Jul 4, 2014 | Article, Volume 4 - Issue 3
Maureen C. Kenny, Mérode Ward-Lichterman, Mona H. Abdelmonem
The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) introduced a chapter titled “Feeding and Eating Disorders,” which takes a life-span approach to diagnosing eating disorders and contains all related diagnoses. Rather than appearing throughout the text, all eating disorders are now contained within their own chapter for ease of review and comparison. Changes to the feeding and eating disorders include diagnostic revisions and the addition of several new disorders, including avoidant/restrictive food intake disorder and binge-eating disorder. While pica and rumination disorder remain unchanged, anorexia nervosa and bulimia nervosa experience some criteria changes. There is now a system for classifying the severity of several eating disorders (mild, moderate and severe) and an emphasis on body mass index for the diagnosis of anorexia nervosa. The DSM-5 also attempted to address the number of cases of eating disorders that did not meet criteria in any one category (e.g., eating disorder not otherwise specified), and the authors discuss the result of this attempt in examining two new disorders. This paper examines these changes and addresses clinical implications, while alerting counselors to important diagnostic information.
Keywords: eating disorders, DSM-5, pica, anorexia nervosa, bulimia nervosa, binge eating
With the publication of the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association [APA], 2013a) in May 2013 came structural changes to the categorization of disorders as well as criteria changes to a variety of disorders. One diagnostic category that experienced multiple changes is eating disorders. As stated in the DSM-5, “feeding and eating disorders are characterized by a persistent disturbance of eating or eating-related behavior that results in the altered consumption or absorption of food and that significantly impairs physical health or psychosocial functioning” (APA, 2013a, p. 329). Previously spread throughout several chapters in the DSM, these disorders are now self-contained in a single, more comprehensive chapter titled “Feeding and Eating Disorders.” This revised diagnostic category includes several new disorders and reflects changes to the criteria and wording of some existing diagnoses. While some of the changes are minor, all are noteworthy (Hartmann, Becker, Hampton, & Bryant-Waugh, 2012) and warrant examination. This article seeks to highlight the changes to this category and assist counselors in a greater understanding of these updated diagnoses.
Prevalence of Eating Disorders
One study by Hudson, Hiripi, Pope, and Kessler (2007) used data from the National Comorbidity Survey Replication to generate estimates of the prevalence of anorexia nervosa (AN), bulimia nervosa (BN) and binge-eating disorder (BED) among adults in the United States. The researchers based these estimates on the criteria found in the DSM-IV (Hudson et al., 2007). The authors report the following lifetime prevalence rates for AN, BN and BED, respectively: 0.9% among females and 0.3% among males, 1.5% among females and 0.5% among males, and 3.5% among females and 2.0% among males (Hudson et al., 2007). Of note is that BED, a new diagnosis in the DSM-5 (but one for which criteria appeared in the appendices of DSM-IV-TR), is by far the most prevalent of these three eating disorders. Also worth noting is the fact that the statistics for women, specifically for women under age 20, indicate that eating disorders are common among this subset of the population; young women appear to be afflicted at dramatically higher rates than the population at large. Using the DSM-5 criteria, Stice, Marti, and Rohde (2013) found a lifetime prevalence of 13.1% among this population, concluding that “one in eight young women” (p. 455) will have some form of diagnosable eating disorder.
Not represented in the figures above is the fact that in the past, the most common eating disorder diagnosis has been the DSM-IV and the DSM-IV-TR category eating disorder not otherwise specified (EDNOS; Fairburn & Cooper, 2011; Machado, Gonҫalves, & Hoek, 2013). EDNOS cases may represent as many as 60% of eating disorder diagnoses (Fairburn et al., 2007). As Smink, van Hoeken, and Hoek (2012) pointed out, a “major goal” (p. 407) of the revisions reflected among eating disorders in DSM-5 was to decrease significantly the number of EDNOS or unspecified diagnoses. The addition of BED and the changes to AN and BN (which resulted in generally less stringent criteria) reflect this aim (Smink et al., 2012). Studies concluded that the DSM-5 criteria will, in fact, reduce the number of EDNOS diagnoses considerably (Allen, Byrne, Oddy, & Crosby, 2013; Fairburn & Cooper, 2011; Machado et al., 2013). The authors in all three studies determined, however, that the number of cases that will not meet the revised DSM-5 criteria for AN, BN or BED is still sizable (Allen et al., 2013; Fairburn & Cooper, 2011; Machado et al., 2013).
While the prevalence of AN and BN are reasonably well established, the DSM-5 cites the prevalence of pica as unclear (APA, 2013a). It is predominantly recognized among children, most notably those with intellectual disabilities (Mash & Wolfe, 2013); pregnant women (Geissler, Mwaniki, Thiong’o, & Friis, 1998; Khan et al., 2009); adults with iron deficiency (Moore & Sears, 1994); and institutionalized persons (McAlpine & Singh, 1986). The prevalence of rumination disorder is also inconclusive, but believed to be higher in individuals with intellectual disabilities than the general population (APA, 2013a). Similarly, there are no reported prevalence rates for avoidant/restrictive food intake disorder (APA, 2013a).
Overview of Changes in DSM-5
Before the current edition of the DSM, feeding and eating disorders were in two main sections of the manual: (1) Disorders Usually First Diagnosed in Infancy, Childhood or Adolescence and (2) Eating Disorders (APA, 2013a). The former no longer appears in the DSM-5. With the removal of a separate section describing disorders that were most likely to occur in childhood or adolescence, the DSM-5 now contains chapters for each diagnostic category, which include both disorders that may first manifest during youth and others that may not surface until adulthood. In line with one objective of the DSM-5, the placement of eating and feeding disorders in their own chapter ensures that diagnoses are applicable across the life span (Bryant-Waugh & Kreipe, 2012), and helps bring attention to the development and presentation of symptoms at various points in the life span; this reflects what some refer to as the age and stage approach (Bryant-Waugh, 2013). The childhood section that was removed had previously contained several eating disorders (e.g., pica and rumination). The new chapter in the DSM-5 now contains eight eating disorders (APA, 2013a), including several new disorders, among which are avoidant/restrictive food intake disorder (which replaces, but significantly expands on, feeding disorder of infancy or early childhood) and BED. The diagnoses of other specified feeding or eating disorders and unspecified feeding or eating disorders are new and replace the diagnosis of EDNOS. The already existing disorders of pica, rumination disorder, AN and BN reflect some minor changes as well. While many feeding and eating disorders share symptoms or behaviors, it is important to note that an individual can receive only one diagnosis (Dailey et al., 2014). The feeding and eating disorders diagnostic criteria are mutually exclusive, meaning that if a client is diagnosed with one disorder in this chapter, the client cannot be diagnosed with another (with pica as the only exception). The DSM-5 wants to ensure differentiation of each disorder and help counselors plan treatment that targets the unique features of a disorder (APA, 2013a). See Table 1 for a review of DSM-IV-TR and DSM-5 classification of eating disorders.
Table 1
Past and Current Feeding and Eating Disorder Diagnoses
|
DSM- IV-TR
|
DSM-5
|
| Pica |
Pica |
| Rumination Disorder |
Rumination Disorder |
| Feeding Disorder of Infancy or Early Childhood |
Avoidant/Restrictive Food Intake Disorder |
| Anorexia Nervosa |
Anorexia Nervosa |
| Bulimia Nervosa |
Bulimia Nervosa |
|
Binge-Eating Disorder |
| Eating Disorder Not Otherwise Specified (EDNOS) |
Other Specified Feeding or Eating Disorder |
|
Unspecified Feeding or Eating Disorder |
Specific Changes to Eating Disorder Diagnoses
Pica and Rumination Disorder
Pica and rumination disorder are two eating disorders that often receive less clinical attention from counselors than other eating disorders. This is probably due to the fact that these disorders are likely to be observed in institutionalized settings, and that treatment may necessitate the expertise of behavioral analysts or therapists highly trained in working with developmental disabilities (Williams & McAdam, 2012). Only the locations of pica and rumination have changed in the DSM-5: These disorders now appear in the chapter on feeding and eating disorders. With this change, these diagnoses are now applicable to individuals across the life span. The criteria for these disorders did not change.
Pica is the ingestion of non-nutritive substances (e.g., hair, chalk, paint chips) over at least a one-month period. Availability and the age of the affected individual often determine what substances a person will consume (Hartmann et al., 2012). Some reports have included individuals eating paper, tissues, wood, metal, small rocks, carpet and soap (Matson, Belva, Hattier, & Matson, 2011). The eating of these non-food substances is deemed to be inappropriate to the developmental level of the individual and is not part of a cultural or socially accepted practice (APA, 2013a). Generally, clinicians see this disorder in children with intellectual disabilities (Mash & Wolfe, 2013). However, the fourth criterion of the diagnosis notes that if this condition does occur within the context of a developmental or intellectual disability, it should be sufficiently severe to warrant clinical attention.
Children with pica eat normal foods as well as non-nutritive foods. In most cases, the disorder remits on its own, or will cease with improved environmental conditions or added infant stimulation (Mash & Wolfe, 2013). One common thought is that this disorder presents in children who do not have sufficiently stimulating environments. Hartmann et al. (2012) reported that some clinicians regard pica as a form of self-soothing behavior, employed when one’s arousal reaches a certain level. However, for children with intellectual disabilities, it may be life-threatening (Matson et al., 2011). Ingestion of metal or other items with high toxicity pose a threat to the developing child (Hartmann et al., 2012). There are multiple treatments available for such individuals including punishment, overcorrection, restraint, positive reinforcement, psychopharmacology and time out (Matson et al., 2013). There is some literature that discusses the presence of pica in pregnant women, which may cause lead poisoning or other health issues for the developing fetus (Thihalolipavan, Candalla, & Ehrlich, 2013).
There were no major changes to the diagnosis of rumination disorder in the DSM-5. Rumination disorder is repeated regurgitation (e.g., spewing up or spitting up of food) for a period of at least one month (APA, 2013a). This regurgitation of food is not attributable to any related medical or gastrointestinal condition. Thus, the regurgitation is voluntary and distinguished from vomiting or gastroesophageal reflux. Similar to pica, the fourth criterion of this diagnosis notes that if this condition does occur within the context of a developmental or intellectual disability, it is sufficiently severe to warrant clinical attention. Some individuals with rumination disorder appear to engage in the behavior for self-soothing effects, while for others it is habitual and a difficult behavior to reduce (Hartmann et al., 2012). Certainly, this disorder reduces the social functioning of an individual, as it is a socially undesirable behavior.
The DSM-5 reports that both pica and rumination disorder are generally first observable in infancy, but onset can occur in childhood, adolescence or adulthood. Another commonality of these diagnoses in DSM-5 is that they both now have a specifier of in remission. This is reserved for individuals who may have previously met the criteria of the disorder, but have not “for a sustained period of time” (APA, 2013a, p. 330). Additionally, pica and rumination disorder are concurrently diagnosable. Another commonality of these disorders is that they often occur in secret and are difficult to detect (Hartmann et al., 2012). Individuals are not likely to disclose their engagement in these behaviors. For young children, parental report is critical in assessment.
Avoidant Restrictive Food Intake Disorder
An interesting addition to the DSM-5 is the diagnosis of avoidant restrictive food intake disorder (ARFID). The essence of this disorder is a disturbance in eating or feeding characterized by inadequate food intake (Bryant-Waugh & Kreipe, 2012). This inadequacy may mean that the individual does not meet necessary energy intake needs for the day (i.e., by consuming too few calories from food), or has an insufficient nutritional diet, or both. This disorder replaces feeding disorder of infancy or early childhood, but also adds significant new criteria. As Kreipe and Palomaki (2012) stated, “Although it has somewhat awkward phrasing, the name captures the key clinical features of non-eating disorder eating disturbances: avoiding (not necessarily ‘refusing’) foods for a variety of reasons, and restricting intake in the amount and/or range of foods eaten” (p. 428). In the DSM-IV-TR (APA, 2000), feeding disorder of infancy or early childhood primarily emphasized the child’s persistent failure to eat adequately, with significant failure to gain weight or significant loss of weight over at least one month. The primary symptom was a disturbance in eating or feeding not attributable to an associated medical or gastrointestinal condition, and the disorder was required to have an onset before six years of age. With the addition of ARFID, those criteria remain the same, but there is the additive criterion of significant nutritional deficiency, and dependence on enteral feeding (i.e., tube feeding) or oral nutritional supplements. The diagnosis is more specific in stating that the eating or feeding disturbance may be related to the sensory characteristics of food or a concern about aversive consequences of eating (e.g., nausea). The second criterion (a new addition) also mentions that a lack of available food or an associated, culturally sanctioned practice cannot account for the disturbance. The other criteria remain the same (e.g., ARFID cannot occur during the course of AN or BN; the condition cannot be related to a medical condition). It is, however, likely to co-occur with autism spectrum disorder or other neurodevelopmental disorders. Similar to other disorders in the DSM-5, one can apply in remission here if the individual previously met the full criteria for the disorder, but now has not met these criteria for a sustained period.
Sometimes the individual with ARFID restricts certain foods, and at other times, there is an inadequate intake of vitamins and minerals. The inadequacy of energy intake may result in a child’s poor growth, weight loss or low weight. In their study on picky eating among children, Jacobi, Schmitz, and Agras (2008) pointed out that the longer the duration of the pickiness, the more avoidant the child becomes to trying new foods. However, children with ARFID are more than just picky eaters, as they suffer from failure to meet nutritional and/or energy needs that may result in weight loss. As the criteria imply, some of these individuals must rely on enteral feeding.
The clinical presentation of ARFID is quite variable (Bryant-Waugh & Kreipe, 2012). Over time, there may be evidence that subgroups of the disorder are present, requiring further classification. Bryant-Waugh and Kreipe (2012) describe several presentations that include some of the ARFID symptoms. For example, some children (and some adults) eat only certain-colored foods or foods with a particular texture, thus ingesting only a narrow range of foods. Others may avoid certain foods based on past negative experiences with them, usually gastrointestinal problems. While there is no specific assessment for ARFID, careful clinical interviewing, including parental observations and a medical evaluation, are necessary for diagnosis. Because ARFID and AN share many common symptoms in childhood and young adulthood (e.g., low weight, food avoidance), differential diagnosis may be difficult (APA, 2013a). The DSM-5 reminds counselors that in AN, the individual has a persistent fear of becoming fat and/or gaining weight, which is not present in ARFID. We refer readers to Bryant-Waugh (2013) for a case study of a child with ARFID, including assessment questions and treatment.
Anorexia Nervosa
The DSM-5 diagnostic criteria for AN reflect several significant changes from the criteria outlined in DSM-IV-TR. There are two particularly noteworthy changes to the first criterion for an AN diagnosis in DSM-5. The first of these is that what was described as “refusal to maintain body weight” in the DSM-IV-TR (APA, 2000, p. 589) has been reframed as “restriction of energy intake relative to requirements” in the DSM-5 (APA, 2013a, p. 338). The removal of the word refusal, which has negative connotations, results in a more neutrally worded criterion. Moreover, the new phrasing of this criterion in DSM-5 focuses specifically on the central behavioral component of AN (i.e., restriction of intake), rather than upon the results of this behavior (i.e., body weight).
The second key change to this first criterion is that the specific guideline provided in DSM-IV-TR as a definition of a less than “minimally normal” body weight (i.e., below “85% of that expected”; APA, 2000, p. 589) no longer appears in the DSM-5. The new criterion instead highlights the essential role of context (e.g., age, sex, developmental status) in determining whether a particular individual is at a “significantly low weight” for his or her own body (APA, 2013a, p. 338). This change is particularly important because, while the DSM-IV-TR clarifies that 85% is intended as a guideline, once incorporated into the criteria, it became in many cases a requirement for insurance reimbursement (Hebebrand & Bulik, 2011).
The second criterion for AN previously included only the cognitive symptom of “intense fear of gaining weight or becoming fat” (APA, 2000, p. 589). That same language appears in the DSM-5, but the new criterion includes a behavioral component as well. Moreover, because the word or is used rather than and, the behavioral manifestation of this criterion can actually stand in for other, more overt expressions of the cognitive component. In other words, according to the DSM-5, an individual engaging in “persistent behavior that interferes with weight gain” (APA, 2013a, p. 338) can now meet this second criterion even if he or she does not explicitly communicate anxiety around weight gain. This change may have particular relevance in pediatric cases, because some children with AN have not yet developed the cognitive abilities required either to have or to express this intense fear (Bravender et al., 2010; Reierson & Houlihan, 2008; Workgroup for Classification of Eating Disorders in Children and Adolescents, 2007).
The third criterion in the DSM-5 is very similar to that of the previous edition, aside from one notable distinction. In the new DSM, the phrase “persistent lack of recognition” (APA, 2013a, p. 339) replaces “denial” (APA, 2000, p. 589) in describing the anorexic individual’s perspective on the risks posed by his or her underweight status. As with the change to criterion one, the result of this rewording is more value-neutral (like refusal, the word denial has negative connotations). The resulting criterion may also be more accurate, in that the focus is on an inability of the anorexic individual to recognize the inherent dangers of his or her condition, rather than a conscious repudiation of the truth.
Although these small linguistic changes may not seem especially significant, the outcome is a set of criteria that is, on the whole, less stigmatizing. This is important because research indicates that many clinicians have negative biases toward individuals with eating disorders. This may be especially true in the case of those with AN, and the stigma appears to impact the availability of quality treatment for the disorder (Thompson-Brenner, Satir, Franko, & Herzog, 2012).
The fourth criterion for AN, which appears in the previous edition, was removed altogether from the DSM-5, so that there are now only three criteria for a diagnosis of AN. This previous criterion, amenorrhea (the cessation of menstruation), applied only to females who had achieved menarche (APA, 2000). By definition, then, this criterion inherently excluded all males, as well as pre-pubertal and post-menopausal females. Also excluded were females taking hormonal contraceptives (APA, 2013b). The removal of amenorrhea therefore results in a more inclusive set of criteria, reflective of the APA’s (2013a) stated goal of avoiding “overly narrow” diagnostic categories (p. 12), which in the past have contributed to an excess of EDNOS diagnoses (Fairburn & Cooper, 2011; Machado et al., 2013).
As in the DSM-IV-TR, the criteria for AN in the DSM-5 include specifiers of restricting or binge-eating/purging types (APA, 2000, 2013a). The language in the new edition is similar to that of the previous edition, but clarifies that the specifier applies to the last 3 months (APA, 2013a), rather than the DSM-IV-TR’s more vaguely stated “current episode” (APA, 2000, p. 589). This change is relevant because the empirical evidence indicates that crossover between subtypes is frequent (Eddy et al., 2008). The DSM-5 reflects this research, and the text in the manual cautions that because such crossover occurs, “subtype description should be used to describe current symptoms rather than longitudinal course” (APA, 2013a, p. 339). It may be worth noting that some in the field have concluded that these diagnostic subtypes of AN are not actually clinically relevant (e.g., Eddy et al., 2008), although clearly the DSM-5 does not reflect this thinking.
Like other disorders in the DSM-5, the diagnostic criteria for AN now include additional specifiers regarding remission status (partial or full) and severity (APA, 2013a). The remission specifier may be especially useful for clinicians working with individuals with eating disorders, AN in particular. For example, with regard to the weight criterion, an individual who reaches “normal” weight will no longer meet the full criteria for an AN diagnosis, but may still be struggling with other key components of the disorder (e.g., intense fear of weight gain). Such a scenario may be particularly likely with this disorder, especially because a change in weight status can be the result of outside intervention rather than internal motivation (Nicholls, Lynn, & Viner, 2011).
Finally, the DSM-5 includes a severity specifier that uses the individual’s body mass index (BMI). There are three levels of severity: extreme (BMI < 15 kg/m2), severe (BMI 15–15.99 kg/m2), moderate (BMI 16–16.99 kg/m2) and mild (BMI > 17 kg/m2). As the manual states, the ranges are from the World Health Organization categories for thinness in adults. For children and adolescents, clinicians are encouraged to use the BMI percentiles. These levels of severity help indicate the clinical symptoms, the potential need for supervision and the degree of functional disability (APA, 2013a).
Bulimia Nervosa
The diagnosis of BN remains largely the same in the DSM-5, although there are some modifications to the criteria. BN is characterized by repeated, uncontrollable binge-eating episodes (criterion A) accompanied by ongoing compensatory behaviors to avoid weight gain (criterion B). These behaviors to avoid weight gain include “self-induced vomiting; misuse of laxatives, diuretics, or other medications; fasting; or excessive exercise” (APA, 2013a, p. 345). The DSM-5 brings no changes to these first two criteria from the DSM-IV-TR. Also unchanged in the new edition is the fourth criterion, the following key cognitive symptom: “self-evaluation is unduly influenced by body shape and weight” (APA, 2013a, p. 345).
The major change to BN in the DSM-5 is in criterion C, the frequency of the compensatory behaviors required for diagnosis. In the DSM-5, this frequency has been reduced from an average of twice weekly to an average of only once per week. The required duration of these behaviors, however, remains the same in DSM-5: three months. Research indicates that individuals who display these behaviors at this new, lower threshold of once per week experience similar levels of pathology and distress (Wilson & Sysko, 2009). This decrease in frequency is likely to result in more diagnoses of BN; as stated, “increased prevalence rates are the result of a general lowering of diagnostic thresholds for eating disorders” (Dailey et al., 2014, p. 180).
A secondary change to the BN criteria is the removal of the specifier regarding purging and nonpurging types of BN (APA, 2000). In the past, these specifiers described the type of compensatory behavior used by the individual. In the DSM-5, the criterion for compensatory behavior includes both types, so no further specifier is necessary. This change reflects the research indicating that many individuals with BN regularly engage in both purging and nonpurging compensatory behaviors, making this specifier insignificant (Ekeroth, Clinton, Norring, & Birgegård, 2013; Vaz, Peñas, Ramos, López-Ibor, & Guisado, 2001).
BN, like the other disorders in the DSM-5, now has severity specifiers. For this diagnosis, the assessment of severity depends upon the frequency of inappropriate compensatory behaviors (e.g., the average number of times an individual purges in a given week). Depending on the frequency of compensatory behaviors per week, a case may be categorized as one the following: mild (1–3 episodes), moderate (4–7 episodes), severe (8–13 episodes) or extreme (14 or more episodes) (APA, 2013a). Finally, as with other disorders in the DSM-5, clinicians can apply the specifiers of partial or full remission to BN.
Binge-Eating Disorder
The diagnosis of BED is new to the DSM-5. First mentioned in the DSM-IV (Striegel-Moore & Franko, 2008), the disorder appeared in that edition and the subsequent text revision under EDNOS, with research criteria outlined in the appendices (APA, 2000). With the publication of the DSM-5, BED was promoted from “criteria sets . . . for further study” (APA, 2000, p. 759) to being a full-fledged diagnosis. This addition is highly significant because BED is likely to be the most prevalent eating disorder (Striegel-Moore & Franko, 2008).
BED shares the binge-eating criterion of BN (i.e., consuming an objectively large quantity of food in a relatively short time while experiencing a loss of control). The disorder differs from BN, however, in that individuals with BED do not engage in compensatory behaviors (e.g., vomiting or laxative use) after binge eating. An additional distinction is that BED does not include a key cognitive criterion necessary for a diagnosis of BN—the undue influence of weight and shape on self-concept (APA, 2013a).
The second criterion for BED describes behaviors, emotions and cognitions associated with binge eating. The criterion includes five items and specifies that individuals must display a minimum of three to qualify for diagnosis. Examples are eating in the absence of physical hunger, eating unusually quickly and experiencing feelings of guilt and disgust around eating. Although a diagnosis of BN does require the presence of binge eating, that diagnosis does not include these additional criteria.
As is the case with other eating disorders, the diagnostic criteria for BED in the DSM-5 reflect reduced requirements for duration and frequency. Whereas the research criteria in the DSM-IV-TR specified that bingeing must take place at least two days a week for six months (APA, 2000), the DSM-5 diagnostic criterion is that binge eating must occur an average of once per week, for a minimum of three months (APA, 2013a). In the DSM-5, frequency is measured in times—rather than days—per week (for discussion, see DSM-IV-TR Appendix B, APA, 2000). In keeping with the other eating disorders, DSM-5 includes a severity specifier for BED, with, for example, between one and three episodes per week constituting mild BED, and 14 or more episodes per week qualifying as extreme (APA, 2013a). The addition of this severity rating is very helpful, as it will allow clinicians to determine the seriousness of the individual’s disorder in order to assist in treatment planning. Clinicians should also now specify whether an individual is in partial or full remission from BED.
Obesity
The introduction to the chapter on feeding and eating disorders explicitly addresses the decision not to include obesity as a diagnosis in the DSM-5. This statement outlines the reasons that obesity itself does not constitute a mental disorder: “Obesity (excess body fat) results from the long-term excess of energy intake relative to energy expenditure. A range of genetic, physiological, behavioral, and environmental factors that vary across individuals contributes to the development of obesity” (APA, 2013a, p. 329). In other words, obesity is a physical condition caused by a number of contributing factors and is not, therefore, simply the embodiment of a psychological state. The introduction goes on to clarify, however, that there exist complex relationships between obesity and several psychiatric conditions. This section also refers to the connection between obesity and medications used to treat mental disorders (APA, 2013a).
One of the disorders described by the DSM-5 as having a “robust association” with obesity is BED (APA, 2013a, p. 329). The relationship between obesity and BED is complicated. The manual specifies, on the one hand, that while some obese individuals suffer from BED, the majority do not. Moreover, individuals with BED are not necessarily obese; they may be overweight, or their weight may fall in the normal range (Striegel-Moore & Franko, 2008). On the other hand, obesity is a risk factor for BED (Decaluwé & Braet, 2003), and “the risk of presenting with BED increases with increasing obesity” (Hill, 2007, p. 151). One might assume that binge eating would precede obesity, but the relationship appears to move in the opposite direction (Decaluwé & Braet, 2003). Obesity also is a risk factor for the development of BN (Decaluwé & Braet, 2003; Hill, 2007).
Other Specified Feeding or Eating Disorder and Unspecified Feeding or Eating Disorder
Whereas the DSM-IV-TR contained the catchall diagnostic category of EDNOS, this category no longer appears in the DSM-5. The EDNOS category previously was reserved for individuals who did not meet the full criteria for an eating disorder (e.g., a woman who meets all criteria for AN except that she has regular menses). It has been reported that this diagnosis was overly used by practitioners (Bryant-Waugh & Kreipe, 2012), so the changes in the DSM-5 attempt to address this problem. The literature indicates that many individuals who were being treated for an eating disorder received this diagnosis because they did not meet the stringent criteria for AN or BN (e.g., Sysko & Walsh, 2011). As mentioned previously, researchers have reported that EDNOS represented as many as 60% of all eating disorder diagnoses (Fairburn et al., 2007).
In the DSM-5, two new diagnostic categories replace EDNOS: other specified feeding or eating disorder and unspecified feeding or eating disorder. Other specified feeding or eating disorder refers to individuals who present symptoms characteristic of a feeding or eating disorder that causes clinically significant impairment, but does not meet the full criteria for any of the disorders in this section. However, when applying this diagnosis, the clinician is able to specify or state the specific reason that the presentation does not meet the full criteria. Thus, the specific reason should follow the diagnosis. An example of this diagnosis would be BN (of low frequency and/or limited duration). In this example, the individual meets all of the criteria of BN except that the inappropriate compensatory behavior and binge eating occur at a frequency less than once a week and/or for less than 3 months.
This diagnosis presents a contrast with another new diagnosis, unspecified feeding or eating disorder. In using this designation, the clinician is unable to provide the specific reason why the clinical presentation does not meet full criteria. This may be because of insufficient information from the client, such as may occur when a client obtains treatment in an emergency setting or a clinician fails to gather enough information during intake. In these cases, the client displays symptoms of an eating or feeding disorder that is causing clinically significant impairment, but does not meet the full criteria for any disorder.
Implications for Counselors
Given the prevalence of some eating disorders, as well as their presence across the life span, counselors will likely encounter individuals suffering from a diagnosable eating disorder at some point in their career. In fact, research suggests that DSM-5 criteria will result in a rise in the prevalence of diagnosable eating disorders (Allen et al., 2013). This prediction underscores the importance of those in the counseling profession becoming well-informed regarding these revised criteria. New, broader criteria, when implemented by well-informed professionals, will likely increase the chances that a greater portion of the individuals suffering from these disorders will receive the help they need.
Feeding and eating disorders appear to exist on a continuum, with some related behaviors frequently occurring in the population at large. The skilled counselor will be able to differentiate between behaviors that would not be considered pathological (e.g., overeating or typical “dieting”), or are developmentally appropriate (e.g., picky eating), and those that are indicative of greater dysfunction (e.g., binge eating, dramatically restricting calories). Counselors should be aware, however, that clients with eating disorders may not be forthcoming about their symptoms, hide their behaviors and display resistance to seeking help (Abbate-Daga, Amianto, Delsedime, De-Bacco, & Fassino, 2013). Also, many individuals who are at risk for developing eating disorders or who have them may never seek help (Dailey et al., 2014). In addition, full recovery from eating disorders is the outcome in only about 50% of cases, while 20% of individuals make no improvement (Schlozman, 2002). Thus, many individuals have a lifelong battle with eating disorders and relapse is common. It is critical, therefore, that counselors screen all clients for potential eating disorders. Careful assessment of the client’s underlying thoughts, symptom presentation and impairment will help counselors make a correct diagnosis.
Eating disorders can be damaging to one’s physical well-being, emotional health and interpersonal relationships (Dailey et al., 2014). These factors, coupled with the possible medical consequences and potential fatality of some eating disorders, highlight the need for counselors who work with these clients to have specialized training. If a counselor does not have the appropriate background in eating disorders, it is vital that he or she refer the client to an eating disorders specialist. Moreover, individuals with eating disorders must consult a physician for a comprehensive physical assessment and intervention (Piran, 2013). Given the complexity of the symptom presentation, treatment is likely to involve a multidisciplinary team approach for treatment of eating disorders (Dailey et al., 2014) and counselors would be wise to familiarize themselves with treatment resources in their community.
Conflict of Interest and Funding Disclosure
The author reported no conflict of interest or funding contributions for the development of this manuscript.
References
Abbate-Daga, G., Amianto, F., Delsedime, N., De-Bacco, C., & Fassino, S. (2013). Resistance to treatment and change in anorexia nervosa: A clinical overview. BMC Psychiatry, 13, 294–311. doi:10.1186/1471-244X-13-294
Allen, K. L., Byrne, S. M., Oddy, W. H., & Crosby, R. D. (2013). DSM-IV-TR and DSM-5 eating disorders in adolescents: Prevalence, stability and psychosocial correlates in a population-based sample of male and female adolescents. Journal of Abnormal Psychology, 122, 720–732. doi:10.1037/a0034004
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author.
American Psychiatric Association. (2013a). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: Author.
American Psychiatric Association. (2013b). Highlights of changes from DSM-IV-TR to DSM-5. Retrieved from http://www.dsm5.org/Documents/changes%20from%20dsm-iv-tr%20to%20dsm-5.pdf
Bravender, T., Bryant-Waugh, R., Herzog, D., Katzman, D., Kriepe, R. D., Lask, B., . . . Zucker, N. (2010). Classification of eating disturbances in children and adolescents: Proposed changes for the DSM-V. European Eating Disorders Review, 18, 79–89. doi:10.1002/erv.994
Bryant-Waugh, R. (2013). Avoidant restrictive food intake disorder: An illustrative case example. International Journal of Eating Disorders, 46, 420–423. doi:10.1002/eat.22093
Bryant-Waugh, R., & Kreipe, R. E. (2012). Avoidant/restrictive food intake disorder in DSM-5. Psychiatric Annals, 42, 402–405. doi:10.3928/00485713-20121105-04
Dailey, S. F., Gill, C. S., Karl, S. L., & Barrio Minton, C. A. (2014). DSM-5 learning companion for counselors. Alexandria, VA: American Counseling Association.
Decaluwé, V., & Braet, C. (2003). Prevalence of binge-eating disorder in obese children and adolescents seeking weight-loss treatment. International Journal of Obesity, 27, 404–409. doi:10.1038/sj.ijo.0802233
Eddy, K. T., Dorer, D. J., Franko, D. L., Tahilani, K., Thompson-Brenner, H., & Herzog, D. B. (2008). Diagnostic crossover in anorexia nervosa and bulimia nervosa: Implications for DSM-V. The American Journal of Psychiatry, 165, 245–250. doi:10.1176/appi.ajp.2007.07060951
Ekeroth, K., Clinton, D., Norring, C., & Birgegård, A. (2013). Clinical characteristics and distinctiveness of DSM-5 eating disorder diagnoses: Findings from a large naturalistic clinical database. Journal of Eating Disorders, 1, 31–41. doi:10.1186/2050-2974-1-31
Fairburn, C. G., & Cooper, Z. (2011). Eating disorders, DSM-5 and clinical reality. The British Journal of Psychiatry, 198, 8–10. doi:10.1192/bjp.bp.110.083881
Fairburn, C. G., Cooper, Z., Bohn, K., O’Connor, M. E., Doll, H. A., & Palmer, R. L. (2007). The severity and status of eating disorders NOS: Implications for DSM-V. Behaviour Research and Therapy, 45, 1705–1715. doi:10.1016/j.brat.2007.01.010
Geissler, P. W., Mwaniki, D., Thiong’o, F., & Friis, H. (1998). Geophagy as a risk factor for geohelminth infections: A longitudinal study of Kenyan primary schoolchildren. Transactions of the Royal Society of Tropical Medicine and Hygiene, 92, 7–11. doi:10.1016/S0035-9203(98)90934-8
Hartmann, A. S., Becker, A. E., Hampton, C., & Bryant-Waugh, R. (2012). Pica and rumination disorder in DSM-5. Psychiatric Annals, 42, 426–430. doi:10.3928/00485713-20121105-09
Hebebrand, J., & Bulik, C. M. (2011). Critical appraisal of the provisional DSM-5 criteria for anorexia nervosa and an alternative proposal. International Journal of Eating Disorders, 44, 665–678. doi:10.1002/eat.20875
Hill, A. J. (2007). Obesity and eating disorders. Obesity Reviews, 8, 151–155. doi:10.1111/j.1467-789X.2007.00335.x
Hudson, J. I., Hiripi, E., Pope, H. G., Jr., & Kessler, R. C. (2007). The prevalence and correlates of eating disorders in the national comorbidity survey replication. Biological Psychiatry, 61, 348–358. doi:10.1016/j.biopsych.2006.03.040
Jacobi, C., Schmitz, G., & Agras, W. S. (2008). Is picky eating an eating disorder? International Journal of Eating Disorders, 41, 626–634. doi:10.1002/eat.20545
Khan, N. Z., Ferdous, S., Islam, R., Sultana, A., Durkin, M., & McConachie, H. (2009). Behaviour problems in young children in rural Bangladesh. Journal of Tropical Pediatrics, 55, 177–182. doi:10.1093/tropej/fmn108
Kreipe, R. E., & Palomaki, A. (2012). Beyond picky eating: Avoidant/restrictive food intake disorder. Current Psychiatry Report, 14, 421–431. doi:10.1007/s11920-012-0293-8
Machado, P. P. P., Gonçalves, S., & Hoek, H. W. (2013). DSM-5 reduces the proportion of EDNOS cases: Evidence from community samples. International Journal of Eating Disorders, 46, 60–65. doi:10.1002/eat.22040
Mash, E. J., & Wolfe, D. A. (2013). Abnormal child psychology (5th ed.). Belmont, CA: Wadsworth.
Matson, J. L., Belva, B., Hattier, M. A., & Matson, M. L. (2011). Pica in persons with developmental disabilities: Characteristics, diagnosis, and assessment. Research in Autism Spectrum Disorders, 5, 1459–1464. doi:10.1016/j.rasd.2011.02.006
McAlpine, C., & Singh, N. N. (1986). Pica in institutionalized mentally retarded persons. Journal of Mental Deficiency Research, 30, 171–178. doi:10.1111/j.1365-2788.1986.tb01309.x
Moore, D. F., Jr., & Sears, D. A. (1994). Pica, iron deficiency, and the medical history. The American Journal of Medicine, 97, 390–393. doi:10.1016/0002-9343(94)90309-3
Nicholls, D. E., Lynn, R., & Viner, R. M. (2011). Childhood eating disorders: British national surveillance study. The British Journal of Psychiatry, 198, 295–301. doi:10.1192/bjp.bp.110.081356
Piran, N. (2013). Prevention of eating disorders in children: The role of the counselor. In L. H. Choate (Ed.), Eating disorders and obesity: A counselor’s guide to prevention and treatment (pp. 201–219). Alexandria, VA: American Counseling Association.
Reierson, A. R., & Houlihan, D. D. (2008). Childhood onset of anorexia nervosa. Gundersen Lutheran Medical Journal, 5, 9–12.
Schlozman, S. (2002, March). The shrink in the classroom: Feast or famine. Educational Leadership, 59(6), 86–87. Retrieved from http://www.ascd.org/publications/educational-leadership/mar02/vol59/num06/Feast-or-Famine.aspx
Smink, F. R. E., van Hoeken, D., & Hoek, H. W. (2012). Epidemiology of eating disorders: Incidence, prevalence and mortality rates. Current Psychiatry Reports, 14, 406–414. doi:10.1007/s11920-012-0282-y
Stice, E., Marti, C. N., & Rohde, P. (2013). Prevalence, incidence, impairment, and course of the proposed DSM-5 eating disorder diagnoses in an 8-year prospective community study of young women. Journal of Abnormal Psychology, 122, 445–447. doi:10.1037/a0030679
Striegel-Moore, R. H., & Franko, D. L. (2008). Should binge eating disorder be included in DSM-V? A critical review of the state of the evidence. Annual Review of Clinical Psychology, 4, 305–324. doi:10.1146/annurev.clinpsy.4.022007.141149
Sysko, R., & Walsh, B. T. (2011). Does the broad categories for the diagnosis of eating disorders (BCD-ED) scheme reduce the frequency of eating disorder not otherwise specified? International Journal of Eating Disorders, 44, 625–629. doi:10.1002/eat.20860
Thihalolipavan, S., Candalla, B. M., & Ehrlich, J. (2013). Examining pica in NYC pregnant women with elevated blood lead levels. Maternal and Child Health Journal, 17, 49–55. doi:10.1007/s10995-012-0947-5
Thompson-Brenner, H., Satir, D. A., Franko, D. L., & Herzog, D. B. (2012). Clinician reactions to patients with eating disorders: A review of the literature. Psychiatric Services, 63, 73–78. doi:10.1176/appi.ps.201100050
Vaz, F. J., Peñas, E. M., Ramos, M. I., López-Ibor, J. J., & Guisado, J. A. (2001). Subtype criteria for bulimia nervosa: Short- versus long-term compensatory behaviors. Eating Disorders, 9, 301–311. doi:10.1080/106402601753454877
Williams, D. E., & McAdam, D. (2012). Assessment, behavioral treatment, and prevention of pica: Clinical guidelines and recommendations for practitioners. Research in Developmental Disabilities, 33, 2050–2057. doi:10.1016/j.ridd.2012.04.001
Wilson, G. T., & Sysko, R. (2009). Frequency of binge eating episodes in bulimia nervosa and binge eating disorder: Diagnostic considerations. International Journal of Eating Disorders, 42, 603–610. doi:10.1002/eat.20726
Workgroup for Classification of Eating Disorders in Children and Adolescents. (2007). Classification of child and adolescent eating disturbances. International Journal of Eating Disorders, 40(S3), S117–S122. doi:10.1002/eat.20458
Maureen C. Kenny, NCC, is a Professor at Florida International University. Mérode Ward-Lichterman is a graduate student at Florida International University. Mona H. Abdelmonem is an alumna of Florida International University. Correspondence can be addressed to Maureen C. Kenny, 11200 SW 8th Street, ZEB 247A, Miami, Florida 33199, kennym@fiu.edu.
Jul 3, 2014 | Article, Volume 4 - Issue 3
Laura K. Jones, Jenny L. Cureton
Trauma survivors are a unique population of clients that represent nearly 80% of clients at mental health clinics and require specialized knowledge on behalf of counselors. Researchers and trauma theorists agree that, with the exception of dissociative identity disorder, no other diagnostic condition in the history of the Diagnostic and Statistical Manual of Mental Disorders (DSM) has created more controversy with respect to the boundaries of the condition, diagnostic criteria, central assumptions and clinical utility than post-traumatic stress disorder. However, this mutable conceptualization of trauma and its aftermath have considerable implications for counseling practice. With the recently released fifth edition of the DSM (DSM-5), the definition of trauma and the diagnostic criteria for post-traumatic stress disorder have changed considerably. This article highlights the changing conceptualization of trauma and how the DSM-5 definition impacts effective practices for assessing, conceptualizing and treating traumatized clients.
Keywords: trauma, post-traumatic stress disorder, PTSD, DSM-5, diagnostic, clinical utility
Nearly 80% of clients seen in community mental health clinics have experienced at least one incident of trauma during their lifetime, representing roughly five out of every six clients (Breslau & Kessler, 2001). Over the past 15 years, between increases in school and community violence in the United States and unrelenting wars overseas, overt exposure to traumatic events has become an epidemic. Such events affect individuals across the life span and precipitate numerous diagnoses within the Diagnostic and Statistical Manual of Mental Disorders (DSM), most notably post-traumatic stress disorder (PTSD; Breslau & Kessler, 2001).
Survivors of trauma are a unique population of clients who require specialized knowledge and multifaceted considerations on behalf of counselors (Briere & Scott, 2006). The Council for Accreditation of Counseling and Related Educational Programs (CACREP) reiterates across both master’s and doctoral training levels the importance of understanding the implications of trauma theory, research and practice in counselor preparation and ultimately practice. CACREP (2009) standards incorporate trauma training within all eight core curricular areas of demonstrated knowledge and within each core counseling track. Section II, Professional Identity, says that counselors should understand the “effects of … trauma-causing events on persons of all ages” (CACREP, 2009, p. 10). However, even with the notable rates of trauma exposure, the deleterious outcomes faced by survivors and the call for counselor training in this area, counselors report feeling unprepared to work with survivors (Parker & Henfield, 2012). Over 60% of practicing therapists reported wanting additional support and education in their trauma work (Cook, Dinnen, Rehman, Bufka, & Courtois, 2011).
Trauma theorists agree that, with the exception of dissociative identity disorder, no other diagnostic condition in the history of the DSM has created more controversy about boundaries of the condition, symptomatological profile, central assumptions, clinical utility and prevalence than PTSD (Brewin, Lanius, Novac, Schnyder, & Galea, 2009). Changing definitions and the rationale for such shifts have significant implications for counselors. The fifth edition of the DSM (DSM-5), released in May 2013 (American Psychiatric Association [APA], 2013a), contains substantial changes, including the reorganization of “Trauma- and Stressor-Related Disorders” (TSRDs) into a new category and chapter distinct from “Anxiety Disorders,” the restructuring of factors, the modification of symptoms and specifiers, and the addition of a new subtype of PTSD in children.
The highly debated and variable definition of trauma and the diagnostic criteria for psychological responses to traumatic events may contribute to low counselor efficacy in trauma practice. Without a clear understanding of the latest views and requirements for trauma diagnosis using DSM-5, counselors may feel tentative about assessing for trauma and selecting efficacious interventions. This manuscript explores the changing definitions of trauma over time, implications of such changes on counseling practice and areas of needed growth and research. While this article’s core focus is on PTSD, we also briefly describe other TSRDs. By outlining DSM-5 changes, reviewing recent research substantiating such modifications and providing practical suggestions for practitioners, we hope to mitigate confusion and enhance efficacy in counselors working with trauma clients during this crucial diagnostic transition.
History of Trauma
Derived from the Greek word for “wound,” tales of trauma and the its profound consequences thereof date back to writings in antiquity. Only in the late 19th century did Pierre Janet and Sigmund Freud provide the first writings on the characterizations and clinical implications of traumatic events. In the mid-1890s, both practitioners developed similar theories of the etiology of hysteria, namely experiences of psychological trauma, particularly sexual trauma (Herman, 1992a). The theories presented in Freud’s The Aetiology of Hysteria (1962), however, were met with vehement contention, and such censuring stifled potential ramifications of his discoveries. Consequently, contemporary theories and definitions of trauma became largely fashioned from studies of male soldiers’ reactions to the horrors of war. Investigations of traumatic stress and apposite interventions for survivors emerged following World War I, purportedly as a means of rehabilitating soldiers for redeployment (van der Kolk, 2007). This attention waned during times of peace, but took command of the mental health research and literature during the Vietnam War. Concurrently, marked attention again became drawn to the consequences of sexual and domestic violence against women and children owing to the Women’s Movement (Herman, 1992a).
The examination of traumatic responses on both fronts (i.e., combat and interpersonal violence) led to the inclusion of a distinct PTSD diagnosis in the third edition of the DSM (DSM-III; APA, 1980). Previous iterations of the DSM recognized reactions to stressful experiences as a “transient situational disturbance,” suggesting that without an underlying psychological condition, the individual’s psychological experiences would wane as the stressor subsided (Yehuda & Bierer, 2009). However, the DSM-III classified trauma as an event existing “outside the range of usual human experience” (APA, 1980, p. 236) and provided legitimization for the potential pervasive and deleterious effects of exposure. As research continues, however, both the definitions of what constitutes a traumatic experience and what characterizes the symptoms of PTSD have rapidly transformed.
The publications of the DSM-IV and DSM-IV-TR brought a considerably more inclusive definition of trauma (APA, 1994, 2000).Varied events as a car accident, a natural disaster, learning about a death of a loved one, and even a particularly difficult divorce were considered variations of traumatic experience. This expanded definition engendered a 59% increase in trauma diagnoses (Breslau & Kessler, 2001). Modern trauma theory conceptualizes trauma and traumatic responses as occurring along a continuum (Breslau & Kessler, 2001), with researchers elucidating the importance of differentiating between traumatic experiences when investigating the etiology, physiological responses, course and efficacious therapeutic interventions for the range of potential traumatic responses (Breslau & Kessler, 2001; Kelley, Weathers, McDevitt-Murphy, Eakin, & Flood, 2009). The unique consequences of these diverse populations may be obscured if survivors of disparate populations are combined in research or excluded from trauma definitions altogether.
Primary Challenges to the DSM-IV-TR
The 13 years between the DSM-IV-TR (2000) and the DSM-5 (2013a) engendered considerable debate regarding how trauma was defined and the core criteria of PTSD. In the DSM-IV-TR, the presence of at least six symptoms (out of 17) distributed among three core symptom clusters served as a basis for diagnosing PTSD. This three-factor model stipulated that following a traumatic event, which induced fear, helplessness or horror, a survivor must experience at least one symptom of persistent re-experiencing (criterion B), three symptoms of avoidance or emotional numbing (criterion C), and two indicators of increased arousal (criterion D), all of which must persist for at least 1 month. Further, a clinician could specify whether the condition was acute, chronic and/or with delayed onset. An examination of the challenges surrounding this diagnosis follows.
Is Trauma an Anxiety Disorder?
PTSD was historically characterized as an anxiety disorder within the DSM. Authors supporting this view reference the pronounced fear and classical conditioning believed central among survivor experiences and treatment approaches that aim to extinguish such fear-based responses (i.e., exposure therapies; Zoellner, Rothbaum, & Feeny, 2011). Zoellner et al. (2011) branded PTSD a “quintessential anxiety disorder” (p. 853), arguing that the co-occurrence of PTSD with other anxiety disorders suggests common core constructs. These authors warned that reclassifying PTSD would suggest incorrectly to clinicians and researchers that “fear and anxiety are not critical in understanding PTSD” (p. 855). However, other researchers promoted making trauma-related disorders a new diagnostic category, suggesting that the traumatic event and not the symptoms demarcate such disorders (Nemeroff et al., 2013). Nemeroff et al. (2013) suggested that using the traumatic event as the foundation for the diagnosis respects the intensely heterogeneous nature and symptomatic presentation of the disorder.
Precipitating Events and Subjective Response
Also termed the stressor criterion, PTSD criterion A stipulated two requirements. An individual must first experience a traumatic episode (A1), defined as:
A direct personal experience of an event that involves actual or threatened death or serious injury, or other threat to one’s physical integrity; or witnessing an event that involves death, injury, or a threat to the physical integrity of another person; or learning about an unexpected or violent death, serious harm, or threat of death or injury experienced by a family member or other close associate (APA, 2000, p. 463).
The second prerequisite (A2) required that the survivor must have experienced “intense fear, helplessness, or horror” (p. 467) following the event. Clinicians and researchers have criticized both requirements (Breslau & Kessler, 2001; Friedman, Resick, Bryant, & Brewin, 2011).
The debate over what constitutes a traumatic event emerged with the first inclusion of the diagnosis into the DSM-III, and has persisted. Some researchers argued that the DSM-IV’s broad definition of trauma led to “bracket creep” (McNally, 2009, p. 598) and overdiagnosis of PTSD resulting from less threatening events. McNally (2009) questioned the ramifications of having equivalent diagnoses for a traumatized individual who watched the World Trade Center collapse from thousands of miles away and a survivor who escaped the building directly. Some postulated that weakening the A1 criteria had detrimental outcomes in client care and in forensic and disability settings and supported a narrower definition of trauma (Rosen & Lilienfeld, 2008). Others starkly disagreed, suggesting that what may be traumatic for one individual may not be for another, and that an attempt to include all possible traumatic events within the context of a diagnosis was futile (Brewin et al., 2009). Numerous researchers and clinicians have remarked that for no other diagnosis in the DSM is a specific precursory event stipulated, and they have argued for the removal of the A1 event altogether (Brewin et al., 2009), questioning the compulsory relationship between a traumatic event and PTSD (i.e., other disorders may result from such an event) and asserting that minor events, repeated over time, can likewise lead to PTSD.
More prominent was dispute over the latter stressor requirement (A2). Friedman et al. (2011) emphasized that the presence of a subjective response did not predict that an individual who would go on to develop PTSD. Although these subjective responses are characteristic trauma reactions, limiting the range of psychological responses may discount subpopulations, most notably survivors of sexual and partner violence, military and first responders (Friedman et al., 2011). The predominant post-traumatic reactions of interpersonal violence survivors include anger, guilt and shame; the military and first responders often report not having an immediate emotional reaction to traumatic exposure as a result of their training. In a sample of adult sexual assault survivors, over 75% endorsed shame as a leading psychological response (Vidal & Petrak, 2007). Over 20% of survivors were misdiagnosed due to not meeting the A2 criteria (Creamer, McFarlane, & Burgess, 2005).
Three-factor Model: The Avoidance and Numbing Debate
The third criterion for a PTSD diagnosis in DSM-IV-TR included experiencing at least three symptoms related to either behavioral avoidance or affective numbing (APA, 2000). Having a double-barreled criterion engendered considerable disagreement in trauma research and clinical practice. Although these two constructs were initially considered synonymous, with emotional numbing serving as a volitional form of emotional avoidance, research has elucidated differences in their bases, functions and neurophysiological underpinnings (Asmundson, Stapleton, & Taylor, 2004). Foa, Riggs, and Gershuny (1995) further determined that emotional numbing, over and above avoidance or another symptomatic feature of PTSD, best distinguishes PTSD from other diagnostic categories. Conceptually, authors (Foa, Zinbarg, & Rothbaum, 1992; Ullman & Long, 2008) frequently distinguished avoidance and numbing by examining the intentionality behind the event: whereas avoidance represents conscious attempts to escape trauma-related stimuli or responses, numbing is an unconscious and automatic physiological response to trauma exposure. Confirmatory factor analyses substantiated such claims and repeatedly demarcated a four-factor rather than a three-factor model of PTSD that differentiates avoidance and numbing (Friedman et al., 2011).
The integrated conceptualization of numbing and avoidance had marked significance on clinical practice. It was often difficult to confirm three of the seven conditions (Schützwohl & Maercker, 1999), leading to subthreshold diagnoses or underdiagnosis. Further, the severity of numbing precipitated a category of trauma survivors marked by the most chronic and pervasive disturbances following trauma and most pronounced disruptions in daily life (Breslau, Reboussin, Anthony, & Storr, 2005). In addition, Asmundson et al. (2004) determined that symptoms of avoidance and numbing are differentially influenced by treatment approaches, reinforcing the notion that avoidance and numbing should be considered and clinically addressed as distinct symptomatic concerns. Further, using the DSM-IV, a clinician treating an unconscious response (i.e., numbing) as an intentional action (i.e., avoidance) could unintentionally lead to treatment that was ineffective, blaming, disempowering or even re-traumatizing to clients.
Subthreshold Diagnoses
Several of the aforementioned considerations denote concern around subthreshold or subsyndromal survivors, namely individuals whose trauma did not match the A1 or A2 events or whose symptoms did not fulfill the restrictive criterion C. These survivors, potentially facing grossly impaired functioning, did not fulfill PTSD criteria and thus may have been prohibited from receiving any services, appropriate services or related validation of their experiences (Cukor, Wyka, Jayasinghe, & Difede, 2010; Schützwohl & Maercker, 1999). Problems with subthreshold diagnoses and misdiagnoses under the DSM-IV guidelines were particularly notable among children (Pynoos et al., 2009; Scheeringa, Zeanah, & Cohen, 2011). Using DSM-IV criteria, over 30% of children with pervasive symptoms and severe functional impairment did not meet criteria (Scheeringa, Myers, Putnam, & Zeanah, 2012). Although notes regarding symptom presentation in children were presented, the DSM-IV did not identify a separate diagnosis for preschool post-traumatic reactions. Researchers argued that the DSM-IV criteria were not attentive to developmental considerations, owing largely to the linguistic and introspective differences of young children, and provided unrepresentative criteria for this population (Pynoos et al., 2009; Scheeringa et al., 2011). Consequently, researchers highlighted the need for child-specific PTSD criteria. Underdiagnosis in children and adults is particularly troubling given that these populations of survivors have long been misdiagnosed and stigmatized by the DSM (Fish, 2004; Rojas & Lee, 2004). Drawing on both behavioral and neurological research, these challenges to the DSM-IV PTSD diagnosis touched at the core of trauma theory and resulted in many shifting perspectives in the fifth edition. Given the historical complications in trauma theory and recent reformulations of trauma, it is important that counselors receive guidance on trauma-informed practice using the DSM-5 (APA, 2013a).
Shifting Perspectives and New DSM-5 Diagnostic Criteria
In the DSM-5, PTSD now serves as the cornerstone of a new category of diagnoses, TSRD. Within the new category, the definition of trauma is more explicit, and the symptomatic profile was expanded from a three- to four-factor structure. Subjective responses following a traumatic event are no longer required, and a separate preschool diagnosis for children 6 years old and younger is now available. The modifications to the PTSD diagnosis in the DSM-5 are delineated in Table 1.
Exemption from Anxiety Disorders
The foremost change in the DSM-5 diagnosis of PTSD is its assignment to an innovative diagnostic category, TSRDs. Throughout the review period, members of the Trauma and Stressor-Related and Dissociative Disorders (TSRDD) Sub-Work Group of the DSM-5 (Friedman, 2013) determined that PTSD did not “fit neatly into the anxiety disorder niche to which it had been assigned since DSM-III” (p. 549). This redefining of PTSD marks a significant shift from its former conceptualization and highlights the central importance of the predisposing stressor. Exposure to a traumatic or aversive event is now recognized as a vital cause of an entire class of conditions affecting mental well-being. Before the DSM-5, trauma exposure was an accepted catalyst of Acute Stress Disorder and PTSD, yet the explicit influence of such aversive events on numerous other disorders went largely unacknowledged.
Restructuring the Stressor Criterion
Emphasis on the precipitating traumatic event called for reconsideration of the definition of trauma. Despite the argument by Brewin et al. (2009) that what is or is not considered a traumatic event should be defined by the individual rather than a committee, the DSM-5 retained criterion A1, with modifications to the breadth of the definition. Trauma is now defined as exposure to actual or threatened death, serious injury or sexual violence in one or more of four ways: (a) directly experiencing the event; (b) witnessing, in person, the event occurring to others; (c) learning that such an event happened to a close family member or friend; and (d) experiencing repeated or extreme exposure to aversive details of such events, such as with first responders. Actual or threatened death must have occurred in a violent or accidental manner; and experiencing cannot include exposure through electronic media, television, movies or pictures, unless it is work-related.
Table 1
Key Modifications to PTSD in DSM-5
|
PTSD Modifications
|
| Location |
New category: “Trauma- and Stressor-Related Disorders”No longer a subcategory of “Anxiety Disorders” |
| Criteria |
|
| A. Exposure |
Included sexual violence as a traumatic event
Exposure refined to include:
- Learning the event(s) occurred to close family or frienda,
- Repeated or extreme exposure to details of the event(s)b, i.e., vicarious trauma.
Removed A2, subjective response (i.e., fear, helplessness, horror) |
| B. Intrusion(1 of 5) |
No major changes |
C. Avoidance
(1 of 2) |
New separate criterion (factor) for avoidance symptoms
No major changes to symptoms |
D. Negative Alterations in Mood/cognition
(2 of 7) |
New criterion (factor) for numbing symptoms
Two new symptoms:
- Persistent negative emotional states
- Persistent blame
|
E. Arousal and Reactivity
(2 of 6) |
One new symptom:
- Reckless or self-destructive behavior
|
| F. Duration |
No change: Still 1 month since stressor |
| G. Significance |
No change |
| H. Not substance or medical |
Added criterion |
| Specifiers |
Two types available:
- With dissociative sx, i.e., depersonalization or derealization
- With delayed expression of 6 or more months
|
| Subtype |
For children 6 years or younger (Preschool subtype)
Separate criteria |
Note. sx = symptoms. Adapted from DSM-5 (APA, 2013a, p. 272).
aActual or threatened death must have been violent or accidental.
bSuch exposure through media, television, movies or pictures does not qualify unless for work.
Several changes in the DSM-5 definition stand out immediately, such as the inclusion of sexual violence within the core premise of trauma. Experiencing sexual violence may precipitate PTSD, as can witnessing it, learning about it and experiencing repeated exposure to stories of such acts. Furthermore, loss of a loved one to natural causes is no longer considered a causal factor. For example, now a client whose partner unexpectedly died of a heart attack no longer fits PTSD criteria. Lastly, a new subset of possible exposure has been established, namely vicarious trauma. This is the first time that DSM criteria have included deleterious effects of repeatedly witnessing or hearing stories regarding the aftermath of trauma. This inclusion may not be surprising to trauma counselors, as nearly 15–20 % develop PTSD symptoms from hearing and sharing in the stories of survivors; this inclusion may help to legitimize the gravity of counselors’ reactions (Arvay & Uhlemann, 1996; Meldrum, King, & Spooner, 2002). The inclusion also may serve to de-stigmatize the reactions of first responders and reinforce the need for wellness training and post-exposure care (Royle, Keenan, & Farrell, 2009). However, the DSM-5 clearly states that vicarious trauma cannot be the result of repeated exposure via electronic or print media. This precludes, for example, McNally’s (2009) case example of an individual with trauma symptoms who repeatedly witnessed the attacks on the World Trade Center by way of television monitors.
Removal of Subjective Response
Along with changes to the definition of trauma, the DSM-5 now excludes the A2 subjective response. The PTSD diagnosis now represents survivors who experience reactions other than fear, helplessness or horror, or who exhibit no pronounced emotional response. For example, a client who witnessed a fatal car accident and predominantly feels pervasive guilt for not offering support could be diagnosable. This change has great significance for numerous populations and may lead to more survivors gaining access to efficacious mental health care.
A Four-Factor Approach
In accordance with evidence supporting a four-factor model of PTSD, the APA (2013a) split the previous criterion C into two distinct categories within the DSM-5: (a) avoidance and (b) negative reactivity and related numbing. The new criterion C (i.e., persistent avoidance) requires only one of the two original avoidance symptoms. The new criterion D in DSM-5, “negative alterations in cognitions and mood” (p. 271, APA, 2013a), underscores the notion that trauma leads to unconscious numbing of positive emotions and increased negative affect overall (Frewen et al., 2010). Persistent negative emotionality and persistent blame are additions to the original symptom profile, the latter of which predicts PTSD severity and chronicity (Moser, Hajcak, Simons, & Foa, 2007). Two of seven symptoms must be endorsed in the new criterion D.
Criterion B (i.e., presence of intrusive symptoms) remains unchanged from the DSM-IV, and requires only one of five symptoms. The new criterion E, persistent alterations in arousal, reflects the previous criterion D and includes one additional symptom, reckless or self-destructive behaviors. Self-destructive behaviors comprise anything from hazardous driving to suicidal behavior (Friedman, 2013). Two of the now six symptoms of altered arousal are required. Despite refinements to criteria, considerable overlap remains across and within PTSD symptoms, such as between intrusion and the dissociative-depersonalization specifier.
Dissociative Specifier
In addition to delayed expression, the DSM-5 includes specifiers for dissociative symptoms in PTSD, with either depersonalization or derealization constituting the primary presentation. Dissociation often predicts significantly greater severity, chronicity and impairment in survivors, as well as decreased responsiveness to common treatment approaches (Lanius, Brand, Vermetten, Frewen, & Spiegel, 2012). The inclusion of this subtype acknowledges differences in neurological and physiological functioning among this population (Felmingham et al., 2008) and relevant needs and clinical considerations (Lanius et al., 2012).
Post-traumatic Stress Disorder in Children
In recognizing the gross oversights in previous iterations of the DSM regarding developmental considerations in PTSD, the DSM-5 explicitly provides a preschool subtype for children 6 years and younger. This new diagnosis honors the unique trauma experiences and responses of children, with symptoms that are behaviorally based and thus not reliant upon the cognitive or linguistic complexity absent in young survivors. For example, symptoms include restless sleep, temper tantrums or decreased participation in play. Children may express symptoms through behavior or play reenactment, which may or may not appear related to the traumatic event. The preschool subtype retains the three-factor model that combines avoidance and negative alterations of mood and cognition. To circumvent concerns related to children not meeting criterion C requirements, only one of six symptoms is necessary. These changes have pronounced implications for counseling adult and child survivors of trauma.
Implications for Counseling Practice
Understanding these changes and the rationale behind them is essential to thorough client conceptualization and efficacious counseling. Otherwise, counselors may feel tentative about key areas of care, such as assessing for trauma exposure, making accurate diagnoses, selecting efficacious interventions and filing reimbursement claims. A consideration of specific ways the new that the DSM-5 PTSD diagnosis impacts counselors, clients and clinical practice follows.
Multifarious Symptom Structure and Trauma Prevalence
The expanded PTSD symptom set in the DSM-5 set leads to extensive variations in possible trauma responses. The increase in symptoms from 17 in the DSM-IV-TR to 20 in the DSM-5 now yields over 600,000 possible symptom combinations (Galatzer-Levy & Bryant, 2013). Consider this number in comparison to the potential 70,000 combinations possible in the DSM-IV-TR (2000), a number already criticized for its expansiveness, and the meager 256 possible for depression (Zoellner et al., 2011). This marked increase in symptom patterns calls into question prevalence rates for trauma under the new DSM. A recent study established similar prevalence rates using DSM-5 and DSM-IV-TR criteria, 39.8% and 37.5%, respectively, and an overall 87% consistency between the two versions (Carmassi et al., 2013). Carmassi et al. (2013) determined that the discrepancy was due primarily to individuals not fulfilling criterion C within the DSM-IV-TR. This finding illustrates the impact of modifications related to the bifurcation of avoidance and numbing. Kilpatrick et al. (2013), however, found marginally decreased prevalence with the DSM-5, citing constraints on the A1 definition of trauma. However, both studies found significantly increased prevalence among females than males using DSM-5 (Carmassi et al., 2013; Kilpatrick et al., 2013).
Although heterogeneity may provide a more thorough scope and representation of traumatic responses, the considerable variation in behavioral presentation may lead to confusion among both counselors and clients (Friedman, 2013). Two clients may present in drastically different manners, but receive the same diagnosis. One client with PTSD may be distrustful, experience violent nightmares and behave aggressively, while another with a PTSD diagnosis is more withdrawn and self-blaming, with internally directed negative emotionality. Conversely, a counselor could have two clients who present analogously; and yet, due to the nature of the traumatic event, one could be diagnosable and the other not. This may cause complications for counselors in providing psychoeducation or in determining appropriate clinical interventions.
Counselors will encounter many questions with the changing and heterogeneous face of PTSD. For instance, would a counselor work differently with the client with a PTSD diagnosis than with a client having an analogous presentation, but no PTSD diagnosis? Do neurological ramifications differ dramatically now given the shifting labels, and thus call for varied interventions? How does a counselor explain to a client who had PTSD under the DSM-IV that she or he no longer meets criteria nor qualifies for reimbursement with the new diagnosis of adjustment disorder? Or will adjustment disorder, re-categorized as a TSRD in DSM-5, now be recognized by third-party payment systems as a reimbursable disorder? Although some answers are beginning to unfold, an increased awareness and adaption of trauma assessment, treatment and administration can help counselors navigate such questions and effectively work with clients.
Client Assessment
Changes precipitated by the DSM-5 require counselors be acutely aware of the modified PTSD diagnostic criteria for careful assessment of survivors. Thorough assessment includes applying both informal and formal approaches, using multiple sources of information, and conducting initial and ongoing screenings. During the present transition, informal assessment becomes especially important as efforts to revise and validate formal assessment tools continue.
Informal assessment. Given the central importance of trauma exposure in client care, counselors may continue to struggle to sensitively solicit needed information early in the counseling process. Honed skills for developing and continually fostering the therapeutic alliance are essential to client disclosure and in conscientiously deciphering such information. Some clients may be more reticent to share information, while others may reveal very detailed accounts of their story. In either case, counselors need to remain cognizant of the risk for re-traumatization during this process and pace sessions accordingly. Friedman (2013) also recognized that the current conceptualization of trauma in the DSM-5 insinuates the trauma has already happened, and that the individual is now “in a context of relative safety” (p. 763). This assumption may complicate assessment of individuals in enduring traumatic environments (e.g., partner violence).
During informal assessment with adults, counselors should practice acute observation skills for nonverbal clues that may signal present intrusive, numbing, arousal and dissociative symptomatology. Reported experiences of feeling detached from body or mind and reports of the world seeming dreamlike or unreal are primary indicators of dissociative experiences. Objective cues of dissociative responses also may be present, such as the client appearing to space out (Briere & Scott, 2013). Further, behavioral responses such as reckless and self-destructive behavior must also be recognized as potential trauma responses. The two new criterion D symptoms related to client cognitions, however, require counselors to determine a survivor’s cognitive perception of the event, self and world, and how perceptions of the latter two may have shifted post-trauma. Moreover, given the current distinction between numbing and avoidance symptoms, counselors may need to discern conscious from unconscious motivations behind client behaviors.
In children, informal assessment of traumatic responses, although now facilitated by developmentally appropriate criteria, may be particularly challenging. This requires keen observation of behavior, interpersonal interactions, sleep patterns and play. Cohen et al. (2010) suggested that child assessments must account for the onset of symptoms and changing patterns therein to avoid potential misdiagnoses. Recognizing how trauma responses manifest in children will help counselors correctly identify child survivors and help children get the mental health care needed to avert potentially protracted concerns across the life span.
Formal assessment. Formal assessment methods consistent with the revised diagnostic criteria are an essential adjunct to a counselor’s informal assessment. A notable addition to the DSM-5 is the provision of diagnostic assessments. Many are still considered “emerging,” as the APA continues to gather feedback from clinicians (APA, 2014). Counselors can familiarize themselves with these measures and stay updated on their availability and validation through the DSM-5 website (www.psych.org/practice/dsm/dsm5).
Relevant formal measures of PTSD for the DSM-5 include the following: Level 1 Cross-Cutting Symptom Measures for brief assessment, Level 2 measures for in-depth domain-specific assessment, disorder-specific Severity Measures, and potentially Early Development and Home Background Forms (APA, 2014). Level 1 surveys include questions related to avoidance, sleep quality, repetitive unpleasant thoughts and other symptoms found in DSM-5 PTSD criteria. This level provides a measure for adults, a self-rated measure for children ages 11 to 17, and a guardian-rated measure for children ages 6 to 17. Level 2 Cross-Cutting Symptom Measures allow for more in-depth explorations of symptoms. Disorder-Specific Severity Measures contain the National Stressful Events Survey PTSD Short Scales for adults and for children ages 11-17. Although guardian measures are available, the applicable age range is limited from 6 to 17 years. Thus these measures are not appropriate for assessing symptoms in preschool children, despite the addition of distinct diagnostic criteria for this population.
In addition to the DSM-5 measures provided by the APA, the National Center for PTSD updated three measures to include DSM-5 criteria: the Clinician-Administered PTSD Scale for DSM-5 (CAPS-5), the PTSD Checklist for DSM-5 (PCL-5), and the Life Events Checklist for DSM-5 (LEC-5). Counselors wanting to access these measures can submit requests on the National Center for PTSD’s website (www.ptsd.va.gov/).
Differential diagnosis: A resource with limitations. Another component of assessment is differential diagnosis. The use of updated measures for formal assessment may not always resolve confusion engendered by facets of DSM-5 diagnosis such as overlapping criteria. Selecting among the Level 2 cross-cutting measures may be challenging, as many currently focus on anxiety, anger and inattention, which may not be applicable or adequate in assessing PTSD. Differential diagnosis may help counselors gain needed clarity and is often considered integral to every initial clinical encounter and the basis for treatment planning (First, 2014).
Decision trees allow for diagnostic determination based on the entirety of a client’s presenting symptoms and assist in identifying diagnostic options by using lists of symptoms relevant to PTSD, including distractibility, mood concerns, suicidal behavior, anxiety, avoidance and insomnia. Out of the 29 available decision trees in the DSM-5 Handbook of Differential Diagnosis (First, 2014), nine include decisions that may result in an accurate diagnosis of PTSD or another TSRD, not including lists with adjustment disorder as the sole TSRD.
However, some decision trees, which include symptoms reflective of PTSD criteria, do not include the disorder as a possible conclusion. For instance, criterion D covers “negative alterations in cognitions and mood,” though none of the three decision trees associated with mood include PTSD. The new symptom in criterion E is “self-destructive or reckless behavior,” yet the Decision Tree for Suicidal Ideation or Behavior does not include PTSD as a possible diagnosis, nor does its counterpart for self-injury or self-mutilation. Thus, in the initial absence of information about a precipitating event, well-developed informal assessment skills for PTSD may be the best tool a counselor can use to form initial hypotheses for client conceptualization and associated treatment planning.
Treatment
New changes to the DSM also engender implications for PTSD treatment. As noted, the four-factor model of PTSD discriminates between avoidance and negative emotionality/numbing. This transition emphasizes the need to address these two constructs as unique symptom sets in survivors and highlights the influence of neuroscience research on best practices in trauma care. For instance, positive emotional numbing is considered a neurologically based symptom outside the conscious control of survivors, as opposed to the conscious or conditioned behavioral-based responses of effortful avoidance used to decrease arousal (Asmundson et al., 2004). The degree of emotional numbing versus avoidance in clients (or vice versa) suggests differential subpopulations of survivors and thus treatment approaches. For example, exposure therapy has proven particularly beneficial for avoidance symptoms (Asmundson et al., 2004). However, given the longstanding conceptual overlap in avoidance and numbing symptoms, optimal measures to assess treatment responses to emotional numbing have been limited (Orsillo, Theodore-Oklota, Luterek, & Plumb, 2007). Such findings suggest that effective treatment for trauma clients may become increasingly multidimensional and multidisciplinary.
The addition of new symptoms within criterion E and subtypes of PTSD calls for modified treatment approaches and goals for survivors who fulfill such criteria. For example, the inclusion of reckless or self-destructive behaviors as a feature of hyperarousal in criterion E now encompasses suicidal behavior (Friedman, 2013). Researchers have long denoted strong correlations between PTSD and suicide risk (Krysinka & Lester, 2010). The inclusion of self-destructive behavior as a symptom finally gives credence to this relationship. Counselors should practice vigilance and responsiveness to warning signs of suicidality. Regarding treatment, distress tolerance was shown to moderate PTSD and suicidal behavior (Anestis, Tull, Bagge, & Gratz, 2012), although perceived social support may buffer the impact of trauma symptoms on such behavior (Panagioti, Gooding, Taylor, & Tarrier, 2014). Similarly, the addition of dissociative subtypes highlights the severity and uniqueness of this subpopulation and the need for appropriate treatment considerations. Cloitre et al. (2012) endorsed a staged treatment emphasizing affective and interpersonal regulation as one option for treating dissociation in PTSD.
The addition of a preschool PTSD diagnosis increases the discernible importance of trauma-informed counseling with children and families. Research on best practices with children 6 years old and younger supports the use of cognitive-behavioral therapy (CBT), individually or in groups, most notably Trauma-Focused CBT; as well as child-parent relational psychotherapy; EMDR; and play therapy (Scheeringa, 2014). Scheeringa stressed that the key to working with this age group is engaging the child in developmentally appropriate methods that respect linguistic and introspective abilites (2014). Although some treatment implications stemming from the DSM-5 are presently discernible, additional research on best practices for addressing novel symptoms and symptom patterns of PTSD in children and adults will further inform practice.
Reimbursement and Legal Ramifications
Additional implications of DSM-5 modifications, such as healthcare consequences, remain largely unknown. General healthcare implications are explored in a file provided on the DSM-5 website (APA, 2013b), with the major foci including International Classification of Diseases (ICD) coding and assessment of disability and functioning. The APA (2013b) assured “periodic updates of agreements with federal agencies, private insurance companies, and medical examination boards as they become available” (p. 4). It can be expected that insurance companies will continue to reimburse for PTSD. However, a parallel expectation or hope is for companies to begin reimbursing more consistently for subthreshold PTSD, adjustment disorder and related diagnoses.
Conclusion
Although the changes to PTSD in the DSM-5 were empirically based and arose after considerable analysis and debate, several areas of concern and oversight still stand. Research remains mixed about overall prevalence rates of vicarious trauma (VT) in mental health practitioners (Kadambi & Ennis, 2004). Given the inclusion of VT in trauma definitions, the expected increase of PTSD diagnoses in clients, and the related potential for reimbursement and access to care for a broader range of traumatized clients, the prevalence of VT in clinicians may increase as well. Further research is needed on prevalence, risk and protective factors, and effective help for counselors experiencing VT. The addition of VT in the DSM-5 provides a diagnostic construct, yet future research will yield notable contributions to conceptualization and inform counseling practices for individuals experiencing VT.
Furthermore, a growing body of evidence suggests that a traditional diagnosis of PTSD is not sufficient to describe the range and intensity of symptomatology experienced in survivors of unremitting and recurrent abuse, notably abuse during early stages of development. Research has determined that such iterative and early trauma engenders symptomatic sequelae divergent from adult onset or isolated acts of violence (Herman, 1992b; van der Kolk, Roth, Pelcovitz, Sunday, & Spinazzola, 2005). Herman (1992b) and van der Kolk et al. (2005) proposed a diagnostic formulation distinct from PTSD: complex PTSD or disorders of extreme stress not otherwise specified (DESNOS). The profoundly disruptive nature of DESNOS led researchers to characterize complex PTSD as an experience of “mental death” (p. 617; Ebert & Dyck, 2004). In field trials on the addition of complex PTSD in forthcoming editions of DSM, 68% of children who experienced sexual abuse were found to have complex PTSD over and above an expression of PTSD alone (Roth, Newman, Pelcovitz, van der Kolk, & Mandel, 1997). In a follow-up to earlier field trial studies, van der Kolk et al. (2005) found early interpersonal trauma gives rise to more complex pathology than later interpersonal victimization, and that the younger the age of onset of the trauma, the more likely the individual is to suffer from C-PTSD. However, at the time of the DSM-5’s publication, the TSRDD Sub-Work Group of the DSM-5 determined that there was not currently enough information on the distinctiveness and pervasiveness of the disorder to warrant a formal diagnosis (Friedman, 2013). However, the group incorporated certain proposed DESNOS symptoms (e.g., self-destructive behavior, dissociative subtype) into the reformulated diagnosis (Friedman et al., 2011). Given evidence of uniquely deleterious consequences of early and repeated trauma, ongoing conceptualization and validation of DESNOS will be essential.
Although the DSM-5 provides improvements to PTSD diagnoses, it also presents notable challenges and engenders numerous unanswered questions for counselors and other mental health professionals. Counselor experiences in the field will inform practice, and continued research will provide more coherent understanding of criteria such as negative emotionality and numbing, accurate assessment of TSRDs, and ramifications in legal, health care and forensic settings. To continue to work ethically within their scope of practice (American Counseling Association, 2014), counselors must ensure that they are trained in the area of trauma and continue to seek professional education and guidance on the ongoing developments in this topic.
Conflict of Interest and Funding Disclosure
The author reported no conflict of interest or funding contributions for the development of this manuscript.
References
American Counseling Association. (2014). 2014 ACA code of ethics. Alexandria, VA: Author.
American Psychiatric Association. (1980). Diagnostic and statistical manual of mental disorders (3rd ed.). Washington, DC: Author.
American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author.
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author.
American Psychiatric Association. (2013a). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: Author.
American Psychiatric Association. (2013b). Insurance implications of DSM-5. Retrieved from http://www.psychiatry.org/File%20Library/Practice/DSM/DSM-5/Insurance-Implications-of-DSM-5.pdf
American Psychiatric Association. (2014). Online assessment measures. Retrieved from http://www.psychiatry.org/practice/dsm/dsm5/online-assessment-measures
Anestis, M. D., Tull, M. T., Bagge, C. L., & Gratz, K. L. (2012). The moderating role of distress tolerance in the relationship between posttraumatic stress disorder symptom clusters and suicidal behavior among trauma exposed substance users in residential treatment. Archives of Suicide Research, 16, 198–211. doi:10.1080/13811118.2012.695269
Arvay, M. J., & Uhlemann, M. R. (1996). Counsellor stress in the field of trauma: A preliminary study. Canadian Journal of Counselling and Psychotherapy, 30, 193–210.
Asmundson, G. J. G., Stapleton, J. A., & Taylor, S. (2004). Are avoidance and numbing distinct PTSD symptom clusters? Journal of Traumatic Stress, 17, 467–475. doi:10.1007/s10960-004-5795-7
Breslau, N., & Kessler, R. C. (2001). The stressor criterion in DSM-IV posttraumatic stress disorder: An empirical investigation. Biological Psychiatry, 50, 699–704. doi:10.1016/s0006-3223(01)01167-2
Breslau, N., Reboussin, B. A., Anthony, J. C., & Storr, C. L. (2005). The structure of posttraumatic stress disorder: Latent class analysis in 2 community samples. Archives of General Psychiatry, 62, 1343–1351. doi:10.1001/archpsyc.62.12.1343
Brewin, C. R., Lanius, R. A., Novac, A., Schnyder, U., & Galea, S. (2009). Reformulating PTSD for DSM-V: Life after Criterion A. Journal of Traumatic Stress, 22, 366–373. doi:10.1002/jts.20443
Briere, J., & Scott, C. (2006). Principles of trauma therapy: A guide to symptoms, evaluation and treatment. Thousand Oaks, CA: Sage.
Briere, J. N., & Scott, C. (2013). Principles of trauma therapy: A guide to symptoms, evaluation and treatment (2nd ed.). Thousand Oaks, CA: Sage.
Carmassi, C., Akiskal, H. S., Yong, S. S., Stratta, P., Calderani, E., Massimetti, E., . . . Dell’Osso, L. (2013). Post-traumatic stress disorder in DSM-5: Estimates of prevalence and criteria comparison versus DSM-IV-TR in a non-clinical sample of earthquake survivors. Journal of Affective Disorders, 151, 843–848. doi:10.1016/j.jad.2013.07.020
Cloitre, M., Petkova, E., Wang, J., & Lu, F. (2012). An examination of the influence of a sequential treatment on the course and impact of dissociation among women with PTSD related to childhood abuse. Depression and Anxiety, 29, 709–717. doi:10.1002/da.21920
Cohen, J. A., Bukstein, O., Walter, H., Benson, R. S., Chrisman, A., Farchione, T. R., . . . Medicus, J. (2010). Practice parameter for the assessment and treatment of children and adolescents with posttraumatic stress disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 49, 414–430.
Cook, J. M., Rehman, O., Bufka, L., Dinnen, S., & Courtois, C. (2011). Responses of a sample of practicing psychologists to questions about clinical work with trauma and interest in specialized training. Psychological Trauma: Theory, Research, Practice, and Policy, 3, 253–257. doi:10.1037/a0025048
Council for Accreditation of Counseling and Related Educational Programs. (2009). 2009 standards. Retrieved from http://www.cacrep.org/wp-content/uploads/2013/12/2009-Standards.pdf
Creamer, M., McFarlane, A. C., & Burgess, P. (2005). Psychopathology following trauma: The role of subjective experience. Journal of Affective Disorders, 86, 175–182. doi:10.1016/j.jad.2005.01.015
Cukor, J., Wyka, K., Jayasinghe, N., & Difede, J. (2010). The nature and course of subthreshold PTSD. Journal of Anxiety Disorders, 24, 918–923. doi:10.1016/j.janxdis.2010.06.017
Ebert, A., & Dyck, M. J. (2004). The experience of mental death: The core feature of complex posttraumatic stress disorder. Clinical Psychology Review, 24, 617–635. doi:10.1016/j.cpr.2004.06.002
Felmingham, K., Kemp, A. H., Williams, L., Falconer, E., Olivieri, G., Peduto, A., & Bryant, R. (2008). Dissociative responses to conscious and non-conscious fear impact underlying brain function in post-traumatic stress disorder. Psychological Medicine, 38, 1771–1780. doi:10.1017/S0033291708002742
First, M. B. (2014). DSM-5 Handbook of Differential Diagnosis. Arlington, VA: American Psychiatric Association.
Fish, V. (2004). Some gender biases in diagnosing traumatized women. In P. J. Caplan & L. Cosgrove (Eds.), Bias in psychiatric diagnosis (pp. 213–220). Lanham, MD: Rowman & Littlefield.
Foa, E. B., Riggs, D. S., & Gershuny, B. S. (1995). Arousal, numbing, and intrusion: Symptom structure of PTSD following assault. The American Journal of Psychiatry, 152, 116–120.
Foa, E. B., Zinbarg, R., & Rothbaum, B. O. (1992). Uncontrollability and unpredictability in post-traumatic stress disorder: An animal model. Psychological Bulletin, 112, 218–238. doi:10.1037/0033-2909.112.2.218
Freud, S. (1962). The aetiology of hysteria. In J. Strachey (Ed.), The standard edition of the complete psychological works of Sigmund Freud, Volume III (1893-1899): Early psycho-analytic publications (pp. 187–221). London, England: Hogarth Press.
Frewen, P. A., Dozois, D. J. A., Neufeld, R. W. J., Densmore, M., Stevens, T. K., & Lanius, R. A. (2010). Social emotions and emotional valence during imagery in women with PTSD: Affective and neural correlates. Psychological Trauma: Theory, Research, Practice, and Policy, 2, 145–157. doi:10.1037/a0019154
Friedman, M. J. (2013). Finalizing PTSD in DSM-5: Getting here from there and where to go next. Journal of Traumatic Stress, 26, 548–556. doi:10.1002/jts.21840
Friedman, M. J., Resick, P. A., Bryant, R. A., & Brewin, C. R. (2011). Considering PTSD for DSM-5. Depression and Anxiety, 28, 750–769. doi:10.1002/da.20767
Galatzer-Levy, I. R., & Bryant, R. A. (2013). 636,120 ways to have posttraumatic stress disorder. Perspectives on Psychological Science, 8, 651–662. doi:10.1177/1745691613504115
Herman, J. L. (1992a). Trauma and recovery: The aftermath of violence—from domestic abuse to political terror. New York, NY: Basic Books.
Herman, J. L. (1992b). Complex PTSD: A syndrome in survivors of prolonged and repeated trauma. Journal of Traumatic Stress, 5, 377–391. doi:10.1002/jts.2490050305
Kadambi, M. A., & Ennis, L. (2004). Reconsidering vicarious trauma: A review of the literature and its’ [sic] limitations. Journal of Trauma Practice, 3, 1–21. doi:10.1300/J189v03n02_01
Kelley, L. P., Weathers, F. W., McDevitt-Murphy, M. E., Eakin, D. E., & Flood, A. M. (2009). A comparison of PTSD symptom patterns in three types of civilian trauma. Journal of Traumatic Stress, 22, 227–235. doi:10.1002/jts.20406
Kilpatrick, D. G., Resnick, H. S., Milanak, M. E., Miller, M. W., Keyes, K. M., & Friedman, M. J. (2013). National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. Journal of Traumatic Stress, 26, 537–547. doi:10.1002/jts.21848
Krysinska, K., & Lester, D. (2010). Post-traumatic stress disorder and suicide risk: A systematic review. Archives of Suicide Research, 14, 1–23. doi:10.1080/13811110903478997
Lanius, R. A., Brand, B., Vermetten, E., Frewen, P. A., & Spiegel, D. (2012). The dissociative subtype of posttraumatic stress disorder: Rationale, clinical and neurobiological evidence, and implications. Depression and Anxiety, 29, 701–708. doi:10.1002/da.21889
McNally, R. J. (2009). Can we fix PTSD in DSM-V? Depression and Anxiety, 26, 597–600. doi:10.1002/da.20586
Meldrum, L., King, R., & Spooner, D. (2002). Secondary traumatic stress in case managers working in community mental health services. In C. R. Figley (Ed.), Treating compassion fatigue (pp. 85–106). New York, NY: Brunner-Routledge.
Moser, J. S., Hajcak, G., Simons, R. F., & Foa, E. B. (2007). Posttraumatic stress disorder symptoms in trauma-exposed college students: The role of trauma-related cognitions, gender, and negative affect. Journal of Anxiety Disorders, 21, 1039–1049. doi:10.1016/j.janxdis.2006.10.009
Nemeroff, C. B., Weinberger, D., Rutter, M., MacMillan, H. L., Bryant, R. A., Wessely, S., . . . Lysaker, P. (2013). DSM-5: A collection of psychiatrist views on the changes, controversies, and future directions. BMC Medicine, 11, 1–19. doi:10.1186/1741-7015-11-202
Orsillo, S. M., Theodore-Oklota, C., Luterek, J. A., & Plumb, J. (2007). The development and psychometric evaluation of the Emotional Reactivity and Numbing Scale. Journal of Nervous & Mental Disease, 195, 830–836. doi:10.1097/NMD.0b013e318156816f
Panagioti, M., Gooding, P. A., Taylor, P. J., & Tarrier, N. (2014). Perceived social support buffers the impact of PTSD symptoms on suicidal behavior: Implications into suicide resilience research. Comprehensive Psychiatry, 55, 104–112. doi:10.1016/j.comppsych.2013.06.004
Parker, M., & Henfield, M. S. (2012). Exploring school counselors’ perceptions of vicarious trauma: A qualitative study. The Professional Counselor, 2, 134–142.
Pynoos, R. S., Steinberg, A. M., Layne, C. M., Briggs, E. C., Ostrowski, S. A., & Fairbank, J. A. (2009). DSM-V PTSD diagnostic criteria for children and adolescents: A developmental perspective and recommendations. Journal of Traumatic Stress, 22, 391–398. doi:10.1002/jts.20450
Rojas, V. M., & Lee, T. N. (2004). Childhood vs. adult PTSD. In R. R. Silva (Ed.), Posttraumatic stress disorders in children and adolescents: Handbook (pp. 237–256). New York, NY: Norton.
Rosen, G. M., & Lilienfeld, S. O. (2008). Posttraumatic stress disorder: An empirical evaluation of core assumptions. Clinical Psychology Review, 28, 837–868. doi:10.1016/j.cpr.2007.12.002
Roth, S., Newman, E., Pelcovitz, D., van der Kolk, B., & Mandel, F. S. (1997). Complex PTSD in victims exposed to sexual and physical abuse: Results from the DSM-IV field trial for posttraumatic stress disorder. Journal of Traumatic Stress, 10, 539–555. doi:10.1002/jts.2490100403
Royle, L., Keenan, P., & Farrell, D. (2009). Issues of stigma for first responders accessing support for post traumatic stress. International Journal of Emergency Mental Health, 11, 79–85.
Scheeringa, M. S. (2014). PTSD for children 6 years and younger. Retrieved from http://www.ptsd.va.gov/professional/PTSD-overview/ptsd_children_6_and_younger.asp
Scheeringa, M. S., Myers, L., Putnam, F. W., & Zeanah, C. H. (2012). Diagnosing PTSD in early childhood: An empirical assessment of four approaches. Journal of Traumatic Stress, 25, 359–367. doi:10.1002/jts.21723
Scheeringa, M. S., Zeanah, C. H., & Cohen, J. A. (2011). PTSD in children and adolescents: Toward an empirically based algorithma. Depression and Anxiety, 28, 770–782. doi:10.1002/da.20736
Schützwohl, M., & Maercker, A. (1999). Effects of varying diagnostic criteria for posttraumatic stress disorder are endorsing the concept of partial PTSD. Journal of Traumatic Stress, 12, 155–165. doi:10.1023/a:1024706702133
Ullman, S. E., & Long, S. M. (2008). Factor structure of PTSD in a community sample of sexual assault survivors. Journal of Trauma & Dissociation, 9, 507–524. doi:10.1080/15299730802223370
van der Kolk, B. A. (2007). The history of trauma in psychiatry. In M. J. Friedman, T. M. Keane, & P. A. Resick (Eds.), Handbook of PTSD: Science and practice (pp. 19–36). New York, NY: The Guilford Press.
van der Kolk, B. A., Roth, S., Pelcovitz, D., Sunday, S., & Spinazzola, J. (2005). Disorders of extreme stress: The empirical foundation of a complex adaptation to trauma. Journal of Traumatic Stress, 18, 389–399. doi:10.1002/jts.20047
Vidal, M. E., & Petrak, J. (2007). Shame and adult sexual assault: A study with a group of female survivors recruited from an East London population. Sexual and Relationship Therapy, 22, 159–171. doi:10.1080/14681990600784143
Yehuda, R., & Bierer, L. M. (2009). The relevance of epigenetics to PTSD: Implications for the DSM-V. Journal of Traumatic Stress, 22, 427–434. doi:10.1002/jts.20448
Zoellner, L. A., Rothbaum, B. O., & Feeny, N. C. (2011). PTSD not an anxiety disorder? DSM committee proposal turns back the hands of time. Depression and Anxiety, 28, 853–856. doi:10.1002/da.20899
Laura K. Jones, NCC, is an Assistant Professor at the University of Northern Colorado. Jenny L. Cureton, NCC, is a doctoral student at the University of Northern Colorado. Correspondence can be addressed to Laura K. Jones, University of Northern Colorado, Department of Applied Psychology and Counselor Education, Box 131, Greeley, CO 80639, laura.jones@unco.edu.
Jul 2, 2014 | Article, Volume 4 - Issue 3
Saundra M. Tomlinson-Clarke, Colleen M. Georges
The 2013 publication of the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5) marked the reemergence of issues related to the appropriateness of diagnosis and the uses of the DSM-5 within the counseling profession. Concerns focus on the implications of the DSM-5 for counseling professionals whose professional identity is grounded in a prevention and wellness model, and the impact of the diagnostic process on counseling ethical practice. In this article, the authors explore the use of the DSM-5 in counseling training and practice. The authors also discuss integrating DSM-5 diagnosis into a counselor training framework while maintaining a wellness orientation. Multicultural and strength-based considerations are recommended when using the DSM-5 in counseling training and practice, while maintaining consistency with a philosophical orientation focused on development and wellness and delivering services that are indicative of a unified counseling professional identity.
Keywords: diagnosis, DSM-5, strengths, wellness, counselor training, multicultural
The history of the counseling profession dates back to the vocational guidance movement of the early 1900s. As society became increasingly industrialized, a need arose to improve individuals’ vocational choices (Whiteley, 1984). With a focus on helping people to resolve problems in living, the counseling profession has maintained an emphasis on growth, prevention and early intervention across the life span (Gladding, 2013). Counseling is defined as “a professional relationship that empowers diverse individuals, families, and groups to accomplish mental health, wellness, education, and career goals” (Kaplan, Tarvydas, & Gladding, 2013). According to Remley and Herlihy (2014), many problems and issues that people face are developmental in nature. A wellness orientation toward helping and help seeking and the use of holistic approaches to treatment distinguish professional counselors from other mental health professionals (Mellin, Hunt, & Nichols, 2011). A focus on normal development and positive lifestyles promotes counselor professional identity and unifies the counseling profession (Gale & Austin, 2003). Given its common historical roots of assisting individuals with educational, occupational and emotional well-being (Whiteley, 1984), the field of counseling psychology also “maintains a focus on facilitating personal and interpersonal functioning across the life span. . . [with] particular attention to emotional, social, vocational, educational, health-related, developmental, and organizational concerns” (Society of Counseling Psychology, American Psychological Association, Division 17, 2014). Therefore, counselors, counseling psychologists and counselor educators benefit from understanding the dynamics of human growth and development in developing responsive interventions for clients with mental health concerns (Ibrahim, 1991). Furthermore, in creating a shared vision for supporting counselors, services to clients and the counseling profession, “advocat[ing] for optimal human development by promoting prevention and wellness” was among the six critical themes identified at the Counselor Advocacy Leadership Conference (Kaplan & Gladding, 2011, p. 368).
With the publication of the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5; American Psychiatric Association [APA], 2013), issues related to counselor professional identity, diagnosis and the use of the DSM-5 within the counseling profession have reemerged. Concerns focus on the implications of the DSM-5 for counseling professionals who advocate prevention and wellness, and the impact of the diagnostic process on counseling ethical practice (Kress, Hoffman, Adamson, & Eriksen, 2013). Also, multicultural and contextual considerations may be ignored when adhering to a medical model implied by the DSM system. Despite these criticisms, few models exist for integrating diagnosis using the DSM-5 into a wellness and prevention orientation, which is central to professional counseling training and practice. Our goal is to explore the use of the DSM-5 in counseling training and practice, and to suggest ways that DSM-5 diagnosis might be integrated into a counselor training framework while maintaining a wellness orientation.
DSM and Counseling Training
Distinguishing counseling from other mental health professions by a focus on human development, prevention and wellness does not exclude counseling professionals and trainees from acquiring an understanding of behavior across the adaptive-maladaptive continuum. In promoting a counselor professional identity, and reinforcing the consensus definition of professional counseling as empowering individuals, families and groups, teaching diagnosis using the DSM-5 to counseling trainees requires a cultural and contextual understanding of individuals and their concerns. Providing counseling trainees with learning experiences designed to foster knowledge and skills extends beyond exposure to the DSM-5 classification systems for categorizing behavior identified as disordered. Successfully integrating knowledge, skills and practices of diagnosis and the DSM-5 into counselor education involves a review of counselor common core curricular and professional practice (Council for Accreditation of Counseling and Related Educational Programs [CACREP], 2009).
In the requirements for common core curricular experiences and demonstrated knowledge, CACREP (2009) requires that all counseling trainees learn about “the nature and needs of persons at all developmental levels and in multicultural contexts” (II.G.3, p. 10), including “theories for facilitating optimal development and wellness over the life span” (II.G.3.h, p. 10) and about “human behavior, including an understanding of developmental crises, disability, psychopathology, and situational and environmental factors that affect both normal and abnormal behavior” (II.G.3.f, p. 10). Furthermore, the standards for Addiction Counseling and Clinical Mental Health Counseling specifically require demonstrated “professional knowledge, skills, and practices” (CACREP, 2009, III, p. 17; p. 29), use of the current DSM and use of other diagnostic tools. Therefore, in addition to common core curricular experiences that develop knowledge and skills needed for “facilitating optimal development and wellness over the life span” (CACREP, 2009, II.G.3.h, p. 10), professional counselors must have diagnostic knowledge, skills and practices. This includes understanding “etiology, the diagnostic process and nomenclature, treatment, referral, and prevention of mental and emotional disorders” (CACREP, 2009, III.C.2, p. 30) and “the range of mental health service delivery” (III.C.5, p. 30). Specifically, CACREP (2009) standards require that counseling trainees must evidence knowledge, relevant skills and practices that include the following: knowledge of the use of the current edition of the DSM (i.e., DSM-5), an understanding of possible biases that might occur when using diagnostic tools with culturally diverse clients, knowledge of the correct use of diagnosis during a traumatic event, and the ability to differentiate “between diagnosis and developmentally appropriate reactions” to traumatic events (CACREP, 2009, III.L.3, p. 34). Moreover, in demonstrating knowledge, skills and practices of the diagnostic process, counseling trainees must understand the implications of diagnosis and treatment interventions. To this end, Kress et al. (2013) stressed the importance of weighing both the benefits and risks of diagnosis when working with clients.
DSM-5 and Counseling Practice
Despite goals of revising the diagnostic classification scheme to make it “more clinically valuable and more biologically valid” (Nemeroff et al., 2013, p. 2), and of acknowledging cultural variations in clients’ expressions of their concerns (Brown & Lewis-Fernández, 2011), the DSM-5 has been criticized from within and beyond the psychiatric community. Released in May 2013, the DSM-5 was met with controversy from mental health professionals and organizations representing their interest in providing effective clinical mental health services to clients (Washburn, 2013). Many viewed the DSM-5 as an extension of the traditional medical model of diagnosis. For example, Ladd (2013) criticized DSM diagnosis for (1) ignoring the therapeutic alliance as a critical aspect of treatment; (2) depending on “statistically acquired symptoms” and “specific rules and timelines” created by Task Force/Work Group professional experts (p. 2); and (3) gearing its usefulness toward “insurance companies, managed care agencies and other professionals in the health care system” (p. 3). The American Mental Health Counselors Association (AMHCA) DSM-5 Task Force (2012), among other groups, submitted feedback to improve the DSM-5 draft. Although the DSM provides a common language for presenting client problems (Hinkle, 1999), the language and assumptions associated with the criteria for diagnosis became the focus of criticism. Stressing the important distinction of “separating the art of mental health diagnosis and complying with the mental health diagnosis business,” Ladd (2013, p. 3) described the DSM as “the diagnostic instrument for the ‘mental health diagnosis business’ with categories and labels used as the language for insurance reimbursement, pharmaceutical treatment, and collaboration between experts” (p. 3).
Due to a growing need for quality mental health services, counseling professionals are providing services to clients presenting with a diverse range of concerns. Counselors are often required to diagnose clients’ problems using the DSM-5 (Miller & Prosek, 2013). DSM diagnosis is necessary for counselors to access managed care and insurance company reimbursements (Hinkle, 1999). However, a traditional use of the DSM may pathologize behavior and separate diagnosis from treatment interventions (Ivey & Ivey, 1999). Counselors faced with these ethical dilemmas may question their professional identity, the usefulness of a wellness orientation and the effectiveness of counseling-related tasks (McAuliffe & Eriksen, 1999; Mellin et al., 2011). Counselors’ challenge to adhere to a wellness orientation as the foundation of their professional identity may be further tested by other mental health professionals’ tendency to conceptualize health and illness using models of pathology and remediation (McAuliffe & Eriksen, 1999). These dilemmas in counseling practice are more likely to become problematic when counselors are not grounded in a strong professional identity. Gale and Austin (2003) encouraged counselors to embrace a wellness model rather than an illness or deficit model of help seeking and treatment planning. Counselor clinical judgment is critical to the diagnostic process. Notwithstanding criticisms of the DSM, Johnson (2013) asserted that diagnosis is directly related to the philosophical and theoretical orientations of the clinician. The medical model used in diagnosis negatively impacts clients’ willingness to seek help for their concerns, and also influences mental health professionals’ orientations toward deficit models (McAuliffe & Eriksen, 1999).
Important considerations for teaching the DSM are directly related to understanding the diagnostic process and implications for models of helping used to conceptualize counseling goals and interventions with clients. Given the focus on prevention, wellness and health across the life span, key questions arise when teaching the DSM-5 to counseling trainees from a traditional medical model that is “focused disproportionately on the physical aspects of illness” (Ingersoll, 2002, p. 115). A traditional disease model views the helper as the expert responsible for healing the client (McAuliffe & Eriksen, 1999). Brickman et al. (1982) viewed this model of helping as deficient in that the helper fosters dependency, which is antithetical to an empowering therapeutic relationship. Teaching the DSM-5 to counseling students requires an understanding of a developmental and wellness orientation. Models of helping must be philosophically and theoretically congruent with a professional counseling identity. To this end, counseling trainees must be challenged to examine their beliefs about seeking help and their view of a helper in the counseling relationship. Diagnosis and treatment should not be separate; rather, diagnosis should occur in conjunction with treatment (Ivey & Ivey, 1999). Viewing clients from a holistic perspective assumes that the greatest source of information lies within the client, not a manual or system of classifying disorders. Focusing on clients’ strengths rather than deficiencies helps to empower clients as part of their learning and development. Integrating multicultural and strength-based considerations as part of the diagnostic process helps to ensure that clients receive culturally responsive counseling interventions.
Integrating Multicultural and Strength-Based Considerations
Counselors, counseling psychologists and counselor educators have been instrumental in recognizing the role of culture and integrating multicultural perspectives in an attempt to understand behavior more fully (Pedersen, 1991; Sue, Sue, Sue, & Sue, 2014). Although racial-ethnic minority groups remained underrepresented in research examining psychopathology, African-American and Hispanic or Latino clients are more likely to be diagnosed, to receive diagnoses of greater severity and to experience less effective treatment outcomes than are White clients (Johnson, 2013; Sue & Sue, 2013). Consequently, multicultural counselor competencies are necessary to address counselors’ culturally biased assumptions and to increase counseling effectiveness in a society changing in culture and diversity (Arredondo et al., 1996; Pedersen, 1987, 2003; Sue, Arredondo, & McDavis, 1992; Sue et al., 1982; Sue & Sue, 2013). Multiculturalism integrates culturally specific and universal perspectives in explaining the dynamics of behavior and developing culturally responsive approaches to treatment. However, counselors may ignore multicultural considerations when adhering to a medical model implied by the DSM. Ivey and Ivey (1999) called on counseling professionals to apply multicultural perspectives when using the DSM. In advancing a contextual understanding of behavior and disorders, Sue et al. (2014) developed a multipath model using four dimensions (i.e., biological, psychological, social and sociocultural) to describe etiological explanations of abnormal behavior.
Social, cultural and economic considerations must be acknowledged when attempting to identify and classify behavior diagnosed as maladaptive. Sue et al. (2014) distinguished cultural universality from cultural relativity in describing behavior within a sociocultural context. Important cultural nuances may be misunderstood when viewed by others who are culturally dissimilar. The result is the labeling of culturally normal behavior as maladaptive. To this end, myths associated with abnormal behavior have led to the social construction of diagnostic categories, which have been cited as major criticisms of using the DSM. Among these faulty assumptions is the belief that abnormal behavior can be readily recognized, distinguished from normal behavior and therefore categorized according to a diagnostic classification scheme (Maddux, 2002; Sue et al., 2014). Maddux (2002) further stated that diagnostic categories used in making biased clinical judgments lead to culturally unresponsive treatment interventions. Inherent in this approach is the basis of the medical model, in which clients are more often treated for pathological behavior (McAuliffe & Eriksen, 1999).
A step toward more holistic diagnostic practices appeared in the DSM-5 in the form of dimensional rather than categorical assessments. These dimensional assessments of every categorical diagnosis were designed to assist counselors with diagnosis and treatment planning (Jones, 2012). Unlike previous versions of the DSM that used a categorical system, dimensional assessments view disorders on a continuum, representing varying degrees of a behavior (Sue et al., 2014). The dimensional assessment also allows counselors to consider individual differences and the influences of race and culture (Johnson, 2013). With the dimensional model, counselors are able to determine whether a diagnostic criterion is present and rate its severity (Brown & Lewis-Fernández, 2011). Viewing disorders on a continuum of behavior may decrease comorbidity; however, it also may affect clients’ accessibility to services by eliminating clients who might have formerly met the criteria for diagnosis or diagnosing clients with a disorder that would have been excluded based on the former criteria. Examples include autism spectrum disorder and depression resulting from bereavement, respectively. Given these changes, the effect of the DSM-5 on diagnosis may impact clients’ access to mental health services and create ethical dilemmas for counselors related to over- and undertreatment.
In addition to the dimensional assessments, the DSM-5 also contains disorders associated with cultural issues. Psychosocial factors are included by using V codes from the World Health Organization’s (WHO) International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM; WHO, 1979) and Z codes from the International Classification of Diseases, Tenth Revision (ICD-10; WHO,1992), as well as three new terms: cultural syndrome, cultural idiom of distress and cultural explanation or perceived cause (Pomeroy & Anderson, 2013). Counselors must become familiar with the ICD-10-CM diagnostic codes, which will become the standard medical coding system in the United States beginning October 1, 2015. Inclusion of psychosocial factors evidences the relationship between psychosocial factors and mental health. Multicultural considerations in diagnosis allow mental health practitioners to understand cultural and individual characteristics that define identity and experience. These characteristics of a client’s identity are multiple and interlocking. The uniqueness that defines a client may be lost if group generalizations as represented by the DSM-5 are used as the only means of understanding a client’s experiences. Critical to understanding clients and their stories is the ability to conceptualize clients as individuals interacting within the sociocultural context in which they live. This also involves hearing clients’ stories from their perspective, using their own words.
The importance of cultural influences on mental health diagnosis also is demonstrated by the inclusion of the Cultural Formulation Interview (CFI; Pomeroy & Anderson, 2013). The CFI was developed to improve cross-cultural diagnostic assessment and was created from the Outline for Cultural Formulation (OCF) of the DSM-IV (Aggarwal, Nicasio, DeSilva, Boiler, & Lewis-Fernández, 2013). In keeping with multicultural competency models, the CFI provides a way for counselors to explore and understand clients’ experiences and worldviews, as well as clients’ cultural explanations and interpretations of their concerns. However, Aggarwal et al. (2013) cautioned that the overstandardization of the CFI may result in counselor and client barriers such as the following: a counselor misunderstanding the problem and the problem severity, a lack of conceptual relevance between the client’s concern and counseling interventions, and a counselor and client’s lack of acceptance and unwillingness to engage in the process. Counselors’ ability to develop authentic and caring relationships is essential to accurate diagnosis and relevant counseling interventions. When clients are viewed as unique and counselors understand their experiences, accurate diagnosis and ethical practice are ensured (Swartz-Kulstad & Martin, 1999).
Moving beyond an illness model toward a counselor-client collaborative wellness model begins with a process of engaging with the client, gathering the information needed for assessing the client and trusting in the therapeutic alliance to accomplish the goals of treatment (Ivey & Ivey, 1999). Contrary to the medical or illness model, in which the client’s weaknesses or deficiencies precipitate the diagnosis, treatment and policy decisions, the integration of a strength-based framework and counselor preparation ensures a holistic approach to assessment and treatment (Wright & Lopez, 2002). Working with clients from a holistic perspective requires knowledge and skills that preserve the integrity of the counseling profession by embracing multicultural and strength-based considerations. A framework adapted from positive psychology, defined as “the study of . . . what is ‘right’ about people––their positive attributes, psychological assets, and strengths” (Kobau et al., 2011, p. e1), assists in bolstering resilience and promoting mental health.
Strength-Based Approaches to Diagnosis
Character Strengths and Virtues
Character Strengths and Virtues: A Handbook and Classification (CSV; Peterson & Seligman, 2004), which its authors dub a “Manual of the Sanities” (p. 3) in the introductory chapter, was developed in part as a companion to the DSM that focuses on classifying what is right about people. It includes explicit criteria for character strengths and launched the development of several assessment tools that aid in diagnosing one’s strengths in the way that the DSM diagnoses one’s limitations. Character strengths are the foundation of strength-based approaches and provide a way to assess client functioning from a wellness orientation (O’Hanlon & Bertolino, 2012). The CSV distinguishes three conceptual levels: (1) virtues: core characteristics that moral and religious philosophers esteem; (2) character strengths: processes that define virtues; and (3) situational themes: practices that lead people to establish specific character strengths in certain situations.
Parallel to the DSM, the CSV outlines 10 specific criteria that must be satisfied to warrant inclusion as a character strength. Using these criteria, 24 character strengths were identified under the respective umbrellas of six core virtues: (1) wisdom and knowledge (creativity, curiosity, open-mindedness, love of learning, and perspective); (2) courage (bravery, persistence, integrity, and vitality); (3) humanity (love, kindness, and social intelligence); (4) justice (citizenship, fairness, and leadership); (5) temperance (forgiveness and mercy, humility and modesty, prudence, and self-regulation); and (6) transcendence (appreciation of beauty and excellence, gratitude, hope, humor, and spirituality). The CSV also broadly outlines strength assessment strategies, as well as interventions that further cultivate strengths. For example, counselors might assist clients in realizing or reaffirming their virtue of strength of courage by exploring the will to achieve goals while facing external or internal opposition (O’Hanlon & Bertolino, 2012). This exercise empowers clients and provides counselors with a positive rather than a negative assessment of client behavior. Similarly, the use of positive talk moves clients away from a perspective of deficiency and illness toward encouragement and motivation for change.
Using the CSV in conjunction with the DSM enables counselors to help their clients identify, take pride in and use their character strengths and virtues to enhance well-being in all areas of their lives. Gander, Proyer, Ruch and Wyss (2013) found that using one’s signature strengths in a different way lowered depression and boosted happiness for six months. Wood, Linley, Matlby, Kashdan and Hurling’s (2011) longitudinal study determined that using one’s strengths was correlated with well-being; decreased stress; and greater self-esteem, positive affect and vitality, with the effects still present at three-month and six-month follow-ups. Furthermore, the majority of positive counseling interventions focus on character strength interventions, which have been found to benefit both adults and children dealing with depression and anxiety (Rashid & Anjum, 2008; Seligman, Rashid, & Parks, 2006).
Client diagnosis and conceptualization using the DSM-5 may be incomplete if clinicians do not consider clients’ environmental resources, well-being and strengths (Snyder et al., 2003). Minor alterations to this diagnostic system could promote emphasis on positive functioning and provide information that could contribute to a more complete client picture and conceptualization. Recommendations for rescaling the Axis V Global Assessment of Functioning (GAF) Scale of the DSM-IV-TR included creating a functioning baseline, with the current GAF level of 100 (absence of symptomatology) rescaled to a midpoint of 50. This would have encouraged practitioners to identify and use client strengths, with a GAF of 1 representing severely impaired functioning, 50 representing good health and 100 representing optimal functioning. Snyder et al. (2003) also suggested adding personal strengths and growth facilitators through three brief questions and four positive psychology assessments that measure hope, optimism, personal growth initiative and subjective well-being. Similarly, Magyar-Moe (2009) suggested using a seven-axis system of positive psychological assessment that included documenting positive and negative aspects of clients’ cultural identities, as well as clients’ personal strengths as facilitators of growth.
These exercises, based in positive well-being, are consistent with a wellness orientation of helping and should not be solely limited to clients’ growth and development. Counseling trainees and professional counselors benefit personally and professionally when functioning from a strength-based orientation. For example, based on findings from attribution theory, negative labels affect motivation for change (O’Hanlon & Bertolino, 2012). Therefore, O’Hanlon and Bertolino cautioned against using negative diagnostic labels that may communicate a belief that clients are unable to change. From this perspective, counselors must continually examine their own behavior and the subtle messages that clients might receive during counseling. Through strength-based exercises, counselors are encouraged to promote strengths and resilience as part of an ongoing reflective practice.
Conclusion
Teaching the process of diagnosis using the DSM-5 to counseling trainees is not an easy undertaking. Developed as a tool that promotes a language for use in the larger mental health system (Hinkle, 1999), the DSM is required learning for counseling trainees, and demonstrating professional knowledge, skills and practices is required for professional counselors. Teaching the basic vocabulary and criteria associated with disorders is only the first level of discussion. Effectively teaching diagnosis informed by multicultural and strength-based perspectives includes acknowledging the purpose and limitations of the DSM-5, and examining beliefs about helping, and the role and behavior of helpers. Counselors must explore the concept of normal behavior and their ability to identify abnormal behavior, as well as factors influencing growth and change.
Peterson (2013) stated, “we have developed a wonderful vocabulary that explains what goes wrong with folks and we have almost nothing to say about what can go right with folks” (p. 7). Teaching diagnosis and the DSM-5 integrated with multicultural and strength-based considerations helps counselors to understand what goes right with clients. Through this understanding, clients’ strengths, character and virtues become the support for growth and change within the counseling relationship. Rather than focusing on illness and deficiencies, counselors and clients acknowledge strengths and use them to assist clients in resolving problems in life. Informing the diagnostic process with multicultural and strength-based considerations fosters a holistic view of clients and reinforces counselor advocacy of optimal human functioning. Counselors must consider culture, context and strengths for the diagnostic process to be useful in working with clients from a wellness orientation (Adams & Quartiroli, 2010).
Furthermore, multicultural and strength-based practice considerations encourage reflection and counselor reflective practice, which challenge culturally biased assumptions that negatively affect counselor judgments about clients and the diagnostic process. As a result, counseling professionals do not view clients as confined and limited to a diagnosis; rather, they conceptualize clients as resilient and evolving (Adams & Quartiroli, 2010). Recognizing limitations and possibilities of the DSM-5, embracing a wellness and holistic orientation, and understanding clients from their cultural and situational contexts with a focus on strengths are critical factors that reduce ethical dilemmas and support the use of the DSM-5 in counseling training and practice (Adams & Quartiroli, 2010; Gale & Austin, 2003; McAuliffe & Eriksen, 1999). Integrating multicultural and strength-based considerations into counseling training and practice increases the likelihood that counselors will embrace a professional identity congruent with a wellness orientation when using the DSM-5 as a tool in the diagnostic process (Mannarino, Loughran, & Hamilton, 2007).
Conflict of Interest and Funding Disclosure
The author reported no conflict of interest or funding contributions for the development of this manuscript.
References
Adams, J. R., & Quartiroli, A. (2010). Critical considerations of the diagnostic and statistical manual: Importance of the inclusion of cultural and contextual factors. Journal of Humanistic Counseling, Education and Development, 49, 84–97. doi:10.1002/j.2161-1939.2010.tb00089.x
Aggarwal, N. K., Nicasio, A. V., DeSilva, R., Boiler, M., & Lewis-Fernández, R. (2013). Barriers to implementing the DSM-5 Cultural Formulation Interview: A qualitative study. Culture, Medicine, and Psychiatry, 37, 505–533. doi:10.1007/s11013-013-9325-z
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
Arredondo, P., Toporek, R., Pack Brown, S., Jones, J., Locke, D. C., Sanchez, J., & Stadler, H. (1996). Operationalization of the multicultural counseling competencies. Journal of Multicultural Counseling and Development, 24, 42–78. doi:10.1002/j.2161-1912.1996.tb00288.x
Brickman, P., Rabinowitz, V. C., Karuza, J., Jr., Coates, D., Cohn, E., & Kidder, L. (1982). Models of helping and coping. American Psychologist, 37, 368–384.
Brown, R. J., & Lewis-Fernández, R. (2011). Culture and conversion disorder: Implications for the DSM-5. Psychiatry, 74, 187–206. doi:10.1521/psyc.2011.74.3.187
Council for Accreditation of Counseling and Related Educational Programs. (2009). 2009 CACREP standards. Alexandria, VA: Author.
Gale, A. U., & Austin, B. D. (2003). Professionalism’s challenges to professional counselors’ collective identity. Journal of Counseling & Development, 81, 3–10. doi:10.1002/j.1556-6678.2003.tb00219.x
Gander, F., Proyer, R. T., Ruch, W., & Wyss, T. (2013). Strength-based positive interventions: Further evidence for their potential in enhancing well-being and alleviating depression. Journal of Happiness Studies, 14, 1241–1259. doi:10.1007/s10902-012-9380-0
Gladding, S. T. (2013). Counseling: A comprehensive profession (7th ed.). Upper Saddle River, NJ: Pearson.
Hinkle, J. S. (1999). A voice from the trenches: A reaction to Ivey and Ivey (1998). Journal of Counseling & Development, 77, 474–483. doi:10.1002/j.1556-6676.1999.tb02475.x
Ibrahim, F.A. (1991). Contribution of cultural worldview to generic counseling and development. Journal of Counseling & Development, 70, 13–19. doi:10.1002/j.1556-6676.1991.tb01556.x
Ingersoll, R. E. (2002). An integral approach for teaching and practicing diagnosis. The Journal of Transpersonal Psychology, 34, 115–127.
Ivey, A. E., & Ivey, M. B. (1999). Toward a developmental diagnostic and statistical manual: The vitality of a contextual framework. Journal of Counseling & Development, 77, 484–490. doi:10.1002/j.1556-6676.1999.tb02476.x
Johnson, R. (2013). Forensic and culturally responsive approach for the DSM-5: Just the FACTS. The Journal of Theory Construction & Testing, 17, 18–22.
Jones, K. D. (2012). Dimensional and cross-cutting assessment in the DSM-5. Journal of Counseling & Development, 90, 481–487. doi:10.1002/j.1556-6676.2012.00059.x
Kaplan, D. M., & Gladding, S. T. (2011). A vision for the future of counseling: The 20/20 Principles for Unifying and Strengthening the Profession. Journal of Counseling & Development, 89, 367–372.
Kaplan, D. M., Tarvydas, V. M., & Gladding, S. T. (2013). 20/20: A vision for the future of counseling: The new consensus definition of counseling. Retrieved from http://www.counseling.org/docs/david-kaplan’s-files/consensus-definition-of-counseling.docx?sfvrsn=2
Kobau, R., Seligman, M. E. P., Peterson, C., Diener, E., Zack, M. M., Chapman, D., & Thompson, W. (2011). Mental health promotion in public health: Perspectives and strategies from positive psychology. American Journal of Public Health, 101, e1–e9. doi:10.2105/AJPH.2010.300083
Kress, V. E., Hoffman, R. M., Adamson, N., & Eriksen, K. (2013). Informed consent, confidentiality, and diagnosing: Ethical guidelines for counselor practice. Journal of Mental Health Counseling, 35, 15–28.
Ladd, P. D. (2013). Knowledge vs. wisdom in DSM diagnosis: A person-centered perspective. In Ideas and research you can use: VISTAS 2013. Retrieved from http://www.counselingoutfitters.com/vistas/vistas13/Article_6.pdf
Maddux, J. E. (2002). Stopping the “madness”: Positive psychology and the deconstruction of the illness ideology and the DSM. In C. R. Snyder & S. J. Lopez (Eds.), Handbook of Positive Psychology (pp.13–25). New York, NY: Oxford University Press.
Magyar-Moe, J. L. (2009). Therapist’s guide to positive psychological interventions. San Diego, CA: Elsevier Academic Press.
Mannarino, M. B., Loughran, M. J., & Hamilton, D. (2007, October). The professional counselor and the diagnostic process: Challenges and opportunities for education and training. Paper based on a program presented at the conference of the Association for Counselor Education and Supervision, Columbus, OH.
McAuliffe, G. J., & Eriksen, K. P. (1999). Toward a constructivist and developmental identity for the counseling profession: The context-phase-stage-style model. Journal of Counseling & Development, 77, 267–280. doi:10.1002/j.1556-6676.1999.tb02450.x
Mellin, E. A., Hunt, B., & Nichols, L. M. (2011). Counselor professional identity: Findings and implications for counseling and interprofessional collaboration. Journal of Counseling & Development, 89, 140–147. doi:10.1002/j.1556-6678.2011.tb00071.x
Miller, R., & Prosek, E. A. (2013). Trends and implications of proposed changes to the DSM-5 for vulnerable populations. Journal of Counseling & Development, 91, 359–366. doi:10.1002/j.1556-6676.2013.00106.x
Moss, J. M., Gibson, D. M., & Dollarhide, C. T. (2014). Professional identity development: A grounded theory of transformational tasks of counselors. Journal of Counseling & Development, 92, 3–12. doi:10.1002/j.1556-6676.2014.00124.x
Nemeroff, C. B., Weinberger, D., Rutter, M., MacMillan, H. L., Bryant, R. A., Wessely, S., . . . Lysaker, P. (2013). DSM-5: A collection of psychiatrist views on the changes, controversies, and future directions. BMC Medicine, 11, 1–19. doi:10.1186/1741-7015-11-202
O’Hanlon, B., & Bertolino, B. (2012). The therapist’s notebook on positive psychology: Activities, exercises, and handouts. New York, NY: Routledge.
Pedersen, P. (1987). Ten frequent assumptions of cultural bias in counseling. Journal of Multicultural Counseling and Development, 15, 16–24.
Pedersen, P. B. (1991). Multiculturalism as a generic approach to counseling. Journal of Counseling & Development, 70, 6–12. doi:10.1002/j.1556-6676.1991.tb01555.x
Pedersen, P. B. (2003). Culturally biased assumptions in counseling psychology. The Counseling Psychologist, 31, 396–403. doi:10.1177/0011000003031004002
Peterson, C. (2013). The strengths revolution: A positive psychology perspective. Reclaiming Children and Youth, 21, 7–14.
Peterson, C., & Seligman, M. E. P. (2004). Character strengths and virtues: A handbook and classification. New York, NY: Oxford University Press and Washington, DC: American Psychological Association.
Pomeroy, E. C., & Anderson, K. (2013). The DSM-5 has arrived. Social Work, 58, 197–200. doi:10.1093/sw/swt028
Rashid, T., & Anjum, A. (2008). Positive psychotherapy for young adults and children. In J. R. Z. Abela & B. L. Hankin (Eds.), Handbook of depression in children and adolescents (pp. 250–287). New York, NY: Guilford Press.
Remley, T. P., Jr., & Herlihy, B. P. (2014). Ethical, legal, and professional issues in counseling (4th ed.). Upper Saddle River, NJ: Pearson.
Seligman, M. E. P, Rashid, T., & Parks, A. C. (2006). Positive psychotherapy. American Psychologist, 61, 774–788. doi:10.1037/0003-066X.61.8.774
Snyder, C. R., Lopez, S. J., Edwards, L. M., Pedrotti, J. T., Prosser, E. C., Walton, S. L., . . . Ulven, J. C. (2003). Measuring and labeling the positive and the negative. In S. J. Lopez & C. R. Snyder (Eds.), Positive psychological assessment: A handbook of models and measures (pp. 21–39). Washington, DC: American Psychological Association.
Society of Counseling Psychology, American Psychological Association, Division 17. (2014). What is Counseling Psychology. Retrieved from http://www.div17.org/about/what-is-counseling-psychology/
Sue, D. W., Arredondo, P., & McDavis, R. J. (l992). Multicultural competencies and standards: A call to the profession. Journal of Counseling & Development, 70, 477–486. doi:10.1002/j.1556-6676.1992.tb01642.x
Sue, D. W., Bernier, J. E., Durran, A., Feinberg, L., Pedersen, P., Smith E. J., & Vasquez-Nuttall, E. (1982). Position paper: Cross-cultural counseling competencies. The Counseling Psychologist, 10, 45–52. doi:10.1177/0011000082102008
Sue, D. W., & Sue, D. (2013). Counseling the culturally diverse: Theory and practice (6th ed.). New York, NY: Wiley & Sons.
Sue, D., Sue, D. W., Sue, D., & Sue, S. (2014). Essentials of understanding abnormal behavior (2nd ed.). Belmont, CA: Cengage Learning.
Swartz-Kulstad, J. L., & Martin, W. E. (1999). Impact of culture and context on psychosocial adaptation: The cultural and contextual guide process. Journal of Counseling & Development, 77, 281–293. doi:10.1002/j.1556-6676.1999.tb02451.x
Washburn, M. (2013). Five things social workers should know about the DSM-5. Social Work, 58, 373–376. doi:10.1093/sw/swt030
Whiteley, J. M. (1984). A historical perspective on the development of counseling psychology as a profession. In S. D. Brown & R. W. Lent (Eds.), Handbook of counseling psychology (pp. 3–55). New York, NY: Wiley and Sons.
Wood, A. M., Linley, P. A., Maltby, J., Kashdan, T. B., & Hurling, R. (2011). Using personal and psychological strengths leads to increases in well-being over time: A longitudinal study and the development of the strengths use questionnaire. Personality and Individual Differences, 50, 15–19. doi:10.1016/j.paid.2010.08.004
World Health Organization. (1979). International statistical classification of diseases and related health problems, clinical modification (9th rev.). Geneva, Switzerland: Author.
World Health Organization. (1992). International statistical classification of diseases and related health problems (10th rev.). Geneva, Switzerland: Author.
Wright, B. A., & Lopez, S. J. (2002). Widening the diagnostic focus: A case for including human strengths and environmental resources. In C. R. Snyder & S. J. Lopez (Eds.), Handbook of Positive Psychology (pp. 26–44). New York, NY: Oxford University Press.
Saundra M. Tomlinson-Clarke is an Associate Professor at Rutgers University. Colleen M. Georges is an Adjunct Professor at Rutgers University. Correspondence can be addressed to Saundra Tomlinson-Clarke, 10 Seminary Place, New Brunswick, NJ 08901-1183, saundra.tomlinson-clarke@gse.rutgers.edu.
Jul 1, 2014 | Article, Volume 4 - Issue 3
Let us start with two important disclaimers. First, I will be identifying the many ways that the Diagnostic and Statistical Manual of Mental Disorders (DSM) system has been detrimental to psychotherapy and how the fifth edition (DSM-5; American Psychiatric Association [APA], 2013) will make the current situation even worse. However, this does not mean that I consider DSM diagnosis irrelevant to psychotherapy and counseling, nor do I believe that psychotherapists and counselors should neglect learning about diagnosis. I do not trust therapists who focus their contact with the client exclusively around the DSM diagnosis. Hippocrates believed that it is more important to know the person who has the disease than the disease the person has. Nevertheless, I also do not trust therapists who are completely free-form, impressionistic and idiosyncratic in their approach to clients. DSM diagnosis is only a small part of what goes into therapy, but it is often a crucial part. We need to know what makes each person different and unique; on the other hand, we also need to group clients with similar problems as a way of choosing interventions and predicting the treatment course.
The second disclaimer relates to the proper roles of medication, psychotherapy and counseling. The DSM has promoted a reductionistic medicalization of mental illness that, in combination with misleading drug company marketing strategies, has created a strong bias toward treatment with medication and against treatment with psychotherapy and counseling. I am greatly disturbed by the resulting enormous overuse of psychotropic drugs among both adults and children, many of whom do not need psychotropic drugs and would do much better without them. However, we must be equally alert to the fact that many people who need medication do not receive it. Psychotherapists and counselors are important gatekeepers who should recognize when medication is needed and when it is not. It makes no sense to be for or against medicating clients. It is crucial that medication not be used carelessly, but also essential to realize that it is sometimes absolutely necessary.
I will offer a brief history. Before the publication of the DSM-III (APA) in 1980, psychiatric diagnosis was a subject of little interest or importance because it was unreliable and not particularly useful for treatment planning. The DSM-III marked a sudden and dramatic change—it made diagnosis a major focus of clinical attention and the starting point of all treatment guidelines. Its provision of clearly defined criteria allowed for reasonably reliable diagnosis and for targeting specific symptoms that became the focus of treatment. The DSM-III’s influence exceeded all expectations, in some ways useful, but also with a significant defect. The prevailing mental health approach before the DSM-III was the well-rounded biopsychosocial model. At that time, clinicians conceptualized symptoms as arising from the complex interplay of brain functioning, psychological factors, and familial and social contexts. Perhaps without intention, the DSM-III downgraded the psychological and social factors and promoted undue emphasis on the biological factors. The DSM-III was advertised as “atheoretical” and neutral, usable by practitioners of all professional orientations. To some small degree, this was true; yet the DSM-III’s emphasis on purely descriptive psychiatry strongly favored biological treatments over cognitive-behavioral treatments. This bias proved to be irrelevant and eventually destructive to family and psychodynamic therapies. The descriptive DSM-III method focused attention on surface symptoms in the individual and ignored both deeper psychological understanding and the social and familial contexts. Clinicians often adopted a symptom checklist approach to evaluation and forgot that a complete evaluation must account for psychological factors, social supports and stressors.
In addition to its considerable impact on the mental health profession, the DSM-III also significantly affected the pharmaceutical industry. Drug companies benefited greatly from the DSM-III approach, particularly since 1987 when Prozac established the template for promoting blockbuster psychiatric drugs. Pharma realized that the best way to sell pills is to promote disease-mongering. Their marketing campaign offers the misleading idea that mental disorders are underdiagnosed, easy to diagnose due to chemical imbalances in the brain and best treated with a pill. The marketing targeted psychiatrists first, then primary care physicians and, since 1997, the general public. In the United States and New Zealand, drug companies have successfully bullied the government into allowing direct advertising to consumers on television, in print and on the Internet. Use of medication has skyrocketed as a result of these billion-dollar marketing budgets, turning us into a pill-popping society. This increase in drug use is great for Pharma shareholders and executives, but often inappropriate for clients and terribly costly to the economy. More than $40 billion a year are spent on psychiatric drugs. Most of these (80%) are prescribed by primary care doctors with little training or interest in psychiatric diagnosis or treatment, while under strong pressure from patients and drug company representatives, and after only seven minutes of evaluation on average. During the last decade, many drug companies have received enormous fines (e.g., one fine was $3.3 billion) for illegal marketing practices, but they continue because the rewards are so great.
For mild to moderate psychiatric problems, psychotherapy and counseling are just as effective as medication, and their effects are much more enduring. Most people taking medication would probably have been better off had they received psychotherapy or counseling. Unfortunately, psychotherapy and counseling suffer from two great disadvantages in their competition with drug treatment. Drug companies are enormously profitable industrial giants with billion-dollar budgets to push their products. In contrast, the mental health field is more of a nickel-and-dime, mom-and-pop operation with absolutely no marketing punch. Insurance companies further tilt the playing field by consistently favoring medication management over psychotherapy and counseling based on the mistaken assumption that it will be cheaper. In fact, brief treatments are often much more cost-effective because their effects are lasting, whereas medication may be necessary for years or a lifetime.
The medicalization of mental illness has had a dire impact on our clients and our society. Twenty percent of the population regularly takes a psychiatric drug, many for problems of everyday life more amenable to watchful waiting or psychotherapy and counseling than to drug treatment. It is astounding that there are now more overdoses and deaths from prescription drugs than street drugs. The tremendous societal investment in psychiatric drugs also misallocates resources much better spent on terribly underfunded social investments. Would it not be better for children to have smaller classes and more gym periods than for so many of them to be on pills for ADHD?
In preparing the DSM-IV (APA, 1994), we attempted to hold the line against diagnostic inflation and the medicalization of normality; however, we failed. During the past 20 years, the United States has experienced fad epidemics of ADHD, autism and bipolar disorder. We were conservative in writing the DSM-IV, but failed to anticipate or prevent its careless misuse under external pressure, particularly drug company marketing and the requirement of a psychiatric diagnosis for clients to qualify for school services and disability benefits. The quick fix is to give a diagnosis, but often this does more harm than good in the long run. Inaccurate diagnoses are easy to give but hard to remove. Often they haunt the client for life with stigma, unnecessary treatments and reduced expectations. Making an accurate diagnosis requires really knowing one’s client, which may take weeks or even months. In uncertain situations, it is better to underdiagnose than overdiagnose a symptom pattern, and better to be safe than sorry.
The DSM-5 will considerably increase medicalization and may turn our current diagnostic inflation into hyperinflation. Overdiagnosis transforms normal grief into major depressive disorder, normal temper tantrums into disruptive mood dysregulation disorder, normal forgetfulness of old age into minor neurocognitive disorder, poor eating habits into binge eating disorder, and expectable worry about physical symptoms into somatic symptom disorder. It also further loosens the already far too slack criteria for attention deficit disorder and contains a completely confusing definition of autism. Experience teaches that whenever the diagnostic spigot is unrestricted, drug company revenues increase, and less funding is available to support psychotherapy and counseling visits.
The DSM is only one guide to diagnosis—it is not a bible or official manual of diagnosis. The DSM codes that clinicians routinely use for reimbursement are in fact all International Classification of Diseases, Clinical Modification (ICD-CM) codes that are available for free on the Internet. DSM-5 is one suggested way to arrive at an ICD-CM diagnosis, but it is not the only or best way. Other more reliable guides to psychiatric diagnosis are available. Therapists do not have to buy or use the DSM-5 unless they work for an institution that requires it.
Receiving a psychiatric diagnosis can be a turning point in a client’s life. An accurate diagnosis can lead to an effective treatment plan; an inaccurate diagnosis can lead to side effects, stigma, high costs, reduced opportunities and needless suffering. Severe and classic presentations require quick diagnosis and immediate intervention, usually including medication. Milder, equivocal presentations allow for and require a more cautious approach. Therefore, watchful waiting or brief counseling is usually best.
Conflict of Interest and Funding Disclosure
The author published two books that critically
review the DSM-5, titled Saving Normal and
Essentials of Psychiatric Diagnosis.
References
American Psychiatric Association. (1980). Diagnostic and statistical manual of mental disorders (3rd ed.). Washington, DC: Author.
American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
Jun 5, 2014 | Video Reviews
 In this 4-hour and 16-minute video, psychotherapist Otto Kernberg demonstrates Transference-Focused Psychotherapy (TFP) in three live sessions with a 40-year-old patient named Alfred (portrayed by an actor). TFP is an evidence-based treatment that is effective for individuals struggling with personality disorders. It is specifically helpful for individuals with borderline and narcissistic personality disorders, and focuses on treating the individual’s entire personality.
In this 4-hour and 16-minute video, psychotherapist Otto Kernberg demonstrates Transference-Focused Psychotherapy (TFP) in three live sessions with a 40-year-old patient named Alfred (portrayed by an actor). TFP is an evidence-based treatment that is effective for individuals struggling with personality disorders. It is specifically helpful for individuals with borderline and narcissistic personality disorders, and focuses on treating the individual’s entire personality.
Kernberg engages in TFP with Alfred, who suffers from a personality disorder. Using a psychodynamic TFP approach, Kernberg demonstrates how therapists can conduct treatment. From the TFP perspective, personality disorders develop due to dysfunction in early life as well as genetic factors. They can specifically occur due to insecure attachment to a caregiver, severe trauma and/or severe family pathology that is transmitted in the interaction between family members. TFP focuses on helping patients change their distorted perceptions of others, internalized messages, and self-image. Dr. Kernberg builds a relationship with Alfred to demonstrate how this can be accomplished in a therapeutic setting, by using transference analysis, interpretation, and technical neutrality.
For example, during the first session, Alfred becomes suspicious of Dr. Kernberg because he perceives him as taking the side of his previous therapist. Dr. Kernberg confronts the patient about his contradictory attitudes and reinforces the realistic side of Alfred’s statement. He also interprets Alfred’s desire to leave therapy as a fear of attack and betrayal by everyone, including the therapist.
In subsequent sessions, Kernberg responds to Alfred’s distorted views of his relationships, particularly with his ex-girlfriend. Kernberg intermittently interjects his commentary for the viewer throughout the sessions. He helps explain common symptoms of personality disorders and applies them directly to what transpires within each session. He also explains each session’s progress as well as the reasoning for his questions, which helps the viewer understand the theory and how to use it.
The video is supplemented with an instructor’s manual which offers valuable tips for making the best use of the video. The instructor’s manual contains a transcript of the sessions, which helps highlight key moments in the video. It also contains discussion questions that can be used to facilitate dialogue. For example, in session two, one of the discussion questions addresses the patient’s feelings of betrayal as follows: “What do you think of Kernberg’s straightforward way of interpreting Alfred’s avoidance of feelings of betrayal? How do you imagine different clients responding to this style? How does it match or differ from your own?” The instructor’s manual also contains suggestions for activities related to the video, such as a reaction paper and role-play exercise. The instructor’s manual is useful, but a little difficult to navigate.
This video seems appropriate for a relatively higher-level mental health professional or student. It offers a unique perspective on the therapeutic techniques of TFP. Unlike reading a textbook, watching this video gives the viewer a comprehensive understanding of the theory, effectively bringing it theory to life. The video could be a useful teaching tool for instructors and learning tool for students.
Reviewed by: Nicole Berry, Barry University.
Yalom, V. (2007). Psychoanalytic Psychotherapy with Otto Kernberg, MD [DVD]. Mill Valley, CA: Psychotherapy.net.
Available at http://www.psychotherapy.net
Jun 5, 2014 | Book Reviews
 Set against a backdrop of survival, Michael Bloom’s Thinking Like a Therapist provides readers with a different approach to the typical case study. The author follows a young couple through an immense tragedy and subsequent strife, inviting the reader on a journey through isolation and its effects on the couple’s relationship. In a unique conceptualization of a case study, the author juxtaposes scenes of the couple fighting for their lives with scenes of the couple in therapy sessions, as though they can magic themselves from the wilderness to the therapist’s office. Each chapter has three sections: journal entries narrating part of the couple’s adventures, a dialogue between the couple and the therapist, and a discussion of the therapist’s goals and interventions in the preceding therapy session. The book offers a new approach to discussing mental health therapy in a more entertaining fashion than typical counseling books.
Set against a backdrop of survival, Michael Bloom’s Thinking Like a Therapist provides readers with a different approach to the typical case study. The author follows a young couple through an immense tragedy and subsequent strife, inviting the reader on a journey through isolation and its effects on the couple’s relationship. In a unique conceptualization of a case study, the author juxtaposes scenes of the couple fighting for their lives with scenes of the couple in therapy sessions, as though they can magic themselves from the wilderness to the therapist’s office. Each chapter has three sections: journal entries narrating part of the couple’s adventures, a dialogue between the couple and the therapist, and a discussion of the therapist’s goals and interventions in the preceding therapy session. The book offers a new approach to discussing mental health therapy in a more entertaining fashion than typical counseling books.
What Bloom does exceptionally well is illuminate the inner workings of a therapist’s mind. He offers readers well-articulated insights into the mind of a highly competent therapist, which is an excellent learning tool for those studying the art of counseling. The therapist acts with intentionality, and Bloom clearly demonstrates the process of translating thought into action. Novice counselors will learn the importance of intentionality as well as the importance of implementing structure into counseling.
Readers unfamiliar with the counseling field will be introduced to what counseling looks like and how the process of change manifests itself outside sessions. Even though the events surrounding the young couple are extreme in nature, what surfaces during their excursion is highly relatable to anyone who has been in an intimate relationship. Among the many issues the couple work through are joint decision making, depression, differentiation, boundaries, jealousy, and sexual intimacy. Bloom describes the couple’s struggles and successes with the eye of a behavioral expert. Ultimately, all readers will find the implications of Bloom’s book realistic and applicable.
Reviewed by: Joseph M. Graham, Jr., doctoral student in counselor education, University of Central Florida, Orlando, FL.
Bloom, M. (2013). Thinking like a therapist: A novel overview of psychotherapy. Sioux Falls, SD: Cogitavi.
Jun 5, 2014 | Book Reviews
 In A Counselor’s Introduction to Neuroscience, the authors claim that “neurocounseling” is the fifth force in the history of psychology and counseling. Although a precise and detailed definition of neurocounseling is elusive (both in this book and in the professional literature), it is described as the marriage of counseling and neurobiology. They offer a crash course in brain anatomy, function and development in order to lay the groundwork for how neurocounseling can be used effectively with clients. Several chapters focus on the ways the brain is affected by certain mental disorders, and how specific counseling approaches address various brain regions and functions. The remainder of the book focuses on assessment of brain function and fictional cases to illustrate neurocounseling techniques. The chapters include numerous tables, figures, cases and opportunities to stop and reflect. The overall intent of the book is to arm counselors “with yet another highly effective and efficient way to help clients cope with (overcome, etc.) their personal psychological distress.”
In A Counselor’s Introduction to Neuroscience, the authors claim that “neurocounseling” is the fifth force in the history of psychology and counseling. Although a precise and detailed definition of neurocounseling is elusive (both in this book and in the professional literature), it is described as the marriage of counseling and neurobiology. They offer a crash course in brain anatomy, function and development in order to lay the groundwork for how neurocounseling can be used effectively with clients. Several chapters focus on the ways the brain is affected by certain mental disorders, and how specific counseling approaches address various brain regions and functions. The remainder of the book focuses on assessment of brain function and fictional cases to illustrate neurocounseling techniques. The chapters include numerous tables, figures, cases and opportunities to stop and reflect. The overall intent of the book is to arm counselors “with yet another highly effective and efficient way to help clients cope with (overcome, etc.) their personal psychological distress.”
Although the authors are clearly enamored with the interaction between neurobiology and counseling, they purposefully offer honest words of caution regarding the nascent and speculative nature of contemporary brain science. However, on occasion, they also make promising statements without citing scientific evidence and generalize results from animal studies (including rodents) to humans without offering their reasoning for doing so. As with any other resource, practitioners are responsible for weighing information and evaluating whether it is accurate and whether it will be helpful in their work. It is important to note that this book bills itself as an “introduction”—readers should not expect concrete or realistic examples of how professional counselors can use their new neuroscience knowledge to understand and enhance client functioning.
A Counselor’s Introduction to Neuroscience will help counselors begin to grapple with the implications of neuroscience for our profession. Although the neuroscience knowledge base that the authors provide is a good start, scientific rigor in terms of concrete application would be useful. Years from now, neurocounseling may well be a new force in counseling, but presenting it to the counseling community as an effective and efficient way to help clients today is premature. In the end, it is best to consider this book as a reasonable beginning and food for thought rather than a how-to guide for counselors seeking neurocounseling training. Hopefully in the ensuing years, there will be clearer guidance available to help professional counselors integrate neuroscience into their practice.
Reviewed by: Tara Smart and John Sommers-Flanagan, University of Montana.
McHenry, B., Sikorski, A. M., & McHenry, J. (2014). A counselor’s introduction to neuroscience. New York, NY: Routledge.
Available at http://www.routledge.com/books/details/9780415662284/
Apr 8, 2014 | International, Volume 4 - Issue 1
J. Scott Hinkle
Abstract: The World Health Organization (WHO) estimates that at least 450 million people worldwide live with unmet mental health problems. Additionally, one in four people will experience psychological distress and meet criteria for a diagnosable mental health disorder at some point in their lives. This data speaks to the need for accessible, effective and equitable global mental health care. Available mental health resources are inequitably distributed, with low- to middle-income countries showing significantly fewer mental health human resources than high-income countries. The need to proactively address this care-need gap has been identified by WHO and various national organizations, including NBCC International (NBCC-I). NBCC-I’s Mental Health Facilitator (MHF) program addresses the global need for community-based mental health training that can be adapted to reflect the social, cultural, economic and political climate of any population, nation or region.
Keywords: global, mental health, international, mental health facilitator, MHF, population, community, WHO
Pages 1–18
Developing and promoting mental health services at the grassroots level while also maintaining a global perspective is, to say the least, an overwhelming task. The National Board for Certified Counselors’ International division (NBCC-I) has responded to this task in two deliberate steps. Initially, NBCC-I collaborated with the World Health Organization’s (WHO) Department of Mental Health and Substance Abuse to establish the global Mental Health Facilitator (MHF) training program. The MHF program addresses the international need for population-based mental health training that can be adapted to reflect the social, cultural, economic and political realities of any country or region. Once the program was effectively addressed by WHO and NBCC-I as a viable strategy to reduce mental health issues on a global basis, NBCC-I independently developed a curriculum and implementation method that has begun to make a promising global impact (Hinkle, 2006, 2007, 2009, 2010a, 2010b, 2012a, 2012b, 2012c, 2013; Hinkle & Henderson, 2007; Hinkle & Schweiger, 2012; Schweiger & Hinkle, 2013).
For years the global burden of mental disorders on individuals, families, communities and health services has been considerably underestimated (Chisholm et al., 2000; Murray & López, 1996a, 1996b; Ustün & Sartorius, 1995). Resources for mental, neurological, and substance use disorders have been slow in development, insufficient, constrained, fragmented, inequitably distributed, and ineffectively implemented (Becker & Kleinman, 2013; Chen et al., 2004; Gulbenkian Global Mental Health Platform [GGMHP], 2013a; Hinkle & Saxena, 2006). While mental and neurological disorders comprise only 1% of deaths worldwide, they account for 8–28% of the disease burden (GGMHP, 2013a; Murray et al., 2012; Prince et al., 2007; WHO, 2004a), with the majority of these disorders occurring in low- to middle-income countries.
Mental Health: An International Problem
Most mental disorders are highly prevalent in all societies, remain largely undetected and untreated, and result in a substantial burden to families and communities. Although many mental disorders can be mitigated or are avoidable, they continue to be overlooked by the international community and produce significant economic and social hardship. Moreover, in all countries there is an enormous gap between the prevalence of mental disorders and the number of people receiving care (Becker & Kleinman, 2013; Saraceno et al., 2007; Weissman et al., 1994; Weissman et al., 1996; Weissman et al., 1997; WHO, 2010a, 2010b). In less-developed countries, more than 75% of persons with serious mental disorders do not receive treatment (Demyttenaere et al., 2004). Unfortunately, psychiatry’s best efforts at training physicians to provide mental health care within the global context are simply too small for such a large, global problem (Furtos, 2013; Hinkle, 2009, 2010b, 2012b, 2012c; Patel, 2013). The focus has been too long on medicine and not on local communities (Patel, 2013). In fact, every person’s health care is local (Unützer, 2013). The major issue with the current provision of care is, therefore, the limited size and training of the community health care workforce (Becker & Kleinman, 2013).
Globally, one in four people will experience psychological distress and meet criteria for a diagnosable mental disorder at some point in their lives (WHO, 2005). This ominous data speaks to the need for accessible, effective and socially equitable mental health care (Hinkle & Saxena, 2006). WHO estimates that more than 450 million people worldwide live with mental health problems; these numbers are no doubt bleak. More specifically, WHO estimates that globally more than 154 million people suffer from depression, 100 million are affected by alcohol use disorders, 25 million have schizophrenia, 15 million experience drug abuse, and nearly one million people die each year by suicide (Saraceno et al., 2007). Depending on the source, unipolar depression has been estimated to be in the top four causes of loss of disability-adjusted life years across the six socially diverse continents (Murray & López, 1996a, 1996b; Vos et al., 2012).
Furthermore, it has been estimated that as many as 25% of all primary care consultations have a mental health component (Goldberg & Huxley, 1992; Warner & Ford, 1998; WHO, 2006a). Mental disorders are related to a range of problems, from poverty, marginalization, and social disadvantage, to relationship issues such as divorce, physical conditions such as heart disease, reductions in economic productivity, and interruption of child and adolescent educational processes (see Alonso, Chatterji, He, & Kessler, 2013; Breslau et al., 2013). At the developmental level, at least 10% of children are considered to have mental health problems, but pediatricians and general medical practitioners are not typically equipped to provide effective treatment (Craft, 2005). With mental disorders contributing to an average of 20% of disabilities at the societal level, the evidence is clear that these disorders pose a major challenge to global health (Alonso, Chatterji, et al., 2013; Alonso, Petukhova, et al., 2013). Moreover, the associated economic burden exceeds that of the top four non-communicable diseases (i.e., diabetes, cardiovascular, respiratory and cancer; Bloom et al., 2011).
Unfortunately, most international mental health systems are dominated by custodial psychiatric hospitals that deplete resources for treatments with little efficacy (WHO, 2005). In contrast, governments and nongovernmental organizations (NGOs) should scale up services for community mental health with programs that reflect credible evidence of effectiveness (see Patel, 2013; Patel, Araya, et al., 2007). Murthy (2006) has indicated that there is no global community mental health blueprint to achieve universal mental health access, and that effective community workforce strategies need to be matched to each country’s unique situation. It is an ecological fallacy to try to understand people and mental health issues outside the environments in which they exist (Galea, 2013). Thus, a radical shift is urgently needed in the way mental disorders are managed, and this clearly includes community-based care that can be effectively implemented via non-health as well as health sectors (GGMHP, 2013a, 2013b; Hinkle, 2012b).
Global Community Mental Health
Serious mental disorders are generally associated with substantial role disability within the community. About 35–50% of mental health cases in developed countries and approximately 75–85% in less-developed countries have received no treatment in the 12 months preceding a clinical interview. Due to the high prevalence of mild and sub-threshold cases, the number of untreated cases is estimated to be even larger. These milder cases, which can be found in communities all over the world, require careful consideration because they are prone to progress to serious mental disorders (WHO, 2010a, 2010b; WHO World Mental Health Survey Consortium, 2004).
It is important to note that in most low- to middle-income countries, community workers are often the people’s first line of contact with the health care system (Anand & Bärnighausen, 2004; Hongoro & McPake, 2004). However, there is a long history of issues with the sustainability of community programs (Walt, 1988), and the lack of community service providers with the necessary competencies to address needs remains the most significant barrier to the provision of mental health services. Although human resources are the crucial core of health systems, they have been a neglected developmental component (Hongoro & McPake, 2004), particularly in the field of mental health. WHO’s “Mental Health Atlas” (2005) specifies a critical global shortage of mental health professionals (e.g., psychiatrists, psychiatric nurses, psychologists, social workers, neurologists). Similarly, an informal international survey of clinical mental health, school, and career and work counselors by NBCC-I indicated that the professional counselor workforce has yet to be adequately identified on a global scale (Hinkle, 2010b). Moreover, extant mental health services are inequitably distributed; lower-income countries, where behavioral risk factors tend to cluster among people of lower socioeconomic status, have significantly fewer mental health human resources than higher-income countries (Coups, Gaba, & Orleans, 2004; WHO, 2005; WHO World Mental Health Survey Consortium, 2004).
In low- to middle-income countries, human resources are clearly limited, and the quality and productivity of the existing workforce is often challenged. Investment in human resources for community mental health care is insufficient in absolute terms as well as in distribution (Hongoro & McPake, 2004). For instance, the global average for physicians is 170 per 100,000 people, but in Nepal and Papua New Guinea there have been as few as five doctors for this ratio (WHO, 2004a). In 2003, approximately 36% of doctors’ posts and 18% of nurses’ posts were unfilled around the world (Bach, 2004). Moreover, general practitioners are not typically adept at providing mental health care, including detection, referral and management of mental disorders (Chisholm et al., 2000). Therefore, partnerships between formal primary and informal community health care systems need to be more prevalent, effective and integrated.
Two facets for integrating mental health into primary care are (a) financial and human resources and (b) collaboration with non-health sectors. NGOs, community workers and volunteers can play a significant role in supporting formal primary care systems for mental health. For example, village health workers in Argentina, India and the Islamic Republic of Iran have been trained to identify and refer people for medical assistance. Even countries that have adequate services, like Australia, use local informal services to support mental health patients (see WHO, 2006b). Because psychiatric hospital beds are extremely limited, the demand for mental health services within communities becomes even more critical (Forchuk, Martin, Chan, & Jensen, 2005). Furthermore, early detection and treatment of mental disorders and co-occurring emotional and behavioral problems not only decreases the chance of lower physical health later in life, but also associated costly hospitalizations (Alonso, Chatterji, et al., 2013; Alonso, Petukhova, et al., 2013; Scott et al., 2013).
An urgent, radical change in the way mental disorders are managed and monitored—one that moves away from lengthy institutional hospitalizations and toward population-based mental health care in the community—is needed (GGMHP, 2013a, 2013b; Hinkle, 2009). The need to proactively address this care-need gap from a praxis, or practical, rather than a theoretical approach has been repeatedly identified by WHO and various national and international organizations, including NBCC-I (Hinkle & Schweiger, 2012). Communities in developing countries have historically lacked opportunities for mental health training, skill development, and capacity building (Abarquez & Murshed, 2004); however, long years of training are not necessary for learning how to provide fundamental help for people who are emotionally distressed.
Volunteer community workers are a large untapped community resource of potential service providers for people suffering from problems associated with mental health (Hoff, Hallisey, & Hoff, 2009). Chan (2010) has reported that “there is a widely shared but mistaken idea that improvements in mental health require sophisticated and expensive technologies and highly specialized staff. The reality is that most of the mental, neurological and substance use conditions that result in high morbidity and mortality can be managed by non-specialist health-care providers” (p. iii). The research has substantiated that it is feasible to deliver psychosocial-type interventions in non-specialized health care settings (WHO, 2010a, 2010b). Enhancing basic community mental health services, both informally and formally, is a viable way to assist the never-served. The MHF program is part of a grassroots implementation trend that has already begun in communities around the globe (e.g., Canada, Europe, Africa, Asia, United States; see Hinkle, 2007, 2013; Hoff, 1993; Hoff et al., 2009; Marks & Scott, 1990; McKee, Ferlie, & Hyde, 2008; Mosher & Burti, 1994; Patel, 2013; Rachlis & Kushner, 1994).
A Brief Review of Grassroots Community Mental Health Approaches
Unfortunately, governmental psychiatric hospitals have a long history of human rights violations and poor clinical outcomes (Hinkle, 2010b). They also are costly and consume a disproportionate amount of mental health care monies. In contrast, informal community caregivers are not generally part of the formal health care system; examples include traditional healers, professionals such as teachers, police and various community workers, NGOs, consumer and family associations, as well as laypeople. Informal care is typically accessible because it is an integral part of the community. However informal, this care should not replace the core of formal mental health service provision (Saraceno et al., 2007; WHO, 2010a, 2010b), but serve as a grassroots, adjunctive care system.
For example, beginning as early as 1963, the work of Rioch et al. portrayed community paraprofessionals serving as in- and out-patient “therapists.” Similarly, as far back as 50 years, Albee (1967) reported that the dearth of manpower in mental health services could be lessened by the use of paraprofessionals who could arrange for neighborhood outreach and basic psychiatric evaluations (Hines, 1970).
Likewise, in 1969 Vidaver suggested the development of mental health technicians with generalist skills for lateral and vertical mental health employment mobility. Vidaver (1969) further commented that community colleges were able to train local community helpers for a variety of informal roles in mental health services without years of higher education. Interviewing (i.e., communication), consultation, and community liaison techniques (i.e., referral) were depicted by Vidaver as important general skills for community helpers. One year later, Lynch and Gardner (1970) developed a training program with the goal of training laypeople to be “helpers in a psychiatric setting” (p. 1476), emphasizing communication skills training with a focus on the “front line of operation” (p. 1475) provided by paraprofessionals and professionals providing backup services.
Also in 1970, the U.S. military addressed mental health manpower shortages by increasing the use of paraprofessional specialists who were taught entry-level skills to help soldiers in need (Nolan & Cooke, 1970). Training included conducting interviews, collecting historical, situational and observational data, and developing referral skills to connect the soldier with professional mental health resources. Identifying common mental health problems and relating to problems in a realistic way were included in the training. Program evaluations indicated that trainees “quickly and confidently transpose their course-acquired skills to the job situation” (Nolan & Cooke, 1970, p. 79).
More recently, basic psychological first aid programs have been effective in Bangladesh, where psychosocial support is used in emergency situations (Kabir, 2011). As well, nurses and health care staff have been trained as mental health facilitators in the United Kingdom to recognize depression, anxiety, stress, drug and alcohol problems, grief reactions, and domestic violence; make referrals; and provide support and aftercare. These nurses also assist people with co-occurring disorders and provid mental health promotion in the schools. Furthermore, the nursing profession in the United Kingdom has noted that community mental health care is a particular problem area, resulting in the development of the mental health assistant practitioner as a creative practice strategy to reduce the costs of services as well as improve multi-professional communication based on local needs (Warner & Ford, 1998; Warne & McAndrew, 2004).
Although implementing such grassroots community mental health programs is not easy, global health care organizations have demonstrated greater need to develop innovative uses of informal mental health assistants and facilitators to establish community mental health services (Warne & McAndrew, 2004). In the long run, if the gap in mental health services is sufficiently closed, it must include the use of non-specialists to deliver care (Eaton, 2013; Eaton et al., 2011; Hinkle, 2006, 2009). Such non-specialized workers will have received novel training in identifying mental stress, distress and disorders; providing fundamental care; monitoring strategies; and making appropriate referrals (see Becker & Kleinman, 2013; Hinkle & Schweiger, 2012; Hinkle, Kutcher, & Chehil, 2006; Jorm, 2012; Saraceno et al., 2007).
The Mental Health Facilitator Training Program
Existing data speaks loudly to the need for accessible, effective and equitable global mental health care. However, a common barrier to mental health care is a lack of providers who have the necessary competencies to address basic community psychosocial needs. This barrier has been clearly identified by WHO and various national and international organizations, including NBCC-I (Eaton, 2013; Hinkle, 2006, 2009, 2012c; Hinkle & Saxena, 2006; Patel, 2013; WHO World Mental Health Survey Consortium, 2004; WHO, 2005, 2010a, 2010b).
General MHF Background Information and Rationale
In 2005, officers from NBCC-I met with the director of the WHO Department of Mental Health and Substance Abuse to discuss the challenges of international mental health care. As a result of these meetings, WHO selected 32 international mental health professionals to evaluate NBCC-I’s proposed MHF program, with almost 100% supporting its development. Subsequently, the curriculum and master training guide were completed by NBCC-I in 2007. Drafts of the curriculum and proposed teaching methods were piloted on two occasions in Mexico City with mental health professionals from Europe, the Caribbean, Africa and the United States. Additional subject matter experts facilitating pilot development included mental health professionals from Malaysia, Canada, Trinidad, St. Lucia, Turkey, India, Mexico, Botswana, Romania and Venezuela.
The resulting MHF training program draws on a variety of competencies derived from related disciplines, including but not limited to psychiatry, psychology, social work, psychiatric nursing, and counseling. Its eclectic programming and international composition allowed for a flexible training model with expertise drawn from global practices. Because MHF training is transdisciplinary, traditional professional helping silos are not reinforced; skills and competencies are linked instead to population-based mental health needs rather than professional ideologies. Thus, individuals with MHF training (MHFs) can effectively identify and meet community mental health needs in a standardized manner, regardless of where these needs are manifested and how they are interpreted. Mental health and the process of facilitating it is based on developing community relationships that promote a state of well-being, enabling individuals to realize their abilities, cope with the normal and less-than-normal stresses of life, work productively, and make a contribution to their communities.
The MHF training program was first taught in Lilongwe, Malawi in 2008 and has since been taught approximately 108 times by 435 trainers, including 181 master trainers in 20 countries. The MHF program recently expanded to provide mental health assistance in more established countries, as manifested in the program’s current popularity in the United States (Schweiger & Hinkle, 2013). This expansion also marks the completion of an educators’ edition of the MHF curriculum for use in schools with a focus on students, teachers and schooling.
To date, the MHF training program has been implemented globally to enhance mental health care at various levels. At the formal, primary health care level, general medical practitioners provide acute and long-term treatment to individuals with a variety of mental disorders, supplemented by the efforts of individuals with MHF training. MHFs also augment specialized services by functioning within a mental health care team to provide support, targeted assistance, referral and follow-up monitoring (Paredes, Schweiger, Hinkle, Kutcher, & Chehil, 2008). Likewise, informal community care is characterized by community members without formal mental health education or training providing much-needed services. At this level, nonclinical forms of mental health care such as psychological support or strategic problem solving by community leaders, family groups, and local elders (including indigenous healers) are emphasized. MHF training has been used to bridge the gap between formal and informal mental health care where MHFs work within both systems and do so simultaneously (Hinkle, Kutcher, & Chehil, 2006). With due respect to horizontal and vertical considerations, MHFs have augmented traditional, formal inpatient services by working with mental health teams to provide family support and education, monitor follow-ups, and provide practical “in the trenches” assistance (see Figure 1). This is where informal care, including self-care, becomes critical (Murthy, 2006).
Contextualizing the MHF Program
Most importantly, it is ill-advised to attempt to understand people outside their environments; people must be considered within the characteristics of their respective populations (Galea, 2013). The MHF program is designed to be flexible so local experts can modify components of the training to reflect the realities of their situation. Local stakeholders then identify and include specific competencies in their MHF trainings. As a consequence, consumers and policymakers ensure that MHF trainings provide culturally relevant services to the local population. Furthermore, the MHF training curriculum was conceived as a dynamic document and is revised once each year based on input from local institutions and individuals who provide MHF training. This contextual, organic approach grounds the MHF program in the principle that mental health care is a combination of both universally applicable and context-specific knowledge and skills (Furtos, 2013; Hinkle, 2012a; Paredes et al., 2008). The program consists of integrated knowledge ranging from basic mental health information and promotion to specific, local, culturally relevant helping strategies. The global MHF program
Figure 1. Modified WHO Pyramid Framework: MHF (Hinkle, 2013b)
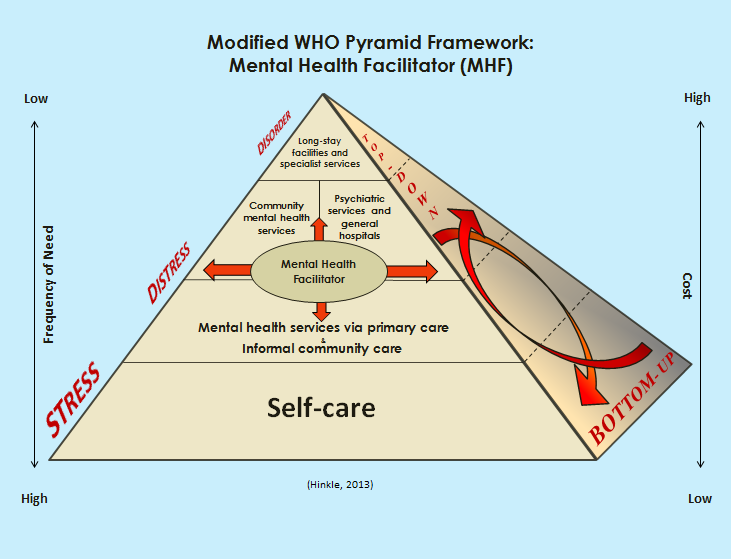
provides equitable access to quality first-contact interventions, including but not limited to mental health advocacy, helping skills, and monitoring and referral, all of which respect human dignity and rights, and meet local population needs.
Individuals receiving MHF training represent a broad cross section of the community. Diverse trainee backgrounds increase the possibility of addressing the various gaps in local mental health care, which helps local policy makers, service providers, NGOs and communities meet mental health needs without costly infrastructural investments. Moreover, contextualized MHF training facilitates further development and delivery of community-based care consistent with WHO recommendations for addressing the gap in global mental health services.
Bottom-Up vs. Top-Down Community Strategies
It is commonly known that top-down approaches across public services generally have limited success. Conversely, long-term strategies that enhance the successful implementation of public mental health services are best when they are centrally facilitated from a locally directed, bottom-up approach (Rock, Combrinck, & Groves, 2001). From both a service delivery and administrative perspective, a bottom-up strategy has its advantages. One obvious benefit is that it requires local stakeholders to articulate objective and verifiable goals that use a “common currency” (p. 44) or terminology (Rock et al., 2001).
Similarly, MHFs have the advantage of serving as community leaders developing “upstream” versus “downstream” care, as well as providing important links to professional mental health care (Hinkle, Kutcher, & Chehil, 2006; Hoff et al., 2009; McKinlay, 1990). MHFs working in communities apply primary prevention principles by anticipating mental health services for people who may be vulnerable. For instance, MHFs in Bhutan provide drop-in peer assistance for young people challenged by rapid changes in their society. When MHF services are available at the secondary prevention level, people with mental health issues can often avoid disruptive and costly hospitalization. MHFs can assist with reducing long-term disabling effects among people recovering from a mental disorder by applying tertiary prevention measures from the bottom up (Hinkle & Saxena, 2006; Hoff et al., 2009). Furthermore, governmental direction from the top needs to intersect with community efforts from the bottom (Isaac, 2013; see Figure 1); and once programs are vetted from the top, they need to be diverted to bottom-up management (Eaton, 2013).
Although community mental health programs may achieve local success, few have been systematically scaled up to serve the needs of national populations. Despite the array of treatments for mental health, little evidence exists regarding their feasibility and effectiveness when integrated into routine care settings among low- and middle-income countries. Even though bottom-up approaches offer advantages, they also require outcome measurements, something that mental health workers have found traditionally burdensome (Rock et al., 2001). For example, evidence-based mental health interventions for people exposed to conflict and other disasters are weak, especially for strategies implemented in the midst of emergencies (Patel, Araya, et al., 2007). Only a small fraction of the clinical research trials regarding mental health treatment have been administered in low-income countries, resulting in a dearth of knowledge about treatment effectiveness in poor, culturally diverse settings (Becker & Kleinmen, 2013). Consequently, the MHF process is currently undergoing an evaluation in two diverse countries on two separate continents to seek evidence for the effectiveness of this training program. This is a critical step in the program’s continued development, because empirical evaluation of lay health workers’ implementation of community mental health services in low- and middle-income countries has been historically insufficient (Lewin et al., 2005). However, if the global strategy is only to collect more information and add to data resources, there will continue to be a gap in human resources.
As planned, individuals seeking MHF training have represented a broad cross section of local society, ranging from school teachers and principals to business owners, clergy and neighborhood workers. MHF volunteers are also police officers, neighborhood workers, community leaders, NGO employees, elders and indigenous healers. In fact, such healers in Malawi, Africa have learned to apply their first-contact mental health skills to identify, assess, support and refer people in need of acute mental health care through the MHF program. This diversity of trainee backgrounds at the grassroots level increases possibilities for addressing as many gaps as possible in community mental health care. Indeed, grassroots efforts emanate from the ground level (Eaton, 2013; Hinkle, 2010b, 2012a; Hinkle & Schweiger, 2012; Schweiger & Hinkle, 2013).
The Global MHF Partnership
Partnerships among NGOs, governments, agencies and academia can make a difference in the mental health workforce capacity by integrating global expertise with local knowledge (Fricchione, Borba, Alem, Shibre, Carney, & Henderson, 2012; WHO, 2009). As countries recognize the dearth of community health services and attempt to develop fundamental services with a mental health focus, the MHF training program is appealing because of its emphasis at the “street” or “trenches” level (Hinkle, 2012a). This is a critical component of the MHF training program since local stakeholders always have more at stake in risk reduction and capacity building than agencies outside the local neighborhood, village or barrio (Abarquez & Murshed, 2004). For example, MHF training has benefited the people of Mexico City, who have had historically limited access to mental health services (Suck, Kleinberg, & Hinkle, 2013a).
The initial stage of the MHF training process identifies local partners who have the willingness and ability to increase local mental health care capacity. NBCC-I negotiates MHF training with partners such as educational institutions, government agencies, NGOs, private companies or other entities capable of managing a training. An ideal global partner has the capacity and ability to maintain the MHF program and promote continuing mental health education. NBCC-I and respective training partners identify master trainers who can train more trainers, ensuring a multiplier effect (NBCC-I, 2013). In countries where English is not a primary or spoken language, it is necessary to translate and adapt the MHF curriculum and materials. Thus far, MHF partnerships have resulted in the curriculum being translated into 10 languages:Arabic, Bahasa Malaysian, Bhutanese [Dzongka], Chinese, German, Greek, Japanese, Portuguese, Spanish and Swahili.
The MHF Curriculum: General Features
NBCC-I has responded to the care-need gap challenge, and developed and standardized the MHF curriculum drawing on a variety of competencies derived from related mental health disciplines within a cultural context. General, nonclinical, first-responder forms of community mental health care such as basic assessment, social support and referral are included in the MHF curriculum. Similar models that include assessment, advising, agreement on goals, interventions, support and follow-up have been used successfully in mental health care (Fiore et al., 2000; Hinkle, 2012b, 2012c; Whitlock, Orleans, Pender, & Allan, 2002). Currently there are MHFs on five continents, with new trainings being coordinated almost weekly. In developing the curriculum, an eclectic group of professional contributors allowed for a flexible training model with expertise drawn from various international practices. The training consists of 30 hours that can be taught on consecutive days, or divided into its 20 modules and taught over several weeks, depending on the needs of the local community (Hinkle & Henderson, 2007). As local stakeholders are identified and trained using the MHF curriculum, they become the foundation on which to build community mental health care.
The MHF training includes a certificate of completion for anyone successfully completing the program, and additional certificates of completion for trainers and master trainers. Trainers are required to hold a bachelor’s degree or its equivalent, and master trainers must have a master’s degree or its equivalent in a mental health–related discipline. One affirming by-product of the training is the identification of individuals who desire more training and education in mental health services. For example, the MHF program in Bhutan has led to specified substance abuse training in several communities, as well as two students seeking graduate studies in counseling in the United States.
Specific Features of the MHF Curriculum
The MHF curriculum is based on the universality of mental stress, distress and disorders (Desjarlais, Eisenberg, Good, & Kleinman, 1995; Hinkle & Henderson, 2007). MHF training includes numerous topics such as basic helping skills, coping with stress, and community mental health services. The program consists of fundamental, integrated mental health knowledge and skills ranging from community advocacy and commitment, to specified interventions such as suicide mitigation. Also included in the curriculum are segments on working with integrity and not providing services outside the limits of training and experience (Hinkle, 2010a; Reyes & Elhai, 2004). In general, MHFs are taught that negative and unhealthy assumptions about life and living contribute to additional mental and emotional stress (Browne & Winkelman, 2007; Feiring, Taska, & Chen, 2002; Sonne, 2012).
More specifically, the curriculum begins with a section on the benefits of investing in mental health, cost-effective interventions, impacts of mental disorders on families, barriers to mental health care, confidentiality and privacy, and the goals of the MHF program. Understanding perspectives regarding human feelings, effective nonverbal and verbal communication, and using questions effectively in the helping process also are covered in the curriculum, as well as how to assess problems, identify mental health issues, and provide support (Hinkle & Henderson, 2007). Making effective referrals is a crucial segment of the curriculum because this skill also serves the purpose of steering people to physicians for co-occurring physical disorders such as diabetes, heart disease and chronic pain (Gureje, 2013).
MHF trainees also learn how to effectively end a helping relationship—an essential skill taught to mental health workers for the past 40 years (Hines, 1970; Hinkle & Henderson, 2007). MHFs learn that the helping process involves joining with the person seeking assistance, identifying specific concerns, assessing the level of difficulty, surveying the possibilities, solving problems and making choices, and referring to more formal care where appropriate. This is accomplished within a simple framework emphasizing personal strengths and mitigation of significant stress.
Following the basic helping skills section of the curriculum, which emphasizes the age-old but important phenomena of human development and diversity, trainees concentrate on the abilities, needs and preferences that all people possess and how these are integrated in various cultures (Elder & Shanahan, 2007; Huston & Bentley, 2010; Lerner, 2007). A section on understanding various types of encountered problems introduces trainees to the concept of a balanced, less balanced, little balanced, or off balance mental health continuum, alongside how to solve problems and set goals with people experiencing difficulty coping with life (Hinkle & Henderson, 2007). Similarly, trainees learn about stress, distress and basic mental disorders including anxiety and post-traumatic stress disorder (PTSD), depression and mania, psychosis and schizophrenia, substance abuse and dependence, delirium and dementia, mental retardation (intellectual disability), chronic pain, and epilepsy. Child reactions to trauma (van Wesel, Boeije, Alisic, & Drost, 2012) and child maltreatment (Wekerle, 2011) also are covered in the MHF curriculum, which emphasizes helping children and adolescents in the least restrictive environment and as close to their communities as possible (Hinkle & Henderson, 2007).
Preventing suicide and effectively dealing with an actual suicide are two topics of relevance covered in MHF training. Suicide is a leading cause of death in low- and middle-income countries, especially among young people (WHO, 2006a). Self-poisoning using pesticides is common, with estimates of 300,000 of these deaths a year in the Asia-Pacific region alone (Patel, Araya, et al., 2007), validating the need for suicide’s inclusion in the curriculum.
In the 1990s, humanitarian organizations began to recognize the increased need for psychosocial support after various types of disasters (Barron, 2004; Wells, 2006). Disasters result in tremendous loss of property, resources and life. In addition, political, economic and social disruptions are common consequences that have mental health–related implications. Therefore, information about assisting individuals and families in the aftermath of disasters is included in the MHF curriculum (Hinkle & Henderson, 2007; Wells, 2006). The MHF training also emphasizes ways to assist with situations involving domestic violence, refugees, migrants and victims of human trafficking and war, as well as other unfortunate forms of crisis.
Stress-related disorders, as depicted in the MHF curriculum, go largely untreated in many areas of the world, especially when crises and disasters strike. It is all too often the scenario that an earthquake, typhoon, hurricane or human-made crisis has occurred, and limited or no mental health care services are available following the event. Attempts to provide assistance in the aftermath of these disasters have come from governmental responses, NGOs, and community and religious organizations, but it is important to note that even professional mental health workers receive cursory instruction in disaster interventions (Hinkle, 2010a). The need for greater mental health response services is apparent; MHFs from Lebanon to Liberia have assisted communities following civil war and refugee crises, and MHFs in China have assisted in the aftermath of a major earthquake using the basic mental health training they received from the MHF curriculum.
Regardless of their genesis, many mental health–related concerns are largely dependent on problem-solving abilities, a focus on cultural values regarding mental health functioning, and social and economic support (Hinkle et al., 2006; Hoff et al., 2009), all of which are addressed in the MHF curriculum. Studies from stress-related literature suggest that a fundamental problem-solving coping approach is generally associated with positive outcomes (Benight, 2012; Taylor & Stanton, 2007), whereas avoidant-related coping is associated with negative outcomes (Littleton, Horsley, John, & Nelson, 2007); thus the emphasis on problem-solving skills in the MHF curriculum.
Lastly, consulting with helping professionals during mental health emergencies and recognizing the importance of self-care when working in crisis situations also are part of the MHF curriculum. The curriculum culminates with the all-important local contextualizing of what trainees have learned during their MHF training (Hinkle & Henderson, 2007; Sonne, 2012).
Potential Limitations
Unfortunately, organizational, cultural, and professional concerns coinciding with the often ambiguous role and purpose of mental health care can beset the expanding use of community helpers and may have an unintended impact on role identities among the general health workforce (see Warne & McAndrew, 2004). Possibly complicating matters further, the MHF program is a set of concepts and skills, not a professional designation. One concern associated with the MHF program is therefore its potential for propagating invisibly and resulting in new worker roles that cause confusion within standardized health care. Although “the potential of the fully visible and verbal paraprofessional to effect changes in the delivery of psychiatric care is vast” (Lynch & Gardner, 1970, p. 1478), it could become problematic in some locations if MHFs are not strategically blended into community health services. It has long been known that without a viable, transparent strategy, the utilization of MHFs could make for strained relationships in places where the program is not fully vetted. Furthermore, organizational structures that are not flexible or willing to pursue institutional change and innovation may have more difficulty accepting the MHF program (Hinkle, 2012b). Therefore, local and global political and networking skills are critical to the MHF program’s sustainability.
Working conditions and available remuneration for community programs and workers raises several questions that will need to be addressed at some point (Hongoro & McPake, 2004). For instance, could municipalities and governments make MHF a job classification with an upwardly mobile career ladder within existing mental health services? Where financial incentives are not possible, could ad hoc benefits such as access to more training be feasible? How will MHF trainings be sustained in communities over time? Will volunteers be able to conduct the MHF program with limited resources? Additionally, for the program to be sustainable, trainers must have incentives to train more MHFs as community service providers. Without trainers teaching more programs, it is likely that a multiplier strategy will have limited success.
Another potential criticism of the MHF program is that the quality and safety of care could be compromised using community workers. However, the more critical point remains that providing basic assistance is much safer and salubrious than providing no care at all (see Hongoro & McPake, 2004). As in mental health nursing, supervision and mentoring of MHFs will at some point become an issue (Eaton, 2013; Warne & McAndrew, 2004). Furthermore, supportive supervisory relationships are important because supervisors are perceived as role models (Thigpen, 1979) in addition to providing needed guidance for informal community mental health workers.
Future MHF training strategies will need to incorporate continuing community educational development in mental health. Twinning or pairing universities in developing countries with those in less-developed countries is one method for increasing continuing education efforts. Distance learning can be an effective delivery method as well. However, twinning and distance education are all too often not core interests in developing nations, which tend to lack expertise in managing such partnerships (see Fricchione et al., 2012; Hongoro & McPake, 2004).
Conclusion
For the MHF program to proliferate, it will take not only training, education and implementation in often less than optimal working conditions, but also savvy negotiation of often poorly managed political systems that experience some level of corruption and inability to impact the universal stigma that plagues mental illness. To manage the program effectively, the global MHF strategy will need to continue to be accessible from the bottom up and maintain an uncomplicated implementation process. Patel (2013) has advocated that community mental health must be simplified, available where people live, locally contextualized, affordable and sustainable. The MHF program has met all of these criteria with the exception of sustainability, and only more time will tell the level of program longevity.
Advances in alleviating the costs of mental disorders have been limited and slow in coming (Becker & Kleinman, 2013). It is abundantly obvious that the challenges of unmet mental health needs negatively impact societies and economies around the globe. Becker and Kleinman (2013) have recently reported that “according to virtually any metric, grave concern is warranted with regard to the high global burden of mental disorders, the associated intransigent, unmet needs, and the unacceptable toll of human suffering” (p. 71). The burden of mental disorders at the social and individual level is comparable to that of physical disorders and substantially impacts the capital of all countries. Social factors are critical to the promotion and prevention of mental health (GGMHP, 2013b). Furthermore, children exposed to adult mental health disorders among their caregivers, as well as emotional psychological trauma, are predicted to have higher risks of mental disorders in adulthood, further compounding the problem (Chatterji, He, & Alonso, 2013; Patel, Araya, et al., 2007; Patel, Flisher, Hetrick, & McGorry, 2007). WHO (2010a, 2010b) has recommended bridging the care-need gap; however, this will not occur while services are embedded in professional silos rather than being population-centered (Chatterji & Alonso, 2013; Hinkle, 2012c).
The need to address workforce issues affects the quality and quantity of international mental health services (Warne & McAndrew, 2004); there is a clear link between human resources and population health. Community and family caregiving for mental disorders, often uncompensated, has a “tremendous value from a public health perspective by way of offsetting the costs and services of expensive and critically shorthanded healthcare professionals” (Viana et al., 2013, p. 134). At the American Psychiatric Association’s annual convention in 2013, Galea reported that the social aspects of mental health are not a sideshow, but at the very core and not being paid attention to. Unfortunately, not even the laudable efforts of the WHO or United Nations have been able to bring countries that are in desperate need of basic mental health care together effectively. Sadly, psychiatry alone cannot do enough in the global context; world mental health is a social issue (Galea, 2013) and much larger than any one profession (Furtos, 2013). This reality underscores the need for urgent development of grassroots community mental health programs.
For over 40 years, community mental health workers have known that a key component of any program’s design is its ability to be flexible (see Lynch & Gardner, 1970). Flexibility allows for the modification and contextualization of programs by local leaders to reflect realities of current social contexts and circumstances (Furtos, 2013; Rock et al., 2001). As aforementioned, this approach grounds the MHF program on the principle that mental health care is a combination of basic, universally applicable and context-specific knowledge and skills. Supportive social networks in the community result in less need for expensive professional treatments and hospitalizations (Forchuk et al., 2005). Moreover, grassroots approaches will aid global attempts at deinstitutionalization.
Governments of low-income countries are constrained by a lack of resources. In fact, in 85% of low-income countries, essential psychotropic medications are not available (Becker & Kleinman, 2013); monies for mental health care are disproportionately lacking even though their associated burden is tremendous (WHO, 2004a). Wider horizontal approaches to global community health care have been successful in the management of childhood illness (Gwatkin, 2004) and can likewise be successful in general mental health care. Furthermore, the benefits of essential psychotropic medications can be greatly enhanced by adjunctive psychosocial treatments including population-based models of mental health care (Patel, Araya, et al., 2007; Patel, Flisher, et al., 2007).
In summary, the MHF program is making an impact from Bhutan to Berlin and from Botswana to Bulgaria. Its training process provides equitable access to first-responder interventions including mental health promotion, advocacy, monitoring and referral, and the implementation of community MHF training furthers the development and delivery of community-based care consistent with WHO’s recommendations for addressing global mental health needs. The population-based, transdisciplinary MHF training model provides countries with a workable human resource development strategy to effectively and equitably bridge the mental health need-care service gap, one country at a time.
Conflict of Interest and Funding Disclosure
The author reported no conflict of interest or funding contributions for the development of this manuscript.
References
Abarquez, I., & Murshed, Z. (2004). Field practitioner’s handbook. Bangkok, Thailand: Asian Disaster Preparedness Center.
Albee, G. W. (1967). The relationship of conceptual models to manpower needs. In E. L. Cowen, E. Gardner, & M. Zax (Eds.), Emergent approaches to mental health problems (pp. 63–73). New York, NY: Appleton-Century-Crofts.
Alonso, J., Chatterji, S., He, Y., & Kessler, R. C. (2013). Burdens of mental disorders: The approach of the World Mental Health (WMH) surveys. In J. Alonso, S. Chatterji, & Y. He (Eds.), The burdens of mental disorders: Global perspectives from the WHO World Mental Health surveys (pp. 1–6). Cambridge, United Kingdom: Cambridge University Press.
Alonso, J., Petukhova, M. V., Vilagut, G., Bromet, E. J., Hinkov, H., Karam, E. G.,…Stein, D. J. (2013). Days totally out of role associated with common mental and physical disorders. In J. Alonso, S. Chatterji, & Y. He (Eds.), The burdens of mental disorders: Global perspectives from the WHO World Mental Health surveys (pp. 137–148). Cambridge, United Kingdom: Cambridge University Press.
Anand, S., & Bärnighausen, T. (2004). Human resources and health outcomes: Cross-country econometric study. The Lancet, 364, 1603–1609.
Bach, S. (2004). Migration patterns of physicians and nurses: Still the same story? Bulletin of the World Health Organization, 82, 624–625.
Barron, R. A. (2004). International disaster mental health. Psychiatric Clinics of North America, 27, 505–519.
Becker, A. E., & Kleinman, A. (2013). Mental health and the global agenda. New England Journal of Medicine, 369, 66–73.
Benight, C. C. (2012). Understanding human adaptation to traumatic stress exposure: Beyond the medical model. Psychological Trauma: Theory, Research, Practice, and Policy, 4, 1–8.
Bloom, D. E., Cafiero, E. T., Jané-Llopis, E., Abrahams-Gesse, S., Bloom, L. R., Fathima, S., … Weiss, A. (2011). The Global Economic Burden of Non-communicable Diseases. Geneva, Switzerland: World Economic Forum.
Breslau, J., Lee, S., Tsang, A., Lane, M. C., Aguilar-Gaxiola, S., Alonso., J.,…Williams, D. R. (2013). Associations between mental disorders and early termination of education. In J. Alonso, S. Chatterji, & Y. He (Eds.), The burdens of mental disorders: Global perspectives from the WHO World Mental Health surveys (pp. 56–65). Cambridge, United Kingdom: Cambridge University Press.
Browne, C., & Winkleman, C. (2007). The effect of childhood trauma on later psychological adjustment. Journal of Interpersonal Violence, 22, 684–697.
Chan, M. (2010). Foreword. In mhGAP intervention guide for mental, neurological and substance use disorders in non-specialized health settings (p. iii). Geneva, Switzerland: World Health Organization.
Chatterji, S., He, Y., & Alonso, J. (2013). Conclusions and future directions. In J. Alonso, S. Chatterji, & Y. He (Eds.), The burdens of mental disorders: Global perspectives from the WHO World Mental Health surveys (pp. 244–247). Cambridge, United Kingdom: Cambridge University Press.
Chen, L., Evans, T., Anand, S., Boufford, J. I., Brown, H., Chowdhury, M.,…Wibulpolprasert, S. (2004). Human resources for health: Overcoming the crisis. The Lancet, 364, 1984–1990.
Chisholm, D., James, S., Sekar, K., Kumar, K. K., Murthy, S., Saeed, K., & Mubbashar, M. (2000). Integration of mental health care into primary care. The British Journal of Psychiatry, 176, 581–588.
Coups, E. J., Gaba, A., & Orleans, T. (2004). Physician screening for multiple behavioral health risk factors. American Journal of Preventive Medicine, 27, 34–41.
Craft, A. (2005). What are the priorities for child health in 2004? Child: Care, Health and Development, 31, 1–2.
Demyttenaere, K., Brufferts, R., Posada-Villa, J., Gasquet, I., Kovess, V., Lepine, J. P.,… Chatterji, S. (2004). Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization Mental Health Surveys. Journal of the American Medical Association, 291, 2581–2590.
Desjarlais, R., Eisenberg, L., Good, B., & Kleinman, A. (1995). World mental health. Oxford, United Kingdom: Oxford University Press.
Eaton, J. (2013, October). Document two. In J. de Almeida (Chair), Innovation in deinstitutionalization: A WHO expert survey. Symposium conducted at the International Forum on Innovation in Mental Health, Gulbenkian Global Mental Health Platform, Lisbon, Portugal.
Eaton, J., McCay, L., Semrau, M., Chatterjee, S., Baingana, F., Araya, R.,… & Saxena, S. (2011). Scale up of services for mental health in low-income and middle-income countries, The Lancet, 378, 1592–1603.
Elder, G. H., & Shanahan, M. J. (2007). The life course and human development. In R. M. Lerner & W. Damon (Eds.), Handbook of child psychology. (Vol. 1, pp. 665–715). Hoboken, NJ: John Wiley & Sons.
Feiring, C., Taska, L., & Chen, K. (2002). Trying to understand why horrible things happen: Attribution, shame, and symptom development following sexual abuse. Child Maltreatment, 7, 25–39.
Fiore, M. C., Bailey, W. C., Cohen, S. J., Dorfman, S. F., Goldstein, M. G., Gritz, E. R., …Wewers, M. E. (2000). Treating tobacco dependence and use: Clinical practice guideline. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service.
Forchuk, C., Martin, M. L., Chan, Y. L., & Jensen, E. (2005). Therapeutic relationships: From psychiatric hospital to community. Journal of Psychiatric and Mental Health Nursing, 12, 556–564.
Fricchione, G. L., Borba, C. P. C., Alem, A., Shibre, T., Carney, J. R., & Henderson, D. C. (2012). Capacity building in global mental health: Professional training. Harvard Review of Psychiatry, 20, 47–57.
Furtos, J. (2013, May). Globalization and mental health: The weight of the world, the size of the sky. Presidential symposium conducted at the American Psychiatric Association Annual Meeting, San Francisco, CA.
Galea, S. (2013, May). Re-emerging research around the social and economic production of mental health: Toward a comprehensive model of mental health. Presidential symposium conducted at the American Psychiatric Association Annual Meeting, San Francisco, CA.
Goldberg, D., & Huxley, P. (1992). Common mental disorders: A bio-social model. London, England: Routledge.
Gulbenkian Global Mental Health Platform. (2013a). Integrating mental and physical health, promoting social inclusion, humanizing mental health care. Retrieved from http://www.gulbenkianmhplatform.com/
Gulbenkian Global Mental Health Platform. (2013b). International forum on innovation in mental health. Lisbon, Portugal: Author.
Gureje, O. (2013, October). Document one. In B. Saraceno (Chair), Integrating the response to mental disorders and other chronic diseases in health care systems. Symposium conducted at the International Forum on Innovation in Mental Health, Gulbenkian Global Mental Health Platform, Lisbon, Portugal.
Gwatkin, D. R. (2004). Integrating the management of childhood illness. The Lancet, 364, 1557–1558.
Hines, L. (1970). A nonprofessional discusses her role in mental health. American Journal of Psychiatry, 126, 1467–1472.
Hinkle, J. S. (2006, October). MHF town meeting: Ideas/questions. Presentation at the NBCC Global Mental Health Conference: Focus on the Never Served, New Delhi, India.
Hinkle, J. S. (2007, June). The mental health facilitator training: Ongoing developments. Presentation at the 12th International Counseling Conference, Shanghai, China.
Hinkle, J. S. (2009, July). Mental health facilitation: The challenge and a strategy. Keynote address at the Association for Multicultural Counseling and Development/Association for Counselor Education and Supervision 2nd Annual Conference on Culturally Competent Disaster Response, Gabarone, Botswana.
Hinkle, J. S. (2010a). International disaster counseling: Today’s reflections, tomorrow’s needs. In J. Webber & J. B. Mascari (Eds.), Terrorism, trauma, and tragedies: A counselor’s guide to preparing and responding (3rd ed., pp. 179–184). Alexandria, VA: American Counseling Association.
Hinkle, J. S. (2010b, August). Mental health facilitation: A global challenge and workable strategy. Manuscript presented at the 18th Asian Pacific Education Counseling Association Biennial Conference-Workshop, Penang, Malaysia.
Hinkle, J. S. (2012a, September). The Mental Health Facilitator program: Optimizing global emotional health one country at a time. Retrieved from http://www.revistaenfoquehumanistico.com/#!Scott Hinkle/c1lbz
Hinkle, J. S. (2012b, May). Mental health facilitation: A global strategy. Manuscript presented at the Asian Pacific Educational Counseling Association Conference, Tokyo, Japan.
Hinkle, J. S. (2012c, October). Population-based mental health facilitation (MHF): A strategy that works. Manuscript presented at the Seventh World Conference on the Promotion of Mental Health and the Prevention of Mental and Behavioural Disorders, Perth, Australia.
Hinkle, J. S. (2013a, February). Population-based mental health facilitation (MHF): Community empowerment and a vision that works. Manuscript presented at the North Carolina Counseling Association 2013 Conference, Greensboro, NC.
Hinkle, J. S. (2013b, November). La salud mental en e mundo. Presentation at the Old Dominion University Counseling Institute, Buenos Aires, Argentina.
Hinkle, J. S., & Henderson, D. (2007). Mental health facilitation. Greensboro, NC: NBCC-I.
Hinkle, J. S., Kutcher, S. P., & Chehil, S. (2006, October). Mental health facilitator: Curriculum development. Presentation at the NBCC International Global Mental Health Congress, New Delhi, India.
Hinkle, J. S., & Saxena, S. (2006, October). ATLAS: Mapping international mental health care. Presentation at the NBCC International Global Mental Health Congress, New Delhi, India.
Hinkle, J. S., & Schweiger, W. (2012, September). Mental health facilitation around the world. Manuscript presented at HOLAS Second Counseling Conference of the Americas, Buenos Aires, Argentina.
Hoff, L. A. (1993). Review essay: Health policy and the plight of the mentally ill. Psychiatry, 56, 400–419.
Hoff, L. A., Hallisey B. J., & Hoff, M. (2009). People in crisis: Clinical and diversity perspectives (6th ed.). New York, NY: Routledge.
Hongoro, C., & McPake, B. (2004). How to bridge the gap in human resources for health. The Lancet, 364, 1451–1456.
Huston, A. C., & Bentley, A. C. (2010). Human development in societal context. Annual Review of Psychology, 61, 411–437.
Isaac, M. (2013, October). Document two. In J. de Almeida (Chair), Innovation in deinstitutionalization: A WHO expert survey. Symposium conducted at the International Forum on Innovation in Mental Health, Gulbenkian Global Mental Health Platform, Lisbon, Portugal.
Jorm, A. F. (2012). Mental health literacy: Empowering the community to take action for better mental health. American Psychologist, 67, 231–243.
Kabir, B. (2011, January–May). Compassionate and dignified emergency health service delivery in Bangladesh. Asian Disaster Management News, 17(1), 4–6.
Lerner, R. M. (2007). Developmental science, developmental systems, and contemporary theories of human development. In R. M. Lerner & W. Damon (Eds.), Handbook of child psychology (Vol. 1, pp. 1–17). Hoboken, NJ: John Wiley & Sons.
Lewin, S. A., Dick, J., Pond, P., Zwarenstein, M., Aja, G., Van Wyk, B.,…Patrick, M. (2005). Lay health workers in primary and community health care. The Cochrane Database of Systematic Reviews, 2005(1), CD004015.
Littleton, H. L., Horsley, S., John, S., & Nelson, D. V. (2007). Trauma coping strategies and psychological distress: A meta-analysis. Journal of Traumatic Stress, 20, 977–988.
Lynch, M., & Gardner, E. A. (1970). Some issues raised in the training of paraprofessional personnel as clinic therapists. American Journal of Psychiatry, 126, 1473–1479.
Marks, I., & Scott, R. (Eds.). (1990). Mental health care delivery, impediments and implementation. Cambridge, United Kingdom: Cambridge University Press.
McKee, L., Ferlie, E., & Hyde, P. (2008). Organizing and reorganizing: Power and change in health care organizations. Houndmills, Bastingstoke, Hampshire, United Kingdom: Palgrave MacMillan.
McKinlay, J. B. (1990). A case for refocusing upstream: The political economy of illness. In P. Conrad & R. Kern (Eds.), The sociology of health and illness: Critical perspectives (3rd ed., pp. 502–516). New York, NY: St. Martin’s Press.
Mosher, L. R., & Burti, L. (1994). Community mental health: A practical guide. New York, NY: W. W. Norton.
Murray, C. J. L., & López, A. D. (1996a). Evidence-based health policy: Lessons from the Global Burden of Disease study, Science, 274, 740–743.
Murray, C. J. L., & López, A. D. (1996b). The global burden of diseases: A comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. Boston, MA: Harvard School of Public Health, WHO and World Bank.
Murray, C. J. L., Vos, T., Lozano, R., Naghavi, M., Flaxman, A. D., Michaud, M.,…Andrews, K. G. (2012). Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. The Lancet, 380, 2197–2223.
Murthy, R. S. (Ed.). (2006). Mental health by the “people.” Peoples Action for Mental Health, Bangalore, India.
National Board for Certified Counselors-International. (2013). Mental health facilitator (MHF). Retrieved from http://www.nbccinternational.org/What_we_do/MHF
Nolan, K. J., & Cooke, E. T. (1970). The training and utilization of the mental health paraprofessional within the military: The social work/psychology specialist. American Journal of Psychiatry, 127, 74–79.
Paredes, D., Schweiger, W., Hinkle, S., Kutcher, S., & Chehil, S. (2008). The mental health facilitator program: An approach to meet global mental health care needs, Orientacion Psychologica, 3, 73–80.
Patel, V. (2013, October). Integrating mental health care in priority health programs: Addressing a grand challenge in global mental health. Manuscript presented at the International Forum on Innovation in Mental Health, Gulbenkian Global Mental Health Platform, Lisbon, Portugal.
Patel, V., Araya, R., Chatterjee, S., Chisholom, D., Cohen, A., DeSilva, M.,…Van Ommeren, M. (2007). Treatment and prevention of mental disorders in low-income and middle-income countries. The Lancet, 370, 991–1005.
Patel, V., Flisher, A. J., Hetrick, S., & McGorry, P. (2007). Mental health of young people: A global public-health challenge. The Lancet, 369, 1302–1313.
Prince, M., Patel, V., Saxena, S., Maj, M., Maselko, J., Phillips, M. R., & Rahman, A. (2007). No health without mental health. The Lancet, 370, 859–877.
Rachlis, M., & Kushner, C. (1994). Strong medicine: How to save Canada’s health care system. New York, NY: HarperCollins.
Reyes, G., & Elhai, J. D. (2004). Psychosocial interventions in the early phases of disasters. Psychotherapy: Theory, Research, Practice, Training, 41, 399–411.
Rioch, M. J., Elkes, C., Flint, A. A., Usdansky, B. S., Newman, R. G., & Silber, E. (1963). National institute of mental health pilot study in training mental health counselors. American Journal of Orthopsychiatry, 33, 678–689.
Rock, D., Combrinck, J., & Groves, A. (2001). Issues associated with the implementation of routine outcome measures in public mental health services. Australasian Psychiatry, 9, 43–46.
Saraceno, B., van Ommeren, M., Batniji, R., Cohen, A., Gureje, O., Mahoney, J.,…Underhill, C. (2007). Barriers to improvement of mental health services in low-income and middle-income countries. The Lancet, 370, 1164–1174.
Schweiger, W. K., & Hinkle, J. S. (2013, October). The Mental Health Facilitator (MHF): A program to meet diverse international and domestic needs. Presentation at the 2013 Association for Counselor Educators and Supervisors Conference, Denver, CO.
Scott, K. M., Wu, B., Saunders, K., Benjet, C., He, Y., Lépine, J.-P.,…Von Korff, M. (2013). Early-onset mental disorders and their links to chronic physical conditions in adulthood. In J. Alonso, S. Chatterji, & Y. He (Eds.), The burdens of mental disorders: Global perspectives from the WHO World Mental Health surveys (pp. 87–96). Cambridge, United Kingdom: Cambridge University Press.
Sonne, J. L. (2012). PsychEssentials: A pocket resource for mental health practitioners. Washington, DC: American Psychological Association.
Suck, A. T., Kleinberg, E., & Hinkle, J. S. (2013). Counseling in Mexico. In T. H. Hohenshil, N. E. Amundson, & S. G. Niles (Eds.), Counseling around the world: An international handbook (pp. 315–322). Alexandria, VA: American Counseling Association.
Taylor, S., & Stanton, A. L. (2007). Coping resource, coping processes, and mental health. Annual Review of Clinical Psychology, 3, 377–401. doi:10.1146/annurev.clinpsy.3.022806.091.520
Thigpen, J. D. (1979). Perceptional differences in the supervision of paraprofessional mental health workers. Community Mental Health Journal, 15, 139–148.
Unützer, J. (2013, October). Document one. In B. Saraceno (Chair), Integrating the response to mental disorders and other chronic diseases in health care systems. Symposium conducted at the International Forum on Innovation in Mental Health, Gulbenkian Global Mental Health Platform, Lisbon, Portugal.
Ustün, T. B., & Sartorius, N. (Eds.). (1995). Mental illness in general health care: An international study. Chichester, England: John Wiley and Sons.
van Wesel, F., Boeije, H., Alisic, E., & Drost, S. (2012). I’ll be working my way back: A qualitative synthesis on the trauma experience of children. Psychological Trauma: Theory, Research, Practice, and Policy, 4, 516–526.
Viana, M. C., Gruber, M. J., Shahly, V., de Jonge, P., He, Y., Hinkov, H., & Kessler, R. C. (2013). Family burden associated with mental and physical disorders. In J. Alonso, S. Chatterji, & Y. He (Eds.), The burdens of mental disorders: Global perspectives from the WHO World Mental Health surveys (pp. 122–135). Cambridge, United Kingdom: Cambridge University Press.
Vidaver, R. M. (1969). The mental health technician: Maryland’s design for a new health career. American Journal of Psychiatry, 125, 1013–1023.
Vos, T., Flaxman, A. D., Naghavi, M., Lozano, R., Michaud, C., Ezzati, M.,…Murray, C. J. L. (2012). Years lied with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: A systemic analysis for the Global Burden of Disease Study 2010. The Lancet, 380, 2163–2196.
Walt, G. (1988). Community health workers: Policy and practice in national programmes. London, England: London School of Hygiene and Tropical Medicine, EPC publication number 16.
Warne, T., & McAndrew, S. (2004). The mental health assistant practitioner: An oxymoron. Journal of Psychiatric and Mental Health Nursing, 11, 179–184.
Warner, L., & Ford, R. (1998, October). Mental health facilitators in primary care. Nursing Standard, 13, 36–40.
Weissman, M. M., Bland, R. C., Canino, G. J., Faravelli, C., Greenwald, S., Hwu, H. G.,…Yeh, E. K. (1994). The cross national epidemiology of obsessive compulsive disorder. Journal of Clinical Psychiatry, 55, 5–10.
Weissman, M. M., Bland, R. C., Canino, G. J., Faravelli, C., Greenwald, S., Hwu, H. G.,…Yeh, E. K. (1997). The cross-national epidemiology of panic disorder. Archives of General Psychiatry, 54, 305.
Weissman, M. M., Bland, R., Canino, G., Greenwald, S., Lee, C., Newman, S.,…Wickramaratne, P. J. (1996). The cross-national epidemiology of social phobia: A preliminary report. International Clinical Psychopharmacology, 11, Suppl: 3, 9–14.
Wekerle, C. (2011). Emotionally maltreated: The under-current of impairment? Child Abuse & Neglect, 35, 899–903. doi:10.1016/j.chiabu.2011.09.002
Wells, M. E. (2006). Psychotherapy for families in the aftermath of a disaster. Journal of Clinical Psychology: In Session, 62, 1017–1027.
Whitlock, E. P., Orleans, C. T., Pender, N., & Allan, J. (2002). Evaluating primary care behavioral counseling interventions: An evidenced-based approach. American Journal of Preventive Medicine, 22, 267–284.
WHO World Mental Health Survey Consortium. (2004). Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization world mental health surveys. Journal of the American Medical Association, 291, 2581–2590.
World Health Organization (2004a). Atlas: Country resources for neurological disorders. Geneva, Switzerland: Author.
World Health Organization. (2005). Mental health atlas. Geneva, Switzerland: Author.
World Health Organization. (2006a). Integrating mental health into primary care: A global perspective. Geneva, Switzerland: Author.
World Health Organization. (2006b). Preventing suicide: A resource for counsellors. Geneva, Switzerland: Author.
World Health Organization. (2009). Scaling up nursing & medical education: Report on the WHO/PEPFAR planning meeting on scaling up nursing and medical education. Geneva, Switzerland: Author.
World Health Organization. (2010a). Mental health and development: Targeting people with mental health conditions as a vulnerable group. Geneva, Switzerland: Author.
World Health Organization. (2010b). mhGAP intervention guide for mental, neurological and substance use disorders in non-specialized health settings. Geneva, Switzerland: Author.
Dr. J. Scott Hinkle is the Director of Professional Development at NBCC-I. For further information on the MHF program, please contact Adriana Petrini at petrini@nbcc.org. The author appreciates editorial contributions from Laura Jones, Katherine Clark, Ryan Vale, Traci Collins, Allison Jones, and Keith Jones. A version of this article was originally presented at the World Mental Health Congress, August 28, 2013, Buenos Aires, Argentina (Spanish: “Facilitación de Salud Mental (MHF): Una Estrategia Comunal”). Correspondence can be addressed to J. Scott Hinkle, NBCC, 3 Terrace Way, Greensboro, NC 27403, hinkle@nbcc.org.
Apr 7, 2014 | Author Videos, Volume 4 - Issue 1
Thomas A. Field
Abstract: Based on emerging findings from neuroscience, the counseling professional can consider a different approach to research-informed practice, by integrating left- and right-brain processing in client care. This new model is commensurate with counseling’s historical lineage of valuing the counseling relationship as the core ingredient of effective counseling.
Keywords: counseling, neuroscience, evidence-based, effectiveness, right-hemisphere, intuition
During the past decade, the field of counseling has considered the notion of identifying effective counseling practices. In 2005, the American Counseling Association’s (ACA) Code of Ethics included a recommendation to use therapies that “have an empirical or scientific foundation” (C.6.e). The Journal of Counseling & Development introduced a new journal feature in 2007, entitled “Best Practices.” In 2009, the Council for the Accreditation of Counseling and Related Educational Programs (CACREP) modified their Standards for addiction counseling (I.3., p. 22), clinical mental health counseling (I.3., p. 34), and marriage, couple, and family counseling (I.3., p. 39) to require that the student “knows evidence-based treatments” (EBTs; p. 5). In the September 2012 edition of Counseling Today, Dr. Bradley Erford, the current ACA President, asserted the following in his monthly column:
If professional counselors use the best available research-based approaches to help clients and students, then counselor effectiveness, client satisfaction and third-party insurer satisfaction all improve. When professional counselors provide effective services, it also helps our professional advocacy and lobbying efforts with federal, state, and local politicians and bureaucrats, and leads to more counseling jobs and higher pay scales.(p. 5)
Erford argues that counselors must use research to inform practice—the public, insurance companies, and clients demand it. Yet until recently, only one approach to research-informed practice has been available to the counseling profession—namely the EBT movement that originated in the field of psychology. Many techniques and theories exist outside of the EBT movement, in addition to other models for best practices such as the common factors movement (Duncan, Miller, Wampold, & Hubble, 2010). Counselors may feel confused about which model to follow. An approach to research-informed practice that is more commensurate with the counseling profession’s values and identity is the application of research evidence from neuroscience to inform counseling interventions.
Current Direction: The Left-Brain Pathway
The left side of the brain is responsible for rational, logical, and abstract cognition and conscious knowledge. Neuroscientists such as Allan Schore (2012) have suggested that activities associated with the left hemisphere (LH) currently dominate mental health services. This is evidenced by the current reliance upon psychopharmacology over counseling services, the manualization of counseling, a reductionist and idealistic view of “evidence-based practice,” and a lack of respect for the counseling relationship in client outcomes despite a large body of evidence. McGilchrist (2009) takes this argument further: if left unchecked, the modern world will increase its reliance upon the LH compared to the than right hemisphere (RH), with disastrous consequences. A “left-brain world” would lead to increased bureaucracy, a focus on quantity and efficiency over quality, and a valuing of technology over human interaction, and uniformity over individualization. While this dystopia has not been fully realized yet, one could argue that the field’s current reductionist and cookie-cutter approach to mental health services and reliance on quantitative over qualitative research all point in one direction.
To understand the importance of the association between the LH and the current mental health system, the author reviews the history of the counseling effectiveness movement, along with the counseling profession’s gradual adherence to this left-brain movement.
The History of “Effectiveness”
It is hard to know when the term effectiveness was first used in counseling circles. A long history of competition exists between different theoretical schools that sought to find evidence for the efficacy of their theory and discredit (or at least, disprove) all pretenders. Eventually, in 1995, the American Psychological Association (APA) defined effectiveness by identifying counseling interventions that were considered to have adequate research support (Task Force for Promotion and Dissemination of Psychological Procedures, 1995). The criteria for delineation were narrow: at least two randomized controlled studies or multiple pre-and post- individual studies, and the existence of a treatment manual. This model of efficacy was based on the Federal Drug Administration’s (FDA) criteria for what constituted acceptable research evidence for a new medication’s efficacy. The field of psychology was concerned at the time about medications being considered the “first line of treatment” for mental disorders instead of counseling and psychotherapy, thus wanting to provide empirical evidence for counseling efficacy that could be used for political and financial leverage in the marketplace (LaRoche & Christopher, 2009). Various terms were used for this movement: psychological treatments, empirically validated treatments, empirically supported treatments, and EBT. This movement soon became synonymous with the definition of effectiveness in counseling and psychotherapy.
Criticisms abounded throughout the mental health services community. It became apparent that these interventions were difficult to implement, or else that practitioners were resistant (Becker, Stice, Shaw, & Woda, 2009). Criticisms focused on the inadequate representation of certain demographic and minority groups, the disregard for the predominance of co-occurring disorders within client populations, the exclusionary definition of “research evidence,” and the lack of consideration for clinical expertise and judgment (Bernal & Scharró-del-Rio, 2001; LaRoche & Christopher, 2009).
Training programs in the mental health services field have also been resistant to training students in EBTs. Weissman et al. (2006) found that only 28.1% of psychiatry preparation programs and 9.8% of social work preparation programs required both didactic instruction and clinical supervision in EBT use. In clinical psychology preparation programs, 16.5% (PhD) and 11.5% (PsyD) required didactic instruction and clinical supervision in EBTs. This is a low rate, considering that the inclusion of training in psychological treatments is required for APA doctoral program accreditation (Chambless, 1999). No data are currently available on the percentage of counselor education programs that require both didactic instruction and clinical supervision in EBT use. However, one could argue that the 2009 CACREP Standards mandate instruction and supervision in the use of EBTs. If counselors do not find another path, counselor education may adhere to the training model of psychology, requiring a greater emphasis on teaching techniques rather than relational skills, and inflexibly following standards of practice rather than individualized instruction. Counselor education may become a left-brain discipline.
Counseling Approaches and the Left-Brain
Counselors are already using EBTs in practice settings. Field, Farnsworth, and Nielsen (2011) conducted a small unpublished national pilot study in the use of EBTs by National Certified Counselors (NCCs; n = 76). Demographics were consistent with the most recent demographical survey of NCCs (National Board of Certified Counselors, 2000). The majority of participants reported utilizing EBTs within the past year (69.4%), and the number of EBTs utilized was surprisingly high (M = 9.17, SD = 6.94, SEM = 0.97) for those who utilized EBTs. Furthermore, of those who used EBTs, only 6% (n = 3) did not report using a form of cognitive-behavioral therapy (CBT). Although this was a small pilot study, and thus results cannot be wholly generalized to the counselor population, initial findings seem to indicate that EBT utilization may be practically synonymous with CBT utilization. This is alarming, since research has shown that when psychotherapies are directly compared to one another, studies in which CBT is claimed to be more beneficial than other treatments subsequently achieved comparative outcomes (e.g., Wampold, Minami, Baskin, & Tierney, 2002). The apparent “fit” between CBT and the EBT movement can be elucidated when considering that following a manualized protocol and using conscious verbal analysis (CBT) are both LH functions, and studies have found a link between CBT and activation in the dorsolateral prefrontal cortex of the LH (Siegle, Steinhauer, Friedman, Thompson, & Thase, 2011). Put simply, CBT activates the LH, and the EBT movement values LH over RH processing.
It could be argued that the emergence of the EBT movement has propelled CBT into first place among interventions used in practice settings. Structured interventions that can be easily manualized and measured such as CBT seem to correspond with strict and rigid guidelines for empiricism compared to therapies that are more abstract and unstructured (e.g., humanistic-existential and relational forms of counseling). The dominance of CBT may only solidify following the initiation of EBT training within graduate programs. Yet even Aaron T. Beck, the founder of cognitive therapy, asserted that “you can’t do cognitive therapy from a manual any more than you can do surgery from a manual” (Carey, 2004, p. F06). In other words, the purely LH approach of rigidly following a treatment manual is not sufficient for effective counseling practice.
The Right-Brain Pathway
The right side of the brain is associated with unconscious social and emotional learning, and includes intuition, empathy, creativity, and flexibility. Some may argue that counseling has always been associated with RH processes (J. Presbury, personal communication, November 25, 2012). There are signs that the field of counseling is moving toward the valuing of RH processes during interventions, evidenced by the empirical respect attributed to the therapeutic relationship (e.g., Magnavita, 2006; Norcross & Wampold, 2011; Orlinsky, Ronnestad, & Willutzki, 2004), and the admission that EBTs are unsuccessful if applied rigidly. The APA Task Force on Evidence-Based Practice (2006) intoned that “sensitivity and flexibility in the administration of therapeutic interventions produces better outcomes than rigid application of…principles” (p. 278). A purely LH counseling approach may be overly rigid, problematic since counselor rigidity has been found to impair the counselor-client relationship (Ackerman & Hilsenroth, 2001).
Clinical Judgment vs. Intuition
In 2006, the APA issued a new definition of evidence-based practice, derived largely from the definition provided in 2001 by the Institute of Medicine (APA, 2006). Evidence-based practice was redefined as consisting of three elements: research evidence, clinical judgment, and client contextual variables (APA, 2006; Institute of Medicine, 2001). Yet the APA’s revised definition of evidence-based practice still privileged LH processing. Whereas clinical judgment can be defined as the application of rational and analytical reasoning when working with clients (LH function), clinical intuition can be described as the attunement to unconscious and implicit knowledge when working with clients, and has been associated with activation in areas of the RH (Bolte & Goschke, 2005). Often difficult to articulate, intuition has been commonly described as “the unthought known,” a “gut feeling,” and “a working hypothesis” (Bollas, 1987). Lieberman (2000) defined clinical intuition as “the subjective experience associated with the use of knowledge gained through implicit learning” (p. 109). It is now known that effective counseling requires both conscious reasoning and unconscious intuition—in other words, the integration of the LH and RH of the brain. As the famous attachment theorist John Bowlby (1991) once wrote, “clearly the best therapy is done by the therapist who is naturally intuitive and also guided by the appropriate theory” (p. 16).
Studies on counselor development have found that experienced counselors tend to rely more on intuition than manualized protocols (Rønnestad & Skovolt, 2003; Stoltenberg, McNeill, & Delworth, 1998). As any experienced practitioner can attest, counselors tend to learn intuitive skills such as timing and word choice with experience. Welling (2005) wrote, “no therapist can reasonably deny following hunches, experiencing sudden insights, choosing directions without really knowing why, or having uncanny feelings that turn out to be of great importance for therapy” (p. 19). Volz and von Cramon (2008) concluded that the counselor’s intuition is often reliable and accurate during the counseling process. The difference between novice and experienced counselors can be understood as a difference in amount of accumulated experiences from prior client encounters within the unconscious, which informs intuitive clinical judgments (Schore, 2012). Less-experienced counselors are prone to make more inaccurate intuitive clinical decisions given their lesser clinical experience and, therefore, their less sculpted unconscious intuition.
Creativity vs. Replication
Creativity in the counseling process allows clinicians to individualize treatment, and consider the client’s contextual values during decision making (APA, 2006). This is the third part of the APA’s definition of evidence-based practice. Creativity has also been associated with the RH (Grabner, Fink, & Neubauer, 2007), and occurs when counselors are attuned to implicit memories. Creativity occurs when counselors trust their unconscious, where novel ideas are generated, based on environmental cues. Creativity is typically an emergent and unconscious process, unfolding in the immediacy of the counseling room. Counselors often cannot fully prepare for what the client brings to the session. Every session therefore requires some degree of creativity by the counselor, whose flexible response to the interpersonal contact with the client is crucial to establishing a deep and sustained therapeutic bond. For this reason, there is no existing evidence-based protocol for nonverbal body language or affective response by the counselor; these behaviors and responses are highly individualized and contextual, and thus cannot be manualized. Without creativity, the counselor is reduced to the role of technician, administering treatments in a consistent yet rote and rigid manner. The manualization of counseling naturally limits the creative process and RH processing for both counselor and client. While studies are needed, it is possible that a rigid LH approach to the counseling process would restrict rather than enhance the creative capacities of counselor and client, and neglect the client’s natural problem-solving ability (Bohart & Tallman, 2010).
To take a purely LH approach to counseling is to negate the importance of unconscious intuition and clinical experience in counselor effectiveness. Shrinking clinical expertise to merely conscious decision making is reductionist and misses a large body of evidence suggesting that unconscious information also guides clinical decisions. It is entirely possible that many clinical decisions are based more on RH than LH processes. For example, some counselors have experienced moments with clients when they instinctively know the diagnosis or what problem a client is experiencing, without formally checking off symptoms from diagnostic criteria. Counselor educators and supervisors can help trainees to hone unconscious intuition by asking questions such as the following: What is your gut feeling about this client? What prior clinical experiences may have led you to that conclusion? What unconscious decisions have you made that you were satisfied with? What unconscious information are you ignoring or suppressing.
The Centrality of the Counseling Relationship
The importance of RH processing extends to the counseling relationship, which is considered to have a central role in client outcomes. In 2001, the APA formed a Task Force on Evidence-Based Therapy Relationships, concluding in 2011 that the counseling relationship was central to client outcomes to an equivalent or greater extent as the treatment method, and “efforts to promulgate best practices or evidence-based practices (EBPs) without including the relationship are seriously incomplete and potentially misleading” (Norcross & Wampold, 2011, p. 98). Fifty years of research support the centrality of the counseling relationship in client outcomes (Orlinsky et al., 2004). Magnavita (2006) concluded, “the quality of the therapeutic relationship is probably the most robust aspect of therapeutic outcome” (p. 888). By the end of the 1990s, counseling was beginning to move toward a two-person interpersonal model in place of a one-person intrapersonal model for conceptualizing client problems and planning treatment (Cozolino, 2010). Some have argued that identifying and utilizing specialized treatments for certain disorders is therefore misleading, since research studies have consistently found that the “confounding variable” of the therapeutic relationship is the primary factor for counseling efficacy (Norcross & Wampold, 2011).
During counselor-client interactions, the level of intersubjective attunement and engagement strongly influences the quality of this interpersonal contact. As Bromberg (2006) wrote, when counselors try to “know” their clients instead of “understand” their clients through their engagement in the shared intersubjective field of the here and now, “an act of recognition (not understanding) takes place in which words and thoughts come to symbolize experience instead of substitute for it” (p. 11). When this moment of meeting occurs, the client can safely contact, describe, and regulate inner experience. During the client’s heightened emotional states, the counselor can model healthy emotional regulation for the client. This secure holding environment enables clients to experience and cope with their own dysregulated emotions and thus serves as a corrective emotional experience. Because the LH is specialized to manage “ordinary and familiar circumstances” while the RH is specialized to manage emotional arousal and interpersonal interactions (MacNeilage, Rogers, & Vallortigara, 2009), many if not most counseling interventions enhance RH processing for both counselor and client.
Neuroscience supports the integration of both the LH and RH in interactions between counselor and client. The counseling relationship is informed by linguistic content and auditory input (LH function), in addition to visual-facial input, tactile input, proprioceptive input (the body’s movement in space), nonverbal gestures, and body language (RH function). Whereas the LH is involved in conscious processing of language, the RH is responsible for a large amount of social and emotional behavior that occurs during the counseling relationship, such as the moment of contact between counselor and client (Stern, 2004), attention to the external environment (Raz, 2004), empathic resonance of both linguistic content and nonverbal behavior (Keenan, Rubio, Racipoppi, Johnson, & Barnacz, 2005), mental creativity (Asari, Konishi, Jimura, Chikazoe, Nakamura, & Miyashita, 2008), social learning (Cozolino, 2010), emotional words (Kuchinke, Jacobs, Võ, Conrad, Grubich, & Herrmann, 2006), and emotional arousal (MacNeilage et al., 2009). Clearly, all of these RH functions are crucial to the development of a strong counseling relationship. One cannot establish an effective counseling relationship by merely attending to verbal content (LH); a strong counseling relationship requires the integration of both LH and RH processes. Approximately 60% of communication is nonverbal (Burgoon, 1985), which is a RH function (Benowitz, Bear, Rosenthal, Mesulam, Zaidel, & Sperry, 1983). Since so much of counseling is nonverbal and unspoken, yet “known” to the counselor, the practice can be better understood as a communication cure rather than a talking cure (Schore, 2012).
Proposed Direction: Integration of Left- and Right-Brain Pathways
A balance needs to be struck between the extreme polarities of creative vs. structured and repetitive approaches, individualization vs. fidelity to manuals, flexibility vs. rigidity, unconscious vs. conscious, emotions vs. cognitions, and RH vs. LH. Radical adherence to either polarity is less effective. At one polarity, fidelity to a structured, rigid, conscious, LH-activating manualized treatment would lack the flexibility and individualization necessary to establish a strong counseling relationship. At the other extreme, fidelity to a purely spontaneous, flexible, unconscious and RH-activating individualized approach would result in the impossibility of research evidence and thus be unproven. This has been a criticism of some theoretical approaches, such as psychoanalysis (Modell, 2012). Counselors can avoid rigidly following treatment manuals, and avoid completely spontaneous approaches that lack research evidence. According to emerging evidence from neuroscience, an integrated approach to client care seems necessary for effective counseling practice (Schore, 2012). The RH and LH seem equally important to human functioning and survival. These often function in tandem with one another. For example, both hemispheres are integral to problem solving; the RH generates solutions, while the LH decides on a single solution to best fit a problem (Cozolino, 2010).
Conclusion
Counseling effectiveness requires the integration of both right- and left-brain processing. Effective counseling is determined not only by what the counselor does or says; it is determined also by the quality of the counselor’s interaction with the client (Bromberg, 2006). In a two-person relational system, the interaction between counselor and client is at the core of effective counseling. The neuroscience literature suggests that hemispheric processing for both counselor and client is bidirectional. The counselor’s RH-to-RH attunement to the client’s subjective experience in the here-and-now encounter of the counseling room informs unconscious intuition and creativity for both counselor and client.
The counselor develops an implicit understanding of the client’s inner world and generates clinical intuitions that guide the counselor’s decision making. The client is provided with a RH-to-RH holding environment from which deep emotions and sectioned-off past experiences can be explored, and creativity is sparked by the need to respond to the uniqueness of the counseling environment. In cases when clients seem to benefit from interventions that target LH processing, the counselor’s often intuitive and unconscious adjustment is a result of the RH-to-RH interaction between counselor and client. Integrating LH interventions may provide a helpful structure to address client problems and facilitate RH processing when the counselor and client both expect change to occur and demonstrate belief in the chosen intervention, which further strengthens the therapeutic bond (Frank & Frank, 1991).
Prior to incorporating a manualized protocol, counselors can therefore establish rapport and attend to the therapeutic alliance and counseling relationship. This attention to RH processing provides a foundation from which the structure of a LH-activating, manualized treatment can be provided, thus mitigating potential ruptures to the therapeutic relationship that occur when counselors abruptly or rigidly apply treatment manuals in a rote fashion. In this manner, both LH and RH processing is enhanced, which is crucial to successful counseling outcomes.
Taking such an approach would integrate the left and right brain in counselor practice. By incorporating research evidence from neuroscience, counselors have a new model for research-informed counseling practice that fits the historical lineage of prizing the counseling relationship as the core ingredient in therapeutic change. While it is not easy to value both structure and spontaneity, or uniformity and individuality, achieving this balance will result in practice behaviors that are more commensurate with the counseling profession’s values and identity.
Conflict of Interest and Funding Disclosure
The author reported no conflict of interest or funding contributions for the development of this manuscript.
References
Ackerman, S. J., & Hilsenroth, M. J. (2001). A review of therapist characteristics and techniques negatively impacting the therapeutic alliance. Psychotherapy, 38, 171–185. doi: 10.1037/0033-3204.38.2.171
American Counseling Association. (2005). ACA code of ethics. Alexandria, VA: Author.
American Psychological Association Presidential Task Force on Evidence-Based Practice. (2006). Evidence-based practice in psychology. The American Psychologist, 61, 271–285.
Asari, T., Konishi, S., Jimura, K., Chikazoe, J., Nakamura, N., & Miyashita, Y. (2008). Right temporopolar activation associated with unique perception. NeuroImage, 41, 145–152. doi: 10.1016/j.pscychresns.2010.01.002
Carey, B. (2004, June 8). Pills or talk? If you’re confused, no wonder. The New York Times. Retrieved from http://www.nytimes.com/2004/06/08/health/pills-or-talk-if-you-re-confused-no-wonder.html?pagewanted=2
Becker, C. B., Stice, E., Shaw, H., & Woda, S. (2009). Use of empirically supported interventions for psychopathology: Can the participatory approach move us beyond the research-to-practice gap? Behaviour Research and Therapy, 47, 265–274. doi: 10.1016/j.brat.2009.02.007
Benowitz, L. I., Bear, D. M., Rosenthal, R., Mesulam, M-M., Zaidel, E., & Sperry, R. W. (1983). Hemispheric specialization in nonverbal communication. Cortex, 19, 5–11.
Bernal, G., & Scharró-del-Rio, M. R. (2001). Are empirically supported treatments valid for ethnic minorities? Toward an alternative approach for treatment research. Cultural Diversity and Ethnic Minority Psychology, 7, 328–342. doi: 10.1037/1099-9809.7.4.328
Bohart, A. C., & Tallman, K. (2010). Clients: The neglected common factor of psychotherapy. In B. L. Duncan, S. D. Miller, B. E. Wampold, & M. A. Hubble (Eds.), The heart & soul of change: Delivering what works in therapy (2nd ed.). Washington, DC: American Psychological Association.
Bollas, C. (1987). The shadow of the object: Psychoanalysis of the unthought known. New York, NY: Columbia University Press.
Bolte, A., & Goschke, T. (2005). On the speed of intuition: Intuitive judgments of semantic coherence under different response deadlines. Memory & Cognition, 33, 1248–1255. doi: 10.3758/BF03193226
Bowlby, J. (1991, Autumn). The role of the psychotherapist’s personal resources in the therapeutic situation. Tavistock Gazette.
Bromberg, P. M. (2006). Awakening the dreamer: Clinical journeys. Mahwah, NJ: Analytic Press.
Burgoon, J. K. (1985). Nonverbal signals. In M. L. Knapp & C. R. Miller (Eds.), Handbook of interpersonal communication (pp. 344–390). Thousand Oaks, CA: Sage.
Chambless, D. L. (1999). Empirically supported treatments—What now? Applied Preventative Psychology, 8, 281–284. doi: 10.1016/S0962-1849(05)80043-5
Council for Accreditation of Counseling and Related Educational Programs. 2009 Standards. Retrieved from http://www.cacrep.org
Cozolino, L. (2010). The neuroscience of psychotherapy: Healing the social brain (2nd ed.). New York, NY: Norton.
Duncan, B. L., Miller, S. D., Wampold, B. E,. & Hubble, M. A. (Eds.). (2010). The heart and soul of change: Delivering what works in therapy (2nd ed.). Washington, DC: American Psychological Association.
Erford, B. T. (2012, September). Where’s the beef?! Counseling Today, 55(3), 5.
Field, T. A., Farnsworth, E. B., & Nielsen, S. K. (2011). Do counselors use evidenced-based treatments? Results from a national pilot survey. Unpublished manuscript.
Frank, J. D., & Frank, J. B. (1991). Persuasion and healing: A comparative study of psychotherapy. Baltimore, MD: Johns Hopkins Press.
Grabner, R. H., Fink, A., & Neubauer, A. C. (2007). Brain correlates of self-related originality of ideas: Evidence from event-related power and phase-locking changes in the EEG. Behavioral Neuroscience, 121, 224–230. doi: 10.1037/0735-7044.121.1.224
Institute of Medicine. (2001). Crossing the quality chasm: The new health system for the 21st century. Washington, DC: National Academy of Sciences.
Keenan, J. P., Rubio, J., Racioppi, C., Johnson, A., & Barnacz, A. (2005). The right hemisphere and the dark side of consciousness. Cortex, 41, 695–704. doi: 10.1016/S0010-9452(08)70286-7
Kuchinke, L., Jacobs, A. M., Võ, M. L.-H., Conrad, M., Grubich, C., & Herrmann, M. (2006). Modulation of prefrontal cortex activation by emotional words in recognition memory. NeuroReport, 17, 1037–1041. doi: 10.1097/01.wnr.0000221838.27879.fe
La Roche, M. J., & Christopher, M. S. (2009). Changing paradigms from empirically supported treatment to evidence-based practice: A cultural perspective. Professional Psychology: Research and Practice, 40(4), 396–402. doi: 10.1037/a0015240
Lieberman, M. D. (2000). Intuition: A social neuroscience approach. Psychological Bulletin, 126, 109–137. doi: 10.1037/0033-2909.126.1.109
MacNeilage, P. F., Rogers, L., & Vallortigara, G. (2009, June). Origins of the left and right brain. Scientific American, 301, 160–167.
Magnavita, J. J. (2006). In search of the unifying principles of psychotherapy: Conceptual, empirical, and clinical convergence. American Psychologist, 61, 882–892. doi: 10.1037/0003-066X.61.8.882
McGilchrist, I. (2009). The master and his emissary. New Haven, CT: Yale University Press.
Modell, A. H. (2012). Science confirms psychoanalytic theory: Commentary on Howard Shrevin’s paper. Psychoanalytic Review, 99, 511–551.
National Board of Certified Counselors. (2000). Gracefully aging at NBCC. The National Certified Counselor, 17(1), 1–2.
Norcross, J. C., & Wampold, B. E. (2011). Evidence-based therapy relationships: Research conclusions and clinical practices. Psychotherapy, 48(1), 98-102. doi: 10.1037/a0022161
Orlinsky, D. E., Ronnestad, M. H., & Willutzki, U. (2004). Fifty years of psychotherapy process-outcome research: Continuity and change. In M. J. Lambert (Ed.), Handbook of psychotherapy and behavior change (5th ed.). New York, NY: Wiley.
Raz, A. (2004). Anatomy of attentional networks. Anatomical Records, 281B, 21–36.
Rønnestad, M. H., & Skovolt, T. M. (2003). The journey of the counselor and therapist: Research findings and perspectives on professional development. Journal of Career Development, 30(1), 5–44. doi: 10.1023/A:1025173508081
Schore, A. N. (2012). The science of the art of psychotherapy. New York, NY: Norton.
Siegle, G. J., Steinhauer, S. R., Friedman, E. S., Thompson, W. S., & Thase, M. E. (2011). Remission prognosis for cognitive therapy for recurrent depression using the pupil: Utility and neural correlates. Biological Psychiatry, 69, 726–733.
Stern, D. N. (2004). The present moment in psychotherapy and everyday life. New York: Norton.
Stoltenberg, C. D., McNeill, B. W., & Delworth, U. (1998). IDM: An integrated developmental model for supervising counselors and therapists. San Francisco, CA: Jossey-Bass.
Task Force on Promotion and Dissemination of Psychological Procedures. (1995). Training in and dissemination of empirically supported treatments: Report and recommendations. Clinical Psychologist, 48(1), 2–23.
Volz, K. G., & von Cramon, D. Y. (2008). Cortical regions activated by the subjective sense of perceptual coherence of environmental sounds: A proposal for the neuroscience of intuition. Cognitive Affective & Behavioral Neuroscience, 18, 2077–2087. doi: 10.3758/CABN.8.3.318
Wampold, B. E., Minami, T., Baskin, T. W., & Tierney, S. C. (2002). A meta-(re)analysis of the effects of cognitive therapy versus “other therapies” for depression. Journal of Affective Disorders, 68, 159–165.
Weissman, M. M., Verdeli, H., Gameroff, M. J., Bledsoe, S. E., Betts, K., . . . & Wickramaratne, P. (2006). National survey of psychotherapy training in psychiatry, psychology and social work. Archives of General Psychiatry, 63, 925–934.
Welling, H. (2005). The intuitive process: The case of psychotherapy. Journal of Psychotherapy Integration, 15, 19–47.
Thomas A. Field, M.Ed., NCC, LPC is a Faculty/Program Coordinator for the Masters of Arts in Counseling program at City University of Seattle and Ph.D. candidate in the counseling and supervision program at James Madison University. Correspondence can be addressed to Thomas A. Field, City University of Seattle, 521 Wall Street, Seattle, WA 98121, tfield@cityu.edu.
Apr 7, 2014 | Article, Volume 4 - Issue 2
Elizabeth A. Prosek, Jessica M. Holm
The U.S. Department of Veterans Affairs (VA) and TRICARE have approved professional counselors to work within the military system. Counselors need to be aware of potential ethical conflicts between counselor ethical guidelines and military protocol. This article examines confidentiality, multiple relationships and cultural competency, as well as ethical models to navigate potential dilemmas with veterans. The first model describes three approaches for navigating the ethical quandaries: military manual approach, stealth approach, and best interest approach. The second model describes 10-stages to follow when navigating ethical dilemmas. A case study is used for analysis.
Keywords: military, ethics, veterans, counselors, competency, confidentiality
The American Community Survey (ACS; U.S. Census Bureau, 2011) estimated that 21.5 million veterans live in the United States. A reported 1.6 million veterans served in the Gulf War operations that began post-9/11 in 2001 (U.S. Census Bureau, 2011). Gulf War post-9/11 veterans served mainly in Iraq and Afghanistan, in operations including but not limited to Operations Enduring Freedom (OEF), Iraqi Freedom (OIF), and New Dawn (OND) (M. E. Otey, personal communication, October 23, 2012). Holder (2007) estimated that veterans represent 10% of the total U.S. population ages 17 years and older. Pre-9/11 data suggested that 11% of military service members utilized mental health services in the year 2000 (Garvey Wilson, Messer, & Hoge, 2009). In 2003, post-9/11 comparative data reported that 19% of veterans deployed to Iraq accessed mental health services within one year of return (Hoge, Auchterlonie, & Milliken, 2006). Recognizing the increased need for mental health assessment, the U.S. Department of Defense (DOD) mandated the Post-Deployment Health Assessment (PDHA) for all returning service members (Hoge et al., 2006). The PDHA is a brief three-page self-report screening of symptoms to include post-traumatic stress, depression, suicidal ideation and aggression (U.S. DOD, n.d.). The assessment also indicates service member self-report interest in accessing mental health services.
Military service members access mental health services for a variety of reasons. In a qualitative study of veterans who accessed services at a Veterans Affairs (VA) mental health clinic, 48% of participants reported seeking treatment because of relational problems, and 44% sought treatment because of anger and/or irritable mood (Snell & Tusaie, 2008). Veterans may also present with mental health symptoms related to post-traumatic stress disorder (PTSD), depression, and suicidal ideation (Hoge et al., 2006). Depression is considered a common risk factor of suicide among the general population, and veterans are additionally at risk due to combat exposure (Martin, Ghahramanlou-Holloway, Lou, & Tucciarone, 2009). The DOD (2012) confirmed that 165 active-duty Army service members committed suicide in 2011. Furthermore, researchers asserted that suicide caused service member deaths more often than combat (O’Gorman, 2012). Hoge et al. (2004) reported that veterans were most likely to access mental health services 3–4 months post-deployment. Unfortunately, researchers suggested that service members were hesitant to access mental health treatment, citing the stigma of labels (Kim, Britt, Klocko, Riviere, & Adler, 2011). Studies indicated that mental health service needs are underestimated among the military population and are therefore a potential burden to an understaffed helping profession (Garvey Wilson et al., 2009; Hoge et al., 2006). In May of 2013, the DOD and VA created 1,400 new positions for mental health providers to serve military personnel (DOD, 2013). Moreover, as of March 2013, the DOD-sponsored veterans crisis line reported more than 800,000 calls (DOD, 2013). It is evident that the veteran population remains at risk for problems related to optimal mental health functioning and therefore requires assistance from trained helping professionals.
Historically, the DOD employed social workers and psychologists almost exclusively to provide mental health services in the military setting. Recently, the DOD and VA expanded services and created more positions for mental health clinicians (U.S. VA, 2012). Because licensed professional counselors (LPCs) are now employable by VA service providers (e.g., VA hospitals) and approved TRICARE providers (Barstow & Terrazas, 2012), it is imperative to develop an understanding of the military system, especially of the potential conflict that may exist between military protocol and counselor ethical guidelines. The military health system requires mental health professionals to be appropriately credentialed (e.g., licensed), and credentialing results in the mandatory adherence to a set of professional ethical standards (Johnson, Grasso, & Maslowski, 2010). However, there may be times when professional ethical standards do not align with military regulations. Thus, an analysis of the counselor ethical codes relevant to the military population is presented. At times, discrepancies between military protocol and counselor ethical codes may emerge; therefore, recommendations for navigating such ethical dilemmas are provided. A case study and analysis from the perspective of two ethical decision-making models are presented.
Ethical Considerations for Counselors
The mission of the American Counseling Association (ACA) Code of Ethics (2005) is to establish a set of standards for professional counselors, which ensure that the counseling profession continues to enhance the profession and quality of care with regard to diversity. As professional counselors become employed by various VA mental health agencies or apply for TRICARE provider status, it is important to identify specific ethical codes relevant to the military population. Therefore, three categories of ethical considerations pertinent to working with military service members are presented: confidentiality, multiple relationships, and cultural competence.
Confidentiality
The ACA Code of Ethics (2005) suggests that informed consent (A.2.a., p. 4) be a written and verbal discussion of rights and responsibilities in the counseling relationship. This document includes the client right for confidentiality (B.1.c., p. 7) with explanation of limitations (B.1.d., p. 7). The limitations, or exceptions, to confidentiality include harm to self, harm to others and illegal substance use. In the military setting, counselors may need to consider other exceptions to confidentiality including domestic violence (Reger, Etherage, Reger, & Gahm, 2008), harassment, criminal activity and areas associated with fitness for duty (Kennedy & Johnson, 2009). Also, military administrators may require mandated reporting when service members are referred for substance abuse treatment (Reger et al., 2008). When these conditions arise in counseling, the military may require reporting beyond the standard ethical protocol to which counselors are accustomed.
Counselors working in the VA mental health system or within TRICARE may need to be flexible with informed consent documents, depending on the purpose of services sought. Historically, veterans represented those who returned from deployment and stayed home. Currently, military members may serve multiple tours of combat duty; therefore, the definition of veterans now includes active-duty personnel. This modern definition of veteran speaks to issues of fitness for duty, where the goal is to return service members ready for combat. Informed consent documents may need to outline disclosures to commanding officers. For example, if a service member is in need of a Command-Directed Evaluation (CDE), then the commander is authorized to see the results of the assessment (Reger et al., 2008). Fitness for duty is also relevant when service members are mandated to the Soldier Readiness Program (SRP) to determine their readiness for deployment. In these situations, counselors need to clearly explain the exception to confidentiality before conducting the assessment. Depending on the type of agency and its connection to the DOD, active-duty veterans’ health records may be considered government property, not the property of the service provider (McCauley, Hacker Hughes, & Liebling-Kalifani, 2008). It is imperative that counselors are educated on the protocols of the setting or assessments, because “providing feedback to a commander in the wrong situation can be an ethical violation that is reviewable by a state licensing authority” (Reger et al., 2008, p. 30). Thus, in order to protect the client and the counselor, limitations to confidentiality within the military setting must be accurately observed at all times. Knowledge of appropriate communication between the counselor and military system also speaks to the issue of multiple relationships.
Multiple Relationships
Kennedy and Johnson (2009) suggested creating collaborative relationships with interdisciplinary teams in a military setting in order to create a network of consultants (e.g., lawyers, psychologists, psychiatrists), which is consistent with ACA ethical code D.1.b to develop interdisciplinary relationships (2005, p. 11). However, when interdisciplinary teams are formed, there are ACA (2005) ethical guidelines that must be considered. These guidelines state that interdisciplinary teams must focus on collaboratively helping the client by utilizing the knowledge of each professional on the team (D.1.c., p. 11). Counselors also must make the other members of the team aware of the constraints of confidentiality that may arise (D.1.d., p. 11). In addition, counselors should adhere to employer policies (D.1.g., p. 11), openly communicating with VA superiors to navigate potential discrepancies between employers’ expectations and counselors’ roles in best helping the client.
In the military environment, case transfers are common because of the high incidence of client relocation, which increases the need for the interdisciplinary teams to develop time-sensitive treatment plans (Reger et al., 2008). Therefore, treatment plans not only need to follow the guidelines of A.1.c., in which counseling plans “offer reasonable promise of success and are consistent with abilities and circumstances of clients” (ACA, 2005, p. 4), but they also need to reflect brief interventions or treatment modalities that can be easily transferred to a new professional. Mental health professionals may work together to best utilize their specialized services in order to meet the needs of military service members in a minimal time allowance.
For those working with military service members, consideration of multiple relationships in terms of client caseload also is important. Service members who work together within the same unit may seek mental health services at the same agency. Members of a military unit may be considered a support network which, according to ethical code A.1.d., may be used as a resource for the client and/or counselor (ACA, 2005, p. 4). However, learning about a military unit as a network from multiple member perspectives may also create a dilemma. Service members within a unit may be tempted to probe the counselor for information about other service members, or tempt the counselor to become involved in the unit dynamic. McCauley et al. (2008) recommended that mental health professionals avoid mediating conflicts between service members in order to remain neutral in the agency setting.
However, there are times when the unit cohesion may be used to support the therapeutic relationship. Basic military training for service members emphasizes the value of teamwork and the collective mind as essential to success (Strom et al., 2012). It is important for counselors to approach military service member clients from this perspective, not from a traditional Western individualistic lens. Mental health professionals also are warned not to be discouraged if rapport is more challenging to build than expected. Hall (2011) suggested that the importance of secrecy in the military setting might make it more difficult for service members to readily share in the therapeutic relationship. Researchers noted that military service members easily built rapport with each other in a group therapy session, often leaving out the civilian group leader (Strom et al., 2012). It might behoove counselors to build upon the framework of collectivism in order to earn the trust of members of the military population. Navigating the dynamic of a unit or the population of service members accessing care at the agency may be a challenge; however, counselors are able to alleviate this challenge with increased knowledge of the military culture in general.
Cultural Competence
The military population represents a group of people with a unique “language, a code of manners, norms of behavior, belief systems, dress, and rituals” and therefore can be considered a cultural group (Reger et al., 2008, p. 22). Reger et al. (2008) suggested that many clinical psychologists learned about military culture as active service members themselves. While there may be many veterans currently working as professional counselors, civilian counselors also serve the mental health needs of the military population; and as civilians, they require further training. The ACA Code of Ethics (2005) suggests that counselors communicate with their clients in ways that are culturally appropriate to ensure understanding (A.2.c., p. 4). This can be achieved by prolonged exposure to military culture or by seeking supervision from a professional involved with the military mental health system (Reger et al., 2008). Strom et al. (2012) outlined examples of military-specific cultural components for professionals to learn: importance of rank, unique terminology and value of teamwork. It behooves counselors intending to work with the military population to learn terminology in order to understand service members. For example, R&R refers to vacation leave and MOS or rate refers to a job category (Strom et al., 2012).
Personal values may cause dilemmas for a mental health professional working within the VA system. This can be especially true during times of war. Stone (2008) suggested that treating veterans of past wars may be easier than working with military service members during current combat because politics may be intensified. A counselor who does not support the current wartime mission may be conflicted when clients are mandated to return to active-duty assignments (Stone, 2008). The ACA Code of Ethics (2005) addresses the impact of counselors’ personal values (A.4.b., pp. 4–5) on the therapeutic relationship. It is recommended that counselors be aware of their own values and beliefs and respect the diversity of their clients. Counselors need to find a way to value the contributions of their client when personal or political opinion conflicts with the DOD’s plans or efforts overseas. If one wants to be successful with this population, Johnson (2008) suggested the foundational importance of accepting the military mission. If this is in direct conflict with the counselor’s values, it may be recommended for the counselor to consider the client’s value of the mission.
The ACA ethical code stresses the importance of mental health professionals practicing within the boundaries of their competence and continuing to broaden their knowledge to work with diverse clients (ACA, 2005, C.2.a., p. 9). Counselors should only develop new specialty areas after appropriate training and supervised experience (ACA, 2005, C.2.b., p. 9). Working within the VA mental health system, mental health professionals may be asked to provide a service in which they are not competent (Kennedy & Johnson, 2009). Such a request may occur more frequently here than in other settings, due to the high demand of mental health services and low availability of trained professionals (Garvey Wilson et al., 2009; Hoge et al., 2006). Counselors must determine if their experience and training can be generalized to working with military service members (Kennedy & Johnson, 2009), and may be their own best advocate for receiving appropriate training.
Awareness of when and how military service members access mental health services also might be important to consider. Reger et al. (2008) reported that military personnel were more likely to access services before and after a deployment. Researchers specified a higher prevalence rate of access 3–4 months after a deployment (Hoge et al., 2004). The relationship of time between deployment and help-seeking behaviors suggests that counselors should be prepared for issues related to trauma. For women, combat-related trauma is compounded with increased rates of reported military sexual trauma (Kelly et al., 2008). Counselors would benefit from additional trainings in trauma intervention strategies. The VA and related military organizations offer many resources online to educate professionals working with military members with identified trauma symptoms (U.S. VA., n.d.).
Advocating for appropriate training in areas of incompetence is the responsibility of the professional, who should pursue such training in order to best meet the needs of the military population. It is best practice for mental health professionals to be engaged in ongoing trainings to ensure utilization of the latest protocols and treatment modalities (McCauley et al., 2008). Trainings may need to extend beyond general military culture, because each branch of service (e.g., Army, Marines, Navy) could be considered a cultural subgroup with unique language and standards. For example, service members in the Army are soldiers, whereas members of the Navy are sailors (Strom et al., 2012).
This article has outlined many ACA (2005) ethical guidelines pertinent to working with the military population. However, as presented, there are times when counselor ethical codes conflict with military regulations. Counselors interested in working in the military setting or with military personnel may consider decision-making models to address ethical dilemmas.
Recommendations for Counselors
The military mental health system has almost exclusively employed psychologists and social workers. Counselors interested in employment within VA agencies or as TRICARE providers may utilize the resources created by these practitioners to better serve the military population. Two ethical decision-making models are presented, and a case study is provided to demonstrate how to implement the models.
Ethical Models
The ACA Code of Ethics (2005) advises counselors to adhere to the code of ethics whenever possible, working towards a resolution of the conflict (H.1.b., p. 19). If a favorable resolution cannot be formed, counselors have the choice to act in accordance with the law or regulation. Psychology researchers have suggested ethical models for professionals to use during times of dilemma within the military setting. The first model presented considers three overarching approaches to address ethical dilemmas; and the second model presented is a more specific stage model with which to approach dilemmas. These models may serve to assist counselors as the counseling profession gains more experience in the VA system and eventually develops counselor-specific decision-making models.
Approach model. Johnson and Wilson (1993) identified three approaches for psychologists to consider when navigating the ethical quandaries of the military mental health system. The first, the military manual approach, occurs when professionals adhere strictly to military regulations without consideration for the specific client’s needs. The second, the stealth approach, occurs when there is strict adherence to the mental health professionals’ code of ethics, regardless of the legalities surrounding the circumstances. While the client’s best interests may be at the forefront in this approach, the counselor must also take into account the possibility of being the subject of legal action for not adhering to the standards set by the military. For example, the counselor may use ambiguous wording within the client file or leave some information out altogether, so that if the files were requested, the client’s information would be protected (Johnson & Wilson, 1993). The third, the best interest approach, occurs when the counselor maintains focus on the client’s best interest while also adhering to the standards of the military. This may require professionals to adhere to the minimum professional standards in order to accommodate the client’s best interest. Although most professionals have deemed this approach the best option, it also leads to the most ambiguity. Under certain circumstances, the counselor also must take into account what is in the best interest for society as a whole, while also navigating a responsibility to the client and the military mental health system. Researchers in psychology responded to the ambiguity of this model by developing a more specific stage model to assist professionals with ethical dilemmas.
Stage model. Barnett and Johnson (2008) proposed a 10-stage model to follow when navigating an ethical dilemma. They advise that professionals must do the following:
1. Clearly define the situation.
2. Determine what parties could be affected.
3. Reference the pertinent ethical codes.
4. Reference the pertinent laws and regulations.
5. Reflect on personal thoughts and competencies on the issue.
6. Select knowledgeable colleagues with whom to consult.
7. Develop alternate courses of action.
8. Evaluate the impact on all parties involved.
9. Consult with professional organizations, ethics committees and colleagues.
10. Decide on a course of action.
Barnett and Johnson (2008) also noted that once a decision is made, the process does not end. It is best practice to monitor the implications and, if necessary, modify the plan. Documentation throughout this entire process is necessary for the protection of the counselor, the client and other involved stakeholders. Counselors working in the military mental health system may find this 10-stage model helpful when navigating ethical dilemmas.
To better understand the implementation of the two presented ethical decision-making models, a case study was developed. The case is then conceptualized from both the approach model and stage model, and the ethical dilemmas associated with the case are discussed.
Case Study
Megan is a licensed professional counselor employed at a clinic that serves military service members. She provides individual outpatient counseling to veterans and family members, as well as facilitates veteran support groups. Megan’s client, Robert, is a Petty Officer First Class in the Navy. Robert is married with two children. In recent sessions, Megan became concerned with Robert’s increased alcohol use. Recently, Robert described a weekend of heavy drinking at the local bar. Although Robert drove after leaving the bar both nights, Megan suspected that he was not sober enough to drive. In a follow-up session, Robert reported that his binge-drinking weekend caused friction at home with his wife, and that he missed his children’s soccer games. During his most recent session, Robert was visibly distressed as he disclosed to Megan that he received orders for a deployment in 3 months. Robert is anxious about informing his wife and children of the pending 6-month deployment, as he knows it will only increase conflict at home. Robert reported that his family could use the increase in pay associated with family separation and tax-free wages during deployment. However, he also knows that deployments cause tension with his wife, which has already increased due to Robert’s recent drinking binges. While leaving the session, he mentioned with a laugh that he would rather go to the bar than go home.
Analysis from approach model. Megan may consider using Johnson and Wilson’s (1993) ethical approach model as she conceptualizes the potential ethical dilemma presented in Robert’s case. From a military manual approach, Megan may need to report Robert’s recent alcohol abuse behavior to his superior, as it may impact his fitness for duty on his next deployment. And although Robert has not been caught drinking and driving or charged with a crime, his behavior also puts him at risk of military conduct violations. However, when Robert originally came to the clinic, he did so of his own accord, not under orders, which could mean that notifying a commanding officer is an ethical violation. In consideration of the stealth approach, Megan may review the ACA (2005) ethical guidelines and conclude that there are no violations at risk if she chooses not to report Robert’s drinking habits. However, Megan contemplates whether addressing Robert’s drinking binges is in his best interest overall. She understands that the money associated with deployment is important to Robert’s family at this time; however, his drinking may put him at increased risk during deployment. Finally, Megan applies the best-interest approach to Robert’s situation. Megan may refer Robert to the center’s substance use support group. This referral will be reflected in Robert’s records, but if he begins receiving treatment for his alcohol abuse now (3 months before deployment), there may be time for Robert to demonstrate significant progress before his fitness for duty assessment.
Analysis from stage model. Megan may consider her ethical dilemma from Barnett and Johnson’s (2008) 10-stage model. In stage 1, she clearly defines the situation as Robert’s alcohol abuse and pending deployment. In stage 2, Megan considers who may be affected in this situation. She understands that Robert’s family would benefit from the extra money associated with the deployment, and therefore the family may be impacted if Robert is not deployed. Megan also notes that the family is already negatively impacted by his recent drinking binge (e.g., conflict with his wife, missed soccer games). If Robert’s problematic drinking continues, he is at risk for evaluation and promotion issues. In stage 3, Megan reflects upon the ACA (2005) ethical codes in order to better understand her dilemma from a counselor’s view. Robert has a right to confidentiality (B.1.c., p. 7) with limitations including illegal substance use (B.1.d., p. 7). However, Robert’s current substance is alcohol, which is a legal substance. Megan considers the importance of his support network (A.1.d., p. 4) including his family and unit, but she does not have the ethical right to disclose her concerns about his substance abuse. In stage 4, Megan considers the pertinent laws and regulations of the dilemma. As per the clinic regulations, she is aware that if she makes a substance use program referral, it will be reflected in Robert’s record, which is the property of the military. Megan also is aware that Robert has not committed a documented crime of driving under the influence.
In stage 5 of the 10-stage ethical decision-making model, Megan must reflect on her personal thoughts and competencies. She is very concerned about Robert’s increased use of alcohol and is worried for his safety if deployed. Megan feels less confident in her ability to accurately assess for substance use problems. She facilitates the PTSD support group for the clinic, which is her specialty area. Megan recognizes that she is fond of Robert as a client and is disappointed that he could be jeopardizing his family and career with his alcohol abuse. She considers whether she is overreacting to his binge-drinking incident because of her higher expectations of him. In stage 6, Megan consults with her colleague who leads the substance use support groups at the clinic. She describes Robert’s recent abuse of alcohol and inquires as to whether he is a good candidate for the substance use group, needs more intense treatment, or needs no treatment at all. The colleague suggests that the group would be a very appropriate fit for someone with Robert’s symptoms.
In stage 7, Megan develops her course of action to refer Robert to the substance use group. Then, in stage 8, she evaluates the plan for potential impact on parties involved. Megan conceptualizes that Robert may be at risk for losing his deployment orders if he is accessing substance use treatment. Megan believes she has reduced this potential impact by referring to the substance support group, rather than an inpatient treatment facility, which may be more appropriate for a dependence issue. Megan recognizes that attending a 90-minute group each week will take Robert away from his family, but she also realizes that the 90-minute commitment is less than his current time spent away from the family when binge drinking. Megan reflects upon how her therapeutic relationship with Robert may be strained at the time of referral, and is prepared for a potential negative response from her client. She trusts in their therapeutic relationship and moves forward. In stage 9, Megan presents her planned course of action to her supervisor at the clinic. The supervisor approves the referral for the support group, but also suggests that Megan consider a referral to couples counseling for Robert and his wife, which may assist with resolving conflicts before the deployment.
In the final stage, Megan proposes the treatment plan of action to Robert in their next session. Megan explains that she feels ethically obligated to refer Robert to the substance use support group, and that as of now, Robert may make this choice for himself. Megan and Robert discuss the potential that substance use treatment may no longer be a choice in the future if his current drinking behavior continues. There is more discussion of fitness for duty and how participation in the support group will positively reflect upon the assessment in the future. Megan also presents Robert with the recommendation of couples counseling to help mediate relationship conflicts before deployment. She reports that if Robert and his wife decide to receive couples counseling, she can provide a referral for them at that time.
With the ethical decision-making models presented, the counselor is able to successfully navigate the military mental health system, while still maintaining the professional standards of the counseling profession. In each model, the situation is resolved with considerable attention to the client’s best interest, while maintaining the expectations of the military clinic. Psychologists developed the two ethical models presented, and counselors may choose to utilize these approaches until more counselor-specific ethical processes are created. As counselors become more permanent fixtures in the VA mental health system and as TRICARE providers, opportunities to develop an ethical decision-making model will likely arise.
Conclusion
The recent inclusion of counselors as mental health professionals within the VA system and as TRICARE providers allows for new employment opportunities with the military population. However, these new opportunities are not without potential dilemmas. Counselors interested in working with service members need to be educated on the potential conflict between counselor professional ethical guidelines and military protocols. Future research in the counseling field may develop a counselor-specific ethical decision-making model. In the meantime, counselors may utilize or adapt the ethical decision-making models created by other mental health professionals, who have a longer history working with the military population.
References
American Counseling Association. (2005). ACA code of ethics. Retrieved from http://www.counseling.org/Resources/aca-code-of-ethics.pdf
Barnett, J. E., & Johnson, W. B. (2008). The ethics desk reference for psychologists. Washington DC: American Psychological Association.
Barstow, S., & Terrazas, A. (2012, February). DoD releases TRICARE rule on independent practice for counselors. Counseling Today, 54(8), 10. Retrieved from
http://ct.counseling.org/2012/02/dod-releases-tricare-rule-on-independent-practice-for-counselors/
Garvey Wilson, A. L., Messer, S. C., & Hoge, C. W. (2009). U.S. military mental health care utilization and attrition prior to the wars in Iraq and Afghanistan. Social Psychiatry and Psychiatric Epidemiology, 44, 473–481. doi:10.1007/s00127-008-0461-7
Hall, L. (2011). The importance of understanding military culture. Social Work in Health Care, 50, 4–18. doi:10.1080/00981389.2010.513914
Hoge, C. W., Auchterlonie, J. L., & Milliken, C. S. (2006). Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. The Journal of the American Medical Association, 295(9), 1023–1032. doi:10.1001/jama.295.9.1023
Hoge, C. W., Castro, C. A., Messer, S. C., McGurk, D., Cotting, D. I., & Koffman, R. L. (2004). Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. The New England Journal of Medicine, 351(1), 13–22. doi:10.1056/NEJMoa040603
Holder, K. A. (2007). Comparison of ACS and ASEC data on veteran status and period of military service: 2007. U.S. Census Bureau: Housing and Household Economics Statistics Division. Retrieved from http://www.census.gov/hhes/veterans/files/comparison_report.pdf
Johnson, W. B. (2008). Top ethical challenges for military clinical psychologists. Military Psychology, 20, 49–62. doi:10.1080/08995600701753185
Johnson, W. B., Grasso, I., & Maslowski, K. (2010). Conflicts between ethics and law for military mental health providers. Military Medicine, 175, 548–553.
Johnson, W., & Wilson, K. (1993). The military internship: A retrospective analysis. Professional Psychology: Research and Practice, 24(3), 312–318. doi:10.1037/0735-7028.24.3.312
Kelly, M. M., Vogt, D. S., Scheiderer, E. M., Ouimette, P., Daley, J., & Wolfe, J. (2008). Effects of military trauma exposure on women veterans’ use and perceptions of Veterans Health Administration care. Journal of General Internal Medicine, 23, 741–747. doi:10.1007/s11606-008-0589-x
Kennedy, C. H., & Johnson, W. B. (2009). Mixed agency in military psychology: Applying the American Psychological Association ethics code. Psychological Services, 6(1), 22–31. doi:10.1037/a0014602
Kim, P. Y., Britt, T. W., Klocko, R. P., Riviere, L. A., & Adler, A. B. (2011). Stigma, negative attitudes about treatment, and utilization of mental health care among soldiers. Military Psychology, 23, 65–81. doi:10.1080/08995605.2011.534415
Martin, J., Ghahramanlou-Holloway, M., Lou, K., & Tucciarone, P. (2009). A comparative review of U.S. military and civilian suicide behavior: Implications for OEF/OIF suicide prevention efforts. Journal of Mental Health Counseling, 31(2), 101–118.
McCauley, M., Hacker Hughes, J., & Liebling-Kalifani, H. (2008). Ethical considerations for military clinical psychologists: A review of selected literature. Military Psychology, 20, 7–20. doi:10.1080/08995600701753128
O’Gorman, K. (2012, August 16). Army reports record suicides in July [Blog post]. Retrieved from http://iava.org/blog/army-reports-record-high-suicides-july
Reger, M. A., Etherage, J. R., Reger, G. M., & Gahm, G. A. (2008). Civilian psychologists in an army culture: The ethical challenge of cultural competence. Military Psychology, 20, 21–35. doi:10.1080/08995600701753144
Snell, F., & Tusaie, K. R. (2008). Veterans reported reasons for seeking mental health treatment. Archives of Psychiatric Nursing, 22(5), 313–314. doi:10.1016/j.apnu.2008.06.003
Stone, A. M. (2008). Dual agency for VA clinicians: Defining an evolving ethical question. Military Psychology, 20, 37–48. doi:10.1080/08995600701753177
Strom, T. Q., Gavian, M. E., Possis, E., Loughlin, J., Bui, T., Linardatos, E.,…Siegel, W. (2012). Cultural and ethical considerations when working with military personnel and veterans: A primer for VA training programs. Training and Education in Professional Psychology, 6(2), 67–75. doi:10.1037/a0028275
U.S. Census Bureau, American Community Survey. (2011). B21002: Period of military service for civilian veterans 18 years and over (2011 American Community Survey 1-year estimates). Retrieved from http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_11_1YR_B21002&prodType=table
U.S. Department of Defense. (n.d.). Enhanced post-deployment health assessment (PDHA) process (DD Form 2796). Retrieved from http://www.pdhealth.mil/dcs/dd_form_2796.asp
U.S. Department of Defense. (2012). Army releases July suicide data, No. 683-12. Retrieved from http://www.defense.gov/releases/release.aspx?releaseid=15517
U.S. Department of Defense. (2013). DOD, VA and HHS partner to expand access to mental health services for veterans, service members, and families, No. 353-13. Retrieved from http://www.defense.gov/releases/release.aspx?releaseid=16024
U.S. Department of Veterans Affairs. (n.d.). PTSD: National center for PTSD. Retrieved from http://www.ptsd.va.gov/professional/index.asp
U.S. Department of Veterans Affairs (2012, April). VA adding family therapists and mental health counselors to workforce. Retrieved from http://www.va.gov/opa/pressrel/pressrelease.cfm?id=2303
Elizabeth A. Prosek, NCC, is an Assistant Professor at the University of North Texas. Jessica M. Holm is a doctoral student at the University of North Texas. Correspondence can be addressed to Elizabeth A. Prosek, University of North Texas, 1155 Union Circle #310829, Denton, TX 76203-5017, elizabeth.prosek@unt.edu.
 In this 4-hour and 16-minute video, psychotherapist Otto Kernberg demonstrates Transference-Focused Psychotherapy (TFP) in three live sessions with a 40-year-old patient named Alfred (portrayed by an actor). TFP is an evidence-based treatment that is effective for individuals struggling with personality disorders. It is specifically helpful for individuals with borderline and narcissistic personality disorders, and focuses on treating the individual’s entire personality.
In this 4-hour and 16-minute video, psychotherapist Otto Kernberg demonstrates Transference-Focused Psychotherapy (TFP) in three live sessions with a 40-year-old patient named Alfred (portrayed by an actor). TFP is an evidence-based treatment that is effective for individuals struggling with personality disorders. It is specifically helpful for individuals with borderline and narcissistic personality disorders, and focuses on treating the individual’s entire personality. Set against a backdrop of survival, Michael Bloom’s Thinking Like a Therapist provides readers with a different approach to the typical case study. The author follows a young couple through an immense tragedy and subsequent strife, inviting the reader on a journey through isolation and its effects on the couple’s relationship. In a unique conceptualization of a case study, the author juxtaposes scenes of the couple fighting for their lives with scenes of the couple in therapy sessions, as though they can magic themselves from the wilderness to the therapist’s office. Each chapter has three sections: journal entries narrating part of the couple’s adventures, a dialogue between the couple and the therapist, and a discussion of the therapist’s goals and interventions in the preceding therapy session. The book offers a new approach to discussing mental health therapy in a more entertaining fashion than typical counseling books.
Set against a backdrop of survival, Michael Bloom’s Thinking Like a Therapist provides readers with a different approach to the typical case study. The author follows a young couple through an immense tragedy and subsequent strife, inviting the reader on a journey through isolation and its effects on the couple’s relationship. In a unique conceptualization of a case study, the author juxtaposes scenes of the couple fighting for their lives with scenes of the couple in therapy sessions, as though they can magic themselves from the wilderness to the therapist’s office. Each chapter has three sections: journal entries narrating part of the couple’s adventures, a dialogue between the couple and the therapist, and a discussion of the therapist’s goals and interventions in the preceding therapy session. The book offers a new approach to discussing mental health therapy in a more entertaining fashion than typical counseling books. In A Counselor’s Introduction to Neuroscience, the authors claim that “neurocounseling” is the fifth force in the history of psychology and counseling. Although a precise and detailed definition of neurocounseling is elusive (both in this book and in the professional literature), it is described as the marriage of counseling and neurobiology. They offer a crash course in brain anatomy, function and development in order to lay the groundwork for how neurocounseling can be used effectively with clients. Several chapters focus on the ways the brain is affected by certain mental disorders, and how specific counseling approaches address various brain regions and functions. The remainder of the book focuses on assessment of brain function and fictional cases to illustrate neurocounseling techniques. The chapters include numerous tables, figures, cases and opportunities to stop and reflect. The overall intent of the book is to arm counselors “with yet another highly effective and efficient way to help clients cope with (overcome, etc.) their personal psychological distress.”
In A Counselor’s Introduction to Neuroscience, the authors claim that “neurocounseling” is the fifth force in the history of psychology and counseling. Although a precise and detailed definition of neurocounseling is elusive (both in this book and in the professional literature), it is described as the marriage of counseling and neurobiology. They offer a crash course in brain anatomy, function and development in order to lay the groundwork for how neurocounseling can be used effectively with clients. Several chapters focus on the ways the brain is affected by certain mental disorders, and how specific counseling approaches address various brain regions and functions. The remainder of the book focuses on assessment of brain function and fictional cases to illustrate neurocounseling techniques. The chapters include numerous tables, figures, cases and opportunities to stop and reflect. The overall intent of the book is to arm counselors “with yet another highly effective and efficient way to help clients cope with (overcome, etc.) their personal psychological distress.”