Dec 9, 2015 | Article, Volume 5 - Issue 4
Lindsey Mitchell
The purpose of this study was to explore the relationship of five variables—primary appraisal, secondary appraisal, coping skills, social support and stigma—to bereavement among women whose military spouses had completed suicide. Four correlations to bereavement (primary appraisal, secondary appraisal, coping skills and stigma) were significant. Hierarchical multiple regression analysis assessed the overall relationship of bereavement (the criterion variable) to the five predictor variables, along with the unique contribution of each predictor variable. In the regression, five of six models (all except Model 4) showed significance. The dissertation on which this manuscript is based has the following practical implications: statistically significant correlations between bereavement and constructs of Lazarus’ Cognitive Model of Stress (LCMS), as well as the significance of Lazarus’ construct of primary appraisal within Model 6, indicate that LCMS holds promise for understanding symptoms of bereavement in women whose military spouses have completed suicide.
Keywords: suicide, bereavement, military, spouse, Lazarus
Reports indicate that suicides in the U.S. military surged to a record number of 349 in 2013. This figure far exceeds the 295 American combat deaths in Afghanistan in 2012 and compares with the 201 military suicides in 2011 (National Institute of Mental Health [NIMH], 2013). Some private experts predict that the trend will worsen this year (Miles, 2010).
From 2008–2010, the Army reported the highest number of suicides (n = 182) among active duty troops; whereas the Navy and Air Force reported 60 and 59 respectively (National Institute of Mental Health [NIMH], 2013). The Marine Corps had the largest percentage increase in suicides in a period of 2 years (Lamorie, 2011). U.S. veterans accounted for 20% of the more than 30,000 suicide deaths in the United States in 2009. Between 2003 and 2009, approximately 6,000 veterans committed suicide annually, an average of 18 suicides each day (Congressional Quarterly, 2010; Miles, 2010). During the 2009 fiscal year, 707 members of the veteran population committed suicide, and another 10,665 made unsuccessful suicide attempts (Miles, 2010). Certain experiences of military service members (e.g., exposure to violence, act of killing the enemy, risk of injury, exposure to trauma) increase suicidal tendencies (Zamorski, 2011).
For every person who completes suicide, an estimated 20 people experience trauma related to the death (NIMH, 2010). This suggests that from the 349 military suicides in 2013, approximately 7,000 people have experienced related trauma. Suicide survivors are family members and friends whose lives significantly change because of the suicide of a loved one (Andriessen, 2009; Jordan & McIntosh, 2011; McIntosh, 1993). Survivors of suicide may have higher risk for a variety of psychological complications, including elevated rates of complicated grief and even reactive suicide (Agerbo, 2005).
It is also important to note that suicide survivors might not differ significantly from other bereaved groups regarding general mental health, depression, post-traumatic stress disorder symptoms and anxiety (Sveen & Walby, 2008). Examining the impact of suicide on surviving military family members may provide important information on minimizing negative consequences, including possible survivor suicide.
Military deaths are often sudden, unexpected, traumatic and/or violent in nature, and the family is conditioned to anticipate these types of deaths. In contrast, death by suicide is not anticipated and might not be handled well among military families (Martin, Ghahramanlou-Holloway, Lou, & Tucciarone, 2009). Suicide within the military culture is a traumatic as well as a unique experience. Service members and their families struggle with the visible and invisible wounds of war and the aftermath that combat deaths leave for the survivors. When a service member’s trauma leads to suicide, the military community is less trained and conditioned to process the grief than when death occurs as a direct result of military service (Zhang & Jia, 2009).
Stress plays a role in the grief process within the military culture when it relates to suicide. The chief identifying feature of military culture is warfare, which in turn leads to the claiming of human lives (Siebrecht, 2011). Siebrecht argued that bereavement can only be overcome if people adopt a more rational attitude and grant death its natural place in life. Association with the military ensures that most families will have to experience some form of bereavement and many forms of loss during times of war (Audoin-Rouzeau & Becker, 2002). Military men and woman are less equipped than the general population when it comes to their culture’s acceptance of outward demonstration or sharing of the emotional experience of grief (Doka, 2005).
Stigma
Historically, the stigma of suicide has been present in society (Cvinar, 2005). The biggest obstacles that families with members who have completed suicide confront are acts of informal social disapproval. The surviving family may be suspected of being partly blameworthy in a suicide death and consequently may be subjected to informal isolation and shunning (Bleed, 2007). The stigma of suicide can be subtle. It can be manifested in overt actions taken against the survivors (i.e., placing blame on the family), as well as by omitted actions (i.e., not receiving life insurance), which are probably far more common. When people experience the untimely loss of a family member, there can be feelings of being offended, wounded or abandoned (Neimeyer & Jordan, 2002). The stigmatization experienced by survivors may complicate their bereavement process (Cvinar, 2005; Jordan, 2001; McIntosh, 1993). This complexity results in communication issues, social isolation, projection of guilt, blaming of others and scapegoating (Harwood, Hawton, Hope, & Jacoby, 2002; Lindemann & Greer, 1953). There is a lack of research in the professional literature addressing the grief of surviving military family members impacted by the death, including suicide, of a loved one (Lamorie, 2011).
Suicide and Bereavement
Jordan (2001) researched suicide bereavement and concluded that there are several underlying reasons that it differs from other types of mourning. Jordan summarized that “there is considerable evidence that suicide survivors are viewed more negatively by others and by themselves” (p. 93) and that suicide “is distinct in three significant ways: the thematic content of grief, the social processes surrounding the survivor, and the impact suicide has on family systems” (p. 91). In reviewing the social processes surrounding suicide, Jordan’s analysis supports those of Worden (1991) and Ness and Pfeffer (1990), saying that “there is considerable evidence that survivors feel more isolated and stigmatized than other mourners, and may be viewed more negatively by others in their social network” (p. 93). Most traumatic death survivors will face questions regarding their own culpability in their loved one’s decision to take his or her own life. Survivors may find themselves repeatedly pondering missed warning signs and risk factors (Parrish & Tunkle, 2005). Four primary factors that distinguish the complexities of suicide bereavement for families include stigma, questions about reasons, issues of remorse and guilt, and various logistical and legal factors unique to suicide that necessarily influence the events and processes following death (Minois,1999). The question of why often comes up given the pervasive sense that suicide is a preventable event. This line of thought can often define the grief process. Combined with factors of shock from the sudden, often violent nature of the death, these questions are virtually unavoidable. In some cases, answers to questions of why may never be forthcoming or satisfactory (Steel, Dunlavy, Stillman, & Pape, 2011). Among military families, bereavement is complex. A military death often has circumstances not normally found in the civilian world. It is most likely unexpected, potentially traumatic, occurring in another country, publicized by the media, and enveloped in the commitment to duty and country. Surviving family members of military personnel are often parents, siblings, grandparents and spouses. Military widows are young, often with young families, and are living at a duty station, far away from family and longtime friends (Katzenell, Ash, Tapia, Campino, & Glassberg, 2012).
Bereavement in the Military Culture
Bereavement is a part of the military culture but is often misinterpreted as a weakness that will elicit limited outside support. Military men and women in general are uninformed about the cultural acceptability of outwardly demonstrating their grief or sharing the emotional experience of the loss (Doka, 2005). Although traditional mental health treatments predominantly encourage emotional vulnerability, the military culture values emotional toughness (Kang, Natelson, Mahan, Lee, & Murphy, 2003) and stigmatizes mental illness (Doka, 2005). These attitudes can often deter service members from seeking assistance that could help them to overcome physical and mental health issues. Military culture affects the impact of suicide on families. Each spouse and family has a different bereavement process, and this process is influenced by stigma, social support and ability to cope. In the U.S. military, these issues can be a hindrance to seeking services and can lead to feelings of isolation, which in turn are a risk factor for suicide (Christensen & Yaffe, 2012).
Conceptual Framework
The conceptual framework of Lazarus’ Cognitive Model of Stress (LCMS) was used to frame this study. The underlying construct of this model states that times of uncertainty and difficulty may assist in understanding a person’s ability and capacity to cope with the suicide of a loved one. In general, when people encounter a difficult situation, they employ strategies for dealing with and lessening perceived stress (Groomes & Leahy, 2002).
LCMS (Lazarus & Folkman, 1984) has served as a useful lens for examining the interaction between a person and situational demands. Burton, Farley, and Rhea (2009) used LCMS to frame a study of the relationship between level of perceived stress and extent of physical symptoms of stress, or somatization, among spouses of deployed versus non-deployed servicemen. Eberhardt and associates (2006) examined Lazarus and Folkman’s 1984 stress theory regarding the ways that stress mediators and perceived social support may affect anxiety (as a stress response). The above studies show the usefulness of LCMS in depicting the impact of stress and coping on perceived anxiety, acceptance, ability to lead mentally and physically satisfactory lives, and perception of social support.
LCMS includes primary appraisal, secondary appraisal, coping and perceived social support. Stress is defined as a person’s relationship to his or her environment, specifically a relationship that the person perceives as exceeding his or her resources and endangering well-being. This model supports that the person and the environment are in a dynamic, reciprocal and multidimensional relationship. This conceptualization suggests that people’s perception of stress is related to the way they evaluate, appraise and cope with difficulties.
Stress can be measured by the way an individual appraises a specific encounter. Lazarus and Folkman (1984) presented two types of appraisal. The first is primary appraisal, defined as an individual’s expressed concern in terms of harm, loss, threat or challenge. Harm and loss appraisals refer to loss or damage that has already taken place; threat appraisal refers to harm or loss that has not yet occurred (i.e., anticipatory loss); and challenge appraisal refers to the opportunity for mastery or growth (Lazarus & Folkman, 1984). The second type is secondary appraisal, defined as the focus on what the individual can do to overcome or prevent harm. Lazarus and Folkman suggested that an appraisal of threat is associated with coping resources that can mediate the relationship between stressful events (e.g., loss of spouse to suicide) and outcomes (e.g., ability to seek mental health services).
Coping resources are the personal factors that people use to help them manage situations that are appraised as stressful (Lazarus & Folkman, 1984). Coping resources can be available to the person during the grief process or can be obtained as needed. This fact suggests that the grief process following a suicide is stressful and imposes demands on coping as the bereavement process evolves. Lazarus and Folkman (1984) defined coping as “constantly changing cognitive and behavioral efforts to manage specific external or internal demands that are appraised as exceeding the resources of the person” (p. 141). Coping is a dynamic process that is called into action whenever people are faced with a situation that requires them to engage in some special effort to manage that situation (Lazarus & Folkman, 1984). The ability to cope impacts a person’s bereavement process, and the ways and ability to cope vary with each individual. Stigma and the amount of perceived social support also influence the ability to cope (Bandura, 1997). These variables impact the bereavement process, especially with the added variable of death by suicide.
Social support can strengthen an individual’s position against the stressor and reduce the level of threat (Lazarus, 1996). Research suggests there are specific reasons why survivors do not seek out social support. McMenamy, Jordan, and Mitchell (2008) identified depression and a lack of energy as substantial barriers to obtaining social support.
People who experience a traumatic event are more likely to perceive barriers and not request medical and mental health services due to this lack of energy, lack of trust in professionals and depression (Amaya-Jackson et al., 1999). Provini, Everett, and Pfeffer (2000) stated that the stigma and social isolation that survivors experience can interfere with seeking social support and the willingness of social support networks to come to the aid of the survivor. A lack of social support can increase depression, a lack of energy to complete daily tasks and isolation. Limited social support is especially common for suicide survivors. Shame and guilt surrounding a suicide can impact survivors’ ability to seek social support; however, high social support can be linked to positive mental health.
Barriers to Bereavement
Many suicide survivors struggle with questions about the meaning of life and death, report feeling more isolated and stigmatized, and have greater feelings of abandonment and anger compared with other sudden death survivors (Callahan, 2000). Moreover, the feeling of relief from no longer having to worry about the deceased may distinguish survivors of suicide from survivors of other types of sudden death (Jordan, 2001). Experiencing suicide in one’s family increases risks for family members’ mental health and family relationships (Jordan, 2001). Despite the frequency of suicide, there is limited research focusing on the needs of surviving spouses (Miers, Abbott, & Springer, 2012).
The family system in which the spouses existed as a couple is destabilized by suicide, but the survivor must continue to function. Tasks that were carried out in the relationship must now be carried out by the survivor (Murray, Terry, Vance, Battistutta, & Connolly, 2000). Cerel, Jordan, and Duberstein (2008) stated that because suicide occurs within families, the focus on the aftermath of suicide within families and the impact on the spouse are important areas to investigate in order to determine exactly how to help survivors. Helping survivors to address practical, economic and legal issues, in addition to providing information and therapeutic intervention, is important (Dyregrov, 2002; Provini et al., 2000).
Purpose of the Study
Because of the frequency of suicide in the United States, the increased number of suicides within the U.S. military, and the impact of suicide on the family, the bereavement process among female spousal survivors of military suicides deserves further exploration. The purpose of this study was to explore bereavement in female spousal survivors of military suicides. Using LCMS, the study explored the relationship of bereavement and stigma, social support, primary appraisal, secondary appraisal, and coping skills among women whose military spouse had completed suicide.
Summary of the Study and Methodology
This study investigated the linear relationship between the dependent variable of bereavement and each of five independent variables—primary appraisal, secondary appraisal, coping skills, perceived social support and stigma—among women whose military spouses had completed suicide. The following hypotheses guided the study. Hypothesis 1 stated that there would be a relationship between bereavement and stigma; this positive relationship was significant. Hypothesis 2 stated that there would be a relationship between bereavement and social support; the relationship was not statistically significant. Hypothesis 3 stated that there would be a relationship between bereavement and primary appraisal; this positive relationship was significant. Hypothesis 4 stated that there would be a relationship between bereavement and secondary appraisal; this negative relationship was significant. Hypothesis 5 stated that there would be a relationship between bereavement and coping skills; this negative relationship was significant.
Using hierarchical regression analysis, the researcher examined the relationship of five independent variables—primary appraisal, secondary appraisal, coping skills, social support and stigma—to bereavement. The relationship was statistically significant. The model was a good fit and controlled for time since death (i.e., number of years since the person completed suicide). Therefore, for this sample, the five independent variables are components of a statistically significant model.
Participants and Recruitment
The participants in this study were women aged 18 and older who had lost a military spouse to suicide. Criteria for inclusion were that (a) the service member who had completed suicide had been either on active duty or of veteran status, (b) the survivor was female and 18 years of age or older, and (c) the survivor was considered a spouse. A spouse was defined as legally married to another person or living and cohabiting with another person in a marriage-like relationship, including a marriage-like relationship between persons of the same gender. Participants were chosen from seven national organizations serving veterans. The researcher recruited participants from these organizations by explaining the study and asking for volunteers. The director or assistant director of each organization distributed study information and materials through listservs and posted them on their Web sites. Once prospective participants received an e-mail, they decided whether they wanted to participate and whether they met the eligibility requirements. If the spouses decided to participate in the study, they would complete the survey through Survey Monkey.
Variables
Demographic variables included age, race/ethnicity, length of relationship with the deceased partner, the decedent’s military status (active or retired), the decedent’s length of service, and time elapsed since death. The survey also asked about the deceased’s rank, education level, surviving children and prior suicide attempts.
A self-report online survey was constructed using the following five instruments: the Core Bereavement Items (CBI; Holland, Futterman, Thompson, Moran, & Gallagher-Thompson, 2013), the Stigma of Suicide and Suicide Survivor Scale (STOSASS; Scocco, Castriotta, Toffol, & Preti, 2012), the Coping Self-Efficacy Scale (CSES; Chesney, Neilands, Chambers, Taylor, & Folkman, 2006), the Multidimensional Scale of Perceived Social Support (MSPSS; Zimet, 1988), and the Stress Appraisal Measure (SAM; Peacock & Wong, 1990). The SAM is one measure. However, the variables of primary stress appraisal and secondary stress appraisal within it were separated, and the questions within the SAM regarding primary stress appraisal were referred to as the primary stress appraisal measure (PSAM), and the remaining questions of the SAM were referred to as the secondary stress appraisal measure (SSAM). In addition to these assessments, participants would also answer 11 demographic questions and three open-ended questions. The survey was split into seven sections.
The first section had 11 demographic questions. The second section, comprised of the MSPSS, had 12 questions regarding social support of the participant and used a 7-point Likert scale. The third section, comprised of the CBI, had 26 questions regarding the participant’s ability to cope and used a 10-point Likert scale. The fourth section, comprised of the SAM, had 19 questions regarding participant’s stress appraisal measures and used a 4-point Likert scale. The fifth section, comprised of the STOSASS, had 17 questions regarding the participant’s perceived stigma and used a 4-point Likert scale. The sixth section, comprised of the CBI, had 17 questions regarding the participant’s bereavement process and used a 4-point Likert scale. The survey included the three following open-ended questions that were derived from the Grief Evaluation Measure (GEM) and reviewed by three licensed professional counselors working in the field of suicide bereavement: (1) What do you recall about how you responded to the death of your spouse at the time?; (2) What was the most painful part of the experience to you?; and (3) How has this experience affected your view of yourself or your view of your world? To analyze the qualitative responses, the researcher identified the most commonly recurring words or phrases used by participants for each question. Three experts in the field of grief and loss were consulted and confirmed the content and face validity of the survey.
Data Analysis
The Statistical Package for the Social Sciences (SPSS), a statistical software package, generated all of the statistics for this research investigation. A Pearson correlation analysis was conducted to determine whether there was a linear relationship between primary appraisal, secondary appraisal, social support, coping skills, stigma and bereavement for women whose military spouse had completed suicide. Following this analysis, a multiple regression was used to describe the relationships of the independent or predictor variables to the dependent or criterion variable (Lussier & Sonfield, 2004). Because LCMS states that it is possible to discern the order in which a person experiences each variable with regard to a particular event, the variables were entered into the regression using the following equation: Bereavement = {time since death} + {primary appraisal} + {secondary appraisal} + {coping skills} + {perceived social support} + {perceived stigma}.
Results
Descriptive Statistics
Descriptive statistics provided simple summaries of the demographic characteristics of the sample, as well as descriptors such as means and standard deviations for these characteristics. The sample was a well-educated, racially diverse group of women who had lost their military spouses to suicide. The majority of participants were non-Hispanic White females who had attended at least some college. Most were affiliated with the Army and had been married to the military member who had completed suicide. The majority of the partners had committed suicide while on active duty. The mean age of respondents was 33.48 years (SD = 5.20; SE = .373); their ages ranged from 23–50 years. The mean number of children aged 17 or under that were a product of the relationship with the service member was 1.12 (SD = .79; SE = .064); the range was 0–4 children. The mean number of prior suicide attempts by the service member (known/confirmed by the surviving female spouse) was 1.31 (SD = 1.06; SE = .096); the range was 0–4 prior suicide attempts.
Correlation Results
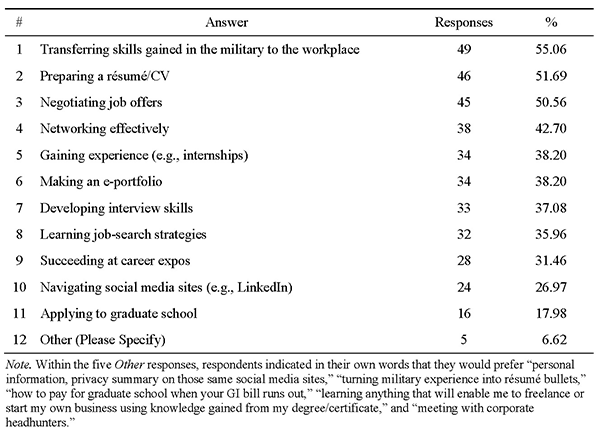
Using SPSS Student Version 22.0 software, a Pearson correlation coefficient was used to measure the relationship of bereavement, primary appraisals, secondary appraisals, coping skills, social support, and stigma among women whose military spouses had completed suicide. The correlation coefficient measures the strength and direction of the relationship among variables. When conducting a correlational analysis of two co-occurring variables, the researcher can indicate whether change in one is accompanied by systematic change in the other. Examination of intercorrelations among study variables indicated statistically significant correlations between bereavement and each of four independent variables: primary appraisal, secondary appraisal, coping skill, and stigma. The results for each correlation are presented separately and summarized below as well as in Table 1.
Control variable. There was a statistically significant relationship between time since death and bereavement for women whose military spouse had completed suicide, r(194) = .277, p < .01. The shorter the amount of time elapsed, the higher the bereavement scores.
Independent variables. Primary stress appraisal, r(193) = -.309, p < .01: There is a weak negative linear relationship between bereavement and primary stress appraisal. Secondary stress appraisal, r(193) = -.309, p < .01: There is a weak negative linear relationship between secondary stress appraisal and bereavement. Coping skills, r(193) = -.174, p = .015: There is a weak negative linear relationship between coping skills and bereavement. Social support, r(193) = -.039, p = .594: There is no linear relationship between perceived social support and bereavement. Stigma, r(193) = .252, p < .01: There is a weak positive linear relationship between perceived stigma and bereavement.
Table 1
Correlations for Independent, Dependent and Control Variables
CBI TSD PSAM SSAM MSPSS CSES
1. TSD .277*
2. PSAM -.309* -.167
3. SSAM -.309* -.151 .602*
4. MSPSS -.039 .032 .379* .172*
5. CSES -.174* -.167* .494* .473* .585*
6. STOSASS .252* .095 -.196* -.221* .022 -.253
Note: N = 194; CBI = Core Bereavement Items; TSD = Time Since Death (in months);
PSAM = Primary Stress Appraisal Measure; SSAM = Secondary Stress Appraisal Measure;
CSES = Coping Self-Efficacy Scale; MSPSS = Multidimensional Scale of Perceived Social Support; STOSASS = Stigma of Suicide and Suicide Survivor Scale.
*Significant at p < .05.
Multiple Regression
Following the correlational analysis, a multiple regression was utilized. This analysis was appropriate to describe the relationships between the independent or predictor and dependent or criterion variables in an objective manner (Lussier & Sonfield, 2004). The design was appropriate because the purpose of the study was to explain the relationships between variables.
Model 1 (TSD onto bereavement) yielded R = .277, R2 = .077, F(1, 125), p < .001. The portion of the variance explained was 7%. Model 2 (TSD and primary appraisal) yielded R = .431, R2 = .186, F(2, 124), p < .001. The portion of variance explained was 18.6%. Model 3 (TSD, primary appraisal and secondary appraisal) yielded R = .454, R2 = .206, F(3, 123), p < .001. The portion of variance explained was 20.6%. Model 4 (time since death, primary appraisal, secondary appraisal and coping skills) yielded R = .455, R2 = .207, F(4, 122), p < .001. The portion of variance explained was 20.7%. Model 5 (time since death, primary appraisal, secondary appraisal, coping skills and social support) yielded R = .471, R2 = .221, F(5, 121), p < .001. The portion of variance explained was 22.1%. Model 6 (time since death, primary appraisal, secondary appraisal, coping skills, social support, and stigma) yielded R = .482, R2 = .232, F(6, 120), p < .001. The portion of variance explained was 23.2% (see Table 2).
Table 2
Hierarchical Multiple Regression
| Model |
R |
R2 |
t |
p |
B |
β |
R2 Change |
| Model 1TSD |
.277
|
.077
|
61.600
3.228
|
.000
.002
|
.049
|
.277
|
0
|
| Model 2TSDPSAM |
.431
|
.186
|
19.482
2.696
-4.074
|
.000
.008
.000
|
.039
-.406
|
.222
-.335
|
.109
|
| Model 3TSDPSAMSSAM |
.454
|
.206
|
19.646
2.618
-1.947
-1.782
|
.000
.010
.054
.077
|
.038
-.254
-.192
|
.214
-.209
-.191
|
.02
|
| Model 4TSDPSAMSSAMCSES |
.455
|
.207
|
16.971
2.622
-1.952
-1.788
.266
|
.000
.010
.053
.076
.791
|
.038
-.262
-.199
.004
|
.216
-.216
-.198
.025
|
.001
|
| Model 5TSDPSAMSSAMCSESMSPSS |
.471
|
.221
|
12.989
2.307
-2.359
-1.111
-0.710
1.505
|
.000
.023
.020
.269
.479
.135
|
.034
-.335
-.132
-.012
.091
|
.192
-.276
-.132
-.083
.167
|
.015
|
| Model 6 TSDPSAMSSAMCSESMSPSSSTOSASS |
.482
|
.232
|
9.026
2.329
-2.187
-1.105
-0.320
1.107
1.280
|
.000
.022
.031
.271
.750
.271
.203
|
.034
-.312
-.131
-.006
.069
.086
|
.194
-.257
-.131
-.039
.128
.112
|
.010
|
Note: TSD = Time Since Death (in months); PSAM = Primary Stress Appraisal Measure; SSAM = Secondary Stress Appraisal Measure; CSES = Coping Self-Efficacy Scale; MSPSS = Multidimensional Scale of Perceived Social Support; STOSASS = Stigma of Suicide and Suicide Survivor Scale.
Qualitative Component
There is a growing interest in integrating qualitative data across quantitative studies to discover patterns and common threads within a specific topic or issue (Erwin, Brotherson, & Summers, 2011). The main aim of the qualitative questions within the survey is to gain insight into the participants’ world and capture their unique experiences (e.g., naturally occurring events and/or social or human problems) and their interpretations of these experiences (Jones, 1995; Sarantakos, 1993).
A total of 55 (28.4%) participants responded to the question, “What do you recall about how you responded to the death of your spouse at the time?” Of these, 24 stated recalling “sadness” as most frequent. Fifteen participants indicated disbelief, shock, feelings of helplessness or feelings of fear. Other participants’ responses included “trying not to think about what had happened,” crying, sobbing, physical symptoms, physical pain, collapsing, fainting, being unable to forget what happened, and being unable to recall or process the event. A total of 68 (35.1%) participants responded to the question, “What was the most painful part of the experience to you?” Of these, 50 reported physical and emotional numbness and only partial recollection of learning about the death (e.g., who told them, where they were when notified, immediate responses). These participants indicated that they could recall parts of the experience but struggled with identifying feelings or emotions directly following the event. Other responses included being hospitalized, contemplating suicide, refraining from eating, and feeling that their future had been lost. Although four reported contemplating suicide following the death of their spouse, no participants reported attempting suicide at any point. A total of 36 (18.6%) participants responded to the question, “How has this experience affected your view of yourself or your view of your world?” Of these, 15 participants indicated that they no longer feared death, while seven reported having a negative reaction to relationships. Eleven participants reported that they perceived stress as more threatening than before the suicide of their spouse and were unaware of the triggers that brought on stress during the bereavement process. Ten participants indicated that their view of love had changed since the loss of their spouse. Nine participants wrote about making an effort to enjoy life after the suicide of their spouse.
Discussion
This study investigated the relationships between bereavement and primary appraisal, secondary appraisal, coping skills, perceived social support and stigma among women whose military spouses had completed suicide. There are several study findings that deserve further exploration.
First, there was a statistically significant positive relationship between stigma and bereavement, suggesting that as female survivors perceive increased stigma regarding the suicide of their spouse, they present more symptoms of bereavement. Knieper (1999) suggested that bereavement following suicide is not the same as that following natural death. He reported that stigma and avoidance continue to be central issues for suicide survivors. Psychological projection of feelings of rejection and the actual social response to the survivor interact in a complicated manner. Worden (2009) also noted a difference between suicide bereavement and other forms of bereavement, suggesting that suicide is often associated with stigma and a sense of shame. Such shame can result in the complete isolation of the bereaved during the period immediately following the suicide event. Eaton and associates (2008) examined survivors’ barriers to seeking mental health treatment after the suicide of their partners and found that spouses were 70% less likely to seek treatment following a suicide, as compared to a natural death, and that stigma was a recurrent theme in the qualitative analysis. However, Eaton et al.’s study did not directly examine the impact of stigma on bereavement. It did show that stigma is an important variable that needs to be investigated further. The present study showed similar results to Eaton et al.’s (2008) research.
The qualitative comments recorded in the open-ended question section of the survey supported the study findings. For example, one participant responded, “I blamed myself for not doing more, not being there enough, or not being there when the death happened.” Another participant noted, “Suicide is one of the most difficult and painful ways to lose someone we love, because we are left with so many unanswerable questions.” One participant expressed the following:
[I felt] anger at family members for not assisting me with my husband and anger at physicians that treated my husband and were not able to see the warning signs or provide assistance in caring for them properly. I was then left with the scars after the death and had to explain to people what happened. I felt I got blamed and it was not my fault.
Several participants expressed “numbness and isolation.” Responding to stigma, people with mental health problems often internalize public attitudes and become embarrassed or ashamed. These feelings can lead them to conceal symptoms and fail to seek treatment (President’s New Freedom Commission on Mental Health, 2003). These survey responses assist in understanding the impact of stigma upon the military spouse survivors and imply that unanswered questions, as well as guilt, are important factors to explore in the grief process following a suicide.
Second, a statistically significant relationship between primary appraisal and bereavement was reported, suggesting that survivors who perceive the death of a spouse to be stressful are more likely to experience bereavement. This result is supported by the bereavement literature (Cvinar, 2005; Jordan, 2001; McIntosh, 1993). Lazarus (2005) argued that primary appraisal shows that it is not the situation, but the way a person interprets the situation, that affects the person’s experience. The way a person appraises a situation can impact the way the person reacts to it. Primary appraisal is an important step in processing the stress of bereavement, since grieving is such an individualized experience.
The qualitative comments recorded in the open-ended question portion of the survey supported the statistical relationship between primary appraisal and bereavement. For example, one participant indicated that her worldview had changed when she responded, “My world has become gray; I have made myself closed. I live in a rain cloud and now know that good people do bad things that change lives.” The participant had changed her worldview such that her world became a smaller, more restricted place. Another stated, “This death, this loss, makes small things seem insignificant. Material things are insignificant. Relationships with people are more important. I don’t have a fear of dying and in fact, feel like I will die at a young age.” This concept of primary appraisal is based on the idea that emotional processes are dependent on a person’s expectancies about the significance and outcome of a specific event. The same event within the same community (in this case, suicide within the military) can elicit responses of different quality, intensity and duration due to individuality in experiences and personality (Krohne, Pieper, Knoll, & Breimer, 2002). The different kinds of stress identified by the primary appraisal may be embedded in specific types of emotional reactions, thus illustrating the close conjunction of the fields of stress and emotion (Lazarus & Folkman, 1984).
Third, a statistically significant negative relationship was reported between secondary appraisal and bereavement, suggesting that survivors who make a negative appraisal of their ability to control the outcomes of their spouse’s death are more likely to experience bereavement. In the future, when examining outcomes of interventions that impact coping, beliefs about a person’s ability to perform specific behaviors related to coping would need to be highlighted. This concept is known as specific coping behaviors and is also pertinent to stress, coping theory and secondary appraisal (Chesney et al., 2006). Part of secondary appraisal is the judgment that an outcome is controllable through coping; another part addresses the question of whether or not the individual believes he or she can carry out the requisite coping strategy (Chesney et al., 2006; DiClemente, 1986; Hofstetter, Sallis, & Hovell, 1990).
The qualitative comments recorded in the open-ended section of the survey supported this finding. For example, one participant indicated her appraisal of the situation by stating, “Everyone must learn to face the misfortune, because life on the road will not be smooth.” Another stated that “time can dilute all and I must face life and accept my reality;” yet another wrote, “I want to work on longer range goals to give myself some structure and direction to my life and not focus on my loss. I am only interested in rebuilding my life.” However, other participants stated that it was harder to assess the loss and to move forward after the suicide. One participant stated the following:
I often find myself complaining to God about what seems senseless or unjust and unfair. I find myself bogged down in fear and even anger at myself or the person who died and “left” me. I do not accept what happen[ed] to me and my children.
Some participants reported not knowing what to do. An example of this feeling is the statement, “I perceive stress as threatening. I feel totally helpless.” Perceived self-efficacy, defined as a belief about one’s ability to perform a specific behavior, is a salient component of this theory. It highlights the importance of personal efficacy in determining the acquisition of knowledge on which skills are founded (Bandura, 1997; Chesney et al., 2006).
Fourth, a statistically significant negative relationship between coping skills and bereavement was reported, suggesting that survivors who believe they have a low ability to cope with their spouses’ death are more likely to experience bereavement. Although it is important for survivors to become familiar with the stress appraisal process, the way they assign meaning to their spouse’s death and their past experience with death also are important in their primary appraisal to the overall coping effort. One model of this process is the transactional model of coping (Lazarus & Folkman, 1984). This model of coping implies that a person’s appraisal of his or her interaction with a difficult event naturally evokes a coping response for dealing with the situation. Experiencing a suicide or living in a social environment that hinders, stigmatizes or isolates a person who has experienced a suicidal death may cause demands to exceed his or her resources for dealing with certain situations. Few studies have examined the natural coping efforts used by suicide survivors, or have identified specific problems and needs that survivors experience following the suicide of a significant other (McMenamy et al., 2008). Interventions with suicide survivors have limited effectiveness (Jordan & McMenamy, 2004). Provini et al. (2000) presented four categories of concerns for suicide survivors: concerns related to (a) family relationships, (b) psychiatric symptoms, (c) bereavement and (d) stress. Family-related problems were the most frequently mentioned type of concerns (Provini et al., 2000). Examples of family relationship concerns included inability to maintain parenting roles, inability to maintain family routines, existence of different coping styles within the family, and inability to provide appropriate emotional support to family members.
Qualitative comments recorded in the open-ended section of the survey supported this study finding. For example, one participant stated, “I often feel distracted, forgetful, irritable, disoriented, or confused. I try to remember how I got over a death in the past, sometimes it helps and sometimes it does not.” Another participant stated, “I know I need to start to form new relationships or attachments in my life but my mind [is] telling me ‘there must be some mistake,’ or ‘this can’t be true.’ ” Regarding bereavement, one participant wrote, “Grief is perhaps the most painful companion to death.” Addressing coping, one participant stated, “I must also adjust to working or returning to work after the death. I know things can’t go back to the way they were before, very difficult and painful to deal with and I better adjust to life.” These statements support the need to further explore the relationship between one’s ability to cope with the suicide of a spouse and one’s ability to experience and acknowledge feelings and move forward with everyday life activities (e.g., employment, childcare, financial obligations). Ability to cope impacts a person’s bereavement process; the ways and ability to cope vary with the individual. Stigma and amount of perceived social support have been correlated with ability to cope (Bandura, 1997). It is important to understand the individual impacts that stigma, social support, primary appraisal, secondary appraisal and coping have on bereavement. However, it is equally important to examine the relationships of these variables within the context of a model in order to establish future interventions for bereavement within the context of a suicide.
Fifth, results indicated that the model is statistically significant in predicting bereavement outcomes and provides considerable support for using the Lazarus model as a means of understanding the relationship between stress and bereavement when placed into the equation in a particular order: CBI = TSD + PSAM + SSAM + CSES + MSPSS + STOSASS.
This study suggests that the proposed model, using LCMS and assessment of stress, identifies the constructs associated with bereavement among women whose military spouses completed suicide. Future research could further explore the assessment of primary and secondary appraisal processes, coping, stigma, and social support enhancement programs and interventions to improve the bereavement process for military spouses. When survivors can identify and address their needs, the bereavement process following a suicide can begin (Christensen & Yaffe, 2012).
Limitations
First, the majority of the sample (54.1%) were non-Hispanic White, or Euro-American. Second, there is limited representation across military branches. Third, the study collected data from a self-administered electronic survey. Fourth, although the social support measure (i.e., MSPSS) has good reliability and measures social support as a general feeling of belonging to a social network that one can turn to for advice and assistance in times of need (Uchino, 2006), it does not delineate various types of social support. Finally, most of the sample consisted of women whose spouses had completed suicide while on active duty. Active duty members typically live on base and are well connected to the military community. When the military spouse dies, these supports are often no longer available, and the stigma of a suicide could strongly affect these women.
Recommendations for Future Studies
There are several practice implications from this study. The statistically significant correlations between bereavement and four other variables (primary appraisal, secondary appraisal, coping skills and stigma), as well as the significance of the LCMS construct of primary appraisal within Model 6, indicate that LCMS holds promise for understanding symptoms of bereavement in females following the suicide of a military spouse. Primary appraisal, the most significant variable within this study, could be highlighted within bereavement research on women whose military spouses have completed suicide. When conceptualizing the responses of these women, counselors and clinicians could use LCMS, examining the three components of primary appraisal (goal relevance, goal congruence and ego involvement) and exploring the ways these components present during the client’s bereavement process. The approach would focus on the role of maladaptive cognitions during times of stress (Sudak, 2009).
The reluctance of the military community to seek mental health support contributes to an inability to move through the bereavement process in a healthy way. Within the military community, it can be quite difficult to deal with the ambiguity of bereavement that is typically associated with emotional vulnerability (Lamorie, 2011). However, the current study suggests that four constructs—primary appraisal, secondary appraisal, coping and stigma—are significant when addressing the issues of bereavement in females who have lost a military spouse to suicide. Using LCMS to address cognitions, counselors might be able to assist a population whose members have been reluctant to seek mental health services in the past. Because the components of LCMS are correlated with bereavement, clinicians could use LCMS and cognitive stress research, which together seem to be a promising direction, when assisting women who have lost a military spouse to suicide.
Conflict of Interest and Funding Disclosure
The author reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Agerbo, E. (2005). Midlife suicide risk, partner’s psychiatric illness, spouse and child bereavement by suicide or other modes of death: A gender specific study. Journal of Epidemiology and Community Health, 59, 407–412. doi:10.1136/jech.2004.024950
Amaya-Jackson, L., Davidson, J. R., Hughes, D. C., Swartz, M., Reynolds, V., George, L. K., & Blazer, D. G. (1999). Functional impairment and utilization of services associated with posttraumatic stress in the community. Journal of Traumatic Stress, 12, 709–724. doi:10.1023/A:1024781504756
Andriessen, K. (2009). Can postvention be prevention? Crisis: The Journal of Crisis Intervention and Suicide Prevention, 30, 43–47. doi:10.1027/0227-5910.30.1.43
Audoin-Rouzeau, A., & Becker, S. (2002). 14–18: Understanding the great war. New York, NY: Hill and Wang.
Bandura, A. (1997). Self-efficacy: The exercise of control. New York, NY: Worth.
Bleed, J. (2007, February 19). Howell’s life insurance payout not a sure bet. Arkansas Democrat-Gazette.
Retrieved from http://www.arkansasonline.com/
Burton, T., Farley, D., & Rhea, A. (2009). Stress-induced somatization in spouses of deployed and nondeployed servicemen. Journal of the American Academy of Nurse Practitioners, 21, 332–339. doi:10.1111/j.1745-7599.2009.00411.x
Callahan, J. (2000). Predictors and correlates of bereavement in suicide support group participants. Suicide & Life-Threatening Behavior, 30, 104–124. doi:10.1111/j.1943-278X.2000.tb01070.x
Cerel, J., Jordan, J. R., & Duberstein, P. R. (2008). The impact of suicide on the family. Crisis: The Journal of Crisis Intervention and Suicide Prevention, 29, 38–44. doi:10.1027/0227-5910.29.1.38
Chesney, M. A., Neilands, T. B., Chambers, D. B., Taylor, J. M., & Folkman, S. (2006). A validity and reliability study of the coping self-efficacy scale. British Journal of Health Psychology, 11, 421–337. doi:10.1348/135910705X53155
Christensen, B. N., & Yaffe, J. (2012). Factors affecting mental health service utilization among deployed military personnel. Military Medicine, 177, 278–283.
Congressional Quarterly. (2010). Rising military suicide: The pace is faster than combat death in Iraq and Afghanistan. Retrieved from http://www.infiniteunknown.net/2010/01/01/rising-us-military-suicides-the-pace-is-faster-than-combat-deaths-in-iraq-or-afghanistan/
Cvinar, J. C. (2005). Do suicide survivors suffer social stigma: a review of the literature. Perspectives in Psychiatric Care, 41, 14–21. doi:10.1111/j.0031-5990.2005.00004.x
DiClemente, C. C. (1986). Self-efficacy and the addictive behaviors. Journal of Social and Clinical Psychology, 4, 302–315. doi:10.1521/jscp.1986.4.3.302
Doka, K. J. (2005). Ethics, end-of-life decisions and grief. Mortality, 10, 83–90. doi:10.1080/13576270500031105
Dyregrov, K. (2002). Assistance from local authorities versus survivors’ needs for support after suicide. Death Studies, 26, 647–668. doi:10.1080/07481180290088356
Eaton, K. M., Hoge, C. W., Messer, S. C., Whitt, A. A., Cabrera, O. A., McGurk, D., . . . Castro, C. A. (2008). Prevalence of mental health problems, treatment need, and barriers to care among primary care-seeking spouses of military service members involved in Iraq and Afghanistan deployments. Military Medicine, 173, 1051–1056.
Eberhardt, B., Dilger, S., Musial, F., Wedding, U., Weiss, T., & Miltner, W. H. (2006). Short-term monitoring of cognitive functions before and during the first course of treatment. Journal of Cancer Research & Clinical Oncology, 132, 234–240. doi:10.1007/s00432-005-0070-8
Erwin, E. J., Brotherson, M. J., & Summers, J. A. (2011). Understanding qualitative metasynthesis: Issues and opportunities in early childhood intervention research. Journal of Early Intervention, 33, 186–200. doi:10.1177/1053815111425493
Groomes, D. A. G., & Leahy, M. J. (2002). The relationships among the stress appraisal process, coping disposition, and level of acceptance of disability. Rehabilitation Counseling Bulletin, 46, 15–24.
Harwood, D., Hawton, K., Hope, T., & Jacoby, R. (2002). The grief experiences and needs of bereaved relatives and friends of older people dying through suicide: A descriptive and case-control study. Journal of Affective Disorders, 72, 185–194. doi:10.1016/S0165-0327(01)00462-1
Hofstetter, C. R., Sallis, J. F., & Hovell, M. F. (1990). Some health dimensions of self-efficacy: Analysis of theoretical specificity. Social Science & Medicine, 31, 1051–1056.
Holland, J. M., Futterman, A., Thompson, L. W., Moran, C., & Gallagher-Thompson, D. (2013). Difficulties accepting the loss of a spouse: A precursor for intensified grieving among widowed older adults. Death Studies, 37, 126–144. doi:10.1080/07481187.2011.617489
Jones, R. (1995). Why do qualitative research? British Medical Journal, 311(6996), 2–3. doi:10.1136/bmj.311.6996.2
Jordan, J. R. (2001). Is suicide bereavement different? A reassessment of the literature. Suicide and Life-Threatening Behavior, 31, 91–102. doi:10.1521/suli.31.1.91.21310
Jordan, J. R., & McIntosh, J. L. (2011). Grief after suicide: Understanding the consequences and caring for the survivors. New York, NY: Routledge.
Jordan, J. R., & McMenamy, J. (2004). Interventions for suicide survivors: A review of the literature. Suicide and Life-Threatening Behavior, 34, 337–349. doi:10.1521/suli.34.4.337.53742
Kang, H. K., Natelson, B. H., Mahan, C. M., Lee, K. Y., & Murphy, F. M. (2003). Post-Traumatic stress disorder and chronic fatigue syndrome-like illness among Gulf War veterans: A population-based survey of 30,000 veterans. American Journal of Epidemiology, 157, 141–148. doi:10.1093/aje/kwf187
Katzenell, U., Ash, N., Tapia, A. L., Campino, G. A., & Glassberg, E. (2012). Analysis of the causes of death of casualties in field military setting. Military Medical Journal, 177, 1065–1068.
Knieper, A. J. (1999). The suicide survivor’s grief and recovery. Suicide and Life-Threatening Behavior, 29, 353–364. doi: 10.1111/j.1943-278X.1999.tb00530.x
Krohne, H. W., Pieper, M., Knoll, N., & Breimer, N. (2002). The cognitive regulation of emotions: The role of success versus failure experience and coping dispositions. Cognition & Emotion, 16, 217–243. doi:10.1080/02699930143000301
Lamorie, J. (2011). Operation Iraqi Freedom/Operation Enduring Freedom: Exploring wartime death and bereavement. Social Work in Health Care, 50, 543–563. doi:10.1080/00981389.2010.532050
Lazarus, A. A. (2005). Is there still a need for psychotherapy integration? Current Psychology, 24, 149–152. doi:10.1007/s12144-005-1018-5
Lazarus, A. A. (1996). Behavior therapy & beyond. New York, NY: McGraw-Hill.
Lazarus, R. S., & Folkman, S. (1984). Stress, appraisal, and coping. New York, NY: Springer.
Lindemann, E., & Greer, I. M. (1953). A study of grief: Emotional responses to suicide. Pastoral Psychology, 4, 9–13.
Lussier, R. N., & Sonfield, M. C. (2004). Family business management activities, styles and characteristics: A correlational study. Mid-American Journal of Business, 19, 47–53.
Martin, J., Ghahramanlou-Holloway, M., Lou, K., & Tucciarone, P. (2009). A comparative review of U.S. military and civilian suicide behavior: Implications for OEF/OIF suicide prevention efforts. Journal of Mental Health Counseling, 31, 101–118.
McIntosh, J. L. (1993). Control group studies of suicide survivors: A review and critique. Suicide and Life-Threatening Behavior, 23,146–161. doi:10.1111/j.1943-278X.1993.tb00379.x
McMenamy, J. M., Jordan, J. R., & Mitchell, A. M. (2008). What do suicide survivors tell us they need? Results of a pilot study. Suicide and Life-Threatening Behavior, 38, 375–389. doi:10.1521/suli.2008.38.4.375
Miers, D., Abbott, D., & Springer, P. R. (2012). A phenomenological study of family needs following the suicide of a teenager. Death Studies, 36, 118–133. doi:10.1080/07481187.2011.553341
Miles, D. (2010). VA strives to prevent veteran suicides. Retrieved from http://www.defense.gov/news/newsarticle.aspx?id=58879
Minois, G. (1999). History of suicide: Voluntary death in western culture (L. G. Cochrane, Trans.). Baltimore, MD: Johns Hopkins University Press.
Murray, J. A., Terry, D. J., Vance, J. C., Battistutta, D., & Connolly, Y. (2000). Effects of a program of intervention on parental distress following infant death. Death Studies, 24, 275–305. doi:10.1080/074811800200469
National Institute of Mental Health. (2010). Statistics. http://www.nimh.nih.gov/health/statistics/index.shtml
National Institute of Mental Health. (2013). Suicide prevention. http://www.nimh.nih.gov/health/topics/suicide-prevention/index.shtml
Neimeyer, R. A., & Jordan, J. R. (2002). Disenfranchisement as empathic failure: Grief therapy and the co-construction of meaning. In K. J. Doka (Ed.), Disenfranchised grief: New directions, challenges, and strategies for practice (pp. 95–117). Champaign, IL: Research Press.
Ness, D. E., & Pfeffer, C. R. (1990). Sequelae of bereavement resulting from suicide. American Journal of Psychiatry, 147, 279–285.
Parrish, M., & Tunkle, J. (2005). Clinical challenges following an adolescent’s death by suicide: Bereavement issues faced by family, friends, schools, and clinicians. Clinical Social Work Journal, 33, 81–102. doi:10.1007/s10615-005-2621-5
Peacock, E. J., & Wong, P. T. P. (1990). The stress appraisal measure (SAM): A multidimensional approach to cognitive appraisal. Stress Medicine, 6, 227–236. doi:10.1002/smi.2460060308
President’s New Freedom Commission on Mental Health. (2003). New freedom commission on mental health report. Retrieved from http://govinfo.library.unt.edu/mentalhealthcommission/reports/FinalReport/downloads/FinalReport.pdf
Provini, C., Everett, J. R., & Pfeffer, C. R. (2000). Adults mourning suicide: Self-Reported concerns about bereavement, needs for assistance, and help-seeking behavior. Death Studies, 24, 1–19. doi:10.1080/074811800200667
Sarantakos, S. (1993). Social research. Basingstoke, England: Macmillan.
Scocco, P., Castriotta, C., Toffol, E., & Preti, A. (2012). Stigma of Suicide Attempt (STOSA) scale and Stigma of Suicide and Suicide Survivor (STOSASS) scale: Two new assessment tools. Psychiatry Research, 200, 872–878. doi:10.1016/j.psychres.2012.06.033
Siebrecht, C. (2011). Imagining the absent dead: Rituals of bereavement and the place of the war dead in German women’s art during the First World War. German History, 29, 202–223.
Steel, J. L., Dunlavy, A. C., Stillman, J., & Pape, H. C. (2011). Measuring depression and PTSD after trauma: Common scales and checklists. Injury, 42, 288–300. doi:10.1016/j.injury.2010.11.045
Sudak, D. (2009). Training in cognitive behavioral therapy in psychiatry residency: An overview for educators. Behavior Modification, 33, 124–137. doi:10.1177/1059601108322626
Sveen, C.-A., & Walby, F. A. (2008). Suicide survivors’ mental health and grief reactions: A systematic review of controlled studies. Suicide and Life-Threatening Behavior, 38, 13–29. doi:10.1521/suli.2008.38.1.13
Uchino, B. N. (2006). Social support and health: A review of physiological processes potentially underlying links to disease outcomes. Journal of Behavior Medicine, 29, 377–387. doi:10.1007/s10865-006-9056-5
Worden, J. W. (1991). Grief counseling & grief therapy: A handbook for the mental health practitioner (2nd ed.). New York, NY: Springer.
Worden, J. W. (2009). Grief counseling and grief therapy: A handbook for the mental health practitioner (4th ed.) New York, NY: Springer.
Zamorski, M. A. (2011). Suicide prevention in military organizations. International Review of Psychiatry, 23, 173–180. doi:10.3109/09540261.2011.562186
Zhang, J., & Jia, C.-X. (2009). Attitudes toward suicide: The effect of suicide death in the family. Omega, 60, 365–382. doi:10.2190/OM.60.4.d307.
Zimet, G. D., Dahlem, N. W., Zimet, S. G., Farley, G. K. (1988). The multidimensional scale of perceived social support. Journal of Personality Assessment, 52, 30–41. doi:10.1207/s15327752jpa5201_2
Lindsey Mitchell, NCC, is the recipient of the 2015 Outstanding Dissertation Award for The Professional Counselor and a licensed counselor in both Texas and Washington, D.C. Correspondence may be addressed to Lindsey Mitchell at lmitch26@gwmail.gwu.edu.
Apr 7, 2014 | Article, Volume 4 - Issue 2
Elizabeth A. Prosek, Jessica M. Holm
The U.S. Department of Veterans Affairs (VA) and TRICARE have approved professional counselors to work within the military system. Counselors need to be aware of potential ethical conflicts between counselor ethical guidelines and military protocol. This article examines confidentiality, multiple relationships and cultural competency, as well as ethical models to navigate potential dilemmas with veterans. The first model describes three approaches for navigating the ethical quandaries: military manual approach, stealth approach, and best interest approach. The second model describes 10-stages to follow when navigating ethical dilemmas. A case study is used for analysis.
Keywords: military, ethics, veterans, counselors, competency, confidentiality
The American Community Survey (ACS; U.S. Census Bureau, 2011) estimated that 21.5 million veterans live in the United States. A reported 1.6 million veterans served in the Gulf War operations that began post-9/11 in 2001 (U.S. Census Bureau, 2011). Gulf War post-9/11 veterans served mainly in Iraq and Afghanistan, in operations including but not limited to Operations Enduring Freedom (OEF), Iraqi Freedom (OIF), and New Dawn (OND) (M. E. Otey, personal communication, October 23, 2012). Holder (2007) estimated that veterans represent 10% of the total U.S. population ages 17 years and older. Pre-9/11 data suggested that 11% of military service members utilized mental health services in the year 2000 (Garvey Wilson, Messer, & Hoge, 2009). In 2003, post-9/11 comparative data reported that 19% of veterans deployed to Iraq accessed mental health services within one year of return (Hoge, Auchterlonie, & Milliken, 2006). Recognizing the increased need for mental health assessment, the U.S. Department of Defense (DOD) mandated the Post-Deployment Health Assessment (PDHA) for all returning service members (Hoge et al., 2006). The PDHA is a brief three-page self-report screening of symptoms to include post-traumatic stress, depression, suicidal ideation and aggression (U.S. DOD, n.d.). The assessment also indicates service member self-report interest in accessing mental health services.
Military service members access mental health services for a variety of reasons. In a qualitative study of veterans who accessed services at a Veterans Affairs (VA) mental health clinic, 48% of participants reported seeking treatment because of relational problems, and 44% sought treatment because of anger and/or irritable mood (Snell & Tusaie, 2008). Veterans may also present with mental health symptoms related to post-traumatic stress disorder (PTSD), depression, and suicidal ideation (Hoge et al., 2006). Depression is considered a common risk factor of suicide among the general population, and veterans are additionally at risk due to combat exposure (Martin, Ghahramanlou-Holloway, Lou, & Tucciarone, 2009). The DOD (2012) confirmed that 165 active-duty Army service members committed suicide in 2011. Furthermore, researchers asserted that suicide caused service member deaths more often than combat (O’Gorman, 2012). Hoge et al. (2004) reported that veterans were most likely to access mental health services 3–4 months post-deployment. Unfortunately, researchers suggested that service members were hesitant to access mental health treatment, citing the stigma of labels (Kim, Britt, Klocko, Riviere, & Adler, 2011). Studies indicated that mental health service needs are underestimated among the military population and are therefore a potential burden to an understaffed helping profession (Garvey Wilson et al., 2009; Hoge et al., 2006). In May of 2013, the DOD and VA created 1,400 new positions for mental health providers to serve military personnel (DOD, 2013). Moreover, as of March 2013, the DOD-sponsored veterans crisis line reported more than 800,000 calls (DOD, 2013). It is evident that the veteran population remains at risk for problems related to optimal mental health functioning and therefore requires assistance from trained helping professionals.
Historically, the DOD employed social workers and psychologists almost exclusively to provide mental health services in the military setting. Recently, the DOD and VA expanded services and created more positions for mental health clinicians (U.S. VA, 2012). Because licensed professional counselors (LPCs) are now employable by VA service providers (e.g., VA hospitals) and approved TRICARE providers (Barstow & Terrazas, 2012), it is imperative to develop an understanding of the military system, especially of the potential conflict that may exist between military protocol and counselor ethical guidelines. The military health system requires mental health professionals to be appropriately credentialed (e.g., licensed), and credentialing results in the mandatory adherence to a set of professional ethical standards (Johnson, Grasso, & Maslowski, 2010). However, there may be times when professional ethical standards do not align with military regulations. Thus, an analysis of the counselor ethical codes relevant to the military population is presented. At times, discrepancies between military protocol and counselor ethical codes may emerge; therefore, recommendations for navigating such ethical dilemmas are provided. A case study and analysis from the perspective of two ethical decision-making models are presented.
Ethical Considerations for Counselors
The mission of the American Counseling Association (ACA) Code of Ethics (2005) is to establish a set of standards for professional counselors, which ensure that the counseling profession continues to enhance the profession and quality of care with regard to diversity. As professional counselors become employed by various VA mental health agencies or apply for TRICARE provider status, it is important to identify specific ethical codes relevant to the military population. Therefore, three categories of ethical considerations pertinent to working with military service members are presented: confidentiality, multiple relationships, and cultural competence.
Confidentiality
The ACA Code of Ethics (2005) suggests that informed consent (A.2.a., p. 4) be a written and verbal discussion of rights and responsibilities in the counseling relationship. This document includes the client right for confidentiality (B.1.c., p. 7) with explanation of limitations (B.1.d., p. 7). The limitations, or exceptions, to confidentiality include harm to self, harm to others and illegal substance use. In the military setting, counselors may need to consider other exceptions to confidentiality including domestic violence (Reger, Etherage, Reger, & Gahm, 2008), harassment, criminal activity and areas associated with fitness for duty (Kennedy & Johnson, 2009). Also, military administrators may require mandated reporting when service members are referred for substance abuse treatment (Reger et al., 2008). When these conditions arise in counseling, the military may require reporting beyond the standard ethical protocol to which counselors are accustomed.
Counselors working in the VA mental health system or within TRICARE may need to be flexible with informed consent documents, depending on the purpose of services sought. Historically, veterans represented those who returned from deployment and stayed home. Currently, military members may serve multiple tours of combat duty; therefore, the definition of veterans now includes active-duty personnel. This modern definition of veteran speaks to issues of fitness for duty, where the goal is to return service members ready for combat. Informed consent documents may need to outline disclosures to commanding officers. For example, if a service member is in need of a Command-Directed Evaluation (CDE), then the commander is authorized to see the results of the assessment (Reger et al., 2008). Fitness for duty is also relevant when service members are mandated to the Soldier Readiness Program (SRP) to determine their readiness for deployment. In these situations, counselors need to clearly explain the exception to confidentiality before conducting the assessment. Depending on the type of agency and its connection to the DOD, active-duty veterans’ health records may be considered government property, not the property of the service provider (McCauley, Hacker Hughes, & Liebling-Kalifani, 2008). It is imperative that counselors are educated on the protocols of the setting or assessments, because “providing feedback to a commander in the wrong situation can be an ethical violation that is reviewable by a state licensing authority” (Reger et al., 2008, p. 30). Thus, in order to protect the client and the counselor, limitations to confidentiality within the military setting must be accurately observed at all times. Knowledge of appropriate communication between the counselor and military system also speaks to the issue of multiple relationships.
Multiple Relationships
Kennedy and Johnson (2009) suggested creating collaborative relationships with interdisciplinary teams in a military setting in order to create a network of consultants (e.g., lawyers, psychologists, psychiatrists), which is consistent with ACA ethical code D.1.b to develop interdisciplinary relationships (2005, p. 11). However, when interdisciplinary teams are formed, there are ACA (2005) ethical guidelines that must be considered. These guidelines state that interdisciplinary teams must focus on collaboratively helping the client by utilizing the knowledge of each professional on the team (D.1.c., p. 11). Counselors also must make the other members of the team aware of the constraints of confidentiality that may arise (D.1.d., p. 11). In addition, counselors should adhere to employer policies (D.1.g., p. 11), openly communicating with VA superiors to navigate potential discrepancies between employers’ expectations and counselors’ roles in best helping the client.
In the military environment, case transfers are common because of the high incidence of client relocation, which increases the need for the interdisciplinary teams to develop time-sensitive treatment plans (Reger et al., 2008). Therefore, treatment plans not only need to follow the guidelines of A.1.c., in which counseling plans “offer reasonable promise of success and are consistent with abilities and circumstances of clients” (ACA, 2005, p. 4), but they also need to reflect brief interventions or treatment modalities that can be easily transferred to a new professional. Mental health professionals may work together to best utilize their specialized services in order to meet the needs of military service members in a minimal time allowance.
For those working with military service members, consideration of multiple relationships in terms of client caseload also is important. Service members who work together within the same unit may seek mental health services at the same agency. Members of a military unit may be considered a support network which, according to ethical code A.1.d., may be used as a resource for the client and/or counselor (ACA, 2005, p. 4). However, learning about a military unit as a network from multiple member perspectives may also create a dilemma. Service members within a unit may be tempted to probe the counselor for information about other service members, or tempt the counselor to become involved in the unit dynamic. McCauley et al. (2008) recommended that mental health professionals avoid mediating conflicts between service members in order to remain neutral in the agency setting.
However, there are times when the unit cohesion may be used to support the therapeutic relationship. Basic military training for service members emphasizes the value of teamwork and the collective mind as essential to success (Strom et al., 2012). It is important for counselors to approach military service member clients from this perspective, not from a traditional Western individualistic lens. Mental health professionals also are warned not to be discouraged if rapport is more challenging to build than expected. Hall (2011) suggested that the importance of secrecy in the military setting might make it more difficult for service members to readily share in the therapeutic relationship. Researchers noted that military service members easily built rapport with each other in a group therapy session, often leaving out the civilian group leader (Strom et al., 2012). It might behoove counselors to build upon the framework of collectivism in order to earn the trust of members of the military population. Navigating the dynamic of a unit or the population of service members accessing care at the agency may be a challenge; however, counselors are able to alleviate this challenge with increased knowledge of the military culture in general.
Cultural Competence
The military population represents a group of people with a unique “language, a code of manners, norms of behavior, belief systems, dress, and rituals” and therefore can be considered a cultural group (Reger et al., 2008, p. 22). Reger et al. (2008) suggested that many clinical psychologists learned about military culture as active service members themselves. While there may be many veterans currently working as professional counselors, civilian counselors also serve the mental health needs of the military population; and as civilians, they require further training. The ACA Code of Ethics (2005) suggests that counselors communicate with their clients in ways that are culturally appropriate to ensure understanding (A.2.c., p. 4). This can be achieved by prolonged exposure to military culture or by seeking supervision from a professional involved with the military mental health system (Reger et al., 2008). Strom et al. (2012) outlined examples of military-specific cultural components for professionals to learn: importance of rank, unique terminology and value of teamwork. It behooves counselors intending to work with the military population to learn terminology in order to understand service members. For example, R&R refers to vacation leave and MOS or rate refers to a job category (Strom et al., 2012).
Personal values may cause dilemmas for a mental health professional working within the VA system. This can be especially true during times of war. Stone (2008) suggested that treating veterans of past wars may be easier than working with military service members during current combat because politics may be intensified. A counselor who does not support the current wartime mission may be conflicted when clients are mandated to return to active-duty assignments (Stone, 2008). The ACA Code of Ethics (2005) addresses the impact of counselors’ personal values (A.4.b., pp. 4–5) on the therapeutic relationship. It is recommended that counselors be aware of their own values and beliefs and respect the diversity of their clients. Counselors need to find a way to value the contributions of their client when personal or political opinion conflicts with the DOD’s plans or efforts overseas. If one wants to be successful with this population, Johnson (2008) suggested the foundational importance of accepting the military mission. If this is in direct conflict with the counselor’s values, it may be recommended for the counselor to consider the client’s value of the mission.
The ACA ethical code stresses the importance of mental health professionals practicing within the boundaries of their competence and continuing to broaden their knowledge to work with diverse clients (ACA, 2005, C.2.a., p. 9). Counselors should only develop new specialty areas after appropriate training and supervised experience (ACA, 2005, C.2.b., p. 9). Working within the VA mental health system, mental health professionals may be asked to provide a service in which they are not competent (Kennedy & Johnson, 2009). Such a request may occur more frequently here than in other settings, due to the high demand of mental health services and low availability of trained professionals (Garvey Wilson et al., 2009; Hoge et al., 2006). Counselors must determine if their experience and training can be generalized to working with military service members (Kennedy & Johnson, 2009), and may be their own best advocate for receiving appropriate training.
Awareness of when and how military service members access mental health services also might be important to consider. Reger et al. (2008) reported that military personnel were more likely to access services before and after a deployment. Researchers specified a higher prevalence rate of access 3–4 months after a deployment (Hoge et al., 2004). The relationship of time between deployment and help-seeking behaviors suggests that counselors should be prepared for issues related to trauma. For women, combat-related trauma is compounded with increased rates of reported military sexual trauma (Kelly et al., 2008). Counselors would benefit from additional trainings in trauma intervention strategies. The VA and related military organizations offer many resources online to educate professionals working with military members with identified trauma symptoms (U.S. VA., n.d.).
Advocating for appropriate training in areas of incompetence is the responsibility of the professional, who should pursue such training in order to best meet the needs of the military population. It is best practice for mental health professionals to be engaged in ongoing trainings to ensure utilization of the latest protocols and treatment modalities (McCauley et al., 2008). Trainings may need to extend beyond general military culture, because each branch of service (e.g., Army, Marines, Navy) could be considered a cultural subgroup with unique language and standards. For example, service members in the Army are soldiers, whereas members of the Navy are sailors (Strom et al., 2012).
This article has outlined many ACA (2005) ethical guidelines pertinent to working with the military population. However, as presented, there are times when counselor ethical codes conflict with military regulations. Counselors interested in working in the military setting or with military personnel may consider decision-making models to address ethical dilemmas.
Recommendations for Counselors
The military mental health system has almost exclusively employed psychologists and social workers. Counselors interested in employment within VA agencies or as TRICARE providers may utilize the resources created by these practitioners to better serve the military population. Two ethical decision-making models are presented, and a case study is provided to demonstrate how to implement the models.
Ethical Models
The ACA Code of Ethics (2005) advises counselors to adhere to the code of ethics whenever possible, working towards a resolution of the conflict (H.1.b., p. 19). If a favorable resolution cannot be formed, counselors have the choice to act in accordance with the law or regulation. Psychology researchers have suggested ethical models for professionals to use during times of dilemma within the military setting. The first model presented considers three overarching approaches to address ethical dilemmas; and the second model presented is a more specific stage model with which to approach dilemmas. These models may serve to assist counselors as the counseling profession gains more experience in the VA system and eventually develops counselor-specific decision-making models.
Approach model. Johnson and Wilson (1993) identified three approaches for psychologists to consider when navigating the ethical quandaries of the military mental health system. The first, the military manual approach, occurs when professionals adhere strictly to military regulations without consideration for the specific client’s needs. The second, the stealth approach, occurs when there is strict adherence to the mental health professionals’ code of ethics, regardless of the legalities surrounding the circumstances. While the client’s best interests may be at the forefront in this approach, the counselor must also take into account the possibility of being the subject of legal action for not adhering to the standards set by the military. For example, the counselor may use ambiguous wording within the client file or leave some information out altogether, so that if the files were requested, the client’s information would be protected (Johnson & Wilson, 1993). The third, the best interest approach, occurs when the counselor maintains focus on the client’s best interest while also adhering to the standards of the military. This may require professionals to adhere to the minimum professional standards in order to accommodate the client’s best interest. Although most professionals have deemed this approach the best option, it also leads to the most ambiguity. Under certain circumstances, the counselor also must take into account what is in the best interest for society as a whole, while also navigating a responsibility to the client and the military mental health system. Researchers in psychology responded to the ambiguity of this model by developing a more specific stage model to assist professionals with ethical dilemmas.
Stage model. Barnett and Johnson (2008) proposed a 10-stage model to follow when navigating an ethical dilemma. They advise that professionals must do the following:
1. Clearly define the situation.
2. Determine what parties could be affected.
3. Reference the pertinent ethical codes.
4. Reference the pertinent laws and regulations.
5. Reflect on personal thoughts and competencies on the issue.
6. Select knowledgeable colleagues with whom to consult.
7. Develop alternate courses of action.
8. Evaluate the impact on all parties involved.
9. Consult with professional organizations, ethics committees and colleagues.
10. Decide on a course of action.
Barnett and Johnson (2008) also noted that once a decision is made, the process does not end. It is best practice to monitor the implications and, if necessary, modify the plan. Documentation throughout this entire process is necessary for the protection of the counselor, the client and other involved stakeholders. Counselors working in the military mental health system may find this 10-stage model helpful when navigating ethical dilemmas.
To better understand the implementation of the two presented ethical decision-making models, a case study was developed. The case is then conceptualized from both the approach model and stage model, and the ethical dilemmas associated with the case are discussed.
Case Study
Megan is a licensed professional counselor employed at a clinic that serves military service members. She provides individual outpatient counseling to veterans and family members, as well as facilitates veteran support groups. Megan’s client, Robert, is a Petty Officer First Class in the Navy. Robert is married with two children. In recent sessions, Megan became concerned with Robert’s increased alcohol use. Recently, Robert described a weekend of heavy drinking at the local bar. Although Robert drove after leaving the bar both nights, Megan suspected that he was not sober enough to drive. In a follow-up session, Robert reported that his binge-drinking weekend caused friction at home with his wife, and that he missed his children’s soccer games. During his most recent session, Robert was visibly distressed as he disclosed to Megan that he received orders for a deployment in 3 months. Robert is anxious about informing his wife and children of the pending 6-month deployment, as he knows it will only increase conflict at home. Robert reported that his family could use the increase in pay associated with family separation and tax-free wages during deployment. However, he also knows that deployments cause tension with his wife, which has already increased due to Robert’s recent drinking binges. While leaving the session, he mentioned with a laugh that he would rather go to the bar than go home.
Analysis from approach model. Megan may consider using Johnson and Wilson’s (1993) ethical approach model as she conceptualizes the potential ethical dilemma presented in Robert’s case. From a military manual approach, Megan may need to report Robert’s recent alcohol abuse behavior to his superior, as it may impact his fitness for duty on his next deployment. And although Robert has not been caught drinking and driving or charged with a crime, his behavior also puts him at risk of military conduct violations. However, when Robert originally came to the clinic, he did so of his own accord, not under orders, which could mean that notifying a commanding officer is an ethical violation. In consideration of the stealth approach, Megan may review the ACA (2005) ethical guidelines and conclude that there are no violations at risk if she chooses not to report Robert’s drinking habits. However, Megan contemplates whether addressing Robert’s drinking binges is in his best interest overall. She understands that the money associated with deployment is important to Robert’s family at this time; however, his drinking may put him at increased risk during deployment. Finally, Megan applies the best-interest approach to Robert’s situation. Megan may refer Robert to the center’s substance use support group. This referral will be reflected in Robert’s records, but if he begins receiving treatment for his alcohol abuse now (3 months before deployment), there may be time for Robert to demonstrate significant progress before his fitness for duty assessment.
Analysis from stage model. Megan may consider her ethical dilemma from Barnett and Johnson’s (2008) 10-stage model. In stage 1, she clearly defines the situation as Robert’s alcohol abuse and pending deployment. In stage 2, Megan considers who may be affected in this situation. She understands that Robert’s family would benefit from the extra money associated with the deployment, and therefore the family may be impacted if Robert is not deployed. Megan also notes that the family is already negatively impacted by his recent drinking binge (e.g., conflict with his wife, missed soccer games). If Robert’s problematic drinking continues, he is at risk for evaluation and promotion issues. In stage 3, Megan reflects upon the ACA (2005) ethical codes in order to better understand her dilemma from a counselor’s view. Robert has a right to confidentiality (B.1.c., p. 7) with limitations including illegal substance use (B.1.d., p. 7). However, Robert’s current substance is alcohol, which is a legal substance. Megan considers the importance of his support network (A.1.d., p. 4) including his family and unit, but she does not have the ethical right to disclose her concerns about his substance abuse. In stage 4, Megan considers the pertinent laws and regulations of the dilemma. As per the clinic regulations, she is aware that if she makes a substance use program referral, it will be reflected in Robert’s record, which is the property of the military. Megan also is aware that Robert has not committed a documented crime of driving under the influence.
In stage 5 of the 10-stage ethical decision-making model, Megan must reflect on her personal thoughts and competencies. She is very concerned about Robert’s increased use of alcohol and is worried for his safety if deployed. Megan feels less confident in her ability to accurately assess for substance use problems. She facilitates the PTSD support group for the clinic, which is her specialty area. Megan recognizes that she is fond of Robert as a client and is disappointed that he could be jeopardizing his family and career with his alcohol abuse. She considers whether she is overreacting to his binge-drinking incident because of her higher expectations of him. In stage 6, Megan consults with her colleague who leads the substance use support groups at the clinic. She describes Robert’s recent abuse of alcohol and inquires as to whether he is a good candidate for the substance use group, needs more intense treatment, or needs no treatment at all. The colleague suggests that the group would be a very appropriate fit for someone with Robert’s symptoms.
In stage 7, Megan develops her course of action to refer Robert to the substance use group. Then, in stage 8, she evaluates the plan for potential impact on parties involved. Megan conceptualizes that Robert may be at risk for losing his deployment orders if he is accessing substance use treatment. Megan believes she has reduced this potential impact by referring to the substance support group, rather than an inpatient treatment facility, which may be more appropriate for a dependence issue. Megan recognizes that attending a 90-minute group each week will take Robert away from his family, but she also realizes that the 90-minute commitment is less than his current time spent away from the family when binge drinking. Megan reflects upon how her therapeutic relationship with Robert may be strained at the time of referral, and is prepared for a potential negative response from her client. She trusts in their therapeutic relationship and moves forward. In stage 9, Megan presents her planned course of action to her supervisor at the clinic. The supervisor approves the referral for the support group, but also suggests that Megan consider a referral to couples counseling for Robert and his wife, which may assist with resolving conflicts before the deployment.
In the final stage, Megan proposes the treatment plan of action to Robert in their next session. Megan explains that she feels ethically obligated to refer Robert to the substance use support group, and that as of now, Robert may make this choice for himself. Megan and Robert discuss the potential that substance use treatment may no longer be a choice in the future if his current drinking behavior continues. There is more discussion of fitness for duty and how participation in the support group will positively reflect upon the assessment in the future. Megan also presents Robert with the recommendation of couples counseling to help mediate relationship conflicts before deployment. She reports that if Robert and his wife decide to receive couples counseling, she can provide a referral for them at that time.
With the ethical decision-making models presented, the counselor is able to successfully navigate the military mental health system, while still maintaining the professional standards of the counseling profession. In each model, the situation is resolved with considerable attention to the client’s best interest, while maintaining the expectations of the military clinic. Psychologists developed the two ethical models presented, and counselors may choose to utilize these approaches until more counselor-specific ethical processes are created. As counselors become more permanent fixtures in the VA mental health system and as TRICARE providers, opportunities to develop an ethical decision-making model will likely arise.
Conclusion
The recent inclusion of counselors as mental health professionals within the VA system and as TRICARE providers allows for new employment opportunities with the military population. However, these new opportunities are not without potential dilemmas. Counselors interested in working with service members need to be educated on the potential conflict between counselor professional ethical guidelines and military protocols. Future research in the counseling field may develop a counselor-specific ethical decision-making model. In the meantime, counselors may utilize or adapt the ethical decision-making models created by other mental health professionals, who have a longer history working with the military population.
References
American Counseling Association. (2005). ACA code of ethics. Retrieved from http://www.counseling.org/Resources/aca-code-of-ethics.pdf
Barnett, J. E., & Johnson, W. B. (2008). The ethics desk reference for psychologists. Washington DC: American Psychological Association.
Barstow, S., & Terrazas, A. (2012, February). DoD releases TRICARE rule on independent practice for counselors. Counseling Today, 54(8), 10. Retrieved from
http://ct.counseling.org/2012/02/dod-releases-tricare-rule-on-independent-practice-for-counselors/
Garvey Wilson, A. L., Messer, S. C., & Hoge, C. W. (2009). U.S. military mental health care utilization and attrition prior to the wars in Iraq and Afghanistan. Social Psychiatry and Psychiatric Epidemiology, 44, 473–481. doi:10.1007/s00127-008-0461-7
Hall, L. (2011). The importance of understanding military culture. Social Work in Health Care, 50, 4–18. doi:10.1080/00981389.2010.513914
Hoge, C. W., Auchterlonie, J. L., & Milliken, C. S. (2006). Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. The Journal of the American Medical Association, 295(9), 1023–1032. doi:10.1001/jama.295.9.1023
Hoge, C. W., Castro, C. A., Messer, S. C., McGurk, D., Cotting, D. I., & Koffman, R. L. (2004). Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. The New England Journal of Medicine, 351(1), 13–22. doi:10.1056/NEJMoa040603
Holder, K. A. (2007). Comparison of ACS and ASEC data on veteran status and period of military service: 2007. U.S. Census Bureau: Housing and Household Economics Statistics Division. Retrieved from http://www.census.gov/hhes/veterans/files/comparison_report.pdf
Johnson, W. B. (2008). Top ethical challenges for military clinical psychologists. Military Psychology, 20, 49–62. doi:10.1080/08995600701753185
Johnson, W. B., Grasso, I., & Maslowski, K. (2010). Conflicts between ethics and law for military mental health providers. Military Medicine, 175, 548–553.
Johnson, W., & Wilson, K. (1993). The military internship: A retrospective analysis. Professional Psychology: Research and Practice, 24(3), 312–318. doi:10.1037/0735-7028.24.3.312
Kelly, M. M., Vogt, D. S., Scheiderer, E. M., Ouimette, P., Daley, J., & Wolfe, J. (2008). Effects of military trauma exposure on women veterans’ use and perceptions of Veterans Health Administration care. Journal of General Internal Medicine, 23, 741–747. doi:10.1007/s11606-008-0589-x
Kennedy, C. H., & Johnson, W. B. (2009). Mixed agency in military psychology: Applying the American Psychological Association ethics code. Psychological Services, 6(1), 22–31. doi:10.1037/a0014602
Kim, P. Y., Britt, T. W., Klocko, R. P., Riviere, L. A., & Adler, A. B. (2011). Stigma, negative attitudes about treatment, and utilization of mental health care among soldiers. Military Psychology, 23, 65–81. doi:10.1080/08995605.2011.534415
Martin, J., Ghahramanlou-Holloway, M., Lou, K., & Tucciarone, P. (2009). A comparative review of U.S. military and civilian suicide behavior: Implications for OEF/OIF suicide prevention efforts. Journal of Mental Health Counseling, 31(2), 101–118.
McCauley, M., Hacker Hughes, J., & Liebling-Kalifani, H. (2008). Ethical considerations for military clinical psychologists: A review of selected literature. Military Psychology, 20, 7–20. doi:10.1080/08995600701753128
O’Gorman, K. (2012, August 16). Army reports record suicides in July [Blog post]. Retrieved from http://iava.org/blog/army-reports-record-high-suicides-july
Reger, M. A., Etherage, J. R., Reger, G. M., & Gahm, G. A. (2008). Civilian psychologists in an army culture: The ethical challenge of cultural competence. Military Psychology, 20, 21–35. doi:10.1080/08995600701753144
Snell, F., & Tusaie, K. R. (2008). Veterans reported reasons for seeking mental health treatment. Archives of Psychiatric Nursing, 22(5), 313–314. doi:10.1016/j.apnu.2008.06.003
Stone, A. M. (2008). Dual agency for VA clinicians: Defining an evolving ethical question. Military Psychology, 20, 37–48. doi:10.1080/08995600701753177
Strom, T. Q., Gavian, M. E., Possis, E., Loughlin, J., Bui, T., Linardatos, E.,…Siegel, W. (2012). Cultural and ethical considerations when working with military personnel and veterans: A primer for VA training programs. Training and Education in Professional Psychology, 6(2), 67–75. doi:10.1037/a0028275
U.S. Census Bureau, American Community Survey. (2011). B21002: Period of military service for civilian veterans 18 years and over (2011 American Community Survey 1-year estimates). Retrieved from http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_11_1YR_B21002&prodType=table
U.S. Department of Defense. (n.d.). Enhanced post-deployment health assessment (PDHA) process (DD Form 2796). Retrieved from http://www.pdhealth.mil/dcs/dd_form_2796.asp
U.S. Department of Defense. (2012). Army releases July suicide data, No. 683-12. Retrieved from http://www.defense.gov/releases/release.aspx?releaseid=15517
U.S. Department of Defense. (2013). DOD, VA and HHS partner to expand access to mental health services for veterans, service members, and families, No. 353-13. Retrieved from http://www.defense.gov/releases/release.aspx?releaseid=16024
U.S. Department of Veterans Affairs. (n.d.). PTSD: National center for PTSD. Retrieved from http://www.ptsd.va.gov/professional/index.asp
U.S. Department of Veterans Affairs (2012, April). VA adding family therapists and mental health counselors to workforce. Retrieved from http://www.va.gov/opa/pressrel/pressrelease.cfm?id=2303
Elizabeth A. Prosek, NCC, is an Assistant Professor at the University of North Texas. Jessica M. Holm is a doctoral student at the University of North Texas. Correspondence can be addressed to Elizabeth A. Prosek, University of North Texas, 1155 Union Circle #310829, Denton, TX 76203-5017, elizabeth.prosek@unt.edu.
Apr 3, 2014 | Article, Volume 4 - Issue 2
Seth Hayden, Kathy Ledwith, Shengli Dong, Mary Buzzetta
Student veterans often encounter unique challenges related to career development. The significant number of student veterans entering postsecondary environments requires career-development professionals addressing the needs of this population to decide upon appropriate career intervention topics. This study utilized a career-needs assessment survey to determine the appropriate needs of student veterans in a university setting. Student veterans indicated a desire to focus on the following topics within career intervention: transitioning military experience to civilian work, developing skills in résumé-building and networking, and negotiating job offers. Results of the needs survey can be used in the development of a career-related assessment.
Keywords: student veterans, career development, needs assessment, military, career-related assessment
In 2013, there were 21.4 million male and female veterans aged 18 and older in the civilian noninstitutional population (U.S. Bureau of Labor Statistics, 2014a). The post-9/11 GI Bill, authorized by Congress in 2008, has contributed to a large number of veterans seeking postsecondary degrees (Sander, 2012). Since 2008, more than 817,000 military veterans have used the bill to attend U.S. colleges (Sander, 2013). Student veterans face many challenges on college campuses, including transition issues, relational challenges, feelings of isolation, and lingering effects of combat-related injuries (Green & Hayden, 2013).
One of the most significant concerns is that veterans typically experience unemployment at a higher rate than their civilian counterparts (U.S. Bureau of Labor Statistics, 2014b). In 2013, the unemployment rate for Gulf War II-era veterans was 10.1 %; Gulf War I-era veterans 5.5%; and World War II, Korean War, and Vietnam War veterans 5.5% (U.S. Bureau of Labor Statistics, 2014b). Younger veterans in particular struggled with unemployment. As of 2013, about 2.8 million of the nation’s veterans had served during the Gulf War II era (September 2001–present; U.S. Bureau of Labor Statistics, 2014a). The unemployment rate for the Gulf War II-era veterans (10.1%) is significantly higher than their civilian counterparts (6.8%; U.S. Bureau of Labor Statistics, 2014b). As young military personnel continue to return to college campuses, it is important to address the career-readiness needs of this population utilizing evidence-based practices.
Cognitive Information Processing
The Cognitive Information Processing (CIP) approach to career decision making (Sampson, Reardon, Peterson, & Lenz, 2004) has been suggested as a way to aid veterans as they transition into the civilian workforce (Bullock, Braud, Andrews, & Phillips, 2009; Buzzetta & Rowe, 2012; Clemens & Milsom, 2008; Hayden, Green, & Dorsett, in press; Phillips, Braud, Andrews, & Bullock, 2007; Stein-McCormick, Osborn, Hayden, & Van Hoose, 2013). The CIP approach is designed to assist individuals in making both current and future career choices (Sampson et al., 2004; Buzzetta & Rowe, 2012). This theoretical approach states that career problem solving and decision making are skills that can be learned and practiced (Sampson et al., 2004). Once clients have improved their problem-solving and decision-making skills, then they can apply these same skills to choices they make in the future. According to the CIP approach, the key aspects of career problem solving and decision making are self-knowledge, occupational knowledge, decision-making skills, and metacognitions (Sampson et al., 2004). Engels and Harris (2002) suggest that military individuals would benefit from understanding their self-knowledge, occupational information and decision-making skills.
Pyramid of Information Processing
The CIP approach consists of two key components: the pyramid of information processing, or the knowing, and the CASVE cycle, or the doing. The interactive elements are analogous to a recipe used in cooking. The pyramid is like the ingredients for the dish, while the CASVE cycle reflects the necessary steps to make the dish. Both are critical for effective career decision making and problem solving (Sampson et al., 2004). The pyramid of information processing includes three domains involved in career decision making: knowledge, decision-making skills, and executive processing (Sampson et al., 2004). Sampson et al. (2004) theorized that all components of the pyramid are affected by dysfunctional thinking and negative self-talk. The knowledge domain consists of two main areas: self-knowledge and occupational knowledge. Self-knowledge is the cornerstone of a client’s career-planning process, and is comprised of an individual’s knowledge of his or her values, interests, skills, and employment preferences (Reardon, Lenz, Peterson, & Sampson, 2012; Sampson et al., 2004). Occupational knowledge is the second cornerstone of a client’s career-planning process; it encompasses knowledge of options, including educational, leisure, and occupational alternatives, as well as how occupations can be organized.
The decision-making skills domain consists of a systematic process to help clients improve their problem-solving and decision-making skills, and includes the CASVE cycle, which is a multi-phase decision-making process, intended to increase client awareness and improve a client’s decision-making skills. The executive processing domain includes metacognitions, which include an individual’s thoughts about the decision-making process. There are three cognitive strategies included in the executive processing domain: self-talk, self-awareness, and monitoring and controlling an individual’s progress in the problem-solving process. Metacognitions can include dysfunctional career thinking, which can present problems in career decision making, influence other domains in the pyramid, and impact individuals’ perceptions of their capabilities to perform well (Sampson et al., 2004).
CASVE Cycle
The CASVE cycle is used as a means of approaching a career problem or decision, and consists of five sequential stages (communication, analysis, synthesis, valuing, and execution), with repeated circuits when the problem still exists or new problems arise (Sampson et al., 2004). An individual enters the CASVE cycle after receiving either internal or external cues that he or she must make a career decision. In the communication stage, individuals are required to examine these prompts, and identify a gap that exists between where they are currently and where they would like to be. In the analysis phase, individuals clarify their existing self-knowledge by determining their occupational preferences, abilities, interests and values. The process of clarifying existing knowledge and gaining new information about potential options also is included. In the synthesis phase, individuals narrow down and further develop the options they are considering.
In the valuing phase, individuals assess the costs and benefits of each remaining alternative. This task involves prioritizing the alternatives, as well as selecting a tentative primary and secondary choice. In the execution phase, individuals create and commit to a plan of action for accomplishing their first choice. Upon completion of the execution phase, individuals return to the communication phase to determine whether the gap has been filled. The CASVE cycle is recursive in nature. Therefore, if the gap has not been removed and problems still exist, an individual will progress through the CASVE cycle again (Sampson et al., 2004).
Negative Thinking
Several studies have found that negative thoughts are related to career decision-making difficulties (Kleiman et al., 2004; Sampson, Peterson, Lenz, Reardon, & Saunders, 1996; Sampson et al., 2004). Kleiman et al. (2004) examined the relationship between dysfunctional thoughts and an individual’s degree of career decidedness in a sample of 192 college students enrolled in an undergraduate career-planning course. The researchers found that dysfunctional thinking during the decision-making process can negatively influence rational decisions. Assessing for dysfunctional career thoughts and working with individuals to reduce negative career thinking can have a positive impact on the knowledge and decision-making skills domains of the pyramid of information processing. More importantly, utilizing a theoretical approach can provide a structure in which to address the needs of student veterans.
Needs Assessment Survey
In order to address the needs of student veterans, counselors must first assess what these needs are. Student veterans offer a unique subset of our veteran population in that they operate within an educational environment while possessing diverse life experiences, and are therefore often unique in relation to their peers (Cook & Kim, 2009). Given the aforementioned employment difficulties for younger veterans (U.S. Bureau of Labor Statistics, 2014b), a need for career-focused interventions designed to assist this population is apparent.
While various supportive services for veterans are available, determining an appropriate allocation of resources and time to address the needs of this population can enhance the quality of services. To match intervention with need, the authors created a needs survey designed to inform the development of a theoretically based career intervention, the purpose of which is assisting student veterans in developing skills in career decision making and problem solving.
Sample
The sample for this needs assessment was collected from a sample of student veterans attending a large southeastern university (n = 92). Currently, this university has approximately 317 student veterans enrolled and receiving educational benefits through either the Montgomery GI Bill or post-9/11 GI Bill. This means of identifying veterans is imperfect, as there may be student veterans attending the university who do not utilize educational benefits. However, this is a common method of identifying veterans within university settings (University of Arizona, 2007). The participants were asked to complete the needs survey by both the university veterans association and the veterans benefit officer. Both social media and e-mail were used to elicit participation.
All 317 identified members of the population receiving education benefits were provided the opportunity to respond to the survey, via both an e-mail request with the electronic survey attached and a post on the student veteran organization’s social media Web page. A total of 92 (29%) completed surveys were collected. Of the 92 respondents, a majority identified as graduate students (47; 51%). The remaining respondents indicated their classifications as undergraduate students with the classifications of junior (25; 23%), senior (18; 20%), and sophomore (2; 2%). No students classified as freshmen responded to the survey.
Instrument
The research team constructed the Veterans Needs Survey after examining the common career-development needs of both veterans and nonveterans encountered in the university’s career center. The instrument was created via a Qualtrics survey management system and attached to an electronic communication addressed to the potential respondents, as well as embedded in a social media thread of the university’s student veteran organization. The measure inquired about whether respondents had heard of the university career center; whether they had previously visited the university career center; what they would like to learn more about related to the career-development process; what modalities of treatment they were most interested in attending (e.g., group counseling, workshop series); how likely they were to attend the option indicated; education status; major/field of study; additional comments related to their career development; and an opportunity to participate in an intervention (an e-mail address was requested). The authors did not collect significant demographic information, instead focusing on variables like utilization of services (e.g., contact with the career center) and students’ academic classification, as these factors appear directly connected with career-development concerns.
Results
The survey examined utilization and perceptions of career-development needs. The majority of respondents (80; 87%) indicated that they had heard of the career center, but a smaller number indicated actually visiting the career center (66; 73%). The question pertaining to perceived career-development needs provided a multiple-option response set in which one could indicate several options. The most frequently indicated response was transferring skills gained in the military to the workplace (49; 55.06%). The second most frequently indicated response was preparing a résumé/CV (46; 51.69%), followed by negotiating a job offer (45; 50.56%). Table 1 provides a detailed description of additional responses regarding the career-development process.
A significant majority (54; 61%) indicated that they would be most interested in attending a group format, and fewer respondents selected the workshop series as their first choice (24; 27%). Respondents indicating the other category specified that they would attend career fairs, take advantage of individual counseling, and utilize online workshops. Following up on the previous question, one item inquired how likely a respondent would be to attend the option indicated. The most frequently indicated response was somewhat likely (42; 47%) followed by very likely (34; 38%) with unlikely (14; 16%) being the least frequently indicated response. The majors/fields of study with a significant number of responses were law (9), business-related (undergraduate and graduate; 9), social work (7), and criminology (8).
Participants provided diverse general comments related to their career development. One student veteran stated, “I have an associates [sic] degree in Laboratory Technology from the military and would also like assistance building a résumé trying to find employment now.” Another shared, “As a distance learner, it is possible to feel out of reach when it comes to on-campus resources. But, I know we can overcome that. I may be a combat disabled veteran. But, I won’t let disabilities stop my self-actualization quest.”
The information obtained from the needs survey can be utilized to inform an intervention designed to assist student veterans in their career development, which will provide a grounded approach in addressing these issues. The following section offers a proposal for meeting student veteran needs with a career-development intervention.
Table 1
Perceived Career-Development Needs
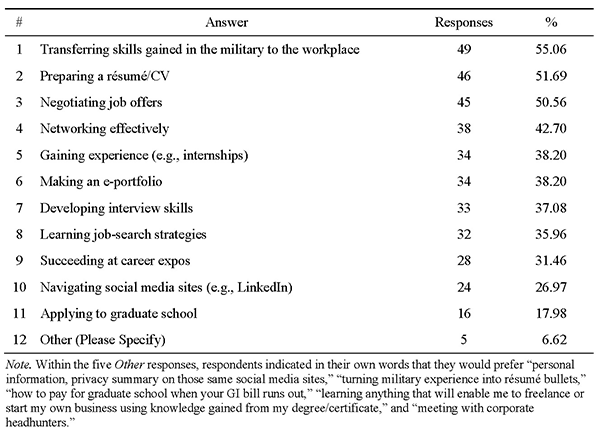
A Proposed Theoretically Based Career Intervention
Based upon the CIP theoretical framework (Sampson et al., 2004) and the feedback received from the needs assessment, psychoeducational groups will be conducted in order to achieve the following goals: expanding student veteran self-knowledge and career options through the CIP approach, exploring transferable skills gained through military experiences, gaining knowledge of resources that can assist student veterans in the job search and application processes, and identifying and decreasing negative metacognitions and dysfunctional career thoughts.
The psychoeducational group will meet once a week for 4 weeks. The group is open to all student veteran members attending the university through a campus-wide recruitment effort. Considering the tight connections between each CIP component, the group will be conducted in a closed-group format. The group facilitators will be graduate students pursuing doctoral degrees in counseling psychology or school psychology, and/or master’s students studying career counseling.
The group activities will center on the student veterans’ needs obtained through the needs assessment survey and the CIP components that have been proposed to serve the needs of veterans (Bullock et al., 2009; Clemens & Milsom, 2008). The structure of the psychoeducational group is based on the CIP model and five stages of the CASVE cycle diagram: communication, analysis, synthesis, valuing, and execution.
During the first session (communication), the group leader(s) will help to identify gaps between where group members are currently and where they aspire to be. Group members’ baseline information will be obtained by completing the Career Thoughts Inventory (CTI; Sampson, Peterson, Lenz, Reardon, & Saunders, 1996/1998) and My Vocational Situation (MVS; Holland, Daiger, & Power, 1991). The group leader(s) will explain the CIP Pyramid, CASVE Cycle Diagram, Self-Directed Search (SDS; Holland 1985) and assessment procedures. Group members will have an opportunity to interact with each other and complete one section of the Guide to Good Decision Making (Sampson, Peterson, Lenz, & Reardon, 1992). As a part of the homework assignment listed on the Individual Learning Plan (ILP), a document designed to identify career-related goals and associated action steps, group members will complete the SDS, and bring a copy of their current résumé to the next session.
During the second session (analysis/synthesis), the group leader(s) will help the student veterans examine and identify their interests, values, and skills (including transferable skills). The group leader(s) will assist group members in interpreting their SDS results, and examine any potential dysfunctional career thoughts that may be impacting group members’ career choices and decision-making abilities. To expand their career options, group members will be exposed to career-related resources such as the Occupational Outlook Handbook (U.S. Bureau of Labor Statistics, 2014c) and the Military Crosswalk Search via O*Net Online (National Center for O*NET Development, n.d.). In addition to gaining self-knowledge and occupational information in the analysis process, group members will have opportunities to practice synthesis skills. Group members will improve their résumé-writing skills through practice and feedback from peers and the group leader(s). Exploring and highlighting transferable skills is another important component. As part of their assignment listed on the ILP, group members will enhance their career networking skills by accessing supportive professionals via an alumni network and the Student Veterans Association, among other resources. Group members will also conduct an informational interview to gain firsthand experiences for their chosen career options. They will bring updated versions of their résumés and cover letters for the next session to obtain feedback from the group.
During the third session (valuing and execution), group members will present reflections on their informational interviews and provide feedback on their peers’ résumés and cover letters. In addition, group members will be exposed to various career resources such as VetJobs (VetJobs, Inc., 2014), Feds Hire Vets (U.S. Office of Personnel Management, n.d.), Job-hunt.org (NETability, Inc., 2014), the Riley Guide (Riley Guide, 2014), and the National Resource Directory (U.S. Departments of Defense, Labor and Veterans Affairs, n.d.). The group leader(s) will explain the “elevator speech” exercise and ask group members to practice this exercise in order to maximize their interview skill development. The group will also enhance members’ ability to use social networking to optimize their job search and applications. All activities aim to help members weigh their career options and execute their career decision making through careful planning. The group leader(s) will encourage members to initiate career networking and start exploring job and career opportunities.
During the last session (communication), group members will share what they originally included in their ILPs and what they have achieved, and offer suggestions and feedback to one another. They will retake the CTI and MVS and compare their new and initial results. Group leaders will help group members examine whether the gaps identified at the communication stage have successfully been closed, and suggest further measures to close gaps if necessary.
Discussion
The information gathered from the needs survey provides a thorough description of student veterans’ career-development needs. Interventions designed to support this population by determining appropriate interventions are often constructed using anecdotal information rather than objective needs. Student veteran responses to the survey indicate that veterans are concerned about transitioning their military experiences to civilian employment opportunities. In addition, student veterans appear to desire assistance with practical elements of the career-development process such as creating a résumé, negotiating a job offer, and networking. The purpose of this study is to develop a theoretically based intervention, and the study offers a framework in which to create effective career-development interventions for student veteran population.
Student veterans appear to engage in a wide array of academic programs, with a significant portion of veterans selecting majors within the realm of business, law, sociology, social work and criminology. These survey results provide a snapshot of the majors/fields of study that student veterans seem to gravitate toward. These preferences could be attributed to the hierarchical and meritocratic nature of some of these fields, which are somewhat analogous to the culture of the military.
Responses to the survey also provided a glimpse into the preferred modality of receiving career-related assistance. Oftentimes, military transition programs are designed to serve a large number of people, using seminar or workshop modalities in which to provide information. Student veterans indicated a strong preference for a smaller group counseling format that would provide more individual career-development support.
An additional important consideration for future interventions is the high number of respondents who identified themselves as distance learners in the needs assessment (some of them may have been on active service, whereas others were simply enrolled in the university from a remote location). Given the technological capabilities that allow online learning environments, it is reasonable that student veterans could utilize e-learning opportunities. Designing online interventions could be helpful in determining appropriate modalities by which to deliver services.
The student veterans’ comments and responses regarding their desired areas of focus for career development indicate a preference for a balanced approach of skill development. Ensuring that interventions focus on practical elements such as résumés and networking skill development, while also addressing broader topics such as transitioning from the military to the civilian workforce, appears to be a desired method for addressing the career-development needs of student veterans.
Limitations
The needs survey is limited in generalizability, as the results were collected from one educational institution, confining interpretations to the student veterans in this institution. Despite this limitation, the career-development concerns of student veterans provide a snapshot of the needs of this unique subset of the veteran population. Given the paucity of research in this area, it seemed necessary to facilitate an in-depth examination of this population’s career-development concerns, allowing the development of an informed intervention and establishing replicable protocol for future needs surveys.
The low response rate to the online survey also limits the application of findings. Though the response rate of 29% may be considered reasonable for an online assessment, having a large portion of the sample disregard the assessment presents a gap in fully substantiated information on this topic. Developing methods for collecting more information would enhance the validity of the data.
Finally, the high rate of graduate students who responded to the survey presents a challenge in applying the results to a primarily undergraduate institution. While there may be analogous experiences between graduate and undergraduate students, specific aspects of undergraduate student veterans’ career development may need additional evaluation.
Implications for Practice and Research
In this needs assessment, collaborative efforts between career services professionals at the institution and the university veterans’ center resulted in informative data on the career concerns of student veterans. Co-sponsored initiatives targeting these expressed needs could increase the number of student veterans impacted by career services. Survey respondents, along with group or workshop participants, could be recruited to provide feedback as part of a career-development focus group, further informing research and application for student veterans’ career concerns. Survey results could also be useful for marketing career services to student veterans. In addition, career centers or university libraries could acquire career resources such as books and print materials on topics that survey respondents considered desirable, especially those specifically tailored for veterans.
At the larger university level, major data on their students’ career-development concerns would be valuable information for college and department academic advisors and other university stakeholders. Career center staff members focus on various academic units as part of their career outreach, but further research regarding the unique career concerns of student veterans in specific majors could allow career center liaisons to impact veterans more effectively in their designated areas. As previously stated, since the survey was conducted at one higher education institution, duplicating the needs survey across a larger sample of colleges and universities would provide additional data sets for analysis, as well as broader application possibilities. Survey data could also be applied outside the institution to identify the most optimal partnerships in order to meet the comprehensive needs of student veterans. For example, career counselors might collaborate with mental health professionals, school counselors, and rehabilitation professionals to identify challenges and provide resources in order to maximize development for student veterans.
The results of this survey also support future research on the efficacy and suitability of online career-development options. There are many online programs designed to provide veterans the opportunity to pursue their education while in active duty. While the convenience of remote educational options for a mobile population is understood, ensuring that universities also provide career-development resources to distance learners is an important consideration in addressing the needs of veterans. Career-development opportunities such as webinars and online workshops offer the flexibility of distance learning. For example, online formats could provide veterans an opportunity to participate in such workshops collaboratively. Possible areas of research would include effective use of distance learning for veterans and comparative benefits and costs of in-person versus distance formats.
Based on the information collected, in future needs surveys, adjusting the survey items to detail reasons for certain item selections could allow greater understanding of both the responses and student veterans’ career thinking in general. Resulting career interventions would provide additional opportunities for further research to investigate aspects of career decision making and CIP theory, including relationships between student veterans’ self-knowledge, options knowledge, decision-making skills and metacognitions.
Conclusion
While veterans’ needs receive significant attention, programs are often created based on anecdotal and intuitive information. Developing needs assessments to solicit veterans’ perceptions of career development can inform interventions. Specifically regarding career development, utilizing a theoretically based, researched approach offers a framework to guide practice and research. Ongoing assessment of needs and services that utilizes established approaches will ensure quality services for those who have sacrificed greatly in service of their country.
References
Bullock, E. E., Braud, J., Andrews, L., & Phillips, J. (2009). Career concerns of unemployed U.S. war veterans: Suggestions from a Cognitive Information Processing approach. Journal of Employment Counseling, 46, 171–181. doi:10.1002/j.2161-1920.2009.tb00080.x
Buzzetta, M., & Rowe, S. (2012, November 1). Today’s veterans: Using Cognitive Information Processing (CIP) approach to build upon their career dreams. Career Convergence Magazine. Retrieved from http://www.ncda.org/aws/NCDA/pt/sd/news_article/66290/_self/layout_details/false
Clemens, E. V., & Milsom, A. S. (2008). Enlisted service members’ transition into the civilian world of work: A cognitive information processing approach. The Career Development Quarterly, 56, 246–256. doi:10.1002/j.2161-0045.2008.tb00039.x
Cook, B. J., & Kim, Y. (2009). From soldier to student: Easing the transition of service members on campus. Retrieved from http://www.acenet.edu/news-room/Documents/From-Soldier-to-Student-Easing-the-Transition-of-Service-Members-on-Campus.pdf
Engels, D. W., & Harris, H. L. (2002). Career counseling with military personnel and their dependents. In S. G. Niles (Ed.), Adult career development: Concepts, issues, and practices (3rd ed., pp. 253–266). Tulsa, OK: National Career Development Association.
Green, L., & Hayden, S. (2013). Supporting student veterans: Current landscape and future directions. Journal of Military and Government Counseling, 1, 89–100.
Hayden, S., Green, L., & Dorsett, K. (in press). Perseverance and progress: Career counseling for military personnel with traumatic brain injury. VISTAS. Retrieved from http://www.counselingoutfitters.com/vistas/vistas_2013_TOC-QR3-section_01.htm
Holland, J. L. (1985). Making Vocational Choices: A theory of vocational personalities and work environments. Englewood Cliffs, NJ: Prentice Hall.
Holland, J. L., Daiger, D. C., & Power, P. G. (1991). My Vocational Situation. Mountain View, CA: Consulting Psychologists Press.
Kleiman, T., Gati, I., Peterson, G., Sampson, J., Reardon, R., & Lenz, J. (2004). Dysfunctional
thinking and difficulties in career decision making. Journal of Career Assessment, 12,
312–331. doi:10.1177/1069072704266673
National Center for O*NET Development. (n.d.). Military crosswalk search [Database]. O*NET Online. Retrieved from http://www.onetonline.org/crosswalk/MOC/
NETability, Inc. (2014). How to succeed in your job search today. Job-hunt.org. Retrieved from http://www.job-hunt.org
Phillips, J., Braud, J., Andrews, L., & Bullock, E. E. (2007, November 1). Bridging the gap from job to career for U.S. veterans. Career Convergence Magazine. Retrieved from
http://associationdatabase.com/aws/NCDA/pt/sd/news_article/5412/_PARENT/layout_details_cc/false
Reardon, R. C., Lenz, J. G., Peterson, G. W., & Sampson, J. P., Jr. (2012). Career development and planning: A comprehensive approach (4th ed.). Dubuque, IA: Kendall Hunt Publishing.
Riley Guide. (2014). The Riley Guide. Retrieved from http://www.rileyguide.com/
Sampson, J. P., Jr., Peterson, G. W., Lenz, J. G., & Reardon, R. C. (1992). A cognitive approach
to career services: Translating concepts into practice. The Career Development Quarterly, 41, 67–74.
Sampson, J. P., Jr., Peterson, G. W., Lenz, J. G., Reardon, R. C., & Saunders, D. E. (1996). Career Thoughts Inventory: Professional manual. Odessa, FL: Psychological Assessment Resources.
Sampson, J. P., Jr., Peterson, G. W., Lenz, J. G., Reardon, R. C., & Saunders, D. E. (1998). The design and use of a measure of dysfunctional career thoughts among adults, college students, and high school, students: The Career Thoughts Inventory. Journal of Career Assessment, 6, 115–134. doi:10.1177/106907279800600201
Sampson, J. P., Jr., Reardon, R. C., Peterson, G. W., & Lenz, J. G. (2004). Career counseling & services: A cognitive information processing approach. Belmont, CA: Brooks/Cole.
Sander, L. (2012, July). Colleges expand services for veterans, but lag in educating faculty on veterans’ needs. The Chronicle of Higher Education. Retrieved from https://chronicle.com/
Sander, L. (2013, January). Veterans tell elite colleges: ‘We Belong’. The Chronicle of Higher Education. Retrieved from https://chronicle.com/
Stein-McCormick, C., Osborn, D. S., Hayden, S. C. W., & Van Hoose, D. (2013). Career development for transitioning veterans. Broken Arrow, OK: National Career Development Association.
U.S. Bureau of Labor Statistics. (2014a). Employment situation of veterans – 2012 [News release]. Retrieved from http://www.bls.gov/news.release/pdf/vet.pdf
U.S. Bureau of Labor Statistics. (2014b). Table A-5. Employment status of the civilian population 18 years and over by veteran status, period of service, and sex, not seasonally adjusted [Economic news release]. Retrieved from http://data.bls.gov/cgi-bin/print.pl/news.release/empsit.t05.htm
U.S. Bureau of Labor Statistics. (2014c). 2014–2015 Occupational outlook handbook. Retrieved from http://www.bls.gov/ooh/
U.S. Departments of Defense, Labor and Veterans Affairs. (n.d.). National resource directory. Retrieved from https://www.nrd.gov/
U.S. Office of Personnel Management. (n.d.). Feds hire vets. Retrieved from http://www.fedshirevets.gov/Index.aspx
University of Arizona. (2007). Student veteran needs assessment survey. Retrieved from https://studentaffairs.arizona.edu/assessment/documents/VETS_Needs7-2012FINAL.pdf
VetJobs, Inc. (2014). VetJobs: Veterans make the best employees. Retrieved from https://www.vetjobs.com/
Seth Hayden, NCC, is the Program Director of Career Advising, Counseling and Programming at Florida State University. Kathy Ledwith, NCC, is the Assistant Director for Career Counseling, Advising and Programming at Florida State University. Shengli Dong is an Assistant Professor at Florida State University. Mary Buzzetta, NCC, is a doctoral student at Florida State University. Correspondence can be addressed to Seth Hayden, 100 S. Woodward Avenue, Tallahassee, FL 32308, scwhayden@fsu.edu.