Sep 13, 2024 | Volume 14 - Issue 2
Sapna B. Chopra, Rebekah Smart, Yuying Tsong, Olga L. Mejía, Eric W. Price
This mixed methods program evaluation study was designed to assist faculty in better understanding students’ multicultural and social justice training experiences, with the goal of improving program curriculum and instruction. It also offers a model for counselor educators to assess student experiences and to make changes that center social justice. A total of 139 first-semester students and advanced practicum students responded to an online survey. The Consensual Qualitative Research-Modified (CQR-M) method was used to analyze brief written narratives. The Multicultural Counseling Competence and Training Survey (MCCTS) and the Advocacy Competencies Self-Assessment Survey (ACSA) were used to triangulate the qualitative data. Qualitative findings revealed student growth in awareness, knowledge, skills, and action, particularly for advanced students, with many students reporting a desire for more social justice instruction. Some students of color reported microaggressions and concerns that training centers White students. Quantitative analyses generally supported the qualitative findings and showed advanced students reporting higher multicultural and advocacy competencies compared to beginning students. Implications for counselor education are discussed.
Keywords: social justice, program evaluation, training, multicultural counseling, counselor education
In the midst of the COVID-19 pandemic and the long-standing inequities it brought to light, many universities began examining the ways that injustice unfolds within their institutions (Mull, 2020). Arredondo et al. (2020) noted that counseling and counselor education continue to uphold white supremacy and center the experiences of White people within theories, training, and research. White supremacy culture promotes Whiteness as the norm and standard, intersects with and reinforces other forms of oppression, and shows up in institutions in both overt and covert ways, such as emphasis on individualism, avoidance of conflict, and prioritizing White comfort (Okun, 2021). Arredondo et al. (2020) called for counselor educators to engage in social justice advocacy and to unpack covert White supremacy in training programs. The present study investigated the multicultural and social justice training experiences of students in a Western United States counseling program so that counseling faculty can be empowered to uncover biases and better integrate social justice in the curriculum.
Counselor education programs are products of the larger sociopolitical environment and dominant patriarchal, cis-heteronormative, Eurocentric culture that often fails to “challenge the hegemonic views that marginalize groups of people” which “perpetuate deficit-based ideologies” (Goodman et al., 2015, p. 148). For example, the focus on the individual in traditional counseling theories can reinforce oppression by failing to address the role of systemic oppression in a client’s distress (Singh et al., 2020). Counseling theory textbooks usually provide an ancillary section at the end of each chapter focusing on multicultural issues (Cross & Reinhardt, 2017). White supremacy culture is so ubiquitous that it is typically invisible to those immersed within it (DiAngelo, 2018). It is not surprising then that counseling is often viewed as a White, middle-class endeavor, and BIPOC (Black, Indigenous, and People of Color) clients frequently perceive that they should leave their cultural identities and experiences outside the counseling session (Turner, 2018). Counselor educators have been encouraged to reflect on how Eurocentric curricula and pedagogy may marginalize students and seek liberatory teaching practices that promote critical consciousness (Sharma & Hipolito-Delgado, 2021).
Students’ Perceptions of Their Growth, Learning Process, and Critiques of Their Training
Studies of mostly White graduate students show gains in expanding awareness of their own biases and privilege, knowledge about other cultures and experiences of oppression, as well as the importance of empowering and advocating for clients (Beer et al., 2012; Collins et al., 2015; Sanabria & DeLorenzi, 2019; Singh et al., 2010). Others indicated the benefits of integrating feminist principles in treatment (Hoover & Morrow, 2016; Singh et al., 2010). Consciousness-raising and self-reflection were key parts of multicultural and social justice learning (Collins et al., 2015; Hoover & Morrow, 2016), and could be emotionally challenging. Indeed, Goodman et al. (2018) identified a theme of internal grappling reflecting students’ experiences of intellectual and emotional struggle; others noted students’ experiences of overwhelm and isolation (Singh et al., 2010), as well as resistance, such as withdrawing or dismissing information that challenged their existing belief system (Seward, 2019). Researchers have also documented student complaints about their social justice training; for example, that social justice is not well integrated or that there was inadequate coverage of skills and action (Collins et al., 2015). Kozan and Blustein (2018) found that even among programs that espouse social justice, there was a lack of training in macro level advocacy skills. Barriers to engaging in advocacy included: lack of time (Field et al., 2019; Singh et al., 2010), emotional exhaustion stemming from observations of the harms caused by systemic inequities (Sanabria & DeLorenzi, 2019), and ill-informed supervisors (Sanabria & DeLorenzi, 2019).
The studies reviewed thus relied on samples of mainly White, cisgender, heterosexual women. Some noted that education on social justice is often centered on helping White students expand their awareness (Haskins & Singh, 2015). In one study focused on challenges faced by students of color, participants expressed frustration with the lack of diversity among their professors, classmates, and curriculum (Seward, 2019). Participants also experienced marginalization and disconnection when professors and students made offensive or culturally uninformed comments and when course content focused on teaching students with privileged identities. Students from marginalized communities also face isolation in academic settings and sometimes question the multicultural competence of their professors (Haskins & Singh, 2015), which in turn contributes to the underrepresentation of students of color in counseling and psychology (Arney et al., 2019).
The Present Study
Counselor educators must critically examine their curriculum, course materials, and overall learning climate for students (Haskins & Singh, 2015). Listening to students’ experiences and perceptions of their training offers faculty an opportunity to model cultural humility, gain useful feedback, and make necessary changes. Given the increased recognition of racial trauma and societal inequities, it is critical that counseling programs engage with students of diverse backgrounds as they seek to shift their pedagogy. Historically, academic institutions have responded to student demands with performative action rather than meaningful change (Zetzer, 2021). This mixed methods study is part of a larger process of counseling faculty working to invite student feedback and question internalized assumptions and biases in order to implement real change. The goal of program evaluation is to investigate strengths and weaknesses in order to improve the program (Royse et al., 2010). According to the 2024 Council for Accreditation of Counseling and Related Educational Programs (CACREP) standards, program evaluation is essential to assess and improve the program (CACREP, 2023). Thus, the purpose of this program evaluation study was to understand students’ self-assessment and experiences with the counseling program’s curriculum in the area of multicultural and social justice advocacy, with the overarching goal of program curriculum and instruction improvement. This article offers counselor educators a model of how to assess program effectiveness in multicultural and social justice teaching and practical suggestions based on the findings. The research questions were: What are beginning and advanced students’ self-perceptions regarding their multicultural and social justice advocacy competencies? What are beginning and advanced students’ perceptions of the multicultural and social justice advocacy competencies training they are receiving in their program?
Method
We employed a mixed method, embedded design in which the quantitative data offered a supportive and secondary role to the qualitative results (Creswell et al., 2003). Qualitative and mixed methods research designs are particularly useful in program evaluation (Royse et al., 2010). Mixed method approaches also offer value in research that centers social justice advocacy, as the integration of diverse methodological techniques within a single study fosters the understanding of multiple perspectives and facilitates a deeper comprehension of intricate issues (Ponterotto et al., 2013). We used an online survey to collect written narratives (qualitative) and survey data (quantitative) from two counseling courses: a beginning counseling course in the first semester (beginning students), and an advanced practicum course, taken by those who had completed at least part of their year-long practicum (advanced students).
Participants
Participants were counseling students enrolled in a CACREP-accredited program at a large West Coast public university in the United States that is both a federally designated Hispanic-serving institution and an Asian American and Native American Pacific Islander–serving institution. Responses were collected from two courses, which included 94 beginning students (84% response rate) and 62 advanced students (71% response rate). Twelve percent of the advanced practicum students also completed the survey when they were first-semester (beginning) students. The mean age of the 139 participants was 27.7 (SD = 7.11), ranging from 20 to 58 years. Racial identifications were 40.3% White, 33.1% Latinx, 14.4% Asian, 7.2% Biracial or Multiracial, 2.9% Black, 0.7% Middle Eastern, 0.7% American Indian/Alaska Native, and 0.7% Native Hawaiian/Pacific Islander. The majority identified as women (82.0%), followed by 14.4% as men, and 2.9% as nonbinary/queer. Students self-identified as heterosexual (71.2%), bisexual (11.5%), lesbian/gay (6.5%), queer (4.3%), pansexual (1.4%), and about 1% each as asexual, heteroflexible, and unsure. About 19.4% of students were enrolled in a bilingual/bicultural (Spanish/Latinx) emphasis within the program.
Procedure
After receiving university IRB approval, graduate students enrolled in the first-semester beginning counseling course (fall 2018 and 2019) or the advanced practicum course (summer 2019 and 2020) were asked to complete an online survey through Qualtrics with both quantitative measures and open-ended questions as part of their preparation for class discussion. Students were informed that this homework would not be graded and was not intended to “test” their knowledge but rather would serve as an opportunity to reflect on their experience of the program’s multicultural and social justice training. Students were also given the option to participate in the current study by giving permission for their answers to be used. Those who consented were asked to continue to complete the demographic questionnaire. In accordance with the American Counseling Association Code of Ethics (2014), students were informed that there would be no repercussions for not participating. A faculty member outside the counseling program managed the collection of and access to the raw data in order to protect the identities of the students and ensure that their participation or lack of participation in the study could not affect their grade for the course or standing in the program. All students, regardless of participation status, were given the option to enter an opportunity drawing for a small cash prize ($20 for data collection in 2018 and 2019, $25 for 2020) through a separate link not connected to their survey responses.
Data Collection
We collected brief written qualitative data and responses to two quantitative measures from both beginning and advanced students.
Qualitative Data
The faculty developed open-ended questions that would elicit student feedback on their multicultural and social justice training. Prior to beginning the counseling program, first-semester students were asked two questions about their experiences and impressions: How would you describe your knowledge about and interest in multiculturalism/diversity and social justice from a personal and/or academic perspective? and How would you describe your initial impressions or experience of the focus on multicultural and social justice in the program so far? They were also asked, if it was relevant, to include their experience in the Latinx counseling emphasis program component. Advanced students, who were seeing clients, were asked the same questions and also asked to: Consider/describe how this experience of multiculturalism and social justice in the program may impact you personally and professionally (particularly in work with clients) in the future.
Quantitative Data
Two instruments were selected to quantitatively assess students’ perceptions of their own multicultural and advocacy competencies. The Multicultural Counseling Competence and Training Survey (MCCTS; Holcomb-McCoy & Myers, 1999) is designed to assess counselors’ perceptions of their multicultural competence and the effectiveness of their training. The survey contains 32 statements for which participants answer on a 4-point Likert scale (not competent, somewhat competent, competent, extremely competent). Sample items include: “I can discuss family therapy from a cultural/ethnic perspective” and “I am able to discuss how my culture has influenced the way I think.” The reliability coefficients for each of the five components of the MCCTS ranged from .66 to .92: Multicultural Knowledge (.92), Multicultural Awareness (.92), Definitions of Terms (.79), Knowledge of Racial Identity Development Theories (.66), and Multicultural Skills (.91; Holcomb-McCoy & Myers, 1999). In this study, the Cronbach’s alpha coefficients ranged from .75 to .96.
The Advocacy Competencies Self-Assessment Survey (ACSA; Ratts & Ford, 2010) assesses for competency and effectiveness across six domains: (a) client/student empowerment, (b) community collaboration, (c) public information, (d) client/student advocacy, (e) systems advocacy, and (f) social/political advocacy. It contains 30 statements that ask participants to respond with “almost always,” “sometimes,” or “almost never.” Sample questions include “I help clients identify external barriers that affect their development” and “I lobby legislators and policy makers to create social change.” Although Ratts and Ford (2010) did not provide psychometrics of the original ACSA, it was validated with mental health counselors (Bvunzawabaya, 2012), suggesting an adequate internal consistency for the overall measure, but not the specific domains. In this study, the Cronbach’s alpha coefficients ranged from .69 to.79 for the six domains, and .94 for the overall scale. For the purposes of this study, we were not interested in specific domains and used the overall scale to assess students’ overall social justice/advocacy competencies.
Data Analysis
Qualitative Data Analysis
To analyze the qualitative data, we used Consensual Qualitative Research-Modified (CQR-M; Spangler et al., 2012), which was based on Hill et al.’s (2005) CQR but modified for larger numbers of participants with briefer responses. In contrast to the in-depth analysis of a small number of interviews, CQR-M was ideal for our data, which consisted of brief written responses from 139 participants. CQR-M involves a consensus process rather than interrater reliability among judges, who discuss and code the narratives, and relies on a bottom-up approach, in which categories
(i.e., themes) are derived directly from the data rather than using a pre-existing thematic structure. Frequencies (i.e., how many participants were represented in each category) are then calculated. We analyzed the beginning and advanced students’ responses separately, as the questions were adjusted for their time spent in the program.
After immersing themselves in the data, the first two authors, Sapna B. Chopra and Rebekah Smart, met to outline a preliminary coding structure, then met repeatedly to revise the coding into more abstract categories and subcategories. The computer program NVivo was used to organize the coding process and determine frequencies. After all data were coded, the fifth author, Eric W. Price, served as auditor and provided feedback on the overall coding structure. Both the consensus process and use of an auditor are helpful in countering biases and preconceptions. Brief quantitative data, as used in this study, can be used effectively as a means of triangulation (Spangler et al., 2012).
Quantitative Data Analysis
To examine for significant differences in the self-perceptions of multicultural competencies and advocacy competencies between White and BIPOC students as well as between beginning and advanced students, a two-way (2×2) ANOVA was conducted with the overall MCCT as the criterion variable and student levels (beginning, advanced) and race (White, BIPOC) as the two independent variables. In addition, two (5×2) multivariate analyses of variances (MANOVAs) were conducted with the five factors of multicultural competencies (knowledge, awareness, definition of terms, racial identity, and skills) as criterion variables and with student levels (beginning, advanced) and student races (White, BIPOC) as independent variables in each analysis. Data for beginning and advanced students were analyzed separately to assess whether time in the counseling program helped to expand their interest and commitment to social justice.
Research Team
We were intentional in examining our own social identities and potential biases throughout the research process. Chopra is a second-generation South Asian American, heterosexual, cisgender woman. Smart is a White European American, heterosexual, cisgender woman. Yuying Tsong identifies as a genderqueer first-generation Taiwanese and Chinese American immigrant. Olga L. Mejía is an Indigenous-identified Mexican immigrant, bisexual, cisgender woman. Price is a White, gay, cisgender male. All have experience as counselor educators and in qualitative research methods, and all have been actively engaged in decolonizing their syllabi and incorporating multicultural and social justice into their pedagogy.
Results
The research process was guided by the overarching question: What are beginning and advanced counseling students’ perceptions of their multicultural and social justice competencies and training and how can their feedback be used to improve their counselor education program? We explore the qualitative findings first, as the primary data for the study, followed by the quantitative data.
Qualitative Findings for Beginning Counseling Students
Two higher-order categories emerged from the beginning students’ narratives: developing competencies and learning process so far.
Developing Competencies
Students’ descriptions of the competencies they were developing included themes of awareness, knowledge, and skills and action. Some students entered the program with an already heightened awareness, while others were making new discoveries. Awareness included subthemes of humility (24.5%), awareness of own privilege (6.4%), and awareness of bias (3.2%). “There’s a lot to learn” was a typical sentiment, particularly from White students. One White female student wrote: “I definitely need more and I believe that open discussions, even hard ones would be some of the best ways to go about this.” A large group expressed knowledge of oppression and systemic inequities (33%); a smaller group referenced intersectionality (3.2%). Within skills and action, some students expressed specific intentions in allyship (11.7%); a number of students expressed commitment to social action but felt unsure how to engage in social justice (11.7%).
Learning Process So Far
Central themes in this category were support for growth, concerns in training, and internal challenges. Some students felt excited and supported, while some were cautiously optimistic or concerned. Support for growth was a strong theme that reflected excited and enthusiastic to learn (22.3%); appreciation for the Latinx emphasis (18.1%); and receiving support from professors and program (17.0%). For example, one Mexican student in the Latinx emphasis who noted that mental health was rarely discussed in her family shared: “For me to see that there is a program that teaches students how to communicate to individuals who are unsure of what counseling is about, gave me a sense of happiness and relief.”
A few students were adopting a wait-and-see attitude and expressed some concerns about their training. Although the percentage for these subthemes is low, they provide an important experience that we want to amplify. This theme had multiple subthemes. The subtheme concerns from students of color included centering White students (3.2%), microaggressions (3.2%), and lack of representation (1.1%). A student who identified as a Mexican immigrant shared experiences of microaggressions, including classmates using a hurtful derogatory phrase referring to immigrants with no comment from the professor until the student raised the issue. Concerns in training also included the subtheme concerns with how material is presented in classes (7.0%). For some, the concern related to the potential for harm in classes in which White and BIPOC students were encouraged to process issues of privilege and oppression. For example, one Asian Pacific Islander student wrote that although they appreciated the emphasis on social justice, “Time always runs out and I believe it’s careless and dangerous to cut off these types of conversations in a rushed manner.” A small minority seemed to suggest a backlash to the emphasis on social justice, stating that the content was presented in ways that were too “politically correct,” “biased,” or “repetitive.”
Multiple subthemes emerged from the theme of internal challenges. Both BIPOC and White students shared feeling afraid to speak up (5.3%). BIPOC students expressed struggling with confidence or wanting to avoid conflict, while White students’ fear of speaking up was also connected to discomfort and uncertainty as a White person (2.1%). A small minority of White students did not express explicit discomfort but seemed to engage in a color-blind strategy, as indicated in the theme of people are people (2.1%): “I find people are people, regardless of any differences, and love hearing the good and bad about everybody’s experiences.” Some students of color expressed limited knowledge about cultures other than one’s own (4.3%). For example, an Asian American student stated that they had gravitated to “those who were most similar to me” growing up. Lastly, a few students shared feeling overwhelmed and exhausted (3.2%).
Qualitative Findings for Advanced Counseling Students
Four higher-order themes emerged: competencies in process, multiculturalism and diversity in the program, social justice in the program, and the learning process.
Competencies in Process
Similar to beginning students, advanced students described growing self-awareness, knowledge and awareness of others, skills, and action. Their disclosures often related to clinical work, now that they had been seeing clients. Self-awareness included strong subthemes of: humility and desire to keep learning (25.8%); increased open-mindedness, acceptance of others, and compassion (22.6%); awareness of personal privilege and oppression (17.7%); awareness of personal bias and value systems (17.7%); and awareness of personal cultural identity (14.5%). One Mexican American student wrote: “I have also gained an increased awareness of how my prejudices can impact my work with clients and learned about how to check-in with myself.”
Knowledge and awareness of others had subthemes of privilege and oppression (19.4%) and increased knowledge of culture (14.5%), with awareness of the potential impact on clients. The advanced students also had more to say about skills, which included subthemes of diversity considerations in conceptualization (29%), and in treatment (12.9%), and cultural conversations in the therapy room (21%). One White student wrote: “I have been able to have difficult conversations that once were unheard of. I have also been able to bring culture, ethnicity, and oppression into the room so that my clients can feel understood and safe.” Within the theme of action, 52% wrote about their commitment to social justice and intention to advocate. Although this strongest subtheme suggested action was still more aspirational than currently enacted, a smaller group also wrote about the experiences that they have already had with client advocacy (12.9%), community and/or political action (12.9%), and unspecified action (11.3%).
Multiculturalism and Diversity in the Program
Many students (44%) indicated that they appreciated that multicultural issues were integrated or addressed well within the program. However, with more time spent in the program, 26% felt that there was more nuance, depth, or scope needed. Some wanted more attention to specific issues, such as disability, gender identity, and religion/spirituality. One Asian American student wrote that the focus had been “basic and surface-level,” adding “I feel like it has also generally catered to the protection of White feelings and voices, which is inherently complicit in the system of White supremacy, especially in higher ed.” Others (9.7%) said more training in clinical application was needed.
Social Justice in the Program
Students expressed a variety of opinions. The largest number (29%) were satisfied that social justice issues were well integrated into the program. Although more students were satisfied than not, many (24%) noted that social justice is addressed but not demonstrated. Similarly, 24% noted minimal attention, specifically that social justice was not addressed much beyond the one course focused on culture, and 24% noted a desire for more opportunities within the program to engage in advocacy. Some suggested requiring social justice work rather than leaving it as an optional activity. Others (13%), mostly from 2020, noted the relevance of current events and sociopolitical climate. One White student shared about a presentation on Black Lives Matter: “This project opened my eyes to my limited knowledge of systemic oppression in the U.S. and impacted me in ways that I will NEVER be the same.” A small number of students (3%) reported that there was no need or room for more training in social justice. One White student wrote that they felt “frustrated” and that the social justice “agenda is so in my face all the time,” adding “sometimes I feel like I am being trained to be an advocate and an activist, which is/are a different job.”
The Learning Process
Three central themes emerged: enrichment experienced, challenges, and suggestions for change. Many students were appreciative of their experience. A strong subtheme within enrichment experienced was professors’ encouragement and modeling (24%). Others commented on how much came from learning from peers (21%). Some shared feeling personally empowered (14.5%). For example, a student who identified as coming from an Asian culture wrote about the hesitancy to be an activist, stating, “There is an underlying belief that our voices will not really ever be heard which is strongly tied to systemic oppression and racism throughout history. Consequently, I appreciate this challenge to grow more in social justice issues.” Others shared ways that the program prompted them to engage in social justice outside the classroom (11.3%). For example, one student wrote: “This program gave me the knowledge and education I needed to make sure that when I did speak out I wasn’t just talking to talk. I would actually have facts, stats, evidence-based research to back up my argument.” A number of students noted the unique benefits of the Latinx program (9.7%). One Mexican American student reflected that they had learned about diversity within Latinx cultures, and that, “As a result, I feel more confident in being able to serve clients from various Latinx cultures or at least know where to obtain relevant information when needed.” Many students expressed a sense of belonging (8.1%).
Challenges. Nearly 10% wrote about struggling to make time [for social justice] and 6.5% noted the emotional impact. For example, one White student wrote: “It was a rude and brutal awakening, to say the least. It was riddled with emotion and heartache but was worth the process.” A few had conflicted or mixed feelings (8.1%)—they felt appreciative but wanted more. A few noted possible harm to marginalized students (6.5%). One Asian American student wrote that faculty should be “calling out microaggressions . . . otherwise, their stance on social justice feels more performative and about protecting their own liability rather than caring for their students of color.” A smaller number (4.8%) struggled with peers and colleagues who seemed uninformed.
Suggestions for Change. Students offered suggestions for improvement, with a strong theme to develop more diverse representation (16.1%), including more representation in faculty, students, case examples, and class discussions. Some comments were specifically about needed attention to Black experiences; one concerned teaching about resiliencies and strengths in the face of oppression. Almost 15% suggested making changes to courses or curriculum. One White student wrote: “If it were me running the program (lol) I would . . . remove the culture class and have all those topics embedded into the fabric of each class because culture and diversity are in all those topics.” A few suggested that faculty require social justice assignments (8.1%), adding that many students will not act unless required. A few also suggested that the program provide more education of White students (8.1%).
Quantitative Findings
Quantitative analyses were conducted to provide triangulation for the qualitative findings and a different view of the data, including possible differences between BIPOC and White students and beginning and advanced students. Table 1 includes descriptive statistics providing an overview of beginning and advanced students’ self-perception of their multicultural and social justice competencies.
Table 1
Descriptive Statistics of Competencies
|
|
|
Multicultural |
Social Justice/Advocacy |
|
|
N |
Mean |
SD |
Mean |
SD |
| White |
Beginning |
35 |
2.58 |
.50 |
62.97 |
24.23 |
| Advanced |
27 |
3.09 |
.38 |
76.07 |
19.11 |
| Total |
62 |
2.80 |
.52 |
68.68 |
22.93 |
| BIPOC |
Beginning |
59 |
2.66 |
.56 |
63.05 |
29.30 |
| Advanced |
35 |
3.01 |
.30 |
77.14 |
20.71 |
| Total |
94 |
2.79 |
.51 |
68.30 |
27.19 |
| Total |
Beginning |
94 |
2.63 |
.54 |
63.02 |
27.39 |
| Advanced |
62 |
3.05 |
.34 |
76.68 |
19.87 |
| Total |
156 |
2.80 |
.51 |
68.45 |
25.51 |
To examine if there were discernable differences between the beginning and advanced students’ perceptions of their competencies, and if there were differences between White and BIPOC students, a two-way (2×2) ANOVA was conducted with the overall MCCT as the criterion variable and student levels (beginning, advanced) and race (White, BIPOC) as the two independent variables. Results indicated that although there were no interaction effects between race and student levels, there were significant differences in overall multicultural competencies between beginning and advanced students, F(1, 152) = 30.54, p < .001, indicating that advanced practicum students reported significantly higher overall multicultural competencies than beginning students. There were no statistically significant differences between White and BIPOC students in their overall multicultural competencies. Two (5×2) MANOVAs were conducted with the five factors of multicultural competencies as criterion variables (knowledge, awareness, definition of terms, racial identity, and skills). Student levels (beginning, advanced) and student race (White, BIPOC) were independent variables. Results indicated that there were significant differences between beginning and advanced students in at least one of the multicultural competencies components, Wilks’ Lambda = .72, F(5, 150) = 11.97, p < .001. More specifically, follow-up univariate ANOVAs indicated that advanced students reported significantly higher multicultural competencies in their knowledge, F(1, 154) = 43.74, p < .001, µ2 = .22; awareness, F(1, 154) = 6.20, p = .014, µ2 = .04; and racial identity, F(1, 154) = 43.17, p < .001, µ2 = .21. However, there were no significant differences in definitions of terms or skills. Even though there were no significant differences between White and BIPOC students in their overall multicultural competencies, the results of the 5×2 MANOVA indicated that there were significant differences in at least one of the components, Wilks’ Lambda = .87, F(5, 150) = 4.49, p = .001. Follow-up univariate ANOVAs indicated that White students reported higher multicultural competencies in racial identity than BIPOC students in this study, F(1, 154) = 4.51, p = .035, µ2 = .03. There were no differences in the other areas.
A two-way (2×2) ANOVA was conducted with the overall ACSA as the criterion variable and student levels (beginning, advanced) and race (White, BIPOC) as the two independent variables. Results indicated that while there were no interaction effects between race and student levels, there were significant differences in overall advocacy competencies between beginning and advanced students, F(1, 152) = 10.78, p = .001, indicating that advanced students reported significantly higher overall advocacy competencies (M = 76.68) than beginning students (M = 63.02). There were no statistically significant differences between White and BIPOC students in their overall advocacy competencies.
Discussion
This study was designed to examine students’ experiences of their multicultural and social justice training as an aspect of program evaluation, specifically to assist faculty in improving curriculum and instruction with regard to multicultural and advocacy competencies; the study also offers a unique contribution to existing literature by including a more racially diverse (60% BIPOC) sample. Students reported growth in the core areas of multicultural and social justice competency as outlined by Ratts et al. (2016): awareness, knowledge, skills, and action. Consistent with Field et al.’s (2019) findings, students reported more growth in awareness and knowledge than in social justice action, with some differences as students moved through the program. Although beginning students identified personal biases, the theme of self-awareness was more complex for them later in the program. This suggests that a longer time spent in the program contributed to personal growth; although this seems expected, these outcomes have not necessarily been examined before and confirm that the programs’ increasing effort on multiculturalism and social justice are showing gains. The advanced students wrote about clinical application as well and made overt statements of their commitment to social justice. The quantitative results supported these qualitative findings, with advanced students reporting higher multicultural competencies in knowledge, awareness, and racial identity and higher overall advocacy competencies compared to beginning students. With one exception, there were no significant differences between White and BIPOC students in their self-assessment of multicultural or advocacy competencies. Across racial groups, students expressed humility and desire to learn more.
Although students expressed mixed opinions about their experience of the multicultural and social justice training, a greater number of advanced students reported that they thought multicultural (44%) and social justice issues (30%) were well integrated into the program compared to the number of students with critiques. Students reported that support from faculty and peers facilitated their growth and learning, consistent with previous research (e.g., Beer et al., 2012; Keum & Miller, 2020). Some students noted a sense of belonging, particularly those in the Latinx emphasis.
Similar to other researchers, we found that many students wanted social justice issues to be integrated across the curriculum rather than into one course (Beer et al., 2012; Collins et al., 2015); they also wanted more focus on skills and action (Collins et al., 2015; Kozan & Blustein, 2018). Students’ scores on the ACSA advocacy competencies scale reflect this gap in training as well. Though fewer students offered critiques of their training, these responses are important to amplify because some of these concerns are rarely solicited or acknowledged. For example, BIPOC students echoed the challenges faced by students in Seward’s (2019) study, including lack of representation in their faculty, classmates, and curriculum as well as feelings of marginalization when microaggressions in the classroom went unchecked and when instruction centered the needs of White students. Additionally, a few advanced students from 2020, during a time of significant racial-sociopolitical uprising in the United States, expressed concern that class discussions potentially caused harm to students from marginalized communities. Though more students expressed a desire for greater in-depth training, a small minority of mostly White students indicated that they did not want more social justice training and would rather focus solely on traditional counseling skills. These different student perspectives point to the challenges of teaching social justice amidst diverse political and ideological backgrounds and the need to increase community and collaboration.
Listening to Student Feedback and Implications for Decolonizing Program Curriculum
This study’s findings support the benefits of listening to students’ voices related to multicultural and social justice to inform counselor educators on program strengths and areas for growth. Although student feedback was not the sole impetus for making program changes, accessing this more detailed response was helpful in refining our purpose and direction, as well as highlighting weaknesses. Perhaps more important was the faculty’s willingness to engage in this self-reflective process and to take necessary actions. Rather than waiting for exit interview feedback from graduating students, counselor educators can conduct ongoing program evaluations through anonymous online surveys as well as town hall meetings that invite students to share their process of learning, perceptions of the cultural climate, and experiences of microaggressions. We have a growing understanding that during such evaluations great care needs to be taken for building safety, so as not to retraumatize students from marginalized communities. Based on the results and a series of Zoom town hall meetings, we have implemented changes, such as more consistent integration of social justice across the curriculum; training and day-long retreats focused on increasing faculty competence; faculty participation in Academics for Black Survival and Wellness, an intensive training led by Dr. Della Mosely and Pearis Bellamy; accountability support groups in social justice work; and decolonizing syllabi and class content (e.g., including BIPOC voices and non–APA-style writing assignments). Faculty have also made significant modifications to course materials. For example, beginning students complete weekly modules that include readings and exercises from The Racial Healing Handbook (Singh, 2019), and students study Liberation Psychology during the first week of theories class so they can consider ways to decolonize more traditional models throughout the semester. These strategies have been helpful in preparing students for more difficult conversations surrounding anti-racism in more advanced courses throughout the program. Forming faculty accountability partners or small groups is helpful so that faculty can support each other as a part of their ongoing development in addressing internalized White supremacy and avoiding harm to students.
Student feedback also called attention to the need for self-care, which our program continues to explore. Consistent with previous research (Collins et al., 2015; L. A. Goodman et al., 2018; Hoover & Morrow, 2016; Singh et al., 2010), students reported that their multicultural and social justice learning was often accompanied by moments of overwhelm, hopelessness, and despair. Without tools to manage these emotions, some students may retreat into defensiveness and withdrawal (Seward, 2019), and some may experience activist burnout (Gorski, 2019). Sustainability is necessary for effective social change efforts (Toporek & Ahluwalia, 2021). Counseling programs can offer resources and guidance for students to practice self-care with counselor educators modeling self-care behavior. For example, the Psychology of Radical Healing Collective (Chen et al., 2019) offered strategies to practice radical self-care, including making space for one’s own healing, finding joy and a sense of belonging, and engaging in advocacy at the local community level. Mindfulness practices can be integrated into social justice education to help students and counselor educators manage difficult emotions, increase their ability to be present, and strengthen compassion and curiosity (Berila, 2016). In addition to individual self-care practices, counselor educators can advocate for community care by tending to the community’s needs and drawing on collective experience and wisdom (Gorski, 2019).
The findings point to the need for counselor educators to better address Whiteness and White supremacy, as well as to center the experiences of students from marginalized communities. Counselor educators may be able to mobilize and direct White students’ feelings of guilt into racial consciousness and action by helping them explore Whiteness, White privilege, and what it means to them while allowing and confronting feelings that arise (Grzanka et al., 2019). It may be helpful for educators to read and assign books on White fragility and ways to address it (DiAngelo, 2018; Helms, 2020; Saad, 2020), so that they can assist White students in managing these emotions. It is important that educators explicitly name and recognize White supremacy as it shows up in counseling theory and practice, and to include a shift from the primary focus on the individual to understanding and dismantling oppressive systems. Counselor educators must also attend to the ways in which they center the comfort of White students over the needs of BIPOC students, so that they do not perpetuate harm and trauma (Galán et al., 2021). Although students with privileged identities may learn powerful lessons about oppression from their classmates, it is important that such learning does not occur at the expense of students with marginalized identities. Offering spaces for White students, especially those who are new to conversations about race and racism, to process their feelings may be helpful to avoid harm to BIPOC students who have experienced racial trauma. Similarly, BIPOC students may benefit from spaces in which they can talk freely and support each other as they unpack their own experiences of microaggressions and trauma (Galán et al., 2021).
Based on the finding that support from faculty was important in facilitating student growth and learning, counselor educators may benefit from implementing strategies informed by relational pedagogy and relational–cultural theory (Dorn-Medeiros et al., 2020). Relational pedagogy centers the relationship between teachers and students and posits that all learning takes place in relationships. Relational–cultural theory emphasizes mutual empathy and empowerment and is rooted in feminist multicultural principles. Practices grounded in these approaches include professors’ use of self-disclosure to model openness, vulnerability, and self-reflection; and their work to reduce power imbalances and invite student feedback at multiple points in time through anonymous surveys and one-on-one meetings. Counselor educators can uplift students as the experts of their experience (Sharma & Hipolito-Delgado, 2021).
Limitations and Future Research
The results of this study must be considered in light of a number of limitations. The use of the online survey meant that we were not able to follow up with students for further discussion or clarification of their responses. Adding focus groups or interviews to this methodology would likely provide a more thorough picture. In spite of assurances to the contrary, some students may have been hesitant to be honest out of concern that their own professors would be reading their feedback. It is possible that different themes would have emerged if all students had participated. In addition, 12% of the advanced students had participated as beginning students and therefore were previously exposed to the survey materials. Although this could have impacted their later responses, we suspect that given the nearly 2-year time lapse this may not have been meaningful. Nevertheless, future research and program evaluation would be strengthened with longitudinal analyses. Lastly, the reliability for the ACSA was relatively low, so conclusions are tentative; however, the results support the qualitative data. Despite these limitations, this study offers a model for assessing students’ learning and experiences with the goal of program improvement. The process of counselor educators humbling themselves and inviting and integrating student feedback is an important step in decolonizing counselor education and better serving students and the clients and communities that they will serve.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
American Counseling Association. (2014). ACA code of ethics. https://www.counseling.org/docs/default-source/default-document-library/ethics/2014-aca-code-of-ethics.pdf?sfvrsn=55ab73d0_1
Arney, E. N., Lee, S. Y., Printz, D. M. B., Stewart, C. E., & Shuttleworth, S. P. (2019). Strategies for increased racial diversity and inclusion in graduate psychology programs. In M. T. Williams, D. C. Rosen, & J. W. Kanter (Eds.), Eliminating race-based mental health disparities: Promoting equity and culturally responsive care across settings (pp. 227–242). Context Press.
Arredondo, P., D’Andrea, M., & Lee, C. (2020). Unmasking White supremacy and racism in the counseling profession. Counseling Today. https://ctarchive.counseling.org/2020/09/unmasking-white-supremacy-and-racism-in-the-counseling-profession
Beer, A. M., Spanierman, L. B., Greene, J. C., & Todd, N. R. (2012). Counseling psychology trainees’ perceptions of training and commitments to social justice. Journal of Counseling Psychology, 59(1), 120–133. https://doi.org/10.1037/a0026325
Berila, B. (2016). Integrating mindfulness into anti-oppression pedagogy: Social justice in higher education. Routledge.
Bvunzawabaya, B. (2012). Social justice counseling: Establishing psychometric properties for the Advocacy Competencies Self-Assessment Survey (Doctoral dissertation, Auburn University). https://etd.auburn.edu/handle/10415/3369
Chen, G. A., Neville, H. A., Lewis, J. A., Adames, H. Y., Chavez-Dueñas, N. Y., Mosley, D. V., & French, B. H. (2019). Radical self-care in the face of mounting racial stress: Cultivating hope through acts of affirmation. Psychology Today. https://www.psychologytoday.com/us/blog/healing-through-social-justice/201911/radical-self-care-in-the-face-mounting-racial-stress
Collins, S., Arthur, N., Brown, C., & Kennedy, B. (2015). Student perspectives: Graduate education facilitation of multicultural counseling and social justice competency. Training and Education in Professional Psychology, 9(2), 153–160. https://doi.org/10.1037/tep0000070
Council for the Accreditation of Counseling and Related Educational Programs. (2023). 2024 CACREP standards.
https://www.cacrep.org/wp-content/uploads/2023/06/2024-Standards-Combined-Version-6.27.23.pdf
Creswell, J. W., Plano Clark, V. L., Gutmann, M. L., & Hanson, W. E. (2003). Advanced mixed methods research designs. In A. Tashakkori & C. Teddlie (Eds.), SAGE handbook of mixed methods in social and behavioral research (1st ed.; pp. 209–240). SAGE.
Cross, W. E., Jr., & Reinhardt, J. S. (2017). Whiteness and serendipity. The Counseling Psychologist, 45(5), 697–705. https://doi.org/10.1177/0011000017719551
DiAngelo, R. (2018). White fragility: Why it’s so hard for White people to talk about racism. Beacon Press.
Dorn-Medeiros, C. M., Christensen, J. K., Lértora, I. M., & Croffie, A. L. (2020). Relational strategies for teaching multicultural courses in counselor education. Journal of Multicultural Counseling and Development, 48(3), 149–160. https://doi.org/10.1002/jmcd.12174
Field, T. A., Ghoston, M. R., Grimes, T. O., Sturm, D. C., Kaur, M., Aninditya, A., & Toomey, M. (2019). Trainee counselor development of social justice counseling competencies. Journal for Social Action in Counseling and Psychology, 11(1), 33–50. https://doi.org/10.33043/JSACP.11.1.33-50
Galán, C. A., Bekele, B., Boness, C., Bowdring, M., Call, C., Hails, K., McPhee, J., Mendes, S. H., Moses, J., Northrup, J., Rupert, P., Savell, S., Sequeira, S., Tervo-Clemmens, B., Tung, I., Vanwoerden, S., Womack, S., & Yilmaz, B. (2021). Editorial: A call to action for an antiracist clinical science. Journal of Clinical Child and Adolescent Psychology, 50(1), 12–57. https://doi.org/10.1080/15374416.2020.1860066
Goodman, L. A., Wilson, J. M., Helms, J. E., Greenstein, N., & Medzhitova, J. (2018). Becoming an advocate: Processes and outcomes of a relationship-centered advocacy training model. The Counseling Psychologist, 46(2), 122–153. https://doi.org/10.1177/0011000018757168
Goodman, R. D., Williams, J. M., Chung, R. C.-Y., Talleyrand, R. M., Douglass, A. M., McMahon, H. G., & Bemak, F. (2015). Decolonizing traditional pedagogies and practices in counseling and psychology education: A move towards social justice and action. In R. D. Goodman & P. C. Gorski (Eds.), Decolonizing “multicultural” counseling through social justice (pp. 147–164). Springer.
Gorski, P. C. (2019). Fighting racism, battling burnout: Causes of activist burnout in US racial justice activists. Ethnic and Racial Studies, 42(5), 667–687. https://doi.org/10.1080/01419870.2018.1439981
Grzanka, P. R., Gonzalez, K. A., & Spanierman, L. B. (2019). White supremacy and counseling psychology: A critical–conceptual framework. The Counseling Psychologist, 47(4), 478–529. https://doi.org/10.1177/0011000019880843
Haskins, N. H., & Singh, A. (2015). Critical race theory and counselor education pedagogy: Creating equitable training. Counselor Education and Supervision, 54(4), 288–301. https://doi.org/10.1002/ceas.12027
Helms, J. E. (2020). A race is a nice thing to have: A guide to being a White person or understanding the White persons in your life (3rd ed.). Cognella.
Hill, C. E., Knox, S., Thompson, B. J., Williams, E. N., Hess, S. A., & Ladany, N. (2005). Consensual qualitative research: An update. Journal of Counseling Psychology, 52(2), 196–205. https://doi.org/10.1037/0022-0167.52.2.196
Holcomb-McCoy, C. C., & Myers, J. E. (1999). Multicultural competence and counselor training: A national survey. Journal of Counseling & Development, 77(3), 294–302. https://doi.org/10.1002/j.1556-6676.1999.tb02452.x
Hoover, S. M., & Morrow, S. L. (2016). A qualitative study of feminist multicultural trainees’ social justice development. Journal of Counseling & Development, 94(3), 306–318. https://doi.org/10.1002/jcad.12087
Keum, B. T., & Miller, M. J. (2020). Social justice interdependence among students in counseling psychology training programs: Group actor-partner interdependence model of social justice attitudes, training program norms, advocacy intentions, and peer relationships. Journal of Counseling Psychology, 67(2), 141–155. https://doi.org/10.1037/cou0000390
Kozan, S., & Blustein, D. L. (2018). Implementing social change: A qualitative analysis of counseling psychologists’ engagement in advocacy. The Counseling Psychologist, 46(2), 154–189. https://doi.org/10.1177/0011000018756882
Mull, R. C. (2020). Colleges are in for a racial reckoning. The Chronicle of Higher Education. https://www.chronicle.com/article/colleges-are-in-for-a-racial-reckoning
Okun, T. (2021). White supremacy culture – Still here. https://drive.google.com/file/d/1XR_7M_9qa64zZ00_JyFVTAjmjVU-uSz8/view
Ponterotto, J. G., Mathew, J. T., & Raughley, B. (2013). The value of mixed methods designs to social justice research in counseling and psychology. Journal for Social Action in Counseling and Psychology, 5(2), 42–68. https://doi.org/10.33043/JSACP.5.2.42-68
Ratts, M. J., & Ford, A. (2010). Advocacy Competencies Self-Assessment (ACSA) Survey©: A tool for measuring advocacy competence. In M. J. Ratts, R. L. Toporek, & J. A. Lewis (Eds.), ACA advocacy competencies: A social justice framework for counselors (pp. 21–26). American Counseling Association.
Ratts, M. J., Singh, A. A., Nassar-McMillan, S., Butler, S. K., & McCullough, J. R. (2016). Multicultural and social justice counseling competencies: Guidelines for the counseling profession. Journal of Multicultural Counseling and Development, 44(1), 28–48. https://doi.org/10.1002/jmcd.12035
Royse, D., Thyer, B. A., & Padgett, D. K. (2010). Program evaluation: An introduction (5th ed.). Cengage.
Saad, L. F. (2020). Me and White supremacy: Combat racism, change the world, and become a good ancestor. Sourcebooks.
Sanabria, S., & DeLorenzi, L. (2019). Social justice pre-practicum: Enhancing social justice identity through experiential learning. Journal for Social Action in Counseling and Psychology, 11(2), 35–53. https://doi.org/10.33043/JSACP.11.2.35-53
Seward, D. X. (2019). Multicultural training resistances: Critical incidents for students of color. Counselor Education and Supervision, 58(1), 33–48. https://doi.org/10.1002/ceas.12122
Sharma, J., & Hipolito-Delgado, C. P. (2021). Promoting anti-racism and critical consciousness through a critical counseling theories course. Teaching and Supervision in Counseling, 3(2), 15–25. https://doi.org/10.7290/tsc030203
Singh, A. A. (2019). The racial healing handbook: Practical activities to help you challenge privilege, confront systemic racism, and engage in collective healing. New Harbinger.
Singh, A. A., Appling, B., & Trepal, H. (2020). Using the multicultural and social justice counseling competencies to decolonize counseling practice: The important roles of theory, power, and action. Journal of Counseling & Development, 98(3), 261–271. https://doi.org/10.1002/jcad.12321
Singh, A. A., Hofsess, C. D., Boyer, E. M., Kwong, A., Lau, A. S. M., McLain, M., & Haggins, K. L. (2010). Social justice and counseling psychology: Listening to the voices of doctoral trainees. The Counseling Psychologist, 38(6), 766–795. https://doi.org/10.1177/0011000010362559
Spangler, P. T., Liu, J., & Hill, C. E. (2012). Consensual qualitative research for simple qualitative data: An introduction to CQR-M. In C. E. Hill (Ed.), Consensual qualitative research: A practical resource for investigating social science phenomena (pp. 269–283). American Psychological Association.
Toporek, R. L., & Ahluwalia, M. K. (2021). Taking action: Creating social change through strength, solidarity, strategy, and sustainability. Cognella Press.
Turner, D. (2018). “You shall not replace us!” White supremacy, psychotherapy and decolonisation. Journal of Critical Psychology, Counselling and Psychotherapy, 18(1), 1–12. https://cris.brighton.ac.uk/ws/portalfiles/portal/495044/JCPCP+18-1+-+Turner+article.pdf
Zetzer, H. A. (2021). Decolonizing the curriculum in health service psychology. Association of Psychology Training Clinics Bulletin: Practicum Education & Training, 20–22. https://aptc.org/images/File/newsletter/APTC_Bulletin_PET_2021_Spring%20FINAL.pdf
Sapna B. Chopra, PhD, is an associate professor at California State University, Fullerton. Rebekah Smart, PhD, is a professor at California State University, Fullerton. Yuying Tsong, PhD, is a professor and Associate Vice President for Student Academic Support at California State University, Fullerton. Olga L. Mejía, PhD, is a licensed psychologist and an associate professor at California State University, Fullerton. Eric W. Price, PhD, is an associate professor at California State University, Fullerton. Correspondence may be addressed to Sapna B. Chopra, Department of Human Services, California State University, Fullerton, P.O. Box 6868, Fullerton, CA 92834-6868, sapnachopra@fullerton.edu.
Aug 10, 2022 | Volume 12 - Issue 2
Lacey Ricks, Malti Tuttle, Sara E. Ellison
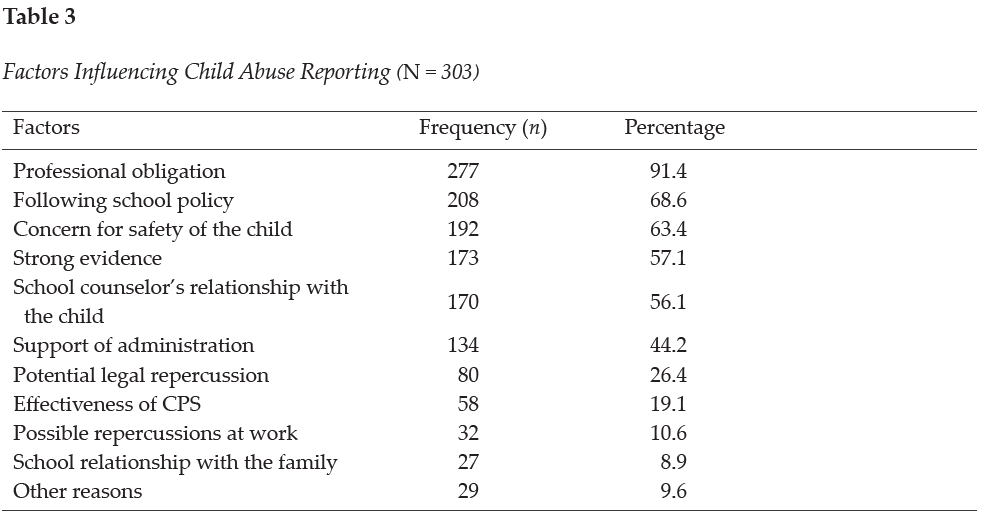
Quantitative methodology was utilized to assess factors influencing veteran school counselors’ decisions to report suspected child abuse. Veteran school counselors were defined as having 6 or more years of experience working as a school counselor within a public or private school. This study is a focused examination of the responses of veteran school counselors from a larger data set. The results of the analysis revealed that academic setting, number of students within the school, and students’ engagement in the free or reduced lunch program were significantly correlated with higher reporting among veteran school counselors. Moreover, veteran school counselors’ self-efficacy levels were moderately correlated with their decision to report. Highly rated reasons for choosing to report suspected child abuse included professional obligation, following school protocol, and concern for the safety of the child. The highest rated reason for choosing not to report was lack of evidence. Implications for training and advocacy for veteran school counselors are discussed.
Keywords: child abuse, reporting, veteran school counselors, self-efficacy, training
In 2019, approximately 4.4 million reports alleging maltreatment were made to U.S. child protective services (U.S. Department of Health & Human Services [HHS] et al., 2021). Of these reports, nearly two thirds were made by professionals who encounter children as a part of their occupation. Child maltreatment is identified as all types of abuse against a child under the age of 18 by a parent, caregiver, or person in a custodial role, and includes physical abuse, sexual abuse, emotional abuse, and neglect (Fortson et al., 2016). Public health emergencies, such as the continued COVID-19 pandemic, increase the risk for child abuse and neglect due to increased stressors (Swedo et al., 2020). Factors such as financial hardship, exacerbated mental health issues, lack of support, and loneliness may contribute to increased caregiver distress, ultimately resulting in negative outcomes for children and adolescents (Collin-Vézina et al., 2020).
The psychological impact of child abuse and neglect on victims can increase the risk of mental health disorders such as depression, anxiety, eating disorders, and post-traumatic stress disorder (Heim et al., 2010; Klassen & Hickman, 2022). Similarly, trauma experienced in childhood is associated with higher rates of long-term physical health issues when compared to individuals with less trauma; these include cancer (2.4 times more likely to develop), diabetes (3.0 times as likely to develop), and stroke (5.8 times more likely to experience; Bellis et al., 2015). Children who are victims of child abuse and neglect may also experience educational difficulties, low self-esteem, and trouble forming and maintaining relationships (Child Welfare Information Gateway, 2019).
Voluntary disclosure of childhood abuse is relatively uncommon; one study found that less than half of adults with histories of abuse reported disclosing the abuse to anyone during childhood, and only 8%–16% of those disclosures resulted in reporting to authorities (McGuire & London, 2020). For this reason, mandated reporting by professionals is an integral piece of child abuse prevention. School counselors, by virtue of their ongoing contact with children, are uniquely positioned to identify and report child abuse (Behun et al., 2019). We recognize that school-based professionals such as teachers, administrators, and other school-based staff are mandated reporters as well. However, for the purpose of this article, we specifically focus on school counselors based on their role, responsibility, and training that best equips them to fulfill this expectation. School counselors have a unique role within the school system and play a critical role in ensuring schools are a safe, caring environment for all students (American School Counselor Association [ASCA], 2017). School counselors also work to identify the impact of abuse and neglect on students as well as ensure the necessary supports for students are in place (ASCA, 2021).
Ethical and Legal Mandates for Reporting Suspected Child Abuse
Although current estimates for the reporting frequency within schools are not available, it appears likely that high numbers of school counselors encounter the decision to report suspected child abuse each year. In fact, a 2019 survey of 262 school counselors indicated that 1,494 cases of child abuse had been reported by participants over a 12-month period (Ricks et al., 2019). Despite the frequency with which it occurs, reporting can be a distressing part of school counselors’ responsibilities (Remley et al., 2017); this could be because of limited knowledge or competency in reporting procedures, unfamiliarity with the law, or potential repercussions for the child (Bryant, 2009; Bryant & Milsom, 2005; Lambie, 2005). Additionally, laws, definitions, and mandates of child abuse and neglect vary by state; therefore, confusion may arise when school counselors relocate to another area (ASCA, 2021; Hogelin, 2013; Lambie, 2005; Tuttle et al., 2019). School counselors need to identify and familiarize themselves with the unique laws in their state in addition to reviewing federal law and ethical codes.
Federally, school counselors are mandated by the Child Abuse Prevention and Treatment Act of 1974, Public Law 93-247, to report suspected abuse and neglect to proper authorities (ASCA, 2021). Failure to report suspected abuse could result in civil or criminal liability (Remley et al., 2017; White & Flynt, 2000). ASCA Ethical Standards echo this mandate, directing school counselors to report suspected child abuse and neglect while protecting the privacy of the student (ASCA, 2022a, A.12.a). School counselors should also assist students who have experienced abuse and neglect by connecting them with appropriate services (ASCA, 2022a). Moreover, school counselors should work to create a safe environment free from abuse, bullying, harassment, and other forms of violence for students while promoting autonomy and justice (ASCA, 2022a).
School Counselors as Advocates in Mandated Reporting
Barrett et al. (2011) recognized school counselors as social justice leaders based on their role to advocate for students who are underserved, disadvantaged, maltreated, or living in abusive situations. Child abuse impacts children and adolescents from every race, socioeconomic status, gender, and age (Lambie, 2005; Tillman et al., 2015). School counselors who are trained to provide culturally sustaining school counseling will work with students and families from all demographics to promote student wellness within their comprehensive school counseling program (ASCA, 2021). As leaders within the school, school counselors, and especially veteran school counselors, can work to educate all stakeholders on the implications of child abuse.
School counselors not only are legally positioned to serve as mandated reporters but also ethically positioned to train school personnel in recognizing and identifying child abuse symptoms and in reporting procedures (Hodges & McDonald, 2019). Training of school personnel, such as teachers, to identify and report suspected child abuse is essential because they are also recognized legally as mandated reporters (Hupe & Stevenson, 2019) and they interact with students daily. It is vital that school counselors advocate for ongoing comprehensive training related to child abuse because their knowledge affects many stakeholders in the school setting (ASCA, 2021; Tuttle et al., 2019).
Self-Efficacy Among Veteran School Counselors
Previous literature from this data set highlighted the reporting behaviors of early career school counselors (Ricks et al., 2019), and a framework was developed to assist new professionals in reporting (Tuttle et al., 2019). However, the child abuse reporting behaviors and needs of veteran school counselors are understudied. Therefore, this article focuses on veteran school counselors. For the purpose of this study, veteran school counselors are considered licensed school counselors having 6 or more years of experience. Professional literature has highlighted the unique needs and experiences of novice counselors as compared to veteran school counselors (Buchanan et al., 2017; Johnson et al., 2017). One study (Mishak, 2007) examined differences in instructional strategies for early career and veteran school counselors in elementary schools in Iowa. Although that study does not specifically address child abuse reporting, it does highlight differences found among the respondents based on their experience level.
One factor supporting the unique needs of veteran school counselors is self-efficacy. Self-efficacy theory posits that an individual’s expectations of mastery are strongly influenced by personal experience and indirect exposure to a phenomenon (Bandura, 1977, 1997). Veteran school counselors, based on their years of experience in a school setting, are likely to have multiple exposures to child abuse reporting. They may have filed reports themselves, spoken to peers about their reporting experiences, or assisted other professionals in the school with reporting. Bandura (1997) suggested that self-efficacy is supported when individuals not only possess the skill and ability to complete a task, but also have the confidence and motivation to execute it.
Veteran school counselors can receive ongoing training from workshops, university courses, webinars, district training, or other professional organizations that may further impact self-efficacy levels. Previous research has shown that as an individual’s knowledge of child abuse increases, their levels of self-efficacy in recognizing or reporting child abuse also increases (Balkaran, 2015; Jordan et al., 2017). However, little research linking school counselors’ self-efficacy levels to child abuse reporting has been published. Despite the paucity of research on this topic, Ricks et al. (2019) found a moderate relationship between early career school counselors’ self-efficacy and their ability to identify types of abuse. Additionally, Tang (2020) found that school counseling supervision increased school counselor self-efficacy; differences between early career and veteran school counselors were not addressed in Tang’s study. Although the positive correlation found by Tang did not directly address child abuse reporting, assisting students with crisis situations was one of the principal components of the analysis. Even though veteran school counselors have experience serving as mandated reporters, they require ongoing professional development in this area to effectively fulfill their roles as advocates in maintaining the welfare and safety of students (ASCA, 2021; Tuttle et al., 2019). Therefore, we seek to utilize this article as a form of advocacy on behalf of veteran school counselors by providing additional research and literature in the field.
Purpose of the Present Study
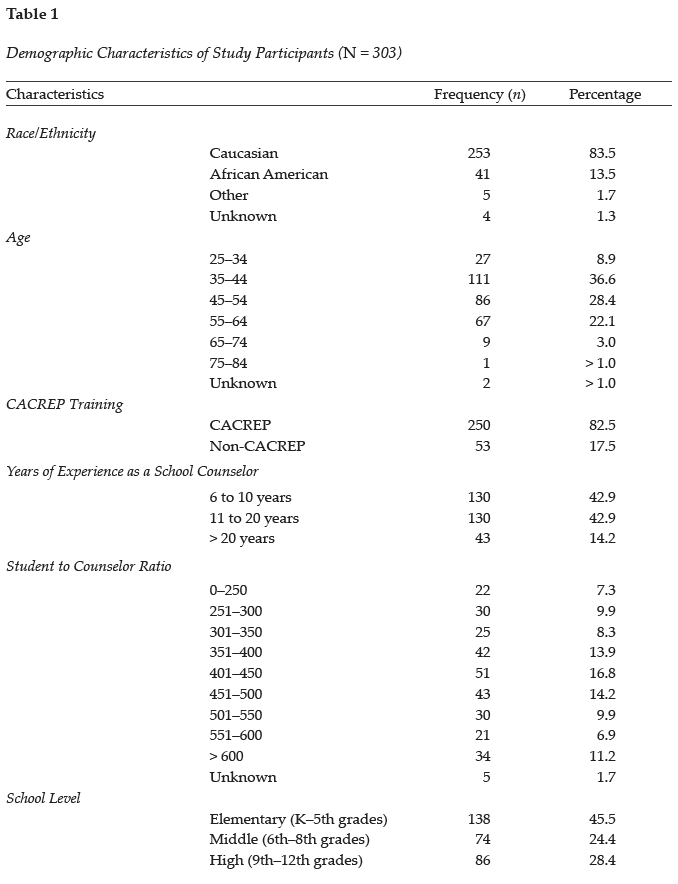
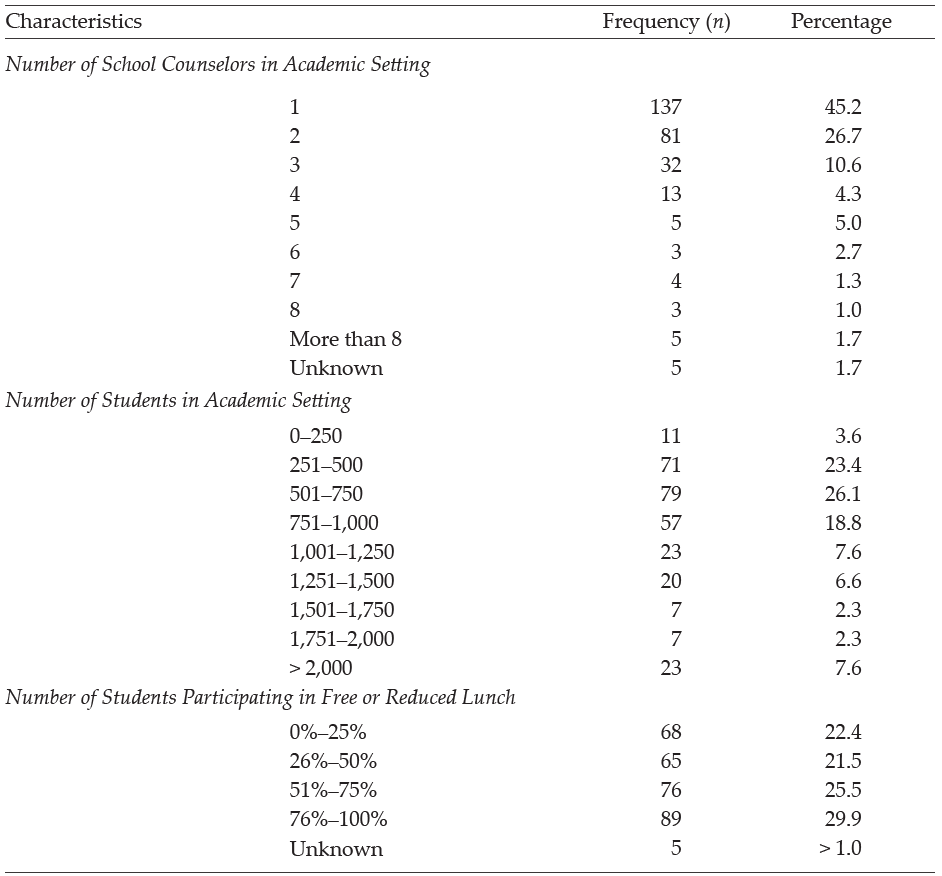
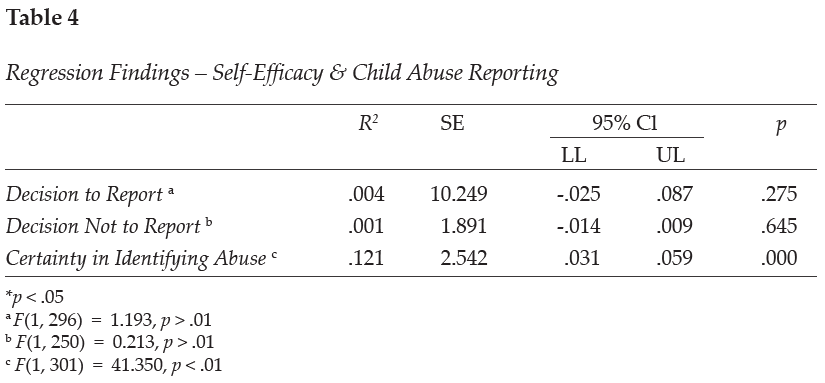
The purpose of this quantitative study is to examine (a) the prevalence of child abuse reporting by veteran school counselors within the school year; (b) the factors affecting veteran school counselors’ decisions to report or not report suspected child abuse; (c) reasons for reporting or not reporting suspected child abuse by veteran school counselors; and (d) veteran school counselors’ self-efficacy levels related to child abuse reporting. Our intent was to build upon an initial larger study to examine veteran school counselors’ knowledge of procedures and experiences with child abuse reporting. The present study is a focused examination of the data collected from veteran school counselors as part of the primary study, which solicited data from school counselors across their careers related to their experiences with child abuse reporting (see Ricks et al., 2019). Demographic variables were collected from participants to assess their impact on child abuse reporting; see Table 1 for a complete list of variables.
Methods
Multiple correlation and regression analyses were conducted to assess factors influencing veteran school counselors’ decisions to report suspected child abuse. After obtaining IRB approval, the authors recruited school counselors in the Southeastern United States (Alabama, Arkansas, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, South Carolina, Tennessee, Texas, Virginia, and West Virginia). Participants were recruited using a professional school counseling association membership list, a southeastern state counseling association listserv, and social media. Participants were informed that participation in the online study was voluntary and that they could withdraw from the study at any time. Participants were also informed that the survey would take between 10–15 minutes and that the information collected in the survey would remain anonymous.
Participants
A total of 848 surveys were collected from participants. Veteran school counselor data was extracted from the total sample and analyzed to assess the unique experiences of these individuals in child abuse reporting. Veteran school counselors were defined as having 6 or more years of experience working as a school counselor within a public or private school. Four hundred and twenty-eight veteran school counselors began the survey, but data from 125 participants was excluded from the analysis for incomplete responses, resulting in a final sample of 303 participants. Most participants (n = 265, 87.5%) reported being licensed/certified as a school counselor. Some participants may not have possessed a license because of working in the private school sector or working on a provisional basis. See Table 1 for all demographic frequencies and percentages related to participants in the study.
Measures
Three measures were selected and employed as part of the larger study. These included the Child Abuse Reporting Questionnaire (Bryant & Milsom, 2005), the School Counselor Self-Efficacy Scale (Bodenhorn & Skaggs, 2005), and the Knowledge of Child Abuse Reporting Questionnaire (Ricks et al., 2019). Each measure is described below as previously reported in Ricks et al. (2019).
Child Abuse Reporting Questionnaire
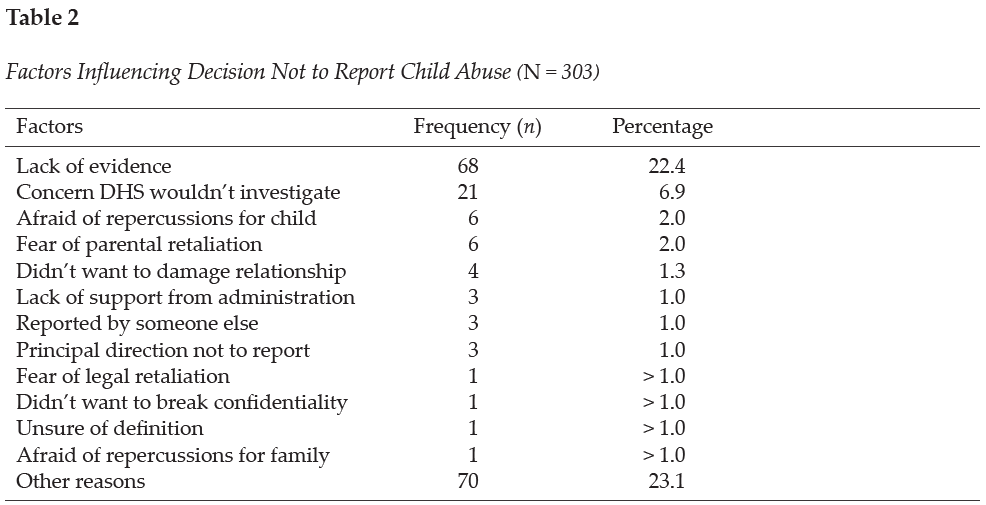
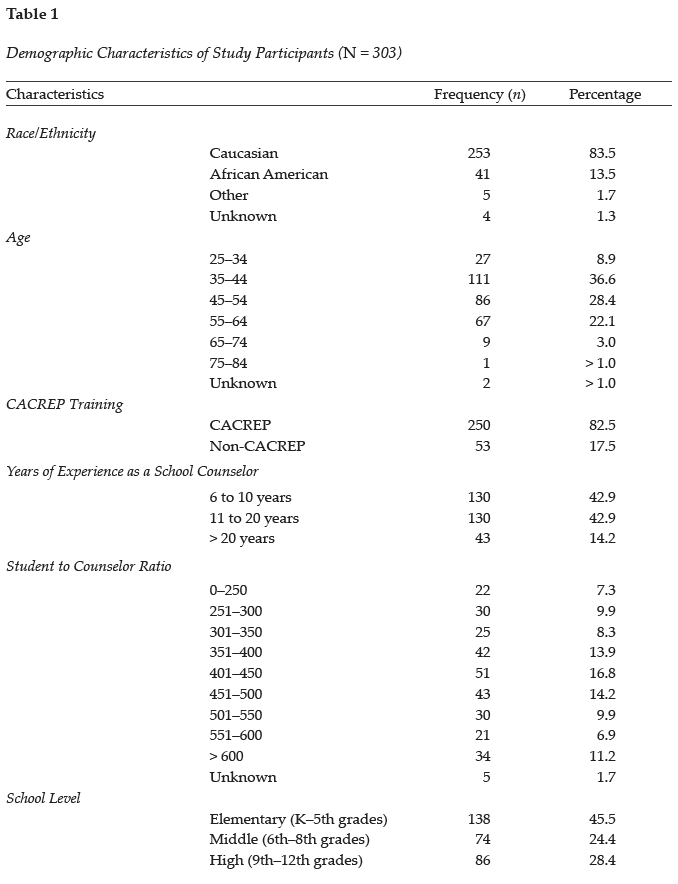
The Child Abuse Reporting Questionnaire was developed to assess three domains, including school counselor General Information, Training in Child Abuse Reporting, and Child Abuse Reporting Experience (Bryant & Milsom, 2005). In the first section of the questionnaire, Training in Child Abuse Reporting, participants were asked to list where they obtained their knowledge of child abuse reporting and to assess four different types (physical, sexual, neglect, emotional) of child abuse. In the Child Abuse Reporting Experience section, the participants were asked two questions. The first question asked participants to recall the number of suspected child abuse cases they encountered during the preceding school year and the number of child abuse cases they reported. The next question asked participants how many cases of suspected child abuse they did not report. Participants were also asked in the survey to indicate reasons for choosing not to report suspected child abuse cases based on 12 commonly reported barriers or to list other reasons for not reporting the suspected cases. See Table 2 for a complete list of the common reasons given for not reporting suspected child abuse cases. Internal consistency measures were not obtained for this questionnaire because of the demographic nature of assessing participants’ personal experiences with child abuse reporting.
School Counselor Self-Efficacy Scale
The School Counselor Self-Efficacy Scale (SCSE) was used to assess school counselors’ self-efficacy and to link their personal attributes to their career performance (Bodenhorn & Skaggs, 2005). Participants completed Likert scale questions to indicate their confidence in performing school counseling tasks for 43 scale items. An example question would ask school counselors to indicate their confidence in advocating for integration of student academic, career, and personal development into the mission of their school. A rating of 1 indicated not confident and a rating of 5 indicated highly confident. The coefficient alpha for the scale score was found to be .95 (Bodenhorn & Skaggs, 2005). The SCSE subscales include five domains: Personal and Social Development (12 items), Leadership and Assessment (9 items), Career and Academic Development (7 items), Collaboration and Consultation (11 items), and Cultural Acceptance (4 items). The correlations of the subscales ranged from .27 to .43.
Knowledge of Child Abuse Reporting Questionnaire
The Knowledge of Child Abuse Reporting Questionnaire was developed to assess respondents’ knowledge of child abuse reporting and procedures within three areas (Ricks et al., 2019). To develop the survey, the researchers and outside counselor educators reviewed the questionnaire to determine if it clearly measured the constructs. In the first section of the questionnaire, Identifying Types of Abuse, participants’ perceptions of their ability to identify the four different types of child abuse were assessed. To complete this section, participants rated their comfort level using a 4-point Likert scale. A rating of 1 indicated very uncertain and a rating of 4 indicated very certain. The coefficient alpha for the scale score was found to be .902. The Knowledge of Guidelines section assessed participants’ knowledge of the state rules, ASCA Ethical Standards, and child abuse reporting protocol within their current school and district. To complete this section, participants rated their comfort level using a 5-point Likert scale. A rating of 1 indicated not knowledgeable and a rating of 5 indicated extremely knowledgeable. The coefficient alpha for the scale score was found to be .799. Lastly, the Child Abuse Training section assessed where participants received training on general knowledge of child abuse reporting, how to make a referral, and indicators of child abuse. To complete this section, participants selected options from a dropdown menu based on commonly reported agencies or listed an organization not provided. Options included in the survey list were universities or colleges, schools or districts, conferences or workshops, colleagues, journals, professional organizations, or the state department of education.
Data Analysis
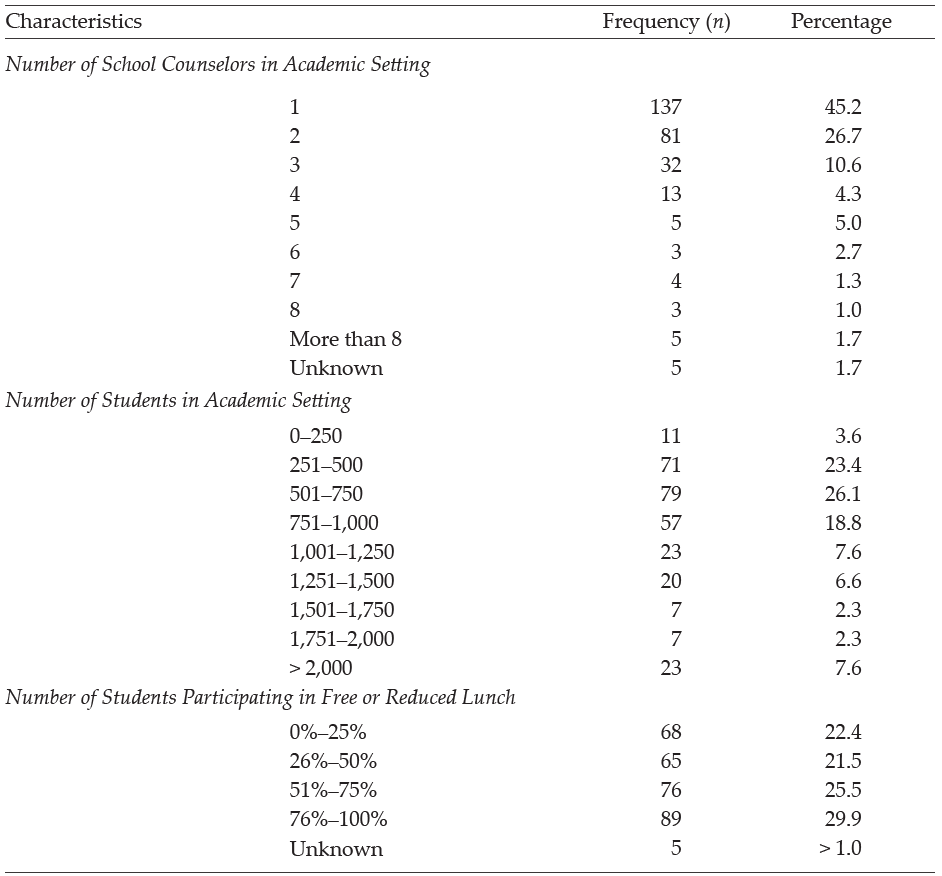
SPSS Statistics 27 was used to analyze data within this study. First, a correlation analysis was executed to assess the strength of the relationship across variables. Next, analyses of variance (ANOVAs) were performed to assess the relationship between the number of reported child abuse cases and five demographic variables, which included academic setting (elementary, middle, high); number of students participating in the school’s free or reduced lunch program; number of school counselors working in a school setting; years of experience as a school counselor; and number of students enrolled in a school setting. Lastly, regression analyses were used to determine the relationship between school counselors’ self-efficacy and their decisions to report or not report suspected child abuse cases as well as to assess the relationship between school counselors’ self-efficacy and their certainty in identifying types of abuse.
Results
Suspected and Reported Cases of Abuse
Descriptive statistics generated from the child abuse survey included the participants (N = 303) suspecting 2,289 cases of child abuse during the school year. Scores reported by participants ranged from 0 to 100 (M = 7.71, SD = 10.58). Seven participants omitted this question within the questionnaire. Participants indicated reporting a total of 2,140 cases of suspected child abuse; individual frequency ranged from 0 to 100 (M = 7.21, SD = 10.25). Physical child abuse cases (M = 4.03, SD = 7.12) were reported at a higher rate than cases of neglect (M = 2.72, SD = 5.10), emotional abuse (M = 0.56, SD = 1.52), and sexual abuse (M = 0.57, SD = 1.37).
School Demographics
The relationship between the number of reported child abuse cases and demographic variables was examined using a bivariate correlation. Results indicated a negative correlation between the number of child abuse reports and the academic level of students the school counselor works with (elementary, middle, or high school), r(293) = −.283, p < .001, with elementary school counselors reporting child abuse at a higher rate than high school counselors. An additional negative correlation was found between the number of child abuse reports and the number of school counselors working within the school, r(293) = −.164, p < .001. Results indicated a positive significant relationship between the number of reported child abuse cases and the number of students who participate in the school’s free or reduced lunch program, r(293) = .225, p < .001. Weaker negative relationships were also found between the number of child abuse reports and the participants’ years of experience as a school counselor, r(297) = −.115, p < .05, as well as how many students are enrolled in a school, r(293) = −.127, p < .06. No other significant relationships were found among the variables and reported cases.
An ANOVA was conducted to examine the relationship between the academic level of students (elementary, middle, and high) the participants worked with and the number of child abuse cases reported. Results showed a significant relationship among the variables, f(2, 290) = 13.021, p > .00. A follow-up test was used to evaluate pairwise differences among the means. Results of a Tukey HSD indicated a significant difference between elementary (M = 10.314) and high school (M = 3.58) counselors who reported child abuse. A difference was also found between elementary and middle school (M = 5.86) reporting levels. No other significant differences were found between variables.
An ANOVA was also conducted to evaluate the differences between child abuse reporting and the percentage (0%–25%, 26%–50%, 51%–75%, 76%–100%) of students who participated in free or reduced lunch. Results showed a significant relationship among the variables, f(3, 289) = 5.22, p = .002. A Tukey HSD post hoc test was used to make a pairwise comparison and statistically significant mean differences were found between the 0%–25% (M = 2.33) group and the 51%–75% (M = 7.78) group. Additionally, a difference was found between the 0%–25% group and the 76%–100% (M = 10.12) group. Lastly, a difference was found between the 26%–50% (M = 6.54) group and the 76%–100% group. No other significant differences were found between the groups.
An ANOVA was conducted to examine the relationship between how many school counselors are working in a school setting and the differences in child abuse reporting. Analysis of the ANOVA found no significant difference (p < .05) between the groups (one counselor, M = 8.26; two counselors, M = 7.81; three counselors, M = 7.69; four counselors, M = 5.00; five counselors, M = 2.80; six counselors, M = 2.25; seven counselors, M = 3.50; eight counselors, M = 2.33; more than eight counselors, M = 2.20), but a downward trend can be seen in the number of cases reported with the increase in the number of school counselors within a school.
Likewise, an ANOVA was used to examine the relationship between years of experience as a school counselor and the differences in child abuse reporting, but no significant difference (p < .05) was found between groups (6 to 10 years, M = 8.58; 11 to 20 years, M = 6.36; above 20 years, M = 5.57); however, a slight trend can be seen with participants who have less experience reporting at higher rates. A larger sample size may have yielded significant results, but additional research is needed in this area.
Lastly, an ANOVA was also executed to assess the differences in child abuse reporting and the number of students enrolled in a school setting. A significant difference was found between schools with more than 2,000 students (M = 3.00) and schools with 251–500 students (M = 8.07) as well as schools with 501–750 students (M = 8.63). This difference suggests school counselors who work in schools with more students tend to report child abuse at a lower rate than those who work in smaller schools. A downward trend can be seen in reporting of cases as student numbers increase (751–1,000 students, M = 7.62; 1,001–1,250 students, M = 7.39; 1,251–1,500 students, M = 6.68; 1,501–1,750 students, M = 6.00; 1,751–2,000 students, M = 2.57), with the exception of the 0–250 students (M = 4.82) school classification. Differences in the sample sizes of classification categories could have impacted significance outcomes. No other significant differences were found between the groups.
The Decision to Report
On the Child Abuse Reporting Survey, participants (N = 303) were asked to indicate what factors influenced their decision to report child abuse. Participants indicated the number one factor was following the law (professional obligation; 91.4%, n = 277). Other reasons cited by over half of school counselors included following school policy (68.6%, n = 208), concern for safety of the child (63.4%, n = 192), strong evidence that abuse had occurred (57.1%, n = 173), and the school counselor’s relationship with the child (56.1%, n = 173). See Table 3 for factors influencing child abuse reporting. Further, participants indicated reasons why they chose not to report suspected child abuse. Participants specified inadequate evidence as the primary reason for not reporting suspected child abuse (22.4%, n = 68). Another notable influence included concern that DHS would not investigate the reported case (6.9%, n = 21). See Table 2 for factors influencing the decision not to report child abuse.
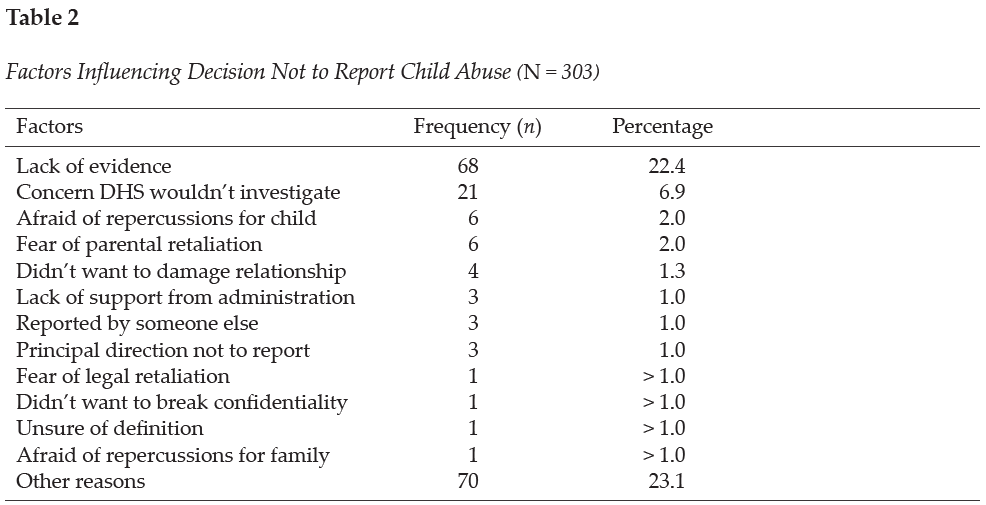
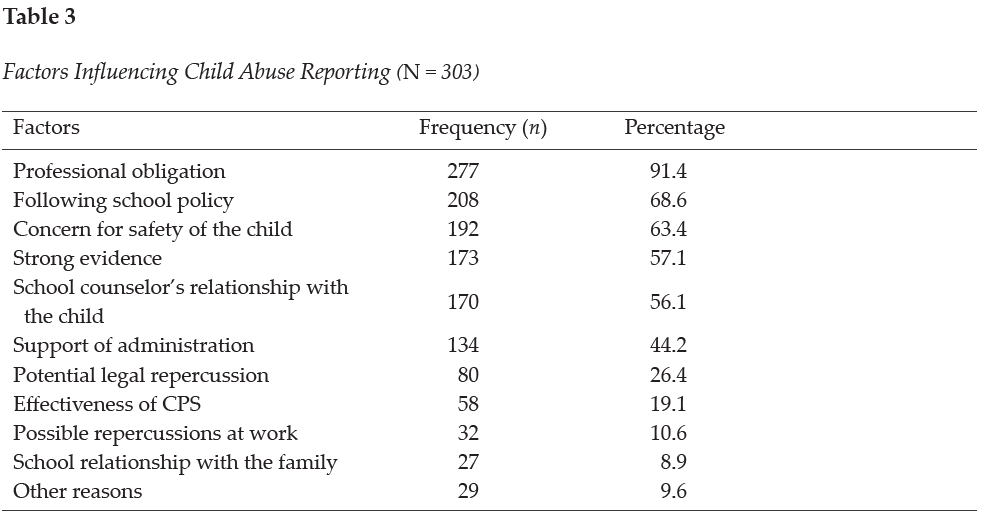
Knowledge and Training
On the Knowledge of Child Abuse Reporting Questionnaire, participants were asked to rate how certain they feel about their abilities to identify types of abuse on a 4-point Likert scale with 1 indicating very uncertain and 4 indicating very certain. Participants reported most confidence in their ability to identify physical abuse (M = 3.49, Mdn = 4), followed by neglect (M = 3.30, Mdn = 3), sexual abuse (M = 3.20, Mdn = 3), and emotional abuse (M = 3.06, Mdn = 3). When participants (N = 303) were asked where they gained knowledge about child abuse, most reported receiving training from professional experiences (88.4%, n = 268), mandated reporting training at school (79.5%, n = 241), workshops (72.3%, n = 219), discussion with colleagues (61.4%, n = 186), or literature (58.1%, n = 176). Additionally, participants indicated gaining knowledge from university courses (46.5%, n = 141), media (9.2%, n = 28), or other avenues unlisted in the survey (12.2%, n = 37).
Participants were asked where they received training on how to make a referral for a child abuse case. Most of the school counselors responded that they received the training from a school/district training (87.5%, n = 265), conference/workshop (57.4%, n = 174), or university class (42.9%, n = 130). Other responses included from a colleague (38.9%, n = 118), professional organization (32.7%, n = 99), Department of Education website (20.5%, n = 62), journal (10.9%, n = 33), or other sources (11.2%, n = 34). Lastly, veteran counselors were asked where they received training about the indicators of child abuse. The majority of the respondents reported learning in a school/district training (87.1%, n = 264), conference/workshop (77.9%, n = 236), or university/college course (67.3%, n = 204). Other responses included learning from a professional organization (38%, n = 115), colleague (30%, n = 91), journal (23.4%, n = 71), Department of Education website (21.5%, n = 65), or other sources (9.9%, n = 30).
Veteran school counselors reported that 88.1% (n = 267) of schools/districts provided them with training on local abuse reporting policies. Therefore, 11.9% did not receive training from their local school system. Additionally, 60.1% (n = 182) of the school counselors reported their school/district had a handbook/resource outlining the steps for mandated reporter training within their school system. Consequently, 39.9% of the school counselors reported not having a handbook/resource to reference outlining steps for mandated reporting.
Self-Efficacy and Child Abuse Reporting
A regression analysis was used to examine the relationship between veteran school counselors’ self-efficacy and three variables, including the number of reported child abuse cases, the decision not to report suspicion of child abuse, and certainty in identifying types of child abuse. Results showed the strength of the relationship between self-efficacy and certainty in identifying types of child abuse was moderately related, F(1, 301) = 41.350, p < .01. Over 12% (r2 = 0.121) of the variance of the school counselors’ self-efficacy level was associated with certainty in identifying child abuse. No other significant results were found among the variables. See Table 4 for the regression analysis related to self-efficacy and child abuse reporting.
Discussion
Given the well-documented negative impact of child abuse on the emotional, physical, and academic well-being of children, it is essential to understand how school counselors are trained to identify and report child abuse. Understanding trends and research in child abuse reporting can help schools prepare school counselors and other staff members. It is imperative for veteran school counselors to receive ongoing training to best serve as advocates for students, maintain relevancy in their roles as mandated reporters by staying current on laws and policies, and further their ability to work within their scope of practice. Ongoing training may also help alleviate difficulties that arise because of terminology differing from state to state and district to district (ASCA, 2021; Hogelin, 2013; Lambie, 2005; Tuttle et al., 2019).
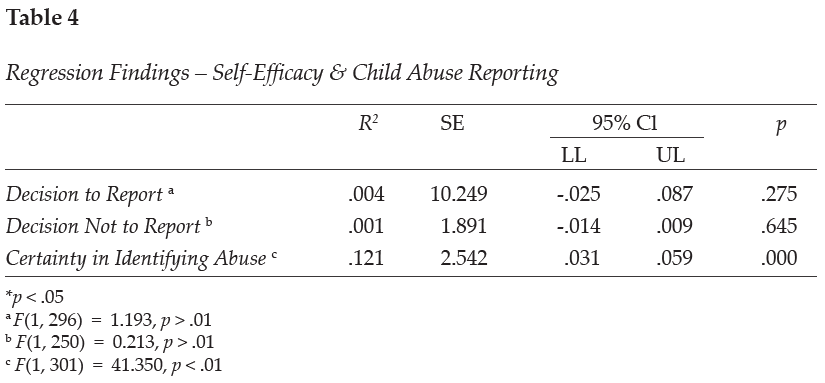
In this study, veteran school counselors’ reporting frequency is shown to differ based on various school demographics. Veteran school counselors were specifically targeted in this analysis to examine their experiences related to child abuse reporting. Although these findings may not show direct causation to child abuse reporting among veteran school counselors, they can help us better understand school and school counselor demographics that need to be evaluated further. The findings can also be used to guide professional development training needed for school counselors as well as additional training needs for counselors-in-training.
Elementary school counselors were found to report child abuse at a higher rate than middle or high school counselors; however, this is anticipated because studies show that younger children experience higher rates of maltreatment than older children (HHS et al., 2021). In fact, rates of maltreatment seem to decrease as age increases. Children who are 6 years old have victimization rates of 9.0 per 1,000 children compared to children who are 16 years of age who have a victimization rate of 5.5 per 1,000 children (HHS et al., 2021). Higher maltreatment levels in younger children may be because of increased caregiver burden (Fortson et al., 2016); as children get older, they are better able to care for themselves and avoid parental confrontation. In addition, older students may be more likely to hide abuse and more astute when dealing with disclosure protocol (Bryant & Milsom, 2005). Knowledge of the signs and symptoms of child abuse and neglect can help school counselors identify children suffering from maltreatment.
Within this study on veteran school counselors, a slight trend can be seen with participants with less experience reporting suspected child abuse at a higher rate. Differences of reporting rates by years of experience may be because of higher ego maturity in less experienced school counselors because of more recent training in their graduate programs (Lambie et al., 2011). According to Lambie et al. (2011), ego development predicts an individual’s level of ethical and legal knowledge, which has been found to be higher in counselors-in-training than the average school counselor. Ego development has also been correlated with greater degrees of self-efficacy (Singleton et al., 2021), which can impact school counselors’ actions when making decisions related to child abuse reporting. Tuttle et al. (2019) also emphasized the need for continuous training to increase school counselors’ self-efficacy as mandated reporters, although more research is needed to understand the impact of self-efficacy on school counselor action. These findings highlight the need for continued assessment of training needs for school counselors of various experience levels.
Although age has been associated with varying levels of child abuse victimization, low socioeconomic status within the home environment has also been identified as a high risk factor for child abuse (Bryant, 2009; Bryant & Milsom, 2005; Ricks et al., 2019; Sedlak et al., 2010). Specifically, the higher the percentage of students participating in the school’s free or reduced lunch program, the more child abuse cases the school counselor reported (Bryant, 2009; Bryant & Milsom, 2005; Ricks et al., 2019). Although most children in low-income families do not experience child abuse, one study estimated that 22.5 children per 1,000 in low-income families experience maltreatment as compared to 4.4 per 1,000 in more affluent families (Sedlak et al., 2010). However, it is important to note the disproportionality that exists within child welfare reporting; non-White children and children of low socioeconomic status are reported to child protective services at a higher rate than their peers (Krase, 2015; Luken et al., 2021). School counselors working in low-income schools need to be aware of the increased risk factors of low socioeconomic status as well as the racial and economic disproportionality that occurs within child maltreatment reporting as a result of possible bias. School counselors should work to be aware of potential biases they may hold with regard to over-reporting certain groups of children and under-reporting others (Tillman et al., 2015).
When examining the current practices of veteran school counselors, participants reported professional obligation as the number one reason they reported suspected child abuse. The primary reason given for failing to report suspected abuse was inadequate evidence. These findings are similar to prior research that shows lack of evidence as an influencing factor in school counselors’ decisions not to report suspected abuse (Bryant, 2009; Bryant & Milsom, 2005; Tillman et al., 2015); this is concerning because some cases of abuse may go unreported. As Tuttle et al. (2019) have stated, “the school counselor’s responsibility is to follow legal and ethical obligations as a mandated reporter by reporting all suspected child abuse” (p. 242). Although concern that DHS would not investigate is denoted as an important factor for why school counselors choose not to report, school counselors must recognize they do not have the proper resources or training to lead a child abuse investigation on their own (Tuttle et al., 2019). As a result, school counselors are ethically and legally mandated to report all suspected cases of abuse to the proper authorities defined by their state, school policies, and ethical codes. Failure to report cases could lead to legal ramifications for the school counselor (Remley et al., 2017; White & Flynt, 2000) and continued maltreatment for the student.
School counselors should strive to “understand child abuse and neglect and its impact on children’s social/emotional, physical and mental well-being” (ASCA, 2021, para. 6). Veteran school counselors completing this survey were most confident in their ability to identify physical abuse and less confident in their ability to identify emotional abuse. This finding supports the assertion that types of abuse with visible evidence are more identifiable than other types of abuse such as emotional or sexual abuse (Bryant, 2009; Bryant & Milsom, 2005). Cases of suspected abuse in which a child reports physical abuse are less likely to be reported if there is no evidence of bodily harm (Tillman et al., 2015). Although school counselors report physical abuse as the most easily identifiable type of abuse, child protective services report neglect as the most common type of maltreatment (Child Welfare Information Gateway, 2021).
Results from this study show that veteran school counselors reported receiving their knowledge on child abuse from professional experiences and mandated reporter training at their school; comparatively, early career school counselors reported most of their knowledge came from professional experience and university courses (Ricks et al., 2019). Reported differences were also observed between veteran school counselors and early career school counselors in terms of sources of knowledge on how to make a referral and learn about indicators of abuse (Ricks et al., 2019). Differences may exist because of variable school district policies regarding ongoing mandated reporter training frequency and practices.
When assessing training needs, participants indicated that most veteran school counselors do receive training from their school district on how to make a referral, indicators of child abuse, and local abuse reporting procedures. In fact, 25% more veteran school counselors reported receiving training from their district than early career school counselors (Ricks et al., 2019). Additionally, approximately 40% of veteran school counselors reported not having a handbook or resource to reference outlining the mandated reporting protocol for their district/school. This result is slightly lower than that reported in research on early career school counselors showing approximately half of school counselors not having a handbook/resource (Ricks et al., 2019). The lack of access to a set protocol outlined by the district is concerning because of the inconsistencies that exist within protocols across states and school districts. Confusion may arise as to timeliness and manner of reporting as well as to who must make the actual report (Kenny & McEachern, 2002). As compared to novice school counselors, veteran counselors appear to report receiving training and/or a handbook/resources related to child abuse reporting in higher numbers. Discrepancies in reported training may indicate a delay in training provided to new school counselors or that training on child abuse is not occurring annually. Although the majority of veteran school counselors did report receiving some training from their school districts, it is important to have “established protocols [to] help address concerns over quality control, fear of lawsuits, and the protection of staff in reporting cases, as well as ensure that there are effective steps for helping children” (Crosson-Tower, 2003, p. 29).
Previous research (Kenny & McEachern, 2002) has indicated that school counselors with more years of experience report less adequate pre-service training in child abuse reporting and that school counselors with in-service training in the last 12 months are less concerned about the consequences of making a report (Behun et al., 2019). This might be due to recently trained school counselors having greater awareness about current information and procedures, which supports the need for participation in continuous ongoing education on this topic. Although the veteran school counselors surveyed in this study indicated experience in child abuse reporting, continued updates to the law highlight the need for current and well-defined guidelines within each school system. Ongoing training is recommended for all school counselors to ensure they stay informed on updated protocols and research (Kenny & Abreu, 2016; Tuttle et al., 2019).
Results of the data analysis also indicated a moderately significant relationship between veteran school counselor self-efficacy and their certainty identifying types of abuse. These findings echo other research indicating that school counselors’ self-efficacy levels may influence their decisions to report suspected abuse (Ricks et al., 2019; Tuttle et al., 2019). According to Larson and Daniels (1998), counselor self-efficacy beliefs are the main factor contributing to effective counseling action. Given the impact of counselor self-efficacy on effective action, it is important to understand how self-efficacy impacts school counselors’ decision-making processes. Experience and training are two factors that have been found to increase school counselor self-efficacy (Morrison & Lent, 2018). Veteran school counselors, who already have years of experience on their side, may benefit most from additional training opportunities. Increased support should be provided to all school counselors to enhance their counseling self-efficacy (Schiele et al., 2014) and contribute to positive school counseling outcomes.
Implications
Lack of knowledge related to reporting policies has been identified as a key barrier in reporting child abuse (Kenny, 2001; Petersen et al., 2014). School counselors should advocate for standardization in reporting policies. Understanding each state’s unique child abuse prevention statutes can help school counselors best serve their clients (Remley et al., 2017). Given that laws and definitions pertaining to child abuse and neglect vary among states (ASCA, 2021), school counselors should identify collaborative relationships to navigate these legal and ethical parameters. Key collaborations may include those with the school social worker, the school district’s attorney, law enforcement, child protective services, parents/guardians, and community members (Tuttle et al., 2019). Working together, in conjunction with administration and other school stakeholders, school counselors can help establish or update written guidelines and implement ongoing professional development in mandated reporting within their school district. Additionally, developing a positive working relationship with law enforcement and child protective services can help ensure that child abuse cases are reported and documented properly, which can promote positive outcomes for students and families. Moreover, based on the findings from this research study, school counseling certification organizations (i.e., state departments of education/licensure boards) may want to increase or update current training policies for professional school counselors. An area for further study would be examining school districts’ training and protocols for child abuse reporting.
Higher reporting trends in low socioeconomic settings highlight the need for additional mental health services in low-income school districts. School counselors may need more training on the risk factors associated with poverty as well as to be reminded that abuse occurs in all types of families (Bryant, 2009; Tillman et al., 2015). Practicing school counselors working with students living in poverty are often in schools where there are significantly limited resources. School counselors report that “working in schools with high poverty means academic services and the school counseling program itself are limited” (Ricks et al., 2020, p. 61). More research is needed to assess how to support school counselors working in low-income schools; however, school counselors should remain cognizant and demonstrate cultural competency. It is also important for veteran school counselors to continue to assess self-bias as a factor in identifying and reporting suspected child abuse cases (Tillman et al., 2015). Further, it is essential that school counselors emerge as advocates for students in these low socioeconomic settings by pushing for more resources for mental health services as well as changes to policies that negatively impact students’ success. School counselors can work with a task force or advisory committee within the school to examine current practices on child abuse identification and reporting (Temkin et al., 2020). The task force could look for systemic barriers that are impacting students related to child abuse reporting and trauma support; these include current school policies, reporting procedures, teacher and staff training protocols, school counselor professional development, access to mental health services, community resources, direct and indirect school counseling protocols, and other factors impacting student identification and support.
Given the higher number of child abuse cases in the elementary grade levels, more school counselors are needed to adequately identify child abuse and provide services for these students. Despite these needs, the school counselor-to-student ratio varies in each state and is higher in elementary schools (ASCA, 2022b); the national state averages for the school counselor-to-student ratio in grades kindergarten through eighth ranges from 1:419 to 1:1,135 as compared to 1:164 to 1:347 in grades nine through 12 (ASCA, 2022b). Moreover, 20 states currently have no school counseling mandates that require school counselors to be present within the schools (ASCA, 2022c). Of the 30 states that do have mandated counseling, seven do not have mandated counseling for elementary-level students (ASCA, 2022c). School counselors should advocate for more school counselors within their districts and state. Moreover, school administrations and state departments of education should consider hiring additional school counselors to address ongoing mental health needs. Recent research has shown that as a result of the COVID-19 pandemic, students may be experiencing no motivation to do schoolwork, difficulty concentrating, concern for falling behind in school, concern for getting sick, or other stress-related factors (Styck et al., 2021), as well as an increased risk for child abuse and neglect (Swedo et al., 2020). Elementary school counselors, who are uniquely trained in child development, can implement prevention and intervention programs to address these ongoing needs (ASCA, 2019). Elementary school counselors are essential in providing early intervention and prevention services for students.
Further research is needed in understanding how self-efficacy impacts school counselors’ decision-making process. The variation of confidence in identifying abuse as well as variance in reporting patterns among school counselors with differing years of experience are indicators that further professional development and training is needed within schools. It is also important to examine how school support can increase school counselors’ self-efficacy levels (Schiele et al., 2014). Current research shows that a school counselor’s level of self-efficacy predicts quality of practice and knowledge of evidence-based practices (Schiele et al., 2014).
Limitations
Although measures were used to reduce confounding variables, limitations exist in the methodological design of the study that could impact the validity of the findings. Firstly, this study obtained a sample size from a limited geographic area (Southeastern United States). Secondly, self-reported data was used. Although participants were informed their answers would remain anonymous, they may have answered based on what they perceived as acceptable and appropriate. School counselors may not be inclined to admit they did not report suspected child abuse for fear of legal or ethical violations. Likewise, selective memory may impact participants’ ability to effectively recall events that happened over a year ago. Additionally, many of the participants were White; responses from participants of color were limited. Further research with a more diverse sample would be beneficial to gain a comprehensive understanding of school counselors’ self-efficacy in identifying and reporting child abuse.
Conclusion
School counselors are mandated to report suspected child abuse and neglect cases to authorities and are key school personnel in early detection and recognition of abuse (ASCA, 2021). In this study, differing school demographics were associated with varying reporting practices among veteran school counselors. Continued professional development training, by virtue of its ability to increase veteran school counselors’ self-efficacy and knowledge of identification and reporting protocols, represents a promising possible pathway to improving outcomes among maltreated children.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
American School Counselor Association. (2017). The school counselor and academic development. https://www.schoolcounselor.org/Standards-Positions/Position-Statements/ASCA-Position-Statements/The-School-Counselor-and-Academic-Development
American School Counselor Association. (2019). The essential role of elementary school counselors. https://www.schoolcounselor.org/getmedia/1691fcb1-2dbf-49fc-9629-278610aedeaa/Why-Elem.pdf
American School Counselor Association. (2021). The school counselor and child abuse and neglect prevention. https://schoolcounselor.org/Standards-Positions/Position-Statements/ASCA-Position-Statements/The-School-Counselor-and-Child-Abuse-and-Neglect-P
American School Counselor Association. (2022a). ASCA ethical standards for school counselors. https://www.school
counselor.org/About-School-Counseling/Ethical-Legal-Responsibilities/ASCA-Ethical-Standards-for-School-Counselors-(1)
American School Counselor Association. (2022b). School counselor roles & ratios. https://www.schoolcounselor.org/About-School-Counseling/School-Counselor-Roles-Ratios
American School Counselor Association. (2022c). State school counseling mandates & legislation. https://www.school
counselor.org/About-School-Counseling/State-Requirements-Programs/State-School-Counseling-Man
dates-Legislation
Balkaran, S. (2015). Impact of child abuse education on parent’s self-efficacy: An experimental study. Walden Dissertations and Doctoral Studies, 1432.
Bandura, A. (1977). Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review, 84(2),
191–215. https://doi.org/10.1037/0033-295X.84.2.191
Bandura, A. (1997). Self-efficacy: The exercise of control. W. H. Freeman.
Barrett, K. M., Lester, S. V., & Durham, J. C. (2011). Child maltreatment and the advocacy role of professional school counselors. Journal for Social Action in Counseling and Psychology, 3(2), 86–103.
https://doi.org/10.33043/JSACP.3.2.86-103
Behun, R. J., Cerrito, J. A., Delmonico, D. L., & Kolbert, J. B. (2019). The influence of personal and professional characteristics on school counselors’ recognition and reporting of child sexual abuse. Journal of School Counseling, 17(13), 1–34.
Bellis, M. A., Hughes, K., Leckenby, N., Hardcastle, K. A., Perkins, C., & Lowey, H. (2015). Measuring mortality and the burden of adult disease associated with adverse childhood experiences in England: A national survey. Journal of Public Health, 37(3), 445–454. https://doi.org/10.1093/pubmed/fdu065
Bodenhorn, N., & Skaggs, G. (2005). Development of the school counselor self-efficacy scale. Measurement and Evaluation in Counseling and Development, 38(1), 14–28. https://doi.org/10.1080/07481756.2005.11909766
Bryant, J. K. (2009). School counselors and child abuse reporting: A national survey. Professional School Counseling, 12(5), 333–342. https://doi.org/10.1177/2156759X0901200501
Bryant, J., & Milsom, A. (2005). Child abuse reporting by school counselors. Professional School Counseling, 9(1), 63–71.
Buchanan, D. K., Mynatt, B. S., & Woodside, M. (2017). Novice school counselors’ experience in classroom management. The Journal of Counselor Preparation and Supervision, 9(1). https://doi.org/10.7729/91.1146
Child Welfare Information Gateway. (2019). Long-term consequences of child abuse and neglect. U.S. Department of Health and Human Services, Administration for Children and Families, Children’s Bureau. https://www.childwelfare.gov/pubpdfs/long_term_consequences.pdf
Child Welfare Information Gateway. (2021). Child maltreatment 2019: Summary of key findings. U.S. Department of Health and Human Services, Administration for Children and Families, Children’s Bureau. https://www.childwelfare.gov/pubs/factsheets/canstats
Collin-Vézina, D., Brend, D., & Beeman, I. (2020). When it counts the most: Trauma-informed care and the
COVID-19 global pandemic. Developmental Child Welfare, 2(3), 172–179.
https://doi.org/10.1177/2516103220942530
Crosson-Tower, C. (2003). The role of educators in preventing and responding to child abuse and neglect. U.S. Department of Health and Human Services, Administration for Children and Families, Administration on Children, Youth and Families, Children’s Bureau, Office on Child Abuse and Neglect. https://www.childwelfare.gov/pubpdfs/educator.pdf
Fortson, B. L., Klevens, J., Merrick, M. T., Gilbert, L. K., & Alexander, S. P. (2016). Preventing child abuse and neglect: A technical package for policy, norm, and programmatic activities. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. https://www.cdc.gov/violenceprevention/pdf/can-prevention-technical-package.pdf
Heim, C., Shugart, M., Craighead, W. E., & Nemeroff, C. B. (2010). Neurobiological and psychiatric consequences of child abuse and neglect. Developmental Psychobiology, 52(7), 671–690. https://doi.org/10.1002/dev.20494
Hodges, L. I., & McDonald, K. (2019). An organized approach: Reporting child abuse. Journal of Professional Counseling: Practice, Theory, & Research, 46(1–2), 14–26. https://doi.org/10.1080/15566382.2019.1673093
Hogelin, J. M. (2013). To prevent and to protect: The reporting of child abuse by educators. Brigham Young University Education and Law Journal, 2013(2), 225–252. https://digitalcommons.law.byu.edu/elj/vol2013/iss2/3
Hupe, T. M., & Stevenson, M. C. (2019). Teachers’ intentions to report suspected child abuse: The influence of compassion fatigue. Journal of Child Custody, 16(4), 364–386. https://doi.org/10.1080/15379418.2019.1663334
Johnson, G., Nelson, J., & Henriksen, R. (2017). Mentoring novice school counselors: A grounded theory. In G. R. Walz & J. Bleuer (Eds.), Ideas and research you can use: VISTAS 2017 (pp. 1–16). Counseling Outfitters.
Jordan, K. S., MacKay, P., & Woods, S. J. (2017). Child maltreatment: Optimizing recognition and reporting by school nurses. NASN School Nurse, 32(3), 192–199. https://doi.org/10.1177/1942602X16675932
Kenny, M. C. (2001). Child abuse reporting: Teachers’ perceived deterrents. Child Abuse and Neglect, 25(1), 81–92. https://doi.org/10.1016/s0145(00)00218-0
Kenny, M. C, & Abreu, R. L. (2016). Mandatory reporting of child maltreatment for counselors: An innovative training program. Journal of Child and Adolescent Counseling, 2(2), 112–124.
https://doi.org/10.1080/23727810.2016.1228770
Kenny, M. C., & McEachern, A. G. (2002). Reporting suspected child abuse: A pilot comparison of middle and high school counselors and principals. Journal of Child Sexual Abuse, 11(2), 59–75.
https://doi.org/10.1300/J070v11n02_04
Klassen, S. L., & Hickman, D. L. (2022). Reporting child abuse and neglect on K-12 campuses. In A. M. Powell (Ed.), Best practices for trauma-informed school counseling. IGI Global.
https://doi.org/10.4018/978-1-7998-9785-9.ch010
Krase, K. S. (2015). Child maltreatment reporting by educational personnel: Implications for racial disproportionality in the child welfare system. Children & Schools, 37(2), 89–99.
https://doi.org/10.1093/cs/cdv005
Lambie, G. W. (2005). Child abuse and neglect: A practical guide for professional school counselors. Professional School Counseling, 8(3), 249–258. http://www.jstor.org/stable/42732466
Lambie, G. W., Ieva, K. P., Mullen, P. R., & Hayes, B. G. (2011). Ego development, ethical decision-making, and legal and ethical knowledge in school counselors. Journal of Adult Development, 18(1), 50–59.
https://doi.org/10.1007/s10804-010-9105-8
Larson, L. M., & Daniels, J. A. (1998). Review of the counseling self-efficacy literature. The Counseling Psychologist, 26(2), 179–218. https://doi.org/10.1177/0011000098262001
Luken, A., Nair, R., & Fix, R. L. (2021). On racial disparities in child abuse reports: Exploratory mapping the 2018 NCANDS. Child Maltreatment, 26(3), 267–281. https://doi.org/10.1177/10775595211001926
McGuire, K., & London, K. (2020). A retrospective approach to examining child abuse disclosure. Child Abuse and Neglect, 99, 1–16. https://doi.org/10.1016/j.chiabu.2019.104263
Mishak, D. A. (2007). An investigation of early career and veteran Iowa elementary school counselors and their classroom guidance programs (Order No. 3265967). Available from ProQuest Dissertations & Theses Global. (304858653).
Morrison, M. A., & Lent, R. W. (2018). The working alliance, beliefs about the supervisor, and counseling self-efficacy: Applying the relational efficacy model to counselor supervision. Journal of Counseling Psychology, 65(4), 512–522. https://doi.org/10.1037/cou0000267
Petersen, A. C., Joseph, J., & Feit, M. (Eds.). (2014). New directions in child abuse and neglect research. The National Academies Press.
Remley, T. P., Jr., Rock, D. W., & Reed, R. M. (2017). Ethical and legal issues in school counseling (4th ed.). American School Counselor Association.
Ricks, L., Carney, J., & Lanier, B. (2020). Attributes, attitudes, and perceived self-efficacy levels of school counselors toward poverty. Georgia School Counselors Association Journal, 27, 51–68.
Ricks, L., Tuttle, M., Land, C., & Chibbaro, J. (2019). Trends and influential factors in child abuse reporting: Implications for early career school counselors. Journal of School Counseling, 17(16). http://www.jsc.montana.edu/articles/v17n16.pdf
Schiele, B. E., Weist, M. D., Youngstrom, E. A., Stephan, S. H., & Lever, N. A. (2014). Counseling self-efficacy, quality of services and knowledge of evidence-based practices in school mental health. The Professional Counselor, 4(5), 467–480. https://doi.org/10.15241/bes.4.5.467
Sedlak, A. J., Mettenburg, J., Basena, M., Petta, I., McPherson, K., Greene, A., & Li, S. (2010). Fourth national incidence study of child abuse and neglect (NIS-4): Report to Congress. U.S. Department of Health and Human Services, Administration for Children and Families. https://www.acf.hhs.gov/sites/default/files/documents/opre/nis4_report_congress_full_pdf_jan2010.pdf
Singleton, O., Newlon, M., Fossas, A., Sharma, B., Cook-Greuter, S. R., & Lazar, S. W. (2021). Brain structure and functional connectivity correlate with psychosocial development in contemplative practitioners and controls. Brain Sciences, 11(6), 728. https://doi.org/10.3390/brainsci11060728
Styck, K. M., Malecki, C. K., Ogg, J., & Demaray, M. K. (2021). Measuring COVID-19-related stress among 4th through 12th grade students. School Psychology Review, 50(4), 530–545.
https://doi.org/10.1080/2372966X.2020.1857658
Swedo, E., Idaikkadar, N., Lemmis, R., Dias, T., Radhakrishnan, L., Stein, Z., Chen, M., Agathis, N., & Holland, K. (2020). Trends in U.S. emergency department visits related to suspected or confirmed child abuse and neglect among children and adolescents aged <18 years before and during the COVID-19 pandemic—United States, January 2019–September 2020. Morbidity and Mortality Weekly Report, 69(49), 1841–1847. https://doi.org/10.15585/mmwr.mm6949al
Tang, A. (2020). The impact of school counseling supervision on practicing school counselors’ self-efficacy in building a comprehensive school counseling program. Professional School Counseling, 23(1).
https://doi.org/10.1177/2156759X20947723
Temkin, D., Harper, K., Stratford, B., Sacks, V., Rodriguez, Y., & Bartlett, J. D. (2020). Moving policy toward a whole school, whole community, whole child approach to support children who have experienced trauma. The Journal of School Health, 90(12), 940–947. https://doi.org/10.1111/josh.12957
Tillman, K. S., Prazak, M. D., Burrier, L., Miller, S., Benezra, M., & Lynch, L. (2015). Factors influencing school counselors’ suspecting and reporting of childhood physical abuse: Investigating child, parent, school, and abuse characteristics. Professional School Counseling, 19(1), 103–115. https://doi.org/10.5330/1096-2409-19.1.103
Tuttle, M., Ricks, L., & Taylor, M. (2019). A child abuse reporting framework for early career school counselors. The Professional Counselor, 9(3), 238–251. https://doi.org/10.15241/mt.9.3.238
U.S. Department of Health & Human Services, Administration for Children and Families, Administration on Children, Youth and Families, Children’s Bureau. (2021). Child maltreatment 2019. https://www.acf.hhs.gov/sites/default/files/documents/cb/cm2019.pdf
White, J., & Flynt, M. (2000). The school counselor’s role in prevention and remediation of child abuse. In J. Wittmer (Ed.), Managing your school counseling program: K-12 developmental strategies (pp. 149–160). Educational Media.
Lacey Ricks, PhD, NCC, NCSC, is an associate professor at Liberty University. Malti Tuttle, PhD, NCC, NCSC, LPC, is an associate professor at Auburn University. Sara E. Ellison, MS, NCC, LAPC, is a doctoral student at Auburn University. Correspondence may be addressed to Lacey Ricks, 1971 University Blvd, Lynchburg, VA 24515, lricks1@liberty.edu.
Apr 29, 2020 | Volume 10 - Issue 2
Amanda Giordano, Lindsay A. Lundeen, Chelsea M. Scoffone, Erin P. Kilpatrick, Frank B. Gorritz
Nonsuicidal self-injury (NSSI) is a common clinical concern. We surveyed a national sample of 94 licensed clinicians to better understand their work with clients who self-injure. Our data revealed that over the past year, 95.7% (n = 90) of the sample reported working with at least one client who self-injured. Thirty-six clinicians (38%) reported that most or all of their clients who self-injured were adolescents, 61 (64.9%) reported that most or all clients who self-injured were female, and 43 (45.7%) reported that most or all clients who self-injured engaged in cutting as the primary NSSI method. About 35% (n = 33) of the clinicians in our sample indicated they have never asked clients who self-injured about their online activity related to NSSI. The majority of our participants (n = 78; 83%) supported the notion that NSSI could be an addictive behavior for some clients and less than half (n = 42; 44.7%) received NSSI training in their graduate coursework.
Keywords: nonsuicidal self-injury, NSSI, licensed clinicians, training, behavioral addiction
Nonsuicidal self-injury (NSSI) is a complex phenomenon. Favazza (1998) defined NSSI as “the deliberate, direct destruction or alteration of body tissue without conscious suicidal intent” (p. 260). The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association [APA], 2013) noted that NSSI is intentional and self-inflicted body damage that is not socially sanctioned (e.g., piercings or tattoos) and lacks suicidal intent. The fact that NSSI is intentional and direct distinguishes it from unplanned or indirect forms of self-harm such as disordered eating or substance abuse (Favazza, 1998; Walsh, 2012). Furthermore, although a relationship exists, NSSI is distinct from suicide attempts in that it is a means of seeking relief and coping, thereby sustaining rather than ending one’s life (Walsh, 2012; Wester & Trepal, 2017). NSSI has been conceptualized as a behavioral addiction (Buser & Buser, 2013) given that some clients demonstrate a loss of control over NSSI, continued engagement despite negative consequences, craving to engage in NSSI, and compulsivity, which are hallmarks of addiction. Also, researchers have found evidence for NSSI contagion, in which the behavior is imitated by others in a specific community (Walsh, 2012; Walsh & Rosen, 1985). Given these complexities, it is imperative that clinicians are adequately trained to assess and treat NSSI.
In light of previously published prevalence rates, it is likely that most clinicians will work with clients who self-injure at some point in their careers. Indeed, 21%–80% of inpatient clients and 22%–40% of outpatient clients have reported engagement in self-injurious behavior (Wester & Trepal, 2017). Moreover, in a national sample of 74 clinical practitioners, 60 (81%) reported working with clients who self-injured (Trepal & Wester, 2007), and among 443 school counselors, 357 (81%) reported working with at least one student engaged in self-injury (Roberts-Dobie & Donatelle, 2007). Much has changed, however, in the social landscape related to self-injury, including the popularity of sharing NSSI images online; television shows, movies, and songs depicting NSSI; and celebrities disclosing NSSI behavior. Thus, we sought to investigate licensed clinicians’ experiences working with clients who self-injure to provide updated information and better inform the profession of counseling.
Terminology and Prevalence of NSSI
NSSI is not a new abnormal behavior. Indeed, it was documented in the gospel account of Mark written between A.D. 55 and 65, in which the author described a man cutting himself with stones (Mark 5:5; NIV Life Application Study Bible, 1984). Self-injurious behavior has been labeled self-mutilation, self-harm, deliberate self-harm, parasuicide, cutting, and non-suicidal self-directed violence (Wester & Trepal, 2017). In this paper, we use the term nonsuicidal self-injury (NSSI) as it is currently listed as the proposed diagnosis in the DSM-5 (Section III, Conditions for Further Study; APA, 2013).
Current prevalence rates indicate that NSSI affects a substantial portion of the population, particularly female adolescents (Nock, 2009; Wester & Trepal, 2017). For example, in a study of 665 adolescents, researchers determined that 8% engaged in NSSI at some point in their lives, which included 9% of the females in the sample and 6.7% of the males (Barrocas et al., 2012). Furthermore, Doyle and colleagues (2017) surveyed adolescents in Ireland and found that 12% had engaged in NSSI, the majority (72.8%) of which were female. Moreover, the examination of data from emergency room visits among youth in the United States (10–24 years of age) indicated a rise in non-fatal self-inflicted injury among females (with and without suicidal intent) from 2001 to 2015 (Mercado et al., 2017). Specifically, self-inflicted injuries with a sharp object rose from 261 incidents in 2001 to 1,021 incidents in 2015 (Mercado et al., 2017). Along with adolescent populations, NSSI is a growing concern among young adults. Wester et al. (2018) examined NSSI among three cohorts of freshman college students and found that lifetime NSSI increased from 16% in the 2008 cohort to 45% in the 2015 cohort. Additionally, current NSSI increased from 2.6% in the 2008 cohort to 19.4% in the 2015 cohort (Wester et al., 2018).
Motives for NSSI
The function of NSSI can be challenging to comprehend among those who do not engage in the behavior. Criterion B in the proposed criteria for NSSI Disorder in the DSM-5 (APA, 2013) highlighted three potential functions: (a) to relieve negative feelings and cognitions, (b) to address relational difficulties, and (c) to stimulate positive feelings. Indeed, emotion regulation is a primary motivation for NSSI (Nock, 2009). Among 108 adolescents in inpatient treatment who engaged in self-injurious thoughts or behaviors, Nock and Prinstein (2004) found 52.9% engaged in NSSI to relieve negative emotions, 34.1% engaged to feel something, and 30.6% engaged as a form of self-punishment. Doyle et al. (2017) found 79% of adolescents who engaged in NSSI did so to find relief from negative emotions or cognitions, 38% engaged to punish themselves, and 35% sought to communicate the extent of their distress. In light of the many means of emotion regulation that exist, Nock (2009) identified three reasons why some individuals choose NSSI: (a) as a result of social learning from the media, friends, and family; (b) as a form of punishment via self-directed abuse; and (c) as a means of social signaling, or communicating with others (particularly when other forms of communication were ineffective). Engaging in NSSI may be a more accessible, affordable, and easy-to-hide method of emotion regulation compared to other strategies such as substance abuse (Nock, 2009).
NSSI Social Contagion
One important consideration related to NSSI is social contagion, or the engagement in a behavior by at least two people in a group within 24 hours (Jarvi et al., 2013; Walsh, 2012; Walsh & Rosen, 1985; Wester & Trepal, 2017). Individuals can become exposed to NSSI through peers, family members, media, and song lyrics, which contribute to social learning (Jarvi et al., 2013; Nock, 2009) and potentially sensationalize the behavior (Walsh, 2012). In a review of the literature, researchers found 16 studies supporting the association between social contagion and NSSI (Jarvi et al., 2013). In a seminal work, Walsh and Rosen (1985) studied the behavior of 25 adolescents in treatment for various mental health diagnoses for one year. The researchers analyzed the frequency and timing of particular behaviors, including NSSI, and found significant clustering of self-injurious incidents, supporting contagion for NSSI among the group. Furthermore, researchers have found that a small portion of those who engage in NSSI do so to influence others (e.g., get the attention of a particular person, manipulate others, or elicit care; Doyle et al., 2017; Nock, 2008).
In light of the ubiquitous nature of the internet, NSSI social contagion may occur among online groups, as well as those that exist offline. Walsh (2012) noted that factors contributing to social contagion offline can also occur online within the context of social networking sites, message boards, chat rooms, and YouTube. Researchers have confirmed the prevalence of NSSI images and videos online. Lewis and colleagues (2011) investigated NSSI videos on YouTube and found that the top 100 NSSI videos were viewed over 2 million times. Miguel et al. (2017) found 770 NSSI-related images on three social media platforms in a 6-month period using one search term (#cutting). The researchers classified 59.5% of the images as graphic in nature (Miguel et al., 2017). Although there are potential benefits of online communication about NSSI, such as encouraging help-seeking and support, online NSSI-related images and videos pose risks as well. Lewis et al. (2012) noted that online mediums may provide reinforcement for NSSI, provide tips and strategies (such as first aid considerations), and trigger urges among users to engage in NSSI.
NSSI as a Behavioral Addiction
Given its seemingly compulsive nature, some authors have proposed the conceptualization of NSSI as a behavioral addiction (Buser & Buser, 2013; Davis & Lewis, 2019). Indeed, Buser and Buser (2013) posited that for some individuals, NSSI reflects the commonly used criteria for addiction, including compulsivity, loss of control, continuation despite negative consequences, relief from negative emotions, and tolerance. Specifically, tolerance to NSSI can develop as a result of frequent activation of the endogenous opioid system, to which the individual becomes less sensitive (Buser & Buser, 2013; Walsh, 2012). Tolerance among those who self-injure may manifest as increased frequency of NSSI, increased severity of skin tissue damage, or the use of additional NSSI methods (Wester & Trepal, 2017). In the content analysis of 500 posts on NSSI online message boards, Davis and Lewis (2019) determined six themes that underscored the addictive nature of NSSI: urge/obsession, relapse, can’t/don’t want to stop, coping mechanism, hiding shame, and getting worse/not enough. These themes indicate that some individuals who engage in NSSI experience cravings, a loss of control, urges, and relapse—all common features of addictive behaviors (American Society of Addiction Medicine, 2019). Given the growing acceptance of behavioral addictions, as evidenced by recent changes and additions to both the DSM-5 (APA, 2013) and the International Classification of Diseases (ICD-11; World Health Organization, 2018), it is important to assess whether clinicians working with clients who self-injure conceptualize the behavior as addictive.
Purpose of the Study
Although some researchers have investigated the experience of clinicians addressing clients who self-injure (Roberts-Dobie & Donatelle, 2007; Trepal & Wester, 2007), the growing prevalence of NSSI (Mercado et al., 2017; Wester et al., 2018) warrants updated information. Therefore, we designed the current study to explore licensed clinicians’ experiences with clients who engage in self-injurious behaviors. Specifically, we sought to examine the frequency of addressing NSSI in clinical work, characteristics of clients who self-injure, NSSI assessment practices, the role of the internet in NSSI, clinicians’ beliefs pertaining to NSSI, and clinical training and competence.
Method
Sample
Our sample consisted of 94 licensed clinicians in the United States. Participants ranged in age from 26 to 70 years old with a mean age of 45 (SD = 11.06). Eighty (85.1%) participants identified as White, six (6.4%) as Black/African American, three (3.2%) as biracial/multiracial, three (3.2%) as other, and two (2.1%) as Latino(a)/Hispanic. With regard to gender, 79 (84%) participants identified as female, 13 (13.8%) as male, one (1.1%) as transgender, and one (1.1%) as other. Of the 94 participants, 82 (87.2%) identified as heterosexual, five (5.3%) as bisexual, three (3.2%) as queer, two (2.1%) as lesbian, and one (1.1%) each as gay and other.
In relation to professional background, the clinicians represented varying degree levels and educational fields of study. Most of the participants’ highest degree was a master’s (n = 86; 91.5%), while seven (7.4%) earned a doctoral degree, and one (1.1%) participant earned a specialist degree. Fifty-six (59.6%) of the participants reported that their highest degree was from a CACREP-accredited program, while 26 (27.7%) of the participants came from a non–CACREP-accredited program, and 12 (12.8%) did not answer the question. Some diversity existed among participants’ programs of study and licensure: 51 (54.3%) participants studied professional counseling or counselor education, 27 (28.7%) studied counseling psychology, seven (7.4%) studied clinical psychology, six (6.4%) studied other areas not listed, and three (3.2%) studied rehabilitation counseling. In terms of licensure, 47 (50%) participants were licensed professional counselors (LPCs), 19 (20.2%) were licensed mental health counselors (LMHCs), 15 (16%) were licensed professional clinical counselors (LPCCs), 11 (11.7%) held licensures not listed in our questionnaire, 11 (11.7%) were licensed clinical professional counselors (LCPCs), seven (7.4%) were licensed clinical mental health counselors (LCMHCs), four (4.3%) were licensed professional counselors of mental health (LPCMHs), three (3.2%) were licensed marriage and family therapists (LMFTs), and one (1.1%) was a licensed chemical dependency counselor (LCDC).
The participants had varying years of clinical experience. Eighteen (19.1%) participants had been counseling clients for 1–5 years, 43 (45.7%) for 6–10 years, 17 (18.1%) for 11–15 years, six (6.4%) for 16–20 years, three (3.2%) for 21–25 years, five (5.3%) for 26–30 years, and two (2.1%) for more than 30 years. All participants stated they were currently seeing clients. We asked participants to describe their typical client base by selecting all applicable responses: 84 (89.4%) of the participants counseled adults, 37 (39.4%) counseled adolescents, 37 (39.4%) counseled college students, 27 (28.7%) counseled couples, 19 (20.2%) counseled children, and 12 (12.8%) counseled families.
Instrument
Similar to the approach employed by Trepal and Wester (2007), our questionnaire consisted of two sections: participants’ demographics and clinical experiences with NSSI. In the demographics section, we assessed participants’ age, race, ethnicity, gender, sexual orientation, education, clinical license, and typical client base. Next, to better understand clinical work with clients who self-injure, we compiled a series of descriptive, Likert-type assessment items. Specifically, the questionnaire items explored how often clinicians addressed issues of NSSI in counseling, characteristics of clients who self-injured, methods of assessing NSSI, clients’ internet and social networking activity pertaining to self-injury, the extent to which clinicians conceptualized NSSI as an addiction and whether NSSI should be a formal diagnosis included in the DSM proper (rather than as an appendix), extent of clinical training pertaining to NSSI, and perceived clinical competence when working with issues of NSSI among clients. In sum, the questionnaire contained 22 items related to clinical work with NSSI.
Design
We acquired our national sample of licensed clinical participants using the clinician database on the Psychology Today website. Specifically, we conducted a search of clinicians with experience addressing a general clinical issue (i.e., anxiety) within each of the 50 states. We identified the names of the first 13 licensed clinicians from each state and searched the internet for their email addresses. If an email address could not be found, we replaced this clinician with the next licensed clinician listed on the Psychology Today website for that particular state. We continued this process until we had names and email addresses for 13 licensed clinicians from each state, yielding 650 potential participants.
We calculated a desired sample of 650 given that researchers purported an average response rate of 15.7% for online research surveys sent to professional counselors in the “other” category (members of state-level associations), which most closely reflected our sample (Poynton et al., 2019). After receiving approval from the Institutional Review Board, we emailed the questionnaire link utilizing the Qualtrics software program to the 650 potential participants. Fifty-two emails were undeliverable, resulting in 598 emails sent. We sent participants three reminder emails over the course of three weeks. We received 102 questionnaires (17.1% response rate) from our national sample of licensed clinicians. After removing eight unfinished questionnaires, our final sample consisted of 94 participants (adjusted response rate = 15.7%).
Results
To answer our research questions regarding licensed clinicians’ experiences with client NSSI, we assessed descriptive data resulting from responses to our questionnaire. The data fell into six broad categories: (a) frequency of NSSI in clinical work, (b) descriptions of clients who self-injure, (c) assessment of NSSI, (d) role of the internet, (e) clinicians’ beliefs about NSSI as an addiction and formal diagnosis, and (f) NSSI-related training and perceived competence.
Frequency of NSSI in Clinical Work
We first sought to examine how frequently licensed clinicians worked with clients who self-injured. Specifically, we asked our sample how often in the totality of their clinical work they addressed client NSSI. Results indicated that only two (2.1%) clinicians had never worked with a client reporting NSSI, 37 (39.4%) addressed NSSI rarely (about 10% of the time), 33 (35.1%) addressed NSSI occasionally (about 30% of the time), 13 (13.8%) addressed NSSI a moderate amount (about 50% of the time), five (5.3%) addressed NSSI frequently (about 70% of the time), and four (4.3%) addressed NSSI almost always (about 90% of the time). Thus, among a national sample of 94 licensed clinicians, 92 (97.9%) reported working with NSSI at some point in their careers, with 55 (58.5%) reporting that they addressed NSSI 30% of the time or more.
We also assessed frequency of NSSI among clients in the past year. Only one (1.1%) clinician reported not having self-injuring clients in the previous 12 months. Fifty-one (54.3%) clinicians worked with 1–5 clients who self-injured, 24 (25.5%) worked with 6–10 clients who self-injured, six (6.4%) worked with 11–15 clients who self-injured, and nine (9.6%) worked with more than 15 clients who self-injured. Three (3.2%) participants did not respond to this item.
Descriptions of Clients Who Self-Injure
We then examined clinicians’ descriptions of clients who reported NSSI. Specifically, we inquired about age, gender, race, and method of self-harm by asking clinicians what portion of their clients who self-injured fell into various categories (Table 1). Sixty-one (64.9%) clinicians reported that most or all of their clients who self-injured were female, five (5.3%) reported that most or all of their clients who self-injured were transgender, and one (1.1%) reported that most or all clients who self-injured were male. With regard to race, 63 (67.0%) clinicians reported that most or all of their clients who self-injured were White and nine (9.6%) clinicians reported that most or all of their clients who self-injured were members of a marginalized racial group. With regard to age, 36 (38.3%) clinicians reported that most or all of their clients who self-injured were adolescents, 31 (33.0%) reported that most or all of their clients who self-injured were adults, and one (1.1%) reported that most or all of their clients who self-injured were children. In terms of method of self-injury, 43 (45.7%) clinicians reported that most or all of their clients who self-injured engaged in cutting and seven (7.4%) clinicians reported that most or all of their clients who self-injured engaged in self-injurious behavior other than cutting (e.g., burning, hitting, scratching, punching). Therefore, the experience of NSSI is diverse. Although a substantial portion of clinicians reported that the majority of clients presenting with NSSI were White female adolescents who engaged in cutting, numerous clinicians indicated some clients (up to 50%) were male or transgender, children or adults, clients of color, and engaged in methods other than cutting.
Table 1
Number of Clinicians Endorsing Each Response
| Item: Among your clients who self-injure, what portion are: |
None
(0%) |
Some
( < 50%) |
About half (50%) |
Most
( > 50%) |
All
(100%) |
| Female |
1 (1.1%) |
17 (18.1%) |
12 (12.8%) |
43 (45.7%) |
18 (19.1%) |
| Male |
21 (22.3%) |
57 (60.6%) |
11 (11.7%) |
1 (1.1%) |
0 |
| Transgender |
39 (41.5%) |
37 (39.4%) |
9 (9.6%) |
3 (3.2%) |
2 (2.1%) |
| White |
2 (2.1%) |
20 (21.3%) |
6 (6.4%) |
45 (47.9%) |
18 (19.1%) |
| Person of Color |
25 (26.6%) |
51 (54.3%) |
7 (7.4%) |
6 (6.4%) |
3 (3.2%) |
| Children |
64 (68.1%) |
24 (25.5%) |
0 |
0 |
1 (1.1%) |
| Adolescents |
19 (20.2%) |
22 (23.4%) |
15 (16.0%) |
31 (33.0%) |
5 (5.3%) |
| Adults |
7 (7.4%) |
39 (41.5%) |
13 (13.8%) |
22 (23.4%) |
9 (9.6%) |
| Engaged primarily in cutting |
2 (2.1%) |
32 (34.0%) |
14 (14.9%) |
35 (37.2%) |
8 (8.5%) |
| Engaged primarily in self-injurious behavior other than cutting |
19 (20.2%) |
52 (55.3%) |
14 (14.9%) |
6 (6.4%) |
1 (1.1%) |
Note. Numerical values refer to number of clinicians endorsing that response, followed by percent of clinicians out of the total (N = 94); percentages do not equate to 100 because of missing items: female (missing 3), male (missing 4), transgender (missing 4), White (missing 3), person of color (missing 2), children (missing 5), adolescents (missing 2), adults (missing 4), primarily cutting (missing 3), primarily other behavior (missing 2).
Assessment of NSSI
We also examined data related to the clinical assessment of NSSI. The most commonly endorsed form of assessing NSSI among clinicians was informal assessment through dialogue (n = 83, 88.3%), followed by the use of formal NSSI assessment instruments (n = 21, 22.3%). One (1.1%) clinician reported never assessing NSSI in their clinical work. We also inquired as to whether or not clinicians’ intake forms contained items related to NSSI. Forty-six (48.9%) reported yes, the NSSI item was separate from suicide items; 22 (23.4%) reported yes, the NSSI item was in conjunction with suicide attempts; 16 (17.0%) clinicians reported no, their intake form did not have an item related to NSSI; and 10 (10.6%) did not know or did not answer this question.
Role of the Internet in Client Self-Injurious Behavior
We investigated participants’ responses to items related to clients’ internet use related to NSSI. Specifically, we asked clinicians what portion of their clients engaging in NSSI utilized the internet or social networking sites (SNS) to share pictures of self-injury. Forty-two (44.7%) clinicians reported they did not know because they never discussed the issue with their clients who self-injured. Twenty-six (27.7%) clinicians reported that some (up to 50%) of their clients who self-injured shared NSSI pictures online, 20 (21.3%) reported none of their clients who self-injured shared NSSI pictures online, and three (3.2%) reported that half to all of their clients who self-injured shared NSSI pictures online. In response to the item assessing the frequency in which clinicians asked clients who self-injured about their internet and SNS use related to self-injury, 33 (35.1%) clinicians reported they never asked about this topic, 27 (28.7%) asked sometimes (less than 50% of the time), seven (7.4%) asked about half the time, 17 (18.1%) asked most of the time (more than 50%), and eight (8.5%) always asked. Therefore, it appears that clinicians do not consistently inquire about clients’ internet and SNS use as it relates to NSSI, but those who do find that some of their clients share pictures of self-injury online.
Clinicians’ Beliefs About NSSI
In light of the current status of NSSI Disorder as a condition for further study in the DSM-5 (APA, 2013) and debate about the addictive nature of NSSI, we asked clinicians to share their beliefs on these two topics. With regard to diagnostic status, 32 (34%) clinicians believed NSSI Disorder should be a formal diagnosis in the next edition of the DSM, 24 (25.5%) did not have a preference, and 13 (13.8%) did not believe it should be a diagnosis. Twenty-five (26.6%) participants did not respond to this item. Pertaining to the conceptualization of NSSI as an addiction, 78 (83.0%) clinicians believed that for some individuals, NSSI can be an addiction; eight (8.5%) did not believe NSSI could be an addiction; six (6.4%) stated they did not know; and two (2.1%) did not answer this item. Thus, it appears that one third of the sample supported a formal diagnosis of NSSI Disorder in the DSM proper and a large majority of the sample agreed that NSSI could be an addictive behavior.
NSSI-Related Training and Competence
Finally, participants reported settings in which they received training to address NSSI in clinical work (participants could select all modalities that applied). The most common training modality was continuing education (e.g., conference presentations, workshops, seminars), which was endorsed by 55 (58.5%) clinicians. On-the-job training was the second most common modality, endorsed by 47 (50.0%) clinicians, followed by graduate school coursework, endorsed by 42 (44.7%) clinicians; self-study, endorsed by 38 (40.4%) clinicians; and graduate school internships, endorsed by 28 (29.8%) clinicians. Three (3.2%) clinicians reported that they had never received NSSI training. Clinicians further reported the extent to which they felt competent addressing NSSI in counseling. Four (4.3%) clinicians felt extremely incompetent, eight (8.5%) felt somewhat incompetent, 10 (10.6%) felt neither competent nor incompetent, 54 (57.4%) felt somewhat competent, and 17 (18.1%) felt extremely competent. One (1.1%) clinician did not respond to this item. Overall, clinicians primarily received NSSI training via continuing education workshops and on-the-job experiences. About half of our sample felt somewhat competent to address NSSI, indicating opportunities to improve NSSI training and competence among clinicians.
Discussion
Given the rising prevalence of NSSI (Mercado et al., 2017; Wester et al., 2018) and new considerations such as social contagion (Walsh, 2012; Walsh & Rosen, 1985) and sharing NSSI images online (Lewis et al., 2011; Miguel et al., 2017), continued research is needed related to clinical work with self-injury. We disseminated a questionnaire among a national sample of licensed clinicians to examine the prevalence of NSSI, descriptions of clients who engage in NSSI, means of assessing NSSI, role of the internet in NSSI behaviors, clinicians’ beliefs about NSSI, and NSSI training and perceived competence. Our results indicated that most clinicians surveyed (n = 92, 97.9%) have worked with at least one client who engaged in NSSI. This prevalence rate suggests a potential increase in the presenting concern since Trepal and Wester’s (2007) study, in which 81% of practicing counselors reported working with a client who self-injured during their careers. Furthermore, our results revealed that 95.7% (n = 90) of clinicians treated at least one client participating in NSSI within the past year. Although researchers have determined that 8% of adolescents (Barrocas et al., 2012) and 45% of college freshman (Wester et al., 2018) in naturalistic samples engaged in NSSI at some point in their lifetimes, it appears the frequency might be higher among clients seeking counseling services.
Previous researchers have established that NSSI is more prevalent among females than males (Barrocas et al., 2012; Doyle et al., 2017; Mercado et al., 2017). Our results confirmed these findings as 61 (64.9%) of the clinicians in our sample indicated that most or all of their clients who self-injured were female, as compared to only one (1.1%) who said most or all were male. It is important to note, however, the prevalence of clinicians who reported working with male clients who self-injured. Specifically, 57 (60.6%) noted that some of their clients who self-injured were male and 11 (11.7%) reported that about half of their clients who self-injured were male. Thus, these results indicate that although NSSI is more prevalent among females, it also occurs among male populations. Additionally, although NSSI typically begins in adolescence (Nock & Prinstein, 2004; Wester & Trepal, 2017), 31 (33%) of the clinicians in our sample reported that most or all of their clients who engaged in NSSI were adults. It is imperative, therefore, that clinicians who work with both adolescents and adults are prepared to effectively screen for and treat NSSI.
Regarding the assessment of self-injurious behaviors, our results revealed that only 21 (22.3%) clinicians utilized formal NSSI assessments. Although informal assessment measures often are effective, clinicians could benefit from reviewing psychometrically sound NSSI assessment instruments such as the Deliberate Self-Harm Inventory (Gratz, 2001), the Alexian Brothers Urge to Self-Injure Scale (ABUSI; Washburn et al., 2010), or the Non-Suicidal Self-Injury-Assessment Tool (Whitlock et al., 2014; see Wester & Trepal, 2017, for an extensive description of multiple NSSI assessments).White Kress (2003) summarized that clinicians should assess the function, severity, and dynamics of NSSI, including age of onset, emotions while engaging in NSSI, antecedents to NSSI, desire and efforts to stop or control NSSI, use of substances while self-injuring, medical complications, and changes over time.
We also sought to understand the role of the internet and SNS in NSSI behaviors. Specifically, we inquired of licensed clinicians the extent to which their clients utilized the internet or SNS to share NSSI images and the frequency in which they asked clients who self-injured about their internet behavior. According to the results of our survey, almost half of clinicians surveyed (n = 42; 44.7%) did not know about the role of the internet or SNS among clients who self-injured because they did not ask. Twenty-nine (30.9%) clinicians reported that at least some of their clients used the internet to share pictures. Furthermore, 33 (35.1%) of the clinicians in our study disclosed they had never asked about SNS or the internet when assessing and treating clients engaging in NSSI, and 27 (28.7% ) reported asking less than 50% of the time. These numbers indicate a need for clinicians to have access to current research related to the prevalence of viewing and sharing NSSI images online (Lewis et al., 2011; Miguel et al., 2017). For example, Lewis and Seko (2016) thematically examined 27 empirical studies investigating the perceived effects of online behavior among those who self-injure. The authors reported both perceived benefits of online NSSI activity (i.e., mitigation of social isolation, recovery encouragement, emotional self-disclosure, and curbing NSSI urges) as well as perceived risks (i.e., NSSI reinforcement, triggering NSSI urges, and stigmatization of NSSI; Lewis & Seko, 2016). In addition, previous researchers have found that a portion of individuals engaging in NSSI do so to influence others (Doyle et al., 2017; Nock, 2008), and thus may be particularly attracted to sharing NSSI images online. Given the complex role of the internet in self-injury, it seems imperative that clinicians broach the subject with clients who self-injure.
Our results also demonstrated a strong belief among clinicians (n = 78; 83%) that NSSI can be an addictive behavior for some clients, which supports the stance of previous researchers who conceptualize NSSI as a behavioral addiction (Buser & Buser, 2013). The conceptualization of NSSI as an addictive behavior, with particular emphasis on the stimulation of the endogenous opioid system, has important implications for treatment. Evidence-based addictions treatment strategies such as 12-step support group attendance (Connors et al., 2001) and motivational interviewing (Miller & Rollnick, 2013) can be helpful approaches for working with client NSSI.
Finally, we examined clinicians’ training experience and perceived competence related to NSSI. Less than half of our participants (n = 42; 44.7%) received NSSI training in their graduate-level coursework. The number of clinicians seeking NSSI training via continuing education (n = 55; 58.5%) and self-study (n = 38; 40.4%) is indicative of the desire for more knowledge related to self-injury. In addition, roughly 23% (n = 22) of our sample felt less than “somewhat competent” when addressing NSSI in their clinical work. This perceived incompetency reflects the reported lack of training related to NSSI treatment. Ultimately, this data highlights the opportunity to substantially improve NSSI training to increase clinical competence.
Implications for Counselors
The results of the current study have implications for clinical work with NSSI, specifically in the realms of assessment and treatment. Although many clinicians in our study reported effective assessment measures related to NSSI, an important step for improving assessment might be to include a separate NSSI item on intake forms distinct from suicidal behavior. Sixteen clinicians (17%) in our study said their intake form did not inquire about NSSI, and 22 (23.4%) said the item was written in conjunction with suicidal ideation and attempts. The combination of NSSI and suicidal thoughts or ideations on an intake form can make client conceptualization and treatment goals challenging. NSSI and suicide attempts have markedly different motives (Favazza, 1998; Walsh, 2012; Wester & Trepal, 2017); therefore, listing the behaviors as two separate intake items may best serve both clinicians and clients. Specifically, clinicians could provide a definition of NSSI (Favazza, 1998) on the form to help clients understand the terminology. For clients who indicate that they are engaging in NSSI, clinicians can then utilize formal assessment instruments or the proposed NSSI Disorder diagnostic criteria in the DSM-5 (APA, 2013) to gain a thorough understanding of the behavior. Additionally, clinicians may best serve clients by assessing NSSI with all individuals, regardless of gender, age, racial, or ethnic identification, by asking a broad question such as “Have you ever deliberately hurt yourself?” rather than “Have you ever cut yourself?” to be inclusive of multiple forms of NSSI.
With regard to treatment strategies for NSSI, several useful approaches exist. Dialectical behavior therapy (Linehan, 1993) is a counseling method combining cognitive-behavioral and mindfulness techniques for work with clients diagnosed with borderline personality disorder (BPD). NSSI can be associated with BPD given that self-mutilation is listed as a diagnostic criterion for the disorder (APA, 2013). Researchers have found empirical support for the efficacy of dialectical behavior therapy with regard to NSSI (Choate, 2012; Muehlenkamp, 2006); thus, this treatment approach may be useful for clients with BPD and NSSI. Self-injury also can exist apart from a BPD diagnosis (Muehlenkamp, 2005). In these instances, treatment for self-injurious behavior (T-SIB; Andover et al., 2015) may be a useful approach. T-SIB is a 9-week intervention designed for young adults who self-injure. The intervention includes providing psychoeducation, increasing motivation to change, conducting functional analysis, developing replacement behaviors, increasing distress tolerance, and cognitive restructuring (Andover et al., 2015, 2017). Some empirical support exists for the efficacy of T-SIB among young adults, and the treatment manual provides detailed information for clinicians using the approach (Andover et al., 2015, 2017).
Regardless of the therapeutic intervention, it would behoove clinicians to inquire about clients’ online activities related to NSSI to inform treatment plans and goals. Clients’ online activities could include watching NSSI videos; viewing NSSI images; posting and sharing NSSI images on SNS; communicating with others who self-injure via chatrooms and NSSI websites; or seeking information related to how to conceal, clean, or perform NSSI. As part of their recovery plan, it may be helpful for clients and counselors to develop strategies for healthy online behaviors to minimize triggers, urges, or the normalization of NSSI. Even for clients who describe using the internet to find support for their NSSI, clinicians have the opportunity to describe potential risks with NSSI online activity as well (Lewis & Seko, 2016).
Limitations and Future Research
This study is not without limitations. First, our final participant sample consisted of only 94 licensed clinicians, which reflected a 15.7% response rate. Although this is fairly typical for online surveys (Poynton et al., 2019), there were many potential respondents who did not participate, and we were unable to determine if non-respondents differed significantly from respondents. Additionally, in order to obtain a nationally representative sample, we utilized the clinician database found on Psychology Today. Thus, our participants were limited to only those clinicians who registered for that particular website. Furthermore, although our questionnaire was robust, we did not inquire about the nature of internet use among clients with NSSI. Future researchers may choose to assess whether clients primarily use the internet for education related to NSSI, to find support, to share images, or to read others’ accounts of NSSI behaviors. Finally, we utilized only licensed clinicians for this study. Future researchers may choose to replicate this study with specific types of counselors such as school counselors, inpatient counselors, and outpatient counselors to assess experiences with individuals who self-injure. In these various settings, researchers may inquire as to how clinicians code for NSSI, given that it is not included in the DSM-5 proper.
Conclusion
Nonsuicidal self-injury is a prevalent concern among clients seeking clinical services. We sought to understand clinicians’ experiences working with NSSI by surveying a national sample of licensed practitioners (N = 94). As demonstrated by our results, NSSI affects individuals across age ranges and gender identifications, although it is most prevalent among White female adolescents. Our findings indicate that the majority of clinicians (97.9%) worked with at least one client who engaged in NSSI in the past year. Furthermore, the majority of our sample (83.0%) supported the stance that NSSI can be an addictive behavior. Finally, our study indicates a need for more training related to NSSI in graduate programs and an emphasis on differentiating between NSSI and suicide attempts on intake forms and in clinical work.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
American Society of Addiction Medicine (2019). Definition of addiction. https://www.asam.org/resources/definition-of-addiction
Andover, M. S., Schatten, H. T., Morris, B. W., Holman, C. S., & Miller, I. W. (2017). An intervention for nonsuicidal self-injury in young adults: A pilot randomized controlled trial. Journal of Consulting and Clinical Psychology, 85(6), 620–631. http://doi.org/10.1037/ccp0000206
Andover, M. S., Schatten, H. T., Morris, B. W., & Miller, I. W. (2015). Development of an intervention for nonsuicidal self-injury in young adults: An open pilot trial. Cognitive and Behavioral Practice, 22(4), 491–503. https://doi.org/10.1016/j.cbpra.2014.05.003
Barrocas, A. L., Hankin, B. L., Young, J. F., & Abela, J. R. Z. (2012). Rates of nonsuicidal self-injury in youth: Age, sex, and behavioral methods in a community sample. Pediatrics, 130(1), 39–45.
https://doi.org/10.1542/peds.2011-2094
Buser, T. J., & Buser, J. K. (2013). Conceptualizing nonsuicidal self-injury as a process addiction: Review of research and implications for counselor training and practice. Journal of Addiction & Offender Counseling, 34(1), 16–29. https://doi.org/10.1002/j.2161-1874.2013.00011.x
Choate, L. H. (2012). Counseling adolescents who engage in nonsuicidal self-injury: A dialectical behavior therapy approach. Journal of Mental Health Counseling, 34(1), 56–71.
https://doi.org/10.17744/mehc.34.1.506780307v16m402
Connors, G. J., Tonigan, J. S., & Miller, W. R. (2001). A longitudinal model of intake symptomatology, AA participation and outcome: Retrospective study of the Project MATCH outpatient and aftercare samples. Journal of Studies on Alcohol, 62(6), 817–825. https://doi.org/10.15288/jsa.2001.62.817
Davis, S., & Lewis, C. A. (2019). Addicted to self-harm? The case of online postings on self-harm message boards. International Journal of Mental Health and Addiction, 17, 1020–1035.
https://doi.org/10.1007/s11469-018-9975-8
Doyle, L., Sheridan, A., & Treacy, M. P. (2017). Motivations for adolescent self-harm and the implications for mental health nurses. Journal of Psychiatric and Mental Health Nursing, 24(2-3), 134–142. https://doi.org/10.1111/jpm.12360
Favazza, A. R. (1998). The coming of age of self-mutilation. The Journal of Nervous and Mental Disease, 186(5), 259–268. https://doi.org/10.1097/00005053-199805000-00001
Gratz, K. L. (2001). Measurement of deliberate self-harm: Preliminary data on the Deliberate Self-Harm Inventory. Journal of Psychopathology and Behavioral Assessment, 23, 253–263.
https://doi.org/10.1023/A:1012779403943
Jarvi, S., Jackson, B., Swenson, L., & Crawford, H. (2013). The impact of social contagion on non-suicidal self-injury: A review of the literature. Archives of Suicide Research, 17(1), 1–19.
https://doi.org/10.1080/13811118.2013.748404
Lewis, S. P., Heath, N. L., Michal, N. J., & Duggan, J. M. (2012). Non-suicidal self-injury youth and the internet: What mental health professionals need to know. Child and Adolescent Psychiatry and Mental Health, 6, 13–21. https://doi.org/10.1186/1753-2000-6-13
Lewis, S. P., Heath, N. L., St. Denis, J. M., & Noble, R. (2011). The scope of nonsuicidal self-injury on YouTube. Pediatrics, 127(3), e552–e557. https://doi.org/10.1542/peds.2010-2317
Lewis, S. P., & Seko, Y. (2016). A double-edged sword: A review of benefits and risks of online nonsuicidal self-injury activities. Journal of Clinical Psychology, 72(3), 249–262. https://doi.org/10.1002/jclp.22242
Linehan, M. M. (1993). Cognitive-behavioral treatment of borderline personality disorder. Guilford.
Mercado, M. C., Holland, K., Leemis, R. W., Stone, D. M., & Wang, J. (2017). Trends in emergency department visits for nonfatal self-inflicted injuries among youth aged 10 to 24 years in the United States, 2001–2015. JAMA, 318(19), 1931–1933. https://doi.org/10.1001/jama.2017.13317
Miguel, E. M., Chou, T., Golik, A., Cornacchio, D., Sanchez, A. L., DeSerisy, M., & Comer, J. S. (2017). Examining the scope and patterns of deliberate self-injurious cutting content on popular social media. Depression and Anxiety, 34(9), 786–793. https://doi.org/10.1002/da.22668
Miller, W. R., & Rollnick, S. (2013). Motivational interviewing: Helping people change (3rd ed.). Guilford.
Muehlenkamp, J. J. (2005). Self-injurious behavior as a separate clinical syndrome. American Journal of Orthopsychiatry, 75(2), 324–333. https://doi.org/10.1037/0002-9432.75.2.324
Muehlenkamp, J. J. (2006). Empirically supported treatments and general therapy guidelines for non-suicidal self-injury. Journal of Mental Health Counseling, 28(2), 166–185.
https://doi.org/10.17744/mehc.28.2.6w61cut2lxjdg3m7
NIV Life Application Study Bible. (1984). Tyndale House Publishers.
Nock, M. K. (2008). Actions speak louder than words: An elaborated theoretical model of the social functions of self-injury and other harmful behaviors. Applied and Preventive Psychology, 12(4), 159–168. https://doi.org/10.1016/j.appsy.2008.05.002
Nock, M. K. (2009). Why do people hurt themselves? New insights into the nature and functions of self-injury. Current Directions in Psychological Science, 18(2), 78–83.
https://doi.org/10.1111/j.1467-8721.2009.01613.x
Nock, M. K., & Prinstein, M. J. (2004). A functional approach to the assessment of self-mutilative behavior. Journal of Consulting and Clinical Psychology, 72(5), 885–890. https://doi.org/10.1037/0022-006X.72.5.885
Poynton, T. A., DeFouw, E. R., & Morizio, L. J. (2019). A systematic review of online response rates in four counseling journals. Journal of Counseling & Development, 97(1), 33–42. https://doi.org/10.1002/jcad.12233
Roberts-Dobie, S., & Donatelle, R. J. (2007). School counselors and student self-injury. Journal of School Health, 77(5), 257–264. https://doi.org/10.1111/j.1746-1561.2007.00201.x
Trepal, H. C., & Wester, K. L. (2007). Self-injurious behaviors, diagnoses, and treatment methods: What mental health professional are reporting. Journal of Mental Health Counseling, 29(4), 363–375. https://doi.org/10.17744/mehc.29.4.d277t298667q5367
Walsh, B. W. (2012). Treating self-injury: A practical guide (2nd ed.). Guilford.
Walsh, B. W., & Rosen, P. (1985). Self-mutilation and contagion: An empirical test. The American Journal of Psychiatry, 142(1), 119–120. https://doi.org/10.1176/ajp.142.1.119
Washburn, J. J., Juzwin, K. R., Styer, D. M., & Aldridge, D. (2010). Measuring the urge to self-injure: Preliminary data from a clinical sample. Psychiatry Research, 178(3), 540–544.
https://doi.org/10.1016/j.psychres.2010.05.018
Wester, K., & Trepal, H. C. (2017). Non-suicidal self-injury: Wellness perspectives on behaviors, symptoms, and diagnosis. Routledge.
Wester, K., Trepal, H., & King, K. (2018). Nonsuicidal self-injury: Increased prevalence in engagement. Suicide and Life-Threatening Behavior, 48(6), 690–698. https://doi.org/10.1111/sltb.12389
White Kress, V. E. (2003). Self-injurious behaviors: Assessment and diagnosis. Journal of Counseling & Development, 81(4), 490–496. https://doi.org/10.1002/j.1556-6678.2003.tb00276.x
Whitlock, J., Exner-Cortens, D., & Purington, A. (2014). Assessment of nonsuicidal self-injury: Development and initial validation of the Non-Suicidal Self-Injury–Assessment Tool (NSSI-AT). Psychological Assessment, 26(3), 935–946. https://doi.org/10.1037/a0036611
World Health Organization. (2018). International statistical classification of diseases and related health problems (11th Revision). https://icd.who.int/en
Amanda Giordano, PhD, LPC, is an assistant professor at the University of Georgia. Lindsay A. Lundeen, MS, NCC, is a doctoral student at the University of Georgia. Chelsea M. Scoffone, MEd, is a doctoral student at the University of Georgia. Erin P. Kilpatrick, MS, NCC, LPC, is a doctoral student at the University of Georgia. Frank B. Gorritz, MS, NCC, is a doctoral student at the University of Georgia. Correspondence may be addressed to Amanda Giordano, 422G Aderhold Hall, 110 Carlton Street, Athens, GA 30602, amanda.giordano@uga.edu.