Feb 26, 2021 | Volume 11 - Issue 1
Priscilla Rose Prasath, Peter C. Mather, Christine Suniti Bhat, Justine K. James
This study examined the relationships between psychological capital (PsyCap), coping strategies, and well-being among 609 university students using self-report measures. Results revealed that well-being was significantly lower during COVID-19 compared to before the onset of the pandemic. Multiple linear regression analyses indicated that PsyCap predicted well-being, and structural equation modeling demonstrated the mediating role of coping strategies between PsyCap and well-being. Prior to COVID-19, the PsyCap dimensions of optimism and self-efficacy were significant predictors of well-being. During the pandemic, optimism, hope, and resiliency have been significant predictors of well-being. Adaptive coping strategies were also conducive to well-being. Implications and recommendations for psychoeducation and counseling interventions to promote PsyCap and adaptive coping strategies in university students are presented.
Keywords: university students, psychological capital, well-being, coping strategies, COVID-19
In January 2020, the World Health Organization declared the outbreak of a new coronavirus disease, COVID-19, to be a public health emergency of international concern, and the effects continue to be widespread and ongoing. For university students, the pandemic brought about disruptions to life as they knew it. For example, students had to stay home, adapt to online learning, modify internship placements, and/or reconsider graduation plans and jobs. The aim of this study was to understand how the sudden changes and uncertainty resulting from the pandemic affected the well-being of university students during the early period of the pandemic. Specifically, the study addresses coping strategies and psychological capital (PsyCap; F. Luthans et al., 2007) and how they relate to levels of well-being.
University Students and Mental Health
Although mental health distress has been an issue on college campuses prior to the pandemic (Flatt, 2013; Lipson et al., 2019), COVID-19 has and will continue to magnify this phenomenon. Experts are projecting increases in depression, anxiety, post-traumatic stress disorder, and suicide in the United States (Wan, 2020). Johnson (2020) indicated that 35% of students reported increased anxiety associated with a move from face-to-face to online learning in the spring 2020 semester, matching the early phases of the COVID-19 outbreak. Stress associated with adapting to online learning presented particular challenges for students who did not have adequate internet access in their homes (Hoover, 2020).
Researchers have reported that high levels of technology and social media use are associated with depression and anxiety among adolescents and young adults (Huckins et al., 2020; Primack et al., 2017; Twenge, 2017). Given the current realities of physical distancing, there are fewer opportunities for traditional-age university students attending primarily residential campuses to maintain social connections, resulting in social fragmentation and isolation. Research has demonstrated that this exacerbates existing mental health concerns among university students (Klussman et al., 2020).
The uncertainties arising from COVID-19 have added to anticipatory anxiety regarding the future (Ray, 2019; Witters & Harter, 2020). From the Great Depression to 9/11 and Hurricane Katrina, victims of these life-shattering events have had to deal with their present circumstances and were also left with worries about how life and society would be inexorably altered in the future. University students are dealing with uncertain current realities and futures and may need to bolster their internal resources to face the challenges ahead. In this context, positive coping strategies and PsyCap may be increasingly valuable assets for university students to address the psychological challenges associated with this pandemic and to maintain or enhance their well-being.
Coping Strategies
Coping is often defined as “efforts to prevent or diminish the threat, harm, and loss, or to reduce associated distress” (Carver & Connor-Smith, 2010, p. 685). There are many ways to categorize coping responses (e.g., engagement coping and disengagement coping, problem-focused coping and emotion-focused coping, accommodative coping and meaning-focused coping, proactive coping). Engagement coping includes problem-focused coping and some forms of emotion-focused coping, such as support seeking, emotion regulation, acceptance, and cognitive restructuring. Disengagement coping includes responses such as avoidance, denial, and wishful thinking, as well as aspects of emotion-focused coping, because it involves an attempt to escape feelings of distress (Carver & Connor-Smith, 2010; de la Fuente et al., 2020). Findings on the effectiveness of problem-focused coping strategies versus emotion-focused coping strategies suggest the effectiveness of the particular strategy is contingent on the context, with controllable issues being better addressed through problem-focused strategies, while emotion-focused strategies are more effective with circumstances that cannot be controlled (Finkelstein-Fox & Park, 2019). In general, problem-focused coping strategies, also known as adaptive coping strategies, include planning, active coping, positive reframing, acceptance, and humor (Carver & Connor-Smith, 2010). Other coping strategies, such as denial, self-blame, distraction, and substance use, are more often associated with negative emotions, such as shame, guilt, lower perception of self-efficacy, and psychological distress, rather than making efforts to remediate them (Billings & Moos, 1984). These strategies can be harmful and unhealthy with regard to effectively coping with stressors. Researchers have recommended coping skills training for university students to modify maladaptive coping strategies and enhance pre-existing adaptive coping styles to optimal levels (Madhyastha et al., 2014).
Flourishing: The PERMA Well-Being Model
Positive psychologists have asserted that studies of wellness and flourishing are important in understanding adaptive behaviors and the potential for growth from challenging circumstances (Joseph & Linley, 2008; Seligman, 2011). Flourishing (or well-being) is defined as “a dynamic optimal state of psychosocial functioning that arises from functioning well across multiple psychosocial domains” (Butler & Kern, 2016, p. 2). Seligman (2011) proposed a theory of well-being stipulating that well-being was not simply the absence of mental illness (Keyes, 2002), but also the presence of five pillars with the acronym of PERMA (Seligman, 2002, 2011). The first pillar, positive emotion (P), is the affective component comprising the feelings of joy, hope, pleasure, rapture, happiness, and contentment. Next are engagement (E), the act of being highly interested, absorbed, or focused in daily life activities, and relationships (R), the feelings of being cared about by others and authentically and securely connected to others. The final two pillars are meaning (M), a sense of purpose in life that is derived from something greater than oneself, and accomplishment (A), a persistent drive that helps one progress toward personal goals and provides one with a sense of achievement in life. Seligman’s (2011) PERMA model is one of the most highly regarded models of well-being.
Seligman’s multidimensional model integrates both hedonic and eudaimonic views of well-being, and each of the well-being components is seen to have the following three properties: (a) it contributes to well-being, (b) it is pursued for its own sake, and (c) it is defined and measured independently from the other components (Seligman, 2011). Studies show that all five pillars of well-being in the PERMA model are associated with better academic outcomes in students, such as improved college life adjustment, achievement, and overall life satisfaction (Butler & Kern, 2016; DeWitz et al., 2009; Tansey et al., 2018). Additionally, each pillar of PERMA has been shown to be positively associated with physical health, optimal well-being, and life satisfaction and negatively correlated with depression, fatigue, anxiety, perceived stress, loneliness, and negative emotion (Butler & Kern, 2016). At a time of significant stress, promoting the highest human performance and adaptation not only helps with well-being in the midst of the challenge but also can provide a foundation for future potential for optimal well-being (Joseph & Linley, 2008).
Psychological Capital (PsyCap)
PsyCap is a state-like construct that consists of four dimensions: hope (H), self-efficacy (E), resilience (R), and optimism (O), often referred to by the acronym HERO (F. Luthans et al., 2007). F. Luthans et al. (2007) developed PsyCap from research in positive organizational behavior and positive psychology. PsyCap is defined as an
individual’s positive psychological state of development characterized by (1) having confidence (self-efficacy) to take on and put in the necessary effort to succeed at challenging tasks; (2) making a positive attribution (optimism) about succeeding now and in the future; (3) persevering toward goals and, when necessary, redirecting paths to goals (hope) in order to succeed; and (4) when beset by problems and adversity, sustaining and bouncing back and even beyond (resilience) to attain success. (F. Luthans et al., 2015, p. 2)
Over the past decade, PsyCap has been applied to university student development and mental health. There is robust empirical support suggesting that individuals with higher PsyCap have higher levels of performance (job and academic); satisfaction; engagement; attitudinal, behavioral, and relational outcomes; and physical and psychological health and well-being outcomes. Further, they have negative associations with stress, burnout, negative health outcomes, and undesirable behaviors at the individual, team, and organizational levels (Avey, Reichard, et al., 2011; Newman et al., 2014). Researchers have also examined the mediating role of PsyCap in the relationship between positive emotion and academic performance (Carmona-Halty et al., 2019; Hazan Liran & Miller, 2019; B. C. Luthans et al., 2012; K. W. Luthans et al., 2016); relationships and predictions between PsyCap and mental health in university students (Selvaraj & Bhat, 2018); and relationships between PsyCap, well-being, and coping (Rabenu et al., 2017).
Aim of the Study and Research Questions
The aim of the current study was to examine the relationships among well-being in university students before and during the onset of COVID-19 with PsyCap and coping strategies. The following research questions guided our work:
- Is there a significant difference in the well-being of university students prior to the onset of COVID-19 (reported retrospectively) and after the onset of COVID-19?
- What is the predictive relationship of PsyCap on well-being prior to the onset of COVID-19 and after the onset of COVID-19?
- Do coping strategies play a mediating role in the relationship between PsyCap and well-being?
Method
Participants
A total of 806 university students from the United States participated in the study. After cleaning the data, 197 surveys were excluded from the data analyses. Of the final 609 participants, 73.7% (n = 449) identified as female, 22% (n = 139) identified as male, and 4.3% (n = 26) identified as non-binary. The age of participants ranged from 18 to 66 (M = 27.36, SD = 9.9). Regarding race/ethnicity, most participants identified as Caucasian (83.6%, n = 509), while the remaining participants identified as African American (5.3%, n = 32), Hispanic or Latina/o (9.5%, n = 58), American Indian (0.8%, n = 5), Asian (3.6%, n = 22), or Other (2.7%, n = 17). Fifty-four percent of the participants were undergraduate students (n = 326), and the remaining 46% were graduate students (n = 283). The majority of the participants were full time students (82%, n = 498) compared to part-time students (18%, n = 111). Sixty-three percent of the students were employed (n = 384) and the remaining 37% were unemployed (n = 225).
Data Collection Procedures
After a thorough review of the literature, three standardized measures were identified for use in the study along with a brief survey for demographic information. Instruments utilized in the study measured psychological capital (Psychological Capital Questionnaire [PCQ-12]; Avey, Avolio et al., 2011), coping (Brief COPE; Carver, 1997), and well-being (PERMA-Profiler; Butler & Kern, 2016). Data were collected online in May and June 2020 using Qualtrics after obtaining approval from the IRBs of our respective universities. An invitation to participate, which included a link to an informed consent form and the survey, was distributed to all university students at two large U.S. public institutions in the Midwest and the South via campus-wide electronic mailing lists. The survey link was also distributed via a national counselor education listserv, and it was shared on the authors’ social media platforms. Participants were asked to complete the well-being assessment twice—first, by responding as they recalled their well-being prior to COVID-19, and second, by responding as they reflected on their well-being during the pandemic.
Instruments
Demographic Questionnaire
A brief questionnaire was used to capture participant information. The questionnaire included items related to age, gender, race/ethnicity, relationship status, education classification, and employment status.
Psychological Capital Questionnaire – Short Version (PCQ-12)
The PCQ-12 (Avey, Avolio et al., 2011), the shortened version of PCQ-24 (F. Luthans et al., 2007), consists of 12 items that measure four HERO dimensions: hope (four items), self-efficacy (three items), resilience (three items), and optimism (two items), together forming the construct of psychological capital (PsyCap). The PCQ-12 utilizes a 6-point Likert scale with response options ranging from strongly disagree to strongly agree. Cronbach’s alpha coefficients as a measure of internal consistency of the HERO subscales in the current study were high—hope (α = .86), self-efficacy (α = .86), resilience (α = .73), and optimism (α = .83)—consistent with the previous studies.
Brief COPE Questionnaire
Coping strategies were evaluated using the Brief COPE questionnaire (Carver, 1997), which is a short form (28 items) of the original COPE inventory (Carver et al., 1989). The Brief COPE is a multidimensional inventory used to assess the different ways in which people generally respond to stressful situations. This instrument is used widely in studies with university students (e.g., Madhyastha et al., 2014; Miyazaki et al., 2008). Fourteen conceptually differentiable coping strategies are measured by the Brief COPE (Carver, 1997): active coping, planning, using emotional support, using instrumental support, venting, positive reframing, acceptance, denial, self-blame, humor, religion, self-distraction, substance use, and behavioral disengagement. The 14 subscales may be broadly classified into two types of responses—“adaptive” and “problematic” (Carver, 1997, p. 98). Each subscale is measured by two items and is assessed on a 5-point Likert scale. Thus, in general, internal consistency reliability coefficients tend to be relatively smaller (α = .5 to .9).
PERMA-Profiler
The PERMA-Profiler (Butler & Kern, 2016) is a 23-item self-report measure that assesses the level of well-being across five well-being domains (i.e., positive emotion, engagement, relationships, meaning, accomplishment) and additional subscales that measure negative emotion, loneliness, and physical health. Each item is rated on an 11-point scale ranging from never (0) to always (10), or not at all (0) to completely (10). The five pillars of well-being are defined and measured separately but are correlated constructs that together are considered to result in flourishing (Seligman, 2011). A single overall flourishing score provides a global indication of well-being, and at the same time, the domain-specific PERMA scores provide meaningful and practical benefits with regard to the possibility of targeted interventions. The measure demonstrates acceptable reliability, cross-time stability, and evidence for convergent and divergent validity (Butler & Kern, 2016). For the present study, reliability scores were high for four pillars—positive emotion (α = .88), relationships (α = .83), meaning (α = .89), accomplishment (α = .82); high for the subscales of negative emotion (α = .73) and physical health (α = .85); and moderate for the pillar of engagement (α = .65). The overall reliability coefficient of well-being items is very high (α = .94).
Data Analysis Procedure
The data were screened and analyzed using Statistical Package for the Social Sciences (SPSS, v25). Changes in PERMA elements were calculated by subtracting PERMA scores reported retrospectively by participants before the pandemic from scores reported at the time of data collection during COVID-19, and a repeated-measures ANOVA was conducted to examine the difference. Point-biserial correlation and Pearson product moment correlation coefficients were calculated to examine the relationships of demographic variables, PsyCap, and coping strategies with change in PERMA scores. Multivariate multiple regression was carried out to understand the predictive role of PsyCap on PERMA at two time points (before and during COVID-19). Structural equation modeling in Analysis of Moment Structures (AMOS, v23) software was used to test the mediating role of coping strategies on the relationship between PsyCap and change in PERMA scores. Mediation models were carried out with bootstrapping procedure with a 95% confidence interval.
Results
Prior to exploring the role of PsyCap and coping strategies on change in well-being due to COVID-19, an initial analysis was conducted to understand the characteristics and relationships of constructs in the study. Correlation analyses (see Table 1) revealed significant and positive correlations between four PsyCap HERO dimensions (i.e., hope, self-efficacy, resilience, and optimism; Avey, Avolio et al., 2011) and the six PERMA elements (i.e., positive emotion, engagement, relationships, meaning, accomplishment, and physical health; Butler & Kern, 2016). Further, PsyCap HERO dimensions were negatively correlated to negative emotion and loneliness. Age was positively correlated with change in PERMA elements, but not gender. Similarly, approach coping strategies such as active coping, positive reframing, and acceptance (Carver, 1997) were resilient strategies to handle pandemic stress whereas using emotional support and planning showed weaker but significant roles. Similarly, religion also tended to be an adaptive coping strategy during the pandemic. Behavioral disengagement and self-blame (Carver, 1997) were found to be the dominant avoidant coping strategies that were adopted by students, which led to a significant decrease in well-being during the pandemic. Overall, as seen in Table 1, all three variables studied—PsyCap HERO dimensions, eight PERMA elements, and coping strategies—were highly related.
Table 1
Relationship of Demographic Factors, Psychological Capital, and Coping Strategies With Change in PERMA Elements
| Variables |
Mean |
SD |
P |
E |
R |
M |
A |
N |
H |
L |
| Age |
27.36 |
9.91 |
.15** |
.11** |
.14** |
.16** |
.14** |
.01 |
.03 |
-.17** |
| Course Ф |
– |
– |
.19** |
.10* |
.19** |
.16** |
.06 |
-.05 |
.09* |
-.14** |
| Nature of course Ф |
– |
– |
.06 |
.06 |
.12** |
.13** |
.09* |
.03 |
.03 |
-.10** |
| Gender Ф |
– |
– |
-.01 |
-.06 |
.01 |
-.02 |
-.02 |
.02 |
-.02 |
.03 |
| Employment Ф |
– |
– |
-.17** |
-.11** |
-.13** |
-.19** |
-.10* |
.04 |
-.11** |
.11** |
| Self-Efficacy |
13.80 |
3.21 |
.11** |
.13** |
.14** |
.18** |
.16** |
-.05 |
.15** |
-.03 |
| Hope |
18.68 |
3.92 |
.24** |
.26** |
.20** |
.34** |
.40** |
-.17** |
.21** |
-.10* |
| Resilience |
13.41 |
3.08 |
.23** |
.22** |
.20** |
.32** |
.33** |
-.16** |
.15** |
-.13** |
| Optimism |
8.61 |
2.39 |
.21** |
.27** |
.23** |
.32** |
.30** |
-.11** |
.16** |
-.10* |
| Self-Distraction |
6.32 |
1.41 |
-.09* |
.01 |
.03 |
-.02 |
.01 |
.08* |
.02 |
.11** |
| Active Coping |
5.83 |
2.01 |
.24** |
.28** |
.20** |
.28** |
.32** |
-.09* |
.23** |
-.08* |
| Denial |
2.96 |
1.42 |
-.19** |
-.14** |
-.18** |
-.16** |
-.16** |
.24** |
-.16** |
.12** |
| Substance Use |
3.60 |
2.02 |
-.18** |
-.15** |
-.15** |
-.20** |
-.20** |
.11** |
-.09* |
.17** |
| Using Emotional Support |
5.07 |
1.81 |
.12** |
.11** |
.32** |
.18** |
.11** |
.04 |
.10* |
-.02 |
| Using Instrumental Support |
4.35 |
1.70 |
.01 |
.04 |
.20** |
.07 |
.02 |
.10* |
.04 |
.07 |
| Behavioral Disengagement |
3.96 |
2.11 |
-.43** |
-.37** |
-.40** |
-.46** |
-.44** |
.31** |
-.26** |
.27** |
| Venting |
4.58 |
1.54 |
-.24** |
-.16** |
-.08* |
-.17** |
-.16** |
.29** |
-.09* |
.16** |
| Positive Reframing |
5.12 |
1.78 |
.28** |
.27** |
.21** |
.26** |
.25** |
-.15** |
.18** |
-.14** |
| Planning |
5.42 |
1.75 |
.07 |
.12** |
.11** |
.13** |
.11** |
.08 |
.08* |
-.04 |
| Humor |
4.93 |
2.00 |
-.02 |
-.02 |
-.02 |
-.04 |
-.06 |
-.02 |
.02 |
.05 |
| Acceptance |
6.47 |
1.43 |
.33** |
.27** |
.27** |
.34** |
.31** |
-.25** |
.21** |
-.15** |
| Religion |
3.93 |
2.03 |
.21** |
.16** |
.16** |
.22** |
.13** |
-.08 |
.15** |
-.05 |
| Self-Blame |
4.08 |
1.72 |
-.33** |
-.27** |
-.29** |
-.36** |
-.36** |
.29** |
-.22** |
.20** |
Note. P = Positive Emotion, E = Engagement, R = Relationships, M = Meaning, A = Accomplishment, N = Negative Emotion, H = Physical Health, L = Loneliness.
Ф Point-biserial correlation
* p < .05, ** p < .01
Research Question 1
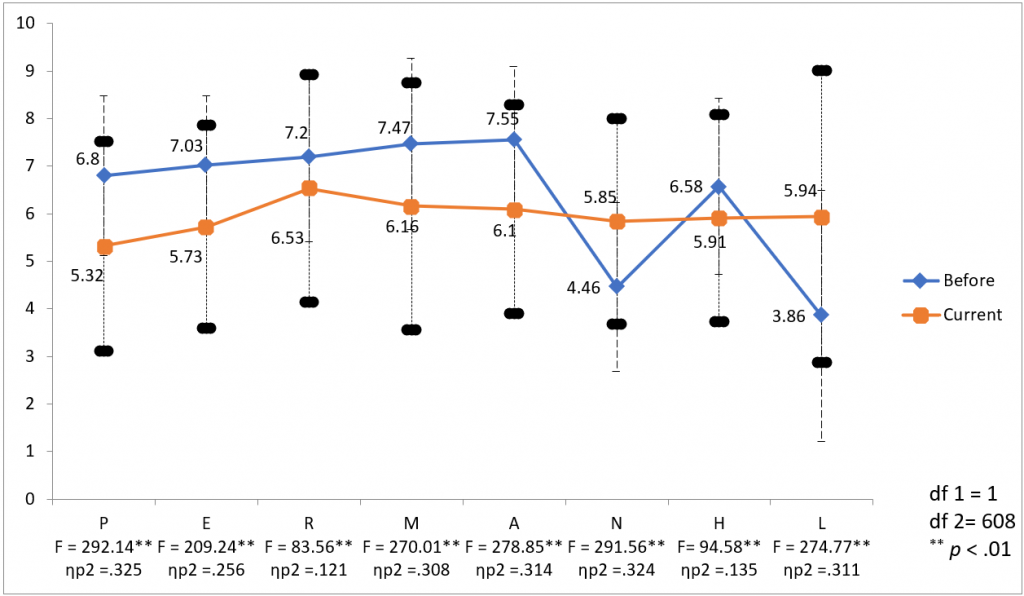
Results of a repeated-measures ANOVA presented in Figure 1 indicate that mean scores of PERMA decreased significantly during COVID-19: λ = .620; F (5,604) = 73.99, p < .001. Partial eta squared was reported as the measure of effect size. The effect size of the change in well-being for PERMA elements was 38%, ηp2 = .380, a high effect size (Cohen, 1988). As expected, negative emotion and loneliness significantly increased during the period of COVID-19, impacting overall well-being in an adverse manner. The average scores of negative emotion and loneliness increased from 4.46 and 3.86 to 5.85 and 5.94, respectively. Physical health significantly reduced from 6.58 to 5.91. The effect size of the change in the scores of individual PERMA elements ranged between 12.1% and 32.5%. Among the PERMA elements, engagement and physical health were least impacted by COVID-19, whereas students’ experiences of positive emotion and negative emotion were the factors that were largely affected.
Figure 1
Changes in the PERMA Prior to the Onset of COVID-19 and After the Onset of COVID-19
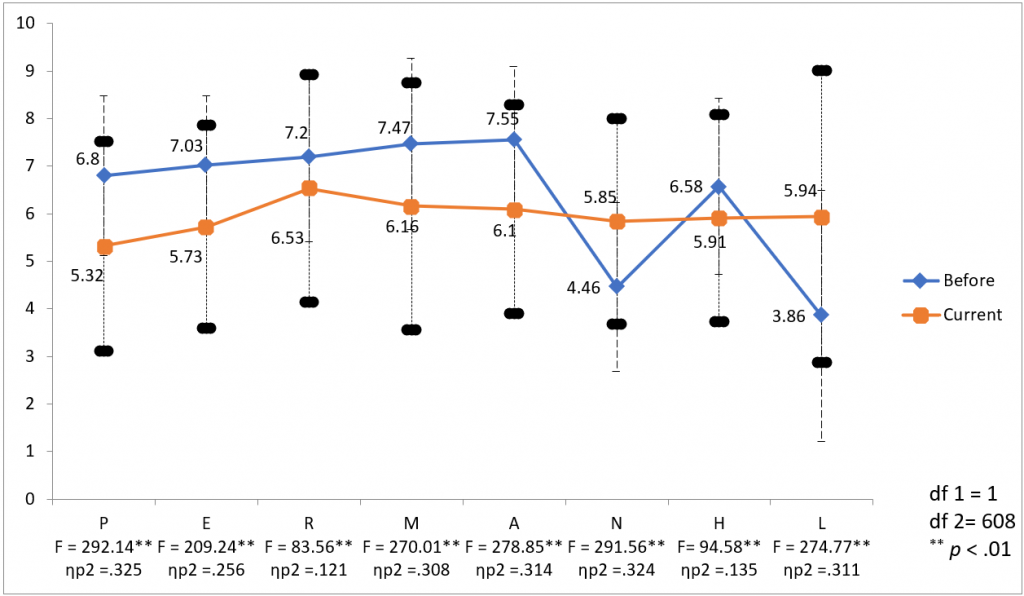
Note. P = Positive Emotion, E = Engagement, R = Relationships, M = Meaning, A = Accomplishment, N = Negative Emotion, H = Physical Health, L = Loneliness.
Research Question 2
The predictive role of PsyCap on well-being at two time points (before and after the onset of COVID-19) was analyzed using multivariate multiple regression (see Table 2). Coefficients of determination for models predicting well-being from PsyCap dimensions ranged from 4% to 28%. Before the onset of COVID-19, 23% of the variance in well-being was explained by the PsyCap dimensions (R2 = .23, p < .001), with self-efficacy and optimism as the most significant predictors of well-being. However, during the pandemic, the covariance of the PsyCap dimensions with well-being increased to 39% (R2 = .39, p < .01). Interestingly, after the onset of the pandemic, the predictor role of certain PsyCap dimensions shifted. For example, optimism became the strongest predictor of overall well-being and hope emerged as a predictor of engagement, meaning, accomplishment, and physical health during the pandemic. The predictive role of hope was negligible before COVID-19. The predictive role of resilience on positive emotion, accomplishment, negative emotion, and loneliness also became significant during COVID-19. Self-efficacy was a consistent predictor of PERMA elements before COVID-19. But during COVID-19, the relevance of self-efficacy in predicting PERMA elements was limited to controllable factors—relationships, meaning, and physical health—and the predictive role of self-efficacy overall was no longer significant (see Table 2).
Table 2
Predicting PERMA Elements From Psychological Capital Prior to the Onset of COVID-19 and After the Onset of COVID-19
|
PERMA |
Self-Efficacy |
Hope |
Resilience |
Optimism |
Adj. R2 |
F |
| Before COVID-19 |
|
|
|
|
|
|
|
Positive Emotion |
.10* |
-.06 |
-.01 |
.44** |
.19 |
37.66** |
| Engagement |
.10* |
.06 |
.01 |
.11* |
.05 |
8.80** |
| Relationships |
.10* |
.07 |
-.09 |
.29** |
.12 |
21.33** |
| Meaning |
.21** |
.06 |
-.03 |
.38** |
.28 |
58.68** |
| Accomplishment |
.24** |
.06 |
.04 |
.13* |
.14 |
25.62** |
| Negative Emotion |
-.13** |
.10 |
-.05 |
-.29** |
.11 |
18.97** |
| Physical Health |
.16** |
.08 |
-.04 |
.12* |
.07 |
12.16** |
| Loneliness |
-.10* |
0 |
-.01 |
-.19** |
.04 |
7.36** |
| Well-Being |
.19** |
.04 |
-.02 |
.35** |
.23 |
45.41** |
| During COVID-19 |
|
|
|
|
|
|
|
Positive Emotion |
.04 |
.09 |
.10* |
.41** |
.30 |
67.05** |
| Engagement |
.02 |
.21** |
.05 |
.26** |
.21 |
40.86** |
| Relationships |
.09* |
.1 |
-.01 |
.33** |
.19 |
36.72** |
| Meaning |
.11** |
.18** |
.09 |
.38** |
.39 |
99.93** |
| Accomplishment |
.05 |
.37** |
.14** |
.17** |
.39 |
96.96** |
| Negative Emotion |
-.03 |
-.07 |
-.13* |
-.23** |
.14 |
26.80** |
| Physical Health |
.16** |
.19** |
-.03 |
.14** |
.15 |
27.25** |
| Loneliness |
-.04 |
.01 |
-.11* |
-.20** |
.08 |
13.34** |
| Well-Being |
.07 |
.22** |
.08 |
.37** |
.39 |
97.48** |
* p < .05, ** p < .01
Research Question 3
Structural equation modeling was used to examine whether coping strategies mediate PsyCap’s effect on well-being. Coping strategies that predicted change in PERMA were used for mediation analysis. Indirect effects describing pathways from PsyCap factors to PERMA factors through identified coping strategies were tested for mediating roles. Results indicated that PsyCap affected well-being both directly and indirectly through coping strategies. Optimism had a significant indirect effect on change in well-being compared to hope and resilience (see Table 3). Among adaptive coping strategies, active coping, positive reframing, and using emotional support mediated the relationship between optimism and overall well-being. Interestingly, using emotional support also showed a similar mediating link between resilience and PERMA, but not for the factors of loneliness and negative emotion. On the other hand, self-blame and behavioral disengagement were two problematic coping strategies that mediated the relationship between optimism and all PERMA elements. Specifically, we found coping through self-blame playing a mediating role between PERMA factors and two of the HERO dimensions—resilience and hope.
Table 3
Indirect Effect of Psychological Capital on PERMA Factors Through Coping Strategies (Mediators)
| PsyCap |
Standardized Beta (ß, Indirect effect) |
| L |
H |
N |
A |
M |
R |
E |
P |
| Active Coping Ф |
|
|
|
|
|
|
|
|
Optimism |
-.016* |
.043** |
-.017* |
.06** |
.052** |
.037** |
.052** |
.044** |
|
Resilience |
-.005 |
.014 |
-.006 |
.02 |
.017 |
.012 |
.017 |
.015 |
|
Hope |
-.007 |
.018 |
-.007 |
.025 |
.022 |
.015 |
.022 |
.018 |
|
Self-Efficacy |
-.009 |
.025 |
-.01 |
.034 |
.03 |
.021 |
.03 |
.025 |
| Positive Reframing Ф |
|
|
|
|
|
|
|
|
|
Optimism |
-.047** |
.06** |
-.05** |
.085** |
.088** |
.07** |
.094** |
.096** |
|
Resilience |
-.005 |
.007 |
-.006 |
.01 |
.01 |
.008 |
.011 |
.011 |
|
Hope |
.003 |
-.003 |
.003 |
-.005 |
-.005 |
-.004 |
-.005 |
-.005 |
|
Self-Efficacy |
-.005 |
.006 |
-.005 |
.009 |
.009 |
.007 |
.01 |
.01 |
| Using Emotional Support Ф |
|
|
|
|
|
|
|
|
Optimism |
-.007 |
.02* |
.012 |
.03* |
.049** |
.086** |
.029* |
.032** |
|
Resilience |
.003 |
-.012 |
-.005 |
-.013* |
-.021* |
-.037* |
-.012* |
-.014* |
|
Hope |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
|
Self-Efficacy |
-.001 |
.006 |
.002 |
.006 |
.01 |
.018 |
.006 |
.007 |
| Self-Blame Ф |
|
|
|
|
|
|
|
|
|
Optimism |
-.038** |
.043** |
-.056** |
.07** |
.07** |
.056** |
.054** |
.065** |
|
Resilience |
-.03** |
.034** |
-.044** |
.055** |
.055** |
.044** |
.042** |
.051** |
|
Hope |
-.023* |
.025* |
-.033* |
.042* |
.041* |
.033* |
.032* |
.038** |
|
Self-Efficacy |
-.005 |
.006 |
-.007 |
.009 |
.009 |
.007 |
.007 |
.008 |
| Behavioral Disengagement Ф |
|
|
|
|
|
|
|
Optimism |
-.07** |
.067** |
-.081** |
.113** |
.118** |
.104** |
.097** |
.112** |
|
Resilience |
-.02 |
.02 |
-.023 |
.033 |
.034 |
.03 |
.028 |
.033 |
|
Hope |
-.032 |
.03 |
-.036 |
.051 |
.053 |
.047 |
.044 |
.051 |
|
Self-Efficacy |
-.009 |
.009 |
-.011 |
.015 |
.016 |
.014 |
.013 |
.015 |
Note. Coping strategies with insignificant mediating role are not included in the table. P = Positive Emotion,
E = Engagement, R = Relationships, M = Meaning, A = Accomplishment, N = Negative Emotion, H = Physical Health,
L = Loneliness.
Ф Mediator coping strategies.
* p < .05, ** p < .01
Discussion
The current study investigated the PERMA model of well-being (Seligman, 2011) with university students before and during the COVID-19 pandemic, as well as the relationships between PsyCap (F. Luthans et al., 2007), coping strategies, and well-being of university students. We examined whether the COVID-19 context shaped the efficacy of particular strategies to promote well-being. Findings are discussed in three areas: reduction in well-being related to COVID-19, shift in predictive roles of PsyCap HERO dimensions, and coping strategies as a mediator.
Reduction in Well-Being Related to COVID-19
Well-being scores across all PERMA elements, including physical health, were lower than those reported retrospectively prior to the pandemic. Such a decline in well-being following a pandemic is consistent with previous occurrences of public health crises or natural disasters (Deaton, 2012). Participants reported higher levels of negative emotion and loneliness after the onset of COVID-19, and a decrease in positive emotion. It is this balance of positive and negative emotions that contributes to life satisfaction (Diener & Larsen, 1993), and our findings support the notion that fostering particular positive psychological states (PsyCap), as well as engaging in related coping strategies, promotes well-being in the context of this large-scale crisis.
Shift in Predictive Roles of PsyCap HERO Dimensions
Consistent with prior research (Avey, Reichard et al., 2011; F. Luthans & Youssef-Morgan, 2017; Youssef-Morgan & Luthans, 2015), we found that PsyCap predicted well-being. PsyCap’s positive psychological resources (HERO dimensions) may enable students to have a “positive appraisal of circumstances” (F. Luthans et al., 2007, p. 550) by providing mechanisms for reframing and reinterpreting potentially negative or neutral situations. There was however an interesting shift in the predictive role of PsyCap dimensions before and after the onset of COVID-19. Prior to COVID-19, self-efficacy and optimism were the two major psychological resources that predicted university student well-being. However, after COVID-19, self-efficacy did not present as a predictor of well-being in this study. Although the reason for this result is uncertain, it is conceivable that attending to an uncertain future (i.e., hope) and recovering from immediate losses (i.e., resilience) became more salient, and one’s self-efficacy in managing normal, everyday challenges receded in importance. Indeed, optimism and hope each uniquely predict a major proportion of variance of the change in well-being and may together help students to face an uncertain future (M. W. Gallagher & Lopez, 2009). Resilience, the ability to recover from setbacks when pathways are blocked (Masten, 2001), had a predictive role on positive emotion and accomplishment in this study.
Coping Strategies as a Mediator
While PsyCap directly relates to well-being and coping strategies relate to well-being, our findings indicated that coping strategies also played a significant mediating role in the relationship between PsyCap and well-being. Specifically, adaptive coping strategies played a significant role in enhancing the positive effects of PsyCap on well-being. Adaptive coping strategies—such as active coping, acceptance, using emotional support, and positive reframing—were found to better aid in predicting well-being. In this study, accepting the realities, using alternative affirmative explanations, seeking social support for meeting emotional needs, and engaging in active problem-focused coping behaviors seem to be the most helpful ways to counter the negative effects of the pandemic on well-being. Conversely, when individuals employed problematic coping strategies such as behavioral disengagement and self-blame (Carver, 1997), the negative impacts were much stronger than the positive effect of adaptive coping strategies.
Implications for Counselors
Given findings of the relationship between PsyCap and well-being in the current study, as well as in prior research (F. Luthans et al., 2006; F. Luthans et al., 2015; McGonigal, 2015), counselors may wish to focus on developing PsyCap to help university students flourish both during the pandemic and in a post-pandemic world. Two significant challenges to counseling professionals on college campuses are the lack of resources to adequately respond to mental health concerns among students and the stigma associated with accessing services (R. P. Gallagher, 2014; Michaels et al., 2015). Thus, efficient interventions that are not likely to trigger stigma responses are helpful in this context. Several researchers have found that relatively short training in PsyCap interventions, including web-based platforms (Dello Russo & Stoykova, 2015; Demerouti et al., 2011; Ertosun et al., 2015; B. C. Luthans et al., 2012, 2013) have been effective. Recently, the use of positive psychology smartphone apps such as Happify and resilience-building video games such as SuperBetter have been suggested and tested as motivational tools, especially with younger adults, to foster sustained and continued engagement with PsyCap development (F. Luthans & Youssef-Morgan, 2017; McGonigal, 2015). These are potential areas of practice for college counselors and counselors serving university students.
Interventions that are described as well-being approaches rather than those that highlight pathologies are less stigmatizing (Hunt & Eisenberg, 2010; Umucu et al., 2020) than traditional deficit-based therapeutic approaches. There are a number of research-based approaches offered in the field of positive psychology to guide mental health professionals to facilitate development of PsyCap and other important well-being correlates. These include approaches to building positive emotions (Fredrickson, 2009); coping strategies, which were found in this study to boost well-being (Jardin et al., 2018; Lyubomirsky, 2008); and effective goal pursuits (F. Luthans & Youssef-Morgan, 2017). One of the distinguishing characteristics of PsyCap is its malleability and openness to change and development (Avey, Reichard et al., 2011; F. Luthans et al., 2006). Thus, there is potential for counselors to develop well-being promotion initiatives for students on university campuses targeting PsyCap and its constituting positive psychological HERO resources with the end goal of strengthening well-being (Avey, Avolio et al., 2011; F. Luthans et al., 2015; F. Luthans & Youssef-Morgan, 2017).
Strategies and programming to develop wellness can be delivered in one-on-one sessions with students, as well as in group settings, and may have either a prevention or intervention focus. They could also be adapted to provide services online. A variety of free online assessments are also available for use by counselors, including tools that measure well-being, positive psychological resources, and character strengths of university students in addition to existing assessment batteries. By administering the PERMA-Profiler to university students, counselors could identify and understand what dimension of well-being should be further developed (Umucu et al., 2020). With each PERMA element individually rendering to flourishing mental health, specific targeted positive psychology interventions might be offered as domain-specific interventions.
Counselors could help university students benefit from attending to, appreciating, and attaining life’s positives (Sin & Lyubomirsky, 2009) and from enhancing the strength and frequency of employing positive coping strategies through targeted psychoeducational or counseling interventions. Teaching university students active coping strategies, such as positive reframing and how to access emotional support, could help them cope with adverse situations. Sheldon and Lyubomirsky (2006) indicated that practicing gratitude helps people to cope with negative situations because it enables them to view such situations through a more positive lens. Among university students, healthy coping strategies could buffer them from some of the unique challenges associated with acculturating and adjusting to college experiences (Jardin et al., 2018), especially during a pandemic.
Limitations and Directions for Future Research
The findings of this study should be considered in light of certain limitations. Foremost among these is that data were collected using self-report measures, and in the case of the PERMA-Profiler, data were collected using the retrospective recall of participants as they considered their well-being prior to the onset of COVID-19. Retrospective recall may be inaccurate (Gilbert, 2007) with participants under- or overestimating their well-being. Given the ongoing repercussions of the pandemic, we recommend continued and longitudinal studies on well-being, coping strategies, and PsyCap. Additionally, data collection methods and sample demographics would likely limit generalizability. We utilized a correlational cross-sectional study design; therefore, although PsyCap was predictive of change in well-being before and during COVID-19, neither causation nor directionality can be assumed. In future, researchers may wish to investigate whether PsyCap predicts longitudinal changes in well-being in the COVID-19 context.
A further consideration is that the PERMA model of well-being (Seligman, 2011) may not be associated with similar outcomes for people of other cultures and backgrounds during COVID-19. Future researchers examining well-being in university students in different regions of the country or internationally may wish to further investigate the applicability of the PERMA model as a measure of university students’ well-being during the pandemic. Finally, the moderate Cronbach’s alpha reliability scores of < .70 (Field, 2013) for the subscales of the Brief COPE inventory and the engagement subscale of the PERMA-Profiler are of concern, which has also been expressed by prior researchers (Goodman et al., 2018; Iasiello et al., 2017). Future researchers should consider issues of internal consistency as they choose scales and interpret results.
Conclusion
To conclude, the present findings contribute to existing literature on PsyCap and well-being, using the PERMA model of well-being (Seligman, 2011) among university students in the United States in the context of COVID-19. Key findings are that the optimism, hope, and resilience dimensions of PsyCap are significant predictors of well-being, explaining a large amount of variance, with adaptive coping being conducive to flourishing. Further, the present findings highlight the importance of examining the relationships between each element of well-being and with each HERO dimension. Both individual counseling and group-based programming focused on PsyCap and positive coping strategies could support the well-being of university students as they experience ongoing stressors related to the pandemic or as they face other setbacks.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Avey, J. B., Avolio, B. J., & Luthans, F. (2011). Experimentally analyzing the impact of leader positivity on follower positivity and performance. The Leadership Quarterly, 22(2), 282–294.
https://doi.org/10.1016/j.leaqua.2011.02.004
Avey, J. B., Reichard, R. J., Luthans, F., & Mhatre, K. H. (2011). Meta-analysis of the impact of positive psychological capital on employee attitudes, behaviors, and performance. Human Resource Development Quarterly, 22(2), 127–152. https://doi.org/10.1002/hrdq.20070
Billings, A. G., & Moos, R. H. (1984). Coping, stress, and social resources among adults with unipolar depression. Journal of Personality and Social Psychology, 46(4), 877–891. https://doi.org/10.1037//0022-3514.46.4.877
Butler, J., & Kern, M. L. (2016). The PERMA-Profiler: A brief multidimensional measure of flourishing. International Journal of Wellbeing, 6(3), 1–48. https://doi.org/10.5502/ijw.v6i3.526
Carmona-Halty, M., Schaufeli, W. B., & Salanova, M. (2019). Good relationships, good performance: The mediating role of psychological capital: A three-wave study among students. Frontiers in Psychology, 10, 306. https://doi.org/10.3389/fpsyg.2019.00306
Carver, C. S. (1997). You want to measure coping but your protocol’s too long: Consider the Brief COPE. International Journal of Behavioral Medicine, 4(1), 92–100. https://doi.org/10.1207/s15327558ijbm0401_6
Carver, C. S., & Connor-Smith, J. (2010). Personality and coping. Annual Review of Psychology, 61, 679–704.
https://doi.org/10.1146/annurev.psych.093008.100352
Carver, C. S., Scheier, M. F., & Weintraub, J. K. (1989). Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology, 56(2), 267–283. https://doi.org/10.1037//0022-3514.56.2.267
Cohen, J. (1988). Statistical power analysis for the behavioral sciences. Routledge Academic.
de la Fuente, J., Lahortiga-Ramos, F., Laspra-Solis, C., Maestro-Martin, C., Alustiza, I., Auba, E., & Martin-Lanas, R. (2020). A structural equation model of achievement emotions, coping strategies and engagement-burnout in undergraduate students: A possible underlying mechanism in facets of perfectionism. International Journal of Environmental Research and Public Health, 17(6). https://doi.org/10.3390/ijerph17062106
Deaton, A. (2012). The financial crisis and the well-being of Americans: 2011 OEP Hicks lecture. Oxford Economic Papers, 64(1), 1–26. https://doi.org/10.1093/oep/gpr051
Dello Russo, S., & Stoykova, P. (2015). Psychological capital intervention (PCI): A replication and extension. Human Resource Development Quarterly, 26(3), 329–347. https://doi.org/10.1002/hrdq.21212
Demerouti, E., van Eeuwijk, E., Snelder, M., & Wild, U. (2011). Assessing the effects of a “personal effectiveness” training on psychological capital, assertiveness and self-awareness using self-other agreement. The Career Development International, 16(1), 60–81. https://doi.org/10.1108/13620431111107810
DeWitz, S. J., Woolsey, M. L., & Walsh, W. B. (2009). College student retention: An exploration of the relationship between self-efficacy beliefs and purpose in life among university students. Journal of College Student Development, 50(1), 19–34. https://doi.org/10.1353/csd.0.0049
Diener, E., & Larsen, R. J. (1993). The experience of emotional wellbeing. In M. Lewis & J. M. Haviland (Eds.), Handbook of emotions (pp. 405–415). Guilford.
Ertosun, Ö. G., Erdil, O., Deniz, N., & Alpkan, L. (2015). Positive psychological capital development: A field study by the Solomon four group design. International Business Research, 8(10), 102–111.
https://doi.org/10.5539/ibr.v8n10p102
Field, A. (2013). Discovering statistics using IBM SPSS statistics. SAGE.
Finkelstein-Fox, L., & Park, C. L. (2019). Control-coping goodness-of-fit and chronic illness: A systematic review of the literature. Health Psychology Review, 13(2), 137–162. https://doi.org/10.1080/17437199.2018.1560229
Flatt, A. K. (2013). A suffering generation: Six factors contributing to the mental health crisis in North American higher education. College Quarterly, 16(1).
Fredrickson, B. L. (2009). Positivity: Groundbreaking research reveals how to embrace the hidden strength of positive emotions, overcome negativity, and thrive. Crown.
Gallagher, M. W., & Lopez, S. J. (2009). Positive expectancies and mental health: Identifying the unique contributions of hope and optimism. The Journal of Positive Psychology, 4(6), 548–556.
https://doi.org/10.1080/17439760903157166
Gallagher, R. P. (2014). National Survey of College Counseling Centers 2014. International Association of Counseling Services, Inc. http://d-scholarship.pitt.edu/28178
Gilbert, D. (2007). Stumbling on happiness. Random House.
Goodman, F. R., Disabato, D. J., Kashdan, T. B., & Kauffman, S. B. (2018). Measuring well-being: A comparison of subjective well-being and PERMA. The Journal of Positive Psychology, 13(4), 321–332.
https://doi.org/10.1080/17439760.2017.1388434
Hazan Liran, B., & Miller, P. (2019). The role of psychological capital in academic adjustment among university students. Journal of Happiness Studies: An Interdisciplinary Forum on Subjective Well-Being, 20(1), 51–65. https://doi.org/10.1007/s10902-017-9933-3
Hoover, E. (2020). Distanced learning. Chronicle of Higher Education. https://www.chronicle.com/article/distanced-learning
Huckins, J. F., DaSilva, A. W., Wang, W., Hedlund, E., Rogers, C., Nepal, S. K., Wu, J., Obuchi, M., Murphy, E. I.,
Meyer, M. L., Wagner, D. D., Holtzheimer, P. E., & Campbell, A. T. (2020). Mental health and behavior of college students during the early phases of the COVID-19 pandemic: Longitudinal smartphone and ecological momentary assessment study. Journal of Medical Internet Research, 22(6), e20185.
https://doi.org/10.2196/20185
Hunt, J., & Eisenberg, D. (2010). Mental health problems and help-seeking behavior among college students. Journal of Adolescent Health, 46(1), 3–10. https://doi.org/10.1016/j.jadohealth.2009.08.008
Iasiello, M., Bartholomaeus, J., Jarden, A., & Kelly, G. (2017). Measuring PERMA+ in South Australia, the State of Wellbeing: A comparison with national and international norms. Journal of Positive Psychology and Wellbeing, 1(2), 53–72.
Jardin, C., Mayorga, N. A., Bakhshaie, J., Garey, L., Viana, A. G., Sharp, C., Cardoso, J. B., & Zvolensky, M. J.
(2018). Clarifying the relation of acculturative stress and anxiety/depressive symptoms: The role of anxiety sensitivity among Hispanic college students. Cultural Diversity and Ethnic Minority Psychology, 24(2), 221–230. https://doi.org/10.1037/cdp0000175
Johnson, R. (2020). Students stressed out due to coronavirus, new survey finds. Best Colleges (April 20, 2020).
https://www.bestcolleges.com/blog/coronavirus-survey
Joseph, S., & Linley, P. A. (Eds.). (2008). Trauma, recovery, and growth: Positive psychological perspectives on posttraumatic stress. Wiley.
Keyes, C. L. M. (2002). The mental health continuum: From languishing to flourishing in life. Journal of Health and Social Behavior, 43(2), 207–222. https://doi.org/10.2307/3090197
Klussman, K., Nichols, A. L., Langer, J., & Curtin, N. (2020). Connection and disconnection as predictors of mental health and wellbeing. International Journal of Wellbeing, 10(2). https://doi.org/10.5502/ijw.v10i2.855
Lipson, S. K., Lattie, E. G., & Eisenberg, D. (2019). Increased rates of mental health service utilization by U.S. college students: 10-year population-level trends (2007–2017). Psychiatric Services, 70(1), 60–63.
https://doi.org/10.1176/appi.ps.201800332
Luthans, B. C., Luthans, K. W., & Avey, J. B. (2013). Building the leaders of tomorrow: The development of academic psychological capital. Journal of Leadership & Organizational Studies, 21(2), 191–199.
https://doi.org/10.1177/1548051813517003
Luthans, B. C., Luthans, K. W., & Jensen, S. M. (2012). The impact of business school students’ psychological capital on academic performance. The Journal of Education for Business, 87(5), 253–259.
https://doi.org/10.1080/08832323.2011.609844
Luthans, F., Avey, J. B., Avolio, B. J., Norman, S. M., & Combs, G. M. (2006). Psychological capital development: Toward a micro-intervention. Journal of Organizational Behavior, 27(3), 387–393.
https://doi.org/10.1002/job.373
Luthans, F., Avolio, B. J., Avey, J. B., & Norman, S. M. (2007). Positive psychological capital: Measurement and relationship with performance and satisfaction. Personnel Psychology, 60(3), 541–572.
https://doi.org/10.1111/j.1744-6570.2007.00083.x
Luthans, F., & Youssef-Morgan, C. M. (2017). Psychological capital: An evidence-based positive approach. Annual Review of Organizational Psychology and Organizational Behavior, 4, 339–366.
Luthans, F., Youssef-Morgan, C. M., & Avolio, B. J. (2015). Psychological capital and beyond. Oxford University Press.
Luthans, K. W., Luthans, B. C., & Palmer, N. F. (2016). A positive approach to management education: The relationship between academic PsyCap and student engagement. Journal of Management Development, 35(9), 1098–1118. https://doi.org/10.1108/JMD-06-2015-0091
Lyubomirsky, S. (2008). The how of happiness: A scientific approach to getting the life you want. Penguin.
Madhyastha, S., Latha, K. S., & Kamath, A. (2014). Stress, coping and gender differences in third year medical students. Journal of Health Management, 16(2), 315–326. https://doi.org/10.1177/0972063414526124
Masten, A. S. (2001). Ordinary magic: Resilience processes in development. American Psychologist, 56(3), 227–238. https://doi.org/10.1037//0003-066x.56.3.227
McGonigal, J. (2015). SuperBetter: A revolutionary approach to getting stronger, happier, braver and more resilient. Penguin Press.
Michaels, P. J., Corrigan, P. W., Kanodia, N., Buchholz, B., & Abelson, S. (2015). Mental health priorities: Stigma elimination and community advocacy in college settings. Journal of College Student Development, 56(8), 872–875. https://doi.org/10.1353/csd.2015.0088
Miyazaki, Y., Bodenhorn, N., Zalaquett, C., & Ng, K.-M. (2008). Factorial structure of Brief COPE for international students attending U.S. colleges. College Student Journal, 42(3), 795-806.
Newman, A., Ucbasaran, D., Zhu, F., & Hirst, G. (2014). Psychological capital: A review and synthesis. Journal of Organizational Behavior, 35(S1), S120–S138. https://doi.org/10.1002/job.1916
Primack, B. A., Shensa, A., Escobar-Viera, C. G., Barrett, E. L., Sidani, J. E, Colditz, J. B., & Everette James, A. (2017). Use of multiple social media platforms and symptoms of depression and anxiety: A nationally-representative study among U.S. young adults. Computer Human Behavior, 69, 1–9.
https://doi.org/10.1016/j.chb.2016.11.013
Rabenu, E., Yaniv, E., & Elizur, D. (2017). The relationship between psychological capital, coping with stress, well-being, and performance. Current Psychology, 36(4), 875–887. https://doi.org/10.1007/s12144-016-9477-4
Ray, J. (2019). Americans’ stress, worry and anger intensified in 2018. Gallup. https://news.gallup.com/poll/249098/americans-stress-worry-anger-intensified-2018.aspx
Seligman, M. E. P. (2002). Authentic happiness: Using the new positive psychology to realize your potential for lasting fulfillment. Simon & Schuster.
Seligman, M. E. P. (2011). Flourish: A visionary new understanding of happiness and well-being. Simon & Schuster.
Selvaraj, P. R., & Bhat, C. S. (2018). Predicting the mental health of college students with psychological capital. Journal of Mental Health, 27(3), 279–287. https://doi.org/10.1080/09638237.2018.1469738
Sheldon, K. M., & Lyubomirsky, S. (2006). How to increase and sustain positive emotion: The effects of expressing gratitude and visualizing best possible selves. The Journal of Positive Psychology, 1(2), 73–82. https://doi.org/10.1080/17439760500510676
Sin, N. L., & Lyubomirsky, S. (2009). Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: A practice-friendly meta-analysis. Journal of Clinical Psychology, 65(5), 467–487. https://doi.org/10.1002/jclp.20593
Tansey, T. N., Smedema, S., Umucu, E., Iwanaga, K., Wu, J.-R., Cardoso, E. D. S., & Strauser, D. (2018). Assessing college life adjustment of students with disabilities: Application of the PERMA framework. Rehabilitation Counseling Bulletin, 61(3), 131–142. https://doi.org/10.1177/0034355217702136
Twenge, J. M. (2017). iGen: Why today’s super-connected kids are growing up less rebellious, more tolerant, less happy—and completely unprepared for adulthood—and what that means for the rest of us. Atria Books.
Umucu, E., Wu, J.-R., Sanchez, J., Brooks, J. M., Chiu, C.-Y., Tu, W.-M., & Chan, F. (2020). Psychometric validation of the PERMA-profiler as a well-being measure for student veterans. Journal of American College Health, 68(3), 271–277. https://doi.org/10.1080/07448481.2018.1546182
Wan, W. (2020). The coronavirus pandemic is pushing America into a mental health crisis. Washington Post. https://www.washingtonpost.com/health/2020/05/04/mental-health-coronavirus
Witters, D., & Harter, J. (2020). Worry and stress fuel record drop in U.S. life satisfaction. Gallup.
https://news.gallup.com/poll/310250/worry-stress-fuel-record-drop-life-satisfaction.aspx
Youssef-Morgan, C. M., & Luthans, F. (2015). Psychological capital and well-being. Stress Health, 31(3), 180–188. https://doi.org/10.1002/smi.2623
Priscilla Rose Prasath, PhD, MBA, LPC (TX), is an assistant professor at the University of Texas at San Antonio. Peter C. Mather, PhD, is a professor and department chair at Ohio University. Christine Suniti Bhat, PhD, LPC, LSC (OH), is a professor and the interim director of the George E. Hill Center for Counseling & Research at Ohio University. Justine K. James, PhD, is an assistant professor at University College in Kerala, India. Correspondence may be addressed to Priscilla Rose Prasath, 501 W. Cesar E. Chavez Boulevard, Durango Building, University of Texas at San Antonio, San Antonio, TX 78207, priscilla.prasath@utsa.edu.
Feb 26, 2021 | Volume 11 - Issue 1
Christian D. Chan, Stacey Diane Arañez Litam
The emergence and global spread of COVID-19 precipitated a massive public health crisis combined with multiple incidents of racial discrimination and violence toward Asian American and Pacific Islander (AAPI) communities. Although East Asian communities are more frequently targeted for instances of pandemic-related racial discrimination, multiple disparities converge upon Filipino communities that affect their access to mental health care in light of COVID-19. This article empowers professional counselors to support the Filipino community by addressing three main areas: (a) describing how COVID-19 contributes to racial microaggressions and institutional racism toward Filipino communities; (b) underscoring how COVID-19 exacerbates exposure to stressors and disparities that influence help-seeking behaviors and utilization of counseling among Filipinos; and (c) outlining how professional counselors can promote racial socialization, outreach, and mental health equity with Filipino communities to mitigate the effects of COVID-19.
Keywords: Asian American, Filipino, mental health equity, COVID-19, discrimination
Asian Americans represent the fastest-growing ethnic group in the United States (Budiman et al., 2019). Following the global outbreak of COVID-19, many Asian Americans and Pacific Islanders (AAPIs) have experienced a substantial increase in race-based hate incidents. These incidents of racial discrimination have included verbal harassment, physical attacks, and discrimination against Asian-owned businesses (Jeung & Nham, 2020), which multiply the harmful effects on psychological well-being and life satisfaction among AAPIs (Litam & Oh, 2020). According to Pew Research Center trends (Ruiz et al., 2020), about three in 10 Asian adults reported they experienced racial discrimination since the outbreak began. Proliferation of anti-Chinese and xenophobic hate speech from political leaders, news outlets, and social media, which touted COVID-19 as the “Chinese virus,” further exacerbate instances of race-based discrimination (U.S. Department of Justice, 2020) and echo the Yellow Peril discourse from the late 19th century (Litam, 2020; Poon, 2020).
Although the community is often aggregated, Asian Americans are not a monolithic entity (Choi et al., 2017; Jones-Smith, 2019; Sue et al., 2019). The term Asian American encompasses over 40 distinct subgroups, each with distinct languages, cultures, beliefs, and migration histories (Pew Research Center, 2013; Sue et al., 2019). It is no surprise, therefore, that specific ethnic subgroups would be more affected by the pandemic than others. For example, instances of COVID-19–related racial discrimination disproportionately affect East Asian communities, specifically Chinese migrants and Chinese Americans. An analysis of nearly 1,500 reports of anti-Asian hate incidents indicated approximately 40% of Chinese individuals reported experiences of discrimination as compared to 16% of Korean individuals and 5.5% of Filipinos (Jeung & Nham, 2020). Although Chinese individuals disproportionately experience overt forms of COVID-19–related discrimination, Filipino migrants and Filipino Americans are not immune to the deleterious effects of the pandemic.
With over 4 million people of Filipino descent residing in the United States (Asian Journal Press, 2018), it is of paramount importance for professional counselors to recognize how the Filipino American experience may compound with additional COVID-19 exposure and related stressors in unique ways that distinctively impact their experiences of stress and mental health. The current article identifies how the racialized climate of COVID-19 influences Filipino-specific microaggressions and the presence of systemic and institutional racism toward Filipino communities. The ways in which COVID-19 exacerbates existing racial disparities across social determinants of health, help-seeking behaviors, and utilization of counseling services are described. Finally, the implications for counseling practice and advocacy are presented in ways that can embolden professional counselors to promote racial socialization, outreach, and health equity with Filipino communities to mitigate the effects of COVID-19.
Health Disparities Among Filipino Americans
The unprecedented emergence of COVID-19 has affected the global community. As of January 5, 2021, a total of 21,382,296 cases were confirmed and 362,972 deaths had been reported in the United States (Worldometer, n.d.). Although information about how racial and ethnic groups are affected by the pandemic is forthcoming, emerging data suggests that specific groups are disproportionately affected. Professional counselors must be prepared to support communities that may be more vulnerable to pandemic-related stress and face challenges related to medical and mental health care access because of intersecting marginalized identities, such as age, race, ethnicity, gender identity, sexual identity, social class, and migration history (Chan & Henesy, 2018; Chan et al., 2019; Litam & Hipolito-Delgado, 2021). For example, the AAPI population may be especially in need of mental health support because of ongoing xenophobic sentiments from political leaders that combine with intergenerational trauma, racial discrimination, and racial trauma (Litam, 2020).
Underutilization of Mental Health Services
Compared to other Asian American subgroups, Filipinos are the least likely to seek professional mental health services. In a study of 2,230 Filipinos, approximately 73% had never used any type of mental health service and only 17% sought help from friends, community members, peers, and religious or spiritual leaders (Gong et al., 2003). Since the Gong et al. (2003) study, a multitude of researchers have documented the persistent disparity of mental health usage and unfavorable attitudes toward professional help-seeking among Filipinos (David & Nadal, 2013; David et al., 2019; Nadal, 2021; Tuazon et al., 2019), despite high rates of psychological distress (Martinez et al., 2020).
The experiences of Filipino communities uniquely influence aspects of mental health and wellness. Compared to other subgroups of Asian Americans, Filipino Americans with post-traumatic stress experiences tend to exhibit poorer health (Kim et al., 2012; Klest et al., 2013), and report higher rates of racial discrimination (Li, 2014). As a subgroup, Filipino Americans present to mental health counseling settings with high rates of depression, suicide, HIV, unintended pregnancy, eating disorders, and drug use (David et al., 2017; Klest et al., 2013; Nadal, 2000, 2021). Compared to other Asian subgroups, Filipinos may experience lower social class and employment statuses, which may increase the prevalence of mental health issues (Araneta, 1993). Among Filipinos, intergenerational cultural conflicts and experiences of racial discrimination were identified as significant contributors to depression and suicidal ideation (Choi et al., 2020). The underutilization of professional mental health services and help-seeking among Filipino communities is unusual because of their familiarity with Western notions, systems, and institutions, which surface as traits that are typically associated with mental health help-seeking within the broader AAPI community (Abe-Kim et al., 2002, 2004; Shea & Yeh, 2008).
Distinct Experiences of Oppression
Aspects of Filipino history are characterized by colonization, oppression, and intergenerational racial trauma (David & Nadal, 2013) and have been rewritten by White voices in ways that communicate how America saved the Philippines from Spanish rule through colonization (Ocampo, 2016). These sentiments remain deeply entrenched within the mindset of many Filipinos in the form of colonial mentality (David & Nadal, 2013; Tuazon et al., 2019). Colonial mentality refers to the socialized and oppressive mindset characterized by beliefs about the superiority of American values and denigration of Filipino culture and self (David & Okazaki, 2006a, 2006b). Colonial mentality is the insidious aftermath galvanized through years of intergenerational trauma, U.S. occupation, and socialization under White supremacy (David et al., 2017). Professional counselors must recognize the interplay between colonial mentality and the mental health and well-being of Filipino clients to best support this unique population.
The internalized experiences of oppression perpetuate the denigration of Filipinos by Filipinos as a result of the internalized anti-Black sentiments and notions of White supremacy that remain at the forefront of American history (Ocampo, 2016). The Filipino experience is one that is characterized by forms of discrimination by individuals who reside both within and outside of the Filipino community (Nadal, 2021). For example, Filipinos who espouse a colonial mentality disparage those with Indigenous Filipino traits (i.e., dark skin and textured hair) as unattractive, undesirable, and worthy of shame (Angan, 2013; David, 2020; Mendoza, 2014). Filipinos also experience a sense of otherness within the AAPI community and from other communities of color because their history, culture, and phenotype combine in ways that “break the rules of race” (Ocampo, 2016, p. 13). Although Filipinos are sometimes confused with individuals from Chinese communities, they are not typically perceived as Asian or East Asian (Lee, 2020) and are often mistaken for Black or Latinx (Ocampo, 2016; Sanchez & Gaw, 2007). These pervasive experiences render the Filipino identity invisible (Nadal, 2021). Ultimately, Filipinos remain among the most mislabeled and culturally marginalized of Asian Americans (Sanchez & Gaw, 2007). Professional counselors who work with Filipino clients must obtain a deeper understanding of how these unique experiences of invisibility and colonial mentality continue to affect the minds and the worldviews of Filipinos and Filipino Americans.
Risk Factors for COVID-19 Exposure
The burgeoning rate of COVID-19 cases has devastated hospitals and medical settings. The overwhelming strain faced by medical communities uniquely affects Filipino migrants and Filipino Americans who are overrepresented in health care and disproportionately at risk of COVID-19 exposure (National Nurses United, 2020). The overrepresentation of Filipinos in health care, particularly within the nursing profession, is directly tied to the history of U.S. colonization. Following the U.S. occupation of the Philippines from 1899 to 1946, the Filipino zeitgeist became imbued with profound cultural notions of American superiority and affinity for Westernized attitudes, behaviors, and values (David et al., 2017). For example, the introduction of the American nursing curricula by U.S. Army personnel during the Spanish-American war (McFarling, 2020) instilled pervasive cultural influences that positioned the nursing profession as a viable strategy to escape political and economic instability in pursuit of a better life in the United States (Choy, 2003). These cultural notions have culminated to make the Philippines the leading exporter of nurses in the world (Choy, 2003; Espiritu, 2016). Of the immigrant health care workers across the United States, an estimated 28% of registered nurses, 4% of physicians and surgeons, and 12% of home health aides are Filipinos (Batalova, 2020). About 150,000 registered nurses in the United States are Filipino, equating to about 4% of the overall nursing population (McFarling, 2020; National Nurses United, 2020). According to the National Nurses United (2020) report, 31.5% of deaths among registered nurses and 54% of deaths among registered nurses of color were Filipinos. Based on these statistics, Filipinos face disproportionate exposure to pandemic-related stressors and death that may increase the risk for mental health issues.
Individuals of Filipino descent may also face significant COVID-19–related challenges, as they are predisposed to several health conditions that have been linked with poorer treatment prognosis and outcomes (Ghimire et al., 2018; Maxwell et al., 2012). Compared to other racial and ethnic subgroups, Filipinos residing in California had higher rates of type II diabetes, asthma, and cardiovascular disease (Adia et al., 2020). High rates of hypertension, cholesterol, and diabetes were also noted in studies of Filipino Americans residing in the greater Philadelphia region (Bhimla et al., 2017) and in Las Vegas, Nevada (Ghimire et al., 2018). One study of Filipinos residing in the New York metropolitan area indicated rates of obesity significantly increased the longer Filipino immigrants resided in the United States (Afable et al., 2016). The Centers for Disease Control and Prevention (2021) associated each of these underlying medical conditions with a greater likelihood for hospitalization, intensive care, use of a ventilator, and increased mortality. Filipino Americans also tend to report lower social class and employment statuses as compared to other Asian Americans, which may contribute to higher rates of mental health issues and create barriers to health care access (Adia et al., 2020; Sue et al., 2019).
Cultural Barriers to Professional Mental Health Services
Filipinos face culturally rooted barriers to seeking professional mental health services that may include fears related to reputation, endorsement of fatalistic attitudes, religiousness, communication barriers, and lack of culturally competent services (Gong et al., 2003; Nadal, 2021; Pacquiao, 2004). The presence of mental illness stigma is also deeply entrenched within Filipino communities (Appel et al., 2011; Augsberger et al., 2015; Tuazon et al., 2019). In many traditional Filipino families, mental illness is mitigated by addressing personal and emotional problems with family and close friends, and through faith in God (David & Nadal, 2013). Rejection of mental illness is based on the belief that individuals who receive counseling or therapy are crazy, dangerous, and unpredictable (de Torres, 2002; Nadal, 2021).
Connection and Kinship
Given the central prominence of family, it is no surprise that Filipino individuals’ mental health begins to suffer when their connection to community and kinship is compromised. Although relatively few studies on Filipino mental health exist, Filipinos and Filipino Americans consistently report family-related issues as among the most stressful. In one study of Filipino and Korean families in the Midwest (N = 1,574), the presence of intergenerational family conflict significantly contributed to an increase in depressive symptoms and suicidal ideation (Choi et al., 2020). In another study of Filipino Americans, quality time with family, friends, and community was identified as an important factor in mitigating the effects of depression (Edman & Johnson, 1999). The centralized role of Filipino families uniquely combines with a group mentality in ways that may additionally hinder rates of professional help-seeking.
Hiya and Amor Propio
Notions of hiya and amor propio each represent culturally specific barriers to seeking mental health care. According to Gong and colleagues (2003), hiya and amor propio are related to the East Asian notions of saving face. While hiya emphasizes the more extensive experience of shame that arises from fear of losing face, amor propio is associated with concepts of self-esteem linked to the desire to maintain social acceptance. A loss of amor propio would result in a loss of face and may compromise the cherished position of community acceptance (Gong et al., 2003). Filipino Americans may thus avoid seeking professional mental health services because of combined feelings of shame (hiya) linked to beliefs that one has failed or is unable to overcome their problems independently, and fears of losing social positioning within one’s community (amor propio). To experience amor propio would put a Filipino—or worse, their family—at risk for tsismis, or gossip. Indeed, avoiding behaviors that may lead others within the Filipino community to engage in tsismis about the client or their family is a significant factor that guides choices and behaviors. Engaging in behaviors that result in one’s family becoming the focus of tsismis is considered highly shameful and reprehensible among Filipino communities.
Bahala Na
The Tagalog term bahala na refers to the sense of optimistic fatalism that characterizes the shared experiences of many Filipinos and Filipino Americans. Bahala na can be evidenced through Filipino cultural expectations to endure emotional problems and avoid discussion of personal issues. This core attitude may have deleterious effects on mental health and help-seeking, as many Filipinos are socialized to deny or minimize stressful experiences or to simply endure emotional problems (Araneta, 1993; Sanchez & Gaw, 2007). A qualitative analysis of 33 interviews and 18 focus groups of Filipino Americans indicated bahala na may combine with religious beliefs to create additional barriers to addressing mental health problems (Javier et al., 2014). For example, virtuous and religious Filipinos and Filipino Americans may endorse bahala na attitudes by believing their higher power has instilled purposeful challenges that can be overcome by sufficient faith and endurance (Javier et al., 2014).
Hindi Ibang Tao
Moreover, many Filipinos and Filipino Americans demonstrate hesitance to trust individuals who are considered outsiders. When interactions with those considered other cannot be avoided, traditional Filipinos tend to be reticent, conceal their real emotions, and avoid disclosure of personal thoughts, needs, and beliefs (Pasco et al., 2004). Filipino community members place a large value on in-group versus out-group members and largely prefer to seek support from helping professionals within the Filipino community, rather than from others outside of the group (Gong et al., 2003). Individuals who are hindi ibang tao (in Tagalog, “one of us”) are differentiated from those who are ibang tao (in Tagalog, “not one of us”), which influences interactions and amount of trust given to health care providers (Sanchez & Gaw, 2007). White counselors may be able to bridge the cultural gap with Filipino clients to become hindi ibang tao by exhibiting respect, approachability, and a willingness to consider the specific influences of Filipino history and the importance of family (Sanchez & Gaw, 2007). Professional counselors who overlook, minimize, or disregard these cultural values risk higher rates of early termination and may experience their Filipino clients as exhibiting little emotion (Nadal, 2021). Filipino clients who are not yet comfortable with professional counselors may interact in a polite, yet superficial manner because culturally responsive relationships and trust have not been developed (Gong et al., 2003; Pasco et al., 2004; Tuazon et al., 2019).
Pakikisama and Kapwa
Another Filipino cultural barrier is pakikisama, or the notion that when one belongs to a group, one should be wholly dedicated to pleasing the group (Bautista, 1999; Nadal, 2021). Filipino core values extend beyond the general notion of collectivism and include kapwa, an Indigenous worldview in which the self is not distinguished from others (David et al., 2017; Enriquez, 2010). Thus, Filipinos do not solely act in ways that benefit the group; they are also expected to make decisions that please other group members, even at the expense of their own desires, needs, or mental health (Nadal, 2021). The cultural notions of pakikisama and kapwa interplay with amor propio in ways that have detrimental effects on Filipinos in dire need of mental health support. For example, a second-generation Filipino American may recognize that their suicidal thoughts and experiences of depression may be worthy of mental health support, but recognition of cultural mistrust toward those deemed other may risk their family’s social acceptance (amor propio). Risking the family’s social acceptance could ultimately violate group wishes (pakikisama) and may subject their family to stigma and gossip (tsismis).
Implications for Practice and Advocacy in Professional Counseling
The COVID-19 pandemic and increased visibility to discrimination against Asian Americans illuminates the importance of addressing the presence of mental health barriers among Filipino communities. Filipino communities face complex barriers rooted in colonialism, racism, and colorism that negatively affect their overall mental health (David & Nadal, 2013; Tuazon et al., 2019; Woo et al., 2020). The combination of educational, health, and welfare disparities culminate in poorer health outcomes for Filipino American communities compared to other ethnic Asian groups (Adia et al., 2020). Many of these identifiable barriers and forces of oppression increase the racial trauma narratives incurred among Filipino communities (David et al., 2017; Klest et al., 2013); deny the impact of microaggressions and discrimination (Nadal et al., 2014); divest resources that support economic, educational, and social well-being (Nadal, 2021; Smith & Weinstock, 2019); and discourage the utilization of needed counseling spaces (Tuazon et al., 2019).
Cultivating cultural sensitivity in health care providers can buffer the psychological toll and emotional consequences of negative health care encounters for historically marginalized communities (Flynn et al., 2020), including Filipinos. Findings associated with health equity and help-seeking behaviors (e.g., Flynn et al., 2020; Ghimire et al., 2018) have significant ramifications for Filipino communities that face a litany of barriers to counseling services (Gong et al., 2003; Tuazon et al., 2019). In light of COVID-19, professional counselors are encouraged to employ culturally responsive interpersonal and systemic interventions that promote the sustainable mental health equity of Filipino communities.
Promoting Racial Socialization and Critical Consciousness
Reducing barriers for mental health access is connected to protective factors, actions, and cultural capital instilled across generations of Filipino communities (David et al., 2017). Filipino communities draw from several generations of colonization, which continues to affect second-generation Filipinos living in the United States (David & Okazaki, 2006a, 2006b). Experiences of historical colonization, forced assimilation into other cultures, and the erasure of Filipino cultural values have resulted in a range of Eurocentrically biased and historically oppressive experiences (Choi et al., 2020; David & Nadal, 2013). These experiences have prepared Filipino communities, intergenerationally and collectively, to respond to experiences of discrimination in ways that preserve their cultural values (David et al., 2017). The preservation of Filipino cultural values across generations has bolstered a type of protective factor through racial socialization, where parents and families teach future generations of children about race and racism (Juang et al., 2017). Ultimately, preparing future generations of Filipinos to respond to racial oppression can protect cultural assets (David et al., 2017). In fact, a study by Woo and colleagues (2020) indicated Filipino parents who prepared their children to respond to racial discrimination prepared them for bias and strengthened their ethnic identity.
One strategy that professional counselors can use to infuse social justice in their work is to help Filipino clients raise their critical consciousness. Critical consciousness is an approach that helps clients to recognize the systemic factors contributing to their barriers with mental health utilization and mental health stressors (David et al., 2019; Diemer et al., 2016; Ratts & Greenleaf, 2018; Seider et al., 2020) and to feel empowered to take part in action (Ratts et al., 2016; Watts & Hipolito-Delgado, 2015). Professional counselors can raise Filipino clients’ critical consciousness by engaging in conversations about how the history of colonization, endorsement of colonial mentality, and systemic factors continue to marginalize Filipinos (David et al., 2019). Connecting critical consciousness to COVID-19, professional counselors can highlight how public anti-Asian discourse echoes centuries of oppression and leads to cultural mistrust of health care providers, particularly professional counselors (Litam, 2020; Ratts & Greenleaf, 2018; Tuazon et al., 2019). Similarly, professional counselors can raise the critical consciousness of Filipino clients by discussing the effects of race-based trauma and racial violence as a result of COVID-19 (Litam, 2020; Nadal, 2021). Including these topics during counseling can be instrumental for detecting the effects of race-based trauma, such as somatic symptoms, while grasping the manifestation of pandemic stress (Taylor et al., 2020). As health care providers focus predominantly on wellness, professional counselors play a significant part in deconstructing the connections and nuances among race-based traumatic stress and pandemic stress (Ratts & Greenleaf, 2018).
Additionally, professional counselors can raise the critical consciousness of Filipino clients by examining the intersection of underlying health disparities, Filipino core values, and overrepresentation of Filipinos working in health care positions during COVID-19 through a trauma-informed lens. Aligned with this perspective, professional counselors can identify and discuss how intergenerational trauma narratives may have persisted across generations of Filipino communities (David & Okazaki, 2006b; David et al., 2019; Nadal, 2021; Tuazon et al., 2019) in ways that have adverse effects on mental health. For example, professional counselors may support Filipino clients to critically reflect on how socialized messages from parents and elders with intergenerational trauma may have contributed to the internalization of colonial mentality. Professional counselors may also broach these cultural factors by promoting discussions within clients’ families and communities about the cultural preservation of Filipino identities (Choi et al., 2017, 2020; David et al., 2017).
Culturally Congruent Coping Responses Among Filipino Clients
Professional counselors can help Filipino clients who seek counseling during COVID-19 by empowering them to engage in coping responses that cultivate their cultural assets and strengthen their ethnic identity (David et al., 2017, 2019; Woo et al., 2020). Before implementing these culturally sensitive strategies, professional counselors must reflect on whether they hold individualistic notions and Western attitudes about which coping responses are deemed helpful or unhelpful to mitigate the effects of racial discrimination (Oh et al., in press; Sue et al., 2019). Following experiences of racial discrimination and stress, Filipinos tend to use disengagement coping responses (Centeno & Fernandez, 2020; Tuason et al., 2007). Following an assessment of coping responses, professional counselors can support Filipino clients by reinforcing culturally responsive disengagement coping strategies, such as tiyaga (Tagalog for “patience and endurance”) and lakas ng loob (Tagalog for “inner strength and hardiness”), to promote resilience and demonstrate flexibility.
Given these central cultural values, professional counselors must be cautioned from solely using emotion-centered counseling strategies that center experiences of stress, racial trauma, or COVID-19–related discrimination (Litam, 2020). Instead, Filipino clients may benefit from interventions that draw from their cultural values of endurance (tiyaga) and inner strength (lakas ng loob) to refocus energy toward cultivating meaningful relationships and roles (David & Nadal, 2013; David et al., 2017). For example, Filipino clients who are concerned about the wellness of their community may experience a heightened sense of purpose and inner strength by reflecting on how their actions have already benefitted their families rather than focusing on their fears. Indeed, when stressful experiences occur, Filipinos have a long history of demonstrating resilience. Empowering Filipino clients to reflect on the historical ways that the Filipino community has evidenced resilience and inner strength may cultivate a strong sense of Filipino pride and strengthen ethnic identity as protective factors to mental health distress (Choi et al., 2020; David et al., 2019; Tuazon et al., 2019).
Filipinos may also benefit from engagement coping strategies, such as prayer, employing religious and spiritual resources, and responding with humor, to promote health and wellness (Nadal, 2021; Sanchez & Gaw, 2007). Counselors can help Filipino clients leverage engagement coping strategies by reflecting on existing responses to stress. Counselors may ask, “How have you intentionally responded to stressful events in the past?” and “How did these ways of coping impact your levels of stress?” Counselors can also demonstrate culturally sensitive strategies and lines of questioning that move from general, shared Filipino values to specific client experiences. For example, counselors can state: “Many Filipinos find peace of mind through prayer, religious practices, and humor. I’m wondering if this is true for you?” Because of the community orientation and collectivism embedded within Filipino culture, it may be helpful for counselors to elaborate on cultural contexts and relationships that inform coping strategies: “I am wondering how you may have seen some of these coping strategies in your home, family, or community. How might you have experienced a coping strategy like humor within your own community?” This statement communicates a familiarity with Filipino cultural values and creates an invitation for clients to explore their coping resources.
Creating Outreach Initiatives and Partnerships
For counselors placed in school and community settings, challenging the systemic effects of COVID-19 among Filipino communities necessitates community partnerships and integrated care settings to achieve health equity (Adia et al., 2019). Health equity initiatives call for two types of overarching efforts to sustain long-term benefits and changes. One aspect of health equity relates to developing community partnerships as a method to intentionally increase health literacy within the community (Guo et al., 2018). Increasing mental health literacy, including education about counseling services and a comprehensive approach to wellness, operates as a direct intervention to cultural and linguistic barriers that precede negative health care experiences (Flynn et al., 2020). Increasing mental health literacy in Filipino communities may also normalize the process of professional mental health services, challenge the cultural notion that those who seek mental health care are crazy, and offer strength-based language related to counseling services (Ghimire et al., 2018; Maxwell et al., 2012; Nadal, 2021). Expanding on recommendations by Tuazon and colleagues (2019), professional counselors can challenge the systemic effects of COVID-19 in Filipino communities by helping community stakeholders understand culturally responsive practices for seeking professional mental health services. Professional counselors employed in community settings can leverage opportunities to liaise with Filipino community organizations and leaders to increase the utilization of counseling services as a preventive method (Graham et al., 2018; Maxwell et al., 2012), especially in response to the increased mental health issues in Filipinos following COVID-19. Professional counselors employed in community settings are therefore uniquely positioned to broach cultural factors of colonialism and systemic racism while addressing the urgency of mental health services for Filipino communities during COVID-19 (Day-Vines et al., 2018, 2020).
Increasing Visibility of Filipino Counselors
The second aspect of health equity initiatives focuses on increasing representation in the pipeline of providers. Although Flynn and colleagues (2020) documented the importance of culturally responsive practices to buffer negative health care experiences, public health scholars have generally identified that the representation of professional counselors is crucial for encouraging historically marginalized communities to seek services (Campbell, 2019; Graham et al., 2018; Griffith, 2018). According to Campbell (2019), historically marginalized clients are more likely to pursue services and demonstrate an openness to speak with professional counselors who are representative of their communities. In addition to increasing Filipino counselors and counselor educators in the pipeline (Tuazon et al., 2019), professional counselors can enact community-based initiatives that position Filipino leaders to support the larger Filipino community (Guo et al., 2018; Maxwell et al., 2012; Nadal, 2021). For example, professional counselors can train Filipino leaders and community members to share information about coping responses (e.g., mindfulness, yoga, and diaphragmatic breathing) that mitigate the deleterious effects of racism, colonialism, and COVID-19–related stress. Professional counselors can also work with community members to establish Filipino-led wellness groups that frame discussions about stress within the broader context of health and wellness. Assessing for previous assumptions about mental health literacy may be helpful to normalize group discussions about stress and mental health. As outreach initiatives and community partnerships are established within the context of COVID-19, professional counselors must consider how they develop marketing materials for counseling services that appropriately reflect the cultural and linguistic diversity of Filipinos and invite input from Filipino community leaders (Campbell, 2019; Graham et al., 2018).
Conclusion
The cumulative effects of colonialism and racism continue to influence the mental health and visibility of Filipino communities within the global crisis of COVID-19. Unlike other AAPI subgroups, experiences of pandemic-related distress in Filipinos are additionally compounded by their distinct history of colonization, cultural values, and low levels of help-seeking behaviors. Specific interventions for culturally responsive counseling and outreach for Filipino communities are critical (Choi et al., 2017; David & Nadal, 2013; David et al., 2017; Tuazon et al., 2019) and were outlined in this article. Professional counselors, especially those in community settings, have numerous opportunities to enact a systematic plan of action that integrates culture, health, and policy (Chan & Henesy, 2018; Nadal, 2021). These interventions illuminate a longstanding and never more urgent call to action for extending efforts and initiatives to increase the visibility of Filipino communities and support individuals of Filipino descent in counseling.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Abe-Kim, J., Gong, F., & Takeuchi, D. (2004). Religiosity, spirituality, and help-seeking among Filipino Americans: Religious clergy or mental health professionals? Journal of Community Psychology, 32(6), 675–689. https://doi.org/10.1002/jcop.20026
Abe-Kim, J., Takeuchi, D. T., & Hwang, W.-C. (2002). Predictors of help seeking for emotional distress among Chinese Americans: Family matters. Journal of Consulting and Clinical Psychology, 70(5), 1186–1190.
https://doi.org/10.1037/0022-006X.70.5.1186
Adia, A. C., Nazareno, J., Operario, D., & Ponce, N. A. (2020). Health conditions, outcomes, and service access among Filipino, Vietnamese, Chinese, Japanese, and Korean adults in California, 2011–2017. American Journal of Public Health, 110(4), 520–526. https://doi.org/10.2105/AJPH.2019.305523
Adia, A. C., Ng, M. J., Quilantang, M. I., Restar, A. J., Hernandez, L. I., Imperial, R. H., Nazareno, J., & Operario, D. (2019). Collective coping strategies for HIV-related challenges among men who have sex with men in Manila, Philippines. AIDS Education and Prevention, 31(5), 479–490.
https://doi.org/10.1521/aeap.2019.31.5.479
Afable, A., Ursua, R., Wyatt, L. C., Aguilar, D., Kwon, S. C., Islam, N. S., & Trinh-Shevrin, C. (2016). Duration of US residence is associated with overweight risk in Filipino immigrants living in New York metro area. Family and Community Health, 39(1), 13–23. https://doi.org/10.1097/FCH.0000000000000086
Angan, J. (2013). Beyond the beach: The untold story of Boracay’s Ati tribe. GMA News Online. https://www.gmanet
work.com/news/lifestyle/artandculture/313920/beyond-the-beach-the-untold-story-of-boracay-s-ati-tribe/story
Appel, H. B., Huang, B., Ai, A. L., & Lin, C. J. (2011). Physical, behavioral, and mental health issues in Asian American women: Results from the National Latino Asian American Study. Journal of Women’s Health, 20(11), 1703–1711. https://doi.org/10.1089/jwh.2010.2726
Araneta, E. G. (1993). Psychiatric care of Filipino Americans. In A. C. Gaw (Ed.), Culture, Ethnicity, and Mental Illness (pp. 377–411). American Psychiatric Association.
Asian Journal Press. (2018). New census data shows more than four million Filipinos in the US. https://www.asian
journal.com/usa/dateline-usa/new-census-data-shows-more-than-four-million-filipinos-in-the-us
Augsberger, A., Yeung, A., Dougher, M., & Hahn, H. C. (2015). Factors influencing the underutilization of mental health services among Asian American women with a history of depression and suicide. BMC Health Services Research, 15(1), 1–11. https://doi.org/10.1186/s12913-015-1191-7
Batalova, J. (2020). Immigrant health-care workers in the United States. Migration Policy Institute. https://www.migrationpolicy.org/article/immigrant-health-care-workers-united-states-2018
Bautista, V. (1999). The Filipino Americans: From 1763 to the present: Their history, culture, and traditions. Bookhaus.
Bhimla, A., Yap, L., Lee, M., Seals, B., Aczon, H., & Ma, G. X. (2017). Addressing the health needs of high-risk Filipino Americans in the greater Philadelphia region. Journal of Community Health, 42(2), 269–277.
https://doi.org/10.1007/s10900-016-0252-0
Budiman, A., Cilluffo, A., & Ruiz, N. G. (2019). Key facts about Asian origin groups in the U.S. Pew Research Center. https://www.pewresearch.org/fact-tank/2019/05/22/key-facts-about-asian-origin-groups-in-the-u-s
Campbell, K. M. (2019). Race, gender, and health equity. Journal of Best Practices in Health Professions Diversity, 11(2), 155–157.
Centeno, R. P. R., & Fernandez, K. T. G. (2020). Effect of mindfulness on empathy and self-compassion: An adapted MBCT program on Filipino college students. Behavioral Sciences, 10(3), 1–15.
https://doi.org/10.3390/bs10030061
Centers for Disease Control and Prevention. (2021). People with certain medical conditions. Retrieved March 14, 2021, from https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fneed-extra-precautions%2Fgroups-at-higher-risk.html
Chan, C. D., & Henesy, R. K. (2018). Navigating intersectional approaches, methods, and interdisciplinarity to health equity in LGBTQ+ communities. Journal of LGBT Issues in Counseling, 12(4), 230–247.
https://doi.org/10.1080/15538605.2018.1526157
Chan, C. D., Henesy, R. K., & Erby, A. N. (2019). Toward praxis, promise, and futures of intersectionality in multimethod counseling research. Counseling Outcome Research and Evaluation, 10(1), 12–18.
https://doi.org/10.1080/21501378.2018.1562845
Choi, Y., Park, M., Lee, J. P., Kim, T. Y., & Tan, K. (2017). Culture and family process: Examination of culture-specific family process via development of new parenting measures among Filipino and Korean American families with adolescents. In Y. Choi & H. C. Hahm (Eds.), Asian American parenting: Family process and intervention (pp. 37–68). Springer. https://doi.org/10.1007/978-3-319-63136-3_3
Choi, Y., Park, M., Noh, S., Lee, J. P., & Takeuchi, D. (2020). Asian American mental health: Longitudinal trend and explanatory factors among young Filipino- and Korean Americans. SSM – Population Health, 10, 1–10. https://doi.org/10.1016/j.ssmph.2020.100542
Choy, C. C. (2003). Empire of care: Nursing and migration in Filipino American history. Duke University Press.
David, E. J. R. (2020). Addressing anti-Black microaggressions in Filipino families. Psychology Today. https://www.psychologytoday.com/us/blog/unseen-and-unheard/202006/addressing-anti-black-microaggressions-in-filipino-families-0
David, E. J. R., & Nadal, K. L. (2013). The colonial context of Filipino American immigrants’ psychological experiences. Cultural Diversity and Ethnic Minority Psychology, 19(3), 298–309.
https://doi.org/10.1037/a0032903
David, E. J. R., & Okazaki, S. (2006a). Colonial mentality: A review and recommendation for Filipino American psychology. Cultural Diversity and Ethnic Minority Psychology, 12(1), 1–16.
https://doi.org/10.1037/1099-9809.12.1.1
David, E. J. R., & Okazaki, S. (2006b). The Colonial Mentality Scale (CMS) for Filipino Americans: Scale construction and psychological implications. Journal of Counseling Psychology, 53(2), 241–252.
https://doi.org/10.1037/0022-0167.53.2.241
David, E. J. R., Sharma, D. K. B., & Petalio, J. (2017). Losing kapwa: Colonial legacies and the Filipino American family. Asian American Journal of Psychology, 8(1), 43–55. https://doi.org/10.1037/aap0000068
David, E. J. R., Schroeder, T. M., & Fernandez, J. (2019). Internalized racism: A systematic review of the psychological literature on racism’s most insidious consequence. Journal of Social Issues, 75(4), 1057–1086. https://doi.org/10.1111/josi.12350
Day-Vines, N. L., Booker Ammah, B., Steen, S., & Arnold, K. M. (2018). Getting comfortable with discomfort: Preparing counselor trainees to broach racial, ethnic, and cultural factors with clients during counseling. International Journal for the Advancement of Counselling, 40(2), 89–104.
https://doi.org/10.1007/s10447-017-9308-9
Day-Vines, N. L., Cluxton-Keller, F., Agorsor, C., Gubara, S., & Otabil, N. A. A. (2020). The multidimensional model of broaching behavior. Journal of Counseling & Development, 98(1), 107–118. https://doi.org/10.1002/jcad.12304
de Torres, S. (2002). Understanding persons of Philippine origin: A primer for rehabilitation service providers. Center for Institutional Rehabilitation Research Information and Exchange. http://cirrie-sphhp.webapps.buffalo.edu/culture/monographs/philippines.php
Diemer, M. A., Rapa, L. J., Voight, A. M., & McWhirter, E. H. (2016). Critical consciousness: A developmental approach to addressing marginalization and oppression. Child Development Perspectives, 10(4), 216–221. https://doi.org/10.1111/cdep.12193
Edman, J. L., & Johnson, R. C. (1999). Filipino American and Caucasian American beliefs about the causes and treatment of mental problems. Cultural Diversity and Ethnic Minority Psychology, 5(4), 380–386.
https://doi.org/10.1037/1099-9809.5.4.380
Enriquez, V. G. (2010). From colonial to liberation psychology: The Philippine experience (2nd ed.). University of the Philippines Press.
Espiritu, Y. L. (2016). Gender, migration, and work: Filipina health care professionals to the United States. In M. Zhou & A. C. Ocampo (Eds.), Contemporary Asian America: A multidisciplinary reader (3rd ed., pp. 236–256). New York University Press.
Flynn, P. M., Betancourt, H., Emerson, N. D., Nunez, E. I., & Nance, C. M. (2020). Health professional cultural competence reduces the psychological and behavioral impact of negative healthcare encounters. Cultural Diversity and Ethnic Minority Psychology, 26(3), 271–279. https://doi.org/10.1037/cdp0000295
Ghimire, S., Cheong, P., Sagadraca, L., Chien, L.-C., & Sy, F. S. (2018). A health needs assessment of the Filipino American community in the greater Las Vegas area. Health Equity, 2(1), 334–348.
https://doi.org/10.1089/heq.2018.0042
Gong, F., Gage, S.-J. L., & Tacata, L. A., Jr. (2003). Helpseeking behavior among Filipino Americans: A cultural analysis of face and language. Journal of Community Psychology, 31(5), 469–488.
https://doi.org/10.1002/jcop.10063
Graham, L. F., Scott, L., Lopeyok, E., Douglas, H., Gubrium, A., & Buchanan, D. (2018). Outreach strategies to recruit low-income African American men to participate in health promotion programs and research: Lessons from the Men of Color Health Awareness (MOCHA) project. American Journal of Men’s Health, 12(5), 1307–1316. https://doi.org/10.1177/1557988318768602
Griffith, D. M. (2018). “Centering the margins”: Moving equity to the center of men’s health research. American Journal of Men’s Health, 12(5), 1317–1327. https://doi.org/10.1177/1557988318773973
Guo, M., Quensell, M., Chang, A., Miyamura, J., & Sentell, T. (2018). Understanding of key obstetric quality terminology by Asian and Pacific Islander subgroups: Implications for patient engagement and health equity. Maternal and Child Health Journal, 22(11), 1543–1549. https://doi.org/10.1007/s10995-018-2597-8
Javier, J. R., Supan, J., Lansang, A., Beyer, W., Kubicek, K., & Palinkas, L. A. (2014). Preventing Filipino mental health disparities: Perspectives from adolescents, caregivers, providers, and advocates. Asian American Journal of Psychology, 5(4), 316–324. https://doi.org/10.1037/a0036479
Jeung, R., & Nham, K. (2020). Incidents of Coronavirus-related discrimination. Asian Pacific Policy & Planning Council. http://www.asianpacificpolicyandplanningcouncil.org/wp-content/uploads/STOP_AAPI_HATE_MONTHLY_REPORT_4_23_20.pdf
Jones-Smith, E. (2019). Culturally diverse counseling: Theory and practice. SAGE.
Juang, L. P., Yoo, H. C., & Atkin, A. (2017). A critical race perspective on an empirical review of Asian American parental racial-ethnic socialization. In Y. Choi & H. C. Hahm (Eds.), Asian American parenting: Family process and intervention (pp. 11–35). Springer. https://doi.org/10.1007/978-3-319-63136-3_2
Kim, G., Chiriboga, D. A., Bryant, A., Huang, C.-H., Crowther, M., & Ma, G. X. (2012). Self-rated mental health among Asian American adults: Association with psychiatric disorders. Asian American Journal of Psychology, 3(1), 44–52. https://doi.org/10.1037/a0024318BB
Klest, B., Freyd, J. J., Hampson, S. E., & Dubanoski, J. P. (2013). Trauma, socioeconomic resources, and self-rated health in an ethnically diverse adult cohort. Ethnicity & Health, 18(1), 97–113.
https://doi.org/10.1080/13557858.2012.700916
Li, M. (2014). Discrimination and psychiatric disorder among Asian American immigrants: A national analysis by subgroups. Journal of Immigrant and Minority Health, 16, 1157–1166.
https://doi.org/10.1007/s10903-013-9920-7
Litam, S. D. A. (2020). “Take your Kung-Flu back to Wuhan”: Counseling Asians, Asian Americans, and Pacific Islanders with race-based trauma related to COVID-19. The Professional Counselor, 10(2), 144–156.
https://doi.org/10.15241/sdal.10.2.144
Litam, S. D. A., & Hipolito-Delgado, C. P. (2021). When being “essential” illuminates disparities: Counseling clients affected by COVID-19. Journal of Counseling & Development, 99(1), 3–10. https://doi.org/10.1002/jcad.12349
Litam, S. D. A., & Oh, S. (2020). Ethnic identity and coping strategies as moderators of COVID-19 racial discrimination experiences among Chinese Americans. Counseling Outcome Research and Evaluation. Online publication. https://doi.org/10.1080/21501378.2020.1814138
Martinez, A. B., Co, M., Lau, J., & Brown, J. S. L. (2020). Filipino help-seeking for mental health problems and associated barriers and facilitators: A systematic review. Social Psychiatry and Psychiatric Epidemiology, 55, 1397–1413. https://doi.org/10.1007/s00127-020-01937-2
Maxwell, A. E., Danao, L. L., Cayetano, R. T., Crespi, C. M., & Bastani, R. (2012). Evaluating the training of Filipino American community health advisors to disseminate colorectal cancer screening. Journal of Community Health, 37(6), 1218–1225. https://doi.org/10.1007/s10900-012-9557-9
McFarling, U. L. (2020). Nursing ranks are filled with Filipino Americans. The pandemic is taking an outsized toll on them. Stat. https://www.statnews.com/2020/04/28/coronavirus-taking-outsized-toll-on-filipino-american-nurses
Mendoza, R. L. (2014). The skin whitening industry in the Philippines. Journal of Public Health Policy, 35(2), 219–238. https://doi.org/10.1057/jphp.2013.50
Nadal, K. L. (2000). F/Pilipino American substance abuse: Sociocultural factors and methods of treatment. Journal of Alcohol and Drug Education, 46(2), 26–36.
Nadal, K. L. (2021). Filipino American psychology: A handbook of theory, research, and clinical practice (2nd ed.). Wiley. https://doi.org/10.1002/9781119677109
Nadal, K. L., Griffin, K. E., Wong, Y., Hamit, S., & Rasmus, M. (2014). The impact of racial microaggressions on mental health: Counseling implications for clients of color. Journal of Counseling & Development, 92(1), 57–66. https://doi.org/10.1002/j.1556-6676.2014.00130.x
National Nurses United. (2020). Sins of omission: How government failures to track COVID-19 data have led to more than 1,700 health care worker deaths and jeopardize public health. https://www.nationalnursesunited.org/sites/default/files/nnu/graphics/documents/0920_Covid19_SinsOfOmission_Data_Report.pdf
Ocampo, A. C. (2016). The Latinos of Asia: How Filipino Americans break the rules of race. Stanford University Press.
Oh, S., Litam, S. D. A., & Chang, C. (in press). COVID-19 fueled subtle and blatant racism and stress-related growth among international Asians in the United States: The roles of ethnic identity, resiliency, and coping. Asian American Journal of Psychology.
Pacquiao, D. (2004). Overcoming stigma and mental illness among Filipinos. Presentation at the National Conference of the New York Coalition for Asian Mental Health. New York Academic of Medicine, New York.
Pasco, A. C. Y., Morse, J. M., & Olson, J. K. (2004). Cross-cultural relationships between nurses and Filipino Canadian patients. Journal of Nursing Scholarship, 36(3), 239–246.
https://doi.org/10.1111/j.1547-5069.2004.04044.x
Pew Research Center. (2013). The rise of Asian Americans. https://www.pewsocialtrends.org/2012/06/19/the-rise-of-asian-americans
Poon, L. (2020, April 7). What bigotry looks like during social distancing. Citylab. https://www.citylab.com/equity/
2020/04/coronavirus-racism-hate-crimes-asian-americans-xenophobia/609517
Ratts, M. J., & Greenleaf, A. T. (2018). Counselor–advocate–scholar model: Changing the dominant discourse in counseling. Journal of Multicultural Counseling and Development, 46(2), 78–96.
https://doi.org/10.1002/jmcd.12094
Ratts, M. J., Singh, A. A., Nassar-McMillan, S., Butler, S. K., & McCullough, J. R. (2016). Multicultural and social justice counseling competencies: Guidelines for the counseling profession. Journal of Multicultural Counseling and Development, 44(1), 28–48. https://doi.org/10.1002/jmcd.12035
Ruiz, N. G., Horowitz, J. M., & Tamir, C. (2020). Many Black and Asian Americans say they have experienced discrimination amid the COVID-19 outbreak. Pew Research Center. https://www.pewsocialtrends.org/2020/07/01/many-black-and-asian-americans-say-they-have-experienced-discrimination-amid-the-covid-19-outbreak
Sanchez, F., & Gaw, A. (2007). Mental health care of Filipino Americans. Psychiatric Services, 58(6), 810–815. https://doi.org/10.1176/ps.2007.58.6.810
Seider, S., Clark, S., & Graves, D. (2020). The development of critical consciousness and its relation to academic achievement in adolescents of color. Child Development, 91(2), e451–e474. https://doi.org/10.1111/cdev.13262
Shea, M., & Yeh, C. (2008). Asian American students’ cultural values, stigma, and relational self-construal: Correlates of attitudes toward professional help-seeking. Journal of Mental Health Counseling, 30(2), 157–172. https://doi.org/10.17744/mehc.30.2.g662g5l2r1352198
Smith, M. J., & Weinstock, D. (2019). Reducing health inequities through intersectoral action: Balancing equity in health with equity for other social goods. International Journal of Health Policy and Management, 8(1), 1–3. https://doi.org/10.15171/IJHPM.2018.103
Sue, D. W., Sue, D., Neville, H. A., & Smith, L. (2019). Counseling the culturally diverse: Theory and practice (8th ed.). Wiley.
Taylor, S., Landry, C. A., Paluszek, M. M., Fergus, T. A., McKay, D., & Asmundson, G. J. G. (2020). Development and initial validation of the COVID Stress Scales. Journal of Anxiety Disorders, 72(2020), 1–7.
https://doi.org/10.1016/j.janxdis.2020.102232
Tuason, M. T. G., Taylor, A. R., Rollings, L., Harris, T., & Martin, C. (2007). On both sides of the hyphen: Exploring the Filipino-American identity. Journal of Counseling Psychology, 54(4), 362–372.
https://doi.org/10.1037/0022-0167.54.4.362
Tuazon, V. E., Gonzalez, E., Gutierrez, D., & Nelson, L. (2019). Colonial mentality and mental health help-seeking of Filipino Americans. Journal of Counseling & Development, 97(4), 352–363. https://doi.org/10.1002/jcad.12284
U.S. Department of Justice. (2020). Coronavirus is no excuse for hate: Remembering Vincent Chin. Department of Justice, U.S. Attorneys’ Office, District of Idaho. https://www.justice.gov/usao-id/pr/coronavirus-no-excuse-hate
Watts, R. J., & Hipolito-Delgado, C. P. (2015). Thinking ourselves to liberation? Advancing sociopolitical action in critical consciousness. The Urban Review, 47(5), 847–867. https://doi.org/10.1007/s11256-015-0341-x
Woo, B., Maglalang, D. D., Ko, S., Park, M., Choi, Y., & Takeuchi, D. T. (2020). Racial discrimination, ethnic-racial socialization, and cultural identities among Asian American youths. Cultural Diversity & Ethnic Minority Psychology, 26(4), 447–459. https://doi.org/10.1037/cdp0000327
Worldometer. (n.d.). Covid-19 coronavirus pandemic. https://www.worldometers.info/coronavirus/#countries
Christian D. Chan, PhD, NCC, is an assistant professor at the University of North Carolina at Greensboro. Stacey Diane Arañez Litam, PhD, NCC, CCMHC, LPCC-S, is an assistant professor at Cleveland State University. Correspondence may be addressed to Christian D. Chan, Department of Counseling and Educational Development, The University of North Carolina at Greensboro, P.O. Box 26170, Greensboro, NC 27402, cdchan@uncg.edu.
Aug 18, 2020 | Volume 10 - Issue 3
S Anandavalli, John J. S. Harrichand, Stacey Diane Arañez Litam
Amidst the global health crisis of COVID-19, international students’ safety and well-being is threatened by community- and policy-level animus. In addition to adjusting to a foreign culture, a series of draconian policies and communal hate crimes during the pandemic have placed international students in an especially vulnerable position. In this context, professional counselors must be well prepared to support this community. The authors describe the current sociopolitical events that have adversely impacted international students in the United States. Next, challenges to international students’ mental health are identified to aid counselors’ understanding of this community’s needs. Finally, recommendations grounded in critical feminist and bioecological approaches are offered to facilitate counselors’ clinical and advocacy work with international students.
Keywords: COVID-19, international students, critical feminist, bioecological, advocacy
COVID-19–related fears have resulted in social and political responses characterized by racial discrimination and xenophobia toward marginalized groups (Devakumar et al., 2020; Litam, 2020; Litam & Hipolito-Delgado, in press), including international students (Anandavalli, 2020; Zhai & Du, 2020). Rates of misleading media portrayals and xenophobic rhetoric substantially increased after President Trump referred to COVID-19 as the “Chinese virus” on March 16, 2020, and have steadily risen across social media platforms (Lyu et al., 2020). Exposure to COVID-19–related racial discrimination has deleterious effects on the mental health and life satisfaction of racial minorities (Litam, 2020; Litam & Oh, in press; Wen et al., 2020), including international students residing in the United States (Zhai & Du, 2020). The extant body of literature has clearly established lower levels of help seeking, barriers to counseling, and increased rates of mental health distress among international students compared to their domestic counterparts (Auerbach et al., 2018; Clough et al., 2018; Sawir et al., 2008; Zhai & Du, 2020). These existing challenges and psychosocial stressors may uniquely combine with current sociopolitical messages and policies to further exacerbate the unique developmental and cultural stressors encountered by international students. Thus, counselors working in various roles (e.g., college counselors, private practitioners) are called to develop a deeper understanding of the ways in which international students are negatively affected by xenophobic policies following COVID-19 and to employ culturally sensitive strategies grounded in systems approaches.
Although all counselors working with international students must consider the impact of larger systemic issues on international students’ mental health, college counselors might be in a unique position to support this population because of their close proximity. Counselors must consider how the combined effects of sociopolitical influences, systemic inequity, intersectionality, and COVID-19–related experiences of xenophobia uniquely contribute to the mental health disparities of international students in a post-pandemic reality. It is vital that counselors consider the impact of social and political structures, as Anandavalli (2020) found that contextual and systemic influences (e.g., elections, travel bans, anti-immigrant sentiment) have a profound impact on international students’ mental health. Unfortunately, despite repeated calls to action, counselors may be unprepared to support international students in the United States (e.g., Kim et al., 2019). Even years after Yoon and Portman’s (2004) critique, accredited counseling programs continue to offer little to no training to students to work effectively with international students. Perhaps as a result of years of limited training and research on international students’ mental health experiences, counselors continue to have inadequate cultural competence when working with international students. In a recent study, Liu et al. (2020) noted that although Korean and Chinese international students in their study had a cautiously optimistic attitude toward their college counselors, a third of them felt hurt and disappointed by their college counselors’ cultural incompetence and reported incidents of counselors’ cultural ignorance and stereotyping. With limited attention to social justice and equity issues, counselors can further traumatize and alienate some international students (Jones et al., 2017).
Within the counseling literature, even the few studies that explored the mental health of international students from a relational and systemic perspective (e.g., Lértora & Croffie, 2020; Page et al., 2019) have failed to adopt a critical lens and examine the impact and accountability of larger social institutions on the community’s well-being. At present, a review on PsycINFO, Google Scholar, and SocINDEX using the search terms international student mental health, international students counseling bioecological model, and international students multicultural critical race theory yielded no counseling literature that addressed strategies to support the mental health of international students in the United States from a critical perspective. Thus, the following article contributes to the extant body of literature on the topic by (a) describing the ways in which current sociopolitical events and policies send denigrating messages that devalue international students, (b) outlining the mental health challenges of international students, and (c) offering specific suggestions for counselors working with this vulnerable population through a critical feminist and bioecological lens.
Sociopolitical Policies Affecting International Students
According to the Institute of International Education (IIE; 2019), as the most popular study abroad destination, the United States hosts more than 1 million international (foreign-born) students. However, in the context of the racialized COVID-19 pandemic, Chirikov and Soria (2020) found that as many as 17% of the surveyed international students have experienced xenophobic actions that threaten their safety and presence. Further, they found these rates were higher among students from East Asian and Southeast Asian countries such as Japan, China, and Vietnam (22%–30%), given increasing Sinophobia (anti-Chinese sentiment) in the country. In addition to pursuing higher education, each year thousands of international students seek post-education professional experiences to receive practical training through an H-1B visa. An H-1B visa authorizes international students and professionals to work in the United States because of their experience in specialty occupations of distinguished merit and ability (U.S. Department of Labor, n.d.). On June 22, 2020, H-1B visa holders were notified that effective June 24, 2020, the U.S. embassy would not be issuing new H-1B visa stamps; additionally, the ruling dictated that without a valid H-1B visa stamp, individuals could not enter the United States until December 31, 2020 (The White House, 2020). This xenophobic proclamation left thousands of international professionals stranded and placed them at risk of losing their employment. The announcement to ban H-1B visa holders devalued international students and professionals in the United States and reminded international students of their fragile futures and conditional status.
The most recent incident in the upsurge of xenophobic sociopolitical messages negatively affecting international students was introduced by the U.S. Immigration and Customs Enforcement (ICE) on July 6, 2020. A few weeks prior to the fall 2020 semester, international students were informed that they would be deported to their home countries if they were enrolled in fully online programs (ICE, 2020). International students became tasked with an impossible decision to either prioritize their health or their education. Unlike domestic students, who could safely attend programs online, the proclamation required international students to attend in-person classes to remain in the country (ICE, 2020). Although the proclamation was later amended to allow international students to attend online courses without deportation (ICE, 2020), the disparaging messages toward international students could not be overlooked. The presence of a discriminatory order that forced international students to choose between their safety and educational training is reflective of larger anti-immigration sentiments that push many students toward an emotional breakdown (Garcini et al., 2020).
Mental Health Challenges for International Students
Although international students contributed about $45 billion to the U.S. economy and to the development of 450,000 new jobs in the United States in 2018–19 (National Association of Foreign Student Advisers [NAFSA], 2020), worldviews that position international students as harbingers of innovation, intellectual diversity, economic success, and a necessity for sustaining higher education institutions are uncommon within American society (Williams & Johnson, 2011). Sadly, experiences of hate crimes are so frequent that many international students perceive them as normal consequences of being an international person in the United States (Lee & Rice, 2007; Pottie-Sherman, 2018). According to George Mwangi et al. (2019), for many international students, universities are far from being spaces of inclusivity and openness. Often, they were described as sites of oppression and “Americanization.” Interviews with international students from Africa indicated that due to their intersecting identities as racial and cultural minorities, participants in the study endured constant messages and actions undermining their culture and knowledge. In fact, persistent incidents of prejudice and discrimination made the participants feel “crazy” (George Mwangi et al., 2019). Chronic exposure to xenophobia, discrimination, and anti-immigrant sentiments has been documented to have profound impacts on international students’ psychological well-being (Houshmand et al., 2014; Ong et al., 2013). As a result of multiple factors, including xenophobia, international students suffer from severe psychological symptoms. One example is a recent study by Dovchin (2020), who found that parochial attitudes toward non-native English speakers and embedded linguistic racism had “serious ‘psychological damages’” (p. 815) on the international students’ mental health. Notably, the impact of “ethnic accent bullying” (p. 815) on her international student participants included development of social anxiety symptoms and suicidal ideation. Given that many of the instances of linguistic racism were found within classrooms, it is imperative that college counselors consider the pervasive influence of systemic inequities on international students’ mental health.
Critical Feminist Perspectives
Critical feminist paradigms acknowledge the powerful role of systemic influences and focus on change at structural levels. These paradigms challenge larger social structures (e.g., national and institutional policies) and promote the pursuit of social justice through clinical practice and inquiry (Moradi & Grzanka, 2017; Mosley et al., 2020). Thus, critical feminist paradigms are grounded in the philosophy that current social landscapes are inequitable and therefore unjust (Bonilla-Silva, 2013). Specifically, the critical feminist theory of intersectionality describes how systems of oppression and the social constructions of race, socioeconomic class, gender, and other identities interact in ways that influence one’s social positioning (Crenshaw, 1989). Given many international students’ intersecting identities as linguistic, racial, and ethnic minorities, counselors must consider how their unique combination of marginalized and privileged identities contribute to their social position and worldview as outlined in the Multicultural and Social Justice Counseling Competencies (MSJCC; Ratts et al., 2015). Consistent with the focus on addressing the pervasive role of sociopolitical systemic influences, the analysis and recommendations offered in this article are grounded in the critical feminist paradigm.
Bioecological Systems Theory
Oppression and change occur across multiple levels of human interactions, and each level may require varied strategies for advocacy on the part of the counselor (Ratts et al., 2015). These interactions range from everyday occurrences in one’s immediate surroundings (e.g., classrooms) to international policies (e.g., travel bans). To address the powerful influence of multiple systems on the mental health of international students, a critical feminist paradigm was applied to Bronfenbrenner’s (1979) bioecological systems theory. The bioecological systems theory outlines how systems and environment interact with an individual in ways that impact their overall well-being. According to the model (Bronfenbrenner, 1994), individuals experience a bidirectional relationship (directly and indirectly) as a result of interacting with environmental systems where the impact of the relationship is dependent on the amount of interaction taking place. The bioecological theory is represented by five concentric circles that expand to represent multiple levels of permeable systems that affect one’s development (Bronfenbrenner, 1994). The systems within Bronfenbrenner’s model include: (a) microsystem, the immediate environment (e.g., family, school, peer group, neighborhood); (b), mesosytem, connections within the immediate environment, such as college campus and roommates; (c) exosystem, external environmental settings that only indirectly affect development, such as religious institutions outside of one’s faith; (d) macrosystem, which refers to one’s larger cultural context; and (e) chronosystem, encompassing patterns and transitions over the course of time and development (Bronfenbrenner, 1994).
Although the bioecological model represents a relatively robust theory, the model is not without its limitations. Christensen (2016) noted that the theory fails to account for the effects of globalization and technological developments that affect various parts of the world differently. These disparities can be addressed by combining the bioecological model with the critical feminist paradigm, which challenges institutions and structures that cut across national boundaries. Both models combine to create a unique framework that may guide concrete recommendations for counselors actively seeking to support and advocate for international students.
Implications for Counseling International Students
As the extant counseling literature on international students suffers from a limited emphasis on a critical feminist and bioecological lens, the current manuscript offers a systemic framework for counseling international students. We invite college counselors to adopt a critical feminist and systems perspective to hold larger systems accountable for their harmful role in international students’ mental health concerns (e.g., a university’s unwillingness to engage in culturally responsive and linguistically inclusive teaching strategies; Archer, 2007). The following counseling recommendations were developed from the authors’ direct experiences through counseling international students, and through a review of relevant literature. Although these recommendations may apply to all counselors irrespective of their settings, some may be specific to a particular role (e.g., college counselor).
Microsystem
The microsystem level includes the bidirectional relationships between the international student and the people with whom they regularly interact (Bronfenbrenner, 1979). College counselors and community counselors working with this population can support international students at the microsystem level by asking them to identify and deeply explore “safe” and “unsafe” relationships that exist within their college/university campus, neighborhood, and relevant religious group. Next, counselors can empower international students by framing their concerns as part of a larger systemic issue to minimize self-blame (i.e., seeing themselves as the cause of their challenges; Sue & Sue, 1990). Here, the focus is placed on empowering international students to engage in self-advocacy within the systems they occupy (Haskins & Singh, 2015). The reframe may also aid in enhancing the international student’s critical consciousness (Ratts, 2017; Ratts & Greenleaf, 2017) and help them shift their perspectives from self-blame to acknowledging the role(s) of external oppressive forces (e.g., racism, xenophobia, Sinophobia; Manzano et al., 2017). Indeed, engaging in the internalization of problems in response to stressors is prevalent among many international cultures (Wong et al., 2013).
Interventions at this level might involve the use of microinterventions (Sue et al., 2019) to empower international students. Sue et al. (2019) defined microinterventions as deeds and interactions that communicate affirmation and validation to targets of microaggressions. These interventions have the potential to enhance the psychological well-being and self-efficacy of the target and disarm the effects of microaggressions by challenging the perpetrator. Counselors can provide psychoeducation on microinterventions, using caution and clinical judgment to avoid further harm to the student. It is imperative that counselors recognize and educate the international student that it could be dangerous to employ microinterventions without understanding the specificities of the context. Sue et al. noted that the minoritized individual (target) employing microinterventions must be intentional about picking their battles, as endless responses to each encountered incident of microaggression can be damaging to the target’s well-being. The target should be aware of the context of the microaggression and modify their response as the situation requires. Given that racism and oppression permeate classroom spaces, college counselors can also provide opportunities for practicing microinterventions through role plays (Litam, 2020). One microintervention is making the “invisible” visible by responding to instances of racial discrimination on campus, making the offending party (e.g., domestic students, staff) aware of their offensive actions or words, and/or compelling them to consider their impact (Sue et al., 2019). Counselors may further guide international students in educating the offender (Sue et al., 2019). Litam (2020) noted that although it is of critical importance to avoid placing the onus of responsibility on minoritized individuals (e.g., international students) to educate and/or confront their offenders, when they do engage in thoughtful responses the opportunity to educate can result in positive changes and healthier relationships.
Finally, counselors can support international students to incorporate mindfulness and self-compassion as culturally sensitive tools to address the xenophobic experiences of COVID-19–related racial discrimination (Litam, 2020). Compassion meditation may help international students release their feelings of anger and intentionally cultivate experiences of self-compassion and positive regard toward self and others. Self-compassion may be cultivated by encouraging international students to attend to their immediate needs by remaining present and non-judgmental (Germer & Neff, 2015). Grounded in the Buddhist concept of loving-kindness, international students may be trained to pay attention to their somatic experiences with a non-judgmental curiosity. For instance, as these students confront chronic racism, they may benefit from opportunities to be kind to themselves. Counselors may also guide them to engage in mindful breathing to ground themselves in the face of chronic stress (Germer & Neff, 2015).
Additionally, empowering international students to cultivate a strong sense of ethnic identity may also represent an important strategy at this level. Extant research continues to identify the role of ethnic identity as a protective factor for experiences of racial discrimination (Carter et al., 2019; Chae & Foley, 2010; Choi et al., 2016; Tran & Sangalang, 2016), including experiences of COVID-19–related racial discrimination (Litam & Oh, in press).
Mesosystem
Counselors working with international students at the mesosystem level may continue to strengthen the interventions at the microsystem level while exploring mental health stressors that may arise through interactions between the student and their peers and/or members of the college/university campus community. Counselors who interact with various social groups uniquely position themselves in ways that establish new relationships, building support with spiritual and religious leaders (Sue et al., 2019) and mid- and senior-level administrators who are then able to directly or indirectly support international students on and off campus (Mac et al., 2019).
Leveraging their network within the university system, college counselors can explore how faculty members, administrators, and staff may improve their cultural humility and competence by collaborating with them in efforts to support international students within the campus (Hook et al., 2013). For instance, faculty members and staff could be invited to on-campus ethnic interest groups, cultural festivals, or language clubs on a regular basis to immerse themselves in their students’ cultural practices. Additionally, many international students on campus occupy shared housing. College counselors can teach international students’ roommates, peers, and resident advisors to detect signs of distress and isolation. This can potentially help student leaders and other residents better support international students and promote wellness in the student body more broadly. Engaging the community in culturally relevant strategies for promoting the mental health of international students and recognizing their distress may help college counselors in early detection of distress for this community.
Exosystem
The exosystem level examines social settings that indirectly impact the student but in which the student has no direct impacts (e.g., local politics, medical and social services; Bronfenbrenner, 1979). Interventions at the exosystem level might examine how educational training grounded in Eurocentrism may further marginalize international students and negatively impact their academic standing and their overall mental health and well-being (George Mwangi et al., 2019; Ploner & Nada, 2020). Counselors working with international students at the exosystem level must shift their perspectives from interpersonal interventions toward a greater examination of systemic influences. Counselors may utilize the MSJCC (Ratts et al., 2015) to consider the intersecting ways in which the privileged and oppressed identities of international students uniquely influence their mental health experiences. A detailed description of how counselors can apply the MSJCC to counseling international students can be found in Kim et al. (2019).
College counselors working at the exosystem level must play an active role in advocating on behalf of international students by working to dismantle White supremacy in college/university counseling settings (Ratts, 2017) and academic settings (Haskins & Singh, 2015). Furthermore, counselors working at the exosystem level are called to advocate for inclusive spaces and educational curricula that incorporate diversity of thought and pedagogical practices that cater to all student groups. Other examples of exosystem-level advocacy include involvement with academic units, institutions, organizations such as NAFSA and the American College Personnel Association, and communities that indirectly impact international students (Manzano et al., 2017). Trainings for educators and staff at colleges/universities about the importance of dismantling systemic racism and facilitating anti-oppressive pedagogy may also be provided (Berlak, 2004).
Furthermore, community counselors working with this population may collaborate with various social groups (e.g., host families) to develop antiracist approaches that address internalized racism and White supremacy (Kendi, 2019; Singh, 2019). These collaborations may also aid in facilitating the help-seeking behavior of international students and countering the embedded stigma against seeking mental health support (Liu et al., 2020).
Macrosystem
The macrosystem-level focus is on cultural norms, values, and laws that influence the international student without being directly influenced by the student (Bronfenbrenner, 1979). At this level, college counselors may collaborate with other health specialists (e.g., community mental health counselors, social workers, medical doctors) and explore how current U.S. political structures impact the mental health and well-being of international students. These alliances can help students as counselors engage in advocacy initiatives and tackle public policy on behalf of the student (Chan et al., 2019). For example, college counselors can engage in advocacy efforts similar to those that encouraged college and university administrators to oppose the ICE policy by President Trump that targeted international students.
In addition to seeking change to public policies that discriminate against international students, college counselors working at the macrosystem level can also advocate for equitable practices within college and university systems and promote an educational climate that celebrates international students on campuses. Forming alliances with stakeholders (e.g., administrators, legislators, legislative staff) who directly and indirectly impact cultural norms and values in society could also be a helpful strategy for counselors supporting international students at the macrosystem level (Mac et al., 2019). Similarly, community counselors can offer cultural sensitivity training programs to members of local government agencies (e.g., credit unions, DMV). Knowledge of how visa regulations and cultural norms operate can help state and national organizations better serve this population. Finally, platforms such as the National Association for College Admission Counseling and The Chronicle of Higher Education may offer unique spaces for collaboration among counselors, educators, and allies to advocate for this community.
Chronosystem
The chronosystem encompasses all other societal systems that directly and indirectly impact the international student over time (e.g., federal employment policies; Bronfenbrenner, 1979). Interventions at the chronosystem level could address how the transition from an international student to worker in the United States (e.g., H-1B visa–holding professional) impacts how they are perceived by American society. For example, counselors can design programs that identify and address the needs of international students based on past and current sociopolitical events (e.g., 9/11 attacks, COVID-19 pandemic). Furthermore, college counselors may consider how these sociopolitical events might lead to disparaging attitudes toward international students and actively work to facilitate workshops, webinars, or trainings that identify and dispel harmful notions. Both college and community counselors must critically consider how systems continue to evolve over time (Chan et al., 2019). Therefore, they need to be actively attuned to the needs of international students, stay abreast of the current events that affect them, and actively participate in professional advocacy efforts across various systemic levels (e.g., institutional, state, national) to continue supporting this vulnerable community.
Future Directions
Using the search terms listed earlier, we completed an extensive review of the counseling literature. A paucity of empirical research exists in the counseling profession on international students’ mental health needs and experiences from a critical and systemic perspective. Empirical data can help counselors discern which types of interventions are most effective for international students within the counseling setting across various systems. In this article, we highlight that because of racial, linguistic, gender, and other differences within the international student community, an intersectional approach to inquiry is necessary. For instance, the experiences of a White, German, male international student will be vastly different from the experiences of a Black, Ghanaian, female student. Thus, inquiry on the experiences of this community must be positioned in the intersectionality framework (Crenshaw, 1989). Limited access to critical scholarship on the mental health experiences of international students within the counseling setting puts counselors at risk for retraumatizing their minoritized clients (Jones et al., 2017) through potential use of microaggressions and stereotypes, as shared by participants in the study by Liu et al. (2020). Thus, a tutorial stance grounded in cultural humility (Hook et al., 2013) and openness may be needed to build a safe and meaningful therapeutic relationship (Gonzalez et al., 2020). Future inquiries may help practitioners develop training modules and culturally responsive resources to improve their counseling skills and advocacy work with international students.
Conclusion
This article outlines a critical feminist and bioecological systems approach to supporting international students who are at higher risk for mental health distress because of xenophobic policies, racial discrimination, and systemic barriers. Discriminatory attitudes and behaviors toward international students have heightened during the current COVID-19 pandemic. Amidst this burgeoning crisis, counselors practicing in all settings are called to consider how each of these factors uniquely contribute to the mental health and overall well-being of this vulnerable population. Future research is needed to establish specific interventions that are most effective in mitigating the effects of pandemic-related stressors on the mental health of international students. Counselors are called to engage in advocacy efforts that dismantle systems of oppression at various levels, including within the community, in university/college settings, and in state and federal policies.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Archer, L. (2007). Diversity, equality and higher education: A critical reflection on the ab/uses of equity
discourse within widening participation. Teaching in Higher Education, 12(5–6), 635–653.
https://doi.org/10.1080/13562510701595325
Anandavalli, S. (2020). Lived experiences of international graduate students of color and their cultural capital: A critical
perspective [Doctoral dissertation, The University of North Carolina at Greensboro]. Dissertation
Abstracts International Section A: Humanities and Social Sciences. https://libres.uncg.edu/ir/uncg/f/
Anandavalli_uncg_0154D_12696.pdf
Auerbach, R. P., Mortier, P., Bruffaerts, R., Alonso, J., Benjet, C., Cuijpers, P., Demyttenaere, K., Ebert, D. D., Green, J. G., Hasking, P., Lee, S., Lochner, C., McLafferty, M., Nock, M. K., Petukhova, M. V., Pinder-Amaker, S., Rosellini, A. J., Sampson, N. A., Vilagut, G., Zaslavsky, A. M., & Kessler, R. C. (2018). Mental disorder comorbidity and suicidal thoughts and behaviors in the World Health Organization World Mental Health Surveys International College Student Initiative. International Journal of Methods in Psychiatric Research, 28(2), 1–16. https://doi.org/10.1002/mpr.1752
Berlak, A. C. (2004). Confrontation and pedagogy: Cultural secrets, trauma, and emotion in antioppressive pedagogies. Counterpoints, 240, 123–144. www.jstor.org/stable/42978384
Bonilla-Silva, E. (2013). Racism without racists: Color-blind racism and the persistence of racial inequality in America (4th ed.). Rowman & Littlefield.
Bronfenbrenner, U. (1979). The ecology of human development: Experiments by nature and design. Harvard University Press.
Bronfenbrenner, U. (1994). Ecological models of human development. In International Encyclopedia of Education (Vol. 3, 2nd ed., pp. 37–43). Elsevier.
Carter, R. T., Johnson, V. E., Kirkinis, K., Roberson, K., Muchow, C., & Galgay, C. (2019). A meta-analytic review of racial discrimination: Relationships to health and culture. Race and Social Problems, 11, 15–32. https://doi.org/10.1007/s12552-018-9256-y
Chae, M. H., & Foley, P. F. (2010). Relationship of ethnic identity, acculturation, and psychological well-being among Chinese, Japanese, and Korean Americans. Journal of Counseling & Development, 88(4), 466–476. https://doi.org/10.1002/j.1556-6678.2010.tb00047.x
Chan, C. D., DeDiego, A. C., & Band, M. P. (2019). Moving counselor educators to influential roles as advocates: An ecological systems approach to student-focused advocacy. Journal of Counselor Leadership and Advocacy, 6(1), 30–41. https://doi.org/10.1080/2326716X.2018.1545614
Chirikov, I., & Soria, K. M. (2020). International students’ experiences and concerns during the pandemic. SERU Consortium, University of California – Berkeley and University of Minnesota. https://docs.google.com/document/d/1lZdc4dWiX9C_8o1vH-4H7XokIHoJ4yjjVNRv0vS3tBE/edit#headin
g=h.ivkygr983tef
Choi, S., Lewis, J. A., Harwood, S., Mendenhall, R., & Huntt, M. B. (2016). Is ethnic identity a buffer? Exploring the relations between racial microaggressions and depressive symptoms among Asian-American individuals. Journal of Ethnic & Cultural Diversity in Social Work, 26(1–2), 18–29. http://doi.org/10.1080/15313204.2016.1263815
Christensen, J. (2016). A critical reflection of Bronfenbrenner’s development ecology model. Problems of Education in the 21st Century, 69, 22–28. https://doi.org/10.13140/RG.2.1.2959.7681
Clough, B. A., Nazareth, S. M., Day, J. J., & Casey, L. M. (2018). A comparison of mental health literacy, attitudes, and help-seeking intentions among domestic and international tertiary students. British Journal of Guidance & Counselling, 47(1), 123–135. https://doi.org/10.1080/03069885.2018.1459473
Crenshaw, K. W. (1989). Demarginalizing the intersection of race and sex: A Black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. University of Chicago Legal Forum, 1989(1), 139–167.
Devakumar, D., Shannon, G., Bhopal, S. S., & Abubakar, I. (2020). Racism and discrimination in COVID-19 responses. The Lancet, 395(10231), 1194. https://doi.org/10.1016/S0140-6736(20)30792-3
Dovchin, S. (2020). The psychological damages of linguistic racism and international students in Australia. International Journal of Bilingual Education and Bilingualism, 23(7), 804–818. https://doi.org/10.1080/13670050.2020.1759504
Garcini, L. M., Domenech Rodríguez, M. M., Mercado, A., & Paris, M. (2020). A tale of two crises: The compounded effect of COVID-19 and anti-immigration policy in the United States. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S230–S232. https://doi.org/10.1037/tra0000775
George Mwangi, C. A., Changamire, N., & Mosselson, J. (2019). An intersectional understanding of African international graduate students’ experiences in U.S. higher education. Journal of Diversity in Higher Education, 12(1), 52–64. https://doi.org/10.1037/dhe0000076
Germer, C. K., & Neff, K. D. (2015). Cultivating self-compassion in trauma survivors. In V. M. Follette, J. Briere, D. Rozelle, J. W. Hopper, & D. I. Rome (Eds.), Mindfulness-oriented interventions for trauma: Integrating contemplative practices (pp. 43–58). Guilford.
Gonzalez, E., Sperandio, K. R., Mullen, P. R., & Tuazon, V. E. (2020). Development and initial testing of the Multidimensional Cultural Humility Scale. Measurement and Evaluation in Counseling and Development, 1–16. https://doi.org/10.1080/07481756.2020.1745648
Haskins, N. H., & Singh, A. (2015). Critical race theory and counselor education pedagogy: Creating equitable training. Counselor Education and Supervision, 54(4), 288–301. https://doi.org/10.1002/ceas.12027
Hook, J. N., Davis, D. E., Owen, J., Worthington, E. L., Jr., & Utsey, S. O. (2013). Cultural humility: Measuring openness to culturally diverse clients. Journal of Counseling Psychology, 60(3), 353–366. https://doi.org/10.1037/a0032595
Houshmand, S., Spanierman, L. B., & Tafarodi, R. W. (2014). Excluded and avoided: Racial microaggressions targeting Asian international students in Canada. Cultural Diversity and Ethnic Minority Psychology, 20(3), 377–388. https://doi.org/10.1037/a0035404
Institute of International Education. (2019). Fast facts Open Doors 2019. https://opendoorsdata.org/fast_facts/fast-facts-2019
Jones, L. K., Rybak, C., & Russell-Chapin, L. A. (2017). Neurophysiology of traumatic stress. In T. A. Field, L. K. Jones, & L. A. Russell-Chapin (Eds.), Neurocounseling: Brain-based clinical approaches (pp. 61–80). American Counseling Association. https://doi.org/10.1002/9781119375487.ch4
Kendi, I. X. (2019). How to be an antiracist. One World.
Kim, N., Oh, S., & Mumbauer, J. (2019). Supporting international students: Enhancing college counselors’ multicultural counseling competence. Journal of College Counseling, 22(2), 179–192. https://doi.org/10.1002/jocc.12129
Lee, J. J., & Rice, C. (2007). Welcome to America? International student perceptions of discrimination. Higher Education, 53(3), 381–409. https://doi.org/10.1007/s10734-005-4508-3
Lértora, I. M., & Croffie, A. L. (2020). Using relational-cultural theory to conceptualize international student transitions. Journal of Creativity in Mental Health, 15(1), 30–42. https://doi.org/10.1080/15401383.2019.1638862
Litam, S. D. A. (2020). “Take your Kung Flu back to Wuhan”: Counseling Asians, Asian Americans, and Pacific Islanders with race-based trauma related to COVID-19. The Professional Counselor, 10(2), 144–156. https://doi.org/10.15241/sdal.10.2.144
Litam, S. D. A., & Hipolito-Delgado, C. P. (in press). When being “essential” illuminates disparities: Counseling clients affected by COVID-19. Journal of Counseling & Development, 99(1).
Litam, S. D. A., & Oh, S. (in press). Ethnic identity and coping strategies as moderators of COVID-19 racial discrimination experiences among Chinese Americans. Counseling Outcome Research and Evaluation.
Liu, H., Wong, Y. J., Mitts, N. G., Li, P. F. J., & Cheng, J. (2020). A phenomenological study of East Asian international students’ experience of counseling. International Journal for the Advancement of Counselling, 42(3), 269–291. https://doi.org/10.1007/s10447-020-09399-6
Lyu, H., Chen, L., Luo, J., & Wang, Y. (2020). Sense and sensibility: Characterizing social media users regarding the use of controversial terms for COVID-19. https://covid-19.conacyt.mx/jspui/bitstream/1000/1890/1/1100781.pdf
Mac, J., Sarreal, A. D., Wang, A. C., & Museus, S. D. (2019). Conditions that catalyze the emergence of Asian American and Native American Pacific Islander serving institutions. New Directions for Higher Education, 2019(186), 67–77. https://doi.org/10.1002/he.20324
Manzano, L. J., Poon, O. A., & Na, V. S. (2017). Asian American student engagement in student leadership and activism. New Directions for Student Services, 2017(160), 65–79. https://doi.org/10.1002/ss.20244
Moradi, B., & Grzanka, P. R. (2017). Using intersectionality responsibly: Toward critical epistemology, structural analysis, and social justice activism. Journal of Counseling Psychology, 64(5), 500–513.
https://doi.org/10.1037/cou0000203
Mosley, D. V., Hargons, C. N., Meiller, C., Angyal, B., Wheeler, P., Davis, C., & Stevens-Watkins, D. (2020). Critical consciousness of anti-Black racism: A practical model to prevent and resist racial trauma. Journal of Counseling Psychology. https://doi.org/10.1037/cou0000430
National Association of Foreign Student Advisers: Association of International Educators. (2020). Losing talent 2020: An economic and foreign policy risk America can’t ignore. https://www.nafsa.org/sites/default/files/media/document/nafsa-losing-talent.pdf
Ong, A. D., Burrow, A. L., Fuller-Rowell, T. E., Ja, N. M., & Sue, D. W. (2013). Racial microaggressions and daily well-being among Asian Americans. Journal of Counseling Psychology, 60(2), 188–199.
https://doi.org/10.1037/a0031736
Page, N., Beecher, M. E., Griner, D., Smith, T. B., Jackson, A. P., Hobbs, K., & Kirchhoefer, J. (2019). International student support groups: Learning from experienced group members and leaders. Journal of College Student Psychotherapy, 33(3), 180–198. https://doi.org/10.1080/87568225.2018.1450106
Ploner, J., & Nada, C. (2020). International student migration and the postcolonial heritage of European higher education: Perspectives from Portugal and the UK. Higher Education, 80(2), 373–389.
https://doi.org/10.1007/s10734-019-00485-2
Pottie-Sherman, Y. (2018). Retaining international students in northeast Ohio: Opportunities and challenges in the ‘age of Trump.’ Geoforum, 96, 32–40. https://doi.org/10.1016/j.geoforum.2018.07.015
Ratts, M. J. (2017). Charting the center and the margins: Addressing identity, marginalization, and privilege in counseling. Journal of Mental Health Counseling, 39(2), 87–103. https://doi.org/10.17744/mehc.39.2.01
Ratts, M. J., & Greenleaf, A. T. (2017). Multicultural and social justice counseling competencies: A leadership framework for professional school counselors. Professional School Counseling, 21(1b), 1–9.
https://doi.org/10.1177/2156759X18773582
Ratts, M. J., Singh, A. A., Nassar-McMillan, S., Butler, S. K., & McCullough, J. R. (2015). Multicultural and social justice counseling competencies. https://www.counseling.org/docs/default-source/competencies/multicultural-and-social-justice-counseling-competencies.pdf?sfvrsn=8573422c_20
Sawir, E., Marginson, S., Deumert, A., Nyland, C., & Ramia, G. (2008). Loneliness and international students: An Australian study. Journal of Studies in International Education, 12(2), 148–180.
https://doi.org/10.1177/1028315307299699
Singh, A. A. (2019). The racial healing handbook: Practical activities to help you challenge privilege, confront systemic racism & engage in collective healing. New Harbinger.
Sue, D. W., Alsaidi, S., Awad, M. N., Glaeser, E., Calle, C. Z., & Mendez, N. (2019). Disarming racial microaggressions: Microintervention strategies for targets, White allies, and bystanders. American Psychologist, 74(1), 128–142. https://doi.org/10.1037/amp0000296
Sue, D. W., & Sue, D. (1990). Counseling the culturally different: Theory and practice (2nd ed.). Wiley.
Tran, A. G. T. T., & Sangalang, C. C. (2016). Personal discrimination and satisfaction with life: Exploring
perceived functional effects of Asian American race/ethnicity as a moderator. Cultural Diversity and
Ethnic Minority Psychology, 22(1), 83–92. https://doi.org/10.1037/cdp0000052
U.S. Department of Labor. (n.d.). H-1B Program. https://www.dol.gov/agencies/whd/immigration/h1b
U.S. Immigration and Customs Enforcement. (2020, July 6). SEVP modifies temporary exemptions for nonimmigrant students taking online courses during fall 2020 semester. https://www.ice.gov/news/releases/sevp-modifies-temporary-exemptions-nonimmigrant-students-taking-online-courses-during
Wen, J., Aston, J., Liu, X., & Ying, T. (2020). Effects of misleading media coverage on public health crisis: A case of the 2019 novel coronavirus outbreak in China. Anatolia: An International Journal of Tourism and Hospitality Research, 31(2), 331–336. https://doi.org/10.1080/13032917.2020.1730621
The White House. (2020, June 22). Proclamation suspending entry of aliens who present a risk to the U.S. labor market following the Coronavirus outbreak. https://www.whitehouse.gov/presidential-actions/proclamation-suspending-entry-aliens-present-risk-u-s-labor-market-following-coronavirus-outbreak
Williams, C. T., & Johnson, L. R. (2011). Why can’t we be friends?: Multicultural attitudes and friendships with international students. International Journal of Intercultural Relations, 35(1), 41–48.
https://doi.org/10.1016/j.ijintrel.2010.11.001
Wong, Y. J., Wang, K. T., & Maffini, C. S. (2013). Asian international students’ mental health-related outcomes: A person × context cultural framework. The Counseling Psychologist, 42(2), 278–305.
https://doi.org/10.1177/0011000013482592
Yoon, E., & Portman, T. A. A. (2004). Critical issues of literature on counseling international students. Journal of Multicultural Counseling and Development, 32(1), 33–44. https://doi.org/10.1002/j.2161-1912.2004.tb00359.x
Zhai, Y., & Du, X. (2020). Mental health care for international Chinese students affected by the COVID-19
outbreak. The Lancet Psychiatry, 7(4), E22. https://doi.org/10.1016/S2215-0366(20)30089-4
S Anandavalli, PhD, NCC, LPC-I, is an assistant professor at Southern Oregon University. John J. S. Harrichand, PhD, NCC, CCMHC, ACS, LPC, LMHC, is an assistant professor at State University of New York at Brockport. Stacey Diane Arañez Litam, PhD, NCC, CCMHC, LPCC, is an assistant professor at Cleveland State University. Correspondence may be addressed to S Anandavalli, Clinical Mental Health Counseling, Southern Oregon University, 1250 Siskiyou Blvd, Ashland, OR 97520, anandavas@sou.edu.