Mar 3, 2015 | Article, Volume 5 - Issue 2
Emily Goodman-Scott, Simone F. Lambert
Sensory processing disorder is a complex neurological disorder affecting approximately 5–17% of the population, yet professional counselors often misunderstand and misdiagnose this disorder. A child’s academic, emotional and social functioning can be substantially impacted by sensory processing disorder; early diagnosis and treatment is crucial. In this article, the authors describe the disorder, discuss its impact on children and their families, and provide recommendations and resources for both mental health counselors and school counselors to utilize when serving this unique population with special needs. A case study is included, in addition to suggestions for treatment collaboration and advocacy on behalf of clients with sensory processing disorder.
Keywords: Sensory processing disorder, special needs, children, school counselors, mental health counselors
Children experience the world through their senses—the sound of the air conditioner running in their classroom, the feel of a chair under their legs, the sight of a colorful wall, the smell of food cooking, the muscle movement used to pick up a toy. The typical child can accurately perceive, process and respond to the myriad stimuli in their environment, focusing on important stimuli, such as a parent’s voice, and filtering out unimportant ones, such as a humming refrigerator. For other children, the same environment and accompanying stimuli can be uncomfortable, overwhelming, unnoticeable and even frightening. Researchers estimate that approximately 5–17% of the population has sensory processing disorder (SPD), a neurological disorder in which sensory input is irregularly sensed, processed, organized, and responded to, creating sensory challenges that negatively impact daily functioning (Ahn, Miller, Milberger, & McIntosh, 2004; Ben-Sasson, Carter, & Briggs-Gowan, 2009). As a result of poor sensory processing, individuals with SPD may overreact or underreact to stimuli (Byrne, 2009; Dunn, 1997, 2001; James, Miller, Schaaf, Nielsen, & Schoen, 2011; Katz, 2006; Miller, Anzalone, Lane, Cermak, & Osten 2007; Walbam, 2013; Withrow, 2007). SPD is a lifelong disorder; while typically developing children gain the ability to increasingly suppress stimuli with age, children with SPD tend to struggle throughout their lifetime (Davies & Gavin, 2007), particularly if SPD is unidentified, misdiagnosed or inaccurately treated.
Professional counselors are called to accurately diagnose and treat clients’ mental health and co-occurring disorders (American Counseling Association [ACA], 2014). However, SPD is widely unrecognized and misdiagnosed in the counseling field (Collier & Falls, 2010; Katz, 2006; Murphy, 2011; Withrow, 2007). With increasing research supporting the legitimacy of the SPD diagnosis (e.g., Chang et al., 2014; Davies & Gavin, 2007; Owen et al., 2013), counselors can be on the forefront of screening and providing counseling services to children with SPD. This article will provide readers with background information on SPD, implications for clinical mental health and school counseling practice, a case study example, and recommendations for future professional education, advocacy and research. In the literature, SPD has been referred to by similar terms such as sensory integration disorder or categorized by subtype (e.g., sensory modulation disorder). However, the term sensory processing disorder (SPD) will be utilized in this article, since SPD is the most prevalent term used in recent years (Miller, Nielsen, Schoen, & Brett-Green, 2009). Similarly, we will use the term sensory processing to also encompass sensory integration, as they are often used interchangeably in the literature.
Background
The most commonly known senses are auditory (sound), olfactory (smell), tactile (touch), visual (sight) and gustatory (taste); two less known senses are proprioception and the vestibular sense (James et al., 2011; Katz, 2006; Withrow, 2007). Proprioception is a sense found in muscles, tendons and joints that deciphers bodily awareness and coordinated movements. The vestibular sense is located in the inner ear and provides sensory input regarding one’s balance and gravity. Sensory processing is a complex neurobiological process in which individuals’ seven senses perceive information or stimuli from the environment, sending data to the brain to interpret, process and respond to; the senses and brain are constantly engaged in a process of perceiving, interpreting, processing, and responding to environmental stimuli (Byrne, 2009; Katz, 2006; Miller et al., 2009; Parham & Mailloux, 2015; Walbam, 2013; Withrow, 2007). Sensory processing is a developmental process, and thus especially crucial in the children’s first 10 years of life (Ayres, 1979). In summary, a typically developing child may easily and accurately perceive and process environmental stimuli, yet this is not the case for all children.
Sensory processing has been well studied in the occupational therapy profession during the last 50 years, beginning with the groundbreaking work of Dr. A. Jean Ayres, occupational therapist, psychologist and neuroscientist (Parham & Mailloux, 2015). During the last several decades Ayres and others discovered patterns of atypical sensory processing in children, which have collectively come to be labeled as SPD. “Sensory processing disorder is a heterogeneous condition that includes a variety of subtypes. Individuals with the disorder have impaired responses to, processing of, and/or organization of sensory information that effects [sic] participation in functional daily life routines and activities” (Miller et al., 2009, p. 1). Further, Parham and Mailloux (2015) described SPD as “patterns that emerge developmentally . . . and are thought to reflect subtle neural processing differences involving sensory and motor systems” (p. 266). Thus, children with SPD struggle with the neurobiological cycle of receiving, sending, processing and responding to stimuli, and they experience a severity that negatively impacts their daily functioning (Ayres, 1979; Davies & Gavin, 2007; Owen et al., 2013; Parham & Mailloux, 2015). As a result of skewed sensory processing, individuals with SPD may overreact or underreact to stimuli, perceiving stimuli to much greater or lesser degrees than peers (Byrne, 2009; Dunn, 1997, 2001; James et al., 2011; Katz, 2006; Miller et al., 2007; Walbam, 2013; Withrow, 2007). For example, a crowded indoor playground could be loud to one child, but frightening or even physically painful for a child with auditory sensitivities. While a typical child may get dizzy from spinning around, a child with an underdeveloped vestibular system may rarely become dizzy and seek spinning to feel soothed.
Although children with SPD may have neurological similarities, SPD is a highly individualistic disorder that presents differently in each child and can be described by corresponding subtypes (Dunn, 1997, 2001; James et al., 2011; Murphy, 2011; Walbam, 2013; Withrow, 2007). While there is consensus on an overarching definition for SPD, there is not a consistent nosology for describing the subtypes (Miller et al., 2009). Proposed nosologies of SPD subtypes typically include hyposensitivity, hypersensitivity and sensory-seeking subtypes (Ayres, 1979; Dunn, 1997, 2001; Interdisciplinary Council on Developmental and Learning Disorders, 2012; James et al., 2011; Katz, 2006; Miller et al., 2007; Walbam, 2013; Zero to Three, National Center for Infants, Toddlers and Families, 2005).
Subtypes
Those with hyposensitivities, one subtype of SPD, often have a high threshold for sensation, are under-sensitive, and receive or process too few stimuli (Dunn, 1997, 2001; James et al., 2011; Katz, 2006; Walbam, 2013; Withrow, 2007). A child with hyposensitivities may seem to have poor social skills and miss social cues; some behavioral examples include not hearing a teacher calling his or her name, being unaware of food on the face, or lacking culturally appropriate personal space. Social skill deficits can negatively impact children’s friendships and group participation in both academic and social environments (Dunn, 1997; Kranowitz, 2005; Withrow, 2007).
Children with hypersensitivities, a second subtype of SPD, have a low threshold for sensation and may receive an overwhelming amount of stimuli, be unable to prioritize their sensory messages and be easily overstimulated (Dunn, 1997, 2001; James et al., 2011; Katz, 2006; Walbam, 2013; Withrow, 2007). As a coping technique against stimuli perceived as uncomfortable and even painful, children with hypersensitivies may have heightened alertness, act aggressively toward others in response to perceived threats, and engage in behavioral outbursts and rigid routines in attempts to avoid or escape stimuli (Dunn, 1997; Withrow, 2007). These children may be described as generally anxious, aggressive, distracted or unfocused, or as picky eaters.
Lastly, some children with a third subtype of SPD crave and actively seek sensory input and increased stimuli (Dunn, 1997, 2001). These children may seek constant movement to receive sensations from their environment, and exhibit behaviors including running, jumping, chewing, tapping, humming and squeezing (Dunn, 1997, 2001). Individuals with sensory-seeking behaviors may appear impulsive, unpredictable, and have inappropriate personal space which may negatively impact academics and social relationships. Children who seek sensations may be described as rambunctious, aggressive, or bouncing off the walls (sometimes literally). They may seek spicy foods and not be bothered by intense flavors.
Sensitivities and sensation seeking occur on a spectrum from mild to severe (James et al., 2011). Furthermore, these variations can present differently in each of the seven senses (Dunn, 1997, 2001), and children can even experience both hypersensitivities and hyposensitivities within the same sense (Withrow, 2007). This circumstance may baffle parents, who question how a child can watch a movie at a loud volume at home, yet be unable to tolerate the noise of a crowded restaurant. Children and the adults around them may need assistance recognizing children’s placement on the hyposensitivity, hypersensitivity and sensory-seeking spectrums before, during and after an event which can facilitate children successfully coping and thriving in various settings.
Prevalence
Researchers have estimated that SPD occurs in approximately 5–17% of children (Ahn et al., 2004; Ben-Sasson et al., 2009). In one study examining the prevalence of SPD in children 4–6 years old, the parents of incoming kindergarten students in one U.S. school district (N = 1,796) were asked to complete the Short Sensory Profile, a parental-report screening tool used to determine parents’ perceptions of SPD correlates (Ahn et al., 2004). Approximately 14% of those who completed the survey (with a 39% return rate) met the criteria for SPD. However, researchers conservatively estimated that if all non-responders were free from meeting the SPD criteria, then approximately 5% of this population would meet the screening criteria for SPD. Thus, the number of incoming kindergarten students who met the criteria for SPD based on parental perceptions ranged from 5–14%. Similarly, Ben-Sasson et al. (2009) used a longitudinal birth cohort sample of children to study sensory over-responsivity (SOR) and related correlates. They found that nearly 17% of the 7–11 year olds in their study (N = 925) had clinically significant elevated SOR scores. However, these researchers believe the number to be a conservative estimate of the population, as children with diagnosed medical and developmental conditions were excluded from the study.
Secondary Symptoms
All areas of a child’s life can be impacted by SPD (Walbam, 2013; Withrow, 2007). In addition to children presenting primary symptoms of the disorder, they often face a host of secondary emotional and behavioral difficulties as a result of the disorder, such as frustration, loneliness, low self-esteem, a greater risk for strained peer relationships, discouragement, and social, emotional and academic challenges (Champagne & Koomar, 2012; Katz, 2006; Miller, Nielsen, & Schoen, 2012; Walbam, 2013; Withrow, 2007). Also, those with SPD tend to be more likely to struggle with depression and anxiety than their typically developing peers (Miller et al., 2012) and may need assistance with self-regulation (Katz, 2006). These secondary symptoms may result from attempted self-regulation due to negatively perceived sensory stimuli as well as feelings of isolation and being misunderstood due to undiagnosed, untreated and mistaken symptoms (Miller et al., 2012; Withrow, 2007). In this article, we describe the experiences of children with SPD as comparable to those of children with special needs including disabilities and chronic illnesses.
Diagnosis and Treatment
Early SPD diagnosis and treatment is crucial in assisting children with both primary and secondary SPD symptoms (Ben-Sasson et al., 2009; Byrne, 2009; Miller, 2006). SPD diagnosis and treatment early in life is highly impactful on a child’s developing brain and behavioral symptoms (Ben-Sasson, et al., 2009; Miller, 2006). While occupational therapists (OTs) are charged with diagnosing and treating the primary symptoms and underlying conditions associated with SPD, counselors need to be aware of SPD in order to appropriately screen for, avoid misdiagnosing, make appropriate referrals for, and treat the secondary symptoms related to SPD.
Occupational therapy. Typically, OTs evaluate for and treat SPD (Castaneda, Olson, & Radley, 2013; Champagne & Koomar, 2012; Katz, 2006; Parham & Mailloux, 2015; Walbam, 2013). Children are often referred to OTs by parents, teachers and physicians (Parham & Mailloux, 2015); however, before making an OT referral, physicians need to rule out medical conditions and medication side effects. OTs assist people with daily living and occupational skills, and they are trained in mental and physical disorders (Castaneda et al., 2013). Since school is “work” for children, OTs help children with SPD to function more effectively in their academic work and social living skills. OTs can be school-based or work in community or hospital settings (Castaneda et al., 2013).
OTs use several strategies to assess for SPD, including interviews and questionnaires, direct observations (e.g., naturalistic and structured clinical) and standardized testing (Parham & Mailloux, 2015). SPD diagnoses often begin with the use of a screening tool to determine the existence of symptoms signifying possible sensory irregularities. The Sensory Profile 2 (Dunn, 2014) is a standardized, parental-report tool for evaluating children’s sensory processing patterns in various environments and requires a B-level qualification to administer (Dunn, 2014). The Sensory Integration and Praxis Tests (SIPT) is a popular, recommended and standardized comprehensive test for measuring sensory integration and requires a C-level qualification to administer (Ayres, 1989). The SIPT was normed on approximately 2,000 children in North America and is considered a valid and reliable assessment.
The sensory integration approach to occupational therapy is commonly used to treat SPD; the overarching goal of this intervention is to enable a child’s nervous system to more efficiently process and respond to sensory information (Parham & Mailloux, 2015). Occupational therapy is highly specialized based on the child’s unique needs and diagnosis. Further, occupational therapy also may include the use of a sensory diet—an individualized program for children with sensory challenges including a specific combination of sensory activities throughout the day (Parham & Mailloux, 2015). A sensory diet provides a wide range of sensory input; for example, activities may evoke the senses through music, new smells, visual stimulus, as well as “movement, heavy work, or tactile stimulation” (Hall & Case-Smith, 2007, p. 212).
Clinical diagnosis. The occupational therapy profession has treated SPD for decades. Furthermore, the SPD Scientific Work Group, including approximately 40 interdisciplinary research scientists from various specialties (e.g., neurology, pediatrics, occupational therapy, psychiatry, autism, psychology) has regularly met since 2002 with the aim of studying SPD; members’ efforts have been funded through both the Wallace Research Foundation and National Institutes of Health (SPD Foundation, 2014). However, much controversy has existed regarding SPD as an independent disorder, particularly in the psychiatry and psychology professions, whose members have raised the following criticisms: “(1) an absence of formal diagnostic criteria, (2) high prevalence among children with developmental disorders such as autism spectrum disorders . . . (3) unknown etiology, and (4) lack of epidemiological evidence related to this condition” (Ben-Sasson et al., 2009, p. 706). These criticisms will be addressed in the subsequent paragraphs.
Diagnostic criteria. Sensory disorders are found both in the Diagnostic Manual for Infancy and Early Childhood (Interdisciplinary Council on Developmental and Learning Disorders, 2012) and the Zero to Three’s Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood-Revised (Zero to Three, 2005). For example, the Zero to Three was created by an interdisciplinary group of researchers and clinicians to complement the American Psychiatric Association’s (APA) Diagnostic and Statistical Manual of Mental Disorders (DSM) with a specific focus on the unique development of and disorders found among infants and young children. This nosology includes two sensory-related disorders: Hyposensitive/Underresponsive (420) and Sensory Stimulation-Seeking/Impulsive (430), describing the sensory reactivity patterns, motor patterns and behavioral patterns of each disorder (Zero to Three, 2005).
The APA reviewed SPD for consideration in the DSM-5 (Levingston, 2014; Murphy, 2011) and groups such as the SPD Scientific Work Group lobbied for its inclusion (SPD, 2012, 2014). The full diagnosis of SPD was not included in DSM-5 reportedly due to lack of research (Levingston, 2014). However, the new Avoidant/Restrictive Food Intake Disorder does recognize that sensory aspects of food can cause a significant food disturbance (e.g., texture, smell, spiciness; APA, 2013). Further, in the DSM-5 the APA recognized sensory issues as a part of autism spectrum disorder (ASD), including: “hyper- or hyporeactivity to sensory input or unusual interest in sensory aspects of the environment” (APA, 2013, p. 50). While the DSM-5 does not recognize SPD as an individual disorder, we find it promising that SPD was considered for inclusion and that sensory issues were added to the most recent DSM. The DSM has evolved and will likely continue to evolve based on research advances (APA, 2013) and we are hopeful that SPD will be considered for inclusion in the next edition of the DSM, especially with recent research advances (e.g., Chang et al., 2014; Owen et al., 2013).
In addition to the DSM, the 10th revision of the International Statistical Classification of Diseases (ICD-10; World Health Organization, 2013) and the ICD-9 (Centers for Disease Control and Prevention, National Center for Health Statistics, 1991) are other commonly used nosologies. Although the ICD does not specifically identify sensory issues, OTs may use the following codes to diagnose clients: lack of normal physiological development, unspecified (783.40; ICD-9); other symptoms involving nervous and musculoskeletal systems (781.99; ICD-9), and unspecified lack of expected normal physiological development in childhood (R62.50; ICD-10; E. Smolak, personal communication, January 15, 2015). Thus, professionals can use ICD codes related to SPD.
SPD research. Researchers have determined distinct patterns among children with SPD varying from those among their typically developing peers. Specifically, when comparing children with clinically determined atypical sensory processing to their typically developing peers, researchers found that the former exhibited differences in their physiological responses to sensory stimuli (McIntosh, Miller, Shyu, & Hagerman, 1999), parasympathetic nervous system functioning (Schaaf et al., 2010; Schaaf, Miller, Seawell, & O’Keefe, 2003), and differences in both behavioral and physiological measures (Schoen, Miller, Brett-Green, & Nielsen, 2009). Additionally, Davies and Gavin (2007) and Gavin et al. (2011) found differences in brain activity between children with and without SPD using electroencephalography. In fact, “brain activity correctly distinguished children with SPD from children who were typically developing with 86% accuracy” (Davies & Gavin, 2007, p. 176). Finally, in a recent study (N = 40), Owen et al. (2013) found neurological differences in brain structure between children with and without SPD, specifically stating:
Children with SPD show specific reduction in the white matter microstructure primarily affecting posterior cerebral tracts. . . . These findings suggest that children with SPD have a specific imaging biomarker for their clinical disorder and the pattern of their shared structural difference. (p. 850)
Significant sensory abnormalities (e.g., SPD) can be comorbid with several childhood clinical disorders such as ASD, attention-deficit/hyperactivity disorder (ADHD), anxiety disorders, depression, Fragile X syndrome and obsessive-compulsive disorder (Ghanizadeh, 2011; Goldsmith, Van Hulle, Arneson, Schreiber, & Gernsbacher, 2006; Tomchek & Dunn, 2007; Van Hulle, Schmidt, & Goldsmith, 2011). At the same time, researchers are suggesting that SPD is a separate and distinct disorder. For example, when studying youth with ASD and SPD, Schoen et al. (2009) demonstrated differences in sympathetic nervous system functions and sensory-related behaviors between children in the two samples, while Chang et al. (2014) reported differing patterns of brain connectivity in adolescents with the two separate diagnoses. In addition, Miller et al. (2012) studied differences between youth with SPD, ADHD and the two dual diagnoses by using several parental-report instruments and measuring physiological reactions to sensory stimuli by electrodermal response. They found that participants with ADHD had greater inattention and participants with SPD had the most sensory issues, while those with both diagnoses experienced inattention and fewer sensory issues than those who only had SPD. Further, participants with SPD had greater physiological or electrodermal reactivity to sensory stimuli than participants with ADHD (Miller et al., 2012). Overall, differences seem to exist between participants with SPD and those with similar but varying clinical diagnoses (e.g., ADHD and ASD), suggesting SPD as an individual disorder.
Etiology. While the etiology of SPD is still largely unknown, several researchers believe that SPD may have a genetic basis (e.g., Goldsmith et al., 2006; Miller et al., 2009; Owen et al., 2013; Van Hulle et al., 2011). For example, Goldsmith et al. (2006) studied the tactile and auditory defensiveness, temperament, and behavior problems of toddler-aged twins as determined by parent reports. Researchers determined moderate genetic influences with tactile defensiveness, leading them to suggest more research investigating the heritability of SPD and sensory issues.
Overall, although SPD is controversial, there is substantial evidence for SPD as a distinct disorder in children. According to the APA (2013),
A mental disorder is a syndrome characterized by clinically significant disturbance in an individual’s cognition, emotion regulation, or behavior that reflects a dysfunction in the psychological, biological, or developmental processes underlying mental functioning. Mental disorders are usually associated with significant distress or disability in social, occupational, or other important activities. (p. 20)
Based on the literature review, we believe that SPD meets the APA’s criteria for a mental health disorder, due to an irregular neurological pattern of receiving, sending, processing and responding to stimuli, which results in impairment to an individual’s regular behavioral and emotional functioning.
Professional counseling. SPD has received some, albeit limited recognition in the counseling field (e.g., Collier & Falls, 2010; Katz, 2006; Withrow, 2007), including an article featured in Counseling Today (Murphy, 2011). However, SPD seems to be widely unrecognized in the counseling profession. Counselors may often misdiagnose this neurological condition due to clients’ highly individualized presentations, as well as SPD symptoms mirroring those of other disorders (Collier & Falls, 2010; Katz, 2006; Murphy, 2011; Walbam, 2013). SPD can present as ADHD through impulsive and inattentive behaviors; ASD through social deficits, rigidity and sensory symptoms; and depression and anxiety through withdrawn and lethargic behaviors. Well-known author and OT Carol Kranowitz wrote the following:
Many parents, educators, doctors, and mental health professionals have difficulty recognizing SPD. When they don’t recognize the problem, they may mistake a child’s behavior, low self-esteem, or reluctance to participate in ordinary childhood experiences for hyperactivity, learning disabilities, or emotional problems. Unless they are educated about SPD, few people understand that bewildering behavior may stem from a poorly functioning nervous system. (2005, p. xxiv)
SPD and sensory challenges are often unrecognized, misdiagnosed and considered solely behavioral, psychological or emotional issues (Parham & Mailloux, 2015).
An accurate diagnosis is imperative for client treatment and is included as follows in the 2014 ACA Code of Ethics, section E.5.a.: “Counselors take special care to provide proper diagnosis of mental disorders” (ACA, 2014, p. 11). Counselors are ethically required to thoughtfully consider mental diagnostic possibilities and to accurately diagnose clients. However, medical and mental disorders can be commonly misdiagnosed, especially when many disorders have similar symptoms and overlapping criteria (Pollak, Levy, & Breitholtz, 1999). Misdiagnoses may have long-term ramifications for individuals, including ineffective treatment and secondary concerns due to unmet needs, such as anxiety, depression, low self-esteem, and poor academic and social functioning (Katz, 2006; Kinnealey & Fuiek, 1999; Miller, 2006, Miller et al., 2012; Withrow, 2007). Lack of an accurate diagnosis also can lead to poor use of resources and harmful or even fatal client outcomes (Pollak et al., 1999). In order to uphold the ACA’s ethical standards for accurately diagnosing clients, as well as to meet clients’ needs, it is imperative that counselors are aware of SPD and work in tandem with other service providers when warranted in order to ensure that each client receives an accurate diagnosis and treatment.
Counselor Implications
All Professional Counselors
Given the prevalence of SPD, counselors are likely already working with clients who have SPD. Thus, counselors across settings need to be aware of SPD and related counseling implications. Since early intervention is preferred, counselors who work with children should be at the forefront for recognizing and addressing SPD in session. This section will focus on the following: awareness and education, screening and diagnosis, treatment team, treatment goals, counseling strategies, and counseling accommodations.
Awareness and education. First and foremost, counselors must possess knowledge of SPD as a neurological disorder and awareness of SPD characteristics in children. There is limited counseling-related SPD literature (e.g., Collier & Falls, 2010; Katz, 2006; Murphy, 2011; Withrow, 2007), and in our experiences as counselor educators and practitioners, we have seen very little SPD information in counseling textbooks or at counseling conferences. Thus, counselors may need to seek educational and training opportunities outside the counseling field in order to stay abreast of SPD.
Screening and diagnosis. Counselors can screen for SPD through the process of differential diagnosis to see if the symptoms (a) are part of a separate mental health diagnosis, (b) indicate SPD misdiagnosed as another disorder or (c) are co-occurring (Byrne, 2009). Screening and diagnosis are complicated due to SPD often co-occurring with other mental health disorders (Walbam, 2013). Additionally, context is critically important when counselors identify diagnostic criteria, as well as triggers and antecedents to emotional and behavioral responses. For example, a child who presents characteristics of ADHD (e.g., impulsiveness and hyperactivity) also should be considered for SPD, as this child could lack physical stimulation and seek sensory input to self-modulate. Dr. Roianne Ahn, a licensed psychologist, SPD researcher and staff member at the Sensory Therapies and Research Center provides training to mental health clinicians regarding recognizing SPD in clients. When clinicians suspect that a child has sensory abnormalities, Dr. Ahn encourages them to use a parental-report screening checklist (e.g., Appendix A: Sensory Processing Disorder Checklist or the Sensory Profile 2) to initially screen for SPD symptoms and then recommend a formal occupational therapy evaluation (R. Ahn, personal communication, November 7, 2014). With the high prevalence of SPD, professional counselors may want to consider including a screening checklist in initial client paperwork.
Treatment team. Counselors can consult and collaborate with stakeholders through the use of a treatment team (Katz, 2006; Murphy, 2011; Walbam, 2013). The purpose of the treatment team is to collaborate on the child’s needs and treatment across various settings, gaining the perspectives of diverse stakeholders. A treatment team can be comprised of the counselor (e.g., school counselor, mental health counselor), OT, parents or caregivers, and teachers. The treatment team may include the child’s pediatrician and potentially a nutritionist when appropriate. Counselors can play a vital role as part of a treatment team by coordinating the interdisciplinary team. Also, family involvement is crucial—parents or caretakers often know their child best, children are heavily impacted by their families, and parents or caretakers often advocate for their child on a long-term basis.
Through the collaborative treatment team, counselors can identify and advocate for resources for children with SPD and their families in order to improve their daily functioning (Walbam, 2013; Withrow, 2007). Treatment teams can discuss children’s needs, accommodations and resources, ensuring that stakeholders are working collaboratively to serve the child. For example, one function of the treatment team may be consultation to discuss the child’s sensory diet in multiple settings, such as chewing gum to remain attentive in class or receiving calming deep pressure before school in the morning (Parham & Mailloux, 2015).
Treatment goals. Counseling treatment goals can incorporate suggestions from the treatment team. For instance, counseling treatment goals may focus on children’s emotions, cognitions and behaviors pertaining to SPD (Kranowitz, 2005). Children with SPD may have a number of mental health concerns including anxiety, depression, low self-esteem, poor social skills and frustration (Champagne & Koomar, 2012; Katz, 2006; Miller et al., 2012; Walbam, 2013; Withrow, 2007). Similar to those with chronic illness (Cheu, 2013), children with SPD may have additional concerns including fear, grief, shame, anger or frustration. Furthermore, children may misunderstand SPD; thus, educating children and normalizing their experiences may be appropriate treatment goals (Withrow, 2007).
Other treatment goals can include the child adjusting to the diagnosis of SPD and identifying strategies for coping in social situations when SPD symptoms often occur (Murphy, 2011). For example, although home environments may be easily controlled to meet the child’s sensory needs, children with SPD may need to cope with uncontrolled environments, such as a crowded grocery store or an odorous and loud public restroom. Thus, counseling treatment may include systematic desensitization—children increasingly coping with uncomfortable stimuli through increased exposure. Counseling can assist with behavioral, social and emotional symptoms related to SPD (Kranowitz, 2005), in addition to other disorders that may co-occur including anxiety, depression, ASD, attention-deficit disorder and learning disorders (Ostovar, 2009). Further, one disorder can exasperate another (i.e., the child may have difficulty adjusting to a new environment if there is a change in sensory input, such as street noise by the child’s bedroom window).
Counseling strategies. Counselors can provide individual, group and family counseling modalities (Withrow, 2007) using solution-focused and cognitive-behavioral techniques to address children’s mental health needs and co-occurring disorders. For example, through individual counseling, children may increase their coping skills and self-esteem; through group counseling, children can improve their social skills. Further, counselors can assist clients to understand their disorder (Withrow, 2007), adjust to their limitations and capitalize on their strengths (Miller, 2006). Through the use of psychoeducation and bibliotherapy (see Appendix B), counselors can educate children about SPD, normalizing their experience. Further, by focusing on the child’s strengths, counselors can emphasize the positives of SPD. For example, children who seek sensory input from spinning may excel in gymnastics or ice skating, while those who need physical input may thrive in contact sports.
Some mental health issues, such as children’s anxiety, can be exacerbated by contextual factors like an unpredictable environment that may occur in everyday life situations as well as at special events (Ostovar, 2009). Taking a systems approach, counselors can work with family members and other service providers (e.g., teachers) to increase the predictability and children’s understanding of their environment (Withrow, 2007). Thus, counselors can assist in identifying sensory triggers and establishing accommodations, while simultaneously addressing secondary emotional and behavioral symptoms that occur in various settings and situations.
Counseling accommodations. In conjunction with the treatment team’s recommendations, counselors can make a number of small accommodations during their counseling sessions to support children with SPD as they engage in the counseling process (Withrow, 2007). First, counselors should be mindful of environmental stimuli in their offices, such as bright lights, highly decorated offices or intense smells, which may be distracting for a child with SPD. Counselors can keep smells to a minimum, for example, by not wearing perfume and asking office mates to refrain from using incense or scented candles. Next, varied seating options can increase children’s comfort, as their needs may vary from firm to soft cushions and from smooth to more textured upholstery.
Similar to OTs (Kranowitz, 2005), counselors working with young children typically have numerous toys and materials to use in therapy (Landreth, Ray, & Bratton, 2009). Counselors may find that covering a shelf and only displaying a couple of items at once reduces children’s feelings of being overwhelmed. Likewise, many children may enjoy a variety of arts and crafts materials, yet some children with SPD may not be able to tolerate getting glue or paint on their hands. Using a paintbrush for glue application and using hand wipes or a nearby sink to clean their hands may allow children to fully engage in the activity. In consultation with an OT, alternative materials can be selected. Based on the client’s needs, therapeutic putty could be substituted for a regular modeling compound to provide more sensory input; a dry food box (e.g., uncooked rice, beans, pastas) could be substituted for a traditional sand tray to provide more tactile input through different textures; and markers with or without scents could be used as part of a child’s sensory diet.
In consulting with the treatment team, the counselor may learn of the child’s need to implement other movement strategies as part of a sensory diet to increase his or her participation during counseling. These movements may include use of a rocking chair, proprioceptive exercises or a fidget. Balancing counseling interventions with attending to sensory inputs may help the child best focus during counseling sessions.
Mental Health Counselors
Play-based strategies. Children, particularly young children, express their emotions, thoughts and experiences through the language of play (Trice-Black, Bailey, & Riechel, 2013). Children with SPD may have qualitatively different playing styles, which may affect their social development (Cosbey, Johnston, Dunn, & Bauman, 2012). Counselors can foster the achievement of social development therapeutic goals by examining the nature of children’s play and the activities that children find most fulfilling. Cosbey et al. (2012) reported that children with SPD tend to participate in more solitary play, less complex play and greater overall conflict in play when compared to peers’ play. Therefore, social development and play strategies may be a focus of counseling for children with SPD. Furthermore, Cosbey, Johnston, and Dunn (2010) recommended three potential goals in working with children with SPD: (a) identify activities that bring joy and meaning to the individual child, (b) strategize ways that the child can successfully engage in the activity, and (c) use these activities to build his or her social circles with peers. Similarly, counselors may use such activities to assist children with SPD in improving relationships and interactions with family members.
Family counseling strategies. A substantial aspect of serving a child with SPD involves working with and supporting the people important in the child’s life, such as parents, siblings and other family members (Parham & Mailloux, 2015). When working from a family systems perspective, counselors should recognize the adjustment process for both parents and siblings. Just as children with SPD need to adjust to the diagnosis, so do their family members. The SPD diagnosis may bring a sense of relief to parents who have spent a long journey attempting to find an accurate diagnosis for their child (Parham & Mailloux, 2015). Some parents may feel grief and loss when their child is diagnosed with special needs, guilt for not obtaining the diagnosis sooner, and overwhelmed by navigating a new world of treatment expenses and accommodations (Anderson & Davis, 2011; Grossman & Okun, 2009; Marshak, Dandeneau, Prezant, & L’Amoreaux, 2010). Gourley, Wind, Henninger, and Chinitz (2013) found that parental stress was positively correlated with SPD severity, and that parents whose children had SPD had greater stress than those who had children without SPD. Thus, counselors can assist parents in processing their emotions, learning coping strategies, developing a plan of action and gaining a better understanding of SPD. Through psychoeducation (see suggestions in Appendix B), parents can learn about SPD and counselors can teach parents how to advocate for their children in various settings and situations (e.g., birthday parties, classroom activities, family gatherings; Ostovar, 2009; Withrow, 2007).
Another of the counselor’s essential tasks may be providing support for parents (Cohn, May-Benson, & Teasdale, 2011), which can be accomplished through a local support group for parents of children with SPD or through family therapy. As the severity of SPD increases, so does the level of support needed by parents (Cohn et al., 2011). Cohn et al. (2011) found a significant correlation between an increase in a child’s SPD severity and a decrease in parents’ perceived parental competence. Informing parents about the benefits of proper treatment may not only increase the likelihood of children receiving the needed treatment, but also decrease parents’ stress and anxiety related to parenting a child with special needs. Finally, family counseling may include treatment goals that center on establishing balance for the family system, as many families may have spent a large amount of family time and resources seeking an accurate diagnosis for their child (Gladding, 2015).
Siblings of children with special needs such as SPD may be negatively impacted in various ways, including greater likelihood of psychological or behavioral concerns, stressed relationships with parents, and missing parental attention (Anderson & Davis, 2011; Cohen, 1999). Engaging siblings in counseling can assist all the children in the family with adapting to the new family norms, routines and rules. For example, siblings can benefit from learning more about SPD (Parham & Mailloux, 2015) and processing their reactions to the SPD diagnosis, treatment and changes to the family system. Depending on the siblings’ ages and developmental levels, understanding SPD and the related issues may be difficult for them to comprehend. For example, siblings’ interactive play may change significantly once triggers are identified for the child with SPD. Siblings may need to process their emotions in their own space; thus, a referral to a sibling support group or individual counseling may be warranted.
School Counselors
According to the American School Counselor Association (ASCA, 2013), school counselors are charged with serving all students, including students with disabilities and special needs. School counselors can serve students through increasing their own awareness of SPD, consulting and collaborating with stakeholders, advocating for necessary student services and accommodations, and providing students with individual and small group counseling (ASCA, 2013). Thus, school counselors can apply these strategies to their work with children who have SPD.
Education, consultation and collaboration. To serve students with SPD, school counselors should educate themselves about the disorder and be vigilant about the signs and symptoms. School counselors can consult with other school professionals such as the OT and parents or caretakers if they suspect SPD. As teachers and family members may possess little knowledge of SPD, school counselors can educate, consult and collaborate with these stakeholders (ASCA, 2013) to increase their understanding of the disorder and to learn to best support the child with SPD.
Accommodations. The 2008 amendments of Section 504 of the Rehabilitation Act of 1973 constitute a “federal law designed to protect the rights of individuals with disabilities in programs and activities that receive Federal financial assistance from the U.S. Department of Education” (U.S. Department of Education, 2013, Introduction, para. 2), including students in public schools. To be eligible under Section 504, students must have a confirmed physical or mental impairment that substantially impacts their functioning (U.S. Department of Education, 2013). If a student’s SPD significantly impedes his or her school participation and learning, that student may be eligible for Section 504, including relevant accommodations, supports and a documented plan. School counselors can advocate for students receiving services under Section 504, as well as assist students and parents in navigating the educational system as they seek services.
To promote academic performance and social and emotional functioning in schools, 504 services vary based on the unique needs of each student. Accommodations should be individualized and based on information gathered from the student, family, teacher and diagnosing professionals. Once the student’s sensory triggers are identified, the school counselor can examine each aspect of the child’s day for potential triggers and modifications; small changes can make a significant difference. SPD accommodations in the classroom may include preferential seating, possibly with a larger personal space circumference (e.g., the student’s own table for classroom work and testing), sensory breaks in the classroom, “heavy work” (e.g., delivering books to the library), increased time for assignments and tests, and a quiet location for testing. Some students with poor muscle coordination may require accommodations for underdeveloped fine motor skills, such as using a mechanical pencil for short assignments, a computer for longer writing assignments and pencil grips. In coordination with an OT, other accommodations may include a weighted vest or lap pillow, a balance ball chair instead of a traditional seat, and fidgets or stress balls to help increase attending behavior, reduce stress and increase hand muscle strength. If available and as needed, students can meet with a school-based OT to further address SPD symptoms in the classroom.
In addition to focusing on student accommodations for accessing the core curriculum, students with SPD may struggle with the elective or “specials” classes, unplanned situations, transitions and unstructured time outside of the classroom. While many children love playing tag during recess or physical education (P.E.), a student who is sensory defensive may dread this and similar activities. Thus, a P.E. accommodation may be engaging in a different noncontact sport. Alternatively, children who need sensory input may have accommodations to complete additional jumping jacks or wall pushes beyond P.E. class. In addition, a child with gross motor skill challenges could receive accommodations to strengthen and develop those areas without being penalized for failure to meet grade-level expectations. With any sport, an OT can assess a child’s physical strengths and challenges, working with P.E. teachers, coaches and parents to select appropriate individual or group activities based on the SPD presentation in each child (Kirkpatrick, 2012).
As previously mentioned regarding play-based techniques, some creative arts activities may be troublesome for children with SPD. Accommodations in art class should ensure that students with SPD participate to the best of their ability, and receive modified assignments and grading protocols (e.g., extra time to complete assignments). Likewise, students in music class may need to utilize their noise reduction headphones. Finally, school counselors should be mindful of students’ schedules, advocating for “specials” classes to be spaced out and at the end of the day when possible, as children with SPD who have multiple triggers are apt to have challenges concentrating once back in their regular classroom.
Children with SPD may be fearful of unexpected situations due to concern that a sensory trigger will occur. Providing students with advance warning can assist them during these situations. For instance, students can receive advance notice for fire drills and prearranged substitute teachers. The school counselor can check on the students during such triggering events to determine their reactions and ensure that accommodations are implemented. The school counselor can coach children to advocate for themselves in these situations, for example, by asking a substitute teacher to reduce the classroom noise level, or wearing noise-canceling headphones during fire drills.
Students with SPD may benefit from accommodations assisting them with daily school transitions. For example, a visual reminder (e.g., written schedule) may help reduce students’ anxiety surrounding transitions. To preserve personal space when transitioning between classes, younger students can receive preferential order in line, while older students can receive permission to walk in the hallways immediately before or after their peers.
Children with SPD may find unstructured school time to be difficult due to the magnitude of overwhelming sensory input. School counselors can assist students with SPD by collaborating with them and other stakeholders to create modifications for unstructured school times (e.g., recess, lunch, school assemblies, class parties, bathroom breaks, transportation to and from school). Accommodations may include preferential seating, noise-canceling headphones and decreased time in such situations. Further, students should be provided a safe place to decompress when overstimulated.
When annually reviewing 504 plans and adjusting accommodations, school counselors need to be aware that students’ triggers and challenges may change at different developmental and chronological ages. For example, high school students with SPD may require unique accommodations in various situations such as the following: during driver’s education (e.g., not driving with other students in the car), while dissecting frogs in biology or when using odorous chemicals in chemistry. Biological changes in adolescence produce new and potentially triggering smells, such as the P.E. locker room at the secondary level. Thus, school counselors may need to (a) advocate for accommodations to counter these scenarios that may emerge in middle and high school, and (b) further address the emotions related to dealing with SPD symptoms in the classroom and in social situations with classmates that may occur with the onset of adolescence.
Counseling. In addition to assisting with accommodations, school counselors can conduct individual and small group counseling for students with SPD in order to help them succeed in school (Collier & Falls, 2010). School counselors can provide counseling to address students’ emotional and mental health concerns, which may include anxiety, depression, low self-esteem, poor social skills and frustration (Champagne & Koomar, 2012; Katz, 2006; Miller et al., 2012; Walbam, 2013; Withrow, 2007). School counseling may address students’ anxiety about school transitions and school-related sensory reactions by teaching students coping skills. School counselor-led counseling can normalize the experience of children with SPD, combating potential feelings of self-consciousness and isolation. Through the use of bibliotherapy and psychoeducation (see Appendix B), students can learn improved self-regulation and organization skills as well as self-advocacy and assertiveness. For example, students can learn to advocate for themselves by participating in their 504 plan meeting, as well as learn to develop strategies for communicating with teachers when becoming overwhelmed by sensory stimuli.
When students with SPD receive accommodations and counseling, classmates may express jealousy or frustration, similar to siblings. The school counselor can help process these situations and role-play social interactions in individual or group settings. Further, school counselors can assist teachers in offering sensory modulation strategies for an entire class, in order to prevent the child with SPD from being singled out. The following is a case study of how a counselor can intervene with a child who has SPD.
Case Study
Euna is a 6-year-old, second-generation Korean American attending her first year of school as a first-grade student in public school. Her parents are professionals, and she is an only child who had an in-home nanny and no formal preschool. At school, she shows little variation in affect and rarely speaks to peers. However, she and her parents speak at home, often in quiet voices. Euna flinches when touched and her parents describe her as a picky eater and uncoordinated. She does not like school; at home she has daily outbursts prior to departing for the school bus. Euna does not have reciprocal friendships in school and often sits alone in the cafeteria during lunch. Often she requests to visit the nurse to avoid the cafeteria during lunch.
Euna visits a mental health counselor for anxiety; this counselor has basic awareness of SPD. After the intake and initial counseling session with Euna, the mental health counselor suspects SPD and gathers additional background information from Euna’s parents as well as a release of information to speak to Euna’s teacher and school counselor. Next, the mental health counselor gathers background information from Euna’s school counselor and teacher about her school functioning. After completing screening checklists (e.g., Appendix A: Sensory Processing Disorder Checklist or the Sensory Profile 2), the mental health counselor and school counselor provide Euna’s parents with an OT referral for formal evaluation and recommend that her parents first speak to the pediatrician; the counselors obtain a release of information to be able to speak with the OT and pediatrician. The OT determines that Euna does have SPD, and through the physical examination, Euna’s pediatrician rules out other potential physiological causes for symptoms. The pediatrician also provides a referral to a nutritionist who can ensure that Euna is obtaining proper nutrition and gradually increase the types and textures of food in Euna’s diet.
After consulting with the OT and pediatrician, the school and mental health counselors work together to provide bibliotherapy resources for the family, education for the teacher and school staff, and coping strategies for Euna in school, at home and in the community. They collaborate with the OT to incorporate sensory strategies that will enhance counseling sessions with Euna. Lastly, the school counselor invites the OT and mental health counselor to participate in the development of the 504 plan to provide accommodations for Euna to be successful in school.
During the last several years, authors have presented variations of the Euna case study to audiences in counseling classes and conferences, asking for participants’ thoughts on a preliminary diagnosis for further exploration. Common participant responses include trauma, anxiety and school phobia; this is not surprising, as SPD can be easily misdiagnosed as other disorders.
Summary and Recommendations
SPD is a neurological disorder that impacts the daily functioning of children across settings. Thus, to advocate on behalf of children with SPD in mental health and school settings, counselors need to increase their SPD-related education, advocacy, screening, treatment, stakeholder collaboration and research. First, counselors should become increasingly knowledgeable about and advocate for an increased awareness of SPD within the counseling profession. We recommend that counselors advocate for the inclusion of SPD in diagnostic standards, such as the future edition of the DSM, and in counselor education, professional development and counseling literature. By increasing the counseling profession’s knowledge of SPD, counselors can provide children with more appropriate and earlier treatment interventions.
Next, counselors need to effectively screen for SPD and collaborate with parents and other professionals to treat the primary and secondary needs of children with this disorder. Also, counselors can educate stakeholders on SPD, including teachers and parents. By further demystifying and clarifying SPD for professionals and family members, these stakeholders can best support children with SPD, improving their quality of life and achieving treatment goals.
Conducting and publishing counseling-related SPD research can add professional credibility and recognition of SPD. In the future, researchers should investigate the following: (a) counselors’ awareness of SPD; (b) mental health, school, and family counseling interventions used for children with SPD; (c) consultation practices with other service providers to serve children with SPD; and (d) perceptions and outcomes of clients with SPD receiving counseling services in an effort to develop future evidence-based best practices. Also, researchers can explore the psychometric properties of instruments used to screen for SPD, perceptions regarding these instruments, and effectiveness of counselors using these instruments. Finally, counselors can conduct interdisciplinary research with OTs, as future SPD research areas outlined by the American Occupational Therapy Association (2014) are related to counseling treatment goals pertaining to SPD (e.g., social communication, anger management, academic performance, behavior issues). When counselors and researchers engage in self-education and professional education, more accurate screening, evidence-based counseling treatment strategies, stakeholder education and collaboration, and research, they advocate for children with SPD across settings and have the potential to dramatically improve the lives of many children.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of
interest or funding contributions for
the development of this manuscript.
References
Ahn, R. R., Miller, L. J., Milberger, S., & McIntosh, D. N. (2004). Prevalence of parents’ perceptions of sensory processing disorders among kindergarten children. American Journal of Occupational Therapy, 58, 287–293. doi:10.5014/ajot.58.3.287
American Counseling Association. (2014). ACA code of ethics. Alexandria, VA: Author.
American Occupational Therapy Association. (2014). Research opportunities in the area of children and adolescents with challenges in sensory processing and sensory integration. American Journal of Occupational Therapy, 68, 242–244. doi:10.5014/ajot.2014.682003
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
American School Counselor Association. (2013). The professional school counselor and students with disabilities. Retrieved from http://www.schoolcounselor.org/asca/media/asca/PositionStatements/PS_Disabilities.pdf
Anderson, T., & Davis, C. (2011). Evidence-based practice with families of chronically ill children: A critical literature review. Journal of Evidence-Based Social Work, 8, 416–425. doi10.1080/15433710903269172
Ayres, A. J. (1979). Sensory integration and the child. Los Angeles, CA: Western Psychological Services.
Ayres, A. J. (1989). Sensory integration and Praxis tests (SIPT) [Measurement instrument]. Torrance, CA: Western Psychological Services. Retrieved from http://www.wpspublish.com/store/p/2971/sensory-integration-and-praxis-test-sipt
Ben-Sasson, A., Carter, A. S., & Briggs-Gowan, M. J. (2009). Sensory over-responsivity in elementary school: Prevalence and social-emotional correlates. Journal of Abnormal Child Psychology, 37, 705–716.
doi:10.1007/s10802-008-9295-8
Byrne, M. W. (2009). Sensory processing disorder: Any of a nurse practitioner’s business? Journal of the American Academy of Nurse Practitioners, 21, 314–321. doi:10.1111/j.1745-7599.2009.00417.x
Castaneda, R., Olson, L. M., & Radley, L. C. (2013). Occupational therapy’s role in community mental health. Retrieved from http://www.aota.org/About-Occupational-Therapy/Professionals/MH/Community-Mental-Health.aspx#sthash.7aYvMJBy.dpuf
Centers for Disease Control and Prevention, National Center for Health Statistics. (1991). The international classification of diseases, 9th revision, clinical modification (ICD-9-CM). Washington, DC: US Department of Health and Human Services, Health Care Financing Administration.
Champagne, T., & Koomar, J. (2012). Evaluating sensory processing in mental health occupational therapy practice. OT Practice, 17(5), CE-1–CE-8.
Chang, Y.-S., Owen, J. P., Desai, S. S., Hill, S. S., Arnett, A. B., Harris, J., . . . Mukherjee, P. (2014). Autism and sensory processing disorders: Shared white matter disruption in sensory pathways but divergent connectivity in social-emotional pathways. PLOS ONE, 9(7), 1–17. doi:10.1371/journal.pone.0103038
Cheu, R. (2013). Living well with chronic illness: Natural ways to maintain and restore mental and spiritual well-being. Alternative Medicine, 11, 60–62.
Cohen, M. S. (1999). Families coping with childhood chronic illness: A research review. Families, Systems, & Health, 17, 149–164. doi:10.1037/h0089879
Cohn, E., May-Benson, T. A., & Teasdale, A. (2011). The relationship between behaviors associated with sensory processing and parental sense of competence. OTJR: Occupation, Participation and Health, 31, 172–181. doi:10.3928/15394492-20110304-01
Collier, N. R., & Falls, L. A. (2010). Making sense out of sensory processing disorder. ASCA School Counselor. Retrieved from http://www.schoolcounselor.org/school-counselors-members/professional-development/learn-more/student-mental-health-resources
Cosbey, J., Johnston, S. S., & Dunn, M. L. (2010). Sensory processing disorders and social participation. American Journal of Occupational Therapy, 64(3), 462–473. doi:10.5014/ajot.2010.09076
Cosbey, J., Johnston, S. S., Dunn, M. L., & Bauman, M. (2012). Playground behaviors of children with and without sensory processing disorders. OTJR: Occupation, Participation and Health, 32(2), 39–47.
doi:10.3928/15394492-20110930-01
Davies, P. L., & Gavin, W. J. (2007). Validating the diagnosis of sensory processing disorders using EEG technology. American Journal of Occupational Therapy, 61(2), 176–189. doi:10.5014/ajot.61.2.176
Dunn, W. (1997). The impact of sensory processing abilities on the daily lives of young children and families: A conceptual model. Infants &Young Children, 9, 23–35.
Dunn, W. (2001). The sensations of everyday life: Empirical, theoretical, and pragmatic considerations. American Journal of Occupational Therapy, 55(6), 608–620. doi:10.5014/ajot.55.6.608
Dunn, W. (2014). Sensory Profile 2 [Clinical assessment]. Retrieved from http://www.pearsonclinical.com/psychology/products/100000822/sensory-profile-2.html#tab-details
Gavin, W. J., Dotseth, A., Roush, K. K., Smith, C. A., Spain, H. D., & Davies, P. L. (2011). Electroencephalography in children with and without sensory processing disorders during auditory perception. American Journal of Occupational Therapy, 65, 370–377. doi:10.5014/ajot.2011.002055
Ghanizadeh, A. (2011). Sensory processing problems in children with ADHD, a systematic review. Psychiatry Investigation, 8(2), 89–94. doi:10.4306/pi.2011.8.2.89
Gladding, S. T. (2015). Family therapy: History, theory, and practice (6th ed.). Upper Saddle River, NJ: Pearson.
Goldsmith, H. H., Van Hulle, C. A., Arneson, C. L., Schreiber, J. E., & Gernsbacher, M. A. (2006). A population-based twin study of parentally reported tactile and auditory defensiveness in young children. Journal of Abnormal Child Psychology, 34, 393–407. doi:10.1007/s10802-006-9024-0
Gourley, L., Wind, C., Henninger, E. M., & Chinitz, S. (2013). Sensory processing difficulties, behavioral problems, and parental stress in a clinical population of young children. Journal of Child and Family Studies, 22, 912–921. doi:10.1007/s10826-012-9650-9
Grossman, N. S., & Okun, B. F. (2009). Challenges in family forensic psychology: Families with special-needs children II. The Family Psychologist, 25(2), 19–20.
Hall, L., & Case-Smith, J. (2007). The effect of sound-based intervention on children with sensory processing disorders and visual-motor delays. American Journal of Occupational Therapy, 61, 209–215.
Interdisciplinary Council on Developmental and Learning Disorders. (2012). Diagnostic manual for infancy and early childhood: Mental health disorders, developmental disorders, regulatory-sensory processing disorders, language disorders, and learning challenges. Bethesda, MD: ICDL-DMIC Work Groups.
James, K., Miller, L. J., Schaaf, R., Nielsen, D. M., & Schoen, S. A. (2011). Phenotypes within sensory modulation dysfunction. Comprehensive Psychiatry, 52, 715–724. doi:10.1016/j.comppsych.2010.11.010
Katz, I. (2006). Students with sensory integration dysfunctions: Issues for school counselors. Journal of School Counseling, 4(22), 1–22. Retrieved from http://jsc.montana.edu/articles/v4n22.pdf
Kinnealey, M., & Fuiek, M. (1999). The relationship between sensory defensiveness, anxiety, depression and perception of pain in adults. Occupational Therapy International, 6, 195–206. doi:10.1002/oti.97
Kirkpatrick, J. (2012). Sports for children with sensory processing disorders: A guide for occupational therapy practitioners. OT Practice, 17(10), 8–13.
Kranowitz, C. S. (2005). The out-of-sync child: Recognizing and coping with sensory processing disorder. New York, NY: Penguin Group.
Landreth, G. L., Ray, D. C., & Bratton, S. C. (2009). Play therapy in elementary schools. Psychology in the Schools, 46, 281–289. doi:10.1002/pits.20374
Levingston, S. A. (2014). The debate over sensory processing disorder: Are some kids really ‘out of sync’? The Washington Post. Retrieved from http://www.washingtonpost.com/national/health-science/the-debate-over-sensory-processing-disorder-are-some-kids-really-out-of-sync/2014/05/12/fca2d338-d521-11e3-8a78-8fe50322a72c_story.html
Marshak, L. E., Dandeneau, C. J., Prezant, F. P., & L’Amoreaux, N. A. (2010). The school counselor’s guide to helping students with disabilities. San Francisco, CA: Jossey-Bass.
McIntosh, D. N., Miller, L. J., Shyu, V., & Hagerman, R. J. (1999). Sensory-modulation disruption, electrodermal responses, and functional behaviors. Developmental Medicine & Child Neurology, 41, 608–615.
Miller, L. J. (2006). Sensational kids: Hope and help for children with sensory processing disorder (SPD). New York, NY: Penguin Group.
Miller, L. J., Anzalone, M. E., Lane, S. J., Cermak, S. A., & Osten, E. T. (2007). Concept evolution in sensory integration: A proposed nosology for diagnosis. American Journal of Occupational Therapy, 61, 135–140.
doi:10.5014/ajot.61.2.135
Miller, L. J., Nielsen, D. M., & Schoen, S. A., (2012). Attention deficit hyperactivity disorder and sensory modulation disorder: A comparison of behavior and physiology. Research in Developmental Disabilities, 33, 804–818. doi:10.1016/j.ridd.2011.12.005
Miller, L. J., Nielsen, D. M., Schoen, S. A., & Brett-Green, B. A. (2009). Perspectives on sensory processing disorder: A call for translational research. Frontiers in Integrative Neuroscience, 3(22), 1–12. doi:10.3389/neuro.07.022.2009
Murphy, S. N. (2011). Don’t touch me. Counseling Today, 53(10), 40–44.
Ostovar, R. (2009). The ultimate guide to sensory processing disorder: Easy, everyday solutions to sensory challenges. Arlington, TX: Sensory World.
Owen, J. P., Marco, E. J., Desai, S., Fourie, E., Harris, J., Hill, S. S., . . . Mukherjee, P. (2013). Abnormal white matter microstructure in children with sensory processing disorders. NeuroImage: Clinical, 2, 844–853.
doi:10.1016/j.nicl.2013.06.009
Parham, L. D., & Mailloux, Z. (2015). Sensory integration. In J. Case-Smith & J. C. O’Brien (Eds.), Occupational therapy for children and adolescents (7th ed., pp. 258–303). St. Louis, MO: Mosby.
Pollak, J., Levy, S., & Breitholtz, T. (1999). Screening for medical and neurodevelopmental disorders for the professional counselor. Journal of Counseling & Development, 77, 350–358. doi:10.1002/j.1556-6676.1999.tb02459.x
Schaaf, R. C., Benevides, T., Blanche, E. I., Brett-Green, B. A., Burke, J. P., Cohn, E. S., & … Schoen, A. S. (2010). Parasympathetic functions in children with sensory processing disorder. Frontiers in Integrative Neuroscience, 4(4), 1–10. doi:10.3389/fnint.2010.00004
Schaaf, R. C., Miller, L. J., Seawell, D., & O’Keefe, S. (2003). Children with disturbances in sensory processing: A pilot study examining the role of the parasympathetic nervous system. American Journal of Occupational Therapy, 57, 442–449.
Schoen, S. A., Miller, L. J., Brett-Green, B. A., & Nielsen, D. M. (2009). Physiological and behavioral differences in sensory processing: A comparison of children with autism spectrum disorder and sensory modulation disorder. Frontiers in Integrative Neuroscience, 3(29), 1–11. doi:10.3389/neuro.07.029.2009
Sensory Processing Disorder Foundation. (2012). Final decision for DSM-V. Retrieved from http://spdfoundation.net/sensory-processing-blog/2012/12/05/final-decision-for-dsm-v/
Sensory Processing Disorder Foundation. (2014). SPD scientific work group. Retrieved from http://www.spdfoundation.net/collaborations.html
Tomchek, S. D., & Dunn, W. (2007). Sensory processing in children with and without autism: A comparative study using the Short Sensory Profile. American Journal of Occupational Therapy, 61, 190–200.
Trice-Black, S., Bailey, C. L., & Riechel, M. E. K. (2013). Play therapy in school counseling. Professional School Counseling, 16, 303–312.
U.S. Department of Education, Office for Civil Rights. (2013). Protecting students with disabilities: Frequently asked questions about Section 504 and the education of children with disabilities. Retrieved from http://www2.ed.gov/about/offices/list/ocr/504faq.html
Van Hulle, C. A., Schmidt, N. L., & Goldsmith, H. H. (2012). Is sensory over-responsivity distinguishable from childhood behavior problems? A phenotypic and genetic analysis. The Journal of Child Psychology and Psychiatry, 53, 64–72. doi:10.1111/j.1469-7610.2011.02432.x
Walbam, K. M. (2014). The relevance of sensory processing disorder to social work practice: An interdisciplinary approach. Child and Adolescent Social Work Journal, 31, 61–70. doi:10.1007/s10560-013-0308-2
Withrow, R. L. (2007). Sensory integration dysfunction: Implications for counselors working with children. Journal of School Counseling, 5(18), 1–24.
World Health Organization. (2013). International statistical classification of diseases and related health problems (10th rev., 2014 ed.). Geneva, Switzerland: Author.
Zero to Three, National Center for Infants, Toddlers, and Families. (2005). DC:0-3R: Diagnostic classification of mental health and developmental disorders of infancy and early childhood. Washington, DC: Zero To Three Press.
Appendix A
Sensory Processing Disorder Checklist
© Sensory Therapies And Research (STAR) Center, 2006
Retrieved from http://spdfoundation.net/library/checklist.html
Many of the symptoms listed in the following categories are common to that particular age group. Where more than a few symptoms are found in a child, we recommend you talk to your doctor or check the SPD Foundation’s Treatment Directory for a professional experienced with treating Sensory Processing Disorder.*
Infant/ Toddler Checklist:
____ My infant/toddler has problems eating.
____ My infant/toddler refused to go to anyone but me.
____ My infant/toddler has trouble falling asleep or staying asleep
____ My infant/toddler is extremely irritable when I dress him/her; seems to be uncomfortable in clothes.
____ My infant/toddler rarely plays with toys, especially those requiring dexterity.
____ My infant/toddler has difficulty shifting focus from one object/activity to another.
____ My infant/toddler does not notice pain or is slow to respond when hurt.
____ My infant/toddler resists cuddling, arches back away from the person holding him.
____ My infant/toddler cannot calm self by sucking on a pacifier, looking at toys, or listening to my voice.
____ My infant/toddler has a “floppy” body, bumps into things and has poor balance.
____ My infant/toddler does little or no babbling, vocalizing.
____ My infant/toddler is easily startled.
____ My infant/toddler is extremely active and is constantly moving body/limbs or runs endlessly.
____ My infant/toddler seems to be delayed in crawling, standing, walking or running.
Pre-School Checklist:
____ My child has difficulty being toilet trained.
____ My child is overly sensitive to stimulation, overreacts to or does not like touch, noise, smells, etc.
____ My child is unaware of being touched/bumped unless done with extreme force/intensity.
____ My child has difficulty learning and/or avoids performing fine motor tasks such as using crayons and
fasteners on clothing.
____ My child seems unsure how to move his/her body in space, is clumsy and awkward.
____ My child has difficulty learning new motor tasks.
____ My child is in constant motion.
____ My child gets in everyone else’s space and/or touches everything around him.
____ My child has difficulty making friends (overly aggressive or passive/ withdrawn).
____ My child is intense, demanding or hard to calm and has difficulty with transitions.
____ My child has sudden mood changes and temper tantrums that are unexpected.
____ My child seems weak, slumps when sitting/standing; prefers sedentary activities.
____ It is hard to understand my child’s speech.
____ My child does not seem to understand verbal instructions.
School Age:
___ My child is overly sensitive to stimulation, overreacts to or does not like touch, noise, smells, etc.
___ My child is easily distracted in the classroom, often out of his/her seat, fidgety.
___ My child is easily overwhelmed at the playground, during recess and in class.
___ My child is slow to perform tasks.
___ My child has difficulty performing or avoids fine motor tasks such as handwriting.
___ My child appears clumsy and stumbles often, slouches in chair.
___ My child craves rough housing, tackling/wrestling games.
___ My child is slow to learn new activities.
___ My child is in constant motion.
___ My child has difficulty learning new motor tasks and prefers sedentary activities.
___ My child has difficulty making friends (overly aggressive or passive/ withdrawn).
___ My child gets stuck on tasks and has difficulty changing to another task.
___ My child confuses similar sounding words, misinterprets questions or requests.
___ My child has difficulty reading, especially aloud.
___ My child stumbles over words; speech lacks fluency, and rhythm is hesitant.
Adolescent/Adult:
___ I am over-sensitive to environmental stimulation: I do not like being touched.
___ I avoid visually stimulating environments and/or I am sensitive to sounds.
___ I often feel lethargic and slow in starting my day.
___ I often begin new tasks simultaneously and leave many of them uncompleted.
___ I use an inappropriate amount of force when handling objects.
___ I often bump into things or develop bruises that I cannot recall.
___ I have difficulty learning new motor tasks, or sequencing steps of a task.
___ I need physical activities to help me maintain my focus throughout the day.
___ I have difficulty staying focused at work and in meetings.
___ I misinterpret questions and requests, requiring more clarification than usual.
___ I have difficulty reading, especially aloud.
___ My speech lacks fluency, I stumble over words.
___ I must read material several times to absorb the content.
___ I have trouble forming thoughts and ideas in oral presentations.
*While this checklist can’t diagnose a child with SPD, it can be a helpful guide to see if additional testing should be done. When filling out this checklist, think about the child’s behavior during the past six months.
Appendix B
Abbreviated List of Sensory Processing Disorder Resources
Resources for Parents, Teachers and Counselors
- Answers to Questions Teachers Ask about Sensory Integration: Forms, Checklists, and Practical Tools for Teachers and Parents by Jane Koomar, Carol Kranowitz, Stacey Szklut, Lynn Balzer-Martin, Elizabeth Haber, Deanna Iris Sava
- Building Sensory Friendly Classrooms to Support Children with Challenging Behaviors: Implementing Data Driven Strategies! by Rebecca A. Moyes
- The Out-of-Sync Child Has Fun, Revised Edition: Activities for Kids with Sensory Processing Disorder by Carol Stock Kranowitz
- The Out-of-Sync Child: Recognizing and Coping with Sensory Processing Disorder, Revised Edition by Carol Kranowitz and Lucy Jane Miller
- Parenting a Child with Sensory Processing Disorder: A Family Guide to Understanding and Supporting Your Sensory-Sensitive Child by Christopher R. Auer
- Raising a Sensory Smart Child: The Definitive Handbook for Helping Your Child with Sensory Integration Issues by Lindsey Biel and Nancy Peske
- Sensational Kids: Hope and Help for Children with Sensory Processing Disorder by Lucy Jane Miller and Doris A. Fuller
- Sensory Parenting, From Newborns to Toddlers: Everything is Easier When Your Child’s Senses are Happy! by Britt Collins and Jackie Linder Olson
- Sensory Parenting, The Elementary Years: School Years Are Easier when Your Child’s Senses Are Happy! by Britt Collins and Jackie Linder Olson
- Sensory Processing Disorder Foundation: http://www.spdfoundation.net/index.html
- Starting Sensory Therapy: Fun Activities for the Home and Classroom! by Bonnie Arnwine
- The Survival Guide for Travelling with a Sensory Kiddo: From Amusement Parks, to the Beach or a Weekend Road Trip to Visit Relatives…Sensory Help is Here! by Angie Voss
- Too Loud, Too Bright, Too Fast, Too Tight: What to Do If You Are Sensory Defensive in an Overstimulating World by Sharon Heller
- Understanding Your Child’s Sensory Signals: A Practical Daily Use Handbook for Parents and Teachers by Angie Voss
- Your Essential Guide to Understanding Sensory Processing Disorder: When You See a Child Through Sensory Goggles…It ALL Makes More “Sense”! by Angie Voss
Sensory Processing Disorder Checklists
- http://www.sensory-processing-disorder.com/sensory-processing-disorder-checklist.html
- http://sinetwork.org/library/checklist.html
- http://www.sensationalbrain.com/sensory-activities-6-quick-ideas/
For Children
- The Adventures of Sensory Avoider Allie: Allie Only Eats Three Foods by Angie Voss and Dillon Seglem
- Arnie and His School Tools: Simple Sensory Solutions That Build Success by Jennifer Veenendall
- Ellie Bean the Drama Queen: A Children’s Book about Sensory Processing Disorder by Jennie Harding and Dave Padgett
- I’m Not Weird, I Have Sensory Processing Disorder (SPD): Alexandra’s Journey (Growing with Love) by Chynna T. Laird
- Meghan’s World: The Story of One Girl’s Triumph over Sensory Processing Disorder by Diane M. Renna and Regina Stark
- Picky, Picky Pete by Michele Griffin
- Sensitive Sam: Sam’s Sensory Adventure has a Happy Ending! by Marla Roth-Fisch
- Squirmy Wormy: How I Learned to Help Myself by Lynda Farrington Wilson
- This is Gabriel Making Sense of School: A Book About Sensory Processing Disorder by Hartley Steiner
- Why Does Izzy Cover Her Ears? Dealing with Sensory Overload by Jennifer Veenendall
Emily Goodman-Scott, NCC, is an Assistant Professor at Old Dominion University. Simone F. Lambert, NCC, is the Counseling Department Chair and Associate Professor at Argosy University. Correspondence may be addressed to Emily Goodman-Scott, 110 Education Building, Old Dominion University, Norfolk, VA 23529, egscott@odu.edu.
Mar 2, 2015 | Article, Volume 5 - Issue 2
Cassandra A. Storlie, Eric R. Baltrinic
Cystic fibrosis is a progressive, chronic disease that affects approximately 30,000 adults and children in the United States. Counseling children with the special needs specific to cystic fibrosis can be overwhelming for mental health professionals due to the progressive and deteriorating nature of the illness, long-term contact with clients, and discouraging prognosis. Being exposed to long-term therapeutic relationships with chronically ill children and witnessing treatment failure can contribute to burnout, compassion fatigue and vicarious trauma in counselors, highlighting the need for targeted literature addressing holistic self-care strategies. The purpose of this manuscript is to provide a review of the current literature illuminating the challenges facing children with cystic fibrosis and to provide targeted self-care suggestions for professional counselors working with this population.
Keywords: children, chronic disease, compassion fatigue, cystic fibrosis, self-care
Cystic fibrosis (CF) is a chronic, terminal disease targeting most organ systems (Withers, 2012) and affects approximately 30,000 children and adults nationwide (Cystic Fibrosis Foundation [CFF], 2014a). CF primarily affects the gastrointestinal and respiratory systems (Withers, 2012), and although the life expectancy has greatly improved, CF is fatal and there is no known cure (CFF, 2014a). Counseling children with chronic illnesses, such as CF, presents special challenges for mental health professionals (Sidell, 1997), including professional counselors. As the nature and severity of clients’ problems impact levels of counselor burnout or compassion fatigue (Figley, 2002), it is essential that professional counselors working with children with CF maintain healthy self-care practices.
There is an abundance of information examining the physiological aspects of CF that clients experience throughout the disease progression (CFF, 2014a; Pearson, Pumariega, & Seilheimer, 1991; Sawicki, Sellers, & Robinson, 2009; Sawicki & Tiddens, 2012). However, there is limited literature on the special considerations that need to be taken when counseling children with CF. Furthermore, there is a paucity of counseling literature targeting how professional counselors can foster personal self-care while working with young clients with special needs and chronic conditions. The purpose of this manuscript is to provide a review of literature that illuminates the challenges facing children with CF and provides a primer for self-care suggestions for professional counselors who work with these children.
Special Needs of Children with Cystic Fibrosis
Physiological Challenges Facing Children with Cystic Fibrosis
Professional counselors need to be knowledgeable of chronic diseases affecting their clients in order to be sensitive to the traumas experienced by children and families coping with illness (Thompson & Henderson, 2007). CF is most commonly diagnosed during newborn screening and severely affects the exocrine system (CFF, 2014b). Within the exocrine system, there is a lack of appropriate enzymes available during digestion, so children with CF are unable to properly digest their food and absorb essential nutrients for healthy growth and development. They experience recurrent gastrointestinal distress such as issues of diarrhea and constipation with foul-smelling stools due to poor absorption (CF Living, 2014). As such, children with CF often suffer from malnutrition and an inability to maintain a healthy weight. However, the most notable signs and symptoms affecting children with CF result from chronic lung and respiratory infections that lead to frequent coughing spells to clear the lungs of thick mucus. This inability to clear the lungs requires multiple episodes of daily chest physiotherapy (Berge & Patterson, 2004). Over time, the respiratory infections produce lung damage that appears cyst-like, giving name to the disease cystic fibrosis (CFF, 2014a).
Children with CF can spend hours per day on medical treatments such as nebulizer treatments to improve breathing, medications prior to meals to improve digestion, and oral, inhaled or intravenous antibiotics to treat respiratory infections (CF Living, 2014). However, disabilities from CF are not often visibly apparent until later stages of the disease. Decreased mobility and debilitating side effects from long-term medications, along with decreased lung capacity, all contribute to clients with CF requiring oxygen therapy for survival (Withers, 2012). The later stages of CF are inundated with frequent hospitalizations. Treatment during end-stage CF is palliative rather than curative (Lowton & Gabe, 2003), and without lung transplantation, CF remains a fatal disease due to respiratory failure (Hayes, Anstead, Warner, Kuhn, & Ballard, 2010). Nevertheless, medical breakthroughs have increased the survival rate of children with CF (Blum, 1992) and now many children are living into adulthood. Advanced clinical drug trials, aggressive antibiotic medications and innovative gene therapy research have been successful with CF clients of all ages. In 1955, children with CF were not expected to live to attend grade school. Children born with CF in this decade are projected to live into their 40s (CFF, 2014a). With this increase in life expectancy, health care teams are faced with unique challenges specific to the turbulence of adolescence and treatment compliance (Withers, 2012). Although there has been a predominant focus on treating CF based on medical science (Chesson, Chisholm, & Zaw, 2004), there is a strong interconnection of the psychosocial and physical challenges facing children and adolescents with CF. As such, professional counselors are called to increase their knowledge, skill and awareness of not just the physical challenges affecting children with CF, but also the emotional obstacles facing this population.
Psychosocial Challenges Facing Children with Cystic Fibrosis
Emotional and behavioral health disorders affect approximately 20% of all children and adolescents nationwide (Canning, Haner, Shade, & Boyce, 1992), and children with chronic illness may exhibit even higher incidences of mental health and psychosocial issues (Barnes, Eisenberg, & Resnick, 2010). For example, children with CF may experience extreme psychological challenges (e.g., depression, hopelessness, suicidal ideation) and physical complications (e.g., poor lung functioning, malnutrition) throughout the progression of their chronic condition. Taken together, these comorbidities contribute to the complexity of supporting an intense treatment modality (Anderson, Flume, & Hardy, 2001; Withers, 2012) that also promotes healthy psychosocial development and family system functioning (O’Haver et al., 2010).
In order to provide evidenced-based practices to clients with CF, as well as their families and loved ones, professional counselors need to be current on mental health research related to this special population. Studies have identified that children with CF may be predisposed to psychological issues and attachment and behavioral problems (Berge & Patterson, 2004) that may require additional training for professional counselors to effectively and efficiently counsel this population. When compared to healthy peers, children with chronic health conditions also have been found to have a slightly higher risk of attempting suicide (Barnes et al., 2010). Grief and loss, internal and external stress, negative body image, and difficulty managing emotions are common challenges experienced by children with CF (Berge & Patterson, 2004; Withers, 2012). In managing these difficulties, internalizing behaviors and anxiety also have been found prominent among this population (Berge & Patterson, 2004). Younger male children with CF have been found to exhibit higher levels of anxiety (Bregnballe, Thastum, & Schiøtz, 2007) and female children with CF have demonstrated internalizing behaviors by expressing less anger than female children without CF (Bregnballe et al., 2007).
Although research supports the idea that individuals with chronic illnesses are at increased risk for depression (Quittner et al., 2008), studies conducted on individuals with CF have provided mixed results (Pearson et al., 1991; Thompson, Hodges, & Hamlet, 1990). Berge and Patterson (2004) identified higher incidences of depression among youth with CF, whereas Tluczek et al. (2014) found that patients with CF report similar psychosocial functioning as their healthy peers. One possible factor affecting the mixed reports of depression among children with CF may include the level of disease acceptance. Previous investigations have identified that the level of disease acceptance among youth with CF can significantly lessen levels of anxiety, depression and disability in adolescents with CF (Casier et al., 2008). Nonetheless, depression and depressive symptoms have been shown to impact the progression of chronic diseases, such as CF, by increasing the likelihood that clients will be less compliant with treatment regimens and partake in risky behaviors (Quittner et al., 2008; Withers, 2012). Hence, we recommend assessing and screening for depressive symptoms frequently and examining the level of disease acceptance in clients with CF. Professional counselors working with children with CF will need to further tailor interventions based on the client’s symptom patterns (Chesson et al., 2004), while accounting for changes typical of childhood development.
Recently, scholars have researched the experiences of adolescents with CF in their transition to adulthood. This turbulent time (Withers, 2012) may need special consideration by professional counselors. Qualitative research on the experiences of adolescents with CF who were transitioning to adulthood generated the following three emerging themes: treatment compliance, health-related problems and future outlook concerning their disease (Berge, Patterson, Goetz, & Milla, 2007). Male participants described being more independent with treatment compliance, whereas females desired an accountability partner for their treatment regimen. Female participants expressed issues with depression, negative body image and fear of diabetes as a complication from CF, whereas males only disclosed their fear of acquiring diabetes as the disease progressed. Interestingly, both male and female participants expressed a positive outlook concerning CF regarding identity and acceptance of the disease (Berge et al., 2007). Identifying and maintaining a positive outlook while dealing with a chronic and debilitating illness can be a challenge for children with CF and their parents and families. Professional counselors working with youth with CF need to consider these findings. Special attention may be given to issues of treatment compliance, further physical complications from CF and maintaining a positive outlook.
Regarding risky behaviors (Quittner et al., 2008), teenagers with CF have admitted to using alcohol and drugs to seek relief from the challenges of CF (Vaeth & Martins, 2015). As such, professional counselors working with children with CF need to tailor interventions to the individuals’ symptom-specific patterns (Chesson et al., 2004) and be mindful of behaviors that may hasten the disease process. The use of alcohol and drugs may hasten the disease’s progression because of the ways in which these substances can interact with the client’s current prescription medication regimen. Alcohol use may result in pancreatitis and a hypoglycemic reaction (Withers, 2012). Likewise, clients who smoke legal and illegal substances contribute to the deterioration of lung functioning. We recommend frequently assessing and screening for substance abuse and depressive symptoms and exploring the level of disease acceptance among youth with CF in creative, developmentally appropriate ways. Importantly, professional counselors preparing counseling interventions for children with CF need to account for the added psychosocial and developmental challenges that are typical in childhood development.
Special Considerations When Counseling Children with Cystic Fibrosis
Many children share similar psychological and developmental needs as they grow (Thompson & Henderson, 2007). However, children with chronic illness may struggle to be emotionally mature, while simultaneously managing the physical symptoms of their conditions (Dahlbeck & Lightsey, 2008). Furthermore, the psychosocial complexities and the chronic nature of CF may create unique challenges for professional counselors providing services to children and their families, such as the deteriorating nature of CF, frequent hospitalizations and the life-threatening prognosis (Frels, Leggett, & Larocca, 2009; Morison, Bromfield, & Cameron, 2003). Counseling professionals’ increased sensitivity to the progression and impact of this disease can help guide their intervening efforts (Chesson et al., 2004) by leading them to consider the physiological and psychological trauma caused by CF. Professional counselors must ensure that they have developed rapport with the child as an individual, instead of a child with a disability (Thompson & Henderson, 2007).
Counseling interventions for children with CF begin with recognizing that children with CF are not adults with CF. Therefore, treatment and counseling efforts need to allow for special consideration of childhood development and understanding (Chesson et al., 2004; Geldard & Geldard, 2008). Chesson et al. (2004) offered suggestions for meeting the needs of children with chronic illnesses through counseling. First, counselors need to obtain the child’s understanding of counseling (e.g., what it is, how it will help, roles, communication). Although parental support and involvement is important when counseling children (Geldard & Geldard, 2008; Morison et al., 2003), relying solely on parental reports is not a replacement for exploring the child’s perspective of counseling (Geldard & Geldard, 2008). Chronic illnesses such as CF impact the whole family system (Kirk et al., 2013). However, within the therapeutic counseling relationship, children with CF must feel as if they are the experts on their lives and their mental health, regardless of age.
Second, counselors working with children should limit the amount of talking they do in session (Chesson et al., 2004) in favor of engaging children through natural modes of expression such as play, drawing and games. We recommend structuring counseling sessions to include discussions alongside an activity, versus a sole reliance on face-to-face conversation, in order to improve rapport building within the therapeutic relationship. Children engaging in healthy interdependent relationships with counselors can begin to develop a sense of independence and trust (Juntunen & Atkinson, 2002) within the counseling process, despite the tumultuous times during the disease progression. The adverse impact of chronic illness on social functioning (Last, Stam, Onland-van Nieuwenhuizen, & Grootenhuis, 2007) can lead to social withdrawal (Dahlbeck & Lightsey, 2008), which can be intensified when there is a concentrated focus on the child via adult approaches to counseling (e.g., making the child the center of attention to discuss his or her illness). As such, we recommend that professional counselors make age-appropriate and developmental adjustments to the counseling session and consider instituting group counseling modalities to counter the regularity of social isolation among these children.
Third, professional counselors developing a therapeutic relationship with a child experiencing CF must incorporate interactions that address the traumatic impact of living with the illness. Children with CF undergo physically stressful and painful experiences during medical treatment. Geldard and Geldard (2008) suggested that professional counselors clarify the nature of counseling and differentiate it from medical treatments. They also suggested maintaining an environment that provides acceptance and invites free disclosure. Professional counselors are urged to explain the distinction between counseling and medical procedures (e.g., there are no needles or painful medical procedures in counseling). Professional counselors also are encouraged to engage children in activities and play to reduce their level of anxiety and guardedness (Chesson et al., 2004). These targeted counseling strategies can promote resiliency factors such as self-efficacy and empowerment so that children may cope with adversity throughout the illness (Dahlbeck & Lightsey, 2008; Luszczynska, Gutiérrez-Doña, & Schwarzer, 2005). Chesson et al. (2004) further suggested that counselors gradually establish the therapeutic relationship over a number of shorter sessions in order to establish trust with the child. We caution against rushing the counseling relationship-building process and encourage professional counselors to listen openly in order to understand the child’s world.
As children struggle with chronic illnesses such as CF, acute emotional reactions are invariably triggered, which may increase the propensity for children to act out in self-injurious ways (Vaeth & Martins, 2015). The counseling process requires consistency and transparency when discussing how a child’s treatment progress will be shared among adults. Accordingly, a fourth special consideration needs to be illuminated—the limits of confidentiality. Professional counselors must illustrate the circumstances when parents will be notified of instances of self-harm or suicidal and homicidal ideation. Given the susceptibility of children with chronic illnesses to depression (Quittner et al., 2008) and suicidal ideation (Barnes et al., 2010), coping with the challenges and effects of CF are constantly in the minds of these children. Rebecca Mueller (2001) illustrated this point as a young person struggling with the illness as follows:
All the information I have about my disease has been dispersed in small pieces over time. The idea that [when] a child with CF reaches a certain age, truth and honest answers should suddenly be given is awful. With the many different sides and aspects of CF or other diseases, the information needs to come out over time, giving the person time to react and contemplate. (p. 43)
Professional counselors working with children with CF understand the need for a collaborative approach in supporting individuals and families experiencing the trauma of chronic illness. Children with chronic diseases are involved with multiple treatment professionals (e.g., dieticians, respiratory therapists, physicians, nurses, case managers, mental health and school counselors). Chesson et al. (2004) recommended that counselors assist children with understanding the decisions made by their parents, doctors and other professionals about their treatment. This task can be done by assessing the child’s knowledge of the disease process and treatment and initiating family sessions or sessions with other health care professionals when warranted. Ultimately, children who protest treatment interventions can be overridden by a caregiver’s decision. When children have a history of adult-driven decisions related to life-preserving medical treatments, this experience can make behavioral counseling interventions difficult. We suggest that counselors make every effort to respect the feelings and wishes of children with CF, including helping to “coordinate services, rearranging physical environments, removing barriers and inconveniences, and securing special equipment and materials” (Thompson & Henderson, 2007, p. 713). Professional counselors can further facilitate this supportive process by empowering children to identify and articulate their perspectives on medical treatments, given their limited choices (Chesson et al., 2004; Morison et al., 2003).
Family Involvement
Family involvement is critical to all aspects of treatment of children with CF, starting with diagnosis. Parents and families are significantly affected when their child is diagnosed with a chronic illness (Anderson et al., 2001; O’Haver et al., 2010). Thompson and Henderson (2007) explained, “The demands for energy, time, and financial resources may add a heavy burden of stress to families” (p. 602). It is essential to note that families and children face myriad stressors related to the “uncertainty and uncontrollability” of chronic illness, along with “restrictions on their freedom” (Last et al., 2007, p. 102). However, family members (particularly parents) are often responsible for providing an environment in which children can develop resiliency and independence. Family members provide a supportive environment and help to promote children’s sense of self-worth and ability to cope with challenging life situations (Juntunen & Atkinson, 2002). These tasks may be especially difficult for parents of children with CF in that they too are more vulnerable to higher incidences of depression (Quittner et al., 2008; Tluczek et al., 2014). Hence, we recommend that professional counselors working with the family system ensure that parents of children with CF have access to the emotional supports necessary to sustain family functioning and equilibrium, including participation in their own counseling as needed (Tluczek et al., 2014). Similarly, professional counselors may find it necessary to provide parent education about the CF disease process in order to help parents identify strategies to enhance resiliency in their child (Juntunen & Atkinson, 2002).
Counseling children with CF involves implementing prolonged and gradual approaches to relationship building, increasing one’s knowledge of the illness, adapting treatment approaches to account for the impact of invasive medical procedures, and involving parents, guardians and other professionals in the counseling process. Above all, honoring the perspective of the child is central to success in counseling this population, which can be easier said than done. The chronic and complex nature of CF and its treatment requires a great deal of effort and presents additional clinical challenges for professional counselors. Over time, the challenges of working with children with special needs can affect the wellness of professional counselors providing services. Therefore, it is important for counselors to recognize the factors contributing to impairment and burnout, particularly among counselors who work with children experiencing chronic illnesses like CF.
A Self-Care Primer for Professional Counselors
Professional counselors and other health professionals engaged in prolonged therapeutic contact with clients with CF are vulnerable to burnout, compassion fatigue and vicarious trauma (Coady, Kent, & Davis, 1990; Lewiston, Conley, & Blessing-Moore, 1981; Savicki & Cooley, 1987), potentially leading to impairment. Counselors have an ethical obligation to recognize their state of wellness and potential impairment (American Counseling Association [ACA], 2011), which may be impacted by burnout, compassion fatigue or vicarious trauma while working with children experiencing chronic conditions (Angerer, 2003; Kalliath, O’Driscoll, Gillespie, & Bluedorn, 2000; Najjar, Davis, Beck-Coon, & Doebbeling, 2009; Sexton, 1999) such as CF. Such occupational risks may be heightened when professionals work with clients with a poor prognosis associated with chronic illness, including CF (Coady et al., 1990).
Counselors and other mental health professionals experience occupational stressors such as long working hours, work with challenging clients, poor interdisciplinary support and poor supervision (Coady et al., 1990). Lewiston et al. (1981) examined burnout among health care providers working with clients experiencing CF. They found high levels of emotional exhaustion and client depersonalization (i.e., a sense of inability to impact clients’ improvement while watching clients’ illness progress), and a lower sense of accomplishment among health care providers working with this population. The implications of these results are intensified because “psychotherapists who work with chronic illnesses tend to disregard their own self-care needs when focusing on the needs of clients” (Figley, 2002, p. 1433).
Children with CF and their families are survivors of both medical and psychosocial traumas. Frequent trips to the emergency room, an inability to breathe, surgeries, and understanding the unpredictable and fatal progression of CF are among the traumas endured by this special population. Professional counselors who hear these traumatic stories within the therapeutic milieu must understand that vicarious trauma can occur for even the most experienced counselor. Sommer (2008) clarified that vicarious traumatization is not inadequacy on behalf of the counselor or emotional damage of the client but can be considered an “occupational hazard” (p. 52). Vicarious trauma, defined as “a traumatic reaction to specific client-presented information” (Trippany, Kress, & Wilcoxon, 2004, p. 32), also may occur among professional counselors working with children who have CF due to the erratic and terminal progression of the illness.
Professional counselors serving the CF community must recognize their vulnerabilities to burnout, compassion fatigue and vicarious trauma. Given the realities of clinical practice and responsibilities of everyday living (e.g., busy schedules, high caseloads, supervision barriers, family responsibilities, maintaining relationships), poor self-care and wellness may be easy to identify but difficult to change. In order to prevent issues of burnout, compassion fatigue and vicarious trauma, the following self-care strategies are suggested for professional counselors who work with this special population.
Self-Care Strategies for Professional Counselors
Although counselors are taught to utilize a developmental and wellness approach when working with clients (Myers & Sweeney, 2005), they often neglect their own health and well-being. Self-care strategies embedded in a wellness philosophy may help to prevent incidences of burnout among those working with the unique emotional and psychosocial stressors affecting children with CF and their families. Myers and Sweeney (2005) identified wellness as both a process and an outcome in that it is an “overarching goal for living and a day-by-day, minute-by-minute way of being” (p. 9). Self-care strategies involve managing stress in ways that limit the impact on the individual (Young, 2005). Within the counseling literature, wellness is depicted as incorporating social, emotional, physical, intellectual and spiritual dimensions (Roscoe, 2009). Counseling wellness models have been empirically supported in the counseling literature (Myers & Sweeney, 2005; Myers, Sweeney, & Witmer, 2000; Sweeney & Witmer, 1991; Witmer & Sweeney, 1992) and inform individuals about methods to limit their stress and maintain a healthy sense of well-being. Hence, we recommend that professional counselors use multidimensional, holistic self-care strategies to maintain a sense of wellness when working with youth experiencing special needs. The following section provides physiological, cognitive and spiritual wellness strategies for professional counselors to use while working with children with CF and other chronic conditions.
Physiological self-care strategies. Professional counselors are accustomed to working with clients regarding wellness and self-care but may not always practice their own healthy suggestions. Self-care strategies that are body-focused may help alleviate the impact of stress (Young, 2005), particularly among those working with children with special needs such as CF. Young (2005) recommended approaches such as progressive relaxation, balanced exercise and nutrition, and adequate rest to assist with integrating a wellness focus and enhancing self-care. A healthy diet and physical activity are readily known to prevent physical and mental health conditions, while also increasing energy levels. Furthermore, “minding the body” and having adequate sleep and bodily rest are additional suggestions for restoring self-care as a priority for professional counselors (Norcross & Guy, 2007, pp. 64–65). Professional counselors interested in implementing physiological self-care strategies to address potential issues of vicarious trauma while working with children diagnosed with CF may consider simple tasks such as taking a brisk walk during their lunch break, joining a gym, or being more intentional with their diet and bedtime routines. In addition to focusing on physical health and wellness, self-care in the cognitive domain is equally important for fostering a sense of well-being.
Cognitive self-care strategies. Stress from occupational risks accumulated through working with youth with special needs may be further prevented if counselors utilize cognitive approaches to support their own self-care. Professional counselors interested in improving their self-care in cognitive ways may consider cognitive restructuring to formulate new thinking patterns and assertiveness training to bring about direct changes in behaviors that may have been impacted by stress (Young, 2005), which often accumulates during the long-term therapeutic relationship with children and families affected by CF. Moreover, the use of guided imagery may provide both cognitive and physical benefits in helping to create a cognitive break from daily stress inside and outside the workplace. Notably, cognitive self-care strategies begin with self-monitoring, insight and self-awareness (Norcross & Guy, 2007). Despite counselors’ close therapeutic connection to clients with CF and their families, healthy boundaries are imperative to prevent issues of burnout and compassion fatigue. Norcross and Guy (2007) noted that “setting boundaries consistently emerges in the research as one of the most frequently used and one of the most highly effective self-care principles” (p. 94). Due to counselors’ innate desire to help others, they often take on too many clients or are mandated to do so by agency policies. Counselors may provide extra time to ancillary responsibilities and have unrealistic expectations of themselves. As such, we recommend that professional counselors obtain good supervision to help manage and maintain work–life balance, particularly when working with children with special needs. In addition to the benefits of physical and cognitive self-care strategies, spirituality also has been shown to enhance levels of wellness and thus decrease the potential for burnout and compassion fatigue.
Spiritual self-care strategies. Spirituality comes in many forms and there is no finite definition of how one engages in his or her spiritual self. Many counselors and psychotherapists identify their own career path as a calling to care for others and commitment to growth and self- knowledge (Norcross & Guy, 2007). Research supports that spirituality, prayer and meditation are positive manners in which to promote wellness and augment self-care (Cashwell, 2005). Spiritual beliefs, practices and experiences are intricately connected and may continue to foster support from communities and individuals, along with reinforcing healthy emotions. While working with children experiencing the later stages of CF, professional counselors’ spirituality may help them connect with clients on a more meaningful level. Taking a spiritual perspective can further shape counselors’ perspective on life events (Young, 2005), particularly when they are grieving the death of a child with CF. In seeking a spiritual connection to a higher power, the negative responses to stressful events may be limited (Young, Cashwell, & Shcherbakova, 2000), strengthening one’s wellness and ability to care for oneself. These actions, along with discussing spirituality with the child and family affected by CF, may further model healthy practices during difficult times in the disease process.
Spiritual self-care can include the use of mindfulness, which can be viewed as the nonjudgmental awareness of one’s own inner suffering (Birnie, Speca, & Carlson, 2010) and reflections on self-compassion (Neff, 2003). Birnie et al. (2010) described self-compassion as the awareness of “feelings of caring and kindness towards oneself in the face of personal suffering” and the “recognition that one’s suffering, failures, and inadequacies are part of the human condition” (p. 2). When counseling children with CF, professional counselors may consider routinely expressing self-compassion as part of their inner dialogue. The following mantra used by the second author may be of assistance to professional counselors implementing spiritual self-care:
Suffering is part of life. My clients suffer, but did not choose this illness. They are walking in its wake and I will walk alongside them. I will extend loving kindness in all the work I do, despite the pain and suffering I experience and witness.
We highlight the following three essential components of self-compassion: (a) extending kindness and understanding toward oneself rather than harsh judgments or criticism, (b) recognizing that suffering (even chronic illness) is a part of the larger human condition, and (c) not overidentifying with the awareness of one’s painful thoughts (Birnie et al., 2010; Neff, 2003). By engaging in self-compassion and mindfulness, professional counselors may help to prevent incidences of compassion fatigue while working with children and families affected by CF by recognizing that this illness has a role in their humanity.
Conclusion
Professional counselors working with children and families affected by CF should consider the physical and psychosocial challenges facing this special-needs population. With the discouraging nature of the disease progression, professional counselors must have a basic understanding of the client’s chronic condition (Thompson & Henderson, 2007) and how the progression of the illness affects the child’s emotional state. Professional counselors must further explore how to limit the impact of occupational stress that may lead to burnout, compassion fatigue and vicarious trauma. This article provides a primer on the physiological, psychosocial and special needs specific to youth with CF and offers targeted self-care strategies for professional counselors. Children with CF are a special population and professional counselors are called to implement these special considerations in their thoughtful practice. There is an abundance of literature examining the physiological aspects of CF (CFF, 2014a; Pearson et al., 1991; Sawicki et al., 2009; Sawicki & Tiddens, 2012). However, more research is warranted to examine the salient factors that affect the therapeutic relationship between professional counselors and children with CF. Meanwhile, professional counselors can develop and implement individualized, multidimensional self-care strategies to counter the effects of this difficult yet rewarding work.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of
interest or funding contributions for
the development of this manuscript.
References
American Counseling Association. (2011). ACA’s taskforce on counselor wellness and impairment. Retrieved from http://www.counseling.org/knowledge-center/counselor-wellness
Anderson, D. L., Flume, P. A., & Hardy, K. K. (2001). Psychological functioning of adults with cystic fibrosis. Chest, 119, 1079–1084.
Angerer, J. M. (2003). Job burnout. Journal of Employment Counseling, 40, 98–107.
doi:10.1002/j.2161-1920.2003.tb00860.x
Barnes, A. J., Eisenberg, M. E., & Resnick, M. D. (2010). Suicide and self-injury among children and youth with chronic health conditions. Pediatrics, 125, 889–895. doi:10.1542/peds.2009-1814
Berge, J. M., & Patterson, J. M. (2004). Cystic fibrosis and the family: A review and critique of the literature. Families, Systems and Health, 22, 74–100. doi:10.1037/1091-7527.221.74
Berge, J. M., Patterson, J. M., Goetz, D., & Milla, C. (2007). Gender differences in young adults’ perceptions of living with cystic fibrosis during the transition to adulthood: A qualitative investigation. Families, Systems, and Health, 25, 190–203. doi:10.1037/1091-7527.25.2.190
Birnie, K., Speca, M., & Carlson, L. E. (2010). Exploring self-compassion and empathy in the context of mindfulness-based stress reduction (MBSR). Stress and Health, 26, 359–371. doi:10.1002/smi.1305
Blum, R. W. (1992). Chronic illness and disability in adolescence. Journal of Adolescent Health, 13, 364–368. doi:10.1016/1054-139X(92)90029-B
Bregnballe, V., Thastum, M., & Schiøtz, P. O. (2007). Psychosocial problems in children with cystic fibrosis. Acta Pædiatrica, 96, 58–61. doi:10.1111/j.1651-2227.2006.00014.x
Canning, E. H., Haner, S. B., Shade, K. A., & Boyce, W. T. (1992). Mental disorders in chronically ill children: Parent-child discrepancy and physician identification. Pediatrics, 90, 692–696.
Cashwell, C. S. (2005). Spirituality and wellness. In J. E. Myers & T. J. Sweeney (Eds.), Counseling for wellness: Theory, research, and practice (pp. 197–205). Alexandria, VA: American Counseling Association.
Casier, A., Goubert, L., Huse, D., Theunis, M., Franckx, H., Robberecht, E., . . . Crombez, G. (2008). The role of acceptance in psychological functioning in adolescents with cystic fibrosis: A preliminary study. Psychology and Health, 23, 629–638. doi:10.1080/08870440802040269
CF Living. (2014). About CF. Retrieved from http://www.cfliving.com/newly-diagnosed/living-with-cf/about-cf.jsp
Chesson, R. A., Chisholm, D., & Zaw, W. (2004). Counseling children with chronic physical illness. Patient Education and Counseling, 55, 331–338. doi:10.1016/j.pec.2003.04.002
Coady, C. A., Kent, V. D., & Davis, P. W. (1990). Burnout among social workers working with patients with cystic fibrosis. Health and Social Work, 15, 116–124.
Cystic Fibrosis Foundation. (2014a). About cystic fibrosis. Retrieved from http://www.cff.org/AboutCF/
Cystic Fibrosis Foundation. (2014b). Newborn screening: Info for new parents. Retrieved from http://www.cff.org/AboutCF/Testing/NewbornScreening/
Dahlbeck, D. T., & Lightsey, O. R., Jr. (2008). Generalized self-efficacy, coping, and self-esteem as predictors of psychological adjustment among children with disabilities or chronic illnesses. Children’s Health Care, 37, 293–315. doi:10.1080/02739610802437509
Figley, C. R. (2002). Compassion fatigue: Psychotherapists’ chronic lack of self care. Journal of Clinical Psychology, 58, 1433–1441. doi:10.1002/jclp.10090
Frels, R. K., Leggett, E. S., & Larocca, P. S. (2009). Creativity and solution-focused counseling for a child with chronic illness. Journal of Creativity in Mental Health, 4, 308–319. doi:10.1080/15401380903372646
Geldard, K., & Geldard, D. (2008). Counselling children: A practical introduction (3rd ed.). London, England: Sage.
Hayes, D., Jr., Anstead, M. I., Warner, R. T., Kuhn, R. J., & Ballard, H. O. (2010). Inhaled morphine for palliation of dyspnea in end-stage cystic fibrosis. American Journal of Health-System Pharmacy, 67, 737–740.
doi:10.2146/ajhp080188
Juntunen, C. L., & Atkinson, D. R. (Eds.). (2002). Counseling across the lifespan: Prevention and treatment. Thousand Oaks, CA: Sage.
Kalliath, T. J., O’Driscoll, M. P., Gillespie, D. F., & Bluedorn, A. C. (2000). A test of the Maslach burnout inventory in three samples of healthcare professionals. Work and Stress, 14, 35–50. doi:10.1080/026783700417212
Kirk, S., Beatty, S., Callery, P., Gellatly, J., Milnes, L., & Pryjmachuk, S. (2013). The effectiveness of self-care support interventions for children and young people with long-term conditions: A systematic review. Child: Care, Health and Development, 39, 305–324. doi:10.1111/j.1365-2214.2012.01395.x
Last, B. F., Stam, H., Onland-van Nieuwenhuizen, A.-M., & Grootenhuis, M. A. (2007). Positive effects of a psycho-educational group intervention for children with a chronic disease: First results. Patient Education and Counseling, 65, 101–112. doi:10.1016/j.pec.2006.06.017
Lewiston, N. J., Conley, J., & Blessing-Moore, J. (1981). Measurement of hypothetical burnout in cystic fibrosis caregivers. Acta Pædiatrica, 70, 935–939. doi:10.1111/j.1651-2227.1981.tb06254.x
Lowton, K., & Gabe, J. (2003). Life on a slippery slope: Perceptions of health in adults with cystic fibrosis. Sociology of Health and Illness, 25, 289–319. doi:10.1111/1467-9566.00348
Luszczynska, A., Gutiérrez-Doña, B., & Schwarzer, R. (2005). General self-efficacy in various domains of human functioning: Evidence from five countries. International Journal of Psychology, 40, 80–89. doi:10.1080/00207590444000041
Morison, J. E., Bromfield, L. M., & Cameron, H. J. (2003). A therapeutic model for supporting families of children with a chronic illness or disability. Child and Adolescent Mental Health, 8, 125–130. doi:10.1111/1475-3588.00058
Mueller, R. (2001). The child’s perspective. In M. Bluebond-Langner, B. Lask, & D. B. Angst (Eds.), Psychological aspects of cystic fibrosis (pp. 37–44). New York, NY: Arnold.
Myers, J. E., & Sweeney, T. J. (Eds.). (2005). Counseling for wellness: Theory, research, and practice. Alexandria, VA: American Counseling Association.
Myers, J. E., Sweeney, T. J., & Witmer, J. M. (2000). The wheel of wellness counseling for wellness: A holistic model for treatment planning. Journal of Counseling & Development, 78, 251–266. doi:10.1002/j.1556-6676.2000.tb01906.x
Najjar, N., Davis, L. W., Beck-Coon, K., & Doebbeling, C. C. (2009). Compassion fatigue: A review of the research to date and relevance to cancer-care providers. Journal of Health Psychology, 14, 267–277. doi:10.1177/1359105308100211
Neff, K. (2003). Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and Identity, 2, 85–102. doi:10.1080/15298860309032
Norcross, J. C., & Guy, J. D., Jr. (2007). Leaving it at the office: A guide to psychotherapist self-care. New York, NY: Guilford Press.
O’Haver, J., Moore, I. M., Insel, K. C., Reed, P. G., Melnyk, B. M., & Lavoie, M. (2010). Parental perceptions of risk and protective factors associated with the adaptation of siblings of children with cystic fibrosis. Pediatric Nursing, 36, 284-–292.
Pearson, D. A., Pumariega, A. J., & Seilheimer, D. K. (1991). The development of psychiatric symptomatology in patients with cystic fibrosis. Journal of the American Academy of Child & Adolescent Psychiatry, 30, 290–297.
Quittner, A. L., Barker, D. H., Snell, C., Grimley, M. E., Marciel, K., & Cruz I. (2008). Prevalence and impact of depression in cystic fibrosis. Current Opinion in Pulmonary Medicine, 14, 582–588. doi:10.1097/MCP.0b013e3283121cf1
Roscoe, L. J. (2009). Wellness: A review of theory and measurement for counselors. Journal of Counseling & Development, 87, 216–226. doi:10.1002/j.1556-6678.2009.tb00570.x
Savicki, V., & Cooley, E. (1987). The relationship of work environment and client contact to burnout in mental health professionals. Journal of Counseling & Development, 65, 249–252.
Sawicki, G. S., Sellers, D. E., & Robinson, W. M. (2009). High treatment burden in adults with cystic fibrosis: Challenges to disease self-management. Journal of Cystic Fibrosis, 8, 91–96. doi:10.1016/j.jcf.2008.09.007
Sawicki, G. S., & Tiddens, H. (2012). Managing treatment complexity in cystic fibrosis: Challenges and opportunities. Pediatric Pulmonology, 47, 523–533. doi:10.1002/ppul.22546
Sexton, L. (1999). Vicarious traumatisation of counsellors and effects on their workplaces. British Journal of Guidance and Counselling, 27, 393–403. doi:10.1080/03069889908256279
Sidell, N. L. (1997). Adult adjustment to chronic illness: A review of the literature. Health & Social Work, 22, 5–11. doi:10.1093/hsw/22.1.5
Sommer, C. A. (2008). Vicarious traumatization, trauma-sensitive supervision, and counselor preparation. Counselor Education and Supervision, 48, 61–71. doi:10.1002/j.1556-6978.2008.tb00062.x
Sweeney, T. J., & Witmer, J. M. (1991). Beyond social interest: Striving toward optimum health and wellness. Individual Psychology: The Journal of Adlerian Theory, Research & Practice, 47, 527–540.
Thompson, C. L., & Henderson, D. A. (2007). Counseling children (7th ed.). Belmont, CA: Thomson.
Thompson, R. J., Jr., Hodges, K., & Hamlett, K. W. (1990). A matched comparison of adjustment in children with cystic fibrosis and psychiatrically referred and nonreferred children. Journal of Pediatric Psychology, 15, 745–759. doi:10.1093/jpepsy/15.6.745
Tluczek, A., Laxova, A., Grieve, A., Heun, A., Brown, R. L., Rock, M. J., . . . Farrell, P. M. (2014). Long-term follow-up of cystic fibrosis newborn screening: Psychosocial functioning of adolescents and young adults. Journal of Cystic Fibrosis, 13, 227–234. doi:10.1016/j.jcf.2013.10.001
Trippany, R. L., Kress, V. E. W., & Wilcoxon, S. A. (2004). Preventing vicarious trauma: What counselors should know when working with trauma survivors. Journal of Counseling & Development, 82, 31–37. doi:10.1002/j.1556-6678.2004.tb00283.x
Vaeth, S., & Martins, L. (2015). Teens, cystic fibrosis and emotional health. Retrieved from http://cfcenter.stanford.edu/teens/CysticFibrosisandEmotionalHealth_000.html
Withers, A. L. (2012). Management issues for adolescents with cystic fibrosis. Pulmonary Medicine, 2012, 1–10. doi:10.1155/2012/134132
Witmer, J. M., & Sweeney, T. J. (1992). A holistic model for wellness and prevention over the life span. Journal of Counseling & Development, 71, 140–148.
Young, J. S. (2005). A wellness perspective on the management of stress. In J. E. Myers & T. J. Sweeney (Eds.), Counseling for wellness: Theory, research, and practice (pp. 207-–215). Alexandria, VA: American Counseling Association.
Young, J. S., Cashwell, C. S., & Shcherbakova J. (2000). The moderating relationship of spirituality on negative life events and psychological adjustment. Counseling and Values, 45, 49–57.
Cassandra A. Storlie, NCC, is an Assistant Professor at Kent State University. Eric R. Baltrinic is an Assistant Professor at the University of Toledo. Correspondence may be addressed to Cassandra Storlie, 310 White Hall, PO Box 5190, Kent, OH 44242, cstorlie@kent.edu.
Mar 1, 2015 | Article, Volume 5 - Issue 2
Sherry Richmond-Frank
This article, written by a parent of an adult child with spina bifida, invites counselors into the life experiences of children with handicaps and their families. The description of these experiences highlights current problems with the stigma this population experiences. The author describes the varying disability identities and orientations that have evolved within the disability culture and wider society. Counselors are encouraged to use unbiased terminology in both research and clinical work with children with disabilities. Solutions are offered for counselors to implement in practice and research to further overcome stereotypes, develop disability awareness and provide helpful counseling. The author provides practical interventions for a variety of challenges where counselors may be useful to children with disabilities and their families.
Keywords: children, disabilities, stereotypes, stigma, handicaps
I am a counselor, a life coach and the parent of an individual with a disability. Since entering the disability community 28 years ago with the birth of my daughter, I have attended both workshops and seminars designed to assist parents concerning children with disabilities or chronic illness. In 2005, I attended eight monthly sessions of Partners in Policymaking, a national leadership training program for people with developmental disorders and family members of young children with disabilities, designed to achieve productive partnerships between people needing and using services and those who make public policy and laws. In this article, I provide information about children with disabilities and their family systems and offer recommendations for counselors working with children with disabilities and their families.
Disability Identity and Orientation
I use the term disability in this article, while the preferable word to describe differences is variation, a more neutral term that lacks negative connotations for children in society. Variations provide richness and diversity in life that can be noted without being denigrated or overemphasized. Depending on how children or adults identify with and orient themselves to the impact of their disabilities, both personally and with respect to society at large, they may have varying preferences for acceptable terms. The reader can consult Gilson and DePoy (2004) for a discussion on disability identities and orientations.
The saying “Nothing about us without us” is an informal one within the disability community. Hahn (1993), a social scientist with over 10 years of research experience in the disability field and personal experience using crutches and a wheelchair since the age of 6, has spoken of a minority model of disability that has its origins in a sociopolitical model. This model arose when individuals with non-transient or lifelong disabilities stated that research using prior models did not seem relevant to their lived experience. Thus, policies and services that arose from these models did not result in meaningful life improvements. Attitudinal variation has arisen within the disability subculture regarding identities and orientations toward disabilities. A sociological ideology for conceptualizing individuals with disabilities and their families has emerged, which varies from the older entrenched medical model that regards disability as illness, tragedy or a negative situation requiring treatment and rehabilitation. Using the medical model, people with disabilities and their families are conceptualized based on their acceptance of and adaptation to disabilities. The sociological model focuses on the larger society or system and its reaction to the individual, rather than examining the person with the disability as the identified patient. Impairment and dysfunction are conceptualized as part of the larger system, with its handicapping environment and public attitudinal barriers, rather than within the individual who has varying abilities and is referred to by this larger system as a person with a disability.
A wide range of models have evolved to the point that Darling (2003) proposed an exploration of disability orientations that include normalization, crusadership, affirmation, isolated affirmation, situational identification, resignation and apathy. Familiarity with these orientations will help counselors understand the disability identities and orientations of their clients and their family members. It is beneficial to acquire a clearer understanding of disabilities and their actual rather than imagined impact on clients in order to improve one’s diversity awareness.
Eliminating Ableism and Pity
Professionals entering the multilayered maze of counseling children with disabilities must honestly explore their positive and negative preconceptions about people with disabilities. Counselors should understand and confront ableism, defined as “the discrimination or prejudice against individuals with disabilities” (Ableism, 2015). Furthermore, counselors should examine and challenge their own disability stereotypes prior to entering the counseling room with clients impacted by disability. Scope (2014), a disability-related charity in the United Kingdom, challenges ableism in the initiative “End the Awkward” found on the their website (http://www.scope.org.uk/awkward). This site allows readers to take an informal quiz to see if they are an “ambassador of cool” or a “captain awkward” around people with disabilities and also a link to watch short television advertisements designed to decrease awkwardness around individuals with disabilities. Helping professionals need to internally clarify the distinction between empathy and sympathy. Counselors can invite open discussion about the disability, as they would invite clients to share information about any subculture, so they feel free to clarify pertinent aspects of their lives and disability in counseling that might otherwise go unaddressed.
Helping professionals also should use non-handicapping language to affirm the individuality and personhood of clients. The Publication Manual of the American Psychological Association (American Psychological Association, 2010) has provided the following recommendations for unbiased terminology in research and academic writing:
The overall principle for “nonhandicapping language” is to maintain the integrity (worth) of all individuals as human beings. Avoid language that objectifies a person by her or his condition (e.g., autistic, neurotic), that uses pictorial metaphors (e.g., wheelchair bound or confined to a wheelchair), that uses excessive and negative labels (e.g., AIDS victim, brain damaged), or that can be regarded as a slur (e.g., cripple, invalid). Use people-first language, and do not focus on the individual’s disabling or chronic condition (e.g., person with paraplegia, youth with autism). Also use people-first language to describe groups of people with disabilities. For instance, say people with intellectual disabilities in contrast to the retarded (University of Kansas, Research and Training Center on Independent Living, 2008).
Avoid euphemisms that are condescending when describing individuals with disabilities (e.g., special, physically challenged, handi-capable). Some people with disabilities consider these terms patronizing and offensive. When writing about populations with disabilities or participants, emphasize both capabilities and concerns to avoid reducing them to a “bundle of deficiencies” (Rappaport, 1977). Do not refer to individuals with disabilities as patients or cases unless the context is within a hospital or clinical setting. (p. 76)
Children with Disabilities and the Family System
The family of a newborn diagnosed with a disability attempts to become acquainted with the infant and gain parenting skills, while still in a bustling neonatal intensive care unit. The family may be experiencing what McHugh (1968) called anomie, which is the idea that life is no longer normal, does not make sense, and is out of one’s control. The family’s experience may include focusing on the physician’s words, hearing the startling news that their child is receiving the diagnosis of lifelong disability, and considering what impact the disability will have on their child and family. Simultaneously, numerous specialists and nurses may be verbally giving the parents large amounts of vital, unfamiliar information in complex medical terminology, while evaluating how the parents are adjusting. The parents may be asked to make urgent life-altering medical decisions about surgeries that will affect their child’s well-being. Helping professionals must realize that parents need time to adapt to this life-changing situation.
Normalization
Parents who have not lived with a disability as a part of their lives need time to absorb the impact of the disability on their child and family as they move through anomie into the period that Seligman and Darling (2007) called normalization and resume the activities that were punctuated by the adjustment to the disability. Families acclimate to a new normal that contains a member with a disability. Gradually parents become capable of a knowledgeable dialogue with the medical community and may even inform physicians of promising treatments for their child, eventually realizing that they and their child(ren) are capably managing the practicalities of the disability, gaining needed services, and coping when unexpected changes and challenges arise.
During normalization, family members strive to help each other, and they build satisfying experiences and memories as they travel through the family life cycle. This process is neither easy nor quick; it can be gut-wrenchingly painful. However, it can produce much personal growth, the shifting of previously held values and priorities, and the satisfaction of a job well done. The process of normalization is not, as some assume, an insurmountable burden to bear, but rather a growth-producing challenge that can be met, sometimes joyfully. Counselors should beware of assuming that all children with disabilities and their families contain pathology. Many families have the internal and external resources to adapt to the disability over time without the need for professional intervention. Helping professionals should avoid referring to these families and children as special, as this term minimizes and unintentionally disrespects the effort required by ordinary people who face extraordinary challenges while meeting the other demands of daily living.
Parents’ Adjustment to the Diagnosis
People assume that parents whose children receive a disability diagnosis at birth are grieving the loss of an ideal perfect child. I suggest that the parents have grown to love the child prenatally and are grieving what their actual child is experiencing or may experience throughout life. The parents may struggle with the pain of relaying the diagnosis to siblings, grandparents and extended family members. Olshansky (1962), one of the initial researchers of families of children who have cognitive disabilities, recommended that chronic grief is an expected reaction of a caring parent to parenting a child with a disability and much more useful than the oversimplified idea of acceptance or rejection.
Some developmental disabilities are discovered prenatally or shortly after birth, or result from premature birth. Some disabilities are diagnosed later in childhood, as parents notice missed developmental milestones or the child loses previously-acquired skills through illness, accident or physical abuse. Other parents may suspect a disability in their child prior to receiving an official diagnosis. Counselors should remember that the pang of sadness a parent may feel when his or her child misses a developmental milestone or experiences social stigma is normal and does not mean that parents are coping poorly.
Parents who are trying to be hopeful are not necessarily denying the disability. Automatically applying diagnoses from the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, 2013) to the parent’s reaction to an initial diagnosis of disability in their child can add additional stress to the family system. Family members of children with disabilities may be inclined toward mental health difficulties that do not interfere with normal life functioning until the additional stress of the disability and the requirements for managing it overload the person’s coping skills, either temporarily or over time. The process of normalization takes time to unfold. Helping professionals should build a caring relationship with the family at the time of diagnosis and be available later if mental health issues begin to interfere with normal functioning. Counselors should use their clinical skills of differential diagnosis to understand and unearth the interplay between the parent’s orientation to disability and his or her conceptualization of disability identity to avoid framing a mindset as a mental health disorder.
The child’s parents or siblings may have psychiatric diagnoses or relational difficulties that predate the child’s disability diagnosis. Such issues may interfere with family resilience and the process of normalizing the disability and promoting healthy child development. Addictions, anxiety, depression, adult attention-deficit/hyperactivity disorder and other diagnoses can impede parental well-being and effective parenting. Thompson and Gustafson (1996) suggested that improved child development and adaptation to chronic childhood illness are associated with parental social support, adjustment and decreased stress. Elman (1991) suggested the need for counseling depressed family members. Crnic and Greenberg (1990) indicated that decreased competence in children is related to parental personal stress that interferes with effective parent–child communication. After many years of counseling families, I have come to believe that the family system can operate more smoothly if the individual members address mental health issues that impede marital satisfaction, family cohesion, conflict resolution, stress management, child rearing, medical management and other positive coping skills.
The birth order of a child with a disability can change the future family structure as the parents contemplate whether to have additional children. If the child with a disability is the parents’ firstborn and the disability has a genetic component, additional children may share the same disability, in a milder or more severe form. Parents may consult geneticists to explore the probabilities of a recurrence of the disability while they consider their ability to incorporate various scenarios into their lives. Childhood disabilities have direct and indirect psychosocial and financial costs for families. Seligman and Darling (2007) discussed direct costs of adaptive equipment, therapy and child care, and indirect costs like fees for housing modifications, work absences, and parental difficulty for career advancement. Sometimes one parent chooses not to work outside the home in order to be available for tasks related to managing the disability, a decision that reduces the family’s income. Regardless of the counselor’s or geneticist’s viewpoints, the decision to pursue additional children can be a complex, grueling decision for individuals whose convictions do not give them the option of attempting to conceive and then terminating a life prenatally if a disability is detected, especially for parents who already love a prior child with that or another disability.
Self-Concept Development among Children with Disabilities
The child with the disability develops opinions about the family and himself or herself. Children create a sense of self from the reflections they see in their interactions with others. Unfortunately, people with cognitive, emotional or physical differences encounter distorted mirrors daily. The communication they have with others often is filtered through an unspoken screen of ableism and stigma. In Disability Is Natural: Revolutionary Common Sense for Raising Successful Children with Disabilities, Snow (2001) described the Euro-American history of disability and myths. When the child encounters a person who has not had close friendships with anyone with disabilities, the person may display uncomfortable, awkward behavior around the child. The person may stare, avoid eye contact, treat the child with pity, act like the child is “special,” speak to the parents instead of the child or act in other confusing ways that pose barriers to intimacy. Children with disabilities sometimes do not question the interpretations of others and may begin to believe that anomalies are bad and that they are inherently bad, rather than just different. Children with disabilities also may not realize that the awkwardness in the room arises from discomfort in the other person and may wonder what is wrong with them.
Though people with disabilities are a natural part of society, they continually encounter barriers to full participation in society. In a society containing environmental and attitudinal barriers—for example, the lack of ramps or curb cuts necessary for people in wheelchairs to navigate their community—the simplest of tasks can be continually inconvenient.
Counselors must recognize that the disability is the child’s constant companion, 24 hours a day, 7 days a week, which may include a complex medical condition that affects various parts of the body and its functions, possibly resulting in pain. The vocabularies of children with disabilities may include medical terminology and treatments that are complicated to understand and time consuming to accomplish. The child may have a visible disability that is always on display for others’ comments and stares; alternatively, the child may have a disability that is hidden and misinterpreted by people in the community. Until one accompanies a person with a visible disability in public, one does not even realize what a luxury it is to go about daily tasks without others stopping to look for extended amounts of time with expressions of wide-eyed shock or curiosity. Counselors can teach children without disabilities to react less awkwardly around children who have disabilities.
Counselors should remember that each child and family is unique, but be aware that children with disabilities are more like children without disabilities than they are different. They simply vary in some way. The child may be in counseling because of internal challenges resulting from the disability or external emotional, social, attitudinal, educational or physical barriers to inclusion. However, the child may be in counseling for a difficulty that would arise even if there were no disability. It is helpful for children with disabilities to realize that some of the struggles they encounter are common to all children.
The Emotional Toll of Services
Community services, such as Respite Care and Individual Education Plans, are available to assist children with disabilities and their families with some of the challenges presented by the disability. People are vetted to see if they qualify for services and terms from the medical model of disability are utilized. Unfortunately, in order to receive services designed to maximize potential, children with disabilities must interact with agency staff members who discuss and emphasize deficits and rehabilitation in their presence. Children with disabilities may find the language and terminology insulting and demoralizing, considering that they have not had an accident and do not feel the need to be compared or repaired.
The disability subculture is not homogenous. Developmental disabilities include spina bifida, cerebral palsy, diseases of the muscles and bones, neurological disorders, craniofacial deformities, metabolic disorders, endocrine disorders, seizure disorders, cleft palate, cleft lip, visual impairment and blindness, hearing impairment and deafness, mental retardation, attention-deficit/hyperactivity disorder, learning disabilities, autism, chromosome and genetic disorders, and numerous others, including those that are extremely rare and possibly unnamed. Children and families in these various subgroups have some experiences in common and other distinct differences due to the various traits, challenges, onset and societal reactions to their particular disabilities.
Complex Client Group
Counseling children with developmental disabilities is like working a complex three-dimensional puzzle. Each individual child is as distinctive as a fingerprint. The child is a member of a family that has its own characteristics, rules and roles. The child and his or her family members’ temperaments affect reactions to a disability. Within any given family, there may be varying opinions among members about how to handle the disability or avoid dealing with it, which can impact family interactions. Children with handicaps come from a variety of ethnic cultures and heritages that influence the adjustment of the family members’ reactions to the child’s differences.
Spirituality
Counselors should not underestimate the benefits that some children with disabilities and their families derive from strong connections to their faith or other forms of spirituality, if they are not part of a religious community. Seligman and Darling (2007) wrote that some religious communities contribute a great deal of support to the families of children with disabilities. Poston and Turnbull (2004) discovered that other families have difficulty finding a religious group that will incorporate their child and family into the faith community. They reported that having a child with a disability, at times, is the precipitating factor to the development of spirituality in family members. Schiele (2000) and Parham (2002) proposed that aspects of the Afrocentric service models are beneficial when working with African Americans since these models incorporate interdependence, collectivity, affect and spirituality. These benefits may be generalizable to other ethnic groups. McCarthy (1995) encouraged counselors to explore and use spiritual ideas and techniques to benefit the physical and mental well-being of clients.
Belief in a benevolent power or ideological concept can sustain exhausted, discouraged individuals when situations are beyond their control despite their sincere proactive efforts. During those moments when they feel that they cannot continue without despair, they can let go and allow God, a higher power or whatever spirituality they cling to for sustenance intervene. For example, when sending their day-old neonate into spinal surgery, religious parents may draw comfort from the belief that a divine being continues with their infant and the surgeon beyond the operating room doors that separate them from their child. Children whom physicians predict will die continue against all scientific evidence to live and thrive; sometimes parents have supernatural theories about these outcomes. Turnbull, Turnbull, Erwin, and Soodak (2006) referred to spirituality as the way that people derive meaning in their lives and interact with the sacred. According to Skinner, Correa, Skinner, and Bailey (2001), spirituality can influence whether a family considers the addition of a member with a disability to be a blessing or retribution for an offense (Chan, 1998; Chan & Lee 2004; Rolland, 2003). Frisco (as cited in Seligman & Darling, 2007) indicated that the majority of the grandparents surveyed reported that religion and belief in God helped them more comfortably accept a disability in their grandchild.
Multiple Interconnecting Systems
The child and his or her family have multiple interconnecting systems to navigate, while attempting to achieve the normal activities of being a family and helping the child accomplish typical developmental tasks, without reducing this goal to a tedious, life-draining behavioral chart that devalues the child’s personhood and the spontaneity and freedom of childhood. Nichols (1984) considered an open system to be a group of interconnected parts of a whole that interact with each other and the larger environment around information, material and energy. General systems theory and cybernetics provide concepts that assist counselors in studying the multiple elements that constitute the collective experience of living with a disability. These systems may include physicians, therapists, schools, tutors, insurance companies, respite care services, disability advocacy and support groups, community activities, neighbors, playmates, extended family, and other groups of people who make up the ever-evolving gears of an interacting environment that contains the child and his or her nuclear family subsystem. Miller (1995) affirmed that a well-functioning psychosocial environment is vital to the child’s healthy maturation, and counselors can work with children and their families to reduce feelings of being overwhelmed.
Disabilities are not as inherently stressful as what parents go through while trying to help their child with optimal growth and development. Acquiring adaptive equipment, services, educational accommodations and community participation can be tedious and frustrating. Parents often are required to contact busy physicians, educators, automated insurance provider telephone messages and agency coordinators to get documentation for equipment that they need in order to accomplish simple tasks that the dominant culture takes for granted. Normal activities like comfortable body positioning, eating, toileting, ambulating and being integrated into school classrooms can be prolonged, inordinately exhausting, emotionally draining and time consuming.
Once services and equipment are acquired, the family unit may become part of a large, complex, constantly evolving system including, depending on the particular disability, educators, adapted physical educators, therapists (e.g., physical, occupational, speech, respiratory), tutors, dieticians and medical specialists (e.g., pediatricians, gastroenterologists, orthopedic surgeons, cardiologists, urologists, audiologists). Many disabilities require adaptive equipment that is initially unfamiliar to the family. Medical professionals tell parents and their children about assistive health devices that others with similar disabilities have found helpful. The family may need time to adjust to the reality that their child has to use the device, to examine the risks and benefits of equipment and treatments for the disability, and to find someone who provides the service locally.
Health devices are often expensive and must be paid for through insurance, government programs or private payments. Obtaining the equipment may be a lengthy, convoluted process that involves repeated negotiation with insurance providers and resubmitting payment requests or searching out alternative funding sources if insurance payment is denied. Once the adaptive equipment arrives, there are often therapy appointments to individualize the fit of the equipment to the child, teach the parents and child how to use the product, coax the child to use the aids, and check to see that the product is doing no harm to the child. It can take weeks of trial and error to modify equipment that is problematic. This process may repeat often as the child grows older.
Children may want to participate in activities that are outside the realm of the Americans with Disabilities Act. Parents may find themselves having to reassure and encourage the people who run these programs to include their child. This process may involve educating Scout leaders, religion teachers, preschool staff, parents of the child’s classmates, camp staff and others about the disability and how to make modifications to include the child, and also may involve calming fears that it will be too difficult for the staff or the child to manage or too dangerous for the child to participate. Most children with limitations want the same independent adventure opportunities as other children; to try new experiences; risk, fail, try again and succeed; and sometimes surpass others’ expectations for them.
It is important to help families see that their child needs to be surrounded by a support system that has challenged negative assumptions about people with disabilities. Children with an observable disability do not have the gift of anonymity that most people take for granted. They need comfortable places to just be themselves, recharge emotionally and exist as a member of the group. They need the enduring support and friendship from others who are easy, normal and natural in their interactions with the children, to inoculate them against assaults to their worth that they can encounter in the larger society. On some level, children may think that their parents are giving them affirmation because of their roles as parents. Children need to know that people other than their parents also acknowledge their skills, temperament, accomplishments and personhood. Children need interactions with people who allow them to be authentic and respond genuinely and honestly; thus, children learn how to be in healthy relationships.
Interventions to Disable Ableism and Promote Friendships
Parents of children without disabilities sometimes tell their children not to stare at children with disabilities but may not make a suggestion for a replacement behavior, like saying, “hello.” Thus normal opportunities to interact are missed and taboos that encourage shunning and bullying continue. This behavior can contribute to unnecessary adjustment problems in adulthood that Cadman, Boyle, Szatmari, and Offord (1987) and Rutter, Tizard, and Whitmore (1970) have suggested are related to experiencing social rejection early in one’s life. To promote integration and change attitudes, it would be helpful for school counselors to offer diversity training concerning disabilities for students and parents throughout the school population. Informational sheets could be sent home in the beginning of the school year or brief presentations could be included at parent meetings. Some of the child’s classmates may grow up and one day become parents of children with disabilities.
Social Skills Development
Miller (1995) reminded us that the peer social system is the main area where children develop and hone relationship-building and social problem-solving skills. However, some children with disabilities have trouble forming relationships with their peers for a variety of reasons. They may lack the opportunity to socialize with peers in a regular setting or have trouble ambulating to where children are playing. They may have a human aide who impedes normal peer interactions, tagging along to manage a healthcare issue. They may not understand the social mores of others their age because of so much time spent with parents and adult health care providers or due to aspects of their disability. In addition, service providers may talk to parents about the child as if the child is not present. Parents can learn to redirect physicians, nurses and other service providers to speak to the child in age-appropriate language.
Tovray and Wilson-Portuondo (1995) suggested that children may need formal help to learn social skills for developing friendships if they do not notice or understand social cues and nonverbal messages from others. Children with disabilities may struggle with nonverbal learning issues or characteristics on the autism spectrum, making engaging or understanding others difficult. They also may have behavioral disabilities that alienate other children or result in the continual loss of recess privileges. They may have medical therapies after school and daily tasks to complete between visits. Children with disabilities may spend an unreasonable amount of time trying unsuccessfully to complete homework assignments. Counselors can help a child with a disability by making a referral to a neuropsychologist to determine strengths and weaknesses, and then the counselor, parents, neuropsychologist, teachers and tutors can help the child develop more effective study and executive functioning skills that match his or her temperament and learning style. Parents and counselors can work together so that children with disabilities have opportunities to be and not just do activities.
Educating Peers to Reduce Isolation
Sometimes children ask questions undiplomatically. For example, a preschooler with spina bifida might be asked, “Why do you walk weird?” Some parents of children with disabilities visit the school on the child’s first day and speak to the child’s classmates in an attempt to decrease painful queries that can invite social anxiety. Preparing the class as a group also frees peers from being preoccupied with unanswered questions. If professionals help the child and family create and practice an elevator speech, perhaps these unhelpful questions will occur less often. The elevator speech can be a few sentences to explain the disability when meeting new people, which could prevent the disability from becoming a taboo subject. Talking openly can relieve other children’s unrealistic fears of catching the disability.
Returning to the previous example of a preschooler with spina bifida, the child could introduce herself by name and say something to let her classmates know what they have in common, like, “I am 5 years old. I have a brother and sister, and two dogs. Who else has a brother and sister? Does anyone else have a dog? I like to play, read books and eat ice cream. I am looking forward to being your friend.” After this joining statement, she could then give a brief age-appropriate description naming her disability and saying how it affects her and others, as follows: “I have spina bifida, so some of the nerves in my back don’t talk to my legs to tell them to feel or move. The other parts of my legs have to work harder, so I walk differently. I’ll pass around my old braces, like the ones I wear to help me walk. Please don’t mess with my wheelchair unless I ask for help. You can’t catch spina bifida like you do a cold. I don’t run so please walk slower, so I can keep up. Let’s talk and see how we can all play together.” Sometimes the child may not have the social or cognitive skills for public speaking or may simply prefer that the parent give the elevator speech. However, the child can learn self-advocacy by sharing some part of the elevator talk. After the elevator speech, the parent can ask if anyone has any questions. Parents sometimes ask educators to send a letter home to the parents of their child’s typical classmates with a brief description of the disability so that parents understand and include the child in after-school invitations that are extended to the rest of the class. Then the child and peers can begin the school year ready to focus on getting to know each other, forming friendships and learning classroom content.
This introduction could reduce the isolation of children with disabilities by demystifying their differences and allowing them to assimilate into the group. Children with disabilities, their classmates, school staff and families need practical skills for dealing with bullies. Parents can search for schools that take bullying and violence prevention seriously and have a school strategy in place to discourage bullying. Bullies may try their unacceptable behaviors on various class members; however, they tend to choose people who are alone to be their victims of repetitive bullying. Children with disabilities can learn strategies for standing up to the bully. Classmates of children with disabilities can acquire the information necessary to become friends and allies for the student in areas where there may be less adult supervision such as the lunchroom, bathrooms, hallways, or on the playground. They can help intervene to include the child with a disability in pleasant encounters with children from other classrooms and also speak on behalf of their friend when others ask questions or make nasty comments. Counselors can work with the school staff, parents and children to develop school-wide anti-bullying campaigns that teach children to counteract bullying and become allies for one another.
Preventing Isolation by Building Peer Support
The child and family may share their culture, religion and other signs of unity and cohesion. However, if the child’s exceptionality is not inherited, he or she may have the difficult experience of being the only member of his family with the anomaly. The child may benefit from the support of peers with the same disability to spend time with and compare experiences; or just be with colleagues who are already familiar with the disability and do not require explanations. Counselors can help parents find camps and support groups for both the family and child that include both children with disabilities and typical peers. Children need older, successful role models with disabilities who inspire them to persevere when they are discouraged. They need mentors, with and without disabilities, who challenge them to dream and make continual progress to accomplish their dreams.
Recommendations for Counselors
Counselors can be more aware of areas in which they can be quite helpful. Counselors can intervene in the medical system to provide newborns with disabilities and their parents with natural settings that allow relaxed time together to promote attachment and bonding. Counselors also can operate from a systemic, strengths-based model in order to best respect and support the child and family. Throughout the child’s development, counselors and families can collaborate to promote the development of age-appropriate skill acquisition, protective yet permeable personal boundaries, self-awareness, positive self-esteem, social skills, relationship development, the ability to be resilient in the face of stigma, and the opportunity to transition to the adult roles of employment, independent living, dating and family formation.
Systemic, Strengths-Based Counseling Models
Allen (1994) indicated that counselors and theorists operating from various individually oriented counseling perspectives assume that the origin of dysfunction and self-destructive behaviors in an individual is an internally defective self, psyche or physiological flaw. Hahn (1993) noted that the medical understanding of disability relates to organic pathology or impairment. Counselors who operate from a family systems model believe that difficult individual behavior is best understood as one piece of a larger interacting whole, such as the family or society, which is greater than the sum of its parts. The behaviors of individual members of the system are considered reflections of what is happening in the larger system. Rather than identifying the individual as a patient to be fixed, Nichols (1984) stated that the system should be explored to identify pathology in the interactions between people. Oliver (1996) did not believe that disabilities are intrinsically bad, and Linton (1998) reported that many people have disability pride. Disability pride refers to recognition that society is enriched by the distinctive positive voices, identities, thoughts, awareness, lifestyle examples and literature produced by individuals with disabilities. Seligman and Darling (2007) suggested that professionals who adopt a medical model of pathology may presume that the birth of a child with a disability will lead to maladaptive family functioning and therefore the implementation of intrusive, undesired interventions from service providers. I advocate the use of a collaborative, systemic, strengths-based counseling model due to the complex interconnected systems that make up the environment of children with disabilities and because it is more respectful of the child and family’s disability orientations and ability to prosper within a complicated context. It is erroneous, unkind and disrespectful to label a child who is capably using his resources to the best of his ability as unhealthy simply because he varies from the norm.
A systemic, strengths-based counseling model also respects the inherent worth of the child with a disability by not presuming that he or she is the identified patient. He or she is incredibly resilient in the face of daily challenges that would make many adults cower and yet gets up each day with renewed hope and moves forward into the future. Not only does this child face the same developmental tasks of childhood as his or her peers, but he or she must use additional thought, energy and time to develop and implement strategies to compensate for personal variations that may make the accomplishment of these tasks extremely difficult and time consuming.
One goal of counselors working with children with disabilities is to acknowledge the personhood and accomplishments of the children and their incredible inner fortitude, without categorizing them as more special than any other child. In a society where people are compared to a perceived norm, this child was either born with or acquired a variation that has been characterized as less than the norm, and labeled a disability, impairment, handicap or developmental disorder. The terms are pejorative; the connotations of the words just mentioned are as follows: not able, broken, defective, of lesser quality and developing incorrectly.
Counselors might also wonder how separation experiences impact attachment and bonding from the child’s perspective. Does the child experience feelings of abandonment and fear at a time when he or she lacks the ability to conceptualize or express them? A question for counselors and researchers to consider is whether there is an enduring impact from these experiences. Some parents initially reject the child with a disability or fear that they will not be able to manage the infant’s medical needs. Family members who have access to each other usually bond. Seligman and Darling (2007) reported that attachment can be difficult for some parents when aspects of the child’s disability interfere with the baby responding positively to his or her parents’ overtures.
Parents and counselors can help children with disabilities develop a healthy sense of self and determine what behavior is acceptable in others, and under what conditions. With so many people entering and leaving the child’s life, it is helpful for parents and counselors to help children understand different types of relationships and what to expect from them. They need to be protected from physical, sexual and emotional abuse and learn refusal skills in situations where their trust and cooperation are exploited.
Promoting Self-Awareness
Children with disabilities need self-awareness. Counselors have the opportunity to assist parents of young children with disabilities by suggesting that parents play games with their toddlers to help them learn body parts and their functions, including the terms that name their disability since it is also a natural part of them. It is not a defining part, but rather an aspect of themselves that they can become aware of and discuss, such as being adopted or having green eyes. Once the disability is assimilated into the family, family members go about the business of life; their child with a disability is just another member of the family.
Helping Children with Disabilities, Siblings and Parents Deal with Stigma
Siblings can help children with disabilities begin to interact differently with peers by accustoming them to the support, disagreements and jealously common between brothers and sisters. Children with disabilities encounter people within the larger community who may not be familiar with disabilities or the concept that disabilities occur among regular people. Children with disabilities and their siblings need to be prepared ahead of time for ableism so that they are not surprised or heartbroken by the reactions they receive from people outside their home. At home, no one stares at children with disabilities, mocks their disability-related differences or calls them negative names. Unfortunately, well-adjusted children with disabilities may encounter cruelty from other children whom they meet outside their homes and primary social networks. They need to know that the dysfunction in these interactions does not originate in them, but rather are due to a lack of knowledge in other people. Children, parents and siblings need help interacting with the larger society around issues of being different and educating others about their disabilities. Sibling groups can be helpful for children who sometimes feel torn between conflicting emotions about their sibling with a disability. Goffman (1963) said that family members of children with disabilities sometimes receive courtesy stigma when they are in public with their family member who has a disability. Children have reported feeling embarrassed by their sibling or guilty for excluding them or not defending them. At other times children have been shunned for standing up for their sibling. Siblings may sometimes be jealous of the extra attention their sibling’s disability requires, assist with their sibling’s care or operate independently.
The Importance of Being, While Also Acquiring Skills
Children need time for unstructured play to develop their imagination, gain independence, explore hobbies and experience leisure. They need opportunities to develop the daily living skills necessary to achieve autonomy by adulthood. In addition to learning to prepare food, clean, do laundry, manage money, monitor appointments and keep a home from dissolving into chaos, they will need to gradually take over the medical management of their disability if they intend to maintain their health. Children with disabilities and their families need extreme time-management skills in order to accomplish this herculean task. Counselors or life coaches can help families develop a long-term family vision. They also can help the child and family develop short-term and long-term goals for the child with the disability and problem-solving skills to overcome obstacles to their vision and goals. Parents and children may find it helpful to learn assertiveness skills so they can coordinate homework tasks assigned by support services and say no to excessive demands from numerous systems that add up to more than a 24-hour day.
Helping Adolescents Progress to Adulthood
When a disability is added to the list of difficulties Haley (1997) described, one may discover additional requirements for launching a young adult with disabilities. Some states require adolescents with disabilities to be evaluated before they can apply for a driver’s license, and their vehicles may need costly accommodations. Some people with disabilities are refused the opportunity to obtain a driver’s license and must make other plans for transportation. A young person with a disability needs a plan for vocational career development, job training, higher education or some means of financial support. Plans for independent living, a group home, or a nursing home, must be made prior to leaving the family home. Such plans often include meetings with a team to develop an individual education transition plan during secondary school, and meetings with rehabilitation counselors after high school to plan for college, vocational training or employment. Parents and students spend additional time and energy to acquire the documentation required to obtain these services. Counselors and life coaches can help the family members prioritize the various activities competing for their time, energy and financial resources. Professionals may encourage creativity around informal methods of achieving formal goals that do not require the child and family to expend more energy acquiring and maintaining the services than warranted by the potential relief obtained from the services.
Other Counseling Services
Counselors have so many tools to offer children with disabilities and their families throughout the family life cycle. They can offer concepts and techniques to deal with grief and anomie at the initial diagnosis of a disability, the chronic grief that emerges when a developmental milestone is missed, repeated encounters with ableism, or unsuccessful operations and physical therapy. Some childhood disabilities and chronic illnesses end in death at an early age. Counselors and hospice staff can help families prepare for this untimely departure.
Relaxation exercises can be helpful to families after a busy day of preoperative medical appointments, immediately prior to a surgery or while waiting for a surgery to end. A child having a painful medical procedure or frightening experience like Magnetic Resonance Imaging also can use relaxation as a method to cope. Cognitive therapy can help children and families reframe complex medical issues and disabilities from seemingly overwhelming tragedies to neutral manageable situations within their capabilities. Reframing can allow parents who regret missing work to spend hours in physician’s offices, X-ray labs or therapy appointments to see the experiences as valuable times—opportunities to really get to know the child and bond around lived experiences.
Learning to use communication skills allows parents to request that nonurgent operations and treatments be scheduled at times that do not interrupt other activities, such as birthdays, weddings and exciting field trips with classmates. Counselors can teach communication skills that can be used within the family to explore rigid roles that may not allow members the flexibility to effectively cope with the added chores that accompany a disability without sacrificing the real needs of any one family member.
Counselors can assist families and children in learning vital time-management and decision-making skills. They can help parents see that self-care is useful and that it is fine to ask for help from each other and use resources outside the family to relieve caregiver stress. Counselors can help families learn to develop a stress management plan that utilizes positive rather than negative coping skills during times of extreme stress. If families and children learn assertiveness skills, they may be able to release passivity or aggression. Counselors can help children and families reduce anxiety and depression throughout the lifespan, cultivate humor and gratitude, and juggle a variety of activities and emotions in the pursuit of a balanced life. Counselors may use their own creativity to generate original ideas for assisting children with disabilities and their families.
Conclusion
This article provides significant ideas to consider when working with individuals with disabilities and their families; there is much to learn through exploring relevant research and anecdotal information regarding disability awareness. An understanding of systemic theory is invaluable when working with the complex interconnecting systems that make up the environment of a child with a disability. Counselors may explore disability identities and orientations within the individual with a disability, the family and society. Professionals can consider interventions concerning identity formation in the person with a disability by promoting self-awareness, boundary development, and the understanding of and externalization of ableism for both the child and family members. Mental health professionals have the opportunity to confront the stigma associated with disabilities and service acquisition. Counselors can use reframing to normalize variations within students and decrease pity. They can partner with the child and his or her parents to educate the child’s classmates and their parents, school personnel, and community about the disability and inclusive practices that prevent social isolation and encourage interactions that disarm bullying and myths about people with disabilities. Counselors can offer practical help to children who may struggle with social skills, study skills, communication, assertiveness, stress management, spirituality, transitioning from childhood to adulthood, and the importance of being or experiencing one’s humanity rather than just accomplishing tasks. In addition to using the introductory ideas provided in the article, counselors are invited to creatively adapt additional theories and techniques to support children with disabilities and their families.
Conflict of Interest and Funding Disclosure
The author reported no conflict of
interest or funding contributions for
the development of this manuscript.
References
Ableism. (2015). In Merriam-Webster’s online dictionary. Retrieved from http://www.merriam-webster.com/dictionary/ableism
Allen, D. M. (1994). A family systems approach to individual psychotherapy therapy. Northvale, NJ: Aronson.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
American Psychological Association. (2010). Publication manual of the American Psychological Association (6th ed.). Washington, DC: Author.
Cadman, D., Boyle, M., Szatmari, P., & Offord, D. R. (1987). Chronic illness, disability, and mental and social well-being: Findings of the Ontario Child Health Study. Pediatrics, 79, 805–813.
Chan, S. (1998). Families with Asian roots. In E. W. Lynch & M. J. Hanson (Eds.), Developing cross-cultural competence: A guide for working with children and their families (2nd ed., pp. 251–354). Baltimore, MD: Brookes.
Chan, S., & Lee, E. (2004). Families with Asian roots. In E. W. Lynch & M. J. Hanson (Eds.), Developing cross-cultural competence: A guide for working with children and their families (3rd ed., pp. 219–298). Baltimore, MD: Brookes.
Crnic, K. A., & Greenberg, M. T. (1990). Minor parenting stresses with young children. Child Development, 61, 1628–1637.
Darling, R. B. (2003). Toward a model of changing disability identities: A proposed typology and research agenda. Disability & Society, 18, 881–895. doi:10.1080/0968759032000127308
Elman, N. S. (1991). Family therapy. In M. Seligman (Ed.), The family with a handicapped child (2nd ed., pp. 369–406). Boston, MA: Allyn & Bacon.
Gilson, S. F., & DePoy, E. (2004). Disability, identity, and cultural diversity. Review of Disability Studies, 1, 16–23.
Goffman, E. (1963). Stigma: Notes on the management of spoiled identity. Englewood Cliffs, NJ: Prentice Hall.
Hahn, H. (1993). The political implications of disability definitions and data. Journal of Disability Policy Studies, 4, 41–52. doi:10.1177/104420739300400203
Haley, J. (1997). Leaving home: The therapy of disturbed young people (2nd ed.). Levittown, PA: Brunner/Mazel.
Linton, S. (1998). Claiming disability: Knowledge and identity. New York, NY: New York University Press.
McCarthy, H. (1995). Integrating spirituality into rehabilitation in a technocratic society. Rehabilitation Education, 9, 87–95.
McHugh, P. (1968). Defining the situation: The organization of meaning in social interaction. Indianapolis, IN: Bobbs-Merrill.
Miller, B. D. (1995). Promoting healthy function and development in chronically ill children: A primary care approach. Family Systems Medicine, 13, 187–200.
Nichols, M. (1984). Family therapy: Concepts and methods. New York, NY: Gardner Press.
Oliver, M. (1996). Understanding disability: From theory to practice. New York, NY: St. Martin’s Press.
Olshansky, S. (1962). Chronic sorrow: A response to having a mentally defective child. Social Casework, 43, 190–193.
Parham, T. A. (2002). Counseling models for African Americans. In T. A. Parham (Ed.), Counseling persons of African descent: Raising the bar of practitioner competence (pp. 100–118). Thousand Oaks, CA: Sage.
Poston, D. J., & Turnbull, A. P. (2004). Role of spirituality and religion in family quality of life for families of children with disabilities. Education and Training in Developmental Disabilities, 39, 95–108.
Rolland, J. S. (2003). Mastering family challenges in illness and disability. In F. Walsh (Ed.), Normal family processes: Growing diversity and complexity (3rd ed., pp. 611–630). New York, NY: Guilford Press.
Rutter, M., Tizard, J., & Whitmore, K. (1970). Education, health, and behavior. London, England: Longman.
Schiele, J. H. (2000). Human services and the Afrocentric paradigm. New York, NY: Haworth Press.
Scope. (2014). End the awkward. Retrieved from http://www.scope.org.uk/awkward
Seligman, M., & Darling, R. B. (2007). Ordinary families, special children: A systems approach to childhood disability (3rd. ed.). New York, NY: Guilford Press.
Skinner, D. G., Correa, V., Skinner, M., & Bailey, D. B., Jr. (2001). Role of religion in the lives of Latino families of young children with developmental delays. American Journal on Mental Retardation, 106, 297–313.
Snow, K. (2001). Disability is natural: Revolutionary common sense for raising successful children with disabilities. Woodland Park, CO: BraveHeart Press.
Thompson, R. J., Jr., & Gustafson, K. E. (1996). Adaptation to chronic childhood illness. Washington, DC: American Psychological Association.
Tovray, S., & Wilson-Portuondo, M. (1995). Helping your special needs child: A practical and reassuring resource guide. Rocklin, CA: Prima.
Turnbull, A. P., Turnbull, H. R., Erwin, E. J., & Soodak, L. C. (2006). Families, professionals, and exceptionality: Positive outcomes through partnerships and trust. (5th ed.). Upper Saddle River, NJ: Prentice Hall.
Sherry Richmond-Frank, NCC, is the President of Creative Growth Counseling & Coaching, Inc. in Destrehan, LA. Correspondence may be addressed to Sherry Richmond-Frank, PO Box 1033, Destrehan, LA 70047, sherry@creative-growth.com.
Feb 9, 2015 | Article, Volume 5 - Issue 1
Mary-Catherine McClain, Robert C. Reardon
In this article, the authors analyze ways of categorizing civilian occupations and employment data collected by the U.S. Census Bureau over 6 decades (1960–2010) with respect to six kinds of work (Holland’s RIASEC classification), occupational titles used, employment and income. O*NET provided data for the 2010 census regarding employment and income. The authors discuss the distribution of employment changes over time and the examination of findings in relation to science, technology, engineering and mathematics fields. The article concludes with practical implications for counseling and guidance practice.
Keywords: Holland, RIASEC, census, employment, occupations, income
Holland’s (1997) RIASEC theory is generally recognized as one of the most important and influential in the field of counseling and career development. Foutch, McHugh, Bertoch, and Reardon (2014) sought to verify such an observation by using bibliographic research tools and identified all publications based on this theory from 1953–2011. They found over 1,970 reference citations to Holland’s theory and applications, and categorized them in terms of practice, specific populations (e.g., K–12), instruments, diverse populations and theory. These citations appeared in 275 publications (e.g., books, journals, periodicals, reports) produced in varied professional fields and disciplines worldwide.
Many counselors know relatively more about Holland’s RIASEC personality typology than corresponding environmental models (Reardon & Lenz, 1998). From the outset, Holland believed that the environmental aspects of the typology needed further examination (Weinrach, 1980). Occupations, fields of study or academic disciplines, organizations, leisure activities, and jobs (positions) are aspects of the environment included in the theory. In this article, we address the interaction between RIASEC theory and the environment by examining 2010 census data and updating prior studies of occupational employment in 1960, 1970, 1980, 1990 and 2000 in relation to RIASEC codes and Holland’s theory (Reardon, Bullock, & Meyer, 2007).
Various people contemplating career decisions can benefit from understanding the scope and nature of the labor force and employment from this psychological, counseling-based point of view. Moreover, given characteristics of the contemporary U.S. economy, it is important to know how the distribution of jobs is changing over time. For example, the distribution of jobs across the RIASEC categories has changed from 1960–2010 in some ways, but not in others. An analysis of occupational employment, then, can be beneficial to counselors and career services providers assisting those who are unemployed, displaced or exploring the labor force. This work is important for both theoretical and practical reasons. For example, the number of annual job openings is strongly related to the number of people currently working in an occupation, so knowing the number employed is of practical importance in job hunting because of the need to replace workers.
Authors of recent literature have identified concerns about the use of outmoded concepts such as occupation in career/life counseling at a time of unprecedented socioeconomic change in the global economy. For example, Savickas et al. (2009) noted that new social arrangements for work and the digital revolution have led to unstable occupations and frequent job transitions for individuals: “Today, occupational prospects seem far less definable and predictable, with job transitions more frequent and difficult” (Savickas et al., 2009, p. 240). Sampson and Reardon (2011) summarized these ideas: “Occupations have changed in fundamental ways as technology and globalization have reshaped the workplace. Occupations have become fluid and organizations are evolving rapidly, adapting their workforce to respond to a rapidly evolving marketplace” (p. 41). We agree that some occupations are changing but conclude that the concept of an occupation remains common and useful in the social sciences as a way of categorizing work activities and employment.
In contrast to this view, Murray (2012) suggested that the workplace has not transformed for the 82% of American workers in occupations other than managerial professional positions. Teachers, police, plumbing contractors, insurance agents and carpenters have the same duties and routines that these occupations have always required, although some of the work tasks may have been affected by technology. Sampson and Reardon (2011) noted that the perception of massive occupational change has been exacerbated by inaccuracies in media presentations and the failure to use career theory to examine occupational changes.
In the present article, we examine occupational information using Holland’s (1997) RIASEC theory. This theory rests on four basic assumptions: (a) individuals can be categorized into Realistic (R), Investigative (I), Artistic (A), Social (S), Enterprising (E) and Conventional (C) types; (b) environments (i.e., occupations) also can be categorized into these same six types; (c) individuals tend to choose environments that fit their personality types; and (d) behavior is determined by the fit between an individual’s personality and environment. Examination of the occupational titles used to describe current work in the United States, including information about employment and income, can increase understanding of the workplace from this theoretical perspective.
Holland’s (1997) typological theory specifies a theoretical connection between vocational personalities and work environments that makes it possible to use the same RIASEC classification system for both persons and occupations. Many inventories and assessment tools also use the typology to enable individuals to categorize their interests and personal characteristics in terms of the six types and combinations of the types. These six types are briefly defined as follows:
- Realistic (R) types are found in occupations such as auto mechanic, surveyor, electrician and farmer. The R type usually has mechanical and athletic abilities, likes to work outdoors and with tools and machines, and might be described as conforming, hardheaded, honest, humble, materialistic, practical and thrifty.
- Investigative (I) types like occupations such as a biologist, chemist, geologist, anthropologist and medical technician. The I type usually has math and science abilities, and likes to work alone and to solve problems. The I type might be described as analytical, critical, curious, independent, intellectual, pessimistic and rational.
- Artistic (A) types are found in occupations such as musician, dancer, interior decorator, actor and writer. The A type usually has artistic skills, enjoys creating original work and has a good imagination. The A type may be described as disorderly, emotional, idealistic, imaginative, impulsive, independent, introspective and original.
- Social (S) types like occupations such as teacher, speech therapist, counselor, clinical psychologist and nurse. The S type generally likes to help, teach and counsel people, and may be described as friendly, generous, helpful, idealistic, kind, responsible, tactful, understanding and warm.
- Enterprising (E) types like occupations such as buyer, sports promoter, business executive, salesperson, supervisor and manager. The E type usually has leadership and public speaking abilities, is interested in money and politics, and likes to influence people. The E type is described as acquisitive, ambitious, domineering, extroverted, optimistic, self-confident and sociable.
- Conventional (C) types are found in occupations such as bookkeeper, financial analyst, banker and secretary. The C type has clerical and math abilities, likes to work indoors and to organize things. The C type is described as conforming, efficient, obedient, orderly, persistent, practical and unimaginative.
The six RIASEC types are optimally represented by a circular order, also commonly referred to as the hexagonal model. Holland’s (1997) structure of the six types as a hexagon is one of the most well-replicated findings in the history of vocational psychology (Rounds, 1995). The six domains are arranged according to their relative similarity in a hexagonal formation of R-I-A-S-E-C. For example, according to Holland’s theory, the Social and Enterprising types appear in adjacent positions on the hexagon because they are alike; in contrast, the Social and Realistic types are dissimilar and appear in opposite positions from one another on the hexagon.
Prior Studies
In the early 1970s, researchers began to examine the U.S. labor market using the RIASEC classification system (Reardon et al., 2007), and the present study is a continuation of that line of research. Using data provided by the decennial census in 1960, 1970 and 1980, researchers (G. D. Gottfredson & Daiger, 1977; G. D. Gottfredson & Holland, 1996; G. D. Gottfredson, Holland, & Gottfredson, 1975; L. S. Gottfredson, 1978; L. S. Gottfredson, 1980; L. S. Gottfredson & Brown, 1978) analyzed U.S. employment patterns using Holland’s theory. These studies examined a number of variables with respect to the Holland RIASEC classification, including the percentages of men and women working in hundreds of occupations, salaries earned during the preceding year by incumbents, educational and training levels associated with occupations, occupational prestige, and the education levels or cognitive complexity ratings for occupations. These studies provided practitioners and scholars with more theory-based, detailed information about work environments and the characteristics of workers.
After a 15-year hiatus in research on census employment and Holland codes, Reardon, Vernick, and Reed (2004) analyzed the 1990 census data in relation to data from 1960, 1970 and 1980. They considered the variables of gender, income and cognitive complexity and reported stability in the census data for occupational titles and six kinds of work from 1960–1990. For example, the Realistic area included many more named occupations in the census than the other five areas, averaging between 46% and 50% of all named occupations over the 40-year period.
Reardon et al. (2004) found that while employment declined by 18% in the Realistic area relative to other Holland types, it remained the largest area of employment and actually increased in real numbers through 1990. Only 1% of employment was in the Artistic area. Reardon et al. (2004) also reported marked differences in employment between men and women across the six areas from 1960–1990. Reardon et al. (2004) further examined income and gender by six kinds of work and found that the average income profile ranging from highest to lowest was IESARC. The discrepancy across the six areas was very large, with the average Investigative income being two times the average Conventional income.
In a later study, Reardon et al. (2007) examined trends in labor market characteristics using census data from 1960–2000. They found stability in occupational constructs for six kinds of work from 1960–2000; for instance, the Realistic area included many more named occupations in the census than the other five areas, ranging between 43% and 50% of all occupations included over the five census periods. Reardon et al. (2007) reported that although employment in the Realistic area declined by 25% from 1960–2000, this area remained the largest area of employment and actually increased in real numbers from 1960–2000. As before, only 1% of employment was in the Artistic area. Finally, Reardon et al. (2007) examined income and gender by kinds of work and found that the average income profile for six kinds of work ranging from highest to lowest was IESARC in 1990 and ISEARC in 2000. The discrepancy across the six areas was very large, with the average Investigative income about twice as large as the average Conventional income.
In summary, the data included in these studies (Reardon et al., 2007; Reardon et al., 2004) were unique in several ways and have special implications for counselors. First, as an independent branch of the federal government, the U.S. Census Bureau reported actual numbers of people working in different occupations based on an accounting of persons in households. Second, these data provided a retrospective look at the labor markets, and by examining them over time it was possible to view changes in the economic lives of persons in the United States. Third, the occupational titles included in the census have remained constant over the years, reinforcing the use of the occupational schema in matching persons and environments. Fourth, these studies were conducted by researchers in the counseling field rather than economists or sociologists, which helps counselors use occupational data organized by Holland codes to illustrate and explain where jobs exist in relation to their clients’ interests. For example, a client may have a strong interest in Artistic occupations, and census data may help a counselor explain the relatively small number of persons working in Artistic fields.
The Present Study
We examined the employment trends reported in earlier research and added a new analysis based on the 2010 census and O*NET data. Research questions included the following:
- What were the numbers of occupational titles reported in the census from 1960–2010 relative to the six areas of work?
- What were the numbers and percentages of occupational employment in 1960, 1970, 1980, 1990, 2000 and 2010 in relation to six kinds of work?
- What were the mean incomes for six different kinds of work in 1990, 2000 and 2010?
Methods
Procedures and Research Tools
Varied procedures have been used to collect occupational data for the decennial census over the past 6 decades.
1960, 1970, 1980 census. In the 1960 census, the sampling unit was the housing unit, or the person in the case of group housing. This method provided information about 297 detailed occupational categories. L. S. Gottfredson and Brown (1978) described the methods they used to derive Holland codes for the 1960 census data using 1970 census data as a point of reference. In the 1970 census, the sampling unit again was the housing unit, and 440 detailed occupational titles were included in these data, 143 more than in 1960. As with the 1960 census, the data included only employed persons and excluded members of the armed forces. G. D. Gottfredson, Holland, and Gottfredson (1975) analyzed data from the 1970 census involving 424 occupations, and excluded men (5.6%) and women (6.6%) not classified according to one of the detailed occupations. Information about the 1980 census was taken primarily from G. D. Gottfredson and Holland (1989) and G. D. Gottfredson (1984). The 1980 analysis was based on 503 selected occupations.
1990 census. Comprehensive information about the 1990 census was provided by the U.S. Census Bureau (1992a, 1992b), and was based on 500 selected occupations. G. D. Gottfredson and Holland (1996) indicated that this classification was most closely related to the Standard Occupational Classification (SOC; U.S. Department of Commerce, 1980). The U.S. population count in 1990 was 283,928,233 (U.S. Census Bureau, 1992b). Four new categories of work were added to the 1990 census while six from the 1980 census were eliminated.
2000 census. The 2000 census counted 281,421,906 people in the 50 states and the District of Columbia. As in the past, short and long forms were used with about 17% (1 in 6 households) receiving the latter (U.S. Census Bureau, 2002). The 2000 census included 471 occupations classified using the SOC (U.S. Department of Labor, 2000).
2010 census. The 2010 census counted 308,745,538 people in the 50 states and the District of Columbia. This census included 539 occupations, including those with “all other” titles representing occupations with a wide range of characteristics not fitting into one of the O*NET detailed occupations. However, as in prior studies, the focus was on the detailed occupations in the 2010 census (N = 494) and excluded military-based occupations.
The information collected in the 2010 census was based on the short form rather than the long form, which means that demographic information about gender, salary and age was not collected relative to occupations. Lowe (2010) noted that the introduction of the American Community Survey by the U.S. Census Bureau provided the most sweeping change in census data collection in 60 years. The American Community Survey is a nationwide, continuous survey designed to provide reliable and timely demographic housing, social and economic data every year, in contrast to the long form, which provided data only at the beginning of each decade.
After locating the 2010 census data from the U.S. Census Bureau with lists of occupations categorized with census and SOC codes, we organized the information into a spreadsheet using the following headings: Occupation 2010 category description (e.g., management occupations), Occupation (e.g., chief executive), 2010 Census Code (e.g., 0010) and 2010 SOC Code (e.g., 11-1011). Additional columns were created to incorporate Holland code information for 2010 employment data and mean annual wages. The SOC (U.S. Department of Labor, 2010) was used to collect employment and salary information from the O*NET system (http://online.onetcenter.org/). O*NET is a comprehensive database that provides information on 780 occupations, worker skills and job training requirements. O*NET is sponsored by the U.S. Department of Labor’s Employment and Training Administration. The Self-Directed Search Occupations Finder—Revised Edition (OF; Holland & PAR Staff, 2010) and the Dictionary of Holland Occupational Codes (DHOC; G. D. Gottfredson & Holland, 1996) also were used to obtain the first-letter Holland code for each specific occupation. Employment data and mean annual wages for census occupations were found in O*NET.
A Note about Data Analysis
Previous studies of employment using census data and Holland codes have reported frequency and percentage distributions, and this study continued that approach. As earlier researchers have noted (G. D. Gottfredson & Daiger, 1977), the sample sizes are so large that the magnitude of observed differences is more important than statistical differences. Rounded numbers are used in this report to the nearest percent or thousand in order to avoid communicating a misplaced sense of precision in the findings.
Results
Occupational Titles in the Census for Six Kinds of Work, 1960–2010
For the first question, we examined the number of occupational titles used in the census and O*NET, and categorized these in relation to the six areas of work. Occupational titles provide schemas for career exploration using Holland’s (1997) RIASEC codes—tools for the exploration and examination of occupational information. As in previous studies (Reardon et al., 2007), the Realistic area included many more named occupations in the census than the other five areas (see Table 1, updated with 2010 data). For example, the 2010 census specified 211 occupations in the Realistic area and 283 occupations in the other five areas combined. Only 19 occupations were identified in the Artistic area. Overall, occupations in the Enterprising area increased from 27 in 1960 to 88 in 2010. Finally, 282 occupations were included in the 1960 analysis, which increased to 465 in 1970, 502 in 1980 and 500 in 1990, dropped to 434 in 2000, and increased again to 494 in 2010.
Table 1 also shows that occupational titles were not equally distributed across the six areas of work over the past six decades and have changed very little during this period. For example, the Realistic area consistently has the most occupational titles and the Artistic area the fewest. Figure 1 shows the average percentages of occupational titles in the census across six decades, as follows: Realistic 46%, Investigative 12%, Artistic 3%, Social 12%, Enterprising 18% and Conventional 9%. This distribution is similar to what was found in 2010: Realistic 43%, Investigative 11%, Artistic 4%, Social 13%, Enterprising 18% and Conventional 11%. Figure 1 shows in graphic form that the schemas used to describe work activities in the U.S. economy have remained relatively stable over 6 decades.
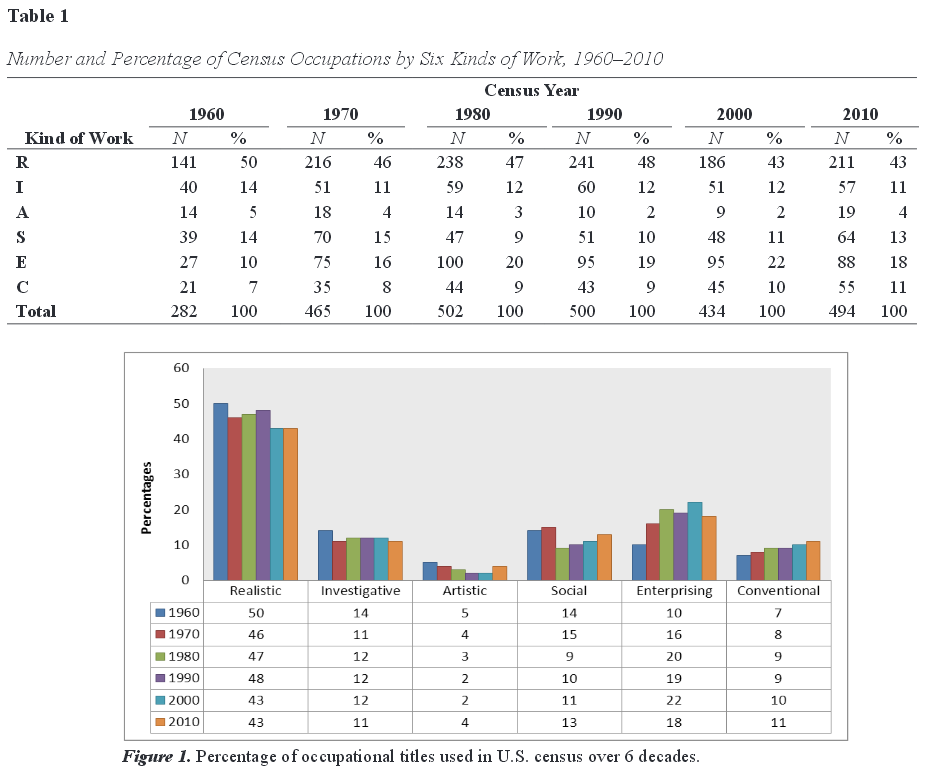
Employment in Six Kinds of Work, 1960–2010
In analyzing U.S. employment data over 6 decades, we focused on the detailed occupations as in previous census studies (Reardon et al., 2007). Table 2 indicates that the total estimated employment increased over the 6 decades from 64.1 million in 1960 to 119.8 million in 2010. Table 2 and Figure 2 reveal that the percentage of Realistic employment declined 28% from 1960–2010, an average of about 4.7% for each decade. However, and in spite of this decline, the Realistic area showed that 31.9 million persons were employed in 2010, and the Realistic area had the highest level of employment across the six RIASEC areas in each census period. The Artistic area had the fewest number employed in 2010 with 2.0 million. Table 2 and Figure 2 show that the percentage of employment in the Social area increased from 9% in 1960 to 24% in 2010, or 5.6 million to 29.6 million persons. During the same period, employment in the Investigative area increased from 3% in 1960 to 10% in 2010, or 2.0 million to 11.5 million persons. Employment in the other four areas remained more stable. Figure 2 graphically shows that the RIASEC employment profile for highest to lowest areas was RSECIA in 1960 compared to RECSIA in 2010. The Realistic, Investigative, and Artistic areas maintained their positions over this time period.
Table 2
Number and Percentage of Persons Employed in Six Kinds of Work, 1960–2010
|
Census Year (Detailed Occupations)
|
|
| Kind of Work |
1960a |
1970a |
1980 |
1990 |
2000 |
2010 |
|
|
|
|
|
|
|
| R |
35,029
|
34,342
|
42,253
|
42,711
|
36,700
|
31,868
|
|
55%
|
48%
|
42%
|
37%
|
30%
|
27%
|
| I |
1,986
|
3,690
|
4,169
|
6,738
|
9,315
|
11,457
|
|
3%
|
5%
|
4%
|
6%
|
8%
|
10%
|
| A |
756
|
975
|
1,277
|
1,552
|
1,622
|
2,027
|
|
1%
|
1%
|
1%
|
1%
|
1%
|
2%
|
| S |
5,611
|
8,390
|
10,815
|
14,983
|
18,821
|
29,563
|
|
9%
|
12%
|
11%
|
13%
|
16%
|
24%
|
| E |
11,106
|
12,153
|
25,920
|
29,668
|
35,946
|
23,991
|
|
17%
|
17%
|
25%
|
26%
|
30%
|
20%
|
| C |
9,569
|
12,658
|
17,540
|
20,086
|
18,574
|
20,878
|
|
15%
|
17%
|
17%
|
17%
|
15%
|
17%
|
| Total |
64,057
|
72,208
|
101,974
|
115,738
|
120,978
|
119,784
|
|
|
|
|
|
|
|
|
Note. Employment numbers are in millions rounded to the nearest thousand.
aUsed by permission of Academic Press Inc., Journal of Vocational Behavior, 10, p. 131. Copyright 1977 Academic Press Inc.
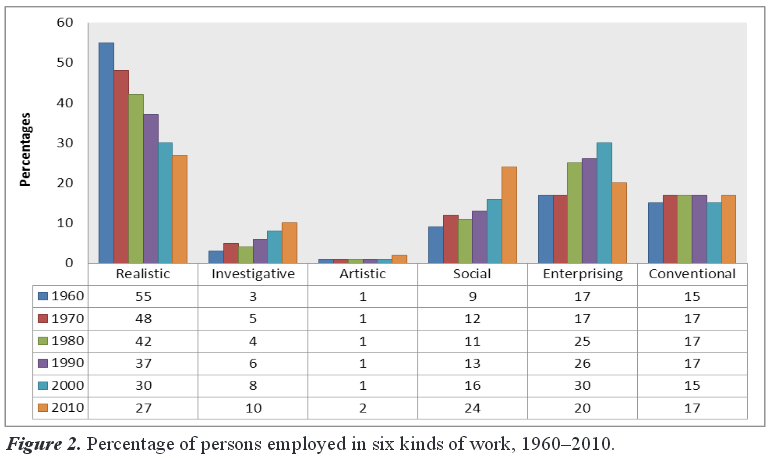
Income and Kinds of Work, 1990–2010
For the third question, we focused on mean income levels for persons employed in six kinds of work in 1990, 2000 and 2010. Inspection of Figure 3 shows the results of this analysis. These data reveal the continued discrepancy with regard to income among the Holland types across the three most recent census periods. The RIASEC profiles for highest to lowest income were IESARC, ISEARC and IEASRC in 1990, 2000 and 2010, respectively. The Investigative area consistently showed the highest income levels over the 3 decades, while the Conventional and Realistic areas tended to show the lowest. The average income over the 3 decades for the Investigative area was $54,587, compared to Conventional, $28,047 and Realistic, $27,981. Data in Figure 3 continue to show wide variations in income levels among the six RIASEC groups. For example, in 2010 the income in the Investigative area was almost double that of the Conventional area.
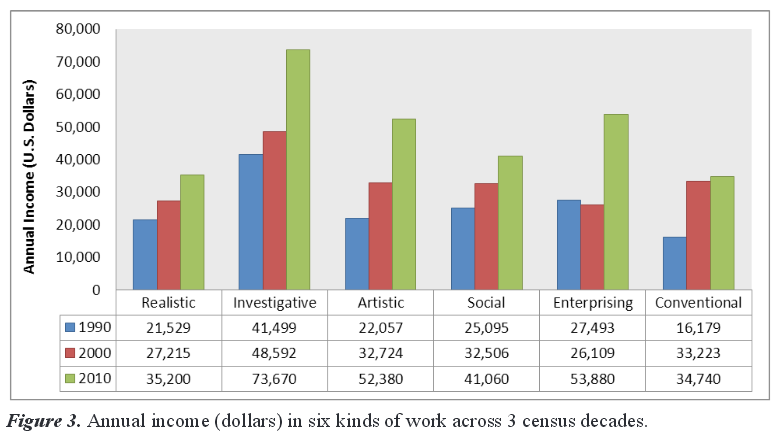
Discussion
The principal findings of this study are examined in terms of the three questions that guided the research, followed by a discussion of the study’s limitations and implications for counseling practice.
Occupational Titles by RIASEC Code
Information about jobs and employment used in counseling may be affected by the uneven distribution of occupational titles describing work across RIASEC areas. Over 60% of the titles used in 2010 were in the Realistic and Enterprising areas, and this distribution has been consistent over the past 6 decades. It is noteworthy that the percentages of occupational titles in the Investigative and Conventional areas in 2010 were the same, but the income reported across the six areas was the most discrepant between these two areas. Labor market information across the six areas is not always equivalent.
G. D. Gottfredson and Holland (1989) reported that the Dictionary of Occupational Titles also showed variations in the distribution of RIASEC codes for occupational titles. They were interested in the number of times each RIASEC letter appeared somewhere in the three-letter code for each occupation in the Dictionary of Occupational Titles and reported the following: Realistic, 10,708 times; Investigative, 2,551; Artistic, 570; Social, 6,606; Enterprising, 10,405; and Conventional, 5,999. These data reveal that upon examining the world of work from a RIASEC perspective, counselors can obtain a theory-based view of work environments that is not equitable across the six areas. Counselors can use RIASEC codes to inform clients about work and to increase their understanding of occupations and employment.
Information about jobs and employing organizations changes more frequently than information about occupations (e.g., typical work duties, training requirements, working conditions; Reardon, Lenz, Sampson, & Peterson, 2012). Perhaps lessons from the field of general semantics (Johnson, 1946) can be useful here. For example, the word chair can communicate information about the arrangement of furniture in a room, but this word does not communicate everything known about chairs, which in reality may take many different forms and be built of varied kinds of materials. The same is true for occupational terms. There are many different carpenters working in varied job positions and for varied employers, but the term carpenter still has meaning in communications because it is generally understood that not all carpenters are the same.
Over the 6 decades of this analysis, the number of census occupations in each RIASEC area has been relatively static. This stability indicates that there is considerable permanence in the array of the named occupations in the census reports about the workforce. This finding is contrary to the observations by Savickas (2012) and Savickas et al. (2009) regarding instability of the concept of an occupation in the contemporary global economy.
Employment in Six Areas of Work
The findings of this study report both the numbers of persons employed and the percentages of employment across RIASEC areas for six census periods. We believe that information about employment in the past can be instructive for future career planning. Table 2 reports the numeric and percentage changes in employment over 6 decades. The table shows the actual number of persons employed according to the decennial censuses over the 60-year period. This table and Figure 2 show the percentage changes—the distribution of the workforce within the RIASEC categories. Occupations that employ the largest numbers of people are in the Realistic, Social and Enterprising areas, with less employment in the Investigative and Artistic areas. The latter two areas report both the fewest numbers employed and the smallest percentages of employment across the six RIASEC areas.
The current emphasis on preparation for careers in science, technology, engineering and mathematics (STEM) fields involves occupations that do not employ large numbers of people. These occupations, often found in the Investigative and Artistic areas, employed relatively small numbers of people in 2010 compared to the other four areas: 12% versus 88%. The STEM fields are not big-growth occupational areas that employ many hundreds of thousands or millions of people (e.g., nurses, retail salespersons, office clerks, teachers). However, the STEM fields are generally characterized by fast growth that involves a few thousand or more persons (e.g., biomedical engineers, veterinary technicians, glaziers, physical therapists). Persons in these occupations typically have higher salaries and better employment opportunities (Horrigan, 2003–2004).
The findings of the present study indicate that most people are employed in Realistic, Enterprising and Conventional (REC) occupations. Public attention to employment and career preparation often is directed at occupations with code combinations in the Investigative, Artistic and Social (IAS) areas because the percentage rate of employment growth is often greater there than in the REC areas (Reardon et al., 2012). The IAS areas provide higher levels of prestige and income, but employ fewer people (Reardon et al., 2004). One must remember that these are projected new jobs, which seem to capture more public attention and interest than the census data regarding actual employment.
A large number of jobs actually involve replacement of older workers, perhaps as much as one-third of employment (Mittelhauser, 1998). The U.S. Bureau of Labor Statistics (BLS; 2012) used data from the Current Population Survey and found that the replacements provide many more job openings in most occupations than straight employment growth does.
While the census data provide information about past employment that can inform career planning, the U.S. BLS provides additional labor market forecast information based on occupational projections. Lockard and Wolf (2012) identified the 20 occupations expected to have the most job openings each year through 2020 (big-growth occupations). Four of these occupations—registered nurses, retail salespeople, home health aides and personal care aides—will add more than half a million jobs each through 2020. These occupations are not new, different or unique, and they are unrelated to STEM fields. Reardon et al. (2012) noted that the Holland summary code order for these 20 big-growth occupations was SREICA. In the current study, the profile for employment in the 2010 census was RECSIA. It is not surprising that the Realistic area is prominent in both of these projections, because according to the census, it is the area of largest employment in the economy.
Given the overall increase in actual employment from 64.1 million in 1960 to 119.8 million in 2010, there has been a corresponding increase in employment across the six areas of work. For example, the number of persons employed in the Investigative area has grown from over 1.9 million in 1960 to 11.5 million in 2010, and in the Social area from 5.6 million in 1960 to 29.6 million in 2010. Employment growth has been less dramatic in the Artistic, Enterprising and Conventional areas, and growth has declined slightly in the Realistic area from 35.0 million in 1960 to 31.9 million in 2010.
In addition, the percentages of the U.S. population employed in the six areas of work also have changed from 1960–2010, but in a less dramatic way (see Figure 2). For example, the employment percent profile from highest to lowest employment in 1960 was RECSIA, and in 2010 it was RSECIA, with only the ECS areas alternating in order. However, the percentage difference between the Realistic and Artistic areas was greater in 1960 (54%) than in 2010 (25%). This may be evidence of a decline in manufacturing.
Income Across Six Areas of Work
Our findings indicate that income is not equitable across the six RIASEC areas, with the Investigative area consistently having the highest income and the Realistic and Conventional areas the lowest. Research using census data by Huang and Pearce (2013), Reardon et al. (2004), and Reardon et al. (2007) revealed similar findings. We find that although the RIASEC schema is familiar to counselors using the Self-Directed Search, the Strong Interest Inventory and many other career assessments, the idea of using this schema to analyze occupational information is more novel. For example, thinking of income levels in terms of the RIASEC schema means using an order of IEASRC per the 2010 census data when discussing occupational information with clients.
Reardon et al. (2007) reported that examining levels of cognitive complexity associated with occupations may provide an explanation for the income disparity among the six RIASEC areas. G. D. Gottfredson and Holland (1996) created the Complexity Rating (Cx) to estimate the cognitive skill and ability associated with an occupation. In developing the Cx, the authors wanted to make greater use of job analysis ratings obtained by the U.S. BLS and also create a single measure of cognitive or substantive complexity associated with an occupation. They noted that cognitive complexity of work demands (G. D. Gottfredson & Holland, 1996) might be an appropriate term for the Cx. A Cx rating of 65 or higher could be associated with an occupation requiring a college degree and possibly postgraduate work and on-the-job training of 4–10 years, while a Cx level of 50 might characterize an occupation requiring a high school diploma and a year or more of on-the-job training. Reardon et al. (2007) found that Cx levels were highest in the Investigative and Artistic areas and that the Conventional area was associated with the lowest ratings. They found that employment in the Investigative area occurred only at the highest two levels of Cx (i.e., baccalaureate or higher) while the other four areas—Realistic, Social, Enterprising and Conventional—showed employment at all six levels of Cx.
Huang and Pearce (2013) reported that higher annual incomes in 2010 were found in occupations associated with greater Investigative and Enterprising traits. In addition, they found that the differentiation of an occupational interest profile positively predicted median annual income and moderated the effect across each of the six RIASEC areas. In other words, the more the occupation was characterized by a single, robust RIASEC code letter, the greater the income level for the occupation.
Reardon et al. (2007) examined income by kinds of work and found that the average income profile for six kinds of work ranging from highest to lowest was IESARC. In the current study, the income profile was almost identical—IEASRC. These findings are very similar to those reported by Huang and Pearce (2013). Given that the Investigative area of work requires more education and training than the other five areas, these findings from census data provide evidence that education pays. Reardon et al. (2012) reported that the unemployment rate is clearly related to educational attainment. Those with more education are less frequently unemployed and have higher weekly earnings—more education is connected to more income.
Limitations
As with earlier studies (Reardon et al., 2007; Reardon et al., 2004), several limitations in the present study should be noted. First, the occupational titles included in the census have changed only slightly over the years. The U.S. BLS conducts extensive research to determine whether a new occupation should be added to its list of detailed occupations. A new occupation is one that includes duties not previously identified, one that has been recognized in small numbers and continues to grow (e.g., now has its own professional association or trade group), or one that is evolving and whose tasks have changed significantly. These new occupations arise from technological advances, new laws or regulations, or changing demographics. However, we believe that this issue has minimal impact on the findings of the present study because changes in occupational codes are unlikely to affect the first letter of a code. First-letter codes of occupations are much more stable over time and across industries than second or third letters.
A second limitation of this study is related to the classification of hundreds of thousands of jobs into 350–500 occupational categories, which requires considerable judgment and skill by occupational analysts. These specialists base their judgments on the application of classification criteria, and there is the possibility of error in the use of this system of analysis. Third, we used the first letter in each Holland code in our analysis in order to simplify reporting. While this decision reduced some of the precision inherent in the Holland classification when three-letter codes are used, it increased the accuracy of occupational classification.
Fourth, our analysis was based on a sampling procedure used by the U.S. Census Bureau over 6 decades, and we generalized from this sample to the entire U.S. population. We assumed that the sampling procedure used by the U.S. Census Bureau was appropriate for this study. Fifth, the method for calculating the income levels reported in this study differed across the 3 decades, and comparisons should be made with caution. We used mean levels rather than median levels, and information about the skew of the distribution is not provided in this study. For example, Lowe (2010) noted that while the American Community Survey data are more current, they are not as precise (margins of error are generally higher) as data obtained in the long form used by the U.S. Census Bureau previously. Finally, it is possible that occupations may be shifting within or among industry groups, which would mask some of the findings regarding income reported in the present analysis.
Implications for Counseling Practice
Limitations notwithstanding, the results of this analysis of six kinds of work and employment over 6 decades have implications for counselors. Holland (1997) noted several rules to use in interpreting the Self-Directed Search interest inventory, such as the Rule of Asymmetrical Distribution of Types and Subtypes. This rule reminds both counselor and client that the distribution of types across the six RIASEC areas is very uneven and unequal; moreover, the distribution of jobs across the six types is not symmetrical or equal. Codes associated with small employment numbers may have fewer positions and fewer openings. The research in the present article underscores the validity of this rule. In each census period, the Artistic area was the smallest area of employment at 1% or 2%. At the other extreme, the Realistic area was the largest area of employment, ranging from 55% in 1960 to 27% in 2010. Career counselors should be cautious in advising workers to look for employment outside the Realistic area, because it has been the largest area of employment for the past 6 decades, with ongoing replacement needs (Reardon et al., 2007).
We can add that even the numbers of named census occupations are extremely uneven across six kinds of work. For example, the schema based on RIASEC types used in 2010 to examine occupations was heavily skewed in the direction of the Realistic area (N = 211), with very few occupational titles associated with the Artistic area (N = 19). We surmise that these findings reveal little evidence of instability and change in the use of the occupational schema by the U.S. Census Bureau, at least from a RIASEC perspective.
Some of these findings may be interpreted in different ways. For example, the Realistic area employed the most persons in 2010, but employment in that area has dropped 28% over the 6 decades. The loss of jobs in the Realistic area is greater than the changes in any other area, decreasing from 42.7 million in 1990 to 31.8 million in 2010. The Investigative area almost tripled in employment from 1960–2010, from 3% to 10%, but fewer than 10% of total U.S. jobs are in the Investigative area (11.5 million). These findings seem related to the issue of big-growth and fast-growth jobs described by Horrigan (2003–2004), in which very few occupations appear at the top of both lists. For example, only home health aides and personal care aides are included in both the top 20 big-growth and fast-growth employment areas. This information underscores the importance of understanding demography and an aging population in using labor market information. The information used in career guidance programs often touts the rapid growth in information and technology jobs; however, this information must be balanced with the understanding that only 8% of U.S. employment is in the Investigative area.
The findings of the current study can update and enhance a counselor’s view of labor market information based on Holland’s career theory. We suggest that a RIASEC perspective on jobs in the labor market indicates that things are not really changing as much as others sometimes discuss. U.S. census data compiled over 6 decades (1960–2010) can inform counseling practice and career interventions for students and others exploring occupational changes. These findings can assist counselors and their clients in better matching personal characteristics with occupational and work environments.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of
interest or funding contributions for
the development of this manuscript.
References
Foutch, H., McHugh, E. R., Bertoch, S. C., & Reardon, R. C. (2014). Creating and using a database on Holland’s theory and practical tools. Journal of Career Assessment, 22, 188–202. doi:10.1177/1069072713492947
Gottfredson, G. D. (1984, August). An empirical classification of occupations based on job analysis data: Development and applications. Paper presented at the meeting of the American Psychological Association, Toronto, Canada.
Gottfredson, G. D., & Daiger, D. C. (1977). Using a classification of occupations to describe age, sex, and time differences in employment patterns. Journal of Vocational Behavior, 10, 121–138.
Gottfredson, G. D., & Holland, J. L. (1989). Dictionary of Holland occupational codes (2nd ed.). Odessa, FL: Psychological Assessment Resources.
Gottfredson, G. D., & Holland, J. L. (1996). Dictionary of Holland occupational codes (3rd ed.). Odessa, FL: Psychological Assessment Resources.
Gottfredson, G. D., Holland, J. L., & Gottfredson, L. S. (1975). The relation of vocational aspirations and assessments to employment reality. Journal of Vocational Behavior, 7, 135–148. doi:10.1016/0001-8791(75)90040-8
Gottfredson, L. S. (1978). An analytical description of employment according to race, sex, prestige, and Holland type of work. Journal of Vocational Behavior, 13, 210–221. doi:10.1016/0001-8791(78)90046-5
Gottfredson, L. S. (1980). Construct validity of Holland’s occupational typology in terms of prestige, census, Department of Labor, and other classification systems. Journal of Applied Psychology, 65, 697–714. doi:10.1037/0021-9010.65.6.697
Gottfredson, L. S., & Brown, V. C. (1978). Holland codes for the 1960 and 1970 census detailed occupational titles. Journal Supplement Abstract Service Catalog of Selected Documents in Psychology, 8, 22. (MS. No. 1660)
Holland, J. L. (1997). Making vocational choices. Odessa, FL: Psychological Assessment Resources.
Holland, J. L., & PAR Staff. (2010). The self-directed search occupations finder—revised edition. Odessa, FL: Psychological Assessment Resources.
Horrigan, M. W. (2003–2004). Introduction to the projections. Occupational Outlook Quarterly, 47, 1–4.
Huang, J. L., & Pearce, M. (2013). The other side of the coin: Vocational interests, interest differentiation and annual income at the occupation level of analysis. Journal of Vocational Behavior, 83, 315–326. doi:10.1016/j.jvb.2013.06.003
Johnson, W. (1946). People in quandaries: The semantics of personal adjustment. New York, NY: Harper & Row.
Lockard, C. B., & Wolf, M. (2012). Occupational employment projections to 2020. Monthly Labor Review, 84, 84–108.
Lowe, S. (2010). How the American community survey will improve census statistics. Retrieved from http://www.census.gov/newsroom/releases/pdf/09ACS_improve.pdf .
Mittelhauser, M. (1998). The outlook for college graduates, 1996–2006: Prepare yourself. Occupational Outlook Quarterly, 42, 2–9.
Murray, C. (2012). Coming apart: The state of white America, 1960–2010. New York, NY: Crown Forum.
Reardon, R. C., Bullock, E. E., & Meyer, K. E. (2007). A Holland perspective on the U.S. workforce from 1960 to 2000. Career Development Quarterly, 55, 262–274. doi:10.1002/j.2161-0045.2007.tb00082.x
Reardon, R. C., & Lenz, J. G. (1998). The self-directed search and related Holland career materials: A practitioner’s guide. Odessa, FL: Psychological Assessment Resources.
Reardon, R. C., Lenz, J. G., Sampson, J. P., Jr., & Peterson, G. W. (2012). Career development and planning: A comprehensive approach (4th ed.). Dubuque, IA: Kendall-Hunt.
Reardon, R. C., Vernick, S. H., & Reed, C. A. (2004). A Holland perspective on the U.S. workforce from 1960 to 1990. Journal of Career Assessment, 12, 99–112.
Rounds, J. (1995). Vocational interests: Evaluating structural hypotheses. In D. J. Lubinski & R. V. Dawis (Eds.), Assessing individual differences in human behavior: New concepts, methods, and findings (pp. 177–232). Palo Alto, CA: Davies-Black.
Sampson, J. P., Jr., & Reardon, R. C. (2011). Changes in occupations? A commentary and implications for practice. The Professional Counselor, 1, 41–45.
Savickas, M. L. (2012). Life design: A paradigm for career intervention in the 21st century. Journal of Counseling & Development, 90, 13–19. doi:10.1111/j.1556-6676.2012.00002.x
Savickas, M. L., Nota, L., Rossier, J., Dauwalder, J.-P., Duarte, M. E., Guicharad, J., . . . van Vianen, A. E. M. (2009). Life designing: A paradigm for career construction in the 21st century. Journal of Vocational Behavior, 75, 239–250. doi:10.1016/j.jvb.2009.04.004
U.S. Bureau of Labor Statistics. (2012, February). Estimating occupational replacement needs. Retrieved from http://www.bls.gov/emp/ep_replacements.htm
U.S. Census Bureau. (1992a). 1990 census of population alphabetical index of industries and occupations. Washington, DC: U.S. Government Printing Office.
U.S. Census Bureau. (1992b). Census of population and housing, 1990: Summary Tape File 3 on CD-ROM. [Machine-readable data file]. Washington, DC: Author.
U.S. Census Bureau. (2002). Census 2000 basics. Washington, DC: U.S. Government Printing Office.
U.S. Department of Commerce. (1980). Standard occupational classification manual. Washington, DC: U.S. Government Printing Office.
U.S. Department of Labor. (2010). Standard occupational classification (SOC) system manual. Washington, DC: U.S. Government Printing Office.
Weinrach, S. G. (1980). Have hexagon will travel: An interview with John Holland. The Personnel and Guidance Journal, 58, 406–414. doi:10.1002/j.2164-4918.1980.tb00420.x
Mary-Catherine McClain is a postdoctoral fellow at the University of Georgia. Robert C. Reardon is a professor emeritus at Florida State University. Correspondence can be addressed to Robert C. Reardon, FSU Career Center, PO Box 3064162, 100 South Woodward Avenue, Tallahassee, FL 32306-4162, rreardon@admin.fsu.edu.
Feb 9, 2015 | Article, Volume 5 - Issue 1
Joel A. Lane
Today’s emerging adults (i.e., individuals between the ages of 18 and 29) in industrialized nations navigate multiple significant life transitions (e.g., entering career life), and do so in a rapidly changing society. While these transitions pose psychological difficulties, a growing body of research has identified attachment and social support as two notably salient protective factors in emerging adulthood. The purpose of the present article is to explore the counseling of emerging adult clients, particularly those in the midst of one or more transitions. The concept of emerging adulthood represents a relatively recent phenomenon that the counseling community has been slow to acknowledge. Specifically, this author reviews literature pertaining to emerging adulthood, attachment and social support, and uses this literature to provide clinicians with practical recommendations for counseling emerging adults.
Keywords: emerging adulthood, life transitions, attachment, social support, counseling
Emerging adulthood is a stage of life resulting from recent societal trends in industrialized nations, occurring between the ages of 18 and 29 (Arnett, 2000, 2004, 2007). These trends include the proliferation of college enrollment, significant delays in settling down and high unemployment compared to prior generations of young adults (Furstenberg, Rumbaut, & Settersten, 2005). Corresponding with these changes is an evolution of the psychosocial development of current emerging adults, who engage in extended identity exploration and report subjectively feeling in between adolescence and adulthood (Arnett, 2001). While the benefits and drawbacks of these changes are a source of frequent and intense debate (Arnett, 2013; Twenge, 2013), few would disagree that being twenty-something today is a drastically different experience than it was several decades ago.
Emerging adulthood presents many life transitions and significant mental health risk. In the midst of prolonged identity experimentation and subjectivity, emerging adults navigate a multitude of major life and role changes, such as leaving home, entering and leaving educational settings, and starting a career. The convergence of these factors—the subjective feeling of not being an adult and near-constant life changes propelling one toward adulthood—seems to contribute to critical periods of identity crisis and various psychological difficulties (Lane, 2013b; Lee & Gramotnev, 2007; Weiss, Freund, & Wiese, 2012). Though not all emerging adults experience difficulties during these transitions (Buhl, 2007; Galambos, Barker, & Krahn, 2006), some respond with significant distress (Murphy, Blustein, Bohlig, & Platt, 2010; Perrone & Vickers, 2003; Polach, 2004), which is problematic given that the emerging adult years are considered a critical juncture in the development of mental illness (American Psychiatric Association [APA], 2013; Ingram & Gallagher, 2010) and substance abuse (APA, 2013; Chassin, Pitts, & Prost, 2002; Ingram & Gallagher, 2010). Elevated distress also has been shown to increase impulsivity and risk-taking behaviors in emerging adulthood (Scott-Parker, Watson, King, & Hyde, 2011). The distress accompanying these transitions, therefore, poses a considerable threat to emerging adult well-being.
Despite these changes and risk factors, the counseling community has been slow to acknowledge the evolving landscapes of the late teens and twenties. Counselor training programs continue to prominently feature theories of development contending that identity development is a task completed by the end of the teenage years (i.e., Erikson, 1959/1994). It seems likely that many counselors face the challenge of using outdated developmental models to conceptualize their emerging adult clients. For counselors to work effectively with the many challenges and risks that emerging adults face, they must have an increased awareness of emerging adulthood and better understand factors that predict well-being and stability during the numerous transitions commonly experienced. To address this concern, the author provides an overview of emerging adult theory and research describing the significance of emerging adult life transitions; reviews literature examining the importance of attachment and social relationships in emerging adulthood, which appear to especially salient sources of risk resilience during this period of life; and considers implications for counseling professionals to utilize when working with emerging adults.
Emerging Adulthood
Current societal expectations regarding normative life trajectories in the early-to-mid 20s—being finished with education, marrying, acclimating to a professional setting and adjusting to life as a parent—do not seem fully applicable to today’s emerging adults in most industrialized nations. Arnett (2000) described emerging adulthood as a period of feeling “in between” (p. 471), during which individuals are no longer adolescents, but do not yet identify as adults. Thus, the normative developmental tasks for individuals in their 20s seem to have shifted from objective tasks like attaining work, settling down and becoming financially independent, to more subjective tasks like considering the question, Who am I and what do I want my life to look like? This shift is reflected in several factors that distinguish emerging adulthood from other life stages and from prior young adult generations. Of these distinctions, the three most prominent pertain to demographic instability, changes in subjective self-perceptions and extended periods of identity testing (Arnett, 2000).
Characteristics of Emerging Adulthood
One way that emerging adulthood is distinct from other life stages is with regard to demographics. The past several decades correspond with higher proportions of 18- to 25-year-olds leaving home and periodically moving back home several times (Goldscheider & Goldscheider, 1999), attending college immediately after high school (Arnett, 2004), delaying marriage and childbirth (Arnett, 2000), spending more time in college (Arnett, 2004; Mortimer, Zimmer-Gembeck, Holmes, & Shanahan, 2002) and changing careers (Wendlandt & Rochlen, 2008). In comparison to other age groups, the demographic statuses of emerging adults today vary with little predictability (Arnett, 2000; Cohen, Kasen, Chen, Hartmark, & Gordon, 2003); however, the demographic factor that is most predictable is frequent residential change (Arnett, 2000, 2007; Shulman & Nurmi, 2010). All of these trends indicate the changing demographic landscapes of today’s late teens and early 20s compared to those of prior generations.
Another changing landscape of emerging adulthood is a trend toward increasingly vague and subjective self-perceptions (Arnett, 2000; Fussell & Furstenberg, 2005). Emerging adults view their progression into adulthood as long and gradual. When a sample of emerging adults were asked if they felt they had reached adulthood, over 50% selected the answer choice “in some respects yes, in some respects no,” and fewer than 5% selected “yes” (Arnett, 2001, p. 140). Moreover, emerging adults seem to consider individual character qualities (e.g., accepting responsibility) to be more salient indicators of having reached adulthood than objective milestones, such as completing education or becoming a parent (Lopez, Chervinko, Strom, Kinney, & Bradley, 2005). In short, emerging adults perceive themselves as no longer adolescents, but also not quite adults, and report vague perceptions of what it will take to feel more like adults.
A third distinction of emerging adulthood is a prolonged period of identity exploration (Arnett, 2000; Gerstacker, 2010). Given the relative freedom from life obligations, in tandem with the long-term implications of many of the decisions that will be made during emerging adulthood, this stage of life represents an opportunity for significant identity development to occur (Gerstacker, 2010). The freedom to engage in identity exploration results in the delay of firm decisions regarding adult roles (Schulenberg, Bryant, & O’Malley, 2004). These factors also contribute to an increased self-focus during emerging adulthood (Arnett, 2004). While some researchers have interpreted these features as resulting from increased narcissism among emerging adults (e.g., Twenge, 2013), Arnett (2004) conceptualized them as temporary and developmentally normative qualities.
The three most common areas of emerging adult identity exploration are love, work and worldviews (Arnett, 2000). First, emerging adults use their freedom to explore varying levels of commitment with regard to sexual and romantic relationships (Arnett, 2004), and do so in a time period with unprecedented societal acceptance of differing sexual and romantic preferences (Garcia, Reiber, Massey, & Merriwether, 2012). Second, significant identity exploration occurs with regard to professional identity, for which evidence can be found in several college trends. Emerging adults are increasingly likely to change their majors more than once (Arnett, 2000), report negative attitudes toward graduation (Lane, 2013a, in press-a; Yazedjian, Kielaszek, & Toews, 2010), spend more time in college (Arnett, 2004) and experience more career turnover (Wendlandt & Rochlen, 2008) than prior generations. Finally, worldviews represent a third area of identity exploration. With today’s unprecedented higher education enrollment (National Center for Education Statistics, 2014; Weber, 2012), a growing number of emerging adults are gaining a more complex understanding of the world around them via higher education experiences. The impact of the college environment on moral reasoning and cross-cultural experiences is well documented (e.g., Bowman, 2010). These trends may explain the observations of several scholars that today’s emerging adults share an unprecedented passion for social justice and community well-being (e.g., Arnett, 2007), especially in urban areas.
Emerging Adult Transitions
A central feature of emerging adulthood is the frequent occurrence of significant life transitions. Each of these transitions initiates significant role changes that impact social networks, familial support and autonomy. The influence of life transition on well-being has been well documented and frequently results in periods of self-doubt, immobilization and denial (Brammer & Abrego, 1981). In contrast to common assumptions that the transitions associated with emerging adulthood (e.g., college graduation, obtaining employment) are positive life events, these transitions represent periods of loss (Vickio, 1990) that consist of considerable psychological distress for some individuals (Lane, in press-a, in press-b; Lee & Gramotnev, 2007). The proceeding section reviews a growing body of recent research suggesting that the characteristic delay in adult identity formation in emerging adulthood may increase the degree of loss and difficulty experienced during several normative transitions.
High school graduation. Conclusions are mixed regarding the assertion that high school graduation is a critical emerging adult transition. Though some have reported that graduation is associated with increased quality of parental relationships and decreased depressed mood and delinquent behaviors (Aseltine & Gore, 1993), others have reported significant differences in these trajectories as a function of race and college attendance (Gore & Aseltine, 2003). Similarly, social and institutional support predicts whether deviant behaviors increase or decrease after high school (Sampson & Laub, 1990). These findings suggest that the transition of high school graduation is a positive experience for some emerging adults, but a psychologically distressing experience for others, especially those who lack social support, do not attend college, or identify as African American or Latino.
The transition to professional life among non-college attendees. After high school, the two most common trajectories are to enter either postsecondary education or the workforce (Arnett, 2004). The transition to work can be particularly difficult for those who forgo college. These emerging adults attempt to transition into professional life without the advantage of higher education—a psychologically beneficial resource that provides important institutional and social support (Raymore, Barber, & Eccles, 2001). Among individuals with high school diplomas, unemployment rates are highest between the ages of 18 and 19, approaching 20% in 2014 (Bureau of Labor Statistics, 2014). Those who do find work are unlikely to receive a sustainable income, as mean incomes among emerging adults are drastically lower than for other adult age groups (U.S. Census Bureau, 2012). Such difficulties are particularly problematic given that unemployment and economically inadequate employment have been implicated as mental health risks (Dooley, Prause, & Ham-Rowbottom, 2000).
The freshman transition. For those emerging adults who decide to attend college, their adjustment to college life also represents a significant life transition. In particular, the first year of college is a risk factor for psychological distress. Bowman (2010) found that among first-generation college freshmen, psychological well-being significantly decreased throughout the course of the freshman academic year. Similarly, Sharma (2012) demonstrated that first-year undergraduates experienced significantly greater emotional and social difficulties than other college students. A prominent focus of first-year transition literature is the important role of attachment relationships, a construct that will be discussed in greater depth later in this article. In short, the attachment security of incoming freshmen predicts their overall well-being, as well as their social and academic adjustment (Kenny & Donaldson, 1991; Larose & Boivin, 1998).
The senior year experience. A small but growing body of recent research has identified potential difficulties for college seniors preparing to transition out of school (Lane, 2013a, in press-a). The college experience represents a period of moratorium from many adult responsibilities (Fasick, 1988) and is associated with increased leisure behaviors compared to individuals who do not attend college (Raymore, Barber, Eccles, & Godbey, 1999). Given the subjective experience among emerging adults that they have not yet reached adulthood (Arnett, 2001) and the prevailing societal expectation that college graduation is associated with adult roles (e.g., entering the workforce, settling down), it is likely that emerging adults increasingly view graduation as an important signifier of impending life changes for which they do not feel ready (Lane, 2013a). For example, ambivalence about graduating was one of the primary themes to emerge from a qualitative study of college seniors (Yazedjian et al., 2010). Other qualitative studies of college seniors have found that students are frequently anxious about graduating due to the impending changes they will experience in priorities (Overton-Healy, 2010) and the sense that they lack direction regarding the next phase of life (Allen & Taylor, 2006). Factor analyses of surveys given to college seniors uncovered domains of concern about graduation, including leaving behind the student lifestyle, the impending loss of friendships and support, the process of obtaining employment, and the process of applying to graduate school (Pistilli, Taub, & Bennett, 2003). A recent path analysis revealed significant relationships between these domains of concern and factors such as life satisfaction, psychological health and attachment security (Lane, in press-a).
Life after college. Given the psychological implications of preparing to leave the college environment, it is not surprising that the time immediately following college life often presents psychological difficulties as well. A sample of Australian college graduates voiced concerns about adjusting to life after college and to work life, referring to this period as a low point of their lives (Perrone & Vickers, 2003). Chickering and Schlossberg (1998) found that well-being suffered when emerging adult graduates encountered difficulties obtaining employment. Such findings are especially significant since they contrast overall trends toward increased well-being throughout emerging adulthood (Galambos et al., 2006). That is, while emerging adulthood is associated with upward trends in well-being, the time immediately following graduation can alter this trajectory, especially when emerging adults experience difficulties obtaining employment.
However, emerging adults who do secure postcollege employment are not exempt from transition-related distress. This transition involves significant changes in attitudes, expectations and levels of preparedness compared to college life (Polach, 2004; Wendlandt & Rochlen, 2008). Transitioning to the world of work can be particularly difficult since emerging adults are typically leaving an environment in which they felt experienced (e.g., high school, college) and becoming inexperienced professionals (Lane, in press-b). More than half of all college graduates leave their initial place of postcollege employment within two years of graduating (Wendlandt & Rochlen, 2008), and there is evidence suggesting that this turnover is due to difficulties in adjusting to professional life for the first time (Sturges & Guest, 2001). Such difficulties seem to frequently result in experiences of imposter syndrome (i.e., perceiving oneself as incompetent despite evidence of competence) among emerging adults entering professional life (Lane, in press-b). Other related difficulties include significant learning curves, less feedback and structure than afforded by the college environment, guilt about initial levels of work production, and difficulties forming new social networks (Polach, 2004). Similarly, the results of a survey conducted by Sleap and Reed (2006) suggested that most graduates possess limited awareness of the impending culture changes they will experience as a result of leaving higher education and entering the workplace. The importance of this awareness was demonstrated in a longitudinal study in which emerging adults were tested as college seniors regarding their knowledge about workplace culture, and then were subsequently tested both six months and one year after entering professional life (Gardner & Lambert, 1993). Those who had more accurate information as seniors were more likely to report job satisfaction at both subsequent intervals. Buhl (2007) conducted a similar longitudinal study, finding that the subjective quality of participant parental relationships predicted well-being trajectories during the initial three years of professional life.
In sum, it is clear that the common transitions experienced during emerging adulthood pose threats to well-being due to role confusion and psychological distress. Given the risks associated with psychological distress, it is paramount to better understand factors that might promote the maintenance of well-being during periods of transition in emerging adulthood. Accordingly, a focus of emerging adult research has been examining constructs that predict positive developmental progressions through these periods of transition. Two such constructs that have received considerable attention are attachment (e.g., Kenny & Sirin, 2006) and social support (e.g., Murphy et al., 2010). It seems that emerging adults who feel secure in their relational attachments and supported by social networks are able to face the developmental challenges of emerging adulthood with greater confidence and well-being than those who lack support and secure attachments. To better explain the impact of these constructs on emerging adult development and well-being, the proceeding sections of this article examine attachment and social support literature pertaining to emerging adulthood.
Attachment
Attachment theory contends that the early relationships people develop with their caregivers inform attitudes toward help seeking and new learning in times of distress across the lifespan (Bowlby, 1969/1982). Attachment is defined as the emotional bonds that develop between children and their caregivers beginning in infancy. Based on repeated experiences of caregiver responsiveness, infants begin to develop beliefs and expectations regarding the degree to which their physical and emotional needs will be satisfied. According to attachment theory, these beliefs become internalized as subconscious representations of self and other, which continue to increase in complexity and broadly inform social interactions throughout the lifespan. Those whose representations are based on consistent and sufficient caregiver responsiveness are considered securely attached and are likely to trust their ability to resolve future needs, either by themselves or by relying on caregivers. Insecurely attached children, on the other hand, develop expectations that their caregivers cannot be adequately relied upon in times of need; these children are likely to react to perceived threats with inappropriate levels of affect (i.e., overactivation or deactivation). These reactions interfere with the children’s development of effective emotional regulation and with the successful resolution of stressful situations, thereby continuing to reinforce such responses to future stressful situations (Guttmann-Steinmetz & Crowell, 2006).
This idea positions early attachment relationships as a likely influence on psychological health in emerging adulthood. The years of later adolescence and early emerging adulthood are a time in which attachment needs are increasingly fulfilled by peers and romantic partners, as opposed to caregivers (Fraley & Davis, 1997). Thus, the relative security of parental attachment representations is likely to inform interpersonal trust and intimacy, as well as the ability to seek the meeting of attachment needs from others (Schnyders & Lane, 2014). In fact, frequency of contact with parents during emerging adulthood is negatively associated with subjective closeness to parents (Hiester, Nordstrom, & Swenson, 2009), while geographical distance from parents is positively associated with psychological adjustment (Dubas & Petersen, 1996). Younger emerging adults are likely to begin experimenting with independence, though they often still use parents or caregivers as attachment figures in times of distress (Fraley & Davis, 1997; Kenny, 1987).
Bartholomew and Horowitz (1991) conducted what was perhaps the first study to consider the relevance of attachment to the unique needs of young adult populations. They demonstrated several trajectories in interpersonal functioning on the basis of attachment functioning. In the study, attachment was conceptualized as occurring across dimensions of self and other: secure (positive representations of self and other), anxious (negative representations of self, positive representations of other), dismissive-avoidant (positive representations of self, negative representations of other), and fearful-avoidant (negative representations of self and other). Such a conceptualization has become a standard for contemporary adult attachment research (Brennan, Clark, & Shaver, 1998). Fearful-avoidant participants seemed to struggle with interpersonal passivity. Dismissive-avoidance was “related to a lack of warmth in social interactions” (Bartholomew & Horowitz, 1991, p. 234). The interpersonal problems of anxious participants suggested control seeking or overinvolvement in the affairs of their peers. These findings corroborate more recent conceptualizations of insecure attachments in adulthood (Brennan et al., 1998; Mallinckrodt, 2000). Specifically, individuals with elevated attachment anxiety are likely to respond to distress with a hyperactivated strategy, heightening awareness of their distress and causing them to seek inappropriate levels of interpersonal dependence. Conversely, individuals with elevated attachment avoidance are likely to respond to distress with a deactivated strategy, inhibiting awareness of negative affect and preventing them from seeking support from others.
A growing body of emerging adult research supports the importance of healthy attachment functioning for various psychological outcomes during emerging adulthood. Attachment is a crucial predictor of well-being trajectories at many key emerging adult transition points (Lane, 2014), including the first year of college (Kenny & Donaldson, 1991), the last year of college (Lane, in press-a) and the postcollege years (Kenny & Sirin, 2006). For example, one study tracked Israeli males from their final year of high school through their third year away from home for compulsory military service (Scharf, Mayseless, & Kivenson-Baron, 2004). Securely attached individuals demonstrated better coping strategies and higher capacity for intimacy during their military service than those with insecure attachments. More generally, attachment security in emerging adulthood also influences self-reinforcement capacity and reassurance needs (Wei, Mallinckrodt, Larson, & Zakalik, 2005), affect regulation and resilience (Karreman & Vingerhoets, 2012), perceived self-worth (Kenny & Sirin, 2006), dysfunctional attitudes and self-esteem (Roberts, Gotlib, & Kassel, 1996), self-compassion and empathy toward others (Wei, Liao, Ku, & Shaffer, 2011), self-organization strategies (Lopez, Mitchell, & Gormley, 2002), and identification with emerging adulthood (Schnyders, 2014; Schnyders & Lane, 2014). Many of these factors illustrate the importance of attachment functioning in developing healthy and supportive interpersonal social networks.
Social Support
The construct of social support refers to social relationships or interactions that provide individuals with actual or perceived assistance (Sarason et al., 1991). Social support is psychologically beneficial in its capacity to mitigate stress during stressful situations (e.g., Ditzen et al., 2008), an idea commonly referred to as the stress buffering hypothesis (Cohen & McKay, 1984). A wealth of recent research has strongly suggested that social support is particularly salient during emerging adulthood, as this is a life period marked with numerous transitions and opportunities to experience distress. In a qualitative study of emerging adults who had recently transitioned into professional life, social support was the most prominent theme related to adjustment (Murphy et al., 2010); those who reported relational isolation also struggled with unpreparedness for new financial obligations and feeling that their expectations about life after college were left unfulfilled. Mortimer et al. (2002) reported similar findings. Wendlandt and Rochlen (2008), noting that social support is often lacking in the transition out of college and into the work force, urged college counselors to develop interventions aimed at increasing perceived support. This idea was supported in a study of college graduates who had recently relocated to a metropolitan area and were adjusting to their first year of professional life (Polach, 2004). Participants reported frustration and difficulties trying to establish new peer groups outside the college environment. They also cited the importance of a sense of belonging as the primary reason for moving to a city after graduating. Clearly, ample evidence supports the protective qualities of social support for emerging adults transitioning into professional life.
Moreover, social support also seems to be important during other emerging adult transitions. In one qualitative study, emerging adult participants described the ability to understand friendship dynamics as an important component in the subjective experience of reaching adulthood (Lopez et al., 2005). Examples of understanding friendship dynamics included the maintenance of preexisting friendships, changes in friendships based on varying maturation rates, and understanding the importance of the social network. In another study, first-year college students seemed to adjust more effectively to college life when the support they received from family members shifted from actions consistent with parental attachment to actions consistent with social support (Kenny, 1987). In a multiethnic sample of urban high school students, perceived social support predicted aspirations for career success, positive beliefs pertaining to achieving career goals and the importance of work in the future (Kenny, Blustein, Chaves, Grossman, & Gallagher, 2003).
Several longitudinal studies also have demonstrated relationships between aspects of social support and various elements of positive adjustment in emerging adulthood. A large study that tracked individuals for nearly 30 years beginning at age 7 (Masten et al., 2004) found that social quality was an aspect of resilience and predicted success in various emerging adult developmental tasks (e.g., academic attainment). Moreover, success with these tasks predicted success in postemerging adult developmental tasks (e.g., parenting quality, romantic success, work success). O’Connor et al. (2011) found perceived quality of peer relationships to predict positive development in emerging adulthood, which they conceptualized to include life satisfaction, trust and civic engagement. Galambos et al. (2006), in a longitudinal study tracking nearly 1,000 Canadian participants throughout the course of emerging adulthood, found that increases in social support were significantly correlated with increases in well-being.
These findings suggest that the degree to which emerging adults are able to develop and rely upon support networks directly impacts their ability to adapt to various normative experiences and transitions. Given the aforementioned discussion regarding emerging adult attachment, it is likely that these two constructs (attachment and social support) are of shared importance during such transitions. That is, attachment representations inform one’s capacity for positive interpersonal interactions (Mallinckrodt & Wei, 2005), and in this way, attachment and social support collectively facilitate transition processes in emerging adulthood (Lane, 2014; Larose & Boivin, 1998).
Implications for Counseling Emerging Adults
Counseling professionals who work in mental health or university settings are uniquely positioned to intervene with emerging adult clients and to foster resilience and well-being during this turbulent life phase. If counselors are to be effective working with the many challenges that emerging adults face, it is necessary to better understand factors that predict well-being during life transition. The aforementioned literature demonstrates the protective qualities of social support for emerging adults in transition. Emerging adults who are able to rely on positive social relationships during life transitions derive higher psychological well-being, life satisfaction and positive affect (Lane, 2014). Accordingly, counselors would be wise to assist their emerging adult clients in cultivating supportive social relationships. While counseling is a supportive relationship unto itself (Slade, 2008), the degree to which emerging adults in transition are able to derive satisfaction from a number of supportive relationships seems to directly impact the experience of well-being during transition. In this regard, counselors are encouraged to recognize the unprecedented complexity of emerging adult support networks (Arnett, 2007; Garcia et al., 2012; Manago, Taylor, & Greenfield, 2012) due to the proliferation of social media and changing attitudes toward romantic relationships.
Moreover, social support is not limited to interpersonal relationships, but also includes structural and institutional forms of support (Masten et al., 2004). Thus, possessing knowledge of community programs and resources available to emerging adults also is imperative when working with this age group. Support can be enhanced through transition-specific programs (e.g., Lane, 2013a; Yeadon, 2010) that provide information about future expectations and strengthen coping skills (Wendlandt & Rochlen, 2008). Further benefits can be derived as counselors work with their clients to rely on these support systems during times of transition.
As the literature further suggests, one’s degree of attachment security will impact the ability to develop and rely upon social support. Thus, excessive attachment anxiety or avoidance could pose challenges to working with emerging adults on support utilization. Accordingly, counselors of emerging adults should be aware of this potential therapeutic roadblock; they also should be prepared to intervene to develop corrective attachment experiences with their clients. Mallinckrodt (2000) suggested an approach in which clinicians utilize the therapeutic relationship to promote secure attachment strategies. The focus of this approach is maintaining relational boundaries through anticipating how clients might resist such boundaries. That is, because elevated attachment anxiety promotes a desire for maladaptive interpersonal dependence (Brennan et al., 1998), counselors should work to establish greater interpersonal distance than their anxiously attached clients would prefer (Mallinckrodt, 2000). Similarly, since elevated attachment avoidance promotes a desire for maladaptive interpersonal isolation, counselors should seek greater interpersonal closeness than their avoidant-attached clients would prefer. While doing so, clinicians should monitor the affective experience of their clients as a result of the therapeutic relationship, and should assist their clients in self-monitoring as well. This process can facilitate client awareness of attachment tendencies and enhance mindfulness about communicating future relational needs.
Other helpful suggestions come from a qualitative study of experienced therapists who worked toward corrective attachment experiences with their clients (Daly & Mallinckrodt, 2009). The therapists in the sample suggested that therapeutic boundaries should be reevaluated over the course of therapy. These therapists also emphasized the importance of sensitivity to client defenses early in the therapeutic relationship, and suggested several strategies for both managing boundaries and combating resistance. Such strategies included intentional disclosure of feelings toward client patterns, fostering a sense of consistency and dependability about counseling, and developing an awareness of the temporary nature of the therapeutic relationship, beginning at the onset of therapy. These considerations may aid counselors in helping emerging adult clients work past insecure attachment patterns to develop healthy social relationships that can be utilized to facilitate emerging adult transition.
More broadly, the preceding literature review speaks to the importance of counselors acknowledging the changing landscapes of young adulthood. Current trends in the media seem to advance a narrative that today’s young adults are narcissistic, entitled and lazy. While the veracity of such labels is a focus of current debate in the research community (for an overview of this debate, see Arnett, 2013 and Twenge, 2013), the narrative that these labels perpetuate is not conducive to an empathic understanding of the needs of those in this age group. Thus, counselors are encouraged to consider Arnett’s (2004) theory of emerging adulthood when conceptualizing their work with emerging adult clients. This theory indirectly encourages counselors to honor the process of emerging adulthood, during which it is normative to engage in numerous behaviors that are often negatively misconstrued. Specifically, emerging adults are likely to (a) frequently move out and back into the parental household (which could be construed as parental enmeshment), (b) engage in prolonged identity exploration (which could be construed as laziness), (c) possess vague subjective understandings regarding the realization of adult identities (which could be construed as lack of direction), (d) think optimistically about the future (which could be construed as entitlement) and (e) temporarily possess a heightened self-focus (which could be construed as narcissism). Thus, acknowledging and normalizing these characteristics, even if they might constitute relatively recent phenomena, is important for fostering empathic understanding between counselors and their emerging adult clients.
Conclusions
Emerging adults navigate many significant life and role transitions with important long-term implications. These transitions can induce great pressure and distress for some emerging adults, increasing their likelihood of experiencing many of the risks commonly associated with this age group. Thus, it is important that counselors understand the unique dynamics of emerging adulthood, especially given the myriad ways that this group has changed and evolved compared to prior young adult generations. In particular, the aforementioned literature suggests that counselors may find success with their emerging adult clients by working to enhance social support and correct potential insecure attachment behaviors, as well as by incorporating emerging adult theory to conceptualize client behaviors and perspectives. Though emerging adulthood is often a time of turmoil and instability, it is also a period rife with opportunities and possibilities, thus providing the potential for deeply rewarding and transformative counseling experiences.
Conflict of Interest and Funding Disclosure
The author reported no conflict of
interest or funding contributions for
the development of this manuscript.
References
Allen, J. K., & Taylor, K. (2006). The senior year transition: Women undergraduates search for a path. Journal of College Student Development, 47, 595–608.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
Arnett, J. J. (2000). Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist, 55, 469–480. doi:10.1037/0003-066X.55.5.469
Arnett, J. J. (2001). Conceptions of the transition to adulthood: Perspectives from adolescence through midlife. Journal of Adult Development, 8, 133–143. doi:10.1023/A:1026450103225
Arnett, J. J. (2004). Emerging adulthood: The winding road from the late teens through the twenties. New York, NY: Oxford University Press.
Arnett, J. J. (2007). Socialization in emerging adulthood: From the family to the wider world, from socialization to self-socialization. In J. E. Grusec & P. D. Hastings (Eds.), Handbook of socialization: Theory and research (pp. 208–231). New York, NY: Guilford Press.
Arnett, J. J. (2013). The evidence for generation we and against generation me. Emerging Adulthood, 1, 5–10. doi:10.1177/2167696812466842
Aseltine, R. H., Jr., & Gore, S. (1993). Mental health and social adaptation following the transition from high school. Journal of Research on Adolescence, 3, 247–270. doi:10.1207/s15327795jra0303_3
Bartholomew, K., & Horowitz, L. M. (1991). Attachment styles among young adults: A test of a four-category model. Journal of Personality and Social Psychology, 61, 226–244. doi:10.1037//0022-3514.61.2.226
Bowlby, J. (1982). Attachment and loss: Vol. 1. Attachment. New York, NY: Basic Books. (Original work published 1969)
Bowman, N. A. (2010). The development of psychological well-being among first-year college students. Journal of College Student Development, 51, 180–200. doi:10.1353/csd.0.0118
Brammer, L. M., & Abrego, P. J. (1981). Intervention strategies for coping with transition. The Counseling Psychologist, 9, 19–36. doi:10.1177/001100008100900203
Brennan, K. A., Clark, C. L., & Shaver, P. R. (1998). Self-report measurement of adult attachment: An integrative overview. In J. A. Simpson & W. S. Rholes (Eds.), Attachment theory and close relationships (pp. 46–76). New York, NY: Guilford Press.
Buhl, H. M. (2007). Well-being and the child–parent relationship at the transition from university to work life. Journal of Adolescent Research, 22, 550–571. doi:10.1177/0743558407305415
Bureau of Labor Statistics. (2014, October). Unemployment rates by age, sex, race, and Hispanic or Latino ethnicity. Washington, DC: U.S. Department of Labor. Retrieved from http://www.bls.gov/web/empsit/cpsee_e16.htm
Chassin, L., Pitts, S. C., & Prost, J. (2002). Binge drinking trajectories from adolescence to emerging adulthood in a high-risk sample: Predictors and substance abuse outcomes. Journal of Consulting and Clinical Psychology, 70, 67–78. doi:10.1037/0022-006X.70.1.67
Chickering, A. W., & Schlossberg, N. K. (1998). Moving on: Seniors as people in transition. In J. N. Gardner, G. Van der Veer, & Associates (Eds.), The senior year experience: Facilitating integration, reflection, closure, and transition (pp. 37–50). San Francisco, CA: Jossey-Bass.
Cohen, P., Kasen, S., Chen, H., Hartmark, C., & Gordon, K. (2003). Variations in patterns of developmental transitions in the emerging adulthood period. Developmental Psychology, 39, 657–669. doi:10.1037/0012-1649.39.4.657
Cohen, S., & McKay, G. (1984). Social support, stress and the buffering hypothesis: A theoretical analysis. In A. Baum, S. E. Taylor, & J. E. Singer (Eds.), Handbook of psychology and health (Vol. 4, pp. 253–267). Hillsdale, NJ: Erlbaum.
Daly, K. D., & Mallinckrodt, B. (2009). Experienced therapists’ approach to psychotherapy for adults with attachment avoidance or attachment anxiety. Journal of Counseling Psychology, 56, 549–563. doi:10.1037/a0016695
Ditzen, B., Schmidt, S., Strauss, B., Nater, U. M., Ehlert, U., & Heinrichs, M. (2008). Adult attachment and social support interact to reduce psychological but not cortisol responses to stress. Journal of Psychosomatic Research, 64, 479–486. doi:10.1016/j.jpsychores.2007.11.011.
Dooley, D., Prause, J., & Ham-Rowbottom, K. A. (2000). Underemployment and depression: Longitudinal relationships. Journal of Health and Social Behavior, 41, 421–436.
Dubas, J. S., & Petersen, A. C. (1996). Geographical distance from parents and adjustment during adolescence and young adulthood. New Directions for Child and Adolescent Development, 71, 3–19. doi:10.1002/cd.23219967103
Erikson, E. H. (1994). Identity and the life cycle. New York, NY: Norton. (Original work published 1959)
Fasick, F. A. (1988). Patterns of formal education in high school as rites de passage. Adolescence, 23, 457–468.
Fraley, R. C., & Davis, K. E. (1997). Attachment formation and transfer in young adults’ close friendships and romantic relationships. Personal Relationships, 4, 131–144. doi:10.1111/j.1475-6811.1997.tb00135.x
Furstenberg, F. F., Jr., Rumbaut, R. G., & Settersten, R. A., Jr. (2005). On the frontier of adulthood: Emerging themes and new directions. In R. A. Settersten, Jr., F. F. Furstenberg, Jr., & R. G. Rumbaut (Eds.), On the frontier of adulthood: Theory, research, and public policy (pp. 3–28). Chicago, IL: University of Chicago Press.
Fussell, E., & Furstenberg, F. F., Jr. (2005). The transition to adulthood during the twentieth century: Race, nativity and gender. In R. A. Settersten, Jr., F. F. Furstenberg, Jr., & R. G. Rumbaut (Eds.), On the frontier of adulthood: Theory, research, and public policy (pp. 29–75). Chicago, IL: University of Chicago Press.
Galambos, N. L., Barker, E. T., & Krahn, H. J. (2006). Depression, self-esteem, and anger in emerging adulthood: Seven-year trajectories. Developmental Psychology, 42, 350–365. doi:10.1037/0012-1649.42.2.350
Garcia, J. R., Reiber, C., Massey, S. G., & Merriwether, A. M. (2012). Sexual hook-up culture: A review. Review of General Psychology, 16, 161–176. doi:10.1037/a0027911
Gardner, P. D., & Lambert, S. E. (1993). It’s a hard, hard, hard, hard, hard, hard world. Journal of Career Planning and Employment, 53, 40–49.
Gerstacker, M. D. (2010). Becoming an emerging adult: Demographic and cultural factors, coping style, and coping self-efficacy as predictors of exploration and commitment during the resolution of an emerging adult’s identity crisis (Doctoral dissertation). Retrieved from repository.lib.ncsu.edu/ir/bitstream/1840.16/5134/1/etd.pdf
Goldscheider, F., & Goldscheider, C. (1999). The changing transition to adulthood: Leaving and returning home. Thousand Oaks, CA: Sage.
Gore, S., & Aseltine, R. H., Jr. (2003). Race and ethnic differences in depressed mood following the transition from high school. Journal of Health and Social Behavior, 44, 370–389.
Guttmann-Steinmetz, S., & Crowell, J. A. (2006). Attachment and externalizing disorders: A developmental psychopathology perspective. Journal of the American Academy of Child and Adolescent Psychiatry, 45, 440–451. doi:10.1097/01.chi.0000196422.42599.63
Hiester, M., Nordstrom, A., & Swenson, L. M. (2009). Stability and change in parental attachment and adjustment outcomes during the first semester transition to college life. Journal of College Student Development, 50, 521–538. doi:10.1353/csd.0.0089
Ingram, R. E., & Gallagher, M. W. (2010). The nature of adult vulnerability: History and definitions. In R. E. Ingram & J. M. Price (Eds.), Vulnerability to psychopathology: Risks across the lifespan (2nd ed., pp. 39–56). New York, NY: Guilford Press.
Karreman, A., & Vingerhoets, A. J. J. M. (2012). Attachment and well-being: The mediating role of emotion regulation and resilience. Personality and Individual Differences, 53, 821–826. doi:10.1016/j.paid.2012.06.014
Kenny, M. E. (1987). The extent and function of parental attachment among first-year college students. Journal of Youth and Adolescence, 16, 17–29. doi:10.1007/BF02141544
Kenny, M. E., Blustein, D. L., Chaves, A., Grossman, J. M., & Gallagher, L. A. (2003). The role of perceived barriers and relational support in the educational and vocational lives of urban high school students. Journal of Counseling Psychology, 50, 142–155. doi:10.1037/0022-0167.50.2.142
Kenny, M. E., & Donaldson, G. A. (1991). Contributions of parental attachment and family structure to the social and psychological functioning of first-year college students. Journal of Counseling Psychology, 38, 479–486.
Kenny, M. E., & Sirin, S. R. (2006). Parental attachment, self-worth, and depressive symptoms among emerging adults. Journal of Counseling & Development, 84, 61–71. doi:10.1002/j.1556-6678.2006.tb00380.x
Lane, J. A. (2013a). Group counseling for students transitioning out of postsecondary education: A narrative approach. Groupwork: An Interdisciplinary Journal for Working With Groups, 23, 34–55. doi:10.1921/1501230103
Lane, J. A. (2013b). The impact of attachment working models and social support on the subjective and psychological well-being of emerging adults in transition: Testing a theoretical mediation model (Unpublished doctoral dissertation). Oakland University, Rochester, MI.
Lane, J. A. (2014). Attachment, social support, and well-being during life transition in emerging adulthood. Manuscript submitted for publication.
Lane, J. A. (in press-a). Attachment, well-being, and college senior concerns about the transition out of college. Journal of College Counseling.
Lane, J. A. (in press-b). The imposter phenomenon among emerging adults transitioning into professional life. Adultspan Journal.
Larose, S., & Boivin, M. (1998). Attachment to parents, social support expectations, and socioemotional adjustment during the high school-college transition. Journal of Research on Adolescence, 8, 1–27. doi:10.1207/s15327795jra0801_1
Lee, C., & Gramotnev, H. (2007). Life transitions and mental health in a national cohort of young Australian women. Developmental Psychology, 43, 877–888. doi:10.1037/0012-1649.43.4.877
Lopez, F. G., Chervinko, S., Strom, T., Kinney, J., & Bradley, M. (2005). What does it mean to be an adult? A qualitative study of college students’ perceptions and coping processes. Journal of College and Character, 6(4), 1– 31. doi:10.2202/1940-1639.1424
Lopez, F. G., Mitchell, P., & Gormley, B. (2002). Adult attachment and college student distress: Test of a mediational model. Journal of Counseling Psychology, 49, 460–467. doi:10.1037/0022-0167.49.4.460
Mallinckrodt, B. (2000). Attachment, social competencies, social support, and interpersonal process in psychotherapy. Psychotherapy Research, 10, 239–266. doi:10.1093/ptr/10.3.239
Mallinckrodt, B., & Wei, M. (2005). Attachment, social competencies, social support, and psychological distress. Journal of Counseling Psychology, 52, 358–367. doi:10.1037/0022-0167.52.3.358
Manago, A. M., Taylor, T., & Greenfield, P. M. (2012). Me and my 400 friends: The anatomy of college students’ Facebook networks, their communication patterns, and well-being. Developmental Psychology, 48, 369–380. doi:10.1037/a0026338
Masten, A. S., Burt, K. B., Roisman, G. I., Obradović, J., Long, J. D., & Tellegen, A. (2004). Resources and resilience in the transition to adulthood: Continuity and change. Development and Psychopathology, 16, 1071–1094. doi:10.1017/S0954579404040143
Mortimer, J. T., Zimmer-Gembeck, M. J., Holmes, M., & Shanahan, M. J. (2002). The process of occupational decision making: Patterns during the transition to adulthood. Journal of Vocational Behavior, 61, 439–465. doi:10.1006/jvbe.2002.1885
Murphy, K. A., Blustein, D. L., Bohlig, A. J., & Platt, M. G. (2010). The college-to-career transition: An exploration of emerging adulthood. Journal of Counseling & Development, 88, 174–181. doi:10.1002/j.1556-6678.2010.tb00006.x
National Center for Education Statistics. (2014). Degrees conferred by sex and race. Washington, DC: U.S. Department of Education, Institute of Education Sciences. Retrieved from http://nces.ed.gov/fastfacts/display.asp?id=72
O’Connor, M., Sanson, A., Hawkins, M. T., Letcher, P., Toumbourou, J. W., Smart, D., . . . Olsson, C. A. (2011). Predictors of positive development in emerging adulthood. Journal of Youth and Adolescence, 40, 860–874. doi:10.1007/s10964-010-9593-7
Overton-Healy, J. (2010). First-generation college seniors: A phenomenological exploration of the transitional experience of the final college year (Doctoral dissertation). Retrieved from dspace.iup.edu/bitstream/handle/2069/249/Julia Overton-Healy.pdf?sequence=1
Perrone, L., & Vickers, M. H. (2003). Life after graduation as a “very uncomfortable world”: An Australian case study. Education and Training, 45, 69–78. doi:10.1108/00400910310464044
Pistilli, M. D., Taub, D. J., & Bennett, D. E. (2003). Development of the senior concerns survey: An exploratory factor analysis. Journal of the First-Year Experience, 15, 39–52.
Polach, J. L. (2004). Understanding the experience of college graduates during their first year of employment. Human Resource Development Quarterly, 15, 5–23. doi:10.1002/hrdq.1084
Raymore, L. A., Barber, B. L., & Eccles, J. S. (2001). Leaving home, attending college, partnership and parenthood: The role of life transition events in leisure pattern stability from adolescence to young adulthood. Journal of Youth and Adolescence, 30, 197–223. doi:10.1023/A:1010345825065
Raymore, L. A., Barber, B. L., Eccles, J. S., & Godbey, G. C. (1999). Leisure behavior pattern stability during the transition from adolescence to young adulthood. Journal of Youth and Adolescence, 28, 79–103. doi:10.1023/A:1021624609006
Roberts, J. E., Gotlib, I. H. & Kassel, J. D. (1996). Adult attachment security and symptoms of depression: The mediating roles of dysfunctional attitudes and low self-esteem. Journal of Personality and Social Psychology, 70, 310–320. doi:10.1037/0022-3514.70.2.310
Sampson, R. J., & Laub, J. H. (1990). Crime and deviance in the life course: The salience of adult social bonds. American Sociological Review, 55, 609–627. doi:10.2307/2095859
Sarason, B. R., Pierce, G. R., Shearin, E. N., Sarason, I. G., Waltz, J. A., & Poppe, L. (1991). Perceived social support and working models of self and actual others. Journal of Personality and Social Psychology, 60, 273–287. doi:10.1037/0022-3514.60.2.273
Scharf, M., Mayseless, O., & Kivenson-Baron, I. (2004). Adolescents’ attachment representations and developmental tasks in emerging adulthood. Developmental Psychology, 40, 430–444.
Schnyders, C. M. (2014). Parent and peer attachment as predictors of the perceived experience of emerging adulthood. Manuscript submitted for publication.
Schnyders, C. M., & Lane, J. A. (2014). Gender differences regarding attachment relationships in perceptions of early emerging adulthood experiences. Manuscript submitted for publication.
Schulenberg, J. E., Bryant, A. L., & O’Malley, P. M. (2004). Taking hold of some kind of life: How developmental tasks relate to trajectories of well-being during the transition to adulthood. Development and Psychopathology, 16, 1119–1140. doi:10.1017/S0954579404040167
Scott-Parker, B., Watson, B. C., King, M. J., & Hyde, M. K. (2011). The psychological distress of the young driver: A brief report. Injury Prevention, 17, 275–277. doi:10.1136/ip.2010.031328.
Sharma, B. (2012). Adjustment and emotional maturity among first year college students. Pakistan Journal of Social and Clinical Psychology, 9, 32–37.
Shulman, S., & Nurmi, J.-E. (2010). Dynamics of goal pursuit and personality make-up among emerging adults: Typology, change over time, and adaptation. In S. Shulman & J.-E. Nurmi (Eds.), The role of goals in navigating individual lives during emerging adulthood: New directions for child and adolescent development, number 130 (pp. 57–70). San Francisco, CA: Wiley.
Slade, A. (2008). The implications of attachment theory and research for adult psychotherapy: Research and clinical perspectives. In J. Cassidy & P. R. Shaver (Eds.), Handbook of attachment: Theory, research, and clinical applications (2nd ed., pp. 762–782). New York, NY: Guilford Press.
Sleap, M., & Reed, H. (2006). Views of sport science graduates regarding work skills developed at university. Teaching in Higher Education, 11, 47–61. doi:10.1080/13562510500400123
Sturges, J., & Guest, D. (2001). Don’t leave me this way! A qualitative study of influences on the organisational commitment and turnover intentions of graduates early in their career. British Journal of Guidance and Counselling, 29, 447–462. doi:10.1080/03069880120085992
Twenge, J. M. (2013). The evidence for generation me and against generation we. Emerging Adulthood, 1, 11–16. doi:10.1177/2167696812466548
U.S. Census Bureau. (2012, September). Table P-10. Age—people (both sexes combined) by median and mean. Washington, DC: Author. Retrieved from https://www.census.gov/hhes/www/income/data/historical/people/
Vickio, C. J. (1990). The goodbye brochure: Helping students to cope with transition and loss. Journal of Counseling & Development, 68, 575–577. doi:10.1002/j.1556-6676.1990.tb01414.x
Weber, L. (2012, June 21). Do too many young people go to college? The Wall Street Journal. Retrieved from http://online.wsj.com/article/SB10001424052970203960804577239253121093694.html
Wei, M., Liao, K. Y.-H., Ku, T.-Y., & Shaffer, P. A. (2011). Attachment, self-compassion, empathy, and subjective well-being among college students and community adults. Journal of Personality, 79, 191–221. doi:10.1111/j.1467-6494.2010.00677.x
Wei, M., Mallinckrodt, B., Larson, L. M., & Zakalik, R. A. (2005). Adult attachment, depressive symptoms, and validation from self versus others. Journal of Counseling Psychology, 52, 368–377. doi:10.1037/0022-0167.52.3.368
Weiss, D., Freund, A. M., & Wiese, B. S. (2012). Mastering developmental transitions in young and middle adulthood: The interplay of openness to experience and traditional gender ideology on women’s self-efficacy and subjective well-being. Developmental Psychology, 48, 1774–1784. doi:10.1037/a0028893
Wendlandt, N. M., & Rochlen, A. B. (2008). Addressing the college-to-work transition: Implications for university career counselors. Journal of Career Development, 35, 151–165. doi:10.1177/0894845308325646
Yazedjian, A., Kielaszek, B. J., & Toews, M. L. (2010). Students’ perceptions regarding their impending transition out of college. Journal of the First-Year Experience & Students in Transition, 22, 33–48.
Yeadon, C. (2010). College senior transition programs: Transitioning from college to the workplace. Journal of Student Affairs, 19, 44–50.
Joel A. Lane, NCC, is the recipient of the 2014 Outstanding Dissertation Award for The Professional Counselor and an Assistant Professor at Portland State University. Correspondence can be addressed to Joel A. Lane, Department of Counselor Education, Portland State University, Graduate School of Education, PO Box 751, Portland, OR 97207, lanejoel@pdx.edu.
Feb 9, 2015 | Article, Volume 5 - Issue 1
Miles Matise
This article describes a qualitative interview study of 11 counselors’ personal experiences of crying in session with a client and their perception of its effects on the therapeutic relationship. Semistructured interviews with counselors at a mid-sized university in the Midwest found that tears could be an appropriate response to a client’s unique situation and helpful in empathizing with the client. Themes of awareness, empathy, modeling and authenticity as well as implications for counselors are discussed.
Keywords: crying, empathy, self-disclosure, authenticity, therapeutic relationship
Crying is a response that all people have in common and one of the most powerful demonstrations of emotional expression in humans. Darwin’s (1872) early theories of emotions have greatly influenced the significance of studying tears. Emotional expression seems to be universal among humans and the expression of tears is innate, serving an important function for our welfare, as well as a form of non-verbal communication. The words “crying” and “tears” are used synonymously in this study to mean tearing up, as in the eyes filling with tears or running over as an expression of empathy.
Counselors are faced with a variety of emotionally charged situations that at times might be uncomfortable and unpleasant and, as a result, influence counseling behavior during a session. The rationale for this study was based on the paucity of research on counselors’ tearing up as an appropriate form of self-disclosure, when it genuinely and spontaneously occurs and is not the result of the counselor’s unresolved issues.
The main purposes for exploring the phenomenon of counselors’ crying were as follows: (a) to increase counselor self-awareness and reactions in emotionally intense situations, (b) to promote dialogue for counseling supervisors and educators, and (c) to discover the meaning a counselor places on personally significant crying experiences. Cornelius (1981) noted that researchers are a long way from developing a comprehensive theory of crying and that there is a need for more descriptive data before construction of a theory. The current study is a step toward providing such data on the phenomenon of counselors’ crying in session.
Individuals in helping roles are vulnerable to a wide variety of emotionally charged situations, which can be defined situations in which there is high potential for reactionary behaviors. These behaviors can lead to overt expressions, such as crying, screaming, angry outbursts and sometimes seemingly irrational demonstrations of emotion. Emotionally charged situations can be uncomfortable and unpleasant and can induce a state of anxiety, especially in professional situations such as counseling. When a counselor has an emotionally charged response to a client, feelings can intensify, resulting in a spontaneous reaction, even crying. However, a study by Curtis, Matise, and Glass (2003) suggested that crying with clients could be a genuine expression of emotions and facilitate the therapeutic relationship.
Crying has several advantages. Crying is a natural coping mechanism that helps to buffer against the pathogenic effects of stress (Davis, 1990; Frey, Desota-Johnson, Hoffman, & McCall, 1981). Crying not only has certain health benefits (Davis, 1990; Frey, Desota-Johnson, Hoffman, & McCall, 1981) such as relieving stress caused by the buildup of emotions, but also can enhance empathy and facilitate the therapeutic alliance (Horvath, 2001). Waldman (1995) suggested that a counselor’s crying could be therapeutic to a client. According to Frey et al. (1981), emotional stress alters the chemical balance of the human body. When the stimulation of the lacrimal gland in the brain increases due to emotional intensity, it results in the production of tears. Although the social expression of crying has differences in degree, for this study crying is defined as the state of lachrymose secretions pouring from the eyes in response to emotional stimulation.
Crying and Stress in the Counseling Situation
The connection between emotional stress and the biological process suggests that crying is a function of the body to maintain homeostasis by helping to relieve emotional stress. In a study on why adults cry, emotional tears seemed to be associated with tension reduction (Efran & Spangler, 1979). The researchers focused on the recovery aspect of tears and suggested that crying happens when a psychological barrier or perturbation disappears, signifying recovery and adaptation rather than continuation of distress or arousal, thus permitting the system to shift into recovery
Hill, Mahalik, and Thompson (1989) offered two explanations for a counselor’s emotional reaction of crying during a session. The first is self-disclosure, which refers to a counselor’s personal emotional response to the client. When self-disclosure is appropriate, the counselor shares a segment from his or her own life with the client for the purpose of either reassuring or challenging the client’s experience. Yet, the focus in this situation is on the client and not the counselor. When a counselor is in a situation that stirs powerful emotions, self-disclosure can deepen the counselor–client connection or can reflect the counselor’s inability to contain his or her own feelings.
A second explanation for a counselor’s emotional reaction of crying during a session is empathy, which refers to one’s active attention toward the feelings of others (Rogers, 1980). This concept emphasizes the therapeutic function of a counselor’s ability to fully experience the attitude expressed by the client and reflect to the client what he or she is experiencing. Empathy is considered a significant way to enhance and deepen the therapeutic relationship.
Sometimes counselors might discount the behavior of crying as an inappropriate reaction triggered by the experience of anxiety and discomfort or an overly sympathetic response. In order to reduce his or her reaction to an emotionally charged situation, a counselor might emotionally detach from the client in order to quell his or her own discomfort and limit a reactionary response in return. While the intention of this emotional detachment may help the counselor maintain a more objective perspective toward the client’s reaction, the result also may be to limit the counselor’s emotional availability and thus protect the counselor’s own needs over the needs of the client. By detaching, the counselor can unintentionally emotionally abandon the client at a time when the client most needs support.
The Therapeutic Effectiveness of Crying
Few studies have examined the effectiveness of counselors’ crying in session. Waldman (1995) and Counselman (1997) suggested that counselors’ emotional tears could be therapeutic to a client. Waldman (1995) interviewed ten licensed psychologists with at least 5 years of clinical experience each. Each psychologist discussed his or her perceptions and feelings related to an incident in which he or she cried with a client during a session. Waldman found that nine of the participants believed that their emotional tears were helpful in facilitating the therapeutic process. In contrast, one participant reported that emotional crying was the result of personal unresolved issues, which was not helpful to the client. With this in mind, it is possible that counselors’ crying can be the result of the counselor’s own struggles and countertransference. In this instance, objectivity could be lost and the therapeutic relationship hindered. Therefore, counselors might perceive crying as nontherapeutic and even unethical. Nevertheless, Waldman (1995) concluded that crying with clients enhanced the counselor–client connection and facilitated the client’s work in session.
Counselman (1997) conducted a case study exploring the therapeutic effectiveness of a counselor crying in session with a client. She reported on her work with a couple in which the wife was dying of cancer. After several sessions of marriage counseling relating to an affair by the husband, the author described crying when the couple disclosed that the wife’s breast cancer had recurred. Counselman (1997) admitted that her greatest fear was that she would not be able to stop crying and presumably might be viewed as unprofessional. However, she decided that her first priority was to be fully present with the couple, even if this meant crying with them in session. She reported that her willingness to share her emotions with this couple deepened the therapeutic relationship and facilitated the couple’s counseling goals all the way to her client’s death. She also indicated that this self-exposure “was healing for me in the way our work as counselors often is” (p. 237). Corey (2001) suggested, “If you use your own feelings as a way of understanding yourself, your client, and the relationship between the two of you, these feelings can be a positive and healing force” (p. 108).
Men in our society have consistently been taught not to cry and to downplay emotions. Counselors who find themselves on the verge of emotional tears may find the experience more profitable if they have had access to images that portrayed this behavior as acceptable and natural rather than a shameful and weak demonstration of emotions, especially for male counselors (Hoover-Dempsey, Plas, & Wallston, 1986).
Given that much therapeutic work is dedicated to helping clients express their deepest feelings, the lack of research regarding counselors’ tearing up in session lends significance to the study of professionals who encounter emotionally charged situations and their emotional availability to respond in authentic ways without diminishing their credibility.
Methods
Study Design
The present study was informed by life-world phenomenology (Ashworth, 2003) in order to gain information and to give voice to the lived experiences of counselors around the issue of intense emotional experiences in the counseling situation, which sometimes includes crying. A phenomenological approach with oral responses was consistent with the goals of the study and sensitive to the needs of the participants. Phenomenological research originated from Edmund Husserl’s phenomenology philosophy and aims to clarify a person’s lived experience through everyday life situations (Giorgi & Giorgi, 2008). The root of phenomenology is that of intentionality, which allows objects to appear as phenomena because the self and the world are inseparable components of meaning. The idea is to suspend all presuppositions and biases and closely capture an experience within the context that the experience takes place. This is attempted through the three steps of epoche, phenomenological reduction and imaginative variation (Willig, 2001).
Participants and Setting
Potential participants were contacted either by email or in person and asked to volunteer for a brief interview concerning crying with clients while in a session. The criteria for inclusion were based on licensure, certification and experience, as well as the ability to provide full descriptions of one’s personal experiences of crying in session. In total, 11 counselors and professionals with related experience were included in this study. Participants were between 25 and 71 years old; four participants were males and the remainder female. The sample consisted of licensed professional counselors, school counselors, national certified counselors, a licensed marriage and family counselor, and a psychologist, with a combined average of 15 years’ experience in their related fields. The participant’s theoretical perspectives were varied and consisted of the following: cognitive behavioral, family systems, existential, Adlerian and person centered. Open-ended questions provided a general guide to the interviews (see Appendix), while allowing for discussion of relevant material.
Data Collection
Data collection consisted of semistructured interviews varying in length from 30–120 minutes. Interviews were chosen in order to open up topics and receive the participants’ stories of crying in session with clients. Each interview was audio recorded and notes were taken during the interviews to facilitate transcription and future analysis. Repeat interviews were conducted with all but three of the participants, thus contributing to richer descriptions. The following topic areas were covered in the interviews: (1) What issues would make you cry in session? (2) What is your response to a client who starts crying in session? (3) How would crying be beneficial to the therapeutic relationship? (4) How do you keep yourself from crying in session with a client? (For more complete information, see Appendix.)
The data were processed in order to discern meanings and actions by first using a central idea or question relating to the research. The central questions used to guide this analysis were as follows:
What is the counselor’s internal experience of a client who cries in session?
What is the counselor’s internal experience of allowing him or herself to cry in session with a client?
Second, the author and a colleague brainstormed other terms that relate to the central concept of crying. This process led to further questions and terms, such as awareness, empathy, crying as choice, loss, grief, genuineness, control, equality, acceptance and permission. Third, connections were drawn among the various terms based on how the ideas related to each other, until ideas were exhausted about the central topic. Fourth, the findings were summarized and a graphical representation of the data was used to draw themes at face value, rather than explain or interpret at that point. Fifth, the author discussed the findings with a non-biased professional colleague in order to interpret how the data were linked to the big picture, theoretical perspectives and previous literature.
Data Analysis
Following the qualitative guidelines proposed by Creswell (1998) and Moustakas (1994), phenomenological analysis proceeded through several stages. The first was horizonalization of the data, in which the researcher read through the data and identified statements that described how the participants experienced the phenomenon of crying. Moustakas (1994) called these meaning statements and Creswell (1998) called them significant statements. For instance, one participant contributed a significant statement by describing crying as a genuine and spontaneous response:
I see it [crying] as an expression of a deep emotion and a genuine or real thing that happens. The client can see how I’m experiencing what they’ve told me. If that involves crying, that means that’s how I experience their story.
The second stage was transcribing the statements into separate themes. Third, phenomenological reduction was used to group the meaning statements thematically by coding them with short descriptions for each theme. Lastly, imaginative variation was used to vividly capture the textures of the themes. Through intuitive thinking, imaginative variation enables the researcher to derive structural themes from the textural descriptions (Moustakas, 1994). An overall description of the themes that illustrated the essential meaning of the experience was concluded.
Audio-recorded interviews were transcribed verbatim for each participant and the transcripts were analyzed by the author and cross-analyzed for consistency by a professional colleague who was not a member of the counseling profession. All of the interviews were thematically and categorically analyzed for commonalities in the phenomenon of crying, and regular discussions were held to achieve consensus on emerging themes from the descriptive to the analytic stages.
Three main phases of data collection and analysis occurred over the course of 32 weeks. The first phase was an initial analysis that took place during data collection. The second was a content analysis conducted after the study was completed. The final analysis was thematic, in which categories were used to organize contributions.
Categorical analytic procedures described by Creswell (1998) and Merriam (1998) guided analysis of the interview data and narrative questionnaire data, which were combined for analysis. During the interviews, the author bracketed (epoche) experiences that may have contaminated collection, interpretation and analysis of the data. Bracketing is performed by examining possible researcher biases and then setting those biases aside (Moustakas, 1994). This challenge was addressed by the researcher maintaining a journal of thoughts and reactions in order to increase his awareness of and accountability to the process of epoche. Potential researcher biases consisted of the researcher’s personal experiences with crying, his own values and opinions concerning the phenomenon of crying, and his own professional ethics related to crying with a client.
During data collection, there was a continuous cycle in which the researcher read, reread, reflected on and interpreted the data. Constant comparison (Merriam, 1998) was practiced, in which multiple readings of the data set were examined and compared with the next piece of data. Unique responses and isolated situations also were identified and analyzed.
Ethical Considerations
As a professional counselor, the researcher has been conditioned by his training and abides by ethical codes of conduct from professional organizations, most of which do not address the issue of a counselor’s crying in session with a client. These measures were taken during data analysis so as not to interfere with the accurate telling of each participant’s personal experiences of the phenomenon of crying.
Ethical approval was granted by the Internal Review Board of the university where participants were solicited. Participants were asked to consent to a voluntary interview about the nature of their experience of crying in session with a client and notified of the estimated time of participation. The results of the interviews were confidential and no personal identification was requested of the participants.
Procedures to Ensure Trustworthiness
A variety of strategies were used to ensure the credibility, confirmability (validity) and trustworthiness (reliability) of this study. First, a purposeful sample was selected for this investigation to ensure that the participants had a wide range of experiences as counselors in a therapeutic milieu, and in order to increase the probability of participants having experienced the phenomenon of crying in a session.
An audit trail (Lincoln & Guba, 1985) was created to ensure that the participants felt confident that the research data showed a fully accurate description of their experiences of crying in session. Records were kept in the form of raw data (e.g., field notes), data reduction (e.g., summaries of theoretical notes), data reconstruction (e.g., structure of categories, themes, relationships, definitions, conclusions), and process notes (e.g., trustworthiness notes relating to credibility and dependability).
Data triangulation (Thurmond, 2001) was implemented by soliciting feedback from participants during the analysis stage of data collection. The participants’ diversity of experience, theoretical perspectives, demographic variability and length of experience as licensed professionals in their fields helped the researcher gain a clearer understanding of the phenomenon of crying and how it applies to counseling. Participants were allowed to see the interview questions prior to the interview, in order to provide more in-depth and thoughtful answers regarding the phenomenon being investigated.
Member checking was implemented to test the accuracy of the categories, interpretations and conclusions of the researcher with the participants from whom the data were originally obtained. This procedure was conducted informally during the normal course of observation and conversation with the participants at the time of their interviews. A more formal procedure was implemented after the researcher transcribed the interviews and sent them to participants for investigation. After the evaluation stage was complete and themes were established for the phenomenon of crying in session with clients, an email was sent to participants with a summary of the thematic conclusions, soliciting feedback, challenges or additional information from participants.
An external audit was conducted throughout the evaluation and analysis stages, in which the author discussed the data with a colleague who was not a part of the mental health profession. The purpose of choosing this colleague was to have an unbiased person who would not be swayed by training as a counselor and the ethics of the profession. The researcher’s assumption was that mental health professionals would be more prone to accept, tolerate and be nonjudgmental toward clients’ intense emotional experiences, even to the point of crying with them. Another external audit conducted to foster the accuracy and validity of the present study included advising from a faculty member in the applied statistics and research methods department of the university where the participants were sampled.
Results
Through analysis of the participants’ interviews, invariant horizons were identified and themes were extracted and clustered through the reduction process (Moustakas, 1994). Following are textual descriptions of the prominent identified themes that emerged, including awareness, empathy, modeling and authenticity. An examination of participants’ experiences also was extrapolated from the data.
Theme 1: Awareness
Each of the participants spoke about the skill of awareness as a decisive factor as to whether they would cry in session. Awareness was described as a skill that could be learned and used by the counselor, not only to determine whether to cry in session, but whether the voluntary nature of crying as an emotional response could be used to facilitate a therapeutic interaction. One male counselor-participant described crying as follows:
Crying means different things in different cultures. Some cultures and people may see crying as a sign of weakness, whereas others encourage its expression to practice being humble and exercise social kindness. As part of being culturally sensitive, a counselor needs to pay attention and try to explore with the client about this behavior. Crying is like a universal language that involves a list of vocabulary from different cultures and persons.
Awareness was an essential component of whether crying was considered therapeutic for the client. Even though all participants had cried to some degree or another in session, their respective levels of comfort and opinions of what could help counselors-in-training prepare for such emotionally charged issues varied. One participant spoke of not being able to turn her crying on or off, but said that if she felt it was not appropriate because it took the focus off the client, then she tried to block herself from crying or tearing up:
If I cry in session, I open it up and tell the client that this is how I’m experiencing your situation and I’m crying, how does that feel to you? If they say it’s not ok, then I’ll tell them that I’ll try to block it, but I’m not sure if I’ll always be able to.
One interview question asked whether counseling programs could do anything different in terms of preparing counselors-in-training to deal with emotionally intense situations in which crying might occur. There was consensus among more than half of the participants that they had had no formal training in dealing with such emotionally intense situations, largely because this training is not something that can be taught from a textbook. One can read about an issue, but experiencing it is something quite different. To know oneself was said to be more pertinent, in terms of knowing how one would react to a particular situation. All of the participants made this statement, though they had no formal training in dealing with emotionally intense situations in which crying might occur. A male marriage and family counselor stated:
You can read the kinds of things we’re talking about in a book, but I think the best way to teach people is in experiential situations. To have some knowledge that these things are going to happen and that it’s ok to deal with it, that’s the cognitive piece that you can teach people. The emotional piece, that you can’t teach people, is how to handle it.
Another participant, a licensed professional counselor, stated that she was in fact overprepared. She continued, “My master’s program was in the day [1970s] when there was a lot of therapy. It was about intensity and our own comfort with intensity.” She felt that the pendulum had swung too far the other way, stating, “I think we ought to do a lot more personal growth in our [training] programs than we do.”
Theme 2: Empathy
A predominant issue for the participants was that of crying linked with empathy. All participants felt that crying demonstrated a deeper form of empathy toward the client. Empathy is the experience of being in the client’s shoes and tapping into the present felt experience of the situation. One of the most effective ways a counselor can help a client change is to affirm his or her subjective experience. Empathy is an essential skill for helping clients feel that they are being validated and understood (Teyber, 2000). For a counselor, knowing the issues that touch his or her own personal soft spots (countertransference) is important in order to inform a counselor’s interaction with a client. One participant said, “I think it [crying] may be the ultimate empathy, if the tears are genuine. I’m sure Carl Rogers would have cried with clients.” The researcher challenged the participant by asking, “I wonder if he [Carl Rogers] ever did cry with a client?” Her response was as follows:
How could he not, because when we’re really in psychological contact we don’t absorb their stuff; we experience it with them for a short time. I don’t think we leave unscathed. I think clients change from our work with them and we change from our work with our clients.
Empathy points to an invisible element that leads to a deeper connection with an individual. Crying with a client in session, if genuine, was deemed a deeper kind of empathy, beyond words, that demonstrates a validating connection and recognition of the client’s subjective experience.
Theme 3: Modeling
As a result of specialized training, counselors may be regarded as more competent in human relation skills such as emotional expression, and thus bear a responsibility to model positive and appropriate expressions of intense emotions to clients. Modeling relates to how the client interprets and integrates the influence of the counselor’s actions into his or her daily activities of emotional expression. Because of training in interpersonal effectiveness, counselors may be more adept at emotional expression, and thus there may exist a higher expectation from others regarding trained mental health professionals’ reactions to such emotionally intense situations. A school counselor stated:
By acknowledging crying, you don’t have to pull back, because what I’ve seen with therapists is they pull back in an attempt to control it, so they lose contact with the client and the situation. They’re also modeling for the client that it [crying]’s not ok and whatever it is they’re experiencing is not okay to share with other people, because it makes people uncomfortable.
Counselors can have a significant influence on clients and model a corrective emotional experience. If counselors are not to be merely conduits for cultural values, in terms of what the socially acceptable response is for emotional expressions, then a counselor modeling authenticity is most effective when it is a genuine act of responding to an emotionally intense situation.
Theme 4: Authenticity
All participants came from a counseling perspective that was relationally based. One counselor came from a cognitive-behavioral theoretical approach, four came from a family systems perspective, one from an existential approach, one from an Adlerian approach, and the remainder from a person-centered perspective. What these theoretical perspectives have in common is that the relationship with the client forms the foundation of the theory. Being genuine was correlated with authenticity and therapeutic effectiveness. Crying might have an equalizing effect, confirming to clients that the counselor is human and understands their experience.
It was found that among participants the range of and comfort with emotional expression varied by age. Older participants (> 40 years old) with more experience had become more comfortable with the way in which they expressed their emotions. Younger participants (< 40 years old) felt that it was acceptable to cry as long as it was appropriate in their estimation, but were less likely to do so while in session with a client.
A technique called immediacy can have an equalizing effect on the relationship and induce a therapeutic moment by revealing the counselor’s immediate perspective on the situation at hand. One female participant clarified, “Usually when I cry I will say something regarding the tears and have a discussion whether they are helpful or disturbing to the client.” While authenticity is not the sole determining factor of whether or not a counselor cries, according to participants, crying is a strong indicator of the authenticity of a therapeutic interaction. For one counselor, her authenticity took the form of a countercultural response:
When I went to my dad’s funeral, I was thinking, if I don’t cry then they’re going to think something is wrong with me, so I hope I can cry. . . . Sometimes you’re in a situation where you feel it’s expected.
Despite cultural expectations, authenticity represents characteristics that are unique to every individual and is an internal experience of an outward expression. What is a genuine emotional expression to one counselor might look different to another.
Discussion
The outward expression of crying in a counseling session and whether tears flow as a result of a counselor’s unresolved issues versus an empathetic response to a client’s situation is critical for determining the effectiveness of the crying response. The studies reviewed and the participants interviewed varied in their conclusions about whether to cry with a client while in session and whether it is helpful to the client. Whether it is helpful to the client for the counselor to cry with him or her depends upon certain factors, including the degree and timing of the counselor’s tears, the cultural acceptableness of this type of emotional expression, and even gender. There are unforeseen factors that only a counselor can experience with a client based on the conditions of that exact moment. That being said, whether or not to cry with a client is a choice made based on the professional judgment of the counselor.
One way to measure the appropriateness of crying in session with a client is by the generally accepted practices of professionals in the mental health field. A counselor’s professional judgment has some link to the larger profession and the generally accepted practices of other professionals, as long as they adhere to the ethical standards of the prominent organizations of the field. However, this strategy may not always yield a conclusive answer. A counselor’s oath to do no harm should be a guiding factor, as well as obtaining supervision in order to work out these unique situations with clients.
The theme of authenticity and the desire to be oneself in the counseling session was consistent among the participants of this study. It has been suggested that hiding behind technical expertise and leaving one’s genuineness out of the relationship may not create the most therapeutic environment (Corey, 2001). Considerable research indicates that the counseling relationship is more important than technique in predicting client outcomes (Lambert & Cattani-Thompson, 1996; Nelson & Neufeldt, 1996). Thus, counseling by its very nature requires counselors to undertake the difficult task of managing countertransference while maintaining a genuine and open relationship with clients. To be authentic in session may mean to cry with a client or it may not, even if the emotional expression is intentionally held back. There may be no conclusively right or wrong way to be with a client, only a list of ethical guidelines to which to adhere.
Another important concept that is becoming more useful in the field of counseling is mindfulness. Mindfulness is much like this study’s theme of awareness, which the participants in this study recognized as an important aspect of determining whether to cry with a client. Self-awareness is considered not only a vital part of a counselor’s development, but also an important goal for the client who engages in counseling. Mindful attention helps distinguish between distorted thoughts and emotional patterns that entrap, in order to free the counselor (Bennett-Goleman, 2001). By practicing mindfulness, the counselor strengthens personal attention as a protection against being hijacked by a schema or distortion of thoughts. A mindful counselor can be more aware of thought patterns and catch him or herself from reacting to certain stimuli, such as a client’s tears. By not reacting, a counselor can make a wise choice as to the most appropriate response for a given situation. Because a goal of mindfulness is to be more fully present in the moment, a counselor who is mindful may be more aware of the subtleties between the counselor and client and be less judgmental. The mindful counselor may be slightly detached and more objective in an assessment of the situation and therefore less triggered by rogue feelings and judgments, while allowing for clarity of the situation and an authentic emotional response that may include crying.
Conclusion
A lack of clarity remains around the issue of intense emotional experiences in the counseling situation, which often includes crying or tearing up to some degree, as well as a lack of training in counselor education programs to deal with such situations. This study employed methods adopted from the phenomenological research tradition to generate data with which to interpret the crying event. The phenomenological method served as a starting point for exploration, and through this investigation, a rich description of the textural and structural aspects of each counselor’s experience was developed, as well as a final synthesized description of each participant’s unique set of circumstances. The findings of this investigation may prove useful for counseling faculty, supervisors, counselors and other mental health professionals.
Conflict of Interest and Funding Disclosure
The author reported no conflict of interest or funding contributions for the development of this manuscript.
References
Ashworth, P. D. (2003). The phenomenology of the lifeworld and social psychology. Social Psychological Review, 5, 18–34.
Bennett-Goleman, T. (2001). Emotional alchemy: How the mind can heal the heart. New York, NY: Three Rivers Press.
Corey, G. (2001). Theory and practice of counseling and psychotherapy (6th ed.). Belmont, CA: Wadsworth.
Cornelius, R. R. (1981). Weeping as social interaction: The interpersonal logic of the moist eye. Dissertation Abstracts International, 42(8), 3491B–3492B.
Counselman, E. F. (1997). Self-disclosure, tears, and the dying client. Psychotherapy, 34, 233–237.
Creswell, J. W. (1998). Qualitative inquiry and research design: Choosing among five traditions. Thousand Oaks, CA: Sage.
Curtis, R., Matise, M., & Glass, S. (2003). Counseling students’ views and concerns about weeping with clients: A pilot study. Counselling and Psychotherapy Research, 3, 300–306. doi:10.1080/14733140312331384303
Darwin, C. (1872). The expression of the emotions in man and animals. London, England: Murray.
Davis, W. E. (1990). Crying it out: The role of tears in stress and coping of college students (Unpublished doctoral dissertation). University of Colorado, Boulder, CO.
Efran, J. S., & Spangler, T. J. (1979). Why grown-ups cry: A two-factor theory and evidence from The Miracle Worker. Motivation and Emotion, 3, 63–72.
Frey, W. H., II, Desota-Johnson, D., Hoffman, C., & McCall, J. T. (1981). Effect of stimulus on the chemical composition of human tears. American Journal of Ophthalmology, 92, 559–567. doi:10.1016/0002-9394(81)90651-6
Giorgi, A., & Giorgi, B. (2008). Phenomenology. In J. A. Smith (Ed.), Qualitative psychology: A practical guide to research methods (2nd ed., pp. 26–52). London, England: Sage.
Hill, C. E., Mahalik, J. R., & Thompson, B. J. (1989). Therapist self-disclosure. Psychotherapy, 26, 290–295. doi:10.1037/h0085438
Hoover-Dempsey, K. V., Plas, J. M., & Wallston, B. S. (1986). Tears and weeping among professional women: In search of new understanding. Psychology of Women Quarterly, 10, 19–34. doi:10.1111/j.1471-6402.1986.tb00734.x
Horvath, A. O. (2001). The alliance. Psychotherapy: Theory, Research, Practice, Training, 38, 365–372. doi:10.1037/0033-3204.38.4.365
Lambert, M. J., & Cattani-Thompson, K. (1996). Current findings regarding the effectiveness of counseling: Implications for practice. Journal of Counseling and Development, 74, 601–608. doi:10.1002/j.1556-6676.1996.tb02299.x
Lincoln, Y. S., & Guba, E. G. (1985). Naturalistic inquiry. Newbury Park, CA: Sage.
Merriam, S. B. (1998). Qualitative research and case study applications in education. San Francisco, CA: Jossey-Bass.
Moustakas, C. (1994). Phenomenological research methods. Thousand Oaks, CA: Sage.
Nelson, M. L., & Neufeldt, S. A. (1996). Building on an empirical foundation: Strategies to enhance good practice. Journal of Counseling and Development, 74, 609–615. doi:10.1002/j.1556-6676.1996.tb02300.x
Rogers, C. R. (1980). A way of being. New York, NY: Houghton Mifflin.
Teyber, E. (2000). Interpersonal process in therapy: An integrative model (4th ed.). Belmont, CA, Brooks/Cole.
Thurmond, V. A. (2001). The point of triangulation. Journal of Nursing Scholarship, 33, 253–258. doi:10.1111/j.1547-5069.2001.00253.x
Waldman, J. (1995). Breakthrough or breakdown: When the psychotherapist cries during the therapy session (Unpublished doctoral dissertation). Massachusetts School of Professional Psychology, Boston, MA.
Willig, C. (2001). Introducing qualitative research in psychology: Adventures in theory and method. Buckingham, England: Open University Press.
Appendix
A qualitative interview on personal experiences and effects of counselors’ crying in session.
Tell me why you decided to be a counselor.
Have you ever cried in session with a client? If no, have you ever felt like crying while in session with a client?
What do you think of clients crying in session?
What issues would make you cry in session with a client?
What do you think of other therapists who cry in session?
What is your response to a client who starts crying in session?
What do you do if you feel like crying in session with a client?
What strategies do you use to deal with yourself crying in session?
How would your crying be beneficial to the therapeutic relationship?
How would your crying hinder the therapeutic relationship?
What fears do you have of allowing yourself to cry in session with a client?
How do you keep yourself from crying in session with a client?
How would your controlling your desire to cry affect your relationship with a client?
What else would you like to add?
Miles Matise, NCC, is an Assistant Professor at Troy University. Correspondence should be addressed to 81 Beal Pkwy SE, Fort Walton Beach, Florida, 32548, mmatise@troy.edu.