Jul 25, 2025 | Volume 15 - Issue 2
Sara E. Ellison, Jill M. Meyer, Julia Whisenhunt, Jessica Meléndez Tyler
Nonsuicidal self-injury (NSSI) has historically been associated with deficits in impulse control; however, evidence suggests that individuals high in self-control also self-injure. This constructivist grounded theory study aimed to explore the nature of undercontrolled and overcontrolled self-injury to fill gaps in the literature and to improve clinical understanding and treatment. The resulting Theory of Overcontrolled and Undercontrolled Self-Injury provides a preliminary understanding of the mechanisms that guide overcontrolled and undercontrolled NSSI, the processes that can facilitate individuals switching profiles, and the processes that lead to cessation of self-injurious behavior, thereby contributing to the development of more comprehensive theories of self-harm. Additionally, clinical implications for developing assessments and interventions aimed at preventing and treating NSSI are discussed.
Keywords: nonsuicidal self-injury, self-control, undercontrolled, overcontrolled, self-harm
Nonsuicidal self-injury (NSSI) is the act of intentional, self-inflicted damage of body tissue without the intent to end one’s life and for purposes not socially or culturally sanctioned (Klonsky et al., 2014). NSSI takes many forms including cutting, scratching, piercing, or burning the skin; preventing wounds from healing; and head banging (Favazza, 2011). The functions of NSSI vary considerably between individuals; however, commonly endorsed reasons are emotion regulation, self-punishment, relief from dissociation, and the communication of psychological pain (Doyle et al., 2017; Edmondson et al., 2016).
NSSI affects individuals across the lifespan, but onset frequently begins in adolescence (Brager-Larsen et al., 2022). Prevalence rates in community samples suggest that approximately one in five individuals report a history of self-injury (Andover, 2014; Giordano et al., 2023). Clinically, NSSI is a frequent presenting concern; 97.9% of licensed clinicians reported working with NSSI at some point during their careers (Giordano et al., 2020). Despite this, counselors often experience anxiety and self-doubt when working with clients who self-injure (Whisenhunt et al., 2014), perhaps in part because of the limited scholarly resources available to guide intervention.
NSSI has historically been linked with impulse control problems, largely because of its association with borderline personality disorder (BPD; Hamza et al., 2015). However, recent meta-analyses examining NSSI and impulsivity have produced mixed findings (Hamza et al., 2015; Liu et al., 2017). One study examined the degree of impulsivity and found that 77% of participants waited an average of 15 minutes or less between NSSI thought and action (Glenn & Klonsky, 2010). A positive relationship was also found between the frequency of NSSI and lack of premeditation and perseverance. However, no differences in inhibitory control function were found between individuals who self-injured and those who did not. Before its recent classification as a condition for further study in the DSM-5 (American Psychiatric Association [APA], 2013), NSSI appeared only once in the manual, as a symptom of BPD.
Undercontrol and Overcontrol
Self-control is a multidimensional construct that encompasses the ability to regulate behavior following social norms, moral standards, and long-term goals (Baumeister & Heatherton, 1996). Self-control has been linked to numerous positive outcomes, including superior academic performance, well-being, and relationships (Hofmann et al., 2014; Tangney et al., 2004). However, although many theorists (e.g., Metcalfe & Mischel, 1999; Tangney et al., 2004) posit that high levels of self-control are invariably advantageous, some have argued that the relationship between self-control and well-being is curvilinear, with both the highest and lowest levels of self-control capacity being maladaptive (Block & Block, 1980; Lynch et al., 2015).
Although research on overcontrol (OC; i.e., the excessive presence of self-control) is limited, maladaptive overcontrol is not new. Block and Block developed a theory that focused on individual differences in impulse control, which varies from undercontrol to overcontrol (Block, 2002; Block & Block, 1980). Undercontrolled (UC) individuals struggle with impulse and emotion regulation, exhibiting spontaneity, impulsivity, emotional variability, disregard for social norms, and indifference to ambiguity. In contrast, overcontrolled individuals excessively inhibit their impulses and expressions, which is characterized by emotional restraint, dependability, high organization, and an unnecessary delay of gratification or denial of pleasure. More recently, Lynch (2018) proposed a transdiagnostic model of disorders of overcontrol in conjunction with the development of Radically Open Dialectical Behavioral Therapy (RO DBT). This model suggests that although overcontrolled individuals often achieve measurable success, they frequently experience pervasive loneliness and psychological distress.
Undercontrolled and Overcontrolled NSSI
NSSI has historically been associated with deficits in impulse control (Glenn & Klonsky, 2010); however, evidence suggests that individuals high in self-control also self-injure (Claes et al., 2012; Hempel et al., 2018). Hempel et al. (2018) found that self-injurious behavior in undercontrolled individuals is typically impulsive, emotionally driven, and may involve others. In contrast, overcontrolled individuals tend to engage in planned, rule-governed, and secretive self-injury. Although this study offers compelling evidence of differing self-injurious behaviors based on undercontrol and overcontrol, further research is needed to fully understand these differences.
Purpose of the Study
Despite extensive research on NSSI, much remains to be understood about this behavior. The inclusion of NSSI as a condition for further study in the latest DSM revision (APA, 2022) underscores the need for more research to refine diagnostic criteria and clinical interventions. Significant research has yet to focus on NSSI within the frameworks of undercontrol and overcontrol. Thus, our study aimed to develop a theory about undercontrolled and overcontrolled self-injury in order to fill existing gaps in the literature and to enhance clinical understanding and treatment. Our research question was: What are the experiences, attitudes, and behaviors related to undercontrolled and overcontrolled self-injury?
Method
We selected a constructivist grounded theory approach, which seeks to offer explanations about a phenomenon from the perspective of those who experience it (Charmaz, 2014). This inductive approach facilitates the construction of a theoretical model that systematically describes processes associated with the phenomenon of interest (Charmaz, 2014) and, therefore, is well-suited to helping counselors understand their clients’ experiences and behaviors (Hays & Singh, 2023). Constructivist methodology holds the ontological position that our world is socially constructed through interactions over time; therefore, the researchers and participants are co-creators of knowledge (Charmaz, 2014).
Researcher Reflexivity
Reflexivity is essential if researchers’ experiences and interpretations influence the grounded theories they construct (Charmaz, 2014). Sara E. Ellison is a White cisgender woman, a doctoral student, and a licensed professional counselor (LPC). She has experience working with clients who self-injure in residential and outpatient settings, which sparked her interest in the differences in undercontrolled and overcontrolled NSSI. This clinical experience and her training in dialectical behavior therapy (DBT) and RO DBT influenced the expectation that UC NSSI would align with characteristics such as impulsivity, emotionality, and openness, and that OC NSSI would align with planning, inhibited emotion, and secretiveness. Jill M. Meyer is a White cisgender woman, a professor and Director of Counselor Education at a CACREP-accredited R1 university, and an LCPC. Her education, training, and clinical experiences are outside of this topic area, positioning her to be objective in the study of NSSI. She approached this research with curiosity about whether OC and UC NSSI would reflect characteristics previously described in the literature on OC and UC.
Julia Whisenhunt is a White, cisgender woman and a professor at a regional comprehensive university with a CACREP-accredited program. She is an LPC and a certified professional counselor supervisor who specializes in crisis intervention and has studied NSSI for approximately 15 years. Based on her work with clients who self-injure and her prior research and scholarship on the topic, she entered with core assumptions about NSSI that may have contributed to her conceptualization of the data. Whisenhunt believes that NSSI most often serves as a coping skill for intense intrapersonal experiences (e.g., self-loathing, despair, anger, fear, shame, anxiety, dissociation) and is best treated through a person-centered approach. Jessica Meléndez Tyler is a Latina cisgender woman and a faculty member at a CACREP-accredited R1 institution. She is a licensed counseling supervisor with 15 years of experience working with at-risk adults in outpatient settings. Tyler’s clinical experiences have deepened her understanding of the complexities of NSSI, driving her commitment to advancing knowledge and interventions in this area. She approached this research with the assumption that UC and OC play a significant role in NSSI and that effective and humanistic therapeutic interventions can improve the quality of life for affected individuals. Our values of empathy, compassion, and a nonjudgmental approach to behaviors that have often been misunderstood by the public guided our interpretation of the data, aiming to view NSSI through a lens of human complexity rather than pathology.
This research was completed as a dissertation study with Ellison receiving support and guidance from the other authors throughout the research process. Ellison conducted intensive interviews and coding, with Meyer and Whisenhunt advising and supporting the consideration of multiple perspectives. We met eight times during data collection and analysis, during which we reviewed emerging codes, participant narratives, and developing theory. We also engaged in reflexivity exercises and triangulated the findings with existing NSSI scholarship. Tyler assisted with study conceptualization and manuscript development.
Participants and Procedures
After obtaining institutional review board approval, we used purposeful criterion sampling and theoretical sampling to recruit participants (Timonen et al., 2018). Selection criteria included adults who had self-injured five or more times in their lifetime and self-identified as undercontrolled or overcontrolled. Although qualitative research on NSSI often includes individuals with any NSSI experience (e.g., Hambleton et al., 2022), we chose to recruit those with significant NSSI histories to better understand their behavioral, emotional, and cognitive patterns. This is consistent with previous qualitative research including those who have self-injured five to six times in their lifetime (da Cunha Lewin et al., 2024; Kruzan & Whitlock, 2019).
It is recommended that researchers screen participants for vulnerabilities and balance the need for rich data with potential harm when asking sensitive questions (Hays & Singh, 2023); therefore, we conducted a literature review to assess the potential iatrogenic effects and benefits related to participating in interviews broaching NSSI. Researchers have viewed self-injury in the context of the transtheoretical stages of change model and suggested that individuals enter the termination stage after 3 years of abstinence from NSSI behavior (Kruzan et al., 2020). Previous studies (Muehlenkamp et al., 2015; Whitlock et al., 2013) have indicated that participating in detailed NSSI research did not have significant adverse effects; however, to minimize risk, participant eligibility for the study was based on the absence of any current suicidal ideation and no self-injury in the past 3 years.
In order to reach individuals with meaningful self-injury experience, we posted a recruitment flyer in four Facebook and Reddit support groups related to self-injury. We also emailed calls for participation to experts in the field and shared them on listservs, including Counselor Education and Supervision Network, Georgia Therapist Network, and Radically Open DBT Listserv. Participants received a $25 e-gift card as compensation for their time and contributions.
The 20 study participants all self-identified as undercontrolled (UC; n = 10, 50%) or overcontrolled (OC; n = 10; 50%) as described by Block and Block (1980). Most participants identified as White or Caucasian (n = 14, 70%), with three identifying as Multi-Racial (15%), two identifying as African American and/or Black (10%), and one identifying as Hispanic or Latino/a/x (5%). Likewise, most participants identified as women (n = 18, 90%), with one identifying as a nonbinary woman (5%) and one identifying as a man (5%). Participants ranged in age from 18 to 43, with the mean age being 29.4. The participants lived in various geographic regions, with the most common region being the South (n = 12, 60%), followed by the Midwest (n = 4, 20%), Northeast (n = 2, 10%), and West (n = 2, 10%). We ceased recruiting participants once we achieved comprehensive coverage of emerging categories and new data no longer provided theoretical insights (Charmaz, 2014).
Data Collection
After identifying eligible participants via a screening and demographic questionnaire, Ellison conducted intensive, semi-structured Zoom interviews, each lasting about 60 minutes. The researchers developed the interview protocol after reviewing current qualitative literature and assessment measures on NSSI and consulting with two NSSI subject matter experts with significant qualitative research experience (see Appendix for complete interview protocol). Intensive interviewing relies on the practice of following up on unanticipated areas of inquiry prompted by emerging data (Timonen et al., 2018); therefore, after several participants mentioned their reactions to NSSI in peers or media representations, a question related to perception of others’ NSSI was integrated into subsequent interviews. Participants chose pseudonyms in order to protect their identities; all interviews were audio-recorded and transcribed. Participants were then invited to review their transcripts and make any revisions, redactions, or additions to ensure the accuracy of their voices and experiences.
Data Analysis
Ellison conducted initial coding by labeling data segments to summarize and categorize them. Transcripts were repeatedly read and analyzed as new data were collected to identify similarities and differences in participant narratives. Focused coding then aimed to refine the most salient codes into categories and themes in order to develop a larger theory (Charmaz, 2014). During this phase, Ellison condensed the 38 initial codes into concise descriptions encapsulating participants’ narratives, resulting in 15 themes that explained the relationships between findings. This process moved the analysis from descriptive to conceptual, guiding theory development (Charmaz, 2014). Ellison, Meyer, and Whisenhunt met multiple times to review the developing codebook, connect data, and clarify theory development.
Constant comparative methods (Glaser & Strauss, 1967) were used throughout coding to identify patterns and to ground the theory in participant narratives. Memo writing recorded analytic ideas for later follow-up. Data and codes were organized using Dedoose, a HIPAA-compliant, password-protected online qualitative software. After reaching theoretical saturation we conducted member checks by emailing participants a summary of themes and categories to solicit feedback. All 20 participants confirmed that the emerging theory aligned with their experiences.
Trustworthiness Strategies
Several strategies were employed to enhance rigor and mitigate methodological limitations in this qualitative study. Participant perspectives and the investigated phenomenon’s authenticity are crucial for the study’s validity (Denzin et al., 2023). Member checking was consistently used during data collection and analysis, enabling participants to confirm the relevance of findings to their experiences. Follow-up questions were integrated into interviews to clarify participant responses (Hays & Singh, 2023) and participants reviewed their interview transcripts and initial findings to provide feedback (Charmaz, 2014). Five participants contributed additional insights, enriching the theoretical framework with their unique perspectives. Researcher reflexivity was employed to acknowledge personal beliefs, values, and biases that might influence data interpretation (Hays & Singh, 2023), addressing reactions to participants, insights into potential findings, and adjustments made to the research process.
Findings
The findings of this grounded theory analysis describe the experiences, attitudes, and behaviors related to OC and UC NSSI, including the processes that can facilitate individuals switching profiles and the processes that lead to the cessation of self-injurious behavior.
OC NSSI
Restrained
OC NSSI was associated with high levels of restraint, which allowed participants to mask negative emotions, delay self-injury, and moderate how deeply they cut. Motivated by the highly private nature of OC NSSI, participants often postponed their self-injury for several hours or more to keep it hidden. This time was frequently used to plan when, where, and how self-injury might occur. Emma described this:
There were definitely times where maybe something would happen like at school. Or somewhere out in public or something like that. Where I knew that . . . because I was extremely secretive about what I was doing, that I maybe thought, “well, later I might go home and do that.” I can’t remember ever thinking to myself, “well, I need to go home right now and cut,” you know? That was never crossing my mind.
Participants also used restraint during the behavior, cutting deeply enough to feel relief but not so severely that it resulted in medical attention or attention from others. Jenny shared:
When I was cutting . . . I had to really pay attention. Really focus, laser focus, to not do something wrong or not cause more grievous harm or also to sort of maintain some pain, but maybe not too much pain, not go too deep.
Participants expressed a sense of pride in their ability to utilize restraint related to OC NSSI, which contributed to their sense of identity and differentiated their behavior from impulsive conceptualizations of self-injury.
Highly Private
Participants were highly private about their OC NSSI, prompting them to avoid disclosure experiences, take great care to hide injuries and scars, and avoid medical attention. This desire to conceal their self-injury was often motivated by maintaining a specific image or not burdening others. Emma shared, “I didn’t want to be a burden to anyone or my pain to be a burden to anyone. And so that was my worst nightmare, for someone to know what was going on.” OC NSSI was seen as deeply personal and carried out solely for the benefit of participants. The highly private nature of OC NSSI influenced the location of participants’ self-injury as well as rules that would support keeping it hidden, as Madeline described:
I never . . . very rarely cut on my arms or like even my legs because I [was] training for triathlons and was swimming. And so a lot of it was like on my breasts, on like my pelvic area where it would never be seen.
The avoidance of medical care meant that some participants took responsibility for caring for severe wounds independently. Phoenix described learning to suture her wounds on YouTube. Rex instituted a disinfecting process after a cut on her leg became severely infected: “I didn’t want to end up in the hospital having to have somebody ask a question about [self-injury].” Even after the cessation of NSSI, participants were often reluctant to discuss the behavior. Jenny disclosed that her participation in this study represented more discussion about her self-injury than all her other disclosures combined. The private nature of participants’ OC NSSI made them less likely to seek help, including mental health care.
Guided by Rules and Ritual
Participants describing OC NSSI spoke of rules that dictated their use of specific tools, number of cuts, and locations on the body. Often, these rules were based on a compensatory approach to self-injury in which participants responded to specific wrongdoings or perceived failures with distinct approaches to self-punishment. These rules provided the scaffolding for behavior that became ritualistic. Participants described a structured, disciplined approach to self-injury that was often motivated by upholding established routines rather than emotional dysregulation or NSSI urges. Katie shared that her self-injury occurred nightly around the same time and in the same location: “There were nights where I didn’t really feel like I had like a lot of emotions. And it was more of that secret part of it, where I was keeping a routine. Like, ‘Well, time to go do this.’” Madeline adhered rigidly to the rules and ritual she had established for herself: “I’m not gonna stop. If I’ve decided this is gonna happen 113 times, I’m doing 113. Like, regardless of if I decide halfway through, I don’t wanna keep doing this.”
Participants also described ritualized aftercare, often involving an organized medical supply kit, which became a meaningful part of the self-injury process. In some cases this also involved photographing, writing about, or otherwise documenting their wounds. Phoenix shared that she “always stitched it up, or whatever. In the moment, it was something that was very destructive. But afterwards, it was always taken care of . . . maybe in a way, that was a way of kind of taking care of myself.” The rules and rituals associated with participants’ OC NSSI created order and structure in their lives. They imbued the behavior with meaning that elevated it beyond a simple emotion regulation tool.
Perception of Others’ NSSI as Inferior
Participants describing OC NSSI often expressed feeling as though their self-injury was superior to others’ and were highly judgmental of NSSI that they viewed as impulsive or not intentionally hidden. They eschewed the idea of their own NSSI as attention-seeking and felt a sense of pride in their ability to control their impulses and affect and meticulously hide their behavior. Katie shared, “I think I felt very judgmental of [others who self-injured], like, ‘How come you’re doing this to yourself and then sharing it to everybody?’ Like, ‘I can’t believe you’re using this to get attention and stuff like that.’”
These participants used words such as “correct,” “pious,” “better,” and “right” to describe the way they self-injured, positioning themselves as morally superior and intrinsically dissimilar from others who approached the behavior differently. Emma described this:
Pride is a strange word to describe it, but it was almost sort of like being more pious. It was like . . . I’m holding this big secret. I’m doing this thing, and that’s the way it should be. So I felt like I was doing it correctly.
Participants viewed their OC NSSI as different from what they saw around them, which contributed to both a sense of isolation and a feeling of pride.
Cessation—Loss of Utility and Defined Decision to Stop
Cessation of OC NSSI often occurred when the behavior lost its utility and followed a defined decision to stop. This pragmatic approach meant that once the benefits of self-injury waned, participants saw no reason to continue to engage with it, as Katie described:
I feel like I achieved what I wanted to achieve and now I don’t feel like doing it anymore . . . I remember going into therapy afterwards and thinking, “I don’t know why I’m here because like I don’t even feel these urges anymore. So . . . there’s no point.”
Although cessation experiences sometimes included counseling or other interventions, they often occurred independently, consistent with the highly private nature of OC NSSI.
Scaffolded by their ability to exercise restraint, participants rarely went back on their decision or experienced a lengthy cessation process. Katie stated, “I think that was another part of the control. Like I get to decide when I do this and how I do this and when I stop and stuff like that.” Lauri also identified a defined ending of her self-injurious behavior:
I actually got to a point where I was like, “Okay, I’m in my 30s now. This has like, you know, got to stop. Like, this is not okay.” But I actually went and got a tattoo as a marker that I’m not doing this anymore, and I haven’t.
The resoluteness with which they committed to their decision to stop often felt more salient than any distress they experienced because of cessation.
UC NSSI
Impulsive
UC NSSI was described as occurring in an impulsive and unplanned manner. Participants described an urgency to their self-injurious thoughts that motivated them to seek immediate relief, often within minutes of the decision to self-injure. Lauri stated that when she had an urge to self-injure, “It was kind of like a panic, like trying to get to it as soon as possible to get relief.” To facilitate this, some participants always carried self-injury tools with them. Others used whatever they could find nearby, even it was not their preferred instrument. If these participants delayed their self-injury, it was due to seeking favorable circumstances rather than planning or premeditation. Amy shared: “There wasn’t a premeditated like separate razor blade or anything. It was just, I knew where and when I could do it. And so if I got overwhelmed, I might go take a shower or something.” This impulsiveness sometimes contributed to disclosure experiences because participants could not inhibit their self-injury urges until they reached a private space, or their hastiness contributed to others’ suspicions.
Disclosed Despite Secrecy
UC NSSI was often disclosed despite participants’ desire for secrecy. Participants’ inability to delay their NSSI behavior or mask their emotions sometimes contributed to self-injuring with others present or in manners that were more likely to be discovered. Additionally, participants described conflicting feelings related to disclosure in which they often desired for others to know about their NSSI while simultaneously experiencing shame or embarrassment about the behavior. Rose described wanting to cut in places that could be covered, but also shared that she didn’t hide her self-injury from her friends:
I had a couple of really close friends at college, and I told one of them pretty early on, and that was voluntary . . . I don’t remember how I told the others or if I just said, “it’s okay if you tell the others.” But eventually, my friend group knew.
Lola described hiding her self-injury, but not so deliberately that it didn’t raise people’s suspicions: “I always wore long sleeves, which definitely I guess I could say my parents felt a little bit suspicious of when it was summertime and stuff.” Eventually, Lola’s mom became so suspicious that “she asked to look, and so I showed her, and she found out, and we had a conversation about it and everything.” Jane also shared conflicting thoughts related to disclosure. On one hand, she shared, “I would cut my arms mostly. And that was like a, ‘hey, I’m doing this,’ kind of thing.” At the same time, she remembered thinking:
This is embarrassing. I don’t really want people to know or ask me about it. But it was also like, in a place where like, sometimes I’d be in a t-shirt. So sometimes you would see it. Or sometimes people would notice.
Participants’ ambivalence about disclosure often resulted in inconsistent or disorganized concealment behaviors, making the discovery of their NSSI by others more likely.
Guided by Emotion
Emotion influenced when, where, and how UC NSSI occurred. Participants reported being highly responsive to their mood states and experiencing self-injury as a potent strategy to cope with dysregulation. Because they were typically unable or unwilling to inhibit their impulses, self-injurious behavior often occurred at the peak of emotional distress. Rose reported that “any negative feeling, but especially like guilt or regret [or] shame” might trigger an episode of self-injury, “so it was very much an emotional regulator.”
Pacey described the emotional intensity when he would self-injure: “Definitely [self-injury would occur] at the top. Sometimes I remember crying really hard when it was happening, or feeling so anxious that I was lightheaded. And the cutting would help bring that emotion down.” This connection between emotionality and UC NSSI meant that participants more frequently conceptualized their triggers as interpersonal, resulting from interactions that precipitated emotional distress.
Perception of Others’ NSSI as Superior or Relatable
If participants encountered peers that self-injured or media representations of NSSI, their view was often that others’ NSSI was superior or relatable. Participants sometimes described feeling that others’ self-injury was “cooler,” “better,” “brave,” or more “impactful” than their own and endorsed a desire to emulate this. Jane shared:
There was definitely a period of time where I would see people who maybe were self-injuring in a way that was more aggressive than I was doing it and definitely had some inferiority complex going on like, oh . . . mine’s not impactful . . . I felt like an imposter.
When Pacey joined online support groups, he “felt a lot of similarities to their stories . . . And it was nice to know that I wasn’t alone.” Even when participants identified a misalignment between others’ self-injurious behaviors and their own, they typically remained nonjudgmental and assumed that others were doing the best they could. Rose shared:
In the books I read, it was portrayed really sympathetically. Like, they’re struggling, and so are the friends [I knew that self-injured]. But somehow still, I got that idea of people do it for attention. But my personal experience from books and friends was just like, they’re having a hard time, and that’s the only way they can figure it out.
Participants’ view of others’ NSSI as superior or relatable influenced their willingness to engage in conversations with others who self-injured, further supporting their capacity to seek and receive help.
Cessation—Interpersonal Influence and Protracted Process of Stopping
Interpersonal influence (e.g., therapy or pressure from peers or family) contributed to the cessation of UC NSSI. Jasmine described the support from her inner circle as essential to her self-injury cessation. “They would encourage me to call one of them and just have them come over or have me go to the restroom or outside near a tree and just talk through what my emotions were telling me.” Amy also leaned on support from friends:
Having that friend that knew about it from freshman year that I lived with was also a help in not doing it again because I could go literally right next door to her room and kind of talk about how I was feeling for a second and sit on her floor and just let that feeling pass.
Rose shared that seeing a counselor twice weekly supported her in decreasing and ultimately stopping NSSI. Because participants frequently had already disclosed their UC NSSI, interpersonal support was more likely to be available and, therefore, influential to cessation.
Participants also highlighted the lengthy process of stopping their self-injury. Tricia recalled gradually working on controlling her emotions in other ways:
It wasn’t something that I stopped immediately because, like I said, I tried to work on my emotions. I tried to control my anger. I went back to it and almost went back to it a lot of times. I tried to distract myself from the cause of the pain. . . . It wasn’t a fast process. It was a gradual process.
Participants experiencing a protracted cessation process did not typically memorialize it or assign specific meaning to the final experience.
Processes Supporting Participants Switching Profiles
UC to OC NSSI: Aging and Feedback
Participants reported that getting older and receiving negative feedback influenced their transition from UC NSSI to OC NSSI. Jane shared her feeling that “when you’re in your teens, a lot of people are doing weird self-harm shit. . . . by the time you’re in your 20s, if people see something on your arm, they’re like, ‘what the fuck is wrong with you?’” Shane echoed this: “It was easier to hide when I got older because I understood—cognitively, I was like, ‘well, this isn’t really healthy or appropriate.’ But I still did it.” As participants encountered criticism or judgment related to self-injury, they often became more secretive, restrained, or ritualistic in their behaviors. Roxanne shared how feedback influenced the way she engaged with self-injury:
I had a friend notice, and she told the teacher and I was really embarrassed. And then my grandmother found out and she was really mad. And so I realized that I needed to do a better job hiding it. And so that’s why I moved locations, because I really didn’t want anybody to know. I was embarrassed by it. But it did make me feel a lot better. And so I wanted to keep doing it.
When participants transitioned from a UC NSSI profile to an OC NSSI profile, they typically continued to self-injure in this manner until cessation.
OC to UC NSSI: Intense Interpersonal Distress, Fear, and Shame
Participants described experiences of intense interpersonal distress as a salient factor in their transition from OC NSSI to UC NSSI. During relational conflict that resulted in extreme dysregulation, participants reported losing the ability to moderate their emotions or how severely or impulsively they self-injured. Rex shared an experience of UC NSSI that occurred in the context of an abusive relationship, describing it as a departure from her previous self-injury, which was private, superficial, and very controlled:
and she kept on yelling and yelling and then I did it in front of her and the fat started bleeding out of my arm. . . . It was like scarier and felt way more out of control than anything like I had ever experienced as far as self-harm.
Participants’ impulsivity and emotionality in these moments meant that they might self-injure in the presence of others or reach for tools they didn’t normally use, resulting in wounds that were more severe than they normally experienced.
When participants who typically self-injured in a restrained, private manner experienced UC NSSI, the result was acute feelings of fear and shame. Perhaps because they had previously held judgment of self-injury that occurred impulsively and publicly, self-judgment often occurred in the wake of a transition to UC NSSI. Olive described the fear they felt after the last time they self-injured, which resulted in 17 stitches:
I was having nightmares and flashbacks for three months afterwards. So it was traumatic for me to experience, and I scared myself. I didn’t know that I could do that to myself. I didn’t know that I was capable of causing that kind of harm, and I guess it made me realize how dangerous it was for me to be doing what I was doing because when I actually did it I had a total loss of control in that moment.
These feelings of fear and shame felt by participants, coupled with the loss of equilibrium related to their NSSI identity, prompted them to reconsider the role of NSSI in their lives. Often, this episode of UC NSSI represented the last time they self-injured.
The Theory of Overcontrolled and Undercontrolled Self-Injury, illustrated in Figure 1, was developed based on participant narratives and feedback to represent the experiences, attitudes, and behaviors associated with OC and UC NSSI. Participants were asked to self-identify as UC or OC; however, this classification did not consistently align with their profile of self-injury. For example, three participants identified that their NSSI behavior was markedly different than their behavior in the rest of their lives. Additionally, several participants described transitioning from one profile to another at some point during their self-injury. As a result of this unexpected finding, we categorized participant NSSI based on their descriptions of their self-injurious experiences, attitudes, and behaviors rather than their self-identified personality typology.
Figure 1
Theory of Overcontrolled and Undercontrolled Self-Injury
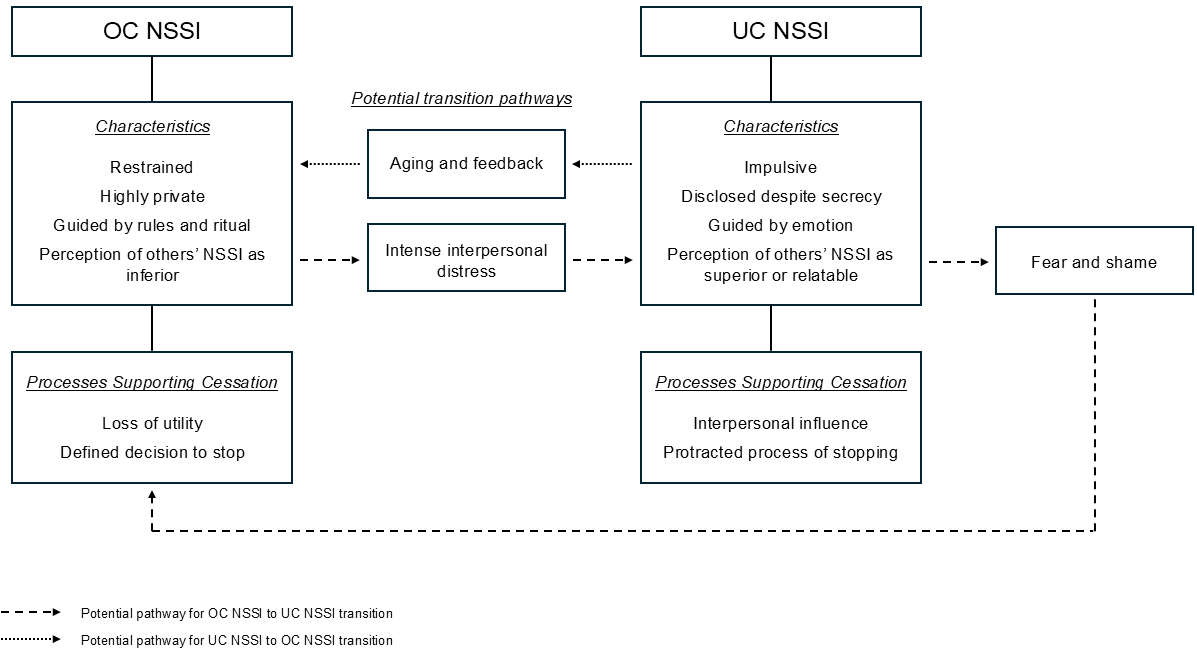
Discussion
This study provides insight into how self-control influences individuals’ experiences of NSSI. The data identified two distinct profiles, which is consistent with prior research indicating the ability to differentiate NSSI behavior based on its occurrence in OC or UC contexts (Hempel et al., 2018). OC NSSI was characterized as restrained, private, and rule-guided, aligning with previous conceptualizations of OC linked to impulse inhibition, high distress tolerance, and rigid behavioral patterns (Block, 2022; Block & Block, 1980; Lynch et al., 2015). Similarly, UC NSSI was described as impulsive, disclosed despite secrecy, and emotion-driven, consistent with literature highlighting heightened emotional fluctuations, low distress tolerance (Block, 2002), and higher levels of openness and expressiveness (Gilmartin, 2024).
Although a desire for secrecy was reported in both OC and UC NSSI, the commitment and dedication to maintaining this privacy varied between groups. This study’s findings differ slightly from those of Hempel et al. (2018), who described UC NSSI as public, lacking nuance regarding participants’ internal conflicts. Participants’ dissonance regarding disclosure may be viewed through a lens of dialectics. Linehan (1993) described BPD, a disorder of UC, as a “dialectical failure” in which individuals vacillate between contradictory viewpoints, rendering their behavior inconsistent and confusing. OC, on the other hand, has been associated with maladaptive perfectionism (Lynch et al., 2015), in which individuals avoid vulnerability to maintain an image of flawless performance (Dunkley et al., 2003). Those striving to appear problem-free may perceive their self-injury as a sign that they are flawed or weak and thus go to great lengths to conceal it. Because both groups describe their NSSI as secretive, further exploration of disclosure patterns is essential to facilitate deeper understanding.
An unexpected finding was that participants’ perceptions of others’ NSSI differed based on whether they engaged in UC or OC NSSI. One explanation for the association between OC NSSI and a perception of others as inferior may lie in a phenomenon described by Lynch (2018) as “the enigma predicament.” The enigma predicament is a self-protective stance in which OC individuals believe they are fundamentally different or more complex than others. This attitude maintains social isolation, aloofness, and a feeling of being misunderstood. Cultural emphasis on self-control may bolster beliefs of superiority among these individuals, fostering a secret sense of pride.
No existing literature was found that explored the judgments of individuals who self-injure related to others’ NSSI; however, viewing these findings through the lens of social norms offers context. OC individuals are sensitive to social pressures and conformity, whereas UC individuals are less concerned with societal norms (Block, 2002). Individuals experiencing UC NSSI may be more likely to disregard prescriptive norms for self-presentation, facilitating empathy or admiration for those openly displaying their NSSI. Those experiencing OC NSSI, which is typically a well-kept secret, may be unlikely to encounter others engaging in NSSI in a like manner.
Another novel finding lies in the shifts participants described in their self-injury profile as a direct result of specific experiences, such as aging and feedback. Although no existing literature was found that examined this phenomenon, UC typically peaks in early to middle adolescence (Hasking & Claes, 2020), suggesting that aging may influence a transition from impulsive to more restrained NSSI for some individuals. It is also plausible that individuals whose self-injury was disclosed (i.e., UC NSSI) would receive more negative feedback than those whose self-injury remained concealed (i.e., OC NSSI). Participants who reported switching from OC to UC NSSI attributed this change to experiences of intense interpersonal distress that appeared to eclipse their high capacity for restraint and control. Lynch (2018) described this phenomenon as “emotional leakage,” in which OC individuals temporarily lose the ability to inhibit their impulses, leading to intense emotional outbursts followed by feelings of shame and self-criticism.
Implications for Counselors
The emergent theory in this study creates a new theoretical model that may provide valuable implications for clinical practice. The identification of two distinct profiles of NSSI supports previous research indicating that individuals with both low and high levels of self-control may engage in self-injurious behavior (Hempel et al., 2018). The current proposed criteria for NSSI disorder, listed in Section III of the DSM-5-TR (APA, 2022) as a condition for further study, would identify both OC and UC NSSI as conceptualized in this study. For instance, criterion C specifies that self-injury may involve “a period of preoccupation with the intended behavior that is difficult to control” or “frequent thoughts about self-injury, even if not acted upon” (p. 923). This expands previous views of NSSI by recognizing behaviors that involve greater restraint alongside those driven by impulse inhibition failures.
Knowing this, counselors may benefit from conducting thorough assessments to accurately diagnose and differentiate between OC and UC NSSI. This can involve using clinical interviews, standardized assessments, and behavioral observations to evaluate clients’ impulse control and emotional regulation abilities. Recommended measures include the Assessing Styles of Coping: Word-Pair Checklist (Lynch, 2018) for adults and the Youth Over- and Under-Control Screening Measure (Lenz et al., 2021) for children and adolescents. To assess OC and UC self-injury specifically, including questions in clinical interviews that evaluate the dimensions explored in this study may be helpful. Clinicians can also inquire specifically about clients’ NSSI impulsivity and emotionality levels, disclosure and aftercare behaviors, and whether any rules or rituals inform the behavior. Questions such as, “When you self-injure, do you tell anyone about it before or afterward?” and “Do you have any rules about when, where, or how you self-injure?” may assist clinicians in developing a deeper understanding of the processes driving the behavior, thereby informing the use of congruent therapeutic interventions.
Participants in this study highlighted distinct processes influencing their NSSI behaviors and cessation, emphasizing the need for tailored treatment approaches based on whether NSSI occurs in an OC or UC context. Traditional therapeutic approaches to treating self-injury, such as DBT (Linehan, 1993) and emotional regulation group therapy (Andover & Morris, 2014), which focus on improving emotional regulation and distress tolerance, may need to be adapted or supplemented to address specific vulnerabilities and underlying mechanisms related to OC NSSI. Interventions targeting UC NSSI should emphasize enhancing inhibitory control and distress tolerance while reducing emotional reactivity. Conversely, interventions treating OC NSSI should aim to relax excessive inhibitory control and rigidity while increasing emotional expressiveness and openness. RO DBT, which was developed specifically to treat disorders of OC by targeting deficits related to excessive inhibitory control (Lynch et al., 2015), represents a promising approach for these clients.
Understanding participants’ perceptions of others’ NSSI behaviors also holds implications for social contagion (Conigliaro & Ward-Ciesielski, 2023). Previous research has implicated identifying or relating with others who self-injure (Whitlock et al., 2009) and a higher need to belong (Conigliaro & Ward-Ciesielski, 2023) as factors increasing vulnerability to social contagion. Because UC NSSI was associated with a perception of others’ NSSI as superior or relatable, individuals exhibiting this self-injury profile may be more vulnerable to the effects of social contagion. Counselors should be aware of these dynamics when formulating interventions.
Lastly, counselors can benefit from considering how the enigma predicament may negatively impact the therapeutic relationship with OC clients who may believe that they are so complex or unique that they will invariably be misunderstood (Lynch, 2018). This may explain why study participants experiencing OC NSSI sometimes found therapy unrewarding or unhelpful, particularly if counselors generalized about self-injury in a way that felt incongruous with their experiences. Knowing this, counselors should aim to set aside their assumptions about self-injury and allow the client to educate them on their experience.
Care should also be taken when asserting that OC NSSI behavior is normal, common, or understandable. Although this might typically be viewed as a positive intervention (i.e., normalizing the behavior), such expressions may cause alliance ruptures in this population (Lynch, 2018). Acknowledging these unique perspectives and avoiding assumptions about the normalcy or commonality of NSSI behaviors can help maintain therapeutic rapport and prevent alliance ruptures. By integrating these implications into clinical practice, counselors can enhance their ability to effectively assess, conceptualize, and intervene with UC and OC NSSI, ultimately promoting resilience and improved psychological well-being.
Limitations and Suggestions for Future Research
Several limitations must be acknowledged in order to interpret this study’s findings. First, because of the absence of validated measures of UC and OC, participants self-identified based on Block and Block’s (1980) conceptualization of these terms. Knowing the challenges associated with the clinical assessment of OC (Hempel et al., 2018) and the subjective nature of self-assessment, it is reasonable to assume that some participants may have self-identified in ways that are incongruent with established criteria for UC and OC. Future studies aimed at the development of instruments capable of effectively measuring and differentiating between OC and UC NSSI would aid mental health and medical professionals in congruent conceptualization and intervention for NSSI. They would also pave the way for quantitative exploration of UC and OC NSSI, potentially fostering greater knowledge, understanding, and generalizability.
The sample in this study was composed predominantly of White women, limiting its ability to encompass a diversity of experiences. It is possible that a more diverse sample would have generated different results. Future studies should intentionally strive to incorporate more diverse samples, specifically focusing on amplifying the voices and experiences of gender-diverse individuals, people of color, and men. Care should be taken in generalizing the results of this analysis, especially in groups underrepresented in sampling. Additionally, participants in this study had not self-injured in the last 3 years, which may have allowed for a greater degree of cognitive processing related to their experiences. Future studies focusing on current self-injurious experiences are needed to support the development of effective interventions in this population.
Finally, this study’s qualitative design has inherent limitations despite efforts to ensure credibility and trustworthiness. The semi-structured interview method used may influence participant responses through question framing, wording, and presentation. Additionally, the research team’s perspective inevitably influences the interpretation of findings, allowing for alternative interpretations by different research teams.
Conclusion
The constructivist grounded theory findings enrich our initial grasp of how self-control influences NSSI experiences, attitudes, and behaviors, offering significant implications for mental health research and clinical practice. Future efforts should focus on translating these insights into evidence-based assessments and interventions that acknowledge individuals’ attitudes, motivations, and vulnerabilities associated with NSSI, aiming to effectively enhance resilience and well-being.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (5th ed., text rev.).
Andover, M. S. (2014). Non-suicidal self-injury disorder in a community sample of adults. Psychiatry Research, 219(2), 305–310. https://doi.org/10.1016/j.psychres.2014.06.001
Andover, M. S., & Morris, B. W. (2014). Expanding and clarifying the role of emotion regulation in nonsuicidal self-injury. Canadian Journal of Psychiatry, 59(11), 569–575. https://doi.org/10.1177/070674371405901102
Baumeister, R. F., & Heatherton, T. F. (1996). Self-regulation failure: An overview. Psychological Inquiry, 7(1), 1–15. https://doi.org/10.1207/s15327965pli0701_1
Block, J. (2002). Personality as an affect-processing system: Toward an integrative theory. Lawrence Erlbaum.
Block, J. H., & Block, J. (1980). The role of ego-control and ego-resiliency in the organization of behavior. In W. A. Collins (Ed.), Development of cognition, affect, and social relations: The Minnesota symposia on child psychology (Vol. 13, pp. 39–101). Lawrence Erlbaum.
Brager-Larsen, A., Zeiner, P., Klungsøyr, O., & Mehlum, L. (2022). Is age of self-harm onset associated with increased frequency of non-suicidal self-injury and suicide attempts in adolescent outpatients? BMC Psychiatry, 22(1), 1–9. https://doi.org/10.1186/s12888-022-03712-w
Charmaz, K. (2014). Constructing grounded theory (2nd ed.). SAGE.
Claes, L., Soenens, B., Vansteenkiste, M., & Vandereycken, W. (2012). The scars of the inner critic: Perfectionism and nonsuicidal self-injury in eating disorders. European Eating Disorders Review, 20(3), 196–202. https://doi.org/10.1002/erv.1158
Conigliaro, A., & Ward-Ciesielski, E. (2023). Associations between social contagion, group conformity characteristics, and non-suicidal self-injury. Journal of American College Health, 71(5), 1427–1435. https://doi.org/10.1080/07448481.2021.1928141
da Cunha Lewin, C., Leamy, M., & Palmer, L. (2024). How do people conceptualize self-harm recovery and what helps in adolescence, young and middle adulthood? A qualitative meta-synthesis. Journal of Clinical Psychology, 80(1), 39–64. https://doi.org/10.1002/jclp.23588
Denzin, N. K., Lincoln, Y. S., Giardina, M. D., & Cannella, G. S. (2023). The SAGE handbook of qualitative research (6th ed.). SAGE.
Doyle, L., Sheridan, A., & Treacy, M. P. (2017). Motivations for adolescent self-harm and the implications for mental health nurses. Journal of Psychiatric and Mental Health Nursing, 24(2–3), 134–142. https://doi.org/10.1111/jpm.12360
Dunkley, D. M., Zuroff, D. C., & Blankstein, K. R. (2003). Self-critical perfectionism and daily affect: Dispositional and situational influences on stress and coping. Journal of Personality and Social Psychology, 84(1), 234–252. https://doi.org/10.1037/0022-3514.84.1.234
Edmondson, A. J., Brennan, C. A., & House, A. O. (2016). Non-suicidal reasons for self-harm: A systematic review of self-reported accounts. Journal of Affective Disorders, 191(1), 109–117. https://doi.org/10.1016/j.jad.2015.11.043
Favazza, A. R. (2011). Bodies under siege: Self-mutilation, nonsuicidal self-injury, and body modification in culture and psychiatry (3rd ed.). John Hopkins University Press.
Gilmartin, T., Dipnall, J. F., Gurvich, C., & Sharp, G. (2024). Identifying overcontrol and undercontrol personality types among young people using the five factor model, and the relationship with disordered eating behaviour, anxiety and depression. Journal of Eating Disorders, 12, Article 16.
https://doi.org/10.1186/s40337-024-00967-4
Giordano, A., Lundeen, L. A., Scoffone, C. M., Kilpatrick, E. P., & Gorritz, F. B. (2020). Clinical work with clients who self-injure: A descriptive study. The Professional Counselor, 10(2), 181–193. https://doi.org/10.15241/ag.10.2.181
Giordano, A. L., Prosek, E. A., Schmit, E. L., & Schmit, M. K. (2023). Examining coping and nonsuicidal self-injury among adolescents: A profile analysis. Journal of Counseling & Development, 101(2), 214–223. https://doi.org/10.1002/jcad.12459
Glaser, B. G., & Strauss, A. L. (1967). The discovery of grounded theory: Strategies for qualitative research. Aldine.
Glenn, C. R., & Klonsky, E. D. (2010). A multimethod analysis of impulsivity in nonsuicidal self-injury. Personality Disorders: Theory, Research, and Treatment, 1(1), 67–75. https://doi.org/10.1037/a0017427
Hambleton, A. L., Hanstock, T. L., Halpin, S., & Dempsey, C. (2022). Initiation, meaning and cessation of self-harm: Australian adults’ retrospective reflections and advice to adolescents who currently self-harm. Counselling Psychology Quarterly, 35(2), 260–283. https://doi.org/10.1080/09515070.2020.1737509
Hamza, C. A., Willoughby, T., & Heffer, T. (2015). Impulsivity and nonsuicidal self-injury: A review and meta-analysis. Clinical Psychology Review, 38(1), 13–24. https://doi.org/10.1016/j.cpr.2015.02.010
Hasking, P., & Claes, L. (2020). Transdiagnostic mechanisms involved in nonsuicidal self-injury, risky drinking, and disordered eating: Impulsivity, emotion regulation, and alexithymia. Journal of American College Health, 68(6), 603–609. https://doi.org/10.1080/07448481.2019.1583661
Hays, D. G., & Singh, A. A. (2023). Qualitative research in education and social sciences (2nd ed). Cognella.
Hempel, R. J., Rushbrook, S., O’Mahen, H. A., & Lynch, T. R. (2018). How to differentiate overcontrol from undercontrol: Findings from the RefraMED study and guidelines from clinical practice. The Behavior Therapist, 41(3), 132–142.
Hofmann, W., Luhmann, M., Fisher, R. R., Vohs, K. D., & Baumeister, R. F. (2014). Yes, but are they happy? Effects of trait self-control on affective well-being and life satisfaction. Journal of Personality, 82(4), 265–277. https://doi.org/10.1111/jopy.12050
Klonsky, E. D., Victor, S. E., & Saffer, B. Y. (2014). Nonsuicial self-injury: What we know, and what we need to know. The Canadian Journal of Psychiatry, 59(11), 565–568. https://doi.org/10.1177%2F070674371405901101
Kruzan, K. P., & Whitlock, J. (2019). Processes of change and nonsuicidal self-injury: A qualitative interview study with individuals at various stages of change. Global Qualitative Nursing Research, 6, 1–15. https://doi.org/10.1177/2333393619852935
Kruzan, K. P., Whitlock, J., & Hasking, P. (2020). Development and initial validation of scales to assess decisional balance (NSSI-DB), processes of change (NSSI-POC), and self-efficacy (NSSI-SE) in a population of young adults engaging in nonsuicidal self-injury. Psychological Assessment, 32(7), 635–648. https://doi.org/10.1037/pas0000821
Lenz, A. S., James, P., Stewart, C., Simic, M., Hempel, R., & Carr, S. (2021). A preliminary validation of the Youth Over- and Under-Control (YOU-C) screening measure with a community sample. International Journal for the Advancement of Counselling, 43(4), 489–503. https://doi.org/10.1007/s10447-021-09439-9
Linehan, M. M. (1993). Cognitive-behavioral treatment of borderline personality disorder. Guilford.
Liu, R. T., Trout, Z. M., Hernandez, E. M., Cheek, S. M., & Gerlus, N. (2017). A behavioral and cognitive neuroscience perspective on impulsivity, suicide, and non-suicidal self-injury: Meta-analysis and recommendations for future research. Neuroscience & Biobehavioral Reviews, 83, 440–450.
https://doi.org/10.1016/j.neubiorev.2017.09.019
Lynch, T. R. (2018). Radically open dialectical behavior therapy: Theory and practice for treating disorders of overcontrol. Context Press.
Lynch, T. R., Hempel, R. J., & Dunkley, C. (2015). Radically open-dialectical behavioral therapy for over-control: Signaling matters. American Journal of Psychotherapy, 69(2), 141–162. https://doi.org/10.1176/appi.psychotherapy.2015.69.2.41
Metcalfe, J., & Mischel, W. (1999). A hot/cool-system analysis of delay of gratification: Dynamics of willpower. Psychological Review, 106(1), 3–19. https://doi.org/10.1037/0033-295X.106.1.3
Muehlenkamp, J. J., Swenson, L. P., Batejan, K. L., & Jarvi, S. M. (2015). Emotional and behavioral effects of participating in an online study of nonsuicidal self-injury: An experimental analysis. Clinical Psychological Science, 3(1), 26–37. https://doi.org/10.1177/2167702614531579
Tangney, J. P., Baumeister, R. F., & Boone, A. L. (2004). High self-control predicts good adjustment, less pathology, better grades, and interpersonal success. Journal of Personality, 72(2), 271–324. https://doi.org/10.1111/j.0022-3506.2004.00263.x
Timonen, V., Foley, G., & Conlon, C. (2018). Challenges when using grounded theory: A pragmatic introduction to doing GT research. International Journal of Qualitative Methods, 17(1), 1–10. https://doi.org/10.1177/1609406918758086
Whisenhunt, J. L., Chang, C. Y., Flowers, L. R., Brack, G. L., O’Hara, C., & Raines, T. C. (2014). Working with clients who self-injure: A grounded theory approach. Journal of Counseling & Development, 92(4), 387–397. https://doi.org/10.1002/j.1556-6676.2014.00165.x
Whitlock, J., Pietrusza, C., & Purington, A. (2013). Young adult respondent experiences of disclosing self-injury, suicide-related behavior, and psychological distress in a web-based survey. Archives of Suicide Research, 17(1), 20–32. https://doi.org/10.1080/13811118.2013.748405
Whitlock, J., Purington, A., & Gershkovich, M. (2009). Media, the internet, and nonsuicidal self-injury. In M. K. Nock (Ed.), Understanding nonsuicidal self-injury: Origins, assessment, and treatment (pp. 139–155). American Psychological Association.
Appendix
Interview Protocol
- Please give me a brief timeline of your experiences with self-injury over the course of your lifetime.
Alternate wording:
I’d like to ask you to think back to the first time you self-injured. Could I ask you to describe what led to that moment?
- Where on your body did you typically self-injure?
- Have you ever hurt yourself during self-injury to the extent that you needed medical assistance, even if you did not receive it?
Follow-up questions:
a. What was the experience of seeking medical help like for you?
b. How did you manage treating the injury without medical professionals?
- What has your experience been with disclosing your self-injury to others?
Follow-up questions:
a. Who are the people in your life that are aware that you have self-injured?
b. Did you choose to tell those people about your self-injury or did they find out in some other way?
c. What were people’s responses when they found out that you had self-injured?
d. What influenced your decision to disclose or not disclose your self-injury?
- Please describe the purpose of your self-injury?
Alternate wording:
How did your self-injury influence your mental health? Relationships?
What did self-injury offer you?
- When you self-injured, to what extent did you plan how, when, or where you were going to do it in advance?
Follow-up questions:
a. How would you describe the period of time between thinking about how or when you were going to self-injure and the self-injurious behavior itself?
b. How long was the period of time, generally, between the thought and the behavior?
- Did you have any rules about when, where, or how you self-injured? If so, could I ask you to describe them to me?
- If you think about your level of distress or emotionality as a wave with a peak where the emotion is most intense, when did your self-injury typically occur along that continuum?
- If a close friend or family member had seen you in the moments before you self-injured, to what extent would they have suspected that you were in distress?
Follow-up question:
What factors would have influenced their idea that you were/were not in distress?
- How would you describe the experiences that led you to stop self-injuring?
Is there anything else you would like to add about your experiences that we haven’t touched on?
Sara E. Ellison, PhD, NCC, ACS, LPC, is adjunct faculty at Auburn University and the University of West Georgia. Jill M. Meyer, PhD, LPCP, CRC, is a professor and Director of Counselor Education at Auburn University. Julia Whisenhunt, PhD, NCC, LPC, CPCS, is a professor, assistant chair, and program director at the University of West Georgia. Jessica Meléndez Tyler, PhD, NCC, BC-TMH, LPC-S, is an associate professor at Vanderbilt University. Correspondence may be addressed to Sara E. Ellison, 3084 Haley Center, Auburn, AL 36849, szm0194@auburn.edu.
Jul 25, 2025 | Volume 15 - Issue 2
Michael T. Kalkbrenner, Shannon Esparza
Physicians in the United States are a client population facing increased risks for mental distress coupled with a reticence to seek professional counseling. Screening tools with valid scores have utility for helping counselors understand why prospective client populations who might benefit from counseling avoid seeking services. The Revised Fit, Stigma, and Value (RFSV) Scale is a screener for measuring barriers to counseling. The primary aims of the present study were to validate RFSV scores with physicians in the United States and to investigate demographic differences in physicians’ RFSV scores. Results revealed that the RFSV Scale and its dimensionality were estimated sufficiently with a national sample of physicians (N = 437). Physicians’ RFSV scores were a significant predictor (p = .002, Nagelkerke R2 = .05) of peer-to-peer referrals to counseling. We also found that male physicians and physicians with help-seeking histories were more sensitive to barriers to counseling than female physicians and physicians without help-seeking histories, respectively. Recommendations for how counselors can use the RFSV Scale when working with physician clients are provided.
Keywords: Revised Fit, Stigma, and Value Scale; counseling; barriers to counseling; help-seeking; physicians
Because of the particularly stressful nature of their work, coupled with the pressure in medical culture to not display psychological vulnerability (Linzer et al., 2016), physicians in the United States must be vigilant about their self-care. Physicians are responsible for treating over 300 million patients in the United States, which can lead to elevated psychological distress that may undermine the quality of patient services and physicians’ personal well-being (Walker & Pine, 2018). Attending personal counseling is associated with a number of personal and professional benefits for physicians (Melnyk et al., 2020). However, a stigma toward seeking counseling and other mental health support services exists in the U.S. medical culture (Dyrbye et al., 2015). Lobelo and de Quevedo (2016) found that physicians are attending counseling at lower rates since 2000, with approximately 40%–70% attending counseling before the year 2000 and only 12%–40% after 2000. One of the next steps in this line of research is gaining a better understanding of barriers to counseling, including reasons why physicians are reluctant to attend.
Screening tools with valid scores are one way to understand why individuals are reticent to attend counseling (Goldman et al., 2018). For example, the Revised Fit, Stigma, and Value (RFSV) Scale is a screening tool with rigorously validated scores for measuring barriers to counseling (Kalkbrenner et al., 2019). Scores on the RFSV Scale have been validated with seven different normative samples since 2018, including adults in the United States (Kalkbrenner & Neukrug, 2018), mental health counselors (Kalkbrenner et al. 2019), counselors-in-training (Kalkbrenner & Neukrug, 2019), college students attending a Hispanic Serving Institution (HSI; Kalkbrenner et al., 2022), and STEM students (Kalkbrenner & Miceli 2022).
At the time of this writing, RFSV scores have not been validated with a normative sample of physicians. Validity evidence of test scores can fluctuate between normative samples (American Educational Research Association [AERA] et al., 2014; Lenz et al., 2022). Accordingly, counseling practitioners, researchers, and students have a responsibility to validate scores with untested populations before using the test in clinical practice or research (Lenz et al., 2022). Validating RFSV scores with a national sample of U.S. physicians may provide professional counselors with a clinically appropriate screening tool for ascertaining what barriers contribute to physicians’ reluctance to attend counseling services. Identifying barriers to counseling within this population may also promote efforts to increase physicians’ support-seeking behaviors (Mortali & Moutier, 2018).
Barriers to Counseling
Counseling interventions provide physicians with protective factors such as promoting overall health and wellness (Major et al., 2021) and decreasing emotional exhaustion associated with burnout (Wiederhold et al., 2018). Despite these correlations, Kase et al. (2020) found that although 43% of a sample of U.S. pediatric physicians had access to professional counseling and support groups, only 17% utilized these services. Participants cited barriers to attending counseling, including inconvenience, time constraints, preference for handling mental health issues on their own, and perceiving mental health services as unhelpful.
A significant barrier contributing to U.S. physicians’ reticence to attend counseling is the influence of medical culture which reinforces physician self-neglect and pressure to maintain an image of invincibility (Shanafelt et al., 2019). This pressure can begin as early as medical school and may lead to a decreased likelihood of seeking counseling, as medical students who endorsed higher perceptions of public stigma within their workplace culture perceived counseling as less efficacious and considered depression a personal weakness (Wimsatt et al., 2015). An association of frailty with mental health diagnoses and treatment may be driven by incongruences in medical culture between espoused values and actual behaviors, such as teaching that self-care is important, yet practicing excessive hours, delaying in seeking preventive health care, and tolerating expectations of perfectionism (Shanafelt et al., 2019). Such hidden curricula may perpetuate the stigma of seeking mental health treatment, which is considered a primary driver of suicide in the health care workforce (American Hospital Association [AHA], 2022).
In addition to the barrier presented by medical culture, the stigmatization and negative impact on licensure of receiving a diagnosis also discourages physicians from seeking care (Mehta & Edwards, 2018). Almost 50% of a sample of female U.S. physicians believed that they met the criteria for a mental health diagnosis but had not sought treatment, citing reasons such as a belief that a diagnosis is embarrassing or shameful and fear of being reported to a medical licensing board (Gold et al., 2016). It is recommended best practice for state medical licensing boards to phrase initial and renewal licensure questions to only inquire about current mental health conditions, to ask only if the physician is impaired by these conditions, to allow for safe havens, and to use supportive language; yet in a review of all 50 states, the District of Columbia, and four U.S. territories, only three states’ or territories’ applications met all four conditions (Douglas et al., 2023). Thus, it is unsurprising that out of a sample of 5,829 U.S. physicians, nearly 40% indicated reluctance to seek formal care for a mental health condition because of licensure concerns (Dyrbye et al., 2017). The barriers of medical culture and its expectations, stigma, and diagnosis are consequential; further research is needed given the pressure physicians may experience to remain silent on these issues (Mehta & Edwards, 2018).
Demographic Differences
A number of demographic variables are related to differences in physicians’ mental health and their attitudes about seeking counseling (Creager et al., 2019; Duarte et al., 2020). For example, demographic differences such as gender and ethnoracial identity can add complexity to physicians’ risk of negative mental health outcomes (Duarte et al., 2020). Sudol et al. (2021) found that female physicians were at higher risk of depersonalization and emotional exhaustion than male physicians, while physicians from racial/ethnic minority backgrounds were more likely to report burnout than White physicians. Gender identity can also affect help-seeking behavior, as female physicians are more likely than male physicians to utilize social and emotional supports and less likely to prefer handling mental health symptoms alone (Kase et al., 2020). Work setting is another demographic variable that is associated with physicians’ mental health wellness, as Creager et al. (2019) identified lower burnout and stress rates among physicians working in private practice than those working in non–private practice settings.
Help-seeking history has become a more frequently examined variable in counseling research, often categorized into two groups: (a) individuals who have attended at least one session of personal counseling or (b) those who have never sought counseling (Cheng et al., 2018). This demographic variable is especially important when evaluating the psychometric properties of screening tools for physicians, who encounter numerous obstacles to accessing counseling services. Help-seeking history is related to more positive attitudes about seeking counseling, as Kevern et al. (2023) found that 80% of a sample of U.S. resident physicians who attended mental health counseling reported their sessions increased their willingness to attend counseling. These collective findings suggest demographic variables such as gender, ethnoracial identity, work setting, and help-seeking history may impact physicians’ mental health and their sensitivity to barriers to attending counseling and thus warrant further investigation.
The Revised Fit, Stigma, and Value Scale
Neukrug et al. (2017) developed and validated scores on the original 32-item Fit, Stigma, and Value (FSV) Scale with a sample of human service professionals in order to appraise barriers to attending personal counseling. The FSV subscales assess sensitivity to three potential barriers to counseling attendance, including fit, the extent to which a respondent trusts the counseling process; stigma, the feelings of shame or embarrassment associated with attending counseling; and value, the perceived benefit of being in counseling. Kalkbrenner et al. (2019) also developed and validated scores on a briefer 14-item version of the FSV Scale (the RFSV Scale), that contains the original three subscales. Additionally, Kalkbrenner and Neukrug (2019) identified a higher-order factor, the Global Barriers to Counseling Scale, which is the composite score of the RFSV’s Fit, Stigma, and Value single-order subscales.
Integrative Behavioral Health Care
Mental health challenges and attitudes toward seeking support are shaped by both individual (microsystemic) and broader societal (macrosystemic) factors, making it impossible for a single discipline to address these issues (Lenz & Lemberger-Truelove, 2023; Pester et al., 2023). As a result, the counseling profession is increasingly adopting interdisciplinary collaboration models, in which mental health professionals work together to deliver holistic care to clients or patients. Emerging research highlights interventions aimed at reducing barriers to accessing counseling services (e.g., Lannin et al., 2019). However, the complex interplay of ecological factors influencing mental health distress and service utilization makes evaluating these interventions challenging. Accordingly, counselors and other members of interdisciplinary teams need screening tools with valid scores to help determine the effectiveness of such interventions.
The primary aims of the present study were to validate RFSV scores with a national sample of physicians in the United States and to investigate demographic differences in physicians’ RFSV scores. The validity and meaning of latent traits (i.e., RFSV scores) can differ between different normative samples (AERA, 2014; Lenz et al., 2022). RFSV scores have not been normed with physicians. Accordingly, testing for factorial invariance of RFSV scores is a pivotal next step in this line of research. In other words, the internal structure validity of RFSV scores must be confirmed with physicians before the scale can be used to measure the intended construct. Although a number of different forms of validity evidence of scores exists, internal structure validity is a crucial consideration when testing the psychometric properties of an inventory with a new normative sample (AERA, 2014; Lenz et al., 2022). If RFSV scores are validated with a national sample of U.S. physicians, counselors can use the scale to better understand why physicians, as a population, are reticent to seek counseling.
Pending at least acceptable validity evidence, we sought to investigate the capacity of physicians’ RFSV scores for predicting referrals to counseling and to examine demographic differences in RFSV scores. Results have the potential to offer professional counselors a screening tool for understanding why physicians might be reticent to seek counseling. Findings also have the potential to reveal subgroups of physicians who might be especially unlikely to access counseling services. To these ends, the following research questions (RQs) were posed:
RQ1. What is the factorial invariance of scores on the RFSV Scale among a national sample of U.S. physicians?
RQ2. Are U.S. physicians’ RFSV scores statistically significant predictors of making at least one referral to counseling?
RQ3. Are there demographic differences to the RFSV barriers among U.S. physicians’ RFSV scores?
Method
Participants and Procedures
A quantitative cross-sectional psychometric research design was utilized to answer the research questions. The current study is part of a larger grant-funded project with an aim to promote health-based screening efforts and wellness among physicians. The aim of the previous study (Kalkbrenner et al., 2025) was to test the psychometric properties of three wellness-based screening tools with physicians. In the present study, we further analyzed the data in Kalkbrenner et al. (2025) to answer different research questions about a different scale (the RFSV Scale) on barriers to counseling. This data set was collected following approval from our IRB. Crowdsourcing is an increasingly common data collection strategy in counseling research with utility for accessing prospective participants on national and global levels (Mullen et al., 2021). Qualtrics Sample Services is a crowdsource solutions service with access to over 90 million prospective participants who voluntarily participate in survey research for monetary compensation. Grant funding was utilized to engage the services of a data collection agency to enlist a nationwide cohort of U.S. physicians. Qualtrics Sample Services was selected because they were the only crowdsource service we came across that could provide a sample of more than 400 licensed U.S. physicians. A sample greater than 400 was necessary for answering the first research question because 200 participants per group is the lower end of acceptable for multiple-group confirmatory factor analysis (MG-CFA; Meade & Kroustalis, 2006). Qualtrics Sample Services provided us with a program manager and a team of analysts who undertook a meticulous quality assessment of the data. This quality assessment involved filtering out respondents exhibiting excessive speed in responding, random response patterns, failed attention checks, and instances of implausible responses (e.g., individuals claiming to be 18 years old with an MD).
A total of N = 437 valid responses that met quality standards were obtained. An analysis of missing values indicated an absence of missing data. Examination of standardized z-scores and Mahalanobis (D) distances identified no univariate outliers (z > ± 3.29) and no multivariate outliers, respectively. Skewness and kurtosis values for physicians’ scores on the RFSV Scale were within the range indicative of a normal distribution of test scores (skewness < ± 2 and kurtosis < ± 7). Participants in the sample (N = 437) ranged in age from 25 to 85 (M = 47.80, SD = 11.74); see Table 1 for the demographic profile of the sample.
Table 1
Demographic Profile of the Sample (N = 437)
| Sample Characteristics |
n |
% |
| Gender |
|
|
| Male |
217 |
49.7 |
| Female |
215 |
49.2 |
| Transgender |
1 |
0.2 |
| Nonbinary |
1 |
0.2 |
| Preferred not to answer |
3 |
0.7 |
| Ethnoracial Identity |
|
|
| American Indian or Alaska Native |
1 |
0.2 |
| Asian or Asian American |
28 |
6.4 |
| Black or African American |
76 |
17.4 |
| Hispanic, Latinx, or Spanish origin |
97 |
22.2 |
| Middle Eastern or North African |
6 |
1.4 |
| Multiethnic |
6 |
1.4 |
| White or European American |
216 |
49.4 |
| Identified as another race, ethnicity, or origin |
1 |
0.2 |
| Preferred not to answer |
4 |
0.9 |
| Help-Seeking History |
|
|
| No help-seeking history |
228 |
52.2 |
| Help-seeking history |
208 |
47.6 |
| Work Setting |
|
|
| Private practice |
202 |
46.2 |
| Non–private practice |
233 |
53.3 |
| Did not report work setting |
2 |
0.5 |
Measures
Prospective participants voluntarily indicated their informed consent and confirmed that they met the eligibility criteria for participation, including being a physician licensed as an MD, treating patients in the United States, and being over 18 years old at the time of data collection. Participants then responded to a demographic questionnaire and completed the RFSV Scale.
The RFSV Scale
The RFSV Scale is a screening tool designed to measure respondents’ sensitivity to barriers to attending counseling (Kalkbrenner et al., 2019) and is comprised of three subscales. Participants respond to a stem (“I am less likely to attend counseling because . . . ”) on the following Likert scale: 1 = Strongly Disagree, 2 = Disagree, 3 = Neither Agree nor Disagree, 4 = Agree, or 5 = Strongly Agree. Higher scores indicate greater reluctance to seek counseling. The Fit subscale measures the degree to which a respondent believes that the counseling process is congruent with their personality, values, or beliefs (e.g. “I couldn’t find a counselor who would understand me”). The Stigma subscale measures one’s reluctance to attend counseling because of shame or embarrassment (e.g. “It would damage my reputation”). The Value subscale appraises the degree to which a respondent perceives the effort required to attend counseling as beneficial (e.g. “It is not an effective use of my time”).
Kalkbrenner et al. (2019) found moderate to strong reliability evidence of scores on the RFSV subscales (Fit α = .82, Stigma α = .91, Value α = .78) and support for the internal structure validity of the RFSV through factor analysis. Additionally, Kalkbrenner and Neukrug (2018) demonstrated evidence of internal structure validity of RFSV scores through confirmatory factor analysis (CFA). Moreover, Kalkbrenner et al. (2022) found internal structure validity and criterion validity evidence of RFSV scores. More specifically, Kalkbrenner et al. (2022) found internal structure validity evidence of RFSV scores via CFA with a normative sample of STEM students. In addition, Kalkbrenner et al. (2022) found that STEM students’ scores on the Value barrier were a statistically significant predictor of a non-test criterion (referrals to the counseling center), which supported criterion validity of RFSV scores.
Cronbach’s alpha (α) and McDonald’s omega (ω) were calculated to estimate the reliability of physicians’ scores on the RFSV Scale. Consistent with the Responsibilities of Users of Standardized Tests (RUST-4E) standards, we computed confidence intervals (CIs) for each point reliability estimate (Lenz et al., 2022). All CIs were estimated at the 95% level. The following interpretive guidelines for internal consistency reliability evidence of test scores were used: α > .70 (Tavakol & Dennick, 2011) and ω > .65 (Nájera Catalán, 2019). Among the sample of physicians in the present study, scores on the Fit subscale showed acceptable internal consistency reliability of scores (α = .819, 95% CI [.789, .846]; ω = .827, 95% CI [.799, .851]). Scores on the Stigma subscale displayed acceptable-to-strong internal consistency reliability evidence of scores (α = .896, 95% CI [.877, .912]; ω =. 902, 95% CI [.885, .918]). Physicians’ scores on the Value subscale displayed acceptable internal consistency reliability of scores (α = .817, 95% CI [.781, .848]; ω =.820, 95% CI [.783, .850]). Finally, we found strong internal consistency reliability estimates of scores on the Global Barriers scale (α = .902, 95% CI [.885, .915]; ω = .897, 95% CI [.887, .911]).
Data Analytic Plan
MG-CFA is an advanced psychometric analysis for determining the extent to which the meaning of latent constructs remain stable across subgroups of a sample (Dimitrov, 2012). MG-CFA is particularly sensitive to sample size (Meade & Kroustalis, 2006). A number of guidelines for MG-CFA sample size exist; however, at least 200 participants per each level of every invariance variable tends to be the minimum. To ensure that the present sample included 200+ participants in each group (see Table 2), the gender identity and ethnoracial identity variables were coded as female or male and White or non-White, respectively, for sample size considerations. This method of dummy coding highlights a frequent sample size–based challenge encountered in survey research, particularly in the context of assessing gender or ethnoracial identity (Ross et al., 2020). However, this coding method can be appropriate for survey research provided that the authors openly acknowledge the limitations inherent in such procedures, and that there is at least some degree of consistency between the dummy-coded groups and both the existing literature and the research questions (Ross et al., 2020). The coded groups are consistent with the literature and RQs, as findings in the extant literature (e.g., Duarte et al., 2022) demonstrated mental health care disparities between White and non-White and between male and female physicians. There are macro- and microlevel inequalities in the U.S. health care system between White and non-White populations (Matthew, 2015). Using the comparative method between participants with White and non-White ethnoracial identifies can have utility for highlighting the discrepancies in the U.S. health care system (Matthew, 2015; Ross et al., 2020). The limitations of this statistical aggregation procedure in terms of external validity will be articulated in the Discussion section.
Table 2
Multiple-Group Confirmatory Factor Analysis: RFSV Scale With U.S. Physicians
| Invariance Forms |
CFI |
∆CFI |
RMSEA |
∆RMSEA |
RMSEA CIs |
SRMR |
∆SRMR |
Model Comparison |
| Ethnoracial Identity: White (n = 216) vs. Non-White (n = 215) |
| Configural |
.934 |
|
.057 |
|
.049; .064 |
.070 |
|
|
| Metric |
.933 |
.001 |
.055 |
.002 |
.048; .063 |
.070 |
< .001 |
Configural |
| Scalar |
.928 |
.005 |
.055 |
< .001 |
.048; .062 |
.071 |
.001 |
Metric |
| Gender Identity: Female (n = 215) vs. Male (n = 217) |
|
| Configural |
.936 |
|
.056 |
|
.048; .063 |
.060 |
|
|
| Metric |
.935 |
.001 |
.055 |
.001 |
.047; .062 |
.066 |
.006 |
Configural |
| Scalar |
.921 |
.014 |
.057 |
.002 |
.051; .064 |
.067 |
.001 |
Metric |
| Help-Seeking History: Yes (n = 208) vs. No (n = 228) |
|
| Configural |
.921 |
|
.062 |
|
.055; .070 |
.080 |
|
|
| Metric |
.921 |
< .001 |
.061 |
.001 |
.053; .068 |
.080 |
< .001 |
Configural |
| Scalar |
.906 |
.015 |
.063 |
.001 |
.057; .070 |
.079 |
.001 |
Metric |
| Work Setting: Private Practice (n = 202) vs. Non-Private Practice (n = 233) |
|
| Configural |
.942 |
|
.053 |
|
.045; .061 |
.062 |
|
|
| Metric |
.937 |
.005 |
.054 |
.001 |
.046; .061 |
.075 |
.013 |
Configural |
| Scalar |
.936 |
.001 |
.052 |
.002 |
.044; .059 |
.075 |
< .001 |
Metric |
|
|
|
|
|
|
|
|
|
|
We computed an MG-CFA to test the factorial invariance of U.S. physicians’ RFSV scores (RQ1). All statistical analyses were computed in IBM SPSS AMOS version 29 with a maximum likelihood estimation method. The fit of the baseline configural models was compared to the following cutoff scores: root mean square error of approximation (RMSEA < .08 = acceptable fit and < .06 = strong fit), standardized root mean square residual (SRMR < .08 = acceptable fit and < .06 = strong fit), and the comparative fit index (CFI, .90 to .95 = acceptable fit and > .95 = strong fit (Dimitrov, 2012; Schreiber et al., 2006). Pending at least acceptable fit of the baseline models, we used the following guidelines for factorial invariance testing: < ∆ 0.010 in the CFI, < ∆ 0.015 in the RMSEA, and < ∆ 0.030 in the SRMR for metric invariance or < ∆ 0.015 in SRMR for scalar invariance (Chen, 2007; Cheung & Rensvold, 2002).
A binary logistic regression analysis was computed to investigate the predictive capacity of physicians’ RFSV scores (RQ2). The predictor variables included physicians’ interval level scores on the RFSV Scale. The criterion variable was whether or not physicians have made at least one referral to counseling (0 = no or 1 = yes). Interscale corrections between the RFSV scales ranged from r = .44 to r = .55, indicating that multicollinearity was not present in the data.
A 2 (gender) X 2 (ethnicity) X 2 (work setting) X 2 (help-seeking history) factorial multivariate analysis of variance (MANOVA) was computed to investigate differences in physicians’ RFSV scores (RQ3). The categorical level independent variables (IVs) included gender (female or male), ethnoracial identity (White or non-White), help-seeking history (yes or no), and work setting (private practice or non–private practice). The dependent variables (DVs) were physicians’ interval level scores on the RFSV Scale. Box’s M test demonstrated that the assumption of equity of covariance matrices was met, F = (90, 73455.60) = 86.28, p = .719.
Results
Factorial Invariance Testing
An MG-CFA was computed to answer the first research question regarding the factorial invariance of U.S. physicians’ scores on the RFSV Scale. First, the baseline configural models were investigated for fit. We then tested for invariance, as the baseline models showed acceptable fit based on the previously cited guidelines provided by Dimitrov (2012) and Schreiber et al. (2006), including gender identity (CFI = .936, RMSEA = .056, 90% CI [.048, .063], and SRMR = .060), ethnoracial identity (CFI = .934, RMSEA = .057, 90% CI [.049, .064], and SRMR = .070), help-seeking history (CFI = .921, RMSEA = .062, 90% CI [.055, .070], and SRMR = .080), and work setting (CFI = .942, RMSEA = .053, 90% CI [.045, .061], and SRMR = .062).
In terms of invariance, all of the fit indices (∆CFI, ∆RMSEA, and ∆SRMR) supported both metric and scalar invariance of scores for ethnoracial identity and work setting (see Table 2). For the gender identity and help-seeking history variables, the ∆RMSEA and ∆SRMR supported both metric and scalar invariance of scores. The ∆CFI supported metric but not scalar invariance of scores for the help-seeking history and gender identity variables. Demonstrating invariance can be deemed acceptable solely based on metric invariance (Dimitrov, 2010). This is particularly true when only a single fit index, such as the CFI, confirms metric invariance but not scalar invariance of scores.
Logistic Regression
A logistic regression analysis was computed to answer the second research question regarding the predictive capacity of physicians’ RFSV scores. The logistic regression model was statistically significant, X2 (3) = 15.36, p = .002, Nagelkerke R2 = .05. The odds ratios, Exp(B), demonstrated that an increase of one unit in physicians’ scores on the Stigma subscale (higher scores = higher barriers to counseling) was associated with a decrease in the odds of having made at least one referral to counseling by a factor of .711, Exp(B) 95% CI [.517, .947], p = .036. In addition, an increase of one unit in physicians’ scores on the Value subscale was associated with a decrease in the odds of having made at least one referral to counseling by a factor of .707, Exp(B) 95% CI [.508, .984], p = .040.
Factorial MANOVA
A 2 (gender) X 2 (ethnicity) X 2 (work setting) X 2 (help-seeking history) factorial MANOVA was computed to investigate differences in physicians’ RFSV scores (RQ3). A significant main effect emerged for gender on the combined DVs, F = (3, 409) = 6.50, p < .001, Λ = 0.95, n2p = .05. The statistically significant findings in the MANOVA were followed up with post-hoc discriminant analyses. The discriminant function significantly discriminated between groups, λ = 0.94, X2 = 25.07, df = 3, Canonical correlation = .29, p < .001. The correlations between the latent factors and discriminant functions showed that Fit (−1.17) loaded more strongly on the function than Stigma (0.68) and Value (0.62), suggesting that Fit contributed the most to group separation in gender identity. The mean discriminant score on the function for male physicians was 0.24 and the mean score for female physicians was −0.25 (higher scores = greater barriers to counseling).
A significant main effect emerged for help-seeking history on the combined DVs, F = (3, 409) = 4.57, p = .004, Λ = 0.95, n2p = .03. The post-hoc discriminant function significantly discriminated between groups, Wilks λ = 0.96, X2 = 19.61, df = 3, Canonical correlation = .21, p < .001. The correlations between the latent factors and discriminant functions showed that Value (1.03) loaded more strongly on the function than Stigma (0.28) and Fit (0.26), suggesting Value contributed the most to group separation in help-seeking history. The mean discriminant score on the function for physicians with a help-seeking history was −0.23 and the mean score was 0.21 for physicians without a help-seeking history.
Discussion
The aims of the present study were to: validate RFSV scores with a national sample of physicians in the United States, investigate the capacity of RFSV scores for predicting physician referrals to counseling, and investigate demographic differences in physicians’ RFSV scores. The findings will be discussed in accordance with the RQs. The model fit estimates for each of the baseline configural models were all in the acceptable range based on the recommendations of Dimitrov (2012) and Schreiber et al. (2006; see Table 2). The acceptable fit of the configural models supported that the RFSV Scale and its dimensionality were estimated adequately with a normative sample of physicians. RFSV scores have been normed with seven different normative samples since 2018, including adults in the United States (Kalkbrenner & Neukrug, 2018), mental health counselors (Kalkbrenner et al., 2019), counselors-in-training (Kalkbrenner & Neukrug, 2019), college students at an HSI (Kalkbrenner et al., 2022), and STEM students (Kalkbrenner & Miceli, 2022). The baseline CFA results in the present study extend the generalizability of RFSV scores to a normative sample of physicians in the United States. Because we found support for the baseline configural models, we proceeded to test for invariance of scores.
Invariance testing via MG-CFA takes internal structure validity testing to a higher level by revealing if the meaning of a latent trait stays consistent (i.e., invariant) between specific groups of a normative sample (Dimitrov, 2012). The results of factorial invariance testing were particularly strong and evidenced both metric and scalar invariance of RFSV scores for the ethnoracial identity and work setting variables. The ∆ in RMSEA and SRMR also supported both metric and scalar invariance for the help-seeking history and gender identity variables. The ∆ in CFI revealed metric, but not scalar invariance of scores for the help-seeking history and gender identity variables. Metric invariance alone can be sufficient for demonstrating invariance of scores across a latent trait (Dimitrov, 2010). This is particularly true when only a single fit index, such as the CFI, supports metric invariance but not scalar invariance of scores. In totality, the MG-CFA results supported invariance of physicians’ RFSV scores by ethnoracial identity, work setting, and, to a lesser but acceptable degree, help-seeking history and gender identity.
The MG-CFA results demonstrated that RFSV scores were valid among a national sample of U.S. physicians (RQ1). This finding adds rigor to the results of RQs 2 and 3 on predictive and demographic differences in physicians’ RFSV scores, as the scale was appropriately calibrated with a new normative sample. A test of the predictive capacity of RFSV scores revealed that physicians’ scores on the Stigma and Value subscales were statistically significant predictors of having made one or more referrals to counseling (RQ2). In other words, lower levels of stigma and higher attributions to the value of counseling were associated with higher odds of physicians making one or more referrals to counseling at a statistically significant level. This finding is consistent with Kalkbrenner and Miceli (2022), who found that scores on the Value subscale were predictors of referrals to counseling among STEM students. Similarly, Kalkbrenner et al. (2022) found that scores on the Value subscale predicted supportive responses to encountering a peer in mental distress among college students attending an HSI. Collectively, the findings of the present study are consistent with past investigators (e.g., Kalkbrenner et al., 2022) who found that more positive attitudes about counseling tend to predict increases in the odds of having made one or more peer referrals to counseling.
The final aim of the present study was to test for demographic differences in physicians’ sensitivity to the RFSV barriers (RQ3). We found statistically significant main effects for the gender identity and help-seeking history variables. Results revealed that male physicians were more sensitive to the Fit barrier than female physicians. This finding suggests that physicians who identify as male might be more skeptical about the counseling process in general and may doubt their chances of finding a counselor they feel comfortable with. This finding adds to the extant literature on physicians’ mental health and attitudes about seeking counseling. Past investigators (e.g., Sudol et al., 2021) documented female physicians’ increased risk for mental health stress when compared to male physicians. The findings of the present study showed that male physicians were more sensitive to the Fit barrier than female physicians. Accordingly, it is possible that female physicians are more likely to report symptoms of and seek support services for mental health issues than male physicians. This might be due, in part, to differences between male and female physicians’ beliefs about the fit of counseling. Future research is needed to test this possible explanation for this finding.
We found that physicians with a help-seeking history (i.e., attended one or more counseling sessions in the past) were less sensitive to the Value barrier when compared to physicians without a help-seeking history. Similarly, past investigators found associations between help-seeking history and more positive attitudes about the value and benefits of seeking counseling, including among STEM students (Kalkbrenner & Miceli 2022), college students at an HSI (Kalkbrenner et al., 2022), and adults living in the United States (Kalkbrenner & Neukrug, 2018). Collectively, the results of the present study are consistent with these existing findings, which suggest that physicians and members of other populations with help-seeking histories tend to attribute more value toward the anticipated benefits of counseling.
Limitations and Future Research
We recommend that readers consider the limitations of the present study before the implications for practice. Causal attributions cannot be drawn from a cross-sectional survey research design. Future researchers can build upon this line of research by testing the RFSV barriers using an experimental approach. Such research could involve administering the scale to physician clients before and after their counseling sessions. Such an approach might yield evidence on how counseling reduces sensitivity to certain barriers. However, it is important to note that pretest/posttest approaches can come with a number of limitations, including attrition, regression to the mean, history, and maturation.
Dummy coding the sociodemographic variables into broader categories to ensure adequate sample sizes for MG-CFA was a particularly challenging decision, especially for the ethnoracial identity variable. Although this statistical aggregation procedure can be useful for making broad and tentative generalizations about ethnicity and other variables (Ross et al., 2020), it limited our ability to explore potential differences in the meaning of the RFSV barriers among physicians with identities beyond White or non-White, and male or female. Future research with a more diverse sample by gender and ethnoracial identity is recommended.
Implications for Practice
The findings from this study provide robust psychometric evidence that supports the dimensionality of U.S. physicians’ scores on the RFSV Scale and carries important implications for counseling professionals. The National Board for Certified Counselors (NBCC; 2023) emphasizes the use of screening tools with valid scores as a means of improving clinical practice. Additionally, ethical guidelines for counselors stress the importance of ensuring that the screening tools that they utilize offer valid and reliable scores, derived from representative client samples, to uphold their effectiveness and proper application (AERA, 2014; Lenz et al., 2022; NBCC, 2023). Mental health issues and attitudes about utilizing mental health support services are influenced by microsystemic and macrosystemic factors (Lenz & Lemberger-Truelove, 2023; Pester et al., 2023). To this end, implications for practice will be discussed on both microsystemic and macrosystemic levels.
The practicality of the RFSV Scale adds to its utility, as it is free to use, simple to score, and typically takes between 5 and 8 minutes to complete. Identifying barriers or doubts that physician clients have about counseling during the intake process might help increase physician client retention. To these ends, counselors can include the RFSV Scale with intake paperwork for physician clients. Counselors can use the results as one way to gather information about doubts that their physician clients might have about attending counseling. Suppose, for example, that a physician client scores higher on the Fit subscale (higher scores = higher barriers to counseling) than the Stigma or Value subscales. It might be helpful for the counselor and client to discuss how they can make the counseling process a good fit (i.e., how and in what ways the counseling process can be congruent with their personality, values, or beliefs). Increasing physician clients’ buy-in regarding the counseling process may increase retention.
Counselors could also administer the RFSV Scale at the beginning, middle, and end of the counseling process when working with clients who are physicians or medical students. Results might reveal the utility of counseling for reducing barriers to counseling among clients who are physicians or medical students. Our results revealed that physicians with help-seeking histories perceived greater value about the benefits of counseling than physicians without help-seeking histories. Mental health support services provided by counselor education students can be a helpful resource for medical students and residents (Gerwe et al., 2017). Accordingly, there may be utility in counselor education programs collaborating with medical colleges and schools to address stigma around seeking counseling that can exist in the medical field. This broader perspective is consistent with the ecological systems direction that the counseling profession spearheaded (Lenz & Lemberger-Truelove, 2023; Pester et al., 2023) and could help address stigma toward seeking counseling before medical students become physicians. More specifically, directors and clinical coordinators of counseling programs can reach out to directors of medical schools to establish collaborative relationships in which counseling interns provide supervised counseling services to medical students and residents. This might have dual benefits because medical schools would be able to offer their students free mental health support services and counseling programs would provide additional internship sites for their students. Early intervention before students become physicians could reduce stigma toward counseling throughout their careers.
Time constraints can be a barrier to counseling among physicians, residents, and medical students (Gerwe et al., 2017; Kase et al., 2020). Accordingly, it could be beneficial for counseling students who are interested in working with medical students or residents to complete their internship placements in the same settings where medical students and residents work. In all likelihood, providing supervised group and individual counseling for medical students at their work sites would increase the accessibility of counseling.
The counseling profession is moving toward interdisciplinary collaboration models that involve teams of mental health professionals working together to provide comprehensive client/patient care (Lenz & Lemberger-Truelove, 2023; Pester et al., 2023). Interventions designed to reduce barriers to counseling are only beginning to appear in the extant literature (e.g., Lannin et al., 2019). The ecological systemic nature of mental health distress and influences on attitudes about accessing mental health support services makes evaluating the utility of reducing barriers to counseling interventions complex. To address this, counselors and interdisciplinary teams need screening tools with reliable and valid scores in order to effectively assess the impact of these interventions.
The results of CFA and MG-CFA in the present study confirmed that the RFSV Scale measured the intended construct of measurement with a national sample of U.S. physicians (RQ1). Thus, the RFSV Scale may have utility as a pretest/posttest for measuring the effectiveness of interventions geared toward reducing barriers to counseling. The extant literature on interventions for reducing barriers to counseling is in its infancy. Lannin et al. (2019) started to fill this gap in the knowledge base by conducting an intervention study with random assignment. Lannin et al. (2019) tested the extent to which contemplation about seeking counseling and self-affirmation were related to seeking mental health screening and general information about mental health support services. Results revealed that participants who used both self-affirming personal values and contemplation were significantly more likely to seek mental health screening and general information about mental health than participants in the contemplation-only group. In addition, participants in the contemplation about seeking counseling group only reported higher self-stigma. Findings indicated that interventions including both contemplation and self-affirmation of participants’ personal values were more likely to increase receptivity to outreach efforts.
Lannin et al. (2019) sampled undergraduate students attending a historically Black college/university. Lannin et al.’s (2019) intervention might have utility with physicians. However, to the best of our knowledge, the screening tools used by Lannin et al. have not been validated with U.S. physicians. Accordingly, professional counselors can use the RFSV Scale as one way to measure potential reductions in barriers to seeking counseling before and after participating in interventions geared toward promoting help-seeking among physicians. Fully developing an intervention that reduces barriers to counseling is beyond the scope of this study. Although future research is needed in this area, the results of this study confirmed that the RFSV Scale measured the intended construct of measurement with a national sample of U.S. physicians. Accordingly, professional counselors can use the RFSV Scale to better understand why prospective or current physician clients are reluctant to seek counseling. For example, professional counselors can work with medical supervisors and the directors of physician residency programs to administer the RFSV Scale at orientations for new physician employees and medical residents. The results could reveal specific barriers that are particularly salient in a given medical setting. Professional counselors can use the results to structure psychoeducation sessions about the utility of counseling for physicians. Suppose, for example, that physicians in a particular setting score higher on the Stigma subscale. A counselor can structure the content of the psychoeducation session on reducing stigma toward counseling. Specifically, the session could involve reframing seeking counseling in the context of the courage it takes for one to reach out to a counselor and the benefits associated with participating in counseling. These sessions may also help strengthen interpersonal bonds among physicians and begin to normalize mental health support within the medical community.
Consistent with the findings of Kalkbrenner and Miceli (2022), we found that lower scores on the Value subscale (lower scores = greater perceived benefits of counseling) was a statistically significant predictor of higher odds of participants having made one or more peer referrals to counseling. This finding, combined with the extant literature on physicians’ vulnerability to mental health distress and reticence to seek counseling (Lobelo & de Quevedo, 2016; Walker & Pine, 2018), suggested that peer-to-peer support may be a valuable resource for counselors who work in medical settings. In other words, we found that greater perceived value of the benefits of counseling was a statistically significant predictor of an increase in the odds of physicians recommending counseling to another physician. Accordingly, professional counselors who work in medical settings are encouraged to organize peer-to-peer support networks among physicians within their work setting. For example, professional counselors can work to promote physicians’ awareness of the value of attending professional counseling, particularly for reducing burnout, grieving the loss of a patient, coping with the demanding work life of physicians, and increasing general health (Major et al., 2021; Trivate et al., 2019; Wiederhold et al., 2018). Our results revealed that when compared to female physicians, male physicians scored higher on the Fit subscale (higher RFSV scores = poorer attitudes about counseling) and physicians with a help-seeking history scored higher on the Value subscale than those without help-seeking histories. To this end, there may be utility in focusing outreach sessions about the benefits of counseling to male physicians. For example, professional counselors could produce short videos, flyers, or other types of media on the benefits that attending counseling can have for physicians. These media sources can be shared with physicians. Such awareness advocacy about the benefits of counseling may result in an increase of peer-to-peer referrals to counseling among physicians.
Summary and Conclusion
Physicians in the United States face increased risks for mental distress and often hesitate to seek professional counseling (Lobelo & de Quevedo, 2016; Walker & Pine, 2018). Screening tools with validated scores are essential resources for helping professional counselors to understand why potential clients avoid seeking counseling services. The RFSV Scale measures barriers to counseling. This study aimed to validate RFSV scores among U.S. physicians and investigated demographic differences in their scores. Results indicated that the RFSV Scale and its dimensions were adequately estimated with a national sample of physicians in the United States. Physicians’ RFSV scores significantly predicted peer-to-peer counseling referrals. We identified demographic differences in sensitivity to barriers to counseling based on gender identity and help-seeking history. Physicians who self-identified as male and those without help-seeking histories were more sensitive to barriers to counseling than female physicians or physicians with help-seeking histories, respectively. At this phase of development, professional counselors can use the RFSV Scale as a tool for understanding barriers to seeking counseling among physicians.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
American Educational Research Association, American Psychological Association, National Council on Measurement in Education, & Joint Committee on Standards for Educational and Psychological Testing (U.S.). (2014). Standards for educational and psychological testing. https://www.apa.org/science/programs/testing/standards
American Hospital Association. (2022). Suicide prevention: Evidence-informed interventions for the health care workforce. https://www.aha.org/system/files/media/file/2022/09/suicide-prevention_evidence-informed-interventions-for-the-health-care-workforce.pdf
Chen, F. F. (2007). Sensitivity of goodness of fit indexes to lack of measurement invariance. Structural Equation Modeling, 14(3), 464–504. https://doi.org/10.1080/10705510701301834
Cheng, H.-L., Wang, C., McDermott, R. C., Kridel, M., & Rislin, J. L. (2018). Self-stigma, mental health literacy, and attitudes toward seeking psychological help. Journal of Counseling & Development, 96(1), 64–74. https://doi.org/10.1002/jcad.12178
Cheung, G. W., & Rensvold, R. B. (2002). Evaluating goodness-of-fit indexes for testing measurement invariance. Structural Equation Modeling, 9(2), 233–255. https://doi.org/10.1207/S15328007SEM0902_5
Creager, J., Coutinho, A. J., & Peterson, L. E. (2019). Associations between burnout and practice organization in family physicians. Annals of Family Medicine, 17(6), 502–509. https://doi.org/10.1370/afm.2448
Dimitrov, D. M. (2010). Testing for factorial invariance in the context of construct validation. Measurement and Evaluation in Counseling and Development, 43(2), 121–149. https://doi.org/10.1177/0748175610373459
Dimitrov, D. M. (2012). Statistical methods for validation of assessment scale data in counseling and related fields. American Counseling Association.
Douglas, R. N., Sharpe, E. E., Kraus, M., Saddawi-Konefka, D., Hanson, A. C., & Pulos, B. (2023). Mental health questions on state medical license applications and evaluation of updates. JAMA Network Open, 6(9), 1–5. https://doi.org/10.1001/jamanetworkopen.2023.33360
Duarte, D., El-Hagrassy, M. M., Castro e Couto, T., Gurgel, W., Fregni, F., & Correa, H. (2020). Male and female physician suicidality: A systematic review and meta-analysis. JAMA Psychiatry, 77(6), 587–597. https://doi.org/10.1001/jamapsychiatry.2020.0011
Duarte, D., El-Hagrassy, M. M., Couto, T., Gurgel, W., Frey, B. N., Kapczinski, F., & Correa, H. (2022). Physician suicide demographics and the COVID-19 pandemic. Brazilian Journal of Psychiatry, 44(2). https://doi.org/10.1590/1516-4446-2021-1865
Dyrbye, L. N., Eacker, A., Durning, S. J., Brazeau, C., Moutier, C., Massie, F. S., Satele, D., Sloan, J. A., & Shanafelt, T. D. (2015). The impact of stigma and personal experiences on the help-seeking behaviors of medical students with burnout. Academic Medicine, 90(7), 961–969. https://doi.org/10.1097/ACM.0000000000000655
Dyrbye, L. N., West, C. P., Sinsky, C. A., Goeders, L. E., Satele, D. V., & Shanafelt, T. D. (2017). Medical licensure questions and physician reluctance to seek care for mental health conditions. Mayo Clinic Proceedings, 92(10), 1486–1493. https://doi.org/10.1016/j.mayocp.2017.06.020
Gerwe, C., Parks-Savage, A. C., Bertolet, C. L., Kalkbrenner, M. T., & Archer, L. (2017). Promoting the wellness of physician-residents: Counselor-delivered coaching. Counseling & Wellness: A Professional Counseling Journal, 6(1), 1–19.
Gold, K. J., Andrew, L. B., Goldman, E. B., & Schwenk, T. L. (2016). “I would never want to have a mental health diagnosis on my record”: A survey of female physicians on mental health diagnosis, treatment, and reporting. General Hospital Psychiatry, 43(1), 51–57. https://doi.org/10.1016/j.genhosppsych.2016.09.004
Goldman, M. L., Bernstein, C. A., & Summers, R. F. (2018). Potential risks and benefits of mental health screenings of physicians. JAMA, 320(24), 2527–2528. https://doi.org/10.1001/jama.2018.18403
Kalkbrenner, M. T., & Miceli, G. (2022). Barriers to seeking counseling among STEM students: The Revised Fit, Stigma, and Value Scale. The Professional Counselor, 12(3), 249–261. https://doi.org/10.15241/mtk.12.3.249
Kalkbrenner, M. T., & Neukrug, E. S. (2018). Identifying barriers to attendance in counseling among adults in the United States: Confirming the factor structure of the Revised Fit, Stigma, & Value Scale. The Professional Counselor, 8(4), 299–313. https://doi.org/10.15241/mtk.8.4.299
Kalkbrenner, M. T., & Neukrug, E. S. (2019). The utility of the Revised Fit, Stigma, and Value Scale with counselor trainees: Implications for enhancing clinical supervision. The Clinical Supervisor, 38(2), 262–280.
https://doi.org/10.1080/07325223.2019.1634665
Kalkbrenner, M. T., Neukrug, E. S., & Esquivel, L. E. (2022). Mental health literacy screening of students in Hispanic Serving Institutions. Journal of Counseling & Development, 100(3), 319–329. https://doi.org/10.1002/jcad.12428
Kalkbrenner, M. T., Neukrug, E. S., & Griffith, S.-A. M. (2019). Appraising counselors’ attendance in counseling: The validation and application of the Revised Fit, Stigma, and Value Scale. Journal of Mental Health Counseling, 41(1), 21–35. https://doi.org/10.17744/mehc.41.1.03
Kalkbrenner, M. T., Sun, H., & Peterson, S. (2025). Psychometric evaluation of wellness-based screeners: National sample of U.S. physicians. Journal of Mental Health Counseling, 47(1), 74–94. https://doi.org/10.1080/07481756.2024.2441135
Kase, S. M., Gribben, J. L., Waldman, E. D., & Weintraub, A. S. (2020). A pilot study exploring interventions for physician distress in pediatric subspecialists. Pediatric Research, 88(1), 398–403. https://doi.org./10.1038/s41390-020-0805-x
Kevern, T., Davies, D. R., Stiel, K., & Raaum, S. (2023). Impact of opt-out therapy appointments on resident physicians’ mental health, well-being, stigma, and willingness to engage. Journal of Graduate Medical Education, 15(6), 734–737. https://doi.org/10.4300/JGME-D-22-00898.1
Lannin, D. G., Ludwikowski, W. M. A., Vogel, D. L., Seidman, A. J., & Anello, K. (2019). Reducing psychological barriers to therapy via contemplation and self-affirmation. Stigma and Health, 4(3), 247–255. https://doi.org/10.1037/sah0000139
Lenz, A. S., Ault, H., Balkin, R. S., Barrio Minton, C., Erford, B. T., Hays, D. G., Kim, B. S. K., & Li, C. (2022). Responsibilities of users of standardized tests (RUST-4E): Prepared for the Association for Assessment and Research in Counseling. Measurement and Evaluation in Counseling and Development, 55(4), 227–235. https://doi.org/10.1080/07481756.2022.2052321
Lenz, A. S., & Lemberger-Truelove, M. E. (2023). The social determinants of mental health and professional counseling: A call to action. Journal of Counseling & Development, 101(4), 375–380. https://doi.org/10.1002/jcad.12489
Linzer, M., Poplau, S., Babbott, S., Collins, T., Guzman-Corrales, L., Menk, J., Murphy, M. L., & Ovington, K. (2016). Worklife and wellness in academic general internal medicine: Results from a national survey. Journal of General Internal Medicine, 31(9), 1004–1010. https://doi.org/10.1007/s11606-016-3720-4
Lobelo, F., & de Quevedo, I. G. (2016). The evidence in support of physicians and health care providers as physical activity role models. American Journal of Lifestyle Medicine, 10(1), 36–52. https://doi.org/10.1177/1559827613520120
Major, A., Williams, J. G., McGuire, W. C., Floyd, E., & Chacko, K. (2021). Removing barriers: A confidential opt-out mental health pilot program for internal medicine interns. Academic Medicine, 96(5), 686–689. https://doi.org/10.1097/ACM.0000000000003965
Matthew, D. B. (2015). Just medicine: A cure for racial inequality in American health care. New York University Press.
Meade, A. W., & Kroustalis, C. M. (2006). Problems with item parceling for confirmatory factor analytic tests of measurement invariance. Organizational Research Methods, 9(3), 369–403. https://doi.org/10.1177/1094428105283384
Mehta, S. S., & Edwards, M. L. (2018). Suffering in silence: Mental health stigma and physicians’ licensing fears. The American Journal of Psychiatry Residents’ Journal, 13(11), 2–4. https://doi.org/10.1176/appi.ajp-rj.2018.131101
Melnyk, B. M., Kelly, S. A., Stephens, J., Dhakal, K., McGovern, C., Tucker, S., Hoying, J., McRae, K., Ault, S., Spurlock, E., & Bird, S. B. (2020). Interventions to improve mental health, well-being, physical health, and lifestyle behaviors in physicians and nurses: A systematic review. American Journal of Health Promotion, 34(8), 929–941. https://doi.org/10.1177/0890117120920451
Mortali, M., & Moutier, C. (2018). Facilitating help-seeking behavior among medical trainees and physicians using the Interactive Screening Program. Journal of Medical Regulation, 104(2), 27–36. https://doi.org/10.30770/2572-1852-104.2.27
Mullen, P. R., Fox, J., Goshorn, J. R., & Warraich, L. K. (2021). Crowdsourcing for online samples in counseling research. Journal of Counseling & Development, 99(2), 221–226. https://doi.org/10.1002/jcad.12369
Nájera Catalán, H. E. (2019). Reliability, population classification and weighting in multidimensional poverty measurement: A Monte Carlo study. Social Indicators Research, 142(3), 887–910. https://doi.org/10.1007/s11205-018-1950-z
National Board for Certified Counselors. (2023). NBCC code of ethics. https://bit.ly/NBCCCodeofEthics
Pester, D. A., Jones, L. K., & Talib, Z. (2023). Social determinants of mental health: Informing counseling practice and professional identity. Journal of Counseling & Development, 101(4), 392–401. https://doi.org/10.1002/jcad.12473
Ross, P. T., Hart-Johnson, T., Santen, S. A., & Zaidi, N. L. B. (2020). Considerations for using race and ethnicity as quantitative variables in medical education research. Perspectives on Medical Education, 9(5), 318–323. https://doi.org/10.1007/s40037-020-00602-3
Schreiber, J. B., Nora, A., Stage, F. K., Barlow, E. A., & King, J. (2006). Reporting structural equation modeling and confirmatory factor analysis results: A review. The Journal of Educational Research, 99(6), 323–338.
https://doi.org/10.3200/JOER.99.6.323-338
Shanafelt, T. D., Schein, E., Minor, L. B., Trockel, M., Schein, P., & Kirch, D. (2019). Healing the professional culture of medicine. Mayo Clinic Proceedings, 94(8), 1556–1566. https://doi.org/10.1016/j.mayocp.2019.03.026
Sudol, N. T., Guaderrama, N. M., Honsberger, P., Weiss, J., Li, Q., & Whitcomb, E. L. (2021). Prevalence and nature of sexist and racial/ethnic microaggressions against surgeons and anesthesiologists. JAMA Surgery, 156(5), 1–10. https://doi.org/10.1001/jamasurg.2021.0265
Tavakol, M., & Dennick, R. (2011). Making sense of Cronbach’s alpha. International Journal of Medical Education, 2(1), 53–55. https://doi.org/10.5116/ijme.4dfb.8dfd
Trivate, T., Dennis, A. A., Sholl, S., & Wilkinson, T. (2019). Learning and coping through reflection: Exploring patient death experiences of medical students. BMC Medical Education, 19(1), 451. https://doi.org/10.1186/s12909-019-1871-9
Walker, R., & Pine, H. (2018). Physician wellness is an ethical and public health issue. Otolaryngology–Head and Neck Surgery, 158(6), 970–971. https://doi.org/10.1177/0194599818773296
Wiederhold, B. K., Cipresso, P., Pizzioli, D., Wiederhold, M., & Riva, G. (2018). Intervention for physician burnout: A systematic review. Open Medicine, 13(1), 253–263. https://doi.org/10.1515/med-2018-0039
Wimsatt, L. A., Schwenk, T. L., & Sen, A. (2015). Predictors of depression stigma in medical students: Potential targets for prevention and education. American Journal of Preventive Medicine, 49(5), 703–714.
https://doi.org/10.1016/j.amepre.2015.03.021
Michael T. Kalkbrenner, PhD, NCC, is a full professor at New Mexico State University. Shannon Esparza, BA, is a graduate student at New Mexico State University. Correspondence may be addressed to Michael T. Kalkbrenner, Department of Counseling and Educational Psychology, New Mexico State University, Las Cruces, NM 88003, mkalk001@nmsu.edu.
Jul 25, 2025 | Volume 15 - Issue 2
Natalie M. Ricciutti, Willough Davis
Substance use disorders (SUDs) and addictions are prevalent client issues that counselors are likely to encounter. Yet, researchers have previously found that counseling journals publish articles about addiction issues at lower rates when compared to other topics. The purpose of this study was to determine recent publication rates of addiction-focused articles in 24 counseling journals between 2016 and 2023. We determined that only 174 (4%) of 4,356 articles published in counseling journals explored addictions-related issues. We conducted a multiple regression analysis and found that the publishing journal had a significant predictive relationship with the publication of addiction-focused articles, while publication year did not. We provide implications for counselors, researchers, reviewers, and journal editors to advocate for the publication of addiction-focused literature for the benefit of the counseling profession.
Keywords: substance use disorders, addictions, counseling journals, publication rates, addiction-focused articles
Addiction treatment is an important and necessary service to both individuals and communities. The 2022 National Survey on Drug Use and Health published by the Substance Abuse and Mental Health Services Administration (SAMHSA; 2024) estimated that 48.7 million people have a substance use disorder (SUD). The same survey also found that approximately 21.5 million adults in the United States have co-occurring substance use and mental health disorders. These figures indicate that SUDs and addictions are prevalent issues that counseling professionals are likely to treat. Accordingly, the U.S. Bureau of Labor Statistics (2024) estimated that the job outlook for substance abuse, behavioral disorder, and mental health counselors is expected to grow by 18% by 2032. This rate of growth is notably faster than the average career growth rate of 5% for those counseling fields. For this reason, it is important that counselors have access to resources that help them learn about addiction issues and treatment in order to better serve their clients. Research articles are one type of resource counselors and counselors-in-training use regularly (Golubovic et al., 2021; Lee, 2014).
Despite the value placed on published counseling literature (Council for the Accreditation of Counseling and Related Educational Programs [CACREP], 2024; Golubovic et al., 2021), counselors have reported difficulty finding articles written about evidence-based addiction treatment practices and research (Doumas et al., 2019; McCuistian et al., 2023; Ricciutti & Storlie, 2024; Sperandio et al., 2023). Previous researchers also found that addiction-focused articles make up a small percentage of the overall counseling literature (Moro et al., 2016; Wahesh et al., 2017). The potential lack of addiction literature in counseling journals may contribute to professionals being uninformed about evidence-based practices and techniques (Golubovic et al., 2021; Lee, 2014). The purpose of this study was to conduct a conceptual content analysis to determine: (a) the rate and frequency of addiction-focused articles that were published in counseling journals from 2016 to 2023, (b) the journals that published the most addiction-focused articles, (c) the most common type of articles published (quantitative, qualitative, mixed methods, conceptual, etc.), and (d) if publishing journal and year of publication predicted the frequency of published addiction-focused articles.
Addiction Issues in Counseling Specialty Areas
SUDs, addictions, and addiction-related issues are prevalent across a variety of populations and age groups and can be common co-occurring disorders (SAMHSA, 2021, 2024). Addictions are also considered to be a continuously growing public health crisis (Matsuzaka & Knapp, 2020; SAMHSA, 2014; Wing Lo et al., 2020). Given the scope and magnitude of addiction prevalence, counselors are likely to work with individuals with an SUD or addiction in treatment, academic, and clinical settings (Chetty et al., 2023). It is vital that counselors across all counseling specialties are informed about addiction-related issues.
One specialty area in which knowledge about SUD and addiction treatment is of the utmost importance is college counseling. According to the American College Health Association (2023), 65.9% of students reported alcohol use and 30.4% reported cannabis use in the previous 3 months. Additionally, 12.8% of the students who reported alcohol use demonstrated moderate or high risk; 20.5% of the students who reported cannabis use demonstrated moderate or high risk. Researchers have found that use of other substances such as opiates (Schulenberg et al., 2019), unprescribed medication (Sharif et al., 2021), and vaping products (National Institutes of Health, 2020) have all recently increased among college students. College students are also susceptible to developing internet addiction (Krishnamurthy & Chetapalli, 2015; Pu et al., 2023) and sex addiction (Giordano & Cashwell, 2018; Giordano et al., 2017), which are categorized as behavioral addictions (American Psychiatric Association, 2022). Counseling services have been found to have a positive impact on college student substance use (Pu et al., 2023; Zhang et al., 2020). However, students enrolled in counseling programs are not required to complete addiction counseling courses (CACREP, 2024). Some college counselors have reported that they lack the addiction counseling training and competence needed to work with students with an SUD or addiction (DePue & Hagedorn, 2015; Giordano & Cashwell, 2018). The prevalence of substance use and addiction issues in university settings suggests that college counselors may benefit from evidence-based addiction counseling literature.
Career counseling is another specialty area in which professionals may work with individuals experiencing SUDs and addictions. Addiction can impact an individual’s occupational wellness as well as their ability to secure and maintain employment (Allen & Bradley, 2015; Siu et al., 2019). Sherba et al. (2018) found that individuals with addictions experienced difficulty finding and sustaining employment. Researchers also identified that employment issues increased relapse rates for individuals in recovery (Sánchez-Hervás et al., 2012). Conversely, individuals with an SUD or addiction who received career counseling services experienced an increase in career maturity and career self-efficacy (Allen & Bradley, 2015) and a decreased risk of relapse (Kim et al., 2022). Yet, similar to college counselors, future career counselors are not required to take an addiction counseling course (CACREP, 2024). Graham (2006) found that this lack of education may cause career counselors to engage in treatment with biases that may negatively impact the therapeutic alliance. Therefore, career counselors need access to addiction counseling information, as it can be a beneficial aspect of an effective and well-rounded treatment plan and potentially decrease counselors’ biases.
Clinical mental health counselors (CMHCs) may often work with individuals with addictions. It is estimated that 7.7 million American adults have both a diagnosable mental health disorder and an SUD or addiction (Han et al., 2017; SAMHSA, 2024). Common comorbidities include mood and anxiety disorders (Kingston et al., 2017), attention-deficit hyperactivity disorder (Harstad et al., 2014), personality disorders (Medeiros & Grant, 2018; Pennay et al., 2011), and schizophrenia (Menne & Chesworth, 2020). For this reason, CMHCs are likely to work with individuals with addictions who initially seek treatment for a mental health disorder. Han et al. (2017) also found that individuals with comorbid mental health disorders and SUDs may seek out different treatment providers for each diagnosable issue. For example, clients may work with a CMHC for a mood disorder and an addiction counselor for an SUD. This dual treatment approach can be problematic because the providers may be unaware of the individual’s co-occurring disorders, and they may provide contradicting information and treatment (Han et al., 2017). Further, comorbid diagnoses have been found to be more effectively treated when one counselor uses integrated therapeutic modalities for both mental health and SUDs (Chetty et al., 2023). Thus, CMHCs must have access to research and information about SUDs and addiction issues to effectively treat individuals with comorbid disorders.
Like other specialties, marriage or couples and family counseling can be impacted by addiction-related issues. Addiction can lead to decreased trust between married or coupled partners (Molla et al., 2018) and an increased risk of marital dissolution and divorce (Torvik et al., 2013). In family systems, researchers found that having a child with an addiction was associated with lower family quality of life and lower marital satisfaction (Hamza et al., 2021). Children are more likely to experience attachment issues and mental health concerns if one or both parents have an addiction (Patton et al., 2019). Marriage or couples and family counselors must be aware of the impact SUD and addiction issues can have on their clients, as well as effective, evidence-based practices in order to support the development of healthy couple and family functioning.
School counselors also face SUD and addiction-related issues among their students and can work in the areas of intervention and prevention. Substance use at an early age may increase the risk of developing an addiction later in life (Nelson et al., 2015). According to the National Institute on Alcohol Abuse and Alcoholism (2024), 29.8% of high school students reported current alcohol use, 13.2% reported current electric vape use, and 19.8% reported current marijuana use. Some students may also be at risk of developing behavioral addictions, such as internet gaming disorder (Chibbaro et al., 2019; Sylvestro et al., 2023). Similar to marriage or couples and family counselors, school counselors may also work with students whose parents have an addiction (Bröning et al., 2012). These children are at a higher risk of experiencing mental health issues (Patton et al., 2019), experimenting with substances, and developing an addiction themselves (Järvinen, 2015; Leijdesdorff et al., 2017). School counselors play a vital role in the early intervention of substance use and the prevention of addictions because of their position as school-based helping professionals (Bröning et al., 2012). Consequently, school counselors, and all counseling professionals, must have access to accurate, peer-reviewed, evidence-based literature about general addiction issues and specific topics relevant to their specialty.
Addiction-Focused Research and Publications
Despite evidence that substance use and addiction issues are common in every area of counseling (Allen & Bradley, 2015; Han et al., 2017; Pu et al., 2023), previous researchers have found that these issues are not reflected in published research (Moro et al., 2016; Wahesh et al., 2017). In 2017, Wahesh et al. reviewed articles published in 23 counseling journals from 2005 to 2014 and found that 4.5% (210 out of 4,640) were focused on addiction-related topics. They also found that an average of 23.33 addiction-focused articles were published each year from 2005 to 2014. Wahesh et al. highlighted that many journals had the capacity to publish more addiction-focused articles but did not. For example, the Journal of Specialists in Group Work published a total of 209 articles between 2005 and 2014. Only five of those articles were focused on addictions or addiction-related issues. The researchers also analyzed changes in publication trends by year and determined that, of the 210 articles focused on addiction-related topics, most were published in 2011 (n = 30) and 2012 (n = 30), while the fewest articles were published in 2008 (n = 14) and 2009 (n = 17). Wahesh et al. concluded that their results may stem from journals rejecting addiction-focused articles and/or addiction counseling researchers submitting their work to journals in other professions (e.g., psychology, social work, public health).
Moro et al. (2016) found similar results when they explored the prevalence of addiction-related articles in four counseling journals published between 2007 and 2011. They found that the Journal of Counseling and Development (JCD) published three (5.1%) addiction-related articles, Measurement and Evaluation in Counseling and Development (MECD) published two (12.9%) articles, Counseling Outcome Research and Evaluation published four (19%) articles, and Counselor Education and Supervision (CES) did not publish any addiction-related articles. Moro et al. also analyzed the frequency of addiction counseling topics presented at the Association for Counselor Education and Supervision conferences during that time frame. Thirty-six out of 1,966 (1.8%) conference presentations discussed addictions, addiction counseling, or addiction counseling education. These results are particularly concerning because many practicing counselors obtain continuing education through reading articles and attending conferences. Counselors may not have other avenues for learning about addiction-related research and evidence-based treatment if the information is not disseminated to the profession via published literature or conference presentations (Moro et al., 2016).
This lack of published literature and conference presentations has led counselors to advocate for more information about addictions and addiction-related issues. Both Moro et al. (2016) and Wahesh et al. (2017) stressed the importance of publishing more addiction-focused articles in counseling journals. Wahesh et al. specifically advocated for research that focuses on how addictions impact diverse groups, subcommunities, and evidence-based practices. Regarding diverse groups, Chaney (2019) explored the degree to which LGBTQ+ populations were included in articles published in the Journal of Addiction and Offender Counseling (JAOC). Chaney found that five (1.78%) out of the 281 articles published since the inauguration of the journal in 1980 to 2018 were focused on LGBTQ+ individuals. Behavioral addictions are another type of addiction that counselors have reported treating (Király et al., 2020; Oka et al., 2021; Ricciutti & Storlie, 2024), yet there is a dearth of published research (Giordano, 2019; Ricciutti, 2023; Wilson & Johnson, 2013). Ricciutti & Storlie (2024) interviewed practicing counselors about their experiences working with clients with process addictions, and all of the participants indicated that they had trouble finding relevant evidence-based practices and techniques in counseling literature. Carlisle et al. (2016) called for more research about the treatment of internet gaming disorder by counselors. Chaney and Burns-Wortham (2014) advocated for more research about sex addiction among the LGBTQ+ community.
Published research is a necessity for the counseling and counselor education professions (Giordano et al., 2021; Golubovic et al., 2021; Lee, 2014). Advancement in counseling practices cannot occur without the constant publication of exemplary research. Some counseling subtopics have seen a surge in published research within the previous decade (i.e., diversity and multicultural issues). Addiction counselors, researchers, and educators have repeatedly called for more addiction counseling information to be published in counseling journals (Golubovic et al., 2021; Moro et al., 2016; Ricciutti & Storlie, 2024; Wahesh et al., 2017). At this time it is unclear if these calls have been answered and if changes have been made. If they have not, it may reflect the lack of addiction-related content being published in counseling journals.
The purpose of this research study was to update the research done by Wahesh et al. (2017) and to determine: (a) the rate and prevalence of addiction articles that have been published in counseling journals between 2016 and 2023, (b) which journals published the most addiction-focused articles, (c) the type of addiction-focused articles (e.g., quantitative, qualitative, mixed methods) published, and (d) if the publishing journal and year of publication predicted the frequency of published addiction-focused articles. We hope that this research will highlight any changes that counseling journals have made to publish more information about addictions and addiction counseling since
the Wahesh et al. review was published in 2017.
Research Questions
Four research questions guided this study:
RQ1: What was the rate and percentage of addiction-focused articles that were published in counseling journals between 2016 and 2023?
RQ2: Which journals published the most addiction-focused articles?
RQ3: What type of article was most commonly published (e.g., quantitative, qualitative, mixed methods, content analysis, literature review)?
RQ4: Did the publishing journal and the year of publication predict the frequency of published addiction-focused articles?
Methodology
We used journal websites and the library resources at the university where the study took place to answer the research questions. We followed Delve et al. (2023) and Hsieh and Shannon’s (2005) recommended guidelines for conducting a conceptual content analysis research study. These guidelines supported our choice to: (a) focus on the concept of addiction-focused counseling research, (b) identify specific words presented in text form (e.g., “addiction,” “substance use,” “addiction counseling”), (c) follow a combined deductive and inductive coding process by categorizing segments of the text that represent the focused concept, (d) take steps to address potential coder disagreements, and (e) use appropriate subjective interpretation based on our expertise.
Our research team included one professor, Natalie M. Ricciutti, and one doctoral-level graduate student, Willough Davis. Ricciutti has a degree in counselor education and supervision, with specializations in addiction counseling and addiction education, and extensive experience conducting content analysis research. At the time of the study, Davis was enrolled in a counselor education and supervision program and has a strong clinical background in addiction counseling. Davis also assisted in the study to fulfill requirements of an independent study about content analyses. We are both White females who have previously completed multiple courses in research methods. Ricciutti determined the purpose of the study, outlined the coding process, and trained Davis to identify and include relevant data prior to and throughout the study. Davis completed the initial review and categorization of the addiction counseling literature and Ricciutti provided feedback weekly.
Journal Search and Data Collection
In an attempt to update Wahesh et al.’s (2017) study with fidelity, the data collection and review processes in the current study remained the same, with a few exceptions. First, we chose a timeline of 8 inclusive years instead of 9 because 8 years had passed since Wahesh et al. ended their data collection in 2015. Second, we selected the same 23 counseling journals for our study and added the Journal of School Counseling, bringing our journal total to 24. We organized the 24 journals into a list for data collection purposes (Table 1). This list included national journals (n = 19, 79.2%), regional journals (n = 3, 12.5%), and international journals (n = 2, 8.3%). National journals included JCD, CES, JAOC, and the Professional School Counselor; regional journals included Counselor Preparation and Supervision and Teaching & Supervision in Counseling; and international journals included the International Journal for the Advancement of Counseling and the Asia Pacific Journal of Counseling & Psychotherapy. We conducted a thorough review of all the articles published in the 24 journals, which resulted in a total of 4,356 articles.
We reviewed the title, abstract, keywords, and full narrative of each of the 4,356 articles to determine whether or not each was about addiction or substance use–related issues. We labeled articles as addiction-focused if they used addiction-related terminology in the title, abstract, keywords, and/or full narrative. Common terminology included specific types of substance or behavioral addictions, addiction recovery, addiction treatment, and addiction counseling. We also included articles if they focused on addictions or addiction-related topics. Common topics included evidence-based addiction treatment practices, issues related to specific SUDs and behavioral addictions, risk and protective factors of addictions, the impact of addiction and/or substance use among specific populations, and addiction counseling education.
We collected data by categorizing each addiction-focused article’s relevant information in an Excel spreadsheet. This included the article title, the publishing journal, year of publication, the article’s keywords, type of article (e.g., original research, conceptual, literature review), and the type of research the article included (if relevant; quantitative, qualitative, mixed methods). Similar to the inclusion process, we excluded articles if they did not have an addiction-related focus, and they did not include addiction-related terminology in the title, abstract, keywords, and full narrative. Ricciutti reviewed Davis’s categorization of articles and data coding during weekly meetings to ensure coder agreement. We both reviewed articles when it was unclear if an article was focused on addiction-related content. When necessary, we discussed an article’s focus until we resolved disagreements and reached consensus on inclusion or exclusion. Lastly, we cross-referenced our collected data with the 4,356 articles to ensure that we included all of the published addiction-focused articles. We determined that no articles needed to be added or removed. The data was transferred into SPSS (Version 28) for analysis.
Data Analysis
We used descriptive statistics to answer the first research question and to determine the rate and percentage of all addiction-focused articles published in counseling journals between 2016 and 2023. For the second research question, we used descriptive statistics to determine the rate and percentage of the addiction-focused articles published in each journal. For the third research question, we used descriptive statistics to determine the rate and percentage of the type of articles and the research methodology researchers used. We also used descriptive statistics to determine the number of the type of article and type of methodology published each year (Figures 1 and 2). We conducted a multiple regression analysis to answer the final research question to determine the predictive relationship between the independent variables of publishing journal and year of publication as well as the dependent variable of frequency of published addiction-focused articles.
Table 1
Addiction-Focused Article Trends per Journal
| Journal |
Total Number of Articles |
Number of Addiction-Focused Articles |
Percentage of Addiction-Focused Articles |
| Adultspan Journal |
62 |
0 |
0% |
| Asia Pacific Journal of Counseling and Psychotherapy |
96 |
0 |
0% |
| Counseling Outcome Research and Evaluation |
79 |
4 |
5.0% |
| Counseling and Values |
107 |
2 |
1.87% |
| Counselor Education and Supervision |
178 |
1 |
0.56% |
| The Family Journal |
448 |
20 |
4.46% |
| International Journal for the Advancement of Counseling |
281 |
7 |
4.49% |
| The Journal for Specialists in Group Work |
141 |
2 |
1.42% |
| Journal of Addiction & Offender Counseling |
67 |
51 |
74.63% |
| Journal of College Counseling |
118 |
15 |
13.56% |
| Journal of Counseling & Development |
324 |
14 |
4.32% |
| Journal of Counselor Preparation and Supervision |
305 |
4 |
1.31% |
| Journal of Creativity in Mental Health |
316 |
12 |
4.11% |
| Journal of Employment Counseling |
114 |
1 |
0.89% |
| Journal of Humanistic Counseling |
117 |
3 |
2.56% |
| Journal of LGBT Issues in Counseling |
155 |
4 |
2.58% |
| Journal of Mental Health Counseling |
182 |
6 |
3.29% |
| Journal of Multicultural Counseling & Development |
148 |
2 |
1.35% |
| Journal of School Counseling |
172 |
3 |
1.74% |
| Journal of Technology in CE&S |
49 |
0 |
0% |
| Measurement and Evaluation in Counseling and Development |
167 |
6 |
3.59% |
| The Professional Counselor |
227 |
11 |
4.85% |
| Professional School Counselor |
408 |
2 |
0.98% |
| Teaching and Supervision in Counseling |
95 |
2 |
2.11% |
Note. Total number of articles is 4,356. Number of addiction-focused articles is 174.
Figure 1
Type of Addiction-Focused Articles Published per Year
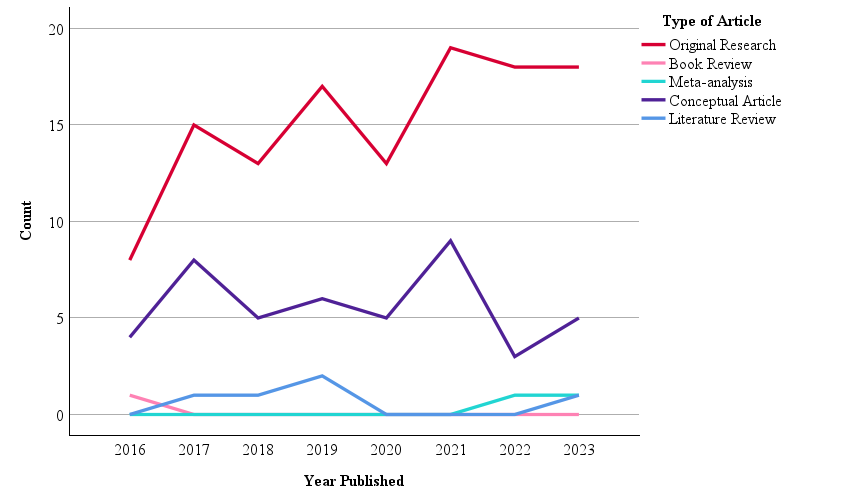 Note. N = 174.
Note. N = 174.
Figure 2
Type of Research in Published Addiction-Focused Articles per Year
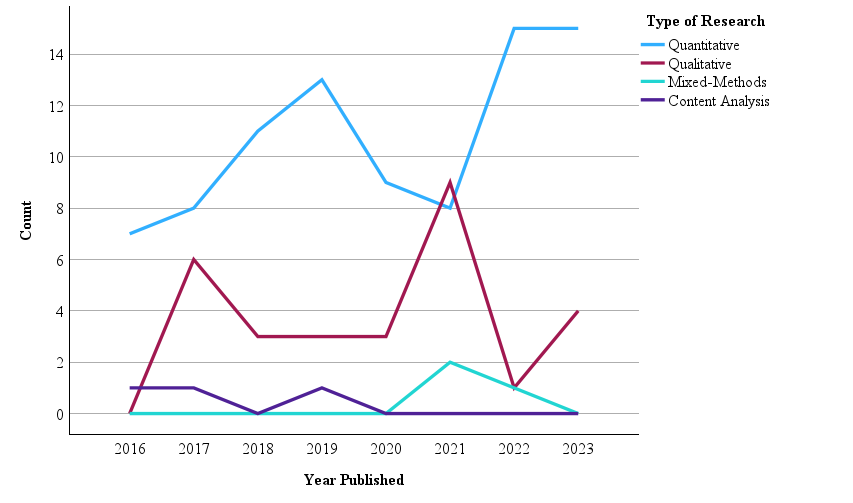
Note. N = 121.
Results
Of the 4,356 articles published in 24 counseling journals from 2016 to 2023, we identified 174 (4%) as focused on addiction counseling or other addiction-related issues (Table 1). Regarding our second research question, JAOC had the highest rate and percentage of addiction-focused articles at 74.63% (n = 51). Adultspan Journal, Asia Pacific Journal of Counseling & Psychotherapy, and Technology in CES were tied with the lowest percentage of addiction-focused articles at 0%. Regarding the third research question, the most common type of article was original research (n = 121, 69.5%). Other types of articles included conceptual pieces (n = 45, 25.9%), literature reviews (n = 5, 2.9%), meta-analyses (n = 2, 1.1%), and book reviews (n = 1, 0.6%). Figure 1 provides a description of the type of addiction-focused articles published during each year. Of the 121 original research articles, 86 (71.1%) were quantitative studies, 29 (24%) were qualitative studies, three (2.5%) were content analyses, and three (2.5%) were mixed method studies. Figure 2 provides a description of the type of research conducted in each addiction-focused published article during each year.
Regarding the fourth research question, we first calculated yearly analyses to determine the number of addiction-focused articles published in counseling journals each year (Table 2). The year 2016 had the lowest number of published addiction-focused articles (n = 13, 7.5%), while 2021 had the highest (n = 28, 16.1%). On average, 21.75 addiction-focused articles were published each year from 2016 to 2023. Next, we conducted a multiple linear regression analysis to determine if journal and year of publication had a predictive relationship with the frequency of published addiction-focused articles. This analysis resulted in a statistically significant regression model, F(2, 187) = 4.134, p = .018, R2 = 0.42. Finally, we examined the individual predictors (i.e., independent variables). We found that publishing journal had a significant predictive relationship with the frequency of published addiction-focused articles, (Beta = −.192, t(189) = −3.682, p = .008). In other words, some journals were significant predictors of being more likely to publish addiction-focused articles than others. We also found that publication year did not have a significant predictive relationship with the frequency of published addiction-focused articles (Beta = .07, t(189) = .973, p = .332).
Table 2
Addictions-Focused Articles Published Per Year
| Year |
n |
% |
| 2016 |
13 |
7.5 |
| 2017 |
24 |
13.8 |
| 2018 |
19 |
10.9 |
| 2019 |
25 |
14.4 |
| 2020 |
18 |
10.3 |
| 2021 |
28 |
16.1 |
| 2022 |
22 |
12.6 |
| 2023 |
25 |
14.4 |
Note. Total N = 174.
Discussion
The purpose of this study was to examine the frequency of addiction-focused articles published in counseling journals in recent years. We reviewed 4,356 articles published in 24 counseling journals from 2016 to 2023 to determine the frequency and percentage of addiction-focused literature in the counseling profession. The results indicate only 174 (4%) of those articles were focused on addiction counseling or other addiction-related issues. This percentage is less than previously identified by Wahesh et al. (2017), who found that 210 (4.5%) out of 4,640 articles published from 2005 to 2014 were about addiction issues. Publication year also did not have a significant, predictive relationship with publication rates. This result suggests that national and global events occurring between 2016 and 2023 (e.g., the opioid epidemic, the COVID-19 pandemic) did not statistically impact the publication of addiction-focused articles in counseling journals.
We also determined that the majority of addiction-focused articles were original research, many of which used quantitative analytic techniques. This result reflects a long-standing trend toward quantitative methodologies in the counseling and other helping professions (Berríos & Lucca, 2006; Marshall et al., 2025; Oh et al., 2017). We also found that only three of the 174 addiction-focused articles used mixed methods techniques. This number is lower than Wahesh et al.’s (2017) finding of six mixed methods studies. Researchers and professionals in counseling have called for more mixed methods research to achieve well-rounded study findings (Ponterotto et al., 2013; Wester & McKibben, 2019). Our results indicate that this change has yet to occur with addiction-focused research published in counseling journals.
It is worth noting the differences we found in publication rates by journal when considering potential reasons for the lack of addiction-focused counseling literature. The specific journal and the publication of addiction-focused articles had a significant, predictive relationship. Unsurprisingly, JAOC published the most addiction-related literature in both number and percentage. Yet, it had one of the lowest numbers of total published articles (67 from 2016 to 2023; Table 1). As discussed, counselors have reported experiencing difficulty finding relevant, evidence-based addiction counseling literature to support their practice (Chaney, 2019; Ricciutti & Storlie, 2024; Wilson & Johnson, 2013). This struggle may be because the only addiction counseling journal has one of the lowest publication rates out of the 24 journals included in this study.
Another reason for the publication rate may be a lack of addiction-focused articles being submitted to counseling journals. Instead, counseling researchers with expertise in addiction issues may be submitting their manuscripts to journals in other professions (e.g., psychology, social work, public health, etc.). We did not find a study exploring the rates of addiction-focused articles in the psychology, social work, or public health professions to compare with our findings. Yet, these professions each have many addiction and substance use–focused journals where researchers can choose to submit their work. A Google Scholar (2024) search of all addiction journals’ h5-indices (i.e., the number of articles published in the last 5 years) and h5-medians (i.e., the median number of citations for articles in the h5-index) shows that the top 20 publications at the time of this writing are the psychology journals the International Journal of Mental Health and Addiction, Drug and Alcohol Dependence, and Addictive Behaviors. JAOC was not included in that list.
The results may also be due to the small number of counseling researchers and educators with expertise in addiction issues compared to the overall profession. A number of studies have found that many counseling students leave their programs without the necessary academic experience to competently practice addiction counseling (Golubovic et al., 2021; Lee, 2014; Ricciutti & Storlie, 2024). As discussed, CACREP (2024) standards do not include addiction counseling content requirements for many of the specialty practice areas. Ricciutti & Storlie (2024) found that the lack of education caused some counselors to report that addiction counseling was not part of their professional identity. For this reason, we join Moro et al. (2016) in advocating for the inclusion of an addictions course into the counseling core curriculum. Requiring a course for all students may help future counselors incorporate addiction counseling into their professional identity. Doing so could instill future counselors with a passion for addiction issues and eventually lead to an increase in addiction-focused manuscripts submitted for publication in counseling journals.
Recommendations for Counselors, Counselor Educators, and Researchers
Addiction-focused literature published in counseling journals is highly relevant for practicing counselors, counseling researchers, and the overall profession. Substantial value is placed on published research to advance the counseling profession (CACREP, 2024; Golubovic et al., 2021). SUD and addictions are common primary and co-occurring disorders (SAMHSA, 2021, 2024) and the job outlook for addiction and substance use counselors is expected to grow rapidly (U.S. Bureau of Labor Statistics, 2024). Counselors in every specialty area need relevant, evidence-based research about SUD and addiction issues to inform their practice. Yet, we found the publication of addiction-focused articles to be low, with some journals failing to publish anything about addiction issues from 2016 to 2023. Journals may want to consider how to solicit addiction-focused content for publication to fill this research gap.
The existing prevalence rates of addiction-focused articles may, in part, stem from researchers not submitting articles about addiction issues to counseling journals. Researchers may believe that their manuscript is likely to be rejected if it is sent to a journal that has not published an addiction-related article in recent years. We encourage authors and researchers to push against this potential belief and consider submitting their addiction-focused manuscripts to journals that have not recently published articles about the topic. This practice could inform editors and reviewers about addiction-related issues in the counseling profession, as well as help authors reach new audiences who may not normally read addiction-focused articles. Counselors and researchers also can attempt to advocate for the inclusion of addiction-focused articles in the journals they frequently read. This advocacy can come in the form of writing letters to journal editors to request more addiction content. Practicing counselors can also work to conduct addiction-focused research studies through their agencies, practices, schools, or universities. The information gleaned from studies that are conducted in novel settings with diverse populations would be highly relevant to the profession and help grow the existing body of literature.
An increase in addiction-focused research studies and submitted manuscripts is only the first step toward a higher prevalence of published articles. Journal review boards and editors must be willing to expand the aims, scope, and acceptable topics to include addiction-related issues. For example, addiction issues are highly relevant in every counseling specialty area, including school counseling (Bröning et al., 2012). Yet, the Professional School Counselor published two addiction-focused articles and the Journal of School Counseling only published three (Table 1). This is despite recent evidence that substance use and addiction issues continue to be a common issue among children and adolescents in the last decade (National Institute on Drug Abuse, 2023). Editors and reviewers expanding journals’ scope and acceptable topics for consideration may allow researchers with an expertise in addiction counseling to feel more confident sending their manuscripts to counseling journals other than JAOC.
Journals can sponsor special issues that are dedicated to addiction-related topics. We urge researchers, writers, journal editors, and reviewers to consider the long-term implications and benefits of providing more addiction-focused articles to the entire counseling profession. These journal practices will help grow the existing literature over time; expand addiction-related topics to a variety of co-occurring disorders and populations; and provide new opportunities for continuing education, much of which can be obtained through reading and contributing to journal articles. For example, Chaney (2019) called for more literature about substance use and addiction among the LGBTQ+ community. The Journal of LGBT Issues in Counseling could combine both topics in a special issue. Finally, we encourage CACREP to consider adding new addiction counseling standards to their next edition at both the master’s and doctoral levels. As discussed, counselors in every specialty area are likely to work with individuals with addictions and SUDs (Bröning et al., 2012; Kim et al., 2022; Patton et al., 2019). Yet, many have reported their training and skills in this area have fallen short of competence (DePue & Hagedorn, 2015; Giordano & Cashwell, 2018; Han et al., 2017). It is necessary that all counselors receive education in addiction counseling in order to better serve their clients or students.
Limitations
This study is not without limitations. First, as with any conceptual content analysis, researcher error and subjective interpretation of the data is a potential limitation. Although we fully reviewed each of the 4,640 articles, we identified addiction-focused articles, in part, through the inclusion of addiction terminology in the title, abstract, keywords, and narrative. It is possible we unintentionally excluded relevant articles or included articles that were irrelevant because we did not use statistical measures of interrater reliability. Similarly, it is possible there was addiction-related language and terminology that we were unfamiliar with, causing us to exclude articles that should have been included. We also may have allowed our unconscious biases to impact our data inclusion process throughout the study. We worked to mitigate this potential limitation by reviewing each article in full and by following recommended guidelines for conducting a conceptual content analysis (Delve et al., 2023; Hsieh & Shannon, 2005).
Second, this study focuses on addiction articles published in 24 counseling journals from 2016 to 2023. For this reason, it is possible that our study may not accurately reflect published addiction-focused articles over a broader period of time or with different journals. We encourage future researchers to review additional counseling journals not included in this study, such as state counseling journals or local university counseling journals. Third, we only collected and analyzed data that was publicly available—published articles in counseling journals. We did not gather data on the number of addiction-focused manuscripts that were submitted to journals but not published. Future researchers may consider contacting counseling journal editors to ascertain the rate of submitted manuscripts that were not published for any reason (e.g., rejected, author pulled their manuscript). Researchers can then compare the number of submitted addiction manuscripts with the number of published articles. Doing so may incorporate data excluded from this study and determine if the small number of addiction-focused articles is due to lack of quality submissions or potential reviewer and editor bias. Researchers could also conduct a similar study with journals in other helping professions (e.g., psychology, social work, public health) to determine if our results reflect a common trend in the publication of addiction-focused articles.
Conclusion
We explored the prevalence of addiction-focused articles published in 24 counseling journals from 2016 to 2023 and found recent publication rates to be low. We reported the journals that have published addiction-focused articles during that time frame, the type of articles published, and the potential impact of journal and year of publication. We compared our findings with Wahesh et al. (2017) and determined that the prevalence and rate of addiction articles has not increased since 2005. The lack of information may make it difficult for counselors in every specialty area to learn about addiction issues relevant to their clients or students. Finally, we provided information about the importance of addiction literature in the counseling profession and the implications of journals expanding their aims and scopes to include addiction issues.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Allen, K. R., & Bradley, L. (2015). Career counseling with juvenile offenders: Effects on self-efficacy and career maturity. Journal of Addictions & Offender Counseling, 36(1), 28–42. https://doi.org/10.1002/j.2161-1874.2015.00033.x
American College Health Association. (2023). National College Health Assessment: Spring 2022 reference group executive summary. https://www.acha.org/ncha/data-results
American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (5th ed., text rev.). https://doi.org/10.1176/appi.books.9780890425787
Berríos, R., & Lucca, N. (2006). Qualitative methodology in counseling research: Recent contributions and challenges for a new century. Journal of Counseling & Development, 84(2), 174–186. https://doi.org/10.1002/j.1556-6678.2006.tb00393.x
Bröning, S., Kumpfer, K., Kruse, K., Sack, P.-M., Schaunig-Busch, I., Ruths, S., Moesgen, D., Pflug, E., Klein, M., & Thomasius, R. (2012). Selective prevention programs for children from substance-affected families: A comprehensive systematic review. Substance Abuse Treatment, Prevention, and Policy, 7(23), 1–17. http://www.substanceabusepolicy.com/content/7/1/23
Carlisle, K. L., Carlisle, R. M., Polychronopoulos, G. B., Goodman-Scott, E., & Kirk-Jenkins, A. (2016). Exploring internet addiction as a process addiction. Journal of Mental Health Counseling, 38(2), 170–182. https://doi.org/10.17744/mehc.38.2.07
Chaney, M. P. (2019). LGBTQ+ addiction research: An analysis of the Journal of Addictions & Offender Counseling. Journal of Addictions & Offender Counseling, 40(1), 2–16. https://doi.org/10.1002/jaoc.12053
Chaney, M. P., & Burns-Wortham, C. M. (2014). The relationship between online sexual compulsivity, dissociation, and past child abuse among men who have sex with men. Journal of LGBT Issues in Counseling, 8(2), 146–163. https://doi.org/10.1080/15538605.2014.895663
Chetty, A., Guse, T., & Malema, M. (2023). Integrated vs non-integrated treatment outcomes in dual diagnosis disorders: A systematic review. Health SA Gesondheid, 28(1), a2094. https://doi.org/10.4102/hsag.v28i0.2094
Chibbaro, J. S., Ricks, L., & Lanier, B. (2019). Digital awareness: A model for school counselors. Journal of School Counseling, 17(22). https://jsc.montana.edu/articles/v17n22.pdf
Council for the Accreditation of Counseling and Related Educational Programs. (2024). 2024 CACREP standards. https://www.cacrep.org/wp-content/uploads/2024/04/2024-Standards-Combined-Version-4.11.2024.pdf
Delve, Ho, L., & Limpaecher, A. (2023, January 25). What is conceptual content analysis in qualitative research? Step-by-step guide. https://delvetool.com/blog/what-is-conceptual-qualitative-content-analysis-step-by-step-guide
DePue, M. K., & Hagedorn, W. B. (2015). Facilitating college students’ recovery through the use of collegiate recovery programs. Journal of College Counseling, 18(1), 66–81. https://doi.org/10.1002/j.2161-1882.2015.00069.x
Doumas, D. M., Miller, R. M., & Esp, S. (2019). Continuing education in motivational interviewing for addiction counselors: Reducing the research-to-practice gap. Journal of Addictions & Offender Counseling, 40(1), 36–51. https://doi.org/10.1002/jaoc.12055
Giordano, A. L., & Cashwell, C. S. (2018). An examination of college counselors’ work with student sex addiction: Training, screening, and referrals. Journal of College Counseling, 21(1), 43–57. https://doi.org/10.1002/jocc.12086
Giordano, A. L., Cashwell, C. S., Lankford, C., King, K., & Henson, R. K. (2017). Collegiate sexual addiction: Exploring religious coping and attachment. Journal of Counseling & Development, 95(2), 135–144. http://doi.org/10.1002/jcad.12126
Giordano, A. L., Malacara, A., & Agarwal, S. (2019). A process addictions course for counselor training programs. Teaching and Supervision in Counseling, 1(1), 47–59. https://doi.org/10.7290/tcs010105
Giordano, A. L., Schmit, M. K., & Schmit, E. L. (2021). Best practice guidelines for publishing rigorous research in counseling. Journal of Counseling & Development, 99(2), 123–133. https://doi.org/10.1002/jcad.12360
Golubovic, N., Dew, B., Rumsey, A., Murphy, T., Dispenza, F., Tabet, S., & Lebensohn-Chialvo, F. (2021). Pedagogical practices for teaching addiction counseling courses in CACREP-accredited programs. Journal of Addictions & Offender Counseling, 42(1), 3–18. http://doi.org/10.1002/jaoc.12086
Google Scholar. (2024). Addiction – Google Scholar Metrics. https://scholar.google.com/citations?view_op=top_venues&hl=en&vq=med_addiction
Graham, M. D. (2006). Addiction, the addict, and career: Considerations for the employment counselor. Journal of Employment Counseling, 43(4), 168–178. https://doi.org/10.1002/j.2161-1920.2006.tb00016.x
Hamza, E. G. A., Gladding, S., & Moustafa, A. A. (2021). The impact of adolescent substance abuse on family quality of life, marital satisfaction, and mental health in Qatar. The Family Journal, 30(1), 85–90. https://doi.org/10.1177/10664807211000720
Han, B., Compton, W. M., Blanco, C., & Colpe, L. J. (2017). Prevalence, treatment, and unmet treatment needs of US adults with mental health and substance use disorders. Health Affairs, 36(10), 1739–1747. https://doi.org/10.1377/hlthaff.2017.0584
Harstad, E., Levy, S., & Committee on Substance Abuse. (2014). Attention-deficit/hyperactivity disorder and substance abuse. Pediatrics, 134(1), e293–e301. https://doi.org/10.1542/peds.2014-0992
Hsieh, H.-F., & Shannon, S. E. (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15(9), 1277–1288. https://doi.org/10.1177/1049732305276687
Järvinen, M. (2015). Understanding addiction: Adult children of alcoholics describing their parents’ drinking problems. Journal of Family Issues, 36(6), 805–825. http://doi.org/10.1177/0192513X13513027
Kim, M., Byrne, A. M., & Jeon, J. (2022). The effect of vocational counseling interventions for adults with substance use disorders: A narrative review. International Journal of Environmental Research and Public Health, 19(8), 4674. https://doi.org/10.3390/ijerph19084674
Kingston, R. E. F., Marel, C., & Mills, K. L. (2017). A systematic review of the prevalence of comorbid mental health disorders in people presenting for substance use treatment in Australia. Drug and Alcohol Review, 36(4), 527–539. https://doi.org/10.1111/dar.12448
Király, O., Potenza, M. N., Stein, D. J., King, D. L., Hodgins, D. C., Saunders, J. B., Griffiths, M. D., Gjoneska, B., Billieux, J., Brand, M., Abbott, M. W., Chamberlain, S. R., Corazza, O., Burkauskas, J., Sales, C. M. D., Montag, C., Lochner, C., Grünblatt, E., Wegmann, E., . . . Demetrovics, Z. (2020). Preventing problematic internet use during the COVID-19 pandemic: Consensus guidance. Comprehensive Psychiatry, 100.
https://doi.org/10.1016/j.comppsych.2020.152180
Krishnamurthy, S., & Chetapalli, S. K. (2015). Internet addiction: Prevalence and risk factors, A cross-sectional study among college students in Bengaluru, the Silicon Valley of India. Indian Journal of Public Health, 59(2), 115–121. https://doi.org/10.4103/0019-557X.157531
Lee, T. K. (2014). Addiction education and training for counselors: A qualitative study of five experts. Journal of Addictions & Offender Counseling, 35(2), 67–80. https://doi.org/10.1002/j.2161-1874.2014.00027.x
Leijdesdorff, S., van Doesum, K., Popma, A., Klaassen, R., & van Amelsvoort, T. (2017). Prevalence of psychopathology in children of parents with mental illness and/or addiction: An up to date narrative review. Current Opinion in Psychiatry, 30(4), 312–317. https://doi.org/10.1097/YCO.0000000000000341
Marshall, D. T., Elmer, J. W., Hebert, C. C., & Barringer, K. E. (2025). Counseling research trends: A content analysis 2016–2020. Journal of Professional Counseling: Practice, Theory & Research, 52(1), 51–65. https://doi.org/10.1080/15566382.2024.2368647
Matsuzaka, S., & Knapp, M. (2020). Anti-racism and substance use treatment: Addiction does not discriminate, but do we? Journal of Ethnicity in Substance Abuse, 19(4), 567–593. https://doi.org/10.1080/15332640.2018.1548323
McCuistian, C., Fokuo, J. K., Dumoit Smith, J., Sorensen, J. L., & Arnold, E. A. (2023). Ethical dilemmas facing substance use counselors during the COVID-19 pandemic. Substance Use: Research and Treatment, 17, 1–19. https://doi.org/10.1177/11782218231158338
Medeiros, G. C., & Grant, J. E. (2018). Gambling disorder and obsessive–compulsive personality disorder: A frequent but understudied comorbidity. Journal of Behavioral Addictions, 7(2), 366–374. https://doi.org/10.1556/2006.7.2018.50
Menne, V., & Chesworth, R. (2020). Schizophrenia and drug addiction comorbidity: Recent advances in our understanding of behavioural susceptibility and neural mechanisms. Neuroanatomy and Behaviour, 2(1), e10. https://doi.org/10.35430/nab.2020.e10
Molla, E., Tadros, E., & Cappetto, M. (2018). The effects of alcohol and substance use on a couple system: A clinical case study. The Family Journal, 26(3), 341–350. https://doi.org/10.1177/1066480718795500
Moro, R. R., Wahesh, E., Likis-Werle, S. E., & Smith, J. E. (2016). Addiction topics in counselor educator professional development: A content analysis. Journal of Addictions & Offender Counseling, 37(1), 2–15. https://doi.org/10.1002/jaoc.12012
National Institute on Alcohol Abuse and Alcoholism. (2024). Underage drinking in the United States (ages 12 to 20). https://www.niaaa.nih.gov/alcohols-effects-health/alcohol-topics/alcohol-facts-and-statistics/underage-drinking-united-states-ages-12-20
National Institute on Drug Abuse. (2023, December 13). Reported drug use among adolescents continued to hold below pre-pandemic levels in 2023. https://nida.nih.gov/news-events/news-releases/2023/12/reported-drug-use-among-adolescents-continued-to-hold-below-pre-pandemic-levels-in-2023
National Institutes of Health. (2020, September 15). Vaping, marijuana use in 2019 rose in college-age adults.
https://www.nih.gov/news-events/news-releases/vaping-marijuana-use-2019-rose-college-age-adults
Nelson, S. E., Van Ryzin, M. J., & Dishion, T. J. (2015). Alcohol, marijuana, and tobacco use trajectories from age 12 to 24 years: Demographic correlates and young adult substance use problems. Development and Psychopathology, 27(1), 253–277. https://doi.org/10.1017/S0954579414000650
Oh, J., Stewart, A. E., & Phelps, R. E. (2017). Topics in the Journal of Counseling Psychology, 1963–2015. Journal of Counseling Psychology, 64(6), 604–615. https://doi.org/10.1037/cou0000218
Oka, T., Hamamura, T., Miyake, Y., Kobayashi, N., Honjo, M., Kawato, M., Kubo, T., & Chiba, T. (2021). Prevalence and risk factors of internet gaming disorder and problematic internet use before and during the COVID-19 pandemic: A large online survey of Japanese adults. Journal of Psychiatric Research, 142, 218–225. https://doi.org/10.1016/j.jpsychires.2021.07.054
Patton, R., Goerke, J., Fye, J., & Katafiasz, H. (2019). Does hazardous alcohol use impact individual and relational functioning among couples seeking couples therapy? The Family Journal, 27(3), 287–292. https://doi.org/10.1177/1066480719844033
Pennay, A., Cameron, J., Reichert, T., Strickland, H., Lee, N. K., Hall, K., & Lubman, D. I. (2011). A systematic review of interventions for co-occurring substance use disorder and borderline personality disorder. Journal of Substance Abuse Treatment, 41(4), 363–373. https://doi.org/10.1016/j.jsat.2011.05.004
Ponterotto, J. G., Mathew, J. T., & Raughley, B. (2013). The value of mixed methods designs to social justice research in counseling and psychology. Journal for Social Action in Counseling & Psychology, 5(2), 42–68. https://doi.org/10.33043/JSACP.5.2.42-68
Pu, Y., Liu, Y., Qi, Y., Yan, Z., Zhang, X., & He, Q. (2023). Five-week of solution-focused group counseling successfully reduces internet addiction among college students: A pilot study. Journal of Behavioral Addictions, 12(4), 964–971. https://doi.org/10.1556/2006.2023.00064
Ricciutti, N. M. (2023). Counselors’ stigma toward addictions: Increasing awareness and decreasing stigma. Journal of Counselor Preparation and Supervision, 17(3). https://digitalcommons.sacredheart.edu/jcps/vol17/iss3/6
Ricciutti, N. M. & Storlie, C. A. (2024). The experiences of clinical mental health counselors treating clients for process/behavioral addictions. Alcoholism Treatment Quarterly, 42(1), 27–44. https://doi.org/10.1080/07347324.2023.2267004
Sánchez-Hervás, E., Gómez, F. J., Villa, R. S., García-Fernández, G., García-Rodríguez, O., & Romaguera, F. Z. (2012). Psychosocial predictors of relapse in cocaine-dependent patients in treatment. The Spanish Journal of Psychology, 15(2), 748–755. https://doi.org/10.5209/rev_SJOP.2012.v15.n2.38886
Schulenberg, J. E., Johnston, L. D., O’Malley, P. M., Bachman, J. G., Miech, R. A., & Patrick, M. E. (2019). Monitoring the Future national survey results on drug use, 1975–2018: Volume 2, College students & adults ages 19–60. Institute for Social Research, The University of Michigan. https://monitoringthefuture.org/wp-content/uploads/2022/08/mtf-vol2_2018.pdf
Sharif, S., Guirguis, A., Fergus, S., & Schifano, F. (2021). The use and impact of cognitive enhancers among university students: A systematic review. Brain Sciences, 11(3), 355. https://doi.org/10.3390/brainsci11030355
Sherba, R. T., Coxe, K. A., Gersper, B. E., & Vinley, J. V. (2018). Employment services and substance abuse treatment. Journal of Substance Abuse Treatment, 87, 70–78. https://doi.org/10.1016/j.jsat.2018.01.015
Siu, A. M. H., Fung, M. S. M., Cheung, P. P. P., Shea, C. K., & Lau, B. W. M. (2019). Vocational evaluation and vocational guidance for young people with a history of drug abuse. WORK: A Journal of Prevention, Assessment & Rehabilitation, 62(2), 327–336. https://doi.org/10.3233/WOR-192867
Sperandio, K. R., Goshorn, J. R., Moh, Y. S., Gonzalez, E., & Johnson, N. G. (2023). Never ready: Addictions counselors dealing with client death. Journal of Counseling & Development, 101(1), 29–45. https://doi.org/10.1002/jcad.12440
Substance Abuse and Mental Health Services Administration. (2014). Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H-48, HHS Publication No. (SMA) 14-4863.
https://www.samhsa.gov/data/sites/default/files/NSDUHresultsPDFWHTML2013/Web/NSDUHresults2013.pdf
Substance Abuse and Mental Health Services Administration. (2021). Key substance use and mental health indicators in the United States: Results from the 2020 National Survey on Drug Use and Health. http://www.samhsa.gov/data/sites/default/files/reports/rpt35325/NSDUHFFRPDFWHTMLFiles2020/2020NSDUHFFR1PDFW102121.pdf
Substance Abuse and Mental Health Services Administration. (2024). 2022 National Survey on Drug Use and Health. https://www.datafiles.samhsa.gov/dataset/national-survey-drug-use-and-health-2022-nsduh-2022-ds0001
Sylvestro, H. M., Glance, D. E., Ripley, D., & Stephenson, R. (2023). Elementary school counselors’ experiences working with children affected by parental substance use. Professional School Counseling, 27(1). https://doi.org/10.1177/2156759X231182142
Torvik, F. A., Røysamb, E., Gustavson, K., Idstad, M., & Tambs, K. (2013). Discordant and concordant alcohol use in spouses as predictors of marital dissolution in the general population: Results from the Hunt Study. Alcoholism: Clinical and Experimental Research, 37(5), 877–884. https://doi.org/10.1111/acer.12029
U.S. Bureau of Labor Statistics. (2024). Substance abuse, behavioral disorder, and mental health counselors.
http://www.bls.gov/ooh/community-and-social-service/substance-abuse-behavioral-disorder-and-mental-health-counselors.htm
Wahesh, E., Likis-Werle, S. E., & Moro, R. R. (2017). Addictions content published in counseling journals: A 10-year content analysis to inform research and practice. The Professional Counselor, 7(1), 89–103. https://doi.org/10.15241/ew.7.1.89
Wester, K., & McKibben, B. (2019). Integrating mixed methods approaches in counseling outcome research. Counseling Outcome Research and Evaluation, 10(1), 1–11. http://doi.org/10.1080/21501378.2018.1531239
Wilson, A. D., & Johnson, P. (2013). Counselors’ understanding of process addiction: A blind spot in the counseling field. The Professional Counselor, 3(1), 16–22. https://doi.org/10.15241/adw.3.1.16
Wing Lo, T., Yeung, J. W. K., & Tam, C. H. L. (2020). Substance abuse and public health: A multilevel perspective and multiple responses. International Journal of Environmental Research and Public Health, 17(7), 2610. https://doi.org/10.3390/ijerph17072610
Zhang, X., Shi, X., Xu, S., Qiu, J., Turel, O., & He, Q. (2020). The effect of solution-focused group counseling intervention on college students’ internet addiction: A pilot study. International Journal of Environmental Research and Public Health, 17(7), 2519. https://doi.org/10.3390/ijerph17072519
Natalie M. Ricciutti, PhD, NCC, LPCC, LCASA, is an assistant professor at the University of North Carolina Charlotte. Willough Davis, MEd, NCC, LCMHC, LCASA, is a doctoral candidate at the University of North Carolina Charlotte. Correspondence may be addressed to Natalie M. Ricciutti, University of North Carolina Charlotte, 9201 University City Blvd., Charlotte, NC 28223, nricciut@charlotte.edu.
Jul 25, 2025 | Volume 15 - Issue 2
Kelly Emelianchik-Key, Adriana C. Labarta, Clara Bossie, Carman S. Gill
Self-compassion, or the ability to show oneself kindness in challenging situations, has various advantages for mental well-being and psychological health, encompassing three interrelated elements: self-kindness, common humanity, and mindfulness. Mothers are an often-overlooked population who face numerous mental health challenges because of socially constructed ideals of motherhood. Therefore, mothers may encounter obstacles in developing self-compassion amid the demands of motherhood, related societal pressures, and other contextual factors, such as the COVID-19 pandemic. This research study utilized a photovoice methodology to investigate how mothers with children ages 5 to 12 experience self-compassion post–COVID-19 pandemic. The findings revealed four main themes with 13 subthemes, illustrating the distinct challenges and benefits associated with self-compassion for mothers. The authors conclude with implications for counseling, including the need for interventions that promote self-compassion and wellness for mothers from culturally and racially diverse communities.
Keywords: mothers, motherhood, self-compassion, photovoice, wellness
Intensive mothering, a term coined by Hays (1996), refers to the socially constructed expectation of motherhood that a mother must meet unrealistic standards to be deemed a good mother. Although societal roles have evolved over the past 30 years, with many mothers working full-time, the unrealistic ideal of motherhood has remained unchanged (Chae, 2014; Forbes et al., 2020; Lamar et al., 2019; Prikhidko & Swank, 2018). Intensive mothering demands that mothers be the central, self-sacrificing caregivers who devote extensive time, energy, and resources to their children’s needs (Hays, 1996). Forbes et al. (2021) asserted that the fact that “the expectations of mothers remain primarily unchanged despite advances made in gender equality in the U.S. as a result of feminist critiques suggests the expectations of mothers are deeply engrained in the fabric of society” (p. 271).
Research indicates that mothers from diverse backgrounds (e.g., race, ethnicity, social class, job status) endorse unrealistic beliefs about intensive mothering (Forbes et al., 2020), though cultural ideals, lack of resources, and structural barriers could impact the extent to which diverse communities endorse intensive mothering (Lankes, 2022). Living up to intensive mothering standards causes mothers to put children (and often the whole family) before their own mental and physical health (Elliot et al., 2015). Mothers who cannot live up to this ideal often face physical and mental health consequences, such as exhaustion, overwhelming anxiety, feelings of isolation and inadequacy, identity challenges and loss of self, self-criticism, and shame and guilt (Forbes et al., 2021; Prikhidko & Swank, 2018). They are also more likely to experience depression, anxiety, and decreased life satisfaction (Forbes et al., 2020; Prikhidko & Swank, 2018).
These pressures may lead mothers to engage in counseling to seek support, build realistic expectations, develop coping skills, and create a working family system that relies on more than one person to meet the needs of a child. Wellness, a cornerstone for effective counseling practice, focuses on the optimal health and well-being of the mind, body, and spirit, allowing individuals to live life more fully (Myers & Sweeney, 2004; Neff & Germer, 2013). Relatedly, maternal health strategies help support the physical, emotional, and mental health of mothers (Mitchell et al., 2018). Research suggests that mothers may benefit from focusing less on developing coping skills and more on developing maternal wellness strategies, such as having a plan and asking for help, which can impact the overall family system and functioning (Currie, 2018). The body of research on maternal wellness promotion in the counseling literature is not extensive, and there is a notable gap in empirical studies investigating how mothers’ well-being has been affected in the aftermath of the COVID-19 pandemic.
Dual Roles of Motherhood Post-Pandemic
The COVID-19 outbreak was declared a pandemic in early March 2020. In late 2021, the World Health Organization (WHO) reported approximately 4.5 million deaths, with over 650,000 deaths in the United States alone (WHO, 2021). The COVID-19 pandemic’s impact ranged from being a manageable inconvenience for some to causing severe loss of lives and livelihoods for others, cutting across class, ethnic, and national boundaries (Park, 2021). As the COVID-19 pandemic became an inevitable daily reality, it increasingly highlighted pre-existing social disparities, including limited access to health care and education, which disproportionately affect marginalized communities. This was evident in the higher rates of cases, hospitalizations, and deaths among these groups (Centers for Disease Control and Prevention [CDC], 2020).
In a society already emphasizing intensive mothering, COVID-19 worsened gender inequalities, forcing women to take on additional home and childcare responsibilities, including homeschooling. More women left jobs because of these role changes (Alon et al., 2020; Bureau of Labor Statistics, 2021) and experienced higher rates of exhaustion, anxiety, and depression (Davenport et al., 2020; Grose, 2021). According to Grose’s (2021) article in The New York Times, 69% of mothers reported adverse health effects from COVID-19 pandemic–related stress, compared to 51% of fathers. The pandemic also intensified job disparities, with women facing more job losses and slower recovery than men, pre– and post–COVID-19 pandemic (Lofton et al., 2021). In dual-income households, mothers assumed greater childcare responsibilities than fathers, a trend that persisted throughout the COVID-19 pandemic (Zamarro et al., 2020). Hupkau and Petrongolo (2020) predicted that an unequal division of labor will perpetuate inequalities in parental roles. Although remote work allows women to balance work and family, it can dilute their workplace presence and negatively impact their careers. Increased domestic labor has led to worsening emotional and financial health for U.S. mothers (Bahn et al., 2020; Ruppanner et al., 2021). Therefore, addressing the intersection of motherhood and mental health is crucial for effectively addressing the post–COVID-19 pandemic impact.
Self-Compassion and Motherhood
Given the prevalent challenges that mothers faced before, during, and after the COVID-19 pandemic, counselors need evidence-based approaches to promote wellness in community and clinical settings. Self-compassion comprises three dichotomous yet related components: mindfulness versus overidentification, common humanity versus isolation, and self-kindness versus self-judgment (Neff & Germer, 2013). Mindfulness is an evidence-based approach that entails nonjudgment and accepting one’s experiences rather than overidentifying or suppressing emotions (Neff, 2011). Common humanity describes the interconnectedness of the human experience and allows individuals to recognize pain and failure as universal struggles. Finally, self-kindness requires treating oneself with kindness, support, and understanding rather than engaging in self-criticism in response to life’s challenges (Neff, 2011).
Research has consistently linked lower levels of self-compassion with a range of mental health issues, including depression and anxiety (Han & Kim, 2023; Neff, 2011). As such, self-compassion may represent a powerful wellness construct because of its effectiveness in treating mental health concerns like anxiety, depression, stress, eating concerns, rumination, and self-criticism (Ferrari et al., 2019). Self-compassion may also represent an effective coping mechanism for mothers experiencing post-traumatic stress symptoms after childbirth (Mitchell et al., 2018), postpartum depression (Fonseca & Canavarro, 2018), and insecure attachment and parenting stress (Moreira et al., 2015; Neff, 2011). Furthermore, self-compassion may help mothers increase mental health, mindful parenting (Moreira et al., 2015; Neff, 2011), and the “ability to respond to the challenges of parenting in ways that are more sensitive and resilient” (Psychogiou et al., 2016, p. 897). Beyond individual benefits, emerging research has considered the intergenerational impacts of self-compassion (Carbonneau et al., 2020; Lathren et al., 2020). Mothers with greater self-compassion may better tolerate difficult emotions through kindness and nonjudgment, thereby better supporting their children in navigating distressing emotional experiences (Lathren et al., 2020).
Present Study
Because of the potential for new roles, increased responsibilities, and decreased support during and post–COVID-19 pandemic, mothers are at greater risk for mental health concerns (Bahn et al., 2020; Ruppanner et al., 2021). We believe that self-compassion is a promising tool for wellness-based counseling with mothers. Although the previous examples presented in our literature review reflected a few benefits of this practice, we sought to further explore the role and impact of self-compassion in mothers’ lives post–COVID-19 pandemic. In this study, we utilized photovoice, a method within community-based participatory research (CBPR) that draws on feminist theory, in order to better understand, empower, raise consciousness, create dialogue, and produce social change on behalf of mothers struggling with mental health and wellness post–COVID-19 pandemic (Wang, 1999; Wang & Burris, 1997).
Method
Grounded in feminism, critical pedagogy, and photography (Wang & Burris, 1997), photovoice is one of several qualitative research methods in CBPR that allows individuals to express their beliefs about community and social issues using photos and personal descriptions. This robust methodology promotes social action, diversity, and advocacy within communities (Smith et al., 2010; Wang & Burris, 1997). Photovoice assumes that participants are the experts in their own lives, with the research process involving three unique components: (a) facilitating a partnership within the community, developing a research question, and training; (b) reflecting on the images, adhering to critical pedagogy while using a structured analytical framework consisting of five questions, called SHOWeD, to guide the analysis and promote meaningful change; and (c) disseminating the findings within the community (Wang & Burris, 1997).
In counseling, photovoice has the power to promote critical ideologies and reflective dialogue that allows for the constructivist creation of meaning around a social construct, promoting social justice and advocacy within the community (Sackett & Jenkins, 2015; Wester et al., 2021). Additionally, research demonstrates that photovoice fosters team building, social skills, self-efficacy, social connectedness, friendship, empowerment, and a sense of community (Wang & Burris, 1997; Wilson et al., 2007). Scholars in the counseling profession have called for the use of photovoice to promote community and advocacy and investigate interventions for issues that inhibit client growth (Sackett & Jenkins, 2015). Because of this call, the strong ties to critical pedagogy, and the underpinnings of feminist theory, we used a photovoice methodology to explore the following research question: How do mothers in our community understand, experience, and enact self-compassion in their daily lives in a post–COVID-19 pandemic world?
Participants
For the present study, the inclusion criteria indicated that participants must (a) be 18 years of age or older, (b) have no history of a personality disorder diagnosis and no severe symptoms of mental illness (e.g., suicidal ideation or psychosis), and (c) have at least one child in the home between the ages of 5 and 12. The rationale for selecting this age range was based on neurological data demonstrating differences in brain development for children over 5 (van der Kolk, 2014) and in Erikson’s psychosocial stages of development that document differences in individuals over 12 (Orenstein & Lewis, 2021). Our target sample size was eight to 12 participants, which was determined based on the standard for photovoice methodology (Wang & Burris, 1997), but additionally, the goal was to capture the depth and breadth of each individual analysis.
After excluding participants who did not complete the study or follow the study guidelines, the final sample consisted of eight women aged 30 to 42 (M = 37.25). Seven participants self-identified as White/Caucasian; one identified as Asian and White/Caucasian. All eight participants indicated that they were married. Participants were asked about their employment status and were given the option to select all applicable options. Five participants selected part-time employment, three marked stay-at-home parent, one indicated being employed full-time, and one indicated being self-employed. Regarding education level, four participants reported earning a bachelor’s degree or higher, two reported completing some college, one reported completing trade school, and one declined to respond. Lastly, concerning mental health concerns, two participants reported struggling with anxiety and depression, one reported struggling with attention-deficit hyperactivity disorder symptoms, three declined to respond, and two denied any mental health concerns.
Procedure
After receiving IRB approval, we collaborated with two local community mental health agencies, including one nonprofit agency and one for-profit agency. These community-based mental health agencies allowed us to advertise and recruit mothers who met the criteria and demonstrated interest in this research. We shared electronic flyers via social media with the study information, including the design, purpose, and participant expectations (i.e., taking photos and discussing the meaning behind them in focus groups). We also provided a small allotment to compensate for participants’ costs, such as internet or cell phone data use. The for-profit agency also offered free self-compassion books to all participants who completed the study. Participants could receive this resource by providing their email addresses after their final interview.
After completing an informed consent form, each participant participated in a 45–60-minute psychoeducational focus group led by one or more members of our research team, where they learned the basic components of self-compassion (i.e., self-kindness, common humanity, and mindfulness) and engaged in discussions about self-compassion with other group members. These psychoeducational groups consisted of two to four participants because of the scheduling needs of participants. Our overarching research question for the study was shared and we engaged in dialogue about changes experienced because of the COVID-19 pandemic. At the end of the session, we provided participants with information about taking photos, directions, and information to assist in maintaining confidentiality (e.g., avoid taking photos of self or others to protect confidentiality). The participants had 10 days to take or select photos to visually describe self-compassion in their own lives. Following, each participant was asked to caption them with a title, respond to the SHOWeD questions, which are unique to the methodology, and send them to us via email. The SHOWeD questions consisted of the following: 1) What do you see in the photo? 2) What is happening in your photograph? 3) How does this photo capture self-compassion in your own life? 4) Why does this photo contribute to the challenge, concern, or strengths that exist in self-compassion? and 5) What can mental health professionals or others do to help foster and support self-compassion in mothers? (Wang & Burris, 1997).
Each participant completed a follow-up photovoice session in which we placed participants’ top two selected photos on a slideshow with their corresponding captions. We followed outlined guidelines for the second photovoice session (Wang & Burris, 1997; Wester et al., 2021) while focusing on the two photos each participant selected, which were used to establish themes. Most of the second photovoice sessions were held individually to give mothers more scheduling flexibility and prevent further attrition. Although these in-depth, semi-structured interviews were individual, participants were encouraged to engage in dialogue with our research team regarding other participants’ photos and captions in order to create shared meaning. Once the meeting ended, we transcribed the entire discussion while focusing on the participants’ meaning of the photos.
Data Analysis
This study used photovoice, a methodology within CBPR (Wang, 1999; Wang & Burris, 1997), and interpretative phenomenological analysis (IPA) to explore participants’ experiences within interview transcripts and photographs (Burton et al., 2017; Griffin & May, 2012). The study emphasized collaboration between researchers and community members throughout the research process, from defining research questions to disseminating findings. This approach ensured the research was relevant to and beneficial for the community it aimed to serve. The feminist framework underpinned the entire process, influencing the focus on gender issues and power dynamics, emphasizing participants’ voices and lived experiences, and promoting social change and empowerment (Wang, 1999). IPA was utilized as the primary analytical approach, aligning with the study’s aim to explore how participants make sense of their experiences (Burton et al., 2017). Participants were viewed as experts in their own experiences, and the analysis focused on understanding their perspectives.
Following the IPA procedures of Griffin and May (2012), the analysis began with thorough familiarization with the data, followed by initial coding, developing emergent themes, searching for connections, and looking for patterns across cases. Recurring patterns and key concepts were identified in each transcript, photo, and responses to the SHOWeD questions. Relationships between themes found in the written dialogue and patterns in photos were extracted, always keeping in mind the true meaning expressed by the participants. We engaged in a double hermeneutic process, interpreting the participants’ interpretations of their experiences. Interpretive themes were developed to analyze deeper meaning. All four of us met weekly during the coding process to discuss each step and reach a consensus before moving on to each next step (Larkin & Thompson, 2011).
Role of the Researcher and Trustworthiness
Trustworthiness is critical in qualitative research. To promote transparency as the research team, we identified our backgrounds and identities, which could impact the study (Creswell, 2020). Our team consisted of four members: three coders and one auditor. Kelly Emelianchik-Key (associate professor), Adriana C. Labarta (assistant professor), and Carman S. Gill (full professor) served as coders and were all counselor educators at Florida Atlantic University during the research process. They are each licensed mental health counselors, National Certified Counselors, and Approved Clinical Supervisors; Emelianchik-Key is also a licensed marriage and family therapist. Emelianchik-Key and Gill identify as White females and Labarta identifies as Latina. Emelianchik-Key also identifies as a mother, which was a critical piece of the study and important to consider to prevent bias. The auditor, Clara Bossie, is a White female and a counselor education doctoral student at Florida Atlantic University; she is a licensed marriage and family therapist with specialized training in dialectical behavioral therapy and as a Mindful Self-Compassion (MSC) teacher. She is also the owner and clinical director of a private practice.
Emelianchik-Key, Labarta, and Gill have extensive experience in qualitative research and coded the data, while Bossie served as an external auditor because of her specialized MSC training in order to provide additional perspectives and feedback, enhancing trustworthiness (Creswell & Báez, 2020). As a team, we discussed biases and assumptions throughout the research and data analysis process, maintaining an audit trail. Peer validation was used to promote trustworthiness (Larkin & Thompson, 2011) while noting intersectionality and privilege within the team. Member checking was conducted after developing the final themes, with participants providing feedback. No objections were raised, and two of the participants responded noting they agreed with the results.
Results
The findings that emerged from the discussion of the SHOWeD questions, participant photos, and corresponding captions included four overarching themes with 13 subthemes. Theme 1, Challenges With Self-Compassion, included subthemes Permission and Justification, Making Time, Self-Worth, and Understanding Self-Compassion. Theme 2, Isolation Versus Common Humanity, included subthemes Social Media, Desire for Connection, and Self-Criticism. Theme 3, Awareness and Education, included the subthemes Self-Awareness, Acknowledgment From Self and Others, and Psychoeducation. Theme 4, Mindfulness, included subthemes Open Awareness, One-Pointed Awareness, and Tactile Experiences.
Theme 1: Challenges With Self-Compassion
The initial theme revolved around mothers’ obstacles and difficulties with integrating self-compassion into their daily lives. These challenges encompassed permission giving, allocating time, grappling with feelings of self-worth, and distinguishing between self-compassion and self-care. The subtheme of Permission and Justification encompassed the hurdles mothers encounter when attempting to incorporate self-compassion into their lives. A common rationale for practicing self-compassion was the significant impact it may have on their children and families. Mothers expressed challenges with practicing self-compassion “just because” and sought justifications for their practice. The second subtheme of Making Time underscored the challenge of making time for self-compassion amid juggling various roles and responsibilities as a mother. Moreover, this subtheme emerged during our study because of the difficulty in finding mothers to participate amidst their many demands. Rather than making time for themselves, mothers described examples of wedging acts of self-compassion into everyday activities, such as morning coffee and reflective moments in the car during Little League practice.
The third subtheme of Self-Worth underscored mothers’ difficulties in recognizing their value, particularly as they navigate societal and familial expectations of the “perfect” mother. Participants expressed sentiments of needing to validate or “prove” their worthiness. The last subtheme of Understanding Self-Compassion shed light on the difficulty of discerning between self-care and self-compassion. Participants frequently equated self-care activities with self-compassion, failing to distinguish between them and often neglecting their needs. The self-compassion practices described by participants were not entirely directed toward their well-being, as evidenced by self-care activities and compassion practices that primarily sought to extend warmth and kindness to others rather than focusing on themselves. Examples from these subthemes are in Table 1.
Table 1
Participant Quotes Related to Subthemes of Theme 1: Challenges With Self-Compassion
| Subthemes |
Participant Quote |
| Permission and Justification |
Participant 3: “It’s been really important for me to find time for myself to do things that I want to do. But then I feel like sometimes, as a mom, you feel like everything revolves around your family, and then, when you take time away from that, it’s like you’re being selfish.” |
| Making Time |
Participant 2: “It’s hard to remember sometimes when you’re on autopilot. Yeah, or things happen like one after another, and then you don’t have that awareness right away sometimes.” |
| Self-Worth |
Participant 3: “I feel like I’m always trying to prove that what I do is important. And it’s not only proving that to other people, but I need to feel it myself.” |
| Understanding Self-Compassion |
Participant 1: “I think even like understanding self-compassion can be kind of strange, because nowadays it’s self-care. Everyone calls it ‛self-care.’ It seems like just everyone is getting their nails done or paying for expensive facials, or whatever, because it’s self-care. I think that’s kind of more of like a superficial thing, where self-compassion is more internal . . . you have to like, you know, be self-aware to know how to be self-compassionate.” |
Theme 2: Isolation Versus Common Humanity
The second theme highlighted one of the central components of the self-compassion model: Isolation Versus Common Humanity (Germer & Neff, 2019; Neff & Germer, 2013). This theme showcased the contrast between participants’ longing for connection while engaging in behaviors that fostered disconnection. The first subtheme was Social Media, including its positive and negative impacts. A significant aspect was the experience of social comparisons, which either provided participants with understanding and validation or left them feeling isolated and separate from others, resulting in self-criticism. Social media had both helpful and harmful influences on participants’ well-being.
The second subtheme of Desire for Connection reflected participants’ deep longing to connect with others and to feel heard, valued, and acknowledged for their efforts. This is especially true when navigating parenting challenges to avoid feelings of isolation. The last subtheme was Self-Criticism. Self-criticism captured instances in which mothers engaged in or exhibited self-critical language. Participants frequently engaged in cognitive distortions such as overgeneralizing, ruminating on “should haves,” and making self-judgments. This tendency toward self-criticism often led to narratives and expressions of isolation or feeling excluded from a group or family. Participant quotes for each of these subthemes are found in Table 2.
Table 2
Participant Quotes Related to Subthemes of Theme 2: Isolation Versus Common Humanity
| Subthemes |
Participant Quote |
| Social Media |
Participant 2: “I think the reason self-compassion isn’t as popular is because a lot of the mainstream help we easily come across makes a profit on people feeling like they’re not good enough. Self-compassion doesn’t count on people needing to take a big action to make a change in their lives.” |
| Desire for Connection |
Participant 5: “The overall experience was good. . . . It’s always nice to hear that you’re not the only person juggling a thousand things and trying to make sense of it.” |
| Self-Criticism |
Participant 6: “Sometimes we all feel like we’re alone in the things that we’re doing and the things that we’re dealing with because we can’t feel like we can talk about it cause then we’re a failure. And that’s like one of the biggest things for moms.” |
Theme 3: Awareness and Education
The third theme encapsulated participants’ journey toward cultivating heightened self-awareness regarding the importance of self-compassion, alongside a plea for counselors to provide enhanced education and incorporate strengths-based, empowering approaches for mothers. The first subtheme of Self-Awareness involved participants recognizing the significance of self-compassion and their ability to prioritize time for engaging in self-compassion and self-care. Participants acknowledged that seeking help is permissible and that the shaming associated with being unable to manage everything should not occur. The second subtheme of Acknowledgment From Self and Others centered around the desire to be recognized and valued for their many roles as mothers, spouses, breadwinners, etc., while embracing self-kindness and self-validation. The last subtheme of Psychoeducation emerged as participants emphasized the necessity for greater awareness and understanding of self-compassion and its relevance in daily life. Specifically, they stressed the importance of making this knowledge more accessible for mothers and the need for others to be educated about the challenges mothers face. Example quotes from these subthemes are in Table 3.
Theme 4: Mindfulness
The fourth theme explored the various methods by which participants incorporated mindfulness activities as part of their practice of self-compassion. The first subtheme, Open Awareness, addressed the specific ways participants engaged in mindfulness activities that allowed them to become more aware of the entire environment. Some participants participated in mindfulness activities that heightened their awareness of their surroundings, although this engagement focused more on relationship mindfulness than self-compassion. The second subtheme of One-Pointed Awareness described participants’ mindfulness practices with focused awareness, concentrating solely on one aspect of the present moment. They fully immersed themselves in the mindfulness practice, recognizing it as a means of personal growth. The last subtheme of Tactile Experiences illustrated participants’ self-soothing or grounding practices involving multiple senses, particularly touch, sensation, smell, and profound observation. These practices typically occurred in the morning and often included enjoying coffee, gardening, or immersing oneself in nature. A sample quote from each subtheme is in Table 4.
Table 3
Participant Quotes Related to Subthemes of Theme 3: Awareness and Education
| Subthemes |
Participant Quote |
| Self-Awareness
|
Participant 7: “We’d taken a picture of my daughter’s little emotion dolls, or like some animals . . . I’m like, ‛well, that’s perfect.’ Because you know, we all have these emotions. . . . So that really stood out to me, because that’s something that I’ve really learned becoming a parent and a mom . . . we are going to have these emotions. It’s okay to have emotions and that’s something I’ve been, you know, trying to teach my kids to a lot of the time . . . that was a big self-compassion thing that stood out to me was, you know, letting myself feel like, you know, anger or frustration, or all the other ones that were lined up in that picture.” |
Acknowledgment From
Self and Others |
Participant 3: “I think, that just hearing like, ‛Hey, I see you. I see that you’re working hard, and you’re doing great,’ you know. So I think that that’s what moms need to hear.” |
| Psychoeducation |
Participant 8: “Just educating mothers more on like the postpartum journey and normalizing, you know, postpartum depression and postpartum anxiety. . . . I don’t necessarily feel like I was properly educated while I was pregnant, and then postpartum on, you know, how much you, your hormones and everything, it affects you mentally, especially in this world with social media. And you know, everyone’s perfect. And you know, everyone wakes up the next day after, you know, not sleeping with a newborn all night and being exhausted. And you’re supposed to look perfect and act perfect. And you know, I just wish there was more acceptance and kind of education and normalizing the raw journey of postpartum.” |
Table 4
Participant Quotes Related to Subthemes of Theme 4: Mindfulness
| Subthemes |
Participant Quote |
| Open Awareness |
Participant 8: “I do struggle a lot with my body image as a woman. And just, you know, after you have children and your body changes. So, for me, this photo is also really powerful in that aspect, because I’ve been doing a lot of work with that as well as just not being as hard on myself. And you know, normally, I would be like super uncomfortable at the beach, and especially because it was like a packed day. It was Mother’s Day, wearing a bathing suit, and I just didn’t give a shit, and it was really cool. And I just, I think, because I was just so immersed with my family and being present.” |
| One-Pointed Awareness |
Participant 2: “Just paying attention to your body. And if I feel I’m breathing a little shallow, sometimes I notice I’m holding my breath, and sometimes I notice that my shoulders are up here, and that’s usually my little sign to like, okay . . . this doesn’t feel good. Let’s fix this for a minute. Do something.” |
| Tactile Experiences |
Participant 4: “We just moved into this house 6 months ago, and I love flowers. And you know, I missed my old house with like my garden, so I had to start over. . . . That’s like my thing. I literally go out there and do that every single morning. I mean, sometimes it’s 3 minutes, sometimes it’s 15 minutes, but mainly it’s 5 minutes. But that’s where I was like, yeah, that’s my time. You know, where I don’t bring the phone out there with me.” |
Data Presentation to Stakeholders
Consistent with CBPR goals and photovoice procedures (Wang & Burris, 1997; Wester et al., 2021), we sought to promote change and advocate for mothers by sharing our findings with stakeholders. The stakeholders included the nonprofit community-based agency and private practice that helped recruit participants, and a group of local counselors affiliated with a large community agency who could further increase awareness, co-create meaning, and facilitate change. The study participants were invited to join our meeting with stakeholders who participated in a presentation of the findings, including PowerPoint slides illustrating the primary themes and participant photos. The last question of the SHOWeD method was especially considered: “What can mental health professionals or others do to help foster and support self-compassion in mothers?” We engaged in a collaborative dialogue on implementing the study’s findings into practice, which are further elaborated in the discussion section of this manuscript.
Discussion
Mothers, often serving as the backbone of their families, face silent battles with mental health and identity, heightened by sociocultural ideals and other contextual factors like the recent COVID-19 pandemic’s isolating conditions (Chae, 2014; Davenport et al., 2020; Grose, 2021; Neff, 2011; Prikhidko & Swank, 2018). Mothers’ quiet struggles illuminate an alarming need for more mental health support tailored to the unique experiences of motherhood. Our study explored mothers’ experiences post–COVID-19 pandemic with cultivating self-compassion using photovoice, revealing four overarching themes: (a) Challenges With Self-Compassion, (b) Isolation Versus Common Humanity, (c) Awareness and Education, and (d) Mindfulness.
The first theme suggests that mothers’ challenges with self-compassion are deeply entangled in the daily realities of motherhood and exacerbated by societal ideals. These difficulties extend beyond finding time (which was extremely limited) for self-care; instead, they reflect more profound issues of how mothers perceive and treat themselves amid overwhelming external expectations, often compromising their well-being and prioritizing their children and families (Forbes et al., 2021; Lamar et al., 2019). Feminist theory recognizes how gendered expectations of motherhood create structural time poverty, but the lack of self-compassionate practices calls attention to the systemic issues about women’s unpaid labor and societal expectations. The subtheme of Permission and Justification manifested itself through the notion of self-compassion to “model it” for their children rather than themselves, which aligns with previous research (Lathren et al., 2020). A complex interplay of self-neglect and societal pressures led mothers to conflate the concept of self-care with self-compassion. Consequently, mothers frequently and erroneously equate self-care activities with self-compassion. This misunderstanding underscores the need for psychoeducation on self-compassion in counseling. Although self-care is essential to address one’s immediate needs, self-compassion embodies a more profound, forgiving, and accepting approach to our limitations and failures (Neff, 2011).
The second theme, Isolation Versus Common Humanity, highlights one of the primary components of the self-compassion model (Germer & Neff, 2019; Neff & Germer, 2013) and extends prior research on the impact of social comparison and media on mothers (Chae, 2014; Prikhidko & Swank, 2018). Participants described a dichotomy between the desire to connect with others while grappling with social comparison, thus leading to feelings of inadequacy and isolation. Participants acknowledged the benefits of social media (e.g., accessibility) while simultaneously struggling with the overwhelmingly “positive” and “happy” images in contrast to content addressing the challenges of motherhood. Mothers sought authentic, meaningful connections beyond social media and surface-level interactions. This finding underscores the need for counselors to foster nonjudgmental and compassionate spaces for mothers to connect on their shared experiences and struggles. Additionally, intentional engagement in mindfulness is critical for feelings of isolation that stem from social media usage. This approach can encourage mothers to become more aware of the images they engage with and facilitate the positive benefits of social media. Feminist frameworks emphasize the importance of recognizing personal struggles as connected to broader social patterns, so difficulties connecting with common humanity may also reflect the individualistic messaging mothers receive about “doing it all.”
Awareness and Education, the third theme of our study, was at the forefront of our interviews with participants. Mothers expressed excitement about the construct of self-compassion, leading to critical discussions on the need for more psychoeducation on this practice. Given the abundant research that supports self-compassion as a means of developing mental health and wellness (Ferrari et al., 2019; Fonseca & Canavarro, 2018; Lathren et al., 2020; Mitchell et al., 2018; Moreira et al., 2015), greater access to treatment and resources is crucial to mitigate mothers’ challenges to practicing self-compassion, particularly at the community level. For instance, counselors can use social media platforms to provide psychoeducation on self-compassion, share helpful resources, and foster supportive communities that challenge the “illusion of perfection” (Neff, 2011, p. 70).
The fourth theme underscores how Mindfulness and Self-Compassion are inextricably linked (Neff, 2011; Neff & Germer, 2013). Regardless of how mothers practiced mindfulness (e.g., Open Awareness, One-Pointed Awareness, or Tactile Experiences), it allows them to connect more deeply with their experiences by accepting difficult emotions, becoming more aware of their environment, or engaging the senses. However, it is essential to note that mindfulness and self-compassion do not automatically co-occur. Neff and Dahm (2015) indicated:
It is possible to be mindfully aware of painful thoughts and feelings without actively soothing and comforting oneself or remembering that these feelings are part of the shared human experience. Sometimes it takes an extra intentional effort to be compassionate toward our own suffering, especially when our painful thoughts and emotions involve self-judgments and feelings of inadequacy. (p. 130)
Neff and Dahm’s assertion highlights that while mindfulness fosters awareness, self-compassion requires additional intentionality, particularly in the face of self-judgment. Building on this, counselors play a vital role in educating mothers on the all-encompassing practice of self-compassion, which goes beyond mindful awareness to include self-kindness and a recognition of common humanity. This is especially important in addressing societal and cultural expectations that are contrary to “slowing down,” being kind to oneself, and recognizing one’s connection with others.
Implications for Counselors
The findings of this study illuminate the need for a multifaceted approach to helping mothers cultivate self-compassion and wellness. Although most participants’ narratives did not explicitly address self-compassion practices and connection to the COVID-19 pandemic, counselors should carefully consider how the additional responsibilities and stressors that emerged during this period may have become normalized and integrated into mothers’ daily lives. The minimal direct pandemic references in participants’ responses may be telling, suggesting that what began as temporary adaptations to crisis have potentially evolved into enduring expectations and workload increases for mothers. This has important implications for how counselors conceptualize and address maternal stress, role strain, and work–life integration in their practice.
Counselors must establish trust, safety, and rapport with mothers to discuss challenging topics such as self-doubt, isolation, and self-worth. Counselors can demonstrate the differences between self-compassion and self-care. For example, although self-care may help to temporarily disconnect after a difficult day (e.g., watching an entertaining television series), self-compassion encourages mothers to become curious about their inner emotional experiences (mindfulness), utilize sources of support (common humanity), and respond to uncomfortable emotions with acceptance and warmth (self-kindness). Counselors may consider various approaches to integrating self-compassion into their work and communities, from offering courses as an MSC-trained teacher (Germer & Neff, 2019) to utilizing The Mindful Self Compassion Workbook: A Proven Way to Accept Yourself, Build Inner Strength, and Thrive (Neff & Germer, 2018) and online resources available through the Center for Mindful Self-Compassion. MSC integrates the practice of mindfulness with the nurturing qualities of self-compassion, creating a potent approach for cultivating emotional resilience. MSC combines mindfulness with nurturing self-compassion to build emotional resilience, improving overall physical wellness while reducing anxiety, depression, and burnout (Germer & Neff, 2019), making it especially valuable for mothers with limited mental health access.
Therapeutic modalities that explore underlying factors contributing to mothers’ reluctance or hesitation to engage in self-compassion practices, such as past experiences, societal expectations, or cultural influences, may increase the effectiveness of programs like MSC. Our participants indicated deeply ingrained negative beliefs about themselves, which can hinder their ability to practice self-compassion. Counselors can help mothers identify and challenge these beliefs, encouraging them to develop more compassionate and realistic self-perceptions through insight-oriented practices, such as Socratic questioning, motivational interviewing, and self-reflective practices.
Though MSC offers therapeutic benefits, it’s not therapy itself. Unlike our study participants who were prepared for vulnerability, counselors must recognize that mothers come with varying needs. Germer and Neff (2019) emphasized that effective MSC delivery depends on a client’s tolerance zone, which includes being in a safe, challenged, or overwhelmed state, with optimal learning occurring in safe or challenged states where clients can progress through acceptance stages while maintaining emotional regulation. Opening oneself to self-compassion may lead to “backdraft,” when individuals encounter previously suppressed painful emotions (Germer & Neff, 2019). Although most mothers can embrace self-compassion practices immediately, some in clinical populations may need deeper therapeutic work as preparation (Neff & Germer, 2018). In addition to the challenges and pressures of motherhood, mothers may arrive with various co-occurring issues such as grief, mental health concerns, complex trauma, or other shame-invoking experiences lying just below the surface (Neff, 2011). It is important that counselors are prepared to utilize evidence-based treatment approaches to help mothers fully access self-compassion practices and handle potential backdrafts.
Theoretical Integration
Integrating a self-compassion–informed approach into counseling is greatly enhanced by drawing from evidence-based approaches that align with the construct of self-compassion, such as acceptance and commitment therapy (ACT), compassion-focused therapy (CFT), mindfulness-based cognitive therapy (MBCT), dialectical behavior therapy (DBT), and Adlerian theory. These therapeutic models support the development of self-compassion, a key aspect of MSC, by promoting emotional resilience, self-awareness, and adaptive coping mechanisms. Gilbert (2014) developed CFT to explicitly target
self-criticism and shame while promoting the cultivation of self-compassion through exercises designed to enhance compassionate self-awareness. CFT provides structured techniques to cultivate a kind and understanding inner voice, benefiting clients with harsh self-judgment. Similarly, Adlerian theory’s holistic social perspective emphasizes social connectedness and community feeling (Adler, 1938), aligning with MSC’s principle of common humanity that recognizes suffering as a shared human experience. By fostering a sense of belonging and encouraging clients to develop self-compassion within the context of their social relationships, Adlerian theory enhances the application of MSC in promoting overall well-being. Moreover, third-wave cognitive-behavioral models are widely praised for integrating validation, mindfulness, and self-acceptance that support self-compassion–informed counseling. ACT’s emphasis on mindfulness and acceptance aligns with self-compassion by encouraging clients to accept their thoughts and feelings without judgment and commit to values-based actions (Hayes et al., 2006). This approach promotes a compassionate stance toward oneself, central to Germer and Neff’s (2019) MSC program. By fostering curiosity and kindness toward internal experiences, ACT helps integrate self-compassion practices into daily life (Hayes et al., 2006). MBCT combines cognitive strategies with mindfulness practices, making it a natural ally to MSC. By teaching clients to recognize and break free from patterns of depressive rumination, MBCT enhances clients’ ability to respond to difficult emotions with mindfulness and self-compassion (Segal et al., 2018). This supports clients in emotional balance and resilience, essential components of MSC (Segal et al., 2018). Lastly, DBT and MSC share core principles. DBT’s mindfulness emphasis and dialectical approach of balancing acceptance with change aligns with MSC, offering robust tools for navigating emotional turbulence through self-acceptance and compassion (Linehan, 2014).
Multicultural Considerations and Future Implications
One important consideration is that we recruited participants from local mental health agencies, with the final sample being predominantly White. Participation challenges arose primarily for women of color recruited via social media, including declining participation and dropout because of time constraints. Forbes et al. (2020) noted that the experience of intensive mothering was consistent across various maternal demographics (i.e., race, ethnicity, social class upbringing, relationship status, number of children, and job status). However, Lankes (2022) distinguished that the significance and impact of intensive mothering can vary depending on cultural ideals, resource availability, and structural barriers. This means that mothers from marginalized or underserved communities who face heightened societal stressors and systemic barriers may experience impediments to engaging in self-care practices and accessing mental health resources. Thus, the compounding effects of racism, discrimination, and the unique pressures associated with motherhood can exacerbate mental health challenges and diminish opportunities for cultivating self-compassion and well-being (Condon et al., 2022). Counselors must provide culturally responsive care that acknowledges their clients’ unique, intersectional identities and the historical and current context of oppression and marginalization. Overall, counselors can advocate for policies and systemic changes for underserved mothers, such as by offering self-compassion workshops for mothers in the community, thus increasing access to services.
Community Conversations
After completing the study, we sought expert validation by presenting our findings to a local community agency through a research presentation and interactive dialogue. We invited clinicians with expertise in self-compassion, family counseling, parenting, women’s issues, and vulnerable populations to share their reactions based on clinical experiences and to offer recommendations. The attending clinicians validated the four overarching themes of our study, sharing stories of motherhood marked by self-criticism, judgment, and expectation. Participants were also invited to this meeting as part of our CBPR methodology. Clinicians who identified as professionals and mothers resonated with the study’s themes, sharing personal narratives that aligned strongly with our findings. They discussed strategies to help their clients, particularly mothers, practice self-compassion, including curating social media feeds (e.g., Instagram) to avoid disempowering content that perpetuates comparison and self-criticism. Additionally, they emphasized the importance of psychoeducation from a systems perspective, suggesting mindfulness and self-compassion as powerful tools for family wellness, and acknowledged the challenges and strengths of mothers. Although no participants opted to attend because of scheduling challenges (finding time was an overarching challenge for participants throughout the study), final thoughts and comments on how this information can impact our work was discussed with community clinicians. Overall, these discussions affirmed the study’s findings and support the need for ongoing research and advocacy initiatives to raise awareness and increase access to self-compassion practices for mothers.
Following expert validation, a nationally recognized treatment center invited us to co-host an experiential seminar open to counselors and community members. The seminar, held in an underserved community, provided an overview of the study’s findings, self-compassion principles, and experiential exercises. We distributed learning materials to participants, and we offered recommendations for integrating self-compassion into daily life, family relationships, and clinical practice. As part of our ongoing efforts to disseminate the findings and advance community advocacy, the research team presented the results at a national conference, which sparked further conscious conversations, reinforcing our commitment to supporting mothers in underserved communities.
Limitations and Future Research
The present study is not without limitations. Although the nature of photovoice calls for focus groups (Wang & Burris, 1997; Wilson et al., 2007), we decided to meet with participants in smaller groups or individually to accommodate busy schedules. Although the format provided flexibility, the individual interviews can limit dialogue and community building. Additionally, our participants were too busy to attend our community meetings—a crucial component of CBPR. Future research can replicate our study using focus groups, which may provide additional insights into mothers’ self-compassion practices. Researchers may want to consider providing childcare to assist with finding time. Another limitation was a lack of racial and ethnic diversity, as our sample mainly included White women connected to counseling communities. Future research can explore the experiences of mothers with diverse racial, sexual, affectional, and marital backgrounds with self-compassion through photovoice. Mothers with intersecting identities face additional challenges, such as discrimination and systemic inequities, further impacting mental health and parenting stress (Condon et al., 2022). Wellness interventions, like self-compassion skills, could help bridge health disparities for diverse mothers.
Conclusion
Self-compassion is essential for psychological well-being. Mothers face numerous mental health challenges due to societal expectations and contextual factors, such as post–COVID-19 pandemic shifts in work–life balance, and may encounter obstacles in cultivating self-compassion. The findings reveal the unique challenges and benefits of self-compassion for mothers and the mismatch between the understanding of self-compassion and its practice in daily life. A comprehensive and multidimensional approach is necessary to assist mothers in developing self-compassion and promoting their overall well-being. Counselors must find ways to educate clients and foster this critical skill in mothers, who can often be overlooked, overburdened, and unintentionally undervalued.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
for the development of this manuscript.
Florida Atlantic University provided a small
grant to the researchers for community-engaged
research projects.
References
Adler, A. (1938). Social interest: A challenge to mankind. Faber & Faber.
Alon, T., Doepke, M., Olmstead-Rumsey, J., & Tertilt, M. (2020). The impact of COVID-19 on gender equality (Working Paper 26947). National Bureau of Economic Research. https://doi.org/10.3386/w26947
Bahn, K., Cohen, J., & van der Meulen Rodgers, Y. (2020). A feminist perspective on COVID-19 and the value of care work globally. Gender, Work, & Organization, 27(5), 695–699. https://doi.org/10.1111/gwao.12459
Bureau of Labor Statistics. (2021). The employment situation—January 2021 (Publication No. USDL-21-0142).
https://www.bls.gov/news.release/archives/empsit_02052021.pdf
Burton, A., Hughes, M., & Dempsey, R. C. (2017). Quality of life research: A case for combining photo-elicitation with interpretative phenomenological analysis. Qualitative Research in Psychology, 14(4), 375–393.
https://doi.org/10.1080/14780887.2017.1322650
Carbonneau, N., Goodman, L. C., Roberts, L. T., Bégin, C., Lussier, Y., & Musher-Eizenman, D. R. (2020). A look at the intergenerational associations between self-compassion, body esteem, and emotional eating within dyads of mothers and their adult daughters. Body Image, 33, 106–114.
https://doi.org/10.1016/j.bodyim.2020.02.007
Centers for Disease Control and Prevention. (2020). COVID-19 hospitalization and death by race/ethnicity.
https://stacks.cdc.gov/view/cdc/97937
Chae, J. (2014). “Am I a better mother than you?” Media and 21st-century motherhood in the context of the social comparison theory. Communication Research, 42(4), 503–525. https://doi.org/10.1177/0093650214534969
Condon, E. M., Barcelona, V., Ibrahim, B. B., Crusto, C. A., & Taylor, J. Y. (2022). Racial discrimination, mental health, and parenting among African American mothers of preschool-aged children. Journal of the American Academy of Child & Adolescent Psychiatry, 61(3), 402–412. https://doi.org/10.1016/j.jaac.2021.05.023
Creswell, J. W., & Báez, J. C. (2020). 30 essential skills for the qualitative researcher. SAGE.
Currie, J. L. (2018). Managing motherhood: A new wellness perspective. Springer.
Davenport, M. H., Meyer, S., Meah, V. L., Strynadka, M. C., & Khurana, R. (2020). Moms are not ok: COVID-19 and maternal mental health. Frontiers in Global Women’s Health, 1. https://doi.org/10.3389/fgwh.2020.00001
Elliott, S., Powell, R., & Brenton, J. (2015). Being a good mom: Low-income, Black single mothers negotiate intensive mothering. Journal of Family Issues, 36(3), 351–370. https://doi.org/10.1177/0192513X13490279
Ferrari, M., Hunt, C., Harrysunker, A., Abbott, M. J., Beath, A. P., & Einstein, D. A. (2019). Self-compassion interventions and psychosocial outcomes: A meta-analysis of RCTs. Mindfulness, 10(8), 1455–1473.
https://doi.org/10.1007/s12671-019-01134-6
Fonseca, A., & Canavarro, M. C. (2018). Exploring the paths between dysfunctional attitudes towards motherhood and postpartum depressive symptoms: The moderating role of self-compassion. Clinical Psychology & Psychotherapy, 25(1), e96–e106. https://doi.org/10.1002/cpp.2145
Forbes, L. K., Donovan, C., & Lamar, M. R. (2020). Differences in intensive parenting attitudes and gender norms among U.S. mothers. The Family Journal, 28(1), 63–71. https://doi.org/10.1177/1066480719893964
Forbes, L. K., Lamar, M. R., & Bornstein, R. S. (2021). Working mothers’ experiences in an intensive mothering culture: A phenomenological qualitative study. Journal of Feminist Family Therapy, 33(3), 270–294.
https://doi.org/10.1080/08952833.2020.1798200
Germer, C. K., & Neff, K. (2019). Teaching the mindful self-compassion program: A guide for professionals. Guilford.
Gilbert, P. (2014). The origins and nature of compassion focused therapy. British Journal of Clinical Psychology, 53(1), 6–41. https://doi.org/10.1111/bjc.12043
Griffin, A., & May, V. (2012). Narrative analysis and interpretative phenomenological analysis. In C. Seale (Ed.), Researching society and culture (3rd ed., pp. 441–458). SAGE.
Grose, J. (2021, February 4). America’s mothers are in crisis. The New York Times. https://www.nytimes.com/spotlight/working-moms-coronavirus
Han, A., & Kim, T. H. (2023). Effects of self-compassion interventions on reducing depressive symptoms, anxiety, and stress: A meta-analysis. Mindfulness, 14, 1553–1581. https://doi.org/10.1007/s12671-023-02148-x
Hayes, S. C., Luoma, J. B., Bond, F. W., Masuda, A., & Lillis, J. (2006). Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy, 44(1), 1–25. https://doi.org/10.1016/j.brat.2005.06.006
Hays, S. (1996). The cultural contradictions of motherhood. Yale University Press.
Hupkau, C., & Petrongolo, B. (2020). Work, care and gender during the COVID-19 crisis. Fiscal Studies, 41(3), 623–651. https://doi.org/10.1111/1475-5890.12245
Lamar, M. R., Forbes, L. K., & Capasso, L. A. (2019). Helping working mothers face the challenges of an intensive mothering culture. Journal of Mental Health Counseling, 41(3), 203–220. https://doi.org/10.17744/mehc.41.3.02
Lankes, J. (2022). Negotiating “impossible” ideals: Latent classes of intensive mothering in the United States. Gender & Society, 36(5), 677–703. https://doi.org/10.1177/08912432221114873
Larkin, M., & Thompson, A. R. (2011). Interpretative phenomenological analysis in mental health and psychotherapy research. In D. Harper & A. R. Thompson (Eds.), Qualitative research methods in mental health and psychotherapy: A guide for students and practitioners (pp. 99–116). Wiley.
Lathren, C., Bluth, K., & Zvara, B. (2020). Parent self-compassion and supportive responses to child difficult emotion: An intergenerational theoretical model rooted in attachment. Journal of Family Theory & Review, 12(3), 368–381. https://doi.org/10.1111/jftr.12388
Linehan, M. M. (2014). DBT® skills training manual. Guilford.
Lofton, O., Petrosky-Nadeau, N., & Seitelman, L. (2021). Parents in a pandemic labor market (Working Paper No. 2021-04). Federal Reserve Bank of San Francisco. https://doi.org/10.24148/wp2021-04
Mitchell, A. E., Whittingham, K., Steindl, S., & Kirby, J. (2018). Feasibility and acceptability of a brief online self-compassion intervention for mothers of infants. Archives of Women’s Mental Health, 21, 553–561.
https://doi.org/10.1007/s00737-018-0829-y
Moreira, H., Gouveia, M. J., Carona, C., Silva, N., & Canavarro, M. C. (2015). Maternal attachment and children’s quality of life: The mediating role of self-compassion and parenting stress. Journal of Child and Family Studies, 24, 2332–2344. https://doi.org/10.1007/s10826-014-0036-z
Myers, J. E., & Sweeney, T. J. (2004). The indivisible self: An evidence-based model of wellness. Journal of Individual Psychology, 60(3), 234–245. https://core.ac.uk/download/pdf/149232976.pdf
Neff, K. (2011). Self-compassion: The proven power of being kind to yourself. HarperCollins.
Neff, K. D., & Dahm, K. A. (2015). Self-compassion: What it is, what it does, and how it relates to mindfulness. In B. D. Ostafin, M. D. Robinson, & B. P. Meier (Eds.), Handbook of mindfulness and self-regulation (pp. 121–137). Springer. https://doi.org/10.1007/978-1-4939-2263-5_10
Neff, K. D., & Germer, C. K. (2013). A pilot study and randomized controlled trial of the mindful self-compassion program. Journal of Clinical Psychology, 69(1), 28–44. https://doi.org/10.1002/jclp.21923
Neff, K., & Germer, C. (2018). The mindful self-compassion workbook: A proven way to accept yourself, build inner strength, and thrive. Guilford.
Orenstein, G. A. & Lewis, L. (2021). Erikson’s stages of psychosocial development. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK556096
Park, J. (2021). Who is hardest hit by a pandemic? Racial disparities in COVID-19 hardship in the U.S. International Journal of Urban Sciences, 25(2), 149–177. https://doi.org/10.1080/12265934.2021.1877566
Prikhidko, A., & Swank, J. M. (2018). Motherhood experiences and expectations: A qualitative exploration of mothers of toddlers. The Family Journal, 26(3), 278–284. https://doi.org/10.1177/1066480718795116
Psychogiou, L., Legge, K., Parry, E., Mann, J., Nath, S., Ford, T., & Kuyken, W. (2016). Self-compassion and parenting in mothers and fathers with depression. Mindfulness, 7, 896–908.
https://doi.org/10.1007/s12671-016-0528-6
Ruppanner, L., Tan, X., Carson, A., & Ratcliff, S. (2021). Emotional and financial health during COVID-19: The role of housework, employment and childcare in Australia and the United States. Gender, Work, & Organization, 28(5), 1937–1955. https://doi.org/10.1111/gwao.12727
Sackett, C. R., & Jenkins, A. M. (2015). Photovoice: Fulfilling the call for advocacy in the counseling field. Journal of Creativity in Mental Health, 10(3), 376–385. https://doi.org/10.1080/15401383.2015.1025173
Segal, Z., Williams, M., & Teasdale, J. (2018). Mindfulness-based cognitive therapy for depression (2nd ed). Guilford.
Smith, L., Davis, K., & Bhowmik, M. (2010). Youth participatory action research groups as school counseling interventions. Professional School Counseling, 14(2), 174–182. http://www.jstor.org/stable/42732946
van der Kolk, B. A. (2014). The body keeps the score: Brain, mind, and body in the healing of trauma. Penguin.
Wang, C. C. (1999). Photovoice: A participatory action research strategy applied to women’s health. Journal of Women’s Health, 8(2), 185–192. https://doi.org/10.1089/jwh.1999.8.185
Wang, C., & Burris, M. A. (1997). Photovoice: Concept, methodology, and use for participatory needs assessment. Health Education & Behavior, 24(3), 369–387. https://doi.org/10.1177/109019819702400309
Wester, K. L., Wachter Morris, C. A., Trustey, C. E., Cory, J. S., & Grossman, L. M. (2021). Promoting rigorous research using innovative qualitative approaches. Journal of Counseling & Development, 99(2), 189–199. https://doi.org/10.1002/jcad.12366
Wilson, N., Dasho, S., Martin, A. C., Wallerstein, N., Wang, C. C., & Minkler, M. (2007). Engaging young adolescents in social action through photovoice: The Youth Empowerment Strategies (YES!) Project. The Journal of Early Adolescence, 27(2), 241–261. https://doi.org/10.1177/0272431606294834
World Health Organization. (2021, May). The true death toll of COVID-19: Estimating global excess mortality.
https://www.who.int/data/stories/the-true-death-toll-of-covid-19-estimating-global-excess-mortality
Zamarro, G., Perez-Arce, F., & Jose Prados, M. (2020). Gender differences in the impact of COVID-19. Center for Economic and Social Research, University of Southern California. https://www.ktla.com/wp-content/uploads/sites/4/2020/06/ZamarroGenderDiffImpactCOVID-19_061820-2.pdf
Kelly Emelianchik-Key, PhD, NCC, ACS, LMFT, LMHC-QS, is an associate professor at Florida Atlantic University. Adriana C. Labarta, PhD, NCC, ACS, LMHC, is an assistant professor at Florida Atlantic University. Clara Bossie, MS, ACS, LMFT-QS, is a doctoral candidate at Florida Atlantic University and Owner and Clinical Director of Wisely Wellness LLC. Carman S. Gill, NCC, ACS, LCMHC, is a professor and department chair at Florida Atlantic University. Correspondence may be addressed to Kelly Emelianchik-Key, Department of Counselor Education, Florida Atlantic University, 777 Glades Rd. Bldg. 47, Rm. 275, Boca Raton, FL 33431-0991, Kemelian@fau.edu.
Jul 25, 2025 | Volume 15 - Issue 2
Alexandra Frank, Amanda C. DeDiego, Isabel C. Farrell, Kirby Jones, Amanda C. Tracy
State policies and school district regulation largely shape the roles and responsibilities of school counselors in the United States. The American School Counselor Association (ASCA) provides guidance on recommendations for school counseling practice; however, state policies may not align with guiding principles. Using a rubric informed by the ASCA National Model, we conducted a problem-driven content analysis to explore state policy alignment with the Define, Manage, Deliver, and Assess components of the model. Our findings indicate state policy differences between K–8 and 9–12 grade levels and within each rubric component. School counselors and school counselor educators can use these findings to support strategic advocacy efforts aimed at increased clarity around school counselors’ roles and responsibilities.
Keywords: content analysis, advocacy, state policy, school counseling, ASCA National Model
What is a school counselor? The profession has a long history of attempting to answer this question, not always successfully. Role confusion in school counseling was highlighted by Murray (1995) who stated that the roles of school counselors often vary from the printed job description. Murray attributed unclear counseling duties to misunderstandings about school counselors’ roles by stakeholders, such as administrators, parents, and students. Murray also found that differences in legislative definitions of school counseling contributed to role confusion. As an early act of advocacy in school counseling, Murray suggested developing a uniform definition of school counseling, advocating for that definition, and engaging in effective communication strategies among stakeholders as solutions to role confusion. Since this early movement to define school counseling roles, professional groups (e.g., The American School Counselor Association [ASCA]), academic organizations (e.g., School Counselors for MTSS), and professional conferences (e.g., The Evidence-Based School Counseling Conference and ASCA conference) have joined in the efforts to describe school counselor identity and roles. Despite these efforts, school counselors across the United States struggle with the lack of clarity in their roles (Bardhoshi & Duncan, 2009; Chandler et al., 2018).
School counselors’ impacts on student outcomes are well-documented (O’Connor, 2018). When describing the role and influence of school counselors, researchers point to improved student outcomes, such as decreased student behavior issues (Reback, 2010), increased student achievement (Carrell & Hoekstra, 2014), and increased college-going behavior (Hurwitz & Howell, 2014). School counselors’ roles in supporting student social–emotional health became particularly important when navigating the effects of COVID-19 (McCoy-Speight, 2021). However, Murray’s (1995) concern about legislative differences in defining the role of a school counselor remains. Despite evidence describing positive impacts of school counselors on student outcomes, the school counselor role is often misunderstood and continues to vary from state to state (Carey & Dimmitt, 2012). Recently, state differences were most pronounced in Texas Senate Bill 763 (2023), which proposed to equip chaplains to serve as school counselors, and in Florida’s emphasis on parents as resiliency coaches (Florida Governor’s Press Office, 2023). Additionally, factors such as organizational constraints (Alexander et al., 2022), student–counselor ratios (Kearney et al., 2021), and engagement in non-counseling duties (Blake, 2020; Camelford & Ebrahim, 2017; Chandler et al., 2018) continue to hinder the impact that school counselors can make within their school settings. Intrigued by Murray’s observation regarding the long-standing issues with school counseling roles and duties differing from state to state and recent state initiatives to supplement the role of a school counselor with chaplains or parents (e.g., Texas and Florida), we sought to explore how state-level policies and statutes define school counselor roles and responsibilities and how they align with national recommendations.
Defining School Counseling
Noting the need for a uniform definition of school counseling, we turned to ASCA. Although ASCA is not the only professional organization supporting school counselors, it has the longest history (formed in 1952) and largest membership (approximately 43,000). Additionally, ASCA exists for the explicit purpose of supporting school counselors by “providing professional development, enhancing school counseling programs, and researching effective school counseling practices” (n.d.-a, About ASCA section). ASCA (2023) defines school counseling as a comprehensive, developmental, and preventative support aimed at improving student outcomes. ASCA (n.d.-b) advocates for a united school counseling vision and voice among stakeholders. Despite their efforts, researchers, educational leaders, and state policymakers continue to hold varied perspectives about the definitions, needs, and roles of school counselors. Although ASCA (2019; 2023) clearly delineates appropriate and inappropriate school counseling roles and responsibilities, school counselors often find themselves asked to engage in activities deemed inappropriate by ASCA (Bardhoshi & Duncan, 2009; Chandler et al., 2018).
School counselors can use collaboration and advocacy to promote a more appropriate use of their time (McConnell et al., 2020) and to mediate feelings of burnout (Holman et al., 2019). Researchers have discussed the importance of advocacy as integral to pre–school counselor training (Havlik et al., 2019), individual school counseling practice (Perry et al., 2020), and system-wide professional unity (Cigrand et al., 2015). However, such efforts are often limited to a single school or district and often do not include state-level advocacy.
The ASCA National Model
To support their mission of improving student outcomes, ASCA (2019) recommends a national model as a framework for school counselors. The ASCA National Model is aligned with school counseling priorities, such as data-informed decision-making, systemic interventions, and developmentally appropriate care considerations. Implementation is associated with both student-facing and school counselor–facing benefits. In an introduction to a special issue on comprehensive school counseling programs, Carey and Dimmitt (2012) described findings across six statewide studies highlighting the relationship between program implementation and positive student outcomes, including improved attendance and decreases in rates of student discipline. Pyne (2011) and more recently Fye and colleagues (2022) demonstrated correlations between program implementation and school counselor job satisfaction. Pyne found that school counselors with administrative support and staff collaboration related to program implementation experienced higher rates of job satisfaction. Fye et al. noted that as implementation of the ASCA National Model increased, role ambiguity decreased and job satisfaction increased.
The ASCA National Model consists of four components: Define, Manage, Deliver, and Assess. We outline the model in Table 1 below.
Table 1
Four Components of The ASCA National Model
| Define |
Standards to support school counselors
School counselors are supported in implementation and assessment of a comprehensive school counseling program by existing standards such as the ASCA Mindsets & Behaviors, the ASCA Ethical Standards for School Counselors, and the ASCA School Counselor Professional Standards & Competencies. |
| Manage |
Effective and efficient implementation of a comprehensive school counseling program
ASCA outlines planning tools to support a program focus, program planning, and appropriate school counseling activities. |
| Deliver |
The actual delivery of a comprehensive school counseling program
School counselors implement developmentally appropriate activities and services to support positive student outcomes. School counselors engage in direct (e.g., instruction, appraisal and advisement, counseling) and indirect (e.g., consultation, collaboration, referrals) student services. ASCA (2019) stipulates that school counselors should spend 80% of their time in direct or indirect student services. School counselors should spend 20% or less of their time on school support activities and/or program planning. |
| Assess |
Data-driven accountability measures to assess the efficacy of program delivery
School counselors are charged with evaluating their program’s efficacy and implementing improvements, based on student needs. School counselors should demonstrate that students are positively impacted because of the counseling program. |
We extend the Assess component to also include research-based examples on factors contributing to a school counselor’s efficacy. Such factors include student–school counselor ratios. For decades, ASCA has advocated for a student–school counselor ratio of 250:1 as well as broader support for school counselor roles (Kearney et al., 2021). Yet, data from the 2021–2022 school year put the average national student–school counselor ratio at 408:1 (National Center for Education Statistics [NCES], 2023). Researchers demonstrate that schools with ASCA-approved ratios experience increased student attendance, higher test scores, and improved graduation rates (e.g., Carey et al., 2012; Carrell & Carrell, 2006; Goodman-Scott et al., 2018; Lapan et al., 2012).
Alternatively, Donohue and colleagues (2022) demonstrated that higher ratios relate to worse outcomes for students. Notably, minoritized students and their school communities often face the brunt of increased student–school counselor ratios (Donohue et al., 2022; Education Trust, 2018). Thus, the ASCA alignment is not only concerned with improved student outcomes but also with the equitable provision of mental health services. Given the role ASCA plays in advocating for and structuring the school counselor’s role and responsibilities, we chose to use the components of the ASCA National Model (2019) as a theoretical framework guiding our study. We have incorporated our theoretical framework throughout, including data collection, data analysis, results, discussion, and implications.
Method
The purpose of our study was to understand how state policies align with the ASCA National Model. We analyzed state policies defining and guiding the practice of school counseling. In any inquiry, the type and characteristics of the data available should dictate the research methods (Flick, 2015). Content analysis allows researchers to identify recurring themes, patterns, and trends (Krippendorff, 2019). By systematically coding and categorizing content, researchers can uncover insights that might not be immediately apparent through casual observation. Additionally, it enables researchers to analyze large volumes of data in a systematic and replicable manner, reducing the impact of personal bias and increasing the reliability of findings. Because of these factors, we found content analysis to be the best method for our inquiry. We chose a subtype of content analysis—problem-driven content analysis (Krippendorff, 2019). Problem-driven content analysis aims to answer a research question. The research question guiding our analysis was: How are state policies aligned or misaligned with the ASCA National Model?
Sample
Using the State Policy Database maintained by the National Association of State Boards of Education (NASBE; 2023), we pulled current policies from all 50 U.S. states and the District of Columbia (N = 51) that dictate the role of school counselors and school counseling services. As ASCA (n.d.-c) describes, terms used for school counseling services can vary, and although “school counselor” is favorable to “guidance counselor,” both terms may be found. However, in NASBE’s State Policy Database, the category was specifically listed as “counseling, psychological, and social services,” and the subcategory was listed as “school counseling—elementary” and “school counseling—secondary” (NASBE, 2023). We included policies that govern kindergarten through eighth grade (K–8) and ninth through 12th grade (9–12). Data included all policies related to school counseling delivery and certification, with State Policy Databases sorted into policies governing K–8 (n = 156, 47.42%) and 9–12 (n = 173, 52.58%) levels, for a total of 329 policies.
Design
From our research question to data reporting, we followed the problem-driven content analysis steps (see Figure 1). We collected language from the policies, including policy type and policy name, and then determined if school counseling was encouraged, recommended, or not specified as either. We built a spreadsheet to divide, define, and identify the state policies into sampling units. We divided them into originating state, policy type, requirements for having school counselors in schools, policy name, and summary of the policy. Additionally, we separated the data into K–8 and 9–12 education designations.
Figure 1
Problem-Driven Content Analysis Process (Krippendorff, 2019)
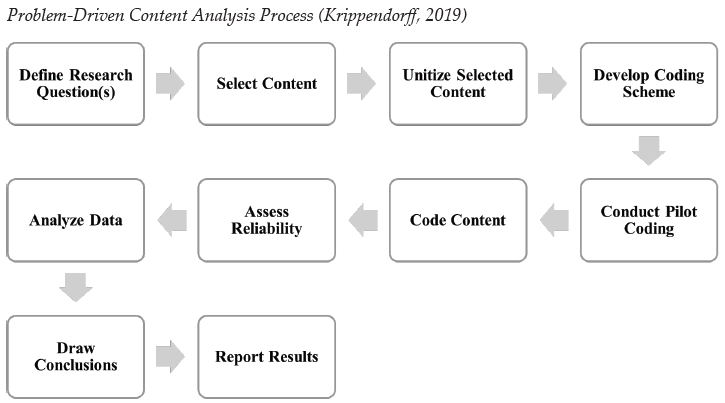
The analytical process began with filtering policies for inclusion outlined in our selection criteria. We built a spreadsheet to divide, define, and identify the legislative bills into sampling units. We focused on dividing them into originating state, bill number, year, subcategory, and summary of the bill. After completing the spreadsheet with all the data, Kirby Jones and Amanda C. Tracy tested our coding frame on a sample of text. Although content analysis does not require piloting, Schreier (2012) suggested piloting around 20% of the data to test the reliability of the coding frame. We used 20% of our data (n = 66) to conduct pilot coding.
We approached the data analysis deductively, with the components of the ASCA National Model (2019) acting as our initial codes. Prior to analysis, we created a coding rubric that we used to analyze each state’s school counseling policy (see Table 2). We used the four components of the ASCA National Model as the rubric criteria: Define, Manage, Deliver, and Assess. Within each criterion, we developed standards ranging from 1 point to 5 points. We chose point ranges based on the information within each criterion. For example, the Define criterion included three standards for 5 total points. We awarded 1 point if a state required (versus recommended) school counselors in school; we awarded 1 point if a state required school counselors to be licensed and/or certified based on a graduate degree; and we awarded 3 points if a state specifically described all three focus areas of school counseling—academic, college/career, and social/emotional.
Alexandra Frank, Amanda C. DeDiego, and Isabel C. Farrell were involved in creating the rubric and completing initial pilot coding to ensure the usability and utility of the rubric. All team members met throughout the process to ensure workability and fidelity. Following initial testing, each coding pair was trained to appropriately analyze state-level policy data using the rubric. Before finalizing rubric metrics for each state, all team members met again to review metrics and to determine final scores for each state. Importantly, individual state-level rubric scores do not indicate grades, but rather demonstrate evidence of alignment between state-level policy as it is written and the ASCA National Model (2019).
Table 2
Rubric to Evaluate State Policy for Adherence to the ASCA National Model
| Aspects of the ASCA National Model |
|
Define
5 points
|
Manage
1 point |
Deliver
1 point |
Assess
2 points |
|
Required
1 point
|
Education
1 point |
Focus
3 points |
Implementation
1 point |
Use of Time
1 point |
Accountability
1 point |
Ratio
1 point
|
| State has provisions requiring school counselors |
Requires school counselors to be licensed/certified |
Areas of focus include:
(1) academic,
(2) college/career,
(3) social/emotional |
Role includes appropriate school counseling activities |
80% of time spent in direct/indirect services supporting student achievement, attendance, and discipline |
Evaluation of school counselor role included |
Maximum
of 250:1
|
Research Team
Our research team consisted of two counselor educators, two counselor education doctoral students, and one master’s-level counseling student. We began meeting as a research team in summer 2023. Conceptualization, data collection, and analysis occurred throughout the fall, ending in December 2023. Frank, DeDiego, and Farrell continued with edits and writing in 2024. Varying counseling backgrounds (including clinical mental health and school counseling), education settings (e.g., urban, rural, research, teaching), and personal identities were represented. All members are united by a passion for mentorship and advocacy. Additionally, DeDiego and Farrell provided expertise in legislative advocacy and content analysis, and Frank and Tracy provided expertise in school counseling. All members are affiliated with counseling programs accredited by the Council for the Accreditation of Counseling and Related Educational Programs. Frank, DeDiego, and Farrell designed the coding frame and trained Jones and Tracy on the coding process. Frank, DeDiego, and Farrell also resolved any coding conflicts. For example, if a state regulation was unclear, Frank, DeDiego, and Farrell met and decided what code would apply. All members of the research team communicated via email, Google Docs, and/or Zoom meetings to build consensus through the data collection and data analysis processes.
Trustworthiness
To enhance trustworthiness in this study, we followed the checklist for content analysis developed by Elo et al. (2014), which includes three phases: preparation, organization, and reporting. The preparation phase involves determining the most appropriate data source to address the research question and the appropriate scope of the content and analysis. In this phase, we determined the focus of the project to be policy defining school counselor roles; thus, state-level legislation was the most appropriate data source. Use of the NASBE (2023) database offered a means of limiting scope and focus of the content. Using deductive coding (McKibben et al., 2022), we first developed the rubric coding framework based on the ASCA National Model (2019) and then conducted pilot coding to test the framework.
During the organization phase, the checklist addresses organizing coding and theming strategies. We first conducted pilot coding to establish how to apply the ASCA National Model (2019) to coding legislation. We evaluated the content using the rubric to determine how the legislation aligned with the ASCA National Model. Elo et al. (2014) suggested researchers also determine how much interpretation will be used to analyze the data. The coding framework using the ASCA National Model offers structure to this interpretation. Data were coded separately for trustworthiness by Jones and Tracy. Then we met to compare coding. If there was discrepancy, one of us reviewed the data in order to reach a two-thirds majority for all of the coding. By the end of the process, all coding met the threshold of two-thirds majority agreement.
In the Elo et al. (2014) checklist, the reporting phase addresses how to represent and share the results of the analysis. This includes ensuring that categories used to report findings capture the data well and that results are clear and understandable for targeted audiences. The use of a rubric framework offers a clear method to represent and share results of the analysis process.
Results
Our results highlighted trends in the scope and practice of school counseling across the United States. We organized results by rubric strands (Table 3) and by state, analyzing results for K–8 (Appendix A) and 9–12 (Appendix B). We further describe our results within each strand of the ASCA National Model (2019): Define, Manage, Deliver, and Assess.
Table 3
Summary of Rubric Outcomes by Category
|
K–8 |
9–12 |
|
Yesa |
Nob |
Yesa |
Nob |
| Required |
37 (72.55%) |
14 (27.45%) |
40 (78.73%) |
11 (21.57%) |
| Education |
40 (78.43%) |
11 (21.57%) |
50 (98.04%) |
1 (1.96%) |
| Focus
Academic
College/Career
Social/Emotional |
35 (68.63%)
37 (72.55%)
35 (68.63%) |
16 (31.37%)
14 (27.45%)
16 (31.37%) |
40 (78.43%)
41 (80.39%)
40 (78.43%) |
11 (21.57%)
10 (19.61%)
11 (21.57%) |
| Implementation |
34 (66.67%) |
17 (33.33%) |
36 (70.59%) |
15 (29.41%) |
| Use of Time |
17 (33.33%) |
34 (66.76%) |
10 (19.61%) |
41 (80.39%) |
| Accountability |
21 (41.18%) |
30 (58.82%) |
29 (56.86%) |
22 (43.14%) |
| Ratio |
2 (3.92%) |
49 (96.08%) |
3 (5.88%) |
48 (94.12%) |
aIndicates awarding of a point, as outcome was represented in the policy.
bIndicates no point was awarded, as outcome was not represented in the policy.
In the state policies, school counselors were designated as required, encouraged, or not specified. For the K–8 level, 72.55% (n = 37) of states required school counselors in schools, 19.61% (n = 10) encouraged the presence of school counselors, and 7.84% (n = 4) of states did not specify a requirement of school counselor presence. At the 9–12 level, 78.73% (n = 40) of states required school counselors in schools, 19.60% (n = 10) encouraged the presence of school counselors, and 1.96% (n = 1) of states did not specify a requirement of school counselor presence.
The category of not specified included policies that were uncodified or policies that did not address the requirement of school counselors at all. The majority of states required school counselors at the K–8 (n = 37, 72.55%) and 9–12 (n = 40, 78.73%) levels. At the K–8 level, one state had a policy that was uncodified (Michigan) and three did not address the requirements of school counselors (i.e., Hawaii, South Dakota, Wyoming). At the 9–12 level, one state had an uncodified policy (Hawaii) and one did not specify a requirement for school counselors (South Dakota). Forty states (80%) for K–8 and 50 states (98.04%) for 9–12 required school counselors to have a license or certification in school counseling. The only state that did not require certification or licensure was Florida. Thirty-five states (70%) for K–8 and 40 states (78.43%) for 9–12 described the role of a school counselor as supporting students’ academic success. Thirty-seven states (72.54%) for K–8 and 41 states (80.39%) for 9–12 described the role of a school counselor as supporting college and career readiness. Finally, 35 states (68.63%) for K–8 and 40 states (78.43%) for 9–12 described the role of a school counselor as supporting students’ social and emotional growth.
Within the Manage aspect of the ASCA National Model (2019), we determined if the state outlined appropriate school counseling activities in alignment with ASCA recommendations in policy or statute (e.g., small groups, counseling, classroom guidance, preventative programs). Thirty-four states (66.67%) for K–8 and 36 states (70.59%) for 9–12 outlined school counseling activities in their policy. For Deliver, only 17 states (33.33%) for K–8 and 10 states (20%) for 9–12 outlined whether or not the majority of school counselors’ time should be spent providing direct and indirect student services.
Moreover, for the Assess category, we evaluated whether the state policy required school counselors to do an evaluation of their role and/or counseling services. Twenty-one states (58.82%) for K–8 and 29 states (56.86%) for 9–12 outlined evaluation requirements. Finally, we evaluated whether the state complied with the ASCA student–school counselor ratio of 250:1. Two states for K–8 (3%; i.e., New Hampshire, Vermont) and three states for 9–12 (5.9%; i.e., Michigan, New Hampshire, Vermont) complied with the recommended ratios. A few states (i.e., Colorado, Illinois, Kentucky, Minnesota, Montana) recommended that state districts follow the ASCA 250:1 recommendation, but it was not a requirement; those state ratios exceeded 250:1.
Next, we examined overall trends of compliance by grade level and by state. For K–8, eight states (15.69%) had higher scores of ASCA National Model (2019) compliance (i.e., Arkansas, Maine, Nevada, New Hampshire, Oregon, Pennsylvania, West Virginia, Wisconsin) compared to other states in our dataset with a score of 8 out of 9. For 9–12, six states (11.76%) scored 8 out of 9 (i.e., Arkansas, Maine, New Hampshire, Pennsylvania, West Virginia, Wisconsin). Excluding Hawaii, South Dakota, and Wyoming, because their state policies did not address the requirements of K–8 school counselors, the states with the lowest scores of ASCA National Model compliance, with 1 out of 9 for K–8 were Alabama, Maryland, Missouri, and North Dakota (n = 4, 7.8%). For 9–12 state policy, two states (3.9%)scored 1 out of 9 (i.e., Massachusetts, South Dakota).
Discussion
Given ASCA’s (n.d.-b) advocacy efforts to develop a unified definition of school counseling, there is a need to assess how those advocacy efforts translate to state policy. Although individual state and district policies shed light on existing discrepancies between school counselor roles and responsibilities, our analysis also provides evidence of alignment with the ASCA National Model (2019) in some areas. These results can inform strategic efforts for further alignment. School counselors can use advocacy to support their role and promote responsibilities more aligned with the ASCA National Model (McConnell et al., 2020). We outline our discussion by again utilizing the four components of the ASCA National Model as a conceptual framework.
Define
Our findings suggest that the Define component of the ASCA National Model (2019) is well-represented in state and district policies. Although our results highlight differences in policy governing practice in K–8 and 9–12 schools, for the most part, all state and district policies required or encouraged the presence of a school counselor. Additionally, the vast majority of states required that individuals practicing as school counselors hold the appropriate licensure and/or certification. Similarly, most state and district policies defined a school counselor’s role as contributing to students’ academic, college/career, and/or social/emotional development. Vigilance in advocacy efforts remains important, as language in policy can change with each legislative session. For example, Texas Senate Bill No. 763 (2023) introduced legislation allowing chaplains to serve in student support roles instead of school counselors. The Lone Star State School Counselor Association (2023) quickly took action with a published brief condemning the language in the bill. As a result of advocacy efforts, lawmakers changed the verbiage in the bill to hire chaplains in addition to school counselors, rather than in lieu of them.
Similarly, Florida’s First Lady, Casey DeSantis (Florida Governor’s Press Office, 2023), announced a shift in counseling services to emphasize resiliency and include resiliency coaches—a role in which “moms, dads, and community members will be able to take training covering counseling standards and resiliency education standards” and provide a “first layer of support to students” (para. 8). Although the Florida School Counselor Association emphasizes advocacy efforts, it has not yet published a response to the changes in Florida’s resilience instruction and support plans (Weatherill, 2023). The legislation in Texas and Florida and the response from state-level school counselor associations highlight, once again, the importance of advocacy for creating and maintaining a uniform definition of school counseling.
Manage
Although ASCA clearly defines appropriate and inappropriate school counseling activities, state policy is less specific on codifying the appropriate use of school counselors’ time and resources. Although most states encouraged appropriate school counseling activities, states did not specifically define appropriate school counseling activities or provide protection around school counselors’ time to implement appropriate school counseling activities. Such findings are consistent with the literature (Bardhoshi & Duncan, 2009; Chandler et al., 2018). Florida’s K–8 policy suggests that school counselors should implement a program that suits the school and department, whereas some states’ K–8 policy, such as New Jersey’s, recommends incorporating the ASCA National Model (2019). Several states include uncodified policy addressing the implementation of a school counseling program. However, as such recommendations are not codified into policy, they do not dictate the day-to-day activities of school counselors. Interestingly, new legislation introducing support roles for chaplains and family/community members only bolsters the need to protect school counselors’ time. Texas Senate Bill No. 763 references the need for support, services, and programming. Florida First Lady Casey DeSantis similarly emphasizes the need for support and mentorship. School counselors are trained professionals equipped to support student outcomes (ASCA, 2019). One wonders whether legislative efforts introducing chaplains and family members would be needed if school counselors’ time was protected in ways to better support students with appropriate school counseling duties. Thus, there remains an opportunity for increased advocacy surrounding the implementation of school counseling programs with specific attention on appropriate versus inappropriate school counseling activities.
Deliver
ASCA suggests that school counselors should spend 80% of their time in direct/indirect services to support student outcomes. Such efforts are pivotal, as research suggests that school counselors play a key role in supporting student outcomes (e.g., Carey & Dimmitt, 2012; O’Connor, 2018). Researchers indicate that school counselors within a comprehensive school counseling program play an integral role in supporting improved student attendance (Carey & Dimmitt, 2012), graduation rates (Hurwitz & Howell, 2014), and academic performance (Carrell & Hoekstra, 2014). However, few states support student outcomes by codifying a school counselor’s use of time into policy. Idaho’s 9–12 policy instructs school counselors to use most of their time on direct services. While not equivalent to ASCA’s 80%, such efforts represent a start to protecting school counselors’ time and ensuring that school counselors are able to make the impact they are well-trained to in their school settings. Similar to Manage, current legislative efforts only highlight the importance of school counselors spending a majority of their time supporting students through direct services.
Assess
ASCA continues to focus their advocacy efforts on student–school counselor ratios with good reason; our findings indicate that 2% of K–8 state and district policies and 3% of 9–12 policies specifically outlined a 250:1 ratio that aligns with ASCA recommendations. Yet, researchers demonstrate that reduced student–counselor ratios support improved student outcomes (Carey et al., 2012; Carrell & Carrell, 2006; Goodman-Scott et al., 2018; Lapan et al., 2012). Further, minoritized students and their communities often face the negative consequences of increased student–counselor ratios (Donohue et al., 2022). As such, further advocacy around student–school counselor ratios is also needed from an equity perspective. Some states, such as Colorado, Illinois, Kentucky, and Montana, recommended ASCA ratios, but as is the case with appropriate versus inappropriate school counseling activities, without policy “teeth” to enforce recommendations, school counselors are often continuing to practice in settings that far exceed ASCA ratios, as is consistent with recent findings (NCES, 2023).
Although many states did not codify policies aligned with the ASCA National Model (2019), several states (North Dakota, New Jersey, Delaware) made reference to the ASCA National Model and recommended alignment. Our analysis supports previous research indicating that advocacy works (Cigrand et al., 2015; Havlik et al., 2019; Holman et al., 2019; McConnell et al., 2020; Perry et al., 2020). Our findings also highlight the value of supporting professional identity through membership in both national organizations and state-level advocacy groups.
Implications
We explored implications for school counselor educators, school counselors, and school counseling advocates. School counselor educators must prepare future school counselors for their roles as advocates. Counselor educators also play an important role in equipping future school counselors with an understanding of the landscape of the profession (McMahon et al., 2009). As such, including state-level policy and district-level conversations in curriculum helps connect counseling students with the evolving policies guiding their work. The rubric created for this research offers a valuable tool to explore state and school district alignment with the ASCA National Model (2019) and demonstrate areas to focus advocacy efforts. Counseling programs often participate in advocacy efforts, such as Hill Day. School counselor educators can use state-level and district-level policy as a springboard to promote specific advocacy efforts with state and local legislation. On a local level, school counselor educators can use our rubric to frame practice conversations for future school counselors to prepare for future conversations with school principals. Finally, school counselor educators can continue engaging in policy-level research to support ongoing school counseling advocacy. School counselor educators can further illuminate the impacts of school counseling policy by describing perspectives of practicing school counselors. School counselor educators can also engage in quantitative research methods to study the relationships between school counselor satisfaction and state policy adherence to the ASCA National Model (2019).
School counselors can use our rubric to analyze alignment of school districts when examining job descriptions during their job searches. School counselors could also use the rubric as part of the evaluation component of a comprehensive school counseling program. From our analysis, it appears most imperative that advocacy efforts focus on school counselors’ use of time and student–counselor ratios. Using data, school counselors can continue to advocate for their role to become more closely aligned to ASCA’s recommendations. Kim et al. (2024) described the “urgent need” (p. 233) for school counselors to engage in outcome research. We hope that our framework provides a tool for school counselors to engage in evaluation and advocacy based on our findings. However, school counselors should not be alone in their advocacy efforts. School counseling advocates, including educational stakeholders, counselors, school counselor educators, and educational policymakers, should continue supporting school counselors by advocating on their behalf at the district, state, and national level.
Future research may focus on the disconnect between state policy and how the districts enact those policies. A content analysis comparing state policy to district rules, regulations, and practices is needed to understand how state policy and district practices align. Finally, although there is frequent legislative advocacy from ASCA, there is a lack of data on state legislators’ knowledge about the ASCA National Model (2019) and ASCA priorities. School counseling researchers can use qualitative methods to interview state legislators, especially after events such as Hill Day, to better detail what legislators understand about the roles and impacts of school counselors.
Limitations
The purpose of content analysis was to discover patterns in large amounts of data through a systematic coding process (Krippendorff, 2019). We are all professional counselors or counselors-in-training with a passion for advocacy. Thus, as with any qualitative work, there is potential for bias in the coding process. Interrater reliability was used to mitigate this risk. There are many factors that impact the practice of school counseling beyond state-level policy. District policies and school leadership vastly impact the ways that state policy is interpreted and enacted in schools. Thus, this content analysis represents only school counseling regulation as described in policy and may not fully represent the day-to-day experiences of school counselors.
Conclusion
Although confusion and role ambiguity muddy the school counseling profession, advocacy efforts and outcome research act as cleansers. By providing a rubric to assess alignment between state policy and the ASCA National Model, we hoped to clarify the current state of school counseling practice and provide a helpful tool for future school counselors, current practitioners, educational leaders, and policymakers.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Alexander, E. R., Savitz-Romer, M., Nicola, T. P., Rowan-Kenyon, H. T., & Carroll, S. (2022). “We are the heartbeat of the school”: How school counselors supported student mental health during the COVID-19 pandemic. Professional School Counseling, 26(1b). https://doi.org/10.1177/2156759X221105557
American School Counselor Association. (n.d.-a). About ASCA. https://www.schoolcounselor.org/About-ASCA
American School Counselor Association. (n.d.-b). Advocacy and legislation. https://bit.ly/ASCAadvocacylegislation
American School Counselor Association (n.d.-c). Guidance counselor vs. school counselor. https://www.schoolcounselor.org/getmedia/c8d97962-905f-4a33-958b-744a770d71c6/Guidance-Counselor-vs-School-Counselor.pdf
American School Counselor Association. (2019). ASCA National Model: A framework for school counseling programs (4th ed.).
American School Counselor Association. (2023). The role of the school counselor. https://www.schoolcounselor.org/getmedia/ee8b2e1b-d021-4575-982c-c84402cb2cd2/Role-Statement.pdf
Bardhoshi, G., & Duncan, K. (2009). Rural school principals’ perception of the school counselor’s role. The Rural Educator, 30(3), 16–24. https://doi.org/10.35608/ruraled.v30i3.445
Blake, M. K. (2020). Other duties as assigned: The ambiguous role of the high school counselor. Sociology of Education, 93(4), 315–330. https://doi.org/10.1177/0038040720932563
Camelford, K. G., & Ebrahim, C. H. (2017). Factors that affect implementation of a comprehensive school counseling program in secondary schools. Vistas Online, 1–10.
Carey, J., & Dimmitt, C. (2012). School counseling and student outcomes: Summary of six statewide studies. Professional School Counseling, 16(2), 146–153. https://doi.org/10.1177/2156759X0001600204
Carey, J., Harrington, K., Martin, I. M., & Hoffman, D. (2012). A statewide evaluation of the outcomes of the implementation of ASCA National Model school counseling programs in rural and suburban Nebraska high schools. Professional School Counseling, 16(2), 89–99. https://doi.org/10.1177/2156759X0001600203
Carrell, S. E., & Carrell, S. A. (2006). Do lower student to counselor ratios reduce school disciplinary problems? The B.E. Journal of Economic Analysis & Policy, 5(1), 1–24. https://doi.org/10.2202/1538-0645.1463
Carrell, S. E., & Hoekstra, M. (2014). Are school counselors an effective education input? Economics Letters, 125(1), 66–69. https://doi.org/10.1016/j.econlet.2014.07.020
Chandler, J. W., Burnham, J. J., Riechel, M. E. K., Dahir, C. A., Stone, C. B., Oliver, D. F., Davis, A. P., & Bledsoe, K. G. (2018). Assessing the counseling and non-counseling roles of school counselors. Journal of School Counseling, 16(7), n7. https://files.eric.ed.gov/fulltext/EJ1182095.pdf
Cigrand, D. L., Havlik, S. G., Malott, K. M., & Jones, S. G. (2015). School counselors united in professional advocacy: A systems model. Journal of School Counseling, 13(8), n8. https://files.eric.ed.gov/fulltext/EJ1066331.pdf
Donohue, P., Parzych, J. L., Chiu, M. M., Goldberg, K., & Nguyen, K. (2022). The impacts of school counselor ratios on student outcomes: A multistate study. Professional School Counseling, 26(1). https://doi.org/10.1177/2156759X221137283
Education Trust. (2018). Funding gaps: An analysis of school funding equity across the U.S. and within each state.
https://edtrust.org/wp-content/uploads/2014/09/FundingGapReport_2018_FINAL.pdf
Elo, S., Kääriäinen, M., Kanste, O., Pölkki, T., Utriainen, K., & Kyngäs, H. (2014). Qualitative content analysis: A focus on trustworthiness. SAGE Open, 4(1). https://doi.org/10.1177/2158244014522633
Flick, U. (2015). Qualitative Inquiry—2.0 at 20? Developments, trends, and challenges for the politics of research. Qualitative Inquiry, 21(7), 599–608. https://doi.org/10.1177/1077800415583296
Florida Governor’s Press Office. (2023, March 22). First lady Casey DeSantis announces next steps in Florida’s first-in-the-nation approach to create a culture of resiliency and incentivize parental involvement in schools [Press release]. https://www.flgov.com/eog/news/press/2023/first-lady-casey-desantis-announces-next-steps-floridas-first-nation-approach
Fye, H. J., Schumacker, R. E., Rainey, J. S., & Guillot Miller, L. (2022). ASCA National Model implementation predicting school counselors’ job satisfaction with role stress mediating variables. Journal of Employment Counseling, 59(3), 111–119. https://doi.org/10.1002/joec.12181
Goodman-Scott, E., Sink, C. A., Cholewa, B. E., & Burgess, M. (2018). An ecological view of school counselor ratios and student academic outcomes: A national investigation. Journal of Counseling & Development, 96(4), 388–398. https://doi.org/10.1002/jcad.12221
Havlik, S. A., Malott, K., Yee, T., DeRosato, M., & Crawford, E. (2019). School counselor training in professional advocacy: The role of the counselor educator. Journal of Counselor Leadership and Advocacy, 6(1), 71–85. https://doi.org/10.1080/2326716X.2018.1564710
Holman, L. F., Nelson, J., & Watts, R. (2019). Organizational variables contributing to school counselor burnout: An opportunity for leadership, advocacy, collaboration, and systemic change. The Professional Counselor, 9(2), 126–141. https://doi.org/10.15241/lfh.9.2.126
Hurwitz, M., & Howell, J. (2014). Estimating causal impacts of school counselors with regression discontinuity designs. Journal of Counseling & Development, 92(3), 316–327. https://doi.org/10.1002/j.1556-6676.2014.00159.x
Kearney, C., Akos, P., Domina, T., & Young, Z. (2021). Student-to-school counselor ratios: A meta-analytic review of the evidence. Journal of Counseling & Development, 99(4), 418–428. https://doi.org/10.1002/jcad.12394
Kim, H., Molina, C. E., Watkinson, J. S., Leigh-Osroosh, K. T., & Li, D. (2024). Theory-informed school counseling: Increasing efficacy through prevention-focused practice and outcome research. Journal of Counseling & Development, 102(2), 226–238. https://doi.org/10.1002/jcad.12507
Krippendorff, K. (2019). Content analysis: An introduction to its methodology (4th ed.). SAGE. https://doi.org/10.4135/9781071878781
Lapan, R. T., Gysbers, N. C., Stanley, B., & Pierce, M. E. (2012). Missouri professional school counselors: Ratios matter, especially in high-poverty schools. Professional School Counseling, 16(2). https://doi.org/10.1177/2156759X0001600207
Lone Star State School Counselor Association. (2023). SB 763 and Texas school counselors. https://www.lonestarstateschoolcounselor.org/news_issues
McConnell, K. R., Geesa, R. L., Mayes, R. D., & Elam, N. P. (2020). Improving school counselor efficacy through principal-counselor collaboration: A comprehensive literature review. Mid-Western Educational Researcher, 32(2). https://scholarworks.bgsu.edu/cgi/viewcontent.cgi?article=1063&context=mwer
McCoy-Speight, A. (2021). The school counselor’s role in a post-COVID-19 era. In I. Fayed & J. Cummings (Eds.), Teaching in the post COVID-19 era (pp. 697–706). Springer. https://doi.org/10.1007/978-3-030-74088-7_68
McKibben, W. B., Cade, R., Purgason, L. L., & Wahesh, E. (2022). How to conduct a deductive content analysis in counseling research. Counseling Outcome Research and Evaluation, 13(2), 156–168. https://doi.org/10.1080/21501378.2020.1846992
McMahon, H. G., Mason, E. C. M., & Paisley, P. O. (2009). School counselor educators as educational leaders promoting systemic change. Professional School Counseling, 13(2). https://doi.org/10.1177/2156759X0901300207
Murray, B. A. (1995). Validating the role of the school counselor. The School Counselor, 43(1), 5–9. https://www.jstor.org/stable/23901422
National Association of State Boards of Education. (2023). State policy database. https://statepolicies.nasbe.org
National Center for Education Statistics. (2023). National teacher and principal survey. Institute of Education Sciences. https://nces.ed.gov/surveys/ntps
O’Connor, P. J. (2018). How school counselors make a world of difference. Phi Delta Kappan, 99(7), 35–39.
https://kappanonline.org/oconnor-school-counselors-make-world-difference
Perry, J., Parikh, S., Vazquez, M., Saunders, R., Bolin, S., & Dameron, M. L. (2020). School counselor self-efficacy in advocating for self: How prepared are we? Journal of Counselor Preparation and Supervision, 13(4), 5. https://research.library.kutztown.edu/jcps/vol13/iss4/5
Pyne, J. R. (2011). Comprehensive school counseling programs, job satisfaction, and the ASCA National Model. Professional School Counseling, 15(2). https://doi.org/10.1177/2156759X1101500202
Reback, R. (2010). Schools’ mental health services and young children’s emotions, behavior, and learning. Journal of Policy Analysis and Management, 29(4), 698–725. https://doi.org/10.1002/pam.20528
S.B. 763, 88th Cong. (2023). https://capitol.texas.gov/BillLookup/History.aspx?LegSess=88R&Bill=SB763
Schreier, M. (2012). Qualitative content analysis in practice. SAGE. https://doi.org/10.4135/9781529682571
Weatherill, A. (2023). Florida Department of Education update. Florida Department of Education. https://www.myflfamilies.com/sites/default/files/2023-11/DOE%20Update-DCF%20committee%20meeting%206-28-23.pdf
Appendix A
Breakdown of State Rubric Scores for ASCA Alignment for K–8 Schools
|
Define
(5 points)
|
Manage
(1 point) |
Deliver
(1 point) |
Assess
(2 points) |
State Score
(9 points) |
|
Required
(1 point)
|
Education
(1 point) |
Focus
(3 points) |
Implementation
(1 point) |
Use of Time
(1 point) |
Accountability
(1 point) |
Ratio
(1 point) |
Total |
| AL |
1 |
0 |
0 |
0 |
0 |
0 |
0 |
1 |
| AK |
0 |
1 |
2 |
1 |
0 |
1 |
0 |
5 |
| AZ |
0 |
1 |
3 |
1 |
0 |
1 |
0 |
6 |
| AR |
1 |
1 |
3 |
1 |
1 |
1 |
0 |
8 |
| CA |
1 |
1 |
3 |
1 |
0 |
1 |
0 |
7 |
| CO |
0 |
1 |
3 |
1 |
0 |
1 |
0 |
6 |
| CT |
0 |
1 |
3 |
1 |
1 |
1 |
0 |
7 |
| DE |
1 |
0 |
3 |
0 |
0 |
0 |
0 |
4 |
| DC |
1 |
1 |
0 |
0 |
0 |
0 |
0 |
2 |
| FL |
0 |
1 |
1 |
0 |
0 |
1 |
0 |
3 |
| GA |
1 |
1 |
3 |
1 |
0 |
0 |
0 |
6 |
| HI |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
| ID |
1 |
1 |
3 |
1 |
1 |
0 |
0 |
7 |
| IL |
0 |
1 |
3 |
1 |
1 |
1 |
0 |
7 |
| IN |
1 |
1 |
3 |
1 |
0 |
0 |
0 |
6 |
| IA |
1 |
1 |
3 |
0 |
0 |
0 |
0 |
5 |
| KA |
1 |
0 |
0 |
1 |
0 |
0 |
0 |
2 |
| KY |
1 |
1 |
0 |
1 |
1 |
0 |
0 |
4 |
| LA |
1 |
1 |
3 |
1 |
1 |
0 |
0 |
7 |
| ME |
1 |
1 |
3 |
1 |
1 |
1 |
0 |
8 |
| MD |
1 |
0 |
0 |
0 |
0 |
0 |
0 |
1 |
| MA |
0 |
0 |
3 |
1 |
0 |
0 |
0 |
4 |
| MI |
0 |
1 |
0 |
1 |
0 |
0 |
0 |
2 |
| MN |
0 |
0 |
3 |
1 |
0 |
0 |
0 |
4 |
| MI |
1 |
1 |
3 |
1 |
1 |
0 |
0 |
7 |
| MO |
1 |
0 |
0 |
0 |
0 |
0 |
0 |
1 |
| MT |
1 |
1 |
3 |
1 |
1 |
0 |
0 |
7 |
| NE |
1 |
1 |
0 |
0 |
0 |
1 |
0 |
3 |
| NV |
1 |
1 |
3 |
1 |
1 |
1 |
0 |
8 |
| NH |
1 |
1 |
3 |
1 |
0 |
1 |
1 |
8 |
| NJ |
1 |
0 |
2 |
0 |
0 |
1 |
0 |
4 |
| NM |
1 |
1 |
3 |
1 |
0 |
1 |
0 |
7 |
| NY |
1 |
1 |
3 |
1 |
0 |
1 |
0 |
7 |
| NC |
1 |
1 |
3 |
1 |
1 |
0 |
0 |
7 |
| ND |
0 |
1 |
0 |
0 |
0 |
0 |
0 |
1 |
| OH |
0 |
1 |
0 |
1 |
0 |
1 |
0 |
3 |
| OK |
1 |
1 |
3 |
1 |
0 |
1 |
0 |
7 |
| OR |
1 |
1 |
3 |
1 |
1 |
1 |
0 |
8 |
| PA |
1 |
1 |
3 |
1 |
1 |
1 |
0 |
8 |
| RI |
1 |
1 |
3 |
0 |
0 |
0 |
0 |
5 |
| SC |
1 |
1 |
3 |
0 |
1 |
0 |
0 |
6 |
| SD |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
| TN |
1 |
1 |
3 |
1 |
0 |
0 |
0 |
6 |
| TX |
1 |
1 |
3 |
1 |
0 |
0 |
0 |
6 |
| UT |
1 |
1 |
0 |
0 |
0 |
0 |
0 |
2 |
| VT |
1 |
1 |
3 |
0 |
0 |
0 |
1 |
6 |
| VA |
1 |
1 |
3 |
1 |
1 |
0 |
0 |
7 |
| WA |
1 |
1 |
3 |
1 |
0 |
0 |
0 |
6 |
| WV |
1 |
1 |
3 |
1 |
1 |
1 |
0 |
8 |
| WI |
1 |
1 |
3 |
1 |
1 |
1 |
0 |
8 |
| WY |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
| Total |
37 |
40 |
107 |
34 |
17 |
21 |
2 |
– |
Note. Categories refer to the ASCA National Model (2019).
Appendix B
Breakdown of State Rubric Scores for ASCA Alignment for 9–12 Schools
|
Define
(5 points)
|
Manage
(1 point) |
Deliver
(1 point) |
Assess
(2 points) |
State Score
(9 points) |
|
Required
(1 point)
|
Education
(1 point) |
Focus
(3 points) |
Implementation
(1 point) |
Use of Time
(1 point) |
Accountability
(1 point) |
Ratio
(1 point) |
Total |
| AL |
1 |
1 |
0 |
0 |
0 |
0 |
0 |
2 |
| AK |
0 |
1 |
3 |
1 |
0 |
0 |
0 |
5 |
| AZ |
0 |
1 |
3 |
1 |
0 |
1 |
0 |
6 |
| AR |
1 |
1 |
3 |
1 |
1 |
1 |
0 |
8 |
| CA |
0 |
1 |
3 |
1 |
0 |
1 |
0 |
6 |
| CO |
0 |
1 |
3 |
1 |
0 |
1 |
0 |
6 |
| CT |
1 |
1 |
3 |
1 |
0 |
1 |
0 |
7 |
| DE |
1 |
1 |
3 |
1 |
0 |
1 |
0 |
7 |
| DC |
1 |
1 |
0 |
0 |
0 |
0 |
0 |
2 |
| FL |
1 |
0 |
1 |
1 |
0 |
1 |
0 |
4 |
| GA |
1 |
1 |
3 |
1 |
0 |
1 |
0 |
7 |
| HI |
0 |
1 |
3 |
0 |
0 |
0 |
0 |
4 |
| ID |
1 |
1 |
3 |
1 |
1 |
0 |
0 |
7 |
| IL |
0 |
1 |
3 |
1 |
1 |
1 |
0 |
7 |
| IN |
1 |
1 |
3 |
1 |
0 |
0 |
0 |
6 |
| IA |
1 |
1 |
3 |
1 |
0 |
1 |
0 |
7 |
| KA |
1 |
1 |
0 |
0 |
0 |
0 |
0 |
2 |
| KY |
1 |
1 |
1 |
0 |
0 |
1 |
0 |
4 |
| LA |
1 |
1 |
3 |
1 |
0 |
0 |
0 |
6 |
| ME |
1 |
1 |
3 |
1 |
1 |
1 |
0 |
8 |
| MD |
1 |
1 |
3 |
0 |
0 |
1 |
0 |
6 |
| MA |
0 |
1 |
0 |
0 |
0 |
0 |
0 |
1 |
| MI |
0 |
1 |
3 |
1 |
0 |
1 |
1 |
7 |
| MN |
0 |
1 |
3 |
1 |
0 |
1 |
0 |
6 |
| MI |
1 |
1 |
3 |
1 |
1 |
0 |
0 |
7 |
| MO |
1 |
1 |
3 |
1 |
0 |
1 |
0 |
7 |
| MT |
1 |
1 |
3 |
1 |
0 |
0 |
0 |
6 |
| NE |
1 |
1 |
3 |
1 |
0 |
0 |
0 |
6 |
| NV |
1 |
1 |
3 |
1 |
0 |
1 |
0 |
7 |
| NH |
1 |
1 |
3 |
1 |
0 |
1 |
1 |
8 |
| NJ |
1 |
1 |
3 |
0 |
0 |
0 |
0 |
5 |
| NM |
1 |
1 |
3 |
1 |
0 |
1 |
0 |
7 |
| NY |
1 |
1 |
3 |
1 |
0 |
1 |
0 |
7 |
| NC |
1 |
1 |
0 |
1 |
0 |
1 |
0 |
4 |
| ND |
1 |
1 |
0 |
0 |
0 |
0 |
0 |
2 |
| OH |
0 |
1 |
0 |
0 |
0 |
1 |
0 |
2 |
| OK |
1 |
1 |
3 |
1 |
0 |
1 |
0 |
7 |
| OR |
1 |
1 |
3 |
1 |
0 |
0 |
0 |
6 |
| PA |
1 |
1 |
3 |
1 |
1 |
1 |
0 |
8 |
| RI |
1 |
1 |
3 |
0 |
0 |
0 |
0 |
5 |
| SC |
1 |
1 |
3 |
1 |
0 |
1 |
0 |
7 |
| SD |
0 |
1 |
0 |
0 |
0 |
0 |
0 |
1 |
| TN |
1 |
1 |
3 |
1 |
0 |
1 |
0 |
7 |
| TX |
1 |
1 |
3 |
1 |
0 |
1 |
0 |
7 |
| UT |
1 |
1 |
0 |
0 |
0 |
0 |
0 |
2 |
| VT |
1 |
1 |
3 |
0 |
0 |
0 |
1 |
6 |
| VA |
1 |
1 |
3 |
1 |
1 |
0 |
0 |
7 |
| WA |
1 |
1 |
3 |
1 |
1 |
0 |
0 |
7 |
| WV |
1 |
1 |
3 |
1 |
1 |
1 |
0 |
8 |
| WI |
1 |
1 |
3 |
1 |
1 |
1 |
0 |
8 |
| WY |
1 |
1 |
2 |
0 |
0 |
0 |
0 |
4 |
| Total |
40 |
50 |
121 |
36 |
10 |
29 |
3 |
– |
Note. Categories refer to the ASCA National Model (2019).
Alexandra Frank, PhD, NCC, is an assistant professor at the University of Tennessee at Chattanooga. Amanda C. DeDiego, PhD, NCC, ACS, BC-TMH, LPC, is an associate professor at the University of Wyoming. Isabel C. Farrell, PhD, NCC, LPC, is an associate professor at Wake Forest University. Kirby Jones, MA, LCMHCA, is a licensed counselor at Camel City Counseling. Amanda C. Tracy, MS, NCC, PPC, is a doctoral candidate at the University of Wyoming. Correspondence may be addressed to Alexandra Frank, University of Tennessee at Chattanooga, School of Professional Studies, 651 McCallie Ave, Room 105D, Chattanooga, TN 37403, Alexandra-Frank@utc.edu.
Jul 25, 2025 | Volume 15 - Issue 2
Wendi L. Ferrell, Joshua D. Smith, Neal D. Gray
Each year TPC presents an interview with an influential veteran in counseling as part of its Lifetime Achievement in Counseling series. This year, Dr. Barbara Herlihy shared insights from her decades-long commitment to the professionalization of counseling and the evolution of the profession’s ethical standards. Dr. Herlihy’s scholarship and service have had a profound effect on how counseling ethics are taught, applied, and revised to remain relevant in an ever-evolving world. In this interview, she connects counselors’ professional ethical obligations to the advancement of social justice and the internationalization of the profession. We are grateful for Dr. Herlihy’s contributions to our profession and for the wisdom that she shared in this interview.
—J. Richelle Joe, Editor
 Barbara Herlihy, PhD, NCC, is Professor Emerita in the counselor education program in the College of Education and Human Development at the University of New Orleans. She is a Fellow of the American Counseling Association and is a recipient of the Chi Sigma Iota Thomas J. Sweeney Professional Leadership Award, the SACES Courtland Lee Social Justice Award, and the ACES Distinguished Mentor Award.
Barbara Herlihy, PhD, NCC, is Professor Emerita in the counselor education program in the College of Education and Human Development at the University of New Orleans. She is a Fellow of the American Counseling Association and is a recipient of the Chi Sigma Iota Thomas J. Sweeney Professional Leadership Award, the SACES Courtland Lee Social Justice Award, and the ACES Distinguished Mentor Award.
A prolific writer, she is co-author (with Dr. Gerald Corey) of the ACA Ethical Standards Casebook and (with Dr. Theodore Remley) of Ethical, Legal, and Professional Issues in Counseling, and co-editor (with Dr. Cassie Storlie) of Counseling Leaders & Advocates. She has authored or co-authored over 100 journal articles and book chapters, primarily on ethics, social justice, and feminist therapy. She serves as Associate Editor for Ethics for Counseling and Values. She has served twice as Chair of the ACA Ethics Committee, and she currently serves as Chair of the ACA Ethics Appeals Committee. In recent years, she has become passionate about furthering the globalization of the counseling profession and has presented seminars and workshops across the United States and in other countries. She currently serves as Co-Director of Global Issues for the International Institute for the Advancement of Counseling Theory.
1. Can you provide more details about your experience as Chair of the ACA Ethics Appeal Committee? What were your key responsibilities, and how did the committee operate in addressing ethical issues in the counseling profession? What drew you to the field of counseling ethics, and what makes this area so meaningful to you, both personally and professionally?
Looking back, I realize I’ve been engaged consistently with the ACA Code of Ethics in some way for several decades now. I’ve served on the ACA Ethics Committee, the ACA Ethics Appeal Committee, and on Ethics Code Revision task forces; co-authored (first with Larry Golden and then with Gerald Corey) the most recent four editions of the ACA Ethical Standards Casebook; and presented on various ethical issues at numerous professional conferences. With this constant engagement, one might think that I can recite the Code of Ethics from memory. No, not even close! However, I do have a feel for how the Code has evolved over the decades to continue to meet the needs of counselors in a constantly changing and increasingly complex world of practice.
That constant evolution is a major reason why ethics has remained interesting and meaningful to me over the years. Opportunities are constantly being created to ponder new and intriguing ethical dilemmas. I’m routinely challenged to refine how I teach ethics to help students develop finely honed ethical reasoning skills, to research and write about ethical issues as they emerge, and to serve the counseling profession through membership on committees and task forces.
Of all the committees on which I have served, I would say that the ACA Ethics Committee and the Ethics Appeal Committee are the most challenging. Ethics and Ethics Appeals Committee members are charged with reviewing all the evidence provided in a complaint or an appeal and then rendering a judgment. If a counselor is found to be in violation of one or more ethical standards, then the appropriate consequence (which can be anything from a recommendation to change a particular practice to permanent expulsion from ACA) must be chosen and applied. Because counselors are trained to be nonjudgmental and because we gravitate toward forgiveness and compassion rather than imposing punishments, the entire process can be very uncomfortable. In my experience, the ACA members who take on these committee assignments take them very seriously and are keenly aware that their decisions can be consequential. Thankfully, these committees typically have only a very small number of complaints to adjudicate over the course of a year. Formal complaints of ethical violations against counselors are rare, considering the thousands of ACA members who are in practice at any given time, and appeals are even more uncommon. This speaks to the integrity of the practitioners of our profession!
2. Given the current climate, ethical concerns are becoming even more pressing. What are your thoughts on the tension between personal and professional values, and how counselors can uphold ethical standards while respecting cultural diversity and individual client autonomy?
Conflicts between personal and professional values is an issue that jumped into bold relief about 15 years ago as a result of two court cases, Ward v. Wilbanks (2010, 2012) and Keeton v. Augusta State University (2011), in which students were dismissed from their master’s programs in counseling after they refused to counsel clients regarding the clients’ same-sex affectional relationships. The students argued that these relationships were not acceptable according to their religious beliefs. These cases spawned considerable discussion about values conflicts in counseling. Counselor educators grappled with how to best teach students to set aside, or “bracket,” their personal values when entering a counseling session. A body of professional literature developed around managing conflicts between personal and professional values and around the ethical decision-making process when values conflicts exist.
The difficulties associated with counseling clients whose values differ from those of the counselor re-emerged during the run-up to the 2024 presidential election, a time when it seemed that most Americans had such strong political feelings that they found it difficult if not impossible to really hear each other’s viewpoints. Again, counselors struggled when clients expressed views with which the counselors strongly disagreed. Although the specific values-laden issues were different from those that emerged around the students who were dismissed from their training programs, counselors sometimes struggled to set aside their personal values so they could be fully present for their clients. To me, it seems inevitable that in our diverse culture, these issues will continue to emerge. Our work as counselors will be challenged by values conflicts, and I believe we will need to remain vigilant to our own experiences, and work to identify both our explicit and implicit biases so that we can continue to honor and respect our clients without judging their personal value systems. We are a richly diverse society, and as I’ve been saying for many years, multicultural competence and ethical practice go hand in hand—neither one can exist without the other.
3. Given your extensive knowledge and experience in counseling, how do you maintain your motivation and enthusiasm for your work, especially during difficult periods? What aspects of counseling resonate most with you, and are there any particular initiatives or methods that you’re currently excited about?
I have been blessed with the incredibly good fortune of working in what is, for me, the perfect profession. Knowing that as a counselor I may have touched some lives in meaningful ways, and that as a counselor educator I’ve had the privilege of mentoring young professionals who went on to make significant contributions, has been more than enough to maintain my motivation and enthusiasm. Seeking out my own counselor whenever I hit a rough spot on my own personal journey has also sustained me.
Ethics, multicultural competence, social justice, and feminist therapy have been consistent themes throughout my work. At this point in my journey, I am also passionate about the internationalization of counseling. I hope to help find ways to extend helping and healing, whether or not the process is formally called “counseling,” to serve marginalized communities across the globe. I’m also intrigued by the broad spectrum of counseling theory, and how we can connect it more directly to effective practice, particularly with culturally diverse client populations in the United States and internationally.
4. Would you take a moment and share your thoughts on the internationalization of counseling—specifically, how counseling practices are expanding across borders and adapting to different cultural contexts? What are the challenges and benefits of these cross-cultural exchanges, and how does the profession develop effective practice across diverse populations?
One of the exciting projects in which I am currently involved is a “world mapping” initiative, sponsored by the International Institute for the Advancement of Counseling Theory and spearheaded by Dr. Ed Neukrug of Old Dominion University. Along with Dr. Courtland C. Lee, I co-chair the Global Subgroup that is engaged in the mapping project. This year we are exploring South America; our incredible graduate assistant, Kacey Bunting, is presently conducting interviews with leaders who engage in and teach counseling/helping/healing in South American countries. (We refer broadly to “counseling/helping/healing” as many countries don’t have formal counseling professions.) As we analyze Kacey’s interviews, we hope to learn about approaches that are unique to these countries and the extent to which and how Euro-American theories and practices are being adapted. We’re eager to see what we can learn about mental health and the helping process in other countries. Of course, many challenges exist, including language barriers and lack of contact information that would enable us to identify and connect with key people. However, the anticipated benefits far outweigh the challenges. In addition to helping counselors and counseling students improve their “global citizenship,” an attribute that Dr. Lee has emphasized in his writings, this project should provide us with a wealth of information that can be used to improve our counseling practices here in the United States, particularly with culturally diverse clients.
5. How have you seen the counseling profession evolve over the years? What changes, either positive or negative, have you observed?
Over my several decades as a counselor and counselor educator, I have witnessed incredible changes in our profession. I think these changes are reflected in the ways that the ACA Code of Ethics has evolved since it was first published in 1961. The original contained no section on technology, of course, but it also made no mention of diversity or multicultural competence. Early versions made what seem now to be rather simplistic statements like “dual relationships should be avoided.” Over the years, the code has been revised periodically to reflect a constantly changing and increasingly complex world of practice.
Overall, I think the most significant change in a positive direction has been the increased professionalization of counseling. Hard-won battles have resulted in the achievement of counselor licensure in all 50 states, the establishment of training standards, and the inclusion of counselors in diverse work settings like the military, inpatient and outpatient mental health facilities, and business and industry.
6. Looking ahead, what do you envision for the future of counseling, and what do you see as potential challenges or boundaries that might delay progress or limit growth in the profession? How do your relationships with counseling associations and organizations influence or shape the evolution of your practice, and do you see any potential challenges or support coming from these affiliations?
The counseling profession in the United States is, inevitably, a microcosm of our society. I am concerned that relationships among our professional associations seem to be divisive in some ways, and that right now our profession does not seem to speak with one voice to our public. My hope is that we will be able to focus on our common purpose and use our united voice to help ensure that social justice issues have a prominent position in our politics, our lives, and our work. Professional associations such as ACA and NBCC have been instrumental in my own professional development, and they continue to be a source of support. I am honored to have had opportunities to give back, in small measure, what I have received, through service to professional associations. If I may end with a word to early-career counselors and counselor educators—those service opportunities exist for you, as well. I hope you will get involved!
This concludes the 10th interview for the annual Lifetime Achievement in Counseling Series. TPC is grateful to Wendi L. Ferrell, Joshua D. Smith, and Neal D. Gray for providing this interview. Wendi L. Ferrell is a graduate candidate at the University of Mount Olive. Joshua D. Smith, PhD, NCC, LCMHC, is an assistant professor at the University of Mount Olive. Neal D. Gray, PhD, LCMHC-S, is a professor at Lenoir-Rhyne University. Correspondence can be emailed to Joshua Smith at jsmith@umo.edu.
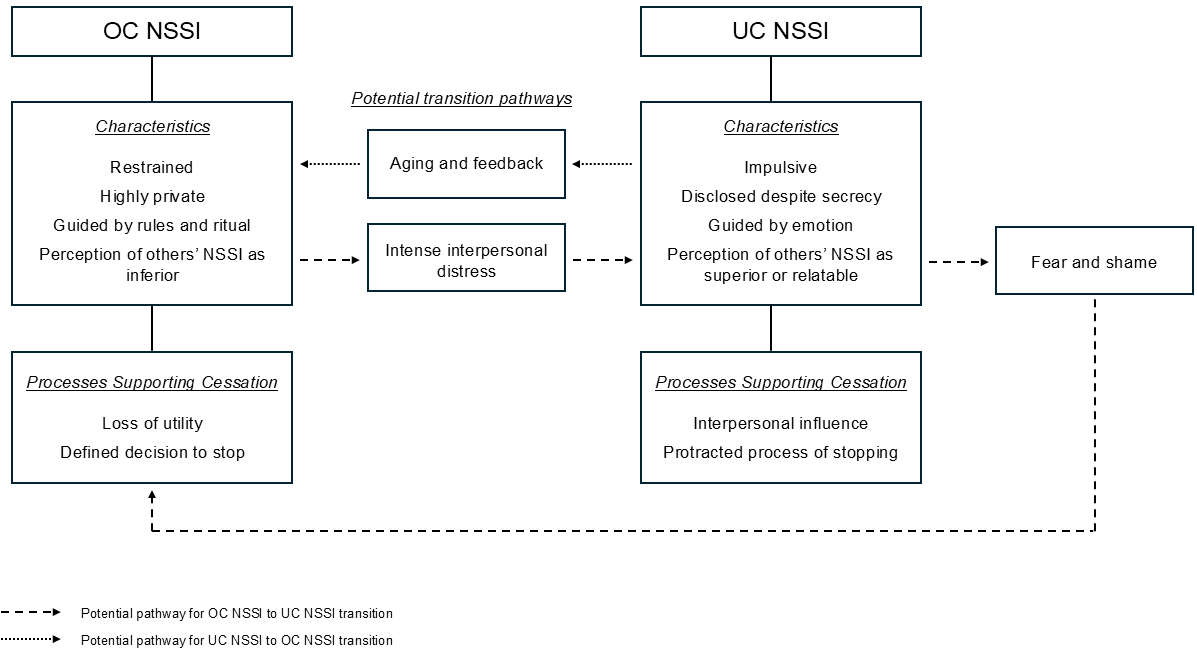
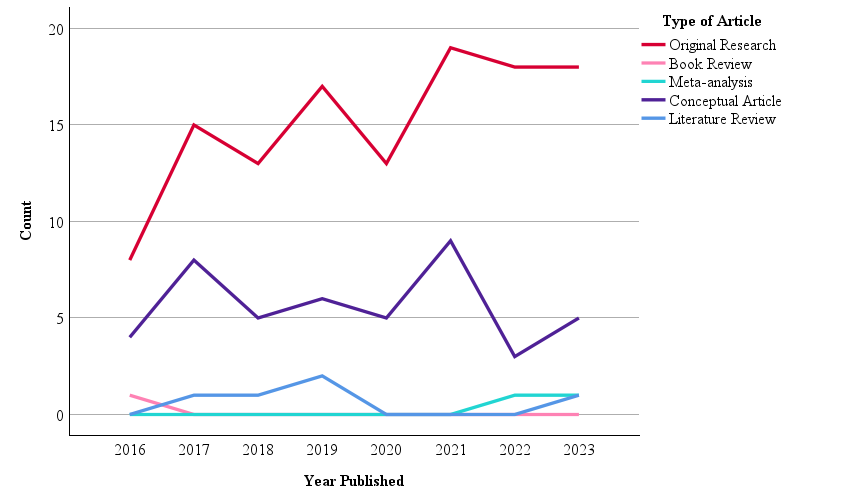 Note. N = 174.
Note. N = 174.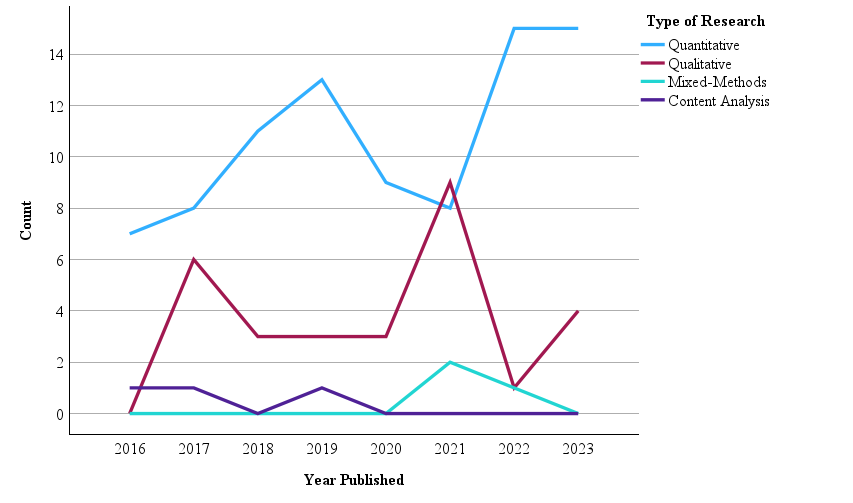
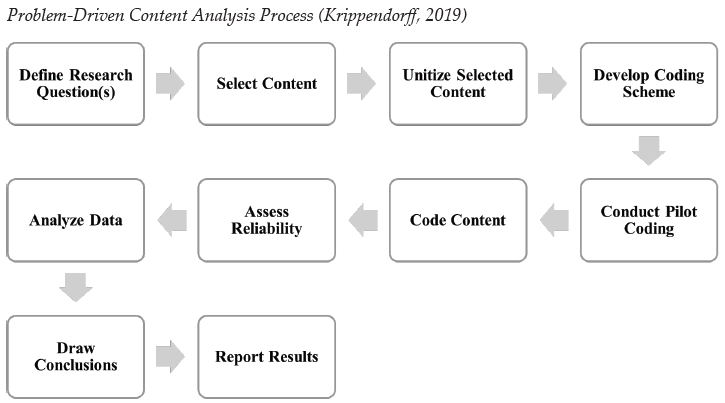
 Barbara Herlihy, PhD, NCC, is Professor Emerita in the counselor education program in the College of Education and Human Development at the University of New Orleans. She is a Fellow of the American Counseling Association and is a recipient of the Chi Sigma Iota Thomas J. Sweeney Professional Leadership Award, the SACES Courtland Lee Social Justice Award, and the ACES Distinguished Mentor Award.
Barbara Herlihy, PhD, NCC, is Professor Emerita in the counselor education program in the College of Education and Human Development at the University of New Orleans. She is a Fellow of the American Counseling Association and is a recipient of the Chi Sigma Iota Thomas J. Sweeney Professional Leadership Award, the SACES Courtland Lee Social Justice Award, and the ACES Distinguished Mentor Award.