Nov 30, 2019 | Volume 9 - Issue 4
Joshua D. Smith, Neal D. Gray
This interview is the fourth in the Lifetime Achievement in Counseling Series at TPC that presents an annual interview with a seminal figure who has attained outstanding achievement in counseling over a career. I am honored to present the interview of Liliana Sznaidman, a professional counselor in North Carolina. Ms. Sznaidman is the second practitioner to be interviewed for this annual series. Ms. Sznaidman is a licensed professional counselor and licensed professional counselor supervisor with over 20 years of clinical experience. She is currently the principal owner of a private practice where she provides counseling, clinical supervision, and consultation services. Joshua Smith and Dr. Neal Gray graciously accepted the assignment to interview Ms. Sznaidman. What follows are Ms. Sznaidman’s reflections on her counseling career and its impact on her clients. —J. Scott Hinkle, Editor
 Liliana Sznaidman has over 20 years of experience as a licensed professional counselor (LPC) and licensed professional counselor supervisor (LPCS) in North Carolina. She currently owns a private practice where she provides counseling and psychotherapy to adults, couples, and young adult clients. She also provides clinical supervision and consultation services to pre-licensed counselors and other mental health professionals.
Liliana Sznaidman has over 20 years of experience as a licensed professional counselor (LPC) and licensed professional counselor supervisor (LPCS) in North Carolina. She currently owns a private practice where she provides counseling and psychotherapy to adults, couples, and young adult clients. She also provides clinical supervision and consultation services to pre-licensed counselors and other mental health professionals.
Ms. Sznaidman received her master’s degree in counseling at the University of North Carolina at Greensboro. Prior to her master’s training, she completed a degree in early childhood education in Buenos Aires, Argentina. In addition to her LPC and LPCS, Ms. Sznaidman holds the credentials of National Certified Counselor and Approved Clinical Supervisor. She also has completed post-master’s training in clinical supervision and has received extensive training in psychoanalytic theory and practice.
Before going into private practice, Ms. Sznaidman worked as an outpatient psychotherapist providing family counseling services, and as a bilingual therapist. Ms. Sznaidman has been an advocate and asset to her community. She has conducted and co-facilitated psychoeducational groups in Spanish for Latinx adolescents and assisted in providing case management and referrals. Ms. Sznaidman has demonstrated service to the profession by serving as a field placement supervisor for master’s-level student interns and provided professional presentations to community agencies.
Ms. Sznaidman is a member of several professional organizations, including the Licensed Professional Counselors Association of North Carolina (LPCANC), where she was the president of the board of directors and helped to advocate for the inclusion of LPCs in continuing education opportunities. She also created the first mentoring program in the association. Ms. Sznaidman is an active member of the American Mental Health Counselors Association (AMHCA); the Pro Bono Counseling Network for Durham, Orange, Person, and Chatham Counties; and the Psychoanalytic Center of the Carolinas. Ms. Sznaidman received both the 2009 Distinguished Practitioner Award and the 2013 Alumni Distinguished Service Award from the University of North Carolina at Greensboro, and was named 2014 Mental Health Counselor of the Year by AMHCA.
In this interview, Ms. Sznaidman shares beneficial insights into her career, her approach to counseling, growth and changes within the counseling profession, her involvement in professional organizations, and the future development of the profession.
- As an LPC and LPCS in North Carolina, what led you to pursue a degree in
counseling compared to other helping professions?
It was in my late high school years when I began to think about engaging in a helping profession due to personal experiences receiving such help and becoming increasingly curious about the human mind.
However, political unrest in my country of origin, Argentina, followed by a couple of moves back and forth to the United States, veered my career in a different direction and affected a delay of my initial plans. It was after I settled more permanently in the United States that a counseling career became a reality.
After examining other specialties within the mental health profession, I decided to pursue professional counseling due to its predominant academic and practice emphasis on the provision of services to clients. Other disciplines seemed to divide their focus between this and macro work in communities, or psychological testing, which was not appealing to me in either the academic or practice realms.
- As a bilingual counselor with clinical interests in diversity and cross-cultural
counseling, what have been your perceptions and observations regarding
multicultural competency in counseling?
I recall taking a multicultural course in graduate school and truly appreciating it, based on how it set the tone for challenging the notion of mainstream cultural values being the guiding principle for helping clients, and erroneous, stereotypical assumptions about other cultures. Yet, it was quite surprising to witness thereafter that more emphasis was not placed on postgraduate continuing education opportunities in multicultural competency.
It seems to me that multiculturalism may be erroneously considered a specialty, particularly in today’s society where cultural differences are embedded in many client–therapist dyads. If we conceptualize multicultural nuances in a more expansive manner, even aspects as subtle as having had an urban upbringing compared to being raised on a farm, it might lead to richer exploration and meaning making in the context of working with clients.
Our profession and the counseling field overall would benefit from incorporating multicultural aspects into virtually every realm of training, rather than considering it a separate and unique body of knowledge. By not doing so, we might shortchange the overall growth of our profession in this area and limit how we serve our clients.
3. As a licensed counselor for over 20 years, what in your opinion are the biggest
changes within the profession? How have these changes impacted your work as a
clinician? Conversely, what are the biggest barriers facing counselors right now?
This is a very good topic to explore because it is easy for professional counselors to forget when there used to be little respect for our profession, despite our graduate training being comparable to that of others in the mental health field. The mental health professional world and the public at large knew very little about our training and our professional license. As a result, employers were quite wary about considering us in their hiring opportunities overall, and particularly while candidates were still accruing full licensure status. Health insurance companies, including those federally or state funded, were not accepting our licensed clinicians on their provider panels.
Being fully aware that the nature of our profession’s historical presence may vary from state to state, I can only speak of it based on my experience practicing in North Carolina. Thanks to the work of a handful of dedicated colleagues, professional counselors gradually but steadily gained acknowledgment by prospective employers and attained full third-party reimbursement status from insurance companies that operate within the state. In North Carolina, we were among the first in the field to institute distinct formal licensing tiers for associate, fully licensed, and supervisory levels. This offers a way to clearly reflect differential levels of training within our profession. However, it is evident that more work needs to be done by our professional associations in educating the public at large about who we are, how we are trained, and what exactly each of these tiered licensure levels means.
Nationally, of course we know that Medicare recognition is the next desired achievement, but we have certainly come a long way as a profession. It behooves us all to look back in gratitude in order to look forward to new horizons. Lastly, I want to say how encouraging it is to see the impetus of several national organizations working together toward a more cohesive licensing nomenclature and criteria, as well as reciprocity across states. Implementing uniformity in licensing standards can only benefit all of us in attaining increased professional recognition throughout the United States.
Witnessing the profession evolve and change throughout the years has been both encouraging and at times concerning. Particularly in private practice, the salient point is the impact of increasing administrative requirements and treatment barriers placed by insurance companies, while compensation for counseling services has remaining unchanged or lowered for over 15 years. Over time, insurers established a fee-for-service model that has resulted in a decline in previously available salaried employment opportunities, giving way to contract-based type arrangements. This model may pose many challenges to new graduates who may not feel fully ready to venture on their own into private practice, while also finding percentage fee-for-service remuneration positions financially unsustainable. At the state level, we also have seen a significant transformation involving the transition of publicly funded county mental health clinics to outsourcing management and provision of all services to large private sector companies. This, too, has impacted the nature of the job market for counselors.
Overall, we have seen an increase in new graduates starting out in private practice immediately after graduation, but for some this might be too soon or too daunting. I think that graduate programs can help pave the way by a two-fold approach: providing students with at least the basics of practice management skills and impressing upon them the importance of ongoing supervision and consultation with peers. It is no secret that private practice can at times feel isolating; thus establishing regular contact with colleagues for support and consultation can make a significant and positive impact.
- I see that you operate from a psychodynamic approach, both as a clinician and as a
supervisor. What does that approach mean to you in each of these roles?
Psychoanalytic psychotherapy operates under the premise that through exploration of the unconscious, conflicts take place. It also works by utilizing transference and countertransference in the client–counselor relationship to identify common threads in people’s lives. Analytic therapy is often criticized in part due to the length of treatment intrinsic to this orientation, misconceptions about it being solely rooted on antiquated and outdated theory and practice, as well as the therapist’s role being perceived as less active. However, contrary to many beliefs, there is a significant body of research in its efficacy and long-term sustained gains, in addition to its well-known years of historical practice and evolving theoretical contributions.
In my work with clients, I try to guide them to identify common themes, which when brought to the conscious level, begin to form a cohesive narrative of the person’s life that they may not have previously realized. In supervision, I attempt to help my supervisees identify themes in their clients, while also remaining attentive to what emerges within them in the context of that dyadic relationship. It is meaningful, transforming work that does not focus on presenting symptoms alone, but rather on the underlying roots most often unbeknownst to the client and on affecting long-lasting change for self-fulfilling lives.
- What has been your experience when interacting with national and local counseling
organizations? Do you feel supported by professional organizations and leaders?
Has support changed in the last 20 years?
I was active for many years within professional organizations, including serving on a state chapter association’s board of directors, LPCANC, for approximately five years. The work of these organizations is remarkable, as are their attainments. I think it was fortunate that my graduate program placed so much emphasis on involvement in these organizations. It was discussed in classes, in workshops, and certainly modeled by faculty in the program. I met our regional association leaders for the first time in one such workshop, and that experience truly made an impression on me as a student. The learning, networking, and growth opportunities that this involvement affords us is likely not available in any other aspect of our professional careers and is invaluable.
- Throughout your years of practice, what has been the role of counselor identity,
and has that changed over time?
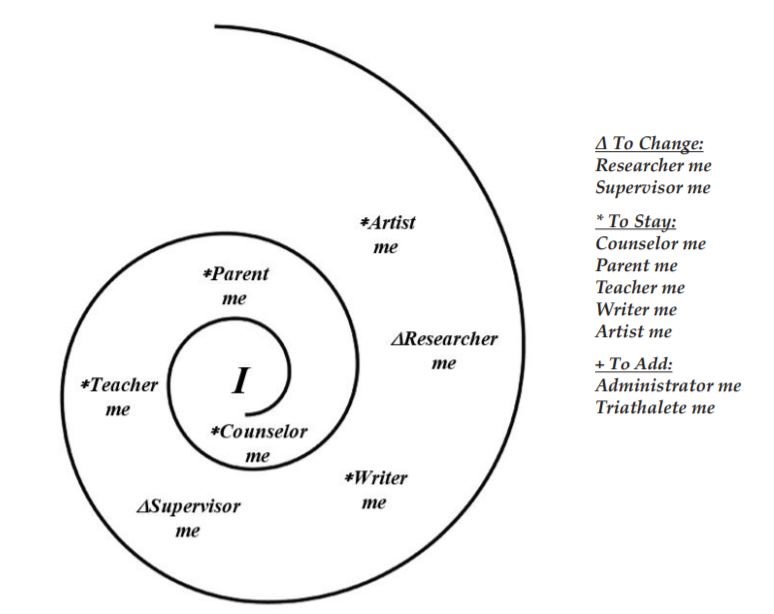
It has been interesting to me to witness my own journey within the profession throughout the years. Certainly, most of us work on getting better at and more experienced in what we are trained to do. It was interesting to me to see this focus and role expand and morph, venturing in different directions, such as advocacy and involvement in professional associations, more intensive clinical training, mentoring and training others via clinical supervision, and combining all of these in my professional life.
- For future counselors, what advice would you have regarding their involvement in
advancement and future development of the profession?
As I mentioned earlier, it was through the work of our dedicated colleagues that we attained the recognitions we now have, and yet more work always needs to be done. It is important that we as a profession make inroads in increasing salaried employment opportunities for our new graduates, as we still witness some hospitals, specific departments, university counseling centers, and the like that do not include professional counselors in their hiring practices. Counselors can certainly enter private practice at any juncture in their career, even while under supervision. Yet, based from my own experience, there is not much better learning than that which takes place when you witness the day-to-day practice of professionals more senior to you. This in my mind translates into full-time employment where excellent role models are available.
Another important aspect of advancing in the profession stems from engaging in lifelong learning and some of the best ways to do so are through continuing education and ongoing supervision. It is not uncommon for new counselors to experience supervision as such a financially burdensome mandate throughout their restricted license period that they tend to discontinue it immediately after full licensure is attained. I see this as depriving themselves of ongoing growth. Clinical supervision can take many different forms and frequency levels after graduation, but it remains an invaluable source of ongoing learning. It has been my own personal choice to remain in some form of clinical supervision throughout the entirety of my 20+ year career thus far, and I have never regretted it.
I would also encourage new counselors to engage in professional associations, volunteering and advocating from the outset. It may seem daunting to have that responsibility on top of learning their way as new professionals. However, it is crucial they know there will most likely be someone in those associations ready to guide them in this endeavor, and as the saying goes, “many hands make light work.”
This concludes the fourth interview for the annual Lifetime Achievement in Counseling Series. TPC is grateful to Joshua D. Smith, NCC, and Dr. Neal D. Gray for providing this interview. Joshua D. Smith is a doctoral student in counselor education and supervision at the University of North Carolina at Charlotte. Neal D. Gray is a professor and Chair of the School of Counseling and Human Services at Lenoir-Rhyne University. Correspondence can be emailed to Joshua Smith at jsmit643@uncc.edu.
Nov 29, 2019 | Volume 9 - Issue 4
Ariann Evans Robino
Explanations of compassion fatigue generally consider the client–counselor relationship as the primary source of challenges to wellness. Because of the nature of the current sociopolitical climate and the increased exposure through media, the counseling profession should consider expanding the influences on compassion fatigue related to current events. This article introduces the concept of global compassion fatigue (GCF), a phenomenon that provides an opportunity for counselor self-awareness. Implications for adopting GCF into the counselor impairment literature include understanding how global events impact counselor development and clinical practice as well as the importance of maintaining a wellness lifestyle to protect against its effects. Counselors’ involvement in advocacy and social justice are also explored as contributors to GCF.
Keywords: global compassion fatigue, counselor impairment, advocacy, self-awareness, wellness
Counselors and counselors-in-training (CITs) feel the weight of societal stressors. According to the ACA Code of Ethics, “promoting social justice” (American Counseling Association [ACA], 2014, p. 3) is a core value of the counseling profession. Furthermore, because of its impact on the profession, scholars have declared social justice as the fifth force in counseling (Ratts, 2009; Ratts, D’Andrea, & Arredondo, 2004). Representatives from ACA have acted in accordance by addressing the federal government’s recent prohibition of specific language associated with diverse populations (Yep, 2017) as well as releasing a statement of support shortly after the 2016 presidential election calling on all counselors to remain strong in their beliefs and actively assist those in need (Roland, 2016). Similarly, the closing keynote speaker at ACA’s Illuminate Symposium on June 10, 2017, Dr. Cheryl Holcomb-McCoy, encouraged attendees to take action against human rights offenses through vocal opposition in multiple settings, including social media (Meyers, 2017). These positions demonstrate the desired role of counselors to engage in advocacy and activism for global issues.
Natural disasters, threats to civil rights, violence, terrorist attacks, and animal welfare concerns are simply a few of the powerful issues that humans face as highly social and emotional beings. Although advocacy is one avenue of handling the emotional unrest related to these events, the complex nature of counselors’ personal and professional identities presents an invitation to consider these sensitive issues currently faced by society. Professional counselor identity allows counselors to make meaning of their work during these times of strong emotion (Solomon, 2007). Considering how these events affect both counselors’ and CITs’ personal lives and clinical practice produces opportunities for counselor professional development and greater self-awareness. The purpose of this article is to explore global compassion fatigue (GCF), a phenomenon related to the human condition and how global events impact professional counselors and other helpers. This article begins with a review of current counselor impairment concepts as well as the role of wellness in managing these conditions. Then, the reader is introduced to GCF and how a review of the literature supports the examination of this new concept. Next, I provide a detailed conceptualization of the phenomenon and implications for the field. Finally, suggestions for future research are provided.
Understanding Compassion Fatigue
Compassion fatigue research spans the literature of multiple disciplines, including nursing, social work, and counseling (Compton, Todd, & Schoenberg, 2017; Lynch & Lobo, 2012; Sorenson, Bolick, Wright, & Hamilton, 2016). Counselors typically understand compassion fatigue as an event occurring as a result of counselor–client interaction. Charles Figley (1995) first defined the concept of compassion fatigue as “a state of exhaustion and dysfunction—biologically, psychologically, and socially—a result of prolonged exposure to companion stress and all that it evokes” (p. 253) and conceptualized it as a response to the emotional demands of hearing and witnessing stories of pain and suffering. Symptoms of compassion fatigue include re-experiencing the client’s traumatic event, avoidance of reminders of the event and/or feeling numb to those reminders, and persistent arousal (Figley, 1995). Researchers carefully note the differences between compassion fatigue, vicarious traumatization, and burnout (Lawson & Venart, 2005; Meadors, Lamson, Swanson, White, & Sira, 2010). Vicarious traumatization, defined as a significant altering of cognitive schemas and a disruption of an individual’s sense of identity, worldview, and meaning, occurs as a result of empathic engagement with the traumatic experiences of a client (McCann & Pearlman, 1990). Vicarious traumatization symptoms involve a more covert change in thought and cognitive schema rather than an observable experiencing of symptomatology (Jenkins & Baird, 2002). Burnout is a process that occurs because of occupational stressors such as high caseloads, low morale, and minimal support (Maslach & Jackson, 1981). It is associated with emotional exhaustion, strain, and overload in addition to a reduction in personal accomplishment and job satisfaction (Maslach, 1982). Counselors are more likely to experience compassion fatigue, vicarious traumatization, and burnout when they have a previous history of personal trauma (Baird & Kracen, 2006), high emotional involvement with clients (Adams, Boscarino, & Figley, 2006), fewer perceived coping mechanisms (Baird & Kracen, 2006), and lower self-awareness (P. Clark, 2009). However, the goal of this article is to expand upon the phenomenon of compassion fatigue as distinguished from these other explanations of impairment to understand better how global events outside of the counselor–client dyad impact counselors. Although other impairment concepts hold value and applicability to counselors, compassion fatigue and its relationship to emotional suffering as a result of a desire to help others most closely aligns with the concept presented in this article. When considered in the context of counselors, an awareness of compassion fatigue, its effects, and how to mitigate those effects is vital for client welfare.
Counselor Impairment and Wellness
According to the ACA Code of Ethics, counselors should “monitor themselves for signs of impairment from their own physical, mental, or emotional problems” (ACA, 2014, p. 9). The ACA Code of Ethics dedicates an entire section to counselor impairment (C.2.g.), which states that, in the interest of client protection, counselors should cease providing services while impaired, seek assistance to solve issues of impairment, and assist colleagues and supervisors in recognizing and rectifying their own impairment (ACA, 2014). When counselors are impaired, it can result in significant harm to clients through an interference with the counseling process, trust violations, and ethical breaches (Lawson, Venart, Hazler, & Kottler, 2007). Adopting an alternative lens for viewing the impairment literature presents an opportunity for counselors to monitor themselves and others for potential issues as indicated by the ACA Code of Ethics (ACA, 2014). In addition, the ACA Code of Ethics guides counselors to “engage in self-care activities to maintain and promote their own emotional, physical, mental, and spiritual well-being to meet their professional responsibilities” (ACA, 2014, p. 8). As self-advocacy for wellness can promote better professional practice within the counseling community (Dang & Sangganjanavanich, 2015), counselors are encouraged to avoid and rectify issues of impairment through positive, health-promoting strategies.
Recognizing this area of need within the profession, ACA established the Taskforce on Counselor Wellness and Impairment in 2003 to address the needs of impaired counselors (Lawson & Venart, 2005). The taskforce identified goals for education for counselors on impairment and how to prevent it, securing treatment for impaired counselors, teaching self-care strategies, and advocating within the organization and at both the state and national levels to address issues associated with impairment. Although the taskforce focused on the broader topic of impairment, compassion fatigue remains a component of this experience. The creation, cultivation, and maintenance of a wellness lifestyle is a primary means of addressing and rectifying counselor impairment and compassion fatigue (Lawson & Venart, 2005).
Wellness is defined as “a way of life oriented toward optimal health and well-being in which body, mind, and spirit are integrated by the individual to live life more fully” (Myers, Sweeney, & Witmer, 2000, p. 252). Wellness and prevention are core components of counselors’ professional identities (Mellin, Hunt, & Nichols, 2011). As a result, researchers have studied the benefits of wellness strategies for counselors (Cummins, Massey, & Jones, 2007), counselor educators (Wester, Trepal, & Myers, 2009), and CITs (Yager & Tovar-Blank, 2007). Additionally, Figley (1995) specifically identified poor self-care as a primary risk factor for experiencing compassion fatigue, and Chi Sigma Iota’s (CSI; n.d.) advocacy themes, specifically Theme 6, outline the need for advocacy related to prevention and wellness for clients and counselors (Lee, 2012). The development of a taskforce, the extensive literature associated with compassion fatigue and wellness, and CSI’s identification of wellness as an area of advocacy indicate a clear relationship between counselor experience and counselor practice. Based on previous research, ACA’s stance on counselor self-care, and humans’ innate desire to engage in complex processes to achieve optimal functioning and well-being, it is beneficial for counselors to consider a new phenomenon related to their consistent exposure to global issues through media and social media. Counselors currently conceptualize compassion fatigue as a linear process occurring as a result of the cumulative direct exposure to clients’ distressing experiences. This article presents an expanded perspective on counselor compassion fatigue occurring as a result of exposure to current events and issues. Furthermore, this article offers a language for this experience as well as a conceptualization of the phenomenon.
GCF
I suggest the term global compassion fatigue to describe the process by which an individual experiences extreme preoccupation and tension as a result of concern for those affected by global events without direct exposure to their traumas through clinical intervention. GCF requires examining compassion fatigue outside of client-specific experiences and within a larger context. This invites counselors and CITs to explore how they are human and existing in a conflicted, polarized, and oftentimes troubling world.
Figure 1 provides a visual depiction of these constructs. After exposure to a traumatic global event, humans experience an acute stress-related psychological response (Holman, Garfin, & Silver, 2013); for counselors this may manifest as GCF because of their foundational helping skills rooted in the ability to feel and exhibit empathy for the issues faced by others (A. J. Clark, 2010). Once this response occurs, counselors can utilize wellness and self-care strategies and engage in social justice advocacy efforts as deterrents to GCF. If they bypass these methods, they might experience the extreme preoccupation and tension that are indicators of GCF. However, counselors can interrupt and manage their GCF by moving to wellness and advocacy strategies.
Figure 1. Process of GCF. After media exposure to a global event and engaging in an emotional response, counselors can immediately experience GCF. Wellness and advocacy are two methods of either addressing GCF after experiencing it or through prevention to deter the experience.
GCF differs from vicarious traumatization in that it does not denote permanent change in cognitive schema; rather, a counselor can experience GCF transiently and in response to significant global and communal events. Counselors experiencing GCF do so outside of clients’ presenting problems. Although no current counseling literature describes this phenomenon, Stebnicki (2007) proposed the concept of empathy fatigue, which “results from a state of emotional, mental, physical, and occupational exhaustion that occurs as the counselors’ own wounds are continually revisited by their clients’ life stories of chronic illness, disability, trauma, grief and loss” (p. 318). Whereas GCF does bear similarity to empathy fatigue, empathy fatigue remains related to an occurrence resulting from direct clinical exposure (Stebnicki, 2007), and GCF involves counselor introspection unrelated to session content. Relatedly, Bayne and Hays (2017) recently conducted a study to conceptualize the conditions of empathy within the counseling process. They developed an exploratory model of counselor empathy that acknowledges the multidimensionality of the empathic process, including the variables associated with counselor impairment. GCF proposes that counselors’ intense emotional experiences related to global concerns are associated with empathy and a desire to help those directly affected. Current events that may cause a counselor to experience GCF include politics, natural disasters, violence (including mass shootings), terrorist attacks, threats to human rights, and animal abuse.
Compassion fatigue research is the best point of reference when considering the experience of GCF. Compassion fatigue manifests through physical, psychological, spiritual, and social symptoms (Lynch & Lobo, 2012), and counselors experiencing GCF also can exhibit these symptoms. However, counselors must consider the source of their feelings of fatigue. For example, Coetzee and Klopper (2010) noted, “compassion fatigue is caused by the prolonged, intense, and continuous care of patients, use of self, and exposure to stress” (p. 239). I suggest that GCF involves a similar experience, although as a result of continuous concern for other beings, a desire to help recover from or solve the issues affecting those beings, and repeated exposure to current events harming individuals on a large scale. Additionally, ACA’s Advocacy Competencies call for professional counselors to engage in systemic and sociopolitical advocacy on a continuum ranging from the microlevel (i.e., the individual) to the macrolevel (i.e., the public; Lewis, Arnold, House, & Toporek, 2003). Therefore, it is a counselor’s duty to remain aware of systemic, environmental, and political factors impacting clients in addition to immersing themselves in advocacy and mechanisms for change. Such actions may leave counselors susceptible to impairment in response to global issues, although moving from awareness to action also can help prevent or mitigate GCF.
Researchers have explored the effects of distressing events on helping professionals. Early research described the relationship between clergy members’ compassion fatigue and their time spent with trauma victims following the September 11th terrorist attacks (Flannelly, Roberts, & Weaver, 2005). Counselors responding after a natural disaster (Lambert & Lawson, 2013) and trauma counselors (Sansbury, Graves, & Scott, 2015) are populations often researched in the compassion fatigue literature. For example, Day, Lawson, and Burge (2017) reported the results of a qualitative research study exploring compassion fatigue and shared trauma in clinicians providing services after the shootings at Virginia Tech in 2007. Day et al. raised an interesting point between a counselor’s direct and indirect exposure to global events as well as the level of impairment resulting from the experience. Given the possibility that unresolved trauma can cause issues in functioning, direct exposure to an event removes the possibility that a counselor is experiencing GCF. This shared trauma may result in similar symptomatology, but these symptoms are attributed to the commonality of the trauma experience (Figley Institute, 2012).
From a different framework, researchers have explored the experiences of non-counselors when exposed indirectly to traumatic global events. Although many Americans were not in New York at the time of the September 11th attacks, nor were they likely to have known someone associated with the attacks, the stress of the event was felt across the country in the form of trauma symptoms (Schuster et al., 2001). Individuals living in Britain also experienced psychological changes as a result of the vicarious media exposure to these terror attacks on America (Linley, Joseph, Cooper, Harris, & Meyer, 2003). Similarly, college students at a separate university described an increase in acute stress symptoms as they learned about the shootings at Virginia Tech on television (Fallahi & Lesik, 2009). This research indicates that individuals can experience emotional duress in response to indirect exposure to global or national issues. Ultimately, it is important to remember that, despite extensive training and experience, counselors are humans navigating a society that can upset them in various ways. GCF awareness furthers counselor insight and promotes opportunities for evaluating self-care, wellness, and efficacy under these conditions. Such awareness requires an understanding of the role media plays in individuals’ experiencing of traumatic global events.
The Impact of Media
Previous researchers evaluated the impact of television viewing on an individual’s stress symptoms and levels of vicarious exposure (Fallahi & Lesik, 2009; Linley et al., 2003), suggesting that the role of technology can significantly affect a counselor’s ability to create boundaries and step away from the tragic circumstances occurring in the world around them. With 62% of adults obtaining their news from social media sites in 2016, an increase from 49% in 2012 (Gottfried & Shearer, 2016), it is clear that regular social media use can result in high levels of exposure to distressing news content. Additionally, four out of five adults in the United States reported constantly “checking” their cellular phones for emails, text messages, and social media (American Psychological Association, 2017). This same survey also described higher stress levels in the “constant checker” population than those using technology less frequently.
Researchers have discovered a link between emotional well-being and use of television media. Schlenger et al. (2002) found a statistically significant relationship between the levels of post-traumatic stress disorder symptoms and the numbers of hours spent watching television coverage of the September 11th terrorist attacks when assessing the psychological reactions of 2,273 adults residing in major metropolitan cities in the United States one to two months after the attacks. Fallahi and Lesik (2009) also identified a problematic association between indirect exposure to a tragic event through news media sources and symptoms of acute stress disorder.
Therefore, if a counselor or CIT is particularly sensitive to the content to which they are exposed through the media, they increase their risk of experiencing GCF. Conversely, social media also might provide an opportunity for community and connection in the face of global issues. The idea of community is no longer constrained within the bounds of physical associations; rather, the internet provides access to distant communities and relationships (Gruzd, Wellman, & Takhteyev, 2011). Supporters and activists involved in the Black Lives Matter movement are an example of such a community. Black Lives Matter erupted on social media as a Twitter hashtag created to raise awareness for and demonstrate protest against police brutality on members of the Black community (Petersen-Smith, 2015). Through this online movement, individuals were able to exhibit solidarity and take a stand against racism toward Black people with their use of social media (Schuschke & Tynes, 2016). Similarly, the #MeToo internet-based movement brought attention to women’s rights and sexual violence (Hostler & O’Neil, 2018), and social media platforms also provide a method of addressing the stigma of mental health and addiction (de la Cretaz, 2017).
ACA has an active social media presence through online pages and forums on their website, Facebook, Twitter, and LinkedIn (ACA, 2017). The ACA Code of Ethics (ACA, 2014) states that counselors will use social media only when it is in the best interest of the client while protecting their identity and well-being (Section H). This is another example in which a position is based on a situation specifically involving the client and counselor. Although researchers have explored the role of social media in counselor education (Tillman, Dinsmore, Chasek, & Hof, 2013) and recommendations have been made for using social media ethically in clinical practice (Giota & Kleftaras, 2014), researchers have yet to explore how social media affects practicing counselors on an emotional level. Adopting GCF into the counselor impairment literature would suggest a need for ACA to also establish recommendations for counselors’ social media use and how excessive exposure to global events can affect their work as counselors.
A New Perspective
As social beings dependent upon one another for survival, humans have an evolutionary and biological drive to feel connected and invested in others. Specifically, humans are interested in the welfare of others on a neurological level (Lieberman, 2013). Counselors and CITs can feel a need to help others based on evolutionary compulsions rooted in social psychology. However, they also can feel this drive to an amplified extent because of their consistent demonstration and use of empathy, a foundational helping skill that allows counselors to “enter the client’s phenomenal world, to experience the client’s world as it were your own without ever losing the ‘as if’ quality” (Rogers, 1961, p. 284). Although all humans are susceptible to experiencing fatigue as a result of high exposure to global issues through media, not all humans work in a helping profession based in the empathic experience. Therefore, similar to the need for counselors to monitor themselves for impairment as a result of direct engagement with clients’ presenting issues, counselors also need to monitor for impairment from global issues. Regardless of continuous exposure to distressing global events, counselors continue to help others on a consistent basis. This indicates a critical need for counselors to understand their relationship to social media and the global events to which they experience an emotional response.
Symptoms of GCF can manifest similarly to traditional compassion fatigue. These symptoms can include emotional and physical exhaustion associated with care for others, desensitization to stories and experiences, poorer quality of care, feelings of depression or anxiety, increased stress, difficulty concentrating, and preoccupation (Figley Institute, 2012). Ultimately, it is the responsibility of the counselor to understand the source of these symptoms. Unlike counselors’ direct work with clients in which there may be greater opportunities to assist in managing or addressing a pain-inducing problem, emotional and cognitive responses to global issues present a different type of challenge. Managing issues in which a person may perceive little control and direct influence can cause responses such as rumination (Nolen-Hoeksma, Wisco, & Lyubomirsky, 2008) and fear (Pain & Smith, 2008). Although counselors can experience these feelings regarding clients (Sansbury et al., 2015), there are greater opportunities for direct interaction with the client needing assistance. In most cases, counselors are unable to directly impact the people involved in the global events to which they are continuously exposed through media and social media. Optimal human functioning involves integration of the mind, body, and spirit (Myers et al., 2000). GCF can impact this integration when counselors are unable to live fully through the exhaustion of exposure to global events. Wellness strategies and forms of advocacy can prevent or rectify these experiences. Myers et al. (2000) acknowledged that “global events, whether of natural (e.g., floods, famines) or human (e.g., wars) origin, have an impact on the life forces and life tasks depicted in [wellness models]” (p. 252). In addition, advocacy in the wake of social events can provide feelings of efficacy and social connection (Scott & Maryman, 2016). This new perspective provides implications for the profession of counseling, including recommendations, cultural considerations, and areas of future research.
Implications for Counselors
In a “plugged-in” society, it is possible to become overwhelmed with the daily stream of news and information. Additionally, counselors can be at higher risk of experiencing impairment because of their empathic nature (Figley, 1995) and ethical duty to engage in social justice for causes that improve equity for individuals and groups (ACA, 2014). As leaders and advocates, GCF may be present in counselors’ daily clinical work. Licensed counselors in private practice may not be receiving ongoing supervision (Bernard & Goodyear; 2014); therefore, no external individual is monitoring how they are managing GCF and its effects. Counselors outside of supervision must exercise great care to practice self-awareness and approach others for assistance. Furthermore, counselors in high-volume settings often work with large caseloads that present with complex issues (Belling et al., 2011; Lombardo, 2018), and it may be easy for them to ignore their own needs while addressing the needs of others. Given the critical period of counselor development, GCF also must be considered within the context of counselor education. GCF during the formative period of graduate-level education in counseling can impede overall skill development. As new counselors find themselves more likely to experience compassion fatigue (Figley, 1995), the same may hold true for GCF. GCF may result in a type of developmental stalling in which counseling students feel an “empathy overload.” Such an overload of empathic emotions may impede the student’s transformation into a counselor. This provides implications for counselor education programs to measure students’ responses to emotionally distressing stimuli (O’Brien & Haaga, 2015) of both clinical and global nature as well as openly and unashamedly discuss signs and symptoms of impairment (Merriman, 2015).
I propose that counselors can manage GCF similarly to compassion fatigue because of the possibility of the two phenomena appearing symptomatically similar. However, GCF requires a greater level of self-awareness, recognition, and acceptance in order to address it. Counselors must learn how to distinguish between the two concepts and understand the possibility for overlap. A number of tools used to manage compassion fatigue can be used for GCF. Supervision, personal counseling, and consultation are all avenues of accountability, monitoring, and fidelity to the profession (Bernard & Goodyear, 2014). Although advocacy can be another tangible method of preventing or mitigating GCF, activism can cause emotional, mental, and physical exhaustion (Chen & Gorski, 2015); therefore, advocacy paired with careful attention to wellness can allow counselors to be most effective in helping to address global issues (Roysircar, 2009). Self-care practices and a wellness lifestyle may also act as protective factors to GCF. Myers et al. (2000) noted, “If one’s spirituality is healthy . . . [it] provides a firm foundation and core for the rest of the components of wellness” (p. 258). This indicates counselors developing an optimistic outlook in response to global events creates greater buffering or management of GCF. Similarly, these authors also state that self-direction allows a person to “move smoothly through time and space”
(p. 258). The cumulative pressure of global stressors necessitates firm self-direction to maintain focus in the chaos of present time and space. Wellness is cumulative and enhances longevity for professional practice (Myers et al., 2000). Ultimately, counselors are ethically responsible for ensuring they practice healthy boundaries and work within their competencies (ACA, 2014). An open dialogue with colleagues, self-awareness of strong responses to global events, pursuing systemic change through advocacy, and cultivating personal wellness encourage management of GCF (Robino & Pignato, 2017).
GCF holds particular relevance for counselors of color. Individuals from historically marginalized populations must understand, identify, and address their experiences and the effects of systemic and individualized racism as well as the psychological trauma of oppression and marginalization (Carter, 2007). The number of publicized events that occur in relation to civil rights issues and social justice concerns warrant additional consideration of GCF in specific populations. For example, police brutality against Black males can cause GCF in many counselors, particularly in counselors of color because of the negative psychological health outcomes for communities of color that stem from racism and discrimination (Carter & Forsyth, 2009; Comas-Díaz, 2016). Furthermore, violence (e.g., the Charleston, South Carolina, shooting targeting a specific religious group consisting of people of color and the Charlottesville, Virginia, protests that resulted in the death of a counter-protester) and localized natural disasters (e.g., fires in Tennessee and the Western United States that affected entire communities and hurricanes like Harvey, Irma, and Maria that caused devastation in the Southern United States and Puerto Rico) also increase the risk of GCF in counselors indirectly or somewhat directly exposed to these events. At the time of this writing, the president of the United States has signed an Immigration Executive Order (Executive Order No. 13,769, 2017) that calls for banning residents of certain Middle Eastern countries from entering the United States. In addition, the public expressed outrage at the removal of children from families seeking asylum at the U.S.–Mexico border (Goldstein, 2018). Such traumatic events become a systemic, multi-level public health issue (Magruder, McLaughlin, & Elmore Borbon, 2017) and increase the possibility of GCF among concerned individuals, including counselors and counseling students.
The emergence of this concept paves the way for a broad range of research avenues. First, I recommend the study of GCF in counselor education programs. With CITs particularly sensitive to the nuances of the counseling profession (Bernard & Goodyear, 2014), the critical period of graduate education requires an examination into how GCF can affect counselor development. Second, the management of GCF calls for greater practice of self-care and exercising of insight. For example, researchers could explore the use of mindfulness and reflexivity in assessing how to treat counselors impacted by global events. Additionally, future research could explore the relationship of counselors’ social media use and GCF experiences. Statistics indicating the increase of social media as a news source (Gottfried & Shearer, 2016) raise questions of how counselors are impacted by their own internet activity. Researchers also could investigate counselor advocacy on social media. Although this article proposes that counselors may experience frustrations that contribute to GCF as a result of social media exposure to distressing global events, Dr. Holcomb-McCoy described social media as a tool for advocacy (Meyers, 2017), which may help in mitigating GCF. Such studies may assist counselors in delineating between GCF and other phenomena of impairment.
Finally, greater research is needed to assess and measure GCF. No accurate measurement yet exists for the phenomenon of GCF. Compassion fatigue measurements assess the negative aspects of helping others through direct contact (Figley, 1996). For GCF, this does not address the negative aspects of compassion for indirect exposure to global events. The Impact of Events Scale-Revised (IES-R; Weiss, 2007) measures the subjective distress associated with a traumatic event. However, the IES-R measures symptoms associated with post-traumatic stress disorder. Although it captures the experience of an external global event, it does not capture the transient, yet profound, emotional experience of GCF. The answer to assessing GCF may lie in the development of an instrument that combines compassion fatigue assessments and the IES-R to measure GCF symptoms as it relates to global events.
Conclusion
This article introduces the concept of GCF into the counseling literature. By expanding the literature on other explanations of impairment, we broaden opportunities for self-awareness and professional development. Previously researched impairment concepts require an expansion into this new perspective by incorporating the effects of exposure to current events. This new phenomenon also contributes to counselor wellness research and the importance of maintaining a healthy wellness lifestyle as a deterrent to GCF. Adopting this concept and language into the literature on impairment and wellness encourages further consideration of counselor health, counselors’ management of distressing global events, and how this may impact both counselors and clients as humans.
As counselors become competent in their roles as advocates for social justice, their involvement in critical global events necessitates attention to the cumulative toll such a role may entail. In addition, consistent exposure to emotionally debilitating global events through social media places counselors in a peculiar position in which they must balance their need to remain informed of events and their need to remain healthy and well. Counselors carry the extra responsibility of remaining present and empathic with their clients while also protecting the empathy they experience for the world around them. Counselors’ marginalized and impacted cultural identities also factor into their experiences of GCF. In this regard, wellness becomes not simply an ethical duty, but also a professional imperative in the interest of both counselor and client welfare.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Adams, R. E., Boscarino, J. A., & Figley, C. R. (2006). Compassion fatigue and psychological distress among social workers: A validation study. American Journal of Orthopsychiatry, 76, 103–108.
doi:10.1037/0002-9432.76.1.103
American Counseling Association. (2014). ACA code of ethics. Alexandria, VA: Author.
American Counseling Association. (2017). Press room. Retrieved from https://www.counseling.org/about-us/about-aca/press-room
American Psychological Association. (2017). Stress in America: Coping with change. Retrieved from https://www.apa.org/news/press/releases/stress/2017/technology-social-media.pdf
Baird, K., & Kracen, A. C. (2006). Vicarious traumatization and secondary traumatic stress: A research synthesis. Counselling Psychology Quarterly, 19, 181–188. doi:10.1080/09515070600811899
Bayne, H. B., & Hays, D. G. (2017). Examining conditions for empathy in counseling: An exploratory model. The Journal of Humanistic Counseling, 56, 32–52. doi:10.1002/johc.12043
Belling, R., Whittock, M., McLaren, S., Burns, T., Catty, J., Jones, I. R., . . . the ECHO Group. (2011). Achieving continuity of care: Facilitators and barriers in community mental health teams. Implementation Science, 6, 23–29. doi:10.1186/1748-5908-6-23
Bernard, J. M., & Goodyear, R. K. (2014). Fundamentals of clinical supervision (5th ed.). Upper Saddle River, NJ: Pearson Education.
Carter, R. T. (2007). Racism and psychological and emotional injury: Recognizing and assessing race-based traumatic stress. The Counseling Psychologist, 35, 13–105. doi:10.1177/0011000006292033
Carter, R. T., & Forsyth, J. M. (2009). A guide to the forensic assessment of race-based traumatic stress reactions. Journal of the American Academy of Psychiatry and the Law, 37, 28–40.
Chen, C. W., & Gorski, P. C. (2015). Burnout in social justice and human rights activists: Symptoms, causes, and implications. Journal of Human Rights Practice, 7, 366–390. doi:10.1093/jhuman/huv011
Chi Sigma Iota. (n.d.). Theme F: Prevention/wellness. Retrieved from http://www.csi-net.org/?Advocacy_Theme_F
Clark, A. J. (2010). Empathy: An integral model in the counseling process. Journal of Counseling & Development, 88, 348–356. doi:10.1002/j.1556-6678.2010.tb00032.x
Clark, P. (2009). Resiliency in the practicing marriage and family therapist. Journal of Marital and Family Therapy, 35, 231–247. doi:10.1111/j.1752-0606.2009.00108.x
Coetzee, S. K., & Klopper, H. C. (2010). Compassion fatigue within nursing practice: A concept analysis. Nursing and Health Science, 12, 235–243. doi:10.1111/j.1442-2018.2010.00526.x
Comas-Díaz, L. (2016). Racial trauma recovery: A race-informed therapeutic approach to racial wounds. In A. N. Alvarez, C. T. H. Liang, & H. A. Neville (Eds.), The cost of racism for people of color: Contextualizing experiences of discrimination (pp. 249–272). Washington, DC: American Psychological Association.
Compton, L., Todd, S., & Schoenberg, C. (2017). Compassion fatigue and satisfaction among Critical Incident Stress Management (CISM) providers: A study on risk and mitigating factors. Virginia Counselors Journal, 35, 20–27.
Cummins, P. N., Massey, L., & Jones, A. (2007). Keeping ourselves well: Strategies for promoting and maintaining counselor wellness. Journal of Humanistic Counseling, Education, and Development, 46, 35–49. doi:10.1002/j.2161-1939.2007.tb00024.x
Dang, Y., & Sangganjanavanich, V. F. (2015). Promoting counselor professional and personal well-being through advocacy. Journal of Counselor Leadership and Advocacy, 2, 1–13. doi:10.1080/2326716X.2015.1007179
Day, K .W., Lawson, G., & Burge, P. (2017). Clinicians’ experiences of shared trauma after the shootings at Virginia Tech. Journal of Counseling & Development, 95, 269–278. doi:10.1002/jcad.12141
de la Cretaz, B. (2017, April 21). The Voices Project is fighting addiction & stigma through social media. Retrieved from https://www.thefix.com/voices-project-fighting-addiction-stigma-through-social-media
Exec. Order No. 13,769, 3 C.F.R. 8977-8982 (2017).
Fallahi, C. R., & Lesik, S. A. (2009). The effect of vicarious exposure to the recent massacre at Virginia Tech. Psychological Trauma: Theory, Research, Practice, and Policy, 1, 220–230. doi:10.1037/a0015052
Figley, C. R. (Ed.). (1995). Compassion fatigue: Coping with secondary traumatic stress disorder in those who treat the traumatized. Philadelphia, PA: Brunner/Mazel.
Figley, C. R. (1996). Review of the Compassion Fatigue Self-Test. In B. H. Stamm (Ed.), Measurement of stress, trauma, and adaptation (pp. 127–130). Baltimore, MD: Sidran Press.
Figley Institute. (2012). Basics of compassion fatigue. Retrieved from http://www.figleyinstitute.com/documents/Workbook_AMEDD_SanAntonio_2012July20_RevAugust2013.pdf
Flannelly, K. J., Roberts, S. B., & Weaver, A. J. (2005). Correlates of compassion fatigue and burnout in chaplains and other clergy who responded to the September 11th attacks in New York City. Journal of Pastoral Care & Counseling, 59, 213–224. doi:10.1177/154230500505900304
Giota, K. G., & Kleftaras, G. (2014). Social media and counseling: Opportunities, risks, and ethical considerations. International Journal of Social, Behavioral, Educational, Economic, Business, and Industrial Engineering, 8, 2378–2380.
Goldstein, J. M. (2018, May 26). As ICE separates children from parents at the border, public outrage grows. Retrieved from https://thinkprogress.org/as-ice-separates-children-from-parents-at-the-border-public-outrage-grows-c624e69cd43f/
Gottfried, J., & Shearer, E. (2016, May 26). News use across social media platforms 2016. Retrieved from www.jour
nalism.org/2016/05/26/news-use-across-social-media-platforms-2016/
Gruzd, A., Wellman, B., & Takhteyev, Y. (2011). Imagining Twitter as an imagined community. American Behavioral Scientist, 55, 1294–1318. doi:10.1177/0002764211409378
Holman, E. A., Garfin, D. R., & Silver, R. C. (2013). Media’s role in broadcasting acute stress following the Boston Marathon bombings. Proceedings of the National Academy of Sciences, 111, 93–98.
doi:10.1073/pnas.1316265110
Hostler, M. J., & O’Neil, M. (2018, April 17). Reframing sexual violence: From #MeToo to Time’s Up. Stanford Social Innovation Review. Retrieved from https://ssir.org/articles/entry/reframing_sexual_violence_from_metoo_to_times_up
Jenkins, S. R., & Baird, S. (2002). Secondary traumatic stress and vicarious trauma: A validational study. Journal of Traumatic Stress, 15, 423–432. doi:10.1023/A:1020193526843
Lambert, S. F., & Lawson, G. (2013). Resilience of professional counselors following Hurricanes Katrina and Rita. Journal of Counseling & Development, 91, 261–268. doi:10.1002/j.1556-6676.2013.00094.x
Lawson, G., & Venart, B. (2005). Preventing counselor impairment: Vulnerability, wellness, and resilience. In VISTAS: Compelling perspectives on counseling. Retrieved from https://www.counseling.org/Resources/Library/VISTAS/
vistas05/Vistas05.art53.pdf
Lawson, G., Venart, E., Hazler, R. J., & Kottler, J. A. (2007). Toward a culture of counselor wellness. The Journal of Humanistic Counseling, Education, and Development, 46, 5–19. doi:10.1002/j.2161-1939.2007.tb00022.x
Lee, C. C. (2012). Social justice as the fifth force in counseling. In C. Y. Chang, C. A. Barrio Minton, A. L. Dixon, J. E. Myers, & T. J. Sweeney (Eds.), Professional counseling excellence through leadership and advocacy (pp. 109–120). New York, NY: Routledge/Taylor & Francis Group.
Lewis, J. A., Arnold, M. S., House, R., & Toporek, R. L. (2003). ACA advocacy competencies. Retrieved from https://www.counseling.org/resources/competencies/advocacy_competencies.pdf
Lieberman, M. D. (2013). Social: Why our brains are wired to connect. New York, NY: Crown.
Linley, P. A., Joseph, S., Cooper, R., Harris, S., & Meyer, C. (2003). Positive and negative changes following vicarious exposure to the September 11 terrorist attacks. Journal of Traumatic Stress, 16, 481–485. doi:10.1023/A:1025710528209
Lombardo, C. (2018, February 26). With hundreds of students, school counselors just try to ‘stay afloat’. Retrieved from https://www.npr.org/sections/ed/2018/02/26/587377711/with-hundreds-of-students-school-counselors-just-try-to-stay-afloat
Lynch, S. H., & Lobo, M. L. (2012). Compassion fatigue in family caregivers: A Wilsonian concept analysis. Journal of Advanced Nursing, 68, 2125–2134. doi:10.1111/j.1365-2648.2012.05985.x
Magruder, K. M., McLaughlin, K. A., & Elmore Borbon, D. L. (2017). Trauma is a public health issue. European Journal of Psychotraumatology, 81, 1375338. doi:10.1080/20008198.2017.1375338
Maslach, C. (1982). Burnout: The cost of caring. Englewood Cliffs, NJ: Prentice-Hall.
Maslach, C., & Jackson, S. E. (1981). The measurement of experienced burnout. Journal of Occupational Behavior, 2(2), 99–113. doi:10.1002/job.4030020205
McCann, I. L., & Pearlman, L. A. (1990). Vicarious traumatization: A framework for understanding the psychological effects of working with victims. Journal of Traumatic Stress, 3, 131–149.
doi:10.1007/BF00975140
Meadors, P., Lamson, A., Swanson, M., White, M., & Sira, N. (2010). Secondary traumatization in pediatric healthcare providers: Compassion fatigue, burnout, and secondary traumatic stress. OMEGA: Journal of Death and Dying, 60(2), 103–128. doi:10.2190/OM.60.2.a
Mellin, E. A., Hunt, B., & Nichols, L. M. (2011). Counselor professional identity: Findings and implications for counseling and interprofessional collaboration. Journal of Counseling & Development, 89, 140–147. doi:10.1002/j.1556-6678.2011.tb00071.x
Merriman, J. (2015). Enhancing counselor supervision through compassion fatigue education. Journal of Counseling & Development, 93, 370–378. doi:10.1002/jcad.12035
Meyers, L. (2017, June 12). Illuminate closing: Less talk, more action. Counseling Today, Online Exclusives. Retrieved from https://ct.counseling.org/2017/06/illuminate-closing-less-talk-action/
Myers, J. E., Sweeney, T. J., & Witmer, J. M. (2000). The Wheel of Wellness counseling for wellness: A holistic
model for treatment planning. Journal of Counseling & Development, 78, 251–266.
doi:10.1002/j.1556-6676.2000.tb01906.x
Nolen-Hoeksema, S., Wisco, B. E., & Lyubomirsky, S. (2008). Rethinking rumination. Perspectives on Psychological Science, 3, 400–424. doi:10.1111/j.1745-6924.2008.00088.x
O’Brien, J. L., & Haaga, D. A. F. (2015). Empathic accuracy and compassion fatigue among therapist trainees. Professional Psychology: Research and Practice, 46, 414–420. doi:10.1037/pro0000037
Pain, R., & Smith, S. J. (Eds.). (2008). Fear: Critical geopolitics and everyday life. New York, NY: Routledge/Taylor & Francis Group.
Petersen-Smith, K. (2015). Black Lives Matter: A new movement takes shape. International Socialist Review, 96. Retrieved from http://isreview.org/issue/96/black-lives-matter
Ratts, M. J. (2009). Social justice counseling: Toward the development of a “fifth force” among counseling paradigms. The Journal of Humanistic Counseling, Education, and Development, 48(2), 160–172.
doi:10.1002/j.2161-1939.2009.tb00076.x
Ratts, M. J., D’Andrea, M., & Arredondo, P. (2004). Social justice counseling: “Fifth force” in the field. Counseling Today, 47, 28–30.
Robino, A., & Pignato, L. (2017, February). Global compassion fatigue: An ethical duty for awareness and action. Paper presented at the Virginia Association for Counselor Education and Supervision (VACES) Conference, Norfolk, VA.
Rogers, C. R. (1961). On becoming a person: A therapist’s view of psychotherapy. Boston, MA: Houghton Mifflin.
Roland, C. B. (2016, November 10). ACA president issues post-election statement of support. Retrieved from https://www.counseling.org/news/updates/2016/11/10/aca-president-issues-post-election-statement-of-support
Roysircar, G. (2009). The big picture of advocacy: Counselor, heal society and thyself. Journal of Counseling & Development, 87, 288–294. doi:10.1002/j.1556-6678.2009.tb00109.x
Sansbury, B. S., Graves, K., & Scott, W. (2015). Managing traumatic stress responses among clinicians: Individual and organizational tools for self-care. Trauma, 17(2), 114–122. doi:10.1177/1460408614551978
Schlenger, W. E., Caddell, J. M., Ebert, L., Jordan, B. K., Rourke, K. M., Wilson, D., . . . Kulka, R. A. (2002). Psychological reactions to terrorist attacks: Findings from the national study of Americans’ reactions to September 11. JAMA: Journal of the American Medical Association, 288, 581–588. doi:10.1001/jama.288.5.581
Schuschke, J., & Tynes, B. M. (2016). Online community empowerment, emotional connection, and armed love in the Black Lives Matter Movement. In S. Y. Tettegah (Ed.), Emotions, technology, and social media (pp. 25–47). San Diego, CA: Academic Press.
Schuster, M. A., Stein, B. D., Jaycox, L. H., Collins, R. L., Marshall, G. N., Elliott, M. N., . . . Berry, S. H. (2001). A national survey of stress reactions after the September 11, 2001, terrorist attacks. The New England Journal of Medicine, 345, 1507–1512. doi:10.1056/NEJM200111153452024
Scott, J. T., & Maryman, J. (2016). Using social media as a tool to complement advocacy efforts. Global Journal of Community Psychology Practice, 7(1S), 1–22. doi:10.7728/0701201603
Solomon, J. (2007). Metaphors at work: Identity and meaning in professional life. Retrieved from http://thegoodproje
ct.org/pdf/JSolomon-Metaphors-at-Work-Manuscript-Nov-2007.pdf
Sorenson, C., Bolick, B., Wright, K., & Hamilton, R. (2016). Understanding compassion fatigue in healthcare providers: A review of current literature. Journal of Nursing Scholarship, 48, 456–465. doi:10.1111/jnu.12229
Stebnicki, M. A. (2007). Empathy fatigue: Healing the mind, body, and spirit of professional counselors. American Journal of Psychiatric Rehabilitation, 10, 317–338. doi:10.1080/15487760701680570
Tillman, D. R., Dinsmore, J. A., Chasek, C. L., & Hof, D. D. (2013). The use of social media in counselor education. In Ideas and Research you can use: VISTAS 2013. Retrieved from http://www.counseling.org/docs/default-source/vistas/the-use-of-social-media-in-counselor-education.pdf?sfvrsn=370433a5_10
Weiss, D. S. (2007). The Impact of Event Scale—Revised. Retrieved from http://www.emdrhap.org/co
ntent/wp-content/uploads/2014/07/VIII-E_Impact_of_Events_Scale_Revised.pdf
Wester, K. L., Trepal, H. C., & Myers, J. E. (2009). Wellness of counselor educators: An initial look. The Journal of Humanistic Counseling, Education, and Development, 48, 91–109. doi:10.1002/j.2161-1939.2009.tb00070.x
Yager, G. G., & Tovar-Blank, Z. G. (2007). Wellness and counselor education. The Journal of Humanistic Counseling, Education, and Development, 46(2), 142–153. doi:10.1002/j.2161-1939.2007.tb00032.x
Yep, R. (2017, December 21). ACA weighs in on wording restrictions at the Centers for Disease Control [Blog post]. Retrieved from https://www.counseling.org/news/aca-blogs/aca-government-affairs-blog/aca-government-affairs-blog/2017/12/20/aca-weighs-in-on-wording-restrictions-at-the-centers-for-disease-control
Ariann Evans Robino, NCC, is an assistant professor at Nova Southeastern University. Correspondence can be addressed to Ariann Robino, 3301 College Avenue, Maltz Building, Fort Lauderdale, FL 33314, arobino@nova.edu.
Nov 28, 2019 | Volume 9 - Issue 4
Nesime Can, Joshua C. Watson
Scholars have described compassion fatigue as the result of chronic exposure to clients’ suffering and traumatic stories. Counselors can struggle when they experience compassion fatigue because of various reasons. As such, an exploration of factors predictive of compassion fatigue may help counselors and supervisors buffer adverse effects. Utilizing a hierarchical linear regression analysis, we examined the association between wellness, resilience, supervisory working alliance, empathy, and compassion fatigue among 86 counselors-in-training (CITs). The research findings revealed that resilience and wellness were significant predictors of compassion fatigue among CITs, whereas empathy and supervisory working alliance were not. Based on our findings, counselor educators might consider enhancing their current training programs by including discussion topics about wellness and resilience, while supervisors consider practicing wellness and resilience strategies in supervision and developing interventions designed to prevent compassion fatigue.
Keywords: compassion fatigue, counselors-in-training, wellness, resilience, supervisory working alliance
Balancing self-care and client care can be a challenge for many counselors. When counselors neglect self-care, they can become vulnerable to several issues, including increased anxiety, distress, burnout, and compassion fatigue (Ray, Wong, White, & Heaslip, 2013). Counselors might be especially prone to experiencing compassion fatigue because they repeatedly hear traumatic stories and clients’ suffering in sessions (Skovholt & Trotter-Mathison, 2016). This phenomenon is likely pronounced among counselors-in-training (CITs), as lack of experience, skillset, knowledge, and support can lead to struggles when working with clients (Skovholt & Trotter-Mathison, 2016). Coupled with the increased anxiety, distress, and disappointment, CITs can experience compassion fatigue early in their career development, which can lead to exhaustion, disengagement, and a decline in therapeutic effectiveness (Rønnestad & Skovholt, 2013). At this developmental stage, negative experiences can lead to feelings of doubt and a lack of confidence among CITs and potentially lead to career dissatisfaction. Therefore, it is essential and necessary to better understand the predictive factors of compassion fatigue among CITs to prevent its early onset.
Compassion Fatigue in Counseling
Counselors listening to their clients’ fear, pain, and suffering can feel similar emotions. Figley (1995) defined this experience as compassion fatigue; it also can be defined as the cost of caring (Figley, 2002). Whether working in mental health agencies, schools, or hospital settings, counselors experience compassion fatigue because of exposure to large caseloads, painful stories, and lack of support and resources (Skovholt & Trotter-Mathison, 2016). Despite this exposure, counselors are expected to place their personal feelings aside and provide the best treatment possible in response to the presenting issues and needs of their clients (Figley, 2002; Ray et al., 2013; Turgoose, Glover, Barker, & Maddox, 2017). Maintaining this sense of detached professionalism has its costs, as a number of counselors find themselves at risk for experiencing physical, mental, and emotional exhaustion, as well as feelings of helplessness, isolation, and confusion—a situation collectively referred to as compassion fatigue (Eastwood & Ecklund, 2008; Thompson, Amatea, & Thompson, 2014).
Merriman (2015b) stated that ongoing compassion fatigue negatively impacts counselors’ health as well as their relationships with others. Additionally, compassion fatigue can lead to a lack of empathy toward clients, decrease in motivation, and performance drop in effectiveness, making even the smallest tasks seem overwhelming (Merriman, 2015b). When this occurs, counselors can project their anger on others, develop trust issues, and experience feelings of loneliness (Harr, 2013). Therefore, the demands of the counseling profession can affect many counselors’ wellness and potentially could hurt the quality of client care provided (Lawson, Venart, Hazler, & Kottler, 2007; Merriman, 2015a). Further, counselors experiencing compassion fatigue might have difficulties making effective clinical decisions and potentially be at risk for harming clients (Eastwood & Ecklund, 2008). Consequently, scholars appear to agree that compassion fatigue is an occupational hazard that mental health care professionals need to address (Figley, 2002; Merriman, 2015a).
Factors Associated With Compassion Fatigue
Many researchers have studied the relationships between compassion fatigue and various constructs, such as empathy, gender, mindfulness, support, and wellness (e.g., Beaumont, Durkin, Martin, & Carson, 2016; Caringi et al., 2016; Ray et al., 2013; Sprang, Clark, & Whitt-Woosley, 2007; Turgoose et al., 2017). Researchers conducted most of these studies among novice and veteran mental health professionals. Scant research among CITs exists. Our research attempts to fill this gap by exploring factors affecting CITs given their unique position as both students and emerging professionals. The following review of the literature supports the inclusion of predictor variables used in this study.
Empathy and Compassion Fatigue
One of the most widely studied concepts across various cultures is empathy, as it has been determined to be one of the major precipitants of compassion fatigue (Figley, 1995). However, findings in the literature regarding the association between compassion fatigue and empathy remain mixed (e.g., MacRitchie & Leibowitz, 2010; O’Brien & Haaga, 2015; Wagaman, Geiger, Shockley, & Segal, 2015). For instance, O’Brien and Haaga (2015) compared trait empathy and empathic accuracy with compassion fatigue after showing a videotaped trauma self-disclosure among therapist trainees (a combined group of advanced and novice graduate students) and non-therapists. The results indicated that there was no significant association between participants’ levels of compassion fatigue and empathy scores. However, MacRitchie and Leibowitz (2010) found a significant relationship between compassion fatigue and empathy after exploring the relation of these variables on trauma workers whose clients were survivors of violent crimes. The mixed results of these previous studies suggest further research is needed to understand better the relationship between empathy and compassion fatigue and how this relationship impacts counseling practice.
Supervisory Working Alliance and Compassion Fatigue
Although reviewed literature addressed studies suggesting supervision and support are related factors to compassion fatigue, research on this relationship is still insufficient. Kapoulitsas and Corcoran (2015) conducted a study and found that a positive supervisory relationship has a significant role in developing resilience and reducing compassion fatigue among counselors. Knight (2010) also found that students uncomfortable talking with their supervisor reported a higher risk for developing compassion fatigue. Additionally, organizational support appears to reduce compassion fatigue, whereas an absence of support increases practitioners’ and interns’ risk of developing compassion fatigue symptoms (Bride, Jones, & MacMaster, 2007). Given the intense need for support and guidance CITs need during their initial work with clients, it is expected that those students who do not actively work with their supervisors can struggle and be more vulnerable for compassion fatigue.
Wellness, Resilience, and Compassion Fatigue
Although counselors are encouraged to practice self-care activities to continue to enhance personal well-being (American Counseling Association [ACA], 2014; Coaston, 2017; H. L. Smith, Robinson, & Young, 2008), not all CITs can balance caring for self and others. When CITs do not receive training in the protective factors for compassion fatigue, they risk becoming more vulnerable to violating the ACA code of ethics (Merriman, 2015a; Merriman, 2015b). Kapoulitsas and Corcoran (2015) and Skovholt and Trotter-Mathison (2016) highlighted the importance of resilience and self-care activities as protective factors for compassion fatigue. Wood et al. (2017) evaluated the effectiveness of a mobile application called Provider Resilience to reduce compassion fatigue scores of mental health professionals. After a month of utilization, the results indicated that the application was effective in reducing compassion fatigue. Additionally, Lawson and Myers (2011) conducted a study with professional counselors to examine counselor wellness about compassion fatigue and found a negative correlation between total wellness scores and compassion fatigue scores. As CITs balance academic, family, and work demands, the probability of decreased wellness and a corresponding increase in compassion fatigue exists.
Compassion Fatigue Among CITs
Most CITs are often unable to master all counselor competencies (Rønnestad & Skovholt, 2013), and therefore they might not know how to deal with possible stressors and the emotional burden of their work (Star, 2013). Although they are learning counseling skills to provide the best care possible to clients, CITs may find themselves working with seriously troubled or traumatized clients without obtaining quality supervision and support (Skovholt & Trotter-Mathison, 2016). Lack of skills and resources increases the likelihood of CITs developing compassion fatigue (Merriman, 2015b). However, there is a lack of focus in compassion fatigue education on preparing CITs to manage compassion fatigue symptoms (Merriman, 2015a). Although scholars have examined compassion fatigue among counselors, there is still a dearth of studies investigating the level of compassion fatigue among CITs and addressing its protective factors within this population (Beaumont et al., 2016; Blount, Bjornsen, & Moore, 2018; Thompson et al., 2014). Subsequently, further research is needed to understand better potential protective factors that can be enhanced to offset the negative impact of compassion fatigue on CITs and the counseling process. Thus, with this study, we aimed at assessing the relationship between resilience, wellness, supervisory working alliance, empathy, and compassion fatigue among CITs in the United States. To accomplish this goal, we sought to answer the following research questions: (1) What is the prevalence of compassion fatigue among CITs? and (2) Do empathy, supervisory working alliance, resilience, and wellness significantly predict levels of compassion fatigue among CITs?
Method
Participants
Participants recruited for this study consisted of master’s-level counseling students who are at least 18 years of age and enrolled in an internship course in the United States through mostly professional listservs (e.g., Counselor Education and Supervision Network Listserv [CESNET-L], Texas Association for Counselor Education and Supervision Network Listserv [TACESNET-L], Counseling Graduate Student Network [COUNSGRADS]). Because of the impossibility of knowing how many individuals received the email invitation, we were unable to calculate and determine a response rate. Accordingly, a total of 114 CITs initially agreed to participate in this study. Before data analysis, we inspected the data set for possible entry errors and missing data. After the inspection, we excluded 28 participants from all subsequent data analyses resulting in the reduced sample of 86 CITs used to address our research questions. Overall, the sample consisted of 78 female (90.7%) and eight male (9.3%) participants, and the mean age of the participants was 32.89 years (SD = 9.72) with participants’ ages ranging between 21 and 62 years. Participants were from diverse ethnic and racial backgrounds, with the sample consisting of White (n = 48, 55.8%), Hispanic/Latino (n = 18, 20.9%), Black/African American (n = 12, 14.0%), and Asian (n = 5, 5.8%) CITs. Three participants (3.5%) listed their ethnicities as “other” when providing demographic information. Participants reported their program enrollment as follows: clinical mental health counseling program (n = 47, 54.7%); school counseling program (n = 23, 26.7%); marriage, couple, and family counseling program (n = 4, 4.7%); college counseling and student affairs program (n = 3, 3.5%); addiction counseling program (n = 2, 2.3%); and other programs (n = 7, 8.1%). Additionally, most of the participants (n = 73, 84.9%) reported enrollment in a CACREP-accredited program with the remaining participants (n = 13, 15.1%) enrolled in a non–CACREP-accredited program.
Procedure
Upon receiving institutional review board approval, we recruited participants from different institutions with the primary researcher contacting professional colleagues at various departments to disseminate the online survey link to potential participants during the 2017 summer and fall semesters. We also recruited participants through professional listservs (e.g., CESNET-L, TACESNET-L, COUNSGRAD), with listserv participants being provided the same informed consent and survey link through a secure website. The survey completion process took approximately 15–20 minutes.
Measures
We used the following self-administered survey questionnaires and a separate demographic data sheet in our data collection.
Professional Quality of Life Scale (ProQOL). This scale is designed to measure the mental and emotional consequences of working with individuals who experienced trauma or painful events (Stamm, 2010). The ProQOL includes two main traits, Compassion Satisfaction (positive) and Compassion Fatigue (negative). Compassion Satisfaction is related to the joy individuals develop when they do their work well (Stamm, 2010). Compassion Fatigue consists of two subscales: Secondary Traumatic Stress (STS) and Burnout. Scholars have defined STS as an emotional state that occurs when an individual becomes upset or traumatized as a result of their exposure to victim experiences (Figley, 2002). The second part of Compassion Fatigue is Burnout, which is a multidimensional syndrome related to the social work environment. Burnout could be related to work overload, lack of control, insufficient rewards, unfairness, and value conflict at a workplace (Skovholt & Trotter-Mathison, 2016).
The ProQOL is a 30-item Likert-type self-report assessment with responses of never, rarely, sometimes, often, and very often for each item. A sample item is “I feel depressed because of the traumatic experiences of the people I [help].” This assessment has 10 questions per each of three main scales measuring separate constructs. However, the Compassion Fatigue scale includes two of these constructs, which are the Burnout and the STS scales. According to Stamm (2010), the ProQOL has good construct validity, as researchers have noted its efficacy in over 200 published articles. Finally, alpha coefficient values for the Burnout and STS scales were .75 and .81, respectively (Stamm, 2010), and are similar (.72 and .79) to the Cronbach’s alpha values from the current study presented in Table 1.
Table 1
Descriptive Statistics of the Study Variables (N = 86)
|
|
|
|
Range |
|
|
| Variable |
M |
SD |
Min |
Max |
Skew |
α |
| Compassion Fatigue |
41.48 |
8.03 |
22 |
60 |
.19 |
|
|
BO |
21.34 |
4.38 |
12 |
32 |
– |
.72 |
|
STS |
20.14 |
4.96 |
10 |
38 |
– |
.79 |
| Empathy |
21.86 |
4.12 |
9 |
28 |
-.51 |
.80 |
| Supervisory Working Alliance |
5.82 |
.97 |
2.16 |
7 |
1.26 |
|
|
CF |
6.65 |
1.30 |
2.17 |
8.17 |
– |
.90 |
|
R |
5.80 |
.96 |
2.33 |
7 |
– |
.93 |
| Resilience |
3.43 |
.79 |
1 |
4.67 |
-.74 |
.89 |
| Wellness |
47.58 |
6.23 |
27 |
56 |
-1.39 |
.86 |
|
|
|
|
|
|
|
|
|
|
|
|
Note. BO = Burnout; STS = Secondary Traumatic Stress; CF = Client Focus; R = Rapport
Interpersonal Reactivity Index (IRI). Davis (1983) developed the IRI to measure the reactions of a person to other individuals’ observed experiences. The 28-item instrument has four subscales: Empathic Concern, Perspective Taking, Fantasy, and Personal Distress (Davis, 1983). Researchers report separate subscale scores, as a total score for the instrument has not been recommended (Davis, 1983). In this study, we only used the Empathic Concern subscale to collect data regarding empathy scores of CITs.
Davis (1983) described empathic concern as an emotional response, such as compassion and sympathy, to someone else in need. The 7-item subscale is a self-report assessment with a 5-point Likert-type scale, ranging from Does not describe me well to Describes me very well. A sample item is “I am often quite touched by things that I see happen.” An alpha coefficient of .77 has been reported for the Empathic Concern subscale (Péloquin & Lafontaine, 2010), while the Cronbach’s alpha value of the IRI in the current study was .80.
Supervisory Working Alliance Inventory: Trainee Form (SWAI-T). Efstation, Patton, and Kardash (1990) developed this inventory to measure supervisees’ perceptions about the effectiveness of the working relationship with their supervisors, and we used the SWAI-T to measure the construct of the supervisory working alliance. With a total of 19 items, the self-report assessment includes a 7-point Likert-type scale with responses ranging from almost never to almost always. A sample item is “When correcting my errors with the client, my supervisor offers alternative ways of intervening with the client.” The SWAI-T has two subscales—Client Focus and Rapport—and the Cronbach alpha coefficients of these scales were .77 and .90, respectively (Efstation et al., 1990). For the current study, we calculated Cronbach alpha values of .90 for the Client Focus subscale and .93 for the Rapport subscale. Because some researchers have found high correlations between these two subscales, they decided to combine them in their studies (e.g., Ganske, 2007; White & Queener, 2003). Therefore, in this study, after conducting a correlation analysis with the subscale scores, we also chose to combine subscales as the results of subscale scores were highly correlated.
Brief Resilience Scale (BRS). The BRS was developed to measure a person’s ability to recover from stress and cope with challenging situations (B. W. Smith et al., 2008). The BRS is used to measure the construct of resilience. As a 6-item self-report assessment, the BRS includes a 5-point Likert-type scale with responses ranging from strongly disagree to strongly agree. A sample item is “I usually come through difficult times with little trouble.” B. W. Smith and colleagues (2008) reported that the Cronbach’s alpha values of the BRS range from .80 to .91, and we calculated a Cronbach alpha of .89 for the current study.
Flourishing Scale (FS). The FS was designed to measure individuals’ self-perceived success in areas like optimism and relationships (Diener et al., 2010) and used to measure the construct of wellness in this study. The FS is an 8-item self-report assessment with a 7-point Likert-type scale with responses ranging from strongly disagree to strongly agree (Diener et al., 2010). A sample item is “I lead a purposeful and meaningful life.” Diener and colleagues (2010) reported moderately high reliability with a .87 Cronbach’s alpha coefficient, and in the current study, the FS had a Cronbach alpha of .86.
Data Analysis
Statistical power analysis. We used an a priori type of the G*Power to set the minimum number of participants needed to detect statistical power for this research design. Based on an alpha of .05, a power level of .90, and four predictors (Faul, Erdfelder, Buchner, & Lang, 2009), the computation results suggested that a minimum of 73 participants was required to detect statistical significance with at least a moderate size effect (.15). We had 86 participants, suggesting adequate power.
Preliminary analyses. We analyzed all data using the Statistical Package for the Social Sciences, Version 20 (SPSS; IBM Corporation, 2011). Before addressing our stated research questions, we cleaned the dataset and addressed missing data. We did not observe any pattern between missing data points. Therefore, the type of missing data was completely random, which was addressed using the series of mean function within the SPSS. Next, we calculated descriptive statistics and alpha coefficients for each scale used in the study (see Table 1). Before performing hierarchical regression analyses, we tested all associated model assumptions. First, we examined study variables based on their types and concluded each utilized a continuous scale. We then assessed normality with the Shapiro-Wilk test of normality (W > .05), indicating data was normally distributed for the dependent variable. To identify outliers, we examined boxplots. Although there were a few mild outliers, no extreme scores were detected. We assessed linearity and homoscedasticity through inspection of standardized residual plots. To assess for the assumption of multicollinearity, we examined the correlation matrix of study variables to determine if any correlated highly. According to Field (2013), correlations above .80 are considered high and may indicate the presence of multicollinearity. In the present study, none of the correlation coefficients were above .50 (see Table 2). Collectively, these findings indicated no evidence suggesting any of the model assumptions had been violated. As a result, the dataset was deemed appropriate for analysis using a hierarchical regression design.
Primary analysis. Descriptive statistics were calculated to organize the data by producing means, mode, median, standard deviations, and minimum and maximum scores for the study variables (Field, 2013). Individually, we reviewed descriptive statistics for the compassion fatigue variable, and results were reported to address the first research question. Next, we performed a three-step hierarchical linear regression to address the second research question.
Table 2
Intercorrelations for Scores on the Study Variables
|
Variable |
1 |
2 |
3 |
4 |
5 |
| 1. |
ProQOL-CF |
– |
|
|
|
|
| 2. |
SWAIT-T |
.04 |
– |
|
|
|
| 3. |
IRI-EC |
-.06 |
.04 |
– |
|
|
| 4. |
BRS |
-.47** |
-.09 |
-.11 |
– |
|
| 5. |
FS |
-.45** |
.12 |
.25* |
.35** |
– |
Note. N = 86; ProQOL = Professional Quality of Life (Compassion Fatigue [CF] subscale score is presented); IRI = Interpersonal Reactivity Index (Empathic Concern [EC] subscale score is presented); SWAI-T = Supervisory Working Alliance Inventory: Trainee Form; BRS = Brief Resilience Scale; FS = Flourishing Scale.
*p < .05. **p < .01.
Results
Compassion fatigue scores of CITs represent the sum of scores of all items on the STS and Burnout subscales. According to the ProQOL administration manual (Stamm, 2010), individuals scoring below 22 may indicate little or no issues with Burnout and STS, while scores between 23 and 41 indicate moderate levels of Burnout and STS, and scores above 42 indicate higher levels of Burnout and STS. For this sample, participants’ Burnout scores ranged from 12 to 32 with a mean of 21.34 (SD = 4.38), and STS scores ranged from 10 to 38 with a mean of 20.14 (SD = 4.96). These results indicated a low risk of both Burnout and STS among CITs.
To address the second research question, we performed a three-step hierarchical linear regression analysis. With this analysis, we aimed to assess the association between resilience, wellness, supervisory working alliance, empathy, and compassion fatigue. We chose to implement a hierarchical multiple regression analysis because scholars previously have highlighted the essential relationship between empathy, supervision, and compassion fatigue (Figley, 2002; MacRitchie & Leibowitz, 2010). In the first step, empathy scores entered the model as a predictor variable, as Figley (1995) stated that empathy is one of the main factors contributing to compassion fatigue. However, among this sample, we found that empathy was not a significant predictor of compassion fatigue: F(1, 84) = .2, p = .66 , R2 = .002 (adjusted R2 = -.01). Then, we added supervisory working alliance scores to the model in the second step, as both Knight (2010) and Miller and Sprang (2017) emphasized the importance of supervisory support for mental health practitioners. Results revealed that the supervisory working alliance variable also was not a significant predictor of compassion fatigue: F(2, 83) = .16, p = .85, R2 = .004 (adjusted R2 = -.02). In the third step, resilience and wellness scores were entered into the model to determine whether these variables significantly improved the amount of explained variance in compassion fatigue. Results showed that this combination of variables significantly predicted 26% of the variance in compassion fatigue: F(4, 81) = 8.57, p < .001, R2 = .30. Therefore, it was concluded that CITs with greater wellness and resilience reported developing less compassion fatigue (see Table 3).
Table 3
Hierarchical Regression Analysis Results for Variables Predicting Compassion Fatigue
| Variables |
B |
SEB |
β |
R2 |
ΔR2 |
| Step 1 |
|
|
|
|
.002 |
-.01 |
| Empathy |
-.09 |
.21 |
-.05 |
|
|
| Step 2 |
|
|
|
|
.004 |
-.02 |
| Empathy |
-.10 |
.21 |
-.05 |
|
|
| SWA |
.33 |
.91 |
.04 |
|
|
| Step 3 |
|
|
|
|
.30* |
.26 |
| Empathy |
-.03 |
.19 |
-.02 |
|
|
| SWA |
.36 |
.78 |
.04 |
|
|
| Wellness |
-.39 |
.14 |
-.30* |
|
|
| Resilience |
-3.66 |
1.05 |
-.36* |
|
|
Note. SWA = Supervisory Working Alliance
*p < .05.
Discussion
In this study, CITs reported having a low risk of compassion fatigue. When we examined the Burnout and STS scores separately, the main contributors of compassion fatigue (Stamm, 2010), both subscale scores indicated participants having a low risk for STS and Burnout. This finding is similar to results found by Beaumont and colleagues (2016) in their study of compassion fatigue, burnout, self-compassion, and well-being relationships among student counselors and student cognitive behavioral psychotherapists. According to their research findings, a total of 54 student participants reported high scores on self-compassion and well-being and reported less compassion fatigue and burnout (Beaumont et al., 2016).
One of the goals of this study was to seek understanding of whether wellness and resilience explain a statistically significant amount of variance in compassion fatigue among CITs after accounting for empathy and supervisory working alliance. The results indicated that empathy and supervisory working alliance were not significant predictors of compassion fatigue. Regarding empathy and compassion fatigue relation results, the findings of this study did not support Figley’s (1995) assumption of empathy as one of the main contributors to compassion fatigue. This result also is inconsistent with Wagaman and colleagues’ (2015) results indicating a significant association between empathy and compassion fatigue among social workers. However, current results aligned with those studies that found no correlation between empathy and compassion fatigue (e.g., O’Brien & Haaga, 2015; Thomas & Otis, 2010). An explanation of the variability between this inquiry and previous studies might lie with the difference between participants’ field of study and measurement differences. Also, none of the previous studies used CITs solely as their sample, nor used a similar way to measure the construct of empathy. Additionally, CITs would have less experience working with clients compared to experienced counselors, and thus less time for feelings of compassion fatigue to build.
Although scholars addressed the importance of supervision and supervisory working alliance to help prevent compassion fatigue (Kapoulitsas & Corcoran, 2015; Merriman, 2015a), this study’s results indicated supervisory working alliance was not a significant predictor of compassion fatigue among CITs. Like current results, Ivicic and Motta (2017) and Williams, Helm, and Clemens (2012) found no statistically significant association between supervisory working alliance and compassion fatigue among mental health practitioners. It is noteworthy that these studies highlighting the importance of supervision and the supervisory relationship are qualitative in design, and participants did not consist solely of CITs. Additionally, their results emphasized the importance of supervision as support to counter the negative impact of trauma exposure (Kapoulitsas & Corcoran, 2015; Ling, Hunter, & Maple, 2014). According to the current study results, CITs did not report experiencing a high level of compassion fatigue. This finding could be interpreted as CITs not yet feeling the need for supervisory support to help with compassion fatigue.
Results also indicated that resilience and wellness were significant predictors of compassion fatigue among CITs. In other words, when reflecting on both the regression and correlation results, CITs with greater resilience and wellness reported lower scores of compassion fatigue and these results were consistent with Tosone, Minami, Bettmann, and Jasperson’s (2010) research findings. Regarding a wellness and compassion fatigue relationship, Beaumont and colleagues (2016) conducted a study with student counselors and student cognitive behavioral psychotherapists. The results of Beaumont et al.’s study revealed that individuals with high scores of self-compassion and well-being reported having less compassion fatigue and burnout. Thomas and Morris (2017) also highlighted the significance of self-care and well-being not only for preventing and helping to manage the potentially damaging impact of practice, but also for facilitating the counselor’s personal and professional growth.
Implications for Counselor Educators and Supervisors
The research findings provide data-driven results regarding compassion fatigue among CITs that have meaningful implications for counselor educators and supervisors. Present study results revealed that CITs indicated experiencing a low risk of compassion fatigue. However, raising awareness on this issue may still help CITs as a preventative measure to cope with possible compassion fatigue experience in the future. To address this issue, counselor educators may consider raising awareness on this topic by reviewing current counseling program curricula to add discussion questions related to compassion fatigue and its empirically predictive factors—wellness and resilience. Roach and Young (2007) stated that students in counseling programs reported group counseling, counseling techniques, legal and ethical issues, practicum, and wellness courses as contributing most to their knowledge and skills regarding wellness. Therefore, counselor educators might use different assignments, including group discussions, projects, and role-playing exercises, to open a discussion about the compassion fatigue phenomenon and the relation with its predictive factors and these courses. Counselor educators may also use the ProQOL scale as an assignment in an assessment and testing course to inform CITs about how to use this instrument as a self-monitoring aid. For example, professional counselors may feel overwhelmed because of working with trauma survivors after graduation and start noticing compassion fatigue symptoms in themselves. These individuals may self-administer the ProQOL scale to determine whether they have developed compassion fatigue. Additionally, in a practicum or an internship course, CITs may fill out the ProQOL as part of their continuing personal wellness plan by comparing personal results over time and sharing their thoughts and reflections about the results.
Supervisors need to find ways to raise awareness of compassion fatigue and its protective factors with CITs. For instance, during internship experience, supervisors may develop a site training including compassion fatigue awareness for CITs, as CITs should be prepared for the possible emotional and psychological consequences in working with trauma survivors. Student counselors also should be encouraged to advocate for themselves when they notice symptoms of compassion fatigue. Supervisors might consider the administration of the ProQOL scale regularly to assess both organizational and individual risks (Newell & MacNeil, 2010). Additionally, supervisors can use the ProQOL scale with their supervisees to start a conversation about compassion fatigue. Although the ProQOL is not a diagnostic test, the 30-item self-report scale can be utilized readily as a conversation starter in supervision sessions.
The results suggested that empathy and supervisory working alliance did not predict CITs’ compassion fatigue level. However, wellness and resilience are significantly related to contributing to it. Therefore, both counselor educators and supervisors might consider enhancing CITs’ resilience and wellness a worthwhile endeavor. For example, Miller and Sprang (2017) developed a component-based practice and supervision model to reduce compassion fatigue for use in training, supervision, and clinical practice. A tool like this one can be added to existing training curricula and supervision practice to improve CITs’ resilience and wellness.
Limitations
The results of this study aim to provide greater clarity regarding the predictive factors of compassion fatigue among CITs. However, interpretation of results should take into consideration the limitations that emerged because of uncontrollable influences and choices we made. The study was limited in its ability to represent all CITs throughout the United States, as we utilized a convenience sampling approach. Additionally, we gathered data through self-report questionnaires, which introduce the possibility of response bias in the findings. Although we assumed participants answered each question honestly, they might not have been honest in their responses because of the fear of being perceived as weak or less competent. It is important to note that being in an internship class might also increase participants’ interest in the profession as they currently are engaged in the practice of counseling. Therefore, participants might have had a higher level of enthusiasm and reported less compassion fatigue. Also, individuals who suffer from compassion fatigue might have preferred not to respond to these items. Finally, although participants were enrolled in an internship class, each participant may have different numbers of hours of client experience.
Future Directions for Research
Additional research should be conducted to expand and clarify the current research findings of compassion fatigue among CITs. A phenomenological study using a qualitative research method is recommended to expand the findings of this current study. Future researchers may use the ProQOL scale to assess CITs’ level of compassion fatigue and then conduct interviews with the volunteer participants reporting a higher level of compassion fatigue to better understand CITs’ experience with compassion fatigue and its contributing factors. The data collected through a qualitative study may provide greater insight into the phenomenon of compassion fatigue among CITs. Additionally, researchers can replicate the present study with early-career counselors who have recently graduated, because of the noted intensity of those first years after graduation (Skovholt & Trotter-Mathison, 2016). Therefore, future researchers exploring novice counselors’ experiences with compassion fatigue will help counselor educators and supervisors better understand when counselors may start developing compassion fatigue symptoms, as well as how they cope with the symptoms.
Conclusion
CITs may struggle when they continuously hear painful stories of clients because of a lack of experience, skillset, or support (Skovholt & Trotter-Mathison, 2016). Researchers have described this experience as compassion fatigue. With this study, we aimed to provide a better understanding of the predictive factors of compassion fatigue among CITs. Using data-driven research results to determine ways to work with CITs on compassion fatigue and its predictive factors can be beneficial in preventing compassion fatigue symptoms from an early onset. CITs may take precautionary measures to ensure they remain enthusiastic and energized by the work they do. Further, implications of the current study may help CITs start their professional careers better prepared to provide their clients with the optimal care needed throughout the counseling relationship by minimizing compassion fatigue.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
American Counseling Association. (2014). ACA code of ethics. Alexandria, VA: Author.
Beaumont, E., Durkin, M., Martin, C. J. H., & Carson, J. (2016). Measuring relationships between self-compassion, compassion fatigue, burnout and well-being in student counsellors and student cognitive behavioural psychotherapists: A quantitative survey. Counselling & Psychotherapy Research, 16, 15–23. doi:10.1002/capr.12054
Blount, A. J., Bjornsen, A. L., & Moore, M. M. (2018). Work values, occupational engagement, and professional quality of life in counselors-in-training: Assessments in a constructivist-based career counseling course. The Professional Counselor, 8, 60–72. doi:10.15241/ajb.8.1.60
Bride, B. E., Jones, J. L., & MacMaster, S.A. (2007). Correlates of secondary traumatic stress in child protective services workers. Journal of Evidence-Based Social Work, 4(3/4), 69–80. doi:10.1300/J394v04n03_05
Caringi, J. C., Hardiman, E. R., Weldon, P., Fletcher, S., Devlin, M., & Stanick, C. (2017). Secondary traumatic stress and licensed clinical social workers. Traumatology, 23(2), 186–195. doi:10.1037/trm0000061
Coaston, S. C. (2017). Self-care through self-compassion: A balm for burnout. The Professional Counselor, 7, 285–297. doi:10.15241/scc.7.3.285
Davis, M. H. (1983). Measuring individual differences in empathy: Evidence for a multidimensional approach. Journal of Personality and Social Psychology, 44, 113–126. doi:10.1037/0022-3514.44.1.113
Diener, E., Wirtz, D., Tov, W., Kim-Prieto, C., Choi, D., Oishi, S., & Biswas-Diener, R. (2010). New measures of well-being: Flourishing and positive and negative feelings. Social Indicators Research, 39, 247–266. doi:10.1007/978-90-481-2354-4_12
Eastwood, C. D., & Ecklund, K. (2008). Compassion fatigue risk and self-care practices among residential treatment center childcare workers. Residential Treatment for Children & Youth, 25, 103–122. doi:10.1080/08865710802309972
Efstation, J. F., Patton, M. J., & Kardash, C. M. (1990). Measuring the working alliance in counselor supervision. Journal of Counseling Psychology, 37, 322–329. doi:10.1037/0022-0167.37.3.322
Faul, F., Erdfelder, E., Buchner, A., & Lang, A.-G. (2009). Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behavior Research Methods, 41, 1149–1160. doi:10.3758/brm.41.4.1149
Field, A. (2013). Discovering statistics using IBM SPSS statistics (4th ed.). Thousand Oaks, CA: SAGE.
Figley, C. R. (Ed.). (1995). Compassion fatigue: Coping with secondary traumatic stress disorder in those who treat the traumatized. New York, NY: Routledge.
Figley, C. R. (Ed.). (2002). Treating compassion fatigue. New York, NY: Brunner-Routledge.
Ganske, K. H. (2007). The relationship between counselor trainee perfectionism and working alliance with supervisor and client. (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3377933)
Harr, C. (2013). Promoting workplace health by diminishing the negative impact of compassion fatigue and increasing compassion satisfaction. Social Work & Christianity, 40, 71–88.
IBM Corporation. (2011). IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: Author.
Ivicic, R., & Motta, R. (2017). Variables associated with secondary traumatic stress among mental health professionals. Traumatology, 23, 196–204. doi:10.1037/trm0000065
Kapoulitsas, M., & Corcoran, T. (2015). Compassion fatigue and resilience: A qualitative analysis of social work practice. Qualitative Social Work: Research and Practice, 14, 86–101. doi:10.1177/1473325014528526
Knight, C. (2010). Indirect trauma in the field practicum: Secondary traumatic stress, vicarious trauma, and compassion fatigue among social work students and their field instructors. The Journal of Baccalaureate Social Work, 15, 31–52.
Lawson, G., & Myers, J. E. (2011). Wellness, professional quality of life, and career-sustaining behaviors: What keeps us well? Journal of Counseling & Development, 89, 163–171. doi:10.1002/j.1556-6678.2011.tb00074.x
Lawson, G., Venart, E., Hazler, R. J., & Kottler, J. A. (2007). Toward a culture of counselor wellness. The Journal of Humanistic Counseling, Education and Development, 46, 5–19. doi:10.1002/j.2161-1939.2007.tb00022.x
Ling, J., Hunter, S. V., & Maple, M. (2014). Navigating the challenges of trauma counselling: How counsellors thrive and sustain their engagement. Australian Social Work, 67, 297–310.
doi:10.1080/0312407X.2013.837188
MacRitchie, V., & Leibowitz, S. (2010). Secondary traumatic stress, level of exposure, empathy and social
support in trauma workers. South African Journal of Psychology, 40, 149–158. doi:10.1177/008124631004000204
Merriman, J. (2015a). Enhancing counselor supervision through compassion fatigue education. Journal of Counseling & Development, 93, 370–378. doi:10.1002/jcad.12035
Merriman, J. (2015b). Prevention-based training for licensed professional counselor interns. Journal of Professional Counseling: Practice, Theory & Research, 42, 40–53.
Miller, B., & Sprang, G. (2017). A components-based practice and supervision model for reducing compassion fatigue by affecting clinician experience. Traumatology, 23, 153–164. doi:10.1037/trm0000058
Newell, J. M., & MacNeil, G. A. (2010). Professional burnout, vicarious trauma, secondary traumatic stress, and compassion fatigue: A review of theoretical terms, risk factors, and preventive methods for clinicians and researchers. Best Practices in Mental Health: An International Journal, 6, 57–68.
O’Brien, J. L., & Haaga, D. A. F. (2015). Empathic accuracy and compassion fatigue among therapist trainees. Professional Psychology: Research and Practice, 46, 414–420. doi:10.1037/pro0000037
Péloquin, K., & Lafontaine, M. (2010). Measuring empathy in couples: Validity and reliability of the
Interpersonal Reactivity Index for couples. Journal of Personality Assessment, 92, 146–157. doi:10.1080/00223890903510399
Ray, S. L., Wong, C., White, D., & Heaslip, K. (2013). Compassion satisfaction, compassion fatigue, work life conditions, and burnout among frontline mental health care professionals. Traumatology, 19, 255–267. doi:10.1177/1534765612471144
Roach, L. F., & Young, M. E. (2007). Do counselor education programs promote wellness in their students? Counselor Education & Supervision, 47, 29–45. doi:10.1002/j.1556-6978.2007.tb00036.x
Rønnestad, M. H., & Skovholt, T. M. (2013). The developing practitioner: Growth and stagnation of therapists and counselors. New York, NY: Routledge.
Skovholt, T. M., & Trotter-Mathison, M. (2016). The resilient practitioner: Burnout and compassion fatigue prevention and self-care strategies for the helping professions (3rd ed.). New York, NY: Routledge.
Smith, B. W., Dalen, J., Wiggins, K., Tooley, E., Christopher, P., & Bernard, J. (2008). The Brief Resilience Scale: Assessing the ability to bounce back. International Journal of Behavioral Medicine, 15, 194–200. doi:10.1080/10705500802222972
Smith, H. L., Robinson, E. H. M., III, & Young, M. E. (2008). The relationship among wellness, psychological distress, and social desirability of entering master’s-level counselor trainees. Counselor Education & Supervision, 47, 96–109. doi:10.1002/j.1556-6978.2007.tb00041.x
Sprang, G., Clark, J. J., & Whitt-Woosley, A. (2007). Compassion fatigue, compassion satisfaction, and burnout: Factors impacting a professional’s quality of life. Journal of Loss and Trauma, 12, 259–280. doi:10.1080/15325020701238093
Stamm, B. H. (2010). The concise ProQOL manual (2nd ed.). Pocatello, ID: ProQOL.org.
Star, K. L. (2013). The relationship between self-care practices, burnout, compassion fatigue, and compassion satisfaction among professional counselors and counselors-in-training. (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3618924)
Thomas, D. A., & Morris, M. H. (2017). Creative counselor self-care. In Ideas and research you can use: VISTAS 2017. Retrieved from https://www.counseling.org/docs/default-source/vistas/creative-counselor-self-care.pdf?sfvrsn=4
Thomas, J. T., & Otis, M. D. (2010). Intrapsychic correlates of professional quality of life: Mindfulness, empathy, and emotional separation. Journal of the Society for Social Work and Research, 1(2), 83–98. doi:10.5243/jsswr.2010.7
Thompson, I. A., Amatea, E. S., & Thompson, E. S. (2014). Personal and contextual predictors of mental health counselors’ compassion fatigue and burnout. Journal of Mental Health Counseling, 36, 58–77. doi:10.17744/mehc.36.1.p61m73373m4617r3
Tosone, C., Bettmann, J. E., Minami, T., & Jasperson, R. A. (2010). New York City social workers after 9/11: Their attachment, resiliency, and compassion fatigue. International Journal of Emergency Mental Health, 12(2), 103–116.
Turgoose, D., Glover, N., Barker, C., & Maddox, L. (2017). Empathy, compassion fatigue, and burnout in police officers working with rape victims. Traumatology, 23, 205–213. doi:10.1037/trm0000118
Wagaman, M. A., Geiger, J. M., Shockley, C., & Segal, E. A. (2015). The role of empathy in burnout, compassion satisfaction, and secondary traumatic stress among social workers. Social Work, 60, 201–209.
doi:10.1093/sw/swv014
White, V. E., & Queener, J. (2003). Supervisor and supervisee attachments and social provisions related to the
supervisory working alliance. Counselor Education and Supervision, 42, 203–218.
doi:10.1002/j.1556-6978.2003.tb01812.x
Williams, A., Helm, H., & Clemens, E. V. (2012). The effect of childhood trauma, personal wellness, supervisory working alliance, and organizational factors on vicarious traumatization. Journal of Mental Health Counseling, 34, 133–153. doi:10.17744/mehc.34.2.j3l62k872325h583
Wood, A. E., Prins, A., Bush, N. E., Hsia, J. F., Bourn, L. E., Earley, M. D., . . . Ruzek, J. (2017). Reduction of
burnout in mental health care providers using the Provider Resilience mobile application. Community
Mental Health Journal, 53, 452–459. doi:10.1007/s10597-016-0076-5
Nesime Can is an instructor at Ankara University in Turkey. Joshua C. Watson, NCC, is a professor and department chair at Texas A&M University–Corpus Christi. Correspondence can be addressed to Nesime Can, Ankara University Faculty of Educational Sciences, Department of Educational Sciences, Program of Counseling and Guidance, Office 3111, Çankaya, Ankara, Turkey 06590, nesime.can@ankara.edu.tr.
Nov 27, 2019 | Volume 9 - Issue 4
Margaret R. Lamar, Elysia Clemens, Adria Shipp Dunbar
Conceptualizing doctoral training programs as research training environments (RTEs) allows for the exploration of theory to help counselor educators facilitate doctoral students’ development from practitioners toward counseling researchers. Researchers have proposed self-concept theory as a way to understand identity development. In this article, the authors applied self-concept theory to understand how researcher identity may develop in a counseling RTE. Organizational theory also is described, as it provides insight for how doctoral students are socialized to the profession. Suggestions are made for how counselor education programs can utilize self-concept theory and organizational theory to create positive RTEs designed to facilitate researcher development.
Keywords: doctoral students, development, researcher identity, research training environments, self-concept theory
Conceptualizing doctoral training programs as research training environments (RTEs) allows for the exploration of theories to help counselor educators facilitate doctoral students’ development from having an identity primarily focused on being a helper toward a research identity (Gelso, 2006). Gelso (2006) defined RTEs as all “forces in graduate training programs . . . that reflect attitudes toward research and science” (p. 6). The RTE includes formal coursework; interactions with faculty, other students, and staff; informal mentoring experiences; and institutional culture that promotes or devalues research. However, there is little information about how counselor educators can practically develop a systematic approach to creating positive RTEs that facilitate the development of counselor education and supervision (CES) doctoral student researchers.
It is important to attend to the RTE because it has an impact on the researcher’s identity, researcher self-efficacy, research interest, and scholarly productivity of CES doctoral students (Borders, Wester, Fickling, & Adamson, 2014; Gelso, 2006; Gelso, Baumann, Chui, & Savela, 2013; Kuo, Woo, & Bang, 2017; Lamar & Helm, 2017; Lambie, Hayes, Griffith, Limberg, & Mullen, 2014; Lambie & Vaccaro, 2011). Researchers have found that CES doctoral student research self-efficacy and research interest were related to productivity (Kuo et al., 2017; Lambie & Vaccaro, 2011). Research self-efficacy is defined as the belief one has in their ability to engage in research tasks (Bishop & Bieschke, 1998). A related but separate construct, research interest is the desire to learn more about research. Lambie and Vaccaro (2011) found that doctoral students with scholarly publications had higher research self-efficacy and research interest, while Kuo et al. (2017) found that scholarly productivity can be predicted by research self-efficacy and intrinsic research motivation. Given that most CES doctoral students enter their programs with little research experience (Borders et al., 2014), the RTE likely contributes to a doctoral student’s ability to gain research and publication experience. However, much of the early exposure to research in counselor education rests primarily on research coursework, not extracurricular experiences, such as working on a manuscript with a faculty member (Borders et al., 2014). Though some programs provide systematic extracurricular non-dissertation research experiences, about half of the CES programs surveyed by Borders et al. (2014) offered no structured research experiences early in the program sequence or relied on doctoral students to create their own opportunities. Lamar and Helm (2017) found that the RTE, including faculty mentoring and research experiences, was an essential part of CES doctoral student researcher identity development. Given prior findings (Borders et al., 2014; Kuo et al., 2017; Lamar & Helm, 2017; Lambie & Vaccaro, 2011), it seems crucial for CES doctoral faculty to systematically create an RTE that is conducive to CES doctoral student researcher identity, research self-efficacy, and research interest development.
Leadership in the counseling field has stressed the importance of research in furthering the profession by stating that “expanding and promoting our research base is essential to the efficacy of professional counselors and to the public perception of the profession” (Kaplan & Gladding, 2011, p. 372). Therefore, it is essential to strengthen the training of future researchers so they are successful at achieving this vision. Thus, there are two primary purposes of this manuscript: 1) propose that the state of research in the field of counselor education is a reflection, in part, of an RTE issue; and 2) provide practical ways for programs to facilitate researcher development among doctoral students. The authors provide insight on how self-concept theory and organizational development theory may be a useful means for conceptualizing researcher development and facilitating change in RTEs.
Self-Concept Theory
Self-concept theory provides a framework for conceptualizing the way a person organizes beliefs about themselves. Purkey and Schmidt (1996) defined self-concept theory as “the totality of a complex and dynamic system of learned beliefs that an individual holds to be true about their personal experience” (p. 31). Learned beliefs are subjective and not necessarily based on reality but instead are reflections of individuals’ perceptions of themselves. These perceptions are related to past experiences and expectations about future goals. Purkey and Schmidt (1996) suggested conceptualizing the self-concept using the following categories: (a) organized, (b) learned, (c) dynamic, and (d) consistent. Discussions of each of these categories are presented in the context of applying self-concept theory to researcher development.
Current counselor training literature has discussed the development of student professional counselor identity (e.g., Prosek & Hurt, 2014); however, until recently (e.g., Jorgensen & Duncan, 2015; Lamar & Helm, 2017), counseling professional identity literature has not included a focus on how research is integrated into a student’s identity. Self-concept theory can be used to conceptualize the inclusion of researcher identity into the professional identity of CES doctoral students.
Organization of the Self-Concept
Purkey and Schmidt (1996) used a spiral as a visual representation of how the self is organized (Figure 1). They referred to the sense of self, or overarching view of who you are, as the central I, and placed it at the very center of the spiral. In addition, people also have other specific identities, or what Purkey and Schmidt termed me’s, that inform their global identity. These multiple identities can be considered hierarchical, meaning that one of the me identities might be more important to a person than another aspect of their identity and is placed more proximal to the central I on the spiral than more distal me’s. Developmentally, it makes sense that a beginning CES doctoral student, for example, may have a stronger counselor me (located closer to their central I), whereas their researcher me might be located closer to the periphery of the spiral. This is confirmed through previous research findings suggesting that CES students enter doctoral programs with stronger helper identities and integrate research into their self-concept throughout their academic experience (Gelso, 2006; Lamar & Helm, 2017; Lambie & Vaccaro, 2011). It would be expected that these me’s would be more likely to shift throughout the course of a doctoral program with greater exposure to a positive RTE. The relative importance of these identities to a doctoral student’s professional identity is illustrated for exemplary purposes in Figure 1. Faculty have a significant role in creating positive RTEs so that a doctoral student’s researcher me can be strengthened and become more fully integrated into their self-concept.
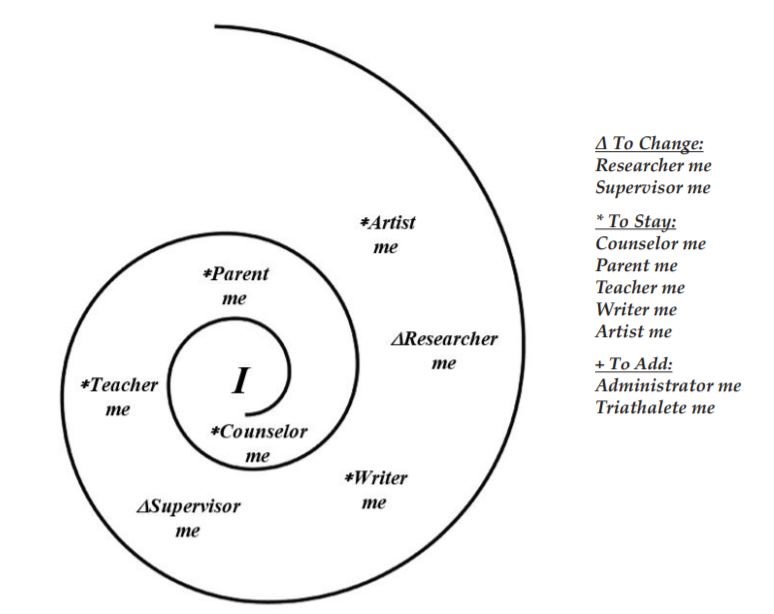
Figure 1. Self-Concept Spiral
Learning for a Lifetime
Developing the self-concept is a task that takes a lifetime of learning (Purkey & Schmidt, 1996). Self-
concept learning occurs in three ways: (a) exciting or devastating events, (b) professional helping relationships, and (c) everyday experiences. Individually, and in combination, these experiences can reorganize and shape a person’s self-concept. For example, receiving a first decision letter from an editor can be an exciting or devastating event that influences a doctoral student’s self-concept. Faculty members can process and contextualize the experience so a doctoral student’s researcher self-concept is positively promoted (e.g., a lengthy revise and resubmit letter can feel overwhelming but is a fantastic outcome; Gelso, 2006; Lamar & Helm, 2017). Similarly, the counseling RTE can promote positive research attitudes for doctoral students on a daily basis (e.g., displaying examples of student and faculty research).
Dynamic and Consistent Self-Concept Processes
Self-concept is dynamic; it is constantly changing and has the potential to propel doctoral student researchers forward (Purkey & Schmidt, 1996). Change occurs when a doctoral student incorporates new beliefs into existing ones. When new information is presented to the doctoral student, contrary to what they currently believe about themselves (e.g., ability to understand the methods section of an article), they are challenged to merge the new information with their current beliefs (e.g., “I’m a clinician,” and skip to the implications section). As they revise their belief system, they may be able to behave in new ways (e.g., making connections between the methods section and clinical application or engaging in critical discussions of research). However, reconciling new beliefs about their self-concept and demonstrating new research skills can be challenging. Consistency is highly valued by doctoral students faced with a need to adopt new ideas into their self-concept (Purkey & Schmidt, 1996). A doctoral student may experience what is commonly known as imposter syndrome, which occurs when a student is unable to internalize their accomplishments and attributes their success to good luck (Parkman, 2016). As CES doctoral students become proficient in research pursuits, they may still have difficulty seeing themselves as researchers (e.g., articulating hesitancy to share findings with peers or at professional conferences). They might tell others they are a counselor, a teacher, or a supervisor and they also conduct research, thus distancing that identity from the core of their self-concept (Lamar & Helm, 2017). They may need to repeatedly have their new researcher identity confirmed by faculty and their own personal experiences before they can communicate a fully integrated self-concept to others.
As learning occurs, the self-concept reorganizes toward a more stable professional identity. Incorporation of a researcher identity into their self-concept is likely to be dynamic, with consistency increasing throughout the doctoral students’ academic program. As CES doctoral students move into new stages of their career, their researcher identity is likely to become a more fixed aspect of their self-concept.
Development of the self-concept occurs in a CES doctoral program, which exists within the larger academic culture. Doctoral students are initially presented with the challenge of navigating a new culture. The culture of academe has its own processes, language, and roles. In addition to development of their researcher self-concept, doctoral students also must integrate their roles within higher education into their self-concept.
Organizational Development
A primary goal of doctoral education is to prepare and acculturate doctoral students to their future professional life as counselor educators (Austin, 2002; Johnson, Ward, & Gardner, 2017; Weidman & Stein, 2003). Many doctoral students in CES programs will pursue a CES faculty position within higher education organizations. Higher education organizations demonstrate various forms of culture and socialization processes (Tierney, 1997). University cultural norms include expectations for how to act, what to strive for, and how to define success and failure. Graduate education literature has included discussions on helping doctoral students transition into faculty life and university organizational culture (e.g., Austin, 2002; Austin & McDaniels, 2006). This socialization process has not been extensively discussed in the counselor training literature, yet there is potential for it to be useful in creating positive RTEs.
Socialization Into the Academy
Socialization is the process by which doctoral students learn the culture of an institution, including both the spoken and unspoken rules (Johnson et al., 2017). The process of socializing doctoral students to graduate school is a part of a greater socialization to higher education (Gardner & Barnes, 2007). Weidman, Twale, and Stein (2001) described four stages and characterized three elements of socialization—knowledge acquisition, investment, and involvement—that are experienced over the four stages. These stages provide insight for doctoral programs looking to provide intentional support for their students acclimating to the RTE within higher education.
Anticipatory stage. Doctoral students begin developing an understanding of the organizational culture even before they start a program of study (Clarke, Hyde, & Drennan, 2013; Weidman et al., 2001). During recruitment and introduction to the program, doctoral students gather information about the program (knowledge acquisition), decide to enroll (investment), and begin to make sense of organizational norms, expectations, and roles (involvement). CES doctoral students are, therefore, entering counseling programs with preconceived ideas about their roles as students, including their function as student researchers.
Formal and informal stages. The formal and informal stages co-occur but are differentiated in that the formal stage is more faculty or program driven, whereas the informal stage is peer socialization (Gardner, 2008; Weidman et al., 2001). Some of the formal stage methods of socialization can include classroom instruction, faculty direction, and focused observation. Courses grounded in the 2016 Council for Accreditation of Counseling and Related Educational Programs (CACREP) standards related to doctoral professional identity or research are part of the formal socialization process. Out-of-classroom conversations with faculty and other university staff orient doctoral students to the value of research in the program and university. Doctoral students learn through faculty direction and observation about networking at conferences, publishing, and what types of research are considered valuable in the field. Students also observe faculty working around obstacles to keep their own research active. These examples are all consistent with knowledge acquisition.
Informal socialization happens as new doctoral students observe and learn how more advanced students and incoming cohorts define norms (Gardner, 2008). This stage has many parallels to existing research about how faculty acculturate to new organizations. Tierney and Rhoads (1994) proposed new faculty members learn the culture of the organization in mostly informal ways. As they observe the established tenured faculty, new faculty learn what is important to the department and develop understanding about the institution’s priorities. This acculturation process is important because it is likely to impact the RTE faculty create for doctoral students.
Similarly, doctoral students learning about culture, investment, and involvement in research are likely guided by the knowledge they acquire through observing and engaging with more advanced doctoral students in their programs of study (Gardner, 2008; Gelso, 2006). Acquisition of knowledge, occurring “through exposure to the opinions and practices of others also working in the same context” (Mathews & Candy, 1999, p. 49), creates norms among doctoral students. Norms regarding participation in research, such as whether it is done only to meet degree requirements or with more intrinsic motivation, may be conveyed across cohorts. Lamar and Helm (2017) found CES doctoral students were intrinsically motivated by their research when it was connected to their counselor identity and they could see how their research would help their clients. Jorgensen and Duncan (2015) identified external facilitators, such as faculty, coursework, and program expectations, that shaped the researcher identity development of master’s counseling students. Faculty communicated the culture of the institution and indirectly communicated their own intrinsic motivation, or lack of it, through their research activity. New students also gain insight from advanced doctoral students about the degree to which research should be aligned with faculty members and the more subtle messages about departmental expectations. For example, is qualitative research supported and valued as much as quantitative? Are certain research methodologies prioritized by faculty or the institution? The combination of formal and informal socialization leads to an understanding of the academic organization and counselor education profession.
Personal stage. During this final stage, doctoral students internalize and act upon the role they have taken within their organization (Gardner, 2008; Weidman et al., 2001). They solidify their professional identity at the student level and have, perhaps, begun to integrate their researcher identity into their self-concept. They also can use the knowledge they have acquired to make purposeful decisions about investment and involvement in research. Doctoral students make decisions about their course of study and the amount of time dedicated to developing as a researcher compared to other aspects of counselor education such as teaching, supervision, and service. In this stage, it is important for faculty to attend to whether doctoral students feel caught in the role they occupy within the program. Some doctoral students might more quickly adopt research into their self-concept and find opportunities to engage in research, while others take longer to develop their researcher identity and might not find themselves with as many options to get involved in faculty research projects. Additionally, those students’ strong helper identities might make them valuable doctoral-level supervisors or clinicians that programs can lean on to train master’s-level students. They may feel stuck in their clinical roles and miss out on opportunities to gain informal research experience. This is not to diminish doctoral students who are primarily interested in a CES degree with the goal of strengthening their clinical work. It is the position of these authors that scholarship is an integral part of all clinical work and, therefore, programs should provide equitable opportunities for all doctoral students, regardless of their professional goals, to engage in the research process.
Implications for Counselor Education RTEs
Thinking about CES programs as RTEs allows for a programmatic approach to researcher identity that can be informed by self-concept identity theory and organizational development literature. Specifically, there are implications for the RTE connected to fostering researcher identity, increasing both research self-efficacy and research interest, and attending to the process of socializing doctoral students to academia (Gelso et al., 2013). The strategies presented in this section are written with the goal of integrating self-concept identity theory and organizational development theory. They are designed based on the assumption that programs want to train researchers and celebrate that aspect of counselor education identity.
Transparency Regarding Identity Development
Formal socialization of doctoral students to the program should include intentional conversations about identity development (Lamar & Helm, 2017; Prosek & Hurt, 2014). Programs can choose to be transparent about the expectation that part of the transition from counseling to counselor education is strengthening their researcher identity. Attending to doctoral student development and class-based activities can be part of monitoring this transition.
Much like counselor educators assess and address the identity development of master’s students through student learning outcomes (CACREP, 2015), programs might choose to intentionally include researcher development in the systematic review of doctoral students’ progress. This could be accomplished through advising conversations, faculty feedback forms, and standardized instruments such as the Interest in Research Questionnaire (Bishop & Bieschke, 1998), Research Identity Scale (Jorgensen & Schweinle, 2018), or the Research Self-Efficacy Scale (Bieschke, Bishop, & Garcia, 1996). Considering this information at the program level, in addition to individual student level, can provide insight into opportunities to improve the RTE for program-level assessment and to impact the broader professional understanding of doctoral research education (e.g., does research interest or research self-efficacy consistently shift at identifiable points in a CES doctoral program?).
One class-based strategy is to use Purkey and Schmidt’s (1996) self-concept spiral to raise doctoral students’ awareness of professional identity transition. Counselor educators can consider asking students as a class to brainstorm all of the me’s that are part of counselor education. Individually, doctoral students can then create a list of me’s that are part of their identity in general (e.g., parent, musician). Once the counselor education and personal identity lists are generated, invite doctoral students to depict on the spiral the me’s from both lists that apply to their identity today and organize them relative to the central I (or center of the spiral). Next, encourage students to indicate with a star or asterisk aspects of their identity they want to remain stable throughout their doctoral program. Use a triangle, which symbolizes delta or change, to identify aspects of their identity they would like to shift as they progress through their doctoral program. Doctoral students might want to indicate in a space near the spiral counselor education me’s that are not currently part of their identity but that they would like to incorporate. Figure 1 is an example of a completed self-concept spiral. This spiral helps doctoral students visualize how their researcher identity relates to their other professional and personal identities. Faculty can facilitate conversation with doctoral students about their hopes, fears, concerns, and anticipation around their researcher identities. It would be even more valuable for doctoral students to hear their faculty’s researcher development using the spiral (e.g., draw one representing their years as a student and draw one where they see themselves now or at other points in their professional development).
Counselor educators can consider assigning research articles that address different aspects of counselor researcher development. Students can read about CES doctoral student researcher identity development (e.g., Jorgensen & Duncan, 2015; Lamar & Helm, 2017), RTEs (e.g., Borders et al., 2014; Gelso, 2006; Gelso et al., 2013), research self-efficacy and research interest (e.g., Kuo et al., 2017; Lambie & Vaccaro, 2011), and counseling research competencies (Wester & Borders, 2014). These articles provide insight for a doctoral student’s individual development and also demonstrate the applicability of research in the profession.
Sequencing of Research Experiences
Most incoming CES doctoral students have little or no research experience, which means their research self-efficacy and research interest is likely to be low and vary substantially (Borders et al., 2014; Gelso at al., 2013; Lambie & Vaccaro, 2011). This makes the sequencing of coursework and extracurricular research experiences important to consider (Borders et al., 2014; Gelso et al., 2013). Students on the extreme ends of research self-efficacy and research interest may see a quicker transition into a stable identity. Those with a higher research self-efficacy and research interest might more quickly identify as a researcher, while those with a lower research self-efficacy and research interest can move away from research toward other areas of focus. It is important, therefore, to sequence research experiences that can help doctoral students with higher levels of both research self-efficacy and research interest capitalize on that momentum without further disenfranchising students with lower research self-efficacy and research interest. The strategies presented in this section are described with the modifiers of higher and lower self-efficacy and interest for clarity purposes; however, individual doctoral student’s research self-efficacy and research interest could be anywhere on the continuum from very high to very low.
Determining a doctoral student’s sequence of research coursework or experiences can be accomplished through advising with the student (Kuo et al., 2017). A positive RTE is one in which care is taken to create developmentally appropriate research opportunities for all doctoral students (Borders et al., 2014; Kuo et al., 2017). Students with higher research self-efficacy and research interest might be ready to engage in a statistics sequence at the start of their program and then transition quickly into conducting independent research or engaging in data analysis. Doctoral students with lower research self-efficacy and research interest might benefit by first being exposed to research in a conceptual rather than technical environment, such as a counseling research seminar. Focusing on developing research ideas and reviewing the literature might be a better introduction to research for lower self-efficacy or interest doctoral students than a statistics course (Gelso, 2006). Kuo et al. (2017) found that it was important for CES programs to offer research opportunities that presented a small risk to doctoral students in order to foster researcher development.
For the optimal researcher development, it is important to provide doctoral students research experiences outside of their coursework (Borders et al., 2014; Kuo et al., 2017; Lamar & Helm, 2017). Providing doctoral students with opportunities to do “minimally threatening” research early in their program is consistent with a positive RTE (Gelso, 2006, p. 6). What each student might consider to be minimally intimidating research is likely connected to research self-efficacy (Kuo et al., 2017). Engaging in conversations with doctoral students about what might be a good first research experience is a way to help students intentionally sequence their experiences. Faculty can take an active role in connecting doctoral students with opportunities that are developmentally appropriate (Borders et al., 2014; Kuo et al., 2017; Lamar & Helm, 2017; Lambie & Vaccaro, 2011). Lambie and Vaccaro (2011) found that doctoral students with published work had higher levels of research self-efficacy than those who did not. This is an important finding for faculty to consider when creating research opportunities for doctoral students. One possible explanation for this result could be that doctoral students with a published work already have higher levels of research self-efficacy prior to their publication. If this is the case, it is important for researchers to investigate what other factors are contributing to their research self-efficacy. Nevertheless, an RTE that facilitates doctoral student confidence around research, regardless of their pre-existing research self-efficacy, is one where faculty are helping students publish, either on their own or in or in partnership with faculty actively engaged in research (Gelso, 2006; Kuo et al., 2017; Lambie & Vaccaro, 2011).
It is important to consider a doctoral student’s level of autonomy when planning sequencing of research experiences. Early experiences might be more positive if there is a community or social aspect to the research experience, rather than independent research projects, which can be isolating (Gelso et al., 2013). Additionally, Cornér, Löfström, and Pyhältö (2017) found that having an increased sense of a scholarly community helps doctoral students feel supported during their dissertations. Love, Bahner, Jones, and Nilsson (2007) found positive social interactions in research teams could positively influence research self-efficacy. Additionally, Kuo et al. (2017) found that the advisory relationship was instrumental in a doctoral student’s engagement in research, suggesting that faculty can make research a fun, social process in which students want to continually engage. It is evident that doctoral students can benefit from experiencing research as a social activity throughout their studies. Therefore, faculty might consider structuring research opportunities that encourage research as a social activity throughout the doctoral program. For example, first-year doctoral students can be encouraged to join research groups that are already in place or join a faculty member working on a manuscript for publication, while students working on a dissertation might create a weekly writing group.
Faculty should be intentionally thoughtful of doctoral student dynamics, including individual student need, research self-efficacy, and research interest, when designing research partnerships. Research partnerships can take the form of class research projects, informal research dyads, or research mentorships (Lamar & Helm, 2017; Lambie & Vaccaro, 2011). When deciding class research groups, faculty can connect doctoral students who can create a positive research group environment for each other (Love et al., 2007). Groups may be based on research interests or personality variables. Advisors might have insight into certain doctoral student characteristics that would negatively impact a research partnership. Negative group experiences, such as group conflict, do not contribute positively to research self-efficacy (Love et al., 2007). However, it is important for faculty to balance letting research groups form organically with formal assignment of such partnerships.
Attending to Subtle Messages About Research
Socialization to a doctoral program occurs formally through faculty- and program-driven processes and informally through interactions with peers (Gardner, 2008; Weidman et al., 2001). Neither formal nor informal socialization is synonymous with intentional socialization. There are likely subtle messages occurring through the socialization processes that contribute to the RTE and impact researcher development (Gelso, 2006). It is important to point out that program faculty and administrators might also send messages about research that are not subtle. These messages (e.g., a good dissertation is a done dissertation, or just get through your stats classes) are likely sent with the best of intention to help a student complete their degree successfully, but communicate values around research that can damage a doctoral student’s researcher identity development, research self-efficacy, and research interest. Recognizing and intentionally attending to all messages sent by students, faculty, and the program are part of shaping the RTE.
Student messages. Individual doctoral student and cohort dynamics may impact students’ research identity development both positively and negatively (Lamar & Helm, 2017). Different career aspirations among cohort individuals can also impact the RTE. For example, doctoral students who are interested in pursuing academic careers might have a higher level of motivation to involve themselves in research early in their graduate program. Students who plan to pursue other careers and do not have a strong interest in research might receive subtle messages from their peers or faculty about a hierarchy within the doctoral student body of “researchers” versus “practitioners.”
It is important for faculty to encourage positive interactions regarding research and to intervene should negative messages damage the RTE (Gelso, 2006; Lamar & Helm, 2017). Continuing with the above example, faculty can facilitate doctoral student discussions around the science–practitioner model. Focusing on the importance of integrating research into practice (and vice versa) can motivate all doctoral students in their research endeavors. The majority of students enter their doctoral program with their identities structured around helping others (Borders et al., 2014; Gelso, 2006). This value can be reinforced throughout the research process (Wachter Morris, Wester, Vaishnav, & Austin, 2018). For instance, faculty can facilitate discussion about how a doctoral student’s research can impact practitioners’ work and, ultimately, a client’s life. Additionally, faculty can reinforce subtle messages that contribute to the development of a positive RTE. For example, intentionally developing a culture of supportive inquiry, talking with each other about idea development, and celebrating each other’s research achievements can be encouraged and lauded (Gelso et al., 2013).
Faculty messages. Subtle messages faculty send about doctoral students’ abilities may influence students’ research self-efficacy and researcher identity development (Gelso, 2006; Lamar & Helm, 2017). Reflecting on the patterns of how research opportunities are provided to doctoral students may yield opportunities to improve the RTE. Consider if the culture to disseminate research-related opportunities includes all doctoral students or if opportunities are offered more frequently to a subset of students. If the latter proves to be true, faculty can send a subtle and unintentional message. Borders et al. (2014) found that doctoral students in many CES programs get involved in research opportunities by coincidence rather than by program intentionality. Students can receive a subtle message that not all doctoral students are welcome to participate in research or that faculty do not engage in research themselves. Similarly, messages about research ability can come in the form of differential faculty responses to doctoral students’ research-related work. Heightening awareness around the balance of feedback that is given to doctoral students when discussing their research ideas can contribute to an improved RTE. In addition, reflection on the rigor of the discussion helps faculty become more intentional about the messages they are sending.
Program messages. While programs often tout research-related accomplishments, faculty can contextualize those celebrations by talking about their process, not just the final products (Gelso, 2006; Gelso et al., 2013; Lamar & Helm, 2017). Orienting doctoral students to the substantial amount of time it takes to conduct research and to write for publication is part of intentionally socializing students to academia. Making the process more visible can be as simple as having a research project list visible in faculty offices or indicating blocks of time on office hour sign-ups that are set aside for writing. These are subtle messages that are designed to indicate that research takes dedicated time and that productivity is more than one manuscript at a time but having a variety of projects at different points in the pipeline. Similarly, Gelso (2006) recommended faculty share their failures as well as successes, as this sends doctoral students a message that research is a process. When faculty are transparent about research outcomes, both good and bad, and still maintain positive attitudes, they communicate subtle but important messages about the process of research (Gelso, 2006; Gelso et al., 2013; Lamar & Helm, 2017).
Directions for Future Research
Researchers (Gelso et al., 2013; Lambie et al., 2014; Lambie & Vaccaro, 2011) to date have focused primarily on identifying constructs that relate to research engagement and productivity of CES doctoral students. Increasing attention to understanding doctoral student researcher developmental processes and connecting those investigations to theory are important next steps. This could come in the form of investigations that explore experiences of doctoral students in the context of their RTEs. It also is important to increase understanding about how counseling master’s-level students and practitioners develop as researchers, specifically around the constructs of researcher identity, research self-efficacy, and research interest, as they provide important information about the state of researchers in the field and of doctoral students entering CES programs. As mentioned above, it would be valuable to understand if researcher identity, research self-efficacy, or research interest develops at specific points in a doctoral program or if certain doctoral benchmarks (e.g., comprehensive exams, dissertation proposal) contribute to the development of those variables. Researchers can look at educational interventions designed to increase research self-efficacy, research interests, and researcher identity for both doctoral and master’s counseling students. This is valuable for program evaluation and for informing the profession at large. Researchers also can test the relevance of the theoretical frameworks applied in this manuscript to the outcomes of the research competencies suggested by Wester and Borders (2014).
Conclusion
Counselor education doctoral programs as RTEs are the foundation for creating a programmatic climate that fosters the development of strong researchers. Faculty members are encouraged to take an intentional approach to promoting the development of researcher identity and research self-efficacy of doctoral students. This intentionality includes assessing the formal and informal socialization that occurs in a doctoral program. Program faculty can actively engage in the research identity development of doctoral students through the use of interventions, including attending to subtle messages, sequencing developmentally appropriate research experiences, and encouraging research as a social activity. Additionally, program faculty should be transparent about the research identity development process and attend to research self-efficacy beliefs through providing interventions designed to boost research self-efficacy and research interest.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Austin, A. E. (2002). Preparing the next generation of faculty: Graduate school as socialization to the academic career. The Journal of Higher Education, 73, 94–122. doi:10.1353/jhe.2002.0001
Austin, A. E., & McDaniels, M. (2006). Using doctoral education to prepare faculty to work within Boyer’s four
domains of scholarship. New Directions for Institutional Research, 2006(129), 51–65. doi:10.1002/ir.171
Bieschke, K. J., Bishop, R. M., & Garcia, V. L. (1996). The utility of the Research Self-Efficacy Scale. Journal of Career Assessment, 4, 59–75. doi:10.1177/106907279600400104
Bishop, R. M., & Bieschke, K. J. (1998). Applying social cognitive theory to interest in research among counseling psychology doctoral students: A path analysis. Journal of Counseling Psychology, 45, 182–188. doi:10.1037/0022-0167.45.2.182
Borders, L. D., Wester, K. L., Fickling, M. J., & Adamson, N. A. (2014). Researching training in doctoral programs accredited by the Council for Accreditation of Counseling and Related Educational Programs. Counselor Education and Supervision, 53, 145–160. doi:10.1002/j.1556-6978.2014.00054.x
Clarke, M., Hyde, A., & Drennan, J. (2013). Professional identity in higher education. In B. M. Kehm & U. Teichler (Eds.), The academic profession in Europe: New tasks and new challenges (pp. 7–22). Dordrecht, Netherlands: Springer.
Cornér, S., Löfström, E., & Pyhältö, K. (2017). The relationship between doctoral students’ perceptions of supervision and burnout. International Journal of Doctoral Studies, 12, 91–106. doi:10.28945/3754
Council for Accreditation of Counseling and Related Educational Programs. (2015). 2016 CACREP
standards. Retrieved from http://www.cacrep.org/wp-content/uploads/2018/05/2016-Standards-with-Glossary-5.3.2018.pdf
Gardner, S. K. (2008). Fitting the mold of graduate school: A qualitative study of socialization in doctoral education. Innovative Higher Education, 33, 125–138. doi:10.1007/s10755-008-9068-x
Gardner, S. K., & Barnes, B. J. (2007). Graduate student involvement: Socialization for the professional role. Journal of College Student Development, 48, 369–387.
Gelso, C. J. (2006). On the making of a scientist–practitioner: A theory of research training in professional psychology. Training and Education in Professional Psychology, S(1), 3–16. doi:10.1037/1931-3918.S.1.3
Gelso, C. J., Baumann, E. C., Chui, H. T., & Savela, A. E. (2013). The making of a scientist–psychotherapist: The
research training environment and the psychotherapist. Psychotherapy, 50(2), 139–149. doi:10.1037/a0028257
Johnson, C. M., Ward, K. A., & Gardner, S. K. (2017). Doctoral student socialization. In J. Shin & P. Teixeira (Eds.), Encyclopedia of international higher education systems and institutions. Dordrecht, Netherlands: Springer.
Jorgensen, M. F., & Duncan, K. (2015). A grounded theory of master’s-level counselor research identity. Counselor Education and Supervision, 54, 17–31. doi:10.1002/j.1556-6978.2015.00067.x
Jorgensen, M. F., & Schweinle, W. E. (2018). The Research Identity Scale: Psychometric analyses and scale refinement. The Professional Counselor, 8, 21–28. doi:10.15241/mfj.8.1.21
Kaplan, D. M., & Gladding, S. T. (2011). A vision for the future of counseling: The 20/20 principles for unifying
and strengthening the profession. Journal of Counseling & Development, 89, 367–372.
doi:10.1002/j.1556-6678.2011.tb00101.x
Kuo, P. B., Woo, H., & Bang, N. M. (2017). Advisory relationship as a moderator between research self-efficacy, motivation, and productivity among counselor education doctoral students. Counselor Education and Supervision, 56(2), 130–144. doi:10.1002/ceas.12067
Lamar, M. R., & Helm, H. M. (2017). Understanding the researcher identity development of counselor education and supervision doctoral students. Counselor Education and Supervision, 56, 2–18. doi:10.1002/ceas.12056
Lambie, G. W., Hayes, B. G., Griffith, C., Limberg, D., & Mullen, P. R. (2014). An exploratory investigation of the research self-efficacy, interest in research, and research knowledge of Ph.D. in education students. Innovative Higher Education, 39, 139–153. doi:10.1007/s10755-013-9264-1
Lambie, G. W., & Vaccaro, N. (2011). Doctoral counselor education students’ level of research self-efficacy, perceptions of the research training environment, and interest in research. Counselor Education and Supervision, 50, 243–258. doi:10.1002/j.1556-6978.2011.tb00122.x
Love, K. M., Bahner, A. D., Jones, L. N., & Nilsson, J. E. (2007). An investigation of early research experience and research self-efficacy. Professional Psychology: Research and Practice, 38, 314–320.
doi:10.1037/0735-7028.38.3.314
Mathews, J. H., & Candy, P. C. (1999). New dimensions in the dynamics of knowledge and learning. In D. Boud & J. Garrick (Eds.), Understanding learning at work (pp. 47–64). London, UK: Routledge.
Parkman, A. W. (2016). The imposter phenomenon in higher education: Incidence and impact. Journal of Higher Education Theory and Practice, 16, 51–60.
Prosek, E. A., & Hurt, K. M. (2014). Measuring professional identity development among counselor trainees. Counselor Education and Supervision, 53, 284–293. doi:10.1002/j.1556-6978.2014.00063.x
Purkey, W. W., & Schmidt, J. J. (1996). Invitational counseling: A self-concept approach to professional practice. Pacific Grove, CA: Brooks Cole.
Tierney, W. G. (1997). Organizational socialization in higher education. The Journal of Higher Education, 68, 1–16. doi:10.1080/00221546.1997.11778975
Tierney, W. G., & Rhoads, R. A. (1994). Faculty socialization as cultural process: A mirror of institutional commitment
(ASHE-ERIC Higher Education Report No. 93-6). Washington, DC: The George Washington University
School of Education and Human Development.
Wachter Morris, C. A., Wester, K. L., Vaishnav, S., & Austin, J. L. (2018). Introduction. In C. A. Wachter Morris & K. L. Wester (Eds.), Making research relevant: Applied research designs for the mental health practitioner (pp. 1–13). New York, NY: Routledge.
Weidman, J. C., & Stein, E. L. (2003). Socialization of doctoral students to academic norms. Research in Higher Education, 44, 641–656. doi:10.1023/A:1026123508335
Weidman, J. C., Twale, D. J., & Stein, E. L. (2001). Socialization of graduate and professional students in higher education: A perilous passage? (ASHE-ERIC Higher Education Report, 28, No. 3). San Francisco, CA: Jossey-Bass.
Wester, K. L., & Borders, L. D. (2014). Research competencies in counseling: A Delphi study. Journal of Counseling & Development, 92, 447–458. doi:10.1002/j.1556-6676.2014.00171.x
Wester, K. L., Borders, L. D., Boul, S., & Horton, E. (2013). Research quality: Critique of quantitative articles in the Journal of Counseling & Development. Journal of Counseling & Development, 91, 280–290.
doi:10.1002/j.1556-6676.2013.00096.x
Margaret R. Lamar, NCC, is an assistant professor at Palo Alto University. Elysia Clemens is Deputy Director of the Colorado Evaluation and Action Lab. Adria Shipp Dunbar is an assistant professor at North Carolina State University. Correspondence may be addressed to Margaret Lamar, Palo Alto University, 1791 Arastradero Road, Palo Alto, CA 94304, mlamar@paloaltou.edu.
Nov 26, 2019 | Volume 9 - Issue 4
Matthew C. Fullen, Jonathan D. Wiley, Amy A. Morgan
This interpretative phenomenological analysis explored licensed professional counselors’ experiences of turning away Medicare beneficiaries because of the current Medicare mental health policy. Researchers used semi-structured interviews to explore the client-level barriers created by federal legislation that determines professional counselors as Medicare-ineligible providers. An in-depth presentation of one superordinate theme, ineffectual policy, along with the emergent themes confounding regulations, programmatic inconsistencies, and impediment to care, illustrates the proximal barriers Medicare beneficiaries experience when actively seeking out licensed professional counselors for mental health care. Licensed professional counselors’ experiences indicate that current Medicare provider regulations interfere with mental health care accessibility and availability for Medicare-insured populations. Implications for advocacy are discussed.
Keywords: Medicare, interpretative phenomenological analysis, mental health, advocacy, federal legislation
Medicare is the primary source of health insurance for 60 million Americans, including adults 65 years and over and younger individuals with a long-term disability; the number of beneficiaries is expected to surpass 80 million by 2030 (Kaiser Family Foundation, 2019; Medicare Payment Advisory Commission, 2015). According to the Center for Medicare Advocacy (2013), approximately 26% of all Medicare beneficiaries experience some form of mental health disorder, including depression and anxiety, mild and major neurocognitive disorder, and serious mental illness such as bipolar disorder and schizophrenia. Among older adults specifically, nearly one in five meets the criteria for a mental health or substance use condition, and if left unaddressed, these issues may lead to consequences such as impaired physical health, hospitalization, and even suicide (Institute of Medicine, 2012).
Past research demonstrates that Medicare-eligible populations respond appropriately to counseling (Roseborough, Luptak, McLeod, & Bradshaw, 2012). Federal agencies such as the Substance Abuse and Mental Health Services Administration (SAMHSA) publish entire guides on how to use counseling to treat depression and related conditions in older adults (SAMHSA, 2011). However, researchers have noted specific challenges that Medicare-eligible populations, such as older adults, face when trying to access mental health services. Stewart, Jameson, and Curtin (2015) described acceptability, accessibility, and availability as three intersecting dimensions that may influence whether an older adult in need of help is able to access care. In contrast to acceptability, which focuses on whether older individuals are willing to participate in specific mental health services, accessibility and availability are both supply-side issues that impede older adults’ engagement with mental health services. Accessibility refers to factors like funding for mental health services and providing transportation support to attend appointments. Availability is used to describe the number of mental health professionals who provide services to older adults within a particular community.
Stewart et al.’s (2015) framework is useful when examining current Medicare policy and its impact on beneficiaries’ ability to participate in mental health treatment when needed. Experts have criticized Medicare for its relative inattention to mental health care (Bartels & Naslund, 2013), noting a remarkably low percentage of its total budget is spent on mental health (1% or $2.4 billion; Institute of Medicine, 2012), as well as a lack of emphasis on prevention services. In terms of accessibility, Congress has made efforts to remove restrictions to using one’s health insurance to access mental health treatment. For example, mental health parity laws were passed in 2008 to ensure that Medicare coverage for mental illness is not more restrictive than coverage for physical health concerns (Medicare Improvements for Patients and Providers Act of 2008, 2008). Yet current Medicare policy may restrict the availability of services at the mental health provider level. For example, the Medicare program has not updated its mental health provider licensure standards since 1989, when licensed clinical social workers were added as independent mental health providers and restrictions on services provided by psychologists were removed (H.R. Rep. No. 101-386, 1989). Although counseling is only one mental health care modality available to Medicare beneficiaries, counselors can play a prominent role in the mental health treatment of older adults and people with long-term disabilities.
Meanwhile, there are references in the literature to a provider gap that may influence the ability of Medicare beneficiaries, including older adults, to access mental health services. A 2012 Institute of Medicine report described the lack of mental health providers as a crisis, and experts on geriatric mental health care have decried the lack of mental health professionals who focus their work on older adults (Bartels & Naslund, 2013). Despite these concerns, relatively little attention has been given to the influence of Medicare provider regulations in limiting the number of available providers. Scholars have noted that a significant proportion of graduate-level mental health professionals are currently excluded from Medicare regulations, despite providing a substantial ratio of community-based mental health services (Christenson & Crane, 2004; Field, 2017; Fullen, 2016; Goodman, Morgan, Hodgson, & Caldwell, 2018). Licensed professional counselors (LPCs) and licensed marriage and family therapists (LMFTs) jointly comprise approximately 200,000 providers (Medicare Mental Health Workforce Coalition, 2019), which means that approximately half of all master’s-level providers are not available to provide services under Medicare. Since their recognition as independent mental health providers by Congress in 1989, only licensed clinical social workers and advanced practice psychiatric nurses have constituted the proportion of master’s-level providers eligible to provide mental health services through Medicare.
Despite current Medicare reimbursement restrictions, Medicare beneficiaries are likely to seek out services from LPCs. Fullen, Lawson, and Sharma (in press-a) found that over 50% of practicing counselors had turned away Medicare-insured individuals who sought counseling services, 40% had used pro bono or sliding scale approaches to provide services, and 39% were forced to refer existing clients once those clients became Medicare-eligible. When this occurs, the Medicare mental health coverage gap (MMHCG) impacts providers and beneficiaries in several distinct ways. First, some beneficiaries may begin treatment only to have services interrupted or stopped altogether once the provider is no longer able to be reimbursed by Medicare. This can occur because of confusion about whether a particular patient’s insurance coverage authorizes treatment by a particular provider type, or when beneficiaries who have successfully used one type of coverage to pay for services transition to Medicare coverage because of advancing age or qualifying for long-term disability.
Most Medicare beneficiaries (81%; Kaiser Family Foundation, 2019) have supplemental insurance, including 22% who have both Medicare and Medicaid. Medicare beneficiaries who are dually eligible for Medicaid may be particularly vulnerable to the MMHCG. In most states, Medicaid authorizes LPCs to provide counseling services; however, in certain cases when these individuals also qualify for Medicare, the inconsistency in provider regulations between these programs can interfere with client care. A similar problem occurs when the Medicare-insured attempt to use supplemental plans (e.g., private insurance, Medigap) because of Medicare functioning as a primary source of insurance, and supplemental plans requiring documentation that a Medicare claim has been denied. Regardless of the reason for having to terminate treatment prematurely, early withdrawal from mental health treatment has been described as inefficient and harmful to both clients and mental health providers (Barrett et al., 2008).
The MMHCG also can interfere with clients’ ability to access services because of a lack of Medicare-eligible providers in a particular geographical region. For example, beneficiaries who reside in rural localities can have more difficulty finding mental health providers because of a general shortage of providers in these areas (Larson, Patterson, Garberson, & Andrilla, 2016). Larson et al. (2016) found that rural communities were less likely to have licensed mental health professionals overall, although these localities were more likely to have a counseling professional than a clinical social worker, psychiatric nurse practitioner, or psychiatrist. Historically, older adults from rural and urban localities experience a comparable prevalence of mental health disorders (Center for Behavioral Health Statistics and Quality, 2018). However, studies consistently describe low rates of mental health services accessibility and availability within rural communities (Smalley & Warren, 2012). Establishing counselors as Medicare-eligible providers can reduce the disparities of mental health services accessibility and availability experienced by older adults in rural communities.
Although it is known that LPCs are currently excluded from Medicare coverage, it is not well understood what sort of impact this has on mental health providers and the Medicare beneficiaries who seek their services. Recent efforts to raise awareness of this issue have emerged in the literature (Field, 2017; Fullen, 2016; Goodman et al., 2018), but there has not yet been an investigation into the phenomenological experiences of mental health providers who are directly impacted by existing Medicare policy. The purpose of this study was to explore the lived experiences of mental health professionals who have turned away clients because of their status as Medicare-ineligible providers. The primary research question for this study was: How do Medicare-ineligible providers make sense of their experiences turning away Medicare beneficiaries and their inability to serve these clients?
Research Design and Methods
This study was executed using interpretive phenomenological analysis (IPA) to guide both data collection and analysis. The study focused on the experiences of Medicare-ineligible mental health professionals as they navigated interactions with Medicare beneficiaries who sought mental health care from them. By using a hermeneutic approach to understand their unique perspectives on this phenomenon, we aimed to remain consistent with the philosophical approach of IPA, which is idiographic in nature (Smith, Flowers, & Larkin, 2009). This study received approval from the Western Institutional Review Board.
IPA focuses on the personal meaning-making of participants who share a particular experience within a specific context (Smith et al., 2009). We determined IPA to be the most appropriate method to answer our research question because of the personal impact on LPCs of turning away Medicare beneficiaries because of Medicare-ineligible provider status. Nationally, LPCs share the experience of being unable to serve Medicare beneficiaries because of the current Medicare mental health policy that establishes these licensed mental health professionals as Medicare-ineligible. IPA also is appropriate for this study because of the positionality of the researchers. The research team consisted of two LPCs and one LMFT who have denied services or had to refer clients because of the current Medicare mental health policy and have engaged in prior research and advocacy related to the professional and clinical implications of the current Medicare mental health policy. We selected IPA for this study because of the shared experience between the researchers and participants as Medicare-ineligible providers. A distinguishing feature of IPA, a variation of hermeneutic phenomenology, is the acknowledgment of a double-interpretative, analytical process: The researchers make sense of how the participants make sense of a shared phenomenon (Smith et al., 2009).
Participants
Participants were screened based on the inclusion criteria of having direct experience with turning away or referring Medicare beneficiaries and holding a mental health license as an LPC. Because states grant licenses to health care providers, we limited participation to LPCs who were practicing in a specific state in the Mid-Atlantic region. This allowed for consistency in licensure requirements, training provided, and current scope of practice across all participants. The nine participants interviewed all held the highest professional counseling license in this state, which allows these individuals to practice independent of supervision after completing 4,000 hours of supervised training. Post-license experience ranged from 6 months to 17 years, and participants practiced in both rural and non-rural settings. Pseudonyms were assigned by the research team (see Table 1 for participant information).
| Table 1
Participant Information
|
| Participant |
License Type |
Rural Statusa |
Years of Licensed Experience |
| Michelle |
LPC |
Rural |
4 years |
| Cecelia |
LPC |
Non-rural |
5 years |
| Mary |
LPC |
Non-rural |
17 years |
| Roger |
LPC |
Non-rural |
2 years |
| Aubrey |
LPC |
Rural |
4 years |
| Donna |
LPC |
Rural |
4 years |
| April |
LPC |
Non-rural |
0.5 years |
| Robert |
LPC/LMFT |
Non-rural |
22 years |
| Brandon |
LPC |
Rural |
5 years |
aThe table displays rural status as designated by the U.S. Department of Health and Human Services Health Resources and Services Administration (2016) according to the practice location of the participant. Non-rural includes metropolitan and micropolitan areas. Rural indicates any locality that is neither metropolitan or micropolitan.
Most participants were identified because of having completed a national survey of mental health providers unable to serve Medicare beneficiaries (Fullen et al., in press-a). Participants in the national survey were provided with a question in which they were able to indicate their openness to participating in follow-up individual interviews regarding their experiences with turning away clients as a result of Medicare policy. Two additional participants had not completed the national survey but were identified locally because of their unique experiences with the phenomenon under investigation. We selected nine participants in accordance with IPA participant selection and data saturation guidelines (Smith et al., 2009). Although the current Medicare policy excludes both LPCs and LMFTs, we chose to focus on the experiences of LPCs to ensure a purposive and homogeneous sample (Smith et al., 2009).
Data Collection
Semi-structured, in-depth interviews of the nine participants were conducted by the research team. All research team members are LPCs or LMFTs. Individual interviews were conducted by a single member of the team who digitally recorded and transcribed verbatim the interview procedure. Consent was obtained from the participants and pseudonyms were used to ensure participant confidentiality. Also, participants were given the option to stop the interview at any time. The elapsed time of each interview ranged between 47 and 66 minutes. The semi-structured interview protocol began with two initial questions to frame the interview: (a) Have you ever had to refer a potential client to another counselor/therapist/agency because of not being able to accept their Medicare insurance coverage? and (b) Have you ever established a working relationship with a client who later transitioned to Medicare insurance coverage?
Based on participant responses to these initial questions, two grand tour questions followed:
(a) Tell me about what typically occurs when someone with Medicare insurance contacts your office in search of counseling? and (b) Tell me about any times when you have had to alter a pre-existing working relationship with a client because of their Medicare coverage? Follow-up questions focused on the impact of current Medicare mental health policy on the interviewees, as well as their perceived impact on clients, local communities, other therapists in the area, and their employment contexts.
Data Analysis
The IPA process outlined by Smith et al. (2009) was employed to analyze the transcribed interview data. The following steps were employed throughout the analysis process: (a) reading and re-reading of transcripts, (b) initial noting, (c) developing emergent themes, (d) searching for connections across emergent themes, (e) moving to the next case, and (f) looking for patterns across cases. Codes and themes developed at each stage of the first transcript analysis required consensus agreement among the authors. After re-reading, initial noting, developing emergent themes, and clustering of superordinate themes for each of the remaining interviews, the authors proceeded to engage in a group-level analysis process of looking for patterns across all interviews. Patterns across all interviews were organized into a concept map to synthesize connections and relationships between the interviews. Connections and relationships identified through this cross-case analysis led to the identification of a group-level clustering of superordinate themes that resulted in the identification of the primary themes.
Trustworthiness
The authors attended to the credibility and trustworthiness of this analysis using four strategies. First, the authors have prolonged engagement in the fields of counseling and marriage and family therapy as licensed professionals. This prolonged engagement has allowed the authors to be situated to the contexts of the participants, account for abnormalities in the data, and transcend their own observations (Lincoln & Guba, 1985). Second, the authors engaged in a team-based reflexive process through the sharing of personal reflections and group discussions about emerging issues (Barry, Britten, Barber, Bradley, & Stevenson, 1999). Third, negative case analysis was used in the analytical process of this study to develop, broaden, and confirm themes that emerged from the data (Lincoln & Guba, 1985; Patton, 1999). The fourth strategy was analyst triangulation (Denzin, 1978; Patton, 1999). All three authors participated in the development of the study, data collection, and data analysis to reduce the potential bias that can emerge from a single researcher performing each of these tasks (Patton, 1999). Each researcher independently analyzed the same data and compared their findings throughout data analysis to check selective perception and interpretive bias.
Results
Three superordinate themes emerged from our interviews with nine mental health professionals who have experience with the Medicare coverage gap: ineffectual policy, difficult transitions, and undue burden. We will discuss one superordinate theme, ineffectual policy, with the emergent themes of confounding regulations, programmatic inconsistencies, and impediment to care. By presenting a single meta-theme, we hope to provide increased depth and the nuanced experiences that our participants shared (see Levitt et al., 2018 for a discussion on dividing qualitative data into multiple manuscripts).
All nine participants expressed concerns about the ineffectiveness of current Medicare policy when it comes to treating people with mental disorders who live in their communities. The disconnect between Medicare’s intended aim—to provide sound health care to beneficiaries—and the present outcome for clients seeking out counseling led us to describe the policy as ineffectual or not producing the intended effect. Our participants perceived that the policy had severe shortcomings in terms of providing access to mental health care, which they viewed as a serious problem with cascading consequences for their clients, communities, and themselves.
Confounding Regulations
Several participants described the Medicare coverage gap as “confusing” and “frustrating” for mental health providers and Medicare beneficiaries who are seeking mental health services. Brandon, an LPC who serves as a director within a Federally Qualified Health Center, stated, “Most people are pretty shocked to realize we are not part of Medicare.” He went on to explain that most medical providers, including psychiatrists, were not aware of LPCs’ Medicare ineligibility when making client referrals. Participants described how the confusion interferes with referrals between medical providers and clients seeking mental health services.
Other participants described how frustrating the policy is, both for themselves and their clients. Robert, an LPC who also is credentialed as an LMFT, stated that “as a provider, it’s frustrating to turn people away,” and “it’s especially concerning for older people who can’t afford to pay out of pocket.” Michelle, who works as an LPC in a rural community, described how the MMHCG influences clients’ views of the larger Medicare system, stating, “[Clients are] very angry—not directed towards me, just the system . . . they’re on Medicare now [and] they have to leave. They paid into a system and then still can’t see the clinician that they want to see.” According to interviewees like Michelle, current Medicare provider regulations do not account for the preponderance of LPCs who provide care, particularly in rural communities. Regulations are then perceived by clients as an additional barrier to getting help at a time when they may be vulnerable.
In fact, in certain cases, current Medicare policy may result in all Medicare beneficiaries within a particular community losing access to mental health care. Brandon described a 4-month period when his Federally Qualified Health Center was unable to serve any Medicare beneficiaries because of job turnover: “[It] took us four months to find an LCSW. . . . We specifically had to weed out some very qualified licensed mental health professionals because they weren’t LCSWs.” Brandon went on to explain that during this 4-month period, his clients were unable to access mental health care at the community clinic. He concluded, “It was pretty disruptive to their care.”
Brandon’s description elucidates the cascading impact of the current policy on clients, community agencies that provide mental health services, and counselors seeking work. When specific providers are excluded from servicing Medicare beneficiaries, older adults with mental health conditions are vulnerable to gaps in coverage, such as the 4-month period that Brandon described.
Programmatic Inconsistencies
Several interviewees referenced confusion about how Medicare interfaces with other insurance programs. Roger and Mary, a couple in joint practice, explained how confusion among clients and health providers in their community is exacerbated by inconsistencies between Medicare and Medicaid, including the fact that in their state LPCs are eligible for reimbursement from Medicaid, but not Medicare. Roger explained, “[The] confusion is not just with clients who have low SES. It’s agency people, it’s case managers in the community, doctors that would make referrals, there really is a misunderstanding . . . and sometimes a disbelief.” They went on to describe their frustration in having to explain to referral sources that Medicare ineligibility has nothing to do with a lack of training. Roger concluded, “Yes, we are trained and . . . virtually every other insurance company accepts licensed professional counselors.”
Mary’s and Roger’s statements are indicative of the confusion that current policy creates among providers and clients. Several interviewees expressed annoyance that they had to explain to prospective clients that they possessed the requisite license and training required by the state to provide counseling and that they were recognized providers by non-Medicare insurance providers (i.e., Medicaid, Tricare, private insurance providers).
Related to the inconsistency between Medicaid and Medicare, several interviewees alluded to the fact that the very circumstances that qualify individuals for government-funded insurance (e.g., poverty, disability) may inadvertently restrict the mental health care that is available to them. Michelle described this phenomenon in the context of having to address clients who were referred to work with her by the local community mental health agency. She alluded to a particularly challenging cycle in which clients who were diagnosed with schizophrenia would be referred to her for counseling while they were also applying for long-term medical disability. She described the challenges of working with these clients, only to have to refer them elsewhere once they became eligible for disability benefits (which include Medicare). Describing her clients, she stated, “[They] applied for disability, they received disability, and now they have to, even though they have established the relationship with me . . . transition over to a different therapist.” Michelle then highlighted what occurs after this transition is initiated: “[One] individual . . . has continued to see me because with that particular diagnosis, he doesn’t trust anyone else. . . . [Another] individual . . . just chooses not to see anyone . . . and then she ends up having to be hospitalized every so often.”
Beyond being discouraged or exasperated, Michelle’s capacity to remain stoic in the face of such a paradox was telling. As she described it, this sequence had happened on multiple occasions and would likely happen again save for a federal policy change. Michelle also alluded to the potential economic detriments of current policy. By foregoing outpatient counseling because of the barriers described above, her patient with schizophrenia must be intermittently hospitalized, which is a much more expensive form of treatment.
Policy-level inconsistencies were confusing to providers as well. April, an LPC who attained her independent license within the past year, stated, “It feels like handcuffs. It’s like here you have this credential that the state says you have earned, but it’s only a half credential because you can’t [accept] one of the main government sponsored programs.” Cecelia, an LPC working in a metropolitan area, expressed similar sentiments as she explained how clients with Medicare and secondary insurance plans are turned away: “I initially bill Anthem first and my claims continue to get denied.” She explained, “Basically what they want me to do is submit the claims to Medicare, allow Medicare to deny the claim, and then submit the claim to them with the denial from Medicare and then they’ll provide reimbursement.” However, Cecelia stated that this process has been halted when Medicare refuses to issue a denial letter because of her status as an LPC. She put it this way: “The struggle that I found with Medicare is that because I’m an LPC, Medicare won’t even recognize me to even allow me to submit a claim . . . so I cannot provide Anthem with the denial that they’re looking for.”
Cecelia’s description of the inconsistency between Medicare and private insurance reflects a particularly problematic experience for her clients. Although they had paid for supplemental private insurance plans to augment their Medicare coverage, they were unable to use these benefits without a denial letter from Medicare. Ironically, according to Cecelia, the Medicare office could not provide the denial to a Medicare-ineligible provider in the first place.
Brandon made a similar statement about the inconsistency in provider regulations between Medicare and Tricare, specifically referencing his own training levels: “I’m shocked. . . . We’re some of the most qualified licensed mental health professionals in the business to provide psychotherapy and treatment for psychiatric diagnoses . . . and yet somehow that doesn’t count . . . somehow we’re not included.” Citing the growing number of insurance providers that do recognize LPCs, including Tricare, he concluded, “So, literally Medicare is the last holdout that I’m aware of.” By describing Medicare as “the last holdout,” Brandon implies that Medicare is the only federal program that has not updated its provider regulations to match the current mental health marketplace. Echoing Brandon, the sentiment that Medicare provider regulations were not in line with the current state of mental health practice was common among our interviewees.
Impediment to Care
The therapeutic working alliance has been shown to be one of the key factors that positively impacts counseling treatment (Wampold, 2015). When existing clients become eligible for Medicare, whether because of increasing age or qualifying for a long-term disability, current policy appears to interfere with continuity of care. Aubrey, an LPC who practices in a rural locality, describes it this way: “I will tell you where the problem arises . . . if I’m assigned a client, and I have the rapport with them, and we’re working together and they become eligible for Medicare . . . then I have to transfer them.” Because of the emphasis within counseling on the working relationship, Aubrey suggested that after building a strong working relationship with a counselor, even referrals within an agency can be disruptive to patient care.
Additionally, several interviewees described the challenges associated with referring Medicare beneficiaries to alternative providers. Some alluded to clients who made an effort to continue working with an LPC, despite not being able to use their Medicare coverage. Eventually, disparities in clients’ financial circumstances resulted in some clients having to forego receiving mental health care. Brandon explained the difficulty that current Medicare policy brings to communities, particularly those in which there are relatively few Medicare-eligible providers relative to LPCs. He described monthly meetings with community private practice providers this way: “[They are] all booked up. There’s just not enough . . . licensed mental health providers in town to see everybody. And . . . because only half of those people can accept Medicare, it has a very particular impact on Medicare recipients.” Citing the shortage of providers, Brandon emphasized the additional burden faced by the Medicare-insured because of having a smaller available provider pool.
The shortage of alternative mental health providers was a common theme among interviewees, especially for those who practiced in rural communities. Michelle explained that there is a misperception that Medicare-eligible providers are available when Medicare beneficiaries seek out help: “I hear . . .
there are so many licensed clinical social workers in this area, but there aren’t.” As a consequence, “[individuals] that are trying to work themselves into the schedule of a licensed clinical social worker, they often wait months before they’re actually able to be seen.”
Donna, an LPC who also works in a rural community, expressed a similar concern about the lack
of options facing beneficiaries who live in rural areas: “I see such a shortage in rural areas of providers across the board. And then when you have to narrow it down even further to limit who they can see, then that makes it even more difficult for them to get the care that they need.”
In fact, the expense of mental health care when insurance coverage is unavailable was a factor that several interviewees described. Robert told the story of a client he had seen for several years who tried to pay out of pocket but could no longer make that financially viable: “[It] was really disappointing because she really wasn’t finished. . . . We had a great working relationship and it was sad to have her stop just because of reimbursement reasons.”
Brandon made a similar comment about an individual who was deterred from seeking treatment because of the cost of paying out of pocket when his Medicare insurance was unable to be used: “I let him know . . . I can’t accept Medicare. And he asked how much it would be. [I said] anywhere from $75 to $125, and . . . he was pretty disheartened by that.”
Mary noted how the MMHCG can result in Medicare beneficiaries not seeking out necessary services. She emphasized that turning people away at the point when they have elected to ask for help can be disconcerting: “Right at a time when they’re willing to reach out and ask for [help]. That’s the worst part. Because I think . . . that discourages clients from seeking services—they have to work too hard . . . finding a provider.” April added a similar sentiment: “It’s heartbreaking . . . [my] emphasis is on those most vulnerable and those most in need of services . . . it is my worst nightmare for a client to walk away . . . because I want them to know they are my priority.” In each of these examples, participants expressed concerns that current policy acted as a deterrent to accessing necessary mental health services because of the burdensome process of having to locate a Medicare-eligible provider.
Discussion
Our findings illuminate how current Medicare mental health policy impacts Medicare beneficiaries’ access to counseling treatment for mental health conditions. Nine mental health providers who are not Medicare-eligible were interviewed to learn about their experiences interacting with Medicare beneficiaries who sought their services. The central phenomenon that all interviewees responded to—their inability to work with Medicare beneficiaries in the same manner that they work with clients who use other forms of insurance—has infrequently been referenced in the extant literature. This phenomenon provides a unique contribution to discussions about the accessibility and availability of mental health services to older adults (Stewart et al., 2015) and people with long-term disabilities. Particularly compelling about what was reported in these interviews is the fact that these individuals were actively seeking out or currently engaged in mental health treatment at the time when they were turned away. In the past, explanations about barriers to mental health care for Medicare-insured populations have focused on systemic factors such as rural geography (Kim et al., 2013) or stigma about mental health (Chapin et al., 2013). While these are certainly relevant factors that provide a broad explanation for why older people are less likely to receive mental health services, the current study illuminates several proximate point-of-service barriers that result in providers having to cease treatment with clients, deny care to clients who were actively seeking it out, or refer clients to relatively long wait-lists in lieu of more prompt treatment by available providers. Given the lack of scholarly attention focused on the MMHCG, the perspectives offered by these participants contributes to a broader discussion about how to increase access to mental health services for older adults, as well as for individuals with long-term disabilities.
Among our interviewees, there was a noticeable amount of concern for how the MMHCG impacts individuals in the community in need of mental health care. Participants’ concerns about the consequences of the MMHCG on their clients may be related to their awareness that mental illness influences other key indicators of well-being. For example, depression reflects a relatively common mental health condition that responds well to treatment but can be problematic for clients when left untreated. Although depression was only one of several types of mental illness described by participants, clinically relevant depressive symptoms affect 10% of males over 65 and 15% of females over 65, and the presence of depressive symptoms is correlated with greater functional disability, dementia, higher rates of physical illness, and higher health care resource utilization (Federal Interagency Forum on Aging-Related Statistics, 2016). As the number of Medicare beneficiaries grows, it is reasonable to assume that there will be corresponding growth in the number of people who meet the criteria for mental health conditions, including depression. Echoing the concern voiced by our participants, we state that the current Medicare policy extends the risk of mental health needs going unmet among Medicare-insured populations.
Additionally, the economic consequences of untreated or undertreated mental illness are worth considering. Each participant described instances of unmet client mental health needs because of a combination of (a) practitioner inability to submit for Medicare reimbursement, (b) client’s inability to pay a sliding scale rate, and (c) lack of follow-through on referrals to mental health providers eligible for Medicare coverage. For example, some participants described this undertreatment as resulting in potential inpatient psychiatric hospitalization because of clients’ inability to utilize their Medicare benefits to seek care within their local communities. Undertreatment of mental health conditions can lead to inefficient administration of health care, including an over-reliance on more expensive mental health services when outpatient services could have been more appropriate. For example, the reimbursement rate for 45 minutes of counseling is $84.74 for doctoral-level providers (see American Psychological Association, 2015, for a critique of this rate), and the rate for master’s-level providers is estimated at 75% of this amount ($63.56). This is in contrast to the cost of a single day in an inpatient psychiatric facility, which is $782.78, or approximately 12 times higher than a single counseling session (Centers for Medicare & Medicaid Services, 2019). Having adequate outpatient services available within a community is traditionally a sound strategy for reducing high-cost treatment; yet this is not occurring as regularly as is needed when Medicare beneficiaries are involved. Although not every person who may be at risk for inpatient hospitalization will benefit solely from weekly outpatient services, several cases referenced by our interviewees (e.g., Michelle’s work with clients with schizophrenia) fit this category. Considering that a single day of inpatient treatment costs the same as a 12-session course of counseling from a master’s-level provider, it stands to reason that there are economic benefits to re-examining current Medicare mental health policy.
The inefficiency of current Medicare policy was highlighted when several participants alluded to inconsistencies between insurance programs, including certain cases in which having Medicare precluded clients from using other forms of insurance (e.g., Medicaid, Tricare, private supplemental plans) that would otherwise cover mental health treatment by LPCs. This feature of the MMHCG has important ramifications given that 81% of Medicare beneficiaries possess a supplemental health plan (Kaiser Family Foundation, 2019), including more than 12 million Americans who are dually covered by Medicare and Medicaid (Centers for Medicare & Medicaid Services, n.d.). For this latter group, dual-eligible adults are more likely to have functional or cognitive impairments, chronic conditions, or conditions that frequently coincide with mental health conditions. In fact, among dual-eligible individuals, 59% of those with disabilities and 20% of those who are 65 years or older self-reported diagnosis of a mental health disorder (Donohue, 2006). This means that some of the most vulnerable Medicare beneficiaries are particularly burdened by current Medicare mental health policy.
Implications for Professional Advocacy
Regarding advocacy on behalf of clients, these findings suggest that Medicare reimbursement for LPCs is urgently needed in order to provide Medicare-insured populations with access to mental health services. Currently, efforts to change Medicare regulations through the legislative process have support from a broad range of professional interest groups, many of which comprise the Medicare Mental Health Workforce Coalition (Medicare Mental Health Workforce Coalition, 2019). Further, there is currently legislation under consideration in both the U.S. Senate (S. 286; Mental Health Access Improvement Act, 2019) and U.S. House of Representatives (H.R. 945; Mental Health Access Improvement Act, 2019) that would include LPCs and LMFTs as Medicare-eligible providers. As of November 2019, these bills had 29 and 96 cosponsors, respectively (U.S. Congress 2019a, 2019b). Despite these efforts, more than half of counseling professionals recently surveyed had not participated in advocacy related to Medicare reimbursement (Fullen, Lawson, & Sharma, in press-b). Therefore, additional work is needed to educate members of the counseling profession about the consequences of current Medicare mental health policy on clients from underserved populations. Fullen et al. (in press-a, in press-b) describe several strategies that can be used to strengthen advocacy efforts among members of the counseling profession, including counselor educators, master’s and doctoral students, and practicing counselors.
Limitations and Future Research
A primary limitation of this study relates to the generalizability of the results. This study reports on a specific and localized account of how Medicare mental health policy impacts Medicare beneficiaries’ access to counseling treatment in a single state. We intentionally focused on a homogenous sample purposefully selected to explore how LPCs are making sense of their inability to provide counseling services to Medicare beneficiaries based on their professional status as Medicare-ineligible. The findings present a narrative account of how these licensed mental health providers make sense of and respond to the experience of not being able to serve Medicare clients because of professional limitations contained within Medicare mental health policy. The utilization of IPA has allowed for the detection of nuance, subtlety, and complexity within the data from the semi-structured interviews with our participants. This specificity allows for an understanding that shows how the coverage gap created by the exclusion of counselors impacts Medicare beneficiaries’ access to counseling services.
An additional limitation of our study is the use of prolonged engagement as a strategy to establish credibility and trustworthiness. Prolonged engagement, traditionally employed in ethnography and
participant observation, requires that researchers spend sufficient time in the field to learn or understand the experiential phenomenon of the study (Lincoln & Guba, 1985). Though we did not spend time with participants within their specific practice settings, we each have practice experience as Medicare-ineligible providers within the field of professional counseling. In a more ethnographic study on the MMHCG, we would be able to employ a more traditional application of prolonged engagement.
Future research should focus on additional qualitative and quantitative data sets that allow for more generalizability of findings. By nature, Medicare policy is consistent across the United States, which leads us to believe that there are likely similarities between the phenomena described by our interviewees and what occurs in other states. Nonetheless, additional inquiry is needed to probe the impact of MMHCG more comprehensively. An empirical investigation into the perspectives of Medicare-insured individuals who have been unable to utilize their Medicare benefits because of the MMHCG may lend an additional lens toward understanding the impact of Medicare mental health policy on clients. Ultimately, this study and subsequent studies focusing on diminishing coverage gaps for Medicare beneficiaries can support progress toward diminishing health inequities because of health care policy restrictions.
Conclusion
This study highlights an existing gap in the administration of Medicare services for clients seeking counseling treatment for mental health conditions. By attending to the theme of ineffectual policy, we have attempted to illuminate how current policy impacts the Medicare-insured, as well as LPCs who are involved in their mental health care. Based on our analysis of the MMHCG, future revisions to Medicare policy allowing for the inclusion of LPCs to provide counseling treatment to Medicare-insured individuals may contribute to a more equitable health care system for Medicare beneficiaries.
Conflict of Interest and Funding Disclosure
This research was supported by the Virginia Tech
Institute for Society, Culture, and Environment.
References
American Psychological Association. (2015). Medicare’s shrinking psychologist reimbursement rates. Retrieved from https://www.apaservices.org/practice/advocacy/state/leadership/medicare-payment
Barrett, M. S., Chua, W.-J., Crits-Christoph, P., Gibbons, M. B., Casiano, D., & Thompson, D. (2008). Early withdrawal from mental health treatment: Implications for psychotherapy practice. Psychotherapy: Theory, Research, Practice, Training, 45, 247–267. doi:10.1037/0033-3204.45.2.247
Barry, C. A., Britten, N., Barber, N., Bradley, C., & Stevenson, F. (1999). Using reflexivity to optimize teamwork in qualitative research. Qualitative Health Research, 9, 26–44. doi:10.1177/104973299129121677
Bartels, S. J., & Naslund, J. A. (2013). The underside of the silver tsunami—Older adults and mental health care. The New England Journal of Medicine, 368, 493–496. doi:10.1056/NEJMp1211456
Center for Behavioral Health Statistics and Quality. (2018). 2017 National survey on drug use and health: Detailed tables. Rockville, MD: Substance Abuse and Mental Health Services Administration. Retrieved from
https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHDetailedTabs2017/NSDUHDeta
iledTabs2017.pdf
Center for Medicare Advocacy. (2013). Medicare and mental health. Retrieved from https://www.medicareadvoca
cy.org/medicare-and-mental-health
Centers for Medicare & Medicaid Services. (n.d.). Seniors & Medicare and Medicaid enrollees. Retrieved from
https://www.medicaid.gov/medicaid/eligibility/medicaid-enrollees/index.html
Centers for Medicare & Medicaid Services. (2019). Fiscal year 2019 inpatient psychiatric facility prospective payment system rates and adjustment factors. In Inpatient psychiatric facility prospective payment system (Addendum A). Retrieved from https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/Inpatient-Psychiatric-Facility-Prospective-Payment-System.pdf
Chapin, R. K., Sergeant, J. F., Landry, S., Leedahl, S. N., Rachlin, R., Koenig, T., & Graham, A. (2013). Reclaiming joy: Pilot evaluation of a mental health peer support program for older adults who receive Medicaid. The Gerontologist, 53, 345–352. doi:10.1093/geront/gns120
Christenson, J. D., & Crane, D. R. (2004). Estimating the cost of direct reimbursement of marriage and family therapy under Medicare. Journal of Marital and Family Therapy, 30, 515–525. doi:10.1111/j.1752-0606.2004.tb01259.x
Denzin, N. K. (Ed.). (1978). Sociological methods: A sourcebook. New York, NY: McGraw-Hill.
Donohue, J. (2006). Mental health in the Medicare Part D drug benefit: A new regulatory model? Health Affairs, 25, 707–719. doi:10.1377/hlthaff.25.3.707
Federal Interagency Forum on Aging-Related Statistics. (2016). Older Americans 2016: Key indicators of well-being. Washington, DC: U.S. Government Printing Office. Retrieved from https://agingstats.gov/docs/LatestReport/Older-Americans-2016-Key-Indicators-of-WellBeing.pdf
Field, T. A. (2017). Clinical mental health counseling: A 40-year retrospective. Journal of Mental Health Counseling, 39, 1–11. doi:10.17744/mehc.39.1.01
Fullen, M. C. (2016). Medicare advocacy for the counselor advocate. Adultspan Journal, 15, 3–12. doi:10.1002/adsp.12015
Fullen, M. C., Lawson, G., & Sharma, J. (in press-a). Analyzing the impact of the Medicare coverage gap on counseling professionals: Results of a national study. Journal of Counseling & Development.
Fullen, M. C., Lawson, G., & Sharma, J. (in press-b). Medicare reimbursement for counselors: Counseling professionals’ advocacy beliefs and behavior. Counselor Education and Supervision.
Goodman, J. M., Morgan, A. A., Hodgson, J. L., & Caldwell, B. E. (2018). From private practice to academia: Integrating social and political advocacy into every MFT identity. Journal of Marital and Family Therapy, 44, 32–45. doi:10.1111/jmft.12298
H.R. Rep. No. 101-386 (1989). Retrieved from https://www.congress.gov/bill/101st-congress/house-bill/3299
Institute of Medicine. (2012). The mental health and substance use workforce for older adults: In whose hands? Washington, DC: National Academies Press.
Kaiser Family Foundation. (2019). An overview of Medicare. Retrieved from https://www.kff.org/medicare/issue-brief/an-overview-of-medicare
Kim, G., Parton, J. M., DeCoster, J., Bryant, A. N., Ford, K. L., & Parmelee, P. A. (2013). Regional variation of racial disparities in mental health service use among older adults. The Gerontologist, 53, 618–626. doi:10.1093/geront/gns107
Larson, E. H., Patterson, D. G., Garberson, L. A., & Andrilla, C. H. A. (2016). Supply and distribution of the behavioral health workforce in rural America. Data Brief #160. Seattle, WA: WWAMI Rural Health Center, University of Washington.
Levitt, H. M., Creswell, J. W., Josselson, R., Bamberg, M., Frost, D. M., & Suárez-Orozco, C. (2018). Journal article reporting standards for qualitative primary, qualitative meta-analytic, and mixed methods research in psychology: The APA Publications and Communications Board task force report. American Psychologist, 73, 26–46. doi:10.1037/amp0000151
Lincoln, Y. S., & Guba, E. G. (1985). Naturalistic inquiry. Newbury Park, CA: SAGE.
Medicare Improvements for Patients and Providers Act of 2008, Pub. L. No. 110-275, 122 Stat. 2494 (2008).
Medicare Mental Health Workforce Coalition. (2019). Expanding the Medicare provider workforce: A solution to the behavioral health crisis. Retrieved from https://centerstone.org/wp-content/uploads/MHAIA-One-Pager-FINAL.pdf
Medicare Payment Advisory Commission. (2015). Chapter 2: The next generation of Medicare beneficiaries. In Report to the Congress: Medicare and the health care delivery system (pp. 35–57). Retrieved from http://www.medpac.gov/docs/default-source/reports/chapter-2-the-next-generation-of-medicare-beneficiaries-june-2015-report-.pdf?sfvrsn=0
Patton, M. Q. (1999). Enhancing the quality and credibility of qualitative analysis. HSR: Health Services Research, 34, 1189–1208.
Roseborough, D. J., Luptak, M., McLeod, J., & Bradshaw, W. (2012). Effectiveness of psychodynamic psychotherapy with older adults: A longitudinal study. Clinical Gerontologist, 36, 1–16.
Smalley, K. B., & Warren, J. C. (2012). The current state of rural mental health. In K. B. Smalley, J. C. Warren, & J. P. Rainer (Eds.), Rural mental health: Issues, policies, and best practices (pp. 3–16). New York, NY: Springer.
Smith, J. A., Flowers, P., & Larkin, M. (2009). Interpretative phenomenological analysis: Theory, method and research. Thousand Oaks, CA: SAGE.
Stewart, H., Jameson, J. P., & Curtin, L. (2015). The relationship between stigma and self-reported willingness to use mental health services among rural and urban older adults. Psychological Services, 12(2), 141–148. doi:10.1037/a0038651
Substance Abuse and Mental Health Services Administration. (2011). Treatment of depression in older adults evidence-based practices (EBP) kit. Retrieved from https://store.samhsa.gov/product/Treatment-of-Depression-in-Older-Adults-Evidence-Based-Practices-EBP-KIT/SMA11-4631CD-DVD
U.S. Congress. (2019a). H.R.945—Mental Health Access Improvement Act of 2019. Retrieved from https://www.congress.gov/bill/116th-congress/house-bill/945
U.S. Congress. (2019b). S.286—Mental Health Access Improvement Act of 2019. Retrieved from https://www.congress.gov/bill/116th-congress/senate-bill/286
U.S. Department of Health and Human Services, Health Resources and Services Administration. (2016). FORHP rural areas [Data file]. Retrieved from https://data.hrsa.gov/data/about#DataUsage
Wampold, B. E. (2015). How important are the common factors in psychotherapy? An update. World Psychiatry, 14, 270–277. doi:10.1002/wps.20238
Matthew C. Fullen is an assistant professor at Virginia Tech. Jonathan D. Wiley, NCC, is a doctoral candidate at Virginia Tech. Amy A. Morgan is a doctoral candidate at Virginia Tech. Correspondence can be addressed to Matthew Fullen, School of Education, College of Liberal Arts and Human Sciences, 1750 Kraft Drive, Suite 2000, Room 2005, Blacksburg, VA 24061, mfullen@vt.edu.
Nov 25, 2019 | Volume 9 - Issue 4
Alwin E. Wagener, Laura K. Jones, J. Scott Hinkle
The global burden of disease related to mental health is astronomical and growing, with underprivileged countries being disproportionately affected. The Mental Health Facilitator (MHF) program was designed by the National Board for Certified Counselors (NBCC) to address the need for greater mental health support within international communities lacking adequate mental health practitioners to provide services. The MHF program trains individuals within communities to provide support and necessary referrals for those struggling with mental health challenges. This study assesses the effectiveness of MHF trainings conducted in a diverse subset of countries and communities. Initial findings from the analyses found significant gains in participants’ knowledge of mental health and mental health facilitation skills across training populations.
Keywords: Mental Health Facilitator, MHF, mental health, NBCC, global
Over 450 million individuals around the world struggle with mental health concerns with 300 million people alone suffering from depression (World Health Organization [WHO], 2018). Mental health is defined as “a state of well-being in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community” (WHO, 2014a, para. 1). Mental disorders account for nearly 30% of the global burden of disease (i.e., what kills, injures, and disables people around the world) in terms of years lived with disability (Kessler et al., 2009; Vigo, Thornicroft, & Atun, 2016). In addition to the hardships that mental disorders place on an individual’s social relationships, occupational opportunities, and physical health, nearly 800,000 people a year die by suicide, with 75% of those individuals residing in developing countries (WHO, 2014b). Such staggering statistics include the rank of suicide as the second most common cause of death among young people globally (WHO, 2014b).
In addition to personal struggles, communities also face economic hardships related to mental disorders. The global cost of mental health was estimated at $2.5 trillion in 2010, with estimates of costs expected to reach as high as $6 trillion by 2030 (Bloom et al., 2011). Such costs can be devastating for individuals and communities alike, especially where resources are limited.
Despite the exorbitant number of individuals around the world struggling with mental health concerns and the associated individual, societal, and economic costs, only a small portion of people receive the support they need (Hinkle, 2014; Kohn, Saxena, Levav, & Saraceno, 2004; Wang et al., 2007). It is important to note that only one third to one half of individuals in high-income countries receive mental health care. This gap is even more pervasive in low- to middle-income countries, with a mere 15%–24% of individuals receiving any form of mental health support (Demyttenaere, 2004). Furthermore, according to WHO (2015), most of the world’s population live in areas where there is an average of less than one psychiatrist per 200,000 people and even fewer individuals trained in psychosocial interventions.
This gap in service provision and treatment stems from both attitudinal (e.g., misinformation about mental health such as low perceived need, stigma, and discrimination) and structural-level (e.g., availability of services, financial considerations, and transportation problems) barriers (Andrade et al., 2014; Hinkle, 2014). Although attitudinal barriers appeared to be more pervasive, overall individuals with more severe mental health conditions and those in low- or lower–middle- income countries cited financial and service availability barriers as being especially problematic. In 2011, WHO detailed the scarcity of resources available to treat and promote mental health across the spectrum of high- to low-income countries, which leads to a gap in the provision of treatment as well as the quality of treatment when it is available. For example, within high-income countries, approximately $44.84 USD is spent per person on annual mental health expenditures, a value which drops to $0.20 USD per person in low-income countries (WHO, 2011). Clearly, a strategy to lessen this gap in global mental health service provision is needed.
A Call to Action
Given the pervasiveness and deleterious consequences of mental health disorders paired with the dearth of individuals receiving treatment, there is a global imperative that countries begin prioritizing mental health awareness, education, and treatment and combatting the noted barriers to individuals seeking and receiving adequate care. Enhancing the awareness and education of not only individuals struggling with mental health difficulties, but also members of the community, would be beneficial in addressing attitudinal barriers, while providing additional resources through increasing the number of both service providers and service centers can help to eliminate structural barriers to services. Such solutions are reflected in the WHO’s (2013) Mental Health Action Plan, which outlines the following four objectives:
(1) to strengthen effective leadership and governance for mental health; (2) to provide comprehensive, integrated and responsive mental health and social care services in community-based settings; (3) to implement strategies for promotion and prevention in mental health; and (4) to strengthen information systems, evidence and research for mental health. (p. 10)
Several approaches exist to address these objectives, yet one program in particular is unique in creatively addressing multiple objectives at once. Developed by the National Board for Certified Counselors (NBCC) and initially endorsed by WHO, the Mental Health Facilitator (MHF) program aims to reduce disparities in mental health care by facilitating access to support individuals and mental health services in underserved populations (Hinkle, 2006, 2014; Hinkle & Saxena, 2006). Specifically, the MHF program trains diverse community members (i.e., mental health laypersons) in the knowledge and skills necessary to identify mental health needs, support those in need of care, work with existing care resources, and make referrals to mental health professionals as needed (Hinkle & Henderson, 2007). The program focuses on creating a culturally appropriate curriculum adaptive to community needs and contexts while also providing fundamental information concerning mental health and basic psychosocial interventions. Also, unlike many other programs, the MHF program is only tailored and implemented into specific communities at the community’s request. In this way, the MHF program content aligns with WHO’s Mental Health Action Plan by working to strengthen culturally appropriate information systems, implementing strategies for promoting mental health and decreasing the severity and pervasiveness of disorders, and enhancing responsive and integrated service provision within community-based settings tailored to the needs of that community (Hinkle, 2014).
Content of the MHF Program
The mission of the MHF program is to provide skilled, responsible access to quality mental health interventions. This is usually accomplished through basic first-contact help and referrals to mental health professionals with respect for human dignity and meeting population needs by balancing globally accepted mental health practices within local norms and conditions (Hinkle, 2014). Cross-disciplinary in nature, the MHF program includes competencies from psychiatry, psychology, social work, psychiatric nursing, and counseling, covering topics such as helping skills, diversity, violence and trauma, suicide prevention, and referral and consultation skills. The design of the training emphasizes important considerations and approaches in addressing mental health concerns while allowing for flexibility in implementation. This flexibility is a key strength of the training program and is necessary given the breadth of cultural and contextual factors affecting mental health and mental health care around the globe. Such flexibility allows local stakeholders to identify and adapt the training to local needs and the knowledge gained from the MHF training program to be implemented within existing care settings or to provide a foundation for care in areas where no established system is present. The information contained within the training and flexibility of implementation constitute a population-based mental health care approach to addressing health care needs across a broad range of social, political, economic, and cultural environments (Hinkle, 2014), and one that is growing in its evidence base.
History and Implementation of the MHF Program
The MHF program is a three-tiered, train-the-trainer implementation model that consists of MHF master trainers, MHF trainers, and mental health facilitators. MHF master trainers are selected by NBCC based on specific criteria, most notably the completion of considerable training and experience in mental health and education. MHF trainers are often professionals or paraprofessionals with mental health and teaching experience located in the community who can train community groups. MHF trainees are typically laypersons with an interest in mental health who then become the first line of support for community members with mental health needs. Following training at each of the levels, individuals are registered in the international MHF registry. Currently there are over 4,774 registered MHF master trainers, MHF trainers, and mental health facilitators located around the world.
The MHF program was first established in 2005, when NBCC worked in collaboration with WHO to establish a panel of experts, including mental health professionals from the United States, Canada, Malaysia, Trinidad, St. Lucia, Turkey, Romania, India, Mexico, Botswana, and Venezuela, who would contribute to the development of the MHF training manual, curriculum, and implementation plans. This approach led to content and delivery plans that represented diverse cultures and thus diverse perspectives on mental health, mental health care, and the role of MHF master trainers, MHF trainers, and mental health facilitators. The curriculum and master training guide were completed and piloted in Mexico City in 2007 and 2008. Later in 2008, the first train-the-trainer program was delivered in Lilongwe, Malawi. To date, NBCC has partnered with 26 countries, including eight countries in Africa, five in Asia, four in the Middle East, and eight in Europe, as well as programs in Mexico and the United States. Furthermore, the MHF curriculum has been translated into Arabic, Chinese, Dzongkha (the language of Bhutan), Estonian, German, Greek, Japanese, Malay, Portuguese, Romanian, Russian, Spanish, and Swahili (Hinkle, 2014).
The MHF Curriculum
When developing a partnership with NBCC, communities can choose one of five MHF curricula to best suit their needs, namely the original MHF training, an abridged MHF training, a training for educators (MHF-EE), an abridged MHF-EE, or a version for first responders (i.e., fire, rescue, and police). The five MHF curricula share core content aimed at helping professionals and paraprofessionals improve communication and helping skills, identify local mental health resources, understand important ethical considerations, and connect health providers with individuals within their community who are in need of mental health services (Hinkle, 2014). In addition to the core content, the curricula directed toward educators and emergency personnel contain tailored modules to best support those populations. With trainings ranging from 6 to 30 hours, the curricula can be delivered over consecutive days or divided into its modules and taught over several weeks, depending on community needs (Hinkle & Henderson, 2007).
The foundation of the MHF curriculum underscores the shared experiences of stress, distress, and disorder (Desjarlais, Eisenberg, Good, & Kleinman, 1995; Hinkle, 2014; Hinkle & Henderson, 2007). Given these theoretical underpinnings, the core modules cover topics such as basic helping skills, coping with stress, community mental health services, and community advocacy skills, and also introduce trainees to considerations around ethical practice and specifics about interventions such as suicide mitigation and trauma responses (Hinkle, 2014). Participants learn the benefits of investing in mental health, barriers to mental health care, cost-effective interventions, how mental health disorders impact families, confidentiality and privacy, and the broad mission of the MHF program (Hinkle, 2014).
In the basic helping skills section of the training, trainees cover development; diversity; verbal and nonverbal communication; facilitative skills such as listening, asking questions, and providing reflections; assessing for mental health concerns; empathy and understanding human feelings; and how to make referrals and effectively terminate relationships (Hinkle, 2014; Hinkle & Henderson, 2007). This information is followed by a discussion of how to understand problems, coping styles, and ways of effectively managing problems. The training then delves into recognizing stress, distress, and various disorders, including risk factors and mental health in children. The core modules conclude with discussions of suicide and trauma. Being the leading cause of death among young people in low- and middle-income countries, suicide is a pressing concern within all communities (WHO, 2006). Similarly, the pervasiveness of natural and human-born disasters and crises, such as war, forced displacement, human trafficking, typhoons, and wildfires, affects individuals of all demographics around the world and often goes untreated (Hinkle, 2014). A final topic covered in the core MHF training is the importance of self-awareness and self-care for mental health facilitators.
Moreover, the content in any of the five MHF curricula can be adapted to best fit the social, cultural, economic, and political realities and needs of any community, country, or region. For example, countries have chosen to add additional modules on child maltreatment in the Syrian region.
Past and Ongoing MHF Research
Building a strong evidence base is imperative to the development of a sustainable program that addresses the staggering gap that exists in mental health service provision. With limited resources spent on mental health, countries and communities cannot afford to implement programs that lack evidence supporting their projected outcomes and benefits. To this end, NBCC has and will continue to emphasize building a solid evidence base for the MHF program. Qualitative studies published to date (Luke, Hinkle, Schweiger, & Henderson, 2016; Van Leeuwen, Adkins, Mirassou-Wolf, Schweiger, & Grundy, 2016) support the perceived value and effectiveness of the program. Luke et al. (2016) reported that among the value and benefits, participants commented on how the program was culturally congruent and beneficially adapted to the needs of their community as well as how the program filled a need in terms of limited mental health resources. Participants further noted the considerable negative implications if the MHF program were to be discontinued (Luke et al., 2016). Van Leeuwen et al. (2016) also found notable positive perceptions of the MHF program. Participants reported that they gained skills in communication and referral. They also noted how they received important education on mental health and causes of mental health problems, and an enhanced awareness of mental health in communication. Finally, participants reported that there were both personal and community benefits to the program, such as an ability to better understand their own mental health and the mental health of family members as well as a reduction in community mental health stigma (Van Leeuwen et al., 2016).
However, to date no study has reported the quantitative outcomes of MHF trainings. Most trainings include pre- and post-training assessments of participants using a true-false, pencil-and-paper–based assessment. The assessment for the original MHF curriculum had three small adaptations involving changing the wording on several questions in 2009, 2011, and 2013. The adaptations were minimal, so all years were included in this study. This study fills the gap in the MHF literature by reporting on the objective data gathered from the pre- and post-training assessments of the original MHF curriculum.
Methods
This study uses a quasi-experimental research design to evaluate whether participants in 88 MHF original trainings demonstrated increased knowledge of mental health issues and approaches to address community mental health concerns. The trainings spanned from 2009–2017 and included all MHF trainings conducted outside of the European Union and the United States. For each MHF training, pre- and post-training assessments were completed by all participants in an effort to evaluate the effectiveness of training. The pre- and post-training assessments contained 50 true-false questions with the pretest administered on the first day of training and the posttest administered at the final training day, 5 days later. The present study analyzed the pretest and posttest evaluations using paired t-tests and a one-way ANOVA.
Participants
Participants who completed all items on both the pretests and posttests were included in the study, resulting in 1,392 participants from 15 countries. Of the 1,392 participants, only 735 provided descriptive information. For those participants, 431 were female (59%) and 304 were male (41%). The age range of participants was 17 to 75 years with a mean age of 36 years. The education of participants ranged from elementary school to doctoral (PhD) and professional degrees (MD and JD). There were 14 participants reporting only an elementary school level of education (2%), 150 with high school (20%), 151 with a 2-year degree (21%), 310 with a 4-year degree (42%), 99 with a master’s degree (13%), and 11 with a PhD or professional degree (1%). Given that trainings were conducted in countries within North America, Africa, Asia, and the Middle East, the data included a diverse range of participants in terms of nationality.
Research Questions
There were two primary questions investigated in this study. The questions were prompted by a desire to better understand the effectiveness of the MHF trainings: (1) Does the MHF program training significantly increase overall knowledge of mental health facilitation from pretest to posttest evaluation for participants? and (2) How does performance on the pretest, or initial mental health knowledge, affect possible training gains made between pretest and posttest scores for the participants?
Data Preparation
Prior to formal data analyses, the authors examined the data to ensure it satisfied the assumptions of the relevant statistical tests. Upon initial data examination, the authors determined that 77 participants of an initial 1,392 were outliers. The outliers were those with scores 1.5 times the interquartile range, either above the third quartile or below the first quartile. Based on this, the data analyses presented in the following sections were run with and without the outliers removed, and it was determined that the outliers did not significantly affect the results (the only exception to the outliers affecting the results is described in the results section). As such, the data analyses presented are using the remaining 1,315 participants after the removal of the outliers.
As the data set is too large for statistical normality tests to be accurate, skewness and kurtosis values were examined. The data set without the outliers had skewness (.208) and kurtosis (-.018), both values within the normal range. A visual inspection of the descriptive q-q line further supported the conclusion that the data is normally distributed.
Results
Overall Mental Health Knowledge Gain
The first research question, asking whether the MHF program training significantly increased overall knowledge of mental health and mental health facilitation, was assessed using a paired sample t-test. The result of this analysis showed that there was a significant difference (t = -35.90, p = 0.000) between pretest (M = 37.64, SD = 5.58) and posttest (M = 41.17, SD = 5.24) scores. This analysis confirms the hypothesis that the MHF program training significantly increases the scores of participants from pretest to posttest evaluation.
Initial Mental Health Knowledge and Training Gains
The second research question investigated whether the starting knowledge of participants, as measured in the pretest, affected the training gains made between the pretest and posttest. To address this research question, four categories based on pretest scores were generated. A descriptive analysis was conducted to determine the quartiles of the pretest scores, and the quartiles were used to define the categories. The authors determined that quartiles are an effective means of dividing the pretest scores into four groups given that the relationships between the groups are clearly linked to the overall distribution of pretest scores. The pretest scores ranged from 15–50 (the range of possible scores was 0–50), and quartiles were generated in order to better understand the effects of MHF training on participants with low, medium-low, medium-high, and high MHF knowledge going into the training. The quartile scores were as follows: low < 34 (N = 317, M = 5.34, SD = 4.23), medium-low = 34 to 38 (N = 369, M = 4.13, SD = 3.62), medium-high = 39 to 42 (N = 340, M = 3.06, SD = 2.69), and high > 42 (N = 289, M = 1.35, SD = 2.04).
To compare the four groups and answer the second research question, a one-way ANOVA was used. The analysis showed that the differences between the scores of the four categories are significant (F[3, 1311] = 81.05, p = 0.000). A post-hoc Tukey HSD test allowed for a more detailed understanding of the difference between the four groups. The Tukey HSD test results indicated significant differences between all four groups. The details of the differences between means in the post-hoc test are as follows. The low score group showed a significant difference between pretest and posttest scores compared to the medium-low test score group (mean difference = 1.21, p = 0.000), the medium-high test score group (mean difference = 2.28, p = 0.000), and the high test score group (mean difference = 3.99, p = 0.00). The medium-low test score group was significantly different from the medium-high (mean difference = 1.07, p = 0.000) and high (mean difference = 2.78, p = 0.000) test score groups, and the medium-high test score group was significantly different from the high test group (mean difference = 1.71, p = 0.000). When running the one-way ANOVA with the outliers included, the only difference in significance found in the results for any of the analyses occurred between the medium-low and medium-high groups. With the outliers included in the analysis, there was no significant difference between those two groups, although all the other significant differences remained, and the overall trend of pretest to posttest score differences decreasing as the pretest score rose remained unchanged. The results of the analyses confirm that the lower the pretest scores, the larger the gain in knowledge from the training.
Post-Hoc Data Analysis
After considering the significant pretest to posttest gains, the authors became curious about whether the content of the pretest and posttest questions might be separated into subscales to better evaluate MHF training effectiveness. The observation that the questions on the MHF pretests and posttests naturally related to either knowledge or skills prompted the authors to separate the questions into the two subscale categories, MHF knowledge and MHF skills.
To generate the two subscales, one author went through the questions independently and categorized them for each of the three test iterations. Then, the second author went through the questions to confirm they fit the subscales. A paired t-test was used to determine whether participants demonstrated equivalent gains in both knowledge and skills.
The results of the analyses showed significant gains on both subscales. The mean gain on MHF knowledge was 1.41 (N = 1315, t = -22.86, p = 0.000), and the mean gain on MHF skills was 2.12 (N = 1315, t = -29.67, p = 0.000). The results of this post-hoc analysis confirm the hypothesis that the MHF program training leads to significant increases in both MHF knowledge and skills.
Discussion
The results of the present study provide further evidence of the effectiveness of the MHF program. Previous studies have examined qualitative accounts of trainees’ experiences and impressions of the program (Luke et al., 2016; Van Leeuwen et al., 2016). The present data, however, provide objective evidence that the program is indeed enhancing trainee knowledge of mental health and MHF skills. This finding suggests that individuals who complete the MHF program have the requisite knowledge and skills to provide frontline interventions and needed referrals for community members struggling with their mental health.
Interestingly, the results also demonstrate that the documented growth in knowledge and skills is relative to the existing knowledge of the participant prior to training, whereby those with less initial training (i.e., lower scores on the pretest) showed greater gains in knowledge and skill from participation in the MHF training. Although somewhat intuitive, this provides evidence that the program is successful at enhancing the knowledge and skills of participants despite previous training in mental health. It brings all participants up to a similar, requisite baseline level of knowledge to perform mental health facilitation. Participants with little to no information regarding mental health can gain the needed knowledge and skills necessary to support the mental health of others in their community, while those with considerable information and training can refine their skills and knowledge for their new role.
Post-hoc analyses assessed whether the MHF program is equally adept at enhancing knowledge related to mental health and mental health struggles as well as the skills needed in mental health facilitation. Findings revealed that participants demonstrated a significant growth in both knowledge and skills. As such, the MHF program not only provides mental health literacy, but also the skills needed to support those in need. This is notable given the significant disparity of mental health literacy in both the developed and developing world (Ganasen et al., 2008; Jorm, 2000). Among professionals and laypersons alike, the lack of knowledge and understanding of mental health not only contributes to the treatment gap, but also the considerable stigma faced by those who struggle with mental health issues.
Taken together, the results suggest that the researchers and program developers can confidently endorse this program as one that leads to an increase in mental health knowledge and skills associated with mental health facilitation among both professionals and laypersons. In this way, the MHF program furthers the WHO’s (2013) Mental Health Action Plan goals of strengthening information systems surrounding mental health and clearly establishing a requisite foundation for the implementation of strategies and services. In its proposed actions for member states, WHO emphasized the importance of human resource development by “build[ing] the knowledge and skills of general and specialized health workers to deliver evidence-based, culturally appropriate and human rights-oriented mental health and social care services” (WHO, 2013, p. 15).
Our findings also complement the positive evaluation feedback of participants. In particular, Van Leeuwen et al. (2016) found that participants appreciated the increased knowledge they gained, noting that it was beneficial to themselves as well as their community. Participants noted that they had an enhanced ability to better understand their personal and family members’ mental health and that the MHF training helped reduce community stigma. Examined in conjunction with the present data, this suggests that not only are participants objectively gaining knowledge about mental health, they are aware of what they learned and actively and intentionally applying that knowledge to help themselves, other individuals, and their overall community better understand mental health. Given that the present study also demonstrated that participants are gaining an enhanced understanding of MHF-related skills, the researchers are hopeful that with their knowledge of mental health, participants are likewise intentionally putting their facilitation skills into action to support those in need within their communities.
Limitations and Future Research
The present study provides a notable step in further documenting the effectiveness of the MHF program, yet the limitations of this research must be taken into consideration and used for ongoing program planning and research development. Using true-false repeated measures pre- and post-training assessment could lend itself to bias. Within such situations, the trainee may recall, implicitly or explicitly, the questions asked in the pre-training assessment and may be primed for remembering the information needed to respond to those questions. Similarly, although the findings were statistically significant, probability suggests that true-false questions are more accessible to educated guesses rather than a depiction of accurate knowledge. In this way, having a multiple-choice format test with possible case scenarios to assess application in greater depth might provide a richer depiction of the knowledge gained. The present means of assessment also are vulnerable to a ceiling effect, whereby those with the most knowledge around mental health would earn the maximum number of points on both the pre- and post-training assessment. Although the present testing level is the most adaptive to all knowledge levels, perhaps a greater breadth of questioning to assess more nuanced components of the MHF skillset might be more helpful in accurately assessing the knowledge and skills gained by those coming into the MHF program with more extensive mental health training. An additional limitation of the assessments specifically was the post-hoc distinction between the skills and knowledge components assessed in the MHF training. In the future, greater attention to developing questions specifically geared toward these two necessary areas will be more effective in discriminating such gains. One final limitation of the present study and an area well positioned for future research is the lack of specific data regarding how the knowledge and skills are being used following the training.
Prior to this study, there was no formal quantitative data analysis to substantiate the reach of the MHF program. In addition to this research assessing the knowledge and skills gained through participation in the MHF program, there is the equally important next step of assessing how that knowledge is being used to address the goals of the program. Research examining the extent to which the MHF program aides in increasing mental health access for individuals in need of support and thereby decreasing the treatment gap among individuals struggling with their mental health would be especially important in addressing the over 70% of individuals in developing countries who do not receive the mental health care they so desperately need (Demyttenaere, 2004).
Conclusion
The growing number of individuals around the world with mental health challenges, coupled with the lack of knowledge, services, access, and fiscal resources to address the growing need, drives mental health to the forefront of worldwide public health challenges. Countries and communities in both developed and developing countries alike must embrace creative, economical, and culturally appropriate population-based solutions. The MHF program developed by NBCC (Hinkle & Henderson, 2007), initially in coordination with WHO and mental health experts from around the world, provides one such solution. Extant research on the MHF program validates the cultural appropriateness of the tailored programs as well as the extent to which community members believe they have benefited from the trainings (Luke et al., 2016; Van Leeuwen et al., 2016). The present findings further this research by providing quantitative data speaking to the effectiveness of the program at enriching participants’ knowledge and skills in relation to mental health. This burgeoning evidence base moves the MHF program one step closer to becoming a global best practice in addressing the notable and growing gap in mental health care around the world.
Conflict of Interest and Funding Disclosure
The first two authors were reimbursed by NBCC
for expenses related to this manuscript.
The third author is an employee of NBCC who
has developed and conducted MHF trainings.
References
Andrade, L. H., Alonso, J., Mneimneh, Z., Wells, J. E., Al-Hamzawi, A., Borges, G., . . . Kessler, R. C. (2014). Barriers to mental health treatment: Results from the WHO World Mental Health surveys. Psychological Medicine, 44, 1303–1317. doi:10.1017/S0033291713001943
Bloom, D. E., Cafiero, E. T., Jané-Llopis, E., Abrahams-Gessel, S., Bloom, L. R., Fathima, S., . . . Weinstein, C. (2011). The global economic burden of non-communicable diseases. Geneva, Switzerland: World Economic Forum.
Demyttenaere, K., Bruffaertts, R., Posada-Villa, J., Gasquet, I., Kovess, V., Lepine, J. P., . . . Chatterji, S. (2004). Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health surveys. JAMA, 291, 2581–2590. doi:10.1001/jama.291.21.2581
Desjarlais, R., Eisenberg, L., Good, B., & Kleinman, A. (1995). World mental health: Problems and priorities in low-income countries. Oxford, England: Oxford University Press.
Ganasen, K. A., Parker, S., Hugo, C. J., Stein, D. J., Emsley, R. A., & Seedat, S. (2008). Mental health literacy: Focus on developing countries. African Journal of Psychiatry, 11, 23–28. doi:10.4314/ajpsy.v11i1.30251
Hinkle, J. S. (2006, October). MHF town meeting: Ideas/questions. Presentation at the NBCC Global Mental Health Conference: Focus on the Never Served, New Delhi, India.
Hinkle, J. S. (2014). Population-based mental health facilitation (MHF): A grassroots strategy that works. The Professional Counselor, 4, 1–18. doi:10.15241/jsh.4.1.1
Hinkle, J. S., & Henderson, D. (2007). Mental health facilitation: Program history and summary. Greensboro, NC: National Board for Certified Counselors. Retrieved from http://mentalhealthfacilitator.com/Assets/Project_Summary.pdf
Hinkle, J. S., & Saxena, S. (2006, October). ATLAS: Mapping international mental health care. Presentation at the NBCC Global Mental Health Conference: Focus on the Never Served, New Delhi, India.
Jorm, A. F. (2000). Mental health literacy: Public knowledge and beliefs about mental disorders. The British Journal of Psychiatry, 177, 396–401. doi:10.1192/bjp.177.5.396
Kessler, R. C., Aguilar-Gaxiola, S., Alonso, J., Chatterji, S., Lee, S., Ormel, J., . . . Wang, P. S. (2009). The global burden of mental disorders: An update from the WHO World Mental Health (WMH) surveys. Epidemiology and Psychiatric Sciences, 18, 23–33. doi:10.1017/S1121189X00001421
Kohn, R., Saxena, S., Levav, I., & Saraceno, B. (2004). The treatment gap in mental health care. Bulletin of the World Health Organization, 82, 858–866. doi:10.1590/S0042-96862004001100011
Luke, M., Hinkle, J. S., Schweiger, W., & Henderson, D. (2016). Mental health facilitator (MHF) service implementation in schools in Malawi, Africa: A strategy for increasing community human resources. The Professional Counselor, 6, 1–21. doi:10.15241/ml.6.1.1
Van Leeuwen, J. M., Adkins, S., Mirassou-Wolf, T., Schweiger, W. K., & Grundy, R. (2016). An evaluation of the Mental Health Facilitator programme in rural Uganda: Successes and recommendations for future implementation. Journal of Psychology in Africa, 26, 288–299. doi:10.1080/14330237.2016.1185919
Vigo, D., Thornicroft, G., & Atun, R. (2016). Estimating the true global burden of mental illness. The Lancet Psychiatry, 3, 171–178. doi:10.1016/S2215-0366(15)00505-2
Wang, P. S., Angermeyer, M., Borges, G., Bruffaerts, R., Chiu, W. T., De Girolamo, G., . . . Usten, T. B. (2007). Delay and failure in treatment seeking after first onset of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry, 6, 177–185.
World Health Organization. (2006). Integrating mental health into primary care: A global perspective. Geneva, Switzerland. Retrieved from https://www.who.int/mental_health/resources/mentalhealth_
PHC_2008.pdf
World Health Organization. (2011). Mental health atlas 2011. Retrieved from https://apps.who.int/iris/
bitstream/handle/10665/44697/9799241564359_eng.pdf;jsessionid=7488A5219E439A1D1D082CCFA2E872E5?sequence=1
World Health Organization. (2013). Mental health action plan 2013–2020. Retrieved from http://www.who.int/mental_health/publications/action_plan/en/
World Health Organization. (2014a). Mental health: A state of well-being. Retrieved from http://www.who.int/features/factfiles/mental_health/en/
World Health Organization. (2014b). 10 facts on mental health. Retrieved from https://www.who.int/features/factfiles/mental_health/mental_health_facts/en/
World Health Organization. (2015). Mental health atlas 2014. Retrieved from http://www.who.int/mental_health/evidence/atlas/mental_health_atlas_2014/en/
World Health Organization. (2018). Mental disorders. Retrieved from
http://www.who.int/mediacentre/factsheets/fs396/en/
Alwin E. Wagener, NCC, is an assistant professor at Fairleigh Dickinson University. Laura K. Jones is an assistant professor at the University of North Carolina Asheville. J. Scott Hinkle is the editor of The Professional Counselor. Correspondence can be addressed to Alwin Wagener, 285 Madison Ave., M-AB2-01, Madison, NJ 07940, awagener@fdu.edu.
 Liliana Sznaidman has over 20 years of experience as a licensed professional counselor (LPC) and licensed professional counselor supervisor (LPCS) in North Carolina. She currently owns a private practice where she provides counseling and psychotherapy to adults, couples, and young adult clients. She also provides clinical supervision and consultation services to pre-licensed counselors and other mental health professionals.
Liliana Sznaidman has over 20 years of experience as a licensed professional counselor (LPC) and licensed professional counselor supervisor (LPCS) in North Carolina. She currently owns a private practice where she provides counseling and psychotherapy to adults, couples, and young adult clients. She also provides clinical supervision and consultation services to pre-licensed counselors and other mental health professionals.