Sep 13, 2024 | Volume 14 - Issue 2
Dax Bevly, Elizabeth A. Prosek
Professional counselors may choose to increase self-awareness and/or engage in self-care through the use of personal therapy. Some counselors may feel reluctant to pursue personal therapy due to stigma related to their professional identity. To date, researchers have paid limited attention to the unique concerns of counselors in personal therapy. The purpose of this descriptive phenomenological study was to explore counselors’ experiences and decision-making in seeking personal therapy. Participants included 13 licensed professional counselors who had attended personal therapy with a licensed mental health professional within the previous 3 years. We identified six emergent themes through adapted classic phenomenological analysis: presenting concerns, therapist attributes, intrapersonal growth, interpersonal growth, therapeutic factors, and challenges. Findings inform mental health professionals and the field about the personal and professional needs of counselors. Limitations and future research directions are discussed.
Keywords: professional counselors, self-awareness, self-care, personal therapy, phenomenological
Self-awareness is a fundamental part of the counseling profession. Not only do professional counselors seek to increase the self-awareness and personal growth of their clients, but counselor educators call upon counselor trainees to increase their own self-awareness before entering the field (Council for the Accreditation of Counseling and Related Educational Programs [CACREP], 2023, Section 3A11). Additionally, counselor educators often recommend self-growth experiences such as personal counseling to increase counselor trainees’ self-awareness in preparation for professional practice (Remley & Herlihy, 2020). Several scholars define counselor self-awareness as the mindfulness of thoughts, feelings, and behaviors in the self and in the counseling relationship (Fulton & Cashwell, 2015; Merriman, 2015; Rosin, 2015). Pompeo and Levitt (2014) asserted that self-awareness parallels awareness of personal values and enables counselors to explore best practices in counseling. However, after training, it becomes less clear how, if at all, counselors access their own counseling for self-growth and self-awareness; therefore, we designed the current study to explore how practicing counselors utilize personal therapy.
Correlates of Self-Awareness Among Counselors
Counselor self-awareness relates to awareness of the counseling relationship, which is helpful to client satisfaction and growth (Pompeo & Levitt, 2014); as such, several researchers have examined the clinical implications of counselor self-awareness, including professional competence, client treatment outcomes, and wellness. For example, Rake and Paley (2009) found that the therapists in their study reported modeling themselves after their own therapist as well as learning about technical aspects of a therapeutic approach. In regard to wellness, Gleason and Hays (2019) found that counselor self-awareness helped identify stressors and needs regarding personal wellness in doctoral-level counselor trainees. Similarly, Merriman (2015) discussed how self-awareness can help prevent burnout or compassion fatigue. Many researchers have investigated the importance of self-awareness as a characteristic of counselors who can competently work with culturally diverse clients (Ivers et al., 2016; Sue et al., 2022). Thus, some evidence of the clinical impact of counselor self-awareness already exists in the literature.
Expanding upon the impacts of self-awareness on the therapeutic relationship, Anderson and Levitt (2015) articulated the importance of self-awareness in how counselors’ social influence impacts the working alliance. Additionally, Tufekcioglu and Muran (2015) described how the working alliance provides a laboratory wherein the client can focus on and more clearly delineate their experience in relation to the therapist’s experience. Thus, the counseling goal of cultivating mindfulness in clients with respect to the details of their own experience involves counselors becoming mindful of the corresponding details of their own experience. Tufekcioglu and Muran argued that every encounter with a client demands the counselor’s self-reflection in the form of greater self-awareness in relation to the working alliance, and maintained that the therapeutic process should involve change for both participants.
Counselors Seeking Mental Health Care
Counselors can gain self-awareness in a variety of ways, including personal therapy. Mearns and Cooper (2017) stated that the term therapy loosely signifies the receiving of mental health services from any mental health professional who holds a license to practice. We use the word therapist in reference to researchers who did not specify the type of mental health professional (e.g., counselor, psychologist, social worker) who provided therapy to the participants in their study. Several scholars have suggested that therapists who participated in their own personal therapy experienced increased professional development as well as positive client outcomes. For example, VanderWal (2015) found that clients of counselor trainees with personal therapy experience demonstrated reduced rates of distress more quickly than clients of counselor trainees without personal therapy experience. Other researchers have noted the impact of therapy on therapists’ personal growth. Although not specific to professional counselors, Moe and Thimm (2021) conducted a systematic review of the literature regarding mental health professionals’ experiences in personal therapy and discovered benefits related to genuineness, empathy, and creation of a working alliance. Outcomes of this previous research support the positive impact of personal therapy for therapists.
Some counselors may seek personal therapy due to mental health concerns. Therefore, it is worth exploring the needs of this unique population. In one study, Orlinsky (2013) reported that therapists’ most frequently cited presenting concerns were resolving personal problems. Additionally, Moore et al. (2020) reported that counselors experienced interpersonal stress as a response to threatening situations in their clinical work and, in order to cope, neglected their own personal needs. Other investigators found a relationship between higher rates of ethical dilemmas in clinical practice and increased stress and burnout among counselors (Mullen et al., 2017). Robino (2019) introduced the concept of global compassion fatigue, a phenomenon wherein counselors experience “extreme preoccupation and tension as a result of concern for those affected by global events without direct exposure to their traumas through clinical intervention” (p. 274). In this conceptual piece, Robino summarized the literature findings on how indirect exposure of distressing events impact the mental well-being of professional helpers and advocated for the role of self-awareness as an important coping skill. Furthermore, Prosek et al. (2013) found that counselor trainees presented with elevated levels of anxiety and depression, providing further evidence that counselors are at risk for mental health concerns related to occupational and personal stressors.
Purpose of the Study
The psychological needs of counselors coupled with the emphasis on gaining self-awareness highlight the necessity for counselors’ personal therapy. Self-awareness is an important component of counselor development due to the personal nature of the profession (Pompeo & Levitt, 2014; Remley & Herlihy, 2020). Personal therapy is one way to enhance counselor self-awareness (Mearns & Cooper, 2017). Additionally, counselors may experience a variety of mental health concerns, including compassion fatigue, interpersonal conflict, depression, and anxiety (Moore et al., 2020; Mullen et al., 2017; Orlinsky, 2013; Prosek et al., 2013; Robino, 2019). Researchers have primarily focused on the perceived outcomes of personal therapy, including personal growth, professional development, and positive client outcomes (Moe & Thimm, 2021; VanderWal, 2015). However, scarce research exists regarding counselors’ decision-making processes in seeking personal therapy. Thus, if counselors could benefit from personal therapy, and if little knowledge exists regarding how counselors decide to seek personal therapy, professional counselors, counselor educators, counselor supervisors, and other mental health providers have limited information regarding how to facilitate that decision-making process.
Researchers employing qualitative investigation typically seek to holistically understand meaning. More specifically, the goal of a phenomenological approach is to capture the experiences and meaning-making from the participants’ perspectives (Creswell & Creswell, 2017). We want to illuminate how professional counselors make meaning of their experiences in personal therapy, as much of the existing literature focuses on trainees, clinical outcomes, or quantitative data. We believe describing the lived experiences, or essence (Moustakas, 1994), of counselors receiving personal therapy may lead to a deeper body of research regarding the perceptions, emotions, and behaviors of this population. The following questions guided our inquiry:
- What contributes to counselors’ decisions to seek personal therapy?
- How do professional counselors make meaning of their experiences in utilizing
personal therapy?
Method
Phenomenologists seek to understand the distinctive characteristics of human behavior and first-person experience (Hays & Singh, 2023). Based on an existentialist research paradigm, we wanted to understand how counselors make meaning of their experiences in personal therapy. Because we aimed to describe the lived experiences of counselors receiving personal therapy, descriptive phenomenology answers the research questions appropriately (Prosek & Gibson, 2021). Consistent with descriptive phenomenology, we used Miles et al.’s (2019) adaptation of classic data analysis, an inductive–deductive approach.
Research Team and Reflexivity
At the time of data collection (pre–COVID pandemic), Dax Bevly, who identifies as a White, Latina cisgender woman in her late 20s, was completing a doctoral degree in counseling. Elizabeth A. Prosek, who identifies as a White, cisgender woman, brought experience in conducting, teaching, and mentoring qualitative research studies. Bevly utilized a research team for data analysis that included four women in their early 20s completing master’s degrees in counseling; three identified as White and one identified as Asian. As instruments in the research themselves, the team needed to embrace their potential influence and impact (Hays & Singh, 2023); therefore, Bevly and Prosek participated in research reflexivity meetings several times during data collection and analysis, where they discussed thoughts and emotions evoked through their participation in the study. Descriptive phenomenology requires researchers to establish epoche, an exchange of assumptions that can be held accountable to bracket or identify throughout the process. Our research team demonstrated epoche by journaling and discussing biases and assumptions regarding the present study throughout the data analysis process. Bevly in particular was especially aware of her own personal biases due to long-term participation in personal therapy, believing it to have highly influenced her personal and professional development in a positive way. Bevly consulted with the research team as we examined experiences, reactions, and any assumptions or biases that could interfere with the coding process during data analysis. The research team members held Bevly accountable for her responses to the research process (Creswell & Creswell, 2017). The four other members of the research team also engaged in the examination of their experiences, reactions, and assumptions or biases during analysis, reporting assumed benefits including increased awareness, higher functioning in relationships, and increased self-esteem. Bevly also utilized the research team for the purpose of engaging in critical discussion during the analysis process in order to develop a trustworthy study. Furthermore, Bevly and Prosek kept a journal in order to document the research team members’ bracketing throughout the study. The journal also noted the connection and validation that Bevly experienced in interviewing participants and the care and mindfulness to not insert her personal experiences, especially regarding the overlapping roles of client and counselor as well as feelings of vulnerability.
Procedure
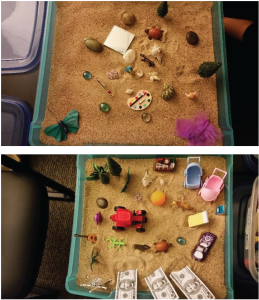
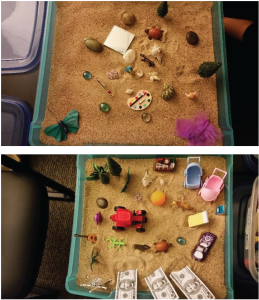
We obtained IRB approval before participant recruitment. Eligibility for the study included identifying as a licensed professional counselor (LPC) aged 18 or older who utilized counseling services with a licensed mental health therapist either currently or within the previous 3 years (similar criteria to Yaites, 2015). We used purposive sampling to select participants for this phenomenological study (Hays & Singh, 2023), recruiting participants through email, word of mouth, and networking with LPCs in a 50-mile radius of our institution, which is located in a large state in the Southwestern United States. This radius allowed us to intentionally reach more diverse areas of the geographical region. We also recruited participants through personal contacts and professional counseling organizations. Potential participants completed an eligibility online survey via Qualtrics. We contacted them via phone or email to explain the study and confirm their eligibility. We excluded participants who reported holding expired LPC licenses, experienced therapy more than 3 years ago, or described personal therapy from an individual without a license in a mental health profession. We scheduled face-to-face meetings with participants in their professional counseling office at their convenience. Although participants read and acknowledged the informed consent before meeting face-to-face, we readdressed informed consent before proceeding. Bevly conducted and audio recorded 60-minute interviews with each participant. At the conclusion of each interview, Bevly also facilitated a sand tray activity with the participant.
Participants
We recruited participants based on gaining depth with adequate sampling (Prosek & Gibson, 2021). Participants (N = 13) identified mostly as White, cisgender women with an average age of 37.23; see Table 1 for complete demographics. Although we sought to recruit participants with diverse social identities, geographic limitations presented a challenge. Thus, our findings should be interpreted with caution, as the external validity, or generalizability, of the findings to other populations or different contexts is impacted by the limited diversity among our participant demographics. Lastly, we asked participants to choose pseudonyms in an effort to protect their anonymity and confidentiality.
Data Sources
Demographic Form
In order to determine eligibility and collect demographic information, we asked potential participants to complete a Qualtrics survey, an online initial screening tool that included questions about age, gender, racial and ethnic identification, sexual orientation, religious/spiritual identity, number of personal therapy sessions completed, length of time since termination of personal therapy (if applicable), number of years as an LPC, disability status, licensure of therapist, therapist demographic information, and whether or not their counseling training program required personal therapy. The online demographic survey also included information about informed consent and confidentiality. Although it was not required for the study, all participants reported that therapy took place face-to-face.
Table 1
Participants of the Study
| Participant |
Age |
Race/Ethnicity |
Gender |
Religious/Spiritual Affiliation |
Sexual Orientation |
| Alma |
37 |
Latina |
Woman |
Christian |
Heterosexual |
| Amy |
30 |
Latina |
Woman |
Christian |
Heterosexual |
| Ashley |
29 |
Multiracial |
Woman |
Spiritual |
Heterosexual |
| Betty |
55 |
White |
Woman |
None |
Heterosexual |
| Elenore |
30 |
Multiracial |
Woman |
Christian |
Queer |
| Felicity |
44 |
White |
Woman |
Christian |
Heterosexual |
| Jennifer |
40 |
White |
Woman |
Christian |
Heterosexual |
| Liz |
35 |
White |
Woman |
Pagan |
Bisexual |
| Lynn |
48 |
White |
Woman |
Christian |
Heterosexual |
| Michelle |
37 |
White |
Woman |
Christian |
Heterosexual |
| Rose |
30 |
White |
Woman |
Christian |
Heterosexual |
| Sophia |
35 |
White |
Woman |
None |
Heterosexual |
| Thomas |
34 |
White |
Man |
None |
Heterosexual |
Semi-Structured Interview Protocol
We developed a semi-structured interview protocol to guide the interviews. We drafted the questions based on existing literature concerning counselors and personal therapy. The protocol consisted of six open-ended questions and follow-up prompts to understand the experiences of professional counselors who have engaged in personal therapy (see Table 2).
Table 2
Interview Protocol
| Grand tour question: |
| Please tell me about your experience in personal therapy in as much detail as you feel comfortable sharing. |
| Follow-up:
What motivated you to seek personal therapy?
What was happening in your life at the time?
How did you go about selecting a therapist?
Can you tell me about what your internal process (thoughts/feelings) was like leading up to your decision to seek personal therapy? |
| What outcomes did you experience as a result of personal therapy? |
| How, if at all, has personal therapy affected your personal growth? |
| How, if at all, has personal therapy affected your own clinical work? |
| Describe the experience of being both a client and a counselor.
Some literature suggests that counselors feel stigmatized when seeking personal therapy. What do you make of this? How is that similar or different for you? |
| Is there anything else that you would like to share? |
Sand Tray Activity
Hays and Singh (2023) stated that “visual methods in general provide participants the opportunity to express themselves in a nonverbal manner that may access deeper aspects of their understanding and/or experience of a phenomenon” (p. 332). After the semi-structured interview, Bevly invited participants to create their personal therapy experience in a sand tray using the figures and materials provided. This method is consistent with Measham and Rousseau (2010), who used sand trays as a method of data collection for understanding the experiences of children with trauma. The sand trays were documented by digital photos (see Appendix), and participants’ discussions about their creations are part of the audio recordings.
Data Analysis
We sent the audio recordings to a professional transcriptionist for transcription of each interview and sand tray session. We reviewed transcripts while listening to the recordings for participants’ tone and to verify accuracy. Consistent with phenomenological procedures, the research team conducted data analysis according to an adaptation of classic analysis (Miles et al., 2019), in which three main activities take place: data reduction, data presentation, and conclusion or verification.
Prior to initial coding, the research team completed several tasks in order to develop the preliminary coding manual: taking notes, summarizing notes, playing with words, and making comparisons (Miles et al., 2019). Taking notes involved the research team as well as Bevly’s own independent analysis of a subset of the first three interviews and sand tray explanation transcripts. We divided the transcripts into 10-line segments and wrote notes in the margins. The research team noted our initial reactions to the material.
Summarizing notes involved discussion between the team regarding our reactions to the interview material. We compared and contrasted our margin notes and highlighted shared perspectives and inconsistent viewpoints in a summary sheet. To play with words, we generated metaphors based on our summary sheet. We developed phrases that represented our interpretation of the participants’ interview responses.
During the making comparisons task, we compared and contrasted the key phrases developed in the previous step and grouped them into categories. The team then facilitated reduction of the data as we combined similar phrases and merged overlapping categories. Hays and Singh (2023) asserted the importance of sieving the data to eliminate redundancy. We continued to merge categories and reformat the category headings. From this process, we developed preliminary themes based on the data. To develop initial codes, we established agreement by independently applying the preliminary codes to a subset of three interviews. The research team met weekly to discuss inconsistencies and points of agreement, adjust the preliminary codes, and reapply them to the data subset. We continued to discuss any remaining discrepancies and concerns until we reached a mean agreement of 86% to 90% (Creswell & Creswell, 2017). We reached a mean agreement of 95.1% and then finalized the codes to use in our coding manual.
It is important to note that the research team sensed that we had reached saturation during the final coding process once we began to read the same comments repeatedly in the participant transcripts. In final coding, we applied the final coding manual to each of the interviews and sand tray explanations. We used the same coding manual for both the interviews and the sand tray explanations. The same research team member coded both the interview and sand tray explanation for the same participant. Bevly coded all 13 interviews and sand tray explanations; all four research team members coded the first three interviews and sand tray explanations. Two research team members coded interviews and sand tray explanations 4 through 8, and the other two research team members coded interviews and sand tray explanations 9 through 13. The research team’s finalized codes included the meaning and depth of participants’ experiences in personal therapy. However, if necessary, researchers could still recode during final coding to maintain consistency with the revised definitions (Creswell & Creswell, 2017). When recoding occurred, we reviewed previously analyzed transcripts with the updated codebook on four occasions. Once we completed final coding, Bevly performed member checks with the participants.
Establishing Trustworthiness
To develop trustworthiness in qualitative research, Lincoln and Guba (1985) presented four criteria: credibility, transferability, dependability, and confirmability. We established credibility in this study through the use of research partners in debriefing, researcher reflexivity, and participant checks. Participant checks occurred after we completed final coding. In this process, we emailed all participants a summary of the identified themes and inquired if the summary portrayed an accurate representation of the experience. Nine out of 13 participants responded and informed Bevly that no adjustments were necessary because the summary adequately captured their experiences. The remaining four participants did not respond to the follow-up email. Additionally, we utilized researcher partners in debriefing and data analysis steps to strengthen the development of the coding manual. In relation to researcher reflexivity, we bracketed our experiences by reflecting on biases and assumptions as counselors who experienced personal therapy through journaling and discussing assumptions with each other, particularly those related to positive personal experience in our own counseling. We demonstrated transferability by openly and honestly providing information about the researchers, the proposed study’s context, the participants, and study methods. This transparency allows readers to have a sense of the context when interpreting findings. We achieved dependability through documenting each task that we completed for the study by keeping an audit trail, allowing for replication. Additionally, the use of multiple data sources, including the demographic survey, interviews, and sand trays, increased the complexity of analysis (i.e., dependability). Also, we provided an in-depth description of our methodology to increase dependability of the study, including information about sample size, data collection, and data analysis that the research team used. Lastly, confirmability was based on an acknowledgement that we, as the primary researchers, cannot be truly objective (Cope, 2014). However, we triangulated the findings using participant checks, consultation with colleagues, and research team consensus to facilitate confirmability.
Findings
The research team identified six major themes and 11 subthemes (see Table 3). The six major themes were: (a) presenting concerns, (b) therapist attributes, (c) intrapersonal growth, (d) interpersonal growth, (e) therapeutic factors, and (f) challenges. We present the subthemes in more detail in the following sections using participant data as supporting evidence.
Table 3
Themes and Subthemes
| Themes |
Subthemes |
| Theme 1: Presenting concerns |
Subtheme 1a: Mental health
Subtheme 2a: Life transitions |
| Theme 2: Therapist attributes |
Subtheme 2a: Practicality
Subtheme 2b: Quality |
| Theme 3: Intrapersonal growth |
Subtheme 3a: Cognitive
Subtheme 3b: Emotional |
| Theme 4: Interpersonal growth |
Subtheme 4a: Personal
Subtheme 4b: Professional |
| Theme 5: Therapeutic factors |
Subtheme 5a: Nurturing
Subtheme 5b: Normalization
Subtheme 5c: Vulnerability
Subtheme 5d: Transference |
| Theme 6: Challenges |
Subtheme 6a: Finances
Subtheme 6b: Stigma
Subtheme 6c: Role adjustment |
Theme 1: Presenting Concerns
Presenting concerns included participants’ thoughts and feelings prior to engaging in personal therapy. Participants shared their decision-making processes and motivations leading to the initiation of personal therapy. Participants described two subthemes that captured their motivation to engage: mental health concerns and life transitions. Mental health concerns represented grief, trauma, anxiety, depression, emotional dysregulation, and relational stressors. For example, Michelle shared:
I would say those were the times when it was like I was pulled to my end, and so the depression, it was like I needed something else more than just the regular support from family and friends and then the miscarriages. It was like I felt so isolated, and then with my dad dying it was like I, gosh, this is . . . it was like both of them dying so close together.
Participants also described life transitions that served as motivation to engage in personal therapy, such as changes in relationships, careers, and living arrangements. As Lynn represented,
some of that was related to like, as a result of the divorce. I’ve moved three times in the past, like sold a house and moved out of it or kind of moved into storage while in that house in order to be able to stage it and sell it. Then out of the house into an apartment, out the apartment into a rent house. And so there’s been a lot of upheaval for me and for my child.
Presenting concerns may also be interactional in nature. For some participants (n = 10), life transitions overlapped with their mental health concerns, such as a career change triggering anxiety. However, the remaining three participants cited either mental health concerns or life transitions as a reason for initiating personal therapy. All participants differentiated their experience of internal mental health distress and external life stressors.
Theme 2: Therapist Attributes
As participants reflected on the different feelings and thought processes they experienced during the initiation of personal therapy, they also shared different attributes they looked for in a therapist. Two subthemes emerged: practicality and quality. Practicality involved factors such as location and affordability. Quality consisted of therapist credentials, training, experience, and specialty areas. All participants shared factors related to both subthemes, including Liz and Alma:
So I was like, “Okay. Well I know this person, I know this person, I know this one. Oh. I don’t know this person, okay. Let’s see if they have an opening.” I wanted someone that was close to my work because it’s easier for me just to go straight from work considering working at a hospital, I can work ridiculously long hours. Sometimes, you know, 12-hour days . . . so I needed someone in [city withheld], and I needed someone I didn’t know. (Laughs) And they took my insurance. (Liz)
I really wanted somebody who was not an intern and not a grad student. I need somebody who was fully licensed. I was looking for somebody who’d done their own work. I wouldn’t really know, but I can kind of tell. I was looking for somebody who had done their own work, their own process, and somebody who’d work with therapists. And so the first therapist that I found, she’d been a therapist for about 12 years. She had a successful private practice on her own. (Alma)
Some participants (n = 8) prioritized affordability and location over other attributes, while other participants (n = 5) emphasized education, specialty area, and recommendations as their way of selecting therapists. Each participant highlighted their need for accessibility and a good fit into their hectic schedules and personal lives. Participants described these factors as a method of narrowing down the pool of possible therapists.
Theme 3: Intrapersonal Growth
All participants expressed changes in thoughts related to self that were associated with increased perspective represented by the theme of intrapersonal growth and narrowed into subthemes of cognitive and emotional. Participants specifically reported cognitive intrapersonal growth through internal changes such as awareness, mindfulness, and a sense of purpose as outcomes of receiving personal therapy. Twelve participants described these cognitive changes as a positive experience. Jennifer described the experience as distressing due to the increased awareness of unpleasant knowledge of self and others:
I think a lot of self-awareness in the sense of why I function the way I function and an understanding of why, not only the why, but what I was needing and what I was seeking. And so, just a greater understanding of those pieces that I really had no awareness of before that. . . . I had a little awareness of it, I should say. I probably knew a little bit, but I don’t think I trusted myself in seeing that, trust in myself, trust in my intuition, and trust in my decision-making.
All participants described emotional intrapersonal growth within themselves related to regulation, stability, and expression as a result of personal therapy. Participants reported a decrease in distressing emotion, increased attunement to their emotional well-being, and an increased ability to express emotions in a healthier manner. Additionally, participants experienced fewer negative feelings toward themselves, including Thomas, who shared, “Back then I was just hiding from a lot of pain. I was hiding a lot of pain. So now I’ve been able to work through that in therapy, I’m just more emotionally attuned in general.”
All participants expressed the overlap between cognitive and emotional intrapersonal growth; furthermore, participants explained how this intrapersonal growth that occurred as a result of personal therapy carried over into other relationships. Participants shared that these internal benefits influenced external factors in their lives. Thus, the theme of intrapersonal growth led directly into the fourth theme, interpersonal growth.
Theme 4: Interpersonal Growth
All participants shared interpersonal growth, changes in relationships, and depth of social connection, both in their personal relationships and their professional relationships with clients. Participants reflected on how their growth affected relationships with romantic partners, family, friends, and clients. As a result, the two subthemes of personal relationships and professional relationships arose in the data, as expressed by Betty and Thomas:
I believe that it helped me connect with people on a deeper level. Because it’s hard to empathize or connect with someone if you can’t feel yourself. ‘Cause if you can’t feel yourself, you can’t feel what they’re feeling either. So, with my kids, I would be able to first of all, set firmer boundaries with them. And they would take me more seriously. And I’ll then also be able to connect more. And in another area, I was able to learn to ask for help. . . . instead of trying to always take care of things and handle things by myself, and to actually feel safe enough to ask for help. (Betty)
I could empathize. I could play the role of counselor and do my job, but I wasn’t doing it, like “for real for real” . . . I was falling out of what I really needed to be doing, and now I’m able to sit with clients, and every now and then my mind wanders to “oh, I gotta do this or that,” but I’m quick, I become aware of it more quickly, and I’m able to feel deeply with clients. . . . I have sessions all the time now where I’m tearing up with my clients and just feeling so moved by them. And also, I cry more in my personal life and professional life. (Thomas)
Twelve participants experienced their interpersonal growth as helpful in alleviating their presenting concerns. The remaining participant described the interpersonal growth as tense and uncomfortable. All participants explained that their interpersonal growth in personal relationships was connected to interpersonal growth in professional relationships with their clients. For example, increased boundaries with family extended to increased boundaries with clients. Participants shared that the relationship with their therapist acted as a surrogate for relationships with other people in their lives, which emerged in the therapeutic factors theme.
Theme 5: Therapeutic Factors
All participants reported avenues of healing within the context of the therapeutic alliance that led to the changes in self and in relationships. Participants reflected on how engaging in the relationship with their therapist facilitated their intrapersonal and interpersonal growth. This theme included four subthemes: nurturing, normalization, vulnerability, and transference. Seven participants described their therapist as nurturing or felt nurtured throughout the process of personal therapy. Participants reported that nurturing meant feeling safe with, trusting of, and cared for by their therapist. This atmosphere of nurturing helped participants foster the courage to take risks without fear of judgment or criticism, as expressed by Jennifer:
I felt prized, and loved, and 100% accepted. And nothing was abnormal or weird, like, what I shared. . . . her response was always super supportive. . . . My schedule was really odd, and so she made it work for my schedule. So, sometimes we met at 7:30 in the morning. Which I really appreciate. Sometimes we met at 8:00, sometimes we met at 2:00 in the afternoon . . . and I never felt like that was a burden . . . she never made it sound like I was burdening her . . . and I’m super appreciative for that.
All participants reported that their therapist, in different ways, normalized their experience. Many participants (n = 12) believed something was atypical or flawed about their personhood for needing personal therapy. Receiving help triggered feelings of stigma, self-rejection, or self-criticism. Thus, a large part of participants’ healing process was feeling normalized by the therapist. Thomas shared:
There’s even been times when I’ve asked her, like, “do I fit a diagnosis? Like, what’s wrong with me?” You know, there’s even been times when I’ve kind of demanded from her, like “what, what’s the deal? I’ve been seeing you for 2 years, tell me what’s wrong with me.” And she won’t do it. She will not do it, and she’s just like, “No, that’s not what I do.” And so that’s helped me immensely. She’s like “everything you’ve told me, every, everything fits.” And it’s helped me to see it that way.
Participants also reported feeling vulnerable as the client and described the feeling of opening themselves to the presence and feedback of another as uncomfortable but also inducing growth. Participants described this level of vulnerability as it related to their counselor identity; they explained that they were most accustomed to structuring the session and managing the time and felt more comfortable in the therapeutic relationship in the role of counselor. As the client, participants experienced a new kind of vulnerability that led to intrapersonal and interpersonal growth due to the reversed power differential, as described by Betty:
When I’m the client, it’s like, “I don’t know where we’re going, I don’t know what’s gonna come up.” It’s kind of scary sometimes. Like you know? He’s the guy with the flashlight, and I don’t know where he’s, what’s gonna happen sometimes. Like what’s going to get uncovered, [what] I’m suddenly gonna become aware of or feel, or something. So it’s a little scary.
Several participants (n = 9) shared that healing occurred as a result of therapeutic transference in the relationship with their therapist. Participants reported perceiving the therapist as a significant relationship in their life, sometimes describing their therapists as a parental presence. At times, the therapists themselves were the healing catalyst, acting as a substitute for redirecting emotional wounds. This subtheme also encompassed feelings of attachment. In many cases, participants’ early attachment figures were either emotionally or physically unavailable or harmful. Participants explained that their therapists acted as a healthy attachment figure and described this aspect of the relationship as reparative. Some participants shared feeling re-parented by their therapist, like Michelle:
She probably was the age of my mom at the time, and so I felt very nurtured by her in a way that, like I always wanted to be nurtured by mom but it hadn’t happened like that. . . . I mean, there was that transference kind of feeling that was happening, but it was very positive and she was very warm, and I feel like that relationship was so healing and allowed me to process through more things, feeling supported and encouraged by someone who is kinda like my mom but not my mom, almost like it was like a reparative thing within the relationship.
Theme 6: Challenges
Two participants shared that personal therapy was a purely positive experience without negative or uncomfortable feelings. However, 11 participants reported challenges during the course of therapy that inhibited their healing processes. These challenges included three subthemes: finances, stigma, and role adjustment, as explained by Felicity, Michelle, and Rose:
Um and then I kind of thought I was done and then I realized it was like, okay I have to add the money aspect, because every time I’m just like ugh, because I am perpetually broke. And so, I added the money like off to the side just like it’s not really part of the process but it’s this thing that exists that I can’t erase. (Felicity)
There is a stigma like that if you need to go see someone that you’re somehow like inadequate to deal with your own stuff, or that you’re crazy or that you’re really far gone, like only people who are really far gone need to do that, but I still think it’s a pride thing, you know? (Michelle)
It’s weird and it’s distracting as a client because . . . I know what she’s doing. Why is she doing that? Huh. Like it’s a good place to run to if you don’t want to go where they’re trying to take you; you can go into your analytical, left brain, logical mode. Oh, I know exactly, and you feel like an expert. You know what they’re doing. They’re not pulling it over on you. (Rose)
Five participants discussed the idea of stigma related to their counselor status. The remaining participants (n = 9) explained that they did not personally feel stigmatized, but were aware of the stigma that existed with regard to counselors who receive personal therapy. All participants shared that they would attend personal therapy longer or more frequently if not for financial barriers. Additionally, each participant described the difficulty of experiencing the identity of both client and counselor.
Discussion
We aimed to answer two overarching research questions: 1) What contributes to counselors’ decisions to seek personal therapy? and 2) How do professional counselors make meaning of their experiences in utilizing personal therapy? The results of the current study are both similar and contradictory to previous literature. For example, many researchers have demonstrated evidence of counselor burnout and compassion fatigue (Moore et al., 2020; Robino, 2019; Thompson et al., 2014). Participants described feeling burned out and lacking in empathy as motivations to seek personal therapy. Additionally, Day and colleagues (2017) outlined behavioral symptoms of burnout and compassion fatigue, including mood changes, sleep disturbances, becoming easily distracted, and increased difficulty concentrating. Many participants shared similar symptoms when discussing thoughts and feelings in their decision-making processes to initiate personal therapy, as well as when describing their mental health concerns. Therefore, it is important to assess counselors for levels of burnout and compassion fatigue in addition to raising awareness of their signs and symptoms.
The subtheme of stigma in participant voices within the current study is consistent with the existing literature. Kalkbrenner et al. (2019) found that stigma was one of three primary barriers to counseling among practicing counselors and human service professionals. Participants in our study described the general stigma and personal shame in seeking mental health treatment. Furthermore, participants differentiated between general stigma regarding mental health and stigma specific to counselors. Based on this finding, counselors may experience greater stigma than the general population when seeking personal therapy due to their professional identity. We would also like to note the research team’s personal reactions of feeling affirmed and normalized, as we had all experienced some level of stigma in seeking our own therapy—hearing and reading the participants’ experience of stigma created increased feelings of universality among our team.
With regard to theories about the working alliance, Mearns and Cooper (2017) described the notion of working at the intimate edge of the ever-shifting interface between client and counselor, referring to both the boundary between self and other and the boundary of self-awareness. Most notably in our study, the subtheme of professional interpersonal growth illuminates how the self-awareness gained in therapy impacted participants’ clinical work, supporting the working alliance theory, outlined by Mearns and Cooper (2017), which posits that expanding self-discovery and becoming more intimate with one’s own experience through the evolving relationship with the other increases intimacy in interpersonal relationships as one becomes more attuned to the self.
Aligned with the concept of professional growth, many researchers have emphasized that personal therapy was an educational or training experience for therapists and added to their professional repertoire of knowledge and skills (Anderson & Levitt, 2015; Moe & Thimm, 2021). However, these findings are not congruent with the experiences of participants in the present study. Although participants reported enhanced professional growth in terms of boundaries with clients and professional advocacy outside of the therapeutic relationship, participants shared that the intellectual aspect of personal therapy within the relationship served as a barrier to the healing process. All participants expressed a desire or intent to release themselves of their counselor identity while experiencing the client role. Thus, some counselors may not see personal therapy as a means for education or professional role modeling and instead find those aspects as distracting to the experience. It is also interesting to note that our research team’s perspectives mirrored this varied experience; through our journaling and discussion, we acknowledged that some research team members shared the experience of participants in our study, while other members felt more similarly to the preexisting literature’s conclusions.
Limitations and Future Research
The current study includes many strengths, such as the rigor we followed and trustworthiness we demonstrated. However, some limitations exist. Firstly, we collected data prior to the pandemic; a replication study post–COVID-19 could shed light on specific factors related to how the pandemic has impacted counselors’ experiences in personal therapy. Additionally, we used a single interview design, which limits the amount of extended field experience with participants. Participants may have offered more intimate and sensitive information after spending more time in the interviewing process. Due to the sensitive nature of the topic of the study, we worked to establish trust and build rapport with the participants by using introductory questions at the beginning of the interview. Researchers may collect richer data through the use of longitudinal studies that examine participants’ experiences in personal therapy over time and with other data sources. Despite plans to recruit a sample that was diverse in terms of age, gender, ethnic identification, sexual orientation, and religious/spiritual orientation, participants in this study were similar to each other. Only one participant identified as a man, and the majority of participants (n = 9) were White. We attempted to rectify the above limitations through networking with licensed professional counselors who worked in a variety of counseling settings. However, future researchers could examine the experience of counselors who identify as men or non-binary, as well as counselors of color.
Implications for Counselors
The knowledge gained from our study offers both suggestions for how clinicians can approach counselors in personal therapy and broader advocacy for the profession to increase engagement in counseling. In terms of clinical practice, participants often emphasized the struggle in assuming the client role, as they were most comfortable with the typical power differential in their professional work. This phenomenon was especially salient in the participant voices of this study; vulnerability and role adjustment were crucial themes of their experience. Therefore, it may behoove clinicians to maintain awareness of this possibility or discuss it within personal therapy. For example, Moore et al. (2020) suggested engaging in conversations about interpersonal stress, self-care, and burnout within the supervision relationship; however, we purport that clinicians of clients who are also counselors could facilitate intentional space to address these issues in counseling. That being said, mental health professionals may find benefit in balancing attending to the person of the counselor with focus on professional identity due to the barrier of role adjustment presented in this study. Neswald-Potter and colleagues (2013) suggested the use of the Wheel of Wellness Model developed by Witmer and Sweeney (1992) to facilitate an integrated approach in promoting wellness in counselors: spirituality, self-direction, work and leisure, friendship, and love. Finding meaning in all life tasks could assist clinicians in balancing professional and personal concerns in working with counselors as clients. Wellness is often associated with self-care practices in counseling.
Self-care is not a novel topic of discussion in counselor training or professional practice. However, in light of this study’s findings, we aim to describe therapeutic interventions for mental health professionals who may have counselors as clients. Coaston (2017) summarized much of the literature on self-care for counselors and recommended several strategies for interventions in three main areas: mind, body, and spirit. Concretely, interventions may include mindfulness, boundary setting, time management, cognitive reappraisal writing activities, stretching, moral inventory, and listing life principles (Coaston, 2017; Posluns & Gall, 2020). Finally, Bradley et al. (2013) outlined a variety of creative approaches to counselor self-care, as well as facilitative questions that may lend well to opening dialogue in a therapy session. Example questions include: (a) What are the indications that you are doing well and healthy? (b) Which things in the environment can be changed to help you continue to grow? and (c) Do you experience this emotion or pattern of emotions frequently? How did you respond? These suggested self-care interventions are only useful if counselors attend personal therapy, and in the results of our study, participants described how stigma remained a barrier.
Clinicians may consider normalizing thoughts and feelings related to stigma in order to encourage engagement in counseling. Sommers-Flanagan and Sommers-Flanagan (2018) defined normalization as the therapist’s use of indirect or direct statements that reframe client problems as contextual responses to the difficulties of life. Therapists use normalization to depathologize client concerns and convey implicit acceptance of the person of the client. Varying degrees of normalization skills include psychoeducation, reframing, and self-disclosure (Sommers-Flanagan & Sommers-Flanagan, 2018). Reducing the stigma of accessing counseling as a counselor may need to begin with normalizing it during training. Knaak et al. (2014) reported that the most effective anti-stigma interventions incorporate social contact, education, personal testimonies, teaching skills, and myth-busting. Therefore, creating space for anti-stigma interventions in professional development activities (e.g., conference presentations, continuing education sessions) as well as incorporating these strategies into counselor training (e.g., class or group supervision) may advocate for engagement in counseling across the counselor profession spectrum. Additionally, a follow-up study examining counselors seeking therapy to improve their own clinical efficacy with clients may also serve as a way to decrease stigma.
Lastly, we believe that the findings of our study support the need for and advocacy of personal therapy after graduate training. Unlike counselor trainee program requirements that often mandate a certain number of hours in personal therapy, fully licensed professional counselors are not regulated by licensing boards with regard to continuing personal therapy. Policy changes that include a personal therapy requirement in a similar vein as continuing education credits may positively impact counselor stigma and wellness.
Conclusion
Counselors face many challenges in their clinical work, including occupational stressors and the need for self-awareness (Moore et al., 2020; Mullen et al., 2017; Prosek et al., 2013; Robino, 2019; Thompson et al., 2014). The current descriptive phenomenological study serves to provide an understanding of the lived experiences of counselors who utilize personal therapy, including their motives to engage and meaning made while engaged. We offer clinical suggestions within the counseling relationship, steps to reduce stigma, and recommendations for facilitating self-care strategies among counselor trainees and professional counselors directly from voices of counselors who have accessed personal therapy.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Anderson, R. S., & Levitt, D. H. (2015). Gender self-confidence and social influence: Impact on working alliance. Journal of Counseling & Development, 93(3), 280–288. https://doi.org/10.1002/jcad.12026
Bradley, N., Whisenhunt, J., Adamson, N., & Kress, V. E. (2013). Creative approaches for promoting counselor self-care. Journal of Creativity in Mental Health, 8(4), 456–469. https://doi.org/10.1080/15401383.2013.844656
Coaston, S. C. (2017). Self-care through self-compassion: A balm for burnout. The Professional Counselor, 7(3), 285–297. https://doi.org/10.15241/scc.7.3.285
Council for the Accreditation of Counseling and Related Educational Programs. (2023). 2024 CACREP standards. https://www.cacrep.org/wp-content/uploads/2023/06/2024-Standards-Combined-Version-6.27.23.pdf
Creswell, J. W., & Creswell, J. D. (2017). Research design: Qualitative, quantitative, and mixed methods approaches (5th ed.). SAGE.
Day, K. W., Lawson, G., & Burge, P. (2017). Clinicians’ experiences of shared trauma after the shootings at Virginia Tech. Journal of Counseling & Development, 95(3), 269–278. https://doi.org/10.1002/jcad.12141
Fulton, C. L., & Cashwell, C. S. (2015). Mindfulness-based awareness and compassion: Predictors of counselor empathy and anxiety. Counselor Education and Supervision, 54(2), 122–133. https://doi.org/10.1002/ceas.12009
Gleason, B. K., & Hays, D. G. (2019). A phenomenological investigation of wellness within counselor education programs. Counselor Education and Supervision, 58(3), 177–194. https://doi.org/10.1002/ceas.12149
Hays, D. G., & Singh, A. A. (2023). Qualitative research in education and social sciences. Cognella.
Ivers, N. N., Johnson, D. A., Clarke, P. B., Newsome, D. W., & Berry, R. A. (2016). The relationship between mindfulness and multicultural counseling competence. Journal of Counseling & Development, 94(1), 72–82. https://doi.org10.1002/jcad.12063
Kalkbrenner, M. T., Neukrug, E. S., & Griffith, S.-A. M. (2019). Appraising counselor attendance in counseling: The validation and application of the Revised Fit, Stigma, and Value Scale. Journal of Mental Health Counseling, 41(1), 21–35. https://doi.org/10.17744/mehc.41.1.03
Knaak, S., Modgill, G., & Patten, S. B. (2014). Key ingredients of anti-stigma programs for health care providers: A data synthesis of evaluative studies. The Canadian Journal of Psychiatry, 59(1 suppl), 19–26. https://doi.org/10.1177/070674371405901S06
Lincoln, Y. S., & Guba, E. G. (1985). Naturalistic inquiry. SAGE.
Mearns, D., & Cooper, M. (2017). Working at relational depth in counselling and psychotherapy (2nd ed.). SAGE.
Measham, T., & Rousseau, C. (2010). Family disclosure of war trauma to children. Traumatology, 16(4), 85–96. https://doi.org/10.1177/1534765610395664
Merriman, J. (2015). Enhancing counselor supervision through compassion fatigue education. Journal of Counseling & Development, 93(3), 370–378. https://doi.org/10.1002/jcad.12035
Miles, M. B., Huberman, A. M., & Saldaña, J. (2019). Qualitative data analysis: A methods sourcebook (4th ed.). SAGE.
Moe, F. D., & Thimm, J. (2021). Personal therapy and the personal therapist. Nordic Psychology, 73(1), 3–28.
https://doi.org/10.1080/19012276.2020.1762713
Moore, C. M., Andrews, S. E., & Parikh-Foxx, S. (2020). “Meeting someone at the edge”: Counselors’ experiences of interpersonal stress. Journal of Counseling & Development, 98(2), 123–135. https://doi.org/10.1002/jcad.12307
Moustakas, C. (1994). Phenomenological research methods. SAGE.
Mullen, P. R., Morris, C., & Lord, M. (2017). The experience of ethical dilemmas, burnout, and stress among practicing counselors. Counseling and Values, 62(1), 37–56. https://doi.org/10.1002/cvj.12048
Neswald-Potter, R. E., Blackburn, S. A., & Noel, J. J. (2013). Revealing the power of practitioner relationships: An action-driven inquiry of counselor wellness. The Journal of Humanistic Counseling, 52(2), 177–190. https://doi.org/10.1002/j.2161-1939.2013.00041.x
Orlinsky, D. E. (2013). Reasons for personal therapy given by psychoanalytically oriented psychotherapists and their effects on personal wellbeing and professional development. Psychoanalytic Psychology, 30(4), 644–662. https://doi.org/10.1037/a0034587
Pompeo, A. M., & Levitt, D. H. (2014). A path of counselor self-awareness. Counseling & Values, 59(1), 80–94. https://doi.org/10.1002/j.2161-007X.2014.00043.x
Posluns, K., & Gall, T. L. (2020). Dear mental health practitioners, take care of yourselves: A literature review on self-care. International Journal for the Advancement of Counselling, 42, 1–20. https://doi.org/10.1007/s10447-019-09382-w
Prosek, E. A., & Gibson, D. M. (2021). Promoting rigorous research by examining lived experiences: A review of four qualitative traditions. Journal of Counseling & Development, 99(2), 167–177. https://doi.org/10.1002/jcad.12364
Prosek, E. A., Holm, J. M., & Daly, C. M. (2013). Benefits of required counseling for counseling students. Counselor Education & Supervision, 52(4), 242–254. https://doi.org/10.1002/j.1556-6978.2013.00040.x
Rake, C., & Paley, G. (2009). Personal therapy for psychotherapists: The impact on therapeutic practice. A qualitative study using interpretative phenomenological analysis. Psychodynamic Practice, 15(3), 275–294. https://doi.org/10.1080/14753630903024481
Remley, T. P., Jr., & Herlihy, B. (2020). Ethical, legal and professional issues in counseling (6th ed.). Merrill.
Robino, A. E. (2019). Global compassion fatigue: A new perspective in counselor wellness. The Professional Counselor, 9(4), 272–284. https://doi.org/10.15241/aer.9.4.272
Rosin, J. (2015). The necessity of counselor individuation for fostering reflective practice. Journal of Counseling & Development, 93(1), 88–95. https://doi.org/10.1002/j.1556-6676.2015.00184.x
Sommers-Flanagan, J., & Sommers-Flanagan, R. (2018). Counseling and psychotherapy theories in context and practice: Skills, strategies, and techniques (3rd ed.). Wiley.
Sue, D. W., Sue, D., Neville, H. A., & Smith, L. (2022). Counseling the culturally diverse: Theory and practice (9th ed.). Wiley.
Thompson, I. A., Amatea, E. S., & Thompson, E. S. (2014). Personal and contextual predictors of mental health counselors’ compassion fatigue and burnout. Journal of Mental Health Counseling, 36(1), 58–77. https://doi.org/10.17744/mehc.36.1.p61m73373m4617r3
Tufekcioglu, S., & Muran, J. C. (2015). Case formulation and the therapeutic relationship: The role of therapist self-reflection and self-revelation. Journal of Clinical Psychology, 71(5), 469–477. https://doi.org/10.1002/jclp.22183
VanderWal, B. L. (2015). The relationship between counselor trainees’ personal therapy experiences and client outcome (Publication No. 1199) [Doctoral dissertation, Western Michigan University]. https://scholarworks.wmich.edu/dissertations/1199
Witmer, J. M., & Sweeney, T. J. (1992). A holistic model for wellness and prevention over the life span. Journal of Counseling & Development, 71(2), 140–148. https://doi.org/10.1002/j.1556-6676.1992.tb02189.x
Yaites, L. D. (2015). The essence of African Americans’ decisions to seek professional counseling services: A phenomenological study [Doctoral dissertation, University of North Texas]. https://digital.library.unt.edu/ark:/67531/metadc804978
Appendix
Dax Bevly, PhD, is core faculty at Antioch University Seattle. Elizabeth A. Prosek, PhD, NCC, LPC, is an associate professor at The Pennsylvania State University. Correspondence may be addressed to Dax Bevly, Antioch University Seattle, School of Applied Psychology, Counseling, and Family Therapy, 2400 3rd Ave #200, Seattle, WA 98121, dbevly@antioch.edu.
Aug 24, 2023 | Volume 13 - Issue 2
Kyoung Mi Choi, Jung H. Hyun
This study, using a transcendental phenomenological approach, explored the perceptions and experiences of school counselor trainees participating in a self-care course grounded in mindfulness and social–emotional learning. Seven students who enrolled in a master’s-level school counseling program and completed a summer self-care course shared their experiences, leading to the identification of five key themes: (a) recognizing the importance and need for self-care, (b) cultivating a nonjudgmental mindset toward challenging emotions, (c) integrating self-care into both personal and professional settings, (d) an increase in compassion and empowerment, and (e) a commitment to ongoing learning and advocacy. The school counselor trainees’ narratives highlight the importance of self-care as a way to reclaim power within themselves and become change agents in their school communities.
Keywords: school counselor trainees, self-care, mindfulness, social–emotional learning, advocacy
The COVID-19 pandemic has dramatically changed the way we live, work, learn, and interact on a daily basis, making self-care a crucial topic of discussion in both schools and workplaces (Harrichand et al., 2021; Norcross & Phillips, 2020). Many K–12 students are facing increased emotional distress and mental health issues, such as high levels of anxiety, depression, and post-traumatic symptoms (Chen et al., 2020; Marques de Miranda et al., 2020; Prime et al., 2020). At the same time, school counselors are also struggling with issues such as fatigue, burnout, and even vicarious trauma (Parker & Henfield, 2012), along with other challenges like high workloads, uncertainty about their role, and a lack of perceived support and professional development opportunities (Savitz-Romer et al., 2021). This makes self-care for school counselors and trainees more critical now than ever before (Harrichand et al., 2021).
Self-care refers to engaging in activities or behaviors that promote one’s overall wellness and prevent burnout (Christopher et al., 2016). This concept can also be expanded to include a larger sense of self-care that encompasses embracing one’s humanity; increasing awareness of internalized negative cultural messages; and fostering a positive cultural identity that embraces one’s heritage and community strengths, assets, traditions, and legacy (Duncan-Andrade & Morrell, 2008). Some scholars view self-care as the start of personal power (hooks, 1994) and a process of humanization in education that is reciprocal, anti-oppressive, and supportive of collective well-being (Paris & Winn, 2013). Additionally, many educators and scholars believe that dismantling oppressive ideologies and power structures is an important objective in the transformative process of self-care, which involves critical self-reflection, recognition of dehumanization, and reclaiming agency (Berila, 2016; Freire, 1970/2000; hooks, 1994; Litam & Hipolito-Delgado, 2021).
The significance of self-care has led to it being viewed not just as an individual responsibility, but also a professional one. Leading counseling organizations, such as the American Counseling Association (ACA) and the Council for the Accreditation of Counseling and Related Educational Programs (CACREP), consider self-care to be a crucial aspect of a mental health professional’s duties. The ACA Code of Ethics (2014) states that “counselors engage in self-care activities to maintain and promote their own emotional, physical, mental, and spiritual well-being to best meet their professional responsibilities” (p. 8). The CACREP (2015) standards, under the Professional Counseling Identity section, include standards for counselor education programs that emphasize self-care strategies appropriate to the counselor role (Section 2.F.1.i). The American School Counselor Association (ASCA; 2019) promotes the monitoring of “emotional and physical health and practice wellness to ensure optimal professional effectiveness” for school counselors (p. 7).
However, despite the recognition of self-care as an ethical responsibility, most counseling training programs do not incorporate it as part of their curriculum (Chen et al., 2020; Christopher & Maris, 2010; Shapiro et al., 2007). Lack of time, academic pressure, and the absence of guidance and faculty role models are cited as barriers (Campbell & Christopher, 2012; Christopher & Maris, 2010; Nelson et al., 2018). Nevertheless, there is a pressing need for self-care strategies to be included in counselor training and curriculum (Mitchell & Binkley, 2021). This study utilized transcendental phenomenology to investigate the essence of self-care experiences among school counseling trainees who participated in a 10-session seminar course that focused on mindfulness and social–emotional learning (SEL).
Literature Review
Mindfulness as Humanizing Process in Self-Care
The integration of mindfulness as a self-care practice into counseling training and programs has been widely adopted over the past three decades (Bohecker & Horn, 2016; Bohecker et al., 2016; Campbell & Christopher, 2012; Christopher & Maris, 2010; Shapiro et al., 2007). Research has shown that mindfulness can lead to numerous benefits, including reduced levels of anxiety and depression, enhanced life satisfaction, increased social connection, optimism, tolerance, empathy, and self-efficacy (Bohecker & Horn, 2016; Bohecker et al., 2016; Brown & Ryan, 2003). Christopher and Maris (2010) asserted that incorporating mindfulness practices into counselor training programs could help reduce burnout, compassion fatigue, and other stress-related physical and psychological symptoms by providing education in self-care and stress management. Furthermore, Shapiro and his team (2007) found that Mindfulness-Based Stress Reduction training had a significant impact, decreasing stress levels, negative affect, rumination, and anxiety, and boosting positive affect and self-compassion.
Moreover, mindfulness is more than just a form of relaxation, but a transformative and proactive approach to self-care. It involves increased awareness of internalized negative cultural messages and the cultivation of a positive cultural identity (Duncan-Andrade & Morrell, 2008). The practice of mindfulness can lead to critical self-reflection and bring to the surface issues of power and privilege, and through deep reflection and honest dialogue, can support the process of humanization and the dismantling of oppressive ideologies (Berila, 2016; del Carmen Salazar, 2013).
Given the high levels of stress and burnout that school counselors commonly experience, prioritizing self-care practices is crucial for maintaining their personal and professional well-being. Mindfulness-based self-care has emerged as a promising approach for addressing these challenges and provides a unique opportunity for school counselors to reflect on their identities within societal and cultural contexts. Additionally, the SEL framework can be helpful in self-care training by outlining specific skills essential for managing stress, fostering well-being, and developing advocacy in both personal and professional contexts.
Social–Emotional Learning
SEL is defined as “the process in which children enhance their ability to integrate thinking, feelings, and behaving to achieve important life tasks” (Zins et al., 2007, p. 194). The Collaborative for Academic, Social, and Emotional Learning (CASEL) outlines five core competencies of SEL: self-awareness, self-management, social awareness, relationship skills, and responsible decision-making (CASEL, 2023a). CASEL’s mission is to make SEL a fundamental aspect of every child’s education through offering training and educational opportunities to advance scientific research, assessment, and implementation of effective SEL practices in schools (CASEL, 2023b). Numerous studies have demonstrated the positive impact of SEL programs on students’ growth (Carrell & Carrell, 2006; Durlak & DuPre, 2008; Lapan & Harrington, 2009).
Despite the positive effects of SEL in education, its traditional definition has faced numerous criticisms for its inadequacy in addressing equity and justice issues in classrooms and the educational system in light of recent racial and gender awareness. Higheagle Strong and McMain (2020) argued that the traditional SEL approach reinforces oppressive ideologies by valuing White, middle-class knowledge systems above others, portraying marginalized students as troubled and incompetent, and perpetuating injustice. With a growing emphasis on cultural responsiveness in the SEL definition (Higheagle Strong & McMain, 2020; Jagers et al., 2019), a critical question arises: “Are we teaching individual students to manage their emotions and behaviors simply for the sake of upward mobility or recognize and reclaim their emotions and relationships as fuel for social and cultural healing and transformation?” (Camangian & Cariaga, 2021, p. 16).
CASEL subsequently revised their definition of SEL and introduced a new concept of transformative SEL, defined as “a process whereby students and teachers build strong, respectful relationships founded on an appreciation of similarities and differences; learn to critically examine root causes of inequity; and develop collaborative solutions to community and social problems” (Jagers et al., 2018, p. 2). This updated definition acknowledges existing educational disparities and places an emphasis on authentic partnerships between schools, families, and communities. It also calls for a re-examination of the curriculum, instructional methods, and evaluation systems. Educators are encouraged to adopt an equity-focused lens when assessing the five core SEL competencies, asking questions such as “What are the social dynamics among students from different backgrounds in your class? Do you view these differences as a liability or an asset?”, “How do you create an inclusive and safe learning environment for all your students?”, and “Are there policies or practices in your school that prevent your students from receiving the quality education they deserve?”
Overall, the principles of SEL are closely aligned with the goals of school counseling, particularly in developing the skills necessary for promoting the social, emotional, and cognitive development of their students and promoting equity, social justice, and cultural competence necessary for supporting diverse student populations. School counselors can leverage SEL strategies to create a welcoming and inclusive environment that fosters learning, resilience, and well-being among students. Van Velsor (2009) emphasized the role of school counselors as SEL consultants, empowering students to achieve their personal goals and promoting prosocial behaviors, with the ultimate aim of improving the well-being of both the school and society.
Self-care has been integrated into the ethical standards of school counselor preparation programs (Christopher et al., 2016; Nelson et al., 2018), and mindfulness is often taught and studied in these programs (Campbell & Christopher, 2012; Christopher & Maris, 2010). However, there has been a lack of research investigating the experiences of school counselor trainees when learning and practicing self-care alongside mindfulness and SEL competencies in counselor education. In this study, we created and implemented a self-care curriculum for school counseling trainees and examined how this curriculum impacted their personal and professional lives through the use of transcendental phenomenology. The goal was to delve into the experiences of master’s students who took part in a summer course on self-care that was grounded in both mindfulness and SEL.
Methodology
The transcendental phenomenological investigation is often used in research to explore individuals’ subjective experiences and perceptions of a particular phenomenon (Giorgi, 2009; Moustakas, 1994). Using this approach, we aimed to explore the school counseling trainees’ thoughts, feelings, and behaviors of the personal and professional changes in the areas of self-awareness, self-management, social awareness, relationship skills, and responsible decision-making. The umbrella research question that guided this study was “What is the essence of the lived experiences of self-care of school counseling trainees who took 10 seminar sessions grounded in mindfulness and SEL in a master’s-level counseling program over a 5-week period?” Semi-structured interview questions were used to explore the participants’ experiences in their own words, which are detailed in Appendix A. After the approval from the IRB, we invited counseling trainees to participate in the study and followed the three steps of Moustakas’s (1994) transcendental approach: (a) the epoche, (b) the eidetic reduction, and (c) the transcendental reduction in data analysis.
Participants
The purposive sampling method outlined by Glesne (2011) was utilized to select participants for the study. Invitations were extended to all 15 students who had completed the EDCO 298 Seminar in Professional Counseling during the summer course. Based on the guidelines set by Polkinghorne (1989), a sample size of 5–25 individuals is recommended for a phenomenological study. Seven participants, who were female graduate students in the counselor education program, agreed to take part in the study through in-depth interviews. The participants were between the ages of 21 and 45 and attended a single, midsized, public university designated as a Hispanic-Serving Institution in Northern California, United States. Five of the participants identified as Hispanic, Mexican, or Latinx, while two identified as White.
Data Collection
The data for this study was collected through qualitative interviews with individuals who had completed a summer course, EDCO 298 Seminar in Professional Counseling, taught by Kyoung Mi Choi. To ensure impartiality and minimize the impact of the professor’s influence, three precautions were taken: (a) participants were contacted at least 14 days after the course had ended and their grades were posted, (b) they were informed that participation in the study was voluntary, and (c) all interviews were conducted by Jung Hee Hyun, who had no association with the program and held no power over the students’ grades.
Description of the Course
In summer 2020, Choi created an online 5-week course called EDCO 298 Seminar in Professional Counseling, which is detailed in Appendix B. The focus of the course was on self-care, combining six mindfulness core values (such as presence, gratitude, and compassion) and the five SEL competencies framework (self-awareness, self-management, social awareness, relationship skills, and responsible decision-making). The course was attended by 15 master’s-level school counseling students. The aim of the class was to encourage and inspire the students to make a deeper connection with their thoughts, emotions, and physical well-being.
The objectives of the course were to (a) explore the five SEL competencies, (b) explore the mindfulness-based self-care and SEL interventions for counseling and personal growth, (c) understand the effectiveness of the SEL tools and practice mindfulness in daily life, and (d) create a workshop that serves the community the student hopes to serve. The instructor’s role was to create a supportive and safe environment in which students could share their personal narratives and experiences, including their strengths, cultural assets, resilience, privilege, discrimination, and oppression. Throughout the course, various mindfulness practices were utilized, such as collective breathing, body scan, mindful walking, mindful eating, mindful speaking, journaling, storytelling, visualization, and meditation.
Individual Interviews
After the summer session was over, Choi’s counselor education department gave permission to announce the research project via email. Those who showed interest in participating were given a research packet containing details of the study, informed consent, and a demographic sheet, as well as contact information for further inquiries. At every stage of the recruitment and research process, it was emphasized that participation or non-participation in the study would not affect the participants’ course credit or final grade. To be eligible for the study, participants had to meet the following criteria: (a) enrolled in the counselor education program, (b) completed the summer seminar, (c) successfully finished the entire course, and (d) willing to participate in a voluntary lengthy interview.
Once students agreed to participate in the study and submitted their informed consent, contact information, and demographic questionnaire (including a pseudonym, gender, age, self-identified ethnicity, and specialization), they were individually interviewed by Hyun through Zoom. The interviews lasted for approximately an hour and followed a semi-structured format consisting of 16 open-ended questions asked in a consistent order (see Appendix A). The interviews were recorded in their entirety and then transcribed by a graduate student who was not affiliated with the study. After being reviewed by the participants and analyzed by the researchers, the audio recordings were deleted. To maintain the confidentiality of the participants, only pseudonyms were used in all written materials.
Data Analysis
The research methodology employed by the team was transcendental phenomenology (Moustakas, 1994), aimed at uncovering the fundamental nature of human experience (Moerer-Urdahl & Creswell, 2004). NVivo12, a qualitative data analysis software by QSR International (2018), was utilized for data storage, coding, and retrieval. To analyze the data, we followed Moustakas’s (1994) steps for data analysis, which involved the following process: (a) the researchers reflected on and recorded their own experiences of self-care, mindfulness, and critical consciousness before, during, and after data collection; (b) the transcripts were imported into NVivo12, and key statements that provided insight into the participants’ experiences of self-care were highlighted (horizontalization); (c) themes were formed by summarizing these significant statements (cluster of meanings); (d) the significant statements and themes were used to describe the participants’ experiences as a collective whole (textural description); (e) the context that influenced the participants’ experiences of self-care was described using the significant statements and themes (imaginative variation/structural description); and (f) a synthesis of the meanings and essence of the experience was provided by integrating all of the textual and structural descriptions into a universal description.
Reflexivity Statement
Choi is a professor and holds a master’s degree in school counseling and international relations, as well as a doctorate in counselor education and supervision. She has been teaching at the master’s level for over a decade and has received extensive training in mindfulness, yoga, and SEL. Hyun is an associate professor specializing in school counseling and holds a master’s degree in school counseling and a doctorate in counselor education. She provides counseling and consultation to children and parents using play therapy and multicultural counseling interventions. Choi taught the course that the study is based on, while Hyun conducted the participant interviews. Both Choi and Hyun have prior experience in qualitative research and are dedicated to promoting multiculturalism and social justice in counselor education.
In our research, we utilized the epoche technique, which involves temporarily setting aside our preconceived beliefs and assumptions about self-care to approach the research with an open mindset. Throughout the research process, we made a conscious effort to examine and clarify our assumptions to avoid potential biases. We also practiced reflexivity by reflecting on our own positionality and how it could affect our assumptions and interpretations of the data. This approach helped us to ensure that our findings were based on the actual experiences and perspectives of the participants, rather than on our own assumptions. Our assumptions about self-care included the following: (a) the importance for counselors to be responsible about self-care; (b) the impact of self-care practice on both personal and professional life; (c) the necessity for counseling programs to provide specific tools and strategies to support students in developing the knowledge and skills for self-care; (d) the holistic approach of self-care, encompassing cognitive, emotional, physical, interpersonal, and spiritual well-being; (e) the gradual development and continual practice required for self-care ability; (f) the possibility of self-care looking different based on individual and cultural backgrounds; and (g) the transformation process of self-care, facilitating the humanization process, increasing awareness of internalized oppressive messages and cultural identities and leading to individual and collective liberation.
Establishing Trustworthiness
In order to enhance the reliability and validity of the study, we employed the use of an external auditor and member checking (Glesne, 2011; Hays & Wood, 2011; Lincoln & Guba, 1985). The external auditor, a research assistant with previous experience in phenomenological approaches but no prior knowledge of self-care or mindfulness research, was appointed to assist in increasing the credibility of the study. The external auditor reviewed the research process, examined the interview process for potential biases, and verified the interpretations of the data. Additionally, we utilized member checking, in which we presented emergent themes and interview content to the participants to ensure their agreement with the written comments and to check for any additional information or edits.
Findings
We identified five themes that reflect the perceptions and experiences of school counseling trainees regarding self-care grounded on mindfulness and SEL: (a) recognizing the importance and need for self-care, (b) cultivating a nonjudgmental mindset toward challenging emotions, (c) integrating self-care into both personal and professional settings, (d) an increase in compassion and empowerment, and (e) a commitment to ongoing learning and advocacy. These themes, which capture the essence of the participants’ experiences, are contextualized as follows.
Theme One: Recognizing the Importance and Need for Self-Care
Participants in a summer course focused on self-care were aware of their motivations and inspiration for registering for the course. They reported their experiences of struggle and challenges in their lives, particularly during the COVID-19 pandemic. Elizabeth stated, “I was facing personal challenges. This course arrived just when I needed it the most.” Sophia added, “I was struggling with intense emotions during the lockdown period and had doubts about myself. But after taking the first class, I felt that it was meant for me.”
Despite the eagerness of all participants to gain knowledge on self-care, they lacked a clear understanding of the concept. The term “self-care” had been mentioned in other classes within the counseling program, but the application of self-care through mindfulness and SEL was unfamiliar to most of them. Daisy expressed:
I never truly comprehended the meaning of connecting with oneself, which requires dedicating time for personal reflection within daily activities and establishing a connection with one’s body and emotions. This was a new idea for me, as I had not previously implemented or even recognized its significance before participating in the course.
The participants were amazed to discover the relationship between their body, mind, emotions, and nature when they made time for self-reflection and self-care. Stacy expressed, “I never considered the idea of self-care before. This class has shown me that some of the things I already do actually fall under the category of self-care.” Sophia also said, “Self-compassion, I did hear about it or read about it, but I never truly dedicated myself to practicing it.” Furthermore, Stacy added, “I never realized the importance of having a complete connection between the body and nature.”
Theme Two: Cultivating a Nonjudgmental Mindset Toward Challenging Emotions
The participants shared their difficulties in managing emotions such as anxiety, depression, anger, disappointment, uncertainty, and shame. They found learning practical mindfulness strategies to recognize and process these emotions without judgment to be helpful. Elizabeth shared how she connected with her body and was able to understand the physical and emotional cues signaling her needs through increased self-awareness:
I have always been constantly on the move and never took the time to acknowledge my physical and emotional well-being. This class taught me the importance of paying attention to my body’s signals, both physical and mental, signaling the need to slow down. I learned to recognize signs, such as backaches, sore muscles, and headaches, and to listen to what they are trying to tell me about my overall well-being.
Sara echoed, saying, “Self-awareness is about embracing and loving myself.” Veronica, who identified as an immigrant, shared her insight on the impact of self-compassion and a shift in perspective:
As an English learner, I often get nervous during public speaking or classroom presentations because I self-doubt. That’s where self-compassion has played a crucial role for me. Instead of viewing myself as someone who doesn’t speak perfect English, I see myself as someone who has accomplished much despite being an immigrant. I used to struggle with low self-confidence, but after being introduced to self-compassion, it has opened my eyes to see everything as a growth opportunity rather than a potential failure. It’s about focusing on what you have, rather than what you lack, and viewing yourself as a human being like any other. This shift in perspective has been healing.
Carol explained how the class aided her in processing challenging emotions, saying “I learned to create space between myself and my emotions, have more control over impulsive emotions, and take breaks to have fun or engage in self-care.” Daisy summarized her approach to dealing with challenging emotions by saying, “The course taught me that it’s okay to accept my feelings, allowing myself to experience them without judgment. I understand that they are temporary and by processing them, I am able to let them go.”
Theme Three: Integrating Self-Care Into Both Personal and Professional Settings
A strong connection between understanding the importance of self-care and its practical application in daily life was evident in the narratives of all participants. They explored, experimented with, and reinforced a variety of self-care strategies both in and outside of class. Sophia stated, “The class helped me to become more patient, and I now practice those techniques daily.” Elizabeth also spoke of the impact of the class and her daily self-care practices:
I realized the enormous benefits of taking time for myself, both in the morning to start my day and in the evening to relax. Practicing mindfulness and self-care, such as staying aware of my body’s signals through yoga, stretching, and breathing, has been incredibly helpful. My physical healing has become a path to emotional healing. I’m making a conscious effort to care for myself. The class was the perfect introduction to this.
Veronica echoed similar experiences in implementing what she learned from the course.
I feel like I gained a lot from this course because we were able to put what we learned into practice. This class provided a deeper understanding of the subject through reading and trying different practices such as meditation and deep breathing. I’ve made a conscious effort to practice mindfulness daily, instead of only when I felt the need. Currently, I’ve been more consistent and practice it at least five times a week.
Positive and affirmative perspectives toward oneself transformed the participants’ relationship with themselves. Sophia described this transformation by saying, “Since taking the class, I have become a different person. By different, I mean that I approach things differently and I don’t feel stressed out as much. I am able to identify and process my emotions, and accept them.” She explained how her 5-minute mindfulness practice changed her challenging relationship:
Mindfulness allows me to connect with myself, to disconnect from external distractions. I only need 5 minutes of silent meditation to feel that inner connection. If I have an issue or conflict with someone in my family, I take those 5 minutes to disconnect from the story, reflect, and become more relaxed.
Theme Four: An Increase in Compassion and Empowerment
The participants, who exuded confidence and a newfound sense of self-care, expressed their eagerness to assist others in their own self-care journeys. They saw their role as school counselors as being further strengthened, and they showed a keen interest in exploring effective mindfulness and self-care techniques. Veronica stated, “I am confident that offering emotional support online will be just as impactful as in person. I now have a wider range of tools and activities to support my students.” Sophia also shared how her newfound sense of empowerment has made her more compassionate toward her students, saying:
I have changed. Our learning has taught me that my students are the most important individuals sitting in front of me in my counseling offices . . . my goal in supporting them is to acknowledge their opinions, feelings, and emotions. I care about all that they are experiencing, not just their issues but also their emotions. I have gained more empathy for them and strive to provide them with the best support I can.
Elizabeth stated, “As a future school counselor, I am confident that incorporating mindfulness practices into my work will have a positive impact on my interactions with students, staff, and teachers. I have learned these techniques in class and am eager to put them into practice.” Daisy shared her engagement with her students, saying:
At times, I can feel overwhelmed by the volume of students I see in a day and the diverse range of topics discussed. However, by taking the time to connect with myself and acknowledge my emotions, I find that I am more grounded after a workday. This has also helped me form stronger connections with my students.
Carol also expressed that mindfulness can rejuvenate one’s energy and foster positive relationships with oneself and others:
When you have a student who requires a lot of your energy, and you find yourself feeling depleted afterwards, it can be challenging to give your best to the next student. I think it’s important to learn how to recharge quickly so that each student receives the best version of you. With the pandemic, it’s even more crucial to meet the students’ needs academically, emotionally, and for career and college planning. What I have found is that students especially need emotional support because of the stress caused by COVID-19.
Theme Five: A Commitment to Ongoing Learning and Advocacy
The participants recognized the significance of self-care and appreciated their capacity to support others with openness, curiosity, and empathy without any judgments. They viewed self-care and mindfulness as a never-ending journey of learning and personal growth. They expressed their determination to continue their mindfulness-based self-care journey. Elizabeth described the process of healing as like a domino effect, in which one positive change can lead to a chain of similar changes in other areas of life: “Healing one aspect of my life has a positive impact on other parts as well. I’m excited to attend workshops and read more to further my mindfulness journey.” Daisy spoke of her strengthened connection with her students, saying “I feel like I am able to better communicate with my students. I strive to offer them a warm and caring presence, and I am being transparent and accepting of their diverse cultural backgrounds.”
Sara explained her practice with her family, saying, “I have been continuing to study and practice throughout the summer and have been sharing and discussing with my family members. This has been a really healing experience for our family.” Sophia also emphasized the importance of continuing her practice, stating:
Healing is a process, and it doesn’t happen overnight. However, it does help us become better people, improve our connections with others, become better listeners, judge less, and listen more to ourselves. This class has had a truly positive impact on me, and I plan to continue my mindfulness practices.
Advocacy is seen as a natural progression. Stacy also expressed her commitment to practicing alongside her students, saying, “It’s important to understand the importance of congruence in both teaching and life. If I just tell my students what to do, they won’t listen. But if I practice alongside them, it’s more effective.” Sophia spoke about the power of sharing mindfulness practices and their impacts with others, stating,
As a counselor and advocate for these techniques, I want to bring them into the K–12 education system at an early age. I hope to introduce these practices wherever I go and to our students, as I believe everyone can benefit from them.
Discussion
The five themes embody the significance and definition of self-care grounded in mindfulness and SEL for graduate students in counseling who took a summer self-care course. Participants reported a new experience in self-discovery through the practice. Despite the difficulties brought by the COVID-19 pandemic and the shift to online education, learning about self-care helped them cope with daily stress. By participating in a group, they discovered their personal and professional understanding of self-care. They learned how to connect with their emotions, physical sensations, thoughts, and others in their relationships. Particularly, they emphasized the importance of embracing difficult emotions. The self-care grounded in mindfulness and SEL taught in the course enabled them to face emotions such as anger, disappointment, anxiety, uncertainty, and shame with nonjudgment and acceptance. The students connected their understanding of self-care with their daily practices both in and outside of the class. The consistent and dedicated practice demonstrated a true embodiment of self-care among the participants.
Along with displaying great confidence in themselves and their self-care practices, the participants strongly expressed their desire to help others in their communities. Their professional identity as school counselors was enhanced, and the participants developed agency to empower underserved students and communities by introducing self-care strategies and mindfulness practices. After completing the course, the participants expressed their intention to continue the practice and viewed self-care and mindfulness as a lifelong journey.
These findings align with previous qualitative studies (Baker, 2016; Bohecker & Horn, 2016; Campbell & Christopher, 2012; Christopher et al., 2011, 2016; Christopher & Maris, 2010) on the experiences of master’s-level students in mindfulness self-care courses. Across these studies, a common theme is that students reported substantial changes in both their personal and professional lives. This included increased confidence in their professional and interpersonal relationships, a greater appreciation for their physical well-being, healthier lifestyle choices, and the ability to handle challenging situations more effectively.
Furthermore, the significance of the current study is to confirm that self-care is imperative for counselor training. As the participants expressed their sense of empowerment and desire to engage in creating and providing workshops for their families, schools, and communities, they demonstrated self-care as part of social and cultural advocacy. There was a clear shift from a deficit- to a strengths-based self-identity regarding linguistic ability, emotional availability, and a healing-focused process. This is consistent with the role of school counselors, as system change agents need to critically examine dominant culture and its impact on their own racial identity development, power, privilege, and oppression in educational settings (Mitchell & Binkley, 2021). Before disrupting and dismantling the oppression and power in the system, school counselors will need to embrace themselves wholly and consider using themselves as a tool in advocating for those in need. When serving diverse students and communities, self-care goes beyond relaxation and self-awareness of one’s own thoughts and emotions. It also involves reclaiming power within oneself—physically, emotionally, spiritually, and culturally.
Implications
The study’s results have significant implications for counselor educators. First, student readiness is crucial for the maximum impact of self-care courses. What is noticeable in the findings is that the students were ready to change as they chose the course and had a strong desire to learn more about self-care. When students are prepared, the impact can be powerful. Additionally, students who accepted themselves, both strengths and weaknesses, and experienced the mind–body–spirit connection had a greater awareness of themselves and felt more prepared to serve others. The study suggests that self-reflection is essential to maintaining an ethical practice when working with people of different identities, values, and cultures. The participants in this study emphasized their humanity by accepting their identities, processing challenging feelings, practicing self-compassion, and sharing their experiences and knowledge to empower others.
Second, the study recommends that counselor education programs incorporate a self-care course or workshop into their curriculum, as it has been shown to have a positive impact on pre-service counselors (Harrichand et al., 2021). Students’ strong desire to learn more about mindfulness and self-care is consistent with the literature (Baker, 2016) and shows the urgency of incorporating mindfulness practice, SEL, and self-care practice in the school counseling curriculum. The participants recommended offering the course every year and an advanced level later in the program. Because of logistical difficulties, it may be more practical to integrate self-care knowledge and practice into existing coursework and programs rather than adding an extra course.
Lastly, many studies on mindfulness, SEL, or self-care do not give enough importance to humanization, agency, inclusion, and equity in the individual and collective self-care process (Mitchell & Binkley, 2021). This study suggests that it is essential to include mindfulness in personal as well as social and cultural transformative processes. Participants expressed increased agency and advocacy during and after learning and practicing self-care. The self-care course can cultivate and strengthen the capacity to imagine a world beyond the current social conditions with confidence in the ability to bring change through individual and collective efforts (Pyles, 2020).
Limitations and Future Research
The authors of the study acknowledge that self-selection may have contributed to biases in the findings, as participants who enrolled voluntarily in the summer elective course showed strong interest in the research topic (Lavrakas, 2008). They also volunteered to share their experiences, which could have resulted in them focusing on positive and socially desirable narratives. The authors of the study also acknowledge that factors such as the class format, selected activities, and instructor’s teaching styles may have contributed to the participants’ experiences, which may not be generalizable to other school counseling trainees and programs. For future research, a study exploring how master’s students with different placements (i.e., pre/post-practicum, internship) or cultural identities (ethnicity, sexual and gender identity, religion, generation) experience and practice self-care could provide valuable insights to counselor educators. Additionally, a quantitative study using pre- and post-surveys to assess progress in the five SEL competencies can provide useful data for counselor educators and researchers to understand students’ social–emotional development.
Conclusion
This study examined the experiences of school counselor trainees in a self-care course based on mindfulness and SEL, consisting of 10 seminar sessions over 5 weeks. The findings revealed information about the transformation process, the importance of self-care in counseling preparation programs, and the empowering effects on graduate students becoming agents of change. Participants experienced a transformation leading to a change in their relationship with their mind, body, and emotions, and this transformation extended to their relationships with family, friends, students, and colleagues, empowering them to be more engaged with their communities and society. They embodied Carl Rogers’s (1980) core conditions for change, including unconditional positive regard, genuineness, and empathy (Campbell & Christopher, 2012), both personally and professionally, describing the experience as encountering a new self through fresh eyes.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
American Counseling Association. (2014). ACA code of ethics. https://www.counseling.org/docs/default-source/default-document-library/2014-code-of-ethics-finaladdress.pdf
American School Counselor Association. (2019). The ASCA national model: A framework for school counseling programs (4th ed.). https://www.schoolcounselor.org/About-School-Counseling/ASCA-National-Model-for-School-Counseling-Programs
Baker, S. (2016). Working in the present moment: The impact of mindfulness on trainee psychotherapists’ experience of relational depth. Counselling and Psychotherapy Research, 16(1), 5–14.
https://doi.org/10.1002/capr.12038
Berila, B. (2016). Mindfulness as a healing, liberatory practice in queer anti-oppression pedagogy. Social Alternatives, 35(3), 5–10. https://socialalternatives.com/wp-content/uploads/2021/02/berila_soc_alt_vol_35_3.pdf
Bohecker, L., & Horn, E. A. D. (2016). Increasing students’ empathy and counseling self-efficacy through a mindfulness experiential small group. The Journal for Specialists in Group Work, 41(4), 312–333.
https://doi.org/10.1080/01933922.2016.1232322
Bohecker, L., Vereen, L. G., Wells, P. C., & Wathen, C. C. (2016). A mindfulness experiential small group to help students tolerate ambiguity. Counselor Education and Supervision, 55(1), 16–30.
https://doi.org/10.1002/ceas.12030
Brown, K. W., & Ryan, R. M. (2003). The benefits of being present: Mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology, 84(4), 822–848. https://doi.org/10.1037/0022-3514.84.4.822
Camangian, P., & Cariaga, S. (2021). Social and emotional learning is hegemonic miseducation: Students deserve humanization instead. Race Ethnicity and Education, 25(7), 901–921.
https://doi.org/10.1080/13613324.2020.1798374
Campbell, J., & Christopher, J. (2012). Teaching mindfulness to create effective counselors. Journal of Mental Health Counseling, 34(3), 213–226. https://doi.org/10.17744/mehc.34.3.j75658520157258l
Carrell, S. E., & Carrell, S. A. (2006). Do lower student to counselor ratios reduce school disciplinary problems? Contributions to Economic Analysis & Policy, 5(1), 1–24. https://www.schoolcounselor-ca.org/files/Advocacy/Lower%20Counselor%20Ratios%20Equal%20Less%20Discipline.pdf
Chen, S., Cheng, Z., & Wu, J. (2020). Risk factors for adolescents’ mental health during the COVID-19 pandemic: A comparison between Wuhan and other urban areas in China. Globalization and Health, 16(1).
https://doi.org/10.1186/s12992-020-00627-7
Christopher, J. C., Chrisman, J. A., Trotter-Mathison, M. J., Schure, M. B., Dahlen, P., & Christopher, S. B. (2011). Perceptions of the long-term influence of mindfulness training on counselors and psychotherapists: A qualitative inquiry. Journal of Humanistic Psychology, 51(3), 318–349.
https://doi.org/10.1177/0022167810381471
Christopher, J. C., Christopher, S. E., Dunnagan, T., & Schure, M. (2016). Teaching self-care through mindfulness practices: The application of yoga, meditation, and qigong to counselor training. Journal of Humanistic Psychology, 46(4), 494–509. https://doi.org/10.1177/0022167806290215
Christopher, J. C., & Maris, J. A. (2010). Integrating mindfulness as self-care into counselling and psychotherapy training. Counselling and Psychotherapy Research, 10(2), 114–125. https://doi.org/10.1080/14733141003750285
Collaborative for Academic, Social, and Emotional Learning. (2023a). What is the CASEL framework? https://casel.org/fundamentals-of-sel/what-is-the-casel-framework
Collaborative for Academic, Social, and Emotional Learning. (2023b). Our mission and work. https://casel.org/about-us/our-mission-work
Council for Accreditation of Counseling and Related Educational Programs. (2015). 2016 CACREP standards. http://www.cacrep.org/wp-content/uploads/2018/05/2016-Standards-with-Glossary-5.3.2018.pdf
del Carmen Salazar, M. (2013). A humanizing pedagogy: Reinventing the principles and practice of education as a journey toward liberation. Review of Research in Education, 37(1), 121–148.
https://doi.org/10.3102/0091732X12464032
Duncan-Andrade, J. M. R., & Morrell, E. (2008). The art of critical pedagogy: Possibilities for moving from theory to practice in urban schools. Peter Lang.
Durlak, J. A., & DuPre, E. P. (2008). Implementation matters: A review of research on the influence of implementation on program outcomes and the factors affecting implementation. American Journal of Community Psychology, 41(3–4), 327–350. https://doi.org/10.1007/s10464-008-9165-0
Freire, P. (2000). Pedagogy of the oppressed. Continuum. (Original work published 1970)
Giorgi, A. (2009). The descriptive phenomenological method in psychology: A modified Husserlian approach. Duquesne University Press.
Glesne, C. (2011). Becoming qualitative researchers: An introduction (4th ed.). Pearson.
Harrichand, J. J. S., Litam, S. D. A., & Ausloos, C. D. (2021). Infusing self-care and wellness into CACREP curricula: Pedagogical recommendations for counselor educators and counselors during COVID-19. International Journal for the Advancement of Counselling, 43(3), 372–385. https://doi.org/10.1007/s10447-021-09423-3
Hays, D. G., & Wood, C. (2011). Infusing qualitative traditions in counseling research designs. Journal of Counseling & Development, 89(3), 288–295. https://doi.org/10.1002/j.1556-6678.2011.tb00091.x
Higheagle Strong, Z., & McMain, E. M. (2020). Social emotional learning for social emotional justice: A conceptual framework for education in the midst of pandemics. Northwest Journal of Teacher Education, 15(2).
https://doi.org/10.15760/nwjte.2020.15.2.6
hooks, b. (1994). Teaching to transgress: Education as the practice of freedom. Routledge.
Jagers, R., Rivas-Drake, D., & Borowski, T. (2018). Toward transformative social and emotional learning: Using an equity lens. https://measuringsel.casel.org/wp-content/uploads/2018/11/Framework_EquitySummary-.pdf
Jagers, R. J., Rivas-Drake, D., & Williams, B. (2019). Transformative social and emotional learning (SEL): Toward SEL in service of educational equity and excellence. Educational Psychologist, 54(3), 162–184.
https://doi.org/10.1080/00461520.2019.1623032
Lapan, R. T., & Harrington, K. M. (2009). Paving the road to college: How school counselors help students succeed. Center for School Counseling Outcome Research.
Lavrakas, P. J. (2008). Encyclopedia of survey research methods. SAGE. https://doi.org/10.4135/9781412963947
Lincoln, Y. S., & Guba, E. G. (1985). Naturalistic inquiry. SAGE.
Litam, S. D. A., & Hipolito-Delgado, C. P. (2021). When being “essential” illuminates disparities: Counseling clients affected by COVID-19. Journal of Counseling & Development, 99(1), 3–10. https://doi.org/10.1002/jcad.12349
Marques de Miranda, D., da Silva Athanasio, B., Sena Oliveira, A. C., & Simoes-e-Silva, A. C. (2020). How is COVID-19 pandemic impacting mental health of children and adolescents? International Journal of Disaster Risk Reduction, 51, 101845. https://doi.org/10.1016/j.ijdrr.2020.101845
Mitchell, M., & Binkley, E. (2021). Self-care: An ethical imperative for anti-racist counselor training. Teaching and Supervision in Counseling, 3(2), Article 5. https://doi.org/10.7290/tsc030205
Moerer-Urdahl, T., & Creswell, J. W. (2004). Using transcendental phenomenology to explore the “ripple effect” in a leadership mentoring program. International Journal of Qualitative Methods, 3(2), 19–35.
https://doi.org/10.1177/160940690400300202
Moustakas, C. E. (1994). Phenomenological research methods. SAGE.
Nelson, J. R., Hall, B. S., Anderson, J. L., Birtles, C., & Hemming, L. (2018). Self–compassion as self-care: A simple and effective tool for counselor educators and counseling students. Journal of Creativity in Mental Health, 13(1), 121–133. https://doi.org/10.1080/15401383.2017.1328292
Norcross, J. C., & Phillips, C. M. (2020). Psychologist self-care during the pandemic: Now more than ever. Journal of Health Service Psychology, 46(2), 59–63. https://doi.org/10.1007/s42843-020-00010-5
Paris, D., & Winn, M. T. (Eds.). (2013). Humanizing research: Decolonizing qualitative inquiry with youth and communities. SAGE.
Parker, M., & Henfield, M. S. (2012). Exploring school counselors’ perceptions of vicarious trauma: A qualitative study. The Professional Counselor, 2(2), 134–142. https://doi.org/10.15241/mpp.2.2.134
Polkinghorne, D. E. (1989). Phenomenological research methods. In R. S. Valle & S. Halling (Eds.), Existential-phenomenological perspectives in psychology: Exploring the breadth of human experience (pp. 41–60). Plenum Press.
Prime, H., Wade, M., & Browne, D. T. (2020). Risk and resilience in family well-being during the COVID-19 pandemic. American Psychologist, 75(5), 631–643. https://doi.org/10.1037/amp0000660
Pyles, L. (2020). Healing justice, transformative justice, and holistic self-care for social workers. Social Work, 65(2), 178–187. https://doi.org/10.1093/sw/swaa013
QSR International Pty Ltd. (2018). NVivo (Version 12) [Software]. https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home
Rogers, C. R. (1980). A way of being. Houghton Mifflin.
Savitz-Romer, M., Rowan-Kenyon, H. T., Nicola, T. P., Alexander, E., & Carroll, S. (2021). When the kids are not alright: School counseling in the time of COVID-19. AERA Open, 7.
https://doi.org/10.1177/23328584211033600
Shapiro, S. L., Brown, K. W., & Biegel, G. M. (2007). Teaching self-care to caregivers: Effects of mindfulness-based stress reduction on the mental health of therapists in training. Training and Education in Professional Psychology, 1(2), 105–115. https://doi.org/10.1037/1931-3918.1.2.105
Van Velsor, P. (2009). School counselors as social-emotional learning consultants: Where do we begin? Professional School Counseling, 13(1), 50–58. https://www.jstor.org/stable/42732919
Zins, J. E., Bloodworth, M. R., Weissberg, R. P., & Walberg, H. J. (2007). The scientific base linking social and emotional learning to school success. Journal of Educational and Psychological Consultation, 17(2–3), 191–210. https://doi.org/10.1080/10474410701413145
Appendix A
Semi-Structured Interview Protocol
Title of the Study: School Counselor Trainees’ Perceptions and Experiences on Self-Care Grounded in Mindfulness and Social–Emotional Learning (SEL)
To be consistent with the goal of qualitative research, all participants will be described through their own viewpoints and in their own words. All questions are open-ended, and these semi-structured interview protocols will guide the researcher throughout the interviews. However, it is not expected that the remaining questions will be asked sequentially, that all questions will be asked of all participants, or that the list of provided questions is exhaustive. Rather, we offer the questions below as representing possible directions in which we anticipate the interviews may proceed.
Introduction
We want to thank you for your willingness to participate in this study. Recently, you completed the course EDCO 298-01 Seminar in Professional Counseling. Today, we would like to take some time to collect information on your perceptions, thoughts, reactions, and follow-up response to your mindfulness-based self-care and SEL practice. If at any time you feel uncomfortable or do not desire to answer a question, please let me know.
Semi-Structured Interview Questions
- What are the most important things you learned regarding mindfulness-based self-care and SEL?
- How have your knowledge and practice of SEL affected your personal and professional life in the area of self-awareness, self-management, responsible decision-making, relationship skills, and social awareness?
- Do you attribute these changes to the class?
- Have these changes stayed with you since you took the class? What has changed?
- Describe the history of your self-care practices.
- What self-care practices do you currently practice? How often for each?
- How did the class influence these practices?
- Describe how your mindfulness-based self-care affects your personal and professional life.
- In what ways do your own practice of mindfulness and self-care change how you think about students’ or clients’ issues or problems? How have your ideas about what is therapeutic, or healing, changed since taking the class? Do you see mindfulness techniques as healing? How?
- Have the mindfulness practices influenced who you are as a counselor, advisor, educator, or therapist or what it’s like for you to be in the role of the counselor, advisor, educator, or therapist? How?
- Have you tried to introduce mindfulness concepts/techniques with a client/student? Which techniques? What was your level of comfort with introducing the mindfulness techniques?
- What are consequences/outcomes from mindfulness-based self-care practices? (elaborate)
General Questions & Feedback
Is there anything you would like to say about your experiences in relation to the course that we have overlooked? What suggestions do you have to make this course a better experience?
Ending
We want to thank you for your participation in this project.
Appendix B
Course Content and Activities
| Week |
Module |
Mindful Theme |
SEL Competencies |
Class Activities |
| One |
1 |
Presence |
Self-Awareness |
Course Overview: Review syllabus, expectations, course
requirements, and online resourcesWhat’s Social and Emotional Learning (SEL)?
Three Collective Breaths
Why Aren’t We Teaching Mindfulness: TED Video
Pre-Training Survey
Small Group with Accountability and Support |
| 2 |
Self-Connection Practice
Mindful Listening and Speaking
Brave Zone
Trauma-Informed Practice: Grounding, Orienting, and Centering
“Seven Up” Film
My Seven Up Writing
Body Scan
Weekly Journal Entry |
| Two |
3 |
Gratitude |
Self-Management |
Setting Intentions
Mind–Body Connection
Non-Violent Communication
Empathy Practice
Appreciation Circle |
| 4 |
Non-Violent Communication Tools: Mourn/Celebrate/Learn (MCL)
Exploring Identities: “I Am”
Thankful Thoughts
Negative Bias
Weekly Journal Entry |
| Three |
5 |
Creativity |
Relationship Skills |
Play Therapy: Foundations and Techniques (1)
Creative Arts
Additional Readings |
| 6 |
Play Therapy: Foundations and Techniques (2)
My Relationships
Community Circle: Appreciation Practice
Weekly Journal Entry |
| Four |
7 |
Compassion |
Social Awareness |
Check-In: Daily Practice
Compassionate Self-Talk
Neuroplasticity
“Into Light” Video
My Life and Vision: Milestones |
| 8 |
Courageous Conversations
Mindful Eating
Sound Healing
Capstone Preparation
Weekly Journal Entry |
| Five |
9 |
Equity & Inclusion |
Responsible Decision-Making |
Giving and Receiving Loving-Kindness
Transformative SEL: Advocacy
Gender Identities and Pronouns
Mindful Breathing
Silent Mindfulness Practice
Yoga and Mindfulness |
| 10 |
Capstone Presentations
Celebration: A Closing Ceremony
Post-Training Survey
Final Journal Entry |
Kyoung Mi Choi, PhD, NCC, is a professor at San José State University. Jung H. Hyun, PhD, NCC, is an associate professor at Nova Southeastern University. Correspondence may be addressed to Kyoung Mi Choi, One Washington Square, San José, CA 95192, kyoungmi.choi@sjsu.edu.
Apr 18, 2017 | Volume 7 - Issue 3
Susannah C. Coaston
Counselors are routinely exposed to painful situations and overwhelming emotions that can, over time, result in burnout. Although counselors routinely promote self-care, many struggle to practice such wellness regularly, putting themselves at increased risk for burning out. Compassion is essential to the helper’s role, as it allows counselors to develop the therapeutic relationship vital for change; however, it is often difficult to direct this compassion inward. Developing an attitude of self-compassion and mindfulness in the context of a self-care plan can create space for an authentic, kind response to the challenges inherent in counseling. This article expands beyond the aspirational aspects of self-compassion and suggests a variety of practices for the mind, body, and spirit, with the intention of supporting the development of an individualized self-care plan for counselors.
Keywords: self-care, self-compassion, burnout, mindfulness, wellness
Wellness, prevention, and human development compose the core of a counselor’s professional identity (Mellin, Hunt, & Nichols, 2011). This fundamental grounding is emphasized within the American Counseling Association’s (ACA) Code of Ethics (ACA, 2014), as well as by the Council for Accreditation of Counseling & Related Education Programs (CACREP; 2016). To fulfill their role in the change process, counselors depend heavily upon compassion, a key component of the therapeutic relationship that—paradoxically—counselors may seldom apply to themselves (Patsiopoulos & Buchanan, 2011). Whereas compassion means being with others in their suffering (Pollack, Pedulla, & Siegel, 2014), self-compassion can be understood as “being touched by and open to one’s own suffering, not avoiding or disconnecting from it, generating the desire to alleviate one’s suffering and to heal oneself with kindness” (Neff, 2003, p. 87). Higher levels of self-compassion can serve as a buffer against burnout (Barnard & Curry, 2011). Therefore, cultivating an attitude of self-compassion may assist counselors in employing self-care practices to refresh, rejuvenate, and recharge their bodies, minds, and souls. The purpose of this manuscript is to reimagine self-care as regular acts of self-compassion that benefit both clients and counselors.
Self-Compassion
Self-compassion, a construct from Buddhist thought, consists of self-kindness, common humanity, and mindfulness, and is characterized by gentleness with oneself when faced with a perceived sense of inadequacy or failure (Neff, 2003). Self-compassion is not based on an evaluation of the self; self-compassion becomes the path to positively relating to oneself (Neff & Costigan, 2014). The concept of self-compassion is consistent with the idea of self-acceptance in the humanistic tradition (Neff, 2003). Carl Rogers (1961) described a successful outcome of psychotherapy as an increase in positive attitudes toward self: “The client not only accepts himself . . . he actually comes to like himself. This is not a bragging or self-assertive liking; it is a rather quiet pleasure in being one’s self” (p. 87). The practice of self-compassion calls for a mindful awareness of emotions, and painful emotions are met with a sense of understanding, connection to our common humanity, and self-kindness (Neff, 2003). Neff and Costigan (2014) described self-compassion’s relationship with pain thusly: “Self-compassion does not avoid pain, but rather embraces it with kindness and goodwill that is rooted in the experience of being fully human” (p. 114). Self-compassion practices have been found to improve psychological functioning in both clinical and non-clinical settings (Neff, Kirkpatrick, & Rude, 2007; Schanche, Stiles, McCullough, Svartberg, & Nielsen, 2011).
Mindfulness is one of the core components of self-compassion and is critical for the awareness of suffering that precedes compassion (Germer & Neff, 2015). Mindfulness is the focusing on the awareness of pain in the present moment, and self-compassion becomes the act of taking that awareness and encouraging kindness toward oneself. The common humanity component of self-compassion becomes one of acknowledgment that, as humans, we are imperfect and make mistakes; recognizing our flawed condition allows for a broader perspective toward our difficulties (Neff, 2003). Adopting such a view of pain reduces the chance of over-identification or getting so wrapped up in one’s emotions that they become exaggerated (Neff & Costigan, 2014). When an individual can recognize pain as a universal occurrence, such a viewpoint then fosters a sense of connection with others who have felt suffering. Pain becomes an uncomfortable but acknowledged part of the human condition. When practicing self-compassion, the self-directed kindness is not done to change the circumstance of suffering, but done because there is suffering. The practitioner asks “What do I need now?” The individual then acts accordingly to provide comfort when experiencing the pain of inadequacy or failure (Germer & Neff, 2015). Learning self-compassion becomes a gift for both clients and the practitioner (Barnett, Baker, Elman, & Schoener, 2007). Making time for one’s self is one way counselors can practice self-care (Patsiopoulos & Buchana, 2011). That self-acceptance can prove vital for counselors, whose work often puts them at a risk for burnout (Yager & Tovar-Blank, 2007).
Counselor Burnout
Burnout is a multidimensional experience consisting of exhaustion, cynicism, and reduced professional efficacy that can result from dissatisfaction with the organizational context of the job position (Maslach, Schaufeli, & Leiter, 2001). Burnout can affect individuals in a variety of ways, with anxiety, irritability, fatigue, withdrawal, and demoralization as major examples (Schaufeli & Enzmann, 1998). Burnout can affect individuals at any point in their career and can hamper productivity and creativity, resulting in a reduction of compassion toward themselves and clients (Grosch & Olsen, 1994). “It is when counseling seems to have little effect that counselors reach despair because their raison d’être for choosing this work—to make a difference in human life—is threatened” (Skovholt, Grier, & Hanson, 2001, p. 171). Caring for others and caring for oneself becomes a difficult balance to achieve for both new and seasoned counselors alike. Carl Rogers (1980) wrote, “I have always been better at caring for and looking after others than I have in caring for myself. But in these later years, I made progress” (p. 80). Self-compassion can serve as a protective factor against such potentially debilitating effects of work-related burnout.
Historically, researchers examined the causes of burnout relating to demographic, personality, or attitudinal differences between individuals (Maslach et al., 2001). Today, burnout is viewed from an organizational standpoint and is concerned with the relationship, or fit, between the person and his or her environment, wherein mismatches can result in burnout over time (Maslach, Leiter, & Jackson, 2012). An individual’s perceptions have a reciprocal relationship with the work environment; how counselors make meaning of their work impacts their satisfaction, commitment, and performance in the workplace (Lindholm, 2003). Counselors experiencing work-related stress and burnout will construct meaning differently and require a tailored self-care plan that reflects their individual assessment of their own fit within their work environment.
Counselor Self-Care
Self-care can be defined as an activity to “refill and refuel oneself in healthy ways” (Gentry, 2002, p. 48). Self-care is vital if we are to remain effective in our role and avoid burnout; however, many counselors do not regularly implement the techniques they recommend to clients in their own lives (O’Halloran & Linton, 2000; Skovholt et al., 2001). Although self-care is widely promoted within the counseling literature, this author contends that inherent in many self-care plans and workplace improvement efforts is the idea that overwhelming work-related stress reflects an inadequacy of the individual. The message in the literature often reflects the view that a counselor’s distress hinges upon inadequate coping resources, poor health practices, or other kinds of personal failing, such as lacking assertiveness or not taking enough time off from work (Bradley, Whisenhunt, Adamson, & Kress, 2013; Killian, 2008; O’Halloran & Linton, 2000). As a result, self-care plans tend to take on the air of a New Year’s resolution, a strategy to get better. This narrow focus reflects the historical view of burnout that focused primarily on its individual dimension, without taking into consideration the organizational, interpersonal, or societal perspectives (Schaufeli & Enzmann, 1998). When self-care plans are written like self-improvement plans, the opportunities for criticism and judgment abound, particularly for new counselors who struggle with anxiety and self-doubt (Skovholt, 2012). When counselors are suffering, experiencing symptoms of burnout, struggling to maintain healthy professional boundaries (i.e., under- or over-involvement), or feeling as though they are not caring for themselves effectively, shame may cause them to be less likely to seek assistance (Graff, 2008). Some counselors may fear negative repercussions as a result of disclosure, such as being perceived as impaired or having professional competency problems (Rust, Raskin, & Hill, 2013).
Self-care is an ethical imperative (ACA, 2014), because utilizing self-care strategies reduces the likelihood of impairment (ACA, 2010). Issues in a counselor’s personal life, burnout in the workplace, mental or physical disability, or substance abuse can result in impairment (ACA, 2010). Sadly, in a survey completed in 2004, nearly two-thirds of participants knew a counselor that they would identify as impaired (ACA, 2010). Counselors who better manage their self-care needs are more likely to set appropriate boundaries with clients and less likely to use clients to meet their own personal or professional needs (Nielsen, 1988). Self-care education has been integrated into the accreditation standards for counselor training (CACREP, 2016), and there are multiple articles discussing how to incorporate the value of wellness and self-care into counselor education programs (Witmer & Young, 1996; Yager & Tovar-Blank, 2007). For counselor educators and supervisors, monitoring counselors-in-training for possible impairment is an important part of the responsibility of gatekeeping (Frame & Stevens-Smith, 1995). However, despite this attention, both students and practicing professional counselors still struggle to implement self-care (Skovholt et al., 2001; E. Thompson, Frick, & Trice-Black, 2011).
Bradley and colleagues (2013) suggested that many of the self-care suggestions in the literature are too general, focusing mainly on general health practices, such as eating healthily and getting enough sleep, or professional recommendations regarding seeking support from colleagues. A case can be made that a counselor would be better served by employing an overall approach to efforts that are based in a self-compassionate mindset. Therefore, actively seeking awareness of one’s own signs and symptoms that indicate suffering can not only help counselors recognize burnout, it also can provide clues toward the first step in soothing.
Mindfulness represents one possible means of increasing such awareness. Mindfulness allows the practitioner to be present in the moment non-judgmentally (Kabat-Zinn, 1994). To practice self-compassion, a counselor needs to be willing to attend to feelings of discomfort, pain, or suffering and acknowledge the experience without self-recrimination (Germer & Neff, 2015). Consider the experience of having a regular client stop attending sessions and returning calls or abruptly discontinuing services. Although common, the ambiguous loss of a connection with a client can be a source of stress and pain (Skovholt et al., 2001). It also can provide an opportunity. Covey (2010) shared the following quote that is often misattributed to Viktor Frankl: “Between stimulus and response there is a space. In that space is our power to choose our response. In our response lies our growth and our freedom” (p. VI). The space Covey describes is our opportunity to be mindful of the stimulus and choose to offer ourselves compassion in response. Choosing to deny, suppress, or distract to avoid these feelings may cause the counselor to miss the trigger to practice self-care. When such feelings are recognized, the counselor may act compassionately toward himself or herself by normalizing or validating the experience. Within self-compassion, the concept of common humanity becomes crucial to precluding the often-automatic tendency to become self-critical for experiencing discomfort (Neff, 2003). Thoughts such as, “I shouldn’t feel this way,” “Just snap out of it; it’s not so bad,” or “What’s wrong with me?” invalidate the sufferer and may cause the counselor to feel as though self-care is an act of indulgence rather than an essential, self-directed gift of kindness. Expressing kindness through self-care acknowledges that counseling can be both difficult and rewarding, a duality representative of the human condition.
When counselors choose to practice self-care, they enhance themselves and their practice. One participant in a narrative inquiry on self-compassion in counseling stated: “What’s so important about self-compassion? Three words: Avoidance of burnout” (Patsiopoulos & Buchanan, 2011, p. 305). Another participant noted, “When we come from a self-compassionate place, self-care is no longer about these sporadic one-time events that you do when you feel burned out and exhausted. Self-care is something you can do all the time” (Patsiopoulos & Buchanan, 2011, p. 305). The consequence of our job as counselors is working compassionately with suffering, and in doing so we suffer (Figley, 2002).
For someone to develop genuine compassion toward others, first he or she must have a basis upon which to cultivate compassion, and that basis is the ability to connect to one’s own feelings and to care for one’s own welfare. . . . Caring for others requires caring for oneself. (Germer & Neff, 2015, p. 48) Self-care, then, is a vital part of a counselor’s responsibilities to clients and to one’s self.
It is important to remember that counseling can be emotionally demanding for counselors in different ways (O’Halloran & Linton, 2000). Self-compassion encourages remembering the shared human experience (Neff, 2003), as the experience of being a professional counselor can be quite isolating, especially for those working in more independent environments (e.g., school counselors, private practitioners; Freadling & Foss-Kelly, 2014; Matthes, 1992). Using mindfulness, counselors can maintain an objective stance that can allow the counselor to view one’s work circumstances with a non-judgmental lens (Newsome, Waldo, & Gruszka, 2012), then act kindly to intervene with a self-care practice that is revitalizing to mind, body, and spirit. Using self-compassion tenets as a guide, self-care plans can be created that are authentic and kind, connect us to the human experience, and reflect a balanced state of self-awareness.
Creating a Self-Compassion–Infused Self-Care Plan
In wellness counseling, optimal functioning of the mind, body, and spirit is the goal for holistic wellness (Myers, Sweeney, & Witmer, 2001). The physical dimension is the most common focus for wellness intervention (Carney, 2007); however, this is quite limiting in a profession that is often sedentary, with long hours and pressure to meet productivity demands (Franco, 2016; Freadling & Foss-Kelly, 2014; Ohrt, Prosek, Ener, & Lindo, 2015). Maintaining one’s health is important but may not be enough to assuage the emotional demands of a high-touch profession in which a strong professional relationship is combined with the often-conflicting pressures of reimbursement; short-term, diagnosis-focused treatment; and behaviorally based outcomes associated with managed care (Cushman & Gilford, 2000; Freadling & Foss-Kelly, 2014). Developing a collaborative treatment plan is a common practice in counseling; it allows the counselor and the client to determine the possible direction and outcomes for their work together (Kress & Paylo, 2015). In the best case, this plan is individualized, specific, and open to revision when necessary. A good self-care plan can follow the same formula.
What follows are specific suggestions regarding self-care practices that stretch beyond the “should,” the “ought to,” and the New Year’s resolution language. When reading the interventions, consider the question Linder, Miller, and Johnson (2000) suggested for clients when encouraging self-care: “How do you reassure yourself?” (p. 4). The suggestions are organized into mind, body, and spirit; however, these are artificial divisions and some interventions may satisfy in multiple ways.
Interventions for the Mind
Mindfulness is a component of self-compassion, but it can also be used intentionally as a regular practice for self-care. Mindfulness can be described as a dispositional trait, a state of being and a practice (Brown, Ryan, & Creswell, 2007). The use of mindfulness has been integrated into many facets of counseling practice (I. Thompson, Amatea, & Thompson, 2014). For those attracted to the practice of mindfulness for self-care, non-judgmental awareness can be integrated as a practice (e.g., a set time for engagement in a particular mindfulness exercise) or as a way of being during particular activities within the day. Exercises such as mindful eating, maintaining sensory awareness while washing dishes, or mindful walking can be helpful for those who are looking for brief, everyday opportunities for self-care. Researchers I. Thompson and colleagues (2014) found that higher levels of mindfulness corresponded with lower levels of burnout. Mindfulness has been suggested as a beneficial way to teach self-care in counselor training (Christopher, Christopher, Dunnagan, & Schure, 2006), and also as a way to reduce stress and increase self-compassion in students training to be in helping professions (Newsome et al., 2012). For any number of reasons, not all counselors may find benefit in mindfulness practices; therefore, some may choose methods of self-care that are more mentally invigorating.
Intellectual stimulation in any endeavor is important to maintain engagement, interest, and enjoyment, but such motivation can be particularly helpful when a work position contains routine, mundane, or downright boring tasks. To create a stimulating work life, seasoned professionals find active ways to continue their professional development, which can decrease the boredom that can lead to burnout (Skovholt et al., 2001). Activities for growth and development can include learning something new within counseling or outside the profession, such as learning a new language, or how to make sushi, write code, or play a strategy game such as the ancient board game, Go.
The role of a counselor involves exposure to circumstances of human suffering, painful emotions, and heartbreaking situations, which increases the risk of burnout due to absorption of the clients’ pain (Ruysschaert, 2009). Finding a way to keep and maintain positive memories, cards and notes, compliments or successes—what this author terms warm and fuzzies—either personally or professionally, in a box, folder, jar, or bulletin board, can be a helpful response. Bradley and colleagues (2013) suggested tracking small changes made by clients when discouraged and sharing the progress with co-workers.
Writing can be a powerful intervention in a counseling setting and can benefit both mental and physical health (Pennebaker & Seagal, 1999; Riordan, 1996). Counselors can use the medium of writing in a multitude of ways. Whether through journaling, narrative, poetry, musical lyrics, or letters, the act of writing can reduce emotional inhibition (Connolly Baker & Mazza, 2004). Creative writing can be used to access the healing benefits of writing without worry about form or audience (Warren, Morgan, Morris, & Morris, 2010).
Warren et al.’s (2010) The Writing Workout is a way to express, validate, and externalize painful emotions. This wellness approach illustrates how creative writing for self-care can cultivate compassion. Narrative writing strategies can allow the writer to change the outcome of a lived experience or reframe a life experience (Connelly Baker & Mazza, 2004). Creating a narrative of an event can help the storyteller organize details and events, reflect and process thoughts and feelings, and derive meaning from experiences (Pennebaker & Seagal, 1999). A creative, mindful writing intervention could be used to examine a clinical situation that may not have gone as the counselor had hoped, or to creatively explore life lessons derived from a clinical encounter. For some clinicians, writing gives voice to emotions too raw to easily speak aloud (Wright, 2003).
Traditional journaling can allow for self-reflection, increased self-awareness, and growth (Lent, 2009; Utley & Garza, 2011). Journal writing can be inherently self-compassionate. Linder et al. (2000) discussed the use of a non-judgmental journaling practice in which there are no wrong words and writers are encouraged to use random sentences and words that do not make sense. Through almost nonsensical form, journaling offers a sense of safety and freedom, while creating a trusting relationship with the journal. Linder et al. (2000) stated, “Journaling finds the meaning in meaninglessness and negates the emptiness through creating writing from the heart. It is an outlet to tell the truth without being judged” (p. 7).
Beyond the traditional journal, counselors may find alternative ways to use journaling for emotional expression, such as use of bullet journaling or a personal blog online. Bullet journaling uses a rapid-logging approach, or a visual code, to represents tasks, events, and notes in a physical notebook (Bullet Journal, 2017). Keeping a bullet journal is a clever way of managing multiple arenas of one’s life in a single place, and the events and notes categories can be particularly helpful in the practice of journaling for self-care. Events are to be written down briefly and objectively despite the degree of emotional content they carry (Bullet Journal, 2017), offering an opportunity to practice the non-reactive skill of mindfulness (Kabat-Zinn, 1994). Once an event has been entered, the counselor can respond mindfully to it by writing at length on the following page. The notes category for bullet journaling consists of ideas, thoughts, or observations (Bullet Journal, 2017), which could include inspirational quotes, eureka moments, or other insights worth reviewing at a later date. The author can use signifiers (i.e., symbols) to create a legend to provide additional context for an event, note, or task. The bullet journal approach for self-expression exemplifies a creative twist on an old concept to better fit the preferences of the writer. Similarly, scrapbook journaling can be used to accommodate the types of expressive media that resonate with the counselor’s personal style or interests (Bradley et al., 2013). Counselors can use photos, poems, song lyrics, and quotes to reflect their emotional state, and then reflect on the emotional patterns or themes that arise. For counselors who prefer to share their thoughts on the Internet, an online blog can be a cost-effective, accessible medium to express oneself emotionally and share thoughts, feelings, and experiences with others (Lent, 2009). Counselors should consider the risks associated with the use of the Internet and maintenance of confidentiality in an online medium in accordance with the ACA Code of Ethics (2014).
Finally, a simple self-care intervention can involve writing oneself a permission slip or prescription for something. This could be the permission to be imperfect, to take a mental health day, or to run through a sprinkler on a hot day. A writing assignment of this sort expresses kindness in providing the very thing that is needed for an emotional recharge. In some cases, this may involve taking a quiet moment to allow one’s mind to wander. This can occur during a warm bath or shower at the end of the day or while savoring a warm cup of coffee or tea in the afternoon. Although mind-wandering can be a threat to effectiveness and productivity when it occurs at inopportune times, taking time for mind-wandering can relieve boredom, stimulate creative thoughts, and facilitate future planning (Smallwood & Schooler, 2015).
Interventions for the Body
Many self-care plans begin and end with a strong concentration on physical self-care, typically involving making nutritional changes and increasing physical activity (Bradley et al., 2013; E. Thompson et al., 2011). These therapeutic lifestyle changes (TLCs) can have a huge impact on health and well-being (Walsh, 2011). Although the mental health benefits of these types of changes are well documented (Walsh, 2011), a myopic focus on physiological wellness may be limiting, and self-care should include a broader range of ways to cope (E. Thompson et al., 2011). For individuals wishing to focus specifically on such changes, using the imagery of caring for oneself as one does a plant may increase self-awareness of bodily self-care needs (Bradley et al., 2013). Considering one’s needs in this metaphorical way may help counselors increase their own self-compassion by considering their unique needs and the changes they are ready and willing to make. A counselor may indicate they require shade from the sun, which could represent reducing over-stimulating environments; good spacing from other plants, indicating healthy boundaries or alone time; and water and nutrients, which may remind the counselor to keep a pitcher of water on the desk and a bag of almonds in a drawer. Externalizing in this way can be particularly helpful when learning self-compassion because often counselors find it easier to care for others than themselves (Patsiopoulos & Buchanan, 2011).
Although exercise has clear mental health benefits (Callaghan, 2004), for some the concept of exercise may lack appeal or may prove difficult to prioritize within a daily work schedule. The use of stretching, walking, or yoga for a short amount of time may be more easily integrated into a hectic schedule. Yoga has been found to be equivalent to exercise in many mental and physical health domains, but not all types of yoga have been found to improve overall physical fitness as compared to more rigorous exercise (Ross & Thomas, 2010). The practice of yoga has been found to increase acceptance of self and others and reduce self-criticism (Valente & Marotta, 2005). Further, the regular practice of yoga can “provide therapists with a discipline capable of fostering a greater sense of self-awareness and helping to develop a lifestyle that is conducive to their own personal growth and the goals of their profession” (Valente & Marotta, 2005, p. 79).
The benefits of movement go beyond improvements in cardiac and musculoskeletal health, while serving to benefit the mind and the spirit. Dance has been used for centuries as a healing practice (Koch, Kunz, Lykou, & Cruz, 2014) and reduces stress, increases stress tolerance, and improves well-being (Bräuninger, 2012). Marich and Howell (2015) developed the practice of dancing mindfulness, which utilizes dance as the medium for practicing meditation. Dancing mindfulness participants report improvement in emotional and spiritual domains, greater acceptance of self, and an increased ability to use mindfulness in everyday life (Marich & Howell, 2015). However, caring for oneself requires more than just nutrition and movement; self-care plans should metaphorically consider the environment.
Skovholt et al. (2001; Skovholt, 2012) uses the concept of a greenhouse to describe the characteristics for a healthy work environment. Plants flourish within a nurturing greenhouse environment. Likewise, counselors thrive within a work environment that is characterized by a sense of autonomy and fairness; growth-promoting and meaningful work; reasonable expectations and remuneration; and trust, support, and respect among colleagues (Skovholt, 2012). The metaphorical work “greenhouse” contains individualized supports and resources that allow for growth and rejuvenation, but can protect the counselor from the harshness that could characterize their work. Examining and adjusting factors that may be under the counselor’s control, such as breaks between clients; scheduling of clients engaged in trauma work; number of assessments, intakes, or group sessions in one day; or other malleable elements can help create a work day that best meets the needs of the counselor. Strategic planning and focused intentionality allows the counselor to engage fully in each client encounter.
Interventions for the Spirit
Religion and spirituality are important factors within the lives of many clients (Cashwell, Bentley, & Bigbee, 2007). Within the United States, 77% of adults identify with some religious faith (Masci & Lipka, 2016). However, the United States is growing in those who identify as spiritual, with 59% of adults reporting a regular “deep sense of ‘spiritual peace and well-being’” (Masci & Lipka, 2016, para. 2). To attend appropriately and fully to clients’ religious and spiritual needs, counselors also need to care for their own spiritual selves.
Humanistic counselors engage fully with clients to create a genuine connection and are most effective as helpers in areas in which they themselves are stronger and more grounded (Baldwin, 2013). Therefore, when addressing the spiritual concerns of a client, counselors need to be aware of where they are on their own spiritual path. Otherwise, there is no assurance their own religious or spiritual concerns will not create an obstacle for their client’s growth (Sori, Biank, & Helmeke, 2006). A counselor’s spiritual concerns can influence the therapeutic alliance in many ways. Influences can include increased reactivity to the spiritual concerns of the client, decreased recognition of how the client values personal spirituality, or inattention to how the client’s spirituality may be a therapeutic resource or contributing factor to distress (Sori et al., 2006). Sori and colleagues (2006) concluded that failure to be aware of spirituality as an aspect of the human condition can create potential boundary issues, limit a counselor’s understanding of the client due to unexamined beliefs rooted in one’s own spiritual background, and result in difficulty managing the emotional uncertainty and pain of clients due to the counselor’s own struggles with faith. Therefore, engaging in reflection, exploration, or a regular spiritual practice can benefit both the counselor and the client.
Spirituality in counseling has been defined as “the capacity and tendency present in all human beings to find and construct meaning about life and existence and to move toward personal growth, responsibility, and relationship with others” (Myers & Williard, 2003, p. 149). This definition conceptualizes spirituality as a central component of wellness that shapes one’s functioning physically, psychologically, and emotionally, not as separate parts of the whole being (Myers & Williard, 2003). Valente and Marotta (2005) asserted that a healthy spiritual life can be emotionally nourishing and keep burnout at bay. Further, greater self-awareness of one’s spirituality may allow practitioners to be more present with their own suffering and that of their clients. Chandler, Miner Holden, and Kolander (1992) stated that attending to spiritual health when making personal change toward wellness will increase the likelihood of self-transformation and greater balance in life. Because there are many expressions of spirituality, individuals wishing to incorporate spirituality into their self-care plan should consider choosing activities that align with personal goals and are consistent with their values (Cashwell et al., 2007).
A spiritual self-care practice can create an inner refuge (Linder et al., 2000) that can offer sanctuary for a counselor when overwhelmed by personal or professional suffering (Sori et al., 2006). Particularly for those in the exploration phase of their own spirituality, but beneficial for all, conducting a moral inventory can assess how individuals are living in accordance with personal beliefs and values (Sori, et al., 2006). Following the moral inventory, a counselor may create a short list of principles to live by (i.e., a distilled list of values consistent with religious and spiritual ideas that are particularly personally valuable; V. Pope, personal communication, August, 2016). Individual research or joining a spiritual community can be helpful for education, support, and guidance in learning more about a particular religious or spiritual tradition (Cashwell et al., 2007). Some religious traditions, such as Seventh-Day Adventists, offer guidelines for physical and mental exercises, as well as nutritional advice that can be translated into intentional counselor self-care practices. Seventh-Day Adventists have a strong focus on wellness and advocate a vegetarian diet and avoidance of tobacco, alcohol, and mind-altering substances (General Conference of Seventh-Day Adventist World Church, 2016). Further, self-reflection may be regularly incorporated into rituals associated with an important time of year such as Lent or the Days of Awe.
For many, prayer can be a powerful practice for connecting with a higher power. Prayer is an integral part of a variety of spiritual traditions and has been associated with a variety of improvements in health and well-being (Granello, 2013). Spending time in communion with a higher power can be integrated into a regular routine for the purpose of self-care. Meditation also can be a spiritual practice and has a long history of applications and associations with health improvement (Granello, 2013). Broadly speaking, there are two types of meditation: concentration, which involves focusing attention (e.g., repeating a mantra, counting, or attending to one’s breath), and mindfulness, which non-judgmentally expands attention to thoughts, sensations, or emotions present at the time (Ivanovski & Malhi, 2007). These quiet practices can allow the participant moments of silence to achieve various ends, such as relaxation, acceptance, or centering.
Connecting with the earth or nature also can be a practice of spiritual self-care. Grounding exercises such as massage, Tai Chi, or gardening can be helpful to encourage a reconnection with the body and the earth (Chandler, et al., 1992). Furthermore, spending time in nature has been found to be rejuvenating both mentally and spiritually (Reese & Myers, 2012).
Engaging in a creative, expressive art activity for the purposes of spiritual practice and healing can be incredibly powerful to heal mind, body, and soul (Lane, 2005). Novelist John Updike has said, “What art offers is space—a certain breathing room for the spirit” (Demakis, 2012, p. 23). Art can come in many forms. Expressive arts can be a powerful tool of self-expression (Snyder, 1997; Wikström, 2005) and provide many options that can easily be used as self-care interventions. Sometimes the inner critic, need for approval, fear of failure, or a fear of the unknown can create barriers to exploring one’s creative energy (N. Rogers, 1993). Maintaining a self-compassionate attitude can allow counselors to create a safe environment to practice self-care free of judgment.
Use of dance, music, art, photography, and other media can be used intentionally for holistic healing. Through the use of clay, paint, charcoal, or other media, the creator can become in touch with feelings, gain insight, release energy, and discover alternative spiritual dimensions of the self, as well as experience another level of consciousness (N. Rogers, 1993). Music has been found to be both therapeutic and transcendental (Knight & Rickard, 2001; Lipe, 2002; Yob, 2010). There are various ways to incorporate music into a self-care plan depending on interest, access, and preference. In many cultures, music and spirituality are integrally linked (Frame & Williams, 1996). Listening to a favorite hymn, gospel music, or other type of liturgical music can be one way to revitalize the spirit during the workday. Relaxing music has been found to prevent physiological responses to stress and subjective experience of anxiety in one study of undergraduates (Knight & Rickard, 2001). Singing is another way of expressing thoughts and feelings, and for some it can provide a vehicle for self-actualization, connection to a higher power, and self-expression (Chong, 2010). After a long day, singing in the office, in the car, or while cooking dinner can be particularly cathartic.
Conclusion
Counselors are routinely exposed to painful situations, traumatic circumstances, and overwhelming emotions. Consequently, they could benefit from creating a safe place for vulnerability, especially when emotionally overwrought after a long day or a particularly difficult counseling session. To thrive as a counselor, self-care is essential, yet many struggle to care for themselves as they care for their clients. To best achieve holistic wellness, counselors must incorporate interventions for the body, mind, and spirit. Counselors can apply self-compassion principles to the creation of an individualized self-care plan, one that functions to rejuvenate flagging professional commitment and soothe potentially debilitating stress. By cultivating an attitude of self-compassion, counselors may be more attentive to their own needs, reducing the risk of developing burnout and benefitting both clients and themselves. These counselors also may be more effective in assisting clients with overcoming their own barriers to self-care. Similarly, counselors who serve as educators or supervisors can model such principles and routinely ask students and supervisees, “What do you need now?” to increase awareness and the practice of tuning in. Consequently, the self-compassionate counselor learns to create a self-care plan that becomes a balm for burnout.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest or funding contributions for the development of this manuscript.
References
American Counseling Association. (2010). American Counseling Association’s Task Force on Counselor Wellness and Impairment. Retrieved from http://www.creating-joy.com/taskforce/tf_history.htm
American Counseling Association. (2014). 2014 ACA code of ethics. Alexandria, VA: Author. Retrieved from https://www.counseling.org/resources/aca-code-of-ethics.pdf
Baldwin, M. (2013). Interview with Carl Rogers on the use of the self in therapy. In M. Baldwin (Ed.), The use of self in therapy (3rd ed., pp. 28–35). New York, NY: Routledge.
Barnard, L. K., & Curry, J. F. (2011). Self-compassion: Conceptualizations, correlates, & interventions. Review of General Psychology, 15, 289–303. doi:10.1007/s11089-011-0377-0
Barnett, J. E., Baker, E. K., Elman, N. S., & Schoener, G. R. (2007). In pursuit of wellness: The self-care imperative. Professional Psychology: Research and Practice, 38, 603–612. doi:10.1037/0735-7028.38.6.603
Bradley, N., Whisenhunt, J., Adamson, N., & Kress, V. E. (2013). Creative approaches for promoting counselor self-care. Journal of Creativity in Mental Health, 8, 456–469. doi:10.1080/15401383.2013.844656
Bräuninger, I. (2012). Dance movement therapy group intervention in stress treatment: A randomized controlled trial (RCT). The Arts in Psychotherapy, 39, 443–450. doi:10.1016/j.aip.2012.07.002
Brown, K. W., Ryan, R. M., & Creswell, J. D. (2007). Mindfulness: Theoretical foundations and evidence for its salutary effects. Psychological Inquiry, 18, 211–237. doi:10.1080/10478400701598298
Bullet Journal. (2017). Getting started. Retrieved from http://bulletjournal.com/get-started/
Callaghan, P. (2004). Exercise: A neglected intervention in mental health care? Journal of Psychiatric and Mental Health Nursing, 11, 476–483. doi:10.1111/j.1365-2850.2004.00751.x
Carney, J. V. (2007). Humanistic wellness services for community mental health providers. The Journal of Humanistic Counseling, 46, 154–171. doi:10.1002/j.2161-1939.2007.tb00033.x
Cashwell, C. S., Bentley, D. P., & Bigbee, A. (2007). Spirituality and counselor wellness. The Journal of Humanistic Counseling, 46, 66–81. doi:10.1002/j.2161-1939.2007.tb00026.x
Chandler, C. K., Holden, J. M., & Kolander, C. A. (1992). Counseling for spiritual wellness: Theory and practice. Journal of Counseling & Development, 71, 168–175. doi:10.1002/j.1556-6676.1992.tb02193.x
Chong, H. J. (2010). Do we all enjoy singing? A content analysis of non-vocalists’ attitudes toward singing. The Arts in Psychotherapy, 37, 120–124. doi:10.1016/j.aip.2010.01.001
Christopher, J. C., Christopher, S. E., Dunnagan, T., & Schure, M. (2006). Teaching self-care through mindfulness practices: The application of yoga, meditation, and qigong to counselor training. Journal of Humanistic Psychology, 46, 494–509. doi:10.1177/0022167806290215
Connolly Baker, K., & Mazza, N. (2004). The healing power of writing: Applying the expressive/creative component of poetry therapy. Journal of Poetry Therapy, 17, 141–154. doi:10.1080/08893670412331311352
Council for Accreditation of Counseling & Related Educational Programs. (2016). 2016 CACREP standards. Alexandria, VA: Author. Retrieved from http://www.cacrep.org/for-programs/2016-cacrep-standards
Covey, S. R. (2010). Foreword. In A. Pattakos (Ed.), Prisoners of our thoughts: Viktor Frankl’s principles for discovering meaning in life and work (2nd ed., pp. V–XI). Oakland, CA: Berrett-Koehler Publishers.
Cushman, P., & Gilford, P. (2000). Will managed care change our way of being? American Psychologist, 55, 985–996. doi:10.1037//0003-066X.55.9.985
Demakis, J. (2012). The ultimate book of quotations. Seattle, WA: CreateSpace.
Figley, C. R. (2002). Compassion fatigue: Psychotherapists’ chronic lack of self-care. Journal of Clinical Psychology, 58, 1433–1441. doi:10.1002/jclp.10090
Frame, M. W., & Stevens-Smith, P. (1995). Out of harm’s way: Enhancing monitoring and dismissal processes in counselor education programs. Counselor Education and Supervision, 35, 118–129. doi:10.1002/j.1556-6978.1995.tb00216.x
Frame, M. W., & Williams, C. B. (1996). Counseling African Americans: Integrating spirituality in therapy. Counseling and Values, 41, 16–28. doi:10.1002/j.2161-007X.1996.tb00859.x
Franco, G. E. (2016). Productivity standards: Do they result in less productive and satisfied therapists? The Psychologist-Manager Journal, 19, 91–106. doi:10.1037/mgr0000041
Freadling, A. H., & Foss-Kelly, L. L. (2014). New counselors’ experiences of community health centers. Counselor Education and Supervision, 53, 219–232. doi:10.1002/j.1556-6978.2014.00059.x
General Conference of Seventh-Day Adventist World Church. (2016). Living a healthful life. Retrieved from https://www.adventist.org/en/vitality/health
Gentry, J. E. (2002). Compassion fatigue: A crucible of transformation. Journal of Trauma Practice, 1(3–4), 37–61. doi:10.1300/J189v01n03_03
Germer, C. K., & Neff, K. D. (2015). Cultivating self-compassion in trauma survivors. In V. M. Follette, J. Briere, D. Rozelle, J. W. Hopper, & D. I. Rome (Eds.), Mindfulness-oriented interventions for trauma: Integrating contemplative practices (pp. 43–58). New York, NY: The Guilford Press.
Graff, G. (2008). Shame in supervision. Issues in Psychoanalytic Psychology, 30, 79–94.
Granello, P. F. (2013). Wellness counseling. Upper Saddle River, NJ: Pearson Education.
Grosch, W. N. & Olsen, D. C. (1994). When helping starts to hurt: A new look at burnout among psychotherapists. New York, NY: W. W. Norton.
Ivanovski, B., & Malhi, G. S. (2007). The psychological and neurophysiological concomitants of mindfulness forms of meditation. Acta Neuropsychiatrica, 19, 76–91. doi:10.1111/j.1601-5215.2007.00175.x
Kabat-Zinn, J. (1994). Wherever you go, there you are: Mindfulness meditation in everyday life. New York, NY: Hyperion.
Killian, K. D. (2008). Helping till it hurts? A multimethod study of compassion fatigue, burnout, and self-care in clinicians working with trauma survivors. Traumatology, 14(2), 32–44. doi:10.1177/1534765608319083
Knight, W. E., & Rickard, N. S. (2001). Relaxing music prevents stress-induced increases in subjective anxiety, systolic blood pressure, and heart rate in healthy males and females. Journal of Music Therapy, 38, 254–272. doi:10.1093/jmt/38.4.254
Koch, S., Kunz, T., Lykou, S., & Cruz, R. (2014). Effects of dance movement therapy and dance on health-related psychological outcomes: A meta-analysis. The Arts in Psychotherapy, 41, 46–64.
doi:10.1016/j.aip.2013.10.004
Kress, V. E., & Paylo, M. J. (2015). Treating those with mental disorders: A comprehensive approach to case conceptualization and treatment. Upper Saddle River, NJ: Pearson Education.
Lane, M. R. (2005). Creativity and spirituality in nursing: Implementing art in healing. Holistic Nursing Practice, 19, 122–125.
Lent, J. (2009). Journaling enters the 21st century: The use of therapeutic blogs in counseling. Journal of Creativity in Mental Health, 4, 67–73. doi:10.1080/15401380802705391
Linder, S., Miller, G., & Johnson, P. (2000, March). Counseling and spirituality: The use of emptiness and the importance of timing. Paper presented at the meeting of the American Counseling Association, Washington, DC.
Lindholm, J. A. (2003). Perceived organizational fit: Nurturing the minds, hearts, and personal ambitions of university faculty. The Review of Higher Education, 27, 125–149. doi:10.1353/rhe.2003.0040
Lipe, A. W. (2002). Beyond therapy: Music, spirituality, and health in human experience: A review of literature. Journal of Music Therapy, 39, 209–240. doi:10.1093/jmt/39.3.209
Marich, J., & Howell, T. (2015). Dancing mindfulness: A phenomenological investigation of the emerging practice. EXPLORE: The Journal of Science and Healing, 11, 346–356. doi:10.1016/j.explore.2015.07.001
Masci, D., & Lipka, M. (2016, January 21). Americans may be getting less religious, but feelings of spirituality are on the rise. Washington, DC: Pew Research Center. Retrieved from http://www.pewresearch.org/fact-tank/2016/01/21/americans-spirituality
Maslach, C., Leiter, M. P., & Jackson, S. E. (2012). Making a significant difference with burnout interventions: Researcher and practitioner collaboration. Journal of Organizational Behavior, 33, 296–300. doi:10.1002/job.784
Maslach, C., Schaufeli, W. B., & Leiter, M. P. (2001). Job burnout. Annual Review of Psychology, 52, 397–422. doi:10.1146/annurev.psych.52.1.397
Matthes, W. A. (1992). Induction of counselors into the profession. The School Counselor, 39, 245–250.
Mellin, E. A., Hunt, B., & Nichols, L. M. (2011). Counselor professional identity: Findings and implications for counseling and interprofessional collaboration. Journal of Counseling & Development, 89, 140–147. doi:10.1002/j.1556-6678.2011.tb00071.x
Myers, J. E., Sweeney, T. J., & Witmer, J. M. (2001). Optimization of behavior: Promotion of wellness. In D. C. Locke, J. E. Myers, & E. L. Herr (Eds.), The handbook of counseling (pp. 641–652). Thousand Oaks, CA: Sage.
Myers, J. E., & Williard, K. (2003). Integrating spirituality into counselor preparation: A developmental, wellness approach. Counseling and Values, 47, 142–155. doi:10.1002/j.2161-007X.2003.tb00231.x
Neff, K. D. (2003). Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and Identity, 2, 85–101. doi:10.1080/15298860390129863
Neff, K. D., & Costigan, A. P. (2014). Self-compassion, wellbeing, and happiness. Psychologie in Österreich, 2(3), 114–119. Retrieved from http://self-compassion.org/wp-content/uploads/publications/Neff&Costigan.pdf
Neff, K. D., Kirkpatrick, K. L., & Rude, S. S. (2007). Self-compassion and adaptive psychological functioning.
Journal of Research in Personality, 41, 139–154. doi:10.1016/j.jrp.2006.03.004
Newsome, S., Waldo, M., & Gruszka, C. (2012). Mindfulness group work: Preventing stress and increasing self-compassion among helping professionals in training. The Journal for Specialists in Group Work, 37, 297–311. doi:10.1080/01933922.2012.690832
Nielsen, L. A. (1988). Substance abuse, shame and professional boundaries and ethics: Disentangling the issues. Alcoholism Treatment Quarterly, 4, 109–137. doi:10.1300/J020v04n02_08
O’Halloran, T. M., & Linton, J. M. (2000). Stress on the job: Self-care resources for counselors. Journal of Mental Health Counseling, 22, 354–364.
Ohrt, J. H., Prosek, E. A., Ener, E., & Lindo, N. (2015). The effects of a group supervision intervention to promote wellness and prevent burnout. The Journal of Humanistic Counseling, 54, 41–58.
doi:10.1002/j.2161-1939.2015.00063.x
Patsiopoulos, A. T., & Buchanan, M. J. (2011). The practice of self-compassion in counseling: A narrative inquiry. Professional Psychology: Research and Practice, 42, 301–307. doi:10.1037/a0024482
Pennebaker, J. W., & Seagal, J. D. (1999). Forming a story: The health benefits of narrative. Journal of Clinical Psychology, 55, 1243–1254. doi:10.1002/(SICI)1097-4679(199910)55:10<1243::AID-JCLP6>3.0.CO;2-N
Pollack, S. M., Pedulla, T., & Siegel, R. D. (2014). Sitting together: Essential skills for mindfulness-based psychotherapy. New York, NY: The Guilford Press.
Reese, R. F., & Myers, J. E. (2012). EcoWellness: The missing factor in holistic wellness models. Journal of Counseling & Development, 90, 400–406. doi:10.1002/j.1556-6676.2012.00050.x
Riordan, R. J. (1996). Scriptotherapy: Therapeutic writing as a counseling adjunct. Journal of Counseling and Development, 74, 263–269. doi:10.1002/j.1556-6676.1996.tb01863.x
Rogers, C. R. (1961). On becoming a person: A therapist’s view of psychotherapy. Boston, MA: Houghton Mifflin.
Rogers, C. R. (1980). A way of being. New York, NY: Houghton Mifflin Harcourt.
Rogers, N. (1993). The creative connection: Expressive arts as healing. Palo Alto, CA: Science and Behavior Books.
Ross, A., & Thomas, S. (2010). The health benefits of yoga and exercise: A review of comparison studies. The Journal of Alternative and Complementary Medicine, 16, 3–12. doi:10.1089=acm.2009.0044
Rust, J. P., Raskin, J. D., & Hill, M. S. (2013). Problems of professional competence among counselor trainees: Programmatic issues and guidelines. Counselor Education and Supervision, 52, 30–42.
doi:10.1002/j.1556-6978.2013.00026.x
Ruysschaert, N. (2009). (Self) hypnosis in the prevention of burnout and compassion fatigue for caregivers: Theory and induction. Contemporary Hypnosis, 26, 159–172. doi:10.1002/ch.382
Schanche, E., Stiles, T. C., McCullough, L., Svartberg, M., & Nielsen, G. H. (2011). The relationship between activating affects, inhibitory affects, and self-compassion in patients with Cluster C personality disorders. Psychotherapy, 48, 293–303. doi:10.1037/a0022012
Schaufeli, W., & Enzmann, D. (1998). The burnout companion to study & practice: A critical analysis. Philadelphia, PA: Taylor and Francis.
Skovholt, T. M. (2012). The counselor’s resilient self. Turkish Psychological Counseling and Guidance Journal, 4(38), 137–146. Retrieved from http://www.pegem.net/dosyalar/dokuman/138861-20140125102831-1.pdf
Skovholt, T. M., Grier, T. L., & Hanson, M. R. (2001). Career counseling for longevity: Self-care and burnout prevention strategies for counselor resilience. Journal of Career Development, 27, 167–176. doi:10.1023/A:1007830908587
Smallwood, J., & Schooler, J. W. (2015). The science of mind wandering. Annual Review of Psychology, 66, 487–518. doi:10.1146/annurev-psych-010814-015331
Snyder, B. A. (1997). Expressive art therapy techniques: Healing the soul through creativity. Journal of Humanistic Education & Development, 36, 74–82. doi:10.1002/j.2164-4683.1997.tb00375.x
Sori, C. F., Biank, N., & Helmeke, K. B. (2006). Spiritual self-care of the therapist. In K. B. Helmeke & C. F. Sori (Eds.), The therapist’s notebook for integrating spirituality in counseling: Homework, handouts, and activities for use in psychotherapy (Vol. 1, pp. 3–18). Binghamton, NY: The Haworth Press.
Thompson, E. H., Frick, M. H., & Trice-Black, S. (2011). Counselor-in-training perceptions of supervision practices related to self-care and burnout. The Professional Counselor, 1, 152–162. doi:10.15241/eht.1.3.152
Thompson, I., Amatea, E., & Thompson, E. (2014). Personal and contextual predictors of mental health counselors’ compassion fatigue and burnout. Journal of Mental Health Counseling, 36, 58–77. doi:10.17744/mehc.36.1.p61m73373m4617r3
Utley, A., & Garza, Y. (2011). The therapeutic use of journaling with adolescents. Journal of Creativity in Mental Health, 6, 29–41. doi:10.1080/15401383.2011.557312
Valente, V., & Marotta, A. (2005). The impact of yoga on the professional and personal life of the psychotherapist. Contemporary Family Therapy, 27, 65–80. doi:10.1007/s10591-004-1971-4
Walsh, R. (2011). Lifestyle and mental health. American Psychologist, 66, 579–592. doi:10.1037/a0021769
Warren, J., Morgan, M. M., Morris, L.-N. B., & Morris, T. M. (2010). Breathing words slowly: Creative writing and counselor self-care—The writing workout. Journal of Creativity in Mental Health, 5, 109–124.
doi:10.1080/15401383.2010.485074
Wikström, B. M. (2005). Communicating via expressive arts: The natural medium of self-expression for hospitalized children. Pediatric Nursing, 31, 480–485.
Witmer, J. M., & Young, M. E. (1996). Preventing counselor impairment: A wellness approach. The Journal of Humanistic Counseling, 34, 141–155. doi:10.1002/j.2164-4683.1996.tb00338.x
Wright, J. K. (2003). Writing for protection: Reflective practice as a counsellor. Journal of Poetry Therapy, 16, 191–198. doi:10.1080/0889367042000197376
Yager, G. G., & Tovar-Blank, Z. G. (2007). Wellness and counselor education. The Journal of Humanistic Counseling, 46, 142–153. doi:10.1002/j.2161-1939.2007.tb00032.x
Yob, I. M. (2010). Why is music a language of spirituality? Philosophy of Music Education Review, 18, 145–151. doi:10.2979/pme.2010.18.2.145
Susannah C. Coaston is an assistant professor at Northern Kentucky University. Correspondence can be addressed to Susannah Coaston, 1 Nunn Drive, MEP 203C, Highland Heights, KY 41099, coastons1@nku.edu.
Mar 2, 2015 | Article, Volume 5 - Issue 2
Cassandra A. Storlie, Eric R. Baltrinic
Cystic fibrosis is a progressive, chronic disease that affects approximately 30,000 adults and children in the United States. Counseling children with the special needs specific to cystic fibrosis can be overwhelming for mental health professionals due to the progressive and deteriorating nature of the illness, long-term contact with clients, and discouraging prognosis. Being exposed to long-term therapeutic relationships with chronically ill children and witnessing treatment failure can contribute to burnout, compassion fatigue and vicarious trauma in counselors, highlighting the need for targeted literature addressing holistic self-care strategies. The purpose of this manuscript is to provide a review of the current literature illuminating the challenges facing children with cystic fibrosis and to provide targeted self-care suggestions for professional counselors working with this population.
Keywords: children, chronic disease, compassion fatigue, cystic fibrosis, self-care
Cystic fibrosis (CF) is a chronic, terminal disease targeting most organ systems (Withers, 2012) and affects approximately 30,000 children and adults nationwide (Cystic Fibrosis Foundation [CFF], 2014a). CF primarily affects the gastrointestinal and respiratory systems (Withers, 2012), and although the life expectancy has greatly improved, CF is fatal and there is no known cure (CFF, 2014a). Counseling children with chronic illnesses, such as CF, presents special challenges for mental health professionals (Sidell, 1997), including professional counselors. As the nature and severity of clients’ problems impact levels of counselor burnout or compassion fatigue (Figley, 2002), it is essential that professional counselors working with children with CF maintain healthy self-care practices.
There is an abundance of information examining the physiological aspects of CF that clients experience throughout the disease progression (CFF, 2014a; Pearson, Pumariega, & Seilheimer, 1991; Sawicki, Sellers, & Robinson, 2009; Sawicki & Tiddens, 2012). However, there is limited literature on the special considerations that need to be taken when counseling children with CF. Furthermore, there is a paucity of counseling literature targeting how professional counselors can foster personal self-care while working with young clients with special needs and chronic conditions. The purpose of this manuscript is to provide a review of literature that illuminates the challenges facing children with CF and provides a primer for self-care suggestions for professional counselors who work with these children.
Special Needs of Children with Cystic Fibrosis
Physiological Challenges Facing Children with Cystic Fibrosis
Professional counselors need to be knowledgeable of chronic diseases affecting their clients in order to be sensitive to the traumas experienced by children and families coping with illness (Thompson & Henderson, 2007). CF is most commonly diagnosed during newborn screening and severely affects the exocrine system (CFF, 2014b). Within the exocrine system, there is a lack of appropriate enzymes available during digestion, so children with CF are unable to properly digest their food and absorb essential nutrients for healthy growth and development. They experience recurrent gastrointestinal distress such as issues of diarrhea and constipation with foul-smelling stools due to poor absorption (CF Living, 2014). As such, children with CF often suffer from malnutrition and an inability to maintain a healthy weight. However, the most notable signs and symptoms affecting children with CF result from chronic lung and respiratory infections that lead to frequent coughing spells to clear the lungs of thick mucus. This inability to clear the lungs requires multiple episodes of daily chest physiotherapy (Berge & Patterson, 2004). Over time, the respiratory infections produce lung damage that appears cyst-like, giving name to the disease cystic fibrosis (CFF, 2014a).
Children with CF can spend hours per day on medical treatments such as nebulizer treatments to improve breathing, medications prior to meals to improve digestion, and oral, inhaled or intravenous antibiotics to treat respiratory infections (CF Living, 2014). However, disabilities from CF are not often visibly apparent until later stages of the disease. Decreased mobility and debilitating side effects from long-term medications, along with decreased lung capacity, all contribute to clients with CF requiring oxygen therapy for survival (Withers, 2012). The later stages of CF are inundated with frequent hospitalizations. Treatment during end-stage CF is palliative rather than curative (Lowton & Gabe, 2003), and without lung transplantation, CF remains a fatal disease due to respiratory failure (Hayes, Anstead, Warner, Kuhn, & Ballard, 2010). Nevertheless, medical breakthroughs have increased the survival rate of children with CF (Blum, 1992) and now many children are living into adulthood. Advanced clinical drug trials, aggressive antibiotic medications and innovative gene therapy research have been successful with CF clients of all ages. In 1955, children with CF were not expected to live to attend grade school. Children born with CF in this decade are projected to live into their 40s (CFF, 2014a). With this increase in life expectancy, health care teams are faced with unique challenges specific to the turbulence of adolescence and treatment compliance (Withers, 2012). Although there has been a predominant focus on treating CF based on medical science (Chesson, Chisholm, & Zaw, 2004), there is a strong interconnection of the psychosocial and physical challenges facing children and adolescents with CF. As such, professional counselors are called to increase their knowledge, skill and awareness of not just the physical challenges affecting children with CF, but also the emotional obstacles facing this population.
Psychosocial Challenges Facing Children with Cystic Fibrosis
Emotional and behavioral health disorders affect approximately 20% of all children and adolescents nationwide (Canning, Haner, Shade, & Boyce, 1992), and children with chronic illness may exhibit even higher incidences of mental health and psychosocial issues (Barnes, Eisenberg, & Resnick, 2010). For example, children with CF may experience extreme psychological challenges (e.g., depression, hopelessness, suicidal ideation) and physical complications (e.g., poor lung functioning, malnutrition) throughout the progression of their chronic condition. Taken together, these comorbidities contribute to the complexity of supporting an intense treatment modality (Anderson, Flume, & Hardy, 2001; Withers, 2012) that also promotes healthy psychosocial development and family system functioning (O’Haver et al., 2010).
In order to provide evidenced-based practices to clients with CF, as well as their families and loved ones, professional counselors need to be current on mental health research related to this special population. Studies have identified that children with CF may be predisposed to psychological issues and attachment and behavioral problems (Berge & Patterson, 2004) that may require additional training for professional counselors to effectively and efficiently counsel this population. When compared to healthy peers, children with chronic health conditions also have been found to have a slightly higher risk of attempting suicide (Barnes et al., 2010). Grief and loss, internal and external stress, negative body image, and difficulty managing emotions are common challenges experienced by children with CF (Berge & Patterson, 2004; Withers, 2012). In managing these difficulties, internalizing behaviors and anxiety also have been found prominent among this population (Berge & Patterson, 2004). Younger male children with CF have been found to exhibit higher levels of anxiety (Bregnballe, Thastum, & Schiøtz, 2007) and female children with CF have demonstrated internalizing behaviors by expressing less anger than female children without CF (Bregnballe et al., 2007).
Although research supports the idea that individuals with chronic illnesses are at increased risk for depression (Quittner et al., 2008), studies conducted on individuals with CF have provided mixed results (Pearson et al., 1991; Thompson, Hodges, & Hamlet, 1990). Berge and Patterson (2004) identified higher incidences of depression among youth with CF, whereas Tluczek et al. (2014) found that patients with CF report similar psychosocial functioning as their healthy peers. One possible factor affecting the mixed reports of depression among children with CF may include the level of disease acceptance. Previous investigations have identified that the level of disease acceptance among youth with CF can significantly lessen levels of anxiety, depression and disability in adolescents with CF (Casier et al., 2008). Nonetheless, depression and depressive symptoms have been shown to impact the progression of chronic diseases, such as CF, by increasing the likelihood that clients will be less compliant with treatment regimens and partake in risky behaviors (Quittner et al., 2008; Withers, 2012). Hence, we recommend assessing and screening for depressive symptoms frequently and examining the level of disease acceptance in clients with CF. Professional counselors working with children with CF will need to further tailor interventions based on the client’s symptom patterns (Chesson et al., 2004), while accounting for changes typical of childhood development.
Recently, scholars have researched the experiences of adolescents with CF in their transition to adulthood. This turbulent time (Withers, 2012) may need special consideration by professional counselors. Qualitative research on the experiences of adolescents with CF who were transitioning to adulthood generated the following three emerging themes: treatment compliance, health-related problems and future outlook concerning their disease (Berge, Patterson, Goetz, & Milla, 2007). Male participants described being more independent with treatment compliance, whereas females desired an accountability partner for their treatment regimen. Female participants expressed issues with depression, negative body image and fear of diabetes as a complication from CF, whereas males only disclosed their fear of acquiring diabetes as the disease progressed. Interestingly, both male and female participants expressed a positive outlook concerning CF regarding identity and acceptance of the disease (Berge et al., 2007). Identifying and maintaining a positive outlook while dealing with a chronic and debilitating illness can be a challenge for children with CF and their parents and families. Professional counselors working with youth with CF need to consider these findings. Special attention may be given to issues of treatment compliance, further physical complications from CF and maintaining a positive outlook.
Regarding risky behaviors (Quittner et al., 2008), teenagers with CF have admitted to using alcohol and drugs to seek relief from the challenges of CF (Vaeth & Martins, 2015). As such, professional counselors working with children with CF need to tailor interventions to the individuals’ symptom-specific patterns (Chesson et al., 2004) and be mindful of behaviors that may hasten the disease process. The use of alcohol and drugs may hasten the disease’s progression because of the ways in which these substances can interact with the client’s current prescription medication regimen. Alcohol use may result in pancreatitis and a hypoglycemic reaction (Withers, 2012). Likewise, clients who smoke legal and illegal substances contribute to the deterioration of lung functioning. We recommend frequently assessing and screening for substance abuse and depressive symptoms and exploring the level of disease acceptance among youth with CF in creative, developmentally appropriate ways. Importantly, professional counselors preparing counseling interventions for children with CF need to account for the added psychosocial and developmental challenges that are typical in childhood development.
Special Considerations When Counseling Children with Cystic Fibrosis
Many children share similar psychological and developmental needs as they grow (Thompson & Henderson, 2007). However, children with chronic illness may struggle to be emotionally mature, while simultaneously managing the physical symptoms of their conditions (Dahlbeck & Lightsey, 2008). Furthermore, the psychosocial complexities and the chronic nature of CF may create unique challenges for professional counselors providing services to children and their families, such as the deteriorating nature of CF, frequent hospitalizations and the life-threatening prognosis (Frels, Leggett, & Larocca, 2009; Morison, Bromfield, & Cameron, 2003). Counseling professionals’ increased sensitivity to the progression and impact of this disease can help guide their intervening efforts (Chesson et al., 2004) by leading them to consider the physiological and psychological trauma caused by CF. Professional counselors must ensure that they have developed rapport with the child as an individual, instead of a child with a disability (Thompson & Henderson, 2007).
Counseling interventions for children with CF begin with recognizing that children with CF are not adults with CF. Therefore, treatment and counseling efforts need to allow for special consideration of childhood development and understanding (Chesson et al., 2004; Geldard & Geldard, 2008). Chesson et al. (2004) offered suggestions for meeting the needs of children with chronic illnesses through counseling. First, counselors need to obtain the child’s understanding of counseling (e.g., what it is, how it will help, roles, communication). Although parental support and involvement is important when counseling children (Geldard & Geldard, 2008; Morison et al., 2003), relying solely on parental reports is not a replacement for exploring the child’s perspective of counseling (Geldard & Geldard, 2008). Chronic illnesses such as CF impact the whole family system (Kirk et al., 2013). However, within the therapeutic counseling relationship, children with CF must feel as if they are the experts on their lives and their mental health, regardless of age.
Second, counselors working with children should limit the amount of talking they do in session (Chesson et al., 2004) in favor of engaging children through natural modes of expression such as play, drawing and games. We recommend structuring counseling sessions to include discussions alongside an activity, versus a sole reliance on face-to-face conversation, in order to improve rapport building within the therapeutic relationship. Children engaging in healthy interdependent relationships with counselors can begin to develop a sense of independence and trust (Juntunen & Atkinson, 2002) within the counseling process, despite the tumultuous times during the disease progression. The adverse impact of chronic illness on social functioning (Last, Stam, Onland-van Nieuwenhuizen, & Grootenhuis, 2007) can lead to social withdrawal (Dahlbeck & Lightsey, 2008), which can be intensified when there is a concentrated focus on the child via adult approaches to counseling (e.g., making the child the center of attention to discuss his or her illness). As such, we recommend that professional counselors make age-appropriate and developmental adjustments to the counseling session and consider instituting group counseling modalities to counter the regularity of social isolation among these children.
Third, professional counselors developing a therapeutic relationship with a child experiencing CF must incorporate interactions that address the traumatic impact of living with the illness. Children with CF undergo physically stressful and painful experiences during medical treatment. Geldard and Geldard (2008) suggested that professional counselors clarify the nature of counseling and differentiate it from medical treatments. They also suggested maintaining an environment that provides acceptance and invites free disclosure. Professional counselors are urged to explain the distinction between counseling and medical procedures (e.g., there are no needles or painful medical procedures in counseling). Professional counselors also are encouraged to engage children in activities and play to reduce their level of anxiety and guardedness (Chesson et al., 2004). These targeted counseling strategies can promote resiliency factors such as self-efficacy and empowerment so that children may cope with adversity throughout the illness (Dahlbeck & Lightsey, 2008; Luszczynska, Gutiérrez-Doña, & Schwarzer, 2005). Chesson et al. (2004) further suggested that counselors gradually establish the therapeutic relationship over a number of shorter sessions in order to establish trust with the child. We caution against rushing the counseling relationship-building process and encourage professional counselors to listen openly in order to understand the child’s world.
As children struggle with chronic illnesses such as CF, acute emotional reactions are invariably triggered, which may increase the propensity for children to act out in self-injurious ways (Vaeth & Martins, 2015). The counseling process requires consistency and transparency when discussing how a child’s treatment progress will be shared among adults. Accordingly, a fourth special consideration needs to be illuminated—the limits of confidentiality. Professional counselors must illustrate the circumstances when parents will be notified of instances of self-harm or suicidal and homicidal ideation. Given the susceptibility of children with chronic illnesses to depression (Quittner et al., 2008) and suicidal ideation (Barnes et al., 2010), coping with the challenges and effects of CF are constantly in the minds of these children. Rebecca Mueller (2001) illustrated this point as a young person struggling with the illness as follows:
All the information I have about my disease has been dispersed in small pieces over time. The idea that [when] a child with CF reaches a certain age, truth and honest answers should suddenly be given is awful. With the many different sides and aspects of CF or other diseases, the information needs to come out over time, giving the person time to react and contemplate. (p. 43)
Professional counselors working with children with CF understand the need for a collaborative approach in supporting individuals and families experiencing the trauma of chronic illness. Children with chronic diseases are involved with multiple treatment professionals (e.g., dieticians, respiratory therapists, physicians, nurses, case managers, mental health and school counselors). Chesson et al. (2004) recommended that counselors assist children with understanding the decisions made by their parents, doctors and other professionals about their treatment. This task can be done by assessing the child’s knowledge of the disease process and treatment and initiating family sessions or sessions with other health care professionals when warranted. Ultimately, children who protest treatment interventions can be overridden by a caregiver’s decision. When children have a history of adult-driven decisions related to life-preserving medical treatments, this experience can make behavioral counseling interventions difficult. We suggest that counselors make every effort to respect the feelings and wishes of children with CF, including helping to “coordinate services, rearranging physical environments, removing barriers and inconveniences, and securing special equipment and materials” (Thompson & Henderson, 2007, p. 713). Professional counselors can further facilitate this supportive process by empowering children to identify and articulate their perspectives on medical treatments, given their limited choices (Chesson et al., 2004; Morison et al., 2003).
Family Involvement
Family involvement is critical to all aspects of treatment of children with CF, starting with diagnosis. Parents and families are significantly affected when their child is diagnosed with a chronic illness (Anderson et al., 2001; O’Haver et al., 2010). Thompson and Henderson (2007) explained, “The demands for energy, time, and financial resources may add a heavy burden of stress to families” (p. 602). It is essential to note that families and children face myriad stressors related to the “uncertainty and uncontrollability” of chronic illness, along with “restrictions on their freedom” (Last et al., 2007, p. 102). However, family members (particularly parents) are often responsible for providing an environment in which children can develop resiliency and independence. Family members provide a supportive environment and help to promote children’s sense of self-worth and ability to cope with challenging life situations (Juntunen & Atkinson, 2002). These tasks may be especially difficult for parents of children with CF in that they too are more vulnerable to higher incidences of depression (Quittner et al., 2008; Tluczek et al., 2014). Hence, we recommend that professional counselors working with the family system ensure that parents of children with CF have access to the emotional supports necessary to sustain family functioning and equilibrium, including participation in their own counseling as needed (Tluczek et al., 2014). Similarly, professional counselors may find it necessary to provide parent education about the CF disease process in order to help parents identify strategies to enhance resiliency in their child (Juntunen & Atkinson, 2002).
Counseling children with CF involves implementing prolonged and gradual approaches to relationship building, increasing one’s knowledge of the illness, adapting treatment approaches to account for the impact of invasive medical procedures, and involving parents, guardians and other professionals in the counseling process. Above all, honoring the perspective of the child is central to success in counseling this population, which can be easier said than done. The chronic and complex nature of CF and its treatment requires a great deal of effort and presents additional clinical challenges for professional counselors. Over time, the challenges of working with children with special needs can affect the wellness of professional counselors providing services. Therefore, it is important for counselors to recognize the factors contributing to impairment and burnout, particularly among counselors who work with children experiencing chronic illnesses like CF.
A Self-Care Primer for Professional Counselors
Professional counselors and other health professionals engaged in prolonged therapeutic contact with clients with CF are vulnerable to burnout, compassion fatigue and vicarious trauma (Coady, Kent, & Davis, 1990; Lewiston, Conley, & Blessing-Moore, 1981; Savicki & Cooley, 1987), potentially leading to impairment. Counselors have an ethical obligation to recognize their state of wellness and potential impairment (American Counseling Association [ACA], 2011), which may be impacted by burnout, compassion fatigue or vicarious trauma while working with children experiencing chronic conditions (Angerer, 2003; Kalliath, O’Driscoll, Gillespie, & Bluedorn, 2000; Najjar, Davis, Beck-Coon, & Doebbeling, 2009; Sexton, 1999) such as CF. Such occupational risks may be heightened when professionals work with clients with a poor prognosis associated with chronic illness, including CF (Coady et al., 1990).
Counselors and other mental health professionals experience occupational stressors such as long working hours, work with challenging clients, poor interdisciplinary support and poor supervision (Coady et al., 1990). Lewiston et al. (1981) examined burnout among health care providers working with clients experiencing CF. They found high levels of emotional exhaustion and client depersonalization (i.e., a sense of inability to impact clients’ improvement while watching clients’ illness progress), and a lower sense of accomplishment among health care providers working with this population. The implications of these results are intensified because “psychotherapists who work with chronic illnesses tend to disregard their own self-care needs when focusing on the needs of clients” (Figley, 2002, p. 1433).
Children with CF and their families are survivors of both medical and psychosocial traumas. Frequent trips to the emergency room, an inability to breathe, surgeries, and understanding the unpredictable and fatal progression of CF are among the traumas endured by this special population. Professional counselors who hear these traumatic stories within the therapeutic milieu must understand that vicarious trauma can occur for even the most experienced counselor. Sommer (2008) clarified that vicarious traumatization is not inadequacy on behalf of the counselor or emotional damage of the client but can be considered an “occupational hazard” (p. 52). Vicarious trauma, defined as “a traumatic reaction to specific client-presented information” (Trippany, Kress, & Wilcoxon, 2004, p. 32), also may occur among professional counselors working with children who have CF due to the erratic and terminal progression of the illness.
Professional counselors serving the CF community must recognize their vulnerabilities to burnout, compassion fatigue and vicarious trauma. Given the realities of clinical practice and responsibilities of everyday living (e.g., busy schedules, high caseloads, supervision barriers, family responsibilities, maintaining relationships), poor self-care and wellness may be easy to identify but difficult to change. In order to prevent issues of burnout, compassion fatigue and vicarious trauma, the following self-care strategies are suggested for professional counselors who work with this special population.
Self-Care Strategies for Professional Counselors
Although counselors are taught to utilize a developmental and wellness approach when working with clients (Myers & Sweeney, 2005), they often neglect their own health and well-being. Self-care strategies embedded in a wellness philosophy may help to prevent incidences of burnout among those working with the unique emotional and psychosocial stressors affecting children with CF and their families. Myers and Sweeney (2005) identified wellness as both a process and an outcome in that it is an “overarching goal for living and a day-by-day, minute-by-minute way of being” (p. 9). Self-care strategies involve managing stress in ways that limit the impact on the individual (Young, 2005). Within the counseling literature, wellness is depicted as incorporating social, emotional, physical, intellectual and spiritual dimensions (Roscoe, 2009). Counseling wellness models have been empirically supported in the counseling literature (Myers & Sweeney, 2005; Myers, Sweeney, & Witmer, 2000; Sweeney & Witmer, 1991; Witmer & Sweeney, 1992) and inform individuals about methods to limit their stress and maintain a healthy sense of well-being. Hence, we recommend that professional counselors use multidimensional, holistic self-care strategies to maintain a sense of wellness when working with youth experiencing special needs. The following section provides physiological, cognitive and spiritual wellness strategies for professional counselors to use while working with children with CF and other chronic conditions.
Physiological self-care strategies. Professional counselors are accustomed to working with clients regarding wellness and self-care but may not always practice their own healthy suggestions. Self-care strategies that are body-focused may help alleviate the impact of stress (Young, 2005), particularly among those working with children with special needs such as CF. Young (2005) recommended approaches such as progressive relaxation, balanced exercise and nutrition, and adequate rest to assist with integrating a wellness focus and enhancing self-care. A healthy diet and physical activity are readily known to prevent physical and mental health conditions, while also increasing energy levels. Furthermore, “minding the body” and having adequate sleep and bodily rest are additional suggestions for restoring self-care as a priority for professional counselors (Norcross & Guy, 2007, pp. 64–65). Professional counselors interested in implementing physiological self-care strategies to address potential issues of vicarious trauma while working with children diagnosed with CF may consider simple tasks such as taking a brisk walk during their lunch break, joining a gym, or being more intentional with their diet and bedtime routines. In addition to focusing on physical health and wellness, self-care in the cognitive domain is equally important for fostering a sense of well-being.
Cognitive self-care strategies. Stress from occupational risks accumulated through working with youth with special needs may be further prevented if counselors utilize cognitive approaches to support their own self-care. Professional counselors interested in improving their self-care in cognitive ways may consider cognitive restructuring to formulate new thinking patterns and assertiveness training to bring about direct changes in behaviors that may have been impacted by stress (Young, 2005), which often accumulates during the long-term therapeutic relationship with children and families affected by CF. Moreover, the use of guided imagery may provide both cognitive and physical benefits in helping to create a cognitive break from daily stress inside and outside the workplace. Notably, cognitive self-care strategies begin with self-monitoring, insight and self-awareness (Norcross & Guy, 2007). Despite counselors’ close therapeutic connection to clients with CF and their families, healthy boundaries are imperative to prevent issues of burnout and compassion fatigue. Norcross and Guy (2007) noted that “setting boundaries consistently emerges in the research as one of the most frequently used and one of the most highly effective self-care principles” (p. 94). Due to counselors’ innate desire to help others, they often take on too many clients or are mandated to do so by agency policies. Counselors may provide extra time to ancillary responsibilities and have unrealistic expectations of themselves. As such, we recommend that professional counselors obtain good supervision to help manage and maintain work–life balance, particularly when working with children with special needs. In addition to the benefits of physical and cognitive self-care strategies, spirituality also has been shown to enhance levels of wellness and thus decrease the potential for burnout and compassion fatigue.
Spiritual self-care strategies. Spirituality comes in many forms and there is no finite definition of how one engages in his or her spiritual self. Many counselors and psychotherapists identify their own career path as a calling to care for others and commitment to growth and self- knowledge (Norcross & Guy, 2007). Research supports that spirituality, prayer and meditation are positive manners in which to promote wellness and augment self-care (Cashwell, 2005). Spiritual beliefs, practices and experiences are intricately connected and may continue to foster support from communities and individuals, along with reinforcing healthy emotions. While working with children experiencing the later stages of CF, professional counselors’ spirituality may help them connect with clients on a more meaningful level. Taking a spiritual perspective can further shape counselors’ perspective on life events (Young, 2005), particularly when they are grieving the death of a child with CF. In seeking a spiritual connection to a higher power, the negative responses to stressful events may be limited (Young, Cashwell, & Shcherbakova, 2000), strengthening one’s wellness and ability to care for oneself. These actions, along with discussing spirituality with the child and family affected by CF, may further model healthy practices during difficult times in the disease process.
Spiritual self-care can include the use of mindfulness, which can be viewed as the nonjudgmental awareness of one’s own inner suffering (Birnie, Speca, & Carlson, 2010) and reflections on self-compassion (Neff, 2003). Birnie et al. (2010) described self-compassion as the awareness of “feelings of caring and kindness towards oneself in the face of personal suffering” and the “recognition that one’s suffering, failures, and inadequacies are part of the human condition” (p. 2). When counseling children with CF, professional counselors may consider routinely expressing self-compassion as part of their inner dialogue. The following mantra used by the second author may be of assistance to professional counselors implementing spiritual self-care:
Suffering is part of life. My clients suffer, but did not choose this illness. They are walking in its wake and I will walk alongside them. I will extend loving kindness in all the work I do, despite the pain and suffering I experience and witness.
We highlight the following three essential components of self-compassion: (a) extending kindness and understanding toward oneself rather than harsh judgments or criticism, (b) recognizing that suffering (even chronic illness) is a part of the larger human condition, and (c) not overidentifying with the awareness of one’s painful thoughts (Birnie et al., 2010; Neff, 2003). By engaging in self-compassion and mindfulness, professional counselors may help to prevent incidences of compassion fatigue while working with children and families affected by CF by recognizing that this illness has a role in their humanity.
Conclusion
Professional counselors working with children and families affected by CF should consider the physical and psychosocial challenges facing this special-needs population. With the discouraging nature of the disease progression, professional counselors must have a basic understanding of the client’s chronic condition (Thompson & Henderson, 2007) and how the progression of the illness affects the child’s emotional state. Professional counselors must further explore how to limit the impact of occupational stress that may lead to burnout, compassion fatigue and vicarious trauma. This article provides a primer on the physiological, psychosocial and special needs specific to youth with CF and offers targeted self-care strategies for professional counselors. Children with CF are a special population and professional counselors are called to implement these special considerations in their thoughtful practice. There is an abundance of literature examining the physiological aspects of CF (CFF, 2014a; Pearson et al., 1991; Sawicki et al., 2009; Sawicki & Tiddens, 2012). However, more research is warranted to examine the salient factors that affect the therapeutic relationship between professional counselors and children with CF. Meanwhile, professional counselors can develop and implement individualized, multidimensional self-care strategies to counter the effects of this difficult yet rewarding work.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of
interest or funding contributions for
the development of this manuscript.
References
American Counseling Association. (2011). ACA’s taskforce on counselor wellness and impairment. Retrieved from http://www.counseling.org/knowledge-center/counselor-wellness
Anderson, D. L., Flume, P. A., & Hardy, K. K. (2001). Psychological functioning of adults with cystic fibrosis. Chest, 119, 1079–1084.
Angerer, J. M. (2003). Job burnout. Journal of Employment Counseling, 40, 98–107.
doi:10.1002/j.2161-1920.2003.tb00860.x
Barnes, A. J., Eisenberg, M. E., & Resnick, M. D. (2010). Suicide and self-injury among children and youth with chronic health conditions. Pediatrics, 125, 889–895. doi:10.1542/peds.2009-1814
Berge, J. M., & Patterson, J. M. (2004). Cystic fibrosis and the family: A review and critique of the literature. Families, Systems and Health, 22, 74–100. doi:10.1037/1091-7527.221.74
Berge, J. M., Patterson, J. M., Goetz, D., & Milla, C. (2007). Gender differences in young adults’ perceptions of living with cystic fibrosis during the transition to adulthood: A qualitative investigation. Families, Systems, and Health, 25, 190–203. doi:10.1037/1091-7527.25.2.190
Birnie, K., Speca, M., & Carlson, L. E. (2010). Exploring self-compassion and empathy in the context of mindfulness-based stress reduction (MBSR). Stress and Health, 26, 359–371. doi:10.1002/smi.1305
Blum, R. W. (1992). Chronic illness and disability in adolescence. Journal of Adolescent Health, 13, 364–368. doi:10.1016/1054-139X(92)90029-B
Bregnballe, V., Thastum, M., & Schiøtz, P. O. (2007). Psychosocial problems in children with cystic fibrosis. Acta Pædiatrica, 96, 58–61. doi:10.1111/j.1651-2227.2006.00014.x
Canning, E. H., Haner, S. B., Shade, K. A., & Boyce, W. T. (1992). Mental disorders in chronically ill children: Parent-child discrepancy and physician identification. Pediatrics, 90, 692–696.
Cashwell, C. S. (2005). Spirituality and wellness. In J. E. Myers & T. J. Sweeney (Eds.), Counseling for wellness: Theory, research, and practice (pp. 197–205). Alexandria, VA: American Counseling Association.
Casier, A., Goubert, L., Huse, D., Theunis, M., Franckx, H., Robberecht, E., . . . Crombez, G. (2008). The role of acceptance in psychological functioning in adolescents with cystic fibrosis: A preliminary study. Psychology and Health, 23, 629–638. doi:10.1080/08870440802040269
CF Living. (2014). About CF. Retrieved from http://www.cfliving.com/newly-diagnosed/living-with-cf/about-cf.jsp
Chesson, R. A., Chisholm, D., & Zaw, W. (2004). Counseling children with chronic physical illness. Patient Education and Counseling, 55, 331–338. doi:10.1016/j.pec.2003.04.002
Coady, C. A., Kent, V. D., & Davis, P. W. (1990). Burnout among social workers working with patients with cystic fibrosis. Health and Social Work, 15, 116–124.
Cystic Fibrosis Foundation. (2014a). About cystic fibrosis. Retrieved from http://www.cff.org/AboutCF/
Cystic Fibrosis Foundation. (2014b). Newborn screening: Info for new parents. Retrieved from http://www.cff.org/AboutCF/Testing/NewbornScreening/
Dahlbeck, D. T., & Lightsey, O. R., Jr. (2008). Generalized self-efficacy, coping, and self-esteem as predictors of psychological adjustment among children with disabilities or chronic illnesses. Children’s Health Care, 37, 293–315. doi:10.1080/02739610802437509
Figley, C. R. (2002). Compassion fatigue: Psychotherapists’ chronic lack of self care. Journal of Clinical Psychology, 58, 1433–1441. doi:10.1002/jclp.10090
Frels, R. K., Leggett, E. S., & Larocca, P. S. (2009). Creativity and solution-focused counseling for a child with chronic illness. Journal of Creativity in Mental Health, 4, 308–319. doi:10.1080/15401380903372646
Geldard, K., & Geldard, D. (2008). Counselling children: A practical introduction (3rd ed.). London, England: Sage.
Hayes, D., Jr., Anstead, M. I., Warner, R. T., Kuhn, R. J., & Ballard, H. O. (2010). Inhaled morphine for palliation of dyspnea in end-stage cystic fibrosis. American Journal of Health-System Pharmacy, 67, 737–740.
doi:10.2146/ajhp080188
Juntunen, C. L., & Atkinson, D. R. (Eds.). (2002). Counseling across the lifespan: Prevention and treatment. Thousand Oaks, CA: Sage.
Kalliath, T. J., O’Driscoll, M. P., Gillespie, D. F., & Bluedorn, A. C. (2000). A test of the Maslach burnout inventory in three samples of healthcare professionals. Work and Stress, 14, 35–50. doi:10.1080/026783700417212
Kirk, S., Beatty, S., Callery, P., Gellatly, J., Milnes, L., & Pryjmachuk, S. (2013). The effectiveness of self-care support interventions for children and young people with long-term conditions: A systematic review. Child: Care, Health and Development, 39, 305–324. doi:10.1111/j.1365-2214.2012.01395.x
Last, B. F., Stam, H., Onland-van Nieuwenhuizen, A.-M., & Grootenhuis, M. A. (2007). Positive effects of a psycho-educational group intervention for children with a chronic disease: First results. Patient Education and Counseling, 65, 101–112. doi:10.1016/j.pec.2006.06.017
Lewiston, N. J., Conley, J., & Blessing-Moore, J. (1981). Measurement of hypothetical burnout in cystic fibrosis caregivers. Acta Pædiatrica, 70, 935–939. doi:10.1111/j.1651-2227.1981.tb06254.x
Lowton, K., & Gabe, J. (2003). Life on a slippery slope: Perceptions of health in adults with cystic fibrosis. Sociology of Health and Illness, 25, 289–319. doi:10.1111/1467-9566.00348
Luszczynska, A., Gutiérrez-Doña, B., & Schwarzer, R. (2005). General self-efficacy in various domains of human functioning: Evidence from five countries. International Journal of Psychology, 40, 80–89. doi:10.1080/00207590444000041
Morison, J. E., Bromfield, L. M., & Cameron, H. J. (2003). A therapeutic model for supporting families of children with a chronic illness or disability. Child and Adolescent Mental Health, 8, 125–130. doi:10.1111/1475-3588.00058
Mueller, R. (2001). The child’s perspective. In M. Bluebond-Langner, B. Lask, & D. B. Angst (Eds.), Psychological aspects of cystic fibrosis (pp. 37–44). New York, NY: Arnold.
Myers, J. E., & Sweeney, T. J. (Eds.). (2005). Counseling for wellness: Theory, research, and practice. Alexandria, VA: American Counseling Association.
Myers, J. E., Sweeney, T. J., & Witmer, J. M. (2000). The wheel of wellness counseling for wellness: A holistic model for treatment planning. Journal of Counseling & Development, 78, 251–266. doi:10.1002/j.1556-6676.2000.tb01906.x
Najjar, N., Davis, L. W., Beck-Coon, K., & Doebbeling, C. C. (2009). Compassion fatigue: A review of the research to date and relevance to cancer-care providers. Journal of Health Psychology, 14, 267–277. doi:10.1177/1359105308100211
Neff, K. (2003). Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and Identity, 2, 85–102. doi:10.1080/15298860309032
Norcross, J. C., & Guy, J. D., Jr. (2007). Leaving it at the office: A guide to psychotherapist self-care. New York, NY: Guilford Press.
O’Haver, J., Moore, I. M., Insel, K. C., Reed, P. G., Melnyk, B. M., & Lavoie, M. (2010). Parental perceptions of risk and protective factors associated with the adaptation of siblings of children with cystic fibrosis. Pediatric Nursing, 36, 284-–292.
Pearson, D. A., Pumariega, A. J., & Seilheimer, D. K. (1991). The development of psychiatric symptomatology in patients with cystic fibrosis. Journal of the American Academy of Child & Adolescent Psychiatry, 30, 290–297.
Quittner, A. L., Barker, D. H., Snell, C., Grimley, M. E., Marciel, K., & Cruz I. (2008). Prevalence and impact of depression in cystic fibrosis. Current Opinion in Pulmonary Medicine, 14, 582–588. doi:10.1097/MCP.0b013e3283121cf1
Roscoe, L. J. (2009). Wellness: A review of theory and measurement for counselors. Journal of Counseling & Development, 87, 216–226. doi:10.1002/j.1556-6678.2009.tb00570.x
Savicki, V., & Cooley, E. (1987). The relationship of work environment and client contact to burnout in mental health professionals. Journal of Counseling & Development, 65, 249–252.
Sawicki, G. S., Sellers, D. E., & Robinson, W. M. (2009). High treatment burden in adults with cystic fibrosis: Challenges to disease self-management. Journal of Cystic Fibrosis, 8, 91–96. doi:10.1016/j.jcf.2008.09.007
Sawicki, G. S., & Tiddens, H. (2012). Managing treatment complexity in cystic fibrosis: Challenges and opportunities. Pediatric Pulmonology, 47, 523–533. doi:10.1002/ppul.22546
Sexton, L. (1999). Vicarious traumatisation of counsellors and effects on their workplaces. British Journal of Guidance and Counselling, 27, 393–403. doi:10.1080/03069889908256279
Sidell, N. L. (1997). Adult adjustment to chronic illness: A review of the literature. Health & Social Work, 22, 5–11. doi:10.1093/hsw/22.1.5
Sommer, C. A. (2008). Vicarious traumatization, trauma-sensitive supervision, and counselor preparation. Counselor Education and Supervision, 48, 61–71. doi:10.1002/j.1556-6978.2008.tb00062.x
Sweeney, T. J., & Witmer, J. M. (1991). Beyond social interest: Striving toward optimum health and wellness. Individual Psychology: The Journal of Adlerian Theory, Research & Practice, 47, 527–540.
Thompson, C. L., & Henderson, D. A. (2007). Counseling children (7th ed.). Belmont, CA: Thomson.
Thompson, R. J., Jr., Hodges, K., & Hamlett, K. W. (1990). A matched comparison of adjustment in children with cystic fibrosis and psychiatrically referred and nonreferred children. Journal of Pediatric Psychology, 15, 745–759. doi:10.1093/jpepsy/15.6.745
Tluczek, A., Laxova, A., Grieve, A., Heun, A., Brown, R. L., Rock, M. J., . . . Farrell, P. M. (2014). Long-term follow-up of cystic fibrosis newborn screening: Psychosocial functioning of adolescents and young adults. Journal of Cystic Fibrosis, 13, 227–234. doi:10.1016/j.jcf.2013.10.001
Trippany, R. L., Kress, V. E. W., & Wilcoxon, S. A. (2004). Preventing vicarious trauma: What counselors should know when working with trauma survivors. Journal of Counseling & Development, 82, 31–37. doi:10.1002/j.1556-6678.2004.tb00283.x
Vaeth, S., & Martins, L. (2015). Teens, cystic fibrosis and emotional health. Retrieved from http://cfcenter.stanford.edu/teens/CysticFibrosisandEmotionalHealth_000.html
Withers, A. L. (2012). Management issues for adolescents with cystic fibrosis. Pulmonary Medicine, 2012, 1–10. doi:10.1155/2012/134132
Witmer, J. M., & Sweeney, T. J. (1992). A holistic model for wellness and prevention over the life span. Journal of Counseling & Development, 71, 140–148.
Young, J. S. (2005). A wellness perspective on the management of stress. In J. E. Myers & T. J. Sweeney (Eds.), Counseling for wellness: Theory, research, and practice (pp. 207-–215). Alexandria, VA: American Counseling Association.
Young, J. S., Cashwell, C. S., & Shcherbakova J. (2000). The moderating relationship of spirituality on negative life events and psychological adjustment. Counseling and Values, 45, 49–57.
Cassandra A. Storlie, NCC, is an Assistant Professor at Kent State University. Eric R. Baltrinic is an Assistant Professor at the University of Toledo. Correspondence may be addressed to Cassandra Storlie, 310 White Hall, PO Box 5190, Kent, OH 44242, cstorlie@kent.edu.