Oct 15, 2014 | Article, Volume 3 - Issue 3
Katie L. Haemmelmann, Mary-Catherine McClain
Research in chronic illness and disability (CID) in college students has demonstrated that students with disabilities encounter more difficulties psychosocially than their nondisabled counterparts. Subsequently, these difficulties impact the ability of these students to successfully adapt. Using the illness intrusiveness model in combination with cognitive behavioral therapy (CBT), the authors propose therapeutic interventions that could be taken with these students to enhance their overall well-being, adaptation and academic success. The authors also provide final thoughts with directions for future research and application.
Keywords: chronic illness, disability, illness intrusiveness model, cognitive behavioral therapy, college students with disabilities
Chronic illness and disability (CID) impact more than 35 million Americans, often interfering with their everyday life (Livneh & Antonak, 1997). The condition is typically accompanied by a prolonged course of treatment, an often uncertain prognosis, constant and intense psychosocial stress, increasing interference with the performance of daily activities and life roles, and conflict with family and friends (Livneh & Antonak, 1997). Approximately 11% of undergraduate students reported having a disability in 2008 (National Center for Education Statistics, 2011) and 88% of colleges are continuing to enroll students with disabilities (The Princeton Review, 2011). In addition to adjusting to the presence of a disability, adjustment to independent living and beginning academic courses at an undergraduate institution can be challenging for someone with a chronic illness or disability.
The severity of the disability and its functional limitations do not always correlate in a uniform pattern with coping and adjustment (Lustig, Rosenthal, Strauser, & Haynes, 2000). Similarly, disability may include permanent and significant changes in an individual’s body appearance, functional capacities, body image and self-concept (Lustig et al., 2000). This variable, typically referred to as psychosocial adaptation, becomes compounded among college students and deserves further investigation. In order to better understand the adaptation process, conceptualize cases, and provide the most effective services to college students with disabilities, it is important for researchers to test comprehensive models specifically designed to aid in the interpretation of illness-induced interference. Similarly, counselors need to understand and implement empirically supported interventions, techniques and related strategies to assist individuals with disabilities in the transition to higher education.
Currently, there is a dearth of information pertaining to the adjustment of young people that can be applied to college students with chronic illness and disabilities. Additionally, theories within the rehabilitation, quality of life, and counseling literature are used to translate theory into practice. After describing the nature of transitions individuals face upon entering college, discussing current legislative policies, and examining identity formation, this article provides an overview of the illness intrusiveness model and theoretical framework for CBT. Next, the article offers strategies for implementing an integrated model, including elements of illness intrusiveness and CBT, with the college population. Treatment strategies and intervention techniques are also described. Finally, accommodations, the importance of social support, and future directions are addressed.
Identity Formation and College Transition
Identity formation typically continues during the late teens and early 20s (Luyckx, Schwartz, Soenens, Vansteenkiste, & Goossens, 2010), which also is the time when youth attend or transition to higher education. During this time, the individual is still a child on one hand, yet an adult on the other hand. According to Wright (1983), this creates an overlapping situation in which the adolescent with the disability is not only struggling with the problematic overlap of “child” and “adult,” but also that of “normal” and “disabled.” This is a complex time filled with instability and uncertainty regarding the years ahead. A synthesized sense of identity can provide beneficial effects on an individual’s adjustment (Luyckx et al., 2010), and a comprehensive sense of self can be facilitated through psychotherapeutic interventions. Also, the process of adaptation is multidimensional, complex and subjective (Smart, 2001). Consequently, a comprehensive framework for assessing and intervening is critical for fostering positive counseling outcomes.
Preparing someone for a career is a task that should not be taken lightly, but given the utmost attention. Career can be defined as the “time extended working out of a purposeful life pattern through work undertaken by the person” (Sampson, Reardon, Peterson, & Lenz, 2004, p. 6).This definition helps clarify the idea that a career is an activity people engage in regularly through a lifetime. Employment opportunities for this population are already limited by job choice (variability), available hours, and reduced salary (Schmidt & Smith, 2007). Also, enhancing potential job opportunities for individuals with disabilities is beneficial, as research has shown that the onset of a disability can negatively influence one’s vocational identity—potentially leading to poor adjustment, limited self-direction and goal setting, and lower career development (Enright, Conyers, & Szymanski, 1996; Skorikov & Vondracek, 2007; Yanchak, Lease, & Strauser, 2005).
According to Kirsh et al. (2009), with the economy becoming increasingly knowledge-based, and as the forces of globalization transform to eliminate entry-level positions, people with limitations in cognitive function may become increasingly marginalized. This is not to say that this population can maintain only entry-level positions, but to reiterate that as there is an increase in students with disabilities attending universities, there is an increase in job requirements, qualifications and performance levels required by all populations. Enhancing education and overall college experience with counseling will assist these students as they acquire new skills to use for the rest of their lives.
Need for Psychotherapeutic Interventions
In the past 20 years, there has been a trend of more persons with disabilities pursing higher education. Based on the National Organization on Disability Harris Survey of Americans with Disabilities conducted in 2000, there was a marked increase in persons with disabilities having graduated from high school (77%) compared to those in 1986 (61%). Based on several legislative and social policies implemented in the 1980s (Canadian Human Rights Act, 1985) and 1990s (Individuals with Disabilities Education Act, 1997 [IDEA]), an estimated 8–18% of students in higher education are students with disabilities (Sachs & Schreuer, 2011). Furthermore, persons with disabilities entering postsecondary education are making significant progress toward successful completion of their program of studies (Stodden & Whelley, 2004). This is why educators, administrators, and policymakers are working to improve services while also providing accommodations, interventions, and support services in postsecondary settings (Barazandeh, 2005; Brinckerhoff, Shaw, & McGuire, 1992; Dowrick, Anderson, Heyer, & Acosta, 2005; Dutta, Kundu, & Schiro-Geist, 2009; Johnson, 2006; Swanson & Hoskyn, 1998; West et al., 1993). Examples of such accommodations include transportation, separate locations for test taking, access to private study rooms, and extended time on exams.
With the reauthorization of the IDEA in 1997 (PL 94-142), there was an increase of higher expectations upon quality preparation to postsecondary education and employment for persons with intellectual disabilities. The Americans with Disabilities Act (ADA) sought to provide reasonable accommodations to ensure equal access to learning and work environments (Jacob & Hartshorne, 2007). The vocational rehabilitation system exists to provide assistance to individuals with disabilities seeking employment. This can be a good support system for those interested in higher education, but only supports eligible consumers (Gilmore & Bose, 2005). While these recent pieces of legislation have been incredibly beneficial and have encouraged individuals and professionals alike to actively engage in advocacy, they do not specifically address the access or right to counseling as an appropriate accommodation.
As students transition to postsecondary education, fear of the unknown affects not only those transitioning, but the people around them (e.g., professors, administrators or counselors) as they experience a change in roles. Parents, for instance, may want to protect their child from the risks of the larger world, and limit them by choosing self-contained and protected programs (Stodden & Whelley, 2004). This approach may deprive students of the opportunity for further education. With optional counseling specifically designed for those individuals with disabilities transitioning into the next phase of life, this may be reassuring not only for the student, but also for the student’s primary support system. One counseling model to implement in such situations is the illness intrusiveness model.
Illness Intrusiveness Model: Theoretical Framework
The illness intrusiveness model was developed based on the idea that illness-induced interference, in addition to interests and valued activities, compromises one’s psychological well-being—ultimately contributing to emotional distress. It is derived from a variety of sources such as functional losses, treatment side effects, disease and treatment-related lifestyle disruptions, and disease-related anatomical changes (Devins, 2010). The model postulates that when there is a decrease in positively reinforcing outcomes from valued activities and limited personal control (e.g., mood level) to obtain positive outcomes and avoid negative ones, significant adaptive changes and coping demands occur (Devins, 2010).
By examining the five factors of disease—that is (1) treatment requirements, (2) personal control, (3) nature of life outcomes, (4) psychological factors, and (5) social factors—one can inspect the level of participation in valued activities, also known as illness intrusiveness. Illness intrusiveness may serve or act as a mediating variable by which unbiased circumstances of disease and treatment influence psychosocial well-being and emotional distress. Specifically, illness intrusiveness is based not only on the experience of the person, but also the psychological characteristics based on objective and subjective concepts (Roessler, 2004).
This model posits that social and psychological factors have a direct effect on life outcomes. Time spent transitioning into college is heavily influenced by social factors, which can create positive or negative experiences in the individual. If the social factors weigh heavily on the individual’s psychological factors in a maladaptive way, the person’s coping abilities and adaptation skills may be compromised and lead to undesirable outcomes. The model also encompasses the idea of locus of control, presented as personal control of self-efficacy (similar to what was described earlier in this article), the idea being that low levels of personal control result in learned helplessness (Roessler, 2004). Furthermore, the theoretical framework hypothesizes that intrusiveness mediates the psychosocial effect of chronic conditions. Indirectly through the effects on intrusiveness, illness and treatment variables are believed to impact subjective well-being (Bettazzonie, Zipursky, Friedland, & Devins, 2008). Incorporation of the illness intrusiveness model can assist professional counselors and clients alike in laying out a clear path of focus (i.e., the five factors of disease; Roessler, 2004) while simultaneously increasing one’s coping and adaptation skills, as well as external allocation of self-efficacy. After describing an assessment tool and following a review of ways in which the illness intrusiveness model has been applied to specific illnesses and populations, the authors provide a rationale for implementing this model among college students with disabilities.
Application of the Illness Intrusiveness Model
Previous research suggests that applying various components of the illness intrusiveness model (e.g., examination of domains) in end-of-stage renal disease clients is effective in objectively measuring varying modes of treatment (e.g., transplantation, dialysis; Devins, et al., 1983). Furthermore, the levels of illness intrusiveness directly affected the psychosocial impact of the condition. Additionally, it was noted that severity levels of hyperhidrosis shared a significant positive correlation with scores on the Illness Intrusiveness Rating Scale (IIRS) (Devins et al., 1983). Intrusiveness scores were weakly related to efforts to control the condition (i.e., medications and ointments), which is indicative of the value of knowledge of self-care techniques and action-based knowledge (Roessler, 2004). Empirical support also has pointed to illness intrusiveness as a precipitant for depression and for feeling a loss of control. This has been observed in persons with arthritis, cancer, diabetes and multiple sclerosis (Roessler, 2004). Furthermore, Devins (2010) notes that levels of illness intrusiveness vary according to illness severity, and weigh in differently for valued activities. This is of particular importance when collaborating therapeutically with college students with disabilities, since there are a wide range of disabilities (e.g., learning disabilities, physical disabilities, mental illness) and they vary in severity (e.g., psychiatric symptoms, functional ability). Subsequently, even among college students with disabilities, there is a wide array of differences; one would expect a shift in valued activities based on transitioning (e.g., social support, school involvement) and disability interference.
The illness intrusiveness model is ideal for working with college students with disabilities because it focuses on improving psychosocial adaptation outcomes. Specifically, it stresses the effect of psychological, social and environmental variables on the interpretation of the disease (Roessler, 2004). This is essential knowledge for implementing effective therapeutic interventions for this population, because often the transition into the college atmosphere impacts the interpretation of the individual and the disability. Additionally, the theoretical framework helps to estimate the effect of disease interpretation and the intrusiveness of treatment factors (Roessler, 2004).
As mentioned previously, the college student population typically struggles to form self-identity in terms of a developmental framework, and intrusiveness is presented in this model as both an objective and subjective concept. This is noteworthy since these individuals are still processing their identity, their life goals, and their viewpoints. With a helping professional, they can work collaboratively to change perspectives that may be distorted or need reframing. Finally, the illness intrusiveness model implies that intrusiveness has a direct effect on both personal control and life outcomes (Roessler, 2004). Through prevention or early intervention, college students with disabilities will realize and begin to feel empowered as they recognize their ability to take control of their lives. This can further be reinforced by seeing positive outcomes almost immediately when collaborating with the practitioner. Before discussing how the illness intrusiveness model can be integrated with other treatment approaches and how it can be applied to college students with disabilities, it is useful to provide a brief history of general psychotherapy with disabled persons and core principles of CBT with this population.
History of Counseling with Persons with Disabilities
Over the past several decades, four basic approaches to adjustment services (e.g., work acclimation) have emerged in disability literature. While the approaches are not mutually exclusive, each offers a new viewpoint on adjustment for persons with disabilities and sheds perspective on both the client and practitioner.
The work acclimation approach utilizes the psychological principle that the greater degree to which a current environment resembles a future environment, the more likely an individual would behave in the same manner in the future environmental setting. Programs utilized almost exclusively in work centers were pay incentives, peer and supervisory work pressure, production rate feedback, lead workers, and status-promotion incentives.
The problem-solving approach to adjustment services represents the second model. It begins by obtaining baseline measures of the problem and delineates adjustment services to any treatment and training modalities necessary to ameliorate the problem, thus allowing the student to succeed academically and vocationally. It is within this model that the approach employs behavioral counseling and behavioral modification techniques that can be applied in multiple settings or situations (Couch, 1984). For example, in a university setting, students with disabilities can be seen for brief or extended psychological services, in which baseline and outcome data are used to encourage behavioral modification and monitor intrusiveness.
In the developmental approach, clients are viewed as capable, problem-solving individuals, fully qualified to accept responsibility for life and determine personal direction. They are taught self-responsibility and self-potency, as well as beliefs, values, and skills, all of which will enable them to solve problems, maintain a sense of self-worth, and enhance personal identity.
Finally, the education approach takes on a different perspective and focuses on skill deficits. This helps the client to engage in remedial education, learn about available resources, and conquer tasks. Examples of such tasks include acquiring a driver’s license or earning a college degree (Couch, 1984). A focus on skill deficits blends well with the theoretical origins of CBT. The following section briefly describes the framework of CBT.
Theoretical Framework for CBT
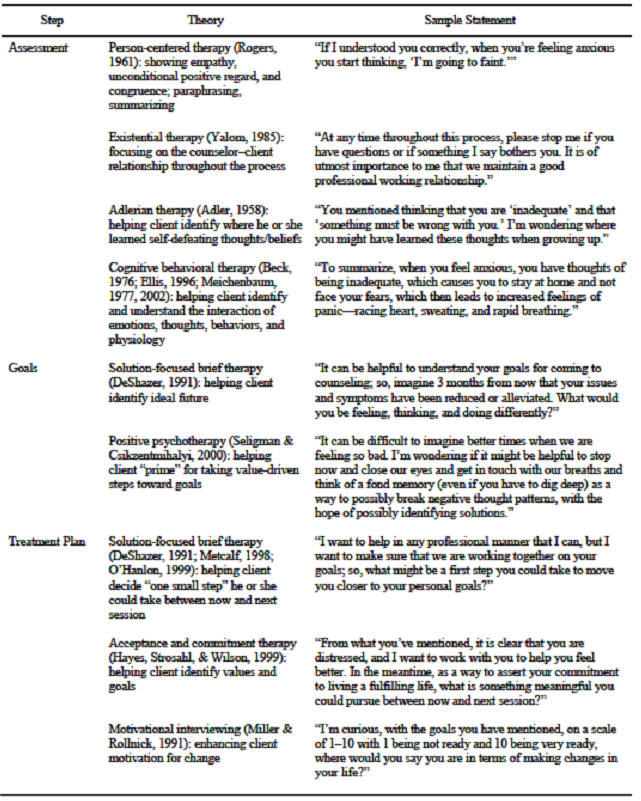
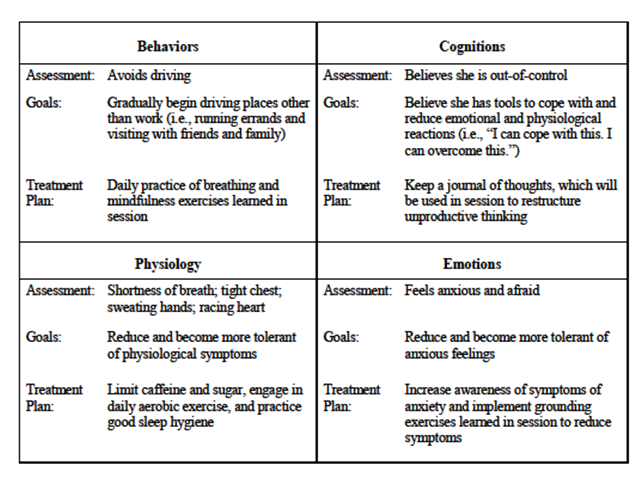
Three main goals set forth in the field of rehabilitation counseling pertain to affective goals, cognitive goals, and behavioral goals (Parker, Szymanski, & Patterson, 2005). This is similar to taking a holistic or ecological approach in the field of counseling. It is important to treat not just specific aspects of individuals, but to treat the individuals as humans in their entirety. Thus, when addressing college students with disabilities, it could be important to integrate the illness intrusiveness model with that of CBT. The model itself enables the counselor to apply cognitive and behavioral interventions in order to reduce illness intrusiveness strategically, which could encourage the client to participate in valued activities, redefine personal goals, and restructure irrational beliefs related to intrusiveness (Roessler, 2004).
Furthermore, the counselor is able to provide knowledge of self-management and self-care skills, which is facilitated by task-focused coping and problem-solving skills, both of which are central constructs from CBT and can lead to a positive impact on illness intrusiveness. Finally, by including personal control or self-efficacy as critical variables in the illness intrusiveness model, and as a way to better understand life outcomes, individuals are supported in impacting their perceived self-control on life outcomes related to educational achievement and overall well-being (Roessler, 2004).
Integrating the Illness Intrusiveness Model and CBT
Prior to discussing techniques and skills that can be utilized within this framework and among this population, the present article discusses the importance of incorporating specific concepts or tasks within the realm of a client’s goals. Examining client outcomes of counseling interventions is necessary in the field of mental health and other related fields to acquire knowledge on effective treatments, obtain financial funds, establish accountability, and achieve long-term positive results. In addition to cognitive behavioral techniques, client variables with this population may impact the outcome of therapy. For example, Ju (1982) discovered that clients having 12 years of education do not seem to benefit from receiving information and exploring feelings. Rather, they tend to benefit from counselors who predominantly listen attentively and focus on the facilitation of client expression and concern. Additionally, clients with more than 12 years of education tend to reap the most benefits from counselors who not only emphasize the processing of information, but also share personal values, opinions and experiences with the client. This has potential treatment implications from the start of counseling, because to be a viable candidate for collegiate studies, the individual has to successfully complete 12 years of prior education (either formally or in an alternative manner). As students attending school will always vary widely in age, this factor should be kept in the forefront of the counselor’s mind.
Rehabilitation counseling has a history of being goal directed and behaviorally oriented as opposed to a psychodynamically oriented treatment (Ju, 1982). Similarly, a defining characteristic of CBT is the proposal that symptoms and dysfunctional behaviors are often cognitively mediated; thus, modifying dysfunctional thinking and beliefs can lead to improvement (Butler, Chapman, Forman, & Beck, 2006). By following a psychoeducational model, emphasizing therapy as a learning process that includes acquiring and practicing new skills, learning new ways of thinking, and obtaining more effective ways of coping (Corey, 2005), students with disabilities can benefit from improved adjustment to the college atmosphere.
A central role in CBT is the treatment rationale, which provides clients and counselors with a model of etiology and treatment (Addis & Carpenter, 2000). It is within this framework that the counselor teaches the client to identify, evaluate and change dysfunctional thinking patterns so therapeutic changes in mood and behavior can occur (Padesky & Greenberger, 1995). Additionally, it is imperative to address an individual’s metacognitions, or understanding of self-knowledge, in order to grasp the process of cognition and its outcomes (Hresko & Reid, 1988).
Thomas and Parker (1984) remark on the need for effective counseling with persons with disabilities, identifying the following two main focuses: career and psychosocial issues. This only reiterates the need for therapeutic intervention for this specific population who is trying to further education in order to obtain chosen careers while simultaneously adapting to a new lifestyle and appropriately managing the disabilities. It is by weaving together the major tenets presented in CBT (e.g., thoughts, moods, behaviors, biology, and environment; Padesky & Greenberger, 1995), with the five factors of disease (Roessler, 2004) in the illness intrusiveness model that practitioners will be better able to serve this population. This is not to say that all ten areas will need to be remedied or addressed for each individual seeking treatment. Rather, counselors need to be aware that each individual will have different needs to meet or areas to improve.
Akridge (1981) stated that psychological adjustment is an ongoing process of evaluating the self-in-situation to adaptation. A comprehensive self-assessment in the psychosocial domain is the process of summarizing one’s satisfactions and dissatisfactions within the self and the personally relevant aspects of one’s situation. This could be undertaken within the realm of the therapeutic alliance as the client and counselor are working collaboratively toward agreed-upon goals and a focus on improvement. One could suggest the completion of a prescribed homework assignment addressing the area needing further investigation. The client could then experience an increase in self-confidence through exploring each domain, thus decreasing the impact of intrusiveness.
To begin treatment successfully, the counselor and client need to establish a positive, collaborative working relationship. Aaron Beck emphasized the quality of the therapeutic relationship as basic to the application of cognitive therapy (Corey, 2005). The core therapeutic conditions described by Carl Rogers in his person-centered approach are viewed by cognitive therapists as being necessary, but not sufficient, in producing optimal therapeutic effects (Corey, 2005).
The collaborative relationship is essential because it conveys to clients that they possess important information that must be shared to solve problems. Counselors employ general strategies and treatment models while clients are keepers of all the information about unique experiences—only clients can describe thoughts and moods (Padesky & Greenberger, 1995). This again enables clients to build self-esteem and feelings of self-worth so they begin to feel confident in skills and abilities in areas they may doubt. This in turn impacts the domains of career choice, personal control, life outcomes, and psychological and social factors.
In order to be successful at the collegiate level, one must possess sufficient organizational skills. When working with students with disabilities, it is important to address this topic and readdress it throughout the psychotherapeutic process. This approach is key to assist clients in learning to control the things they can in regards to homework assignments, readings, and note-taking, so that if something unexpected or overwhelming becomes more pertinent in unpreventable circumstances, clients will be able to recognize that they have done what they can to contain circumstances within their personal control.
This also relates back to the topic of increasing awareness of metacognition and the cognitive processes. For example, a student may begin to recognize trouble learning a particular topic or realize that there is a need to double-check written work. Similarly, a student may know to review all potential answers before choosing one as the correct option and understand the need to write a task down in order to remember it—essentially working to improve study skills (Hresko & Reid, 1988). Another concept or task that needs to be addressed with this population is that of appropriate accommodations within the university.
Accommodations
The Americans with Disabilities Act states that a disability is “a physical or mental impairment that substantially limits the individual in one or more major life activities” (Jacob & Hartshorne, 2007, p. 209). In such instances, in order for the students to receive and begin using the resources available within the setting and circumstances of the disability, they most likely will need to provide appropriate documentation. This may be an instance in which the therapist needs to take on a more pragmatic role and point the students to the designated resources so they can begin partaking in services. In addition, this simple task models advocacy for the individual. Once the client has taken the required steps to establish services, the practitioner will need to discuss with the client what kinds of services or accommodations may be needed, not only in the classroom, but also for transportation, living, studying, or choosing a career path. A client may need extra time taking tests, to meet with a class note-taker, or require special transportation or access within living space. Addressing organizational skills, as stated previously, may be a way to lead into the topic of study habits or assistance required in completing homework. Clients with mobility limitations or attention deficits may need instruction in specialized computer programs when required to write their thoughts on paper.
Altering Social Factors
Another task or concept that could be discussed within the counseling sessions is social support outside of the therapeutic alliance. Counselors should discuss with the client what types of support have been used in the past, what has worked, what did not work, and what could be modified. In some cases, clients may rely solely on their family for social support while others may rely on both family and friends. It would be beneficial to discuss the client’s preferred approach, to lay out the necessary steps, and to discuss the practicality of accomplishing the support. Some students may find it helpful to join various clubs or organizations, while others may wish to take part in a support group for persons with disabilities who are experiencing similar struggles. One option may be attending a counseling group offered at a university counseling center in which aspects of CBT and illness intrusiveness are addressed. Regardless of the outlet clients require to reach the most beneficial level of social support, they need a realistic understanding of the work required to reach the goal, a picture of what that process looks like, and a comprehensive understanding of why a good support system is necessary. This process will most likely be an ongoing learning experience for both the counselor and client as appropriate adjustments are made and learning and growth are facilitated.
Corey (2005) stated that the goal of CBT is to challenge the client to confront faulty beliefs with contradictory evidence that is gathered and can be evaluated (e.g., thought record). Another important aspect of CBT is goal setting. Padesky and Greenberger (1995) identified five key points about the importance of goal setting. First, setting goals helps identify what clients want to change, and provides guideposts to track progress. Charting such changes within the realm of the illness intrusiveness model can be done by utilizing the IIRS. This method helps the counselor gather baseline data at the onset of therapy, as well as monitor progress and present problems and symptoms.
Second, breaking general goals into specific goals simplifies the process into step-by-step plans for achieving general goals. Third, prioritizing goals helps the client and practitioner to decide which goals should be addressed first to provide the most beneficial outcome from therapy. Fourth, charting emotional changes helps monitor progress toward reaching goals. One can track changes based on emotional intensity and frequency, as well as specific mood-related symptoms. Finally, if the client is not making progress toward the goals, the counselor should consider breaking goals into even smaller steps, thus addressing the impediment to progress and considering changes in the treatment plan (Padesky & Greenberger, 1995).
One of the many reasons that agreement and clarity in goal setting is important is that regardless of individual differences, therapeutic outcomes are more apt to be positive when the counselor and client move toward the same goals (Ju, 1982). It is important that, when a client with specific disabilities makes progress toward and ultimately accomplishes each goal, reinforcement is applied by the practitioner. Reinforcement should be put into practice with intentionality and only when it promotes the attainment of skills and behaviors that the client needs to meet objectives. This skill needs to be used systematically rather than randomly (Thomas & Parker, 1984).
Other techniques that can be employed during the therapeutic process are that of Socratic questioning and activity scheduling. The first occurs by having the practitioner facilitate the telling and retelling of the story until opportunities for new meaning and story content develop (Corey, 2005). The use of Socratic questioning with students with disabilities enables these clients to realize they possess an understanding of their problems and preconceived notions, thoughts, or beliefs, and can alter them by elaborating and discussing matters further. In sum, the use of one simple technique could have a profound impact on illness intrusiveness factors such as personal control, social and psychological factors, and life outcomes.
Activity scheduling is not only another important aspect of CBT, but also an effective tool for decreasing illness intrusiveness. By engaging the client in planned activities, the client is encouraged to take an active role in life, as well as rediscover activities that may have previously been enjoyed. By discerning likes and dislikes, the client is able to increase personal insight and lower levels of depression. Activity scheduling also enables clients to see that they are capable of not just choosing the level and type of daily activities, but also seeing the big picture in choosing the direction of life outcomes. By realizing that they are able to control these tasks, the clients will also begin to reframe their locus of control from external to internal.
Finally, cognitive behavioral counselors aim to teach clients how to be their own therapist (Corey, 2005). As with any case, the hope is that the client can walk away from counseling and make use of skills acquired throughout the therapy process, applying them in daily living without therapeutic assistance. Whether treatment is permanently terminated or titrated down, the outcome will directly impact illness intrusiveness through treatment factors, feelings of personal control, life outcomes, and psychological and social factors.
While research within this specific population is lacking, the application of CBT among persons with intellectual disabilities has shown varied results. For example, Gustafsson et al. (2009) found weak correlations between behavioral therapy, CBT, and other forms of integrated support, while others (Oathamshaw & Haddock, 2006) showed that persons with intellectual disabilities and psychosis could link events and emotions, and differentiate feelings from behaviors—all skills necessary to engage in CBT. While effectiveness among those with intellectual disabilities may or may not be applicable to other types of disabilities, it is worthy to note that evidence exists. It would be beneficial to add to this evidence by supporting the use of CBT in combination with the illness intrusiveness model among students with disabilities transitioning into postsecondary education. Furthermore, by implementing this treatment modality among all college students with disabilities, researchers and counselors would be able to establish whether this model is effective with specific disabilities, cases in which it may not be as useful, and ways treatment can be modified or enhanced. Utilizing the authors’ presented model, future research could aim to investigate treatment of different types of college students with disabilities (e.g., learning disabilities, psychiatric disabilities, attention deficit hyperactivity disorder [ADHD]) and examine the effectiveness, similarities, differences, or any future directions. Treatment may be implemented in both the individual and group setting, and individual changes should be monitored by means of the IIRS.
Summary
The use of CBT among college students with disabilities transitioning into the college atmosphere could have a vast impact on illness intrusiveness. While, to the current authors’ knowledge, no recent studies have looked at implementing this model and mode of treatment, it would be an area worth investigating. The convergence of an empirically supported model such as the illness intrusiveness model, as well as a theory having a preponderance of empirical evidence such as CBT, would be a solid foundation to begin implementation of therapeutic intervention.
The college student population will have to face many potentially problematic situations when transitioning into the world of continued education. Some struggles that may be encountered when assisting college students in transition who also have disabilities may relate to homework completion, organizational stills, appropriate accommodations (e.g., extended test taking time, use of a note-taker, use of assistive computer technology), transportation and living accommodations, and reliable social support systems. By addressing the above areas of concern, an efficacious treatment could be set into practice in order to adhere to professional and personal standards.
Kirsh et al. (2009) found that “disabled adults are twice as likely to be in a household with lower
incomes, and disabled people of working age are more than twice as likely as nondisabled people to have no employment-related qualifications” (p. 392). This is an essential point when discussing the importance of secondary schooling and continued education for persons with disabilities. If the statistics show that disabled persons are twice as likely as those without disabilities to have no employment-related qualifications, then accommodating them in the transition to the college environment seems appropriate. It makes sense to aid others in engaging and succeeding at their endeavors rather than waiting for them to fail or not assisting in the process at all. Counseling intervention and prevention could benefit those who may be struggling to persevere on their own, and implementation of the illness intrusiveness model in combination with CBT may provide to incoming college students with disabilities the appropriate coping skills to transition adaptively to the next phase of their life.
References
Addis, M. E., & Carpenter, K. M. (2000). The treatment rationale in cognitive behavioral therapy: Psychological mechanisms and clinical guidelines. Cognitive and Behavioral Practice, 7(2), 147–156. doi:10.1016/S1077-7229(00)80025-5
Akridge, R.L. (1981). Psychosocial assessment in rehabilitation. Journal of Applied Rehabilitation Counseling, 12(1), 36–39.
Barazandeh, G. (2005). Attitudes toward disabilities and reasonable accommodation at the university. The UCI Undergraduate Research Journal, 8, 1–12.
Bettazzoni, M., Zipursky, R. B., Friedland, J., & Devins, G. M. (2008). Illness intrusiveness and subjective well-being in schizophrenia. The Journal of Nervous and Mental Disease, 196, 798–805.
Brinckerhoff, L. C., McGuire, J. M., & Shaw, S. F. (2002). Postsecondary education and transition for students with learning disabilities (2nd ed.). Austin, TX: PRO-ED.
Butler, A. C., Chapman, J. E., Forman, E. M., & Beck, A. T. (2006). The empirical status of cognitive-behavioral therapy: A review of meta-analyses. Clinical Psychology Review, 26, 17–31.
Canadian Human Rights Act (December 15, 2012). Retrieved from http://laws-lois.justice.gc.ca
Corey, G. (2005). Theory and practice of counseling and psychotherapy. Belmont, CA: Brooks/Cole.
Couch, R. H. (1984). Basic approaches to adjustment services in rehabilitation. Journal of Applied Rehabilitation Counseling, 15, 20–23.
Devins, G. M. (2010). Using the Illness Intrusiveness Ratings Scale to understand health-related quality of life in chronic disease. Journal of Psychosomatic Research, 68, 591–602.
Devins, G. M., Binik, Y. M., Hutchinson, T. A., Hollomby, D. J., Barré, P. E., & Guttmann, R. D. (1983). The emotional impact of end-stage renal disease: Importance of patients’ perceptions of intrusiveness and control. The International Journal of Psychiatry in Medicine, 13, 327–343.
Dowrick, P.W., Anderson, J., Heyer, K., Acosta, J. (2005). Postsecondary education across the
USA: Experience of adults with disabilities. Journal of Vocational Rehabilitation, 22, 41–47.
Dutta, A., Kundu, M., & Schiro-Geist, C. (2009). Coordination of postsecondary transition services for students with disabilities. Journal of Rehabilitation, 75(1), 10–17.
Enright, M. S., Conyers, L. M., & Szymanski, E. M. (1996). Career and career-related educational concerns of college students with disabilities. Journal of Counseling & Development, 75, 103–114.
Gilmore, D. S., & Bose, J. (2005). Trends in postsecondary education: Participation within the vocational rehabilitation system. Journal of Vocational Rehabilitation, 22, 33–40.
Gustafsson, C., Öjehagen, A., Hansson, L., Sandlund, M., Nyström, M., Glad, J., … Fredriksson, M. (2009). Effects of psychosocial interventions for people with intellectual disabilities and mental health problems: A survey of systematic reviews. Research on Social Work Practice, 19(3), 281–290. doi:10.1177/1049731508329403
Hresko, W. P., & Reid, D. K. (1988). Five faces of cognition: Theoretical influences on approaches to learning disabilities. Learning Disability Quarterly, 11, 211–216.
Individuals with Disability Education Act Amendments of 1997 [IDEA]. (1997). Retrieved from http://thomas.loc.gov/home/thomas.php
Jacob, S., & Hartshorne, T. S. (2007). Ethics and law for school psychologists (5thed.). Hoboken, NJ: John Wiley.
Johnson, A. L. (2006). Students with disabilities in postsecondary education: Barriers to Success
and implication to professionals. Vistas Online. Retrieved from http://www.counseling.org/knowledge-center/vistas/vistas-2006
Ju, J. J. (1982). Counselor variables and rehabilitation outcomes: A literature overview. Journal of Applied Rehabilitation Counseling, 13, 28–31.
Kirsh, B., Stergiou-Kita, M., Gewurtz, R., Dawson, D., Krupa, T., Lysaght, R., & Shaw, L. (2009). From margins to mainstream: What do we know about work integration for persons with brain injury, mental illness and intellectual disability? Work: A Journal of Prevention, Assessment and Rehabilitation, 32(4), 391–405. doi:10.3233/WOR-2009-0851
Livneh, H., & Antonak, R. F. (1997). Psychosocial adaptation to chronic illness and disability. Gaithersburg, MD: Aspen.
Lustig, D. C., Rosenthal, D. A., Strauser, D. R., & Haynes, K. (2000). The relationship between sense of coherence and adjustment in persons with disabilities. Rehabilitation Counseling Bulletin, 43, 134–141.
Luyckx, K., Schwartz, S. J., Soenens, B., Vansteenkiste, M., & Goossens, L. (2010). The path from identify commitments to adjustment: Motivational underpinnings and mediating mechanisms. Journal of Counseling & Development, 88, 52–60.
National Organization on Disability/Louis Harris & Associates, Inc. (2000). Key findings: 2000 N.O.D./Harris survey of Americans with disabilities. Retrieved from National Organization on Disability Web site: http://nod.org/assets/downloads/2000-key-findings.pdf
Oathamshaw, S. C., & Haddock, G. (2006). Do people with intellectual disabilities and psychosis have the cognitive skills required to undertake cognitive behavioural therapy? Journal of Applied Research in Intellectual Disabilities, 19, 35–46.
Padesky, C. A., & Greenberger, D. (1995). Clinician’s guide to mind over mood. New York, NY: Guilford Press.
Parker, R. M., Szymanski, E. M., & Patterson, J. B. (2005). Rehabilitation counseling: Basics and beyond (4th ed.). Austin, TX: PRO-ED.
Roessler, R. T. (2004). The illness intrusiveness model: Rehabilitation implications. Journal of Applied Rehabilitation Counseling, 35, 22–27.
Sachs, D., & Schreuer, N. (2011). Inclusion of students with disabilities in higher education: Performance and participation in student’s experiences. Disability Studies Quarterly, 31(2), 1–19.
Sampson, J. P., Reardon, R. C., Peterson, G. W., & Lenz, J. G. (2004). Career counseling & services: A cognitive information processing approach. Belmont, CA: Brooks/Cole.
Schmidt, M. A., & Smith, D. L. (2007). Individuals with disabilities perceptions on preparedness for the workforce and factors that limit employment. Work: A Journal of Prevention, Assessment and Rehabilitation, 28, 13–21.
Skorikov, V. B., & Vondracek, F. W. (2007). Vocational identity. In V. B. Skorikov & W. Patton (Eds.), Career development in childhood and adolescence (pp. 143–168). Rotterdam, The Netherlands: Sense.
Smart, J. (2001). Disability, society, and the individual. Gaithersburg, MD: Aspen.
Stodden, R. A., & Whelley, T. (2004). Postsecondary education and persons with intellectual disabilities: An introduction. Education and Training in Developmental Disabilities, 39, 6–15.
Swanson, H. L., & Hoskyn, M. (1998). Experimental intervention research on students with
learning disabilities: A meta-analysis of treatment outcomes. Review of Educational Research, 68, 277–321.
The Princeton Review (2011, July 1). Many students with disabilities attending college. Retrieved from http://in.princetonreview.com/in/2011/07/many-students-with-disabilities-attending-college.html
Thomas, K. R., & Parker, R. M. (1984). Counseling interventions. Journal of Applied Rehabilitation Counseling, 15, 15–19.
U.S. Department of Education. Institute of Education Sciences, National Center for Education Statistics (2011). Fast facts: Students with disabilities. Retrieved from http://nces.ed.gov/fastfacts/display.asp?id=60
West, M., Kregel, J., Getzel, E. E., Ming, Z., Ipsen, S. M., & Martin, E. D. (1993). Beyond section 504: Satisfaction and empowerment of students with disabilities in higher education. Exceptional Children, 59, 456–467.
Wright, B. A., (1983). Physical disability—A psychosocial approach (2nd ed.). New York, NY: Harper Collins.
Yanchak, K. V., Lease, S. H., & Strauser, D. R. (2005). Relation of disability type and career thoughts to vocational identity. Rehabilitation Counseling Bulletin, 48, 130–138.
Katie L. Haemmelmann, NCC, is a predoctoral intern at All Children’s Hospital and the Rothman Center for Pediatric Neuropsychiatry in St. Petersburg, FL. Mary-Catherine McClain is a predoctoral intern at Johns Hopkins University Counseling Center in Baltimore, MD. Correspondence can be addressed to Katie L. Haemmelmann, 3210 Stone Building, 1114 West Call Street, Tallahassee, FL 32306, klh08d@my.fsu.edu.
Oct 15, 2014 | Article, Volume 3 - Issue 3
Kathleen Brown-Rice
The theory of historical trauma was developed to explain the current problems facing many Native Americans. This theory purports that some Native Americans are experiencing historical loss symptoms (e.g., depression, substance dependence, diabetes, dysfunctional parenting, unemployment) as a result of the cross-generational transmission of trauma from historical losses (e.g., loss of population, land, and culture). However, there has been skepticism by mental health professionals about the validity of this concept. The purpose of this article is to systematically examine the theoretical underpinnings of historical trauma among Native Americans. The author seeks to add clarity to this theory to assist professional counselors in understanding how traumas that occurred decades ago continue to impact Native American clients today.
Keywords: historical trauma, Native Americans, American Indian, historical losses, cross-generational trauma, historical loss symptoms
Compared with all other racial groups, non-Hispanic Native American adults are at greater risk of experiencing feelings of psychological distress and more likely to have poorer overall physical and mental health and unmet medical and psychological needs (Barnes, Adams, & Powell-Griner, 2010). Suicide rates for Native American adults and youth are higher than the national average, with suicide being the second leading cause of death for Native Americans from 10–34 years of age (Centers for Disease Control and Prevention [CDC], 2007). Given that there are approximately 566 federally recognized tribes located in 35 states, and 60% of Native Americans in the United States reside in urban areas (Indian Health Services, 2009), there is much diversity within the Native American population. Therefore, it is difficult to make overall generalizations regarding this population (Gone, 2009), and it is important to not stereotype all Native American people. Still, Native American individuals are reported as having the lowest income, least education, and highest poverty level of any group—minority or majority—in the United States (Denny, Holtzman, Goins, & Croft, 2005) and the lowest life expectancy of any other population in the United States (CDC, 2010).
To explain why some Native American individuals are subjected to substantial difficulties, Brave Heart and Debruyn (1998) utilized the literature on Jewish Holocaust survivors and their decedents and pioneered the concept of historical trauma. The current problems facing the Native American people may be the result of “a legacy of chronic trauma and unresolved grief across generations” enacted on them by the European dominant culture (Brave Heart & DeBruyn, 1998, p. 60). The primary feature of historical trauma is that the trauma is transferred to subsequent generations through biological, psychological, environmental, and social means, resulting in a cross-generational cycle of trauma (Sotero, 2006). The theory of historical trauma has been considered clinically applicable to Native American individuals by counselors, psychologists, and psychiatrists (Brave Heart, Chase, Elkins, & Altschul, 2011; Goodkind, LaNoue, Lee, Freeland, & Freund, 2012; Myhra, 2011). However, there has been uncertainty about the validity of this theory due to the ambiguity of some of the concepts with little empirical evidence (Evans-Campbell, 2008; Gone, 2009). Specifically, there has been a lack of research about how the past atrocities suffered by the Native American people are connected with the current problems in the Native American community. The intent of this article is to examine the theoretical framework of historical trauma and apply recent research regarding the impact of trauma on an individual’s physiological functioning and cross-generational transmission of trauma. Through this analysis, the author seeks to assist professional counselors in their clinical practice and future research.
Core Concepts of Historical Trauma
Sotero (2006) provided a conceptual framework of historical trauma that includes three successive phases. The first phase entails the dominant culture perpetrating mass traumas on a population, resulting in cultural, familial, societal and economic devastation for the population. The second phase occurs when the original generation of the population responds to the trauma showing biological, societal and psychological symptoms. The final phase is when the initial responses to trauma are conveyed to successive generations through environmental and psychological factors, and prejudice and discrimination. Based on the theory, Native Americans were subjected to traumas that are defined in specific historical losses of population, land, family and culture. These traumas resulted in historical loss symptoms related to social-environmental and psychological functioning that continue today (Whitbeck, Adams, Hoyt, & Chen, 2004).
Historical Losses
For the last 500 years, individuals from the dominant European cultures have engaged in behaviors that have resulted in the purposeful and systematic destruction of the Native American people (Plous, 2003). Native Americans have been subjected to traumas that have resulted in specific historical losses. These losses include loss of people, loss of land, and loss of family and culture (Brave Heart & Debruyn, 1998; Garrett & Pichette, 2000; Whitbeck et al., 2004).
The population of Native Americans in North America decreased by 95% from the time Columbus came to America in 1492 and the establishment of the United States in 1776 (Plous, 2003). This decline can be explained by two main factors: the intentional killing of Native Americans and the exposure of Native Americans to European diseases (Trusty, Looby, & Sandhu, 2002). The majority of the Native American population died due to its lack of resistance to “diseases such as smallpox, diphtheria, measles, and cholera” that Europeans brought to North America (Trusty et al., 2002, p. 7). While some of the exposure to these illnesses was unintentional on the part of the Europeans, it has been documented that many times the Native American people were purposely subjected to these diseases. In 1763, for instance, Lord Jeffrey Amherst ordered his subordinates to introduce smallpox to the Native American people through blankets offered to them (Plous, 2003).
This loss of population further impacted the Native American community due to the lack of public acknowledgment of these deaths by the dominant culture and the denial of Native Americans to properly mourn their losses. Mourning practices were disrupted when an 1883 federal law prohibited Native Americans from practicing traditional ceremonies (Brave Heart, Chase, Elkins, & Altschul, 2011). This law remained in effect until 1978, when the American Indian Religious Freedom Act was enacted. This disenfranchised grief has resulted in the Native American people not being able to display traditional grief practices (Brave Heart et al., 2011; Sotero, 2006). As a result, subsequent generations have been left with feelings of shame, powerlessness and subordination (Brave Heart & DeBruyn, 1998).
The taking of Native American lands was a primary agenda for the majority of the United States government officials in the 19th century (Duran, 2006; Sue & Sue, 2012). President Andrew Jackson approved the Indian Removal Act of 1830, initiating the use of treaties in exchange for Native American land east of the Mississippi River and forcing the relocation of as many as 100,000 Native Americans (Plous, 2003). The motivation for the confiscation of the lands was often driven by economics (e.g., Fort Laramie Treaty of 1868; Trusty et al., 2002). By 1876, the U.S. government had obtained the majority of Native American land and the Native American people were forced to either live on reservations or relocate to urban areas (Brave Heart & Debruyn, 1998; Trusty et al., 2002). Reservations, for the most part, were not the best lands for agriculture and hunting. Further, being relocated to urban areas removed Native American people from all the lives they were familiar with. Leaving their domestic lands led to a decline in socioeconomic status as Native American men were not able to provide for their families, and the families became dependent on goods provided by the U.S. government (Brave Heart & Debruyn, 1998). These relocations resulted in the death of thousands of Native Americans and the disruption of families.
The agenda throughout the majority of history by U.S. government agencies, churches, and other organizations was to encroach on the Native American population and lands, leading to a disruption to the Native American culture for the preponderance of the Native population (Brave Heart & DeBruyn, 1998; Garrett & Pichette, 2000). Principally, the intent was to force the Native American people to fully assimilate to the dominant European-American culture and completely abandon their own culture. In 1871 the U.S. congress declared Native Americans wards of the U.S. government, and the U.S. government’s goal became to civilize Native Americans and assimilate them to the dominant White culture (Trusty et al., 2002). Government and church-run boarding schools would take Native American children from their families at the age of 4 or 5 and not allow any contact with their Native American relations for a minimum of 8 years (Brave Heart & Debruyn, 1998; Garrett & Pichette, 2000). In the boarding schools, Native American children had their hair cut and were dressed like European American children; additionally, all sacred items were taken from them and they were forbidden to use their Native language or practice traditional rituals and religions (Brave Heart & Debruyn, 1998; Garrett & Pichette, 2000). Many children were abused physically and sexually and developed a variety of problematic coping strategies (e.g., learned helplessness, manipulative tendencies, compulsive gambling, alcohol and drug use, suicide, denial, and scapegoating other Native American children) (Brave Heart & Debruyn, 1998; Garrett & Pichette, 2000). Such circumstances led many Native Americans to not engage in traditional ways and religious practices, which led to a loss of ethnic identity (Garrett & Pichette, 2000). The removal of children from their families is considered one of the most devastating traumas that occurred to the Native American people because it resulted in the disruption of the family structure, forced assimilation of children, and a disruption in the Native American community. This situation is considered the crucial precursor to many of the existing problems for some Native Americans (Brave Heart & Debruyn, 1998; Duran & Duran, 1995).
Historical Loss Symptoms
The second core concept of the theory of historical trauma relates to the current social-environmental, psychological and physiological distress in Native American communities, in that these difficulties are a direct result of the historical losses this population has suffered. Specifically, these traumatic historical losses result in historical loss symptoms.
Societal-environmental concerns. Domestic violence and physical and sexual assault are three-and-a-half times higher than the national average in Native American communities; however, this number may be low, as many assaults are not reported (Sue & Sue, 2012). Cole (2006) proposed that the breakdown in Native American families due to the forced removal of Native American children can be seen as the reason for the high number of child abuse and domestic violence incidents reported in these families. Additionally, Native American children are one of the most overrepresented groups in the care of child protective services (Hill, 2008). Further, fewer Native Americans have a high school education than the total U.S. population; an even smaller percentage has obtained a bachelor’s degree: 11% compared with 24% of the total population. Almost 26% of Native Americans live in poverty compared to 12% for the entire U.S. population (U.S. Census Bureau, 2006). Native Americans residing on reservations have double the unemployment rate compared to the rest of the U.S. population (U.S. Census Bureau, 2006).
Psychological concerns. Native Americans have the highest weekly alcohol consumption of any ethnic group (Chartier & Caetano, 2010). Native American adults reported that in the last 30 days, 44% used alcohol, 31% engaged in binge drinking, and 11% used an illicit drug (National Survey on Drug Use and Health, 2010). Many Native American adolescents have co-occurring disorders related to substance abuse and mental health disorders (Abbott, 2006). Abuse of alcohol by Native individuals may be related to low self-esteem, loss of cultural identity, lack of positive role models, history of abuse and neglect, self-medication due to feelings of hopelessness, and loss of family and tribal connections (Sue & Sue, 2012).
Statistics indicate that a proportionally high level of Native Americans have mood disorders and posttraumatic stress disorder (PTSD; CDC, 2007; Dickerson & Johnson, 2012). Suicide rates among Native Americans are 3.2 times higher than the national average (CDC, 2007). For males ages 15–19, Native American suicide rates were 32.7 per 100,000, compared to non-Hispanic White (14.2), Black (7.4), Hispanic (9.9), and Asian or Pacific Islander (8.5) [CDC, 2007]. Studies have shown family disruptions and loss of ethnic identity places Native American adolescents at higher risk for alcoholism, depression and suicide (May, Van Winkle, Williams, McFeeley, DeBruyn, & Serma, 2002). It has been found that an increase in the number of suicides corresponds to a lack of linkage between the adolescents and their cultural past and their ability to relate their past to their current situation and the future (Chandler, Lalonde, Sokol, & Hallet, 2003).
Physiological concerns. The life expectancy at birth for the Native American population is 2.4 years less than that of all U.S. populations combined (CDC, 2010). Further, Native American individuals are overrepresented in the areas of heart disease, tuberculosis, sexually transmitted diseases, and injuries with, diabetes being more prevalent with this population than any other racial or ethnic group in the United States (Barnes et al., 2010). Only 28% of Native Americans under the age of 65 have health insurance (CDC, 2010).
The majority (60%) of Native Americans receive behavioral and medical health services from Indian Health Services (IHS, 2013a). IHS was established and funded by the U.S. government in 1955 to uphold treaty obligations to provide healthcare services to members of federally recognized Native American tribes (Jones, 2006). Three branches of service exist within IHS: (a) an independent, federally operated direct care system, (b) tribal operated health care services, and (c) urban Indian health care services (Sequist, Cullen, & Acton, 2011). However, according to the IHS (2009), the Native American people “have long experienced lower health status when compared with other Americans.” This is substantiated by the IHS (2013a) report that $2,741 is spent per IHS recipient in comparison to $7,239 for the general population; of that, less than 10% of these funds were utilized for mental health and substance abuse treatment in 2010 even though the rates of mental health and substance abuse issues are prominent. This disparity in medical and behavioral health services is due to “inadequate education, disproportionate poverty, discrimination in the delivery of health services, and cultural differences” (IHS, 2013b). Further, Barnes and colleagues (2010) reported that the inequality may not only be related to the above factors, but epigenetic and behavioral influences. There may be environmental factors that alter the way genes are expressed (Francis, 2009) and behavioral patterns that further negatively influence the situation. In order to gain a better understanding of relationship epigenetic component, it is important to recognize how trauma impacts a person’s physical as well as mental functioning.
The Impact of Trauma on Physiological Functioning
“Traumatic experiences cause traumatic stress, which disrupts homeostasis” in the body (Solomon & Heide, 2005, p. 52). People who have experienced traumatic events have higher rates than the general population for cardiovascular disease, diabetes, cancer and gastrointestinal disorders (Kendall-Tackett, 2009). Specifically, trauma affects the functioning of the sympathetic nervous system and the endocrine system (Solomon & Heide, 2005). When the body is experiencing stress, it needs oxygen and glucose in order to fight or flee from the perceived danger. The brain then sends a message to the adrenal glands telling, them to release epinephrine (Kendall-Tackett, 2009). Epinephrine increases the amount of sugar in the blood stream, increases the heart rate and raises blood pressure. The brain also sends a signal to the pituitary gland to stimulate the adrenal cortex to produce cortisol that keeps the blood sugar high in order to give the body energy to be able to escape the stressor (Solomon & Heide, 2005). This physiological response to stress is created for a short-term remedy. Additionally, it has been found that in people who have experienced a prior trauma, their bodies react quicker to new stressors and thus cortisol and epinephrine are released at a faster rate (Kendall-Tackett, 2009).
Amygdala and Hypothalamic-Pituitary-Adrenal Axis
Experiencing trauma can impact a person’s neurological functioning. After a traumatic event, many people have an overactive amygdala (Brohawn, Offringa, Pfaff, Hughes, & Shin, 2010). This hyperactivation of the amygdala “may be responsible for symptoms of hyperarousal in PTSD, including exaggerated startle responses, irritability, anger outbursts, and general hypervigilance,” and may be the reason for a person re-experiencing the event due to a trauma reminder (Weiss, 2007, p. 116). After the original trauma takes place, any perceived external threat that reminds the body of the original trauma (e.g., sound, face, smell, gesture) will cause the body, through the amygdala, to automatically respond to the perceived threat by producing epinephrine and cortisol (Weiss, 2007). This biological response happens without the person consciously being aware of it. It has been found that “emotionally arousing stimuli are generally better remembered than emotionally neutral stimuli, and the amygdala is responsible for this emotional memory enhancement” (Koenigs & Grafman, 2009, p. 546). The amygdala is responsible for giving emotional meaning to the external stimuli; however, the hippocampus provides contextual meaning to the stimuli (Brohawn et al., 2010).
Ganzel, Casey, Glover, Voss, and Temple (2007) examined whether trauma exposure has long-term effects on the brain and behavior in healthy individuals. These researchers compared a group of people who lived within 1.5 miles of the World Trade Center on 9/11 (Ground Zero) and a group of people who lived 200 miles away from Ground Zero. More than three years after the events of 9/11, both groups were shown pictures of fearful and calm faces; the amygdala activation of the group members was measured utilizing functional Magnetic Resonance Imaging (fMRI; Ganzel et al., 2007). The results indicated that the group that resided closer to Ground Zero had heightened amygdala reactivity when shown images of people in fear.
In another study, researchers utilized fMRI to examine amygdala and hippocampus activation in 18 trauma-exposed non-PTSD control subjects and 18 individuals with PTSD (Brohawn et al., 2010). The results of this study indicated that there was hyperactive amygdala activation when negative emotional stimuli were introduced to the PTSD group. Additionally, when a person is exposed to traumatic events during development, the hypothalamic-pituitary-adrenal (HPA) axis can be altered, which may increase susceptibility to disease, including PTSD and other mood and anxiety disorders (Gillespie, Phifer, Bradley, & Ressler, 2009). The HPA axis is the part of the neuroendocrine system that controls reactions to stress as well as regulates digestion, the immune system, mood and emotions, and sexuality. This overactivation of the amygdala and HPA axis due to re-experiencing the initial trauma sends the message to the adrenal glands to release epinephrine and cortisol (Kendall-Tackett, 2009; Solomon & Heide, 2005). Current research has shown that the continual release of cortisol due to exposure to recurrent stressors, particularly during development, can cause the HPA axis to shutdown, which results in low cortisol levels (Neigh, Gillespie, & Nemeroff, 2009). Therefore, chronic exposure to stressors can relate to either a hypo- or hyper-stress response in the HPA axis.
This impact on the HPA axis functioning may explain why researchers have found a relationship between PTSD and physical illnesses. Weisberg et al. (2003) performed a study of 502 adults; 17% had no history of trauma, 46% had a history of trauma but no PTSD, and 37% were diagnosed with PTSD. The researchers found that individuals with PTSD reported a significantly larger number of current and lifetime medical conditions than did other participants, including anemia, arthritis, asthma, back pain, diabetes, eczema, kidney disease, lung disease, and ulcers (Schnurr & Green, 2004; Weisberg et al., 2003). Specifically, a multiple regression indicated that PTSD was a stronger predictor of medical difficulties than physical injury, lifestyle factors, or comorbid depression (Weisberg et al., 2003). A study of veterans found that those participants with PTSD were more likely to have the medical conditions of osteoarthritis, diabetes, heart disease, comorbid depression, and obesity (David, Woodward, Esquenazi, & Mellman, 2004). Additionally, Goodwin and Davidson (2005) conducted a survey study of over 5,500 subjects and found that there was an association between a diagnosis of diabetes and having PTSD.
Integrating Historical Trauma Theory
As evidenced above, the traumas inflicted on the Native American people (historical losses) are well documented and the literature provides significant information regarding the current psychological, environmental-societal, and physiological problems facing the Native American people (historical loss symptoms). The literature also supports the conceptualization of a relationship between experiencing trauma and the brain remembering the trauma when confronted by an emotional meaning stimulus (Brohawn et al., 2010; Weiss, 2007). Further, a relationship between PTSD and physiological functioning has been found (David et al., 2004; Weisberg et al., 2003). Therefore, it can be surmised that, given the substantial historical traumas Native Americans have experienced, they would be at greater risk of developing physical and emotional concerns related to re-experiencing these traumas. However, the question remains whether some Native American people are being confronted by emotionally significant stimuli in the present day that causes them to reflect about the historical traumas that occurred many generations ago.
In answer to this question, Whitbeck and colleagues (2004) developed the Historical Loss Scale and the Historical Loss Associated Symptoms Scale. Whitbeck et al. (2004) surveyed Native American adult parents of children for their perceptions of historical events. These participants were generations removed from many of the historical traumas that had been inflicted on the Native American people. However, 36% had daily thoughts about the loss of traditional language in their community and 34% experienced daily thoughts about the loss of culture (Whitbeck et al., 2004). Additionally, 24% reported feeling angry regarding historical losses, and 49% provided they had disturbing thoughts related to these losses. Almost half (46%) of the participants had daily thoughts about alcohol dependency and its impact on their community. Further, 22% of the respondents indicated they felt discomfort with White people, and 35% were distrustful of the intentions of the dominant White culture due to the historical losses the Native American people had suffered (Whitbeck et al, 2004).
Ehlers, Gizer, Gilder, Ellingson, & Yehuda (2013) utilized the Historical Loss Scale and Historical Loss Associated Symptoms Scale to survey 306 Native American adults. The majority of the participants thought about historical losses at least occasionally and these thoughts caused them distress. In particular, how frequent a person thought about historical losses was linked with not being married, high degrees of Native heritage and cultural identification. When comparing the Whitbeck et al. (2004) and Ehlers et al. (2013) studies, about the same percentage of participants thought about the losses several times a day; however, respondents reported less daily and weekly thoughts of historical losses in the Ehlers et al. (2013) results. The differences between the two studies could be a result of “the extent of historical losses suffered by each individual Native community, the impact of current trauma, levels of acculturation, population norms about historical losses, and population admixture” (Ehlers et al., 2013, p. 6). Therefore, it is important to recognize there are differences in how historical losses are impacting Native American communities.
The above findings may clarify one reason why some populations in the Native American community are suffering from such severe emotional, physical and social-environmental consequences related to past traumas. Specifically, their bodies’ ability to deal with stress has been overwhelmed by the reoccurring thoughts related to historical losses they have suffered. However, it is important not to make generalizations and to remember not all of the Native American people have been experiencing severe historical loss symptoms (Evans-Campbell, 2008). These within-group differences in the Native American population would explain the variances in rates of disease, child abuse and neglect, violence, suicide, unemployment, familial disruption, and poverty between tribal affiliations.
Another important consideration is an individual’s perception of being discriminated against. Perceived discrimination has been associated with negative health consequences (Bogart, Wagner, Galvan, Landrine, Klein, & Sticklor, 2011). In particular, Capezza, Zlotnick, Kohn, Vicente, and Saldivia (2012) administered structured diagnostic assessments for major depressive disorder (MDD) and PTSD and the Alcohol Use Disorders Identification Test (AUDIT) to 2,839 participants in Concepción and Talcahuano, Chile. These researchers found that controlling for demographic variables and previous trauma, participants who reported discrimination in the preceding six months were significantly more likely to participate in risky alcohol use, illegal drug use, and be diagnosed with MDD and PTSD than respondents not reporting discrimination.
Another study examined the relationships between neglect and abuse, PTSD symptoms, ethnicity-specific factors (e.g., ethnic orientation, ethnic identity, perceived discrimination), and alcohol and drug problems within adolescent girls (Gray & Montgomery, 2012). These researchers found that abuse and neglect were correlated to alcohol and drug problems, but only in relation with PTSD symptoms. It also was found that greater perceived discrimination was related with an increased influence of abuse and neglect on PTSD symptoms (Gray & Montgomery, 2012). Given the generations of persecution, discrimination, and oppression suffered by the Native American people (Brave Heart et al., 2011), it is reasonable that perceived discrimination could be an aggravating factor.
Cross-Generational Trauma Transmission
As a result of the loss of people, land, and culture, a systematic transmission of trauma to subsequent generations occurred that has resulted in historical loss symptoms for many Native American individuals (Brave Heart et al., 2011; Whitbeck et al., 2004). Specifically, the traumatic events suffered during previous generations creates a pathway that results in the current generation being at an increased risk of experiencing mental and physical distress that leaves them unable to gain strength from their indigenous culture or utilize their natural familial and tribal support system (Big Foot & Braden, 2007). Therefore, the next step in investigating the theory of historical trauma is to understand how the generational transmission of trauma transpires. Significant research has been completed on the cross-generational transmission of trauma regarding Holocaust victims and their descendants (Doucet & Rovers, 2010; Jacobs, 2011; Neigh et al., 2009; Yehuda, Schmeidler, Wainberg, Binder-Brynes, & Duvdevani, 1998).
Based upon this research, three means by which trauma is transmitted to subsequent generations have been identified: (a) children identifying with their parents’ suffering, (b) children being influenced by the style of communication caregivers use to describe the trauma, and (c) children being influenced by particular parenting styles (Doucet & Rovers, 2010). Parental identification is a form of vicarious learning in which the child identifies with trauma and takes on the historical loss symptoms. Lichenstein and Annas (2000) found there is a relationship between a parent having a fear and children developing the same fear due to vicarious learning. This seems to be substantiated by Myhra’s (2011) findings that all 13 participants in a qualitative study examining the relationship between substance use and historical trauma in Native American adults believed that historical trauma was key to their elders’ dysfunctional behavior—in particular, substance abuse. One participant characterized it as “monkey see, monkey do,” in that she was following her family’s pattern of abusing substances and being involved in abusive interpersonal relationships (Myhra, 2011, p. 26). However, it is important to mention that participants also expressed a great respect and admiration for their elders due to their strength and resiliency.
Lichenstein and Annas (2000) also examined if the way parents relayed information to children regarding a stimulus impacted the development of a fear or phobia in the children. The researchers found that there was a relationship between children developing a fear or phobia when parents engaged in negative talk with children regarding the stimulus. In the Native American culture, information and history is often passed down from generation to generation in a narrative summary. Given that the atrocities that were inflicted on the Native American people were substantive, it seems understandable that transmission of historical loss symptoms could occur via this pathway to the children. In fact, Myhra (2011) found that Native American participants connected “the impact of elders’ stories of historical trauma and loss, and their own traumatic experiences, to intrusive thoughts about these ordeals and to fear that trauma will continue for future generations” (p. 25).
Parenting style also can be impacted as a result of trauma. Walker (1999), in completing an extensive literature review of this subject, found that parenting can be impacted as a result of the parental exposure to trauma. First, parents may have difficulty with trust and intimacy as a result of their experiences of being victimized. Therefore, it may be a challenge for them to develop a healthy attachment with their children. Second, many adults who have been subjected to abuse and neglect may in turn unintentionally enter into a cycle of violence with their own children (Walker, 1999). Due to the forced removal of Native children from their homes and tribal communities, the familial structure was interrupted and many suffered extreme abuse and neglect (Cole, 2006). Therefore, subsequent generations of Native Americans may have not been able to develop healthy parenting styles and inadvertently continued a cycle of violence and abuse. A relationship between a parent’s diagnosis of PTSD and abuse and neglect of children also has been found. Children of Holocaust survivors diagnosed with PTSD report more neglect and emotional abuse than demographically similar children of parents who were not diagnosed with PTSD (Neigh et al., 2009; Yehuda, Bierer, Schmeidler, Aferiat, Breslau, & Dolan, 2000). The reasons why Native American children stand overrepresented in the U.S. foster care system (Hill, 2008) may be related to the abuse suffered by many Native Americans while in boarding schools and the high number of Native Americans displaying PTSD symptoms.
As mentioned previously, experiencing traumatic events during development can alter the HPA axis, which may increase susceptibility to disease (e.g., PTSD, mood and anxiety disorders) (Gillespie et al., 2009). Specifically, it has been found that children of Holocaust survivors have significantly lower cortisol levels when compared with control groups (Yehuda et al., 2000). Further, children of parents who developed PTSD after surviving the Holocaust had reduced cortisol levels when compared to children of Holocaust survivors that did not have PTSD. The results of this study provide that trauma exposure can change how the HPA axis functions and increase risk of PTSD symptoms at least one generation removed from the initial trauma experience (Neigh et al., 2009; Yehuda et al., 2000).
Other studies have found that adult children of Holocaust survivors have a greater lifespan occurrence of PTSD, as well as other mood and anxiety disorders, than demographically comparable individuals who reported a similar exposure to trauma (Neigh et al., 2009; Yehuda et al., 1998). Further, children of trauma-exposed Holocaust survivors who did not develop PTSD were at an increased risk of manifesting other mental health disorders (e.g., depression, anxiety, PTSD) when compared to individuals whose parents were not exposed to trauma (Yehuda, Halligan, & Bierer, 2001). Additionally, researchers have looked at the impact of maternal trauma on the unborn child. Nine-month-old infants born to mothers who were diagnosed with PTSD as a result of trauma-exposure related to the September 11, 2001 attacks had lower cortisol levels than infants born to unexposed mothers (Neigh et al., 2009; Yehuda et al., 2005). The results were more significant with infants whose mothers were in their third trimester when the attacks occurred.
Based upon the above cited research, it can be surmised that parents’ exposure to trauma does form a passageway to subsequent generations that results in an increased risk of negative mental health symptoms. In fact, the latest version of the American Psychiatric Association (APA, 2013) Diagnostic and Statistical Manual of Mental Disorders (DSM-5) includes a stressor criterion for adults, adolescents, and children older than six years related to learning that a close relative or close friend was exposed to trauma. Additionally, the DSM-5 added a PTSD diagnosis for a child six years or younger. One of the triggering events is a child learning that a traumatic event has occurred to a parent or caregiving figure (APA, 2013).
Implications for Professional Counselors
The results of this analysis of historical trauma assist in removing some of the ambiguity regarding this theory. Specifically, a link between neurological functioning and trauma and cross-generational trauma transmission were conceptualized and applied to the theory of historical trauma. This comprehensive examination provides professional counselors with an increased understanding of how traumas that occurred within the Native American population generations ago continue to impact clients today. This information is critical to enhance clinicians’ clinical skills when working with Native American clients. Having an understanding of historical trauma will assist professional counselors in being more responsive to the unique needs of members of this population and incorporating historical trauma in their clinical work.
Dionne, Davis, Sheeber, and Madrigal (2009) provide that integrating mainstream mental health intervention in Native American individuals should involve two phases: (a) motivational phase (i.e., historical context around current difficulties in Native American communities is discussed); and (b) intervention phase (i.e., utilizing mainstream evidence-based interventions). Not only do clinicians and interventions need to be culturally competent, but conventional counseling theories need to be adjusted to be culturally appropriate (Wendt & Gone, 2012). Thus, traditional counseling theories should be integrated with elements of historical trauma and the Native American holistic view of the person.
First, professional counselors should reframe historical loss symptoms in terms of collective responses that are employed to assist clients in alleviating symptoms (Brave Heart & DeBruyn, 1998). Thus, the psychological, social-environmental, and physiological concerns that plague many Native people are signs and symptoms of a communal reaction to generations of persecution, discrimination, and oppression. Specifically, historical trauma differs from the diagnosis of PTSD in that many of the traumas that occurred were systemic in nature (e.g., massacres, Trail of Tears, mass removal of children), which led to collective subjugated grief. Brave Heart and DeBruyn (1998) in their pioneering writings on historical trauma proposed that the initial disenfranchised grief of the Native American people resulted in historical unresolved grief. Therefore, a second intervention is the need for clinicians to validate the existence of not only the initial historical losses that occurred but the continued discrimination and oppression that has impacted the Native American people (Brave Heart et al., 2011). Therapeutic change may be difficult for Native American clients to engage in without validation of not only the past atrocities that occurred to Native American communities, but acknowledgment of the current discriminatory environment that many Native people still endure. Given that the dominant European culture has been the perpetrator of many of the historical losses, this validation is especially important when the professional counselor is a member of the White dominant culture. Third, clients should be educated regarding historical trauma to enhance awareness about its impact and the associated grief and loss that can occur (Brave Heart & DeBruyn, 1998). The Native American people are well aware of the history of the traumas of their people; however, they might not have insight about how the events of the past may impact them today.
Finally, professional counselors need to understand that historical trauma permeates all domains of existence (e.g., personal identity, interpersonal relationships, collective memory, cultural and spiritual worldviews; Weisband, 2009). Clinicians need to have knowledge that historical losses impact all facets of a client. This can be explained to the client by use of the Medicine Wheel Model of Wellness, Balance, and Healing (The Medicine Wheel). According to this model, a person is interconnected through the spiritual, physical, emotional and mental. The Medicine Wheel has been found to be an effective tool in working with Native American individuals (Gray & Rose, 2012).
Implications and Directions for Future Research
This article provides needed insight regarding historical trauma; however, future research regarding this concept is needed, as Native Americans are underrepresented in mental health research (Echo-Hawk, 2011). Gone and Alcántara (2007) completed an extensive review of the literature on evidence-based mental health interventions with Native Americans and found 3 randomized or controlled outcome studies, 6 nonrandomized or uncontrolled outcome studies, 16 studies related to intervention descriptions, 7 clinical case studies, and 24 intervention approaches. The majority of these articles did not address assessment of therapeutic outcomes, but were more theoretically based or provided recommendations for working with Native American clients. The 9 outcome studies described pre- and post-intervention results for a treatment group with no control group for comparison, leaving questions about the validity of the treatment intervention. Specifically, there is no proven empirically based treatment modality to utilize when addressing the distinctive mental health needs of Native American clients. Given the severe mental health problems that plague many of the Native American people, determining effective psychological treatments is vital (Gone & Alcántara, 2007). This can be accomplished through future empirical research.
However, the Native people have a history of being devalued and marginalized in the interest of research (Walters & Simoni, 2009). Therefore, research should be conducted in a culturally sensitive and ethical manner. This is best accomplished by utilizing a collaborative approach (Waiters & Simoni, 2009). Therefore, researchers should work in partnership with tribal elders, healers, officials, health administrators and mental health providers. Specifically, future research should utilize a collective approach and take into account the diversity in tribal affiliations of clients (Hartmann & Gone, 2012).
The first area in need of research attention relates to the fact that the majority of the scholarship on historical trauma has been theoretical in nature. Therefore, there is a need to have empirical evidence to substantiate this concept. First, beneficial research would demonstrate a relationship between individuals reflecting on their historical losses (e.g., loss of people, land, family and culture) and suffering from historical loss symptoms (e.g., psychological distress, social-environmental problems, physiological concerns). Given that Whitbeck and colleagues (2004) have created scales to measure historical trauma, other self-report measures (e.g., depression, anxiety, self-efficacy inventories) could be utilized to determine a relationship between positive and negative affect and a person’s degree of historical trauma. Second, this author suggests that the previous research regarding the impact of trauma on physiological functioning can be a catalyst for future research on historical trauma. Specifically, future studies can focus on determining if there is a correlation between neural activity and clients’ self-reported level of historical trauma. In these studies, fMRI technology and Whitbeck et al. (2004) scales can be utilized to determine the relationship between clients’ self-reported level of historical trauma and amygdala and hippocampus activity.
The second area of research should examine the effectiveness of incorporating indigenous healing methods with mainstream counseling approaches. Utilizing a collaborative approach, researchers would utilize the expertise and guidance of culture keepers (e.g., tribal elders, traditional healers) (Hartmann & Gone, 2012) to incorporate indigenous healing methods with mainstream counseling theories. Given that no evidence-based treatment modality has been established for clinicians to utilize when treating Native American clients, additional research in this area is crucial. This article provides clarity on the theory of historical trauma, but there is a need for empirical research in order to improve the understanding of how atrocities perpetuated on the Native American people generations ago continue to manifest today by psychological, social-environmental and physiological means.
Conclusion
Large numbers of the Native American population continue to suffer from severe psychological, economic, social, environmental and physical distress. The theory of historical trauma provides professional counselors a framework to understanding the current issues that are invading the Native American people and their culture. Specifically, practitioners working with this population should have an understanding of how the historical losses suffered generations ago have resulted in historical loss symptoms being transferred to subsequent and current generations of Native Americans. The concept of historical trauma is “collective and multilayered rather than being solely centered on an individual” and this differs from a “typical Eurocentric perspective of illness and treatment, which tends to reduce suffering to discrete illnesses with individual causes and solutions” (Goodkind, Hess, Gorman, & Parker, 2012, p. 1021). Therefore, professional counselors should adapt evidence-based practices by applying tribal-specific healing strategies, community support, and approaches that incorporate validation of grief and loss associated with historical traumas (Brave Heart et al., 2011). Failure of professional counselors to deepen their understanding of this population would continue the disparity of Native clients receiving competent behavioral health services and facilitate the continuation of the cycle of historical trauma to future generations.
References
Abbott, P. J. (2007). Co-morbid alcohol/other drug abuse/dependence and psychiatric disorders in adolescent American Indian and Alaska Natives. Alcoholism Treatment Quarterly, 24(4), 3–21. doi:10.1300/J020v24n04_02
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental health disorders. (5th ed.). Arlington, VA: Author.
Barnes, P. M., Adams, P. F., & Powell-Griner, E. (2010). Health characteristics of the American Indian or Alaska Native adult population: United States, 2004–2008. National Health Statistics Reports, No. 20. Hyattsville, MD: National Center for Health Statistics.
BigFoot, D., & Braden, J. (2007, Winter). Adapting evidence-based treatments for use with American Indian and Native Alaskan children and youth. Focal Point, 21(1), 19–22. Retrieved from http://www.rtc.pdx.edu/PDF/fpW0706.pdf
Bogart, L. M., Wagner, G. J., Galvan, F. H., Landrine, H., Klein, D. J., & Sticklor, L. A. (2011). Perceived discrimination and mental health symptoms among Black men with HIV. Cultural Diversity and Ethnic Minority Psychology, 17(3), 295–302. doi:10.1037/a0024056
Brave Heart, M., Chase, J., Elkins, J., & Altschul, D. B. (2011). Historical trauma among indigenous peoples of the Americas: Concepts, research, and clinical considerations. Journal of Psychoactive Drugs, 43(4), 282–290. doi:10.1080/02791072.2011.628913
Brave Heart, M. Y. H., & DeBruyn, L. M. (1998). The American Indian holocaust: Healing historical unresolved grief. American Indian and Alaska Native Mental Health Research, 8(2), 60–82.
Brohawn, K., Offringa, R., Pfaff, D. L., Hughes, K. C., & Shin, L. M. (2010). The neural correlates of emotional memory in posttraumatic stress disorder. Biological Psychiatry, 68(11), 1023–1030. doi:10.1016/j.biopsych.2010.07.018
Capezza, N. M., Zlotnick, C., Kohn, R., Vicente, B., & Saldivia, S. (2012). Perceived discrimination is a potential contributing factor to substance use and mental health problems among primary care patients in Chile. Journal of Addiction Medicine, 6(4), 297–303. doi:10.1097/ADM.0b013e3182664d80
Centers for Disease Control and Prevention (CDC), Office of Minority Health & Health Equity. (2010). American Indian & Alaska Native populations. Retrieved from http://www.cdc.gov/omhd/populations/aian/aian.htm#Disparities
Centers for Disease Control and Prevention (CDC). (2007). Web-based Injury Statistics Query and Reporting System. Retrieved from http://www.cdc.gov/injury/wisqars/index.html
Chandler, M. J., Lalonde, C. E., Sokol, B. W., & Hallett, D. (2003). Personal persistence, identity development, and suicide: A study of Native and non-Native North American adolescents. Monographs of the Society for Research in Child Development, 68(2, Serial No. 273).
Chartier, K., & Caetano, R. (2010). Ethnicity and health disparities in alcohol research. Alcohol Research & Health, 33(1-2), 152–160.
Cole, N. (2006). Trauma and the American Indian. In T. Witko (Ed.), Mental health care for urban Indians: Clinical insights from Native practitioners (pp. 115–130). Washington, DC: American Psychological Association.
David, D., Woodward, C., Esquenazi, J., & Mellman, T. A. (2004). Comparison of comorbid physical illnesses among veterans with PTSD and veterans with alcohol dependence. Psychiatric Services, 55(1), 82–85.
Denny, C. H., Holtzman, D., Goins, T., & Croft, J. B. (2005). Disparities in chronic disease risk factors and health status between American Indian/Alaska Native and White elders: Findings from a telephone survey, 2001 and 2002. American Journal of Public Health, 95(5), 825–827. doi:10.2105/AJPH.2004.043489
Dickerson, D. L., & Johnson, C. L. (2012). Mental health and substance abuse characteristics among a clinical sample of urban American Indian/Alaska Native youths in a large California Metropolitan area: A descriptive study. Community Mental Health Journal, 48(1), 56–62. doi:10.1007/s10597-010-9368-3
Dionne, R., Davis, B., Sheeber, L., & Madrigal, L. (2009). Initial evaluation of a cultural approach to implementation of evidence-based parenting interventions in American Indian communities. Journal of Community Psychology, 37(7), 911–921. doi:10.1002/jcop.20336
Doucet, M., & Rovers, M. (2010). Generational trauma, attachment, and spiritual/religious interventions. Journal of Loss & Trauma, 15, 93–105. doi: 10.1080/15325 020903373078
Duran, E. (2006). Healing the soul wound: Counseling with American Indians and other Native peoples. New York, NY: Teachers College Press.
Duran, E., & Duran, B. (1995). Native American postcolonial psychology. Albany, NY: State University of New York Press.
Echo-Hawk, H. (2011). Indigenous communities and evidence building. Journal of Psychoactive Drugs, 43(4), 269–275. doi:10.1080/02791072.2011.628920
Evans-Campbell, T. (2008). Historical trauma in American Indian/Native Alaska communities: A multilevel framework for exploring impacts on individuals, families, and communities. Journal of Interpersonal Violence, 23(3), 316–338. doi:10.1177/0886260507312290
Francis, D. D. (2009). Conceptualizing child health disparities: A role for developmental neurogenomics. Pediatrics, 124, 196–202. doi:10.1542/peds.2009-1100G
Ganzel, B., Casey, B. J., Glover, G., Voss, H. U., & Temple, E. (2007). The aftermath of 9/11: Effect of intensity and recency of trauma on outcome. Emotion, 7(2), 227–238. doi:10.1037/1528-3542.7.2.227
Garrett, M. T., & Pichette, E. F. (2000). Red as an apple: Native American acculturation and counseling with or without reservation. Journal of Counseling & Development, 78(1), 3–13.
Gillespie, C. F., Phifer, J., Bradley, B., & Ressler, K. J. (2009). Risk and resilience: Genetic and environmental influences on development of the stress response. Depression and Anxiety, 26(11), 984–992. doi:10.1002/da.20605
Goodkind, J. R., Hess, J. M., Gorman, B., & Parker, D. P. (2012). “We’re still in a struggle”: Diné resilience, survival, historical trauma, and healing. Qualitative Health Research, 22(8), 1019–1036. doi:10.1177/1049732312450324
Goodkind, J., LaNoue, M., Lee, C., Freeland, L., & Freund, R. (2012). Involving parents in a community-based, culturally grounded mental health intervention for American Indian youth: Parent perspectives, challenges, and results. Journal of Community Psychology, 40(4), 468–478. doi:10.1002/jcop.21480
Goodwin, R. D, & Davidson, J. R. (2005). Self-reported diabetes and posttraumatic stress disorder among adults in the community. Preventive Medicine, 40(5), 570–574.
Gone, J. P. (2009). A community-based treatment for Native American historical trauma: Prospects for evidence-based practice. Journal of Counseling and Clinical Psychology, 77(4), 751–762. doi:10.1037/a0015390
Gone, J. P., & Alcántara, C. (2007). Identifying effective mental health interventions for American Indians and Alaska Natives: A review of the literature. Cultural Diversity & Ethnic Minority Psychology, 13(4), 356–363. doi:10.1037/1099-9809.13.4.356
Gray, C. M., & Montgomery, M. J. (2012). Links between alcohol and other drug problems and maltreatment among adolescent girls: Perceived discrimination, ethnic identity, and ethnic orientation as moderators. Child Abuse & Neglect, 36(5), 449–460. doi:10.1016/j.chiabu.2012.03.002
Gray, J. S., & Rose, W. J. (2012). Cultural adaptation for therapy with American Indians and Alaska Natives. Journal of Multicultural Counseling and Development, 40(2), 82–92. doi:10.1002/j.2161-1912.2012.00008.x
Hartmann, W. E., & Gone, J. P. (2012). Incorporating traditional healing into an urban American Indian health organization: A case study of community member perspectives. Journal of Counseling Psychology, 59(4), 542–554. doi:10.1037/a0029067
Hill, R. B. (2008). Gaps in research and public policies. Child Welfare, 87(2), 359–367.
Indian Health Service (IHS). (2009). IHS fact sheets: Indian health disparities. Retrieved from http://www.ihs.gov/newsroom/includes/themes/newihstheme/display_objects/documents/factsheets/Disparities_2013.pdf
Indian Health Service (IHS). (2013a). IHS year 2013 profile. Retrieved from http://www.ihs.gov/newsroom/includes/themes/newihstheme/display_objects/documents/factsheets/ProfileSheet_2013.pdf
Indian Health Service (IHS). (2013b). Disparities. Retrieved from http://www.ihs.gov/newsroom/factsheets/disparities/
Jacobs, J. (2011). The cross-generational transmission of trauma: Ritual and emotion among survivors of the Holocaust. Journal of Contemporary Ethnography, 40(3), 342–361. doi:10.1177/0891241610387279
Jones, D. S. (2006). The persistence of American Indian health disparities. American Journal of Public Health, 96(12), 2122–2134. doi:10.2105/AJPH.2004.054262
Lichtenstein, P., & Annas, P. (2000). Heritability and prevalence of specific fears and phobias in childhood. Journal of Child Psychology and Psychiatry, 41(7), 927–937.
Kendall-Tackett, K. (2009). Psychological trauma and physical health: A psychoneuroimmunology approach to etiology of negative health effects and possible interventions. Psychological Trauma: Theory, Research, Practice, and Policy, 1(1), 35–48. doi:10.1037/a0015128
Koenigs, M., & Grafman, J. (2009). Posttraumatic stress disorder: The role of medial prefrontal cortex and amygdala. Neuroscientist, 15(5), 540–548. doi: 10.1177/1073858409333072
May, P. A., Van Winkle, N. W., Williams, N. B., McFeeley, P. J., DeBruyn, L. M., & Serma, P. (2002). Alcohol and suicide death among American Indians of New Mexico 1980–1998. Suicide and Life-Threatening Behavior, 32(3), 240–255.
Myhra, L. L. (2011). “It Runs in the Family”: Intergenerational transmission of historical trauma among urban American Indians and Alaska Natives in culturally specific sobriety maintenance programs. American Indian and Alaska Native Mental Health Research, 18, 17–40.
National Survey on Drug Use and Health (NSDUH). (2010). Substance use among American Indian or Alaska Native adults. Office of Applied Studies, Substance Abuse and Mental Health Services Administration. Retrieved from http://www.oas.samhsa.gov/2k10/182/ AmericanIndian.htm#footnote5
Neigh, G., Gillespie, C., & Nemeroff, C. (2009). The neurobiological toll of child abuse and neglect. Trauma, Violence & Abuse, 10(4), 389–410. doi:10.1177/1524838009339758
Plous, S. (2002). Understanding prejudice and discrimination. New York, NY: McGraw-Hill.
Schnurr, P.P., & Green, B. L. (Eds.) (2004). Trauma and health: Physical health consequences of exposure to extreme stress. Washington, DC: American Psychological Association.
Sequist, T. D., Cullen, T., & Acton, K. J. (2011). Indian health service innovations have helped reduce health disparities affecting American Indian and Alaska Native people. Health Affairs, 30(10), 1965–1973. doi:10.1377/hlthaff.2011.0630
Solomon, E. P., & Heide, K. M. (2005). The biology of trauma: Implications for treatment. Journal of Interpersonal Violence, 20(1), 51–60.
Sotero, M. M. (2006). A conceptual model of historical trauma: implications for public health practice and research. Journal of Health Disparities Research and Practice, 1(1), 93–108.
Sue, D. W., & Sue, D. (2012). Counseling the culturally diverse: Theory and practice. (6th ed.). New York, NY: John Wiley & Sons, Inc.
Trusty, J., Looby, E. J., & Sandhu, D. S. (2002). Multicultural counseling: Context, theory and practice, and competence. New York, NY: Nova Science Publishers.
United States Census Bureau. (2006). We the People: American Indians and Alaska Natives in the United States: Census 2000 Special Reports, CENSR-28. Retrieved from http://www.census.gov/prod/2006pubs/censr-28.pdf
Walker, M. (1999). The inter-generational transmission of trauma: The effects of abuse on their survivor’s relationship with their children and on the children themselves. European Journal of Psychotherapy, Counselling and Health, 2(3), 281–296.
Walters, K. L., & Simoni, J. M. (2009). Decolonizing strategies for mentoring American Indians and Alaska Natives in HIV and mental health research. American Journal of Public Health, 99(S1), S71–S76. doi:10.2105/AJPH.2008.136127
Weisband, E. (2009). On the aporetic borderlines of forgiveness: Bereavement as a political form. Alternatives, 34(4), 359–381.
Weiss, S. J. (2007). Neurobiological alterations associated with traumatic stress. Perspectives In Psychiatric Care, 43(3), 114–122. doi:10.1111/j.1744-6163.2007.00120.x
Weisberg, R. B., Bruce, S. E., Bruce, S. E., Machan, J. T., Kessler, R. C., Culpepper, L., & Keller, M. B. (2003). Nonpsychiatric illness among primary care patients with trauma histories and posttraumatic stress disorder. Psychiatric Services, 53(7), 848–854.
Wendt, D. C., & Gone, J. P. (2012). Rethinking cultural competence: Insights from indigenous community treatment settings. Transcultural Psychiatry, 49(2), 206–222. doi:10.1177/1363461511425622
Whitbeck, L. B., Adams, G. W., Hoyt, D. R., & Chen, X. (2004). Conceptualizing and measuring historical trauma among American Indian people. American Journal of Community Psychology, 33(3-4), 119–130. doi:10.1023/B:AJCP.0000027000.77357.31
Yehuda, R., Halligan, S. L., & Bierer, L. M. (2001). Relationship of parental trauma exposure and PTSD to PTSD, depressive and anxiety disorders in offspring. Journal of Psychiatric Research, 35(5), 261–270.
Yehuda, R., Bierer, L. M., Schmeidler, J., Aferiat, D. H., Breslau, I., & Dolan, S. (2000). Low cortisol and risk for PTSD in adult offspring of holocaust survivors. The American Journal of Psychiatry, 157(8), 1252–1259.
Yehuda, R., Schmeidler, J., Wainberg, M., Binder-Brynes, K., & Duvdevani, T. (1998). Vulnerability to posttraumatic stress disorder in adult offspring of Holocaust survivors. American Journal of Psychiatry, 155, 1163.
Kathleen Brown-Rice, NCC, is an Assistant Professor at the University of South Dakota. Correspondence can be addressed to Kathleen Brown-Rice, Division of Counseling and Psychology in Education, School of Education, University of South Dakota, 210E Delzell, Vermillion, SD 57069, kathleen.rice@usd.edu.
Oct 15, 2014 | Article, Volume 3 - Issue 3
Simone Lambert, Emily Goodman-Scott
This article explores a model partnership with a counseling education program and the Peace Corps. Counselor education students in a group counseling course developed and implemented a singular structured group session with clients not typically used (e.g., non-counseling students) to maximize student learning and implement group counseling skills. Group services were provided to returning Peace Corps volunteers with diverse cultural experiences who were in career and life transitions. In addition, the authors provide strategies for developing similar partnerships between counselor education programs and other agencies.
Keywords: group counseling, counselor education, Peace Corps, volunteers, student learning
Group counseling is a core element of accredited master’s-level counselor education programs, as noted in the Council for Accreditation of Counseling and Related Programs Training Standards (CACREP, 2009). During the group counseling course, students often learn the process of participating in and leading experiential process groups, typically with other counseling students (McDonnell, Toth, & Aldarondo, 2005). While process groups are beneficial to student learning, student learning could be maximized by going one step further and providing group counseling to non-counseling students. The authors propose that rather than waiting until students’ clinical coursework (e.g., practicum, internship) to provide counseling services to non-counseling students, participating in a model partnership with the Peace Corps could foster such student learning. This experience offers master’s-level group counseling students the opportunity to provide group counseling to non-counseling students under intense supervision. In addition, students provide a service to Returning Peace Corps Volunteers (RPCVs), who traditionally face a myriad of challenges transitioning back into the United States from their international service (Bosustow, 2006; Callahan & Hess, 2012; Christofi & Thompson, 2007; Gaw, 2000; Szkudlarek, 2010).
The first section of this article summarizes the importance of student learning through experiential group counseling, especially with non-counseling students. Additionally, the authors discuss RPCVs and their potential needs following deployment. The second section of this article describes the partnership between a counselor education program and the Peace Corps that has evolved over several years to include group counseling services to RPCVs. The logistical aspects involved (e.g., class assignments) are offered as a model for future adaptation, as well as overall trends in group members’ and facilitators’ feedback. Finally, the authors provide suggestions for counselor education programs to implement similar partnerships with their local organizations and other programs on campus.
Background of Partnership
The partnership between a counselor education program and the Peace Corps developed with consideration of the needs of counselor education students and RPCVs. The authors discuss training standards and ethical considerations in relation to teaching group counseling through the use of experiential groups. Non-peer group members—in this case RPCVs—are described in both their unique diverse experiences and the challenges they face that are suitable for group exploration. Group counseling students and RPCVs are explored through their unique needs from and contributions to the partnership.
Group Counseling Students
Experiential process groups have been used in counselor education programs to help students learn basic group counseling skills and learn about themselves (Anderson & Price, 2001; Lennie, 2007; McDonnell et al., 2005; Osborn, Daninhirsch, & Page, 2003). Group counseling courses should teach students skill sets in group leadership, and also provide students with experiential opportunities to practice the skills they acquire (Furr & Barret, 2000). By incorporating experiential opportunities into a group counseling course, instructors increase student knowledge and understanding of group dynamics, group leadership skills, and group concepts (Akos, Goodnough, & Milsom, 2004).
Both the Association for Specialist in Group Work (ASGW, 2000) and CACREP (2009) recommend that students train in group counseling through participation in experiential learning, such as group leadership and membership roles. Additionally, Shumaker, Ortiz, and Brenninkmeyer (2011) outlined the consensus between counselor educators and accrediting bodies that experiential group participation provides students with greater levels of group process and self-awareness compared to solely didactic instruction. Thus, experiential learning such as group membership and leadership are paramount in training group counseling students.
While group membership can lead to increased “interpersonal learning, self-awareness, and empathy” (Ieva, Ohrt, Swank, & Young, 2009, p. 365) and provide an intrinsic understanding of group process, group counseling students need direct experiences to practice the concepts and skills learned in class (Gillam, 2004). Group leadership experience increases students’ competence and ease in implementing interventions with immediacy (Toth & Stockton, 1996). Group leadership can occur on a rotating basis for group counseling students in their experiential group, yet there are ethical considerations (e.g., programmatic gatekeeping, multiple relationships) when students participate in group counseling with peers, including disclosing intimate details to fellow students and/or faculty members (Furr & Barret, 2000; Shumaker et al., 2011). The American Counseling Association’s Code of Ethics (2005) describes the need to protect the rights of students when groups are led by peers. Thus, alternatives to traditional in-class experiential groups may be helpful to allow students to gain group leadership skills without feeling uncomfortable about personal disclosures or multiple relationships.
Given the limitations and concerns described above, counselor education students who provide group counseling to non-peers may bypass some of the disadvantages of experiential groups with peers (Conyne, Wilson, & Ward, 1997). By recruiting group members from outside of class, ethical dilemmas surrounding multiple relationships amongst peers as well as with students and instructors are negated, and the instructor can focus on evaluating the group leadership skills demonstrated in the session, rather than student self-disclosures (Furr & Barret, 2000). As a result, students leading a group of non-peers may be better able to implement their newly acquired group counseling skills. Additionally, students leading a group of non-peers may gain exposure to a different population and practice serving diverse client needs.
Returning Peace Corps Volunteers (RPCVs)
Both the CACREP (2009) standards and ACA’s Code of Ethics (2005) emphasize the need for counselors to advocate for and serve diverse populations. The CACREP standards state that counselors should be prepared for “promoting cultural social justice, advocacy…and other culturally supported behaviors that promote optimal wellness and growth of the human spirit, mind, or body” (p. 11). Not only should counselors be prepared to work with culturally diverse clients, but they also are charged with advocating and serving diverse clients and supporting their wellness. RPCVs are a diverse population in terms of their acculturation levels and varied service-related cultural identities. They are a population that typically encounters difficulties transitioning back into the United States post-international service, including possible social, emotional, behavioral, cognitive, and career difficulties (Bosustow, 2006; Callahan & Hess, 2012; Christofi & Thompson, 2007; Gaw, 2000; Szkudlarek, 2010). As a result, RPCVs are a population with unique needs that could benefit from counseling services.
During their service, Peace Corps volunteers spend 2–3 years in a host culture with typically only one visit back to the United States (Callahan & Hess, 2012). Additionally, Peace Corps volunteers are encouraged to become fully immersed in their host culture and complete 3 months of intensive cultural and linguistic training in preparation (Callahan & Hess, 2012). When abroad, expatriates (e.g., Peace Corps volunteers) go through an adaptation or acculturation process. Haslberger (2005) described cross-cultural adaptation as “a complex process in which a person becomes capable of functioning effectively in a culture other than the one he or she was originally socialized in” (p. 86). According to Berry (2005), “acculturation is the dual process of cultural and psychological change that takes place as a result of contact between two or more cultural groups and their individual members” (p. 698).
Osland (2000) described the expatriate experience as trifold: (a) separation from the home culture: adventurous and homesick; (b) immersion into the host culture: a transformative struggle to acclimate and enjoy living in the host culture; and (c) return and reintegration into the home culture: often the most challenging stage, as individuals attempt to integrate their new identity into previous roles and relationships. Expatriates’ acculturation in the host culture can be a transformative process of negotiating and letting go of aspects of their home culture and previous identity in exchange for a new cultural identity and norms (Osland, 2000). In a qualitative study, Kohonen (2004) discovered that expatriates encountered identity shifts when living abroad, including developing bicultural identities. Haslberger (2005) echoed similar sentiments, stating that full immersion in a foreign culture impacts the individuals in every aspect of their identity. In a recent study, Callahan and Hess (2012) found that RPCVs reported being more multicultural and developing new ways of thinking, as a result of their time in the host culture. In fact, RPCVs often recounted continuing to practice cultural patterns learned abroad, even after returning to the United States (Callahan & Hess, 2012).
RPCVs are a population with varied needs. One of the challenges facing RPCVs, along with other expatriates who return to their home culture after living abroad for an extended period, is reverse culture shock. “Reverse culture shock is the process of readjusting, reacculturating, and reassimilating into one’s own home culture after living in a different culture for a significant period of time” (Gaw, 2000, pp. 83–84). Reverse culture shock includes (a) feelings of surprise and frustration at the reentry process, when reentry is more challenging than anticipated; (b) feeling disconnected from both home and abroad cultures; and (c) depression, loneliness, anxiety, isolation, and social maladjustment reported by expatriates (Bosustow, 2006; Christofi & Thompson, 2007; Gaw, 2000; Szkudlarek, 2010).
Returning to the home culture can be as stressful as becoming integrated into the host culture, and often more so, as RPCVs do not expect the return home to be so challenging (Callahan & Hess, 2012). Reverse culture shock can occur because not only have the RPCVs changed, so have their home cultures in their absence (Callahan & Hess, 2012). Bosustow (2006) found that RPCVs reported their reentry adjustment taking longer than they initially expected—often a year or longer. Additionally, approximately 25% of the RPCVs in Bosustow’s study stated that the Peace Corps did not adequately address their psychological reentry needs. However, over 77% of these RPCVs reported that the most helpful component of their reentry was talking to other RPCVs about their experiences.
RPCVs have many adjustment needs as they reenter the United States and report a lack of adequate formal support (Bosustow, 2006). Best practices recommend that counselors receive training to meet the diverse and unmet needs of clients such as the RPCVs (ACA, 2005; CACREP, 2009). Additionally, since the RPCVs in Bosustow’s (2006) study found informal support from their peers with shared experiences, group counseling with other RPCVs could be a particularly beneficial counseling intervention for this population. Assisting RPCVs with challenges related to reentry (e.g., career transition, interpersonal concerns) allows counselor education students to provide a needed service while gaining counseling experience with a diverse, non-student population.
The Partnership in Action
The authors have taught a general group counseling class to both school and clinical mental health counseling students. In the first author’s initial years of teaching group counseling, students reported many advantages and disadvantages of utilizing peers with the experiential group as outlined above. Through conversations with students, it became apparent that a different experiential group counseling experience would enhance students’ integration of material presented in the group counseling course. As a result, the first author developed a culminating assignment for the course.
The purpose of the culminating assignment was to integrate student learning from didactic lectures, group counseling observations in the classroom and in the community, group membership, and group leadership with peers. The culminating assignment offered a direct experience with non-peer clients under intense supervision, creating a safe environment for students to experiment with newly obtained group counseling skills. In this instance, students had the opportunity to increase confidence in conducting groups prior to their clinical practicum or internship. This partnership has evolved over the last several years with the process expanding to include doctoral students in both the supervision and instruction process as part of the doctoral students’ supervision and teaching internships. This article will explain the process of designing, implementing, and supervising the RPCVs groups, including (a) describing the class assignment, (b) group member procurement, and (c) group composition and format.
Class Assignments
Furr and Barret (2000) suggested that structured psychoeducational groups can be implemented as a component of an entry-level group counseling course, providing students with the valuable skills of designing and leading groups. Structured psychoeducational groups can be found in a variety of counseling specialties (Gladding, 2012), such as clinical mental health, marriage and family, career, school, college and addictions. In fact, these structured groups are the primary group type utilized by school counselors (Akos et al., 2004). Psychoeducational groups should be customized for different populations (e.g., youth versus adults) (DeLucia-Waack, 2006; Gladding, 2012). Yet there are many similarities between the overall group counseling process for both youth and adult clients, including membership screening and selection, confidentiality issues, group leadership skills, and the value of group work (Gladding, 2012; Steen, Bauman, & Smith, 2007; Van Velsor, 2004). Counseling students are being prepared to work in a multitude of settings with varied client needs (e.g., schools, clinical mental health agencies, colleges). As such, learning fundamental structured psychoeducational group skills is useful for counseling students across specialties, settings and client needs (Conyne et al., 1997).
Leading up to the culminating assignment of designing and conducting a structured psychoeducational group, students completed a number of class assignments in preparation: (1) students became familiar with group concepts by reading their text, listening to lectures, and partaking in class discussions; (2) they observed videotaped demonstrations in class and two group counseling sessions in the community or school settings; (3) they participated in an experiential group with their peers; and (4) they facilitated or co-facilitated the experiential group with classmates on a rotating basis at least once. These assignments were processed in writing as well as verbally with classmates.
ASGW (2000) indicated that competencies need to be gained in planning, implementing, leading and evaluating group interventions. These competencies converged in the culminating assignment divided into two parts: the development of a group counseling proposal and the actual implementation of the proposed psychoeducational group for RPCVs (see Appendix for sample assignment descriptions). By both designing and implementing the group within the course, students immediately applied psychoeducational group proposals they created. By developing their own psychoeducational group, students had high personal investment in both the proposal and its implementation.
For the culminating assignment, students were encouraged to work in pairs; thus, the co-facilitators coauthored the group proposal. The group proposal was due a few weeks prior to the students conducting the structured psychoeducational group, giving the instructor time to coordinate logistics with the RPCV coordinator. The instructor graded the proposals, emphasizing mastery of the assignment with revisions being a part of the process. Svinicki and McKeachie (2014) describe how student anxiety about grades can be lessened by allowing students to resubmit revised work. The instructor could then focus on student anxiety related to student facilitation of the group. In addition, these revised group proposals can be a document added to students’ professional portfolios.
Intensive supervision was provided as the instructor and/or doctoral supervision interns were present for all group sessions. Stockton and Toth (1996) suggested that providing a supervised experiential group experience is a vital element in training group leaders. In addition, Toth and Stockton (1996) stated that observing other students lead a group can be instrumental in attaining group leadership skills. These two factors were combined by providing on-site supervision and reviewing portions of students’ recorded group sessions during the following class session. Also, on-site supervision allowed the instructor to address any client safety concerns that arose (e.g., harm to self or others).
One of the biggest challenges to implementing this learning opportunity was scheduling the groups at a time when supervisors, students and group members were available. Over the past several years, the authors tried a number of configurations for scheduling the psychoeducational groups. Holding multiple sessions concurrently over 3–4 hours was the preferred method.
Osborn et al. (2003) recommended that counseling students engage in instructor-facilitated reflection to debrief and learn from their group leadership experience. Likewise, Luke and Kiweewa (2010) recommended that counselor education programs include reflective journaling to maximize students’ self-awareness in the group work context. After completion of the culminating assignment (the psychoeducational group facilitation), students submitted a reflection paper describing their reaction to their group leadership experience. Student learning continued through receiving and discussing post-session evaluations of RPCVs. Following the group facilitation, students reported having a clearer sense of their strength and growth areas. During students’ subsequent practicum and internship courses, they often reported confidence and skill in group counseling, which they attributed to the culminating assignment in their group counseling course.
Group Member Procurement
The described counselor education program had an established relationship with the local Peace Corps Career Center (PCCC), which was established years prior through a faculty member offering career counseling services to RPCVs. For example, practicum students provided individual counseling sessions to RPCVs during the spring semester. Peace Corps staff expressed an interest in offering year-round services to RPCVs, due to the limited debriefing available to RPCVs (J. Hammer and R. Michon, personal communication, January 8, 2008). As a result, group counseling sessions were a welcome addition during the fall semester. The PCCC coordinator was instrumental in recruiting and screening group members. After counseling students provided a paragraph describing their proposed groups, the coordinator marketed the groups through a RPCV listserv, and flyers were posted throughout the PCCC inviting RPCVs to participate in group sessions. Group members, RPCVs, chose topic area(s) that were appropriate for their personal career and life-transition challenges; there were no fees for group members to attend the sessions. RPCVs were notified in advance that the psychoeducational group would be recorded for instructional purposes, and both informed consent and authorization of recording were secured in writing at the beginning of the group sessions. Students began their group sessions by briefly describing the limits of confidentiality.
Group Composition and Format
The group size was predetermined by the instructor(s), and the coordinator at the PCCC screened and enrolled people accordingly. The preference was to have co-facilitators with no more than 10 RPCVs in each group, with a smaller group number for those groups with only one facilitator (in the instance there was an odd number of students enrolled in the group counseling course). The RPCVs varied in age from mid-twenties to mid-forties and in marital status, although the majority were single. The group members were from varied ethnic and racial backgrounds (predominantly Caucasian). While most of the RPCVs lived near the PCCC where the structured psychoeducational groups were held, prior to their Peace Corps service they lived throughout the United States. The Peace Corps experience had occurred in a wide variety of geographic locations around the globe, where RPCVs had been immersed in another culture—often a culture in the developing world—for an extended period of time. Most of the RPCV group members had returned from their service within the past year, yet some of them had been stateside for up to 5 years.
The number of groups offered to the RPCVs during one semester depended on student enrollment in the group counseling class. Various RPCV group members chose to attend sessions on distinctly different topics and often participated in multiple groups offered by the group counseling students. The structured psychoeducational group topics were offered during late afternoon and evening hours to maximize the opportunity for RPCVs to attend a variety of sessions. Group counseling topics often included career decision-making (making career choices), networking cooperatives (building networking skills for a job search), life transitions (processing readjustment to life back in the United States), work-life balance (developing coping strategies to create manageable lifestyle), interviewing skills (preparing for the interview), and stress management during the job search (learning stress management techniques). The instructor(s) and the on-site PCCC coordinator orchestrated the flow of sessions, keeping group leaders and group members on schedule.
RPCV Feedback About the Groups
Students collected feedback from the RPCVs after each psychoeducational group to identify strengths and suggestions regarding the students as facilitators. Additional anecdotal feedback was solicited from the RPCVs about the overall process; RPCVs typically responded very favorably about the experience. Specifically, the positive highlights from the experience tended to be resources and information, universality and cohesiveness experienced by the RPCVs. The most common complaint expressed was that the 1-hour sessions were not long enough, which may indicate the perceived value of the group experience and actual needs of the RPCVs.
Likewise, students provided anecdotal feedback that the structured psychoeducational group with non-peers helped them to synthesize their learning of group counseling skills and to decrease their overall anxiousness about conducting group counseling. The authors observed increased student confidence and knowledge of group counseling implementation following the group leadership experience with the RPCVs. Students also reported an increased awareness of and appreciation for the service of RPCVs, including learning secondhand about internationally diverse cultures and the unique experience of the RPCVs as expatriates. The combined feedback from RPCVs and students, along with observed increase in students’ confidence and reported skills, may suggest that the culminating assignment did indeed maximize student learning.
Resources for Partnerships
Not every counselor education program is fortunate enough to have a fully operational training clinic where students from the university or members of the community can partake in a group counseling experience on campus. Students may be able to lead groups at other locations, including clinical mental health agencies, schools and other related counseling agencies (Stockton & Toth, 1996). A need exists for counselor educators to identify agencies that could utilize the skills and resources provided by group counseling students, and that would be open to having counseling students provide services to the agency volunteers or employees.
The Peace Corps is certainly a prime example of this type of agency; whereby RPCVs often struggle with reentry issues (e.g., interpersonal concerns, career transition) and could benefit from structured psychoeducational groups. Interacting with the RPCVs reportedly has been a humbling experience for students in the group counseling course, who recognize the talent and sacrifices that these individuals made to serve others. Students often stated that it was an honor to work with RPCVs during the group counseling course.
There are a number of national agencies that, like the Peace Corps, may have a need for debriefing volunteers and employees who have been through some life-changing event as a result of their work with the agency. By teaming up with such agencies, the partnership may become mutually beneficial for volunteers/employees of the agency and the group counseling students. A list of possible agencies and websites is provided for future partnerships with counselor education programs (see Table 1). By visiting these agency websites, counselor educators may find a local or regional office in close proximity to their university and establish a rewarding partnership for all.
Table 1
Potential Agencies for Partnerships
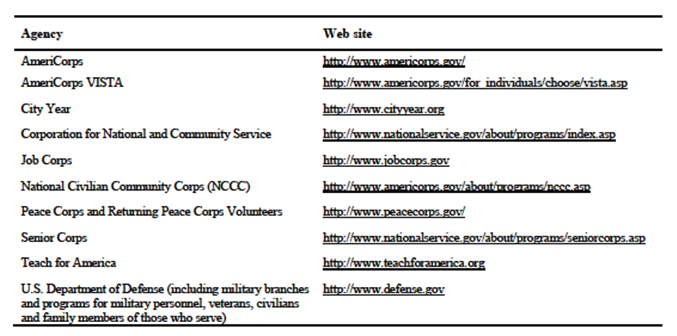
Another possibility for a mutually beneficial partnership is to offer group counseling services to the international student population at the counselor education program’s university. Often-times, international students are dealing with transition and acculturation issues similar to that of the RPCVs. Structured psychoeducational groups could provide needed information and time to process acclimation of international students to a different culture and educational system. Group counseling students would have the opportunity to increase their cultural awareness and develop appropriate culturally-sensitive interventions (Bodenhorn, DeCarla Jackson, & Farrell, 2005). This is just one other example of how group counseling students, group members, and counselor education programs can benefit from such partnerships. Counselor educators are encouraged to explore possible opportunities for similar partnerships with local agencies, schools and universities.
Conclusion
Research, professional standards, and accrediting bodies all indicate that an experiential group process is a crucial dimension of group counseling course curriculum. Group leadership further synthesizes and cements group counseling skills and processes learned throughout a group counseling course. While peer experiential groups are beneficial for students, conducting a structured psychoeducational group with non-peers may maximize student learning by teaching valuable skills that can be transferred to clinical mental health and school settings. Conyne et al. (1997) stated that exemplary preparation programs often included experiential learning opportunities, such as supervised students facilitating group counseling to non-students, and serving the community through their group work, both of which were utilized in the described partnership with the Peace Corps.
Best practices also recommend that students gain experience counseling and serving diverse clients. Collaborating with agencies whose employees and volunteers engaged in an international experience offers counselor educators the opportunity to enter into a mutually beneficial relationship: (a) group counseling students receive valuable supervised clinical experience serving clients with diverse experiences; and (b) clients receive needed assistance through difficult transitions. Partnering with an agency with an international focus may increase students’ multicultural competencies and help recruit diverse counselor education students to the preparation program. Overall, collaborating with the Peace Corp was a win-win situation for the described counselor education program: counseling students maximized their learning of group counseling skills within a multicultural-laden context, and RPCVs gained crucial services to assist in their life transition.
References
Akos, P., Goodnough, G. E., & Milsom, A. S. (2004). Preparing school counselors for group work. The Journal for Specialists in Group Work, 29(1), 127–136. doi:10.1080/01933920490275637
American Counseling Association. (2005). ACA code of ethics. Alexandria, VA: Author.
Anderson, R. D., & Price, G. E. (2001). Experiential groups in counselor education: Student atitudes and instructor participation. Counselor Education and Supervision, 41(2), 111–119. doi:10.1002/j.1556-6978.2001.tb01275.x
Association for Specialists in Group Work. (2000). Professional standards for the training of group workers. Retrieved from http://www.asgw.org/PDF/training_standards.pdf
Berry, J. W. (2005). Acculturation: Living successfully in two cultures. International Journal of Intercultural Relations, 29(6), 697–712. doi:10.1016/j.ijintrel.2005.07.013
Bodenhorn, N., DeCarla Jackson, A., & Farrell, R. (2005). Increasing personal cultural awareness through discussions with international students. International Journal of Teaching and Learning in Higher Education, 17(1), 63–68. Retrieved from http://www.isetl.org/ijtlhe/pdf/IJTLHE7.pdf
Bosustow, N. J. (2006). The reentry experience: An examination of Peace Corps volunteers’ experience of returning home after service. (Unpublished doctoral dissertation). The Wright Institute Graduate School of Psychology, Berkeley, CA.
Callahan, C., & Hess, J. (2012). Experiences of deculturation among United States Peace Corps volunteers. Journal of International Communication, 18(1), 49–62. doi:10.1080/13216597.2012.662167
Christofi, V., & Thompson, C. L. (2007). You cannot go home again: A phenomenological investigation of returning to the sojourn country after studying abroad. Journal of Counseling & Development, 85(1), 53–63. doi:10.1002/j.1556-6678.2007.tb00444.x
Conyne, R. K., Wilson, F. R., & Ward, D. E. (1997). Comprehensive group work: What it means and how to teach it. Alexandria, VA: American Counseling Association.
Council for Accreditation of Counseling and Related Educational Programs. (2009). 2009 CACREP standards. Alexandria, Virginia: Author.
DeLucia-Waack, J. L. (2006). Leading psychoeducational groups for children and adolescents. Thousand Oaks, CA: Sage Publications.
Furr, S. R., & Barret, B. (2000). Teaching group counseling skills: Problems and solutions. Counselor Education and Supervision, 40(2), 94–104. doi:10.1002/j.1556-6978.2000.tb01241.x
Gaw, K. F. (2000). Reverse culture shock in students returning from overseas. International Journal of Intercultural Relations, 24(1), 83–104. doi:10.1016/S0147-1767(99)00024-3
Gillam, S. L. (2004). Preplanning considerations in teaching group counseling courses: Applying a general framework for conceptualizing pedagogy. The Journal for Specialists in Group Work, 29(1), 75–85. doi:10.1080/01933920490275475
Gladding, S. T. (2011). Groups: A counseling specialty (6th ed.). Upper Saddle River, NJ: Pearson.
Haslberger, A. (2005). Facets and dimensions of cross-cultural adaptation: Refining the tools. Personnel Review, 34(1), 85–109. doi:10.1108/00483480510571897
Ieva, K. P., Ohrt, J. H., Swank, J. M., & Young, T. (2009). The impact of experiential groups on master students’ counselor and personal development: A qualitative investigation. The Journal for Specialists in Group Work, 34(4), 351–368. doi:10.1080/01933920903219078
Kohonen, E. (2004). Learning through narratives: About the impact of international assignments on identity. International Studies of Management and Organization, 34(3), 27–45.
Lennie, C. (2007). The role of personal development groups in counselor training: Understanding factors contributing to self-awareness in the personal development group. British Journal of Guidance & Counselling, 35(1), 115–129. doi:10.1080/03069880601106849
Luke, M., & Kiweewa, J. M. (2010). Personal growth and awareness of counseling trainees in an experiential group. The Journal for Specialist in Group Work, 35(4), 365–388. doi:10.1080/01933922.2010.514976
McDonnell, K. A., Toth, P. L., & Aldarondo, F., II. (2005). Rex Stockton’s contributions to group counselor education. The Journal for Specialists in Group Work, 30(3), 221–240. doi:10.1080/01933920591003069
Osborn, C. J., Daninhirsch, C. L., & Page, B. J. (2003). Experiential training in group counseling: Humanistic processes in practice. The Journal of Humanistic Counseling, Education and Development, 42(1), 14–28.
Osland, J. S. (2000). The journey inward: Expatriate hero tales and paradoxes. Human Resource Management, 39(2–3), 227–238. doi:10.1002/1099-050X(200022/23)39:2/3<227::AID-HRM11>3.0.CO;2-R
Shumaker, D., Ortiz, C., & Brenninkmeyer, L. (2011). Revisiting experiential group training in counselor education: A survey of master’s-level programs. The Journal for Specialists in Group Work, 36, 111–128. doi:10.1080/01933922.2011.563142
Steen, S., Bauman, S., & Smith, J. (2007). Professional school counselors and the practice of group work. Professional School Counseling, 11(2), 72–80. doi:10.5330/PSC.n.2010-11.72
Stockton, R., & Toth, P. L. (1996). Teaching group counselors: Recommendations for maximizing preservice instruction. The Journal for Specialists in Group Work, 21(4), 274–282. doi:10.1080/01933929608412259
Svinicki, M. D., & McKeachie, W. J. (2012). McKeachie’s teaching tips: Strategies, research, and theory (14th ed.). Belmont, CA: Wadsworth.
Szkudlarek, B. (2010). Reentry-a review of the literature. International Journal of Intercultural Relations, 34(1), 1–21. doi:10.1016/j.ijintrel.2009.06.006
Toth, P. L., & Stockton, R. (1996). A skill-based approach to teaching group counseling interventions. The Journal for Specialists in Group Work, 21(2), 101–109. doi:10.1080/01933929608412238
Van Velsor, P. (2004). Training for successful group work with children: What and how to teach. The Journal for Specialist in Group Work, 29(1), 137–146. doi:10.1080/01933920490275664
Simone Lambert, NCC, is an Assistant Professor at the Counseling Programs, Argosy University DC. Emily Goodman-Scott, NCC, is an Assistant Professor at Old Dominion University. Correspondence can be addressed to Simone Lambert, Counseling Programs, Argosy DC, 1550 Wilson Blvd., Suite 600, Arlington, VA 22209, sflambert@argosy.edu.
Appendix
Example Assignment Descriptions for Syllabus
I. Group Counseling Proposal Assignment
Students are required to develop a proposal for a 1-hour psychoeducational group to be conducted with RPCVs. The proposal should be 8–10 pages and include current literature. The proposal outline is as follows:
- Purpose and goals of the group
- Eligibility criteria, recruitment strategies, and screening techniques (e.g., RPCVs selected based on interest in program topic, screened by PC staff)
- Length, frequency, duration of group (e.g., a single 1-hour group session)
- Appropriate leadership style and roles
- Appropriate group norms, process, and procedures (e.g., structure and relevant activities)
- Demonstration of the various stages of the group process
- Ethical considerations
- Cultural considerations
- Evaluation criteria: What will determine whether group goals have been met?
- Summary: Briefly summarize your proposal and rationale.
II. Group Leadership/Facilitation/Reflection Paper
Students will co-lead a 1-hour psychoeducational group for RPCVs. The group will be based on your written proposal. Feedback will be provided to you regarding your proposal prior to conducting the group. After the session, you and your co-facilitator will each write a two-page reflection paper on the group process that took place under your leadership. The reflection paper will include your analysis of the following:
- What group stages did the group experience?
- What do you believe would be needed for the group to function more effectively?
- Which techniques did you actually use in the session?
- How did you incorporate a theoretical framework into the session?
- Were the desired group goals/outcomes achieved?
- How did your group leadership influence these goals/outcomes?
- If you were able to have an additional session, what direction would you take the group?
- What were your own strengths and areas of growth as a group leader within the session?
Oct 15, 2014 | Article, Volume 3 - Issue 3
Russ Curtis, Heather Thompson, Gerald A. Juhnke, Melodie H. Frick
Treatment fit is the degree to which the counselor and the client agree upon the presenting issues, counseling goals and the initial treatment plan. Research indicates that treatment fit is one of the strongest predictors of client outcome. As such, a brief functional treatment fit model (TFM) is presented to assist counselors in conducting multidimensional needs assessments and developing co-created treatment plans. Application of this model is demonstrated with a case study. In addition, a link to a video demonstration of this model is included, along with a discussion as to the need for including links to videos in counseling journals.
Keywords: treatment fit, multidimensional needs assessment, treatment plan, counseling goals, video demonstration
This is an exciting time in the mental health profession as health care specialists and policy makers are recognizing the value of counseling in increasing the quality of patient care while decreasing overall health care costs (Burtnett, 2012; Curtis & Christian, 2012; Lee et al., 2012; Wos, 2013). As such, counselors are increasingly being recognized not just as mental health providers, but as viable health care professionals who may well be the crucial link in improving a flawed and exorbitantly expensive health care system (American Psychological Association [APA], 2012; Brill, 2013; Paquette et al., 2003). With this positive momentum, however, it becomes even more imperative for counselors to consistently utilize evidence-based practices (i.e., empirically supported counseling strategies), which include practice-based evidence (i.e., continuous feedback between counselor and client) to ensure optimal treatment. Unfortunately, the utilization rates of evidence-based practices by counselors are minimal and inconsistent (Beutler, 2009; Olmstead, Abraham, Martino, & Roman, 2012), which may in part be the reason why the general public, when surveyed, have indicated that the primary reason for not seeking counseling was their lack of confidence in positive outcomes (Harris Interactive, 2004). One could argue that while it is critically important for counselors to continue conducting innovative treatment research, it is equally imperative that counselors increase efforts in implementing well-established evidence-based counseling strategies (Olmstead et al., 2012).
One of the best predictors of client outcome is treatment fit (APA, 2012; Budd & Hughes, 2009; Kim, Ng, & Ahn, 2009), the process by which the client and counselor collaboratively assess mental health issues, set goals, and create an initial treatment plan. At the heart of treatment fit is the collaboration between client and counselor including continuous feedback about issues, goals and treatment to ensure the optimal provision of care. A parallel to treatment fit in the medical community is the increasing use of checklists to ensure that evidence-based procedures are being properly implemented. In surgical safety research, for instance, Haynes et al. (2009) found in a large multi-site international study that when medical professionals followed a brief surgical checklist (e.g., the patient has verified his or her identity, the surgical site, and procedure and consent), patient deaths decreased from 1.5% to 0.8% and inpatient complications following surgery decreased from 11.0% to 7.0% (Haynes et al., 2009). As demonstrated in this surgical safety study, the consistent application of evidence-based procedures had a significant impact on patients’ lives. Similarly, the purpose of this article is to show how evidence-based counseling strategies that comprise treatment fit can help counselors more consistently and frequently implement treatments that work in order to increase the likelihood of positive client outcomes.
This article is comprised of two primary objectives. The first objective is to describe a brief, functional, first-session counseling protocol for ensuring treatment fit with clients. The second objective is to increase reader and viewer understanding and application of this treatment fit protocol by providing an online video demonstration of the treatment fit process. In so doing, the authors hope that counseling researchers and counselor educators will see the value in providing links of video demonstrations in their academic publications. To accomplish these objectives the authors have organized the article as follows: (a) a definition of treatment fit and a review of its literature, (b) a detailed explanation for how to conduct a treatment fit protocol, (c) evidence supporting the use of accessible online video in training, and (d) methods by which counselor educators can use accessible video to enhance student learning.
Treatment Fit
Treatment fit is the process by which client and counselor collaborate and agree on the issues, goals and treatment plan (Beutler, 2009; Beutler et al., 2003; Kim et al., 2009). Treatment fit is comprised of three empirically supported counseling strategies: (a) assessment of the clients’ concerns to increase the counselor–client shared world view (Keeley, Geffken, Ricketts, McNamara, & Storch, 2011; Spinhoven, Giesen-Bloo, van Dyck, Kooiman, & Arntz, 2007; Westra, Constantino, Arkowitz, & Dozois, 2011), (b) goal setting to increase the transparency of the counseling process and to increase clients’ positive expectations for counseling (Achor, 2010; Bednar & Parker, 1969; Bonner & Everett, 1982; Childress & Gillis, 1977; Constantino, Arnkoff, Glass, Amentrano, & Smith, 2011; Egan, 2007; Grosz, 1968; Hardin & Yanico, 1983; Kim, 2008; Tinsley, Bowman, & Ray, 1988; Ziemelis, 1974), and (c) initial treatment planning that instills hope and encourages clients to practice new behaviors (Duckworth, Grant, Loew, Oettingen, & Gollwitzer, 2011; Hirai & Clum, 2006; Hofmann & Smits, 2008; Norcross & Beutler, 2008).
As a whole, treatment fit is an integral aspect of effective counseling (Sexton, Whiston, Bleuer, & Walz, 1997). Treatment fit has been shown to improve client outcome (Beutler, 2009; Miller, Duncan, Brown, Sorrell, & Chalk, 2006), reduce early termination (Miller et al., 2006), decrease clients’ complaints against therapists (Cummings, O’Donohue, & Cummings, 2009), and reduce treatment costs (Heinssen, Levendusky, & Hunter, 1995). In one study of clients with co-morbid substance dependence and depression where several treatment variables were analyzed (e.g., client coping styles, therapeutic alliance, treatment fit), treatment fit was found to be the best predictor of client outcome (Beutler et al., 2003).
From a cross-cultural perspective, evidence indicates that treatment fit contributes to the counselor-client cultural worldview, or worldview match (Gonzalez, 2002; Kim, Ng, & Ahn, 2005), and is a significant predictor of therapeutic alliance (Kim et al.). This is important due to existing research indicating strong therapeutic alliances increase treatment efficacy (Budd & Hughes, 2009; Connors, DiClemente, Carroll, Longabaugh, & Donovan, 1997; Horvath & Symonds, 1991).
Budd and Hughes (2009) concluded in their review of 30 years of counseling meta-analyses that treatment fit was more important in predicting client outcome than therapeutic modality. And the APA’s Recognition of Psychotherapy Effectiveness (2012) states the following:
In contrast to large differences in outcome between those treated with psychotherapy and those not treated, different forms of psychotherapy typically produce relatively similar outcomes. This research also identifies ways of improving different forms of psychotherapy by attending to how to fit interventions to the particular patient’s needs. (p. 1)
In other words, treatment fit is a more powerful predictor of client outcome than therapeutic modality. Perhaps Beutler et al. (2003) sums it up best: “The addition of patient-treatment fit leads to the conclusion that ‘fit’ of patient and treatment should not be ignored either in studies of treatment effects or in studies of therapeutic alliance” (p. 84).
Despite evidence indicating the importance of treatment fit, there is a dearth of literature explaining how to conduct a brief, functional and collaborative treatment fit protocol in the first counseling session. And, although it is recognized that developing a treatment plan is advisable (Heinssen et al., 1995; Sexton et al., 1997), there is little information describing how to create treatment fit in a brief and practical format that can be used in clinical settings. Early initiation of treatment fit is especially important considering the evidence indicating that clients expect counseling to be brief (Klein, Stone, Hicks, & Pritchard, 2003), and on average attend only 3.5 sessions (Miller et al., 2006). Finally, it is recognized that counselor educators and supervisors need to develop systematic methods for teaching counselors how to build therapeutic alliance and ensure treatment fit (Budd & Hughes, 2009).
The Treatment Fit Model
Before describing the model, it is important for counselors to understand that either before or at the outset of the first counseling session, the client should complete an intake questionnaire that addresses a range of topics including but not limited to presenting symptoms, social support/stressors, legal, trauma, medical, illicit substances, employment and educational history. Thus, when beginning the treatment fit process the counselor is interested in the client’s intrapersonal responses to the aforementioned issues gleaned during intake. Once the intake is completed, the treatment fit process can begin. This treatment fit model (TFM) is a modified version of several existing models (Boffey, 1993; Fong, 1993; Heinssen et al., 1995; Meichenbaum, 2002), but redesigned and enhanced to accomplish several tasks: (a) gather information about the client’s concerns, goals and treatment options, (b) determine how the client’s concerns form multiple intrapersonal perspectives, (c) provide the client with a written summary of concerns, goals and treatment plan, and (d) use the model as a psychoeducational tool to help the client see how emotions, thoughts, behaviors and physiology interact, which can help the client recognize symptoms and develop coping skills before issues become overwhelming.
Facilitation of Treatment Fit Model
All three of the components, referred to as steps in the treatment fit process, can be accomplished within one 50-minute counseling session using the model in Table 1. Within each of the three steps—assessment, goals, and treatment plan—information is gathered about the client’s intrapersonal domains of emotions, cognitions, behaviors and physiology (e.g., racing heart, cold hands) to ensure a comprehensive understanding of the client’s issues and goals so a tentative treatment plan can be co-created with the client.
As seen in Table 1, several theories are integrated into and used with this model to facilitate each step. Although the theories and techniques described in this article have been used by the authors to effectively facilitate the treatment fit process, they are not meant to be prescriptive. Instead, integrative theoretical approaches will vary depending upon the needs of the client and skill level of the counselor.
Table 1
Primary Theories Integrated in the Treatment Fit Model
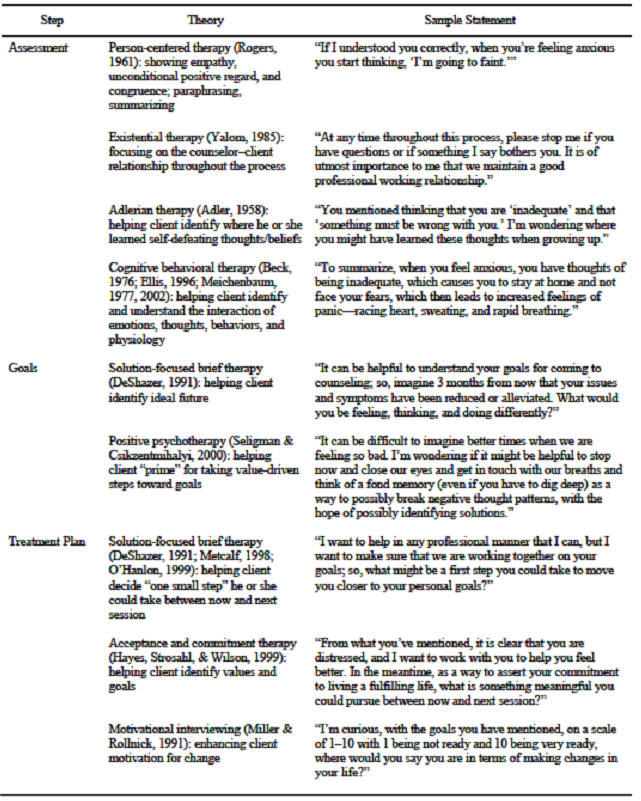
Step 1: Assessment
During the assessment phase of the model, person-centered (Rogers, 1961) and motivational interviewing skills (Miller & Rollnick, 1991) are used to create an environment where clients feel safe to discuss their issues. The assessment phase of the model should provide clients ample opportunity to discuss their concerns in an atmosphere that fosters therapeutic alliance. Anecdotal evidence suggests clients often discuss their emotions, thoughts, behaviors and physiological reactions related to presenting issues without excessive counselor questioning. By utilizing empathy, positive regard, summarization, and open-ended questions; and by clarifying discrepancies and listening for change-words (i.e., words that indicate a client’s needs, desires, abilities and commitment to change), a counselor creates an environment that enhances therapeutic alliance. The following case scenario is described to show how the different components of the TFM are conducted.
Sabine is a 30-year-old female, who was born in Quebec, Canada, and moved to the United States when she was 8 years old. She is a college graduate and has worked for the past eight years in a bank where she is now the branch manager. After witnessing a car accident two months ago, she reports experiencing increasing anxiety when driving, which is now compromising other areas of her life. She reports feeling isolated from friends and family, and for the first time in her professional career, she called in sick to avoid driving to work. After further reflection of content and summarizing, it appears that she is feeling helpless and having thoughts of being “out-of-control” and unable to manage her anxiety. She is scared that she will not be able to drive to see her family, or continue to drive to work. She reports that her anxiety is now causing her to stay at home most of the day and not visit with friends or attend church. Her main anxiety symptoms include rapid pulse, shallow breathing, difficulty with swallowing, and feeling faint. Sabine described herself as a shy child who was always able to overcome her fears. She reports no substance use except for a few glasses of wine with friends on the weekend, and she takes no medication.
From Sabine’s presenting concerns, the assessment phase of the model can be completed. To ensure Sabine’s presenting concerns were fully heard, the model is shown to Sabine, and she is asked what else needs to be added to ensure that her concerns are represented. This process serves two important purposes. First, Sabine sees how the four quadrants are interrelated, a cognitive behavioral technique that serves to teach the client how thoughts, feelings, behaviors and physiology interact. Second, presenting the information in this way helps to establish a good working relationship and treatment fit. It makes Sabine aware that the counselor wants to fully understand her primary concerns.
Step 2: Goal Setting
With the initial assessment complete, Sabine is asked to imagine resolution of her issues in the near future and to describe what she would be feeling, thinking, and doing, and how this might affect her physiological reactions. The following script is one way to begin facilitating the goals step of the process:
Sabine, it is helpful for me as a counselor to understand your life goals and values so we can work together to determine an effective treatment plan. So, keeping the different areas in mind that we discussed earlier, let us assume that three months from now you are feeling much better. What words best describe how you would be feeling in three months?
Thus, if Sabine were to say, “I’d be feeling more self-confident,” the counselor would respond, “When you are feeling self-confident, what kind of thoughts will you have about yourself?”
It can be helpful with some clients to give examples of “thoughts about self” to increase their awareness and help them challenge unproductive self-beliefs. For instance, the counselor could say, “If I were feeling more self-confident, I might be saying to myself ‘I can do it,’ or ‘I can accomplish my goals.’” Such counselor self-disclosure can make it easier for clients to identify positive affirmations. To determine desired behaviors and physiological responses, the counselor asks, “When you are feeling confident and thinking ‘I can handle this,’ what will you be doing differently and how might this affect your physiological symptoms?”
Once goals are generated, it is imperative to assess the client’s readiness to pursue goals so that the appropriate treatment approach can be tailored to meet the client’s stage of change (Hettema & Hendricks, 2010; Lundahl, Kunz, Brownell, Tollefson, & Burke, 2010). One way to assess a client’s readiness is to ask the client:
Sabine, we are all at various stages of change in our lives depending upon a number of factors. I’m curious, with the goals you have mentioned, on a scale of 1–10 with 1 being not ready and 10 being very ready, where would you say you are in terms of making changes in your life?
The counselor then processes the responses; if the client is ready, the counselor helps the client tailor small objectives to reach goals. If the client expresses reluctance toward making change, the counselor can proceed as follows:
It seems you are frustrated being here, and it doesn’t sound like you feel you need to work on anything at this time. I respect your ability and power to choose what is right for you. So, if this needs to be the end of the session, please let me know. However, given we have 20 minutes left in this session, what would be most helpful for you?
Step 3: Treatment Planning
Assuming the client is ready to make changes, the counselor can proceed with the treatment planning phase of the model. To begin this phase the counselor draws from solution-focused brief therapy (DeShazer, 1991; Metcalf, 1998; O’Hanlon, 1999) and asks, “What is a small step you would be willing to take between now and next session that may move you closer to your goals?” It is important to note at this point that goals do not have to be established for each model domain. The idea is to have clients choose their goals and take small steps to ensure forward progress and success, which will hopefully lead to further goal attainment and eventually increased confidence and symptom relief, all based on appropriate treatment fit (see Table 2).
Table 2
Completed Treatment Fit Model
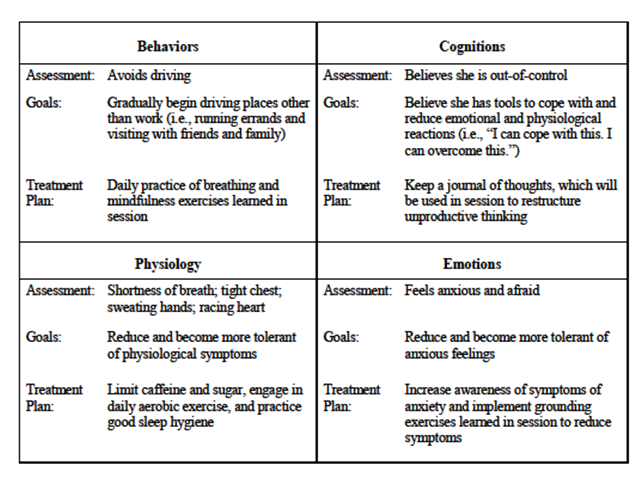
Once one or more goals have been agreed upon, the counselor and client review the document and make any necessary changes. Once the tentative TFM document is agreed upon, the client is given a copy and asked to review it before the next session. The client also is encouraged to make any additions or changes before the next counseling session. The TFM is an organic document that can be reviewed at the beginning of each session to ensure good treatment fit. For further clarification, the application of this TFM can be viewed in a brief online video.
Enhancing Counseling Techniques Through Online Videos
We, the authors, feel at this seminal time in the counseling profession that it is not enough to simply describe the TFM in print materials. Instead, we believe the counseling profession can lead the way in which the effective dissemination and conveyance of counseling techniques and protocols are introduced to the world. Despite more than six billion hours of YouTube videos viewed each month (YouTube Statistics, 2013), websites such as YouTube, Vimeo, and other readily available social media are underutilized by educators (Burden & Atkinson, 2007). There is, however, emerging evidence indicating the potential benefits of utilizing social media video when educating health care professionals (Burke & Snyder, 2008), providing medical information to patients (Murphy, 2011), disseminating public health messages to adolescents (Lite, 2010), modeling pro-social behavior to K–12 students (Shallcross, 2011), and enhancing counselor skill development (Martino, 2010). Social media is an innovative tool for teaching the application of counseling strategies, which can be used at the convenience of the counselor, even on handheld devices between client sessions.
Furthermore, findings suggest that today’s students are virtual learners who enjoy the use of video in their learning experience (Li-Ping Tang & Austin, 2009). Thus, to further enhance counselors’ ability to apply the TFM, and to reach the new generation of counselors and health care providers who rely on the easy access of social media, the authors have provided a link to a video “How to conduct a 1st counseling session,” which demonstrates the process for effectively conducting the TFM: https://www.youtube.com/watch?v=xrHgOoNBiWk
Implications for Counselors and Counselor Educators
Counselors can teach their colleagues and students how to use the TFM by incorporating video demonstrations, such as the aforementioned video link, to provide examples of case scenarios. Viewing video clips at various points can stimulate classroom discussion and group activities, and prompt homework assignments (Agazio & Buckley, 2009) that provide opportunities to practice the model’s steps of assessment, developing goals and treatment planning. For example, after watching a few minutes of the video case scenario, students can discuss the assessment phase by describing what was observed, and work collaboratively with their peers in discerning what behaviors, cognitions, physiological symptoms and emotions can be addressed. Students would then be able to consider how to address goals and treatment plans with the client, and watch the rest of the video to compare their attempts in using the model. Discussion would then ensue on how to effectively use the TFM and improve observation of a client’s verbal and nonverbal communication of her issues.
Further, students can role-play in order to practice demonstrating empathy, asking open-ended questions, and using reflection statements in an effort to build therapeutic alliance with clients when using the TFM. In addition, counselor educators can post videos on their university’s online system, such as Blackboard, and have students develop case scenarios and work through the TFM on their own, with a partner, or for in-class demonstrations.
Mental health counseling trainers and counselor educators may find using social media videos a cost-effective and timely method, as opposed to buying traditional training videos that are often expensive and outdated. Moreover, by using collaborative learning activities such as video and class discussions when teaching students how to develop treatment plans, counselor educators will better match students’ different learning styles, increase learning outcomes (e.g., increase memory of content, focus students’ concentration), and promote deeper understanding (Berk, 2009) of the TFM. Thus, the TFM model coupled with the video demonstration can further enhance counselors’ skills and counseling education by providing a uniform structure by which treatment fit can be established in a timely format. Furthermore, by expanding pedagogical advances with students and readers of academic journals, the inclusion of video demonstrations in counseling academic articles provide advantages by
- enhancing counseling skills by enabling students to view video demonstrations at their convenience, even after graduation;
- increasing a student’s ability to understand the nuances of effective counseling that are difficult to convey in print material;
- increasing professionalism by promoting a uniform yet flexible approach by which first counseling sessions can be conducted; and
- assessing students’ ability to identify counseling skills during exams by identifying theories and techniques in video clips.
Conclusion
Consistently and effectively utilizing strategies that work in counseling to improve the probability of positive client outcomes should be the goal of every counselor. Conducting a brief and functional TFM comprised of empirically supported counseling strategies in the first session should be one of those strategies. The TFM presented in this article is one that counselors can utilize to ensure a mutual understanding of clients’ issues, goals and treatment options.
In an effort to promote accessibility and tap into the immense potential of social media as an educational tool, it is hoped that the video demonstration of this model increases counselors’ ability to apply treatment fit. It also is possible for counselors to collaborate with university faculty and students in the film production department to create professional videos at reasonable costs. Whatever method used, the authors are hopeful that the inclusion of counseling video demonstrations embedded in journal articles will become the norm, which, we believe, will help bridge the gap between cognitive understanding and behavioral application.
References
Achor, S. (2010). The happiness advantage: The seven principles of positive psychology that fuel success and performance at work. New York, NY: Crown Business.
Adler, A. (1958). What life should mean to you. New York, NY: Capricorn Books.
Agazio, J., & Buckley, J. M. (2009). An untapped resource: Using YouTube in nursing education. Nurse Educator, 34(1), 23–28. doi: 10.1097/01.NNE.0000343403.13234.a2
American Psychological Association (2012, August). Recognition of psychotherapy effectiveness. Retrieved from http://www.apa.org/about/policy/ resolution-psychotherapy.aspx
Beck, A. T. (1976). Cognitive therapy and emotional disorders. New York, NY: International Universities Press.
Bednar, R. L., & Parker, C. A. (1969). Client susceptibility to persuasion and counseling outcome. Journal of Counseling Psychology, 16(5), 415–420. doi: 10.1037/h0028000
Berk, R. A. (2009). Multimedia teaching with video clips: TV, movies, YouTube, and mtvU in the college classroom. International Journal of Technology in Teaching and Learning, 5(1), 1–21.
Beutler, L. E. (2009). Making science matter in clinical practice: Redefining psychotherapy. Clinical Psychology: Science and Practice, 16(3), 301–317. doi: 10.1111/j.1468-2850.2009.01168.x
Beutler, L. E., Moleiro, C., Malik, M., Harwood, T. M., Romanelli, R., Gallagher-Thompson, D., & Thompson, L. (2003). A comparison of the Dodo, EST, and ATI factors among comorbid stimulant-dependent, depressed patients. Clinical Psychology and Psychotherapy, 10, 69–85. doi: 10.1002/cpp.354
Boffey, D. B. (1993). Reinventing yourself: A control theory approach to becoming the person you want to be. Chapel Hill, NC: New View.
Bonner, B., & Everett F. (1982). Influence of client preparation and therapist prognostic expectations on children’s attitudes and expectations of psychotherapy. Journal of Clinical Child Psychology, 11, 202–208. doi: 10.1080/15374418209533088
Brill, S. (2013, March 4). Bitter pill: How outrageous pricing and egregious profits are destroying our health care. Time, 181, 17–55.
Budd, R., & Hughes, I. (2009). The dodo bird verdict—controversial, inevitable and important: A commentary on 30 years of meta-analyses. Clinical Psychology and Psychiatry, 16, 510–522. doi: 10.1002/cpp.648
Burden, K., & Atkinson, S. (2007). Jumping on the YouTube bandwagon? Using digital video clips to develop personalized learning strategies. In ICT: Providing choices for learners and learning. Proceedings ascilite Singapore 2007. Retrieved from http://www.ascilite.org.au/conferences/singapore07/procs/burden-poster.pdf
Burke S. C., & Snyder, S. L. (2008). YouTube: An innovative learning resource for college health education courses. International Electronic Journal of Health Education, 11, 39–46.
Burtnett, F. (2012, June). Bridging the separation between behavioral and general health care. Counseling Today, 54(12), 38–39.
Childress, R., & Gillis, J. S. (1977). A study of pretherapy role induction as an influence process. Journal of Clinical Psychology, 33(2), 540–544. doi: 10.1002/1097-4679(197704)
Connors, G. J., Carroll, K. M., DiClemente, C. C., Longabaugh, R., & Donovan, D. M. (1997). The therapeutic alliance and its relationship to alcoholism treatment participation and outcome. Journal of Consulting and Clinical Psychology, 65(4), 588–598. doi: 10.1037/0022-006X.65.4.588
Constantino, M. J., Arnkoff, D. B., Glass, C. R., Ametrano, R. M., & Smith, J. Z. (2011). Expectations. Journal of Clinical Psychology: In Session, 67(2), 184–192. doi: 10.1002/jclp.20754
Cummings, N. A., O’Donohue, W. T., & Cummings, J. L. (2009). The financial dimension of integrated behavioral/primary care. Journal of Clinical Psychology in Medical Settings, 16, 31–39. doi: 10.1007/s10880-008-9139-2
Curtis R., & Christian, E. (2012). Introduction to integrated care. In Curtis & Christian (Eds.), Integrated care: Applying theory to practice (pp. 3–19). New York, NY: Routledge.
DeShazer, S. (1991). Putting difference to work. New York, NY: Norton.
Duckworth, A. L., Grant, H., Loew, B., Oettingen, G., & Gollwitzer, P. M. (2011). Self-regulation strategies improve self-discipline in adolescents: Benefits of mental contrasting and implementation intentions. Journal of Educational Psychology, 31(1), 17–26. doi: 10.1080/01443410.2010.506003
Egan, G. E. (2007). The skilled helper: A problem-management and opportunity development approach to helping (8th ed.). Belmont, CA: Thompson Brooks/Cole.
Ellis, A. (1996). Better, deeper, and more enduring brief therapy: The rational emotive behavior therapy approach. New York, NY: Brunner/Mazel.
Fong, M. L. (1993). Teaching assessment and diagnosis within a DSM-III-R framework. Counselor Education and Supervision, 32, 276–287.
Gonzalez, M. J. (2002). Mental health intervention with Hispanic immigrants: Understanding the influence of the client’s worldview, language, and religion. Journal of Immigrant & Refugee Services, 1, 81–92. doi: 10.1300/J191v01n01_07
Grosz, R. D. (1968). Effect of client expectations on the counseling relationship. Personnel and Guidance Journal, 46, 797–800. doi: 10.1002/j.2164-4918.1968.tb03250.x
Hardin, S., & Yanico, B. (1983). Counselor gender, type of problem, and expectations about counseling. Journal of Counseling Psychology, 30(2), 294–297. doi: 10.1037/0022-0167.30.2.294
Harris Interactive. (2004, April). Therapy in America 2004 (Survey No. 20431). Rochester, NY: Author. Retrieved from http://www.napabipolardepression.org/images/therapy_in_america.pdf
Hayes, S. C., Strosahl, K. D., & Wilson, K. G. (1999). Acceptance and commitment therapy: An experiential approach to behavior change. New York, NY: Guilford.
Haynes, A. B., Weiser, T. G., Berry, W. R., Lipsitz, S. R., Breizat, A. S., Dellinger, E. P., … Gawande, A. A. (2009). A surgical safety checklist to reduce morbidity and mortality in a global population. The New England Journal of Medicine, 360(5), 491–499. doi: 10.1056/NEJMsa0810119
Heinssen, R. K., Levendusky, P. G., & Hunter, R. H. (1995). Client as colleague: Therapeutic contracting with the seriously mentally ill. American Psychologist, 50(7), 522–532. doi: 10.1037/0003-066X.50.7.522
Hettema, J. E., & Hendricks, P. S. (2010). Motivational interviewing for smoking cessation: A meta-analytic review. Journal of Consulting and Clinical Psychology, 78(6), 868–884. doi: 10.1037/a0021498
Hirai, M., & Clum, G. A. (2006). A meta-analytic study of self-help interventions for anxiety disorders. Behavior Therapy, 37(2), 99–111.
Hofmann, S. G., & Smits, J. A. J. (2008). Cognitive-behavioral therapy for adult anxiety disorders: A meta-analysis of randomized placebo controlled trials. Journal of Clinical Psychiatry, 69(4), 621–632. doi: 10.4088/JCP.v69n0415
Horvath, A. O., & Symonds, B. D. (1991). Relation between working alliance and outcome in psychotherapy: A meta-analysis. Journal of Counseling Psychology, 38(2), 139–149. doi: 10.1037/0022-0167.38.2.139
Keeley, M. L., Geffken, G. R., Ricketts, E., McNamara, J. P. H., & Storch, E. A. (2011). The therapeutic alliance in the cognitive behavioral treatment of pediatric obsessive-compulsive disorder. Journal of Anxiety Disorders, 25, 855–863. doi 10.1016/j.janxdis.2011.03.017
Kim, B. S. K., Ng, G. F., & Ahn, A. J. (2005). Effects of client expectation for counseling success, client-counselor worldview match, and client adherence to Asian and European American cultural values on counseling process with Asian Americans. Journal of Counseling Psychology, 52(1), 67–76. doi: 10.1037/0022-0167.52.1.67
Kim, B. S. K., Ng, G. F., & Ahn, A. J. (2009). Client adherence to Asian cultural values, common factors in counseling, and session outcome with Asian American clients at a university counseling center. Journal of Counseling & Development, 87(2), 131–142. doi: 10.1002/j.1556-6678.2009.tb00560.x
Kim, J. S. (2008). Examining the effectiveness of solution-focused brief therapy: A meta-analysis. Research on Social Work Practice, 18(2), 107–116. doi: 10.1177/1049731507307807
Klein, E. B., Stone, W. N., Hicks, M. W., & Pritchard, I. L. (2003). Understanding dropouts. Journal of Mental Health Counseling, 25, 89–100. doi: 10.1080/09515070310001610119
Lee, S., Aos, S., Drake, E., Pennucci, A., Miller, M., & Anderson, L. (2012). Return on investment: Evidence-based options to improve statewide outcomes, April 2012 (Document No. 12-04-1201). Olympia: Washington State Institute for Public Policy. Retrieved from http://www.wsipp.wa.gov/rptfiles/12-04-1201.pdf
Li-Ping Tang, T., & Austin, M. J. (2009). Students’ perceptions of teaching technologies, application of technologies, and academic performance. Computers & Education, 53(4), 1241–1255. doi: 10.1016/j.compedu.2009.06.007
Lite, J. (2010, November–December). When Facebook is your medical record. Miller-McCune, 18–21.
Lundahl, B. W., Kunz, C., Brownell, C., Tollefson, D., & Burke, B. L. (2010). A meta-analysis of motivational interviewing: Twenty-five years of empirical studies. Research on Social Work Practice, 20(2), 137–160. doi: 10.1177/1049731509347850
Martino, S. (2010). Strategies for training counselors in evidence-based treatments. Addiction Science & Clinical Practice, 5(2), 30–40.
Meichenbaum, D. (1977). Cognitive behavior modification: An integrative approach. New York, NY: Plenum Press.
Meichenbaum, D. (2002, December). Core tasks of psychotherapy: What ‘expert’ therapists do. Paper presented at the Brief Therapy Conference, Orlando, FL.
Metcalf, L. (1998). Solution focused brief therapy: Ideas for groups in private practice, schools, agencies and treatment programs. New York, NY: The Free Press.
Miller, S. D., Duncan, B. L., Brown, J., Sorrell, R., & Chalk, M. B. (2006). Using formal client feedback to improve retention and outcome: Making ongoing, real-time assessment feasible. Journal of Brief Therapy, 5(1), 5–22.
Miller, W. R., & Rollnick, S. (1991). Motivational interviewing: Preparing people for change. New York, NY: Guilford.
Murphy, E. T. (2011, September 20). Social media primer for healthcare professionals [Medscape News]. Retrieved from http://www.medscape.com/viewarticle/749576
Norcross, J. C., & Beutler, L. E. (2008). Integrative psychotherapies. In R. J. Corsini & D. Wedding (Eds.), Current Psychotherapies (8th ed., pp. 481–511). Belmont, CA: Brooks/Cole.
O’Hanlon, W. H. (1999). Do one thing different. New York, NY: HarperCollins.
Olmstead, T. A., Abraham, A. J., Martino, S., & Roman, P. M. (2012). Counselor training in several evidence-based psychosocial addiction treatments in private US substance abuse treatment centers. Drug and Alcohol Dependency, 120(1–3), 149–154. doi: 10.1016/j.drugalcdep.2011.07.017
Paquette, V., Lévesque, J., Mensour, B., Leroux, J. M., Beaudoin, G., Bourgouin, P., & Beauregard, M. (2003). “Change the mind and you change the brain”: Effects of cognitive behavioral therapy on the neural correlates of spider phobia. Neuroimage, 18(2), 401–409. doi:10.1016/S1053-8119(02)00030-7
Rogers, C. (1961). On becoming a person: A therapist’s view of psychotherapy. New York, NY: Houghton Mifflin.
Seligman, M. E. P., & Csikzentmihalyi, M. (2000). Positive psychology: An introduction. American Psychologist, 55(1), 5–14. doi: 10.1037/0003-066X.55.1.5
Sexton, T., Whiston, S. C., Bleuer, J. C., & Walz, G. R. (1997). Integrating outcome research into counseling practice and training. Alexandria, VA: American Counseling Association.
Shallcross, L. (2011, October). Finding technology’s role in the counseling relationship. Counseling Today, 54(4), 26–35.
Spinhoven, P., Giesen-Bloo, J., van Dyck, R., Kooiman, K., & Arntz, A. (2007). The therapeutic alliance in schema-focused therapy and transference-focused psychotherapy for borderline personality disorder. Journal of Consulting and Clinical Psychology, 75(1), 104–115. doi: 10.1037/0022-006X.75.1.104
Tinsley, H. E. A., Bowman, S. L., & Ray, S. B. (1988). Manipulation of expectancies about counseling and psychotherapy: Review and analysis of expectancy manipulation strategies and results. Journal of Counseling Psychology, 35(1), 99–108. doi: 10.1037/0022-0167.35.1.99
Westra, H. A., Constantino, M. J., Arkowitz, H., & Dozois, D. J. A. (2011). Therapist differences in cognitive-behavioral psychotherapy for generalized anxiety disorder: A pilot study. Psychotherapy, 48(3), 282–292.
Wos, A. (2013, February). State of mental health in North Carolina. Presented at the North Carolina Counseling Association’s Annual Meeting, Greensboro, NC.
Yalom, I. D. (1985). The theory and practice of group psychotherapy (3rd ed.). New York, NY: Basic Books.
YouTube. (October 19, 2013). Traffic. Retrieved from http://www.youtube.com/yt/press/statistics.html
Ziemelis, A. (1974). Effects of client preference and expectancy upon the initial interview. Journal of Counseling Psychology, 21(1), 23–30. doi: 10.1037/h0036067
Russ Curtis is an Associate Professor and Heather Thompson an Assistant Professor, both at the counseling program at Western Carolina University. Gerald A. Juhnke, NCC, is a Professor in the Counseling Department at The University of Texas at San Antonio; Melodie Frick, NCC, is an Assistant Professor in the counseling program at Western Carolina University. Correspondence can be addressed to Russ Curtis, Department of Human Services, Western Carolina University, 91 Killian Building Lane, Room 208, Cullowhee, NC 28723, curtis@email.wcu.edu.
Oct 15, 2014 | Article, Volume 3 - Issue 3
Monica G. Darcy, Nahid M. Abed-Faghri
A state’s counseling association conducted a study to explore characteristics of its licensed mental health counselors. Responses were collected regarding employment, priorities for the state professional association, competence in professional activities, and sources of professional support. The majority of respondents indicated high job satisfaction with employment in full-time private practice. Peer support from coworkers or from external work settings was indicated as most beneficial to the respondents’ successful practice. The information is explored to determine how the association can better represent the state’s counselors. The authors also discuss ways that professional associations, counselors and counselor education programs can collectively contribute to strong professional identity in mental health counselors.
Keywords: professional association, professional identity, counselor education, peer support, job satisfaction, private practice, licensed mental health counselors, LMHC
The professionalization of counseling is blurred among mental health professionals (e.g., mental health counselors, psychologists, social workers, marriage and family therapists, psychiatrists). This issue is based in large part on shared foundational knowledge, overlapping goals and similar work environments, all of which make it difficult to clearly distinguish a mental health counselor’s identity (Calley & Hawley, 2008; Gale & Austin, 2003; Hanna & Bemak, 1997; Weinrach, 1987). The need for role clarification seems imperative for mental health counselors as a means to carve their own niche in the mental health workforce.
The essential role of a professional association in facilitating role clarification from a practical standpoint is to focus on mental health counselors’ professional identity. With clarity in this area, a professional association can establish the foundation for success in advocacy, provide recognition rights, and serve a crucial role in establishing legitimate positions in the workplace (Myers, Sweeney, & White, 2002). Information about the current employment and expertise of mental health counselors can be useful in increasing visibility of the role counselors play in the field of mental health care (Hawley & Calley, 2009; Rollins, 2007). Stated simply, examining the existing characteristics of mental health counselors with an in-depth description of their work niche can help a professional association understand the unique nature of their constituents’ professional identity.
The Purpose of State Professional Counseling Associations
The development of professional identity for counselors evolves, at least in part, through the presence of professional associations. The contribution of professional associations to establish and maintain the unique identity of counselors has three core components: (a) differentiation of counseling from other helping professions, (b) recognition of the uniqueness of the profession, and (c) representation of the profession of counseling (American Mental Health Counselors Association [AMHCA], 1978). In fact, within their mission, the formal purposes of professional associations center on professional identity by establishing a platform for common professional interests, encouraging professional development through research, acting as a unified voice that represents the profession, providing a forum for enhancing counselor skills and knowledge, and serving as a place to improve professional performance (American Counseling Association [ACA], 2009).
National associations (AMHCA, ACA, NBCC) make efforts on behalf of counseling professionals to address employment obstacles, which improves public and professional awareness of counseling and counselors. Several recent examples include enhancing role distinction for counselors in private practice who experienced unfair consideration by insurance companies (Myers et al., 2002), advocating successfully for professional recognition of insurance reimbursement with TRICARE (AMHCA, 2010b), and continuing to do the same with Medicare (AMHCA, 2010a). In addition, a historic step in the federal recognition of professional counselors occurred with the successful establishment of qualification standards formally recognizing licensed professional counselors as mental health specialists within the Veterans Health Administration (AMHCA, 2010c). Representing professional counseling as worthy of fiscal support on par with other mental health providers is pivotal to promoting the counseling discipline (Hawley & Calley, 2009). These efforts highlight counselor expertise in mental health assessment and treatment, placing them on par with other equally qualified mental health professionals in the helping field.
An Exploratory Study of a State Professional Association
The topic of advocacy has surfaced on the local level with mental health counselors in the state professional associations that are striving to be well-informed representatives of their profession at important state-level meetings. These efforts have been stymied by a waning membership, lack of presence at state level mental health–focused meetings, and lack of knowledge regarding regulatory issues surrounding mental health. In order to improve the capacity of one state association, a research subcommittee was formed to conduct a study to explore the characteristics of professional capacity, and to express the needs of counselors in order to enhance the representation of counselors in the state. Two counseling faculty members worked with other association members on a subcommittee that surveyed all LMHCs in the state. The intent was to investigate the current status of all LMHCs, make recommendations about association mission revisions, and suggest professional development activities.
Several important questions guided the development of an exploratory survey for distribution among licensed mental health counselors (LMHCs) in the state. First, what is the nature of the work of LMHCs; what types of employment do counselors have; is that employment satisfying; and do counselors feel supported in their work? Second, what do LMHCs want from a professional association, and what services do the counselors value from the professional association? Additionally, in what areas do LMHCs feel competent within their profession? These questions were posed with the underlying assumption that there are ways the professional association can improve its efforts to support and advance the professional capacity and identity of the state’s counselors.
Method
Participants
All active licensed mental health counselors in one New England state (N = 358) were included in the survey distribution. Surveys were completed by 55 licensed mental health counselors representing a 15% return rate. The respondents included 45 females (82%) and 10 males (18%). The age ranges and frequencies of the participants were 20–30 (9%), 30–40 (26%), 40–50 (27%), 50–60 (26%), and over 60 (13%). The procedures of this study were approved by the Institutional Review Board of the college of the counselor educators on the research subcommittee.
Instrument and Procedure
Participants responded to a researcher-created online survey with four sections. In Section 1, exploratory questions were designed to gather information on education, training and employment patterns of mental health counselors (work settings, hours, populations of clients, conditions treated, and salary). Section 2 questions focused on satisfaction levels of LMHCs regarding salary, and availability and quality of jobs, as well as professional supports. In Section 3, respondents were asked to record their participation in professional associations and to rank services they valued from the association. The last section prompted participants to respond to selected areas of perceived professional competencies in service to clients, supervisory activities, working with insurance companies, and understanding legislation and guidelines of the profession (College of Psychologists of Ontario, 2009).
Each section of the survey included forced-choice questions, Likert-scale questions in areas of job satisfaction and perceived competence, multiple-choice items, and open-ended questions. Descriptive statistics were used in quantitative data analysis to gain an understanding of the responses (Fink, 2009). Qualitative data from comments on work as a LMHC and professional association membership were analyzed to find general themes (Creswell, 2005).
Since this was a researcher-created survey, the authors conducted a three-stage review process to aid in survey clarity and address any confusing statements (Franklin, 2007). The survey was first tested through a modified pilot with knowledgeable colleagues. Three reviewers responded to the initial draft, their responses were analyzed, and adjustments in the wording of four questions and three response choices were made to improve clarity. Next, cognitive interviews were conducted with three participants who participated in a “think out loud” interview during the time they completed the survey. The interviewer noted any areas that caused hesitation or confusion and the researchers altered phrasing in these sections. The last pilot stage involved three participants doing a retrospective discussion after they finished the survey, which served as a final check to eliminate design errors.
Results
Employment, Education, License and Expertise
Respondents indicated that the period of time since they were granted a license in counseling ranged from 5 months to 32 years with an average of 8 years. Forty-nine respondents (91%) reported being currently employed as a LMHC with the majority of counselors (65%) working in independent practice or a private agency. Other areas of employment included community or state agencies (47%), schools (14%), hospitals (10%), substance abuse treatment centers (8%), employee assistance programs (4%), and group homes (2%).
State requirements for licensing include 60 graduate hours in specific content areas, 2,000 post-master’s clinical hours, and 100 supervision hours. All respondents to this survey hold at least a master’s degree with 41% reporting completion of the 60–semester hour postgraduate degree, Certificate of Advanced Graduate Studies (CAGS), or its equivalent. For those respondents who reported an additional license or certification, 13 noted chemical dependency and 3 were licensed in other states.
Respondents noted that they worked 10–65 hours per week with the average at 38.5 hours. The majority of LMHCs (62%) work full-time with one job while 23% work full-time, but at more than one job. Part-time work at one job described 17% of the respondents with 9% having part-time work at more than one job. Health benefits were available for 65% of the respondents. The most frequent response to salary was 34% earning $60,000 and above, with others reporting below $40,000 (21%), $40,000–$50,000 (25%), and $50,000–$60,000 (19%).
Individual counseling topped the list of services provided, with 94% of participants indicating this response. This was followed by family counseling (65%), group counseling (49%), supervision (43%), and case management (37%). Regarding the type of clients served, respondents noted their work with adults (83%), child/adolescents (70%), families (51%), disabled (19%), elderly (9%), and prisoners (4%).
Anxiety disorders (96%) were the most frequent conditions assessed or treated, with 94% of respondents reporting work with mood disorders and 88% reporting work with trauma. Other responses included stress/life transitions (84%), co-occurring disorders (57%), personality disorders (45%), and psychotic disorders (28%).
Job Satisfaction and Professional Support
Through examination of job satisfaction, 95% of participants reported above moderate to extreme satisfaction in their work as LMHCs (M = 4.1 on 5-point scale), and expressed less satisfaction with their job regarding salary (M = 2.9) and availability of jobs (M = 2.7).
For those respondents who made comments (n = 13) on their work as LMHCs, most (n = 7) commented on compensation issues such as disparate reimbursement from Licensed Independent Clinical Social Workers and lack of recognition for Medicare and government insurance such as TRICARE. Other comments (n = 6) can be categorized as “I love my job” statements that highlighted the pride the respondents have in the important work they do.
Most respondents noted peer support from coworkers (67%) as a source of support that is most beneficial to successful practice. Other sources of support include peer support external from work setting (54%) and individual supervision within agency practice (31%). Paid individual supervision and professional association membership were both reported by 15% of the respondents, with 8% reporting no professional support.
Value of a Professional Association
Respondents’ level of participation in professional associations was highest in the ACA (65%), followed by AMCHA (35%) and American Association for Marriage and Family Therapy (6%). Although 78% of the respondents indicated they were aware of the state association, only 22% indicated they were members.
Members cited some logistical challenges to attending meetings: (a) lack of information about the association (52%), (b) not enough time to attend (30%), (c) dues too costly (27%), (d) time of meeting not fitting schedule (16%) or inconvenient (14%), and (e) location (9%). Other responses included not seeing a purpose for attending (20%) and getting support from other sources (16%).
Respondents ranked the five most valuable services for the state professional association to provide as (1) professional development and education opportunities (83%), (2) information sharing (82%), (3) advocacy (70%), (4) promote visibility and name recognition (50%), and (5) provide liaisons at the state and national level (43%). For respondents who made comments on professional association membership (n = 10), the types of comments were mixed. There was a relatively equal balance of positive, negative and neutral comments about professional involvement.
Perceived Competence
Most respondents (96%) reported working directly with clients, with 98% reporting moderately high to high competence in providing services. Sixty-one percent of respondents indicated that they work with insurance companies, with 43% reporting moderately high to high competence in working with these companies. The perceived competence of respondents with understanding legislation, standards and insurance billing codes was 51% reporting moderately high to high levels of competence. With 40% of respondents reporting work as a counseling supervisor, 68% reported moderately high to high levels of competence.
Discussion
The data gathered in this survey are informative for the state professional counseling association. A more thorough understanding of one core question of the study—the nature of the work of the state’s mental health counselors—can be drawn from the information gathered from respondents. The majority of respondents (95%) indicated high satisfaction with counseling work and reported their work setting as independent or private practice (65%). The data are consistent with a recent national survey of counselors in which private solo practice is the predominantly reported current work setting (Normandy-Dolberg, 2010).
In addition to a clearer picture of the nature of counseling work for LMHCs in the state, the responses in several areas of this survey can be considered to inform the professional association. Specifically, the responses of the state’s LMHCs on sources of support, perceived areas of competence, and services valued from a professional association can be incorporated into a future focus for the association. For example, in light of the prevalence of employment in private practice in which professional isolation is a potential drawback, it is interesting to note the sources of support reported as most beneficial to counselors’ successful practice. Respondents indicated peer support from coworkers (67%) and support external from work settings (54%) as important to their work. This suggests a role for membership in a professional association as a source of supportive relationships, which can ameliorate the potential solitary nature of private practice.
Additionally, responses regarding services valued from a professional association and perceived competence in areas of mental health counselors’ work can be used to suggest priorities for the association to use as a focus. Respondents noted professional development and education, information sharing, advocacy, and promoting visibility and name recognition as the most valuable services of a professional association. These results are consistent with a recent national survey of mental health counselors who also expressed the need for professional associations to advocate for professional visibility and name recognition (Normandy-Dolberg, 2010).
Priorities revealed in the survey indicate unmet needs of the state’s professional counselors. There is a disparity when we consider the respondents who reported high competence in understanding legislation, standards and codes (53%), and competence with insurance companies (43%), as opposed to higher levels of reported competence in direct service to clients (98%) and supervisory activities (67%). This apparent gap in levels of reported competence, when viewed in conjunction with the stated preferences for services valued from a professional association, suggests a possible role for the professional association in bridging this gap.
Limitations
The design of this exploratory study was an online survey distributed to all of the licensed mental health counselors in one state in an attempt to understand counselor characteristics. The small number of responses may not reflect a representative sample of the counselors in the state and precludes any within group analyses of the results (i.e., differences in responses based on years since licensure and place of employment). Additionally, the reasons for which respondents self-selected to complete the survey are unknown. As such, the sample must be viewed in a limited way to reflect the experiences and opinions of counselors in the state.
The results, when used as exploratory findings, have specific utility for the state’s professional association as a first step in refining the ways it serves its possible pool of members. The ensuing discussions about the use of these results have been at the core of ways to strengthen the connection between the state’s professional association and its membership. The low response rate limits broader interpretation of the results; however, the results remind us of the importance to poll members periodically to better understand their professional situations.
Implications for a State Professional Association
The results of this survey have three major implications for the state’s professional association: (a) create an atmosphere of support that addresses LMHCs’ stated priorities; (b) focus on the various needs of the counseling professionals in the state; and (c) provide opportunities to improve competence, specifically in areas such as legislation, standards and codes, and insurance.
Given the large proportion of respondents who work in private practice as well as the reported benefit of peer support as it relates to professional success, the state professional association can be proactive in offering supportive relationship opportunities to LMHCs in the state. Previous research identifies support from coworkers as a work-related social resource (Hobfoll, 1988), and connects higher levels of social integration with less emotional exhaustion and depersonalization (Ross, Altmaier, & Russell, 1989). Similarly, coworkers provide instrumental support in dealing with the demands of work and can buffer stress and reduce vulnerability to professional stress (Ray & Miller, 1994). Although professional association meetings and events do not replicate day-to-day work interactions, they can foster useful professional connections. Following recommendations to promote wellness and self-care strategies for counseling professionals with an active, supportive relationship with supervisors and peers (ACA, 2010), membership in the state professional association can be encouraged as an extended peer group, a means for counselors to find collegial interactions and support, especially for those who are working in independent practice.
Another implication for the association is to use the top five stated preferences for the services of the professional association to create meaningful local visibility of licensed mental health counselors. Using the preferred services, namely (a) professional development and education opportunities, (b) information sharing, (c) advocacy, (d) promoting visibility and name recognition, and (e) providing liaisons at the state (and national) levels, can be a starting point for priorities for the association. These are clear suggestions to revitalize the state association’s mission, and if specific attention is paid to these valued services, it may provide a natural incentive to become a member.
Unfortunately, there is a circular dilemma here: to represent the professional adequately with expertise and vibrancy, an association needs a robust membership; and a robust membership will promote an active and visible association. But, the question remains—where to start? Members have many possible reasons for joining their professional organization with one compelling consideration being the ability to give voice to their own professional identity. Although membership in professional associations is relatively low (22% of the respondents were members in the state association at the time of this research), only 15% of the total mental health counselors in the state were members, and a national survey reports an overall low percentage of counselors who are members of ACA or its divisional affiliates (Hodges, 2011). Half of the respondents expressed desire for professional visibility; this apparent divide between wanting professional representation from an association and finding the incentive to become a member suggests an area of growth for the association.
A further finding has implications for how the professional association relates to the reported low level of perceived competence in understanding legislation, standards and codes, and insurance. Counselors need support to meet post-licensure expectations for ongoing competence across the professional lifespan (Kaslow, et al., 2007). Tasks of the professional state association in this area are twofold: (a) raise awareness of the need to stay abreast of trends in legislation, standards and codes, and insurance as a cornerstone for successful professional practice, and (b) contribute to competence building of LMHCs in the state through professional development and the creation of ongoing networking opportunities.
Next Steps for a State Professional Counseling Association
The implications of these results are big tasks for a small state professional association to undertake. The approach of the board members who began this survey of its members is to discard the approach of “if we are here, they will come,” but rather to focus on growing capacity within the membership and improving relevance to counselors’ needs. These tasks are more easily accomplished if professional associations encourage investment in counselor professionalism. Counselors themselves must be encouraged to promote their profession. One collaborative partner in achieving these results is counselor education programs which have mutual interests in promoting the professional success of counselors.
When viewing professional development as a lifelong process (Ronnestad & Skovholt, 2003), there is a shared responsibility in the ways that counselor education programs launch future counselors and the ways that professional associations extend the learning. Counselors face an important transformational task when they self-locate within a professional community (Gibson, Dollarhide, & Moss, 2010), and the cooperative relationship between counselor education and local professional associations can smooth that transition. When undertaken as a collaborative venture, the professional identity of the counselors will strengthen throughout the pre-service to post-licensure journey. The continuum of pre-service preparation leading to professional involvement that is steeped in active social, legislative and association visibility will prepare counselors to fend for their professional identities at a time when pressures are coming from many directions.
Furthermore, findings from this survey suggest that counselor education programs can support professional association efforts by promoting early involvement of students with the state professional association as a habit of caring for oneself as a professional. The role of counselor education early in the professional development of mental health counselors begins the process by establishing a sense of professional pride (Myers at al., 2002). Establishing a consistent cycle of information sharing between counselors in pre-service training and professional association members begins the process of involvement with professional elders that can fuel professional growth (Ronnestad & Skovholt, 2003). Informal discussions as well as more formal mentoring relationships can serve as an ongoing exchange between counselor preparation and working professionals.
Counselor educators carry a responsibility to be proactive with trends in the field, including ways those trends inform curricula (Darcy, Dalphonse, & Winsor, 2010). The finding in these survey results of a large pool of private practitioners who reported low levels of perceived competence in understanding legislation, standards and codes, and insurance is important feedback for local counselor education programs. Previous commentary noting that counselor programs prepare graduates for leadership and clinical skills, but can improve curricula in political networking and entrepreneurship (Curtis & Sherlock, 2006) is important to consider. Perhaps factors such as those introduced at the preparation stage of a counselor’s development can address these concerns. Counselor education programs and state professional associations can create networks that allow for information sharing in order to keep training opportunities in pre-service and post-licensure stages relevant to counselor professional needs.
Conclusion
There are challenges in the 21st century marketplace for which professional counseling associations can support counselors. Strength can come from counselors’ ability to adapt to external demands (Hodges, 2011), and this can be more easily accomplished when state professional associations collaborate with the professionals they represent and the programs that prepare them. Although there has been tremendous progress in establishing mental health counselors’ professional identity, there remains a need for further advocacy and visibility, since the mental health counseling profession still strives to clearly define and distinguish itself from other mental health professions (Calley & Hawley, 2008; Hanna & Bemak, 1997). Educating members of the counseling profession, other professions involved with mental health, the public, employers, and insurance panels about the differences that exist among mental health professions remains a challenging task (Calley & Hawley, 2008; Mrdjenovich & Moore, 2004). Areas such as reciprocating counselors’ credentials across states (Bemak & Espina, 1999), increasing alliance and unity among counselors (Rollins, 2007), and improving public perception (Gale & Austin, 2003) all merit exploration. Each of these issues can be crucial for state and national initiatives, which call for contributions from professional associations, individual counselors, and counselor education programs to strengthen mental health counseling professional identity.
Collectively, the efforts of professional associations, counselors, and counselor education programs represent ways to transmit a strong professional identity in the counseling field. All of these options protect the professional success of mental health counselors; because of their direct connection to employability in the workforce, a common thread of advocacy binds them. From all perspectives, the need to recognize and promote mental health counseling’s identity is paramount to securing counseling’s role as a distinct discipline.
References
American Counseling Association. (2009). 20/20 statement of principles advances the profession. Retrieved from http://www.counseling.org/news/news-release-archives/by-year/2009/2009/01/20/20-20-statement-of-principles-advances-the-profession
American Counseling Association. (2010). ACA’s taskforce on counselor wellness and impairment: Wellness strategies. Retrieved from http://www.counseling.org/knowledge-center/counselor-wellness
American Mental Health Counselors Association. (1978). Blueprint for the mental health counseling profession. Alexandria, VA: Author.
American Mental Health Counselors Association. (2010a). Health care reform on life support: Urge senators to pass reform and include LMHC Medicare eligibility. Retrieved from http://www.amhca.org/news/detail.aspx?ArticleId=87
American Mental Health Counselors Association. (2010b). AMHCA/ACA/NBCC update: Senate Introduces “TRICARE Mental Health Care Access Act” S. 3371. Retrieved from http://www.amhca.org/news/detail.aspx?ArticleId=161
American Mental Health Counselors Association (2010c). AMHCA/ACA/NBCC update: The Department of Veterans Affairs recognizes licensed professional mental health counselors! Retrieved from http://www.amhca.org/news/detail.aspx?ArticleId=224
Bemak, F., & Espina, M. R. (1999). Professional counseling licensure: Going from state to state. ACES Spectrum, 60(2), 4–6, 11.
Calley, N. G., & Hawley, L. D., (2008). The professional identity of counselor educators. The Clinical Supervisor, 27, 3–16.
College of Psychologists of Ontario. (2009). Self assessment guide and professional development plan: Quality assurance program. Retrieved from http://www.cpo.on.ca/members-of-the-college/quality-assurance/index.aspx?id=124&ekmensel=12_submenu_26_link_2
Creswell, J. W. (2005). Educational research: Planning, conducting, and evaluating quantitative and qualitative research. Upper Saddle River, NJ: Pearson.
Curtis, R., & Sherlock, J. (2006). Wearing two hats: Counselors as managerial leaders in agencies and schools. Journal of Counseling & Development, 84, 120–126. doi: 10.1002/j.1556-6678.2006.tb00386.x
Darcy, M. G., Dalphonse, L., & Winsor, C. (2010, August). Developing a more skilled co-occurring disorders workforce. Counselor Magazine, 11(4), 10–16.
Fink, A. (2009). How to conduct surveys: A step-by-step guide. Los Angeles, CA: Sage.
Franklin, C. (2007). Factors that influence elementary teachers’ use of computers. Journal of Technology and Teacher Education, 15, 267–293.
Gale, A. U., & Austin, B. D. (2003). Professionalism’s challenges to professional counselors’ collective identity. Journal of Counseling & Development, 81, 3–10. doi: 10.1002/j.1556-6678.2003.tb00219.x
Gibson, D. M., Dollarhide, C. T., & Moss, J. M. (2010). Professional identity development: A grounded theory of transformational tasks of new counselors. Counselor Education and Supervision, 50, 21–38.
Hanna, F. J., & Bemak, F. (1997). The quest for identity in the counseling profession. Counselor Education and Supervision, 36, 194–206.
Hawley, L. D., & Calley, N. G. (2009). Professional identity of counseling: A template for action. Michigan Journal of Counseling: Research, Theory & Practice, 36, 1–12.
Hobfoll, S. E. (1988). The ecology of stress. New York, NY: Hemisphere.
Hodges, S. (2011). Through a glass darkly—Envisioning the future of the counseling profession: A commentary. The Professional Counselor, 1, 191–200.
Kaslow, N. L., Rubin, N. J., Bebeau, M. J. , Leigh, I. W., Lichtenberg, J. W.,Nelson, P. D., Portnoy, S. M., & Smith, I. L. (2007). Guiding principles and recommendations for the assessment of competence. Professional Psychology: Research and Practice, 38(5), 441– 451.
Mrdjenovich, A.J. & Moore, B. A. (2004). The professional identity of counseling psychologists in health care: A review and call for research. Counseling Psychology Quarterly, 17, 69–79.
Myers, J. E, Sweeney, T. J., & White, V. E. (2002). Advocacy for counseling and counselors: A professional imperative. Journal of Counseling & Development, 80, 394–402. doi: 10.1002/j.1556-6678.2002.tb00205.x
Normandy-Doelbrg, J. (2010, September 1). AMHCA survey results: Concerns cited with managed care, and with funding retirement. Retrieved from http://www.amhca.org/news/print.aspx?Print=y&F_AdvocateId=17
Ray, E. B., & Miller, K. I. (1994). Social support, home/work stress, and burnout: Who can help? Journal of Applied Behavioral Science, 30, 357–373. doi: 10.1177/0021886394303007
Rollins, J. (2007, May 6). 20/20 delegates start reaching consensus. Counseling Today. Retrieved from http://ct.counseling.org/2007/05/20-20-delegates-start-reaching-consensus/
Ronnestad, M. H., & Skovholt, T. M. (2003). The journey of the counselor and therapist: Research findings and perspectives in professional development. Journal of Career Development, 30, 5–44. doi: 10.1177/089484530303000102
Ross, R. R., Altmaier, E. M., & Russell, D. W. (1989). Job stress, social support and burnout among counseling center staff. Journal of Counseling Psychology, 36, 464–470.
Weinrach, S. D. (1987). Some serious and not so serious reactions to AACD and its journals. Journal of Counseling & Development, 65, 395–399. doi: 10.1002/j.1556-6676.1987.tb00739.x
Monica G. Darcy, NCC, is an Associate Professor and Director of Graduate Programs at Rhode Island College. Nahid M. Abed-Faghri is a member of the Rhode Island Mental Health Counselors Association. Correspondence can be addressed to Monica G. Darcy, Rhode Island College, 600 Mount Pleasant Avenue, Adams 102, Providence, RI 02908, mdarcy@ric.edu.
Oct 15, 2014 | Article, Volume 3 - Issue 3
Melanie H. Iarussi, Jessica M. Tyler, Sarah Littlebear, Michelle S. Hinkle
Motivational interviewing (MI), a humanistic counseling style used to help activate clients’ motivation to change, was integrated into a basic counseling skills course. Nineteen graduate-level counseling students completed the Counselor Estimate of Self-Efficacy at the start and conclusion of the course. Significant differences were found between students’ pre/post measures of self-efficacy (t(18) = –7.055, p = .0005). Qualitative data collected concerning students’ experiences learning counseling skills in the context of MI are described by four main themes: (a) valuable and relevant learning experience, (b) more self-assuredness in working with challenging clients, (c) uncertainty in applying technique, and (d) feelings of restriction with MI application. Implications for integrating MI in skills courses and future directions in research are discussed.
Keywords: counseling skills, counseling students, motivational interviewing, self-efficacy, student experiences
Self-efficacy is an important mediator of performance and involves the degree to which people are capable, diligent and committed in their work (Chen, Casper, & Cortina, 2001). Specific to counselor education, there is a supported relationship between counseling self-efficacy and counselor training (Larson et al., 1992; Nilsson & Duan, 2007). Counseling self-efficacy has been shown to play a fundamental role in counselor development and training (Barnes, 2004; Lent et al., 2006), and higher counseling self-efficacy can be related to greater performance due to motivation factors (Bandura, 1986; Greason & Cashwell, 2009). In this study, the authors explored counselor trainees’ counseling self-efficacy before and after the completion of a counseling skills course that integrated MI. This technique was incorporated into the course to increase students’ humanistic people-responsiveness skills and to expose students to a defined evidence-based practice to help increase their counseling self-efficacy. Students’ experiences in this course were also a focus in the current study.
Counseling Self-Efficacy
Counseling self-efficacy can be defined as a counselor’s belief about his or her ability to effectively counsel a client in the near future (Larson, 1998; Larson & Daniels, 1998; Lent et al., 2006). Based on Bandura’s (1997) theory, this confidence is an important factor in the likelihood of counselor trainees applying specific counseling skills. Counseling skills can be defined as the ability of a counselor to demonstrate attending behavior that displays empathy, support, and a unified effort with the client toward a common goal of resolution and movement forward (Ivey, Packard, & Ivey, 2006; Schaefle et al., 2005; Schaefle, Smaby, Packman, & Maddux, 2007). More specifically, counseling attending behavior can be demonstrated through clarifications, encouragement, paraphrasing, reflecting and summarizing of client statements (Easton et al., 2008; Ivey et al., 2006). Self-efficacy theory states that the ability to thrive in the workplace entails not only content knowledge and appropriate application of required skills, but also the worker’s belief that he or she will use the skills successfully (Barnes, 2004; Melchert, Hays, Wiljanen, & Kolocek, 1996; Tang et al., 2004). Counseling self-efficacy theory holds the assumption that self-efficacy is the instrument through which effective practice occurs and perseverance is strengthened for navigating challenging professional scenarios. The theory also contends that self-efficacy enables an environment where counselor trainees are better able to value feedback in their learning processes (Barnes, 2004; Larson, 1998).
Providing opportunities for students to practice, learn and master counseling skills is a powerful way to develop self-efficacy (Greason & Cashwell, 2009). Within pedagogy literature, researchers suggest that counselor competency can be best developed through critical thinking activities such as role-play, modeling, and receiving practice feedback. Such activities build students’ self-efficacy to help them cope with real-work challenges (Daniels & Larson, 2001; Larson et al., 1992; Duys & Hedstrom, 2000; Tang et al., 2004). These purposeful and challenging interventions, which are important for developing counseling self-efficacy, have also been found to be most effective early in skill training (Barnes, 2004; Larson, 1998; Larson et al., 1999). Although new counselors may not feel confident or be fully prepared in their skills, research has found that experience in the field will likely compensate for any earlier deficiencies (Lent et al., 2006; Tang et al., 2004). As such, self-efficacy has been found to be higher among counselors with more education in counseling, more years of experience practicing counseling, and more hours of supervision (Larson et al., 1992).
When pertaining to counselor training, higher self-efficacy has been associated with greater execution of microskills among counselors-in-training who conducted mock sessions (Larson et al., 1992). Counseling self-efficacy includes having confidence in problem-solving and decision-making skills when working with clients (Easton, Martin, & Wilson, 2008). Self-efficacy is positively related to self-esteem, self-perceived planning effectiveness, and outcome expectations (Easton, Martin, & Wilson, 2008; Larson et al., 1992; Schaefle, Smaby, Maddux, & Cates, 2005; Tang et al., 2004), and negatively related to anxiety (Barnes, 2004; Daniels & Larson, 2001; Larson et al., 1992; Lent et al., 2006; Schaefle et al., 2005). Greason and Cashwell (2009) stated that although self-efficacy and competence are not interchangeable, counselors with strong self-efficacy report less anxiety and interpret their professional concerns as “challenging rather than overwhelming or hindering” (p. 3).
The current study assessed students’ counseling self-efficacy before and after completing a basic counseling skills course that integrated MI. Bandura (1984) described self-efficacy as a “generative capability in which multiple subskills must be flexibly orchestrated in dealing with continuously changing realities, often containing ambiguous, unpredictable, and stressful elements” (p. 233). We assert that integrating MI into a basic counseling skills course can provide counselor trainees with this capability as MI is a structured, evidence-based counseling style that requires the practitioner to approach clients in a humanistic people-responsive manner.
Motivational Interviewing
MI is a collaborative, person-centered counseling style intended to elicit and explore clients’ personal motivations to change in an accepting and compassionate environment (Miller & Rollnick, 2013). MI practice includes an indispensable humanistic “spirit” that contains four components: partnership, acceptance, compassion and evocation (Miller & Rollnick, 2013). Within the client-counselor partnership, or collaboration, the counselor is not doing anything “to” the client, but rather is working “with” or “for” the client, and the client is considered the “expert” on his or her own life. Acceptance is an extension of Rogers’s (1957) concept of unconditional positive regard. Expressions of acceptance in MI include supporting client autonomy, expressing accurate empathy, and reflecting client strengths and attributes through genuine affirmations. Compassion emphasizes the primary focus on the client’s welfare. In regard to evocation, the counselor elicits information about the problem from the client’s perspective, as well as information about the client’s goals, values and struggles. Further, the counselor explores the client’s ambivalence about change and evokes the client’s personal motivations to change. By teaching MI in basic skills courses, graduate counseling students learn to base their practice on these humanistic principles, emphasizing the establishment of a working therapeutic relationship based on empathic acceptance.
In addition to a foundational humanistic spirit, the essential skills of MI derive from person-centered counseling. Open questions, reflective statements, summarizations, and statements of affirmation are heavily utilized and emphasized throughout the four phases of MI: engaging, focusing, evoking and planning (Miller & Rollnick, 2013). Phase one—engaging—requires the establishment of a therapeutic relationship, which may include diminishing any relationship discord (formerly known as “resistance”) that is initially present. In phase two, the counselor guides the focus of the interaction to whatever change the client may be considering. In phase three, the MI counselor focuses on evocation by eliciting the client’s arguments in favor of change and helping guide the client to further develop these ideas based on the client’s personal beliefs, values and goals. Counselor behaviors such as confrontation, persuasion and coercion are the antithesis to evocation and are not utilized in MI practice. Providing unsolicited advice and attempting to impose change are seen as counterproductive as these behaviors tend to result in discord in the therapeutic relationship and inhibit client change (Madson, Loignon, & Lane, 2009).
Instead, MI focuses on strategic use of evocation and reflective listening to help guide clients to consider change as they come to recognize and resolve inconsistencies between their values or goals and current behaviors (i.e., developing discrepancies; Miller & Rollnick, 2013). In this way, MI is goal-directed as the counselor intentionally moves with the client to explore and resolve client ambivalence that is interfering with change, and ultimately assist the client to enhance his or her personal motivations to implement and sustain positive behavior change. Finally, once a sufficient level of motivation is present, the counselor and client collaboratively develop a plan for change (phase four). Throughout the four phases of MI, counselors retain the humanistic spirit, meet clients where they are in their unique process of change, and respond to the individualized needs and circumstances of the client.
Basis for Integrating Motivational Interviewing into a Skills Course
The usefulness of MI and the diversity of its application informed the decision to incorporate MI into a basic counseling skills course. Adhering to the four phases of MI provides a clear blueprint for counselor trainees to engage clients in the counseling process, establish a working therapeutic relationship, focus on specific client goals, and develop a plan for change. Further, learning MI includes learning basic counseling skills such as open-ended questions, summarizations, reflections, and highlighting client strengths (i.e., affirmations); therefore, integration of MI might help strengthen these basic skills (Young & Hagedorn, 2012). In addition to these essential skills, learning MI also provides students with the opportunity to learn how to manage discord in the counseling relationship and help resolve client ambivalence about change—both common clinical challenges, especially for beginning counselors. We anticipated that these factors would lead to enhanced self-efficacy among counselor trainees.
In addition to providing a clear framework for counselor trainees to follow to begin the counseling process and a defined method that requires the practice of a humanistic spirit and skills, MI is considered an evidence-based practice (EBP) in the treatment of substance use disorders, the area in which it originated. In addition to substance-abuse treatment, MI has demonstrated efficacy across diverse populations, symptoms and behaviors (Hettema, Steele, & Miller, 2005; Lundahl, Kunz, Brownell, Tollefson, & Burke, 2010). From hundreds of research studies and several meta-analyses, MI has been found to be efficacious in the areas of chronic mental disorders management, treatment adherence, problem gambling, smoking cessation, generalized anxiety disorder, and co-occurring mental health and substance use disorders, as well as various health issues (Barrowclough et al., 2010; Burke, Arkowitz, & Menchola, 2003; Cleary, Hunt, Matheson, & Walter, 2009; Hettema et al., 2005; Lundahl et al., 2010; Westra, Arkowitz, & Dozois, 2009). MI also has been applied to adolescent counseling (e.g., Knight et al., 2005; Peterson, Baer, Wells, Ginzler, & Garrett, 2006), group therapy (e.g., Walters, Ogle, & Martin, 2002), and couples therapy (e.g., Burke, Vassilev, Kantchelov, & Zweben, 2002). By training counseling students to use an approach that has demonstrated effectiveness with a broad range of clients and issues, it seems likely that students’ self-efficacy with regard to clients would increase. In addition, counselor training programs are encouraged to expose students to EBPs (e.g., Council for Accredited Counseling and Related Educational Programs [CACREP], 2009).
Increasing Counselor Trainee Self-Efficacy Through MI Training
Learning to effectively implement MI is a complex task that requires specific training. Extensive training that includes practice feedback or coaching has been found to be helpful in establishing and maintaining proficient MI practice (Abramowitz, Flattery, Franses, & Berry, 2010; Doran, Hohman, & Koutsenok, 2011; Miller, Yahne, Moyers, Martinez, & Pirritano, 2004). To our knowledge, in the only study that has explored MI training with counselor trainees, researchers implemented a 4-hour MI training with graduate counseling students who were in practicum, which resulted in enhanced MI skills compared to a control group who did not receive the 4-hour MI training (Young & Hagedorn, 2012). In the current study, first-year counseling graduate students were exposed to MI starting in the fourth week of a 15-week semester course on basic counseling skills.
This study responded to two research questions. The first question asked, “Does an introductory counseling skills course that incorporated MI significantly increase counseling students’ self-efficacy?” Further, it was expected that an increase in self-efficacy would occur at rates comparable to or exceeding other skill training methods (e.g., skilled counselor training model; Urbani et al., 2002). Second, the authors sought to gain an understanding about the students’ experiences of learning counseling skills within the context of MI.
Description of the Course
Course Materials and Assignments
Two textbooks were used in the described course: the first was a general interview and counseling skills text (Ivey, Ivey, & Zalaquett, 2010), which was used exclusively for the first three classes and then intermittently throughout the semester. The second textbook was specific to building MI skills (Rosengren, 2009) and introduced in the fourth class meeting and also incorporated throughout the remainder of the semester. The third edition of the Motivational Interviewing: Helping People Change (Miller & Rollnick, 2013) text was scheduled to be released shortly after the end of the course. Therefore, students learned the MI concepts as they were presented in the second edition of the text (Miller & Rollnick, 2002) which was a recommended, not required, text for the course. Additional resources were incorporated into the course throughout the semester including supplemental readings related to MI (e.g., Lundahl et al., 2010; Miller & Rollnick, 2004; Miller & Rose, 2009) and video demonstrations of specific MI skills (Miller, Rollnick & Moyers, 1998). The summary of course content provided in Table 1 shows how MI was integrated into the course week-by-week.
Table 1
Integration of MI in Counseling Course
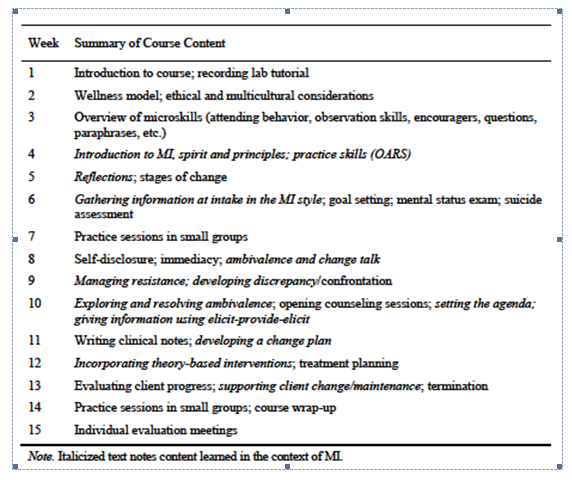
Students were required to complete four video-recorded demonstrations (one 15-minute session, three 45- to 50-minute sessions) of the counseling skills learned in class—with increasing complexity—using role-play with a classmate. Grading rubrics, which were developed by senior faculty and used in this course in previous years and therefore not MI-specific, were used to grade the skill demonstrations. In addition to recorded demonstrations, various written assignments were required throughout the semester, such as reflection papers, a self-evaluation, a completed intake form, a transcribed segment of a recorded mock session, and progress notes.
Course Process
In regard to the process of the course, skill development and practice were emphasized. For each skill presented, a video or interactive demonstration was shown, after which students practiced the skills in dyads or small groups using role-plays. Feedback was provided to the “counselor” from classmates and the instructor and/or a teaching assistant (TA). Three doctoral-level TAs (only one of whom had formal MI training) circulated with the primary instructor (first author) while the students practiced skills in small groups. In the third class meeting, students learned how to give appropriate, constructive feedback to their peers prior to engaging in the first role-play (Ivey, Ivey & Zalaquett, 2010).
Method
A pretest-posttest single group design was employed to investigate the differences in students’ self-efficacy between the start and end of the course, as measured by a self-administered counselor self-efficacy questionnaire. A qualitative case study approach was used to investigate students’ experiences in the course. Qualitative data was collected via an open-ended questionnaire distributed at the final class meeting. All data was collected anonymously and study participation was voluntary.
Participants
This study took place with 19 participants who were graduate students in the counseling programs offered at a large public university in the southern United States. Participants were enrolled in the required Introduction to Counseling Practice course during their second semester of study in their respective counseling programs. Forty-two percent (n = 8) of participants were enrolled in the CACREP-accredited school counseling program, 37% (n = 7) were in the CACREP-accredited clinical mental health counseling program, and 21% (n = 4) were in the APA-accredited counseling psychology program. Twenty-one percent (n = 4) of participants were Black/African American and 79% (n = 15) were White/Caucasian. Sixteen percent (n = 3) of the participants were men and 84% (n = 16) were women. Ages ranged from 22–29 with a mode of 22. All but one of these 19 participants passed this course.
Instruments
The Counselor Estimate of Self-Efficacy (COSE) is a 37-item measure of self-efficacy on a 6-point Likert scale. Sample items include, “When using responses like reflection of feeling, active listening, clarification, probing, I am confident I will be concise and to the point” and “I feel that I have enough fundamental knowledge to do effective counseling.” The COSE has demonstrated reliability and validity as Larson et al., (1992) reported the internal consistency of the COSE was .93 and the test-retest reliability over three weeks was .87. The range for total scores on the COSE is 37–222, with higher scores indicating greater self-efficacy.
The feedback questionnaire distributed at the end of the course consisted of five questions: (a) How would you describe your overall experience of learning counseling skills in the context of MI?; (b) What, if any, were the benefits of learning counseling skills in the context of MI?; (c) What, if any, were the challenges of learning counseling skills in the context of MI?; (d) Would you recommend that this course follow a similar format (integrating MI into the course) for subsequent cohorts? Why or why not?; and (e) Please provide any other comments/suggestions you may have.
Procedure
This counseling course was a required course that met weekly for 2 hours and 50 minutes over the course of a 15-week semester in the Spring of 2012. The course instructor (first author) was an assistant professor and a member of the Motivational Interviewing Network of Trainers (MINT), meaning she had completed a 3-day training to train others in MI. Three doctoral students assisted with the instruction of the course (one of whom is the third author). These TAs taught segments of the course that were not specific to MI, observed and provided students with feedback during class practice sessions, and provided written feedback on students’ recorded skill demonstrations using a grading rubric that was focused on general counseling skill demonstrations (i.e., not specific to MI).
The second author, who was not part of the course instruction, conducted the informed consent and data collection following protocol approval from the Institutional Review Board. Participants completed a demographic form and a pretest COSE on the first day of class. During the final class meeting (week 14), students completed the posttest COSE and the feedback questionnaire. To reduce coercion and protect participant confidentiality, each participant was issued a code that only he or she knew to match his or her pretest and posttest; students completed the qualitative questionnaire anonymously. The course instructor (first author) was not present during the consenting procedures or data collection, and participants were directed not to provide any identifying information on data collection materials. Finally, participants were informed that their decision to participate in the study, not to participate in the study, or to stop participating would not affect their grade in the course, their relationship with the instructor/researchers, or their future relations with the department or university. No incentives were provided for study participation. Nineteen of the 20 students enrolled in the course completed the study in full. One student was absent during the final class meeting, and therefore did not complete the posttest or the qualitative questionnaire. The pretest from this student was destroyed and not used in data analysis.
Case Study Analysis
A case study design was chosen for qualitative portion of this study in order to explore students’ experiences within a bounded system: the counseling skills course that integrated MI (Creswell, Hanson, Plano, & Morales, 2007). The second and third authors completed the qualitative analysis and aimed to arrive at a description of this specific case using case-based themes (Creswell et al., 2007). To do so, the textual data collected via the feedback questionnaire was typed verbatim by the second author. Then, the second and third authors read over participant responses several times to become familiar with the data. Throughout data analysis, these authors engaged in reflexivity and memo writing with the purpose of reflecting on their personal perspectives and experiences in an effort to see the data as it was and to avoid undue influence from their own histories (Morrow, 2005; Patton, 2002), as well as to record and facilitate analytical thinking (Maxwell, 2005).
Consistent with case study research, the second and third authors independently used categorical aggregation to identify patterns and emergent themes from the data (Creswell, 2007). These authors then came together to reach a consensus about the meaning of the data by discussing their independent categories, referring back to the data, and identifying and agreeing upon preliminary categories. The researchers identified major ideas within the data and identified substantiating evidence across participants’ accounts to support each key issue (Creswell, 2007). Through data analysis, the initial 12 categories (practical skills, beneficial experience, client autonomy, helpful experience, enjoyable experience, effective skills, client resistance, client motivation, adaptable skills, difficult clients, ambivalent clients, and client connection) were collapsed into four information-rich themes, one of which contained two subthemes (Creswell, 2007). The authors repeatedly reverted back to the data when considering the wording of the themes and subthemes to confirm that the titles were consistent with the contents.
A peer reviewer (Creswell et al., 2007; Lincoln & Guba, 1985), who is the fourth author and who was familiar with qualitative research, was employed on two occasions in which the themes and analysis process were examined and questioned in terms of rationale, clarity and holistic understanding of the raw data. After each peer review session, the second and third authors discussed the themes and subthemes and made changes to the organization of the themes and their titles. Final themes were agreed upon by the second and third authors as they reflected the overall meaning of the data. These themes served as naturalistic generalizations or descriptions from which others may learn about this case (Creswell, 2007).
Results
Counseling Students’ Self-Efficacy
Participants’ point increases on the COSE ranged from 0 to 74 with the mode being 19 and the mean 30 points. No student showed a decrease in self-efficacy and one student’s score did not change between the pretest and posttest. After determining the assumption of normality was met using normal Q-Q plots, a dependent t-test was used to determine if significant differences existed between the COSE pretest and posttest for these participants. Results showed that a significant improvement occurred at the .0005 level in which the pretest COSE scores had a mean of 144.79±19.6 and the posttest scores averaged at 174.42 ± 16.0, t(18) = –7.055, p = .0005.
Experiences Learning Counseling Skills Using Motivational Interviewing
The feedback questionnaire elicited participants’ perceived benefits and challenges of learning counseling skills in the context of MI. Overall, participants provided more rich descriptions of positive experiences and benefits rather than negative experiences or challenges. Additionally, each participant responded affirmatively to the fourth question, “Would you recommend that this course follow a similar format (integrating MI into the course) for subsequent cohorts?” In response to the second research question, four main themes were identified to capture participants’ experiences of learning counseling skills within the context of MI. Two subthemes also emerged within the first theme. These themes are presented along with corroborating excerpts from the data.
Learning experience valuable and relevant to skill development. According to a majority of participants in this study, learning counseling skills in the context of MI could translate to their future professional experiences and be relevant in working with clients. Two subthemes emerged from this theme: (a) class instruction was useful and valuable, and (b) students felt they had learned practical and effective skills.
Class instruction useful and valuable. Many students conveyed that class instruction was helpful and they expressed confidence in the expertise of their instructor. One student reflected on the overall experience of learning counseling skills in the context of MI and feeling better prepared following the course: “I see MI being very helpful in my profession and in the overall profession of counseling.” In response to the inquiry about challenges experienced, one student indicated that “the professors did a wonderful job breaking down the beginning and basic steps in order to build on them throughout the semester.”
Participant responses also suggested that students found practicing the skills during class time to be beneficial. One student reflected on the experience of practicing skills: “MI has a ton of great tool[s] that help you connect with your client as you work together to help them change. Practicing the skills in class helped me see how effective they can be in the real world.” When asked about the challenges encountered while learning skills in the context of MI, another student responded: “It is a lot of skills, but practicing them helped me remember and understand them.”
Practical and effective skills learned. Within this subtheme, almost all of the comments from participants suggest that the skills learned were versatile and effective. One student noted the versatile application of MI: “I think the skills can be applied to most any counseling session, regardless of the counselor’s theoretical perspective.” The students also appreciated the demonstrated efficacy of MI, perhaps enhancing their own counseling efficacy. For example, one student wrote, “I feel that learning the skills in the context of MI has enabled me to possess a wide variety of skills and interventions that will work effectively with the client while promoting client autonomy.”
Participants’ beliefs that they would be able to connect with clients also were viewed as a valuable and useful part of this experience. For example, one student reported that “the overall experience of learning MI has given me a new outlook and approach that I can use to connect with and help my clients.” Students also seemed to find the MI approach to be practical, as one student reflected: “All the information that goes with MI seems so practical and almost like common sense.” Another student responded, “I really appreciate the strengths-based approach and the empowerment-stance toward clients. I also like that the skills are specific enough to be practical and general enough to be applicable to a variety of clients.”
More self-assuredness about challenging clients. This theme captured participants’ experiences of an increased sense of self-assurance and comfort when working with clients who are not ready to change (e.g., ambivalent), or who might be considered “difficult” or “hesitant” clients. When describing the benefits of learning counseling skills in the context of MI, almost half the students commented on working with challenging clients with more self-assurance or comfort. For example, one student reflected: “MI allows you to understand that you cannot make someone change and this [rolling] with resistance really helps put the counseling skills to effective use.” Students also expressed they would feel more self-assured working with ambivalent clients in the future. One student noted that “MI has taught me how to work with ambivalence and gave me a whole new set of tools to help initiate change from within the client.” Finally, one student wrote, “I feel I am much more prepared with the skills that will help me when working with hesitant clients.”
Uncertainty in applying technique. Almost half of participants expressed a sense of uncertainty in applying techniques learned throughout the course. This uncertainty appeared to be associated with the technical application of the skills that were taught in conjunction with basic counseling skills. One student reflected on the challenges of learning counseling skills in the context of MI: “Sometimes it was hard to tell the difference between MI techniques and basic counseling techniques. There was a lot of overlap.” Another student responded, “I had trouble implementing the skills learned in class into the video tapes [assignments]. Some of the practice sessions were awkward.” Another student commented on the technicality of skill use: “For me, knowing exactly when to use the skills and how to use them so it’s a natural flow to things.”
Restrictions in applying Motivational Interviewing. Finally, a few students conveyed feelings that the application of MI techniques was somewhat rigid. This rigidity included difficulty in using the techniques in various situations and with a variety of clients as well as combining MI skills with other counseling skills. Although MI was introduced in the counseling skills course to provide a structured approach to practicing basic skills, beginning counseling students typically have had limited exposure to counseling approaches, which may be necessary for students to develop their own counseling style. As one student reflected, “I think it was difficult for me to focus the skills if MI is not being used with a client…kind of rigid in that aspect.” According to another student, “The only suggestion I would make is to incorporate other skills outside of MI.” Finally, one student noted a preference for the skills to be more specific to a school setting: “I would recommend maybe some of the taping sessions to be more school focused.”
Discussion
In the current study, significant differences were found between participants’ counseling self-efficacy pretests and posttests, suggesting that the counseling skills course that incorporated MI was effective in enhancing students’ beliefs that they can be successful counseling clients. The average point increase on the COSE was 30, which is comparable to the findings of Larson and colleagues (1992), who found that counselor trainees’ COSE scores increased approximately one standard deviation over the course of their clinical practicum experience and had an average point increase of 30.4. Similarly, the posttest scores of participants of the current study were comparable to those found by Urbani et al. (2002), who examined the self-efficacy of 53 students who learned counseling skills through the skilled counselor training model (SCTM; 176.46 compared to 174.42 in the current study). These comparable increases in student self-efficacy lend support to incorporating MI into counseling skill courses.
Although there is evidence that participants gained self-efficacy in counseling after learning MI skills in conjunction with basic counseling skills, the qualitative findings suggest that some students were uncertain how to directly apply the MI skills. This self-doubt was particularly expressed when students considered how they might incorporate the skills into sessions with “actual clients” and how to utilize the skills across various theoretical orientations. This concern might not be related to the specific integration of MI skills in a techniques course, but rather a reflection of where students are in their process of becoming a counselor and process of learning. Experiencing discomfort may be developmentally appropriate for beginning counselors and can facilitate growth and learning (Griffith & Frieden, 2000; Kember, 2001).
Rønnestad and Skovholt (2003) described Phase 2: The Beginning Student Phase (of their previously formulated eight stages of counselor development) as a time when students feel easily overwhelmed by new skills and information they are learning, and as a result lack confidence in their abilities. The researchers reported that during this stage, the introduction of basic helping skills that can be used with all clients is helpful in providing students with a sense of control and tranquility. Young and Hagedorn (2012) reported that students who had MI skills training had marked improvements in basic counseling microskills (e.g., empathy, open questions, support, evocation) and noted that this outcome might have been due to the overlap of basic counseling skills used in MI. As MI training reiterates the microskills that many counselor educators expect students to learn, its incorporation into a basic skills course might provide students with the practice and confidence needed to ease the anxiety students may experience in the beginning stages of counselor development.
Incorporating MI into a basic counseling skills course provides students with training in an EBP that possesses a humanistic foundation. Further, it may foster people-responsive counseling skills, such as how to respond to clients who are not ready to change (e.g., ambivalent or mandated clients); students might otherwise receive no or minimal exposure to such skills. Responses in the qualitative portion of this study indicated satisfaction and perhaps relief in learning specific skills that might be useful when working with challenging clients (e.g., reluctant, mandated, difficult). This is especially promising when considering that an obstacle for novice counselors is knowing how to respond to stress-invoking situations when clients show behaviors that seem confusing to counselors (e.g., lack of motivation; Skovholt & Rønnstad, 2003).
In their qualitative research on beginning psychotherapists in a counseling psychology doctoral program, Hill and colleagues (2007) identified that students shared similar frustration when working with clients who were reluctant to participate in the counseling process or who were not open to counselor help. Although other counseling methods might conceptualize and provide ways to work with resistant clients, MI offers a humanistic conceptualization and specific skills for counselors to meet and accept clients where they are in their process of change. Many of MI’s components are specific to working with clients who present in earlier stages of change (i.e., precomtemplation and contemplation), particularly those regarding relationship discord and ambivalence. MI also can be useful as clients prepare for change, take action, and work to maintain changes (DiClemente & Velasquez, 2002). As such, MI skills expand beyond a typical basic skill set and beginning counselors can benefit from having MI as part of their repertoire, especially to help them feel more confident when working with clients who are not ready for change.
Limitations
As with any research investigation, the current study has limitations for consideration. First, the primary instructor of the course also was the primary investigator for the study. This dual role may have influenced students’ responses. Second, this study lacked a control group, which would be necessary to determine between group differences. Third, this study was conducted at one university with a small sample size and is therefore limited in generalizability. Fourth and finally, although a case study design will typically incorporate multiple sources of data (Creswell, 2007), this study relied solely on the feedback questionnaire to gather qualitative data, thus limiting the richness of data collected.
Implications for Counselor Education
Results indicated that using MI skills in an introductory level skills course provided enhanced self-efficacy and positive experiences in learning basic counseling skills. These findings suggest that it might behoove counselor educators to utilize the MI spirit and skills as a way for students to gain a humanistic foundation, reiterate basic counseling skills, and prepare students to help clients who are not yet ready to change. However, it is important for counselor educators who choose to integrate MI into a skills course to be trained and competent in MI skills and application. Additionally, they should be prepared to demonstrate these skills to students.
Students reported higher confidence levels in their readiness to use specific counseling skills; however, they indicated uncertainty in how to integrate these skills with other skills they may have been learning specific to particular theoretical orientations. Since MI is a counseling style and not a theoretical approach, it can be used with other counseling approaches (e.g., cognitive behavior therapy) for a potential synergistic effect (Miller & Rose, 2009). In response to the need for a greater integrative understanding, counselor educators might consider providing additional opportunities for students to discuss and self-reflect on their use of MI skills with their preferred theories, and model ways to synthesize these skills cohesively across theories and various problems presented by clients. Such opportunities would likely occur in advanced coursework including practicum and internship when students are engaging with actual clients. In addition, it may be useful to have more experiential practice in integrating the skills rather than having the sole focus be on using a particular MI skill in isolation.
Overall, incorporating MI into an introductory skills course appeared to be helpful for students. The spirit of MI (Miller & Rollnick, 2013) is undeniably humanistic as it emphasizes self-directed growth and people responsiveness within the therapeutic relationship. Fitch, Canada, and Marshall (2001) reported that humanistic theories (person-centered, existential and Gestalt) are influential in practicum courses, perhaps due to their emphasis on relationship building. When considering MI’s humanistic tenets, it might be useful for counselor educators to consider the utility and worthiness of this approach among other influential and well-established humanistic theories in the field.
Future Directions in Research
Ongoing studies are investigating if these students demonstrated MI proficiency on their final recorded skill demonstration required for this course, and the degree to which students maintained use of MI after they learned and integrated cognitive behavior therapy into their practice. Research that includes a control group is needed in order to assess the effect of learning MI on counselor trainees’ self-efficacy and skill development. Future research also might investigate possible associations between student self-efficacy, satisfaction in a counseling skills course, and execution of skills within and beyond the counseling skills course. In addition, research is needed to inform optimal timing of this type of skill training, as students might be better equipped to incorporate such training later in the graduate programs (e.g., during practicum).
Conclusion
This study investigated students’ counseling self-efficacy before and after completing a counseling skills course that integrated MI. Results indicated that students’ self-efficacy increased at rates comparable to alternative counseling skill development models. Further, students reported positive overall experiences when learning MI skills, which were noted in qualitative themes highlighting their skill development and self-assuredness in working with challenging clients. Students also had some lingering questions about the implementation of MI; however, this might be expected given their early stages of counselor development. Given that student self-efficacy increased by the end of the course and students reported overall positive experiences, this study provides preliminary support of the integration of MI into a counseling skills course. Although further investigations are needed, it seems that the inclusion of MI in the course may be useful to reiterate humanistic counseling skills and prepare students to work with clients who are not yet ready to change and who might otherwise overwhelm a novice counselor.
References
Abramowitz, S., Flattery, D., Franses, K., & Berry, L. (2010). Linking a motivational interviewing curriculum to the chronic care model. Journal of General Internal Medicine, 25, 620–626.
Bandura, A. (1984). Recycling misconceptions of perceived self-efficacy. Cognitive Therapy and Research, 8, 231–255.
Bandura, A. (1986). Social foundations of thought and action: A social cognitive theory.Englewood Cliffs, NJ: Prentice Hall.
Bandura, A. (1997). Self-efficacy. Harvard Mental Health Letter, 13(9), 4–7.
Barnes, K. (2004). Applying self-efficacy theory to counselor training and supervision: A comparison of two approaches. Counselor Education and Supervision, 44, 56–69.
Barrowclough, C., Haddock, G., Wykes, T., Beardmore, R., Conrod, P., Craig, T., . . . Tarrier, N. (2010). Integrated motivational interviewing and cognitive behavioural therapy for people with psychosis and comorbid substance misuse: Randomised controlled trial. British Medical Journal, 341, 6325–6337.
Burke, B. L., Arkowitz, H., & Menchola, M. (2003). The efficacy of motivational interviewing: A meta-analysis of controlled clinical trials. Journal of Consulting and Clinical Psychology, 71, 843–861.
Burke, B. L., Vassilev, G., Kantchelov, A., & Zweben, A. (2002). Motivational interviewing with couples. In W. R. Miller & S. Rollnick (Eds.), Motivational interviewing: Preparing people for change (2nd ed., pp. 347–361). New York, NY: Guilford.
Chen, G., Casper, W. J., & Cortina, J. M. (2001). The roles of self-efficacy and task complexity in the relationships among cognitive ability, conscientiousness, and work-related performance: A meta-analytic examination. Human Performance, 14, 209–230.
Cleary, M., Hunt, G. E., Matheson, S., & Walter, G. (2009). Psychosocial treatments for people with co-occurring severe mental illness and substance misuse: Systematic review. Journal of Advanced Nursing, 65, 238–258.
Council for Accreditation of Counseling and Related Educational Programs (CACREP). (2009). 2009 standards. Retrieved from: http://www.cacrep.org
Creswell, J. W. (2007). Qualitative inquiry & research design: Choosing among five approaches (2nd ed.). Thousand Oaks, CA: Sage.
Creswell, J. W., Hanson, W. E., Clark, V. L., & Morales, A. (2007). Qualitative research designs: Selection and implementation. The Counseling Psychologist, 35, 236–264.
Daeppen, J., Fortini, C., Bertholet, N., Bonvin, R., Berney, A., Michaud, P., . . . Gaume, J. (2012). Training medical students to conduct motivational interviewing: A randomized controlled trial. Patient Education & Counseling, 87, 313–318.
Daniels, J. A., & Larson, L. M. (2001). The impact of performance feedback on counseling self-efficacy and counselor anxiety. Counselor Education and Supervision, 41, 120–130.
DiClemente, C. C., & Velasquez, M. M. (2002). Motivational interviewing and the stages of change. In W. R. Miller & S. Rollnick (Eds.), Motivational interviewing: Preparing people for change (2nd ed., pp. 201–216). New York, NY: Guilford.
Doran, N., Hohman, M., & Koutsenok, I. (2011). Linking basic and advances motivational interviewing training outcomes for juvenile correctional staff in California. Journal of Psychoactive Drugs, 43, 19–26.
Duys, D. & Hedstrom, S. (2000). Basic counselor skills training and counselor cognitive complexity. Counselor Education and Supervision, 40, 8–19.
Easton, C., Martin Jr., W., & Wilson, S. (2008). Emotional intelligence and implications for counseling self-efficacy: Phase II. Counselor Education and Supervision, 47, 218–232.
Fitch, T. J., Canada, R., & Marshall, J. L. (2001). The exposure of counseling practicum students to humanistic counseling theories: A survey of CACREP programs. Journal of Humanistic Counseling, 40, 232–242.
Greason, P., & Cashwell, C. (2009). Mindfulness and counseling self-efficacy: The mediating role of attention and empathy. Counselor Education and Supervision, 49, 2–19.
Griffith, B. A., & Frieden, G. (2000). Facilitating reflective thinking in counselor education. Counselor Education and Supervision, 40, 82–94.
Hettema, J., Steele, J., & Miller, W. R. (2005). Motivational interviewing. Annual Review of Clinical Psychology, 1, 91–111.
Hill, C. E., Sullivan, C., Knox, S., & Schlosser, L. Z. (2007). Becoming psychotherapists: Experiences of novice trainees in a beginning graduate class. Psychotherapy: Theory, Research, Practice, Training, 44(4), 434–449. doi 10.1037/0033-3204.44.4.434
Ivey, A. E., Ivey, M. B., & Zalaquett, C. P. (2010). Intentional interviewing & counseling: Facilitating client development in a multicultural society (7th ed.). Belmont, CA: Brooks/Cole.
Ivey, A. E., Packard, N. G., & Ivey, M. B. (2006). Basic attending skills (4th ed.). North Amherst, MA: Microtraining Associates.
Kember, D. (2001). Beliefs about knowledge and the process of teaching and learning as a factor in adjusting to study in higher education. Studies in Higher Education, 26, 205–221. doi:10.1080/03075070120052116
Knight, J. R., Sherritt, L., Hook, S. V., Gates, E. C., Levy, S., & Chang, G. (2005). Motivational interviewing for adolescent substance use: A pilot study. Journal of Adolescent Health, 37, 167–169. doi:10.1016/j.jadohealth.2004.08.020
Larson, L. M. (1998). The SCMCT making it to “the show”: Four criteria to consider. The Counseling Psychologist, 26(2), 324–341. doi:10.1177/0011000098262008
Larson, L. M., Clark, M. P., Wesely, L. H., Koraleski, S. F., Daniels, J. A., & Smith, P. L. (1999). Videos versus role plays to increase counseling self-efficacy in prepractica trainees. Counselor Education and Supervision, 38, 237–248. doi: 10.1002/j.1556-6978.1999.tb00574.x
Larson, L. M., & Daniels, J. A. (1998). Review of the counseling self-efficacy literature. The Counseling Psychologist, 26, 179–218. doi:10.1177/0011000098262001
Larson, L. M., Suzuki, L. A., Gillespie, K. N., Potenza, M. T., Bechtel, M. A., & Toulouse, A. L. (1992). Development and validation of the Counseling Self-Estimate Inventory. Journal of Counseling Psychology, 39, 105–120. doi: 10.1037/0022-0167.39.1.105
Lent, R. W., Hoffman, M. A., Hill, C. E., Treistman, D., Mount, M., & Singley, D. (2006). Client-specific counselor self-efficacy in novice counselors: Relation to perceptions of session quality. Journal of Counseling Psychology, 53, 453–463. doi: 10.1037/0022-0167.53.4.453
Lincoln, Y. S., & Guba, E. G. (1985). Naturalistic inquiry. Newbury Park, CA: Sage.
Lundahl, B. W., Kunz, C., Brownell, C., Tollefson, D., & Burke, B. L. (2010). A meta-analysis of motivational interviewing: Twenty-five years of empirical studies. Research on Social Work Practice, 20, 137–160. doi: 10.1177/1049731509347850
Madson, M. B., Loignon, A. C., & Lane, C. (2009). Training in motivational interviewing: A systematic review. Journal of Substance Abuse Treatment, 36, 101–109. doi: 10.1016/j.jsat.2008.05.005
Maxwell, J. A. (2005). Qualitative research design: An interactive approach (2nd ed.). Thousand Oaks, CA: Sage.
Melchert, T. P., Hays, V. L., Wiljanen, L. M., & Kolocek, A. K. (1996). Testing models of counselor development with a measure of counseling self-efficacy. Journal of Counseling & Development, 74, 640–644. doi: 10.1002/j.1556-6676.1996.tb02304
Miller, W. R., & Rollnick, S. (2002). Motivational interviewing: Preparing people for change (2nd ed.). New York, NY: Guilford.
Miller, W. R., & Rollnick, S. (2004). Talking oneself into change: Motivational interviewing, stages of change, and therapeutic process. Journal of Cognitive Psychotherapy, 18, 299–308. doi: 10.1891/jcop.18.4.299.64003
Miller, W. R., & Rollnick, S. (2013). Motivational interviewing: Helping people change (3rd ed.). New York, NY: Guilford.
Miller, W. R., Rollnick, S., & Moyers, T. B. (1998). Motivational interviewing: Professional training videotape series [DVD]. Albuquerque, NM: The University of New Mexico.
Miller, W. R., & Rose, G. S. (2009). Toward a theory of motivational interviewing. American Psychologist, 64, 527–537. doi: 10.1037/a0016830
Miller, W. R., Yahne, C. E., Moyers, T. B., Martinez, J., & Pirritano, M. (2004). A randomized trial of methods to help clinicians learn motivational interviewing. Journal of Clinical and Consulting Psychology, 72, 1050–1062. doi: 10.1037/0022-006X.72.6.1050
Morrow, S. L. (2005). Quality and trustworthiness in qualitative research in counseling psychology. Journal of Counseling Psychology, 52, 250–260. doi: 10.1037/0022-0167.52.2.250
Nilsson, J. E. & Duan, C. (2007). Experiences of prejudice, role difficulties, and counseling self-efficacy among U.S. racial and ethnic minority supervisees working with white supervisors. Journal of Multicultural Counseling and Development, 35, 219–229. doi: 10.1002/j.2161-1912.2007.tb00062.x
Patton, M. Q. (2002). Qualitative research & evaluation methods (3rd ed.). Thousand Oaks, CA: Sage.
Peterson, P. L., Baer, J. S., Wells, E. A., Ginzler, J. A., & Garrett, S. B. (2006). Short-term effects of a brief motivational intervention to reduce alcohol and drug risk among homeless adolescents. Psychology of Addictive Behaviors, 20, 254–164. doi: 10.1037/0893-164X.20.3.254
Rogers. C. R. (1957). The necessary and sufficient conditions of therapeutic personality change. Journal of Consulting Psychology, 21, 95–103. doi: 10.1037/h0045357
Rosengren, D. B. (2009). Building motivational interviewing skills: A practitioner workbook. New York, NY: Guilford.
Rønnestad, M. H., & Skovholt, T. M. (2003). The journey of the counselor and therapist: Research findings and perspectives on professional development. Journal of Career Development, 30, 5–44. doi:10.1177/089484530303000102
Schaefle, S., Smaby, M. H., Maddux, C. D., & Cates, J. (2005). Counseling skills attainment, retention, and transfer as measured by the skilled counseling scale. Counselor Education and Supervision, 44, 280–292. doi: 10.1002/j.1556-6978.2005.tb01756.x
Schaefle, S., Smaby, M. H., Packman, J., & Maddux, C. D. (2007). Performance assessment of counseling skills based on specific theories: Acquisition, retention, and transfer to actual counseling sessions. Education, 128, 262–273.
Skovholt, T. M., & Rønnestad, M. H. (2003). Struggles of the novice counselor and therapist. Journal of Career Development, 30, 45–58. doi:10.1177/089484530303000103
Tang, M., Addison, K. D., LaSure-Bryant, D., Norman, R., O’Connell, W., & Stewart-Sicking, J. (2004). Factors that influence self-efficacy of counseling students: An exploratory study. Counselor Education and Supervision, 44, 70–80. doi: 10.1002/j.1556-6978.2004.tb01861.x
Urbani, S., Smith, M. R., Maddux, C. D., Smaby, M. H., Torres-Rivera, E., & Crews, J. (2002). Skills-based training and counseling self-efficacy. Counselor Education and Supervision, 42, 92–106. doi: 10.1002/j.1556-6978.2002.tb01802.x
Walters, S. T., Ogle, R., & Martin, J. E. (2002). Perils and possibilities of group-based motivational interviewing. In W. R. Miller & S. Rollnick (Eds.), Motivational interviewing: Preparing people for change (2nd ed., pp. 377–390). New York, NY: Guilford.
Westra, H. A., Arkowitz, H., & Dozois, D. J. A. (2009). Adding a motivational interviewing pretreatment to cognitive behavioral therapy for generalized anxiety disorder: A preliminary randomized controlled trial. Journal of Anxiety Disorders, 23, 1106–1117. doi: 10.1016/j.janxdis.2009.07.014.
Young, T. L., & Hagedorn, W. B. (2012). The effect of a brief training in motivational interviewing on trainee skill development. Counselor Education and Supervision, 51, 82–97. doi: 10.1002/j.1556-6978.2012.00006.x
Melanie H. Iarussi is an Assistant Professor at Auburn University. Jessica M. Tyler, NCC, is Clinical Coordinator at East Alabama Mental Health and Adjunct Professor at Auburn University. Sarah Littlebear, NCC, is a doctoral candidate at Auburn University. Michelle S. Hinkle is an Assistant Professor at William Paterson University. Correspondence can be addressed to Melanie H. Iarussi, Auburn University, 2084 Haley Center, Auburn, AL 36830, miarussi@auburn.edu.