May 10, 2023 | Volume 13 - Issue 1
Shainna Ali, John J. S. Harrichand, M. Ann Shillingford, Lea Herbert
Guyana has the highest rate of suicide in the Western Hemisphere. Despite this statistic, a wide gap exists in the literature regarding the exploration of mental wellness in this population. This article shares the first phase in a phenomenological study in which we explored the lived experiences of 30 Guyanese American individuals to understand how mental health is perceived. The analysis of the data revealed that participants initially perceived mental health as negative and then transitioned to a positive perception of mental health. We discuss how these perceptions affect the lived experience of the participants and present recommendations for counselors and counselor educators assisting Guyanese Americans in cultivating mental wellness.
Keywords: Guyanese American, mental health, phenomenological, mental wellness, perceptions
In 2014, the World Health Organization (WHO) reported Guyana as having the highest suicide rate in the world (44.2 suicides per 100,000 people; global average is 11.4 per 100,000 people). According to World Population Review (2023), within the Western Hemisphere, even after almost 10 years, Guyana remains the country with the highest rate of suicide—a concerning statistic. Responding to the WHO (2014) report, Arora and Persaud (2020) engaged in research to better understand the barriers Guyanese youth experience in relation to mental health help-seeking and suicide. Their research included 17 adult stakeholders (i.e., teachers, administrative staff, community workers) via focus groups, and 40 high school students who engaged in interviews. Arora and Persaud used a grounded theory approach and found the following themes as barriers to mental health help-seeking in Guyanese youth: shame and stigma about mental illness, fear of negative parental response to mental health help-seeking, and limited awareness and negative beliefs about mental health service. They recommended integrating culturally informed suicide prevention programs in schools and communities. In efforts to extend Arora and Persaud’s findings, we sought to further understand how Guyanese Americans define and experience mental health to better serve them in counseling.
Startled by the statistics presented by the WHO (2014) and Arora and Persaud (2020), we were compelled to focus our attention on this unique immigrant subgroup in the United States. It is important to note that between the WHO’s 2014 report and Aurora and Persaud’s research, no other studies related to Guyanese American suicidality are recorded in the literature. However, two studies on Guyanese American mental health emerged by Hosler and Kammer (2018) and Hosler et al. (2019). Our decision to conduct research on the Guyanese American community was further informed by Forte and colleagues’ (2018) review of immigrant literature in the United States, which stated that “immigrants and ethnic minorities may be at a higher risk for suicidal behavior as compared to the general population” (p. 1). Forte et al. found that immigrants, when compared with individuals in their homeland, were at an increased risk of experiencing mental health challenges like depression and other psychotic disorders. Currently, suicide is listed as the 10th leading cause of death overall in the United States (Heron, 2021). More specifically, within ages 10–34 and 35–44, suicide is the second and fourth leading cause of death, respectively. Heron’s (2021) report, referencing the Centers for Disease Control and Prevention (CDC), highlighted that in the United States, death by suicide (47,511) is 2.5 times higher than homicides (19,141). The prevalence of suicide among Guyanese people within and without the United States warranted further exploration of the experiences of this marginalized group.
The Guyanese American Experience
Comparing all countries with a population of at least 750,000 people, Guyana, a Caribbean nation, is said to have “the biggest share of its native-born population—36.4%—living abroad” due to remoteness and limited opportunities within the country to move from a lower to a higher socioeconomic status (Buchholz, 2022, para. 2). It is estimated that the United States is home to approximately 232,000 Guyanese Americans whose ancestry can be traced back to Guyana (United States Census Bureau, 2019), a country in the northeast of South America, bordered by Brazil, Venezuela, and Suriname. Although approximately 50% of all Guyanese immigrants in the United States reside in New York City alone (Indo-Caribbean Alliance, Inc., 2014), Guyanese people can be found across all 50 states and the District of Columbia (Statimetric, 2022). This draw to the United States, an English-speaking nation, might be linked to the fact that Guyana is the only country in South America that recognizes English as its official language (One World Nations Online, n.d.).
Like most immigrants, Guyanese immigrants travel to the United States seeking a better life and opportunities for themselves and their families. However, the process of transplanting can be bittersweet, in that Guyanese immigrants might be forced to relinquish their identity and customs and embrace American customs through assimilation (Arvelo, 2018; Cavalcanti & Schleef, 2001). For many Guyanese immigrants, being caught between leaving their homeland and beginning life in their adoptive home can lead to a cultural clash, resulting in problematic coping mechanisms (e.g., minimizing/hiding mental health challenges, cultural shedding [adopting American identity and losing cultural heritage]; Arvelo, 2018).
As discussed above, suicide in the Guyanese community is unquestionably a serious concern, but the community faces other challenges in the United States as well. For example, Hosler et al. (2019) found a statistically significant association between discrimination experience and major depressive symptoms in a sample of Guyanese Americans. However, Hosler et al. (2019) also found mean scores on the Everyday Discrimination Scale (EDS; Williams et al., 1997) were lower (i.e., less discriminatory experiences in everyday life) for Guyanese Americans when compared to other groups (Black, White, and Hispanic) because Guyanese Americans have a more cohesive interpersonal network. It would appear that Guyanese Americans experience lower everyday discrimination because they operate within interpersonal spaces that are more cohesive, yet their discriminatory experiences are positively associated with depression symptoms, which is a source of concern.
Another area of concern among Guyanese Americans is intimate partner violence (IPV), yet research remains lacking (Baboolal, 2016), leading us to draw directly from Guyanese literature. In Guyana, IPV is one of the most prevalent forms of violence (Parekh et al., 2012). As a country, although Guyana endorses the commitment to gender equality, women are the majority only in the tertiary sector (e.g., education, human services, clerical services, and tourism). Nicolas et al. (2021) stated that “domestic duties, marriage, and child-bearing, particularly for women between the ages of 25–29, have hindered their labor force participation” (p. 147). They documented that 1 in 6 Guyanese women, mostly from rural parts of the country, hold the belief that beating one’s wife is necessary (i.e., husbands are justified in beating their wives, resulting in domestic violence being a relevant mental health issue). In fact, suicide is identified as a public health issue for Guyanese women, who use it as a means of coping “with economic despair, poverty, and hopelessness . . . [and] to escape family turmoil, relationship issues, and domestic violence” (Nicolas et al., 2021, p. 148). However, even with access to mental health services increasing in Guyana, seeking out mental health care is uncommon due to stigma, lack of communication, inadequate financial resources, limited providers, and other barriers related to access (Nicolas et al., 2021). Within the U.S. literature, there remains a dearth of information on the experiences of this group as it relates to suicide and IPV. Most likely, this is a result of racial categorization within the United States, where, based on phenotype and racial composite, individuals are often lumped into one category, such as Black. As important as Guyanese literature on IPV is to inform the work of counselors, we believe it is equally important for us to engage in research regarding IPV and other mental health challenges on Guyanese Americans specifically. Learning about Guyanese Americans’ perceptions of mental health may facilitate closing the gap in the utilization of mental health services, warranting the current investigation.
Recognizing the noticeable research gap related to the mental health experiences of Guyanese Americans, we conducted a thorough review of the literature related to mental health and well-being. Through databases such as PsycINFO, ProQuest Central, Web of Science, MEDLINE, and SocINDEX, using the search terms “Guyanese Americans, Health and Wellbeing, Mental Health of Guyanese Americans, Access to Mental Health,” 54 search results were found. However, only two applicable studies were found to address Guyanese Americans’ mental health specifically (Hosler & Kammer, 2018; Hosler et al., 2019). The other search results were either not research manuscripts (i.e., reflections and newspaper articles) or addressed other constructs specific to the Guyanese people (e.g., family, education). The first study by Hosler and Kammer (2018) focused specifically on the health profiles of Guyanese immigrants in Schenectady, New York. This study was conducted with 1,861 residents between the ages of 18–64 years. Guyanese Americans from Schenectady were mostly from a low socioeconomic status, which resulted in them being less likely to have health insurance coverage, an identified place to receive care, and access to cancer screenings. They were also identified as being more likely to engage in alcohol binge drinking—all conditions of significant concern to us, resulting in the present study. In fact, Hosler and Kammer reported that Guyanese Americans are among the lowest group of those insured in the United States when compared with other minority groups such as Black and Latinx groups. Some researchers believe ethnocentric stereotyping, cultural incompetence by professionals, a lack of steady employment, and poor previous interactions with the health care system are barriers Guyanese immigrants experience when accessing medical and mental health services (Arvelo, 2018; Cheng & Robinson, 2013; Jackson et al., 2007).
The second study of Guyanese immigrants was conducted by Hosler et al. (2019) and explored everyday discrimination experiences and depressive symptoms in relation to urban Black, Hispanic, and White adults. This study included 180 Guyanese Americans (i.e., both citizens by birth and naturalized citizens/immigrants), all 18 years and older, from Schenectady, New York. The researchers found a significant independent association between the EDS score and major depressive symptoms for Guyanese Americans, suggesting that discrimination experiences might be an important social cause for depression within this community. Based on the reported challenges faced by Guyanese Americans, as well as our desire to contribute meaningfully to the extant body of literature on the Guyanese American community, we conducted a phenomenological inquiry. More specifically, we sought to better understand the lived experiences of Guyanese Americans pertaining to mental health (i.e., definitions, beliefs, practices), and how they access and incorporate mental health resources to mitigate the known mental health risks of this population in the United States, in the hopes of creating tailored methods for culturally responsive care.
Method
Because limited mental health research exists on this unique community, the present study, which is part of a larger research endeavor, sought to explore Guyanese Americans’ lived experiences with mental health. To lay the foundation of understanding, the present study focused on Guyanese Americans’ perceptions of mental health. Phenomenology, a constructivist approach, recognizes the existence of multiple realities and provides an understanding of participants’ lived experiences using their own voices (Haskins et al., 2022). We selected transcendental phenomenology (Moustakas, 1994) as the appropriate methodology for answering our research questions, as it is congruent with the counseling profession’s similar objective of understanding the human being. Akin to the practice of counseling, transcendental phenomenology emphasizes methods of the researcher to best set aside the potential clouds caused by bias in an effort to allow the explored phenomenon to surface. Transcendental phenomenology aligns with one of the core professional values in the American Counseling Association’s Code of Ethics (ACA, 2014), that of supporting “the worth, dignity, potential, and uniqueness of people within their social and cultural contexts” (p. 3). It also aligns with Ratts et al.’s (2015) Multicultural and Social Justice Counseling Competencies (MSJCC), specifically understanding the client’s worldview domain. Our focus on Guyanese Americans, an understudied minority group in the United States (Hosler & Kammer, 2018) originating from a country that has been identified as having the world’s highest suicide rate (WHO, 2014), led us to select this method so that we could maintain cognizance of our surroundings, hold respect for the population, and examine participants’ experiences (Haskins et al., 2022; Hays & Singh, 2012; Hays & Wood, 2011).
Participants
Before participants were recruited for the study, IRB approval was obtained from the university with whom Shainna Ali, M. Ann Shillingford, and Lea Herbert are affiliated. Purposive criterion sampling was used to recruit participants, leading to a sample of adults who self-identified as Guyanese American (i.e., either immigrated to the United States themselves or had at least one parent who was born in Guyana). Recruitment materials were shared with Guyanese Americans using counseling listservs (i.e., ACA–AMCD Connect and CESNET) and social media platforms (i.e., LinkedIn, Facebook, and Instagram). Members of the research team contacted all participants using email to share details regarding the study and the informed consent document, collect demographic data, and schedule individual interviews. According to qualitative research, sample size recommendations range from six to 12 participants (Creswell, 2013; Guest et al., 2006; Onwuegbuzie & Leech, 2007). Hence, we sought to recruit 15–20 participants to account for the possibility of attrition.
Our recruitment efforts yielded 73 individuals who expressed interest in the study, 60 of whom met all inclusion criteria and were initially contacted. Forty-three individuals were unable to complete an individual interview due to scheduling conflicts; hence, we secured a total of 30 participants who completed the study. Of this number, 17 participated in individual interviews and a total of 23 individuals participated in a one-time focus group to further clarify data from the individual interviews. It should be noted that 10 of the 23 focus group participants also participated in the individual interview. Further recruitment was deemed unnecessary, as the data analysis reached saturation with data from the individual interviews and focus group. We present demographic data on all participants who engaged in the study, both individual interviews and the focus group (N = 30), in Table 1.
Table 1
Participant Demographic Data
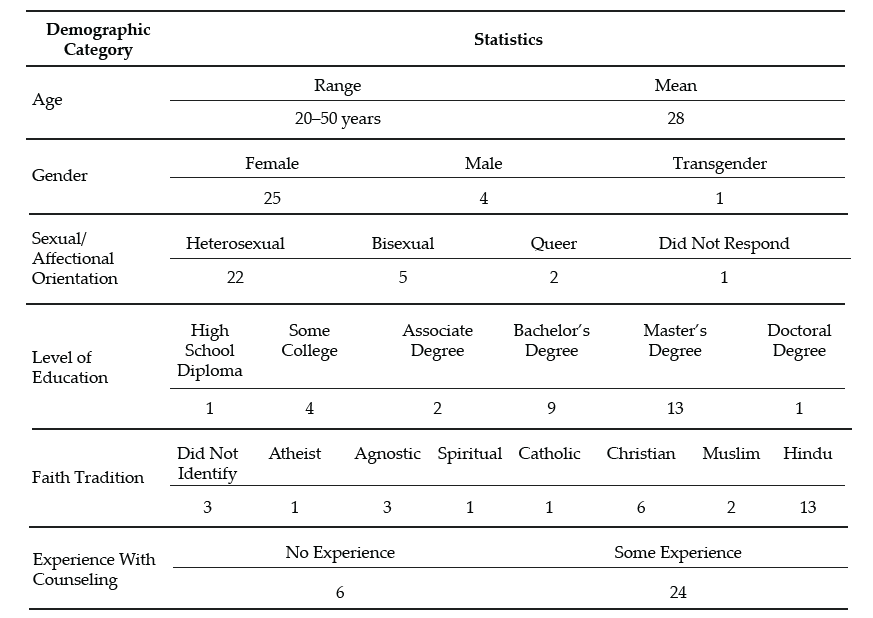
Note. This table provides a breakdown of the demographic characteristics of Guyanese American participants (N = 30).
Data Collection and Analysis
Participants engaged in a semi-structured interview lasting 30–60 minutes, conducted by Ali and Shillingford. Interviews were conducted via Zoom, audio-recorded, and transcribed verbatim. The interview protocol consisted of three primary questions, and sub-questions were used to clarify responses: 1) How do you define mental health?; 2) Who in your life has had experiences with mental health?; and 3) What experiences have you had with mental health? Prior to conducting our study, we included in our IRB documentation that data collection of individual interviews would follow saturation guidelines and that a focus group could be used for further data illumination. Following initial data analysis, we found it necessary to conduct a 1-hour follow-up focus group via Zoom to probe deeper into the data and to allow participants to clarify concepts related to emerging themes. Upon the first round of analysis, it was noted that several participants experienced a shift in perceptions regarding mental health. Focus group probes explored whether participants noticed this shift, what may have contributed to this shift, and when the shift occurred.
After all focus group and individual interviews were transcribed, we used guidelines outlined by Moustakas (1994) to analyze the data. First, we immersed ourselves in the data, reviewing each transcript individually. The transcripts were then divided equally among the four researchers, who read through each to become familiar with the data. With each transcript, we identified relevant statements reflecting participants’ lived experiences (horizontalization) as Guyanese Americans within the contexts of mental health beliefs and experiences.
Following this process, we met multiple times to review all transcripts and confer about the textural descriptions. We identified relevant codes, then synthesized the textural descriptions into themes based on commonalities, distilling the meaning expressed by participants. Then we engaged in reduction and elimination via consensus coding. This process included reading and rereading transcripts together, which followed an iterative process of reviewing the text and code, coding, rereading, and recoding, before determining which thematic content was a new horizon or new dimension of the phenomenon.
After all transcripts were analyzed following this reduction process, clustering and thematizing occurred (i.e., thematic content was clustered into core themes based on participant experiences; Hays & Singh, 2012; Moustakas, 1994). We extracted verbatim examples from the transcripts to generate a thematic and visual description of the phenomenon being examined. After completing the initial data analysis, we conducted member checking by sending each participant their individual transcript as well as the written results section. Participants were requested to provide feedback on the accuracy of their transcripts. Additionally, following the focus group and elucidation of themes all participants were offered an opportunity to member check and clarify the degree to which the results aligned with their lived experiences. The participants did not report any errors; however, clarification was offered by one participant.
Trustworthiness and Positionality
Trustworthiness is a key element of qualitative research in which the research findings accurately reflect the data (Lincoln & Guba, 1985). A critical element of maintaining research credibility is through reflexivity, wherein researchers critically examine procedures employed in relation to power, privilege, and oppression (Hunting, 2014). To safeguard against researcher bias, we worked collaboratively to establish and maintain credibility throughout data collection and analysis processes. Our research team consisted of one Indo-Guyanese American female faculty member, one Afro-Guyanese American female doctoral student, one Black female faculty member, and one Indo-Chinese-Guyanese Canadian male faculty member. All three faculty members belong to CACREP-accredited counselor education programs, and all four researchers have clinical experience working with diverse populations.
To address researcher bias, we engaged in bracketing to minimize the ways in which our experiences influence our approach to research and expectations of the outcomes of the study. Prior to data collection, we discussed our experiences in relation to Guyana, mental health in the Guyanese American community, and our roles as mental health leaders and advocates. We identified our personal experiences, acknowledged our biases, and attempted to bracket while conducting the interviews and focus group. Throughout the data collection and analysis processes, we participated in personal reflection and kept analytic memos documenting our reactions and initial thoughts about the data collected.
Before analyzing the data, we met to confirm analysis procedures, ensuring consistency. We initially analyzed data individually, then determined codes and themes as a team to reduce bias. Throughout the data analysis process, we consulted with each other, addressing questions or concerns related to the data. We also consulted with an outside researcher experienced in qualitative research to obtain critical feedback on the data analysis process and the research findings (Marshall & Rossman, 2006). Our consultant served as an external check of the research methodology and theoretical interpretation of the data.
Findings
The results of the analysis increase understanding of the lived mental health experiences of Guyanese Americans by elucidating perceptions of mental health (Creswell, 2013). All participants shared their beliefs about mental health and the direct and indirect experiences that informed their conceptualization. Three themes surfaced. The first two showed a clear divide in the data: 1) mental health being perceived as negative, stigmatized, elusive, and intimidating; and 2) mental health being perceived as positive, important, helpful, and empowering. It is important to note that these primary themes were not representative of two subsets of participants, and this extracted another theme, which centered on the tendency of participants’ beliefs to transition from negative to positive views of mental health.
The Perception of Mental Health as Negative
When exploring obstacles, subthemes emerged in which hindrances to mental health were acknowledged to exist across three levels: individual, familial, and sociocultural. In parallel, these three subthemes were echoed in the exploration of factors that participants acknowledged have contributed to their mental wellness. The following section explores the primary themes in detail by highlighting the participants’ voices in describing their lived experiences.
Mental Health Concerns Are a Sign of Weakness
All participants in the individual interviews shared that they originally believed that mental health developed out of weakness. This belief was often attributed to minimizing remarks from family members. Oftentimes these comments were paired with other suggestions of how to ameliorate symptoms such as praying more, working harder, or contributing to physical health (e.g., drinking tea). Sharon shared:
It was just like, oh no, you just need to read a book or you just need to go and do something and take your mind off of however it is you’re feeling, like there’s no reason for you to be sad, you have a roof over your head and you’re going to school and you’re doing all of these things, it doesn’t matter. There’s no reason for you to be sad or feel any type of way about anything because we provide everything for you.
Several participants noted that investment in physical wellness was preferable to mental wellness, although physical health was not genuinely prioritized. Participants shared personal and observed maladaptive coping with poor eating habits (i.e., quality and quantity) and excessive substance abuse, namely alcohol. Some participants shared that these tactics were used to manage mental health symptoms or avoidance. Christine shared, “When you’re struggling with things . . . you have nowhere to go to with them except alcohol and the bottom of a rum bottle.” Many participants recognized that coping with alcohol is normalized within the culture. Further, the commonality of these methods normalized consumption and have caused additional issues (e.g., diabetes, heart disease, alcoholism). Arjun noted:
We all have relatives that are kind of stuck on the whole drinking issue. We know a lot of them. They get together with their friends and they “lime,” as we like to call it. They drink in groups and they “gyaff,” they have fun. But it’s a completely different story when they’re by themselves and they’re drinking.
Mental Health Is Taboo
A general consensus was that all participants in the study once believed that mental health was not important and that mental health problems were shameful and not to be discussed. This consistent trend was one of the reasons that we opted to further understand responses through a focus group. Therefore, a direct probe was offered to the focus group participants to explore if they believed discussing mental health was taboo. When delving deeper into these perceptions, participants noted that these thoughts were informed by the beliefs of others and upheld in the wider cultural paradigm. All participants reported that, generally, mental health should not be talked about in order to save face and be respectful. Because mental health issues were seen to be synonymous with weakness, sharing about mental health was equated with the risk of bringing shame to oneself or to one’s family. For example, Chandra shared that “Guyanese people don’t want a kid that’s broken or a little off.” Hence, if someone opts to discuss their mental illness, it is to be done carefully, or secretly.
Most participants shared that typically, when divulging their symptoms, they went to an elder, often a parent, grandparent, or elder sibling, in an effort to keep concerns within the family system. However, many participants noted being minimized or dismissed when sharing their concerns with family members. Ramona explained her feeling that her family
is really strong about, like, don’t be selfish. And I wonder if they would categorize it under that. Like if you’re taking up too much space or time or whatever, you’re trying to center the attention on you or whatever, so that’s a self-serving thing.
A generational rule of discourse emerged from the data. Though the tendency was to keep mental health discussions within the family system, it was also atypical for a younger member to address observed issues with an elder. Several participants noted that this hidden guideline kept informed younger generations from being able to utilize their recognition of warning signs to help the given person and the family system. Arjun shared that as he’s gotten older and has learned more about mental health, he has acquired the courage to address the problems he sees with elders, including his uncle:
I said, “Uncle, what’s wrong?” And he said, “No, nothing is wrong.” But he was crying, you could see tears were streaked on his face, but he wouldn’t talk about it—he wouldn’t say anything. It’s not only one time I saw him, it’s multiple times that I’ve seen him when he has been drinking by himself, that he kind of has the same face all the time. Prior to the times that I asked him, I kind of looked at him and I kind of walked away the first couple of times. Because I was kind of like, this is not something that looked like I should butt in, as a child especially. When you’re younger, your parents tell you, “Mind your business.” Or they say, “You’re not an adult, go with the kids.” So . . . the first couple of times I saw him, I kind of avoided it.
Others Are Not To Be Trusted
Some participants noted that beyond the purpose of family protection, caution to mental health discourse was also due to lack of trust of others. Christine explained: “We had a counseling center on campus, but I was like, ‘Oh, I can’t go talk to anybody,’ because that’s what I was raised with. You don’t talk to strangers about your problems. I had to keep everything inside.” Nevertheless, some families encouraged talking to a religious leader to assist the individual in enhancing devotion and reducing mental health symptoms. Still, regarding professional mental health services, many participants believed, at least at one time, that such services are not helpful, providers are not to be trusted, assistance of that nature is for other (e.g., White) people, and succumbing to that level of desperation is a sign of weakness. When sharing about mistrust in professional mental health assistance, misconceptions and stereotypes surfaced. Ramesh shared:
Oh boy. I have to be honest with you, I feel counseling is, I’ll speak to a shrink and they’ll prescribe drugs to me, like Ritalin or . . . I was like, you know what, I’m better than that. I’m probably totally wrong about it, but that’s just the perception that I have. I’ll be laying on the couch and I’m going to speak into someone and then they’re going to prescribe drugs to me. I don’t want that. I can try to figure this out on myself by talking and trying to do things—positive behavior.
Mental Health Perceived as Positive
All participants in the individual interviews acknowledged a shift in their perceptions of mental health. Their newfound conceptualization included a holistic view of wellness in which mental wellness was seen as an important component to overall well-being and quality of life. In this newer perception, participants acknowledged the ability to consider more variables influencing mental health than they recognized in the past. For example, many participants noted a link between mind and body, versus the previously held notion that physical health is more important than mental health. A few participants noted that mental health can be influenced by genetics, while some noted that it could be influenced by personality, and others noted that it can be influenced by people and the surrounding environment.
All participants, from both the individual interviews and focus group, concurred that everyone feels mental health effects; furthermore, showing signs of a problem is not attributed to weakness. Moreover, because mental health affects everyone, a widespread belief emerged that we all have the responsibility to foster our mental wellness. Additionally, participants shared several examples of what naturally ensued without investing in strategies for mental health such as challenges with emotional regulation, coping, relationships, and worsening mental health problems.
The Transition Between Negative and Positive Perceptions
The transition between old and new conceptualizations of mental health was informed by direct and indirect experiences. All participants shared a transition in beliefs in the individual interviews, and this was explored in the focus group for further clarification. Most participants shared that their personal mental health history informed a change in their beliefs. Many of these participants noted the influence of their healing process, most notably seeking professional help. All participants, from both the individual interviews and the focus group, shared at least one example of learning about mental health by observing another person’s experience. For example, Jessie shared, “Unfortunately, I came from a home of domestic violence . . . I was around maybe six, my dad was bipolar . . . [and] he was just a wife beater. That is probably when I can recall [learning] of mental health.” Another example of learning about mental health from others is captured in Reginald’s comment:
[As] an only child . . . my parents took it upon themselves to [teach me]. . . . It wasn’t like, “Okay, sit down. Let me tell you why these things are.” It was just we’ll be talking about somebody else or going over something that happened and then they’ll explain why, but never directly for me. It was always about other people’s kids.
Many of these individuals emphasized the belief that by paying attention to others, you can learn what is helpful and unhelpful for mental health. Oftentimes this was in their own family; however, extended family and community members were also highlighted. Moreover, a few participants shared their recognition that living with someone who is struggling with their mental health may negatively impact personal wellness (e.g., be triggering). Beyond the family system, some participants noted that exposure to other cultures and perceptions of mental health informed a conceptualization of mental wellness. Seeta shared:
I had friends of other religions or like no religions. And then we would talk about a lot of different things. Like I would ask them questions like, “Oh, so how do things work in your house? Do your parents talk about your God or whatever?” And they’re like, “No.” And I’m like, “So where do your emotions come from?” And they’re like, “Well, you know, we just feel them. Some days I feel angry and some days I feel sad, some days I feel happy.” And I’m just like, “Okay, this is interesting.”
From the quote, it might appear that one’s emotions are in some way connected with God or another higher power; however, this is not something that was observed with other participants of our study. It was more common for participants to share stories of their families using religion as the solution to mental health concerns. For example, Yolanda shared:
My grandmother came when I turned 16 and she kept trying to tell my mom I was showing signs of depression. And my mom was like, “No, she’s like that all the time, like, that’s just how she is.” And my grandma was like, “That’s not normal. You should get her checked out.” And my mom kept saying, “No” and kept denying it. And then my grandma said, “You have to do something.” And then my mom replied, “Oh, I’m going to pray for her.”
In addition to personal experiences and observations of others, participants noted that improved mental health awareness and education prompted them to think critically about their mental health schemas. Ramesh shared:
My education, I always feel like this is what saved me in the end, because I was able to be around other people to know better and to come back home and be like, “Excuse me, this is not how we do things. This is not how we say things. I don’t know what it was like in Guyana.”
Some participants associated this with growing older, and others noted their personal initiative to improve mental health knowledge by following mental health pages on social media, taking a related class, and for some, becoming a part of the mental health field themselves. From this vantage point, many participants were able to equate their previously held notions with beliefs embedded in the culture such as generational rules of respect, gender differences, and the impact of colonialism. Participants, despite their gender differences, noted that within the cultural framework, the rule that mental health should not be discussed is disproportionately applicable to males. Participants shared that this is often due to the perception that it is important for men to be strong, and again, mental illness is a symptom of weakness. This was also linked to the breadwinner role and the pressure to provide for the family. However, this was only noted to have detrimental effects, as anger issues, IPV, and alcoholism were noted to arise out of this rule. Some participants noted that the survival aspect of colonialism may have contributed to the lack of privilege to focus on mental health. In addition, the history of colonialism in Guyana (i.e. slavery, indentured labor) could have informed the lack of trust in professional services.
The change in mental health conceptualization was noted to have benefits beyond the participants themselves. Some participants remarked that the shift in perception was recognized in the wider generation. Ramona reflected:
I will say that a lot of folks from my generation have been a lot more like, “Go to therapy. We should be taking care of our thoughts and our feelings or emotions.” That’s important to you in the same way that if you tore a ligament that you would need to get surgery or do whatever.
Within the newfound conceptualization of mental wellness emerged a vow of social responsibility. All participants, from both the individual interviews and the focus group, shared their intention to help others, and some even noted it as their duty. Ways to help others included advocating for mental health awareness, access, and education; helping to challenge unhelpful cultural beliefs; breaking generational cycles; and protecting others from experiencing similar struggles (e.g., child, sibling).
Discussion
The findings from this study are enlightening, and some are the first to be documented through research, even if they were observed in practice. Initial perceptions of all participants, from both the individual interviews and the focus group, were that mental health is a taboo topic and seeking mental health services is bad. These perceptions stemmed from fear, mistrust, and limited awareness of the benefits of mental health services. This is consistent with findings from Arora and Persaud (2020), who surmised that Guyanese individuals hold negative views of mental health that significantly impact their help-seeking. Furthermore, the findings point to strong familial and sociocultural influences, such as beliefs about mental health, that swayed individual perceptions of mental health, which is in keeping with recent literature on affirming cultural strengths and incorporating familial identity in working with clients of Guyanese descent (Groh et al., 2018; Nicolas et al., 2021).
Discussing issues related to mental health was viewed as a sign of weakness, which translated to help-seeking being a taboo. It would appear that the stigma associated with mental health remains a common experience for Guyanese Americans, and when coupled with limited communication, insufficient funding, and lack of providers, we can see how Nicolas et al. (2021) found this to be concerning. Cultural clash, ethnocentric stereotyping, and cultural incompetency may also be responsible for Guyanese Americans being distrustful of the health care system, leading them to engage in maladaptive behaviors (i.e., avoidance, use of substances, IPV) and not receive the mental health attention and care they need (Arvelo, 2018; Cheng & Robinson, 2013; Jackson et al., 2007).
It appears that even in the face of discrimination and experiences of mental health challenges like alcoholism, depression (Hosler & Kammer, 2018), and IPV (Parekh et al., 2012), leaning on the support of the community serves to buffer against mental health challenges for Guyanese Americans. It also seems that changing mental health perceptions from negative to positive was significantly related to mental health literacy and exposure to other systems such as school, work, and community (i.e., cross-cultural exchange).
Findings that were not previously documented in the literature suggest that an integrated view of wellness enabled participants to augment their negative abstractions of mental health care. These findings serve as an indication that among Guyanese Americans, although mental health has been perceived as negative, weak, and a taboo, the narrative is beginning to shift to make space for mental health awareness, education, access, and functioning, thereby creating unique implications for counselors seeking to meet the needs of this immigrant subgroup.
Implications
In combination with prior literature, the results of this study provide a rationale for mental health counselors, marriage and family counselors, school counselors, and counselor educators to inspire dialogue to foster mental wellness. Based on the findings from this study, when working with Guyanese Americans, counselors should focus on three key strategies to support Guyanese American clients: (a) mental health awareness, (b) mental health education, and (c) mental health experience.
Mental Health Awareness
Participants in this study initially held limited views and awareness of the signs and symptoms of mental health. When awareness was heightened through various means, they were more open to exploring the benefits of services. Counselors can be instrumental in creating awareness by first raising their own awareness pertaining to cultural stigma and its influence on Guyanese Americans’ mental health. For example, unwillingness to attend counseling sessions may be linked to the culturally held perception that discussing mental health, especially beyond the core family system, is taboo. In acknowledging this, counselors can raise awareness of confidentiality, which can be seen as an alignment with the cultural notion that talking about mental health is taboo when it means talking to anyone, and the role of the counselor can be highlighted as a professional collaboration versus communal gossip. Counselors need to be mindful of the collectivistic nature of Guyanese American culture, which causes personal and familial illnesses alike to be perceived as personal problems. Rather than dismiss a client’s concerns about mental health, a counselor can benefit from exploring how the family members’ symptoms, perceptions about mental health, and willingness to adhere to treatment influence the client’s symptoms, perceptions, and commitment to counseling. Further, collectivism spans beyond the protective family system. On one hand, this community orientation can be used to explore a broad range of support, yet on the other hand, depending on the client’s experience, this may also be a widened range of societal pressure (e.g., judgment, criticism, shame).
Mental Health Education
Increased understanding of mental health appeared to have led participants to seek services and resources to increase their mental health literacy, with the hope of improving their well-being. Counselors and counselor educators can be instrumental in offering Guyanese Americans mental health education. To begin, all mental health professionals should demonstrate a posture of cultural humility when engaged in psychoeducation on mental health and wellness for this population. In order to raise awareness through education, mental health professionals are encouraged to model trust, respect, sensitivity, compassion, and a nonjudgmental stance. Within session, counselors should be prepared to offer information regarding early signs of mental illness, compounding factors (e.g., alcohol, suicidal ideation, domestic violence), obstacles (e.g., stigma), and resources. Additionally, counselors may need to offer psychoeducation on the family system, roles, dynamics, beliefs, experiences, and generational patterns that can influence individual mental health. In the event that a family member with mental health problems is unwilling to seek assistance, helping the client to better understand the diagnosis and cope personally can be empowering. Finally, to employ the collectivistic nature of Guyanese American culture, stigma can be confronted, and mental health education can be effectively offered by providing group counseling within this population. Group counseling can offer a variety of therapeutic factors that can benefit Guyanese Americans such as universality, hope, and corrective recapitulation of the primary family group (Yalom & Leszcz, 2005).
Beyond the counseling office, counselors and counselor educators should consider collaborating with culturally supportive organizations. Workshops and information sessions can be tailored to explore and address cultural, religious, ethnic, and generational differences in addition to offering mental health resources (e.g., signs, symptoms, treatment). Several of the participants in our study shared that access to psychology courses in school helped to improve their knowledge about mental health. In addition to these classes continuing to be offered, accessibility to such courses should be expanded. Schools and universities may benefit from offering workshops and other informational sessions to support mental health. Beyond information being offered, a follow-up may be beneficial by linking school or campus counselors in order to connect an improvement in awareness and education to action, change, and health.
Several participants shared that because of a lack of access to mental health education, their knowledge was attained through social media platforms such as Instagram and TikTok. Although the quality of mental health education was not assessed in the present study, the lack of regulation on social platforms could perpetuate misleading, confusing, and stigmatizing misinformation surrounding mental health. Counselor educators should consider their roles beyond the classroom. In addition to empowering counselor trainees to utilize the suggestions above to foster awareness and education, counselor educators can offer responsive and succinct information via social media. Whereas social media is not an appropriate platform for tailored education or services, brief information can be offered to bridge the gap between awareness, education, and access.
Mental Health Experience
Growth in awareness and knowledge around mental health resulted in participants intentionally engaging in positive experiences as a way of resisting past harmful and hurtful practices and generational patterns, reauthoring a new narrative of hope and healing. Being wellness-focused, counselors are uniquely positioned to support this community by facilitating positive experiences impacting overall mental health and well-being.
Counselors can honor clients from this community by creating safe spaces for them to share their narratives without judgment. Counselors can foster healing communities through group counseling, where clients collaboratively share each other’s mental burdens and celebrate successes (Yalom & Leszcz, 2005). Counselors can honor collectivism by encouraging clients to participate in support groups in addition to personal counseling. Counselors and counselor educators can enhance the approachability of counselors by improving their visibility in the community. Examples include a community counselor being involved in outreach with a local cultural center, a school counselor offering mentorship with student clubs, a college counselor guest-speaking at a Guyanese American student organization meeting, or a counselor educator offering tailored workshops for the community.
In addition to the aforementioned implications, we believe that in order for counselors to bridge generational gaps in counselor distrust, counselors must acknowledge the lack of representation of diversity within the profession of counseling, the predominance of Western and European cultural and psychologist-centered curriculum, and lapses in poor bioethics and power dynamics among counselors and marginalized communities (Singh et al., 2020). Next, the specific intersectional impacts suggest counselors must adapt a multicultural orientation and illuminate cultural sensitivity. When a clinician enacts cultural sensitivity in session, clients can examine their perceptions of illness and center their multiple identities (Davis et al., 2018).
Limitations and Future Research
Several limitations that arose from the research process are important to mention. All interviews were conducted virtually. Although secured virtual platforms such as Zoom are considered acceptable for research, lack of face-to-face interviewing may have excluded subtle visual cues and induced video-conferencing fatigue (Spataro, 2020). Though researchers made great attempts to increase participant comfort and review the informed consent before the interview process, it is also plausible that respondents may have censored their responses out of concern for potential breach in confidentiality. A majority of respondents are college-educated, female, first generation, and of Indo-Guyanese descent; hence, the results may not be representative of all Guyanese Americans. Additionally, aligned with phenomenological methods of exploring lived experiences, research prompts were general. Recognizing the concerning statistics surrounding suicide (WHO, 2014), a future study exploring suicidality could be beneficial. Future research might seek to explore a more diverse pool of participants, including diversity in gender, age, ethnicity, and number of years in the United States. To build on the findings from the present study, future studies should explore what factors contribute to Guyanese American mental health as well as what variables may hinder mental wellness. It may also be beneficial to include research from the perspective of children and parents to further understand the influence of family systems and cross-generational norms.
Conclusion
This study highlighted the crucial need to address the mental health literacy of Guyanese Americans. The findings illuminate Guyanese Americans’ perceptions of mental health, including the transition from negative to positive perceptions and its potential influences. Efforts should be made to promote awareness, education, and experience related to mental health awareness for Guyanese Americans. Supporting mental health may help to reduce alarming rates of mental illness in Guyanese Americans and may also have the potential to influence related groups such as Guyanese, American, and Caribbean individuals. Counselors and counselor educators have the potential to play a significant role in supporting these clients by being cognizant and informed about cultural considerations.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
American Counseling Association. (2014). ACA code of ethics. https://www.counseling.org/resources/aca-code-of-ethics.pdf
Arora, P. G., & Persaud, S. (2020). Suicide among Guyanese youth: Barriers to mental health help-seeking and recommendations for suicide prevention. International Journal of School & Educational Psychology, 8(1), 133–145. https://doi.org/10.1080/21683603.2019.1578313
Arvelo, S. D. (2018). Biculturalism: The lived experience of first- and second-generation Guyanese immigrants in the United States (Order No. 10749930) [Doctoral dissertation, Chicago School of Professional Psychology]. ProQuest One Academic. (2027471070).
Baboolal, A. A. (2016). Indo-Caribbean immigrant perspectives on intimate partner violence. International Journal of Criminal Justice Sciences, 11(2), 159–176. https://www.researchgate.net/publication/336926774_Indo-Caribbean_Immigrant_Perspectives_on_Intimate_Partner_Violence
Buchholz, K. (2022, November 11). The world’s biggest diasporas [Infographic]. Forbes. https://www.forbes.com/sites/katharinabuchholz/2022/11/11/the-worlds-biggest-diasporas-infographic/?sh=4185fd634bde
Cavalcanti, H. B., & Schleef, D. (2001). Cultural loss and the American dream: The immigrant experience in Barry Levinson’s Avalon. Journal of American and Comparative Cultures, 24(3–4), 11–22.
https://doi.org/10.1111/j.1537-4726.2001.2403_11.x
Cheng, T. C., & Robinson, M. A. (2013). Factors leading African Americans and Black Caribbeans to use social work services for treating mental and substance use disorders. Health & Social Work, 38(2), 99–109. https://doi.org/10.1093/hsw/hlt005
Creswell, J. W. (2013). Qualitative inquiry and research design: Choosing among five approaches (3rd ed.). SAGE.
Davis, D. E., DeBlaere, C., Owen, J., Hook, J. N., Rivera, D. P., Choe, E., Van Tongeren, D. R., Worthington, E. L., Jr., & Placeres, V. (2018). The multicultural orientation framework: A narrative review. Psychotherapy, 55(1), 89–100. https://doi.org/10.1037/pst0000160
Forte, A., Trobia, F., Gualtieri, F., Lamis, D. A., Cardamone, G., Giallonardo, V., Fiorillo, A., Girardi, P., & Pompili, M. (2018). Suicide risk among immigrants and ethnic minorities: A literature overview. International Journal of Environmental Research and Public Health, 15(7), 1–21. https://doi.org/10.3390/ijerph15071438
Groh, C. J., Anthony, M., & Gash, J. (2018). The aftermath of suicide: A qualitative study with Guyanese families. Archives of Psychiatric Nursing, 32(3), 469–474. https://doi.org/10.1016/j.apnu.2018.01.007
Guest, G., Bunce, A., & Johnson, L. (2006). How many interviews are enough? An experiment with data saturation and variability. Field Methods, 18(1), 59–82. https://doi.org/10.1177/1525822X05279903
Haskins, N. H., Parker, J., Hughes, K. L., & Walker, U. (2022). Phenomenological research. In S. V. Flynn (Ed.), Research design for the behavioral sciences: An applied approach (pp. 299–325). Springer.
Hays, D. G., & Singh, A. A. (2012). Qualitative inquiry in clinical and educational settings. Guilford.
Hays, D. G., & Wood, C. (2011). Infusing qualitative traditions in counseling research designs. Journal of Counseling & Development, 89(3), 288–295. https://doi.org/10.1002/j.1556-6678.2011.tb00091.x
Heron, M. (2021). Deaths: Leading causes for 2019. National Vital Statistics Reports, 70(9), 1–113. https://doi.org/10.15620/cdc:107021
Hosler, A. S., & Kammer, J. R. (2018). A comprehensive health profile of Guyanese immigrants aged 18–64 in Schenectady, New York. Journal of Immigrant and Minority Health, 20(4), 972–980.
https://doi.org/10.1007/s10903-017-0613-5
Hosler, A. S., Kammer, J. R., & Cong, X. (2019). Everyday discrimination experience and depressive symptoms in urban Black, Guyanese, Hispanic, and White adults. Journal of the American Psychiatric Nurses Association, 25(6), 445–452. https://doi.org/10.1177/1078390318814620
Hunting, G. (2014). Intersectionality-informed qualitative research: A primer. The Institute for Intersectionality Research and Policy. https://nanopdf.com/download/intersectionality-informed-qualitative-research-a-primer-gemma-hunting_pdf
Indo-Caribbean Alliance, Inc. (2014, February 3). Population analysis of Guyanese and Trinidadians in NYC.
https://www.indocaribbean.org/blog/population-analysis-of-guyanese-and-trinidadians-in-nyc
Jackson, J. S., Neighbors, H. W., Torres, M., Martin, L. A., Williams, D., & Baser, R. (2007). Use of mental health services and subjective satisfaction with treatment among Black Caribbean immigrants: Results from the National Survey of American Life. American Journal of Public Health, 97(1), 60–67. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1716231/
Lincoln, Y. S., & Guba, E. G. (1985). Naturalistic inquiry. SAGE.
Marshall, C., & Rossman, G. B. (2006). Designing qualitative research (4th ed.). SAGE.
Moustakas, C. (1994). Phenomenological research methods. SAGE.
Nicolas, G., Dudley-Grant, G. R., Maxie-Moreman, A., Liddell-Quintyn, E., Baussan, J., Janac, N., & McKenny, M. (2021). Psychotherapy with Caribbean women: Examples from USVI, Haiti, and Guyana. Women & Therapy, 44(1–2), 136–155. https://doi.org/10.1080/02703149.2020.1775993
One World Nations Online. (n.d.). Guyana. https://www.nationsonline.org/oneworld/guyana.htm
Onwuegbuzie, A. J., & Leech, N. L. (2007). A call for qualitative power analyses. Quality & Quantity, 41, 105–121. https://doi.org/10.1007/s11135-005-1098-1
Parekh, K. P., Russ, S., Amsalem, D. A., Rambaran, N., Langston, S., & Wright, S. W. (2012). Prevalence of intimate partner violence in patients presenting with traumatic injuries to a Guyanese emergency department. International Journal of Emergency Medicine, 5(1), 1–5. https://doi.org/10.1186/1865-1380-5-23
Ratts, M. J., Singh, A. A., Nassar-McMillan, S., Butler, S. K., & McCullough, J. R. (2015). Multicultural and social justice counseling competencies. American Counseling Association. https://www.counseling.org/docs/default-source/competencies/multicultural-and-social-justice-counseling-competencies.pdf
Singh, A. A., Appling, B., & Trepal, H. (2020). Using the Multicultural and Social Justice Counseling Competencies to decolonize counseling practice: The important roles of theory, power, and action. Journal of Counseling & Development, 98(3), 261–271. https://doi.org/10.1002/jcad.12321
Spataro, J. (2020). The future of work—the good, the challenging & the unknown. https://www.microsoft.com/en-us/microsoft-365/blog/2020/07/08/future-work-good-challenging-unknown/
Statimetric. (2022). Distribution of Guyanese people in the US. https://www.statimetric.com/us-ethnicity/Guyanese
United States Census Bureau. (2019). People reporting ancestry: American community survey. http://bit.ly/42RazKC
Williams, D. R., Yu, Y., Jackson, J. S., & Anderson, N. B. (1997). Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of Health Psychology, 2(3), 335–351.
https://doi.org/10.1177/135910539700200305
World Health Organization. (2014). First WHO report on suicide prevention. https://www.who.int/news/item/04-09-2014-first-who-report-on-suicide-prevention
World Population Review. (2023). Suicide rate by country 2023. https://worldpopulationreview.com/country-rankings/suicide-rate-by-country
Yalom, I. D., & Leszcz, M. (2005). The theory and practice of group psychotherapy (5th ed.). Basic Books.
Shainna Ali, PhD, NCC, ACS, LMHC, is the owner of Integrated Counseling Solutions. John J. S. Harrichand, PhD, NCC, ACS, CCMHC, CCTP, LMHC, LPC-S, is an assistant professor at The University of Texas at San Antonio. M. Ann Shillingford, PhD, is an associate professor at the University of Central Florida. Lea Herbert is a doctoral student at the University of Central Florida. Correspondence may be addressed to Shainna Ali, 3222 Corrine Drive, Orlando, FL 32803, hello@drshainna.com.
May 10, 2023 | Volume 13 - Issue 1
Warren Wright, Jennifer Hatchett Stover, Kathleen Brown-Rice
Racial trauma has become a common topic of discussion in professional counseling. This concept is also known as race-based traumatic stress, and it addresses how racially motivated incidents impede emotional and mental health for Black, Indigenous, and people of color (BIPOC). Research about this topic and strategies to reduce its impact are substantial in the field of psychology. However, little research about racial trauma has been published in the counseling literature. The intent of this paper is to provide an in-depth perspective of racial trauma and its impact on BIPOC to enhance professional counselors’ understanding. Strategies for professional counselors to integrate into their clinical practice are provided. In addition, implications for counselor supervisors and educators are also provided.
Keywords: racial trauma, BIPOC, counseling, professional counselors, clinical practice
The impact of racism on the psychological, emotional, and physical well-being of those subjected to it is no secret. In fact, the Centers for Disease Control and Prevention (2021) has declared racism as a public health issue and threat to the health of minoritized individuals. Similarly, the Federal Bureau of Investigation (2019) reported that 5,155 people were targets of racially motivated hate crimes in 2018: 47.1% of the victims identified as Black/African American, 13% as Hispanic/Latino, 4.1% as American Indian/Alaskan Native, and 3.4% as Asian. Daily experiences of racism for Black, Indigenous, and people of color (BIPOC) can lead to an increase in health complications and mental health disparities (French et al., 2020; Williams et al., 2019). Hemmings and Evans (2018) noted that because of racism, BIPOC communities have limited access to resources, which impacts their quality of education and health care. Thus, racially marginalized communities are susceptible to chronic illnesses and mental health concerns such as diabetes, heart disease, depression, and suicide (Hemmings & Evans, 2018). Furthermore, researchers have found that exposure to racism and discrimination increases levels of stress in the body and can lead to chronic illnesses such as high blood pressure, diabetes, and gastrointestinal issues for people of color (Bernier et al., 2021; Chavez-Dueñas et al., 2019; Smith et al., 2011; Wagner et al., 2015), therefore adversely impacting the livelihood and overall well-being of BIPOC communities.
Racism-related stressors can lead to race-based traumatic stress, also known as racial trauma (Carter, 2007; Comas-Díaz et al., 2019). Racial trauma and race-based traumatic stress occur when there is an experience of direct or indirect racism that leads to psychological and emotional injury for BIPOC. Examples include experiencing microaggressions in the workplace (Sue et al., 2019), witnessing an unarmed Black person being killed by law enforcement (Williams et al., 2018), and being physically attacked because others believe a person’s racialized group is the cause of a global pandemic (e.g., Asian American and Pacific Islanders [AAPIs]; Litam, 2020). There is a substantial amount of literature in the field of psychology related to racism, race-based traumatic stress, and racial trauma (Adames et al., 2023; Bryant-Davis & Ocampo, 2006; Carter, 2007; Comas-Díaz et al., 2019; French et al., 2020; Helms et al., 2010; Mosley et al., 2021). However, there is little to no research in the counseling profession related to racial trauma. Therefore, this article provides an overview of racial trauma and implications for the counseling profession.
Race-Based Traumatic Stress and Racial Trauma
Racial trauma is the collective stress experienced by BIPOC directly or indirectly due to continuous racially motivated incidents of microaggressions, exclusion, discrimination, and sociopolitical events that create psychological and emotional harm (Anderson & Stevenson, 2019; Comas-Díaz et al., 2019). Race-based traumatic stress is one of the most common interchangeable terms for racial trauma and refers to the stress response and emotional injury that occur after experiencing a racist encounter (Carter, 2007; Williams et al., 2018). Carter (2007), along with other researchers (Chavez-Dueñas et al., 2019; Helms et al., 2010; Smith et al., 2007, 2016), examined the experiences of BIPOC and the accompanying psychological stress when they experience racism-related incidents. Constant exposure to racially motivated incidents can create and lead to an overwhelming emotional stress response for BIPOC. Bryant-Davis and Ocampo (2005), Hemmings and Evans (2018), and Litam (2020) discussed how racist incidents of physical assaults, verbal attacks, and threats to one’s safety impact a person’s sense of self and can cause a person to present with symptoms of trauma.
It is imperative to note that experiencing racism and presentation of trauma symptoms are not all life threatening. Therefore, racial trauma differs from the traditional diagnosable PTSD criteria as stated in the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association [APA], 2013). Although it is not explicitly stated in the DSM-5, racial trauma encompasses racism-related stressors associated with one’s membership in a racialized social group, historical trauma, and continuous exposure to racism-related violence. Consequently, conceptualizing and diagnosing a client that presents to counseling with trauma symptomology that does not fit the criteria for the PTSD diagnosis can be confusing for mental health professionals. Therefore, it is important for professional mental health counselors to be prepared to assess and treat clients who present to counseling with trauma symptomology related to racist incidents.
Impact of Racism and Racial Trauma
Racial trauma could impact a person’s sense of self, pride in culture, and identity (Brown-Rice, 2013; Skewes & Blume, 2019). Skewes and Blume (2019) found that assimilation, exploitation, and forced relocation led to the loss of spiritual and cultural practices for American Indian and Alaska Native (AI/AN) communities. Additionally, Brown-Rice (2013) stated that loss of cultural traditions and native practices creates a sense of confusion and hopelessness for Native American adults. Thus, racialized trauma can lead to a separation of cultural identity and practices. Similarly, Chavez-Dueñas and colleagues (2019) found that racial trauma has increased psychological distress for Latinx immigrant communities because of anti-immigration policies, opposition to assimilation into the American culture, and fear of deportation. Furthermore, racial trauma can lead to psychological concerns such as anxiety, depression, emotional dysregulation, and suicidal ideation (American Foundation for Suicide Prevention, 2020; Bryant-Davis & Ocampo, 2005; Comas-Díaz et al., 2019; French et al., 2020; Hemmings & Evans, 2018). Additionally, the American Foundation for Suicide Prevention (2020) found suicide rates for minoritized communities have increased. Moreover, racial discrimination has been positively correlated with suicidal ideation among African American young adults (American Foundation for Suicide Prevention, 2020).
Racism is consistently prevalent within American schools and continues to be an issue of concern experienced by BIPOC students (Kohli et al., 2017; Merlin, 2017). The experience of trauma coupled with racism and discriminatory practices in education has shown to impart racial disparities among BIPOC students in the areas of academic achievement, employment, and participation in the criminal justice system (Lebron et al., 2015). Black students are underrepresented in advanced courses, are less likely to be college ready, and spend less time in the classroom because of disciplinary practices (United Negro College Fund, 2020). According to a report on school discipline by the U.S. Department of Education Office for Civil Rights (2018), Black students only account for 18% of preschool enrollment, yet they make up 42% of total suspensions and 3 times more expulsions than their White peers. In addition, Black students are more than twice as likely to be referred to law enforcement and subject to arrest for school-based incidents when compared to their peers (United Negro College Fund, 2020). Furthermore, not only are Black students underrepresented in advanced courses, but they are overrepresented in special education programs and more likely to be identified with a disability (Harper, 2017). Therefore, it is imperative for professional mental health counselors to understand how racial trauma could impact the mental health and well-being of individuals at distinct phases of life span development (e.g., children, college students, etc.).
Currently, racial trauma has been exacerbated by the recent COVID-19 pandemic plaguing the United States and other parts of the world. Liu and Modir (2020) and Fortuna et al. (2020) highlighted the lived experiences within BIPOC communities regarding living in low-income neighborhoods, denial of access to care, and being disproportionately affected by the COVID-19 virus. Black Americans accounted for 34% of confirmed cases in the United States, followed by Latinos at 20%–25% of cases (Fortuna et al., 2020). This demonstrates that health disparities coupled with racism could impact the physical well-being of BIPOC. Racism-related stress impacts the emotional and physical health of BIPOC communities. This includes sense of self (Chavez-Dueñas et al., 2019), culture identity (Skewes & Blume, 2019), and overall wellness (Litam, 2020). Healing racial trauma requires professional mental health counselors working with BIPOC individuals to consider sociocultural factors such as systemic racism, oppression of marginalized communities, and cultural trauma.
Implications for Professional Counselors
The counseling profession highlights the importance of assessment competency as stated in the American Counseling Association (ACA) Code of Ethics (ACA, 2014; e.g., Standard E.5.c: Historical and Social Prejudices in the Diagnosis of Pathology) and the 2016 Council for Accreditation of Counseling and Related Educational Programs (CACREP, 2015) Standards (e.g., Assessment and Testing). In addition, the 2016 CACREP standards emphasized the importance of social and cultural diversity, highlighting strategies and techniques to identify and eliminate barriers of oppression and discrimination (CACREP, 2015). Because racial trauma is invasive and harmful for BIPOC individuals and communities, understanding its impact on psychological and emotional well-being is imperative for all mental health professionals in their respective roles. Thus, counselors must be prepared to provide culturally responsive care to BIPOC individuals who have experienced racism-related trauma.
Licensed Professional Mental Health Counselors
Assessing for racial trauma is of utmost importance when conceptualizing and creating a treatment plan for BIPOC clients. It is imperative for counselors to become familiar with assessments and clinical interventions to inform their approach to treating racial trauma. Williams and colleagues (2018) proposed the UConn Racial/Ethnic Stress and Trauma Survey (UnRESTS) to assist mental health professionals in their case conceptualizations and treatment planning when racial trauma is present in BIPOC individuals. The UnRESTS is a clinician-administered semi-structured interview that is beneficial in case conceptualization to determine the multiple experiences of racism for the client. The interview comprises 6 sections: introduction of the interview, racial and ethnic identity development, experiences of direct overt racism, experiences of racism by loved ones, experiences of vicarious racism, and experiences of covert racism (Williams et al., 2018). Even though this survey is like the DSM-5 Cultural Formulations Interview (APA, 2013) and helps the counselor determine if the client’s symptomology fits criteria for PTSD, it should not be the only assessment tool used to determine a diagnosis of PTSD. Additionally, this interview tends to be lengthy in time; therefore, counselors should consider completing this interview within the first and second sessions. This assessment along with other clinical approaches could be beneficial to understanding the traumatic responses of clients impacted by racism.
Several BIPOC scholars have offered models, theories, and frameworks to heal racial trauma (Adames et al., 2023; Bryant-Davis & Ocampo, 2006; French et al., 2020; Mosley et al., 2021). Counselors must position themselves to consider approaches that go beyond Eurocentric theories and models when addressing and treating racial trauma. These include being critical of sociopolitical structures, awareness of one’s own racial identity, and comfort level when broaching the topic of racism and racial trauma (Adames et al., 2023; Thrower et al., 2020). For instance, Bryant-Davis and Ocampo (2006) provided a foundation for treating racial trauma in a safe environment. Their therapeutic approach included acknowledgment, grieving/mourning loss, analyzing internalized shame and racism, and centering coping and resistance strategies. Supporting clients to name oppressive systems, process their experiences of racist incidents, and deconstruct self-blame narratives because of racism fosters liberation and healing for BIPOC clients who have experienced racism-related stress and trauma (Adames et al., 2023). Thus, counselors must be empathetic and take initiative in helping BIPOC clients shift the focus on harm from self-blame to external oppressive factors. This promotes a strong sense of self and healthy living for BIPOC clients.
Similarly, models offered by Chavez-Dueñas et al. (2019), French et al. (2020), Mosley et al. (2021), and Adames et al. (2023) center the well-being and collective power of BIPOC communities. For example, critical consciousness, Black Psychology, Liberation Psychology, and trauma-informed care influenced these approaches to address racism-related stress and trauma. Subsequently, French and colleagues’ (2020) Radical Healing Framework centers justice and overall wellness for BIPOC communities. This is the intentional practice of going beyond just coping with racism to focus on healing wherein a client can thrive by connecting to community and engaging in resistance against racism-related stressors (French et al., 2020). Thus, helping clients to engage in activism and utilize microinterventions to disarm and address microaggressions can empower clients (Mosley et al., 2021; Sue et al., 2019). Microinterventions help equip clients with tools they can implement to assert boundaries and communicate disagreement with microaggressions (Litam, 2020; Sue et al., 2019). However, counselors must remember that safety is a priority when supporting clients in confronting perpetrators of racism-related trauma (Litam, 2020). Therefore, role-plays in counseling sessions could provide the space and time to strategize when it is and is not appropriate to confront perpetrators of microaggressions.
Utilizing these approaches with clients fosters validation and affirmation of their experiences. Failure to acknowledge and attend to the symptoms and experiences of racism-related stress and trauma can maintain psychological distress for BIPOC clients (Chavez-Dueñas et al., 2019). Furthermore, helping clients process the positive messages they received about their racial identity throughout their life can reinforce these approaches (Anderson & Stevenson, 2019). Thus, counselors should use a strength-based approach when supporting BIPOC clients in healing from racism-related stress and trauma. In addition, consultation with colleagues, supervisors, and counselor educators can provide support and a space to implement best practices to provide the most effective care for BIPOC individuals who have experienced racial trauma, rendering positive mental health outcomes.
Professional School Counselors
Professional school counselors should demonstrate cultural competence and serve as essential stakeholders in identifying and supporting clients impacted by trauma (ACA, 2014; American School Counselor Association [ASCA], 2016; Parikh-Foxx et al., 2020). ASCA specifies these responsibilities and obligations in their ASCA Ethical Standards for School Counselors (ASCA, 2022). These principles serve as a framework in which professional values, norms, and behaviors are referenced. Further, school counselors can help to identify, respond to, and prevent incidents of racism and bias, as well as become resources to help promote systemic change and advocate for social justice within the educational setting (ASCA, 2020). However, ASCA (2021) recognizes the lack of racial literacy and the inherent gaps between racial equity and equality within education, petitioning for school counselors to continually pursue cultural competency and work toward mitigating the negative effects of racism and bias. Subsequently, ASCA guidelines encourage school counselors to examine their own biases and consult with community professionals to engage in immersive experiences and provide support to students and families who have experienced racial trauma or have been negatively impacted by racism (ASCA, 2021; Atkins & Oglesby, 2019; Levy & Adjapong, 2020).
As facilitators of change, school counselors can help to create environments that are safe and inclusive for both students and educators. One approach is to discuss issues of racial trauma using trauma-informed and restorative practices (National Child Traumatic Stress Network [NCTSN], 2018). Trauma-informed practices take on a phenomenological approach, seeking to identify, understand, and address the meaning behind student behaviors and experiences (Steane, 2019). Additionally, restorative practices not only provide an alternative to harsh disciplinary practices, but also create spaces for individuals to share their own perspectives without fear of judgement or ridicule, while being open to listening and validating the values, experiences, and perspectives of others (NCTSN, 2018; United Negro College Fund, 2020). Moreover, Anderson and Stevenson (2019) posited the concept of racial socialization, which is the intentional communication about the system of racism, racial identity, and experiences between parents and their children and others within the family system with similar racial and ethnic identities. Racial socialization aids in the development of a positive sense of self and cultural identity as mitigating forces to racial trauma. Further, the Racial Encounter Coping Appraisal and Socialization Theory (RECAST) helps families and youth prepare for, discuss, and respond to racially stressful experiences appropriately (Anderson & Stevenson, 2019). Thus, this can also prepare students to strategize how to respond to incidents of racism in the school environment.
It is evident that incidents of school-based racism are perpetuated by several factors and continue to negatively impact student performance and affect the health and well-being of BIPOC students (Kohli et al., 2017). The implementation of culturally responsive pedagogy can be used to mitigate this impact, increase academic success, and help students maintain cultural integrity (Ladson-Billings, 1995; Lebron et al., 2015). Counseling professionals can support this effort by engaging in training and professional development to understand racism and its impact on culturally diverse students and by facilitating necessary discussions that help to equip stakeholders with tools to adequately address discrimination, racism, and race-based trauma (NCTSN, 2018; Pietrantoni, 2017).
Counselor Supervisors
The ACA Code of Ethics (2014; e.g., Section F: Supervision, Teaching, and Training) highlights the importance of counselor supervision for the development of counselors seeking licensure as independent mental health practitioners. Additionally, counselor supervision enhances a supervisee’s knowledge, skills, and ability to work with diverse clients (ACA, 2014). Therefore, counselor supervisors and their supervisees should be aware of racial trauma and the effects it could have on BIPOC clients. Pieterse (2018) posited guidelines and considerations for supervisors to follow when attending to racial trauma concerns in clinical supervision. Specifically, supervisors must be reflective of their own racial identity, understand how to assess for racial trauma, and implement effective clinical interventions for their supervisees’ clients impacted by racial trauma (Pieterse, 2018).
Additionally, understanding the concept of racial trauma in the larger context of historical trauma for BIPOC communities creates a learning environment for supervisees to deepen their knowledge of racial trauma (Comas-Díaz, 2000; French et al., 2020; Pieterse, 2018). For example, educating supervisees on historical depictions of racism-related stress and trauma for BIPOC communities, such as internment camps, chattel slavery, and colonization, provides the historical context of psychological wounds impacting BIPOC communities in present day by way of intergenerational trauma (Comas-Díaz et al., 2019; Nagata et al., 2019). Furthermore, clinical supervisors can role-play in supervision meetings with their supervisees to model helping clients process racist-related incidents, assessing for psychological distress, and empowering clients to practice effective coping and resistant strategies (Pieterse, 2018), thus ensuring supervisors’ awareness of multiculturalism and diversity in the supervisory relationship (ACA, 2014; e.g., Section F.2.b.: Multicultural Issues/Diversity in Supervision). It is critical for counselor supervisors to obtain the knowledge, skills, and abilities to best prepare counselor supervisees in addressing and treating racial trauma concerns.
Counselor Educators
Moh and Sperandio (2022) urged the counseling profession to integrate trauma-informed curricula to best prepare counselors-in-training (CITs) to respond effectively to trauma concerns caused by systemic racism in the United States. However, there is hesitancy for counselor educators to teach CITs about racial trauma (VanAusdale & Swank, 2020). Specifically, counselor educators have reported a lack of knowledge and limited ability to teach CITs about racial trauma (VanAusdale & Swank, 2020), futher highlighting the need for trauma-informed curricula to be adopted in the counselor profession to best prepare counselors and educators to address the needs of those impacted by racial trauma. In addition, counselor educators’ lack of knowledge in trauma-informed care and racial trauma does not help prepare future CITs to address this concern once they have graduated from their respective counselor education programs, consequently leading to racial trauma concerns going unaddressed and deepening the wounds of racial trauma for BIPOC (Bryant-Davis & Ocampo, 2005; Comas-Díaz, 2000; Helms, et al., 2010).
However, counselor educators can find creative ways to implement racial trauma education into the classroom. For example, counselor educators can include required readings from BIPOC scholars in their classes that contribute to the racial trauma literature (e.g., Anderson & Stevenson, 2019; French et al., 2020; Mosley et al., 2021). Additionally, counselor educators can demonstrate how to implement the UnRESTS (Williams et al., 2018) for CITs in practicum and internship courses who are practicing conducting clinical interviews. Furthermore, counselor educators can introduce CITs to theories that go beyond the Eurocentric tradition. For example, the first author of this article, Warren Wright, was introduced to queer theory, critical theory, and critical race theory in his master’s-level multicultural counseling (formerly cross-cultural counseling) course. As a student, Wright was assigned to write a social justice and advocacy paper, in which he utilized critical race theory to discuss how adolescents’ responses to experiencing racism in K–12 education could present as behavioral and emotional dysregulation. To mitigate this concern, Wright created an after-school program that utilized dance movement therapy (i.e., stepping) to help Black adolescent males with emotional regulation, personal development, and academic excellence. This approach is an example of a trauma-informed and responsive practice that could reduce harsh disciplinary referrals and increase Black students’ socioemotional development (Stover et al., 2022). If counselor educators feel inadequate to teach trauma counseling or trauma-informed practices, they should seek additional training and consultation to increase their awareness, knowledge, and skills about trauma-informed curricula and approaches (Moh & Sperandio, 2022).
Conclusion
The aim of this article is to provide an understanding of racial trauma and its impact on the psychological and emotional well-being of BIPOC communities and provide recommendations for the counseling profession. Intentional practices, strategies, and approaches are needed to help reduce the impact of racial trauma experienced by BIPOC individuals and communities. Therefore, it is imperative for CITs, licensed professional mental health counselors, school counselors, counselor educators, and supervisors to be well-equipped to address racial trauma concerns. Failure of the counseling profession to address racial trauma concerns deepens the psychological and emotional injuries of racial trauma. Therefore, curricula for CITs should be adapted to best prepare the next generation of counselors to aid with and mitigate the lasting impacts of racially motivated trauma inflicted on BIPOC individuals and communities.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Adames, H. Y., Chavez-Dueñas, N. Y., Lewis, J. A., Neville, H. A., French, B. H., Chen, G. A., & Mosley, D. V. (2023). Radical healing in psychotherapy: Addressing the wounds of racism-related stress and trauma. Psychotherapy, 60(1), 39–50. https://doi.org/10.1037/pst0000435
American Counseling Association. (2014). ACA code of ethics. https://www.counseling.org/resources/aca-code-of-ethics.pdf
American Foundation for Suicide Prevention. (2020). Suicide statistics. https://afsp.org/suicide-statistics
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
American School Counselor Association. (2016). The school counselor and trauma-informed practice. ASCA Position Statements. https://www.schoolcounselor.org/Standards-Positions/Position-Statements/ASCA-Position-Statements/The-School-Counselor-and-Trauma-Informed-Practice
American School Counselor Association. (2020). Eliminating racism and bias in schools: The school counselor’s role. School Counseling Standards in Practice. https://www.schoolcounselor.org/getmedia/542b085a-7eda-48ba-906e-24cd3f08a03f/SIP-Racism-Bias.pdf
American School Counselor Association. (2021). The school counselor and anti-racist practices. ASCA Position Statements. https://www.schoolcounselor.org/Standards-Positions/Position-Statements/ASCA-Position-Statements/The-School-Counselor-and-Anti-Racist-Practices
American School Counselor Association. (2022). ASCA ethical standards for school counselors. https://www.schoolcounselor.org/getmedia/44f30280-ffe8-4b41-9ad8-f15909c3d164/EthicalStandards.pdf
Anderson, R. E., & Stevenson, H. C. (2019). RECASTing racial stress and trauma: Theorizing the healing potential of racial socialization in families. American Psychologist, 74(1), 63–75.
https://doi.org/10.1037/amp0000392
Atkins, R., & Oglesby, A. (2019). Interrupting racism: Equity and social justice in school counseling. Routledge.
Bernier, R. A., Venkatesan, U. M., Soto, J. A., Rabinowitz, A. R., Hong, J. S., & Hillary, F. G. (2021). Perceived discrimination and blood pressure in individuals aging with traumatic brain injury. Rehabilitation Psychology, 66(2), 148–159. https://doi.org/10.1037/rep0000379.supp (Supplemental).
Brown-Rice, K. (2013). Examining the theory of historical trauma among Native Americans. The Professional Counselor, 3(3), 117–130. https://doi.org/10.15241/kbr.3.3.117
Bryant-Davis, T., & Ocampo, C. (2005). Racist incident-based trauma. The Counseling Psychologist, 33(4), 479–500. https://doi.org/10.1177/0011000005276465
Bryant-Davis, T., & Ocampo, C. (2006). A therapeutic approach to the treatment of racist-incident-based trauma. Journal of Emotional Abuse, 6(4), 1–22. https://doi.org/10.1300/J135v06n04_01
Carter, R. T. (2007). Racism and psychological and emotional injury: Recognizing and assessing race-based traumatic stress. The Counseling Psychologist, 35(1), 13–105. https://doi.org/10.1177/0011000006292033
Centers for Disease Control and Prevention. (2021, April 8). Media statement from CDC Director Rochelle P. Walensky, MD, MPH, on racism and health. https://www.cdc.gov/media/releases/2021/s0408-racism-health.html
Chavez-Dueñas, N. Y., Adames, H. Y., Perez-Chavez, J. G., & Salas, S. P. (2019). Healing ethno-racial trauma in Latinx immigrant communities: Cultivating hope, resilience, and action. American Psychologist, 74(1), 49–62. https://doi.org/10.1037/amp0000289
Comas-Díaz, L. (2000). An ethnopolitical approach to working with people of color. American Psychologist, 55(11), 1319–1325. https://doi.org/10.1037/0003-066X.55.11.1319
Comas-Díaz, L., Hall, G. N., & Neville, H. A. (2019). Racial trauma: Theory, research, and healing: Introduction to the special issue. American Psychologist, 74(1), 1–5. https://doi.org/10.1037/amp0000442
Council for Accreditation of Counseling and Related Educational Programs. (2015). 2016 CACREP standards. http://www.cacrep.org/wp-content/uploads/2017/08/2016-Standards-with-citations.pdf
Federal Bureau of Investigation. (2019). 2018 hate crime statistics. https://ucr.fbi.gov/hate-crime/2018/topic-pages/victims.pdf
Fortuna, L. R., Tolou-Shams, M., Robles-Ramamurthy, B., & Porche, M. V. (2020). Inequity and the disproportionate impact of COVID-19 on communities of color in the United States: The need for a trauma-informed social justice response. Psychological Trauma: Theory, Research, Practice, and Policy, 12(5), 443–445. https://doi.org/10.1037/tra0000889
French, B. H., Lewis, J. A., Mosley, D. V., Adames, H. Y., Chavez-Dueñas, N. Y., Chen, G. A., & Neville, H. A. (2020). Toward a psychological framework of radical healing in communities of color. The Counseling Psychologist, 48(1), 14–46. https://doi.org/10.1177/0011000019834506
Harper, K. (2017). The school-to-prison pipeline: The intersections of students of color with disabilities. Child Trends. https://www.childtrends.org/publications/school-prison-pipeline-intersections-students-color-disabilities
Helms, J. E., Nicolas, G., & Green, C. E. (2010). Racism and ethnoviolence as trauma: Enhancing professional training. Traumatology, 16(4), 53–62. https://doi.org/10.1177/1534765610389595
Hemmings, C., & Evans, A. M. (2018). Identifying and treating race-based trauma in counseling. Journal of Multicultural Counseling and Development, 46(1), 20–39. https://doi.org/10.1002/jmcd.12090
Kohli, R., Pizarro, M., & Nevárez, A. (2017). The “new racism” of K-12 schools: Centering critical research on racism. Review of Research in Education, 41, 182–202. http://www.jstor.org/stable/44668692
Ladson-Billings, G. (1995). But that’s just good teaching! The case for culturally relevant pedagogy. Theory into Practice, 34(3), 159–165. https://www.jstor.org/stable/1476635
Lebron, D., Morrison, L., Ferris, D., Alcantara, A., Cummings, D., Parker, G., & McKay, M. (2015). Facts matter! Black lives matter! The trauma of racism. http://mcsilver.nyu.edu/sites/default/files/reports/Trauma-of-Racism-Report.pdf
Levy, I. P., & Adjapong, E. S. (2020). Toward culturally competent school counseling environments: Hip-hop studio construction. The Professional Counselor, 10(2), 266–284. https://doi.org/10.15241/ipl.10.2.266
Litam, S. D. A. (2020). “Take your kung-flu back to Wuhan”: Counseling Asians, Asian Americans, and Pacific Islanders with race-based trauma related to COVID-19. The Professional Counselor, 10(2), 144–156. https://doi.org/10.15241/sdal.10.2.144
Liu, S. R., & Modir, S. (2020). The outbreak that was always here: Racial trauma in the context of COVID-19 and implications for mental health providers. Psychological Trauma: Theory, Research, Practice, and Policy, 12(5), 439–442. https://doi.org/10.1037/tra0000784
Merlin, C. (2017). School counselors and multicultural education: Applying the five dimensions. Journal of School Counselors. https://files.eric.ed.gov/fulltext/EJ1144757.pdf
Moh, Y. S., & Sperandio, K. R. (2022). The need to consider requiring trauma training in entry-level academic training programs in clinical mental health counseling. Journal of Mental Health Counseling, 44(1), 18–31. https://doi.org/10.17744/mehc.44.1.03
Mosley, D. V., Hargons, C. N., Meiller, C., Angyal, B., Wheeler, P., Davis, C., & Stevens-Watkins, D. (2021). Critical consciousness of anti-Black racism: A practical model to prevent and resist racial trauma. Journal of Counseling Psychology, 68(1), 1–16. https://doi.org/10.1037/cou0000430
Nagata, D. K., Kim, J. H. J., & Wu, K. (2019). The Japanese American wartime incarceration: Examining the scope of racial trauma. American Psychologist, 74(1), 36–48. https://doi.org/10.1037/amp0000303
National Child Traumatic Stress Network. (2018). Addressing race and trauma in the classroom: A resource for educators. The National Child Traumatic Stress Network. https://www.nctsn.org/resources/addressing-race-and-trauma-classroom-resource-educators
Parikh-Foxx, S., Martinez, R., Baker, S. B., & Olsen, J. (2020). Self-efficacy for enhancing students’ career and college readiness: A survey of professional school counselors. Journal of Counseling & Development, 98(2), 183–192. https://doi.org/10.1002/jcad.12312
Pieterse, A. L. (2018). Attending to racial trauma in clinical supervision: Enhancing client and supervisee outcomes. The Clinical Supervisor, 37(1), 204–220. https://doi.org/10.1080/07325223.2018.1443304
Pietrantoni, Z. (2017). School counselor multicultural self-efficacy: Educational and training practices. In Ideas and Research You Can Use: VISTAS 2017. https://www.counseling.org/docs/default-source/vistas/school-counselor-multicultural-self-efficacy.pdf?sfvrsn=9e9f4a2c_4
Skewes, M. C., & Blume, A. W. (2019). Understanding the link between racial trauma and substance use among American Indians. American Psychologist, 74(1), 88–100. https://doi.org/10.1037/amp0000331
Smith, W. A., Allen, W. R., & Danley, L. L. (2007). “Assume the position…you fit the description”: Psychosocial experiences and racial battle fatigue among African American male college students. American Behavioral Scientist, 51(4), 551–578. https://doi.org/10.1177/0002764207307742
Smith, W. A., Hung, M., & Franklin, J. D. (2011). Racial battle fatigue and the miseducation of Black men: Racial microaggressions, societal problems, and environmental stress. Journal of Negro Education, 80(1), 63–82.
Smith, W. A, Mustaffa, J. B., Jones, C. M., Curry, T. J., & Allen, W. R. (2016). “You make me wanna holler and throw up both my hands!”: Campus culture, Black misandric microaggressions, and racial battle fatigue. International Journal of Qualitative Studies in Education, 29(9), 1189–1209. https://doi.org/10.1080/09518398.2016.1214296
Steane, B. R. (2019). Removing traumatic barriers to learning: The need for effective trauma-informed approach to learning legislation in Pennsylvania. Temple Law Review, 92(1), 299–330. https://www.templelawreview.org/lawreview/assets/uploads/2020/01/Steane_92-Temp.-L.-Rev.-299.pdf
Stover, J. H., Wright, W. B., & Brown-Rice, K. (2022). Trauma-informed and responsive practices. Counseling Today, 65(2), 20–23.
Sue, D. W., Alsaidi, S., Awad, M. N., Glaeser, E., Calle, C. Z., & Mendez, N. (2019). Disarming racial microaggressions: Microintervention strategies for targets, White allies, and bystanders. American Psychologist, 74(1), 128–142. https://doi.org/10.1037/amp0000296
Thrower, S. J., Helms, J. E., & Price, M. (2020). Racial dynamics in counselor training: The racial identity social interaction model. The Journal of Counselor Preparation and Supervision, 13(1).
United Negro College Fund. (2020). K-12 disparity facts and statistics. https://uncf.org/pages/k-12-disparity-facts-and-stats
U.S. Department of Education Office for Civil Rights. (2018). 2015–16 civil rights data collection: School climate and safety. https://www2.ed.gov/about/offices/list/ocr/docs/school-climate-and-safety.pdf
VanAusdale, S., & Swank, J. M. (2020). Integration of trauma based education in counselor education. The Journal of Counselor Preparation and Supervision, 13(2). https://digitalcommons.sacredheart.edu/cgi/viewcontent.cgi?article=1354&context=jcps
Wagner, J., Lampert, R., Tennen, H., & Feinn, R. (2015). Exposure to discrimination and heart rate variability reactivity to acute stress among women with diabetes. Stress & Health, 31(3), 255–262. https://doi.org/10.1002/smi.2542
Williams, M. T., Metzger, I. W., Leins, C., & DeLapp, C. (2018). Assessing racial trauma within a DSM-5 framework: The UConn Racial/Ethnic Stress and Trauma Survey. Practice Innovations, 3(4), 242–260. https://doi.org/10.1037/pri0000076
Williams, M. T., Rosen, D. C., & Kanter, J. W. (2019). Eliminating race-based mental health disparities: Promoting equity and culturally responsive care across settings. New Harbinger.
Warren Wright, MEd, NCC, LPC, CCTP, is a doctoral student at Sam Houston State University. Jennifer Hatchett Stover, MA, NCC, LPC, CCTP, CSC, is a doctoral student at Sam Houston State University. Kathleen Brown-Rice, PhD, NCC, ACS, LPC, LCMHC, LCAS, is a professor at Sam Houston State University. Correspondence may be addressed to Warren Wright 1932 Bobby K. Marks Drive, Huntsville, TX 77340, wbw007@shsu.edu.
May 10, 2023 | Volume 13 - Issue 1
Erin E. Woods, Alexandra Gantt-Howrey, Amber L. Pope
To better understand how women portray obsessive-compulsive disorder (OCD) on social media, we conducted a critical content analysis of TikTok videos. We examined a sample of 50 TikTok videos tagged with “#OCD” that were created by women, yielding two themes and multiple subthemes: 1) minimizes OCD symptoms and 1a) uses OCD as a synonym for cleanliness and organization; 2) accurately depicts OCD symptoms, 2a) corrects misunderstanding, and 2b) shares obsessive fears. Results revealed that TikToks perpetuating stigma about OCD were prevalent, though women also posted TikToks presenting OCD in more accurate and comprehensive ways. Implications for mental health counselors are explained.
Keywords: obsessive-compulsive disorder, TikTok, women, content analysis, stigma
Obsessive-compulsive disorder (OCD) is often used in the popular vernacular to describe someone who likes things tidy or who is particular about a certain issue. Individuals commonly use phrases like “I’m so OCD” as captions of social media posts (Pavelko & Myrick, 2016), which may perpetuate stigma and misunderstanding about this complicated condition. According to the American Psychiatric Association (APA), OCD is a serious mental health condition that often results in significant impairment and distress due to the presence of time-consuming obsessions and compulsion (APA, 2022; Fennell & Liberato, 2007). Obsessions are urges, images, or thoughts that are unwanted, distressing, intrusive, and repetitive (APA, 2022) and may adhere to certain themes, such as doubt, contamination, harm, religious ideas, unwanted sexual thoughts, perfectionism, or fear of losing control (Clark & Radomsky, 2014; International Obsessive Compulsive Disorder Foundation [IOCDF], n.d.b.). Moreover, due to the distressing nature of obsessions, individuals with OCD often try to ignore, neutralize, or suppress these thoughts through compulsive acts—repeated mental or behavioral actions that individuals feel they must do to reduce the distress associated with obsessions or to prevent an undesirable event from occurring. Compulsions usually adhere to strict rules, are excessive, and are not realistically related to the concern they attempt to prevent or eliminate. Compulsions often are classified into common groupings, such as checking, cleaning, ordering or repeating, and/or mental actions (APA, 2022; Starcevic et al., 2011). According to prevalence data, women are slightly more likely than men to be diagnosed with OCD in adulthood and often experience later symptom onset than men (APA, 2022).
Appropriate diagnosis and effective treatment of OCD often takes an average of 17 years (IOCDF, n.d.a). Individuals with OCD often delay seeking treatment because of concerns of being viewed in a negative manner and the fear of stigma related to being diagnosed with a mental health disorder (Belloch et al., 2009; Steinberg & Wetterneck, 2017). Conceptualization of OCD ranges from viewing OCD as a less serious concern compared to other mental health disorders, to deeming OCD a chronic illness, to considering OCD as a positive trait. The medicalization of OCD may help individuals feel less stigmatized by identifying OCD as an illness (Fennell & Liberato, 2007). As Fennell and Liberato noted, “Societal conceptions [of OCD] are constantly relevant to respondents, affecting their self-conception and anticipated stigma” (p. 327). To this effect, accurate portrayal of OCD and factually based education for the public have been noted as important action steps to reduce stigma (Webb et al., 2016).
The stigma associated with OCD impacts the disclosure of symptoms to others, including social supports as well as mental health providers. Some may hide their OCD symptoms or make excuses for their behavior out of shame or embarrassment. Further, some individuals report negative perceptions or reactions after disclosing their OCD diagnosis to friends, family, or employers (Fennell & Liberato, 2007). However, some individuals benefit from disclosing symptoms of OCD to their support systems, and others find it helpful to engage and interact with people who also have an OCD diagnosis. Hence, societal conceptions of OCD can impact how individuals cope with their symptoms, including help-seeking behaviors (Fennell & Boyd, 2014; Ma, 2017; Steinberg & Wetterneck, 2017).
OCD Representations on Social Media
Researchers have called for continued examination of the representation of OCD in the media, particularly on social media platforms (Pavelko & Myrick, 2016; Robinson et al., 2019). Although increased social media discussions about OCD may decrease stigma, the often trivial nature of such depictions downplays the seriousness of this disorder (Fennell & Liberato, 2007). For instance, Robinson and colleagues (2019) explored attitudes toward five mental health and five physical health diagnoses on Twitter and found OCD to have the highest rate of trivialization of the 10 disorders, concluding that minimization of OCD symptoms and related suffering is a form of stigma.
How individuals describe OCD in the common vernacular on social media impacts societal conceptualizations of OCD (Fennell & Boyd, 2014; Pavelko & Myrick, 2016). In a quantitative study examining the use of “#OCD” on Twitter, Pavelko and Myrick (2016) identified post after post in which Twitter users employed “#OCD” when referring to non-disordered actions, such as organizing pencils. Tweets labeled “#OCD” were presented to participants, assessing their emotional reactions, stereotypes about OCD, and behavioral intentions to support individuals with OCD after reviewing the hashtagged tweets. Participants indicated increased irritation and decreased sympathy when OCD was framed in trivial language (i.e., language downplaying the seriousness of OCD) versus objective clinical language in the tweets. Further, these correlations varied by gender of the tweeter, with participants reporting increased negative emotional reactivity to women who utilized trivial language rather than to men. Pavelko and Myrick concluded that “Messages regarding trifling, detail-oriented behaviors frequently belittle or downplay the severity of OCD in 140 characters or less” (p. 42).
In a qualitative study, Fennell and Boyd (2014) examined how media portrayals of OCD were interpreted by individuals who have been diagnosed with or believe they have OCD. Similar to Pavelko and Myrick’s (2016) findings, participants reported feeling frustrated by the seemingly casual use of “OCD” in the vernacular and by depictions of OCD that were presented in stereotypical and comedic manners, at times making light of the symptoms (Fennell & Boyd, 2014). Participants noted users exhibited certain symptoms of OCD more frequently than others, namely contamination obsessions, washing and cleaning compulsions, and hoarding behaviors, all of which may portray OCD as a habit rather than a disorder. However, participants expressed appreciation for depictions of OCD in the media, acknowledging that media portrayals helped them identify what they were experiencing as OCD. Hence, media representations of OCD are varied and complex, eliciting mixed emotional reactions and divergent understandings of OCD from individuals who are consuming those messages (Fennell & Boyd, 2014; Pavelko & Myrick, 2016).
Moreover, OCD and associated symptoms are frequently misunderstood, even among mental health professionals who are trained to diagnose the disorder. In a quantitative study of mental health counselors and graduate students, participants exhibited stigma toward OCD symptoms related to sexual thoughts, violent thoughts, and contamination (Steinberg & Wetterneck, 2017). Further, Glazier et al. (2013) found issues pertaining to the accurate and timely diagnosis of OCD among APA members due to misidentification of OCD symptoms. In this quantitative study, participants were asked to provide a diagnosis for five case vignettes, each depicting various OCD obsessive symptoms. There was a 38.9% misidentification rate of OCD across the vignettes, with variation in rates based on the symptoms presented in each vignette. The vignette describing symptoms related to contamination was misidentified at the lowest rate of 15.8%, although the vignette describing symptoms of obsessions related to “homosexuality” was misdiagnosed at a rate of 77.0% (Glazier et al., 2013). In sum, OCD is an often stigmatized and misunderstood disorder, resulting in challenges for individuals living with OCD and for mental health counselors attempting to accurately diagnose OCD in their clients (Fennell & Boyd, 2014; Fennell & Liberato, 2007; Glazier et al., 2013; Steinberg & Wetterneck, 2017).
TikTok: Social Media Phenomenon and Social Change Agent
Although researchers have explored the use of the term OCD in the vernacular and on social media, along with associated impacts on people living with OCD (Fennell & Boyd, 2014), researchers have yet to explore how particular mental health diagnoses such as OCD are portrayed and discussed on TikTok, a popular social media application, or “app,” released globally in 2017 (Iqbal, 2022). TikTok’s content consists of brief videos created by users, which can be viewed and interacted with by other users (Anderson, 2020). TikTok uses an algorithm to show users videos that appeal to their interests. Users interact on the platform through likes, comments, reactions, and direct messages. Hashtags are added to videos to help individuals search for specific types of content. To have full access to TikTok, a user must have an active account; individuals with accounts can create a profile page, which can be used with various privacy settings (Anderson, 2020). The scope of TikTok is vast, reaching an average of 689 million users worldwide every month, with 100 million users in the United States (Iqbal, 2022). According to Iqbal (2022), TikTok reached over 1.4 billion users in 2022. The app is frequented by individuals of various ages, nationalities, genders, and socioeconomic statuses and in 2022, TikTok was downloaded over 3.3 billion times (Iqbal, 2022).
Based on TikTok’s wide reach, it is reasonable to assume that content shared on the app has implications for how society views certain topics, including mental health disorders, as meaning is constructed through interactions with others on the application. Vitikainen et al. (2020) described TikTok as a social change agent, noting that despite the app’s ban on political campaign–related content, users have utilized TikTok for political movements, such as joining together to sabotage a Donald Trump rally in 2020 (Lorenz et al., 2020). Further, TikTok videos and hashtags were used to spread information about wearing masks during the COVID-19 pandemic (Basch, Fera, et al., 2021). The World Health Organization TikTok videos related to wearing a mask were viewed over 57 million times, and just 100 TikToks with the hashtag “#WearaMask” were viewed over 500 million times (Basch, Fera, et al., 2021).
As the app has such an extensive user base, “TikTok has great potential in conveying important public health messages to various segments of the population” (Basch, Fera, et al., 2021, para. 18). It stands to reason that if TikTok videos can influence social action and aid in the spread of public health information, they also could be a powerful tool in either upholding or dismantling misunderstanding and stigma around mental health disorders such as OCD. However, researchers have highlighted the existence of misinformation on popular social media platforms, including TikTok (Sharevski et al., 2023). For example, in various studies on COVID-19 information conveyed via TikTok, researchers found that much of the information is misinformation (Basch, Meleo-Erwin, et al., 2021; McCashin & Murphy, 2022). Sharevski et al. (2023) found that in viewing TikToks that included debunked abortion misinformation, approximately 30% of participants believed the information to be true. These findings highlight the prevalence of health-related misinformation on TikTok and related implications for professionals and the general public alike. Therefore, to better understand current social discourse around OCD, we conducted a content analysis to answer the following research question: How are women portraying OCD on TikTok?
Methods
We conducted a deductive, qualitative content analysis of 50 TikTok videos to examine how OCD is being discussed and portrayed by women on the large-scale social media platform of TikTok, which encompasses the power to disrupt stigma and influence the narratives attributed to OCD. Our decision to utilize content analysis was influenced by the use of this methodology in existing literature exploring OCD and media (Fennell & Boyd, 2014; Robinson et al., 2019), and a content analysis aligned with our intent to interpret women’s portrayal of OCD through social discourse on TikTok. A content analysis is a systematic yet flexible process utilized to derive meaning from a set of data (Schreier, 2014). Qualitative content analysis is aligned with social constructivism and is concerned with exploring the “meaning and interpretation . . . of symbolic material, [and] the importance of context in determining meaning” (Schreier, 2014, p. 173). To describe meaning from our sample of TikTok videos, we followed the steps of a qualitative content analysis (Schreier, 2014): define the research question; select the content to analyze; develop a coding frame; segment and trial code the data; evaluate the coding frame; conduct the main analysis; and interpret and present the findings.
After determining our research question, we selected TikTok videos that met the following criteria: a) the TikTok video included the hashtag OCD (#OCD), and b) the primary person in the video presented as a woman and/or included she/her pronouns in their profile bio. We chose to focus on individuals presenting as women in this study because OCD symptomology varies based on gender in studies comparing cisgender women to cisgender men, with women having slightly higher rates of OCD diagnoses than men. Further, women exhibit cleaning-related symptoms more often than men (APA, 2022), and excessive cleanliness is commonly displayed in media depictions of OCD (Fennell & Boyd, 2014). Women also have unique experiences related to the intersectionality of gender, social discourse, and mental health diagnosis and treatment, or lack thereof (Bondi & Burman, 2001; Robinson et al., 2019). Further, women’s trivialization of OCD on social media may elicit stronger negative emotional reactions from consumers, such as annoyance and decreased sympathy toward individuals with OCD (Pavelko & Myrick, 2016).
We chose the 50 TikTok videos with the most views for our sample (Dworkin, 2012). We were able to determine these videos by searching for “#OCD” within the TikTok app in February 2021. The sample was analyzed in March 2021. Similarly, in another content analysis, Fowler et al. (2021) selected the first 50 TikTok videos using a particular hashtag for their sample. They noted the influence of the TikTok algorithm, as the algorithm determines which videos are shown and in which order. Moreover, we determined the sample size based on other studies that engaged qualitative methods to analyze videos on various social media platforms, some of which utilized a sample size of fewer than 50 (Fowler et al., 2021; Johnson et al., 2019, 2021; Wallis, 2011). Next, we deductively determined codes in a concept-driven way (Schreier, 2014) based on the extant literature surrounding OCD, stigma, and popular understanding of the diagnosis. These initial codes were stigma perpetuated and accurate information about OCD shared. It is important to note that at the time of data analysis, the current edition of the Diagnostic and Statistical Manual of Mental Disorders was the DSM-5 (APA, 2013). The DSM-5-TR (APA, 2022) was released in 2022; however, there were no updates to the OCD diagnostic criteria in the text revision.
The research team identified more codes during the review of the data, and we altered codes to be more specific to the data, including daily routine, checking OCD, and feeling misunderstood. During the segmentation phase of the coding process, the research team divided the data into individual units, or segments, based on a thematic criterion. More specifically, we divided the larger chunks of data (i.e., the entirety of what was said in a TikTok) into individual units (i.e., sentences) based on the aforementioned codes. Next, we went through a pilot round of coding using the predetermined codes on approximately 50% of the data. We evaluated and made changes to the coding frame as necessary, developing more specific codes to best represent the data. From there, we proceeded to the main analysis phase, in which the research team coded all data according to our final coding framework and determined themes and subthemes based on the coded data. Each team member individually determined themes, and then the team members met to compare, discuss, and alter the themes until we reached consensus on the themes and subthemes that best represented the data. Of the total sample, 48 videos comprise the two final categories.
Increasing Trustworthiness
The research team for the content analysis consisted of the first two authors of this article, Erin E. Woods and Alexandra Gantt-Howrey, who are cisgender heterosexual (cishet) White women and are mental health counselors familiar with OCD. To increase trustworthiness, Woods and Gantt-Howrey practiced weekly reflexive journaling to become more aware of and bracket our biases throughout the data analysis, with the recognition that bias cannot be completely bracketed (Creswell, 2003). As part of the reflexive journaling process, we recognized and considered various sociocultural factors at play in our own lives, including our existence as cishet White women in the United States. Moreover, we identified various biases and expectations we held, including expectations of seeing OCD used as a non-clinical descriptor, previous knowledge related to OCD misdiagnosis and misunderstanding, and the belief that OCD should be used only in reference to the actual disorder. In an attempt to bracket these biases throughout the data analysis process, we engaged in frequent dialogue with one another to consider and evaluate assumptions that arose during the data analysis. Finally, to increase trustworthiness, the third author, Amber L. Pope, a licensed mental health counselor and counselor educator who identifies as a cishet White woman, acted as an auditor and reviewed the final themes and subthemes according to the data (Creswell, 2003). More specifically, Pope reviewed the data as well as the themes and subthemes developed by Woods and Gantt-Howrey. Pope then offered feedback on the results (e.g., use of theme names to accurately represent the data), and Woods and Gantt-Howrey integrated Pope’s feedback into the final results presented below.
Results
This investigation explored how women communicate about OCD on TikTok. Two themes and three subthemes emerged from the data: 1) minimizes OCD symptoms and 1a) uses OCD as a synonym for cleanliness and organization; 2) accurately depicts OCD symptoms, 2a) corrects misunderstanding, and 2b) shares obsessive fears. A clear dichotomy was found: Many TikTok videos depicted women using OCD as an inaccurate descriptor, perpetuating stigma surrounding the diagnosis, while others shared factually based information in alignment with the DSM-5 description of OCD, often representing their own experiences with OCD. Below, our findings are illustrated with rich descriptions from the data.
Minimizes OCD Symptoms
The first category, minimizes OCD symptoms, describes participants’ portrayals of OCD in a way that either minimized or negated symptom severity, and/or described the disorder in a manner that does not align with the DSM-5 definition of OCD. Twenty-eight videos (56%) from the sample are included in this category. Many TikToks in this category used the term “OCD” as a synonym for being very clean or organized, or to portray an unrelated phenomenon, such as collecting items or creating a spreadsheet. One TikTok of a woman describing her father exemplifies this misuse of the term “OCD”: “This is my dad and he has a problem . . . because he has the OCD. And you might have it too if your 800-count DVD collection is in alphabetical order from ‘8 Mile’ to ‘Young Frankenstein.’” This quote is representative of the trivialization of the OCD diagnosis. Moreover, a TikTok about a mother’s feelings of frustration over her daughter’s messy painting further demonstrates the stigma perpetuated by many TikTok videos, as the mother stated:
Do any other moms relate to the extreme anxiety this gives me? I can sit here and watch but I’m dying on the inside. This is very hard for me. But I will sit here . . . and not let my anxiety and OCD get the best of me.
Uses OCD as a Synonym for Cleanliness and Organization
The subcategory uses OCD as a synonym for cleanliness and organization represents TikTok videos in which women used OCD as a descriptor for a clean person, and includes 10 of the 28 videos in this category. Building upon the first category, minimizes OCD symptoms, this subcategory further demonstrates explanations, examples, and use of the term OCD in ways that do not accurately describe the disorder. A popular audio clip was utilized frequently in our sample and was often paired with visual content of individuals organizing or cleaning various objects and spaces. The woman in the audio stated:
When they come into my house and they also think that I am a sociopath, that I take the time to do this once a month. Like, you know what? You say OCD is a disease, I say it’s a blessing.
Through equating OCD to “a blessing” and also trivializing the term “sociopath” to simply describe someone who is well-organized, such TikTok videos minimize the OCD diagnosis and the experiences of individuals with OCD, equating the disorder to something it is not—a proclivity for cleanliness and organization. Furthermore, other TikToks with #OCD were solely about cleaning or organizing. A woman in one TikTok described a “bathroom hack for a deep clean” as she displayed bleach and a bowl of hot water. In another TikTok, these words crossed the screen for the viewer to read: “*My bff being messy*” and, subsequently, “*My OCD kicking in*,” while the video displays an unmade bed.
Accurately Depicts OCD Symptoms
The second category, accurately depicts OCD symptoms, is defined as women portraying information that aligns with the DSM-5 description of OCD symptom constellations and current research on OCD. Twenty videos (40%) comprise this category. Women in the TikToks in this category typically indicated they had an OCD diagnosis, describing their unique experiences with OCD and explaining how their symptoms align with the DSM-5 definition. For example, TikToks in our sample represented the following aspects of the DSM-5 symptoms of OCD (APA, 2013): recurrent intrusive thoughts, performance of a compulsion, and “clinically significant distress or impairment in social, occupational, or other important areas of functioning” (p. 237). For example, one TikTok begins with the words “Live with ______ for a day” across the screen. A woman is then pictured “selecting” OCD from a variety of mental health diagnoses. In other TikToks, users describe their compulsions, such as a woman narrating her need to perform various rituals like choosing a certain color shirt, or another in which a woman flips a light switch repeatedly.
Corrects Misunderstanding
The first subcategory, corrects misunderstanding, encompasses videos in which women with OCD sought to correct misinformation or inaccurate portrayals about OCD. Eight of the 20 videos from the second category are included in this subcategory. The following quote demonstrates a woman debunking popular misconceptions of OCD symptoms: “What people think OCD is *picture of an organized desk.* What it’s like for me: *woman spraying perfume.* My brain: ‘spray it 3 times or your mum will die.’” In another TikTok, a woman lamented the prevalent, stigmatized view of OCD:
OCD is not cute. She doesn’t wear big glasses and chunky sweaters while she neatly lines up her stationary in color order. She’s probably the most misunderstood disorder, to the point where people nonchalantly use her name to describe a neat person.
Importantly, the speaker describes OCD as “misunderstood,” directly contradicting the previously described “version” of OCD as simply a proclivity for neatness or organization.
Shares Obsessive Fears
In this subcategory, shares obsessive fears, women provided more specific information and details in their TikToks to depict OCD in a more holistic, accurate manner. Eleven videos are included in this subcategory. The fears women shared included the deaths of loved ones, losing one’s job, accidentally setting one’s house on fire, losing a relationship, and not locking one’s front door. One woman’s TikTok portrayed the intrusive thoughts and subsequent fears she experienced frequently:
Documenting a side of OCD that people don’t usually see: Did I tell my mom I love her before she went to bed? What if she dies on the way to work tomorrow? Should I wake her up and tell her just in case? No, that will make her mad. Wait, but did I lock the doors? Did my sister make it home safe? She didn’t text me; her location is off. Oh, she’s fine; she just responded. Should I check the locks?
This quote demonstrates the intrusive thoughts that individuals with OCD often experience. More specifically, the intrusive thoughts in this example include fears such as death of a loved one, uncertainty, and potential lack of safety for self and others.
Discussion
The purpose of this study was to increase understanding of how women are portraying OCD on TikTok to inform counselors on the current social discourse around OCD. Our findings substantiate the extant literature and provide new insight, possibilities, and practice implications given this novel exploration of how women discuss OCD on TikTok. The categories that emerged from our content analysis reveal the variety in the types of TikToks women created and hashtagged with the term “OCD,” with the two main themes being minimizes OCD symptoms, demonstrating the trivialization of OCD by women on TikTok, and accurately depicts OCD symptoms, in which women attempted to correct inaccurate perceptions about OCD by sharing their own experiences and factual information about the diagnosis. Our results also suggested that women with an OCD diagnosis shared more factually based depictions of the disorder than the women who did not indicate a diagnosis in their TikTok videos. Our findings of two dichotomous themes are unsurprising given other findings on health-related misinformation on TikTok (e.g., Basch, Meleo-Erwin, et al., 2021; McCashin & Murphy, 2022), yielding opportunities for professionals to provide accurate information on the platform.
The majority of women whose content fell in the accurately depicts OCD symptoms theme indicated they had an OCD diagnosis. These women corrected misinformation about OCD and also shared their own experiences of living with OCD, depicting the seriousness and pervasiveness of their obsessive thoughts. Our results indicate that women with OCD may desire to see OCD portrayed correctly in the media, in ways that are different from the stereotypical or comedic depictions often prevalent in mainstream media (Fennell & Boyd, 2014). These negative stereotypes may contribute to women’s oppression through the perpetuation of misinformation. Women with OCD also may be motivated by the fear of stigma (Steinberg & Wetterneck, 2017) and the desire to have their mental health diagnosis taken seriously. Fennell and Liberato (2007) noted the importance of societal conceptions of OCD to those with the diagnosis; therefore, the creators in our sample may be motivated to alter the popular understanding and trivialization of OCD (Pavelko & Myrick, 2016; Robinson et al., 2019) through their TikTok content as a result of living with the disorder themselves and the impact of their OCD symptoms on their functioning. Moreover, motivation to post publicly about one’s experience with OCD may help women connect with others (Fennell & Liberato, 2007) through a large social media platform.
Yet our other main theme of minimizes OCD symptoms supports findings from previous research (e.g., Pavelko & Myrick, 2016; Robinson et al., 2019) that OCD is frequently depicted in the media and popular culture in a manner that minimizes the symptomatology or severity of OCD symptoms. Our results illustrate that the content created by women on TikTok often portrays OCD as synonymous with cleanliness and organization, hence trivializing OCD symptoms. Multiple TikToks (n = 4) utilized a popular audio: “You say OCD is a disease; I say it’s a blessing,” over a video of someone organizing, often some sort of household item, which aligns with previous findings that OCD is typically portrayed in the media by characters with washing and cleaning compulsions (Fennell & Boyd, 2014). Additionally, multiple videos in the uses OCD as a synonym for cleanliness or organization subtheme included language and descriptions that stigmatized cleaning symptoms, such as “*My bff being messy*,” *My OCD kicking in*,” and “I literally saved my toothbrush to like get the corners and clean cuz I’m OCD.” Despite cleanliness being the most visible depiction of OCD (Steinberg & Wetterneck, 2017) and more often seen in women with OCD than in men (APA, 2022), the way these symptoms are portrayed do not holistically represent OCD or encompass the potential effects of this disorder and instead contribute to the continued trivialization of this disorder.
Implications
Our findings yield various implications for counselors and future research. Because of the popularity and breadth of TikTok content, both clients and counselors are likely to use the app and subsequently view TikToks that contain minimizing, trivializing, or stigmatizing information about OCD. Counselors are not immune to holding stigmatizing views about OCD (Steinberg & Wetterneck, 2017). Exposure to trivializing content may influence how counselors view OCD symptoms and the severity of OCD with their clients, potentially contributing to misdiagnosing OCD. Our results indicate cleanliness and organization were the common depictions of OCD on TikTok, which could result in counselors having a limited understanding of OCD symptomatology and misidentifying other types of OCD symptoms that fall into groupings such as unwanted sexual thoughts or religious obsessions (Glazier et al., 2013). Mental health counselors responded with social rejection and general concerns to case vignettes of clients with contamination obsessions and cleaning compulsions (Steinberg & Wetterneck, 2017); consumption of social media that equates OCD to cleanliness and organization could perpetuate similar stigmas toward OCD among counselors.
For clients, exposure to content that trivializes and/or stigmatizes OCD may lead to hesitancy to seek treatment (Steinberg & Wetterneck, 2017) or even a failure to recognize one’s symptoms as indicative of a mental health issue (Fennell & Liberato, 2007). Hence, our results stress the importance of counselors increasing their knowledge of OCD in its various presentations and examining their own beliefs and biases toward OCD symptoms, recognizing that our reactions as counselors may impact how clients choose to present or hide their symptoms of OCD out of fear of stigmatization. During the mental health assessment process, counselors may want to ask clients displaying OCD symptoms questions related to their perceptions of the disorder such as, “How have you seen OCD depicted by characters on TV or in the movies?” or “What do you believe about OCD according to what you have seen/read on social media?” For clients who indicate inaccurate or negative conceptualization of OCD, psychoeducation may be useful to correct misinformation or misconceptions about OCD that clients obtained from the media. Counselors also may want to help clients develop media literacy skills, particularly for clients who consume a lot of social media, so clients can effectively analyze and reflect on the messages they encounter regarding OCD.
To enhance counselors’ knowledge of OCD, counselor educators can use the portrayals of OCD on social media to inform classroom discussion and activities when teaching about mental health diagnosis. For example, counselor educators can ask students to describe what they have seen about OCD in the media and explore how these examples do or do not align with the DSM-5 description of OCD. Counselor educators also can encourage students to explore their own biases and perceptions about OCD, which may help reduce the stigma held by mental health counselors related to OCD symptoms (Steinberg & Wetterneck, 2017) and increase accurate diagnosis of OCD (Glazier et al., 2013).
Further, our results demonstrate the importance of public education to decrease stigma related to mental health disorders (Webb et al., 2016), particularly targeted to individuals who do not have an OCD diagnosis, as they may be more likely to share or create trivializing content. As Fennell and Liberato (2007) stated, “the need for more public information on the lived experience of OCD and mental ‘disorders’ cannot be stressed enough” (p. 328). TikTok shows great potential to spread health information (Basch, Fera, et al., 2021), and this social media platform could be utilized to help share more accurate depictions of OCD. For example, counselors, individuals with OCD, and other advocates may consider utilizing the power of a targeted “hashtag” campaign, with the goal of reducing stigma toward OCD through countering the impact of stigmatizing content (Robinson et al., 2019). This type of positive and factual representation of OCD also may help to combat societal inequalities that can be perpetuated through the stigmatization and trivialization of OCD, and hashtag campaigns may be enacted by individuals and larger counseling organizations alike.
TikTok has a unique feature called “stitch” that allows users to combine another user’s video with the one they are creating. Some counselors are already using the “stitch” function as a means of psychoeducation and advocacy to correct misconceptions of mental health in TikTok videos, where counselors can directly connect their educated responses to the original video that contained inaccurate information. To effectively challenge the stigma surrounding mental health diagnoses, counselors need to be aware of the current public discourse occurring on social media platforms and use this information to develop advocacy-based interventions. In line with the American Counseling Association’s Code of Ethics (2014), counselors should consider other means of engaging in advocacy to benefit those diagnosed with OCD, such as providing public education in their local contexts and supporting public policies that could help provide affordable treatment of the disorder. The IOCDF’s Advocate Program (IOCDF, 2022) may prove to be a beneficial resource for such work.
Concerning future research, we suggest utilizing a larger sample of TikTok videos, analyzing social media content on other platforms, and including gender-expansive individuals and cisgender men as part of the sample to gather more perspectives. Additionally, researchers can compare who is creating the social media content and where accurate or inaccurate portrayals of OCD are occurring on social media. Quantitative research may provide more insight into how individuals with an OCD diagnosis create media content compared to those who do not have a diagnosis. Understanding the nuances in how OCD is portrayed across platforms or creators can enhance counselors’ knowledge of how to use social media as appropriate resources or social connections for their clients with OCD. Finally, more information on how OCD is depicted on social media can help counselors better recognize the messages their clients receive about OCD when using social media and improve their ability to correct the unreliable information their clients consume on these platforms.
Limitations
Various limitations should be taken into consideration. Given the nature of qualitative research, the findings of this study cannot be generalized to larger groups. We did not obtain IRB approval for this study, given that we used publicly available information for our data, and we did not directly contact the video creators to clarify gender identity, OCD diagnosis, or other demographic information that would have enhanced the description of our sample or allowed us to explore how intersectionality impacts depictions of OCD. Because we did not gather demographic information, we determined inclusion based on the individuals’ presentation as a woman and/or use of she/her pronouns in their profile, and our results are based solely on the content the women disclosed in their videos. For example, we cannot conclusively determine that women with a diagnosis share more accurate information about OCD on TikTok as compared to those without a diagnosis. Additionally, we did not contact the creators to gain a more thorough understanding of their intended message when creating the video. Finally, it should be noted that by utilizing the 50 most viewed TikToks with #OCD, videos that were less widely viewed and shared were not included in our sample, perhaps limiting our understanding of more nuanced portrayals of OCD on TikTok. Utilizing the most viewed TikToks as our sample may have contributed to the resulting dichotomous themes, capturing only the predominant trends of minimizing or accurately depicting OCD symptoms.
Conclusion
OCD is a serious and often debilitating mental health disorder (APA, 2022) that is frequently misunderstood and misrepresented in mainstream culture (Pavelko & Myrick, 2016; Steinberg & Wetterneck, 2017). Through a content analysis of TikTok videos created by women with the hashtag “OCD,” our resulting themes and subthemes revealed a mix of perpetuating stereotypes and minimizing OCD symptoms and of sharing accurate information and personal experiences concerning OCD. These findings can assist counselors and counselor educators to better understand the types of social media content clients are viewing and potential harmful messages clients may internalize about OCD through exposure to media. Further, counselors should consider their own consumption of social media and examine their perceptions of and biases toward OCD throughout the treatment process. Likewise, counselor educators should adjust their pedagogy to encourage student exploration of misconceptions and enhance training in how to accurately diagnose and treat OCD in their future work as mental health counselors. Although social media can perpetuate stigma, it can also be used as a tool for powerful positive change, and we encourage all readers to consider the accuracy of the content they post on social media when it comes to depicting mental health disorders.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
American Counseling Association. (2014). ACA code of ethics. https://www.counseling.org/docs/default-source/default-document-library/2014-code-of-ethics-finaladdress.pdf
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (5th ed., text rev.). https://doi.org/10.1176/appi.books.9780890425787
Anderson, K. E. (2020). Getting acquainted with social networks and apps: It is time to talk about TikTok. Library Hi Tech News, 37(4), 7–12. https://doi.org/10.1108/LHTN-01-2020-0001
Basch, C. H., Fera, J., Pierce, I., & Basch, C. E. (2021). Promoting mask use on TikTok: Descriptive, cross-sectional study. JMIR Public Health and Surveillance, 7(2), e26392. https://doi.org/10.2196/26392
Basch, C. H., Meleo-Erwin, Z., Fera, J., Jaime, C., & Basch, C. E. (2021). A global pandemic in the time of viral memes: COVID-19 vaccine misinformation and disinformation on TikTok. Human Vaccines & Immunotherapeutics, 17(8), 2373–2377. https://doi.org/10.1080/21645515.2021.1894896
Belloch, A., del Valle, G., Morillo, C., Carrió, C., & Cabedo, E. (2009). To seek advice or not to seek advice about the problem: The help-seeking dilemma for obsessive-compulsive disorder. Social Psychiatry and Psychiatric Epidemiology, 44(4), 257–264. https://doi.org/10.1007/s00127-008-0423-0
Bondi, L., & Burman, E. (2001). Women and mental health A feminist review. Feminist Review, 68(1), 6–33. https://doi.org/10.1080/01417780122133
Clark, D. A., & Radomsky, A. S. (2014). Introduction: A global perspective on unwanted intrusive thoughts. Journal of Obsessive-Compulsive and Related Disorders, 3(3), 265–268. https://doi.org/10.1016/j.jocrd.2014.02.001
Creswell, J. W. (2003). Research design: Qualitative, quantitative, and mixed methods approaches (2nd ed.). SAGE.
Dworkin, S. L. (2012). Sample size policy for qualitative studies using in-depth interviews. Archives of Sexual Behavior, 41, 1319–1320. https://doi.org/10.1007/s10508-012-0016-6
Fennell, D., & Boyd, M. (2014). Obsessive-compulsive disorder in the media. Deviant Behavior, 35(9), 669–686. https://doi.org/10.1080/01639625.2013.872526
Fennell, D., & Liberato, A. S. Q. (2007). Learning to live with OCD: Labeling, the self, and stigma. Deviant Behavior, 28(4), 305–331. https://doi.org/10.1080/01639620701233274
Fowler, L. R., Schoen, L., Stevens Smith, H., & Morain, S. R. (2021). Sex education on TikTok: A content analysis of themes. Health Promotion Practice, 23(5). https://doi.org/10.1177/15248399211031536
Glazier, K., Calixte, R. M., Rothschild, R.2013). High rates of OCD symptom misidentification by mental health professionals. Annals of Clinical Psychiatry, 25(3), 201–209. https://www.ingentaconnect.com/contentone/fmc/acp/2013/00000025/00000003/art00006
International Obsessive Compulsive Disorder Foundation. (2022). IOCDF Advocate Program. https://iocdf.org/advocate-program/#:~:text=The%20IOCDF%20Advocate%20Program%20i
s%20about%20OCD%20and%20related%20disorders
International Obsessive Compulsive Disorder Foundation. (n.d.a). IOCDF Training Institute. https://iocdf.org/professionals/training-institute/
International Obsessive Compulsive Disorder Foundation. (n.d.b.) What is OCD? https://iocdf.org/about-ocd/
Iqbal, M. (2022). TikTok revenue and usage statistics. Business of Apps. https://www.businessofapps.com/data/tik-tok-statistics/
Johnson, K. F., Brookover, D. L., Borden, N. J., Worth, A. K., Temple, P., & Mahan, L. B. (2021). What YouTube narratives reveal about online support, counseling entrance, and how Black Americans manage depression symptomology. Informatics for Health and Social Care, 46(1), 84–99. https://doi.org/10.1080/17538157.2020.1865967
Johnson, K. F., Worth, A., & Brookover, D. (2019). Families facing the opioid crisis: Content and frame analysis of YouTube videos. The Family Journal, 27(2), 1–12. https://doi.org/10.1177/1066480719832507
Lorenz, T., Browning, K., & Frenkel, S. (June, 2020). TikTok teens and K-pop stans say they sank Trump rally. The New York Times. https://www.nytimes.com/2020/06/21/style/tiktok-trump-rally-tulsa.html
Ma, Z. (2017). How the media cover mental illnesses: A review. Health Education, 117(1), 90–109. https://doi.org/10.1108/HE-01-2016-0004
McCashin, D., & Murphy, C. M. (2022). Using TikTok for public and youth mental health—A systematic review and content analysis. Clinical Child Psychology and Psychiatry, 28(1). https://doi.org/10.1177/13591045221106608
Pavelko, R., & Myrick, J. G. (2016). Tweeting and trivializing: How the trivialization of obsessive–compulsive disorder via social media impacts user perceptions, emotions, and behaviors. Imagination, Cognition and Personality, 36(1), 41–63. https://doi.org/10.1177/0276236615598957
Robinson, P., Turk, D., Jilka. S., & Cella, M. (2019). Measuring attitudes towards mental health using social media: Investigating stigma and trivialisation. Social Psychiatry and Psychiatric Epidemiology, 54(1), 51–58. https://doi.org/10.1007/s00127-018-1571-5
Schreier, M. (2014). Qualitative content analysis. In U. Flicke (Ed.), The SAGE handbook of qualitative data analysis (pp. 170–183). SAGE. https://doi.org/10.4135/9781446282243
Sharevski, F., Loop, J. V., Jachim, P., Devine, A., & Pieroni, E. (2023). Abortion misinformation on TikTok: Rampant content, lax moderation, and vivid user experiences. arXiv preprint. https://doi.org/10.48550/arXiv.2301.05128
Starcevic, V., Berle, D., Brakoulias, V., Sammut, P., Moses, K., Milicevic, D., & Hannan, A. (2011). Functions of compulsions in obsessive–compulsive disorder. Australian & New Zealand Journal of Psychiatry, 45(6), 449–457. https://doi.org/10.3109/00048674.2011.567243
Steinberg, D. S., & Wetterneck, C. T. (2017). OCD taboo thoughts and stigmatizing attitudes in clinicians. Community Mental Health Journal, 53, 275–280. https://doi.org/10.1007/s10597-016-0055-x
Vitikainen, S., Buzzell, M., de Regt, L., & Timmermans, L. (2020). “Stop licking the boots and start marching them”—An exploratory research proposal into peer-to-peer political discussion on TikTok. Masters of Media. http://mastersofmedia.hum.uva.nl/blog/2020/10/21/stop-licking-the-boots-and-start-marching-them/
Wallis, C. (2011). Performing gender: A content analysis of gender display in music videos. Sex Roles, 64(3–4), 160–172. https://doi.org/10.1007/s11199-010-9814-2
Webb, M., Peterson, J., Willis, S. C., Rodney, H., Siebert, E., Carlile, J. A., & Stinar, L. (2016). The role of empathy and adult attachment in predicting stigma toward severe and persistent mental illness and other psychosocial or health conditions. Journal of Mental Health Counseling, 38(1), 62–78. https://doi.org/10.17744/mehc.38.1.05
Erin E. Woods, PhD, LPC, serves as Clinic Director at the College of William & Mary. Alexandra Gantt-Howrey, PhD, NCC, is an assistant professor at New Mexico State University. Amber L. Pope, PhD, LPC, LMHC, CCTP, is an assistant professor at the College of William & Mary. Correspondence may be addressed to Alexandra Gantt-Howrey, P.O. Box 30001, MSC 3AC, Las Cruces, New Mexico 88003, aghowrey@nmsu.edu.
May 10, 2023 | Volume 13 - Issue 1
Claudette Brown-Smythe, Shirin Sultana
We examined the extent to which anxious attachment and avoidant attachment predicted loneliness and social self-efficacy among 863 college students. Further, we investigated whether social self-efficacy mediated the relationships between the two insecure attachment styles and loneliness. Pearson correlations and regression analysis showed that anxious and avoidant attachment styles were significant predictors of loneliness and social self-efficacy. Mediation analysis revealed that social self-efficacy fully mediated the relationship between avoidant attachment and loneliness and partially mediated the relationship between anxious attachment and loneliness. Implications for college counseling are discussed, and we propose recommendations for counselors to enhance social self-efficacy and attachment security to decrease loneliness.
Keywords: social self-efficacy, anxious attachment, avoidant attachment, loneliness, attachment security
Existential philosophers, as well as counseling theorists, have alluded to loneliness as a common human condition, one that can lead to mental health challenges like depression and anxiety (Sharf, 2012). Researchers began calling attention to the increase in loneliness across the life span (Cacioppo et al., 2015; Diehl et al., 2018; Mushtaq et al., 2014) prior to the outbreak of the novel coronavirus disease (COVID-19), and the subsequent declaration by the World Health Organization (WHO) that the outbreak was a public health emergency of international concern (Pan American Health Organization, 2020). In 2015, Vivek Murthy (2020), then surgeon general of the United States, identified loneliness as a public health issue, endemic across all ages and socioeconomic groups. As of 2019, three out of every five people, or 61% of the U.S. population, reported feeling lonely, which was a 7% increase from 2018 (Cigna, 2020). Isolation then surged during the COVID-19 pandemic, which contributed to loneliness (Dahlberg, 2021; Holt-Lunstad, 2020).
The Cigna (2020) report noted that 49.9% of emerging adults 18–22 years old and 47.7% of adults 23–37 years old reported feeling lonely. Moreover, the American College Health Association (2017) reported that 64% of college students experienced loneliness, which aligns with the Healthy Minds Study results indicating that 66% of college students struggled with loneliness (Eisenberg et al., 2020). Again, these figures predate the 2020 coronavirus pandemic, and rates of loneliness experienced because of the lockdown and restrictions during that time are projected to increase (Dahlberg, 2021; Holt-Lunstad, 2020).
As the preceding data demonstrate, loneliness is a special concern for the college-age population. Moreover, loneliness is a human challenge that if left unattended can lead to and exacerbate mental health issues. Like Bandura (1977), we believe that individuals who possess strong social self-efficacy can motivate themselves to build connections and engage with others and reduce feelings of loneliness. This study sought to examine the extent to which social self-efficacy serves as a mediator of the two insecure attachment styles on loneliness.
Literature Review
Loneliness
Loneliness is viewed as a complex multidimensional and subjective psychological construct that is seen from an individual’s perspective. DiTommaso et al. (2015) described loneliness as a temporary psychological response to changes in one’s social environment or a stable dissatisfaction with one’s personal network, while Perlman and Peplau (1981) viewed it as a negative feeling that occurs when individuals do not perceive the quality or quantity of their social relationships as satisfying.
Early researchers like Perlman and Peplau (1981) identified three types of loneliness: (a) chronic loneliness, or a long-term experience of feelings of separation and isolation over several years; (b) situation loneliness, or a disruption of one’s social relationship patterns; and (c) transient loneliness, described as the occasional feelings of loneliness experienced at different times when one is making changes throughout the life span. Yanguas et al. (2018) highlighted a dichotomous view of loneliness, identifying social loneliness (lacking a sense of community and connection to social network) and emotional loneliness (lacking attachment figures and companionship), and noting that an individual can experience loneliness in both areas simultaneously.
Loneliness as a developmental issue can occur at different periods in people’s lives. For example, for emerging adults (i.e.,18–25 years old) this period is marked by transitions that can predispose them to experiencing loneliness (Moeller & Seehuus, 2019). Emerging adults overlap two critical stages in Erikson’s (1980) psychosocial development theory. The first stage of identity versus role confusion (12–19 age range) is marked by a sense of ego identity in which the individual seeks balance and congruence between their self-perception and how others perceive them. The second stage is intimacy versus isolation (20–25 age range), in which the goal is to establish committed relationships with friends and develop intimate romantic relationships. Erikson posited that individuals who were unsuccessful at the earlier stages, and were lacking a strong sense of identity, may struggle in building healthy relationships. This in turn can result in emotional distress and isolations, as they will be unable to establish the committed relationships that are needed to resolve this stage and experience loneliness. There are normative transitions many emerging adults make that can precipitate feelings of loneliness, like leaving home, beginning college, or starting a full-time job. Additionally, the maturation changes from adolescence to emerging adulthood (Chickering & Reisser, 1993), along with the psychosocial development crisis of intimacy versus isolation, can impact emerging adults’ self-perception of loneliness (Qualter et al., 2015).
At the beginning of college, students may not have relationships with peers at their institutions and will need to establish connections in this new social context (Thurber & Walton, 2012). This new context may be bigger or smaller than home, or it may be less diverse or more diverse from their home communities, thereby decreasing students’ feelings of connection. Colleges often give much attention to transition issues experienced at the beginning of college (Bruffaerts et al., 2018); however, these experiences can persist throughout the college years. Moeller and Seehuus (2019) noted that students are challenged to build and sustain relationships in this social context while also navigating and balancing a more demanding academic workload, new expectations around academic productivity and engagement, and developmental changes as they transition from adolescence to adulthood. This period of transition and competing priorities can be challenging for students as they attempt new things, try to integrate, and adjust to the changes to their personal and academic lives and make decisions about what is important to them. For some, this can be overwhelming, and their inability to cope with these challenges and form meaningful relationships in this social context can precipitate students’ mental health struggles and loneliness (Thomas et al., 2020). Students’ struggles during this period are linked to attrition, college withdrawal, and dropout rates (Diehl et al., 2018; Fink, 2014).
Social Self-Efficacy
Bandura (1977) defined social self-efficacy as an individual’s beliefs about their skills for success in interpersonal interactions and social situations. He noted that individuals with high social self-efficacy had greater cognitive resourcefulness and flexibility to effectively manage their environment and motivate themselves to achieve a desired goal, which is the opposite for individuals with insecure attachment. Social self-efficacy, then, is about the individual’s perceived confidence in their ability to engage in social interactions and to take the initiative to maintain these interpersonal relationships. Consequently, higher social self-efficacy is important for building and maintaining interpersonal relationships and for engaging in social gatherings (Kim et al., 2020). These engagements can then help in staving off loneliness. People who are lonely are assumed to possess less interpersonal competence than individuals who are not lonely, and research often points to a positive correlation between poor social skills and loneliness (Moeller & Seehuus, 2019).
Attachment Theory
Attachment theory is an established framework that describes the impact of early bonding with caregivers as a foundation for subsequent close relationships across the life span (Ainsworth, 1985; Bowlby, 1973). These theorists posited two major attachment types: secure and insecure attachment. Available, sensitive, and supportive bonding experiences with caregivers contribute to a sense of connectedness and security resulting in the development of secure attachment and a healthy internal model of self and others (Mikulincer & Shaver, 2014). That is, these experiences create a positive view of self and others.
On the other hand, individuals who experienced unsupportive, frustrated, and fractured caregiving emerge with insecure attachment styles, which lead to difficulties with relationships in later life. Insecure attachment is characterized in two dimensions—avoidant and anxious attachment styles. Individuals with high anxious attachment style tend to be fearful of being rejected or abandoned by others and have a negative working model of self; that is, they may hold a negative perception of their worthiness. Those with avoidant attachment fear intimacy and being dependent on others and hold a negative working model of others (Mikulincer & Shaver, 2014; Zhu et al., 2016).
Individuals with insecure attachment styles may lack prosocial skills and engage in negative coping strategies (Mikulincer & Shaver, 2014, 2019). For example, individuals with high anxious attachment may “rely on hyperactivating strategies . . . to achieve support and love,” and when the support and love are not provided, individuals may then experience anger and despair (Mikulincer & Shaver, 2014, p. 36). Conversely, those with high avoidant attachment may use detachment and deactivated strategies to protect themselves; they tend to push others away, “avoiding closeness and interdependence in relationship” (p. 36). These maladaptive behaviors may result in greater feelings of loneliness, as these individuals may experience lower satisfaction in their relationships.
Loneliness, Attachment, and Social Self-Efficacy
The relationship between attachment styles established in early childhood and feelings of loneliness in early adulthood is well documented (Akdoğan, 2017; Benoit & DiTommaso, 2020; Klausli & Caudill, 2021). Higher levels of attachment security correlated with lower levels of loneliness in undergraduate students (Benoit & DiTommaso, 2020). As young adults transition to college life, their social network shifts from the family domain to peers. An individual’s ability to cope with this transition and form meaningful relationships may depend on the adaptiveness of their attachment style. Individuals with a secure attachment style report a stronger sense of self and social competence (Akdoğan, 2017; Klausli & Caudill, 2021), which may counteract feelings of loneliness.
Research on loneliness has frequently pointed to a lack of prosocial skills and social competency to initiate and maintain friendships when addressing the connection between insecure attachment and loneliness (Akdoğan, 2017). Individuals with secure attachment demonstrate strong social skills and social competency and can be said to possess social self-efficacy. “Adult attachment research revealed that attachment insecurities tended to negatively bias cognitions, emotions, and behavior during interpersonal interactions” (Mikulincer & Shaver, 2014, p. 37); therefore, it could be concluded that individuals with attachment insecurities are likely to exhibit low social self-efficacy.
Earlier researchers found conflicting effects of social self-efficacy on loneliness (Mallinckrodt & Wei, 2005; Wei et al., 2005). The results of a longitudinal study of 308 freshmen examining social self-efficacy and self-disclosure as mediators for insecure attachment, loneliness, and depression revealed that a lack of social self-efficacy mediated the relationship between anxious attachment and loneliness after controlling for depression (Wei et al., 2005). However, social self-efficacy was not found to mediate avoidant attachment. In another study with 430 students investigating social self-efficacy as a mediator for insecure attachment, social support, and psychological distress, researchers found that high levels of avoidant attachment were correlated with lower levels of social self-efficacy and perceived social support (Mallinckrodt & Wei, 2005). These competing findings influenced us to further explore the extent to which social self-efficacy would affect loneliness.
The Current Study
For this study, we focused on social and emotional loneliness (Yanguas et al., 2018), holding the view that loneliness is a temporary psychological state due to circumstances (DiTommaso et al., 2015). These two dimensions are considered more salient for college students given their psychosocial developmental levels and societal expectations. Researchers (Akdoğan, 2017; Benoit & DiTommaso, 2020; Mikulincer & Shaver, 2014, 2019) have indicated that primary attachment style impacts social competency, sense of self, and one’s ability to form a supportive network. All of these can affect whether college students experience loneliness and to what degree they experience it.
To date, few researchers have examined how the detrimental effects of loneliness in people with avoidant and anxious attachment styles can be mediated by social self-efficacy. In this study, we examined the triadic relationship between the dimensions of insecure attachment (i.e., anxious attachment and avoidant attachment), loneliness, and social self-efficacy. Three research questions and hypotheses guided this study:
- What is the relationship between social self-efficacy, loneliness, and the types of insecure attachment?
- Do anxious attachment and avoidant attachment predict the levels of social self-efficacy?
- How does social self-efficacy mediate the relationship between loneliness and anxious attachment and avoidant attachment styles?
We hypothesized that a) social self-efficacy, loneliness, and anxiety are correlated; b) anxious attachment and avoidant attachment will predict the levels of social self-efficacy; and c) social self-efficacy will mediate the relationship between loneliness and anxious attachment and avoidant attachment styles.
Methods
Procedure
Upon receiving IRB approval, we collected data during the last 2 months of the fall 2020 semester. At this mid-size comprehensive college in the Northeast, students were on campus until the week before Thanksgiving. After the Thanksgiving break, students were not permitted to return, and all classes transitioned to virtual platforms because of the uptick in the number of cases and deaths as a result of COVID-19. Data collection spanned both class formats. All students 18 years and older who were enrolled in classes for the fall 2020 semester were eligible to participate in this study. Data were collected through the Qualtrics online survey platform. The university enrollment management office distributed the recruitment email inviting students to volunteer to participate in the research. The students who volunteered completed the informed consent with the screening statement, “I am 18 years or older, currently enrolled in classes for the fall 2020 semester.”
Participants
Participants were drawn from 5,838 full-time students attending a medium-sized public college in the northeastern United States. After eliminating participants with more than 10% of missing values throughout the questionnaire (n = 28; Tabachnick & Fidell, 2007) the final sample was N = 863 students. The participants’ ages ranged between 18 and over 40 years, with the majority (n = 79.9%) being between 18 and 25 years old. Of these 863 participants, 153 (17.7%) participants were first-year students, 105 (12.2%) participants were second-year students, 205 (23.8%) were in their third year, 182 (21.1%) were fourth-year students, 43 (4.9%) were fifth-year students (those who added one more year to complete the degree), 163 (18.9%) were graduate students, and 12 (1.4%) were non–degree-seeking students.
Regarding their cultural background, most participants (n = 689; 79.8%) were White European, whereas 51 (5.9%) were African American, 44 (5.1%) were Hispanic/Latinx, 20 (2.3%) were Asian, 17 (2.0%) were Caribbean/West Indian, 11 (1.3%) were Native American or Alaska Native, and two (0.2%) were Native Hawaiian or Pacific Islander. Regarding gender, 647 (75%) identified as women, 197 (22.8%) as men, 6 (0.7%) as transgender, and 13 (1.5%) as other gender. Most of the participants identified as heterosexual (n = 611, 70.8%), whereas 117 (13.6%) identified as bisexual, 37 (4.3%) identified as asexual, 29 (3.4%) identified as lesbian, 12 (1.4%) identified as queer, and 11 (1.3%) identified as homosexual. The relationship status of the participants varied. Most of the participants were single (n = 375, 43.5%), whereas 361 (41.9%) were dating, 80 (9.3%) were married, 37 (4.3%) were engaged, and seven (0.8%) were divorced.
In terms of living arrangements, many participants (n = 204, 23.7%) lived on campus with suitemates, 201 (23.3%) lived with their parents/guardians, 190 (22.0%) lived with their partners or spouses, 102 (11.8%) lived alone, and 36 (4.2%) lived with a non-student roommate. Regarding religious affiliation, 336 (39.3%) of the participants identified as Christian, 250 (29.2%) identified as spiritual/not religious, 129 (15.1%) identified as agnostic, 103 (11.9%) identified as atheist, 11 (1.3%) identified as Buddhist, 11 (1.3%) identified as Jewish, 8 (0.9%) identified as Muslim, and 1 (0.1%) identified as Mormon.
Instruments
Demographic Questionnaire
The demographic questionnaire consisted of 13 questions. These questions addressed age, gender, sexual orientation, class standing, enrollment status, race/ethnicity, and living arrangements. Additional questions asked about marital status, income, religion/spiritual practice, and employment.
UCLA Loneliness Scale
The UCLA Loneliness Scale (Version 3) is a 20-item scale measure of subjective feelings of loneliness and feelings of social isolation (Russell, 1996). Participants are asked to rate how often each of the positively and negatively worded statements describes them on a 4-point Likert scale from 1 (never) to 4 (often). Sample items included, “How often do you feel that there are people that you can talk to?” and “How often do you feel that people are around you but not with you?” Scoring is done by reversing the positively worded items and then summing the scores on each item for a composite score ranging from 20 to 80, with higher scores (> 40) indicating greater degrees of loneliness. Version 3 has been widely used and validated with the college population as well as other adults in the United States and has yielded high reliability with alpha coefficient values ranging from .89 to .94 and test-retest reliability of .73 (Russell, 1996). In the current study, we followed Kalkbrenner’s (2023) recommendation and computed both Cronbach’s alpha value and coefficient omega, as the latter is a robust measure to alpha’s statistical assumptions. For the UCLA Loneliness Scale, both were the same value of .94, indicating strong reliability.
Social Self-Efficacy Scale
The Social Self-Efficacy Scale (SSES) is a 6-item measure subscale from the Self-Efficacy Scale (Sherer et al., 1982) that assesses students’ beliefs in their social competence. Items ask participants to respond on a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree) to statements like “It is difficult for me to make new friends” and “I do not handle myself well in social gatherings.” Reverse scoring is done for the negatively worded items followed by summing the scores of all the items. A higher score indicates higher social self-efficacy. Researchers have indicated coefficient alpha values of .76 and .71 (Sherer et al., 1982; Wei et al., 2005). Construct validity for this measure has demonstrated correlations with measures of ego strength, interpersonal competency, and self-esteem (Sherer et al., 1982). In the current study, Cronbach’s alpha value for the SSES was .60, while the coefficient omega value was .57. Because we used a subscale of the Self-Efficacy Scale, the poor internal consistency reliability estimates of the SSES might, in part, be due to the low number of questions (Tavakoli & Dennick, 2011). Nonetheless, this instrument was chosen because it is a widely used instrument for assessing social self-efficacy and has reported construct validity (Sherer et al., 1982).
The Experiences in Close Relationships—Relationship Structures Questionnaire
The Experiences in Close Relationships—Relationship Structures Questionnaire (ECR-RS; Fraley et al., 2011) is a 9-item measure used to assess attachment patterns with a variety of familiar relationships. For the current study, participants were asked to respond on the basis of close relationships in general as opposed to thinking about a specific person/relationship. The ECR-RS has two fundamental dimensions of underlying attachment patterns: anxious attachment and avoidant attachment. Sample items include “I usually discuss my concerns and problems with this person,” “I find it easy to depend on this person,” and “I worry this person may abandon me.” Participants rate the extent to which they believe each of the nine statements describes their feelings about their close relationships on a 7-point Likert scale from 1 (strongly disagree) to 7 (strongly agree). Items 1, 2, 3, and 4 are reverse scored. Items 1 to 6 make up the Avoidance Attachment scale, and items 7 to 9 comprise the Anxiety Attachment scale (Fraley et al., 2011). Scores for each scale are derived from finding the average of the items.
Researchers noted Cronbach’s alpha reliabilities ranging between .83 and .87 for the Anxiety Attachment scale and .81 to .92 for the Avoidance Attachment scale across multiple domains (Fraley et al., 2011; Klausli & Caudill, 2021). Our study yielded a Cronbach’s alpha score of .88 and a coefficient omega score of .87 on the Avoidance Attachment scale and alpha .76 and omega .82 for the Anxiety Attachment scale. The ECR-RS has been normed on the college-age population, and Varghese and Pistole (2017) demonstrated the usefulness of this instrument with college students.
Data Analyses
SPSS (Version 27) was used to analyze the data. We first examined the data for missing values that are common in survey research and utilized D. A. Bennett’s (2001) recommendation for deleting cases that had 10% of the data missing. For data that were missing at random, these data were replaced using group means for any item that had 15% or less of the cases missing as a way of maintaining the sample size without threatening the validity of the results (George & Mallery, 2010). Descriptive statistics and reliability estimates for all the scales of the sample were calculated to check for errors, statistical assumptions, and violations, and to describe the data distribution. We utilized the guide that a distribution could be approximated to normal if the skewness value was less than or equal to plus or minus two [≤ ±2] (Garson, 2012).
The skewness and kurtosis values for all but the UCLA Loneliness Scale were less than plus or minus two (< ±2), indicating approximately normal distribution (George & Mallery, 2010). It should be noted that the mean, median, and mode for the loneliness measure were similar (47.46), suggesting a fairly normal distribution. Scores were, however, negatively skewed. The data revealed that 15.8% of students scored in the high range for loneliness levels (40–60) and 53.8% were in the very high range (≥ 61). Collinearity statistics were in the acceptable range and met the assumptions for multicollinearity. The means and standard deviation, as well as correlations for the main variables from the SSES, UCLA Loneliness Scale, and Anxiety Attachment and Avoidance Attachment subscales, are presented in Table 1. We used Pearson’s correlation to answer the first research question and regression analyses were used for the other research questions and hypothesis.
Table 1
Pearson Correlations of Study Variables With Means and Standard Deviation
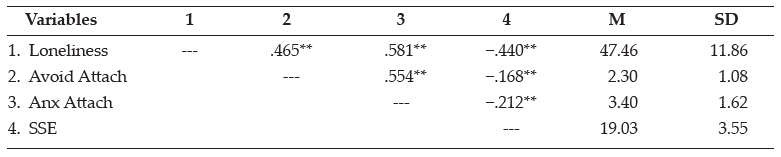
Note. Avoid Attach = Avoidant Attachment, Anx Attach = Anxious Attachment, SSE = Social Self-Efficacy.
**p < .01.
Results
Correlational Analysis
Pearson correlations were computed to answer the first research question: What is the relationship between social self-efficacy, loneliness, and the types of insecure attachment? The results of the Pearson correlation showed a statistically significant positive correlation between loneliness and avoidant attachment (r = .47, p < .001) and loneliness and anxious attachment (r = .58, p < .001), indicating that participants who had higher levels of avoidant attachment and anxious attachment experienced higher levels of loneliness. The results of Pearson correlation analysis showed a statistically significant negative correlation between loneliness and social self-efficacy (r = −.44, p < .001). The findings indicated that participants who experienced higher levels of social self-efficacy experienced lower levels of loneliness. Additionally, the results of Pearson correlation analysis showed a statistically significant, albeit weak, negative correlation between social self-efficacy and anxious attachment (r = −.21, p < .001), as well as avoidant attachment (r = −.17, p < .001).
Both anxious attachment and avoidant attachment explained 34% and 22% of the variances in loneliness, respectively. Additionally, we found that anxious attachment accounted for 4% of the variance, and avoidant attachment explained 3% of the variance in social self-efficacy. When we analyzed the relationship between loneliness, social self-efficacy, avoidant attachment, and anxious attachment, we found that avoidant attachment was significantly negatively associated with loneliness, while all the other variables showed a significant positive (p < .001) association.
Multiple Regression Analysis
Multiple regression was used to answer the second research question: Do anxious attachment and avoidant attachment predict the levels of social self-efficacy? The results indicated that anxious attachment was a statistically significant predictor of social self-efficacy (F = 40.68, p < .001) with a β of .04 (p < .001), accounting for 5% of the variance in social self-efficacy (see Table 2). These results indicate that among students who participated in this study, higher levels of social self-efficacy were a result of lower levels of both anxious attachment and avoidant attachment styles. Overall, the model explains 5% of the variance of anxious attachment in social self-efficacy (r = .39).
Table 2
Multiple Regression Analysis Predictor of Social Self-Efficacy
Factor R R2* β t p F P
Anxious attachment .21 .05 .04 −6.38 < .001 40.68 < .001
*Adjusted R2 = .04
Finally, we examined the third research question and the corresponding hypothesis: How does social self-efficacy mediate the relationship between loneliness and anxious attachment and avoidant attachment styles? In support of our hypothesis that social self-efficacy would mediate the relationship between avoidant attachment and anxious attachment and loneliness, we conducted two regression analyses using Baron and Kenny’s model (1986) for each. In the first model (Figure 1a), in Step 1 the predictor avoidant attachment was regressed on the outcome loneliness. This path provided the coefficient for path c = 5.13 as identified in Figure 1a and was statistically significant {t (861) = 15.42, p = < .001}. In Step 2, the mediator social self-efficacy was regressed against the outcome and provided the path coefficient, denoted a = −.55, with t (862) = −.55, p = < .001. In Step 3, social self-efficacy was regressed on loneliness and the mediator. The significance of the mediation was determined using the Sobel test and was found to be statistically significant at z = −13.54, p = < .001.
Figure 1a
Mediation Path Model for Social Self-Efficacy on Avoidant Attachment on Loneliness
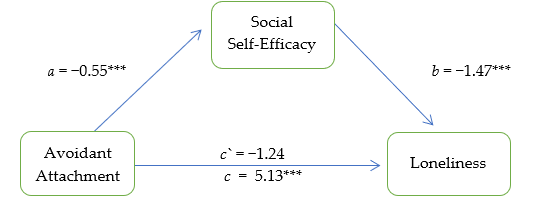
Note. Mediation model testing social self-efficacy as mediator for avoidant attachment and loneliness.
***p < .001
The second path model (Figure 1b) was conducted to ascertain the extent to which social self-efficacy mediated the relationship between anxious attachment and loneliness. Step 1 of the mediation provided the coefficient for path c = 4.25. This was statistically significant {t (861) = 20.945, p = .001}. The mediation path was also statistically significant, signaling partial mediation: c` = 3.73 {t (860) = 19.59, p < .001} with R2 = .442 and adjusted R2 = .441.
Figure 1b
Mediation Path Model for Social Self-Efficacy on Anxious Attachment on Loneliness
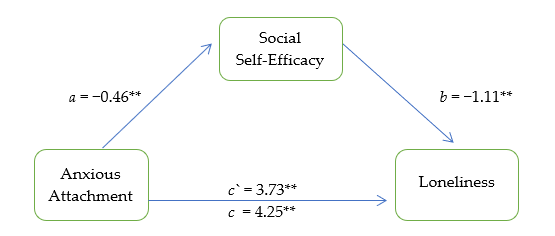
Note. Mediation model testing social self-efficacy as mediator for anxious attachment and loneliness.
**p < .001
Discussion
In the current study, we found statistically significant relationships among anxious attachment, avoidant attachment, social self-efficacy, and loneliness. Higher levels of anxious attachment and avoidant attachment were correlated to higher levels of loneliness, which is consistent with prior studies (Benoit & DiTommaso, 2020; Mikulincer & Shaver, 2014). Individuals with insecure attachment styles are predisposed to feeling lonely and may not be motivated to seek out others and engage in social activities. Conversely, those with secure attachment styles are more likely to engage with others because of their healthy view of themselves and their interpersonal ability to build and maintain relationships (Akdoğan, 2017; DiTommaso et al., 2015; Mikulincer & Shaver, 2019). Additionally, the results indicate that social self-efficacy was negatively associated with both anxious attachment and avoidant attachment, as well as loneliness. Students with higher levels of social self-efficacy did not score as having anxious or avoidant attachment styles. Although the weak correlations mean that the findings should be considered with caution, the negative relationship between insecure attachment styles and social self-efficacy reflects the expectations outlined by attachment theory. Specifically, individuals who demonstrate anxious and avoidant attachments will theoretically experience more social interaction challenges, as they may likely possess less social efficacy.
In college, many young adults struggle to adjust to their new social networks and make meaningful relationships. This can be especially challenging for students with an insecure attachment style and can result in them experiencing both emotional and social loneliness as described by DiTommaso et al. (2015) and Yanguas et al. (2018). The current study findings of a negative association between social self-efficacy and insecure attachment support the notion that students with insecure attachment styles may have deficits in their prosocial skills and their ability to initiate and maintain interactions with others, in part explaining their loneliness (Akdoğan, 2017). Negative social self-efficacy stems from internalized negative views about self-worth and competence, as well as a fear of rejection and distrust of others, which can contribute to feelings of loneliness (Akdoğan, 2017; DiTommaso et al., 2015).
In support of the mediation hypothesis, the relationship between avoidant attachment and loneliness was mediated by social self-efficacy, with high social self-efficacy explaining decreased loneliness in those with avoidant attachment. Interestingly, the relationship between anxious attachment and loneliness was only partially mediated by social self-efficacy. Through the lens of attachment theory, this partial mediation makes sense in that individuals with high anxious attachment tend to be fearful of rejection and abandonment. They tend to be overly self-focused and critical; therefore, they may be more likely to perceive themselves as lonely because these worries undermine the quality of their interpersonal relationships (Akdoğan, 2017; Mikulincer & Shaver, 2014). These individuals may hold a negative working model of self and may be more likely to perceive themselves as low in social self-efficacy, which could account for the partial mediation.
Conversely, individuals with an avoidant attachment style typically have low expectations of others and tend to push people away. However, the findings indicate that when individuals also have strong social self-efficacy, this seems to mediate the desire for detachment and help them in building relationships with others. Social self-efficacy strengthens one’s interpersonal competency and social skills, thereby enhancing coping strategies and self-regulation during relationship challenges. Thus, our findings support the existing literature that social self-efficacy mediates the relationship between anxious attachment and avoidant attachment on loneliness.
Although this study supports the established relationship of insecure attachment styles and high levels of loneliness, as well as the mediation effect of social self-efficacy on insecure attachment and loneliness, we recognize that existing research has examined the mediating effect after controlling for some psychological distress like depression (Wei et al., 2005). As a result, we reviewed the mediating effects of other constructs that are comparable to social self-efficacy. Our study provides support for mediating effects of feelings of inferiority on insecure attachment and loneliness (Akdoğan, 2017), as well as for mediating effects of social support (Benoit & DiTommaso, 2020). We posit that feelings of inferiority and lack of social support are very similar to lack of social self-efficacy and have significant clinical implications.
Implications for Counseling
Our findings suggest that attachment style greatly influences loneliness and the propensity for how one makes and maintains relationships (Akdoğan, 2017; Helm et al., 2020). For emerging adults who are at Erikson’s stage of intimacy versus isolation, loneliness can be understood as a developmental struggle that some students may need help resolving, particularly if they have avoidant or anxious attachment styles (Erikson, 1980). Counselors should therefore broach the subject of loneliness and assess for loneliness and low self-efficacy with clients as well as examine interpersonal difficulties on campus.
College counselors could utilize the Diagnostic and Statistical Manual of Mental Disorders (5th ed.; American Psychiatric Association, 2013) Level 1 and Level 2 cross-cutting symptom measures for adults or the widely used Counseling Center Assessment of Psychological Symptoms (CCAPS; Locke et al., 2011), as well as readily available assessments for depression and anxiety, to collect data on students’ levels of psychological stress. Psychological stress, depression, and anxiety are identified as contributors to and symptoms of loneliness (Cacioppo et al., 2015; Fink, 2014; Moeller & Seehuus, 2019) and can further provide information on social self-efficacy. Additionally, during the normal intake session and risk assessments, counselors should assess for social support, thereby gathering qualitative data on students’ social networks and the quality of their interpersonal relationships.
Because social self-efficacy mediated the relationship between attachment and loneliness, it could prove helpful for counselors to help clients bolster their prosocial skills and interpersonal confidence. This could be done through individual and group counseling interventions based on clients’ assessed needs related to psychological stress and interpersonal difficulties. Furthermore, because counseling promotes a strength-based and wellness philosophy, counselors can work with all students to enhance prosocial skills and interpersonal confidence and resiliency. Bandura (2000) noted that high social self-efficacy requires greater cognitive resourcefulness and flexibility to not only manage the environment but as motivation to achieve a desired goal. For college students, bolstering social self-efficacy might help to build interpersonal confidence, enhance motivation, and give them social capital (Thomas et al., 2020). Our hope is that through these processes, students’ intra- and interpersonal development regarding increased social self-efficacy will translate to academic success, personal success, and a decrease in perceived loneliness.
Because of the interactive nature of group counseling, it may be useful as a therapeutic approach to reducing loneliness in college students. Group counseling may also reveal how those with loneliness approach developing relationships with others in the group. Group work is known to be highly effective and superior to individual therapy, as it provides opportunities for social learning, developing social supports, and improving social networks (Yalom & Leszcz, 2020). For example, personal growth groups (e.g., social support groups or interpersonal process groups) are focused on both the personal and social development of members and can be used as interventions to address insecure attachment and loneliness. Additionally, these groups help members to develop self-awareness and insight while also learning new skills to enhance their interpersonal attractiveness. In short, groups like these have the potential to address members’ interpersonal challenges and disrupt behaviors that impede the building and maintaining of healthy relationships while also enhancing group members’ social self-efficacy. Ultimately, the focus is on relationship building and helping members to feel more connected with each other (Reese, 2011).
Additional ways in which counselors could support students experiencing loneliness is through collaboration with residence life, other social clubs, and groups to help students find connections and learn how to foster and maintain healthy relationships. These approaches support the work of Moeller and Seehuus (2019), reiterating the need to build and enhance college students’ social skills (thereby enhancing social self-efficacy) and facilitating opportunities for greater engagement to reduce loneliness and increase retention (Thomas et al., 2020).
It is noteworthy, but not surprising, that higher anxious and avoidant attachments correlated to higher levels of loneliness in our study. Given this knowledge that students may have negative working models of self and/or others, counselors may need to expand the ways in which they develop rapport and provide supportive spaces for risk-taking where clients may be more willing to explore issues surrounding their insecure attachment. Exploring the impact of the insecure attachment on their sense of self and how it presents as a barrier to initiating and/or maintaining quality social connections could be helpful, in addition to teaching strategies and skills to increase their sense of safety and self-efficacy.
Having conversations about initiating and maintaining meaningful relationships can also allow the counselor to address the risk of rejection and vulnerability inherent in relationships and help the clients develop coping skills to deal with these experiences rather than internalizing negative results. The counseling relationship can serve as a model and as evidence to the students that they have the ability to connect with others. Wei et al. (2005) noted that counselors could help students with high avoidant attachment understand how their reluctance to self-disclose prevents them from developing deeper or emotionally fulfilling relationships. Counselors can help clients with high anxious attachment examine how self-doubts may contribute to their perceptions of loneliness and other mental health challenges and learn strategies to increase self-confidence.
Moreover, the counseling relationship can serve as a model to evaluate the impact of self-doubt and lack of self-disclosure on the relationship and help with insight and self-awareness. As counseling progresses and students begin to address the self-doubt or begin to self-disclose, they will also be able to see how these changes shift the dynamics of the relationship and can lead to a more satisfying relationship. Counselors can incorporate strategies from different modalities, including using cognitive behavioral therapy and narrative therapy to address maladaptive thinking, and can help students explore unique outcomes congruent with their goals. E. D. Bennett et al. (2017) recommended some creative strategies that could be employed (e.g., talk meter, the paper bag story, using music, or modeling interventions using social media models). It is hoped that as students increase their self-awareness and social self-efficacy, they will transfer and integrate these new behaviors in establishing and maintaining relationships outside of the counseling room, thereby strengthening their social networks and decreasing loneliness.
Limitations and Future Research
Though a robust study in terms of the number of participants, this study has several limitations that should be considered. Some of the data collection took place when the college pivoted to online learning and students had to stay home as a result of COVID-19. This time of forced social isolation could have impacted students’ responses. The cross-sectional design of this study is a limitation. Social self-efficacy and perception of loneliness were assessed at one point in time. Social self-efficacy and loneliness are complex constructs that can vary at different time points, so a longitudinal research design is an important next step. Furthermore, a longitudinal design would allow researchers to track changes over time and throughout students’ college experiences, noting changes as a student progresses developmentally.
The self-report nature of the measurements and response bias are limitations that weaken the construct validity of the study. Self-report measures, though used extensively in research, are subject to respondent biases and social desirability (Crowne & Marlowe, 1964), which can limit self-awareness, self-knowledge, and self-report. The poor internal consistency reliability estimates of the SSES in this study is another limitation that might indicate that the SSES failed to capture stability of test scores within our sample. Future researchers may consider using other measures of social self-efficacy.
Although the mediation model provides explanatory effect of social self-efficacy on attachment and loneliness, future studies should examine other related factors such as self-esteem, empathy, or personality traits like Myers-Briggs or the Big Five personality traits. Additionally, the attachment measure was retrospective in nature, and participants were instructed to consider their feelings about close relationships in general rather than on a specific relationship on the Experiences in Close Relationships—Relationship Structures Questionnaire. In retrospect, it might have been more beneficial to have them consider specific relationships at college.
Conclusion
This study further expanded the research on the impact of insecure attachment as a contributor to feelings of loneliness. Further, our study pointed to social self-efficacy as a possible mediator for this relationship. Although attachment styles may be difficult to change, enhancing mediators like social self-efficacy might help individuals with insecure attachment styles to reduce loneliness (Thomas et al., 2020). Helping individuals with insecure attachment styles learn new skills to enhance their interpersonal and intrapersonal skills might enhance their beliefs in others and possibly bolster their self-confidence and competence. In the college setting, enhancing insecure attachment styles may have long-term consequences on reducing feelings of loneliness and may contribute to a sense of belonging and increase retention rates and academic success.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Ainsworth, M. D. (1985). Patterns of infant-mother attachments: Antecedents and effects on development. Bulletin of the New York Academy of Medicine, 61(9), 771–791. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1911899/pdf/bullnyacadmed00065-0005.pdf
Akdoğan, R. (2017). A model proposal on the relationships between loneliness, insecure attachment, and inferiority feelings. Personality and Individual Differences, 111, 19–24. https://doi.org/10.1016/j.paid.2017.01.048
American College Health Association. (2017). American College Health Association – National College Health Assessment II: Fall 2017 Reference Group Executive Summary. https://www.acha.org/documents/ncha/NCHA-II_FALL_2017_REFERENCE_GROUP_EXECUTIVE_SUMMARY.pdf
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
Bandura, A. (1977). Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review, 84(2), 191–215. https://doi.org./10.1037/0033-295X.84.2.191
Bandura, A. (2000). Self-efficacy. In A. E. Kazdin (Ed.), Encyclopedia of psychology (Vol. 7, pp. 212–213). Oxford University Press. https://doi.org/10.1037/10522-094
Baron, R. M., & Kenny, D. A. (1986). The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51(6), 1173–1182. https://doi.org/10.1037//0022-3514.51.6.1173
Bennett, D. A. (2001). How can I deal with missing data in my study? Australian and New Zealand Journal of Public Health, 25(5), 464–469.
Bennett, E. D., Le, K., Lindahl, K., Spencer, W., & Mak, T. W. (2017). Five out of the box techniques for encouraging teenagers to engage in counseling. In Ideas and Research You Can Use: VISTAS 2017, Article 3, 1–17. https://www.counseling.org/docs/default-source/vistas/encouraging-teenagers.pdf
Benoit, A., & DiTommaso, E. (2020). Attachment, loneliness, and online perceived social support. Personality and Individual Differences, 167, 110230. https://doi.org/10.1016/j.paid.2020.110230
Bowlby, J. (1973). Attachment and loss: Separation anxiety and anger. Basic Books.
Bruffaerts, R., Mortier, P., Kiekens, G., Auerbach, R. P., Cuijpers, P., Demyttenaere, K., Green, J. G., Nock, M. K., & Kessler, R. C. (2018). Mental health problems in college freshmen: Prevalence and academic functioning. Journal of Affective Disorders, 225, 97–103. https://doi.org/10.1016/j.jad.2017.07.044
Cacioppo, S., Grippo, A. J., London, S., Goossens, L., & Cacioppo, J. T. (2015). Loneliness: Clinical import and interventions. Perspectives on Psychological Science, 10(2), 238–249. https://doi.org/10.1177/1745691615570616
Chickering, A. W., & Reisser, L. (1993). Education and identity (2nd ed.). Jossey-Bass.
Cigna. (2020). Loneliness and the workplace: 2020 U.S. Report. https://www.cigna.com/static/www-cigna-com/docs/about-us/newsroom/studies-and-reports/combatting-loneliness/cigna-2020-loneliness-report.pdf
Crowne, D. P. and Marlowe, D. (1964). The approval motive: Studies in evaluation dependence. Wiley.
Dahlberg, L. (2021). Loneliness during the COVID-19 pandemic. Aging & Mental Health, 25(7), 1161–1164. https://doi.org/10.1080/13607863.2021.1875195
Diehl, K., Jansen, C., Ishchanova, K., & Hilger-Kolb, J. (2018). Loneliness at universities: Determinants of emotional and social loneliness among students. International Journal of Environmental Research and Public Health, 15(9), 1865. https://doi.org/10.3390/ijerph15091865
DiTommaso, E., Fizell, S. R., & Robinson, B. A. (2015). Chronic loneliness within an attachment framework: Processes and interventions. In A. Sha´ked & A. Rokach (Eds.), Addressing loneliness: Coping prevention and clinical interventions (pp. 241–253). Routledge.
Eisenberg, D., Lipson, S. K., & Heinze, J. (2020). The healthy minds study: Fall 2020 data report. https://healthymindsnetwork.org/wp-content/uploads/2021/02/HMS-Fall-2020-National-Data-Report.pdf
Erikson, E. H. (1980). Identity and the life cycle. W. W. Norton.
Fink, J. E. (2014). Flourishing: Exploring predictors of mental health within the college environment. Journal of American College Health, 62(6), 380–388. https://doi.org/10.1080/07448481.2014.917647
Fraley, R. C., Heffernan, M. E., Vicary, A. M., & Brumbaugh, C. C. (2011). Experiences in Close Relationships—Relationship Structures Questionnaire. APA PsycTests. https://doi.org/10.1037/t08412-000
Garson, G. (2012). Testing statistical assumptions. Statistical Associates Publishing.
George, D., & Mallery, P. (2010). SPSS for Windows step by step: A simple study guide and reference, 17.0 update (10th ed.). Allyn & Bacon.
Helm, P. J., Jimenez, T., Bultmann, M., Lifshin, U., Greenberg, J., & Arndt, J. (2020). Existential isolation, loneliness, and attachment in young adults. Personality and Individual Differences, 159, 109890.
https://doi.org/10.1016/j.paid.2020.109890
Holt-Lunstad, J. (2020, June 22). The double pandemic of social isolation and COVID-19: Cross-sector policy must address both. Health Affairs Forefront. https://doi.org/10.1377/hblog20200609.53823
Kalkbrenner, M. T. (2023). Alpha, omega, and H internal consistency reliability estimates: Reviewing these options and when to use them. Counseling Outcome Research and Evaluation, 14(1), 77–88.
https://doi.org/10.1080/21501378.2021.1940118
Kim, Y., Kim, B., Hwang, H.-S., & Lee, D. (2020). Social media and life satisfaction among college students: A moderated mediation model of SNS communication network heterogeneity and social self-efficacy on satisfaction with campus life. The Social Science Journal, 57(1), 85–100.
https://doi.org/10.1016/j.soscij.2018.12.001
Klausli, J. F., & Caudill, C. (2021). Discerning student depression: Religious coping and social support mediating attachment. Counseling and Values, 66(2), 179–198. https://doi.org/10.1002/cvj.12156
Locke, B. D., Buzolitz, J. S., Lei, P.-W., Boswell, J. F., McAleavey, A. A., Sevig, T. D., Dowis, J. D., & Hayes, J. A. (2011). Development of the Counseling Center Assessment of Psychological Symptoms-62 (CCAPS-62). Journal of Counseling Psychology, 58(1), 97–109. https://doi.org/10.1037/a0021282
Mallinckrodt, B., & Wei, M. (2005). Attachment, social competencies, social support, and psychological distress. Journal of Counseling Psychology, 52(3), 358–367. https://doi.org/10.1037/0022-0167.52.3.358
Mikulincer, M., & Shaver, P. R. (2014). An attachment perspective on loneliness. In R. J. Coplan & J. C. Bowker (Eds), The handbook of solitude: Psychological perspectives on social isolation, social withdrawal, and being alone (pp. 34–50). Wiley.
Mikulincer, M., & Shaver, P. R. (2019). Attachment orientations and emotion regulation. Current Opinion in Psychology, 25, 6–10. https://doi.org/10.1016/j.copsyc.2018.02.006
Moeller, R. W., & Seehuus, M. (2019). Loneliness as a mediator for college students’ social skills and experiences of depression and anxiety. Journal of Adolescence, 73(1), 1–13.
https://doi.org/10.1016/j.adolescence.2019.03.006
Murthy, V. (2020, March 23). Former surgeon general Vivek Murthy: Loneliness is a public health crisis [Interview]. WBUR On Point. https://www.wbur.org/onpoint/2020/03/23/vivek-murthy-loneliness
Mushtaq, R., Shoib, S., Shah, T., & Mushtaq, S. (2014). Relationship between loneliness, psychiatric disorders and physical health? A review on the psychological aspects of loneliness. Journal of Clinical and Diagnostic Research, 8(9), 1–4. https://doi.org/10.7860/JCDR/2014/10077.4828
Pan American Health Organization. (2020, January 30). WHO declares public health emergency on novel coronavirus [Press release]. https://www.paho.org/en/news/30-1-2020-who-declares-public-health-emergency-novel-coronavirus
Perlman, D., & Peplau, L. A. (1981). Toward a social psychology of loneliness. In R. Gilmour & S. Duck (Eds.), Personal Relationships: 3. Relationships in Disorder (pp. 31–56). Academic Press.
Qualter, P., Vanhalst, J., Harris, R., Van Roekel, E., Lodder, G., Bangee, M., Maes, M., & Verhagen, M. (2015). Loneliness across the life span. Perspectives on Psychological Science, 10(2), 250–264.
https://doi.org/10.1177/1745691615568999
Reese, M. K. (2011). Interpersonal process groups in college and university settings. In T. Fitch & J. L. Marshall (Eds.), Group work and outreach plans for college counselors (pp. 87–92). American Counseling Association.
Russell, D. W. (1996). UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. Journal of Personality Assessment, 66(1), 20–40. https://doi.org/10.1207/s15327752jpa6601_2
Sharf, R. S. (2012). Theories of psychotherapy and counseling: Concepts and cases (5th ed.). Cengage.
Sherer, M., Maddux, J. E., Mercandante, B., Prentice-Dunn, S., Jacobs, B., & Rogers, R. W. (1982). The Self-Efficacy Scale: Construction and validation. Psychological Reports, 51(2), 663–671.
https://doi.org/10.2466/pr0.1982.51.2.663
Tabachnick, B. G., & Fidell, L. S. (2007). Using multivariate statistics (5th ed.). Pearson.
Tavakoli, M., & Dennick, R. (2011). Making sense of Cronbach’s alpha. International Journal of Medical Education, 2, 53–55. https://doi.org/10.5116/ijme.4dfb.8dfd
Thomas, L., Orme, E., & Kerrigan, F. (2020). Student loneliness: The role of social media through life transitions. Computers & Education, 146, 103754. https://doi.org/10.1016/j.compedu.2019.103754
Thurber, C. A., & Walton, E. A. (2012). Homesickness and adjustment in university students. Journal of American College Health, 60(5), 415–419. https://doi.org/10.1080/07448481.2012.673520
Varghese, M. E., & Pistole, M. C. (2017). College student cyberbullying: Self-esteem, depression, loneliness, and attachment. Journal of College Counseling, 20(1), 7–21. https://doi.org/10.1002/jocc.12055
Wei, M., Russell, D. W., & Zakalik, R. A. (2005). Adult attachment, social self-efficacy, self-disclosure, loneliness, and subsequent depression for freshman college students: A longitudinal study. Journal of Counseling Psychology, 52(4), 602–614. https://doi.org/10.1037/0022-0167.52.4.602
Yalom, I. D., & Leszcz, M. (2020). The theory and practice of group psychotherapy (6th ed.). Basic Books.
Yanguas, J., Pinazo-Henandis, S., & Tarazona-Santabalbina, F. J. (2018). The complexity of loneliness. Acta Biomedica, 89(2), 302–314. https://doi.org/10.23750/abm.v89i2.7404
Zhu, W., Wang, C. D., & Chong, C. C. (2016). Adult attachment, perceived social support, cultural orientation, and depressive symptoms: A moderated mediation model. Journal of Counseling Psychology, 63(6),
645–655. https://doi.org/10.1037/cou0000161
Claudette Brown-Smythe, PhD, NCC, ACS, LMHC, CRC, is an assistant professor at SUNY Brockport. Shirin Sultana, PhD, MSS, MSSW, is an assistant professor at SUNY Brockport. Correspondence may be addressed to Claudette Brown-Smythe, 350 New Campus Drive, Brockport, NY 14420, cbrownsm@brockport.edu.
May 10, 2023 | Volume 13 - Issue 1
Joshua D. Smith, Neal D. Gray
Each year TPC presents an interview with an influential veteran in counseling as part of its Lifetime Achievement in Counseling series. This year I am honored to introduce Cherylene McClain Tucker, supervisor of a day treatment program and a lifelong learner and advocate. In this interview, she shares how her experiences in criminal justice, addictions counseling, and mental health counseling intersect to support the mental health and wellness of the whole person. I am grateful to Dr. Joshua Smith and Dr. Neal Gray for highlighting the ongoing contributions of leaders in the profession for the TPC readership. —Richelle Joe, Editor
 Cherylene McClain Tucker, NCC, MAC, LPC, LCDC, is a Program Supervisor with the Tarrant County Community Supervision and Corrections Department (CSCD) in Fort Worth, Texas. She holds a Bachelor of Science in criminal justice from St. John’s University, and Master of Arts degrees in both professional counseling and marriage and family therapy from Amberton University.
Cherylene McClain Tucker, NCC, MAC, LPC, LCDC, is a Program Supervisor with the Tarrant County Community Supervision and Corrections Department (CSCD) in Fort Worth, Texas. She holds a Bachelor of Science in criminal justice from St. John’s University, and Master of Arts degrees in both professional counseling and marriage and family therapy from Amberton University.
Tucker is an active member of several organizations. She is a board member of the Texas Certification Board of Addiction Professionals, and she is a member of the Tarrant County College Mental Health Advisor Committee. Recently, she has been selected to be a mentor with the NBCC Foundation and the Association for Addiction Professionals (NAADAC) Minority Fellowship Program for Addiction Counselors, where she will be mentoring future addiction counselors.
Tucker has also received several awards: the 2016 Counselor of the Year Award from the local chapter of the Texas Association of Addiction Professionals; the 2016 Elves Smith Counselor of the Year Award from the State Board of the Texas Association of Addiction Professionals; and the 2017 Lora Roe Memorial Addiction Counselor of the Year Award from NAADAC.
Prior to her current position, Tucker has worked with the addicted population as a case manager, as an addiction counselor in a hospital setting, and in the criminal justice system as a parole officer.
In Tucker’s current position, she is the program supervisor over the day treatment program in an intensive treatment program within adult probation. She currently oversees eight different modalities of treatment that address substance use disorders, mental health issues, and cognitive distortions. Tucker also collaborates with stakeholders in the community to assist probationers with gaining autonomy and becoming pro-social members of their community.
- What led you to pursue a degree in counseling compared to other helping professions?
What initially led me to the helping professions was my academic interest in criminal justice. While pursuing my undergraduate degree at St. John’s University, I completed an internship with Nassau County Probation Department. Here I observed the DWI Unit. It was suggested that if I wanted to pursue a career in probation, I needed some work history in social service. It was suggested the best place to do this was working in foster care. I took the suggestion; I obtained a job at Catholic Home Bureau. This is where my passion was awakened.
I began working with adults caught in the grips of addiction in 1987 as a caseworker in New York City for the Catholic Home Bureau Agency. This was the peak of the crack epidemic. This was also the era when HIV was still an unknown disease. Early on I saw how addiction impacted the lives of people and how their families were being destroyed. Working as a caseworker, I felt I was not doing enough to help and desired to help this population more. I returned to school to acquire my substance abuse training at Molloy College in 1991 as a Credentialed Alcoholism Counselor (CAC). In 1993, I began working in the therapeutic field of addiction as an addiction counselor at Kings County Hospital, in Brooklyn, New York. Here I was able to help those caught in the grips of addiction from various areas of life, not just foster care.
Many of my clients had lengthy histories of abuse, neglect, mental health issues, or involvement in the criminal justice or foster care setting. This encouraged me to want to learn more and pursue my graduate studies. In 2009, I returned to school and obtained my master’s degree in professional counseling, and I returned again in 2016 and obtained my master’s degree in marriage and family therapy. I became a Licensed Professional Counselor in 2018.
- Recently, you were awarded the Lora Roe Memorial Addiction Counselor of the Year Award from NAADAC, the Association for Addiction Professionals. What has been your experience working in both mental health and addiction settings? What challenges or barriers have you encountered as a counselor in this area?
As I mentioned before, working with addiction intrigued me. There were so many different facets of addiction. As I began to understand addiction and alcohol and substance use disorders in the DSM, I noticed clients coming into treatment for their addiction had endured long histories of untreated mental health issues. A lot of the referrals from social service agencies were of people who had endured untreated trauma histories. Those mandated to treatment by the criminal justice system many times had untreated and undiagnosed mental health issues.
One of the barriers I encountered early on was not being a dual-licensed counselor and not being able to address those co-occurring disorders because I was only an addiction counselor, licensed to only treat substance use disorders. I knew in order to be effective, I needed to treat the whole person and not just the addiction portion. This gave me the drive to pursue a higher-level education and licensure in order to treat the whole person. A challenge I recognized was that once a person left to pursue a higher level of education, they would pursue a higher level of pay, which many times is not being offered in a substance use disorder treatment setting. I worked many years in a treatment setting, and because I did not have a master’s-level degree or license, my salary did not match my years of experience. This did not deter me from the field. My passion for helping people causes me to stay in this field. Counseling has given me the ability to help people find their hope and develop coping skills to manage their emotions. However, I know that many of my peers have left the field due to the low level of pay.
- In your view, what can be done, or needs to change, to address or overcome these challenges and barriers? Specifically, there has been a push in more recent years for addiction counseling to require graduate-level training. How does this help or hinder the profession and the clients we serve?
I want to start by saying, I am grateful for my formative years I had at Kings County Hospital. Working as an addiction counselor in the trenches gave me my foundation in addiction counseling. This is where I knew I was called to do this career. What I think needs to happen is that there needs to be more incentives for counselors who are working in addiction, especially those who transition from working as a non–master’s-level counselor to a master’s-level counselor. There is a significant difference in pay when working as a non–master’s-level counselor, as opposed to being a master’s-level counselor working in mental health. While in graduate school, there were not as many conversations about working in addiction as there were about working in mental health once you became a fully licensed counselor. I understand that when you complete graduate school, many students have debt and they are eager to become recognizable therapists. Working in the trenches with people is very hard. However, if there was more emphasis on the rewards of working in addiction as opposed to the war stories, there may be more of an interest for clinicians coming into the field. The rewards of working in addiction are helping the families, not just the identified client, and creating safety in communities. When people get sober, they commit fewer crimes and this reduces recidivism. It creates a better economy. When we diminish drug use in communities, those sober individuals return to the work force. I think it would be great if there was more of an emphasis on addiction counseling in graduate-level training. A higher level of course work brings value. I believe this would allow the retention level of staff to be more consistent. Being a master’s-level counselor also allows insurance companies and consumers to invest in treatment that has higher skilled professionals, and this increases that monetary value of the job—another component that supports staff retention.
- You also have a strong background in the field of criminal justice and corrections. In your opinion, how do drug reformation and policy changes to criminalization impact the criminal justice system and addiction counseling? Have you seen any advancements in care and rehabilitation as a result of these changes?
Drug reformation and policy changes for the use of marijuana and the continuing rise of opioids impact the criminal justice system greatly. Drug addiction impacts a myriad of things. It impacts the individual, their family, the community, the judicial system, and health care, just to name a few. The local criminal justice system is designed to protect and serve the community. In the past, professionals in law enforcement and the criminal justice system lacked education and knowledge about addiction and mental health, which has caused many problems, especially in minority communities. I do believe today that many law enforcement agencies and criminal justice agencies are improving. They are hiring more professionals with knowledge of addiction and mental health and establishing collaborative relationships. SAMHSA offers a training for the criminal justice community, “How Being Trauma-Informed Improves Criminal Justice System Responses.” Several community supervision and corrections departments are now training their staff to be trauma informed. On a local judiciary level, because drug reformation has become an issue, many marijuana laws are being reviewed and how these will be managed legally. This continues to be an ongoing concern.
- As counseling professionals, we have a duty to promote social justice and advocate on behalf of our clients and profession. What has been your experience in this area and what shifts have you noticed within the profession and socially to illustrate this commitment?
As a Licensed Professional Counselor working in the criminal justice system for the past 17 years, I have had the opportunity on a regular basis to advocate for clients. In addition to my various duties as a program supervisor over the intensive treatment program at Tarrant County CSCD, I collaborate with two specific courts: FAIP (Felony Alcohol Intervention Project) Court and DWI Misdemeanor Court. In both courts, I am the therapist that offers input during court discussions with the judiciary, attorneys, and officers regarding substance use disorders and mental health as it pertains to clients/probationers. There are other courts within Tarrant County CSCD that collaborate with the judiciary, attorneys, officers, and counselors. What is most rewarding is that the judiciary welcomes the voice of the clinicians in the courtroom, and they value our feedback.
For example, there have been several clients who were experiencing a lot of anxiety. As a result, they were using illicit substances to manage their anxiety. During different court conferences, the judge asked me for my thoughts and feedback. We agreed that I would meet with these clients while they were in treatment in our Intensive Outpatient Program. Upon meeting with these clients, it was evident that they needed to meet with their medical doctor or psychiatrist. The clients were agreeable to this. Once the client was seen by their primary doctor or psychiatrist, we were able to explore the origin of the anxiety and those things that triggered the anxiety. I was able to share with the judge the progress of the clients. The judge was very patient with these clients and allowed these clients to work through some of these issues. Clients were allowed to heal and improve their cognition, causing them to stop using illicit substances and be successful on their probation.
- What has been your experience when interacting with national and local organizations, such as ACA, NAADAC, NBCC, etc.? Do you feel supported by professional organizations or leaders, and has this changed throughout your career?
I am honored to say that I am a member of TCA (Texas Counselors Association), NAADAC (Addiction Professionals) and its local branch (TAAP-Texas Association of Addiction Professionals), and hold certifications from NBCC (National Board for Certified Counselors). Each of these organizations are diligently working on behalf of the counseling profession and for the counselors. The organizations keep us abreast of legislative changes and create policies and implement trainings that support counselors. I feel these organizations are key elements that help to better our profession.
- Throughout your years of practice, what has been your experience when collaborating with other mental health, addiction, and medical professionals? How would you describe coordination of care and treatment options currently as we continue to navigate COVID-19 pandemic–related concerns?
I believe over the years, mental health, addiction, and medical professionals have become more collaborative. Here in North Texas, there are several collaborations that are working together to serve the client. Recently, I was selected to be a stakeholder and to be on the Community Advisor Board with a research project with Texas Christian University (TCU) that is working with our local city hospital, the mental health community, and the criminal justice community to address issues with those who have been infected with HIV and have an opioid use disorder within the criminal justice system. Here the researchers are looking at creating seamless lines for this population of people to receive services. TCU has created a community medical mobile unit to offer services to people in lower socioeconomic communities that are involved in the criminal justice system and those who are receiving mental health services. As a representative in the criminal justice community that offers therapeutic services, they can offer services to our clients. There are other collaborative services that are being offered in the community—connecting the local city hospitals and the mental health community and bridging these gaps in services. The increase of teletherapy has allowed services to go on uninterrupted during the height of the COVID-19 pandemic.
- For future mental health and/or addiction counselors, what advice would you have regarding their involvement in advancement and future development of the profession?
My advice for future clinicians—once you identify your passion, continue to be a forever learner. Our field is ever evolving. Working in addictions, new drugs are always on the rise. We must stay on top of things as changes are coming about. When I started in this profession in 1987 as a caseworker, the DSM-III was the clinical reference. By the time I became an addiction counselor in 1993, the DSM-III-TR was the clinical reference. Here we are in 2023, and the new clinical reference is the DSM-5-TR. Participating with local or national associations allows us to be a part of transitions within and around our profession. Create a voice in our profession that helps to support future clinicians.
This concludes the eighth interview for the annual Lifetime Achievement in Counseling Series. TPC is grateful to Joshua D. Smith, PhD, NCC, LCMHC, and Neal D. Gray, PhD, LCMHC-S, for providing this interview. Joshua D. Smith is an assistant professor at the University of Mount Olive. Neal D. Gray is a professor at Lenoir-Rhyne University. Correspondence can be emailed to Joshua Smith at jsmith@umo.edu.
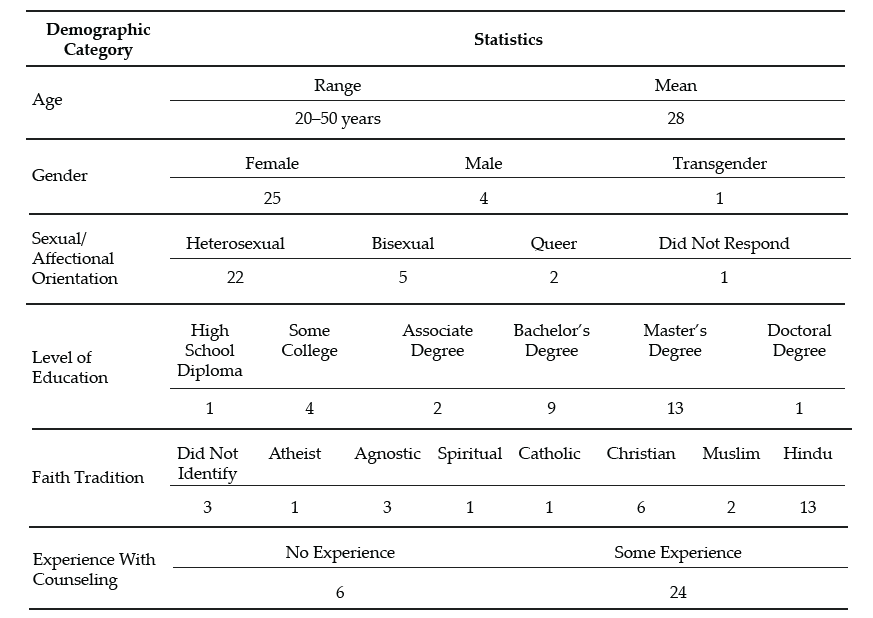
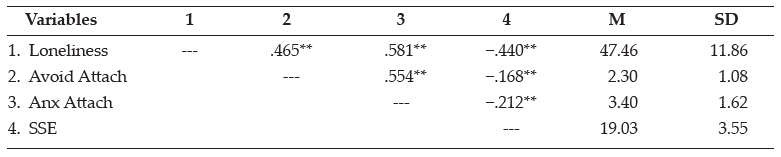
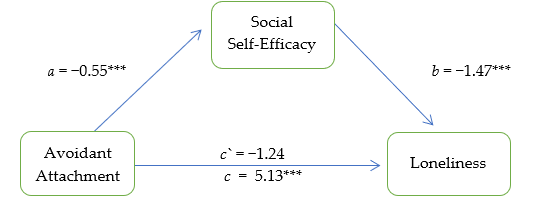
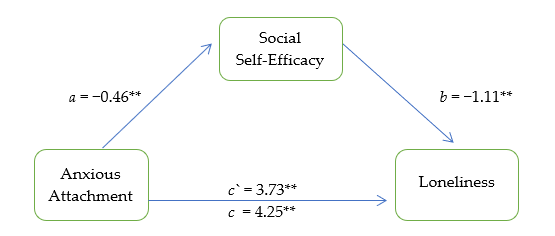
 Cherylene McClain Tucker, NCC, MAC, LPC, LCDC, is a Program Supervisor with the Tarrant County Community Supervision and Corrections Department (CSCD) in Fort Worth, Texas. She holds a Bachelor of Science in criminal justice from St. John’s University, and Master of Arts degrees in both professional counseling and marriage and family therapy from Amberton University.
Cherylene McClain Tucker, NCC, MAC, LPC, LCDC, is a Program Supervisor with the Tarrant County Community Supervision and Corrections Department (CSCD) in Fort Worth, Texas. She holds a Bachelor of Science in criminal justice from St. John’s University, and Master of Arts degrees in both professional counseling and marriage and family therapy from Amberton University.