May 22, 2024 | Volume 14 - Issue 1
William B. Lane, Jr., Timothy J. Hakenewerth, Camille D. Frank, Tessa B. Davis-Price, David M. Kleist, Steven J. Moody
Interpretative phenomenological analysis was used to explore the simultaneous supervision experiences of counselors-in-training. Simultaneous supervision is when a supervisee receives clinical supervision from multiple supervisors. Sometimes this supervision includes a university supervisor and a site supervisor. Other times this supervision occurs when a student has multiple sites in one semester and receives supervision at each site. Counselors-in-training described their experiences with simultaneous supervision during the course of their education. Four superordinate themes emerged: making sense of multiple perspectives, orchestrating the process, supervisory relationship dynamics, and personal dispositions and characteristics. Results indicated that counselors-in-training experienced compounded benefits and challenges. Implications for supervisors, supervisees, and counselor education programs are provided.
Keywords: clinical supervision, simultaneous supervision, counselors-in-training, interpretative phenomenological analysis, counselor education
Supervision is a key component of counselor education in programs accredited by the Council for the Accreditation of Counseling and Related Educational Programs (CACREP; 2015) and an ethical requirement in the ACA Code of Ethics (American Counseling Association, 2014). Supervision of counselors-in-training (CITs) serves the purpose of guiding counselor development, gatekeeping, and, ultimately, ensuring competent client care (Borders et al., 2014). For the present study, we defined simultaneous supervision as a pre-licensure CIT receiving weekly individual or triadic supervision from more than one supervisor over the same time period. At the time of the study, the 2016 CACREP standards required that internship and practicum students receive individual and/or triadic supervision averaging 1 hour per week throughout their clinical experience (Standards 3.L. & 3.H.). Some CITs may gain field experience at multiple clinical sites requiring individual site supervision at each site. Many programs require students to engage in faculty advising meetings (Choate & Granello, 2006), which may take a form analogous to formal supervision. Additionally, supervisees may have clinical supervision, focused on supervisee development and client welfare, as well as administrative supervision, focused on functionality and logistics within an agency; these roles may be fulfilled by the same person or at times by two separate supervisors (Kreider, 2014; Tromski-Klingshirn & Davis, 2007). Consequently, although simultaneous supervision is not required in and of itself, it often occurs in counselor education practice.
Supervision Foundations
Counseling supervision research has increased significantly in the last few decades (Borders et al., 2014). Borders and colleagues (2014) developed best practices for effective supervision, including emphasis on the supervision contract, social justice considerations, ethical guidelines, documentation management, and relational dynamics. Previous research has overwhelmingly demonstrated that a strong supervisory alliance is the bedrock of effective supervision (Bernard & Goodyear, 2019). Sterner (2009) further studied the supervisory relationship as a mediator for supervisee work satisfaction and stress. Lambie and colleagues (2018) developed a CIT clinical evaluation to be used in supervision, with strength in assessing personal dispositions in addition to clinical skills. A review of the supervision literature revealed that a strong supervisory relationship based in goal congruence, empathic rapport, and transparent feedback processes (Bernard & Goodyear, 2019; Borders et al., 2014; Sterner, 2009) generate mutual growth between supervisor and supervisee, enhancing clinical work. Additionally, CACREP mandates that faculty and site supervisors foster CIT professional counselor identity through the supervisory process (Borders, 2006; CACREP, 2015).
Counselor development is also a crucial factor in clinical supervision. An entire category of supervision models centralizes the professional development of supervisees in their approach (Bernard & Goodyear, 2019). One of the most widely known models, the Integrative Developmental Model, plots learning, emotion, and cognitive factors across multiple stages of therapist development (Stoltenberg & McNeill, 2010). By focusing on overarching themes of self–other awareness, autonomy, and motivation, the Integrative Developmental Model (Stoltenberg & McNeill, 2010) illuminates how supervisees fluctuate and grow in their anxiety, self-efficacy, reliance on structure, and independence. All these factors may have substantial impact when considering the complexity that simultaneous supervision brings. Furthermore, professional dispositions of openness to feedback and flexibility and adaptability (Lambie et al., 2018) may have additional developmental implications when considering the complexity of simultaneous supervision.
Ethics similarly serve as a foundation of supervisory experiences. Multiple standards and principles of the ACA Code of Ethics (2014) may be complicated by simultaneous supervision and require special attention. Veracity may be of particular interest given the commonality of supervisee nondisclosure (Kreider, 2014), multiplied by the added number of supervisors in one time period. Furthermore, specific standards in Section D: Relationships With Other Professionals may be implicated by obligations in working with multiple professionals; multiple standards in Section F: Supervision, Training, and Teaching may be indicated because of the convergence of both teaching and clinical supervision in counselor training programs; and, finally, reconciling the additional complexities of simultaneous supervision not explicitly identified elsewhere in the 2014 Code of Ethics may elicit a need to carefully consider Section I: Resolving Ethical Issues. With more parties involved, greater nuance would be expected in ethical decision-making.
Much of the foundational research and reviewed contextual factors have either focused specifically on sole supervision or do not differentiate between sole and simultaneous supervision. When considering best supervision practices, the phenomenon of simultaneous supervision presents distinct practical concerns. Exploration is needed to better understand how supervisees might navigate different but related supervisory relationships, how goals and tasks can be congruent across separate supervisory experiences, and how supervisees would make meaning of multiple sources of feedback. Despite the apparent use of simultaneous supervision in counselor education programs, few researchers have explored these dynamic concerns.
Multiple Supervisors and Multiple Roles
Early researchers began to conceptualize the challenges and strengths inherent in simultaneous supervision in both counseling (Davis & Arvey, 1978) and clinical psychology (Dodds, 1986; Duryee et al., 1996; Nestler, 1990), with mixed results overall. Nestler (1990) identified the difficulties in receiving contradictory feedback from multiple supervisors, reflective of fundamental differences in the supervisors’ approaches. Dodds (1986) similarly identified multiple potential stressors in having concurrent supervisors at agency and training settings. Dodds argued that although the general goals to teach and serve clients overlapped, each had inherent differences in their primary institutional goals and structures. Duryee and colleagues (1996) described a beneficial view of simultaneous supervision, in which supervisees overcome conflicts with site supervisors via support and empowerment from academic program coordinators. Davis and Arvey (1978) presented a case study in which supervisees, in a raw comparison, more highly favored the dual supervision overall. These findings highlight the dynamics that occur in the context of simultaneous supervision and connect with recent findings.
Recent researchers have focused on dual-role supervision, defined as one individual supervisor serving as both a clinical and administrative supervisor to one or more supervisees (Kreider, 2014). Kreider (2014) investigated supervisee self-disclosure as related to three factors: supervisor role (dual role or single role), supervisor training level, and supervisor disclosure. Level of supervisor disclosure was found to be significant in explaining differences in supervisee self-disclosure and was hypothesized as a mitigating factor in supervisor role differences (Kreider, 2014). Tromski-Klingshirn and Davis (2007) surveyed the challenges and benefits unique to dual-role supervision for post-degree supervisees. Most supervisees reported neutral to positive outcomes from a dual-role supervisor, but a minority of supervisees noted power dynamics and fear of disclosure as primarily problematic (Tromski-Klingshirn & Davis, 2007), similar to the earlier hypotheses of Nestler (1990) and Dodds (1986). The small amount of existing research solidifies the prevalence of simultaneous supervision and the challenges and benefits for the supervisees. A missing link emerges in understanding how CITs come to understand their experience in simultaneous supervision from a qualitative perspective.
The distinct focused phenomenon of simultaneous supervision is limited in counseling literature. The few conceptual examinations of simultaneous supervision in the mental health literature have indicated confusion and role ambiguity (Nestler, 1990), while at other times simultaneous supervision has been noted to improve comprehensive learning (Duryee et al., 1996). Our study addresses the gap in the literature regarding current simultaneous supervision in counselor education utilizing qualitative analysis.
Method
Given the limited research on simultaneous supervision and its prevalence within the profession, we decided to explore this phenomenon qualitatively. Our research question was “What is the experience of CITs receiving simultaneous supervision from multiple supervisors?” We used interpretative phenomenological analysis (IPA) to explore this question because of its utility with counseling research, grounded methods of analysis, and emphasis on both contextual individual experiences with the phenomenon and general themes (Miller et al., 2018).
Research Team
At the time of the study, the research team consisted of four doctoral students—William B. Lane, Jr., Timothy J. Hakenewerth, Camille D. Frank, and Tessa B. Davis-Price—who each had previous experience with simultaneous supervision as supervisees and supervisors. The team’s perspective of this phenomenon from both roles informed their interest in and analysis of the phenomenon. The fifth member of the team, David M. Kleist, was our doctoral faculty research advisor. The sixth author, Steven J. Moody, provided support in the writing process.
Participants and Procedure
Our participants were four CITs from CACREP-accredited graduate programs accruing internship hours. Smith et al. (2009) suggested seeking three to six participants for IPA, as this allows researchers to explore the phenomenon with individual participants at a deeper level. All four participants specialized in either addiction, school, or clinical mental health counseling, and identified as White, female CITs ranging from 23 to 37 years old. Additionally, each participant reported receiving supervision from at least two supervisors to include university-affiliated supervisors and site supervisors. Each participant came from a different university representing the Rocky Mountain and North Central regions of the Association for Counselor Education and Supervision. To protect confidentiality, each participant selected a pseudonym for the study.
After securing approval from our university’s review board, we recruited participants through purposive convenience sampling. We posted a recruitment email to the CESNET listserv, an informational listserv for counselor educators and supervisors. This listserv was selected as an initial step of convenience sampling to increase the potential to reach a broad range of counseling programs. Nine individuals responded to the call to participate in the research by taking a participant screening survey that helped us determine suitability for the study. After removing individuals from research consideration because of potential dual relationships, nonresponse, or not meeting inclusion criteria, four individuals were selected as participants. We further planned to engage in serial interviewing to gain richer details of the phenomenon and achieve greater depth with the four participants (Murray et al., 2009; Read, 2018). Prior to data collection, the researchers completed a brief phone screening with each participant to review the interview protocol and explain the phenomenological approach guiding the questions. A $40 gift card was provided as a research incentive to participants. Our selection criteria included (a) being a master’s student within a CACREP counseling program, (b) currently accruing internship hours, and (c) receiving simultaneous supervision. We selected participants in internship only because homogenous sampling helps produce applicable results for a given demographical experience (Smith et al., 2009).
Data Collection
Consistent with the recommendations of Smith et al. (2009), we conducted two semi-structured interviews with each participant lasting between 45–90 minutes. We utilized the online videoconferencing platform Zoom to conduct and record the interviews. First-round interviews consisted of four open-ended questions (see Appendix) that allowed participants to explore the experience of simultaneous supervision in detail (Pietkiewicz & Smith, 2014). These questions were open-ended to allow participants to explore the how of the phenomenon (Miller et al., 2018). The final interview questions were developed through initial generation based off research and personal experiences with the phenomenon, refinement in consultation with the research advisor, and interview piloting with volunteer students who did not participate in the study. Research participants were asked about their overall experience with having multiple supervisors, benefits and detriments of simultaneous supervision, and the meaning they made as a result of experiencing simultaneous supervision. Second-round interview questions were developed based on participant responses to first-round interview questions. After two rounds of interviews and analysis, we conducted a final member check to confirm themes. All participants expressed that the developed themes were illustrative of their lived experiences with simultaneous supervision.
Data Analysis
We followed IPA’s 6-step analysis process as outlined by Smith et al. (2009) and added a seventh step with the use of the U-heuristic analysis for group research teams (Koltz et al., 2010). Our process consisted of first coding and contextualizing the data individually, followed by group analysis, triangulated with the fifth author, Kleist, as research advisor. We completed this process for each participant and then analyzed themes across participants as suggested by Smith et al. We reached consensus that four superordinate themes emerged with 11 subthemes across the two rounds of interviews. All participants endorsed agreement with the themes from their experiences in simultaneous supervision during the member check process.
Trustworthiness
We integrated Lincoln and Guba’s (1985) framework in conducting multiple procedures for establishing trustworthiness and credibility. We demonstrated prolonged engagement and persistent observation through consistent coding meetings over the span of 1 year. Additionally, we adapted the U-heuristic analysis process during data analysis to analyze data individually and collectively to strengthen the credibility of our findings (Koltz et al., 2010). Finally, after we developed the themes, we triangulated the results with participants via a member check, ensuring the individual and group themes matched their idiographic experiences.
We bridled our personal experiences with simultaneous supervision throughout the research process. Bridling recognizes that researchers have had close personal experiences with the phenomenon and that bias is best managed by recognition rather than elimination (Stutey et al., 2020). The four principal investigators, Lane, Hakenewerth, Frank, and Davis-Price, individually engaged in memo writing, discussed personal reactions to the data, and participated in group discussions regarding meaning-making of the phenomenon with Kleist serving as research advisor.
Results
Our data analysis produced four superordinate themes identified across all cases. These themes were (a) making sense of multiple perspectives, (b) orchestrating the process, (c) supervisory relationship dynamics, and (d) personal dispositions and characteristics. In the sections that follow, each theme is described in further detail and exemplar quotes are given to support their development.
Making Sense of Multiple Perspectives
Making sense of multiple perspectives was defined as the receipt and conceptualization of supervisory feedback from multiple supervisors during the same academic semester. Supervisees identified their supervisors as having differing professional orientations. At times, these differing backgrounds led to supervisors providing differing opinions for the same client.
Participants used metaphors to make meaning of the distinct offerings of their supervisors’ feedback. An example of capturing multiple perspectives was one participant, Emma, utilizing the ancient Indian parable of “The Blind Men and the Elephant” (Saxe, 1868): “The point of the story is all the world religions might have a piece of the picture of God, you know. And so between all of us [clinicians and supervisors] together, maybe we have a perspective of truth.” Through retelling of the Indian fable, this participant was able to vividly capture her personal perspective of differing viewpoints through an integrative lens as opposed to a conflict of ideas. Within this superordinate theme, the two subthemes of supervisee framing and safety net vs. minefield emerged.
Supervisee Framing
Supervisee framing focused on the participant’s personal view of hearing multiple perspectives from supervisors within simultaneous supervision. Some participants described hearing varying perspectives as being helpful and valuable, providing support, and increasing confidence. They typically framed the idea of receiving various feedback as a way to gain ideas and then make their own informed decisions. Molly shared this positive perspective when she stated, “I like coming to [my differing supervisors] with different issues I have with different clients because I feel like they both have valuable experience, but in different ways.” In contrast, Hailey identified multiple perspectives as being “really difficult,” and Diana noted they were “more frustrating than beneficial” and confusing. Similarly, Hailey stated, “My supervisors are all very different, so they give me different feedback, and a lot of times it conflicts with what the other one has said.” The supervisee’s framing of discrepant feedback impacted their overall perceptions with simultaneous supervision. Supervisees either valued or were confused by the feedback. Generally, participants spoke of times when multiple perspectives were beneficial and difficult, but it appeared all participants were left with the task of making sense of multiple perspectives while receiving simultaneous supervision.
Safety Net vs. Minefield
Making sense of multiple perspectives was described as creating a safety net of support, while others found the experience to be a minefield that increased confusion, ambiguity, and isolation. Emma and Molly characterized their experience as providing support in an often overwhelming profession. Molly articulated, “I feel like if I didn’t have that good support, that good foundation, I don’t think I could do it because it’s just so much.” She later added, “I feel like getting those different perspectives, getting that support, getting those encouragers is beneficial because I don’t feel as overwhelmed, even though it’s overwhelming.”
Participants also perceived their simultaneous supervision as a minefield wherein they believed they were in double binds. Hailey reflected on an experience when her supervisors contradicted each other and expressed, “It just sucked because I was doing what my supervisor told me to do and suggested I do, and then I was told everything I did was wrong.” Diana echoed that discrepant feedback felt like a constant dilemma needing to be managed “carefully.” In reflecting on contradicting supervision, Diana said, “It’s hard because everybody has their own thing. . . . You just kind of have to appease everyone.” In the face of conflict, it was easier to placate than resolve. Participants’ cognitive framing was a major element of the phenomenon. Whereas making sense of multiple perspectives focused on the cognitive elements of receiving feedback from different supervisors, the next theme focused on the behavioral elements.
Orchestrating the Process
Another theme that emerged in our data analysis was that of supervisees orchestrating the process of simultaneous supervision. This theme revolved around action-oriented steps in supervision. The essence of this theme was captured when Hailey acknowledged the need for “checking her motives” on what she shared with different supervisors. She asked herself, “Am I sharing this with this [supervisor] because I feel like they’re going to answer in the way that I feel like . . . they should answer, because it’s easier for me?” Hailey acknowledged the difficulty in this, countering with, “Or am I just going to them because it’s that person that I’m supposed to see?” Hailey recognized that having options when it came to approaching supervisors meant that disclosure needed to be intentional rather than straightforward as it is when CITs only have one choice. Participants were aware of their process as they picked and chose what to share with whom, through seeking out a preferred supervisor and through managing the practical aspects of having multiple supervisors. The subthemes of picking and choosing, seeking a preferred perspective, and managing practical considerations were a part of orchestrating the process.
Picking and Choosing
The subtheme of picking and choosing emerged in how our participants described what they would share in supervision and the course of action taken in their counseling practice. This subtheme was labeled as an in vivo code, derived from Hailey’s quote: “So I definitely pick and choose what I talk to about each one. Because—this sounds terrible—but I respect the one [supervisor] more.” Hailey also described feelings of vulnerability and self-efficacy from week to week, related to her reactions from feedback: “I knew after having such a hard supervision last week showing tape, I was like, ‘I cannot be super vulnerable right now. I need to choose something that’s more surface level.’” Molly experienced picking and choosing as a means of proactively managing the repetitive nature of supervision: “I think just bringing different things to different supervisors is really helpful, and not constantly talking about the same client or the same situation, because that gets obnoxious and repetitive, and you’re gonna get a hundred different opinions.”
After receiving feedback, participants had varying perspectives on how to integrate and transfer constructs into action. Some participants viewed discrepant feedback as mutually exclusive, whereas others had a more integrative perspective. Molly expressed frustration in choosing between differing feedback from multiple supervisors: “Sometimes I don’t really know which I should go with, which I should choose, and which would be best for the client. . . . It’s like a double-edged sword, like it’s good at some points, but then bad at others.” Diana, who expressed similar frustration in choosing between perspectives, relieved this tension by resolving that, “I have to live with myself at the end of the day, so as long as it’s not unethical, I don’t worry about it too much. And as far as the stuff that I’m told that needs to be done, I do what I can.” Other participants espoused a much more integrative perspective. Emma stated, “I think the thing I like the best about it is actually when [my supervisors] have different advice . . . because then I feel like between the two, I can kind of find what I really like.” All participants spoke about selecting what to share with supervisors and choosing how to integrate feedback into action.
Seeking a Preferred Perspective
Coinciding with picking and choosing, participants also sought a preferred perspective in the process of receiving simultaneous supervision and orchestrating the process. Some reported the decision to go to one supervisor over another was situationally based and determined by clinical skill or specialty of the supervisor. Diana captured this as follows, “Well, I can have a conversation with either. I just get very different answers. If it’s the technical stuff of what has to be done—her. If it’s ‘how would you approach the situation?’ I do tend to talk to him.” Diana also likened seeking a preferred perspective to a child searching for a desired answer: “It’s like, who do I want to talk to? It’s almost like, talk to the person you want for the answer you want. It’s like, ‘Well, if Mom doesn’t have the right answer, go talk to Dad.’”
Managing Practical Considerations
All participants spoke to the practicality of meeting with multiple supervisors. Even though some participants strongly valued having multiple supervisors, all participants spoke to the larger time commitment needed in having simultaneous supervision. Molly captured how simultaneous supervision felt overwhelming, adding to the many other sources of feedback she received: “I already have two group supervisions. I’ve heard opinions about this, and I’m hearing other perspectives of my classmates, of my coworkers. Now I have to have triadic and hear their opinions and have individual. . . . It’s just a lot.” Emma framed this time commitment as detracting from her other obligations: “It just starts adding up. Like, my whole Tuesday evenings are gone, and that’s time I could be seeing clients.” Hailey expressed frustration about the obligatory nature and placating to the program’s requirement to see multiple supervisors: “Honestly, I just give the other supervisor little things because I know I have to talk to him . . . and it’s more, like, checking a box.” Finally, Emma captured how this time commitment was epitomized in documentation: “And the paperwork got exhausting, too, because I had to do everything in triplicate sometimes.” She further talked about the additional mental labor: “And now what are we gonna talk about since I just talked about all of this with [a different supervisor] and feel like I found good solutions, you know?” Supervisees had to manage their time and fit more supervision into their schedules. Simultaneous supervision added complexity, and participants needed to orchestrate this process to manage it efficiently and effectively.
Supervisory Relationship Dynamics
Supervisory relationship dynamics was determined to be a superordinate theme as it reflected on the connecting and disconnecting elements of the supervisory relationship. This theme was broken into three subthemes. The subthemes of vulnerability, power dynamics, and systems of supervision illustrated the relational dynamics within simultaneous supervision.
Vulnerability
In supervisory relationships, feelings of safety and vulnerability influenced interactions with different supervisors. To illustrate, Hailey noted:
There are certain supervisors I feel more safe with. And so those are the ones that I share more with . . . versus some of them I feel less safe with . . . I don’t share as much with them that is vulnerable, or that makes me vulnerable.
Participant experiences highlighted how vulnerability dictated what and how elements were shared in simultaneous supervision.
Power Dynamics
The determination of safety occurred within power dynamics. Diana commented that multiple supervisors serving as evaluators and gatekeepers can create “this weird relationship where you don’t want to be too vulnerable because this person is also your boss and can decide if you are going to stay in that position or not.” Diana and Hailey noted feeling disempowered and disengaged from supervision, referring to supervisors as “bosses” throughout their interviews. When participants perceived their supervision as a firmly directive process, discrepant directives were especially distressing. Diana rephrased this sentiment: “I guess the best thing to compare it to would be if you have more than one boss, but they all give you a different, ‘I want this, I want this, I want this.’” Emma’s experience was more accordant, and she specifically expressed at one time, “None of [my supervisors] are really super bossy either.” Participants identified power dynamics as salient aspects of how they experienced supervision and with whom they connected. Working with more than one supervisor sometimes resulted in characterization of “good” and “bad” supervisors, making individual supervisory relationship dynamics crucial.
Systems of Supervision
Participants conceptualized the phenomenon as broader systems of supervision in which individual supervisors were interacting with each other. Emma noted, “The two faculty supervisors work very closely together and I assume talk all the time.” Emma and Molly provided multiple examples of supervisors working together to best serve clients, thus bolstering supervision through their combined expertise. Molly stated, “It was nice because [my two supervisors] were in agreement and I felt comfortable going into session with [my client].” Even negative experiences contributed to systems of supervision. Hailey reported seeking out additional support when her assigned supervisory relationships did not meet her needs, widening the reach of simultaneous supervision even more: “By not being a good supervisor, he helps me seek out other resources and figure it out for myself.” Finally, Molly noted that supervisor coordination was primarily for evaluation at the end of the semester and only if problems arose. However, she imagined what it would be like if they were more collaborative:
They would have had a better understanding of the way I work in a counseling room. . . . Because my site supervisor really understood how I approached things and the way I would interact with my clients, but I feel like my university supervisor didn’t really, like, she had little snippets of what I was like in a counseling room.
Power, vulnerability, and systems in the supervisory relationship impacted supervisees from multiple levels in their clinical journey.
Personal Dispositions and Characteristics
Personal dispositions and characteristics resulted from participants speaking about the phenomenon as well as what they said about their supervisors. Three dispositions that emerged as relevant were tolerance for ambiguity, curiosity, and availability. The first two subthemes were identified as they spoke about the phenomenon and the third subtheme was a characteristic present because of the nature of simultaneous supervision.
Tolerance for Ambiguity
Tolerance for ambiguity was found to be a critical disposition. This disposition allowed participants to see differences in opinion as helpful. Emma shared that she “very rarely” saw people as giving her “conflicting information.” She said that she saw it as everybody having their own perspective. This connected to her ability to view multiple perspectives as “pieces of the puzzle,” as she expressed earlier in her retelling of the Indian fable. Although participants sometimes expressed concern about direction, Diana shared, “You can ask questions and you can not know and it’s okay.” This disposition directly related to how they reconciled and then reacted to multiple perspectives of simultaneous supervisors.
Curiosity
Curiosity also manifested more implicitly with supervisees. Participants showed curiosity by taking interest in what supervisors had to say, seeking more information, or staying open to difficult feedback. Hailey shared that simultaneous supervision “definitely requires a lot of continuing to look inward and examining your motives and yourself and what the supervisors have said.” In speaking more broadly, Emma shared, “So I don’t think I’ll ever give [simultaneous supervision] up now that I’ve kind of experienced how valuable it is to get another professional opinion.” Curiosity manifested itself as a transient characteristic for other participants. Diana experienced transference with one of her supervisors, which was a barrier to her ability to exhibit this helpful disposition. One of her supervisors suggested that she try and work things out with another supervisor she was having difficulty with, to which Diana said, “No. Who is gonna walk into their supervisor and be like, ‘Okay, so my problem with you is you’re a bitch. You remind me of my abusive ex.’ . . . But at the same time, I have to work with her.” This was an example of Diana demonstrating a closing off to feedback. Both tolerance for ambiguity and curiosity manifested and impacted their experience of multiple perspectives.
Availability
An important disposition was emotional and physical availability. Emma expressed that “there’s always somebody I can get a hold of.” Hailey expressed that she had “more coverage just in general,” but also questioned her supervisors’ true availability: “Do I even need to bring this to supervision or can I work on this on my own? Because sometimes I feel like I annoy them.” All participants expressed that availability was important to their experience, although physical availability did not always translate to being available to discuss what the supervisee wanted. Those participants who identified supervisors within simultaneous supervision as being more available had more positive thoughts regarding simultaneous supervision.
Discussion
All four participants identified the complex position of CITs receiving supervision from more than one supervisor. The results align with the growing body of literature affirming the importance of a positive working relationship between CITs and supervisors (Bernard & Goodyear, 2019; Borders et al., 2014; Sterner, 2009) as well as significant differences between faculty and site supervision (Borders, 2006; Dodds, 1986). The results parallel supervision literature detailing the multiple roles of supervisees (Bernard & Goodyear, 2019) who, unlike supervisors, are not required to have specific education in supervision. The theme of personal dispositions has been studied extensively in counselor education, resulting in prominent placement in clinical assessment instruments (Lambie et al., 2018). The presented themes diverge from the current research base in their construction of a clear model of simultaneous supervision. The subthemes of picking and choosing, seeking a preferred perspective, and systems of supervision illustrate the interpersonal dynamics of simultaneous supervision that is distinct from sole supervision, an underrepresented phenomenon in the supervision literature. Participants in this study reported mixed feelings with simultaneous supervision. Four primary themes emerged from this study: making sense of multiple perspectives, orchestrating the process, supervisory relationship dynamics, and personal dispositions and characteristics. These four themes encompass many areas of the supervisory experience while illuminating guidelines for supervisors engaging in simultaneous supervision.
Implications
Results from this study reinforce the complex levels of integration CITs experience when receiving supervision from multiple supervisors. This process of integration can lead to confusion, ambiguity, and also deeper understanding. The results indicate that the perceived benefit of simultaneous supervision was often based on the relationship between the supervisor and CIT, ability and support to organize the process, and the personal dispositions of the CIT. The implications for this research target three populations.
Supervisors
The findings of this study indicate several implications for supervisors working with clinicians receiving simultaneous supervision. First and foremost, the critical importance of the supervisory relationship to supervision in general (Bernard & Goodyear, 2019) was further substantiated as a foundation for effective simultaneous supervision. Questionable supervisee behaviors such as intentional nondisclosure via seeking a preferred perspective or picking and choosing can be avoided through purposefully fostering trust in the relationship. Similarly, supervisors may support the perspective of simultaneous supervision as a safety net if support for vulnerability is established and the relationship is actively attended to. Supervisors should be mindful of their availability to CITs and periodically check in to see if they are meeting the needs of the supervisee.
Supervisors who are aware of the themes developed from this research may be better equipped to capitalize on benefits and mitigate challenges. One benefit was that simultaneous supervision allowed participants to receive multiple synergistic perspectives regarding their work with clients. Depending on the developmental level of the supervisee and the demeanor of the supervisor, however, these multiple perspectives may present challenges. Supervisors can apply their knowledge of developmental models to tailor their interventions. Supervisors might anticipate that CITs earlier in development (e.g., in practicum) may require structured support in simultaneous supervision to avoid performance anxiety and frustration from rigid applications of multiple perspectives consistent with this stage (Stoltenberg & McNeill, 2010). Supervisors may also wish to focus supervision on interventions that actively facilitate development of these dispositions, such as employing constructivism to elicit greater cognitive flexibility (Bernard & Goodyear, 2019).
Some early-stage supervisees may experience challenges when navigating varying perspectives and feedback provided to them by multiple supervisors. Challenges can be mitigated when supervisors broach the topic of simultaneous supervision with supervisees early. Additionally, when supervisors ensure they respect other supervisors and create collaborative relationships, supervisee difficulty with simultaneous supervision may decrease. When a supervisor learns of a differing opinion of another supervisor, it is important that it is broached as a variance in approach rather than an incorrect practice. Supervisees experiencing difficulties with simultaneous supervision may also benefit from supervisors checking in with them regarding the variable feedback they are receiving. A collaborative supervisory system may strengthen supervisee development and integration of counseling constructs. Counseling programs can play a key role in setting systemic expectations for supervisors and supervisees.
Counselor Education Programs
Accredited counselor education programs have autonomy in how they meet various CACREP (2015) supervision and clinical requirements. Programs may choose to require simultaneous supervision, may require multiple clinical sites, and may utilize faculty advising as supplementary clinical supervision. In unique situations such as students completing two tracks or receiving additional supervision for gatekeeping reasons, how programs manage simultaneous supervision can become complex. Best practice guidelines, policies, and procedures regarding simultaneous supervision can be made clear in clinical handbooks, with clinical coordinators, and in material for site supervisors. This would help to address the supervisee confusion from the programmatic side. Another important implication with simultaneous supervision is to consider the supervisory process through a systemic lens. When simultaneous supervision is utilized, there will be many interactions occurring outside of the dyad or triad apparent to one individual supervisor. When supervisors collaborate and communicate, supervisees may be more likely to receive congruent feedback, understand gatekeeping action, and receive consistent expectations. In particular, communication between academic and clinical supervisors can bridge the gap between idealism and practicality (Bernard & Goodyear, 2019; Choate & Granello, 2006). Programmatically mandated, semesterly site visits and opportunities for regular check-ins could fulfill this purpose.
Supervisees
Participants often spoke to the challenge of organizing simultaneous supervision effectively in relation to feedback, documentation, and case presentation material. Although a certain level of organizational skill is expected of graduate students, the coordination required in simultaneous supervision often seemed unanticipated and unwieldy for students. Preparing for the supervision experience in another course and/or an orientation in lab supervision may aid in this. All participants discussed, at varying distress levels, how having supervision scheduled too close together (e.g., same day or two days in a row) increased repetitiveness and thus made simultaneous supervision feel less efficacious. Supervisees may want to intentionally schedule supervision sessions spaciously to avoid potential repetition or redundancy. With the steady increase in virtual supervision, scheduling supervision in ideal time frames may be easier with increased access and absent travel time. Programmatic preparation, intentional scheduling, and collaborative supervision notes may aid the simultaneous supervision process.
In the areas of core dispositions, CITs who embraced ambiguity and fostered reflexivity, curiosity, and flexibility tended to navigate simultaneous supervision with more ease. Reflexivity, curiosity, and tolerance for ambiguity seemed to strengthen the ability to receive feedback from multiple sources, integrate feedback appropriately, and maintain strong supervisory relationships. A typical guiding question from participants was, “How can I apply this combined feedback to my particular site and client while still maintaining my own clinical identity?” Necessarily, students will enter a program with differing levels of core strengths, yet any student can be encouraged to strengthen their core dispositions. Supervisees are encouraged to think about simultaneous supervision with the same organization and openness required for other courses such as pre-practicum and multicultural counseling. Correspondingly, supervisors have complex responsibilities maintaining ethical competent care, organizing supervision, and fostering these core dispositions.
Ethical Implications of Simultaneous Supervision
In addition to recommendations for the three populations above, findings from this study highlight ethical considerations. Worthington et al. (2002) identified “intentional nondisclosure of important information” (p. 326) and “inappropriate methods of managing conflict with supervisors” (p. 329) as two major ethical issues that are unique to supervisees and correlate with some of the participant supervisees’ experiences of triangulating supervisors, seeking outside consultation to circumvent supervisors, or intentionally withholding information. To ensure client welfare, supervisors and supervisees may benefit from explicitly discussing ethical implications and considerations unique to this phenomenon at the outset of supervision and again when conflicts arise. Future research that addresses limitations of this study will further clarify the role of supervisors, supervisees, and programs in simultaneous supervision as well as specific ethical guidelines.
Limitations and Future Directions
Limited information was gathered about the specific counselor education programs in which our participants were enrolled, restricting the inferences able to be made about simultaneous supervision in context. We also chose a convenience sampling method using CESNET and selected four participants. The choice of indirect sampling, primarily through counselor educators redirecting calls to their students, may have limited participants. Further, all participants of this study identified as the same gender and race, which limits the diversity of experience shared. Future researchers may consider sampling more participants to get a broader exploration of the phenomenon. In doing so, researchers may be able to obtain greater representation in gender and race to increase the transferability of this study.
This study focused on the phenomenon of simultaneous supervision as experienced within individual and triadic supervision. Simultaneous supervision is embedded within the broader experience of supervision, and isolating the phenomenon required vigilance by the researchers. Future researchers would benefit from intentional follow-up questions that better focus participants on simultaneous supervision rather than individual experiences with supervisors. As our study did not explicitly ask participants to distinguish between university-affiliated and site supervisors, future researchers may pursue a qualitative study that highlights the difference. Other research may utilize grounded theory to develop a model of simultaneous supervision for supervisors and supervisees to follow or focus explicitly on supervisors’ perspectives of simultaneous supervision. Quantitative research may illuminate the frequency and use of simultaneous supervision in counselor education programs overall or identify correlations between counselor dispositions such as tolerance for ambiguity and supervision outcomes in simultaneous supervision. Because of the lack of information regarding the phenomenon of simultaneous supervision, many opportunities for research regarding the phenomenon persist.
Conclusion
Overall, the findings from this research indicate CITs valued greater support and thrived when integrating “both/and thinking” in navigating feedback from multiple supervisors. This perspective reinforces the need for systemic communication among counselor educators and supervisors. Additionally, results suggest CITs would benefit from supervisors broaching the topic of simultaneous supervision early in their clinical experience.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
American Counseling Association. (2014). ACA code of ethics. https://www.counseling.org/resources/aca-code-of-ethics.pdf
Bernard, J. M., & Goodyear, R. K. (2019). Fundamentals of clinical supervision (6th ed.). Pearson.
Borders, L. D. (2006). Snapshot of clinical supervision in counseling and counselor education: A five-year review. The Clinical Supervisor, 24(1–2), 69–113. https://doi.org/10.1300/J001v24n01_05
Borders, L. D., Glosoff, H. L., Welfare, L. E., Hays, D. G., DeKruyf, L., Fernando, D. M., & Page, B. (2014). Best practices in clinical supervision: Evolution of a counseling specialty. The Clinical Supervisor, 33(1), 26–44. https://doi.org/10.1080/07325223.2014.905225
Choate, L. H., & Granello, D. H. (2006). Promoting student cognitive development in counselor preparation: A proposed expanded role for faculty advisers. Counselor Education and Supervision, 46(2), 116–130.
https://doi.org/10.1002/j.1556-6978.2006.tb00017.x
Council for the Accreditation of Counseling and Related Educational Programs. (2015). 2016 CACREP standards. https://www.cacrep.org/for-programs/2016-cacrep-standards/
Davis, K. L., & Arvey, H. H. (1978). Dual supervision: A model for counseling and supervision. Counselor Education and Supervision, 17(4), 293–299. https://doi.org/10.1002/j.1556-6978.1978.tb01086.x
Dodds, J. B. (1986). Supervision of psychology trainees in field placements. Professional Psychology: Research and Practice, 17(4), 296–300. https://doi.org/10.1037/0735-7028.17.4.296
Duryee, J., Brymer, M., & Gold, K. (1996). The supervisory needs of neophyte psychotherapy trainees. Journal of Clinical Psychology, 52(6), 663–671. https://doi.org/bmp9p9
Koltz, R. L., Odegard, M. A., Provost, K. B., Smith, T., & Kleist, D. (2010). Picture perfect: Using photo-voice to explore four doctoral students’ comprehensive examination experiences. Journal of Creativity in Mental Health, 5(4), 389–411. https://doi.org/10.1080/15401383.2010.527797
Kreider, H. D. (2014). Administrative and clinical supervision: The impact of dual roles on supervisee disclosure in counseling supervision. The Clinical Supervisor, 33(2), 256–268.
https://doi.org/10.1080/07325223.2014.992292
Lambie, G. W., Mullen, P. R., Swank, J. M., & Blount, A. (2018). The Counseling Competencies Scale: Validation and refinement. Measurement and Evaluation in Counseling and Development, 51(1), 1–15.
https://doi.org/10.1080/07481756.2017.1358964
Lincoln, Y. S., & Guba, E. G. (1985). Naturalistic inquiry. SAGE.
Miller, R. M., Chan, C. D., & Farmer, L. B. (2018). Interpretative phenomenological analysis: A contemporary qualitative approach. Counselor Education and Supervision, 57(4), 240–254. https://doi.org/10.1002/ceas.12114
Murray, S. A., Kendall, M., Carduff, E., Worth, A., Harris, F. M., Lloyd, A., Cavers, D., Grant, L., & Sheikh, A. (2009). Use of serial qualitative interviews to understand patients’ evolving experiences and needs. BMJ, 339, b3702. https://doi.org/10.1136/bmj.b3702
Nestler, E. J. (1990). The case of double supervision: A resident’s perspective on common problems in psychotherapy supervision. Academic Psychiatry, 14(3), 129–136. https://doi.org/10.1007/BF03341284
Pietkiewicz, I., & Smith, J. A. (2014). A practical guide to using interpretative phenomenological analysis in qualitative research psychology. Psychological Journal, 20, 7–14. https://doi.org/10.14691/CPPJ.20.1.7
Read, B. L. (2018). Serial interviews: When and why to talk to someone more than once. International Journal of Qualitative Methods, 17(1), 1–10. https://doi.org/10.1177/1609406918783452
Saxe, J. G. (1868). The poems of John Godfrey Saxe. Ticknor and Fields.
Smith, J. A., Flowers, P., & Larkin, M. (2009). Interpretative phenomenological analysis: Theory, method and research (1st ed.). SAGE.
Sterner, W. (2009). Influence of the supervisory working alliance on supervisee work satisfaction and work-related stress. Journal of Mental Health Counseling, 31(3), 249–263. https://doi.org/10.17744/mehc.31.3.f3544l502401831g
Stoltenberg, C. D., & McNeill, B. W. (2010). IDM supervision: An integrative developmental model for supervising counselors and therapists (3rd ed.). Routledge.
Stutey, D. M., Givens, J., Cureton, J. L., & Henderson, A. J. (2020). The practice of bridling: Maintaining openness in phenomenological research. The Journal of Humanistic Counseling, 59(2), 144–156.
https://doi.org/10.1002/johc.12135
Tromski-Klingshirn, D., & Davis, T. E. (2007). Supervisees’ perceptions of their clinical supervision: A study of the dual role of clinical and administrative supervisor. Counselor Education and Supervision, 46(4), 294–304. https://doi.org/10.1002/j.1556-6978.2007.tb00033.x
Worthington, R. L., Tan, J. A., & Poulin, K. (2002). Ethically questionable behaviors among supervisees: An exploratory investigation. Ethics & Behavior, 12(4), 323–351. https://doi.org/10.1207/S15327019EB1204_02
William B. Lane, Jr., PhD, NCC, BC-TMH, LPCC, is an assistant professor at Western New Mexico University. Timothy J. Hakenewerth, PhD, NCC, LPC, is an assistant professor at the University of Illinois Springfield. Camille D. Frank, PhD, NCC, LMHC, LPC, is an assistant professor at Eastern Washington University. Tessa B. Davis-Price, PhD, LMHC, LCPC, is an assistant professor at Saint Martin’s University. David M. Kleist, PhD, LCPC, is a professor and department chair at Idaho State University. Steven J. Moody, PhD, is a clinical professor at Adams State University. Correspondence may be addressed to William B. Lane, Jr., 1000 W College Ave, Silver City, NM 88061, william.lanejr@wnmu.edu.
Appendix
Interview Protocol
| Interview Questions |
| Round 1 |
| What has been your experience with having multiple simultaneous supervisors?
In your own experience, how has simultaneous supervision been a strength?
In your own experience, how has simultaneous supervision been challenging?
What have you learned about yourself and the counseling profession as you’ve experienced simultaneous supervision? |
| Round 2 |
| How has having simultaneous supervision been different from times when you have only had one supervisor?
What has it been like to have your supervisors interact with each other in regard to the supervision that you have received from them?
What personal dispositions (characteristics/qualities) do you think you have that influenced your experience of simultaneous supervision?
How has simultaneous supervision impacted your experience of safety or vulnerability in supervision?
What practical considerations have you needed to consider for having multiple simultaneous supervisors? |
Nov 26, 2019 | Volume 9 - Issue 4
Matthew C. Fullen, Jonathan D. Wiley, Amy A. Morgan
This interpretative phenomenological analysis explored licensed professional counselors’ experiences of turning away Medicare beneficiaries because of the current Medicare mental health policy. Researchers used semi-structured interviews to explore the client-level barriers created by federal legislation that determines professional counselors as Medicare-ineligible providers. An in-depth presentation of one superordinate theme, ineffectual policy, along with the emergent themes confounding regulations, programmatic inconsistencies, and impediment to care, illustrates the proximal barriers Medicare beneficiaries experience when actively seeking out licensed professional counselors for mental health care. Licensed professional counselors’ experiences indicate that current Medicare provider regulations interfere with mental health care accessibility and availability for Medicare-insured populations. Implications for advocacy are discussed.
Keywords: Medicare, interpretative phenomenological analysis, mental health, advocacy, federal legislation
Medicare is the primary source of health insurance for 60 million Americans, including adults 65 years and over and younger individuals with a long-term disability; the number of beneficiaries is expected to surpass 80 million by 2030 (Kaiser Family Foundation, 2019; Medicare Payment Advisory Commission, 2015). According to the Center for Medicare Advocacy (2013), approximately 26% of all Medicare beneficiaries experience some form of mental health disorder, including depression and anxiety, mild and major neurocognitive disorder, and serious mental illness such as bipolar disorder and schizophrenia. Among older adults specifically, nearly one in five meets the criteria for a mental health or substance use condition, and if left unaddressed, these issues may lead to consequences such as impaired physical health, hospitalization, and even suicide (Institute of Medicine, 2012).
Past research demonstrates that Medicare-eligible populations respond appropriately to counseling (Roseborough, Luptak, McLeod, & Bradshaw, 2012). Federal agencies such as the Substance Abuse and Mental Health Services Administration (SAMHSA) publish entire guides on how to use counseling to treat depression and related conditions in older adults (SAMHSA, 2011). However, researchers have noted specific challenges that Medicare-eligible populations, such as older adults, face when trying to access mental health services. Stewart, Jameson, and Curtin (2015) described acceptability, accessibility, and availability as three intersecting dimensions that may influence whether an older adult in need of help is able to access care. In contrast to acceptability, which focuses on whether older individuals are willing to participate in specific mental health services, accessibility and availability are both supply-side issues that impede older adults’ engagement with mental health services. Accessibility refers to factors like funding for mental health services and providing transportation support to attend appointments. Availability is used to describe the number of mental health professionals who provide services to older adults within a particular community.
Stewart et al.’s (2015) framework is useful when examining current Medicare policy and its impact on beneficiaries’ ability to participate in mental health treatment when needed. Experts have criticized Medicare for its relative inattention to mental health care (Bartels & Naslund, 2013), noting a remarkably low percentage of its total budget is spent on mental health (1% or $2.4 billion; Institute of Medicine, 2012), as well as a lack of emphasis on prevention services. In terms of accessibility, Congress has made efforts to remove restrictions to using one’s health insurance to access mental health treatment. For example, mental health parity laws were passed in 2008 to ensure that Medicare coverage for mental illness is not more restrictive than coverage for physical health concerns (Medicare Improvements for Patients and Providers Act of 2008, 2008). Yet current Medicare policy may restrict the availability of services at the mental health provider level. For example, the Medicare program has not updated its mental health provider licensure standards since 1989, when licensed clinical social workers were added as independent mental health providers and restrictions on services provided by psychologists were removed (H.R. Rep. No. 101-386, 1989). Although counseling is only one mental health care modality available to Medicare beneficiaries, counselors can play a prominent role in the mental health treatment of older adults and people with long-term disabilities.
Meanwhile, there are references in the literature to a provider gap that may influence the ability of Medicare beneficiaries, including older adults, to access mental health services. A 2012 Institute of Medicine report described the lack of mental health providers as a crisis, and experts on geriatric mental health care have decried the lack of mental health professionals who focus their work on older adults (Bartels & Naslund, 2013). Despite these concerns, relatively little attention has been given to the influence of Medicare provider regulations in limiting the number of available providers. Scholars have noted that a significant proportion of graduate-level mental health professionals are currently excluded from Medicare regulations, despite providing a substantial ratio of community-based mental health services (Christenson & Crane, 2004; Field, 2017; Fullen, 2016; Goodman, Morgan, Hodgson, & Caldwell, 2018). Licensed professional counselors (LPCs) and licensed marriage and family therapists (LMFTs) jointly comprise approximately 200,000 providers (Medicare Mental Health Workforce Coalition, 2019), which means that approximately half of all master’s-level providers are not available to provide services under Medicare. Since their recognition as independent mental health providers by Congress in 1989, only licensed clinical social workers and advanced practice psychiatric nurses have constituted the proportion of master’s-level providers eligible to provide mental health services through Medicare.
Despite current Medicare reimbursement restrictions, Medicare beneficiaries are likely to seek out services from LPCs. Fullen, Lawson, and Sharma (in press-a) found that over 50% of practicing counselors had turned away Medicare-insured individuals who sought counseling services, 40% had used pro bono or sliding scale approaches to provide services, and 39% were forced to refer existing clients once those clients became Medicare-eligible. When this occurs, the Medicare mental health coverage gap (MMHCG) impacts providers and beneficiaries in several distinct ways. First, some beneficiaries may begin treatment only to have services interrupted or stopped altogether once the provider is no longer able to be reimbursed by Medicare. This can occur because of confusion about whether a particular patient’s insurance coverage authorizes treatment by a particular provider type, or when beneficiaries who have successfully used one type of coverage to pay for services transition to Medicare coverage because of advancing age or qualifying for long-term disability.
Most Medicare beneficiaries (81%; Kaiser Family Foundation, 2019) have supplemental insurance, including 22% who have both Medicare and Medicaid. Medicare beneficiaries who are dually eligible for Medicaid may be particularly vulnerable to the MMHCG. In most states, Medicaid authorizes LPCs to provide counseling services; however, in certain cases when these individuals also qualify for Medicare, the inconsistency in provider regulations between these programs can interfere with client care. A similar problem occurs when the Medicare-insured attempt to use supplemental plans (e.g., private insurance, Medigap) because of Medicare functioning as a primary source of insurance, and supplemental plans requiring documentation that a Medicare claim has been denied. Regardless of the reason for having to terminate treatment prematurely, early withdrawal from mental health treatment has been described as inefficient and harmful to both clients and mental health providers (Barrett et al., 2008).
The MMHCG also can interfere with clients’ ability to access services because of a lack of Medicare-eligible providers in a particular geographical region. For example, beneficiaries who reside in rural localities can have more difficulty finding mental health providers because of a general shortage of providers in these areas (Larson, Patterson, Garberson, & Andrilla, 2016). Larson et al. (2016) found that rural communities were less likely to have licensed mental health professionals overall, although these localities were more likely to have a counseling professional than a clinical social worker, psychiatric nurse practitioner, or psychiatrist. Historically, older adults from rural and urban localities experience a comparable prevalence of mental health disorders (Center for Behavioral Health Statistics and Quality, 2018). However, studies consistently describe low rates of mental health services accessibility and availability within rural communities (Smalley & Warren, 2012). Establishing counselors as Medicare-eligible providers can reduce the disparities of mental health services accessibility and availability experienced by older adults in rural communities.
Although it is known that LPCs are currently excluded from Medicare coverage, it is not well understood what sort of impact this has on mental health providers and the Medicare beneficiaries who seek their services. Recent efforts to raise awareness of this issue have emerged in the literature (Field, 2017; Fullen, 2016; Goodman et al., 2018), but there has not yet been an investigation into the phenomenological experiences of mental health providers who are directly impacted by existing Medicare policy. The purpose of this study was to explore the lived experiences of mental health professionals who have turned away clients because of their status as Medicare-ineligible providers. The primary research question for this study was: How do Medicare-ineligible providers make sense of their experiences turning away Medicare beneficiaries and their inability to serve these clients?
Research Design and Methods
This study was executed using interpretive phenomenological analysis (IPA) to guide both data collection and analysis. The study focused on the experiences of Medicare-ineligible mental health professionals as they navigated interactions with Medicare beneficiaries who sought mental health care from them. By using a hermeneutic approach to understand their unique perspectives on this phenomenon, we aimed to remain consistent with the philosophical approach of IPA, which is idiographic in nature (Smith, Flowers, & Larkin, 2009). This study received approval from the Western Institutional Review Board.
IPA focuses on the personal meaning-making of participants who share a particular experience within a specific context (Smith et al., 2009). We determined IPA to be the most appropriate method to answer our research question because of the personal impact on LPCs of turning away Medicare beneficiaries because of Medicare-ineligible provider status. Nationally, LPCs share the experience of being unable to serve Medicare beneficiaries because of the current Medicare mental health policy that establishes these licensed mental health professionals as Medicare-ineligible. IPA also is appropriate for this study because of the positionality of the researchers. The research team consisted of two LPCs and one LMFT who have denied services or had to refer clients because of the current Medicare mental health policy and have engaged in prior research and advocacy related to the professional and clinical implications of the current Medicare mental health policy. We selected IPA for this study because of the shared experience between the researchers and participants as Medicare-ineligible providers. A distinguishing feature of IPA, a variation of hermeneutic phenomenology, is the acknowledgment of a double-interpretative, analytical process: The researchers make sense of how the participants make sense of a shared phenomenon (Smith et al., 2009).
Participants
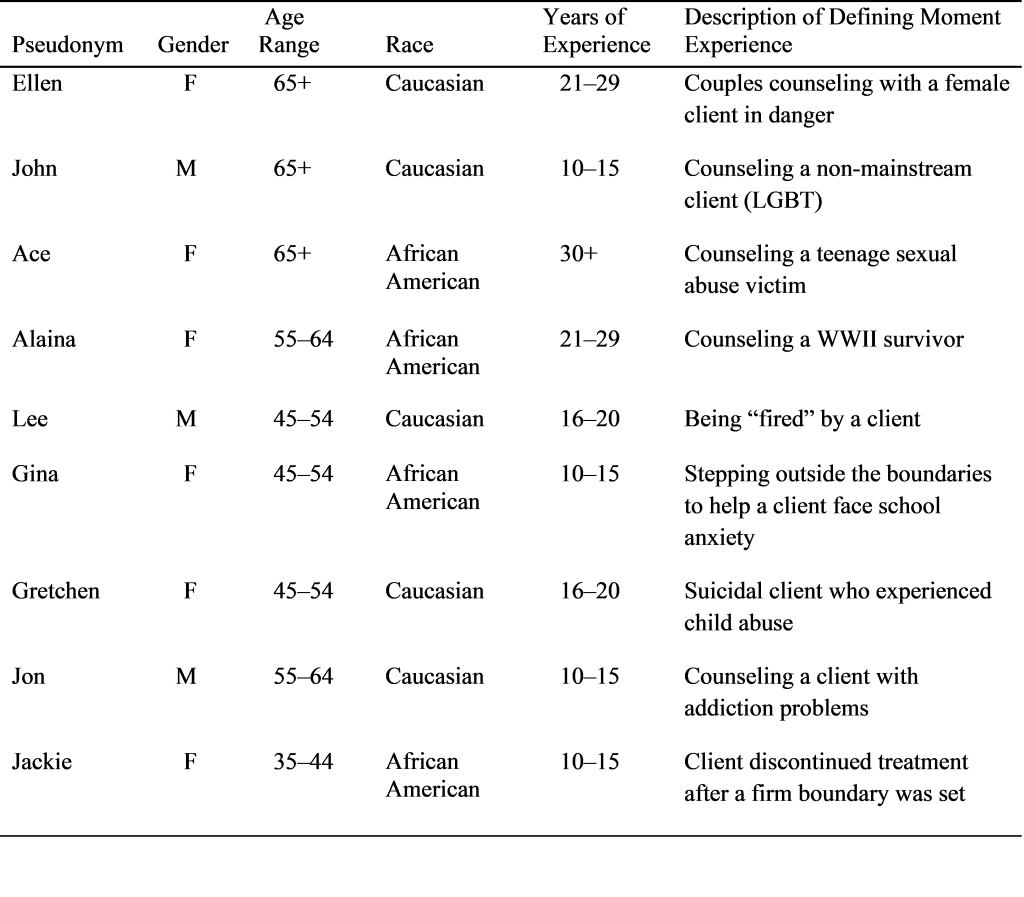
Participants were screened based on the inclusion criteria of having direct experience with turning away or referring Medicare beneficiaries and holding a mental health license as an LPC. Because states grant licenses to health care providers, we limited participation to LPCs who were practicing in a specific state in the Mid-Atlantic region. This allowed for consistency in licensure requirements, training provided, and current scope of practice across all participants. The nine participants interviewed all held the highest professional counseling license in this state, which allows these individuals to practice independent of supervision after completing 4,000 hours of supervised training. Post-license experience ranged from 6 months to 17 years, and participants practiced in both rural and non-rural settings. Pseudonyms were assigned by the research team (see Table 1 for participant information).
| Table 1
Participant Information
|
| Participant |
License Type |
Rural Statusa |
Years of Licensed Experience |
| Michelle |
LPC |
Rural |
4 years |
| Cecelia |
LPC |
Non-rural |
5 years |
| Mary |
LPC |
Non-rural |
17 years |
| Roger |
LPC |
Non-rural |
2 years |
| Aubrey |
LPC |
Rural |
4 years |
| Donna |
LPC |
Rural |
4 years |
| April |
LPC |
Non-rural |
0.5 years |
| Robert |
LPC/LMFT |
Non-rural |
22 years |
| Brandon |
LPC |
Rural |
5 years |
aThe table displays rural status as designated by the U.S. Department of Health and Human Services Health Resources and Services Administration (2016) according to the practice location of the participant. Non-rural includes metropolitan and micropolitan areas. Rural indicates any locality that is neither metropolitan or micropolitan.
Most participants were identified because of having completed a national survey of mental health providers unable to serve Medicare beneficiaries (Fullen et al., in press-a). Participants in the national survey were provided with a question in which they were able to indicate their openness to participating in follow-up individual interviews regarding their experiences with turning away clients as a result of Medicare policy. Two additional participants had not completed the national survey but were identified locally because of their unique experiences with the phenomenon under investigation. We selected nine participants in accordance with IPA participant selection and data saturation guidelines (Smith et al., 2009). Although the current Medicare policy excludes both LPCs and LMFTs, we chose to focus on the experiences of LPCs to ensure a purposive and homogeneous sample (Smith et al., 2009).
Data Collection
Semi-structured, in-depth interviews of the nine participants were conducted by the research team. All research team members are LPCs or LMFTs. Individual interviews were conducted by a single member of the team who digitally recorded and transcribed verbatim the interview procedure. Consent was obtained from the participants and pseudonyms were used to ensure participant confidentiality. Also, participants were given the option to stop the interview at any time. The elapsed time of each interview ranged between 47 and 66 minutes. The semi-structured interview protocol began with two initial questions to frame the interview: (a) Have you ever had to refer a potential client to another counselor/therapist/agency because of not being able to accept their Medicare insurance coverage? and (b) Have you ever established a working relationship with a client who later transitioned to Medicare insurance coverage?
Based on participant responses to these initial questions, two grand tour questions followed:
(a) Tell me about what typically occurs when someone with Medicare insurance contacts your office in search of counseling? and (b) Tell me about any times when you have had to alter a pre-existing working relationship with a client because of their Medicare coverage? Follow-up questions focused on the impact of current Medicare mental health policy on the interviewees, as well as their perceived impact on clients, local communities, other therapists in the area, and their employment contexts.
Data Analysis
The IPA process outlined by Smith et al. (2009) was employed to analyze the transcribed interview data. The following steps were employed throughout the analysis process: (a) reading and re-reading of transcripts, (b) initial noting, (c) developing emergent themes, (d) searching for connections across emergent themes, (e) moving to the next case, and (f) looking for patterns across cases. Codes and themes developed at each stage of the first transcript analysis required consensus agreement among the authors. After re-reading, initial noting, developing emergent themes, and clustering of superordinate themes for each of the remaining interviews, the authors proceeded to engage in a group-level analysis process of looking for patterns across all interviews. Patterns across all interviews were organized into a concept map to synthesize connections and relationships between the interviews. Connections and relationships identified through this cross-case analysis led to the identification of a group-level clustering of superordinate themes that resulted in the identification of the primary themes.
Trustworthiness
The authors attended to the credibility and trustworthiness of this analysis using four strategies. First, the authors have prolonged engagement in the fields of counseling and marriage and family therapy as licensed professionals. This prolonged engagement has allowed the authors to be situated to the contexts of the participants, account for abnormalities in the data, and transcend their own observations (Lincoln & Guba, 1985). Second, the authors engaged in a team-based reflexive process through the sharing of personal reflections and group discussions about emerging issues (Barry, Britten, Barber, Bradley, & Stevenson, 1999). Third, negative case analysis was used in the analytical process of this study to develop, broaden, and confirm themes that emerged from the data (Lincoln & Guba, 1985; Patton, 1999). The fourth strategy was analyst triangulation (Denzin, 1978; Patton, 1999). All three authors participated in the development of the study, data collection, and data analysis to reduce the potential bias that can emerge from a single researcher performing each of these tasks (Patton, 1999). Each researcher independently analyzed the same data and compared their findings throughout data analysis to check selective perception and interpretive bias.
Results
Three superordinate themes emerged from our interviews with nine mental health professionals who have experience with the Medicare coverage gap: ineffectual policy, difficult transitions, and undue burden. We will discuss one superordinate theme, ineffectual policy, with the emergent themes of confounding regulations, programmatic inconsistencies, and impediment to care. By presenting a single meta-theme, we hope to provide increased depth and the nuanced experiences that our participants shared (see Levitt et al., 2018 for a discussion on dividing qualitative data into multiple manuscripts).
All nine participants expressed concerns about the ineffectiveness of current Medicare policy when it comes to treating people with mental disorders who live in their communities. The disconnect between Medicare’s intended aim—to provide sound health care to beneficiaries—and the present outcome for clients seeking out counseling led us to describe the policy as ineffectual or not producing the intended effect. Our participants perceived that the policy had severe shortcomings in terms of providing access to mental health care, which they viewed as a serious problem with cascading consequences for their clients, communities, and themselves.
Confounding Regulations
Several participants described the Medicare coverage gap as “confusing” and “frustrating” for mental health providers and Medicare beneficiaries who are seeking mental health services. Brandon, an LPC who serves as a director within a Federally Qualified Health Center, stated, “Most people are pretty shocked to realize we are not part of Medicare.” He went on to explain that most medical providers, including psychiatrists, were not aware of LPCs’ Medicare ineligibility when making client referrals. Participants described how the confusion interferes with referrals between medical providers and clients seeking mental health services.
Other participants described how frustrating the policy is, both for themselves and their clients. Robert, an LPC who also is credentialed as an LMFT, stated that “as a provider, it’s frustrating to turn people away,” and “it’s especially concerning for older people who can’t afford to pay out of pocket.” Michelle, who works as an LPC in a rural community, described how the MMHCG influences clients’ views of the larger Medicare system, stating, “[Clients are] very angry—not directed towards me, just the system . . . they’re on Medicare now [and] they have to leave. They paid into a system and then still can’t see the clinician that they want to see.” According to interviewees like Michelle, current Medicare provider regulations do not account for the preponderance of LPCs who provide care, particularly in rural communities. Regulations are then perceived by clients as an additional barrier to getting help at a time when they may be vulnerable.
In fact, in certain cases, current Medicare policy may result in all Medicare beneficiaries within a particular community losing access to mental health care. Brandon described a 4-month period when his Federally Qualified Health Center was unable to serve any Medicare beneficiaries because of job turnover: “[It] took us four months to find an LCSW. . . . We specifically had to weed out some very qualified licensed mental health professionals because they weren’t LCSWs.” Brandon went on to explain that during this 4-month period, his clients were unable to access mental health care at the community clinic. He concluded, “It was pretty disruptive to their care.”
Brandon’s description elucidates the cascading impact of the current policy on clients, community agencies that provide mental health services, and counselors seeking work. When specific providers are excluded from servicing Medicare beneficiaries, older adults with mental health conditions are vulnerable to gaps in coverage, such as the 4-month period that Brandon described.
Programmatic Inconsistencies
Several interviewees referenced confusion about how Medicare interfaces with other insurance programs. Roger and Mary, a couple in joint practice, explained how confusion among clients and health providers in their community is exacerbated by inconsistencies between Medicare and Medicaid, including the fact that in their state LPCs are eligible for reimbursement from Medicaid, but not Medicare. Roger explained, “[The] confusion is not just with clients who have low SES. It’s agency people, it’s case managers in the community, doctors that would make referrals, there really is a misunderstanding . . . and sometimes a disbelief.” They went on to describe their frustration in having to explain to referral sources that Medicare ineligibility has nothing to do with a lack of training. Roger concluded, “Yes, we are trained and . . . virtually every other insurance company accepts licensed professional counselors.”
Mary’s and Roger’s statements are indicative of the confusion that current policy creates among providers and clients. Several interviewees expressed annoyance that they had to explain to prospective clients that they possessed the requisite license and training required by the state to provide counseling and that they were recognized providers by non-Medicare insurance providers (i.e., Medicaid, Tricare, private insurance providers).
Related to the inconsistency between Medicaid and Medicare, several interviewees alluded to the fact that the very circumstances that qualify individuals for government-funded insurance (e.g., poverty, disability) may inadvertently restrict the mental health care that is available to them. Michelle described this phenomenon in the context of having to address clients who were referred to work with her by the local community mental health agency. She alluded to a particularly challenging cycle in which clients who were diagnosed with schizophrenia would be referred to her for counseling while they were also applying for long-term medical disability. She described the challenges of working with these clients, only to have to refer them elsewhere once they became eligible for disability benefits (which include Medicare). Describing her clients, she stated, “[They] applied for disability, they received disability, and now they have to, even though they have established the relationship with me . . . transition over to a different therapist.” Michelle then highlighted what occurs after this transition is initiated: “[One] individual . . . has continued to see me because with that particular diagnosis, he doesn’t trust anyone else. . . . [Another] individual . . . just chooses not to see anyone . . . and then she ends up having to be hospitalized every so often.”
Beyond being discouraged or exasperated, Michelle’s capacity to remain stoic in the face of such a paradox was telling. As she described it, this sequence had happened on multiple occasions and would likely happen again save for a federal policy change. Michelle also alluded to the potential economic detriments of current policy. By foregoing outpatient counseling because of the barriers described above, her patient with schizophrenia must be intermittently hospitalized, which is a much more expensive form of treatment.
Policy-level inconsistencies were confusing to providers as well. April, an LPC who attained her independent license within the past year, stated, “It feels like handcuffs. It’s like here you have this credential that the state says you have earned, but it’s only a half credential because you can’t [accept] one of the main government sponsored programs.” Cecelia, an LPC working in a metropolitan area, expressed similar sentiments as she explained how clients with Medicare and secondary insurance plans are turned away: “I initially bill Anthem first and my claims continue to get denied.” She explained, “Basically what they want me to do is submit the claims to Medicare, allow Medicare to deny the claim, and then submit the claim to them with the denial from Medicare and then they’ll provide reimbursement.” However, Cecelia stated that this process has been halted when Medicare refuses to issue a denial letter because of her status as an LPC. She put it this way: “The struggle that I found with Medicare is that because I’m an LPC, Medicare won’t even recognize me to even allow me to submit a claim . . . so I cannot provide Anthem with the denial that they’re looking for.”
Cecelia’s description of the inconsistency between Medicare and private insurance reflects a particularly problematic experience for her clients. Although they had paid for supplemental private insurance plans to augment their Medicare coverage, they were unable to use these benefits without a denial letter from Medicare. Ironically, according to Cecelia, the Medicare office could not provide the denial to a Medicare-ineligible provider in the first place.
Brandon made a similar statement about the inconsistency in provider regulations between Medicare and Tricare, specifically referencing his own training levels: “I’m shocked. . . . We’re some of the most qualified licensed mental health professionals in the business to provide psychotherapy and treatment for psychiatric diagnoses . . . and yet somehow that doesn’t count . . . somehow we’re not included.” Citing the growing number of insurance providers that do recognize LPCs, including Tricare, he concluded, “So, literally Medicare is the last holdout that I’m aware of.” By describing Medicare as “the last holdout,” Brandon implies that Medicare is the only federal program that has not updated its provider regulations to match the current mental health marketplace. Echoing Brandon, the sentiment that Medicare provider regulations were not in line with the current state of mental health practice was common among our interviewees.
Impediment to Care
The therapeutic working alliance has been shown to be one of the key factors that positively impacts counseling treatment (Wampold, 2015). When existing clients become eligible for Medicare, whether because of increasing age or qualifying for a long-term disability, current policy appears to interfere with continuity of care. Aubrey, an LPC who practices in a rural locality, describes it this way: “I will tell you where the problem arises . . . if I’m assigned a client, and I have the rapport with them, and we’re working together and they become eligible for Medicare . . . then I have to transfer them.” Because of the emphasis within counseling on the working relationship, Aubrey suggested that after building a strong working relationship with a counselor, even referrals within an agency can be disruptive to patient care.
Additionally, several interviewees described the challenges associated with referring Medicare beneficiaries to alternative providers. Some alluded to clients who made an effort to continue working with an LPC, despite not being able to use their Medicare coverage. Eventually, disparities in clients’ financial circumstances resulted in some clients having to forego receiving mental health care. Brandon explained the difficulty that current Medicare policy brings to communities, particularly those in which there are relatively few Medicare-eligible providers relative to LPCs. He described monthly meetings with community private practice providers this way: “[They are] all booked up. There’s just not enough . . . licensed mental health providers in town to see everybody. And . . . because only half of those people can accept Medicare, it has a very particular impact on Medicare recipients.” Citing the shortage of providers, Brandon emphasized the additional burden faced by the Medicare-insured because of having a smaller available provider pool.
The shortage of alternative mental health providers was a common theme among interviewees, especially for those who practiced in rural communities. Michelle explained that there is a misperception that Medicare-eligible providers are available when Medicare beneficiaries seek out help: “I hear . . .
there are so many licensed clinical social workers in this area, but there aren’t.” As a consequence, “[individuals] that are trying to work themselves into the schedule of a licensed clinical social worker, they often wait months before they’re actually able to be seen.”
Donna, an LPC who also works in a rural community, expressed a similar concern about the lack
of options facing beneficiaries who live in rural areas: “I see such a shortage in rural areas of providers across the board. And then when you have to narrow it down even further to limit who they can see, then that makes it even more difficult for them to get the care that they need.”
In fact, the expense of mental health care when insurance coverage is unavailable was a factor that several interviewees described. Robert told the story of a client he had seen for several years who tried to pay out of pocket but could no longer make that financially viable: “[It] was really disappointing because she really wasn’t finished. . . . We had a great working relationship and it was sad to have her stop just because of reimbursement reasons.”
Brandon made a similar comment about an individual who was deterred from seeking treatment because of the cost of paying out of pocket when his Medicare insurance was unable to be used: “I let him know . . . I can’t accept Medicare. And he asked how much it would be. [I said] anywhere from $75 to $125, and . . . he was pretty disheartened by that.”
Mary noted how the MMHCG can result in Medicare beneficiaries not seeking out necessary services. She emphasized that turning people away at the point when they have elected to ask for help can be disconcerting: “Right at a time when they’re willing to reach out and ask for [help]. That’s the worst part. Because I think . . . that discourages clients from seeking services—they have to work too hard . . . finding a provider.” April added a similar sentiment: “It’s heartbreaking . . . [my] emphasis is on those most vulnerable and those most in need of services . . . it is my worst nightmare for a client to walk away . . . because I want them to know they are my priority.” In each of these examples, participants expressed concerns that current policy acted as a deterrent to accessing necessary mental health services because of the burdensome process of having to locate a Medicare-eligible provider.
Discussion
Our findings illuminate how current Medicare mental health policy impacts Medicare beneficiaries’ access to counseling treatment for mental health conditions. Nine mental health providers who are not Medicare-eligible were interviewed to learn about their experiences interacting with Medicare beneficiaries who sought their services. The central phenomenon that all interviewees responded to—their inability to work with Medicare beneficiaries in the same manner that they work with clients who use other forms of insurance—has infrequently been referenced in the extant literature. This phenomenon provides a unique contribution to discussions about the accessibility and availability of mental health services to older adults (Stewart et al., 2015) and people with long-term disabilities. Particularly compelling about what was reported in these interviews is the fact that these individuals were actively seeking out or currently engaged in mental health treatment at the time when they were turned away. In the past, explanations about barriers to mental health care for Medicare-insured populations have focused on systemic factors such as rural geography (Kim et al., 2013) or stigma about mental health (Chapin et al., 2013). While these are certainly relevant factors that provide a broad explanation for why older people are less likely to receive mental health services, the current study illuminates several proximate point-of-service barriers that result in providers having to cease treatment with clients, deny care to clients who were actively seeking it out, or refer clients to relatively long wait-lists in lieu of more prompt treatment by available providers. Given the lack of scholarly attention focused on the MMHCG, the perspectives offered by these participants contributes to a broader discussion about how to increase access to mental health services for older adults, as well as for individuals with long-term disabilities.
Among our interviewees, there was a noticeable amount of concern for how the MMHCG impacts individuals in the community in need of mental health care. Participants’ concerns about the consequences of the MMHCG on their clients may be related to their awareness that mental illness influences other key indicators of well-being. For example, depression reflects a relatively common mental health condition that responds well to treatment but can be problematic for clients when left untreated. Although depression was only one of several types of mental illness described by participants, clinically relevant depressive symptoms affect 10% of males over 65 and 15% of females over 65, and the presence of depressive symptoms is correlated with greater functional disability, dementia, higher rates of physical illness, and higher health care resource utilization (Federal Interagency Forum on Aging-Related Statistics, 2016). As the number of Medicare beneficiaries grows, it is reasonable to assume that there will be corresponding growth in the number of people who meet the criteria for mental health conditions, including depression. Echoing the concern voiced by our participants, we state that the current Medicare policy extends the risk of mental health needs going unmet among Medicare-insured populations.
Additionally, the economic consequences of untreated or undertreated mental illness are worth considering. Each participant described instances of unmet client mental health needs because of a combination of (a) practitioner inability to submit for Medicare reimbursement, (b) client’s inability to pay a sliding scale rate, and (c) lack of follow-through on referrals to mental health providers eligible for Medicare coverage. For example, some participants described this undertreatment as resulting in potential inpatient psychiatric hospitalization because of clients’ inability to utilize their Medicare benefits to seek care within their local communities. Undertreatment of mental health conditions can lead to inefficient administration of health care, including an over-reliance on more expensive mental health services when outpatient services could have been more appropriate. For example, the reimbursement rate for 45 minutes of counseling is $84.74 for doctoral-level providers (see American Psychological Association, 2015, for a critique of this rate), and the rate for master’s-level providers is estimated at 75% of this amount ($63.56). This is in contrast to the cost of a single day in an inpatient psychiatric facility, which is $782.78, or approximately 12 times higher than a single counseling session (Centers for Medicare & Medicaid Services, 2019). Having adequate outpatient services available within a community is traditionally a sound strategy for reducing high-cost treatment; yet this is not occurring as regularly as is needed when Medicare beneficiaries are involved. Although not every person who may be at risk for inpatient hospitalization will benefit solely from weekly outpatient services, several cases referenced by our interviewees (e.g., Michelle’s work with clients with schizophrenia) fit this category. Considering that a single day of inpatient treatment costs the same as a 12-session course of counseling from a master’s-level provider, it stands to reason that there are economic benefits to re-examining current Medicare mental health policy.
The inefficiency of current Medicare policy was highlighted when several participants alluded to inconsistencies between insurance programs, including certain cases in which having Medicare precluded clients from using other forms of insurance (e.g., Medicaid, Tricare, private supplemental plans) that would otherwise cover mental health treatment by LPCs. This feature of the MMHCG has important ramifications given that 81% of Medicare beneficiaries possess a supplemental health plan (Kaiser Family Foundation, 2019), including more than 12 million Americans who are dually covered by Medicare and Medicaid (Centers for Medicare & Medicaid Services, n.d.). For this latter group, dual-eligible adults are more likely to have functional or cognitive impairments, chronic conditions, or conditions that frequently coincide with mental health conditions. In fact, among dual-eligible individuals, 59% of those with disabilities and 20% of those who are 65 years or older self-reported diagnosis of a mental health disorder (Donohue, 2006). This means that some of the most vulnerable Medicare beneficiaries are particularly burdened by current Medicare mental health policy.
Implications for Professional Advocacy
Regarding advocacy on behalf of clients, these findings suggest that Medicare reimbursement for LPCs is urgently needed in order to provide Medicare-insured populations with access to mental health services. Currently, efforts to change Medicare regulations through the legislative process have support from a broad range of professional interest groups, many of which comprise the Medicare Mental Health Workforce Coalition (Medicare Mental Health Workforce Coalition, 2019). Further, there is currently legislation under consideration in both the U.S. Senate (S. 286; Mental Health Access Improvement Act, 2019) and U.S. House of Representatives (H.R. 945; Mental Health Access Improvement Act, 2019) that would include LPCs and LMFTs as Medicare-eligible providers. As of November 2019, these bills had 29 and 96 cosponsors, respectively (U.S. Congress 2019a, 2019b). Despite these efforts, more than half of counseling professionals recently surveyed had not participated in advocacy related to Medicare reimbursement (Fullen, Lawson, & Sharma, in press-b). Therefore, additional work is needed to educate members of the counseling profession about the consequences of current Medicare mental health policy on clients from underserved populations. Fullen et al. (in press-a, in press-b) describe several strategies that can be used to strengthen advocacy efforts among members of the counseling profession, including counselor educators, master’s and doctoral students, and practicing counselors.
Limitations and Future Research
A primary limitation of this study relates to the generalizability of the results. This study reports on a specific and localized account of how Medicare mental health policy impacts Medicare beneficiaries’ access to counseling treatment in a single state. We intentionally focused on a homogenous sample purposefully selected to explore how LPCs are making sense of their inability to provide counseling services to Medicare beneficiaries based on their professional status as Medicare-ineligible. The findings present a narrative account of how these licensed mental health providers make sense of and respond to the experience of not being able to serve Medicare clients because of professional limitations contained within Medicare mental health policy. The utilization of IPA has allowed for the detection of nuance, subtlety, and complexity within the data from the semi-structured interviews with our participants. This specificity allows for an understanding that shows how the coverage gap created by the exclusion of counselors impacts Medicare beneficiaries’ access to counseling services.
An additional limitation of our study is the use of prolonged engagement as a strategy to establish credibility and trustworthiness. Prolonged engagement, traditionally employed in ethnography and
participant observation, requires that researchers spend sufficient time in the field to learn or understand the experiential phenomenon of the study (Lincoln & Guba, 1985). Though we did not spend time with participants within their specific practice settings, we each have practice experience as Medicare-ineligible providers within the field of professional counseling. In a more ethnographic study on the MMHCG, we would be able to employ a more traditional application of prolonged engagement.
Future research should focus on additional qualitative and quantitative data sets that allow for more generalizability of findings. By nature, Medicare policy is consistent across the United States, which leads us to believe that there are likely similarities between the phenomena described by our interviewees and what occurs in other states. Nonetheless, additional inquiry is needed to probe the impact of MMHCG more comprehensively. An empirical investigation into the perspectives of Medicare-insured individuals who have been unable to utilize their Medicare benefits because of the MMHCG may lend an additional lens toward understanding the impact of Medicare mental health policy on clients. Ultimately, this study and subsequent studies focusing on diminishing coverage gaps for Medicare beneficiaries can support progress toward diminishing health inequities because of health care policy restrictions.
Conclusion
This study highlights an existing gap in the administration of Medicare services for clients seeking counseling treatment for mental health conditions. By attending to the theme of ineffectual policy, we have attempted to illuminate how current policy impacts the Medicare-insured, as well as LPCs who are involved in their mental health care. Based on our analysis of the MMHCG, future revisions to Medicare policy allowing for the inclusion of LPCs to provide counseling treatment to Medicare-insured individuals may contribute to a more equitable health care system for Medicare beneficiaries.
Conflict of Interest and Funding Disclosure
This research was supported by the Virginia Tech
Institute for Society, Culture, and Environment.
References
American Psychological Association. (2015). Medicare’s shrinking psychologist reimbursement rates. Retrieved from https://www.apaservices.org/practice/advocacy/state/leadership/medicare-payment
Barrett, M. S., Chua, W.-J., Crits-Christoph, P., Gibbons, M. B., Casiano, D., & Thompson, D. (2008). Early withdrawal from mental health treatment: Implications for psychotherapy practice. Psychotherapy: Theory, Research, Practice, Training, 45, 247–267. doi:10.1037/0033-3204.45.2.247
Barry, C. A., Britten, N., Barber, N., Bradley, C., & Stevenson, F. (1999). Using reflexivity to optimize teamwork in qualitative research. Qualitative Health Research, 9, 26–44. doi:10.1177/104973299129121677
Bartels, S. J., & Naslund, J. A. (2013). The underside of the silver tsunami—Older adults and mental health care. The New England Journal of Medicine, 368, 493–496. doi:10.1056/NEJMp1211456
Center for Behavioral Health Statistics and Quality. (2018). 2017 National survey on drug use and health: Detailed tables. Rockville, MD: Substance Abuse and Mental Health Services Administration. Retrieved from
https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHDetailedTabs2017/NSDUHDeta
iledTabs2017.pdf
Center for Medicare Advocacy. (2013). Medicare and mental health. Retrieved from https://www.medicareadvoca
cy.org/medicare-and-mental-health
Centers for Medicare & Medicaid Services. (n.d.). Seniors & Medicare and Medicaid enrollees. Retrieved from
https://www.medicaid.gov/medicaid/eligibility/medicaid-enrollees/index.html
Centers for Medicare & Medicaid Services. (2019). Fiscal year 2019 inpatient psychiatric facility prospective payment system rates and adjustment factors. In Inpatient psychiatric facility prospective payment system (Addendum A). Retrieved from https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/Inpatient-Psychiatric-Facility-Prospective-Payment-System.pdf
Chapin, R. K., Sergeant, J. F., Landry, S., Leedahl, S. N., Rachlin, R., Koenig, T., & Graham, A. (2013). Reclaiming joy: Pilot evaluation of a mental health peer support program for older adults who receive Medicaid. The Gerontologist, 53, 345–352. doi:10.1093/geront/gns120
Christenson, J. D., & Crane, D. R. (2004). Estimating the cost of direct reimbursement of marriage and family therapy under Medicare. Journal of Marital and Family Therapy, 30, 515–525. doi:10.1111/j.1752-0606.2004.tb01259.x
Denzin, N. K. (Ed.). (1978). Sociological methods: A sourcebook. New York, NY: McGraw-Hill.
Donohue, J. (2006). Mental health in the Medicare Part D drug benefit: A new regulatory model? Health Affairs, 25, 707–719. doi:10.1377/hlthaff.25.3.707
Federal Interagency Forum on Aging-Related Statistics. (2016). Older Americans 2016: Key indicators of well-being. Washington, DC: U.S. Government Printing Office. Retrieved from https://agingstats.gov/docs/LatestReport/Older-Americans-2016-Key-Indicators-of-WellBeing.pdf
Field, T. A. (2017). Clinical mental health counseling: A 40-year retrospective. Journal of Mental Health Counseling, 39, 1–11. doi:10.17744/mehc.39.1.01
Fullen, M. C. (2016). Medicare advocacy for the counselor advocate. Adultspan Journal, 15, 3–12. doi:10.1002/adsp.12015
Fullen, M. C., Lawson, G., & Sharma, J. (in press-a). Analyzing the impact of the Medicare coverage gap on counseling professionals: Results of a national study. Journal of Counseling & Development.
Fullen, M. C., Lawson, G., & Sharma, J. (in press-b). Medicare reimbursement for counselors: Counseling professionals’ advocacy beliefs and behavior. Counselor Education and Supervision.
Goodman, J. M., Morgan, A. A., Hodgson, J. L., & Caldwell, B. E. (2018). From private practice to academia: Integrating social and political advocacy into every MFT identity. Journal of Marital and Family Therapy, 44, 32–45. doi:10.1111/jmft.12298
H.R. Rep. No. 101-386 (1989). Retrieved from https://www.congress.gov/bill/101st-congress/house-bill/3299
Institute of Medicine. (2012). The mental health and substance use workforce for older adults: In whose hands? Washington, DC: National Academies Press.
Kaiser Family Foundation. (2019). An overview of Medicare. Retrieved from https://www.kff.org/medicare/issue-brief/an-overview-of-medicare
Kim, G., Parton, J. M., DeCoster, J., Bryant, A. N., Ford, K. L., & Parmelee, P. A. (2013). Regional variation of racial disparities in mental health service use among older adults. The Gerontologist, 53, 618–626. doi:10.1093/geront/gns107
Larson, E. H., Patterson, D. G., Garberson, L. A., & Andrilla, C. H. A. (2016). Supply and distribution of the behavioral health workforce in rural America. Data Brief #160. Seattle, WA: WWAMI Rural Health Center, University of Washington.
Levitt, H. M., Creswell, J. W., Josselson, R., Bamberg, M., Frost, D. M., & Suárez-Orozco, C. (2018). Journal article reporting standards for qualitative primary, qualitative meta-analytic, and mixed methods research in psychology: The APA Publications and Communications Board task force report. American Psychologist, 73, 26–46. doi:10.1037/amp0000151
Lincoln, Y. S., & Guba, E. G. (1985). Naturalistic inquiry. Newbury Park, CA: SAGE.
Medicare Improvements for Patients and Providers Act of 2008, Pub. L. No. 110-275, 122 Stat. 2494 (2008).
Medicare Mental Health Workforce Coalition. (2019). Expanding the Medicare provider workforce: A solution to the behavioral health crisis. Retrieved from https://centerstone.org/wp-content/uploads/MHAIA-One-Pager-FINAL.pdf
Medicare Payment Advisory Commission. (2015). Chapter 2: The next generation of Medicare beneficiaries. In Report to the Congress: Medicare and the health care delivery system (pp. 35–57). Retrieved from http://www.medpac.gov/docs/default-source/reports/chapter-2-the-next-generation-of-medicare-beneficiaries-june-2015-report-.pdf?sfvrsn=0
Patton, M. Q. (1999). Enhancing the quality and credibility of qualitative analysis. HSR: Health Services Research, 34, 1189–1208.
Roseborough, D. J., Luptak, M., McLeod, J., & Bradshaw, W. (2012). Effectiveness of psychodynamic psychotherapy with older adults: A longitudinal study. Clinical Gerontologist, 36, 1–16.
Smalley, K. B., & Warren, J. C. (2012). The current state of rural mental health. In K. B. Smalley, J. C. Warren, & J. P. Rainer (Eds.), Rural mental health: Issues, policies, and best practices (pp. 3–16). New York, NY: Springer.
Smith, J. A., Flowers, P., & Larkin, M. (2009). Interpretative phenomenological analysis: Theory, method and research. Thousand Oaks, CA: SAGE.
Stewart, H., Jameson, J. P., & Curtin, L. (2015). The relationship between stigma and self-reported willingness to use mental health services among rural and urban older adults. Psychological Services, 12(2), 141–148. doi:10.1037/a0038651
Substance Abuse and Mental Health Services Administration. (2011). Treatment of depression in older adults evidence-based practices (EBP) kit. Retrieved from https://store.samhsa.gov/product/Treatment-of-Depression-in-Older-Adults-Evidence-Based-Practices-EBP-KIT/SMA11-4631CD-DVD
U.S. Congress. (2019a). H.R.945—Mental Health Access Improvement Act of 2019. Retrieved from https://www.congress.gov/bill/116th-congress/house-bill/945
U.S. Congress. (2019b). S.286—Mental Health Access Improvement Act of 2019. Retrieved from https://www.congress.gov/bill/116th-congress/senate-bill/286
U.S. Department of Health and Human Services, Health Resources and Services Administration. (2016). FORHP rural areas [Data file]. Retrieved from https://data.hrsa.gov/data/about#DataUsage
Wampold, B. E. (2015). How important are the common factors in psychotherapy? An update. World Psychiatry, 14, 270–277. doi:10.1002/wps.20238
Matthew C. Fullen is an assistant professor at Virginia Tech. Jonathan D. Wiley, NCC, is a doctoral candidate at Virginia Tech. Amy A. Morgan is a doctoral candidate at Virginia Tech. Correspondence can be addressed to Matthew Fullen, School of Education, College of Liberal Arts and Human Sciences, 1750 Kraft Drive, Suite 2000, Room 2005, Blacksburg, VA 24061, mfullen@vt.edu.
Jun 4, 2019 | Volume 9 - Issue 2
Diane M. Coll, Chandra F. Johnson, Chinwé U. Williams, Michael J. Halloran
A defining moment experience is a pinnacle moment or critical incident that occurs within a therapeutic context and contributes significantly to the professional development and personal growth of counselors. The aim of this qualitative study was to investigate how experienced counselors make sense and meaning of their defining moment experiences in terms of developing their clinical attributes. Semi-structured interviews were conducted with nine experienced professional counselors to investigate how defining moment experiences influenced their professional development. Five main themes were derived from analysis via interpretative phenomenological analysis (IPA): acceptance reality, finding a balance, enhanced self-reflection and awareness, reciprocal transformation, and assimilation and integration. These themes provide perspectives on how facilitating conversations and reflection on defining moment experiences may enhance professional development and clinical attributes among counselors.
Keywords: defining moment experiences, professional development, clinical attributes, qualitative study, interpretative phenomenological analysis
The defining moment experience is a contemporary term to describe a pinnacle moment or critical incident that occurs within a therapeutic context and contributes to professional development and the personal growth of professional counselors (Prengel & Somerstein, 2013; Veach & LeRoy, 2012). The defining moment experience typically occurs in the early stages of counselor development and is considered a rite of passage, often serving as a catalyst for significant growth (Furr & Carroll, 2003; Lee, Eppler, Kendal, & Latty, 2001; Skovholt, 2012; Skovholt & McCarthy, 1988). A negative defining moment experience might entail initial exposure to a difficult client, which may have a negative influence on counselor perceptions of clinical competency. In contrast, a positive defining moment experience could involve a novice counselor’s first experience of effectiveness or making a therapeutic breakthrough with a client (Skovholt, 2012). Whether positive or negative, defining moment experiences provide great potential for counselor self-reflection and growth on professional and personal levels (Howard, Inman, & Altman, 2006).
Defining moment experiences are more likely to occur and have greatest influence among novice and early-career counselors from a counselor developmental perspective (Lee et al., 2001). In theory, novice counselors face several stressors, such as performance anxiety, rigid emotional boundaries, an incomplete practitioner-self, glamorized expectations, and inadequate conceptual maps (Skovholt & Rønnestad, 2003). Defining moment experiences are likely to intensify these stressors and existing growing pains in terms of confidence and perceptions of identity within the counseling profession (Patterson & Levitt, 2011). Novice counselors also may find themselves deeply questioning their personal beliefs, biases, and assumptions, which can lead to some level of personal transformation or significant growth (Skovholt, 2012). Nevertheless, Furr and Carroll (2003) argued that the first defining moment experience carries the potential to accelerate counselor development regarding their behaviors (e.g., performance-based skills), cognitions (e.g., simple to complex), and emotions (e.g., feelings of inferiority or self-efficacy).
Several research studies have confirmed these propositions. Indeed, Bischoff, Barton, Thober, and Hawley (2002) reported that the initial counseling session with a client was a defining moment experience among early-career counselors having both a positive and negative influence on their self-efficacy. Similarly, Furr and Carroll (2003) reported direct client experience to be a defining moment in the development of counseling students, leading them to increased self-understanding and confidence as well as recognition of personal deficiencies. A qualitative study by Howard et al. (2006) also investigated defining moment experiences among practicum counseling students as they pertained to their overall professional growth. The findings suggested defining moment experiences influenced their professional identity, personal reactions, competence, supervision processes, and counseling philosophy.
Defining moment experiences also have been found to be important in the ongoing development of professional counselors (Rønnestad & Skovholt, 2003). In their study over 30 years ago, Skovholt and McCarthy (1988) asked 58 mental health professionals with varying degrees of experience and credentials to submit narrative accounts of their own defining moment experiences. Common themes developed from the narratives included feelings of insecurity, learning to accept imperfections and limitations, transforming the experience into a specialty, the attitude of readiness to learn and grow from the experience, and dealing with unexpected events such as the suicide of a client. More recently, Veach and LeRoy (2012) reported several common themes in the defining moment essays of 37 professional counselors, including increased empathy, authenticity, honesty, self-awareness, resilience, compassion, connection, courage, and commitment. Two other publications (Prengel & Somerstein, 2013; Trotter-Mathison, Koch, Sanger, & Skovholt, 2010) have similarly used personal narratives of professional counselors to illustrate the significance of defining moment experiences in the ongoing development of counselors.
Theories of counselor development maintain that the process of growth and change continues throughout the career lifespan of counseling professionals, but may nonetheless entail different challenges at distinct stages of counselor development (Moss, Gibson, & Dollarhide, 2014; Skovholt & Rønnestad, 2003; Zahm, Veach, Martyr, & LeRoy, 2016). For novice counselors, defining moment experiences are likely to intensify pre-existing stressors and provide a significant opportunity for professional development (Skovholt & Rønnestad, 2003). In contrast, experienced counselors are more likely to be able to reflect and process the latent meanings of defining moment experiences for their own ongoing professional growth and development (Moss et al., 2014), making them a valuable resource for understanding the developmental effects of defining moment experiences. Yet there is little systematic research on how defining moment experiences contribute to the practice of experienced professional counselors. This study addressed this shortfall in the research literature by focusing on the following research question: How do experienced counselors make sense and meaning of their defining moment experiences with respect to their professional development and practice?
Method
A qualitative research design was employed in this study and incorporated interpretative phenomenological analysis (IPA) of the defining moment experiences of professional counselors (Smith, 2004; Smith & Osborn, 2008). The IPA approach was considered a suitable methodology to reveal the complex issues associated with the defining moment experiences of counseling professionals, as it enables a rich level of data collection and interpretation by studying people ideographically (Pietkiewicz & Smith, 2012). Semi-structured interviews were employed to collect data by providing participants the opportunity to discuss their defining moment experiences and give voice to their thoughts, beliefs, and attitudes formed as a result of the experience.
Research Team
The research team consisted of the first author, a research assistant, and an external auditor. None of the research team were in a dependent relationship or received monetary compensation for their work, and only the first author was significantly connected to the topic of defining moment experiences. The first author and principal investigator (PI) holds a doctorate in counselor education and supervision and is a licensed professional counselor with over 20 years’ experience. The external auditor is a doctorate-level clinician with over 20 years’ experience, significant knowledge of IPA methods, and no vested interest in the study. The research assistant (RA) is a retired English professor who has familiarity with and understanding of qualitative data analysis. The RA was intentionally selected to provide independent data analysis, as she had no counseling background.
Participants
The study consisted of a purposive sample of nine experienced professional counselors who met the following inclusion criteria: (a) have a minimum of 10 years’ professional counseling experience, (b) be an active licensed professional counselor, and (c) experienced a defining moment in the role of counselor and expressed willingness to share related thoughts, feelings, and attitudes. Participant demographics are displayed in Table 1 with respect to the pseudonym each counselor selected for the study, along with a description of their defining moment experience and their varied backgrounds in terms of gender, age, race, experience, and the nature of their reported defining moment experiences.
Procedure
University IRB approval to conduct the study was received. An invitation to participate in a semi-structured interview on the defining moment experiences of professional counselors was advertised on the state therapist listserv as well as other established mental health agencies and professional counseling listservs limited to the southeast region of the United States. Participants also were recruited via the snowball method by initial contacts for referrals or recommendations for potential interview subjects.
Participants received a paper copy of the informed consent for review and signature prior to the start of each scheduled interview wherein participants were provided with a definition of defining moment experiences. Each participant chose a pseudonym in order to maintain confidentiality and, in accordance with Standard G.2.f. of the American Counseling Association (ACA) Code of Ethics (2014), the location, time, and format (by phone or in-person) of the interview honored each participant’s schedule and preferences. Moreover, interviews were conducted in a private space to maintain confidentiality and be free from distractions. Each interview was audio-recorded using a digital voice recorder and lasted between 60 and 90 minutes. Two interviews were conducted in person, and seven interviews were conducted over the telephone.
Prior to their interview, participants completed a brief demographic questionnaire. Each interview consisted of 12 open-ended questions (see Table 2), with the five main questions being: (1) Tell me about a defining moment that occurred while working with a client(s). (2) How did this experience shape how you saw yourself as a professional counselor? (3) How did this experience shape your sense of clinical competency? (4) How did you regard the therapeutic relationship between client and counselor prior to your defining moment experience? (5) As you reflect on your defining moment experience, how has your perspective changed or not changed? Sub-questions also were asked to illicit the meaning and sense attributed to defining moment experiences. Each interview question was presented in the same order with each participant for consistency (Creswell, 2007). Follow-up impromptu questions were asked in between the established questions to obtain richer, more elaborate details or context, as needed. Each interview progressed at a pace that was set by the participant, allowing for the development of more elaborate data with each question (Hays & Singh, 2012).
Table 1
Participant Demographics and Defining Moment Experience
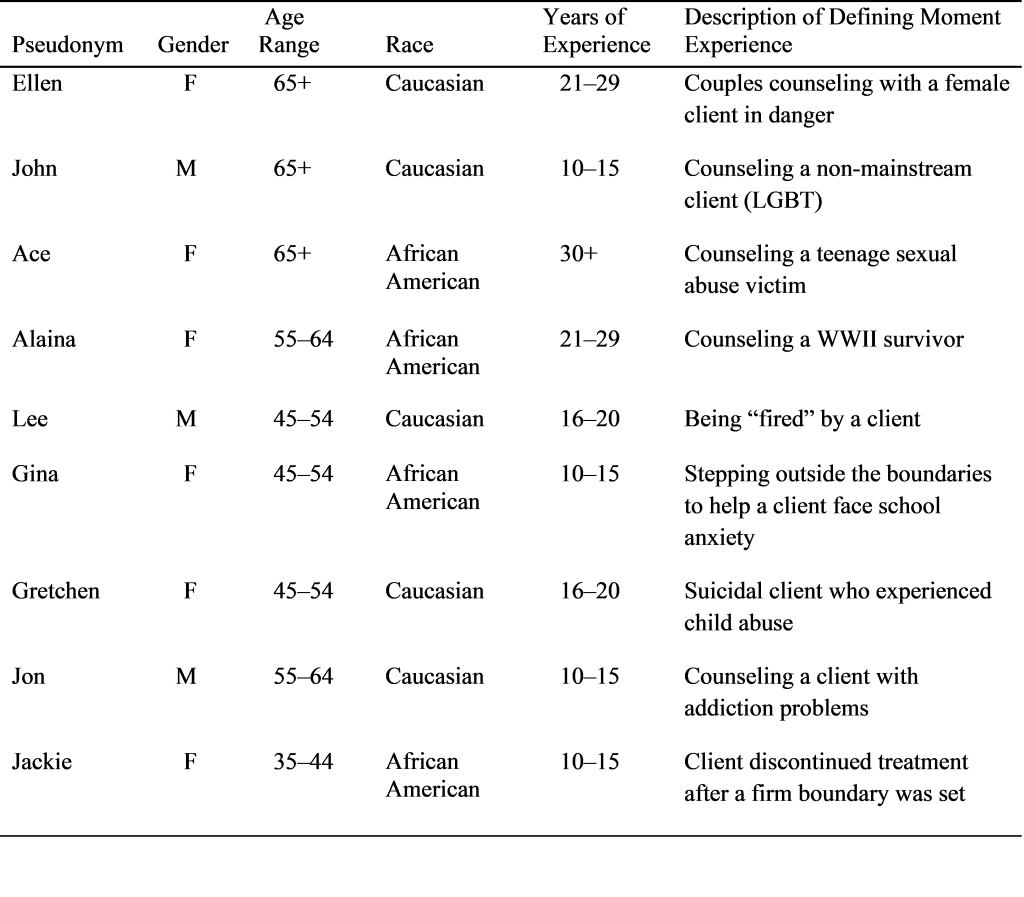
A range of procedural steps were taken to enhance the credibility, dependability, confirmability, and transferability of the data (Lincoln & Guba, 1985) and to counter any potential researcher biases (Morrow, 2005). To establish the credibility of the findings, descriptive field notes were taken during interviews to document observations and add context to the audio data. The field notes emphasized participant content, expressed meaning and PI observations (Creswell, 2007), and provided a means to confirm interpretations of interview data through data triangulation (Anney, 2014). Member checking was used to enhance the credibility of the findings (see Onwuegbuzie & Leech, 2005) by asking participants to check summaries of the interview content. Confirmability of findings entailed the use of analytic memos and a reflexivity journal to ensure objectivity in any interpretations made in the course of data analysis (Smith, Flowers, & Larkin, 2009). Analytic memos were written throughout data analysis to record thoughts about the meaning behind participants’ words (Saldaña, 2009). A reflexivity journal was employed to assist the PI with preparing to interview each participant and enter their subjective reality by writing about her own defining moment experiences as a counselor prior to interviews (Hays & Singh, 2012). Moreover, the PI maintained the reflexivity journal throughout the interviews and data analysis processes. The PI made a consistent effort to bracket assumptions and biases to not superimpose her own experiences or subjective interpretations as a professional counselor (Smith, 2004; Smith & Osborn, 2008). The transferability of research findings was met by purposive sampling of participants based on their capacity to provide relevant knowledge on defining moment experiences (Anney, 2014). The criteria of ensuring dependability was met by employing the Dedoose qualitative research software program (Moylan, Derr, & Lindhorst, 2015) to independently organize, archive, and code interview data and field notes, as well as validate codes and themes derived from interview data (Silver & Lewins, 2014). The dependability of the data was enhanced by having the external auditor confirm the accuracy of (1) interview transcripts, (2) descriptive field notes, (3) the reflexive journal, (4) the theme codebook, and (5) Dedoose summaries and output.
Table 2
Interview Questions for the Study
| Question No. |
Question content |
| 1 |
Tell me about a defining moment that occurred while working with a client(s). This moment could have occurred in the early stages of counselor training or at a later time in your work as a counselor. |
| 1a |
• What made it a defining moment? |
| 1b |
• Do you have a takeaway from this moment? |
| 1c |
• Is there anything else you would like to share about this experience? |
| 2 |
How did this experience shape how you saw yourself as a professional counselor? As a person? |
| 2a |
• What did this experience mean to you as a counselor? |
| 2b |
• What did this experience mean to you on a personal level? |
| 2c |
• What assisted you with making sense out of this experience? |
| 3 |
How did this experience shape your sense of clinical competency? |
| 3a |
• What strengths did you become aware of? |
| 3b |
• What weaknesses or limitations did you become aware of? |
| 4 |
How did you regard the therapeutic relationship between client and counselor prior to your defining moment experience? |
| 4a |
• How did your understanding of the therapeutic relationship change or not change after the
defining moment experience? |
| 4b |
• How would you describe the therapeutic relationship between client and counselor as if you
were describing this to a layperson/non-clinician? |
| 5 |
As you reflect on your defining moment experience, how has your perspective changed or not changed? |
| 5a |
• How did you make sense of the experience then? |
| 5b |
• How do you make sense of the experience now? |
Data Analysis
Data analysis followed a 3-stage process as outlined by Pietkiewicz and Smith (2012): immersion, transformation, and connection. The immersion process began with the PI listening to each interview after its conclusion in order to review the content and record any additional observations in the field notes (Smith & Osborn, 2008). Each interview was transcribed by an independent contractor and the PI reviewed each along with the digital recording to ensure accuracy and facilitate deeper immersion in the data (Pietkiewicz & Smith, 2012). The PI read the participant’s responses along with the recording during the review process to foster deeper immersion and understanding of the experience being shared (Bailey, 2008). The PI documented new observations and insights throughout the immersion process in field notes and via a reflexivity journal (Pietkiewicz & Smith, 2012). The RA also independently engaged in the immersion, transformation, and connection stages with the interview transcripts.
The PI and the RA worked together to review and interpret all their notes about the transcripts and transform them into emergent themes consistent with IPA methodology (Smith & Osborn, 2008). Emergent themes were then connected together according to conceptual similarities to develop a thematic hierarchy (Pietkiewicz & Smith, 2012). The final stage of analysis entailed a narrative account of each theme, including direct passages from the interviews. The PI and the RA also discussed and compared several levels of interpretation of interview content and of interpreted meanings to reach agreement on the final set of distinct themes. Moreover, the transcripts, notes, and themes were submitted to the external auditor, who conducted an independent cross-analysis to ensure their accuracy and clarity.
Results
Data analysis with IPA methods resulted in five themes being identified and labeled based on the meanings associated with professional counselors’ defining moment experiences (see Table 3). The first theme was labeled acceptance of reality and captures how defining moment experiences led professional counselors to the realization that counselors are not always a good match for a client and cannot fully resolve any clinical problem that comes their way. The second theme, finding a balance, addresses how defining moment experiences shaped perceptions of clinical boundaries and the balance between strengths and limitations and external and internal forces. The third theme to be derived from the analysis, enhanced self-reflection and awareness, captures professional counselors’ understanding that defining moment experiences facilitated their own reflection and questioning of their intrapersonal and interpersonal processes. The fourth theme, reciprocal transformation, illustrates how the experiences shaped professional counselors’ understanding of the therapeutic relationship and acted as a mutual change agent for both counselor and client. Lastly, the fifth theme, assimilation and integration, encapsulates how meanings attached to defining moment experiences changed and were incorporated over time.
Table 3
IPA Coding Scheme of the Meaning of Defining Moment Experiences of Professional Counselors
| Theme |
Description |
| Acceptance of reality |
Coming to terms with the realistic, sometimes limiting, aspects of the counselor role |
| Finding a balance |
Perceptions of clinical boundaries and the balance between strengths and limitations and external and internal forces |
| Enhanced self-reflection and awareness |
Facilitated reflection and questioning of intrapersonal and interpersonal processes |
| Reciprocal transformation |
Mutual change agent for both counselor and client |
| Assimilation and integration |
How meanings attached to defining moment experiences changed and were incorporated over time |
Theme 1: Acceptance of Reality
Experienced counselors made meaning of their defining moment experiences in the theme of acceptance of reality. This theme was derived to reflect participants’ thoughts about how their defining moment experience helped them come to terms with the realistic, sometimes limiting, aspects of the counselor role. Specifically, defining moment experiences were understood by counselors to help dispel the myth that counselors are a good match for any client and can “fix” and fully resolve any clinical problem that comes their way. According to Ellen, “some situations are beyond repair. If people wait too long to come to see us, we can’t help, and they can’t even make any changes for themselves.” For Jackie, the defining moment experience meant being comfortable with accepting the reality of the limiting aspects of the counselor role when a client didn’t want to change and wanted Jackie to do all the work. She reflected: “In that moment, I just remembered saying . . . you can’t help everybody. It just means I’m not a good fit (for everybody) and that’s okay.” Similarly, the defining moment experience of Alaina meant accepting the reality that “a client I cannot love is not right for me . . . I don’t agree celebrating [the fact of] working with someone you don’t have a connection with.” It also would appear from these defining moment reflections that the acceptance of reality was associated with deeper knowledge of counselor–client boundary conditions. Indeed, counselor–client boundary issues were a significant factor in the defining moments theme of finding a balance.
Theme 2: Finding a Balance
The theme of finding a balance was identified in participants’ understanding of their defining moment experiences as highlighting different therapeutic boundary conditions and balancing the fine line between internal or external limitations while gaining a sense of finesse and agility between opposing forces. Here, participants identified a dual connection between strengths and limitations, while expressing accountability for establishing a balance between the two factors for client benefit. By taking ownership of a specific personality trait as part of the defining moment experience, Lee came to understand the importance of balance and the potential for possible pitfalls if such a balance is not obtained: “It was my personal disposition to speak with conviction, which is both a strength and limitation. I am still this way of course, but I know when to scale it back—to strike that balance.”
Finding a balance through defining moment experiences was evident in participants sharing their experiences of entering uncharted or unfamiliar territories with some trepidation, only to find their own rhythm through setting boundaries. Alaina shared: “I understood I was really flying by the seat of my pants and the only thing I had that I really understood were my boundaries. It made my boundaries even stronger. They were very heart-wrenching limitations; it was very hard.” Moreover, Ellen conveyed how the defining moment experience highlighted the process of balancing between her own feelings of physical vulnerability and her inner strengths when she was working with a couple in an abusive relationship: “I needed to sit alone with him to keep her safe. It was like walking into the lion’s den; however, my use of self-intuition [and] wisdom was a strength. I was just going to tap dance with him when I saw him.”
Theme 3: Enhanced Self-Reflection and Awareness
Professional counselors understood their defining moment experiences as ones that especially facilitated self-reflection and awareness of intrapersonal and interpersonal processes. At the intrapersonal level, John highlighted how the defining moment experience “increased my awareness and clarity of my own internal processes.” At the interpersonal level, Lee shared: “I made a connection in my personal relationships where I’ve learned to create space for others.” The theme of self-reflection also was manifest in the level of self-questioning prompted by the defining moment experiences of professional counselors. Indeed, Jackie discussed how her defining moment experience led to “a lot of reflection; I started to question my passion and why I wanted to be a therapist.” Similarly, Gina reflected that “I was puzzled and confused; lots of self-doubt [and] reflection. I remember where I would question whether I was a good therapist.” Importantly, the self-reflection and awareness prompted by the defining moment experiences of professional counselors appeared to have confirmed their professional capacities, with Gretchen sharing: “I received affirmation of what I thought I knew—what my gut was telling me.”
Theme 4: Reciprocal Transformation
Professional counselors understood their defining moment experiences as entailing the theme of reciprocal transformation through shared vulnerability and trust. This theme was derived from counselors speaking to their awareness of the dynamic of change within the therapeutic relationship; defining moment experiences generated a broader understanding of the transformative power within the therapeutic bond. For example, Lee shared: “You know, it’s a two-way conversation. This guy came back, taught me a great lesson: just how sacred and fragile the bond can be. I think we both changed after that experience.” Reciprocal transformation was reflected in participants discussing how defining moment experiences were associated with shared feelings of vulnerability and healing. As stated by Ellen, “We work with vulnerable people and if we just pretend we’re not there’s no authentic connection. The relationship is the primary vehicle for healing. Vulnerability is a good thing as a therapist.”
Jackie discussed how her defining moment experience highlighted the importance of disclosure in transforming the therapeutic relationship into one of mutual trust: “You are both engaging in some sense of disclosure and that helps people to build trust. It’s ever-growing, it’s always changing. The relationship can change and grow as the two of you grow and change.” In a similar way, Jon’s understanding of his defining moment experience highlighted the importance of taking risks to transform the therapeutic relationship: “You are risking the possibility that something will happen so then emotionally they won’t go on with you. You need to be willing to clear the air and move forward. I think that’s the place where the relationship deepens.”
Theme 5: Assimilation and Integration
The final theme, assimilation and integration, represents the difference in meaning between how the defining moment experience was initially assimilated by professional counselors and how meanings gleaned from the experience continue to be integrated. Participants discussed the non-static nature of the meanings attached to their defining moment experiences. The meanings continue to be assimilated with time and experience and remain an integral part of their ongoing counselor development. For example, Jackie stated: “I needed to grow as a therapist. Now, I look at the experience differently. It really has evolved into knowing my limitations [and] my strengths.” For Alaina, “the meanings acquired more textures, they got better and continue with me today.” Similarly, Lee used the metaphor of winding a ball of yarn to explain the meaning associated with integrating her defining moment experience over time: “Then, it taught me more about the client. Now, it informs me more. It’s like a ball of yarn. As I acquired experience, there was more yarn to wind. It now informs me how to be with all clients.”
For John, processing the defining moment experience meant he went from a place of anxiety to becoming aware of the spiritual nature of counseling: “At first, the experience relieved some anxiety about whether I was able to do this work. What I appreciate now, that I was too anxious to be aware of at the time, is that this is spiritual work.” Finally, Ace integrated her defining experience of working with a victim of teenage sexual abuse by now conducting advocacy work: “What assisted me with making sense out of my experience was volunteering for child abuse agencies, serving on a board, [and] being an advocate.” Overall, each participant constructed meaningful interpretations of their defining moment experiences that continue to inform their work and passion as counseling professionals, whether as a source of inspiration or affirmation.
Discussion
From novice to seasoned professionals, challenges occur within the therapeutic relationship that can provide growth opportunities to counseling practitioners to develop their clinical attributes (Orlinsky & Rønnestad, 2005; Skovholt & Rønnestad, 2003). The findings from this study support and extend the idea that defining moment experiences represent one such challenge. Professional counselors in this study understood their defining moment experiences as growth opportunities associated with different meanings to their professional practice and clinical skills. The meanings of the defining moment experiences of professional counselors were interpreted to reflect five main themes relevant to counseling practice: acceptance of reality, finding a balance, enhanced self-reflection and awareness, reciprocal transformation, and assimilation and integration.
Professional counselors understood their defining moment experience as one that was a wake-up call to accept the reality that counselors are not ideal for all clients and all presenting problems. This finding supports theory and research that an idealistic and glamorized view of counseling is often a source of stress among developing counselors (Moss et al., 2014; Skovholt & Rønnestad, 2003), wherein supervisors play an important role in guiding novice counselors toward the realistic position that it is not always possible to have a positive impact with clients. Indeed, the findings of this study provide distinct evidence that defining moment experiences of professional counselors bring them to a point in their career when they come to accept that the counselor role may produce limited success with certain clients on different occasions. As suggested by Skovholt and Rønnestad (2003) and the findings of this study, acceptance of reality is paradoxical in a helping profession like counseling; growth as a counselor occurs with the realization that some people and problems cannot be helped. This change of view also meant that the acceptance of reality was associated with deeper knowledge of counselor–client boundary conditions.
The meanings of professional counselors’ defining moment experiences were reflected in the specific theme of finding a balance in terms of participants navigating the boundaries between their strengths and limitations. Previous counselor development research (e.g., Furr & Carroll, 2003; Moss et al., 2014; Trotter-Mathison et al., 2010) has shown that establishing client–counselor boundaries is an important challenge to novice counselors, usually meant in terms of establishing emotional boundaries. To the counselors in this study, establishing such boundaries was about finding the right balance. Nevertheless, the meanings associated with the defining moment experiences of professional counselors extended beyond client–counselor boundaries to include balance between one’s own strengths and weaknesses, internal and external limitations, and finding a rhythm in uncharted or unfamiliar territories. It also was apparent that the participants’ ability for self-reflection and awareness was important for facilitating balance.
Experienced counselors also understood their defining moment experiences to entail enhanced self-reflection and awareness. Indeed, their willingness to self-reflect and take ownership for finding an optimal balance between strengths and limitations that were revealed through defining moment experiences has been clarified elsewhere as an important developmental step toward increased counseling competency (e.g., Skovholt & Rønnestad, 2003; Thériault & Gazzola, 2010; Williams, Hayes, & Fauth, 2008). As identified by Moss et al. (2014), continuous reflection is required for optimal learning. Defining moment experiences for professional counselors meant self-reflection even to the point of questioning their suitability for the profession. Indeed, the best counselors are generally viewed as questioning what they do and why (Kottler, 2017). It would appear from the findings that defining moment experiences appear to bring that level of self-questioning into focus.
The findings also revealed the change-agent quality of defining moment experiences wherein the experiences of counselors led to the development of a broader understanding of the reciprocal and transformative power within the therapeutic bond. In line with previous research (e.g., Orlinsky, Botermans, & Rønnestad, 2001; Skovholt & Rønnestad, 2003), the findings clarified that learning within the counselor–client relationship was a significant influence on career development among experienced counselors. Moreover, reciprocal transformation was reflected in professional counselors acknowledging shared vulnerability within the counselor–client relationship. Other research (e.g., Trotter-Mathison et al., 2010) has similarly found the most powerful defining moments occurred when counselors took risks or a leap of faith and allowed themselves to be vulnerable. Indeed, the defining moment experiences of the professional counselors in this study were reported as opportunities to experience the transformative power of shared vulnerability to establish new learning and growth in both counselor and client alike.
Within the theme of assimilation and integration, professional counselors shared how meanings of their defining moments continue to be a solid foundation of inspiration for their purpose, passion, and advocacy work in the counseling profession. Siegel (2007) referred to this process as the power of recall and repetition, whereby as counselors self-reflect on definitive experiences, the repetition of each memory forges deeper, more meaningful connections in the brain. Whether counselors engage in self-reflection in present time or as retrospection, the repetition of recall begins to move newly acquired data from state to trait, thus furthering the integration of new information or insights (Siegel, 2007). This view is supported in Prengel and Somerstein’s (2013) study of defining moment experiences, which highlights the process of self-reflection as one that requires time and re-examination in order to deepen lessons learned. In kind, the findings of this study suggest it is beneficial for counselors to engage in self-reflective practices throughout their professional life; the practice of self-reflection appears to have facilitated deeper integration of originally assimilated meanings of defining moment experiences by professional counselors. Consistent with the view of Engels, Barrio Minton, and Ray (2009), assimilation and integration of significant meanings appeared to have a positive effect on the competencies of professional counselors in this study.
Altogether, interpretive analysis of the defining moment experiences of professional counselors suggested a set of interrelated meanings and themes that appear to facilitate the development of counselor capacities. Defining moment experiences appear to bring into sharp focus an important transition in counselor thinking—acceptance of the realistic nature of counseling in terms of the sometimes lack of counselor–client-problem fit. In a related way, defining moment experiences of professional counselors facilitated deeper thinking about finding balance in professional practice. Professional counselors reported deeper thinking in the form of heightened self-reflection and self-awareness as meanings they associated with defining moment experiences. One may posit that heightened self-reflection and awareness mediates the relationship between defining moment experiences and acceptance of reality and finding balance in professional counseling. Defining moment experiences of professional counselors also held significant meaning because they highlighted the reciprocal and transformative power within the therapeutic bond and because the meanings continue to be integrated. As shared by Jackie, “This was a great opportunity to reflect on where I was and who I’ve become . . . all with the same lesson from my first client . . . that thread continues to inform me.”
Implications for Counselor Practice
The significance of defining moment experiences to professional counselors raises implications for professional practice and the counselor development process. As suggested by themes identified in the findings of this study, experienced professional counselors appeared to find defining moment experiences helped them accept counseling realities, find balance within the counselor role, and understand the transformative power within the therapeutic bond. At the same time, defining moment experiences facilitated heightened self-awareness, providing professional counselors an opportunity to attune to their own internal processes. As such, the meanings associated with defining moment experiences tie in with standards set forth by the Council for Accreditation of Counseling and Related Educational Programs (2015), which aligns professional competence with counselor self-awareness via self-reflection. Facilitating conversations and reflecting on defining moment experiences may provide a focal point for continuing training of professional counselors consistent with the mission of ACA (2019). The findings of this study underline the potential benefits of practicing and modeling self-reflection throughout the careers of professional counselors, supervisors, and counselor mentors to enhance their ongoing development and clinical expertise.
At the same time, counselor training programs may incorporate the meanings of defining moment experiences into their courses. Indeed, some participants in this study reported on a defining moment experience that occurred as a counselor trainee, and previous research has revealed practicum and novice counselors find great benefit from reflecting on defining experiences when they worked with a challenging client or issue (e.g., Bischoff et al., 2002; Furr & Carroll, 2003; Howard et al., 2006). Providers of counselor education programs and supervisors could develop awareness of the potential for defining moment experiences to raise questions about the realities of counseling, finding a balance in the counselor role, and the transformative power of the therapeutic relationship. This may be facilitated by encouraging novice counselors to employ self-reflection techniques such as journaling, which has been shown in previous research to benefit counselor development (e.g., Burnett & Meacham, 2002). Novice counselors could be asked to self-reflect on a defining moment experience via journaling as a part of their practicum and internship programs and use supervision sessions to connect the meaning and significance of the experience to the development of clinical skills and attributes. The findings of this study provide some insights on what type of meanings may be discussed in such sessions, including how defining moment experiences may relate to acceptance of counseling realities, finding a balance within the counselor role, and understanding the transformative power within the therapeutic bond.
Limitations and Future Research
There are limitations inherent in this study that require acknowledgement. The sample of participants might have invoked a self-selection bias wherein participants who elected to take part in the study may have been more inclined to value and reflect on their defining moment experiences than those who did not elect to participate. The use of semi-structured interviews, whether conducted in person or by phone, could have increased the likelihood of response inhibition (Bischoff et al., 2002). The interview participants could have answered interview questions according to perceived socially desirable responses rather than provide a more accurate and honest account of thoughts and feelings associated with their defining moment experiences. Steps to ensure confidentiality, such as the use of pseudonyms for participants, may have minimized response bias; however, to what degree is uncertain. In addition, the sample of participants was limited to professional counselors who worked in private practice with an expertise in trauma. A final limitation of the study is the potential for researcher subjectivity to influence data collection (interviews) and interpretive analysis (thematic coding). Nevertheless, appropriate methodological steps were taken in this study, such as a reflexivity journal and independent coders, to enhance the objectivity and trustworthiness of the data collection and interpretation procedures and outcomes.
The research findings provide directions for future research on defining moment experiences of professional counselors. To date, there is very little empirical research on defining moment experiences and their significance to professional counselors. Whereas this study provides a unique contribution to the counselor literature, future research may broaden the sample criteria to include not only experienced professionals in other regions of the United States and in other countries, but also licensed clinical social workers, licensed marriage and family therapists, and clinical psychologists. Research with a range of professionals would broaden knowledge about the significance of defining moment experiences to their ongoing professional practice. Moreover, research that broadens the focus on counselors to include an investigation of the role of supervisors in defining moment experiences would be worthwhile. Finally, research may follow up on the revelation from two participants in this study that defining moment experiences led them to question their suitability for the counseling profession. Research on the defining moment experiences of individuals who chose to leave the field may shed light upon the goodness-of-counselor-fit within the counseling profession.
Conclusion
In conclusion, findings from this study support and contribute to the professional counseling literature by revealing the meanings associated with the defining moment experiences of professional counselors. Consistent with models of counselor development (e.g., Moss et al., 2014), experienced counselors showed a comparatively strong capacity to deeply reflect and process the latent meanings and implications of defining moment experiences for their ongoing professional growth and development. Defining moment experiences appear to help professional counselors accept the realities of counseling, find a balance within the counselor role, and understand the transformative power within the therapeutic bond. The findings contribute to existing literature by illustrating how meaningful interpretations of defining moment experiences continue to deepen over time and enhance counselor practice, especially when opportunities are taken for self-reflection. Application of knowledge on the significance, meaning, and implications of defining moment experiences in counselor training programs and supervision sessions provides an opportunity for enhancing the clinical attributes of professional counselors.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
American Counseling Association. (2014). Code of ethics. Alexandria, VA: Author.
American Counseling Association. (2019). Continuing education. Retrieved from https://www.counseling.org /continuing-education
Anney, V. N. (2014). Ensuring the quality of the findings of qualitative research: Looking at trustworthiness criteria. Journal of Emerging Trends in Educational Research and Policy Studies, 5, 272–281.
Bailey, J. (2008). First steps in qualitative data analysis: Transcribing. Family Practice, 25(2), 127–131. doi:10.1093/fampra/cmn003
Bischoff, R. J., Barton, M., Thober, J., & Hawley, R. (2002). Events and experiences impacting the development of clinical self confidence: A study of the first year of clinical contact. Journal of Marital and Family Therapy, 28, 371–382. doi:10.1111/j.1752-0606.2002.tb01193.x
Burnett, P. C., & Meacham, D. (2002). Learning journals as a counseling strategy. Journal of Counseling & Development, 80, 410–415. doi:10.1002/j.1556-6678.2002.tb00207.x
Council for Accreditation of Counseling and Related Educational Programs. (2015). 2016 CACREP standards. Retrieved from https://www.cacrep.org/for-programs/2016-cacrep-standards
Creswell, J. W. (2007). Qualitative inquiry and research design. London, UK: SAGE.
Engels, D. W., Barrio Minton, C. A., & Ray, D. C. (2009). The professional counselor: Portfolio, competencies, guidelines, and assessments. Alexandria, VA: American Counseling Association.
Furr, S. R., & Carroll, J. J. (2003). Critical incidents in student counselor development. Journal of Counseling & Development, 81, 483–489. Hays, D. G., & Singh, A. A. (2012). Qualitative inquiry in clinical and educational settings. New York, NY: Guilford Press.
Howard, E. E., Inman, A. G., & Altman, A. N. (2006). Critical incidents among novice counselors in training. Counselor Education and Supervision, 46(2), 88–102. doi:10.1002/j.1556-6978.2006.tb00015.x
Kottler, J. A. (2017). On being a therapist (5th ed). New York, NY: Oxford University Press.
Lee, R. E., Eppler, C., Kendal, N., & Latty, C. (2001). Critical incidents in the professional lives of first year MFT students. Contemporary Family Therapy, 23, 51–61. doi:10.1023/A:1007872132292
Lincoln, Y. S., & Guba, E. G. (1985). Naturalistic inquiry. Newbury Park, CA: SAGE.
Morrow, S. L. (2005). Quality and trustworthiness in qualitative research in counseling psychology. Journal of Counseling Psychology, 52, 250–260. doi:10.1037/0022-0167.52.2.250
Moss, J. M., Gibson, D. M., & Dollarhide, C. T. (2014). Professional identity development: A grounded theory of transformational tasks of counselors. Journal of Counseling & Development, 92, 3–12.
doi:10.1002/j.1556-6678.2003.tb00275.x
Moylan, C. A., Derr, A. S., & Lindhorst, T. (2015). Increasingly mobile: How new technologies can enhance qualitative research. Qualitative Social Work, 14, 36–47. doi:10.1177/1473325013516988
Onwuegbuzie, A. J., & Leech, N. L. (2005). On becoming a pragmatic researcher: The importance of combining quantitative and qualitative research methodologies. International Journal of Social Research Methodology, 8, 375–387. doi:10.1080/13645570500402447
Orlinsky, D. E., Botermans, J.-F., & Rønnestad, M. H. (2001). Towards an empirically grounded model of psychotherapy training: Four thousand therapists rate influences on their development. Australian Psychologist, 36(2), 139–148. doi:10.1080/00050060108259646
Orlinsky, D. E., & Rønnestad, M. H. (2005). How psychotherapists develop: A study of therapeutic work and professional growth. Washington, DC: American Psychological Association.
Patterson, C. A., & Levitt, D. H. (2011). Student counselor development during the first year: A qualitative study. The Journal of Counselor Preparation and Supervision, 3(2), 6–19.
Pietkiewicz, I., & Smith, J. A. (2012). A practical guide to using interpretative phenomenological analysis in qualitative research psychology. Czasopismo Psychologiczne Psychological Journal, 18, 361–369. doi:10.14691/CPPJ.20.1.7
Prengel, S., & Somerstein, L. (2013). Defining moments for therapists. New York, NY: LifeSherpa.
Rønnestad, M. H., & Skovholt, T. M. (2003). The journey of the counselor and therapist: Research findings and perspectives in professional development. Journal of Career Development, 30, 5–44. doi:10.1177/089484530303000102
Saldaña, J. (2009). The coding manual for qualitative researchers (1st ed.). London, UK: SAGE.
Siegel, D. J. (2007). Mindfulness training and neural integration: Differentiation of distinct streams of awareness and the cultivation of well-being. Social, Cognitive, and Affective Neuroscience, 2, 259–263. doi:10.1093/scan/nsm034
Silver, C., & Lewins, A. (2014). Using software in qualitative research (2nd ed.). Los Angeles, CA: SAGE.
Skovholt, T. M. (2012). Becoming a therapist: On the path to mastery. New York, NY: Wiley & Sons.
Skovholt, T. M., & McCarthy, P. R. (1988). Critical incidents: Catalysts for counselor development. Journal of Counseling & Development, 67(2), 69–72. doi:10.1002/j.1556-6676.1988.tb02016.x
Skovholt, T. M., & Rønnestad, M. H. (2003). Struggles of the novice counselor and therapist. Journal of Career Development, 30, 45–58. doi:10.1023/A:1025125624919
Smith, J. A. (2004). Reflecting on the development of interpretative phenomenological analysis and its contribution to qualitative research in psychology. Qualitative Research in Psychology, 1, 39–54. doi:10.1191/1478088704qp004oa
Smith, J. A., Flowers, P., & Larkin, M. (2009). Interpretative phenomenological analysis: Theory, method and research. London, UK: SAGE.
Smith, J. A., & Osborn, M. (2008). Interpretative phenomenological analysis. In J. A. Smith (Ed.), Qualitative psychology: A practical guide to research methods (pp. 53–80). London, UK: SAGE.
Thériault, A., & Gazzola, N. (2010). Therapist feelings of incompetence and suboptimal processes in psychotherapy. Journal of Contemporary Psychotherapy, 40, 233–243. doi:10.1007/s10879-010-9147-z
Trotter-Mathison, M., Koch, J. M., Sanger, S., & Skovholt, T. M. (2010). Voices from the field: Defining moments in therapist and counselor development. New York, NY: Routledge.
Veach, P. M., & LeRoy, B. S. (2012). Defining moments in genetic counselor professional development: One decade later. Journal of Genetic Counseling, 21, 162–166. doi:10.1007/s10897-011-9427-0
Williams, E. N., Hayes, J. A., & Fauth, J. (2008). Therapist self-awareness: Interdisciplinary connections and future directions. In S. D. Brown & B. Lent (Eds.), Handbook of counseling psychology (4th ed., pp. 303–319). Hoboken, NJ: Wiley.
Zahm, K. W., Veach, P. M., Martyr, M. A., & LeRoy, B. S. (2016). From novice to seasoned practitioner: A qualitative investigation of genetic counselor professional development. Journal of Genetic Counseling, 25, 818–834. doi:10.1007/s10897-015-9900-2
Diane M. Coll is a professional counselor at Argosy University. Chandra F. Johnson is an associate professor at Argosy University. Chinwé U. Williams is an associate professor at Argosy University. Michael J. Halloran is an honorary associate professor at La Trobe University. Correspondence can be addressed to Michael Halloran, School of Psychology and Public Health, La Trobe University, Kingsbury Dr., Bundoora, Australia, 3086, m.halloran@latrobe.edu.au.