Aug 18, 2020 | Volume 10 - Issue 3
Joshua D. Smith, Neal D. Gray
Each year TPC presents an interview with a seminal figure in counseling as part of its Lifetime Achievement in Counseling series. This year I am honored to introduce Dr. Mona Robinson. She identifies as a counselor with expertise in rehabilitation counseling, is among the distinguished faculty at Ohio University, and is an internationally recognized scholar. I am grateful to Dr. Joshua Smith and Dr. Neal Gray, who continue to bring the contributions and wisdom of leaders in the profession to TPC readers. Here they present a view to Dr. Robinson’s accomplishments throughout her career, along with her reflections on the CACREP and CORE merger and the evolution of the profession. —Amie A. Manis, Editor

Mona Robinson, PhD, LPCC-S, LSW, CRC, is a professor at Ohio University and Program Coordinator for both their Counselor Education Program and their Human Services Program. She is the Immediate Past Chair of the Department of Counseling and Higher Education. She holds a BS in psychology, an MA in rehabilitation counseling, and a PhD in rehabilitation services (Rehabilitation Counselor Education) from The Ohio State University. Dr. Robinson is a certified rehabilitation counselor, a licensed professional clinical counselor supervisor, and a licensed social worker.
Prior to her employment at Ohio University, Dr. Robinson served as a counselor and administrator of vocational rehabilitation counseling and employment services to clients with severe mental illness and other barriers to employment. Additionally, she served as a consultant and adjunct professor at Wilberforce University. Her areas of expertise include psychiatric rehabilitation, disability advocacy, multicultural counseling, ethics, and dual diagnosis.
Dr. Robinson serves as the institute director for study abroad programs held in Italy and Botswana. She is currently 1st Vice President for the National Council on Rehabilitation Education, Accessibility Coordinator for the Association for Multicultural Counseling and Development 2019 Summit, and a member of their 2019 Day of Service Committee. She has served as Past President of the National Association of Multicultural Rehabilitation Concerns, Ohio Rehabilitation Association, and Ohio Rehabilitation Counseling Association. She is a past board member of the National Rehabilitation Association and the Ohio Counseling Association Executive Council, and a Past President and Past Secretary of the Central Ohio Counseling Association.
In addition to her extensive professional service, she is also a current member of numerous professional organizations, including but not limited to the American Counseling Association, American Rehabilitation Counseling Association, Association for Multicultural Counseling and Development, National Rehabilitation Counseling Association, Ohio Rehabilitation Association, and Ohio Rehabilitation Counseling Association. She is on the editorial boards of the Journal of Applied Rehabilitation Counseling and the International Journal of Applied Guidance and Counseling, a Vocational Expert for the Social Security Administration Office of Hearing Operations, and a Site Team Chair for the Council for Accreditation of Counseling and Related Educational Programs (CACREP).
Dr. Robinson’s awards and honors include the 2008 and 2014 Ohio University College of Education Distinguished Faculty Graduate Teaching Award; the 2009 Sylvia Walker Multicultural Education Award; and the 2010 Visiting Scholar to South Korea Award, through which she taught global communication at the Kyungpook National University. She was a presenter at the 2012 International Conference on Education in Honolulu, Hawaii, and a speaker at the 2017 4th Biennial Bhutan International Counseling Conference held in Thimphu, Bhutan. Dr. Robinson has been the recipient of the 2014 Ohio University College of Education Distinguished Faculty Outstanding Outreach Award, the 2016 and 2017 Ohio University Faculty Newsmakers Award, the 2017 Virgie Winston-Smith Lifetime Achievement Award, and a 2018 National Association of Multicultural Rehabilitation Concerns Fellow Award. Dr. Robinson was an invited speaker at the University of Botswana in 2017 and 2019 for the Ultimate Motivational Speaker Competition. Lastly, she was the keynote speaker for the Seminar on Guidance and Counseling Conference held in Yogyakarta, Indonesia, in October 2019.
In this interview, Dr. Robinson shares insights on growth and change within the counseling profession, her experience as a woman of color in counselor education, and her outlook on the future development of the profession.
- As a rehabilitation counselor educator, how has the merger between the Council on Rehabilitation Education (CORE) and CACREP impacted your role and the counseling profession?
For me personally, I am pleased to see the merger finally come to fruition. In the past, I worked as a vocational rehabilitation counselor and a licensed professional clinical counselor, so I certainly see the value of both specialty areas. I view myself as a counselor with a specialty area in clinical rehabilitation counseling. I am fortunate to work in a program that has historically integrated clinical mental health counseling, rehabilitation counseling, and school counseling at the master’s level. Holding accreditation with both CORE and CACREP meant we had to go through the accreditation process twice. However, since the merger occurred, we now have one accreditation cycle and our students can obtain credentialing under CACREP for both clinical mental health and rehabilitation counseling.
With respect to the counseling profession, I continue to be involved in discussions regarding the merger, including the revisions to the 2023 CACREP standards, particularly as they relate to clinical rehabilitation counseling. For the purpose of clarification, I think it is noteworthy to mention that rehabilitation counselors receive the same general training as clinical mental health counselors with the exception of diagnosis and treatment of mental and emotional disorders. Traditional rehabilitation counselor training focuses on vocational rehabilitation, specifically as it relates to assisting people with physical and mental disabilities in obtaining meaningful employment and/or independent living opportunities that improve their quality of life. Clinical rehabilitation counselor training would continue to focus on vocational rehabilitation with the inclusion of a clinical mental health counselor curriculum that focuses on treating mental and emotional disorders that lead to licensure as a professional clinical counselor as well as certification as a certified rehabilitation counselor.
Over the years, I presented at national conferences regarding the advantages and disadvantages of the merger. One of the main points of contention in the field of rehabilitation counseling centers around the lack of coursework necessary to treat and diagnose mental and emotional disabilities, including completing an internship in a setting that treats and diagnoses mental and emotional conditions. I firmly believe that the counseling profession as a whole will benefit from the merger with the infusion of clinical rehabilitation standards. This is a first step toward standardization so that all counseling programs can offer the same educational requirements that lead to licensure. Having a standardized counseling program will aid licensure portability as well as serve as a precursor to a national license for counselors. Counseling students reap the benefits of being taught by counselor educators with multiple specialty areas. Rehabilitation counselor educators play a pivotal role in teaching students knowledge from their specialty areas in addition to the clinical mental health competencies.
- What are the benefits and challenges associated with that merger, and where do you see rehabilitation counseling going in the future?
Students in rehabilitation counseling programs will benefit from a more well-rounded education that gives them an opportunity to work with people with physical, mental, and emotional disabilities. Having this additional knowledge will prepare students to work in integrated medical and behavioral settings. Counselor educators who teach from a holistic approach allow students an opportunity to gain skills that will assist them in achieving better outcomes for their clients. In addition to the obvious time considerations, one accreditation cycle for all programs instead of two has positive financial implications for students and institutions alike. Some of the challenges associated with the merger include concerns that rehabilitation counselor educators may need to take additional counseling coursework to become eligible for licensure as a professional clinical counselor. Currently, rehabilitation counseling professionals who teach in rehabilitation counselor programs come from varying backgrounds, including vocational rehabilitation counselors (public and private sector), rehabilitation specialists, physical therapists, and occupational therapists; while beneficial to rehabilitation counseling, they may not be eligible to become licensed as professional clinical counselors without taking additional courses or obtaining another degree. Additionally, there are concerns about rehabilitation counselors losing their professional identity. Therefore, adopting a curriculum that focuses on vocational rehabilitation learning outcomes while infusing clinical mental health learning outcomes will aid in alleviating these fears. Long term, a reunification of the rehabilitation counseling professions (i.e., rehabilitation counselor educators, vocational rehabilitation counselors, rehabilitation specialists, physical therapists, and occupational therapists) will need to happen, as splintering of the profession occurred well before the CORE and CACREP merger process began. It is my hope that the merger will bring about changes in counseling that are beneficial for all counseling professionals.
- What do you consider to be your major contribution to the development of the counseling profession and why?
Increasing faculty diversity as well as student diversity has been a cornerstone of my contribution to the development of the counseling profession. I have been intentional about recruiting AND retaining diverse students and faculty worldwide. The counseling profession has historically been predominantly White. However, the clients that present for counseling continue to come from increasingly diverse backgrounds. Hence, recruitment and retention of African American students and faculty are essential in the 21st century to meet the needs of diverse client populations. Therefore, I will continue to present and publish on the topic of diversity and the need to be responsive to all aspects of diversity. Undertaking my mission to speak about the necessity to respect diversity not only in conversation but also through action is an endeavor that I will continue to pursue.
Another contribution of mine is mentorship. When working in academia, one of the most valuable resources faculty members can acquire is a mentor. Personal relationships and support systems are important factors for a successful career. I believe that participation in formal and informal networks and mentoring relationships is critical in the persistence of African American female faculty in the academy. Mentors provide support, guidance, information, and advice to their mentees who may be struggling with career advancement. A mentor can serve as a support system for a faculty member by providing protection, coaching, and even validation for them through acceptance, friendship, and role modeling.
I believe in the importance of mentoring counselors, students, and faculty. While recruitment is important, retention efforts are even more crucial. I have spent countless hours focusing on the recruitment and retention of African American students and faculty. Additionally, I enjoy speaking locally, nationally, and internationally about issues that affect people of color, including those with varying disabilities. While licensed professional clinical counselors are trained to work with people with mental and emotional conditions, they often lack knowledge to effectively assist people with physical disabilities. I have been fortunate to fill the gap by providing trainings in this area.
- What three challenges to the counseling profession as it exists today concern you most?
Despite the fact that counseling has been a helping profession for decades, it still lags behind social work and psychology in terms of recognition as a profession. If the counseling profession aspires to obtain the same status as other helping professions such as social work and psychology, we must utilize our specialty areas as one cohesive profession. Social workers have done this successfully for decades through being known by the profession first, and then by their specialty areas. For example, someone may seek out a medical social worker that works in a hospital setting. In essence, the setting determines the specialty area of the social worker; counseling should consider adopting the same process. Counselor training is frequently viewed as not being on par with psychology. Therefore, adopting a standardized curriculum for training counselors will aid in eradicating this myth.
Another challenge is the lack of access to billing for Medicare on the part of counselors. Part of the reason for this disparity is that counselors are not viewed as having the appropriate training to serve as professional helpers similar to social workers and psychologists. While the need for trained professionals continues to increase, counseling has not been embraced by the mainstream. Efforts are underway to achieve parity that will allow counselors to bill Medicare—to date, this has not happened. Again, adopting a standardized curriculum will increase the likelihood of counselors serving as vendors for Medicare.
A third area of concern is the looming financial crisis that many institutions of higher learning face. Declining enrollments and increasing tuition costs make recruiting and retaining quality students and faculty a challenge. More attention should be given to offering alternatives to traditional classroom settings as a way to reach more students. Developing and implementing a curriculum that appeals to a broader audience is one way to attract diverse faculty and students. Institutions that offer welcoming environments and appreciate differences will be at the forefront of any future growth.
- What needs to change in the counseling profession for these three concerns to be successfully resolved?
I think it will be important for the counseling profession to take the time to respect diversity in all forms, not only in language but also in action. More unification is necessary between disciplines. Embracing an approach that demonstrates that we are ALL counselors first will be an important first step toward unification of the profession. Professional conferences should be inclusive of all specialty areas when offering sessions. Counselors should take the time to learn about other specialties. We show ourselves as a much stronger profession if we train counselors who can provide services to a diverse population, and that includes meeting the needs of people with disabilities.
With respect to billing parity, counselors should band together to advocate for Medicare. Standing as one unified profession will allow our voices to be heard on a broader scale. Finally, offering a diverse curriculum that meets the needs of underrepresented and underserved populations will aid in increasing enrollment in institutions of higher learning.
- As a woman of color, what has been your experience in counselor education? What advice would you give to others from your experience?
I am thankful for my position and experiences as a counselor educator. I have had many experiences that most counselors do not get to have, and for that I am eternally grateful. I have had the opportunity to travel all over the country and abroad. My entire career as a counselor educator has consisted of working at a predominately White institution (PWI). I believe my training at a Research I PWI contributed to my gaining access to my position. I was fortunate to have mentors who advocated on my behalf and helped open doors that probably would not have been opened otherwise. I worked my way up from an assistant professor to a professor over a 10-year period. I served as the first African American department chair in the College of Education. Throughout my tenure, I actively recruited diverse students and faculty to the university. I had to work harder to prove I was as qualified as the dominant culture. I’ve had decisions challenged as well as faced harassment simply because of the color of my skin. At the end of the day, I’ve learned to do my best and not worry about it. The advice I would give to others based upon my experiences is to be the best you can be and do not let anyone make you feel that you are less—know your self-worth. I always share these words with my mentees: “We have to be better.” Last but not least, self-care!
- If you were advising current counseling leaders, what advice would you give them about moving the counseling profession forward?
Unity makes strength. If we stand together as a profession, we will remain relevant. Advocate for the profession as a whole. Be knowledgeable about Medicare and other issues that affect our profession. Be a part of advocacy efforts that benefit all counselors. Be open-minded to being a counselor first with varying specialty areas. Listen to the concerns of the members of our professional counseling organizations, and finally, recruit students—they are our future!
This concludes the fifth interview for the annual Lifetime Achievement in Counseling Series. TPC is grateful to Joshua D. Smith, PhD, NCC, and Neal D. Gray, PhD, for providing this interview. Joshua D. Smith is a counselor at the Center for Emotional Health in Concord, North Carolina. Neal D. Gray is a professor and Chair of the School of Counseling and Human Services at Lenoir-Rhyne University. Correspondence can be emailed to Joshua Smith at jsmit643@uncc.edu.
Aug 18, 2020 | Volume 10 - Issue 3
Jessica Lloyd-Hazlett, Cory Knight, Stacy Ogbeide, Heather Trepal, Noel Blessing
The coordination of primary and behavioral health care that holistically targets clients’ physical and mental needs is known as integrated care. Primary care is increasingly becoming a de facto mental health system because of behavioral health care shortages and patient preferences. Primary care behavioral health (PCBH) is a gold standard model used to assist in the integration process. Although counselor training addresses some aspects of integrated care, best practices for counselor education and supervision within the PCBH framework are underdeveloped. This article provides an overview of the Program for the Integrated Training of Counselors in Behavioral Health (PITCH). The authors discuss challenges in implementation; solutions; and implications for counselor training, clinical practice, and behavioral health workforce development.
Keywords: integrated care, primary care, counselor training, PITCH, behavioral health workforce development
In 2016, 18.3% of adults were diagnosed with a mental illness and 4.2% of adults were diagnosed with a serious mental illness (SMI; Substance Abuse and Mental Health Services Administration [SAMHSA], 2016). Of those with a mental illness, only 41% received mental health services, leaving more than half unserved (SAMHSA, 2015). Many of these untreated adults turn to their primary care provider (PCP) for help and report preference for behavioral health services within primary care (Ogbeide et al., 2018). In fact, data show that primary care has become the de facto mental health system in the United States (Robinson & Reiter, 2016).
Although PCPs attempt to provide pharmacological interventions and appropriate behavioral health referrals, patients often return still experiencing distress because they are unable to follow through on referrals (Cunningham, 2009; Robinson & Reiter, 2016). On average, this circular process results in substantially longer medical visits (e.g., 20 minutes versus 8 minutes) and fewer billable services (e.g., one versus five or more; Meadows et al., 2011). This also results in a significant increase in health care spending, with patients incurring 30%–40% higher costs because of the presence of a mental health condition (de Oliveira et al., 2016; Wammes et al., 2018). There is a need for professionals trained in behavioral health care working within the primary care setting (Serrano et al., 2018).
Counselor training addresses some aspects of the role of behavioral health professionals in primary care. The most recent version of the Council for Accreditation of Counseling and Related Educational Programs (CACREP) entry-level program standards mandates that all accredited programs, regardless of specialty, orient counseling students to “the multiple professional roles and functions of counselors across specialty areas, and their relationships with human service and integrated behavioral health care systems, including interagency and interorganizational collaboration and consultation” (CACREP, 2016, Standard F.1.b.). As patients’ needs and training mandates increase, there is a demand for counselor training programs to respond with models and practices for counselor training in behavioral health in primary care settings.
The Program for the Integrated Training of Counselors in Behavioral Health (PITCH) is a 4-year project sponsored by a Health Resources and Services Administration (HRSA) Behavioral Health Workforce Education and Training (BHWET) grant received by the Department of Counseling at the University of Texas at San Antonio. The purpose of this article is to describe this innovative program. Toward this end, we briefly outline the Primary Care Behavioral Health (PCBH) consultation model undergirding PITCH. Next, we describe the need for behavioral health integration in primary care settings. Then, we delineate our implementation of PITCH to date, including specialized field placements, training curriculum, and program evaluation methodologies. Following, we discuss challenges and resolutions gleaned from the first 1.5 years of implementation. Finally, we explore implications for counselor education to further enhance counselor preparation and engagement in behavioral health care delivery in primary care settings.
Primary Care Behavioral Health
The coordination of primary and behavioral health care that holistically targets clients’ physical and mental needs is known as integrated care (SAMHSA, 2015). One model used to assist in the integration process is the PCBH consultation model—a team-based and psychologically informed population health approach used to address physical and behavioral health concerns that arise in the primary care setting (Reiter et al., 2018). A hallmark of the PCBH model is integration of behavioral health consultants (BHCs), who dually function as generalist clinicians and as consultants to the primary care team (Serrano et al., 2018).
A BHC is different than a traditional counselor. In fulfilling their roles and functions, a BHC:
Assists in the care of patients of any age and with any health condition (Generalist); strives to intervene with all patients on the day they are referred (Accessible); shares clinic space and resources and assists the team in various ways (Team-based); engages with a large percentage of the clinic population (High volume); helps improve the team’s biopsychosocial assessment and interventions skills and processes (Educator); and is a routine part of psychosocial care (Routine). (Reiter et al., 2018, p. 112)
BHCs conduct brief functional assessments, collaborate with patients on treatment goals, implement evidence-based treatment interventions, and provide PCPs with feedback and recommendations for future patient care and support (Hunter et al., 2018). In addition, BHCs see patients for approximately 15–30-minute visits, with an average range between two and six visits per episode of care (Ray-Sannerud et al., 2012). In many ways, the BHC role involves a new professional identity for mental health professionals (Serrano et al., 2018). To date, BHC training and employment has typically involved social workers and psychologists. However, the counseling profession is increasingly recognized and engaged in integrated PCBH (HRSA, 2017).
Need for Integrated Services
Primary care settings must begin to consider behavioral health integration in order to increase the quality of life of their patients. Over recent years, there has been a significant increase in patients who receive psychotropic medication for mental health complaints in the primary care setting (Olfson et al., 2014). PCPs are managing increasingly complex diagnoses beyond anxiety and depression. These include bipolar, disruptive, and other comorbid disorders (Olfson et al., 2014). Individuals diagnosed with an SMI such as these also show a high prevalence of chronic health conditions, including diabetes and cardiovascular disease. Untreated psychological symptoms can often present themselves in somatic forms and can have a strong impact on chronic health conditions (McGough et al., 2016). People with SMIs prefer behavioral health services from their PCP; however, treatment outcomes for those with SMIs that seek services from their PCP are generally of lesser quality (Viron & Stern, 2010). Patient, provider, and systemic-level factors influence this phenomenon. Relevant factors may include impacts of patients’ mental health diagnoses on treatment adherence, misdiagnosis from PCPs, and minimal collaboration between medical and behavioral health providers (Viron & Stern, 2010).
The PITCH program addresses several critical needs of individuals seeking behavioral health services in the local community, where conditions that necessitate behavioral health services, including mental illness and substance use disorders, are common. In a focus group run in 2011 with members of the community, the group identified mental health as a key concern (Health Collaborative, 2013). Although mental health services were offered in a psychiatric facility for children, adolescents, and adults, members of the focus group reported that the demand for mental health providers and psychiatric beds exceeded the supply. The stigma associated with mental health also was seen as a barrier to care. As a result, many people go undiagnosed and untreated (SAMHSA, 2015).
PITCH also addresses the need for interdisciplinary approaches to behavioral health workforce development. The expansion of PCBH consultation services amplified this need (Robinson & Reiter, 2016). Unlike other models of integrated care (i.e., Collaborative Care Model, Chronic Care Model), the PCBH model makes available primary care–focused behavioral health services across an entire clinic population and across all possible patient presentations. This model also requires a skilled mental health professional adept at a variety of patient presentations and able to manage processes like clinic flow and a new role as consultant—skills and roles not commonly present in training for specialty mental health services (Robinson & Reiter, 2016).
PITCH: An Overview
PITCH is housed within a CACREP-accredited master’s-level clinical mental health counseling (CMHC) program enrolling more than 100 students each year. The principal investigator (PI) of PITCH is a professor specializing in clinical supervision, bilingual counselor education, and professional advocacy. Other PITCH team members include an assistant professor (Co-PI, university liaison) specializing in family counseling, program evaluation, and ethics; an assistant professor and board-certified clinical health psychologist (consultant); and an external project evaluator.
The primary purpose of PITCH is to develop a highly trained workforce of professional counselors to provide integrated behavioral health care (IBH) to rural, vulnerable, and underserved communities in primary care. Sub-goals of the PITCH program include establishing meaningful, longitudinal interdisciplinary partnerships as well as a graduate-level certificate in IBH to support sustainability. Toward this, 12 advanced counseling students enrolled in the aforementioned CMHC program are selected to participate each year from a competitive application pool. Selected trainees are required to complete two specialized IBH courses and two 300-hour clinical rotations in designated primary care settings. In exchange, trainees receive a $5,000 stipend upon completion of each semester rotation. Additionally, PITCH staff coordinate quarterly interprofessional trainings, including workshops focused on primary care, behavioral health, supervision, funding, and policy.
Specialized Field Placements
A unique feature of the PITCH program is the development of specialized field placement sites. Other behavioral health integration projects have relied on existing clinical placement sites (Sampson, 2017). Often these sites have low levels of existing integration, as well as underdeveloped infrastructure to support behavioral health delivery in primary care. When existing clinical site placements do have some integrated services, they are most often co-located services (Peek & the National Integration Academy Council, 2013). Instead of field site development, previous efforts have emphasized student training through workshops (Canada et al., 2018). These workshops are often open to community members. Individuals are then charged to bring knowledge back to extant clinical sites. Although this offers some positive benefits, it may not be as impactful. Further, this approach may fall short of establishing infrastructure to support longitudinal changes (Serrano et al., 2018).
To start development of specialized field placements, we identified potential sites interested in IBH delivery. We then set up initial meetings with sites to discuss the PITCH project and to determine the feasibility of placing a BHC trainee. If sites were amenable, we scheduled a series of follow-up visits to provide orientation to clinic staff on IBH, the PCBH model, and the role and scope of BHCs. During these visits, we also provided consultation on infrastructure components, such as electronic medical record documentation procedures, suggestions for clinic flow, and room spacing (Robinson & Reiter, 2016). Throughout the field placement, we remained active in checking with sites to make workflow adjustments as needed. Trainees complete certificate-based coursework prior to beginning field placements as well as during the clinical rotations.
Trainee Curriculum
Selected trainees are required to complete two specialized courses in IBH, as well as two 300-hour clinical rotations at one of the specialized field placement sites discussed above. The PCBH model scaffolds all aspects of the PITCH training and delivery. We utilize this model to support conceptualization of the BHC role in primary care settings, interventions, and supervision.
As part of the PITCH program, two didactic courses were created to provide training in IBH and PCBH. The courses were developed and instructed by the PITCH IBH consultant. The first course, IBH-I, introduces students to the primary care setting (e.g., family medicine, pediatrics, geriatrics), the PCBH model of care, behavioral health consultation, health behavior change, and common mental and chronic health conditions encountered in primary care, and offers a basic understanding of brief, cognitive-behavioral–based and solution-focused interventions used in primary care (Reiter et al., 2018; Robinson & Reiter, 2016).
Students must complete the following assignments in the course: two exams, an IBH journal article review, a primary care clinic tour, an interview with a PCP, a presentation on one commonly seen problem in primary care (e.g., insomnia, chronic pain, depression), and a term paper highlighting treatment on a common problem in primary care using the 5A’s model (Hunter & Goodie, 2010). The 5A’s is a behavioral change model that includes assessing, advising, agreeing, assisting, and arranging. Upon demonstrating satisfactory performance, students may enroll in IBH-II.
The primary purpose of the second course is to begin applying foundational knowledge of PCBH as well as practice functional and contextual assessment and cognitive-behavioral intervention skills in the primary care setting. Trainees demonstrate their skills through a series of in-class role-plays, leading up to a final evaluation of their performance in a 30-minute initial consultation visit with a standardized patient. Trainees must complete both courses to maintain their status in PITCH. Both courses are open as electives to students enrolled in the counseling program or a related discipline (e.g., social work).
PITCH trainees also complete two semester-long clinical rotations in primary care. Trainees are assigned to one of the specialized field placement sites based on availability, interest, and anticipated fit. Trainees are required to clock 300 hours each semester, 120 of which must represent direct clinical engagement. Direct clinical engagement time includes patient visits, consultation with the primary care team, and facilitating psychoeducational groups tailored to unique clinical populations. Trainees are required to participate in at least 1 hour of clinical supervision with an on-site supervisor each week. Additionally, trainees attend a bi-weekly group supervision course on campus instructed by a CMHC faculty member. After successful completion of didactic and clinical courses of the PITCH program, trainees are eligible to earn a graduate certificate in IBH. Adjustments to specialized field placement sites and the trainee curriculum are made as needed based on ongoing informal and formal evaluation of the program.
Program Evaluation
The HRSA BHWET grant supporting PITCH prioritizes evaluation activities related to workforce training and development effectiveness (HRSA, 2017). In partnership with our external evaluator, we are conducting program evaluation across several domains of PITCH, including evaluations focused on trainees and clinical sites (e.g., level of integration).
Trainee-Focused Metrics
We have several evaluation metrics that are focused on trainees. Trainees complete the Behavioral Health Consultant Core Competency Tool (BHC CC Tool; Robinson & Reiter, 2016) and the Primary Care Brief Intervention Competency Assessment Tool (BI-CAT; Robinson, 2015) at the beginning, midpoint, and conclusion of clinical rotations. The BHC CC Tool measures and tracks skill development across four domains of BHC practice: clinical practice, practice management, consultation, and documentation. The BI-CAT includes domains of practice context, intervention design, intervention delivery, and outcomes-based practice. On-site observations of trainees also are conducted using the PCBH Observation Tool as part of the certificate coursework. These competency tools were developed based on observations of BHC clinical behaviors likely to work effectively in a PCBH model of service delivery. These measures have not yet been formally assessed for psychometric properties or predictive outcomes (Robinson et al., 2018).
In addition to tools that target individual trainee development, program evaluation efforts also attend to the macro experiences of trainees in the program. Specifically, trainees participate in focus groups facilitated by the external evaluator at the end of each semester. Focus groups provide the opportunity to understand pathways and barriers to program development. We also have developed an online database to track trainees’ postgraduation employment trajectories and sustained engagement in PCBH.
Site-Focused Metrics
Although this particular HRSA grant is primarily concerned with trainee-focused outcomes (e.g., employment), we also ask identified clinical site liaisons to complete the Integrated Practice Assessment Tool (IPAT; Waxmonsky et al., 2013) at the start and finish of each rotation. Scores on the IPAT provide a snapshot estimation of the level of integration of clinical sites. Levels of integration correspond to those identified by A Standard Framework for Levels of Integrated Healthcare (Heath et al., 2013) and range from 1–6. Levels 1 and 2 are indicative of minimal, coordinated collaboration, with behavioral health and PCPs maintaining separate facilities and systems. Levels 3 and 4 reflect shared physical space and enhanced communication among behavioral health and PCPs; however, practice change toward system-level integration is underdeveloped. Finally, Levels 5 and 6 are indicative of transformed, team-based approaches in which both “providers and patients view the operation as a single health system treating the whole person” (Heath et al., 2013, p. 6). Focus groups also were conducted with members of selected clinical training sites to explore barriers and pathways to PCBH delivery as a function of level of integration. At this time, the IPAT has not yet been formally assessed for psychometric properties.
Rapid Cycle Quality Improvement
Finally, program evaluation efforts include ongoing rapid cycle quality improvement (RCQI), a quality-improvement method that identifies, implements, and measures changes to improve a process or a system (Center for Health Workforce Studies, 2016). RCQI can be targeted at different aspects of the program. To date, RCQI has targeted trainee competencies related to functional assessment interviews, breadth of referrals concerns, and patient visit length. For example, after tracking trends in daily activity logs submitted by trainees, we noted a majority of referrals centered on anxiety and depression. We then provided supplemental training on identifying behavioral health concerns related to chronic health conditions, such as diabetes and asthma. Following this instruction, we reviewed the daily activity logs and noted greater breadth of referral concerns.
Challenges and Solutions
Best practices for PCBH implementation within the context of workforce development are still developing. Further, available guidelines do not speak to counselor training programs specifically. In the section below, we discuss challenges we have encountered in the first 1.5 years of implementation of the PITCH program. We also share solutions we have generated to support optimal training experiences.
Challenge: On-Site Clinical Supervision
A significant challenge we encountered was related to on-site clinical supervision for the PITCH trainees. National accreditation standards require trainees to participate in regular supervision with both an on-site and university supervisor (CACREP, 2016). The on-site supervisor must have at least 2 years of postgraduate experience, as well as hold a master’s degree in counseling or a related field (e.g., psychology, social work). Furthermore, best practices for BHC training support a scaffolded supervision approach (Dobmeyer et al., 2003), wherein trainees’ initial time is spent completing 360 clinic shadowing visits with an experienced BHC. As trainee skills develop, leadership within patient visits transitions from co-visits to visits. In time, the trainee leads the visits, with an experienced BHC in independent practice shadowing. Additionally, the PCBH model emphasizes preceptor-style supervision, where the supervisor is readily available on-site for patient consultation as needed (Dobmeyer et al., 2003).
Solution: Changes to Specialized Field Placement Sites
During Year 1 of PITCH, almost two thirds of the specialized field placement sites we partnered with did not employ the PCBH model at the time, and thus did not have a BHC available to provide on-site clinical supervision. To meet this need, we provided intensive PCBH and supervision training to four doctoral students enrolled in our counselor education and supervision program. Doctoral student supervisors were asked to spend at least half a day on-site with trainees with this amount tapering off with time and experience.
Although this solution met national accreditation requirements for supervision (CACREP, 2016), we noticed stark differences between the clinical experiences of trainees placed at field sites with an on-site BHC versus doctoral student supervisors. As such, we made the difficult decision in Year 2 to separate from all but two field placement sites that lacked an on-site BHC to provide supervision. The inclusion of a BHC to supervise became a requirement for all the new sites we partnered with in Year 2. Additionally, we made modifications to our grant funding allocations to support graduate assistantships focused on supervision for two of the four doctoral supervisors utilized in Year 1.
Challenge: Knowledge About PCBH and the BHC Role
We encountered internal and external gaps in knowledge about the PCBH model, the BHC role, and the general culture of primary care settings. Internally, members of our faculty less connected to PITCH expressed support but also concern about alignment of PITCH training experiences and the experiences of other counseling students. Specific points of concern related to the brevity of visits, frequency of single encounters with patients, and the underpinning medical model. Additionally, because of patient privacy restrictions, PITCH field placement sites do not permit audio or video recording of clinical work, which is a typical supervision practice for counseling trainees. PITCH trainees also expressed some tension between the professional identity and skills training obtained in the CMHC program to date with the PCBH model and BHC role. Externally, we observed varying degrees of provider knowledge and buy-in about the PCBH approach to integrated practice. Areas of provider disconnect were more prominent at placement sites without existing integrated primary care services.
Solution: Ongoing Education and Advocacy
At the internal level, we provided a brief educational session about the PCBH model at regular faculty meetings. It was important to emphasize PCBH as a different context of practice that, similar to school counseling, requires modes of practice outside of traditional 50-minute sessions. We also sought faculty consultation related to curriculum and structure for our specialized coursework. For example, faculty members expressed concern about missing opportunities for recorded patient visits, so we developed two assignments for the clinical courses that could meet this need. The first was a mock visit with a classmate that was video recorded and transcribed. Students then analyzed micro-skills and reflected. The second assignment consisted of a live observation by the university- or site-based supervisors of the trainee’s work on-site with a patient.
We also encountered various levels of provider buy-in at our different sites. We encouraged students to reframe this resistance as an opportunity for learning and advocacy. As students gained knowledge about what we call the primary care way, students could better contextualize the questions or concerns of providers. For example, students could understand the premiums placed on time and space. From this position, students could tailor their approach to PCPs to enhance the PCP workflow. Additionally, faculty and supervisors emphasized the importance of ongoing psychoeducation about the PCBH model to their teams. Students are encouraged to be proactive in reviewing daily patient schedules for prospective services (i.e., scrubbing the schedule) and educating providers about how BHC services can augment patient care. The use of the BHC competency tools also facilitated this process, which encouraged students to consistently engage in behaviors conducive to BHC practice.
Challenge: Shortage of Spanish-Speaking Service Providers
A final challenge we faced related to a shortage of Spanish-speaking service providers. Some sites offered formal translation services (i.e., in-person medical translator, phone- or tablet-based translators), while others utilized informal resources (i.e., other staff members). When placing students, we prioritized placement of bilingual trainees at locations with the greatest number of Spanish-speaking patients. However, we were not able to accommodate all sites.
Solution: Recruitment and Resources
We have implemented several solutions to address this challenge. Among these, we have moved to weighing Spanish language fluency more heavily in PITCH selection criteria. We also are exploring future partnerships with the bilingual counseling certificate program that is housed in the University of Texas at San Antonio Department of Counseling. Additionally, we provide basic training and support to trainees related to the use of translators (in-person and virtual), and we have employed Spanish-speaking doctoral graduate assistant supervisors where possible for extra support.
Discussion
The implementation of PITCH provides challenges but also solutions to the growing need for counselor education to focus on training in primary care. Patients prefer behavioral health services in primary care (Ogbeide et al., 2018). Thus, equipping the behavioral health workforce to provide services in this setting has proved to be imperative. Although primary care and interprofessional education is relatively new to counselor education, other behaviorally inclined disciplines (e.g., psychology, social work, nursing) have provided a training blueprint for counselor education programs to use and continue developing a place for themselves in primary care (Hooper, 2014; Vogel et al., 2014).
Serrano and colleagues (2018) shared recommendations for PCBH workforce development. These recommendations include: (a) development of an interprofessional certification body; (b) PCBH-specific curricula in graduate studies, including both skills and program development; (c) a national employment clearinghouse; and finally, (d) coalescing knowledge around provision of technical assistance sites. Below we discuss the implications of counselor education programs seeking to advance PCBH workforce development.
Standardized Training Models
An important implication for training future counselors is the use of standardized training models (Tang et al., 2004). Throughout this article, much of the focus has centered on the PCBH consultation model (Reiter et al., 2018). In recent years, training standards have emerged for BHCs in primary care. These standards focus on a psychologically informed, population-based approach to treatment, in which BHCs are trained to create clinical pathways, collaborate with medical providers, conduct a brief functional assessment, and provide a brief behavioral intervention, mostly consisting of skills training and self-management (Reiter et al., 2018)—all of which is done in under 30 minutes. This clinical practice approach has become the de facto model in most BHC preparation programs throughout the United States (Hunter et al., 2018) and is currently endorsed by the Veterans Administration and the Department of Defense for integrated primary care (Funderburk et al., 2013). However, inconsistencies exist in how the PCBH model is taught, and there is a lack of available internship opportunities for master’s-prepared behavioral health providers to receive clinical training (Hall et al., 2015). This challenge is especially relevant to future counselors, who lack a standardized model of training for primary care (Hooper, 2014). Our experience suggests that programs such as PITCH accomplish the joint goals of focusing on instruction and supervised practice in PCBH, developing BHC competencies, and meeting accreditation standards of orienting counselors to their role in integrated care settings (CACREP, 2016).
Behavioral Health Integration
One of the largest challenges facing the PCBH model is behavioral health integration (Hunter & Goodie, 2010). Moreover, the PCBH model requires full integration (e.g., Level 5–6 integration) to be maximally effective. Traditionally, PCPs would refer patients to a local mental health practitioner for issues related to depression or anxiety (Cunningham, 2009). However, these referrals would result in a low rate of success and deter many individuals from seeking out mental health services in the future (Davis et al., 2016). Co-located care (an in-house mental health practitioner conducting traditional psychotherapy or counseling) became the logical next step. This level of integration resulted in quicker referrals but led to poor communication and confidentiality issues between PCPs and mental health providers. This also left out other common, behaviorally influenced conditions in primary care such as diabetes, chronic pain, hypertension, and tobacco cessation (which are not routinely addressed or treated by mental health providers). Full integration (in which PCPs and mental health providers work collaboratively in the same setting) has become the ideal standard for the integration of behavioral health services in primary care (Heath et al., 2013).
Despite the many benefits, full integration might be impractical for clinics just beginning PCBH services. Clinics may not have the staff support, leadership support, and organizational buy-in to be successful because “successful integration is really hard” (deGruy, 2015). Integration, in a sense, causes a necessary disruption in how a clinic functions and serves patients. Although necessary, it is still a disruption and it can take time for a team to normalize their new way of practicing primary care. Clinics may need specific support to help establish pathways for behavioral health referrals (Landis et al., 2013), allow clinic staff more time to adjust to integrated services, and provide a pathway for the development of fully integrated services (Reiter et al., 2018). Investing in technical assistance experts can aid in integration efforts (Serrano et al., 2018). Additionally, clinics that already offer co-located services might benefit from a quality-improvement plan (Wagner et al., 2001) such as a plan-do-study-act model (PDSA; Speroff & O’Connor, 2004) to move to a higher level of integration. A sample PDSA cycle might consist of identifying barriers to improved patient care, creating a team-based plan for addressing barriers, designating a project overseer, tracking outcomes across time, and evaluating project success (Speroff & O’Connor, 2004). Both suggestions are great steps toward full integration and can be performed by counselors and counselor educators with training in PCBH and program evaluation (Newcomer et al., 2015). Funding for counselors in BHC roles would assist in meeting the aforementioned goals.
Funding for Counselors in PCBH
One of the greatest barriers to providing accessible behavioral health services in primary care is funding (Robinson & Reiter, 2016). Insurers are just beginning to reimburse for same-day services (both a PCP and BHC visit; Robinson & Reiter, 2016). However, this recent development has primarily benefited psychologists and social workers in primary care and excludes licensed counselors, who account for 14%–25% of the mental health labor force (U.S. Department of Health and Human Services, 2016). Licensed counselors are a crucial part of the growing behavioral health workforce (Vogel et al., 2014) and bring a strong wellness and systems-based perspective to primary care (Sheperis & Sheperis, 2015). Furthermore, licensed counselors, along with other behavioral health providers, can help in a variety of ways such as reducing patient costs in the medical system (Berwick et al., 2008), reducing patient emergency room visits (Kwan et al., 2015), and implementing continuous quality improvement (Wagner et al., 2001).
Robinson and Reiter (2016) offered several suggestions regarding funding for BHCs unable to conduct same-day billing. The first is for BHCs to understand that PCPs will always be the main source of clinic revenue. Therefore, BHCs can provide support to the primary care team through behavioral consultation; improve screening and clinical pathway procedures; provide support for difficult patients and frequent visitors; and reduce PCP visit time through warm handoffs, with the patient witnessing the transfer of their care between PCP and BHC. Second, BHCs can secure bottom-up support from PCPs by providing “curbside” consultation services (consulting face-to-face with PCPs about a patient without directly treating the patient). It comes as no surprise that PCPs feel more supported when BHCs are an available part of the medical team. Third, BHCs can generate top-down support through billing for group visits such as drop-in group medical appointments and 30-minute follow-up visits (Robinson & Reiter, 2016). Finally, grants represent another potential source of funding for behavioral health implementation (HRSA, 2017, 2018). HRSA and SAMHSA have been a tremendous resource in providing training grants specifically aimed at increasing the BHC workforce (e.g., HRSA, 2017) and addressing the nation’s opioid epidemic (e.g., HRSA, 2018). In Texas, the Hogg Foundation has provided training grants for training future BHCs. Finally, the counseling profession must continue advocacy efforts toward establishing licensed counselors as Medicare providers. With this key change, licensed counselors would be more readily employable in medical settings (Dormond & Afayee, 2016).
Conclusion
Primary care has been the de facto mental health system in the United States for decades. Providing comprehensive primary care to patients is imperative, and in order to do this well, our workforce needs to be equipped to meet the growing behavioral health needs where patients show up to receive care. Given clinical measures such as successful patient outcomes and CACREP accreditation standards targeting integrated health care knowledge, it behooves counselor training programs to consider developing models for BHC training. This article presents the key aspects of the PITCH program in the hopes that our model will be useful to other counselor education programs as the profession moves toward integrated practice models in order to meet the ever-changing needs of the health care landscape.
Conflict of Interest and Funding Disclosure
PITCH is funded by a Behavioral Health Workforce Education
and Training grant from the Health Resources and Services
Administration. There is no known conflict of interest.
References
Berwick, D. M., Nolan, T. W., & Whittington, J. (2008). The triple aim: Care, health, and cost. Health Affairs, 27(3), 759–769. https://doi.org/10.1377/hlthaff.27.3.759
Canada, K. E., Freese, R., & Stone, M. (2018). Integrative behavioral health clinic: A model for social work practice, community engagement, and in vivo learning. Journal of Social Work Education, 54(3), 464–479. https://doi.org/10.1080/10437797.2018.1434442
Center for Health Workforce Studies. (2016). Rapid cycle quality improvement resource guide. http://www.healthworkforceta.org/wp-content/uploads/2016/06/RCQI_Resource_Guide.pdf
Council for Accreditation of Counseling and Related Educational Programs. (2016). CACREP accreditation manual.
Cunningham, P. J. (2009). Beyond parity: Primary care physicians’ perspectives on access to mental health care. Health Affairs, 28(Suppl. 1), 490–501. https://doi.org/10.1377/hlthaff.28.3.w490
Davis, M. J., Moore, K. M., Meyers, K., Mathews, J., & Zerth, E. O. (2016). Engagement in mental health treatment following primary care mental health integration contact. Psychological Services, 13(4), 333–340. http://doi.org/10.1037/ser0000089
deGruy, F. V. (2015). Integrated care: Tools, maps, and leadership. The Journal of the American Board of Family Medicine, 28(Suppl. 1), S107–S110. https://doi.org/10.3122/jabfm.2015.S1.150106
de Oliveira, C., Cheng, J., Vigod, S., Rehm, J., & Kurdyak, P. (2016). Patients with high mental health costs incur over 30 percent more costs than other high-cost patients. Health Affairs, 35(1), 36–43.
https://doi.org/10.1377/hlthaff.2015.0278
Dobmeyer, A. C., Rowan, A. B., Etherage, J. R., & Wilson, R. J. (2003). Training psychology interns in primary behavioral health care. Professional Psychology: Research and Practice, 34(6), 586–594.
https://doi.org/10.1037/0735-7028.34.6.586
Dormond, M., & Afayee, S. (2016, November). Understanding billing restrictions for behavioral health providers.
Behavioral Health Workforce Research Center, University of Michigan. http://www.behavioralhealth
workforce.org/wp-content/uploads/2017/01/FA3P4_Billing-Restrictions_Full-Report.pdf
Funderburk, J. S., Dobmeyer, A. C., Hunter, C. L., Walsh, C. O., & Maisto, S. A. (2013). Provider practices in the
primary care behavioral health (PCBH) model: An initial examination in the Veterans Health Administration and United States Air Force. Families, Systems, & Health, 31(4), 341–353. https://doi.org/10.1037/a0032770
Hall, J., Cohen, D. J., Davis, M., Gunn, R., Blount, A., Pollack, D. A., Miller, W. L., Smith, C., Valentine, N., & Miller, B. F. (2015). Preparing the workforce for behavioral health and primary care integration. The Journal of the American Board of Family Medicine, 28(Suppl. 1), S41–S51. https://doi.org/10.3122/jabfm.2015.S1.150054
Health Collaborative. (2013). 2013 Bexar county community health assessment report. https://iims.uthscsa.edu/sites/iims/files/Newsletters/bexar%20CHA%202013%20final.pdf
Health Resources and Services Administration. (2017). Behavioral health workforce education and training (BHWET) program. https://www.hrsa.gov/grants/find-funding/hrsa-17-070
Health Resources and Services Administration. (2018). FY 2018 expanding access to quality substance use disorder and mental health services (SUD-MH) supplemental funding technical assistance (HRSA-18-118). https://bphc.hrsa.gov/programopportunities/fundingopportunities/sud-mh/
Heath, B., Wise, R. P., & Reynolds, K. (2013). A standard framework for levels of integrated healthcare. SAMHSA-HRSA Center for Integrated Health Solutions. https://www.pcpcc.org/sites/default/files/resources/SAMHSA-HRSA%202013%20Framework%20for%20Levels%20of%20Integrated%20Healthcare.pdf
Hooper, L. (2014). Mental health services in primary care: Implications for clinical mental health counselors and other mental health providers. Journal of Mental Health Counseling, 36(2), 95–98.
https://doi.org/10.17744/mehc.36.2.u756l3l075354625
Hunter, C. L., Funderburk, J. S., Polaha, J., Bauman, D., Goodie, J. L., & Hunter, C. M. (2018). Primary Care Behavioral Health (PCBH) model research: Current state of the science and a call to action. Journal of Clinical Psychology in Medical Settings, 25(2), 127–156. https://doi.org/10.1007/s10880-017-9512-0
Hunter, C. L., & Goodie, J. L. (2010). Operational and clinical components for integrated-collaborative behavioral healthcare in the patient-centered medical home. Families, Systems, & Health, 28(4), 308–321. https://doi.org/10.1037/a0021761
Kwan, B. M., Valeras, A. B., Levey, S. B., Nease, D. E., & Talen, M. E. (2015). An evidence roadmap for implementation of integrated behavioral health under the Affordable Care Act. AIMS Public Health, 2(4), 691–717. https://doi.org/10.3934/publichealth.2015.4.691
Landis, S. E., Barrett, M., & Galvin, S. L. (2013). Effects of different models of integrated collaborative care in a
family medicine residency program. Families, Systems, & Health, 31(3), 264–273.
https://doi.org/10.1037/a0033410
McGough, P. M., Bauer, A. M., Collins, L., & Dugdale, D. C. (2016). Integrating behavioral health into primary care. Population Health Management, 19(2), 81–87. https://doi.org/10.1089/pop.2015.0039
Meadows, T., Valleley, R., Haack, M. K., Thorson, R., & Evans, J. (2011). Physician “costs” in providing behavioral health in primary care. Clinical Pediatrics, 50(5), 447–455. https://doi.org/10.1177/0009922810390676
Newcomer, K. E., Hatry, H. P., & Wholey, J. S. (2015). Handbook of practical program evaluation (4th ed.). Jossey-Bass.
Ogbeide, S. A., Landoll, R. R., Nielsen, M. K., & Kanzler, K. E. (2018). To go or not go: Patient preference in seeking specialty mental health versus behavioral consultation within the Primary Care Behavioral Health Consultation Model. Families, Systems, & Health, 36(4), 513–517. https://doi.org/10.1037/fsh0000374
Olfson, M., Kroenke, K., Wang, S., & Blanco, C. (2014). Trends in office-based mental health care provided by psychiatrists and primary care physicians. The Journal of Clinical Psychiatry, 75(3), 247–253.
https://doi.org/10.4088/JCP.13m08834
Peek, C. J., & the National Integration Academy Council. (2013). Lexicon for behavioral health and primary care integration: Concepts and definitions developed by expert consensus. AHRQ Publication No.13-IP001-EF. Agency for Healthcare Research and Quality. https://integrationacademy.ahrq.gov/sites/default/files/Lexicon.pdf
Ray-Sannerud, B. N., Dolan, D. C., Morrow, C. E., Corso, K. A., Kanzler, K. E., Corso, M. L., Bryan, C. J. (2012). Longitudinal outcomes after brief behavioral health intervention in an integrated primary care clinic. Families, Systems, & Health, 30(1), 60–71. https://doi.org/10.1037/a0027029
Reiter, J. T., Dobmeyer, A. C., & Hunter, C. L. (2018). The Primary Care Behavioral Health (PCBH) model: An overview and operational definition. Journal of Clinical Psychology in Medical Settings, 25(2), 109–126. https://doi.org/10.1007/s10880-017-9531-x
Robinson, P. (2015). PCBH Brief Intervention Competency Assessment Tool (BI-CAT). Mountainview Consulting. http://www.coping.us/images/Robinson_2013_PCBH_BI-CAT.pdf
Robinson, P., Oyemaja, J., Beachy, B., Goodie, J., Sprague, L., Bell, J., Maples, M., & Ward, C. (2018). Creating a primary care workforce: Strategies for leaders, clinicians, and nurses. Journal of Clinical Psychology in Medical Settings, 25(2), 169–186. https://doi.org/10.1007/s10880-017-9530-y
Robinson, P. J., & Reiter, J. T. (2016). Behavioral consultation and primary care: A guide to integrating services (2nd ed.). Springer.
Sampson, M. (2017). Teaching note—Meeting the demand for behavioral health clinicians: Innovative training through the GLOBE project. Journal of Social Work Education, 53(4), 744–750.
https://doi.org/10.1080/10437797.2017.1287024
Serrano, N., Cordes, C., Cubic, B., & Daub, S. (2018). The state and future of the Primary Care Behavioral Health model of service delivery workforce. Journal of Clinical Psychology in Medical Settings, 25(2), 157–168. https://doi.org/10.1007/s10880-017-9491-1
Sheperis, D. S., & Sheperis, C. J. (2015). Clinical mental health counseling: Fundamentals of applied practice (1st ed.). Pearson.
Speroff, T., & O’Connor, G. T. (2004). Study designs for PDSA quality improvement research. Quality Management in Healthcare, 13(1), 17–32. http://innovationlabs.com/r3p_public/rtr3/pre/pre-read/PDSA%20QI%20Research.
Speroff.2004.pdf
Substance Abuse and Mental Health Services Administration. (2015). Behavioral health barometer. https://www.samhsa.gov/data/sites/default/files/2015_National_Barometer.pdf
Substance Abuse and Mental Health Services Administration. (2016). 2016 national survey of drug use and health. http://www.samhsa.gov/data/release/2016-national-survey-drug-use-and-health-nsduh-releases
Tang, M., Addison, K. D., LaSure-Bryant, D., Norman, R., O’Connell, W., & Stewart-Sicking, J. A. (2004). Factors that influence self-efficacy of counseling students: An exploratory study. Counselor Education and Supervision, 44(1), 70–80. https://doi.org/10.1002/j.1556-6978.2004.tb01861.x
U.S. Department of Health and Human Services. (2016). National projections of supply and demand for selected behavioral health practitioners: 2013-2025. https://bhw.hrsa.gov/sites/default/files/bhw/health-workforce-analysis/research/projections/behavioral-health2013-2025.pdf
Viron, M. J., & Stern, T. A. (2010). The impact of serious mental illness on health and healthcare. Psychosomatics, 51(6), 458–465. https://doi.org/10.1016/S0033-3182(10)70737-4
Vogel, M., Malcore, S., Illes, R., & Kirkpatrick, H. (2014). Integrated primary care: Why you should care and how to get started. Journal of Mental Health Counseling, 36(2), 130–144.
https://doi.org/10.17744/mehc.36.2.5312041n10767k51
Wagner, E. H., Glasgow, R. E., Davis, C., Bonomi, A. E., Provost, L., McCulloch, D., Carver, P., & Sixta, C. (2001). Quality improvement in chronic illness care: A collaborative approach. The Joint Commission Journal on Quality Improvement, 27(2), 63–80. https://doi.org/10.1016/S1070-3241(01)27007-2
Wammes, J. J. G., van der Wees, P. J., Tanke, M. A. C., Westert, G. P., & Jeurissen, P. P. T. (2018). Systematic review of high-cost patients’ characteristics and healthcare utilisation. BMJ Open, 8(9), 1–17.
https://doi.org/10.1136/bmjopen-2018-023113
Waxmonsky, J., Auxier, A., Wise-Romero, P., & Heath, B. (2013). Integrated Practice Assessment Tool (IPAT). http://ipat.valueoptions.com/IPAT/
Jessica Lloyd-Hazlett, PhD, NCC, LPC, is an associate professor at the University of Texas at San Antonio. Cory Knight, MS, is a master’s student at the University of Texas at San Antonio. Stacy Ogbeide, PsyD, ABPP, is a behavioral health consultant, licensed psychologist, and associate professor at the University of Texas Health Sciences Center San Antonio. Heather Trepal, PhD, LPC-S, is a professor and coordinator of the Clinical Mental Health Counseling Program at the University of Texas at San Antonio. Noel Blessing, MS, is a doctoral student at the University of Texas at San Antonio. Correspondence may be addressed to Jessica Lloyd-Hazlett, 501 W. Cesar E. Chavez Blvd., DB 4.132, San Antonio, TX 78207, Jessica.lloyd-hazlett@utsa.edu.
Aug 18, 2020 | Volume 10 - Issue 3
Jessica Burkholder, David Burkholder, Stephanie Hall, Victoria Porter
The national epidemic of increasing imprisonment rates in the United States, also known as mass incarceration, disproportionally impacts communities of color. Additionally, the needs of children of incarcerated parents have been neglected. This study examined whether topics pertinent to mass incarceration and the impact on families are being addressed in counselor education programs. Of the 95 counselor educators who participated in the study, results indicated that the majority did not have training to work with families of the incarcerated and did not include information about working with families of the incarcerated in their courses. In addition to exposing students to discussions of implicit bias and data on mass incarceration, specific treatment modalities and protocols need to be developed and validated.
Keywords: mass incarceration, children, counselor education, communities of color, incarcerated parents
The rise of mass incarceration is dramatically affecting families and communities across the nation, with a disproportional impact on communities of color (Glaze & Maruschak, 2008; Graham & Harris, 2013; A. Lopez & Burt, 2013; C. Lopez & Bhat, 2007; Mignon & Ransford, 2012; Western & Smith, 2018). With the increase of persons involved in the criminal justice and legal systems, their families have been found to be more at risk for facing long-lasting life challenges within both the family system and society (Glaze & Maruschak, 2008; Luther, 2016; Mignon & Ransford, 2012; Phillips & Gates, 2011). Client advocacy is one of the most critical roles of the professional counselor (Hipolito-Delgado et al., 2016). The counseling profession is characterized by working with diverse individuals from heterogeneous communities. Counselors are needed to function as advocates, especially when families and communities are facing a sociocultural crisis (American Counseling Association [ACA], 2014; Hipolito-Delgado et al., 2016).
Both ACA and the Council for Accreditation of Counseling and Related Education Programs (CACREP) have identified advocacy, multicultural competence, and social justice as priorities in training and practice (ACA, 2014; CACREP, 2015). The ACA Code of Ethics instructs that “when appropriate, counselors advocate at individual, group, institution, and societal levels to address potential barriers and obstacles that inhibit access and/or the growth and development of clients” (ACA, 2014, Section A.7.a., p. 5). It also directs counselors to gain “knowledge, personal awareness, sensitivity, dispositions, and skills pertinent to being a culturally competent counselor in working with a diverse client population” (ACA, 2014, Section C.2.a., p. 8).
Counselor educators are directed to “infuse material related to multiculturalism/diversity into all courses and workshops” (ACA, 2014, Section F.7.c., p. 14). When describing professional and ethical practice, the CACREP standards require programs to instruct students on “the advocacy processes needed to address institutional and society barriers that impede access, equity, and success for clients” (CACREP, 2015, Standard F.1.e., p. 10). Further, the curriculum guidelines for social and cultural diversity emphasize counselor advocacy when instructing counselor educators to cover “strategies for identifying and eliminating barriers, prejudices and processes of intentional and unintentional oppression and discrimination” (CACREP, 2015, Standard F.2.h., p. 11). Although mass incarceration and its effects are not specifically mentioned in the ACA Code of Ethics or CACREP standards, these broad directives provide support for the specific argument that the scope of this crisis and its impact on families require attention in counselor training. Consequently, the purpose of this research study is to describe the current state of how counselor educators are providing training to counselor trainees to support families of the incarcerated.
The Rise of Mass Incarceration
The national epidemic of increasing imprisonment rates, commonly referred to as mass incarceration, has been a topic of alarm for nearly five decades (Garland, 2001; Glaze & Maruschak, 2008; Graham & Harris, 2013; A. Lopez & Burt, 2013; C. Lopez & Bhat, 2007; National Research Council [NRC], 2014; Sykes & Pettit, 2014). Although the United States accounts for 4.4% of the world’s population, nearly one quarter (22%) of the world’s prisoners are in the United States (American Psychological Association [APA], 2014; NRC, 2014). According to The Sentencing Project (2012), the United States continues to have the highest incarceration rate in the world, consistently increasing since the mid-1970s. The most recent statistics indicate that the United States has an incarcerated population of 2.2 million individuals (APA, 2014; Kaeble & Cowhig, 2018; NRC, 2014). This represents a 500% increase over the last 40 years (The Sentencing Project, 2012). More than 20% of those released return to incarceration within one year (Durose et al., 2014; Western & Smith, 2018). Researchers have found a correlation between imprisonment and individuals belonging to underserved (e.g., lower levels of education, low income, psychiatric treatment and substance abuse histories) and minority populations (Alexander, 2012; Cnaan et al., 2008; NRC, 2014).
Despite the race gap narrowing since 2007, Blacks are imprisoned at a rate 6 times that of Whites and at double the rate for Hispanics (Bronson & Carson, 2019). Because incarceration disproportionately affects minority group members, families of the incarcerated are more likely to be concentrated in minority communities (Graham & Harris, 2013). Consequently, even those children in the community whose parents are not facing incarceration are likely to be impacted by mass incarceration (Wakefield & Wildeman, 2011), as their communities may experience lower incomes, lopsided gender ratios, disrupted social integration and roles, high levels of joblessness, and increased crime (Crutchfield & Weeks, 2015).
An Invisible Group
Results from the National Survey of Children’s Health (U.S. Department of Health and Human Services, 2018) found that more than 7% or 5 million children in the United States have experienced a parent being incarcerated. Gathering current statistics is difficult for researchers. The majority of data on children of incarcerated parents has measured the number of parents in prison, leaving unknown data about the number of parents spending time in jail (Cramer et al., 2017). Because of this, there is reason to believe that the current number of children of incarcerated parents exceeds previous findings of 2.7 million children.
Children of incarcerated parents have frequently been described as an invisible group (Bernstein, 2005; Bouchet, 2008) that bears the collateral consequences of mass incarceration. There are many reasons for the invisibility. Although the children have not committed any crimes, their parent’s incarceration impacts much of what is important to them—family bonds, housing stability, safety, self-image, and social relationships. The criminal justice system does little to support family relationships and there is frequently poor communication between social service organizations and families that may be beneficial for the children (Bernstein, 2005). Those caring for the children often experience high levels of stress (Poehlmann et al., 2010), and families fear stigmatization and may keep secrets or refrain from disclosing an incarceration (Phillips & Gates, 2011).
When a parent is incarcerated, one of the first losses is physical separation between parent and child. Most parents report no physical contact with their children following incarceration (Bocknek et al., 2009). Visitation with parents has been found to be beneficial to the attachment relationship and the child’s overall well-being (Poehlmann et al., 2010) but is often infrequent and not child friendly. Visits can be costly, and relationships may be strained with the child’s caregiver. Children frequently have to travel long distances, endure long wait times, and meet with parents in environments that can feel intimidating and stressful. Mignon and Ransford (2012) found that almost half of the mothers they surveyed never had a visit from their children, and visits became less frequent for those with longer sentences. Yet prisons that implemented child-friendly visitation interventions and allowed for physical interaction demonstrated greater visitation benefits to those children (Poehlmann et al., 2010). Some benefits included improved maternal perceptions of the relationship and improved self-esteem in the children.
This loss associated with the physical separation of parent and child has been discussed in the literature and is commonly referred to as ambiguous loss because children experience the loss without closure. The ambiguity of their parent’s abrupt removal can disrupt children of incarcerated parents from finding meaning in the loss and disrupt the development of coping strategies (Bocknek et al., 2009). Children also experience stigmatization associated with ambiguous loss. In contrast to children who are separated from their caregivers by death, deployment, or divorce, it is often not socially acceptable for children of incarcerated parents to grieve the loss of parents because such parents are viewed as criminals (Phillips & Gates, 2011).
Children of incarcerated parents experience the loss of both fathers and mothers, and there are substantially more fathers in prison than mothers. But since the late 1970s, the growth rate for women in prison is more than double the growth rate for men (Sawyer, 2018). When mothers are incarcerated, the disruptions the child experiences are magnified, as children are more likely to lose their home and their primary support. Children with incarcerated mothers have been found to experience more stress and more risks than those with incarcerated fathers (Poehlmann et al., 2010). Maternal incarceration is often more closely associated with factors such as poverty, substance abuse, and mental health issues (Turney & Goodsell, 2018).
Experiencing the incarceration of a parent has been found to impact the long-term well-being of children (Turney & Goodsell, 2018). Children of incarcerated parents have increased risk for health issues, stigmatization, poverty, negative social interactions, behavior problems, school truancy and failure, and substance abuse (Poehlmann et al., 2010; Turney & Goodsell, 2018). Turney (2018) found that children with incarcerated parents are more than 5 times more likely to face adverse childhood experiences than those without an incarcerated parent. Often these children were already at risk, and the incarceration compounds these inequities. It is important to note that the research on children of incarcerated parents is fraught with selection bias and focus on negative outcomes. Very little research exists that examines protective factors and environments beyond urban, lower-income communities of color. Graham and Harris (2013) cautioned that this narrow research focus can decrease potential positive outcomes. A review of the current literature on children of incarcerated parents revealed that this narrow research trend continues.
Stigmatization and Families of the Incarcerated
Many experts consider stigmatization to be one of the most significant negative consequences of parental incarceration. Families are not stigmatized based on a specific trait they possess, but rather based on being associated with the incarcerated person (Phillips & Gates, 2011). This phenomenon is known as courtesy stigma and results in a spoiled identity for family members (Luther, 2016). The stigmatization may come from other family members, peers, teachers, social service agencies, and mental health providers. Children may be seen as “guilty by association” or perceived as being “deviant” like the parent that is incarcerated (Luther, 2016, p. 1265). In order to avoid stigmatization, families often keep the incarceration a secret, but children tend to fare better when they know the truth. Stigmatization can increase feelings of shame and impact the child’s willingness to reunite with parents (Harris et al., 2010). Foster and Hagan (2015) found parental incarceration leads to social exclusion for children into their 30s, and as a result can contribute to intergenerational socioeconomic inequality.
Purpose of the Research
The longstanding need for increased support in communities impacted by mass incarceration is clear (Harris et al., 2010). Increased awareness of the United States’ imprisonment crisis has prompted research initiatives to better understand community needs. Recent data on adverse childhood experiences suggested that children with incarcerated parents are even more vulnerable than previously thought (Turney, 2018). The developmental needs of families and children of the incarcerated are not being appropriately attended to in the literature (Holmes et al., 2010; Turney, 2018). Although research is clear that children of incarcerated parents and the family system face disequilibrium when parental incarceration occurs (Harris et. al., 2010; Luther, 2016; Phillips & Gates, 2011; Wachter Morris & Barrio Minton, 2012), 58% of new professional counselors reported having either minimal training or no training at all in individual or family-level trauma and crisis preparation (Wachter Morris & Barrio Minton, 2012). Brown and Barrio Minton (2018) found that school counselors wanted more training and resources to work with children of incarcerated parents and their families. This lack of training created barriers and ethical dilemmas in attempting to support children with incarcerated parents. Brown and Barrio Minton recommended counselors learn about families of the incarcerated through reading and participating in professional development opportunities, but the curricular experience of professional counselors working with populations affected by incarceration appears predominantly absent from the literature.
The incongruence between the urgency of mass incarceration affecting communities and the lack of literature exploring how to support families of the incarcerated demands further research. Two key research questions organized our exploration: (1) Are topics pertinent to mass incarceration and its impact on families being addressed in the classroom? (2) If so, how are these topics being included?
Method
Participants
The sample included full-time counseling professors in CACREP-accredited counseling programs in the United States. The researchers compiled an email list of 356 CACREP liaisons from the list of accredited programs on the CACREP website. Upon receiving IRB approval, CACREP liaisons were contacted and asked to forward the email invitation to full-time faculty in their departments. The request for participants was also posted to the Counselor Education and Supervision Network Listserv. The email served as an invitation to participate, contained a synopsis of the purpose of this research, and included an online Survey Monkey link. Informed consent was collected using an electronic consent form. Demographic information was gathered after consent had been obtained.
Ninety-five counselor educators began and completed the survey. Sixty-nine female and 26 male individuals participated, ranging in age from 29 to 78 years. A majority of the participants identified as White or of European descent (n = 61, 64%); 18 (19%) identified as African American/Afro-Caribbean or of African descent; five (5%) identified as Hispanic/Latinx, five (5%) identified as Asian/Polynesian or of Pacific Island descent, and five (5%) identified as multiracial. One person (1%) did not identify a race or ethnicity.
Of the participants, 20 (21%) were full professors, 22 (23%) were associate professors, 43 (45%) were assistant professors, nine (10%) were non–tenure track full-time instructors, and one (1%) was a clinical coordinator. Sixty-five (68%) came from master’s-only programs, and 30 (32%) came from combined master’s and doctoral programs. All CACREP regions were represented with 33 (35%) from the Southern region, 27 (28%) from the North Atlantic region, 21 (22%) from the North Central region, nine (10%) from the Western region, and five (5%) from the Rocky Mountain region.
Survey
The researchers created a brief survey that could lead to a description of the current state of counselor training on issues of mass incarceration and families of the incarcerated. Using broad survey research was necessary because there is currently nothing on this topic in the counseling literature. Eight questions were included in the survey: 1) Do you include the topic of mass incarceration in any of your courses? 2) If yes, what courses? 3) If yes, how do you cover this topic? 4) Do you include working with families of incarcerated persons in any of your courses? 5) If yes, what courses? 6) If yes, how do you cover this topic? 7) Have you received any training on these topics? and 8) If yes, describe.
Results
When asked whether they included the topic of mass incarceration in their courses, only 35 (36.8%) of the counselor educators surveyed answered yes. The most frequently noted course was Multicultural Counseling, under many different titles such as “Social and Cultural Diversity Issues in Counseling” or “Cultural Diversity.” Other courses noted were Foundations of Clinical Mental Health, Career Counseling, Addictions, Diagnosis, Trauma, Practicum, and Internship. Only one participant responded, “every class I teach.” When surveyed whether they included working with families of the incarcerated in their courses, 27 (28.4%) of the counselor educators answered yes. This too was most frequently covered in a multicultural counseling course but also was included in school counseling, child and adolescent counseling, and crisis counseling courses.
Using an open-ended question, participants were asked to describe how they covered the topics. The vast majority of the responses were “discussion.” These discussions were prompted by topics or readings on issues such as “systematic oppression,” “the intersection of race and social class,” “mandated clients,” and “vicarious trauma.” Two participants described developing a special topics course on incarceration and one participant invited a guest speaker related to families of the incarcerated.
When counselor educators were asked whether they had received training on these topics, only 30 (31.58%) reported that they had. But, when the participants described the training that they had received, it is notable that 19 (63.3%) of those reporting training described experiences with incarcerated persons, not specifically the families. Seven (23.3%) of those who responded had attended conference presentations on the topics of incarceration and families of the incarcerated. Two participants (6.7%) had completed research on incarcerated persons. Only one counselor educator (3.3%) described an extended training experience specific to families of the incarcerated. Finally, one (3.3%) participant described the topics being integrated into their doctoral program that was combined with rehabilitation counseling.
Discussion
The purpose of this research was for counselor educators to articulate whether topics relevant to mass incarceration and the effect on families were addressed in their classrooms, and if so, how they were addressed. Because no similar research has been reported, this study was singular in seeking to investigate how or if counseling faculty prepare their students to work with families affected by incarceration. This study did not aim to produce generalizations that apply beyond the research sample.
Nevertheless, it is essential to compare what was discovered in this study with what is documented in the literature. This study found that the majority of counselor educators were not covering mass incarceration or families of the incarcerated in their coursework, nor had they received training to do so. The findings of this study also provide the beginnings of a blueprint for what counseling programs and faculty can do to prepare students to work with children and families affected by incarceration.
For this study, comparing our findings with a body of literature is difficult because such literature does not exist, excepting the study by Wachter Morris and Barrio Minton (2012). Wachter Morris and Barrio Minton reported that 57.51% of professional counselors reported having minimal to no training in working with individual or family-level trauma and crisis preparation. Although Wachter Morris and Barrio Minton’s research did not target families of the incarcerated, this population does fall under the umbrella of individual and family trauma. Like that study, the present study demonstrated that a majority of counseling students are likely not receiving intentional, purposeful training on working with the trauma associated with incarceration. Although close to 30% of our participants did include mass incarceration and families of the incarcerated in their courses, the majority of how the topics were addressed was based on whether it arose out of discussion of broader multicultural topics. It also is reasonable to conclude that because a counseling literature search focused on training students to work with children of incarcerated parents only resulted in one webinar (Brown, 2016), a large majority of professional counselors are not adequately prepared to work with this population.
The findings of the present study may generate discussion of future recommendations and directions that counselor educators and supervisors may explore and implement. The majority of faculty in this research were not trained in the topics of mass incarceration and counseling children and families of the incarcerated, and unsurprisingly the majority did not include any training for their students. As with any topic under the umbrella of multiculturalism, counseling faculty should incorporate mass incarceration and working with children of incarcerated parents when addressing implicit bias with students (Boysen, 2010). In light of the massive numbers impacted by mass incarceration, we recommend this topic be included as required content in counselor education training. One way to ensure its inclusion would be to include persons who are incarcerated and their families in accreditation standards. At a minimum, the topic should be included in textbooks and used in case examples throughout training programs.
Counselor educators should highlight the stigma and spoiled identity that children of incarcerated parents experience and describe stigma management techniques (Luther, 2016) counselors can teach when working with these children. In addition to exposing students to data on mass incarceration and discussions of implicit bias (e.g., Alexander, 2012; Kaeble & Cowhig, 2018; Phillips & Gates, 2011), specific treatment modalities and protocols need to be developed and validated that fulfill the education and ethical expectations (ACA, 2014; CACREP, 2015) to address systemic barriers, advocacy, and cultural competence (Hipolito-Delgado et al., 2016).
Continuing education trainings could provide an opportunity for counseling associations and programs to address important content that may not receive adequate or consistent attention in required coursework. Counseling associations could choose conference themes that would encourage training and research on the needs of families of the incarcerated. Counseling programs could consider continuing education trainings as a method of communicating the program’s values and priorities, such as attention to social justice. Additional benefits may include strengthening their reputation, improving retention, maintaining relationships with alumni, and building relationships with the local clinical community.
Limitations and Future Research
The researchers recognize that the small, purposive, and heterogenous sample limits generalizability of the findings. Additionally, issues with data that rely on self-report have been well documented (Coughlin et al., 2009). Although these limitations make the present study narrow in scope and generalizability, these limitations are features of the positivist tradition aimed at finding “facts” and “truth.” This nascent study sought to establish a beginning understanding of how counselor educators are addressing mass incarceration in the classroom.
There are many directions for future research. It would be valuable to use qualitative research methods to learn from counselor educators who are effectively integrating and instructing on families of the incarcerated to provide a template for pedagogical inclusion. Research focusing on counseling students can serve to further the understanding of curricular experiences with mass incarceration and children of incarcerated parents. Research with practicing counselors can provide insight into the current landscape in the profession, including how families and children of incarcerated parents are affected and how professionals address these concerns. In that vein, outcome research with these children would be useful, as would the development of an instrument that can identify key clinical treatment areas.
Conclusion
Mass incarceration is a national crisis impacting more than 5 million U.S. children and their families (U.S. Department of Health and Human Services, 2018). This study was an attempt to provide a foundational understanding of the preparedness of counseling faculty and how they train students on this issue. The magnitude of the crisis, alongside the absence of counselor training, should cause counselors to consider our responsibility to ensure adequate counselor preparation in this area. By doing so and providing recommendations for programs to consider, it is hoped that more research will be undertaken to further underscore the importance of the topic and illuminate new understandings.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Alexander, M. (2012). The new Jim Crow: Mass incarceration in the age of colorblindness. The New Press.
American Counseling Association. (2014). ACA code of ethics.
American Psychological Association. (2014). Incarceration nation. Monitor on Psychology, 45(9), 56. https://www.apa.org/monitor/2014/10/incarceration
Bernstein, N. (2005). All alone in the world: Children of the incarcerated. The New Press.
Bocknek, E. L., Sanderson, J., & Britner, P. A., IV. (2009). Ambiguous loss and posttraumatic stress in school-age children of prisoners. Journal of Child and Family Studies, 18(3), 323–333.
https://doi.org/10.1007/s10826-008-9233-y
Bouchet, S. M. (2008). Children and families with incarcerated parents: Exploring development in the field and opportunities for growth. The Annie E. Casey Foundation. https://www.aecf.org/resources/children-and-families-with-incarcerated-parents
Boysen, G. A. (2010). Integrating implicit bias into counselor education. Counselor Education and Supervision, 49(4), 210–227. https://doi.org/10.1002/j.1556-6978.2010.tb00099.x
Bronson, J., & Carson, E. A. (2019). Prisoners in 2017. Report prepared for U.S. Department of Justice. Office of Justice Programs. Bureau of Justice Statistics. https://www.bjs.gov/content/pub/pdf/p17.pdf
Brown, E. C. (2016). Help children of incarcerated parents [Webinar]. American School Counselor Association. https://videos.schoolcounselor.org/help-children-of-incarcerated-parents
Brown, E. C., & Barrio Minton, C. A. (2018). Serving children of incarcerated parents. Professional School Counseling, 21(1), 1–11. https://doi.org/10.1177/2156759X18778811
Cnaan, R. A., Draine, J., Frazier, B., & Sinha, J. W. (2008). Ex-prisoners’ re-entry: An emerging frontier and a social work challenge. Journal of Policy Practice, 7(2–3), 178–198.
https://doi.org/10.1080/15588740801938035
Coughlin, M., Cronin, P., & Ryan, F. (2009). Survey research: Process and limitations. International Journal of Therapy and Rehabilitation, 16(1), 9–15. https://doi.org/10.12968/ijtr.2009.16.1.37935
Council for Accreditation of Counseling and Related Educational Programs. (2015). 2016 CACREP standards. http://www.cacrep.org/wp-content/uploads/2018/03/2016-Standards-with-Glossary-3.2018.pdf
Cramer, L., Goff, M., Peterson, B., & Sandstrom, H. (2017). Parent-child visiting practices in prisons and jails: A synthesis of research and practice. Urban Institute. https://www.urban.org/sites/
default/files/publication/89601/parent-child_visiting_practices_in_prisons_and_jails.pdf
Crutchfield, R. D., & Weeks, G. A. (2015). The effects of mass incarceration on communities of color. Issues in Science and Technology, 32(1), 109–119.
Durose, M. R., Cooper, A. D., & Snyder, H. N. (2014). Recidivism of prisoners released in 30 states in 2005: Patterns from 2005 to 2010. Bureau of Justice Statistics Special Report (NCJ 244205), 1–30. https://www.bjs.gov/content/pub/pdf/rprts05p0510.pdf
Foster, H., & Hagan, J. (2015). Maternal and paternal imprisonment and children’s social exclusion in young adulthood. Journal of Criminal Law and Criminology, 105(2), 387–429.
Garland, D. (2001). Introduction: The meaning of mass imprisonment. Punishment & Society, 3(1), 5–7.
https://doi.org/10.1177/14624740122228203
Glaze, L. E., & Maruschak, L. M. (2008). Parents in prison and their minor children. Bureau of Justice Statistics Special Report (NCJ 222984), 1–25. https://www.bjs.gov/content/pub/pdf/pptmc.pdf
Graham, J. A., & Harris, Y. R. (2013). Children of color and parental incarceration: Implications for research, theory, and practice. Journal of Multicultural Counseling and Development, 41(2), 66–81. https://doi.org/10.1002/j.2161-1912.2013.00028.x
Harris, Y. R., Harris, V. A., Graham, J. A., & Oliver Carpenter, G. J. (2010). The challenges of family reunification. In Y. R. Harris, J. A. Graham, & G. J. Oliver Carpenter (Eds.), Children of incarcerated parents: Theoretical, developmental, and clinical issues (pp. 255–275). Springer.
Hipolito-Delgado, C. P., Pharaoh, T., & Hermosillo, J. (2016). Empathy and advocacy: Successfully serving communities of color. The Journal of Humanistic Counseling, 55(1), 37–54.
https://doi.org/10.1002/johc.12023
Holmes, T. R., Belmonte, K., Wentworth, M., & Tillman, K. (2010). Parents “in the system”: An ecological systems approach to the development of children with incarcerated parents. In Y. R. Harris., J. A. Graham, & G. J. Oliver Carpenter (Eds.), Children of incarcerated parents: Theoretical, developmental, and clinical issues (pp. 21–43). Springer.
Kaeble, D., & Cowhig, M. (2018). Correctional populations in the United States, 2016. Bureau of Justice Statistics Special Report (NCJ 251211), 1–13. https://www.bjs.gov/content/pub/pdf/cpus16.pdf
Lopez, A., & Burt, I. (2013). Counseling groups: A creative strategy increasing children of incarcerated parents’ sociorelational interactions. Journal of Creativity in Mental Health, 8(4), 395–415.
https://doi.org/10.1080/15401383.2013.844660
Lopez, C., & Bhat, C. S. (2007). Supporting students with incarcerated parents in schools: A group intervention. The Journal for Specialists in Group Work, 32(2), 139–153. https://doi.org/10.1080/01933920701227125
Luther, K. (2016). Stigma management among children of incarcerated parents. Deviant Behavior, 37(11), 1264–1275. https://doi.org/10.1080/01639625.2016.1170551
Mignon, S. I., & Ransford, P. (2012). Mothers in prison: Maintaining connections with children. Social Work in Public Health, 27(1–2), 69–88. https://doi.org/10.1080/19371918.2012.630965
National Research Council. (2014). The growth of incarceration in the United States: Exploring causes and consequences. The National Academies Press. https://doi.org/10.17226/18613
Phillips, S. D., & Gates, T. (2011). A conceptual framework for understanding the stigmatization of children of incarcerated parents. Journal of Child and Family Studies, 20(3), 286–294.
https://doi.org/10.1007/s10826-010-9391-6
Poehlmann, J., Dallaire, D., Loper, A. B., & Shear, L. D. (2010). Children’s contact with their incarcerated parents: Research findings and recommendations. American Psychologist, 65(6), 575–598.
Sawyer, W. (2018). The gender divide: Tracking women’s state prison growth. https://www.prisonpolicy.org/reports/women_overtime.html
The Sentencing Project. (2009). Incarcerated parents and their children: Trends 1991–2007. https://www.sentencingproject.org/wp-content/uploads/2016/01/Incarcerated-Parents-and-Their-Children-Trends-1991-2007.pdf
The Sentencing Project. (2012). Criminal Justice Facts https://www.sentencingproject.org/criminal-justice-facts
Sykes, B. L., & Pettit, B. (2014). Mass incarceration, family complexity, and the reproduction of childhood disadvantage. The ANNALS of the American Academy of Political and Social Science, 654(1), 127–149. https://doi.org/10.1177/0002716214526345
Turney, K. (2018). Adverse childhood experiences among children of incarcerated parents. Children and Youth Services Review, 89, 218–225. https://doi.org/10.1016/j.childyouth.2018.04.033
Turney, K., & Goodsell, R. (2018). Parental incarceration and children’s wellbeing. The Future of Children, 28(1), 147–164.
U.S. Department of Health and Human Services, Health Resources and Services Administration’s Maternal and Child Health Bureau. (2018). National Survey of Children’s Health (2016–present). https://www.childhealthdata.org/browse/survey
Wachter Morris, C. A., & Barrio Minton, C. A. (2012). Crisis in the curriculum? New counselors’ crisis preparation, experiences, and self-efficacy. Counselor Education and Supervision, 51(4), 256–269. https://doi.org/10.1002/j.1556-6978.2012.00019.x
Wakefield, S., & Wildeman, C. (2011). Mass imprisonment and racial disparities in childhood behavioral problems. Criminology & Public Policy, 10(3), 793–817.
https://doi.org/10.1111/j.1745-9133.2011.00740.x
Western, B., & Smith, N. (2018). Formerly incarcerated parents and their children. Demography, 55(3), 823–847. https://doi.org/10.1007/s13524-018-0677-4
Jessica Burkholder, PhD, NCC, ACS, LPC, is an associate professor at Monmouth University. David Burkholder, PhD, ACS, LPC, is an associate professor and department chair at Monmouth University. Stephanie Hall, PhD, NCC, ACS, LPC, is an associate professor and founding department chair at Emory & Henry College. Victoria Porter is a master’s student at Monmouth University. Correspondence may be addressed to Jessica Burkholder, 400 Cedar Ave, West Long Branch, NJ 07764, jburkhol@monmouth.edu.
Aug 18, 2020 | Volume 10 - Issue 3
Scott W. Peters
Substance use and misuse is exceedingly common and has numerous implications, both individual and societal, impacting millions of Americans directly and indirectly every year. Currently, there are a variety of empirically based interventions for treating clients who engage in substance use and misuse. The Five Ps is an idiographically based framework providing clinicians with a systematic and flexible means of addressing substance use and misuse that can be used in conjunction with standard substance use and misuse interventions. Additionally, its holistic and creative style provides opportunities to address concerns at various points with a variety of strategies and interventions that will best suit clients’ unique situations. It can assist both novice and experienced clinicians working with clients who present for counseling with substance use and misuse. Following a discussion of the Five Ps, a brief case illustration will demonstrate the framework.
Keywords: substance use and misuse, Five Ps, idiographic, systematic, flexible
Substance use and misuse in the United States is extremely common. For the year 2016, the Centers for Disease Control and Prevention (CDC) found that 18% of the U.S. population aged 12 and older had used illicit substances or misused prescription medications (CDC, 2018). The National Survey on Drug Use and Health asserted that close to 30% of respondents aged 12 and older reported use of illicit substances in the past month (Substance Abuse and Mental Health Services Administration [SAMHSA], 2017). Although these statistics are significant, it should be noted that “Most people who use abusable drugs, even most people who use them nonmedically, do so in a reasonably controlled fashion and without much harm to themselves or anyone else” (Kleiman et al., 2011, p. 2). In the context of this article, the word abusable indicates substances that when taken are pleasurable enough to result in excessive dosing or increased frequency of intake (Linden, 2011).
However, there are others who use substances to such an extent that it causes significant distress and impairment in their lives, a phenomenon clinically referred to as a substance use disorder (SUD). The Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-5) bases an SUD on a “pathological pattern related to the use of a substance” (American Psychiatric Association, 2013, p. 483). In his report on alcohol, drugs, and health, the U.S. Surgeon General Vivek Murthy reported that more than 20 million Americans have an SUD (U.S. Department of Health and Human Services, 2016). Clients who engage in substance use and misuse can present with a variety of issues beyond use (Bahorik et al., 2017; Compton et al., 2014; Poorolajal et al., 2016). Thus, there exists a need to concurrently examine and address the potentially complex nature of client substance use and misuse.
Implications of Substance Use and Misuse
Substance use and misuse carries numerous potential repercussions. Societally, substance use and misuse consequences exceed “$400 billion in crime, health, and lost productivity” (U.S. Department of Health and Human Services, 2016, p. 2). Published data on those incarcerated appears to be several years old. However, it does suggest that more than 60% had a substance use disorder and 20% were under the influence at the time of their offense (National Center on Addiction and Substance Abuse at Columbia University, 2010). Regrettably, most do not receive treatment while incarcerated (Belenko et al., 2013). Additionally, many individuals who engage in substance use and misuse have co-occurring major medical conditions, such as cancers, cardiovascular accidents (strokes), and respiratory and cardiac illnesses (Bahorik et al., 2017). This population often experiences stigma and suboptimal health care results (McNeely et al., 2018; van Boekel et al., 2013). Substance use and misuse has significant impact on the occupational sector as well. Substance use and misuse has been correlated with both higher rates of absenteeism and workplace injuries (Bush & Lipari 2015). Those who engage in substance use and misuse often have higher rates of unemployment (Compton et al., 2014; Dieter, 2011). This can result in lack of access to treatment services, contributing to increased stress.
Substance use and misuse also has a negative impact on intimate partners, such as assuming increased responsibility and navigating unpredictability (Hussaarts et al., 2012). More ominously, substance use and misuse has been correlated with intimate partner violence (Murphy & Ting, 2010). Further, substance use and misuse is a significant risk factor for suicidality (Poorolajal et al., 2016). Finally, the number of U.S. adults with a comorbid SUD and mental illness has been shown to be almost 8 million, with only about 5% receiving treatment for both (SAMHSA, 2017). Concurrently treating both is very complex, challenging, and expensive. This can be even more problematic given the lack of health care access for large numbers of Americans (Schoen, 2013).
A Holistic Alternative
Addressing client substance use and misuse can be quite complicated, and as mentioned previously, substance use and misuse impacts users and society in a variety of ways beyond substance intake. There are several approaches to managing client substance use and misuse that have demonstrated effectiveness. Among those are 12-step programs (Humphreys et al., 2004), mindfulness-based interventions (Chiesa & Serretti, 2014), evidence-based approaches such as cognitive behavioral therapy (McHugh et al., 2010), and family counseling (O’Farrell & Clements, 2012). These approaches can be accomplished via outpatient counseling, partial hospitalization programs, inpatient and medically managed substance treatment programs, as well as residential and therapeutic communities. However, each has some shortcomings. Twelve-step attendance is most beneficial with inpatient substance use and misuse treatment (Karriker-Jaffe et al., 2018). Evidence-based approaches, such as cognitive behavioral therapy, tend to be nomothetic, assuming homogeneity and generally geared toward symptom amelioration (Robinson, 2011). Mindfulness-based strategies are not as effective when used alone as when used with other approaches (Sancho et al., 2018). Research on the success of family-based interventions has methodological challenges, such as small sample sizes and the difficulty of examining long-term outcomes (Rowe, 2012).
In addition, using these approaches may result in omitting the uniqueness of clients as a consideration in treatment. SAMHSA (2020) pointed out the significance of addressing clients individually based on their distinctive needs in order to provide the best chance for recovery from substance use and misuse. SAMHSA’s recommendations fit well with a more holistic framework in that such a structure allows clinicians to develop a multidimensional picture of clients. By examining and exploring clients’ use or misuse within the context of a multidimensional framework, interventions can be personalized, and areas of concern can be targeted. Such a framework may enhance the effectiveness of the aforementioned interventions (Wormer & Davis, 2018). Some of these evidence-based approaches will be demonstrated later in a case illustration.
As shown above, there are numerous ways to examine and treat client substance use and misuse. For example, some interventions use an individual lens, such as cognitive behavioral therapy, which examines connections between thoughts, feelings, and behaviors (Morin et al., 2017). Other approaches observe substance use and misuse from a family or systems perspective, looking at familial patterns such as communication and normalization of substance use (Bacon, 2019). Delivery of mindfulness-based interventions may help to address stressful events that previously triggered substance use (Garland et al., 2014). In addition, there are frameworks that use a formulation model examining various aspects of clients (Johnstone & Dallos, 2013) such as causal, contributing, environmental, and personal features, providing a much more expansive view of clients’ concerns.
Client substance use and misuse can be quite challenging for counselors, both novice and experienced. Case formulation, also referred to as conceptualization, is a skill new counselors often lack (Liese & Esterline, 2015). Using a framework to assist in case formulation may prove useful to beginning counselors. Experienced counselors, even with competence in a variety of approaches, can also benefit from using a framework to help address anticipated challenges (Macneil et al., 2012). Case formulations have been used in a number of areas such as those with psychosis, anxiety, and trauma (Chadwick et al., 2003; Ingram, 2012; Persons et al., 2013). One such framework is the Five Ps (Macneil et al., 2012). Macneil and his colleagues (2012) posited that diagnosing was insufficient and it was critical to include other factors such as causal, lifestyle, and personal factors in conceptualizing the case and formulating a plan. Applying this approach with clients who engage in substance use and misuse would allow more individual and flexible ways to intervene with client substance use and misuse. In addition, the collaborative nature of the Five Ps reinforces the concept of an idiographic formulation. This is in keeping with the inherent uniqueness of clients, their concerns, and a variety of factors.
The Five Ps is a type of framework utilizing five factors developed by Macneil et al. (2012). They conceptualized a way to look at clients and their problems, systematically and holistically taking into consideration the (1) Presenting problem, (2) Predisposing factors, (3) Precipitating factors, (4) Perpetuating factors, and (5) Protective factors. Presenting problems are concerns that clients find difficult to manage. Predisposing factors include biological, environmental, or personality considerations that may put clients at risk of further substance use and misuse. Precipitating factors are those that proximally bring about substance use and misuse and its resulting difficulties. Perpetuating factors are those that sustain and possibly reinforce clients’ current substance use and misuse challenges. Protective factors are those that help to moderate actual or potential substance use and misuse impact. The Five Ps framework promotes a very clear and systematic approach to case formulation or assessment that potentially provides a wealth of data. It also provides opportunities for a variety of interventions and strategies targeted to clients and their substance use and misuse or contributing factors.
Given the variations of substances, the level of use, the functional impairment, co-occurrence with other mental disorders, and inherent client differences, an idiographically based framework seems particularly appropriate with this population. The Five Ps permits counselors to both assess and intervene essentially simultaneously. It allows for client individualization, use of a variety of strategies, ongoing assessment, and modifications as needed. Furthermore, the Five Ps helps clients and counselors explore relationships between each factor and the presenting problem. This framework is idiographic in nature, as it looks at clients individually and holistically (Marquis & Holden, 2008). Idiographic case formulation can be useful for complicated cases, such as those encountered with clients engaged in substance use and misuse (Haynes et al., 1997). It is systematic, while allowing for flexibility and creativity. It can be used in outpatient, inpatient, and residential settings and possibly as part of an aftercare program.
Following is a case illustration demonstrating how the Five Ps may be helpful in formulating and engaging in a clinical application. It should be noted that several evidence-based substance use and misuse approaches were integrated in an eclectic approach throughout the case example to demonstrate the idiographic nature of the Five Ps. Many formulation models are administered within a cognitive behavioral grounding (Chadwick et al., 2003; Easden & Kazantzis, 2018; Persons et al., 2013). The Five Ps does not adhere to any particular theoretical orientation, thus allowing for a greater repertoire of strategies to draw from to help clients with substance use and misuse.
Implementing the Five Ps: The Case of Dax
A brief description of Dax, a hypothetical client, and the events that prompted him to seek services is followed by a detailed application of the Five Ps in addressing Dax’s substance use and misuse. It should be noted that the strategies and interventions applied here are used as illustrations and are specific to Dax and his concerns. In addition, the interventions demonstrated are not to be assumed the only ones that can be applied to Dax. They are examples that the author chose to illustrate the Five Ps in practice.
Dax is a 33-year-old married father of two children: a 9-year-old son, Cam, and a 7-year-old daughter, Zoe. He was recently driving home from work in the evening and law enforcement stopped him because of erratic driving. The officers evaluated him, detained him, and subsequently arrested him for driving while intoxicated. As part of his adjudication, Dax was required to attend five counseling sessions and have a clinician’s report provided to the court. Dax presents as extremely frustrated and embarrassed at being mandated to attend counseling sessions. He is confident that he does not have a problem and that counseling should be reserved for those who cannot stop drinking. Dax drinks two to three times a week, usually having one or two shots of whiskey and two to three draft beers. The night he was pulled over, he had had two additional beers and one additional shot of whiskey on top of his usual consumption after a telephone argument with his wife, Sara. Additionally, he reports significant stress and conflict in his marriage as well as concerns over some upcoming diagnostic tests for their daughter related to a heart murmur. Dax denies any other negative consequences from his alcohol use. He denies any significant increase in alcohol use or any other substance use.
Presenting Problem
While being mandated to attend counseling, Dax shares concerns that he is afraid of what his daughter’s test results will show. He fears that she will need open-heart surgery and that she may die. The clinician can intervene here by simply normalizing and validating his fears about the test results. A logical analysis using gentle Socratic dialogue may help to challenge his emotional reactions to his daughter’s heart murmur (Etoom & Ratnapalan, 2014). In addition, mindfulness strategies can assist in helping Dax to cognitively diffuse from present to future events (Harris, 2019). He is also adamant that he does not have a problem with alcohol. Here, a conversation about what counseling entails as well as psychoeducation related to the effects of alcohol on executive functioning may prove beneficial (Day et al., 2015). Acknowledging that his reticence is due to being obligated to attend counseling may assist in relationship building (Tahan & Sminkey, 2012). The clinician may also seek more information on the cause of the reported stress between him and his wife.
Predisposing Factors
Dax reports a strong paternal history of substance use and misuse. His father started out drinking occasionally and over the years slowly developed a dependency on alcohol. Dax further reports his paternal grandfather died from liver failure. Addressing the potential genetic link to substance use and misuse may prove beneficial in raising Dax’s awareness (Dick & Agrawal, 2008). For example, the clinician may ask Dax if they can share how genes are passed on and expressed, like genes for eye color or hypertension. This may open the door to a conversation regarding how his substance use and misuse may progress to alcohol use disorder and its definition as a pattern of alcohol use leading to clinically significant problems, including increase in use, failed attempts to stop, and use leading to an impaired ability to meet role obligations (American Psychiatric Association, 2013). There could be a discussion of alcohol use disorder being a disease, not that different from any other passed-on trait or disease. Additionally, Dax often struggles with strong and painful emotions, and alcohol helps to address them. Here the clinician may utilize strategies drawn from acceptance and commitment therapy related to his control strategy of using alcohol to avoid his emotions (Harris, 2019). The ball in the pool metaphor (i.e., holding a beach ball under the water works temporarily, but eventually it pops back up) can be compared to alcohol temporarily holding those painful emotions down, eventually to resurface. The clinician may also discuss strategies to help Dax regulate his reactions using emotion-focused interventions such as positive reframing to ameliorate the stress of his daughter’s cardiac condition (Plate & Aldao, 2017).
Precipitating Factors
This area explores significant occurrences that preceded or triggered the presenting problem and its consequences. Dax shares that he and his wife are conflicted about how to proceed with their daughter’s medical care. Sara is unequivocal in her confidence in Zoe’s cardiologist and his competence. Dax, however, is hyper-focused on surgery and seems to dismiss Sara’s position. At the end of his workday, he and his wife got into an argument over the phone about an upcoming diagnostic test and the possible results. Dax was quite upset, cursed at her, and then hung up the phone. He then stopped at a local pub and had several drinks.
Here, the clinician may use reality-based strategies that address choice and consequences (Wubbolding & Brickell, 2017). This may include a direct conversation about Dax’s decision to drink, resulting in his becoming impaired, with the consequence of being detained, charged, and adjudicated. Dax can then share his and his wife’s perspectives on their daughter’s care. This conversation can lead to investigating strategies for how each can be heard, including short role-plays with opportunities to practice (Worrell, 2015). The clinician can provide a variety of potential spousal responses, allowing for more adaptability and flexibility in Dax’s responses. The goal here is to build Dax’s competence in communicating, both in listening and expressing. Additionally, there may be a discussion using aspects of existentialism to process inherent anxiety and its connection to unknowable future events (May, 1950; Wu et al., 2015).
Perpetuating Factors
The emphasis here is on features that continue the presenting problem. For Dax, he shares that when he and his wife argue, it follows a very predictable pattern. They disagree, interrupt one another, yell, and he calms down by having several beers. He then withdraws and becomes sullen for a few days. Nothing gets resolved, and this cycle appears once again when they have conflict.
The clinician may discuss the concept of circularity and assist in moving from “vicious cycles” to “virtuous cycles and problem resolution” (Walsh, 2014, p. 162). This involves explaining that interactions can act as a kind of back-and-forth loop of action–reaction–action without any resolution, leaving both parties feeling unheard, misunderstood, and frustrated. The goals here are to both break the pattern and to facilitate healthy conversations. Here the clinician may incorporate a solution-focused strategy exploring a time with Dax when he and his wife have disagreed, but he did not interrupt and the outcome was positive (de Shazer, 1985). If he cannot identify a time, simple role-plays in which Dax does not interrupt or yell and instead experiences different outcomes may provide optimism to Dax. The counselor may also assist Dax in emotional regulation, which may prevent the initiation of arguments (Aldao & Nolen-Hoeksema, 2013). In addition, aspects of narrative therapy may provide an opportunity for Dax to re-author a unique outcome that gives meaning and provides a functional identity to him as a father and husband, thus building a sense of optimism (White & Epston, 1990).
Protective Factors
Here the focus is on investigating resources and/or supports that may help prevent client substance use and misuse from further becoming problematic. This factor has generally been underutilized despite being shown as beneficial to clients (Kuyken et al., 2009). This is often the opportunity for the client to share what may help them move forward, what their assets are, who can support them, and any other self-identified skills (de Shazer, 1985). These can be in the form of personal characteristics such as tenacity, intellect, or insight. They may also present in the form of family, friends, or hobbies. Oftentimes, when the topic of protective factors is used in substance use and misuse, it is related to deterrence of substance use, notably with adolescents (Liao et al., 2018). In the Five Ps context, protective factors are used to potentially prevent substance use and misuse from having more negative impact as well as to increase client resilience. This factor differs markedly from the first four. Protective factors move away from the problem areas that need interventions to hope and optimism and look to future success and competence (Macneil et al., 2012). Once the protective factors are identified, the ensuing conversation provides opportunities to imagine future outcomes in which protective factors may come into play should situations occur that the client finds problematic. Second, it also tends to shift the conversation toward what is present and going well in their lives and away from those areas that cause distress and suffering (de Shazer, 1985).
Discussion
In implementing the Five Ps framework with Dax, the clinician chose to use psychoeducation and strategies borrowed from acceptance and commitment, reality, Bowenian family systems, and solution-focused brief therapies to assist Dax with his substance use and misuse. The choice of the above approaches is only meant as an illustration and not as definitive ways to address this particular client. It is likely that other clinicians presented with Dax would use a different combination of approaches. The Five Ps is a systematic way to look at clients and their presentation, and its idiographic construction takes clients’ uniqueness into account. It also allows clinicians to target specific areas of concern (Macneil et al., 2012) and may be used in a variety of clinical settings. Moreover, the Five Ps align with SAMHSA’s recommendation that clinicians tailor treatment to each client because no single treatment is particularly superior (SAMHSA, 2020).
Limitations and Future Research
There are limitations to the Five Ps framework as a way to formulate and intervene with clients’ substance use and misuse. First and foremost, it should be emphasized that this particular framework has not been empirically tested with client substance use and misuse. However, as mentioned previously, case formulations have been used across a variety of client concerns (Chadwick et al., 2003; Ingram, 2012; Persons et al., 2013). Another potential limitation is that the Five Ps may not be particularly beneficial for substance use and misuse in which there is clinical evidence of an SUD that includes significant withdrawal symptoms. Client substance use and misuse at that level may need medical stabilization and detoxification prior to utilization of the Five Ps. In addition, there may be clients who are simply not ready or able to address some or most of the dimensions of the Five Ps. Furthermore, clients like Dax who are mandated to attend substance-related counseling may have service plans that are not congruent with the Five Ps framework. In spite of these limitations, there may be several potential areas of inquiry.
Previous studies using frameworks to formulate have often used cognitive behavioral therapy as the primary intervention (Chadwick et al., 2003; Persons et al., 2013). Given that client substance use and misuse can be quite complicated, using various approaches within the Five Ps framework may yield positive results. As Chadwick et al. (2003) noted, examining positive client experiences may be one way to discover how to increase client participation in substance use and misuse treatment. Another potential area of study might involve comparing novice counselors to more experienced counselors. As mentioned previously, novice counselors often lack sufficient case formulation skills (Liese & Esterline, 2015). Examining the two groups’ experiences using the Five Ps may provide insight to assist counselor training programs related to substance use and misuse skill development. The implementation of the Five Ps with clients with mild substance use and misuse and those with more significant substance use and misuse, possibly using the DSM-5 diagnosis for SUD, may be another area to explore. This research could point to populations for whom the Five Ps is more and less effective. Studies utilizing the Five Ps with mandated clients may demonstrate its efficacy, notably with agencies that require substance-related counseling.
Conclusion
Client substance use and misuse is a significant problem in the United States, and it continues to cause difficulty for individuals, families, and society. There are numerous methods and combinations of methods to address substance use and misuse, such as family therapy, cognitive behavioral therapy, and self-help groups. Their effectiveness has been well researched, and this paper does not propose a superior way to address substance use and misuse. However, the Five Ps presents a framework in which counselors can examine and intervene with client substance use and misuse using a variety of approaches and strategies. The Five Ps can be used in a variety of settings such as a community mental health agency, primary care clinic, and inpatient or residential treatment centers. The systematic but flexible nature of this framework affords clinicians numerous ways to address substance use and misuse. For some, receiving substance use and misuse services can be stigmatizing. In fact, this stigmatization can come from those who are treating them (Luoma et al., 2007). In addition, the vast majority of those with an SUD never receive treatment (Han et al., 2015). Incorporating the Five Ps, with its holistic framework, may prove attractive to clients and counselors, thus potentially increasing the numbers of clients engaged in substance use and misuse treatment. As mentioned previously, the Five Ps is not meant to replace any other substance use and misuse intervention. It is another way to address the multifaceted and complicated nature of client substance use and misuse. Novice clinicians, who often have a more limited repertoire of strategies, may find the Five Ps valuable because of its systematic framework to clients. Experienced clinicians understandably have a larger catalogue of strategies to choose from. However, they may find this framework valuable as it provides one more way to address the often-encountered complex challenges of substance use and misuse.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Aldao, A., & Nolen-Hoeksema, S. (2013). One versus many: Capturing the use of multiple emotion regulation strategies in response to an emotion-eliciting stimulus. Cognition and Emotion, 27(4), 753–760.
https://doi.org/10.1080/02699931.2012.739998
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
Bacon, M. (Ed.). (2019). Family therapy and the treatment of substance use disorders: The family matters model. Routledge.
Bahorik, A. L., Satre, D. D., Kline-Simon, A. H., Weisner, C. M., & Campbell, C. I. (2017). Alcohol, cannabis, and opioid use disorders, and disease burden in an integrated healthcare system. Journal of Addiction Medicine, 11(1), 3–9. https://doi.org/10.1097/ADM.0000000000000260
Belenko, S., Hiller, M., & Hamilton, L. (2013). Treating substance use disorders in the criminal justice system. Current Psychiatry Reports, 15(11), 2–11. https://doi.org/10.1007/s11920-013-0414-z
Bush, D. M., & Lipari, R. N. (2015, April 16). The CBHSQ report: Substance use and substance use disorder by industry. https://www.ncbi.nlm.nih.gov/books/NBK343542
Centers for Disease Control and Prevention. (2018, August 31). Annual surveillance report of drug-related risks and outcomes. https://www.cdc.gov/drugoverdose/pdf/pubs/2018-cdc-drug-surveillance-report.pdf
Chadwick, P., Williams, C., & Mackenzie, J. (2003). Impact of case formulation in cognitive behaviour
therapy for psychosis. Behaviour and Research Therapy, 41(6), 671–680.
https://doi.org/10.1016/S0005-7967(02)00033-5
Chiesa, A., & Serretti, A. (2014). Are mindfulness-based interventions effective for substance use disorders? A systematic review of the evidence. Substance Use & Misuse, 49(5), 492–512. https://doi.org/10.3109/10826084.2013.770027
Compton, W. M., Gfroerer, J., Conway, K. P., & Finger, M. S. (2014). Unemployment and substance outcomes in the United States 2002–2010. Drug and Alcohol Dependence, 142(1), 350–353.
https://doi.org/10.1016/j.drugalcdep.2014.06.012
Day, A. M., Kahler, C. W., Ahern, D. C., & Clark, U. S. (2015). Executive functioning in alcohol use studies: A brief review of findings and challenges in assessment. Current Drug Abuse Reviews, 8(1), 26–40. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4638323/pdf/nihms734766.pdf
de Shazer, S. (1985). Keys to solution in brief therapy. W. W. Norton.
Dick, D. M., & Agrawal, A. (2008). The genetics of alcohol and other drug dependence. Alcohol Research Current Reviews, 31(2), 111–118. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3860452/
Easden, M. H., & Kazantzis, N. (2018). Case conceptualization research in cognitive behavior therapy: A state of the science review. Journal of Clinical Psychology, 74(3), 356–384. https://doi.org/10.1002/jclp.22516
Etoom, Y., & Ratnapalan, S. (2014). Evaluation of children with heart murmurs. Clinical Pediatrics, 53(2), 111–117. https://doi.org/10.1177/0009922813488653
Garland, E. L., Froeliger, B., & Howard, M. O. (2014). Mindfulness training targets neurocognitive mechanisms of addiction at the attention-appraisal-emotion interface. Frontiers in Psychiatry, 4(173), 1–15.
https://doi.org/10.3389/fpsyt.2013.00173
Han, B., Hedden, S. L., Lipari, R., Copello, E. A. P., & Kroutil, L. A. (2015). Receipt of services for behavioral health problems: Results from the 2014 National Survey on Drug Use and Health. Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/data/sites/default/files/NSDUH-DR-FRR3-2014/NSDUH-DR-FRR3-2014/NSDUH-DR-FRR3-2014.htm
Harris, R. (2019). ACT made simple (2nd ed.). New Harbinger.
Haynes, S. N., Leisen, M. B., & Blaine, D. D. (1997). Design of individualized behavioral treatment programs using functional analytic clinical case models. Psychological Assessment, 9(4), 334–348. https://www.apa.org/pubs/journals/pas/index
Henkel, D. (2011). Unemployment and substance use: A review of the literature (1990–2010). Current Drug Abuse Reviews, 4(1), 4–27. https://doi.org/10.2174/1874473711104010004
Humphreys, K., Wing, S., McCarty, D., Chappel, J., Gallant, L., Haberle, B., Horvath, A. T., Kaskutas, L. A., Kirk, T., Kivlahan, D., Laudet, A., McCrady, B. S., McLellan, A. T., Morganstern, J., Townsend, M., & Weiss, R. (2004). Self-help organizations for alcohol and drug problems: Toward evidence-based practice and policy. Journal of Substance Abuse Treatment, 26(3), 151–158. https://doi.org/10.1016/S0740-5472(03)00212-5
Hussaarts, P., Roozen, H. G., Meyers, R. J., van de Wetering, B. J. M., & McCrady, B. S. (2012). Problem areas reported by substance abusing individuals and their concerned significant others. The American Journal on Addictions, 21(1), 38–46. https://doi.org/10.1111/j.1521-0391.2011.00187.x
Ingram, B. L. (2012). Clinical case formulations: Matching the integrative treatment plan to the client (2nd ed.). Wiley.
Johnstone, L., & Dallos, R. (Eds.). (2013). Formulation in psychology and psychotherapy: Making sense of people’s problems (2nd ed.). Routledge.
Karriker-Jaffe, K. J., Klinger, J. L., Witbrodt, J., & Kaskutas, L. A. (2018). Effects of treatment type on alcohol consumption partially mediated by Alcoholics Anonymous attendance. Substance Use & Misuse, 53(4), 596–605. https://doi.org/10.1080/10826084.2017.1349800
Kleiman, M. A. R., Caulkins, J. P., & Hawken, A. (2011). Drugs and drug policy: What everyone needs to know. Oxford University Press.
Kuyken, W., Padesky, C. A., & Dudley, R. (2009). Collaborative case conceptualization: Working effectively with clients in cognitive-behavioral therapy. Guilford.
Liao, J.-Y., Huang, C.-M., Lee, C. T.-C., Hsu, H.-P., Chang, C.-C., Chuang, C.-J., & Guo, J.-L. (2018). Risk and protective factors for adolescents’ illicit drug use: A population-based study. Health Education Journal, 77(7), 749–761. https://doi.org/10.1177/0017896918763462
Liese, B. S., & Esterline, K. M. (2015). Concept mapping: A supervision strategy for introducing case conceptualization skills to novice therapists. Psychotherapy, 52(2), 190–194. https://doi.org/10.1037/a0038618
Linden, D. J. (2011). The compass of pleasure: How our brains make fatty foods, orgasm, exercise, marijuana, generosity, vodka, learning, and gambling feel so good. Penguin.
Luoma, J. B., Twohig, M. P., Waltz, T., Hayes, S. C., Roget, N., Padilla, M., & Fisher, G. (2007). An investigation of stigma in individuals receiving treatment for substance abuse. Addictive Behaviors, 32(7), 1331–1346. https://doi.org/10.1016/j.addbeh.2006.09.008
Macneil, C. A., Hasty, M. K., Conus, P., & Berk, M. (2012). Is diagnosis enough to guide interventions in mental
health? Using case formulation in clinical practice. BMC Medicine, 10(111), 1–3.
https://doi.org/10.1186/1741-7015-10-111
Marquis, A., & Holden, J. (2008). Mental health professionals’ evaluations of the Integral Intake, a metatheory-based, idiographic intake instrument. Journal of Mental Health Counseling, 30(1), 67–94.
https://doi.org/10.17744/mehc.30.1.j40256207h0581t1
May, R. (1950). The meaning of anxiety. Ronald Press.
McHugh, R. K., Hearon, B. A, & Otto, M. W. (2010). Cognitive behavioral therapy for substance use disorders. Psychiatric Clinics of North America, 33(3), 511–525. https://doi.org/10.1016/j.psc.2010.04.012
McNeely, J., Kumar, P. C., Rieckmann, T., Sedlander, E., Farkas, S., Chollak, C., Kannry, J. L., Vega, A., Waite, E. A., Peccoralo, L. A., Rosenthal, R. N., McCarty, D., & Rotrosen, J. (2018). Barriers and facilitators affecting the implementation of substance use screenings in primary care clinics: A qualitative study of patients, providers, and staff. Addiction Science and Clinical Practice, 13(8), 1–15. https://doi.org/10.1186/s13722-018-0110-8
Morin, J.-F. G., Harris, M., & Conrod, P. J. (2017). A review of CBT treatments for substance use disorders. Oxford Handbooks Online, 1–49. https://doi.org/10.1093/oxfordhb/9780199935291.013.57
Murphy, C. M., & Ting, L. (2010). The effects of treatment for substance use problems on intimate partner violence: A review of empirical data. Aggression and Violent Behavior, 15(5), 325–333.
https://doi.org/10.1016/j.avb.2010.01.006
National Center on Addiction and Substance Abuse at Columbia University. (2010, February). Behind bars II: Substance abuse and America’s prison population. https://www.centeronaddiction.org/addiction-research/reports/behind-bars-ii-substance-abuse-and-america’s-prison-population
O’Farrell, T. J., & Clements, K. (2012). Review of outcome research on marital and family therapy in treatment for alcoholism. Journal of Marital and Family Therapy, 38(1), 122–144.
https://doi.org/10.1111/j.1752-0606.2011.00242.x
Persons, J. B., Lemle Becker, V., & Tompkins, M. A. (2013). Testing case formulation hypotheses in psychotherapy: Two case examples. Cognitive and Behavioral Practice, 20(4), 399–409. https://doi.org/10.1016/j.cbpra.2013.03.004
Plate, A. J., & Aldao, A. (2017). Emotion regulation in cognitive-behavioral therapy: Bridging the gap between treatment studies and laboratory experiments. In S. G. Hofmann & G. J. G. Asmundson (Eds.), The science of cognitive behavioral therapy (pp. 107–127). Academic Press.
Poorolajal, J., Haghtalab, T., Farhadi, M., & Darvishi, N. (2016). Substance use disorder and risk of suicidal ideation, suicide attempt and suicide death: A meta-analysis. Journal of Public Health, 38(3), e282–e291. https://doi.org/10.1093/pubmed/fdv148
Robinson, O. C. (2011). The idiographic/nomothetic dichotomy: Tracing historical origins of contemporary confusions. History & Philosophy of Psychology, 13(2), 32–39.
Rowe, C. L. (2012). Family therapy for drug abuse: Review and updates 2003–2010. Journal of Marital and Family
Therapy, 38(1), 59–81. https://doi.org/10.1111/j.1752-0606.2011.00280.x
Sancho, M., De Gracia, M., Rodríguez, R. C., Mallorquí-Bagué, N., Sánchez-González, J., Trujols, J., Sánchez, I., Jiménez-Murcia, S., & Menchón, J. M. (2018). Mindfulness-based interventions for the treatment of substance and behavioral addictions: A systematic review. Frontiers in Psychiatry, 9, 1–9.
https://doi.org/10.3389/fpsyt.2018.00095
Schoen, C., Osborn, R., Squires, D., & Doty, M. M. (2013). Access, affordability, and insurance complexity are often worse in the United States compared to ten other countries. Health Affairs, 32(12), 2205–2215. https://doi.org/10.1377/hlthaff.2013.0879
Substance Abuse and Mental Health Services Administration. (2017, September 7). Results from the 2016 National Survey on Drug Use and Health: Detailed tables. https://www.samhsa.gov/data/report/results-2016-national-survey-drug-use-and-health-detailed-tables
Substance Abuse and Mental Health Services Administration. (2020, April 21). Behavioral health treatments and services. https://www.samhsa.gov/treatment
Tahan, H. A., & Sminkey, P. V. (2012). Motivational interviewing: Building rapport with clients to encourage desirable behavioral and lifestyle changes. Professional Case Management, 17(4), 164–172.
https://doi.org/10.1097/NCM.0b013e318253f029
U.S. Department of Health and Human Services. (2016). Facing addiction in America: The Surgeon General’s report on alcohol, drugs, and health. https://addiction.surgeongeneral.gov/sites/default/files/surgeon-generals-report.pdf
van Boekel, L. C., Brouwers, E. P. M., van Weeghel, J., & Garretsen, H. F. L. (2013). Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: Systematic review. Drug and Alcohol Dependence, 131(1–2), 23–35. https//doi.org/10.1016/j.drugalcdep.2013.02.018
Van Wormer, K., & Davis, D. R. (2018). Addiction treatment: A strengths perspective (4th ed.). Cengage.
Walsh, F. (2014). Family therapy: Systemic approaches to practice. In J. R. Brandell (Ed.), Essentials of clinical social work (pp. 160–185). SAGE.
White, M., & Epston, D. (1990). Narrative therapy to therapeutic ends. W. W. Norton.
Worrell, M. (2015). Cognitive behavioural couple therapy. Routledge.
Wu, J. Q., Szpunar, K. K., Godovich, S. A., Schacter, D. L., & Hofmann, S. G. (2015). Episodic future thinking in generalized anxiety disorder. Journal of Anxiety Disorders, 36, 1–8. https://doi.org/10.1016/j.janxdis.2015.09.005
Wubbolding, R. E., & Brickell, J. (2017). Counselling with reality therapy (2nd ed.). Routledge.
Scott W. Peters, PhD, LPC-S, is an associate professor at Texas A&M University – San Antonio. Correspondence may be addressed to Scott Peters, One University Way, San Antonio, TX 78224, scott.peters@tamusa.edu.
Aug 18, 2020 | Author Videos, Volume 10 - Issue 3
Curtis Garner, Brenda Freeman, Roger Stewart, Ken Coll
Tools to assess the dispositions of counselor education applicants at the point of program admission are important as mechanisms to screen entrance into the profession. The authors developed the Professional Disposition Competence Assessment—Revised Admission (PDCA-RA) as a screening tool for dispositional assessment in admissions interviews. In this study, 70 participants engaged in a video-based training protocol designed to increase the interrater reliability of the PDCA-RA. An intraclass correlations coefficient was calculated as an index of interrater reliability. Cronbach’s alpha coefficients were calculated for internal consistency, and Fleiss’ kappa, free-marginal kappa, and percent of agreement were calculated for absolute agreement. Calculations were made for pretest and posttest scores. Results of the study suggest that the PDCA-RA demonstrates “good” reliability in terms of interrater reliability and “excellent” reliability in terms of internal consistency. The video-based training improved interrater reliability.
Keywords: dispositions, counselor education, interrater reliability, counseling admissions, PDCA-RA
Beyond ethical codes and standardized education requirements, one criterion understood to be a demarcation of a profession is that it controls entry into its occupation (Miller, 2006). The stature of any profession is heavily influenced by the collective quality, preparation, and professional fit of those who are allowed to enter the profession. In the profession of counseling, counselor preparation programs, practicing counselors, field site supervisors, and state licensure boards share the overarching charge to screen for the profession (Freeman et al., 2016), but counselor educators alone bear the responsibility of initial screening of potential new entrants into the profession. The funnel of individuals seeking entrance into the profession begins with admission to graduate programs. This responsibility is a solemn one because post-admission gatekeeping can lead to high-stakes legal disputes (Dugger & Francis, 2014; Hutchens et al., 2013; McAdams et al., 2007).
Similar to other graduate programs, criteria for entrance into counselor preparation programs generally incorporate academic and career factors, but unlike many other graduate programs, the dispositions (traits and characteristics) of applicants are also critical factors for identifying appropriate candidates for the profession (Hernández et al., 2010). The use of admissions interviews is a common method for observing dispositions (Swank & Smith-Adcock, 2014). Characteristics such as interpersonal skills, warmth, emotional stability, and self-awareness are examples of traits deemed important to many counseling academic programs (Crawford & Gilroy, 2013; McCaughan & Hill, 2015), though counselor educators lack agreement about which dispositions should be screened at admission (Bryant et al., 2013).
Once applicants have been accepted into a counselor education program, if problematic dispositional issues arise the American Counseling Association (ACA) ethical codes require remediation (ACA, 2014), which is sometimes followed by suspension or dismissal. Therefore, gatekeeping, defined as the process of deterring program graduation of those lacking sufficient knowledge or skills (Koerin & Miller, 1995), begins at the point of program screening and admission (Kerl & Eichler, 2005). Bryant et al. (2013) emphasized that effective screening of applicants prior to formal admission into the academic program may greatly reduce the need to address problematic student behaviors after admission.
In addition to conducting admissions screening as a form of gatekeeping, the courts are more likely to support universities in admissions-related legal disputes if screening policies, standards for admission, and admission procedures are clear and fair (Cole, 1991). Legal research also underscores the importance of programs communicating clearly with students about the expected dispositions and other criteria from admission through exit (McCaughan & Hill, 2015). Reliable admissions tools designed to assess dispositions represent one method of showing fidelity in implementing policies (Hutchens et al., 2013). Despite the research support for sound structures to scaffold the admissions process, assessments with published psychometric properties measuring dispositions in admissions interviews are scarce (Hernández et al., 2010).
Jonsson and Svingby (2007) noted that a number of forms of reliability and validity are important in establishing the psychometric properties of admissions tools, but when multiple raters are involved, such as in the admissions process, interrater reliability for rubrics is particularly essential. Specific training in the tool is critical to improving interrater reliability (Jonsson & Svingby, 2007). Video training protocols to increase interrater reliability are becoming more important in professional dispositional research (Kopenhaver Haidet et al., 2009; Rosen et al., 2008). The use of video technology to train raters to capture behavioral observations has two advantages: the opportunity for admissions personnel to practice admissions interview ratings prior to real-time observations, and the relative ease of using modern, sophisticated recording equipment (Kopenhaver Haidet et al., 2009).
Admissions Processes and Criteria
Overwhelmingly, admission criteria and procedures for counselor education programs have focused upon undergraduate grade point average (GPA); standardized test scores, such as the Graduate Record Examination (GRE) or the Miller Analogies Test (MAT); a personal interview; and some form of personal statement (Bryant et al., 2013). Such procedures have been shown to be reasonably predictive of academic success, but less so for counselor development (Smaby et al., 2005). Some programs have utilized Carkhuff’s Rating Scale (Carkhuff, 1969) or Truax’s Relationship Questionnaire (Truax & Carkhuff, 1967) to measure applicants’ ability to communicate the conditions of empathy, genuineness, and respect effectively (Hernández et al., 2010; Swank & Smith-Adcock, 2014). Carkhuff’s Rating Scale and Truax’s Relationship Questionnaire have been found to exhibit good interrater reliability and, when correlated with one another, have been found to exhibit considerable overlap (Engram & Vandergoot, 1978).
Dispositional Assessment
Following the gatekeeping dispute in Ward v. Wilbanks (2010), in which a graduate student in counselor education refused to work with a gay client, and the ensuing litigation upon that student’s dismissal from their program, the need for a reliable method for evaluating counseling student dispositions has become increasingly apparent. This high-profile legal case also highlighted the need to monitor and document student dispositions (Dugger & Francis, 2014; McAdams et al., 2007). Correspondingly, in 2009 the Council for Accreditation of Counseling and Related Educational Programs (CACREP) released standards that made monitoring student dispositions a mandatory aspect of program evaluation. In the 2016 CACREP standards the expectation for the assessment of counselor-in-training dispositions was expanded to include the monitoring of dispositions at multiple points over the duration of time students are enrolled in a counselor education program. The accreditation expectations for screening at the point of admission are found in Section I.L., where the standards delineate the expectation that counseling programs consider dispositions (CACREP, 2015). Dispositions for consideration include relationship skills and cultural sensitivity.
As the need for dispositional appraisal has become increasingly imperative in the counselor education profession, there have been various efforts to design specific approaches to assess student dispositions (Frame & Stevens-Smith, 1995; Kerl et al., 2002; Lumadue & Duffey, 1999; McAdams et al., 2007; Redekop & Wlazelek, 2012; Williams et al., 2014). One early approach was the utilization of standardized personality tests (Demos & Zuwaylif, 1966; Utley Buensuceso, 2008). However, the use of personality tests fell into disfavor because of the potential for conflicts with the Americans with Disabilities Act (U.S. Department of Justice, 2010) as well as for their inherent deficit orientation. Consequently, the use of standardized tests has been generally replaced by rating scales and rubrics (Panadero & Jonsson, 2013).
One reason that rubrics were considered superior to rating scales was their transparency (Panadero & Jonsson, 2013). Transparency empowers students by equipping them with an understanding of expectations for performance prior to their creating a product or performing a skill. Rubrics also have greater potential to align with learning outcomes and they provide useful direct feedback to students (Alexander & Praeger, 2009; Panadero & Jonsson, 2013).
Examples of dispositional assessments for counselors include the Counselor Characteristics Inventory (Pope, 1996), an inventory that assesses personality characteristics of effective counselors. Also, Spurgeon et al. (2012) described a process that includes a Likert-style assessment of dispositional traits. In addition, Swank et al. (2012) developed the Counseling Competencies Scale (CCS), a tool for measuring counselor competence. Frame and Stevens-Smith (1995) developed a 5-point Personal Characteristics Evaluation Form, and finally, Lumadue and Duffey (1999) published a Professional Performance Fitness Evaluation to evaluate specific behaviors of pre-professional counselors. Few studies of the reliability and validity of the tools were found in published research, especially related to admissions. However, some do have limited published psychometric research and in some cases norms (Flynn & Hays, 2015; Pope, 1996; Swank et al., 2012; Taub et al., 2011).
One example of a dispositional tool for counselor education with published psychometrics is the Counselor Personality Assessment (CPA) developed by Halinski (2010). The CPA is a 28-item scale reporting a Cronbach’s alpha reliability score of .82. Another tool, the CCS (Swank et al. 2012), is a 32-item rubric for measuring counseling skills, professional conduct, and professional dispositions in practicum. Cronbach’s alpha for the CCS was reported at .93, and interrater reliability was reported at .57. Criterion validity was established by correlating the CCS score with the semester grade and was reported as moderate. The available psychometric data for the CPA and CCS represent exceptions. In general, lack of psychometric information may result in limited confidence in available assessment tools for appraising counselor student dispositions.
Interrater Reliability
Interrater reliability, essentially the extent to which the raters assign the same scores when observing the same behaviors (McHugh, 2012), is critical for fairness to applicants in counseling admissions interviews. Gwet (2014) stated, “If the inter-rater reliability is high, then raters can be used interchangeably without the researcher having to worry about the categorization being affected by a significant rater factor. Interchangeability of raters is what justifies the importance of inter-rater reliability” (p. 4). Consistency ensures that the data collected are realistic for practical use. When interrater reliability is poor, interviews conducted by overly critical raters (hawks) naturally lead to negative bias against applicants when compared within the same applicant pool with the scores from interviews rated by less critical raters (doves). Epstein and Synhorst (2008) discussed interrater reliability as an approximation in which different people rate the same behavior in the same way. Thus, interrater reliability can also be understood as rater consensus.
Purpose of the Present Study
Effectively screening and selecting new entrants is one of the hallmarks that distinguishes a profession. Unfortunately, there is a dearth of available literature on assessment tools for rating admissions interviews. Further, lack of information on the reliability of the tools that exist represents a significant deficiency in professional literature (Johnson & Campbell, 2002). The Professional Disposition Competence Assessment—Revised Admission (PDCA-RA; Freeman & Garner, 2017; Garner et al., 2016) is a global rubric designed to assess applicant dispositions in brief graduate program interviews. The PDCA-RA includes a video training protocol developed to facilitate consistency across raters in scoring admissions interviews on dispositional domains.
The purpose of the study was to examine the internal stability and the interrater reliability of the PDCA-RA. The rationale for the study was that no similar rubrics assessing dispositions at admissions using training videos were found in published research, suggesting a gap in the literature. Interrater reliability was the key focus of this study because of the importance of interrater reliability for rubrics utilized in situations with multiple raters, a typical scenario for counselor education admissions processes.
Method
Sample
Raters for the study included 70 counselor educators, counseling doctoral students, adjunct faculty, and site supervisors. Counselor educators, doctoral students, and adjunct faculty at two universities were asked to participate in trainings on the new admissions screening tool. Site supervisors providing supervision for practicum and internship students at the two universities were offered training in the PDCA-RA as a component of continued professional development to maintain their supervision status. Training in both instances was free and included professional development credits. Informed consent for participation was obtained from all participants in accordance with ACA ethical codes (ACA, 2014) and IRB oversight at both universities. All participants in the study fully completed the PDCA-RA video-based training. The mean age of the raters was 43.9 (SD = 11.4, range 24–72). Sixty-four percent identified as female and 36% identified as male. Mean average years of experience indicated as a faculty or field supervisor was 12.2 (SD = 9.7, range 1–50). Ninety-three percent identified as White/Caucasian, 6% as Latino/a, and 1% as other ethnicity.
The counselor educators (27% of the sample) were primarily from two CACREP-accredited counseling programs in the Western United States. Participating universities included one private university and a state research university, both with CACREP-accredited programs. Counselor education doctoral students and adjunct faculty participants comprised 7% of the sample. The doctoral students participated in the training because they were involved as raters of master’s-level counselor education applicants in the admissions process at one institution. The remaining 66% of the participants were field site supervisors. Because field site supervisors were involved in gatekeeping, attending training in dispositional assessment was natural to their role as internship site supervisors.
Measure: PDCA-RA
The PDCA-RA was developed on the basis of the Professional Disposition Competence Assessment (PDCA; Garner et al., 2016). The PDCA, a dispositional gatekeeping tool, was revised to the Professional Disposition Competence Assessment-Revised (PDCA-R) after several rounds of use and with feedback from expert panels (Freeman & Garner, 2017). Advice from legal counsel was also reflected in the revision of the PDCA to the PDCA-R. The PDCA-R was originally used for both gatekeeping and admissions purposes, but it was determined that the PDCA-R was best used for gatekeeping, not for admissions screening, because the tool implied that the rater had prior knowledge of the student. Because this is often not the case in admissions screening, the PDCA-RA was developed.
The PDCA, PDCA-R, and PDCA-RA were conceptualized and developed through a comprehensive review of the literature, several rounds of field testing, and adjustments from expert faculty panels at two institutions. In addition to counseling literature on impairment and expert panel feedback, the Five-Factor Model, often referred to as the “Big Five” (Costa & McCrae, 1992), influenced three of the nine dispositional items. The Five-Factor Model consists of five personality traits consistently associated with positive mental health, academic success, and healthy habits and attitudes across the life span: Extraversion, Agreeableness, Conscientiousness, Emotional Stability, and Openness. The PDCA-RA dispositions are identical to the PDCA-R, with the exception of the disposition of Ethics. Ethics was removed from the PDCA-RA because the description assumed knowledge of professional ethical standards, a doubtful expectation for program applicants with no prior training in counseling. The behavioral descriptions in the PDCA-RA were narrowed so they described only those behaviors that can be observed in admissions interviews with no prior knowledge of the applicants. In addition, the rubric item descriptions were shortened to align with the practical context of brief (20- to 30-minute) admissions interviews in which there may be limited time for in-depth assessment.
If dispositions are thought of as traits, as per the definition of dispositions in the CACREP glossary (CACREP, 2015), the PDCA-RA is not technically directly measuring dispositions. Based upon advice from legal counsel, as well as the practicality of assessing applicants during short admissions interviews, the PDCA-RA assessed behaviors associated with dispositions and not the actual dispositions. Behaviors identified for each disposition can be observed during a short admissions interview, whereas personality traits would require a more in-depth assessment approach, one that counselor educators fear might be found legally problematic (Freeman et al., 2019; Schuermann et al., 2018).
The nine dispositions assessed in terms of observable behaviors via the rubric are Conscientiousness, Coping and Self-Care, Openness, Cooperativeness, Moral Reasoning, Interpersonal Skills, Cultural Sensitivity, Self-Awareness, and Emotional Stability. Each disposition in the PDCA-RA is rated on a scale of three levels—developing, meets expectation, and above expectation. The PDCA-RA is described in more detail in a manual that includes the tools as well as three suggested admissions questions for each of the nine dispositions (Freeman & Garner, 2017). The measure of internal consistency for faculty ratings of the original PDCA rubric was a Cronbach’s alpha estimated at .94 (Garner et al., 2016). Cronbach’s alpha for self-ratings was .82, and Cronbach’s alpha for peer ratings was .89. The straightforward modifications from the original PDCA to the PDCA-RA were minimal and unlikely to significantly affect these measures of internal consistency.
Procedure
A video-based training protocol was developed for the purpose of training faculty in counselor education programs, doctoral students, site supervisors, and other admissions raters to use the PDCA-RA to assess the dispositions of graduate program applicants (Freeman & Garner, 2017; Garner et al., 2016). The video was presented to participants by a trainer. The trainer also greeted participants, obtained informed consent, passed out PDCA-RA forms when prompted by the training video, and collected completed PDCA-RA forms for later analysis. Training in the use of the PDCA-RA was important not only as a mechanism to establish interrater reliability but also as a means of informing adjustments to the tool during its initial iterative development process. Development of the video-based training protocol progressed through several stages. At first, the original 90-minute training consisted of a faculty team of seven working together as a group to read and discuss each disposition, followed by each faculty viewing an admissions interview video and rating the applicant independently. Faculty then discussed their ratings, leading to subtle adjustments in the rubric item descriptions. Additional benefits to the training were an increase in faculty self-awareness of dove and hawk tendencies when rating admissions applicants and self-awareness associated with interview bias. With continued training and feedback, the original training protocol was significantly improved.
To complete the next step in the creation of the video-based training protocol, counseling student volunteers were offered a minimal incentive to come to the film studio, and after signing waivers to allow the film clips to be used, the student volunteers were asked to respond to various admissions interview questions. The faculty filming the students instructed them to “give a strong answer” or “give a weak answer.” The researchers treated all responses as unscripted role plays. The questions asked by the interviewer for each disposition were those found in the PDCA-RA materials (Freeman & Garner, 2017). Finally, the authors and developers of the training video reviewed over 100 film clips, removed those in which the acting interfered with the purpose of the video, and rated the remaining clips using the PDCA-RA, resulting in ratings of 1, 3, or 5. These numerical ratings corresponded to descriptive ratings of developing, meets expectation, and above expectation, respectively. Clips in which the researchers found the rating to be difficult were removed from consideration. In selecting the final 18 clips (two for each of nine dispositions), the researchers considered diversity in age, ethnicity, gender, and disability of the student volunteers. The goal was to create video clips of student volunteers with diverse characteristics.
The result was a video-based training protocol that could still be completed by trainees in 90 to 120 minutes. The video training protocol began with an introduction to the PDCA-RA, followed by prompts to rate the video-recorded vignettes using the PDCA-RA prior to receiving training. This initial rating of the vignettes was considered the pretest condition. Training on the application of the PDCA-RA to the vignettes was next. Training included revealing ideal scores as determined by the authors, the reasoning behind the scoring, and opportunities to discuss scoring among participants. Following the training on the PDCA-RA, participants were, once again, given the PDCA-RA rubric along with a new set of video-recorded vignettes. This was considered the posttest condition. Participants were asked to rate the new vignettes using the PDCA-RA.
The video-based training protocol, designed for use in small groups, allowed for group discussion of ratings after each participant completed the PDCA-RA independently. This was indicated by a written message on the video reading, “Pause video for discussion.” The training tape ended with a narrator discussion of how to use the PDCA-RA in actual admissions interviews, including comments on cultural sensitivity in admissions interviews.
The video-based training protocol was used as the means of training participants in dispositional assessment. The purpose of the trainings was to increase consistency of admissions raters in evaluating the admissions interviews of applicants to a master’s-level counselor education program. Typically, participants completed the video training in small groups consisting of approximately six to 10 people. In addition to viewing the training video, participants also took part in group discussion and established a consensus of opinion on group ratings of video clips. Coming to a consensus on ratings, which also included feedback on rubric items and video clips, was an important aspect of the training.
Statistical Analysis
The PDCA-RA scores from the counselor education faculty, adjunct faculty, doctoral students, and site supervisors’ ratings of the vignettes before training were used as the pretest or baseline interrater reliability. The PDCA-RA scores after participants were trained in the tool were used as the posttest. The intraclass correlation coefficient (ICC) was calculated as a measure of interrater reliability. Interrater reliability correlations quantify rater subjectivity (Herman et al., 1992). The ICC was calculated for pretest and posttest scores. Cronbach’s alpha coefficients were calculated for internal consistency, and Fleiss’ kappa (κ) was calculated for absolute agreement. In addition, Fleiss’ free-marginal kappa (κfree) and percent overall agreement were calculated. Calculations were made for both the pretest and posttest ratings, and a t-test was conducted, using SPSS, to determine whether training improved interrater reliability.
Results
The ICC estimates and associated 95% confidence intervals were calculated using SPSS statistical package version 23 and based on an individual rating, absolute agreement, 2-way random-effects model. ICC single measures for absolute agreement were calculated for the pretest administration of the PDCA-RA at .53 (95% CI [0.333–0.807]). The ICC single measures for absolute agreement were calculated for the posttest administration of the PDCA-RA at .76 (95% CI [0.582–0.920]). Cronbach’s alpha was calculated at .99 for both pretest and posttest scores. Pretest and posttest ICCs were compared using a t-test with an a priori significance level set at .05. The test was significant (p < .05), suggesting that there was a difference between the pretest and posttest reliability, with reliability improving from the “moderate” range to the “good” range (Koo & Li, 2016) with training.
Using Excel, kappa (κ) was calculated as a measure of overall agreement for pretest and posttest scores. This particular kappa was extended by Fleiss (1971) and accommodates multiple raters like those rating the PDCA-RA. Assumptions underpinning Fleiss’ kappa include categorical data (i.e., nominal or ordinal) with mutually exclusive categories, symmetrical cross-tabulations, and independence of raters. Data in this study met all assumptions. Data was ordinal with three mutually exclusive response categories for each dispositional area assessed, which resulted in all cross-tabulations being symmetrical. Although raters were trained in a collaborative setting where discussions about ratings were fostered, when the actual ratings of study participants occurred, raters did not discuss their ratings with others and were thus independent of one another. Pretest scores for the nine rubric items reflected a κ of .33, fair agreement according to Landis and Koch (1977). After training, posttest scores on the nine items reflected a κ of .55, moderate agreement according to Landis and Koch.
As an additional analysis, percent overall agreement and κfree was calculated. κfree is appropriate when raters do not know how many cases should be distributed into each category. In addition, κfree is resistant to influence by prevalence and bias (Randolph, 2005). The percent of overall agreement is the measure of agreement between raters and historically has also been used to calculate interrater reliability (McHugh, 2012). Table 1 illustrates that the κfree for the pretest was .36 while the percent of overall agreement was 57.6%. The posttest for the κfree was .56 and the percent of overall agreement was 70.4%. After examining the change in pretest to posttest calculations from both the κfree and the percent of overall agreement, both offer additional support for and provide evidence that training improved the agreement of dispositional ratings on the PDCA-RA.
Table 1
Pre and Post Statistics: Percent Overall Agreement and Free-Marginal Fleiss’ Kappa
| Time of Rating |
Percent Overall Agreement |
Free-Marginal Kappa |
95% CI for Free- Marginal Kappa |
| Before Training: Pre |
57.6 |
.36 |
[.23, .49] |
| After Training: Post |
70.4 |
.56 |
[.31, .80] |
The overall κ, κfree and percent of agreement results were promising, but a comparison of the percent of correct responses (the response intended by the research team) by disposition showed that the ratings of correct responses decreased by more than 2% from pre- to posttesting for three dispositions (Openness, Cooperativeness, and Moral Reasoning). Because this was an unexpected finding, the research team analyzed the ratings for incorrect responses and learned that the raters appeared to be better able to discern the difference between a rating of 1 (developing) and 3 (meets expectation) than between 3 and 5 (above expectation). As a post-hoc analysis, we calculated the percent of agreement with the correct score, collapsing the 3 and 5 ratings. The percent of correct responses with dichotomous categories of 1 and a collapsed category for 3 and 5 are shown in Table 2. As is evident in Table 2, using the collapsed category, the percent of correct responses for eight of the nine dispositions improved from pretest to posttest. The percent of correct responses for one disposition, Cooperativeness, decreased by more than 2% from pretest to posttest.
Table 2
Pre and Post Percent of Correct Responses by Disposition
| Disposition |
Pre Percent
Overall Agreement1, 3, 5
Ratings |
Post Percent Overall Agreement
1, 3, 5
Ratings |
Pre Percent
Overall Agreement1, 3 & 5
Collapsed |
Post Percent Overall Agreement
1, 3 & 5
Collapsed |
| 1. Conscientiousness |
62.0 |
97.1 |
77.1 |
98.6 |
| 2. Coping & Self-Care |
59.9 |
94.4 |
22.9 |
97.1 |
| 3. Openness |
51.0 |
49.4 |
94.3 |
100.0 |
| 4. Cooperativeness |
47.3 |
39.0 |
94.3 |
87.1 |
| 5. Moral Reasoning |
84.1 |
68.8 |
91.4 |
98.6 |
| 6. Interpersonal Skills |
48.0 |
94.4 |
98.6 |
97.1 |
| 7. Cultural Sensitivity |
69.3 |
94.4 |
100.0 |
100.0 |
| 8. Self-Awareness |
40.7 |
40.0 |
54.3 |
64.3 |
| 9. Emotional Stability |
56.3 |
56.5 |
67.1 |
95.7 |
Discussion
The results of the study suggest that the PDCA-RA has potential as a reliable instrument for assessing counseling applicants at the point of program admission. The PDCA-RA demonstrated strong reliability from the standpoint of internal consistency. The interrater reliability, as measured by the ICC, moved from the “moderate” to the “good” range with the application of the standardized training protocol.
The results of the study also provide evidence that counselor educators, supervisors, and doctoral students can improve their agreement on ratings of student dispositions with adequate and appropriate training. Multiple statistical techniques for measuring agreement, including the ICC, κ, κfree, and percent agreement measured under pre-training and post-training conditions demonstrated overall improvement in rater agreement with training. The observed post-training improvement in interrater reliability corroborates the literature, underscoring the necessity of training protocols as the pathway to improved interrater reliability (Jonsson & Svingby, 2007).
The results from the second analysis conducted through collapsing the meets expectation and above expectation categories suggest that the PDCA-RA has higher reliability as a tool to screen out inappropriate candidates than to distinguish excellence within the pool of acceptable candidates. For programs seeking to eliminate problematic applicants, the PDCA-RA could prove reliable. However, for academic programs with large numbers of applicants with an objective to accept a small group of students from a large group of acceptable candidates, the PDCA-RA may be less reliable from an interrater reliability perspective. The PDCA-RA item descriptions for above expectation need further consideration.
The percent of correct responses after training with collapsed categories was over 87% for seven of the nine dispositions. The results suggest that the PDCA-RA or the PDCA-RA training protocol needs revision on two dispositions, Cooperativeness and Self-Awareness. The decrease in correct responses to Cooperativeness may be due to a posttest interview with a higher level of difficulty than the pretest interview. The posttest percent was 87%, suggesting that overall the rubric descriptions functioned as acceptable with this sample of raters, though not excellent. The percent of correct ratings for Self-Awareness increased from pre- to posttesting, but only to 64% agreement. One explanation could be that the Self-Awareness rubric descriptions are behavioral (as recommended by legal counsel), yet Self-Awareness as a trait is difficult to describe in behavioral terms. This could leave raters confused about the difference between their intuitive sense of the self-awareness of the applicant and the narrow behavioral descriptions on the rubric. An alternative explanation is that there is a lack of agreement in the profession on the extent of self-awareness expected from students entering the academic program, leading some raters to find the applicant’s level of self-awareness acceptable, while others found the level unacceptable. In either case, the training protocol for the PDCA-RA and perhaps the rubric description need improvement. The 100% posttest agreement on the dichotomous categories for Openness and Cultural Awareness were encouraging, given the critical importance of these two dispositions (Freeman et al., 2019).
Interrater reliability is of paramount importance for the responsible use of rubrics. To improve the interrater reliability of the PDCA-RA, three issues may need to be addressed. First, the training protocol may need to be lengthened to encompass three rather than two opportunities to rate video clips. Second, structuring the discussion between raters with questions focusing attention on the gaps in ratings could be beneficial. Third, because alternate forms of the videos are being used in the training (different actors with different responses to the same question), a comparison of the complexity of the video clips should be conducted. It may be desirable to revise the training protocol to utilize less complex responses for Part 1 training, followed by equivalent complex interviews for Part 2 training, and more complex interview responses for Part 3. More complex responses, meaning the responses are partially descriptive of two categories on the rubric, are realistic to actual admissions interviews in the field.
In conducting trainings for the PDCA-RA, a potentially interesting observation was that raters appeared predisposed to using their own subjective experience to rate the video interviews instead of applying the item descriptions in the rubric. Often the trainers observed that the disposition title, such as Self-Awareness, triggered an automatic response of high rater confidence in their ability to rate self-awareness without carefully reading the rubric descriptions. The tendency of raters to believe they are “right” rather than applying a rubric description is a potential barrier for any dispositional measure.
Implications of the Study
The implications of this study relate primarily to counselor education programs. As evident from the review of literature, careful admissions processes are critical to prevent or diminish the number of gatekeeping and remediation situations that occur in academic programs after admission. In addition to the importance of fair admissions procedures from a legal perspective, the effort required of applicants to engage in the application process justifies the importance of developing fair processes in which acceptance or denial decisions are not based solely upon the subjectivity of faculty.
For those academic programs utilizing admissions interviews, one important implication of the study is that the results suggest that without training, raters will have high variability in their ratings of admissions applicants, as illustrated by the variability of the pretest scores in this study. Structuring the rating of admissions interviews by using an assessment is one method of mitigating the variability of faculty ratings of applicants. A holistic (global) rubric such as the PDCA-RA is unlikely to ever garner the almost perfect interrater reliability associated with analytic rubrics, but the PDCA-RA is available as one practical, field-tested tool with promising reliability to help facilitate transparent and fair admissions interview rating processes.
Limitations and Future Research
In light of the lack of an established list of professional dispositions, the PDCA-RA’s utility may be limited, as the selected dispositions may not align with the values of all counselor education programs. A second limiting factor is that the sample included both field site supervisors and faculty, and all participants were from the rural Western United States. The reliability of the tool is limited by the demographics of the sample. Another limitation was that the study’s pretest and posttest video clips, although similar, were different from one another. The initial decision to use different pretest and posttest video clips was based on an attempt to reduce the influence of testing as a threat to internal validity. However, this also introduced the possibility that either of the sets of video clips was inherently easier or more difficult to rate than the other. Further research would include randomly juxtaposing pretest and posttest video clips, or perhaps using the same video clips pre- and posttest to eliminate the possibility that differences in pretest and posttest video clips were responsible for the improvements in score reliability rather than the intended independent variable, the training. Another potential limitation to the results is that it is possible that some of the graduate students who were filmed in the vignettes may have been known by six of the faculty members from one of the institutions. The impact of this possibility was reduced by the use of multiple student actors, but prior knowledge of the student could have influenced raters’ scores.
A final issue for consideration is the decision to use site supervisors as raters for the research. Site supervisors more commonly utilize the PDCA-R rather than the PDCA-RA, the version specific to admissions screening. The PDCA-R is used by supervisors to monitor and to communicate with counselor educators and counseling program clinical personnel. Further, at least one of the counselor education programs utilizes site supervisors for the admissions process. The training protocol for both versions of the PDCA is the same, and with site supervisors routinely participating in the training, the decision was made to include site supervisors as raters. It is possible, however, that site supervisors may differ in their abilities to respond to the training protocol when compared to counselor educators, adjunct faculty, and doctoral students.
A possibility for future research is to measure the extent to which the improvement in reliability can be maintained over time. At this point, little is known about whether and how often educators and site supervisors would need training updates to function optimally as raters of student dispositions. Accordingly, rating reliability could be observed at intervals of 3 months, 6 months, or 1 year after training to monitor decay.
Future research is also needed to determine the extent to which the length of the training protocol influences interrater reliability. In addition, cultural and gender bias in the use of the PDCA-RA should be studied, as one criticism of rubrics is the potential for cultural bias.
As a tool for consistently rating counselor education program applicants, the PDCA-RA demonstrates potential, though more research needs to be conducted to increase the interrater reliability. Training improved the interrater reliability results but not to the extent that excellent interrater reliability was achieved. Adjusting the training protocol may be fruitful as a mechanism to improve interrater reliability.
Conclusion
There is a need for reliable admissions tools to assess dispositional behaviors of counseling program applicants. Interrater reliability is an important form of reliability in situations such as admissions interviews in which there are often multiple raters involved in the process. The importance of interrater reliability is founded in the critical premises of fairness and transparency to applicants, though legal protection of counselor education programs is also enhanced by using clear, standardized processes. Dispositional assessment is in its infancy, especially when applied to counselor education in general and to program admissions in particular. How exactly to define dispositions as well as how exactly the role of the counselor will serve as a means of selection and gatekeeping for the profession is yet to be determined. Yet counselor educators perceive both an ethical and professional responsibility for monitoring counseling student dispositions as a means for safeguarding the integrity of the profession (Freeman et al., 2019; Schuermann et al., 2018). The continued development of the PDCA-R and the PDCA-RA, as well as the associated training materials, represents initial steps toward standardizing and improving dispositional appraisal. The video-based training and the exploration of the training as a means of improving rater consistency will potentially increase the ability of counselor educators to consistently assess and monitor developing counseling students. Consistent dispositional ratings can also contribute to the development of a common language for discussing student progress. The current research represents a promising effort to continually improve the dispositions assessment process for counselor educators, counseling programs, and the counseling profession.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Alexander, C. R., & Praeger, S. (2009, June). Smoke gets in your eyes: Using rubrics as a tool for building justice into assessment practices. Paper presented at the Annual Conference of the Australian Teacher Education Association (ATEA). Australian Teacher Education Association. http://files.eric.ed.gov/fulltext/ED524704.pdf
American Counseling Association. (2014). ACA code of ethics.
Bryant, J. K., Druyos, M., & Strabavy, D. (2013). Gatekeeping in counselor education programs: An examination of current trends. In Ideas and research you can use: VISTAS 2013. American Counseling Association. https://www.counseling.org/docs/default-source/vistas/gatekeeping-in-counselor-education-programs.pdf
?sfvrsn=7f6e77b5_13
Carkhuff, R. R. (1969). Critical variables in effective counselor training. Journal of Counseling Psychology, 16(3), 238–245. https://doi.org/10.1037/h0027223
Cole, B. S. (1991). Legal issues related to social work program admissions. Journal of Social Work Education, 27(1), 18–24. https://doi.org/10.1080/10437797.1991.10672165
Costa, P. T., Jr., & McCrae, R. R. (1992). NEO PI-R professional manual. Psychological Assessment Resources, Inc.
Council for Accreditation of Counseling and Related Educational Programs. (2009). CACREP 2009 standards. http://www.cacrep.org/wp-content/uploads/2017/07/2009-Standards.pdf
Council for Accreditation of Counseling and Related Educational Programs. (2015). CACREP 2016 standards. http://www.cacrep.org/forprograms/2016-cacrep-standards
Crawford, M., & Gilroy, P. (2013). Professional impairment and gatekeeping: A survey of master’s level training programs. The Journal of Counselor Preparation and Supervision, 5(1). https://doi.org/10.7729/51.0030
Demos, G. D., & Zuwaylif, F. H. (1966). Characteristics of effective counselors. Counselor Education and Supervision, 5(3), 163–165. https://doi.org/10.1002/j.1556-6978.1966.tb02062.x
Dugger, S. M., & Francis, P. C. (2014). Surviving a lawsuit against a counseling program: Lessons learned from Ward v. Wilbanks. Journal of Counseling & Development, 92(2), 135–141.
https://doi.org/10.1002/j.1556-6676.2014.00139.x
Engram, B. E., & Vandergoot, D. (1978). Correlation between the Truax and Carkhuff scales for measurement of empathy. Journal of Counseling Psychology, 25(4), 349–351. https://doi.org/10.1037/0022-0167.25.4.349
Epstein, M. H., & Synhorst, L. (2008). Preschool behavioral and emotional rating scale (PreBERS): Test–retest reliability and inter-rater reliability. Journal of Child and Family Studies, 17(6), 853–862.
https://doi.org/10.1007/s10826-008-9194-1
Fleiss, J. L. (1971). Measuring nominal scale agreement among many raters. Psychological Bulletin, 76(5), 378–382. https://doi.org/10.1037/h0031619
Flynn, S. V., & Hays, D. G. (2015). The development and validation of the Comprehensive Counseling Skills Rubric. Counseling Outcome Research and Evaluation, 6(2), 87–99. https://doi.org/10.1177/2150137815592216
Frame, M. W., & Stevens-Smith, P. (1995). Out of harm’s way: Enhancing monitoring and dismissal processes in counselor education programs. Counselor Education and Supervision, 35(2), 118–129.
https://doi.org/10.1002/j.1556-6978.1995.tb00216.x
Freeman, B. J., & Garner, C. M. (2017). Professional Dispositions Competency Assessment, Revised. Unpublished instrument, ScholarWorks.
Freeman, B. J., Garner, C. M., Fairgrieve, L. A., & Pitts, M. E. (2016). Gatekeeping in the field: Strategies and practices. Journal of Professional Counseling: Practice, Theory & Research, 43(2), 28–41.
https://doi.org/10.1080/15566382.2016.12033954
Freeman, B. J., Garner, C. M., Scherer, R., & Trachok, K. (2019). Discovering expert perspectives on dispositions and remediation: A qualitative study. Counselor Education and Supervision, 58(3), 209–224.
https://doi.org/10.1002/ceas.12151
Garner, C. M., Freeman, B. J., & Lee, L. (2016). Assessment of student dispositions: The development and psychometric properties of the professional disposition competence assessment (PDCA). In Ideas and research you can use: VISTAS 2016. American Counseling Association. https://www.counseling.org/knowledge-center/vistas/by-year2/vistas-2016/docs/default-source/vistas/article_5235f227f16116603abcacff0000bee5e7
Gwet, K. L. (2014). Handbook of inter-rater reliability: The definitive guide to measuring the extent of agreement among raters (4th ed.). Advanced Analytics.
Halinski, K. H. (2010). Predicting beginning master’s level counselor effectiveness from personal characteristics and admissions data: An exploratory study [Doctoral dissertation, University of North Texas]. https://digital.library.unt.edu/ark:/67531/metadc11038
Herman, J. L., Aschbacher, P. R., & Winters, L. (1992). A practical guide to alternative assessment. Association for Supervision and Curriculum Development.
Hernández, T. J., Seem, S. R., & Shakoor, M. A. (2010). Counselor education admissions: A selection process that highlights candidate self-awareness and personal characteristics. Journal of Counselor Preparation and Supervision, 2(1), 74–87. https://doi.org/10.7729/21.2010
Hutchens, N., Block, J., & Young, M. (2013). Counselor educators’ gatekeeping responsibilities and students’ first amendment rights. Counselor Education and Supervision, 52(2), 82–95.
https://doi.org/10.1002/j.1556-6978.2013.00030.x
Johnson, W. B., & Campbell, C. D. (2002). Character and fitness requirements for professional psychologists: Are there any? Professional Psychology: Research and Practice, 33(1), 46–53. https://doi.org/10.1037/0735-7028.33.1.46
Jonsson, A., & Svingby, G. (2007). The use of scoring rubrics: Reliability, validity and educational consequences. Educational Research Review, 2(2), 130–144. https://doi.org/10.1016/j.edurev.2007.05.002
Kerl, S., & Eichler, M. (2005). The loss of innocence: Emotional costs to serving as gatekeepers to the counseling profession. Journal of Creativity in Mental Health, 1(3–4), 71–88. https://doi.org/10.1300/J456v01n03_05
Kerl, S. B., Garcia, J. L., McCullough, C. S., & Maxwell, M. E. (2002). Systematic evaluation of professional performance: Legally supported procedure and process. Counselor Education and Supervision, 41(4), 321–334. https://doi.org/10.1002/j.1556-6978.2002.tb01294.x
Koerin, B., & Miller, J. (1995). Gatekeeping policies: Terminating students for nonacademic reasons. Journal of Social Work Education, 31(2), 247–260. https://doi.org/10.1080/10437797.1995.10672261
Koo, T. K., & Li, M. Y. (2016). A guideline of selecting and reporting intraclass correlation coefficients for reliability research. Journal of Chiropractic Medicine, 15(2), 155–163. https://doi.org/10.1016/j.jcm.2016.02.012
Kopenhaver Haidet, K., Tate, J., Divirgilio Thomas, D., Kolanowski, A., & Happ, M. B. (2009). Methods to improve reliability of video-recorded behavioral data. Research in Nursing & Health, 32(4), 465–474. http://doi.org/10.1002/nur.20334
Landis, J. R., & Koch, G. G. (1977). The measurement of observer agreement for categorical data. Biometrics, 33(1), 159–174. https://doi.org/10.2307/2529310
Lumadue, C. A., & Duffey, T. H. (1999). The role of graduate programs as gatekeepers: A model for evaluating student counselor competence. Counselor Education and Supervision, 39(2), 101–109.
https://doi.org/10.1002/j.1556-6978.1999.tb01221.x
McAdams, C. R., III, Foster, V. A., & Ward, T. J. (2007). Remediation and dismissal policies in counselor education: Lessons learned from a challenge in federal court. Counselor Education and Supervision, 46(3), 212–229. https://doi.org/10.1002/j.1556-6978.2007.tb00026.x
McCaughan, A. M., & Hill, N. R. (2015). The gatekeeping imperative in counselor education admission protocols: The criticality of personal qualities. International Journal for the Advancement of Counseling, 37, 28–40. https://doi.org/10.1007/s10447-014-9223-2
McHugh, M. L. (2012). Interrater reliability: The kappa statistic. Biochemia Medica, 22(3), 276–282.
https://doi.org/10.11613/BM.2012.031
Miller, S. (2006). Professionalisation, ethics and integrity systems: The promotion of professional ethical standards, and the protection of clients and consumers. A report for the Professional Standards Councils, Centre for Applied Philosophy and Public Ethics, Australia.
Panadero, E., & Jonsson, A. (2013). The use of scoring rubrics for formative assessment purposes revisited: A review. Educational Research Review, 9, 129–144. https://doi.org/10.1016/j.edurev.2013.01.002
Pope, V. T. (1996). Stable personality characteristics of effective counselors: The Counselor Characteristic Inventory (Doctoral dissertation). Retrieved from ProQuest Dissertations & Theses Global (Order No. 9625345).
Randolph, J. J. (2005). Free-marginal multirater kappa (multirater κfree): An alternative to Fleiss’ fixed-marginal multirater kappa. Department of Computer Science, 1, 1–20. http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.59
.8776&rep=rep1&type=pdf
Redekop, F., & Wlazelek, B. (2012). Counselor dispositions: An added dimension for admission decisions. In Ideas and research you can use: VISTAS 2012. American Counseling Association. https://www.counseling.org/knowledge-center/vistas/by-year2/vistas-2012/docs/default-source/vistas/vistas_2012_article_17
Rosen, J., Mulsant, B. H., Marino, P., Groening, C., Young, R. C., & Fox, D. (2008). Web-based training and interrater reliability testing for scoring the Hamilton Depression Rating Scale. Psychiatry Research, 161(1), 126–130. https://doi.org/10.1016/j.psychres.2008.03.001
Schuermann, H., Avent Harris, J. R., & Lloyd-Hazlett, J. (2018). Academic role and perceptions of gatekeeping in counselor education. Counselor Education and Supervision, 57(1), 51–65. https://doi.org/10.1002/ceas.12093
Smaby, M. H., Maddux, C. D., Richmond, A. S., Lepkowski, W. J., & Packman, J. (2005). Academic admission requirements as predictors of counseling knowledge, personal development, and counseling skills. Counselor Education and Supervision, 45(1), 43–57. https://doi.org/10.1002/j.1556-6978.2005.tb00129.x
Spurgeon, S. L., Gibbons, M. M., & Cochran, J. L. (2012). Creating personal dispositions for a professional counseling program. Counseling and Values, 57(1), 96–108. https://doi.org/10.1002/j.2161-007X.2012.00011.x
Swank, J. M., Lambie, G. W., & Witta, E. L. (2012). An exploratory investigation of the counseling competencies scale: A measure of counseling skills, dispositions, and behaviors. Counselor Education and Supervision, 51(3), 189–206. https://doi.org/10.1002/j.1556-6978.2012.00014.x
Swank, J. M., & Smith-Adcock, S. (2014). Gatekeeping during admissions: A survey of counselor education programs. Counselor Education and Supervision, 53(1), 47–61. https://doi.org/10.1002/j.1556-6978.2014.00048.x
Taub, D. J., Servaty-Seib, H. L., Wachter Morris, C. A., Prieto-Welch, S. L., & Werden, D. (2011). Developing skills in providing outreach programs: Construction and use of the POSE (Performance of Outreach Skills Evaluation) rubric. Counseling Outcome Research and Evaluation, 2(1), 59–72. https://doi.org/10.1177/2150137811401019
Truax, C. B., & Carkhuff, R. (1967). Toward effective counseling and psychotherapy: Training and practice. Aldine.
U.S. Department of Justice, Civil Rights Division. (2010). Americans with Disabilities Act Title III Regulations: Part 36 Nondiscrimination on the Basis of Disability in Public Accommodations and Commercial Facilities (CRT Docket No. 106). https://www.ada.gov/regs2010/titleIII_2010/titleIII_2010_regulations.htm
Utley Buensuceso, J. M. (2008). The Sixteen Personality Factor Questionnaire and ratings of counselor effectiveness (Order No. 3341140) [Doctoral dissertation, Azusa Pacific University]. ProQuest Dissertations and Theses Global.
Ward v. Wilbanks. (2010). No. 09-CV-112 37, 2010 U.S. Dist. WL 3026428 (E.D. Michigan, July 26, 2010).
Williams, J. L., Williams, D. D., Kautzman-East, M., Stanley, A. L., Evans, W. J., & Miller, K. L. (2014). Assessing student dispositions in counselor training programs: Implications for supervision, program policy, and legal risk management [PowerPoint slides]. DocPlayer. https://docplayer.net/2862339-Assessing-student-dispositions-in-counselor-training-programs-implications-for-supervision-program-policy-and-legal-risk-management.html
Curtis Garner, EdD, NCC, NCSC, LCPC, is a professor and department chair at Gonzaga University. Brenda Freeman, PhD, is a professor at the University of Nevada, Reno. Roger Stewart, PhD, is a professor at Boise State University. Ken Coll, PhD, is the Dean of the School of Education at the University of Nevada, Reno. Correspondence may be addressed to Curtis Garner, 502 East Boone Ave., Spokane, WA 99258-0102, garnerc@gonzaga.edu.
Aug 18, 2020 | Volume 10 - Issue 3
Melissa Sitton, Tina Du Rocher Schudlich, Christina Byrne, Chase M. Ochrach, Seneca E. A. Erwin
A family systems framework guided our investigation of self-injurious behavior (SIB) in adolescents. As part of a larger study, we collected data examining SIB and family functioning from 29 adolescents (Mage = 15.66) and their caregivers. These adolescents with traits of borderline personality disorder were seeking counseling from community-based practitioners specializing in dialectical behavior therapy. Our primary aim was to better understand the family environment of these adolescents. A second aim was to elucidate interrelations among family communication, roles, problem-solving, affective involvement, affective responsiveness, behavioral control, and conflict and SIB. We found a high rate of SIB among adolescent participants. There was significant congruence between adolescent and caregiver reports of the family environment, with families demonstrating unhealthy levels of functioning in several indicators of family environment. The latent variable of family functioning significantly predicted nonsuicidal and ambivalent SIB. Counselors working with adolescents should consider family functioning when assessing risk for SIB.
Keywords: self-injurious behavior, adolescents, family systems, borderline personality disorder, family functioning
Although emotion dysregulation and unstable personal relationships are common for adolescents, those with symptoms of borderline personality disorder (BPD) often report more extreme experiences (A. L. Miller et al., 2008). BPD is characterized by impaired or unstable emotional and social functioning (American Psychiatric Association, 2013). Individuals with BPD—especially adolescents—may experience impairments in daily functioning as well as within interpersonal relationships (Chanen et al., 2007).
Linehan’s (1993) biosocial theory proposed that BPD can result from an individual’s biological predisposition toward emotion dysregulation and a social environment that amplifies this vulnerability. Given that adolescents spend a substantial amount of time with their family, it is important to examine an adolescent’s familial environment to understand the etiology of BPD symptoms; such examination requires a framework like family systems theory, which emphasizes the relationships between family members rather than focusing on the individual members themselves (Goldenberg & Goldenberg, 2013); this includes family communication, roles, problem-solving, affective involvement, affective responsiveness, and behavioral control (I. W. Miller et al., 2000).
Self-Injurious Behavior (SIB)
Regrettably, it is common for adolescents with BPD to engage in SIB (Kaess et al., 2014). SIB is an umbrella term for all purposeful, self-inflicted acts of bodily harm, whether the intent is suicidal, nonsuicidal (i.e., nonsuicidal self-injury), or ambivalent (i.e., neither strictly suicidal nor nonsuicidal). In fact, SIB is one diagnostic criteria for BPD in adolescents and adults.
Although originally developed to explain the etiology of BPD, the biosocial theory has been applied to the development of SIB as well (Crowell et al., 2009). Countless studies have examined the role of emotion dysregulation and affective reinforcement in SIB, but it is important to also consider the influence of social variables. Indeed, in their four-function model, Nock and Prinstein (2004, 2005) suggested that both affective and social variables can positively and negatively reinforce nonsuicidal SIB. Similarly, Joiner’s (2005) interpersonal theory of suicidal SIB posited that social variables (particularly thwarted belongingness and perceived burdensomeness) drive the desire for suicide. Thus, although there are clear links between affective variables and SIB, social variables are also relevant. For adolescents, an important social variable related to SIB is family environment. From the family systems approach, adolescent SIB is best understood when rooted in the context of family environment. As Levenkron (1998) suggested, “the ways in which all the family members relate to each other… [is] the fuel that drives [SIB]” (pp. 125–126).
Although limited in number, some previous studies have examined family environment and SIB in adolescents. For example, Halstead et al. (2014) found that SIB was related to dysfunctional family environments. Studies have also found relationships between adolescent SIB and familial communication (Halstead et al., 2014; Latina et al., 2015) and conflict (Huang et al., 2017). Additionally, Adrian et al. (2011) demonstrated a link between stress and failure to meet expectations of familial roles. To our knowledge, no studies to date have examined SIB and familial problem-solving, affective involvement, affective responsiveness, and behavioral control. However, studies have linked SIB to an individual’s lack of problem-solving skills (Walker et al., 2017), ability to regulate affective responses (Adrian et al., 2011), and behavioral control related to impulsivity and compulsivity (Hamza et al., 2015).
Current Study
Despite the clear influence of family members on SIB (Halstead et al., 2014) and the significant amount of time adolescents tend to spend with family members, more research is needed to evaluate family environment in relation to SIB. Specifically, we investigated the families of treatment-seeking adolescents with traits of BPD who engage in SIB. Our objectives were to: (a) assess family environment using multiple indicators of family functioning, (b) assess SIB in these treatment-seeking adolescents, including SIB done with suicidal intent, nonsuicidal intent, and ambivalence toward life, and (c) evaluate family functioning as a statistical predictor of lifetime SIB.
Method
Participants and Procedure
We used data from a larger ongoing, unpublished study on dialectical behavior therapy. In the larger study, participants were adolescents and young adults who sought counseling from community-based clinicians specializing in dialectical behavior therapy. Participants sought counseling for symptoms of BPD, particularly SIB. The counselors recruited participants for the research study by explaining voluntary research participation during their standard intake process for new clients at the clinic. The counselors also obtained informed consent for research from the participants. The counselors collaborated with researchers at a local university for this larger study, and the university’s IRB approved the study.
For the current study, we used the existing pretest data from the adolescents only (N = 29; Mage = 15.66, SDage = 1.34, age range = 13–18). A majority of the adolescent sample (82.8%; n = 24) reported no previous experience with counseling. This sample was predominately Caucasian (82.8%; n = 24) and most adolescents identified as female (89.7%; n = 26).
Caregiver participants (N = 29) were involved in the adolescents’ treatment and the accompanying research study. Most caregiver participants were the biological mother (81.5%; n = 22) or adoptive mother (7.4%; n = 2). However, a few adolescents were accompanied by an extended family member (7.4%; n = 2) or their biological father (3.7%; n = 1). A majority of adolescents reported that at least one of their caregivers had attended some (22.2%; n = 6) or all (29.6%; n = 8) of college, or some (3.7%; n = 1) or all (29.6%; n = 8) of graduate school.
Most adolescents reported they currently lived with both biological parents (58.6%; n = 17) or at least one biological parent (31.0%; n = 9), though some lived with non-biological parents or caregivers (10.3%; n = 3). Most adolescents (86.2%; n = 25) also reported having at least one sibling; 58.6% of adolescents (n = 17) reported having at least one biological brother, 37.9% had at least one biological sister (n = 11), and 24.1% had a half- or step-sibling (n = 7). One-way analysis of variance (ANOVA) tests demonstrated that adolescents did not differ in total SIB based on family characteristics (e.g., number of siblings, number of employed caregivers; all values of p > .05).
Measures
Family Functioning
The Family Assessment Device (FAD; Epstein et al., 1983) is a 53-item measure with a 4-point Likert scale used to rate agreement with statements about how the adolescents’ family members interact and relate to each other (e.g., “After our family tries to solve a problem, we usually discuss whether it worked or not”). Both adolescents and caregivers completed the FAD. Subscales of the FAD assess six dimensions of family functioning, including family problem-solving, roles, communication, affective responsiveness, affective involvement, and behavioral control. The scores for each subscale are averaged, with higher scores indicating worse functioning and more problems within families. The FAD has good test-retest reliability and construct validity (I. W. Miller et al., 1985). In this study, the reliability of the FAD was excellent for both samples (Cronbach’s alpha = .95 for adolescents and .96 for caregivers).
The Conflict Behavior Questionnaire (CBQ; Prinz et al., 1979) assesses self-reported familial interactions within the past two weeks. The CBQ has both an adolescent and a caregiver version; both versions consist of 20 true/false items. Scores can range from 0 to 20, with higher scores indicating more conflict between caregiver and adolescent. Studies have shown that CBQ scores delineated between distressed and non-distressed families (Robin & Foster, 1989). The CBQ has good internal consistency and test-retest reliability (Rallis et al., 2015; Robin & Foster, 1989), as well as construct validity (Prinz et al., 1979). In the current study, the reliability of the CBQ was excellent for both samples (Cronbach’s alpha = .88 for adolescents and .92 for caregivers).
Self-Injurious Behavior (SIB)
We used the Lifetime Suicide Attempt Self-Injury Interview (LSASI; Linehan & Comtois, 1996) to assess participants’ history of SIB, including frequency, method, and intent. Using 20 items, the LSASI asks participants to report the dates of the most recent and most severe SIB, as well as their lifetime frequency of 11 different methods of SIB with suicidal intent, without suicidal intent, and with ambivalence. Participants also report the total frequency of each SIB method (combining suicidal, nonsuicidal, and ambivalent), and the number of times medical treatment was received for the SIB method. Higher scores indicate more SIB in the past. In the current study, reliability across all SIB intent types (four variables: suicidal SIB, nonsuicidal SIB, ambivalent SIB, and total SIB) was .65. Because the LSASI was designed for clinical use rather than research, to our knowledge there are no existing studies demonstrating the reliability or validity of the LSASI. Notably, this measure was already in use at the counseling clinic, and the decision to use it for this research study was counselor-driven.
Data Analysis
As part of our preliminary analyses, we first tested all variables for the assumptions of analysis. Specifically, when examining the skew and kurtosis of the composite variables, we used ± 2 as our acceptable range of values. Following advice from Tabachnick and Fidell (2019), we transformed variables that did not meet our criteria for normality.
To better understand family functioning, we conducted descriptive analyses for all seven predictive variables (problem-solving, communication, roles, affective responsiveness, affective involvement, behavioral control, and conflict) separately for adolescent and caregiver scores. We assessed the degree of healthy family functioning using I. W. Miller et al.’s (1985) suggested cut-off scores, which can be used to distinguish between healthy and unhealthy family environments. We also conducted paired sample t-tests to compare the adolescent and caregiver reports of family functioning.
Next, we tested the fit of our theoretical model of family functioning using structural equation modeling (SEM) with maximum likelihood as the method of estimation. We used multiple fit indices to assess the model fit. Specifically, the chi-square statistic assesses absolute model fit, demonstrating good fit when not statistically significant. The chi-square test can also be used to compare the relative fit of two models. Additionally, comparative fit index (CFI), root mean square error of approximation (RMSEA), and standardized root-mean-square residual (SRMR) are all indicators of model fit, with 0.95 or higher, 0.05 or lower, and 0.08 or lower indicating good fit, respectively (for more information on SEM fit indices, see Hooper et al., 2008). Notably, Iacobucci (2010) suggested that researchers can use SEM and establish good model fit even with small samples.
We also conducted descriptive analyses of the participants’ self-reported SIB. We left these variables raw (untransformed) to evaluate how participants viewed their own SIB. We examined the specific SIB methods that participants reported using (e.g., cutting, burning) as well as three outcome variables (suicidal SIB, nonsuicidal SIB, and ambivalent SIB; all transformed because of issues with skew and kurtosis).
Lastly, we used SEM to predict SIB with the proposed model of family functioning. Given our small sample size, we conducted this analysis separately for suicidal SIB, nonsuicidal SIB, and ambivalent SIB. We set alpha at .05 for each model; given the small sample size, we did not apply corrections to the alpha for the multiple analyses.
Results
We used SPSS 24.0 and Amos 24 to analyze our data. Because this study was primarily descriptive, we conducted multiple analyses to better understand the family environment of treatment-seeking adolescents, experiences of SIB for adolescents, and the role of family environment in adolescent engagement in SIB.
Family Characteristics and Functioning
Means, standard deviations, and range of scores for the family functioning variables are shown in Table 1. With the exception of the caregiver reports on affective responsiveness and behavioral control, both adolescent and caregiver reports on every subscale of the FAD fell above the McMaster clinical cut-off (see Table 1) described by I. W. Miller et al.’s (1985) cut-off scores, indicating on average all of the families demonstrated unhealthy functioning. It is worth noting that adolescents and their caregivers reported similar levels in five of the seven indicators of family functioning from the FAD and CBQ (e.g., there was no statistical difference between the two reports, all values of p > .05). As shown in Table 1, adolescent and caregiver reports only statistically differed for behavioral control (t[28] = 4.23, p < .001) and communication (t[28] = 2.96, p = .006). Specifically, adolescents reported higher levels of both behavioral control and communication; these high levels are considered indicative of unhealthy or distressed families (I. W. Miller et al., 1985).
Table 1
Descriptive Statistics and Group Comparisons of Family Functioning Variables as Reported by Adolescents and Caregivers
| Variable |
|
Adolescent |
Caregiver |
|
|
|
Cut-Off |
M |
SD |
Range |
M |
SD |
Range |
t(28) |
p |
| Problem-solving |
2.2 |
2.58 |
0.65 |
1.00–3.80 |
2.29 |
0.57 |
1.40–3.80 |
1.88 |
.071 |
| Communication |
2.2 |
2.56 |
0.37 |
1.83–3.17 |
2.30 |
0.37 |
1.50–3.00 |
2.96 |
.006 |
| Roles |
2.3 |
2.58 |
0.37 |
1.75–3.38 |
2.45 |
0.37 |
1.75–3.38 |
1.57 |
.128 |
| Affective Resp. |
2.2 |
2.34 |
0.68 |
1.00–4.00 |
2.12 |
0.62 |
1.00–3.67 |
1.48 |
.151 |
| Affective Inv. |
2.1 |
2.37 |
0.28 |
1.71–3.00 |
2.44 |
0.23 |
1.86–3.00 |
– 1.61 |
.118 |
| Behav. Control |
1.9 |
2.12 |
0.44 |
1.00–3.11 |
1.77 |
0.41 |
1.00–2.78 |
4.23 |
< .001 |
| Conflict |
— |
9.60 |
4.83 |
0.00–18.00 |
10.05 |
5.67 |
1.00–20.00 |
– 0.46 |
.649 |
Note. Cut-Off = McMaster Cut-Off score; Affective Resp. = Affective responsiveness; Affective Inv. = Affective involvement; Behav. Control = Behavioral control.
We used SEM to test the fit of our theory-driven, congeneric model of family functioning using seven subscales from each source (14 variables; seven for adolescents and seven for caregivers, with the error terms of each subscale correlated between the two sources) to predict family functioning as reported by each source (two latent variables; one for adolescents and one for caregivers). The absolute fit of the model was marginal: χ2(69) = 104.39, p = .004, CFI = 0.79, RMSEA = 0.14, SRMR = 0.14.
In order to reduce variables in our theoretical model, we averaged adolescent and caregiver reports for problem-solving, roles, affective responsiveness, affective involvement, and conflict because these did not statistically differ (all values of p > .05). However, we kept the two reports as separate predictors for communication and behavioral control. This left us with nine predictor variables for subsequent analysis (five averaged predictors and four single-source predictors).
Next, we used SEM to test the fit of the simplified model with the nine observed variables and one latent variable of family functioning. We found that the absolute model fit of this simplified model was acceptable overall. Specifically, the fit indices mostly indicated good fit (χ2[27] = 33.11, p = .194, CFI = 0.93, SRMR = 0.08), though one fit index suggested poor fit (RMSEA = 0.09). Differences in the chi-squares of our two models showed the simplified model was statistically better than the initial model: χ2(42) = 71.28, p = .003. Thus, we selected the simplified model as the final model of family functioning (see Figure 1). See Table 2 for descriptive analyses of the nine predictors in the final model. All variables were positively related to family functioning. The strongest predictors of family functioning in this model were affective responsiveness (average of adolescent and caregiver report; β = .85, B = 1.04, SE B = 0.21, p < .001, R2 = .72), affective involvement (averaged; β = .72, B = 0.88, SE B = 0.22, p < .001, R2 = .51), and problem-solving (averaged; β = .82, R2 = .67; this was the constrained parameter used to identify the regression model).
Figure 1
The Output Structural Regression Model of Family Functioning Developed Using SEM
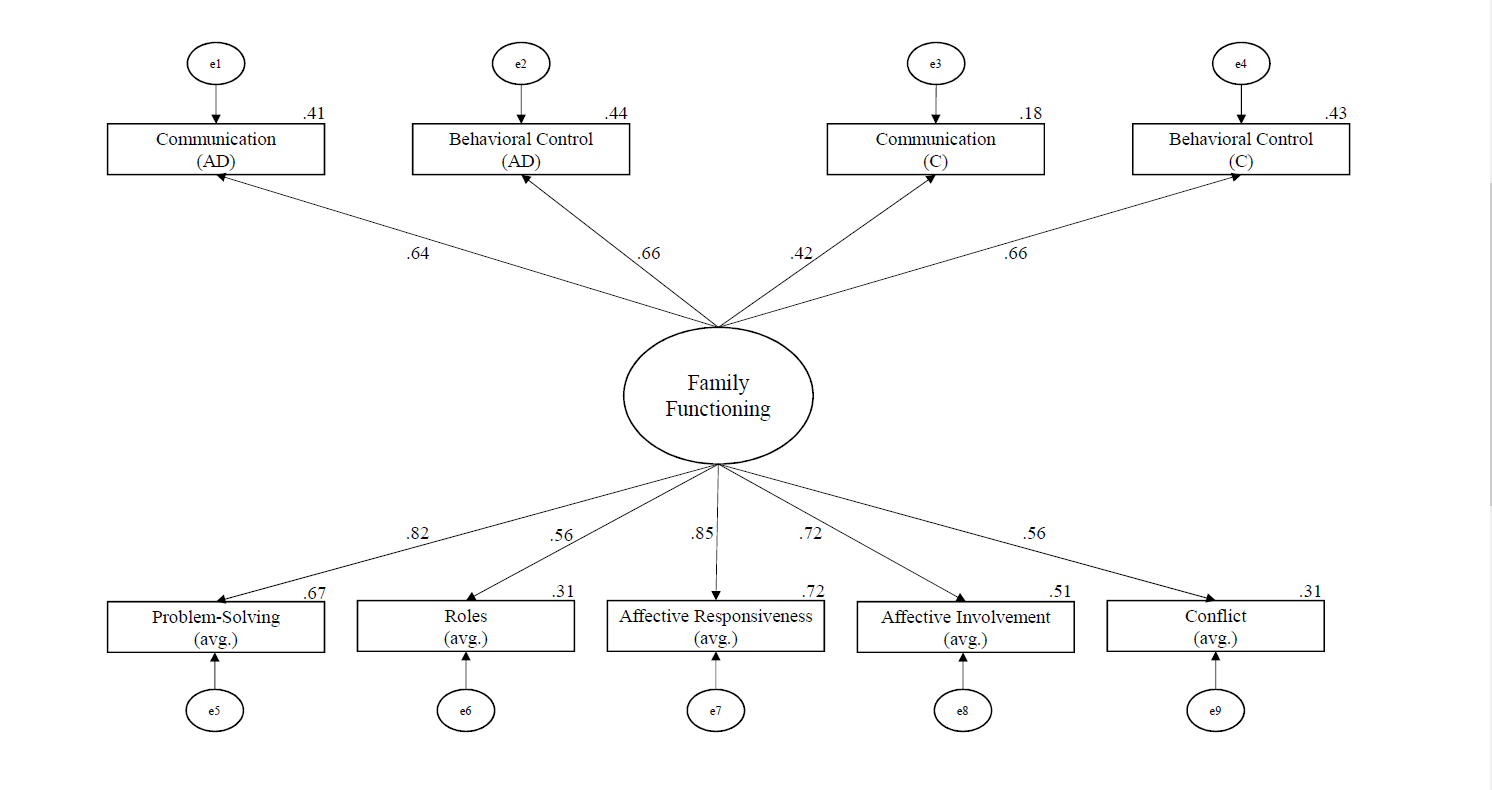
Note. The large circle represents a latent variable, boxes are measured variables, small circles (with “e”) are error terms, and solid lines show regression paths. The numbers on paths are the standardized path coefficients, and the offset values on endogenous variables are the R² effect sizes. (AD) = adolescent report; (C) = caregiver report; (avg.) = averaged score of adolescent and caregiver report.
Table 2
Descriptive Analyses of Predictors of Family Functioning
| Variable |
M |
SD |
| Problem-Solving |
2.43 |
0.44 |
| Roles |
2.51 |
0.29 |
| Affective Responsiveness |
2.23 |
0.51 |
| Affective Involvement |
2.40 |
0.23 |
| Conflict |
9.82 |
4.56 |
| Communication (AD) |
2.56 |
0.37 |
| Communication (C) |
2.30 |
0.37 |
| Behavioral Control (AD) |
2.12 |
0.44 |
| Behavioral Control (C) |
1.77 |
0.41 |
Note. (AD) = adolescent report; (C) = caregiver report.
Adolescent Engagement in SIB
All adolescents reported engaging in SIB in their lifetime, and the average lifetime frequency of SIB was 438.72 (SD = 1,216.65, range = 1–6,079; transformed to address normality: M = 4.41, SD = 1.80). Specifically, most participants reported engaging in nonsuicidal SIB (n = 26) and using it with higher frequency than SIB with other intent (i.e., suicidal or ambivalent SIB), with a lifetime average of 340.16 (SD = 975.22, range = 0–4,565; transformed: M = 3.49, SD = 2.25). Many adolescents also reported engaging in ambivalent SIB (n = 18), with moderate average frequency rates (M = 22.28, SD = 52.02, range = 0–248; transformed: M = 1.62, SD = 1.69). Lastly, fewer adolescents reported engaging in suicidal SIB (n = 18), with the lowest average lifetime frequency (M = 7.34, SD = 25.03, range = 0–136; transformed: M = 0.97, SD = 0.95). See Table 3 for descriptive information on SIB methods (e.g., cutting) used by adolescents in our sample. On average, participants used 3.78 (SD = 2.15) methods of SIB in their lifetime.
Table 3
Descriptive Statistics for All Self-Injurious Behavior Completed in One’s Lifetime (N = 29)
| Variable |
n |
Ma |
SDa |
Rangea |
n of Severe Cases |
| Cutting |
27 |
179.55 |
330.42 |
0–1,500 |
7 |
| Hitting head/body |
16 |
240.90 |
730.59 |
0–3,000 |
0 |
| Overdosing |
13 |
1.88 |
3.59 |
0–15 |
7 |
| Burning |
13 |
6.12 |
14.99 |
0–60 |
1 |
| Strangling/hanging |
8 |
2.18 |
6.42 |
0–30 |
0 |
| Stabbing/puncturing |
8 |
0.80 |
1.64 |
0–7 |
2 |
| Asphyxiating |
7 |
1.66 |
3.90 |
0–15.62 |
0 |
| Other |
6 |
272.92 |
602.33 |
0–1,500 |
2 |
| Jumping |
4 |
1.27 |
5.31 |
0–25 |
1 |
| Drowning |
4 |
0.40 |
.99 |
0–4 |
0 |
| Poisoning |
3 |
0.14 |
.36 |
0–1 |
1 |
Note. The descriptive statistics are based on the total self-injurious behavior, combining acts completed with suicidal intent, nonsuicidal intent, and ambivalence. Other = adolescent-reported participating in a type of self-injury that was not listed; Jumping = jumping from a high place to cause injury; Severe Cases = requiring medical treatment.
a The frequency that adolescents reported engaging in the various methods of self-injury.
Predicting SIB With Family Functioning
To understand the relationships between family functioning and SIB, we conducted correlational analyses of the three outcome variables and nine predictors. As shown in Table 4, problem-solving was moderately associated with ambivalent SIB (r = .44 , p = .018), conflict was moderately associated with nonsuicidal SIB (r = .38 , p = .049), and adolescent-reported communication was moderately to strongly associated with all three SIB variables (suicidal r = .61, p < .001; nonsuicidal r = .47, p = .011; ambivalent r = .56, p = .002). All associations were positive (see Table 4), meaning that worse family functioning scores were associated with more SIB.
Table 4
Bivariate Correlations Between Predictor Variables
|
1. |
2. |
3. |
4. |
5. |
6. |
7. |
8. |
9. |
10. |
11. |
| 1. Nonsuicidal SIB |
– |
|
|
|
|
|
|
|
|
|
|
| 2. Ambivalent SIB |
.35 |
– |
|
|
|
|
|
|
|
|
|
| 3. Suicidal SIB |
.16 |
.46* |
– |
|
|
|
|
|
|
|
|
| 4. Problem-Solving |
.35 |
.44* |
.19 |
– |
|
|
|
|
|
|
|
| 5. Roles |
.21 |
-.01 |
.27 |
.39* |
– |
|
|
|
|
|
|
| 6. Affect. Resp. |
.25 |
.36 |
.28 |
.68*** |
.42* |
– |
|
|
|
|
|
| 7. Affect. Involv. |
.22 |
.13 |
.27 |
.52** |
.43* |
.72*** |
– |
|
|
|
|
| 8. Conflict |
.38* |
.35 |
.26 |
.66*** |
.14 |
.45* |
.15 |
– |
|
|
|
| 9. Comm. (AD) |
.47* |
.56** |
.61*** |
.57** |
.44* |
.51** |
.50** |
.43* |
– |
|
|
| 10. Comm. (C) |
.09 |
.11 |
.04 |
.42* |
.28 |
.29 |
.29 |
.27 |
.17 |
– |
|
| 11. Beh. Cont. (AD) |
.27 |
.06 |
-.21 |
.54** |
.48** |
.51** |
.56** |
.34 |
.41* |
.25 |
– |
| 12. Beh. Cont. (C) |
.27 |
.26 |
.13 |
.49** |
.53** |
.61*** |
.36 |
.38* |
.33 |
.40* |
.47* |
Note. SIB = self-injurious behavior; Affect. Resp. = Affective Responsiveness; Affect. Involv. = Affective Involvement; Comm. = Communication; (AD) = adolescent report; (C) = caregiver report; Beh. Cont. = Behavioral Control.
* p < .05. ** p < .01. *** p < .001.
Next, we used SEM to predict SIB with our simplified model of family functioning. We tested three SIB outcomes separately because of concerns with sample size. For all models predicting SIB, we freed all FAD factors (problem-solving, roles, affective responsiveness, affective involvement, adolescent-reported communication and behavioral control, and caregiver-reported communication and behavioral control) to correlate because variables from the same measure are likely to be related.
The model predicting nonsuicidal SIB had good absolute fit: χ2(7) = 4.28, p = .747, CFI = 1.00, RMSEA = 0.00, SRMR = 0.04. In all, family functioning explains 20% of the variance in nonsuicidal SIB. See Figure 2 for the standardized path coefficients between family functioning variables, the latent variable of family functioning, and nonsuicidal SIB. Notably, family functioning predicted nonsuicidal SIB:
β = .44, B = 1.27, SE B = 0.62, p = .039. Based on effect sizes (see Figure 2), the strongest predictors were problem-solving (averaged; β = .79, B = 0.90, SE B = 0.03, p = .008, R² = .62), communication (adolescent-reported; β = .55, B = 0.05, SE B = 0.03, p = .034, R² = .31), and conflict (averaged; β = .84, R² = .71; this was the constrained parameter used to identify the regression model).
The model predicting ambivalent SIB had good absolute fit: χ²(7) = 5.69, p = .577, CFI = 1.00, RMSEA = 0.00, SRMR = 0.04. In all, family functioning explains 33% of the variance in ambivalent SIB. See Figure 3 for the standardized path coefficients between family functioning variables, the latent variable of family functioning, and ambivalent SIB. Notably, family functioning predicted ambivalent SIB: β = .58, B = 1.04, SE B = 0.46, p = .025. Based on effect sizes (see Figure 3), the strongest predictors were problem-solving (averaged; β = .94, B = 0.15, SE B = 0.07, p = .022, R² = .89), communication (adolescent-reported; β = .83, B = 0.11, SE B = 0.05, p = .030, R² = .69), and affective responsiveness (averaged; β = .69, B = 0.13, SE B = 0.07, p = .049, R² = .47).
Figure 2
The Output Structural Regression Model of Nonsuicidal SIB Developed Using SEM
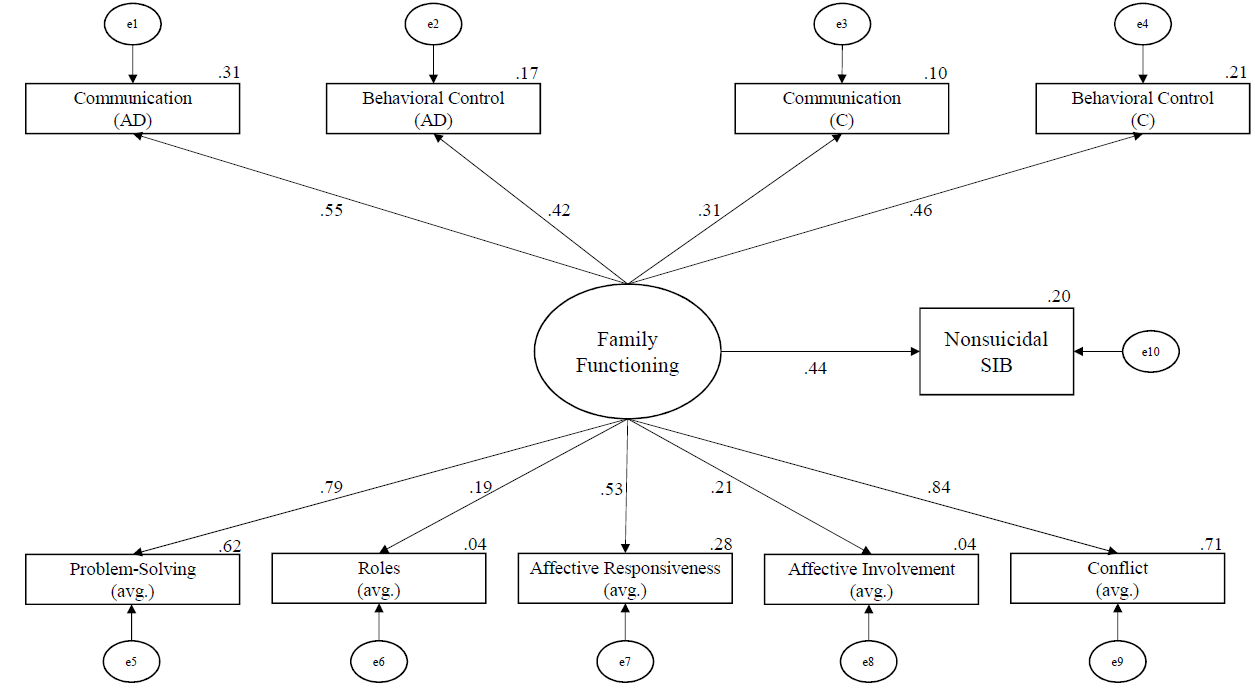
Note. The numbers on paths are the standardized path coefficients, and the offset values on endogenous variables are the R2 effect sizes. (AD) = adolescent report; (C) = caregiver report; (avg.) = averaged score of adolescent and caregiver report.
Figure 3
The Output Structural Regression Model of Ambivalent SIB Developed Using SEM
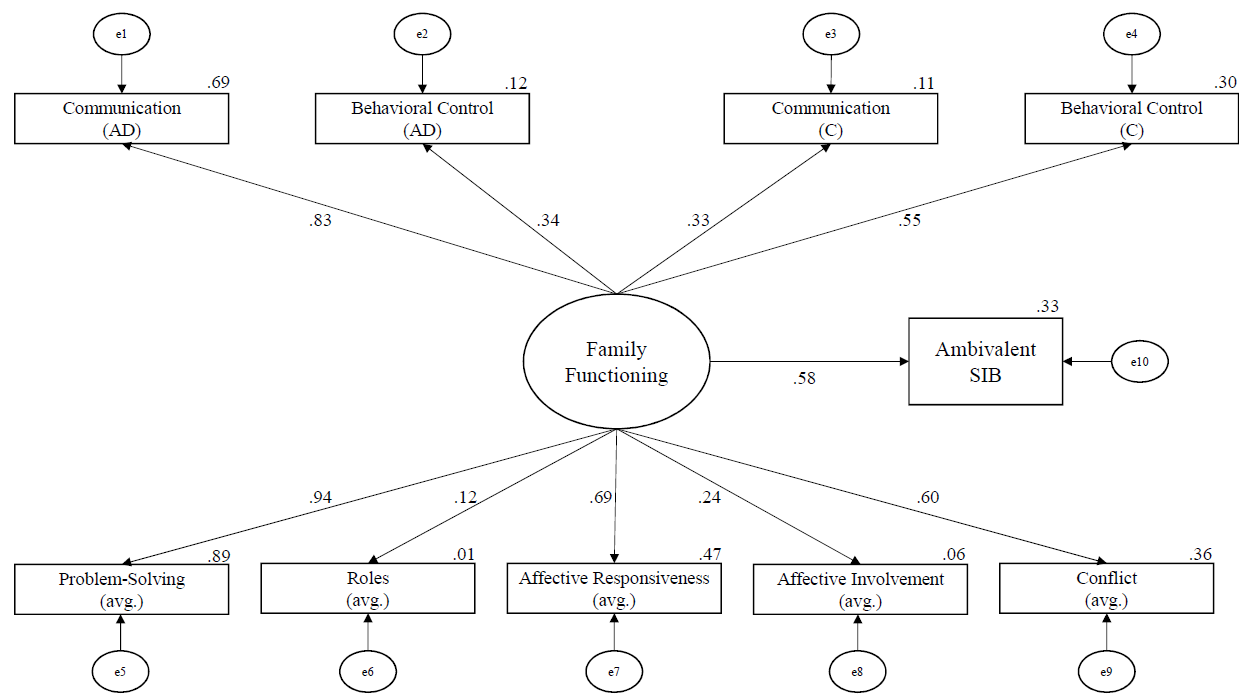
Note. The numbers on paths are the standardized path coefficients, and the offset values on endogenous variables are the R² effect sizes. (AD) = adolescent report; (C) = caregiver report; (avg.) = averaged score of adolescent and caregiver report.
Lastly, the model using family functioning to predict suicidal SIB was not able to successfully converge because of reaching the iteration limit, possibly because of the small sample size. After examining the suggested modification indices, the model was still not able to converge. Thus, we concluded that the suicidal SIB model was a poor model, meaning that family functioning alone was not predictive of suicidal SIB in our sample.
Discussion
The goals of the current study were to examine the family environment of adolescents seeking treatment for symptoms of BPD, as well as their experiences of SIB, and to better understand what aspects of family functioning relate to SIB. Unique strengths of this study include the emphasis on assessing models of family functioning as it relates to SIB and exploring differences between SIB intent types (suicidal SIB, nonsuicidal SIB, and SIB with ambivalence toward life). Further, because participants were clients seeking counseling from community-based master’s-level clinicians and no clients were excluded from participating in this study, results may generalize to other community samples.
We found that adolescents and caregivers often reported family functioning scores that met criteria for distressed families. Interestingly, adolescents and caregivers agreed on a majority of the subscales of family functioning, suggesting that the distress is mutually experienced. Adolescents and their caregivers only differed on reports of behavioral control (e.g., “[my family does not] hold any rules or standards”) and communication (e.g., “when someone [in my family] is upset the others know why”). This self-reported familial distress supports the social component of the biosocial theory (Linehan, 1993) in that the adolescents with traits of BPD engaged in SIB and experienced unhealthy family environments. Additionally, we found high lifetime rates of SIB in our sample of adolescents. As in previous studies (e.g., Anestis et al., 2015), adolescents in the current study engaged in nonsuicidal SIB more frequently than suicidal or ambivalent SIB, and cutting was the most common method.
Notably, our model of family functioning successfully predicted higher levels of both nonsuicidal SIB and ambivalent SIB. In particular, problem-solving, conflict, and adolescent-reported communication had consistently large effect sizes, suggesting that these subscales contributed more to SIB than other subscales. Although no previous studies have examined adolescent SIB and familial problem-solving to our knowledge, the findings that SIB was related to familial conflict (Huang et al., 2017) and communication (Halstead et al., 2014) corroborate the results of previous studies.
The success of the family functioning model in predicting SIB aligns with family systems theory. Specifically, adolescents in our sample may engage in SIB as a coping skill because their family lacks healthy problem-solving skills and thus models poor coping (which aligns with a description by Halstead et al., 2014). Additionally, adolescent SIB may function to temporarily end conflict in the family because it diverts the family’s attention away from the immediate problems. For example, Oldershaw et al. (2008) found that parents avoided conflict and felt like they were “walking on eggshells” (p. 142) after learning of their adolescents’ SIB. Another possible explanation is that the adolescents in our sample may serve as scapegoats within their family, acting as a focal point of a disturbed family system. From a structural family systems perspective, when there are problems within family subsystem relationships, oftentimes the child—typically the most vulnerable one—becomes the focus of the family’s problems (Wetchler, 2003); this trend is consistent with our findings.
It is worth noting that family functioning alone did not sufficiently predict suicidal SIB. One possible explanation is that our family functioning variables did not encompass the factors of thwarted belongingness and perceived burdensomeness, both of which Joiner (2005) suggested may lead to suicide.
Limitations and Future Directions
A strength of this study is that the results may generalize to other real-world settings in which adolescent clients seek counseling services from community-based master’s-level clinicians who specialize in dialectical behavior therapy. However, this ecological validity comes with some relative limitations.
One notable limitation of this study is that we examined family functioning at one point in time, when the adolescent was beginning treatment. Given this single timepoint, we are unable to fully describe the relationship between family functioning and SIB. Considering the biosocial theory, it seems likely that the distressed family environment preceded the SIB; however, it is possible that the SIB caused greater familial distress. Therefore, it would be useful to assess changes in family functioning and SIB across time.
Another limitation is our SIB measure; as Crowell et al. (2013) explained, the LSASI is commonly used in clinical practice but not often in research. In addition to issues with reliability, the LSASI is a lifetime measure as opposed to one focusing on recent behavior. Although all participants reported engaging in SIB in the past year, it is unclear how recently they engaged in SIB relative to the time of the study. Despite the benefit of creating more variability in the data by allowing participants to report their specific frequency of SIB, the alternative of a dichotomous variable of current SIB might be more compatible with our measures of current family functioning.
Additionally, the small sample size limits the power of our analyses as well as the generalizability of our results. A small sample increases the likelihood of a Type II error, meaning an increased likelihood of not finding significant results. However, it is notable that we found statistically significant results (e.g., good model fit of family functioning) despite our low power. Nevertheless, replication studies with much larger samples are needed.
Implications for Practice
Our findings suggest that family functioning is related to SIB in adolescents, particularly nonsuicidal and ambivalent SIB. Although counselors often include families when working with young children, it is common for counselors to work with adolescents individually. This practice is consistent with state laws allowing adolescents to consent to their own mental health treatment, and there are many presenting concerns and situations in which individual counseling may be the most effective modality. However, the connection between family functioning and SIB in adolescents in our sample indicates that it may be important to include family members in treating adolescent SIB; in fact, dialectical behavior therapy for adolescents (originally adapted by A. L. Miller et al., 1997) encourages family involvement in treatment. Counselors therefore need to educate parents and caregivers who may be reluctant to engage in the counseling process with their teen that SIB is an issue for which their participation in counseling could make a positive difference in treatment outcome. Further, from a family systems perspective, it can be challenging for teens to successfully use the coping skills and strategies they learn in counseling if the rest of the family system remains unchanged. Including at least some family members may therefore help adolescents maintain changes gained through the counseling process.
When including family members in counseling with adolescents who have engaged in nonsuicidal and ambivalent SIB, findings from our study suggest that three important targets for assessment and intervention include the domains of familial problem-solving, familial conflict, and adolescent-reported communication. Two of these, conflict and communication, were previously identified in the literature, and our study supports those findings. Our study newly identified familial problem-solving as an additional important predictor of SIB in adolescents. Counselors must keep in mind, however, that these variables were not sufficient in predicting suicidal SIB in adolescents. For these teens, we encourage the use of a broader assessment that includes elements of Joiner et al.’s (2009) interpersonal theory of suicide, especially the crucial interpersonal constructs of thwarted belongingness and perceived burdensomeness.
Conclusion
Based on our findings, it appears there is a relationship between engagement in SIB (especially nonsuicidal and ambivalent SIB) and familial environment for community-based treatment-seeking adolescents with traits of BPD. Additionally, both adolescents and their caregivers in our sample reported distressed levels of multiple indicators of family functioning, suggesting the need for family-based intervention. Counselors and service providers should consider multiple markers of family environment (particularly problem-solving, conflict, and adolescent-reported communication) when assessing risk for and treatment of adolescent SIB.
Conflict of Interest and Funding Disclosure
This study was partially funded by a grant from
Western Washington University awarded to
Dr. Christina Byrne. The authors reported no
conflict of interest for the development of this manuscript.
References
Adrian, M., Zeman, J., Erdley, C., Lisa, L., & Sim, L. (2011). Emotional dysregulation and interpersonal
difficulties as risk factors for nonsuicidal self-injury in adolescent girls. Journal of Abnormal Child
Psychology, 39(3), 389–400. https://doi.org/10.1007/s10802-010-9465-3
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
https://doi.org/10.1176/appi.books.9780890425596
Anestis, M. D., Khazem, L. R., & Law, K. C. (2015). How many times and how many ways: The impact of number of nonsuicidal self-injury methods on the relationship between nonsuicidal self-injury frequency and suicidal behavior. Suicide and Life-Threatening Behavior, 45(2), 164–177. https://doi.org/10.1111/sltb.12120
Chanen, A. M., Jovev, M., & Jackson, H. J. (2007). Adaptive functioning and psychiatric symptoms in adolescents with borderline personality disorder. The Journal of Clinical Psychiatry, 68(2), 297–306.
http://doi.org/10.4088/JCP.v68n0217
Crowell, S. E., Baucom, B. R., McCauley, E., Potapova, N. V., Fitelson, M., Barth, H., Smith, C. J., & Beauchaine, T. P. (2013). Mechanisms of contextual risk for adolescent self-injury: Invalidation and conflict escalation in mother–child interactions. Journal of Clinical Child & Adolescent Psychology, 42(4), 467–480. https://doi.org/10.1080/15374416.2013.785360
Crowell, S. E., Beauchaine, T. P., & Linehan, M. M. (2009). A biosocial developmental model of borderline personality: Elaborating and extending Linehan’s theory. Psychological Bulletin, 135(3), 495–510. https://doi.org/10.1037/a0015616
Epstein, N. B., Baldwin, L. M., & Bishop, D. S. (1983). The McMaster Family Assessment Device. Journal of Marital and Family Therapy, 9(2), 171–180. https://doi.org/10.1111/j.1752-0606.1983.tb01497.x
Goldenberg, H., & Goldenberg, I. (2013). Family therapy: An overview (8th ed.). Brooks/Cole.
Halstead, R. O., Pavkov, T. W., Hecker, L. L., & Seliner, M. M. (2014). Family dynamics and self-injury behaviors: A correlation analysis. Journal of Marital and Family Therapy, 40(2), 246–259.
https://doi.org/10.1111/j.1752-0606.2012.00336.x
Hamza, C. A., Willoughby, T., & Heffer, T. (2015). Impulsivity and nonsuicidal self-injury: A review and meta-analysis. Clinical Psychology Review, 38, 13–24. https://doi.org/10.1016/j.cpr.2015.02.010
Hooper, D., Coughlan, J., & Mullen, M. R. (2008). Structural equation modelling: Guidelines for determining model fit. Electronic Journal of Business Research Methods, 6(1), 53–60. https://doi.org/10.21427/D7CF7R
Huang, Y.-H., Liu, H.-C., Sun, F.-J., Tsai, F.-J., Huang, K.-Y., Chen, T.-C., Huang, Y.-P., & Liu, S.-I. (2017). Relationship between predictors of incident deliberate self-harm and suicide attempts among adolescents. Journal of Adolescent Health, 60(5), 612–618. https://doi.org/10.1016/j.jadohealth.2016.12.005
Iacobucci, D. (2010). Structural equations modeling: Fit indices, sample size, and advanced topics. Journal of Consumer Psychology, 20(1), 90–98. https://doi.org/10.1016/j.jcps.2009.09.003
Joiner, T. E. (2005). Why people die by suicide. Harvard University Press.
Joiner, T. E., Jr., Van Orden, K. A., Witte, T. K., & Rudd, M. D. (2009). The interpersonal theory of suicide: Guidance for working with suicidal clients. American Psychological Association. https://doi.org/10.1037/11869-000
Kaess, M., Brunner, R., & Chanen, A. (2014). Borderline personality disorder in adolescence. Pediatrics, 134(4), 782–793. https://doi.org/10.1542/peds.2013-3677
Latina, D., Giannotta, F., & Rabaglietti, E. (2015). Do friends’ co-rumination and communication with parents prevent depressed adolescents from self-harm? Journal of Applied Developmental Psychology, 41, 120–128. https://doi.org/10.1016/j.appdev.2015.10.001
Levenkron, S. (1998). Cutting: Understanding and overcoming self-mutilation. W. W. Norton.
Linehan, M. M. (1993). Cognitive-behavioral treatment of borderline personality disorder. Guilford.
Linehan, M. M., & Comtois, K. A. (1996). Lifetime parasuicide count. Unpublished manuscript, Department of Psychology, University of Washington, Seattle, Washington.
Miller, A. L., Muehlenkamp, J. J., & Jacobson, C. M. (2008). Fact or fiction: Diagnosing borderline personality disorder in adolescents. Clinical Psychology Review, 28(6), 969–981. https://doi.org/10.1016/j.cpr.2008.02.004
Miller, A. L., Rathus, J. H., Linehan, M. M., Wetzler, S., & Leigh, E. (1997). Dialectical behavior therapy adapted for suicidal adolescents. Journal of Practical Psychiatry and Behavioral Health, 3(2), 78–86.
Miller, I. W., Epstein, N. B., Bishop, D. S., & Keitner, G. I. (1985). The McMaster Family Assessment Device: Reliability and validity. Journal of Marital and Family Therapy, 11(4), 345–356.
https://doi.org/10.1111/j.1752-0606.1985.tb00028.x
Miller, I. W., Ryan, C. E., Keitner, G. I., Bishop, D. S., & Epstein, N. B. (2000). The McMaster approach to families: Theory, assessment, treatment and research. Journal of Family Therapy, 22(2), 168–189.
https://doi.org/10.1111/1467-6427.00145
Nock, M. K., & Prinstein, M. J. (2004). A functional approach to the assessment of self-mutilative behavior. Journal of Consulting and Clinical Psychology, 72(5), 885–890. https://doi.org/10.1037/0022-006X.72.5.885
Nock, M. K., & Prinstein, M. J. (2005). Contextual features and behavioral functions of self-mutilation among adolescents. Journal of Abnormal Psychology, 114(1), 140–146. https://doi.org/10.1037/0021-843X.114.1.140
Oldershaw, A., Richards, C., Simic, M., & Schmidt, U. (2008). Parents’ perspectives on adolescent self-harm: Qualitative study. The British Journal of Psychiatry, 193(2), 140–144. https://doi.org/10.1192/bjp.bp.107.045930
Prinz, R. J., Foster, S. L., Kent, R. N., & O’Leary, K. D. (1979). Multivariate assessment of conflict in distressed and nondistressed mother–adolescent dyads. Journal of Applied Behavior Analysis, 12(4), 691–700.
https://doi.org/10.1901/jaba.1979.12-691
Rallis, B. A., Esposito-Smythers, C., & Mehlenbeck, R. (2015). Family environment as a moderator of the association between conduct disorder and suicidality. Journal of Aggression, Maltreatment & Trauma, 24(2), 150–168. https://doi.org/10.1080/10926771.2015.997909
Robin, A. L., & Foster, S. L. (1989). Negotiating parent–adolescent conflict: A behavioral–family systems approach. Guilford.
Tabachnick, B. G., & Fidell, L. S. (2019). Using multivariate statistics (7th ed.). Pearson Education.
Walker, K. L., Hirsch, J. K., Chang, E. C., & Jeglic, E. L. (2017). Non-suicidal self-injury and suicidal behavior in a diverse sample: The moderating role of social problem-solving ability. International Journal of Mental Health and Addiction, 15(3), 471–484. https://doi.org./10.1007/s11469-017-9755-x
Wetchler, J. L. (2003). Structural family therapy. In L. L. Hecker & J. L. Wetchler (Eds.), An introduction to marriage
and family therapy (pp. 63–93). Haworth Clinical Practice Press.
Melissa Sitton, MS, is a doctoral student at Southern Methodist University. Tina Du Rocher Schudlich, PhD, MHP, is a professor at Western Washington University. Christina Byrne, PhD, is an associate professor at Western Washington University. Chase M. Ochrach, MS, is a doctoral student at the University of Wisconsin–Madison. Seneca E. A. Erwin, BS, is a doctoral student at the University of Northern Colorado. Correspondence may be addressed to Tina Du Rocher Schudlich, 516 High St., MS 9172, Bellingham, WA 98225, tina.schudlich@wwu.edu.