competence, confidence and the ability to engage interpersonally in the spirit of collaboration and collegiality created an opportunity for power sharing. We also noticed in the SBIRT project that when we were flexible and willing to accommodate other’s beliefs and values, they in turn made efforts to accommodate ours.
Conclusion
Counselor educators need to examine pedagogical means of providing counseling students with the knowledge, values and skills to work effectively in interdisciplinary teams. For one counselor education program, the experience of interdisciplinary training provoked passionate dialogue among students and faculty regarding their professional roles, functions, professional advocacy and positioning among other behavioral health professionals. Multiple opportunities for exploring interdisciplinary training and professional identity development processes were evident in the training project described in this article.
Of course, learning about interdisciplinary collaboration does not need to happen solely within a project such as this. Counseling internships typically offer an abundance of opportunities for interdisciplinary collaboration, and the points raised in this article are relevant to all training venues available for counseling students. As mentioned, providing counselors-in-training with a firm foundation in professional orientation both in terms of philosophical underpinnings as well as a clear understanding of their future scope of practice are critical. Additionally, instruction on the scope of practice and roles of other professionals with whom they may be working in practice settings is important. Assuring that counselors enter into internship settings with adequate competence is, of course, critical. But additionally, providing students with positive appropriate feedback so they develop a clear sense of confidence is equally as important for work in collaborative settings. Finally, offering counseling students “pre-training” in collaborative practice, including the requisite skills and attitudes mentioned in this article, is an important component of preparing counselors for interdisciplinary practice. In training sessions such as these, counseling students should be coached to talk about the work they are trained to do, required to assert their perspective in treatment team decision making and offered feedback on the ways in which their voices are heard by others.
In terms of future directions, an exploration of counseling students’ perceptions of the impact of interdisciplinary training on their professional identity development and their ability to work with interdisciplinary teams would be valuable for the field. The outcome of such a study might increase the understanding of the pedagogical experiences that enhance interdisciplinary work competencies for counselors.
STATEMENT OF FUNDING
The interdisciplinary training initiative reported in this publication is part of the Vermont SBIRT Training Collaborative funded by the Substance Abuse and Mental Health Services Administration (SAMHSA), Grant #TI025395-01. The content is solely the responsibility of the authors and does not necessarily represent the official views of SAMHSA.
References
Agerwala, S. M., & McCance-Katz, E. F. (2012). Integrating screening, brief intervention, and referral to treatment (SBIRT) into clinical practice settings: A brief review. Journal of Psychoactive Drugs, 44, 307–317. doi:10.1080/02791072.2012.720169
American Counseling Association. (2014). ACA code of ethics. Alexandria, VA: Author.
Arredondo, P., Shealy, C., Neale, M., & Winfrey, L. L. (2004). Consultation and interprofessional collaboration: Modeling for the future. Journal of Clinical Psychology, 60, 787–800. doi:10.1002/jclp.20015
Bemak, F. (1998). Interdisciplinary collaboration for social change: Redefining the counseling profession. In C. C. Lee & G. R. Walz (Eds.), Social action: A mandate for counselors (pp. 279–292). Greensboro, NC: ERIC/CASS.
Collin, A. (2009). Multidisciplinary, interdisciplinary, and transdisciplinary collaboration: Implications for vocational psychology. International Journal for Education and Vocational Guidance, 9, 101–110. doi:10.1007/s10775-009-9155-2
Council for the Accreditation of Counseling and Related Programs (CACREP). (2009). CACREP accreditation standards and procedures manual. Alexandria, VA: Author.
Davoudi, M., & Rawson, R. A. (2010). Screening, brief intervention, and referral to treatment (SBIRT) initiatives in California: Notable trends, challenges, and recommendations. Journal of Psychoactive Drugs, 42, 239–248. doi:10.1080/02791072.2010.10400547
Delunas, L. R., & Rouse, S. (2014). Nursing and medical student attitudes about communication and collaboration before and after an interprofessional education experience. Nursing Education Perspectives, 35, 100–105. doi:10.548Q/11-716.1
Forrest, L. (2004). Moving out of our comfort zones: School counseling/counseling psychology partnerships. The Counseling Psychologist, 32, 225–234. doi:10.1177/0011000003261368
Gibson, D. M., Dollarhide, C. T., & Moss, J. M. (2010). Professional identity development: A grounded theory of transformational tasks of new counselors. Counselor Education and Supervision, 50, 21–38.
Institute of Medicine (U.S.), Greiner, A., & Knebel, E. (2003). Health professions education: A bridge to quality. Washington, DC: National Academies Press.
Kaplan, D. M., & Gladding, S. T. (2011). A vision for the future of counseling: The 20/20 “Principles for Unifying and Strengthening the Profession.” Journal of Counseling & Development, 89, 367–372. doi:10.1002/j.1556-6678.2011.tb00101.x
Mascari, J. B., & Webber, J. M. (2006). Salting the slippery slope: What licensing violations tell us about preventing dangerous ethical situations. In G. Walz, J. Bleuer, & R. Yep (Eds.), VISTAS: Compelling perspectives on counseling 2006 (pp. 165–168). Alexandria, VA: American Counseling Association.
Mascari, J. B., & Webber, J. (2013) CACREP accreditation: A solution to license portability and counselor identity problems. Journal of Counseling & Development, 91, 15–25. doi:10.1002/j.1556-6676.2013.00066.x
McLean, S. (2012), Barriers to collaboration on behalf of children with challenging behaviours: A large qualitative study of five constituent groups. Child & Family Social Work, 17, 478–486. doi:10.1111/j.1365-2206.2011.00805.x
McNair, R. P. (2005). The case for educating health care students in professionalism as the core content of interprofessional education. Medical Education, 39, 456–464. doi:10.1111/j.1365-2929.2005.02116.x
Mellin, E. A., Hunt, B., & Nichols, L. M. (2011). Counselor professional identity: Findings and implications for counseling and interprofessional collaboration. Journal of Counseling & Development, 89, 140–147. doi:10.1002/j.1556-6678.2011.tb00071.x
Meyers, F. J., Hales, R. E., Young, H. M., Nesbitt, T. S., & Pomeroy, C. (2013). Restructuring academic health centers to advance interdisciplinary collaborations: Opportunities for psychiatry departments. Academic Psychiatry, 37, 72–75. doi:10.1176/appi.ap.11120209
Miller, F. A., & Katz, J. H. (2014). 4 keys to accelerating collaboration. OD Practitioner, 46, 6–11. Retrieved from: https://c.ymcdn.com/sites/odnetwork.site-ym.com/resource/resmgr/2015_Awards/ODP-V46,No1-Miller_and_Katz.pdf
Mitchell, S. G., Gryczynski, J., Gonzales, A., Moseley, A., Peterson, T., O’Grady, K. E., & Schwartz, R. P. (2012). Screening, brief intervention, and referral to treatment (SBIRT) for substance use in a school-based program: Services and outcomes. The American Journal on Addictions, 21, S5–S13. doi:10.1111/j.1521-0391.2012.00299.x
Morphet, J., Hood, K., Cant, R., Baulch, J., Gilbee, A., & Sandry, K. (2014). Teaching teamwork: An evaluation of an interprofessional training ward placement for health care students. Advances in Medical Education and Practice, 5, 197–204. doi:10.2147/AMEP.S61189
Nancarrow, S. A., Booth, A., Ariss, S., Smith, T., Enderby, P., & Roots, A. (2013). Ten principles of good interdisciplinary team work. Human Resources for Health, 11(19), 1–11. doi:10.1186/1478-4491-11-19
O’Brien, B. (Producer & Director). (2013). The hungry heart [Motion picture]. United States: Kingdom County Productions.
Pollard, K. C., & Miers, M. E. (2008). From students to professionals: Results of a longitudinal study of attitudes to pre-qualifying collaborative learning and working in health and social care in the United Kingdom. Journal of Interprofessional Care, 22, 399–416. doi:10.1080/13561820802190483
Reubling, I., Pole, D., Breitbach, A. P., Frager, A., Kettenbach, G., Westhus, N., Kienstra, K., & Carlson, J. (2014). A comparison of student attitudes and perceptions before and after an introductory interprofessional education experience. Journal of Interprofessional Care, 28, 23–27. doi:10.3109/13561820.2013.829421
Wellmon, R., Gilin, B., Knauss, L., & Linn, M. I. (2012). Changes in student attitudes toward interprofessional learning and collaboration arising from a case-based educational experience. Journal of Allied Health, 41, 26–34.
Jane E. Atieno Okech, NCC, and Anne M. Geroski are Associate Professors at the University of Vermont. Correspondence can be addressed to Jane Okech, Mann Hall 101B, 208 Colchester Avenue, Burlington, VT 05405, jokech@uvm.edu.
Dec 7, 2015 | Article, Volume 5 - Issue 4
Corrine R. Sackett, Nadine Hartig, Nancy Bodenhorn, Laura B. Farmer, Michelle R. Ghoston, Jasmine Graham, Jesse Lile
This study explored what faculty members are recommending to counselor education master’s students regarding post-master’s experience when considering doctoral studies and what the current faculty hiring preferences are in reference to the amount of post-master’s experience needed. Advisors in counselor education master’s programs encounter these questions, and the authors believe the findings are beneficial in helping provide answers. Findings indicate faculty members believe post-master’s experience informs supervision, teaching, research and professional identity during the doctoral program and in faculty roles. Findings also indicate faculty members consider the characteristics and circumstances of each individual in determining how important post-master’s experience is prior to entering a doctoral program.
Keywords: counselor education, faculty, supervision, post-master’s experience, doctoral study
An important duty of faculty counselor educators is advising master’s-level students interested in obtaining doctoral education. A doctoral degree is designed to provide the student with advanced competencies in clinical practice, classroom instruction, supervision, research and leadership so that the student may serve as a future leader for the profession of counselor education in academic positions (Bernard, 2006; Goodrich, Shin, & Smith, 2011). While the primary focus of the counselor education doctoral degree is to prepare future leaders in the profession (Goodrich et al., 2011), counselor education has historically lacked clear professional standards regarding the amount or type of necessary counseling experience for admission into doctoral programs (Boes, Ullery, Millner, & Cobia, 1999; Schweiger, Henderson, McCaskill, Clawson, & Collins, 2012; Warnke, Bethany, & Hedstrom, 1999).
When applying for and entering a doctoral-level counselor education and supervision (CES) program, it is assumed that the student has achieved the competencies of an entry-level clinician and has met the requirements of a Council for Accreditation of Counseling and Related Educational Programs (CACREP) accredited master’s program (Goodrich et al., 2011). However, few guidelines have been provided to doctoral applicants about the types or amount of post-master’s experience (PME) necessary or preferred for optimal hiring into a faculty position, for which CES graduates are uniquely qualified. Lack of guidelines can create confusion about how graduate students can best position themselves for successful academic employment (Schweiger et al., 2012; Warnke et al., 1999).
Though conventional wisdom may tell us that the more experience one has, the better, we do not have empirical data in the CES field of how counselor educators are advising master’s students on this issue, or of what faculty search committees prefer in terms of the clinical experience level of candidates. Thus, this study broadly examines the questions: What are faculty members recommending to counselor education master’s students regarding PME when considering doctoral studies? What are current faculty hiring preferences in reference to levels of experience needed? Faculty members, supervisors and advisors frequently encounter these questions from master’s students, and the researchers believe students, faculty and ultimately the counseling field will benefit from information clarifying the current industry standard for counselor education.
Research on CES Preferred Clinical Experience
The field of counselor education lacks clear professional standards regarding the amount or type of necessary counseling experience for admission into doctoral programs (Schweiger et al., 2012; Warnke et al., 1999). One study’s findings concluded that work experience was a necessary component to doctoral admissions (Nelson, Canada, & Lancaster, 2003). Of the 25 CACREP programs that participated in this study, 20 programs rated successful work experience as a criterion for admission to their doctoral programs. In addition, 16 of those reported that work experience is often helpful or always helpful in selecting good doctoral students. One of their respondents reported difficulty in requiring successful work experience because so few applicants had post-master’s counseling experience.
A recent study reviewed the requirements and preferences listed in counselor education faculty position postings on the Counselor Education and Supervision Network (CESNET) between 2005 and 2009 (Bodenhorn et al., 2014). The researchers found 83% of assistant and associate professor position announcements listed counseling experience or licensure as a required or preferred qualification. This remains consistent with a previous finding from Rogers, Gill-Wigal, Harrison, and Abbey-Hines (1998) that counselor education programs ranked clinical experience as the second most important criteria for faculty positions, second only to a PhD in counselor education. Researchers of the 1998 study asserted that although it is clear in their findings that clinical experience is important, whether that clinical experience occurs during internships or outside of coursework is unclear.
These studies showed that experience is prioritized in doctoral admissions (Nelson et al., 2003), as well as in hiring CES faculty members (Bodenhorn et al., 2014; Rogers et al., 1998), yet the counselor education field still lacks important information around this topic. Specifically, the field is lacking data indicating what advice counselor educators give master’s-level students about the amount of experience to obtain prior to entering a doctoral program, and data indicating the amount of post-master’s clinical experience CES faculty search committees prefer in candidates. The current study addresses these gaps in the literature in the exploration of preferences for PME.
Research on Other Helping Professions’ Preferred Clinical Experience
A review of American Psychological Association (APA) accredited clinical psychology programs found academic criteria to be the most important in selecting doctoral students, with achievement of clinical competence also being important (O’Leary-Sargeant, 1996, as cited in Nelson et al., 2003). Another study’s findings included that success in a marriage and family therapy doctoral program correlated positively with age, and students with clinical experience were rated as better clinicians than those who did not have clinical experience (Piercy et al., 1995). It should be noted that researchers did not distinguish between participants who became faculty or expert clinicians in their study.
In the related field of social work, Proctor (1996) and Munson (1996) had opposing viewpoints of whether doctoral programs should admit graduate students with fewer than 2 years of post-master’s in social work (MSW) experience. Proctor argued that doctoral programs in social work should not require PME because it is a detriment to the field. He justified this viewpoint with the idea that by requiring experience, programs are missing out on students who are research-minded and eager to continue with their education; therefore, programs may lose them to other disciplines. Proctor also argued this requirement delays the onset of careers in social work education and research, with educators and researchers starting often in their late thirties and early forties, behind their counterparts in other disciplines. Munson argued that it is not possible for graduates of social work doctoral programs to fulfill the needs of the field, which include building knowledge, conducting practice research and effectively teaching social work practice, without post-MSW experience.
The research in CES and related fields in the area of experience preferred for doctoral programs and faculty positions is dated. Further, the CES field is lacking data on how counselor educators are advising master’s students in terms of amount, if any, of PME that would be beneficial to obtain prior to entering a doctoral program. The field also is lacking clear data on preferences of CES search committees on clinical experience gained outside of program practicum and internships. An exploration of these two questions will equip counselor educators in more effectively advising master’s students who are interested in doctoral programs and faculty careers in CES.
Method
The authors used a survey with both closed and open-ended questions to gain both quantitative and qualitative data about the research questions: What are faculty members recommending to counselor education master’s students regarding PME when considering doctoral studies? What are current faculty hiring preferences regarding levels of experience needed? Surveys were developed by the research team and piloted among CES colleagues with questions about serving on search committees and what priority considerations are given during a search for CES clinical and tenure-track faculty. Hypothetical situations involving a master’s student asking for advice about pursuing a doctoral degree and a search committee situation also were posed in the survey, with space to provide a rationale for the responses, which garnered qualitative data.
Procedure
Access to participants was developed in two different formats, using the same survey. Using a purchased list of 500 randomly selected members of the Association for Counselor Education and Supervision (ACES), half of the names on the list were contacted by postal mail, and half were contacted by e-mail with a request to complete the survey. Response rates have been shown to be higher for surveys sent through postal mail than for surveys sent electronically (Shannon & Bradshaw, 2002) and the researchers aimed to maximize the response rate; however, financial constraints mandated that only half of the surveys be sent through postal mail. Three weeks after the surveys were distributed, a reminder was sent electronically to request completion of the survey, providing the alternative of electronic completion for those who had received the initial request in postal mail. The survey was housed on SurveyMonkey, using the secure feature. The authors input the results in SurveyMonkey for the postal responses.
Simultaneously, the authors sent a survey electronically to the liaison for each of the programs listed on the CACREP Web site as accredited for a doctoral CES program. A question from that survey was used to provide insight about positive and negative impact of post-master’s counseling experience on students’ performance in doctoral classes.
Participants
One hundred and sixty-six respondents completed the ACES survey (33% response rate). In terms of rank, 35 respondents (21%) indicated they were a professor, 53 (32%) associate professor, 49 (30%) assistant professor, 23 (14%) non-tenure track (clinical or adjunct), and 6 (3%) indicated they fell into an other category. About 51% of the respondents had taught a doctoral-level counselor education course before (84), and the other half had not (81), having only taught master’s-level classes. Twenty-seven percent (44) of respondents reported they had never served on a CES faculty search committee. Among the respondents who indicated they had served on CES faculty search committees, 44% (72) served on 1–4 committees, 19% (31) served on 5–8 committees, 4% (7) served on 9–12 committees, and 6% (10) served on more than 12 committees. Eighteen out of 57 CACREP liaisons responded to the survey (32% response rate). Demographic data was not collected from this group.
Survey Design
To respond to the stated research questions, the authors deemed it was important to request demographic information on rank, programs offered, doctoral teaching experience and the number of search committees on which the participants had served. Two questions were developed asking for level of importance of qualifications when considering candidates for a tenure-track position and a non-tenure track (i.e., adjunct or clinical) position. The qualifications the authors identified were: post-master’s counseling, publications, grants, supervision, college teaching, professional organization involvement and professional organization leadership. Participants rated the level of importance as 1 (not at all), 2 (somewhat), 3 (quite a bit) and 4 (extremely). The participants also were asked to provide a minimum quantity for each qualification, if the participant deemed the qualification to be quite a bit or extremely important. The qualifications included were selected based on surveying position announcements for CES positions. Four hypothetical scenarios were presented to the participants that included situations involving serving on a search committee and serving as an advisor to a master’s student with particular questions about pursuing a doctoral degree. Each of the hypothetical scenario questions asked for a response and a rationale for that response. Researchers piloted the survey with three faculty members who all reported that the survey was clear. The pilot participants’ responses were reviewed to ensure survey questions measured what was intended.
Data Analysis
Authors analyzed the demographic and scaling questions by count and percentages using the SurveyMonkey results produced by the software. The results include numerical count of the participant responses.
The authors analyzed responses to the open-ended comment requests using a constant comparative method described by Anfara, Brown, and Mangione (2002), along with a form of check coding described by Miles and Huberman (1994). The first three authors were the analysis team for this process. Two team members independently conducted a first iteration of assigning open codes for each of the five open-ended questions by reading the data from each question broadly and noticing regularities (Anfara et al., 2002). The two authors then conducted a second iteration of comparison within and between codes in order to create categories and identify themes. The constant comparative method of analysis allows a way to make sense of large amounts of data by organizing into manageable parts first and subsequently identifying themes and patterns.
The third team member served in a peer review capacity (Miles & Huberman, 1994) during the categorizing and theme identification for that question. For each question, different team members were assigned as coders and the peer reviewer. Once the team members assigned individually derived themes, the team came together and the peer reviewer for each question led the discussion to arrive at consensus for the categories. Each coder presented individually derived themes, listened to the other and, in areas of difference, the team discussed analysis and wording. During this discussion, the peer reviewer clarified and probed using the original comment wording, and the team came to consensus for the themes through this process. These team members sent the themes and the original data for each of the questions to each of the other authors, who served in another layer of peer review to examine the analysis.
Results
Hiring Preferences and Practices for CES Positions
When evaluating applicants for tenure-track CES positions at the assistant professor level, the largest group of respondents (46%) reported that post-master’s counseling experience was quite a bit important. Forty-four percent of those respondents deemed 2 years to be the minimum number of experience. Also rated quite a bit important by most respondents was supervision experience (40%), with a minimum of 2 years of experience (45%), and professional organization involvement (43%), with a minimum of 2 years of experience (33%). As for publications, grants, college teaching and professional organization leadership experience, most respondents (48%, 55%, 35%, and 57% respectively) reported those qualifications were somewhat important when evaluating applicants for tenure-track positions. Respondents who deemed these areas as important reported a minimum of 2 publications submitted (41%), 1 year of college teaching experience (49%), and 1 year of professional organization leadership experience (71%).
When asking the same question, but when hiring for a non-tenure-track (clinical or adjunct) CES faculty position, respondents reported a different emphasis on priorities. Most respondents (43%) indicated that PME was extremely important, with a minimum number of 2 years (28%), and supervision experience was quite a bit important (43%), with a minimum of 2 years (31%). Most respondents indicated grants and professional organization leadership as not at all important (74% and 50% respectively), and respondents were split between not at all important (48%) and somewhat important (48%) for publications. The majority of respondents indicated college teaching (41%) and professional organization involvement (42%) as somewhat important.
Seventy-two participants responded to a question to indicate the top three priorities of counseling experience preferred for the most recent tenure-track CES assistant or assistant/associate professor faculty search committee they served on. The majority of respondents (64%) indicated school counseling experience was preferred, while 61% preferred experience with populations diverse in culture or ethnic identity, and 59% preferred experience in community-based agencies. Other areas of experience preference included the following: families (25%), addictions (17%), other (13%), private practice (13%), populations diverse in age (11%), play therapy (9%), populations diverse in religious/spiritual identity (9%), populations diverse in sexual identity (7%), inpatient or day treatment (5%), bilingual (2%) and in-home treatment (1%).
Hypothetical Situation Hiring for Tenure Track
Participants were asked which candidate they would prefer to hire for a tenure-track assistant professor position, given two candidates with all things being equal with one exception. Candidate 1 earned a master’s degree, directly entered and completed a doctoral program and then went into the field and gained 3 years of professional experience. Candidate 2 earned a master’s degree, directly went into the field and gained 3 years of professional experience, then entered and completed a doctoral program. One hundred and thirty-eight participants responded to this question. Sixty percent of respondents would prefer candidate 2, 34% would have no preference and 6% would prefer candidate 1. Four themes emerged in the qualitative responses to this question: (1) PME is more relevant and important in training master’s students, (2) PME makes the doctoral program more valuable, (3) research staleness and (4) fit.
PME is more relevant and important in training master’s students relates to what the candidate would be doing in their role as a counselor educator, and participants reported having the clinical experience following their master’s program and prior to their doctoral program was more beneficial in training master’s students. One participant indicated:
This candidate understands what it’s like to work in the field with a master’s degree—a very different experience than working with a PhD. They will be able to better prepare students for the common pressures and issues of working with a master’s (degree) in an agency. This was critical for me as I began teaching.
Another participant spoke to this, specifically in training school counselors:
(The) candidate needs to understand the professional role of a school counselor. This is best accomplished when employed as a school counselor—then a doctoral program afterwards—allows more thorough research on a profession. They understand at a ground level through personal experience.
The second theme, PME makes the doctoral program more valuable, represents participants’ beliefs that having the clinical experience prior to their doctoral studies would make that learning more valuable, as they would have practical experience to help make sense of the abstract learning. One participant illustrated this theme: “I believe the post-master’s degree experience provides candidates with context that helps make doctoral study richer and more relevant to practice.” Another participant pointed to the benefit of PME evident in this theme: “Having experience prior to the PhD allows the (doctoral) student to anchor knowledge and the clinical experiences at the doctoral level, especially courses like supervision.”
The third theme, research staleness, speaks to participants’ concerns that candidates who had been practicing for several years after graduating from a doctoral program would be out of touch with research and writing required in academia. A participant clearly stated this concern: “. . . the candidate that worked after doctoral program may lose scholarly writing and research skills.” Another participant relayed a similar concern:
I think coming right from the doc-level program would provide some of the most current literature/research knowledge for the new faculty, as well as increase the likelihood that the person is poised to submit manuscripts, have a research agenda and probably would have some grant writing experience. I know how busy the counselors in the field are with client productivity, and I think it’s harder to commit to writing and research as a full-time clinician.
Finally, the fourth theme, fit, encompasses participants’ feelings that either candidate would be fine if they were a good fit for the position and program. One participant shared his or her concern for the individual, rather than when they accrued experience:
They have the same amount of professional experience, just at different times in their career. I think there would probably be some pros and cons to each path. I would be more interested in HOW they each spoke about their experiences and the decision-making process they used.
Another participant stated that either candidate would work: “Regardless of order, the applicant received some of the same experience. Either the doctoral work informed their clinical work or their clinical work informed their doctoral work.”
Hypothetical Advising Situations
Researchers asked participants how they would respond to a hypothetical advising situation with a master’s student:
Hypothetically, in October, a master’s-level student who will graduate in May comes to you for advice. The student’s ultimate goal is to be a faculty member and is planning to apply to doctoral programs for entrance in August. Please indicate what your response would be and explain your response in the space below.
One hundred and forty-two participants responded to this question. Twenty-nine percent responded that their recommendation would depend on the quality of the work accomplished by the student. Twenty-seven percent responded that it would depend on the age and maturity of the student. Eighteen percent responded that it would depend on some other factor. Fifteen percent responded they would encourage the student, and 12% responded that they would discourage the student. Three themes emerged from the explanations related to this question: (1) depends on the quality of the student (quality of work, etc. and things related to readiness), (2) need PME and license and (3) encourage student regardless.
The first theme, depends on the quality of the student, includes responses about the quality of the master’s student’s work, maturity level, life experience and readiness. This participant’s response highlights this theme:
It really depends on the quality of work AND the life experiences and maturity level of the student (not the age, but the maturity level). Thus, if (the student) had high levels of quality work, and had experience in a variety of settings (e.g., volunteering, clinical work, GA, etc.) outside of “just” coursework, and seemed to have a breadth of understanding and perspective (i.e., maturity), then I would encourage the doctoral program. However, if any of these areas were lacking I might discuss the possibility of gaining some experience first before applying. It also depends on how active (the student) was in terms of service at the master’s level (e.g., CSI, or community activities).
Although this respondent clearly differentiated maturity from age, other respondents indicated age was a factor, such as this participant: “If the student is younger or has very limited mental health experience, I would probably suggest getting some counseling experience before beginning a doctorate.”
The second theme, needs PME and license, includes the respondents who felt that regardless of the student qualities, PME and licensure are important. The following quote illustrates this theme: “I would encourage the student to work in the field and gain licensure or certification first. I believe that working provides valuable insight into the profession and prepares professors to be more effective when teaching students.”
Finally, on the other end of the spectrum from the previous theme, some respondents said they would encourage any of their students who wished to pursue a doctorate, making up the third theme, encourage student regardless. A respondent expressed the opinion, “One can never know the success level of prospective doctoral student[s]. If they have the desire, they should be encouraged to pursue their goal.”
In another hypothetical situation, researchers asked respondents the following:
Hypothetically, a master’s student who has the GOAL OF becoming a FACULTY MEMBER asks you for advice. The question asked is how many years of post-master’s clinical experience the student should obtain prior to applying to a doctoral program. What would your advice be?
There were 136 respondents to this question. Forty-nine percent would advise at least 2 years of post-master’s clinical experience, 21% would advise the student to enter the doctoral program right away without any experience, 13% would advise obtaining at least 3 years of experience, 14% would advise at least 1 year, 3% would advise at least 5 years, and none would advise more than 5 years. Two themes emerged related to the associated rationale for respondents’ choices to this question: (1) depends on personal factors of the student and (2) enough time to gain experience.
The first theme, depends on personal factors of the student, included factors such as quality of the student, their readiness and maturity level, as well as doctoral program of interest. One respondent spoke to the importance of the student’s readiness:
If the student feels ready to enter the doctoral program, then I would encourage them. I would tell them to trust their own sense of timing. I would not recommend it if they were just trying to get through without being fully interested, eager and invested in the program.
Another respondent stressed the importance of considering each student and the quality of master’s performance and desires for the future:
I did not respond here because it does not include an “it depends” answer, as it depends what experience they have, what they have gained in their master’s program, have they gone above and beyond the call of doing the basic requirements of clinical internship in the master’s program and what type of faculty member are they hoping to be (e.g., teaching only, research heavy, etc.). Thus, it really depends on the uniqueness of each student as to what I would recommend.
Finally in this theme, some respondents referred to the importance of considering which doctoral programs the student is interested in applying to. One respondent spoke to this consideration here:
Doctoral programs are designed differently. Some are designed to have clinical hours built in and are good for individuals going straight through while other programs require 2–5 years of work experience in the field and have less supervision and clinical hours.
Other respondents reported that having experience before entering a doctoral program was critical, regardless of the student, making up the second theme, enough time to gain experience. These respondents spoke to needing enough experience to earn licensure and supervision licensure and to develop a sense of professional identity first. Many also felt students should get a sense of the field before entering a doctoral program to see if they would prefer to practice at the master’s level. The following respondent spoke to the need for experience primarily to aid in his or her future doctoral student role of supervising and teaching master’s students:
In 2 years, a student would have completed or (be) near completion of licensure requirements and thus have some applied knowledge from which to draw upon. In so doing, the prospective doctoral student would bring experience and be better positioned, hierarchically speaking, to work with master’s degree-seeking students. With no experience, the doctoral student may find themselves in a position where they would be supervising or teaching a master’s degree seeking student with greater clinical/life experience creating . . . an interesting power differential.
Similarly, another respondent expressed, “How can one teach or supervise what he or she has not yet experienced?”
Many respondents indicated that gaining licensure before entering a doctoral program was critical: “Licensure in most states requires a minimum of 2 years post-master’s supervised work. I think licensure should be required before proceeding.” Speaking to the need to develop professional identity and to confirm career goals, a respondent said, “(Two years)—this provides enough time to establish a professional identity, create a track record of excellence in the field and clarify their desire to enter the academy.”
Not all respondents believed PME was vital for future faculty members however, as is evident with the following quote: “I entered right away and it worked out fine for me. I don’t think it makes a big difference either way.” Another respondent expressed concern that students who take time away from school often do not return: “I believe that people who go into post-master’s work almost never go back to get their doctorate, no matter how strong the intentions of the person are at graduation.”
In a final hypothetical situation, we asked participants the following:
Hypothetically, a master’s student who has the GOAL of becoming an ADVANCED PRACTITIONER asks you for advice. The question asked is how many years of post-master’s clinical experience the student should obtain prior to applying to a doctoral program. What would your advice be?
There were 134 respondents to this question. Thirty-eight percent would advise at least 2 years of experience, 16% responded there is no need for a doctoral degree in this situation, 10% would advise that no experience is needed and to enter right away, another 13% would advise at least 5 years of experience before applying to a doctoral program, 13% would advise at least 3 years, 9% at least 1 year, and 1% would advise more than 5 years. Four themes emerged related to this question: (1) uncertainty about the purpose of the question, (2) no need for a doctorate to practice, (3) depends on the student and their attributes and (4) desire to specialize.
The first theme, uncertainty about the purpose of the question, encompasses many responses that communicated confusion about the meaning of “advanced practitioner.” This is evident in the following quote: “Not sure what you mean by advanced practitioner.” The intention of the question was to capture potential guidance given to advisees who may seek to obtain a doctoral degree with a goal to enter or return to the clinical field, or to advance into supervision or administrative positions. However, this theme clearly shows there was confusion among respondents over the question and its intent.
The second theme, no need for a doctorate to practice, consists of responses expressing the lack of need for someone to pursue a doctoral degree in order to practice because counselors can become fully licensed at the master’s level. As one respondent stated, “A master’s degree is a terminal degree. Our 60-hour requirement makes our master’s degree an advanced clinical degree. No further coursework is needed for full licensure.” This theme also includes responses indicating that a degree in CES does not prepare you for further clinical practice, as this respondent communicated: “Degrees in counselor education are really about preparing someone for a faculty or supervisor position, in my opinion, and often require little in the way of advanced counseling skill development.”
For this question, as in many of the others, a theme emerged related to the individual student, depends on the student and their attributes. One respondent said that young and bright people can make it happen: “Still believing that bright young people can master most things easily, I don’t believe that waiting to get experience is necessary.”
The final theme, desire to specialize, includes responses indicating the following recommendations: use PME to find a specialization before pursuing a doctorate, PME would make the doctoral program more meaningful, and some students may decide they do not need the doctorate in order to do what they want. A respondent illustrated this theme: “Get some counseling experience and have your counseling license in hand before embarking on doctoral study. Gain some perspective about the areas you want to study in depth, based on what challenges you encounter in actual practice.”
Impact of PME on Doctoral Student Performance
Finally, researchers asked CACREP liaisons about the positive or negative impact of post-master’s counseling experience on their doctoral students’ performance in class. Two themes emerged in the participants’ answers: (1) the more experience the better and (2) experience is valuable, but not essential.
In the first theme, the more experience the better, respondents described the ways that PME helps doctoral students in the classroom. This includes observations from CACREP liaisons that doctoral students who have worked in the field know what mental health issues look like and how to respond. They also are better able to apply content learned in the doctoral program to practice. PME helps doctoral students feel more confident and increases their credibility with master’s students they are teaching and supervising. When doctoral students have PME, they are better equipped to help master’s students in their developmental journey. One respondent illustrated some of these thoughts:
The more experience the better, particularly in terms of supervision and teaching. Without a fairly substantial fund of knowledge about applied practice, doctoral students have difficulty helping master’s counselors-in-training understand abstract concepts in practical terms. What does PTSD look like? How do I respond to a client who becomes suicidal in session? . . . Because our doc students begin providing supervision in the first year of their program, I would be particularly concerned if the ONLY experience they had was in their own master’s internships. They would be essentially just one year (maybe semester) ahead of those they are supervising.
In the second theme, experience is valuable, but not essential, respondents wrote about the experience gained in the master’s and doctoral programs being enough. An example of this rationale is shown here: “. . . although we will admit students without post-master’s experience, we offer deep clinical experience while in our doc program. Many doc students complete two full years of internship while in the program.”
Discussion
The findings of this study help fill a gap in the literature identified by Boes et al. (1999) and Warnke et al. (1999) about the amount of counseling experience needed prior to entering doctoral programs. Goodrich et al. (2011) and Bernard (2006) asserted that doctoral degrees in CES are intended to provide the student with advanced competencies in clinical practice, classroom instruction, supervision, research and leadership so that the student may serve as a future leader for the profession of counselor education in academic positions. Specifically, these findings shed light on what faculty members are recommending to master’s students regarding PME prior to entering a doctoral program and faculty members’ preferences in hiring colleagues with regard to PME.
PME is important both for doctoral students and faculty members, as is indicated by our findings. According to respondents, experience informs supervision, teaching, research and professional identity during the doctoral program and in faculty roles. These findings are compatible with previous research (Bodenhorn et al., 2014; Munson, 1996; Nelson et al., 2003; Rogers et al., 1998). Nelson et al.’s (2003) findings point to the importance of PME in doctoral admissions. They found this was a helpful factor in selecting quality doctoral students, though their participants reported not all applicants have this experience. As for future faculty members, experience has been found to be important as well by Rogers et al. (1998) and Bodenhorn et al. (2014). Bodenhorn established that the majority of assistant and associate professor announcements on CESNET listed counseling experience or licensure as a required or preferred qualification, and Rogers et al. found that counselor education programs ranked clinical experience as their second most important criteria for faculty positions. Similarly, in the social work discipline, Munson (1996) asserted social work PhDs need to have post-MSW experience in order to fulfill the needs of the field, which include teaching master’s-level students and researching to enhance knowledge.
CES faculty spoke to the importance of clinical practice in areas of teaching, supervision and research. Munson (1996) connected clinical experience to research performance in reporting that doctoral students who lack clinical experience tend to avoid practice-related dissertation studies. Similarly, respondents in our study wrote about doctoral students’ clinical experience providing fodder for research ideas. Further, clinical experience may validate teaching credibility (Rogers et al., 1998). This was evident in this study’s findings as well, along with validating supervision credibility. There was concern among respondents about doctoral students providing supervision to master’s students who would possibly be only one semester behind them in experience. In addition, respondents expressed concern that doctoral students and future faculty members with no PME would exhibit rote, by-the-book teaching, rather than drawing on clinical experience to illustrate abstract concepts in counseling.
Though there was much support for PME in our findings, many respondents emphasized evaluating the circumstances of each student individually. Among the circumstances that stood out were age and maturity. Some respondents expressed concern that it can be difficult to return to school once individuals have careers and families. The academic and skill level of the master’s student was another factor emphasized by respondents. Proctor (1996) asserted that the social work field might miss out on academically skilled and eager students by requiring PME. This may be a fear for some in the counselor education field as well. Indeed, within this study’s findings, there was a tension between academically and clinically gifted students entering doctoral programs right away and the importance of getting experience.
For many respondents, the amount of experience obtained during the master’s and doctoral programs is enough, especially in cases where students work in clinical positions while completing their doctoral degrees. Some respondents pointed out that doctoral programs in CES are designed differently, with some emphasizing clinical work as part of the doctoral training and others operating on the assumption that the doctoral student is already an experienced clinician. For example, faculty members might support a master’s student going straight to a doctoral program if the student is applying to a doctoral program with robust opportunities to gain clinical experience.
Implications
These findings will help counselor educators better advise master’s students who have aspirations for doctoral work. Specifically, this study informs the CES field about the value placed on PME. It may be beneficial for advisors to share the findings of this study with advisees who are considering doctoral programs. In addition, advisors may consider the academic and skill level strength of the master’s student and may emphasize more years of clinical experience before applying to doctoral programs to those students who could benefit from the additional experience. Further, students who exhibit more maturity through age and life experience may be perceived as ready to handle doctoral work sooner than those who have entered the master’s program immediately from their undergraduate program.
Responses in this study are in line with Goodrich et al.’s (2011) findings that CACREP-accredited doctoral programs train students in somewhat different ways. Advisors may have familiarity with a variety of doctoral programs and can help their advisees consider the cultures of each to find the best fit in terms of experience, as well as other characteristics.
Finally, it appears clear that experience is valuable; thus, advisors would be wise to encourage students to get PME. The findings of this study show that counselor educators believe experience enriches individuals’ teaching, supervision and research. As such, master’s students will make more effective future doctoral students and faculty members if they gain PME first.
There are limitations to this study that are important to note. While a 33% response rate is considered acceptable, we would prefer to have more than 166 responses. There is likely a portion of professional counselor educators who are not members of ACES and therefore were not included in our sample, and there is no way to determine the numbers or the characteristics of those who choose membership and those who do not. A significant number of the participants had not served on search committees or taught a doctoral class, so those responses might be considered more theoretical than historical. Finally, our hypothetical question related to how participants would advise master’s students with the goal of becoming an advanced practitioner was not clear or well received given the confusion evident in the responses. Regardless of these limitations, the results of this study are compelling. Because of the length of the survey, the demographic questions did not include personal demographics such as gender, age, or ethnicity. Similarly, we did not ask for the type of university at which the participant works (e.g., Carnegie research or teaching designation). There may be intricacies of type of university and relevance of experience or advice that were not identified in this study.
Future research is needed on the role PME plays in the development of the counselor educator as a scholar, teacher and academic leader. Additional research exploring the impact of PME on a CES faculty member’s success in a faculty role, particularly teaching and supervision, would be helpful to the field. Furthermore, research delineating the different types of institutions and possibly different qualifications would assist CES advisors. Lastly, research exploring current practices and potential in the CES field for producing doctoral-trained counselors to represent the counseling discipline at the administrative and supervisory levels of mental health facilities may provide beneficial information for advancing the field.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Anfara, V. A., Jr., Brown, K. M., & Mangione, T. L. (2002). Qualitative analysis on stage: Making the research process more public. Educational Researcher, 31(7), 28–38.
Bernard, J. M. (2006). Tracing the development of clinical supervision. The Clinical Supervisor, 24, 3–21.
Bodenhorn, N., Hartig, N., Ghoston, M. R., Graham, J., Lile, J. J., Sackett, C. R., Farmer, L. B. (2014). Counselor education faculty positions: Requirements and preferences in CESNET announcements 2005–2009. Journal of Counselor Preparation and Supervision, 6, 1–16. doi:10.7729/51.1087
Boes, S. R., Ullery, E. K., Millner, V. S., & Cobia, D. C. (1999). Meeting the challenges of completing a counseling doctoral program. Journal of Humanistic Education and Development, 37, 130–144.
Goodrich, K. M., Shin, R. Q., & Smith, L. C. (2011). The doctorate in counselor education. International Journal for the Advancement of Counselling, 33(3), 184–195.
Miles, M. B., & Huberman, A. M. (1994). Qualitative data analysis: An expanded sourcebook (2nd ed.). Thousand Oaks, CA: Sage.
Munson, C. E. (1996). Should doctoral programs graduate students with fewer than two years of post-MSW practice experience? No! Journal of Social Work Education, 32, 167–172.
Nelson, K. W., Canada, R. M., & Lancaster, L. B. (2003). An investigation of nonacademic admission criteria for doctoral‐level counselor education and similar professional programs. The Journal of Humanistic Counseling, Education and Development, 42, 3–13.
Piercy, F. P., Dickey, M., Case, B., Sprenkle, D., Beer, J., Nelson, T., & McCollum, E. (1995). Admissions criteria as predictors of performance in a family therapy doctoral program. The American Journal of Family Therapy, 23, 251–259. doi:10.1080/01926189508251355
Proctor, E. K. (1996). Should doctoral programs graduate students with fewer than two years of post-MSW practice experience? Yes! Journal of Social Work Education, 32, 161–167. doi:10.1080/10437797.1996.10778446
Rogers, J. R., Gill-Wigal, J. A., Harrigan, M., & Abbey-Hines, J. (1998). Academic hiring policies and projections: A survey of CACREP- and APA-accredited counseling programs. Counselor Education and Supervision, 37(3), 166–178. doi:10.1002/j.1556-6978.1998.tb00542.x
Schweiger, W. K., Henderson, D. A., McCaskill, K., Clawson, T. W., & Collins, D. R. (Eds.). (2012). Counselor preparation: Programs, faculty, trends (13th ed.). New York, NY: Routledge.
Shannon, D. M., & Bradshaw, C. C. (2002). A comparison of response rate, response time, and costs of mail and electronic surveys. The Journal of Experimental Education, 70, 179–192.
Warnke, M. A., Bethany, R. L., & Hedstrom, S. M. (1999). Advising doctoral students seeking counselor education faculty positions. Counselor Education and Supervision, 38, 177–190. doi:10.1002/j.1556-6978.1999.tb00569.x
Corrine R. Sackett is an Assistant Professor at Clemson University. Nadine Hartig is an Associate Professor at Radford University. Nancy Bodenhorn is an Associate Professor at Virginia Tech. Laura B. Farmer is an Assistant Professor at Virginia Tech. Michelle R. Ghoston is an Assistant Professor at Gonzaga University. Jasmine Graham is an Assistant Professor at Gardner-Webb University. Jesse Lile is an Assistant Professor at the University of Saint Joseph. Correspondence can be addressed to Corrine R. Sackett, Clemson University, 307 Tillman Hall, Clemson, SC 29634, csacket@clemson.edu.