May 22, 2024 | Volume 14 - Issue 1
Rebekah Cole, Christine Ward, Taqueena Quintana, Elizabeth Burgin
Military spouses face many challenges as a result of the military lifestyle. Much focus has been placed on enhancing the resilience of military spouses by both the military and civilian communities. However, no research currently exists regarding spouses’ perceptions of their resilience or how they define resilience for themselves and their community. This qualitative study explored the perceptions of eight military spouses regarding their resilience through individual semi-structured interviews. The following themes emerged: 1) shaped by service member and mission priority; 2) challenges within the military lifestyle; 3) outside expectations of spouse resilience; 4) sense of responsibility for family’s resilience; 5) individual resilience; and 6) collective resilience. We discuss ways military leadership and the counseling profession can best understand and enhance the resilience of military spouses.
Keywords: military spouses, resilience, military lifestyle, perceptions, counseling
Because of the unique stressors associated with the military lifestyle, military spouses are at an increased risk for poor mental health (Donoho et al., 2018; Mailey et al., 2018; Numbers & Bruneau, 2017). They may experience mental health concerns, such as anxiety and depression, due to a number of reasons, including separation from their deployed service member, loss of support networks after a relocation, or issues with adjusting to the uncertain and frequent changes of the military (Cole et al., 2021). Additional concerns that arise, such as employment, marital, and financial issues, can also negatively affect the military spouse’s mental health (Cole et al., 2021; Mailey et al., 2018). Dorvil (2017) reported that 51% of active-duty spouses experience more stress than normal. Furthermore, 25% of military spouses meet the criteria for generalized anxiety disorder (Blue Star Families [BSF], 2021). Depression in military spouses is also higher than the rate found within the general population (Verdeli et al., 2011). As a military spouse casts aside their own personal needs to support their service member, stressors may continue to increase, which can contribute to the rise of mental health needs of military spouses (Moustafa et al., 2020).
Resilience and Military Spouses
Nature of Resilience
Given the challenges inherent in the military lifestyle and the associated mental health risks, military spouse resilience is essential. Resilience is a complex and multifaceted construct, significant to researchers, practitioners, and policymakers across numerous disciplines, including mental health and military science. The American Psychological Association (2020) defined resilience as “the process of adapting well in the face of adversity, trauma, tragedy, threats, or even significant sources of stress” (para. 4). Within the military community, resilience has been defined as the ability to withstand, recover, and grow in the face of stressors and changing demands (Meadows et al., 2015). Importantly, determinants of resilience include the interaction of biological, psychological, social, and cultural factors in response to stressors (Southwick et al., 2014). In addition to these salient variables embedded in resilience science, resilience may be operationalized as a trait (e.g., optimism), process (e.g., adaptability in changing conditions), or outcome (e.g., mental health diagnosis, post-traumatic growth; Southwick et al., 2014).
Resilience may also vary on a continuum across domains of functioning (Pietrzak & Southwick, 2011) and change as a function of development and the interaction of systems (Masten, 2014). Accordingly, a definition and operationalization of resilience may vary by population and context (Panter-Brick, 2014). During the post-9/11 era, the resilience of service members and their families received significant attention from stakeholders, including the Department of Defense (DoD) and National Academies of Sciences, Engineering, and Medicine (NASEM), both of which expressed a commitment to conducting research and establishing programming to enhance service member and military family resilience, resulting in increased awareness of the importance of service member and family resilience throughout the military community (NASEM, 2019).
Military Family Resilience
Though military families share the characteristics and challenges of their civilian counterparts, they additionally experience the demanding, high-risk nature of military duties; frequent separation and relocation; and caregiving for injured, ill, and wounded service members and veterans (Joining Forces Interagency Policy Committee, 2021). In recognition of the constellation of military-connected experiences military families face, the Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury (DCoE) commissioned a review of family resilience research and relevant DoD policies to inform a definition of resilience for appropriate application to military spouses and children (Meadows et al., 2015). Meadows and colleagues (2015) proposed family resilience may be best defined as “the ability of a family to respond positively to an adverse situation and emerge from that situation feeling strengthened, more resourceful, and more confident than its prior state” (see Simon et al., 2005, for a further exploration of family resilience). Further, Meadows and colleagues identified two groups of policies delineated at the Joint Chiefs of Staff or DoD levels, or within individual branches of the military: 1) existing programs modified to augment resilience or family readiness, and 2) new programs developed to target family resilience. Programs established by these policies support access to mental health services (e.g., DoD Instruction [DoDI] 6490.06); parenting education (e.g., New Parent Support Program, DoDI 6400.05); child welfare (e.g., Family Advocacy Program, DoD Directive 6400.1); and myriad physical, psychological, social, and spiritual resources. The well-being of military families represents a critical mission for the DoD, extending beyond provision and access for families to meet their basic needs to individual service member and unit readiness, and the performance, recruitment, and retention of military personnel (NASEM, 2019).
Military Spouse Resilience
Though service member and family resilience are critical for accomplishing the DoD’s mission, focusing on the unique nature of military spouse resilience is key for understanding and supporting this population’s resilience. Counseling, psychology, sociology, and military medical professional research related to military spouse resilience has focused primarily on characteristics associated with resilience. In a study by Sinclair et al. (2019), 333 spouse participants completed a survey regarding their resilience, mental health, and well-being. The results revealed that spouses who had children, were a non-minority, had social support, had less work–family conflict, and had a partner with better mental health were more resilient. Another survey study examined the characteristics associated with resilience in Special Operations Forces military spouses, determining that community support and support from the service member was essential for spouse resilience (Richer et al., 2022). A study conducted within the communication field also explored spouses’ communicative construction of resilience during deployments. Qualitative data analysis of interviews with 24 spouses indicated how spouses use communication to reconcile their contradictory realities, which increases their resilience (Villagran et al., 2013). This resilience has also been found to be a protective factor against depression and substance abuse during military deployments (Erbes et al., 2017). Finally, a survey study of Army spouses (N = 3,036) determined that spouses who were less resilient were at higher risk for mental health diagnoses (Sullivan et al., 2021). While these studies explored the nature of resilience demonstrated by military spouses, our searches in JSTOR, PubMed, ERIC, PsycINFO, and Google Scholar did not reveal any studies regarding spouses’ perceptions of their own resilience or how they define this resilience for themselves and their community. Our study fills that research gap by exploring active-duty spouses’ perceptions and definitions of resilience.
Methods
The purpose of this qualitative study was to explore the perceptions of active-duty spouses regarding their resilience. This study was guided by the following research questions: 1) What are military spouses’ perceptions of their own resilience? and 2) How do military spouses define “resilience?” Phenomenology seeks to present a certain phenomenon in its most authentic form (Moustakas, 1994). In order to most authentically and openly describe our participants’ experiences, we chose a qualitative transcendental phenomenological approach to frame our study. This tradition of qualitative research focuses on portraying a genuine representation of the participants’ perceptions and experiences. However, the distinct feature of transcendental phenomenology is its first step, which involves the researchers recognizing and bracketing their biases so they can analyze the data without any interference (Moerer-Urdahl & Creswell, 2004). We selected this design because each of our research team members were military spouses. We therefore recognized the need to mitigate our biases in order to give a true representation of the participants’ perceptions, free from our own preconceived notions.
Participants
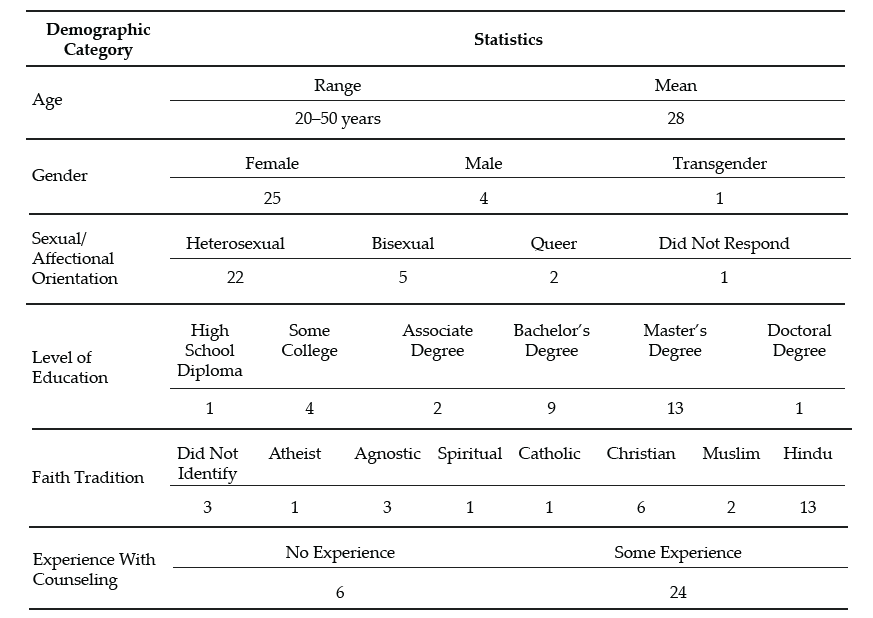
The participants in this study were selected based on their status as active-duty military spouses and their willingness to participate in the study. There were no other inclusion or exclusion criteria for the participants in this study. After gaining IRB approval, we used convenience sampling to recruit eight participants. In qualitative research, convenience sampling is used to recruit participants who are closely accessible to the researchers (Andrade, 2021). Our research team emailed participants that we knew through living, working, and volunteering on military bases throughout the United States and at overseas duty stations who fit the active-duty military spouse criteria for this study and asked them if they were willing to participate in the study. Once the participants expressed interest, they were provided with an information sheet regarding the study’s purpose and the nature of their involvement in the study. Participant demographics are included in Table 1. All of the participants were female and all were between the ages of 30–40. Four branches of the U.S. military, including Army, Navy, Air Force, and Marine Corps, were represented in the sample. No reservist, Coast Guard, or Space Force military spouses participated in our study. Five of our participants were White and three were Black. Their tenure as military spouses ranged from 4 years to 17 years. Five of the spouses were married to a military officer, while three of the participants were married to an enlisted service member. After interviewing these eight participants, our research team met and determined that because of the distinct common patterns we found across each of the participants’ transcripts, we had reached saturation and did not need to recruit any additional participants for our study (Saunders et al., 2018).
Table 1
Participant Demographics
| Participant |
Age |
Ethnicity |
Gender |
Branch |
Spouse’s Rank |
Years as a Spouse |
| 1 |
33 |
Black |
Female |
Air Force |
Enlisted |
4 |
| 2 |
36 |
Black |
Female |
Navy |
Enlisted |
17 |
| 3 |
31 |
White |
Female |
Army |
Officer |
7 |
| 4 |
34 |
Black |
Female |
Navy |
Enlisted |
14 |
| 5 |
36 |
White |
Female |
Marine Corps |
Officer |
12 |
| 6 |
35 |
White |
Female |
Marine Corps |
Officer |
14 |
| 7 |
40 |
White |
Female |
Navy |
Officer |
16 |
| 8 |
34 |
White |
Female |
Navy |
Officer |
10 |
Data Collection
Our research team first developed the interview protocol for the study based on a thorough review of the literature regarding resiliency within military culture as well as the challenges of the military lifestyle for military spouses. Our research team members interviewed each of the participants for 1–2 hours. These semi-structured interviews were audio recorded and transcribed verbatim by an automated transcription service. The interview questions were open-ended and focused on the spouses’ definitions of resilience and their perceptions of their resilience within the military lifestyle and culture (see Appendix for interview protocol). In addition, probing questions such as “Can you explain that a bit more?” or “Can you give any examples of what you mean by that?” were used to gather more in-depth data throughout the interviews.
Data Analysis
We followed the steps of the transcendental phenomenological data analysis process to analyze our study’s results (Moerer-Urdahl, 2004). First, each member of our research team engaged in epoche, in which we bracketed our biases as military spouses so that our own thoughts, feelings, perceptions, and experiences did not influence our interpretation of our participants’ experiences. The next step in the process was horizontalization. During this step, each member of our research team read through the interview transcripts and noted significant statements throughout so we could better understand how the participants perceived, understood, and experienced resilience. Next, we met as a research team to discuss these significant statements and organize them into themes (Moustakas, 1994). Our research team then developed textual and structural descriptions of the themes, describing not only a list of the participants’ perceptions, but also an in-depth analysis of what their perceptions of resilience entailed and how they have experienced it throughout their tenure as military spouses (Moerer-Urdal, 2004; Moustakas, 1994). We then constructed a comprehensive description of the participants’ perceptions of resilience, encapsulating the “essence of the experience” (Moerer-Urdal, 2004, p. 31).
Research Team and Strategies to Increase Trustworthiness
Our research team consisted of four university faculty members, all of whom possessed extensive experience in conducting qualitative research. Three of our research team members possess PhDs in counseling and one research team member possesses an EdD in counseling. All team members had extensive experience conducting research with military-connected communities. In addition, all of our research team members were active-duty military spouses, with years of experience as a military spouse ranging from 1–23 years.
We used several strategies to increase the credibility of our results. First, the use of an experienced research team to collectively analyze the data resulted in diverse perspectives on the emerging themes of the study. However, because each member of our research team was a military spouse, we recognized the need to bracket our own experiences and biases so that they did not interfere with our interpretation of the data. Each team member took notes on their individual biases, and our research team discussed these biases when interpreting themes. Biases held by research team members included a predisposition to believe that spouses of special warfare service members endured greater stressors and were better supported by their military communities; a belief that spouses of higher-ranking service members possessed greater knowledge of and access to resources to support social, behavioral, and mental health needs; and personal experience within the military spouse community. These biases were challenged throughout the research process by each member of the team. As each theme was identified, the team referenced individual transcripts to ensure that the interpretation was justified. We found that our biases were rightfully challenged.
Additionally, to avoid leading questions, our research team made the conscious decision not to define resilience as part of the interview and follow-up process. The team wanted to derive an organic definition of spouse resilience that was not clouded by a formal definition. In addition, we used member checking, in which we emailed the interview transcripts to the participants and asked them to verify the data. The participants responded to our request with minimal change requests related to grammatical errors in the transcriptions and validated our data. Several offered additional insight related to their definition of resilience, which was included in our data analysis.
Results
The following themes emerged from our data: 1) shaped by service member and mission priority; 2) challenges within the military lifestyle; 3) outside expectations of spouse resilience; 4) sense of responsibility for family’s resilience; 5) individual resilience; and 6) collective resilience.
Theme 1: Shaped by Service Member and Mission Priority
Military/Service Member Definition
When discussing their definition of resiliency, the spouses first considered what resiliency meant for their active-duty spouse. The participants varied in their perceptions of what resilience meant for their active-duty service member, though all defined resilience as an active process of adapting or persevering when faced with adversity, rather than a personal trait or characteristic the service member possesses. Participant 3 noted that, for their spouse, resilience was “the ability to adapt to changes that are beyond your control . . . adapting to situations in an optimistic and positive way.” Participant 6 stated that resilience for their spouse meant an “ability to bounce back from a hardship.” One participant asked their spouse to comment specifically about their definition and provided the following definition in a follow-up with the interviewer: “Resilience is how you persevere in difficult circumstances. It’s not about how hard you fall, but how quick you can get back up from being knocked down” (Participant 2 [P2]).
Some participants cited specific notions of resilience that are embedded in the service members’ military community. One Navy spouse remarked that resilience, to their spouse, meant “Don’t give up the ship” (P8). Another Navy spouse mentioned that for their spouse, resilience was “knowing how to weather the storm” (P7). Yet another spouse noted that resilience “the Marine Corps way” meant their service member must “do their job” (P4). Other participants noted that the root of resilience for the military service member stems from a place of selfless service. Participant 8 commented that the resiliency of their spouse was “more about the man standing next to me, the family I’m fighting for at home, the country I’m fighting for at home, than about their own personal needs.”
Adapting, Overcoming, and Persevering
Like their active-duty members, spouses indicated that resilience was about adapting, overcoming, and persevering in the face of obstacles. Resilience to one spouse was “being able to rebound or to overcome an obstacle” (P1); to another, resilience meant they must “be flexible, adapt with whatever, overcome whatever it is that you’re going through” (P2). Spouses noted that resilience was not a one-time event. Instead, spouses suggested that their own resilience stemmed from continually persevering. Participant 6 stated that for them, resilience meant not just “going through something difficult and making it out on the other side,” but that they then had to “keep pushing forward.” One participant indicated that their personal definition of resilience and the notion to persevere stemmed directly from their spouse: “I’ve almost kind of adopted a bit of my husband’s thought process, I guess. You just keep going to get things done” (P8).
Mindset
Our participants indicated that resilience was a mindset that one must choose and that when faced with difficulties, they chose to focus on gratitude, positivity, and growth. For example, Participant 8 stated that, although they had faced and would continue to face challenging and stressful experiences as a result of being a military spouse, they believed that “whatever may come, we’ve been very blessed in our life and we should always be thankful for the life that we have.” Another participant noted that for them, overcoming and persevering meant adopting an optimistic attitude. Specifically, the spouse stated, “sometimes you just have to kinda look at the bright side of things, and you have to find the things that work for you at each place” (P5). One participant drew resilience from a growth mindset:
I think it [resilience] is really a mindset switch. I think it’s changing from “oh this is happening to me, how horrid” to like “how can I take this horrid situation and turn it into something good?” And I think that is a big mindset switch. (P7)
Resilience Variations
Walsh (2012) described risk and resilience as a process of balancing risk and protective factors over the life span. Participants in our study expanded on that idea by suggesting that they reacted to situational challenges along a continuum:
I think what I’m saying is there’s different levels of resilience, like sometimes you have to tap into that different part of yourself. Sometimes you have to let it go and just accept the things that come, and sometimes you just gotta pick yourself up and keep on trucking. (P8)
Likewise, Participant 3 suggested that resilience takes different forms depending on the situation:
Sometimes resiliency just means like surviving day to day and other times, it means figuring out how to continue with your passions to the best of your ability while also supporting your family and your [service member spouse]. I think it’s just super unique to every situation. (P3)
Our participants also recognized that their understanding of resilience was often focused on the here and now of their situation but that their reactions to stressors had long-term effects. One participant indicated that resilience is a learning process and recognized that the stressors they overcome now prepare them to address stressors they will face in the future: “I think being able to come out of extremely, extremely stressful situations, be able to come out on the other side and [know] I’m okay and I survived this, and now I’m kind of better prepared for next time” (P6). Participant 3 wondered about the long-term ramifications of resilience in the face of prolonged adversity, stating “I may be resilient right now in the moment, but in the long term, like, how will this affect me?”
Individualized
Finally, participants defined resilience as an individualized process, stating things such as “everybody has their own unique ways of being resilient, and I think that they do what works best for their families” (P7) and “my resiliency may look different than someone else’s resiliency” (P2). One participant elaborated on this individualized approach to resilience by recognizing that each person has different risk factors that affect their response to stressors, thus affecting the way each person demonstrates resilience. This participant stated that, when viewing resilience among military spouses as a whole, it is important to
take into consideration somebody’s upbringing and the baggage that they bring into this life. We don’t know what people have gone through as kids, and that I think would have a big impact on whether or not someone can be resilient, so I don’t think it’s a one-size-fits-all. (P6)
Theme 2: Challenges Within the Military Lifestyle
Lack of Control
The spouses described the common challenges of the military lifestyle to their resilience. First, they discussed the stress of the feeling of a lack of control in their lives. One participant described how she
just found out yesterday that my husband was getting deployed and he’s leaving Sunday. And I keep hearing people say, “You have to be resilient. You’re gonna be okay!” You’re resilient, but right now, what it feels like is how much can you endure for the sake of the mission? (P1)
Another echoed this sentiment: “I have no control if the Navy says they’re going to deploy my husband. There’s nothing I can do to change that” (P8).
Constant Changes
Another common challenge mentioned among all of the participants was the constant changes they experience in their lives, including moving, career changes, and changes within their family dynamics. Because they move every few years, the spouses described how they are constantly separated from their support systems: “Even though you meet these great people, you don’t get to stay with them . . . and you’re generally not near your family, which is very hard” (P5). Another described how “Once I have started on something and I’m like, ‘This is it, we gon’ be here for a while,’ then my husband is like ‘nope. Military said we got to shift and move again’”(P2).
These constant changes resulted in career struggles for the spouses. One asked, “How can I get this [job] if I’m never at one place for long? . . . How do I uproot everything that I know or everything that I am doing to follow my service member?” (P2). Another described how “moving, changing jobs, not being able to have a secure profession, you do it because you have to . . . but that doesn’t mean that there’s not a whole lot of emotional and mental load that goes with it” (P3).
Another challenge for military spouses was constantly changing family dynamics. One described the difficulty in constantly changing work schedules: “We have to kind of get into this routine without him and then when he comes back, because it’s different while he’s away. We gotta kind of try to fit him back into our routine when he gets back” (P4). Another discussed the challenge of transitioning to being the sole caregiver during a deployment: “If I go down with COVID, what am I going to do? Because, like, I was literally IT. No one is going to want to take my kids. . . . That was the first time I ever felt, like, fearful” (P7).
Mission Priority
In addition to constant change, the spouses also mentioned the challenges of the military’s clear prioritization of the mission above military members and their families: “If something is going on at home, we’re going to take care of our active person first and worry about your family later” (P2). The participants described how this focus on the mission is so intense that it affects service members physically, which increases the burden on military spouses to care for them: “My husband’s health suffers because the mission is most important to him” (P1).
Theme 3: Outside Expectations of Spouse Resilience
Expectation to “Suck It Up”
The spouses described others’ expectations for their resilience. First, they described the military’s expectation that they “suck it up.” One described how “you have a lot of the ‘suck-it-up’ mentality, and I would say when you have the leaders who kind of fall under that, whether it’s seeking the mental health treatment or having stigmas with that” (P6). Another explained that “there’s so much focus and emphasis on just being resilient and sucking it up” so there is often a mindset of “‘Oh well, military spouses are resilient so they signed up for this, they know what it takes and they just have to get over it’” (P3). Another spouse described how “they put so much pressure on you to be like, just make it work, that you’ve gotta figure out the way to make yourself happy, and that’s hard to do” (P5). Participant 7 summed up the military spouse mentality as a whole: “You toughen up and you make it work. You know?”
The participants felt their overall resilience would be enhanced if individuals outside the military community better understood the challenges faced by military families. One participant felt the “suck it up” mentality stemmed less from the military community itself and more from outside communities who might not understand the struggles of military family life: “So when . . . you’re going through another stress of a PCS [permanent change of station], you can’t find a house, they say, well, at least you get a house allowance, at least you get free health care” (P6). Participant 3 expanded on this idea by stating, “I just honestly think that a greater understanding of what sacrifices that military spouses make . . . would increase resiliency, because there’s just so much lack of understanding what it actually entails.” Lastly, one participant mentioned a sentiment they frequently hear from others in a civilian community, expressing that it was frustrating when friends outside the military told her, “I don’t know how you do it,” to which the participant responded, “I don’t know, you just do it!”
Pressure to Be Resilient
The spouses also expressed frustration at others’ misperceptions of the expectation that they and their families demonstrate resilience: “When we call military spouses or children resilient, it just seems like a cop out and relinquishes any type of burden . . . or feeling of guilt about a situation that may cause emotional or mental damage” (P3). Another participant echoed this frustration: “Sometimes I don’t feel like I’m being resilient. Sometimes I feel like I’m just doing what needs to be done because that’s what needs to be done” (P8). Another participant described how her friends
call me Superwoman because I have all these different things going on and I always seem like I got it together. . . . It’s like saying to me that I have to keep going, no matter what, and I think people should be able to just feel defeated sometimes. Or be able to say “that was just too much for me” or “I don’t really feel like being resilient today, I kind of want to lay in bed and just be upset or sad.” (P4)
Given these expectations, one spouse pointed out the danger of expecting military children to consistently demonstrate resilience:
It’s so easy for everyone to say that military kids are always so resilient and sometimes they’re not. Sometimes they are stressed out. They are feeling the crushing weight. They feel sad but everyone keeps telling them that they’re resilient. So it almost makes it seem like . . . they aren’t allowed to feel those hard things or talk about those things or act on those feelings and emotions. (P8)
One spouse proposed a solution to these misperceptions, emphasizing that resilience is unique for military spouses and should be defined to accurately reflect the way they uniquely overcome challenges:
I think it’s important for military spouses to reappropriate that term [resilience] so that it is not weaponized, and I would like to see some sort of guidance as to how we can be resilient but in a way that positively impacts our mental health and physical health and not having to endure all of the things and all of the frustration and uncertainty that comes with the onset of having to be resilient. (P1)
Theme 4: Sense of Responsibility for Family’s Resilience
With their partners focused on the mission, the spouses described their sense of responsibility to maintain their resilience so they can care for their children in the absence of their active-duty spouse: “We have our husband or our spouses gone so much, we need to be a solid parent at home for our kiddos or our family” (P7). Participant 4 likewise described how “I kind of see myself as holding down the fort, you know, because when my husband is not home it is just me and the kids.” Another explained how “I have three little ones that’s looking up to me and I can’t slip away, depressed, because daddy’s not home” (P2). In the end, the spouses defined resilience as an obligation to their families. Participant 3 described that “I have to be that way for my children.” Participant 4 added that “I think that’s what resilience is like, knowing that you kind of have to carry the load, you know, for your whole family to try to keep us afloat.”
The participants described how this resilience is especially obligatory when the active-duty spouse is unable to be resilient:
I’m kind of taking the lead with our kids . . . but I’ve also kind of had to pour into my husband, you know, because he has those times you know where things are really, really hard for him. I’ve also been like his counselor and his doctor sometimes. (P4)
Theme 5: Individual Resilience
In response to being unable to control many aspects of the military lifestyle, most of the spouses described how they have become independent in order to withstand the constantly changing variables within the military lifestyle. One described being “pretty independent, and I think that helps a lot because I don’t rely on my spouse to do all these things I do” (P5). Another described how being independent resulted in self-confidence and resilience:
You gotta figure out how to do all of it just because you can’t ever rely on the spouse being able to help. But I think being able to come out of extremely, extremely stressful situations, be able to come out on the other side and say “I’m okay, and I survived this, and now I’m kind of better prepared for next time.” (P6)
Another spouse described how maintaining an independent identity was key to separating herself from the stressors of the military lifestyle: “That’s a really important part of being a military spouse. It doesn’t have to be a job specifically, but just something that you can be your own person separate from your husband or your spouse’s job” (P8).
The spouses also described the importance of taking care of themselves physically and mentally in order to maintain their resilience. Many described exercise as key to their mental health and wellness: “My biggest coping mechanism is exercise. I’ve found that no matter where I go, I can exercise” (P5). Another spouse described how she “tried to find a kickball team every place we’ve been to since Okinawa because I figured out it’s a stress relief” (P6). Participant 7 echoed that “working out . . . just helps me. It lowers my stress.” One spouse explained how she defaults to exercise when facing the challenges of the military lifestyle because she knows her “ability to recover quickly is directly tied to the way in which I care for myself” (P1).
Theme 6: Collective Resilience
The participants described their reliance on the collective military spouse community for their survival. One spouse, for example, described a connection with other military spouses as the difference between “doing well and barely surviving” (P6). Another spouse described her reliance on the military spouse community: “Community is what it’s all about. I can’t get through anything without community” (P7). Another spouse echoed this survival mechanism: “This is a beautiful community. It’s an amazing place . . . we all get each other. So I think there are times where it’s really hard . . . but we survive, we get through it. We’re resilient. We got the grit” (P7). Participant 1 explained exactly how the military spouse community offers this support to help spouses survive the challenges of the military lifestyle: “When time calls for it, I think, collectively, we bring our resources together to help pull other military spouses up and try to just forewarn them about what the obstacles are and what may have worked for our family” (P1).
The military spouses also described the comfort they found in other military spouses’ understanding of the challenges they face: “I think the most important part and coping is finding your community, so making sure you’re surrounding yourself with women who are going through similar experiences, or who have gone through similar experiences and similar life stages” (P3).
In the midst of this supportive community, the spouses discussed how they actively seek to comfort each other: “You’re not the only one who’s in it who’s having this issue, I understand that you’ll get through this, that we know we’ve been there, we understand how it goes” (P5). This outreach seemed to be especially helpful from spouses who were more experienced with the military lifestyle: “Having that senior spouse example has been so good. . . . She’s always been somebody who said, ‘Hey, I’ve been through a lot. If you ever have any questions, I’m always here for you’” (P8).
In addition to relying on other spouses for their own wellness and resilience, the spouses expressed pride in their ability to contribute to the military spouse community. One described how “I feel like I am a better team player. I feel like I’m more committed to helping others than I have in the past because I know that others will do the same for me” (P7). The participants also described increased self-growth as a result of being a part of a community: “I really don’t think I would have allowed myself to receive help if I hadn’t been part of this phenomenal community that is constantly supporting each other” (P7). Participant 5 echoed this sentiment: “Learning to get that help from other people is something that I feel like you have to kind of get when you are a military spouse because, otherwise, you’re going to have to do everything and you don’t have to.”
Finally, our participants frequently indicated that they felt a “sense of pride” (P7), “connection” (P4), or “camaraderie” (P8) from belonging to a group of military spouses who understood their unique situation. When asked how the military could enhance resilience for military spouses, participants commonly indicated that peer support and fostering connections with senior spouses should be a priority for military commands. One participant noted that their ability to be resilient in difficult times was related to the “opportunities” they had “to connect with other people who are going through similar stuff and who are a part of the same small community” and recommended that the military facilitate more opportunities to connect (P7). Another participant suggested that military commands should “have someone that [the spouse] can talk to” that would “help them to understand the military life whether you are a new spouse or a seasoned spouse” (P2).
Discussion
The purpose of this study was to explore military spouses’ perceptions of their resilience and the ways in which they define resilience for their community. Our study’s results indicate that spouses’ definitions of resilience are currently shaped by service member and mission priority. Our participants also described how they often felt burdened by outside expectations of their resilience as well as by a sense of responsibility for their family’s resilience. Overall, the spouses relied on themselves and the military spouse community to overcome the challenges they faced. Participants expressed a desire for resources aimed specifically at enhancing spouse resilience and more awareness about resilience resources already in place throughout the military.
While past research has examined resilience factors in spouses such as communication skills, social support, and spousal support (Erbes et al., 2017; Richer et al., 2022; Sinclair et al., 2019; Villagran et al., 2013), our study provided new insight into military spouses’ perspectives of their resiliency. This revelation of the spouses’ worldview aids our understanding of ways to best support spouses and areas to focus on to support their resilience. Our participants’ definitions of their resilience were shaped by their relationship with their service member and the influence of the military’s mission. In addition, while past research has indicated that the military lifestyle and culture is challenging for spouses to navigate (Cole et al., 2021; DaLomba et al., 2021; Donoho et al., 2018; Mailey et al. 2018), our participants’ description of their feelings of responsibility for their family’s well-being reveals the added burden that military spouses face as they help their families navigate the military lifestyle. Finally, our participants confirmed that resiliency should be viewed as a variation and is unique to each individual (Pietrzak & Southwick, 2011). As outlined in the professional literature (Masten, 2014; Southwick et al., 2014), the participants confirmed the dynamic nature of resiliency, recognizing that sometimes they felt more resilient than at other times.
In the midst of these challenges, our participants emphasized that the military spouse community serves as a protective factor and a source of their resilience against mental health challenges. This perception of the military spouse community aligns with previous research highlighting the supportive role that spouses play for each other, so much so that it is a protective factor against suicide (Cole et al., 2021). Therefore, military leadership and the counseling community might focus on enhancing this community and connecting spouses with one another—especially more seasoned spouses with newer spouses. In addition, because military-sponsored resilience programs are often targeted to better support service member outcomes, community providers might find ways to focus on supporting the spouses and helping them to overcome the challenges they face in their daily lives.
Finally, the participants discussed how they overcame the challenges of the military lifestyle, including constant moving, deployments, and overall uncertainty, through their own individual and collective resilience. These lifestyle challenges that the participants described correspond to career struggles and shifting family dynamics that cause ongoing stress to the military spouse, both of which have been previously documented in the professional literature (Borah & Fina, 2017; Cole et al., 2021; DaLomba et al., 2021; Donoho et al., 2018; Mailey et al., 2018; Numbers & Bruneau, 2017). Currently, since the withdrawal of troops from Afghanistan, the United States is experiencing peacetime, whereas the nature of future conflicts is uncertain (Marsh & Hampton, 2022). Enhancing the resiliency of military spouses and finding solutions to ongoing stressors is key during this time of peace so that spouses are ready and able to face the stressors of future, potentially large-scale wars (Sefidan et al., 2021).
Implications for Counselors
Professional counselors are called to be trained and ready to meet the unique needs of military spouses, especially in understanding the nature of military culture and its impact on spouse mental health and well-being and enhancing spouse resilience in times of adversity (Cole, 2014). Our study echoes the continued struggles of military spouses described in the professional literature (Cole et al., 2021; Lewy et al., 2014; Runge et al., 2014), suggesting that new and innovative ways of understanding and approaching military spouse resilience is needed within the counseling community. For example, counselors might encourage spouses to explore how their resilience is shaped by the military community in order to increase self-awareness and understanding. They might also help spouses develop their independence and sense of self-efficacy while simultaneously seeking collective support within the military community. Counselors can help spouses examine their social support and help them develop their social skills so they can connect with others around them. Counselors should also help military spouses unpack their perceptions of outsiders’ expectations of their resiliency. Encouraging spouses to reflect on others’ expectations, and the ways in which these expectations impact their sense of well-being, may help define resilience for themselves and capitalize on their unique resiliencies during challenging times. Ultimately, because the military culture is so unique, counselors should seek out professional development so they can better understand how to help military spouses navigate this culture and enhance their resilience. When working with military spouses, professional counselors might explore spouses’ feelings of responsibility for their family members’ health and well-being that were described in our results. In addition, counselors can equip spouses with supportive mental health resources for their family members so they do not feel as if they need to care for them on their own. School counselors, in particular, can provide support for military-connected students at school and can connect military families with resources within both the civilian and military communities to support their mental health and resilience (Cole, 2017; Quintana & Cole, 2021).
Our participants revealed that often the expectation of resilience is burdensome for spouses, which serves as a contradiction to its purposes. Counselors are called to acknowledge the challenges of the military lifestyle and provide support for navigating these challenges, rather than expecting spouses to face these hurdles alone. In addition, counselors might focus on more holistic manifestations of resilience, recognizing that some spouses can be resilient, yet still struggle. Approaching spouses from a strengths-based perspective, rather than from a deficit perspective, can be empowering within the counseling relationship (Smith, 2006).
Limitations
Our recruitment strategy limited our sample size as we only sought participants that we knew through our military spouse networks. In addition, our sample lacked gender diversity, with all of the participants being female. Approximately 91% of active-duty service member spouses are female (DoD, 2022). However, the lack of male participants in the present study is a limitation, and the experience of male spouses is undoubtedly unique and worth exploring in greater depth. Research suggests that stressors and characteristics of resilience transcend gender categories (NASEM, 2019).
Finally, in qualitative research, the researcher’s biases may impact their interpretation of the data. As military spouses, our own experiences may have impacted the way in which we described our participants’ experiences. We took several steps to mitigate these biases, including intentionally bracketing them and engaging in peer debriefing throughout the research process.
Implications for Future Research
The participants in our study described a need for resources and programs geared specifically toward military spouses. Future research might determine how to best develop and implement these programs that will help to enhance spouse resilience. Key areas of focus may be ways to leverage the military spouse community and enhance spouse sense of self, which were two protective factors that emerged from our data. In addition, existing resilience programs within the military that are currently aimed at the active-duty population should undergo a program evaluation to determine their effectiveness with military spouses.
As a follow-up to our qualitative research, future quantitative research studies should address limitations noted previously. Specifically, future research should target a larger sample size and broader demographic of military spouses to further explore their understanding and definition of resilience. This larger and more diverse sample size would allow for greater generalizability and would assist with advocacy within the military. Finally, future qualitative research might explore the perceptions of male spouses, in particular, in order to determine their perception of resiliency and any unique areas of needed support.
Conclusion
Military spouses face a wide range of challenges as a result of the military lifestyle. They are expected to be resilient so as to overcome these challenges. However, our study reveals the often burdensome impact of these expectations on military spouses. Our results also illuminate how spouses uniquely conceptualize their own resilience, recognizing the resilience continuum and focusing on the positive impact of their protective community. Overall, the spouses took pride in themselves and their communities for their ability to overcome obstacles. These revelations are key for both the military and the counseling profession in their work to support military spouses wherever they are on this continuum and enhance their community, which is key to their well-being.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript. The opinions and assertions
expressed herein are those of the authors and
do not reflect the official policy or position of
the Uniformed Services University of the Health
Sciences or the Department of Defense.
References
American Psychological Association. (2020). Building your resilience. https://www.apa.org/topics/resilience/building-your-resilience
Andrade, C. (2021). The inconvenient truth about convenience and purposive samples. Indian Journal of Psychological Medicine, 43(1), 86–88. https://doi.org/10.1177/0253717620977000
Blue Star Families. (2021). Military Family Lifestyle Survey: 2020 comprehensive report. https://bluestarfam.org/wp-content/uploads/2021/03/BSF_MFLS_CompReport_FULL.pdf
Blue Star Families. (2023). Military Family Lifestyle Survey: 2022 comprehensive report. https://bluestarfam.org/wp-content/uploads/2023/03/BSF_MFLS_Spring23_Full_Report_Digital.pdf
Borah, E., & Fina, B. (2017). Military spouses speak up: A qualitative study of military and veteran spouses’ perspectives. Journal of Family Social Work, 20(2), 144–161. https://doi.org/10.1080/10522158.2017.1284702
Cole, R. F. (2014). Understanding military culture: A guide for professional school counselors. The Professional Counselor, 4(5), 497–504. https://doi.org/10.15241/rfc.4.5.497
Cole, R. F. (2017). Supporting students in military families during times of transition: A call for awareness and action. Professional School Counseling, 20(1), 36–43. https://doi.org/10.5330/1096-2409-20.1.36
Cole, R. F., Cowan, R. G., Dunn, H., & Lincoln, T. (2021). Military spouses’ perceptions of suicide in the military spouse community. The Professional Counselor, 11(2), 203–217.
https://doi.org/10.15241/rfc.11.2.203
DaLomba, E., Greer, M. J., Cruz, E., Harris, A., King, C., Laurel, L., McCuaig, T., & Wilder, R. (2021). The experiences of active duty military spouses with advanced degrees in maintaining and advancing their careers. Work, 68(2), 387–398. https://doi.org/10.3233/WOR-203380
Donoho, C. J., LeardMann, C., O’Malley, C. A., Walter, K. H., Riviere, L. A., Curry, J. F., & Adler, A. B. (2018). Depression among military spouses: Demographic, military, and service member psychological health risk factors. Depression and Anxiety, 35(12), 1137–1144. https://doi.org/10.1002/da.22820
Dorvil, M. (2017). 2017 survey of active-duty spouses. Office of People Analytics, U.S. Department of Defense. https://download.militaryones ource.mil/12038/MOS/Surveys/2017-Survey-of-Active-Duty-Spouses-Overview-Briefing.pdf
Erbes, C. R., Kramer, M., Arbisi, P. A., DeGarmo, D., & Polusny, M. A. (2017). Characterizing spouse/partner depression and alcohol problems over the course of military deployment. Journal of Consulting and Clinical Psychology, 85(4), 297–308. https://doi.org/10.1037/ccp0000190
Joining Forces Interagency Policy Committee. (2021). Strengthening America’s military families: Matching their devotion: Deepening our commitment to the families, caregivers, and survivors of service members and veterans. https://www.whitehouse.gov/wp-content/uploads/2021/09/Strengthening_Americas_Military_Families.pdf
Lewy, C. S., Oliver, C. M., & McFarland, B. H. (2014). Barriers to mental health treatment for military wives. Psychiatric Services, 65(9), 1170–1173. https://doi.org/10.1176/appi.ps.201300325
Mailey, E. L., Mershon, C., Joyce, J., & Irwin, B. C. (2018). “Everything else comes first”: A mixed-methods analysis of barriers to health behaviors among military spouses. BMC Public Health, 18(1013), 1–11. https://doi.org/10.1186/s12889-018-5938-z
Marsh, M. K., & Hampton, R. L. (2022). Army medicine’s critical role in large-scale combat operations: Enable the force. Military Review, 102(4), 106–113.
Masten, A. S. (2014). Global perspectives on resilience in children and youth. Child Development, 85(1), 6–20. https://doi.org/10.1111/cdev.12205
Meadows, S. O., Beckett, M. K., Bowling, K., Golinelli, D., Fisher, M. P., Martin, L. T., Meredith, L. S., & Osilla, K. C. (2015). Family resilience in the military: Definitions, models, and policies. RAND Health Quarterly, 5(3).
Moerer-Urdahl, T. & Creswell, J. W. (2004). Using transcendental phenomenology to explore the “ripple effect” in a leadership mentoring program. International Journal of Qualitative Methods, 3(2), 19–35. https://doi.org/10.1177/160940690400300202
Moustafa, A. A., Crouse, J. J., Herzallah, M. M., Salama, M., Mohamed, W., Misiak, B., Frydecka, D., Al-Dosari, N. F., Megreya, A. M., & Mattock, K. (2020). Depression following major life transitions in women: A review and theory. Psychological Reports, 123(5), 1501–1517. https://doi.org/10.1177/0033294119872209
Moustakas, C. (1994). Phenomenological research methods. SAGE.
National Academies of Sciences, Engineering, and Medicine. (2019). Strengthening the military family readiness system for a changing American society. The National Academies Press. https://doi.org/10.17226/25380
Numbers, M., & Bruneau, L. (2017). Creating connections and fostering self-growth: Gestalt group counseling for military spouses. In Ideas and Research You Can Use: VISTAS 2017.
Panter-Brick, C. (2014). Health, risk, and resilience: Interdisciplinary concepts and applications. Annual Review of Anthropology, 43, 431–448. https://doi.org/10.1146/annurev-anthro-102313-025944
Pietrzak, R. H., & Southwick, S. M. (2011). Psychological resilience in OEF-OIF veterans: Application of a novel classification approach and examination of demographic and psychosocial correlates. Journal of Affective Disorders, 133(3), 560–568.
Quintana, T. S., & Cole, R. F. (2021). Forward march: Implementing the ASCA National Model to support military-connected students. Journal of School Counseling, 19(7). http://www.jsc.montana.edu/articles/v19n7.pdf
Richer, I., Frank, C., & Guérin, E. (2022). Understanding Special Operations Forces spouses challenges and resilience: A mixed-method study. Military Behavioral Health, 10(2), 100–111.
https://doi.org/10.1080/21635781.2022.2067921
Runge, C. E., Waller, M., MacKenzie, A., & McGuire, A. C. L. (2014). Spouses of military members’ experiences and insights: Qualitative analysis of responses to an open-ended question in a survey of health and wellbeing. PloS ONE, 9(12), e114755. https://doi.org/10.1371/journal.pone.0114755
Saunders, B., Sim, J., Kingstone, T., Baker, S., Waterfield, J., Bartlam, B., Burroughs, H., & Jinks, C. (2018). Saturation in qualitative research: Exploring its conceptualization and operationalization. Quality & Quantity, 52(4), 1893–1907. https://doi.org/10.1007/s11135-017-0574-8
Sefidan, S., Pramstaller, M., La Marca, R., Wyss, T., Sadeghi-Bahmani, D., Annen, H., & Brand, S. (2021). Resilience as a protective factor in basic military training, a longitudinal study of the Swiss Armed Forces. International Journal of Environmental Research and Public Health, 18(11), 6077. https://doi.org/10.3390/ijerph18116077
Simon, J. B., Murphy, J. J., & Smith, S. M. (2005). Understanding and fostering family resilience. The Family Journal, 13(4), 427–436. https://doi.org/10.1177/1066480705278724
Sinclair, R. R., Paulson, A. L., & Riviere, L. A. (2019). The resilient spouse: Understanding factors associated with dispositional resilience among military spouses. Military Behavioral Health, 7(4), 376–390. https://doi.org/10.1080/21635781.2019.1608876
Smith, E. J. (2006). The strength-based counseling model. The Counseling Psychologist, 34(1), 13–79.
https://doi.org/10.1177/0011000005277018
Southwick, S. M., Bonanno, G. A., Masten, A. S., Panter-Brick, C., & Yehuda, R. (2014). Resilience definitions, theory, and challenges: Interdisciplinary perspectives. European Journal of Psychotraumatology, 5(1), 25338. https://doi.org/10.3402/ejpt.v5.25338
Sullivan, K. S., Hawkins, S. A., Gilreath, T. D., & Castro, C. A. (2021). Mental health outcomes associated with profiles of risk and resilience among U.S. Army spouses. Journal of Family Psychology, 35(1), 33–43. https://doi.org/10.1037/fam0000702
U.S. Department of Defense, Office of the Deputy Assistant Secretary of Defense for Military Community and Family Policy. (2022). 2021 demographics profile: Profile of the military community. https://download.militaryonesource.mil/12038/MOS/Reports/2021-demographics-report.pdf
Verdeli, H., Baily, C., Vousoura, E., Belser, A., Singla, D., & Manos, G. (2011). The case for treating depression in military spouses. Journal of Family Psychology, 25(4), 488–496. https://doi.org/10.1037/a0024525
Villagran, M., Canzona, M. R., & Ledford, C. J. W. (2013). The milspouse battle rhythm: Communicating resilience throughout the deployment cycle. Health Communication, 28(8), 778–788. https://doi.org/10.1080/10410236.2013.800441
Walsh, F. (2012). Family resilience: Strengths forged through adversity. In F. Walsh (Ed.), Normal family processes: Growing diversity and complexity (4th ed.; pp. 399–423). Guilford.
Rebekah Cole, PhD, MEd, NCC, LPC, is a research associate professor at the Uniformed Services University. Christine Ward, PhD, is an associate professor at Walsh University. Taqueena Quintana, EdD, NCC, ACS, BC-TMH, LPC, is an associate professor at Antioch University. Elizabeth Burgin, PhD, NCC, LPC, RPT, CCCPTS, is an assistant professor and program coordinator of the Military and Veterans Counseling program at William & Mary. Correspondence may be addressed to Rebekah Cole, rebekah.cole@usuhs.edu.
Appendix
Interview Protocol
- Tell me a little about your identity as a military spouse?
- What have been some of your rewarding experiences as a military spouse?
- What have been some of your stressful experiences as a military spouse?
- How have you coped with the more stressful experiences as a military spouse?
- How would you describe the military’s definition of “resilience?”
- What does the term “resilience” mean to you?
- What does the term “resilience” mean for your military partner/family?
- How would you describe the resilience of military spouses?
- In what ways have you, personally, been resilient as a military spouse?
- What would enhance the resilience of military spouses and their families, from your perspective?
- How, if at all, has your military experience enhanced your resilience?
- How, if at all, has the military’s focus on resilience presented you with challenges during your military spouse experiences?
- How, if at all, can resilience be a negative way to describe military spouses/families?
- Is there anything else about military resilience that is important to you that I did not ask about?
May 10, 2023 | Volume 13 - Issue 1
Shainna Ali, John J. S. Harrichand, M. Ann Shillingford, Lea Herbert
Guyana has the highest rate of suicide in the Western Hemisphere. Despite this statistic, a wide gap exists in the literature regarding the exploration of mental wellness in this population. This article shares the first phase in a phenomenological study in which we explored the lived experiences of 30 Guyanese American individuals to understand how mental health is perceived. The analysis of the data revealed that participants initially perceived mental health as negative and then transitioned to a positive perception of mental health. We discuss how these perceptions affect the lived experience of the participants and present recommendations for counselors and counselor educators assisting Guyanese Americans in cultivating mental wellness.
Keywords: Guyanese American, mental health, phenomenological, mental wellness, perceptions
In 2014, the World Health Organization (WHO) reported Guyana as having the highest suicide rate in the world (44.2 suicides per 100,000 people; global average is 11.4 per 100,000 people). According to World Population Review (2023), within the Western Hemisphere, even after almost 10 years, Guyana remains the country with the highest rate of suicide—a concerning statistic. Responding to the WHO (2014) report, Arora and Persaud (2020) engaged in research to better understand the barriers Guyanese youth experience in relation to mental health help-seeking and suicide. Their research included 17 adult stakeholders (i.e., teachers, administrative staff, community workers) via focus groups, and 40 high school students who engaged in interviews. Arora and Persaud used a grounded theory approach and found the following themes as barriers to mental health help-seeking in Guyanese youth: shame and stigma about mental illness, fear of negative parental response to mental health help-seeking, and limited awareness and negative beliefs about mental health service. They recommended integrating culturally informed suicide prevention programs in schools and communities. In efforts to extend Arora and Persaud’s findings, we sought to further understand how Guyanese Americans define and experience mental health to better serve them in counseling.
Startled by the statistics presented by the WHO (2014) and Arora and Persaud (2020), we were compelled to focus our attention on this unique immigrant subgroup in the United States. It is important to note that between the WHO’s 2014 report and Aurora and Persaud’s research, no other studies related to Guyanese American suicidality are recorded in the literature. However, two studies on Guyanese American mental health emerged by Hosler and Kammer (2018) and Hosler et al. (2019). Our decision to conduct research on the Guyanese American community was further informed by Forte and colleagues’ (2018) review of immigrant literature in the United States, which stated that “immigrants and ethnic minorities may be at a higher risk for suicidal behavior as compared to the general population” (p. 1). Forte et al. found that immigrants, when compared with individuals in their homeland, were at an increased risk of experiencing mental health challenges like depression and other psychotic disorders. Currently, suicide is listed as the 10th leading cause of death overall in the United States (Heron, 2021). More specifically, within ages 10–34 and 35–44, suicide is the second and fourth leading cause of death, respectively. Heron’s (2021) report, referencing the Centers for Disease Control and Prevention (CDC), highlighted that in the United States, death by suicide (47,511) is 2.5 times higher than homicides (19,141). The prevalence of suicide among Guyanese people within and without the United States warranted further exploration of the experiences of this marginalized group.
The Guyanese American Experience
Comparing all countries with a population of at least 750,000 people, Guyana, a Caribbean nation, is said to have “the biggest share of its native-born population—36.4%—living abroad” due to remoteness and limited opportunities within the country to move from a lower to a higher socioeconomic status (Buchholz, 2022, para. 2). It is estimated that the United States is home to approximately 232,000 Guyanese Americans whose ancestry can be traced back to Guyana (United States Census Bureau, 2019), a country in the northeast of South America, bordered by Brazil, Venezuela, and Suriname. Although approximately 50% of all Guyanese immigrants in the United States reside in New York City alone (Indo-Caribbean Alliance, Inc., 2014), Guyanese people can be found across all 50 states and the District of Columbia (Statimetric, 2022). This draw to the United States, an English-speaking nation, might be linked to the fact that Guyana is the only country in South America that recognizes English as its official language (One World Nations Online, n.d.).
Like most immigrants, Guyanese immigrants travel to the United States seeking a better life and opportunities for themselves and their families. However, the process of transplanting can be bittersweet, in that Guyanese immigrants might be forced to relinquish their identity and customs and embrace American customs through assimilation (Arvelo, 2018; Cavalcanti & Schleef, 2001). For many Guyanese immigrants, being caught between leaving their homeland and beginning life in their adoptive home can lead to a cultural clash, resulting in problematic coping mechanisms (e.g., minimizing/hiding mental health challenges, cultural shedding [adopting American identity and losing cultural heritage]; Arvelo, 2018).
As discussed above, suicide in the Guyanese community is unquestionably a serious concern, but the community faces other challenges in the United States as well. For example, Hosler et al. (2019) found a statistically significant association between discrimination experience and major depressive symptoms in a sample of Guyanese Americans. However, Hosler et al. (2019) also found mean scores on the Everyday Discrimination Scale (EDS; Williams et al., 1997) were lower (i.e., less discriminatory experiences in everyday life) for Guyanese Americans when compared to other groups (Black, White, and Hispanic) because Guyanese Americans have a more cohesive interpersonal network. It would appear that Guyanese Americans experience lower everyday discrimination because they operate within interpersonal spaces that are more cohesive, yet their discriminatory experiences are positively associated with depression symptoms, which is a source of concern.
Another area of concern among Guyanese Americans is intimate partner violence (IPV), yet research remains lacking (Baboolal, 2016), leading us to draw directly from Guyanese literature. In Guyana, IPV is one of the most prevalent forms of violence (Parekh et al., 2012). As a country, although Guyana endorses the commitment to gender equality, women are the majority only in the tertiary sector (e.g., education, human services, clerical services, and tourism). Nicolas et al. (2021) stated that “domestic duties, marriage, and child-bearing, particularly for women between the ages of 25–29, have hindered their labor force participation” (p. 147). They documented that 1 in 6 Guyanese women, mostly from rural parts of the country, hold the belief that beating one’s wife is necessary (i.e., husbands are justified in beating their wives, resulting in domestic violence being a relevant mental health issue). In fact, suicide is identified as a public health issue for Guyanese women, who use it as a means of coping “with economic despair, poverty, and hopelessness . . . [and] to escape family turmoil, relationship issues, and domestic violence” (Nicolas et al., 2021, p. 148). However, even with access to mental health services increasing in Guyana, seeking out mental health care is uncommon due to stigma, lack of communication, inadequate financial resources, limited providers, and other barriers related to access (Nicolas et al., 2021). Within the U.S. literature, there remains a dearth of information on the experiences of this group as it relates to suicide and IPV. Most likely, this is a result of racial categorization within the United States, where, based on phenotype and racial composite, individuals are often lumped into one category, such as Black. As important as Guyanese literature on IPV is to inform the work of counselors, we believe it is equally important for us to engage in research regarding IPV and other mental health challenges on Guyanese Americans specifically. Learning about Guyanese Americans’ perceptions of mental health may facilitate closing the gap in the utilization of mental health services, warranting the current investigation.
Recognizing the noticeable research gap related to the mental health experiences of Guyanese Americans, we conducted a thorough review of the literature related to mental health and well-being. Through databases such as PsycINFO, ProQuest Central, Web of Science, MEDLINE, and SocINDEX, using the search terms “Guyanese Americans, Health and Wellbeing, Mental Health of Guyanese Americans, Access to Mental Health,” 54 search results were found. However, only two applicable studies were found to address Guyanese Americans’ mental health specifically (Hosler & Kammer, 2018; Hosler et al., 2019). The other search results were either not research manuscripts (i.e., reflections and newspaper articles) or addressed other constructs specific to the Guyanese people (e.g., family, education). The first study by Hosler and Kammer (2018) focused specifically on the health profiles of Guyanese immigrants in Schenectady, New York. This study was conducted with 1,861 residents between the ages of 18–64 years. Guyanese Americans from Schenectady were mostly from a low socioeconomic status, which resulted in them being less likely to have health insurance coverage, an identified place to receive care, and access to cancer screenings. They were also identified as being more likely to engage in alcohol binge drinking—all conditions of significant concern to us, resulting in the present study. In fact, Hosler and Kammer reported that Guyanese Americans are among the lowest group of those insured in the United States when compared with other minority groups such as Black and Latinx groups. Some researchers believe ethnocentric stereotyping, cultural incompetence by professionals, a lack of steady employment, and poor previous interactions with the health care system are barriers Guyanese immigrants experience when accessing medical and mental health services (Arvelo, 2018; Cheng & Robinson, 2013; Jackson et al., 2007).
The second study of Guyanese immigrants was conducted by Hosler et al. (2019) and explored everyday discrimination experiences and depressive symptoms in relation to urban Black, Hispanic, and White adults. This study included 180 Guyanese Americans (i.e., both citizens by birth and naturalized citizens/immigrants), all 18 years and older, from Schenectady, New York. The researchers found a significant independent association between the EDS score and major depressive symptoms for Guyanese Americans, suggesting that discrimination experiences might be an important social cause for depression within this community. Based on the reported challenges faced by Guyanese Americans, as well as our desire to contribute meaningfully to the extant body of literature on the Guyanese American community, we conducted a phenomenological inquiry. More specifically, we sought to better understand the lived experiences of Guyanese Americans pertaining to mental health (i.e., definitions, beliefs, practices), and how they access and incorporate mental health resources to mitigate the known mental health risks of this population in the United States, in the hopes of creating tailored methods for culturally responsive care.
Method
Because limited mental health research exists on this unique community, the present study, which is part of a larger research endeavor, sought to explore Guyanese Americans’ lived experiences with mental health. To lay the foundation of understanding, the present study focused on Guyanese Americans’ perceptions of mental health. Phenomenology, a constructivist approach, recognizes the existence of multiple realities and provides an understanding of participants’ lived experiences using their own voices (Haskins et al., 2022). We selected transcendental phenomenology (Moustakas, 1994) as the appropriate methodology for answering our research questions, as it is congruent with the counseling profession’s similar objective of understanding the human being. Akin to the practice of counseling, transcendental phenomenology emphasizes methods of the researcher to best set aside the potential clouds caused by bias in an effort to allow the explored phenomenon to surface. Transcendental phenomenology aligns with one of the core professional values in the American Counseling Association’s Code of Ethics (ACA, 2014), that of supporting “the worth, dignity, potential, and uniqueness of people within their social and cultural contexts” (p. 3). It also aligns with Ratts et al.’s (2015) Multicultural and Social Justice Counseling Competencies (MSJCC), specifically understanding the client’s worldview domain. Our focus on Guyanese Americans, an understudied minority group in the United States (Hosler & Kammer, 2018) originating from a country that has been identified as having the world’s highest suicide rate (WHO, 2014), led us to select this method so that we could maintain cognizance of our surroundings, hold respect for the population, and examine participants’ experiences (Haskins et al., 2022; Hays & Singh, 2012; Hays & Wood, 2011).
Participants
Before participants were recruited for the study, IRB approval was obtained from the university with whom Shainna Ali, M. Ann Shillingford, and Lea Herbert are affiliated. Purposive criterion sampling was used to recruit participants, leading to a sample of adults who self-identified as Guyanese American (i.e., either immigrated to the United States themselves or had at least one parent who was born in Guyana). Recruitment materials were shared with Guyanese Americans using counseling listservs (i.e., ACA–AMCD Connect and CESNET) and social media platforms (i.e., LinkedIn, Facebook, and Instagram). Members of the research team contacted all participants using email to share details regarding the study and the informed consent document, collect demographic data, and schedule individual interviews. According to qualitative research, sample size recommendations range from six to 12 participants (Creswell, 2013; Guest et al., 2006; Onwuegbuzie & Leech, 2007). Hence, we sought to recruit 15–20 participants to account for the possibility of attrition.
Our recruitment efforts yielded 73 individuals who expressed interest in the study, 60 of whom met all inclusion criteria and were initially contacted. Forty-three individuals were unable to complete an individual interview due to scheduling conflicts; hence, we secured a total of 30 participants who completed the study. Of this number, 17 participated in individual interviews and a total of 23 individuals participated in a one-time focus group to further clarify data from the individual interviews. It should be noted that 10 of the 23 focus group participants also participated in the individual interview. Further recruitment was deemed unnecessary, as the data analysis reached saturation with data from the individual interviews and focus group. We present demographic data on all participants who engaged in the study, both individual interviews and the focus group (N = 30), in Table 1.
Table 1
Participant Demographic Data
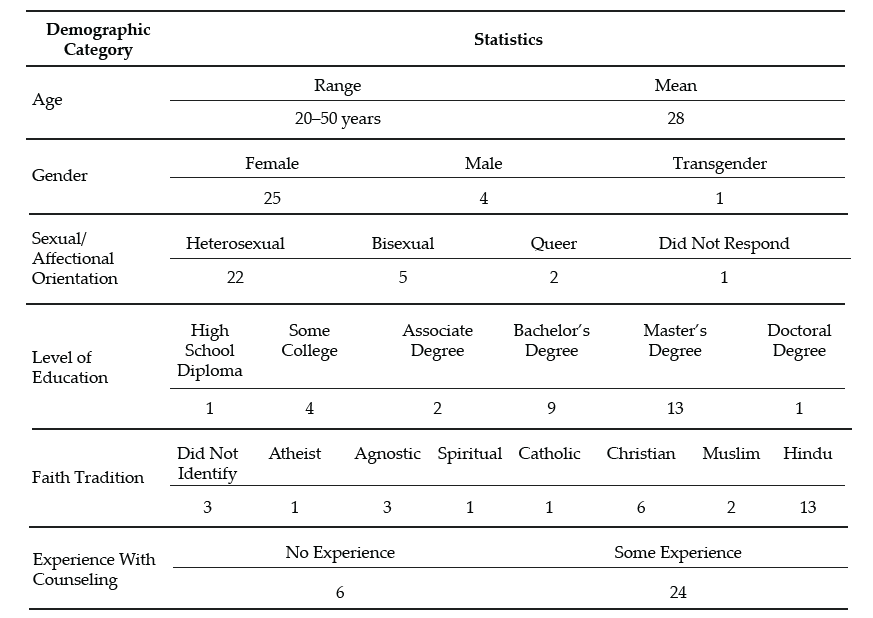
Note. This table provides a breakdown of the demographic characteristics of Guyanese American participants (N = 30).
Data Collection and Analysis
Participants engaged in a semi-structured interview lasting 30–60 minutes, conducted by Ali and Shillingford. Interviews were conducted via Zoom, audio-recorded, and transcribed verbatim. The interview protocol consisted of three primary questions, and sub-questions were used to clarify responses: 1) How do you define mental health?; 2) Who in your life has had experiences with mental health?; and 3) What experiences have you had with mental health? Prior to conducting our study, we included in our IRB documentation that data collection of individual interviews would follow saturation guidelines and that a focus group could be used for further data illumination. Following initial data analysis, we found it necessary to conduct a 1-hour follow-up focus group via Zoom to probe deeper into the data and to allow participants to clarify concepts related to emerging themes. Upon the first round of analysis, it was noted that several participants experienced a shift in perceptions regarding mental health. Focus group probes explored whether participants noticed this shift, what may have contributed to this shift, and when the shift occurred.
After all focus group and individual interviews were transcribed, we used guidelines outlined by Moustakas (1994) to analyze the data. First, we immersed ourselves in the data, reviewing each transcript individually. The transcripts were then divided equally among the four researchers, who read through each to become familiar with the data. With each transcript, we identified relevant statements reflecting participants’ lived experiences (horizontalization) as Guyanese Americans within the contexts of mental health beliefs and experiences.
Following this process, we met multiple times to review all transcripts and confer about the textural descriptions. We identified relevant codes, then synthesized the textural descriptions into themes based on commonalities, distilling the meaning expressed by participants. Then we engaged in reduction and elimination via consensus coding. This process included reading and rereading transcripts together, which followed an iterative process of reviewing the text and code, coding, rereading, and recoding, before determining which thematic content was a new horizon or new dimension of the phenomenon.
After all transcripts were analyzed following this reduction process, clustering and thematizing occurred (i.e., thematic content was clustered into core themes based on participant experiences; Hays & Singh, 2012; Moustakas, 1994). We extracted verbatim examples from the transcripts to generate a thematic and visual description of the phenomenon being examined. After completing the initial data analysis, we conducted member checking by sending each participant their individual transcript as well as the written results section. Participants were requested to provide feedback on the accuracy of their transcripts. Additionally, following the focus group and elucidation of themes all participants were offered an opportunity to member check and clarify the degree to which the results aligned with their lived experiences. The participants did not report any errors; however, clarification was offered by one participant.
Trustworthiness and Positionality
Trustworthiness is a key element of qualitative research in which the research findings accurately reflect the data (Lincoln & Guba, 1985). A critical element of maintaining research credibility is through reflexivity, wherein researchers critically examine procedures employed in relation to power, privilege, and oppression (Hunting, 2014). To safeguard against researcher bias, we worked collaboratively to establish and maintain credibility throughout data collection and analysis processes. Our research team consisted of one Indo-Guyanese American female faculty member, one Afro-Guyanese American female doctoral student, one Black female faculty member, and one Indo-Chinese-Guyanese Canadian male faculty member. All three faculty members belong to CACREP-accredited counselor education programs, and all four researchers have clinical experience working with diverse populations.
To address researcher bias, we engaged in bracketing to minimize the ways in which our experiences influence our approach to research and expectations of the outcomes of the study. Prior to data collection, we discussed our experiences in relation to Guyana, mental health in the Guyanese American community, and our roles as mental health leaders and advocates. We identified our personal experiences, acknowledged our biases, and attempted to bracket while conducting the interviews and focus group. Throughout the data collection and analysis processes, we participated in personal reflection and kept analytic memos documenting our reactions and initial thoughts about the data collected.
Before analyzing the data, we met to confirm analysis procedures, ensuring consistency. We initially analyzed data individually, then determined codes and themes as a team to reduce bias. Throughout the data analysis process, we consulted with each other, addressing questions or concerns related to the data. We also consulted with an outside researcher experienced in qualitative research to obtain critical feedback on the data analysis process and the research findings (Marshall & Rossman, 2006). Our consultant served as an external check of the research methodology and theoretical interpretation of the data.
Findings
The results of the analysis increase understanding of the lived mental health experiences of Guyanese Americans by elucidating perceptions of mental health (Creswell, 2013). All participants shared their beliefs about mental health and the direct and indirect experiences that informed their conceptualization. Three themes surfaced. The first two showed a clear divide in the data: 1) mental health being perceived as negative, stigmatized, elusive, and intimidating; and 2) mental health being perceived as positive, important, helpful, and empowering. It is important to note that these primary themes were not representative of two subsets of participants, and this extracted another theme, which centered on the tendency of participants’ beliefs to transition from negative to positive views of mental health.
The Perception of Mental Health as Negative
When exploring obstacles, subthemes emerged in which hindrances to mental health were acknowledged to exist across three levels: individual, familial, and sociocultural. In parallel, these three subthemes were echoed in the exploration of factors that participants acknowledged have contributed to their mental wellness. The following section explores the primary themes in detail by highlighting the participants’ voices in describing their lived experiences.
Mental Health Concerns Are a Sign of Weakness
All participants in the individual interviews shared that they originally believed that mental health developed out of weakness. This belief was often attributed to minimizing remarks from family members. Oftentimes these comments were paired with other suggestions of how to ameliorate symptoms such as praying more, working harder, or contributing to physical health (e.g., drinking tea). Sharon shared:
It was just like, oh no, you just need to read a book or you just need to go and do something and take your mind off of however it is you’re feeling, like there’s no reason for you to be sad, you have a roof over your head and you’re going to school and you’re doing all of these things, it doesn’t matter. There’s no reason for you to be sad or feel any type of way about anything because we provide everything for you.
Several participants noted that investment in physical wellness was preferable to mental wellness, although physical health was not genuinely prioritized. Participants shared personal and observed maladaptive coping with poor eating habits (i.e., quality and quantity) and excessive substance abuse, namely alcohol. Some participants shared that these tactics were used to manage mental health symptoms or avoidance. Christine shared, “When you’re struggling with things . . . you have nowhere to go to with them except alcohol and the bottom of a rum bottle.” Many participants recognized that coping with alcohol is normalized within the culture. Further, the commonality of these methods normalized consumption and have caused additional issues (e.g., diabetes, heart disease, alcoholism). Arjun noted:
We all have relatives that are kind of stuck on the whole drinking issue. We know a lot of them. They get together with their friends and they “lime,” as we like to call it. They drink in groups and they “gyaff,” they have fun. But it’s a completely different story when they’re by themselves and they’re drinking.
Mental Health Is Taboo
A general consensus was that all participants in the study once believed that mental health was not important and that mental health problems were shameful and not to be discussed. This consistent trend was one of the reasons that we opted to further understand responses through a focus group. Therefore, a direct probe was offered to the focus group participants to explore if they believed discussing mental health was taboo. When delving deeper into these perceptions, participants noted that these thoughts were informed by the beliefs of others and upheld in the wider cultural paradigm. All participants reported that, generally, mental health should not be talked about in order to save face and be respectful. Because mental health issues were seen to be synonymous with weakness, sharing about mental health was equated with the risk of bringing shame to oneself or to one’s family. For example, Chandra shared that “Guyanese people don’t want a kid that’s broken or a little off.” Hence, if someone opts to discuss their mental illness, it is to be done carefully, or secretly.
Most participants shared that typically, when divulging their symptoms, they went to an elder, often a parent, grandparent, or elder sibling, in an effort to keep concerns within the family system. However, many participants noted being minimized or dismissed when sharing their concerns with family members. Ramona explained her feeling that her family
is really strong about, like, don’t be selfish. And I wonder if they would categorize it under that. Like if you’re taking up too much space or time or whatever, you’re trying to center the attention on you or whatever, so that’s a self-serving thing.
A generational rule of discourse emerged from the data. Though the tendency was to keep mental health discussions within the family system, it was also atypical for a younger member to address observed issues with an elder. Several participants noted that this hidden guideline kept informed younger generations from being able to utilize their recognition of warning signs to help the given person and the family system. Arjun shared that as he’s gotten older and has learned more about mental health, he has acquired the courage to address the problems he sees with elders, including his uncle:
I said, “Uncle, what’s wrong?” And he said, “No, nothing is wrong.” But he was crying, you could see tears were streaked on his face, but he wouldn’t talk about it—he wouldn’t say anything. It’s not only one time I saw him, it’s multiple times that I’ve seen him when he has been drinking by himself, that he kind of has the same face all the time. Prior to the times that I asked him, I kind of looked at him and I kind of walked away the first couple of times. Because I was kind of like, this is not something that looked like I should butt in, as a child especially. When you’re younger, your parents tell you, “Mind your business.” Or they say, “You’re not an adult, go with the kids.” So . . . the first couple of times I saw him, I kind of avoided it.
Others Are Not To Be Trusted
Some participants noted that beyond the purpose of family protection, caution to mental health discourse was also due to lack of trust of others. Christine explained: “We had a counseling center on campus, but I was like, ‘Oh, I can’t go talk to anybody,’ because that’s what I was raised with. You don’t talk to strangers about your problems. I had to keep everything inside.” Nevertheless, some families encouraged talking to a religious leader to assist the individual in enhancing devotion and reducing mental health symptoms. Still, regarding professional mental health services, many participants believed, at least at one time, that such services are not helpful, providers are not to be trusted, assistance of that nature is for other (e.g., White) people, and succumbing to that level of desperation is a sign of weakness. When sharing about mistrust in professional mental health assistance, misconceptions and stereotypes surfaced. Ramesh shared:
Oh boy. I have to be honest with you, I feel counseling is, I’ll speak to a shrink and they’ll prescribe drugs to me, like Ritalin or . . . I was like, you know what, I’m better than that. I’m probably totally wrong about it, but that’s just the perception that I have. I’ll be laying on the couch and I’m going to speak into someone and then they’re going to prescribe drugs to me. I don’t want that. I can try to figure this out on myself by talking and trying to do things—positive behavior.
Mental Health Perceived as Positive
All participants in the individual interviews acknowledged a shift in their perceptions of mental health. Their newfound conceptualization included a holistic view of wellness in which mental wellness was seen as an important component to overall well-being and quality of life. In this newer perception, participants acknowledged the ability to consider more variables influencing mental health than they recognized in the past. For example, many participants noted a link between mind and body, versus the previously held notion that physical health is more important than mental health. A few participants noted that mental health can be influenced by genetics, while some noted that it could be influenced by personality, and others noted that it can be influenced by people and the surrounding environment.
All participants, from both the individual interviews and focus group, concurred that everyone feels mental health effects; furthermore, showing signs of a problem is not attributed to weakness. Moreover, because mental health affects everyone, a widespread belief emerged that we all have the responsibility to foster our mental wellness. Additionally, participants shared several examples of what naturally ensued without investing in strategies for mental health such as challenges with emotional regulation, coping, relationships, and worsening mental health problems.
The Transition Between Negative and Positive Perceptions
The transition between old and new conceptualizations of mental health was informed by direct and indirect experiences. All participants shared a transition in beliefs in the individual interviews, and this was explored in the focus group for further clarification. Most participants shared that their personal mental health history informed a change in their beliefs. Many of these participants noted the influence of their healing process, most notably seeking professional help. All participants, from both the individual interviews and the focus group, shared at least one example of learning about mental health by observing another person’s experience. For example, Jessie shared, “Unfortunately, I came from a home of domestic violence . . . I was around maybe six, my dad was bipolar . . . [and] he was just a wife beater. That is probably when I can recall [learning] of mental health.” Another example of learning about mental health from others is captured in Reginald’s comment:
[As] an only child . . . my parents took it upon themselves to [teach me]. . . . It wasn’t like, “Okay, sit down. Let me tell you why these things are.” It was just we’ll be talking about somebody else or going over something that happened and then they’ll explain why, but never directly for me. It was always about other people’s kids.
Many of these individuals emphasized the belief that by paying attention to others, you can learn what is helpful and unhelpful for mental health. Oftentimes this was in their own family; however, extended family and community members were also highlighted. Moreover, a few participants shared their recognition that living with someone who is struggling with their mental health may negatively impact personal wellness (e.g., be triggering). Beyond the family system, some participants noted that exposure to other cultures and perceptions of mental health informed a conceptualization of mental wellness. Seeta shared:
I had friends of other religions or like no religions. And then we would talk about a lot of different things. Like I would ask them questions like, “Oh, so how do things work in your house? Do your parents talk about your God or whatever?” And they’re like, “No.” And I’m like, “So where do your emotions come from?” And they’re like, “Well, you know, we just feel them. Some days I feel angry and some days I feel sad, some days I feel happy.” And I’m just like, “Okay, this is interesting.”
From the quote, it might appear that one’s emotions are in some way connected with God or another higher power; however, this is not something that was observed with other participants of our study. It was more common for participants to share stories of their families using religion as the solution to mental health concerns. For example, Yolanda shared:
My grandmother came when I turned 16 and she kept trying to tell my mom I was showing signs of depression. And my mom was like, “No, she’s like that all the time, like, that’s just how she is.” And my grandma was like, “That’s not normal. You should get her checked out.” And my mom kept saying, “No” and kept denying it. And then my grandma said, “You have to do something.” And then my mom replied, “Oh, I’m going to pray for her.”
In addition to personal experiences and observations of others, participants noted that improved mental health awareness and education prompted them to think critically about their mental health schemas. Ramesh shared:
My education, I always feel like this is what saved me in the end, because I was able to be around other people to know better and to come back home and be like, “Excuse me, this is not how we do things. This is not how we say things. I don’t know what it was like in Guyana.”
Some participants associated this with growing older, and others noted their personal initiative to improve mental health knowledge by following mental health pages on social media, taking a related class, and for some, becoming a part of the mental health field themselves. From this vantage point, many participants were able to equate their previously held notions with beliefs embedded in the culture such as generational rules of respect, gender differences, and the impact of colonialism. Participants, despite their gender differences, noted that within the cultural framework, the rule that mental health should not be discussed is disproportionately applicable to males. Participants shared that this is often due to the perception that it is important for men to be strong, and again, mental illness is a symptom of weakness. This was also linked to the breadwinner role and the pressure to provide for the family. However, this was only noted to have detrimental effects, as anger issues, IPV, and alcoholism were noted to arise out of this rule. Some participants noted that the survival aspect of colonialism may have contributed to the lack of privilege to focus on mental health. In addition, the history of colonialism in Guyana (i.e. slavery, indentured labor) could have informed the lack of trust in professional services.
The change in mental health conceptualization was noted to have benefits beyond the participants themselves. Some participants remarked that the shift in perception was recognized in the wider generation. Ramona reflected:
I will say that a lot of folks from my generation have been a lot more like, “Go to therapy. We should be taking care of our thoughts and our feelings or emotions.” That’s important to you in the same way that if you tore a ligament that you would need to get surgery or do whatever.
Within the newfound conceptualization of mental wellness emerged a vow of social responsibility. All participants, from both the individual interviews and the focus group, shared their intention to help others, and some even noted it as their duty. Ways to help others included advocating for mental health awareness, access, and education; helping to challenge unhelpful cultural beliefs; breaking generational cycles; and protecting others from experiencing similar struggles (e.g., child, sibling).
Discussion
The findings from this study are enlightening, and some are the first to be documented through research, even if they were observed in practice. Initial perceptions of all participants, from both the individual interviews and the focus group, were that mental health is a taboo topic and seeking mental health services is bad. These perceptions stemmed from fear, mistrust, and limited awareness of the benefits of mental health services. This is consistent with findings from Arora and Persaud (2020), who surmised that Guyanese individuals hold negative views of mental health that significantly impact their help-seeking. Furthermore, the findings point to strong familial and sociocultural influences, such as beliefs about mental health, that swayed individual perceptions of mental health, which is in keeping with recent literature on affirming cultural strengths and incorporating familial identity in working with clients of Guyanese descent (Groh et al., 2018; Nicolas et al., 2021).
Discussing issues related to mental health was viewed as a sign of weakness, which translated to help-seeking being a taboo. It would appear that the stigma associated with mental health remains a common experience for Guyanese Americans, and when coupled with limited communication, insufficient funding, and lack of providers, we can see how Nicolas et al. (2021) found this to be concerning. Cultural clash, ethnocentric stereotyping, and cultural incompetency may also be responsible for Guyanese Americans being distrustful of the health care system, leading them to engage in maladaptive behaviors (i.e., avoidance, use of substances, IPV) and not receive the mental health attention and care they need (Arvelo, 2018; Cheng & Robinson, 2013; Jackson et al., 2007).
It appears that even in the face of discrimination and experiences of mental health challenges like alcoholism, depression (Hosler & Kammer, 2018), and IPV (Parekh et al., 2012), leaning on the support of the community serves to buffer against mental health challenges for Guyanese Americans. It also seems that changing mental health perceptions from negative to positive was significantly related to mental health literacy and exposure to other systems such as school, work, and community (i.e., cross-cultural exchange).
Findings that were not previously documented in the literature suggest that an integrated view of wellness enabled participants to augment their negative abstractions of mental health care. These findings serve as an indication that among Guyanese Americans, although mental health has been perceived as negative, weak, and a taboo, the narrative is beginning to shift to make space for mental health awareness, education, access, and functioning, thereby creating unique implications for counselors seeking to meet the needs of this immigrant subgroup.
Implications
In combination with prior literature, the results of this study provide a rationale for mental health counselors, marriage and family counselors, school counselors, and counselor educators to inspire dialogue to foster mental wellness. Based on the findings from this study, when working with Guyanese Americans, counselors should focus on three key strategies to support Guyanese American clients: (a) mental health awareness, (b) mental health education, and (c) mental health experience.
Mental Health Awareness
Participants in this study initially held limited views and awareness of the signs and symptoms of mental health. When awareness was heightened through various means, they were more open to exploring the benefits of services. Counselors can be instrumental in creating awareness by first raising their own awareness pertaining to cultural stigma and its influence on Guyanese Americans’ mental health. For example, unwillingness to attend counseling sessions may be linked to the culturally held perception that discussing mental health, especially beyond the core family system, is taboo. In acknowledging this, counselors can raise awareness of confidentiality, which can be seen as an alignment with the cultural notion that talking about mental health is taboo when it means talking to anyone, and the role of the counselor can be highlighted as a professional collaboration versus communal gossip. Counselors need to be mindful of the collectivistic nature of Guyanese American culture, which causes personal and familial illnesses alike to be perceived as personal problems. Rather than dismiss a client’s concerns about mental health, a counselor can benefit from exploring how the family members’ symptoms, perceptions about mental health, and willingness to adhere to treatment influence the client’s symptoms, perceptions, and commitment to counseling. Further, collectivism spans beyond the protective family system. On one hand, this community orientation can be used to explore a broad range of support, yet on the other hand, depending on the client’s experience, this may also be a widened range of societal pressure (e.g., judgment, criticism, shame).
Mental Health Education
Increased understanding of mental health appeared to have led participants to seek services and resources to increase their mental health literacy, with the hope of improving their well-being. Counselors and counselor educators can be instrumental in offering Guyanese Americans mental health education. To begin, all mental health professionals should demonstrate a posture of cultural humility when engaged in psychoeducation on mental health and wellness for this population. In order to raise awareness through education, mental health professionals are encouraged to model trust, respect, sensitivity, compassion, and a nonjudgmental stance. Within session, counselors should be prepared to offer information regarding early signs of mental illness, compounding factors (e.g., alcohol, suicidal ideation, domestic violence), obstacles (e.g., stigma), and resources. Additionally, counselors may need to offer psychoeducation on the family system, roles, dynamics, beliefs, experiences, and generational patterns that can influence individual mental health. In the event that a family member with mental health problems is unwilling to seek assistance, helping the client to better understand the diagnosis and cope personally can be empowering. Finally, to employ the collectivistic nature of Guyanese American culture, stigma can be confronted, and mental health education can be effectively offered by providing group counseling within this population. Group counseling can offer a variety of therapeutic factors that can benefit Guyanese Americans such as universality, hope, and corrective recapitulation of the primary family group (Yalom & Leszcz, 2005).
Beyond the counseling office, counselors and counselor educators should consider collaborating with culturally supportive organizations. Workshops and information sessions can be tailored to explore and address cultural, religious, ethnic, and generational differences in addition to offering mental health resources (e.g., signs, symptoms, treatment). Several of the participants in our study shared that access to psychology courses in school helped to improve their knowledge about mental health. In addition to these classes continuing to be offered, accessibility to such courses should be expanded. Schools and universities may benefit from offering workshops and other informational sessions to support mental health. Beyond information being offered, a follow-up may be beneficial by linking school or campus counselors in order to connect an improvement in awareness and education to action, change, and health.
Several participants shared that because of a lack of access to mental health education, their knowledge was attained through social media platforms such as Instagram and TikTok. Although the quality of mental health education was not assessed in the present study, the lack of regulation on social platforms could perpetuate misleading, confusing, and stigmatizing misinformation surrounding mental health. Counselor educators should consider their roles beyond the classroom. In addition to empowering counselor trainees to utilize the suggestions above to foster awareness and education, counselor educators can offer responsive and succinct information via social media. Whereas social media is not an appropriate platform for tailored education or services, brief information can be offered to bridge the gap between awareness, education, and access.
Mental Health Experience
Growth in awareness and knowledge around mental health resulted in participants intentionally engaging in positive experiences as a way of resisting past harmful and hurtful practices and generational patterns, reauthoring a new narrative of hope and healing. Being wellness-focused, counselors are uniquely positioned to support this community by facilitating positive experiences impacting overall mental health and well-being.
Counselors can honor clients from this community by creating safe spaces for them to share their narratives without judgment. Counselors can foster healing communities through group counseling, where clients collaboratively share each other’s mental burdens and celebrate successes (Yalom & Leszcz, 2005). Counselors can honor collectivism by encouraging clients to participate in support groups in addition to personal counseling. Counselors and counselor educators can enhance the approachability of counselors by improving their visibility in the community. Examples include a community counselor being involved in outreach with a local cultural center, a school counselor offering mentorship with student clubs, a college counselor guest-speaking at a Guyanese American student organization meeting, or a counselor educator offering tailored workshops for the community.
In addition to the aforementioned implications, we believe that in order for counselors to bridge generational gaps in counselor distrust, counselors must acknowledge the lack of representation of diversity within the profession of counseling, the predominance of Western and European cultural and psychologist-centered curriculum, and lapses in poor bioethics and power dynamics among counselors and marginalized communities (Singh et al., 2020). Next, the specific intersectional impacts suggest counselors must adapt a multicultural orientation and illuminate cultural sensitivity. When a clinician enacts cultural sensitivity in session, clients can examine their perceptions of illness and center their multiple identities (Davis et al., 2018).
Limitations and Future Research
Several limitations that arose from the research process are important to mention. All interviews were conducted virtually. Although secured virtual platforms such as Zoom are considered acceptable for research, lack of face-to-face interviewing may have excluded subtle visual cues and induced video-conferencing fatigue (Spataro, 2020). Though researchers made great attempts to increase participant comfort and review the informed consent before the interview process, it is also plausible that respondents may have censored their responses out of concern for potential breach in confidentiality. A majority of respondents are college-educated, female, first generation, and of Indo-Guyanese descent; hence, the results may not be representative of all Guyanese Americans. Additionally, aligned with phenomenological methods of exploring lived experiences, research prompts were general. Recognizing the concerning statistics surrounding suicide (WHO, 2014), a future study exploring suicidality could be beneficial. Future research might seek to explore a more diverse pool of participants, including diversity in gender, age, ethnicity, and number of years in the United States. To build on the findings from the present study, future studies should explore what factors contribute to Guyanese American mental health as well as what variables may hinder mental wellness. It may also be beneficial to include research from the perspective of children and parents to further understand the influence of family systems and cross-generational norms.
Conclusion
This study highlighted the crucial need to address the mental health literacy of Guyanese Americans. The findings illuminate Guyanese Americans’ perceptions of mental health, including the transition from negative to positive perceptions and its potential influences. Efforts should be made to promote awareness, education, and experience related to mental health awareness for Guyanese Americans. Supporting mental health may help to reduce alarming rates of mental illness in Guyanese Americans and may also have the potential to influence related groups such as Guyanese, American, and Caribbean individuals. Counselors and counselor educators have the potential to play a significant role in supporting these clients by being cognizant and informed about cultural considerations.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
American Counseling Association. (2014). ACA code of ethics. https://www.counseling.org/resources/aca-code-of-ethics.pdf
Arora, P. G., & Persaud, S. (2020). Suicide among Guyanese youth: Barriers to mental health help-seeking and recommendations for suicide prevention. International Journal of School & Educational Psychology, 8(1), 133–145. https://doi.org/10.1080/21683603.2019.1578313
Arvelo, S. D. (2018). Biculturalism: The lived experience of first- and second-generation Guyanese immigrants in the United States (Order No. 10749930) [Doctoral dissertation, Chicago School of Professional Psychology]. ProQuest One Academic. (2027471070).
Baboolal, A. A. (2016). Indo-Caribbean immigrant perspectives on intimate partner violence. International Journal of Criminal Justice Sciences, 11(2), 159–176. https://www.researchgate.net/publication/336926774_Indo-Caribbean_Immigrant_Perspectives_on_Intimate_Partner_Violence
Buchholz, K. (2022, November 11). The world’s biggest diasporas [Infographic]. Forbes. https://www.forbes.com/sites/katharinabuchholz/2022/11/11/the-worlds-biggest-diasporas-infographic/?sh=4185fd634bde
Cavalcanti, H. B., & Schleef, D. (2001). Cultural loss and the American dream: The immigrant experience in Barry Levinson’s Avalon. Journal of American and Comparative Cultures, 24(3–4), 11–22.
https://doi.org/10.1111/j.1537-4726.2001.2403_11.x
Cheng, T. C., & Robinson, M. A. (2013). Factors leading African Americans and Black Caribbeans to use social work services for treating mental and substance use disorders. Health & Social Work, 38(2), 99–109. https://doi.org/10.1093/hsw/hlt005
Creswell, J. W. (2013). Qualitative inquiry and research design: Choosing among five approaches (3rd ed.). SAGE.
Davis, D. E., DeBlaere, C., Owen, J., Hook, J. N., Rivera, D. P., Choe, E., Van Tongeren, D. R., Worthington, E. L., Jr., & Placeres, V. (2018). The multicultural orientation framework: A narrative review. Psychotherapy, 55(1), 89–100. https://doi.org/10.1037/pst0000160
Forte, A., Trobia, F., Gualtieri, F., Lamis, D. A., Cardamone, G., Giallonardo, V., Fiorillo, A., Girardi, P., & Pompili, M. (2018). Suicide risk among immigrants and ethnic minorities: A literature overview. International Journal of Environmental Research and Public Health, 15(7), 1–21. https://doi.org/10.3390/ijerph15071438
Groh, C. J., Anthony, M., & Gash, J. (2018). The aftermath of suicide: A qualitative study with Guyanese families. Archives of Psychiatric Nursing, 32(3), 469–474. https://doi.org/10.1016/j.apnu.2018.01.007
Guest, G., Bunce, A., & Johnson, L. (2006). How many interviews are enough? An experiment with data saturation and variability. Field Methods, 18(1), 59–82. https://doi.org/10.1177/1525822X05279903
Haskins, N. H., Parker, J., Hughes, K. L., & Walker, U. (2022). Phenomenological research. In S. V. Flynn (Ed.), Research design for the behavioral sciences: An applied approach (pp. 299–325). Springer.
Hays, D. G., & Singh, A. A. (2012). Qualitative inquiry in clinical and educational settings. Guilford.
Hays, D. G., & Wood, C. (2011). Infusing qualitative traditions in counseling research designs. Journal of Counseling & Development, 89(3), 288–295. https://doi.org/10.1002/j.1556-6678.2011.tb00091.x
Heron, M. (2021). Deaths: Leading causes for 2019. National Vital Statistics Reports, 70(9), 1–113. https://doi.org/10.15620/cdc:107021
Hosler, A. S., & Kammer, J. R. (2018). A comprehensive health profile of Guyanese immigrants aged 18–64 in Schenectady, New York. Journal of Immigrant and Minority Health, 20(4), 972–980.
https://doi.org/10.1007/s10903-017-0613-5
Hosler, A. S., Kammer, J. R., & Cong, X. (2019). Everyday discrimination experience and depressive symptoms in urban Black, Guyanese, Hispanic, and White adults. Journal of the American Psychiatric Nurses Association, 25(6), 445–452. https://doi.org/10.1177/1078390318814620
Hunting, G. (2014). Intersectionality-informed qualitative research: A primer. The Institute for Intersectionality Research and Policy. https://nanopdf.com/download/intersectionality-informed-qualitative-research-a-primer-gemma-hunting_pdf
Indo-Caribbean Alliance, Inc. (2014, February 3). Population analysis of Guyanese and Trinidadians in NYC.
https://www.indocaribbean.org/blog/population-analysis-of-guyanese-and-trinidadians-in-nyc
Jackson, J. S., Neighbors, H. W., Torres, M., Martin, L. A., Williams, D., & Baser, R. (2007). Use of mental health services and subjective satisfaction with treatment among Black Caribbean immigrants: Results from the National Survey of American Life. American Journal of Public Health, 97(1), 60–67. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1716231/
Lincoln, Y. S., & Guba, E. G. (1985). Naturalistic inquiry. SAGE.
Marshall, C., & Rossman, G. B. (2006). Designing qualitative research (4th ed.). SAGE.
Moustakas, C. (1994). Phenomenological research methods. SAGE.
Nicolas, G., Dudley-Grant, G. R., Maxie-Moreman, A., Liddell-Quintyn, E., Baussan, J., Janac, N., & McKenny, M. (2021). Psychotherapy with Caribbean women: Examples from USVI, Haiti, and Guyana. Women & Therapy, 44(1–2), 136–155. https://doi.org/10.1080/02703149.2020.1775993
One World Nations Online. (n.d.). Guyana. https://www.nationsonline.org/oneworld/guyana.htm
Onwuegbuzie, A. J., & Leech, N. L. (2007). A call for qualitative power analyses. Quality & Quantity, 41, 105–121. https://doi.org/10.1007/s11135-005-1098-1
Parekh, K. P., Russ, S., Amsalem, D. A., Rambaran, N., Langston, S., & Wright, S. W. (2012). Prevalence of intimate partner violence in patients presenting with traumatic injuries to a Guyanese emergency department. International Journal of Emergency Medicine, 5(1), 1–5. https://doi.org/10.1186/1865-1380-5-23
Ratts, M. J., Singh, A. A., Nassar-McMillan, S., Butler, S. K., & McCullough, J. R. (2015). Multicultural and social justice counseling competencies. American Counseling Association. https://www.counseling.org/docs/default-source/competencies/multicultural-and-social-justice-counseling-competencies.pdf
Singh, A. A., Appling, B., & Trepal, H. (2020). Using the Multicultural and Social Justice Counseling Competencies to decolonize counseling practice: The important roles of theory, power, and action. Journal of Counseling & Development, 98(3), 261–271. https://doi.org/10.1002/jcad.12321
Spataro, J. (2020). The future of work—the good, the challenging & the unknown. https://www.microsoft.com/en-us/microsoft-365/blog/2020/07/08/future-work-good-challenging-unknown/
Statimetric. (2022). Distribution of Guyanese people in the US. https://www.statimetric.com/us-ethnicity/Guyanese
United States Census Bureau. (2019). People reporting ancestry: American community survey. http://bit.ly/42RazKC
Williams, D. R., Yu, Y., Jackson, J. S., & Anderson, N. B. (1997). Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of Health Psychology, 2(3), 335–351.
https://doi.org/10.1177/135910539700200305
World Health Organization. (2014). First WHO report on suicide prevention. https://www.who.int/news/item/04-09-2014-first-who-report-on-suicide-prevention
World Population Review. (2023). Suicide rate by country 2023. https://worldpopulationreview.com/country-rankings/suicide-rate-by-country
Yalom, I. D., & Leszcz, M. (2005). The theory and practice of group psychotherapy (5th ed.). Basic Books.
Shainna Ali, PhD, NCC, ACS, LMHC, is the owner of Integrated Counseling Solutions. John J. S. Harrichand, PhD, NCC, ACS, CCMHC, CCTP, LMHC, LPC-S, is an assistant professor at The University of Texas at San Antonio. M. Ann Shillingford, PhD, is an associate professor at the University of Central Florida. Lea Herbert is a doctoral student at the University of Central Florida. Correspondence may be addressed to Shainna Ali, 3222 Corrine Drive, Orlando, FL 32803, hello@drshainna.com.
Feb 26, 2021 | Volume 11 - Issue 1
Lisbeth A. Leagjeld, Phillip L. Waalkes, Maribeth F. Jorgensen
Researchers have frequently described rural women as invisible, yet at 28 million, they represent over half of the rural population in the United States. We conducted a transcendental phenomenological study using semi-structured interviews and artifacts to explore 12 Midwestern rural-based mental health counselors’ experiences counseling rural women through a feminist lens. Overall, we found eight themes organized under two main categories: (a) perceptions of work with rural women (e.g., counselors’ sense of purpose, a rural heritage, a lack of training for work with rural women, and the need for additional research); and (b) perceptions of rural women and mental health (e.g., challenges, resiliency, protective factors, and barriers to mental health services for rural women). We offer specific implications for counselors to address the unique mental health needs of rural women, including hearing their stories through their personal lenses and offering them opportunities for empowerment at their own pace.
Keywords: rural women, mental health counselors, feminist, perceptions, phenomenological
More than 28 million women, ages 18 and older, live in rural America and represent over half of the rural population in the United States (Bennett et al., 2013; U.S. Census Bureau, 2010). Researchers have discussed women’s issues as a distinct category within counseling for over 50 years, yet few counseling programs offer training specific to counseling women (American Psychological Association [APA], 2018; Broverman et al., 1970; Enns, 2017). Rural women have garnered even less attention within counseling literature and training over time (Bennett et al., 2013; Fifield & Oliver, 2016). In addition, rural mental health researchers have focused on rural populations in general, encapsulating women under the entire family unit (U.S. Department of Agriculture, 2015). However, in all environments, women experience mental health needs in unique ways (Mulder & Lambert, 2006; Wong, 2017). Although government agencies have increased efforts to alleviate mental health disparities in rural areas, there is limited research available on rural women’s mental health to guide these efforts (Carlton & Simmons, 2011; Hill et al., 2016). Thus, more studies focused on rural women can assist in comprehensive data-based decision-making efforts of federal, state, and local policymakers (Van Montfoort & Glasser, 2020). Mental health counselors who work with rural women have a unique perspective in understanding the needs of rural women and the disparities they face.
The Invisibility of Rural Women’s Mental Health
Researchers have described rural women as invisible within the mental health literature. Specifically, they have used words such as “unnoticed,” “lack of recognition,” “overlooked,” and “no voice and no choice,” which may illuminate why rural women have less access to appropriate mental health services and may underlie the noticeable absence of rural women as participants within research (Mulder & Lambert, 2006; Weeks et al., 2016). Members of rural communities have traditionally seen women as an extension of their nuclear and extended families and as responsible for involvement in community and church activities (Mulder & Lambert, 2006). Rural women, as a population with unique mental health needs, may need help (i.e., representation in research) getting their voices heard on a more macro level to promote systemic changes (Van Montfoort & Glasser, 2020). A research approach based in feminist theory may amplify the voices of rural women (Schwarz, 2017).
Feminism is a theoretical approach that evolved following the women’s movement in the 1960s, and grew to effect change in social, political, and cultural beliefs about women’s roles (Evans et al., 2005). Many of the early feminist writers spoke of women as “oppressed” and “having no voice” (Evans et al., 2005). Those words have been similarly found throughout the literature on rural women (Weeks et al., 2016). Feminist theory has traditionally challenged the status quo of the patriarchy by working to reduce the invisibility of women’s experiences (Evans et al., 2005; Schwarz, 2017). Further, feminist theory has evolved to amplify voices of all oppressed and marginalized individuals and to promote recognition of the intersectionality of identity. The feminist perspective can facilitate insight into the context of rural women’s experiences (Wong, 2017).
Challenges Faced by Rural Women
The definition of rural areas has historically been based on population size (U.S. Census Bureau, 2010). Some consider rurality a more accurate term than rural, as it may include population density, economic concerns, travel distances to providers, religion, agricultural heritage, behavioral norms, a shared history, and geographical location (Smalley & Warren, 2014). Rural women face unique needs related to the intersection of gender with race, ethnicity, age, and sexual orientation (Barefoot et al., 2015). Rural women have less access to educational opportunities, are often the head of household, and are more likely to live in poverty than urban women (Watson, 2019). Lesbian and bisexual rural women face challenges of bias, lack of support, and increased victimization (Barefoot et al., 2015). Although urban women also experience mental health issues related to motherhood, rural women often must travel long distances to services and have limited access to postpartum care (Radunovich et al., 2017). Residents in many rural communities experience food insecurity and related disordered eating with less proximity to grocery stores and limited food choices (Doudna et al., 2015). Isolation also creates a greater risk for partner abuse that is complicated by long distances to shelters, lack of anonymity, and a widely held view of traditional gender roles (Weeks et al., 2016). The lack of research regarding rural women and mental health compromises the efforts of rural counselors to provide care that is culturally responsive and efficacious (Imig, 2014). In addition, the recognized barriers of accessibility, availability, and acceptability of mental health services in rural areas disproportionally affect rural women (Radunovich et al., 2017).
Barriers to Mental Health Services
A lack of professionals, limited training for work in rural areas, high rates of turnover of mental health professionals, and limited research about rural demographics can negatively impact the quality of services (Smalley & Warren, 2014). In addition, rural residents may experience barriers such as long distances to services, adverse weather conditions, affordability of services, and a lack of insurance coverage (Smalley & Warren, 2014). Rural women may also feel reluctant to seek out mental health services for fear of loss of anonymity and the stigma attached to seeking mental health services in rural areas (Snell-Rood et al., 2019). Approximately 40% of rural residents with mental health issues opt to seek treatment from primary care physicians (PCPs), as these professionals may represent the only health care provider in the area (Snell-Rood et al., 2017). However, these professionals often have limited expertise in diagnosing and treating mental health issues (Hill et al., 2016).
Currently, the Council for Accreditation of Counseling and Related Educational Programs (CACREP; 2015) does not specify rurality or other cultural identities when referencing cultural competence within required curriculum. This omission may contribute to minimal specialized training, in addition to the limited research for mental health counselors to use as a guide for understanding the unique needs of rural women (Watson, 2019). Additionally, agencies have difficulty recruiting mental health counselors because of isolation from colleagues and supervisors, lower salaries, limited social and cultural opportunities, and few training opportunities specific to rural mental health (Fifield & Oliver, 2016).
Addressing Mental Health Needs of Rural Women
Given the limited research about rural women and their unique mental health needs, rural counselors are left with few evidence-based practices to utilize when working with this population (Imig, 2014). Historically, counseling researchers have equated “mentally healthy adults” with “mentally healthy adult males,” resulting in literature that is focused on best practices more appropriate for men (Broverman et al., 1970), and potentially upholding sex-role stereotypes within the fields of psychology, social work, medicine, and mental health counseling (APA, 2018; Schwarz, 2017). More recent researchers have demonstrated the efficacy of gender-specific counseling approaches (Enns, 2017). However, the approaches often do not consider the additional barriers to services that rural women may face, such as long distances to services, limited availability of mental health professionals, and the stigma of seeking services in a rural area (Hill et al., 2016).
In this transcendental phenomenological study, we sought to explore the lived experiences of licensed professional counselors (LPCs) who work with rural women in terms of their perceptions of rural Midwestern women’s mental health, and the academic training they received to prepare them for working with rural women. The study sought to answer the following research questions: (a) What are the lived experiences of LPCs who work with rural women?; (b) What are the challenges and benefits of working with rural women?; (c) How are mental health services perceived by those working with rural women?; and (d) What training, if any, did the participants receive that was specific to work with rural women?
Method
Qualitative research, by its very nature, validates individuals who may be disempowered (Morrow, 2007; Ponterotto, 2010). Phenomenology is a qualitative method that helps researchers describe the common meaning of participants’ lived experiences specific to a particular phenomenon (Creswell & Poth, 2018). In this study, the phenomenon was the lived experiences of LPCs who worked with rural women. Transcendental phenomenology (Moustakas, 1994) provided a framework for the study that began with epoché, a process of bracketing the researchers’ experiences and biases, and the collection of participant stories (Creswell & Poth, 2018). For this study, postpositivist elements of transcendental phenomenology (e.g., bracketing and data analysis) were utilized to reduce researcher biases (Moustakas, 1994). Specifically, we viewed bracketing as essential because participants might not share the feminist viewpoint of the researchers. The infusion of feminism into the study came from a constructivist/interpretivist standpoint as I (i.e., first author and lead researcher) believed—based on literature—the stories of rural women were not being heard and, thus, designed the study to help illuminate the experiences, mental health needs, and resiliency of rural women (Morrow, 2007).
Participants
For this study, participants were recruited using criterion and snowball sampling. Criterion sampling involved selecting individuals on the basis of their shared experiences and their abilities to articulate those experiences (Heppner et al., 2016). Snowball sampling allowed for selecting participants who previously had a demonstrated interest in this area of research based on their connection to other participants. Criteria for participation included a degree from a CACREP-accredited counseling program, licensure within their jurisdiction, current practice, and clinical work that included rural women. To recruit participants, we collected names and emails from a Midwestern state counseling association; however, this method produced only two responses. So, we utilized snowball sampling by asking participants to refer us to others who met our eligibility criteria (Creswell & Poth, 2018). We determined the number of LPCs needed to describe the phenomena by achieving saturation of the data collected (Heppner et al., 2016). This saturation was reflected by eventual redundancy in participant responses.
Following approval from the appropriate IRB, an invitation to participate was emailed to potential participants and included a link to a demographic form and informed consent for those who met the criteria and wished to participate. Rural areas were defined as those geographic areas containing counties with populations of less than 50,000, a definition that did not include population density but was appropriate for the Midwestern areas included in the study (Smalley & Warren, 2014). Twelve mental health counselors met the eligibility criteria for participation and enrolled in the study.
All participants had graduated from a CACREP-accredited counseling program, were licensed to practice within their jurisdiction, were currently practicing privately or in an agency, and had a clinical caseload that included rural women. The designation of LPC was used throughout the study and included all levels of licensure within the various jurisdictions. All of the LPCs reported working with a wide variety of mental health issues; three of the LPCs had addiction counseling credentials. Eleven participants self-identified as female and one self-identified as non-binary. Eleven participants self-identified as Caucasian, and one self-identified as Native American. Years of experience working as a mental health professional ranged from 4 years to 27 years, with an average of approximately 12 years. All participants reported working with both urban and rural clients, and one participant listed a reservation as the primary location for her work. LPCs’ clients included adult rural women from the upper Midwest. The rural women were single or married with children, working or unemployed, Caucasian or Native American. In addition, all the participants expressed a connection to rural areas, either through personal experience of growing up in a rural area or through connections with extended family. Each participant chose a pseudonym that is referred to throughout the manuscript.
Data Collection
We collected data through individual semi-structured interviews and participant artifacts. The semi-structured interview format allowed for more collaboration and interaction between interviewer and interviewee (Creswell & Poth, 2018). In this way, the interview format aligned with a feminist research approach and helped eliminate a power differential between researcher and participant (Heppner et al., 2016). There were 12 interview questions aimed at exploring participants’ work with rural women, participants’ perceptions of the unique mental health needs of rural women, the influence of participants’ rural heritage on their work with rural women, challenges and benefits of participants’ work with rural women, and participants’ training specific to work with rural women (see Appendix for all 12 interview questions). As lead researcher, I conducted all 12 interviews in order to maximize consistency in employing the interview protocol while allowing participants to elaborate on responses. Interviews ranged from 30–45 minutes. All research documents, such as informed consents, demographic questionnaires, and transcriptions, were securely stored on a password-protected device.
Participants were invited to share artifacts that represented their work with rural women. Artifacts could include personal letters, poems, artwork, and photos (Heppner et al., 2016). The artifacts in this study provided an opportunity for broader expression of the counselors’ experiences as well as understanding their connection to rural life. Seven artifacts were pictures of objects or individuals that inspired participants’ work with rural women, two were stories about experiences of rural women, and one was an original poem entitled “Rural Woman.”
Data Analysis
Brown and Gilligan’s (1992) research of young women and relationships utilized a Listener’s Guide for analyzing data. This guide is feminist and relational and allows researchers to pay attention to unheard voices. The Listening Guide is considered a psychological method that reflects the “social and cultural frameworks that affect what can and cannot be spoken or heard” (Gilligan & Eddy, 2017, p. 76). The method included three successive “listenings”—one for plot, one for “I” statements, and one for the individual in relationship to others (Brown & Gilligan, 1992). Throughout the listening process, I looked for and highlighted significant statements the participants made during the interview process that reflected the experiences of the phenomenon. I organized information via a phenomenological template under the heading “Essence of the Phenomenon” and included personal bracketing (epoché), significant statements, meaning units, and textural and structural descriptions (Creswell & Poth, 2018). Although a transcription service was utilized to transcribe the interviews, I read through the transcripts several times and coded data into categories or themes, which emerged organically from the transcripts. An independent peer reviewer then examined the transcriptions and helped to develop the codes and themes. We developed clusters of meaning from the significant statements into themes, followed by a textural and structural description that encompassed the significant statements and related themes. The rich and thick descriptions became the essence of the phenomenon enhanced by continual review of the interview tapes, journal notes, artifacts, and other data collected (Morrow, 2005).
Epoché
The epoché section was written from my perspective as the primary researcher and first author. I was responsible for designing the study, collecting and analyzing data, and writing the manuscript. My co-authors served as consultants in designing the study and helped to write and edit the manuscript. As the primary researcher, I sought to see the lived experiences of participants from a perspective that was free from my assumptions (Creswell & Poth, 2018). I grew up in a Midwestern rural area, steeped in traditional gender roles, while witnessing significant change for all women in expectations and opportunities. During the process of the study, it became apparent that my perceptions of rural women as stay-at-home farmwives have changed to reflect a population more diverse in ethnicity, family structure, and socioeconomic status; however, the traditional patriarchal expectations have not changed. My work as a mental health professional shaped my desire to explore the perceptions of other LPCs’ experiences of their work with rural women. Prior to the data analysis, I bracketed my personal and professional rural experiences about power differentials within rural areas.
Trustworthiness
To promote trustworthiness, I utilized self-reflective journaling, member checks, the achievement of data saturation, independent peer review, and an external audit. I kept a journal and made notes throughout the data collection process to facilitate an awareness of biases and/or assumptions that emerged during the process (Heppner et al., 2016; Morrow, 2005). I also conducted member checks, asking all participants to review and provide feedback via email on descriptions or themes (Creswell & Poth, 2018; Morrow, 2005). Frequently, participants would elaborate on themes by adding clarification to their responses to the interview questions. The “prolonged interaction” (Ponterotto, 2010, p. 583) with participants was significant for developing an egalitarian and unbiased relationship between researcher and participant. This strategy was congruent with feminist theory because it acknowledged the subjectivity of the researcher within the study and facilitated a collaborative relationship between researcher and participant (Morrow, 2007).
Coding the data into categories or themes helped arrange the large amount of data that was collected. The process was made easier by taking notes, or “memoing,” when reading through the information. The peer reviewer evaluated potential researcher bias by checking the coding against all transcripts, serving as a “mirror” that reflected my responses to the research process (Morrow, 2005, p. 254). Next, we discussed possible themes that emerged from the data (Heppner et al., 2016). I also utilized an external auditor to aid in establishing confirmability of the results rather than objectivity (Morrow, 2005). The auditor examined the entire process and determined whether the data supported my interpretations (Creswell & Poth, 2018). Both individuals had participated in phenomenological research and were not authors of this article.
Results
Analysis of the interview transcripts, the artifacts, and the journal reflections resulted in eight themes, organized into two categories. I further categorized each theme as: 1) textural, a subjective experience of the LPC’s experience with rural women; or 2) structural, the context of the experience. According to Moustakas (1994), the textural themes represent phenomenological reduction, a way of understanding that includes an external and internal experience; the structural themes represent imaginative variation, the context of the experience. One of the themes, counselor experience, fit the description of both textural and structural. The categories represented two distinct dimensions of the phenomenon: (a) LPCs’ perceptions of their work with rural women, and (b) LPCs’ perceptions of rural women and issues related to mental health.
Dimension 1: LPCs’ Perceptions of Their Work With Rural Women
Five textural themes emerged from the coding process; I took the names of three of these verbatim from the interviews. The textural themes included 20 codes that represented the subjective experiences of LPCs’ work with rural women. The participants’ pseudonyms were inserted into the direct quotes included in theme descriptions. Artifacts offered by participants were also included.
Bootstraps
Rooted in the familiar saying of “pull yourself up by your bootstraps,” this theme included codes of resilient, stoic, self-sufficient, and independent. According to LPCs’ perceptions of rural women, bootstraps described an acceptance of the current conditions of rural life and a reliance on past experiences for guidance. Many of the LPCs believed that rural women came to counseling with a skill set that, as Nancy said, “can teach us and others about how to be resilient.” Fave commented that working with rural women also required patience:
It’s this sense of “I can do this.” There are more demands with farming, and rural women still believe they should be able to do it all. When they come into counseling it can be difficult because they have worked hard to sort of protect this thing and keep it close to them because they’re pretty sure they can figure it out themselves.
Courtney shared a story about a ranch woman who was grieving the loss of her husband and was struggling with family issues. She remarked in one session, “Today I decided it was time to put on my red cowboy boots.” For Courtney, this represented her client’s resiliency and stoicism—“I’ve got this, and I’ve got my red boots on to prove it.”
Trailblazer
Trailblazer included pioneer, open-minded, resourceful, educated, and empowered; these words described LPCs’ perceptions of rural women’s abilities to move past accepting the realities of rural living and work toward change for improving themselves, their families, and their communities. According to the LPCs, this theme is distinct from bootstraps in that it is future-oriented rather than past-oriented. Elsie first referred to trailblazer when she told a story about a client who began recycling in the early 1980s: “She had bins and bins of recycling because she said, ‘I’m gonna leave this planet in a different shape than I found it.’ Rural women very much can be trailblazers.” The LPCs’ perceptions represented a new perspective that reflected resourceful change-makers, educated and empowered to challenge the status quo.
As one of her artifacts, Courtney offered a story about one woman’s determination to make Christmas special even though there were no resources for gifts and decorations. The woman found a large tumbleweed, covered it with lights and decorations, and declared it beautiful. Courtney said, “She was not just making do, but making things better.”
Challenges of Rural Women
LPCs observed multiple challenges for rural women including isolation, poverty/financial insecurity, role overload, grief, and generational trauma. Layla talked about the complex grief that was experienced by Native American women. She commented that “the death of a family member can mean losing someone from three or four generations. There is grief from loss of jobs, moving from the reservation, and loss of culture.” LPCs cited role overload as one of the most common experiences among rural women. Many rural women worked full-time jobs in addition to caring for family members while contributing to the farm/ranch operation. Jean observed that rural women “are responsible for everyone’s emotions in the family, sometimes leaving them isolated within the family.” LPCs believed that the isolation contributed to vulnerability. Rural women faced domestic violence, anxiety, depression, and addictions, exacerbated by having no one to talk with and long distances to services. Jean noted that resistance to change was perpetuated by the fear and control inherent in domestic abuse for many of her clients and led to complacency in reporting. The challenges of rural women described by participants defined the issues that LPCs faced when working in rural areas and increased their awareness of the critical needs of rural women.
Protective Factors
Protective factors included a sense of identity and the strong support systems of families and community that gave rural women “a lot of people that you can draw upon to help you through hard times,” according to Nancy. Her clients valued the easy access to nature and the opportunity to “immerse yourself in something bigger than yourself. It’s a way to build resilience and find meaning and joy spending time outside.” Layla found a strong sense of identity evident in rural Native women as central to the ability to teach their children cultural beliefs—a protective factor for future generations.
Nancy shared a picture of a family moving their 100-year-old home to a new location as her artifact. Her description of the house and rural heritage symbolized part of what she believed was important for rural women—the connection to family and heritage along with a sense of purpose in maintaining family culture. She said, “It’s a good way to pass down the family stories and even the family culture.”
Counselor Experience
Counselor experience (textural) included the reasons why participants chose to become LPCs. These included the motivations that sustained their work and advice for new counselors. Assumptions about diversity, a sense of purpose, listening, and connections to resources encapsulated this theme.
Layla became a counselor because she wanted “to give back to my Native people.” Nancy believed that the work with rural women helped her build a rural counselor identity. Woods’ early experience with rural women felt profound because of the chaos she observed in the lives of her clients, many of them impoverished single mothers struggling to survive. She was given a sense of purpose in her work saying, “These women are burned into my head.”
When asked about advice for new counselors who anticipate working with rural women, participants offered the following brief statements:
“Don’t make assumptions.” (Courtney)
“Ask to be taught.” (Marie)
“Hear their story without filtering through your own personal lens.” (Nancy)
“There is a difference in working in rural areas—a conservative mind-set, practicality—and you need to meet people where they are.” (Kay)
“Listen more than you talk.” (Suzie)
“Have respect for their culture.” (Layla)
LPCs’ Perceptions of Rural Women and Issues Related to Mental Health
Three structural themes represented what Moustakas (1994) termed imaginative variation, the acknowledgment of the context of multiple perspectives. The themes were derived from nine codes that provided a vital aspect of further describing the phenomenon. The theme descriptions included participants’ quotes and artifacts.
Perceptions of Rural Heritage
This theme represented LPCs’ view of rural life, including traditional values, heritage, and expectations/perfectionism. According to participants, many of the rural women embraced the traditional values of their rural heritage, and the roles of rural life; this theme honors that perspective. Fave talked about the expectations that rural women often have of themselves: “It’s a perfectionist perspective, meaning they can do it all.” Even in light of the increased demands on rural women’s time and energy, Marie found that rural women were often hesitant to seek outside professional mental health counseling, choosing instead to rely on family and community.
Barriers to Mental Health Services
The barriers included codes of lack of resources, stigma, and invisibility. All LPCs felt concerned about the lack of resources for rural women. Suzie talked about the dearth of women’s shelters on the reservation and resources for women who are victims of domestic violence. Suzie said, “They often stay because there are no resources for them to leave, and they can’t afford it.” Woods noted the lack of daycare providers and the fact that many rural women cannot afford these services and depend on family members for childcare. According to several LPCs, rural women do not prioritize their mental health needs, possibly because of the many demands on them.
Kay and Marie practiced in an urban area but saw many rural women who chose to travel long distances for mental health services because it gave them a sense of anonymity. Kay said, “They know if their car is parked at the counselor’s office, it won’t be recognized by everyone in town.” Rural women also feared exposing family secrets if they disclosed something to a counselor who lived in the same area.
Poignantly, LPCs acknowledged the invisibility and minimization of rural women’s mental health needs. The following comments by participants exemplified the rural woman’s experiences of being unnoticed or dismissed. Elsie stated, “Even if rural women are speaking, they don’t have the platform like urban women do, and they feel like nobody gets this life.” Kay stated, “Everything is fine, everything’s great and we’re not going to talk about the fact that Grandma is crying all the time and wearing sunglasses.”
The statements of the participants provided powerful examples of the ramifications of the silencing imposed on rural women through traditional or cultural norms. The stigma of accessing mental health services created a loss of connection between the rural women who needed the services and their community. In addition, rural women often felt selfish in seeking services just for themselves. The consensus among LPCs was that rural women suffer to a greater extent than other rural populations because their needs are minimized or not recognized. Elsie remarked that rural women do not often see their stories in mainstream media, leading them to believe “I’m living this experience that nobody else lives.”
The description of the artifact contributed for this theme may further elucidate the invisibility of rural women. Woods’ artifact was a picture of two locally designed sculptures of women. Woods said, “They are so rooted and earthy.” One sculpture had no arms or legs and, for Woods, that “speaks to the limited access to needed supports and the lack of voice.”
Counselor Experience
Counselor experience (structural) described how LPCs provide mental health services to rural women and included connection to rural life, distances and dual relationships, and lack of academic training/postgraduate training. Although not all the participants grew up in rural areas, many had rural ties through extended family. Marie’s upbringing on a ranch influenced her understanding of rural women: “There is a more intense work ethic; women are very strong and independent and hardworking.”
The LPCs seemed to feel a strong sense of purpose in their work; some of them chose to become counselors and returned to their home communities to work. They discovered that the connections of shared experiences fostered trust in the counseling relationship and process. Most felt that they were helping to make positive change. Although all participants believed the connection to a rural heritage was critical in their work with rural women, some LPCs did not live and work in the same location, saying it helped to reduce the possibility of multiple relationships. Nancy commuted almost an hour to her work “because you really want to have the counseling relationship be through your therapeutic lens and not through the community lens.”
None of the participants recalled receiving academic training specific to rural areas; however, all participants agreed on the need for academic training focused on rural areas and rural women. Elsie believed that textbooks should “include women’s voices and rural voices.” Jean expressed her concern that “We don’t necessarily address rural women or what they need from the communities around them or even what their typical experience is. I think that’s a disservice to our counseling students.”
Two artifacts aligned with this theme: Marie’s picture of a young girl, dressed in overalls, pitching hay, and Mae’s great-grandmother’s writing desk (see Figure 1). Marie’s artifact exemplified the family’s connection to rural life and the physical strength of rural women that she observed in her work. Mae now uses the writing desk in her practice and feels it gives her a strong connection to her rural heritage.
Figure 1
Mae’s Great-Grandmother’s Writing Desk

Note. Mae presented this picture of her great-grandma’s writing desk when asked to provide
an artifact that demonstrated her work with rural women.
Discussion
LPCs described rural women as strong, independent, resourceful, and resilient. However, this image of rural women was not corroborated within the research literature. An APA report on the behavioral health care needs of rural women (Mulder et al., 2000) did not mention resiliency as a coping strategy; however, in 2006, the report’s lead author recognized the need for additional research about resiliency in rural women, saying it would offer “significant potential benefit to rural women” (Mulder & Lambert, 2006, p. 15). In the present study, LPCs’ perceptions of rural women as resilient called attention to the innate strengths of rural women that developed out of necessity, cultivated by connections with family, community, and earth.
Rural heritage represented a dichotomy of rural tradition. From a positive perspective, participants believed the traditional roles of rural women provided a sense of identity and belonging. From a negative perspective, the traditional patriarchy evident in many rural areas dictated social and cultural norms, leaving rural women with the expectation that they should be able to “do it all.” Both perspectives defined a critical aspect of LPCs’ understanding of rural women. Even though many of the rural women participants described worked full-time to contribute to household income and health insurance (in addition to caretaker responsibilities), they faced gender inequities in income, employment, and educational opportunities (Watson, 2019). In addition, rural women have had little political power to effect needed policy changes for better access to care (Van Montfoort & Glasser, 2020).
LPCs highlighted multiple challenges that rural women experience: isolation, poverty, grief, role overload, and generational trauma. Barriers to obtaining services included stigma of mental health issues, loss of anonymity, a lack of resources, invisibility, and minimization of mental health issues. The general population also faces barriers of accessibility, acceptability, and availability of counseling services (Smalley & Warren, 2014); however, there were fewer references to the mental health barriers and challenges specific to rural women (Van Montfoort & Glasser, 2020). This is surprising given that the population of rural women exceeds that of any other population group in rural areas (Bennett et al., 2013). Rural women experience higher risks of depression, domestic violence, and poverty (Snell-Rood et al., 2019). The mental health services available in rural areas, often described as “loosely organized, of uneven quality, and low in resources” (Snell-Rood et al., 2019, p. 63), compound the challenges for rural women.
As evident in the themes of assumptions and diversity, rural women represent a unique population who deserve mental health services that reflect their specific needs. Rural communities and rural women are more diverse than once believed. LPCs’ observations are corroborated by research that acknowledged differences among rural women in socioeconomic status, family structure, age, sexual identity, ethnicity, education, and geographical location (Barefoot et al., 2015). In addition, there remains a misconception that the mental health needs of urban and rural women are the same; in fact, much of the literature about women and mental health is based on an urban context (Weaver & Gjesfjeld, 2014). The findings of the current study support the lack of recognition of the context of rural women’s issues and their status as an invisible population (Bender, 2016). Two LPCs’ observations of the isolation felt by rural women reinforced previous research of the invisibility of rural women. Elsie said, “Rural women don’t see their story a lot,” and Fave shared that “a lot of the women I work with don’t feel like they’re heard.”
None of the participants recalled academic training or postgraduate opportunities specific to work in rural areas or with rural women. Even though rural areas represent the largest population subgroup in the United States (Smalley & Warren, 2014), this study suggests that new counselors may not feel prepared to meet the needs of this underserved population. The shortage of mental health professionals working in rural areas and the lack of counselors who have training specific to rural mental health care suggest a need for rural-based training that might include an elective course in rural mental health and rural internships (Fifield & Oliver, 2016).
Implications
The recognition of the challenges and benefits of working with rural women may validate rural LPCs’ experiences, promote their professional identity as rural counselors, and potentially decrease the isolation felt when working in rural areas. Protective factors, including connections to family, community, and nature, may be critical for building resiliency in both rural women and rural LPCs. The increasing diversity of rural women is often contrary to the traditional stereotype of a stay-at-home farmwife (Carpenter-Song & Snell-Rood, 2017); diverse rural women may face unique barriers to accessing culturally relevant mental health services. In addition, many rural women experience role overload from working full-time and caring for families while contributing to the farm/ranch operation. Counselors should avoid interacting with rural women clients in ways that limit their identities based on stereotypes and work to make their services accessible for all women.
The study results also have implications for counselor educators. Rural-based counselors in this study did not report being taught how to work with rural women. A review of the 2016 CACREP programs found few gender-based counseling courses and none that addressed rural mental health. Programs could offer electives on counseling in rural areas, incorporate the context of gender and rural mental health into current curricula, and encourage rural internships. Collaborating with other rural health professionals may provide more informed approaches to working in rural areas. Rural residents may see their PCPs for mental health–related treatment, as PCPs may be the only health care provider in rural areas (Snell-Rood et al., 2017). Lloyd-Hazlett et al. (2020) suggested creating additional training for LPCs who choose to work in settings offering integrated care. Incorporating LPCs who have the appropriate training and skills into rural medical settings may offer mental health services in a familiar clinical context and one that does not broadcast engagement in mental health care. The collaboration may also provide more awareness of the mental health needs of rural women.
Limitations
The study has several limitations. Although I took measures to reduce any personal bias as a non-traditional rural woman, I do not believe it is possible to eliminate all biases. Many of the participants talked about empowering rural women and working toward making their clients’ voices heard, both tenets of feminist theory (Evans et al., 2005); however, participants rarely used the language of feminism. Several of the participants related personal stories of their connections with rurality and, often, their stories of rural women were from decades ago. Their stories may not have represented the current generation of rural women. Another limitation relates to the demographics of LPCs because a majority of participants self-identified as Caucasian and female and represented rural areas in the Midwest. LPCs working in other areas of the United States may encounter different demographics of rural women, mental health challenges specific to region, and unique intersections of their clients’ identities. Finally, the experiences of rural women were heard through LPCs and not from rural women clients themselves.
Directions for Future Research
This study included a sample of rural LPCs who were primarily Caucasian females from the Midwestern United States; future researchers may seek professional perspectives from participants who represent a blend of race, ethnicities, gender identities, and geographical locations. Research with rural women as participants themselves is also an important opportunity. Based on findings from this study, future researchers might also explore training needs related to work with rural women and rural populations. Studying counselor educators who teach in counseling programs based in rural areas could also offer unique insights. This may reveal information about ways educators currently infuse rural culture and work with rural women into the curriculum. Future researchers may study counselors, health care providers, and rural women in finding ways to integrate health care services in rural areas to provide better access to services and reduce the stigma often associated with mental health. Finally, additional studies about working with rural PCPs may highlight issues (e.g., intimate partner violence) that could benefit from early screening of symptoms.
Conclusion
Gilligan offers these words: “To have something to say is to be a person. But speaking depends on listening and being heard; it is an intensely relational act” (1982/1993, p. xvi). As indicated in our findings, rural women are too often invisible and unheard. This study represents a first step in amplifying the voices of rural women regarding their specific mental health needs. The experiences of the LPCs in this study have illuminated ways to connect with rural women, listen to their stories, and validate unique aspects of their cultural identities that seem to be well illustrated in one participant’s poem:
Rural Women
Resilient; stubborn; motivated
frightened; broken; courageous
Struggling; down-trodden; strong
Relentless in self-expectation
Armed with determination.
A common thread unites us
The heart gently calls, and the
soul asks only—please—listen to me.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
American Psychological Association. (2018). APA guidelines for psychological practice with girls and women.
http://www.apa.org/about/policy/psychological-practice-girls-women.pdf
Barefoot, K. N., Rickard, A., Smalley, K. B., & Warren, J. C. (2015). Rural lesbians: Unique challenges and implications for mental health providers. Journal of Rural Mental Health, 39(1), 22–33.
https://doi.org/10.1037/rmh0000014
Bender, A. K. (2016). Health care experiences of rural women experiencing intimate partner violence and substance abuse. Journal of Social Work Practice in the Addictions, 16(1–2), 202–221.
https://doi.org/10.1080/1533256X.2015.1124783
Bennett, K. J., Lopes, J. E., Jr., Spencer, K., & van Hecke, S. (2013). Rural women’s health. National Rural Health Association Policy Brief. https://www.ruralhealthweb.org/getattachment/Advocate/Policy-Documents/RuralWomensHealth-(1).pdf.aspx
Broverman, I. K., Broverman, D. M., Clarkson, F. E., Rosencrantz, P. S., & Vogel, S. R. (1970). Sex-role stereotypes and clinical judgments of mental health. Journal of Counseling and Clinical Psychology, 34(1), 1–7.
https://doi.org/10.1037/h0028797
Brown, L. M., & Gilligan, C. (1992). Meeting at the crossroads: Women’s psychology and girls’ development. Harvard University Press.
Carlton, E., & Simmons, L. (2011). Health decision-making among rural women: Physician access and prescription adherence. Journal of Rural and Remote Health Research, Education, Practice and Policy, 11, 1–10.
Carpenter-Song, E., & Snell-Rood, C. (2017). The changing context of rural America: A call to examine the impact of social change on mental health and mental health care. Psychiatric Services, 68(5), 503–506.
https://doi.org/10.1176/appi.ps.201600024
Council for Accreditation of Counseling and Related Educational Programs. (2015). 2016 CACREP standards. http://www.cacrep.org/for-programs/2016-cacrep-standards
Creswell, J. W., & Poth, C. N. (2018). Qualitative inquiry & research design: Choosing among five approaches (4th ed.). SAGE.
Doudna, K. D., Reina, A. S., & Greder, K. A. (2015). Longitudinal associations among food insecurity, depressive symptoms, and parenting. Journal of Rural Mental Health, 39(3–4), 178–187.
https://doi.org/10.1037/rmh0000036
Enns, C. Z. (2017). Contemporary adaptations of traditional approaches to counseling women. In M. Kopala & M. Keitel (Eds.), Handbook of counseling women (2nd ed., pp. 51–62). SAGE.
Evans, K. M., Kincade, E. A., Marbley, A. F., & Seem, S. R. (2005). Feminism and feminist therapy: Lessons from the past and hopes for the future. Journal of Counseling & Development, 83(3), 269–277.
https://doi.org/10.1002/j.1556-6678.2005.tb00342.x
Fifield, A. O., & Oliver, K. J. (2016). Enhancing the perceived competence and training of rural mental health practitioners. Journal of Rural Mental Health, 40(1), 77–83. https://doi.org/10.1037/rmh0000040
Gilligan, C. (1993). In a different voice: Psychological theory and women’s development. Harvard University Press. (Original work published 1982)
Gilligan, C., & Eddy, J. (2017). Listening as a path to psychological discovery: An introduction to the Listening Guide. Perspectives on Medical Education, 6, 76–81. https://doi.org/10.1007/s40037-017-0335-3
Heppner, P. P., Wampold, B. E., Owen, J., Thompson, M. N., & Wang, K. T. (2016). Research design in counseling (4th ed.). Cengage.
Hill, S. K., Cantrell, P., Edwards, J., & Dalton, W. (2016). Factors influencing mental health screening and treatment among women in a rural south central Appalachian primary care clinic. Journal of Rural Health, 32(1), 82–91. https://doi.org/10.1111/jrh.12134
Imig, A. (2014). Small but mighty: Perspectives of rural mental health counselors. The Professional Counselor, 4(4), 404–412. https://doi.org/10.15241/aii.4.4.404
Lloyd-Hazlett, J., Knight, C., Ogbeide, S., Trepal, H., & Blessing, N. (2020). Strengthening the behavioral health workforce: Spotlight on PITCH. The Professional Counselor, 10(3), 306–317.
https://doi.org/10.15241/jlh.10.3.306
Morrow, S. L. (2005). Quality and trustworthiness in qualitative research in counseling psychology. Journal of Counseling Psychology, 52(2), 250–260. https://doi.org/10.1037/0022-0167.52.2.250
Morrow, S. L. (2007). Qualitative research in counseling psychology: Conceptual foundations. The Counseling Psychologist, 35(2), 209–235. https://doi.org/10.1177/0011000006286990
Moustakas, C. (1994). Phenomenological research methods. SAGE.
Mulder, P. L., & Lambert, W. (2006). Behavioral health of rural women: Challenges and stressors. In R. T. Coward, L. A. Davis, C. H. Gold, H. Smiciklas-Wright, L. E. Thorndyke, & F. W. Vondracek (Eds.), Rural women’s health: Mental, behavioral, and physical issues (pp. 15–30). Springer.
Mulder, P. L., Shellenberger, S., Streiegel, R., Jumper-Thurman, P., Danda, C. E., Kenkel, M. B., Constantine, M. G., Sears, S. F., Kalodner, M., & Hager, A. (2000). The behavioral healthcare needs of rural women.
http://www.apa.org/practice/programs/rural/rural-women.pdf
Ponterotto, J. G. (2010). Qualitative research in multicultural psychology: Philosophical underpinnings, popular approaches, and ethical considerations. Cultural Diversity and Ethnic Minority Psychology, 16(4), 581–589. https://doi.org/10.1037/a0012051
Radunovich, H. L., Smith, S. R., Ontai, L., Hunter, C., & Cannella, R. (2017). The role of partner support in the physical and mental health of poor, rural mothers. Journal of Rural Mental Health, 41(4), 237–247.
https://doi.org/10.1037/rmh0000077
Schwarz, J. (2017). Counseling women and girls: Introduction to empowerment feminist therapy. In J. E. Schwarz (Ed.), Counseling women across the life span: Empowerment, advocacy, and intervention (pp. 1–20). Springer.
Smalley, K. B., & Warren, J. C. (2014). Mental health in rural areas. In J. C. Warren & K. B. Smalley (Eds.), Rural public health: Best practices and preventive models (pp. 85–93). Springer.
Snell-Rood, C., Feltner, F., & Schoenberg, N. (2019). What role can community health workers play in connecting rural women with depression to the “de facto” mental health care system? Community Mental Health Journal, 55, 63–73. https://doi.org/10.1007/s10597-017-0221-9
Snell-Rood, C., Hauenstein, E., Leukefeld, C., Feltner, F., Marcum, A., & Schoenberg, N. (2017). Mental health treatment seeking patterns and preferences of Appalachian women with depression. American Journal of Orthopsychiatry, 87(3), 233–241. https://doi.org/10.1037/ort0000193
U.S. Census Bureau. (2010). 2010 census urban and rural classification and urban area criteria. http://census.gov/programs-surveys/geography/guidance/geo-areas/urban-rural/2010-urban-rural.html
U.S. Department of Agriculture. (2015). Rural America at a glance. https://www.ers.usda.gov/webdocs/publications/
44015/55581_eib145.pdf?v=751.6
Van Montfoort, A., & Glasser, M. (2020). Rural women’s mental health: Status and need for services. Journal of Depression and Anxiety, 9(3), 1–7.
Watson, D. M. (2019). Counselor knows best: A grounded theory approach to understanding how working class, rural women experience the mental health counseling process. Journal of Rural Mental Health, 43(4), 150–163. https://doi.org/10.1037/rmh0000120
Weaver, A., & Gjesfjeld, C. (2014). Barriers to preventive services use for rural women in the southeastern United States. Social Work Research, 38(4), 225–234. https://doi.org/10.1093/swr/svu023
Weeks, L. E., Macquarrie, C., Begley, L., Gill, C., & Leblanc, K. D. (2016). Strengthening resources for midlife and older rural women who experience intimate partner violence. Journal of Women & Aging, 28(1), 46–57. https://doi.org/10.1080/08952841.2014.950500
Wong, A. (2017). Intersectionality: Understanding power, privilege, and the intersecting identities of women. In J. E. Schwarz (Ed.), Counseling women across the life span: Empowerment, advocacy, and intervention (pp. 39–56). Springer.
Appendix
Twelve Interview Questions
- Tell me about what comes to mind when you think about working with rural women.
- Tell me about where you grew up and how that has influenced your work with rural women.
- Tell me about how you began your work with rural women.
- What have you learned about rural women through your work with them?
- What are the unique mental health needs of rural women that you have seen in your work?
- Tell me about some of the benefits and rewards, if any, you have experienced working with rural women.
- Tell me about some of the challenges, if any, you have experienced working with rural women.
- How have your experiences working with rural women changed you as a mental health counselor?
- Tell me about any academic/classroom experiences in your graduate program that involved the mental health issues of rural women (e.g., class discussions, special projects, conversations with colleagues, internship experiences).
- Tell me about any training experience post-graduation that have involved the mental health issues of rural women (e.g., workshops, conference presentations, webinars, conversations with colleagues).
- What would you like other counselors to know about working with rural women?
- Please describe how the artifact that you have chosen relates to your work with rural women.
Lisbeth A. Leagjeld, PhD, NCC, LCPC, LPC-MH, is a program liaison and faculty member at South Dakota State University – Rapid City. Phillip L. Waalkes, PhD, NCC, ACS, is an assistant professor and doctoral program coordinator at the University of Missouri – St. Louis. Maribeth F. Jorgensen, PhD, NCC, LPC, LMHC, LIMHP, is an assistant professor at Central Washington University. Correspondence may be addressed to Lisbeth A. Leagjeld, 4300 Cheyenne Blvd., Rapid City, SD 57709, Lisbeth.leagjeld@sdstate.edu.