Jun 28, 2018 | Volume 8 - Issue 2
Matthew C. Fullen
As the number of older adults increases, it is important to understand how attitudes toward aging influence society, the aging process, and the counseling profession. Ageism—defined as social stigma associated with old age or older people—has deleterious effects on older adults’ physical health, psychological well-being, and self-perception. In spite of research indicating that the pervasiveness of ageism is growing, there are few studies, whether conceptual or empirical, related to the impact of ageism within the practice of counseling. This article includes an overview of existing literature on the prevalence and impact of ageism, systemic and practitioner-level consequences of ageism, and specific implications for the counseling profession. Discussion of how members of the counseling profession can resist ageism within the contexts of counselor education, gerontological counseling, advocacy, and future research will be addressed.
Keywords: ageism, aging, older adults, gerontological counseling, advocacy
Currently, there are approximately 47.8 million adults age 65 and over living in the United States, and this number is expected to grow to 98 million—or more than one in five Americans—by 2060 (Administration on Aging, 2017). Much of this growth can be attributed to the aging of the boomer generation, the age cohort born between 1946 and 1964. Approximately 10,000 boomers turn 65 every day (Short, 2016). Increases to the average life span also have expanded the number of older Americans, with a person age 65 now living an average of 19.4 additional years, and many living well beyond that age (Administration on Aging, 2017). Nonetheless, many misconceptions remain about the aging process, and recent research demonstrates that the prevalence of ageism is growing (Ng, Allore, Trentalange, Monin, & Levy, 2015). Ageism—defined here as social stigma related to old age or older people (Widrick & Raskin, 2010)—is associated with the lack of mental health services available to older adults (Bartels & Naslund, 2013), and when negative attitudes toward aging are internalized by older adults, significant consequences to health and well-being may occur (Levy, 2009).
Within the counseling literature, there appears to be a lack of research on ageism and its impact on older adulthood. A keyword search of leading counseling journals dating back to 1992 results in a single publication on the topic of ageism within the American Counseling Association’s Journal of Counseling & Development (Saucier, 2004), as well as a single empirical study in Adultspan Journal (McBride & Hays, 2012). Therefore, to elucidate the effects of ageism, as well as its role within the field of professional counseling, this article will provide a review of existing literature on the prevalence of ageism, its consequences among mental health professionals, and the impact of internalized ageism on older adults. The article concludes with recommendations for how counselors, counselor educators, and counseling students can mitigate the effects of ageism and promote positive perceptions of aging.
Prevalence and Impact of Ageism
Prevalence of Ageism
The term “ageism” was first used in the late 1960s to describe discriminatory beliefs or practices that are predicated on the age of a person or group (Butler, 1969). Like racism or sexism, prejudice associated with age is both pernicious and challenging to quantify. Many myths about aging are assumed to be true without additional consideration, leading to a “commonsense reality” about old age or older people that is then perpetuated throughout a society (Angus & Reeve, 2006, p. 141). Moreover, scholars argue that ageism is currently met with less disapproval than racism or sexism (Cuddy & Fiske, 2002; Nelson, 2016; Palmore, 2005), although more recent empirical research is needed to substantiate this hypothesis. Nevertheless, research indicates that views about aging are becoming more negative (Ng et al., 2015). Dominant myths include the notion that older adults are: (a) lonely and depressed; (b) increasingly similar as they grow old; (c) sick, frail, and dependent; (d) cognitively and psychologically impaired; (e) sexless and boring; and (f) unable to learn or change (Thornton, 2002; Whitbourne & Sneed, 2002). These myths persist in spite of research that demonstrates that older adults are heterogeneous, possess many psychosocial resources, frequently have high levels of self-rated and objectively measured health, and mostly do not experience dementia or other forms of cognitive impairment (Whitbourne & Sneed, 2002).
Stereotypes about older adulthood are transmitted throughout society and may lead to detrimental consequences for the health and well-being of older people. For example, media representations of older adults are likely to reinforce negative views about older adulthood. Television shows, movies, and advertising depict older people according to stereotypes about aging—or omit them altogether (North & Fiske, 2012)—and older people who watch more television over the course of their lives tend to view aging in a more negative light (Donlon, Ashman, & Levy, 2005). Ageism is transmitted through social media as well. References to older adults on Facebook are commonly comprised of references to cognitive or physical debilitation, the infantilization of older people, or suggestions that older adults be banned from public activities like driving or shopping (Levy, Chung, Bedford, & Navrazhina, 2014).
Negative stereotypes may lead to age-based discrimination, a phenomenon that experts describe as both “understudied” and “surprisingly pervasive” (North & Fiske, 2012, p. 983). For example, Posthuma and Campion (2009) described several workplace-based stereotypes that exist, in spite of a lack of supporting evidence. These include the notion that older workers have lower levels of ability and motivation, lower productivity, and greater resistance to change. Within the realm of health care, physicians may be less likely to offer particular medical treatments to older patients because of a belief that certain ailments are the inevitable consequences of natural aging (Bowling, 2007). Ageism may result in elder abuse, both within care facilities and among family members; however, it is underreported because of a lack of awareness among health and social service providers (Nelson, 2005).
Negative stereotypes about aging develop in a manner that parallels stereotypes like racism or sexism. Levy’s (2009) stereotype embodiment theory suggests that ageist views may be transmitted culturally and internalized by older adults, leading to significant changes to health and functioning. Older adults are first exposed to negative stereotypes about aging when they are young. As individuals age into older adulthood, their negative beliefs about aging become increasingly salient and self-directed. On the other hand, if an individual is socialized to hold more positive views toward aging, these viewpoints may serve as a buffer against internalized ageism (Levy, 2009).
Furthermore, stereotype embodiment theory (Levy, 2009) suggests that when stereotypes are assimilated from the surrounding culture, they eventually become self-definitions that influence a person’s functioning and health. Stereotype embodiment theory concludes that: (a) stereotypes are internalized throughout the life span; (b) they are likely to operate unconsciously; (c) as views of older age become increasingly relevant to a person’s identity, the age stereotypes become more salient; and (d) self-referential views on aging are developed via pathways that may be both top-down (i.e., societal perspectives are passed on to the individual) and longitudinal (i.e., views on old age begin in childhood).
Cuddy, Norton, and Fiske (2005) argued that groups within a society are often categorized based on two traits—warmth and competence—and the authors found that most participants rated older adults as warm, but incompetent. Contrary to the belief that ageism is only a concern in Western countries, Cuddy et al. reviewed a large-scale international study that included college students in Belgium, Costa Rica, Hong Kong, Japan, and South Korea. Across samples, participants viewed older adults as significantly more warm than competent, non-competitive, and having lower social status. Within their study, this trend persisted even when looking at cultures and countries that are typically described as more collectivist (i.e., Hong Kong, Japan, and South Korea).
Research indicates that ageism is prevalent within environments where older adults receive housing and health care services. In an ethnographic study on the impact of age and illness within a residential care setting, Dobbs et al. (2008) found that some family members, staff, and residents held negative attitudes about aging that resulted in an environment affected by ageism. In their study, examples of negative age bias included neglecting to gather resident input prior to making decisions, using infantilizing speech with older people, and stigmatizing residents because of dementia or physical disability. In a similar study completed within a multi-level care setting, Zimmerman et al. (2016) found that the use of multi-level, stepped care (i.e., adults with differing independence levels residing within the same setting) reinforced stigma related to age and health, with older adults differentiating among themselves based on which levels of care were required.
Impact of Social Forces
Scholars posit a wide range of hypotheses to explain the prevalence of ageism, but two systemic processes—modernization and medicalization—are identified in the literature as the most likely catalysts of negative attitudes toward aging (Cuddy & Fiske, 2002; Ng et al., 2015). In regard to modernization theory, Cuddy and Fiske (2002) explained that views of older adulthood have changed as a result of the shift from an agrarian society to an industrial society. Technological advances, increased literacy rates among young people, and a trend toward urbanization resulted in greater competition between young and old generations, as well as weakened intergenerational social ties between young people and their families of origin. The sum of these social changes led to decreased status for older people, resulting in the “warm, but incompetent” stereotype that is now associated with them (Cuddy et al., 2005).
Relatedly, improvements in health care have extended the life span and increased the ratio of older to younger people. Previous research shows that as the ratio of older adults to younger adults increases, views about older adulthood become increasingly negative (Ng et al., 2015). Given that the number of older people will increase markedly in coming years, it is possible that negative attitudes toward older people will continue to grow unless intervention occurs.
The second major social force described in the literature is the medicalization of aging, which refers to associating old age with a person’s physical health or illness, to the detriment of other aspects of well-being (Ng et al., 2015). The dominance of medical conceptualizations of old age is described as one of the “master narratives” associated with the modern study of aging (Biggs & Powell, 2001, p. 97). Although the causes of medicalization are many and complex, they can be summarized by the shift from viewing old age as a natural part of the life span to the viewpoint that old age, and even death itself, are problems that modern medicine may be able to solve (Ng et al., 2015). Past research indicates that the medicalization of aging predicts negative attitudes toward aging and consequentially leads to “the objectification of older adults as patients rather than as individuals with interesting life experiences” (Ng et al., 2015, p. 2).
Consequences of Ageism
Impact on Older Adults’ Health and Well-Being
There is a substantial body of research indicating that age stereotypes influence older adults’ health and well-being. For instance, older adults’ perceptions of aging are associated with memory performance (Levy, Zonderman, Slade, & Ferrucci, 2011), hearing decline (Levy, Slade, & Gill, 2006), developing Alzheimer’s symptoms (Levy et al., 2016), and dying from respiratory or cardiovascular illnesses (Levy & Myers, 2005). In fact, Levy, Slade, Kunkel, and Kasl (2002) found that even after controlling for age, gender, socioeconomic status, loneliness, and functional health, older adults with more positive self-perceptions of aging lived 7.5 years longer than those with less positive self-perceptions of aging.
Conversely, research indicates that positive perceptions of aging may provide a salutatory effect on health and well-being. Older adults with positive age stereotypes are 44% more likely to fully recover from severe disability compared to those with negative age stereotypes (Levy, Slade, Murphy, & Gill, 2012), and older military veterans who resisted negative age stereotypes had significantly lower rates of mental illness compared to those who fully accepted them (Levy, Pilver, & Pietrzak, 2014). These positive differences were found for suicidal ideation (5.0% vs. 30.1%), anxiety (3.6% vs. 34.9%), and PTSD (2.0% vs. 18.5%), even after controlling for age, combat experience, personality, and physical health. In regard to variables that may influence older adults’ self-perceptions of aging, Fullen, Granello, Richardson, and Granello (in press) found that resilience—the ability to bounce back from adversity—and multidimensional wellness were significant predictors of positive age perception, whereas increased age and decreased physical wellness predicted internalized ageism. Furthermore, resilience appeared to buffer older adults from experiencing internalized ageism as they grew older. However, older adults may not be exposed to interventions to promote resilience and well-being because of ageism’s impact on the availability of mental health services among older adults.
Impact on Mental Health Professionals
The gap between the mental health needs of older adults and the number of mental health professionals with specific training in working with older adults is on the verge of a “crisis” (Institute of Medicine, 2012, p. ix). Scholars provide a variety of explanations to account for this, including systemic factors—such as inadequate funding and a lack of training opportunities within academic programs (Bartels & Naslund, 2013; Gross & Eshbaugh, 2011; Robb, Chen, & Haley, 2002)—and personal factors, including low interest in working with older adults (Tomko, 2008) and therapeutic pessimism (Danzinger & Welfel, 2000; Helmes & Gee, 2003).
Systemic ageism. Although older adults consistently report higher life satisfaction than younger or middle-aged adults (George, 2010), approximately 26% of all Medicare beneficiaries, or more than 13 million Americans, meet the criteria for a mental disorder (Center for Medicare Advocacy, 2013). Yet, mental health services currently account for only 1% of Medicare expenditures (Bartels & Naslund, 2013). Systemic barriers may be partially responsible for the lack of access to mental health services among older adults. For example, inadequate reimbursement rates is cited as one reason for the 19.5% decline in psychiatrists accepting Medicare between 2005–2006 and 2009–2010 (Bishop, Press, Keyhani, & Pincus, 2014). Similarly, Medicare payments to psychologists for psychotherapy decreased by 35% since 2001, after adjusting for inflation (American Psychological Association, 2014). Older adults are currently unable to use Medicare to access services provided by licensed professional counselors (LPCs) or marriage and family therapists (MFTs; Fullen, 2016b). This translates to an estimate of 175,000 mental health professionals who are unavailable to serve as Medicare-eligible providers (American Counseling Association, n.d.). Clients who age into Medicare coverage after working with these professionals face discontinuity of care caused by having to change providers.
Professional training barriers among the helping and health professions also may reflect systemic ageism. Half of the fellowship positions in geriatric medicine and geriatric psychiatry are unfilled each year, and only 4.2% of psychologists focus on geriatric care in clinical practice (Bartels & Naslund, 2013). Institutional barriers that inhibit student interest in careers related to work with older adults include a lack of visibility for multidisciplinary gerontology programs, the absence of gerontological content within textbooks, few faculty who are trained in gerontology, misconceptions about employment opportunities (i.e., the assumption that the only aging sector jobs available are in nursing homes), and a primary focus on the problems associated with old age when later life is discussed within the classroom (Gross & Eshbaugh, 2011).
Within the counseling profession, scholars describe a mixed commitment to gerontological counseling. Going back to 1975, Salisbury (1975) and Blake and Kaplan (1975) described counseling with older adults as an overlooked domain within professional counseling. Twenty years later, Myers (1995) argued that gerontological counseling had evolved from “forgotten and ignored” (p. 143) to a sub-discipline within the profession complete with standards and certification. However, the gerontological counseling specialization that existed between 1992 and 2008 was discontinued in 2009 when only two institutions had applied for accreditation (Bobby, 2013). Perhaps more telling, the 2016 Standards of the Council for Accreditation of Counseling & Related Educational Programs (CACREP) include zero references to the words old, older, older adults, or ageism; only one reference each to the words age and aging; and four references to the phrase life span (CACREP, 2015). Nonetheless, Foster, Kreider, and Waugh (2009) found that many counseling students have interest in topics related to gerontological counseling, including grief counseling (70%), retirement counseling (43%), family counseling with aging parents (64%), and counseling caregivers (55%). The same study found that many respondents were interested in working in a hospice setting (39%), a hospital geriatric unit (29%), a nursing home (25%), private practice with older adults (43%), and a community setting with older adults (45%). However, it is unclear whether students who are interested in working with older adults receive training and employment opportunities within these contexts.
Individual ageism. Research regarding the prevalence of ageism among individual mental health professionals is equivocal. When mental health professionals’ perceptions of clients based on age, gender, and health variables were studied, some researchers found health bias, but not age bias (Robb et al., 2002). Others reported that participants rated older clients as having a greater number of diagnostic problems (Helmes & Gee, 2003) and a worse prognosis than younger clients, in spite of all relevant information being matched across age groups (Danzinger & Welfel, 2000). Helmes and Gee (2003) found large differences in how older people were rated on key therapeutic variables. Older clients were viewed as less able to develop an adequate therapeutic relationship, less appropriate for therapy, and less likely to recover. Respondents in their study also felt less competent in treating older people, and they were less willing to accept older people as clients.
To counteract the potential influence of negative age bias on counseling treatment, McBride and Hays (2012) described the importance of linking work with older adults to multicultural competence. The authors surveyed 360 counselors and counselor trainees and found a significant, negative correlation (r = -.41) between multicultural competence and negative attitude toward aging. Tomko (2008) found that multicultural competence was associated with improved clinical judgment when working with older adults; however, it did not predict global attitudes toward aging. In sum, considerations of both the systemic and individual aspects of ageism have important implications for the counseling profession.
Implications for the Counseling Profession
The rapid growth of the older adult population will impact members of the counseling profession in a variety of ways. Shifting age demographics make it imperative that counselors understand how the pervasiveness of ageism impacts key professional values like diversity, social justice, and client advocacy. Four domains are outlined in which counselors may dedicate their attention to generating positive views of aging. These domains include counselor education, advocacy, research, and counseling practice.
Counteracting Ageism Within Counselor Education
Within counselor training programs, resistance to ageism begins with incorporating discussions about aging and older adulthood into the counselor education curriculum. Therefore, it is important that professional accreditation standards like CACREP adequately reflect the mental health needs of older adults and their families. In its current form, the omission of keywords like aging, older adulthood, and ageism from these standards may send a mixed signal to counselor training programs and their students about social justice and multicultural competencies as they relate to older adults.
Once ageism is identified by a counselor education program as a priority, counselor educators need to develop strategies for incorporating this focus in the existing curriculum. For instance, a life span development course provides ample opportunities to discuss issues such as shifting population demographics, multigenerational families, and how an aging population will impact the counseling profession. Assessing students’ current thoughts about the aging process, including both their own aging and that of family members, may create greater empathy for the needs of older adults. Similarly, when instructing social and cultural diversity courses, counselor educators should consider introducing topics such as ageism and age privilege and juxtaposing these constructs alongside dialogue about diversity and intersectionality (Black & Stone, 2005). Furthermore, when developing practicum or internship sites, counselor educators could make a point of developing placements in which older clients will be served. Identifying potential site supervisors who have experience in working with older adults is an important step, as it ensures that trainees are given adequate opportunities to reflect on their own perspectives on aging, disability, advocacy, and related issues.
Counteracting Ageism Through Advocacy
In regard to advocacy, counselors should resist ageism at national, state, and local levels. At the national level, the omission of counselors as approved Medicare providers limits the availability of mental health services for older adults and reflects the assumption that older adults’ needs are primarily physiological. This issue creates challenges for members of the counseling profession who are interested in providing services across the life span. Mental health advocacy on behalf of older adults includes educating lawmakers about the importance of Medicare reimbursement as a means of creating mental health service access (Fullen, 2016b). Professional organizations continue to support grassroots advocacy, as well as lobbying efforts, to influence Medicare policy on behalf of counselors. In fact, as of this writing there are bills in each chamber of the United States Congress (i.e., S. 1879; H.R. 3032), and a federal advisory group (i.e., the President’s Interdepartmental Serious Mental Illness Coordinating Committee; ISMICC) recently recommended inclusion of counselors within Medicare (National Board for Certified Counselors, n.d.).
At the state and local level, members of the counseling profession should forge partnerships with gerontology professionals. For example, advocacy occurs when professional counselors and counselor educators make connections with members of the local area agency on aging, directors of local assisted living or skilled nursing facilities, or state policymakers who are responsible for budgetary and policy decisions related to aging. These partnerships are mutually beneficial; they provide members of the counseling profession with increased exposure to the diverse needs of older adults in their communities, and they educate local gerontology professionals about the range of mental health services that counselors provide. Additionally, building interprofessional connections may lead to research opportunities that can improve the care received by older adults.
Counteracting Ageism Through Research
In spite of the numerous studies indicating that ageism has detrimental effects on older adults, there are currently very few studies that demonstrate the prevalence and impact of ageism within the counseling profession. For instance, research on in-session dynamics between counselors and much older clients could shed light on the ways in which age is broached in a counseling session. Additionally, research could focus on the benefits of professional counseling for older adult clients, as well as the effectiveness of novel interventions that are grounded in counseling theories or wellness (Fullen & Gorby, 2016; Fullen et al., in press). For instance, the development and validation of a wellness-based approach to counseling older adults might mitigate mental health issues or internalized ageism among older clients (Myers & Sweeney, 2005), and it would serve as additional evidence for the necessity of adding counselors as Medicare providers.
At the institutional level, more research is needed to understand the extent to which counselor training programs address ageism, and in which curricular contexts. It is important to understand which pedagogical strategies are most effective, whether these impacts persist over time, and how well training programs make inroads with local agencies that work with older adults. Research into advocacy efforts related to Medicare reimbursement may also advance the profession. Although Medicare reimbursement is described as a priority for the counseling profession, there is currently little research on counselors’ knowledge about Medicare or participation in Medicare advocacy.
Counteracting Ageism Through Counseling Practice
Finally, it is important to consider how counselors might resist ageism within their counseling practice. Because of the heterogeneity of older adults, counseling services should be tailored to the unique needs of each client. Given that ageism has the potential to influence how older clients are conceptualized by counselors, it is important for counselors to reflect on their own beliefs about aging as well as their assumptions about the ability of older clients to grow and change. Many counselors are not familiar with the wide range of mental health interventions that have been empirically validated with older adults (Myers & Harper, 2004). For example, the SAMHSA-HRSA Center for Integrated Health Solutions (n.d.) provides numerous resources related to providing behavioral health services to older adults. These resources address issues such as evidence-based treatments for late life depression, preventing suicide in older adults, screening for substance misuse, and assessing cognitive functioning.
Given the growing interest in wellness-oriented services for older adults, SAMHSA also provides evidence-based resources related to health promotion and integrated care. Programs that focus on cultivating holistic wellness or resilience are relatively new, but they also may be worth considering as a means of countering ageism within the practice of counseling. Because the wellness approach incorporates multiple dimensions of functioning, older clients who are experiencing deficits in a particular domain (e.g., limited mobility influencing ability to drive) may find that they can use alternative domains as a means of compensating (e.g., greater reliance on social network to carpool to events; Fullen, 2016a). Similarly, discussion of how older clients have used strengths to navigate loss, overcome adversity, and resist ageism in their own lives may prove to be key ingredients in the therapeutic process. Furthermore, incorporating resilience into an older client’s treatment plan may create a buffer against internalized ageism (Fullen et al., in press), as well as an opportunity to highlight older adults’ abilities to adapt in the face of adversity (Fullen & Gorby, 2016).
Conclusion
As the number of older adults grows, members of the counseling profession are increasingly likely to encounter older people who seek to benefit from counseling services. A review of existing research demonstrates that there are numerous causes of ageism, detrimental consequences associated with internalizing negative age stereotypes, and gaps in research related to how the counseling profession should respond. In light of the counseling profession’s commitment to diversity, social justice, and advocacy, it is important to better understand the broad impact of ageism. By combating ageism in the domains of public policy, research, teaching, and direct service with clients, members of the counseling profession have the opportunity to counteract ageism’s deleterious effects and promote more positive perceptions of growing older.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest or funding contributions for the development of this manuscript.
References
Administration on Aging. (2017). A profile of older Americans: 2016. Retrieved from https://www.acl.gov/sites/09default/files/Aging%20and%20Disability%20in%20America/2016-Profile.pdf
American Counseling Association. (n.d.). Medicare, outpatient mental health services, and coverage of licensed professional counselors—S. 562 and H.R. 3662. Retrieved from https://www.counseling.org/docs/public-policy-faqs-and-documents/medicare-briefing-paper.pdf?sfvrsn=6
American Psychological Association. (2014). Congress should halt Medicare’s plummeting psychologist payments. Retrieved from http://www.apapracticecentral.org/advocacy/state/leadership/slc-fact-medicare.aspx
Angus, J., & Reeve, P. (2006). Ageism: A threat to “aging well” in the 21st century. Journal of Applied Gerontology, 25, 137–152. doi:10.1177/0733464805285745
Bartels, S. J., & Naslund, J. A. (2013). The underside of the silver tsunami—Older adults and mental health care. The New England Journal of Medicine, 368, 493–496. doi:10.1056/NEJMp1211456
Biggs, S., & Powell, J. L. (2001). A Foucauldian analysis of old age and the power of social welfare. Journal of Aging & Social Policy, 12, 93–111. doi:10.1300/J031v12n02_06
Bishop, T. F., Press, M. J., Keyhani, S., & Pincus, H. A. (2014). Acceptance of insurance by psychiatrists and the implications for access to mental health care. JAMA Psychiatry, 71, 176–181.
doi:10.1001/jamapsychiatry.2013.2862
Black, L. L., & Stone, D. (2005). Expanding the definition of privilege: The concept of social privilege. Journal of Multicultural Counseling and Development, 33, 243–255. doi:10.1002/j.2161-1912.2005.tb00020.x
Blake, R., & Kaplan, L. S. (1975). Counseling the elderly: An emerging area for counselor education and supervision. Counselor Education and Supervision, 15, 156–157.
Bobby, C. L. (2013). The evolution of specialties in the CACREP Standards: CACREP’s role in unifying the profession. Journal of Counseling & Development, 91,35–43. doi:10.1002/j.1556-6676.2013.00068.x
Bowling, A. (2007). Honour your father and mother: Ageism in medicine. British Journal of General Practice, 57, 347–348.
Butler, R. N. (1969). Age-ism: Another form of bigotry. The Gerontologist, 9, 243–246.
doi:10.1093/geront/9.4_Part_1.243
Center for Medicare Advocacy, Inc. (2013). Medicare and mental health. Retrieved from http://www.medicareadvocacy.org/medicare-and-mental-health/
Council for Accreditation of Counseling & Related Educational Programs. (2015). 2016 CACREP Standards. Alexandria, VA: Author.
Cuddy, A. J. C., & Fiske, S. T. (2002). Doddering but dear: Process, content, and function in stereotyping of older persons. In T. D. Nelson (Ed.), Ageism: Stereotyping and prejudice against older persons (pp. 3–26). Cambridge, MA: MIT Press.
Cuddy, A. J. C., Norton, M. I., & Fiske, S. T. (2005). This old stereotype: The pervasiveness and persistence of the elderly stereotype. Journal of Social Issues, 61, 267–285. doi:10.1111/j.1540-4560.2005.00405.x
Danzinger, P. R., & Welfel, E. R. (2000). Age, gender and health bias in counselors: An empirical analysis. Journal of Mental Health Counseling, 22, 135–149.
Dobbs, D., Eckert, J. K, Rubinstein, B., Keimig, L., Clark, L., Frankowski, A. C., & Zimmerman, S. (2008). An ethnographic study of stigma and ageism in residential care or assisted living. The Gerontologist, 48,
517–526. doi:10.1093/geront/48.4.517
Donlon, M. M., Ashman, O., & Levy, B. R. (2005). Re-vision of older television characters: A stereotype- awareness intervention. Journal of Social Issues, 61, 307–319. doi:10.1111/j.1540-4560.2005.00407.x
Foster, T. W., Kreider, V., & Waugh, J. (2009). Counseling students’ interest in gerocounseling: A survey study. Gerontology & Geriatrics Education, 30, 226–242. doi:10.1080/02701960903133489
Fullen, M. C. (2016a). Counseling for wellness with older adults. Adultspan Journal, 15, 109–123.
doi:10.1002/adsp.12025
Fullen, M. C. (2016b). Medicare advocacy for the counselor-advocate. Adultspan Journal, 15, 3–12.
doi:10.1002/adsp.12015
Fullen, M. C., & Gorby, S. R. (2016). Reframing resilience: Pilot evaluation of a program to promote resilience in marginalized older adults. Educational Gerontology, 42, 660–671. doi:10.1080/03601277.2016.1205409
Fullen, M. C., Granello, D. H., Richardson, V. E., & Granello, P. F. (in press). Using wellness and resilience to predict age perception in older adulthood. Journal of Counseling & Development.
George, L. K. (2010). Still happy after all these years: Research frontiers on subjective well-being in later life. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 65B, 331–339.
doi:10.1093/geronb/gbq006
Gross, P. E., & Eshbaugh, E. M. (2011). Tuning them in versus turning them on: How do we interest students in working with older adults? Gerontology & Geriatrics Education, 32, 122–134.
doi:10.1080/02701960.2011.572037
Helmes, E., & Gee, S. (2003). Attitudes of Australian therapists toward older clients: Educational and training imperatives. Educational Gerontology, 29, 657–670. doi:10.1080/03601270390225640
Institute of Medicine. (2012). The mental health and substance use workforce for older adults: In whose hands? Washington, D.C.: The National Academies Press.
Levy, B. (2009). Stereotype embodiment: A psychosocial approach to aging. Current Directions in Psychological Science, 18, 332–336. doi:10.1111/j.14678721.2009.01662.x
Levy, B. R., Chung, P. H., Bedford, T., & Navrazhina, K. (2014). Facebook as a site for negative age stereotypes. Gerontologist, 54, 172–176. doi:10.1093/geront/gns194
Levy, B. R., Ferrucci, L., Zonderman, A. B., Slade, M. D., Troncoso, J., & Resnick, S. M. (2016). A culture–brain link: Negative age stereotypes predict Alzheimer’s disease biomarkers. Psychology and Aging, 31, 82–88.
doi:10.1037/pag0000062
Levy, B. R., & Myers, L. M. (2005). Relationship between respiratory mortality and self-perceptions of aging. Psychology & Health, 20, 553–564. doi:10.1080/14768320500066381
Levy, B. R., Pilver, C. E., & Pietrzak, R. H. (2014). Lower prevalence of psychiatric conditions when negative age stereotypes are resisted. Social Science & Medicine, 119, 170–174. doi:10.1016/j.socscimed.2014.06.046
Levy, B. R., Slade, M. D., & Gill, T. M. (2006). Hearing decline predicted by elders’ stereotypes. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 61(2), P82–P87.
doi:10.1093/geronb/61.2.P82
Levy, B. R., Slade, M. D., Kunkel, S. R., & Kasl, S. V. (2002). Longevity increased by positive self-perceptions of aging. Journal of Personality and Social Psychology, 83, 261–270. doi:10.1037/0022-3514.83.2.261
Levy, B. R., Slade, M. D., Murphy, T. E., & Gill, T. M. (2012). Association between positive age stereotypes and recovery from disability in older persons. JAMA, 308, 1972–1973. doi:10.1001/jama.2012.14541
Levy, B. R., Zonderman, A. B., Slade, M. D., & Ferrucci, L. (2011). Memory shaped by age stereotypes overtime. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 67, 432–436.
doi:10.1093/geronb/gbr120
McBride, R. G., & Hays, D. G. (2012). Counselor demographics, ageist attitudes, and multicultural counseling competence among counselors and counselor trainees. Adultspan Journal, 11(2), 77–88.
doi:10.1002/j.2161-0029.2012.00007.x
Myers, J. E. (1995). From “forgotten and ignored” to standards and certification: Gerontological counseling comes of age. Journal of Counseling & Development, 74, 143–149. doi:10.1002/j.1556-6676.1995.tb01839.x
Myers, J. E., & Harper, M. C. (2004). Evidence-based effective practices with older adults. Journal of Counseling & Development, 82, 207–218. doi:10.1002/j.1556-6678.2004.tb00304.x
Myers, J. E., & Sweeney, T. J. (2005). Counseling for wellness: Theory, research, and practice. Alexandria, VA: American Counseling Association.
National Board for Certified Counselors. (n.d.). Medicare and professional counselors. Retrieved from http://www.nbcc.org/GovtAffairs/Medicare
Nelson, T. D. (2005). Ageism: Prejudice against our feared future self. Journal of Social Issues, 61, 207–221.
doi:10.1111/j.1540-4560.2005.00402.x
Nelson, T. D. (2016). The age of ageism. Journal of Social Issues, 72, 191–198.
doi:10.1111/josi.12162
Ng, R., Allore, H. G., Trentalange, M., Monin, J. K., & Levy, B. R. (2015). Increasing negativity of age stereotypes across 200 years: Evidence from a database of 400 million words. PLoS One, 10(2), e0117086.
doi:10.1371/journal.pone.0117086
North, M. S., & Fiske, S. T. (2012). An inconvenienced youth? Ageism and its potential intergenerational roots. Psychological Bulletin, 138, 982–997.
doi:10.1037/a0027843
Palmore, E. D. (2005). Three decades of research on ageism. Generations: Journal of the American Society on Aging, 29(3), 87–90.
Posthuma, R. A., & Campion, M. A. (2009). Age stereotypes in the workplace: Common stereotypes, moderators, and future research directions. Journal of Management, 35, 158–188.
doi:10.1177/0149206308318617
Robb, C., Chen, H., & Haley, W. E. (2002). Ageism in mental health and health care: A critical review. Journal of Clinical Geropsychology, 8, 1–12.
doi:10.1023/A:1013013322947
Salisbury, H. (1975). Counseling the elderly: A neglected area in counselor education. Counselor Education and Supervision, 14, 237–238.
doi:10.1002/j.1556-6978.1975.tb00873.x
Saucier, M. G. (2004). Midlife and beyond: Issues for aging women. Journal of Counseling & Development, 82, 420–425.
doi:10.1002/j.1556-6678.2004.tb00329.x
Short, L. (2016). Taking care of the squeaky wheel: Joint replacement long-term issues. The Journal for Nurse Practitioners, 12(4), e175-e176. doi:10.1016/j.nurpra.2016.01.007
SAMHSA-HRSA Center for Integrated Health Solutions. (n.d.). Older adults. Retrieved from www.integration.samhsa.gov/integrated-care-models/older-adults
Thornton, J. E. (2002). Myths of aging or ageist stereotypes. Educational Gerontology, 28, 301–312.
doi:10.1080/036012702753590415
Tomko, J. K. (2008). Predicting counseling psychologists’ attitudes and clinical judgments with respect to older adults (Doctoral dissertation). Retrieved from https://scholarworks.wmich.edu/dissertations/818/
Whitbourne, S. K., & Sneed, J. R. (2002). The paradox of well-being, identity processes, and steretoype threat: Ageism and its potential relationships to the self in later life. In T. D. Nelson (Ed.), Ageism: Stereotyping and prejudice against older persons (pp. 247–273). Cambridge, MA: MIT Press.
Widrick, R. M., & Raskin, J. D. (2010). Age-related stigma and the golden section hypothesis. Aging & Mental Health, 14, 375–385. doi:10.1080/13607860903167846
Zimmerman, S., Dobbs, D., Roth, E. G., Goldman, S., Peeples, A. D., & Wallace, B. (2016). Promoting and protecting against stigma in assisted living and nursing homes. The Gerontologist, 56, 535–547.
doi:10.1093/geronto/gnu058
Jun 28, 2018 | Volume 8 - Issue 2
Ryan M. Cook, Laura E. Welfare, Devon E. Romero
Studies from allied professions suggest that intentional nondisclosure in clinical supervision is common; however, the types of intentional nondisclosure and reasons for nondisclosure have yet to be examined in an adequate sample of counselors-in-training (CITs). The current study examined intentional nondisclosure by CITs during their onsite supervision experience. We utilized content analysis to examine examples of intentional nondisclosure. Sixty-six participants provided examples of intentionally withholding information from their supervisors they perceived as significant. The most common types of information withheld were negative reactions to supervisors, general client observations, and clinical mistakes. The most common reasons cited were impression management, perceived unimportance, negative feelings, and supervisor incompetence. We offer implications for both supervisees and supervisors on how they might mitigate intentional nondisclosure; for example, we present strategies to address ineffective or harmful supervision, discuss techniques to openly address intentional nondisclosure, and explore ways to integrate training on best practices in clinical supervision.
Keywords: intentional nondisclosure, counselors-in-training, supervision, content analysis, best practices in clinical supervision
Counselors-in-training (CITs) in programs accredited by the Council for Accreditation of Counseling & Related Educational Programs (CACREP) are required to complete two supervised onsite field experiences (i.e., practicum and internship) in their area of interest (e.g., clinical mental health, school, rehabilitation; CACREP, 2015). The purpose of this onsite field experience is for CITs to learn the roles and responsibilities of being a professional counselor by applying what they learn in their training programs to their work in a counseling setting (CACREP, 2015). Given CITs’ limited clinical experience, onsite supervisors provide weekly supervision to aid CITs in their professional development (Borders et al., 2011; Borders et al., 2014). Although supervision is a unique opportunity, CITs receive problematic mixed messages about the expectations of the supervisory process (Borders, 2009). CITs are encouraged to discuss the topics and concerns that are the most important to their professional growth (Bordin, 1983), but the information shared is then used by their supervisors to evaluate their clinical performance (Bernard & Goodyear, 2014). These evaluations have a definitive impact on CITs’ ability to pass a practicum or internship course or graduate (CACREP, 2015) and subsequently secure employment in the counseling field. Thus, it is not surprising that studies in allied professions (e.g., clinical psychology, counseling psychology, social work) have shown that trainees commonly withhold potentially unflattering information from their supervisors (Hess et al., 2008; Ladany, Hill, Corbett, & Nutt, 1996; Mehr, Ladany, & Caskie, 2010, 2015; Pisani, 2005). While CITs’ concern to maintain a favorable image in the eyes of their supervisor is understandable, withholding information can result in missed learning opportunities for CITs and negatively impact their clients (Hess et al., 2008).
To date, only two studies have examined supervisee intentional nondisclosure in a sample of counselor education students (Cook & Welfare, 2018; Lonn & Juhnke, 2017). However, neither study examined specific examples of the types and reasons of CIT nondisclosure during onsite supervision. Counselors submit to a unique training model, with specific requirements and goals for master’s-level counselors (e.g., CACREP, 2015). CITs enrolled in CACREP-accredited programs can specialize in one of seven tracks: (a) addictions counseling; (b) career counseling; (c) clinical mental health counseling; (d) clinical rehabilitation counseling; (e) college counseling and student affairs; (f) marriage, couple, and family counseling; (g) school counseling; and (h) rehabilitation counseling. As a result, CITs work in diverse settings with a wide variety of responsibilities that are unique to the counseling profession (CACREP, 2015; Lawson, 2016). Without a study focused on CITs’ experiences in onsite supervision, CITs and supervisors must rely on findings from allied professions that may or may not reflect the counseling training model. Thus, in the current study we aimed to examine the types of intentional nondisclosure and the reasons for the nondisclosure during CITs’ supervised onsite field experience.
Supervised Onsite Field Experience in CACREP-Accredited Programs
Given the growing importance of attending a CACREP-accredited program as an educational requirement for professional counselors (Lawson, 2016), we chose to specifically target intentional nondisclosure by CITs enrolled in CACREP-accredited training programs. State licensure boards are encouraging or mandating that those pursuing professional licensure as counselors must have a degree from a CACREP-accredited program (Lawson, 2016). Additionally, as of January 1, 2022, those applying to be National Certified Counselors (NCCs) will need to graduate from a CACREP-accredited program (National Board for Certified Counselors, 2014). Thus, the standards for onsite field experiences outlined in the 2016 CACREP Standards provide clear guidelines for counselor training. Furthermore, the activities during the onsite field experience are designed to mimic those of a professional counselor in the field (CACREP, 2015). Exploring CIT intentional nondisclosure within the CACREP educational structure can help to inform best practices in counselor training.
Intentional Nondisclosure in Clinical Supervision
The supervision process is reliant on CITs to self-identify important information to share with their supervisors (Ladany et al., 1996); however, identifying this important information is not always clear to CITs given the intricacies of the client–counselor relationship (Farber, 2006; Knox, 2015). Farber (2006) suggested that some nondisclosure “is normative and unavoidable in supervision” (p. 181). Yet, there are instances in which CITs purposefully withhold information they know is relevant because of concerns for what could happen if they shared the information with their supervisor (Hess et al., 2008; Yourman & Farber, 1996).
So why would CITs, who are held to the same ethical standards as practicing counselors (American Counseling Association [ACA], 2014), knowingly choose to withhold information that could be harmful to their professional development or their clients’ treatment? During an onsite field experience, CITs learn the day-to-day tasks of being a professional counselor (e.g., establishing rapport, planning treatment, managing paperwork), but they also must meet the demands of their graduate training programs. Most CITs want to perform counselor functions at a high level, if not perfectly (Rønnestad & Skovholt, 2003). Avoiding clinical mistakes is a dubious belief that CITs hold for themselves (Knox, 2015). These high expectations create a reasonable desire to present oneself favorably to their supervisors, even though supervisors know that perfection is impossible (Farber, 2006). Moreover, CITs are told to share information that is most salient to their personal and professional development with their supervisors, but disclosing information that may be potentially unflattering or embarrassing can then be used by supervisors to evaluate performance (Borders, 2009).
Types and Reasons for Intentional Nondisclosure
In a seminal study on intentional nondisclosure, Ladany et al. (1996) investigated the types and reasons for nondisclosure in a sample of clinical and counseling psychology trainees. Participants were asked to identify instances in which they withheld information from their supervisors and then provide a rationale for why they failed to share that information. The authors found that 97.2% of the participants withheld information from their supervisors.
Through categorizing the content of the nondisclosures, Ladany et al. identified 13 types of nondisclosure, providing definitions and examples of each type: (a) negative reactions to supervisor (e.g., unfavorable thoughts or feelings about supervisors or their actions); (b) personal issues (e.g., information about an individual’s personal life that may not be relevant); (c) clinical mistakes (e.g., an error made by a counselor); (d) evaluation concerns (e.g., worry about the supervisor’s evaluation);
(e) general client observations (e.g., reactions about the client or client treatment); (f) negative reactions to client (e.g., unfavorable thoughts or feelings about clients or clients’ actions); (g) countertransference (e.g., seeing oneself as similar to the client); (h) client–counselor attraction issues (e.g., sexual attraction between client and counselor); (i) positive reactions to supervisor (e.g., favorable thoughts or feelings about supervisors or their actions); (j) supervision setting concerns (e.g., concerns about the placement or tasks required at placement); (k) supervisor appearance (e.g., reactions to supervisor’s outward appearance); (l) supervisee–supervisor attraction issues (e.g., sexual attraction between supervisee and supervisor); and (m) positive reactions to client (e.g., favorable thoughts or feelings about clients or their actions).
They also identified 11 reasons for intentional nondisclosure: (a) perceived unimportance (e.g., information not worth discussing with supervisor); (b) too personal (e.g., information about one’s personal life that is private); (c) negative feelings (e.g., embarrassment, shame, anxiety); (d) poor alliance with supervisor (e.g., poor working relationship with supervisor); (e) deference (e.g., inappropriate for a counselor to bring up because of their role as intern or supervisee); (f) impression management (e.g., desire to be perceived favorably by supervisor); (g) supervisor agenda (e.g., supervisor’s views, roles, and beliefs that guide supervisor’s actions or reactions to supervisee); (h) political suicide (e.g., fear that the disclosure will be disruptive in the workplace and lead to the supervisee being unwelcome or unsupported); (i) pointlessness (e.g., addressing the issue would not influence change); (j) supervisor not competent (e.g., supervisor is inaccessible or unfit for supervisory role); and (k) unclear (e.g., researchers unable to read participants’ statements). The most common types of intentional nondisclosure in the study by Ladany et al. (1996) were negative reactions to supervisor, CITs’ personal issues, clinical mistakes, and evaluation concerns, while the most common reasons for the nondisclosures were perceived unimportance, too personal, negative feelings, and a poor alliance with the supervisor.
Subsequent studies, also from allied professions (e.g., social work, clinical psychology), have found similar results in regard to the types and reasons for intentional nondisclosure (Hess et al., 2008; Mehr et al., 2010; Pisani, 2005). Mehr and colleagues (2010) found 84.2% of psychology trainees reported withholding information from their supervisors, and the most common types of nondisclosures were negative perception of supervision, personal life concerns, and negative perception of the supervisor, while the most common reasons for nondisclosure were impression management, deference, and fear of negative consequences. Additionally, Pisani (2005) found the most commonly withheld information for social work trainees included supervisor–supervisee attraction issues, negative reactions to supervisor, and supervision setting concerns. Finally, in a qualitative study, Hess et al. (2008) explored the differences in a single example of intentional nondisclosure based on psychology trainees’ perceptions of the quality of the supervisory relationship—for example, good (i.e., only one instance of a problem in the supervisory relationship) versus problematic supervisory relationships (i.e., ongoing issues in the supervisory relationship). They found that supervisees in both good and problematic supervisory relationships withheld information about client-related issues. However, supervisees in problematic relationships more commonly withheld supervision-related concerns (e.g., negative reactions to supervisor) compared to supervisees in good relationships. The findings described above provide empirical evidence that nondisclosure in allied professions is common.
The Current Study
Although there is evidence that supervisees from allied professions withhold information, there is currently a dearth of literature regarding intentional nondisclosure by CITs in the field of counseling. Cook and Welfare (2018) found that the quality of the supervisory working alliance and supervisee avoidant attachment style predicted supervisee nondisclosure. In a qualitative study, Lonn and Juhnke (2017) examined supervisee nondisclosure in triadic supervision. They found that the supervisee’s perception of their relationships, the presence of a peer, and opportunity to share were important to whether supervisees withheld information. However, these studies failed to examine the types of information being withheld by CITs as well as their reason for withholding information. Considering that professional counselors have a unique training model (CACREP, 2015), professional identity (Lawson, 2016), and code of ethics (ACA, 2014), the purpose of the current study was to examine the types and reasons of intentional nondisclosure by CITs during their supervised onsite internship experience.
Method
We utilized content analysis (Hsieh & Shannon, 2005) to examine the examples of intentional nondisclosures provided by CITs that occurred in supervision with their onsite internship supervisors. Hsieh and Shannon (2005) defined qualitative content analysis as “a research method for the subjective interpretation of the content of text data through the systematic classification process of coding and identifying themes or patterns” (p. 1278). Our analysis was guided by the findings from Ladany et al. (1996), which allowed us to compare the findings from the current study with those from allied professions while also examining how the phenomenon of intentional nondisclosure might present uniquely in the counseling profession (Hsieh & Shannon, 2005). The current study was designed to answer two research questions: (a) What are the types of information that CITs intentionally withhold from their supervisors during their internship’s onsite supervision? and (b) What are the reasons for their nondisclosure?
Research Team
Our research team included three members. The first and third authors served as coders while the second author served as a peer reviewer. The first and second authors are counselor educators at different universities in the Southeast United States, and the third author was a doctoral student at the same institution as the first author. We all have experience as professional counselors, supervisees, supervisors, and researchers; consequently, we have experienced all parts of the nondisclosure cycle. Prior to the analysis process, we discussed how our previous experiences might impact the analysis. Likewise, we intentionally discussed and bracketed potential influences of bias throughout the project. We also employed triangulation (e.g., multiple coders), utilized frequent peer debriefs, and employed a peer reviewer (Creswell, 2013). Our items also were reviewed by four consultants with counseling, supervision, and research experience to minimize bias and maximize clarity.
Recruitment Procedure and Participants
After securing IRB approval, we recruited participants currently enrolled in internship for the current study through the assistance of counselor education faculty at CACREP-accredited institutions. Fifteen counselor educators at 14 institutions offered paper-and-pencil instrument packets to CITs during one of their class periods. As indicated by the key informants, 152 of the 173 CITs present in class on the day the packets were offered agreed to participate in the study. This resulted in an in-class response rate of 87.86%.
Participants were CITs currently enrolled in internship in a CACREP-accredited program and receiving supervision at their internship sites. The age of the participants ranged from 22 to 60 years old (M = 28.13, SD = 7.43, n = 107). Eighty-eight participants identified as female (80%), 17 participants identified as male (15.5%), three participants identified as nonbinary (gender identity not male and not female, 2.7%), and two participants indicated that they did not want to disclose their gender (1.8%). Regarding race, the majority of participants identified as White (non-Hispanic; n = 71, 64.5%), while 23 participants identified as African American (20.9%), four participants identified as Asian/Pacific Islander (3.6%), three participants identified as Hispanic/Latinx (2.7%), three participants identified as multiracial (2.7%), one participant identified as Native American (0.9%), one participant responded “none of the above categories” (0.9%), and four participants responded that they preferred not to disclose (3.6%). Regarding CACREP track, 64 participants were enrolled in a clinical mental health counseling track (58.2%), 32 participants were enrolled in a school counseling track (29.1%), nine were enrolled in a college counseling and students affairs track (8.2%), and five were enrolled in a marriage, couples, and family track (4.5%).
Instrument
The instrument was designed to gather information about participants’ experiences with their current onsite internship supervisors. Two items were the focus of this study: (a) “Describe a time when you decided not to share something you thought was significant with your current onsite internship supervisor” and (b) “What brought you to that decision to not share it with your current onsite internship supervisor?” In addition, the questionnaire included 15 items to collect demographic information about the participants and their current onsite internship supervisors. Of the 152 participants who began participation, 42 participants (27.6%) were removed from the analysis as they did not complete the open-ended questions, resulting in a final sample of 110 participants. We utilized the demographic variables to check for evidence of nonresponse bias using Chi-square tests of independence and independent t-tests. We did not find evidence of response bias when comparing those who answered the open-ended questions and those who did not.
Data Analysis
We analyzed participants’ responses to the open-ended questions utilizing content analysis. We categorized the types of intentional nondisclosure and the reasons for nondisclosure into categories as recommended by Hsieh and Shannon (2005). For our analysis, we utilized the types of nondisclosure and the reasons for nondisclosure originally identified by Ladany et al. (1996). To reiterate, Ladany et al. identified 13 types of intentional nondisclosure and 11 reasons for nondisclosure (1996). Also, as recommended by Hsieh and Shannon (2005), we allowed for new categories to emerge that did not fit within the categories from Ladany et al. The rationale for this approach was two-fold. First, we could best understand the phenomenon of intentional nondisclosure by comparing our findings to that of previous research from allied professions, while also generating new knowledge of how nondisclosure might uniquely manifest in the counseling profession (Lawson, 2016). Second, utilizing previous research provided structure to our coding procedures and informed the researchers’ interpretation of participant responses (Hsieh & Shannon, 2005).
Coding process. The first and third authors coded the responses of 110 participants for (a) whether or not the participant identified an incident of intentional nondisclosure and (b) to categorize the participant responses that indicated intentional nondisclosure by the type and reasons for the nondisclosure. Each response was coded into one category of type of nondisclosure and one category of reason for the nondisclosure. First, the two coders selected 10 participant responses and coded them as a team. Next, the two coders selected an additional 10 participant responses and coded them independently of each other. They then came together to reach a consensus on the categorization of participant responses. The remaining 90 participant responses were coded independently, and the two coders regularly engaged in peer debriefings throughout the process to ensure consistency (Creswell, 2013). After all 110 participant responses were analyzed, the first and third authors met to finalize the categorization of participant responses and to generate names for the new categories that emerged during the analysis (Hsieh & Shannon, 2005). Regarding the categorization of participant responses in terms of the participant-identified incident of intentional nondisclosure, the coders’ agreement was 100%. Regarding the types and reasons for the nondisclosure, the coders initially disagreed on 15 types of intentional nondisclosure and 23 reasons for the nondisclosure. The two coders established consensus through discussion, resulting in an agreement of 100% (Creswell, 2013). Finally, the second author, serving as a peer reviewer, evaluated the entire coding process. She was chosen based on her expertise with supervision delivery (e.g., protocol, practice) and the topic of intentional nondisclosure. She did not recommend any changes to the categorization of participant responses; however, she recommended renaming two of the new categories for the types of nondisclosures that emerged from the data to better reflect the content of participant responses. Eleven types of intentional nondisclosure and 13 reasons emerged from our analysis.
Results
Forty-four (40%) participants reported that they had never withheld something significant from their current onsite internship supervisors, while 66 (60%) reported that they had. Examples of responses coded as never having withheld something significant from their onsite supervisors include “N/A,” “At this time, I have not withheld any information that I felt was significant with my supervisor,” and “I don’t think there has been one.” For the responses that included an example of intentional nondisclosure (n = 66), 11 types of intentional nondisclosure and 13 reasons for withholding information emerged from the data. The types of intentional nondisclosure included eight types of nondisclosure that were from Ladany et al.’s (1996) research on nondisclosure and three new types of intentional nondisclosure that emerged in this data set: (a) CIT professional developmental needs, (b) a peer’s significant issue, and
(c) experiencing sexual harassment. Regarding the reasons for the intentional nondisclosures, 10 reasons mirrored the findings from Ladany et al. and three reasons were unique to the current study: (a) did not want to harm client or confidentiality concerns, (b) consulted with another supervisor, and (c) issue with other professional in supervision setting.
The Types and Reasons for Intentional Nondisclosures
The most common type of intentional nondisclosures identified by the researchers in the current study were negative reactions to supervisor (n = 18, 27.3%), general client observations (n = 16, 24.2%), and clinical mistakes (n = 15, 22.7%). The most common reasons for intentional nondisclosures were impression management (n = 12, 18.2%), perceived unimportant (n = 8, 12.1%), negative feelings, (n = 8, 12.1%), and supervisor not competent (n = 8, 12.1%). Complete results of the coding and category frequencies of the types of nondisclosures are presented in Table 1, and the final coding and category frequencies of the reasons for nondisclosure are presented in Table 2.
| Table 1
Types of Intentional Nondisclosure |
| Type of Intentional Nondisclosure |
n (%) |
Examples |
| Negative Reactions to Supervisor |
18 (27.3%) |
When my supervisor asked if there is anything that is hindering our relationship, I lied and said that there wasn’t anything and the relationship is fine.
I feel that I am not getting feedback about my counseling from my supervisor in the supervision meetings. Instead I am only getting suggestions of how the supervisor would have handled the client.
Made a comment behind my back. My onsite supervisor is new and so I don’t share too much because he’s easily overwhelmed. |
General Client
Observations |
16 (24.2%) |
I gave [clients] more chances to skip/miss an appointment than [my supervisor] would allow so sometimes don’t let her know when people cancel or no show.
When a client disclosed personal family issues; client’s past trauma. |
| Clinical Mistakes |
15 (22.7%) |
I put a client in danger by a lack of knowledge and being new in a position.
Too much self-disclosure in a session; getting behind on case notes/paperwork.
Having a chronically suicidal client and . . . not assessing for SI in a session and feeling as if when assessed it was not done so well. |
Client–Counselor
Attraction Issues |
4 (6.1%) |
I felt attracted to an assessment client.
During a session, a client told me that he liked how I looked in my pants. He then told me that he got excited at the sound of my voice. |
| Countertransference |
3 (4.5%) |
A client reminded me of my late mother.
Early in internship, I had strong countertransference with a client. |
| Supervision Setting Concerns |
3 (4.5%) |
I was concerned if I was going to have to find another site to finish hours.
Frustration with internship duties. |
| Personal Issues |
2 (3.0%) |
I did not tell my supervisor that I chose to cut it off with a potential romantic partner. |
| CIT Developmental Need |
2 (3.0%) |
When I was first starting out I had a hard time letting my supervisor know when I needed something extra from them whether it be time or information. |
| Negative Reactions to Client |
1 (1.5%) |
Anger toward a student. |
| A Peer’s Significant Issue |
1 (1.5%) |
A client wrote a letter to my co-intern about his sexual desires and love for her. |
| Experiencing Sexual Harassment |
1 (1.5%) |
When I felt sexually harassed by a colleague. |
| Note. Not all types of intentional nondisclosure from Ladany et al. (1996) were present in this sample, and three new types emerged: (a) CIT developmental need, (b) a peer’s significant issue, and (c) experiencing sexual harassment.
|
| Table 2
Reasons for Intentional Nondisclosure |
| Reasons |
n (%) |
Examples |
Impression
Management |
13 (19.7%) |
Concerned about evaluations by those who supervise my supervisors.
Fear of looking bad or being perceived as not being a good counselor.
[Supervisor] might pass judgment because I can’t possibly know what I’m talking about being only an intern.
I worried she will think I’m unprofessional or not trust me with future clients. |
| Negative Feelings |
8 (12.1%) |
Poor self-confidence.
Fear of rejection.
Embarrassment, inferiority felt with supervisor. |
Supervisor Not
Competent |
8 (12.1%) |
I see the way she counsels clients and I know she thinks taking time to establish rapport and positive therapeutic relationships is not always necessary.
Everyone in the office says she is burnt-out and I want to be more compassionate. |
Perceived
Unimportant |
8 (12.1%) |
I did not feel it was necessary.
I was running late to class and I didn’t consult with her because she was in a session with a client so I figured I’d tell her the next day. |
| Deference |
6 (9.1%) |
I did not feel like it would be taken well, and that I am only an intern and should not correct her.
Didn’t want to hurt/upset her or burn a professional relationship. |
| Poor Alliance with Supervisor |
5 (7.6%) |
The power differential.
She berated me in supervision to the point of tears. I feel unsafe with her and our clinical styles contrast.
I knew she would make me feel inferior. |
| Supervisor Agenda |
4 (6.1%) |
I thought he would immediately notify people in charge.
Knowing my supervisor would want to tell [client’s] mother. |
| Political Suicide |
4 (6.1%) |
I want to get hired where I’m working and I don’t feel . . . safe during supervision.
It’s a small practice and I have to share a wall with this offender every day. |
Did Not Want to Harm Client or
Confidentiality
Concerns |
4 (6.1%) |
I didn’t want to put client in a bad situation.
That student was not positive of her status and was not in any danger. Revealing her secret at that point would have damaged the relationship.
Confidentiality issues. |
| Too Personal |
3 (4.5%) |
It was too personal.
I didn’t want to talk about my grief. |
| Pointlessness |
1 (1.5%) |
Thought that was between student and personal physician. |
Consulted with
Another
Supervisor |
1 (1.5%) |
Other supervisor suggestions. |
Issues with Other Professionals in
Supervision Setting |
1 (1.5%) |
The teacher expressed frustration. Hopes to prevent future conflict. |
| Note. Not all categories and reasons from Ladany et al. (1996) were present in this sample, and three new reasons emerged: (a) did not want to harm client or confidentiality concerns, (b) consulted with another supervisor, and (c) issues with other professionals in supervision setting. |
Specific Examples of the Types and Reasons for Intentional Nondisclosure
To provide a more complete picture of the phenomenon of intentional nondisclosure (Hsieh & Shannon, 2005), this section is presented to highlight specific examples provided by participants for each type of nondisclosure and the reasons they withheld the information. Our coded reason for the type of intentional nondisclosure is included in parentheses below (e.g., deference, impression management, political suicide).
Negative reactions to supervisor. One participant stated that she did not disclose that her supervisor “was not helpful during a time that I needed her to be” because the participant “did not want to . . . upset her or burn a professional relationship” (deference). Another participant did not tell her supervisor at her school internship that she disapproved of the way the supervisor addressed a student: “I felt she was being too harsh on a student and not considering other factors.” This participant did not want her supervisor to perceive her as “being wrong” (impression management). A participant stated that even though her supervisor sits in on all of her sessions at her internship site, she still withheld that she is not satisfied with the quality of their relationship and did not share how she felt “in the relationship with her.” She added that she did not disclose this information because “I am afraid she’ll be angry and it will damage the relationship we do have” (negative feelings). Finally, for a clinical mental health CIT, even her supervisor directly asking if she had concerns about the supervisory relationship was not enough to encourage her disclosure: “When my supervisor asked if there is anything that is hindering our relationships I lied and said that there wasn’t anything and the relationship is fine.” The CIT stated she lied because “the power differential, being videotaped, and concerns with confidentiality . . . stopped me from being completely honest about my comfort with our relationship” (poor alliance with supervisor).
General client observations. General client observations differed from clinical mistakes because participants did not self-identify that they perceived the specific examples they provided to be mistakes. Rather, participants indicated that the examples they provided were relevant; however, they failed to disclose this significant information to their supervisors. One school counseling CIT stated that she did not share with her supervisor that she was having trouble “breaking the ice with a client” because she “knew my [supervisor] would make me feel inferior” (poor alliance with supervisor). Another school counseling CIT shared that she failed to disclose that one of her clients was “drinking alcohol on campus” because she thought her supervisor would “immediately notify people in charge of discipline rather than talking to the student first” (supervisor agenda). Finally, another school counseling CIT stated that a client told her she was pregnant, but she failed to notify her supervisor because “that student was not positive of her status and was not in any danger. Revealing her secret at that point would have damaged the relationship” (did not want to harm client; confidentiality concerns).
Clinical mistakes. Participants reported a range of clinical mistakes, from minor clerical errors to potentially more problematic mistakes such as failure to assess for client risk. One clinical mental health CIT did not share that she was “behind on my case notes” because she “did not feel it was necessary” and she “caught up quickly” (perceived unimportant). A student affairs CIT stated that he did not let his supervisor know that he “lacked confidence in theories” because he felt “inadequate” and “embarrassed” (negative feelings). A clinical mental health CIT shared that she failed to disclose something in supervision that her supervisor had previously told her not to do: “My supervisor had previously verbalized that she would be upset.” She withheld this information because “I didn’t want to seem . . . incompetent and I respected her and want her to think I’m doing my best” (impression management). Multiple participants provided specific examples of intentional nondisclosures related to failing to adequately assess for client risk or failing to notify their supervisors that a client was engaging in risk-related behavior. A school counseling CIT shared that she did not discuss with her supervisor that “a client (minor on a school campus) was engaging in [non-suicidal self-injury] again” because “we discussed before how she is obligated to pass that info to school principal who tells parents” (supervisor agenda). This participant added that she decided not to share this information with her supervisor because she perceived the self-injury to be non–life threatening and she wanted to “save rapport” with the client (did not want to harm client; confidentiality concerns). Finally, a school counseling CIT stated that she withheld from her supervisor that she “put a client in danger by my lack of knowledge and being new in my position.” This CIT did not discuss this with her supervisor because “my supervisor wasn’t available” (supervisor not competent).
Client–counselor attraction issues. One clinical mental health counseling CIT stated that her client “told me that he liked how I looked in my pants. He then told me that he got excited at the sound of my voice.” She stated that she did not disclose this information to her supervisor because “I told myself that I did not understand how he meant the comment and I thought he would stop the flirting if I ignored him” (perceived unimportant). Two participants indicated that they experienced sexual attraction to a client but failed to share it with their supervisor. One student affairs CIT stated that she felt “embarrassed” (negative feelings), while a clinical mental health counseling CIT shared that he “did not want anyone to find out and I felt like I handled it fine” (impression management).
Countertransference. One marriage, couples, and family CIT stated that she did not disclose to her supervisor that a client “reminded me of [my] late mother” because she “did not want to talk about [my] grief” (too personal). A clinical mental health counseling CIT echoed the previous participant’s thinking process. She stated she did not tell her supervisor she was experiencing “countertransference” with a client because “it was too personal” (too personal). Finally, another marriage, couples, and family CIT stated that early in her internship she had “strong countertransference with a client” as a result of a personal grieving process. She shared that she did not tell her supervisor because she wasn’t sure “how much I trusted her with this information as it was only several weeks into internship” (poor alliance with supervisor).
Supervision setting concerns. A clinical mental health counseling CIT stated that she did not express her “frustration with internship duties” to her supervisor because “he was unavailable” (supervisor not competent). Another clinical mental health counseling CIT was concerned that she “would need to find another site to finish [internship] hours,” but did not tell her supervisor because “I did not choose to add to stress [of my] site supervisor by posing my concern” (deference).
Personal issues. One participant enrolled in a clinical mental health counseling program withheld from the supervisor that “sad and depressed” feelings because of a “fear of rejection” (negative feelings) arose during supervision. A school counseling CIT did not disclose to her supervisor that she had recently ended a relationship “with a potential romantic partner” even though it was causing her to “feel drained and emotional during the day at her internship” because “I felt that it would be silly to and I thought I did a good enough job ignoring the feelings while with students” (too personal).
CIT developmental need. One clinical mental health counseling CIT shared that she had a difficult time “letting my supervisor know when I needed something extra from them whether it be time or information” because she “felt nervous about [her] position as ‘just an intern’” (negative feelings). Another clinical mental health counseling CIT stated that she failed to let her supervisor know that she is “concerned about being in an individual session with a male client” because she is fearful that her supervisor would think she is “unprofessional or not trust me with future clients” (impression management).
Negative reactions to client. Only one participant indicated that she failed to disclose a negative reaction to a client with her supervisor. This student affairs CIT stated that she did not disclose her “anger towards a client” because she “did not think it was important enough to share” (perceived unimportant).
A peer’s significant issue. One clinical mental health counseling CIT noted that there was a failure to disclose to the supervisor that “a client wrote a letter to my co-intern about his sexual desires and love for her.” This CIT stated that the co-intern did not want this information shared and that the participant “did not think it was my place” (deference).
Experiencing sexual harassment. A clinical mental health counseling CIT stated that she was “sexually harassed by a colleague,” but failed to disclose to her supervisor because “it’s a small practice and I have to share space with this offender every day” (political suicide).
Discussion
The current investigation was designed to examine the types of and reasons for intentional nondisclosure by CITs during their onsite supervision. Sixty percent of the participants provided an example of withholding something significant from their onsite internship supervisors, suggesting that, similar to allied professions, intentional nondisclosure by counseling CITs is common (Ladany et al., 1996; Pisani, 2005; Yourman & Farber, 1996). Participants also provided detailed examples of the types of intentional nondisclosures as well as the reasons they withheld the information. These findings provide insight into the experiences of CITs at their internship placement. In this section, we will connect our findings to those from previous research as well as offer implications for counselors, supervisors, and counselor training programs.
The Types of Intentional Nondisclosure and Reasons for Nondisclosure
Overall, the types of intentional nondisclosure and the reasons for these nondisclosures are comparable to the findings of previous studies in allied professions. There were four categories of the types of intentional nondisclosure that emerged in the study by Ladany et al. (1996) that were not present in the current study: (a) positive reactions to supervisor, (b) supervisor appearance, (c) supervisee–supervisor attraction issues, and (d) positive reactions to client. The category of “unclear” in regard to the reasons for nondisclosure also was not found in the current study, as all participant responses in the current study were legible. Participants of differing CACREP tracks all provided examples of intentional nondisclosure to their supervisors in regard to their field placement. These findings suggest that despite the differences in training models (CACREP, 2015) and professional identities (Lawson, 2016), CITs experience many of the same situations that result in intentional nondisclosure as those from allied professions. The most commonly withheld information in the current study was negative reactions to supervisor, which also was true for psychology trainees in the study by Ladany et al. Supervisees appear most hesitant to discuss their concerns about their supervisor or supervision experience (Hess et al., 2008; Mehr et al., 2010; Pisani, 2005). In addition, CITs also commonly withheld general observations about clients and clinical mistakes similar to allied professions (Hess et al., 2008; Ladany et al., 1996; Mehr et al., 2010; Pisani, 2005).
The CITs in the current study provided many reasons for their intentional nondisclosure, but some reasons were more commonly reported than others. Like the findings from Mehr et al. (2010), participants in the current study most commonly withheld information in order to make a favorable impression on their supervisors. Others reported they withheld because of negative feelings such as “shame” or “embarrassment.” Farber (2006) suggested that internalized negative feelings are often a reason for nondisclosure. Consistent with findings from allied professions (Hess et al., 2008; Ladany et al., 1996), CITs also withheld because (a) they believed a supervisor was not competent, (b) they believed information was not quite important enough to disclose, and (c) they wanted to perform perfectly in their new roles.
Novel Findings Regarding Types and Reasons for Intentional Nondisclosure
An important aspect of content analysis is discussing findings that may extend existing knowledge of a given phenomenon (Hsieh & Shannon, 2005). The current study is the first to examine the types of intentional nondisclosure and reasons for nondisclosure in a sample of CITs. As such, there are several novel findings that warrant discussion. For example, two participants indicated that they did not discuss their professional development needs with their onsite supervisor. This is particularly interesting, given a central function of clinical supervision is to facilitate CIT professional development (Bernard & Goodyear, 2014). CITs who internalize their professional developmental needs as a flaw or who desire to hide these needs for fear of their supervisors’ reactions also may desire to perform perfectly (Rønnestad & Skovholt, 2003). Discussing opportunities for growth as a CIT can be difficult (Mehr et al., 2010); thus, supervisors may need to prompt their supervisees to discuss their needs more directly.
Another novel finding is that one participant indicated that she withheld from her supervisor about her peer’s ethical dilemma (the client letter revealing romantic interest). This participant explained that she did not feel it was her place to share her peer’s information, but all counselors and CITs share some responsibility to address ethical concerns. Ladany et al. (1996) found that 53% of those who withheld information from their supervisors told a peer in the field about their concern. Therefore, it seems likely that other CITs may be placed in a similar position as the participant in the current study. Knowing one’s ethical responsibility to disclose unethical behavior, as in the situation germane to this study, could be prudent (ACA, 2014). Finally, one participant indicated that she was being sexually harassed by a colleague. This report of intentional nondisclosure is particularly concerning given the increased attention to Title IX and attempts to mitigate sexual harassment and sexual assault in university and workplace settings (Welfare, Wagstaff, & Haynes, 2017). This participant’s willingness to share her trauma through the data collection process in this study presents an opportunity for counselor educators and supervisors to explore strategies to prevent these experiences for future CITs.
Regarding the reasons for intentional nondisclosure, there also were novel findings because three new reasons emerged in the current study. First, five participants did not disclose information to their supervisor because they did not want to harm their clients or violate a client’s confidentiality. However, the sharing of information with a supervisor would never violate client confidentiality (ACA, 2014). Perhaps the supervisees’ confusion about the parameters of confidentiality or misdirected efforts to protect clients from the actions of a supervisor they perceived as incompetent led to this decision. A second novel reason for intentional nondisclosure was evidenced by one participant who reported consulting with a supervisor who was not her site supervisor. Ladany et al. (1996) found that 15% of psychology trainees consulted with “another supervisor” outside their primary supervisor (p. 16). Ladany et al. did not ask their participants to clarify the role of another supervisor; however, this finding is relevant to the current study and the training of CITs. Throughout a CIT’s internship experience, they have two supervisors: one onsite supervisor and one university supervisor (CACREP, 2015). It is unclear if the supervisor with whom the participant discussed their concern was another supervisor at the site or the university supervisor. However, this could be an inherent challenge for CITs to identify who to share information with, particularly if there are issues in one of the two relationships. Finally, one school counseling CIT indicated that she had an issue with a teacher and addressed this issue with the teacher directly. Counselors work in diverse settings (ACA, 2014; CACREP, 2015) and may often work with persons outside the counseling profession. Counseling programs and supervisors may need to better prepare students to work with other professionals in their specific setting.
Implications for CITs
The findings from the current study provide empirical evidence that, when faced with the decision to share in clinical supervision, CITs sometimes chose to withhold information from their supervisors despite knowing its relevance. CITs of all CACREP tracks will likely be faced with this difficult decision. We hope that these findings, which offer insights into the experience of intentional nondisclosure, help to normalize the challenges that CITs face and identify strategies to prevent nondisclosure.
Some of the participants described harmful supervision experiences in which they were berated by their supervisors, feared fallout if they were to disclose illegal sexual harassment by another site employee, were concerned about a supervisor’s clinical competence, or did not feel safe to share even blatantly inappropriate client behaviors. Harmful supervision such as this has also been described by Ellis et al. (2014) and is a major concern for counseling and related professions. CITs who find themselves in harmful supervision situations can consider seeking support from another professional, a peer, or a professional association ethics consultant who might help rectify these issues.
Even for those CITs who are not enduring harmful supervision, there are costs to nondisclosure such as stalled development, safety concerns, and ethical or legal violations. Ultimately, the decision to withhold information from one’s clinical supervisor rests with the CIT (Murphy & Wright, 2005). Advocating for a safe and productive supervisory experience may result in a change that serves as a catalyst for supervisee growth or prevents client harm. No supervisee needs to be concerned about burdening a supervisor with disclosures about training issues or ethics; it is the supervisor’s responsibility to address supervisee needs, no matter how burdensome. Relatedly, supervisees who are reluctant to discuss their observations of clients or clinical mistakes for fear of being evaluated poorly or perceived as unqualified should consider ways to demonstrate quality work in order to balance the areas for growth. Making mistakes is expected for all CITs, but it is important to use supervision to learn from these mistakes (Pearson, 2001). In fact, reflecting on previous experiences—and learning from those experiences—is key to becoming a skilled and seasoned counselor (Rønnestad & Skovholt, 2003). CITs also might find it helpful to pursue their own personal counseling as another strategy to facilitate personal and professional growth (Oden, Miner-Holden, & Balkin, 2009).
Several CITs shared their hesitancy in disclosing information to their supervisor for fear of violating their clients’ confidentiality or harming the therapeutic alliance. Although client confidentially is critical, disclosing information to one’s supervisor would not violate a client’s confidentiality (ACA, 2014). In fact, some of the concerns expressed seemed to be more about the limits of confidentiality in the setting more broadly (e.g., high school rules), rather than with the supervisor specifically. Counselors are encouraged to not tell a client that the information shared during the counseling process will remain absolutely confidential. Rather, counselors are encouraged to include a passage in their informed consent about the boundaries of client confidentiality and discuss this information with their clients (ACA, 2014). Finally, predicting when ethical or legal issues will occur may be impossible. Counselors should regularly consult with supervisors to discuss treatment options and legal and ethical issues (ACA, 2014).
Implications for Supervisors and Counselor Education Training Programs
Supervisors and counselor educators play a central role in reducing CIT intentional nondisclosures. The findings from the current study suggest there is a wide range of topics that CITs are reluctant to discuss with their supervisors and a wide range of reasons for withholding. The varying nature of intentional nondisclosures highlights the necessity of individualized interventions. Broadly speaking, supervisors are encouraged to facilitate an open and safe environment that invites disclosure (Bordin, 1983). This might also mean supervisors must be willing to purposefully solicit feedback from their supervisees (Murphy & Wright, 2005). Additionally, supervisors must be proactive in utilizing the knowledge gained from studies like this one to normalize the experiences of their supervisees. Perhaps by discussing each of the types of nondisclosure described above with CITs, supervisors can reduce the pressures associated with performing perfectly (Rønnestad & Skovholt, 2003) or diminish the negative emotions (e.g., shame, embarrassment) associated with making mistakes (Farber, 2006; Knox, 2015).
Finally, some of the experiences described by the participants in the current study are deeply troubling, as they shared specific examples of ineffective and harmful supervision. The burden of providing evidence and reporting instances of harmful supervision is often placed on the CIT (Ellis, Taylor, Corp, Hutman, & Kangos, 2017). We outlined some strategies for CITs in case they were to experience harmful supervision; however, the findings from the current study suggest that CITs are withholding this information for any number of reasons. The participants in this study are not unlike those from other allied professions who have similar supervision experiences (for specific examples of harmful supervision, see Ellis, 2017). Thus, supervisors and counselor education programs must work to prevent CITs from experiencing the damaging effects of ineffective or harmful supervision. We encourage counselor education programs to be proactive by reviewing the signs of ineffective and harmful supervision practices with students before they begin their internships and to regularly check in with students about the supervision experience. Counselor education programs may find it beneficial to solicit student feedback about their practicum/internship site at the end of each term—specifically targeting concerns related to ineffective and harmful supervision.
Encouraging students to disclose their experiences with ineffective or harmful supervision while they are in the process of graded program work might not be possible because of the reasons described above; however, preventing similar experiences for future students may be. Finally, CACREP (2015) requires that all site supervisors receive supervision training prior to serving in this capacity. Accidental instances of ineffective or harmful supervision may be prevented by adding training for site supervisors in this content area (Ellis et al., 2017).
Limitations and Future Research
The current study has limitations that create opportunities for future research. First, we utilized the categories originally identified in the study conducted by Ladany et al. (1996). Although we allowed for the creation of new categories, it is possible that selecting a different study to guide our investigation would have yielded different findings (Hsieh & Shannon, 2005). Also, prompting for a single example of significant intentional nondisclosure may have influenced the findings. Future studies should include the opportunity to provide multiple examples, which could result in different findings. Finally, participants were asked to provide examples of intentional nondisclosure with their onsite supervisors during their internship. These participants were receiving supervision from a university supervisor (CACREP, 2015), meaning the information withheld from the onsite supervisor may have been discussed with the university supervisor. It is also plausible that supervisees withheld the information from both the onsite and university supervisors. Site supervisors and university supervisors might have conflicting agendas, presenting a burden on supervisees to decide what to disclose to whom. Future studies should examine how supervisees decide what to disclose when they have multiple supervisors at one time. Finally, participants in the current study reported they were most hesitant to disclose their negative reactions about their supervisors. Future research should explore how supervisors can better monitor their supervisees’ reactions to them.
Conclusion
Although previous research from allied professions provides evidence of how nondisclosure manifests within those professions, the findings from this study provide empirical evidence of how CIT intentional nondisclosure presents during onsite supervision. These findings provide valuable insights into the types of information that CITs withhold as well as the reasons for their nondisclosure during their onsite supervision. Given that the counseling profession has a unique training model (CACREP, 2015) and professional identity (Lawson, 2016), these findings can be used by CITs, onsite supervisors, and counselor educators to generate targeted solutions to address this critical issue.
Conflict of Interest and Funding Disclosure
This research was supported by a grant from the Association for Counselor Education and Supervision.
References
American Counseling Association. (2014). 2014 ACA code of ethics. Alexandria, VA: Author.
Bernard, J. M., & Goodyear, R. K. (2014). Fundamentals of clinical supervision (5th ed.). Boston, MA: Pearson.
Borders, L. D. (2009). Subtle messages in clinical supervision. The Clinical Supervisor, 28, 200–209. doi:10.1080/07325220903324694
Borders, L. D., DeKruyf, L., Fernando, D. M., Glosoff, H. L., Hays, D. G., Page, B., & Welfare, L. E. (2011). Best practices in clinical supervision. Retrieved from https://www.acesonline.net/sites/default/files/ACES-Best-Practices-in-clinical-supervision-document-FINAL_0_0.pdf
Borders, L. D., Glosoff, H. L., Welfare, L. E., Hays, D. G., DeKruyf, L., Fernando, D. M., & Page, B. (2014). Best practices in clinical supervision: Evolution of a counseling specialty. The Clinical Supervisor, 33, 26–44.
Bordin, E. S. (1983). A working alliance based model of supervision. The Counseling Psychologist, 11, 35–42. doi:10.1177/0011000083111007
Cook, R. M., & Welfare, L. E. (2018). Examining predictors of counselor-in-training intentional nondisclosure. Counselor Education and Supervision, 57, 211–226.
Council for Accreditation of Counseling & Related Educational Programs. (2015). 2016 CACREP standards.
Retrieved from https://www.cacrep.org/for-programs/2016-cacrep-standards
Creswell, J. W. (2013). Qualitative inquiry and research design: Choosing among five approaches (3rd ed.). Thousand Oaks, CA: Sage.
Ellis, M. V. (2017). Narratives of harmful clinical supervision. The Clinical Supervisor, 36, 20–87.
doi:10.1080/07325223.2017.1297752
Ellis, M. V., Berger, L., Hanus, A. E., Ayala, E. E., Swords, B. A., & Siembor, M. (2014). Inadequate and harmful clinical supervision: Testing a revised framework and assessing occurrence. The Counseling Psychologist, 42, 434–472. doi:10.1177/0011000013508656
Ellis, M. V., Taylor, E. J., Corp, D. A., Hutman, H., & Kangos, K. A. (2017). Narratives of harmful clinical supervision: Introduction to the special issue. The Clinical Supervisor, 36, 4–19.
doi:10.1080/07325223.2017.1297753
Farber, B. A. (2006). Self-disclosure in psychotherapy (1st ed.).New York, NY: Guilford Press.
Hess, S. A., Knox, S., Schultz, J. M., Hill, C. E., Sloan, L., Brandt, S., . . . Hoffman, M. A. (2008). Predoctoral interns’ nondisclosure in supervision. Psychotherapy Research, 18, 400–411. doi:10.1080/10503300701697505
Hsieh, H. F., & Shannon, S. E. (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15, 1277–1288. doi:10.1177/1049732305276687
Knox, S. (2015). Disclosure—and lack thereof—in individual supervision. The Clinical Supervisor, 34, 151–163. doi:10.1080/07325223.2015.1086462
Ladany, N., Hill, C. E., Corbett, M. M., & Nutt, E. A. (1996). Nature, extent, and importance of what psychotherapy trainees do not disclose to their supervisors. Journal of Counseling Psychology, 43, 10–24. doi:10.1037/0022-0167.43.1.10
Lawson, G. (2016). On being a profession: A historical perspective on counselor licensure and accreditation. Journal of Counselor Leadership and Advocacy, 3, 71–84. doi:10.1080/2326716X.2016.1169955
Lonn, M. R., & Juhnke, G. (2017). Nondisclosure in triadic supervision: A phenomenological study of counseling students. Counselor Education and Supervision, 56, 82–97. doi:10.1002/ceas.12064
Mehr, K. E., Ladany, N., & Caskie, G. I. L. (2010). Trainee nondisclosure in supervision: What are they not telling you? Counselling & Psychotherapy Research, 10, 103–113. doi:10.1080/14733141003712301
Mehr, K. E., Ladany, N., & Caskie, G. I. L. (2015). Factors influencing trainee willingness to disclose in supervision. Training and Education in Professional Psychology, 9, 44–51. doi:10.1037/tep0000028
Murphy, M. J., & Wright, D. W. (2005). Supervisees’ perspectives of power use in supervision. Journal of Marital and Family Therapy, 31, 283–295. doi:10.1111/j.1752-0606.2005.tb01569.x
National Board for Certified Counselors. (2014). NBCC educational requirements to change in 2022. The National Certified Counselor, 30(3), 1–2.
Oden, K. A., Miner-Holden, J., & Balkin, R. S. (2009). Required counseling for mental health professional trainees: Its perceived effect on self-awareness and other potential benefits. Journal of Mental Health, 18, 441–448. doi:10.3109/09638230902968217
Pearson, Q. M. (2001). A case in clinical supervision: A framework for putting theory into practice. Journal of Mental Health Counseling, 23, 174–183. doi:10.1111/ppc.12003
Pisani, A. (2005). Talk to me: Supervisee disclosure in supervision. Smith College Studies in Social Work, 75, 29–47. doi:10.1300/J497v75n01_03
Rønnestad, M. H., & Skovholt, T. M. (2003). The journey of the counselor and therapist: Research findings and perspectives on professional development. Journal of Career Development, 30, 5–44. doi:10.1177/089484530303000102
Welfare, L. E., Wagstaff, J., & Haynes, J. R. (2017). Counselor education and Title IX: Current perceptions and questions. Counselor Education and Supervision, 56(3), 193–207. doi:10.1002/ceas.12072
Yourman, D. B., & Farber, B. A. (1996). Nondisclosure and distortion in psychotherapy supervision. Psychotherapy: Theory, Research, Practice, Training, 33, 567–575. doi:10.1037/0033-3204.33.4.567
Ryan M. Cook is an assistant professor at The University of Alabama. Laura E. Welfare, NCC, is an associate professor at Virginia Tech. Devon E. Romero, NCC, is an assistant professor at The University of Texas at San Antonio. Correspondence can be addressed to Ryan Cook, 310A Graves Hall, The University of Alabama, Tuscaloosa, AL 35487, rmcook@ua.edu.
Jun 28, 2018 | Volume 8 - Issue 2
William H. Snow, Margaret R. Lamar, J. Scott Hinkle, Megan Speciale
The Council for Accreditation of Counseling & Related Educational Programs (CACREP) database of institutions revealed that as of March 2018 there were 36 CACREP-accredited institutions offering 64 online degree programs. As the number of online programs with CACREP accreditation continues to grow, there is an expanding body of research supporting best practices in digital remote instruction that refutes the ongoing perception that online or remote instruction is inherently inferior to residential programming. The purpose of this article is to explore the current literature, outline the features of current online programs and report the survey results of 31 online counselor educators describing their distance education experience to include the challenges they face and the methods they use to ensure student success.
Keywords: online, distance education, remote instruction, counselor education, CACREP
Counselor education programs are being increasingly offered via distance education, or what is commonly referred to as distance learning or online education. Growth in online counselor education has followed a similar trend to that in higher education in general (Allen & Seaman, 2016). Adult learners prefer varied methods of obtaining education, which is especially important in counselor education among students who work full-time, have families, and prefer the flexibility of distance learning (Renfro-Michel, O’Halloran, & Delaney, 2010). Students choose online counselor education programs for many reasons, including geographic isolation, student immobility, time-intensive work commitments, childcare responsibilities, and physical limitations (The College Atlas, 2017). Others may choose online learning simply because it fits their learning style (Renfro-Michel, O’Halloran, & Delaney, 2010). Additionally, education and training for underserved and marginalized populations may benefit from the flexibility and accessibility of online counselor education.
The Council for Accreditation of Counseling & Related Educational Programs (CACREP; 2015) accredits online programs and has determined that these programs meet the same standards as residential programs. Consequently, counselor education needs a greater awareness of how online programs deliver instruction and actually meet CACREP standards. Specifically, existing online programs will benefit from the experience of other online programs by learning how to exceed and surpass minimum accreditation expectations by utilizing the newest technologies and pedagogical approaches (Furlonger & Gencic, 2014). The current study provides information regarding the current state of online counselor education in the United States by exploring faculty’s descriptions of their online programs, including their current technologies, student and program community building approaches, and challenges faced.
Distance Education Defined
Despite its common usage throughout higher education, the U.S. Department of Education (DOE) does not use the terms distance learning, online learning, or online education; rather, it has adopted the term distance education (DOE, 2012). However, in practice, the terms distance education, distance learning, online learning, and online education are used interchangeably. The DOE has defined distance education as the use of one or more technologies that deliver instruction to students who are separated from the instructor and that supports “regular and substantive interaction between the students and the instructor, either synchronously or asynchronously” (2012, p. 5). The DOE has specified that technologies may include the internet, one-way and two-way transmissions through open broadcast and other communications devices, audioconferencing, videocassettes, DVDs, and CD-ROMs. Programs are considered distance education programs if at least 50% or more of their instruction is via distance learning technologies. Additionally, residential programs may contain distance education elements and still characterize themselves as residential if less than 50% of their instruction is via distance education. Traditional on-ground universities are incorporating online components at increasing rates; in fact, 67% of students in public universities took at least one distance education course in 2014, further reflecting the growth in this teaching modality (Allen & Seaman, 2016).
Enrollment in online education continues to grow, with nearly 6 million students in the United States engaged in distance education courses (Allen & Seaman, 2016). Approximately 2.8 million students are taking online classes exclusively. In a conservative estimate, over 25% of students enrolled in CACREP programs are considered distance learning students. In a March 2018 review of the CACREP database of accredited institutions, there were 36 accredited institutions offering 64 degree programs. Although accurate numbers are not available from any official sources, it is a conservative estimate that over 12,000 students are enrolled in a CACREP-accredited online program. When comparing this estimate to the latest published 2016 CACREP enrollment figure of 45,820 (CACREP, 2017), online students now constitute over 25% of the total. This does not include many other residential counselor education students in hybrid programs who may take one or more classes through distance learning means.
At the time of this writing, an additional three institutions were currently listed as under CACREP review, and soon their students will likely be added to this growing online enrollment. As this trend continues, it is essential for counselor education programs to understand issues, trends, and best practices in online education in order to make informed choices regarding counselor education and training, as well as preparing graduates for employment. It also is important for hiring managers in mental health agencies to understand the nature and quality of the training graduates of these programs have received.
One important factor contributing to the increasing trends in online learning is the accessibility it can bring to diverse populations throughout the world (Sells, Tan, Brogan, Dahlen, & Stupart, 2012). For instance, populations without access to traditional residential, brick-and-mortar classroom experiences can benefit from the greater flexibility and ease of attendance that distance learning has to offer (Bennet-Levy, Cromarty, Hawkins, & Mills, 2012). Remote areas in the United States, including rural and frontier regions, often lack physical access to counselor education programs, which limits the numbers of service providers to remote and traditionally underserved areas of the country. Additionally, the online counselor education environment makes it possible for commuters to take some of their course work remotely, especially in winter when travel can become a safety issue, and in urban areas where travel is lengthy and stressful because of traffic.
The Online Counselor Education Environment
The Association for Counselor Education and Supervision (ACES) Technology Interest Network (2017) recently published guidelines for distance education within counselor education that offer useful suggestions to online counselor education programs or to those programs looking to establish online courses. Current research supports that successful distance education programs include active and engaged faculty–student collaboration, frequent communications, sound pedagogical frameworks, and interactive and technically uncomplicated support and resources (Benshoff & Gibbons, 2011; Murdock & Williams, 2011). Physical distance and the associated lack of student–faculty connection has been a concern in the development of online counselor education programs. In its infancy, videoconferencing was unreliable, unaffordable, and often a technological distraction to the learning process. The newest wave of technology—enhanced distance education—has improved interactions using email, e-learning platforms, and threaded discussion boards to make asynchronous messaging virtually instantaneous (Hall, Nielsen, Nelson, & Buchholz, 2010). Today, with the availability of affordable and reliable technical products such as GoToMeeting, Zoom, and Adobe Connect, online counselor educators are holding live, synchronous meetings with students on a regular basis. This includes individual advising, group supervision, and entire class sessions.
It is important to convey that online interactions are different than face-to-face, but they are not inferior to an in-person faculty–student learning relationship (Hickey, McAleer, & Khalili, 2015). Students and faculty prefer one method to the other, often contingent upon their personal belief in the effectiveness of the modality overall and their belief in their own personal fit for this style of teaching and learning (Watson, 2012). In the actual practice of distance education, professors and students are an email, phone call, or videoconference away; thus, communication with peers and instructors is readily accessible (Murdock & Williams, 2011; Trepal, Haberstroh, Duffey, & Evans, 2007). When communicating online, students may feel more relaxed and less inhibited, which may facilitate more self-disclosure, reflexivity, and rapport via increased dialogue (Cummings, Foels, & Chaffin, 2013; Watson, 2012). Subsequently, faculty who are well-organized, technologically proficient, and more responsive to students’ requests may prefer online teaching opportunities and find their online student connections more engaging and satisfying (Meyer, 2015). Upon Institutional Research Board approval, an exploratory survey of online counselor educators was conducted in 2016 and 2017 to better understand the current state of distance counselor education in the United States.
Method
Participants
Recruitment of participants was conducted via the ACES Listserv (CESNET). No financial incentive or other reward was offered for participation. The 31 participants comprised a sample of convenience, a common first step in preliminary research efforts (Kerlinger & Lee, 1999). Participants of the study categorized themselves as full-time faculty members (55.6%), part-time faculty members (11.1%), academic chairs and department heads (22.2%), academic administrators (3.7%), and serving in other roles (7.4%).
Study Design and Procedure
The survey was written and administered using Qualtrics, a commercial web-based product. The survey contained questions aimed at exploring online counselor education programs, including current technologies utilized, approaches to reducing social distance, development of community among students, major challenges in conducting online counselor education, and current practices in meeting these challenges. The survey was composed of one demographic question, 15 multiple-response questions, and two open-ended survey questions. The demographic question asked about the respondent’s role in the university. The 15 multiple-response questions included items such as: (a) How does online counselor education fit into your department’s educational mission? (b) Do you provide a residential program in which to compare your students? (c) How successful are your online graduates in gaining postgraduate clinical placements and licensure? (d) What is the average size of an online class with one instructor? and (e) How do online students engage with faculty and staff at your university? Two open-ended questions were asked: “What are the top 3 to 5 best practices you believe are most important for the successful online education of counselors?” and “What are the top 3 to 5 lessons learned from your engagement in the online education of counselors?”
Additional questions focused on type of department and its organization, graduates’ acceptance to doctoral programs, amount of time required on the physical campus, e-learning platforms and technologies, online challenges, and best practices for online education and lessons learned. The 18 survey questions were designed for completion in no more than 20 minutes and the survey was active for 10 months, during which time there were three appeals for responses yielding 31 respondents.
Procedure
An initial recruiting email and three follow-ups were sent via CESNET. Potential participants were invited to visit a web page that first led to an introductory paragraph and informed consent page. An embedded skip logic system required consent before allowing access to the actual survey questions.
The results were exported from the Qualtrics web-based survey product, and the analysis of the 15 fixed-response questions produced descriptive statistics. Cross tabulations and chi square statistics further compared the perceptions of faculty and those identifying themselves as departmental chairs and administrators.
The two open-ended questions—“What are the top 3 to 5 best practices you believe are most important for the successful online education of counselors?” and “What are the top 3 to 5 lessons learned from your engagement in the online education of counselors?”—yielded 78 statements about lessons learned and 80 statements about best practices for a total of 158 statements. The analysis of the 158 narrative comments initially consisted of individually analyzing each response by identifying and extracting the common words and phrases. It is noted that many responses contained more than one suggestion or comment. Some responses were a paragraph in length and thus more than one key word or phrase could come from a single narrative response. This first step yielded a master list of 18 common words and phrases. The second step was to again review each comment, compare it to this master list, and place a check mark for each category. The third step was to look for similarities in the 18 common words and group them into a smaller number of meaningful categories. These steps were checked among the researchers for fidelity of reporting and trustworthiness.
Results
Thirty-one distance learning counselor education faculty, department chairs, and administrators responded to the survey. They reported their maximum class sizes ranged from 10 to 40 with a mean of 20.6 (SD = 6.5), and the average class size was 15.5 (SD = 3.7). When asked how online students are organized within their university, 26% reported that students choose classes on an individual basis, 38% said students are individually assigned classes using an organized schedule, and 32% indicated that students take assigned classes together as a cohort.
Additionally, respondents were asked how online students engage with faculty and staff at their university. Email was the most popular, used by all (100%), and second was phone calls (94%). Synchronous live group discussions using videoconferencing technologies were used by 87%, while individual video calls were reported by 77%. Asynchronous electronic discussion boards were utilized by 87% of the counselor education programs.
Ninety percent of respondents indicated that remote or distance counseling students were required to attend the residential campus at least once during their program, with 13% requiring students to come to campus only once, 52% requiring students to attend twice, and 26% requiring students to come to a physical campus location four or more times during their program.
All participants indicated using some form of online learning platform with Blackboard (65%), Canvas (23%), Pearson E-College (6%), and Moodle (3%) among the ones most often listed. Respondents indicated the satisfaction levels of their current online learning platform as: very dissatisfied (6.5%), dissatisfied (3.2%), somewhat dissatisfied (6.5%), neutral (9.7%), somewhat satisfied (16.1%), satisfied (41.9%), and very satisfied (9.7%). There was no significant relationship between the platform used and the level of satisfaction or dissatisfaction (X2 (18,30) = 11.036, p > .05), with all platforms faring equally well. Ninety-seven percent of respondents indicated using videoconferencing for teaching and individual advising using such programs as Adobe Connect (45%), Zoom (26%), or GoToMeeting (11%), while 19% reported using an assortment of other related technologies.
Participants were asked about their university’s greatest challenges in providing quality online counselor education. They were given five pre-defined options and a sixth option of “other” with a text box for further elaboration, and were allowed to choose more than one category. Responses included making online students feel a sense of connection to the university (62%), changing faculty teaching styles from traditional classroom models to those better suited for online coursework (52%), providing experiential clinical training to online students (48%), supporting quality practicum and internship experiences for online students residing at a distance from the physical campus (38%), convincing faculty that quality outcomes are possible with online programs (31%), and other (10%).
Each participant was asked what their institution did to ensure students could succeed in online counselor education. They were given three pre-defined options and a fourth option of “other” with a text box for further elaboration, and were allowed to choose more than one option. The responses included specific screening through the admissions process (58%), technology and learning platform support for online students (48%), and assessment for online learning aptitude (26%). Twenty-three percent chose the category of other and mentioned small classes, individual meetings with students, providing student feedback, offering tutorials, and ensuring accessibility to faculty and institutional resources.
Two open-ended questions were asked and narrative comments were analyzed, sorted, and grouped into categories. The first open-ended question was: “What are the top 3 to 5 best practices that are the most important for the successful online education of counselors?” This yielded 78 narrative comments that fit into the categories of fostering student engagement (n = 19), building community and facilitating dialogue (n = 14), supporting clinical training and supervision (n = 11), ensuring courses are well planned and organized (n = 10), providing timely and robust feedback (n = 6), ensuring excellent student screening and advising (n = 6), investing in technology (n = 6), ensuring expectations are clear and set at a high standard (n = 5), investing in top-quality learning materials (n = 4), believing that online counselor education works (n = 3), and other miscellaneous comments (n = 4). Some narrative responses contained more than one suggestion or comment that fit multiple categories.
The second open-ended question—“What are the top 3 to 5 lessons learned from the online education of counselors?”—yielded 80 narrative comments that fit into the categories of fostering student engagement (n = 11), ensuring excellent student screening and advising (n = 11), recognizing that online learning has its own unique workload challenges for students and faculty (n = 11), providing timely and robust feedback (n = 8), building community and facilitating dialogue (n = 7), ensuring courses are well planned and organized (n = 7), investing in technology (n = 6), believing that online counselor education works (n = 6), ensuring expectations are clear and set at a high standard (n = 5), investing in top-quality learning materials (n = 3), supporting clinical training and supervision (n = 2), and other miscellaneous comments (n = 8).
Each participant was asked how online counselor education fit into their department’s educational mission and was given three categorical choices. Nineteen percent stated it was a minor focus of their department’s educational mission, 48% stated it was a major focus, and 32% stated it was the primary focus of their department’s educational mission.
The 55% of participants indicating they had both residential and online programs were asked to respond to three follow-up multiple-choice questions gauging the success rates of their online graduates (versus residential graduates) in attaining: (1) postgraduate clinical placements, (2) postgraduate clinical licensure, and (3) acceptance into doctoral programs. Ninety-three percent stated that online graduates were as successful as residential students in gaining postgraduate clinical placements. Ninety-three percent stated online graduates were equally successful in obtaining state licensure. Eighty-five percent stated online graduates were equally successful in getting acceptance into doctoral programs.
There were some small differences in perception that were further analyzed. Upon using a chi square analysis, there were no statistically significant differences in the positive perceptions of online graduates in gaining postgraduate clinical placements (X2 (2, 13) = .709, p > .05), the positive perceptions regarding the relative success of online versus residential graduates in gaining postgraduate clinical licensure (X2 (2, 13) = .701, p > .05), or perceptions of the relative success of online graduates in becoming accepted in doctoral programs (X2 (2, 12) = 1.33, p > .05).
Discussion
The respondents reported that their distance learning courses had a mean class size of 15.5. Students in these classes likely benefit from the small class sizes and the relatively low faculty–student ratio. These numbers are lower than many residential classes that can average 25 students or more. It is not clear what the optimal online class size should be, but there is evidence that the challenge of larger classes may introduce burdens difficult for some students to overcome (Chapman & Ludlow, 2010). Beattie and Thiele (2016) found first-generation students in larger classes were less likely to talk to their professor or teaching assistants about class-related ideas. In addition, Black and Latinx students in larger classes were less likely to talk with their professors about their careers and futures (Beattie & Thiele, 2016).
Programs appeared to have no consistent approach to organizing students and scheduling courses. The three dominant models present different balances of flexibility and predictability with advantages and disadvantages for both. Some counselor education programs provide students the utmost flexibility in selecting classes, others assign classes using a more controlled schedule, and others are more rigid and assign students to all classes.
The model for organizing students impacts the social connections students make with one another. In concept, models that provide students with more opportunities to engage each other in a consistent and effective pattern of positive interactions result in students more comfortable working with one another, and requesting and receiving constructive feedback from their peers and instructors.
Cohort models, in which students take all courses together over the life of a degree program, are the least flexible but most predictable and have the greatest potential for fostering strong connections. When effectively implemented, cohort models can foster a supportive learning environment and greater student collaboration and cohesion with higher rates of student retention and ultimately higher graduation rates (Barnett & Muse, 1993; Maher, 2005). Advising loads can decrease as cohort students support one another as informal peer mentors. However, cohorts are not without their disadvantages and can develop problematic interpersonal dynamics, splinter into sub-groups, and lead to students assuming negative roles (Hubbell & Hubbell, 2010; Pemberton & Akkary, 2010). An alternative model in which students make their own schedules and choose their own classes provides greater flexibility but fewer opportunities to build social cohesion with others in their program. At the same time, these students may not demonstrate the negative dynamics regarding interpersonal engagement that can occur with close cohort groups.
Faculty–Student Engagement
Remote students want to stay in touch with their faculty advisors, course instructors, and fellow students. Numerous social engagement opportunities exist through technological tools including email, cell phone texts, phone calls, and videoconference advising. These fast and efficient tools provide the same benefits of in-person meetings without the lag time and commute requirements. Faculty and staff obviously need to make this a priority to use these tools and respond to online students in a timely manner.
All technological tools referred to in the survey responses provide excellent connectivity and communication if used appropriately. Students want timely responses, but for a busy faculty or staff member it is easy to allow emails and voicemails to go unattended. Emails not responded to and unanswered voicemail messages can create anxiety for students whose only interaction is through electronic means. This also might reinforce a sense of isolation for students who are just “hanging out there” on their own and having to be resourceful to get their needs met. It is recommended that the term timely needs to be defined and communicated so faculty and students understand response expectations. It is less important that responses are expected in 24, 48, or even 72 hours; what students need to know is when to expect a response.
Survey responses indicated that remote counselor education students are dependent upon technology, including the internet and associated web-based e-learning platforms. When the internet is down, passwords do not work, or computers fail, the remote student’s learning is stalled. Counselor education programs offering online programming must provide administrative services, technology, and learning support for online students in order to quickly remediate technology issues when they occur. It is imperative that standard practice for institutions include the provision of robust technology support to reduce down-time and ensure continuity of operations and connection for remote students.
Fostering Program and Institutional Connections
Faculty were asked how often online students were required to come to a physical campus location as part of their program. Programs often refer to short-term campus visits as limited residencies to clarify that students will need to come to the campus. Limited residencies are standard, with 90% responding that students were required to come to campus at least once. Short-term intensive residencies are excellent opportunities for online students to make connections with their faculty and fellow students (Kops, 2014). Residential intensives also provide opportunities for the university student life office, alumni department, business office, financial aid office, registrar, and other university personnel to connect with students and link a human face to an email address.
Distance learning students want to engage with their university, as well as fellow students and faculty. They want to feel a sense of connection in a similar manner as residential students (Murdock & Williams, 2011). Institutions should think creatively about opportunities to include online learners in activities beyond the classroom. An example of promoting inclusiveness is when one university moved the traditional weekday residential town halls to a Sunday evening teleconference webinar. This allowed for greater access, boosted attendance, and served to make online counselor education students feel like a part of the larger institution.
As brick-and-mortar institutions consider how to better engage distance learning students, they need to understand that a majority of students (53%) taking exclusively distance education courses reside in the same state as the university they are attending (Allen & Seaman, 2016). Given that most are within driving distance of the physical campus, students are more open to coming to campus for special events, feel their presence is valued, and know that they are not just part of an electronic platform (Murdock & Williams, 2011).
E-Learning Platforms as Critical Online Infrastructure
All participants (100%) reported using an online learning platform. E-learning platforms are standard for sharing syllabi, course organization, schedules, announcements, assignments, discussion boards, homework submissions, tests, and grades. They are foundational in supporting faculty instruction and student success with numerous quality options available. Overall, online faculty were pleased with their technological platforms and there was no clear best platform.
Online learning platforms are rich in technological features. For example, threaded discussions allow for rich, thoughtful dialogue among students and faculty, and they are often valued by less verbally competitive students who might express reluctance to speak up in class but are willing to share their comments in writing. Course examinations and quizzes in a variety of formats can be produced and delivered online through e-learning platforms such as Blackboard, Canvas, and Moodle. Faculty have flexibility for when exams are offered and how much time students have to complete them. When used in conjunction with proctoring services such as Respondus, ProctorU, and B-Virtual, integrity in the examination process can be assured. Once students complete their exam, software can automatically score and grade objective questions, and provide immediate feedback to students.
Videoconferencing and Virtual Remote Classrooms
Videoconferencing for teaching and individual advising through Adobe Connect, Zoom, GoToMeeting, and related technologies is now standard practice and changing the nature of remote learning. Distance learning can now employ virtual classroom models with synchronous audio and video communication that closely parallels what occurs in a residential classroom. Videoconferencing platforms provide tools to share PowerPoints, graphics, and videos as might occur in a residential class. Class participants can write on virtual whiteboards with color markers, annotating almost anything on their screen. Group and private chat functionality can provide faculty with real-time feedback during a class session. Newer videoconferencing features now allow faculty to break students into smaller, private discussion groups and move around to each group virtually, just like what often occurs in a residential classroom. With preparation, faculty can execute integrated survey polls during a video class session. Essentially, videoconferencing tools reduce the distance in distance education.
Videoconference platforms allow faculty to teach clinical skills in nearly the same manner as in residential programs. Counselor education faculty can model skills such as active listening in real time to their online class. Faculty can then have students individually demonstrate those skills while being observed. Embedded features allow faculty to record the video and audio features of any conversation for playback and analysis. Videoconference platforms now offer “breakout” rooms to place students in sub-groups for skills practice and debriefing, similar to working in small groups in residential classrooms. Faculty members and teaching assistants can visit each breakout room to ensure students are on task and properly demonstrating counseling skills. Just as in a residential class, students can reconvene and share the challenges and lessons learned from their small group experience.
Challenges in Providing Remote Counselor Education
Participants were asked to select one or more of their top challenges in providing quality online counselor education. In order of frequency, they reported the greatest challenges as making online students feel a sense of connection to the university (62%), changing faculty teaching styles from brick-and-mortar classroom models to those better suited for online coursework (52%), providing experiential clinical training to online students (48%), supporting quality practicum and internship experiences for online students residing at a distance from the physical campus (38%), and convincing faculty members that quality outcomes are possible with online programs (31%).
Creating a sense of university connection. Counselor education faculty did not report having major concerns with faculty–student engagement. Faculty seemed confident with student learning outcomes using e-learning platforms and videoconferencing tools that serve to reduce social distance between faculty and students and facilitate quality learning experiences. This confidence could be the result of counselor educators’ focus on fostering relationships as a foundational counseling skill (Kaplan, Tarvydas, & Gladding, 2014).
However, faculty felt challenged to foster a student’s sense of connection with the larger university. For example, remote students not receiving emails and announcements about opportunities available only to residential students can feel left out. Remote students might find it difficult to navigate the university student life office, business department, financial aid office, registration system, and other university systems initially designed for residential students. Highly dependent on their smartphone and computer, remote students can feel neglected as they anxiously wait for responses to email and voicemail inquiries (Milman, Posey, Pintz, Wright, & Zhou, 2015).
In the online environment, there are extracurricular options for participating in town halls, special webinars, and open discussion forums with departmental and university leaders. Ninety percent of the programs require students to come to their physical campus one or more times. These short-term residencies are opportunities for students to meet the faculty, departmental chairs, and university leaders face-to-face and further build a sense of connection.
A majority of online students (53%) reside in the same state as the university they are attending (Allen & Seaman, 2016), with many within commuting distance of their brick-and- mortar campus. These students will appreciate hearing about the same opportunities afforded to residential students, and under the right circumstances and scheduling they will participate.
Changing faculty teaching styles. Not all residential teaching styles and methods, such as authority-based lecture formats, work well with all students (Donche, Maeyer, Coertjens, Van Daal, & Van Petegem, 2013). Distance learning students present their own challenges and preferences. Successful distance education programs require active and engaged faculty who frequently communicate with their students, use sound pedagogical frameworks, and maintain a collaborative and interactive style (Benshoff & Gibbons, 2011; Murdock & Williams, 2011). Discovery orientation, discussion, debriefing, action research, and flipped classrooms where content is delivered outside the classroom and the classroom is used to discuss the material are good examples of more collaborative styles (Brewer & Movahedazarhouligh, 2018; Donche et al., 2013).
Organization is critical for all students, but more so for remote students who often are working adults with busy schedules. They want to integrate their coursework into other life commitments and want a clear, well-organized, and thoughtfully planned course with all the requirements published in advance, including specific assignment due dates. Distance counselor education faculty will find their syllabi growing longer with more detail as they work to integrate traditional assignments with the e-learning and videoconferencing tools in order to create engaging, predictable, and enjoyable interactive learning experiences.
Providing experiential clinical training. Counselor educators ideally provide multimodal learning opportunities for counseling students to understand, internalize, and demonstrate clinical skills for a diverse clientele. In residential classrooms, the knowledge component is usually imparted through textbooks, supplemental readings, course assignments, video demonstration, and instructor-led lecture and discussions. All remote programs provide similar opportunities for students and replicate residential teaching models with their use of asynchronous e-learning platforms and synchronous videoconferencing technologies.
Asynchronous methods are not well suited for modeling, teaching, and assessing interpersonal skills. However, synchronous videoconferencing technologies provide the same opportunity as residential settings to conduct “fishbowl” class exercises, break students into groups to practice clinical skills, conduct role plays, apply procedural learning, and give students immediate, meaningful feedback about their skills development.
The majority of surveyed programs required remote students to come to campus at least once to assess students for clinical potential, impart critical skills, and monitor student progress in achieving prerequisite clinical competencies required to start practicum. Courses that teach and assess clinical interviewing skills are well suited for these intensive experiences and provide an important gatekeeping function. Faculty not only have the opportunity to see and hear students engage in role plays, but also to see them interact with other students.
Supporting quality practicum and internship experiences. Remote counselor educators report that their programs are challenged in supporting quality practicum and internship experiences. Residential students benefit from the relationships universities develop over time with local public and nonprofit mental health agencies in which practicum and internship students may cluster at one or more sites. Although online students living close enough to the residential campus may benefit from the same opportunities, remote students living at a distance typically do not experience this benefit. They often have to seek out, interview, and compete for a clinical position at a site unfamiliar to their academic program’s field placement coordinator. Thus, online counselor education students will need field placement coordination that can help with unique practicum and internship requirements. The placement coordinator will need to know how to review and approve distance sites without a physical assessment. Relationships with placement sites will need to rely upon email, phone, and teleconference meetings. Furthermore, online students can live in a state other than where the university is located, requiring the field placement coordinator to be aware of various state laws and regulations.
Convincing faculty that quality outcomes are possible. Approximately one-third of the surveyed counselor education faculty reported the need to convince other faculty that quality outcomes are possible with remote counselor education. Changing the minds of skeptical colleagues is challenging but naturally subject to improvement over time as online learning increases, matures, and becomes integrated into the fabric of counselor education. In the interim, programs would be wise to invest in assisting faculty skeptics to understand that online counselor education can be managed effectively (Sibley & Whitaker, 2015). First, rather than just telling faculty that online counselor education works, programs should demonstrate high levels of interactivity that are comparable to face-to-face engagement by using state-of-the-art videoconferencing platforms. Second, it is worth sharing positive research outcomes related to remote education. Third, it is best to start small by encouraging residential faculty to first try a hybrid course by holding only one or two of their total class sessions online. Fourth, it is important to provide robust support for reluctant but willing faculty who agree to integrate at least one or two online sessions into their residential coursework. Finally, institutions will find more willing faculty if they offer incentives for those who give online counselor education a chance.
Ensuring Online Student Success
Student success is defined by the DOE as related to student retention, graduation rates, time to completion, academic success, and gainful employment (Bailey et al., 2011). Counselor education programs would likely add clinical success in practicum and internship and post-master’s licensure to these critical success outcomes.
The survey respondents reported that student success begins with making sure that the students they accept have the aptitude to learn via online distance education. Students may have unrealistic perceptions that remote distance education is somehow less academically strenuous. Programs need to ensure students are prepared for the unique aspects of online versus residential learning. Fifty-eight percent of the programs engaged in student screening beginning with the admissions process. A quarter of the respondents used a formal assessment tool to assess students for success factors such as motivation, learning style, study habits, access to technology, and technological skills. A commonly used instrument was the Online Readiness Assessment developed by Williams (2017).
Lessons Learned and Best Practices
The 158 statements regarding best practices and lessons learned were further refined to yield the top six imperatives for success in online counselor education, namely: (1) fostering student–faculty–community engagement (57.4%); (2) providing high expectations, excellent screening, advising, and feedback (36%); (3) investing in quality instructional materials, course development, and technology support (30.5%); (4) providing excellent support for online clinical training and supervision (14.6%); (5) recognizing the workload requirements and time constraints of online students; (6) working to instill the belief in others that quality outcomes are possible with online counselor education programs (10.1%); and (7) other assorted responses (13.5%).
An indicator of success for many counselor education programs is the rate at which students graduate, obtain clinical placement, and become licensed. There is also an interest in how successful graduates are in becoming admitted into doctoral programs. For online programs, a further benchmark test is to compare online student graduation, licensure, and doctoral admissions rates to those in residential programs. Fifty-five percent of the respondents served in programs with residential as well as online students. These respondents were able to compare their online student outcomes to residential student outcomes. Their perception was that online graduates were as successful as residential students in gaining postgraduate clinical placements (93%), obtaining state licensure (93%), and acceptance into doctoral programs (85%). They generally believed online graduates were competitive with residential graduates.
Limitations, Recommendations, and Conclusion
Limitations of the Study
When this study began in 2016, there were 11 CACREP-accredited institutions offering online counselor education programs, and by March 2018, there were 36. This study represents a single snapshot of the online counselor education experience during a time of tremendous growth.
This study focused on the reported experience of faculty, departmental chairs, and administrators who have some commitment and investment in online learning. Some would point out the bias of those who advocate for remote counselor education in relaying their own experiences, anecdotal evidence, and personal comparisons of online and residential teaching.
The exploratory nature of this study was clearly not comprehensive in its inclusion of all the factors associated with online counselor education. Specific details of online counselor education programs were not emphasized and could have offered more information about university and departmental resources for remote education, faculty training for online educational formats, and student evaluations of online courses. The numerous technologies used were identified, but this says nothing about their differential effectiveness. Future studies should include these variables as well as other factors that will provide further information about the successes and challenges of online counselor education.
This survey assessed the informed opinions of counselor education faculty and administrators who responded that they were generally satisfied with the various aspects of their programs, including student outcomes. What was not assessed was the actual quality of the education itself. In order to change the mind of skeptics, more than opinions and testimonies will be needed. Future studies need to objectively compare learning outcomes, demonstrate quality, and delineate how remote counselor education programs are meeting the challenges of training counselors within distance learning modalities.
Recommendations
The dynamic nature of the field of online counselor education requires ongoing study. As more programs offer courses and full programs through distance learning modalities, they can contribute their own unique expertise and lessons learned to inform and enrich the broader field.
The challenge of faculty skepticism and possible mixed motives regarding online learning will continue to be problematic. There is a lingering perception by some faculty that online counselor education programs are not equivalent to residential training. An inherent faculty bias might exist in which residential means higher quality and online means lower quality. Some faculty may teach online courses only for additional compensation while privately having reservations. In contrast, departmental chairs and academic administrators might want the same high levels of quality, but may find themselves more driven by the responsibility for meeting enrollment numbers and budgets. In times of scarcity, these individuals may see online counselor education as the answer for new revenue sources (Jones, 2015). For others, online education may present concerns while providing an appeal for its innovative qualities or providing social justice through increasing access to higher education by underserved populations. The best way to clarify the issues and better inform the minds of skeptics is to present them with objective data regarding the nature and positive contributions of remote counselor education learning outcomes.
Aside from the modality of their instructional platform, it is important to understand if effective remote counselor educators are different from equally effective residential course instructors. Remote teaching effectiveness might be associated with some combination of attributes, interests, and motivations, and thus self-selection to teach remote students. Further studies will need to tease out what works, what does not work, and what type of faculty and faculty training make someone best suited for participation in remote counselor education.
Technology is critical to the advances in remote counselor education. Email, smartphones, texting, and e-learning platforms have helped faculty create engaging courses with extensive faculty–student interactions. Videoconferencing in particular has served to reduce the social distance between faculty and remote students. As aforementioned, innovative programs are taking the distance out of distance counselor education, where the virtual remote classroom modality provides similar experiences to those of residential classes. The nature of these technologically facilitated online relationships deserves further study to determine which technologies and related protocols enhance learning and which impede it.
A logical next step is to build on the work that has been accomplished and conduct more head-to-head comparisons of student outcomes among remote and residential programs. This is very feasible, as 34 of the 36 institutions currently offering online counselor education programs also have a residential program with which to make comparisons. These within-institution comparisons will be inherently quasi-experimental. Effective program comparisons of delivery models will require systematically implemented reliable and valid measures of student learning outcomes at strategic points in the counselor training program. The Counselor Competency Scale (Lambie, Mullen, Swank, & Blount, 2018) is a commonly used standardized assessment for graduate students engaged in clinical practicum and internship. The National Counseling Exam scores of current students and recent graduates can provide standardized measures to compare outcomes of graduates across programs.
Finally, although we can learn from institutional best practices and student success stories, we also could benefit from understanding why some programs, faculty, and students struggle. Challenges are certainly faced in remote counselor education and training, but it is likely that one or more programs have developed innovative concepts to surmount these obstacles. The 31 respondents were able to articulate many best practices to manage challenges and believed they were achieving the same learning objectives achieved by residential counseling students. Many faculty members, departmental chairs, and administrators believed that remote counselor education graduates are as successful as those attending residential programs, but this opinion is not universally shared. What is clear is that despite some reservations, a growing number of counselors are trained via a remote modality. It is time to embrace distance counselor education; learn from best practices, successes, and struggles; and continue to improve outcomes for the benefit of programs, the profession of counseling, and the consumers of the services our graduates provide.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest or funding contributions for the development of this manuscript.
References
Allen, I. E., & Seaman, J. (2016). Online report card: Tracking online education in the United States. Babson Survey Research Group. Retrieved from https://onlinelearningsurvey.com/reports/onlinereportcard.pdf
Association for Counselor Education and Supervision Technology Interest Network. (2017). ACES guidelines for online learning in counselor education. Retrieved from https://www.acesonline.net/sites/default/files/Online%20Learning%20CES%20Guidelines%20May%202017%20(1).pdf
Bailey, M., Benitiz, M., Burton, W., Carey, K., Cunningham, A., Fraire, J., . . . Wheelan, B. (2011). Committee on measures of student success: A report to Secretary of Education Arne Duncan. U.S. Department of Education. Retrieved from https://www2.ed.gov/about/bdscomm/list/cmss-committee-report-final.pdf
Barnett, B. G., & Muse, I. D. (1993). Cohort groups in educational administration: Promises and challenges. Journal of School Leadership, 3, 400–415.
Beattie, I. R., & Thiele, M. (2016). Connecting in class? College class size and inequality in academic social capital. The Journal of Higher Education, 87, 332–362.
Bennett-Levy, J., Hawkins, R., Perry, H., Cromarty, P., & Mills, J. (2012). Online cognitive behavioural therapy training for therapists: Outcomes, acceptability, and impact of support: Online CBT training. Australian Psychologist, 47(3), 174–182. doi:10.1111/j.1742-9544.2012.00089.x
Benshoff, J. M., & Gibbons, M. M. (2011). Bringing life to e-learning: Incorporating a synchronous approach to online teaching in counselor education. The Professional Counselor, 1, 21–28. doi:10.15241/jmb.1.1.21
Brewer, R., & Movahedazarhouligh, S. (2018). Successful stories and conflicts: A literature review on the effectiveness of flipped learning in higher education. Journal of Computer Assisted Learning, 1–8. doi:10.1111/jcal.12250
Chapman, L., & Ludlow, L. (2010). Can downsizing college class sizes augment student outcomes? An investigation of the effects of class size on student learning. Journal of General Education, 59(2), 105–123. doi:10.5325/jgeneeduc.59.2.0105
The College Atlas. (2017). 41 facts about online students. Retrieved from https://www.collegeatlas.org/41-surprising-facts-about-online-students.html
Council for Accreditation of Counseling & Related Educational Programs. (2015). 2016 CACREP standards. Washington, DC: Author.
Council for Accreditation of Counseling & Related Educational Programs. (2017). Annual report 2016. Washington, DC: Author.
Cummings, S. M., Foels, L., & Chaffin, K. M. (2013). Comparative analysis of distance education and classroom-based formats for a clinical social work practice course. Social Work Education, 32, 68–80.
doi:10.1080/02615479.2011.648179
Donche, V., De Maeyer, S., Coertjens, L., Van Daal, T., & Van Petegem, P. (2013). Differential use of learning strategies in first-year higher education: The impact of personality, academic motivation, and teaching strategies. British Journal of Educational Psychology, 83, 238–251. doi:10.1111/bjep.12016
Furlonger, B., & Gencic, E. (2014). Comparing satisfaction, life-stress, coping and academic performance of counselling students in on-campus and distance education learning environments. Australian Journal of Guidance and Counselling, 24, 76–89. doi:10.1017/jgc.2014.2
Hall, B. S., Nielsen, R. C., Nelson, J. R., & Buchholz, C. E. (2010). A humanistic framework for distance education. The Journal of Humanistic Counseling, 49, 45–57. doi:10.1002/j.2161-1939.2010.tb00086.x
Hickey, C., McAleer, S. J., & Khalili, D. (2015). E-learning and traditional approaches in psychotherapy education: Comparison. Archives of Psychiatry and Psychotherapy, 4, 48–52.
Hubbell, L., & Hubbell, K. (2010). When a college class becomes a mob: Coping with student cohorts. College Student Journal, 44, 340–353.
Jones, C. (2015). Openness, technologies, business models and austerity. Learning, Media and Technology, 40, 328–349. doi:10.1080/17439884.2015.1051307
Kaplan, D. M., Tarvydas, V. M., & Gladding, S. T. (2014). 20/20: A vision for the future of counseling: The new consensus definition of counseling. Journal of Counseling & Development, 92, 366–372.
doi:10.1002/j.1556-6676.2014.00164.x
Kerlinger, F. N., & Lee, H. B. (1999). Foundations of behavioral research (4th ed). Fort Worth, TX: Wadsworth.
Kops, W. J. (2014). Teaching compressed-format courses: Teacher-based best practices. Canadian Journal of University Continuing Education, 40, 1–18.
Lambie, G. W., Mullen, P. R., Swank, J. M., & Blount, A. (2018). The Counseling Competencies Scale: Validation and refinement. Measurement and Evaluation in Counseling and Development, 51, 1–15.
doi:10.1080/07481756.2017.1358964
Maher, M. A. (2005). The evolving meaning and influence of cohort membership. Innovative Higher Education, 30(3), 195–211.
Meyer, J. M. (2015). Counseling self-efficacy: On-campus and distance education students. Rehabilitation Counseling Bulletin, 58(3), 165–172. doi:10.1177/0034355214537385
Milman, N. B., Posey, L., Pintz, C., Wright, K., & Zhou, P. (2015). Online master’s students’ perceptions of institutional supports and resources: Initial survey results. Online Learning, 19(4), 45–66.
Murdock, J. L., & Williams, A. M. (2011). Creating an online learning community: Is it possible? Innovative Higher Education, 36, 305–315. doi:10.1007/s10755-011-9188-6
Pemberton, C. L. A., & Akkary, R. K. (2010). A cohort, is a cohort, is a cohort . . . Or is it? Journal of Research on Leadership Education, 5(5), 179–208.
Renfro-Michel, E. L., O’Halloran, K. C., & Delaney, M. E. (2010). Using technology to enhance adult learning in the counselor education classroom. Adultspan Journal, 9, 14–25. doi:10.1002/j.2161-0029.2010.tb00068.x
Sells, J., Tan, A., Brogan, J., Dahlen, U., & Stupart, Y. (2012). Preparing international counselor educators through online distance learning. International Journal for the Advancement of Counselling, 34, 39–54. doi:10.1007/s10447-011-9126-4
Sibley, K., & Whitaker, R. (2015, March 16). Engaging faculty in online education. Educause Review. Retrieved from https://er.educause.edu/articles/2015/3/engaging-faculty-in-online-education
Trepal, H., Haberstroh, S., Duffey, T., & Evans, M. (2007). Considerations and strategies for teaching online counseling skills: Establishing relationships in cyberspace. Counselor Education and Supervision, 46(4), 266–279. doi:10.1002/j.1556-6978.2007.tb00031.x
U.S. Department of Education Office of Postsecondary Education Accreditation Division. (2012). Guidelines for Preparing/Reviewing Petitions and Compliance Reports. Retrieved from https://www.asccc.org/sites/default/files/USDE%20_agency-guidelines.pdf
Watson, J. C. (2012). Online learning and the development of counseling self-efficacy beliefs. The Professional Counselor, 2, 143–151. doi:10.15241/jcw.2.2.143
Williams, V. (2017). Online readiness assessment. Penn State University. Retrieved from https://pennstate.qualtrics.com/jfe/form/SV_7QCNUPsyH9f012B
William H. Snow is an associate professor at Palo Alto University. Margaret R. Lamar is an assistant professor at Palo Alto University. J. Scott Hinkle, NCC, is Director of Professional Development at the National Board for Certified Counselors. Megan Speciale, NCC, is an assistant professor at Palo Alto University. Correspondence can be addressed to William Snow, 1791 Arastradero Road, Palo Alto, CA 94304, wsnow@paloaltou.edu.
Jun 28, 2018 | Volume 8 - Issue 2
Kristi A. Lee, Daniel J. Kelley-Petersen
The focus on human development is foundational to the field of counseling, with its importance codified in guiding documents and frameworks, such as the American Counseling Association’s Code of Ethics (2014). Many developmental theories have been established using single-gender or single-culture groups, yet they claim universal application to all humans. Although counseling students must learn these theories because of accreditation standards and licensure requirements, counselor educators need to prepare students for practice in a multicultural world. Counselors are now called to act as social justice advocates, and teaching strategies are needed to prepare students for this role. This study’s focus is on the use of service learning with community counseling students in a human development course. Results from a content analysis demonstrate how service learning enhances learning and broadens students’ perceptions of themselves, others, and social justice in counseling. Findings indicate a shift in participants’ perception of social justice in counseling.
Keywords: service learning, social justice, human development, developmental theories, content analysis
Distinct from the medical model that underlies psychology, the field of counseling has historically focused on developmental processes as the foundation to understanding what makes human life function well (Brady-Amoon, 2011; Kraus, 2008; Lewis, 2011; Stennbarger & LeClair, 1995). These processes of development are explained through theories about learning, normal personality development, and individual and family development, among others (Council for the Accreditation of Counseling & Related Educational Programs [CACREP], 2015). The American Counseling Association (ACA) identified “enhancing human development throughout the lifespan” as the first core value of the counseling profession (2014, p. 3). Further, human development has been established as one of eight knowledge areas by CACREP (2015), the national accrediting body for counselor education programs. Additionally, standardized tests, such as the National Counselor Examination for Licensure and Certification, require students to demonstrate mastery of studies that provide an understanding of the nature and needs of individuals at all developmental levels (National Board for Certified Counselors [NBCC], 2015).
Although understanding and promoting healthy human development across the lifespan are central themes in counselor education, there are critiques of the study of human development (Brady-Amoon, 2011). Many theories and models of human development reflect middle-class, Caucasian-American value systems and culture (Brady-Amoon, 2011; Broderick & Blewitt, 2015; Dixon, 2001; Henrich, Heine, & Norenzayan, 2010), and thus lack utility in developing both a robust and a nuanced understanding of groups who are outside of this demographic. Broderick and Blewitt (2015) stated that there is a “growing concern that traditional theories are insufficient to explain development because they are biased in favor of single-culture or single-gender models” (p. 351). The role of culture in human development is crucial to consider (Rogoff, 2003), yet many theories consider culture an extraneous variable. Systematic misapplication of theories designed for the dominant population may not adequately account for the accepted indicators of development for diverse cultural and societal contexts (Broderick & Blewitt, 2015;
Dixon, 2001; Kraus, 2008). Recognizing challenges in applying developmental theories to diverse populations is critical for counselors who promote social justice in counseling and in society (Kiselica & Robinson, 2001; MacLeod, 2013).
The Movement Toward a Social Justice Perspective in Counseling
Counselors have a unique position as frontline witnesses to how social inequities impact clients. Individual, couples, family, and group counseling are critical in helping clients in non-dominant groups navigate and survive systems of oppression and opportunity. However, these modalities of counseling may not be sufficient to prevent or meaningfully address mental health issues that have systemic causes (Toporek, Gerstein, Fouad, Roysircar, & Israel, 2006). The recognition for the need to adjust counseling approaches to work with issues of healthy human development in a pluralistic society has contributed to the growth of the social justice movement within the field of counseling (Ratts & Wood, 2011). At times identified as the “fifth force” (Ratts, 2009) in counseling, the social justice perspective not only addresses the individual needs of clients, but also seeks to change systems that inhibit human development for oppressed groups. Counselors are challenged to determine how to balance individual counseling interventions with advocacy interventions on local, state, or national levels. A social justice approach to counseling emphasizes the importance of healthy human development for individuals and social groups and necessitates a broader array of skills, knowledge, and perspectives, including advocacy skills (Bemak & Chung, 2011; Brady-Amoon, 2011; Lewis, 2011; Ratts, 2009).
Acceptance of the social justice counseling perspective is evidenced by its codification in important documents that guide many practitioners and educators in the field of counseling. In the preamble to the 2014 Code of Ethics, ACA identified “promoting social justice” (p. 3) as a core principle. Ethical counselors are called to “advocate at individual, group, institutional, and societal levels to address potential barriers and obstacles that inhibit access and/or the growth and development of clients” (2014, p. 5). In 2003, ACA endorsed the Advocacy Competencies (Lewis, Arnold, House, & Toporek, 2002), a document that describes skills and activities for counselor advocacy. Additionally, the 2016 CACREP standards call for preparation of counselors in “advocacy processes needed to address institutional and social barriers that impede access, equity, and success for clients” (2015, p. 10). These documents provide evidence that segments of the profession of counseling, particularly some counselor education programs, are embracing a social justice perspective that can be enacted through counselor advocacy.
Although many counselors may want to advocate for marginalized populations, they may not be comfortable doing so or they may not know how (West-Olatunji, 2010). Further, it is unclear whether counselor educators are adequately preparing students with the skills necessary to practice from a social justice perspective upon graduation (Bemak & Chung, 2011; Constantine, Hage, Kindaichi, & Bryant, 2007). Preparing counselors with effective and culturally relevant advocacy skills for work in today’s pluralistic society requires that counselor educators rethink historically used teaching methods (Brady-Amoon, Makhija, Dixit, & Dator, 2012; Burnett, Long, & Horne, 2005; Herlihy & Watson, 2007; Hoover & Morrow, 2016; Manis, 2012). Rethinking traditional teaching methods and curricula is particularly important for courses such as human development, which have traditionally focused on universalist theories established using single-gender or single-culture groups (Broderick & Blewitt, 2015). However, for the foreseeable future students will be required to demonstrate their mastery of these traditional theories on licensing exams (NBCC, 2015). To meet the dual challenge of preparing students for licensure and preparing them for practice in a pluralistic society, new teaching approaches are needed. The role of social justice advocacy has been conceptualized as central for counselors (Chang, Crethar, & Ratts, 2010; Lewis, Lewis, Daniels, & D’Andrea, 1998), yet few studies have demonstrated how to prepare students for this role.
Service Learning: A Pedagogy for Counselor Education
Defining Service Learning
Teaching that is active, experiential, and addresses real-world problems is needed to meet the call to prepare students as social justice advocates in the context of rapidly changing and diversifying demographics (Bemak, Chung, Talleyrand, Jones, & Daquin, 2011; Constantine et al., 2007; Manis, 2012). As an experiential teaching strategy that combines academic content learned in the classroom with activities in the community that address “human and community needs” (Jacoby, 2015, p. 6), service learning provides a potential avenue for more adequately preparing counseling students for work in today’s pluralistic society.
Although similar to experiential learning, service learning has a set of characteristics that make it distinct from internships and volunteerism (Furco, 2002). With an emphasis on collaboration with community partners (CPs) who represent historically marginalized communities, all participants enter the service-learning experience as learners and as contributors. Community members and students benefit from a collaborative learning partnership through which a solution to a community-articulated problem is developed (Warter & Grossman, 2002).
Service learning can take two forms: placement-based and project-based. Placement-based service learning usually involves a requirement for students to spend a set number of hours at a community organization where a student completes agreed-upon tasks (Parker-Gwin & Mabry, 1998). In project-based service learning, small student groups work with CP organizations on specific projects that help to meet a need or solve a community-articulated problem (Hugg & Wurdinger, 2007).
Service Learning in Counselor Education
A growing number of counselor educators have called for the use of service learning within counselor education to provide students with an avenue for understanding complex systemic social inequities (Bemak & Chung, 2011; Bemak et al., 2011; Constantine et al., 2007; Manis, 2012). Additionally, the use of service learning within counselor education has been the focus of a limited number of studies. A qualitative study by Jett and Delgado-Romero (2009) focused on the impact of using service learning with pre-practicum counseling students. Results showed that service learning “was perceived to facilitate student counselors’ professional development” (p. 116) through promoting a deeper understanding of counselors’ roles and contexts. Exposure to counseling environments promoted student counselors’ understanding of what counseling is, as opposed to what they imagined it to be (Jett & Delgado-Romero, 2009).
Service learning also has been found to increase multicultural competencies in counseling students. In utilizing service learning in a multicultural counseling class, Burnett, Hamel, and Long (2004) found that it provided “an opportunity to build community learning and cultural sensitivity” (p. 190). They found that service learning had merit in multicultural counseling competency training and in reducing a “missionary ideology” (p. 191) in students. These results suggest that service learning can be a useful strategy for helping students understand how to advocate with and on behalf of marginalized communities. In addition, service learning may give students the opportunity to practice advocacy skills in real-world contexts.
In order to explore the relationship between service learning and students’ understanding of the role of social justice advocacy in counseling, the present study documented and analyzed community counseling students’ experiences in project-based service learning in a human development course in a CACREP-accredited program. The study’s research question has four foci: In what ways does the use of service learning in a human development course impact students’ (a) understanding of course content; (b) understanding of development of people in non-dominant populations; (c) perceptions of themselves; and (d) understanding of a social justice perspective in counseling?
Method
Description of Participants and Sampling Procedures
The study included data from 40 participants. Seventy-six percent of participants identified as female, 24% identified as male, and no participant identified as “other,” an option allowing for non-binary gender identities. Participants’ age range was 22 to 56 with an average age of 31, and they identified with the following race or ethnic categories: Black, 5%; Hispanic, 22%; Native American, 2%; Two or More Races, 10%; White, 49%; and No Response, 12%.
To gain a broad understanding of students’ experiences, data from nearly all community counseling students (hereafter called participants) who participated in the course over four academic terms were included in the study. The data for one student was left out of the study because of participation in the research process. Each participant was in the first of a three-year community counseling program while enrolled in the course with service learning. The program was in its final cycle of CACREP
re-accreditation as a community counseling program at the time the data were collected. This study was approved by its host institution’s Internal Review Board.
Class as Context
Service learning is grounded in a specific “academic house” (Lee & McAdams, 2017) that informs the type of service activities. The academic house for the current research project was a course designed to meet the CACREP human growth and development curriculum requirement. Entitled Counseling Across the Lifespan, it was positioned as the first course in a three-year community counseling program located in a private, urban, medium-sized university in the northwest region of the United States. Taught over a 10-week academic term, the course utilized a text that covered theories and models of human development across the lifespan (i.e., theories of learning, personality development, cognitive development, ecological models). Course elements included reading, class lectures, small and large group discussions, papers, and quizzes. Many theories of development included in the course to help students meet the requirements of licensure were developed using a single-gender, monocultural group. To incorporate a social justice perspective, the course instructor (first author) believed it was essential for students to understand how Euro-Western theories of development may or may not apply to populations for whom they were not developed. To provide context for critical analysis of class content, students engaged in a major class project, the Developmental Service-Learning Project (DSLP).
Developmental service-learning projects. In keeping with high-quality service-learning pedagogy with a social justice focus, the DSLPs were designed in collaboration with CP organizations working with marginalized populations. The primary instructor worked with a center on campus that supported faculty in developing service-learning courses to identify potential partners whose organizations serve people across the lifespan. Project examples included needs assessments, resource manual development, and socio-emotional lesson plan development. All project ideas were suggested by CPs and planned collaboratively with the course instructor. CPs visited class to introduce their organizations and projects to students during the second class session. Students then selected a project and met with their CPs during class time to launch the collaborative project work.
The DSLP had several requirements. For students to gain an understanding of the organization and the population with whom they were working, students visited the site under the supervision of the CP. Each project included the development of a product that could go into immediate use at the CP organizations and that would continue to benefit the site after the project ended. Students also were required to read, analyze, and report how relevant scholarly literature informed their project work. A project proposal detailing what would be accomplished during the DSLP was submitted for approval to the CP and the course instructor. Upon approval, students carried out their projects while remaining in contact with their CPs. During the study’s time period, there were a total of 24 completed DSLP projects. In collaboration with CPs, students completed projects on curriculum development, program evaluations, needs assessments through focus groups and interviews, and intake process development, among others. CP organizations served individuals across the lifespan and in historically marginalized communities ranging from a program on kindergarten readiness with refugee families, to developing resources for housing for an older African immigrant community.
CPs attended the final class session for DSLP group presentations. Partners asked questions, gave verbal feedback, and completed formal written evaluations of the projects. Project groups wrote a final report for their CP detailing their work and product. Digital and physical copies of all products were given to CPs for their continued use. The last class session served to celebrate partnerships and accomplishments. After the term ended, the course instructor met with each CP to discuss the experience, solicit feedback, and plan future collaborations; several CPs collaborated on projects over multiple academic terms.
Data Collection and Analysis
Data were collected from three sources, each a required class assignment. The first two sources were reflection papers—one written by participants at midterm, and one at the end of the term. The third assignment was a self-evaluation completed by participants at the end of the DSLP experience. Participants responded to specific prompts such as “Did your experience with the Developmental Service-Learning Project impact your comprehension of the material from the text and lectures? If so, how?” and “Through the Developmental Service-Learning Project, what did you learn about: Yourself? Your community? Working with people who may have had a different developmental trajectory than you?”
Content analysis is a qualitative methodology that can be used for analyzing and drawing meaning from large amounts of textual data. It allows for the “subjective interpretation of the content of text or data through the systematic classification process of coding and identifying themes or patterns” (Hsieh & Shannon, 2005, p. 1278). This methodology has been widely used in counselor education research (Avent, Wahesh, Purgason, Borders, & Mobley, 2015; Burkholder, Hall, & Burkholder, 2014; Cook, Hayden, Gracia, & Tyrrell, 2015).
Using content analysis of secondary data, researchers analyzed existing textual data collected from study participants enrolled in the course over four academic terms, for a total of 120 documents (N = 40 students with three documents each). To maintain participants’ confidentiality and to minimize possible researcher bias, all identifying information was removed from the data sources by the first author prior to analysis. Each participant was assigned a numerical identifier linking them to the course section in which they participated. These identifiers were kept in an Excel file that was password protected and was kept away from the rest of the data in order to reduce bias.
Data were analyzed in two phases to identify central themes associated with the participants’ experiences and perceptions with DSLP. First, data corresponding to each of the four foci of the research question were grouped into the following a priori categories: (a) understanding of course content,
(b) understanding of human development in non-dominant groups, (c) perception of self, and (d) a social justice perspective in counseling. During the second phase of analysis, data within each category were coded by meaning units, which was defined as a collection of words, sentences, or paragraphs that referred to a discrete idea. Closely related codes were collapsed into themes. Researchers used NVivo 10 (QSR International, 2012) for the coding process and to calculate interrater reliability statistics.
Trustworthiness
During the study, the researchers engaged in several strategies to ensure the study’s trustworthiness. The research team consisted of the course instructor and a graduate student research assistant who was trained in the research procedures. Prior to the study’s design and again before data analysis, researchers examined their potential biases. As recommended by Rossman and Rallis (2003), researchers engaged in reflexivity through writing, discussing, and revising researcher-as-instrument statements throughout the process. This process was done to bracket the researchers’ beliefs and opinions to ensure that the participants’ voices could be heard fairly and clearly.
Data were collected from documents that participants completed at two different points during the academic term (midterm and end of term), providing the basis of a longitudinal analysis. At the beginning of data analysis, researchers spent several hours coding data together to support shared meaning of codes and ensure credibility of the analysis. Additionally, researchers engaged in peer debriefing of codes and the coding process at weekly research meetings. Within each phase of coding, the researchers calculated interrater reliability statistics in NVivo 10 (QSR International, 2012) to determine the credibility of the analysis. After each coding session, researchers documented their reflections, questions, and ideas in a reflexive journal designed to document decision making related to the analysis. An audit trail was kept ensuring confirmability of the study’s findings.
Interrater Reliability
During each phase of coding, researchers conducted interrater reliability testing using NVivo 10 (QSR International, 2012) to ensure credibility of the coding process. In the first phase of grouping data into four a priori categories for further coding, an interrater reliability test resulted in a kappa coefficient of .68. This outcome is considered a “substantial” benchmark for kappa coefficients by Landis and Koch (1977). During the second phase of coding into emergent categories, the kappa coefficient for data that was coded by both researchers was .96. This is an “almost perfect” benchmark for kappa coefficients (Landis & Koch, 1977). These results demonstrated that raters consistently coded the data in a similar matter and increased the data’s credibility.
Results
The study’s results indicated the level of impact the DSLP experience had on participants’ understanding of course content, understanding of people in non-dominant groups, perceptions of themselves, and what social justice in a counseling context meant to them. For participants, the DSLP experience became a lens to look at the world in a different way and was a primary frame of reference for the course. In this section, results for each of the four a priori categories is reported, including qualitative results from the content analysis, as well as a narrative description of the data’s emergent themes.
Understanding of Course Content
The first a priori category focused on the impact of the DSLP on participants’ understanding of content in the human development course. Content analysis resulted in 374 meaning units that coalesced into two themes: connecting class material and reflections on learning.
Participants articulated coming away with a more complex and nuanced understanding of seemingly straightforward developmental theories because of the DSLP experience. The messiness of lived experience became real in a way participants did not believe the theories always described. For example, one participant stated that the DSLP experience “muddied the overly clear waters of the text’s simplistic approach to the behavior of complex systems. The service-learning project was a much more realistic approach, introducing us to complex systems and their interactions.” The hands-on nature of the DSLP, as well as the real-world context it provided, facilitated learning that participants described as broader, deeper, and more relevant to their professional futures. Participants reported that the class content was more accessible, more understandable, and easier to absorb because of the DSLP experience. One participant stated that the service-learning experience “required me to broaden my scope of what we were learning in the class. The focus can often be narrow in the classroom setting, but we were able to consider the ‘big picture’ in a realistic way because of this project.”
Further, the context provided by the service-learning experience offered the opportunity for critical analysis of class content. Consistencies and inconsistencies between class content and the lives of the people at their DSLP sites became apparent to participants. Many times, students came away realizing the gaps between theoretical models and lived experiences, particularly for people in non-dominant groups. One participant stated that the experience “made me more critical of the dominant views of development presented in our text. . . . While I understand there are certain fundamental human needs, I really believe in thinking about context as much as content.”
Human Development in Non-Dominant Groups
The next a priori category focused on how the experience with the DSLP impacted participants’ understanding of development of people in non-dominant groups. As CP agencies worked with populations outside the dominant culture, the DSLP provided an opportunity for participants to learn about these groups. Data analysis resulted in 291 meaning units in five themes: access to resources, creating community, cultural awareness, cultural differences, and systems of oppression.
Because of the DSLP experience, participants noted better understanding of the challenges a person in a non-dominant group faces when creating or maintaining their identity. Several participants reported seeing community members’ struggles by incorporating a social construct or standard that did not fit with their own cultural experiences. One participant stated, “As an immigrant parent, the stress is likely increased because the ‘outside influences’ are coming from a culture that is at the very least unfamiliar, and at worst, in conflict with cultural values important to the parents.”
Participants observed a strong sense of resiliency in community members as they overcame obstacles to seek out support. Participants identified that engaging in wellness activities and having a sense of purpose and pride in their lives contributed to resiliency for community members. These wellness activities included groups offered at mental health agencies and informal gatherings where stories and experiences were shared. A participant stated that at her DSLP site she witnessed “strength and resiliency with which people can create meaning and community that is not based on dominant cultural values.”
Furthermore, participants witnessed that when faced with conflicts or challenges, community members found support by referring to their own cultural values and norms. A participant stated, “For an immigrant in a new country, believing that there are others around who not only speak the same language, but have the same values and interests can be powerful in promoting feelings of efficacy instead of helplessness.”
Perceptions of Self
The third a priori category focused on how the DSLP experience impacted participants’ perceptions of themselves. Content analysis resulted in 227 meaning units with three themes that focused on working with new populations, their personal role in social justice, and specific work-related skills.
As CP organizations worked with marginalized communities, such as the East African immigrant community and the youth of the Asian and Pacific Islander community, most participants interfaced with communities with whom they had not previously worked. These interactions spurred participant reflection on the similarities and differences between themselves and those with whom they were working. Participants expressed surprise in what they learned about communities new to them, expecting to find more similarities or more differences. One participant stated, “As a first-generation person, I assumed that I could relate to the issues that the families face. However, I learned that their experience here in (location) is much different than the one I had growing up.” Another participant stated, “Although the students that were in the (CP program) may have a different developmental trajectory than me, there were still many similarities between us. Their values and work ethic reflected the same as mine.”
The interaction with CPs and clients through the DSLP provided a lens for participants to see how structural inequities in society impact the health and development of people in marginalized groups. Because of this, participants were better able to see and understand their own privilege, whether that privilege was related to race, gender, socioeconomic status, or educational attainment. One participant stated, “To be able to briefly see through the eyes of another individual who does not have the same background or privilege as I do, I am better able to understand my own privilege.” Another participant stated, “We all have our own biases and stereotypes and maybe even racist ideologies that we need to get rid of.”
Many participants articulated their perspectives on what social justice meant to them personally and how to move social justice goals in society forward. These were general definitions of social justice not specific to how social justice related to counseling. One participant said, “I believe that being an advocate for social justice involves understanding that many factors in people’s lives influence their development, and that not everyone has equal opportunity to environments conducive to healthy development.” Another participant stated, “To me, social justice means recognizing human dignity across social categories and engaging in some way to distribute power more equitably among people.”
A Social Justice Perspective in Counseling
The final a priori category was focused on how engagement in the DSLP experience impacted participants’ understanding of a social justice perspective in counseling. Data analysis resulted in 416 meaning units with three themes: definitions of social justice in counseling, counselor social justice knowledge, and counselor action through advocacy.
Participants articulated what social justice in the counseling sphere meant to them. One participant stated, “In order to successfully incorporate a social justice approach to counseling, socioeconomic status, culture, academic proficiencies and group membership must be considered.” Empowerment was identified by multiple participants as key to social justice approaches to counseling. According to one participant, “Empowering individuals is at the heart of social justice.” Additionally, participants pointed to understanding each client as a whole individual, including their unique social location, as important in counseling from a social justice perspective.
Participants shared new knowledge of recognizing systems that impacted people in non-dominant groups and acknowledging that the external factors of barriers and injustices may play a role in the need for mental health services. One participant said, “A counselor can promote social justice by helping clients identify the foundation of their behavior and understand that their feelings of insecurity are valid.”
Participants identified that a social justice perspective in counseling included a call to advocate for clients. One participant defined advocacy as, “Part of being a therapist who believes in social justice is advocating for and empowering those individuals who feel they have no voice or feel their voice has been extinguished through societal or institutional oppression.” Participants stated that the goal of social justice counseling was, in fact, to strengthen and support the resiliency of their clients who experience challenges brought on by external factors. One person said, “Social justice advocacy seeks not only to fight oppression but to empower individuals and communities that have been historically oppressed to be self-determinant to live lives of meaning and hope through equitable redistribution of resources, power, and opportunities.”
Discussion
The results of this study offer insight about how using service learning in a human development course impacted community counseling students. Because these findings document a shift in understanding the nature of human development in a pluralistic society, they may be useful for counselor educators who teach human development and who strive to prepare counseling students with a social justice perspective.
The Teaching and Learning of Human Development
As a core curricular area of accredited programs, coursework in human development is required for all counseling students (CACREP, 2015). Students who seek to become licensed counselors must demonstrate their mastery of this content area on national exams (NBCC, 2015). Therefore, counselor educators have an obligation to prepare students with this knowledge base. However, universalist theories of human development may not sufficiently explain development of all groups in a society (Broderick & Blewitt, 2015; Henrich et al., 2010). There is growing acknowledgement that often embedded in models are the worldviews of those who developed them (Rogoff, 2003). Counselor educators are called to teach human developmental theory in such a way that students will be able to responsibly apply (or not apply) theories to clients from whom and for whom they were not developed.
This study’s findings demonstrate that service learning provides participants with a deeper and more nuanced understanding of human development course content through its application in real settings. Participants witnessed how theories did not always match the lives of people at their service-learning sites. Further, participants articulated witnessing how systems of oppression negatively impacted the development of marginalized people. These results build on the evidence that the use of service learning can promote multicultural competence (Burnett et al., 2004) and help students be more prepared to move into the professional role of counselor with a more realistic perspective of what the role means (Jett & Delgado-Romero, 2009).
Preparing Counseling Students as Social Justice Advocates
According to the Code of Ethics (ACA, 2014), counselors should be ready to advocate for removing barriers to healthy growth and development, yet specific strategies for preparing students to do so are lacking. Participation in collaborative service learning focused on important issues for marginalized populations facilitates new awareness of what social justice counseling means. The need for counselors to be aware of their own privilege was stated clearly by participants. In addition, being a counselor for social justice also meant advocating for clients at multiple levels. Working with CPs provided opportunities to witness important work in the community and to practice enacting social justice advocacy. The results demonstrate that service learning can be used as a teaching strategy to meet CACREP requirements and to meet the call for using new “structures, requirements, and goals” (Constantine et al., 2007, p. 27) to prepare students as social justice advocates.
Limitations and Future Research
This study’s findings demonstrated that service learning can be used to teach academic content as well as promote students’ understanding of social justice and advocacy. However, limitations are important to note. First, the primary researcher was the course instructor and the co-researcher participated in the class as a student, although data for the co-researcher was not included in the analysis. Although steps were taken to ensure trustworthiness and authenticity, future studies should include an outside researcher to strengthen the methodology. Second, data for the study was drawn from written text. As such, there were no opportunities to ask participants follow-up or clarifying questions. Although content analysis was chosen to examine the participants’ experiences of the DSLP while they were occurring, future studies using interviews or focus groups could provide more sources of data. Third, the current study focused only on the student experience in the DSLP. Although CPs were involved in every aspect of project creation, execution, and evaluation, they were not included in the systematic study of outcomes. Future studies should examine the impact of service learning on CPs, clients, and communities.
Conclusion
The demographics of the United States are rapidly changing, and soon there will be no one majority group (Cárdenas, Ajinkya, & Gibbs Léger, 2011). Continuing to teach monocultural theories is no longer sufficient; it risks further marginalizing non-dominant groups in society. If we were to better understand how different groups and cultures experience development through their own lenses and a shared pluralistic lens, the problem of applying theories to those from whom and for whom they were not developed would be eliminated. Counselor educators should work with CPs and community members to develop, research, and apply culturally appropriate theories of human development. Until that time, counselor educators must use effective teaching strategies that prepare students to work responsibly and competently in a multicultural world. Service learning, as an educational tool for social justice in counselor education, can contribute to meeting this need.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest or funding contributions for the development of this manuscript.
References
American Counseling Association. (2014). 2014 ACA code of ethics. Retrieved from http://www.counseling.org/docs/ethics/2014-aca-code-of-ethics.pdf?sfvrsn=4
Avent, J. R., Wahesh, E., Purgason, L. L., Borders, L. D., & Mobley, A. K. (2015). A content analysis of peer feedback in triadic supervision. Counselor Education and Supervision, 54, 68–80.
doi:10.1002/j.1556-6978.2015.00071.x
Bemak, F., & Chung, R. C. (2011). Application in social justice counselor training: Classroom without walls. The Journal of Humanistic Counseling, 50, 204–219. doi:10.1002/j.2161-1939.2011.tb00119.x
Bemak, F., Chung, R. C., Talleyrand, R. M., Jones, H., & Daquin, J. (2011). Implementing multicultural social justice strategies in counselor education training programs. Journal for Social Action in Counseling & Psychology, 3, 29–43.
Brady-Amoon, P. (2011). Humanism, feminism, and multiculturalism: Essential elements of social justice
in counseling, education, and advocacy. Journal of Humanistic Counseling, 50, 135–148. doi:10.1002/j.2161-1939.2011.tb00113.x
Brady-Amoon, P., Makhija, N., Dixit, V., & Dator, J. (2012). Social justice: Pushing past boundaries in graduate training. Journal for Social Action in Counseling & Psychology, 4, 85–98.
Broderick, P. C., & Blewitt, P. (2015). The life span: Human development for the helping professions (4th ed). Boston, MA: Pearson.
Burkholder, D., Hall, S. F., & Burkholder, J. (2014). Ward v. Wilbanks: Counselor educators respond. Counselor Education and Supervision, 53, 267–283. doi:10.1002/j.1556-6978.2014.00062.x
Burnett, J. A., Hamel, D., & Long, L. L. (2004). Service learning in graduate counselor education: Developing multicultural counseling competency. Journal of Multicultural Counseling and Development, 32, 180–191. doi:10.1002/j.2161-1912.2004.tb00370.x
Burnett, J. A., Long, L. L., & Horne, H. L. (2005). Service-learning for counselors: Integrating education, training, and the community. The Journal of Humanistic Counseling, Education, and Development, 44, 158–167. doi:10.1002/j.2164-490X.2005.tb00028.x
Cárdenas, V., Ajinkya, J., & Gibbs Léger, D. (2011). Progress 2050: New ideas for a diverse America. Retrieved from https://cdn.americanprogress.org/wp-content/uploads/issues/2011/10/pdf/progress_2050.pdf
Chang, C. Y., Crethar, H. C., & Ratts, M. J. (2010). Social justice: A national imperative for counselor education and supervision. Counselor Education and Supervision, 50(2), 82–87.
doi:10.1002/j.1556-6978.2010.tb00110.x
Constantine, M. G., Hage, S. M., Kindaichi, M. M., & Bryant, R. M. (2007). Social justice and multicultural issues: Implications for the practice and training of counselors and counseling psychologists. Journal of Counseling & Development, 85, 24–29. doi:10.1002/j.1556-6678.2007.tb00440.x
Cook, A. L., Hayden, L. A., Gracia, R., & Tyrrell, R. (2015). Exploring outcomes of a targeted supervisory training curriculum on developing multicultural competency and social justice advocacy. Outcome-Based Program Evaluation, 6(2), 126–140. doi:10.1177/2150137815594201
Council for the Accreditation of Counseling & Related Educational Programs. (2015). 2016 CACREP standards. Retrieved from http://www.cacrep.org/wp-content/uploads/2018/05/2016-Standards-with-Glossary-5.3.2018.pdf
Dixon, G. (2001). The development of course content: Teaching child development from a multicultural perspective. National Association of African American Studies & National Association of Hispanic and Latino Studies: 2000 Literature Monograph Series. Retrieved from https://files.eric.ed.gov/fulltext/ED456182.pdf
Furco, A. (2002). Is service-learning really better than community service? A study of high school service program outcomes. In A. Furco & S. H. Billig (Eds.), Service-learning: The essence of the pedagogy (pp. 23–50). Greenwich, CT: Information Age Publishing.
Henrich, J., Heine, S. J., & Norenzayan, A. (2010). The weirdest people in the world? Behavioral and Brain Sciences, 33(2/3), 61–83. doi:10.1017/S0140525X0999152X
Herlihy, B. R., & Watson, Z. E. P. (2007). Social justice and counseling ethics. In C. C. Lee (Ed.), Counseling for social justice (2nd ed., pp. 181–198). Alexandria, VA: American Counseling Association.
Hoover, S. M., & Morrow, S. L. (2016). A qualitative study of feminist multicultural trainees’ social justice development. Journal of Counseling & Development, 94, 306–318. doi:10.1002/jcad.12087
Hsieh, H. F., & Shannon, S. E. (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15, 1277–1288. doi:10.1177/1049732305276687
Hugg, R., & Wurdinger, S. (2007). A practical and progressive pedagogy for project based service learning. International Journal of Teaching and Learning in Higher Education, 19, 191–204.
Jacoby, B. (2015). Service-learning essentials. San Francisco, CA: Jossey-Bass.
Jett, S. T., & Delgado-Romero, E. A. (2009). Prepracticum service-learning in counselor education: A qualitative case study. Counselor Education and Supervision, 49, 106–121. doi:10.1002/j.1556-6978.2009.tb00091.x
Kiselica, M. S., & Robinson, M. (2001). Bringing advocacy counseling to life: The history, issues, and human dramas of social justice work in counseling. Journal of Counseling & Development, 79, 387–397. doi:10.1002/j.1556-6676.2001.tb01985.x
Kraus, K. L. (2008). Lenses: Applying lifespan development theories in counseling. Boston, MA: Houghton Mifflin Company.
Landis, J. R., & Koch, G. G. (1977). The measurement of observer agreement for categorical data. Biometrics, 33, 159–174. doi:10.2307/2529310
Lee, K. A., & McAdams, C. R. (2017). Promoting social justice advocacy competency and cognitive development among counselor trainees in internship: A service-learning approach. Manuscript submitted for publication.
Lewis, J. A. (2011). Operationalizing social justice counseling: Paradigm to practice. The Journal of Humanistic Counseling, 50, 183–191. doi:10.1002/j.2161-1939.2011.tb00117.x
Lewis, J., Arnold, M. S., House, R., & Toporek, R. I. (2002). ACA advocacy competencies. Retrieved from https://www.counseling.org/Resources/Competencies/Advocacy_Competencies.pdf
Lewis, J. A., Lewis, M. D., Daniels, J. A., & D’Andrea, M. J. (1998). Community counseling: Empowerment strategies for a diverse society (2nd ed.). Pacific Grove, CA: Brooks/Cole.
MacLeod, B. P. (2013). Social justice at the microlevel: Working with clients’ prejudices. Journal of Multicultural Counseling and Development, 41, 169–184. doi:10.1002/j.2161-1912.2013.00035.x
Manis, A. A. (2012). A review of the literature on promoting cultural competence and social justice agency among students and counselor trainees: Piecing the evidence together to advance pedagogy and research. The Professional Counselor, 2, 48–57. doi:10.15241/aam.2.1.48
National Board for Certified Counselors. (2015). Candidate handbook for national certification with the National Counselor Examination for licensure and certification (NCE). Retrieved from http://www.nbcc.org/Assets/Exam/Handbooks/NCE.pdf
Parker-Gwin, R., & Mabry, J. B. (1998). Service-learning as pedagogy and civic education: Comparing outcomes for three models. Teaching Sociology, 26, 276–291. doi:10.2307/1318768
QSR International. (2012). NVivo 10 [Computer software]. Available from http://www.qsrinternational.com
Ratts, M. J. (2009). Social justice counseling: Toward the development of a fifth force among counseling paradigms. The Journal of Humanistic Counseling, Education and Development, 48, 160–172. doi:10.1002/j.2161-1939.2009.tb00076.x
Ratts, M. J., & Wood, C. (2011). The fierce urgency of now: Diffusion of innovation as a mechanism to integrate social justice in counselor education. Counselor Education and Supervision, 50, 207–223. doi:10.1002/j.1556-6978.2011.tb00120.x
Rogoff, B. (2003). The cultural nature of human development. New York, NY: Oxford University Press.
Rossman, G. B., & Rallis, S. F. (2003). Learning in the field: An introduction to qualitative research (2nd ed.). Thousand Oaks, CA: Sage.
Stennbarger, B. N., & LeClair, S. (1995). Beyond remediation and development: Mental health counseling in context. Journal of Mental Health Counseling, 17, 173–187.
Toporek, R. L., Gerstein, L. H., Fouad, N. A., Roysircar, G., & Israel, T. (Eds.). (2006). Handbook for social justice in counseling psychology: Leadership, vision, and action. Thousand Oaks, CA: Sage.
Warter, E. H., & Grossman, J. M. (2002). An application of developmental-contextualism to service-learning. In A. Furco & S. H. Billig (Eds.), Service-learning: The essence of the pedagogy (pp. 83–102). Greenwich, CT: Information Age Publishing.
West-Olatunji, C. (2010). If not now, when? Advocacy, social justice, and counselor education. Counseling and
Human Development, 42(8), 1–12.
Kristi A. Lee, NCC, is an associate professor at Seattle University. Daniel J. Kelley-Petersen, NCC, is an adjunct faculty member at Seattle University. Correspondence can be addressed to Kristi Lee, College of Education, 901 Twelfth Avenue, Seattle, WA 98122, leekrist@seattleu.edu.
Jun 28, 2018 | Volume 8 - Issue 2
Regina Gavin Williams, Stanley B. Baker, ClarLynda R. Williams-DeVane
Three female foster care youth, aged 15, 17, and 17, volunteered to participate in customized counseling interventions. A theory-based presentation framework was used to conduct an A-B-A single-case research design. A female licensed professional counselor collaborated with the participants in customizing interventions, delivering the intervention, and collecting the outcome data, with the three participants engaging in self-monitoring to provide outcome data. Four career and college readiness self-efficacy factor scores were used to determine the components of the customized interventions and to assess the participants’ progress. The factors were: (a) college knowledge, (b) positive personal characteristics, (c) academic competence, and (d) potential to set and achieve future goals. Positive trends occurred for each participant, although different factor-specific outcome data patterns occurred for each participant. Effect sizes ranged from small to large across the participants and factors, and the participants found value in their respective customized interventions.
Keywords: foster care youth, customized counseling interventions, single-case research design, career readiness self-efficacy, college readiness self-efficacy
Appropriate assistance is important for effective navigation of the demanding postsecondary education preparation process and is vital for attaining admittance into higher education (Pecora, Williams, et al., 2006). Youth who are academic low achievers from middle-to-low income families, underrepresented minorities, the disabled, and youth from families in which no one has previously attended college find it especially difficult to navigate access to higher education (College Board, 2006). Moreover, youth in the foster care system potentially face all of the listed access challenges.
Foster care youth have been removed from their family units through decisions determined in the courts. Judges may decide to place youth in foster homes, in group homes, or with their relatives (i.e., kinship foster care; C. M. Kirk, Lewis, Nilsen, & Colvin, 2013). More long-term placement outcomes include adoption or aging out of foster care. According to statistics from the Adoption and Foster Care Analysis and Reporting System (AFCARS; 2013), there were approximately 402,378 youth in foster care, and 47% of these youth resided in non-relative foster care homes. Additionally, foster placements spent 20 months on average in multiple placement settings (AFCARS, 2013). These circumstances create various multiple educational attainment barriers for foster care youth.
According to C. M. Kirk et al. (2013), about 10% of former foster care youth were enrolled in college, and only 4% of these youth obtained a bachelor’s degree. Youth in foster care are more likely to drop out of high school, repeat a grade, or be suspended or expelled (Unrau, Font, & Rawls, 2012). Only one third of foster care youth who age out of the foster care system after their 18th birthday possess a driver’s license, own basic necessities for living, or have money upon leaving the foster system (Pecora, Kessler, et al., 2006). Furthermore, very little is known about the readiness of foster care youth to undertake a postsecondary education, the developmental necessities of these youth during their transition to postsecondary education, and ways professionals in the child welfare system and in higher education can be of assistance (Unrau et al., 2012).
- Kirk et al. (2013) found indications that many youth in foster care have aspirations to pursue a postsecondary education. There is a dearth of information about foster care youth who have become successful in adulthood (Hudson, 2013), or their readiness to make a successful transition to adulthood (Lemon, Hines, & Merdinger, 2005). R. Kirk and Day (2011) found that an experiential learning program for youth aging out of foster care located in a college setting increased their knowledge about college admissions and campus life. Pecora, Williams, et al. (2006) found from a survey of 1,609 foster care alumni that foster care youth who received tutoring and independent living training and had employment experiences had high postsecondary education graduation rates.
Lemon et al. (2005) compared former foster care youth who experienced independent living programs (ILPs) and were attending 11 different colleges with former foster care youth not attending colleges and individuals with low-income backgrounds who were attending colleges. The findings indicated that the ILP participants were more likely to have acquired concrete skills such as finding employment; managing budgets; attaining housing; developing psycho-emotional skills, such as goal setting; and discovering opportunities for training and education (Lemon et al., 2005). Related recommendations for improving the career and college readiness of foster care youth include individual and group counseling focused on adjustment challenges and negative educational attitudes (Geroski & Knauss, 2000). Kaplan, Skolnik, and Turnbull (2009) also recommended career and college readiness counseling interventions.
Conley (2010) defined career ready as possessing the content knowledge and key learning skills and techniques to begin studies in a career pathway. Achieve, Inc. (n.d.) defined college ready as being prepared for postsecondary education training experiences that lead to obtaining credentials such as a bachelor’s or associate degree, a license, or a certificate. The reviewed literature cited above presented foster care youth as being at risk because they lacked the career and college readiness preparation needed for successful transitions from foster care to the postsecondary education opportunities essential for successful futures in the 21st century. Fortunately, there is evidence that group and individual counseling interventions can be helpful (Geroski & Knauss, 2000; Kaplan et al., 2009). The literature cited above also indicated that interventions based on an understanding of the unique circumstances foster care youth experience and focused on enhancing their career and college readiness may improve their potential to have access to postsecondary education opportunities.
A critical component of the challenge to achieve career and college readiness seems to be whether or not foster care youth believe they can successfully attain postsecondary education and develop meaningful careers. The general dependent variable in the present study was self-efficacy—that is, an individual’s personal beliefs about his or her ability to perform a specific behavior or achieve a specific personal goal (Bandura, 1997). The specific self-efficacy variable in the present study was career and college readiness self-efficacy (Baker & Parikh Foxx, 2012). The readiness construct was derived from Savickas’ (2011) career construction theory, built on the classic career readiness construct by Super (1990). The goal for the treatment approach in the study was to help foster care youth connect insights with future work and career opportunities and take possession of their lives.
The authors’ purpose in conducting the present study was to examine the effects of customized individual counseling interventions on the career and college readiness self-efficacy of a small sample of foster care youth. The research hypotheses for all three participants were focused on the effects of the respective customized interventions across baseline, intervention, and withdrawal phases in a single-case research design.
Method
Research Design
An A-B-A single-case experimental research design (SCRD) was employed in the present study. Components of the design were A1 = baseline phase, B = treatment phase, and A2 = withdrawal of treatment phase. The study participants’ responses during the clinical withdrawal phase provided evidence of the effect of the intervention after it had been withdrawn (Engel & Schutt, 2013; Hinkle, 1992; Martin-Causey & Hinkle, 1995).
Participants
The three participants were attending a voluntary, state-funded, county-administered life-skills development program in a Southeastern metropolitan county. The intervention focus of the program was on helping foster care youth transition to adulthood. The program served foster care youth from age 13 to 18 years old, those who aged out of foster care on their 18th birthday, and those voluntarily remaining in foster care after their 18th birthday. Approximately 50 foster care youth were enrolled in the program, although only six to 12 attended monthly meetings at any given time.
The first author had served as a volunteer for the program prior to providing the customized interventions in the present study. Following approval by the university institutional review board, the first author recruited participants for the intervention while attending one of the monthly skills development programs. Initially, four participants volunteered, and one withdrew after the second individual counseling session; being 18 and eligible to leave the system, this participant moved elsewhere. The three continuing participants professed an interest in pursuing postsecondary education. They were interested in exploring career and academic options and in becoming more confident that they could achieve future success in spite of their familial circumstances. Individual information about the participants is given below (pseudonyms are used in place of their real names).
Rose. Rose was a 17-year-old African American female high school senior enrolled in a non-traditional high school in a Southeastern city that served as a gateway to a community college. She decided to attend the community college because of the advantages of the gateway arrangement. Her current grade point average (GPA) was 2.6. She lived in a stable home, although she often had disagreements with her foster parents. Several other foster care youth lived in the same apartment, making privacy difficult to achieve.
Janelle. Janelle was a 15-year-old biracial (Caucasian/African American) female 10th grade student enrolled in a traditional public high school in a Southeastern city. She was an honor roll student with a 3.9 GPA. Her sexual orientation was lesbian, and she believed her foster parents would not accept her if they knew her orientation. She wanted to attend a four-year college and was uncertain about fields of study and potential career goals.
Kara. Kara was a 17-year-old African American female high school senior enrolled in a large comprehensive Southeastern urban high school. She had a 3.4 GPA and planned to attend college following graduation. Deciding on a major was her primary goal. She lived in a kinship foster care setting with two aunts and appeared to have considerable support at home.
The Counselor
The intervention was designed by the first author, who also served as the counselor presenting the customized interventions to the three participants. She was a 30-year-old African American female with a bachelor’s degree in psychology and a master’s degree in school counseling. She was a licensed professional counselor, a National Certified Counselor, and a recipient of a National Board for Certified Counselors minority fellowship. Her professional experience has included college access interventions, outpatient therapy employment, student services in higher education, and transitional living intervention programming. She previously served children and adolescents from underserved backgrounds, a significant number of whom were in foster care. She has had previous research experience; however, the present study was her first SCRD experience.
Instrumentation
Career and college readiness self-efficacy. The Career and College Readiness Self-Efficacy Inventory (CCRSI; Baker & Parikh Foxx, 2012) was completed by participants across all three phases of the study. The CCRSI readiness construct is based on Savickas’ (2011) career constructivist theory, and the self-efficacy concept was derived from Bandura’s (1997) social cognitive theory. Item content represents broad contextual goals (e.g., “I have confidence in being able to achieve a good life 10 years from now”) and specific content (e.g., “I know about various ways to pay for post-high school education”). Responses to each item range from strongly agree (5 points) to strongly disagree (1 point). There are 14 items in the total scale with scores ranging from 14 to 70. Higher scores indicate higher levels of self-efficacy.
In the present study, the customized interventions were based on the four CCRSI factors, and the factor scores were used in the data analyses. The CCRSI factors are: (a) college knowledge (5 items; scores ranging from 5 to 25); (b) positive personal characteristics (4 items; scores ranging from 4 to 20); (c) academic competence (3 items; scores ranging from 3 to 15); and (d) potential to set and achieve future goals (2 items; scores ranging from 2 to 10). An exploratory factor analysis of the CCRSI identified the four factors as accounting for 51% of the variance (Baker et al., 2017), and a confirmatory factor analysis supported the four-factor model (Martinez, Baker, & Young, 2017). Alpha reliability estimates for the total scale from two previous studies were .86 and .87. For the factor scales, they were: (a) college knowledge (.76 and .80), (b) positive personal characteristics (.69 and .70), (c) academic competence (.75 and .75), and (d) potential to set and achieve future goals (.46 and .51; Baker et al., 2017).
Social validity measure. Social validity refers to the social significance of the intervention (Wolf, 1978). According to Hott, Limberg, Ohrt, and Schmit (2015), evidence of social validity serves as a quality indicator in SCRDs and should be presented clearly in the results sections of said studies. Client satisfaction is one of the indicators of social validity recommended by Hott et al. (2015). An extant self-report measure designed to assess participants’ attitudes about research interventions upon their completion was used in the present study.
The Attitude Toward Treatment (ATT; Baker, 1983) scale was used to assess satisfaction with the intervention in the present study. The ATT was used previously as a post-treatment measure of satisfaction with psychoeducational group intervention. Content validity for using the ATT to assess client attitudes toward the interventions they received in clinical settings, as was the case in the present research, had been established in previous studies. The ATT consists of 14 seven-point Likert items with the wording presented in the past tense (e.g., How beneficial do you think this program was for you?). Scores range from a low of 14 to a high of 98.
Assessing unforeseen participant and setting changes. To control for threats to internal validity caused by unforeseen changes in the participants, the counselor-investigator kept field notes for each participant throughout the study (Hott et al., 2015).
Procedure
Customized interventions framework. The independent variables were the customized interventions for each participant. The customized intervention framework was entitled Students That Are Achieving Success (S.T.A.R.S). Explicating the foundations of the customized intervention process is necessary for establishing the fidelity of the treatment (Hott et al., 2015). All three customized interventions were embedded in a single conceptual framework. The conceptual framework was based on an integration of tenets of social cognitive career theory (SCCT; Lent, Brown, & Hackett, 1994), cognitive information processing (CIP; Peterson, Sampson, Lenz & Reardon, 2002), and the American School Counselor Association’s National Model (ASCA; 2012). The SCCT (Lent et al., 1994) is a useful instrument for researchers wishing to stress the importance of addressing external factors that influence career self-efficacy beliefs and outcome expectations. Therefore, the interventions were designed to identify external barriers for each participant and attempt to introduce ways to overcome them. The CIP (Peterson et al., 2002) was designed to help individuals understand the content and process of career decision-making and problem solving. The ILP component of the CIP framework was used during the initial meeting with each participant to identify at least three goals and establish mutually agreed-upon action steps. A focus on helping participants establish personal academic, career, and social goals; develop future plans; and monitor their learning aligned with the individual student planning component of the ASCA National Model.
Specific customizing strategies for each participant. Activities listed on the ILPs reflected the participants’ postsecondary education and career-related needs based on CCRSI (Baker & Parikh Foxx, 2012) scores acquired a week prior to the initial meetings. The counselor and each participant identified the desired activities and related outcomes, estimated time needed to complete activities, matched activities and goals, and prioritized the activities. CCRSI (Baker & Parikh Foxx, 2012) pre-treatment factor scores for each participant were used in the customizing process.
Rose’s customized goals. The pre-treatment CCRSI scores for Rose indicated that she needed assistance in believing in her academic competence and potential to achieve future goals. She already knew she would attend a community college; however, she had difficulty meeting academic expectations while in high school. Consequently, she wanted to explore strategies to help her improve academically and be eligible for admission to the community college. Not knowing what her major would be or how she would pay for college seemed to be interfering with her future goals. Her customized goals were exploring: (a) ways to improve her academic performance, (b) potential academic majors, and (c) ways to pay for college.
Janelle’s customized goals. The pre-treatment CCRSI scores for Janelle indicated that she needed assistance with believing in her academic competence and potential to achieve future goals. As a high school sophomore with no family focus on higher education, Janelle was uninformed about postsecondary education. She indicated that her time-management skills related to academic work were deficient. Consequently, her customized goals were: (a) understanding the college application and admission process, ways to receive financial aid, requirements for academic success in college, and cultural differences between high school and college; (b) exploring college majors and career choices; (c) learning to set short- and long-term goals; and (d) improving her time-management skills.
Kara’s customized goals. The pre-treatment CCRSI scores for Kara indicated that she needed assistance with believing in her academic competence and potential to achieve future goals. Although planning to attend college after graduation, Kara was struggling to maintain academic motivation while balancing academic and extracurricular activities. She also experienced doubts about future goals and achieving them. These circumstances led to the following customized goals: (a) enhancing her time-management skills, (b) engaging in short- and long-term goal setting, (c) exploring potential academic majors, (d) learning more about how to pay for college, and (e) understanding how college education influences one’s future income and lifestyle.
Data collection. The CCRSI (Baker & Parikh Foxx, 2012) was distributed electronically via Qualtrics survey software to the participants upon their submission of the informed consent forms. The pre-treatment CCRSI data served as the baseline (Phase A1) for the study. A common self-monitoring schedule was distributed with instructions for each participant to complete the CCRSI four times during the 2 weeks prior to the beginning of the intervention. The intervention (Phase B) lasted 8 weeks for each participant. Participants completed the CCRSI at the end of each weekly session. During the 2-week withdrawal phase (A2) following the last intervention session, participants were again instructed to follow a common self-monitoring schedule for completing the CCRSI four times. The three participants received a dinner, a gift card, and a certificate of completion from the counselor-investigator at the end of the study.
Data analysis. Visual and non-parametric analyses were used to assess the outcomes for each experiment, and non-parametric analyses provided information about the effects of the treatments (Hott et al., 2015).
Temporal analysis. The time series data were plotted graphically on x (temporal independent variable) and y (dependent variable) axes for each participant and CCRSI factor. Autocorrelation and regression analyses were used to determine the appropriate statistical analysis procedure. Autocorrelation analysis was used to determine whether each observation within each phase and factor of the study was truly independent. Observations that were not correlated to each other could not be predicted (Bloom, Fischer, & Orme, 2006). Regression analysis was used to determine whether significant trends were present for each phase of each CCRSI factor for each participant (alpha <.05). In cases where there was significant trend and autocorrelation, as well as outliers within each phase, the Robust Conservative Dual-Criteria (RCDC; Borckardt, 2008) method was used as the primary statistical analysis tool. RCDC was used to compare differences between phases for each participant as opposed to traditional parametric methods like the student’s t-test and analysis of variance (ANOVA).
Intervention effects. Providing effect sizes in addition to visual analyses enhances the credibility, reliability, and defensibility of single-case research findings (Vannest & Ninci, 2015). Vannest and Ninci (2015) reported that there are several strategies available to estimate effect sizes for SCRD studies. In cases where there is a significant trend and autocorrelation, the G-index (Cohen, 1988) is used to estimate effect sizes. The G-index results were determined by using the regression line and the mean or median from the baseline. The effect size was calculated by using the proportion of participants’ scores in the desired zone above the regression line, which was an expected increase in scores from the baseline to treatment phases. The baseline average was then subtracted from the intervention average, with a positive value indicating improved effects and a negative value indicating decreased effects. Metrics for interpreting G-index effect sizes are: small (< 0.3), medium (0.31 to 0.50), and large (> 0.51).
Assessing social validity and unforeseen changes in participants. Each participant completed the ATT measure following the final session of their respective interventions. The counselor-investigator kept field notes for each participant throughout the study.
Results
Statistical Analyses
Descriptive statistics. Descriptive statistics were computed for each of the participants across each of the factors which are presented in Table 1. Rose’s responses were very stable as indicated by the consistent means and medians across all phases of the study. Further, the standard deviation values were close to zero, indicating a lack of variation in stability. Janelle’s responses were less stable. The large range in the treatment phase is indicative of the presence of outliers in the treatment phase for Janelle. Kara exhibited more variability than Rose, but there were no outliers.
Table 1
Descriptive Statistics
| Participant |
|
n |
Mean |
Median |
SD |
Range (min, max) |
| A1 |
B |
A2 |
A1 |
B |
A2 |
A1 |
B |
A2 |
A1 |
B |
A2 |
A1 |
B |
A2 |
| Rose |
College Knowledge |
4 |
12 |
4 |
24.75 |
25.00 |
25.00 |
25 |
25 |
25 |
0.5 |
0.0 |
0.0 |
(24,25) |
(25,25) |
(25,25) |
| Positive Personal Characteristics |
4 |
12 |
4 |
20.00 |
19.91 |
20.00 |
20 |
20 |
20 |
0.00 |
0.29 |
0.000 |
(20,20) |
(19,20) |
(20,20) |
| Academic Competence |
4 |
12 |
4 |
13.0 |
14.5 |
15.0 |
13 |
15 |
15 |
0.00 |
0.67 |
0.000 |
(13,13) |
(13,15) |
(15,15) |
| Potential to Achieve Future Goals |
4 |
12 |
4 |
10 |
9.91 |
10 |
10 |
10 |
10 |
0.00 |
0.29 |
0.000 |
(10,10) |
(9,10) |
(10,10) |
| All Factors |
4 |
12 |
4 |
67.75 |
69.33 |
70.00 |
68.0 |
69.5 |
70.0 |
0.50 |
0.78 |
0.000 |
(67,68) |
(68,70) |
(70,70) |
| Janelle |
College Knowledge |
4 |
12 |
4 |
13.00 |
17.17 |
25.00 |
12 |
19 |
25 |
2.71 |
7.38 |
0.00 |
(11,17) |
(5,25) |
(25,25) |
| Positive Personal Characteristics |
4 |
12 |
4 |
16.25 |
15.42 |
20.00 |
16 |
19 |
20 |
0.50 |
0.68 |
0.00 |
(16,17) |
(4,20) |
(20,20) |
| Academic Competence |
4 |
12 |
4 |
14.25 |
12.00 |
15.00 |
14 |
15 |
15 |
0.50 |
5.43 |
0.00 |
(14,15) |
(3,15) |
(15,15) |
| Potential to Achieve Future Goals |
4 |
12 |
4 |
9.75 |
8.00 |
10.00 |
10 |
10 |
10 |
0.50 |
3.62 |
0.00 |
(9,10) |
(2,10) |
(10,10) |
| All Factors |
4 |
12 |
4 |
53.25 |
52.58 |
70.00 |
52.0 |
63.5 |
70.0 |
3.20 |
22.67 |
0.00 |
(51,58) |
(14,69) |
(70,70) |
| Kara |
College Knowledge |
4 |
12 |
4 |
17.00 |
21.33 |
23.75 |
17.5 |
21.0 |
24.0 |
2.45 |
2.39 |
0.50 |
(14,19) |
(23,24) |
(19,25) |
| Positive Personal Characteristics |
4 |
12 |
4 |
14.50 |
17.83 |
18.25 |
14.5 |
17.5 |
18.0 |
0.58 |
1.03 |
0.50 |
(14,15) |
(17,20) |
(18,19) |
| Academic Competence |
4 |
12 |
4 |
10.25 |
13.08 |
13.50 |
1.5 |
13.0 |
13.5 |
0.96 |
1.08 |
0.58 |
(9,11) |
(12,15) |
(13,14) |
| Potential to Achieve Future Goals |
4 |
12 |
4 |
9.25 |
9.58 |
10.00 |
9.5 |
10.0 |
10.0 |
.96 |
0.67 |
0.00 |
(8.10) |
(8,10) |
(10,10) |
| All Factors |
4 |
12 |
4 |
51.00 |
61.83 |
65.50 |
50.0 |
60.5 |
65.5 |
2.71 |
4.67 |
1.29 |
(49,55) |
(57,70) |
(64,67) |
Note. The descriptive statistics show stability for both Rose and Kara. More variability was present for Janelle, indicative of outliers leading to the use of non-parametric analysis methods.
Autocorrelation. Autocorrelation was measured and evaluated at the .05 significance level. There was significant autocorrelation for Rose for the Academic Competence factor (p = 0) in the treatment phase. There was no significant correlation for Janelle. There was significant autocorrelation in several areas for Kara: college knowledge (p = 0.003), positive personal characteristics (p = 0.001), and academic competence (p = 0) in the treatment phase. No transformations were applied to correct for autocorrelation because of lack of independence between data points, the small sample size, and the significant trends in some of the phases; therefore, non-parametric data analyses were used.
Regression. Regression was measured for each participant, factor, and phase to determine if there is a trend in each phase of the study. All three participants exhibited unique trend patterns for each of the factors. Rose exhibited a significant trend for academic competence in the treatment phase. The strong positive slope (R2 = 0.7399, Slope = 0.16084, p = .000332) suggested a steady increase during the treatment phase. Janelle exhibited negative treatment phase trends for positive personal characteristics (R2 = 0.3392, Slope = -1.094, p = 0.049), academic competence (R2 = 0.411, Slope = -0.9650, p = 0.0247), and potential to achieve future goals (R2 = 0.411, Slope = -0.6434, p = 0.0247). The negative slopes suggest a decrease in self-efficacy across all factors except college knowledge. Lastly, Kara exhibited significant positive trends for college knowledge (R2 = 0.7142, Slope = 0.5594, p = 0.000538), positive personal characteristics (R2 = 0.6138, Slope = 0.22378, p = 0.00257), and academic competence (R2 = 0.6823, Slope = 0.24825, p = 0.00093) in the treatment phase, suggesting a steady increase in these factors. The overall findings indicated that further parametric data analyses (e.g., ANOVAs) would not be appropriate because of the significant trends in various factors.
RCDC. The autocorrelation indications, regression trends, and additional complexity of outlier scores indicated that the RCDC (Borckardt, 2008), a robust non-parametric method, should be used rather than the Conservative Dual-Criteria method (Fisher, Kelley, & Lomas, 2003; Swoboda, Kratochwill, & Levin, 2010) and parametric methods such as student’s t-test and ANOVA. The RCDC significance threshold is based on the mean and regression lines and the number of comparisons in the comparison phase. Datum that fall above or below the desired zone, as determined by the mean and regression lines, are considered significant. The sign of the slope determines the direction of the difference. For Rose, there were significant increases in the academic competence scores in the treatment phase. Enhancing her academic competence was one of the customized goals set at the beginning of the treatment phase. For Janelle, college knowledge and academic competence scores improved significantly in the treatment phase. These were the two customized goal categories for Janelle. For Kara, positive personal characteristics and academic competence scores improved significantly. Enhancing academic competence was one of the customizing goals set for Kara.
Visual Analyses
The graphic data are presented in Figure 1. The baseline, treatment, and withdrawal phase CCRSI factor scores for each participant are presented visually. The visual analysis confirmed the findings of the RCDC analyses.
Effect Sizes
Cohen’s (1988) G-index effect size findings varied across the three participants, indicating that the interventions had differential treatment effects. For Rose, there was a large effect size (1.00) for academic competence from baseline to end of treatment, with a medium negative effect size from end of treatment to end of withdrawal (-0.5). In her case, the treatment effect appears to have decreased somewhat after the intervention was withdrawn.
Janelle experienced large treatment effect sizes on college knowledge (0.75), positive personal characteristics (0.75), and academic competence (0.75) from the baseline to end of withdrawal, with a negative medium effect size for potential to achieve future goals (-0.5). All four effect sizes were medium (0.5) from end of treatment to end of withdrawal phases. The treatment effect appeared to have declined somewhat during withdrawal for the first three factors, while the effect for potential to achieve future goals appeared to have improved during withdrawal.
Kara’s data indicated effects on three CCRSI factors from baseline to end of treatment: college knowledge (0.25; small), positive personal characteristics (0.5; medium), and academic competence (0.5; medium). All of the effect sizes were negative (-0.5) at the end of the withdrawal phase. Her findings indicated treatment effects across all four CCRSI factors during the intervention with a clear drop off after withdrawal of the intervention.
Social Validity
As stated above, client satisfaction was assessed as an indicator of social validity (Hott et al. 2015). The ATT (Baker, 1983) scores for all three participants were quite high, with Rose scoring 97, Janelle 89, and Kara 89 on a scale ranging from 14 to 98. These findings were assumed to represent evidence of social validity for the study.
Unforeseen Changes in Participants
The counselor-investigator’s field notes provided important information that helped to explain unclear or puzzling visual findings, especially for Janelle. Her scores across all four self-efficacy factors were either quite high or increasing from the beginning of the intervention to the fifth session, and then the scores dropped dramatically over the next three sessions only to dramatically rise to very high levels at the end of the treatment phase. Observing the graphic visual representation of her data was indeed puzzling and would have remained puzzling without the field notes data. Fortunately, the counselor-investigator had recorded Janelle’s sharing of a significant current personal problem that caused concern about the impact of the issue on her future beyond high school. The circumstances led to Janelle’s being in a negative mood that the counselor-investigator was eventually able to help her address in addition to continuing the customized treatment protocol.
Rose informed the counselor-investigator that she lacked privacy in her foster home, and arrangements were made to meet with her for the treatment sessions in a community setting. She eventually decided to join an independent living program and was excited about being on her own with limited assistance.
Summary of the Results
The data indicated that positive trends occurred for each participant. Although the trends were positive, different CCRSI factor-specific outcome data patterns occurred for each participant. The effect sizes ranged from small to large across the participants and factors. There was evidence of statistical effects for each participant; however, the effect-size patterns differed across the three participants.
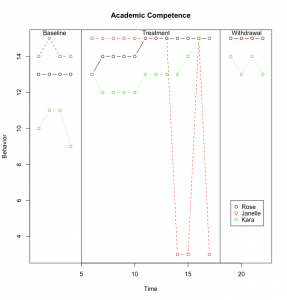
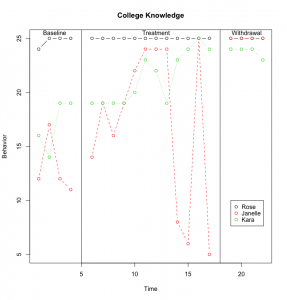
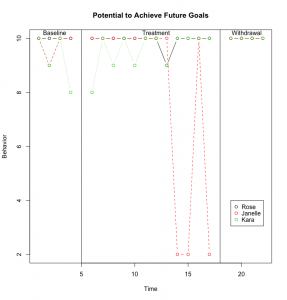
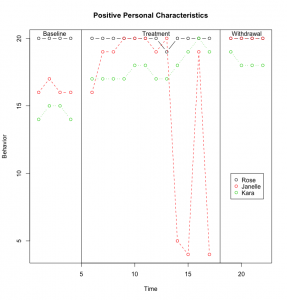
Figure 1. Baseline, Treatment, and Withdrawal Phase CCRSI Data for Each Participant
Discussion
The social validity data was analytically useful in determining that the participants believed they received something of value from their respective customized interventions. The CCRSI data were supportive of each participant, providing some evidence of enhanced career and college readiness self-efficacy during the intervention. The baseline data over 2 weeks for the three foster care participants indicated neither a decline nor an improvement during that phase, leading to an inference that, where there were significant positive changes during the treatment phase, the intervention likely caused them (Ray, 2015). The theory-based framework for the interventions provided an important structure for the counselor when attempting to design customized interventions for each participant. Given the differences in pre-treatment demographic characteristics across the three participants and the differences in CCRSI data for each of them, customizing the interventions seemed to be an appropriate strategy, and the two research strategies seemed to complement each other. Customized treatment interventions allow counselors to focus on specific goals for individual clients. Likewise, a theory-based framework provides a common client treatment process for a broad range of customized interventions. Additional important ingredients are independent and dependent variables that can be clearly defined, translated into intervention strategies, and measured objectively over time.
Although sharing a status—being in foster care—the three participants were not mirror images of each other. Rose was a high school senior with a relatively low GPA who had identified a postsecondary gateway to a community college. Her baseline scores were high on all four CCRSI factors. They remained high throughout the intervention with a statistically significant enhancement on the academic competence self-efficacy factor. The effect size for that factor was large, and her ATT score was categorized as very high.
Janelle was younger than the other participants, had a relatively high GPA, and wanted to attend a four-year college. She had negative treatment trends on all of the factors except college knowledge during the treatment phase, yet an upward trend became statistically significant at the end of the withdrawal phase for the positive personal characteristics and academic competence factors as well. A dramatic drop in her scores near the end of the treatment phase accounted for the negative trend. Significant personal challenges, documented by the counselor’s notes, were problematic for Janelle during treatment. The counselor was able to successfully address Janelle’s concerns and her CCRSI data improved. Her ATT score was high as well. Her lower scores on the college knowledge factor seemed indicative of being a 15-year-old high school student. The less effective impact on the potential to achieve future goals factor may have reflected the ongoing sexual orientation challenge she was experiencing.
Kara was a senior in a comprehensive high school with a strong GPA who wanted to attend college. Her baseline data across the four CCRSI factors was low enough to provide room for a positive trend during the treatment phase, and statistically significant trends occurred on the positive personal characteristics and academic competence factors during the treatment phase. Those effect sizes were medium. There also was a small effect size for the college knowledge factor. The findings indicated that the effects of the treatment dropped off somewhat during the withdrawal phase for Kara. Her ATT score was high.
Having at least three participants in an SCRD study is a recommended criterion (Lenz, 2015; Ray, 2015). This criterion is viewed as a safeguard against attrition and allows for inclusion of diverse participant characteristics. Having multiple participants enhances the opportunity to better understand the phenomenon being studied and supports attempted generalizations. Common findings across the three participants were as follows: (a) all three foster care participants experienced significant positive trends on at least one CCRSI factor in spite of relatively high baseline scores; (b) all participants rated the value of their respective customized interventions highly; (c) field notes were important for counselors when engaged in SCRD interventions; (d) the participants’ demographic differences demonstrated at the beginning of the present study supported the customized intervention idea; and
(e) combining inferential statistical and visual analyses of the data provided important information when the visual data alone were unclear.
Limitations
Although the treatments were customized, the duration of the baseline, treatment, and withdrawal phases were similar for all participants. Consequently, because the three treatment interventions had to be the same length of time within the A-B-A single-case design, the counselor was unable to customize the duration of the interventions. Each foster care participant may have benefitted from being able to engage in the treatment phase as long as needed. Unfortunately, the scheduling circumstances did not allow for this option. Scheduling challenges also forced restricted time frames for the baseline and withdrawal phases. The data collection process required participants to follow a prescribed self-monitoring schedule. They did not consistently conform to it, especially during the baseline and withdrawal phases. This inconsistency caused the counselor to issue reminders more often than desired and led to some inconsistencies in data collection protocols. The varied settings in which the interventions occurred may have caused a reactive effect. Regarding the generally high baseline scores, the participants may have been influenced by a halo effect at the outset. The gender and ethnicity of the participants, two African American females and one Caucasian/African American female, caused the sample to be somewhat homogeneous. During the repeated collections of the CCRSI data, the items were presented in the same order. Consequently, the internal validity of the study may have been enhanced if the items were presented randomly each time.
The study was conducted in the field setting rather than in a laboratory. Although field settings are more realistic than laboratory research, it is more difficult to control events that may reduce the internal validity of a study (Heppner, Wampold, Owen, Thompson, & Wang, 2016). Therefore, the limitations cited above are not unusual for experimental field studies.
Recommendations for Future Research
The recommendations focus on further research using the SCRD model. Two SCRD experimental research thrusts are presented herein. One focuses on serving foster care youth, and the other focuses on understanding and enhancing career and college readiness self-efficacy for diverse populations.
Assuming that the usefulness of a customized approach with a common framework similar to the S.T.A.R.S. model has been established in this study, additional independent variables that have potential for enhancing the postsecondary education readiness of foster care youth can be developed. Self-efficacy represents an attitude or belief variable, and other interventions can be developed to address either additional attitudinal variables (e.g., aspirations) or knowledge and behavior variables that are important for successful access to postsecondary education.
Given that the customized intervention approach with the independent and dependent variables derived from the career and college readiness self-efficacy construct proved useful for a sample of foster care adolescents, applying the same approach to more diverse populations is recommended. All K–12 students can benefit from interventions designed to enhance their career and college readiness self-efficacy. Can this be accomplished across other populations?
Efforts to pursue research related to both foci presented above can benefit from more sophisticated SCRDs and more temporally flexible experimental interventions. More sophisticated designs can enhance the internal validity of SCRD studies. For example, multiple baseline designs (e.g., A-B-A-B) provide for multiple relevant outcomes and increased data points (e.g., A-B-A-B-A-B), and allow researchers to replicate the intervention effects within one study (Lenz, 2015). Also, a combination of statistical and visual data analyses will enhance the probability of finding trends when they are difficult to see visually.
Recommendations for Practice
Recommendations for serving foster care youth herein might be generalizable to some extent for serving all youth. The individual student planning component of the ASCA National Model (2012) will be a useful framework for customizing interventions, providing ongoing activities that will help students with goal setting and planning for the future, and developing learning and graduation plans. Furthermore, school counselors can use appraisal and advisement strategies to enhance career and college readiness by helping students to evaluate their own interests, skills, and abilities in order to make informed decisions about their future (ASCA, 2012).
School counselors are encouraged to create support and educational programming for students in foster care. Because multiple foster care placement switches may serve as an impediment to high school completion and, overall, cause a disruption to educational progression, school counselors are challenged to organize career and college readiness programming that will permit foster care youth to receive a satisfactory amount of information regardless of when they arrive at their schools. School counselors may also engage in and coordinate legislative or policy-level advocacy efforts by organizing social and political advocacy endeavors, such as a legislative day, that tackle the educational needs of foster care youth and assemble individuals to get involved in these efforts. Counselors in the schools can accomplish this goal through participation in either state- or national-level counseling-specific organizations.
Community and school counselors can collaborate with stakeholders to familiarize foster care youth with programs that will aid them with their transition into institutions of postsecondary education. They can acquaint themselves with programs geared toward providing postsecondary education services to both current and former foster care youth who are in college. College counselors can create support groups for adolescents aging out of foster care that address and normalize the transition challenges they face, provide academic and personal support services and resources, and help incoming students build community in their new environment.
Furthermore, counselor educators can inform their students about the career and college readiness self-efficacy construct and how multiple barriers impact the postsecondary education aspirations of all students. In so doing, they also can include career and college readiness enhancement strategies for working with underserved student populations within their course curriculums. Counselors in school, community, and college settings can contribute to enhancing the postsecondary education access of foster care youth specifically, and all youth generally. In so doing, counselors often find themselves providing individualized student planning or counseling services. Within the broad context of career and college readiness, individual student clients, including foster care youth, present varied access circumstances that challenge counselors to customize their responsive services in order to address situation-specific needs.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest or funding contributions for the development of this manuscript.
References
Achieve, Inc. (n.d.). College and career readiness. Washington, DC: Author. Retrieved from https://www.achieve.org/college-and-career-readiness
Administration for Children and Families. (2013). The AFCARS report. Retrieved from https://www.acf.hhs.gov/sites/default/files/cb/afcarsreport21.pdf
American School Counselor Association. (2012). ASCA national model: A framework for school counseling programs (3rd ed.). Alexandria, VA: Author.
Baker, S. B. (1983). Attitude Toward Treatment. Unpublished scale. Raleigh, NC: Counselor Education Program, North Carolina State University.
Baker, S. B., & Parikh Foxx, S. (2012). Career College Readiness Self-Efficacy Inventory. Raleigh, NC: North Carolina State University.
Baker, S. B., Parikh Foxx, S., Akcan-Aydin, P., Gavin Williams, R., Ashraf, A., & Martinez, R. R. (2017). Psychometric properties of the Career and College Readiness Self-Efficacy Inventory. In Ideas and research you can use: VISTAS 2017. Retrieved from https://www.counseling.org/docs/default-source/vistas/article_3166ce2bf16116603abcacff0000bee5e7.pdf?sfvrsn=f8d84b2c_4
Bandura, A. (1997). Self-efficacy: The exercise of control. New York, NY: Freeman.
Bloom, M., Fischer, J., & Orme, J. G. (2006). Evaluating practice: Guidelines for the accountable professional (5th ed.). Needham Heights, MA: Allyn & Bacon.
Borckardt, J. J. (2008). User’s guide: Simulation modeling analysis: Time series analysis program for short time series data streams: Version 8.3.3. Retrieved from http://www.clinicalresearcher.org/SMA_Guide.pdf
Bragg, D. D., Kim, E., & Barnett, E. A. (2006). Creating access and success: Academic pathways reaching underserved students. New Directions for Community Colleges, 135, 5–19.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillside, NJ: Lawrence Erlbaum Associates, Inc.
College Board. (2006). College Ed: Creating a college-going culture guide. Retrieved from http://www.collegeboard.com/prod_downloads/collegeed/collegeEd-create-college-going-culture.pdf
Conley, D. T. (2010). College and career ready: Helping all students succeed beyond high school. San Francisco, CA: Jossey-Bass.
Engel, R. J., & Schutt, R. K. (2013). The practice of research in social work (3rd ed). Thousand Oaks, CA: Sage.
Fisher, W. W., Kelley, M. E., & Lomas, J. E. (2003). Visual aids and structured criteria for improving visual inspection ad interpretation of single-case design. Journal of Applied Behavior Analysis, 36, 387–406. doi:10.1901/jaba.2003.36-387
Geroski, A. M., & Knauss, L. (2000). Addressing the needs of foster children within a school counseling program. Professional School Counseling, 3(3), 152–161.
Heppner, P. P., Wampold, B. E., Owen, J., Thompson, M. N., & Wang, K. T. (2016). Research design in counseling (4th ed.). Boston, MA: Cengage Learning.
Hinkle, J. S. (1992). Computer-assisted career guidance and single-subject research: A scientist-practitioner approach to accountability. Journal of Counseling & Development, 70, 391–395. doi:10.1002/j.1556-6676.1992.tb01622.x
Hott, B. L., Limberg, D., Ohrt, J. H., & Schmit, M. K. (2015). Reporting results of single-case studies. Journal of Counseling & Development, 93, 412–417. doi:10.1002/jcad.12039
Hudson, A. L. (2013). Career mentoring needs of youths in foster care: Voices for change. Journal of Child and Adolescent Psychiatric Nursing, 26, 131–137. doi:10.1111/jcap.12032
Kaplan, S. J., Skolnik, L., & Turnbull, A. (2009). Enhancing the empowerment of youth in foster care: Supportive services. Child Welfare, 88, 133–161.
Kirk, C. M., Lewis, R. K., Nilsen, C., & Colvin, D. Q. (2013). Foster care and college: The educational aspirations and expectations of youth in the foster care system. Youth & Society, 45, 307–323. doi:10.1177/0044118X11417734
Kirk, R., & Day, A. (2011). Increasing college access for youth aging out of foster care: Evaluation of a summer camp program for foster youth transitioning from high school to college. Children and Youth Services Review, 33, 1173–1180. doi:10.1016/j.childyouth.2011.02.018
Lemon, K., Hines, A. M., & Merdinger, J. (2005). From foster care to young adulthood: The role of independent living programs in supporting successful transitions. Children and Youth Services Review, 27, 251–270. doi:10.1016/j.childyouth.2004.09.005
Lent, R. W., Brown, S. D., & Hackett, G. (1994). Toward a unifying social cognitive theory of career and academic interest, choice, and performance [Monograph]. Journal of Vocational Behavior, 45, 79–122. doi:10.1006/jvbe.1994.1027
Lenz, A. S. (2015). Using single-case research designs to demonstrate evidence for counseling practices. Journal of Counseling & Development, 93, 387–393. doi:10.1002/jcad.12036
Martin-Causey, T., & Hinkle, J. S. (1995). Multimodal therapy with an aggressive preadolescent: A demonstration of effectiveness and accountability. Journal of Counseling & Development, 73, 306–310. doi:10.1002/j.1556-6676.1995.tb01753.x
Martinez, R. R., Baker, S. B., & Young, T. (2017). Promoting career and college readiness, aspirations, and self-efficacy: Curriculum field test. The Career Development Quarterly, 65(2), 173–188. doi:10.1002/cdq.12090
Pecora, P. J., Kessler, R. C., O’Brien, K., White, C. R., Williams, J., Hiripi, E., . . . Herrick, M. A. (2006). Educational and employment outcomes of adults formerly placed in foster care: Results from the Northwest Foster Care Alumni Study. Children and Youth Services Review, 28, 1459–1481.
doi:10.1016/j.childyouth.2006.04.003
Pecora, P. J., Williams, J., Kessler, R. C., Hiripi, E., O’Brien, K., Emerson, J., . . . Torres, D. (2006). Assessing the educational achievements of adults who were formerly placed in family foster care. Child & Family Social Work, 11, 220–231. doi:10.1111/j.1365-2206.2006.00429.x
Peterson, G. W., Sampson, J. P., Jr., Lenz, J. G., & Reardon, R. C. (2002). A cognitive information processing approach to career problem solving and decision making. In D. Brown and Associates (Eds.), Career choice and development (pp. 312–369). San Francisco, CA: Jossey-Bass.
Ray, D. C. (2015). Single-case research design and analysis: Counseling applications. Journal of Counseling & Development, 93, 394–402. doi:10.1002/jcad.12037
Savickas, M. L. (2011). Career counseling. Washington, DC: American Psychological Association.
Super, D. E. (1990). A life-span, life space approach to career development. In D. Brown & L. Brooks (Eds.), Career choice and development: Applying contemporary theories to practice (2nd ed., pp. 197–261). San Francisco, CA: Jossey-Bass.
Swoboda, C. M., Kratochwill, T. R., & Levin, J. R. (2010). Conservative dual-criterion method for single-case research: A guide for visual analysis of AB, ABAB, and multiple-baseline designs. Wisconsin Center for Education Research Working Paper No.13, 495–512.
Unrau, Y. A., Font, S. A., & Rawls, G. (2012). Readiness for college engagement among students who have aged out of foster care. Children and Youth Services Review, 34, 76–83. doi:10.1016/j.childyouth.2011.09.002
Vannest, K. J., & Ninci, J. (2015). Evaluating intervention effects in single-case research designs. Journal of Counseling & Development, 93, 403–411. doi:10.1002/jcad.12038
Wolf, M. M. (1978). Social validity: The case for subjective measurement or how applied behavioral analysis is finding its heart. Journal of Applied Behavioral Analysis, 11, 203–214. doi:10.1901/jaba.1978.11-203
Regina Gavin Williams, NCC, is the Director of Student Engagement and Diversity Coordinator at North Carolina State University. Stanley B. Baker, NCC, is a professor at North Carolina State University. ClarLynda R. Williams-DeVane is an associate professor at North Carolina Central University. Correspondence can be addressed to Regina Gavin Williams, 2310 Stinson Dr., CB 7801, North Carolina State University, Raleigh, NC 27695-7801, rjgavin@ncsu.edu.