Feb 26, 2021 | Volume 11 - Issue 1
Lisbeth A. Leagjeld, Phillip L. Waalkes, Maribeth F. Jorgensen
Researchers have frequently described rural women as invisible, yet at 28 million, they represent over half of the rural population in the United States. We conducted a transcendental phenomenological study using semi-structured interviews and artifacts to explore 12 Midwestern rural-based mental health counselors’ experiences counseling rural women through a feminist lens. Overall, we found eight themes organized under two main categories: (a) perceptions of work with rural women (e.g., counselors’ sense of purpose, a rural heritage, a lack of training for work with rural women, and the need for additional research); and (b) perceptions of rural women and mental health (e.g., challenges, resiliency, protective factors, and barriers to mental health services for rural women). We offer specific implications for counselors to address the unique mental health needs of rural women, including hearing their stories through their personal lenses and offering them opportunities for empowerment at their own pace.
Keywords: rural women, mental health counselors, feminist, perceptions, phenomenological
More than 28 million women, ages 18 and older, live in rural America and represent over half of the rural population in the United States (Bennett et al., 2013; U.S. Census Bureau, 2010). Researchers have discussed women’s issues as a distinct category within counseling for over 50 years, yet few counseling programs offer training specific to counseling women (American Psychological Association [APA], 2018; Broverman et al., 1970; Enns, 2017). Rural women have garnered even less attention within counseling literature and training over time (Bennett et al., 2013; Fifield & Oliver, 2016). In addition, rural mental health researchers have focused on rural populations in general, encapsulating women under the entire family unit (U.S. Department of Agriculture, 2015). However, in all environments, women experience mental health needs in unique ways (Mulder & Lambert, 2006; Wong, 2017). Although government agencies have increased efforts to alleviate mental health disparities in rural areas, there is limited research available on rural women’s mental health to guide these efforts (Carlton & Simmons, 2011; Hill et al., 2016). Thus, more studies focused on rural women can assist in comprehensive data-based decision-making efforts of federal, state, and local policymakers (Van Montfoort & Glasser, 2020). Mental health counselors who work with rural women have a unique perspective in understanding the needs of rural women and the disparities they face.
The Invisibility of Rural Women’s Mental Health
Researchers have described rural women as invisible within the mental health literature. Specifically, they have used words such as “unnoticed,” “lack of recognition,” “overlooked,” and “no voice and no choice,” which may illuminate why rural women have less access to appropriate mental health services and may underlie the noticeable absence of rural women as participants within research (Mulder & Lambert, 2006; Weeks et al., 2016). Members of rural communities have traditionally seen women as an extension of their nuclear and extended families and as responsible for involvement in community and church activities (Mulder & Lambert, 2006). Rural women, as a population with unique mental health needs, may need help (i.e., representation in research) getting their voices heard on a more macro level to promote systemic changes (Van Montfoort & Glasser, 2020). A research approach based in feminist theory may amplify the voices of rural women (Schwarz, 2017).
Feminism is a theoretical approach that evolved following the women’s movement in the 1960s, and grew to effect change in social, political, and cultural beliefs about women’s roles (Evans et al., 2005). Many of the early feminist writers spoke of women as “oppressed” and “having no voice” (Evans et al., 2005). Those words have been similarly found throughout the literature on rural women (Weeks et al., 2016). Feminist theory has traditionally challenged the status quo of the patriarchy by working to reduce the invisibility of women’s experiences (Evans et al., 2005; Schwarz, 2017). Further, feminist theory has evolved to amplify voices of all oppressed and marginalized individuals and to promote recognition of the intersectionality of identity. The feminist perspective can facilitate insight into the context of rural women’s experiences (Wong, 2017).
Challenges Faced by Rural Women
The definition of rural areas has historically been based on population size (U.S. Census Bureau, 2010). Some consider rurality a more accurate term than rural, as it may include population density, economic concerns, travel distances to providers, religion, agricultural heritage, behavioral norms, a shared history, and geographical location (Smalley & Warren, 2014). Rural women face unique needs related to the intersection of gender with race, ethnicity, age, and sexual orientation (Barefoot et al., 2015). Rural women have less access to educational opportunities, are often the head of household, and are more likely to live in poverty than urban women (Watson, 2019). Lesbian and bisexual rural women face challenges of bias, lack of support, and increased victimization (Barefoot et al., 2015). Although urban women also experience mental health issues related to motherhood, rural women often must travel long distances to services and have limited access to postpartum care (Radunovich et al., 2017). Residents in many rural communities experience food insecurity and related disordered eating with less proximity to grocery stores and limited food choices (Doudna et al., 2015). Isolation also creates a greater risk for partner abuse that is complicated by long distances to shelters, lack of anonymity, and a widely held view of traditional gender roles (Weeks et al., 2016). The lack of research regarding rural women and mental health compromises the efforts of rural counselors to provide care that is culturally responsive and efficacious (Imig, 2014). In addition, the recognized barriers of accessibility, availability, and acceptability of mental health services in rural areas disproportionally affect rural women (Radunovich et al., 2017).
Barriers to Mental Health Services
A lack of professionals, limited training for work in rural areas, high rates of turnover of mental health professionals, and limited research about rural demographics can negatively impact the quality of services (Smalley & Warren, 2014). In addition, rural residents may experience barriers such as long distances to services, adverse weather conditions, affordability of services, and a lack of insurance coverage (Smalley & Warren, 2014). Rural women may also feel reluctant to seek out mental health services for fear of loss of anonymity and the stigma attached to seeking mental health services in rural areas (Snell-Rood et al., 2019). Approximately 40% of rural residents with mental health issues opt to seek treatment from primary care physicians (PCPs), as these professionals may represent the only health care provider in the area (Snell-Rood et al., 2017). However, these professionals often have limited expertise in diagnosing and treating mental health issues (Hill et al., 2016).
Currently, the Council for Accreditation of Counseling and Related Educational Programs (CACREP; 2015) does not specify rurality or other cultural identities when referencing cultural competence within required curriculum. This omission may contribute to minimal specialized training, in addition to the limited research for mental health counselors to use as a guide for understanding the unique needs of rural women (Watson, 2019). Additionally, agencies have difficulty recruiting mental health counselors because of isolation from colleagues and supervisors, lower salaries, limited social and cultural opportunities, and few training opportunities specific to rural mental health (Fifield & Oliver, 2016).
Addressing Mental Health Needs of Rural Women
Given the limited research about rural women and their unique mental health needs, rural counselors are left with few evidence-based practices to utilize when working with this population (Imig, 2014). Historically, counseling researchers have equated “mentally healthy adults” with “mentally healthy adult males,” resulting in literature that is focused on best practices more appropriate for men (Broverman et al., 1970), and potentially upholding sex-role stereotypes within the fields of psychology, social work, medicine, and mental health counseling (APA, 2018; Schwarz, 2017). More recent researchers have demonstrated the efficacy of gender-specific counseling approaches (Enns, 2017). However, the approaches often do not consider the additional barriers to services that rural women may face, such as long distances to services, limited availability of mental health professionals, and the stigma of seeking services in a rural area (Hill et al., 2016).
In this transcendental phenomenological study, we sought to explore the lived experiences of licensed professional counselors (LPCs) who work with rural women in terms of their perceptions of rural Midwestern women’s mental health, and the academic training they received to prepare them for working with rural women. The study sought to answer the following research questions: (a) What are the lived experiences of LPCs who work with rural women?; (b) What are the challenges and benefits of working with rural women?; (c) How are mental health services perceived by those working with rural women?; and (d) What training, if any, did the participants receive that was specific to work with rural women?
Method
Qualitative research, by its very nature, validates individuals who may be disempowered (Morrow, 2007; Ponterotto, 2010). Phenomenology is a qualitative method that helps researchers describe the common meaning of participants’ lived experiences specific to a particular phenomenon (Creswell & Poth, 2018). In this study, the phenomenon was the lived experiences of LPCs who worked with rural women. Transcendental phenomenology (Moustakas, 1994) provided a framework for the study that began with epoché, a process of bracketing the researchers’ experiences and biases, and the collection of participant stories (Creswell & Poth, 2018). For this study, postpositivist elements of transcendental phenomenology (e.g., bracketing and data analysis) were utilized to reduce researcher biases (Moustakas, 1994). Specifically, we viewed bracketing as essential because participants might not share the feminist viewpoint of the researchers. The infusion of feminism into the study came from a constructivist/interpretivist standpoint as I (i.e., first author and lead researcher) believed—based on literature—the stories of rural women were not being heard and, thus, designed the study to help illuminate the experiences, mental health needs, and resiliency of rural women (Morrow, 2007).
Participants
For this study, participants were recruited using criterion and snowball sampling. Criterion sampling involved selecting individuals on the basis of their shared experiences and their abilities to articulate those experiences (Heppner et al., 2016). Snowball sampling allowed for selecting participants who previously had a demonstrated interest in this area of research based on their connection to other participants. Criteria for participation included a degree from a CACREP-accredited counseling program, licensure within their jurisdiction, current practice, and clinical work that included rural women. To recruit participants, we collected names and emails from a Midwestern state counseling association; however, this method produced only two responses. So, we utilized snowball sampling by asking participants to refer us to others who met our eligibility criteria (Creswell & Poth, 2018). We determined the number of LPCs needed to describe the phenomena by achieving saturation of the data collected (Heppner et al., 2016). This saturation was reflected by eventual redundancy in participant responses.
Following approval from the appropriate IRB, an invitation to participate was emailed to potential participants and included a link to a demographic form and informed consent for those who met the criteria and wished to participate. Rural areas were defined as those geographic areas containing counties with populations of less than 50,000, a definition that did not include population density but was appropriate for the Midwestern areas included in the study (Smalley & Warren, 2014). Twelve mental health counselors met the eligibility criteria for participation and enrolled in the study.
All participants had graduated from a CACREP-accredited counseling program, were licensed to practice within their jurisdiction, were currently practicing privately or in an agency, and had a clinical caseload that included rural women. The designation of LPC was used throughout the study and included all levels of licensure within the various jurisdictions. All of the LPCs reported working with a wide variety of mental health issues; three of the LPCs had addiction counseling credentials. Eleven participants self-identified as female and one self-identified as non-binary. Eleven participants self-identified as Caucasian, and one self-identified as Native American. Years of experience working as a mental health professional ranged from 4 years to 27 years, with an average of approximately 12 years. All participants reported working with both urban and rural clients, and one participant listed a reservation as the primary location for her work. LPCs’ clients included adult rural women from the upper Midwest. The rural women were single or married with children, working or unemployed, Caucasian or Native American. In addition, all the participants expressed a connection to rural areas, either through personal experience of growing up in a rural area or through connections with extended family. Each participant chose a pseudonym that is referred to throughout the manuscript.
Data Collection
We collected data through individual semi-structured interviews and participant artifacts. The semi-structured interview format allowed for more collaboration and interaction between interviewer and interviewee (Creswell & Poth, 2018). In this way, the interview format aligned with a feminist research approach and helped eliminate a power differential between researcher and participant (Heppner et al., 2016). There were 12 interview questions aimed at exploring participants’ work with rural women, participants’ perceptions of the unique mental health needs of rural women, the influence of participants’ rural heritage on their work with rural women, challenges and benefits of participants’ work with rural women, and participants’ training specific to work with rural women (see Appendix for all 12 interview questions). As lead researcher, I conducted all 12 interviews in order to maximize consistency in employing the interview protocol while allowing participants to elaborate on responses. Interviews ranged from 30–45 minutes. All research documents, such as informed consents, demographic questionnaires, and transcriptions, were securely stored on a password-protected device.
Participants were invited to share artifacts that represented their work with rural women. Artifacts could include personal letters, poems, artwork, and photos (Heppner et al., 2016). The artifacts in this study provided an opportunity for broader expression of the counselors’ experiences as well as understanding their connection to rural life. Seven artifacts were pictures of objects or individuals that inspired participants’ work with rural women, two were stories about experiences of rural women, and one was an original poem entitled “Rural Woman.”
Data Analysis
Brown and Gilligan’s (1992) research of young women and relationships utilized a Listener’s Guide for analyzing data. This guide is feminist and relational and allows researchers to pay attention to unheard voices. The Listening Guide is considered a psychological method that reflects the “social and cultural frameworks that affect what can and cannot be spoken or heard” (Gilligan & Eddy, 2017, p. 76). The method included three successive “listenings”—one for plot, one for “I” statements, and one for the individual in relationship to others (Brown & Gilligan, 1992). Throughout the listening process, I looked for and highlighted significant statements the participants made during the interview process that reflected the experiences of the phenomenon. I organized information via a phenomenological template under the heading “Essence of the Phenomenon” and included personal bracketing (epoché), significant statements, meaning units, and textural and structural descriptions (Creswell & Poth, 2018). Although a transcription service was utilized to transcribe the interviews, I read through the transcripts several times and coded data into categories or themes, which emerged organically from the transcripts. An independent peer reviewer then examined the transcriptions and helped to develop the codes and themes. We developed clusters of meaning from the significant statements into themes, followed by a textural and structural description that encompassed the significant statements and related themes. The rich and thick descriptions became the essence of the phenomenon enhanced by continual review of the interview tapes, journal notes, artifacts, and other data collected (Morrow, 2005).
Epoché
The epoché section was written from my perspective as the primary researcher and first author. I was responsible for designing the study, collecting and analyzing data, and writing the manuscript. My co-authors served as consultants in designing the study and helped to write and edit the manuscript. As the primary researcher, I sought to see the lived experiences of participants from a perspective that was free from my assumptions (Creswell & Poth, 2018). I grew up in a Midwestern rural area, steeped in traditional gender roles, while witnessing significant change for all women in expectations and opportunities. During the process of the study, it became apparent that my perceptions of rural women as stay-at-home farmwives have changed to reflect a population more diverse in ethnicity, family structure, and socioeconomic status; however, the traditional patriarchal expectations have not changed. My work as a mental health professional shaped my desire to explore the perceptions of other LPCs’ experiences of their work with rural women. Prior to the data analysis, I bracketed my personal and professional rural experiences about power differentials within rural areas.
Trustworthiness
To promote trustworthiness, I utilized self-reflective journaling, member checks, the achievement of data saturation, independent peer review, and an external audit. I kept a journal and made notes throughout the data collection process to facilitate an awareness of biases and/or assumptions that emerged during the process (Heppner et al., 2016; Morrow, 2005). I also conducted member checks, asking all participants to review and provide feedback via email on descriptions or themes (Creswell & Poth, 2018; Morrow, 2005). Frequently, participants would elaborate on themes by adding clarification to their responses to the interview questions. The “prolonged interaction” (Ponterotto, 2010, p. 583) with participants was significant for developing an egalitarian and unbiased relationship between researcher and participant. This strategy was congruent with feminist theory because it acknowledged the subjectivity of the researcher within the study and facilitated a collaborative relationship between researcher and participant (Morrow, 2007).
Coding the data into categories or themes helped arrange the large amount of data that was collected. The process was made easier by taking notes, or “memoing,” when reading through the information. The peer reviewer evaluated potential researcher bias by checking the coding against all transcripts, serving as a “mirror” that reflected my responses to the research process (Morrow, 2005, p. 254). Next, we discussed possible themes that emerged from the data (Heppner et al., 2016). I also utilized an external auditor to aid in establishing confirmability of the results rather than objectivity (Morrow, 2005). The auditor examined the entire process and determined whether the data supported my interpretations (Creswell & Poth, 2018). Both individuals had participated in phenomenological research and were not authors of this article.
Results
Analysis of the interview transcripts, the artifacts, and the journal reflections resulted in eight themes, organized into two categories. I further categorized each theme as: 1) textural, a subjective experience of the LPC’s experience with rural women; or 2) structural, the context of the experience. According to Moustakas (1994), the textural themes represent phenomenological reduction, a way of understanding that includes an external and internal experience; the structural themes represent imaginative variation, the context of the experience. One of the themes, counselor experience, fit the description of both textural and structural. The categories represented two distinct dimensions of the phenomenon: (a) LPCs’ perceptions of their work with rural women, and (b) LPCs’ perceptions of rural women and issues related to mental health.
Dimension 1: LPCs’ Perceptions of Their Work With Rural Women
Five textural themes emerged from the coding process; I took the names of three of these verbatim from the interviews. The textural themes included 20 codes that represented the subjective experiences of LPCs’ work with rural women. The participants’ pseudonyms were inserted into the direct quotes included in theme descriptions. Artifacts offered by participants were also included.
Bootstraps
Rooted in the familiar saying of “pull yourself up by your bootstraps,” this theme included codes of resilient, stoic, self-sufficient, and independent. According to LPCs’ perceptions of rural women, bootstraps described an acceptance of the current conditions of rural life and a reliance on past experiences for guidance. Many of the LPCs believed that rural women came to counseling with a skill set that, as Nancy said, “can teach us and others about how to be resilient.” Fave commented that working with rural women also required patience:
It’s this sense of “I can do this.” There are more demands with farming, and rural women still believe they should be able to do it all. When they come into counseling it can be difficult because they have worked hard to sort of protect this thing and keep it close to them because they’re pretty sure they can figure it out themselves.
Courtney shared a story about a ranch woman who was grieving the loss of her husband and was struggling with family issues. She remarked in one session, “Today I decided it was time to put on my red cowboy boots.” For Courtney, this represented her client’s resiliency and stoicism—“I’ve got this, and I’ve got my red boots on to prove it.”
Trailblazer
Trailblazer included pioneer, open-minded, resourceful, educated, and empowered; these words described LPCs’ perceptions of rural women’s abilities to move past accepting the realities of rural living and work toward change for improving themselves, their families, and their communities. According to the LPCs, this theme is distinct from bootstraps in that it is future-oriented rather than past-oriented. Elsie first referred to trailblazer when she told a story about a client who began recycling in the early 1980s: “She had bins and bins of recycling because she said, ‘I’m gonna leave this planet in a different shape than I found it.’ Rural women very much can be trailblazers.” The LPCs’ perceptions represented a new perspective that reflected resourceful change-makers, educated and empowered to challenge the status quo.
As one of her artifacts, Courtney offered a story about one woman’s determination to make Christmas special even though there were no resources for gifts and decorations. The woman found a large tumbleweed, covered it with lights and decorations, and declared it beautiful. Courtney said, “She was not just making do, but making things better.”
Challenges of Rural Women
LPCs observed multiple challenges for rural women including isolation, poverty/financial insecurity, role overload, grief, and generational trauma. Layla talked about the complex grief that was experienced by Native American women. She commented that “the death of a family member can mean losing someone from three or four generations. There is grief from loss of jobs, moving from the reservation, and loss of culture.” LPCs cited role overload as one of the most common experiences among rural women. Many rural women worked full-time jobs in addition to caring for family members while contributing to the farm/ranch operation. Jean observed that rural women “are responsible for everyone’s emotions in the family, sometimes leaving them isolated within the family.” LPCs believed that the isolation contributed to vulnerability. Rural women faced domestic violence, anxiety, depression, and addictions, exacerbated by having no one to talk with and long distances to services. Jean noted that resistance to change was perpetuated by the fear and control inherent in domestic abuse for many of her clients and led to complacency in reporting. The challenges of rural women described by participants defined the issues that LPCs faced when working in rural areas and increased their awareness of the critical needs of rural women.
Protective Factors
Protective factors included a sense of identity and the strong support systems of families and community that gave rural women “a lot of people that you can draw upon to help you through hard times,” according to Nancy. Her clients valued the easy access to nature and the opportunity to “immerse yourself in something bigger than yourself. It’s a way to build resilience and find meaning and joy spending time outside.” Layla found a strong sense of identity evident in rural Native women as central to the ability to teach their children cultural beliefs—a protective factor for future generations.
Nancy shared a picture of a family moving their 100-year-old home to a new location as her artifact. Her description of the house and rural heritage symbolized part of what she believed was important for rural women—the connection to family and heritage along with a sense of purpose in maintaining family culture. She said, “It’s a good way to pass down the family stories and even the family culture.”
Counselor Experience
Counselor experience (textural) included the reasons why participants chose to become LPCs. These included the motivations that sustained their work and advice for new counselors. Assumptions about diversity, a sense of purpose, listening, and connections to resources encapsulated this theme.
Layla became a counselor because she wanted “to give back to my Native people.” Nancy believed that the work with rural women helped her build a rural counselor identity. Woods’ early experience with rural women felt profound because of the chaos she observed in the lives of her clients, many of them impoverished single mothers struggling to survive. She was given a sense of purpose in her work saying, “These women are burned into my head.”
When asked about advice for new counselors who anticipate working with rural women, participants offered the following brief statements:
“Don’t make assumptions.” (Courtney)
“Ask to be taught.” (Marie)
“Hear their story without filtering through your own personal lens.” (Nancy)
“There is a difference in working in rural areas—a conservative mind-set, practicality—and you need to meet people where they are.” (Kay)
“Listen more than you talk.” (Suzie)
“Have respect for their culture.” (Layla)
LPCs’ Perceptions of Rural Women and Issues Related to Mental Health
Three structural themes represented what Moustakas (1994) termed imaginative variation, the acknowledgment of the context of multiple perspectives. The themes were derived from nine codes that provided a vital aspect of further describing the phenomenon. The theme descriptions included participants’ quotes and artifacts.
Perceptions of Rural Heritage
This theme represented LPCs’ view of rural life, including traditional values, heritage, and expectations/perfectionism. According to participants, many of the rural women embraced the traditional values of their rural heritage, and the roles of rural life; this theme honors that perspective. Fave talked about the expectations that rural women often have of themselves: “It’s a perfectionist perspective, meaning they can do it all.” Even in light of the increased demands on rural women’s time and energy, Marie found that rural women were often hesitant to seek outside professional mental health counseling, choosing instead to rely on family and community.
Barriers to Mental Health Services
The barriers included codes of lack of resources, stigma, and invisibility. All LPCs felt concerned about the lack of resources for rural women. Suzie talked about the dearth of women’s shelters on the reservation and resources for women who are victims of domestic violence. Suzie said, “They often stay because there are no resources for them to leave, and they can’t afford it.” Woods noted the lack of daycare providers and the fact that many rural women cannot afford these services and depend on family members for childcare. According to several LPCs, rural women do not prioritize their mental health needs, possibly because of the many demands on them.
Kay and Marie practiced in an urban area but saw many rural women who chose to travel long distances for mental health services because it gave them a sense of anonymity. Kay said, “They know if their car is parked at the counselor’s office, it won’t be recognized by everyone in town.” Rural women also feared exposing family secrets if they disclosed something to a counselor who lived in the same area.
Poignantly, LPCs acknowledged the invisibility and minimization of rural women’s mental health needs. The following comments by participants exemplified the rural woman’s experiences of being unnoticed or dismissed. Elsie stated, “Even if rural women are speaking, they don’t have the platform like urban women do, and they feel like nobody gets this life.” Kay stated, “Everything is fine, everything’s great and we’re not going to talk about the fact that Grandma is crying all the time and wearing sunglasses.”
The statements of the participants provided powerful examples of the ramifications of the silencing imposed on rural women through traditional or cultural norms. The stigma of accessing mental health services created a loss of connection between the rural women who needed the services and their community. In addition, rural women often felt selfish in seeking services just for themselves. The consensus among LPCs was that rural women suffer to a greater extent than other rural populations because their needs are minimized or not recognized. Elsie remarked that rural women do not often see their stories in mainstream media, leading them to believe “I’m living this experience that nobody else lives.”
The description of the artifact contributed for this theme may further elucidate the invisibility of rural women. Woods’ artifact was a picture of two locally designed sculptures of women. Woods said, “They are so rooted and earthy.” One sculpture had no arms or legs and, for Woods, that “speaks to the limited access to needed supports and the lack of voice.”
Counselor Experience
Counselor experience (structural) described how LPCs provide mental health services to rural women and included connection to rural life, distances and dual relationships, and lack of academic training/postgraduate training. Although not all the participants grew up in rural areas, many had rural ties through extended family. Marie’s upbringing on a ranch influenced her understanding of rural women: “There is a more intense work ethic; women are very strong and independent and hardworking.”
The LPCs seemed to feel a strong sense of purpose in their work; some of them chose to become counselors and returned to their home communities to work. They discovered that the connections of shared experiences fostered trust in the counseling relationship and process. Most felt that they were helping to make positive change. Although all participants believed the connection to a rural heritage was critical in their work with rural women, some LPCs did not live and work in the same location, saying it helped to reduce the possibility of multiple relationships. Nancy commuted almost an hour to her work “because you really want to have the counseling relationship be through your therapeutic lens and not through the community lens.”
None of the participants recalled receiving academic training specific to rural areas; however, all participants agreed on the need for academic training focused on rural areas and rural women. Elsie believed that textbooks should “include women’s voices and rural voices.” Jean expressed her concern that “We don’t necessarily address rural women or what they need from the communities around them or even what their typical experience is. I think that’s a disservice to our counseling students.”
Two artifacts aligned with this theme: Marie’s picture of a young girl, dressed in overalls, pitching hay, and Mae’s great-grandmother’s writing desk (see Figure 1). Marie’s artifact exemplified the family’s connection to rural life and the physical strength of rural women that she observed in her work. Mae now uses the writing desk in her practice and feels it gives her a strong connection to her rural heritage.
Figure 1
Mae’s Great-Grandmother’s Writing Desk

Note. Mae presented this picture of her great-grandma’s writing desk when asked to provide
an artifact that demonstrated her work with rural women.
Discussion
LPCs described rural women as strong, independent, resourceful, and resilient. However, this image of rural women was not corroborated within the research literature. An APA report on the behavioral health care needs of rural women (Mulder et al., 2000) did not mention resiliency as a coping strategy; however, in 2006, the report’s lead author recognized the need for additional research about resiliency in rural women, saying it would offer “significant potential benefit to rural women” (Mulder & Lambert, 2006, p. 15). In the present study, LPCs’ perceptions of rural women as resilient called attention to the innate strengths of rural women that developed out of necessity, cultivated by connections with family, community, and earth.
Rural heritage represented a dichotomy of rural tradition. From a positive perspective, participants believed the traditional roles of rural women provided a sense of identity and belonging. From a negative perspective, the traditional patriarchy evident in many rural areas dictated social and cultural norms, leaving rural women with the expectation that they should be able to “do it all.” Both perspectives defined a critical aspect of LPCs’ understanding of rural women. Even though many of the rural women participants described worked full-time to contribute to household income and health insurance (in addition to caretaker responsibilities), they faced gender inequities in income, employment, and educational opportunities (Watson, 2019). In addition, rural women have had little political power to effect needed policy changes for better access to care (Van Montfoort & Glasser, 2020).
LPCs highlighted multiple challenges that rural women experience: isolation, poverty, grief, role overload, and generational trauma. Barriers to obtaining services included stigma of mental health issues, loss of anonymity, a lack of resources, invisibility, and minimization of mental health issues. The general population also faces barriers of accessibility, acceptability, and availability of counseling services (Smalley & Warren, 2014); however, there were fewer references to the mental health barriers and challenges specific to rural women (Van Montfoort & Glasser, 2020). This is surprising given that the population of rural women exceeds that of any other population group in rural areas (Bennett et al., 2013). Rural women experience higher risks of depression, domestic violence, and poverty (Snell-Rood et al., 2019). The mental health services available in rural areas, often described as “loosely organized, of uneven quality, and low in resources” (Snell-Rood et al., 2019, p. 63), compound the challenges for rural women.
As evident in the themes of assumptions and diversity, rural women represent a unique population who deserve mental health services that reflect their specific needs. Rural communities and rural women are more diverse than once believed. LPCs’ observations are corroborated by research that acknowledged differences among rural women in socioeconomic status, family structure, age, sexual identity, ethnicity, education, and geographical location (Barefoot et al., 2015). In addition, there remains a misconception that the mental health needs of urban and rural women are the same; in fact, much of the literature about women and mental health is based on an urban context (Weaver & Gjesfjeld, 2014). The findings of the current study support the lack of recognition of the context of rural women’s issues and their status as an invisible population (Bender, 2016). Two LPCs’ observations of the isolation felt by rural women reinforced previous research of the invisibility of rural women. Elsie said, “Rural women don’t see their story a lot,” and Fave shared that “a lot of the women I work with don’t feel like they’re heard.”
None of the participants recalled academic training or postgraduate opportunities specific to work in rural areas or with rural women. Even though rural areas represent the largest population subgroup in the United States (Smalley & Warren, 2014), this study suggests that new counselors may not feel prepared to meet the needs of this underserved population. The shortage of mental health professionals working in rural areas and the lack of counselors who have training specific to rural mental health care suggest a need for rural-based training that might include an elective course in rural mental health and rural internships (Fifield & Oliver, 2016).
Implications
The recognition of the challenges and benefits of working with rural women may validate rural LPCs’ experiences, promote their professional identity as rural counselors, and potentially decrease the isolation felt when working in rural areas. Protective factors, including connections to family, community, and nature, may be critical for building resiliency in both rural women and rural LPCs. The increasing diversity of rural women is often contrary to the traditional stereotype of a stay-at-home farmwife (Carpenter-Song & Snell-Rood, 2017); diverse rural women may face unique barriers to accessing culturally relevant mental health services. In addition, many rural women experience role overload from working full-time and caring for families while contributing to the farm/ranch operation. Counselors should avoid interacting with rural women clients in ways that limit their identities based on stereotypes and work to make their services accessible for all women.
The study results also have implications for counselor educators. Rural-based counselors in this study did not report being taught how to work with rural women. A review of the 2016 CACREP programs found few gender-based counseling courses and none that addressed rural mental health. Programs could offer electives on counseling in rural areas, incorporate the context of gender and rural mental health into current curricula, and encourage rural internships. Collaborating with other rural health professionals may provide more informed approaches to working in rural areas. Rural residents may see their PCPs for mental health–related treatment, as PCPs may be the only health care provider in rural areas (Snell-Rood et al., 2017). Lloyd-Hazlett et al. (2020) suggested creating additional training for LPCs who choose to work in settings offering integrated care. Incorporating LPCs who have the appropriate training and skills into rural medical settings may offer mental health services in a familiar clinical context and one that does not broadcast engagement in mental health care. The collaboration may also provide more awareness of the mental health needs of rural women.
Limitations
The study has several limitations. Although I took measures to reduce any personal bias as a non-traditional rural woman, I do not believe it is possible to eliminate all biases. Many of the participants talked about empowering rural women and working toward making their clients’ voices heard, both tenets of feminist theory (Evans et al., 2005); however, participants rarely used the language of feminism. Several of the participants related personal stories of their connections with rurality and, often, their stories of rural women were from decades ago. Their stories may not have represented the current generation of rural women. Another limitation relates to the demographics of LPCs because a majority of participants self-identified as Caucasian and female and represented rural areas in the Midwest. LPCs working in other areas of the United States may encounter different demographics of rural women, mental health challenges specific to region, and unique intersections of their clients’ identities. Finally, the experiences of rural women were heard through LPCs and not from rural women clients themselves.
Directions for Future Research
This study included a sample of rural LPCs who were primarily Caucasian females from the Midwestern United States; future researchers may seek professional perspectives from participants who represent a blend of race, ethnicities, gender identities, and geographical locations. Research with rural women as participants themselves is also an important opportunity. Based on findings from this study, future researchers might also explore training needs related to work with rural women and rural populations. Studying counselor educators who teach in counseling programs based in rural areas could also offer unique insights. This may reveal information about ways educators currently infuse rural culture and work with rural women into the curriculum. Future researchers may study counselors, health care providers, and rural women in finding ways to integrate health care services in rural areas to provide better access to services and reduce the stigma often associated with mental health. Finally, additional studies about working with rural PCPs may highlight issues (e.g., intimate partner violence) that could benefit from early screening of symptoms.
Conclusion
Gilligan offers these words: “To have something to say is to be a person. But speaking depends on listening and being heard; it is an intensely relational act” (1982/1993, p. xvi). As indicated in our findings, rural women are too often invisible and unheard. This study represents a first step in amplifying the voices of rural women regarding their specific mental health needs. The experiences of the LPCs in this study have illuminated ways to connect with rural women, listen to their stories, and validate unique aspects of their cultural identities that seem to be well illustrated in one participant’s poem:
Rural Women
Resilient; stubborn; motivated
frightened; broken; courageous
Struggling; down-trodden; strong
Relentless in self-expectation
Armed with determination.
A common thread unites us
The heart gently calls, and the
soul asks only—please—listen to me.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
American Psychological Association. (2018). APA guidelines for psychological practice with girls and women.
http://www.apa.org/about/policy/psychological-practice-girls-women.pdf
Barefoot, K. N., Rickard, A., Smalley, K. B., & Warren, J. C. (2015). Rural lesbians: Unique challenges and implications for mental health providers. Journal of Rural Mental Health, 39(1), 22–33.
https://doi.org/10.1037/rmh0000014
Bender, A. K. (2016). Health care experiences of rural women experiencing intimate partner violence and substance abuse. Journal of Social Work Practice in the Addictions, 16(1–2), 202–221.
https://doi.org/10.1080/1533256X.2015.1124783
Bennett, K. J., Lopes, J. E., Jr., Spencer, K., & van Hecke, S. (2013). Rural women’s health. National Rural Health Association Policy Brief. https://www.ruralhealthweb.org/getattachment/Advocate/Policy-Documents/RuralWomensHealth-(1).pdf.aspx
Broverman, I. K., Broverman, D. M., Clarkson, F. E., Rosencrantz, P. S., & Vogel, S. R. (1970). Sex-role stereotypes and clinical judgments of mental health. Journal of Counseling and Clinical Psychology, 34(1), 1–7.
https://doi.org/10.1037/h0028797
Brown, L. M., & Gilligan, C. (1992). Meeting at the crossroads: Women’s psychology and girls’ development. Harvard University Press.
Carlton, E., & Simmons, L. (2011). Health decision-making among rural women: Physician access and prescription adherence. Journal of Rural and Remote Health Research, Education, Practice and Policy, 11, 1–10.
Carpenter-Song, E., & Snell-Rood, C. (2017). The changing context of rural America: A call to examine the impact of social change on mental health and mental health care. Psychiatric Services, 68(5), 503–506.
https://doi.org/10.1176/appi.ps.201600024
Council for Accreditation of Counseling and Related Educational Programs. (2015). 2016 CACREP standards. http://www.cacrep.org/for-programs/2016-cacrep-standards
Creswell, J. W., & Poth, C. N. (2018). Qualitative inquiry & research design: Choosing among five approaches (4th ed.). SAGE.
Doudna, K. D., Reina, A. S., & Greder, K. A. (2015). Longitudinal associations among food insecurity, depressive symptoms, and parenting. Journal of Rural Mental Health, 39(3–4), 178–187.
https://doi.org/10.1037/rmh0000036
Enns, C. Z. (2017). Contemporary adaptations of traditional approaches to counseling women. In M. Kopala & M. Keitel (Eds.), Handbook of counseling women (2nd ed., pp. 51–62). SAGE.
Evans, K. M., Kincade, E. A., Marbley, A. F., & Seem, S. R. (2005). Feminism and feminist therapy: Lessons from the past and hopes for the future. Journal of Counseling & Development, 83(3), 269–277.
https://doi.org/10.1002/j.1556-6678.2005.tb00342.x
Fifield, A. O., & Oliver, K. J. (2016). Enhancing the perceived competence and training of rural mental health practitioners. Journal of Rural Mental Health, 40(1), 77–83. https://doi.org/10.1037/rmh0000040
Gilligan, C. (1993). In a different voice: Psychological theory and women’s development. Harvard University Press. (Original work published 1982)
Gilligan, C., & Eddy, J. (2017). Listening as a path to psychological discovery: An introduction to the Listening Guide. Perspectives on Medical Education, 6, 76–81. https://doi.org/10.1007/s40037-017-0335-3
Heppner, P. P., Wampold, B. E., Owen, J., Thompson, M. N., & Wang, K. T. (2016). Research design in counseling (4th ed.). Cengage.
Hill, S. K., Cantrell, P., Edwards, J., & Dalton, W. (2016). Factors influencing mental health screening and treatment among women in a rural south central Appalachian primary care clinic. Journal of Rural Health, 32(1), 82–91. https://doi.org/10.1111/jrh.12134
Imig, A. (2014). Small but mighty: Perspectives of rural mental health counselors. The Professional Counselor, 4(4), 404–412. https://doi.org/10.15241/aii.4.4.404
Lloyd-Hazlett, J., Knight, C., Ogbeide, S., Trepal, H., & Blessing, N. (2020). Strengthening the behavioral health workforce: Spotlight on PITCH. The Professional Counselor, 10(3), 306–317.
https://doi.org/10.15241/jlh.10.3.306
Morrow, S. L. (2005). Quality and trustworthiness in qualitative research in counseling psychology. Journal of Counseling Psychology, 52(2), 250–260. https://doi.org/10.1037/0022-0167.52.2.250
Morrow, S. L. (2007). Qualitative research in counseling psychology: Conceptual foundations. The Counseling Psychologist, 35(2), 209–235. https://doi.org/10.1177/0011000006286990
Moustakas, C. (1994). Phenomenological research methods. SAGE.
Mulder, P. L., & Lambert, W. (2006). Behavioral health of rural women: Challenges and stressors. In R. T. Coward, L. A. Davis, C. H. Gold, H. Smiciklas-Wright, L. E. Thorndyke, & F. W. Vondracek (Eds.), Rural women’s health: Mental, behavioral, and physical issues (pp. 15–30). Springer.
Mulder, P. L., Shellenberger, S., Streiegel, R., Jumper-Thurman, P., Danda, C. E., Kenkel, M. B., Constantine, M. G., Sears, S. F., Kalodner, M., & Hager, A. (2000). The behavioral healthcare needs of rural women.
http://www.apa.org/practice/programs/rural/rural-women.pdf
Ponterotto, J. G. (2010). Qualitative research in multicultural psychology: Philosophical underpinnings, popular approaches, and ethical considerations. Cultural Diversity and Ethnic Minority Psychology, 16(4), 581–589. https://doi.org/10.1037/a0012051
Radunovich, H. L., Smith, S. R., Ontai, L., Hunter, C., & Cannella, R. (2017). The role of partner support in the physical and mental health of poor, rural mothers. Journal of Rural Mental Health, 41(4), 237–247.
https://doi.org/10.1037/rmh0000077
Schwarz, J. (2017). Counseling women and girls: Introduction to empowerment feminist therapy. In J. E. Schwarz (Ed.), Counseling women across the life span: Empowerment, advocacy, and intervention (pp. 1–20). Springer.
Smalley, K. B., & Warren, J. C. (2014). Mental health in rural areas. In J. C. Warren & K. B. Smalley (Eds.), Rural public health: Best practices and preventive models (pp. 85–93). Springer.
Snell-Rood, C., Feltner, F., & Schoenberg, N. (2019). What role can community health workers play in connecting rural women with depression to the “de facto” mental health care system? Community Mental Health Journal, 55, 63–73. https://doi.org/10.1007/s10597-017-0221-9
Snell-Rood, C., Hauenstein, E., Leukefeld, C., Feltner, F., Marcum, A., & Schoenberg, N. (2017). Mental health treatment seeking patterns and preferences of Appalachian women with depression. American Journal of Orthopsychiatry, 87(3), 233–241. https://doi.org/10.1037/ort0000193
U.S. Census Bureau. (2010). 2010 census urban and rural classification and urban area criteria. http://census.gov/programs-surveys/geography/guidance/geo-areas/urban-rural/2010-urban-rural.html
U.S. Department of Agriculture. (2015). Rural America at a glance. https://www.ers.usda.gov/webdocs/publications/
44015/55581_eib145.pdf?v=751.6
Van Montfoort, A., & Glasser, M. (2020). Rural women’s mental health: Status and need for services. Journal of Depression and Anxiety, 9(3), 1–7.
Watson, D. M. (2019). Counselor knows best: A grounded theory approach to understanding how working class, rural women experience the mental health counseling process. Journal of Rural Mental Health, 43(4), 150–163. https://doi.org/10.1037/rmh0000120
Weaver, A., & Gjesfjeld, C. (2014). Barriers to preventive services use for rural women in the southeastern United States. Social Work Research, 38(4), 225–234. https://doi.org/10.1093/swr/svu023
Weeks, L. E., Macquarrie, C., Begley, L., Gill, C., & Leblanc, K. D. (2016). Strengthening resources for midlife and older rural women who experience intimate partner violence. Journal of Women & Aging, 28(1), 46–57. https://doi.org/10.1080/08952841.2014.950500
Wong, A. (2017). Intersectionality: Understanding power, privilege, and the intersecting identities of women. In J. E. Schwarz (Ed.), Counseling women across the life span: Empowerment, advocacy, and intervention (pp. 39–56). Springer.
Appendix
Twelve Interview Questions
- Tell me about what comes to mind when you think about working with rural women.
- Tell me about where you grew up and how that has influenced your work with rural women.
- Tell me about how you began your work with rural women.
- What have you learned about rural women through your work with them?
- What are the unique mental health needs of rural women that you have seen in your work?
- Tell me about some of the benefits and rewards, if any, you have experienced working with rural women.
- Tell me about some of the challenges, if any, you have experienced working with rural women.
- How have your experiences working with rural women changed you as a mental health counselor?
- Tell me about any academic/classroom experiences in your graduate program that involved the mental health issues of rural women (e.g., class discussions, special projects, conversations with colleagues, internship experiences).
- Tell me about any training experience post-graduation that have involved the mental health issues of rural women (e.g., workshops, conference presentations, webinars, conversations with colleagues).
- What would you like other counselors to know about working with rural women?
- Please describe how the artifact that you have chosen relates to your work with rural women.
Lisbeth A. Leagjeld, PhD, NCC, LCPC, LPC-MH, is a program liaison and faculty member at South Dakota State University – Rapid City. Phillip L. Waalkes, PhD, NCC, ACS, is an assistant professor and doctoral program coordinator at the University of Missouri – St. Louis. Maribeth F. Jorgensen, PhD, NCC, LPC, LMHC, LIMHP, is an assistant professor at Central Washington University. Correspondence may be addressed to Lisbeth A. Leagjeld, 4300 Cheyenne Blvd., Rapid City, SD 57709, Lisbeth.leagjeld@sdstate.edu.
Feb 26, 2021 | Volume 11 - Issue 1
David E. Jones, Jennifer S. Park, Katie Gamby, Taylor M. Bigelow, Tesfaye B. Mersha, Alonzo T. Folger
Epigenetics is the study of modifications to gene expression without an alteration to the DNA sequence. Currently there is limited translation of epigenetics to the counseling profession. The purpose of this article is to inform counseling practitioners and counselor educators about the potential role epigenetics plays in mental health. Current mental health epigenetic research supports that adverse psychosocial experiences are associated with mental health disorders such as schizophrenia, anxiety, depression, and addiction. There are also positive epigenetic associations with counseling interventions, including cognitive behavioral therapy, mindfulness, diet, and exercise. These mental health epigenetic findings have implications for the counseling profession such as engaging in early life span health prevention and wellness, attending to micro and macro environmental influences during assessment and treatment, collaborating with other health professionals in epigenetic research, and incorporating epigenetic findings into counselor education curricula that meet the standards of the Council for Accreditation of Counseling and Related Educational Programs (CACREP).
Keywords: epigenetics, mental health, counseling, prevention and wellness, counselor education
Epigenetics, defined as the study of chemical changes at the cellular level that alter gene expression but do not alter the genetic code (T.-Y. Zhang & Meaney, 2010), has emerging significance for the profession of counseling. Historically, people who studied abnormal behavior focused on determining whether the cause of poor mental health outcomes was either “nature or nurture” (i.e., either genetics or environmental factors). What we now understand is that both nature and nurture, or the interaction between the individual and their environment (e.g., neglect, trauma, substance abuse, diet, social support, exercise), can modify gene expression positively or negatively (Cohen et al., 2017; Suderman et al., 2014).
In the concept of nature and nurture, there is evidence that psychosocial experiences can change the landscape of epigenetic chemical tags across the genome. This change in landscape influences mental health concerns, such as addiction, anxiety, and depression, that are addressed by counseling practitioners (Lester et al., 2016; Provençal & Binder, 2015; Szyf et al., 2016). Because the field of epigenetics is evolving and there is limited attention to epigenetics in the counseling profession, our purpose is to inform counseling practitioners and educators about the role epigenetics may play in clinical mental health counseling.
Though many counselors and counselor educators may have taken a biology class that covered genetics sometime during their professional education, we provide pedagogical scaffolding from genetics to epigenetics. Care was taken to ensure accessibility of information for readers across this continuum of genetics knowledge. Much of what we offer below on genetics is putative knowledge, as we desire to establish a foundation for the reader in genetics so they may be able to have a greater understanding of epigenetics and a clearer comprehension of the implications we offer leading to application in counseling. We suggest readers review Brooker (2017) for more detailed information on genetics. We will present an overview of genetics and epigenetics, an examination of mental health epigenetics, and implications for the counseling profession.
Genetics
Genetics is the study of heredity (Brooker, 2017) and the cellular process by which parents pass on biological information via genes. The child inherits genetic coding from both parents. One can think of these parental genes as a recipe book for molecular operations such as the development of proteins, structure of neurons, and other functions across the human body. This total collection of the combination of genes in the human body is called the genome or genotype. The presentation of observable human traits (e.g., eye color, height, blood type) is called the phenotype. Phenotypes can be seen in our clinical work through behavior (e.g., self-injury, aggression, depression, anxiety, inattentiveness).
Before going further, it is important to establish a fundamental understanding of genetics by examining the varied molecular components and their relationships (Figure 1). Deoxyribonucleic acid (DNA) is a long-strand molecule that takes the famous double helix or ladder configuration. DNA is made up of four chemical bases called adenine (A), guanine (G), cytosine (C), and thymine (T). These form base pairs—A with T and C with G—creating a nucleic acid. The DNA is also wrapped around a specialized protein called a histone. The collection of DNA wrapped around multiple histones is called the chromatin. This wrapping process is essential for the DNA to fit within the cell nucleus. Finally, as this chromatin continues to grow, it develops a structure called a chromosome. Within every human cell nucleus, there are 23 chromosomes from each parent, totaling 46 chromosomes.
Figure 1
Gene Structure and Epigenetics
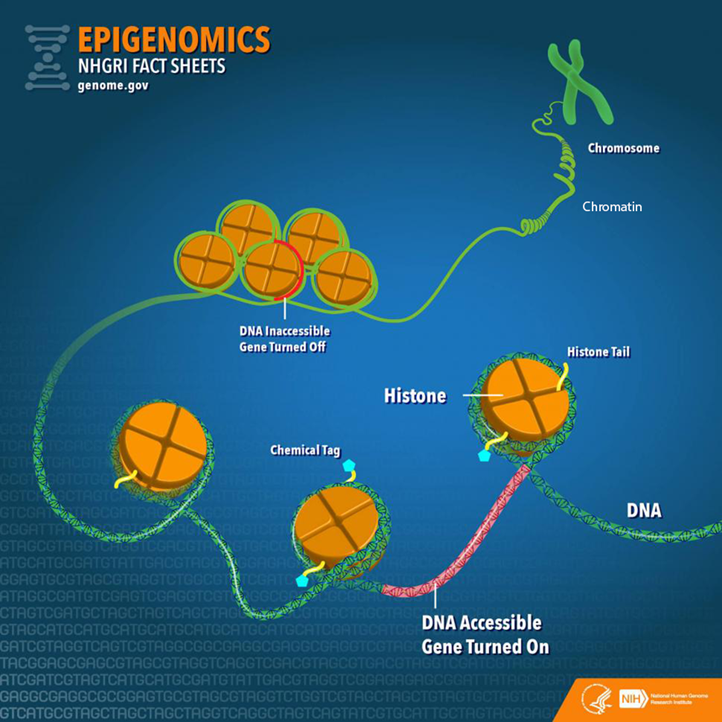
From “Epigenomics Fact Sheet,” by National Human Genome Research Institute, 2020
(https://www.genome.gov/about-genomics/fact-sheets/Epigenomics-Fact-Sheet). In the public domain.
Beyond the chromosomes, chromatin, histones, DNA, and genes, there is another key component in genetics: ribonucleic acid (RNA). RNA can be a cellular messenger that carries instructions from a DNA sequence (specific genes) to other parts of the cell (i.e., messenger RNA [mRNA]). RNA can come in several other forms as well, including transfer RNA (tRNA), microRNA (miRNA), and non-coding RNA (ncRNA). In the sections below, we elaborate on mRNA and tRNA and their impact on the genetic processes. Later in the epigenetics section, we provide fuller details on miRNA and ncRNA.
Besides the aforementioned biological aspects, it is important to understand that a child inherits genes from both parents, but they are not exactly the same genes, (i.e., alternative forms of the same gene may have differing expression). Different versions of the same gene are called alleles. Variation in an allele is one reason why we see phenotypic variation between our clients—height, weight, eye color—and this variation can contribute to mental disease susceptibility. Although there are many potential causes of poor mental health, family history is often one of the strongest risk factors because family members most closely represent the unique genetic and environmental interactions that an individual may experience. We also see this as a function of intergenerational epigenetic effects, which are covered later in this paper.
Transcription and Translation
Now that we have provided a foundation of the genetic components, we move toward the primary two-stage processes of genetics: transcription and translation (Brooker, 2017). The first step in the process of gene expression is called transcription. Transcription occurs when a sequence of DNA is copied using RNA polymerase (“ase” notes that it is an enzyme) to make mRNA for protein synthesis. We can liken transcription to the process of someone taking down information from a client’s voicemail message. In this visualization, DNA is the caller, the person writing down the message is the RNA polymerase, and the actual written message is the RNA.
A particular section of a gene, called a promotor region, is bound by the RNA polymerase (Brooker, 2017). The RNA polymerase acts like scissors to separate the double-stranded DNA helix into two strands. One of the strands, called the template, is where the RNA polymerase will read the DNA code A to T, and G to C to build mRNA. There are other modifications that must occur in eukaryotic cells such as splicing introns and exons. In short, sections of unwanted DNA, called introns, are removed by the process of splicing, and the remaining DNA codes are connected back together (exons).
Now that the mRNA has been created by the process of transcription, the next step is for the mRNA to build a protein necessary for the main functions of the body, in a process known as translation (Brooker, 2017). Here, translation is the process in which tRNA decodes or translates the mRNA into a protein in a mobile cellular factory called the ribosome. It is translating the language of a DNA sequence (gene) into the language of a protein. To do this, the tRNA uses a translation device called an anticodon. This anticodon links to the mRNA-based pairs called a codon. A codon is a trinucleotide sequence of DNA or RNA that corresponds to a specific amino acid, or building block of a protein. This process then continues to translate and connect many amino acids together until a polypeptide (a long chain of amino acids) is created. Later, these polypeptides join to form proteins. Depending on the type of cell, the protein may function in a variety of ways. For example, the neuron has several proteins for its function, and different proteins are used for memory, learning, and neuroplasticity.
Epigenetics
There is a wealth of research conducted on genetics, yet the understanding of epigenetics is more limited when focusing on mental health (Huang et al., 2017). Though the term epigenetics has been around since the 1940s, the “science” of epigenetics is in its youth. Epigenetic research in humans has grown in the last 10 years and continues to expand rapidly (Januar et al., 2015). The key concept for counselors to remember about epigenetics is that epigenetics supports the idea of coaction. Factors present in the client’s external environment (e.g., stress from caregiver neglect, foods consumed, drug intake like cigarettes) influence the expression of their genes (transcription and translation) and thus cell activity and related behavioral phenotypes. In the sections below, we will dive deeper into the understanding of epigenetic mechanisms and define key terms including epigenome, chromatin, and chemical modifications.
To start, the more formal definition of epigenetics is the differentiation of gene expression via chemical modifications upon the epigenome that do not alter the genetic code (i.e., the DNA sequence; Szyf et al., 2007). The epigenome, which is composed of chromatin (the combination of DNA and protein forming the chromosomes) and modification of DNA by chemical mechanisms (e.g., DNA methylation, histone modification), programs the process of gene expression (Szyf et al., 2007). The epigenome differs from the genome in that the chemical actions or modifications are on the outside of the genome (i.e., the DNA) or “upon” the genome. Specifically, epigenetic processes act “upon” the genome, which may open or close the chromatin to various degrees to govern access for reading DNA sequences (Figure 1). When the chromatin is opened, transcription and translation can take place; however, when the chromatin is closed, gene expression is silenced (Syzf et al., 2007).
It is important for counselors to conceptualize their client’s psychosocial environment in conjunction with the observed behavioral phenotypes, in that the client’s psychosocial environment may have partially mediated epigenetic expression (Januar et al., 2015). For example, with schizophrenia, a client’s adverse environment (e.g., early childhood trauma) influences the epigenome, or gene expression, which may contribute up to 60% of this disorder’s development (Gejman et al., 2011). Other adverse environmental influences have been associated with the development of schizophrenia, including complications during client’s prenatal development and birth, place and season of client’s birth, abuse, and parental loss (Benros et al., 2011). As we highlight below, epigenetic mechanisms (e.g., DNA methylation) may mediate between these environmental influences and genes with outcomes like schizophrenia (Cariaga-Martinez & Alelú-Paz, 2018; Tsankova et al., 2007).
Epigenetic Mechanisms
There are a variety of chemical mechanisms or tags that change the chromatin structure (either opening for expression or closing to inhibit expression). Some of the most investigated mechanisms for changes in chromatin structure are DNA methylation, histone modification, and microRNA (Benoit & Turecki, 2010; Maze & Nestler, 2011).
DNA Methylation. Methylation is the most studied epigenetic modification (Nestler et al., 2016). It occurs when a methyl group binds to a cytosine base (C) of DNA to form 5-methylcytosine. A methyl group is three hydrogens bonded to a carbon, identified as CH3. Most often, the methyl group is attached to a C followed by a G, called a CpG. These methylation changes are carried out by specific enzymes called DNA methyltransferase. These enzymes add the methyl group to the C base at the CpG site.
Methylation was initially considered irreversible, but recent research has shown that DNA methylation is more stable compared to other chemical modifications like histone modification and is therefore reversible (Nestler et al., 2016). This DNA methylation adaptability evidence is important, conceivably supporting counseling efficacy across the life span. If methylation is indeed reversible beyond 0 to 5 years of age, counseling efforts hold promise to influence mental health outcomes across the life span.
Beyond noted stability, DNA methylation is also important in that it is tissue-specific, meaning it assists in cell differentiation; it may regulate gene expression up or down and is influenced by different environmental exposures (Monk et al., 2012). For example, DNA methylation represses specific areas of a neuron’s genes, thus “turning off” their function. This stabilizes the cell by preventing any tissue-specific cell differentiation and inhibits the neuron from changing into another cell type (Szyf et al., 2016), such as becoming a lung cell later in development.
When looking at up- or downregulation, Oberlander et al. (2008) provided an example from a study using mice. When examining attachment style in mice, they found that decreased quality of mothering to offspring increased risk of anxiety, in part, because of the methylation at the glucocorticoid receptor (GR) gene and fewer GR proteins produced by the hippocampus. This change may lead to lifelong silencing or downregulation with an increased risk of anxiety to the mouse over its life span. Stevens et al. (2018) also established a link between diet, epigenetics, and DNA methylation. They found an epigenetic connection between poor dietary intake with increased risk of behavioral problems and poor mental health outcomes such as autism. The authors also remarked that further investigation is required for a clearer picture of this link and potential effects.
Histone Modification. Another process that has been extensively researched is post-translational histone modification, or changes in the histone after the translation process. The most understood histone modifications are acetylation, methylation, and phosphorylation (Nestler et al., 2016). Acetylation, the most common post-translational modification, occurs by adding an acetyl group to the histone tail, such as the amino acid lysine. The enzymes responsible for histone acetylation are histone acetyltransferases or HATs (Haggarty & Tsai, 2011). Conversely, histone deacetylases (HDACs) are enzymes that remove acetyl groups (Saavedra et al., 2016). The acetylation process promotes gene expression (Nestler et al., 2016).
Through histone methyltransferases (HMTs), histone methylation increases methylation, thereby reducing gene expression. Histone demethylases (HDMs) remove methyl groups to increase gene activity. Phosphorylation can increase or decrease gene expression. Overall, there are more than 50 known histone modifications (Nestler et al., 2016).
From a counseling perspective, it is important to note that histone modification is flexible. Unlike DNA methylation, which is more stable over a lifetime, histone modifications are more transient. To illustrate, if an acetyl group is added to a histone, it may loosen the binding between the DNA and histone, increasing transcription and thereby allowing gene expression across the life span (Nestler et al., 2016). Such acetylation processes have been found in maternal neglect to offspring (early in the life span) and mindfulness practices in adult clients (Chaix et al., 2020; Devlin et al., 2010). Yet, although histone modification can be changed across the life span (Nestler et al., 2016), it is still important for counselors to recognize the importance of early counseling interventions because of how highly active epigenetics mechanisms (e.g., DNA methylation) are in children 0 to 5 years of age.
MicroRNA. Beyond histone modification, another known mechanism is microRNA (miRNA), which is the least understood and most recently investigated epigenetic mechanism when compared to DNA methylation and histone modification (Saavedra et al., 2016). miRNA is one type of non-coding RNA (ncRNA), or RNA that is changed into proteins. Around 98% of the genome does not code for proteins, leading to a supporting hypothesis that ncRNAs play a significant role in gene expression. For example, humans and chimpanzees share 98.8% of the same DNA code. However, epigenetics and specifically ncRNA contribute to the wide phenotypic variation between the species (Zheng & Xiao, 2016). Further, Zheng and Xiao (2016) estimated that miRNA regulates up to 60% of gene expression.
miRNA has also been found to suppress and activate gene expression at the levels of transcription and translation (Saavedra et al., 2016). miRNAs affect gene expression by directly influencing mRNA. Specifically, the miRNA may attach to mRNA and “block” the mRNA from creating proteins or it may directly degrade mRNA. This then decreases the surplus of mRNA in the cell. If the miRNA binds partially with the mRNA, then it inhibits protein production; but if it binds completely, it is marked for destruction. Once the mRNA is identified for destruction, other proteins and enzymes are attracted to the mRNA, and they degrade the mRNA and eliminate it (Zheng & Xiao, 2016). Moreover, when compared to DNA methylation, which may be isolated to a single gene sequence, miRNA can target hundreds of genes (Lewis et al., 2005). Researchers have discovered that miRNA may mediate anxiety-like symptoms (Cohen et al., 2017).
Human Development and Epigenetics
Over the life of an individual, there are critical or sensitive periods in which epigenetic modifications are more heavily influenced by environmental factors (Mulligan, 2016). Early life (ages 0 to 5 years) appears to be one of the most critical time periods when epigenetics is more active. An example of this is the Dutch Famine of 1944–45, also known as the Dutch Hunger Winter (Champagne, 2010; Szyf, 2009). The Nazis occupied the Netherlands and restricted food to the country, bringing about a famine. The individual daily caloric intake estimate varied between 400 and 1800 calories at the climax of the famine. Most notably, women who gave birth during this time experienced the impact of low maternal caloric intake, which impacted their child and the child’s health outcomes into adulthood. One discovery was that male children had a higher risk of adulthood obesity if their famine exposure occurred early in gestation versus a male fetus who experienced famine in late gestation. Findings suggested that fetuses who experienced restricted caloric intake during the development of their autonomic nervous system may have an increased risk of heart disease in adulthood. The findings of epigenetic mechanisms at work between mother and child during a famine are flagrant enough, yet epigenetic researchers have also discovered that epigenetic tags carry across generations, called genomic imprinting (Arnaud, 2010; Yehuda et al., 2016; T.-Y. Zhang & Meaney, 2010).
Genomic imprinting can be defined as the passing on of certain epigenetic modifications to the fetus by parents (Arnaud, 2010). It is allele-specific, and approximately half of the imprinting an offspring receives is from the mother. The imprinting mechanism marks certain areas, or loci, of offspring’s genes as active or repressed. For instance, the loci may exhibit increased or decreased methylation.
An imprinting example is evident in the IGF-2 (insulin-like growth factor II) gene and those fetuses exposed to the Dutch Hunger Winter (Heijmans et al., 2008). Sixty years after the famine, a decrease in DNA methylation on IGF-2 was found in adults with fetal exposure during the famine compared to their older siblings. Researchers also found these intergenerational imprinting effects associated with the grandchildren of women who were pregnant during the Dutch Hunger Winter. Similar imprinting is also apparent in Holocaust survivors (Yehuda et al., 2016) and children born to mothers who experienced PTSD from the World Trade Center collapse of 9/11 (Yehuda et al., 2005). These imprinting mechanisms are important for counselors to understand in that we see the interplay between the client and the environment across generations. The client becomes the embodiment of their environment at the cellular level. This is no longer the dichotomous “nature vs. nurture” debate but the passing on of biological effects from one generation to another through the interplay of nature and nurture.
Epigenetics and Mental Health Disorders
Now we turn our focus to the influence of epigenetics on the profession of counseling. What we do know is that epigenetic mechanisms, (e.g., DNA methylation, histone modifications, miRNA) are associated with various mental health disorders. It is hypothesized that epigenetics contributes to the development of mental disorders after exposure to environmental stressors, such as traumatic life events, but it may also have positive effects based on salutary environments (Syzf, 2009; Yehuda et al., 2005). We will review only those mental health epigenetic findings that have significant implications relative to clinical disorders such as stress, anxiety, childhood maltreatment, depression, schizophrenia, and addiction. We will also offer epigenetic outcomes associated with treatment, including cognitive behavioral therapy (CBT; Roberts et al., 2015), meditation (Chaix et al., 2020), and antidepressants (Lüscher & Möhler, 2019).
Stress and Anxiety
Stress, especially during early life stages, causes long-term effects for neuronal pathways and gene expression (Lester et al., 2016; Palmisano & Pandey, 2017; Perroud et al., 2011; Roberts et al., 2015; Szyf, 2009; T.-Y. Zhang & Meaney, 2010). Currently, research supports the mediating effects of stress on epigenetics through DNA methylation, especially within the gestational environment (Lester & Marsit, 2018). DNA methylation has been associated with upregulation of the hypothalamic-pituitary-adrenal (HPA) axis, increasing anxiety symptoms (McGowan et al., 2009; Oberlander et al., 2008; Romens et al., 2015; Shimada-Sugimoto et al., 2015; Tsankova et al., 2007). DNA methylation has also been linked with increased levels of cortisol for newborns of depressed mothers. This points to an increased HPA stress response in the newborn (Oberlander et al., 2008). Ouellet-Morin et al. (2013) also looked at DNA methylation and stress. They conducted a longitudinal twin study on the effect of bullying on the serotonin transporter gene (SERT) for monozygotic twins and found increased levels of SERT DNA methylation in victims compared to their non-bullied monozygotic co-twin. Finally, Roberts et al. (2015) examined the effect of CBT on DNA methylation for children with severe anxiety, specifically testing changes in the FKBP5 gene. Although the results were not statistically significant, they may be clinically significant. Research participants with a higher DNA methylation on the FKBP5 gene had poorer response to CBT treatment.
Beyond DNA methylation, other researchers have investigated miRNA and its association with stress and anxiety. A study by Harris and Seckl (2011) found that fetal rodents with increased exposure to maternal cortisol suffered from lower birth weights and heightened anxiety. Similarly, Cohen et al. (2017) investigated anxiety in rats for a specific miRNA called miR-101a-3p. The researchers selectively bred rats, one group with low anxiety and the other with high anxiety traits. They then overexpressed miR-101a-3p in low-anxiety rats to see if that would induce greater expressions of anxiety symptomatology. The investigators observed increased anxiety behaviors when increasing the expression of miR-101a-3p in low-anxiety rats. The researchers postulated that miRNA may be a mediator of anxiety-like behaviors. Finally, paternal chronic stress in rats has been associated with intergenerational impact on offspring’s HPA axis with sperm cells having increased miRNAs, potentially indicating susceptibility of epigenetic preprogramming in male germ cells post-fertilization (Rodgers et al., 2013). The evidence suggests that paternal stress reprograms the HPA stress response during conception. This reprogramming may begin a cascading effect on the offspring’s HPA, creating dysregulation that is associated with disorders like schizophrenia, autism, and depression later in adulthood.
Though some researchers have indicated a negative association between anxiety and epigenetics, others have found positive effects between epigenetics and anxiety. A seminal study by Weaver et al. (2005) illustrated the flexibility of an offspring’s biological system to negative and positive environmental cues. Weaver et al. looked at HPA response of rodent pups who received low licking and grooming from their mother (a negative environmental effect) who exhibited higher HPA response to environmental cues in adulthood. Epigenetically, they found lower DNA methylation in a specific promotor region in these adult rodents. They hypothesized that they could reverse this hypomethylation by giving an infusion of methionine, an essential amino acid that is a methyl group donor. They discovered the ability to reverse low methylation, which improved the minimally licked and groomed adult rodents’ response to stress. This connects with counseling in that epigenetic information is not set for life but reversible through interventions such as diet.
Others have investigated mindfulness and its epigenetic effects on stress. Chaix et al. (2020) looked at DNA methylation at the genome level for differences between skilled meditators who meditated for an 8-hour interval compared to members of a control group who engaged in leisure activities for 8 hours. The control group did not have any changes in genome DNA methylation, but the skilled meditators showed 61 differentially methylated sites post-intervention. This evidence can potentially support the use of mindfulness with our clients as an intervention for treatment of stress.
Childhood Maltreatment
Childhood maltreatment includes sexual abuse, physical abuse and/or neglect, and emotional abuse and/or neglect. Through this lens, Suderman et al. (2014) examined differences in 45-year-old males’ blood samples between those who experienced abuse in childhood and those who did not, with the aim of determining whether gene promoter DNA methylation is linked with child abuse. After 30 years, the researchers found different DNA methylation patterns between abused versus non-abused individuals and that a specific hypermethylation of a gene was linked with the adults who experienced child abuse. Suderman et al. (2014) believed that adversity, such as child abuse, reorganizes biological pathways that last into adulthood. These DNA methylation differences have been associated with biological pathways leading to cancer, obesity, diabetes, and other inflammatory paths.
Other researchers have also found epigenetic interactions at CpG sites predicting depression and anxiety in participants who experienced abuse. Though these interactions were not statistically significant (Smearman et al., 2016), increased methylation at specific promoter regions was discovered (Perroud et al., 2011; Romens et al., 2015). Furthermore, in a hallmark study, McGowan et al. (2009) discovered that people with child abuse histories who completed suicide possessed hypermethylation of a particular promotor region when compared to controls. Perroud et al. (2011) noted that frequency, age of onset, and severity of maltreatment correlated positively with increased methylation in adult participants suffering from borderline personality disorder, depression, and PTSD. Yehuda et al. (2016) reported that in a smaller subset of an overall sample of Holocaust survivors, the impact of trauma was intergenerationally associated with increased DNA methylation. Continued study of these particular regions may provide evidence of DNA methylation as a predictor of risk in developing anxiety or depressive disorders.
Major Depressive Disorder
Most studies of mental illness, genetics, and depression have used stress animal models. Through these models, histone modification, chromatin remodeling, miRNA, and DNA methylation mechanisms have been found in rats and mice (Albert et al., 2019; Nestler et al., 2016). When an animal or human experiences early life stress, epigenetic biomarkers may serve to detect the development or progression of major depressive disorder (Saavedra et al., 2016). Additionally, histone modification markers may also indicate an increase in depression (Tsankova et al., 2007; Turecki, 2014). Beyond animal models, Januar et al. (2015) found that buccal tissue in older patients with major depressive disorder provided evidence that the BDNF gene modulates depression through hypermethylation of specific CpGs in promoter regions.
Lastly, certain miRNAs may serve as potential biomarkers for major depressive disorder. miRNA may be used in the pharmacologic treatment of depressive disorders (Saavedra et al., 2016). Tsankova et al. (2007) and Saavedra et al. (2016) noted that certain epigenetic mechanisms that influence gene expression may be useful as antidepressant treatments. Medication may induce neurogenesis and greater plasticity in synapses through upregulation and downregulation of miRNAs (Bocchio-Chiavetto et al., 2013; Lüscher & Möhler, 2019). This points to the potential use of epigenetic “engineering” for reducing depression progression and symptomology where a counselor could refer a client for epigenetic antidepressant treatments.
Maternal Depression
Maternal prenatal depression may program the postnatal HPA axis in infants’ responses to the caretaking environment. Such programming may result in decreased expression of certain genes associated with lesser DNA methylation in infants, depending on which trimester maternal depression was most severe, and increased HPA reactivity (Devlin et al., 2010). Further, Devlin et al. discovered that maternal depression in the second trimester affected newborns’ DNA methylation patterns. However, the authors offered key limitations in their study, namely the sample was predominantly male and depressive characteristics differed based on age. Conradt et al. (2016) reported that prenatal depression in mothers may be associated with higher DNA methylation in infants. However, maternal sensitivity (i.e., ability of mother to respond to infants’ needs positively, such as positive touch, attending to distress, and basic social-emotional needs) toward infants buffered the extent of methylation, which points to environmental influences. This finding highlights the risk of infant exposure to maternal depression in conjunction with maternal sensitivity. Yet, overall, the evidence suggests that epigenetic mechanisms are at play across critical periods—prenatal, postnatal, and beyond—that have implications for offspring. When a fetus or offspring experiences adverse conditions, such as maternal depression, there is an increased likelihood of “impaired cognitive, behavioral, and social functioning . . . [including] psychiatric disorders throughout the adult life” (Vaiserman & Koliada, 2017, p. 1). For the practicing counselor, we suggest that clinical work with expecting mothers has the potential to reduce such risk based on these epigenetic findings.
Schizophrenia
Accumulated evidence suggests that schizophrenia arises from the interaction between genetics and the client’s environment (Smigielski et al., 2020). Epigenetics is considered a mediator between a client’s genetics and environment with research showing moderate support for this position. DNA methylation, histone modifications, mRNA, and miRNA epigenetic mechanisms have been linked with schizophrenia (Boks et al., 2018; Cheah et al., 2017; Okazaki et al., 2019).
DNA methylation is a main focus in schizophrenia epigenetic research (Cariaga-Martinez & Alelú-Paz , 2018). For example, Fisher et al. (2015) conducted a longitudinal study investigating epigenetic differences between monozygotic twins who demonstrated differences in psychotic symptoms; at age 12, one twin was symptomatic and the other was asymptomatic. Fisher et al. found DNA methylation differences between these twins. The longitudinal twin study design allowed for the control of genetic contributions to the outcome as well as other internal and external threats. Further, it pointed to a stronger association between epigenetics and schizophrenia.
From a clinical perspective, Ma et al. (2018) identified a potential epigenetic biomarker for detecting schizophrenia. The authors were able to identify three specific miRNAs that may work in combination as a biomarker for the condition. According to the authors, this finding may be helpful in the future for diagnosis and monitoring treatment outcomes. We speculate that future counselors may have biomarker tests conducted as part of the diagnostic process and in monitoring treatment effectiveness with alternation in miRNA levels.
Addiction
In addictions, a diversity of epigenetic mechanisms have been identified (e.g., DNA methylation, histone acetylation, mRNA, miRNA) across various substance use disorders: cocaine, amphetamine, methamphetamine, and alcohol (Hamilton & Nestler, 2019). Moreover, these epigenetic processes have been hypothesized to contribute to the addiction process by mediating seeking behaviors via dopamine in the neurological system. Also, Hamilton and Nestler (2019) found that epigenetic mechanisms have the potential to combat addiction processes, but further research is needed.
Cadet et al. (2016) conducted a review of cocaine, methamphetamine, and epigenetics in animal models (mice and rats). Chronic cocaine use was linked with histone acetylation in the dopamine system and DNA methylation for both chronic and acute administrations. They concluded that epigenetics may be a facilitating factor for cocaine abuse. Others have supported this conclusion for cocaine specifically, in that cocaine alters the chromatin structure by increasing histone acetylation, thereby temporarily inducing addictive behaviors (Maze & Nestler, 2011; Tsankova et al., 2007). From a treatment perspective, Wright et al. (2015) reported, in a sample of rats, that an injected methyl supplementation appeared to attenuate cocaine-seeking behavior when compared to the control group associated with cocaine-induced DNA methylation.
Regarding methamphetamines, during their review, Cadet et al. (2016) discovered that there were only a few extant studies on epigenetics and methamphetamines. Numachi et al. (2004) linked extended use of methamphetamines to changes in DNA methylation patterns, which seemed to increase vulnerability to neurochemical effects. More recently, Jayanthi et al. (2014) discovered that chronic methamphetamine use in rats induced histone hypoacetylation, making it more difficult for transcription to occur and potentially supporting the addiction process. To counter this histone hypoacetylation, the authors treated the mice with valproic acid, which inhibited the histone hypoacetylation. This study may evidence potential psychopharmacological treatments in the future at the epigenetic level for methamphetamine addiction.
H. Zhang and Gelernter (2017) reviewed the literature on DNA methylation and alcohol use disorder (AUD) and found mixed results. The authors discovered that individuals with an AUD exhibited DNA hypermethylation and hypomethylation in a variety of promoter regions. They also noted generalization limitations due to small tissue samples from the same regions of postmortem brains. They suggested that DNA methylation may account for “missing heritability” (p. 510) among individuals with AUDs.
Histone deacetylation has also been connected to chromatin closing or silencing for chronic users of alcohol, which may be involved in the maintenance of an AUD. Palmisano and Pandey (2017) suggested that there are epigenetic mediating factors between comorbidity of AUDs and anxiety disorders. On a positive note, exercise has been found to have opposite epigenetic modifications when comparing a healthy exercise group to a group who experience AUDs in terms of DNA methylation at CpG sites (Chen et al., 2018). Thus, counselors may incorporate such aspects in psychoeducation when recommending exercise in goal setting and other treatment interventions.
To summarize, epigenetics has been linked to several disorders such as anxiety, stress, depression, schizophrenia, and addiction (Albert et al., 2019; Cadet et al., 2016; Lester et al., 2016; Palmisano & Pandey, 2017; Smigielski et al., 2020). DNA methylation and miRNA may have mediating effects for mental health concerns such as anxiety (Harris & Seckl, 2011; Romens et al., 2015). Additionally, epigenetic mediating effects have also been discovered in major depressive disorder, maternal depression, and addiction (Albert et al., 2019; Conradt et al., 2016; Hamilton & Nestler, 2019). Moreover, epigenetic imprinting has been associated with trauma and stress, as found in Holocaust survivors and their children (Yehuda et al., 2016). Overall, “evidence accumulates that exposure to social stressors in [childhood], puberty, adolescence, and adulthood can influence behavioral, cellular, and molecular phenotypes and . . . are mediated by epigenetic mechanisms” (Pishva et al., 2014, p. 342).
Implications
A key aim in providing a primer on epigenetics, specifically the coaction between a client’s biology and environment on gene expression, is to illuminate opportunities for counselors to prevent and intervene upon mental health concerns. This is most relevant based on the evidence that epigenetic processes change over a client’s lifetime because of environmental influences, meaning that the client is not in a fixed state per traditional gene theory (Nestler et al., 2016). Epigenetics provides an alternate view of nature and nurture, demonstrating that epigenetic tags may not only be influenced by unfavorable environmental influences (e.g., maternal depression, trauma, bullying, child abuse and neglect) but also by favorable environments and activities (e.g., mindfulness, CBT, exercise, diet, nurturing; Chaix et al., 2020; Chen et al., 2018; Conradt et al., 2016; Roberts et al., 2015; Stevens et al., 2018). Understanding the flexibility of epigenetics has the potential to engender hope for our clients and to guide our work as counselors and counselor educators, because our genetic destinies are not fixed as we once theorized in gene theory.
Bioecological Conceptualization: Proximal and Distal Impact and Interventions
The impact of epigenetics on the counseling profession can be understood using Bronfenbrenner’s (1979) bioecological model. The bioecological model conceptualizes a client’s function over time based on the coaction between the client and their environment (Broderick & Blewitt, 2015; Jones & Tang, 2015). The client’s environment can have both beneficial and deleterious proximal and distal effects. These effects are like concentric rings around the client, which Bronfenbrenner called “subsystems.” The most proximate subsystem is the microsystem, the environment that has a direct influence on the client, such as parents, teachers, classmates, coworkers, relatives, etc. The next level is the mesosystem, in which the micro entities interact with one another or intersect with influence on the client (e.g., school and home intersect to influence client’s thinking and behavior). The next system, called the exosystem, begins the level of indirect influence. This may include neighborhood factors such as the availability of fresh produce, safe neighborhoods, social safety net programs, and employment opportunities. The last subsystem is the macrosystem. This system consists of the cultural norms, values, and biases that influence all other systems. The final aspect of this model, called the chronosystem, takes into account development over time. The chronosystem directs the counselor’s attention to developmental periods that have differing risks and opportunities, or what can be called “critical” developmental periods.
Below we conceptualize epigenetic counseling implications using Bronfenbrenner’s model but simplify it by grouping systems: proximal effects (micro/meso level) labeled as micro effects and distal effects (exo/macro level) labeled as macro effects. We will also apply the chronosystem by focusing on critical developmental periods that are salient when applying epigenetics to counseling. Ultimately, our central focus is the client and the concentric influences of micro and macro effects. To begin, we will first focus on the important contribution of epigenetics during the critical developmental period of 0 to 5 years of age with implications at the micro and macro levels.
Epigenetics Supports Early Life Span Interventions
Though the evidence does support epigenetic flexibility across a client’s life span, we know that early adverse life events may alter a child’s epigenome with mediating effects on development and behavior (Lester & Marsit, 2018). We also know that epigenetic processes are most active in the first 5 years of life (Mulligan, 2016; Syzf et al., 2016). These early insults to the genome may elicit poor mental health into adulthood such as anxiety, depression, schizophrenia, and addiction. For example, a client who grew up in an urban environment with a traditionally marginalized group status and parents who experienced drug dependence has an increased risk for schizophrenia above and beyond the genetic, inherited risk. These adverse childhood experiences have the potential to modify the epigenome, increasing the likelihood of developing mental health concerns, including schizophrenia (Cariaga-Martinez & Alelú-Paz, 2018).
At the micro level, the caregiver can be a salutary effect against adverse environmental conditions (Oberlander et al. 2008; Weaver et al., 2005). Prenatally, counseling can work with parents before birth to generate healthy coping strategies (e.g., reduce substance abuse), flexible and adaptive caregiver functioning, and effective parenting strategies. An example of this is to use parent–child interactive therapy (PCIT) pre-clinically, or before the child evidences a disorder (Lieneman et al., 2017). Preventive services using PCIT have been documented as effective with externalizing behaviors, child maltreatment, and developmental delays. Additional micro-level interventions can be found in the use of home-visiting programs to improve child outcomes prenatally to 5 years of age where positive parenting and other combined interventions are utilized to improve the health of mother, father, and child (Every Child Succeeds, 2019; Healthy Families New York, 2021).
Clinically, epigenetics points to earlier care and treatment to prevent the emergence of mental disorders (e.g., major depressive disorder, schizophrenia). Also, epigenetic research has provided evidence that environmental change can be equally important as client change. Regarding treatment planning, examining the client’s individual level factors or microsystem (e.g., physical health, mental status, education, race, gender) as well as their macrosystem (e.g., social stigma, poverty, housing quality, green space, pollution) may be crucial before considering what kind of modifications and/or interventions are most appropriate. For example, if a 9-year-old White female presents to a counselor for behavioral concerns in school, it is important for the counselor to gather a holistic life history to build an informed picture of the many variables collectively impacting the child’s behavior at each level. At the micro level, a counselor will evaluate for childhood maltreatment, but from an epigenetic lens, other proximal environmental factors could be important to screen for such as poverty, maternal depression, nutrition, classroom dynamics, and exercise (McEwen & McEwen, 2017; Mulligan, 2016). If the 9-year-old child is experiencing parental neglect and food insecurity, the clinician can treat the client’s individual needs at the micro level (i.e., working with the family system to overcome any neglect by using treatments such as PCIT, and direct referral to social workers and other agencies to provide food and shelter to meet basic needs).
The science of epigenetics may also inform action taken during assessment and case conceptualization based on the coaction of environment with a client over time. Although intervention at 0–5 years of age is most preventative, it is not practical in all cases. Using assessments that collect information on an adult client’s early life may help inform case conceptualization and allow the integration of epigenetics into counseling theories to better understand the etiology of a client’s presenting problem(s). For example, using an adverse childhood experiences assessment may help identify individuals at higher risk of epigenetic concerns. Epigenetics highlights the impact of client–environment interaction and its influence (positive or negative) on overall health. Additionally, early life adversity increases the likelihood of poor health outcomes such as heart disease, anxiety, and depression. However, these poor consequences could be mediated by talking with clients about the importance of exercise and its benefit on epigenetics and, by extension, mental health.
At the macro level, examples could include the reduction of hostile environments (e.g., institutional racism, neighborhood violence, limited employment opportunities, low wages, air pollutants, water pollutants), advocacy for statutes, regulations to decrease instability such as unfair housing in low-income neighborhoods, establishing partnerships in the development of community-based and school-based prevention programs, and applying early interventions such as mindfulness to reduce the effects of stress (Chaix et al., 2020). To illustrate, postnatal depression symptom severity has been associated with residential stability (Jones et al., 2018). By developing policies that would increase housing security, a reduction in maternal depression symptom severity could potentially reduce the DNA methylation that is associated with upregulation of the HPA and child reactivity, but this would need to be investigated further for confirmation. According to Rutten et al. (2013), this change may also increase the resiliency of children by reducing their experience of chronic stress, as sustained maternal depression severity often impacts caregiving because of unstable housing.
Although members of the counseling profession have known the significance of early intervention for years, this epigenetic understanding confirms why human growth and development is a core component of our counseling professional identity (Remley & Herlihy, 2020) and provides a supporting rationale for our efforts. Additionally, epigenetic tags have the potential to cross generations via the process of imprinting (Yehuda et al., 2016). This has potential implications across the life span.
In summary, critical developmental periods must be a focal point for counseling interventions, necessitating upstream action rather than our current dominant approach of downstream activities and a shift toward primary prevention over predominantly tertiary prevention. Such primary prevention would reduce stress and trauma for children before signs and symptoms become apparent and attend to the development and sustainability of healthy environments that would increase both client and community wellness.
Epigenetics Supports Counseling Advocacy and Social Justice Efforts
When reflecting on the implications of epigenetics, it is apparent that place, context, and the client’s environment are critical factors for best positioning them for healthy outcomes, engendering a push for advocacy and social justice for clients. Because environments have no boundaries, it is important to think of advocacy across many systems: towns, counties, states, countries, and the world. This reinforces the call for counselors and counselor educators to move beyond the walls of their workplaces in order to collaborate within the larger mental health field (e.g., clinical mental health, school, marriage and family, addiction, rehabilitation). Additionally, said knowledge compels connection with other professions—such as social workers, physicians, psychologists, engineers, housing developers, public health administrators, and members of nonprofit and faith-based organizations, etc.—to enact change on a wider scale and to improve the conditions for clients at a systemic level.
This collaboration also calls for engaging at local and international levels. Global human rights issues such as sex trafficking cross countries, regions, and local communities and necessitate collaboration to ameliorate these practices and the associated trauma. For starters, the American Counseling Association and the International Association for Counseling could partner with other organizations such as the Child Defense Fund to assist in meeting their mission to level the playing field for all children in the United States. At the local level, counselors and counselor educators could collaborate with local children’s hospitals and configure a plan to meet common goals to improve children’s health and wellness.
Counseling Research and Epigenetics
Research primarily affects clients on a macro level but can trickle down to directly engage clients within our clinical work and practice. Counselors and counselor educators can partner with members of other disciplines to further the work with epigenetic biomarkers (e.g., depression and DNA methylation). Counseling researchers can also investigate how talk therapy and other adjuncts, such as diet and exercise, may improve our clients’ treatment outcomes. As counseling researchers, we can develop research agendas around intervention and prevention for those 0–5 years of age and create and evaluate programs for this age group while also creating community partnerships as noted above. An example of this partnership is The John Hopkins Center for Prevention and Early Intervention. The creators of this program developed sustainable partnerships with public schools, mental health systems, state-level educational programs, universities, and federal programs to focus on early interventions that are school-based and beyond. They collaborated to develop, evaluate, and deliver a variety of programs and research activities to improve outcomes for children and adolescents. They have created dozens of publications based on these efforts that help move the discipline forward. In one such publication, Guintivano et al. (2014) looked at epigenetic and genetic biomarkers for predicting suicide.
Counselor Education, CACREP, and Epigenetics
The counselor educational system affects clients distally but also holds implications for the work counselors conduct at the client level. Counselor educators can provide a more robust understanding of epigenetics to counseling students across the counselor education curriculum. These efforts can include introducing epigenetics in theories, diagnosis, treatment, human and family development, practicum and internship, assessment, professional orientation, and social and cultural foundations courses. By assisting counseling students to comprehend the relationship between client and environment, as well as the importance of prevention, educators will increase their students’ ability to carry out a holistic approach with clients and attend to the foundational emphases of the counseling profession on wellness and prevention. Moreover, by learning to include epigenetics in case conceptualization, students can gain a more robust understanding of the determinants of symptomology, potential etiology at the cellular level, and epigenetically supported treatments such as CBT and mindfulness.
It is fairly simple to integrate epigenetics education into programs accredited by the Council for Accreditation of Counseling and Related Educational Programs (CACREP; 2015). To begin, counselor educators can integrate epigenetics education into professional counseling orientation and ethical practice courses. As counselor educators discuss the history and philosophy of the counseling profession, particularly from a wellness and prevention lens (CACREP, 2015, 2.F.1.a), counselor educators can discuss the connection between epigenetics and wellness. Wellness is a foundational value for the counseling profession and is a part of the definition of counseling (Kaplan et al., 2014). Many wellness models (both theoretical and evidence-based) are rooted in the promotion of a holistic balance of the client in a variety of facets and contexts (Myers & Sweeney, 2011). We can continue to support these findings by integrating epigenetics within our conversations about wellness, as we have epigenetic evidence that the positive or negative coaction between the individual and their environment can impact a person toward increased or decreased wellness.
Counselor educators can also integrate epigenetics education into Social and Cultural Diversity and Human Growth and Development courses. Within Social and Cultural Diversity courses, counselor educators can address how negative environmental conditions have negative influences on offspring. This is evidenced by the discrimination against Jews and its imprinting that crosses generations (Yehuda et al., 2016). Counselor educators can discuss how discrimination and barriers to positive environmental conditions can impact someone at the epigenetic level (CACREP, 2015, 2.F.2.h). Within Human Growth and Development, counselor educators can discuss how the study of epigenetics provides us a biological theory to understand how development is influenced by environment across the life span (CACREP, 2015, 2.F.3.a, c, d, f). In particular, it can provide an etiology of how negative factors change epigenetic tags, which are correlated with negative mental health that may become full-blown mental health disorders later in adulthood (CACREP, 2015, 2.F.3.c, d, e, g).
Additionally, counselor educators can integrate epigenetic education within specialty counseling areas. Several studies (Maze & Nestler, 2011; Palmisano & Pandey, 2017; Tsankova et al., 2007; Wong et al., 2011; H. Zhang & Gelernter, 2017) have noted how epigenetic mechanisms may support the addiction process and counselor educators can interweave this information when discussing theories and models of addiction and mental health problems (CACREP, 2015, 5.A.1.b; 5.C.1.d; 5.C.2.g). Counselor educators can also discuss epigenetics as it applies to counseling practice. Because epigenetics research supports treatments like CBT, mindfulness, nutrition, and exercise (Chaix et al., 2020; Chen et al., 2018; Roberts et al., 2015; Stevens et al., 2018), counselor educators can address these topics in courses when discussing techniques and interventions that work toward prevention and treatment of mental health issues (CACREP, 2015, 5.C.3.b).
Generally, CACREP (2015) standards support programs that infuse counseling-related research into the curriculum (2.E). We support the integration of articles, books, websites, and videos that will engender an understanding of epigenetics across the curriculum, so long as the integration supports student learning and practice.
Conclusion and Future Directions
In summary, there are numerous epigenetic processes at work in the symptoms we attend to as counselors. We have provided information that illustrates how epigenetics may mediate outcomes such as depression, anxiety, schizophrenia, and addiction. We have also illustrated how CBT, exercise, diet, and meditation may have positive epigenetic influences supporting our craft. We have discovered that epigenetic processes are most malleable in early life. This information offers incremental evidence for our actions as professional counselors, educators, and researchers, leading to a potential examination of our efforts in areas of prevention, social justice, clinical practice, and counseling program development. However, we must note that epigenetics as a science is relatively new and much of the research is correlational.
Based on the current limits of epigenetic science and a lack of investigation of mental health epigenetics in professional counseling, one of our first recommendations for future research efforts is to collaborate across professions with other researchers such as geneticists, as we did for this manuscript. From this partnership, our profession’s connection to epigenetics is elucidated. Interdisciplinary collaboration allows the professional counselor to offer their expertise in mental health and the geneticist their deep understanding of epigenetics and the tools to examine the nature and nurture relationships in mental health outcomes. We can also make efforts to look at our wellness-based preventions and interventions to document changes at the epigenetic level in our clients and communities. Ideally, as the science of epigenetics advances, we will have epigenetic research in our profession of counseling that is beyond correlation and evidences the effectiveness of our work down to the cellular level.
Conflict of Interest and Funding Disclosure
The development of this manuscript was supported
in part by a Cincinnati Children’s Hospital Medical
Center Trustee Award and by a grant from the
National Heart, Lung, and Blood Institute (HL132344).
The authors reported no conflict of interest.
References
Albert, P. R., Le François, B., & Vahid-Ansari, F. (2019). Genetic, epigenetic and posttranscriptional mechanisms for treatment of major depression: The 5-HT1A receptor gene as a paradigm. Journal of Psychiatry & Neuroscience, 44(3), 164–176. https://doi.org/10.1503/jpn.180209
Arnaud, P. (2010). Genomic imprinting in germ cells: Imprints are under control. Reproduction, 140(3), 411–423. https://doi.org/10.1530/REP-10-0173
Benoit, L., & Turecki, G. (2010). The epigenetics of suicide: Explaining the biological effects of early life environmental adversity. Archives of Suicide Research, 14(4), 291–310.
https://doi.org/10.1080/13811118.2010.524025
Benros, M. E., Nielsen, P. R., Nordentoft, M., Eaton, W. W., Dalton, S. O., & Mortensen, P. B. (2011). Autoimmune diseases and severe infections as risk factors for schizophrenia: A 30-year population-based register study. The American Journal of Psychiatry, 168(12), 1303–1310. https://doi.org/10.1176/appi.ajp.2011.11030516
Bocchio-Chiavetto, L., Maffioletti, E., Bettinsoli, P., Giovannini, C., Bignotti, S., Tardito, D., Corrada, D., Milanesi, L., & Gennarelli, M. (2013). Blood microRNA changes in depressed patients during antidepressant treatment. European Neuropsychopharmacology, 23(7), 602–611. https://doi.org/10.1016/j.euroneuro.2012.06.013
Boks, M. P., Houtepen, L. C., Xu, Z., He, Y., Ursini, G., Maihofer, A. X., Rajarajan, P., Yu, Q., Xu, H., Wu, Y., Wang, S., Shi, J. P., Hulshoff Pol, H. E., Strengman, E., Rutten, B. P. F., Jaffe, A. E., Kleinman, J. E., Baker, D. G., Hol, E. M., . . . Kahn, R. S. (2018). Genetic vulnerability to DUSP22 promoter hypermethylation is involved in the relation between in utero famine exposure and schizophrenia. Nature Partner Journals Schizophrenia, 4(1), 1–8. https://doi.org/10.1038/s41537-018-0058-4
Broderick, P. C., & Blewitt, P. (2015). The life span: Human development for helping professionals (4th ed.). Pearson.
Bronfenbrenner, U. (1979). The ecology of human development: Experiments by nature and design. Harvard University Press.
Brooker, R. J. (2017). Genetics: Analysis and principles (6th ed.). McGraw-Hill.
Cadet, J. L., McCoy, M. T., & Jayanthi, S. (2016). Epigenetics and addiction. Clinical Pharmacology & Therapeutics, 99(5), 502–511. https://doi.org/10.1002/cpt.345
Cariaga-Martinez, A., & Alelú-Paz, R. (2018). Epigenetic and schizophrenia. In F. Durbano (Ed.), Psychotic disorders – An update (pp. 147–162). IntechOpen. https://doi.org/10.5772/intechopen.73242
Chaix, R., Fagny, M., Cosin-Tomás, M., Alvarez-López, M., Lemee, L., Regnault, B., Davidson, R. J., Lutz, A., & Kaliman, P. (2020). Differential DNA methylation in experienced meditators after an intensive day of mindfulness-based practice: Implications for immune-related pathways. Brain, Behavior, and Immunity, 84, 36–44. https://doi.org/10.1016/j.bbi.2019.11.003
Champagne, F. A. (2010). Early adversity and developmental outcomes: Interaction between genetics, epigenetics, and social experiences across the life span. Perspectives on Psychological Science, 5(5), 564–574.
https://doi.org/10.1177/1745691610383494
Cheah, S.-Y., Lawford, B. R., Young, R. M., Morris, C. P., & Voisey, J. (2017). mRNA expression and DNA methylation analysis of serotonin receptor 2A (HTR2A) in the human schizophrenic brain. Genes, 8(1), 1–11. https://doi.org/10.3390/genes8010014
Chen, J., Hutchinson, K. E., Bryan, A. D., Filbey, F. M., Calhoun, V. D., Claus, E. D., Lin, D., Sui, J., Du, Y., & Liu, J. (2018). Opposite epigenetic associations with alcohol use and exercise intervention. Frontiers in Psychiatry, 9(594), 1–12. https://doi.org/10.3389/fpsyt.2018.00594
Cohen, J. L., Jackson, N. L., Ballestas, M. E., Webb, W. M., Lubin, F. D., & Clinton, S. M. (2017). miR-101a-3p and Ezh2 modulate anxiety-like behavior in high-responder rats. European Journal of Neuroscience, 46(7), 2241–2252.
Conradt, E., Hawes, K., Guerin, D., Armstrong, D. A., Marsit, C. J., Tronick, E., & Lester, B. M. (2016). The contributions of maternal sensitivity and maternal depressive symptoms to epigenetic processes and neuroendocrine functioning. Child Development, 87(1), 73–85. https://doi.org/10.1111/cdev.12483
Council for Accreditation of Counseling and Related Educational Programs. (2015). 2016 CACREP standards. http://www.cacrep.org/wp-content/uploads/2017/08/2016-Standards-with-citations.pdf
Devlin, A. M., Brain, U., Austin, J., & Oberlander, T. F. (2010). Prenatal exposure to maternal depressed mood and the MTHFR C677T variant affect SLC6A4 methylation in infants at birth. PloS ONE, 5(8), e12201.
https://doi.org/10.1371/journal.pone.0012201
Every Child Succeeds. (2019). 2019 report to the community. https://static1.squarespace.com/static/5df9251a492
ba56bc96bc96f/t/5e73b2a333e8127c09daabf2/1584640684722/Final2019Report.pdf
Fisher, H. L., Murphy, T. M., Arseneault, L., Caspi, A., Moffitt, T. E., Viana, J., Hannon, E., Pidsley, R., Burrage, J., Dempster, E. L., Wong, C. C. Y., Pariante, C. M., & Mill, J. (2015). Methylomic analysis of monozygotic twins discordant for childhood psychotic symptoms. Epigenetics, 10(11), 1014–1023.
https://doi.org/10.1080/15592294.2015.1099797
Gejman, P. V., Sanders, A. R., & Kendler, K. S. (2011). Genetics of schizophrenia: New findings and challenges. Annual Review of Genomics and Human Genetics, 12, 121–144.
https://doi.org/10.1146/annurev-genom-082410-101459
Guintivano, J., Brown, T., Newcomer, A., Jones, M., Cox, O., Maher, B. S., Eaton, W. W., Payne, J. L., Wilcox, H. C., & Kaminsky, Z. A. (2014). Identification and replication of a combined epigenetic and genetic biomarker predicting suicide and suicidal behaviors. The American Journal of Psychiatry, 171(12), 1287–1296.
https://doi.org/10.1176/appi.ajp.2014.14010008
Haggarty, S. J., & Tsai, L.-H. (2011). Probing the role of HDACs and mechanisms of chromatin-mediated neuroplasticity. Neurobiology of Learning and Memory, 96(1), 41–52. https://doi.org/10.1016/j.nlm.2011.04.009
Hamilton, P. J., & Nestler, E. J. (2019). Epigenetics and addiction. Current Opinion in Neurobiology, 59, 128–136. https://doi.org/10.1016/j.conb.2019.05.005
Harris, A., & Seckl, J. (2011). Glucocorticoids, prenatal stress and the programming of disease. Hormones and Behavior, 59(3), 279–289. https://doi.org/10.1016/j.yhbeh.2010.06.007
Healthy Families New York. (2021, January 4). [Website.] https://www.healthyfamiliesnewyork.org
Heijmans, B. T., Tobi, E. W., Stein, A. D., Putter, H., Blauw, G. J., Susser, E. S., Slagboom, P. E., & Lumey, L. H. (2008). Persistent epigenetic differences associated with prenatal exposure to famine in humans. Proceedings of the National Academy of Sciences, 105(44), 17046–17049. https://doi.org/10.1073/pnas.0806560105
Huang, W.-C., Ferris, E., Cheng, T., Hörndli, C. S., Gleason, K., Tamminga, C., Wagner, J. D., Boucher, K. M., Christian, J. L., & Gregg, C. (2017). Diverse non-genetic, allele-specific expression effects shape genetic architecture at the cellular level in the mammalian brain. Neuron, 93(5), 1094–1109.e7.
https://doi.org/10.1016/j.neuron.2017.01.033
Januar, V., Ancelin, M.-L., Ritchie, K., Saffery, R., & Ryan, J. (2015). BDNF promoter methylation and genetic variation in late-life depression. Translational Psychiatry, 5, e619. https://doi.org/10.1038/tp.2015.114
Jayanthi, S., McCoy, M. T., Chen, B., Britt, J. P., Kourrich, S., Yau, H.-J., Ladenheim, B., Krasnova, I. N., Bonci, A., & Cadet, J. L. (2014). Methamphetamine downregulates striatal glutamate receptors via diverse epigenetic mechanisms. Biological Psychiatry, 76(1), 47–56. https://doi.org/10.1016/j.biopsych.2013.09.034
Jones, D. E., & Tang, M. (2015). Health inequality: What counselors need to know to act. In Ideas and research you can use: VISTAS 2015. https://www.counseling.org/docs/default-source/vistas/article_60785a22f16116603abcacff0000bee5e7.pdf?sfvrsn=4
Jones, D. E., Tang, M., Folger, A., Ammerman, R. T., Hossain, M. M., Short, J. A., & Van Ginkel, J. B. (2018). Neighborhood effects on PND symptom severity for women enrolled in a home visiting program. Community Mental Health Journal, 54(4), 420–428. https://doi.org/10.1007/s10597-017-0175-y
Kaplan, D. M., Tarvydas, V. M., & Gladding, S. T. (2014). 20/20: A vision for the future of counseling: The new consensus definition of counseling. Journaling of Counseling & Development, 92, 366–372. https://www.counseling.org/docs/default-source/20-20/2020-jcd-article-consensus-definition.pdf?sfvrsn=76017f2c_2
Lester, B. M., Conradt, E., & Marsit, C. (2016). Introduction to the special section on epigenetics. Child Development, 87(1), 29–37. https://doi.org/10.1111/cdev.12489
Lester, B. M., & Marsit, C. J. (2018). Epigenetic mechanisms in the placenta related to infant neurodevelopment. Epigenomics, 10(3), 321–333. https://doi.org/10.2217/epi-2016-0171
Lewis, B. P., Burge, C. B., & Bartel, D. P. (2005). Conserved seed pairing, often flanked by adenosines, indicates that thousands of human genes are microRNA targets. Cell, 120(1), 15–20.
https://doi.org/10.1016/j.cell.2004.12.035
Lieneman, C. C., Brabson, L. A., Highlander, A., Wallace, N. M., & McNeil, C. B. (2017). Parent–child interaction therapy: Current perspectives. Psychology Research and Behavior Management, 10, 239–256.
https://doi.org/10.2147/PRBM.S91200
Lüscher, B., & Möhler, H. (2019). Brexanolone, a neurosteroid antidepressant, vindicates the GABAergic deficit hypothesis of depression and may foster resilience. F1000Research, 8(May), 1–14.
https://doi.org/10.12688/f1000research.18758.1
Ma, J., Shang, S., Wang, J., Zhang, T., Nie, F., Song, X., Zhao, H., Zhu, C., Zhang, R., & Hao, D. (2018). Identification of miR-22-3p, miR-92a-3p, and miR-137 in peripheral blood as biomarker for schizophrenia. Psychiatry Research, 265, 70–76. https://doi.org/10.1016/j.psychres.2018.03.080
Maze, I., & Nestler, E. J. (2011). The epigenetic landscape of addiction. Annals of the New York Academy of Sciences, 1216(1), 99–113. https://doi.org/10.1111/j.1749-6632.2010.05893.x
McEwen, C. A., & McEwen, B. S. (2017). Social structure, adversity, toxic stress, and intergenerational poverty: An early childhood model. Annual Review of Sociology, 43, 445–472.
https://doi.org/10.1146/annurev-soc-060116-053252
McGowan, P. O., Sasaki, A., D’Alessio, A. C., Dymov, S., Labonté, B., Szyf, M., Turecki, G., & Meaney, M. J. (2009). Epigenetic regulation of the glucocorticoid receptor in human brain associates with childhood abuse. Nature Neuroscience, 12(3), 342–348. https://doi.org/10.1038/nn.2270
Monk, C., Spicer, J., & Champagne, F. A. (2012). Linking prenatal maternal adversity to developmental outcomes in infants: The role of epigenetic pathways. Development and Psychopathology, 24(4), 1361–1376.
https://doi.org/10.1017/S0954579412000764
Mulligan, C. J. (2016). Early environments, stress, and the epigenetics of human health. Annual Review of Anthropology, 45(1), 233–249. https://doi.org/10.1146/annurev-anthro-102215-095954
Myers, J. E., & Sweeney, T. J. (2011). Wellness counseling: The evidence base for practice. Journal of Counseling & Development, 86(4), 482–493. https://doi.org/10.1002/j.1556-6678.2008.tb00536.x
National Human Genome Research Institute. (2020). Epigenomics fact sheet. https://www.genome.gov/about-genomics/fact-sheets/Epigenomics-Fact-Sheet
Nestler, E. J., Peña, C. J., Kundakovic, M., Mitchell, A., & Akbarian, S. (2016). Epigenetic basis of mental illness. The Neuroscientist, 22(5), 447–463. https://doi.org/10.1177/1073858415608147
Numachi, Y., Yoshida, S., Yamashita, M., Fujiyama, K., Naka, M., Matsuoka, H., Sato, M., & Sora, I. (2004). Psychostimulant alters expression of DNA methlytransferase mRNA in the rat brain. Annals of the New York Academy of Sciences, 1025(1), 102–109. https://doi.org/10.1196/annals.1316.013
Oberlander, T. F., Weinberg, J., Papsdorf, M., Grunau, R., Misri, S., & Devlin, A. M. (2008). Prenatal exposure to maternal depression, neonatal methylation of human glucocorticoid receptor gene (NR3C1) and infant cortisol stress responses. Epigenetics, 3(2), 97–106. https://doi.org/10.4161/epi.3.2.6034
Okazaki, S., Otsuka, I., Numata, S., Horai, T., Mouri, K., Boku, S., Ohmori, T., Sora, I., & Hishimoto, A. (2019). Epigenetic clock analysis of blood samples from Japanese schizophrenia patients. npj Schizophrenia, 5(9), 1–7. https://doi.org/10.1038/s41537-019-0072-1
Ouellet-Morin, I., Wong, C. C. Y., Danese, A., Pariante, C. M., Papadopoulos, A. S., Mill, J., & Arseneault, L. (2013). Increased serotonin transporter gene (SERT) DNA methylation is associated with bullying victimization and blunted cortisol response to stress in childhood: A longitudinal study of discordant monozygotic twins. Psychology of Medicine, 43(9), 1813–1823. https://doi.org/10.107/S0033291712002784
Palmisano, M., & Pandey, S. C. (2017). Epigenetic mechanisms of alcoholism and stress-related disorders. Alcohol, 60, 7–18. https://doi.org/10.1016/j.alcohol.2017.01.001
Perroud, N., Paoloni-Giacobino, A., Prada, P., Olié, E., Salzmann, A., Nicastro, R., Guillaume, S., Mouthon, D.,
Stouder, C., Dieben, K., Huguelet, P., Courtet, P., & Malafosse, A. (2011). Increased methylation of glucocorticoid receptor gene (NR3C1) in adults with a history of childhood maltreatment: A link with the severity and type of trauma. Translational Psychiatry, 1, e59. https://doi.org/10.1038/tp.2011.60
Pishva, E., Kenis, G., van den Hove, D., Lesch, K.-P., Boks, M. P. M., van Os, J., & Rutten, B. P. F. (2014). The epigenome and postnatal environmental influences in psychotic disorders. Social Psychiatry and Psychiatric Epidemiology, 49, 337–348. https://doi.org/10.1007/s00127-014-0831-2
Provençal, N., & Binder, E. B. (2015). The effects of early life stress on the epigenome: From the womb to adulthood and even before. Experimental Neurology, 268, 10–20. https://doi.org/10.1016/j.expneurol.2014.09.001
Remley, T. P., Jr., & Herlihy, B. (2020). Ethical, legal, and professional issues in counseling (6th ed.). Pearson.
Roberts, S., Keers, R., Lester, K. J., Coleman, J. R. I., Breen, G., Arendt, K., Blatter-Meunier, J., Cooper, P., Creswell, C., Fjermestad, K., Havik, O. E., Herren, C., Hogendoorn, S. M., Hudson, J. L., Krause, K., Lyneham, H. J., Morris, T., Nauta, M., Rapee, R. M., . . . Wong, C. C. Y. (2015). HPA axis related genes and response to psychological therapies: Genetics and epigenetics. Depression and Anxiety, 32(12), 861–870.
https://doi.org/10.1002/da.22430
Rodgers, A. B., Morgan, C. P., Bronson, S. L., Revello, S., & Bale, T. L. (2013). Paternal stress exposure alters sperm microRNA content and reprograms offspring HPA stress axis regulation. Journal of Neuroscience, 33(21), 9003–9012. https://doi.org/10.1523/JNEUROSCI.0914-13.2013
Romens, S. E., McDonald, J., Svaren, J., & Pollak, S. D. (2015). Associations between early life stress and gene methylation in children. Child Development, 86(1), 303–309. https://doi.org/10.1111/cdev.12270
Rutten, B. P. F., Hammels, C., Geschwind, N., Menne-Lothmann, C., Pishva, E., Schruers, K., van den Hove, D.,
Kenis, G., van Os, J., & Wichers, M. (2013). Resilence in mental health: Linking psychological and neurobiological perspectives. Acta Psychiatrica Scandinavica, 128(1), 3–20. https://doi.org/10.1111/acps.12095
Saavedra, K., Molina-Márquez, A. M., Saavedra, N., Zambrano, T., & Salazar, L. A. (2016). Epigenetic modifications of major depressive disorder. International Journal of Molecular Sciences, 17(8), 1279.
https://doi.org/10.3390/ijms17081279
Shimada-Sugimoto, M., Otowa, T., & Hettema, J. M. (2015). Genetics of anxiety disorders: Genetic epidemiological and molecular studies in humans. Psychiatry and Clinical Neurosciences, 69(7), 388–401.
https://doi.org/10.1111/pcn.12291
Smearman, E. L., Almli, L. M., Conneely, K. N., Brody, G. H., Sales, J. M., Bradley, B., Ressler, K. J., & Smith, A. K.
(2016). Oxytocin receptor genetic and epigenetic variations: Association with child abuse and adult psychiatric symptoms. Child Development, 87(1), 122–134. https://doi.org/10.1111/cdev.12493
Smigielski, L., Jagannath, V., Rössler, W., Walitza, S., & Grünblatt, E. (2020). Epigenetic mechanisms in schizophrenia and other psychotic disorders: A systematic review of empirical human findings. Molecular Psychiatry, 25, 1718–1748. https://doi.org/10.1038/s41380-019-0601-3
Stevens, A. J., Rucklidge, J. J., & Kennedy, M. A. (2018). Epigenetics, nutrition and mental health: Is there a relationship? Nutritional Neuroscience, 21(9), 602–613. https://doi.org/10.1080/1028415X.2017.1331524
Suderman, M., Borghol, N., Pappas, J. J., Pinto Pereira, S. M., Pembrey, M., Hertzman, C., Power, C., & Szyf, M. (2014). Childhood abuse is associated with methylation of multiple loci in adult DNA. BMC Medical Genomics, 7, 1–12. https://doi.org/10.1186/1755-8794-7-13
Szyf, M. (2009). The early life environment and the epigenome. Biochimica et Biophysica Acta, 1790(9), 878–885. https://doi.org/10.1016/j.bbagen.2009.01.009
Szyf, M., Tang, Y.-Y., Hill, K. G., & Musci, R. (2016). The dynamic epigenome and its implications for behavioral interventions: A role for epigenetics to inform disorder prevention and health promotion. Translational Behavioral Medicine, 6(1), 55–62. https://doi.org/10.1007/s13142-016-0387-7
Szyf, M., Weaver, I., & Meaney, M. (2007). Maternal care, the epigenome and phenotypic differences in behavior. Reproductive Toxicology, 24(1), 9–19. https://doi.org/10.1016/j.reprotox.2007.05.001
Tsankova, N., Renthal, W., Kumar, A., & Nestler, E. J. (2007). Epigenetic regulation in psychiatric disorders. Nature Reviews Neuroscience, 8, 355–367. https://doi.org/10.1038/nrn2132
Turecki, G. (2014). Epigenetics and suicidal behavior research pathways. American Journal of Preventive Medicine, 47(3), S144–S151. https://doi.org/10.1016/j.amepre.2014.06.011
Vaiserman, A. M., & Koliada, A. K. (2017). Early-life adversity and long-term neurobehavioral outcomes: Epigenome as a bridge? Human Genomics, 11(34), 1–15. https://doi.org/10.1186/s40246-017-0129-z
Weaver, I. C. G., Champagne, F. A., Brown, S. E., Dymov, S., Sharma, S., Meaney, M. J., & Szyf, M. (2005). Reversal of maternal programming of stress responses in adult offspring through methyl supplementation: Altering epigenetic marking later in life. Journal of Neuroscience, 25(47), 11045–11054.
https://doi.org/10.1523/JNEUROSCI.3652-05.2005
Wong, C. C. Y., Mill, J., & Fernandes, C. (2011). Drugs and addiction: An introduction to epigenetics. Addiction, 106(3), 480–489. https://doi.org/10.1111/j.1360-0443.2010.03321.x
Wright, K. N., Hollis, F., Duclot, F., Dossat, A. M., Strong, C. E., Francis, T. C., Mercer, R., Feng, J., Dietz, D. M., Lobo, M. K., Nestler, E. J., & Kabbaj, M. (2015). Methyl supplementation attenuates cocaine-seeking behaviors and cocaine-induced c-Fos activation in a DNA methylation-dependent manner. The Journal of Neuroscience, 35(23), 8948–8958. https://doi.org/10.1523/JNEUROSCI.5227-14.2015
Yehuda, R., Daskalakis, N. P., Bierer, L. M., Bader, H. N., Klengel, T., Holsboer, F., & Binder, E. B. (2016). Holocaust exposure induced intergenerational effects on FKBP5 methylation. Biological Psychiatry, 80, 372–380. https://doi.org/10.1016/j.biopsych.2015.08.005
Yehuda, R., Engel, S. M., Brand, S. R., Seckl, J., Marcus, S. M., & Berkowitz, G. S. (2005). Transgenerational effects of posttraumatic stress disorder in babies of mothers exposed to the World Trade Center attacks during pregnancy. The Journal of Clinical Endocrinology & Metabolism, 90(7), 4115–4118.
https://doi.org/10.1210/jc.2005-0550
Zhang, H., & Gelernter, J. (2017). Review: DNA methylation and alcohol use disorders: Progress and challenges. The American Journal on Addictions, 26(5), 502–515. https://doi.org/10.1111/ajad.12465
Zhang, T.-Y., & Meaney, M. J. (2010). Epigenetics and the environmental regulation of the genome and its function. Annual Review of Psychology, 61, 439–466. https://doi.org/10.1146/annurev.psych.60.110707.163625
Zheng, J., & Xiao, X. (2016). Epigenetic modifications and developmental origin of health and diseases (DOHaD). In Y. Dincer (Ed.), Epigenetics: Mechanisms and clinical perspectives (pp. 1–14). Nova Biomedical.
David E. Jones, EdD, NCC, LPC, is an assistant professor at Liberty University. Jennifer S. Park, PhD, NCC, ACS, LPC, is an assistant professor at Colorado Christian University. Katie Gamby, PhD, LPC, CWC, is an assistant professor at Malone University. Taylor M. Bigelow, PhD, is an assistant professor at the University of New Haven. Tesfaye B. Mersha, PhD, is an associate professor at the Cincinnati Children’s Hospital Medical Center (CCMHC), University of Cincinnati College of Medicine. Alonzo T. Folger, PhD, MS, is an assistant professor at the CCMHC, University of Cincinnati College of Medicine. Correspondence may be addressed to David E. Jones, 1971 University Blvd., Lynchburg, VA 24515, dejones14@liberty.edu.

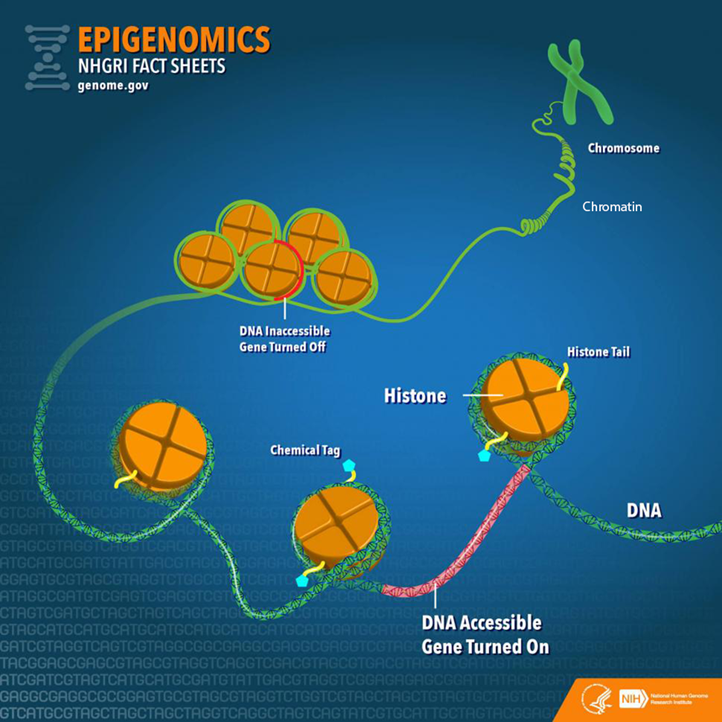
 Michael Ryan, MEd, NCC, is a certified school counselor and currently is the Coordinator of Student Supports for Monongalia County Schools in Morgantown, West Virginia. He holds a BA in psychology from West Virginia University, an MEd with a school counseling concentration from California University of Pennsylvania, and a higher education certification from Salem International University with his Principal, District Administrator, and Superintendent certification.
Michael Ryan, MEd, NCC, is a certified school counselor and currently is the Coordinator of Student Supports for Monongalia County Schools in Morgantown, West Virginia. He holds a BA in psychology from West Virginia University, an MEd with a school counseling concentration from California University of Pennsylvania, and a higher education certification from Salem International University with his Principal, District Administrator, and Superintendent certification.