Mary Alice Fernandez, Melissa Short
This article offers mental health counselors a compilation of best practices and technology in the treatment of combat veterans suffering from post-traumatic stress disorder (PTSD). The goal is to increase counselors’ awareness of the resources available to enhance their repertoire of tools and techniques to assess, diagnose, case-conceptualize and treat the growing population of combat veterans with PTSD. The National Center for PTSD provides guidelines for diagnosing PTSD using the DSM-5. PTSD is now recognized as a trauma disorder related to an external event rather than an anxiety disorder associated with mental illness. The authors describe assessment tools and treatment strategies for PTSD validated on veteran populations. The paper also highlights new technology and mobile apps designed to assist in the treatment of combat PTSD.
Keywords: combat PTSD, trauma disorder, treatment of combat veterans, National Center for PTSD, mobile apps
Volunteering to serve one’s country during wartime is an act of heroism, and counselors working with combat veterans are in a unique position to honor these heroes. Combat veterans have offered the supreme sacrifice and some are paying a price by suffering from combat post-traumatic stress disorder (PTSD). The task of providing mental health services to a growing veteran population and their immediate family members is complicated by the lack of accessible services and the complexities of the disorder. To begin to address this challenge, Senator Jon Tester (D-MT) recently introduced legislation focused on improving access to mental health counselors by tasking the Department of Veterans Affairs (VA) with recruiting more licensed professional mental health counselors (Tester, 2013).
This article offers an overview of resources available to mental health counselors to assess, case-conceptualize, diagnose and treat a growing population of combat veterans with PTSD. The goal is to increase the awareness of both beginning counselors and more experienced counselors of new therapies as well as best practices in treating combat PTSD. The compilation of resources begins with diagnostic criteria, assessment tools, and evidence-based practices, including new technologies for treating PTSD, and culminates with a list of resources available to counselors and veterans.
Diagnosing PTSD
Changes in the Diagnostic and Statistical Manual for Mental Disorders, Fifth Edition (DSM-5) place PTSD under a new heading, Trauma and Stressor-Related Disorders, and remove it from the DSM-4 anxiety category. This new DSM-5 categorization de-stigmatizes PTSD because it recognizes PTSD as a trauma disorder related to an external event rather than an anxiety related to mental illness (Staggs, 2014). The DSM-5 provides eight clear criteria for diagnosing PTSD, beginning with identifying a traumatic event (criterion A) and then noting behavioral symptoms related to PTSD. It organizes symptoms into four clusters: intrusions (criterion B), avoidance (criterion C), negative symptoms (criterion D), and arousal (criterion E) (American Psychological Association, 2013). In order for a client to meet the full criteria for a PTSD diagnosis, his or her symptoms must last longer than a month (criterion F), must prevent him or her from functioning well in significant area(s) of life (criterion G), and cannot be due to physical factors such as a medical condition or substance use (criterion H).
The National Center for PTSD (2014a) provides guidelines for diagnosing PTSD using the DSM-5. Criterion A (stressor) indicates that the person was exposed to at least one of the following: death, threatened death, actual or threatened serious injury, or actual or threatened sexual violence. The person must persistently re-experience at least one of the intrusion symptoms (criterion B) of the traumatic event and one of the avoidance efforts (criterion C) of distressing trauma-related stimuli. Two negative symptoms or alterations in cognition or mood (criterion D) and two alterations in arousal and reactivity (criterion E) that began or worsened after the traumatic event must be present for a diagnosis of PTSD. Although symptoms may occur soon after the event, a person does not qualify for a PTSD diagnosis until at least six months after the traumatic event. An individual with PTSD will experience high levels of either depersonalization or derealization (National Center for PTSD, 2014a).
Nussbaum’s (2013) brief version for diagnosing PTSD begins by asking the following:
What is the worst thing that has ever happened to you? Have you ever experienced or witnessed an event in which you were seriously injured or your life was in danger, or you thought you were going to be seriously injured or endangered? (p. 90)
If the client answers in the affirmative, the counselor is to ask these questions: “Do you think about or re-experience these events? Does thinking about these experiences ever cause significant trouble with your friends or family, at work, or in another setting?” (Nussbaum, 2013, p. 90). Nussbaum (2013) provides a set of questions for each cluster and its associated symptoms to guide the process of diagnosis.
Assessment Tools
Ottati and Ferraro (2009) describe three assessment tools, validated on veteran populations, to screen for combat-related PTSD: the 17-item self-report PTSD Checklist (PCL), the 35-item self-report Mississippi Scale for Combat-Related PTSD (M-PTSD), and the Clinician-Administered PTSD Scale (CAPS). The PCL was recently updated to 20 items to reflect the changes in DSM-5. PCL-5 is a self-report measure that takes 5–10 minutes to complete and may be used to screen, diagnose and monitor changes during and after treatment of PTSD (Weathers et al., 2013). The M-PTSD uses a 5-point Likert scale to rate PTSD symptoms and related symptoms of substance abuse, suicidal ideation, and depression. It provides a PTSD symptom severity index with scores ranging from 35–175. The M-PTSD has not been revised since DSM-3, but may still be useful since it was normed with veteran populations (National Center for PTSD, 2014b). CAPS is a diagnostic structured interview that also measures the severity of symptoms and was recently revised to assess the DSM-5 PTSD symptoms. CAPS-5 is a 30-item questionnaire that takes 45–60 minutes to administer and yields a single score of PTSD severity (Weathers et al., 2013).
Other instruments are available to counselors for consideration. The PTSD Symptom Scale, Interview Version (PSS-I) with 17 items is a shorter clinical interview comparable to CAPS (Peterson, Luethcke, Borah, Borah, & Young-McCaughan, 2011). The PSS-I can be administered in about 20 minutes by a trained lay interviewer, and each item consists of a brief question so that an initial assessment can be made in shorter time (Peterson et al., 2011).The Emotion Regulation Questionnaire (ERQ) assesses differences between expressive suppression and cognitive reappraisal during treatment intake and discharge (Boden et al., 2013). The ERQ assessment assists the counselor in targeting and reducing maladaptive regulation strategies within the context of PTSD treatment in order to help the veteran develop alternative coping skills (Boden et al., 2013). The Quick Test for PTSD (Q-PTSD) is useful for identifying individuals with a true disability (Morel, 2008). Q-PTSD is a time-efficient method of detecting malingering in veterans applying for disability; it may be used by the counselor as an initial assessment of the disorder (Morel, 2008).
Other useful instruments can be incorporated into a treatment plan, such as a strengths-based assessment, depression inventory, substance abuse assessment, and insomnia inventory. Seligman (2011) also recommends the Post-Traumatic Growth Inventory (PTGI) for use with veterans. The 21-item PTGI “measures the extent to which survivors of traumatic events perceive personal benefits, including changes in perceptions of self, relationships with others, and philosophy of life accruing with their attempt to cope with trauma and its aftermath” (Tedeschi & Calhoun, 1996, p. 458). Seligman (2011) suggests that trauma often sets the stage for growth; a counselor may use the PTGI to facilitate veterans’ understanding of the conditions under which growth can happen.
Making a diagnosis of PTSD requires assessing symptoms and also gathering data from multiple assessments, a structured interview, and other knowledge of the client in order to make an evaluative judgment that leads to the development of a sound treatment plan (Ottati & Ferraro, 2009).
PTSD Treatment
Cognitive behavioral therapy (CBT) is unanimously endorsed as the best-practice treatment for PTSD by the VA and the Department of Defense (DOD; U.S. VA & U.S. DOD, 2010), the International Society for Traumatic Stress Studies (Foa, Keane, & Friedman, 2000), and the American Psychiatric Association (Ursano et al., 2010). Tramontin (2010) specifically states that the VA supports Prolonged Exposure (PE) therapy and Cognitive Processing Therapy (CPT).
In CPT and CBT, counselors challenge clients’ automatic thoughts connected with trauma. Through the use of written narratives in CPT, counselors target issues of safety, trust, power, control and self-esteem. Counselors also work with veterans to identify and label feelings as they work through impasses in their stories (Moran, Schmidt, & Burker, 2013). Exposure therapy is an evidence-based practice for many types of trauma including PTSD. According to Rauch, Eftekhari, and Ruzek (2012), PE therapy reduces PTSD symptoms and aids in treating comorbid issues. Rauch et al. (2012) explain that PE therapy consists of four components: psychoeducation, in vivo exposure, imaginal exposure, and emotional processing. Psychoeducation can help those suffering from trauma to understand their PTSD (Rauch et al., 2012). In vivo exposure consists of literally confronting the variables associated with the trauma (i.e., people, places and things; Rauch et al., 2012). Imaginal exposure involves reliving the memories associated with the trauma and engaging the accompanying emotions (Rauch et al., 2012). Emotional processing involves the counselor posing open-ended questions to the client in order to elicit both the emotions the client felt associated with the trauma and present emotions (Rauch et al., 2012).
Virtual reality exposure. In recent years, a new development of a virtual reality exposure therapy has surfaced. Albert “Skip” Rizzo developed a program titled “Virtual Iraq,” a virtual reality simulation designed to assist in the treatment of PTSD (Virtually Better, Inc., 2013). Rizzo developed the program after stumbling upon a video game called “Full Spectrum Warrior” that was originally created to train military service men and women. According to Rothbaum, Rizzo and Difede (2010), the current generation of military service members may be more comfortable participating in virtual reality treatment than conventional talk therapy, due to its similarity to gaming. After viewing several videos that demonstrate the Virtual Iraq system, the authors understand the connection between the exposure to trauma variables in PE and the exposure to trauma variables in virtual reality programs. Sharpless and Barber (2011) found several studies demonstrating the efficacy of virtual reality in treating veterans.
The protocol for virtual reality treatment involves veterans selecting a traumatic combat experience that relates closely to their most severe PTSD symptoms (McLay et al., 2012). Counselors create a realistic experience for the veteran by utilizing various sensory components of the virtual reality environment. Clients then use their senses and are immersed into the virtual reality world where they relive their trauma. Following the treatment, the counselor and the veteran process the material that surfaced in the exposure (McLay et al., 2012). In a study using virtual reality exposure therapy, McLay et al. (2012) found that “75% of participants experienced at least a 50% reduction in PTSD symptoms” (p. 635).
In addition to Virtual Iraq, Virtually Better, Inc. (2013) has developed other programs, including Virtual Vietnam, Afghanistan, Airports, and the World Trade Center. During a phone interview with Emilio Coirini, Director and Business Developer at Virtually Better, Inc., the interviewee stated that a soldier who suffers PTSD costs the government about $50,000 a year to treat, with the average treatment lasting 20 years. In contrast, the virtual reality system costs only about $30,000 with clinical training (E. Coirini, personal communication, November 16, 2012). At the time of the interview, there were about 70 systems installed throughout the United States, and Coirini explained that it is possible to receive grants for the cost of the system.
Animal-assisted treatment. In contrast to the relatively new use of virtual reality technology, animals have been assisting persons with disabilities for many years; there are a growing number of organizations that provide trained animals, specifically canines, to veterans who suffer from PTSD. According to Thompson (2010), in order to qualify as a service animal, the animal must undergo training to do work or perform helpful tasks. McConnell (2011) conducted a study that found that having a pet can provide meaningful social support that improves lives. One organization, Pets for Vets, provides animal companions to veterans with PTSD who are capable of caring for a pet. Pets for Vets states the following (2014):
Our goal is to help heal the emotional wounds of military veterans by pairing them with a shelter animal that is specially selected to match his or her personality. Professional animal trainers rehabilitate the animals and teach them good manners to fit into the veteran’s lifestyle. Training can also include desensitization to wheel chairs or crutches as well as recognizing panic or anxiety disorder behaviors. (para. 2)
Animals have been therapeutic partners to persons with disabilities for generations, and they are now serving wounded warriors.
Utilization of mobile phone applications. While researching other tools to help in treating PTSD, the authors discovered a few mobile applications available for both the iPhone and the Android that are well-developed, user-friendly and comprehensive. The first application, PTSD Coach (U.S. VA, 2014b), is elaborate in design, taking into account potential areas of concern for those who suffer from PTSD. The four main divisions of the application include Learn, Self-Assessment, Manage Symptoms and Find Support. The learning division of the application provides a comprehensive base and answers questions such as What is PTSD? and Who develops PTSD? In addition, the learning division includes answers regarding who should seek professional assistance and possible treatment protocols. The questions in the professional care subsection include Will it really work? and What if I am embarrassed about seeking help? The self-assessment section gives a person insight into the possibility of having PTSD. An example of an evaluative question is, “In the past month how often have you been bothered by disturbing memories, thoughts or images of the traumatic experience?” Users can track the history of their symptoms and schedule assessments to take periodically to provide a comparison of improvement or decline. When utilizing the manage symptoms option, users can select a mental state such as sadness or hopelessness, and the application will provide a suggestion to improve mood, depending on mood severity. Finally, users can set up their own support network, get support immediately or find professional care by choosing the finding support option. (The Apple phone app version may be found at https://itunes.apple.com/us/app/ptsd-coach/id430646302?mt=8, and the Android version may be found at https://play.google.com/store/apps/details?id=gov.va.ptsd.ptsdcoach.)
Another application, T2 Mood Tracker (The National Center for Telehealth and Technology, 2014), aids individuals in keeping track of their moods, which they can then report to their medical or mental health professional(s). The application can be used as a daily tool to track a client’s mood, keep notes regarding stressors, and chart a graph of the information provided. The initial screen asks whether the user would like to rate anxiety, depression, general well-being, head injury, post-traumatic stress, or general stress. The user selects one of the previously stated fields and is then required to rate several factors associated with the chosen field. The user can then graph results, create reports, save reports, or view notes. The application is user-friendly and simple in design, yet intricate enough to help the user and counselor in developing treatment protocols. (The Apple phone app version may be found at https://itunes.apple.com/us/app/t2-mood-tracker/id428373825?mt=8, and the Android version may be found at https://play.google.com/store/apps/details?id=com.t2.vas.)
A third application worthy of acknowledgement is the PE Coach, developed by the VA (2014a). The PE Coach requires a counselor trained in PE therapy. According to the National Center for PTSD (2014c), the PE Coach is a treatment companion that helps the client and counselor work through the PE treatment manual. The features of this application include the following: learning about PE therapy and the most common reactions to trauma, recording therapy sessions for personal use, setting reminders for homework and future therapy appointments, tracking tasks between sessions, practicing breathing exercises, and tracking PTSD symptoms. Currently, anecdotal accounts from veterans indicate that the mobile applications are helpful (U.S. DOD, American Forces Press Service, 2012). (The Apple phone app version may be found at https://itunes.apple.com/us/app/pe-coach/id507357193?mt=8, and the Android version may be found at https://play.google.com/store/apps/details?id=org.t2health.pe.)
Conclusion
Wendling (2008) reported results from an online survey administered to mental health practitioners after they had attended a conference called “Healing the Scars of War.” She found that most counselors did not understand military culture or appear to follow best-practice guidelines. The authors hope this paper serves to increase understanding of this critical area.
Technology makes it possible to access information about military families and resources to serve this special population. The VA has PTSD videos, training courses, and other materials available to inform counselors of the needs and unique cultural experiences of a diverse veteran population experiencing PTSD.
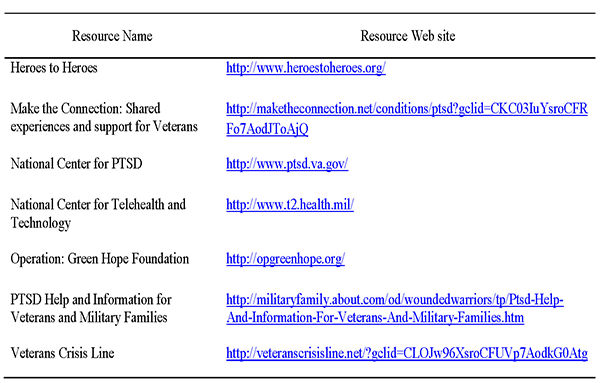
The resources identified (see Table 1) can be readily accessed by counselors and veterans to begin the therapeutic journey. We, the authors, salute the wounded warriors and continue to fight for their healing as they have fought for freedom.
Table 1
Informative Resources about Veterans and PTSD
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5 (5th ed.). Washington, DC: American Psychiatric Publishing.
Boden, M. T., Westermann, S., McRae, K., Kuo, J., Alvarez, J., Kulkarni, M. R., … Bonn-Miller, M. O. (2013). Emotion regulation and posttraumatic stress disorder: A prospective investigation. Journal of Social & Clinical Psychology, 32(3), 296–314. doi:10.1521/jscp.2013.32.3.296
Foa, E. B., Keane, T. M., & Friedman, M. J. (Eds.). (2000). Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies. New York, NY: The Guilford Press.
McConnell, A. R. (2011, July 11). Friends with benefits: Pets make us happier, healthier. Psychology Today. Retrieved from http://www.psychologytoday.com/blog/the-social-self/201107/friends-benefits-pets-make-us-happier-healthier
McLay, R. N., Graap, K., Spira, J., Perlman, K., Johnston, S., Rothbaum, B. O., … Rizzo, A. (2012). Development and testing of virtual reality exposure therapy for post-traumatic stress disorder in active duty service members who served in Iraq and Afghanistan. Military Medicine, 177(6), 635–642.
Moran, S., Schmidt, J., & Burker, E. J. (2013). Posttraumatic growth and posttraumatic stress disorder in veterans. Journal of Rehabilitation, 79(2), 34–43.
Morel, K. R. (2008). Development of a validity scale for combat-related posttraumatic stress disorder: Evidence from simulated malingerers and actual disability claimants. Journal of Forensic Psychiatry & Psychology, 19(1), 52–63. doi:10.1080/14789940701594645
National Center for PTSD. (2014a, January 3). DSM-5 criteria for PTSD. Retrieved from http://www.ptsd.va.gov/professional/PTSD-overview/dsm5_criteria_ptsd.asp
National Center for PTSD. (2014b, January 3). Mississippi Scale for Combat-Related PTSD (M-PTSD). Retrieved from http://www.ptsd.va.gov/professional/assessment/adult-sr/mississippi-scale-m-ptsd.asp
National Center for PTSD. (2014c, January 28). Mobile app: PE coach. Retrieved from http://www.ptsd.va.gov/public/materials/apps/pecoach_mobileapp-public.asp
The National Center for Telehealth and Technology. (2014). T2 Mood Tracker [Mobile application software]. Available from https://itunes.apple.com/us/app/t2-mood-tracker/id428373825?mt=8 or https://play.google.com/store/apps/details?id=com.t2.vas
Nussbaum, A.M. (2013). The Pocket Guide to the DSM-5 Diagnostic Exam. Washington, DC: American Psychiatric Publishing.
Ottati, A., & Ferraro, F. R. (2009). Combat-related PTSD treatment: Indications for exercise therapy. Psychology Journal, 6(4), 184–196.
Peterson, A. L., Luethcke, C. A., Borah, E. V., Borah, A. M., & Young-McCaughan, S. (2011). Assessment and treatment of combat-related PTSD in returning war veterans. Journal of Clinical Psychology in Medical Settings, 18(2), 164–175. doi:10.1007/s10880-011-9238-3
Pets for Vets. (2014). Healing vets and saving pets. Retrieved from http://pets-for-vets.com
Rauch, S. A. M., Eftekhari, A., & Ruzek, J. I. (2012). Review of exposure therapy: A gold standard for PTSD treatment. Journal of Rehabilitation Research & Development, 49(6), 679–687.
Rothbaum, B. O., Rizzo, A., & Difede, J. (2010). Virtual reality exposure therapy for combat-related posttraumatic stress disorder. Annals of the New York Academy of Sciences, 1208, 126–132. doi:10.1111/j.1749-6632.2010.05691.x
Seligman, M. E. P. (2011). Flourish: A visionary new understanding of happiness and well-being. New York, NY: Free Press.
Sharpless, B. A., & Barber, J. P. (2011). A clinician’s guide to PTSD treatment for returning veterans. Professional Psychology: Research and Practice, 42(1), 8–15. doi:10.1037/a0022351
Staggs, S. (2014). Symptoms & diagnosis of PTSD. Retrieved from http://psychcentral.com/lib/symptoms-and-diagnosis-of-ptsd/000158
Tedeschi, R. G., & Calhoun, L. G. (1996). The posttraumatic growth inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress, 9(3), 455–471. doi:10.1002/jts.2490090305
Tester, J. (2013, June 13). Tester introduces comprehensive veterans’ health care legislation [Press release]. Retrieved from http://www.tester.senate.gov/?p=press_release&id=2965
Thompson, M. (2010, November 22). Bringing dogs to heal. Time, 176(21), 54–57. Retrieved from http://p2v.org/wp-content/uploads/2010/11/p2v-time-web.pdf
Tramontin, M. (2010). Exit wounds: current issues pertaining to combat-related PTSD of relevance to the legal system. Developments in Mental Health Law, 29, 23–47.
U.S. Department of Defense, American Forces Press Service. (2012, July 31). DOD, VA release mobile app targeting post-traumatic stress [News release]. Retrieved from http://www.defense.gov/news/newsarticle.aspx?id=117339
U.S. Department of Veterans Affairs. (2014a). PE coach [Mobile application software]. Available from https://itunes.apple.com/us/app/pe-coach/id507357193?mt=8 or https://play.google.com/store/apps/details?id=org.t2health.pe
U.S. Department of Veterans Affairs. (2014b). PTSD coach [Mobile application software]. Available from https://itunes.apple.com/us/app/ptsd-coach/id430646302?mt=8 or https://play.google.com/store/apps/details?id=gov.va.ptsd.ptsdcoach
U.S. Department of Veterans Affairs, & U.S. Department of Defense. (2010). VA/DoD clinical practice guideline for management of post-traumatic stress. Washington, DC: Management of Post-Traumatic Stress Working Group. Retrieved from http://www.healthquality.va.gov/ptsd/cpg_PTSD-FULL-201011612.pdf
Ursano, R. J., Bell, C., Eth, S., Friedman, M., Norwood, A., Pfefferbaum, B., … Benedek, D. M. (2010). Practice guideline for the treatment of patients with acute stress disorder and posttraumatic stress disorder. Arlington, VA: American Psychiatric Association. Retrieved from http://psychiatryonline.org/pdfaccess.ashx?ResourceID=243186&PDFSource=6
Virtually Better, Inc. (2013). Virtual Iraq. Retrieved from http://www.virtuallybetter.com/virtual-iraq/
Weathers, F. W., Blake, D. D., Schnurr, P. P., Kaloupek, D. G., Marx, B. P. & Keane, T. M. (2013). The clinician-administered PTSD scale for DSM-5 (CAP-5). Retrieved from http://www.ptsd.va.gov/professional/assessment/adult-int/caps.asp
Wendling, P. (2008). Knowledge gap exists on best practices for PTSD. Retrieved from http://www.thefreelibrary.com/Knowledge gap exists on best practices for PTSD.-a0199814983
Mary Alice Fernandez, NCC, is an assistant professor at Texas A&M University – Corpus Christi. Melissa Short is a doctoral student at Walden University Online. Correspondence can be addressed to Mary Alice Fernandez, 6300 Ocean Drive, Unit 5834, Corpus Christi, TX 78412-5834, mary.fernandez@tamucc.edu.
