Russ Curtis, Heather Thompson, Gerald A. Juhnke, Melodie H. Frick
Treatment fit is the degree to which the counselor and the client agree upon the presenting issues, counseling goals and the initial treatment plan. Research indicates that treatment fit is one of the strongest predictors of client outcome. As such, a brief functional treatment fit model (TFM) is presented to assist counselors in conducting multidimensional needs assessments and developing co-created treatment plans. Application of this model is demonstrated with a case study. In addition, a link to a video demonstration of this model is included, along with a discussion as to the need for including links to videos in counseling journals.
Keywords: treatment fit, multidimensional needs assessment, treatment plan, counseling goals, video demonstration
This is an exciting time in the mental health profession as health care specialists and policy makers are recognizing the value of counseling in increasing the quality of patient care while decreasing overall health care costs (Burtnett, 2012; Curtis & Christian, 2012; Lee et al., 2012; Wos, 2013). As such, counselors are increasingly being recognized not just as mental health providers, but as viable health care professionals who may well be the crucial link in improving a flawed and exorbitantly expensive health care system (American Psychological Association [APA], 2012; Brill, 2013; Paquette et al., 2003). With this positive momentum, however, it becomes even more imperative for counselors to consistently utilize evidence-based practices (i.e., empirically supported counseling strategies), which include practice-based evidence (i.e., continuous feedback between counselor and client) to ensure optimal treatment. Unfortunately, the utilization rates of evidence-based practices by counselors are minimal and inconsistent (Beutler, 2009; Olmstead, Abraham, Martino, & Roman, 2012), which may in part be the reason why the general public, when surveyed, have indicated that the primary reason for not seeking counseling was their lack of confidence in positive outcomes (Harris Interactive, 2004). One could argue that while it is critically important for counselors to continue conducting innovative treatment research, it is equally imperative that counselors increase efforts in implementing well-established evidence-based counseling strategies (Olmstead et al., 2012).
One of the best predictors of client outcome is treatment fit (APA, 2012; Budd & Hughes, 2009; Kim, Ng, & Ahn, 2009), the process by which the client and counselor collaboratively assess mental health issues, set goals, and create an initial treatment plan. At the heart of treatment fit is the collaboration between client and counselor including continuous feedback about issues, goals and treatment to ensure the optimal provision of care. A parallel to treatment fit in the medical community is the increasing use of checklists to ensure that evidence-based procedures are being properly implemented. In surgical safety research, for instance, Haynes et al. (2009) found in a large multi-site international study that when medical professionals followed a brief surgical checklist (e.g., the patient has verified his or her identity, the surgical site, and procedure and consent), patient deaths decreased from 1.5% to 0.8% and inpatient complications following surgery decreased from 11.0% to 7.0% (Haynes et al., 2009). As demonstrated in this surgical safety study, the consistent application of evidence-based procedures had a significant impact on patients’ lives. Similarly, the purpose of this article is to show how evidence-based counseling strategies that comprise treatment fit can help counselors more consistently and frequently implement treatments that work in order to increase the likelihood of positive client outcomes.
This article is comprised of two primary objectives. The first objective is to describe a brief, functional, first-session counseling protocol for ensuring treatment fit with clients. The second objective is to increase reader and viewer understanding and application of this treatment fit protocol by providing an online video demonstration of the treatment fit process. In so doing, the authors hope that counseling researchers and counselor educators will see the value in providing links of video demonstrations in their academic publications. To accomplish these objectives the authors have organized the article as follows: (a) a definition of treatment fit and a review of its literature, (b) a detailed explanation for how to conduct a treatment fit protocol, (c) evidence supporting the use of accessible online video in training, and (d) methods by which counselor educators can use accessible video to enhance student learning.
Treatment Fit
Treatment fit is the process by which client and counselor collaborate and agree on the issues, goals and treatment plan (Beutler, 2009; Beutler et al., 2003; Kim et al., 2009). Treatment fit is comprised of three empirically supported counseling strategies: (a) assessment of the clients’ concerns to increase the counselor–client shared world view (Keeley, Geffken, Ricketts, McNamara, & Storch, 2011; Spinhoven, Giesen-Bloo, van Dyck, Kooiman, & Arntz, 2007; Westra, Constantino, Arkowitz, & Dozois, 2011), (b) goal setting to increase the transparency of the counseling process and to increase clients’ positive expectations for counseling (Achor, 2010; Bednar & Parker, 1969; Bonner & Everett, 1982; Childress & Gillis, 1977; Constantino, Arnkoff, Glass, Amentrano, & Smith, 2011; Egan, 2007; Grosz, 1968; Hardin & Yanico, 1983; Kim, 2008; Tinsley, Bowman, & Ray, 1988; Ziemelis, 1974), and (c) initial treatment planning that instills hope and encourages clients to practice new behaviors (Duckworth, Grant, Loew, Oettingen, & Gollwitzer, 2011; Hirai & Clum, 2006; Hofmann & Smits, 2008; Norcross & Beutler, 2008).
As a whole, treatment fit is an integral aspect of effective counseling (Sexton, Whiston, Bleuer, & Walz, 1997). Treatment fit has been shown to improve client outcome (Beutler, 2009; Miller, Duncan, Brown, Sorrell, & Chalk, 2006), reduce early termination (Miller et al., 2006), decrease clients’ complaints against therapists (Cummings, O’Donohue, & Cummings, 2009), and reduce treatment costs (Heinssen, Levendusky, & Hunter, 1995). In one study of clients with co-morbid substance dependence and depression where several treatment variables were analyzed (e.g., client coping styles, therapeutic alliance, treatment fit), treatment fit was found to be the best predictor of client outcome (Beutler et al., 2003).
From a cross-cultural perspective, evidence indicates that treatment fit contributes to the counselor-client cultural worldview, or worldview match (Gonzalez, 2002; Kim, Ng, & Ahn, 2005), and is a significant predictor of therapeutic alliance (Kim et al.). This is important due to existing research indicating strong therapeutic alliances increase treatment efficacy (Budd & Hughes, 2009; Connors, DiClemente, Carroll, Longabaugh, & Donovan, 1997; Horvath & Symonds, 1991).
Budd and Hughes (2009) concluded in their review of 30 years of counseling meta-analyses that treatment fit was more important in predicting client outcome than therapeutic modality. And the APA’s Recognition of Psychotherapy Effectiveness (2012) states the following:
In contrast to large differences in outcome between those treated with psychotherapy and those not treated, different forms of psychotherapy typically produce relatively similar outcomes. This research also identifies ways of improving different forms of psychotherapy by attending to how to fit interventions to the particular patient’s needs. (p. 1)
In other words, treatment fit is a more powerful predictor of client outcome than therapeutic modality. Perhaps Beutler et al. (2003) sums it up best: “The addition of patient-treatment fit leads to the conclusion that ‘fit’ of patient and treatment should not be ignored either in studies of treatment effects or in studies of therapeutic alliance” (p. 84).
Despite evidence indicating the importance of treatment fit, there is a dearth of literature explaining how to conduct a brief, functional and collaborative treatment fit protocol in the first counseling session. And, although it is recognized that developing a treatment plan is advisable (Heinssen et al., 1995; Sexton et al., 1997), there is little information describing how to create treatment fit in a brief and practical format that can be used in clinical settings. Early initiation of treatment fit is especially important considering the evidence indicating that clients expect counseling to be brief (Klein, Stone, Hicks, & Pritchard, 2003), and on average attend only 3.5 sessions (Miller et al., 2006). Finally, it is recognized that counselor educators and supervisors need to develop systematic methods for teaching counselors how to build therapeutic alliance and ensure treatment fit (Budd & Hughes, 2009).
The Treatment Fit Model
Before describing the model, it is important for counselors to understand that either before or at the outset of the first counseling session, the client should complete an intake questionnaire that addresses a range of topics including but not limited to presenting symptoms, social support/stressors, legal, trauma, medical, illicit substances, employment and educational history. Thus, when beginning the treatment fit process the counselor is interested in the client’s intrapersonal responses to the aforementioned issues gleaned during intake. Once the intake is completed, the treatment fit process can begin. This treatment fit model (TFM) is a modified version of several existing models (Boffey, 1993; Fong, 1993; Heinssen et al., 1995; Meichenbaum, 2002), but redesigned and enhanced to accomplish several tasks: (a) gather information about the client’s concerns, goals and treatment options, (b) determine how the client’s concerns form multiple intrapersonal perspectives, (c) provide the client with a written summary of concerns, goals and treatment plan, and (d) use the model as a psychoeducational tool to help the client see how emotions, thoughts, behaviors and physiology interact, which can help the client recognize symptoms and develop coping skills before issues become overwhelming.
Facilitation of Treatment Fit Model
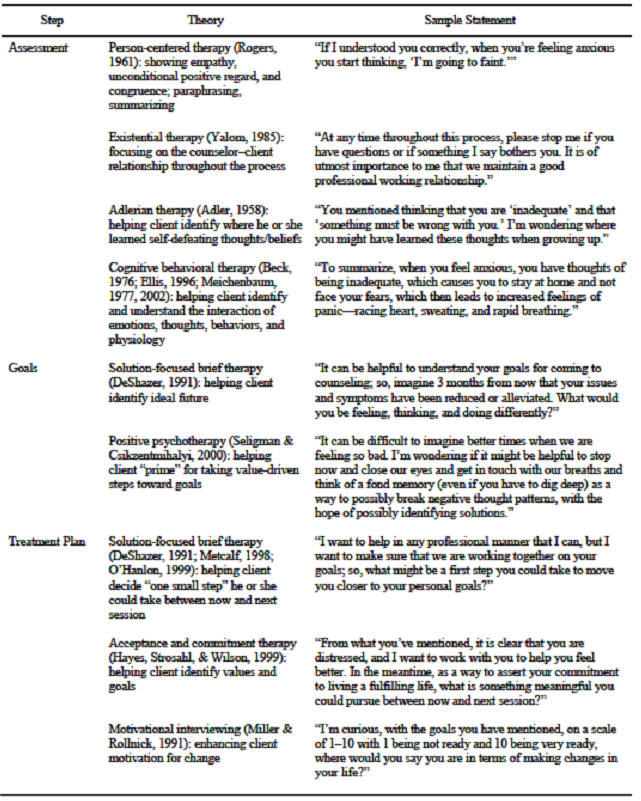
All three of the components, referred to as steps in the treatment fit process, can be accomplished within one 50-minute counseling session using the model in Table 1. Within each of the three steps—assessment, goals, and treatment plan—information is gathered about the client’s intrapersonal domains of emotions, cognitions, behaviors and physiology (e.g., racing heart, cold hands) to ensure a comprehensive understanding of the client’s issues and goals so a tentative treatment plan can be co-created with the client.
As seen in Table 1, several theories are integrated into and used with this model to facilitate each step. Although the theories and techniques described in this article have been used by the authors to effectively facilitate the treatment fit process, they are not meant to be prescriptive. Instead, integrative theoretical approaches will vary depending upon the needs of the client and skill level of the counselor.
Table 1
Primary Theories Integrated in the Treatment Fit Model
Step 1: Assessment
During the assessment phase of the model, person-centered (Rogers, 1961) and motivational interviewing skills (Miller & Rollnick, 1991) are used to create an environment where clients feel safe to discuss their issues. The assessment phase of the model should provide clients ample opportunity to discuss their concerns in an atmosphere that fosters therapeutic alliance. Anecdotal evidence suggests clients often discuss their emotions, thoughts, behaviors and physiological reactions related to presenting issues without excessive counselor questioning. By utilizing empathy, positive regard, summarization, and open-ended questions; and by clarifying discrepancies and listening for change-words (i.e., words that indicate a client’s needs, desires, abilities and commitment to change), a counselor creates an environment that enhances therapeutic alliance. The following case scenario is described to show how the different components of the TFM are conducted.
Sabine is a 30-year-old female, who was born in Quebec, Canada, and moved to the United States when she was 8 years old. She is a college graduate and has worked for the past eight years in a bank where she is now the branch manager. After witnessing a car accident two months ago, she reports experiencing increasing anxiety when driving, which is now compromising other areas of her life. She reports feeling isolated from friends and family, and for the first time in her professional career, she called in sick to avoid driving to work. After further reflection of content and summarizing, it appears that she is feeling helpless and having thoughts of being “out-of-control” and unable to manage her anxiety. She is scared that she will not be able to drive to see her family, or continue to drive to work. She reports that her anxiety is now causing her to stay at home most of the day and not visit with friends or attend church. Her main anxiety symptoms include rapid pulse, shallow breathing, difficulty with swallowing, and feeling faint. Sabine described herself as a shy child who was always able to overcome her fears. She reports no substance use except for a few glasses of wine with friends on the weekend, and she takes no medication.
From Sabine’s presenting concerns, the assessment phase of the model can be completed. To ensure Sabine’s presenting concerns were fully heard, the model is shown to Sabine, and she is asked what else needs to be added to ensure that her concerns are represented. This process serves two important purposes. First, Sabine sees how the four quadrants are interrelated, a cognitive behavioral technique that serves to teach the client how thoughts, feelings, behaviors and physiology interact. Second, presenting the information in this way helps to establish a good working relationship and treatment fit. It makes Sabine aware that the counselor wants to fully understand her primary concerns.
Step 2: Goal Setting
With the initial assessment complete, Sabine is asked to imagine resolution of her issues in the near future and to describe what she would be feeling, thinking, and doing, and how this might affect her physiological reactions. The following script is one way to begin facilitating the goals step of the process:
Sabine, it is helpful for me as a counselor to understand your life goals and values so we can work together to determine an effective treatment plan. So, keeping the different areas in mind that we discussed earlier, let us assume that three months from now you are feeling much better. What words best describe how you would be feeling in three months?
Thus, if Sabine were to say, “I’d be feeling more self-confident,” the counselor would respond, “When you are feeling self-confident, what kind of thoughts will you have about yourself?”
It can be helpful with some clients to give examples of “thoughts about self” to increase their awareness and help them challenge unproductive self-beliefs. For instance, the counselor could say, “If I were feeling more self-confident, I might be saying to myself ‘I can do it,’ or ‘I can accomplish my goals.’” Such counselor self-disclosure can make it easier for clients to identify positive affirmations. To determine desired behaviors and physiological responses, the counselor asks, “When you are feeling confident and thinking ‘I can handle this,’ what will you be doing differently and how might this affect your physiological symptoms?”
Once goals are generated, it is imperative to assess the client’s readiness to pursue goals so that the appropriate treatment approach can be tailored to meet the client’s stage of change (Hettema & Hendricks, 2010; Lundahl, Kunz, Brownell, Tollefson, & Burke, 2010). One way to assess a client’s readiness is to ask the client:
Sabine, we are all at various stages of change in our lives depending upon a number of factors. I’m curious, with the goals you have mentioned, on a scale of 1–10 with 1 being not ready and 10 being very ready, where would you say you are in terms of making changes in your life?
The counselor then processes the responses; if the client is ready, the counselor helps the client tailor small objectives to reach goals. If the client expresses reluctance toward making change, the counselor can proceed as follows:
It seems you are frustrated being here, and it doesn’t sound like you feel you need to work on anything at this time. I respect your ability and power to choose what is right for you. So, if this needs to be the end of the session, please let me know. However, given we have 20 minutes left in this session, what would be most helpful for you?
Step 3: Treatment Planning
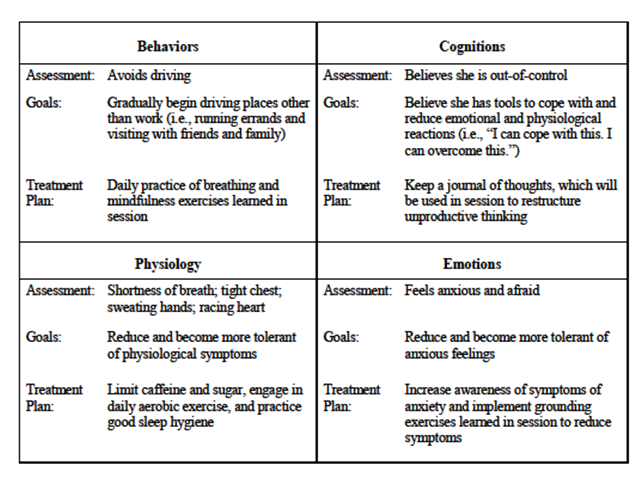
Assuming the client is ready to make changes, the counselor can proceed with the treatment planning phase of the model. To begin this phase the counselor draws from solution-focused brief therapy (DeShazer, 1991; Metcalf, 1998; O’Hanlon, 1999) and asks, “What is a small step you would be willing to take between now and next session that may move you closer to your goals?” It is important to note at this point that goals do not have to be established for each model domain. The idea is to have clients choose their goals and take small steps to ensure forward progress and success, which will hopefully lead to further goal attainment and eventually increased confidence and symptom relief, all based on appropriate treatment fit (see Table 2).
Table 2
Completed Treatment Fit Model
Once one or more goals have been agreed upon, the counselor and client review the document and make any necessary changes. Once the tentative TFM document is agreed upon, the client is given a copy and asked to review it before the next session. The client also is encouraged to make any additions or changes before the next counseling session. The TFM is an organic document that can be reviewed at the beginning of each session to ensure good treatment fit. For further clarification, the application of this TFM can be viewed in a brief online video.
Enhancing Counseling Techniques Through Online Videos
We, the authors, feel at this seminal time in the counseling profession that it is not enough to simply describe the TFM in print materials. Instead, we believe the counseling profession can lead the way in which the effective dissemination and conveyance of counseling techniques and protocols are introduced to the world. Despite more than six billion hours of YouTube videos viewed each month (YouTube Statistics, 2013), websites such as YouTube, Vimeo, and other readily available social media are underutilized by educators (Burden & Atkinson, 2007). There is, however, emerging evidence indicating the potential benefits of utilizing social media video when educating health care professionals (Burke & Snyder, 2008), providing medical information to patients (Murphy, 2011), disseminating public health messages to adolescents (Lite, 2010), modeling pro-social behavior to K–12 students (Shallcross, 2011), and enhancing counselor skill development (Martino, 2010). Social media is an innovative tool for teaching the application of counseling strategies, which can be used at the convenience of the counselor, even on handheld devices between client sessions.
Furthermore, findings suggest that today’s students are virtual learners who enjoy the use of video in their learning experience (Li-Ping Tang & Austin, 2009). Thus, to further enhance counselors’ ability to apply the TFM, and to reach the new generation of counselors and health care providers who rely on the easy access of social media, the authors have provided a link to a video “How to conduct a 1st counseling session,” which demonstrates the process for effectively conducting the TFM: https://www.youtube.com/watch?v=xrHgOoNBiWk
Implications for Counselors and Counselor Educators
Counselors can teach their colleagues and students how to use the TFM by incorporating video demonstrations, such as the aforementioned video link, to provide examples of case scenarios. Viewing video clips at various points can stimulate classroom discussion and group activities, and prompt homework assignments (Agazio & Buckley, 2009) that provide opportunities to practice the model’s steps of assessment, developing goals and treatment planning. For example, after watching a few minutes of the video case scenario, students can discuss the assessment phase by describing what was observed, and work collaboratively with their peers in discerning what behaviors, cognitions, physiological symptoms and emotions can be addressed. Students would then be able to consider how to address goals and treatment plans with the client, and watch the rest of the video to compare their attempts in using the model. Discussion would then ensue on how to effectively use the TFM and improve observation of a client’s verbal and nonverbal communication of her issues.
Further, students can role-play in order to practice demonstrating empathy, asking open-ended questions, and using reflection statements in an effort to build therapeutic alliance with clients when using the TFM. In addition, counselor educators can post videos on their university’s online system, such as Blackboard, and have students develop case scenarios and work through the TFM on their own, with a partner, or for in-class demonstrations.
Mental health counseling trainers and counselor educators may find using social media videos a cost-effective and timely method, as opposed to buying traditional training videos that are often expensive and outdated. Moreover, by using collaborative learning activities such as video and class discussions when teaching students how to develop treatment plans, counselor educators will better match students’ different learning styles, increase learning outcomes (e.g., increase memory of content, focus students’ concentration), and promote deeper understanding (Berk, 2009) of the TFM. Thus, the TFM model coupled with the video demonstration can further enhance counselors’ skills and counseling education by providing a uniform structure by which treatment fit can be established in a timely format. Furthermore, by expanding pedagogical advances with students and readers of academic journals, the inclusion of video demonstrations in counseling academic articles provide advantages by
- enhancing counseling skills by enabling students to view video demonstrations at their convenience, even after graduation;
- increasing a student’s ability to understand the nuances of effective counseling that are difficult to convey in print material;
- increasing professionalism by promoting a uniform yet flexible approach by which first counseling sessions can be conducted; and
- assessing students’ ability to identify counseling skills during exams by identifying theories and techniques in video clips.
Conclusion
Consistently and effectively utilizing strategies that work in counseling to improve the probability of positive client outcomes should be the goal of every counselor. Conducting a brief and functional TFM comprised of empirically supported counseling strategies in the first session should be one of those strategies. The TFM presented in this article is one that counselors can utilize to ensure a mutual understanding of clients’ issues, goals and treatment options.
In an effort to promote accessibility and tap into the immense potential of social media as an educational tool, it is hoped that the video demonstration of this model increases counselors’ ability to apply treatment fit. It also is possible for counselors to collaborate with university faculty and students in the film production department to create professional videos at reasonable costs. Whatever method used, the authors are hopeful that the inclusion of counseling video demonstrations embedded in journal articles will become the norm, which, we believe, will help bridge the gap between cognitive understanding and behavioral application.
References
Achor, S. (2010). The happiness advantage: The seven principles of positive psychology that fuel success and performance at work. New York, NY: Crown Business.
Adler, A. (1958). What life should mean to you. New York, NY: Capricorn Books.
Agazio, J., & Buckley, J. M. (2009). An untapped resource: Using YouTube in nursing education. Nurse Educator, 34(1), 23–28. doi: 10.1097/01.NNE.0000343403.13234.a2
American Psychological Association (2012, August). Recognition of psychotherapy effectiveness. Retrieved from http://www.apa.org/about/policy/ resolution-psychotherapy.aspx
Beck, A. T. (1976). Cognitive therapy and emotional disorders. New York, NY: International Universities Press.
Bednar, R. L., & Parker, C. A. (1969). Client susceptibility to persuasion and counseling outcome. Journal of Counseling Psychology, 16(5), 415–420. doi: 10.1037/h0028000
Berk, R. A. (2009). Multimedia teaching with video clips: TV, movies, YouTube, and mtvU in the college classroom. International Journal of Technology in Teaching and Learning, 5(1), 1–21.
Beutler, L. E. (2009). Making science matter in clinical practice: Redefining psychotherapy. Clinical Psychology: Science and Practice, 16(3), 301–317. doi: 10.1111/j.1468-2850.2009.01168.x
Beutler, L. E., Moleiro, C., Malik, M., Harwood, T. M., Romanelli, R., Gallagher-Thompson, D., & Thompson, L. (2003). A comparison of the Dodo, EST, and ATI factors among comorbid stimulant-dependent, depressed patients. Clinical Psychology and Psychotherapy, 10, 69–85. doi: 10.1002/cpp.354
Boffey, D. B. (1993). Reinventing yourself: A control theory approach to becoming the person you want to be. Chapel Hill, NC: New View.
Bonner, B., & Everett F. (1982). Influence of client preparation and therapist prognostic expectations on children’s attitudes and expectations of psychotherapy. Journal of Clinical Child Psychology, 11, 202–208. doi: 10.1080/15374418209533088
Brill, S. (2013, March 4). Bitter pill: How outrageous pricing and egregious profits are destroying our health care. Time, 181, 17–55.
Budd, R., & Hughes, I. (2009). The dodo bird verdict—controversial, inevitable and important: A commentary on 30 years of meta-analyses. Clinical Psychology and Psychiatry, 16, 510–522. doi: 10.1002/cpp.648
Burden, K., & Atkinson, S. (2007). Jumping on the YouTube bandwagon? Using digital video clips to develop personalized learning strategies. In ICT: Providing choices for learners and learning. Proceedings ascilite Singapore 2007. Retrieved from http://www.ascilite.org.au/conferences/singapore07/procs/burden-poster.pdf
Burke S. C., & Snyder, S. L. (2008). YouTube: An innovative learning resource for college health education courses. International Electronic Journal of Health Education, 11, 39–46.
Burtnett, F. (2012, June). Bridging the separation between behavioral and general health care. Counseling Today, 54(12), 38–39.
Childress, R., & Gillis, J. S. (1977). A study of pretherapy role induction as an influence process. Journal of Clinical Psychology, 33(2), 540–544. doi: 10.1002/1097-4679(197704)
Connors, G. J., Carroll, K. M., DiClemente, C. C., Longabaugh, R., & Donovan, D. M. (1997). The therapeutic alliance and its relationship to alcoholism treatment participation and outcome. Journal of Consulting and Clinical Psychology, 65(4), 588–598. doi: 10.1037/0022-006X.65.4.588
Constantino, M. J., Arnkoff, D. B., Glass, C. R., Ametrano, R. M., & Smith, J. Z. (2011). Expectations. Journal of Clinical Psychology: In Session, 67(2), 184–192. doi: 10.1002/jclp.20754
Cummings, N. A., O’Donohue, W. T., & Cummings, J. L. (2009). The financial dimension of integrated behavioral/primary care. Journal of Clinical Psychology in Medical Settings, 16, 31–39. doi: 10.1007/s10880-008-9139-2
Curtis R., & Christian, E. (2012). Introduction to integrated care. In Curtis & Christian (Eds.), Integrated care: Applying theory to practice (pp. 3–19). New York, NY: Routledge.
DeShazer, S. (1991). Putting difference to work. New York, NY: Norton.
Duckworth, A. L., Grant, H., Loew, B., Oettingen, G., & Gollwitzer, P. M. (2011). Self-regulation strategies improve self-discipline in adolescents: Benefits of mental contrasting and implementation intentions. Journal of Educational Psychology, 31(1), 17–26. doi: 10.1080/01443410.2010.506003
Egan, G. E. (2007). The skilled helper: A problem-management and opportunity development approach to helping (8th ed.). Belmont, CA: Thompson Brooks/Cole.
Ellis, A. (1996). Better, deeper, and more enduring brief therapy: The rational emotive behavior therapy approach. New York, NY: Brunner/Mazel.
Fong, M. L. (1993). Teaching assessment and diagnosis within a DSM-III-R framework. Counselor Education and Supervision, 32, 276–287.
Gonzalez, M. J. (2002). Mental health intervention with Hispanic immigrants: Understanding the influence of the client’s worldview, language, and religion. Journal of Immigrant & Refugee Services, 1, 81–92. doi: 10.1300/J191v01n01_07
Grosz, R. D. (1968). Effect of client expectations on the counseling relationship. Personnel and Guidance Journal, 46, 797–800. doi: 10.1002/j.2164-4918.1968.tb03250.x
Hardin, S., & Yanico, B. (1983). Counselor gender, type of problem, and expectations about counseling. Journal of Counseling Psychology, 30(2), 294–297. doi: 10.1037/0022-0167.30.2.294
Harris Interactive. (2004, April). Therapy in America 2004 (Survey No. 20431). Rochester, NY: Author. Retrieved from http://www.napabipolardepression.org/images/therapy_in_america.pdf
Hayes, S. C., Strosahl, K. D., & Wilson, K. G. (1999). Acceptance and commitment therapy: An experiential approach to behavior change. New York, NY: Guilford.
Haynes, A. B., Weiser, T. G., Berry, W. R., Lipsitz, S. R., Breizat, A. S., Dellinger, E. P., … Gawande, A. A. (2009). A surgical safety checklist to reduce morbidity and mortality in a global population. The New England Journal of Medicine, 360(5), 491–499. doi: 10.1056/NEJMsa0810119
Heinssen, R. K., Levendusky, P. G., & Hunter, R. H. (1995). Client as colleague: Therapeutic contracting with the seriously mentally ill. American Psychologist, 50(7), 522–532. doi: 10.1037/0003-066X.50.7.522
Hettema, J. E., & Hendricks, P. S. (2010). Motivational interviewing for smoking cessation: A meta-analytic review. Journal of Consulting and Clinical Psychology, 78(6), 868–884. doi: 10.1037/a0021498
Hirai, M., & Clum, G. A. (2006). A meta-analytic study of self-help interventions for anxiety disorders. Behavior Therapy, 37(2), 99–111.
Hofmann, S. G., & Smits, J. A. J. (2008). Cognitive-behavioral therapy for adult anxiety disorders: A meta-analysis of randomized placebo controlled trials. Journal of Clinical Psychiatry, 69(4), 621–632. doi: 10.4088/JCP.v69n0415
Horvath, A. O., & Symonds, B. D. (1991). Relation between working alliance and outcome in psychotherapy: A meta-analysis. Journal of Counseling Psychology, 38(2), 139–149. doi: 10.1037/0022-0167.38.2.139
Keeley, M. L., Geffken, G. R., Ricketts, E., McNamara, J. P. H., & Storch, E. A. (2011). The therapeutic alliance in the cognitive behavioral treatment of pediatric obsessive-compulsive disorder. Journal of Anxiety Disorders, 25, 855–863. doi 10.1016/j.janxdis.2011.03.017
Kim, B. S. K., Ng, G. F., & Ahn, A. J. (2005). Effects of client expectation for counseling success, client-counselor worldview match, and client adherence to Asian and European American cultural values on counseling process with Asian Americans. Journal of Counseling Psychology, 52(1), 67–76. doi: 10.1037/0022-0167.52.1.67
Kim, B. S. K., Ng, G. F., & Ahn, A. J. (2009). Client adherence to Asian cultural values, common factors in counseling, and session outcome with Asian American clients at a university counseling center. Journal of Counseling & Development, 87(2), 131–142. doi: 10.1002/j.1556-6678.2009.tb00560.x
Kim, J. S. (2008). Examining the effectiveness of solution-focused brief therapy: A meta-analysis. Research on Social Work Practice, 18(2), 107–116. doi: 10.1177/1049731507307807
Klein, E. B., Stone, W. N., Hicks, M. W., & Pritchard, I. L. (2003). Understanding dropouts. Journal of Mental Health Counseling, 25, 89–100. doi: 10.1080/09515070310001610119
Lee, S., Aos, S., Drake, E., Pennucci, A., Miller, M., & Anderson, L. (2012). Return on investment: Evidence-based options to improve statewide outcomes, April 2012 (Document No. 12-04-1201). Olympia: Washington State Institute for Public Policy. Retrieved from http://www.wsipp.wa.gov/rptfiles/12-04-1201.pdf
Li-Ping Tang, T., & Austin, M. J. (2009). Students’ perceptions of teaching technologies, application of technologies, and academic performance. Computers & Education, 53(4), 1241–1255. doi: 10.1016/j.compedu.2009.06.007
Lite, J. (2010, November–December). When Facebook is your medical record. Miller-McCune, 18–21.
Lundahl, B. W., Kunz, C., Brownell, C., Tollefson, D., & Burke, B. L. (2010). A meta-analysis of motivational interviewing: Twenty-five years of empirical studies. Research on Social Work Practice, 20(2), 137–160. doi: 10.1177/1049731509347850
Martino, S. (2010). Strategies for training counselors in evidence-based treatments. Addiction Science & Clinical Practice, 5(2), 30–40.
Meichenbaum, D. (1977). Cognitive behavior modification: An integrative approach. New York, NY: Plenum Press.
Meichenbaum, D. (2002, December). Core tasks of psychotherapy: What ‘expert’ therapists do. Paper presented at the Brief Therapy Conference, Orlando, FL.
Metcalf, L. (1998). Solution focused brief therapy: Ideas for groups in private practice, schools, agencies and treatment programs. New York, NY: The Free Press.
Miller, S. D., Duncan, B. L., Brown, J., Sorrell, R., & Chalk, M. B. (2006). Using formal client feedback to improve retention and outcome: Making ongoing, real-time assessment feasible. Journal of Brief Therapy, 5(1), 5–22.
Miller, W. R., & Rollnick, S. (1991). Motivational interviewing: Preparing people for change. New York, NY: Guilford.
Murphy, E. T. (2011, September 20). Social media primer for healthcare professionals [Medscape News]. Retrieved from http://www.medscape.com/viewarticle/749576
Norcross, J. C., & Beutler, L. E. (2008). Integrative psychotherapies. In R. J. Corsini & D. Wedding (Eds.), Current Psychotherapies (8th ed., pp. 481–511). Belmont, CA: Brooks/Cole.
O’Hanlon, W. H. (1999). Do one thing different. New York, NY: HarperCollins.
Olmstead, T. A., Abraham, A. J., Martino, S., & Roman, P. M. (2012). Counselor training in several evidence-based psychosocial addiction treatments in private US substance abuse treatment centers. Drug and Alcohol Dependency, 120(1–3), 149–154. doi: 10.1016/j.drugalcdep.2011.07.017
Paquette, V., Lévesque, J., Mensour, B., Leroux, J. M., Beaudoin, G., Bourgouin, P., & Beauregard, M. (2003). “Change the mind and you change the brain”: Effects of cognitive behavioral therapy on the neural correlates of spider phobia. Neuroimage, 18(2), 401–409. doi:10.1016/S1053-8119(02)00030-7
Rogers, C. (1961). On becoming a person: A therapist’s view of psychotherapy. New York, NY: Houghton Mifflin.
Seligman, M. E. P., & Csikzentmihalyi, M. (2000). Positive psychology: An introduction. American Psychologist, 55(1), 5–14. doi: 10.1037/0003-066X.55.1.5
Sexton, T., Whiston, S. C., Bleuer, J. C., & Walz, G. R. (1997). Integrating outcome research into counseling practice and training. Alexandria, VA: American Counseling Association.
Shallcross, L. (2011, October). Finding technology’s role in the counseling relationship. Counseling Today, 54(4), 26–35.
Spinhoven, P., Giesen-Bloo, J., van Dyck, R., Kooiman, K., & Arntz, A. (2007). The therapeutic alliance in schema-focused therapy and transference-focused psychotherapy for borderline personality disorder. Journal of Consulting and Clinical Psychology, 75(1), 104–115. doi: 10.1037/0022-006X.75.1.104
Tinsley, H. E. A., Bowman, S. L., & Ray, S. B. (1988). Manipulation of expectancies about counseling and psychotherapy: Review and analysis of expectancy manipulation strategies and results. Journal of Counseling Psychology, 35(1), 99–108. doi: 10.1037/0022-0167.35.1.99
Westra, H. A., Constantino, M. J., Arkowitz, H., & Dozois, D. J. A. (2011). Therapist differences in cognitive-behavioral psychotherapy for generalized anxiety disorder: A pilot study. Psychotherapy, 48(3), 282–292.
Wos, A. (2013, February). State of mental health in North Carolina. Presented at the North Carolina Counseling Association’s Annual Meeting, Greensboro, NC.
Yalom, I. D. (1985). The theory and practice of group psychotherapy (3rd ed.). New York, NY: Basic Books.
YouTube. (October 19, 2013). Traffic. Retrieved from http://www.youtube.com/yt/press/statistics.html
Ziemelis, A. (1974). Effects of client preference and expectancy upon the initial interview. Journal of Counseling Psychology, 21(1), 23–30. doi: 10.1037/h0036067
Russ Curtis is an Associate Professor and Heather Thompson an Assistant Professor, both at the counseling program at Western Carolina University. Gerald A. Juhnke, NCC, is a Professor in the Counseling Department at The University of Texas at San Antonio; Melodie Frick, NCC, is an Assistant Professor in the counseling program at Western Carolina University. Correspondence can be addressed to Russ Curtis, Department of Human Services, Western Carolina University, 91 Killian Building Lane, Room 208, Cullowhee, NC 28723, curtis@email.wcu.edu.