Dec 5, 2024 | Volume 14 - Issue 3
Fei Shen, Ying Zhang, Xiafei Wang
Intimate partner violence (IPV) has consistently been shown to have deleterious effects on survivors’ interpersonal and intrapersonal relationships. Despite the negative outcomes of IPV, distress after IPV varies widely, and not all IPV survivors show a significant degree of distress. The present study examined the impact of IPV on adult attachment and self-esteem, as well as the moderating role of childhood attachment on the relationships between IPV, adult attachment, and self-esteem using path analysis. A total of 1,708 adult participants were included in this study. As hypothesized, we found that IPV survivors had significantly higher levels of anxious and avoidant adult attachment than participants without a history of IPV. Additionally, childhood attachment buffered the relationship between IPV and self-esteem. We did not find that childhood attachment moderated the relationship between IPV and adult attachment. These results provide insight on attachment-based interventions that can mitigate the negative effects of IPV on people’s perceptions of self.
Keywords: intimate partner violence, childhood attachment, adult attachment, self-esteem, moderation
More than 10 million adults experience intimate partner violence (IPV) victimization annually in the United States (Black et al., 2011); therefore, it undoubtedly remains a prominent public health concern. IPV victimization has been consistently associated with deleterious effects on survivors’ physical and mental health. It is well established that IPV survivors demonstrated increased risks for chronic pain, injury, insomnia, disabilities, post-traumatic stress disorder, depression, and suicidality (Burke et al., 2005; Gilbert et al., 2023; Matheson et al., 2015; McLaughlin et al., 2012). Historically, empirical studies on trauma and violence have focused on psychopathology and symptoms (McLaughlin et al., 2012; Sayed et al., 2015). However, there is limited research on exploring the link between IPV victimization and intrapersonal and interpersonal relationship outcomes. Attachment theory (Bowlby, 1969) not only provides a rich theoretical framework for conceptualizing an individual’s psychopathology, but also establishes a foundation for understanding the intrapersonal and relational sequelae of IPV (Levendosky et al., 2012; Sutton, 2019). IPV survivors often experience a violation of trust and a sense of betrayal in the aftermath and develop ineffective coping mechanisms (e.g., distancing themselves emotionally), which could potentially impact their new intimate relationships (St. Vil et al., 2021).
Despite the negative outcomes of IPV victimization, the levels of distress following such incidents can vary (Scott & Babcock, 2010). Although evidence has implicated numerous risk factors related to IPV victimization (e.g., childhood trauma, gender inequity; Jewkes et al., 2017; Meeker et al., 2020), limited effort has been put forth to recognize protective factors that contribute to IPV survivors’ coping and healing processes. Childhood attachment has been proposed as a potential protective factor for IPV survivors’ coping with traumatic experiences and a moderator for buffering the negative psychological outcomes of IPV (Pang & Thomas, 2020), which provides a meaningful foundation for us to further investigate childhood attachment as a moderator buffering relational outcomes. To our knowledge, no study to date has investigated the potential moderating role of childhood attachment security on the association between IPV, interpersonal outcomes (e.g., adult attachment), and intrapersonal outcomes (e.g., self-esteem) in a non-clinical sample. Understanding the moderating role of childhood attachment can potentially provide further directions toward protecting survivors from negative outcomes and creating interventions that foster healthier interpersonal relationships. In tackling the gaps in the literature, we aim to: (a) investigate the impact of IPV on adult attachment and self-esteem; and (b) examine the moderating role of childhood attachment on the relationships between IPV, adult attachment, and self-esteem.
Theoretical Framework—Attachment Theory
Attachment theory (Bowlby, 1969) offers an explanation of how the relationship between children and their primary caregiver(s) develops and how it impacts children’s subsequent developmental process. According to Bowlby (1973), children develop mental representations of themselves and others, known as internal working models, through their interactions with their primary caregiver(s). Children with secure attachment are more likely to form positive self-perceptions and relationships with others (Bowlby, 1969). In contrast, children who develop insecure attachment are more likely to struggle with coping with distress and form poor relationships with others, resulting from caregivers responding to their needs insensitively.
Although evidence suggests the continuity of attachment from childhood to adulthood (Bowlby, 1969), there are distinctions between these two variables based on individuals’ attachment needs, developmental stages, and characteristics of different relationships. As children grow into adolescents and emerging adults, they often continue to maintain connections with their primary caregivers while exploring new social roles outside of the family and forming close relationships with peers and romantic partners to develop adult attachment (Moretti & Peled, 2004). Secure adult attachment is generally characterized by flexibility, the ability to work independently and cooperatively with others, the ability to seek support from intimate partners, and the capacity to manage loss in a healthy manner (Brennan et al., 1998). Adult romantic relationships are thought to be underlined by two fundamental attachment-related dimensions: anxiety and avoidance. Adults with anxious attachment tend to experience worry and fear regarding abandonment or rejection by their partner, leading them to seek constant reassurance and validation from their partner. On the other hand, avoidant-attached individuals often feel uncomfortable with being close to their partner, which can lead them to withdraw from intimacy and emotional closeness in the relationship (Brennan et al., 1998). Thus, understanding the similarities and differences of attachment categories as well as dynamics of the attachment system is warranted (Lopez & Brennan, 2000).
Childhood Attachment, IPV Victimization, and Adult Attachment
Various researchers have extensively investigated the significant association between attachment developed with romantic partners and its involvement in IPV dynamics (Bradshaw & Garbarino, 2004; Duru et al., 2019; Levendosky et al., 2012). However, most studies explored the relationship between adult attachment and IPV perpetration (Gormley & Lopez, 2010; McClure & Parmenter, 2020). Specifically, individuals with insecure attachment present intense fear of abandonment or rejection and activate their aggressive behaviors to control their partners (Gormley & Lopez, 2010). Regarding IPV victimization circumstances, few studies have examined attachment security among IPV survivors. Specifically, simultaneously exploring attachment with primary caregivers in childhood and attachment with romantic partners in adulthood could capture the complexity of the impact of IPV victimization experiences on relational and emotional outcomes. Ponti and Tani (2019) investigated both childhood attachment and adult attachment among 60 women who experienced IPV and indicated that the attachment to the mother could influence IPV victimization both directly and indirectly through the mediation effect of adult attachment with romantic partners. In other words, attachment with the mother could serve as a protector for not entering a violent romantic relationship or healthily managing the aftermath of traumatic experiences.
Childhood attachment has been identified as a potential moderator that may contribute to the variations of the healing process among IPV survivors in a small but growing number of studies (e.g., Scott & Babcock, 2010). Pang and Thomas (2020) examined the moderating role of childhood attachment on the relationship between exposure to domestic violence in adolescence and psychological outcomes and adult life satisfaction with a sample of 351 adult college students. They found that childhood attachment moderated the relationship between IPV exposure and adult life satisfaction but not psychological outcomes. This study provides empirical support for the moderating role of childhood attachment on early IPV exposure and later adult psychological and relationship outcomes. Given the context in which IPV occurs in the intimate relationships, not addressing the association between childhood attachment and adult attachment together would not fully capture the complexity of the attachment process in the adult population. It is possible that the relationship between IPV victimization and adult attachment security would be attenuated in conditions of childhood attachment. Therefore, the moderation effect of childhood attachment in the context of IPV needs to be empirically substantiated.
Childhood Attachment, IPV Victimization, and Self-Esteem
Self-esteem generally refers to a person’s overall evaluation and attitude toward themself (Rosenberg, 1965). Experiencing IPV was found to have detrimental effects on an individual’s self-esteem; IPV survivors often have lower levels of self-esteem than non-abused individuals (Childress, 2013; Karakurt et al., 2014; Tariq, 2013). Experiencing IPV (e.g., emotional and psychological abuse) can lead to feelings of worthlessness and hopelessness, making it difficult for survivors to maintain autonomy and make decisions that are in their best interest (Tariq, 2013). IPV survivors consistently reported feeling burdened with a sense of guilt, shame, and self-blame for being victimized (Lindgren & Renck, 2008). Unfortunately, this can contribute to a vicious cycle, as survivors who have low self-esteem are less likely to take steps to leave abusive relationships (Karakurt et al., 2014), which leads to further victimization (Eddleston et al., 1998). Understanding the link between IPV victimization and self-esteem is crucial, as rebuilding self-esteem can also help survivors develop stronger relationships with others, gain strength toward ending abusive relationships, reduce risks of mental health problems, and feel more empowered to seek help and support (Karakurt et al., 2022).
The development of the self can be seen to unfold in the context of attachment and the internalization of important others’ perceptions and expectations. Numerous studies have shed some light on the association between childhood attachment and self-esteem, suggesting that secure attachment with primary caregivers can serve as a key protective factor for developing higher levels of self-esteem (Shen et al., 2021; Wilkinson, 2004). In contrast, individuals who reported insecure attachment with their primary caregivers tended to demonstrate lower levels of self-esteem (Gamble & Roberts, 2005). However, interpersonal trauma such as IPV can produce long-term dysfunctions of self (Childress, 2013). Although no study has directly explored the moderating role of childhood attachment buffering the relationship between IPV and self-esteem, several studies have indicated that parental support serves as a moderator role in the relationship between interpersonal violence and self-esteem (Duru et al., 2019). Indeed, if a person had secure attachment experiences in childhood, they may have developed a positive sense of self-worth and the belief that they deserve love and respect, which could buffer the negative effects of IPV on their self-esteem. Considering the existing literature and theoretical explanations as a whole, it seems reasonable to postulate that childhood attachment might serve as a potential moderator of the association between IPV and self-esteem.
Taken together, the literature consistently supports the significance of exploring protective factors contributing to IPV survivors’ healing process, yet no study to date has investigated the potential moderating role of childhood attachment on the association between IPV, adult attachment, and self-esteem in a non-clinical diverse sample. In tackling these gaps, we pose two research questions (RQs):
RQ1: How is IPV associated with adult attachment and self-esteem?
RQ2: How does childhood attachment moderate the relationships between IPV, adult
attachment, and self-esteem?
We hypothesized that: 1) IPV victimization is significantly positively associated with adult attachment (i.e., anxious attachment, avoidant attachment) and negatively associated with self-esteem; 2) Childhood attachment moderates the relationship between IPV victimization and adult attachment (i.e., anxious attachment, avoidant attachment); and 3) Childhood attachment moderates the relationship between IPV victimization and self-esteem.
Method
Sampling Procedures
With approval from the university IRB, research recruitment information was posted on various social media platforms (e.g., Facebook, Craigslist, university announcement boards). Individuals who were 18 years of age or older and able to fill out the questionnaire in English were eligible for the study. Participants were directed to an online Qualtrics survey to voluntarily complete the informed consent and the measures listed in the following section. At the end of the survey, participants were prompted to enter their email addresses to win one of 10 $15 e-gift cards. Their email addresses were not included for data analysis.
Participants
Of the 2,373 voluntary adult participants who took the survey, 1,708 (71.76%) individuals were retained for the final analysis, including 507 (29.68%) participants who experienced IPV in adulthood and 1,191 (69.73%) participants without a history of IPV in adulthood. We eliminated participants who either did not consent to the study (n = 36, 1.51%), were younger than 18 years old (n = 33, 1.39%), or did not complete 95% of the survey questions (n = 596, 25.11%). We examined whether those who were excluded from the sample because of missing or invalid data differed from those who were retained. There was a significant difference in age between the included sample (M = 28.89, SD = 12.38) and excluded sample (M = 32.10, SD = 13.51); t (2,255) = −3.48, p = 0.001. Therefore, excluding participants with missing data was less likely to significantly impact our results. Table 1 shows that 76.23% of the participants were female. The age range of the sample was broad, from 18 to 89 years old, with an average age of 30.
Table 1
Demographic and Key Variables Information (N = 1,708)
| Variables |
N |
Percent |
Range |
M(SD) |
| Childhood attachment |
1,708 |
100% |
1–5 |
3.34(0.92) |
| IPV status
IPV
Non-IPV |
1,698
507
1,191 |
99.41%
29.68%
69.73% |
0–1 |
|
| Self-Esteem |
1,704 |
99.77% |
3–40 |
26.98(7.46) |
| Anxious Attachment |
1,708 |
100% |
1–7 |
4.11(1.26) |
| Avoidant Attachment |
1,708 |
100% |
1–7 |
3.71(1.16) |
| Control Variables |
|
|
|
|
| Gender
Male
Female |
1,683
381
1,302 |
98.54%
22.31%
76.23% |
|
|
| Household Income
Less than $5,000
$5,000–$9,999
$10,000–$14,999
$15,000–$19,999
$20,000–$24,999
$25,000–$29,999
$30,000–$39,999
$40,000–$49,999
$50,000–$74,999
$75,000–$99,999
$100,000–$149,999
$150,000 or more |
1,514
183
96
119
83
98
78
128
141
239
143
139
67 |
88.64%
10.70%
5.60%
7.00%
4.90%
5.70%
4.60%
7.50%
8.30%
14.00%
8.40%
8.10%
3.90% |
|
|
Measures
Childhood Attachment
The parental attachment subscale of the Inventory of Parent and Peer Attachment (Armsden & Greenberg, 1987) was used to measure childhood attachment. Participants rated their attachment to their parent(s) or caregiver(s) who had the most influence on them during their childhood. The subscale consists of 25 items divided into three dimensions, including 10 items on Trust (e.g., “My mother/father trusts my judgment”), nine items on Communication (e.g., “I can count on my mother/father when I need to get something off my chest”), and six items on Alienation (e.g., “I don’t get much attention from my mother/father”). Participants rated the items using a 5-point Likert scale ranging from 1 (almost never or never true) to 5 (almost always or always true). Responses were averaged, with a higher score reflecting more secure childhood attachment. This subscale has demonstrated relatively high internal consistency, with a Cronbach’s alpha of .93 (Armsden & Greenberg, 1987), and construct validity (Cherrier et al., 2023; Gomez & McLaren, 2007). In the present study, the Cronbach’s alpha coefficient for this subscale was .96.
Intimate Partner Violence
Participants’ experiences of IPV were assessed through the question “Have you ever experienced intimate partner violence (physical, sexual, or psychological harm) by a current or former partner or spouse since the age of 18?” Responses were coded as 1 = Yes, 0 = No.
Adult Attachment
Adult attachment was measured using the Experience in Close Relationships Scale (ECR; Brennan et al., 1998). The ECR consists of 36 items with 18 items assessing each of the two dimensions: anxious attachment (e.g., “I worry about being abandoned”) and avoidant attachment (e.g., “I try to avoid getting too close to my partner/friends”). To reduce confounding factors with childhood attachment with their parent(s) or primary caregiver(s), we only assessed adult attachment with close friends and/or romantic partners. Responses were rated on a 7-point Likert scale ranging from 1 (strongly disagree) to 7 (strongly agree). Two scores were computed by averaging items on each subscale, with a higher score reflecting a higher level of anxious or avoidant attachment. Two subscales demonstrated high construct validity in various studies (Gormley & Lopez, 2010; Ponti & Tani, 2019) and a relatively high consistency for anxiety (α = .91) and avoidance (α = .94; Brennan et al., 1998). Cronbach’s alpha coefficients for the present study were .93 for anxiety and .92 for avoidance.
Self-Esteem
The Rosenberg Self-Esteem Scale (RSES; Rosenberg, 1965) is a 10-item self-report measure of overall feelings of self-worth or self-acceptance (e.g., “I am satisfied with myself”). All items were coded using a 4-point Likert scale ranging from 1 (strongly disagree) to 4 (strongly agree). Items were summed, with a higher score indicating a higher level of self-esteem. RSES has been frequently used in various studies, demonstrating high reliability and validity (Brennan & Morris, 1997; Rosenberg, 1979). The Cronbach’s alpha for the present study was .89.
Control Variables
To make more accurate estimates, we included control variables that are potentially associated with IPV exposures, such as gender and household income. Gender was dummy coded as 1 = Male, 2 = Female.
Data Analysis
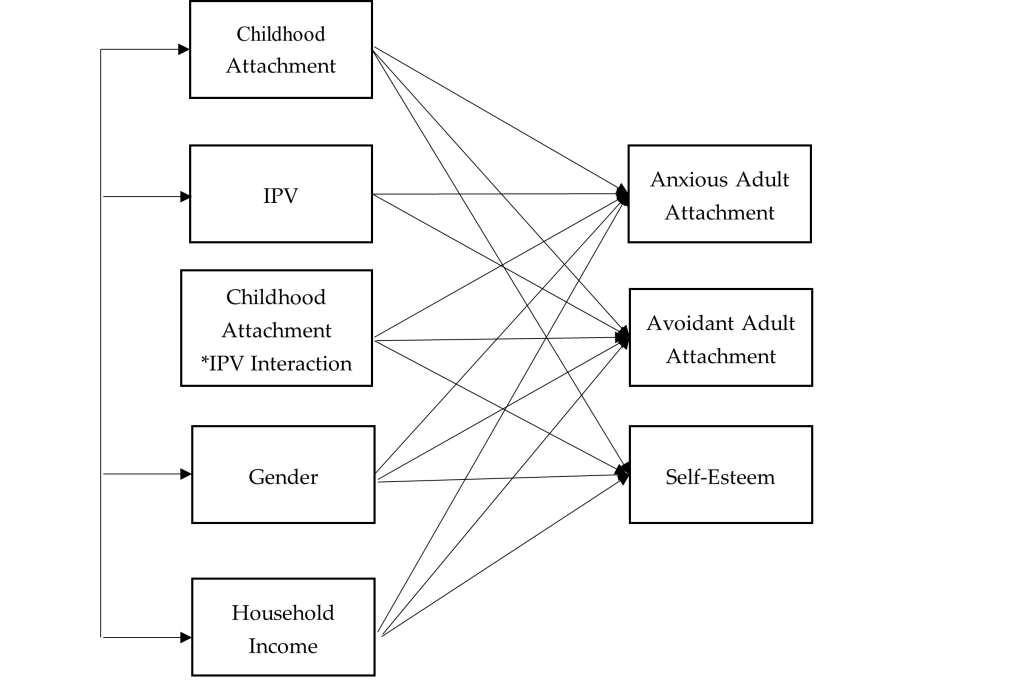
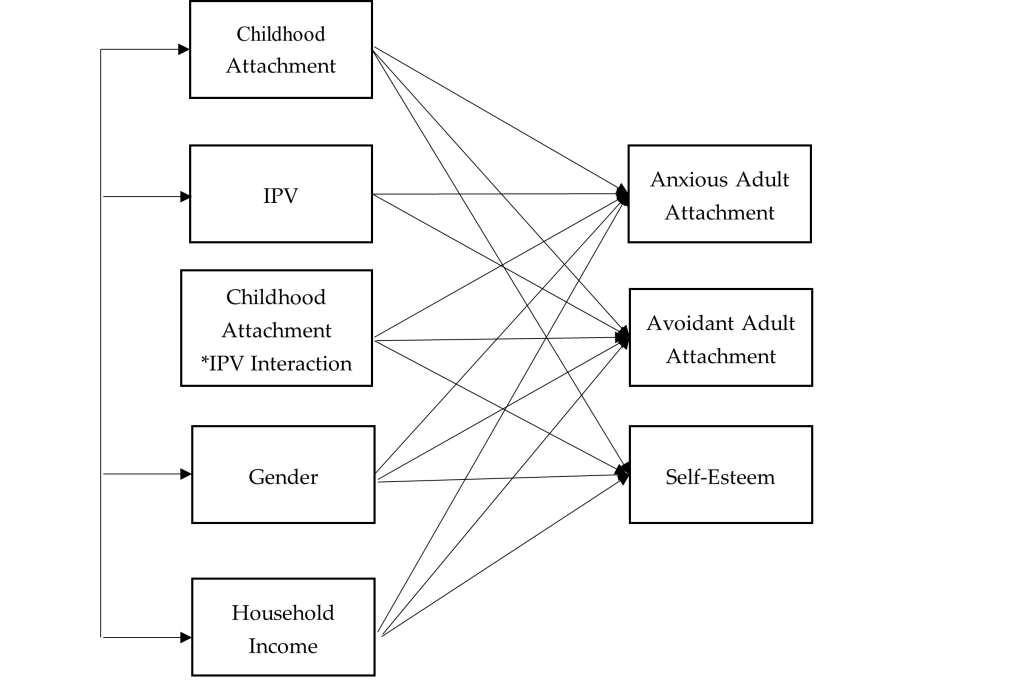
We used SPSS 27 for data preparation and Mplus 8 for data analysis. Missing data were treated with the full information maximum likelihood in Mplus as recommended (Acock, 2005). We examined all the bivariate relationships between all the variables within our study including IPV, childhood attachment, adult attachment (anxious and avoidant attachment), self-esteem, and control variables (i.e., gender and household income). We conducted path analysis to examine the moderating role of childhood attachment between IPV, self-esteem, and adult attachment (see Figure 1). We computed an interaction term by multiplying the predictor (IPV) and the moderator (childhood attachment). A moderation relationship is identified if the interaction item significantly predicts the dependent variables (Baron & Kenny, 1986). The goodness of model fit was evaluated by recommended indices with a non-significant chi-square value, RMSEA < .08, CFI > .90, TLI > .90, and SRMR < .05 (Hooper et al., 2008).
Figure 1
Path Analysis: Moderating Effect of Childhood Attachment on the Relationship Between IPV, Self-Esteem, and Adult Attachment
Results
Descriptive statistics and bivariate correlations of the study variables are demonstrated in Tables 1 and 2. Our model demonstrated good fit to the data, with χ2(4) = 41.90, p = .001, RMSEA = .07, 90% CI [.05, .08], CFI = .99, TLI = .99, SRMR = .02.
The standardized coefficients of the path model revealed that IPV survivors tended to have higher levels of anxious adult attachment (b = .67, p < .001) and avoidant adult attachment (b = .62, p < .001), and lower levels of self-esteem (b = −.29, p < .001) compared with participants without a history of IPV (see Table 3). Individuals with more secure childhood attachment tended to have lower levels of anxious adult attachment (b = −.38, p < .001) and avoidant adult attachment (b = −.31, p < .001), and higher levels of self-esteem (b = .22, p < .001). We found that childhood attachment buffered the relationship between IPV and self-esteem (b = .12, p < .001). Specifically, IPV survivors with more secure childhood attachment demonstrated higher levels of self-esteem. Although the moderation effect was statistically significant, the magnitude of the effect was small. Moreover, IPV survivors with more secure childhood attachment did not demonstrate significant differences on anxious or avoidant adult attachment compared to participants without a history of IPV.
Table 2
Bivariate Correlation Matrix of Variables
| |
1 |
2 |
3 |
4 |
5 |
6 |
7 |
| 1. Anxious Adult Attachment |
– |
|
|
|
|
|
|
| 2. Avoidant Adult Attachment |
.40*** |
– |
|
|
|
|
|
| 3. Self-Esteem |
−.18*** |
−.15*** |
– |
|
|
|
|
| 4. Childhood Attachment |
−.45*** |
−.47*** |
.18*** |
– |
|
|
|
| 5. IPV |
.26*** |
.54*** |
−.17*** |
−.31*** |
– |
|
|
| 6. Gender |
−.10*** |
−.06** |
.14*** |
−.01 |
−.08*** |
– |
|
| 7. Household Income |
.03 |
.08*** |
−.05* |
−.08** |
−.06* |
−.01 |
– |
*p < .05 (two-tailed). **p < .01. ***p < .001.
Table 3
Unstandardized and Standardized Path Coefficients (Standard Errors) for Path Analysis
| Parameter Estimates |
|
Anxious Adult
Attachment |
Avoidant Adult
Attachment |
Self-esteem |
| Childhood Attachment |
Unstandardized |
−.37(.01)*** |
−.33(.02)*** |
.26(.04)*** |
| |
Standardized |
−.38(.01)*** |
−.31(.02)*** |
.22(.03)*** |
| IPV |
Unstandardized |
.61(.01)*** |
.62(.02)*** |
−.33(.04)*** |
| |
Standardized |
.67(.01)*** |
.62(.02)*** |
−.29(.03)*** |
| IPV*Childhood Attachment
Interaction |
Unstandardized |
.00(.00) |
.01(.01) |
.10(.02)*** |
| Standardized |
.01(.01) |
.01(.01) |
.12(.02)*** |
| Control Variables |
| Gender |
Unstandardized |
−.03(.01)** |
−.08(.03)** |
.18(.06)** |
| |
Standardized |
−.02(.01)** |
−.04(.01)** |
.07(.02)** |
| Household Income |
Unstandardized |
.01(.00)*** |
.01(.00)*** |
−.02(.01)** |
| |
Standardized |
.02(.01)*** |
.04(.01)*** |
−.06(.02)** |
*p < .05 (two-tailed). **p < .01. ***p < .001.
Female participants tended to have lower levels of anxious (b = −.02, p < .01) or avoidant adult attachment (b = −.04, p < .01), and higher levels of self-esteem (b = .07, p < .01). Individuals with higher household income reported higher levels of anxious adult attachment (b = .02, p < .001), avoidant adult attachment (b = .04, p < .001), and lower levels of self-esteem (b = −.06, p < .01).
Discussion
Although most existing literature predominantly focuses on revealing how the attachment style of the IPV perpetrators may influence their behavior (Velotti et al., 2018), our study contributes to the field by exploring the potential association between IPV victimization and adult attachment. Using a non-clinical sample, this study identified a positive association between IPV victimization and adult insecure attachment, including both anxious and avoidant dimensions. Meanwhile, a negative association was observed between IPV victimization and self-esteem. These findings concur with the tenets of attachment theory, which posits that individuals who experienced IPV would have a sense of betrayal of trust within intimate relationships. Rather than serving a secure attachment base in intimate adult relationships, IPV experience altered internal models of self as a victim and the other as perpetrator if the individuals stay in the abusive relationships for long enough (Levendosky et al., 2012). IPV survivors may adopt maladaptive coping strategies to mitigate the distress stemming from such intimate relationships. Consequently, these individuals might manifest anxious or avoidant attachment (Levendosky et al., 2012). At the same time, our results indicating reduced self-esteem among IPV victims resonates with previous studies, underscoring the detrimental effects of IPV on self-esteem (Childress, 2013; Karakurt et al., 2014). Enduring undeserved maltreatment from partners can persistently undermine an individual’s sense of self-efficacy and competency (Tariq, 2013).
Our findings do not identify childhood attachment as a significant moderating factor between IPV victimization and insecure attachment in adulthood. There is currently no study to compare with this finding, as the present study is the first to investigate the moderating role of childhood attachment on the relationship between adult IPV victimization and adult attachment.
Although previous research implied that childhood attachment can mitigate the adverse effects of IPV on psychological health and adult life satisfaction (Pang & Thomas, 2020), those studies assessed IPV experiences during an individual’s childhood. Nevertheless, we speculate that IPV targets an individual’s sense of security, which is predominantly influenced by adult romantic relationships (Dutton & White, 2012). This IPV-related sense of security distinguishes itself from childhood attachment, which primarily arises from interactions between parents and children. For instance, the fear associated with intimate relationships and feelings of betrayal, as a result of sustained physical and emotional abuse from an intimate partner, may not be readily alleviated by the sense of security instilled by one’s primary caregivers during childhood. Survivors who were abused by their partner may attempt to manage their distress by deactivating their attachment system, which would reflect more insecure working models of self and others, less self-confidence, and lack of trust in others (Kobayashi et al., 2021).
Conversely, our research determined that childhood attachment acts as a moderator between IPV victimization and self-esteem, aligning with previous studies showing parental support as a vital protective mechanism for the self-esteem of individuals subjected to interpersonal violence (Duru et al., 2019). As posited by attachment theory, secure childhood attachment fosters a robust self-concept, equipping individuals with the belief that they are valuable and deserving of love (Bowlby, 1969). This foundational belief may serve as an effective counterbalance, attenuating the damage to self-esteem precipitated by IPV. We acknowledge that although the moderating effect of childhood attachment on the relationship between IPV victimization and self-esteem was statistically significant, the magnitude standardized coefficients were fairly low. One possible explanation could be that when transitioning to adulthood, individuals expand their social relationships with their peers, romantic partners, and offspring, which may increasingly take on their attachment organizations (Allen et al., 2018; Guarnieri et al., 2015). Future studies could further explore the level of effectiveness of childhood attachment mitigating the negative impact of IPV experience on interpersonal and intrapersonal outcomes in adulthood.
Limitations and Future Directions
Although the present study adds important contributions to the literature on IPV victimization and attachment, several limitations must be acknowledged. First, the dichotomous question of IPV could not fully capture all of the complexity of IPV victimization experiences. Future research should consider other factors related to IPV, including severity of the violence, types of IPV, age of onset, frequency, and duration. Second, retrospective reporting of childhood attachment with the primary caregiver(s) may lead to bias, or distortion in the recall of traumatic events from family of origin. However, previous studies have shown that retrospective reports only have a small amount of bias and that it is not strong enough to invalidate the results for adverse childhood experiences (Hardt & Rutter, 2004).
A growing body of literature has identified adult attachment as a risk factor of IPV (Doumas et al., 2008); here, we were not able to determine the causal relationship between adult attachment and IPV. We did conduct a path analysis using childhood attachment and adult attachment to predict IPV and self-esteem, but the model did not demonstrate a good fit. It is possible that attachment and IPV do not have a simple causal relationship; other childhood trauma experiences may contribute to the complexity of the IPV (Li et al., 2019).
Finally, not knowing the types of attachment in childhood limited our exploration regarding the changes of attachment styles from childhood to adulthood. The cross-sectional design of assessing childhood attachment and adult attachment concurrently did not provide sufficient evidence to determine the cause and effect. Bowlby (1969) believed that there is a continuity between childhood attachment and adult attachment over the life course. An individual’s security in adult relationships may be a partial reflection of their experiences with primary caregivers in early childhood (Ammaniti et al., 2000). However, one of the common misconceptions about attachment theory is that attachment is always stable from infancy to adulthood (Hazan & Shaver, 1994). It is possible that adults’ attachment patterns would change if their relational experiences were disturbed by relational trauma such as IPV (West & George, 1999) or childhood trauma (Shen & Soloski, 2024), which partially explains that childhood attachment is not a significant moderator between IPV and adult attachment from our findings. Future research could conduct longitudinal studies to examine the changes of attachment and how childhood trauma and IPV influences attachment over time.
Implications
The findings of the present study provide insights that may inform clinical interventions for adult survivors who have experienced IPV to rebuild trusting interpersonal relationships and relationships with self. First, IPV experiences were significantly associated with anxious and avoidant adult attachment. During a traumatic experience, such as IPV, the attachment security system is activated, and survivors are in a surviving mode and tend to seek protection. Unfortunately, IPV involves power, control, and betrayal within an intimate relationship, which may damage internal working models of self and others if they stay for long enough (Levendosky et al., 2012). Thus, clinical interventions could focus on altering survivors’ negative internal working models to increase security within non-abusive close relationships. Close friends and family members could remain as a secure base for IPV survivors while they rebuild their personal and social lives that IPV have damaged. Additionally, therapeutic relationships could potentially serve as a secure base for survivors to explore their attachment behaviors. Survivors with avoidant attachment demonstrate deactivation attachment behaviors (Brenner et al., 2021), such as minimizing the impact of their trauma experiences, having a tendency to perceive and present themselves as strong, or avoiding discussing their trauma experiences to avoid the possible pain (Muller, 2009). Therefore, clinicians need to hold a safe space to challenge survivors with avoidant attachment to reactivate their attachment systems, such as by validating their avoidance and ambivalence or facilitating conversations to turn toward trauma-related experiences and emotions instead of turning away. Survivors with anxious attachment, on the other hand, demonstrate hyperactivation attachment behaviors, including fear of rejection and abandonment, hypersensitivity to and preoccupation with relationships and intimacy, utilization of negative emotional regulation strategies, as well as difficulties with leaving abusive relationships (Kural & Kovacs, 2022; Velotti et al., 2018). Clinicians could teach anxious-attached survivors some effective coping strategies, including self-regulation skills, creating boundaries, establishing safety plans, maintaining relationships with others, and increasing self-compassion (Rizo et al., 2017), which may help them to perceive themselves as worthy, lovable, and less dependent on others.
Furthermore, group counseling is a powerful way to learn about trusting oneself and others and to improve interpersonal relationship skills. Clients’ attachment patterns will be activated through interactions with the group members and the facilitators. Clients with anxious attachment tend to react to group members’ rejections, while clients with avoidant attachment tend to demonstrate withdrawal behaviors (e.g., disengagement; Zorzella et al., 2014). Therefore, when working with these clients, clinicians should stimulate the change of internal working models by using the group as a secure base to foster corrective emotional exchanges that challenge group members’ maladaptive beliefs about themselves and others (Marmarosh et al., 2013).
One of the important findings of the current study is that childhood attachment with the primary caregiver(s) buffered the relationship between IPV and self-esteem. From a clinical point of view, the result may bring hope for adult survivors of interpersonal violence regarding their healing process; primary caregivers could still serve as a secure base to offer a crucial opportunity to strengthen the internal working models that would positively affect later adjustment. Counselors could assess survivors’ attachment with their primary caregivers and give them autonomy to determine if it is beneficial to get their non-abusive primary caregivers involved in the treatment to provide support. Although the moderation result from the present study was statistically significant, the magnitude of moderating effect was small. During adulthood, individuals expand their relationship networks with their peers (e.g., friends) and romantic partners, as these relationships become more central in their daily life (Guarnieri et al., 2015). Therefore, the effectiveness of childhood attachment mitigating the adverse effect of IPV in adulthood clinically needs to be further investigated.
Conclusion
The present study empirically examines the moderation role of childhood attachment on the association between IPV, adult attachment, and self-esteem. Specifically, we found that childhood attachment was a significant moderator buffering the relationship between the experience of IPV and self-esteem. A theoretical and empirical understanding of the role of attachment in the context of IPV has implications for researchers and clinicians working with survivors and their families.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Acock, A. C. (2005). Working with missing values. Journal of Marriage and Family, 67(4), 1012–1028.
https://doi.org/10.1111/j.1741-3737.2005.00191.x
Allen, J. P., Grande, L., Tan, J., & Leob, E. (2018). Parent and peer predictors of change in attachment security from adolescence to adulthood. Child Development, 89(4), 1120–1132. https://doi.org/10.1111/cdev.12840
Ammaniti, M., Van Ijzendoorn, M. H., Speranza, A. M., & Tambelli, R. (2000). Internal working models of attachment during late childhood and early adolescence: An exploration of stability and change. Attachment & Human Development, 2(3), 328–346. https://doi.org/10.1080/14616730010001587
Armsden, G. C., & Greenberg, M. T. (1987). The inventory of parent and peer attachment: Individual differences and their relationship to psychological well-being in adolescence. Journal of Youth and Adolescence, 16(5), 427–454. https://doi.org/10.1007/BF02202939
Baron, R. M., & Kenny, D. A. (1986). The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51(6), 1173–1182. https://doi.org/10.1037/0022-3514.51.6.1173
Black, M. C., Basile, K. C., Breiding, M. J., Smith, S. G., Walters, M. L., Merrick, M. T., Chen, J., & Stevens, M. R. (2011). The National Intimate Partner and Sexual Violence Survey: 2010 summary report. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention.
Bowlby, J. (1969). Attachment and loss, Vol. 1: Attachment. Basic Books.
Bowlby, J. (1973). Attachment and loss, Vol. 2: Separation: Anxiety and anger. Basic Books.
Bradshaw, C. P., & Garbarino, J. (2004). Social cognition as a mediator of the influence of family and community violence on adolescent development: Implications for intervention. In J. Devine, J. Gilligan, K. A. Miczek, R. Shaikh, & D. Pfaff (Eds.), Youth violence: Scientific approaches to prevention (pp. 85–105). New York Academy of Sciences.
Brennan, K. A., Clark, C. L., & Shaver, P. R. (1998). Self-report measurement of adult attachment: An integrative overview. In J. A. Simpson & W. S. Rholes (Eds.), Attachment theory and close relationships (pp. 46–76). Guilford.
Brennan, K. A., & Morris, K. A. (1997). Attachment styles, self-esteem, and patterns of seeking feedback from romantic partners. Personality and Social Psychology Bulletin, 23(1), 23–31. https://doi.org/10.1177/0146167297231003
Brenner, I., Bachner-Melman, R., Lev-Ari, L., Levi-Ogolnic, M., Tolmacz, R., & Ben-Amitay, G. (2021). Attachment, sense of entitlement in romantic relationships, and sexual revictimization among adult CSA survivors. Journal of Interpersonal Violence, 36(19–20), NP10720–NP10743. https://doi.org/10.1177/0886260519875558
Burke, J. G., Thieman, L. K., Gielen, A. C., O’Campo, P., & McDonnell, K. A. (2005). Intimate partner violence, substance use, and HIV among low-income women: Taking a closer look. Violence Against Women, 11(9), 1140–1161. https://doi.org/10.1177/1077801205276943
Cherrier, C., Courtois, R., Rusch, E., & Potard, C. (2023). Parental attachment, self-esteem, social problem-solving, intimate partner violence victimization in emerging adulthood. The Journal of Psychology, 157(7), 451–471. https://doi.org/10.1080/00223980.2023.2242561
Childress, S. (2013). A meta-summary of qualitative findings on the lived experience among culturally diverse domestic violence survivors. Issues in Mental Health Nursing, 34(9), 693–705. https://doi.org/10.3109/01612840.2013.791735
Doumas, D. M., Pearson, C. L., Elgin, J. E., & McKinley, L. L. (2008). Adult attachment as a risk factor for intimate partner violence: The “mispairing” of partners’ attachment styles. Journal of Interpersonal Violence, 23(5), 616–634. https://doi.org/10.1177/0886260507313526
Duru, E., Balkis, M., & Turkdoğan, T. (2019). Relational violence, social support, self-esteem, depression and anxiety: A moderated mediation model. Journal of Child and Family Studies, 28, 2404–2414.
https://doi.org/10.1007/s10826-019-01509-2
Dutton, D. G., & White, K. R. (2012). Attachment insecurity and intimate partner violence. Aggression and Violent Behavior, 17(5), 475–481. https://doi.org/10.1016/j.avb.2012.07.003
Gamble, S. A., & Roberts, J. E. (2005). Adolescents’ perceptions of primary caregivers and cognitive style: The roles of attachment security and gender. Cognitive Therapy and Research, 29, 123–141. https://doi.org/10.1007/s10608-005-3160-7
Gilbert, L. K., Zhang, X., Basile, K. C., Breiding, M., & Kresnow, M. (2023). Intimate partner violence and health conditions among U. S. adults—National Intimate Partner Violence Survey, 2010–2012. Journal of Interpersonal Violence, 38(1–2), 237–261. https://doi.org/10.1177/08862605221080147
Gomez, R., & McLaren, S. (2007). The inter-relations of mother and father attachment, self-esteem and aggression during late adolescence. Aggressive Behavior, 33(2), 160–169. https://doi.org/10.1002/ab.20181
Gormley, B., & Lopez, F. G. (2010). Psychological abuse perpetration in college dating relationships: Contributions of gender, stress, and adult attachment orientations. Journal of Interpersonal Violence, 25(2), 204–218. https://doi.org/10.1177/0886260509334404
Guarnieri, S., Smorti, M., & Tani, F. (2015). Attachment relationships and life satisfaction during emerging adulthood. Social Indicators Research, 121(3), 833–847. https://doi.org/10.1007/s11205-014-0655-1
Hardt, J., & Rutter, M. (2004). Validity of adult retrospective reports of adverse childhood experiences: Review of the evidence. Journal of Child Psychology and Psychiatry, 45(2), 260–273. https://doi.org/10.1111/j.1469-7610.2004.00218.x
Hazan, C., & Shaver, P. R. (1994). Deeper into attachment theory. Psychological Inquiry, 5(1), 68–79. https://doi.org/10.1207/s15327965pli0501_15
Hooper, D., Coughlan, J., & Mullen, M. (2008). Structural equation modeling: Guidelines for determining model fit. Electronic Journal of Business Research Methods, 6(1), 53–60. https://doi.org/10.21427/D7CF7R
Jewkes, R., Fulu, E., Tabassam Naved, R., Chirwa, E., Dunkle, K., Haardörfer, R., Garcia-Moreno, C., & the UN Multi-country Study on Men and Violence Study Team. (2017). Women’s and men’s reports of past-year prevalence of intimate partner violence and rape and women’s risk factors for intimate partner violence: A multicountry cross-sectional study in Asia and the Pacific. PloS Medicine, 14(9), e1002381. https://doi.org/10.1371/journal.pmed.1002381
Karakurt, G., Koç, E., Katta, P., Jones, N., & Bolen, S. D. (2022). Treatments for female victims of intimate partner violence: Systematic review and meta-analysis. Frontiers in Psychology, 13, 793021. https://doi.org/10.3389/fpsyg.2022.793021
Karakurt, G., Smith, D., & Whiting, J. (2014). Impact of intimate partner violence on women’s mental health. Journal of Family Violence, 29(7), 693–702. https://doi.org/10.1007/s10896-014-9633-2
Kobayashi, J. E., Levendosky, A. A., Bogat, G. A., & Weatherill, R. P. (2021). Romantic attachment as a mediator of the relationships between interpersonal trauma and prenatal representations. Psychology of Violence, 11(2), 133–143. https://doi.org/10.1037/vio0000361
Kural, A. I., & Kovacs, M. (2022). The role of anxious attachment in the continuation of abusive relationships: The potential for strengthening a secure attachment schema as a tool of empowerment. Acta Psychologica, 225, 103537. https://doi.org/10.1016/j.actpsy.2022.103537
Levendosky, A. A., Lannert, B., & Yalch, M. (2012). The effects of intimate partner violence on women and child survivors: An attachment perspective. Psychodynamic Psychiatry, 40(3), 397–433.
https://doi.org/10.1521/pdps.2012.40.3.397
Li, S., Zhao, F., & Yu, G. (2019). Childhood maltreatment and intimate partner violence victimization: A meta-analysis. Child Abuse & Neglect, 88, 212–224. https://doi.org/10.1016/j.chiabu.2018.11.012
Lindgren, M. S., & Renck, B. (2008). “It is still so deep-seated, the fear”: Psychological stress reactions as consequences of intimate partner violence. Journal of Psychiatric and Mental Health Nursing, 15(3), 219–228. https://doi.org/10.1111/j.1365-2850.2007.01215.x
Lopez, F. G., & Brennan, K. A. (2000). Dynamic processes underlying adult attachment organization: Toward an attachment theoretical perspective on the healthy and effective self. Journal of Counseling Psychology, 47(3), 283–300. https://doi.org/10.1037/0022-0167.47.3.283
Marmarosh, C. L., Markin, R. D., & Spiegel, E. B. (2013). Attachment in group psychotherapy. American Psychological Association. https://doi.org/10.1037/14186-000
Matheson, F. I., Daoud, N., Hamilton-Wright, S., Borenstein, H., Pedersen, C., & O’Campo, P. (2015). Where did she go? The transformation of self-esteem, self-identity, and mental well-being among women who have experienced intimate partner violence. Women’s Health Issues, 25(5), 561–569. https://doi.org/10.1016/j.whi.2015.04.006
McClure, M. M., & Parmenter, M. (2020). Childhood trauma, trait anxiety, and anxious attachment as predictors of intimate partner violence in college students. Journal of Interpersonal Violence, 35(23–24), 6067–6082. https://doi.org/10.1177/0886260517721894
McLaughlin, J., O’Carroll, R. E., & O’Connor, R. C. (2012). Intimate partner abuse and suicidality: A systemic review. Clinical Psychology Review, 32(8), 677–689. https://doi.org/10.1016/j.cpr.2012.08.002
Meeker, K. A., Hayes, B. E., Randa, R., & Saunders, J. (2020). Examining risk factors of intimate partner violence victimization in Central America: A snapshot of Guatemala and Honduras. International Journal of Offender Therapy and Comparative Criminology, 68(5), 468–487. https://doi.org/10.1177/0306624X20981049
Moretti, M. M., & Peled, M. (2004). Adolescent-parent attachment: Bonds that support healthy development. Paediatrics & Child Health, 9(8), 551–555. https://doi.org/10.1093/pch/9.8.551
Muller, R. T. (2009). Trauma and dismissing (avoidant) attachment: Intervention strategies in individual psychotherapy. Psychotherapy: Theory, Research, Practice, Training, 46(1), 68–81. https://doi.org/10.1037/a0015135
Pang, L. H. G., & Thomas, S. J. (2020). Exposure to domestic violence during adolescence: Coping strategies and attachment styles as early moderators and their relationship to functioning during adulthood. Journal of Child & Adolescent Trauma, 13(2), 185–198. https://doi.org/10.1007/s40653-019-00279-9
Ponti, L., & Tani, F. (2019). Attachment bonds as risk factors of intimate partner violence. Journal of Child and Family Studies, 28, 1425–1432. https://doi.org/10.1007/s10826-019-01361-4
Rizo, C. F., Givens, A., & Lombardi, B. (2017). A systematic review of coping among heterosexual female IPV survivors in the United States with a focus on the conceptualization and measurement of coping. Aggression and Violent Behavior, 34, 35–50. https://doi.org/10.1016/j.avb.2017.03.006
Rosenberg, M. (1965). Society and the adolescent self-image. Princeton University Press.
Rosenberg, M. (1979). Conceiving the self. Basic Books.
Sayed, S., Iacoviello, B. M., & Charney, D. S. (2015). Risk factors for the development of psychopathology following trauma. Current Psychiatry Reports, 17, 70. https://doi.org/10.1007/s11920-015-0612-y
Scott, S., & Babcock, J. C. (2010). Attachment as a moderator between intimate partner violence and PTSD symptoms. Journal of Family Violence, 25(1), 1–9. https://doi.org/10.1007/s10896-009-9264-1
Shen, F., Liu, Y, & Brat, M. (2021). Attachment, self-esteem, and psychological distress: A multiple-mediator model. The Professional Counselor, 11(2), 129–142. https://doi.org/10.15241/fs.11.2.129
Shen, F., & Soloski, K. L. (2024). Examining the moderating role of childhood attachment for the relationship between child sexual abuse and adult attachment. Journal of Family Violence, 39, 347–357.
https://doi.org/10.1007/s10896-022-00456-9
St. Vil, N. M., Carter, T., & Johnson, S. (2021). Betrayal trauma and barriers to forming new intimate relationships among survivors of intimate partner violence. Journal of Interpersonal Violence, 36(7–8), NP3495–NP3509. https://doi.org/10.1177/0886260518779596
Sutton, T. E. (2019). Review of attachment theory: Familial predictors, continuity and change, and intrapersonal and relational outcomes. Marriage & Family Review, 55(1), 1–22. https://doi.org/10.1080/01494929.2018.1458001
Tariq, Q. (2013). Impact of intimate partner violence on self esteem of women in Pakistan. American Journal of Humanities and Social Sciences, 1(1), 25–30. https://doi.org/10.11634/232907811604271
Velotti, P., Beomonte Zobel, S., Rogier, G., & Tambelli, R. (2018). Exploring relationships: A systematic review on intimate partner violence and attachment. Frontiers in Psychology, 9, 1166. https://doi.org/10.3389/fpsyg.2018.01166
West, M., & George, C. (1999). Abuse and violence in intimate adult relationships: New perspectives from attachment theory. Attachment & Human Development, 1(2), 137–156. https://doi.org/10.1080/14616739900134201
Wilkinson, R. B. (2004). The role of parental and peer attachment in the psychological health and self-esteem of adolescents. Journal of Youth and Adolescence, 33, 479–493. https://doi.org/10.1023/B:JOYO.0000048063.59425.20
Zorzella, K. P. M., Muller, R. T., & Classen, C. C. (2014). Trauma group therapy: The role of attachment and therapeutic alliance. International Journal of Group Psychotherapy, 64(1), 24–47. https://doi.org/10.1521/ijgp.2014.64.1.24
Fei Shen, PhD, LMFT, is an assistant professor at Kean University. Ying Zhang, PhD, is an assistant professor at Clarkson University. Xiafei Wang, PhD, is an assistant professor at Syracuse University. Correspondence may be addressed to Fei Shen, 1000 Morris Ave., Union, NJ 07083, fshen@kean.edu.
Mar 30, 2018 | Volume 8 - Issue 1
Trish J. Smith, Courtney M. Holmes
Intimate partner violence (IPV) is a public health concern that affects millions of people. Physical violence is one type of IPV and has myriad consequences for survivors, including traumatic brain injury (TBI) and post-traumatic stress disorder (PTSD). It is estimated that as many as 23,000,000 women in the United States who have experienced IPV live with brain injury. This article overviews the intersection of TBI and PTSD as a result of IPV. Implications for counselors treating women impacted by IPV suggest counselors incorporate an initial screening for TBI and consider TBI- and PTSD-specific trauma-informed approaches within therapy to ensure best practices. A case study demonstrating the importance of the awareness of the potential for TBI in clients who experience IPV is included.
Keywords: intimate partner violence, traumatic brain injury, post-traumatic stress disorder, PTSD, public health
In 1981, the U.S. Congress declared October as Domestic Violence Awareness Month, marking a celebratory hallmark for advocates and survivors nationwide (National Resource Center on Domestic Violence, 2012). Since this time, similar social and legislative initiatives have increased overall awareness of gender inequality, thus influencing a decline in women’s risk for intimate partner violence (IPV; Powers & Kaukinen, 2012). Recent initiatives, such as a national briefing focused on brain injury and domestic violence hosted by the Congressional Brain Injury Task Force, continue to call increased attention to the various intersections and implications of this national public health epidemic (Brain Injury Association of America, 2017). Unfortunately, despite various social advocacy movements, IPV remains an underrepresented problem in the United States (Chapman & Monk, 2015). As a result, IPV and related mental and physical health consequences continue to exist at alarmingly high rates (Chapman & Monk, 2015).
IPV refers to any act of physical or sexual violence, stalking, or psychological aggression by a current or previous intimate partner. An intimate partner is an individual with whom someone has close relations with, in which relations are characterized by the identity as a couple and emotional connectedness (Breiding, Basile, Smith, Black, & Mahendra, 2015). An intimate partner may include but is not limited to a spouse, boyfriend, girlfriend, or ongoing sexual partner (Breiding et al., 2015). Physical violence is the intentional use of force that can result in death, disability, injury, or harm and can include the threat of using violence (Breiding et al., 2015). Sexual, emotional, and verbal abuse are often perpetrated in conjunction with physical violence in relationships (Krebs, Breiding, Browne, & Warner, 2011).
Heterosexual and same-sex couples experience IPV at similar rates (Association of Women’s Health, Obstetric and Neonatal Nurses, 2015). Researchers estimate that more than one in every three women and at least one in four men have experienced IPV (Sugg, 2015). These rates likely underestimate the true prevalence of IPV, given that populations with traditionally high incidences of abuse (e.g., poor, hospitalized, homeless, and incarcerated women) may not be included in survey samples (Scordato, 2013; Tramayne, 2012). Additionally, fear and shame often serve as a deterrent to reporting abuse (Scordato, 2013). Although both men and women are victims of IPV, women are abused at a disproportionate rate (Association of Women’s Health, Obstetric and Neonatal Nurses, 2015) and have a greater risk than men of acquiring injury as a result of physical violence (Scordato, 2013; Sillito, 2012). Data have shown that 2–12% of injuries among women brought into U.S. emergency departments are related to IPV (Goldin, Haag, & Trott, 2016), 35% of all homicides against women are IPV-related (Krebs et al., 2011), and approximately 22% of women have experienced physical IPV, averaging 7.1 incidences of violence across their lifespan (Sherrill, Bell, & Wyngarden, 2016). IPV is a pervasive relational problem that creates a myriad of complex mental and physical health issues for female survivors (Sugg, 2015). One health issue commonly experienced by female survivors of IPV is post-traumatic stress disorder (PTSD; Black et al., 2011).
PTSD and IPV
A Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-5; American Psychiatric Association, 2013) diagnosis of PTSD is based on the client’s exposure to a dangerous or life-threatening stressor and consists of the following symptomology: intrusion of thoughts or re-experiencing of the event, including flashbacks; avoidance of experiences or thoughts related to the stressor; negative alterations in cognition and mood; and changes in reactivity, including hypervigilance or hyperarousal. According to Bourne, Mackay, and Holmes (2013), flashbacks are the hallmark symptom of PTSD and involve a process in which the individual dissociates and feels as though they are re-experiencing the traumatic event through involuntary, vivid, and emotional memories. Although PTSD symptoms may occur immediately after a traumatic event, symptoms may have a delayed onset in which the full range of symptoms can manifest even 6 months after the event, showing only partial symptom criteria in the preceding months (Utzon-Frank et al., 2014).
Experiencing IPV increases risk for developing PTSD (National Center on Domestic Violence, Trauma, and Mental Health, 2014). In a national sample of 9,000 women, 62% who experienced some form of IPV reported at least one PTSD symptom (Black et al., 2011). Women who experience IPV are almost three times as likely to meet criteria for PTSD when compared with those who have not had such experiences (Fedovskiy, Higgins, & Paranjape, 2008). Although PTSD is a common manifestation of IPV, another condition, traumatic brain injury (TBI), also is prevalent in survivors (Sherrill et al., 2016). The symptomology of TBI mirrors that of PTSD, rendering the clinical tasks of appropriate diagnosis and treatment planning especially difficult (McFadgion, 2013).
TBI and IPV
TBI is defined as a change in brain function caused by an external force (e.g., strike to the head or strangulation; Murray, Lundgren, Olson, & Hunnicutt, 2016). Symptoms include headaches, dizziness, fatigue, difficulty concentrating, irritability, and perceptual difficulties with noise and light (Zollman, 2016). Other symptoms can include problems with attention, memory, processing speed, decision making, and mood (Jeter et al., 2013). Professionals can use computerized tomography (CT) scans to find contusions, hematomas, diffuse axonal injury, and secondary brain injuries, which aid in the medical diagnosis of TBI (Currie et al., 2016). Although CT is widely used in assisting with the identification of TBI, a final diagnosis is most often made in a clinical interview with the patient, treating physician, and if feasible, those who observed the violent incident or responded to it (Zollman, 2016). Violence that causes TBI may or may not leave internal or external physical evidence of trauma (e.g., bruising, scarring); thus it is crucial that assessment and screening attempts take place beyond neuroimaging technology and are included as a part of a comprehensive evaluation (Joshi, Thomas, & Sorenson, 2012).
Researchers indicate that over 60% of women, with estimates as high as 96%, who experience IPV sustain injury to the face or head areas, including attempted strangulation (McFadgion, 2013; Sherrill et al., 2016; St. Ivany & Schminkey, 2016). Acquired TBI through IPV can complicate the therapeutic treatment of women (Murray et al., 2016). Brain injury shares similar symptomology with PTSD, increasing likelihood for misdiagnosis, complications with care, and long-term brain damage (McFadgion, 2013). Additionally, TBI and PTSD are often comorbid diagnoses, and those who survive physical trauma and incur a TBI suffer negative mental health impacts such as depression, anxiety, and suicidal ideation (Smith, Mills, & Taliaferro, 2001).
PTSD and TBI have an extensive impact on brain functioning (Boals & Banks, 2012; Saar-Ashkenazy et al., 2016). Individuals with PTSD experience daily cognitive failures in memory, perception, and motor function (Boals & Banks, 2012; Saar-Ashkenazy et al., 2016). Other researchers have shown that PTSD negatively impacts brain functioning on multiple levels, including stimuli recognition, and overall cognitive functioning (Saar-Ashkenazy et al., 2016). Similarly, individuals with TBI may experience physical, sensory, cognitive, and social difficulties as a result of their brain injury (Brain Injury Association of Virginia , 2010). Given the overlapping symptoms of PTSD and TBI, and the overall impact on functioning, it is critical for counselors to consider these factors when diagnosing and treating women who have experienced IPV.
In sum, IPV is a widespread public health issue with a multitude of negative consequences related to human functioning. Incidences of TBI in women who have experienced IPV cannot be overlooked. A framework for mental health counselors that includes awareness of the overlapping symptoms between two likely outcomes of IPV and their manifestation is crucial for successful case conceptualization and treatment.
Counseling Implications
PTSD and TBI have extensive impact on human functioning, and it is critical that counselors examine appropriate responses and considerations for therapeutic treatment of female survivors of physical violence resulting from IPV. Clinical considerations should be incorporated into initial screening, therapeutic approaches, and communication with clients.
Screening and Assessment
McLeod, Hays, and Chang (2010) suggested that counselors universally screen clients for a current or past history of IPV. Based on the literature, survivors of IPV face various challenges when seeking services and either reporting or disclosing abuse, including: self-blame for the abuse; fear of the perpetrator; internalized shame; lack of acknowledgement of the level of danger; perception that community services are not helpful; lack of housing, child care, and transportation; access to money; and lack of educational opportunities (Fúgate, Landis, Riordan, Naureckas, & Engel, 2005; Lutenbacher, Cohen, & Mitzel, 2003; McLeod et al., 2010; Scordato, 2013). Minority populations experience additional challenges, including fear of prejudice and systemic oppression (Scordato, 2013). Thus, counselors carry the responsibility to broach screening with all clients. With an intentional screening for IPV, counselors are able to further identify TBI as a result of physical violence in IPV to ascertain medical and related concerns. Given the statistical probability that a woman who experienced physical IPV sustained past injury to the head or neck, initial screening is critical (Murray et al., 2016). The Pennsylvania Coalition Against Domestic Violence (PCADV; 2011) provides a guide based on a classic TBI screening called HELPS. The guide asks questions in the context of IPV, including if the person has ever been: (a) hit on the head, mouth, or other places on the face; (b) pushed so hard the head strikes a hard or firm surface; (c) shaken violently; (d) injured to the head or neck, including strangulation, choking, or suffocating that restricted breathing; and (e) nearly drowned, electrocuted, or intentionally given something allergic. These questions serve as a guide in detecting if the survivor has acquired TBI; however, they should not be used in place of a medical assessment (PCADV, 2011).
The Brain Injury Association of America (2015) describes symptoms of TBI as including: headaches, dizziness, lack of awareness of surroundings, vomiting, lightheadedness, poor attention and concentration, fatigue, and ringing in the ears. Impairments involving functions related to memory, decision making, and processing speed may be indicators of brain injury (Jeter et al., 2013). Recognizing TBI allows for the appropriate response in treatment, including identifying necessary medical consultations and referrals.
Therapeutic Approaches to IPV
After the brain is injured, a recovery process involving three stages is prompted, including: cell repair, functional cell plasticity, and neuroplasticity (Villamar, Santos Portilla, Fregni, & Zafonte, 2012). Zasler, Katz, Zafonte, and Arciniegas (2007) described neuroplasticity as the process in which spared healthy brain regions compensate for the loss of functioning in damaged regions. Kimberley, Samargia, Moore, Shakya, and Lang (2010) suggested that repetition of activities is required to induce neuroplasticity, or recovery of the brain.
Researchers have shown that certain techniques in talk therapy can aid in the recovery of the brain, serving to benefit both the treatment of PTSD as well as the alleviation of symptoms in TBI (Chard, Schumm, McIlvain, Bailey, & Parkinson, 2011). For example, Chard et al. (2011) compared two therapies: (a) cognitive processing therapy (CPT), a form of cognitive behavioral therapy effective in treating PTSD; and (b) an alternate version of CPT, CPT-cognitive only (CPT-C), which omits the writing and reading of one’s trauma narrative and instead emphasizes cognitive challenging and rehearsal. Both approaches were applied to a sample of 42 male veterans who met criteria for PTSD, had history of TBI, and were compared across four groups based on severity and treatment approach (Chard et al., 2011). In addition to speech therapy two to three times a week and a psychoeducation group 23 hours a week, CPT-C individual sessions and group sessions were each held twice a week as a part of a residential treatment program (Chard et al., 2011). Chard et al. identified a significant main effect across PTSD and depression measures for both groups, indicating CPT-C as a plausible treatment for clients with TBI.
Another therapeutic approach includes CRATER therapy, which is an acronym that encompasses six targets for therapy: catastrophic reaction, regularization, alliance, triangulation, externalization, and resilience (Block & West, 2013). The first target, catastrophic reaction, is based on targeting the explosive reaction that is in response to overwhelming environmental stimuli; regularization is the therapist’s approach to establishing a regular daily routine for the client (e.g., sleep–wake cycle, meal times); alliance is the relationship between the professional and survivor; triangulate is the relationship expanded beyond the client to include a family member or friend; externalize negates self-blame; and resilience promotes the use of effective coping skills (Block & West, 2013). The individual’s family members and friends are specifically targeted in the approach to account for ecological validity and provide support. Block and West (2013) stated, “CRATER therapy targets the formation of a good working alliance, teaches the survivor to perform skills without cues from the provider and integrates both cognitive and therapy interventions” (p. 777). Overall, this theory infuses cognitive restructuring into individual psychotherapy and assists the client in developing effective coping strategies.
In addition to the implementation of specific therapeutic approaches in counseling, the counselor can incorporate management strategies to accommodate survivors’ brain injury symptoms in counseling sessions. For example, a client who takes longer to complete tasks and answer questions because of an impaired information processing speed can be accommodated by the counselor doing the following: (a) allowing extra time for responses, (b) presenting one thing at a time, and (c) not answering for them during the lapse in response time (BIAV, 2010). The PCADV (2011) also recommends speaking in a clear and literal sense as well as providing tasks in short increments. If memory is impaired, the counselor can make it a point to repeat information as necessary, encourage the use of external memory aids (e.g., journals, calendars), and give reminders and prompts to assist with recall (Block & West, 2013). In the case in which the client shows poor self-monitoring skills and lacks adherence to social rules or consistently dominates the dialogue in sessions, the counselor can provide feedback, encourage turn-taking, and gently provide redirection of behavior (BIAV, 2010). Implementing techniques that involve feedback and redirection also can decrease chances of oversharing that might re-traumatize the survivor (Clark, Classen, Fourt, & Shetty, 2014). Utilizing compensatory strategies such as these can ensure the accessibility and efficacy of counseling sessions to survivors with TBI.
Therapeutic Communication With IPV Clients
Aside from specific counseling approaches and management strategies, several considerations can be made by the counselor to ensure an informed response in communication and chosen interventions. Building a therapeutic relationship, including instilling hope for possible change, is especially useful with complex PTSD diagnoses (Marotta, 2000). Additionally, researchers suggest that receiving social support is a resiliency factor in trauma recovery (Shakespeare-Finch, Rees, & Armstrong, 2015; Zhou, Wu, Li, & Zhen, 2016). However, data suggest that women with brain injury, when compared with male counterparts, experience more negative alterations to social and play behavior, including more exclusion and rejection in social situations (Mychasiuk, Hehar, Farran, & Esser, 2014). Mychasiuk et al. (2014) indicated that group therapy or other social types of interventions related to social support building and safety planning may be contraindicated until these specific challenges can be addressed in individual counseling.
Counselors should be aware of the cyclical nature of abusive relationships that can result in multiple brain injuries over time (Murray et al., 2016). Additionally, counselors should understand complex PTSD, which is associated with prolonged exposure to severe trauma; alterations to affect and impulses, self-perception, interactions with others, and increased somatization; and medical problems (Pill, Day, & Mildred, 2017). Consideration of the potential impact that cumulative brain injuries and prolonged trauma have on health outcomes is critical for effective clinical intervention (Kwako et al., 2011), as myriad aspects of a woman’s ability to identify and understand her situation may be negatively impacted. A critical skill for women in violent relationships includes the need to account for, and effectively assess, one’s physical environment at the time of abuse. A client can take the following precautions to protect herself from future violence: (a) making herself a smaller target by curling up into a ball in a corner, (b) avoiding wearing scarves or necklaces that can be used in strangulation attempts, (c) guarding her head with her arms around each side of her head, and
(d) hiding guns or knives (PCADV, 2011). Furthermore, it is imperative that the counselor actively assist in the safety planning process given that head injury and trauma often impair cognitive processes such as a person’s ability to plan and organize (PCADV, 2011). Initiating the safety planning process as a psychoeducational component of treatment could serve to counter shame and self-blame for the survivor, ensuring that a trauma-informed approach and best practices are maintained (Clark et al., 2014).
Ethical Implications
Client cases that include current or past IPV are often fraught with numerous ethical considerations (McLaughlin, 2017). Perhaps the most pervasive ethical issue is the responsibility of mandated reporting. Counselors must be aware of the intricacies of such responsibility and understand the limits of reporting as it pertains to survivors of IPV (American Counseling Association, 2014). Clinicians should become skilled at assessing for violence in relationships so that reporting can occur if one of the following situations arise: abuse of children, older adults, or other vulnerable populations; duty to warn situations; or risk of suicide. The responsibility to report must be discussed with clients during the informed consent process and throughout treatment (American Counseling Association, 2014, B.1.d).
IPV presents additional complications for treatment providers. Researchers suggest that more than 50% of couples in therapy report at least one incident of physical aggression against their partner (O’Leary, Tintle, & Bromet, 2014). Despite this implication, counselors fail to adequately assess for violence or intervene when violence is present. Once a thorough assessment has taken place, clinicians can evaluate the most appropriate and safe course of treatment for each individual and the couple together. Treatment options include continued couples work (when appropriate), separate individual therapy, or group work that may include anger management or other behavioral-change strategies (Lawson, 2003).
Counselors working with survivors of IPV should expect to regularly determine how to “maximize benefit and minimize harm” for each client (McLaughlin, 2017, p. 45). Counselors may find themselves working with clients who want or need to stay in the relationship or those who want or need to leave the relationship. Each situation is complicated with a variety of personal factors such as level of violent threat and access to financial and other types of resources. Individual assessment in collaboration with the client to determine the best therapeutic strategy is necessary (McLaughlin, 2017).
Finally, counselors may hold overt or covert personal biases toward IPV clients and violence against women. Counselors should evaluate personal feelings toward both victims and perpetrators of IPV prior to working with them and throughout the course of treatment. McLeod et al. (2010) developed a competency checklist for counselors to assist in necessary self-reflection and self-evaluation of their level of competency when working with this population. Finally, counselors should understand the critical nature of supervision and consultation and seek it out when necessary (McLaughlin, 2017).
Case Study
The following case study is a hypothetical case based loosely on the first author’s experience as a counselor in a domestic violence shelter. The case and treatment description are meant to provide a general overview of how counselors might implement an overarching lens of screening and treatment when working with survivors of IPV.
A 48-year-old Caucasian woman sat across from her counselor, elated as she described the sense of relief she felt to finally receive counseling support during what she explained to be the worst time of her life. In disclosing several accounts of physical, sexual, and emotional abuse, she described times in which her ex-partner had blackened her eye, broken bones, and strangled her. Knowing the various causes of TBI in IPV, the counselor started a conversation about the possibility of brain injury. The client denied going to the emergency room to be assessed for injuries, a process that would have likely detected contusions or swelling of brain tissue. The absence of medical treatment was not surprising to the counselor, given the numerous barriers that often leave survivors of IPV without medical attention, including fear of further harm. Knowing this, the counselor was careful in her communication so as to not suggest blame or judgement for the client’s decisions to not seek past medical assistance. The counselor proceeded to ask questions related to whether or not the client perceived any changes to physical or cognitive functioning in comparison to life before her abusive relationship, with focus on memory, attention, and learning experiences. The client found it very difficult to answer these questions in detail, indicating that her memory was potentially impaired because of either PTSD or brain injury. A neutral, yet warm and understanding, therapeutic stance was critical for the counselor to keep the client engaged in the therapeutic process.
Following the detection of probable TBI, the counselor provided psychoeducation to promote awareness on the nature of the injury as well as referrals to various local and state resources. The counselor and client then discussed the client’s experience of PTSD symptoms and how these symptoms could mirror the symptoms of brain injury. Education is a recommended strategy when working with clients with PTSD (Marotta, 2000). The counselor knew that helping the client to differentiate between the two would help her monitor and document symptoms for the journaling homework that would eventually be assigned to her. At this time, the counselor provided the client with a handout with a t-chart comparing PTSD and TBI symptoms, knowing that a concrete, visual representation might be a helpful accommodation. For her journaling homework, the counselor instructed the client to record the following: symptom type, duration, intensity, and any contextual details. This recording would benefit the client in multiple ways, including increasing personal awareness and attention to symptoms, indicating the necessity of additional referral sources, and providing a record for discussion with future medical professionals.
At the beginning of the next several sessions, the counselor followed up on the client’s journaling homework. During these check-ins, the client reported times of forgetfulness, difficulty with attention, and problems staying organized and making decisions. One particular incident allowed the counselor and client to actively probe through differences between PTSD and TBI when the client reported a time in which she “zoned out” while running errands. They explored the event, discussing duration and contextual details. It was in this conversation that the client mentioned a glass item having fallen nearby and shattering loudly just moments before she “zoned out.” From this detail, especially noting the infrequency of her zoning out day-to-day, the counselor discussed the likelihood of it being trauma-related, connecting it to the many nights of domestic disturbances with her abuser that ended in various household items being destroyed. On the other hand, the counselor associated her increased forgetfulness, headaches, and a distorted sense of smell with possible manifestations of brain injury. The counselor recommended that the client call the state’s brain injury association to learn about medical providers who had extensive experience treating TBI.
Noting shattering glass as one of her triggers, the counselor and client discussed what she could do after perceiving this stimulus to reorient to the present. Grounding techniques such as deep breathing were discussed. To address forgetfulness, the counselor implemented compensatory strategies that included shorter responses and questions, utilization of the present time frame, and repetition of responses provided by the counselor. To encourage further assessment and treatment, the counselor followed up on the client’s contact with experienced TBI medical professionals.
Clients may be involved in both individual and group counseling simultaneously. However, group counseling may be contraindicated for women who have experienced a TBI until social and relational challenges can be addressed in individual counseling (Mychasiuk et al., 2014). Therefore, before recommending entry into a counseling group, the counselor first assessed the client’s day-to-day interactions with individuals and how her social network changed before and after sustaining TBI. This assessment allowed the counselor an opportunity to both gauge the appropriateness of group therapy and identify possible barriers to group that might be assisted with accommodation. With careful consideration and assessment, counselors can maximize the use of group therapeutic factors such as interpersonal learning, socializing techniques, and imitative behavior.
Conclusion
PV is a prevalent public health issue that impacts the development of a wide range of mental and physical health diagnoses, in which PTSD and TBI are two pervasive complications that often affect survivors of IPV. Recent initiatives, such as the national briefing hosted by the Congressional Brain Injury Task Force, are indicative of the work still needed to properly address this underrepresented national issue (Brain Injury Association of America, 2017). Counselors should understand the intersectionality of PTSD and TBI and how such experiences can complicate treatment. This article has provided several suggestions for counselors to improve their clinical practice to better accommodate survivors of IPV, including screening and assessment techniques, therapeutic approaches, and communication suggestions. Counselors should be aware of the need to adopt specific therapeutic approaches and strategies in counseling that compensate for cognitive impairments so as to avoid gaps in the delivery of services and adhere to best treatment practices. Counselors also are required to abide by ethical codes and guidelines and are urged to continually seek supervision and consultation when working with this population to ensure that the various aspects of this complicated category of violence are thoroughly considered.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest or funding contributions for the development of this manuscript.
References
American Counseling Association. (2014). 2014 ACA Code of ethics. Retrieved from https://www.counseling.org/resources/aca-code-of-ethics.pdf
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
Association of Women’s Health, Obstetric and Neonatal Nurses. (2015). Intimate partner violence. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 44, 405–408. doi:10.1111/1552-6909.12567
Black, M. C., Basile, K. C., Breiding, M. J., Smith, S. G., Walters, M. L., Merrick, M. T., . . . Stevens, M. R. (2011). The National Intimate Partner and Sexual Violence Survey: 2010 Summary Report. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. Retrieved from https://www.cdc.gov/violenceprevention/pdf/nisvs_report2010-a.pdf
Block, C. K., & West, S. E. (2013). Psychotherapeutic treatment of survivors of traumatic brain injury: review of the literature and special considerations. Brain Injury, 27, 775–788. doi:10.3109/02699052.2013.775487
Boals, A., & Banks, J. B. (2012). Effects of traumatic stress and perceived stress on everyday cognitive functioning. Cognition and Emotion, 26, 1335–1343. doi:10.1080/02699931.2011.651100
Bourne, C., Mackay, C. E., & Holmes, E. A. (2013). The neural basis of flashback formation: The impact of viewing trauma. Psychological Medicine, 43, 1521–1532. doi:10.1017/S0033291712002358
Brain Injury Association of America. (2015). About brain injury: Concussion/Mild TBI. Retrieved from
http://www.biausa.org/mild-brain-injury.htm
Brain Injury Association of America. (2017, October 17). Briefing: The silent epidemic in America – brain injury and domestic violence. Retrieved from https://www.biausa.org/public-affairs/public-awareness/news/briefing-the-silent-epidemic-in-america-brain-injury-and-domestic-violence
Brain Injury Association of Virginia. (2010). Working with individuals with brain injury: A professional’s guide. Richmond, VA: Author.
Breiding, M. J., Basile, K. C., Smith, S. G., Black, M. C., & Mahendra, R. (2015). Intimate partner violence surveillance: Uniform definitions and recommended data elements. Retrieved from https://www.cdc.gov/violenceprevention/pdf/intimatepartnerviolence.pdf
Chapman, A., & Monk, C. (2015). Domestic violence awareness. American Journal of Psychiatry, 172, 944–945. doi:10.1176/appi.ajp.2015.15070853
Chard, K. M., Schumm, J. A., McIlvain, S. M., Bailey, G. W., & Parkinson, R. B. (2011). Exploring the efficacy of a residential treatment program incorporating cognitive processing therapy-cognitive for veterans with PTSD and traumatic brain injury. Journal of Traumatic Stress, 24, 347–351. doi:10.1002/jts.20644
Clark, C., Classen, C. C., Fourt, A., & Shetty, M. (2014). Treating the trauma survivor: An essential guide to trauma-informed care. New York, NY: Taylor and Francis.
Currie, S., Saleem, N., Straiton, J. A., Macmullen-Price, J., Warren, D. J., & Craven, I. J. (2016). Imaging assessment of traumatic brain injury. Postgraduate Medical Journal, 92, 41–50.
doi:10.1136/postgradmedj-2014-133211
Fedovskiy, K., Higgins, S., & Paranjape, A. (2008). Intimate partner violence: How does it impact major depressive disorder and post-traumatic stress disorder among immigrant Latinas? Journal of Immigrant and Minority Health, 10, 45–51. doi:10.1007/s10903-007-9049-7
Fúgate, M., Landis, L., Riordan, K., Naureckas, S., & Engel, B. (2005). Barriers to domestic violence help seeking: Implications for intervention. Violence Against Women, 11, 290–310.
Goldin, Y., Haag, H. L., & Trott, C. T. (2016). Screening for history of traumatic brain injury among women exposed to intimate partner violence. PM&R, 8(11), 1–7. doi:10.1016/j.pmrj.2016.05.006
Jeter, C. B., Hergenroeder, G. W., Hylin, M. J., Redell, J. B., Moore, A. N., & Dash, P. K. (2013). Biomarkers for the diagnosis and prognosis of mild traumatic brain injury/concussion. Journal of Neurotrauma, 30, 657–670. doi:10.1089/neu.2012.2439
Joshi, M., Thomas, K. A., & Sorenson, S. B. (2012). “I Didn’t Know I Could Turn Colors”: Health problems and health care experiences of women strangled by an intimate partner. Social Work in Health Care, 51, 798–814. doi:10.1080/00981389.2012.692352
Kimberley, T. J., Samargia, S., Moore, L. G., Shakya, J. K., & Lang, C. E. (2010). Comparison of amounts and types of practice during rehabilitation for traumatic brain injury and stroke. Journal of Rehabilitation Research & Development, 47, 851–861. doi:10.1682/JRRD.2010.02.0019
Krebs, C., Breiding, M. J., Browne, A., & Warner, T. (2011). The association between different types of intimate partner violence experienced by women. Journal of Family Violence, 26, 487–500.
doi:10.1007/s10896-011-9383-3
Kwako, L. E., Glass, N., Campbell, J., Melvin, K. C., Barr, T., & Gill, J. M. (2011). Traumatic brain injury in intimate partner violence: A critical review of outcomes and mechanisms. Trauma, Violence, & Abuse, 12(3), 115–126. doi:10.1177/1524838011404251
Lawson, D. M. (2003). Incidence, explanations, and treatment of partner violence. Journal of Counseling & Development, 81, 19–32. doi:10.1002/j.1556-6678.2003.tb00221.x
Lutenbacher, M., Cohen, A., & Mitzel, J. (2003). Do we really help? Perspectives of abused women. Public Health Nursing, 20, 56–64. doi:10.1046/j.1525-1446.2003.20108.x
Marotta, S. A. (2000). Best practices for counselors who treat posttraumatic stress disorder. Journal of Counseling & Development, 78, 492–495. doi:10.1002/j.1556-6676.2000.tb01933.x
McFadgion, A. (2013). Intimate partner violence and probable traumatic brain injury: Manifestations in the lives of abused women (Doctoral dissertation). Retrieved from ProQuest Dissertations Publishing. (Order No. 3613786)
McLaughlin, K. D. (2017). Ethical considerations for clinicians treating victims and perpetrators of intimate partner violence. Ethics & Behavior, 27, 43–52, doi:10.1080/10508422.2016.1185012
McLeod, A. L., Hays, D. G., & Chang, C. Y. (2010). Female intimate partner violence survivors’ experiences with accessing resources. Journal of Counseling & Development, 88, 303–310.
doi:10.1002/j.1556-6678.2010.tb00026.x
Murray, C. E., Lundgren, K., Olson, L. N., & Hunnicutt, G. (2016). Practice update: What professionals who are not brain injury specialists need to know about intimate partner violence-related traumatic brain injury. Trauma, Violence, & Abuse, 17, 298–305. doi:10.1177/1524838015584364
Mychasiuk, R., Hehar, H., Farran, A., & Esser, M. J. (2014). Mean girls: Sex differences in the effects of mild traumatic brain injury on the social dynamics of juvenile rat play behaviour. Behavioural Brain Research, 259, 284–291. doi:10.1016/j.bbr.2013.10.048
National Center on Domestic Violence, Trauma, & Mental Health. (2014). Current evidence: Intimate partner
violence, trauma-related mental health conditions & chronic illness. Retrieved from http://www.national
centerdvtraumamh.org/wp-content/uploads/2014/10/FactSheet_IPVTraumaMHChronicIllness_2014_Final.pdf
National Resource Center on Domestic Violence. (2012). DVAM history. Retrieved from http://www.nrcdv.org/dvam/DVAM-history
O’Leary, K. D., Tintle, N., & Bromet, E. (2014). Risk factors for physical violence against partners in the U.S. Psychology of Violence, 4, 65–77. doi:10.1037/a0034537
Pennsylvania Coalition Against Domestic Violence. (2011). Traumatic brain injury as a result of domestic violence: Information, screening and model practices. Harrisburg, PA: Fern Gilkerson.
Pill, N., Day, A., & Mildred, H. (2017). Trauma responses to intimate partner violence: A review of current knowledge. Aggression and Violent Behavior, 34, 178–184. doi:10.1016/j.avb.2017.01.014
Powers, R. A., & Kaukinen, C. E. (2012). Trends in intimate partner violence: 1980-2008. Journal of Interpersonal Violence, 27, 3072–3090. doi:10.1177/0886260512441077
Saar-Ashkenazy, R., Veksler, R., Guez, J., Jacob, Y., Shelef, I., Shalev, H., . . . Cohen, J. E. (2016). Breakdown of inter-hemispheric connectivity is associated with posttraumatic symptomatology and memory impairment. PLOS One, 11(2), 1–14. doi:10.1371/journal.pone.0144766
Scordato, M. M. (2013). Use of services by female survivors of intimate partner violence: In their own words (Doctoral dissertation). Retrieved from ProQuest Dissertations Publishing. (Order No. 3604177).
Shakespeare-Finch, J., Rees, A., & Armstrong, D. (2015). Social support, self-efficacy, trauma and well-being in emergency medical dispatchers. Social Indicators Research, 123, 549–565. doi:10.1007/s11205-014-0749-9
Sherrill, A. M., Bell, K. M., & Wyngarden, N. (2016). A qualitative examination of situational risk recognition among female victims of physical intimate partner violence. Violence Against Women, 22, 966–985. doi:10.1177/1077801215616706
Sillito, C. L. (2012). Physical health effects of intimate partner abuse. Journal of Family Issues, 33, 1520–1539. doi:10.1177/0192513X12448742
Smith, D. J., Mills, T., & Taliaferro, E. H. (2001). Frequency and relationship of reported symptomology in victims of intimate partner violence: The effect of multiple strangulation attacks. The Journal of Emergency Medicine, 21, 323–329. doi:10.1016/S0736-4679(01)00402-4
St. Ivany, A., & Schminkey, D. (2016). Intimate partner violence and traumatic brain injury. Family and Community Health, 39(2), 129–137. doi:10.1097/FCH.0000000000000094
Sugg, N. (2015). Intimate partner violence: Prevalence, health consequences, and intervention. Medical Clinics of North America, 99, 629–649. doi:10.1016/j.mcna.2015.01.012
Tramayne, S. R. (2012). Intimate partner violence as a risk factor for PTSD in female survivors of domestic violence: A meta-analysis (Doctoral dissertation). Retrieved from ProQuest Dissertations Publishing. (Order No. 3509648).
Utzon-Frank, N., Breinegaard, N., Bertelsen, M., Borritz, M., Eller, N. H., Nordentoft, M., . . . Bonde, J. P. (2014). Occurrence of delayed-onset post-traumatic stress disorder: A systematic review and meta-analysis of prospective studies. Scandinavian Journal of Work, Environment & Health, 40, 215–229. doi:10.5271/sjweh.3420
Villamar, M. F., Santos Portilla, A., Fregni, F., & Zafonte, R. (2012). Noninvasive brain stimulation to modulate neuroplasticity in traumatic brain injury. Neuromodulation: Technology at the Neural Interface, 15, 326–338. doi:10.1111/j.1525-1403.2012.00474.x
Zasler, N. D., Katz, D. I., & Zafonte, R. D. (2007). Brain injury medicine: Principles and practice. New York, NY: Demos Medical.
Zhou, X., Wu, X., Li, X., & Zhen, R. (2016). The role of posttraumatic fear and social support in the relationship between trauma severity and posttraumatic growth among adolescent survivors of the Yaan earthquake. International Journal of Psychology. doi:10.1002/ijop.12281
Zollman, F. S. (2016). Manual of traumatic brain injury: Assessment and management (2nd ed.). New York, NY: Demos Medical.
Trish J. Smith is a resident in counseling and a senior client services advocate at Safe Harbor Shelter in Richmond, Virginia. Courtney M. Holmes, NCC, is an assistant professor at Virginia Commonwealth University. Correspondence can be addressed to Trish Smith, Safe Harbor Shelter, P.O. Box 17996, Richmond, VA 23226, trish@safeharborshelter.com
Jun 26, 2015 | Article, Volume 5 - Issue 3
Ryan G. Carlson, Jessica Fripp, Christopher Cook, Viki Kelchner
Intimate partner violence is a problem among young adults and may be exacerbated through the use of technology. Scant research exists examining the influence of technology on intimate partner violence in young adults. Furthermore, young adult couples on university campuses experience additional stressors associated with coursework that may influence their risk of partner violence. We surveyed 138 young adults (ages 18–25) at a large university and examined the relationships between stress, intimate partner violence and technology. Results indicated that those who use technology less frequently are more likely to report inequality in the relationship, thus suggesting a higher risk for partner violence. An exception applies to those who use technology to argue or monitor partner whereabouts. Implications for counseling young adult couples are discussed.
Keywords: intimate partner violence, stress, young adults, technology, couples
Intimate partner violence (IPV) occurs among young adults (ages 18–24) at a comparable rate with the general population. IPV in the general population occurs among 25%–33% of both men and women (National Intimate Partner and Sexual Violence Survey, 2010), with studies estimating the prevalence of physical violence among college students to be between 20% and 30% (Fass, Benson, & Leggett, 2008; Shook, Gerrity, Jurich, & Segrist, 2000; Spencer & Bryant, 2000). Additionally, IPV is regularly underreported due to the embarrassment and shame victims may feel (Bureau of Justice Statistics, 2003). While causes of IPV are not completely understood, its prevalence among both victims and victimizers has been linked to those who witnessed parental violence as children (Straus, Gelles, & Smith, 1995). However, the increase in college student IPV could be provoked by stress associated with the demands of academics (Mason & Smithey, 2012). IPV victims are more likely to experience symptoms of depression and anxiety, with male victims expressing more shame related to the victimization (Shorey et al., 2011).
In the late 1980s and 1990s, researchers identified types of partner violence within adult relationships (e.g., Gottman et al., 1995; Holtzworth-Munroe & Stuart, 1994; Johnson, 1995). Researchers coined these differences as IPV typologies, which helped researchers and practitioners understand that partner violence is heterogeneous, and thus treatment should be tailored to meet the specific needs of the couple (Carlson & Jones, 2010). This perspective differed from the traditional practice of treating all relationship violence as homogeneous, presuming it to be the result of power and control. Additionally, traditional perspectives on IPV assumed that perpetrators were men trying to assert dominance. Typology researchers refuted this perspective, stating that although some violence is male-on-female, the majority is gender mutual and may have more to do with conflict resolution skills than with asserting control. IPV typology research has gained traction due to its potential treatment implications. However, there is a dearth of research examining IPV typologies among young adults and its relationship to the increased use of technology among this population.
IPV Typologies
Traditionally, relationship violence was more popularly termed domestic violence and deemed homogenous among couple relationships. Thus, all violence was thought to originate from a batterer’s attempt to establish or maintain power and control over a victim. Such violence typically occurred with men as the batterers and women as the victims (in heterosexual relationships). This philosophy gained traction with most practitioners, who assumed that all relationship violence resulted from power and control.
Over the past 15 to 20 years, researchers identified types of relationship violence (e.g., Gottman et al., 1995; Holtzworth-Munroe & Stuart, 1994; Johnson, 1995; & Johnson & Ferraro, 2000). Researchers utilized studies indicating that violence is likely to vary in severity, and often the motive is not to establish power and control over one’s partner. As such, relationship violence was deemed heterogeneous among couples. Therefore, researchers began using the term intimate partner violence as a broader term for describing the variances in violence that occur within relationships, as well as the notion that the violence can be gender mutual in some typologies, meaning that violence is just as likely to be female-on-male as male-on-female in heterosexual relationships. Examples of some of Johnson’s (1995) IPV typologies include the following: (a) situational couple violence, marked by violence that is gender mutual and has lower levels of severity; (b) intimate terrorist, marked by violence that is typically male-on-female, the result of one partner establishing power and control over another, and includes higher levels of lethality (e.g., choking); and (c) violent resistance, when the victim attempts to fight back. Other researchers have established typologies (e.g., Gottman et al., 1995; Holtzworth-Munroe & Stuart, 1994); however, Johnson’s appear to be the most recognized.
Carlson and Jones (2010) developed the continuum of conflict and control to synthesize violence typology research. They asserted that violence typologies could be conceptualized through variances in the type and severity of violence, characteristics of the victimizer, and perceptions of the victim. Assessing information across those three domains can help determine the nature and severity of the violence, and have potential treatment implications. For example, some researchers have examined the effectiveness of relationship interventions when couples present with lower levels of severity in relationship violence (e.g., Bradley, Friend, & Gottman, 2011; Braithwaite & Fincham, 2014; Simpson, Atkins, Gattis, & Christensen, 2008). However, such interventions require counselors to make informed and intentional treatment decisions that consider the safety of the couple.
Counselors may not typically screen for partner violence or make treatment decisions based on the safety of a victim (Schacht, Dimidjian, George, & Berns, 2009). Partner violence screening protocols are beyond the scope of this paper; however, readers are referred to Daire, Carlson, Barden, and Jacobson (2014). Counselors who become aware of partner violence typically refer their clients, with the assumption that treatment is contraindicated. However, couples counseling and other relationship interventions, such as relationship education, appear to reduce overall levels of relationship violence and increase relationship satisfaction (Bradley et al., 2011; Simpson et al., 2008). Couples who participated in this research were identified as having low levels of aggression, and as not attempting to establish power and control over their respective partners. Our review of the literature did not yield any research discussing how IPV typologies translate to young adult relationships, and what effect technology might have on the types of violence. Thus, it is not clear what evidence exists supporting best practice guidelines for counselors who work with young adults experiencing IPV in their relationships.
Dating Violence
The Centers for Disease Control and Prevention (CDC) has defined dating violence as the consistent act of physical and/or sexual violence, as well as the possible emotional or psychological distress perpetrated by a current or previous dating partner (CDC, 2014). Additionally, the CDC has reported that dating violence contributes to health risks including, but not limited to, injury, heavy drinking, suicidal ideation, promiscuity, substance use, issues with self-esteem and perpetuating the act of violence in future relationships. When violence is enacted toward adolescents, healthy development of intimacy, identity and sexuality is hindered (Foshee & Reyes, 2009).
Draucker, Martsolf, and Stephenson (2012) studied the history of dating violence among the adolescent population and found that the risk factors correlating with later dating violence include parenting issues, such as inconsistent parental supervision, discipline and warmth. In addition to identifying factors that contribute to violence (e.g., exposure to violence at a young age, experiencing varying styles of parenting), Stephenson, Martsolf, and Draucker (2012) recognized the role of peers in exacerbating dating violence in young adulthood. Adelman and Kil (2007) purported that peers are directly and indirectly involved in adolescent dating violence, including assisting in the confrontation of a friend’s partner or helping a friend make his or her partner jealous. According to Banister and Jakubec (2004), females often feel isolated by their peers in adolescent dating violence, as many of their friends may not approve of the relationship. Thus, it is possible they may not disclose the nature of the violence within the relationship.
Technology and Conflict Resolution
Cyber aggression has been more thoroughly researched in child and adolescent populations than in young adult populations. Among children and adolescents, technology offers young people an additional medium for aggression, but does not appear to contribute directly to the development of cyber aggression among those who are not aggressive in non-cyber roles (Burton, Florell, & Wygant, 2013; Dempsey, Sulkowski, Dempsey, & Storch, 2011; Werner, Bumpus, & Rock, 2010). Werner et al. (2010) demonstrated that among sixth, seventh and eighth graders, higher rates of relational aggression approval predicted higher rates of Internet aggression. Peer attachment, however, is negatively correlated with both cyber aggression and non-cyber aggression (Burton et al., 2013). In addition to correlations between user beliefs and use of technology, Draucker and Martsolf (2010) found that many individuals who experienced dating violence as adolescents described technology as a medium for violence. Among 56 emerging adults who were interviewed about their adolescent dating violence experiences, participants reported technology use for arguing (6), perpetrating verbal or emotional aggression (30), monitoring or controlling (30), and limiting a partner’s access to self (e.g., avoiding partner; 29). It is unclear whether these same patterns hold true for young adults’ dating experiences, as the members of this sample were asked to reflect on their experiences as adolescents.
In addition to studies focused on children and adolescents, research demonstrates a link between individual beliefs about aggression and the use of technology in a way that is consistent with those beliefs among emerging adults. Thompson and Morrison (2013) studied the relationships between several individual-, social- and community-level predictors of technology-based sexually coercive behavior (TBC) among college students. Thompson and Morrison’s (2013) findings suggest that rape-supportive beliefs and peer approval of forced sex were significant predictors of TBC. However, women who are more assertive in the relationship appear to mitigate cyber aggression (Schnurr, Mahatmya, & Basche, 2013).
Technology use has been identified as a key component in conflict resolution strategies and romantic relationship mediation among young adults as well. Weisskirch and Delevi (2013) found that college students who had positive feelings about conflict resolution were more likely to use technology, specifically text messaging, to terminate relationships. Text messaging was the most commonly cited use of technology for the purpose of initiating or receiving a relationship-ending message. In a study of 1,039 adults aged 17 and older, Coyne, Stockdale, Busby, Iverson, and Grant (2011) found that younger participants were more likely to use technology in communicating with their romantic partner, and that technology was used to communicate in a variety of ways within the romantic relationship, including the expression of affection (75%), discussion of serious issues (25%), apologizing (12%) and hurting their partner (3%). Given the extent to which young adults use technology as a medium for relationship communication, and the prevalence of dating violence, more research is needed to understand how technology use may be correlated with risks of partner violence.
Research Questions
Despite researchers’ attempts to understand IPV among college-aged students, as well as to identify primary prevention interventions, IPV typologies have not been determined among the college student population. Further, the emergence of social media has provided a new mechanism for IPV implementation. Schnurr et al. (2013) found that cyber aggression mitigates physical IPV for men. However, few studies have examined the prevalence of cyber aggression in college students or considered the role of cyber aggression within the IPV typology framework. Thus, the current study aims to explore college students’ perceptions of how technology is used in their relationships, as well as the influence of technology, stress and attitudes toward violence on overall risk for IPV. As such, we examined the following research questions: (a) What relationship exists between young adults’ perceptions of partners’ technology use in relationships, risk for partner violence, acceptance of couple violence and perceived stress?; (b) Can perceptions of partners’ technology use, acceptance of couple violence or perceived stress be considered predictors of risk for partner violence? If so, which exerts the most influence on risk for partner violence?; and (c) What differences exist between individual responses (i.e., yes/no) regarding perceptions of partners’ use of technology in relationships and outcomes (i.e., risk for violence, perceived stress, acceptance of violence)?
Method
Participants
Data collection occurred at a large university in the Southeast region of the United States. We invited undergraduate and graduate students aged 18–25 who were currently in a relationship or had recently been in a relationship to participate. We utilized a convenience sampling approach and recruited participants through both active and passive methods (Yancey, Ortega, & Kumanyika, 2006). Active methods included acquiring instructor permission and speaking briefly to students during class about the study. Passive methods comprised posting study flyers around campus, as well as contacting various departments and programs requesting that they send study information to students on their e-mail listserv. All eligible students were invited to complete the assessment packet online using Survey Monkey. Students began the survey by reading the study information form, which included a warning about the sensitive nature of the questions. At the conclusion of the survey, we provided all participants with a list of domestic violence resources.
Recruitment efforts resulted in 155 students attempting to complete the survey. However, we removed 17 participants, 11 of whom indicated an age of 26 or older (making them ineligible) and six of whom did not complete any of the survey questions. We did not offer any incentives for survey completion as participation was voluntary, but it is possible that instructors provided incentives of their own accord. Instructor-initiated incentives could explain the six participants who did not answer any questions. Therefore, the total sample for the study was 138 participants.
Eighty-six participants (62%) indicated currently being in a relationship, with relationships lasting an average of 30 months. Others were recently in a relationship (n = 49; three participants did not indicate relationship status), reporting an average of 20 months since their last relationship. Women (n = 119; 87%) comprised the majority of the sample. The sample included mostly heterosexual participants (n = 127), with some same-sex participants (n = 10; one person did not report). Participants ranged in grade level; most were graduate students (n = 48; 35%), followed by seniors (n = 42; 30%), juniors (n = 28; 20%), sophomores (n = 17; 12%) and freshmen (n = 3; 2%). See Table 1 for additional demographic information and descriptive statistics for constructs of interest.
Table 1
Descriptive Statistics for Study Constructs
| Constructs |
M
|
SD
|
Range
|
| Age |
21.45
|
1.53
|
18–25
|
| Credit hours |
14.67
|
3.04
|
3–23
|
| Perceived stress (PSS) |
6.31
|
2.77
|
1–13
|
| Intimate justice (IJS) |
26.97
|
10.96
|
15–64
|
| Acceptance of violence (ACV) |
5.61
|
1.22
|
5–12
|
| Use of technology (UTR) |
8.96
|
1.15
|
5–10
|
| Note. M = mean; SD = standard deviation; PSS = Perceived Stress Scale (Cohen, Kamarck, & Mermelstein, 1983; Cohen & Williamson, 1988); IJS = Intimate Justice Scale (Jory, 2004); ACV = Acceptance of Couple Violence (Foshee, Fothergill, & Stuart, 1992); UTR = Use of Technology in Relationships (Draucker & Martsolf, 2010; Schnurr et al., 2013). |
Instruments
Demographic information. The demographic information form consisted of 13 questions and asked participants about basic information such as age, gender, grade, current relationship status, length of relationship (if current) and length of previous relationship (as well as length of time since previous relationship). Participants completed the demographic information form prior to completing the other study assessments.
Perceived Stress Scale. The Perceived Stress Scale (PSS; Cohen, Kamarck, & Mermelstein, 1983; Cohen & Williamson, 1988) is a 10-item measure assessing the perception of stress. We incorporated the PSS to examine the relationship of respondents’ perceived stress to relationship violence (or risk of violent behaviors). Respondents indicate on a five-point Likert scale (0 = Never, 1 = Almost Never, 2 = Sometimes, 3 = Fairly Often and 4 = Very Often) the extent to which situations in life are deemed stressful. The PSS asks general questions, such as “In the last month, how often have you been upset because of something that happened unexpectedly?” The PSS is scored by summing the item responses. The factor structure of the PSS has been supported in a sample of community participants as well as college students (Cohen et al., 1983; Roberti, Harrington, & Storch, 2006). There are several versions of the PSS (each consisting of 14, 10 or four items). The short four-item scale comprises items 2, 4, 5 and 10 of the PSS and has shown support in use with data collected during telephone interviews. We utilized the short form in the current study to reduce the overall number of questions asked of each participant. Cohen et al. (1983) reported an alpha coefficient in their study of .84 for the PSS with 14 items. They examined the test-retest reliability utilizing 65 college students and identified an alpha of .85. The PSS 10-item instrument has demonstrated sound reliability in a sample of college students as well (Dehle, Larsen, & Landers, 2001). Cronbach’s alpha was low (.58) for participants in the current study. However, the PSS short form demonstrated better reliability (.72) in the study conducted by Cohen et al. (1983).
Acceptance of Couple Violence. We incorporated the Acceptance of Couple Violence (ACV; Foshee, Fothergill, & Stuart, 1992) questionnaire to assess for attitudes toward violence in couple relationships. Participants received an adapted version of the ACV to include same-sex relationships. The adapted ACV contains 17 items and comprises five subscales (acceptance of male-on-female violence, acceptance of female-on-male violence, acceptance of male-on-male violence, acceptance of female-on-female violence and acceptance of general dating violence). Scores are summed across responses to calculate a total score within each subscale. We used only acceptance of general dating violence for the current analyses. Cronbach’s alpha reliability for participant scores in the current study was .67.
Use of Technology in Relationships. We used questions adapted by Schnurr et al. (2013) from Draucker and Martsolf (2010) to examine how participants perceived their partners’ use of technology in their relationships (UTR). As such, participants were asked whether their partners used technology in the following ways: (a) to embarrass them, (b) to make them feel bad, (c) to control them, (d) to monitor them and (e) to argue with them. Participants responded by indicating either “yes” (1) or “no” (0) and the responses were summed to acquire a total score. Reliability was low (α = .54) in the current study. However, Schnurr et al. (2013) reported internal consistencies of .76 for men and .71 for women in their sample of dating, emerging adult couples.
Intimate Justice Scale. The Intimate Justice Scale (IJS; Jory, 2004) is a 15-item instrument designed for use in clinical practice to screen for psychological abuse and physical violence. The purpose of the instrument is to aid clinicians in identifying violations of intimate justices (e.g., equity, fairness) that are believed to contribute to relationship violence so that appropriate treatment decisions can be rendered. Participants respond to items on a Likert scale of 1–5, with 1 indicating “I do not agree at all” and 5 indicating “I strongly agree.” Scores are summed across responses, with a minimum possible score of 15 and a maximum possible score of 75. Higher scores indicate violations of intimate justice and a likelihood of relationship abuse. Jory (2004) provided the following guidelines when interpreting total IJS scores: “Scores 15 to 29 may suggest little risk of violence, scores between 30 and 45 may indicate a likelihood of minor violence, and scores > 45 may be a predictor of severe violence” (p. 39). To our knowledge, no assessment currently exists to classify specific IPV typologies. Other popular assessments of IPV exist, such as the Revised Conflict Tactics Scale (CTS; Straus, Hamby, Boney-McCoy, & Sugarman, 1996), but the CTS results do not classify types of IPV behavior with considerations for the victim or the victimizer. The IJS has potential to distinguish between degrees of violence severity, and has been used in studies to differentiate between lower levels and higher levels of violence aggression (e.g., Friend, Bradley, Thatcher, & Gottman, 2011). Scores in the current study ranged from 15–64 (M = 27.02). Alpha reliabilities for participants in the current study were .92.
Results
Preliminary Analysis
Prior to data analyses, we conducted preliminary analyses to test for assumptions, outliers and missing data. The ACV, IJS, and UTR did not meet the assumption of normality, with K-S p values falling below .001. The ACV and IJS resulted in a positive skew, while the UTR resulted in a negative skew. The distributions indicated that most respondents did not report favorable attitudes toward violence, the overall existence of relationship inequality (risk for IPV) or perceptions of partners using technology in an unhealthy manner. This finding is consistent with the mean IJS score (27.02), indicating minimal risk of violence in the sample. Thus, we did not implement any transformation procedures. Potential outliers existed for the ACV and IJS scores. However, examination of the 5% trimmed mean indicated minimal influence on the mean score. Furthermore, these scores represented participants reporting different attitudes and experiences with IPV.
Sixteen participants had missing data points. We created a dummy variable to compare some demographics for those who had complete data versus those who did not. No differences existed between those with and without missing data on age and credit hours taken during the semester of survey administration. We determined that the data were likely missing at random, although it is possible data were missing due to some variable not measured. We used hot deck imputation to address the missing variables (Andridge & Little, 2010; Myers, 2011). Hot deck imputation calculates an average score on an identified outcome variable by matching the score to like variables in the sample (i.e., donor variables). We used participants’ gender, grade level and current relationship status as the donor variables. SPSS averaged the score for matching participants and imputed. Matches existed for 13 of the 16 missing scores. Hot deck imputation provides less bias than mean imputation, and is deemed a better overall solution than the oft-used listwise deletion (Andridge & Little, 2010; Myers, 2011).
Primary Analysis
To begin testing the research questions, we conducted Pearson correlations to examine the relationships between demographics and other constructs of interest (i.e., PSS, IJS, ACV and UTR). Pearson correlation indicated (a) a significant positive correlation between gender and IJS scores, (b) a significant negative correlation between gender and UTR scores, (c) a significant positive correlation between PSS scores and IJS scores, (d) a significant positive correlation between the ACV and IJS scores and (e) a significant negative correlation between UTR scores and IJS scores (See Table 2 for correlations). A scatterplot matrix indicated that (a) increases in stress correlate to increases in intimate justice scores, (b) more favorable attitudes toward couple violence correlate to increases in intimate justice scores; and (c) lower perceived use of technology (i.e., more responses of “no”) correlates with higher intimate justice scores.
Table 2
Correlations Between Constructs of Interest
|
1 |
2 |
3 |
4 |
5 |
| 1. Gender |
1 |
.02 |
.22* |
.13 |
-.17* |
| 2. Perceived stress (PSS) |
|
1 |
.19* |
.05 |
-.04 |
| 3. Intimate justice (IJS) |
|
|
1 |
.26** |
-.05** |
| 4. Acceptance of violence (ACV) |
|
|
|
1 |
-.05 |
| 5. Use of technology (UTR) |
|
|
|
|
1 |
| Note. PSS = Perceived Stress Scale (Cohen, Kamarck, & Mermelstein, 1983; Cohen & Williamson, 1988); IJS = Intimate Justice Scale (Jory, 2004); ACV = Acceptance of Couple Violence (Foshee, Fothergill, & Stuart, 1992); UTR = Use of Technology in Relationships (Draucker & Martsolf, 2010; Schnurr et al., 2013). |
* p < .05. ** p < .001.
The significant correlations supported a hierarchical linear regression analysis to examine the predictive relationships between variables. The IJS served as the dependent variable, while PSS, ACV and UTR scores served as independent variables. The model included three steps, adding predictor variables one step at a time to examine the contribution of each variable. Model one included ACV scores, contributing 6.8% of the variance and demonstrating statistical significance; F(1, 133) = 9.70, p = .002. Model two included UTR scores, adding 18.9% of the variance and achieving significance; F(1, 132) = 33.65, p < .001. Finally, model three added PSS, contributing 2.5% of variance and also achieving significance; F(1, 131) = 4.54, p = .035 (See Table 3). The model as a whole contributed to 26.6% of the variance, although UTR contributed the most variance to IJS scores.
Table 3
Predictors of Partner Violence Risk (Intimate Justice)
| Variable |
Δ R2
|
β
|
p
|
| Model 1: ACV |
.068
|
.261
|
.002
|
| Model 2: UTR |
.189
|
-.435
|
< .001
|
| Model 3: PSS |
.025
|
.158
|
.035
|
| Note. ACV = Acceptance of Couple Violence (Foshee, Fothergill, & Stuart, 1992); UTR = Use of Technology in Relationships (Draucker & Martsolf, 2010; Schnurr et al., 2013); PSS = Perceived Stress Scale (Cohen, Kamarck, & Mermelstein, 1983; Cohen & Williamson, 1988). |
Next, we examined differences between individuals’ responses (i.e., yes/no) regarding perceptions of their partners’ use of technology in the relationships (UTR) and outcome variables (i.e., IJS, ACV and PSS scores). Table 4 presents the frequency of responses for each of the five items on the UTR. A MANOVA indicated that the only significant differences between responses on all five UTR questions and outcomes existed for question four (“Has your partner ever used technology to monitor you?”), F(1, 112) = 4.08, p = .04, = .04, and question five (“Has your partner ever used technology to argue with you?”), F(1, 112) = 5.12, p = .03, = .04. Simple effects revealed that respondents who indicated “yes” to UTR question four had significantly higher IJS scores (M = 33.38, SD = 11.09) than those who indicated “no” (M = 24.71, SD = 9.81); F(1, 129) = 19.81, p < .001, = .13. Participants who indicated “yes” to UTR question five had significantly higher IJS scores (M = 30.79, SD = 11.13) than those who indicated “no” (M = 24.14, SD = 9.78); F(1, 129) = 13.24, p < .001, = .09. Therefore, use of technology to argue with a partner and monitor a partner’s location appear associated with increases in relationship inequality, and place the young couples in our sample at a higher risk of experiencing partner violence.
Table 4
Frequency of Responses to Questions Regarding Use of Technology
| Question (Has partner used technology to . . .) |
% “Yes”
|
% “No”
|
| 1. Embarrass you? |
6.5
|
89.1
|
| 2. Make you feel bad? |
15.2
|
15.9
|
| 3. Control you? |
5.1
|
94.7
|
| 4. Monitor you? |
28.3
|
67.4
|
| 5. Argue with you? |
44.9
|
50.7
|
Discussion
The purpose of this study was to understand the influence of young adults’ use of technology in intimate relationships and examine relationships among stress, attitudes toward violence and overall risk for IPV. First, we examined the relationships among the variables, then we used a regression analysis to understand the contribution of each variable to risk for partner violence. Finally, we explored differences between responses regarding partners’ perceptions of technology use and other outcomes.
Results indicate positive correlations between participants’ stress scores and intimate justice scores, suggesting that as stress increases, so too does risk for partner violence. This finding is similar to the conclusions of Mason and Smithey (2012), who utilized Merton’s Classical Strain Theory as the foundation for testing the influence of life strain on IPV among college students. Their results indicated that some forms of strain increased dating violence among college students. However, the results of our study do not suggest the existence of any relationship between technology use and stress. A potential explanation is that increases in IPV-related behaviors associated with increases in stress may present during face-to-face interactions.
We also found that participants who reported perceptions that partners used technology (e.g., to monitor, argue, embarrass, control, make them feel bad) less frequently were associated with increased intimate justice scores, or risk for partner violence. Although initially suprising, this result appears somewhat consistent with the findings of Coyne et al. (2011) indicating that younger participants are more likely to use technology to communicate in a variety of ways. In fact, it could be that communication via technology is an expectation in young adult relationships, and when that expectation is not met, tension arises. However, further research is needed to explore this conclusion.
Perceived stress (PSS: 2.4% of variance), acceptance of violence (ACV: 6.8% of variance) and use of technology (UTR: 18.9% of variance) were all significant predictors of risk for partner violence (IJS), with UTR contributing the most variance in IJS. This finding is consistent with the correlation and appears to support the notion that a lack of communication via technology may contribute to problems in young adult relationships. In fact, 45% of our sample indicated that their current or past partner used technology to argue with them. Again, this finding could support the notion that conflict resolution via technology is normal or expected in young adult relationships. However, results indicate that participants who perceived their partners as using technology as a means of arguing and monitoring them had higher risk for partner violence (i.e., IJS). The IPV typology literature has identified various characteristics associated with types of violence in couple relationships. A more controlling type, such as Johnson’s (1995) intimate terrorist, may exhibit nonviolent control tactics such as monitoring his or her partner’s location. Thus, it is possible that this behavior is more indicative of controlling IPV typologies. However, more research is needed to understand the influence of using technology to monitor a partner on overall risk for IPV.
Implications for Practice
According to Bergdall et al. (2012), emerging adults frequently use technology to establish relationships with others. Conversely, technology use has been a common medium for sustaining and terminating romantic or intimate relationships. Young adults between the ages of 18 and 29 typically use social media, cell phones and the Internet to communicate (Coyne et al., 2011). Although Bergdall et al. (2012) confirmed that young adults rely heavily on technology to form and dissolve relationships, the authors did not factor in the effect technology may have on psychosocial development, sexual behavior or dating violence.
The findings from our study, as well as from others, indicate that technology is frequently used in young adult relationships. Therefore, when screening for IPV, counselors should consider questions related to how partners use technology in their relationship (e.g., for communicating, announcing the relationship, resolving conflict). Daire et al. (2014) described an IPV protocol for community agencies and practitioners that includes screening clients. Such a protocol also should include technology and consider its overall influence on the functioning of the couple.
Continued research in this area may reveal the ways in which young adults communicate with each other via technology. Individuals who have grown up amidst advances in technology have adapted to a lifestyle in which the ability to communicate with friends and gain entry into one’s personal life is readily available. Due to this factor, the ability to communicate with, gain access to or monitor a partner has increased. Draucker and Martsolf (2010) indicated that technology has changed the course of relationship quality and communication because boundaries have shifted. Counselors can incorporate healthy technology communication into their treatment plans. Bergdall et al. (2012) reported that technology does close the social gap between all people, but if utilized in efforts to educate young adults about healthy and safe ways to communicate with each other, it may have a positive effect on intimate relationships and the potential to reduce violence.
Limitations
This study’s findings should be considered with caution because there are limitations to consider. We did not incorporate a random sampling method, as there were no large student lists or databases for generating random samples. We were unable to calculate a response rate due to the nature of our convenience sampling approach. Thus, the study results might not be representative of the young adult population at all colleges and universities. Additionally, the majority of the sample was comprised of white, heterosexual females.
Another limitation is that two of the assessments we used revealed low Cronbach’s alpha scores (PSS and UTR), while the ACV had a Cronbach’s alpha just below the accepted cutoff. Cronbach’s alpha is not a measure of the overall assessment’s internal consistency as much as it is a measure of the sample’s consistent responses to items (Helms, Henze, Sass, & Mifsud, 2006; Lance, Butts, & Michels, 2006). Thus, the low Cronbach’s alpha suggests diversity in responses to items among the study sample. However, the low Cronbach’s alpha scores may indicate higher measurement error, and results should be considered with caution.
This study also is limited because it incorporated self-report measures, with some participants reflecting on past relationships. Self-report, especially when thinking about a relationship that did not work out, may not provide accurate information. Additionally, we did not collect data from both members of a couple. Finally, there were missing data because participants skipped items, marked two items instead of one or skipped enough items that their results were not interpretable. We used a data imputation method with reduced bias, but there is no certainty in the accuracy of the imputed responses.
Conclusion
Recent research has contributed to the formation of IPV typologies and has challenged traditional models, yet much remains unknown about partner violence among young adults. The use of technology in relationship communication and conflict resolution is an expanding area of research due to technology’s increased use in daily living. Given the need for more information about both IPV and the use of technology in relationship communication, this study looked at technology use as a risk factor for IPV among young adults. Our study both confirmed prior results and contributed new results. Results suggest that emerging adults may expect technology to be an important means of relationship communication. Those counseling college-aged couples should consider discussing healthy avenues for incorporating technology. Furthermore, technology use should be considered when counselors screen couples for risk factors associated with IPV. However, more research is warranted regarding the use of technology in young adult relationships.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Adelman, M., & Kil, S. H. (2007). Dating conflicts: Rethinking dating violence and youth conflict. Violence Against Women, 13, 1296–1318. doi:10.1177/1077801207310800
Andridge, R. R., & Little, R. J. A. (2010). A review of hot deck imputation for survey non-response. International Statistical Review, 78, 40–64. doi:10.1111/j.1751-5823.2010.00103.x
Banister, E., & Jakubec, S. (2004). “I’m stuck as far as relationships go”: Dilemmas of voice in girls’ dating relationships. Child & Youth Services, 26, 33–52. doi:10.1300/J024v26n02_03
Bergdall, A. R., Kraft, J. M., Andes, K., Carter, M., Hatfield-Timajchy, K., & Hock-Long, L. (2012). Love and hooking up in the new millennium: Communication technology and relationships among urban African American and Puerto Rican young adults. Journal of Sex Research, 49, 570–582. doi:10.1080/00224499.2011.604748
Bradley, R. P. C., Friend, D. J., & Gottman, J. M. (2011). Supporting healthy relationships in low-income, violent couples: Reducing conflict and strengthening relationship skills and satisfaction. Journal of Couple & Relationship Therapy, 10, 97–116. doi:10.1080/15332691.2011.562808
Braithwaite, S. R., & Fincham, F. D. (2014). Computer-based prevention of intimate partner violence in marriage. Behaviour Research and Therapy, 54, 12–21. doi:10.1016/j.brat.2013.12.006
Bureau of Justice Statistics. (2003). Family violence statistics. Retrieved from http://www.bjs.gov/content/pub/pdf/fvs.pdf
Burton, K. A., Florell, D., & Wygant, D. B. (2013). The role of peer attachment and normative beliefs about aggression on traditional bullying and cyberbullying. Psychology in the Schools, 50, 103–115. doi:10.1002/pits.21663
Carlson, R. G., & Jones, K. D. (2010). Continuum of conflict and control: A conceptualization of intimate partner violence typologies. The Family Journal, 18, 248–254. doi:10.1177/1066480710371795
Centers for Disease Control and Prevention. (2014). Understanding teen dating violence. National Center for Injury Prevention and Control, Division of Violence Prevention. Retrieved from http://www.cdc.gov/violenceprevention/pdf/teen-dating-violence-factsheet-a.pdf
Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24, 385–396.
Cohen, S., & Williamson, G. M. (1988). Perceived stress in a probability sample of the United States. S. Spacapan & S. Oskamp (Eds.), The Social Psychology of Health (pp. 31–67). Newbury Park, CA: Sage.
Coyne, S. M., Stockdale, L., Busby, D., Iverson, B., & Grant, D. M. (2011). “I luv u :)!”: A descriptive study of the media use of individuals in romantic relationships. Family Relations, 60, 150–162. doi:10.1111/j.1741-3729.2010.00639.x
Daire, A. P., Carlson, R. G., Barden, S. M, & Jacobson, L. (2014). An intimate partner violence (IPV) protocol readiness model. The Family Journal, 22, 170–178. doi:10.1177/1066480713513708
Dehle, C., Larsen, D., & Landers, J. E. (2001). Social support in marriage. American Journal of Family Therapy, 29, 307–324. doi:10.1080/01926180126500
Dempsey, A. G., Sulkowski, M. L., Dempsey, J., & Storch, E. A. (2011). Has cyber technology produced a new group of peer aggressors? Cyberpsychology, Behavior, and Social Networking, 14, 297–302. doi:10.1089/cyber.2010.0108
Draucker, C. B., & Martsolf, D. S. (2010). The role of electronic communication technology in adolescent dating violence. Journal of Child and Adolescent Psychiatric Nursing, 23, 133–142. doi:10.1111/j.1744-6171.2010.00235.x
Draucker, C. B., Martsolf, D., & Stephenson, P. M. (2012). Ambiguity and violence in adolescent dating relationships. Journal of Child and Adolescent Psychiatric Nursing, 25, 149–157. doi:10.1111/j.1744-6171.2012.00338.x
Fass, D. F., Benson, R. I., & Leggett, D. G. (2008). Assessing prevalence and awareness of violent behaviors in the intimate partner relationships of college students using internet sampling. Journal of College Student Psychotherapy, 22(4), 66–75. doi:10.1080/87568220801952248
Foshee, V. A., Fothergill, K., & Stuart, J. (1992). Results from the teenage dating abuse study conducted in Githens Middle School and Southern High School Unpublished technical report. Chapel Hill, NC: University of North Carolina.
Foshee, V. A., & Reyes, H. L. M. (2009). Primary prevention of adolescent dating abuse perpetration: When to begin, whom to target, and how to do it. In D. J. Whitaker & J. R. Lutzker (Eds.), Preventing partner violence: Research and evidence-based intervention strategies (pp. 141–168). Washington, DC: American Psychological Association.
Friend, D. J., Bradley, R. P. C., Thatcher, R., & Gottman, J. M. (2011). Typologies of intimate partner violence: Evaluation of a screening instrument for differentiation. Journal of Family Violence, 26, 551–563. doi:10.1007/s10896-011-9392-2
Gottman, J. M., Jacobson, N. S., Rushe, R. H., Shortt, J. W., Babcock, J., La Taillade, J. J., & Waltz, J. (1995). The relationship between heart rate reactivity, emotionally aggressive behavior, and general violence in batterers. Journal of Family Psychology, 9, 227–248. doi:10.1037/0893-3200.9.3.227
Helms, J. E., Henze, K. T., Sass, T. L., & Mifsud, V. A. (2006). Treating Cronbach’s alpha reliability coefficients as data in counseling research. The Counseling Psychologist, 34, 630–660. doi:10.1177/0011000006288308
Holtzworth-Munroe, A., & Stuart, G. L. (1994). Typologies of male batterers: Three subtypes and the differences among them. Psychological Bulletin, 116, 476–497. doi:10.1037/0033-2909.116.3.476
Johnson, M. P. (1995). Patriarchal terrorism and common couple violence: Two forms of violence against women. Journal of Marriage and Family, 57, 283–294.
Johnson, M. P., & Ferraro, K. J. (2000). Research on domestic violence in the 1990s: Making distinctions. Journal of Marriage and Family, 62, 948–963. doi:10.1111/j.1741-3737.2000.00948.x
Jory, B. (2004). The intimate justice scale: An instrument to screen for psychological abuse and physical violence in clinical practice. Journal of Marital and Family Therapy, 30, 29–44. doi:10.1111/j.1752-0606.2004.tb01220.x
Lance, C. E., Butts, M. M., & Michels, L. C. (2006). The sources of four commonly reported cutoff criteria: What did they really say? Organizational Research Methods, 9, 202–220. doi:10.1177/1094428105284919
Mason, B., & Smithey, M. (2012). The effects of academic and interpersonal stress on dating violence among college students: A test of classical strain theory. Journal of Interpersonal Violence, 27, 974–986. doi:10.1177/0886260511423257
Myers, T. A. (2011). Goodbye, listwise deletion: Presenting hot deck imputation as an easy and effective tool for handling missing data. Communication Methods and Measures, 5, 297–310. doi:10.1080/19312458.2011.624490
Roberti, J. W., Harrington, L. N., & Storch, E. A. (2006). Further psychometric support for the 10-item version of the perceived stress scale. Journal of College Counseling, 9, 135–147. doi:10.1002/j.2161-1882.2006.tb00100.x
Schacht, R. L., Dimidjian, S., George, W. H., & Berns, S. B. (2009). Domestic violence assessment procedures among couple therapists. Journal of Marital and Family Therapy, 35, 47–59. doi:10.1111/j.1752-0606.2008.00095.x
Schnurr, M. P., Mahatmya, D., & Basche, R. A., III. (2013). The role of dominance, cyber aggression perpetration, and gender on emerging adults’ perpetration of intimate partner violence. Psychology of Violence, 3, 70–83. doi:10.1037/a0030601
Shook, N. J., Gerrity, D. A., Jurich, J., & Segrist, A. E. (2000) Courtship violence among college students: A comparison of verbally and physically abusive couples. Journal of Family Violence, 15, 1–22. doi:10.1023/A:1007532718917
Shorey, R. C., Sherman, A. E., Kivisto, A. J., Elkins, S. R., Rhatigan, D. L., & Moore, T. M. (2011). Gender differences in depression and anxiety among victims of intimate partner violence: The moderating effect of shame proneness. Journal of Interpersonal Violence, 26, 1834–1850. doi:10.1177/0886260510372949
Simpson, L. E., Atkins, D. C., Gattis, K. S., & Christensen, A. (2008). Low-level relationship aggression and couple therapy outcomes. Journal of Family Psychology, 22, 102–111. doi:10.1037/0893-3200.22.1.102
Spencer, G. A., & Bryant, S. A. (2000). University students’ dating violence behaviors. Journal of the New York State Nurses Association, 31(2), 15–20.
Stephenson, P. S., Martsolf, D., & Draucker, C. B. (2012). Peer involvement in adolescent dating violence. The Journal of School Nursing, 29, 204–211. doi:10.1177/1059840512469232
Straus, M. A., Gelles, R. J., & Smith, C. (Eds.). (1995). Physical violence in American families: Risk factors and adaptations to violence in 8,145 families. New Brunswick, NJ: Transaction.
Straus, M. A., Hamby, S. L., Boney-McCoy, S., & Sugarman, D. B. (1996). The revised conflict tactics scales (CTS2): Development and preliminary psychometric data. Journal of Family Issues, 17, 283–316. doi:10.1177/019251396017003001
Thompson, M. P., & Morrison, D. J. (2013). Prospective predictors of technology-based sexual coercion by college males. Psychology of Violence, 3, 233–246. doi:10.1037/a0030904
Weisskirch, R. S., & Delevi, R. (2013). Attachment style and conflict resolution skills predicting technology use in relationship dissolution. Computers in Human Behavior, 29, 2530–2534. doi:10.1016/j.chb.2013.06.027
Werner, N. E., Bumpus, M. F., & Rock, D. (2010). Involvement in internet aggression during early adolescence. Journal of Youth and Adolescence, 39, 607–619. doi:10.1007/s10964-009-9419-7
Yancey, A. K., Ortega, A. N., & Kumanyika, S. K. (2006). Effective recruitment and retention of minority research participants. Annual Review of Public Health, 27, 1–28. doi:10.1146/annurev.publhealth.27.021405.102113
Ryan G. Carlson, NCC, is an Assistant Professor at the University of South Carolina. Jessica Fripp is a doctoral candidate at the University of South Carolina. Christopher Cook is a doctoral candidate at the University of South Carolina. Viki Kelchner, NCC, is a doctoral candidate at the University of South Carolina. Correspondence may be addressed to Ryan G. Carlson, University of South Carolina, College of Education, Wardlaw 258, Columbia, SC 29208, rcarlson@sc.edu.