Family Functioning and Self-Injury in Treatment-Seeking Adolescents: Implications for Counselors
Melissa Sitton, Tina Du Rocher Schudlich, Christina Byrne, Chase M. Ochrach, Seneca E. A. Erwin
A family systems framework guided our investigation of self-injurious behavior (SIB) in adolescents. As part of a larger study, we collected data examining SIB and family functioning from 29 adolescents (Mage = 15.66) and their caregivers. These adolescents with traits of borderline personality disorder were seeking counseling from community-based practitioners specializing in dialectical behavior therapy. Our primary aim was to better understand the family environment of these adolescents. A second aim was to elucidate interrelations among family communication, roles, problem-solving, affective involvement, affective responsiveness, behavioral control, and conflict and SIB. We found a high rate of SIB among adolescent participants. There was significant congruence between adolescent and caregiver reports of the family environment, with families demonstrating unhealthy levels of functioning in several indicators of family environment. The latent variable of family functioning significantly predicted nonsuicidal and ambivalent SIB. Counselors working with adolescents should consider family functioning when assessing risk for SIB.
Keywords: self-injurious behavior, adolescents, family systems, borderline personality disorder, family functioning
Although emotion dysregulation and unstable personal relationships are common for adolescents, those with symptoms of borderline personality disorder (BPD) often report more extreme experiences (A. L. Miller et al., 2008). BPD is characterized by impaired or unstable emotional and social functioning (American Psychiatric Association, 2013). Individuals with BPD—especially adolescents—may experience impairments in daily functioning as well as within interpersonal relationships (Chanen et al., 2007).
Linehan’s (1993) biosocial theory proposed that BPD can result from an individual’s biological predisposition toward emotion dysregulation and a social environment that amplifies this vulnerability. Given that adolescents spend a substantial amount of time with their family, it is important to examine an adolescent’s familial environment to understand the etiology of BPD symptoms; such examination requires a framework like family systems theory, which emphasizes the relationships between family members rather than focusing on the individual members themselves (Goldenberg & Goldenberg, 2013); this includes family communication, roles, problem-solving, affective involvement, affective responsiveness, and behavioral control (I. W. Miller et al., 2000).
Self-Injurious Behavior (SIB)
Regrettably, it is common for adolescents with BPD to engage in SIB (Kaess et al., 2014). SIB is an umbrella term for all purposeful, self-inflicted acts of bodily harm, whether the intent is suicidal, nonsuicidal (i.e., nonsuicidal self-injury), or ambivalent (i.e., neither strictly suicidal nor nonsuicidal). In fact, SIB is one diagnostic criteria for BPD in adolescents and adults.
Although originally developed to explain the etiology of BPD, the biosocial theory has been applied to the development of SIB as well (Crowell et al., 2009). Countless studies have examined the role of emotion dysregulation and affective reinforcement in SIB, but it is important to also consider the influence of social variables. Indeed, in their four-function model, Nock and Prinstein (2004, 2005) suggested that both affective and social variables can positively and negatively reinforce nonsuicidal SIB. Similarly, Joiner’s (2005) interpersonal theory of suicidal SIB posited that social variables (particularly thwarted belongingness and perceived burdensomeness) drive the desire for suicide. Thus, although there are clear links between affective variables and SIB, social variables are also relevant. For adolescents, an important social variable related to SIB is family environment. From the family systems approach, adolescent SIB is best understood when rooted in the context of family environment. As Levenkron (1998) suggested, “the ways in which all the family members relate to each other… [is] the fuel that drives [SIB]” (pp. 125–126).
Although limited in number, some previous studies have examined family environment and SIB in adolescents. For example, Halstead et al. (2014) found that SIB was related to dysfunctional family environments. Studies have also found relationships between adolescent SIB and familial communication (Halstead et al., 2014; Latina et al., 2015) and conflict (Huang et al., 2017). Additionally, Adrian et al. (2011) demonstrated a link between stress and failure to meet expectations of familial roles. To our knowledge, no studies to date have examined SIB and familial problem-solving, affective involvement, affective responsiveness, and behavioral control. However, studies have linked SIB to an individual’s lack of problem-solving skills (Walker et al., 2017), ability to regulate affective responses (Adrian et al., 2011), and behavioral control related to impulsivity and compulsivity (Hamza et al., 2015).
Current Study
Despite the clear influence of family members on SIB (Halstead et al., 2014) and the significant amount of time adolescents tend to spend with family members, more research is needed to evaluate family environment in relation to SIB. Specifically, we investigated the families of treatment-seeking adolescents with traits of BPD who engage in SIB. Our objectives were to: (a) assess family environment using multiple indicators of family functioning, (b) assess SIB in these treatment-seeking adolescents, including SIB done with suicidal intent, nonsuicidal intent, and ambivalence toward life, and (c) evaluate family functioning as a statistical predictor of lifetime SIB.
Method
Participants and Procedure
We used data from a larger ongoing, unpublished study on dialectical behavior therapy. In the larger study, participants were adolescents and young adults who sought counseling from community-based clinicians specializing in dialectical behavior therapy. Participants sought counseling for symptoms of BPD, particularly SIB. The counselors recruited participants for the research study by explaining voluntary research participation during their standard intake process for new clients at the clinic. The counselors also obtained informed consent for research from the participants. The counselors collaborated with researchers at a local university for this larger study, and the university’s IRB approved the study.
For the current study, we used the existing pretest data from the adolescents only (N = 29; Mage = 15.66, SDage = 1.34, age range = 13–18). A majority of the adolescent sample (82.8%; n = 24) reported no previous experience with counseling. This sample was predominately Caucasian (82.8%; n = 24) and most adolescents identified as female (89.7%; n = 26).
Caregiver participants (N = 29) were involved in the adolescents’ treatment and the accompanying research study. Most caregiver participants were the biological mother (81.5%; n = 22) or adoptive mother (7.4%; n = 2). However, a few adolescents were accompanied by an extended family member (7.4%; n = 2) or their biological father (3.7%; n = 1). A majority of adolescents reported that at least one of their caregivers had attended some (22.2%; n = 6) or all (29.6%; n = 8) of college, or some (3.7%; n = 1) or all (29.6%; n = 8) of graduate school.
Most adolescents reported they currently lived with both biological parents (58.6%; n = 17) or at least one biological parent (31.0%; n = 9), though some lived with non-biological parents or caregivers (10.3%; n = 3). Most adolescents (86.2%; n = 25) also reported having at least one sibling; 58.6% of adolescents (n = 17) reported having at least one biological brother, 37.9% had at least one biological sister (n = 11), and 24.1% had a half- or step-sibling (n = 7). One-way analysis of variance (ANOVA) tests demonstrated that adolescents did not differ in total SIB based on family characteristics (e.g., number of siblings, number of employed caregivers; all values of p > .05).
Measures
Family Functioning
The Family Assessment Device (FAD; Epstein et al., 1983) is a 53-item measure with a 4-point Likert scale used to rate agreement with statements about how the adolescents’ family members interact and relate to each other (e.g., “After our family tries to solve a problem, we usually discuss whether it worked or not”). Both adolescents and caregivers completed the FAD. Subscales of the FAD assess six dimensions of family functioning, including family problem-solving, roles, communication, affective responsiveness, affective involvement, and behavioral control. The scores for each subscale are averaged, with higher scores indicating worse functioning and more problems within families. The FAD has good test-retest reliability and construct validity (I. W. Miller et al., 1985). In this study, the reliability of the FAD was excellent for both samples (Cronbach’s alpha = .95 for adolescents and .96 for caregivers).
The Conflict Behavior Questionnaire (CBQ; Prinz et al., 1979) assesses self-reported familial interactions within the past two weeks. The CBQ has both an adolescent and a caregiver version; both versions consist of 20 true/false items. Scores can range from 0 to 20, with higher scores indicating more conflict between caregiver and adolescent. Studies have shown that CBQ scores delineated between distressed and non-distressed families (Robin & Foster, 1989). The CBQ has good internal consistency and test-retest reliability (Rallis et al., 2015; Robin & Foster, 1989), as well as construct validity (Prinz et al., 1979). In the current study, the reliability of the CBQ was excellent for both samples (Cronbach’s alpha = .88 for adolescents and .92 for caregivers).
Self-Injurious Behavior (SIB)
We used the Lifetime Suicide Attempt Self-Injury Interview (LSASI; Linehan & Comtois, 1996) to assess participants’ history of SIB, including frequency, method, and intent. Using 20 items, the LSASI asks participants to report the dates of the most recent and most severe SIB, as well as their lifetime frequency of 11 different methods of SIB with suicidal intent, without suicidal intent, and with ambivalence. Participants also report the total frequency of each SIB method (combining suicidal, nonsuicidal, and ambivalent), and the number of times medical treatment was received for the SIB method. Higher scores indicate more SIB in the past. In the current study, reliability across all SIB intent types (four variables: suicidal SIB, nonsuicidal SIB, ambivalent SIB, and total SIB) was .65. Because the LSASI was designed for clinical use rather than research, to our knowledge there are no existing studies demonstrating the reliability or validity of the LSASI. Notably, this measure was already in use at the counseling clinic, and the decision to use it for this research study was counselor-driven.
Data Analysis
As part of our preliminary analyses, we first tested all variables for the assumptions of analysis. Specifically, when examining the skew and kurtosis of the composite variables, we used ± 2 as our acceptable range of values. Following advice from Tabachnick and Fidell (2019), we transformed variables that did not meet our criteria for normality.
To better understand family functioning, we conducted descriptive analyses for all seven predictive variables (problem-solving, communication, roles, affective responsiveness, affective involvement, behavioral control, and conflict) separately for adolescent and caregiver scores. We assessed the degree of healthy family functioning using I. W. Miller et al.’s (1985) suggested cut-off scores, which can be used to distinguish between healthy and unhealthy family environments. We also conducted paired sample t-tests to compare the adolescent and caregiver reports of family functioning.
Next, we tested the fit of our theoretical model of family functioning using structural equation modeling (SEM) with maximum likelihood as the method of estimation. We used multiple fit indices to assess the model fit. Specifically, the chi-square statistic assesses absolute model fit, demonstrating good fit when not statistically significant. The chi-square test can also be used to compare the relative fit of two models. Additionally, comparative fit index (CFI), root mean square error of approximation (RMSEA), and standardized root-mean-square residual (SRMR) are all indicators of model fit, with 0.95 or higher, 0.05 or lower, and 0.08 or lower indicating good fit, respectively (for more information on SEM fit indices, see Hooper et al., 2008). Notably, Iacobucci (2010) suggested that researchers can use SEM and establish good model fit even with small samples.
We also conducted descriptive analyses of the participants’ self-reported SIB. We left these variables raw (untransformed) to evaluate how participants viewed their own SIB. We examined the specific SIB methods that participants reported using (e.g., cutting, burning) as well as three outcome variables (suicidal SIB, nonsuicidal SIB, and ambivalent SIB; all transformed because of issues with skew and kurtosis).
Lastly, we used SEM to predict SIB with the proposed model of family functioning. Given our small sample size, we conducted this analysis separately for suicidal SIB, nonsuicidal SIB, and ambivalent SIB. We set alpha at .05 for each model; given the small sample size, we did not apply corrections to the alpha for the multiple analyses.
Results
We used SPSS 24.0 and Amos 24 to analyze our data. Because this study was primarily descriptive, we conducted multiple analyses to better understand the family environment of treatment-seeking adolescents, experiences of SIB for adolescents, and the role of family environment in adolescent engagement in SIB.
Family Characteristics and Functioning
Means, standard deviations, and range of scores for the family functioning variables are shown in Table 1. With the exception of the caregiver reports on affective responsiveness and behavioral control, both adolescent and caregiver reports on every subscale of the FAD fell above the McMaster clinical cut-off (see Table 1) described by I. W. Miller et al.’s (1985) cut-off scores, indicating on average all of the families demonstrated unhealthy functioning. It is worth noting that adolescents and their caregivers reported similar levels in five of the seven indicators of family functioning from the FAD and CBQ (e.g., there was no statistical difference between the two reports, all values of p > .05). As shown in Table 1, adolescent and caregiver reports only statistically differed for behavioral control (t[28] = 4.23, p < .001) and communication (t[28] = 2.96, p = .006). Specifically, adolescents reported higher levels of both behavioral control and communication; these high levels are considered indicative of unhealthy or distressed families (I. W. Miller et al., 1985).
Table 1
Descriptive Statistics and Group Comparisons of Family Functioning Variables as Reported by Adolescents and Caregivers
| Variable | Adolescent | Caregiver | |||||||
| Cut-Off | M | SD | Range | M | SD | Range | t(28) | p | |
| Problem-solving | 2.2 | 2.58 | 0.65 | 1.00–3.80 | 2.29 | 0.57 | 1.40–3.80 | 1.88 | .071 |
| Communication | 2.2 | 2.56 | 0.37 | 1.83–3.17 | 2.30 | 0.37 | 1.50–3.00 | 2.96 | .006 |
| Roles | 2.3 | 2.58 | 0.37 | 1.75–3.38 | 2.45 | 0.37 | 1.75–3.38 | 1.57 | .128 |
| Affective Resp. | 2.2 | 2.34 | 0.68 | 1.00–4.00 | 2.12 | 0.62 | 1.00–3.67 | 1.48 | .151 |
| Affective Inv. | 2.1 | 2.37 | 0.28 | 1.71–3.00 | 2.44 | 0.23 | 1.86–3.00 | – 1.61 | .118 |
| Behav. Control | 1.9 | 2.12 | 0.44 | 1.00–3.11 | 1.77 | 0.41 | 1.00–2.78 | 4.23 | < .001 |
| Conflict | — | 9.60 | 4.83 | 0.00–18.00 | 10.05 | 5.67 | 1.00–20.00 | – 0.46 | .649 |
Note. Cut-Off = McMaster Cut-Off score; Affective Resp. = Affective responsiveness; Affective Inv. = Affective involvement; Behav. Control = Behavioral control.
We used SEM to test the fit of our theory-driven, congeneric model of family functioning using seven subscales from each source (14 variables; seven for adolescents and seven for caregivers, with the error terms of each subscale correlated between the two sources) to predict family functioning as reported by each source (two latent variables; one for adolescents and one for caregivers). The absolute fit of the model was marginal: χ2(69) = 104.39, p = .004, CFI = 0.79, RMSEA = 0.14, SRMR = 0.14.
In order to reduce variables in our theoretical model, we averaged adolescent and caregiver reports for problem-solving, roles, affective responsiveness, affective involvement, and conflict because these did not statistically differ (all values of p > .05). However, we kept the two reports as separate predictors for communication and behavioral control. This left us with nine predictor variables for subsequent analysis (five averaged predictors and four single-source predictors).
Next, we used SEM to test the fit of the simplified model with the nine observed variables and one latent variable of family functioning. We found that the absolute model fit of this simplified model was acceptable overall. Specifically, the fit indices mostly indicated good fit (χ2[27] = 33.11, p = .194, CFI = 0.93, SRMR = 0.08), though one fit index suggested poor fit (RMSEA = 0.09). Differences in the chi-squares of our two models showed the simplified model was statistically better than the initial model: χ2(42) = 71.28, p = .003. Thus, we selected the simplified model as the final model of family functioning (see Figure 1). See Table 2 for descriptive analyses of the nine predictors in the final model. All variables were positively related to family functioning. The strongest predictors of family functioning in this model were affective responsiveness (average of adolescent and caregiver report; β = .85, B = 1.04, SE B = 0.21, p < .001, R2 = .72), affective involvement (averaged; β = .72, B = 0.88, SE B = 0.22, p < .001, R2 = .51), and problem-solving (averaged; β = .82, R2 = .67; this was the constrained parameter used to identify the regression model).
Figure 1
The Output Structural Regression Model of Family Functioning Developed Using SEM
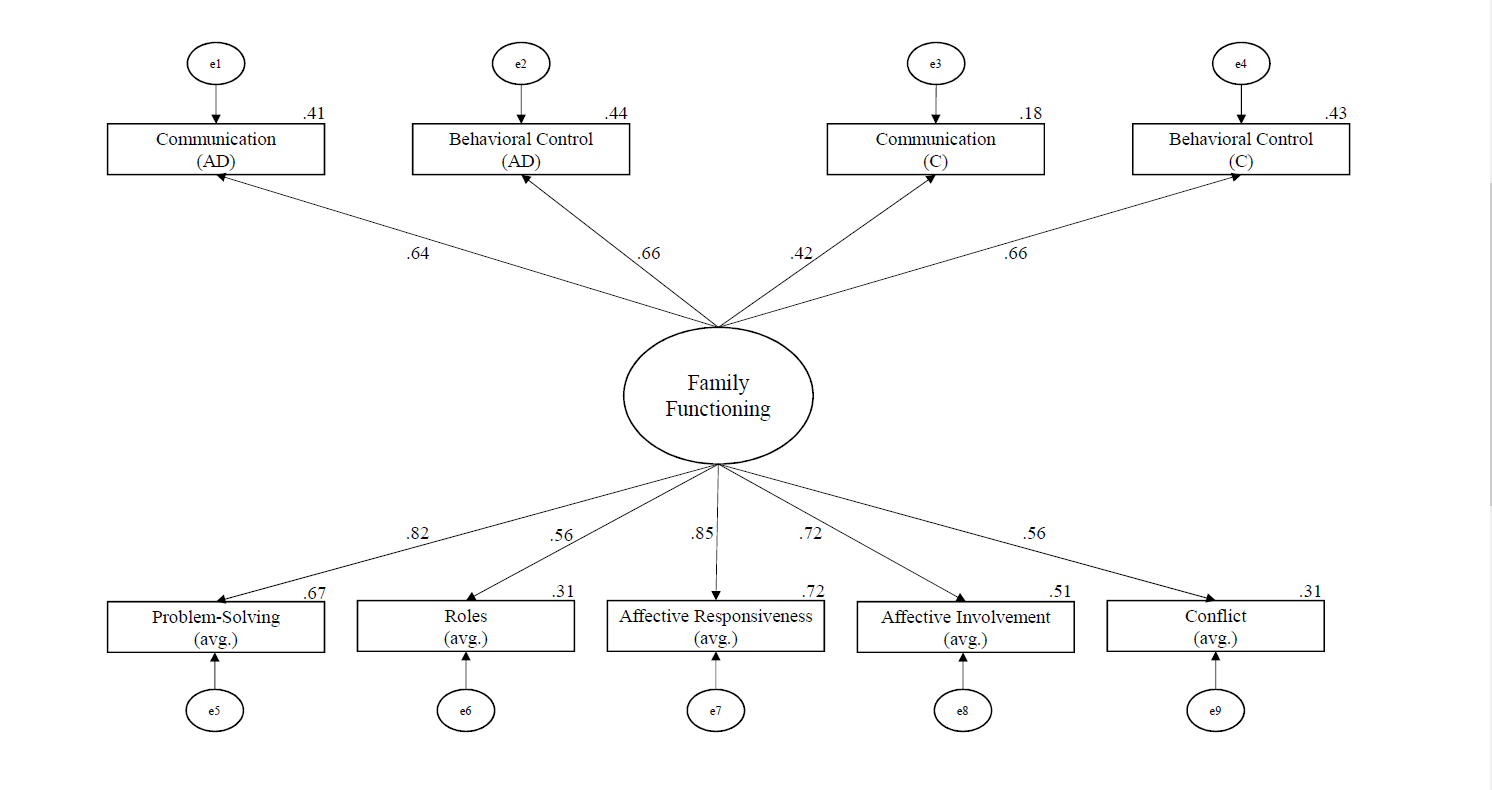
Note. The large circle represents a latent variable, boxes are measured variables, small circles (with “e”) are error terms, and solid lines show regression paths. The numbers on paths are the standardized path coefficients, and the offset values on endogenous variables are the R² effect sizes. (AD) = adolescent report; (C) = caregiver report; (avg.) = averaged score of adolescent and caregiver report.
Table 2
Descriptive Analyses of Predictors of Family Functioning
| Variable | M | SD |
| Problem-Solving | 2.43 | 0.44 |
| Roles | 2.51 | 0.29 |
| Affective Responsiveness | 2.23 | 0.51 |
| Affective Involvement | 2.40 | 0.23 |
| Conflict | 9.82 | 4.56 |
| Communication (AD) | 2.56 | 0.37 |
| Communication (C) | 2.30 | 0.37 |
| Behavioral Control (AD) | 2.12 | 0.44 |
| Behavioral Control (C) | 1.77 | 0.41 |
Note. (AD) = adolescent report; (C) = caregiver report.
Adolescent Engagement in SIB
All adolescents reported engaging in SIB in their lifetime, and the average lifetime frequency of SIB was 438.72 (SD = 1,216.65, range = 1–6,079; transformed to address normality: M = 4.41, SD = 1.80). Specifically, most participants reported engaging in nonsuicidal SIB (n = 26) and using it with higher frequency than SIB with other intent (i.e., suicidal or ambivalent SIB), with a lifetime average of 340.16 (SD = 975.22, range = 0–4,565; transformed: M = 3.49, SD = 2.25). Many adolescents also reported engaging in ambivalent SIB (n = 18), with moderate average frequency rates (M = 22.28, SD = 52.02, range = 0–248; transformed: M = 1.62, SD = 1.69). Lastly, fewer adolescents reported engaging in suicidal SIB (n = 18), with the lowest average lifetime frequency (M = 7.34, SD = 25.03, range = 0–136; transformed: M = 0.97, SD = 0.95). See Table 3 for descriptive information on SIB methods (e.g., cutting) used by adolescents in our sample. On average, participants used 3.78 (SD = 2.15) methods of SIB in their lifetime.
Table 3
Descriptive Statistics for All Self-Injurious Behavior Completed in One’s Lifetime (N = 29)
| Variable | n | Ma | SDa | Rangea | n of Severe Cases |
| Cutting | 27 | 179.55 | 330.42 | 0–1,500 | 7 |
| Hitting head/body | 16 | 240.90 | 730.59 | 0–3,000 | 0 |
| Overdosing | 13 | 1.88 | 3.59 | 0–15 | 7 |
| Burning | 13 | 6.12 | 14.99 | 0–60 | 1 |
| Strangling/hanging | 8 | 2.18 | 6.42 | 0–30 | 0 |
| Stabbing/puncturing | 8 | 0.80 | 1.64 | 0–7 | 2 |
| Asphyxiating | 7 | 1.66 | 3.90 | 0–15.62 | 0 |
| Other | 6 | 272.92 | 602.33 | 0–1,500 | 2 |
| Jumping | 4 | 1.27 | 5.31 | 0–25 | 1 |
| Drowning | 4 | 0.40 | .99 | 0–4 | 0 |
| Poisoning | 3 | 0.14 | .36 | 0–1 | 1 |
Note. The descriptive statistics are based on the total self-injurious behavior, combining acts completed with suicidal intent, nonsuicidal intent, and ambivalence. Other = adolescent-reported participating in a type of self-injury that was not listed; Jumping = jumping from a high place to cause injury; Severe Cases = requiring medical treatment.
a The frequency that adolescents reported engaging in the various methods of self-injury.
Predicting SIB With Family Functioning
To understand the relationships between family functioning and SIB, we conducted correlational analyses of the three outcome variables and nine predictors. As shown in Table 4, problem-solving was moderately associated with ambivalent SIB (r = .44 , p = .018), conflict was moderately associated with nonsuicidal SIB (r = .38 , p = .049), and adolescent-reported communication was moderately to strongly associated with all three SIB variables (suicidal r = .61, p < .001; nonsuicidal r = .47, p = .011; ambivalent r = .56, p = .002). All associations were positive (see Table 4), meaning that worse family functioning scores were associated with more SIB.
Table 4
Bivariate Correlations Between Predictor Variables
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | |
| 1. Nonsuicidal SIB | – | ||||||||||
| 2. Ambivalent SIB | .35 | – | |||||||||
| 3. Suicidal SIB | .16 | .46* | – | ||||||||
| 4. Problem-Solving | .35 | .44* | .19 | – | |||||||
| 5. Roles | .21 | -.01 | .27 | .39* | – | ||||||
| 6. Affect. Resp. | .25 | .36 | .28 | .68*** | .42* | – | |||||
| 7. Affect. Involv. | .22 | .13 | .27 | .52** | .43* | .72*** | – | ||||
| 8. Conflict | .38* | .35 | .26 | .66*** | .14 | .45* | .15 | – | |||
| 9. Comm. (AD) | .47* | .56** | .61*** | .57** | .44* | .51** | .50** | .43* | – | ||
| 10. Comm. (C) | .09 | .11 | .04 | .42* | .28 | .29 | .29 | .27 | .17 | – | |
| 11. Beh. Cont. (AD) | .27 | .06 | -.21 | .54** | .48** | .51** | .56** | .34 | .41* | .25 | – |
| 12. Beh. Cont. (C) | .27 | .26 | .13 | .49** | .53** | .61*** | .36 | .38* | .33 | .40* | .47* |
Note. SIB = self-injurious behavior; Affect. Resp. = Affective Responsiveness; Affect. Involv. = Affective Involvement; Comm. = Communication; (AD) = adolescent report; (C) = caregiver report; Beh. Cont. = Behavioral Control.
* p < .05. ** p < .01. *** p < .001.
Next, we used SEM to predict SIB with our simplified model of family functioning. We tested three SIB outcomes separately because of concerns with sample size. For all models predicting SIB, we freed all FAD factors (problem-solving, roles, affective responsiveness, affective involvement, adolescent-reported communication and behavioral control, and caregiver-reported communication and behavioral control) to correlate because variables from the same measure are likely to be related.
The model predicting nonsuicidal SIB had good absolute fit: χ2(7) = 4.28, p = .747, CFI = 1.00, RMSEA = 0.00, SRMR = 0.04. In all, family functioning explains 20% of the variance in nonsuicidal SIB. See Figure 2 for the standardized path coefficients between family functioning variables, the latent variable of family functioning, and nonsuicidal SIB. Notably, family functioning predicted nonsuicidal SIB:
β = .44, B = 1.27, SE B = 0.62, p = .039. Based on effect sizes (see Figure 2), the strongest predictors were problem-solving (averaged; β = .79, B = 0.90, SE B = 0.03, p = .008, R² = .62), communication (adolescent-reported; β = .55, B = 0.05, SE B = 0.03, p = .034, R² = .31), and conflict (averaged; β = .84, R² = .71; this was the constrained parameter used to identify the regression model).
The model predicting ambivalent SIB had good absolute fit: χ²(7) = 5.69, p = .577, CFI = 1.00, RMSEA = 0.00, SRMR = 0.04. In all, family functioning explains 33% of the variance in ambivalent SIB. See Figure 3 for the standardized path coefficients between family functioning variables, the latent variable of family functioning, and ambivalent SIB. Notably, family functioning predicted ambivalent SIB: β = .58, B = 1.04, SE B = 0.46, p = .025. Based on effect sizes (see Figure 3), the strongest predictors were problem-solving (averaged; β = .94, B = 0.15, SE B = 0.07, p = .022, R² = .89), communication (adolescent-reported; β = .83, B = 0.11, SE B = 0.05, p = .030, R² = .69), and affective responsiveness (averaged; β = .69, B = 0.13, SE B = 0.07, p = .049, R² = .47).
Figure 2
The Output Structural Regression Model of Nonsuicidal SIB Developed Using SEM
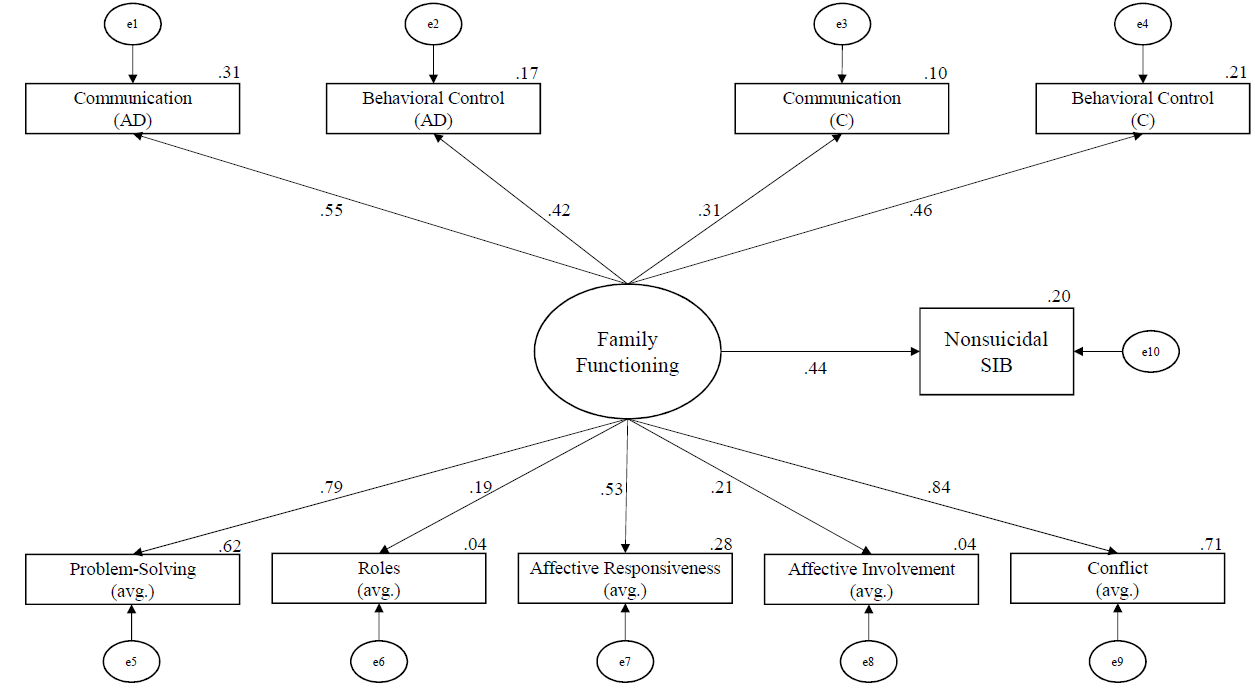
Note. The numbers on paths are the standardized path coefficients, and the offset values on endogenous variables are the R2 effect sizes. (AD) = adolescent report; (C) = caregiver report; (avg.) = averaged score of adolescent and caregiver report.
Figure 3
The Output Structural Regression Model of Ambivalent SIB Developed Using SEM
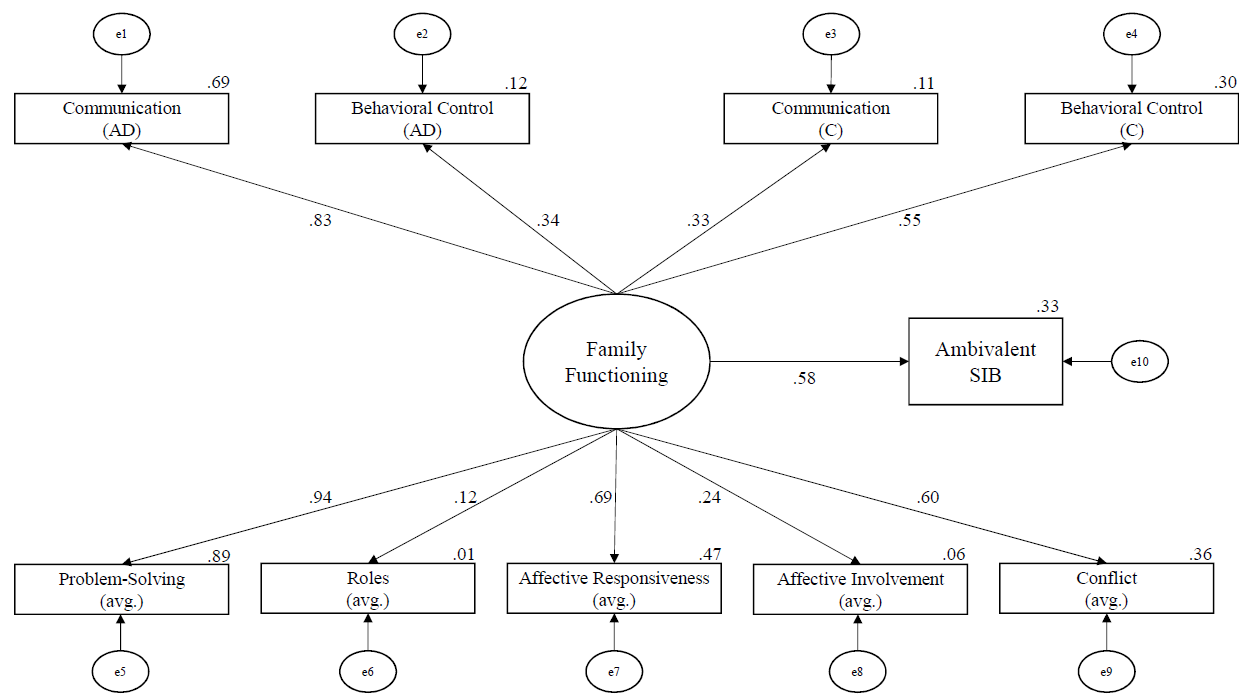
Note. The numbers on paths are the standardized path coefficients, and the offset values on endogenous variables are the R² effect sizes. (AD) = adolescent report; (C) = caregiver report; (avg.) = averaged score of adolescent and caregiver report.
Lastly, the model using family functioning to predict suicidal SIB was not able to successfully converge because of reaching the iteration limit, possibly because of the small sample size. After examining the suggested modification indices, the model was still not able to converge. Thus, we concluded that the suicidal SIB model was a poor model, meaning that family functioning alone was not predictive of suicidal SIB in our sample.
Discussion
The goals of the current study were to examine the family environment of adolescents seeking treatment for symptoms of BPD, as well as their experiences of SIB, and to better understand what aspects of family functioning relate to SIB. Unique strengths of this study include the emphasis on assessing models of family functioning as it relates to SIB and exploring differences between SIB intent types (suicidal SIB, nonsuicidal SIB, and SIB with ambivalence toward life). Further, because participants were clients seeking counseling from community-based master’s-level clinicians and no clients were excluded from participating in this study, results may generalize to other community samples.
We found that adolescents and caregivers often reported family functioning scores that met criteria for distressed families. Interestingly, adolescents and caregivers agreed on a majority of the subscales of family functioning, suggesting that the distress is mutually experienced. Adolescents and their caregivers only differed on reports of behavioral control (e.g., “[my family does not] hold any rules or standards”) and communication (e.g., “when someone [in my family] is upset the others know why”). This self-reported familial distress supports the social component of the biosocial theory (Linehan, 1993) in that the adolescents with traits of BPD engaged in SIB and experienced unhealthy family environments. Additionally, we found high lifetime rates of SIB in our sample of adolescents. As in previous studies (e.g., Anestis et al., 2015), adolescents in the current study engaged in nonsuicidal SIB more frequently than suicidal or ambivalent SIB, and cutting was the most common method.
Notably, our model of family functioning successfully predicted higher levels of both nonsuicidal SIB and ambivalent SIB. In particular, problem-solving, conflict, and adolescent-reported communication had consistently large effect sizes, suggesting that these subscales contributed more to SIB than other subscales. Although no previous studies have examined adolescent SIB and familial problem-solving to our knowledge, the findings that SIB was related to familial conflict (Huang et al., 2017) and communication (Halstead et al., 2014) corroborate the results of previous studies.
The success of the family functioning model in predicting SIB aligns with family systems theory. Specifically, adolescents in our sample may engage in SIB as a coping skill because their family lacks healthy problem-solving skills and thus models poor coping (which aligns with a description by Halstead et al., 2014). Additionally, adolescent SIB may function to temporarily end conflict in the family because it diverts the family’s attention away from the immediate problems. For example, Oldershaw et al. (2008) found that parents avoided conflict and felt like they were “walking on eggshells” (p. 142) after learning of their adolescents’ SIB. Another possible explanation is that the adolescents in our sample may serve as scapegoats within their family, acting as a focal point of a disturbed family system. From a structural family systems perspective, when there are problems within family subsystem relationships, oftentimes the child—typically the most vulnerable one—becomes the focus of the family’s problems (Wetchler, 2003); this trend is consistent with our findings.
It is worth noting that family functioning alone did not sufficiently predict suicidal SIB. One possible explanation is that our family functioning variables did not encompass the factors of thwarted belongingness and perceived burdensomeness, both of which Joiner (2005) suggested may lead to suicide.
Limitations and Future Directions
A strength of this study is that the results may generalize to other real-world settings in which adolescent clients seek counseling services from community-based master’s-level clinicians who specialize in dialectical behavior therapy. However, this ecological validity comes with some relative limitations.
One notable limitation of this study is that we examined family functioning at one point in time, when the adolescent was beginning treatment. Given this single timepoint, we are unable to fully describe the relationship between family functioning and SIB. Considering the biosocial theory, it seems likely that the distressed family environment preceded the SIB; however, it is possible that the SIB caused greater familial distress. Therefore, it would be useful to assess changes in family functioning and SIB across time.
Another limitation is our SIB measure; as Crowell et al. (2013) explained, the LSASI is commonly used in clinical practice but not often in research. In addition to issues with reliability, the LSASI is a lifetime measure as opposed to one focusing on recent behavior. Although all participants reported engaging in SIB in the past year, it is unclear how recently they engaged in SIB relative to the time of the study. Despite the benefit of creating more variability in the data by allowing participants to report their specific frequency of SIB, the alternative of a dichotomous variable of current SIB might be more compatible with our measures of current family functioning.
Additionally, the small sample size limits the power of our analyses as well as the generalizability of our results. A small sample increases the likelihood of a Type II error, meaning an increased likelihood of not finding significant results. However, it is notable that we found statistically significant results (e.g., good model fit of family functioning) despite our low power. Nevertheless, replication studies with much larger samples are needed.
Implications for Practice
Our findings suggest that family functioning is related to SIB in adolescents, particularly nonsuicidal and ambivalent SIB. Although counselors often include families when working with young children, it is common for counselors to work with adolescents individually. This practice is consistent with state laws allowing adolescents to consent to their own mental health treatment, and there are many presenting concerns and situations in which individual counseling may be the most effective modality. However, the connection between family functioning and SIB in adolescents in our sample indicates that it may be important to include family members in treating adolescent SIB; in fact, dialectical behavior therapy for adolescents (originally adapted by A. L. Miller et al., 1997) encourages family involvement in treatment. Counselors therefore need to educate parents and caregivers who may be reluctant to engage in the counseling process with their teen that SIB is an issue for which their participation in counseling could make a positive difference in treatment outcome. Further, from a family systems perspective, it can be challenging for teens to successfully use the coping skills and strategies they learn in counseling if the rest of the family system remains unchanged. Including at least some family members may therefore help adolescents maintain changes gained through the counseling process.
When including family members in counseling with adolescents who have engaged in nonsuicidal and ambivalent SIB, findings from our study suggest that three important targets for assessment and intervention include the domains of familial problem-solving, familial conflict, and adolescent-reported communication. Two of these, conflict and communication, were previously identified in the literature, and our study supports those findings. Our study newly identified familial problem-solving as an additional important predictor of SIB in adolescents. Counselors must keep in mind, however, that these variables were not sufficient in predicting suicidal SIB in adolescents. For these teens, we encourage the use of a broader assessment that includes elements of Joiner et al.’s (2009) interpersonal theory of suicide, especially the crucial interpersonal constructs of thwarted belongingness and perceived burdensomeness.
Conclusion
Based on our findings, it appears there is a relationship between engagement in SIB (especially nonsuicidal and ambivalent SIB) and familial environment for community-based treatment-seeking adolescents with traits of BPD. Additionally, both adolescents and their caregivers in our sample reported distressed levels of multiple indicators of family functioning, suggesting the need for family-based intervention. Counselors and service providers should consider multiple markers of family environment (particularly problem-solving, conflict, and adolescent-reported communication) when assessing risk for and treatment of adolescent SIB.
Conflict of Interest and Funding Disclosure
This study was partially funded by a grant from
Western Washington University awarded to
Dr. Christina Byrne. The authors reported no
conflict of interest for the development of this manuscript.
References
Adrian, M., Zeman, J., Erdley, C., Lisa, L., & Sim, L. (2011). Emotional dysregulation and interpersonal
difficulties as risk factors for nonsuicidal self-injury in adolescent girls. Journal of Abnormal Child
Psychology, 39(3), 389–400. https://doi.org/10.1007/s10802-010-9465-3
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
https://doi.org/10.1176/appi.books.9780890425596
Anestis, M. D., Khazem, L. R., & Law, K. C. (2015). How many times and how many ways: The impact of number of nonsuicidal self-injury methods on the relationship between nonsuicidal self-injury frequency and suicidal behavior. Suicide and Life-Threatening Behavior, 45(2), 164–177. https://doi.org/10.1111/sltb.12120
Chanen, A. M., Jovev, M., & Jackson, H. J. (2007). Adaptive functioning and psychiatric symptoms in adolescents with borderline personality disorder. The Journal of Clinical Psychiatry, 68(2), 297–306.
http://doi.org/10.4088/JCP.v68n0217
Crowell, S. E., Baucom, B. R., McCauley, E., Potapova, N. V., Fitelson, M., Barth, H., Smith, C. J., & Beauchaine, T. P. (2013). Mechanisms of contextual risk for adolescent self-injury: Invalidation and conflict escalation in mother–child interactions. Journal of Clinical Child & Adolescent Psychology, 42(4), 467–480. https://doi.org/10.1080/15374416.2013.785360
Crowell, S. E., Beauchaine, T. P., & Linehan, M. M. (2009). A biosocial developmental model of borderline personality: Elaborating and extending Linehan’s theory. Psychological Bulletin, 135(3), 495–510. https://doi.org/10.1037/a0015616
Epstein, N. B., Baldwin, L. M., & Bishop, D. S. (1983). The McMaster Family Assessment Device. Journal of Marital and Family Therapy, 9(2), 171–180. https://doi.org/10.1111/j.1752-0606.1983.tb01497.x
Goldenberg, H., & Goldenberg, I. (2013). Family therapy: An overview (8th ed.). Brooks/Cole.
Halstead, R. O., Pavkov, T. W., Hecker, L. L., & Seliner, M. M. (2014). Family dynamics and self-injury behaviors: A correlation analysis. Journal of Marital and Family Therapy, 40(2), 246–259.
https://doi.org/10.1111/j.1752-0606.2012.00336.x
Hamza, C. A., Willoughby, T., & Heffer, T. (2015). Impulsivity and nonsuicidal self-injury: A review and meta-analysis. Clinical Psychology Review, 38, 13–24. https://doi.org/10.1016/j.cpr.2015.02.010
Hooper, D., Coughlan, J., & Mullen, M. R. (2008). Structural equation modelling: Guidelines for determining model fit. Electronic Journal of Business Research Methods, 6(1), 53–60. https://doi.org/10.21427/D7CF7R
Huang, Y.-H., Liu, H.-C., Sun, F.-J., Tsai, F.-J., Huang, K.-Y., Chen, T.-C., Huang, Y.-P., & Liu, S.-I. (2017). Relationship between predictors of incident deliberate self-harm and suicide attempts among adolescents. Journal of Adolescent Health, 60(5), 612–618. https://doi.org/10.1016/j.jadohealth.2016.12.005
Iacobucci, D. (2010). Structural equations modeling: Fit indices, sample size, and advanced topics. Journal of Consumer Psychology, 20(1), 90–98. https://doi.org/10.1016/j.jcps.2009.09.003
Joiner, T. E. (2005). Why people die by suicide. Harvard University Press.
Joiner, T. E., Jr., Van Orden, K. A., Witte, T. K., & Rudd, M. D. (2009). The interpersonal theory of suicide: Guidance for working with suicidal clients. American Psychological Association. https://doi.org/10.1037/11869-000
Kaess, M., Brunner, R., & Chanen, A. (2014). Borderline personality disorder in adolescence. Pediatrics, 134(4), 782–793. https://doi.org/10.1542/peds.2013-3677
Latina, D., Giannotta, F., & Rabaglietti, E. (2015). Do friends’ co-rumination and communication with parents prevent depressed adolescents from self-harm? Journal of Applied Developmental Psychology, 41, 120–128. https://doi.org/10.1016/j.appdev.2015.10.001
Levenkron, S. (1998). Cutting: Understanding and overcoming self-mutilation. W. W. Norton.
Linehan, M. M. (1993). Cognitive-behavioral treatment of borderline personality disorder. Guilford.
Linehan, M. M., & Comtois, K. A. (1996). Lifetime parasuicide count. Unpublished manuscript, Department of Psychology, University of Washington, Seattle, Washington.
Miller, A. L., Muehlenkamp, J. J., & Jacobson, C. M. (2008). Fact or fiction: Diagnosing borderline personality disorder in adolescents. Clinical Psychology Review, 28(6), 969–981. https://doi.org/10.1016/j.cpr.2008.02.004
Miller, A. L., Rathus, J. H., Linehan, M. M., Wetzler, S., & Leigh, E. (1997). Dialectical behavior therapy adapted for suicidal adolescents. Journal of Practical Psychiatry and Behavioral Health, 3(2), 78–86.
Miller, I. W., Epstein, N. B., Bishop, D. S., & Keitner, G. I. (1985). The McMaster Family Assessment Device: Reliability and validity. Journal of Marital and Family Therapy, 11(4), 345–356.
https://doi.org/10.1111/j.1752-0606.1985.tb00028.x
Miller, I. W., Ryan, C. E., Keitner, G. I., Bishop, D. S., & Epstein, N. B. (2000). The McMaster approach to families: Theory, assessment, treatment and research. Journal of Family Therapy, 22(2), 168–189.
https://doi.org/10.1111/1467-6427.00145
Nock, M. K., & Prinstein, M. J. (2004). A functional approach to the assessment of self-mutilative behavior. Journal of Consulting and Clinical Psychology, 72(5), 885–890. https://doi.org/10.1037/0022-006X.72.5.885
Nock, M. K., & Prinstein, M. J. (2005). Contextual features and behavioral functions of self-mutilation among adolescents. Journal of Abnormal Psychology, 114(1), 140–146. https://doi.org/10.1037/0021-843X.114.1.140
Oldershaw, A., Richards, C., Simic, M., & Schmidt, U. (2008). Parents’ perspectives on adolescent self-harm: Qualitative study. The British Journal of Psychiatry, 193(2), 140–144. https://doi.org/10.1192/bjp.bp.107.045930
Prinz, R. J., Foster, S. L., Kent, R. N., & O’Leary, K. D. (1979). Multivariate assessment of conflict in distressed and nondistressed mother–adolescent dyads. Journal of Applied Behavior Analysis, 12(4), 691–700.
https://doi.org/10.1901/jaba.1979.12-691
Rallis, B. A., Esposito-Smythers, C., & Mehlenbeck, R. (2015). Family environment as a moderator of the association between conduct disorder and suicidality. Journal of Aggression, Maltreatment & Trauma, 24(2), 150–168. https://doi.org/10.1080/10926771.2015.997909
Robin, A. L., & Foster, S. L. (1989). Negotiating parent–adolescent conflict: A behavioral–family systems approach. Guilford.
Tabachnick, B. G., & Fidell, L. S. (2019). Using multivariate statistics (7th ed.). Pearson Education.
Walker, K. L., Hirsch, J. K., Chang, E. C., & Jeglic, E. L. (2017). Non-suicidal self-injury and suicidal behavior in a diverse sample: The moderating role of social problem-solving ability. International Journal of Mental Health and Addiction, 15(3), 471–484. https://doi.org./10.1007/s11469-017-9755-x
Wetchler, J. L. (2003). Structural family therapy. In L. L. Hecker & J. L. Wetchler (Eds.), An introduction to marriage
and family therapy (pp. 63–93). Haworth Clinical Practice Press.
Melissa Sitton, MS, is a doctoral student at Southern Methodist University. Tina Du Rocher Schudlich, PhD, MHP, is a professor at Western Washington University. Christina Byrne, PhD, is an associate professor at Western Washington University. Chase M. Ochrach, MS, is a doctoral student at the University of Wisconsin–Madison. Seneca E. A. Erwin, BS, is a doctoral student at the University of Northern Colorado. Correspondence may be addressed to Tina Du Rocher Schudlich, 516 High St., MS 9172, Bellingham, WA 98225, tina.schudlich@wwu.edu.
