Oct 31, 2023 | Volume 13 - Issue 3
Wesley B. Webber, W. Leigh Atherton, Kelli S. Russell, Hilary J. Flint, Stephen J. Leierer
The COVID-19 pandemic and efforts to manage it have affected mental health around the world. Although early research on the COVID-19 pandemic showed a general decline in mental health after the pandemic began, mental health in later stages of the pandemic might be improving alongside other changes (e.g., availability of vaccines, return to in-person activities). The present study utilized data from a mental health service intervention for individuals at a southeastern university who were exposed to COVID-19 following the university’s return to in-person operations. This study tested whether time period (August–September 2021 vs. January–February 2022) predicted individuals’ likelihood of being mild or above in depression and anxiety ratings. Results showed that individuals were more likely to be mild or above in both depression and anxiety ratings during August–September of 2021 than January–February of 2022. Suggestions for future research and implications for professional counselors are discussed.
Keywords: COVID-19, mental health, depression, anxiety, university
The novel coronavirus (COVID-19), first detected in 2019, spread globally at a rapid pace, with the first confirmed case in the United States occurring on January 20, 2020, in the state of Washington (Centers for Disease Control and Prevention [CDC], 2023). By April 2020, the United States had the most reported deaths in the world due to COVID-19. It was not until December of 2020 that the first round of vaccines, authorized under emergency use authorization, was made available (Food and Drug Administration [FDA], 2021). As of October 2022 in the United States, a total of 97,063,357 cases of COVID-19 had been reported, from which there were 1,065,152 COVID-19–related deaths (CDC, 2023). A reported 111,367,843 individuals aged 5 and above in the United States had received their first booster dose of a COVID-19 vaccine as of October 2022 (CDC, 2023). Previous research has shown that the COVID-19 pandemic and efforts to manage it (e.g., lockdowns, quarantine, isolation) had negative effects on mental health in the United States and internationally (Huckins et al., 2020; Pierce et al., 2020; Son et al., 2020). Based on the extended duration of the pandemic and changes that have occurred during it (e.g., vaccine availability, lessening of initial social restrictions), more recent research has investigated possible changes in mental health in later stages of the COVID-19 pandemic (Fioravanti et al., 2022; McLeish et al., 2022; Tang et al., 2022). The present study adds to this literature by exploring whether psychosocial symptomatology (i.e., depression and anxiety) at a university in the Southeastern United States differed in individuals exposed to COVID-19 during August–September 2021 as compared to individuals exposed to COVID-19 during January–February 2022 (following the university’s return to on-campus operations in August 2021).
Challenges to Mental Health During the COVID-19 Pandemic
Since the beginning of the COVID-19 pandemic, conceptual and empirical research has focused on ways in which the pandemic and associated stressors might impact mental health (Bzdok & Dunbar, 2020; Marroquín et al., 2020; Şimşir et al., 2022). Implementation of lockdowns to deter spread of the virus led to concerns that social isolation might have severe impacts on mental health (Bzdok & Dunbar, 2020). This hypothesis was empirically supported, as stay-at-home orders and individuals’ reported levels of social distancing were positively associated with depression and anxiety (Marroquín et al., 2020). Individuals’ views on the COVID-19 pandemic evolved quickly at the outset of the pandemic, and perceptions of risk were shown to increase during the pandemic’s first week in the United States (Wise et al., 2020). Growing awareness of the dangers of the virus likely had deleterious effects on mental health; Şimşir et al. (2022) found through a meta-analysis that fear of COVID-19 was associated with a variety of mental health problems. Mental health was also negatively affected by stigmatization associated with the COVID-19 pandemic, as was the case for those exposed to COVID-19 while at their place of work (Schubert et al., 2021). Such stigmatization associated with COVID-19 exposure was found to increase risk for depression and anxiety (Schubert et al., 2021).
The lockdowns and social distancing measures that accompanied early stages of the COVID-19 pandemic also resulted in changes to routines that likely impacted mental health. For some individuals facing lockdowns or other disruptions to typical routines, reductions in physical activity occurred. Individuals who reported greater impact of COVID-19 on their level of physical activity showed greater symptoms of depression and anxiety (Silva et al., 2022). Early in the COVID-19 pandemic, based on people’s increased time spent at home and their concerns about COVID-19 developments, some people increased their media usage (e.g., news outlets, social media). Such increases in media usage were associated with decreases in mental health (Meyer et al., 2020; Riehm et al., 2020). The COVID-19 pandemic had less significant impact on mental health for those with greater tolerance of uncertainty (Rettie & Daniels, 2021) and psychological flexibility (Dawson & Golijani-Moghaddam, 2020). Thus, some individuals were uniquely suited to face the many changes and stressors brought about by the COVID-19 pandemic.
One population that previous research has identified as being especially at risk for negative mental health outcomes during the COVID-19 pandemic is college students (Xiong et al., 2020). For college students, the COVID-19 pandemic occurred alongside other stressors known to be typical for this population such as adjusting to leaving home, navigating new peer groups, and making career decisions (Beiter et al., 2015; Liu et al., 2019). Thus, for many college students, the COVID-19 pandemic disrupted a period of life already filled with many transitions. For example, shortly after the COVID-19 pandemic began, many college students were forced to leave their dormitories and peers as universities transitioned to online delivery of classes (Copeland et al., 2021). Xiong et al. (2020) found through a systematic review that college students were especially vulnerable to negative mental health outcomes at the outset of the COVID-19 pandemic as compared to others in the general population. In the United States, college students’ reported degree of life disruption due to the COVID-19 pandemic was positively associated with depression at the conclusion of the spring 2020 semester (Stamatis et al., 2022). During fall 2020, COVID-19 concerns and previous COVID-19 infection were each found to be associated with higher levels of depression and anxiety among U.S. college students (Oh et al., 2021). Overall, previous research has supported the notion that changes associated with the COVID-19 pandemic had general negative effects on mental health in the general population and in college students specifically.
Changes in Psychosocial Symptomatology Across the COVID-19 Pandemic
Although research has shown that the COVID-19 pandemic introduced unprecedented challenges and stressors that were associated with mental health problems, another important direction for research has been to characterize overall changes in psychosocial symptomatology as the COVID-19 pandemic progressed. Such research is important given that individuals might psychologically adapt to constant COVID-19 stressors or might benefit from changes that have occurred as the COVID-19 pandemic has progressed (e.g., vaccine availability, lessening of societal restrictions). Initial longitudinal studies comparing individuals’ symptomatology before the COVID-19 pandemic and after its beginning showed that mental health deteriorated after the COVID-19 pandemic began (Elmer et al., 2020; Huckins et al., 2020; Pierce et al., 2020). Prati and Mancini (2021) conducted a meta-analysis of 28 studies that used longitudinal or natural experimental designs and found that depression and anxiety showed small but statistically significant increases after implementation of the initial lockdowns in response to COVID-19. The various changes to ways of life associated with the COVID-19 pandemic appeared to result in a general deterioration in mental health.
Previous research has also explored possible changes in mental health beyond those that were observed in the initial phase of the COVID-19 pandemic. In support of the notion that individuals adapted to changes associated with the COVID-19 pandemic, Fancourt et al. (2021) found that anxiety and depression decreased across the initial lockdown period in the United Kingdom. In contrast, Ozamiz-Etxebarria et al. (2020) found that levels of depression and anxiety were higher 3 weeks into the initial lockdown period in Spain as compared to the beginning of the lockdown. Fioravanti et al. (2022) assessed psychological symptoms longitudinally in an Italian sample at three time points—the beginning of the COVID-19 pandemic and first lockdown (March 2020), the end of the first lockdown phase (May 2020), and during a second wave of COVID-19 with increased societal restrictions (November 2020). Their findings pointed to possible influences of COVID-19 waves and societal restrictions on specific psychosocial symptoms. Specifically, depression, anxiety, obsessive-compulsive disorder, and post-traumatic stress disorder all decreased at the end of the first lockdown phase (Fioravanti et al., 2022). However, all symptoms besides obsessive-compulsive disorder significantly increased from the end of the first lockdown phase to the second wave of COVID-19 (Fioravanti et al., 2022).
Recent research on mental health among college students in later stages of the COVID-19 pandemic has also focused on possible mental health changes over time (McLeish et al., 2022; Tang et al., 2022). Tang et al. (2022) reported reductions in anxiety and depression in a longitudinal study of university students in the United Kingdom between a first time point (July–September 2020, after the end of lockdown) and a second time point (January–March 2021, when vaccinations were becoming available). In contrast, McLeish et al. (2022) found through a repeated cross-sectional study that depression and anxiety among students at a specific university increased from spring 2020 to fall 2020, with the increases being maintained in spring 2021. The authors noted that vaccines were not widely available at the university until the end of spring 2021 (McLeish et al., 2022). Thus, recent studies have found mixed results as to whether psychosocial symptomatology improved over time during the COVID-19 pandemic. These discrepancies may be due to contextual differences between studies (e.g., differences in data collection time periods, availability of vaccines, or levels of COVID-19 restrictions being implemented during data collection).
The Present Study
The present study was conducted based on the need for continued research on mental health across the evolving COVID-19 pandemic and based on previous conflicting findings on possible mental health changes in later stages of the COVID-19 pandemic. Given previous research showing detrimental effects of the COVID-19 pandemic on mental health in the general population and in college students, the present study utilized data from a university population. Specifically, an archival dataset was used in the present study to examine data collected during 2021–2022 at a university in the Southeastern United States and to test whether time period would predict severity of depression and anxiety symptoms. Individuals in the study had been exposed to COVID-19 between August–September 2021 or between January–February 2022 and had requested a mental health contact during university-conducted contact tracing. These two time periods corresponded to surges in COVID-19 cases at the university due to the delta and omicron COVID-19 variants, respectively. August–September 2021 also coincided with a return to on-campus operations at the university and therefore captured psychosocial symptomatology at the beginning of a significant transition in the COVID-19 pandemic (i.e., a return to organized in-person activities on a college campus during the evolving pandemic). This study was designed to answer the following research questions:
- Among those requesting mental health contact after COVID-19 exposure, was the likelihood of having at least mild depression symptoms different for those whose contact occurred between August–September 2021 as compared to those whose contact occurred between January–February 2022?
- Among those requesting mental health contact after COVID-19 exposure, was the likelihood of having at least mild anxiety symptoms different for those whose contact occurred between August–September 2021 as compared to those whose contact occurred between January–February 2022?
Method
Design
A retrospective research design was used to analyze the possible effect of time period on severity of depression and anxiety symptoms among members of a university population who had been exposed to COVID-19 and requested a mental health check-in. The study used a de-identified dataset obtained from the service providers who completed the mental health check-in. We confirmed through consultation with the IRB that the use of archival, de-identified data does not necessitate IRB review.
COVID-19 Mental Health Check-In Dataset
The archival, de-identified dataset used in the present study was compiled as part of a mental health service occurring between February 2021 and February 2022. Participants in the dataset had tested positive for COVID-19 or been exposed to COVID-19 without a positive test. During university-conducted contact tracing, they were offered and elected to receive a subsequent mental health check-in. Individuals who were contact traced and thereby offered a mental health check-in had become known to contact tracers through one of two routes: (a) they reported their own COVID-19 diagnosis or exposure through a self-reporting mechanism as instructed by the university, or (b) they were reported by another individual as having been diagnosed with or exposed to COVID-19. The dataset used in this study included data collected during the mental health check-ins for those who elected to receive them. This data was collected over the phone and documented in RedCap (a secure web browser–based survey protocol designed for clinical research) at the time of the phone call or within 24 hours. The dataset consisted of data for 211 individuals’ check-ins. For each check-in, the dataset included participants’ demographic information, screening data (for depression, anxiety, and trauma), identified needs of the participant, resources shared with the participant, and the date of data entry.
The present study focused on check-in data for all individuals from the COVID-19 Mental Health Check-in Dataset whose check-in had occurred during one of the two time periods of focus—August–September 2021 or January–February 2022. These two time periods corresponded to surges in COVID-19 cases at the university associated with the delta and omicron COVID-19 variants, respectively. The 149 individuals who checked in during these 4 months represented 70.62% of the total number of check-ins over the 12-month dataset (N = 211), reflecting the surges in COVID-19 cases during these two periods. Of the 149 individuals in the present study, 96 (64.43%) received their check-in during August–September 2021, and 53 (35.57%) received their check-in during January–February 2022. The selection of these two time periods from the larger dataset allowed for comparison of psychosocial symptomatology during comparable levels of COVID-19 infection (i.e., surges associated with two subsequent COVID-19 variants) at comparable points in subsequent academic semesters (i.e., the first 2 months of the fall 2021 and spring 2022 semesters). The present study used only the screening data for depression and anxiety, as the scales for each of these constructs showed good internal consistency (Cronbach’s alpha > .80).
Participants
The sample in the present study consisted of 149 individuals. The selected individuals’ ages ranged from 17 to 52 (M = 22.21, SD = 7.43). With regard to gender, 67.11% identified as female, 32.21% as male, and 0.67% as non-binary. The reported races of individuals in the study were as follows: 60.4% White, 20.13% African American, 6.71% Hispanic, 3.36% Other, 2.68% Two or more races, 1.34% Middle Eastern, 1.34% Native American, and 0.67% Asian. Some participants preferred not to indicate their race (3.36%). In responding to a question about their ethnicity, 87.25% of individuals identified as not Latinx, 9.40% identified as Latinx, and 3.36% preferred not to answer. With regard to academic level/job title, 32.89% were freshmen, 20.13% were sophomores, 14.09% were juniors, 15.44% were seniors, 7.38% were graduate students, 8.05% were faculty/staff, and 2.01% preferred not to answer. Regarding employment, 53.69% were not employed (including students), 30.20% were employed part-time, 12.75% were employed full-time, and 3.36% preferred not to answer. The relationship statuses of individuals were reported as the following: 87.92% single (never married), 4.7% married, 2.01% single but cohabitating with a significant other, 1.34% in a domestic partnership or civil union, 1.34% separated, 0.67% divorced, and 2.01% preferred not to answer. Table 1 summarizes demographic responses within each of the two time periods and for the full sample.
Measures
Demographic Questionnaire
Participants responded to seven demographic questions (age, gender, race, ethnicity, academic year/job title, current employment status, and relationship status). They were informed that this information was optional and that they could choose not to answer particular questions.
Table 1
Demographic Characteristics of the Sample
|
Demographic
Characteristic |
|
| August–September 2021 |
January–February 2022 |
Full Sample |
|
n |
% |
n |
% |
n |
% |
| Gender |
|
|
|
|
|
|
| Female |
69 |
71.88 |
31 |
58.49 |
100 |
67.11 |
| Male |
27 |
28.13 |
21 |
39.62 |
48 |
32.21 |
| Non-binary |
0 |
0 |
1 |
1.89 |
1 |
0.67 |
| Race |
|
|
|
|
|
|
| White |
56 |
58.33 |
34 |
64.15 |
90 |
60.40 |
| African American |
23 |
23.96 |
7 |
13.21 |
30 |
20.13 |
| Hispanic |
8 |
8.33 |
2 |
3.77 |
10 |
6.71 |
| Other race |
1 |
1.04 |
4 |
7.55 |
5 |
3.36 |
| Two or more races |
4 |
4.17 |
0 |
0 |
4 |
2.68 |
| Middle Eastern |
2 |
2.08 |
0 |
0 |
2 |
1.34 |
| Native American |
1 |
1.04 |
1 |
1.89 |
2 |
1.34 |
| Asian |
1 |
1.04 |
0 |
0 |
1 |
0.67 |
| Prefer not to answer |
0 |
0 |
5 |
9.43 |
5 |
3.36 |
| Ethnicity |
|
|
|
|
|
|
| Not Latinx |
82 |
85.42 |
48 |
90.57 |
130 |
87.25 |
| Latinx |
12 |
12.50 |
2 |
3.77 |
14 |
9.40 |
| Prefer not to answer |
2 |
2.08 |
3 |
5.66 |
5 |
3.36 |
| Academic Year / Job Title |
|
|
|
|
|
|
| Freshman |
38 |
39.58 |
11 |
20.75 |
49 |
32.89 |
| Sophomore |
18 |
18.75 |
12 |
22.64 |
30 |
20.13 |
| Junior |
15 |
15.63 |
6 |
11.32 |
21 |
14.09 |
| Senior |
15 |
15.63 |
8 |
15.09 |
23 |
15.44 |
| Graduate Student |
6 |
6.25 |
5 |
9.43 |
11 |
7.38 |
| Faculty/Staff |
4 |
4.17 |
8 |
15.09 |
12 |
8.05 |
| Prefer not to answer |
0 |
0 |
3 |
5.66 |
3 |
2.01 |
| Employment |
|
|
|
|
|
|
| Not Employed (including student) |
62 |
64.58 |
18 |
33.96 |
80 |
53.69 |
| Employed Part-Time |
26 |
27.08 |
19 |
35.85 |
45 |
30.20 |
| Employed Full-Time |
8 |
8.33 |
11 |
20.75 |
19 |
12.75 |
| Prefer not to answer |
0 |
0 |
5 |
9.43 |
5 |
3.36 |
| Relationship Status |
|
|
|
|
|
|
| Single, never married |
87 |
90.63 |
44 |
83.02 |
131 |
87.92 |
| Married |
3 |
3.13 |
4 |
7.55 |
7 |
4.70 |
| Single, but cohabitating with a
significant other |
2 |
2.08 |
1 |
1.89 |
3 |
2.01 |
| In a domestic partnership or civil union |
2 |
2.08 |
0 |
0 |
2 |
1.34 |
| Separated |
2 |
2.08 |
0 |
0 |
2 |
1.34 |
| Divorced |
0 |
0 |
1 |
1.89 |
1 |
0.67 |
| Prefer not to answer |
0 |
0 |
3 |
5.66 |
3 |
2.01 |
| Note. Average age was 21.51 (SD = 6.98) in August–September 2021 group, 23.49 (SD = 8.11) in January–February 2022 group, and 22.21 (SD = 7.43) in the full sample. |
Patient Health Questionnaire-9 (PHQ-9)
The Patient Health Questionnaire-9 (PHQ-9; Kroenke et al., 2001) is a 9-item self-report questionnaire that measures the frequency and severity of depression symptoms over the past 2 weeks. The PHQ-9 has been validated for screening for depression in the general population (Kroenke et al., 2001; Martin et al., 2006). The questionnaire measures frequency of symptoms such as “feeling down, depressed, or hopeless,” and “little interest or pleasure in doing things.” The PHQ-9 uses a 4-point Likert scale to measure frequency of symptoms over the past 2 weeks with the response options of not at all, several days, more than half the days, and nearly every day. Scores of 0, 1, 2, and 3 are assigned to each of the four response categories, and a PHQ-9 total score is derived by adding the scores for each of the nine PHQ-9 items. Minimal depression is indicated by PHQ-9 total scores of 0–4, mild depression by scores of 5–9, moderate depression by scores of 10–14, moderately severe depression by scores of 15–19, and severe depression by scores of 20–27. Question 9 on the PHQ-9 is a single screening question assessing suicide risk. Interviewers were trained in appropriate protocol in the event of a positive screen for this question. Cronbach’s alpha for the PHQ-9 in the present study was .86.
Generalized Anxiety Disorder 7-Item Scale (GAD-7)
The Generalized Anxiety Disorder 7-Item Scale (GAD-7; Spitzer et al., 2006) is a 7-item self-report anxiety questionnaire that measures the frequency and severity of anxiety symptoms over the past 2 weeks. The GAD-7 has demonstrated reliability and validity as a measure of anxiety in the general population (Löwe et al., 2008). The questionnaire measures symptoms such as “feeling nervous, anxious, or on edge,” and “not being able to stop or control worrying.” The format of the GAD-7 is similar to the PHQ-9, using a 4-point Likert scale to measure frequency of symptoms over the past 2 weeks with response options of not at all, several days, more than half the days, and nearly every day. GAD-7 scores are calculated by assigning scores of 0, 1, 2, and 3 for response categories and then adding the scores from the 7 items to derive a total score ranging from 0 to 21. Minimal anxiety is indicated by total scores of 0–4, mild anxiety by scores of 5–9, moderate anxiety by scores of 10–14, and severe anxiety by scores of 15– 21. Cronbach’s alpha for the GAD-7 in the present study was .86.
Analytic Strategy
Total scores for the PHQ-9 and GAD-7 were found to be positively skewed for both groups of participants. Binary logistic regression was therefore an appropriate method of analysis for this dataset, as binary logistic regression does not require normality of dependent variables (Tabachnick & Fidell, 2019). For two separate binary logistic regression models, individuals were classified as being either minimal or mild or above in depression (PHQ-9) and anxiety (GAD-7) to create binary outcome variables. This choice of cutoff allowed each model (with time period as predictor) to satisfy the recommendation of Peduzzi et al. (1996) that there be at least 10 cases per outcome per predictor in binary logistic regression.
Prior to performing these intended primary analyses to answer the research questions, preliminary analyses were conducted to determine whether adding control variables to the logistic regression models was warranted. Chi-square tests of independence, Fisher-Freeman-Halton Exact tests, Fisher’s Exact tests, and an independent samples t-test were used to test for possible differences between the two time periods in individuals’ responses to demographic questions. In cases in which responses to demographic questions were shown to be significantly different across the two groups, appropriate tests were used to determine whether the demographic responses in question were associated with either of the two intended dependent variables.
Following the preliminary analyses, the intended two binary logistic regressions were conducted to answer the research questions. In the first binary logistic regression, time period was the predictor
(1 = August–September 2021, 0 = January–February 2022) and PHQ-9 depression category was the outcome (1 = mild or above, 0 = minimal). In the second logistic regression, time period was the predictor (1 = August–September 2021, 0 = January–February 2022) and GAD-7 anxiety category was the outcome (1 = mild or above, 0 = minimal). All analyses were conducted using SPSS Version 28.
Results
Preliminary Demographic Analyses
Prior to the primary analyses, preliminary analyses were conducted to determine whether the two groups differed in their responses to demographic questions. Fisher-Freeman-Halton Exact tests and an independent samples t-test were used to test for differences between groups in their responses to the seven demographic questions. Two of the seven tests were statistically significant at Bonferroni-corrected alpha level. Specifically, Fisher-Freeman-Halton Exact tests found significant differences between time periods on the race (p = .004) and employment (p < .001) demographic variables.
Based on the above significant results for the race and employment variables across the time periods, 2 x 2 tests were conducted to test for differences between specific race responses and specific employment responses across the two time periods. For these 2 x 2 tests, a chi-square test of independence was used when all expected cell counts were 5 or greater and Fisher’s Exact test was used when any expected cell counts were less than 5. To follow up the significant result for race, 2 x 2 tests were conducted for all pairs of race responses in which 2 x 2 tests were possible (i.e., in which there was at least one observation for each of the two race responses at both time periods). These follow-up 2 x 2 tests of responses to the race question across time periods found no statistically significant differences between pairs of race responses across time periods using Bonferroni-corrected alpha level. Follow-up 2 x 2 tests comparing all pairs of responses to the employment question across time periods found two statistically significant differences using Bonferroni-corrected alpha level. A chi-square test of independence showed that individuals were more likely to be employed full-time during January–February 2022 than August–September 2021 as compared to those not employed (including students), X2 (1, N = 99) = 9.29, p = .002. Fisher’s Exact test showed that individuals were more likely to indicate “prefer not to answer” during January–February 2022 than during August–September 2021 as compared to those indicating “not employed (including students),” p = .001.
The statistically significant tests for race and employment across time periods were followed up with additional tests to determine if depression or anxiety category (minimal vs. mild or above for each) was associated with individuals’ responses to the relevant race and employment questions. A Fisher-Freeman-Halton Exact test showed that depression category was not associated with individuals’ responses to the race question, p = .099. A Fisher-Freeman-Halton Exact test also showed that individuals’ anxiety category was not associated with individuals’ responses to the race question,
p = .386. With regard to employment, tests of association were conducted between the intended dependent variables and the specific employment responses that were found to differ between the two groups. A chi-square test of independence showed that individuals’ status as “not employed” vs. “employed full-time” was not associated with depression category, X2 (1, N = 99) = .63, p = .429. A chi-square test of independence also showed that these employment statuses were not associated with anxiety category, X2 (1, N = 99) = .27, p = .601. Similarly, Fisher’s Exact tests showed that individuals’ employment responses of “prefer not to answer” vs. “not employed (including students)” were not associated with depression category (p = .156) or anxiety category (p = .317). These results were interpreted as indicating that the ways in which individuals in the two time periods differed demographically did not have significant impact on the study’s dependent variables of interest. Therefore, binary logistic regressions were conducted with only time period as a predictor of each dependent variable.
Relationship Between Time Period and Severity of Depression Symptoms
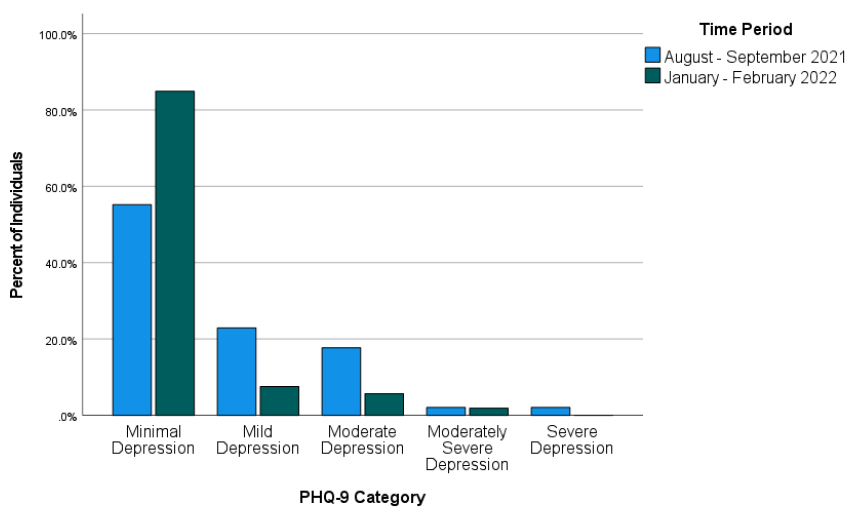
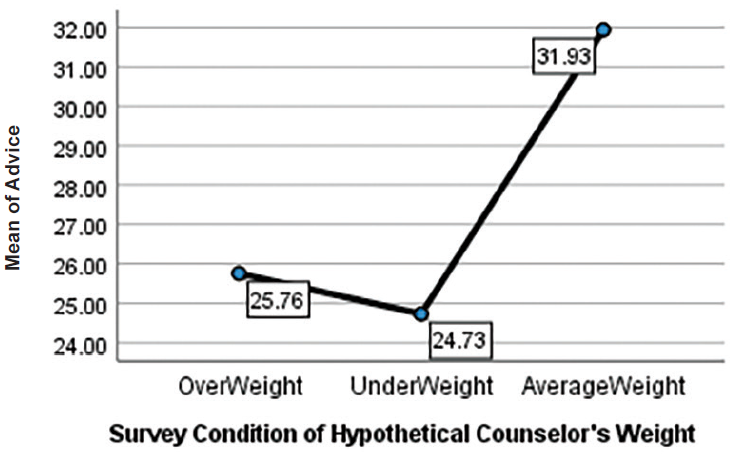
Most individuals in the study were in the minimal depression range on the PHQ-9 as compared to the other four categories. Figure 1 shows the percentage of individuals falling into each of the five PHQ-9 categories during each of the two time periods.
Figure 1
Percentages of Individuals Falling Into Each of the PHQ-9 Categories for Each of the Two Time Periods
Across both time periods combined (August–September 2021 and January–February 2022), 51 individuals (34.23%) were mild or above in depression while 98 (65.77%) were in the minimal range. Binary logistic regression was used to test whether time period predicted severity of depression symptoms. Time period was entered as a predictor (1 = August–September 2021, 0 = January–February 2022) of depression (1 = mild or above, 0 = minimal depression). The overall binary logistic regression model was found to be statistically significant, χ2(1) = 14.46, p < .001, Cox & Snell R2 = .092, Nagelkerke R2 = .128. In the model, time period was found to be a significant predictor of depression, Wald χ2(1) = 12.17, B = 1.52, SE = .44, p < .001. The model estimated that the odds of being mild or above in depression were 4.56 times higher during August–September 2021 than during January–February 2022 for individuals requesting a mental health check-in following COVID-19 exposure. Specifically, the predicted odds of being mild or above in depression were .81 during August–September 2021 and .18 during January–February 2022.
Relationship Between Time Period and Severity of Anxiety Symptoms
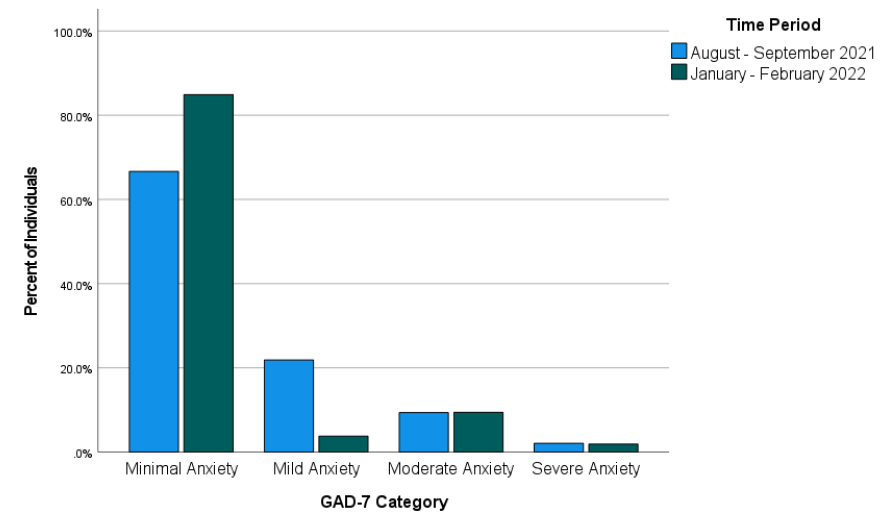
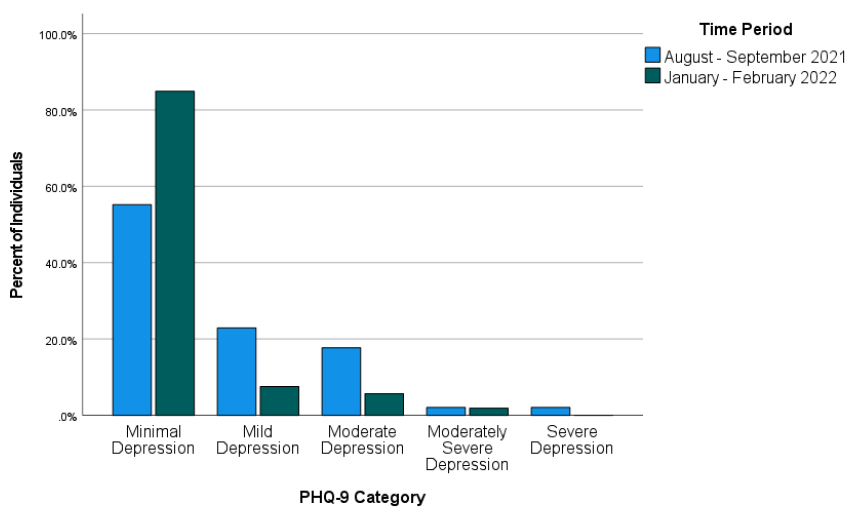
Most individuals in the study were in the minimal anxiety range on the GAD-7 as compared to the other three categories. Figure 2 shows the percentage of individuals falling into each of the four GAD-7 categories during each of the two time periods.
Figure 2
Percentages of Individuals Falling Into Each of the GAD-7 Categories for Each of the Two Time Periods
Across both time periods combined, 40 individuals (26.85%) reported anxiety at levels of mild or above and 109 individuals (73.15%) reported minimal anxiety. Binary logistic regression was used to test whether time period predicted severity of anxiety symptoms. Time period was entered as a predictor (1 = August–September 2021, 0 = January–February 2022) of anxiety (1 = mild or above, 0 = minimal anxiety). The overall binary logistic regression model was statistically significant, χ2(1) = 6.16, p = .013, Cox & Snell R2 = .041, Nagelkerke R2 = .059. In the model, time period was a significant predictor of anxiety, Wald χ2(1) = 5.51, B = 1.03, SE = .44, p = .019. Odds of being mild or above in anxiety were estimated by the model to be 2.81 times higher during August–September 2021 than during January–February 2022 for individuals requesting a mental health check-in after exposure to COVID-19. Specifically, the predicted odds of being mild or above in anxiety were .50 during August–September 2021 and .18 during January–February 2022.
Discussion
This study examined whether time period would predict severity of depression and anxiety symptoms in a sample of individuals exposed to COVID-19 at a university in the Southeastern United States. More specifically, the study addressed the possibility that the likelihood of being mild or above in depression and anxiety would differ between two time periods following the university’s return to in-person operations in August 2021. The results of the study showed that the likelihood of being mild or above in depression and the likelihood of being mild or above in anxiety after exposure to COVID-19 were both higher during August–September 2021 than during January–February 2022. This finding is in line with previous research that found improvements in psychosocial symptomatology in later stages of the COVID-19 pandemic (Tang et al., 2022) and in contrast to research that did not find such improvements (McLeish et al., 2022). Based on the results of the present study, it appears likely that factors that differed between the two assessed time periods (first two months of fall 2021 vs. first two months of spring 2022) contributed to the observed difference in likelihood of depression and anxiety symptoms. McLeish et al. (2022) noted that vaccines were not widely available in their study that did not find such differences, while Tang et al. (2022), who did find significant differences, noted that vaccines were available at their second data collection point (January–March 2021). For individuals in the present study, COVID-19 vaccinations were available. Vaccination was strongly encouraged by university administrators following the return to campus, and more individuals on campus were vaccinated in spring 2022 than in fall 2021. Vaccinations might have lessened individuals’ COVID-19 concerns and contributed to more positive psychosocial outcomes during spring 2022 than fall 2021.
Besides vaccinations possibly lessening depression and anxiety symptoms, other environmental circumstances might also have played a role. The two time periods on which this study focused also differed in their proximity to a significant environmental event—a return to in-person operations on the campus where the individuals studied and/or worked. Early research on the mental health impact of COVID-19 highlighted the negative mental health effects of factors such as reduced physical activity (Silva et al., 2022), life disruptions due to the COVID-19 pandemic (Stamatis et al., 2022), and social distancing (Marroquín et al., 2020). Therefore, it is possible that symptoms of depression and anxiety in spring 2022 were affected by changes in specific circumstances known to have negatively impacted mental health earlier in the COVID-19 pandemic. For example, individuals’ physical activity likely increased because of a return to campus, and they might have perceived less disruption to their lives through being able to resume in-person activities. Although individuals in the present study who were exposed to COVID-19 during the first 2 months after the return to campus might have reaped some benefits from the return to more normal environmental circumstances, they might also have faced a period of adjustment. In contrast, individuals exposed to COVID-19 between January and February 2022 might have been more readjusted and reaped greater benefits from the return to campus, thereby reducing depression and anxiety symptoms.
Implications
This study’s findings on psychosocial symptomatology across time during the COVID-19 pandemic have important implications for the work of counselors. Based on the results of the present study, counselors planning outreach efforts to individuals exposed to COVID-19 should consider that as time passes, these individuals might be more stable with regard to symptoms of depression and anxiety. However, some individuals directly affected by COVID-19 might still be interested in receiving mental health information despite low levels of depression and anxiety. Many individuals in the present study scored as minimal in depression and anxiety but were still interested in receiving a mental health check-in. Thus, counselors should advocate for mental health information and resources to be made available to individuals who are known to be facing stressors related to COVID-19. Counselors should be prepared to have conversations to determine the contextual needs of individuals exposed to COVID-19 rather than relying only on standardized measures of psychosocial symptomatology. For example, counselors working with employees (such as university employees in the present study) should be attentive to the possibility that employees exposed to COVID-19 may be concerned about facing stigma in their workplace due to their exposure (Schubert et al., 2021).
Given that the present study focused on individuals from a university population, the study’s results also have specific implications for college counselors. College counselors should develop approaches to reach students during circumstances that might make traditional outreach challenging. For example, the present study used data from a mental health intervention in which service providers collaborated with university contact tracers to safely provide mental health resources by telephone to individuals exposed to COVID-19. College counselors should be prepared to connect clients with services at a distance. Previous research during the COVID-19 pandemic found that college students were interested in using teletherapy and online self-help resources, particularly if such services were made available for free (Ahuvia et al., 2022).
Besides preparing for flexible modes of service delivery, college counselors should be prepared to deliver interventions most likely to be useful to college students during the COVID-19 pandemic or similar pandemics. Those recently exposed to COVID-19 might benefit from discussing possible fears associated with COVID-19, experiences of stigmatization they might have experienced due to their exposure, and ways to maintain mental health during any period of quarantine or isolation that might be required. Those not recently exposed to COVID-19 might instead benefit from interventions that address other issues that might have resulted from the COVID-19 pandemic or societal responses to it. For example, if circumstances associated with the COVID-19 pandemic led to reductions in a client’s amount of exercise, a counselor can help the client identify ways they might increase their physical activity. Interventions promoting physical activity were found to reduce anxiety and depression in college students during the COVID-19 pandemic (Luo et al., 2022).
Limitations
This study had limitations that should be considered. First, with the study being retrospective and using secondary data from a clinical intervention, it was not possible to include measures that might have better clarified mechanisms of the changes that were observed in psychosocial symptoms. Thus, the possible explanations above of what might have driven these changes are tentative and future research should test them more directly. Second, individuals in the present study were likely to have been in greater distress than the general university population based on their exposure to COVID-19, which might limit the generalizability of the study’s findings. Third, individuals in the present study were from a single university in the Southeastern United States. Thus, our findings might not generalize to other regions where university-related COVID-19 policies might have differed. Fourth, the decision to create a binary independent variable to reflect time periods (August–September 2021 and January–February 2022) in the present study also entails a limitation. This decision was justifiable on the basis that it allowed for comparisons of individuals at similar points in academic semesters and during comparable periods of COVID-19 infection. However, this analysis decision means that inferences from the study’s results are limited to the two specific time periods that were analyzed. Fifth, individuals in the present study responded to items on the GAD-7 and PHQ-9 through a phone conversation with interviewers. Interviewer-administered surveys have been previously associated with greater tendencies toward socially desirable responses than self-administered surveys (Bowling, 2005). This might limit the present study’s generalizability in contexts where self-administrations of the GAD-7 and PHQ-9 are used.
Future Research
The results of this study provide important directions for future research. Future researchers who can conduct prospective studies or who have access to larger retrospective datasets should aim to determine specific factors that might lead to improvement in mental health outcomes over time during the COVID-19 pandemic. Knowledge produced by such studies could contribute to clinical applications in the future regarding COVID-19 or other pandemics that might occur. Relatedly, future research with larger samples of demographically diverse participants should explore possible demographic differences in specific mental health trajectories in later stages of the COVID-19 pandemic.
Future research should continue to focus specifically on those who are interested in mental health information and interventions during the COVID-19 pandemic. To follow up this study’s findings, future quantitative and qualitative studies should aim to identify which individuals are interested in receiving mental health services and determine the best ways to deliver services to them. As a globally experienced stressor, the COVID-19 pandemic might have changed some individuals’ views of mental health and/or their receptiveness to mental health outreach. More specifically, some might be more receptive to available mental health information even at lower thresholds of anxiety, depression, or other psychosocial symptoms. Such clients might be interested in preventive services or their interest in mental health information might be driven by other factors. Future studies should address these possibilities more directly than was possible in the present retrospective study.
Conclusion
Overall, the present study provided a positive picture regarding psychosocial symptomatology in later stages of the COVID-19 pandemic. Results from this study of students and employees at a university in the Southeastern Unites States following their return to campus found that many individuals requesting mental health information after exposure to COVID-19 showed minimal levels of depression and anxiety. Individuals in the study were more likely to be in these minimal ranges during January–February 2022 than August–September 2021. COVID-19 will continue to have effects in individuals’ lives through future infections and potentially through lasting effects of previous stages of the COVID-19 pandemic. As organized in-person activities resume and COVID-19 infections continue, counseling researchers and practitioners should continue efforts to best characterize and address individuals’ mental health needs associated with the COVID-19 pandemic.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Ahuvia, I. L., Sung, J. Y., Dobias, M. L., Nelson, B. D., Richmond, L. L., London, B., & Schleider, J. L. (2022). College student interest in teletherapy and self-guided mental health supports during the COVID-19 pandemic. Journal of American College Health. Advance online publication.
https://doi.org/10.1080/07448481.2022.2062245
Beiter, R., Nash, R., McCrady, M., Rhoades, D., Linscomb, M., Clarahan, M., & Sammut, S. (2015). The prevalence and correlates of depression, anxiety, and stress in a sample of college students. Journal of Affective Disorders, 173, 90–96. https://doi.org/10.1016/j.jad.2014.10.054
Bowling, A. (2005). Mode of questionnaire administration can have serious effects on data quality. Journal of Public Health, 27(3), 281–291. https://doi.org/10.1093/pubmed/fdi031
Bzdok, D., & Dunbar, R. I. M. (2020). The neurobiology of social distance. Trends in Cognitive Sciences, 24(9), 717–733. https://doi.org/10.1016/j.tics.2020.05.016
Centers for Disease Control and Prevention. (2023, March 15). COVID-19 timeline. https://www.cdc.gov/museum/timeline/covid19.html
Copeland, W. E., McGinnis, E., Bai, Y., Adams, Z., Nardone, H., Devadanam, V., Rettew, J., & Hudziak, J. J. (2021). Impact of COVID-19 pandemic on college student mental health and wellness. Journal of the American Academy of Child & Adolescent Psychiatry, 60(1), 134–141.e2. https://doi.org/10.1016/j.jaac.2020.08.466
Dawson, D. L., & Golijani-Moghaddam, N. (2020). COVID-19: Psychological flexibility, coping, mental health, and wellbeing in the UK during the pandemic. Journal of Contextual Behavioral Science, 17, 126–134.
https://doi.org/10.1016/j.jcbs.2020.07.010
Elmer, T., Mepham, K., & Stadtfeld, C. (2020). Students under lockdown: Comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS ONE, 15(7), Article e0236337. https://doi.org/10.1371/journal.pone.0236337
Fancourt, D., Steptoe, A., & Bu, F. (2021). Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: A longitudinal observational study. The Lancet Psychiatry, 8(2), 141–149. https://doi.org/10.1016/S2215-0366(20)30482-X
Fioravanti, G., Benucci, S. B., Prostamo, A., Banchi, V., & Casale, S. (2022). Effects of the COVID-19 pandemic on psychological health in a sample of Italian adults: A three-wave longitudinal study. Psychiatry Research, 315, Article 114705. https://doi.org/10.1016/j.psychres.2022.114705
Food and Drug Administration. (2021, August 23). FDA approves first COVID-19 vaccine. https://www.fda.gov/news-events/press-announcements/fda-approves-first-covid-19-vaccine
Huckins, J. F., daSilva, A. W., Wang, W., Hedlund, E., Rogers, C., Nepal, S. K., Wu, J., Obuchi, M., Murphy, E. I., Meyer, M. L., Wagner, D. D., Holtzheimer, P. E., & Campbell, A. T. (2020). Mental health and behavior of college students during the early phases of the COVID-19 pandemic: Longitudinal smartphone and ecological momentary assessment study. Journal of Medical Internet Research, 22(6), Article e20185.
https://doi.org/10.2196/20185
Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Liu, C. H., Stevens, C., Wong, S. H. M., Yasui, M., & Chen, J. A. (2019). The prevalence and predictors of mental health diagnoses and suicide among U.S. college students: Implications for addressing disparities in service use. Depression and Anxiety, 36(1), 8–17. https://doi.org/10.1002/da.22830
Löwe, B., Decker, O., Müller, S., Brähler, E., Schellberg, D., Herzog, W., & Herzberg, P. Y. (2008). Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Medical Care, 46(3), 266–274. https://doi.org/10.1097/MLR.0b013e318160d093
Luo, Q., Zhang, P., Liu, Y., Ma, X., & Jennings, G. (2022). Intervention of physical activity for university students with anxiety and depression during the COVID-19 pandemic prevention and control period: A systematic review and meta-analysis. International Journal of Environmental Research and Public Health, 19(22), 15338. https://doi.org/10.3390/ijerph192215338
Marroquín, B., Vine, V., & Morgan, R. (2020). Mental health during the COVID-19 pandemic: Effects of stay-at-home policies, social distancing behavior, and social resources. Psychiatry Research, 293, Article 113419. https://doi.org/10.1016/j.psychres.2020.113419
Martin, A., Rief, W., Klaiberg, A., & Braehler, E. (2006). Validity of the Brief Patient Health Questionnaire Mood Scale (PHQ-9) in the general population. General Hospital Psychiatry, 28(1), 71–77.
https://doi.org/10.1016/j.genhosppsych.2005.07.003
McLeish, A. C., Walker, K. L., & Hart, J. L. (2022). Changes in internalizing symptoms and anxiety sensitivity among college students during the COVID-19 pandemic. Journal of Psychopathology and Behavioral Assessment, 44, 1021–1028. https://doi.org/10.1007/s10862-022-09990-8
Meyer, J., McDowell, C., Lansing, J., Brower, C., Smith, L., Tully, M., & Herring, M. (2020). Changes in physical activity and sedentary behavior in response to COVID-19 and their associations with mental health in 3052 US adults. International Journal of Environmental Research and Public Health, 17(18), Article 6469.
https://doi.org/10.3390/ijerph17186469
Oh, H., Marinovich, C., Rajkumar, R., Besecker, M., Zhou, S., Jacob, L., Koyanagi, A., & Smith, L. (2021). COVID-19 dimensions are related to depression and anxiety among US college students: Findings from the Healthy Minds Survey 2020. Journal of Affective Disorders, 292, 270–275. https://doi.org/10.1016/j.jad.2021.05.121
Ozamiz-Etxebarria, N., Idoiaga Mondragon, N., Dosil Santamaría, M., & Picaza Gorrotxategi, M. (2020). Psychological symptoms during the two stages of lockdown in response to the COVID-19 outbreak: An investigation in a sample of citizens in Northern Spain. Frontiers in Psychology, 11, Article 1491.
https://doi.org/10.3389/fpsyg.2020.01491
Peduzzi, P., Concato, J., Kemper, E., Holford, T. R., & Feinstein, A. R. (1996). A simulation study of the number of events per variable in logistic regression analysis. Journal of Clinical Epidemiology, 49(12), 1373–1379. https://doi.org/10.1016/S0895-4356(96)00236-3
Pierce, M., Hope, H., Ford, T., Hatch, S., Hotopf, M., John, A., Kontopantelis, E., Webb, R., Wessely, S., McManus, S., & Abel, K. M. (2020). Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population. The Lancet Psychiatry, 7(10), 883–892.
https://doi.org/10.1016/S2215-0366(20)30308-4
Prati, G., & Mancini, A. D. (2021). The psychological impact of COVID-19 pandemic lockdowns: A review and meta-analysis of longitudinal studies and natural experiments. Psychological Medicine, 51(2), 201–211. https://doi.org/10.1017/S0033291721000015
Rettie, H., & Daniels, J. (2021). Coping and tolerance of uncertainty: Predictors and mediators of mental health during the COVID-19 pandemic. American Psychologist, 76(3), 427–437. https://doi.org/10.1037/amp0000710
Riehm, K. E., Holingue, C., Kalb, L. G., Bennett, D., Kapteyn, A., Jiang, Q., Veldhuis, C. B., Johnson, R. M., Fallin, M. D., Kreuter, F., Stuart, E. A., & Thrul, J. (2020). Associations between media exposure and mental distress among U.S. adults at the beginning of the COVID-19 pandemic. American Journal of Preventive Medicine, 59(5), 630–638. https://doi.org/10.1016/j.amepre.2020.06.008
Schubert, M., Ludwig, J., Freiberg, A., Hahne, T. M., Romero Starke, K., Girbig, M., Faller, G., Apfelbacher, C., von dem Knesebeck, O., & Seidler, A. (2021). Stigmatization from work-related COVID-19 exposure: A systematic review with meta-analysis. International Journal of Environmental Research and Public Health, 18(12), 6183. https://doi.org/10.3390/ijerph18126183
Silva, D. T. C., Prado, W. L., Cucato, G. G., Correia, M. A., Ritti-Dias, R. M., Lofrano-Prado, M. C., Tebar, W. R., & Christofaro, D. G. D. (2022). Impact of COVID-19 pandemic on physical activity level and screen time is associated with decreased mental health in Brazillian adults: A cross-sectional epidemiological study. Psychiatry Research, 314, Article 114657. https://doi.org/10.1016/j.psychres.2022.114657
Şimşir, Z., Koç, H., Seki, T., & Griffiths, M. D. (2022). The relationship between fear of COVID-19 and mental health problems: A meta-analysis. Death Studies, 46(3), 515–523. https://doi.org/10.1080/07481187.2021.1889097
Son, C., Hegde, S., Smith, A., Wang, X., & Sasangohar, F. (2020). Effects of COVID-19 on college students’ mental health in the United States: Interview survey study. Journal of Medical Internet Research, 22(9), Article e21279. https://doi.org/10.2196/21279
Spitzer, R. L., Kroenke, K., Williams, J. B. W., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097.
https://doi.org/10.1001/archinte.166.10.1092
Stamatis, C. A., Broos, H. C., Hudiburgh, S. E., Dale, S. K., & Timpano, K. R. (2022). A longitudinal investigation of COVID-19 pandemic experiences and mental health among university students. British Journal of Clinical Psychology, 61(2), 385–404. https://doi.org/10.1111/bjc.12351
Tabachnick, B. G., & Fidell, L. S. (2019). Using multivariate statistics (7th ed.). Pearson.
Tang, N. K. Y., McEnery, K. A. M., Chandler, L., Toro, C., Walasek, L., Friend, H., Gu, S., Singh, S. P., & Meyer, C. (2022). Pandemic and student mental health: Mental health symptoms amongst university students and young adults after the first cycle of lockdown in the UK. BJPsych Open, 8(4), Article e138.
https://doi.org/10.1192/bjo.2022.523
Wise, T., Zbozinek, T. D., Michelini, G., Hagan, C. C., & Mobbs, D. (2020). Changes in risk perception and self-reported protective behaviour during the first week of the COVID-19 pandemic in the United States.
Royal Society Open Science, 7(9), Article 200742. https://doi.org/10.1098/rsos.200742
Xiong, J., Lipsitz, O., Nasri, F., Lui, L. M. W., Gill, H., Phan, L., Chen-Li, D., Iacobucci, M., Ho, R., Majeed, A., & McIntyre, R. S. (2020). Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders, 277, 55–64. https://doi.org/10.1016/j.jad.2020.08.001
Wesley B. Webber, PhD, NCC, is a postdoctoral scholar at East Carolina University. W. Leigh Atherton, PhD, LCMHCS, LCAS, CCS, CRC, is an associate professor and program director at East Carolina University. Kelli S. Russell, MPH, RHEd, is a teaching assistant professor at East Carolina University. Hilary J. Flint, NCC, LCMHCA, is a clinical counselor at C&C Betterworks. Stephen J. Leierer, PhD, is a research associate at the Florida State University Career Center. Correspondence may be addressed to Wesley B. Webber, Department of Addictions and Rehabilitation Studies, Mail Stop 677, East Carolina University, 1000 East 5th Street, Greenville, NC 27858-4353, webberw21@ecu.edu.
Oct 31, 2023 | Volume 13 - Issue 3
Byeolbee Um, Lindsay Woodbridge, Susannah M. Wood
This content analysis examined articles on international counseling students published in selected counseling journals between 2006 and 2021. Results of this study provide an overview of 18 articles, including publication trends, methodological designs, and content areas. We identified three major themes from multiple categories, including professional practices and development, diverse challenges, and personal and social resources. Implications for counseling researchers and counselor education programs to increase understanding and support for international counseling students are provided.
Keywords: international counseling students, counseling journals, content analysis, publication trends, counseling researchers
International counseling students (ICSs) can be defined as individuals from outside the United States who seek professional training by enrolling in counselor education programs in the United States. After graduation, they often keep contributing to the counseling field as professional counselors or counselor educators, either in the United States or their home countries (Behl et al., 2017). In 2021, non-resident international students accounted for 1.02% of master’s students and 3.81% of doctoral students in counseling programs accredited by the Council for Accreditation of Counseling and Related Educational Programs (CACREP; 2022). However, because these percentages do not include international students who have resident alien status in the United States (Karaman et al., 2018), the actual numbers of international students in counseling programs may be higher. Despite the underestimated number of ICSs in CACREP-accredited programs, Ng (2006) found that at least one international student was enrolled in 41% of CACREP-accredited programs, which suggested that many counselor education programs already had some degree of global cultural diversity. Considering that the number of ICSs in the United States has risen within a few decades (CACREP, 2022; Ng, 2006), additional research is needed on this population and how best to prepare them for professional practice.
Research on International Students in Counseling Programs
While in training, ICSs, like domestic students, experience pressure to perform across academic, practical, and personal contexts (Thompson et al., 2011). However, ICSs face the additional challenges of adapting to a new culture and practicing counseling in that culture (Ju et al., 2020; Kuo et al., 2021; Ng & Smith, 2009). These challenges stem from having varying levels of experience using English in an academic context, adapting to new sociocultural and interpersonal patterns, and navigating key clinical factors of counselor education such as supervision and therapeutic relationships (Jang et al., 2014; C. Li et al., 2018; Y. Mori et al., 2009). Researchers have found that ICSs perceive more barriers and concerns regarding their training, such as academic problems and role ambiguity in supervision (Akkurt et al., 2018; Ng & Smith, 2009).
Regarding the experiences of ICSs, researchers have paid scholarly attention to the concept of acculturation, which is the assimilation process an individual experiences in response to the psychological, social, and cultural forces they are exposed to in a new dominant culture (C. Li et al., 2018; Ng & Smith, 2012). According to counseling studies, ICSs’ levels of acculturation and acculturative stress were associated with several variables related to their professional development, including counseling self-efficacy, language anxiety, and diverse academic and life needs (Behl et al., 2017; Interiano-Shiverdecker et al., 2019; C. Li et al., 2018). For example, Interiano-Shiverdecker et al. (2019) found that two domains of acculturation—ethnic identity and individualistic values—were positively associated with counseling self-efficacy for international counseling master’s students. Researchers have also uncovered the potential issues ICSs can experience related to a lack of acculturation: Behl et al. (2017) found that students’ acculturative stress was positively associated with their academic, social, cultural, and language needs.
With goals of uncovering effective coping strategies and identifying characteristics of high-quality training environments, researchers have investigated the personal and academic experiences of ICSs (Lau & Ng, 2012; Nilsson & Wang, 2008; Park et al., 2017; Woo et al., 2015). Woo and colleagues (2015) identified several coping tools of ICSs. These tools included self-directed strategies such as engaging in reflection and keeping up with the latest literature, support from mentors, and networking among international students and graduates (Woo et al., 2015). Researchers have attended to strategies that support ICSs’ development of cultural competence and commitment to social justice (Delgado-Romero & Wu, 2010; Karaman et al., 2018; Ng & Smith, 2012). For example, Delgado-Romero and Wu (2010) piloted a social justice group intervention with six Asian ICS participants and found the intervention to be a useful way to empower students and enhance their critical consciousness about inequity.
Supervision has been another area of focus in ICS research. Through interviews and surveys of ICSs, researchers have identified supervision strategies that support ICSs’ developing cultural competence, professional development, and self-efficacy (Mori et al., 2009; Ng & Smith, 2012; Park et al., 2017). A shared theme across these studies is the importance of clear communication. Findings of two studies (Mori et al., 2009; Ng & Smith, 2012) support supervisors engaging ICS supervisees in communication about critical topics such as cultural differences and the purpose and expectations of supervision. Based on a consensual qualitative analysis of interviews with 10 ICS participants, Park et al. (2017) recommended that programs and supervisors make sure to share basic information about systems of counseling, health care, and social welfare in the United States.
Necessity of ICS Research
Across academic units, there has been a growing attention to international graduate students (Anandavalli et al., 2021; Vakkai et al., 2020). Given the increasing representation of international students in counseling programs, researchers have called for academic and practical strategies to support ICSs’ success in training (Lertora & Croffie, 2020; Woo et al., 2015). These calls are aligned with the values of professional counseling organizations. Specifically, the American Counseling Association (ACA; 2014) endorsed respect for diversity and multiculturalism as elements of counselor competence. This value is reflected in the ACA Code of Ethics, including Standard F.11.b, which urges counselor educators to value a diverse student body in counseling programs. Similarly, the CACREP standards have identified counseling programs as responsible for working to include “a diverse group of students and to create and support an inclusive learning community” (CACREP, 2015, p. 6). Because counselors must have a profound comprehension of and commitment to diversity, experiences with multiculturalism during professional training programs are essential (O’Hara et al., 2021; Ratts et al., 2016). In this vein, the presence of international students in counseling programs can be beneficial for both domestic and international students by enhancing trainees’ understanding of diversity and multicultural counseling competencies (Behl et al., 2017; Luo & Jamieson-Drake, 2013). Given that there is a substantially increasing need for addressing multiculturalism, diversity, and social justice in the counseling profession, counseling programs’ efforts to recruit various minority student groups, including ICSs, will contribute to not only counselor training but also client outcomes in the long term.
However, despite the importance of the topic, researchers have consistently indicated that research on ICSs has been quite limited (Behl et al., 2017; Lau et al., 2019). In counseling research, there is a history of researchers using content analysis to provide a comprehensive overview of topics that are underrepresented but have growing importance. For example, Singh and Shelton (2011) published a content analysis of qualitative research related to counseling lesbian, gay, bisexual, transgender, and queer clients. Involving the summarization of findings from a body of literature into a few key categories or content areas (Stemler, 2001), content analysis is a useful methodology for expanding the field’s knowledge and understanding of the topic. Considering ICSs’ unique challenges and their potential contributions to enriching diversity in counseling programs and in the profession (Park et al., 2017), a comprehensive understanding of the current ICS literature is needed. This content analysis can identify how the research on ICSs has progressed and what remains unexplored or underexplored, which can provide meaningful implications for researchers interested in conducting ICS research in the future.
Purpose of the Study
The purpose of this study is to identify major findings in literature recently published on ICSs in the United States and to draw useful implications for counseling researchers and counseling programs seeking to better understand and support international students in counseling programs. Our content analysis, which focused on ICS research published between 2006 and 2021 in selected counseling journals, was driven by the following research questions: 1) What are the publication trends in ICS research, such as prevalence, publication outlets, authorship, methodological design, and sample size and characteristics?; and 2) What is the content of the ICS research published in counseling journals? Based on the findings, this study aimed to suggest recommendations for counseling researchers to fill the scholarly gap in ICS research and for counselor education programs to provide more effective training experiences to their international trainees.
Method
Content analysis is a useful methodology to expand our knowledge and understanding of the field through an overview of the current literature (Stemler, 2001). This approach makes it possible to effectively summarize a large amount of data using a few categories or content areas. In counseling research, content analysis has been used to provide an overview of a profession that is underrepresented but with growing importance (e.g., LGBTQ; Singh & Shelton, 2011), which is aligned with the aim of this study. This study employed both quantitative and qualitative content analysis to provide an overview of ICS research. Quantitative content analysis refers to analyzing the data in mathematical ways and applying predetermined categories that do not derive from the data (Forman & Damschroder, 2007). After reviewing existing content analysis articles in the counseling field, Byeolbee Um and Susannah M. Wood determined the scope of our quantitative analysis as: (a) journal and authorship, (b) research design, (c) participant characteristics, and (d) data collection methods.
Research Team
The research team consisted of two doctoral candidates and one full professor, all of whom were affiliated with the same CACREP-accredited counselor education and supervision program at a Midwestern university. Um and Lindsay Woodbridge were doctoral candidates in counselor education and supervision when conducting this research project and are currently counselor educators. Um is an international scholar from an East Asian country. She has drawn on her experiences in quantitative and qualitative courses and research projects to engage in research of marginalized counseling students, including ICSs. Woodbridge is a domestic scholar who has taken classes and collaborated with international student peers and worked with international students in instructional and clinical capacities. She has taken quantitative and qualitative research courses and completed several research projects. The first and second authors met regularly to establish the scope of the investigation, collect data, and form a consensus on coding emerging categories and sorting them into themes. Wood, an experienced researcher and instructor, has worked as a counselor educator for more than 15 years. She has worked with international students in teaching, supervision, advising, and mentoring capacities. She audited the research process, reviewed emergent categories and themes, and provided constructive feedback at each phase of the study.
Data Collection
To identify a full list of ICS studies that satisfy the scope of this study, Um and Woodbridge independently performed electronic searches using research databases including EBSCO, PsycINFO, and ERIC. Because ICSs have attracted scholarly attention relatively recently and because Ng’s (2006) study that estimated the number of ICSs in CACREP-accredited programs was the first published research on ICSs in counselor education programs, we set 2006 as the initial year of our search. We used the following search criteria to identify candidate articles: (a) published between 2006 and 2021 in ACA division, branch, and state journals and major journals under the auspices of professional counseling organizations; (b) containing one or more of the following keywords: international students, international counseling students, international counseling trainees, international counseling programs, counselor education; and (c) involving original empirical findings from ICSs in the United States.
We conducted an extensive search of ICS research across various journals in the counselor education field and identified ICS articles from several ACA-related journals, including Counselor Education and Supervision (CES), Journal of Multicultural Counseling and Development (JMCD), The Journal of Counselor Preparation and Supervision (JCPS), The Journal for Specialists in Group Work (JSGW), and the Journal of Professional Counseling: Practice, Theory & Research (JPC). Additionally, we found ICS articles from the International Journal for the Advancement of Counselling (IJAC) and the Journal of Counselor Leadership and Advocacy (JCLA), which are associated with the International Association for Counselling and Chi Sigma Iota, respectively. Although they are not under the broader umbrella of ACA, these journals have contributed to enriching scholarship in the counseling field.
After the initial searches, Um and Woodbridge made a preliminary list of the articles identified based on the search results. Subsequently, they re-screened the articles independently. Among the 27 identified articles, we excluded five conceptual papers, three articles that examined counselors’ or counselor educators’ experiences after graduation, and one article about ICSs in Turkey. Consequently, the final data consisted of 18 articles published by seven selected counseling journals.
Data Analysis
The research team analyzed content areas of the ICS research as an extension of qualitative content analysis, which requires performing the systematical coding and identifying categories/themes (Cho & Lee, 2014). We followed a series of steps suggested by Downe-Wamboldt (1992), which included selecting the unit of analysis, developing and modifying categories, and coding data. Several methods were used to ensure the trustworthiness of this content analysis study (Kyngäs et al., 2020). For credibility, Um and Woodbridge conducted multiple rounds of review on determining an adequate unit of analysis and tracked all discussions and modifications in great detail. For dependability, we calculated interrater reliability coefficients and Wood provided feedback about the results. Um also secured confirmability by utilizing audit trails, which described the specific steps and reflections of the project. Finally, to support transferability, we carefully examined other content analysis articles, reflected core aspects in the current study, and depicted the research process transparently.
Coding Protocol
After completing the quantitative content analysis, we conducted the qualitative content analysis as Downe-Wamboldt (1992) suggested. In so doing, we applied the inductive category development process suggested by Mayring (2000), which features a systematic categorization process of identifying tentative categories, coding units, and extracting themes from established categories. Specifically, after discussing the research question and levels of abstraction for categories, Um and Woodbridge determined the preliminary categories based on the text of the 18 ICS articles. We practiced coding the data using two articles and then performed independent coding of the remaining articles. Using a constructivist approach, we agreed to add additional categories as needed. Subsequently, the categories were revised until we reached a consensus. In the final step, established categories were sorted into three themes to identify the latent meaning of qualitative materials (Cho & Lee, 2014; Forman & Damschroder, 2007). Regarding validity, the congruence between existing conceptual themes and results of data coding secures external validity, which is regarded as the purpose of content analysis (Downe-Wamboldt, 1992).
Interrater Reliability
We used various indices of interrater reliability to assess the overall congruence between the researchers who performed the qualitative analysis and ensure trustworthiness. In this study, we used the kappa statistic (κ) suggested by Cohen (1960), which shows the extent of consensus among raters for selecting an article or coding texts (Stemler, 2001). Cohen’s kappa has been used extensively across various academic fields to measure the degree of agreement between raters. More specifically, the kappa statistic was calculated in two phases: 1) after screening articles and 2) after coding the texts according to the categories. The kappa results between Um and Woodbridge were .68 for screening articles and .71 for coding the text, both of which are considered substantial (.61–.80; Stemler, 2004).
Results
Results of Quantitative Content Analysis
Based on our electronic search, we identified a total of 18 ICS articles published between 2006 and 2021 in seven selected counseling journals, including three ACA division journals, one ACA state-branch journal, one ACES regional journal, and two journals from professional counseling associations (see Table 1). Specifically, two articles were published in CES, three in JMCD, one in JCPS, one in JSGW, three in JPC, seven in IJAC, and one in JCLA. Across the 18 ICS articles, a total of 35 researchers were identified as authors or co-authors with six authoring more than one article. According to researchers’ positionality statements in qualitative articles, eight researchers reported that they were previous or current ICSs in the United States. The institutional affiliations of researchers include 22 U.S. universities and two international universities, with three institutional affiliations appearing more than once across the studies.
Table 1
Summary of International Counseling Student Research in Selected Counseling Journals Between 2006 and 2021
| Journal and Author |
Research Design |
Participants |
Data Collection |
Topic |
| Counselor Education and Supervision (CES) |
Behl et al.
(2017) |
Quantitative
(Pearson product-moment correlations) |
38 counseling master’s and doctoral students |
Online survey |
Stress related to acculturation and students’ language, academic, social, and cultural needs |
D. Li & Liu
(2020) |
Qualitative (Phenomenology) |
11 doctoral students |
Semi-structured interview |
ICSs’ experiences with teaching preparation |
| Journal of Multicultural Counseling and Development (JMCD) |
Kuo et al.
(2021) |
Qualitative (Consensual
qualitative research) |
13 doctoral students |
Semi-structured interview |
ICSs’ professional identity development influenced by their multicultural identity and experience |
Nilsson &
Dodds (2006) |
Quantitative (Exploratory factor analysis, ANOVA, and hierarchical multiple regression analysis) |
115 master’s and doctoral students in counseling and psychology |
Online survey |
Development of a scale to measure issues in supervision |
Woo et al.
(2015) |
Qualitative (Consensual qualitative research) |
8 counselor education doctoral students |
Semi-structured interview |
Coping strategies used during training in supervision |
| The Journal of Counselor Preparation and Supervision (JCPS) |
Park et al.
(2017) |
Qualitative (Consensual qualitative research) |
10 counseling master’s and doctoral students |
Semi-structured interview |
Practicum and internship experiences of ICSs |
| The Journal for Specialists in Group Work (JSGW) |
Delgado-Romero
& Wu (2010) |
Qualitative
(Not identified) |
6 Asian counseling graduate students |
Counseling
practice |
Social justice–focused group intervention |
| Journal of Professional Counseling: Practice, Theory & Research (JPC) |
Interiano-
Shiverdecker
et al. (2019) |
Quantitative (Hierarchical multiple regression analysis) |
94 counseling master’s and doctoral students |
Online survey |
Relationship between acculturation and self-efficacy |
| Ng (2006) |
Quantitative (Descriptive analysis) |
96 CACREP-accredited
counseling programs |
Responses via email/telephone |
Enrollment in CACREP-accredited programs |
Sangganjanavanich
& Black (2009) |
Qualitative (Phenomenology) |
4 master’s students
and 1 doctoral student
in counseling |
Semi-structured interview |
Perceptions of supervision |
|
|
|
|
|
| International Journal for the Advancement of Counselling (IJAC) |
|
|
Akkurt et al.
(2018) |
Quantitative (Moderation analysis) |
71 counseling master’s and doctoral students |
Online survey |
Relationships between acculturation, counselor self-efficacy, supervisory working alliance, and role ambiguity moderated by frequency of multicultural discussion |
Interiano & Lim
(2018) |
Qualitative (Interpretive phenomenology) |
8 foreign-born doctoral students |
Semi-structured interview |
Influence of acculturation on ICSs’ professional development |
Lertora & Croffie
(2020) |
Qualitative (Phenomenology) |
6 counseling master’s students |
Demographics survey, focus
group, and semi-structured
interview |
Lived experiences of master’s-level ICSs in counseling program, including challenges and support, cultural differences, and future career paths |
C. Li et al.
(2018) |
Quantitative
(Linear regression analysis) |
72 counseling master’s and doctoral students |
Online survey |
Influence of acculturation and foreign language anxiety on ICSs’ counseling self-efficacy |
Ng & Smith
(2009) |
Quantitative
(F-tests) |
56 international counseling students
82 domestic
counseling students |
Survey |
Perceived barriers and concerns of ICSs in their training compared to domestic counseling students |
Ng & Smith
(2012) |
Quantitative (Hierarchical regression analysis) |
71 counseling master’s and doctoral students |
Online survey |
Relationships among ICSs’ training level, acculturation, counselor self-efficacy, supervisory working alliance, role ambiguity, and multicultural discussion |
Smith & Ng
(2009) |
Mixed methods (Descriptive analysis, constant comparative method of analysis, and phenomenology) |
11 master’s students and 10 doctoral students (including 7 recent graduates) |
Online survey |
ICSs’ experiences, resources, hindrances, and recommendations regarding multicultural counseling training |
| Journal of Counselor Leadership and Advocacy (JCLA) |
Kuo et al.
(2018) |
Qualitative (Consensual qualitative research) |
13 doctoral students |
Semi-structured interview |
ICSs’ professional identity development influenced by their multicultural identity and experience |
Note. ICS = international counseling student.
In terms of research design, eight articles employed quantitative research designs with diverse statistical methods including hierarchical multiple regression analysis, ANOVA, exploratory factor analysis, descriptive analysis, linear regression analysis, and moderation analysis. Another nine articles used qualitative approaches including phenomenology and consensual qualitative research, while one article (Smith & Ng, 2009) applied mixed methods design including both quantitative and qualitative analyses. Regarding participants, eight quantitative studies reported having between 38 to 115 ICS participants, including Ng’s (2006) study in which the author collected information on ICSs from 96 CACREP-accredited counseling programs. The numbers of participants in the eight qualitative ICS articles were relatively smaller, ranging from 5 to 13, which is natural given the characteristics of quantitative and qualitative research designs. Finally, the mixed methods study included 21 ICS participants. Quantitative researchers most frequently used online surveys to collect data, although one researcher (Ng, 2006) gathered information via email or telephone. Researchers using qualitative methodologies primarily used semi-structured interviews to collect data, while Delgado-Romero and Wu (2010) performed a group counseling intervention and interpreted the results, including the feedback of group members.
Results of Qualitative Content Analysis
The content areas of the ICS research included personal and professional aspects of ICSs’ adjustment and development. These aspects were influenced by ICSs’ unique circumstances along with their needs, potential stressors, and accessible resources and strategies. During qualitative content analysis, we generated and established preliminary categories. We then developed the preliminary categories into three main themes encompassing ICS research: (a) professional practices and professional development, (b) academic, social, and cultural challenges, and (c) personal and social resources. Each theme consisted of several identified categories.
Professional Practices and Professional Development
Many studies examined ICSs’ perceptions, concerns, needs, and suggestions of professional training experiences, including practicum and internship (e.g., Lertora & Croffie, 2020; Park et al., 2017), supervision (e.g., Ng & Smith, 2012; Nilsson & Dodds, 2006), multicultural training (e.g., Akkurt et al., 2018; Smith & Ng, 2009), social justice group intervention (Delgado-Romero & Wu, 2010), and teaching preparation (D. Li & Liu, 2020) from the unique perspective of ICSs. Furthermore, in relation to the professional practices, several categories of ICSs’ professional development were identified, such as counseling self-efficacy (e.g., Interiano-Shiverdecker et al., 2019; C. Li et al., 2018), professional identity development (e.g., Kuo et al., 2018, 2021), role ambiguity (Akkurt et al., 2018; Ng & Smith, 2012), and multicultural competencies (Smith & Ng, 2009).
Academic, Social, and Cultural Challenges
The second theme included unique challenges that ICSs encountered across academic, social, and cultural domains. The most commonly identified category from 12 studies was acculturation (e.g., Behl et al., 2017; Interiano & Lim, 2018; Lertora & Croffie, 2020). In addition, ICSs faced other cultural barriers involving cultural differences (e.g., Behl et al., 2017; Woo et al., 2015), difficulties in performing teaching and supervision practices (e.g., Li & Liu, 2020; Woo et al., 2015), and struggles in understanding cultural values and U.S. culture (e.g., Kuo et al., 2021; Sangganjanavanich & Black, 2009). ICSs reported that their academic and social concerns included English proficiency (e.g., Kuo et al., 2021; Nilsson & Dodds, 2006) and experiences of language anxiety (C. Li et al., 2018); stigma, biases, and discrimination (e.g., Ng & Smith, 2009; Sangganjanavanich & Black, 2009); and interpersonal isolation (e.g., Behl et al., 2017).
Personal and Social Resources
The third theme emerged from multiple categories of personal and social resources that supported ICSs. In terms of personal resources, researchers identified several characteristics such as self-reflection, self-regulation, and self-efficacy, which contributed to ICSs’ professional development (e.g., Delgado-Romero & Wu, 2010; Interiano-Shiverdecker et al., 2019; Woo et al., 2015). Additionally, the sources of social support for ICSs included their peers and other ICSs (e.g., D. Li & Liu, 2020; Woo et al., 2015), faculty and mentors (e.g., Smith & Ng, 2009; Woo et al., 2015), department and college (e.g., Delgado-Romero & Wu, 2010; D. Li & Liu, 2020), and family (Kuo et al., 2018).
Discussion
The purpose of this content analysis was to provide an organized overview of counseling studies conducted for ICSs over the past 16 years both from quantitative and qualitative perspectives. The aggregated findings, including publication trends and content areas of ICS research, are expected to present the missing pieces in research to better understand and support ICSs and provide meaningful recommendations to better support their professional development. Specifically, we identified 18 articles published in selected counseling journals during the 16-year period from 2006 to 2021. Our findings included the journals, authorship and affiliation, research orientation, participant characteristics, data collection method, and content areas. In general, researchers from many educational institutions have conducted collaborative research focusing on ICSs, with a balance of quantitative and qualitative methodologies. Research participants were ICSs at master’s and doctoral levels, with larger participant groups for quantitative studies and smaller groups for qualitative studies. The most frequently employed methods for data collection were online surveys and semi-structured interviews. Among the 18 identified ICS articles, three main content themes emerged, with each theme consisting of several categories.
In terms of the content, counseling researchers have consistently examined the professional practices of ICSs in their programs. Our findings indicate that many researchers were interested in supervision as an essential aspect of counselor education. Supervision involves intricate dynamics between the supervisor, supervisee, and client, and it can have a substantial influence on counselor competency development (Falender & Shafranske, 2007; Nilsson & Dodds, 2006). For this reason, ICS research has focused not only on investigating the supervisory concerns, needs, and satisfaction of ICSs, but on providing an integrative supervision model for this population (Nilsson & Dodds, 2006; Park et al., 2017; Sangganjanavanich & Black, 2009). Beyond supervision, researchers have also explored other topics, including teaching preparation and social justice counseling (Delgado-Romero & Wu, 2010;
D. Li & Liu, 2020). We found that researchers have attended to ICSs’ professional competencies as well as their training processes, including counseling self-efficacy, professional identity, and multicultural and social justice competencies (Kuo et al., 2021; C. Li et al., 2018; Smith & Ng, 2009). These professional competencies and training processes are regarded as important indices of successful and effective counselor training (Center for Substance Abuse Treatment, 2014; Woo et al., 2015). As a whole, ICS research has addressed diverse student training experiences and resultant developmental outcomes, although the absolute number of studies remains limited.
Our results highlight cultural and language differences as a primary barrier for many ICSs when they initiated their study in a foreign country. This finding is consistent with previous studies, including Mori’s (2000) seminal work. Most studies we examined identified acculturation as a key construct of ICSs’ adjustment and growth in a foreign country (Interiano & Lim, 2018; Ng & Smith, 2012). Many ICS participants sought to maintain a balance between engaging in U.S. language and culture and sustaining their own cultural identity (Interiano-Shiverdecker et al., 2019; D. Li & Liu, 2020; Sangganjanavanich & Black, 2009). Specifically, ICSs reported cultural challenges in several areas, including the educational system, teaching styles, personal interactions, social justice issues, and cultural values and practices (Behl et al., 2017; Delgado-Romero & Wu, 2010; D. Li & Liu, 2020). One study found that doctoral-level ICSs experienced greater cultural adjustment problems and conflicts compared to master’s-level ICSs (Ng & Smith, 2009), which implies that differentiated understanding and approaches may be required according to ICSs’ developmental stages. Also, our findings echoed the existing literature that one of the main obstacles for international students is language proficiency (Kuo et al., 2021; C. Li et al., 2018), as ICSs who had difficulty using English reported greater academic needs and concerns than their peers (Behl et al., 2017).
A notable finding is that the cultural barriers ICSs experienced were intertwined with their social concerns. ICSs are exposed to social dangers involving stigma, discrimination, and interpersonal isolation (Behl et al., 2017; Delgado-Romero & Wu, 2010). Although several researchers explored the potential relationship between ICSs’ length of time in the United States and their stress and cultural development (Behl et al., 2017; Nilsson & Dodds, 2006), their findings did not indicate any significant relationship. This lack of an effect may imply that other risks and protective factors have more influence on the successful adjustment and achievement of ICSs regardless of the amount of time they have spent in the United States. As such, our findings have shown that ICSs face unique challenges across their professional and personal lives in acculturating to two or more cultures and satisfying counseling training requirements.
Corresponding to these challenges, various personal and social resources have been regarded as protective factors of ICS development. Specifically, in terms of social support, researchers identified the importance of support from mentors, supervisors, peers, and other international graduate students (e.g., Woo et al., 2015). Given that ICSs often experience a lack of social support, it is noteworthy that the current ICS literature highlights the need for counselor training programs to promote students’ personal strengths and social connections.
Overall, we identified patterns and trends in research on international students in counseling programs based on studies published in selected counseling journals. Despite our efforts to reflect on diverse ICS experiences, the paucity of ICS research across selected counseling journals, particularly ACA journals, is notable. Given the increasing representation of ICSs in the wider counseling student body (Ng, 2006), further studies addressing the resources and barriers of this student population are needed. Furthermore, international students were exposed to unprecedented difficulties and mental health threats during the COVID-19 pandemic (Chen et al., 2020). These challenges necessitate more scholarly attention toward supporting and advocating for ICSs, including their adjustment, professional development, and transition from training to practice.
Implications
Because members of the counseling profession have expressly emphasized the importance of enriching multiculturalism and diversity (D. Li & Liu, 2020), we expect our findings to provide meaningful implications for counselor education programs. First, counseling researchers are encouraged to conduct more ICS research given the limited available studies and the increasing representation of international students in counseling programs. Even though they attempted to examine diverse training experiences and competency development of ICSs, many areas are understudied, such as their teaching and social justice practices. The existing ICS research mostly concentrated on identifying factors that influence ICSs’ academic and social lives. However, given the continuous increase of ICSs in the counseling field, research about strengths and support strategies of counselor education programs having many ICSs is worth studying. Also, in future studies, researchers can try to reflect the actual voices of ICSs about what they want from their training programs, whether they feel their program is affordable, and whether their program is effective in supporting their professional development. In addition, counseling researchers can develop projects considering cultural differences of ICSs in order to better understand them not as a single group but as multiple individuals having unique cultural backgrounds. Overall, this content analysis study underscores the need for more research on this student population.
Regarding counselor education programs, programs can provide specific resources to support the professional development of ICSs. To help ICSs overcome language barriers, for instance, institutions can provide professional assistance in the use of English, such as writing centers and speaking centers. Departments can provide language support specifically relevant to counseling, including workshops and seminars about practical language tips for counseling practice and research writing. For example, Jang and colleagues (2014) recommended instituting mock supervision sessions before practicum and/or internship to further prepare international counseling trainees for their duties. Counselor education programs are expected to address the unique language and academic needs of ICSs.
Counselor education programs should also facilitate ICSs’ cultural understanding and adjustment. Counselor education programs can design and provide opportunities for ICSs to socially interact with colleagues and faculty members in the program. Existing studies that highlight the importance of mentoring (e.g., Delgado-Romero & Wu, 2010; Ng, 2006; Woo et al., 2015) are further proof that faculty members in counselor education programs can play a significant role in the personal and professional development of ICSs. Because ICSs share unique challenges and learning experiences (D. Li & Liu, 2020; Sangganjanavanich & Black, 2009), faculty members who were ICSs or have experience advising or collaborating with ICSs can serve as essential mentors for this population.
Counselor education programs might benefit from developing and employing curriculum and courses that apply the empirical findings of ICS research, including the results of this study. These studies serve as a reference for designing more effective counselor training. Programs that design their training to support the needs of ICSs may also find that they are more effective in recruiting and retaining international students. For example, faculty members can respond to ICSs’ anxiety and concerns before they enter clinical practice (Ellis et al., 2015; Nilsson & Wang, 2008). Also, ICSs are expected to benefit from synthesized results about ICS research, promoting a deeper understanding of themselves and enabling them to develop their own coping strategies and access potential resources. Furthermore, counselor education programs need to prepare different training trajectories for master’s students and doctoral students. Compared to ICSs in doctoral programs, ICSs are relatively rare at the master’s level, comprising only 1% of master’s-level counseling trainees (CACREP, 2015). Because master’s-level ICSs may feel like they belong to the minority, helping them feel connected is an essential task for counselor education programs. Therefore, programs are required to prioritize the effective delivery of knowledge and adequate practical opportunities for supervisees at the master’s level.
Finally, counselor education programs should work toward a program culture that supports diversity. Although fostering multiculturalism has emerged as a priority for counselor education programs, more work is needed to support internationally diverse perspectives. For example, Taephant and colleagues (2015) examined the experiences of U.S.-educated international counselors practicing in non-Western counseling environments. Drawing upon these findings and other relevant references, counselor educators may design a class discussing the limitations of Western-style training. As is evidenced by existing literature, open discussions about cultural differences can be effective for the psychosocial adjustment and professional development of ICSs.
Limitations and Future Research
This study includes some limitations to note. The first and most important limitation is the concerning lack of research focusing on international students in the counseling profession (D. Li & Liu, 2020; Nilsson & Dodds, 2006; Woo et al., 2015). Even though ICSs have recently begun to attract scholarly attention (Lau et al., 2019), the number of articles published recently may not be sufficient to discuss the diverse purposes and areas of focus for ICS research. Although our study specifically highlighted the need for more research on ICSs, an extensive range of discussion was not possible due to the limited number of articles. Thus, we encourage more professional counseling organizations and counseling researchers to consider ICSs’ professional development as a research topic. Also, because this study was limited to articles published in journals related to ACA and selected other professional organizations, future research with a more comprehensive search may elicit rich and diverse discussion. Finally, content analysis has a few methodological limitations, such as no existence of unified rules and a precise analytical process, and potential biases in coding, which necessitates further research on ICSs using other methodologies for more in-depth investigations.
Conclusion
ICSs can contribute to increasing program diversity and cultivating students’ multicultural counseling competency but have been understudied despite their growing representation. This study provided a comprehensive overview of ICS research across 18 articles within a 16-year period, using both quantitative and qualitative content analysis. Counseling researchers can pay more scholarly attention to the academic and social lives of ICSs from a strength-based approach. Counseling programs and counselor educators can support ICSs by providing resources for adjustment, developing curricular and extracurricular activities involving ICSs, and working toward a more multicultural and inclusive program environment.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Akkurt, M. N., Ng, K.-M., & Kolbert, J. (2018). Multicultural discussion as a moderator of counseling supervision-related constructs. International Journal for the Advancement of Counselling, 40(4), 455–468.
https://doi.org/10.1007/s10447-018-9337-z
American Counseling Association. (2014). ACA code of ethics. https://www.counseling.org/resources/aca-code-of-ethics.pdf
Anandavalli, S., Borders, L. D., & Kniffin, L. E. (2021). “I am strong. Mentally strong!”: Psychosocial strengths of international graduate students of color. The Professional Counselor, 11(2), 173–187.
https://doi.org/10.15241/sa.11.2.173
Behl, M., Laux, J. M., Roseman, C. P., Tiamiyu, M., & Spann, S. (2017). Needs and acculturative stress of international students in CACREP programs. Counselor Education and Supervision, 56(4), 305–318.
https://doi.org/10.1002/ceas.12087
Center for Substance Abuse Treatment. (2014). A treatment improvement protocol: Improving cultural competence. Substance Abuse and Mental Health Services Administration.
Chen, J. H., Li, Y., Wu, A. M. S., & Tong, K. K. (2020). The overlooked minority: Mental health of international students worldwide under the COVID-19 pandemic and beyond. Asian Journal of Psychiatry, 54, 102333. https://doi.org/10.1016/j.ajp.2020.102333
Cho, J. Y., & Lee, E.-H. (2014). Reducing confusion about grounded theory and qualitative content analysis: Similarities and differences. The Qualitative Report, 19(32), 1–20. https://doi.org/10.46743/2160-3715/2014.1028
Cohen, J. (1960). A coefficient of agreement for nominal scales. Educational and Psychological Measurement, 20(1), 37–46. https://doi.org/10.1177/001316446002000104
Council for Accreditation of Counseling and Related Educational Programs. (2015). 2016 CACREP standards. http://www.cacrep.org/wp-content/uploads/2018/05/2016-Standards-with-Glossary-5.3.2018.pdf
Council for Accreditation of Counseling and Related Educational Programs. (2022). CACREP vital statistics 2021. https://www.cacrep.org/wp-content/uploads/2023/01/vital-statistics-report-2021.pdf
Delgado-Romero, E. A., & Wu, Y.-C. (2010). Asian international students in counseling programs: A group intervention to promote social justice. The Journal for Specialists in Group Work, 35(3), 290–298.
https://doi.org/10.1080/01933922.2010.492896
Downe-Wamboldt, B. (1992). Content analysis: Method, applications, and issues. Health Care for Women International, 13(3), 313–321. https://doi.org/10.1080/07399339209516006
Ellis, M. V., Hutman, H., & Chapin, J. (2015). Reducing supervisee anxiety: Effects of a role induction intervention for clinical supervision. Journal of Counseling Psychology, 62(4), 608–620. https://doi.org/10.1037/cou0000099
Falender, C. A., & Shafranske, E. P. (2007). Competence in competency-based supervision practice: Construct and application. Professional Psychology: Research and Practice, 38(3), 232–240.
https://doi.org/10.1037/0735-7028.38.3.232
Forman, J., & Damschroder, L. (2007). Qualitative content analysis. In L. Jacoby & L. A. Siminoff (Eds.), Empirical methods for bioethics: A primer (pp. 39–62). Elsevier.
Interiano, C. G., & Lim, J. H. (2018). A “chameleonic” identity: Foreign-born doctoral students in U.S. counselor education. International Journal for the Advancement of Counselling, 40(3), 310–325.
https://doi.org/10.1007/s10447-018-9328-0
Interiano-Shiverdecker, C. G., Foxx, S. P., & Flowers, C. (2019). Acculturation domains and counselor self-efficacy. Journal of Professional Counseling: Practice, Theory & Research, 46(1–2), 48–63.
https://doi.org/10.1080/15566382.2019.1669373
Jang, Y. J., Woo, H., & Henfield, M. S. (2014). A qualitative study of challenges faced by international doctoral students in counselor education supervision courses. Asia Pacific Education Review, 15(4), 561–572.
https://doi.org/10.1007/s12564-014-9342-9
Ju, J., Merrell-James, R., Coker, J. K., Ghoston, M., Pérez, J. F. C., & Field, T. A. (2020). Recruiting, retaining, and supporting students from underrepresented racial minority backgrounds in doctoral counselor education. The Professional Counselor, 10(4), 581–602. https://doi.org/10.15241/jj.10.4.581
Karaman, M. A., Schmit, M. K., Ulus, I. C., & Oliver, M. (2018). International counseling students’ perception of ethics. Journal of International Students, 8(2), 677–695. https://doi.org/10.5281/zenodo.1250370
Kuo, P., Washington, A., & Woo, H. (2021). Professional identity development and multicultural identity among international counselor education doctoral students. Journal of Multicultural Counseling and Development, 49(2), 116–128. https://doi.org/10.1002/jmcd.12210
Kuo, P., Woo, H., & Washington, A. (2018). Professional identity development of international counselor education doctoral students. Journal of Counselor Leadership and Advocacy, 5(2), 153–169.
https://doi.org/10.1080/2326716X.2018.1452079
Kyngäs, H., Kääriäinen, M., & Elo, S. (2020). The trustworthiness of content analysis. In H. Kyngäs, K. Mikkonen, & M. Kääriäinen (Eds), The application of content analysis in nursing science research (pp. 41–48). Springer. https://doi.org/10.1007/978-3-030-30199-6_5
Lau, J., & Ng, K.-M. (2012). Effectiveness and relevance of training for international counseling graduates: A qualitative inquiry. International Journal for the Advancement of Counselling, 34(1), 87–105.
https://doi.org/10.1007/s10447-011-9128-2
Lau, J., Su, Y.-W., Chen, C.-C., & Dai, C.-L. (2019). Using a collaborative model in supervision with international counseling students. The Journal of Humanistic Counseling, 58(2), 150–164. https://doi.org/10.1002/johc.12103
Lertora, I. M., & Croffie, A. L. (2020). The lived experiences of international students in a CACREP counseling program. International Journal for the Advancement of Counselling, 42(2), 174–190.
https://doi.org/10.1007/s10447-019-09394-6
Li, C., Lu, J., Bernstein, B., & Bang, N. M. (2018). Counseling self-efficacy of international counseling students in the U.S.: The impact of foreign language anxiety and acculturation. International Journal for the Advancement of Counselling, 40(3), 267–278. https://doi.org/10.1007/s10447-018-9325-3
Li, D., & Liu, Y. (2020). International counseling doctoral students’ teaching preparation: A phenomenological study. Counselor Education and Supervision, 59(3), 200–215. https://doi.org/10.1002/ceas.12184
Luo, J., & Jamieson-Drake, D. (2013). Examining the educational benefits of interacting with international students. Journal of International Students, 3(2), 85–101. https://files.eric.ed.gov/fulltext/EJ1056457.pdf
Mayring, P. (2000). Qualitative content analysis. Forum: Qualitative Social Research, 1(2).
Mori, S. C. (2000). Addressing the mental health concerns of international students. Journal of Counseling & Development, 78(2), 137–144. https://doi.org/10.1002/j.1556-6676.2000.tb02571.x
Mori, Y., Inman, A. G., & Caskie, G. I. L. (2009). Supervising international students: Relationship between acculturation, supervisor multicultural competence, cultural discussions, and supervision satisfaction. Training and Education in Professional Psychology, 3(1), 10–18. https://doi.org/10.1037/a0013072
Nilsson, J. E., & Dodds, A. K. (2006). A pilot phase in the development of the International Student Supervision Scale. Journal of Multicultural Counseling and Development, 34(1), 50–62.
https://doi.org/10.1002/j.2161-1912.2006.tb00026.x
Nilsson, J. E., & Wang, C. (2008). Supervising international students in counseling and psychology training. In A. K. Hess, K. D. Hess, & T. H. Hess (Eds.), Psychotherapy supervision: Theory, research, and practice
(2nd ed.; pp. 70–81). Wiley.
Ng, K.-M. (2006). International students in CACREP-accredited counseling programs. Journal of Professional Counseling: Practice, Theory & Research, 34(1–2), 20–32. https://doi.org/10.1080/15566382.2006.12033821
Ng, K.-M., & Smith, S. D. (2009). Perceptions and experiences of international trainees in counseling and related programs. International Journal for the Advancement of Counselling, 31(1), 57–70.
https://doi.org/10.1007/s10447-008-9068-7
Ng, K.-M., & Smith, S. D. (2012). Training level, acculturation, role ambiguity, and multicultural discussions in training and supervising international counseling students in the United States. International Journal for the Advancement of Counselling, 34(1), 72–86. https://doi.org/10.1007/s10447-011-9130-8
O’Hara, C., Chang, C. Y., & Giordano, A. L. (2021). Multicultural competence in counseling research: The cornerstone of scholarship. Journal of Counseling & Development, 99(2), 200–209.
https://doi.org/10.1002/jcad.12367
Park, S., Lee, J. H., & Wood, S. M. (2017). Experiences of international students in practicum and internship courses: A consensus qualitative research. The Journal of Counselor Preparation and Supervision, 9(2).
https://digitalcommons.sacredheart.edu/cgi/viewcontent.cgi?article=1137&context=jcps
Ratts, M. J., Singh, A. A., Nassar-McMillan, S., Butler, S. K., & McCullough, J. R. (2016). Multicultural and social justice counseling competencies: Guidelines for the counseling profession. Journal of Multicultural Counseling and Development, 44(1), 28–48. https://doi.org/10.1002/jmcd.12035
Sangganjanavanich, V. F., & Black, L. L. (2009). Clinical supervision for international counselors-in-training: Implications for supervisors. Journal of Professional Counseling: Practice, Theory & Research, 37(2), 52–65. https://doi.org/10.1080/15566382.2009.12033860
Singh, A. A., & Shelton, K. (2011). A content analysis of LGBTQ qualitative research in counseling: A ten-year review. Journal of Counseling & Development, 89(2), 217–226.
https://doi.org/10.1002/j.1556-6678.2011.tb00080.x
Smith, S. D., & Ng, K.-M. (2009). International counseling trainees’ experiences and perceptions of their multicultural counseling training in the United States: A mixed method inquiry. International Journal for the Advancement of Counselling, 31(4), 271–285. https://doi.org/10.1007/s10447-009-9083-3
Stemler, S. (2001). An overview of content analysis. Practical Assessment, Research, and Evaluation, 7(17). https://doi.org/10.7275/z6fm-2e34
Stemler, S. E. (2004). A comparison of consensus, consistency, and measurement approaches to estimating interrater reliability. Practical Assessment, Research, and Evaluation, 9(1).
https://doi.org/10.7275/96jp-xz07
Taephant, N., Rubel, D., & Champe, J. (2015). A grounded theory of Western-trained Asian group leaders leading groups in Asia. The Journal for Specialists in Group Work, 40(1), 74–101.
https://doi.org/10.1080/01933922.2014.993054
Thompson, E. H., Frick, M. H., & Trice-Black, S. (2011). Counselor-in-training perceptions of supervision practices related to self-care and burnout. The Professional Counselor, 1(3), 152–162. https://doi.org/10.15241/eht.1.3.152
Vakkai, R. J. Y., Harris, K., Chaplin, K. S., Crabbe, J. J., & Reynolds, M. (2020). Sociocultural factors that impact the health status, quality of life, and academic achievement of international graduate students: A literature review. Journal of International Students, 10(3), 758–775. https://files.eric.ed.gov/fulltext/EJ1265821.pdf
Woo, H., Jang, Y. J., & Henfield, M. S. (2015). International doctoral students in counselor education: Coping strategies in supervision training. Journal of Multicultural Counseling and Development, 43(4), 288–304. https://doi.org/10.1002/jmcd.12022
Byeolbee Um, PhD, is an assistant professor at the University of Oklahoma. Lindsay Woodbridge, PhD, LMHC, LPC, is an assistant professor at the University of Wisconsin-Stout. Susannah M. Wood, PhD, NCC, is a professor at the University of Iowa. Correspondence may be addressed to Byeolbee Um, 820 Van Vleet Oval, Rm 303, Norman, OK 73019, byeolbee.um-1@ou.edu.
Oct 31, 2023 | Volume 13 - Issue 3
Nancy Chae, Adrienne Backer, Patrick R. Mullen
All counseling graduate students participate in fieldwork experiences and engage in supervision to promote their professional development. School counseling trainees complete these experiences in the unique context of elementary and secondary school settings. As such, school counselors-in-training (SCITs) may seek to approach supervision with specific strategies tailored for the roles, responsibilities, and dispositions required of competent future school counselors. This article suggests practical strategies for SCITs, including engaging in reflection; navigating feelings of vulnerability in supervision; developing appropriate professional dispositions for school counseling practice; and practicing self-advocacy, broaching, and self-care. Counselor educators can share these strategies to help students identify their needs for their field experiences and prepare for their professional careers as school counselors.
Keywords: supervision, professional development, school counseling, school counselors-in-training, strategies
School counselors-in-training (SCITs) are trainees enrolled in graduate-level counselor education programs and receive supervision as an integral component of their training (Bernard & Goodyear, 2019). Although the supervision relationship is often characterized as hierarchical, trainees must actively participate in the supervision process to develop competency as counseling professionals (Stark, 2017). Despite this, trainees in counseling programs generally receive little guidance on understanding their roles in supervision or how to make the most of their supervision experience to contribute to their learning (Pearson, 2004; Stark, 2017). Although Pearson (2004) offered suggestions for mental health counseling students to optimize their supervision experiences, there is limited literature about how school counseling students can maximize their supervision experiences. The intention of this article is to share strategies for SCITs to take the initiative to approach supervisors with questions and ideas about their overall supervision experience, though these suggestions are not limited to SCITs and may also be useful for trainees across other counseling disciplines.
School counseling site supervision is distinguishable from supervision in other helping professions in that the roles and responsibilities of professional school counselors extend beyond the individual and group counseling services that their community counseling partners provide (American School Counselor Association [ASCA], 2019a, 2021; Quintana & Gooden-Alexis, 2020). For example, comprehensive school counseling programming encompasses direct counseling services with students and families in addition to broader systemic consultation, advocacy, and support for school communities (ASCA, 2019a). School counselors encounter unique challenges in schools regarding student and staff mental health, issues related to equity and access, and navigating the political landscapes of school systems (Bemak & Chung, 2008). Even with an understanding of these distinct themes in school counseling, there is a lack of significance placed on supervision in school counseling within research and in practice to adequately respond to contemporary school counseling issues (Bledsoe et al., 2019). Examining how SCITs can approach supervision and their roles as trainees can ensure their own learning and developmental needs are met, along with the needs of their school communities.
Contexts of School Counseling Supervision
Supervision for SCITs is provided by experienced professional school counselors and characterized by an intentional balance of hierarchy, evaluation, and support during their practicum and internship fieldwork experiences (Bernard & Goodyear, 2019; Borders & Brown, 2005). School counselor supervision serves three primary purposes: (a) promoting competency in effective and ethical school counseling practice; (b) facilitating SCITs’ personal and professional development; and (c) upholding accountability of services and programs for the greater profession and the schools, students, and families receiving services (ASCA, 2021; L. J. Bradley et al., 2010). School counseling site supervisors utilize their training and experiences to guide SCITs through their induction to the profession and development of initial skills and dispositions.
ASCA (2021) compels school counseling supervisors to address the complexities specific to educational settings as they support the professional development of SCITs, which sets school counseling supervision apart from supervision in other clinical counseling disciplines. School counselors facilitate instruction and classroom management, provide appraisal and advisement, and support the developmental and social–emotional needs of students through data-informed school counseling programs (ASCA, 2019a). Within school and community settings, they also navigate systems with an advocacy and social justice orientation and attend to cultural competence and anti-racist work. Although there are school counseling–specific supervision models that address some of the complexities inherent in the work of school counselors (e.g., Lambie & Sias, 2009; Luke & Bernard, 2006; S. Murphy & Kaffenberger, 2007; Wood & Rayle, 2006), there is currently a gap in the school counseling literature about effectively addressing the unique supervision needs of SCITs. Therefore, school counselor practitioners and counselor educators may refer to professional standards for supervision to inform how they supervise and support the developmental needs of SCITs, which may also help SCITs to understand what they might expect to encounter in graduate-level supervision.
Professional Standards for School Counseling Supervision
School counseling professional standards underscore the need for school counselor supervisors to seek supervision and training (ASCA, 2019b; Council for Accreditation of Counseling and Related Educational Programs [CACREP], 2015; Quintana & Gooden-Alexis, 2020). Professional associations and accrediting organizations (e.g., ASCA, CACREP) promote adherence to and integration of school counselor standards and competencies related to leadership, advocacy, collaboration, systemic change, and ethical practice (ASCA, 2022; CACREP, 2015; Quintana & Gooden-Alexis, 2020). As such, school counseling supervision facilitates ethical and professional skill development through school counselor standards and competencies, such as the ASCA School Counselor Professional Standards & Competencies (ASCA, 2019c) and the ASCA Ethical Standards for School Counselors (ASCA, 2022).
School counseling supervisors can support SCITs’ professional growth and development by aligning supervision activities with specific standards and competencies (Quintana & Gooden-Alexis, 2020). For example, a supervisor seeking to model the school counselor mindset and behavior standards focused on collaborative partnerships (i.e., M 5, B-SS 6; ASCA, 2019c) might provide opportunities for SCITs to develop relationships with stakeholders (e.g., families, administrators, community) while supporting student achievement. Similarly, an example of aligning supervision activities with ethical standards might involve guiding an SCIT through the process of utilizing an ethical decision-making model to resolve a potential dilemma (see Section F; ASCA, 2022).
Supervision in School Counseling
Supervision in school counseling ensures that new professionals enter the field prepared to understand and support the needs of students by effectively applying ethical standards and best practices of the profession. As such, gatekeeping is a crucial component of supervision. As gatekeepers, counselor educators or supervisors exercise their professional authority to take action that prevents a trainee who does not enact the required professional dispositions and ethical practices from entering the profession of counseling (Bernard & Goodyear, 2019). When a trainee is identified as unable to achieve counseling competencies or likely to harm others, ethical practice guides counselor educators to provide developmental or remedial services to work toward improvements before dismissal from a counseling program (American Counseling Association [ACA], 2014; Foster & McAdams, 2009).
Although supervised fieldwork experiences during graduate education and training are needed for accreditation (CACREP, 2015) and state certification, professional school counselors employed in the field may not be required to participate in any form of post-master’s clinical supervision for initial school counseling certification or renewal of their certification, unlike professional clinical mental health counselors, who require post-master’s supervision to attain licensure (Dollarhide & Saginak, 2017; Mecadon-Mann & Tuttle, 2023). Administrative supervision provided by a school administrator is more common for school counselors than clinical supervision, which promotes the competence of counselors by focusing on the development and refinement of counseling skills (Herlihy et al., 2002). In other words, though school counselors routinely encounter complex situations that involve supporting students with acute needs and responding to crises, they likely do not receive the clinical supervision needed to enhance their judgment, skills, and ethical decision-making (Bledsoe et al., 2019; Brott et al., 2021; Herlihy et al., 2002; McKibben et al., 2022; Sutton & Page, 1994). Given the reality that school counselors may not access or receive opportunities for postgraduate clinical supervision, it is important that SCITs experience robust supervision during their graduate training programs with the support of qualified site and university supervisors. This sets the stage for SCITs to effectively engage with the challenges of their future school counseling careers.
Expectations of Site and University Supervisors
For SCITs who are new to the experience of supervision in their fieldwork, it is helpful to understand what they may expect from their respective site and university supervisors. Borders et al. (2014) recommended that supervisors initiate supervision, set goals with trainees, provide feedback, facilitate the supervisory relationship, and attend to diversity, as well as engage in advocacy, ethical consideration, documentation, and evaluation. Supervisors select supervision interventions that attend to the developmental needs of trainees, and they also serve as gatekeepers for the profession (Bernard & Goodyear, 2019; Borders et al., 2014). Furthermore, supervisors facilitate an effective relationship with their trainees, characterized by empowerment, encouragement, and safety (Dressel et al., 2007; Ladany et al., 2013; M. J. Murphy & Wright, 2005). Supervisors provide a balance of support and challenge in their feedback and interactions with trainees (Bernard & Goodyear, 2019) and attend to multicultural issues by broaching with their trainees about their intersecting identities and experiences of power, privilege, and marginalization (Dressel et al., 2007; Jones et al., 2019; M. J. Murphy & Wright, 2005). Supervisors also validate trainees’ experiences by acknowledging any emergent issues of vicarious trauma and encouraging self-care (K. Jordan, 2018).
Supervisors and trainees have mutual responsibilities to facilitate an effective supervision experience. Although supervisors may hold a more significant stake of power in the relationship, trainees’ willingness to take an active role also matters. School counseling trainees are not passive bystanders in the learning process; instead, they can be thoughtful learners yearning to take full advantage of the growth from their clinical experiences. To help illuminate the opportunities and expectations SCITs can seek during supervision, the subsequent strategies from school counseling supervision research serve as suggested approaches for SCITs to make the most of this fundamental and practical learning experience.
Strategies for School Counseling Trainees
School counseling trainees can take an active role to ensure that their supervision experiences are relevant to their personal and professional development. The following approaches do not constitute an all-encompassing list but provide a foundation and guidelines rooted in existing research to get the most out of the supervision experience, including engaging in reflection and vulnerability, practicing self-advocacy, broaching, and maintaining personal wellness.
Reflection in Supervision
Reflection is key to school counselor development, especially in supervision. Researchers have reported that continuous reflection helps novice counselors move toward higher levels of cognitive complexity and expertise (Borders & Brown, 2005; Skovholt & Rønnestad, 1992). A reflective trainee demonstrates openness to understanding; avoids being defensive; and engages in profound thought processes that lead to changes in their perceptions, practice, and complexity (Neufeldt et al., 1996). Through reflection, trainees consider troubling, confusing, or uncertain experiences or thoughts and then reframe them to problem-solve and guide future actions (Ward & House, 1998; Young et al., 2011). Further, by developing relationships with supervisors, trainees become open to receiving and integrating feedback to support their development (Borders & Brown, 2005). Reflection becomes an ongoing process and practice throughout trainees’ academic and field experiences and postgraduation.
Trainees can engage in self-reflective practices in various ways over the course of their graduate training. First, trainees can use a journal to record thoughts, feelings, and events throughout their school counseling field experiences. Research has shown that written or video journaling can help trainees to reflect on the highs and lows of counseling training and foster self-awareness (Parikh et al., 2012; Storlie et al., 2018; Woodbridge & O’Beirne, 2017). For example, trainees can connect their practical experiences with knowledge from academic learning to note discrepancies and consistencies (e.g., learning about the ASCA National Model and the extent to which a school chooses to implement the model; navigating the bureaucracy of school systems that often dictate roles and responsibilities of school counselors). Trainees can also challenge their thoughts by exploring difficult experiences using reflective journaling. They can journal about the different perspectives of those involved in the situation (e.g., students, parents/guardians, teachers, administrators), process ethical dilemmas, and gauge and manage any emotional experiences attached to grappling with challenges. Trainees desiring structured prompts can consider writing about specific developmental, emotional, and interpersonal experiences to process events related to counselor and client interactions (Storlie et al., 2018).
Second, trainees can consult with their supervisors to seek guidance and constructive feedback about challenging experiences (Borders & Brown, 2005). Hamlet (2022) recommended using the S.K.A.T.E.S. form to reflect on issues related to trainees’ Skills, Knowledge, Attitudes, Thoughts, Ethics, and Supervision needs. Using S.K.A.T.E.S., for example, a school counseling intern may reflect on how they incorporated motivational interviewing counseling skills to support a student struggling with their declining grades (North, 2017). They might seek supervision about a challenging crisis response at the school and process how they might have responded differently. Even after supervision sessions, trainees should engage in continued self-reflection and apply new learning to their clinical practice.
Third, trainees can utilize the Johari window as a tool to reflect upon the knowledge, awareness, and skills required for school counseling practice (Halpern, 2009). Trainees work with supervisors to consider questions or experiences to identify: (a) open areas (i.e., things known to everyone, such as critically discussing school- and district-wide policies that contribute to inequitable access to college preparatory courses); (b) hidden areas (i.e., things only known to the trainee to be shared in supervision, such as the trainee’s hesitations about leading a group counseling session with middle school students independently for the first time); (c) blind spots (i.e., things that the supervisor is aware of that the trainee may not be, such as personal biases, prejudices, stereotypes, and discriminatory attitudes that may affect the trainee’s conceptualizations and interactions with students and families); and (d) undiscovered potential (i.e., things that the supervisor and trainee can experience and learn together, such as engaging in professional learning together to align school counseling programming with a school-wide movement toward implementing restorative justice practices). This strategy also compels trainees to align their supervision goals with ethical codes (see A.4.b., F.8.c., and F.8.d in the ACA Code of Ethics) and standards for professional practice (ACA, 2014). Trainees can feel empowered to utilize the Johari window with supervisors and peers to guide conversations, generate questions, and develop insights to inform school counseling practice and explore ethical dilemmas.
Vulnerability in Supervision
Vulnerability is an essential yet challenging experience within the hierarchical nature of supervision. Being vulnerable involves feelings of uncertainty, reluctance, and exposure; hence, trainees require a sense of psychological safety and support to explore their needs and areas of weakness (Bradley et al., 2019; Giordano et al., 2018; J. V. Jordan, 2003). Although site supervisors hold the primary responsibility for facilitating supervision relationships characterized by safety and support (Bernard & Goodyear, 2019), trainees can feel empowered to advocate for supervision environments that encourage authenticity and vulnerability, which are conducive to growth and development.
First, trainees can discuss with their supervisors and peers to define feelings of vulnerability and create group norms to promote supported vulnerability (Bradley et al., 2019). With a shared understanding, trainees, supervisors, and peers create an environment for continued growth and risk-taking. For example, during the first group supervision meeting, trainees can suggest norms that will individually and collectively sustain a safe classroom community for sharing and learning. A lack of clear norms about how to communicate feedback may result in experiences of shame and affect trainees’ confidence (J. V. Jordan, 2003; Ratts & Greenleaf, 2018). To mitigate this, trainees, supervisors, and peers can collaboratively discuss appropriate and preferred ways of giving and receiving feedback that is supportive, productive, and meaningful (Ladany et al., 2013). For example, trainees may prefer specific comments rather than general praise: “When the client expressed their frustration, you did well to remain calm and reflect content and feelings in that moment,” instead of “You did a great job.” This exchange among trainees, supervisors, and peers offers a constructive and engaging experience in which individuals can appropriately support and challenge one another.
Second, reviewing recordings offers a learning opportunity for trainees to reflect upon and critique their own skills and dispositions (Borders & Brown, 2005). When presenting recorded case presentations, trainees can practice vulnerability by selecting and presenting recordings that highlight challenging areas that may require constructive feedback (i.e., show their worst rather than their best). Trainees can identify portions of recordings that exemplify where they need the most help, such as a challenging experience during an individual counseling session with a student. Further, when presenting their recordings, trainees can also ask for suggestions to improve consultation work with caregivers when discussing college and career planning issues or innovative instructional strategies for teaching a classroom lesson in response to challenging situations. Vulnerability also occurs when trainees seek support from supervisors and peers about blind spots and areas of strength and growth regarding skill development and self-awareness issues in the recorded session or role-play. For instance, a trainee may express concern about the increasing academic counseling referrals of ninth-grade students who are struggling with the transition to high school and ask for guidance about how to more effectively respond systemically and individually.
Self-Advocacy in Supervision
Self-advocacy is another empowering practice for trainees to identify their needs and seek support. Researchers have defined self-advocacy as understanding one’s rights and responsibilities, communicating needs, and negotiating for support, which helps trainees proactively approach supervision (Astramovich & Harris, 2007; Pocock et al., 2002). Although supervision is characterized as hierarchical, it is also a relationship based on mutual participation, with inherent expectations for trainees (Stark, 2017). Within the evaluative nature of a supervision relationship, trainees may reasonably feel intimidated about practicing self-advocacy. However, trainees can feel empowered to self-advocate when building rapport with supervisors in an environment characterized by safety and support.
To prepare to self-advocate, trainees should continue engaging in self-reflection on their gaps in knowledge, awareness, and skills related to school counseling practice and then consider the types of resources and supports needed from their supervisor to bridge such gaps. In alignment with their learning goals, trainees can self-advocate by taking the initiative to request support for what they would like to achieve during the supervision experience (Storlie et al., 2019). For example, trainees may inquire about logistical concerns, such as seeking guidance about appropriate and creative ways to ensure that they earn sufficient direct and indirect hours, or evaluative concerns, like asking how to improve in specific school counseling skill areas after mid- and end-of-semester evaluations. Trainees can also seek support with conceptualization (e.g., applying a theoretical orientation when understanding the potential contributors to a student’s feeling of anxiety), skill development (e.g., experience with advocating for students receiving special education services in an Individualized Educational Plan [IEP] meeting), and countertransference issues (e.g., emotional reactions that may arise when supporting a grieving student coping with a loss; Pearson, 2004). Trainees should prepare specific questions that communicate their needs and explicitly request resources, opportunities, or next steps for continued improvement and development.
Trainees may also self-advocate through positive communication, which is a critical skill for helping professionals and in maintaining relationships (Biganeh & Young, 2021). Positive communication may involve actively listening to their supervisor’s insights, presenting statements that paraphrase their supervisor’s key points, and asking open-ended questions to elicit mutual exploration of topics of interest. For instance, after observing a crisis response to a student expressing suicidal ideation, the trainee can debrief about their experiences with their supervisor by summarizing key observations and protocol followed, while also asking what steps could be added or reconsidered if the trainee were leading the crisis response. Additionally, practicing communication skills in the context of supervision may enhance trainees’ competence and confidence when interacting with students and stakeholders, including caregivers, teachers, and administrators (Heaven et al., 2006). For example, trainees can request to observe and later role-play how they might facilitate a consultation meeting with a student and their parent to discuss the importance of consistent attendance and academic development.
Trainees can get the most out of their supervision experience by self-advocating and taking initiative to describe their unique learning styles and needs (Storlie et al., 2019). This provides an opportunity for trainees to proactively convey their goals and concerns about students and stakeholders at their sites (Baltrinic et al., 2021; Cook & Sackett, 2018). For example, if the trainee has become increasingly comfortable with co-leading a group counseling session, the trainee can communicate a desire to design and independently lead a group counseling session and then seek feedback about the curriculum plans or recordings of the session for continued improvement in group facilitation skills. Ultimately, engaging in self-advocacy skills during fieldwork helps trainees prepare for their careers as school counselors, in which self-advocacy is necessary when seeking professional development, resources for school counseling program development, and navigating school systems and politics to support their students and school counseling programs (Oehrtman & Dollarhide, 2021).
Broaching
Broaching is an ongoing behavior in which counselors invite conversations to explore race, ethnicity, and culture with clients, which can strengthen the counseling relationship and enhance cultural responsiveness and therapeutic benefits (Day-Vines et al., 2007, 2013). Likewise, in supervisory relationships, broaching helps supervisors and trainees to understand how cultural factors affect the supervisory relationship (Jones et al., 2019). Without broaching, both supervisors and trainees may miss meaningful contexts and realities, potentially rupturing the supervisory relationship (Jones et al., 2019). Broaching is also a key demonstration of commitment to culturally informed clinical supervision that promotes cultural humility and anti-racist counseling and supervision practice (Cartwright et al., 2021).
Although supervisors are charged with the responsibility of broaching based on the hierarchical nature of the supervisory relationship and its inherent power dynamics, they may not consistently incorporate broaching as part of their regular supervision behaviors (Bernard & Goodyear, 2019; King & Jones, 2019). Trainees who feel empowered to discuss issues of identity and power in supervision are more likely to initiate broaching conversations with their supervisors (King & Jones, 2019). As such, trainees should feel encouraged to engage in discussions with their supervisors to openly address cultural identities that may impact the supervisory relationship and their work with students and stakeholders in schools. King and Jones (2019) suggested that trainees can broach topics that they feel comfortable discussing within the context of their supervision relationship. It is necessary to note that the process and outcome of broaching in supervision are not only contingent upon the diverse sociocultural and sociopolitical contexts of individuals, but also on where the trainee and supervisor lie within the continuum of broaching styles and their own racial identity development as well as the power and hierarchy dynamics of the supervisory relationship (Bernard & Goodyear, 2019; Day-Vines et al., 2007; Jones et al., 2019). Just as for any novice counselor and individuals in the early stages of the broaching styles continuum, there may be hesitation, anxiousness, misunderstanding, or intimidation about engaging in broaching skills, especially considering the power dynamic of supervision. Trainees can self-assess their broaching style by using the Broaching Attitudes and Behavior Survey (Day-Vines et al., 2007, 2013), which might provide them with insight about their own level of comfort with broaching in supervision.
Trainees can seek continuing education and support from supervisors and peers about developing and strengthening their understanding of cultural diversity, race, oppression, and privilege related to school counseling. If a trainee feels nervous about broaching with their supervisor, the trainee can express their desire to practice broaching and seek feedback from their supervisor after broaching has taken place (e.g., “I would like to try broaching about a student’s cultural identities, and I was wondering if you could share your thoughts with me.”). Trainees can also directly express curiosities, observations, or questions about how any cultural differences and similarities between the supervisor and trainee may impact and inform the supervisory relationship. For example, a trainee and supervisor can discuss prior supervisory relationships, such as in academic or employment experiences, and identify the shared or different intersectional cultural identities to understand how this new supervisory relationship can be a meaningful relationship and safe space for learning. This exercise demonstrates cultural humility in which trainees engage in respectful curiosity, a stance of openness, and cultural awareness that enhances the supervisory working alliance (Watkins et al., 2019).
Broaching can also help school counseling trainees move beyond the nice counselor syndrome—a phenomenon in which stakeholders may often view school counselors as harmonious and unengaged in conflict, which supersedes their position as social justice advocates and instead perpetuates the status quo and reinforces inequities (Bemak & Chung, 2008). Because broaching invites discussion about multicultural and social justice issues, trainees can initiate conversations about personal obstacles (e.g., apathy, anxiety, guilt, discomfort) and professional obstacles (e.g., professional paralysis, resistance, job security) during supervision (Bemak & Chung, 2008). For example, a trainee can seek guidance about how to present a proposal to administrators about an affinity group for LGBTQ+ students and allies in the school. They can discuss potential personal and professional obstacles, how to overcome such obstacles to promote the group, and how to advocate for inclusion of LGBTQ+ students. It is important for trainees to engage in advocacy during their fieldwork experiences because social justice is inherent to school counselor identity and comprehensive school counseling programs (Glosoff & Durham, 2010).
Personal Well-Being
Self-care and personal wellness are necessary not only for counseling practice but also for supervision experiences; these contribute to personal and professional development and ethical practice, promote positive outcomes with students/clients, and mitigate issues of burnout and turnover (Blount et al., 2016; Branco & Patton-Scott, 2020; Mullen et al., 2020). For trainees, it is typical yet challenging to balance an academic workload; the demands of fieldwork; and other personal, social, and emotional experiences. Trainees can utilize supervision to maintain accountability for self-assessing their wellness practices that support their continued effective and ethical counseling practice. Marley (2011) found that self-help strategies can reduce emotional distress and offer coping skills to manage difficulties, which can help trainees maintain their self-care and develop skills for continued wellness.
Blount et al. (2016) suggested developing a wellness identity in supervision. Trainees can develop a wellness identity by acknowledging the wellness practices they already engage in and continuing practices that help to maintain self-care. Moreover, Mullen et al. (2020) found that engaging in problem-solving pondering (e.g., planning or developing a strategy to complete a task or address a problem within fieldwork), as opposed to negative work-related rumination, supported well-being, higher job satisfaction, and work engagement for school counselors. For example, rather than ruminating about a disagreement with a teacher regarding recommending a student for the gifted program, the trainee can consider ways to turn future conversations into partnership opportunities with the teacher—while also consulting with the supervisor, administrator, and parent about considering additional data points to advocate for the student’s enrollment in the gifted program.
Another way for trainees to support their well-being is to acknowledge their strengths (Wiley et al., 2021) related to their clinical knowledge, awareness, and skills in live and recorded sessions with students. This can be challenging yet empowering for trainees who are quick to self-criticize. For instance, before jumping to areas for improvement, trainees are encouraged to first ask, “What did I do well here?” and also request recommendations for additional wellness strategies to strengthen their school counseling practice. Additional resources, such as readings or role-plays, may help trainees
re-center themselves after difficult or challenging scenarios. For example, after making their first report to child protective services about a suspected physical abuse case, the trainee can process with their supervisor and discuss potential self-care strategies and resources to manage the difficult emotions arising from the challenging experience.
Moreover, researchers suggested utilizing self-compassion as a means of self-care for counseling graduate students (Nelson et al., 2018). Trainees can intentionally practice being kind to oneself; normalizing and humanizing the experience of challenges; and being aware of one’s own feelings, thoughts, and reactions, which can enhance their well-being and reduce potential fatigue and burnout (Nelson et al., 2018; Pearson, 2004). For example, after hearing difficult feedback from their supervisor about improving a lesson plan, a trainee can try reframing weaknesses as areas for continued growth. Or, when reviewing a mid- or end-of-semester evaluation with their supervisor, a trainee can practice being present and open to feedback while also monitoring and taking the initiative to share feelings, insights, and questions. After a supervision session or evaluative experience, a trainee can also engage in journaling or compassionate letter writing (Nelson et al., 2018) to be mindfully aware of their emotions and normalize the challenging growth experiences of a developing counselor.
Overall, trainees deserve meaningful, supportive, and responsive supervision, yet they commonly (mis)perceive themselves as in positions of less power in supervision and their fieldwork sites. Trainees should feel empowered to consult with others at their sites and universities to address issues of concern and seek clarification from supervisors about the expectations of supervision; this supports an effective, collaborative supervision experience. Together with supervisors, trainees can review the strategies throughout supervision sessions. With guidance and support, trainees can attempt such strategies within the safety of the supervisory relationship.
Implications for Site Supervisors and Counselor Educators
There are several implications for site supervisors and counselor educators when considering strategies to empower trainees to maximize their supervision experience. Although trainees can take the initiative to implement such strategies independently, some suggestions may require additional collaborative support and guidance from site supervisors and counselor educators. For example, site supervisors and counselor educators could consider introducing the strategies posed in this article during supervision sessions or as assigned reading for discussion. Altogether, engaging in and facilitating these strategies contributes to the development of important dispositional characteristics required of professional school counselors.
Site supervisors and counselor educators have the responsibility to facilitate a supervision environment in which trainees feel empowered to utilize the suggested strategies. This requires them to intentionally balance safety and support with challenge and high expectations (Stoltenberg, 1981). When trainees lack a sense of safety, they may be less likely to self-disclose dilemmas or concerns and more likely to feel shame, which jeopardizes the overall supervision experience and relationship (J. V. Jordan, 2003; Murphy & Wright, 2005). When trainees experience inclusivity in their training programs and move past the discomfort of vulnerability, they can experience growth, strengthen the supervisory relationship, and address their learning goals (Bradley et al., 2019; Giordano et al., 2018). For example, although trainees can take the initiative to suggest norms for supervision, we encourage supervisors to invite or prompt discussions related to trainees’ learning needs and expectations for the supervisory relationship.
Reflection and vulnerability also require rapport and trust for trainees to self-advocate. Further, when trainees can communicate with their supervisors about their needs, supervisors can respond by appropriately facilitating their request for support (Stoltenberg, 1981). During supervision, supervisors also model, teach, and monitor wellness strategies to support trainees’ ethical and professional school counseling practice (Blount et al., 2016). For instance, site supervisors and counselor educators may need to introduce the Johari window framework as a structured reflective exercise, if trainees are not already aware of this tool (Halpern, 2009).
Finally, broaching within supervision may offer a proactive means of exploring dynamics, power, and cultural differences that can bolster the quality and longevity of the supervision experience. However, the onus is typically on supervisors to initiate broaching conversations after they have facilitated a supervision relationship characterized by trust, acceptance, and inclusion (Jones et al., 2019). Supervisors model how to broach topics of race and culture within the dynamics of the supervisory relationship so that trainees can feel empowered to incorporate broaching as an ongoing professional disposition during and beyond supervision. For example, trainees and supervisors are encouraged to explore, model, and role-play recommendations from Bemak and Chung (2008) to move beyond nice counselor syndrome in school counseling practice.
Limitations and Future Research
Although this article provided a variety of practical strategies for SCITs to navigate supervision, it is not intended to be comprehensive and is not without limitations. The suggested strategies have been informed by research to support the supervision process and overall trainee development but may not necessarily be empirically supported. In addition, the strategies may not apply across all supervision contexts, relationships, and circumstances; thus, we encourage trainees to use their best judgment to consider which strategies may be most feasible and useful within their given contexts. Although this article attempted to provide examples specific to the unique work environment and responsibilities that SCITs will encounter, several suggestions provided herein may also apply to counseling trainees working outside of school counseling contexts. Knowing that supervision is an evaluative and hierarchical process, there may be dynamics of power and privilege present that may intimidate or hinder trainees from autonomously attempting and engaging in such strategies. Thus, the power dynamics of supervision may present a barrier for some trainees to self-advocate.
Future research is needed about the characteristics and contributions of trainees that can enhance the supervisory relationship and competence of the supervisor. Researchers could consider a qualitative study to explore SCITs’ experiences of autonomously implemented strategies during supervision as well as a quantitative intervention study to assess the effectiveness of specific strategies to enhance trainee and supervisor development, self-efficacy, and competence. Researchers could also consider strategies specific to site- and university-based supervision that offer evidence for trainees’ growth and competence and later longitudinal impacts of such strategies on personal and professional development.
Conclusion
Considering that supervision is a time-limited experience, these suggested strategies for approaching supervision can inform SCITs (and trainees from other counseling disciplines) about ways to advocate for a quality supervision experience. When trainees are prepared for supervision, they may feel less anxious and more empowered to approach and shape supervision to meet their developmental needs. When trainees are mindful of and actively engaged in reflection, vulnerability, self-advocacy, broaching, and wellness, they can feel empowered to seek support and resources to bridge gaps in their learning and development during the supervision experience. Site supervisors and counselor educators can also share these strategies with trainees and encourage trainees to implement them in fieldwork and university contexts.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
American Counseling Association. (2014). ACA code of ethics. https://www.counseling.org/resources/aca-code-of-ethics.pdf
American School Counselor Association. (2019a). The ASCA national model: A framework for school counseling programs (4th ed.).
American School Counselor Association. (2019b). ASCA standards for school counselor preparation programs. https://www.schoolcounselor.org/getmedia/573d7c2c-1622-4d25-a5ac-ac74d2e614ca/ASCA-Standards-for-School-Counselor-Preparation-Programs.pdf
American School Counselor Association. (2019c). ASCA school counselor professional standards & competencies. https://www.schoolcounselor.org/getmedia/a8d59c2c-51de-4ec3-a565-a3235f3b93c3/SC-Competencies.pdf
American School Counselor Association. (2021). The school counselor and school counselor supervision. https://www.schoolcounselor.org/Standards-Positions/Position-Statements/ASCA-Position-Statements/The-School-Counselor-and-School-Counselor-Supervis
American School Counselor Association. (2022). ASCA ethical standards for school counselors. https://www.schoolcounselor.org/getmedia/44f30280-ffe8-4b41-9ad8-f15909c3d164/EthicalStandards.pdf
Astramovich, R. L., & Harris, K. R. (2007). Promoting self-advocacy among minority students in school counseling. Journal of Counseling & Development, 85(3), 269–276. https://doi.org/10.1002/j.1556-6678.2007.tb00474.x
Baltrinic, E. R., Cook, R. M., & Fye, H. J. (2021). A Q methodology study of supervisee roles within a counseling practicum course. The Professional Counselor, 11(1), 1–15. https://doi.org/10.15241/erb.11.1.1
Bemak, F., & Chung, R. C.-Y. (2008). New professional roles and advocacy strategies for school counselors: A multicultural/social justice perspective to move beyond the Nice Counselor Syndrome. Journal of Counseling & Development, 86(3), 372–381. https://doi.org/10.1002/j.1556-6678.2008.tb00522.x
Bernard, J. M., & Goodyear, R. K. (2019). Fundamentals of clinical supervision (6th ed.). Pearson.
Biganeh, M., & Young, S. L. (2021). Followers’ perceptions of positive communication practices in leadership: What matters and surprisingly what does not. International Journal of Business Communication, 0(0).
https://doi.org/10.1177/2329488420987277
Bledsoe, K. G., Logan-McKibben, S., McKibben, W. B., & Cook, R. M. (2019). A content analysis of school counseling supervision. Professional School Counseling, 22(1), 1–8. https://doi.org/10.1177/2156759X19838454
Blount, A. J., Taylor, D. D., Lambie, G. W., & Anwell, A. N. (2016). Clinical supervisors’ perceptions of wellness: A phenomenological view on supervisee wellness. The Professional Counselor, 6(4), 360–374.
https://doi.org/10.15241/ab.6.4.360
Borders, L. D., & Brown, L. L. (2005). The new handbook of counseling supervision (1st ed.). Routledge.
Borders, L. D., Glosoff, H. L., Welfare, L. E., Hays, D. G., DeKruyf, L., Fernando, D. M., & Page, B. (2014). Best practices in clinical supervision: Evolution of a counseling specialty. The Clinical Supervisor, 33(1), 26–44. https://doi.org/10.1080/07325223.2014.905225
Bradley, L. J., Ladany, N., Hendricks, B., Whiting, P. P., & Rhode, K. M. (2010). Overview of counseling supervision. In N. Ladany & L. J. Bradley (Eds.), Counselor supervision (4th ed.). Routledge.
Bradley, N., Stargell, N., Craigen, L., Whisenhunt, J., Campbell, E., & Kress, V. (2019). Creative approaches for promoting vulnerability in supervision: A relational-cultural approach. Journal of Creativity in Mental Health, 14(3), 391–404. https://doi.org/10.1080/15401383.2018.1562395
Branco, S. F., & Patton-Scott, V. (2020). Practice what we teach: Promoting wellness in a clinical mental health counseling master’s program. Journal of Creativity in Mental Health, 15(3), 405–412.
https://doi.org/10.1080/15401383.2019.1696260
Brott, P. E., DeKruyf, L., Hyun, J. H., LaFever, C. R., Patterson-Mills, S., Cook Sandifer, M. I., & Stone, V. (2021). The critical need for peer clinical supervision among school counselors. Journal of School-Based Counseling Policy and Evaluation, 3(2), 51–60. https://doi.org/10.25774/nr5m-mq71
Cartwright, A. D., Carey, C. D., Chen, H., Hammonds, D., Reyes, A. G., & White, M. E. (2021). Multi-tiered intensive supervision: A culturally-informed method of clinical supervision. Teaching and Supervision in Counseling, 3(2), Article 8. https://doi.org/10.7290/tsc030208
Cook, R. M., & Sackett, C. R. (2018). Exploration of prelicensed counselors’ experiences prioritizing information for clinical supervision. Journal of Counseling & Development, 96(4), 449–460. https://doi.org/10.1002/jcad.12226
Council for Accreditation of Counseling and Related Educational Programs. (2015). 2016 CACREP standards. http://www.cacrep.org/wp-content/uploads/2017/08/2016-Standards-with-citations.pdf
Day-Vines, N. L., Bryan, J., & Griffin, D. (2013). The Broaching Attitudes and Behavior Survey (BABS): An exploratory assessment of its dimensionality. Journal of Multicultural Counseling and Development, 41(4), 210–223. https://doi.org/10.1002/j.2161-1912.2013.00037.x
Day-Vines, N. L., Wood, S. M., Grothaus, T., Craigen, L., Holman, A., Dotson-Blake, K., & Douglass, M. J. (2007). Broaching the subjects of race, ethnicity, and culture during the counseling process. Journal of Counseling & Development, 85(4), 401–409. https://doi.org/10.1002/j.1556-6678.2007.tb00608.x
Dollarhide, C. T., & Saginak, K. A. (2017). Comprehensive school counseling programs: K-12 delivery systems in action (3rd ed.). Pearson.
Dressel, J. L., Consoli, A. J., Kim, B. S. K., & Atkinson, D. R. (2007). Successful and unsuccessful multicultural supervisory behaviors: A Delphi poll. Journal of Multicultural Counseling and Development, 35(1), 51–64. https://doi.org/10.1002/j.2161-1912.2007.tb00049.x
Foster, V. A., & McAdams, C. R., III. (2009). A framework for creating a climate of transparency for professional performance assessment: Fostering student investment in gatekeeping. Counselor Education & Supervision, 48(4), 271–284. https://doi.org/10.1002/j.1556-6978.2009.tb00080.x
Giordano, A. L., Bevly, C. M., Tucker, S., & Prosek, E. A. (2018). Psychological safety and appreciation of differences in counselor training programs: Examining religion, spirituality, and political beliefs. Journal of Counseling & Development, 96(3), 278–288. https://doi.org/10.1002/jcad.12202
Glosoff, H. L., & Durham, J. C. (2010). Using supervision to prepare social justice counseling advocates. Counselor Education and Supervision, 50(2), 116–129. https://doi.org/10.1002/j.1556-6978.2010.tb00113.x
Halpern, H. (2009). Supervision and the Johari window: A framework for asking questions. Education for Primary Care, 20(1), 10–14. https://doi.org/10.1080/14739879.2009.11493757
Hamlet, H. S. (2022). School counseling practicum and internship: 30+ essential lessons (2nd ed.). Cognella Academic Publishing.
Heaven, C., Clegg, J., & Maguire, P. (2006). Transfer of communication skills training from workshop to workplace: The impact of clinical supervision. Patient Education and Counseling, 60(3), 313–325.
https://doi.org/10.1016/j.pec.2005.08.008
Herlihy, B. J., Gray, N., & McCollum, V. (2002). Legal and ethical issues in school counselor supervision. Professional School Counseling, 6(1), 55–60.
Jones, C. T., Welfare, L. E., Melchior, S., & Cash, R. M. (2019). Broaching as a strategy for intercultural understanding in clinical supervision. The Clinical Supervisor, 38(1), 1–16.
https://doi.org/10.1080/07325223.2018.1560384
Jordan, J. V. (2003). Valuing vulnerability: New definitions of courage. Women in Therapy, 31(2–4), 209–233. https://doi.org/10.1080/02703140802146399
Jordan, K. (2018). Trauma-informed counseling supervision: Something every counselor should know about. Asia Pacific Journal of Counseling and Psychotherapy, 9(2), 127–142. https://doi.org/10.1080/21507686.2018.1450274
King, K. M., & Jones, K. (2019). An autoethnography of broaching in supervision: Joining supervisee and supervisor perspectives on addressing identity, power, and difference. The Clinical Supervisor, 38(1), 17–37. https://doi.org/10.1080/07325223.2018.1525597
Ladany, N., Mori, Y., & Mehr, K. E. (2013). Effective and ineffective supervision. The Counseling Psychologist, 41(1), 28–47. https://doi.org/10.1177/0011000012442648
Lambie, G. W., & Sias, S. M. (2009). An integrative psychological developmental model of supervision for professional school counselors-in-training. Journal of Counseling & Development, 87(3), 349–356.
https://doi.org/10.1002/j.1556-6678.2009.tb00116.x
Luke, M., & Bernard, J. M. (2006). The School Counseling Supervision Model: An extension of the Discrimination Model. Counselor Education and Supervision, 45(4), 282–295. https://doi.org/10.1002/j.1556-6978.2006.tb00004.x
Marley, E. (2011). Self-help strategies to reduce emotional distress: What do people do and why? A qualitative study. Counselling and Psychotherapy Research, 11(4), 317–324. https://doi.org/10.1080/14733145.2010.533780
McKibben, W. B., George, A. L., Gonzalez, O., & Powell, P. W. (2022). Exploring how counselor education programs support site supervisors. Journal of Counselor Preparation and Supervision, 15(2). https://digital
commons.sacredheart.edu/jcps/vol15/iss2/1
Mecadon-Mann, M., & Tuttle, M. (2023). School counselor professional identity in relation to post-master’s supervision. Professional School Counseling, 27(1), 1–11. https://doi.org/10.1177/2156759X221143932
Mullen, P. R., Backer, A., Chae, N., & Li, H. (2020). School counselors’ work-related rumination as a predictor of burnout, turnover intentions, job satisfaction, and work engagement. Professional School Counseling, 24(1), 1–10. https://doi.org/10.1177/2156759X20957253
Murphy, M. J., & Wright, D. W. (2005). Supervisees’ perspectives of power use in supervision. Journal of Marital and Family Therapy, 31(3), 283–295. https://doi.org/10.1111/j.1752-0606.2005.tb01569.x
Murphy, S., & Kaffenberger, C. (2007). ASCA National Model: The foundation for supervision of practicum and internship students. Professional School Counseling, 10(3), 289–296.
https://doi.org/10.1177/2156759X0701000311
Nelson, J. R., Hall, B. S., Anderson, J. L., Birtles, C., & Hemming, L. (2018). Self-compassion as self-care: A simple and effective tool for counselor educators and counseling students. Journal of Creativity in Mental Health, 13(1), 121–133. https://doi.org/10.1080/15401383.2017.1328292
Neufeldt, S. A., Karno, M. P., & Nelson, M. L. (1996). A qualitative study of experts’ conceptualizations of supervisee reflectivity. Journal of Counseling Psychology, 43(1), 3–9. https://doi.org/10.1037/0022-0167.43.1.3
North, R. A. (2017). Motivational interviewing for school counselors. Independently Published.
Oehrtman, J. P., & Dollarhide, C. T. (2021). Advocacy without adversity: Developing an understanding of micropolitical theory to promote a comprehensive school counseling program. Professional School Counseling, 25(1), 1–9. https://doi.org/10.1177/2156759X211006623
Parikh, S. B., Janson, C., & Singleton, T. (2012). Video journaling as a method of reflective practice. Counselor Education and Supervision, 51(1), 33–49. https://doi.org/10.1002/j.1556-6978.2012.00003.x
Pearson, Q. M. (2004). Getting the most out of clinical supervision: Strategies for mental health. Journal of Mental Health Counseling, 26(4), 361–373. https://doi.org/10.17744/mehc.26.4.tttju8539ke8xuq6
Pocock, A., Lambros, S., Karvonen, M., Test, D. W., Algozzine, B., Wood, W., & Martin, J. E. (2002). Successful strategies for promoting self-advocacy among students with LD: The LEAD group. Intervention in School and Clinic, 37(4), 209–216. https://doi.org/10.1177/105345120203700403
Quintana, T. S., & Gooden-Alexis, S. (2020). Making supervision work. American School Counselor Association.
Ratts, M. J., & Greenleaf, A. T. (2018). Multicultural and social justice counseling competencies: A leadership framework for professional school counselors. Professional School Counseling, 21(1b), 1–9.
https://doi.org/10.1177/2156759X18773582
Skovholt, T. M., & Rønnestad, M. H. (1992). Themes in therapist and counselor development. Journal of Counseling & Development, 70(4), 505–515. https://doi.org/10.1002/j.1556-6676.1992.tb01646.x
Stark, M. D. (2017). Assessing counselor supervisee contribution. Measurement and Evaluation in Counseling and Development, 50(3), 170–182. https://doi.org/10.1080/07481756.2017.1308224
Stoltenberg, C. (1981). Approaching supervision from a developmental perspective: The counselor complexity model. Journal of Counseling Psychology, 28(1), 59–65. https://doi.org/10.1037/0022-0167.28.1.59
Storlie, C. A., Baltrinic, E., Fye, M. A., Wood, S. M., & Cox, J. (2019). Making room for leadership and advocacy in site supervision. Journal of Counselor Leadership and Advocacy, 6(1), 1–15.
https://doi.org/10.1080/2326716X.2019.1575778
Storlie, C. A., Giegerich, V., Stoner-Harris, T., & Byrd, J. (2018). Conceptual metaphors in internship: Creative journeys in counselor development. Journal of Creativity in Mental Health, 13(3), 331–343.
https://doi.org/10.1080/15401383.2018.1439790
Sutton, J. M., Jr., & Page, B. J. (1994). Post-degree clinical supervision of school counselors. The School Counselor, 42(1), 32–39. https://www.jstor.org/stable/23901709
Ward, C. C., & House, R. M. (1998). Counseling supervision: A reflective model. Counselor Education and Supervision, 38, 23–33. https://doi.org/10.1002/j.1556-6978.1998.tb00554.x
Watkins, C. E., Jr., Hook, J. N., Mosher, D. K., & Callahan, J. L. (2019). Humility in clinical supervision: Fundamental, foundational, and transformational. The Clinical Supervisor, 38(1), 58–78.
https://doi.org/10.1080/07325223.2018.1487355
Wiley, E. D., Phillips, J. C., & Palladino Schultheiss, D. E. (2021). Supervisors’ perceptions of their integration of strength-based and multicultural approaches to supervision. The Counseling Psychologist, 49(7), 1038–1069. https://doi.org/10.1177/00110000211024595
Wood, C., & Rayle, A. D. (2006). A model of school counseling supervision: The Goals, Functions, Roles, and Systems Model. Counselor Education and Supervision, 45(4), 253–266.
https://doi.org/10.1002/j.1556-6978.2006.tb00002.x
Woodbridge, L., & O’Beirne, B. R. (2017). Counseling students’ perceptions of journaling as a tool for developing reflective thinking. The Journal of Counselor Preparation and Supervision, 9(2), Article 12.
https://doi.org/10.7729/92.1198
Young, T. L., Lambie, G. W., Hutchinson, T., & Thurston-Dyer, J. (2011). The integration of reflectivity in developmental supervision: Implications for clinical supervisors. The Clinical Supervisor, 30(1), 1–18. https://doi.org/10.1080/07325223.2011.532019
Nancy Chae, PhD, NCC, NCSC, ACS, LCPC, is an assistant professor at the University of San Diego. Adrienne Backer, PhD, is an assistant professor at Texas A&M University–Corpus Christi. Patrick R. Mullen, PhD, NCC, NCSC, ACS, is an associate professor and department chair at Virginia Commonwealth University. Correspondence may be addressed to Nancy Chae, University of San Diego, Mother Rosalie Hill Hall, 5998 Alcalá Park, San Diego, CA 92110, nchae@sandiego.edu.
Aug 24, 2023 | Volume 13 - Issue 2
Chloe Lancaster, Michelle W. Brasfield
The COVID-19 pandemic led to an unparalleled disruption of student learning, disengaged students from school and peers, increased exposure to trauma, and had a negative impact on students’ mental health and well-being. School counselors are the most accessible mental health care professionals in a school, providing support for all students’ social and emotional needs and academic success. This study used an exploratory survey design to investigate the perspectives of 207 school counselors in Tennessee regarding students’ COVID-19–related mental health, academic functioning, and interpersonal skills; interventions school counselors have deployed to support students; and barriers they have encountered. Results indicate that students’ mental health has significantly declined across all grade levels and is interconnected with academic, social, and behavioral problems; school counselors have provided support consistent with crisis counseling; and caseload and non-counseling duties have created significant barriers in the provision of care.
Keywords: COVID-19, school counselors, student mental health, interventions, barriers
The psychological cost of the COVID-19 pandemic has been profound and wide-reaching. Although the K–12 population has been less susceptible to the adverse physical effects of COVID-19, for many, the pandemic has left an indelible mark on their mental health (Karaman et al., 2021). Before the outbreak of COVID-19 in 2020, youth mental health had become an issue of national concern, with one in six minors struggling with mental illness (Whitney & Peterson, 2019). Research has emerged to indicate that COVID-19 has further elevated the mental health problems of K–12 students across the nation (Ellis et al., 2020; Karaman et al., 2021; Magson et al., 2021). The end of COVID-19 lockdown restrictions may have alleviated immediate issues associated with social isolation and online learning; however, for those students experiencing COVID-19–related trauma and crisis, symptomatology has persisted beyond school reentry (Centers for Disease Control and Prevention [CDC], 2022; Patterson, 2022). As frontline helping professionals with training in mental health and school systems, school counselors are often the first responders to students in crisis (Karaman et al., 2021; Lambie et al., 2019), yet researchers have not explored reentry problems from the school counselor’s perspective. We conducted this study to understand school counselors’ experience of COVID-19–related student issues, their strategies to assist students, and their encountered barriers. We theorized that persistent problems related to the organizational structures within which counselors work, such as large caseloads, assignment of non-counseling duties, and under-resourced schools and communities (Lambie et al., 2019), may have greatly impacted their ability to meaningfully help students in high need of mental health support.
Literature Review
Students and COVID-19–Related Distress
From the outset of the COVID-19 pandemic, scholars predicted that disruptions to schooling, COVID-19–related stress, family conflict, and frequent media exposure to the pandemic would amplify mental health problems in children and youth (Imran et al., 2020). Empirical studies published in 2020 and 2021 have substantiated this concern, with findings indicating that COVID-19 restrictions adversely affected youth in multiple ways, including the development of unhealthy eating habits, increased screen time, reduced physical activity, sleep disturbances, academic delays, social problems, and an overall escalation in mental health concerns (Ellis et al., 2020; Karaman et al., 2021; Magson et al., 2021). The preponderance of research focused on adolescents, particularly as extended time in social isolation disrupted their developmental reliance on peer interactions for social and emotional support (Imran et al., 2020). Multiple studies found that not feeling connected to friends, high social media usage, and general COVID-19–related fears were associated with higher levels of depression and anxiety (Ellis et al., 2020; Karaman et al., 2021; Magson et al., 2021).
Although less is known about the impact of COVID-19 on younger children, evidence is emerging to indicate that the COVID-19 pandemic has elevated adverse childhood experiences (ACEs; Bryant et al., 2020). From a developmental perspective, children are less able to communicate and process their thoughts and feelings and are greatly affected by the emotional state of their caregivers (Zimmer-Gembeck & Skinner, 2011). Thus, exposure to parental anxieties related to housing, food, and economic insecurity likely exerted a destabilizing effect on children during the stay-at-home mandate and beyond (Imran et al., 2020). Further, children in poverty may be particularly vulnerable to an amplification of ACEs due to their families being disproportionately impacted by economic hardships and family mortality during the pandemic (Bryant et al., 2020).
Students’ Mental Health Pre-Pandemic
The COVID-19 pandemic increased intra-family adversity, which has long-term implications for the well-being of children and adolescents (CDC, 2022). However, in pre–COVID-19 times, with the rise in school shootings and teen suicide, the mental health of K–12 populations had already become a public health concern. According to the National Alliance on Mental Illness, one in six children aged 6–17 experienced a mental health disorder (Whitney & Peterson, 2019). Since reentry following COVID-19 shutdowns, indicators suggest the COVID-19 pandemic has worsened children’s mental health (CDC, 2022; Karaman et al., 2021), with widespread reports of student learning gaps, chronic absenteeism, declines in social skills, and increased behavior problems (CDC, 2022; Patterson, 2022). Further, previous research on children’s responses to a variety of traumatic events has found that children and adolescents can develop long-term mental illness following a traumatic experience, which is unlikely to abate without intervention (Udwin et al., 2000). For youth, the experience of mental health problems increases their risk factors in other areas, such as a decline in academic performance, poor decision-making, drug use, and high-risk sexual behaviors (CDC, 2022). In this regard, the responsiveness of schools to flex their organizational resources to address the psychological changes in their student body seems instrumental in assuaging the long-term effects of COVID-related trauma and the mitigation of adverse educational outcomes (Savitz-Romer et al., 2021).
School Counselors’ Role in Provision of Mental Health Services
Schools have long been discussed as a primary access point for mental health services, given that children spend much of their day in school, and children and adolescents in need of mental health care are more likely to receive assistance in a school as opposed to a clinical setting (Lambie et al., 2019). Conversations about students’ access to mental health care in school settings segue to the role of school counselors and students’ access to school counseling services. School counselors are the most accessible mental health care professionals in schools, with 80.7% of schools employing full-time or part-time school counselors (Lambie et al., 2019). By contrast, only 66.5% employ a school psychologist, and 41.5% employ a school social worker (National Center for Educational Statistics, 2016). Further, school counselors are trained in crisis prevention and responsive services, including individual and group counseling; consultation with administrators, teachers, parents, and professionals; and coordination of services within a multi-tiered system of supports (MTSS; Pincus et al., 2020).
Evidence to support school counselors’ work in times of crisis comes from multiple sources. Salloum and Overstreet (2008) found that a school counselor–led small group implemented after Hurricane Katrina improved PTSD symptoms among elementary school students. Similarly, Udwin and colleagues (2000) found that students who received psychological support at school following a national crisis experienced a reduction in PTSD symptomology. Additionally, scholars have proposed that school counselors utilize their skill set in assessment to administer universal mental health screenings to identify students at greater risk of having or developing mental health concerns (Lambie et al., 2019; Pincus et al., 2020).
Barriers School Counselors Face in the Provision of Services
Although school counselors have the training and skills necessary to assist students transitioning back to school from a disruption like COVID-19, they face multiple barriers to their work. Most notably, they struggle with unmanageable caseloads. The American School Counselor Association (ASCA) recommends that counselor-to-student ratios not exceed 1:250 (ASCA, 2019). Yet, the average ratio in the United States is 1:455, with Tennessee experiencing an average ratio of 1:450 (Patel & Clinedinst, 2021). Research indicates that large school counselor caseloads adversely affect student outcomes, insofar as attendance, graduation, and disciplinary problems are more prevalent in schools with high school counselor caseloads (Parzych et al., 2019). Unfortunately, minority students in under-resourced schools are disproportionately impacted by high counselor ratios (Whitney & Peterson, 2019) and are more likely to experience adverse educational outcomes, as well as unmet mental health needs (Kaffenberger & O’Rorke-Trigiani, 2013). These findings raise concern for students whose mental health and academics have declined since the emergence of COVID-19 who attend schools with overstretched counselors struggling to meet the needs of their student body. This study was conducted in part to explore if caseload correlates to school counselors’ perceived ability to attend to students’ COVID-related problems and if differences were more pronounced in schools with lower socioeconomic status (SES).
In addition to ratios, ASCA recommends that school counselors spend 80% of their time providing direct and indirect services to students. Program elements within direct service include curriculum delivery, individual student planning, and responsive services. Indirect services include referrals to other agencies and programs within and outside the school system and consultation and collaboration with stakeholders, particularly for crisis response (ASCA, 2019). Researchers have documented the favorable effects on student academics and behaviors when school counselors follow these national guidelines for time and role allocations (Cholewa et al., 2015). Nonetheless, school counselors are often assigned non-counseling duties by their campus and district administrators (Gysbers & Henderson, 2012), preventing them from fulfilling their appropriate roles. These duties include test coordination, record keeping, attendance monitoring, substitute teaching, and student discipline (ASCA, 2019). Data indicate that non-counseling duties may be more problematic at the secondary level, with high school counselors over-reporting non-counseling duties, when compared to elementary school counselors (Chandler et al., 2018). Geographic differences have also been documented, with rural school counselors reporting higher levels of non-counseling duties in comparison to urban school counselors (Chandler et al., 2018). In the current study, we were curious to understand the impact of non-counseling duties on school counselors’ response to students’ COVID-19 concerns and to explore the intersection of counselor responsiveness to COVID-19 by non-counseling duties, grade level, and geographic region (e.g., urban, suburban, rural), respectively.
School Responses to COVID-19 in Tennessee
In response to the COVID-19 pandemic, Tennessee’s governor ordered all Tennessee public schools closed from March 20 until March 31, 2020, and extended this closure through the end of the 2019–2020 school year. To complete the school year outside of the physical educational space, districts created their own plans to address student learning, often dependent on available technology and resources (Tennessee Office of the Governor, 2020). Districts made decisions for returning in the fall 2020 semester based on guidelines from the Tennessee Department of Education (DOE), which included social distancing, smaller class size, assigned seats, and alternating in-person days with distance learning (Tennessee DOE, 2020). To provide further context to our survey responses, in 2019, the state DOE (Tennessee State Board of Education, 2017) updated its school counseling policy and standards to require school counselors to spend 80% of their time in direct service to students, a specification consistent with the ASCA National Model for allocation of school counselor time. Although the policy stated counselor ratios should not exceed 1:500 in elementary and 1:350 in secondary schools, this specification falls short of the ASCA 1:250 recommendation. Further, because of the state funding formula that permits school districts to hire administrators in lieu of school counselors, depending on school needs, we expected many of the school counselors would have caseloads that exceeded DOE policy.
Purpose of Study
School counselors are uniquely positioned to assist students with their mental health, including COVID-19–related concerns, in a school context (Pincus et al., 2020). Yet, even before the COVID-19 pandemic, school counseling programs were frequently under-equipped to meet the magnitude of students’ mental health needs (DeKruyf et al., 2013). This study was conducted to understand, from the perspective of school counselors in Tennessee, the ongoing impact of COVID-19 upon students’ mental health, examine strategies they have deployed to assist students, and discover barriers encountered in providing care to meet their students’ needs. Because poor mental health manifests in a plethora of academic, behavior, and social skill adjustment issues for children and adolescents (CDC, 2022), we also examined school counselors’ perceptions of changes in those domains from pre-pandemic to current times. Given documented patterns of variability in school counselor programs, we also investigated school counselors’ perceived barriers to assisting students by location, SES, and assigned non-counseling duties. To address the aim of the study, we posited three related research questions (RQs):
| RQ1: |
How has COVID-19 affected students’ mental health, academics, and social skills in Tennessee? What issues presented the greatest concern, and how did interventions differ by grade level (elementary, middle, or high school)? |
| RQ2: |
What interventions do school counselors in Tennessee use to assist students with their COVID-19–related concerns, and how do interventions differ by grade level (elementary, middle, or high school)? |
| RQ3: |
What barriers do school counselors in Tennessee report as interfering with their ability to address students’ COVID-19 concerns? Do reported barriers differ by grade level (elementary, middle, or high), location (urban, suburban, or rural), socioeconomic status, non-counseling duties, size of caseload (small, medium, or large), or following the state guideline for spending 80% of the time in student services? |
Method
Study Design and Instrumentation
Given the absence of research examining school counselors’ perspectives of how the pandemic has affected student mental health, their response to students’ COVID-19 issues, and barriers encountered in their efforts, we employed an exploratory research design. Exploratory designs are used when there is limited prior research to warrant the examination of a directional hypothesis (Swedberg, 2020). Within the framework of an exploratory design, we developed a non-standardized instrument to answer the three research questions. Although this constitutes a limitation of the study, we endeavored to address validity concerns by following the principles of the tailored design method of survey research (Dillman, 2007). Prior to constructing the survey, we reviewed the extant literature on students’ COVID-19–related issues, school counselors’ roles, and professional issues, in addition to conducting a focus group (N = 7) with school counselors and school counseling supervisors from across the state in which the study was conducted to explore their perceptions in changes to student functioning, strategies they have deployed to assist students, and obstacles they have encountered. Focus group data were used to inform the development of survey items and ensure the instrument covered relevant content. For example, the focus group provided expert insight into the non-counseling duties that are frequently assigned to counselors in the state, as well as the nature of students’ psychological, academic, and behavioral problems witnessed since the onset of COVID-19. Before launching the survey, we piloted the survey with 19 school counselors in Tennessee to elicit feedback about the flow and coverage of the survey. Based on their responses, we added an item addressing universal intervention and edited language on multiple items to align with state-specific terminology (e.g., “MTSS coordination” was expanded to “RTI2B/MTSS/PBIS coordinator” to reflect more state-recognized school counselor titles when operating in these capacities).
The final survey consisted of 64 items in predominantly binary, checkbox, and Likert scale formats. Demographic items were informed by categories outlined by the U.S. Census, the Tennessee DOE, and inclusive practices for data collection (Fernandez et al., 2016). Twenty-one items gathered demographic data related to school counselor characteristics (e.g., age, race, gender), counseling program variables (e.g., caseload, division of time, non-counseling duties, fair-share responsibilities), and school variables (e.g., school level, Title I status, location, staffing patterns). SES was measured using a school’s designated Title I status, with response categories of “yes,” “no,” and “unsure.” Likewise, to determine if school counselors dedicated 80% of their time to direct service, we created a multiple-choice item with the options of “yes,” “no,” and “unsure.” A concise description of the state guidelines was embedded into the survey to promote accurate responses to this item. We gathered data on counselors’ perspectives of their students’ current functioning in areas of mental health, academics, social skills, and behaviors through multiple-choice items with a 5-point range of “much better” to “much worse.” For each area of functioning, school counselors were required to indicate the areas of concern via a checkbox item. Additionally, checkbox items were used to identify school counselors’ strategies to assist students, barriers encountered, and needed resources. As noted, these response categories were based on extant literature and expert input.
Cronbach’s alphas were computed to determine the reliability of the survey items in indicating overall post–COVID-19 functioning of students according to school counselors. These values indicate that these four areas were moderately related with acceptable consistency (α = .653). When making additional comparisons among the four constructs, two areas—behavior and social skills—were found to be more consistent (α = .705; Sheperis et al., 2020). Further, reliability scores likely reflect the exploratory design, which requested participants respond to conceptually related but not converging constructs (e.g., academics, mental health, social skills, and behavior). For example, a change in student academics would not necessarily signify a change in student mental health and vice versa. Thus, participant responses would not necessarily be uniform across items measuring students’ mental health, academics, and social skills, and overall instrument consistency would not be affected in turn.
Participants
We recruited a state-level sample of professional school counselors employed in K–12 public schools in Tennessee. Following the pilot study, in December 2021, we recruited participants through an anonymous Qualtrics link utilizing multiple platforms: the state school counselor association’s listserv, social media, respondent referrals, and dissemination via school counseling supervisors. Participants were eligible to complete the survey if they were currently employed in a K–12 public school in Tennessee. Upon examination of our survey data, we found 276 total responses with 220 complete for a completion rate of 79.7%. Because the survey was distributed through the above-mentioned methods, we were unable to calculate the response rate without knowing how many of the approximately 2,000 public school counselors in Tennessee received the survey. Upon further examination of the survey respondents, we removed one school counseling supervisor; four school counselors whose students were remote/hybrid; and eight school counselors in private, charter, or alternative schools to maintain focus on the experiences of traditional public school counselors working with students in person during the ongoing COVID-19 pandemic for a final sample of 207 participants. An examination of the respondents’ demographics revealed a sample that was predominantly female and White/Caucasian and worked in Title I, suburban, or rural elementary schools. The sample’s mean years serving as a school counselor was 11.7 (SD = 7.5), with mean years at current school of 6.8 (SD = 6.4). See Table 1 for more demographic information. For analysis purposes, we divided the school counselors into three groups by the size of their reported caseload. These categories were informed by a national study of school counselor ratios (National Association of College Admission Counselors, 2019) and consisted of ratios in the range of small (1:100–1:300; 14.0%, n = 29), medium (1:301–1:550; 69.6%, n = 144), and large (1:551 and higher; 15.0%, n = 31).
Table 1
Demographic Characteristics of the Sample
| Characteristic |
n |
% |
| Age |
|
|
| 18–24 years |
3 |
1.4 |
| 25–44 years |
99 |
47.8 |
| 45–64 years |
102 |
49.3 |
| 65 years plus |
3 |
1.4 |
| Race/Ethnicity |
|
|
| Black/African American |
17 |
8.2 |
| Latinx/Hispanic |
1 |
0.5 |
| White/Caucasian |
183 |
88.4 |
| American Indian/Alaskan Native |
1 |
0.5 |
| Other |
5 |
2.4 |
| Gender |
|
|
| Female |
192 |
92.8 |
| Male |
15 |
7.2 |
Note. N = 207.
Data Analysis
We ran a post hoc power analysis using the G*Power 3.1.9.7 statistical software to determine if our sample size was sufficient at the .80 power level with α = .05 and found that a minimum sample size of 100 was required for our analyses. Given our sample size of 207 participants, the power analysis indicated that our sample size was sufficient (Faul et al., 2007). We utilized SPSS version 26 to calculate the following analyses for this study: (a) descriptive statistics; (b) Fisher’s exact test for two dichotomous nominal variables; (c) an extension of Fisher’s exact test, the Freeman-Halton exact test, for one dichotomous nominal variable and one nominal variable with three levels; and (d) point-biserial correlation analysis for one nominal variable and one interval variable (Frey, 2018). We also examined effect size to determine practical importance using the following levels for examining nominal data (Rea & Parker, 1992), precedence for which has been established by complementary studies in educational research (K. Erickson & Quick, 2017; Kotrlik et al., 2011): negligible [0, .1), weak [.1, .2), moderate [.2, .4), relatively strong [.4, .6), strong [.6, .8), and very strong [.8, 1.0). Phi (ϕ) indicates the effect size for the exact tests, and the correlation is the effect size for the point-biserial correlation. We only included statistical analyses that resulted in moderate associations or higher. Three school counselors (1.4%) who reported caseloads that were unusually small (< 100) and outside our specified caseload parameters were removed from the analysis. Additionally, we excluded school counselors who indicated “unsure” in the categories of location (rural, suburban, urban), Title I status, and adherence to state policy for direct service to students. See Table 2 for school characteristics.
Results
Research Question 1
RQ1 examined school counselors’ perspectives of the impact of COVID-19 on students’ mental health, academics, and social skills as well as variation by grade level (elementary, middle, or high school). When asked about the mental health changes they have witnessed in their students post–COVID-19 pandemic, 93.7% (n = 194) of school counselors reported negative changes with 42.5% (n = 88) reporting “much worse” and 51.2% (n = 106) reporting “somewhat worse” changes. Specifically, school counselors reported issues regarding anxiety (92.8%, n = 192), depression (77.3%, n = 160), family dysfunction (71.0%, n = 147), COVID-19–related grief and loss (63.8%, n = 132), technology addiction (52.7%, n = 109), suicidality (50.7%, n = 105), fear of COVID-19 (49.8%, n = 103), substance use issues (21.7%, n = 45), and other issues (12.6%, n = 26) such as separation anxiety, self-harm, and anger. The Freeman-Halton exact test revealed a significant relationship between grade level (n = 183) and depression (p < .001, ϕ = .301) with a moderate positive association, suicidality (p < .001, ϕ = .499) with a relatively strong positive association, and substance use (p < .001, ϕ = .583) with a relatively strong positive association. For depression, 90.0% (n = 54) of high school counselors and 85.7% (n = 36) of middle school counselors reported this issue as compared to 63.0% (n = 51) of elementary school counselors. For suicidality, 76.2% (n = 32) of middle school counselors and 71.7% (n = 43) of high school counselors reported this concern as compared to 23.5% (n = 19) of elementary school counselors. For substance use, 58.3% (n = 35) of high school counselors and 20.0% (n = 8) of middle school counselors reported this concern as compared to 1.2% (n = 1) of elementary school counselors. All other mental health concerns were not significant with grade level.
When queried regarding academic changes post–COVID-19, 90.3% (n = 187) of school counselors reported negative changes to students’ academics with 35.3% (n = 73) reporting “much worse” and 55.1% (n = 114) reporting “somewhat worse” changes. School counselors reported an overall decline across all subjects (80.7%, n = 167). Additionally, school counselors reported non-cognitive factors regarding lack of motivation (84.1%, n = 174), lack of parental support during the school day (75.4%, n = 156), attention issues (71.0%, n = 147), poor mental health (64.7%, n = 134), sleep deprivation (41.1%, n = 85), limited technology during virtual learning (33.3%, n = 69), lack of space to work at home during virtual learning (30.4%, n = 63), poor physical health (17.9%, n = 37), and other (3.9%, n = 8). The Freeman-Halton exact test revealed a significant relationship between grade level (n = 183) and lack of motivation (p = .001, ϕ = .265), poor mental health (p = .001, ϕ = .269), and attention issues (p = .009, ϕ = .232), all with positive moderate associations. For lack of motivation, 96.7% (n = 58) of high school counselors and 88.1% (n = 37) of middle school counselors reported this issue as compared to 75.3% (n = 61) of elementary school counselors. For poor mental health, 78.3% (n = 47) of high school counselors and 69.0% (n = 29) of middle school counselors reported this outcome as compared with 49.4% (n = 40) of elementary school counselors. For attention issues, 79.0% (n = 64) of elementary school counselors and 73.8% (n = 31) of middle school counselors reported concerns as compared to 55.0% (n =33) of high school counselors.
Table 2
School/Program Characteristics
| Characteristic |
n |
% |
| Location |
|
|
| Urban |
31 |
15.0 |
| Suburban |
95 |
45.9 |
| Rural |
72 |
34.8 |
| Unsure |
9 |
4.3 |
| Title I Status |
|
|
| Yes |
121 |
58.5 |
| No |
57 |
27.5 |
| Unsure |
29 |
14.0 |
| Grade Level |
|
|
| Elementary |
81 |
39.1 |
| Middle |
42 |
20.3 |
| High |
60 |
29.0 |
| Other |
24 |
11.6 |
| Follows 80% Direct Service Guideline |
|
|
| Yes |
112 |
54.1 |
| No |
65 |
31.4 |
| Unsure |
30 |
14.5 |
| School Counselor-to-Student Ratio (caseload) |
|
|
| 1:1–1:300 |
29 |
14.0 |
| 1:301–1:550 |
144 |
69.6 |
| 1:551 and higher |
31 |
15.0 |
| Other |
3 |
1.4 |
Note. N = 207
When asked about behavioral changes, 87.4% (n = 181) of school counselors reported negative changes to behaviors with 30.4% (n = 63) reporting “much worse” and 57.0% (n = 118) reporting “moderately worse” changes. Comparably, when asked about social skills changes, 87.0% (n = 180) of school counselors reported negative changes to students’ social skills with 36.2% (n = 75) reporting “much worse” and 50.7% (n = 105) reporting “moderately worse” changes. Specifically, school counselors reported trouble socializing with peers (84.1%, n = 174), absence of social flexibility (58.0 %, n = 120), increase of physical aggression (55.1%, n = 114), increase in relational aggression (50.7%, n = 105), increase in cyberbullying (23.7%, n = 49), increase in bullying (19.3%, n = 40), and other (8.2%, n = 17) such as issues with conflict resolution and preference for technology. The Freeman-Halton exact test revealed a significant relationship between grade level (n = 183) and cyberbullying (p = .003, ϕ = .255), with a moderate positive association with 42.9% (n = 18) of middle school counselors, 23.3% (n = 14) of high school counselors, and 14.8% (n = 12) of elementary school counselors reporting an increase in this area. All other social skills changes were not significant with grade level.
Research Question 2
RQ2 examined the interventions that school counselors used in assisting students with their COVID-19–related concerns and if this differed by grade level. School counselors reported the various supports that they provided to their students who struggled with COVID-19–related issues, including individual counseling (95.7%, n = 198), consultation with parents/teachers (85.5%, n = 177), referrals (80.7%, n = 167), collaboration with other school-based helpers (77.3%, n = 160), coping skills instruction (71.5%, n = 148), group counseling (44.0%, n = 91), universal health screenings (17.9%, n = 37), and other interventions (4.3%, n = 9) such as food programs, holiday donation programs, peer support, and academic support meetings. We used the Freeman-Halton exact test to examine the relationship between grade level (n = 183) and these supports and found that small group counseling (p < .001, ϕ = .405) and coping skills instruction (p = .028, ϕ = .200) were significant, both with moderate positive association. For small group counseling, 63.0% (n = 51) of elementary school counselors and 45.2% (n = 19) of middle school counselors provided this support as compared to 16.7% (n = 10) of high school counselors. For coping skills instruction, 77.8% (n = 63) of elementary school counselors and 71.4% (n = 30) of middle school counselors reported this intervention as compared to 56.7% (n = 34) of high school counselors.
Research Question 3
RQ3 examined the barriers school counselors encountered in their ability to provide services and if this differed by grade level, SES, location, number of non-counseling duties, caseload size, and following the state guideline to spend 80% of time providing student services. When asked if they had encountered barriers to assisting their students with their COVID-19–related needs, 54.6% (n = 113) of school counselors reported that they had experienced barriers, and 45.4% (n = 94) reported that they had not. For those counselors who answered “yes,” barriers included: high caseload (44.4%, n = 92), number of non-counseling duties (20.3%, n = 42), lack of administrator support (12.1%, n = 25), being included on master schedule for guidance classes (10.1%, n = 21), lack of training to address COVID-19 needs (8.2%, n = 17), too much time coordinating the MTSS program (7.7%, n = 16), and other reasons (9.7%, n = 20). Examples of other reasons include students’ attendance, lack of resources (both space and personnel), and focus on academics over mental health. Of note, 47.3% (n = 98) of school counselors reported an increase in non-counseling duties since COVID-19, ranging from a substantial to a slight increase.
We used the Freeman-Halton exact test to examine the aforementioned barriers by grade level (n = 183) and found that being on the master schedule (p < .001, ϕ = .297) was significant with moderate positive association with 19.8% (n = 16) of elementary school counselors reporting this task as compared to 2.4 % (n = 1) of middle school counselors and 1.7% (n = 1) of high school counselors. We used point-biserial correlation analysis to examine how the number of new post–COVID-19 non-counseling duties related to the perceived barriers to providing services to students and found this to be significant (rpb = .211, p = .002) with a positive moderate association. School counselors who reported barriers to providing services had been allocated more non-counseling duties since the pandemic (n = 113, M = 1.22, SD = 1.49) than those who did not report barriers (n = 94, M = .66, SD = 1.04). We used a Freeman-Halton exact test to examine the specific barriers by caseload (n = 204) and found school counselors with a high caseload reported significantly more difficulty in addressing students’ COVID-19–related needs (p < .001, ϕ = .284), with a moderate positive association for large (58.1%, n =18) and medium (47.2%, n = 68) caseloads, as compared to those with a small (10.4%, n = 3) caseload. Investigating the state DOE guideline for 80% of time in service to students (n = 177), excluding those who were unsure, revealed that 63.3% (n = 112) followed the guideline and 36.7% did not (n = 65). We used a Fisher’s exact test to examine the relationship between following the 80% guideline and specific barriers and found that reporting too many non-counseling duties (p < .001, ϕ = -.358) was significant, with a moderate negative association for those who did not follow the guideline (41.5%, n = 27) in comparison to those who did follow the 80% guideline (10.7%, n = 12). All other barriers were not significant with grade level, SES, location, number of non-counseling duties, caseload size, and following the 80% state guideline. We used a Fisher’s exact test to examine SES by Title I (n = 178) classification and found that it was not significant with any of the barriers.
Discussion
Our results render a disturbing picture of students’ post–COVID-19 mental health functioning and school counselors’ perceived ability to effectively meet their students’ needs since a return to in-person learning, as reported by this sample of 207 school counselors in Tennessee. For RQ1, over 93% of our respondents indicated that their students’ mental health had worsened, with anxiety and depression identified as the most pronounced psychological concern, followed by family dysfunction, grief, technology addiction, and suicidality. These results confirm our predictions that the COVID-19 pandemic would exert a harmful impact on the mental health of children and adolescents (Bryant et al., 2020; Cénat & Dalexis, 2020). Depression and suicidality were significant concerns for middle and high school counselors, and substance abuse was significant at the high school level. The reported spike in diagnosable mental health problems by secondary school counselors aligns with research indicating that half of all mental health and substance use disorders begin at 14 (Quinn et al., 2016). The CDC recently reported that depression, substance abuse, and suicide have increased among adult populations since COVID-19, with young adults presenting the most significant risk (Czeisler et al., 2020). Our results provide preliminary evidence indicating that COVID-19–related trends have similarly impacted adolescents. Further, given the relationship between ACEs and substance misuse (CDC, 2022; Quinn et al., 2016), it may be reasonable to conjecture that an increase in family dysfunction, grief, fear of COVID-19, and severance of social relationships underscored a rise in substance use problems, particularly among high school students.
In addition to mental health, student academics notably declined according to school counselors in Tennessee, with 90.3% of participants reporting negative changes to students’ academics. Previous research attributed students’ COVID-19 pandemic–related academic issues to the vagaries of online instruction, a lack of parental supervision, inadequate technology, and limited workspace, among other factors (Ellis et al., 2020; Karaman et al., 2021; Magson et al., 2021). Our results aligned with these findings by explicitly connecting delays in students’ academic progress to psychological factors. Of note, we found a significant relationship between grade level, lack of motivation, poor mental health, and attention issues, with middle and high school counselors reporting greater concerns in the areas of motivation and mental health, and elementary and middle school counselors identifying attention problems as the greatest concern. The developmental onset of mental health disorders (Lambie et al., 2019) likely accounts for increased student mental health problems reported by middle and high school counselors. However, motivation and attentional issues across the grades were problematic, and because both are symptomatic of depression and anxiety, they raise a red flag for the mental health of all K–12 students in Tennessee.
Alongside academics, 87.0% of school counselors reported negative changes in students’ social skills and 87.4% reported worsened behaviors among students, with trouble socializing with peers, absence of social flexibility, and an increase in physical and relational aggression being the most pronounced problems. Declines in students’ ability to get along with peers may be uniquely linked to social isolation during lockdown (Ellis et al., 2020; Karaman et al., 2021); however, of great concern is the increase in all forms of bullying, with cyberbullying being particularly problematic in middle school. Youth aggression is a long-term consequence of ACEs and has implications for overall school safety, with victimization and perpetration both positively associated with school violence (Forster et al., 2020).
RQ2 investigated what interventions school counselors used to assist students with their COVID-19–related concerns and examined interventions by grade level. The preponderance of school counselors relied on individual counseling (95.7%), consultation (85.5%), referrals (80.7%), collaboration with other school-based helpers (77.3%), and coping skills instruction (71.5%), all of which are consistent with crisis-level supports. Nonetheless, only 44% of the sample, primarily elementary school counselors, had used small group counseling, despite its proven efficacy with children exposed to trauma (Salloum & Overstreet, 2008). The underutilization of group work at the high school level presents a concern, given that group work provides context for peer support and social learning, both considered critical therapeutic factors for adolescents (Gysbers & Henderson, 2012). Nonetheless, this finding resonates with previous results that high school counselors are more apt to assume administrative roles in place of the provision of direct student services (Chandler et al., 2018). Universal assessment has been proffered as an efficient and empirically grounded method for the early identification of at-risk students in need of COVID-19–related interventions (A. Erickson & Abel, 2013; Karaman et al., 2021; Pincus et al., 2020). Unfortunately, only 17.9% of the sample reported administering universal mental health screeners, a finding aligned with other studies that indicate schools have resisted adopting mental health screeners because of inadequate resources and related concerns about following up with students identified as being at risk (Burns & Rapee, 2022).
For RQ3, we explored the school counselors’ perspectives of the barriers they have encountered in assisting their students with their COVID-19 concerns. The proliferation of barriers reported by school counselors (high caseload, non-counseling duties, lack of administrator support, being on the master schedule for guidance classes, and a lack of training) verifies our concern that school counselors in Tennessee did not receive the support instrumental to their ability to provide effective student services at this critical time. Our state-level findings resonate with studies conducted in other states that indicate school counselors’ non-counseling duties increased during the pandemic while administrator support declined (Savitz-Romer et al., 2021). Other studies have also drawn attention to widespread staffing shortages associated with COVID-related absences and a reduced pool of substitute teachers (Patterson, 2022). Although we did not examine staff resources explicitly, with almost 50% of our Tennessee sample witnessing an increase in their non-counseling duties, it would be reasonable to infer that campus administrators are deploying school counselors to triage critical gaps in staffing patterns. Interestingly, despite a widespread increase in non-counseling duties post–COVID-19, only 20.3% of counselors reported non-counseling duties as a barrier to providing care. The discrepancy between these two results may be indicative of the phenomenon of role diffusion in school counseling, a problem that emerges when school counselors begin to integrate non-counseling duties as part of their accepted role and thus do not perceive them as antithetical to their professional identity (Astramovich et al., 2013). Furthermore, neither SES (Title I) nor location (rural, suburban, urban) were significant with barriers, and although this could reflect our relatively small sample, it could also be indicative of staff shortages adversely affecting the role of school counselors across all settings, regardless of the school’s demographic status.
The most notable barrier reported by respondents was a large caseload. School counselors with large and medium-sized caseloads reported more barriers and were less likely to follow the 80% guideline. Thus, those students who were negatively impacted by large counselor caseloads before COVID-19 faced further obstacles in accessing their school counseling services despite an overall increase in their mental health and academic needs. Further, elementary school counselors listed on the master schedule for guidance classes faced additional barriers to addressing their students’ needs outside of their prevention-focused (Tier 1) activities. Classroom guidance is considered helpful in elementary school for building social skills and study habits; however, when counselors are placed on the master schedule, it can impact their ability to provide responsive student services (Gysbers & Henderson, 2012) which seemed to be the case with our respondents.
Implications for Professional Advocacy
The results of this study illustrate a decline in student functioning, pronounced in the area of mental health, and have implications for school counselor advocacy in the areas of policy and practice. Advocating for policy change takes time and is beyond the individual efforts of school counselors, who are often beholden to their principal’s limited understanding of school counselors’ appropriate role and function (Lancaster & Reiner, 2022) and subsumed by untenable caseloads in under-resourced schools (Lambie et al., 2019). We, therefore, assert that advocacy is the professional imperative for all vested school counseling professionals (state counseling associations, school counselor educators, school counseling supervisors, and school counselors), all of whom could be working in tandem to advance the profession.
At the policy level, state and national counseling associations should reconsider the important role school counselors play in supporting students’ mental well-being and re-examine policies that delineate the appropriate use of school counselors’ time. Currently, the state school counseling model (Tennessee Policy 5.103) mirrors the national model (ASCA, 2019), perennially focusing on school counselors’ role in supporting student academics and delimiting their counseling role to prevention services, crisis counseling, and referrals to other mental health professionals. For state and national counseling associations, positioning school counselors as primarily focused on student academics demonstrated their value during the No Child Left Behind Act (NCLB; 2001) era, which prioritized unidimensional outcome measures of student success, particularly in math and reading (Savitz-Romer, 2019). However, the Every Student Succeeds Act (ESSA) replaced NCLB in 2015 and emphasizes more holistic aspects of student development and school climate. Many scholars argue that the ESSA (2015) combined with the rise in mental health issues has created a policy window for school counselors, led by their state and national professional associations (Savitz-Romer, 2019), to focus on the non-cognitive aspects that undergird healthy student development and to reclaim mental health as a domain central to school counselor practice (Lambie et al., 2019).
Redefining school counselors’ role in terms of mental health would require them to receive more clinical supervision (Lambie et al., 2019). In comparison to counselors in clinical settings, school counselors receive little to no supervision for their clinical efforts, which affects their clinical identity and weakens their counseling skills over time (Lancaster & Reiner, 2022). To address this gap, symbiotic partnerships could be formed with counselor education programs, particularly those that offer doctoral degrees in counselor education and supervision, to provide clinical supervision to local school counselors. Progress in this area may be forthcoming in the state, as institutions of higher education that operate school counseling, school psychology, and school social work programs have been invited to apply for grants funded through COVID-19 relief funding to support student internships in high-need schools. In addition, funds are available to support clinical supervision experiences that extend beyond students’ graduate training programs (Tennessee DOE, 2023).
MTSS programs also offer a promising prevention and intervention framework for meeting students’ comprehensive needs, including mental health, and align to both state and national school counseling models (Goodman-Scott et al., 2019). Further, the Tennessee DOE (2018) has developed a resource guide based on a tiered model for supporting students’ differential mental health needs, which school counselors could efficiently implement within their existing MTSS programs. Of note, within the Tennessee model, Tier 1 mental health practices build a foundation for mental wellness for all students. Advanced supports at Tiers 2 and 3 provide students who are at risk because of behavioral and/or mental health concerns with access to small groups and mental health interventions. One dimension of the state’s tiered mental health model is universal screening to identify students with internalizing behavioral disorders. Although few counselors in this study utilized universal screening, we recommend school counselors and their supervisors leverage the preexisting Tennessee DOE guidelines to petition their districts to adopt universal mental health screening.
Although the state mandated reduced counselor ratios in 2017 (Policy 5.103.), the funding formula allowed for uneven adoption of this policy (Tennessee Comptroller of the Treasury, n.d.), and target ratios fell short of national recommendations (ASCA, 2019). Thus, a function of this research was to utilize results in policy contexts to advocate for ratio realignments. In partnership with the state school counselor association, we produced a one-page results summary, written in simple language, to disseminate to state politicians to illuminate the acuity of mental health issues faced by K–12 students and proposed a solution through increased school counselor access. An advocacy effort led by the state association resulted in proposed legislation TN HB0364/SB0348, which would require one licensed full-time professional school counselor position for every 250 students and is currently advancing through the state Senate and House committees. A significant takeaway from this study is the importance and potency of coordinated partnerships between researchers, state counseling associations, and school counselors—an alliance that could be replicated in other states by school counselor stakeholders to advocate for the profession.
Limitations
The generalizability of these findings is limited because of the use of a state-level sample and a non-standardized, self-report survey. First, self-report surveys are sensitive to respondents’ tendency to rate themselves more favorably. Thus, it would be reasonable to conjecture that school counselors overestimated their adherence to the state guideline to spend 80% of their time in service to students and underreported their non-counseling duties. Second, although the items were informed by previous research on the psychological issues faced by children and adolescents during COVID-19 (Ellis et al., 2020; Karaman et al., 2021; Magson et al., 2021) and those factors that affect school counselors’ ability to provide direct services (Kaffenberger & O’Rorke-Trigiani, 2013; Parzych et al., 2019; Whitney & Peterson, 2019), the use of an ad hoc survey precluded us from performing more robust analyses (e.g., regression analysis). Third, because we only gathered data on students’ mental health issues and academic functioning post–COVID-19 pandemic, we have no benchmark data of students’ pre–COVID-19 functioning with which to make objective comparisons.
Fourth, although the sample was large enough to find some significant results, it was a small percentage of the state’s total population of public school counselors, which is estimated to be over 2,000. A larger sample would have increased the generalizability of findings and impacted the significance levels and practical importance of the results. Fifth, our sample lacks racial and gender diversity; however, it does align with the state’s overall population of educators (Tennessee DOE, 2021). Finally, regarding data analysis, interpreting correlations on a small population sample needs to be performed cautiously because of the possibility of sampling error. Additionally, point-biserial correlation can be impacted by the dichotomous nature of one of the variables, which constrains the variability of the results (Hinkle et al., 2002). Nonetheless, correlational analyses of ordinal and nominal variables in small-scale research are consistent with our exploratory design, and the results provide evidence that the variables examined share some type of relationship and provide direction for future research.
Future Research
Given that we conducted this study in the aftermath of the COVID-19 pandemic and have utilized data and policy to advocate for expanded student access to school counseling services in Tennessee, this study design could be replicated by future researchers in the event that another pandemic or crisis of similar scale affects K–12 populations. Nonetheless, our exploratory design is an inherent limitation with the preponderance of our findings based on correlational analysis of largely non-parametric data. Future studies could explore dimensions of students’ mental health utilizing student data from empirical inventories. Rather than relying on school counselor perception data, researchers could use results from universal screenings, such as the Behavior Assessment System for Children-3rd edition (BASC-3), to better understand the nature of student issues and examine differential risk by demographic factors (e.g., age, gender, ethnicity), which could be used to inform evidence-based interventions with at-risk and high-risk populations. Further, researchers could employ quasi-experimental designs to assess outcomes of school counselor-led interventions, such as small groups, with students who have scored as being at risk based on universal screening. Studies of this nature can help build a case for the efficacy of school counselors and, in turn, protect them from role misallocation. Qualitative research could also be conducted in those schools in which school counselors implement a universal screening, intervention, and referral system to glean an implementation blueprint practical to other school counselors within and outside the state.
Conclusion
With elevated rates of depression, anxiety, substance use, and bullying, it is reasonable to conjecture that students in Tennessee have experienced COVID-19–related trauma, which according to research is unlikely to abate without intervention (CDC, 2022; Savitz-Romer et al., 2021). Although our state-level respondents indicated that they provided services consistent with crisis counseling (e.g., individual counseling, group counseling, consultation, and referrals), almost 50% of the counselors had been burdened with additional non-counseling duties, which could reduce their capacity to work with students at different levels of risk. Large caseload was a significant barrier, leaving counselors struggling to provide an appropriate level of care. This finding raises considerable concern about the risk faced by students who have experienced deterioration in their mental health and academics since the onset of COVID-19, yet attend schools in Tennessee with elevated school counselor-to-student caseloads. Nationally and at the state level, school counselors are the most prevalent mental health professionals in schools and are trained in crisis response (National Center for Education Statistics, 2016). Unfortunately, Tennessee school counselors appear to be facing barriers in the provision of student services related to high caseload and non-counseling duties, which presents cause for professional advocacy within the state and beyond.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
American School Counselor Association. (2019). ASCA national model: A framework for school counseling programs (4th ed.).
Astramovich, R. L., Hoskins, W. J., Gutierrez, A. P., & Bartlett, K. A. (2013). Identifying role diffusion in school counseling. The Professional Counselor, 3(3), 175–184. https://doi.org/10.15241/rla.3.3.175
Bryant, D. J., Oo, M., & Damian, A. J. (2020). The rise of adverse childhood experiences during the COVID-19 pandemic. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S193–S194.
https://doi.org/10.1037/tra0000711
Burns, J. R., & Rapee, R. M. (2022). Barriers to universal mental health screening in schools: The perspective of school psychologists. Journal of Applied School Psychology, 38(3), 1–18.
https://doi.org/10.1080/15377903.2021.1941470
Cénat, J. M., & Dalexis, R. D. (2020). The complex trauma spectrum during the COVID-19 pandemic: A threat for children and adolescents’ physical and mental health. Psychiatry Research, 293, 113473.
https://doi.org/10.1016/j.psychres.2020.113473
Centers for Disease Control and Prevention. (2022, March 31). New CDC data illuminate youth mental health threats during the COVID-19 pandemic [Press release]. https://tinyurl.com/yckv6v9d
Chandler, J. W., Burnham, J. J., Riechel, M. E. K., Dahir, C. A., Stone, C. B., Oliver, D. F., Davis, A. P., & Bledsoe, K. G. (2018). Assessing the counseling and non-counseling roles of school counselors. Journal of School Counseling, 16(7), 1–33. https://files.eric.ed.gov/fulltext/EJ1182095.pdf
Cholewa, B., Burkhardt, C. K., & Hull, M. F. (2015). Are school counselors impacting underrepresented students’ thinking about postsecondary education? A nationally representative study. Professional School Counseling, 19(1), 144–154. https://doi.org/10.5330/1096-2409-19.1.144
Czeisler, M. É., Lane, R. I., Petrosky, E., Wiley, J. F., Christensen, A., Njai, R., Weaver, M. D., Robbins, R., Facer-Childs, E. R., Barger, L. K., Czeisler, C. A., Howard, M. E., & Rajaratnam, S. M. W. (2020). Mental health, substance use, and suicidal ideation during the COVID-19 pandemic. Morbidity & Mortality Weekly Report, 69(32), 1049–1057. https://www.cdc.gov/mmwr/volumes/69/wr/mm6932a1.htm
DeKruyf, L., Auger, R. W., & Trice-Black, S. (2013). The role of school counselors in meeting students’ mental health needs: Examining issues of professional identity. Professional School Counseling, 16(5), 271–282. https://doi.org/10.1177/2156759X0001600502
Dillman, D. A. (2007). Mail and internet surveys: The tailored design method (2nd ed.). Wiley.
Ellis, W. E., Dumas, T. M., & Forbes, L. M. (2020). Physically isolated but socially connected: Psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Canadian Journal of Behavioural Science/Revue canadienne des sciences du comportement, 52(3), 177–187.
https://doi.org/10.1037/cbs0000215
Erickson, A., & Abel, N. R. (2013). A high school counselor’s leadership in providing school-wide screenings for depression and enhancing suicide awareness. Professional School Counseling, 16(5), 283–289.
https://doi.org/10.1177/2156759X1201600501
Erickson, K., & Quick, N. (2017). The profiles of students with significant cognitive disabilities and known hearing loss. The Journal of Deaf Studies & Deaf Education, 22(1), 35–48.
https://doi.org/10.1093/deafed/enw052
Every Student Succeeds Act, Pub. L. No. 114–95 § 114 Stat. 1177 (2015, Dec. 10). https://www.congress.gov/114/plaws/publ95/PLAW-114publ95.pdf
Faul, F., Erdfelder, E., Lang, A.-G., & Buchner, A. (2007). G*Power 3: A flexible statistical power analysis for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39, 175–191.
https://doi.org/10.3758/bf03193146
Fernandez, T., Godwin, A., Doyle, J., Verdin, D., Boone, H., Kirn, A., Benson, L., & Potvin, G. (2016). More comprehensive and inclusive approaches to demographic data collection. School of Engineering Education Graduate Student Series. Paper 60. https://tinyurl.com/2p9p2ct7
Forster, M., Gower, A. L., McMorris, B. J., & Borowsky, I. W. (2020). Adverse childhood experiences and school-based victimization and perpetration. Journal of Interpersonal Violence, 35(3–4), 662–681.
https://doi.org/10.1177/0886260517689885
Frey, B. B. (2018). The SAGE encyclopedia of educational research, measurement, and evaluation. SAGE.
Goodman-Scott, E., Betters-Bubon, J., & Donohue, P. (Eds.). (2019). The school counselor’s guide to multi-tiered systems of support. Routledge.
Gysbers, N. C., & Henderson, P. (2012). Developing and managing your school guidance and counseling program (5th ed.). American Counseling Association.
Hinkle, D. E., Wiersma, W., & Jurs, S. G. (2002). Applied statistics for the behavioral sciences (5th ed.). Houghton Mifflin Company.
Imran, N., Zeshan, M., & Pervaiz, Z. (2020). Mental health considerations for children & adolescents in COVID-19 pandemic. Pakistan Journal of Medical Sciences, 36(COVID19-S4), S67–S72.
https://doi.org/10.12669/pjms.36.COVID19-S4.2759
Kaffenberger, C. J., & O’Rorke-Trigiani, J. (2013). Addressing student mental health needs by providing direct and indirect services and building alliances in the community. Professional School Counseling, 16(5), 323–332. https://doi.org/10.1177/2156759X1201600505
Karaman, M. A., Eşici, H., Tomar, İ. H., & Aliyev, R. (2021). COVID-19: Are school counseling services ready? Students’ psychological symptoms, school counselors’ views, and solutions. Frontiers in Psychology, 12. https://doi.org/10.3389/fpsyg.2021.647740
Kotrlik, J. W., Williams, H. A., & Jabor, M. K. (2011). Reporting and interpreting effect size in quantitative agricultural education research. Journal of Agricultural Education, 52(1), 132–142.
https://doi.org/10.5032/jae.2011.01132
Lambie, G. W., Stickl Haugen, J., Borland, J. R., & Campbell, L. O. (2019). Who took “counseling” out of the role of professional school counselors in the United States? Journal of School-Based Counseling Policy and Evaluation, 1(3), 51–61. https://doi.org/10.25774/7kjb-bt85
Lancaster, C., & Reiner, S. (2022). Supervision in K–12 school settings. In A. S. Lenz & B. Flamez (Eds.), Practical approaches to clinical supervision across settings: Theory, practice, and research (pp. 223–241). Pearson.
Magson, N. R., Freeman, J. Y. A., Rapee, R. M., Richardson, C. E., Oar, E. L., & Fardouly, J. (2021). Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. Journal of Youth and Adolescence, 50(1), 44–57. https://doi.org/10.1007/s10964-020-01332-9
National Association for College Admission Counseling. (2019). State-by-state student-to-counselor ratio maps by school district: Data visualizations. https://public.tableau.com/profile/nacac.research#!
National Center for Education Statistics. (2016). National teacher and principal survey. https://nces.ed.gov/surveys/ntps
No Child Left Behind Act of 2001, Pub. L. No. 107–110, 115 Stat. 1425 (2002). https://www.congress.gov/107/plaws/publ110/PLAW-107publ110.htm
Parzych, J. L., Donohue, P., Gaesser, A., & Chiu, M. M. (2019). Measuring the impact of school counselor ratios on student outcomes. ASCA Research Report. https://tinyurl.com/3sbuk5dd
Patel, P., & Clinedinst, M. (2021). State-by-state student-to-counselor ratio maps by school district. National Association for College Admission Counseling. https://files.eric.ed.gov/fulltext/ED615227.pdf
Patterson, J. (2022, March 4). School counselors and social workers struggle to meet student needs. National Education Association Today. https://tinyurl.com/yckwhhc4
Pincus, R., Hannor-Walker, T., Wright, L., & Justice, J. (2020). COVID-19’s effect on students: How school counselors rise to the rescue. NASSP Bulletin, 104(4), 241–256. https://doi.org/10.1177/0192636520975866
Quinn, K., Boone, L., Scheidell, J. D., Mateu-Gelabert, P., McGorray, S. P., Beharie, N., Cottler, L. B., & Khan, M. R. (2016). The relationships of childhood trauma and adulthood prescription pain reliever misuse and injection drug use. Drug and Alcohol Dependence, 169, 190–198. https://doi.org/10.1016/j.drugalcdep.2016.09.021
Rea, L. M., & Parker, R. A. (1992). Designing and conducting survey research: A comprehensive guide. Jossey-Bass.
Salloum, A., & Overstreet, S. (2008). Evaluation of individual and group grief and trauma interventions for children post disaster. Journal of Clinical Child & Adolescent Psychology, 37(3), 495–507.
https://doi.org/10.1080/15374410802148194
Savitz-Romer, M. (2019). Fulfilling the promise: Reimagining school counseling to advance student success. Harvard Education Press.
Savitz-Romer, M., Rowan-Kenyon, H. T., Nicola, T. P., Alexander, E., & Carroll, S. (2021). When the kids are not alright: School counseling in the time of COVID-19. AERA Open, 7. https://doi.org/10.1177/23328584211033600
Sheperis, C., Drummond, R. J., & Jones, K. D. (2020). Assessment procedures for counselors and helping professionals (9th ed.). Pearson.
Swedberg, R. (2020). Exploratory research. In C. Elman, J. Gerring, & J. Mahoney (Eds.), The production of knowledge: Enhancing progress in social science (pp. 17–37). Cambridge University Press.
Tennessee Comptroller of the Treasury. (n.d.). Tennessee basic education program: Handbook for computation. https://tinyurl.com/twazjrut
Tennessee Department of Education. (2018). Tennessee comprehensive school-based mental health resource guide. https://tinyurl.com/2bfetw3t
Tennessee Department of Education. (2020). Reopening schools: Overview guide for LEAs. https://tinyurl.com/2hry8hs6
Tennessee Department of Education. (2021). TDOE, TERA releases 2021 Tennessee Educator Survey results. https://tinyurl.com/523b5hmn
Tennessee Department of Education. (2023). Project RAISE internship opportunities. https://web.cvent.com/event/c34c10c7-31e5-48ec-aaa2-7d343e00af77/websitePage:fa84d4fc-c565-4872-98eb-86552d79a670
Tennessee Office of the Governor. (n.d.). COVID-19 timeline. https://www.tn.gov/governor/covid-19/covid19timeline.html
Tennessee State Board of Education. (2017). School counseling model & standards policy 5.103. https://tinyurl.com/39a7jhyx
Udwin, O., Boyle, S., Yule, W., Bolton, D., & O’Ryan, D. (2000). Risk factors for long-term psychological effects of a disaster experienced in adolescence: Predictors of post traumatic stress disorder. Journal of Child Psychology & Psychiatry, 41(8), 969–979. https://doi.org/10.1111/1469-7610.00685
Whitney, D. G., & Peterson, M. D. (2019, February 11). US national and state-level prevalence of mental health disorders and disparities of mental health care use in children. JAMA Pediatrics, 173(4), 389–391.
https://doi.org/10.1001/jamapediatrics.2018.5399
Zimmer-Gembeck, M. J., & Skinner, E. A. (2011). Review: The development of coping across childhood and adolescence: An integrative review and critique of research. International Journal of Behavioral Development, 35(1), 1–17. https://doi.org/10.1177/0165025410384923
Chloe Lancaster, PhD, is an associate professor at the University of South Florida. Michelle W. Brasfield, EdD, LPSC, is an assistant professor at the University of Memphis. Correspondence may be addressed to Chloe Lancaster, 422 E. Fowler Ave, EDU 105, Tampa, FL 33620, clancaster2@usf.edu.
Aug 24, 2023 | Volume 13 - Issue 2
Amy Biang, Clare Merlin-Knoblich, Stella Y. Kim
Although researchers have found that patient weight bias negatively impacts health care professionals, research is limited on client weight bias toward counselors. Given that a client’s perception of their counselor impacts the therapeutic alliance, more research is needed to understand client weight bias toward counselors. To fill this research gap, we conducted a quasi-experimental study examining people’s weight bias toward a hypothetical counselor who was overweight, average weight, or underweight. Participants (N = 189) received a random assignment to a questionnaire featuring one of the three hypothetical counselors. Participants indicated their willingness to trust them, select them as a counselor, and follow their counsel. Results from a Welch ANOVA analysis showed a statistically significantly greater preference for average-weight and overweight counselors than those who are underweight. Additionally, the participants were less willing to follow counsel from overweight and underweight counselors. Implications for counselors are discussed.
Keywords: client weight bias, overweight, underweight, average weight, counselors
Body weight can inform a client’s perception of a health professional’s level of authority, trust, and competence (Hutson, 2013; Schwartz et al., 2006). Researchers have found that overweight bias toward health professionals like fitness instructors and medical physicians results in negative impressions (Hutson, 2013; Puhl et al., 2013; Puhl & Heuer, 2010). Clients may perceive lower competence, conscientiousness, personal grooming, and intrapersonal ability for overweight individuals compared to average-weight ones (Allison & Lee, 2015). When people seek mental health treatment, these perceptions may hinder their selection of a counselor who is perceived as overweight. Additionally, research on underweight bias has emerged that shows adverse outcomes toward underweight individuals (Allison & Lee, 2015; Beggan & DeAngelis, 2015; Davies et al., 2020a). Despite research on overweight and underweight bias in health professionals, limited research on either topic exists in the counseling profession.
Research on weight bias is necessary for counseling given that counselor attributes have the potential to be an integral part of a client’s decision-making and change process (Hauser & Hays, 2010). Attributes of a counselor that may affect client impressions, such as attractiveness (Grimes & Murdock, 1989) or race (Kim & Kang, 2018; Meyer & Zane, 2013), illuminate the social influence process of counseling (McKee & Smouse, 1983). Social influence is pervasive in the judgments of people everywhere. Weight bias continues to be a product of social influence and, as such, weaves stereotypes into the minds of those who consume the message of weight as a moral indiscretion (Beggan & DeAngelis, 2015). As clients search for, build trust with, and consider life changes with a counselor, weight bias ought to be explored as a potential issue for counselors.
In the past 35 years, researchers published only one study about weight perceptions toward overweight counselors (Moller & Tischner, 2019). Furthermore, there were no published studies about underweight counselors found. This gap in research is notable, as body weight can influence clients’ first impressions of a counselor and their expectations of the ensuing relationship (Moller & Tischner, 2019). Understanding how weight bias may impact this relationship is vital to building an authentic therapeutic relationship, which may otherwise be hindered by weight bias, which inaccurately frames a counselor’s competence (McKee & Smouse, 1983). Thus, we examined client weight bias toward overweight, underweight, and average-weight counselors in the current study.
Literature Review
Weight Bias
The term weight bias indicates a negative attitude about the perceived weight of an individual (Christensen, 2021). Historically, weight bias has been directed at people perceived as overweight; however, recent evidence suggests that underweight bodies generate weight bias as well (Allison & Lee, 2015; Beggan & DeAngelis, 2015; Christensen, 2021; Davies et al., 2020a, 2020b). Weight bias is pervasive throughout the United States (McHugh & Kasardo, 2012; Puhl et al., 2014). Negative stereotypes associated with being overweight include laziness, lack of motivation, psychological instability, social rejection, and incompetence in the workforce (Hinman et al., 2015; Lewis et al., 1997; Moller & Tischner, 2019). Likewise, incorrect stereotypes about underweight people include psychological instability or weakness (Marini, 2017). Body weight is not explicitly identified as an issue in the multicultural and social justice competencies (Ratts et al., 2016). However, weight bias is similar to sexism, racism, and classism in its harmful impact on people (Bucchianeri et al., 2013). It is still a common form of prejudice (McHugh & Kasardo, 2012).
Weight bias has become a social justice issue because of how it negatively impacts the lived experiences of people across social contexts (Nutter et al., 2018). Similar to other identities that elicit prejudice, weight bias impacts an individual’s opportunities in the workforce (Hutson, 2013), quality of mental health care (Puhl et al., 2014), and interpersonal relationships (Puhl & Heuer, 2010). Oppression from weight bias may deter a person from forming relationships or making connections with others out of fear of rejection or discrimination based on weight. Likewise, a person with weight bias may struggle to overlook the body of their counselor because of their worldview of weight and health. Even if the client remains in counseling, this initial bias may impede the therapeutic alliance process.
Therapeutic Alliance
The therapeutic alliance is a key variable in predicting client outcomes in counseling (Ackerman & Hilsenroth, 2001). This alliance represents the degree to which the client and counselor are engaged in collaboration, their commitment to one another, and their understanding of the counseling process (Allen et al., 2017; Lorr, 1965). Clients are as important as counselors in building this alliance, which involves their impression of and reaction to the counselor (Tudor, 2011). Disruptions in the therapeutic alliance can be generated from the client’s adverse reaction to the counselor, which thus impacts client outcomes (Ackerman & Hilsenroth, 2001). Weight can be a disruption, as some clients see a counselor being overweight as a barrier to opening up and engaging in counseling (Moller & Tischner, 2019). As the therapeutic alliance impacts clients remaining in counseling (Sharf et al., 2010), biases toward the counselor may hinder building the relationship, leading to early termination. Clients discriminating against counselors may limit capable counselors who fall outside socially acceptable weights from co-building the therapeutic alliance (McKee & Smouse, 1983).
Even with weight bias possibly diminishing the initial therapeutic relationship, Allen et al. (2017) found that communication on tasks/goals was a predictor of a strong therapeutic alliance and activation (i.e., the clients’ readiness and willingness to take on the management of their mental health care). Allen et al. found that alliance around the tasks/goals of therapy had long-term benefits, while an initial therapeutic bond was only associated with activation at the beginning of therapy. These findings suggest that despite client bias, a strong alliance may still form if there is a connection between counselor and client on their treatment goals and plan.
Despite a client and counselor’s mutual investment in a counseling relationship, research about weight bias in counseling has focused solely on counselors’ perceptions of clients’ weight and its influence on the therapeutic alliance (Kinavey & Cool, 2019; McHugh & Kasardo, 2012; Puhl et al., 2014). Thus, research has insufficiently examined how a counselor’s weight may hinder this alliance (Moller & Tischner, 2019). This gap is further concerning given that researchers have found that professionals in other disciplines identified as overweight or underweight face discrimination in the workplace (Beggan & DeAngelis, 2015; Hutson, 2013).
Overweight Bias Toward Counselors
Researchers have found that counselors are subject to weight bias from clients. Moller and Tischner (2019) examined client perceptions of counselors by specifically examining counselor weight. They conducted a qualitative story completion task with students from Great Britain aged 15–24 (N = 203) and found that participants perceived overweight counselors as incompetent. Counselors’ competence came into question because of the perception that being overweight implies a lack of emotional stability, personal discipline, and mental stability (Moller & Tischner, 2019). Participants also reported perceiving overweight counselors as distracting because of their physical appearance. Additionally, participants viewed an overweight counselor as having poor psychological health. Some participants noted that being overweight suggested an eating disorder (ED), such as bulimia or binge eating disorder. Furthermore, responses indicated that weight bias would impact the therapeutic relationship, and many participants would not want to work with an overweight counselor (Moller & Tischner, 2019).
These results are striking, and further research is needed to corroborate their value, as they point to a high level of bias toward overweight counselors. These types of inaccuracies can perpetuate prejudice and discrimination that may also hurt potential clients who would otherwise not have access to a counselor. Stereotypes and biases impact those who choose to work in this profession and could struggle to feel they belong in the helping professions.
Underweight Bias
Research geared toward overweight bias is well established in the health professions; however, evidence suggests that underweight health professionals also experience bias and discrimination (Allison & Lee, 2015; Beggan & DeAngelis, 2015; Davies et al., 2020a, 2020b). Researchers have noted stereotypes suggesting that extreme thinness may indicate a lack of wellness or the presence of a mental health issue like anorexia (Davies et al., 2020a). Furthermore, implicit bias toward underweight people may also come from the survival instinct that hunger, poverty, and war create underfed people, and we want to be with those who can help us survive (Marini, 2017).
Interestingly, scholars have noted that if being underweight is not perceived as stemming from health issues or an ED, people possess more favoritism toward underweight persons, limiting institutional discrimination toward them (Allison & Lee, 2015; Beggan & DeAngelis, 2015). In some social settings, a slender appearance of health follows socially accepted norms and may supersede the importance of actual health (Moller & Tischner, 2019). This leads to what is known as thin privilege; hence the possibility that there is enough benefit to being thin that it negates any negative attitudes or behaviors by others.
This thin privilege allows others to overstep the concept of civil inattention, which is how people are recognized appropriately in polite society. Civil inattention warrants people to be discrete in commenting on or noticing differences among those around them (e.g., those with disabilities, obesity, low socioeconomic status, or other marginalized identities). Some people believe that being underweight may invite a breakdown of civil inattention (Beggan & DeAngelis, 2015). This breakdown may lead a client to comment on a counselor’s body, such as “You are so skinny; how can you understand anything I am feeling about my body” or “If I were as thin as you, I would…” These types of comments are seen as acceptable because they infer a compliment about a socially desirable attribute. However, they can invite feelings of judgment and unease for the counselor, perpetuating a rupture in the therapeutic alliance. As we continue to understand that weight bias exists along a spectrum, counselors may feel prepared to broach the topic of weight regardless of where they fall.
One last finding that significantly impacts weight bias toward counselors comes from a qualitative study of adults (N = 18) with an average female body mass index (BMI) of 18.80 or male BMI of 21.68, both of which fall within the normal range of 18.5 to 24.9 (Centers for Disease Control and Prevention [CDC], 2022). Beggan and DeAngelis (2015) found that participants believed that underweight people lack empathy for others who struggle with weight. Such a belief would be impactful for a counselor, given that empathy is integral for a successful counseling relationship (Clark, 2010).
Empathy
Empathy is one of the six core conditions necessary for client change and contributes significantly to therapeutic outcomes. Clients can perceive empathy from counselors when counselors act in ways consistent with their frame of reference (Feller & Cottone, 2003).
Empathy is a deep understanding of the client’s circumstances. When there is weight bias, the client may not believe their counselor can understand their frame of reference if they are of differing body weights, especially if the client is coming in for body image concerns or health concerns. Even though the counselor has empathy, the client may not accept this as truth, hindering the building of a solid therapeutic alliance.
Weight as Credibility
Whether professionals are overweight or underweight, their bodies are part of their résumé. The term bodily capital describes one’s credibility as portrayed by the body and can influence how professionals are judged by their physical appearance (Hutson, 2013; Moller & Tischner, 2019). The body can be viewed as a symbolic container that indicates the investment of time and resources into health and well-being (Hutson, 2013). Previous scholars have asserted that the healthier a professional appears, the more likely clients and patients will accept their advice and trust their counsel (Hutson, 2013; Puhl et al., 2013). Health expectations are amplified for health professionals, as overweightness can be seen by some as a moral transgression and an inadequacy that may translate into their work (Beggan & DeAngelis, 2015). Some people believe that to be psychologically healthy, a person must appear to be of an appropriate weight; this indicates willpower, discipline, and self-control (Tischner, 2019). Though these ideas are inaccurate for psychological health, they may influence how clients see counselors on the far ends of the weight spectrum.
Antifat Attitudes
Antifat attitudes are a different but related construct to weight bias. An antifat attitude is “a negative attitude toward (dislike of), belief about (stereotype), or behavior against (discrimination) people perceived as being ‘fat’” (Meadows & Daníelsdóttir, 2016, p. 47). Weight bias refers to a negative attitude toward any size body (Christensen, 2021), whereas antifat attitudes describe dislike and discrimination toward people perceived as overweight (Meadows & Daníelsdóttir, 2016). Antifat attitudes have created a marginalized group that faces external stigma throughout society, with some individuals feeling internal stigma due to personal experiences.
Despite encounters with prejudice, some clients who are overweight will still prefer an average-weight counselor because of their own bias toward being overweight (Moller & Tischner, 2019) and will have similar antifat attitudes as average-weight individuals (Schwartz et al., 2006). Contingencies of self-worth encompass the domains in a person’s life that create self-esteem (Clabaugh et al., 2008). When body weight is a domain, success or failure in their ability to lose or gain weight can lead to lower self-worth. Because of weight bias, working with a counselor who mirrors the client’s undesired body weight may impact the client’s willingness to work with the counselor. Examining weight bias across the spectrum and correlating BMI with antifat attitudes will give us further insight into these findings and if they influence client bias toward counselors.
Purpose of the Study
This study examined if client weight bias influences a client’s trust in a counselor’s competence, willingness to follow a counselor’s advice, and desire to select a counselor for therapy. We further examined if a client’s antifat attitudes are associated with their weight bias toward counselors. The following research questions guided this study: 1) Does a counselor’s weight impact a client’s decision to trust, follow advice, and select the counselor? 2) Is there an association between a client’s antifat attitudes and weight bias toward counselors? 3) Are there differences in weight bias toward counselors based on the socio-demographics of the clients using their services? and 4) Do participants with eating disorders have similar perceptions of counselors due to weight bias as those without eating disorders?
Methodology
Recruitment
At the time the research was conducted, the researchers—Amy Biang, Clare Merlin-Knoblich, and Stella Kim—were affiliated with the same university; as such, IRB approval was obtained from that university before recruiting participants. People were eligible to participate in this study if they were 18 years or older and signed an electronic consent form indicating their willingness to participate. We recruited participants through purposive and snowball sampling in three ways. First, Biang emailed a compiled database of counseling professionals within their acquaintance to request they send the survey to previous clients in an effort to obtain sufficient participation from people who have received counseling. In addition, requested participation through two research boards of counseling associations (Academy of Eating Disorders and International Association of Eating Disorder Professionals) allowed us to recruit sufficient participation from previous clients with EDs, as well as other diagnoses, as we requested they send the survey to their former clients. Second, to obtain participation from people with and without experience in counseling, Biang posted calls for participation on social media accounts (i.e., Instagram and Facebook). Third, to further increase participation, Merlin-Knoblich forwarded a participation request to their university’s counseling program listserv. After 2 weeks of data collection, we sent a second follow-up call for participation and then continued data collection for an additional week.
To prevent recruitment bias and confirmation bias during data collection, we omitted the terms weight and weight bias and modified the study title to read “Counselor Attributes that Impact Client’s Selection, Trust, and Advice Following.” The call for participation informed potential participants that we were conducting a study about the attributes of a hypothetical counselor. The end of the questionnaire contained a full disclosure of the study’s purpose. Of the 255 participants who began the study questionnaire, 189 completed the study, representing a 74% completion rate. No data was collected from the 66 non-completers other than an average of 76 seconds with the survey open before ending the survey.
Participants
A sample of 189 participants from 26 states participated in the study. Table 1 presents a summary of the sample characteristics. The majority of participants were from North Carolina (n = 72, 38%),
Ohio (n = 23, 12%), California (n = 19, 10%), Utah (n = 11, 6%), and New York (n = 10, 5%). Participants primarily identified as female (n = 158, 84%). The majority of participants identified as White (n = 153, 81.4%), with other participants identifying as Asian (n = 13, 6.9%), Black/African American (n = 12, 6.4%), Latine/Hispanic (n = 5, 2.7%), and American Indian (n = 3, 1.6%). The majority of participants were over the age of 30 (n = 139, 74%), more than half had previously participated in personal counseling (n = 135, 71.8%), and just over a quarter indicated a previous ED diagnosis (n = 52, 27.7%).
Given the focus of this study, all participants were asked to indicate their height and weight but were informed that such information (like all demographic information) was optional to submit. One hundred and eighty-four participants (97%) shared their height and weight, from which we calculated their BMI—a person’s weight in kilograms divided by the square of height in meters. The mean BMI was 28 (SD = 6.8) among the participants who shared their height and weight. This BMI is designated as “overweight” by the CDC (2022).
Study Design and Instrumentation
Physician Weight Survey Revised
We used a quasi-experimental research design in this study. With permission from Puhl and colleagues (2013), we revised the Physician Weight Survey (PWS), a 44-item questionnaire designed to assess patient weight bias of physicians who are obese, overweight, or seen as average weight. The instrument measures five constructs: physician health behaviors, physician selection, physician compassion, physician trust, and adherence to physician advice. Cronbach’s alpha tests instrument reliability and the internal consistency of the questions on a scale. Alpha scores over .70 are considered acceptable (Taber, 2018). Each subscale of the PWS has demonstrated sufficient internal consistency, with a Cronbach’s alpha of at least .90 (Puhl et al., 2013).
We adapted the questionnaire to address participants’ willingness to trust, follow the advice of, and select a hypothetical counselor based on the weight of that counselor. We replaced the term, physician with counselor and added the underweight category instead of the obese category. Using the underweight category allowed for consideration that weight bias exists on both ends of the weight spectrum. Because
of differences in occupational responsibilities and limiting the dependent variables of our study, we did not use the subscales for health behaviors or compassion. The Health Behavior subscale incorporated the physicians’ use of substances, health screenings, and illness prevention. The Compassion subscale measured the physician’s bedside manner. Without those two additional subscales, our revised measure had 23 items.
Table 1
Participant Demographic Data
| Demographics |
n |
% |
| Gender |
|
|
| Female |
158 |
84.0 |
| Male |
27 |
14.4 |
| Non-Binary |
1 |
0.05 |
| Race/Ethnicity |
|
|
| White |
153 |
81.4 |
| Black/African American |
12 |
6.4 |
| Latine/Hispanic |
5 |
2.7 |
| Asian |
13 |
6.9 |
| American Indian |
3 |
1.6 |
| Age Range |
|
|
| 18–29 |
48 |
25.6 |
| 30–42 |
64 |
34.1 |
| 43 and older |
74 |
39.4 |
| Prior History of Counseling |
|
|
| Yes |
135 |
71.8 |
| No |
51 |
27.1 |
| Prior History of Eating Disorder |
|
|
| Yes |
52 |
27.7 |
| No |
134 |
74.3 |
| BMI Range |
|
|
| Underweight |
4 |
2.1 |
| Average |
64 |
34.0 |
| Overweight |
54 |
28.7 |
| Obese |
60 |
31.9 |
Note. N = 189.
The subscales of Counselor Trust and Counselor Selection align well with our study. The subscale of Advice Following may seem counterintuitive when used with the counseling profession. The term advice equates to the construct of counseling together and incorporates the concept of counselors helping clients create and follow treatment goals, exploring ideas together for change, and even assigning homework. Advice aligns with how clients perceive what counselors do rather than the skills they use. For example, counselors using motivational interviewing and questions such as “What would it take for you to go from a 2 to a 4 in your willingness to reduce your alcohol consumption?” can be seen as advising clients to reduce their alcohol consumption. We chose to use the term advice instead of counsel so all participants, regardless of their experience with counseling, would understand the questions.
Parallel to Puhl and colleagues’ (2013) study, we then created three different versions of the questionnaire. Using Qualtrics, an electronic survey platform, consenting participants received a random assignment to one of three questionnaire versions. Seventy (37%) of the study participants completed the first version of the questionnaire, which described a hypothetical counselor as an overweight counselor. Fifty-eight (31%) participants completed the second questionnaire version, which described a hypothetical counselor as having average weight. And 61 (32%) of the participants completed the third version of the questionnaire, which described a hypothetical counselor as underweight. Participants responded to all items on a Likert scale ranging from 1 (strongly disagree/extremely unlikely) to 7 (strongly agree/extremely likely), with seven questions reverse scored.
Counselor Trust Subscale. The Counselor Trust subscale of the revised PWS consisted of nine questions focused on skills and competence (e.g., “If my counselor was [overweight/underweight/average weight], I would not trust them,” and “If my counselor was [overweight/underweight/average weight], I would have doubts about their credibility”). Other questions focused on believing the counselor would listen or understand their needs (e.g., “I believe an [overweight/underweight/average weight] counselor would listen carefully to what I have to say”). The scale demonstrated good internal consistency (α = .81) with this sample. Higher scores reflect greater trust in the counselor.
Counselor Advice Following Subscale. The Advice Following subscale contained six items. These items indicated making changes to diet, losing weight, and advice in general (e.g., “In general, my counselor’s weight affects whether I listen to their advice” and “If my counselor were [overweight/underweight/average weight], I would feel embarrassed when talking about losing weight”). Though counselors are not medical doctors, many clients explore topics associated with their bodies, exercise, and overall physical health (e.g., sleep issues, pain management, substance use, and daily routines), indicating relevance to counseling for the survey questions. Higher scores suggest more willingness to follow the advice (counsel) of the counselor. Cronbach’s alpha for this scale was .83 with this sample.
Counselor Selection Subscale. The Counselor Selection subscale had seven items indicating a willingness to select the counselor based on their appearance of weight (e.g., “If I went to a new counselor, and the counselor appeared [overweight/underweight/average weight], I would change counselors,” or “If my counselor was [overweight/underweight/average weight], I would not recommend them to my friends”). Similar to the other subscales, higher scores indicate more willingness to select the counselor. For this sample, Cronbach’s alpha was .71.
Antifat Attitudes Questionnaire
In addition to the revised PWS, participants completed the Antifat Attitudes Questionnaire (AFA; Crandall, 1994). The AFA assesses participants’ beliefs about overweight people and their feelings about becoming overweight. Three subscales, Dislike (α = .84), Fear of Fat (α = .79), and Willpower (α = .66), are combined for a composite antifat attitude score. Despite the low Cronbach’s alpha coefficient for the Willpower subscale, it positively correlates with the Dislike subscale (r = .43, p < .001), whereas the Fear of Fat subscale remains uncorrelated with both subscales, suggesting discriminate validity (Lacroix et al., 2017; Ruggs et al., 2010). Both the reliability and validity of the AFA have been extensively assessed by researchers, and the AFA has been found to be a psychometrically sound measure (Ruggs et al., 2010). The Cronbach’s alpha internal consistency reliability was acceptable, with a value of .87 for the data used in the current study. Participants indicated agreement (e.g., “I really don’t like fat people much”) on a Likert scale ranging from 1 (strongly disagree) to 7 (strongly agree), with higher composite scores suggesting stronger negative antifat attitudes. Higher scores may correlate to weight bias toward the overweight counselor. Scores on the Fear of Fat subscale are directed toward a personal antifat fear and not toward others.
The AFA was also used to test the equivalence of groups and any effect of social desirability. Lastly, participants completed a voluntary 8-item demographic questionnaire describing their race/ethnicity, age, gender, height, weight, and experience with receiving counseling or having an ED.
Data Analysis
We conducted all analyses using SPSS Version 27. The first analysis had the four dependent variables of Counselor Trust, Counselor Selection, Advice Following, and Weight Bias, with the independent variable of Weight (overweight, underweight, and average weight). We conducted a series of assumption-checking procedures to draw valid interpretations of the findings. Engaging the Shapiro-Wilk test as a test of normality yielded a significant result (W = 0.92, p < .001) for the overweight counselor, indicating the sample was not normally distributed. After removing outliers, the sample for the overweight survey condition did not meet the assumption of normality. A test for homogeneity of variance yielded a statistically significant Levine’s score of F(2, 168) = .46, p = .013; degrees of freedom were adjusted due to unequal sample sizes for each survey condition.
Conducting a MANOVA yielded statistically significant results; however, not meeting the assumptions of multivariate normality and homogeneity of variance required, we used the Welch ANOVA, which is recommended for non-normal distributions. Using a Welch ANOVA is also a best practice when the homogeneity of variances test fails; it controls the type I error and gives more power in many instances (Liu, 2015). Although a parametric test such as a typical ANOVA or MANOVA is known to be more powerful than a non-parametric test (e.g., Welch ANOVA), it can lead to erroneous results if required assumptions are not satisfactorily met (Zar, 1998). Considering unequal variances and sample sizes across groups, we used Games-Howell for post hoc testing. We used G*Power version 3.1.9.7 (Faul et al., 2007) to perform the power analysis. For the Welch ANOVA test, the minimum sample size was 157, with a medium effect size of .25, a desired statistical power level of .8, and an alpha level of .05. Lastly, we measured the effect size using partial eta squared (ꞃ²), showing the strength of association as a proportion of variance in the dependent variable explained by group membership (Coladarci et al., 2011).
Table 2
Descriptive Statistics for Outcome Variables
|
n |
Mean |
Std.
Deviation |
Std. Error |
95% Confidence Interval for Mean |
Minimum |
Maximum |
| Lower Bound |
Upper Bound |
| Trust |
OW |
70 |
49.70 |
9.89 |
1.18 |
47.34 |
52.06 |
16.00 |
63.00 |
| UW |
59 |
41.15 |
10.72 |
1.40 |
38.36 |
43.95 |
17.00 |
63.00 |
| AW |
60 |
47.48 |
7.75 |
1.00 |
45.48 |
49.49 |
29.00 |
63.00 |
| Total |
189 |
46.33 |
10.16 |
0.74 |
44.87 |
47.79 |
16.00 |
63.00 |
| Selection |
OW |
70 |
32.41 |
5.40 |
0.64 |
31.13 |
33.70 |
19.00 |
40.00 |
| UW |
59 |
30.00 |
5.12 |
0.67 |
28.67 |
31.33 |
21.00 |
40.00 |
| AW |
60 |
31.42 |
4.92 |
0.63 |
30.15 |
32.69 |
16.00 |
40.00 |
| Total |
189 |
31.34 |
5.23 |
0.38 |
30.59 |
32.09 |
16.00 |
40.00 |
| Advice |
OW |
70 |
25.76 |
8.72 |
1.04 |
23.68 |
27.84 |
8.00 |
42.00 |
| UW |
59 |
24.73 |
7.33 |
0.95 |
22.82 |
26.64 |
8.00 |
42.00 |
| AW |
60 |
31.93 |
4.64 |
0.60 |
30.73 |
33.13 |
23.00 |
42.00 |
| Total |
189 |
27.40 |
7.81 |
0.57 |
26.28 |
28.52 |
8.00 |
42.00 |
| Note. OW = overweight; UW = underweight; AW = average weight. |
In the second data analysis, we used the Pearson correlation to assess an association between data sets from the AFA and Composite Weight Bias. Composite Weight Bias was calculated by summing the scales of the revised PWS. Before computing a correlation, we examined the scatter plot between the independent and dependent variables to check the linearity between the two variables and the existence of outliers. We found less than three outliers on all four graphs and identified negative linearity. Using G*Power (Faul et al., 2007), we obtained the estimated sample size necessary to run the correlation analysis, which was 64 with a medium effect size of .3, an alpha level of .05, and power of .8. Lastly, we explored the relationships between demographics and weight bias toward counselors using a one-way ANOVA or an independent t-test. We selected statistical methods based on the number of categories of each demographic variable. See Table 2 for descriptive statistics of the outcome variables.
Results
Areas of Trust, Advice, and Selection
We found significantly different levels of trust, advice following, and counselor selection behaviors among participants assigned to hypothetical counselors of different weights.
Welch ANOVA test results indicated a statistical significance in all three areas between groups, F(2, 120.60) = 12.89, p < .001 with a medium effect size (ꞃ² = .11). Post hoc comparisons using Games-Howell showed the following results at the significance level of α = .05. Counselor Trust for average-weight counselors (M = 47.48, SD = 7.75) was significantly higher than Counselor Trust for underweight counselors (M = 41.15, SD = 10.72) at p = .001. Counselor Trust of overweight counselors (M = 49.70, SD = 9.89) was also significantly higher than Counselor Trust for underweight counselors at p < .001. There was no statistical significance for Counselor Trust between average and overweight counselors. Advice Following for average-weight counselors (M = 31.93, SD = 4.65) was significantly higher than Advice Following for underweight counselors (M = 24.72, SD = 7.28) and Advice Following for overweight counselors (M = 25.75, SD = 8.72) at p < .001 for both. Finally, Counselor Selection for an overweight counselor (M = 32.41, SD = 5.73) was statistically higher than Counselor Selection for an underweight counselor (M = 30.00, SD = 5.59) with p = .028. There was no statistical significance in the Counselor Selection of average-weight counselors (M = 31.41, SD = 4.91) compared to overweight or underweight counselors. See Table 3 and Figures 1–3.
Next, we conducted a Welch ANOVA between overall composite scores and the three weight groups (see Table 4). Again, Welch test results indicated a statistical significance between groups, F(2, 118.73) = 11.71, p < .001 with a medium effect size (² = .10). Post hoc comparisons using Games-Howell showed statistical significance between overweight counselors (M = 107.87, SD = 21.68) and underweight counselors (M = 95.88, SD = 20.00). Underweight counselors were also significantly lower on the overall composite than average-weight counselors (M = 110.83, SD = 19.97). There was no statistical significance between overweight and average-weight counselors for their overall composite scores, which include all three variables.
Figure 1
Willingness to Trust Counselor
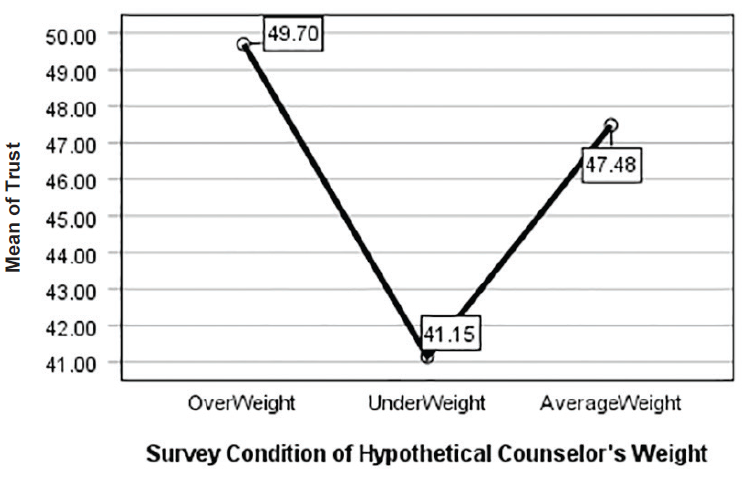
Figure 2
Willingness to Select Counselor
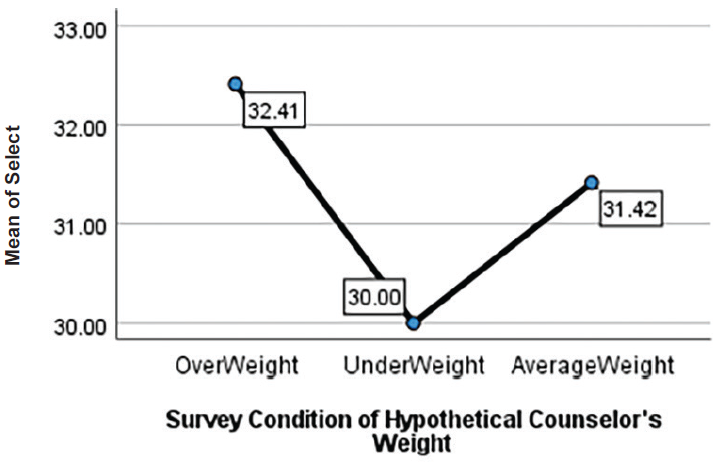
Figure 3
Following Counselor Advice
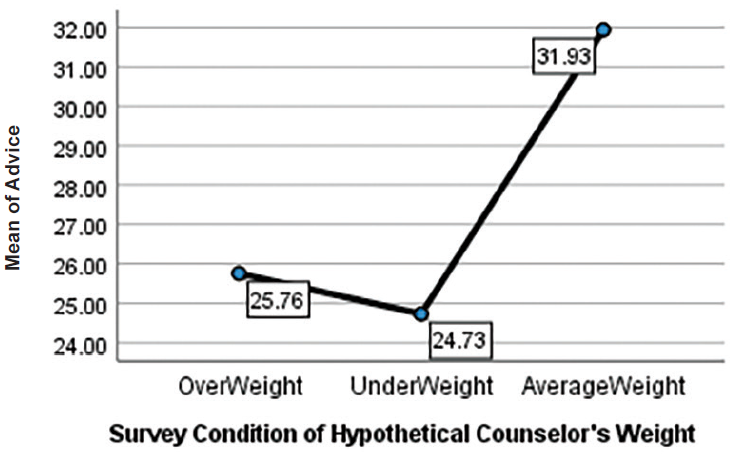
Table 3
Post Hoc Outcome Variables
|
| Dependent Variable |
Mean Difference (I-J) |
Std. Error |
Sig. |
95% Confidence Interval |
| Lower Bound |
Upper Bound |
| Trust |
OW |
UW |
8.547a |
1.829 |
0.00 |
4.206 |
12.888 |
| AW |
2.216 |
1.548 |
0.32 |
−1.456 |
5.889 |
| UW |
OW |
−8.547a |
1.829 |
0.00 |
−12.888 |
−4.206 |
| AW |
−6.330a |
1.717 |
0.00 |
−10.414 |
−2.247 |
| AW |
OW |
−2.216 |
1.548 |
0.32 |
−5.889 |
1.456 |
| UW |
6.330a |
1.717 |
0.00 |
2.247 |
10.414 |
| Selection |
OW |
UW |
2.414a |
0.927 |
0.02 |
0.215 |
4.613 |
| AW |
0.997 |
0.904 |
0.51 |
−1.144 |
3.143 |
| UW |
OW |
−2.414a |
0.927 |
0.02 |
−4.613 |
−0.215 |
| AW |
−1.416 |
0.920 |
0.27 |
−3.601 |
0.767 |
| AW |
OW |
−0.997 |
0.904 |
0.51 |
−3.143 |
1.148 |
| UW |
1.416 |
0.920 |
0.27 |
−0.767 |
3.601 |
| Advice |
OW |
UW |
1.028 |
1.413 |
0.74 |
−2.323 |
4.379 |
| AW |
−6.176a |
1.202 |
0.00 |
−9.034 |
−3.313 |
| UW |
OW |
−1.028 |
1.413 |
0.74 |
−4.379 |
2.323 |
| AW |
−7.204a |
1.126 |
0.00 |
−9.885 |
−4.523 |
| AW |
OW |
6.176a |
1.202 |
0.00 |
3.318 |
9.034 |
| UW |
7.204a |
1.126 |
0.00 |
4.523 |
9.885 |
| Note. The mean difference is significant at the 0.05 level. OW = overweight; UW = underweight; AW = average weight. Welch’s ANOVAs with Games-Howell post hoc tests were run owing to violations of the equality of variances assumption. |
Table 4
Post Hoc Composite Weight Bias
|
| (I) Group |
Mean Difference (I-J) |
Std. Error |
Sig. |
95% Confidence Interval |
| Lower Bound |
Upper Bound |
| OW |
UW |
11.99a |
3.67 |
0.004 |
3.28 |
20.70 |
| AW |
−2.96 |
3.09 |
0.604 |
−10.29 |
4.36 |
| UW |
OW |
−11.99a |
3.67 |
0.004 |
−20.70 |
−3.28 |
| AW |
−14.95a |
3.10 |
0.000 |
−22.32 |
−7.58 |
| AW |
OW |
2.96 |
3.09 |
0.604 |
−4.36 |
10.29 |
| UW |
14.95a |
3.10 |
0.000 |
7.58 |
22.32 |
| Note. The mean difference is significant at the 0.05 level. OW = overweight; UW = underweight; AW = average weight. Welch’s ANOVAs with Games-Howell post hoc tests were run owing to violations of the equality of variances assumption. |
|
In addition to statistical significance, we also examined effect size to quantify the significance found. Results indicated that Advice Following showed a large effect of association with the independent variable of Weight (² = .16). Counselor Trust had a medium effect size (² = .13), and Counselor Selection yielded a small effect size (² = .04). These results suggest that the weight of a counselor has a high association with clients following counselor advice, with average-weight counselors faring the best. Additionally, participants indicated they would trust average and overweight counselors more than underweight counselors. Lastly, overweight counselors were more favorable in Counselor Selection than underweight counselors.
Antifat Attitudes and a Correlation With Counselor Trust, Advice Following, and Counselor Selection
We used Pearson correlations to examine associations between antifat attitudes and weight bias toward counselors (see Table 5). To do so, we examined data from participants assigned to all three counselor conditions in the study. Each group showed a significant relationship between antifat attitudes and weight bias toward counselors; thus, we combined data to attain a larger sample size. The Pearson correlations between the independent variable of antifat attitudes and dependent variables of Counselor Trust, Advice Following, Counselor Selection, and Composite Weight Bias score were significant at α = .05. We found positive correlations between antifat attitudes and Counselor Selection, r(186) = .400, p < .001, and Counselor Trust, r(186) = .211, p = .004. These results indicate that as antifat attitudes increase, participants’ trust in and selection of a counselor based on weight also increase. We found no significant correlation between Advice Following and Composite Weight Bias score with antifat attitudes.
Table 5
Correlation of AFA With Outcome Variables |
|
|
|
|
|
|
AFA |
Trust |
Selection |
| AFA |
Pearson Correlation |
1.000 |
0.211** |
0.400** |
| Sig. |
|
0.004 |
0.000 |
| N |
188.000 |
188.000 |
188.000 |
| Trust |
Pearson Correlation |
0.211** |
1.000 |
0.349** |
| Sig. |
0.004 |
|
0.000 |
| N |
188.000 |
188.000 |
188.000 |
| Selection |
Pearson Correlation |
0.400** |
0.349** |
1.000 |
| Sig. |
0.000 |
0.000 |
|
| N |
188.000 |
188.000 |
188.000 |
Note. AFA = Antifat Attitude. Advice was not statistically significantly correlated with AFA. One participant of the total study sample (N = 189) did not complete this portion and is not included in the table.
*Correlation is significant at the 0.01 level (two-tailed). |
Socio-Demographic Categories
We found no statistically significant differences in weight bias toward counselors based on ethnicity F(4, 181) = .037, p = .997; age F(4, 181) = 1.71, p = .149; BMI F(4, 177) = .193, p = .942; counseling status t(184) = .798, p = .426; eating disorder t(184) = 1.055. p = .137; or gender F(2, 183) = 1.423, p = .426. Additionally, we tested for Pearson correlations between BMI and antifat attitudes. Results indicated that BMI and antifat attitudes had no significant correlation, r(N = 187) = .004, p = .958.
Antifat Attitudes by Survey Condition
To test for undue influence from survey design or responses that stem from social desirability, we ran an ANOVA comparing participants in each questionnaire condition (i.e., underweight, average weight, and overweight counselor) and their scores on the AFA. We found no statistically significant differences between the three groups, F(2, 181) = 2.74, p = .067. For the AFA scores, M = 40.22 and SD = 12.57. However, with the results of the AFA correlation with Counselor Trust and Counselor Selection, these findings may indicate that there was social desirability across all three survey conditions.
Discussion
Contrary to previous research from McKee and Smouse (1983) that suggested counselors of any weight could address personal concerns, our study results indicated that clients might use weight to select a counselor, trust the counselors’ skills, and follow their counsel. When asked about weight, participants in this study slightly preferred to select and trust the average-weight and overweight counselors, with weight bias directed mainly at the underweight counselor. Like previous research about weight bias toward physicians (Puhl et al., 2013) and personal trainers (Hutson, 2013), our results showed some weight bias toward overweight counselors when following advice. For underweight counselors, weight bias was present in all three subscales and mirrored findings that underweight persons are not immune to weight discrimination (Beggan & DeAngelis, 2015).
Overweight Counselors
Our results yielded only one finding that supported the theme from Moller and Tischner’s (2019) study that “fat counselors cannot help” (p. 14). Statistically significant results from the present study showed less willingness to follow the advice of overweight counselors. Similar to the findings from Puhl et al. (2013), taking advice or counsel from an overweight health care professional may prove more difficult than trusting they can perform their job or being willing to work with them. With two-thirds of adults in the United States considered overweight or obese (CDC, 2022), these findings may reflect cause for concern that some clients may not perceive competence in counselors who are overweight.
The correlation between the AFA with Counselor Trust and Counselor Selection can give insight into the findings. The positive correlation between AFA and Counselor Trust was low but significant. With 60% of participants in the overweight-to-obese category, there could be an underlying factor that needs further exploration. There was no correlation between BMI and AFA. However, as Schwartz et al. (2006) suggested, overweight people have similar antifat attitudes as average-weight individuals. The slight correlation potentially relates to most participants having larger bodies and knowing that being in larger bodies does not equate to untrustworthiness. Likewise, for Counselor Selection, we should consider the concept of similar attraction. This concept posits that people associate with those perceived as similar to them and who have similar physical attributes (Montoya & Horton, 2013). Relating to this concept of similar attraction, the positive correlation between AFA and Counselor Selection could be attributed to the high percentage of larger-body participants feeling more comfortable selecting the overweight counselor.
Unlike findings from other studies (Moller & Tischner, 2019; Puhl et al., 2013), our results did not indicate that Counselor Trust or Counselor Selection were negatively related to being overweight. However, when looking at the Advice Following subscale, there was a marked difference in the scores. The hypothetical overweight counselor had higher mean scores than underweight counselors on all three subscales and overall composite scores. On the upside, weight may not be an issue for many clients seeking counseling. Despite continued weight bias and stigma in social media and society, people might recognize that overweight counselors’ skills and knowledge are more important than perceived body weight. On the downside, clients may hesitate to follow counsel associated with issues concerning their own physical well-being from a perceived overweight counselor. To combat this, counselors need to be willing to broach the issue of weight if they feel it is hindering the therapeutic alliance. Similar to other multicultural topics, differences in body weight between the counselor and client may be a potential barrier for the free expression of client concerns. The willingness of the counselor to explore this topic may put the client at ease and make them able to further explore their concerns in a nonjudgmental, therapeutic manner.
Underweight Counselors
We found surprising results suggesting that participants in our study would prefer an overweight or average-weight counselor to an underweight counselor. Participants scored counselors perceived as underweight significantly lower on a client’s willingness to select, trust, and follow a counselor’s advice than average-weight and overweight counselors. These results supported the decision to add this variable to our study and indicate the need for more research on weight bias toward underweight professionals.
The underweight variable yielded results that complement previous research on weight bias, indicating that people can be biased against underweight professionals (Allison & Lee, 2015; Davies et al., 2020b). Because of the persistent social desirability to be thin or underweight, research indicates that people may be pro-underweight on an explicit level; however, they implicitly prefer an average-weight person (Marini, 2017). In our findings, participants somewhat preferred to select an overweight counselor instead of an underweight counselor, upholding the notion that people do not necessarily trust those who are underweight despite the social pressure to be thin. This result highlights a striking mismatch in thought: people may prefer to be underweight because of social pressures but not fully trust an underweight counselor. It could indicate that societal pressures to be underweight are not as strong as once thought or it may suggest that people possess complicated views on being underweight in general.
These results reflect those found by Marini (2017), in which individuals implicitly preferred an overweight individual over an underweight individual, implying maladaptive behaviors and dangerous consequences. Additionally, with body positivity and body acceptance movements, underweight persons may be overlooked as recipients of negative weight bias (Beggan & DeAngelis, 2015). These results may give underweight counselors pause about how clients perceive them in session and the notion that experiences of thin privilege may not transfer into their professional identity. In response to these possible perceptions from clients, underweight counselors may benefit from seeking professional supervision or consulting with colleagues about the topic.
Antifat Attitudes
The AFA results indicated that as a person’s negative attitudes toward overweight people decrease, they disregard weight as a factor for selecting and trusting the skills of counselors. Currently, there is no measure for anti-thin attitudes to analyze whether this bias would yield similar results. Despite the lack of an anti-thin measure, these results reiterate the belief that we judge others based on what attributes are important to us or differentiate us from others (Cermák et al., 1993). When body weight is not an attribute of self-judgment, a person may not use it as a criterion toward others or in working with professionals. As a profession, we must continue supporting movements that promote acceptance of all bodies and destigmatize weight. With strong social media campaigns against weight bias, we can dispel the stereotypes about those who fall outside socially acceptable standards and replace them with acceptance.
Demographics
In addition to antifat attitudes, we chose to study socio-demographics because weight bias may fluctuate based on various group identities. Our results showed no statistically significant differences in age, gender, ethnicity, or BMI. These findings are relevant as they imply that weight bias may exist throughout all groups. However, we interpret these results cautiously, as the sample population was predominantly female, with fewer ethnically diverse participants, and more participation from people over 30. Notably, results for ethnicity were similar to previous research indicating that Black and White women had the same bias and weight stigma toward others who were overweight and underweight (Davies et al., 2020b).
Eating Disorder Consideration
Because of the nature of EDs, we added this category to the study to explore if a counselor’s weight would impact participants with an ED more. As counselors working with EDs often explore issues around weight, exercise, and eating concerns, we hypothesized that these participants might have a higher bias toward underweight and overweight counselors. We found that participants with EDs were not significantly different from participants without EDs in weight bias toward counselors in any of the variables. This finding is favorable information for counselors in this specialty, as it does not align with the findings from Moller and Tischner (2019) that suggest that the weight of a counselor is a barrier to treatment.
Experience of Counseling
A final surprising finding revealed in our results was that people with previous counseling experience had similar levels of weight bias to those who had not worked with a counselor. Participants who previously participated in counseling may recognize attributes, such as expertise, empathy, and compassion of a counselor, as more valuable in their relationship than weight. Because attributes such as genuineness, empathy, unconditional positive regard (Nienhuis et al., 2018) build the therapeutic relationship, it is feasible to see counselor weight as a non-factor. However, we found that prior experience in counseling did not mediate the weight bias participants demonstrated. This result gives room for concern that weight bias may diminish the initial value of core conditions and counselor attributes studied in the past. Perhaps weight bias is pervasive in the decision to work with a counselor.
Implications
Despite years of education and experience, weight bias may rule out competent counselors. Professionals who fall outside the average body weight are hyper-visible (Beggan & DeAngelis, 2015) and prone to judgment of their weight. This study fills a gap in the research pertaining to the way weight bias influences a client’s willingness to trust, follow counselor advice, and select their counselors. Knowing how weight bias impacts the counseling profession can help counselors become aware of an issue that may affect the therapeutic alliance. In response to the study results, we identified two key implications for the counseling profession.
First, the results are indicative of a multicultural issue. Many people see weight as a medical concern instead of a social justice issue (Christensen, 2021). This idea limits the amount of education and training counseling graduate students receive on the topic of weight, leading to the request to address weight in multicultural courses as a core topic. Weight becomes intersectional among identities, and counselors must train to be sensitive to and inclusive of the topic of weight. Broaching weight may feel uncomfortable but be necessary to strengthen the therapeutic relationship.
Second, recognizing that weight bias may impact a client’s willingness to select, follow the counsel of, or trust a counselor reiterates the importance of knowing the factors influencing the counseling relationship. Counselors should acknowledge that stereotypes, discrimination, and oppression influence the counseling relationship (Ratts et al., 2016). Counselors should not ignore weight bias as a possible stereotype and should be comfortable discussing it with their clients. Additionally, the multicultural competencies note that “Counselors know when to initiate discussions with regard to the influences of identity development, power, privilege, and oppression within the counseling relationship” (Ratts et al., 2016, p. 41). As society continues to push the thin ideal while simultaneously pushing body acceptance at any size, these contradictory messages will keep weight bias at the forefront of how others are judged.
Until weight bias is erased, counselors must be vigilant in understanding how they show up in the session, what message a client may perceive by their body weight, and how to broach the topic to strengthen the therapeutic alliance. If counselors seek to help reduce weight bias in society, they may benefit from reflecting on their own biases, privileges, and experiences with oppression in this area. They also may consider challenging potential biases through professional development, group or individual counseling supervision, or literature about weight bias in society.
Limitations
Like all studies, this study contains limitations. One limitation is the subjectivity of weight. Without guidelines for what constitutes overweight and underweight, this study heavily relied on participants’ perceptions of these variables, which may be inconsistent across participants. Not specifying these variables opened interpretation for the overlapping areas of overweight versus obese or underweight versus extremely thin. Participants in each treatment condition may have visualized different hypothetical counselors than peers in the same treatment group. Using images may improve the specificity of the variable in future studies.
Additionally, there was no identified gender for the hypothetical counselors in each treatment condition, allowing participants to visualize any gender of counselor they chose. This lack of specificity may have created a moderating variable. Women represent higher numbers in the counseling profession. Women experience more discrimination than men (McHugh & Kasardo, 2012; Roehling et al., 2007), and it is unknown if people who identify as gender non-binary experience more or less weight bias. By not distinguishing the gender of the counselor, our ability to make inferences across genders is limited. Creating a study that specifies multiple genders may yield more representative results.
Another limitation is that a non-parametric test (e.g., Welch’s ANOVA) was used instead of parametric tests with more statistical power. The decision to use the non-parametric test was unavoidable because of violating the required assumptions. At the same time, future research may corroborate our findings using a parametric test if data allow. Future research may also replicate this study using multivariate ANOVA (MANOVA), which considers correlations of dependent variables.
Lastly, social desirability and self-reporting may have impacted responses. While completing the questionnaire, feelings about weight bias may have occurred outside of participants’ awareness, causing cognitive dissonance. To resolve this dissonance, responses may have overtly favored accepting the overweight counselor or selecting fewer negative answers on the AFA. Participants also reported their own weight bias, which may have presented a self-report limitation. The results of overweight counselors having higher mean scores on Trust and Selection than average-weight counselors give room for consideration that social desirability may have influenced some of the participants’ answers. Future studies may benefit from including a test for social desirability or implicit association tests to increase the study’s validity.
Future Considerations
Future considerations for research encompassing weight bias across the spectrum would require developing an anti-thin attitude measure to identify weight attitudes toward underweight individuals accurately. This measure would be beneficial for bringing more awareness to underweight discrimination and measuring its impact on professionals and members of society. As society continues to push the thin ideal, people will strive to fit that ideal. However, as our results suggest, underweight counselors may face significant weight bias from clients. Consequently, counselors would benefit from a measure created to address underweight bias.
The counseling profession lacks extensive, meaningful research regarding the physical and educational factors that clients find most important in selecting, trusting, and following the advice of a counselor. Another factor to incorporate in future research is a counselor’s level of education and expertise. Clients may more favorably evaluate an average weight counselor with a specialist or doctoral degree than an underweight or overweight colleague with the same credentials. If weight bias influences these variables despite the skill level of the counselor, clients may miss receiving help from highly trained and educated people. Additionally, directly exploring the role that empathy, congruence, and strengths-based counseling have compared to weight bias may yield significant findings.
A final consideration for future research involves focusing on counselors who work in the ED field, a specialty that deals with eating, weight, body image, and exercise. Though we did not find significant differences in this study between those with and without an ED, our hypothetical counselor was not an ED counselor. These counselors may experience more judgment and assumptions of lifestyle choices by their clients, as they are considered specialists in EDs. Studies show that being underweight may indicate an ED, such as anorexia or binge eating disorder (Davies et al., 2020a; Marini, 2017). It is unknown if clients would replicate the results found in this study regarding counselors in the ED field.
Conclusion
This study examined participants’ weight bias toward hypothetical counselors of different weights. Our results highlight the existence of weight bias toward counselors on both ends of the weight spectrum. Even with strengthening the counseling relationship through empathy, congruence, and unconditional positive regard, counselors may benefit from reflecting on potential client weight bias and its impact on their therapeutic alliance. Additionally, weight as a multicultural issue increases counselors’ competence in addressing the prejudice and stereotypes that may limit their client’s willingness to trust them, follow their advice, or select them as their counselor.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Ackerman, S. J., & Hilsenroth, M. J. (2001). A review of therapist characteristics and techniques negatively impacting the therapeutic alliance. Psychotherapy: Theory, Research, Practice, Training, 38(2), 171–185.
https://doi.org/10.1037/0033-3204.38.2.171
Allen, M. L., Cook, B. L., Carson, N., Interian, A., La Roche, M., & Alegría, M. (2017). Patient-provider therapeutic alliance contributes to patient activation in community mental health clinics. Administration and Policy in Mental Health and Mental Health Services Research, 44(4), 431–440. https://doi.org/10.1007/s10488-015-0655-8
Allison, M., & Lee, C. (2015). Too fat too thin: Understanding bias against overweight and underweight in an Australian female university student sample. Psychology & Health, 30(2), 189–202.
https://doi.org/10.1080/08870446.2014.954575
Beggan, J. K., & DeAngelis, M. (2015). “Oh, my God, I hate you”: The felt experience of being othered for being thin. Symbolic Interaction, 38(3), 371–392. https://doi.org/10.1002/SYMB.162
Bucchianeri, M. M., Eisenberg, M. E., & Neumark-Sztainer, D. (2013). Weightism, racism, classism, and sexism: Shared forms of harassment in adolescents. Journal of Adolescent Health, 53(1), 47–53.
https://doi.org/10.1016/j.jadohealth.2013.01.006
Centers for Disease Control and Prevention. (2022, June 3). Defining adult overweight & obesity. https://www.cdc.gov/obesity/basics/adult-defining.html
Cermák, I., Osecká, L., Rehulková, O., & Blatný, M. (1993). Judging others according to yourself: II. Interpersonal characteristics of personality and the structure of interpersonal attributions. Studia Psychologica, 35(2), 185. https://librarylink.uncc.edu/login?url=https://www.proquest.com/scholarly-journals/judging-others-according-yourself-ii/docview/1306142557/se-2?accountid=14605
Christensen, K. N. (2021). Factors related to weight-bias among counselors (Order No. 28541740). Available from Dissertations & Theses @ University of North Carolina Charlotte. (2562239518).
Clabaugh, A., Karpinski, A., & Griffin, K. (2008). Body weight contingency of self-worth. Self and Identity, 7(4), 337–359. https://doi.org/10.1080/15298860701665032
Clark, A. J. (2010). Empathy: An integral model in the counseling process. Journal of Counseling & Development, 88(3), 348–356. https://doi.org/10.1002/j.1556-6678.2010.tb00032.x
Coladarci, T., Cobb, C. D., Minium, E. W., & Clarke, R. B. (2011). Fundamentals of statistical reasoning in education (3rd ed.). Wiley.
Crandall, C. S. (1994). Prejudice against fat people: Ideology and self-interest. Journal of Personality and Social Psychology, 66(5), 882–894. https://doi.org/10.1037/0022-3514.66.5.882
Davies, A., Burnette, C. B., & Mazzeo, S. E. (2020a). Real women have (just the right) curves: Investigating anti-thin bias in college women. Eating and Weight Disorders, 25, 1711–1718.
https://doi.org/10.1007/s40519-019-00812-7
Davies, A., Burnette, C. B., & Mazzeo, S. (2020b). Black and White women’s attributions of women with underweight. Eating Behaviors, 39, 101446. https://doi.org/10.1016/j.eatbeh.2020.101446
Faul, F., Erdfelder, E., Lang, A.-G., & Buchner, A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39, 175–191.
https://doi.org/10.3758/BF03193146
Feller, C. P., & Cottone, R. R. (2003). The importance of empathy in the therapeutic alliance. The Journal of Humanistic Counseling, Education and Development, 42(1), 53–61.
https://doi.org/10.1002/j.2164-490x.2003.tb00168.x
Grimes, W. R., & Murdock, N. L. (1989). Social influence revisited: Effects of counselor influence on outcome variables. Psychotherapy: Theory, Research, Practice, Training, 26(4), 469–474. https://doi.org/10.1037/h0085465
Hauser, M., & Hays, D. G. (2010). The slaying of a beautiful hypothesis: The efficacy of counseling and the therapeutic process. The Journal of Humanistic Counseling, Education and Development, 49(1), 32–44.
https://doi.org/10.1002/j.2161-1939.2010.tb00085.x
Hinman, N. G., Burmeister, J. M., Kiefner, A. E., Borushok, J., & Carels, R. A. (2015). Stereotypical portrayals of obesity and the expression of implicit weight bias. Body Image, 12, 32–35.
https://doi.org/10.1016/j.bodyim.2014.09.002
Hutson, D. J. (2013). “Your body is your business card”: Bodily capital and health authority in the fitness industry. Social Science & Medicine, 90, 63–71. https://doi.org/10.1016/j.socscimed.2013.05.003
Kim, E., & Kang, M. (2018). The effects of client–counselor racial matching on therapeutic outcome. Asia Pacific Education Review, 19(1), 103–110. https://doi.org/10.1007/s12564-018-9518-9
Kinavey, H., & Cool, C. (2019). The broken lens: How anti-fat bias in psychotherapy is harming our clients and what to do about it. Women & Therapy, 42(1–2), 116–130. https://doi.org/10.1080/02703149.2018.1524070
Lacroix, E., Alberga, A., Russell-Mathew, S., McLaren, L., & von Ranson, K. (2017). Weight bias: A systematic review of characteristics and psychometric properties of self-report questionnaires. Obesity Facts, 10(3), 223–237. https://doi.org/10.1159/000475716
Lewis, R. J., Cash, T. F., & Bubb-Lewis, C. (1997). Prejudice toward fat people: The development and validation of the Antifat Attitudes Test. Obesity Research, 5(4), 297–307. https://doi.org/10.1002/j.1550-8528.1997.tb00555.x
Liu, H. (2015). Comparing Welch ANOVA, a Kruskal-Wallis test, and traditional ANOVA in case of heterogeneity of variance. https://doi.org/10.25772/BWFP-YE95
Lorr, M. (1965). Client perceptions of therapists: A study of the therapeutic relation. Journal of Consulting Psychology, 29(2), 146–149. https://doi.org/10.1037/h0021924
Marini, M. (2017). Underweight vs. overweight/obese: Which weight category do we prefer? Dissociation of weight-related preferences at the explicit and implicit level. Obesity Science & Practice, 3(4), 390–398. https://doi.org/10.1002/osp4.136
McHugh, M. C., & Kasardo, A. E. (2012). Anti-fat prejudice: The role of psychology in explication, education and eradication. Sex Roles, 66(9–10), 617–627. https://doi.org/10.1007/s11199-011-0099-x
McKee, K., & Smouse, A. D. (1983). Clients’ perceptions of counselor expertness, attractiveness, and trustworthiness: Initial impact of counselor status and weight. Journal of Counseling Psychology, 30(3),
332–338. https://doi.org/10.1037/0022-0167.30.3.332
Meadows, A., & Daníelsdóttir, S. (2016). What’s in a word? On weight stigma and terminology. Frontiers in Psychology, 7, 1527. https://doi.org/10.3389/fpsyg.2016.01527
Meyer, O. L., & Zane, N. (2013). The influence of race and ethnicity in clients’ experiences of mental health treatment. Journal of Community Psychology, 41(7), 884–901. https://doi.org/10.1002/jcop.21580
Moller, N., & Tischner, I. (2019). Young people’s perceptions of fat counsellors: “How can THAT help me?” Qualitative Research in Psychology, 16(1), 34–53. https://doi.org/10.1080/14780887.2018.1536384
Montoya, R. M., & Horton, R. S. (2013). A meta-analytic investigation of the processes underlying the similarity-attraction effect. Journal of Social and Personal Relationships, 30(1), 64–94.
https://doi.org/10.1177/0265407512452989
Nienhuis, J. B., Owen, J., Valentine, J. C., Winkeljohn Black, S., Halford, T. C., Parazak, S. E., Budge, S., & Hilsenroth, M. (2018). Therapeutic alliance, empathy, and genuineness in individual adult psychotherapy: A meta-analytic review. Psychotherapy Research, 28(4), 593–605. https://doi.org/10.1080/10503307.2016.1204023
Nutter, S., Russell-Mayhew, S., Arthur, N., & Ellard, J. H. (2018). Weight bias and social justice: Implications for education and practice. International Journal for the Advancement of Counselling, 40(3), 213–226.
https://doi.org/10.1007/s10447-018-9320-8
Puhl, R. M., Gold, J. A., Luedicke, J., & DePierre, J. A. (2013). The effect of physicians’ body weight on patient attitudes: Implications for physician selection, trust and adherence to medical advice. International Journal of Obesity, 37(11), 1415–1421. https://doi.org/10.1038/ijo.2013.33
Puhl, R. M., & Heuer, C. A. (2010). Obesity stigma: Important considerations for public health. American Journal of Public Health, 100, 1019–1028. https://doi.org/10.2105/AJPH.2009.159491
Puhl, R. M., Latner, J. D., King, K. M., & Luedicke, J. (2014). Weight bias among professionals treating eating disorders: Attitudes about treatment and perceived patient outcomes. International Journal of Eating Disorders, 47(1), 65–75. https://doi.org/10.1002/eat.22186
Ratts, M. J., Singh, A. A., Nassar-McMillan, S., Butler, S. K., & McCullough, J. R. (2016). Multicultural and social justice counseling competencies: Guidelines for the counseling profession. Journal of Multicultural Counseling and Development, 44(1), 28–48. https://doi.org/10.1002/jmcd.12035
Roehling, M. V., Roehling, P. V., & Pichler, S. (2007). The relationship between body weight and perceived weight-related employment discrimination: The role of sex and race. Journal of Vocational Behavior, 71(2), 300–318. https://doi.org/10.1016/j.jvb.2007.04.008
Ruggs, E. N., King, E. B., Hebl, M., & Fitzsimmons, M. (2010). Assessment of weight stigma. Obesity Facts, 3(1), 60–69. https://doi.org/10.1159/000273208
Schwartz, M. B., Vartanian, L. R., Nosek, B. A., & Brownell, K. D. (2006). The influence of one’s own body weight on implicit and explicit anti-fat bias. Obesity, 14(3), 440–447. https://doi.org/10.1038/oby.2006.58
Sharf, J., Primavera, L. H., & Diener, M. J. (2010). Dropout and therapeutic alliance: A meta-analysis of adult individual psychotherapy. Psychotherapy: Theory, Research, Practice, Training, 47(4), 637–645.
https://doi.org/10.1037/a0021175
Taber, K. S. (2018). The use of Cronbach’s alpha when developing and reporting research instruments in science education. Research in Science Education, 48, 1273–1296. https://doi.org/10.1007/s11165-016-9602-2
Tischner, I. (2019). Tomorrow is the start of the rest of their life—so who cares about health? Exploring constructions of weight-loss motivations and health using story completion. Qualitative Research in Psychology, 16(1), 54–73. https://doi.org/10.1080/14780887.2018.1536385
Tudor, K. (2011). Rogers’ therapeutic conditions: A relational conceptualization. Person-Centered & Experiential Psychotherapies, 10(3), 165–180. https://doi.org/10.1080/14779757.2011.599513
Zar, J. H. (1998). Biostatistical analysis (4th ed.). Prentice Hall.
Amy Biang, PhD, LCMHC, CEDS, is an assistant professor at Northern Arizona University. Clare Merlin-Knoblich, PhD, is an associate professor at the University of North Carolina at Charlotte. Stella Y. Kim, PhD, is an assistant professor at the University of North Carolina at Charlotte. Correspondence may be addressed to Amy Biang, 15451 N 28th Ave, Phoenix, AZ 85053, amy.biang@nau.edu.