Michael T. Kalkbrenner, Edward S. Neukrug
The primary aim of this study was to cross-validate the Revised Fit, Stigma, & Value (FSV) Scale, a questionnaire for measuring barriers to counseling, using a stratified random sample of adults in the United States. Researchers also investigated the percentage of adults living in the United States that had previously attended counseling and examined demographic differences in participants’ sensitivity to barriers to counseling. The results of a confirmatory factor analysis supported the factorial validity of the three-dimensional FSV model. Results also revealed that close to one-third of adults in the United States have attended counseling, with women attending counseling at higher rates (35%) than men (28%). Implications for practice, including how professional counselors, counseling agencies, and counseling professional organizations can use the FSV Scale to appraise and reduce barriers to counseling among prospective clients are discussed.
Keywords: barriers to counseling, FSV Scale, confirmatory factor analysis, attendance in counseling, factorial validity
According to the World Health Organization (WHO), mental health disorders are widespread, with over 300 million people struggling with depressive disorders, 260 million living with anxiety disorders, and hundreds of millions having any of a number of other mental health disorders (WHO, 2017, 2018). The symptoms of anxiety and depressive disorders can be dire and include hopelessness, sadness, sleep disturbances, motivational impairment, relationship difficulties, and suicide in the most severe cases (American Psychiatric Association, 2013). Worldwide, one in four individuals will be impacted by a mental health disorder in their lifetime, which leads to over a trillion dollars in lost job productivity each year (WHO, 2018). In the United States, approximately one in five adults has a diagnosable mental illness each year, and about 20% of children and teens will develop a mental disorder that is disabling (Centers for Disease Control, 2018).
Substantial increases in mental health distress among the U.S. and global populations have impacted the clinical practice of counseling practitioners who work in a wide range of settings, including schools, social service agencies, and colleges (National Institute of Mental Health, 2017; Twenge, Joiner, Rogers, & Martin, 2017). Identifying the percentage of adults in the United States who attend counseling, as well as the reasons why many do not, can help counselors develop strategies that can make counseling more inviting and, ultimately, relieve struggles that people face. Although perceived stigma and not having health insurance have been associated with reticence to seek counseling (Han, Hedden, Lipari, Copello, & Kroutil, 2014; Norcross, 2010; University of Phoenix, 2013), the literature on barriers to counseling among people in the United States is sparse. Appraising barriers to counseling using a psychometrically sound instrument is the first step toward counteracting such barriers and making counseling more inviting for prospective clients. Evaluating barriers to counseling, with special attention to cultural differences, has the potential to help understand differences in attendance to counseling and can help develop mechanisms that promote counseling for all individuals. This is particularly important as research has shown that there are differences in help-seeking behavior as a function of gender identity and ethnicity (Hatzenbuehler, Keyes, Narrow, Grant, & Hasin, 2008).
Attendance in Counseling by Gender and Ethnicity
Previous investigations on attendance in counseling indicated that 15–38% of adults in the United States had sought counseling at some point in their lives (Han et al., 2014; University of Phoenix, 2013), with discrepancies in counselor-seeking behavior found as a function of gender and ethnicity (Han et al., 2014; Lindinger-Sternart, 2015). For instance, women are more likely to seek counseling compared to men (Abrams, 2014; J. Kim, 2017). In addition, individuals who identify as White tend to seek personal counseling at higher rates compared to those who identify with other ethnic backgrounds (Hatzenbuehler et al., 2008; Seidler, Rice, River, Oliffe, & Dhillon, 2017). Parent, Hammer, Bradstreet, Schwartz, and Jobe (2018) examined the intersection of gender, race, ethnicity, and poverty with help-seeking behavior and found the income-to-poverty ratio to be positively related to help-seeking for White males and negatively associated for African American males. In other words, as White males gained in income, they were more likely to seek counseling, whereas the opposite was true for males who identified as African American (Parent et al., 2018).
Barriers to Mental Health Treatment and Attendance in Counseling
Despite the fact that large numbers of individuals in the United States and worldwide will develop a mental disorder in their lifetime, two-thirds of them will avoid or do not have access to mental health treatment (WHO, 2018). In wealthier countries, there is one mental health worker per 2,000 people (WHO, 2015); however, in poorer countries, this drops to 1 in 100,000, and such disparities need to be addressed (Hinkle, 2014; WHO, 2015). Although the lack of attendance in counseling and related services in poorer countries is explained by lack of services, in the United States and other wealthy countries, the availability of mental health services is relatively high, and the lack of attendance is usually explained by other reasons (Neukrug, Kalkbrenner, & Griffith, 2017; WHO, 2015). Research on the lack of attendance in counseling by the general public shows adults in the United States might be reticent to seek counseling because of perceived stigma, financial burden, lack of health insurance, uncertainty about how to find a counselor, and suspicion that counseling will not be helpful (Han et al., 2014; Norcross, 2010; University of Phoenix, 2013).
Appraising Barriers to Counseling
The quantification and appraisal of barriers to counseling is a nuanced and complex construct to measure and has been previously assessed with populations of mental health professionals and with counseling students (Kalkbrenner & Neukrug, 2018; Kalkbrenner, Neukrug, & Griffith, in press; Neukrug et al., 2017). Knowing that personal counseling is a valuable self-care strategy for mental health professionals (Whitfield & Kanter, 2014), Neukrug et al. (2017) developed the original version of the Fit, Stigma, & Value (FSV) Scale, which is comprised of three latent variables, or subscales, of barriers to counseling for human service professionals: fit (the degree to which one trusts the process of counseling), stigma (hesitation to seek counseling because of feelings of embarrassment), and value (the extent to which a respondent thinks that attending personal counseling will be beneficial). Kalkbrenner et al. (in press) extended and validated a revised version of the FSV Scale with a sample of professional counselors, and Kalkbrenner and Neukrug (2018) validated the Revised FSV Scale with a sample of counselor trainees. Although the FSV Scale appears to have utility for appraising barriers to counseling among mental health professionals (Neukrug et al., 2017; Kalkbrenner et al., in press) the factorial validity of the measure has only been tested with helping professionals and counseling students. The appraisal of barriers to seeking counseling among adults in the United States is an essential first step in understanding why prospective clients do, or do not, seek counseling. If validated, researchers and practitioners can potentially use the results of the Revised FSV Scale to aid in the early identification of specific barriers and to inform the development of interventions geared toward reducing barriers to counseling among adults in the United States. Thus, we sought to answer the following research questions (RQs): RQ 1: Is the three-dimensional hypothesized model of the Revised FSV scale confirmed with a stratified random sample of adults in the United States? RQ 2: To what extent do adults in the United States attend counseling? RQ 3: Are there demographic differences to the FSV barriers among adults in the United States?
Method
The psychometric properties of the Revised FSV Scale were tested with a confirmatory factor analysis (CFA) based on structural equation modeling (RQ 1). Descriptive statistics were used to compute participants’ frequency of attendance in counseling (RQ 2). A factorial multivariate analysis of variance (MANOVA) was computed to investigate demographic differences in respondents’ sensitivity to the FSV barriers (RQ 3). A minimum sample size of 320 (10 participants for each estimated parameter) was determined to be sufficient for computing a CFA (Mvududu & Sink, 2013). An a priori power analysis was conducted using G*Power to determine the sample size for the factorial MANOVA (Faul, Erdfelder, Lang, & Buchner, 2007). Results revealed that a minimum sample size of 269 would provide an 80% power estimate (α = .05), with a moderate effect size, f 2 = 0.25 (Cohen, 1988).
Participants and Procedures
After obtaining IRB approval, an online sampling service (Qualtrics, 2018) was contracted to survey a stratified random sample (stratified by age, gender, and ethnicity) of the general U.S. population based on the 2016–2017 census data. A Qualtrics project management team generated a list of parameters and sample quota constraints for data collection. Once the researchers reviewed and confirmed these parameters, a project manager initiated the stratified random sampling procedure and data collection by sending an electronic link to the questionnaire to prospective participants. A pilot study was conducted using 41 participants and no formatting or imputation errors were found. Data collection for the main study was initiated and was completed in less than one week.
A total of 431 individuals responded to the survey. Of these, 21 responses were omitted because of missing data, yielding a useable sample of 410. Participants ranged in ages from 18 to 84 (M = 45,
SD = 15). The demographic profile included the following: 52% (n = 213) identified as female, 44%
(n = 181) as male, 0.5% (n = 2) as transgender, and 3.4% (n = 14) did not specify their gender. For ethnicity, 63% (n = 258) identified as White, 17% (n = 69) as Hispanic/Latinx, 12% (n = 49) as African American, 5% (n = 21) as Asian, 1% (n = 5) as American Indian or Alaska Native, 0.5% (n = 2) as Native Hawaiian or Pacific Islander, and 1.5% (n = 6) did not specify their ethnicity. For highest degree completed, 1% (n = 5) held a doctoral degree, 7% (n = 29) held a master’s degree, 24% (n = 98) held a bachelor’s degree, 16% (n = 65) had completed an associate degree, 49% (n = 199) had a high school diploma, and 3% (n = 14) did not specify their highest level of education. Eighty-four percent (n = 343) of participants had health insurance at the time of data collection. The demographic profile of our sample is consistent with those found in recent surveys of the general U.S. population (Lumina Foundation, 2017; U.S. Census Bureau, 2017).
Instrumentation
Using the Qualtrics e-survey platform (Qualtrics, 2018), participants were asked to respond to a series of demographic questions as well as the Revised FSV Scale.
Demographic questionnaire. Participants responded to a series of demographic items about their age, ethnicity, gender, highest level of education completed, and if they had health insurance. They also were asked to indicate if they had ever recommended counseling to another person and if they had ever participated in at least one session of counseling as defined by the American Counseling Association (ACA) in the 20/20: Consensus Definition of Counseling: “counseling is a professional relationship that empowers diverse individuals, families, and groups to accomplish mental health, wellness, education, and career goals” (2010, para. 2).
The FSV Scale. The original version of the FSV Scale contained 32 items that comprise three subscales (Fit, Stigma, and Value) for appraising barriers to counselor seeking behavior (Neukrug et al., 2017). Kalkbrenner et al. (in press) developed and validated the Revised FSV Scale by reducing the number of items to 14 (of the original 32) and confirmed the same 3-factor structure of the scale. The Revised FSV Scale (see Table 1) was used in the present study for temporal validity, as it is more current and because it is likely to reduce respondent fatigue, because it is shorter than the original. The Fit subscale appraises the degree to which one trusts the process of counseling (e.g., item 11: “I couldn’t find a counselor who would understand me.”). The Stigma subscale measures respondents’ hesitation to seek counseling because of feelings of embarrassment (e.g., item 1: “My friends would think negatively of me.”). The Value scale reflects the extent to which a respondent thinks that attending personal counseling will be beneficial (e.g., item 8: “It is not an effective use of my time.”). For each item, respondents were prompted with the stem, “I am less likely to attend counseling because . . . ” and asked to rate each item on a Likert-type scale: 1 (strongly disagree), 2 (disagree), 3 (neither agree or disagree), 4 (agree), or 5 (strongly agree). Higher scores designate a greater sensitivity to each barrier. Previous investigators demonstrated adequate to strong internal consistency reliability coefficients for the Revised FSV Scale: α = .82, α = .91, and α = .78, respectively (Kalkbrenner et al., in press) and α = .81, α = .87, and α = .77 (Kalkbrenner & Neukrug, 2018). Past investigators found validity evidence for the 3-dimensional factor structure of the original and revised versions of the FSV Scale through rigorous psychometric testing (factor analysis) with populations of human services professionals (Neukrug et al., 2017), professional counselors (Kalkbrenner et al., in press), and counseling students (Kalkbrenner & Neukrug, 2018).
Results
CFA
A review of skewness and kurtosis values (see Table 1) indicated that the 14 items on the revised FSV scale were largely within the acceptable range of a normal distribution (absolute value < 1; Field, 2013). Mahalanobis d2 indices showed no extreme multivariate outliers. An inter-item correlation matrix (see Table 2) was computed to investigate the suitability of the data for factor analysis. Inter-item correlations were favorable and ranged from r = 0.42 to r = 0.82 (see Table 2).
Table 1
Descriptive Statistics: The Revised Version of the FSV Scale (N = 410)
| Items | M | SD | Skew | Kurtosis |
| My friends would think negatively of me. (Stigma) | 2.27 | 1.18 | 0.63 | -0.50 |
| It would suggest I am unstable. (Stigma) | 2.55 | 1.25 | 0.29 | -0.97 |
| I would feel embarrassed. (Stigma) | 2.72 | 1.20 | -0.02 | -1.00 |
| It would damage my reputation. (Stigma) | 2.43 | 1.20 | 0.41 | -0.78 |
| It would be of no benefit. (Value) | 2.46 | 1.20 | 0.39 | -0.71 |
| I would feel badly about myself if I saw a counselor. (Stigma) | 2.35 | 1.13 | 0.45 | -0.61 |
| The financial cost of participating is not worth the personal benefits. (Value) | 2.61 | 1.18 | 0.25 | -0.68 |
| It is not an effective use of my time. (Value) | 2.40 | 1.16 | 0.45 | -0.57 |
| I couldn’t find a counselor with my theoretical orientation (personal style of counseling). (Fit) |
2.42 | 1.12 | 0.62 | -0.68 |
| I couldn’t find a counselor competent enough to work with me. (Fit) | 2.31 | 1.12 | 0.50 | -0.47 |
| I couldn’t find a counselor who would understand me. (Fit) | 2.41 | 1.20 | 0.48 | -0.66 |
| I don’t trust a counselor to keep my matters just between us. (Fit) | 2.50 | 1.21 | 0.33 | -0.82 |
| Counseling is unnecessary because my problems will resolve naturally. (Value) | 2.56 | 1.31 | 0.22 | -0.61 |
| I have had a bad experience with a previous counselor in the past. (Fit) | 2.34 | 1.17 | 0.44 | -0.71 |
Table 2
Inter-Item Correlation Matrix
| Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 | Q14 | |
| Q1 | 1 | 0.70 | 0.64 | 0.72 | 0.54 | 0.63 | 0.53 | 0.57 | 0.57 | 0.60 | 0.60 | 0.53 | 0.47 | 0.53 |
| Q2 | 1 | 0.76 | 0.72 | 0.51 | 0.61 | 0.52 | 0.54 | 0.55 | 0.58 | 0.60 | 0.57 | 0.42 | 0.46 | |
| Q3 | 1 | 0.68 | 0.51 | 0.64 | 0.54 | 0.53 | 0.53 | 0.55 | 0.58 | 0.57 | 0.50 | 0.43 | ||
| Q4 | 1 | 0.62 | 0.68 | 0.55 | 0.59 | 0.58 | 0.61 | 0.63 | 0.61 | 0.51 | 0.53 | |||
| Q5 | 1 | 0.67 | 0.58 | 0.69 | 0.52 | 0.59 | 0.59 | 0.48 | 0.57 | 0.49 | ||||
| Q6 | 1 | 0.58 | 0.68 | 0.59 | 0.68 | 0.69 | 0.60 | 0.56 | 0.48 | |||||
| Q7 | 1 | 0.72 | 0.60 | 0.60 | 0.57 | 0.58 | 0.59 | 0.53 | ||||||
| Q8 | 1 | 0.64 | 0.66 | 0.68 | 0.61 | 0.64 | 0.54 | |||||||
| Q9 | 1 | 0.71 | 0.71 | 0.61 | 0.56 | 0.57 | ||||||||
| Q10 | 1 | 0.82 | 0.65 | 0.56 | 0.56 | |||||||||
| Q11 | 1 | 0.65 | 0.52 | 0.58 | ||||||||||
| Q12 | 1 | 0.57 | 0.52 | |||||||||||
| Q13 | 1 | 0.44 | ||||||||||||
| Q14 | 1 |
A CFA based on structural equation modeling was computed using IBM SPSS Amos version 25 to test the psychometric properties of the revised 14-item scale with adults in the United States (RQ1). A number of goodness-of-fit (GOF) indices recommended by Byrne (2016) were investigated to determine model fit. The Chi Square CMIN absolute fit index was statistically significant: χ2 (74) = 3.54, p < 0.001. More suitable GOF indices for large sample sizes (N > 200) were examined and revealed adequate model fit: comparative fit index (CFI = .96); root mean square error of approximation (RMSEA = .07); 90% confidence interval [.06, .08]; standardized root mean square residual (SRMR = .038); incremental fit index (IFI = .96); and normed fit index (NFI = .94). Collectively, the GOF indices above demonstrated adequate model fit based on the guidelines provided by Byrne. The path model with standardized coefficients is displayed in Figure 1. Tests of internal consistency reliability (Cronbach’s Alpha) revealed strong reliability coefficients for all three FSV subscales: α = .90, α = .91, and α = .87, respectively. An investigation of the path model coefficients (see Figure 1) revealed a moderate to strong association between the FSV barriers. Consequently, researchers computed a follow-up CFA to test if a single-factor model solution for the FSV Scale was a better fit with the data. Results revealed a poor model fit for the single-factor solution, suggesting that retaining the 3-factor model was appropriate for the data.
Figure 1. Confirmatory Factor Analysis Path Model (N = 410)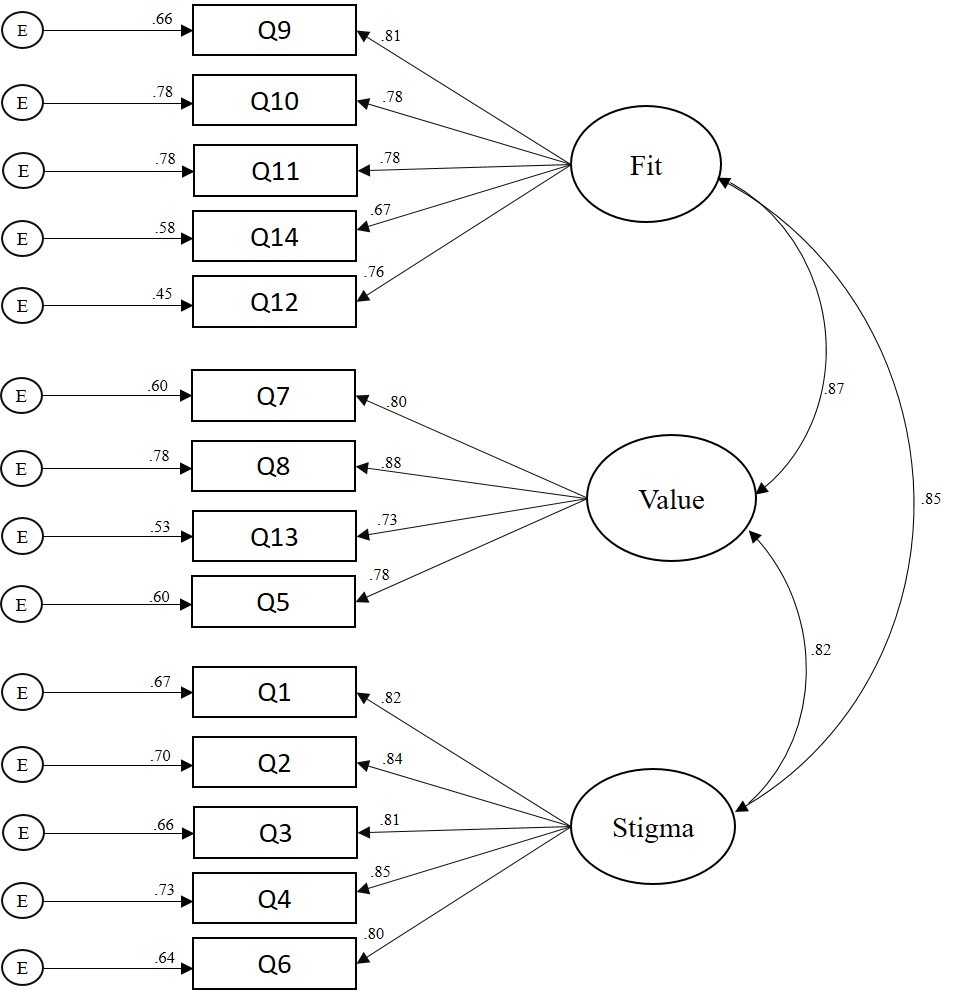
Figure 1. Confirmatory Factor Analysis Path Model (N = 410)
Frequency and Multivariate Analyses
Of the 374 participants who responded to the item regarding whether they had previously attended counseling, 32% (n = 121) indicated they had. A total of 362 participants specified both their gender and past attendance in counseling. Females’ (n = 199) rate of attendance in counseling was 35% (n = 70) and males’ (n = 163) rate of attendance in counseling was 28% (n = 45). Eleven percent
(n = 45) of participants were attending counseling at the time of data collection.
A factorial 2 (gender) X 2 (attendance in counseling) X 2 (ethnicity) MANOVA was computed to examine demographic differences in participants’ sensitivity to barriers to counseling. All three independent variables had two levels: gender (male or female), attendance in counseling (no previous attendance in counseling or previous attendance in counseling), and ethnicity (White or non-White). Based on the recommendations of Kaneshiro, Geling, Gellert, and Millar (2011), the second level of the ethnicity independent variable, non-White, was aggregated by merging all participants who did not identify as White; this ensured comparable groups for statistical analyses. The dependent variables consisted of respondents’ composite scores on each of the three FSV barriers. Because we were interested in investigating all significant main effects and interaction effects across the univariate and multivariate nature of the data, both MANOVA and follow-up univariate ANOVAs were computed (Field, 2013). Bonferroni corrections were applied to control for the familywise error rate.
A significant main effect emerged for gender: F = (7, 354) = 4.73, p = 0.003, Wilks’ Λ = 0.96, η2p = 0.04. The univariate ANOVAs (see Table 3) revealed significant main effects for all three FSV barriers:
Fit: [F = (7, 354) = 6.26, p = 0.013, η2p = 0.02]; Stigma: [F = (7, 354) = 13.71, p < 0.001, η2p = .04]; and
Value: [F = (7, 354) = 5.52, p = 0.02, η2p = .02]. Males (M = 2.56, M = 2.73, M = 2.60) scored higher than females (M = 2.25, M = 2.24, M = 2.23) on Fit, Stigma, and Value, respectively. A significant multivariate main effect also emerged for attendance in counseling: F = (7, 354) = 3.80, p = 0.01, Wilks’ Λ = 0.97, η2p = 0.031. The univariate ANOVA revealed that participants who had not attended counseling (M = 2.60) scored higher than participants who had attended counseling (M = 2.30) on the Value barrier: F = (7, 354) = 4.65, p = 0.03, η2p = 0.01. There were no other statistically significant main effects or any interaction effects (see Table 3). That is, there were no other significant group differences in respondents’ sensitivity to the FSV barriers by gender, attendance in counseling, or ethnicity.
Discussion
The primary aim of the present study was to validate the revised version of the FSV Scale with adults in the United States. Researchers also investigated the percentage of adults that have attended counseling and examined demographic differences in participants’ sensitivity to barriers to counseling. Frequency analyses revealed that 32% of our sample had attended at least one session of personal counseling, and among those who did, females reported a higher rate of attendance (35%) than males (28%). At the time of data collection, 11% of participants were seeing a counselor. Our findings are largely consistent with previous investigations that suggested 15–38% of adults in the United States had sought counseling at some point in their lives (Hann et al., 2014; University of Phoenix, 2013).
Table 3
Demographic Differences in Sensitivity to Barriers to Counseling
2 (gender) X 2 (attendance in counseling) X 2 (ethnicity) Analysis of Variance
| Independent Variable Barrier | F | Sig. | Partial Eta Squared | |||
| Gender | *Fit | 6.26 | 0.01 | 0.02 | ||
| **Stigma | 13.71 | 0.00 | 0.04 | |||
| *Value | 5.52 | 0.02 | 0.02 | |||
| Ethnicity | Fit | 0.34 | 0.56 | 0.00 | ||
| Stigma | 0.00 | 0.96 | 0.00 | |||
| Value | 0.11 | 0.74 | 0.00 | |||
| Attendance in Counseling | Fit | 0.69 | 0.41 | 0.00 | ||
| Stigma | 0.01 | 0.93 | 0.00 | |||
| *Value | 4.65 | 0.03 | 0.01 | |||
| Gender X Ethnicity | Fit | 0.00 | 0.96 | 0.00 | ||
| Stigma | 0.12 | 0.73 | 0.00 | |||
| Value | 0.14 | 0.71 | 0.01 | |||
| Gender X Counseling | Fit | 1.38 | 0.24 | 0.01 | ||
| Stigma | 3.00 | 0.08 | 0.01 | |||
| Value | 1.32 | 0.25 | 0.00 | |||
| Ethnicity X Counseling | Fit | 0.07 | 0.79 | 0.00 | ||
| Stigma | 0.00 | 0.98 | 0.00 | |||
| Value | 0.21 | 0.65 | 0.00 | |||
| Gender X Ethnicity X Counseling | Fit | 0.81 | 0.37 | 0.00 | ||
| Stigma | 1.19 | 0.28 | 0.00 | |||
| Value | 0.24 | 0.62 | 0.00 | |||
df = (1, 354) Note: 0.00 denotes values < 0.01. *Indicates statistical significance at the p < 0.05 level (2-tailed). ** Indicates statistical significance at the p < 0.01 level (2-tailed).
Similar to previous literature on attendance in counseling and congruent with gender theory (Levant, Wimer, & Williams, 2011; Seidler et al., 2017; Vogel, Heimerdinger-Edwards, Hammer, & Hubbard, 2011), we found that males were less likely to seek counseling and were particularly susceptible to the Stigma, Fit, and Value barriers when compared to females. Susceptibility to the Stigma barrier suggests that men might be less likely to attend counseling because of feelings of shame or embarrassment (Cheng, Kwan, & Sevig, 2013; Cheng, Wang, McDermott, Kridel, & Rislin, 2018; J. E. Kim, Saw, & Zane, 2015). Males also reported a higher sensitivity to the Fit and Value barriers as compared to women, suggesting they might place less worth on the anticipated benefits of counseling, and if they were to enter counseling, they may be particularly concerned about finding a counselor with whom they are compatible. It is possible that men’s sensitivity to all FSV barriers may simply be related to their underutilization of counseling services when compared to women, although other explanations also might be plausible.
Consistent with Kalkbrenner et al. (in press), we found that independent of gender, participants who had not attended at least one session of personal counseling placed less value on its potential benefits as compared to those who had attended counseling. This finding suggests that to some extent, attendance in personal counseling might moderate the aforementioned gender differences in participants’ sensitivity to the Value barrier. It is possible that attendance in counseling accounts for a more meaningful amount of the variance in sensitivity to the Value barrier to counseling than gender. Also, consistent with the findings of Kalkbrenner et al. (in press) and Kalkbrenner and Neukrug (2018), we found psychometric support for the factorial validity of the revised version of the FSV scale. Similar to these previous investigations (Kalkbrenner & Neukrug, 2018; Kalkbrenner et al., in press), tests of internal consistency revealed strong reliability coefficients for all three FSV scales. The findings of the present investigators add to the growing body of literature on Fit, Stigma, and Value as three primary barriers to seeking counseling among a variety of populations, including human services professionals (Neukrug et al., 2017), professional counselors (Kalkbrenner et al., in press), counselor trainees (Kalkbrenner & Neukrug, 2018), and now with members of the general U.S. population.
An investigation of the path model coefficients (see Figure 1) revealed moderate to strong associations between the FSV barriers, higher compared to past investigations (Kalkbrenner & Neukrug, 2018; Kalkbrenner et al., in press). A follow-up CFA was computed to test if a single-factor model (aggregated FSV barriers into a single scale) was a better factor solution for the data. However, the follow-up CFA revealed poor model fit for the single factor solution, suggesting that Fit, Stigma, and Value comprise three separate dimensions of a related construct. The differences in the strength of association between the FSV scales in the present study and in the studies by Kalkbrenner et al. (in press) and Kalkbrenner and Neukrug (2018) might be explained by differences between the samples. These investigators validated the FSV barriers with populations of professional counselors and counseling students. It is possible that professional counselors and counseling students were better able to discriminate between different types of barriers to counseling compared to members of the general U.S. population because of the clinical nature of their training. In addition, minor discrepancies are expected in any psychometric study in which authors are attempting to confirm the dimensionality of an attitudinal measure with a new sample (Hendrick, Fischer, Tobi, & Frewer, 2013).
To summarize, the results of internal consistency reliability and CFA indicated that the Revised FSV Scale and its dimensions were estimated adequately with a stratified random sample of adults in the United States. We found close to one-third of our sample had attended counseling, 11% were in counseling at the time of data collection, and there were demographic differences in participants’ sensitivity to barriers to counseling by gender and past attendance in counseling. A number of implications for enhancing counseling practice have emerged from these findings.
Implications for Counseling Practice
With 20% of individuals in the general U.S. population living with a mental disorder, 11% in counseling, 32% having attended counseling, and others wanting counseling but wary of attending, counselors, counseling programs, and counseling organizations can all play a part in reducing the barriers that the public faces when deciding whether or not they should attend counseling. Professional counselors can become leaders in reducing barriers to attending counseling among the general U.S. population through outreach and advocacy. The implications of the following strategies for outreach and advocacy are discussed in the subsequent sub-sections: connecting prospective clients with counselors, interprofessional communication, mobile health, and reducing stigma toward seeking counseling.
Connecting Prospective Clients With Counselors
Nationally, counseling organizations can operate campaigns aimed at reducing the stigma associated with counseling and speaking to its value. The National Board for Certified Counselors (NBCC) advocates for the development and implementation of grassroots community mental health approaches for supporting the accessibility of mental health services on both national and international levels (Hinkle, 2014). Like NBCC, other professional organizations (e.g., ACA and the American Mental Health Counselors Association) might include a directory of professional counselors on their website, along with their specialty areas, who work in a variety of geographic locations to help connect prospective clients with services. On a local level, it is recommended that professional counselors engage in outreach with members of their community to identify the potential unique mental health needs of people in their community and learn about potential barriers to counseling in their local area. Specifically, professional counselors can attend town board meetings and other public events to briefly introduce themselves and use their active listening skills to better understand the needs of the local community. The Revised FSV Scale is one potential tool that professional counselors might use when engaging in outreach with members of their community to gain a better understanding about local barriers to counseling.
We found that participants who had previously attended at least one session of personal counseling reported a higher perceived value of the benefits of counseling compared to those who did not attend counseling. It is possible that individuals’ attendance in counseling is related to their attributing a higher value to the anticipated benefits of counseling. Thus, we suggest community mental health counselors consider offering one free counseling session to promote prospective clients’ attendance in counseling. Just one free session might have the benefit of adding value to a client’s perceived worth of the counseling relationship and increase the likelihood of continued attendance in counseling. Offering one free session may be particularly important for men and minorities, who have traditionally attended counseling at lower rates (Hatzenbuehler et al., 2008; Seidler et al., 2017).
Interprofessional Communication
The flourishing of integrated behavioral health and interprofessional practice across the health care system might provide professional counselors with an opportunity to identify and reduce barriers to seeking counseling among the general U.S. population. In particular, integrated behavioral health involves infusing the delivery of physical and mental health care through interprofessional collaborations or teamwork among a variety of different professionals, thus providing a more holistic model for the patient (Johnson, Sparkman-Key, & Kalkbrenner, 2017). Professional counselors can collaborate with primary care physicians and consider the utility of administering the FSV Scale to patients while they are in the waiting room, as the FSV Scale can be accessed electronically via a tablet or smart phone. We recommend that counseling practitioners reach out to local primary care physicians to discuss the utility of integrated behavioral health and make themselves available to physicians for consultation on how to recognize and refer patients to counseling.
Mobile Health (mHealth)
mHealth refers to the delivery of interventions geared toward promoting physical or mental health by means of a cellular phone (Johnson & Kalkbrenner, 2017). Professional counselors can use mHealth to provide prospective clients with a brief overview of counseling, address prominent barriers to counseling faced by students, and provide mental health resources that are available to students. mHealth might be particularly useful for college and school counselors as academic institutions typically have access to students’ cell phone numbers, and students “appear to be open and responsive to the utilization of mHealth” (Johnson & Kalkbrenner, 2017, p. 323). The campus counseling center is underutilized on some college campuses because of stigma (Rosenthal & Wilson, 2016) and students’ unawareness of the services that are available at the counseling center (Dobmeier, Kalkbrenner, Hill, & Hernández, 2013). College counselors might consider using mHealth as a platform for both reducing stigma toward counselor-seeking behavior and for spreading students’ awareness of the services that are available to them for reduced or no fees at the counseling center.
Reducing Stigma Toward Seeking Counseling
Our results are consistent with the body of evidence indicating that when compared to women, men are less likely to attend counseling, more susceptible to barriers to attending counseling, and more likely to terminate counseling early (Levant et al., 2011; Seidler et al., 2017). Consistent with Vogel et al. (2011), we found that stigma was a predominant barrier to counseling among male participants. It is recommended that counseling practitioners focus on normalizing common presenting concerns that men are facing and find venues (e.g., barber shops, sports arenas) where they can reach out to men and lessen their concerns about attending counseling (Neukrug, Britton, & Crews, 2013).
Professional counselors can become leaders in reducing stigma toward help-seeking among men by normalizing common presenting concerns. As one example, the stress, anxiety, and depression men face when given a diagnosis of prostate cancer can potentially be reduced by counselors and their professional associations. By developing ways for the public to understand prostate cancer and its related mental health concerns, counselors and their professional associations can lessen the stigma of the disease. Promoting public awareness also can increase men’s likelihood of talking about a diagnosis of prostate cancer with friends, loved ones, and counselors, in a similar way that a diagnosis of breast cancer has been destigmatized over the past few decades. Professional counselors should consider other strategies that can be utilized to enhance the likelihood for men to attend counseling, such as group counseling or an informal setting.
Limitations and Future Research
Because causal attributions cannot be inferred from a cross-sectional survey research design, future researchers can extend the line of research on the FSV barriers using an experimental design by administering the scale to clients prior to and following attendance in counseling. Results might provide evidence of how counseling lessens one’s sensitivity to some barriers. Consistent with the U.S. Census Bureau (2017), the ethnic identity of the majority of participants in our sample was White. Thus, future research should replicate the present study using a more ethnically diverse sample, especially because individuals who identify with ethnicities other than White tend to seek counseling at lower rates (Hatzenbuehler et al., 2008; Vogel et al., 2011). In addition, despite having used a rigorous stratified random sampling procedure, it is possible that because of the sample size, this sample is not representative of adults in the United States. In addition, self-report bias is a limitation of the present study.
Our findings, coupled with existing findings in the literature (Kalkbrenner & Neukrug, 2018; Kalkbrenner et al., in press), suggest that the psychometric properties of the revised version of the FSV Scale are adequate for appraising barriers to seeking counseling among mental health professionals and adults in the United States. The next step in this line of research is to confirm the 3-factor structure of the FSV Scale with populations that are susceptible to mental health disorders and who might be reticent to seek counseling (e.g., veterans, high school students, non-White populations, and the older adult population; Akanwa, 2015; American Public Health Association, 2014; Bartels et al., 2003). Because we did not place any restrictions on sampling based on prospective participants’ history of mental illness, it is possible that the mean differences between participants’ sensitivity to the FSV barriers were influenced by the extent to which they were living with clinical problems at the time of data collection. Thus, future researchers should validate the FSV barriers with participants who are living with psychiatric conditions. Future researchers might also investigate the extent to which there might be differences in participants’ sensitivity to the FSV barriers based on the amount of time they have been in counseling (e.g., the number of sessions).
Because of the global increase in mental distress (WHO, 2018), future researchers should consider confirming the psychometric properties of the FSV Scale with international populations. In addition, we found that when gender, ethnicity, and previous attendance in counseling were entered into the MANOVA as independent variables, significant differences in the Value barrier only emerged for attendance in counseling. Therefore, previous attendance in counseling might account for a more substantial portion of the variance in barriers to counseling than gender and ethnicity. Future researchers can test this hypothesis using a path analysis.
Summary and Conclusion
Attendance in counseling among members of the general U.S. population has become increasingly important because of the frequency and complexity of mental disorders within the U.S. and global populations (WHO, 2017). The primary aim of the present study was to test the psychometric properties of the Revised FSV Scale, a questionnaire for measuring barriers to counseling using a stratified random sample of U.S. adults. The results of a CFA indicated that the Revised FSV Scale and its dimensions were estimated adequately with a stratified random sample of adults in the United States. The appraisal of barriers to seeking counseling is an essential first step in understanding why prospective clients do or do not seek counseling. At this stage of development, the Revised FSV Scale appears to have utility for screening sensitivity to three primary barriers (Fit, Stigma, and Value) to seeking counseling among mental health professionals and adults in the United States. Further, the Revised FSV Scale can be used tentatively by counseling practitioners who work in a variety of settings as one way to measure and potentially reduce barriers associated with counseling among prospective clients.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest or funding contributions for the development of this manuscript.
References
Abrams, A. (2014). Women more likely than men to seek mental health help, study finds. TIME Health. Retrieved from
http://time.com/2928046/mental-health-services-women/
Akanwa, E. E. (2015). International students in Western developed countries: History, challenges, and
prospects. Journal of International Students, 5, 271–284.
American Counseling Association. (2010). 20/20: Consensus definition of counseling. Retrieved from https://www.counseling.org/knowledge-center/20-20-a-vision-for-the-future-of-counseling/consensus-definition-of-counseling
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
American Public Health Association. (2014). Removing barriers to mental health services for veterans. Retrieved from https://www.apha.org/policies-and-advocacy/public-health-policy-statements/policy-database/2015/01/28/14/51/removing-barriers-to-mental-health-services-for-veterans
Bartels, S. J., Dums, A. R., Oxman, T. E., Schneider, L. S., Areán, P. A., Alexopoulos, G. S., & Jeste, D. V. (2003). Evidence-based practices in geriatric mental health care: An overview of systematic reviews and meta-analyses. Psychiatric Clinics of North America, 26, 971–990, x–xi. doi:10.1016/S0193-953X(03)00072-8
Byrne, B. M. (2016). Structural equation modeling with AMOS: Basic concepts, applications, and programming (3rd ed.). New York, NY: Routledge.
Centers for Disease Control and Prevention. (2018). Learn about mental health. Retrieved from https://www.cdc.gov/mentalhealth/learn/index.htm
Cheng, H.-L., Kwan, K.-L. K., & Sevig, T. (2013). Racial and ethnic minority college students’ stigma associated with seeking psychological help: Examining psychocultural correlates. Journal of Counseling Psychology, 60, 98–111. doi:10.1037/a0031169
Cheng, H.-L., Wang, C., McDermott, R. C., Kridel, M., & Rislin, J. L. (2018). Self-stigma, mental health literacy, and attitudes toward seeking psychological help. Journal of Counseling & Development, 96, 64–74. doi:10.1002/jcad.12178
Cohen, J. E. (1988). Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc.
Dobmeier, R. A., Kalkbrenner, M. T., Hill, T. L., & Hernández, T. J. (2013). Residential community college student awareness of mental health problems and resources. New York Journal of Student Affairs, 13(2), 15–28.
Faul, F., Erdfelder, E., Lang, A.-G., & Buchner, A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39, 175–191.
Field, A. (2013). Discovering statistics using IBM SPSS Statistics (4th ed.). Thousand Oaks, CA: Sage.
Han, B., Hedden, S. L., Lipari, R., Copello, E. A. P., & Kroutil, L. A. (2014). Receipt of services for behavioral health problems: Results from the 2014 National Survey on Drug Use and Health. Retrieved from https://www.samh sa.gov/data/sites/default/files/NSDUH-DR-FRR3-2014/NSDUH-DR-FRR3-2014/NSDUH-DR-FRR3-2014.htm
Hatzenbuehler, M. L., Keyes, K. M., Narrow, W. E., Grant, B. F., &, Hasin, D. S. (2008). Racial/ethnic disparities in service utilization for individuals with co-occurring mental health and substance use disorders in the general population: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. The Journal of Clinical Psychiatry, 69, 1112–1121.
Hendrick, T. A. M., Fischer, A. R. H., Tobi, H., & Frewer, L. J. (2013). Self-reported attitude scales: Current practice in adequate assessment of reliability, validity, and dimensionality. Journal of Applied Social Psychology, 43, 1538–1552. doi:10.1111/jasp.12147
Hinkle, J. S. (2014). Population-based mental health facilitation (MHF): A grassroots strategy that works. The Professional Counselor, 4, 1–18. doi:10.15241/jsh.4.1.1
Johnson, K. F., & Kalkbrenner, M. T. (2017). The utilization of technological innovations to support college student mental health: Mobile health communication. Journal of Technology in Human Services, 35(4), 1–26. doi:10.1080/15228835.2017.1368428
Johnson, K. F., Sparkman-Key, N., & Kalkbrenner, M. T. (2017). Human service students’ and professionals’ knowledge and experiences of interprofessionalism: Implications for education. Journal of Human Services, 37, 5–13.
Kalkbrenner, M. T., & Neukrug, E. S. (2018). A confirmatory factor analysis of the Revised FSV Scale with counselor trainees. Manuscript submitted for publication.
Kalkbrenner, M. T., Neukrug, E. S., & Griffith, S. A. (in press). Barriers to counselors seeking counseling: Cross validation and predictive validity of the Fit, Stigma, & Value (FSV) Scale. Journal of Mental Health Counseling.
Kaneshiro, B., Geling, O., Gellert, K., & Millar, L. (2011). The challenges of collecting data on race and ethnicity in a diverse, multiethnic state. Hawai’i Medical Journal, 70(8), 168–171.
Kim, J. (2017, January 30). Why I think all men need therapy: A good read for women too. Psychology Today. Retrieved from https://www.psychologytoday.com/us/blog/the-angry-therapist/201701/why-i-think-all-men-need-therapy
Kim, J. E., Saw, A., & Zane, N. (2015). The influence of psychological symptoms on mental health literacy of college students. American Journal of Orthopsychiatry, 85, 620–630. doi:10.1037/ort0000074
Levant, R. F., Wimer, D. J., & Williams, C. M. (2011). An evaluation of the Health Behavior Inventory-20 (HBI-20) and its relationship to masculinity and attitudes towards seeking psychological help among college men. Psychology of Men & Masculinity, 12, 26–41. doi:10.1037/a0021014
Lindinger-Sternart, S. (2015). Help-seeking behaviors of men for mental health and the impact of diverse cultural backgrounds. International Journal of Social Science Studies, 3, 1–6. doi:10.11114/ijsss.v3i1.519
Lumina Foundation. (2017). A stronger nation: Learning beyond high schools builds American talent. Retrieved from http://strongernation.luminafoundation.org/report/2018/#nation
Mvududu, N. H., & Sink, C. A. (2013). Factor analysis in counseling research and practice. Counseling Outcome Research and Evaluation, 4(2), 75–98. doi:10.1177/2150137813494766
National Institute of Mental Health. (2017). Mental Illnesses. Retrieved from https://www.nimh.nih.gov/health/statistics/mental-illness.shtml#part_154787
Neukrug, E., Britton, B. S., & Crews, R. C. (2013). Common health-related concerns of men: Implications for counselors. Journal of Counseling & Development, 91, 390–397. doi:10.1002/j.1556-6676.2013.00109
Neukrug, E., Kalkbrenner, M. T., & Griffith, S. A. (2017). Barriers to counseling among human service professionals: The development and validation of the Fit, Stigma, & Value Scale. Journal of Human Services, 37, 27–40.
Norcross, A. E. (2010). A case for personal therapy in counselor education. Counseling Today, 53(2), 40–42.
Parent, M. C., Hammer, J. H., Bradstreet, T. C., Schwartz, E. N., & Jobe, T. (2018). Men’s mental health help-seeking behaviors: An intersectional analysis. American Journal of Men’s Health, 12, 64–73. doi:10.1177/1557988315625776
Qualtrics [Online survey platform software]. (2018). Provo, UT. Retrieved from https://www.qualtrics.com/
Qualtrics Sample Services [Online sampling service service]. (2018). Provo, UT. Retrieved from https://www.qualtrics.com/online-sample/
Rosenthal, B. S., & Wilson, W. C. (2016). Psychosocial dynamics of college students’ use of mental health services. Journal of College Counseling, 19(3), 194–204. doi:10.1002/jocc.12043
Seidler, Z. E., Rice, S. M., River, J., Oliffe, J. L., & Dhillon, H. M. (2017). Men’s mental health services: The case for a masculinities model. Journal of Men’s Studies, 25, 92–104. doi:10.1177/1060826517729406
Twenge, J. M., Joiner, T. E., Rogers, M. L., & Martin, G. N. (2017). Increases in depressive symptoms, suicide-related outcomes, and suicide rates among U.S. adolescents after 2010 and links to increased new media screen time. Clinical Psychological Science, Advanced online publication. doi:10.1177/2167702617723376
University of Phoenix. (2013). University of Phoenix survey reveals 38 percent of individuals who seek mental health counseling experience barriers. Retrieved from http://www.phoenix.edu/news/releases/2013/05/university-of-phoenix-survey-reveals-38-percent-of-individuals-who-seek-mental-health-counseling-experience-barriers.html
U.S. Census Bureau. (2017). Population estimates, July 1, 2017. Retrieved from https://www.census.gov/quick facts/fact/table/US/PST045216
Vogel, D. L., Heimerdinger-Edwards, S. R., Hammer, J. H., & Hubbard, A. (2011). “Boys don’t cry”: Examination of the links between endorsement of masculine norms, self-stigma, and help-seeking attitudes for men from diverse backgrounds. Journal of Counseling Psychology, 58, 368–382.
doi:10.1037/a0023688
Whitfield, N., & Kanter, D. (2014). Helpers in distress: Preventing secondary trauma. Reclaiming Children and Youth, 22(4), 59–61.
World Health Organization. (2015). Global health workforce, finances remain low for mental health. Retrieved from http://www.who.int/mediacentre/news/notes/2015/finances-mental-health/en/
World Health Organization. (2017). World mental health day, 2017: Mental health in the workplace. Retrieved from http://www.who.int/mental_health/world-mental-health-day/2017/en/
World Health Organization. (2018). World health report: Mental disorders affect one in four people. Retrieved from http://www.who.int/whr/2001/media_centre/press_release/en/
