Feb 7, 2022 | Volume 12 - Issue 1
Emily Sallee, Abraham Cazares-Cervantes, Kok-Mun Ng
Suicide is the second leading cause of death in adolescents (ages 12–19) in the United States, and more work is needed to shed light on the interpersonal protective factors associated with adolescent suicidality. To address this gap in the empirical literature, we examined the application of the Interpersonal Theory of Suicide (IPTS) to the middle adolescent population. We analyzed survey data using the 2017 Oregon Healthy Teen dataset, which included 10,703 students in 11th grade. Binary logistic regressions were used to examine the extent to which the IPTS constructs of perceived burdensomeness and thwarted belongingness predicted middle adolescent suicide ideation and attempt. Findings indicate that three of the five proxy items were statistically significant in each model, with consistent mediators for each. These findings have the potential to guide development of appropriate treatment strategies based on the interpersonal constructs of the IPTS for clinicians working with this population.
Keywords: adolescents, suicide ideation, suicide attempt, suicidality, Interpersonal Theory of Suicide
Suicide is a leading cause of death worldwide, spanning across all ages, ethnicities, genders, cultures, and religions. In the United States from 2000 to 2015, suicide rates increased 28%, with 44,193 people dying by suicide yearly, equating to about one death every 12 minutes. Nationally, statistics now identify suicide as the second leading cause of death in adolescent populations (Centers for Disease Control and Prevention [CDC], 2017). Specific to the state of Oregon, over 500 youth between the ages of 10–24 were hospitalized each year because of self-harm, including suicide attempts. In 2017 alone, more than 750 youth were hospitalized and 107 suicides were completed; considering that many ideations and attempts do not result in hospitalization, it is likely that there were more Oregonian youth who had attempted suicide but were never hospitalized, and an even greater number who had contemplated suicide (Oregon Suicide Prevention, n.d.).
Unfortunately, studies on suicide, particularly adolescent suicide, are rarely driven by theory. This results in a lack of integration between research findings and clinical practice (King et al., 2018). Clinicians working with the adolescent population are in need of research- and evidence-based practices ready for implementation. Although the Interpersonal Theory of Suicide (IPTS; Joiner et al., 2009) was initially developed for and then applied to adult populations, it has the potential to inform clinicians in preventative and intervention efforts in other populations, offering an evidence-based framework to understand and address suicide prevention and intervention. In an earlier study (Sallee et al., 2021), we found evidence to support its use with the early adolescent (ages 11–14) population. The present study utilizes the IPTS as a framework to examine the interpersonal drivers of suicidality among middle adolescents (ages 14–17) in Oregon.
Joiner et al.’s (2009) IPTS offers a theoretical lens to explain suicide ideation and behavior in three dynamic constructs: perceived burdensomeness, thwarted belongingness, and acquired capability. The first two are influential in suicidal desire. The dynamicity of the constructs is related to the fluctuation of interpersonal needs and cognitions over time. Together they contribute to significant risk for suicide ideation. Acquired capability is static and believed to develop in response to exposure to provocative, painful, and/or violent experiences, overpowering the human survival need of self-preservation. Acquired capability, in tandem with thwarted belongingness and perceived burdensomeness, results in a high risk for suicidal behavior/attempt (King et al., 2018).
This field of research uses terms like suicide ideation, suicidal behavior, suicidology, self-harm, self-injury, and self-inflicted death to describe the thoughts and behaviors of a person ending their own life. The CDC defines suicide ideation within a broader class of behavior called self-directed violence, referring to “behaviors directed at oneself that deliberately results in injury or the potential for injury . . . [it] may be suicidal or non-suicidal in nature” (Stone et al., 2017, p. 7). The intent of suicidal self-directed violence is death, while the intent of non-suicidal self-directed violence is not. A suicide attempt may or may not result in death or other injuries. Because we held a particular interest in adolescent suicide ideation and behavior, its differentiation of lethal intent from non-suicidal self-injury (NSSI) led us to leave NSSI ideation and/or behavior out of the scope of the study. However, recent studies addressing IPTS have included self-harm as an indicator of acquired capability (e.g., Barzilay et al., 2019) and should be included in future studies involving this construct.
Suicide ideation and attempt in adolescent populations is a serious public health concern in the United States that is growing in frequency and intensity every year. National statistics suggest that 17.2% of adolescents have experienced or currently experience suicide ideation, and 7.4% of adolescents have made a suicide attempt (CDC, 2017). Despite this growing health concern, most research in this body of work has focused primarily on adult populations (Horton et al., 2016; Stone et al., 2017). Limitations in the extant empirical literature include a lack of emphasis on theory as well as a lack of quantitative research on large samples in non-inpatient treatment settings (Czyz et al., 2015; Horton et al., 2016; Miller et al., 2014). In clinical practice, this challenges mental health practitioners’ ability to rely on evidence to serve their clients. Becker et al. (2020) found significant evidence of the applicability of IPTS to a large undergraduate (ages 18–29) population, suggesting that the interpersonal constructs might be applicable to younger non-inpatient groups. Based on the IPTS, this study examined the extent to which a specific set of interpersonal predictors of perceived burdensomeness and thwarted belonging were associated with suicide ideation and attempt in a large non-clinical sample of middle adolescents.
Adolescents and Suicidality
Adolescence marks the developmental period between childhood and adulthood, corresponding to the time from pubertal onset to guardian independence. This period is associated with increased risk-taking behaviors as well as increased emotional reactivity, occurring in the context of developmental changes influenced by external and internal factors that elicit and reinforce behaviors. Cognitively, over the course of adolescence, the prefrontal cortex of the brain continues to develop and is responsible for impulse control and delayed gratification in favor of more goal-directed choices and behaviors (Jaworska & MacQueen, 2015). One apparent risk factor for suicide ideation and behavior in adolescents is their impaired decision-making. In addition, this developmental period also accounts for half of all emotional and behavioral disorder diagnoses and the highest rates of suicide with subsequent higher risks for suicidal behavior during their lifetime (Wyman, 2014). Wasserman et al. (2015) metabolized research supporting the theory that most pathological changes occur in childhood and adolescence, suggesting that it is during this developmental time period that prevention and intervention is imperative, as the adolescent years themselves prove to be a risk factor for suicide ideation and behavior.
The typical age of 11th grade students is 16 or 17, and these students are characterized as being in the developmental period known as “middle adolescence.” By this age, puberty is typically completed for both males and females, and adolescents begin setting long-term goals, concurrently becoming more interested in the meaning of life and moral reasoning. They experience an increased drive for independence and increased self-involvement. During the overall developmental stage of adolescence, youth must adjust to their physically and sexually maturing bodies and feelings; define their personal sense of identity and adopt a personal value system; renegotiate their relationships with parents, family, and caregivers; and develop stable and productive peer relationships (Teipel, 2013).
Of relevance to the present study, it is important to note that according to Teipel (2013), adolescents in 11th grade (ages 16–17) experience an increased concern with their appearances and bodies, incorporating a personal sense of masculinity or femininity into their identities and establishing values and preferences of sexual behavior. This period of self-involvement results in high expectations of self and low self-concept, coinciding with an increased drive for peer acceptance and reliance (American Academy of Child & Adolescent Psychiatry, 2021). Additionally, as the typical adolescent is tasked with gaining autonomy and independence from the nuclear family, they will likely experience periods of sadness as the psychological loss, not so unlike grief, takes place (Teipel, 2013). Adolescents in the 11th grade school environment are preparing for the final year of high school and potentially postsecondary education after graduation, creating unique stressors related to increasing autonomy and independence as they approach the formidable ascent into adulthood.
The IPTS
Theories of suicide have evolved over the past 70 years to reflect research and societal influences and implications, yet they all seem to agree that “perceived disruption of interpersonal relationships may serve as one potential mechanism of the association between child maltreatment and [suicide ideation]” (Miller et al., 2014, p. 999). Durkheim and Simpson (1951) suggested that suicide was the result of social causes like isolation, altruism, and anger/frustration. Behavioral theorists like Lester (1987) believed that suicide was a learned behavior, resulting from adverse childhood experiences and psychosocial environmental factors. Schneidman (1993) thought suicidal behaviors were motivated by the desire to escape emotional pain caused by the lack of socially supportive and nurturing relationships. Joiner’s IPTS focuses on the importance of interpersonal relationships, characterized by the confluence of two negative interpersonal states (i.e., perceived burdensomeness and thwarted belongingness; Miller et al., 2014).
The present study was guided by several gaps in the literature related to the application of the IPTS to adolescent populations. Initially, the IPTS was constructed by Joiner and his colleagues (2009) through studying adults engaging in suicidal behaviors. Since its development, the theory has been studied primarily in its application to adult and college student populations (Horton et al., 2016). The lack of research on the application of the IPTS to non-inpatient adolescents may suggest its incompatibility to the uniqueness of adolescent suicidality; however, Horton et al. (2016) argued that the constructs of the theory are relevant in adolescence regardless of setting and presentation, though they may manifest in slightly different ways based on differences in developmental context. As such, they proposed that perceived burdensomeness in adolescents may manifest as low academic competency or social disconnection and thwarted belongingness may manifest as social isolation from peers or poor family cohesion. Adolescence is also a developmental period when children may begin to engage in health-risk behaviors, are particularly prone to impulsivity because of the immature nature of their prefrontal cortex, and have the increased pressure of peer behavior on their own, as well as a sense of invulnerability to consequences (Horton et al., 2016). Though adolescent suicide–related research based on the IPTS to date remains sparse, the theory’s focus on the dynamic constructs of perceived burdensomeness and thwarted belongingness appears attractive in consideration of potential application to preventative and responsive efforts.
Perceived Burdensomeness
Perceived burdensomeness is characterized by self-hatred and the belief that one is a burden to others, including family and friends, leading to the idea that they would be better off without them. It deals with the misperceptions of being a liability for family and intimate peers. As a dynamic interpersonal construct, it responds well to both interpersonal and intrapersonal interventions. However, although perceived burdensomeness responds more slowly to intervention, it may be a more significant predictor of suicide ideation and behavior than thwarted belongingness. There is also research that suggests that thwarted belongingness and perceived burdensomeness are more enmeshed in adolescents, suggesting that only one of the dynamic interpersonal constructs is necessary to be coupled with acquired capability and lead to suicidal behavior (Chu et al., 2016; Joiner et al., 2012; Stewart et al., 2017).
Thwarted Belongingness
Thwarted belongingness is a dynamic condition of social disconnection described by the interpersonal state of loneliness in which the psychological need to belong is not met. Of the two dynamic interpersonal constructs within the IPTS that respond to both interpersonal and intrapersonal interventions (thwarted belongingness and perceived burdensomeness), research suggests that thwarted belongingness may be easier to treat and respond more quickly to intervention than perceived burdensomeness (Chu et al., 2016; Joiner et al., 2012; Stewart et al., 2017). It has been well established that positive and negative effects of close relationships are particularly formative in the adolescent years, and therein lies the difficult developmental task of establishing strong peer relationships while also maintaining familial bonds (Miller et al., 2014). Relatedly, adolescents with histories of abuse or other maltreatment are at particular risk. It has been shown that low perceived quality of family and peer connectedness and belonging contribute to thwarted belongingness and its dynamic interpersonal state.
Acquired Capability
Acquired capability is a static construct in the IPTS, describing a decrease in or lack of fear about death and an elevated tolerance of physical pain. It is suggested to be developed through repeated exposure to painful and provocative events (Chu et al., 2016; Joiner et al., 2012; Stewart et al., 2017). Stewart et al. (2017) characterized it as “the combination of increased pain tolerance and decreased fear of death [that] results in progression from suicide intent to suicidal behavior, culminating in a suicide attempt” (p. 438). This construct’s combination of pain tolerance and fearlessness about death is significant in current conversations around adolescents engaging in violent video games, which could correlate to fearlessness about death but not necessarily pain tolerance (Stewart et al., 2017). Acquired capability as the combination of pain tolerance and fearlessness is also significant to other mental health disorders, including anorexia nervosa, in which risk factors for suicide ideation and behavior are prevalent and are characterized by increased pain tolerance and fearlessness about death.
According to the IPTS, these three constructs are proximal to suicidal behavior. Horton et al. (2016) suggested that “an important strength of the theory is that it explains the lower frequency of more severe levels of suicidality (such as suicide attempt) compared to less severe levels (such as passive suicide ideation)” (p. 1134) because it is the combination of the three constructs that leads to suicidal behavior. The theory also posits that the difference between passive and active suicide ideation is the difference between the presence of one or both of the dynamic interpersonal states of thwarted belongingness and perceived burdensomeness. In other words, one dynamic interpersonal construct suggests passive ideation, two suggest active ideation, and all three constructs lead to suicidal behavior.
Purpose of the Present Study
Most previous studies that applied the IPTS to suicidal adolescents of this specific age group only addressed inpatient populations (e.g., Czyz et al., 2015; Horton et al., 2016; Miller et al., 2014). However, our recent study (Sallee et al., 2021) indicated support for using this theory in understanding suicide ideation and attempts among non-inpatient early adolescents. Specifically, the findings revealed significance in multiple mediators representing the IPTS constructs of perceived burdensomeness and thwarted belongingness. The significant drivers for suicide ideation included emotional/mental health and feeling sad/hopeless as the proxy items for perceived burdensomeness, and not straight and bullied as the proxy items for thwarted belongingness. Similarly, the significant drivers for suicide attempt included emotional/mental health and feeling sad/hopeless as the proxy items for perceived burdensomeness, and non-binary and bullied as the proxy items for thwarted belongingness. The current study extends the efforts of using the IPTS in studying suicidality among adolescents to an older age range (ages 16–17). Using the theory to examine suicidal behavior among middle adolescents in school settings can potentially extend its utility and inform practitioners who are working with youth in this age group who struggle with suicide ideation and behavior in various settings such as mental health and medical.
Based on the IPTS, the focus of this study was to examine the extent to which the interpersonal constructs of perceived burdensomeness and thwarted belongingness predict adolescent suicide ideation and attempt. In consideration of the aforementioned needs and gaps in this field of study, we formulated two research questions: 1) To what extent do feelings of perceived burdensomeness and thwarted belongingness predict suicide ideation among 11th grade students (a middle adolescent population) in Oregon? and 2) To what extent do feelings of perceived burdensomeness and thwarted belongingness predict suicide attempts among 11th grade students (a middle adolescent population) in Oregon? We hypothesized that the two dynamic IPTS constructs would both statistically significantly predict suicide ideation and suicide attempts in this population.
Method
Participants
A dataset of 10,703 participants was selected from the randomized weighted sample of 11,895 students in 11th grade who participated in the 2017 Oregon Healthy Teen (OHT) survey, a comprehensive assessment measuring risk factors and assets shown to impact successful development (Oregon Health Authority [OHA], 2017). This dataset was selected for its representation of middle adolescents at the cusp of a monumental transition in life—finishing K–12 education and embarking on what is to come. Participants’ ages ranged from 16 to 17 years (M = 16.7 years). In terms of gender identity, 48.9% self-identified as female, 45.6% as male, and 5.5% as non-binary/gender nonconforming, which included those who identified as “transgender, gender nonconforming, genderqueer, gender fluid, intersex/intergender, or something else.” Among the participants, 85.9% spoke English at home. The racial/ethnic composition was as follows: 62.9% White, 25% Hispanic/Latino, 3.6% Asian, 2.2% Black or African American, 5.5% other, and 0.8% multiple.
Procedures
We conducted a secondary analysis of archival survey data collected in the 2017 OHT survey. The 2017 OHT study utilized a probability design (i.e., all participants’ datasets had equal chances to be selected for the sample) to minimize possible selection biases and a randomization process (lottery method or computer-generated random list) to minimize sampling error with stratification of school regions. The survey was administered by school officials during one designated school period, utilizing standardized procedures to protect student privacy and facilitate anonymous participation. The researchers obtained IRB approval prior to requesting and receiving the data in SPSS format from the OHA.
The OHT Dataset
The OHT survey has origins in the Youth Risk Behavior Survey, a biennial national survey developed by the CDC. The 2017 OHT survey, administered to volunteering eighth and 11th grade students with a school response rate of 83% (R. Boyd personal communication, February 22, 2019), was chosen for this study because it explores a variety of health-related items, including suicidality, and has additional items deemed suitable for proxy descriptors of the IPTS constructs. The 11th grade dataset was selected for the study to target this specific developmental period because of its characteristic of impaired decision-making serving as a risk factor for ideation and behavior. Additionally, adolescents who experience suicidality during this age range are at a higher risk of suicide ideation and attempt in subsequent life stages compared to adolescents who did not experience suicidality at this time (Wyman, 2014).
In this study, the dynamic interpersonal constructs of the IPTS—perceived burdensomeness and thwarted belongingness—served as variables predicting the two outcome variables of suicide ideation and suicide behavior/attempt. The third construct of the IPTS, acquired capability, was not included as a predictor variable because of its staticity and ineffective response to intervention. We were also unable to locate items in the OHT survey that could be used as proxy items for acquired capability. The two predictor variables were measured with proxy items in the OHT survey (OHA, 2017). The proxy items for each predictor variable were chosen based on empirical research (Horton et al., 2016; Miller et al., 2014; Seelman & Walker, 2018; Zhao et al., 2010). Both outcome variables (suicide ideation and suicide behavior/attempt) were direct questions in the survey, surveyed as follows: 1) “During the past 12 months, did you ever seriously consider attempting suicide?” (Yes/No), and 2) “During the past 12 months, how many times did you actually attempt suicide?” (0, 1 time, 2 or 3 times, 4 or 5 times, 6 or more times). The second question was recorded to combine any number of times larger than zero, reflecting the response that either the participant had not attempted suicide (0) or had attempted suicide (1).
Instrumentation
As previously noted, the selection of proxy items was based on previous empirical research on suicidality, adolescent suicidality, and the IPTS (Horton et al., 2016; Miller et al., 2014; Seelman & Walker, 2018; Zhao et al., 2010). The proxy items selected for this specific study differed slightly from the researchers’ previous study with a younger population (early adolescents) because of the developmentally appropriate differences in the eighth and 11th grade OHT survey tools.
The first predictor variable (perceived burdensomeness) was measured with two proxy survey items: emotional/mental health and sad/hopeless feelings. Emotional/mental health was chosen as a proxy item for the predictor variable of perceived burdensomeness because of the research connecting mental health challenges to emotional strain in the family setting, suggesting a potential perception of being a burden on loved ones (Miller et al., 2014). The survey item for emotional/mental health read: “Would you say that in general your emotional and mental health . . .” with the answer options including: 1) Excellent, 2) Very good, 3) Good, 4) Fair, and 5) Poor. The proxy item of sad/hopeless feelings was chosen because of its inclusion in the definition of perceived burdensomeness but exclusion from many studies of the IPTS (Horton et al., 2016). The survey item for sad/hopeless feelings read: “During the past 12 months, did you ever feel so sad or hopeless almost every day for two weeks or more in a row that you stopped doing some usual activities?” with the answer options of simply Yes or No.
The second predictor variable (thwarted belongingness) was measured with three proxy survey items: sexual orientation, sexual identity, and volunteering (inverse). As previously described, thwarted belongingness constitutes the interpersonal state of loneliness and lack of social connection. Sexual orientation and sexual identity were chosen as proxy items for the variable of thwarted belongingness because sexual minority students experience higher rates of bullying and a greater likelihood of suicidal behaviors (Seelman & Walker, 2018); gay, lesbian, and bisexual adolescents attempt suicide at 2 to 6 times the rate of non–gay, lesbian, and bisexual adolescents, suggesting that a sexual minority status is in itself a risk factor for suicidal behaviors, and a child identifying as gay, lesbian, or bisexual and/or as a non-cisgender youth may experience feelings of thwarted belongingness among a peer group (Zhao et al., 2010). The survey item for sexual orientation read: “Do you think of yourself as . . .” with the answer options including: 1) Lesbian or gay; 2) Straight, that is, not lesbian or gay; 3) Bisexual; 4) Something else (Specify); and 5) Don’t know/Not sure. The survey item for sexual identity read: “How do you identify? (Select one or more responses)” with the answer options including: 1) Female, 2) Male, 3) Transgender,
4) Gender nonconforming/Genderqueer, 5) Intersex/Intergender, 6) Something else fits better (Specify), 7) I am not sure of my gender identity, and 8) I do not know what this question is asking. Volunteering (inverse) was chosen because of its suggestion of contributing to society and feeling a sense of belonging and value within the community. The survey item for volunteering read: “I volunteer to help others in my community” with the answer options including: 1) Very much true, 2) Pretty much true, 3) A little true, and 4) Not at all true. Data from this final question was inversely recoded in order to be comparable to the other proxy items.
The CDC utilized existing empirical literature to analyze the self-reported survey data, assessing for cognitive and situational factors that might affect the validity of adolescent self-reporting of behaviors. Through analysis, it was determined that self-reports are in fact affected by both cognitive and situational factors, but the factors do not threaten the validity of self-reports of each behavior equally (Brener et al., 2013).
Data Analysis
This study addresses what impact the predictor variables of perceived burdensomeness and thwarted belongingness have on the outcome variables of suicide ideation and suicide attempt in this particular adolescent population. The selected proxy items had variable answer options (ranging from binary choice to a 7-point Likert scale), so each proxy item for the predictor variables was individually entered with the intention of disaggregating to assess whether or not different combinations of the variables are better predictors of the outcome variables.
The two outcome variables were surveyed as follows: (a) suicide ideation (“During the past 12 months, did you ever seriously consider attempting suicide?”) and (b) suicide attempt (“During the past 12 months, how many times did you actually attempt suicide?”; OHA, 2017). The second question was recoded to allow both questions to be assessed on a binary scale (no/yes), with no equaling 0 and yes equaling 1.
With binary scaled data for the outcome variables, we decided to utilize a binomial logistic regression statistical test to assess the research questions. Additionally, each predictor variable was separately analyzed in order to isolate each outcome variable and consider how the predictor variables influenced each other.
In sum, we examined the descriptive statistics of the survey, created variables based on the selected proxy survey items, and tested the assumptions for utilizing a binomial logistic regression statistical test. Finally, we executed two logistic regression models to determine the relationships between the predictor variables and the two outcome variables—suicide ideation and suicide attempt.
Descriptive Statistics
Table 1 presents the descriptive statistics of the study variables. Although 11,868 students in the 11th grade completed the 2017 OHT survey, data from only 10,703 students were included in the analysis because of recording and data collection errors on those excluded from the analyses, due to missing or incomplete data. Therefore, the descriptive statistics of the study variables reported in the table reflect the data of the 10,703 students applicable for use in the logistic regression model of this study. Given the large sample size, we utilized a p-value threshold of less than 0.01.
Table 1
Descriptive Statistics
| Variable |
M or %a |
SD (if applicable) |
| Emotional/Mental Health |
2.92 |
1.22 |
| Felt Sad/Hopeless (Yes) |
1.68 |
0.47 |
| Not Straight |
17.0% |
N/A |
| Non-Binary |
5.5% |
N/A |
| Volunteer |
2.38 |
0.99 |
| Consider Suicide |
18.0% |
N/A |
| Attempt Suicide |
6.6% |
N/A |
a Some variables were reported as means, and some variables were reported as percentages.
Results
A binomial logistic regression was conducted to quantify the effects of the individual proxy items measuring the predictor variables of perceived burdensomeness and thwarted belongingness on students experiencing suicide ideation (Research Question 1). All five proxy items were entered into the model for the outcome variable. During the data screening process, two proxy items were eliminated (i.e., non-binary, volunteer), as they did not indicate significant results. Regression results indicated the overall model of the three remaining predictors (emotional/mental health, felt sad/hopeless, not straight) was statistically reliable in distinguishing between 11th grade students who did not experience suicide ideation and those who did (Nagelkerke R2 = .413; p < .001). As such, the suicide ideation model was deemed statistically significant—X2(5) = 3104.194—with an overall positive predictive value of 85.5%.
Of the two proxy items for the perceived burdensomeness variable, both proved to be statistically significant (Table 2). Specifically, increased poor emotional/mental health was related to the increased likelihood and occurrence of suicide ideation. Additionally, participants who reported feeling sad or hopeless for at least 2 weeks were over twice as likely to experience suicide ideation than those who did not report feeling sad or hopeless. Of the three proxy items for the thwarted belongingness variable, only one proved to be statistically significant: Students who reported as not straight were more than twice as likely to experience suicide ideation as students who reported as straight.
Table 2
Logistic Regression Predicting Likelihood of Suicide Ideation
| Variable |
B |
SE |
Wald |
df |
p |
Odds |
| Perceived Burdensomeness |
| Emotional/Mental Health |
0.775 |
.033 |
535.821 |
1 |
< .001 |
2.170 |
| Felt Sad/Hopeless |
−1.694 |
.069 |
609.681 |
1 |
< .001 |
0.184 |
| Thwarted Belongingness |
| Not Straight |
0.705 |
.072 |
95.460 |
1 |
< .001 |
2.025 |
| Non-Binary |
0.149 |
.120 |
1.546 |
1 |
.214 |
1.160 |
| Volunteer |
−0.03 |
.031 |
0.949 |
1 |
.330 |
0.970 |
| Constant |
−1.716 |
.189 |
82.107 |
1 |
< .001 |
0.180 |
Similarly, a binomial logistic regression test was conducted to determine the effects of the proxy items measuring the predictor variables of perceived burdensomeness and thwarted belongingness on suicide attempt (Research Question 2). Again, all five items were entered into the model for the outcome variable of suicide attempt. During the data screening process, two proxy items were eliminated (i.e., non-binary, volunteer), as they did not indicate significant results. Regression results indicated that the overall model of the three remaining predictors (emotional/mental health, felt sad/hopeless, not straight) was statistically reliable in distinguishing between 11th grade students who did not attempt suicide and those who did (Nagelkerke R2 = .271; p < .001). The suicide attempt model was deemed statistically significant—X2(5) = 1182.692—with an overall positive predictive value of 93.4%. Both proxy items for the perceived burdensomeness variable proved to be statistically significant (Table 3).
Based on the overall regression analyses, increased poor emotional/mental health was related to the increased likelihood and occurrence of suicide attempt; however, students who reported feeling sad or hopeless for at least 2 weeks were nearly twice as likely to attempt suicide than students who did not report feeling sad or hopeless. Of the three proxy items for the thwarted belongingness variable, only one proved to be statistically significant (Table 3). Students who reported as not straight were nearly twice as likely as students who reported as straight to attempt suicide.
Table 3
Logistic Regression Predicting Likelihood of Suicide Attempt
| Variable |
B |
SE |
Wald |
df |
p |
Odds |
| Perceived Burdensomeness |
| Emotional/Mental Health |
0.599 |
.49 |
149.806 |
1 |
< .001 |
1.820 |
| Felt Sad/Helpless |
−1.856 |
.119 |
242.389 |
1 |
< .001 |
0.156 |
| Thwarted Belongingness |
| Not Straight |
0.533 |
.094 |
31.895 |
1 |
< .001 |
1.704 |
| Non-Binary |
0.055 |
.143 |
0.149 |
1 |
.700 |
1.057 |
| Volunteer |
−0.029 |
.042 |
0.490 |
1 |
.484 |
0.971 |
| Constant |
−2.222 |
.296 |
56.368 |
1 |
< .001 |
0.108 |
These results indicated that there were significant similarities between the predictors of suicide ideation and suicide attempt, supporting our hypotheses. The proxy items that comprised perceived burdensomeness (poor emotional health [odds = 1.820] and feeling sad/hopeless [odds = 6.410]) in conjunction with the proxy item that comprised thwarted belongingness (not straight [odds = 1.704]) all factored into increased likelihood of suicide ideation and suicide attempt. In other words, the mediators of suicide ideation were similar to the mediators of suicide attempt.
Discussion
In discussing the results of the study, it is important to first contextualize the descriptive statistics, as we were studying and applying results to adolescent students in Oregon. The dataset reports 18% of the participants as experiencing suicide ideation, which equates to 1,927 students in the 11th grade. This statistic for suicide ideation is a little higher than the national percentage of 17.2% (CDC, 2017). The dataset also reports 6.6% of the participants as attempting suicide, which equates to 703 students in the 11th grade. This statistic for suicide attempt is a little lower than the national 7.4% (CDC, 2017). In terms of our dataset, Oregon 11th graders were slightly higher than expected for suicide ideation and slightly lower than expected for suicide attempt.
Results from our binomial logistic regression analyses uncovered a model supporting our hypothesis that perceived burdensomeness and thwarted belongingness would significantly predict suicide ideation and attempt in 11th grade students. Further, both variables representing perceived burdensomeness were statistically significant for both suicide ideation and attempt, as was one of the three proxy variables representing thwarted belongingness. These findings align with the IPTS, proposing that perceived burdensomeness and thwarted belongingness are not only important predictors of suicidal behaviors, but are significant elements for both ideation and attempt (with the addition of acquired capability for attempt; Horton et al., 2016; King et al., 2018).
Though not a predetermined hypothesis, it seems reasonable to expect that there would be fewer predictors of suicide attempt, condensed from the predictors of suicide ideation, but that is not the case in our findings. It begs the question: What variables drove students in this population from ideation to attempt? According to the data, 18% of the 11th graders experienced suicide ideation, but only 6.6% reported being driven to attempt suicide. The IPTS would suggest that the missing component was a measure of acquired capability that moves a person from ideation to attempt (Joiner et al., 2009). According to the IPTS (Joiner et al., 2009), experiencing perceived burdensomeness and thwarted belongingness without acquired capability leads to suicide ideation, but the presence of acquired capability is needed to result in suicide attempt. This will be discussed further as a limitation of this study.
These results corroborate previous literature on adolescence and suicidality. Horton et al. (2016) described adolescent perceived burdensomeness as social disconnection and adolescent thwarted belongingness as social isolation from peers. As previously described, with regard to poor emotional/mental health and feeling sad/hopeless, Jaworska and MacQueen (2015) highlighted the increased reactivity of adolescence, and Wyman (2014) indicated that half of the diagnoses of emotional and behavioral disorders take place during this age period (highlighting the importance of mental health clinicians being aware of these findings). With regard to not being straight, this time period also includes establishing values and preferences for sexual behavior and affective orientation (Teipel, 2013). These results also corroborate our previous findings on the application of the IPTS to early adolescents (ages 13–14), suggesting similar significant mediators for both suicide ideation (perceived burdensomeness: emotional/mental health, feeling sad/hopeless; thwarted belongingness: not straight, bullied) and suicide attempt (perceived burdensomeness: emotional/mental health, feeling sad/hopeless; thwarted belongingness: non-binary, bullied; Sallee et al., 2021).
Relative to the literature on suicidality and its role in our selection of proxy items within the OHT survey, research on the connection between poor emotional/mental health and emotional strain in the family setting supports our findings of its significance within the predictor variable of perceived burdensomeness (Miller et al., 2014). The significance of feeling sad/hopeless is supported by previous research discussing its inclusion in the definition of perceived burdensomeness itself (Horton et al., 2016). Sexual minority students experience higher rates of suicidal behaviors, attempting suicide at rates of 2 to 6 times that of straight adolescents (Seelman & Walker, 2018; Zhao et al., 2010). Our findings support this body of research in the significance of being not straight in relation to mental health wellness.
The other proxy predictors examined—being non-binary and volunteering—were not statistically predictive of suicidal behavior. This may be due in part to the developmental tasks and goals characteristic of the period of middle adolescence, or the proxy items themselves may not be significant indicators of the predictor variables in the study, or the wrong indicators were chosen or were conceptualized inaccurately. If that is the case, there would be concerns regarding the construct validity of these indicators and subsequent measures, and because that cannot be proven otherwise, it is a considerable limitation to the study. If the developmental tasks and goals of middle adolescence provide the most insight into the insignificance of being non-binary and volunteering, it is important to consider the developmental period of self-involvement resulting in high expectations of self in combination with low self-concept, impacting an increased drive for peer acceptance (American Academy of Child & Adolescent Psychiatry, 2021). Eleventh grade students are also preparing for their final year of high school and making plans for what their lives will look like after graduation, requiring a high degree of autonomy and independence. It is interesting to consider the insignificant predictors through this developmental lens. Although 11th grade students are seeking peer acceptance, being non-binary may not be a driver because of developing autonomy and independence.
We consider how the findings of this study might relate to research indicating a higher rate of suicide for sexual/gender minorities compared to youth from historically well-represented communities (Teipel, 2013), but perhaps disaggregating sexual/gender minority and focusing on non-binary youth in particular may impact that conversation. Volunteering could prove to be a protective factor but drive for peer acceptance and reliance on peers may determine whether or not a student in the 11th grade chooses to volunteer as opposed to self-motivation or fulfillment.
Limitations and Suggestions for Future Research
Several limitations must be considered when evaluating the findings of this study. First, because of their correlational nature, we were unable to draw any causal conclusions from the results. Relatedly, the results from this study, despite being based on a large sample, described 11th grade students in Oregon who elected to take the survey and had a complete dataset necessary for analysis; the sample was one of convenience, and the extraction of missing datasets impacted the researchers’ ability to gauge the sample’s ability to represent the whole population. As such, generalization of the results to the larger population of adolescents is limited.
Additionally, the data was taken retrospectively from a survey managed by a state government agency; it would have been preferable for us to have input on the questions included in the 2017 OHT survey. Instead, we were forced to select best-fit proxy items that might or might not have been most representative of the predictor variables. Relatedly, and as previously mentioned, there is cause to question the construct validity of these measures, particularly because the selected proxy items do not correlate to other measures of thwarted belongingness in particular. Because we relied on the 2017 OHT survey data, the models for examining the IPTS constructs were incomplete. Lastly, there is a lack of data about unique stressors experienced by students of color related to their social locations, particularly valuable because 25% of the participants were Hispanic/Latino.
Based on our results, despite the limitations previously discussed, there are a variety of avenues for further research on this topic. The first avenue would be to analyze similar data from another state survey or the national Youth Risk Behavior Survey. This would allow researchers to compare results with this study in order to offer more supported generalization to the adolescent population. Another avenue would be to revisit this dataset and theory to consider how they might apply to other behaviors of the adolescent population, such as NSSI and school violence. Further research could revisit this study by creating a survey that would more fully target the interpersonal constructs of the IPTS or create a qualitative or mixed-methods study incorporating additional data sources to examine more in-depth the suicide-related factors and experiences during adolescence.
Another avenue for future research may be to examine additional prospective mediators that may predict the evolution from ideation to attempt because our results presented the exact same predictors for both. Finally, a valuable possibility for future research would be to study factors that might differentially affect students of color and adolescents from sexual minority groups.
Implications
This particular study offers valuable support for the application of the IPTS in working with middle adolescents as well as useful implications for targeting specific interpersonal needs when working with this population. Perceived burdensomeness and thwarted belongingness may be significant construct predictors of suicide ideation and attempt in adolescents according to the findings. Implications for clinical mental health counselors and other professionals working with this population support the importance of taking a systemic and unique approach to working with adolescents and their families that prioritizes and addresses these specific interpersonal needs individually and collectively.
Specific interventions addressing adolescent interpersonal needs of perceived burdensomeness and thwarted belongingness include an array of clinical practices, such as using a suicide screener as part of intake assessments or well-child checks that include items related to these two constructs. Existing suicide intervention modalities need to incorporate and/or integrate the constructs of the IPTS, utilizing counseling goals and interventions that specifically target belongingness and personal value. Further, clinicians must have a basic understanding of the developmental tasks of this period to attend to an adolescent’s stable and productive peer relationships, adoption of personal value systems, and renegotiation of relationships with parents/caregivers, realizing that this transitional stage is also characterized by feelings of grief and loss (Teipel, 2013).
Group counseling is an effective and efficient modality through which a mental health professional can bring together a number of adolescents and facilitate sessions normalizing these developmental tasks and associated feelings. Mental health literacy and bibliotherapy can be used in combination with group counseling, as research has demonstrated their effectiveness on providing structure in the group process, educating adolescents, and fostering connections among the group (Mumbauer & Kelchner, 2017). Groups can also offer parents and caregivers a safe space to navigate family complexities around adolescent suicidality and learn ways to promote a sense of belonging and reduce feelings of burdensomeness among adolescents.
Broader systemic outreach can involve community mental health providers and other professionals collaborating with school stakeholders to offer services such as parent workshops and educator professional development opportunities on understanding suicidality and evidence-based prevention, intervention, and postvention. Partnering with school stakeholders can include consulting on systemic interventions and programming, such as individual student behavior plans, IEPs, and 504 plans, in addition to school- or grade-wide postsecondary transition activities. These consultation and collaboration efforts are often interdependent, in the sense that clinical professionals gain referrals from school stakeholders, and school stakeholders help inform the work of clinical professionals with their adolescent clients.
Through engaging parents, families, school personnel, and their adolescent clients, clinical mental health counselors can work holistically to prevent and intervene in suicidal behaviors by targeting fulfillment and development of interpersonal needs. These findings may have the potential to inform laws and policies through legislative efforts to address adolescent suicide. Clinical mental health counselors have a professional obligation to utilize outcome data to advocate for systemic change to impact clients (Montague et al., 2016), and in this context they may also draw on these findings to provide information to society to assist in advocacy efforts and extend recommendations to professionals working with this population.
Conclusion
The findings of our study support the application of the IPTS in understanding suicidality among middle adolescents, particularly in the ideation model, and are significant in several ways. First, the IPTS has the potential to inform therapeutic interventions in clinical settings, as well as parents and social institutions (e.g., schools and youth development centers), on how best to support youth who experience suicidality. Another focus of our study was on interpersonal factors that are dynamic, rather than static risk factors that may not necessarily be venues for intervention and change for clinicians (e.g., family factors). Third, adolescent clients engaging in suicide ideation and behaviors require interventions that are unique from their adult counterparts and often require environmental and familial interventions as well as individual. Lastly, our findings may serve to provide information to society to assist in advocacy efforts and recommendations for serving adolescent populations within all systems, including laws and policies to address adolescent suicide. Overall, the findings of our study underscore the uniqueness and complexity of this developmental period of adolescence and the importance of theory- and research-based practices. We hope that our findings will inform mental health clinicians, educators, school counselors, parents, and policymakers in their efforts to meet adolescent mental health needs.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
American Academy of Child & Adolescent Psychiatry. (2021). Facts for families guide. https://www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/Layout/FFF_Guide-01.aspx
Barzilay, S., Apter, A., Snir, A., Carli, V., Hoven, C. W., Sarchiapone, M., Hadlaczky, G., Balazs, J., Kereszteny, A., Brunner, R., Kaess, M., Bobes, J., Saiz, P. A., Cosman, D., Haring, C., Banzer, R., McMahon, E., Keeley, H., Kahn, J.-P., . . . Wasserman, D. (2019). A longitudinal examination of the interpersonal theory of suicide and effects of school-based suicide prevention interventions in a multinational study of adolescents. Journal of Child Psychology and Psychiatry, 60(10), 1104–1111. https://doi.org/10.1111/jcpp.13119
Becker, S. P., Foster, J. A., & Luebbe, A. M. (2020). A test of the interpersonal theory of suicide in college students. Journal of Affective Disorders, 260, 73–76. https://doi.org/10.1010/j/jad.2019.09.005
Brener, N. D., Kann, L., Shanklin, S., Kinchen, S., Eaton, D. K., Hawkins, J., & Flint, K. H. (2013, March 1). Methodology of the Youth Risk Behavior Surveillance System—2013. Recommendations and Reports, 62(1), 1–23. Centers for Disease Control and Prevention. https://www.cdc.gov/mmwr/preview/mmwrhtml/rr6201a1.htm
Centers for Disease Control and Prevention. (2017). Trends in the prevalence of suicide-related behaviors. National YRBS: 1991–2017. https://www.cdc.gov/healthyyouth/data/yrbs/pdf/trends/2017_suicide_trend_yrbs.pdf
Chu, C., Rogers, M. L., & Joiner, T. E. (2016). Cross-sectional and temporal association between non-suicidal self-injury and suicidal ideation in young adults: The explanatory roles of thwarted belongingness and perceived burdensomeness. Psychiatry Research, 246, 573–580. https://doi.org/10.1016/j.psychres.2016.07.061
Czyz, E. K., Berona, J., & King, C. A. (2015). A prospective examination of the interpersonal-psychological theory of suicidal behavior among psychiatric adolescent inpatients. Suicide and Life-Threatening Behavior, 45(2), 243–260. https://doi.org/10.1111/sltb.12125
Durkheim, É. (1951). Suicide: A study in sociology. Free Press.
Horton, S. E., Hughes, J. L., King, J. D., Kennard, B. D., Westers, N. J., Mayes, T. L., & Stewart, S. M. (2016). Preliminary examination of the interpersonal psychological theory of suicide in an adolescent clinical sample, Journal of Abnormal Child Psychology, 44, 1133–1144. https://doi.org/10.1007/s10802-015-0109-5
Jaworska, N., & MacQueen, G. (2015). Adolescence as a unique developmental period. Journal of Psychiatry & Neuroscience, 40(5), 291–293. https://doi.org/10.1503/jpn.150268
Joiner, T. E., Ribeiro, J. D., & Silva, C. (2012). Nonsuicidal self-injury, suicidal behavior, and their co-occurrence as viewed through the lens of the interpersonal theory of suicide. Current Directions in Psychological Science, 21(5), 342–347. https://doi.org/10.1177/0963721412454873
Joiner, T. E., Van Orden, K. A., Witte, T. K., & Rudd, M. D. (2009). The interpersonal theory of suicide: Guidance for working with suicidal clients. American Psychological Association.
King, J. D., Horton, S. E., Hughes, J. L, Eaddy, M., Kennard, B. D., Emslie, G. J., & Stewart, S. M. (2018, June). The interpersonal–psychological theory of suicide in adolescents: A preliminary report of changes following treatment. Suicide and Life-Threatening Behavior, 48(3), 294–304. https://doi.org/10.1111/sltb.12352
Lester, D. (1987). Murders and suicide: Are they polar opposites? Behavioral Sciences & the Law, 5(1), 49–60.
https://doi.org/10.1002/bsl.2370050106
Miller, A. B., Adams, L. M., Esposito-Smythers, C., Thompson, R., & Proctor, L. J. (2014). Parents and friendships: A longitudinal examination of interpersonal mediators of the relationship between child maltreatment and suicidal ideation. Psychiatry Research, 220(3), 998–1006. https://doi.org/10.1016/j.psychres.2014.10.009
Montague, K. T., Cassidy, R. R., & Liles, R. G. (2016). Counselor training in suicide assessment, prevention, and management. In G. R. Walz & J. C. Bleuer (Eds). Ideas and research you can use: VISTAS 2016. https://bit.ly/Vistas2016
Mumbauer, J., & Kelchner, V. (2017). Promoting mental health literacy through bibliotherapy in school-based settings. Professional School Counseling, 21(1), 85–94. https://doi.org/10.5330/1096-2409-21.1.85
Oregon Health Authority. (2017). Oregon Healthy Teens Survey. https://bit.ly/OHTsurvey2017
Oregon Suicide Prevention. (n.d.). Youth. https://www.oregonsuicideprevention.org/community/youth
Sallee, E., Ng, K.-M., & Cazares-Cervantes, A. (2021). Interpersonal predictors of suicide ideation and attempt among early adolescents. Professional School Counseling, 25(1), 1–11. https://doi.org/10.1177/2156759X211018653
Schneidman, D. (1993). 1993 health care reforms at the state level: An update. Bulletin of the American College of Surgeons, 78(12), 17–22. https://pubmed.ncbi.nlm.nih.gov/10130176
Seelman, K. L, & Walker, M. B. (2018). Do anti-bullying laws reduce in-school victimization, fear-based absenteeism, and suicidality for lesbian, gay, bisexual, and questioning youth. Journal of Youth and Adolescence, 47, 2301–2319. https://doi.org/10.1007/s10964-018-0904-8
Stewart, S. M., Eaddy, M., Horton, S. E., Hughes, J., & Kennard, B. (2017). The validity of the interpersonal theory of suicide in adolescence: A review. Journal of Clinical Child and Adolescent Psychology, 46(3), 437–449. https://doi.org/10.1080/15374416.2015.1020542
Stone, D., Holland, K., Bartholow, B., Crosby, A., Davis, S., & Wilkins, N. (2017). Preventing suicide: A technical package of policy, programs, and practices. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. https://www.cdc.gov/violenceprevention/pdf/suicidetechnicalpackage.pdf
Teipel, K. (2013, June). Understanding adolescence: Seeing through a developmental lens. State Adolescent Health Resource Center. http://www.amchp.org/programsandtopics/AdolescentHealth/projects/Documents
/SAHRC%20AYADevelopment%20MiddleAdolescence.pdf
Wasserman, D., Hoven, C. W., Wasserman, C., Wall, M., Eisenberg, R., Hadlaczky, G., Kelleher, I., Sarchiapone, M., Apter, A., Balazs, J., Bobes, J., Brunner, R., Corcoran, P., Cosman, D., Guillemin, F., Haring, C., Iosue, M., Kaess, M., Kahn, J.-P., . . . Carli, V. (2015). School-based suicide prevention programmes: The SEYLE cluster-randomized, controlled trial. The Lancet, 385(9977), 1536–1544. https://doi.org/10.1016/S0140-6736(14)61213-7
Wyman, P. A. (2014). Developmental approach to prevent adolescent suicides: Research pathways to effective upstream preventative interventions. American Journal of Preventative Medicine, 47(3S2), S251–S256. https://doi.org/10.1016/ampere.2014.05.039
Zhao, Y., Montoro, R., Igartua, K., & Thombs, B. D. (2010). Suicidal ideation and attempt among adolescents reporting “unsure” sexual identity or heterosexual identity plus same-sex attraction or behavior: Forgotten groups? Journal of the American Academy of Child & Adolescent Psychiatry, 49(2), 104–113.
https://doi.org/10.1016/j.jaac.2009.11.003
Emily Sallee, PhD, BC-TMH, LSC, PCLC, is an assistant professor at the University of Montana. Abraham Cazares-Cervantes, PhD, LSC, is an assistant clinical professor at Oregon State University. Kok-Mun Ng, PhD, NCC, ACS, LPC, is a professor at Oregon State University. Correspondence may be addressed to Emily Sallee, 32 Campus Drive #335, Missoula, MT 59834, emily.sallee@umontana.edu.
Feb 7, 2022 | Volume 12 - Issue 1
Diane M. Stutey, Abigail E. Solis, Kim Severn, Lori Notestine, Kodi L. Enkler, Joseph Wehrman, Molly Cammell
There is a need for mental health interventions for youth in the United States. Youth mentoring programs have proven to be successful in helping in a variety of aspects. The purpose of this phenomenological study was to gain insight into the lived experiences of participants in a therapeutic youth mentoring program. In addition to being paired 1:1 with a mentor, all of the youth had access to individual counseling with counselors-in-training throughout the program. The participants in this study were 14 youth, ages 11–15, who were considered “at-promise youth” if they were not reaching their full potential in the school setting and might be vulnerable to school dropout, substance use/misuse, and/or criminal behavior. All participants were interviewed at the beginning and end of a 12-week therapeutic mentoring program. Five themes emerged from the data: life stressors, self-awareness, trusting others, adaptability and resiliency, and hope for the future. Researchers observed an increase in participants’ self-esteem, self-efficacy, and problem-solving and coping skills. Implications for counselors, particularly those interested in adding a therapeutic component to traditional mentoring programs, are discussed along with suggestions for future research.
Keywords: mentoring programs, therapeutic, mental health interventions, at-promise youth, phenomenological
Because of a staggering dropout rate of 1.2 million students a year, as well as an increase of juvenile delinquency in the United States, there is a need for interventions that will help youth stay in school and out of the juvenile justice system (Weiler, Chesmore, et al., 2019; Weiss et al., 2019). Researchers have indicated that the absence of education, including students who do not graduate from high school, has led to an increase of youth experiencing health complications, substance abuse, social skill deficits, and premature death (Schoeneberger, 2012; Weiler, Chesmore, et al., 2019; Weiler et al., 2015; Weiss et al., 2019). In the past, youth exhibiting behaviors that might lead to juvenile delinquency were referred to as at risk. However, the term at promise is now utilized by organizations such as the California Education Code (McKenzie, 2019). The phrase at-promise youth describes youth who have the ability to reach their full potential with additional time and resources.
One way to help at-promise youth reach their full potential and feel more engaged at school might be connecting them with a young adult who understands their struggles. Youth benefit from enhanced connectedness to adults outside their immediate family to help them navigate through difficult times, and this relationship can be protective against suicidal behavior (King et al., 2018; Rhodes, 2002). Individuals within adolescent ecosystems have voiced the positive changes youth have experienced by participating in youth mentoring programs (Raposa et al., 2019). At-promise youth might benefit even more from youth mentoring programs that incorporate a therapeutic component to address mental health concerns they may be experiencing (Liang et al., 2013).
Youth Mentoring Programs
Youth mentoring is a psychosocial intervention in which a nonparental adult and a younger individual aim to develop a supportive relationship (Karcher et al., 2005; Lund et al., 2019; Sacco et al., 2014; Weiler et al., 2013). During the mentoring program, the youth mentees experience a healthy environment, which often leads to them seeking out and learning to cultivate a healthier environment beyond the youth mentoring program. This shift in environment has allowed researchers to observe improvement in self-perception, social acceptance, parent–child interaction, and academic performance of youth participating in mentoring programs (Anastasia et al., 2012). Researchers have found that mentoring programs may also buffer against the impacts of youth exposed to adverse childhood experiences and improve behavioral, social, emotional, and academic outcomes (Centers for Disease Control and Prevention, 2019; David-Ferdon et al., 2016; Durlak et al., 2010; Tolan et al., 2014). The relationship between mentor and mentee is heavily credited to the success of youth mentoring, signifying the importance of the mentee picking a mentor similar to them (e.g., appearance, culture, interests).
Researchers discovered that both mentor and mentee benefit from the dyadic relationship when there is trust and the mentor is consistent, supportive, and encouraging instead of controlling (Marshall et al., 2016; Rhodes, 2002; Weiler, Boat, & Haddock, 2019; Weiler et al., 2015; Weiss et al., 2019). A mentor should be supportive and encouraging, especially when giving advice, which helps the youth to be open to a new perspective (Lund et al., 2019; Rhodes, 2002). Youth who participated in a positive mentoring relationship had increased feelings of connectedness with a trusted adult and higher rates of pursuing purpose (Lund et al., 2019). In addition, by the end of youth mentoring programs, the majority of mentees achieved a sense of self-worth and increased levels of intimacy, communication, and trust because of the dyadic relationship they had established with their mentors (Keller & Pryce, 2012; Rhodes, 2002).
Mentors and Youth Mentees
Research on youth mentoring programs has described mentees as individuals who are at risk, may have been in the juvenile justice system, or are in danger of offending or reoffending because of a variety of variables (e.g., substance use, academic failure, absences, aggressive behavior, family stressors) present in their lives (Cavell et al., 2009; Haddock et al., 2017; Weiler et al., 2013). Weiler et al. (2013) noted that more than 60% of the youth who participated in a mentoring program in their study had acquired at least a single charge with the juvenile justice system. Numerous researchers have discussed how the role of a mentor in a mentee’s life helped the mentee with improved self-esteem, enhanced health, instilled hope for the future, and reduced reoffending behaviors (Raposa et al., 2019; Rhodes, 2002; Weiler, Boat, & Haddock, 2019; Weiss et al., 2019).
Training is required before being paired with a mentee to ensure the competency of the adult who will be mentoring the youth facing hardships. Anastasia et al. (2012) emphasized the importance of preparatory training and ongoing training so that mentors, who are not in a helping profession, will have the tools necessary to mentor an adolescent successfully. In the preparatory stage of training, mentors learn about maintaining safety, program rules, child-focused social problem–solving skills, and the activities that will be used throughout the program (Anastasia et al., 2012; Cavell et al., 2009).
At the same time, mentors may feel overwhelmed when mentees exhibit mental health issues, behavioral issues, or racial or socioeconomic differences that surpass their basic training and expertise (Marshall et al., 2016; Weiler et al., 2013). With a majority of the adolescents facing difficulties, it can be daunting for the mentor to provide adequate mentoring; therefore, ongoing training is imperative. Ongoing training is meant to help the mentor increase their effectiveness with their mentee (Anastasia et al., 2012), allowing the adult to seek guidance when they start feeling overwhelmed with their mentee’s behavior and actions (Keller & Pryce, 2012). Through ongoing training and interaction with their paired youth, the adult mentor gains a new level of insight and improved health, self-esteem, and self-awareness that they did not have before (Rhodes, 2002).
However, even with ongoing training, mentees may exhibit mental health needs that are beyond the average mentor’s training and skill set. Liang et al. (2013) highlighted that mentees might benefit from receiving traditional therapy to help with their hardships. Therefore, some mentoring programs have added a therapeutic component incorporating trained mental health personnel to positively support both mentors and mentees (Weiler et al., 2013).
Therapeutic Component to Mentoring
Mental health professionals (e.g., counselors, social workers, psychologists) learn through their education how to be culturally competent, preserve client autonomy, and maintain an unbiased perspective that is crucial when trying to develop a mentoring relationship (Anastasia et al., 2012). Liang and colleagues (2013) emphasized how youth with therapeutic needs benefit from the way therapeutic guidance and a mentoring program complement each other. For instance, if a child is stressed about how to pay for college, then a mentor can help their mentee find resources, while a therapist could focus on teaching healthier coping skills to manage stress (Liang et al., 2013). Working in tandem allows for a two-dimensional approach, a noteworthy difference between therapeutic mentoring and traditional mentoring programs (Sacco et al., 2014).
Some therapeutic mentoring programs select mentors from a helping profession and provide additional training and supervision from trained mental health clinicians to create a more therapeutic setting for mentees (Johnson & Pryce, 2013). Other youth mentoring programs include a therapeutic component by incorporating additional staff consisting of mental health professionals, such as counselors-in-training (CITs), to directly address the mental health needs of mentees and support mentors (Sacco et al., 2014; Stark et al., 2021; Weiler et al., 2013). Therapeutic mentoring programs function as an intervention for youth who are engaging in risky behavior or have experienced trauma and other developmental issues (Johnson & Pryce, 2013; Sacco et al., 2014).
Litam and Hipolito-Delgado (2021) discussed how COVID-19 highlighted that communities of color have limited access to health care and education. Marginalized youth and their families may not seek mental health services at all or may be more prone to accept help from non–mental health professionals such as mentors (Dashiff et al., 2009). Therefore, an ideal youth mentoring program might have trained mentors from a helping profession who are supervised by mental health professionals, such as counselors, who are also available to meet with youth throughout the mentoring sessions. However, many mentoring programs are volunteer-based and this may limit access to mental health professionals. In addition, there is a shortage of mental health professionals prepared to work with youth (Dashiff et al., 2009) and there is a treatment gap for mental disorders in children (Patel et al., 2013).
Often youth have access to counselors in their schools, but researchers have found that school counselors report that they have limited time to address ongoing mental health needs (Carlson & Kees, 2013). Litam and Hipolito-Delgado (2021) encouraged counselors to use creative strategies such as reduced or no-cost services when working with communities of color. Dashiff and colleagues (2009) stressed that “innovative strategies of service delivery are needed” when working with youth who may come from poverty or areas with limited access to mental health services (p. 29). Partnering with a university, with a plethora of CITs needing supervised client hours, is an innovative and low- or no-cost approach. In this scenario, the mentor takes on a therapeutic role with their mentee, but the CIT is available to address and process ongoing mental health concerns. Incorporating CITs in a youth mentoring program allows both mentor and CIT to work together to create an environment in which youth feel safe, encompassing a secure attachment to the therapeutic program (Sacco et al., 2014).
The CIT’s position facilitates insight and awareness for the youth while offering tools that will help them reach their therapeutic goals (Johnson & Pryce, 2013; Sacco et al., 2014). The role of the mentor is to serve as a role model and advocate while maintaining open communication with the CIT to facilitate necessary therapeutic modifications (Sacco et al., 2014). Some researchers have found that as the mentor models healthy behavior, the youth will eventually begin to display a healthier interpersonal and intrapersonal self (Johnson & Pryce, 2013; Sacco et al., 2014). Overall, mentoring programs appear to be an effective intervention for youth that could also benefit from the incorporation of a therapeutic component.
Despite the amount of research being done to understand the relationship between mentor and mentee from different perspectives, there is less data that examines the participants’ lived experiences of a therapeutic youth mentoring program that includes CITs. The purpose of this study was to examine and gain further insight into participants’ lived experiences with a therapeutic youth mentoring program—specifically, a therapeutic youth mentoring program in which the mentors had additional training and supervision in mental health areas and additional support was provided by CITs while under supervision. The overarching question for this study was: What were participants’ lived experiences prior to and after participating in a therapeutic youth mentoring program?
Methodology
Phenomenology was utilized in this study to gather and analyze data in order to better understand participants’ lived experiences in a therapeutic youth mentoring program. According to Trusty (2011), “if little is known about a research area or target population, it is likely that a qualitative study would be needed first” (p. 262). Although some research has been conducted with participant perceptions of youth mentoring programs, there is less research with therapeutic mentoring programs; therefore, a qualitative approach was deemed appropriate.
Therapeutic Youth Mentoring Program
The therapeutic youth mentoring program in this study was at a university in the Rocky Mountain region of the United States and utilized the theoretical framework of Campus Corps (Weiler et al., 2013, 2014), now called Campus Connections (CC). CC is an innovative licensed program combining practices from mentoring, after-school programming, and integrated mental health. CC mentors were recruited and selected from a variety of undergraduate disciplines across campus, with more than half being from counseling and human services, psychology, or education majors. All mentors attended an orientation and background screening prior to being accepted for the program. The mentors who were selected spent the first 3 weeks of the semester in intensive training with counselor educators, who were also licensed professional counselors, to learn about child abuse reporting, ethics of working with minors, crises and trauma, and basic counseling skills. Potential mentees were referred by local school counselors and attended an intake with their guardians to go over the format of the program. Mentors created profiles about themselves that were utilized during the intake so that mentees could select their mentor based on preferences.
Once mentees were paired with mentors, the faculty and staff looked at the information provided by caregivers and counselors, demographics, and other relevant information to create diverse mentor families. Each mentor family consisted of approximately three mentor/mentee pairs. In this study, there were a total of three mentor families and each family was assigned a mentor coach. The mentor coaches were graduate-level counseling students who provided their mentor family with support throughout the semester. In addition, four graduate-level CITs were selected to provide ongoing counseling to mentees throughout the therapeutic mentoring program. All CITs were in their last semester of graduate studies and met weekly with counselor educators for supervision. Two counselor educators and supervisors, also licensed professional counselors, were also present each evening of CC to support mentees, mentors, and CITs.
All youth participated in the 12-week CC therapeutic youth mentoring program that met on the university campus, once a week for 4 hours. This therapeutic youth mentoring program was designed to bring youth to a college campus to help them become more comfortable and familiar with future college and career goals. Youth followed a schedule that consisted of:
- working for 60 minutes with their mentor on academic and study skills.
- going on a 30-minute “walk and talk” to learn about different locations on the university campus each week.
- participating in a 30-minute family-style meal at the dining hall with their mentor family.
- choosing two 45-minute prosocial or social justice activities.
The prosocial and social justice activities were directed at helping youth learn skills and concepts such as resiliency, coping, inclusiveness, and empathy. These activities were adapted from a manual created by the founders of CC. Each evening, two 45-minute lessons were facilitated by our graduate assistants and CITs and covered topics around the “Big 8” identities (i.e., gender/sex, race, class/socioeconomic status, sexual orientation, ethnicity, religion, age, and ability). Some examples of the activities included: Backpack, an activity adopted from Peggy Mcintosh’s (2003) The Knapsack, that examines privilege and societal benefits; Build a House, an activity designed to illustrate the differences in resources that people have based on socioeconomic status; and Pink, Blue and Purple, an activity designed to discuss assumptions made about gender.
At any point throughout their time on campus, mentors or mentees could request for the youth to have time to meet with a CIT. CITs also routinely set up check-ins with all mentees and were present throughout the entire process. Often the CITs would help with the after-dinner activities if youth weren’t requesting to meet 1:1. The participants in this study engaged in a total of 720 minutes of counseling with the average youth receiving 50 minutes of individual counseling.
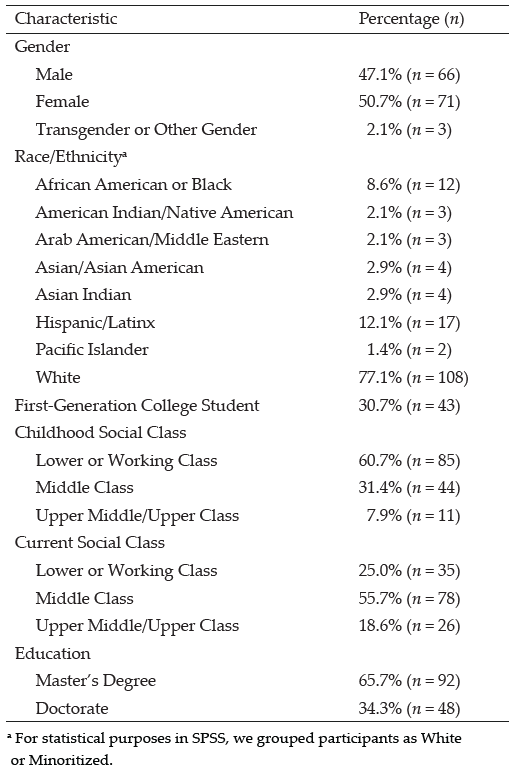
Participants
This was a purposeful sample of at-promise youth participating in the same CC therapeutic youth mentoring program in the spring of 2019. Of the 18 youth enrolled in CC, 14 youth agreed to participate in the research study. The participants in this study consisted of 14 youth, ages 11–15, with the following demographics: 71% male, 21% female, and 7% transgender/gender-expansive; 57% White, 29% Black/African American, 21% Hispanic/Latino, 14% American Indian/Alaska Native, and 7% Asian; and approximately half on free and reduced lunch. School district partners were asked to consider and recommend at-promise youth if they were not reaching their full potential and might be vulnerable to school dropout, substance use/misuse, and/or criminal behavior. Local school counselors submitted referrals based on this criterion for youth to participate in CC. Participation was voluntary and participants could remove themselves from the study at any time throughout the process.
Procedures
At-promise youth are considered a vulnerable population and therefore researchers must contemplate ethical considerations. Our research team went through a full IRB process to ensure youth participants were being treated with the highest ethical considerations. After obtaining IRB approval, informed consent and assent was secured and two audiotaped interviews were conducted with all participants—one at the beginning of the 12-week mentoring program and one 12 weeks later at the end. Semistructured interviews are progressive in design (Merriam, 1998); they allow the researcher to formulate questions ahead of time and adjust the questions based on the participants’ responses (Guba & Lincoln, 1989). Participants were asked a series of open-ended questions that were similar across interviews, such as how a mentor has helped them, their feelings about being on a college campus, and thoughts on meeting with a CIT (see Appendix for a complete list of interview questions). The final interview allowed the participants to describe their experience working with a mentor and CIT and their perceptions of meeting on a university campus each week for 12 weeks.
Our research team consisted of three PhD-level counselor educators, Diane Stutey, Lori Notestine, and Joseph Wehrman; one counselor education doctoral student, Kim Severn; one staff member in master’s-level student affairs and higher education, Molly Cammell; and two graduate students in counseling, Abigail E. Solis and Kodi L. Enkler. All members of the research team were present throughout the 12-week therapeutic youth mentoring program. We met on a regular basis to discuss the research protocol and any potential conflicts of interest or ethical concerns, ensuring trustworthiness of the study.
Data Analysis and Trustworthiness
All data were collected by the research team and Solis transcribed all the interviews. Data were analyzed and independently coded by Stutey, Solis, and Severn, utilizing Merriam’s (1998) two-level approach. After each researcher independently coded all the transcripts, we met to discuss and agree upon emerging themes. After data was further analyzed and organized to support each of the themes, we met again to come to consensus on the themes. Any disagreement of themes or supporting data was discussed until consensus was reached.
Several techniques were used to ensure the trustworthiness and rigor of data collection and analysis (Guba & Lincoln, 1989; Merriam, 1998). Stutey, Solis, and Severn independently coded the data and each kept their own researcher journal. To establish dependability and conformability, an audit trail was created (Lincoln & Guba, 1985). Notestine and Enkler served as peer reviewers and assisted Stutey, Solis, and Severn by providing feedback at various points. Peer reviewers were given access to initial emerging themes, final themes, researchers’ journals, and coding documentation to inform the feedback provided to Stutey, Solis, and Severn throughout the data collection and analysis process.
We also used bridling to establish trustworthiness and acknowledge the researchers’ prior and current experiences. Often qualitative researchers will use bracketing in an attempt to manage their understanding of or experience with a phenomenon. However, bridling encourages ongoing researcher reflexivity and is meant to be more intentional, with researchers maintaining openness and revisiting assumptions throughout the research process (Dahlberg, 2006; Vagle, 2009). Stutey et al. (2020) described bridling as “an ongoing reflective practice that takes place before, during, and after data collection” (p. 124). Bridling was chosen over bracketing because the researchers had personal and professional experiences with at-promise youth, making it unlikely to put aside all biases and assumptions. Development of a researcher’s stance and review of researchers’ journals were utilized throughout the data collection and analysis to bridle and manage researchers’ biases and assumptions.
Findings
In total, five themes emerged from the participant interview data: life stressors, self-awareness, trusting others, adaptability and resiliency, and hope for the future. In order to be considered a theme, at least seven out of the 14 participants had to endorse the theme. Within each theme, there were two to three aspects that were discussed by participants. Each of the themes is discussed in this section, and a sample of participant quotes is provided as evidence of each aspect of the theme. Participants all chose pseudonyms that were used throughout the research study.
Figure 1
Summary of Themes
| Themes |
Aspects of Themes |
| Life Stressors |
· School
· Peers/Bullying
· Mental Health |
| Self-Awareness |
· Positive Self-Image
· Accomplishments |
| Trusting Others |
· Qualities of a Trusted Mentor/Adult
· Feeling Understood or Heard |
| Adaptability and Resiliency |
· Social-Emotional Growth
· Coping Skills |
| Hope for the Future |
· Realistic Goals for School
· Future Careers
· Impact on Others |
Life Stressors
The first theme of life stressors was endorsed by all 14 participants. This theme was defined as participants’ lived experiences of how stressors in their lives were negatively impacting them. Many of the participants shared in the first interview that they were overwhelmed and a bit confused about being on a college campus. Participants were not sure why they were selected for the therapeutic mentoring program or what they might need help with beyond academics. Participants endorsed three aspects of life stressors in the areas of school, peers/bullying, and mental health.
School
In the initial interview, participants discussed wanting to get straight As and that math was a particularly tough subject area for them. Ball stated, “I really struggle with math. I don’t know why it’s always been something that’s really hard for me.” JT shared that they “have to get straight As” and indicated that if they did not, they would “get kicked out.” Tristonion said, “Right now, I really don’t have the motivation to try in school.”
Other participants struggled with certain teachers, behavior at school, or homework. Josh Billups shared, “Sometimes I’m afraid to talk to my teachers . . . talking to adults is kind of hard.” Drift King stated that they had problems in several areas, such as “not studying, not getting most of the work done, not understanding the work, too afraid to ask teachers, raise my hand, or [ask] questions.” Many participants said that they “don’t like homework” and that they also struggle in school because they “talk too much,” are “not turning in assignments,” and find it “really hard . . . to focus.” School and academic success were important to the majority of the participants in this study.
Peers/Bullying
Besides academic stressors at schools, participants shared that they sometimes struggled with bullies and many shared having a lack of peer or other support in school. Bam shared that they struggle at school because of “getting bullied and having nobody to talk to . . . somebody told me to go commit suicide.” Isabel stated that there is a lot of “drama . . . and getting bullied” at their school. Isaiah shared feelings of isolation: “Kids were being mean and stuff so I just went and sat [alone].” Others shared that they have been called “a snitch,” “Bible head,” and “God” by students in their schools that they perceive as bullies. Participants felt they could discuss these matters with their mentors and/or CIT and seek their advice.
Mental Health
Participants also discussed areas of stress that impact them at school such as learning difficulties and specific physical and mental health issues. DTS shared, “I have ADHD . . . and it’s hard getting back on the schedule taking pills every day.” Several participants mentioned struggling with symptoms associated with depression. Isabel stated, “I’ve had a lot of surgeries and I have really bad anxiety and depression.” Isaiah discussed that “everyone is mean to me” and shared that they “don’t have a good memory.” Many participants mentioned that they were using the mental health services of their school counselor and/or the CIT provided through CC but sometimes felt just as comfortable talking to their mentor.
Self-Awareness
The second theme that emerged from this study was self-awareness. This theme was endorsed by 13 of the 14 participants and is defined as participants’ lived experiences of becoming more self-aware after participating in the 12-week therapeutic mentoring program. When asked about how others perceived them, participants tended to initially interpret that teachers and caregivers might have negative views; often these views were opposite of those that they held about themselves or they perceived peers had about them. After participating in the therapeutic mentoring program, youth seemed more open to talking about their strengths and shared more positive comments about themselves and their accomplishments. Participants endorsed two aspects of self-awareness: positive self-image and awareness of accomplishments.
Positive Self-Image
Many of the participants shared a negative self-image in the initial interview. After spending time in the therapeutic mentoring program, they viewed themselves, and perceived that others also viewed them, in a more positive light. Andrew shared, “I learned you don’t have to be bad to get where you need to be. You don’t have to be dangerous for people to like you.” Jeffy stated, “I’ve been focusing on my schoolwork instead of messing around all the time. And [I’m] thinking before I do something . . . less getting in trouble.” Josh discussed how their image had changed since participating: “Back then I was kind of mean, but [the program] kind of helped me change that . . . I have a lot more friends now.” Several participants shared that they were getting along better with others and being “more social now,” were “able to talk and interact with other people,” and were “opening up to more people.” Several participants attributed this shift in their self-image to having a mentor and/or CIT who unconditionally accepted them.
Accomplishments
Along with viewing themselves in more positive ways, many participants shared what they had accomplished during this semester. Andrew stated, “I used to fight a lot and now we [mentor and me] have a goal not to fight. I haven’t fought since.” Drift King shared, “I know that I’ve got to take it [school] seriously. There’s a lot more stuff that I can accomplish in life.” Isaiah discussed that their grades had improved and “I just got accepted to be a web leader.” In fact, many participants shared improvement in their overall well-being, grades, and relationships with peers: “I’ve been more happy,” “Now I have three As and four Bs,” and “I would describe myself as really helpful and caring about other people.” Participants seemed proud to share these accomplishments and were often smiling during the final interview as they discussed ways they had seen improvement.
Trusting Others
The third theme to emerge was trusting others. This theme was endorsed by 12 of the 14 participants and is defined as participants’ lived experiences with learning to trust others, especially adults. In the initial interview, the participants were unsure of some of their relationships and especially expressed a disconnect with adults. Many participants said that they did not always ask for help or they had some past negative experiences with adults and peers. After participating in the therapeutic youth mentoring program, many participants reported having a trusting relationship with their mentor, and a few with other adults supporting the program, such as mentor coaches and CITs. There also seemed to be some shift in participants having better relationships with peers and other adults outside of the therapeutic youth mentoring program. Participants shared two aspects of trusting others: qualities of a trusted mentor/adult and feeling understood or heard.
Qualities of a Trusted Mentor/Adult
Many participants shared that they perceived their mentors as someone who will “always be there for you.” Andrew shared, “We had a lot in common. So, I can talk to her and she’ll know the answer.” Ball shared, “I just get someone to talk to other than my parents and friends . . . [he’s] a helpful person that gets you through bad times.” Drift King stated, “They help you with anything I need: anger management, class, social skills, school, someone to talk to like a counselor.” Participants described mentors as “cool,” “funny,” “nice,” “friendly,” “chill,” and “helpful.”
Participants were also asked about their perceptions of meeting with a counselor before and after participating in the therapeutic mentoring program. The majority of the participants shared positive experiences they have had with counselors both at school and during the therapeutic mentoring program, stating they helped “when I’m having a bad day,” “after my Grandpa died,” and “when I was being bullied.” Only one participant, Isabel, mentioned that she trusted the CIT more than her mentor: “She’s super there for me, and I only want to talk to her about my problems, because I don’t feel like I really know any other counselors.” Andrew seemed confused about the roles of the different adults at the therapeutic mentoring program: “I thought they were all like mentor and mentor coaches.” After clarification, he shared that the CITs “bring you up . . . if you are feeling down or unhappy.” Although there may have been some initial confusion about the difference between the CITs and coaches, it seemed that most participants felt comfortable seeking counseling support as needed.
Feeling Understood or Heard
In addition to sharing qualities that they appreciated about their mentors, participants shared that a mentor is someone who understands them and makes them feel heard. Drift King shared, “I feel like they’ve been through it too, tough times and they succeed . . . I feel they can help you.” Jeffy stated, “We’re really similar, he’s kind of like me. They talk about your weekend . . . and make you feel happier if you had a bad day.” Rene discussed how her mentor “supports me, like if I have a really bad day she helps me out to have a better rest of my day.”
Adaptability and Resiliency
The fourth theme that emerged was adaptability and resiliency. This theme was endorsed by 10 out of the 14 participants and is defined as participants’ lived experiences of the ways in which they were adapting to some of the stressors that they had shared in the first interview. Participants discussed what they had learned in the therapeutic mentoring program, and often the new resiliency skills seemed connected to experiences with their individual mentor. Participants endorsed two major aspects of this theme: social-emotional growth and coping skills.
Social-Emotional Growth
Participants shared ways in which they had grown socially and emotionally over the semester. DTS shared, “I made some new friends.” Isaiah stated, “I open up to new people.” Bam discussed how their mentor helped them “get through rough times.” Many participants shared that working with their mentors helped them “deal with stress,” “learn how to socialize,” and “make the right decisions.” Several participants were hesitant to even attend CC initially and by the end, they expressed that they were sad to leave because of the social and emotional connections.
Coping Skills
Participants also perceived they had better coping skills and strategies for how to approach a variety of problems. Andrew stated, “Yesterday there was a fight, and I didn’t go . . . [my mentor] said, ‘You can always walk away.’” Josh shared that they learned various coping skills such as better “communication skills and knowing people who will help me and be respectful . . . it’s helped me be able to talk and interact with other people.” Tristonion added, “Well, this place teaches us to calm down.” Participants shared that they also “started focusing,” “doing good deeds,” and “hang[ing] with other people.” Several participants shared that the coping skills they were using they had learned either from their mentor or the CITs during 1:1 time or in prosocial activity time.
Hope for the Future
The fifth and final theme that emerged was hope for the future. This theme was endorsed by 13 of the 14 participants and is defined as participants’ lived experiences surrounding their future hopes and plans. Many participants in the initial interview had lofty goals that did not always seem realistic (e.g., become an NBA or NFL player). Participants also emphasized the importance of having perfect grades and that this is how they would know they were successful. After participating in the therapeutic mentoring program, participants shared what they had learned and their hopes for the future. The three aspects of this theme centered around setting realistic goals for school, the importance of future careers, and the impact they could have on others.
Realistic Goals for School
At the end of this study, many participants reported improvement in grades but were not stressing about perfection as much. Participants were setting more realistic goals for themselves with school. Drift King shared they were planning ahead for high school and would “take it more seriously than middle school . . . to get the credit to actually graduate.” Super J stated about meeting with his mentor, “It’s probably going to help me be successful at college because they show you how important it is to not give up.” JT discussed how doing well in school would allow them to continue to wrestle and “get first place again.” Many participants seemed to have learned from their mentor and/or CIT more about the college process and what they needed to do now in order to reach future goals.
Future Careers
Participants were also more interested in what it might take for them to meet their future career goals. Isabel stated, “In September I’m getting my first job . . . and once I graduate high school, I want to be a lawyer in the Air Force.” Josh stated, “I want to get the highest grades I can so I can do activities and get into higher classes to set myself on the right foot for the future.” Josh mentioned the importance of “getting a good education . . . going to college and get[ting] a job.” This youth was considering a variety of occupations such as construction worker or firefighter. Some of the participants even mentioned that after working with their mentor they wanted to “go to college here” and realized that college might help them “be able to have a good job and a good house.” Participants seemed to be making the connection between college and career based on conversations with their mentor and/or CIT.
Impact on Others
At the same time that participants were discussing their hopes for the future, there were many who also wanted to have an impact on others. Isaiah knew that they wanted to help people and discussed a variety of ways they might do this by being a “teacher, nurse, or school counselor.” Rene was not sure if they wanted to help people or animals, so they were considering “being a veterinarian or a doctor.” Finally, Super J shared, “I kind of want to help other kids—like to be an orthodontist and help kids and fix their teeth.” It is important to note that the majority of the undergraduate mentors are in human services and helping degrees so this may have influenced their mentees on some level.
Discussion
The overarching question for this study was: What were participants’ lived experiences prior to and after participating in a therapeutic youth mentoring program? In this section, the findings are discussed as they relate to answering this overarching question. Furthermore, a discussion of how these findings support and add to the literature on therapeutic mentoring programs is provided.
Consistent with prior research studies on mentoring programs, the participants in this study shared that having a mentor had a positive impact on their overall behavior (DuBois et al., 2011; Tolan et al., 2014; Weiler et al., 2015). Specifically, participants indicated more adaptive and resilient thinking after participating in the youth mentoring program. Lee et al. (2012) indicated that resilience is not fixed but can be learned and fostered through the protective factors in a child or adolescent’s life. Being able to walk away from a fight or potentially violent situation and asking adults for help were two of the outcomes participants described. A few participants even cited the therapeutic youth mentoring program as the reason why they have developed better coping strategies to better handle the stress they feel in their daily lives.
Another finding consistent with the research on mentoring programs was that participants acknowledged the significance of the primary mentoring relationship (Weiler et al., 2015; Weiss et al., 2019). One significant finding between the initial and final interview was the participants’ shared perspective that they trusted their mentor and the other adults supporting the youth mentoring program (e.g., mentor coaches and counselors). Griffith and Larson (2015) stated that when youth have trusting relationships with adults they become “deliberate agents of their own development” (p. 791). Mentors and CITs supporting the youth mentoring program helped to facilitate this development of trust by being present, participating in dialogue, and leading prosocial activities with the youth.
Many participants also described that because of the trust they developed with their mentor, they were able to also trust other adults in their lives, specifically parents, counselors, and teachers. When adolescents have a trusting relationship with at least one adult in their life, help-seeking behavior increases for the youth as well as their immediate peer group (DeLay et al., 2016). Although the majority of the participants shared the positive impact of having a therapeutic component to this youth mentoring program, five of the 14 participants still shared in the final interview that they were hesitant to meet with a counselor (either at school or at the therapeutic mentoring program). Haddock and colleagues (2017) posited that youth who participated in CC might be embarrassed to share about their experiences with counselors. It is important to note that some of the youth participants also did not make the distinction between CITs and mentor coaches. So, more clarity on the role of CITs in youth mentoring programs may be needed.
However, the mentors in the CC therapeutic mentoring program do learn some basic counseling skills and are also trained in crisis intervention. Although development of the relationship with the counselor may be an area of further examination with therapeutic mentoring programs, it seemed that many of the participants felt comfortable discussing mental health issues with their mentors who were being supported by counseling professionals.
Researchers have discovered that when mentees do develop a positive perception of support, this can lead to an increase in academic attitudes and self-esteem, lower frequencies of problem behaviors, and thinking more positively about the future (Chan et al., 2013; Haddock et al., 2017; Raposa et al., 2019; Weiler et al., 2014). In this current study, not only did participants indicate that their grades improved, but they also began to develop a more balanced outlook concerning school and their future college and career goals. Similarly, Weiss and colleagues (2019) discovered that positive academic mentoring relationships help youth find hope for the future and instill a belief that college and career goals can be reached.
In the initial interview, many participants discussed their perceived barriers and stressors to academic and life success, such as learning and mental health challenges. Haft and colleagues (2019) discovered that participation in a peer-mentoring program resulted in reduced depressive symptoms and increased self-esteem in youth with ADHD and learning disabilities. Relatedly, participants in our current study talked more openly about their strengths and hopes in the final interviews, demonstrating more self-awareness, fewer depressive indicators, and a higher sense of self. Perhaps gaining more hope and a higher sense of self led the participants to also focus on ways in which they might positively impact others. This finding is interesting considering that Briggs et al. (2007) posited that some youth might seek out opportunities to volunteer to help others in order to increase their self-worth.
Implications
There are a number of implications of these findings for counselors, particularly those interested in adding a therapeutic component to traditional mentoring programs. First, although many youth mentoring programs have historically focused on the connection between mentor and mentee (Marshall et al., 2016; Rhodes, 2002; Weiss et al., 2019), the results of this study indicate a significant benefit related to the additional attention to the mental health needs of mentees. Throughout the 12-week period, mentees had the opportunity to engage with mental health professionals in a non-threatening context. This added therapeutic component appeared to provide an additional support toward the connections the youth developed with trusted adults.
Another important implication emerging from the results points to the increase in self-esteem and self-efficacy in the context of the variety of relationships and settings available to the youth mentees. A number of youth reported they could envision themselves going to college in the future after having spent time on a college campus and being exposed to a wider variety of career options. Mentoring programs may find value in creating pathways to career and college exposure supported by trusted adults, such as mental health counselors.
An increase in problem-solving and coping skills is an additional finding with significant implications for youth mentoring programs. Most of the youth interviewed shared varied experiences in the program that resulted in developing new ways of adapting to life stressors. This theme emerged in various ways for the youth, indicating that it may be effective for other programs to integrate a variety of experiences, such as psychoeducational and therapeutic components, that focus on adaptive and resiliency skills.
Mentoring programs are important in aiding struggling youth but often fall short because of a lack of resources and consistency and an inability to address the mental health needs of mentees (Weiler et al., 2013). Including counselors and incorporating a therapeutic component in youth mentoring programs may be beneficial to both youth and their mentors. The implications of adding a therapeutic component in youth mentoring programs and psychoeducational activities on a college campus are extensive and indicate that further development and research are imperative.
Limitations and Future Research
There are several limitations within this current study. One limitation is that youth reported initial reluctance to participate in the research portion of the program. For many youth, participating in an individual qualitative interview was a novel experience and establishing rapport was often contingent on the overall volume of engagement. It may be helpful to allow the youth to have their mentors present during the interview because they are a trusted adult.
Further, a few participants expressed confusion regarding the difference in roles between the mentors, CITs, and mentor coaches. Youth and their caregivers do go through a formal intake process, but perhaps further psychoeducation or an orientation for youth on the different roles, in particular of the CITs, would be helpful. In addition, youth only participated in an average of 50 minutes of 1:1 counseling across the 12 weeks. However, there were many times they were interacting with CITs in small groups and large classroom guidance, similar to school counseling. Future studies with therapeutic mentoring programs could provide better clarification on the role of CITs and perhaps provide more structured weekly 1:1 counseling time with all participants.
Additionally, follow-up interviews with youth participants could help determine if identified change behaviors and attitudes continue to persist over time. In particular, it would be interesting to see if youth were more likely to reach out to their school counselor and/or counselors in the community after participating in a therapeutic youth mentoring program. Several participants mentioned they had never met with their school counselor and/or an outside counselor and that meeting with the CIT at CC was their first experience with individual counseling.
Lastly, future research regarding the experiences of mentors, parents, and key stakeholders in participants’ lives (e.g., teachers, parole officers, case workers, school counselors) could provide greater validity and confirmation of universal themes and experiences generated by the therapeutic youth mentoring program. A follow-up quantitative or mixed methods study could confirm and further validate key findings.
Conclusion
Mentoring programs are an effective mental health intervention for at-promise youth, and the addition of a therapeutic component might further enhance this intervention. A qualitative study was conducted to analyze youth’s lived experiences before and after participating in a therapeutic youth mentoring program. The participants in this study consisted of a diverse group of youth who were interviewed at the beginning and end of a 12-week therapeutic mentoring program. In addition to being paired 1:1 with a mentor, all of the youth had access to individual counseling with CITs throughout the program. The five themes that emerged from the data were life stressors, self-awareness, trusting others, adaptability and resiliency, and hope for the future. Some aspects discussed within these themes included peers/bullying, positive self-image, feeling heard or understood, social-emotional skills, and future careers. Researchers observed an increase in self-esteem, self-efficacy, and problem-solving and coping skills in the youth. Finally, youth participating in the therapeutic mentoring program perceived a benefit of having additional attention given to their mental health needs.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Anastasia, T. T., Skinner, R. L., & Mundhenk, S. E. (2012). Youth mentoring: Program and mentor best practices. Journal of Family & Consumer Sciences, 104(2), 38–44. https://extension.colostate.edu/docs/4h/youth-mentor-practice.pdf
Briggs, E., Landry, T., & Wood, C. (2007). Beyond just being there: An examination of the impact of attitudes, materialism, and self-esteem on the quality of helping behavior in youth volunteers. Journal of Nonprofit & Public Sector Marketing, 18(2), 27–45. https://doi.org/10.1300/J054v18n02_02
Carlson, L. A., & Kees, N. L. (2013). Mental health services in public schools: A preliminary study of school counselor perceptions. Professional School Counseling, 16(4), 211–221. https://doi.org/10.1177/2156759X150160401
Cavell, T. A., Elledge, L. C., Malcolm, K. T., Faith, M. A., & Hughes, J. N. (2009). Relationship quality and the mentoring of aggressive, high-risk children. Journal of Clinical Child & Adolescent Psychology, 38(2), 185–198. https://doi.org/10.1080/15374410802698420
Centers for Disease Control and Prevention. (2019). Preventing adverse childhood experiences: Leveraging the best available evidence. National Center for Injury Prevention and Control.
Chan, C. S., Rhodes, J. E., Howard, W. J., Lowe, S. R., Schwartz, S. E. O., & Herrera, C. (2013). Pathways of influence in school-based mentoring: The mediating role of parent and teacher relationships. Journal of School Psychology, 51(1), 129–142. https://doi.org/10.1016/j.jsp.2012.10.001
Dahlberg, K. (2006). The essence of essences: The search for meaning structures in phenomenological analysis of lifeworld phenomena. International Journal of Qualitative Studies on Health and Well-Being, 1(1), 11–19. https://doi.org/10.1080/17482620500478405
Dashiff, C., DiMicco, W., Myers, B., & Sheppard, K. (2009). Poverty and adolescent mental health. Journal of Child and Adolescent Psychiatric Nursing, 22(1), 23–32. https://doi.org/10.1111/j.1744-6171.2008.00166.x
David-Ferdon, C., Vivolo-Kantor, A. M., Dahlberg, L. L., Marshall, K. J., Rainford, N. & Hall, J. E. (2016). A comprehensive technical package for the prevention of youth violence and associated risk behaviors. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. https://www.cdc.gov/violenceprevention/pdf/yv-technicalpackage.pdf
DeLay, D., Ha, T., Van Ryzin, M., Winter, C., & Dishion, T. (2016). Changing friend selection in middle school: A social network analysis of a randomized intervention study designed to prevent adolescent problem behavior. Prevention Science, 17, 285–294. https://doi.org/10.1007/s11121-015-0605-4
DuBois, D. L., Portillo, N., Rhodes, J. E., Silverthorn, N., & Valentine, J. C. (2011). How effective are mentoring programs for youth? A systematic assessment of the evidence. Psychological Science in the Public Interest, 12(2), 57–91. https://doi.org/10.1177/1529100611414806
Durlak, J. A., Weissberg, R. P., & Pachan, M. (2010). A meta-analysis of after-school programs that seek to promote personal and social skills in children and adolescents. American Journal of Community Psychology, 45(3–4), 294–309. https://doi.org/10.1007/s10464-010-9300-6
Griffith, A. N., & Larson, R. W. (2015). Why trust matters: How confidence in leaders transforms what adolescents gain from youth programs. Journal of Research on Adolescence, 26(4), 790–804. https://doi.org/10.1111/jora.12230
Guba, E. G., & Lincoln, Y. S. (1989). Fourth generation evaluation. SAGE.
Haddock, S., Weiler, L., Krafchick, J., Zimmerman, T. S., McLure, M., & Rudisill, S. (2013). Campus Corps therapeutic mentoring: Making a difference for mentors. Journal of Higher Education Outreach and Engagement, 17(4), 225–256. https://files.eric.ed.gov/fulltext/EJ1018626.pdf
Haddock, S. A., Zimmerman, T. S., Thomas, A. G., Weiler, L. M., Krafchick, J., & Fredrickson, G. J. (2017). A qualitative analysis of mentee experiences in a campus-based mentoring program. Journal of Youth Development, 12(4), 61–80. https://doi.org/10.5195/jyd.2017.496
Haft, S. L., Chen, T., LeBlanc, C., Tencza, F., & Hoeft, F. (2019). Impact of mentoring on socio-emotional and mental health outcomes of youth with learning disabilities and attention-deficit hyperactivity disorder. Child and Adolescent Mental Health, 24(4), 318–328. https://doi.org/10.1111/camh.12331
Johnson, S. B., & Pryce, J. M. (2013). Therapeutic mentoring: Reducing the impact of trauma for foster youth. Child Welfare, 92(3), 9–25.
Karcher, M. J., Nakkula, M. J., & Harris, J. (2005). Developmental mentoring match characteristics: Correspondence between mentors’ and mentees’ assessments of relationship quality. Journal of Primary Prevention, 26(2), 93–110. https://doi.org/10.1007/s10935-005-1847-x
Keller, T. E., & Pryce, J. M. (2012). Different roles and different results: How activity orientations correspond to relationship quality and student outcomes in school-based mentoring. The Journal of Primary Prevention, 33(1), 47–64. https://doi.org/10.1007/s10935-012-0264-1
King, C. A., Gipson, P. Y., Arango, A., Foster, C. E., Clark, M., Ghaziuddin, N., & Stone, D. (2018). LET’s CONNECT community mentorship program for youths with peer social problems: Preliminary findings from a randomized effectiveness trial. Journal of Community Psychology, 46(7), 885–902. https://doi.org/10.1002/jcop.21979
Lee, J. H., Nam, S. K., Kim, A.-R., Kim, B., Lee, M. Y., & Lee, S. M. (2012). Resilience: A meta-analytic approach. Journal of Counseling & Development, 91(3), 269–279. https://doi.org/10.1002/j.1556-6676.2013.00095.x
Liang, B., Spencer, R., West, J., & Rappaport, N. (2013). Expanding the reach of youth mentoring: Partnering with youth for personal growth and social change. Journal of Adolescence, 36(2), 257–267. https://doi.org/10.1016/j.adolescence.2012.10.002
Lincoln, Y. S., & Guba, E. G. (1985). Naturalistic inquiry. SAGE.
Litam, S. D. A., & Hipolito-Delgado, C. P. (2021). When being “essential” illuminates disparities: Counseling clients affected by COVID-19. Journal of Counseling & Development, 99(1), 3–10. https://doi.org/10.1002/jcad.12349
Lund, T. J., Liang, B., Konowitz, L., White, A. E., & DeSilva Mousseau, A. (2019). Quality over quantity?: Mentoring relationships and purpose development among college students. Psychology in the Schools, 56(9), 1472–1481. https://doi.org/10.1002/pits.22284
Marshall, J. H., Davis, M. C., Lawrence, E. C., Peugh, J. L., & Toland, M. D. (2016). Mentors’ perceived program support scale: Development and initial validation. Journal of Community Psychology, 44(3), 342–357.
McIntosh, P. (2003). White privilege: Unpacking the invisible knapsack. In S. Plous (Ed.), Understanding prejudice and discrimination (pp. 191–196). McGraw-Hill.
McKenzie, L. (2019). No more ‘at-risk’ students in California. Inside Higher Ed. https://bit.ly/InsideHigherEdatrisk
Merriam, S. B. (1998). Qualitative research and case study applications in education (1st ed.). Jossey-Bass.
Patel, V., Kieling, C., Maulik, P. K., & Divan, G. (2013). Improving access to care for children with mental disorders: A global perspective. Archives of Disease in Childhood, 98(5), 323–327. https://doi.org/10.1136/archdischild-2012-302079
Raposa, E. B., Rhodes, J., Stams, G. J. J. M., Card, N., Burton, S., Schwartz, S., Yoviene Sykes, L. A., Kanchewa, S., Kupersmidt, J., & Hussain, S. (2019). The effects of youth mentoring programs: A meta-analysis of outcome studies. Journal of Youth and Adolescence, 48(3), 423–443. https://doi.org/10.1007/s10964-019-00982-8
Rhodes, J. E. (2002). Stand by me: The risks and rewards of mentoring today’s youth. Harvard University Press.
Sacco, F., Jr., Pike, N., & Bourque, J. L. (2014). Therapeutic mentoring: Mentalization training in the community. International Journal of Applied Psychoanalytic Studies, 11(2), 138–150. https://doi.org/10.1002/aps.1405
Schoeneberger, J. A. (2012). Longitudinal attendance patterns: Developing high school dropouts. The Clearing House, 85(1), 7–14.
Stark, C., Wehrman, J., Stutey, D. M., Solis, A., Severn, K., Cammell, M., Gloden, H., Enkler, K., Notestine, L., & Palacios, A. (2021). Therapeutic mentoring for at-promise youth: A grounded theory study of mentors’ adaptation during the COVID-19 crisis. Journal of Human Services: Special Interdisciplinary Issue, 40(2), 116–132.
Stutey, D. M., Givens, J., Cureton, J. L., & Henderson, A. J. (2020). The practice of bridling: Maintaining openness in phenomenological research. Journal of Humanistic Counseling, 59(2), 144–156. https://doi.org/10.1002/johc.12135
Tolan, P. H., Henry, D. B., Schoeny, M. S., Lovegrove, P., & Nichols, E. (2014). Mentoring programs to affect delinquency and associated outcomes of youth at risk: A comprehensive meta-analytic review. Journal of Experimental Criminology, 10, 179–206. https://doi.org/10.1007/s11292-013-9181-4
Trusty, J. (2011). Quantitative articles: Developing studies for publication in counseling journals. Journal of Counseling & Development, 89(3), 261–267. https://doi.org/10.1002/j.1556-6678.2011.tb00087.x
Vagle, M. D. (2009). Validity as intended: ‘Bursting forth toward’ bridling in phenomenological research. International Journal of Qualitative Studies in Education, 22(5), 585–605. https://doi.org/10.1080/09518390903048784
Weiler, L. M., Boat, A. A., & Haddock, S. A. (2019). Youth risk and mentoring relationship quality: The moderating effect of program experiences. American Journal of Community Psychology, 63(1–2), 73–87. https://doi.org/10.1002/ajcp.12304
Weiler, L. M., Chesmore, A. A., Pryce, J., Haddock, S. A., & Rhodes, T. (2019). Mentor response to youth academic support–seeking behavior: Does attunement matter? Youth & Society, 51(4), 548–569. https://doi.org/10.1177/0044118X17697235
Weiler, L. M., Haddock, S. A., Zimmerman, T. S., Henry, K. L., Krafchick, J. L., & Youngblade, L. M. (2015). Time-limited, structured youth mentoring and adolescent problem behaviors. Applied Developmental Science, 19(4), 196–205. https://doi.org/10.1080/10888691.2015.1014484
Weiler, L., Haddock, S., Zimmerman, T. S., Krafchick, J., Henry, K., & Rudisill, S. (2013). Benefits derived by college students from mentoring at-risk youth in a service-learning course. American Journal of Community Psychology, 52(3–4), 236–248. https://doi.org/10.1007/s10464-013-9589-z
Weiler, L. M., Zarich, K. J., Haddock, S. A., Krafchick, J. L., & Zimmerman, T. S. (2014). A comprehensive model of mentor experiences: Perceptions, strategies, and outcomes. Journal of Community Psychology, 42(5), 593–608. https://doi.org/10.1002/jcop.21640
Weiss, S., Harder, J., Bratiotis, C., & Nguyen, E. (2019). Youth perceptions of a school-based mentoring program. Education and Urban Society, 51(3), 423–437. https://doi.org/10.1177/0013124517722830
Appendix
Pre Semi-Structured Interview
- Tell me what you already know about Campus Connections or having a mentor.
- Describe a typical day or week at school.
- What do you enjoy?
- What is something you struggle with?
- What are some ways you think having a mentor could help you (at school, home, in life)?
- What are your future goals or plans?
- For middle school
- High school
- After high school
- What is something that is preventing you from achieving your goals or future plans?
- How could your mentor help you with these challenges?
- Tell me about your thoughts/feelings about being on a college campus.
- What kind of jobs or careers are you thinking about?
- What are your thoughts on meeting with a counselor?
- Can you describe a time when a counselor helped you?
- How do you think people would describe you?
- Teachers?
- Parent or guardians?
- Peers?
- How would you describe yourself?
- What is something you wish people knew about you?
Post Semi-Structured Interview
** Remind the student of the pseudonym they chose and ask if they want to keep or change this.
- Tell me what you now know about Campus Connections and having a mentor.
- How would you describe your mentor?
- Tell me a story about your favorite thing about Campus Connections? Least favorite?
- Describe a typical day or week at school.
- What do you enjoy?
- What is something you struggle with?
- What are some ways you think having a mentor and participating in Campus Connections helped you?
- At school
- At home
- In life
- What are your future goals or plans?
- For middle school
- High school
- After high school
- What is something that has been preventing you from achieving your goals or future plans?
- Describe how your mentor helped you with these challenges.
- Tell me about your thoughts/feelings about being on a college campus.
- What kind of jobs or careers are you thinking about?
- What are your thoughts on meeting with a counselor?
- Can you describe a time when a counselor helped you?
- How do you think people would describe you?
- Teachers?
- Parent or guardians?
- Peers?
- Mentor?
- Counselor?
- How would you describe yourself?
- Are there things about you that you think have changed/improved since joining Campus Connections?
- What is something you wish people knew about you?
- What else would you like me or others to know about Campus Connections?
Diane M. Stutey, PhD, NCC, LPC, RPT-S, is an assistant professor and department chair at the University of Colorado Colorado Springs. Abigail E. Solis, MA, is a clinical mental health counselor at Colorado Motion. Kim Severn, MA, LPC, is an instructor at the University of Colorado Colorado Springs. Lori Notestine, PhD, LPC, is an instructor and program coordinator at the University of Colorado Colorado Springs. Kodi L. Enkler is a licensed school counselor at Swigert Aerospace Academy. Joseph Wehrman, PhD, LPC, is a professor at the University of Colorado Colorado Springs. Molly Cammell, MA, is Campus Connections program manager at the University of Colorado Colorado Springs. Correspondence may be addressed to Diane M. Stutey, 1420 Austin Bluffs Parkway, Colorado Springs, CO 80918, dstutey@uccs.edu.
Feb 7, 2022 | Volume 12 - Issue 1
Gregory T. Hatchett
The addition of disruptive mood dysregulation disorder (DMDD) to the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) was a controversial decision in 2013 and one that continues to the present. Researchers have found that DMDD exhibits both poor interrater reliability and discriminant validity from other common childhood-onset disorders, most notably oppositional defiant disorder (ODD). Research also indicates that DMDD might be better conceptualized as a component of ODD, and consistent with such a conceptualization, experts have recommended that effective treatments for ODD be applied to youth who fit the diagnostic pattern of DMDD. The purpose of this article is to help readers understand the problematic diagnostic validity associated with DMDD and to present recommended treatment strategies for working with youth who fit this challenging symptom profile.
Keywords: disruptive mood dysregulation disorder, oppositional defiant disorder, conceptualization, diagnostic validity, youth
A pattern of emotional and behavioral dysregulation—characterized by severe irritability, temper outbursts, and aggressive behavior—is one of the most common reasons that children and adolescents are referred to mental health service providers (Axelson et al., 2012; Brotman et al., 2017; Stringaris et al., 2018) and a common antecedent to inpatient hospitalization (Chase et al., 2020; Rao, 2014). Despite the prevalence and severity of these associated symptoms, mental health professionals have often disagreed as to how children and adolescents who fit this symptom profile should be conceptualized and properly diagnosed. Over the years, chronic irritability and temper dysregulation have been conceptualized as associated features of externalizing disorders (Carlson, 1998), developmental variations of early-onset bipolar disorder (Biederman et al., 2000), and core features of an experimental research phenotype (Leibenluft et al., 2003; Rich et al., 2005; Stringaris et al., 2010).
In 2013, the American Psychiatric Association (APA) provided a new diagnostic home for youth with chronic and severe irritability in the depressive disorders chapter in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; APA, 2013). This new disorder—disruptive mood dysregulation disorder (DMDD)—was specifically added to the DSM-5 to prevent clinicians from overdiagnosing a bipolar and related disorder in children and adolescents who exhibited non-episodic irritability and temper outbursts. Beginning in the 1990s, there began an exponential increase in the number of children and adolescents who were diagnosed with bipolar disorder. As just one example of this pattern, Moreno et al. (2007) reported a 40-fold increase of the number of outpatient office visits for children and adolescents treated for bipolar disorder between 1995–1996 and 2002–2003. Not only was this increase unusual from an epidemiological perspective (Van Meter et al., 2011), but researchers also began to accumulate evidence that these youth did not match the profile of either youth or adults with traditional bipolar disorder (Leibenluft, 2011; Towbin et al., 2013). To better characterize children and adolescents who exhibited chronic irritability and temper outbursts, researchers at the National Institute of Mental Health (Leibenluft et al., 2003) developed a new diagnostic phenotype, severe emotional dysregulation (SMD), to differentiate this symptom pattern from traditional bipolar disorder. SMD subsequently became the foundation for the inclusion of DMDD in the DSM-5 (APA, 2013).
Many experts disagree about DMDD as a valid and coherent diagnostic category. However, there seems to be a strong consensus that many children and adolescents are severely impaired because of chronic irritability and severe temper dysregulation (Copeland et al., 2014; Rao, 2014). Although early estimates indicate that only 1%–3% of children and adolescents may meet the full diagnostic criteria for DMDD (Copeland et al., 2013), many more may present with at least subthreshold symptoms of the disorder (Baweja, Mayes, et al., 2016; Freeman et al., 2016). Thus, counselors, especially those working in clinical settings, will likely find themselves working with many children and adolescents who exhibit symptoms of DMDD, symptoms which need to be carefully evaluated as part of any differential diagnostic process. To provide the best possible services for this population, counselors need to be familiar with the current literature on both the diagnosis and treatment of DMDD. Consequently, this article summarizes these current DMDD topics and presents treatment recommendations for working with youth diagnosed with DMDD. Because it is important for counselors to understand the questionable diagnostic validity of DMDD and how these diagnostic limitations should inform the treatment planning process, this topic will be preceded by criticisms of DMDD as a valid mental disorder. Also discussed are the challenges of diagnosing youth who present with chronic emotional and behavioral dysregulation.
The Diagnosis of DMDD
The diagnostic criteria and decisional rules for DMDD in the DSM-5 (APA, 2013) are rather detailed, so only a summary will be provided here. (Readers should consult pages 156–160 in the DSM-5 for more detailed information.) The core diagnostic features for DMDD include recurrent (3 or more times a week) temper outbursts that are developmentally inappropriate, severe, and disproportionate to any identifiable stressor along with the persistence of a chronically irritable or angry mood between these temper outbursts—a disruption in mood that is noticeable by others. These symptoms must have begun before the age of 10, persist for a minimum of a year (with no more than 3 consecutive months of symptom-free periods), and be present in at least two out of three settings (i.e., home, school, peer relationships). According to the DSM-5, this diagnosis should not be made if these symptoms occur exclusively during a major depressive episode or if the symptoms are better explained by another mental disorder, such as autism spectrum disorder. Also, a diagnosis of DMDD cannot be given concurrently with oppositional defiant disorder (ODD), bipolar disorder, or intermittent explosive disorder. If a child meets the diagnostic criteria for both DMDD and ODD, only DMDD should be given. As mentioned previously, DMDD was specifically added to the DSM-5 to prevent clinicians from overdiagnosing bipolar and related disorder in children and adolescents who exhibit non-episodic irritability and temper outbursts. However, at first glance, a youth who meets the diagnostic criteria for DMDD may be suspected of having a bipolar and related disorder. Thus, it is important for counselors to recognize the fundamental differences between the two disorder classifications.
As explained above, in DMDD, a child or adolescent experiences non-episodic irritability that is punctuated by severe and disproportionate temper outbursts. This symptom presentation must occur for at least 365 days, and during the year, have no more than a 3-month period in which the child or adolescent does not experience the core features of the disorder. In contrast, youth who meet the diagnostic criteria for bipolar disorder experience distinctive episodes of mania (at least 7 days), hypomania (at least 4 days), or depression (at least 14 days). Although irritability and temper outbursts can certainly occur in the context of a manic or hypomanic episode, there are additional symptoms that must also be present. Specifically, the irritability or temper outbursts should be episodic, accompanied by an increase in goal-directed activity/energy, and include additional symptoms, such as grandiosity, decreased need for sleep, pressured speech, racing thoughts, or reckless impulsivity (APA, 2013). More information on the differential diagnosis of bipolar disorder from DMDD and other conditions can be found in Hatchett and Motley (2016).
Diagnostic Validity of DMDD
Many have argued that adding DMDD to the DSM-5 traded one problem—overdiagnosis of bipolar disorder—for another: a poorly conceptualized diagnostic construct lacking any evidence-based treatments (e.g., S. C. Evans et al., 2017; Freeman et al., 2016; Parker & Tavella, 2018). As Malhi and Bell (2019) recently observed, “more than half a decade later, the ‘creation’ of this new diagnostic entity [DMDD] has not provided any novel insights or greater understanding and is yet to demonstrate any tangible benefits” (p. 706).
Though DMDD has been criticized for its poor interrater reliability (Regier et al., 2013) and low temporal stability across time (e.g., Axelson et al., 2012), the strongest criticism of DMDD has been directed toward its standing as an independent and coherent diagnostic construct, a concern that was not only present at the time of its introduction in the DSM-5, but one that has been bolstered by subsequent research since the publication of the DSM-5 in 2013. Ironically, the evidentiary basis for including DMDD in the DSM-5 was not based on studies of children and adolescents who actually matched the specific diagnostic criteria for DMDD. Instead, the research support for DMDD was inferred from research conducted on SMD (Baweja, Mayes, et al., 2016; Bruno et al., 2019; Rao, 2014; Towbin et al., 2013). As mentioned previously, the phenotype of SMD was developed by researchers at the National Institute of Mental Health (Leibenluft et al., 2003) to provide an alternative conceptualization to bipolar disorder for youth who exhibited chronic and severe irritability, temper dysregulation, and hyperarousal. However, there are important differences between the diagnostic criteria for SMD and DMDD. Compared to the diagnostic criteria for DMDD, SMD includes different age parameters, the presence of an abnormal mood characterized by anger or sadness, different exclusion criteria, and most importantly, the presence of hyperarousal (e.g., insomnia, agitation, distractibility; Leibenluft, 2011). As S. C. Evans et al. (2017) pointed out, “Given the differences between the operationalization of SMD in the literature and the definition of DMDD, virtually no evidence regarding DMDD existed at the time of its inclusion in DSM-5” (p. 33).
Consistent with these differences, researchers have found low levels of correspondence between the two syndromes. For example, Copeland et al. (2013) reported that only 38.9% of those who met the criteria for SMD also met the diagnostic criteria for DMDD. These differences have important implications for the treatment planning process. Specifically, it is unclear whether any of the interventions that have been found to be helpful for youth with SMD (e.g., Towbin et al., 2020) will generalize to youth who match the different diagnostic profile for DMDD (Benarous et al., 2017).
Furthermore, since the publication of the DSM-5 in 2013, researchers have increasingly challenged the validity of DMDD as a stand-alone diagnostic construct (Freeman et al., 2016). For one, there is very little evidence to suggest that DMDD can be reliably differentiated from other common childhood-onset disorders (S. C. Evans et al., 2017; Malhi & Bell, 2019). Several of the core symptoms of DMDD—chronic irritability and recurrent temper outbursts—are not exclusive to DMDD, but rather represent transdiagnostic symptoms often present in many other disorders, such as ODD, generalized anxiety disorder, depression, autism spectrum disorder, bipolar disorder, and post-traumatic stress disorder (e.g., Stringaris et al., 2018). As Parker and Tavella (2018) pointed out, “Those who meet the criteria for DMDD may in fact have a conduct disorder, ODD, attention deficit hyperactivity disorder (ADHD), or any of myriad other behavioral disorders” (p. 815). However, on the one hand, the diagnostic criteria for DMDD in the DSM-5 is very extensive and detailed, especially compared to what is commonly delineated for many other disorders in the DSM-5. Clinicians who carefully follow these detailed criteria and decisional rules should, in theory, arrive at valid and reliable diagnoses of DMDD. Yet, in real practice, the diagnostic process is often plagued by careless errors and clinician biases (Garb, 1998; Lacasse, 2014). Consequently, the issue becomes how well clinicians can apply these criteria in often complex clinical situations.
More research is needed on how well counselors and other clinicians can reliably diagnose DMDD and differentiate it from other conditions in ordinary practice settings. Concerns about the diagnostic validity of DMDD have been most pronounced in the differentiation of DMDD from ODD. In the DSM-5 (APA, 2013), a diagnosis of DMDD automatically supersedes a diagnosis of ODD; thus, these two diagnoses cannot be given concurrently. However, when researchers have removed this exclusionary rule, they have found that nearly all the children and adolescents who met the diagnostic criteria for DMDD also met the diagnostic criteria for ODD (Axelson et al., 2012; Freeman et al., 2016; Mayes et al., 2016). As just one example, Mayes, Waxmonsky, et al. (2015) reported that 91% of the children who met the criteria for DMDD in their study also qualified for a diagnosis of ODD. However, the reverse is not true. Researchers have found that diagnoses of ODD commonly occur in the absence of DMDD. Approximately one-third of children and adolescents who meet diagnostic criteria for ODD do not have significant symptoms of DMDD (Mayes et al., 2016).
According to the hierarchy or parsimony principle in the DSM-5 (APA, 2013), a clinician should diagnose the most severe disorder that best captures the multitude of symptoms that a client is experiencing instead of adding on several more minor diagnoses to the diagnostic record. For example, children and adolescents who meet the diagnostic criteria for autism spectrum disorder simultaneously meet the diagnostic criteria for social communication disorder. Therefore, an additional diagnosis of social communication disorder is unnecessary. Likewise, in the DSM-5, a diagnosis of DMDD is higher on the diagnostic hierarchy than ODD, and thus many of the symptoms of ODD are subsumed under a diagnosis of DMDD. For clinicians who carefully follow the diagnostic rules of the DSM-5, both negative affectivity and oppositional behavior can be recognized and targeted as part of a treatment plan for a youth with DMDD.
For an alternative point of view, some researchers have expressed the concern that a single, overruling diagnosis of DMDD will fail to adequately acknowledge the behavioral problems associated with ODD, resulting in suboptimal treatment planning decisions (S. C. Evans et al., 2017; Mayes et al., 2016). Mayes et al. (2016) pointed out that a diagnosis of DMDD fails to acknowledge many of the disruptive behavioral components of ODD that are nearly always present in children and adolescents who meet the diagnostic criteria for DMDD. Likewise, S. C. Evans et al. (2017) argued that
treating DMDD as a Depressive Disorder—and withholding a diagnosis of ODD, per DSM-5 hierarchical rules—may lead clinicians to conceptualize these youth as having a mood disorder rather than a behavior disorder. For primary care providers and pediatricians, treating DMDD as a mood disorder and removing the ODD label may both decrease referrals for behavioral interventions that are well established (e.g., parent management training) and increase the administration of psychotropic medications such as antidepressants, antipsychotics, and mood stabilizers, for which evidence is limited. (p. 39)
However, the concerns just mentioned may reveal more about problems in the correct use and application of the DSM-5 by clinicians rather than problems inherent in diagnostic rules prescribed by the DSM-5.
Because of the transdiagnostic nature of DMDD symptoms (e.g., Parker & Tavella, 2018), several experts have recommended that DMDD be recognized as either a subtype or specifier under other DSM-5 diagnoses (Mayes, Mathiowetz, et al., 2015), most often as a subtype or specifier under ODD (S. C. Evans et al., 2017; Malhi & Bell, 2019; Mayes et al., 2016; Mayes, Waxmonsky, et al., 2015). This was the approach recently taken by the World Health Organization (2019) in the 11th edition of the International Statistical Classification of Diseases and Related Health Problems (ICD-11). In the ICD-11, clinicians have the option to diagnose a youth with oppositional defiant disorder with or without chronic irritability-anger. Thus, this diagnostic code allows clinicians to concurrently recognize both symptoms of emotional dysregulation and symptoms of argumentative, oppositional, and vindictive behavior. However, at the time of this writing, the ICD-11 has not been adopted in the United States, so counselors in the United States are still using the DSM-5 (APA, 2013) and the ICD-10 (World Health Organization, 2016).
On the other hand, some have cautioned against the use of DMDD as only a subtype or specifier under ODD (e.g., Benarous et al., 2017; Stringaris et al., 2018). Brotman et al. (2017) expressed the concern that many clinicians do not record available specifiers in diagnostic records, and consequently, children and adolescents who are diagnosed with ODD under the DSM-5 might not receive targeted interventions for symptoms of severe irritability and temper outbursts. At the very least, perhaps clinicians should be allowed to diagnose DMDD and ODD concurrently.
Another concern in the differential diagnosis of DMDD is potential racial/ethnic bias. As a depressive disorder in the DSM-5 (APA, 2013), DMDD is conceptualized as an internalizing disorder, whereas ODD is conceptualized as an externalizing or disruptive behavior disorder. Researchers have found that African American youth are more likely to be diagnosed with externalizing disorders, whereas European American youth are more likely to be diagnosed with internalizing disorders (e.g., Fadus et al., 2020; Minsky et al., 2006). Though this research has not yet been replicated specifically in the diagnosis of DMDD, prior research indicates that African American youth may be less likely to be identified as having DMDD and may not receive adequate treatment for potential depressive symptoms. Furthermore, researchers have found that African Americans and other minority groups who experience higher rates of racial/ethnic discrimination also experience more mental health and psychosocial functioning difficulties compared to those with lower experienced rates of racial/ethnic discrimination (Tobler et al., 2013). Consequently, counselors should evaluate the extent to which irritability and aggression among minority youth are associated with experiences of discrimination as opposed to internal psychopathology implicit in the DSM framework (e.g., Carter et al., 2019; Mouzon et al., 2017).
Treatment Planning Strategies
Diagnostic Considerations
Certainly, the main source of information for the proper diagnosis of DMDD is the explicit diagnostic criteria and decision rules in the DSM-5 (APA, 2013). To document these diagnostic criteria, counselors might consider using one or more of the cross-cutting measures included in Section III of the DSM-5 (pp. 733–741). Outside the DSM-5, there are currently few diagnostic tools for counselors to use in confirming a diagnosis of DMDD (Baweja, Mayes, et al., 2016). The assessment tools most often used in the research literature measure general irritability, such as the Affective Reactivity Index (Stringaris et al., 2012) or the Clinician Affective Reactivity Index (Haller et al., 2020). Specific to the diagnosis of DMDD, Wiggins et al. (2016) developed a DMDD module that was used in conjunction with the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children–Present and Lifetime Version (K-SADS-PL; Kaufman et al., 1997). However, this is a new module that has not undergone extensive psychometric evaluation.
In addition to confirming a diagnosis of DMDD, counselors should also assess for common comorbid mental disorders (Mayes et al., 2016). Youth who meet the diagnostic criteria for DMDD almost always have comorbid disorders, most often attention-deficit/hyperactivity disorder (ADHD), conduct disorder, and specific learning disorders (Althoff et al., 2016; Bruno et al., 2019). Though one cannot technically diagnose DMDD and ODD concurrently under DSM-5 rules, counselors should also carefully assess and document symptoms of ODD, which will likely be appropriate targets in the treatment planning process (e.g., S. C. Evans et al., 2017).
Though there are currently not any clearly validated inventories for directly assessing DMDD, there are several inventories available for assessing the comorbid conditions that often accompany the DMDD symptom profile. In addition to the previously mentioned cross-cutting measures in Section III of the DSM-5 (APA, 2013), there are several commercially available inventories for assessing symptoms of ODD, such as the Achenbach Series (Achenbach & Rescorla, 2006) or the Child and Adolescent Disruptive Behavior Inventory (Cianchetti et al., 2013). Again, though a diagnosis of DMDD technically overrides a diagnosis of ODD, symptoms of ODD will likely be present and a major target area of a counseling plan. Administration of a validated measure of ODD will not only help counselors identify symptom severity at the beginning of the counseling process, but can also be repeatedly administered throughout the counseling process to evaluate areas of improvement and areas that need additional attention. This same assessment process could also be used for other conditions comorbid with DMDD. Counselors might use the Conner’s Rating Scales (Conners, 1999) to assess for ADHD and other associated symptoms, such as aggression and learning problems. Symptoms of depression can be evaluated through administering the Children’s Depression Inventory (Sitarenios & Kovacs, 1999) or the Beck Depression Inventory with older adolescents (Beck et al., 1996). As is often the case, an assessment and treatment protocol that targets specific symptoms may be more effective than one that tries to remediate global diagnostic constructs, such as DMDD (e.g., Weisz & Kazdin, 2017).
Evidence-Based Treatments for DMDD
This next section will review the currently available research on both the use of pharmacotherapy and psychosocial interventions in working with youth who meet the diagnostic criteria for DMDD. This will be followed by a review of evidence-based treatments for related clinical conditions and will end with a summary of general treatment recommendations for working with youth diagnosed with DMDD.
Psychopharmacology
Researchers have conducted only a few studies on the effectiveness of pharmacotherapy in reducing symptoms of DMDD. For youth diagnosed with both DMDD and ADHD, researchers have found some evidence for the effectiveness of psychostimulant monotherapy (Baweja, Belin, et al., 2016; Winters et al., 2018) as well as the combination of methylphenidate with aripiprazole (Pan et al., 2018); however, in a small (n = 12) retrospective study, Ozyurt et al. (2017) found that methylphenidate resulted in increased irritability in children diagnosed with both DMDD and ADHD. Most recently, Rice et al. (2019) found some effectiveness for the use of amantadine with a 12-year-old diagnosed with DMDD who was admitted to a psychiatric hospital. Consistent with this limited research base, there are currently not any medications that have received Food and Drug Administration approval for treating children and adolescents specifically diagnosed with DMDD.
Psychosocial Interventions
Parallel to the research on pharmacological interventions, very little research has been published on the use of psychosocial interventions with youth who meet the diagnostic criteria for DMDD. Perepletchikova et al. (2017) reported that a modified version of dialectical behavior therapy, which also included a parent training module, was more effective than treatment as usual (TAU) in improving irritability, temper outbursts, and overall functioning among youth diagnosed with DMDD. In a subsequent study, Miller et al. (2018) reported that a modified version of interpersonal psychotherapy—interpersonal psychotherapy for mood and behavior dysregulation (IPT-MBD)—was more effective than TAU in reducing irritability and angry outbursts. However, both treatment groups had equivalent scores on measures of depression and anxiety by the end of treatment. There have also been a couple of case studies published in the literature. Tudor et al. (2016) reported that cognitive behavioral therapy was effective in reducing irritability and aggression in a 9-year-old girl diagnosed with DMDD and ADHD. In another case study report, Linke et al. (2020) reported that an exposure-based, cognitive behavioral model was effective in treating an 11-year-old boy diagnosed with both DMDD and ADHD.
Interventions for Comorbid Disorders
In the absence of evidence-based treatments for DMDD, many experts have recommended that clinicians select evidence-based treatments for disorders that are often comorbid with DMDD, most commonly ODD (Baweja, Mayes, et al., 2016). As Freeman et al. (2016) recommended, “Until a better evidence base exists, clinicians should be cautious when diagnosing youth with DMDD, and treatment often might best start with using evidence-based practices for ODD” (p. 129). This recommendation is also consistent with the ICD-11, in which the core features of DMDD are conceptualized as a potential subtype of ODD. There are several evidence-based interventions for oppositional behavior in general and ODD in particular, such as cognitive therapy (Greene et al., 2004), parent management training (Costin & Chambers, 2007), and multisystemic therapy (Asscher et al., 2013). There are also several established treatments for ADHD, a condition that is also often comorbid with DMDD. Effective interventions include the use of psychostimulants (Castells et al., 2020) as well as several variations of behavior therapy (S. W. Evans et al., 2014).
Treatments for General Irritability
Another source of information for selecting potentially effective treatments for youth with DMDD may be found in research programs that have targeted transdiagnostic symptoms of irritability and aggressive behavior (Roy et al., 2014). Some evidence suggests that cognitive behavior therapy may be effective in reducing general symptoms of irritability in youth (Derella et al., 2020; S. C. Evans et al., 2020; Sukhodolsky et al., 2016). Along this line, Sukhodolsky and Scahill (2012) have published a treatment manual for working with youth and their families who struggle with anger and aggression. The competencies covered in this manual include, but are not limited to, relaxation training, emotional regulation, problem solving, and social skills training. With regard to pharmacotherapy, Tourian et al. (2015) conducted a literature review on the use of pharmacological agents in reducing symptoms of chronic irritability, aggression, and temper outbursts in children and adolescents. Based on their review, they found that methylphenidate, risperidone, and divalproex may offer some measure of effectiveness in reducing irritability and aggressive behavior.
General Treatment Recommendations
As mentioned earlier, one of the criticisms of adding DMDD to the DSM-5 was that DMDD provided clinicians with a new diagnostic label in the absence of any evidence-based treatments (e.g., Parker & Tavella, 2018). As evidenced by this review, this criticism continues to be valid. Based on the limited treatment literature for DMDD and the larger literature for disruptive behavior disorders, only a few general guidelines seem suitable at this time. For one, experts generally recommend that treatment commence with the use of cognitive behavior therapy combined with parent management training (Brotman et al., 2017; Bruno et al., 2019; Roy et al., 2014; Stringaris et al., 2018). As previously mentioned, recent research indicates that dialectical behavior therapy (Perepletchikova et al., 2017) and interpersonal therapy (Miller et al., 2018) may also be promising. Second, if there is comorbid ADHD, it is recommended that pharmacotherapy begin with the use of a psychostimulant (Blader et al., 2016; Roy et al., 2014). Mood stabilizers and atypical antipsychotics may also be considered if psychostimulants prove ineffective or in cases where there is a need for a quick reduction in severe irritability or aggressive behavior (e.g., Baweja, Mayes, et al., 2016; Roy et al., 2014). Stringaris et al. (2018) recommended that these medications should be used very cautiously:
Our recommendation is that antipsychotic prescriptions be reserved for those young people who have not responded to a series of other treatments and that the prescription be for a short period of time during which health indicators such as weight are tightly monitored. (p. 733)
Third, as mentioned previously, counselors should also consider the use of evidence-based interventions for ODD, a disorder that substantially overlaps with DMDD (e.g., Freeman et al., 2016).
Concluding Comments
The addition of DMDD to the fifth edition of the DSM was a controversial decision, a dispute that continues to the present. At the time of its inclusion in the DSM-5, there was no solid evidentiary foundation for including DMDD as a new diagnostic category (S. C. Evans et al., 2017). Evidence for the validity of DMDD was inferred from the research on SMD, a distinct phenotype (Bruno et al., 2019). Subsequent research since the publication of the DSM-5 in 2013 on the nature of DMDD has demonstrated that DMDD lacks discriminant validity from other common disorders, most notably ODD (Parker & Tavella, 2018).
As this literature has revealed, there continues to be a paucity of evidence-based treatments for children and adolescents who fit the common symptom profile of DMDD. Although evidence-based treatments for comorbid disorders offer promise, it is important that clinicians and researchers develop and validate psychosocial and pharmacological treatments that directly target the core symptoms of DMDD (Baweja, Mayes, et al., 2016). Yet, in addition to more effective remediation strategies (i.e., tertiary prevention), there is also a clear need for prevention processes that can identify and effectively help those children and adolescents who exhibit severe and chronic irritability (Stringaris & Goodman, 2009). Though research is still emerging, a diagnosis of DMDD seems to be a precursor for a lifetime of impairment. Youth with DMDD are at high risk for developing numerous mental health problems in adulthood, including major depressive disorder, persistent depressive disorder (dysthymia), and generalized anxiety disorder (Copeland et al., 2014; Stringaris et al., 2009; Stringaris & Goodman, 2009). The development and evaluation of such prevention processes should be taken up by professional counselors in both school and community settings, a responsibility that is part of our professional identity (Albee & Ryan-Finn, 1993).
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Achenbach, T. M., & Rescorla, L. A. (2006). The Achenbach System of Empirically Based Assessment. In R. P. Archer (Ed.), Forensic uses of clinical assessment instruments (pp. 229–262). Routledge.
Albee, G. W., & Ryan-Finn, K. D. (1993). An overview of primary prevention. Journal of Counseling & Development, 72(2), 115–123. https://doi.org/10.1002/j.1556-6676.1993.tb00909.x
Althoff, R. R., Crehan, E. T., He, J.-P., Burstein, M., Hudziak, J. J., & Merikangas, K. R. (2016). Disruptive mood dysregulation disorder at ages 13–18: Results from the National Comorbidity Survey—Adolescent Supplement. Journal of Child and Adolescent Psychopharmacology, 26(2), 107–113. https://doi.org/10.1089/cap.2015.0038
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
Asscher, J. J., Deković, M., Manders, W. A., van der Laan, P. H., Prins, P. J. M., & Dutch MST Cost-Effectiveness Study Group. (2013). A randomized controlled trial of the effectiveness of multisystemic therapy in the Netherlands: Post-treatment changes and moderator effects. Journal of Experimental Criminology, 9, 169–187. https://doi.org/10.1007/s11292-012-9165-9
Axelson, D., Findling, R. L., Fristad, M. A., Kowatch, R. A., Youngstrom, E. A., Horwitz, S. M., Arnold, L. E., Frazier, T. W., Ryan, N., Demeter, C., Gill, M. K., Hauser-Harrington, J. C., Depew, J., Kennedy, S. M., Gron, B. A., Rowles, B. M., & Birmaher, B. (2012). Examining the proposed disruptive mood dysregulation disorder diagnosis in children in the Longitudinal Assessment of Manic Symptoms Study. The Journal of Clinical Psychiatry, 73(10), 1342–1350. https://doi.org/10.4088/JCP.12m07674
Baweja, R., Belin, P. J., Humphrey, H. H., Babocsai, L., Pariseau, M. E., Waschbusch, D. A., Hoffman, M. T., Akinnusi, O. O., Haak, J. L., Pelham, W. E., & Waxmonsky, J. G. (2016). The effectiveness and tolerability of central nervous system stimulants in school-age children with attention-deficit/hyperactivity disorder and disruptive mood dysregulation disorder across home and school. Journal of Child and Adolescent Psychopharmacology, 26(2), 154–163. https://doi.org/10.1089/cap.2015.0053
Baweja, R., Mayes, S. D., Hameed, U., & Waxmonsky, J. G. (2016). Disruptive mood dysregulation disorder: Current insights. Neuropsychiatric Disease and Treatment, 12, 2115–2124. https://doi.org/10.2147/NDT.S100312
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Manual for the Beck Depression Inventory-II (2nd ed.). Psychological Corporation.
Benarous, X., Consoli, A., Guilé, J.-M., de La Rivière, S. G., Cohen, D., & Olliac, B. (2017). Evidence-based treatments for youths with severely dysregulated mood: A qualitative systematic review of trials for SMD and DMDD. European Child & Adolescent Psychiatry, 26, 5–23. https://doi.org/10.1007/s00787-016-0907-5
Biederman, J., Mick, E., Faraone, S. V., Spencer, T., Wilens, T. E., & Wozniak, J. (2000). Pediatric mania: A developmental subtype of bipolar disorder? Biological Psychiatry, 48(6), 458–466.
https://doi.org/10.1016/S0006-3223(00)00911-2
Blader, J. C., Pliszka, S. R., Kafantaris, V., Sauder, C., Posner, J., Foley, C. A., Carlson, G. A., Crowell, J. A., & Margulies, D. M. (2016). Prevalence and treatment outcomes of persistent negative mood among children with attention-deficit/hyperactivity disorder and aggressive behavior. Journal of Child and Adolescent Psychopharmacology, 26(2), 164–173. https://doi.org/10.1089/cap.2015.0112
Brotman, M. A., Kircanski, K., & Leibenluft, E. (2017). Irritability in children and adolescents. Annual Review of Clinical Psychology, 13, 317–341. https://doi.org/10.1146/annurev-clinpsy-032816-044941
Bruno, A., Celebre, L., Torre, G., Pandolfo, G., Mento, C., Cedro, C., Zoccali, R. A., & Muscatello, M. R. A. (2019). Focus on disruptive mood dysregulation disorder: A review of the literature. Psychiatry Research, 279, 323–330. https://doi.org/10.1016/j.psychres.2019.05.043
Carlson, G. A. (1998). Mania and ADHD: Comorbidity or confusion. Journal of Affective Disorders, 51(2), 177–187. https://doi.org/10.1016/s0165-0327(98)00179-7
Carter, S. E., Ong, M. L., Simons, R. L., Gibbons, F. X., Lei, M. K., & Beach, S. R. H. (2019). The effect of early discrimination on accelerated aging among African Americans. Health Psychology, 38(11), 1010–1013. https://doi.org/10.1037/hea0000788
Castells, X., Ramon, M., Cunill, R., Olivé, C., & Serrano, D. (2020). Relationship between treatment duration and efficacy of pharmacological treatment for ADHD: A meta-analysis and meta-regression of 87 randomized controlled clinical trials. Journal of Attention Disorders, 25(10), 1352–1361.
https://doi.org/10.1177/1087054720903372
Chase, D., Harvey, P. D., & Pogge, D. L. (2020). Disruptive mood dysregulation disorder (DMDD) in psychiatric inpatient child admissions: Prevalence among consecutive admissions and in children receiving NOS diagnoses. Neurology, Psychiatry and Brain Research, 38, 102–106. https://doi.org/10.1016/j.npbr.2020.11.001
Cianchetti, C., Pittau, A., Carta, V., Campus, G., Littarru, R., Ledda, M. G., Zuddas, A., & Fancello, G. S. (2013). Child and Adolescent Behavior Inventory (CABI): A new instrument for epidemiological studies and pre-clinical evaluation. Clinical Practice and Epidemiology in Mental Health, 9, 51–61. https://doi.org/10.2174/1745017901309010051
Conners, C. K. (1999). Conners Rating Scales-Revised. In M. E. Maruish (Ed.), The use of psychological testing for treatment planning and outcomes assessment (1st ed., pp. 467–495). Lawrence Erlbaum.
Copeland, W. E., Angold, A., Costello, E. J., & Egger, H. (2013). Prevalence, comorbidity, and correlates of DSM-5 proposed disruptive mood dysregulation disorder. The American Journal of Psychiatry, 170(2), 173–179. https://doi.org/10.1176/appi.ajp.2012.12010132
Copeland, W. E., Shanahan, L., Egger, H., Angold, A., & Costello, E. J. (2014). Adult diagnostic and functional outcomes of DSM-5 disruptive mood dysregulation disorder. American Journal of Psychiatry, 171(6), 668–674. https://doi.org/10.1176/appi.ajp.2014.13091213
Costin, J., & Chambers, S. M. (2007). Parent management training as a treatment for children with oppositional defiant disorder referred to a mental health clinic. Clinical Child Psychology and Psychiatry, 12(4), 511–524. https://doi.org/10.1177/1359104507080979
Derella, O. J., Burke, J. D., Romano-Verthelyi, A. M., Butler, E. J., & Johnston, O. G. (2020). Feasibility and acceptability of a brief cognitive-behavioral group intervention for chronic irritability in youth. Clinical Child Psychology and Psychiatry, 25(4), 778–789. https://doi.org/10.1177/1359104520918331
Evans, S. C., Burke, J. D., Roberts, M. C., Fite, P. J., Lochman, J. E., de la Pena, F. R., & Reed, G. M. (2017). Irritability in child and adolescent psychopathology: An integrative review for ICD-11. Clinical Psychology Review, 53, 29–45. https://doi.org/10.1016/j.cpr.2017.01.004
Evans, S. C., Weisz, J. R., Carvalho, A. C., Garibaldi, P. M., Bearman, S. K., Chorpita, B. F., & The Research Network on Youth Mental Health. (2020). Effects of standard and modular psychotherapies in the treatment of youth with severe irritability. Journal of Consulting and Clinical Psychology, 88(3), 255–268. https://doi.org/10.1037/ccp0000456
Evans, S. W., Owens, J. S., & Bunford, N. (2014). Evidence-based psychosocial treatments for children and adolescents with attention-deficit/hyperactivity disorder. Journal of Clinical Child & Adolescent Psychology, 43(4), 527–551. https://doi.org/10.1080/15374416.2013.850700
Fadus, M. C., Ginsburg, K. R., Sobowale, K., Halliday-Boykins, C. A., Bryant, B. E., Gray, K. M., & Squeglia, L. M. (2020). Unconscious bias and the diagnosis of disruptive behavior disorders and ADHD in African American and Hispanic youth. Academic Psychiatry, 44, 95–102. https://doi.org/10.1007/s40596-019-01127-6
Freeman, A. J., Youngstrom, E. A., Youngstrom, J. K., & Findling, R. L. (2016). Disruptive mood dysregulation disorder in a community mental health clinic: Prevalence, comorbidity and correlates. Journal of Child and Adolescent Psychopharmacology, 26(2), 123–130. https://doi.org/10.1089/cap.2015.0061
Garb, H. N. (1998). Studying the clinician: Judgment research and psychological assessment. American Psychological Association.
Greene, R. W., Ablon, J. S., Goring, J. C., Raezer-Blakely, L., Markey, J., Monuteaux, M. C., Henin, A., Edwards, G., & Rabbitt, S. (2004). Effectiveness of collaborative problem solving in affectively dysregulated children with oppositional-defiant disorder: Initial findings. Journal of Consulting and Clinical Psychology, 72(6), 1157–1164. https://doi.org/10.1037/0022-006X.72.6.1157
Haller, S. P., Kircanski, K., Stringaris, A., Clayton, M., Bui, H., Agorsor, C., Cardenas, S. I., Towbin, K. E., Pine, D. S., Leibenluft, E., & Brotman, M. A. (2020). The Clinician Affective Reactivity Index: Validity and reliability of a clinician-rated assessment of irritability. Behavior Therapy, 51(2), 283–293. https://doi.org/10.1016/j.beth.2019.10.005
Hatchett, G. T., & Motley, N. R. (2016). Bipolar and related disorders. In B. Flamez and C. J. Sheperis (Eds.), Diagnosing and treating children and adolescents: A guide for mental health professionals (pp. 177–202). Wiley.
Kaufman, J., Birmaher, B., Brent, D., Rao, U., Flynn, C., Moreci, P., Williamson, D., & Ryan, N. (1997). Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child & Adolescent Psychiatry, 36(7), 980–988. https://doi.org/10.1097/00004583-199707000-00021
Lacasse, J. R. (2014). After DSM-5: A critical mental health research agenda for the 21st century. Research on Social Work Practice, 24(1), 5–10. https://doi.org/10.1177/1049731513510048
Leibenluft, E. (2011). Severe mood dysregulation, irritability, and the diagnostic boundaries of bipolar disorder in youths. The American Journal of Psychiatry, 168(2), 129–142. https://doi.org/10.1176/appi.ajp.2010.10050766
Leibenluft, E., Charney, D. S., Towbin, K. E., Bhangoo, R. K., & Pine, D. S. (2003). Defining clinical phenotypes of juvenile mania. The American Journal of Psychiatry, 160(3), 430–437. https://doi.org/10.1176/appi.ajp.160.3.430
Linke, J., Kircanski, K., Brooks, J., Perhamus, G., Gold, A. L., & Brotman, M. A. (2020). Exposure-based cognitive-behavioral therapy for disruptive mood dysregulation disorder: An evidence-based case study. Behavior Therapy, 51(2), 320–333. https://doi.org/10.1016/j.beth.2019.05.007
Malhi, G. S., & Bell, E. (2019). Fake views: DMDD, indeed! Australian & New Zealand Journal of Psychiatry, 53(7), 706–710. https://doi.org/10.1177/0004867419863162
Mayes, S. D., Mathiowetz, C., Kokotovich, C., Waxmonsky, J., Baweja, R., Calhoun, S. L., & Bixler, E. O. (2015). Stability of disruptive mood dysregulation disorder symptoms (irritable-angry mood and temper outbursts) throughout childhood and adolescence in a general population sample. Journal of Abnormal Child Psychology, 43, 1543–1549. https://doi.org/10.1007/s10802-015-0033-8
Mayes, S. D., Waxmonsky, J. D., Calhoun, S. L., & Bixler, E. O. (2016). Disruptive mood dysregulation disorder symptoms and association with oppositional defiant and other disorders in a general population child sample. Journal of Child and Adolescent Psychopharmacology, 26(2), 101–106. https://doi.org/10.1089/cap.2015.0074
Mayes, S. D., Waxmonsky, J., Calhoun, S. L., Kokotovich, C., Mathiowetz, C., & Baweja, R. (2015). Disruptive mood dysregulation disorder (DMDD) symptoms in children with autism, ADHD, and neurotypical development and impact of co-occurring ODD, depression, and anxiety. Research in Autism Spectrum Disorders, 18, 64–72. https://doi.org/10.1016/j.rasd.2015.07.003
Miller, L., Hlastala, S. A., Mufson, L., Leibenluft, E., Yenokyan, G., & Riddle, M. (2018). Interpersonal psychotherapy for mood and behavior dysregulation: Pilot randomized trial. Depression and Anxiety, 35(6), 574–582. https://doi.org/10.1002/da.22761
Minsky, S., Petti, T., Gara, M., Vega, W., Lu, W., & Kiely, G. (2006). Ethnicity and clinical psychiatric diagnosis in childhood. Administration and Policy in Mental Health and Mental Health Services Research, 33, 558–567. https://doi.org/10.1007/s10488-006-0069-8
Moreno, C., Laje, G., Blanco, C., Jiang, H., Schmidt, A. B., & Olfson, M. (2007). National trends in the outpatient diagnosis and treatment of bipolar disorder in youth. Archives of General Psychiatry, 64(9), 1032–1039. https://doi.org/10.1001/archpsyc.64.9.1032
Mouzon, D. M., Taylor, R. J., Woodward, A. T., & Chatters, L. M. (2017). Everyday racial discrimination, everyday non-racial discrimination, and physical health among African-Americans. Journal of Ethnic & Cultural Diversity in Social Work, 26(1–2), 68–80. https://doi.org/10.1080/15313204.2016.1187103
Ozyurt, G., Emiroglu, N., Baykara, B., & Akay Pekcanlar, A. (2017). Effectiveness and adverse effects of methylphenidate treatment in children diagnosed with disruptive mood dysregulation disorder and attention-deficit hyperactivity disorder: A preliminary report. Psychiatry and Clinical Psychopharmacology, 27(1), 99–100. https://doi.org/10.1080/24750573.2017.1293252
Pan, P.-Y., Fu, A.-T., & Yeh, C.-B. (2018). Aripiprazole/methylphenidate combination in children and adolescents with disruptive mood dysregulation disorder and attention-deficit/hyperactivity disorder: An open-label study. Journal of Child and Adolescent Psychopharmacology, 28(10), 682–689. https://doi.org/10.1089/cap.2018.0068
Parker, G., & Tavella, G. (2018). Disruptive mood dysregulation disorder: A critical perspective. The Canadian Journal of Psychiatry, 63(12), 813–815. https://doi.org/10.1177/0706743718789900
Perepletchikova, F., Nathanson, D., Axelrod, S. R., Merrill, C., Walker, A., Grossman, M., Rebeta, J., Scahill, L., Kaufman, J., Flye, B., Mauer, E., & Walkup, J. (2017). Randomized clinical trial of dialectical behavior therapy for preadolescent children with disruptive mood dysregulation disorder: Feasibility and outcomes. Journal of the American Academy of Child & Adolescent Psychiatry, 56(10), 832–840. https://doi.org/10.1016/j.jaac.2017.07.789
Rao, U. (2014). DSM-5: Disruptive mood dysregulation disorder. Asian Journal of Psychiatry, 11, 119–123. https://doi.org/10.1016/j.ajp.2014.03.002
Regier, D. A., Narrow, W. E., Clarke, D. E., Kraemer, H. C., Kuramoto, S. J., Kuhl, E. A., & Kupfer, D. J. (2013). DSM-5 field trials in the United States and Canada, part II: Test-retest reliability of selected categorical diagnoses. The American Journal of Psychiatry, 170(1), 59–70. https://doi.org/10.1176/appi.ajp.2012.12070999
Rice, T., Simon, H., Barcak, D., Maiyuran, H., Chan, V., Hassan, Y., Tatum, J., & Coffey, B. J. (2019). Amantadine for treatment of disruptive mood dysregulation disorder symptoms. Journal of Child and Adolescent Psychopharmacology, 29(8), 642–646. https://doi.org/10.1089/cap.2019.29172.bjc
Rich, B. A., Bhangoo, R. K., Vinton, D. T., Berghorst, L. H., Dickstein, D. P., Grillon, C., Davidson, R. J., & Leibenluft, E. (2005). Using affect-modulated startle to study phenotypes of pediatric bipolar disorder. Bipolar Disorders, 7(6), 536–545. https://doi.org/10.1111/j.1399-5618.2005.00265.x
Roy, A. K., Lopes, V., & Klein, R. G. (2014). Disruptive mood dysregulation disorder: A new diagnostic approach to chronic irritability in youth. American Journal of Psychiatry, 171(9), 918–924.
https://doi.org/10.1176/appi.ajp.2014.13101301
Sitarenios, G., & Kovacs, M. (1999). Use of the Children’s Depression Inventory. In M. E. Maruish (Ed.), The use of psychological testing for treatment planning and outcomes assessment (1st ed., pp. 267–298). Lawrence Erlbaum.
Stringaris, A., Baroni, A., Haimm, C., Brotman, M., Lowe, C. H., Myers, F., Rustgi, E., Wheeler, W., Kayser, R., Towbin, K., & Leibenluft, E. (2010). Pediatric bipolar disorder versus severe mood dysregulation: Risk for manic episodes on follow-up. Journal of the American Academy of Child & Adolescent Psychiatry, 49(4), 397–405. https://doi.org/10.1016/j.jaac.2010.01.013
Stringaris, A., Cohen, P., Pine, D. S., & Leibenluft, E. (2009). Adult outcomes of youth irritability: A 20-year prospective community-based study. The American Journal of Psychiatry, 166(9), 1048–1054.
https://doi.org/10.1176/appi.ajp.2009.08121849
Stringaris, A., & Goodman, R. (2009). Longitudinal outcome of youth oppositionality: Irritable, headstrong, and hurtful behaviors have distinctive predictions. Journal of the American Academy of Child & Adolescent Psychiatry, 48(4), 404–412. https://doi.org/10.1097/CHI.0b013e3181984f30
Stringaris, A., Goodman, R., Ferdinando, S., Razdan, V., Muhrer, E., Leibenluft, E., & Brotman, M. A. (2012). The Affective Reactivity Index: A concise irritability scale for clinical and research settings. Journal of Child Psychology and Psychiatry, 53(11), 1109–1117. https://doi.org/10.1111/j.1469-7610.2012.02561.x
Stringaris, A., Vidal-Ribas, P., Brotman, M. A., & Leibenluft, E. (2018). Practitioner review: Definition, recognition, and treatment challenges of irritability in young people. Journal of Child Psychology and Psychiatry, 59(7), 721–739. https://doi.org/10.1111/jcpp.12823
Sukhodolsky, D. G., & Scahill, L. (2012). Cognitive-behavioral therapy for anger and aggression in children. Guilford.
Sukhodolsky, D. G., Smith, S. D., McCauley, S. A., Ibrahim, K., & Piasecka, J. B. (2016). Behavioral interventions for anger, irritability, and aggression in children and adolescents. Journal of Child and Adolescent Psychopharmacology, 26(1), 58–64. https://doi.org/10.1089/cap.2015.0120
Tobler, A. L., Maldonado-Molina, M. M., Staras, S. A. S., O’Mara, R. J., Livingston, M. D., & Komro, K. A. (2013). Perceived racial/ethnic discrimination, problem behaviors, and mental health among minority urban youth. Ethnicity & Health, 18(4), 337–349. https://doi.org/10.1080/13557858.2012.730609
Tourian, L., LeBoeuf, A., Breton, J.-J., Cohen, D., Gignac, M., Labelle, R., Guile, J.-M., & Renaud, J. (2015). Treatment options for the cardinal symptoms of disruptive mood dysregulation disorder. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 24(1), 41–54.
Towbin, K., Axelson, D., Leibenluft, E., & Birmaher, B. (2013). Differentiating bipolar disorder–not otherwise specified and severe mood dysregulation. Journal of the American Academy of Child & Adolescent Psychiatry, 52(5), 466–481. https://doi.org/10.1016/j.jaac.2013.02.006
Towbin, K., Vidal-Ribas, P., Brotman, M. A., Pickles, A., Miller, K. V., Kaiser, A., Vitale, A. D., Engel, C., Overman, G. P., Davis, M., Lee, B., McNeil, C., Wheeler, W., Yokum, C. H., Haring, C. T., Roule, A., Wambach, C. G., Sharif-Askary, B., Pine, D. S, . . . Stringaris, A. (2020). A double-blind randomized placebo-controlled trial of citalopram adjunctive to stimulant medication in youth with chronic severe irritability. Journal of the American Academy of Child & Adolescent Psychiatry, 59(3), 350–361. https://doi.org/10.1016/j.jaac.2019.05.015
Tudor, M. E., Ibrahim, K., Bertschinger, E., Piasecka, J., & Sukhodolsky, D. G. (2016). Cognitive-behavioral therapy for a 9-year-old girl with disruptive mood dysregulation disorder. Clinical Case Studies, 15(6), 459–475. https://doi.org/10.1177/1534650116669431
Van Meter, A. R., Moreira, A. L. R., & Youngstrom, E. A. (2011). Meta-analysis of epidemiologic studies of pediatric bipolar disorder. The Journal of Clinical Psychiatry, 72(9), 1250–1256. https://doi.org/10.4088/JCP.10m06290
Weisz, J. R., & Kazdin, A. E. (Eds.). (2017). Evidence-based psychotherapies for children and adolescents (3rd ed.). Guilford.
Wiggins, J. L., Brotman, M. A., Adleman, N. E., Kim, P., Oakes, A. H., Reynolds, R. C., Chen, G., Pine, D. S., & Leibenluft, E. (2016). Neural correlates of irritability in disruptive mood dysregulation and bipolar disorders. The American Journal of Psychiatry, 173(7), 722–730. https://doi.org/10.1176/appi.ajp.2015.15060833
Winters, D. E., Fukui, S., Leibenluft, E., & Hulvershorn, L. A. (2018). Improvements in irritability with open-label methylphenidate treatment in youth with comorbid attention deficit/hyperactivity disorder and disruptive mood dysregulation disorder. Journal of Child and Adolescent Psychopharmacology, 28(5), 298–305. https://doi.org/10.1089/cap.2017.0124
World Health Organization. (2016). International statistical classification of diseases and related health problems (10th ed.). https://icd.who.int/browse10/2016/en
World Health Organization. (2019). International statistical classification of diseases and related health problems (11th ed.). https://icd.who.int
Gregory T. Hatchett, PhD, NCC, LPCC-S, is a professor at Northern Kentucky University. Correspondence may be addressed to Gregory T. Hatchett, MEP 211, Highland Heights, KY 41099, hatchettg@nku.edu.
Feb 7, 2022 | Volume 12 - Issue 1
Eric M. Brown, Kristy L. Carlisle, Melanie Burgess, Jacob Clark, Ariel Hutcheon
Despite an emphasis on self-care to avoid burnout and increase compassion satisfaction within the counseling profession, there is a dearth of research on the developmental experiences of counselors that may increase the likelihood of burnout. We examined the impact of mental health counselors’ (N = 140) experiences of adverse childhood experiences and positive childhood experiences on their present rates of compassion satisfaction, burnout, and secondary traumatic stress. We used a cross-sectional, non-experimental correlational design and reported descriptive statistics as well as results of multiple regression models. Results indicated significant relationships among counselors’ rates of adverse childhood experiences, positive childhood experiences, and compassion satisfaction and burnout. We include implications for the use of both the adverse and positive childhood experiences assessments in the training of counseling students and supervisees.
Keywords: counselors, burnout, childhood experiences, compassion satisfaction, secondary traumatic stress
Over the past 20 years, public health research on adverse childhood experiences (ACEs) and their deleterious effects on physical and mental health has proliferated and branched out to various disciplines (Campbell et al., 2016; Frampton et al., 2018). More recently, the importance of understanding the implications of ACEs for the mental health of clients has entered the counseling literature (Wheeler et al., 2021; Zyromski et al., 2020), yet the ways in which a counselor’s own experience of ACEs may affect their work have not been examined. The absence of such research is significant given the report that mental health workers have the highest rates of ACEs among those in the helping professions (Redford, 2016).
A thorough literature search of PsycINFO, ProQuest, and Google Scholar using terms including, but not limited to, adverse childhood experiences, positive childhood experiences (PCEs), compassion satisfaction (CS), burnout, secondary traumatic stress (STS), and mental health counselors (MHCs), found no peer-reviewed articles that examined the relationship between ACEs or PCEs and counselors’ rates of CS and burnout. Therefore, we chose to examine the effects of early developmental adversity, as well as early protective factors, on the professional quality of life of counselors, as measured by assessing the counselor’s levels of CS, burnout, and STS.
Adverse Childhood Experiences (ACEs)
In the mid-nineties, Felitti et al. (1998), with the support of the Centers for Disease Control, created the ACE Study Questionnaire to study early childhood trauma and deprivation experiences. The ACE Study Questionnaire consists of 10 questions related to whether a person before the age of 18 experienced emotional or physical abuse, substance addiction in the home, parental divorce or separation, a caretaker with mental illness, or emotional deprivation. Each question that is answered in the affirmative results in one “ACE,” with respondents’ scores ranging from 1 to 10. Studies have found that ACEs have a dose-response effect; therefore, every point increase can significantly raise the chance of experiencing negative mental and physical health effects into adulthood (Boullier & Blair, 2018; Campbell et al., 2016; Merrick et al., 2017). Additionally, individuals with four or more ACEs are significantly more likely to suffer from mental illness or substance addiction, be further traumatized as adults, and succumb to an early death (Anda et al., 2007; Metzler et al., 2017).
More recently, researchers have found that Black and Latinx individuals have significantly higher rates of ACEs compared to White individuals (R. D. Lee & Chen, 2017; Merrick et al., 2017; Strompolis et al., 2019). In a study involving 60,598 participants, R. D. Lee and Chen (2017) discovered not only that Black and Hispanic participants had higher rates of ACEs, but also that there was a correlation between ACEs and drinking alcohol heavily. In a sample of 214,517 participants across 23 states in the United States, Merrick et al. (2017) found that racially minoritized individuals, sexual minorities, the unemployed, those with less than a high school education, and those making less than $15,000 a year had significantly higher rates of ACEs than White individuals, heterosexuals, the employed, and those with higher education and income, respectively. Zyromski et al. (2020) noted that the preponderance of ACEs within marginalized communities, such as ethnic minority populations, make ACEs “a social justice issue” (p. 352).
There is scarce research related to the potential impact of ACEs on practitioners and graduate students in helping professions. Thomas (2016) evaluated the rates of ACEs with Master of Social Work (MSW) students, discovering that MSW students were 3.3 times more likely to have four or more ACEs compared to a general sample of university students. Similarly, counselors-in-training are not immune to the effects of childhood adversity; in fact, researchers noted that counselors-in-training may pursue a counseling degree because of personal trauma that drives their aspirations to help others (Conteh et al., 2017). Evans (1997) found that 93% of counselors-in-training reported at least one traumatic experience in their lives, while Conteh et al. (2017) discovered that 95% of counselors-in-training reported between one and eight traumas throughout their lifetime. Considering these results, researchers have suggested that practitioners with a history of trauma may be vulnerable to re-experiencing trauma with clients, which could negatively impact client care and increase the rate of counselor burnout (Conteh et al., 2017; Thomas, 2016). Because the rates of ACEs in practicing MHCs are unknown, it is difficult to determine how ACEs may play a role in impacting CS, burnout, and STS. Furthermore, we lack research on early developmental factors that may contribute to CS, burnout, and STS.
Positive Childhood Experiences (PCEs)
In recent years, childhood development researchers have explored protective factors that may reduce the harmful effects of ACEs. In 2018, Crouch et al. (2019) examined the relationship between two protective factors and their mitigating effects on individuals reporting at least four ACEs. In a sample of 7,079 respondents, the researchers discovered that individuals who reported growing up “with an adult who made them feel safe and protected were less likely to report frequent mental distress or poor health” (Crouch et al., 2019, p. 165). Bethell et al. (2019) found significant correlations between seven positive interpersonal experiences with family and friends and decreased negative effects of ACEs. They also discovered that these factors have a dose-response effect in relation to ACEs so that with each additional PCEs, the harmful effects of ACEs are lessened. The discovery of PCEs has become important in understanding developmentally protective factors that guard from the damaging effects of childhood adversity. Specifically, higher rates of PCEs decrease the chances of mental health disorders of adults, even in those with higher numbers of ACEs (Bethell et al., 2019). An examination of the rates of PCEs in MHCs may provide insight into the well-being of counselors.
Counselor Well-Being
As defined by the American Counseling Association (ACA; 2014), professional counselors work to empower diverse clients to achieve their personal goals. Specifically, MHCs provide client-driven services in agencies, hospitals, and private practices (American Mental Health Counselors Association [AMHCA], 2020). Counselors are trained to cultivate and monitor their own sense of well-being while providing their expertise and leadership to clients and students who have experienced difficulties related to trauma, injustice, abuse, loss, violence, and distress (Council for Accreditation of Counseling and Related Educational Programs [CACREP], 2015; S. M. Lee et al., 2010). Self-care, or the act of cultivating a subjectively defined state of health, is now ubiquitous in counselor education programs and promoted among practitioners (ACA, 2014; CACREP, 2015); however, scholars note that many counselors do not routinely prioritize their own sense of well-being and monitor CS, burnout, and STS (Coaston, 2017). While working closely with clients, practitioners may benefit from reflecting on how their own experiences of personal adversity may influence their work and possibly create a predisposition toward burnout.
Burnout of Counselors
Burnout is defined as the emotional and physical response to chronic stressors in the workplace that lead to substantial negative consequences (Maslach et al., 2001). Scholars have evaluated the external facets of professional counselors’ work that lead to increased burnout, such as time spent on non-counseling duties, lack of on-the-job support, and negative working environments (Thompson et al., 2014); however, internal factors that lead to burnout, such as counselors’ experiences of adversity, remain unstudied. The ubiquitous nature of trauma and its lifelong impact on clients has gained more attention over the past 20 years (Bemak & Chung, 2017; Debellis, 2001; Webber et al., 2017), yet researchers are only beginning to explore the impact of trauma on the lives and professional experiences of counselors (Conteh et al., 2017; McKim & Smith-Adcock, 2014).
Recently, scholars have sought to understand contributing factors that diminish CS and increase burnout (S. M. Lee et al., 2010). In a study of 86 counselors-in-training, Can and Watson (2019) found that a trainee’s degree of resilience and wellness predicted burnout, whereas empathy and supervisory working alliance did not. They did not assess for internal or experiential factors that may have contributed to burnout.
Cook et al. (2021) conducted a qualitative inquiry with 246 novice counselors to explore symptoms of burnout that may not be captured in commonly used assessments. The researchers found several predominant themes, including negative emotional experiences such as anxiety, depression and crying spells; fatigue and tiredness; and unfulfillment in work. Participants also reported physical illness and weight gain or loss, self-perceived ineffectiveness as a counselor, and cognitive impairment. Close to 10% of participants stated that an unhealthy environment contributed to their experience of burnout. Cook et al. did not inquire about any personal history that may have also contributed to symptoms of burnout.
Counselors and STS
Distinct from but related to burnout, STS has been discussed in the literature relating to the well-being of helping professions across numerous disciplines (Branson, 2019; Butler et al., 2017; Molnar et al., 2017). Secondary traumatic stress, also called vicarious trauma, is distinguished from burnout by its symptoms overlapping with post-traumatic stress disorder (PTSD), such as intrusive thoughts, hypervigilance, and avoidance of distressing memories (Ivicic & Motta, 2017; Molnar et al., 2017). In a study of 220 counselors, Lanier and Carney (2019) discovered that 49.5% of counselors experienced symptoms of vicarious trauma, with 85.5% reporting “I thought about my work with clients when I didn’t intend to” and 80.5% confirming that “I felt emotionally numb” (p. 339). Lakioti et al. (2020) found in a study of 163 Greek mental health practitioners that there was a significant positive correlation between burnout and STS (r = .48) and that practitioners who scored high in empathy also scored high in STS (r = .34). In their meta-analysis of 38 studies examining risk factors for STS in therapeutic work, Hensel et al. (2015) found small yet significant effect sizes for “trauma caseload volume (r = .16), caseload frequency (r = .12), caseload ratio (r = .19), and having a personal trauma history (r = .19)” in relation to STS (p. 83).
Research regarding counselors’ own personal trauma is still emerging and a consensus is not yet formed. In a recent study of 90 psychotherapy trainees, Klasen et al. (2019) indicated that secure attachments play a modifying role in limiting the severity of trauma’s expression. McKim and Smith-Adcock (2014) evaluated characteristics of trauma counselors to understand how frequent exposure to indirect trauma might influence burnout and CS, as assessed by the Professional Quality of Life Scale (ProQOL; Stamm, 2010). Their results indicated that higher levels of exposure to client trauma, in combination with less perceived control over the workplace, led to increased burnout (McKim & Smith-Adcock, 2014). Consistent with the ACA Code of Ethics (2014), counselors are expected to self-monitor for impairment issues that could impact clients such as burnout, STS, and the decrease of CS.
Compassion Satisfaction
CS has been studied nominally and may serve as a protective factor against burnout (Coaston, 2017). Compassion satisfaction is defined as a psychological benefit derived from working effectively with clients to produce meaningful and positive change in their lives (McKim & Smith-Adcock, 2014; Stamm, 2010). McKim and Smith-Adcock (2014) discovered that trauma counselors who experienced higher levels of personal trauma also exhibited higher levels of CS or fulfillment derived from their role in the helping alliance. Although these emergent results contradict older literature that demonstrates how counselors with more personal trauma have higher levels of burnout (Baird & Kracen, 2006; Nelson-Gardell & Harris, 2003), presently, the relationship between CS, burnout, and STS in counselors in relation to ACEs is still unclear.
Purpose of Study
The purpose of this study was to examine the effects of early developmental adversity as well as early protective factors on the CS, burnout, and STS of MHCs. Despite the ongoing concern for factors that contribute to the CS, burnout, and STS of counselors, there is a dearth of research on personal experiences that may predispose counselors to burnout (Conteh et al., 2017; McKim & Smith-Adcock, 2014). Considering the detrimental effects of burnout on counselors’ health and well-being, as well as the decrease in empathy that often accompanies burnout, it is imperative that we understand the various causes of burnout (Can & Watson, 2019; Cook et al., 2021; Maslach et al., 2001). This knowledge will assist clinical MHCs, supervisors, and counselor educators in knowing which professional counselors or counselors-in-training may be more susceptible to burnout, STS, and decreased CS.
Research on ACEs within the counseling profession, as proposed by the original Felitti et al. (1998) study, is scant. Zyromski et al. (2020) discovered in their content analysis of ACA and American School Counselor Association journals that only three articles contained any focus on ACEs as defined in the original study. They suggested that by incorporating such a well-defined and researched concept as ACEs, counselors will be better equipped to address the deleterious effects of early adverse experiences. In order to address the gap within the literature, we chose to focus on the rates of ACEs and PCEs of counselors and how they potentially impact CS, burnout, and STS. After conducting an exhaustive search of the literature, we found no other study that examined the potential relationship between counselors’ developmental history using the ACEs and PCEs assessments and their levels of burnout, CS, and STS.
Method
This study entailed a cross-sectional, non-experimental correlational design and reported descriptive statistics, as well as results of multiple regression models. Relationships among MHCs’ ACEs, PCEs, CS, burnout, and STS were examined. Research questions (RQs) guiding the study were: RQ1 (descriptive): What are the mean scores of MHCs for ACEs, PCEs, CS, burnout, and STS constructs? and RQ2 (regression): To what extent do MHCs’ ACEs, PCEs, gender, race, socioeconomic status, and educational level predict CS, burnout, and STS?
Power Analysis
The target number of participants for the study was at least N = 138, based on a power analysis. Researchers used G*Power 3.1.9.6 (Faul et al., 2009) to calculate an a priori power analysis with a .05 alpha level (Cohen, 1988, 1992), a medium effect size for multiple R2 of .09 (Cohen, 1988), and a power of .80 (Cohen, 1992).
Participants
The eligibility criteria for this study were to be a clinical MHC, 18 years or older, who worked 30 hours or more per week in the field of mental health counseling. After soliciting participants nationally through emails, we collected data from 140 participants who met the criteria. MHCs ranged in age from 22 to 72 years old with an average age of 38 (SD = 11.01). Table 1 shows the diverse sample. Slightly more than half (n = 71) identified as female and a little less than half (n = 66) as male. More than three-quarters (n = 108) identified as White. The majority of participants (n = 85) reported their childhood SES as lower or working class, while more than half (n = 78) reported their current social class as middle class. Our sample with predominantly female and predominantly White participants is similar both to known counselor demographics (Norton & Tan, 2019) and to the Felitti et al. (1998) ACEs study.
Instrumentation
Three instruments with good validity and reliability were used to measure ACEs, PCEs, CS, burnout, and STS. We created a demographic questionnaire to collect information on participants’ identities (e.g., race, gender) and childhood backgrounds (e.g., ACEs, PCEs, SES).
Adverse Childhood Experiences (ACE) Study Questionnaire
The ACE Study Questionnaire (Felitti et al., 1998) is a 10-item survey of the most common examples of childhood abuse and neglect. It was developed out of research that connected childhood trauma to subsequent mental and physical ailments. Subsequent research found good test-retest reliability of the measure in an adult population (Dube et al., 2004; Frampton et al., 2018) and a Cronbach’s alpha score of .78 (Ford et al., 2014). The survey produces self-report scores between 0 and 10. The higher the score, the greater the risk for mental and physical health issues as well as decreased quality of life. Consistent research (e.g., Anda et al., 2006; Dube et al., 2004; Hughes et al., 2017) shows that a score of 4 or more indicates serious risk.
Table 1
Participant Demographics
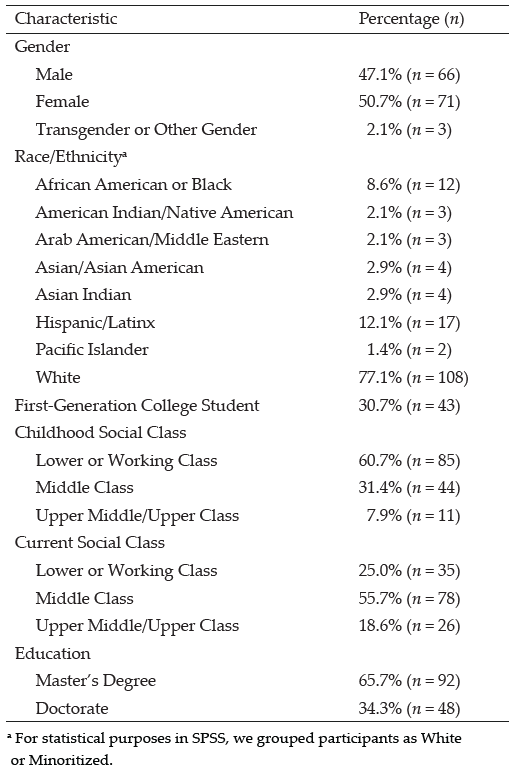
Positive Childhood Experiences (PCE) Questionnaire
The PCE Questionnaire (Bethell et al., 2019) is a 7-item survey of PCEs (i.e., connection with family, friends, and community) that are statistically predictive of good mental health in adulthood. After accounting for ACEs, higher PCE scores reduce mental health and interpersonal problems later in life. Specifically, scores in the 6 to 7 range are most protective from harmful effects of ACEs, and scores in the 3 to 5 range are moderately protective. A Cronbach’s alpha score of .77 reported in the original 2019 study indicates good reliability.
Professional Quality of Life Scale (ProQOL)
The ProQOL (Stamm, 2010) is a 30-item survey with good construct validity measuring both positive and negative responses to the work of helping professionals. It measures three constructs: CS, which has a Cronbach’s alpha score of .88; burnout, which has a Cronbach’s alpha score of .75; and STS, which has a Cronbach’s alpha score of .81. For CS, or positive feelings about one’s ability to help, a score below 23 indicates problems at work. For burnout, or feelings of exhaustion, frustration, anger, or depression, scores below 23 indicate feeling good about work, while scores above 41 indicate feeling ineffective. For STS, or feelings of fear related to trauma in the workplace, scores above 43 indicate something frightening at work.
Procedure
After IRB approval, we used purposeful sampling methods to recruit participants. We emailed over 6,000 MHCs from a data set purchased from a national data bank. Furthermore, we posted invitations to participate on Facebook groups for MHCs. Invitations included informed consent, as well as a link to a Qualtrics survey containing all instruments and demographic questions. Researchers cleaned all collected data leading to 140 usable cases, computed instruments and transformed variables into usable form, and checked for assumptions for multiple regression. For each instrument, we assessed for reliability with Cronbach’s alpha tests. The ACEs instrument produced a Cronbach’s alpha of .89, the PCEs instrument produced .81, and the ProQOL produced .79, all within the good to excellent range. We used SPSS 28 for all analyses.
Data Analysis and Results
To answer our first research question, we evaluated the mean scores for ACEs, PCEs, CS, burnout, and STS. Respondents in the study had a mean ACE score of 3.42, 95% CI [2.8577, 3.9852], beneath the threshold of 4 and just below the range for significant risk. Their mean PCE score of 5.34, 95% CI [5.0006, 5.6957], was at the upper end of moderately protective. White MHCs had a lower average ACE score and higher average PCE score than minoritized MHCs. Male MHCs had higher average ACE and PCE scores than females, and MHCs with lower childhood SES had lower average ACE scores and higher average PCE scores than those with higher SES (see Tables 2 and 3).
Table 2
Average Adverse Childhood Experience Scores by Demographics
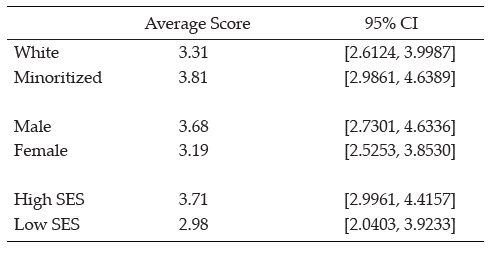
Table 3
Average Positive Childhood Experience Scores by Demographics
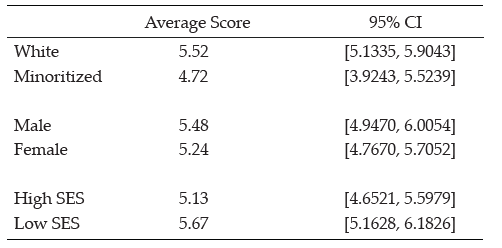
Type of scores are shown in percentages for each type of ACE and PCE to show what percentage of MHCs reported an adverse or protective childhood experience (see Tables 4 and 5).
Table 4
Type of Adverse Childhood Experience Score
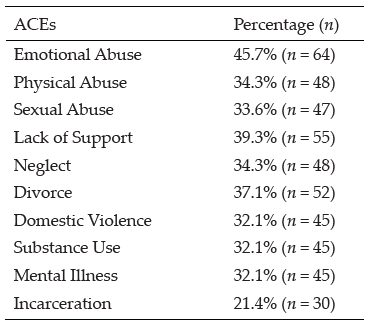
Table 5
Type of Positive Childhood Experience Score
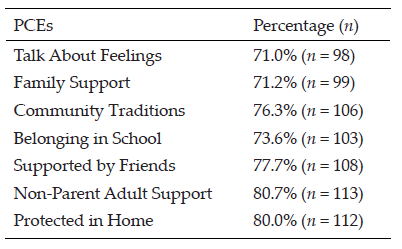
Next, we analyzed MHCs’ scores related to CS, burnout, and STS. Participants’ mean CS score of 31.81, 95% CI [30.6005, 33.0138], was well above the threshold of 23, which indicates a positive level of CS. Their overall mean burnout score of 24.59, 95% CI [23.5793, 25.5921], was well below the threshold of 41, which indicates that the average MHC was not suffering from burnout. Their overall mean STS score of 26.37, 95% CI [25.0346, 27.7083], was also well below the threshold of 43, which indicates the average MHC was not experiencing STS.
For RQ 2, we also tested whether and to what extent MHCs’ ACEs, PCEs, and demographic variables predict CS, burnout, and STS. We ran three linear regression models to assess significant predictors of CS, burnout, and STS. In the first model, a regression of CS on ACEs, PCEs, gender, race/ethnicity, and childhood SES explained a significant 40.5% of the variance in CS, F (5, 134) = 17.558, p < .001. Specifically, significant predictors of CS were ACEs (β = −.550), gender (β = −.218), race/ethnicity (β = −.160), and childhood SES (β = −.171). PCEs were nonsignificant in relation to CS. Items negatively related to CS were ACEs (i.e., higher ACE scores predicted lower CS), gender (i.e., being female predicted higher CS), race/ethnicity (i.e., being minoritized predicted higher CS), and childhood SES (i.e., lower levels of SES predicted higher CS; see Table 6).
In the second model, a regression of burnout on ACEs, PCEs, gender, race/ethnicity, and childhood SES explained a significant 18.9% of the variance in burnout, F (5, 134) = 6.032, p < .001. Specifically, both ACEs and PCEs were significant predictors of burnout (β = .309 and β= −.197, respectively). Gender, race/ethnicity, and SES were nonsignificant predictors of burnout. ACEs were positively related to burnout (i.e., higher ACE scores indicated higher burnout), and PCEs were negatively related to burnout (i.e., higher PCEs indicated lower burnout; see Table 7).
In the third model, a regression of STS on ACEs, PCEs, gender, race/ethnicity, and childhood SES explained a significant 8.5% of variance in STS, F (5, 134) = 2.402, p < .001. Only race/ethnicity was a significant predictor of STS (β= −.222; i.e., being White indicated lower STS). ACEs, PCEs, gender, and SES produced nonsignificant results related to STS (see Table 8).
Table 6
Regression Results Using Compassion Satisfaction as the Criterion
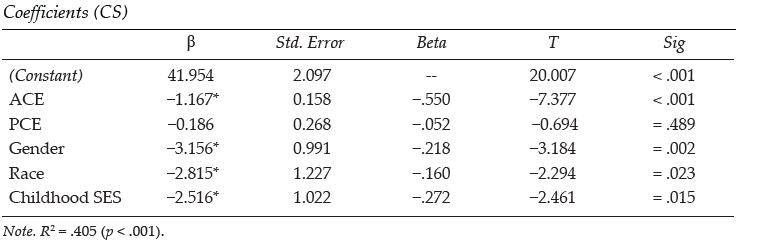
Table 7
Regression Results Using Burnout as the Criterion
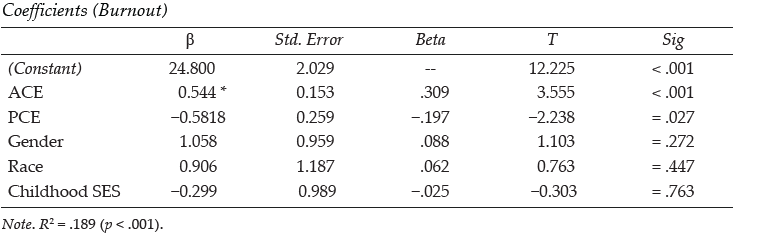
Table 8
Regression Results Using Secondary Traumatic Stress as the Criterion
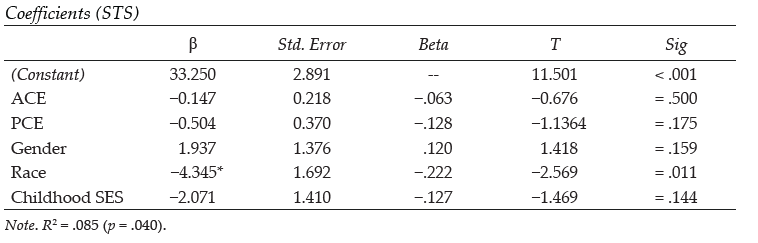
Discussion
After conducting an exhaustive literature review, we found no other study that examined the relationship between a counselor’s personal history of childhood adversity and protective factors (i.e., ACEs and PCEs) and their professional experience with burnout, STS, and CS. As the counseling profession is placing a greater emphasis on counselors becoming trauma-informed (e.g., Bemak & Chung, 2017; Debellis, 2001; Webber et al., 2017), recent research has examined counselor wellness, burnout, PTSD symptoms, and possible contributing factors (Can & Watson, 2019; Cook et al., 2021; Lanier & Carney, 2019). In line with other studies, we found that some individuals drawn to the profession of counseling are more likely to have had adversity and hardship events in their personal histories (Conteh et al., 2017; McKim & Smith-Adcock, 2014). What is unique in this study is the examination of how both adverse and positive childhood experiences may impact the CS, burnout, and STS of MHCs.
Similar to Thomas (2016), who found that social work students had higher rates of ACEs than the general population, the results of this study indicated that counselor participants had higher rates of ACEs for all 10 experiences than the original Felitti et al. (1998) ACEs study. This was also aligned with Conteh and colleagues (2017), who found that counselors-in-training may have higher rates of trauma than the average population. The results also indicated that almost 43% (n = 60) of MHCs scored four or more ACEs, which placed them at high risk for mental and physical health problems (Boullier & Blair, 2018; Campbell et al., 2016; Merrick et al., 2017). As may be surmised from other studies on the deleterious effects of ACEs on emotional well-being, having higher numbers of ACEs was a significant predictor of burnout. Lower ACEs scores also significantly predicted CS with a high effect size (.55). Similarly, higher PCEs were linked to lower burnout. However, PCEs were not found to significantly predict CS.
We examined the average rates of and relationships between ACEs, PCEs, CS, burnout, and STS in a sample of MHCs. McKim and Smith-Adcock (2014) examined the burnout rates of trauma counselors, finding that counselors with more personal trauma had an increase in CS, perhaps due to personal growth. In contrast, this study found that counselors with more ACEs were more likely to experience less CS. This difference may be a result of this study utilizing the ACE Study Questionnaire (Felitti et al., 1998) whereas McKim and Smith-Adcock (2014) used Stamm’s (2008) Stressful Life Experiences – Short Form to assess for experiences that may have happened in adulthood or to someone outside of the family. Developmentally, painful childhood experiences may be harder to process, which may in turn produce further-reaching negative outcomes. McKim and Smith-Adcock also found that having a sense of control in the workplace and the number of years of experience as a counselor also positively correlated with CS. The results from our analysis indicated that greater attention needs to be given to the traumatic experiences of counselors and how these events may impact professional resilience.
This study may also be the first to examine the demographic factors of counselors, including gender, racial identity, and childhood SES, as potential predictive factors of burnout, STS, and CS. All three demographic variables were found to be predictive of CS, but none were predictive of burnout. The results from our analysis indicated that greater attention needs to be given to the traumatic experiences of counselors and how these events may impact CS, burnout, and STS.
It should be noted that ethnically minoritized counselors had higher rates of CS than their White peers. Given that higher ACEs scores had a negative relationship with CS with a high effect size, and that minoritized counselors had higher average rates of ACEs and lower average rates of PCEs when compared to White counselors, we expected minoritized counselors to experience lower CS. However, the current study found that being a minoritized counselor actually predicted higher CS and lower burnout. It may encourage all counselors to know that greater CS among minoritized counselors indicates that ACEs and PCEs are not determinative of whether a person experiences burnout or satisfaction.
Our findings that female counselors were more likely to have higher CS than their male peers, and that counselors from low-income or working-class SES had higher CS than those from middle and upper classes, are also noteworthy. It is possible that the more collectivist tendencies of minoritized individuals in general, and of female counselors regardless of race, may help foster greater professional resilience or quality of life (Graham et al., 2020; Jordan, 2017). Counselors from lower- or working-class childhood SES may also maintain the collectivist orientation of their upbringing. This proposition is supported by previous research, which indicates that social support is a significant factor that promotes CS in therapists (Ducharme et al., 2008). This may also relate to Crouch et al.’s (2019) finding that the most significant PCE that mitigates the effects of ACEs is having a safe relationship with an adult. These results are further supported by research indicating that secure attachments in adulthood moderate the effect of childhood adversity (Klasen et al., 2019). Despite a limited sample size, Conteh et al. (2017) found that 95% of their sample of 86 counselors-in-training reported having experienced at least one trauma. Although male participants in Conteh’s study were significantly more likely to report more traumas than women—4.93 to 3.46 respectively—women reported more post-traumatic growth than men. Similar to our findings, this may indicate why female counselors were more likely to experience greater CS than male counselors.
Although close to half of our participants (42.9%) met the critical threshold of four ACEs, it is encouraging that the average participant indicated that they were not experiencing burnout. This may be the result of more than half of our participants having five or more PCEs, with PCEs predicting lower burnout. It should also be noted that in this study, ACEs were not significantly correlated with STS, which may be counterintuitive as one may assume that childhood adversity may leave one more susceptible to STS. The strongest findings in the current study, as demonstrated by high effect sizes, are that lower ACE scores predict higher CS and lower burnout. However, the potentially mitigating influence of PCEs only predicted burnout, not CS, with a lower effect size.
Limitations
Threats to internal and external validity are unavoidable in descriptive studies. As such, one limitation of this study is that it focused on descriptive and predictive relationships and therefore does not describe causation. Furthermore, this study used self-report data which may threaten internal validity. Finally, selection bias may be a risk to generalizability. However, the sample in this study is demographically similar to other studies examining the counseling population, so this risk may be minimal.
Implications
Both professional organizations (e.g., ACA, AMHCA) and CACREP can promote counselor wellness by putting policies in place recognizing that individuals going into the counseling profession are likely to have personal histories shaped by adverse experiences. These policies may include a more systemic understanding of wellness strategies for counselors. Self-care is often conceptualized as a personal endeavor achieved outside of work hours, yet policies may be put in place to promote organizational wellness by providing space and emotional support for counselor wellness. For example, far too often grants require caseloads that are too heavy to foster and maintain the well-being of counselors.
The results of this study may also have implications for counselor education. Given that 42% of our participants had four or more ACEs, it may be likely that close to half of students within counseling programs have also suffered from a significant amount of childhood adversity. This may have implications for how we educate counselors to work with trauma. Trauma-informed training generally focuses on the effects of trauma on the life of clients and supports evidence-based practices that aid in recovery, resilience, and improved quality of life. Training that is trauma-attuned may focus more on the counselor’s awareness of how their own history of adversity may shape their professional stamina. This may also lead to more research on trauma-attuned supervision.
Considering the substantial percentage of MHCs who may have four or more ACEs, it is possible that many clinical supervisors have also been greatly affected by their personal histories. Trauma-attuned supervisors will continually reflect on how their past adversity may be influencing the supervisory relationship while also monitoring both their own as well as their supervisee’s levels of burnout and emotional reactivity toward clients.
As Zyromski et al. (2020) posited, the use of ACEs as a construct can provide clarity and focus to the harmful experiences that may impede the healthy development of a client. Likewise, knowledge about ACEs and PCEs can help supervisors and counselor educators train counselors who are at greater risk for burnout. It is important that the privacy of the counselor’s childhood experiences be protected, but trainees can be given the ACE and PCE assessments and told of the risk factors that high ACE and low PCE scores have with regard to burnout and CS. Furthermore, clinical and faculty supervisors can provide assessments for CS and burnout at key points during a trainee’s internship or first few years of postgraduate experience. Counselor educators and supervisors may then help trainees develop a self-care plan that will help to foster CS.
Directions for Future Research
Future studies may further examine the difference between demographic groups based on gender, race, and education in relation to potential protective factors that female and minoritized MHCs have that may decrease the likelihood they will experience burnout. Further research may also examine which ACEs, if any, may have higher correlations with burnout and which PCEs are more likely to serve as protective factors. Furthermore, our results indicate a need to study the CS and burnout of minoritized counselors, female counselors, and those coming from lower childhood SES. Examination of potential cultural and protective factors of these groups may contribute significantly to the literature on burnout prevention.
Given the percentage of counselors who have ACE scores that fall within the range of concern, future research may examine potential differences of counselors who are trauma-attuned and not simply trauma-informed. As stated above, ACEs were not significantly correlated with STS. It may be helpful for future researchers to use different measurements of secondary stress to further assess whether there is any correlation between ACEs and STS.
Conclusion
The purpose of this study was to examine personal factors in the developmental history of clinical MHCs that may influence their likelihood of experiencing professional burnout. This is the first known study we can identify using the ACE Study Questionnaire as a measure to inquire about a potential relationship between the counselors’ developmental adversity and their rates of burnout, CS, and STS. Results indicated that higher ACE scores correlate positively with burnout, and yet PCEs may serve as protective factors. Finally, we found that women and minoritized counselors were less likely to experience burnout than males and White individuals. This was true for minoritized counselors despite their having slightly higher rates of ACEs and lower rates of PCEs. We recommend that counselors become aware of how their own experiences of ACEs and PCEs may be impacting their current practice.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
American Counseling Association. (2014). ACA code of ethics. www.counseling.org/docs/default-source/default-document-library/2014-code-of-ethics-finaladdress.pdf
American Mental Health Counselors Association. (2020). AMHCA code of ethics. https://bit.ly/AMHCAcodeofethics
Anda, R. F., Brown, D. W., Felitti, V. J., Bremner, J. D., Dube, S. R., & Giles, W. H. (2007). Adverse childhood experiences and prescribed psychotropic medications in adults. American Journal of Preventive Medicine, 32(5), 389–394. https://doi.org/10.1016/j.amepre.2007.01.005
Anda, R. F., Felitti, V. J., Bremner, J. D., Walker, J. D., Whitfield, C., Perry, B. D., Dube, S. R., & Giles, W. H. (2006). The enduring effects of abuse and related adverse experiences in childhood: A convergence of evidence from neurobiology and epidemiology. European Archives of Psychiatry and Clinical Neuroscience, 256, 174–186. https://doi.org/10.1007/s00406-005-0624-4
Baird, K., & Kracen, A. C. (2006). Vicarious traumatization and secondary traumatic stress: A research synthesis. Counselling Psychology Quarterly, 19(2), 181–188. https://doi.org/10.1080/09515070600811899
Bemak, F., & Chung, R. C.-Y. (2017). Refugee trauma: Culturally responsive counseling interventions. Journal of Counseling & Development, 95(3), 299–308. https://doi.org/10.1002/jcad.12144
Bethell, C., Jones, J., Gombojav, N., Linkenbach, J., & Sege, R. (2019). Positive childhood experiences and adult mental and relational health in a statewide sample: Associations across adverse childhood experiences levels. JAMA Pediatrics, 173(11), e193007. https://doi.org/10.1001/jamapediatrics.2019.3007
Boullier, M., & Blair, M. (2018). Adverse childhood experiences. Pediatrics and Child Health, 28(3), 132–137. https://doi.org/10.1016/j.paed.2017.12.008
Branson, D. C. (2019). Vicarious trauma, themes in research, and terminology: A review of literature. Traumatology, 25(1), 2–10. https://doi.org/10.1037/trm0000161
Butler, L. D., Carello, J., & Maguin, E. (2017). Trauma, stress, and self-care in clinical training: Predictors of burnout, decline in health status, secondary traumatic stress symptoms, and compassion satisfaction. Psychological Trauma: Theory, Research, Practice, and Policy, 9(4), 416–424. https://doi.org/10.1037/tra0000187
Campbell, J. A., Walker, R. J., & Egede, L. E. (2016). Associations between adverse childhood experiences, high- risk behaviors, and morbidity in adulthood. American Journal of Preventive Medicine, 50(3), 344–352. https://doi.org/10.1016/j.amepre.2015.07.022
Can, N., & Watson, J. C. (2019). Individual and relational predictors of compassion fatigue among counselors-in-training. The Professional Counselor, 9(4), 285–297. https://doi.org/10.15241/nc.9.4.285
Coaston, S. C. (2017). Self-care through self-compassion: A balm for burnout. The Professional Counselor, 7(3), 285–297. https://doi.org/10.15241/scc.7.3.285
Cohen, J. (1988). Statistical power analysis for the behavioral sciences. (2nd ed.) Routledge.
Cohen, J. (1992). Statistical power analysis. Current Directions in Psychological Science, 1(3), 98–101. https://doi.org/10.1111/1467-8721.ep10768783
Conteh, J. A., Huber, M. J., & Bashir, H. A. (2017). Examining the relationship between traumatic experiences and posttraumatic growth among counselors-in-training. The Practitioner Scholar: Journal of Counseling and Professional Psychology, 6, 32–36.
Cook, R. M., Fye, H. J., Jones, J. L., & Baltrinic, E. R. (2021). Self-reported symptoms of burnout in novice professional counselors: A content analysis. The Professional Counselor, 11(1), 31–45. https://doi.org/10.15241/rmc.11.1.31
Council for Accreditation of Counseling and Related Educational Programs. (2015). 2016 CACREP standards. http://www.cacrep.org/wp-content/uploads/2018/05/2016-Standards-with-Glossary-5.3.2018.pdf
Crouch, E., Radcliff, E., Strompolis, M., & Srivastav, A. (2019). Safe, stable, and nurtured: Protective factors against poor physical and mental health outcomes following exposure to adverse childhood experiences (ACEs). Journal of Child & Adolescent Trauma, 12, 165–173. https://doi.org/10.1007/s40653-018-0217-9
Debellis, M. D. (2001). Developmental traumatology: the psychobiological development of maltreated children and its implications for research, treatment, and policy. Development and Psychopathology, 13(3), 539–564. https://doi.org/10.1017/s0954579401003078
Dube, S. R., Williamson, D. F., Thompson, T., Felitti, V. J., & Anda, R. F. (2004). Assessing the reliability of retrospective reports of adverse childhood experiences among adult HMO members attending a primary care clinic. Child Abuse & Neglect, 28(7), 729–737. https://doi.org/10.1016/j.chiabu.2003.08.009
Ducharme, L. J., Knudsen, H. K., & Roman, P. M. (2008). Emotional exhaustion and turnover intention in human service occupations: The protective role of coworker support. Sociological Spectrum, 28(1), 81–104. https://doi.org/10.1080/02732170701675268
Evans, J. H. (1997). Trauma and post-traumatic growth among graduate level counselor education students: What is their relative incidence and what relationships do they share? (Order No. 9732654) [Doctoral dissertation, Ohio University]. ProQuest Dissertations & Theses Global.
Faul, F., Erdfelder, E., Buchner, A., & Lang, A.-G. (2009). Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behavior Research Methods, 41(4), 1149–1160. https://doi.org/10.3758/brm.41.4.1149
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., Koss, M. P., & Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine, 14(4), 245–258. https://doi.org/10.1016/s0749-3797(98)00017-8
Ford, D. C., Merrick, M. T., Parks, S. E., Breiding, M. J., Gilbert, L. K., Edwards, V. J., Dhingra, S. S., Barile, J. P., & Thompson, W. W. (2014). Examination of the factorial structure of adverse childhood experiences and recommendations for three subscale scores. Psychology of Violence, 4(4), 432–444. https://doi.org/10.1037/a0037723
Frampton, N. M. A., Poole, J. C., Dobson, K. S., & Pusch, D. (2018). The effects of adult depression on the recollection of adverse childhood experiences. Child Abuse & Neglect, 86, 45–54. https://doi.org/10.1016/j.chiabu.2018.09.006
Graham, C., Chun, Y., Grinstein-Weiss, M., & Roll, S. (2020, June 24). Well-being and mental health amid COVID-19: Differences in resilience across minorities and whites. Brookings. https://www.brookings.edu/research/well-being-and-mental-health-amid-covid-19-differences-in-resilience-across-minorities-and-whites
Hensel, J. M., Ruiz, C., Finney, C., & Dewa, C. S. (2015). Meta-analysis of risk factors for secondary traumatic stress in therapeutic work with trauma victims. Journal of Traumatic Stress, 28(2), 83–91. https://doi.org/10.1002/jts.21998
Hughes, K., Bellis, M. A., Hardcastle, K. A., Sethi, D., Butchart, A., Mikton, C., Jones, L., & Dunne, M. P. (2017). The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. The Lancet Public Health, 2(8), 356–366. https://doi.org/10.1016/S2468-2667(17)30118-4
Ivicic, R., & Motta, R. (2017). Variables associated with secondary traumatic stress among mental health professionals. Traumatology, 23(2), 196–204. https://doi.org/10.1037/trm0000065
Jordan, J. V. (2017). Relational–cultural theory: The power of connection to transform our lives. The Journal of Humanistic Counseling, 56(3), 228–243. https://doi.org/10.1002/johc.12055
Klasen, J., Nolte, T., Möller, H., & Taubner, S. (2019). Aversive kindheitserfahrungen, bindungsrepräsentationen und mentalisierungsfähigkeit von psychotherapeuten in ausbildung [Adverse childhood experiences, attachment representations and mentalizing capacity of psychotherapists in training]. Zeitschrift für Psychosomatische Medizin und Psychotherapie, 65(4), 353–371. https://doi.org/10.13109/zptm.2019.65.4.353
Lakioti, A., Stalikas, A., & Pezirkianidis, C. (2020). The role of personal, professional, and psychological factors in therapists’ resilience. Professional Psychology: Research and Practice, 51(6), 560–570. https://doi.org/10.1037/pro0000306
Lanier, B. A., & Carney, J. S. (2019). Practicing counselors, vicarious trauma, and subthreshold PTSD: Implications for counselor educators. The Professional Counselor, 9(4), 334–346. https://doi.org/10.15241/bal.9.4.334
Lee, R. D., & Chen, J. (2017). Adverse childhood experiences, mental health, and excessive alcohol use: Examination of race/ethnicity and sex differences. Child Abuse & Neglect, 69, 40–48. https://doi.org/10.1016/j.chiabu.2017.04.004
Lee, S. M., Cho, S. H., Kissinger, D., & Ogle, N. T. (2010). A typology of burnout in professional counselors. Journal of Counseling & Development, 88(2), 131–138. https://doi.org/10.1002/j.1556-6678.2010.tb00001.x
Maslach, C., Schaufeli, W. B., & Leiter, M. P. (2001). Job burnout. Annual Review of Psychology, 52, 397–422. https://doi.org/10.1146/annurev.psych.52.1.397
McKim, L. L., & Smith-Adcock, S. (2014). Trauma counsellors’ quality of life. International Journal for the Advancement of Counselling, 36, 58–69. https://doi.org/10.1007/s10447-013-9190-z
Merrick, M. T., Ports, K. A., Ford, D. C., Afifi, T. O., Gershoff, E. T., & Grogan-Kaylor, A. (2017). Unpacking the impact of adverse childhood experiences on adult mental health. Child Abuse & Neglect, 69, 10–19. https://doi.org/10.1016/j.chiabu.2017.03.016
Metzler, M., Merrick, M. T., Klevens, J., Ports, K. A., & Ford, D. C. (2017). Adverse childhood experiences and life opportunities: Shifting the narrative. Children and Youth Services Review, 72, 141–149.
Molnar, B. E., Sprang, G., Killian, K. D., Gottfried, R., Emery, V., & Bride, B. E. (2017). Advancing science and practice for vicarious traumatization/secondary traumatic stress: A research agenda. Traumatology, 23(2), 129–142. https://doi.org/10.1037/trm0000122
Nelson-Gardell, D., & Harris, D. (2003). Childhood abuse history, secondary traumatic stress, and child welfare workers. Child Welfare, 82(1), 5–26.
Norton, A. L., & Tan, T. X. (2019). The relationship between licensed mental health counselors’ political ideology and counseling theory preference. American Journal of Orthopsychiatry, 89(1), 86–94. https://doi.org/10.1037/ort0000339
Redford, J. (Director). (2016). Resilience: The biology of stress and the science of hope [Film]. KPJR Films. https://kpjrfilms.co/resilience/
Stamm, B. H. (2008). Design theory and psychometrics of the stressful life experiences screening (SLES). https://bit.ly/StammSLES
Stamm, B. H. (2010). The concise manual for the professional quality of life scale (ProQOL). https://proqol.org/proqol-manual
Strompolis, M., Tucker, W., Crouch, E., & Radcliff, E. (2019). The intersectionality of adverse childhood experiences, race/ethnicity, and income: Implications for policy. Journal of Prevention & Intervention in the Community, 47(4), 310–324. https://doi.org/10.1080/10852352.2019.1617387
Thomas, J. T. (2016). Adverse childhood experiences among MSW students. Journal of Teaching in Social Work, 36(3), 235–255. https://doi.org/10.1080/08841233.2016.1182609
Thompson, I., Amatea, E., & Thompson, E. (2014). Personal and contextual predictors of mental health counselors’ compassion fatigue and burnout. Journal of Mental Health Counseling, 36(1), 58–77. https://doi.org/10.17744/mehc.36.1.p61m73373m4617r3
Webber, J. M., Kitzinger, R., Runte, J. K., Smith, C. M., & Mascari, J. B. (2017). Traumatology trends: A content analysis of three counseling journals from 1994 to 2014. Journal of Counseling & Development, 95(3), 249–259. https://doi.org/10.1002/jcad.12139
Wheeler, N. J., Regal, R. A., Griffith, S.-A. M., & Barden, S. M. (2021). Dyadic influence of adverse childhood experiences: Counseling implications for mental and relational health. Journal of Counseling & Development, 99(1), 24–36. https://doi.org/10.1002/jcad.12351
Zyromski, B., Baker, E., Betters-Bubon, J., Dollarhide, C. T., & Antonides, J. (2020). Adverse childhood experiences: A 20-year content analysis of American Counseling Association and American School Counselor Association journals. Journal of Counseling & Development, 98(4), 351–362. https://doi.org/10.1002/jcad.12338
Eric M. Brown, PhD, LPC, is an assistant professor at DePaul University. Kristy L. Carlisle, PhD, is an assistant professor at Old Dominion University. Melanie Burgess, PhD, is an assistant professor at the University of Memphis. Jacob Clark, BS, is a graduate student at Old Dominion University. Ariel Hutcheon, MA, is a doctoral student at Old Dominion University. Correspondence may be addressed to Eric M. Brown, 2247 N. Halsted St., Chicago, IL 60614, ebrow107@depaul.edu.
Feb 7, 2022 | Volume 12 - Issue 1
Clark D. Ausloos, Madeline Clark, Hansori Jang, Tahani Dari, Stacey Diane Arañez Litam
Trans youth experience discrimination and marginalization in their homes, communities, and schools. Professional school counselors (PSCs) are positioned to support and advocate for trans youth as dictated by professional standards. However, an extensive review of literature revealed a lack of confidence and competence in counselors working with trans youth and their families. Further, there is a dearth of literature that addresses factors leading to increased school counselor competence with trans students. The current study uses a cross-sectional survey design to contribute to the extant literature and explore how PSCs in the United States work with students in the K–12 public school system. Results from multiple regression analyses indicate that PSCs who have had postgraduate training and report personal and professional experiences with trans students are more competent in working with trans students. Implications for PSCs and school counselor education programs are discussed.
Keywords: trans youth, school counselors, competence, counselor education, multiple regression analysis
Trans people experience an incongruence between their sex assigned at birth and their gender identity (GI; Ginicola et al., 2017; McBee, 2013). The term trans encompasses a wide range of gender-expansive identities, including trans (transgender), nonbinary (one who identifies outside the gender binary of male or female), genderqueer or gender-fluid (one who identifies with gender in a fluid, dynamic way) and agender (one who does not identify as having a gender). Trans people face pervasive discrimination and marginalization (Whitman & Han, 2017), leading to severe physical and mental health disparities, like depression, anxiety, and suicidality (James et al., 2016). In schools, trans students face 4 times higher rates of discrimination when compared with cisgender peers (Kosciw et al., 2020; Williams et al., 2021). Trans students are more vulnerable to mental health disorders, a lack of social support, and an increase in self-harm, suicidal ideations, and suicide attempts (Kosciw et al., 2020; Reisner et al., 2014), especially among transmale and nonbinary students (Toomey et al., 2018). These rates are increasing in national trends and are even higher among Black and Latinx trans students (Vance et al., 2021). The COVID-19 pandemic further exacerbated barriers and inequities for trans students, with increasing health concerns, isolation, economic hardships, issues with housing, and limited access to essential clinical care (Burgess et al., 2021).
Increasingly, trans students face systemic legal barriers to their health and well-being (Wang et al., 2016). States including Arkansas, Idaho, Montana, South Dakota, and Tennessee have introduced bills that ban trans students from participating in sports that are congruent with their GI (Transgender Law Center, 2021). In April of 2021, Arkansas banned medical gender-affirming services to students under 18 years of age (American Civil Liberties Union [ACLU], 2021). New Hampshire’s House Bill 68 proposed adding gender-affirming treatments to the definition of child abuse (ACLU, 2021). Beyond political oppression, trans youth experience overt discrimination, verbal abuse, physical and sexual assault, and marginalization within their homes, schools, and places of employment (Human Rights Campaign [HRC], 2018; James et al., 2016). Trans youth additionally face disaffirming and incompetent teachers and medical professionals (Grant et al., 2011; James et al., 2016; Whitman & Han, 2017) and embedded systemic transmisia (the hatred of trans persons; Simmons University Library, 2019). Despite the pervasive mental health concerns faced by trans students (i.e., depression, anxiety, disordered eating, self-harm, suicide), professional school counselors (PSCs) continue to be ill equipped in supporting and advocating for this marginalized population within schools (Simons, 2021). Based upon an analysis of the extant body of research, we found that counselor education training programs lack rigor in working with trans students (O’Hara et al., 2013; Salpietro et al., 2019), counselor educators may hold biased views about trans students (Frank & Cannon, 2010), and there is an absence of quality professional development opportunities on trans issues (Salpietro et al., 2019; Shi & Doud, 2017). It is therefore of paramount importance for PSCs and counselor education programs to obtain a deeper understanding of how to better prepare for and support trans students in schools.
Professional School Counselors and Trans Students
PSCs focus on academic, career, and social-emotional growth and work as leaders alongside teachers, administration, families, and other stakeholders. PSCs are therefore well positioned to provide safety and support for trans students, promote change, and act as social justice advocates within schools (Bemak & Chung, 2008). The American School Counselor Association (ASCA) mandates that PSCs “promote affirmation, respect, and equal opportunity for all individuals regardless of . . . gender identity, or gender expression . . . and promote awareness of and education on issues related to LGBT students” (2016a, p. 37). PSCs who work with trans students may provide services through the Multitiered Systems of Support lens (MTSS; ASCA, 2019), through collaboration, by supporting school administration and staff (e.g., trainings, meetings, workshops), and through provision of direct student services (e.g., individual and group counseling, working with families). More specifically, PSCs advocate for and with students for name and pronoun changes within schools, trans-inclusive school policies, and increased visibility and normalization of trans people and issues.
ASCA (2016b) adopted a position that PSCs recognize that “the responsibility for determining a student’s gender identity rests with the student rather than outside confirmation from medical practitioners . . . or documentation of legal changes” (p. 64). It is clear that PSCs should possess knowledge and skills in working with and advocating for trans youth through a range of services at various levels and in coordination with other stakeholders in schools, all while respecting students’ autonomy and authenticity (ASCA, 2016a, 2016b, 2019; Bemak & Chung, 2008).
Counselor Education Programs
Although professional standards provide best practices (ALGBTIC LGBQQIA Competencies Taskforce, 2013; ASCA, 2016a), many PSCs never receive the training necessary to effectively serve trans students (Bidell, 2012; O’Hara et al., 2013; Salpietro et al., 2019). Salpietro and colleagues (2019) reported that counselor incompetence was related to a lack of rigorous training that attends to family systems, intersectionality, and medical issues through gender-affirming therapies (i.e., blockers, hormones, or surgeries). These researchers indicated a need for comprehensive, standardized, and thorough formal training (i.e., graduate school) and informal professional development opportunities. These findings are consistent with Shi and Doud (2017), who recommended PSCs specifically take advantage of conferences and workshops to supplement formal educational curricula. The Gay, Lesbian, and Straight Education Network (GLSEN) conducted a survey that reported about 81% of school mental health professionals received “little to no competency training in their graduate programs related to working with [trans] populations,” and about 74% of participants rated their graduate training programs as “fair or poor” in preparing them for work with trans students (GLSEN et al., 2019, p. xviii). GLSEN and other professional organizations additionally reported about two-thirds of school professionals do not feel prepared to work with trans students (GLSEN et al., 2019). Although there are some professional development opportunities, such as those offered through the World Professional Association for Transgender Health (WPATH), the HRC, and the Society for Sexual, Affectional, Intersex, and Gender-Expansive Identities (SAIGE), there is still a lack of concrete training within graduate programs and through fieldwork experiences and an overall lack of accessible, professional trainings. There is a clear need for increased attention to trans issues in formal educational programs and professional development offerings.
Purpose of the Study and Research Questions
This study examines factors that contribute to PSC competence in working with trans students in K–12 public schools. We highlight the need for PSCs and counselor education training programs to better focus on and support trans students. More specifically, we examine the following PSC factors: (a) the PSC’s GI, (b) whether the PSC has received postgraduate training on trans issues or populations, (c) whether the PSC has worked with self-identified trans students, and (d) whether the PSC knows someone who identifies as trans outside of the school setting.
PSC Gender Identity
Researchers recommend that special attention is given within a category of interest (i.e., gender identity) to historically marginalized groups, encouraging counselor-researchers to view all samples “in terms of their particularity and to attend to diversity within samples” (Cole, 2009, p. 176). We were intentional in using PSC GI demographic factors in data analysis, attending to diversity among PSC gender identities, as research indicates there may be relationships between counselor GI, privilege and oppression, and multicultural counselor competence (Cole, 2009). Culturally competent counselors engage in self-reflection, examine their own biases and stereotypes, consider how their positions of privilege or oppression impact the therapeutic alliance, and deliver culturally responsive counseling interventions.
Postgraduate Training Addressing Trans Issues
Researchers note that graduate programs in counselor education are not adequately preparing school counseling students to work with trans students (Bidell, 2012; Farmer et al., 2013; Frank & Cannon, 2010; GLSEN et al., 2019; O’Hara et al., 2013) and that much of the awareness, knowledge, and skills gained in working with this population are result of counselors’ self-seeking professional trainings, education, and workshops that are focused on trans issues and students (Salpietro et al., 2019; Shi & Doud, 2017).
Professional Experiences With Trans Students
O’Hara and colleagues (2013) reported no significance on scores of competence in working with trans clients between counseling students who completed practicum or internship and those who did not. In the present study, our variable relates to PSCs who have already graduated, reflecting on their professional tenure as PSCs, and if these experiences provided opportunities to work with trans students.
Personal Relationships With Trans People
O’Hara and colleagues (2013) reported that participants in their study identified informal sources as necessary for gaining trans-affirming knowledge and skills, such as “exposure to or personally knowing someone who [is trans]” (p. 246). Research supports the concept that increasing affirming attitudes and mitigating negative attitudes and beliefs toward trans individuals can be accomplished by exposure and intentional engagement in fostering personal and professional relationships with trans people (Salpietro et al., 2019; Simons, 2021). In forming relationships with trans people, we can listen to and learn from the lived experiences of this community, examine our own biases, and position ourselves as supportive allies, personally and professionally.
Research Questions
With these factors in mind, the following research questions were identified:
- What is the relationship between PSC factors (GI, postgraduate training, PSC work with trans students, and PSC personally knowing someone who is trans) and levels of PSC self-perceived competence in working with trans students in schools?
- What is the relationship between PSC factors (GI, postgraduate training, PSC work with trans students, and PSC personally knowing someone who is trans) and PSC awareness in working with trans students in schools?
- What is the relationship between PSC factors (GI, postgraduate training, PSC work with trans students, and PSC personally knowing someone who is trans) and PSC knowledge in working with trans students in schools?
- What is the relationship between PSC factors (GI, postgraduate training, PSC work with trans students, and PSC personally knowing someone who is trans) and PSC skills in working with trans students in schools?
We hypothesized there would be a statistically significance difference (p > .05) between PSC factors (GI, postgraduate training, PSC work with trans students, and PSC personally knowing someone who is trans) and levels of PSC self-perceived competence in working with trans students in schools. More specifically, we hypothesized that cisfemale PSCs who have had postgraduate training on trans issues, who have worked with trans students, and who personally know someone who is trans, would report higher scores in measures of awareness, knowledge, skills, and overall competence. Cisgender (cis) refers to someone who experiences congruence between their sex assigned at birth and their GI. Research demonstrates that cismales may express more negative attitudes and hold restrictive views toward queer and trans people when compared with cisfemales (Landén & Innala, 2000; Norton & Herek, 2012).
Method
Participants
With an anticipated medium effect size of 0.15, a desired statistical power level of 0.95, and desired probability level of 0.05 (Israel, 2013), we determined an appropriate minimum sample size for the proposed study was 120 PSCs. Initially, 499 responses were recorded. Of those, 110 were incomplete or had missing data, yielding a total of 389 fully completed surveys. Participants in this study (N = 389) were PSCs with a valid school counseling license working in a public school setting, from kindergarten through 12th grade, in the United States. Participant demographic information can be found in Table 1.
Table 1
Demographic Characteristics of Professional School Counselors (PSCs)
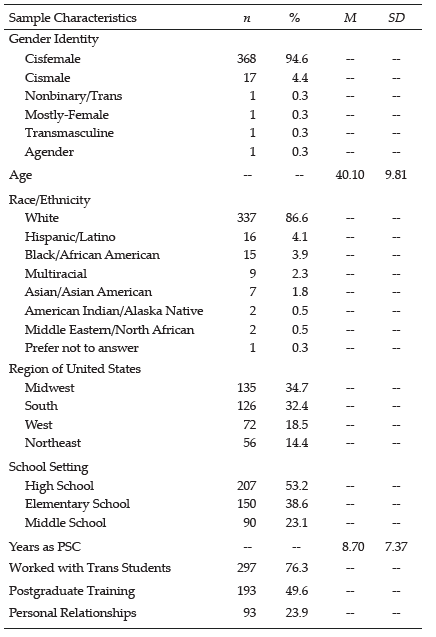
Procedures
For ease of use and accuracy of representation, we used probability sampling, more specifically, a simple random sample selection process (Creswell, 2013). Upon approval by the IRB, we posted a series of three recruitment letters (with 2 weeks between each posting) to PSCs through an online professional forum, ASCA Scene. We also posted our recruitment letter on ASCA Aspects, a monthly e-newsletter. Data were collected over a period of 6 weeks. PSCs who elected to participate were directed to the electronic informed consent document and the survey.
Instrumentation
Demographic Questionnaire
Participants completed a questionnaire with write-in options for both age and gender and forced-choice responses to gather racial-ethnic identity, years working as a licensed school counselor, the region in which they practiced, and grade levels in which the participants worked. Our four independent variables were collected through the demographic questionnaire. Participants indicated their experiences, if any, with trans students, experiences with postgraduate training on trans issues, and personal relationships with trans people.
Gender Identity Counselor Competency Scale
The Gender Identity Counselor Competency Scale (GICCS), a revised version of the Sexual Orientation Counselor Competency Scale (Bidell, 2005), was used to assess PSC competence, the dependent variable in the study. This is the instrument best suited for intended measurement of self-perceived competence (Bidell, 2012; O’Hara et al., 2013). Bidell (2005) developed the instrument based on Sue and colleagues’ (1992) research of multicultural counseling competencies, with the domains of attitudinal awareness, knowledge, and skills. Bidell (2005) reported the Cronbach’s alpha of .90, with subscale scores for internal consistency of .88 for the Awareness subscale, .71 for the Knowledge subscale, and .91 for the Skills subscale (Bidell, 2005, 2012). Test-retest reliability for the overall instrument was found to be .84, with .85 for the Awareness subscale, .84 for the Knowledge subscale, and .83 for the Skills subscale (Bidell, 2005). The GICCS is a 29-item self-report assessment on a 7-point Likert scale (where 1 is not at all true and 7 is totally true). Examples of questions include: “I have received adequate clinical training and supervision to counsel transgender clients” and “The lifestyle of a transgender client is unnatural or immoral” (O’Hara et al., 2013, p. 242). Cronbach’s alpha in the present study was .70, adequate for our analysis.
Awareness Subscale. The Awareness subscale consists of 10 items focused on counselors’ attitudinal awareness and prejudice about trans clients, including statements like “It would be best if my clients viewed a [cisgender] lifestyle as ideal” and “I think that my clients should accept some degree of conformity to traditional [gender] values” (Bidell, 2005, p. 273). Cronbach’s alpha for the Awareness subscale has been reported as .88 (Bidell, 2005) and was .89 in the present sample. Self-awareness and reflection are critical skills for counselors in examining deeply held biases and beliefs and in asking culturally responsive questions to strengthen the therapeutic alliance.
Knowledge Subscale. This subscale of the GICCS consists of eight items focused on counselors’ experiences and skills with trans clients, including statements like “I am aware that counselors frequently impose their values concerning [gender] upon [trans] clients” and “I am aware of institutional barriers that may inhibit [trans] clients from using mental health services” (Bidell, 2005, p. 273). Cronbach’s alpha for the Knowledge subscale was reported as .76 (Bidell, 2005), and was .73 in the present sample. Counselors who impose their own values on a client may cause rifts in the therapeutic alliance and could potentially even harm clients.
Skills Subscale. This subscale of the GICCS consists of 11 items focused on counselors’ experiences and skills with trans clients, including statements like “I have experience counseling [trans male] clients” and “I have received adequate clinical training and supervision to counsel [trans] clients” (Bidell, 2005, p. 273). Cronbach’s alpha for the Skills subscale was reported as .91 (Bidell, 2005) but was .75 in the present sample. Counselors working with trans students need to understand the importance of evolving language and terminologies; utilize affirmative, celebratory, and liberating counseling; and have knowledge of and connection to medical providers who support gender-affirming interventions.
Data Analysis Procedures
Data Cleaning
We first screened the data to ensure it was usable, reliable, and valid to proceed with statistical analyses. We continued data cleaning by coding the demographic variable of GI 1 through 4: cisfemale (1); cismale (2); nonbinary, trans, and/or genderqueer (3); and agender (4). Racial-ethnic identities were coded 1 through 10: American Indian or Alaska Native (1); Asian or Asian American (2); Black or African American (3); Hispanic, Latino, or Spanish Origin (4); Middle Eastern or North African (5); Native Hawaiian or Other Pacific Islander (6); White (7); Some Other Race, Ethnicity, or Origin (8); Prefer Not to Answer (9); and Multiracial Identity (10). PSC location was also coded 1 through 6: Midwest (1), Northeast (2), South (3), West (4), Puerto Rico or other U.S. Territories (5), and Other (6). Last of the demographic variables, we coded PSC School Level 1 through 4: Elementary (1), Middle School (2), High School (3), and Other (4). In addition, we cleaned variables highlighting PSC professional and personal training and experiences with trans persons. The first variable was dummy coded to reflect participants who had worked with trans students (1; n = 297, 76.3%) and participants who indicated not working with trans students (0; n = 92, 23.7%). The next variable, PSC postgraduate training, was dummy coded for use in data analyses, reflecting those who indicated they engaged in postgraduate training (1; n = 193, 49.6%) and participants who indicated they did not engage in postgraduate training (0; n = 196, 50.4%). The final variable was dummy coded to reflect participants who know someone who is trans outside of the school setting (1; n = 93, 23.9%) and those participants who do not know someone who is trans outside of the school setting (0; n = 296, 76.1%). Per Bidell (2005), we started by reverse scoring coded GICCS items and created new variables for the GICCS total mean score, attitudinal Awareness, Skills, and Knowledge subscales.
Data Analysis
Post–data cleaning, we entered all the data from the demographic questionnaire and the GICCS into SPSS 26. To best answer the research questions, we used a series of standard multiple regression analyses to determine “the existence of a relationship and the extent to which variables are related, including statistical significance” (Sheperis et al., 2017, p. 131). Although multiple regression analysis can be used in prediction studies, it can also be used to determine how much of the variation in a dependent variable is explained by the independent variables, which is what we intended to measure (Johnson, 2001). Our independent variables were four categorical variables measured by our demographic questionnaire: PSC GI, postgraduate training, PSC work with trans students, and PSC personal relationships with someone who is trans. Our dependent variable was school counselor competence in working with trans students, as measured by the GICCS (Bidell, 2005).
There are many assumptions to consider when conducting a multiple regression analysis, including (a) two or more continuous or categorical independent variables, (b) a continuous dependent variable, (c) independence of residuals (or observations), (d) linearity (both between dependent variable and each of the independent variables, and between the dependent variable and the independent variables as a whole), (e) homoscedasticity, (f) absence of multicollinearity, (g) no significant outliers, and (h) normally distributed residuals (Flatt & Jacobs, 2019). The research variables met assumptions (a) and (b) in conducting multiple regressions. In analyzing data in SPSS, independence of residuals was determined by using the Durbin-Watson statistic, which ranges in value from 0 to 4, with a value near 2 indicating no correlation between residuals. Assumption (c) was met, as the Durbin-Watson value found was 1.46 (Savin & White, 1977). Additionally, we plotted a scatterplot using variables, as well as a partial regression with each of the independent variables and the dependent variable, and observed linear relationships, attending to the assumptions of linearity (d; i.e., a linear relationship between dependent and independent variables) and homoscedasticity (e; i.e., residuals are equal for all values of the predicted dependent variable). Homoscedasticity was also assessed by visual inspection of a plot of studentized residuals versus unstandardized predicted values. To assess the absence of multicollinearity (f), we considered the variance inflation factors (VIF) indicated in the coefficients table (Flatt & Jacobs, 2019). We found VIF values ranging from 1.01 to 1.05, indicating an absence of multicollinearity (f). VIF is a measure of the amount of multicollinearity in a set of multiple regression variables (Flatt & Jacobs, 2019). We checked for unusual points (g): outliers, high leverage points, and highly influential points. We did identify a significant outlier (−3.10) in case number 133 by examining the range of standardized residuals ([−3.10 to 2.34]), which is outside the common cut-off range of three standard deviations (SD). We then inspected the studentized deleted residual values and found a value in case number 133 (−3.15), which falls outside the common cut-off range of 3 SD.
Additionally, we determined two cases of problematic leverage values that were greater than the safe value of 0.2 (0.36 and 0.23). The cases that violated assumptions were filtered out and the standard multiple regression analysis was run again. This time, the data did not violate assumptions (a) through (g). Last, we observed normally distributed standardized residuals (h). To determine if any cases were influential in the data, we examined the Cook’s Distance values, which ranged from .000 to .090. As there were no values above 1, there were no highly influential points. To answer the first research question (the relationship between PSC factors and levels of PSC self-perceived competence in working with trans students in schools as measured by total scores on the GICCS), we used a standard multiple regression analysis (Sheperis et al., 2017). To answer research questions 2 through 4, we conducted standard multiple regression analyses using the Awareness, Knowledge, and Skills subscales as the dependent variables, respectively.
Results
Correlations Between Variables of Interest
Prior to the regression analysis, we examined correlations between the variables: PSC GI (cisfemale, cismale, trans, agender), having worked with trans students, postgraduate training experiences, personally knowing someone who is trans, the GICCS Awareness subscale, the GICCS Skills subscale, the GICCS Knowledge subscale, and the GICCS total score. Correlations of variables of interest are found in Table 2. There were multiple significant correlations as determined by Pearson product moment correlations (r). The GICCS total score was significantly correlated with the Awareness subscale (r = −.65, p < .001), the Skills subscale (r = .83, p < .001), and the Knowledge subscale (r = .66, p < .001). The Awareness subscale was significantly correlated with the Skills subscale (r = −.26, p < .001) and the Knowledge subscale (r = .30, p < .001). The Knowledge subscale was also significantly correlated with the Skills subscale (r = .30, p < .001). In examining demographic factors, cisfemale GI was significantly correlated with cismale GI (r = −.90, p < .001), trans GI (r = −.37, p < .001), and agender GI (r = −.21, p < .001). Additionally, cisfemale GI was significantly correlated with having worked with trans students (r = −.12, p = .036), as well as the GICCS total score (r = −.14, p = .005), the Skills subscale (r = −.14, p = .005), and the Knowledge subscale (r = −.15, p = .003). Cismale GI was significantly correlated with the GICCS total score (r = .11, p = .038), the Skills subscale (r = .12, p = .017), and the Knowledge subscale (r = .11, p = .003). Trans GI was significantly correlated with personally knowing someone who is trans (r = .12, p = .002), as well as with the GICCS total score (r = .12, p = .034). Having worked with trans students was significantly correlated with the GICCS total score (r = .41, p <.001), the Skills subscale (r = .55, p < .001), and the Awareness subscale (r = −.11,
p = .032). Postgraduate training was significantly correlated with many variables, including personally knowing someone who is trans (r = .14, p = .005), and with the GICCS total scores (r = .36, p < .001), the Skills subscale (r = .41, p < .001), the Knowledge subscale (r = .19, p < .001), and the Awareness subscale (r = −.10, p = .040). Last, personally knowing someone who is trans was significantly correlated with the GICCS total score (r = .35, p < .001), the Skills subscale (r = .29, p < .001), the Knowledge subscale
(r = .25, p < .001), and the Awareness subscale (r = −.22, p < .001).
Table 2
Correlation Table for Variables of Interest
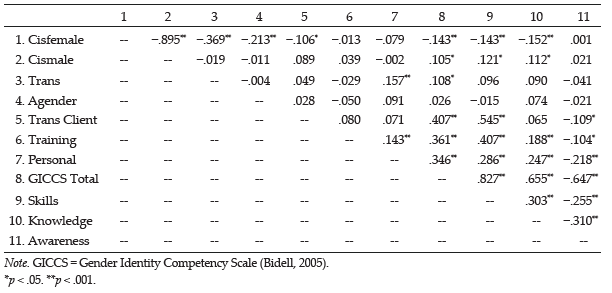
Model 1: PSC Competency
R² for the overall model was 35.2%, with an adjusted R² of 34.1%, a small to moderate size according to Cohen (1988). PSC factors significantly predicted levels of PSC self-perceived competence in working with trans students in schools, F(6, 381) = 34.430, p < .001. In examining beta weights (β), having worked with trans students received the strongest weight in the model (β = .35), followed by postgraduate training (β = .29) and personally knowing someone who is trans (β = .27). The variable with the most weight, having worked with trans students, had a structure coefficient (rs) of .67, and rs2 was 45.2%, meaning that of the 35.2% effect (R2), this variable accounts for 45.2% of the explained variance by itself. This shows that PSCs’ competence is increased by experiences with trans students, engaging in postgraduate trainings, and personally knowing someone who is trans. A summary of regression coefficients and standard errors can be found in Table 3.
Table 3
Multiple Linear Regression Analyses Exploring Professional School Counselor Competence
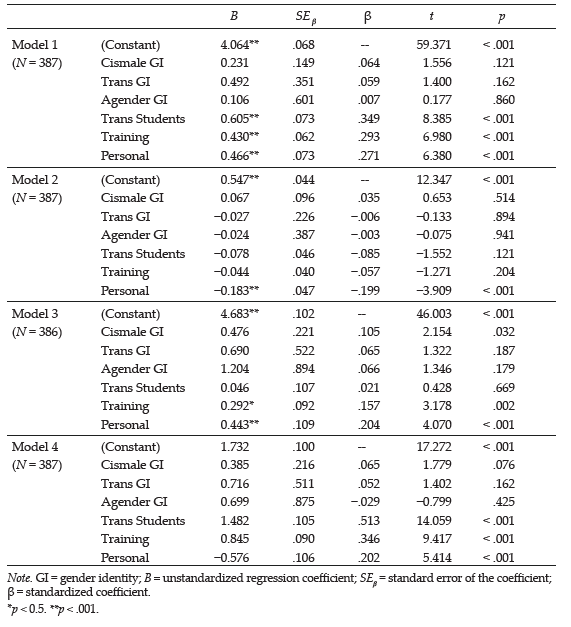
Model 2: PSC Awareness
R² for the overall model was 5.8%, with an adjusted R² of 6.2%, a very small effect size (Cohen, 1988). PSC factors (GI, postgraduate training, PSC work with trans students, and PSC personal relationship with someone who is trans) significantly predicted awareness of PSC self-perceived competence in working with trans students in schools, F(6, 380) = 3.873, p = .001. Personally knowing someone who is trans was the only significant predictor in this model. We examined the regression coefficients and corresponding data (β = −.20, rs = −0.90, rs2 = 80%). Of the 5.8% effect (R²), personally knowing someone who is trans accounted for 80% of the explained variance by itself.
Model 3: PSC Knowledge
R² for the overall model was 10.3%, with an adjusted R² of 8.9%, a small effect size (Cohen, 1988). PSC factors (GI, postgraduate training, PSC work with trans students, and PSC personal relationship with someone who is trans) significantly predicted knowledge of PSC self-perceived competence in working with trans students in schools, F(6, 379) = 7.257, p < .001. Personally knowing someone who is trans, postgraduate training, and cismale GI were all significant in this model. Personally knowing someone who is trans received the strongest weight in the model (β = .20, rs = .76), followed by postgraduate training (β = .16, rs = .58) and cismale GI (β = .12, rs = .35). After examining regression coefficients and corresponding data, we determined that of the 10.3% effect (R2), personally knowing someone who is trans accounted for 58.3% of the explained variance by itself. These findings demonstrate that PSC knowledge is strongly supported through fostering personal relationships with trans people.
Model 4: PSC Skills
R² for the overall model was 50.2%, with an adjusted R² of 49.5%, a medium effect size according to Cohen (1988). PSC factors (GI, postgraduate training, PSC work with trans students, and PSC personal relationship with someone who is trans) significantly predicted self-perceived PSC skills in working with trans students in schools, F(6, 380) = 63.945, p < .001. Having worked with trans students, postgraduate training, and personally knowing someone who is trans were all significant in this model. Having worked with trans students received the strongest weight in the model (β = .51), followed by postgraduate training (β = .35) and personally knowing someone who is trans (β = .20). After examining regression coefficients and corresponding data, we determined that of the 50.2% effect (R2), having worked with trans students accounted for 79% of the explained variance by itself. Counselors can augment their skills by staying updated on appropriate language and terminologies and by fostering relationships with affirming providers and medical professionals in the community.
Discussion
The most salient finding in this model is that PSCs who worked with trans students were strongly positively correlated with GICCS total scores (r = .61, p < .001). This finding may indicate that increased exposure to trans students may subsequently increase competency in working with trans populations. Our research findings supplement existing studies that reported a relationship between affirming attitudes toward trans students and professional exposure to trans people (Salpietro et al., 2019; Simons, 2021). Avoidance of counseling trans students because of discomfort is not only unethical (ASCA, 2016b) but inhibits a PSC’s ability to develop their GI competence (Henry & Grubbs, 2017). Thus, it is imperative that PSCs receive opportunities to work with trans students (through practicum or internship experiences); consult with experienced, gender-affirming PSCs who have worked with trans students; and “expose themselves to published texts . . . films . . . [and] service-learning activities . . . to gain a better understanding of the experiences of [trans] persons” (O’Hara et al., 2013, p. 251). Additionally, PSCs must engage in constant self-reflection, introspection, and processing of biases and worldviews to provide culturally competent care to trans students.
Counseling Competence
Postgraduate training was moderately positively correlated with GICCS total score (r = .43, p < .001), indicating that additional postgraduate training in trans issues increased competence in the present sample (Model 1). This is consistent with extant literature, which demonstrated that PSCs who received postgraduate training were more competent in providing affirming services to trans students compared to PSCs who had not received the training (Salpietro et al., 2019; Shi & Doud, 2017). Finally, the presence of personal relationships with trans people was moderately positively correlated with GICCS total scores (r = .47, p < .001). These results support current literature in that PSCs who currently have or have had personal relationships with trans people were more competent in providing affirming services to trans students (GLSEN et al., 2019; O’Hara et al., 2013; Salpietro et al., 2019; Simons, 2021).
Awareness
We explored the relationship between PSC factors on the Awareness subscale of the GICCS in the second research question (Model 2). In examining coefficients for the model, having personal relationships with trans people is associated with a decrease in GICCS Awareness subscale scores, a weak, negative correlation (r = −.19, p = .001). This finding may indicate that people who did not know someone personally who is trans would score slightly higher on the Awareness subscale. These unexpected findings are contrary to existing research, which reported that engaging in personal relationships with trans people increased affirming attitudes and mitigated negative attitudes (Henry & Grubbs, 2017; Salpietro et al., 2019). Because of the lack of practical significance of PSC factors (i.e., GI, postgraduate training, PSC work with trans students, and PSC personal relationship with someone who is trans) on the Awareness subscale, these results should be considered with caution.
Knowledge
In the third research question, we explored the relationship between PSC factors on the Knowledge subscale of the GICCS (Model 3). In examining coefficients for the model, PSC cisgender male GI was moderately positively correlated with the Knowledge subscale scores (r = .476, p = .032), indicating that cismale PSCs scored moderately higher on the Knowledge subscale when compared with other PSC gender identities in the present sample. One possible explanation is the present study’s sample of cisfemales (N = 368, 94.6%) and cismales (N = 17, 4.4%). Within this sample, the ages of the cismale PSCs could reflect a time in which counselor education programs increased attention to diversity, whereas this was not always a main tenet in training among older PSCs (who may be more represented by cisfemale PSCs in this sample [Bemak & Chung, 2008]). Presently, the Council for Accreditation of Counseling and Related Educational Programs (CACREP; 2015) requires accredited counselor education programs to deliver a counseling curriculum that includes specific attention to social and cultural diversity, an essential foundation of competent counselors. Additionally, PSC postgraduate training was weakly positively correlated with Knowledge subscale scores (r = .292, p = .002), which supports the literature that PSCs who engage in professional training opportunities outside of graduate school increase their knowledge of trans students and trans issues (Salpietro et al., 2019; Shi & Doud, 2017). Having personal experiences with trans people was moderately positively correlated with Knowledge subscale scores (r = .434, p < .001), indicating that those PSCs who personally knew a trans person felt more confident and competent in their knowledge about trans students and issues. This supports current literature (GLSEN et al., 2019; Henry & Grubbs, 2017; O’Hara et al., 2013; Salpietro et al., 2019) showing that PSCs who intentionally engaged in and fostered personal relationships with trans people reported greater competence.
Skills
Finally, we explored the relationship between PSC factors (GI, postgraduate training, PSC work with trans students, and PSC personal relationship with someone who is trans) on the Skills subscale of the GICCS in research question 4 (Model 4). In examining coefficients for the model, having worked with trans students was moderately positively correlated with Skills subscale scores (r = .545, p < .001), which may indicate that PSCs who work with trans students will be more likely to employ the necessary supports to ensure growth in “academic, career and social/emotional development” (ASCA, 2016a, para. 1). This is supported by literature in which researchers reported number of students worked with and “interpersonal contact” (personal exposure) as positive predictors of affirmative counselor competence (Bidell, 2012; Farmer et al., 2013). PSCs play an essential role in advocating for and removing barriers for trans students, which improves trans students’ well-being, academic success, and interpersonal growth. PSC postgraduate training was strongly positively correlated with Skills subscale scores (r = .845, p < .001), which may indicate that PSCs who engage in professional development opportunities and trainings gain essential skills for working with trans students. This finding is consistent with extant research that reported the importance of postgraduate training and professional development opportunities on trans topics (Bidell, 2012; Frank & Cannon, 2010; GLSEN et al., 2019; O’Hara et al., 2013). Finally, knowing someone personally who is trans was moderately positively correlated with Skills subscale scores (r = .576, p < .000), which may mean that having familiarity and exposure to trans folks increases PSC’s self-perceived skills.
Implications
Professional School Counselors
Based on the results of our study, PSCs who worked with trans students reported significantly higher scores of overall self-perceived competence compared to PSCs who had not worked with trans students. Specifically, our results indicate a link between PSCs having worked with trans students and higher scores on the Knowledge subscale. The GICCS Knowledge subscale addresses PSC knowledge of trans psychosocial issues (Bidell, 2005). This supports the idea that PSCs who work with self-identified trans students have a deeper understanding of the social and psychological challenges faced by trans people, and these experiences increase their comfort in working with trans students. All PSCs are required to protect and support the well-being of queer and trans youth and must have foundational knowledge and familiarity with trans students and issues (ASCA, 2016b). PSCs must attend professional development offerings on trans issues, and counselor education programs must provide increased time and attention to discussing trans issues, clients, and students.
PSC postgraduate training experiences are significantly linked to an overall increase in scores on the GICCS, indicating that PSC postgraduate experiences contribute to PSCs feeling more confident and competent in working with trans students. We conceptualized postgraduate training experiences as any training or education focused on trans persons or issues that a PSC received after their graduate program education. These results indicate that to increase competence and provide affirming, ethical care to trans students, PSCs should engage in some type of postgraduate training on trans issues and students, especially if they are unfamiliar with trans issues. These results are congruent with other studies, which found no significance in the relationship between groups on the Awareness subscale, but significant relationships on both the Knowledge and Skills subscales, with professional training experiences (Bidell, 2005; Rutter et al., 2008). PSCs are therefore encouraged to join professional organizations that promote best practices in working with trans students, like WPATH, the HRC, and SAIGE, as these organizations often offer professional development opportunities. It is essential that PSCs seek out trainings that are specific to trans students and issues, attend to unique psychosocial barriers, outline best practices, describe social/medical affirming care, and provide an overview of ethical and legal issues.
Of all the variables in the present study, PSCs knowing someone who identifies as trans was significantly linked to an increase in overall confidence and competence, as well as a significant increase in both Knowledge and Skills. Surprisingly, PSCs who indicated they did not know someone who identified as trans scored slightly higher on the Awareness subscale scores when compared with PSCs who did. The Awareness subscale of the GICCS examines a PSC’s self-awareness of anti-trans biases and stigmatization (Bidell, 2005). This result is contrary to existing research, which reported that engaging in personal relationships with trans folks increased affirming attitudes and mitigated negative attitudes (Henry & Grubbs, 2017; Salpietro et al., 2019). The link between a PSC personally knowing someone who is trans and a counselor’s competence in knowledge and skills supports extant literature that speaks to the importance of non–work-related experiences with trans people (e.g., personal, familial, social) and an increase in counselors’ competence in working with trans students (Whitman & Han, 2017). It is important that PSCs continue to monitor and increase their personal engagement with trans communities, as this significantly links to PSCs feeling more comfortable and more competent in working with trans students. Personal experiences may include fostering connections to trans family members, friends, and trans people through community organizations (GLSEN et al., 2019; Henry & Grubbs, 2017; Salpietro et al., 2019). Given the findings of our study, it is important for PSCs to connect to affirming resources in their communities. PSCs may consider exploring the multitude of resources offered by GLAAD (glaad.org), the National Center for Transgender Equality (NCTE; transequality.org), and PFLAG (pflag.org).
Counselor Education Programs
Our results indicate that those PSCs who engage in professional development are more competent than those who do not. Professional counseling organizations (i.e., ASCA) and accrediting bodies (i.e., CACREP) mandate that school counselors-in-training receive formal training in social and cultural diversity (F.2; CACREP, 2015), including multicultural counseling competencies (F.2.c.; CACREP, 2015), and deliver a comprehensive “counseling program that advocates for and affirms all students . . . including . . . gender, gender identity and expression” (ASCA, 2016a, para. 3). Although current standards call for the inclusion of LGBTQIA+ issues within counselor education curricula, the reality is that counselors-in-training receive minimal training in working with trans and gender-expansive students (Frank & Cannon, 2010; O’Hara et al., 2013). It is imperative that CE programs and counselor educators broaden the scope of learning about trans issues, going beyond the minimal requirements (CACREP, 2015) and providing depth and rigor in gender-related coursework in diversity courses. This research supports other emergent literature which recommends that counselor education programs offer additional, specific courses related to affectional and sexual identities (LGBQ+), and gender-expansive identities (trans, nonbinary), as covering specific issues and populations increases counselor competency (Bidell, 2012; Henry & Grubbs, 2017; O’Hara et al., 2013, Salpietro et al., 2019).
Limitations and Directions for Future Research
Limitations of the study include potential social desirability factors and inattentive responding, which may influence the quality of the data, as the study relied on self-report. Particularly, we note that the findings of higher self-awareness for PSCs who did not know someone who identified as trans could be a potential result of social desirability factors. Although the present study confirms that certain professional and personal factors contribute to PSCs increased competence in working with trans students in the present sample, additional research should be conducted. Also, much of our sample consisted of White ciswomen and, therefore, we caution readers about generalizing these findings to school counselors outside of those identities. The revised GICCS has not been used in many studies focusing on trans populations and additional research is needed to assess its validity with PSCs and trans youth (Bidell, 2005, 2012). Future researchers should consider additive studies that more deeply examine the types of professional development opportunities that promote PSC competency, including length, location, modality, themes, and expertise of presenter(s). Knowing these factors is important for crafting and delivering meaningful and competence-fostering professional development opportunities for PSCs. Also, future studies should examine unique nuances within trans groups, such as nonbinary and gender-fluid students (Toomey et al., 2018), and highlight the voices of trans students of color (Vance et al., 2021). Finally, future studies should also include demographic factors like religiosity and spirituality and their correlation to PSC GI competence, building on the work of Farmer and colleagues (2013).
Conclusion
This study highlights the need for increased attention to trans issues in many domains: among PSCs, within school counseling training programs, and in existing professional development offerings. ASCA mandates that PSCs be advocates for trans students, but there is a lack of attention to trans issues in school counseling training programs, leading PSCs to feel unprepared and to seek outside professional development offerings. The study also highlights the importance of building community and connections with trans people in and outside of professional settings, leading to increased PSC competence in professional settings. PSCs should continue to learn about the evolving language, trends, and needs of the trans community, ideally from those who are part of that community. Additionally, PSCs should engage with and use resources from professional trans-affirming organizations, such as WPATH, HRC, SAIGE, GLAAD, NCTE, and PFLAG.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
ALGBTIC LGBQQIA Competencies Taskforce. (2013). Association for Lesbian, Gay, Bisexual, and Transgender Issues in counseling competencies for counseling with Lesbian, Gay, Bisexual, Queer, Questioning, Intersex, and Ally individuals. Journal of LGBT Issues in Counseling, 7(1), 2–43. https://doi.org/10.1080/15538605.2013.755444
American Civil Liberties Union. (2021). Legislation affecting LGBTQ rights across the country 2021.
https://www.aclu.org/legislation-affecting-lgbt-rights-across-country
American School Counselor Association. (2016a). ASCA ethical standards for school counselors. https://www.schoolcounselor.org/getmedia/f041cbd0-7004-47a5-ba01-3a5d657c6743/Ethical-Standards.pdf
American School Counselor Association. (2016b). The school counselor and transgender/gender-nonconforming youth. https://schoolcounselor.org/Standards-Positions/Position-Statements/ASCA-Position-Statements/The-School-Counselor-and-Transgender-Gender-noncon
American School Counselor Association. (2019). ASCA school counselor professional standards & competencies.
https://www.schoolcounselor.org/getmedia/a8d59c2c-51de-4ec3-a565-a3235f3b93c3/SC-Competencies.pdf
Bemak, F., & Chung, R. C.-Y. (2008). New professional roles and advocacy strategies for school counselors: A multicultural/social justice perspective to move beyond the nice counselor syndrome. Journal of Counseling & Development, 86(3), 372–381. https://doi.org/10.1002/j.1556-6678.2008.tb00522.x
Bidell, M. P. (2005). The Sexual Orientation Counselor Competency Scale: Assessing attitudes, skills, and knowledge of counselors working with lesbian, gay, and bisexual clients. Journal of Counselor Education and Supervision, 44(4), 267–279. https://doi.org/10.1002/j.1556-6978.2005.tb01755.x
Bidell, M. P. (2012). Examining school counseling students’ multicultural and sexual orientation competencies through a cross-specialization comparison. Journal of Counseling & Development, 90(2), 200–207.
https://doi.org/10.1111/j.1556-6676.2012.00025.x
Burgess, C. M., Batchelder, A. W., Sloan, C. A., Ieong, M., & Streed, C. G., Jr. (2021). Impact of the COVID-19 pandemic on transgender and gender diverse health care. The Lancet, 9(11), 729–731.
https://doi.org/10.1016/S2213-8587(21)00266-7
Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed). Routledge.
Cole, E. R. (2009). Intersectionality and research in psychology. American Psychologist, 64(3), 170–180. https://doi.org/10.1037/a0014564
Council for Accreditation of Counseling and Related Educational Programs. (2015). 2016 CACREP standards. https://www.cacrep.org/for-programs/2016-cacrep-standards
Creswell, J. W. (2013). Research design: Qualitative, quantitative, and mixed methods approaches (4th ed.). SAGE.
Farmer, L. B., Welfare, L. E., & Burge, P. L. (2013). Counselor competence with lesbian, gay, and bisexual clients: Differences among practice settings. Journal of Multicultural Counseling and Development, 41(4), 194–209. https://doi.org/10.1002/j.2161-1912.2013.00036.x
Flatt, C., & Jacobs, R. L. (2019). Principle assumptions of regression analysis: Testing, techniques, and statistical reporting of imperfect data sets. Advances in Developing Human Resources, 21(4), 484–502.
https://doi.org/10.1177/1523422319869915
Frank, D. A., II, & Cannon, E. P. (2010). Queer theory as pedagogy in counselor education: A framework for diversity training. Journal of LGBT Issues in Counseling, 4(1), 18–31. https://doi.org/10.1080/15538600903552731
Ginicola, M. M., Smith, C., & Filmore, J. M. (2017). Affirmative counseling with LGBTQI+ people. American Counseling Association.
Gay, Lesbian, & Straight Education Network, American School Counselor Association, American Council for School Social Work, & School Social Work Association of America. (2019). Supporting safe and healthy schools for lesbian, gay, bisexual, transgender, and queer students: A national survey of school counselors, social workers, and psychologists. GLSEN. https://www.glsen.org/sites/default/files/2019-11/Supporting_Saf
e_and_Healthy_Schools_%20Mental_Health_Professionals_2019.pdf
Grant, J. M., Mottet, L. A., Tanis, J., Harrison, J., Herman, J. L., & Keisling, M. (2011). Injustice at every turn: A report of the National Transgender Discrimination Survey. National Center for Transgender Equality and National Gay and Lesbian Task Force. https://transequality.org/sites/default/files/docs/resources/NTDS_Report.pdf
Henry, H. L., & Grubbs, L. (2017). Best practices for school counselors working with transgender students. In G. R. Walz & J. C. Bleuer (Eds), Ideas and research you can use: VISTAS 2016. https://bit.ly/HenryTrans2017
Human Rights Campaign. (2018). 2018 LGBTQ Youth Report. https://bit.ly/HRCLGBTQReport
Israel, G. D. (2013). Determining sample size. Agricultural Education and Communication Department, UF/IFAS Extension. https://bit.ly/Israel2013SampleSize
James, S. E., Herman, J. L., Rankin, S., Keisling, M., Mottet, L., & Anafi, M. (2016). The report of the 2015 U.S. Transgender Survey. National Center for Transgender Equality. https://transequality.org/sites/default/file
s/docs/usts/USTS-Full-Report-Dec17.pdf
Johnson, B. (2001). Toward a new classification of nonexperimental quantitative research. Educational Researcher, 30(2), 3–13. https://doi.org/10.3102/0013189X030002003
Kosciw, J. G., Clark, C. M., Truong, N. L., & Zongrone, A. D. (2020). The 2019 National School Climate Survey: The experiences of lesbian, gay, bisexual, transgender, and queer youth in our nation’s schools. GLSEN. https://www.glsen.org/sites/default/files/2020-10/NSCS-2019-Full-Report_0.pdf
Landén, M., & Innala, S. (2000). Attitudes toward transsexualism in a Swedish national survey. Archives of Sexual Behavior, 29(4), 375–388. https://doi.org/10.1023/A:1001970521182
McBee, C. (2013). Towards a more affirming perspective: Contemporary psychodynamic practice with trans* and gender non-conforming individuals. The University of Chicago School of Social Service Administration (Org.) Advocates’ Forum: The University of Chicago, 37–52. The University of Chicago. https://crownschool.uchicago.edu/contemporary-psychodynamic-trans-and-gender-non-conforming-individuals
Norton, A. T., & Herek, G. M. (2012). Heterosexuals’ attitudes toward transgender people: Findings from a national probability sample of U.S. adults. Sex Roles, 68, 738–753. https://doi.org/10.1007/s11199-011-0110-6
O’Hara, C., Dispenza, F., Brack, G., & Blood, R. A. C. (2013). The preparedness of counselors in training to work with transgender clients: A mixed methods investigation. Journal of LGBT Issues in Counseling, 7(3), 236–256. https://doi.org/10.1080/15538605.2013.812929
Reisner, S. L., White, J. M., Dunham, E. E., Heflin, K., Begenyi, J., Cahill, S., & Project VOICE Team. (2014). Discrimination and health in Massachusetts: A statewide survey of transgender and gender nonconforming adults. The Fenway Institute. http://fenwayfocus.org/wp-content/uploads/2014/07/The-Fenway-Institut
e-MTPC-Project-VOICE-Report-July-2014.pdf
Rutter, P. A., Estrada, D., Ferguson, L. K., & Diggs, G. A. (2008). Sexual orientation and counselor competency: The impact of training on enhancing awareness, knowledge and skills. Journal of LGBT Issues in Counseling, 2(2), 109–125. https://doi.org/10.1080/15538600802125472
Salpietro, L., Ausloos, C., & Clark, M. (2019). Cisgender professional counselors’ experiences with trans* clients. Journal of LGBT Issues in Counseling, 13(3), 198–215. https://doi.org/10.1080/15538605.2019.1627975
Savin, N. E., & White, K. J. (1977). The Durbin-Watson Test for serial correlation with extreme sample sizes or many regressors. Econometrica, 45(8), 1989–1996. https://doi.org/10.2307/1914122
Sheperis, C. J., Young, J. S., & Daniels, M. H. (2017). Counseling research: Quantitative, qualitative, and mixed methods (2nd ed.). Pearson.
Shi, Q., & Doud, S. (2017). An examination of school counselors’ competency working with lesbian, gay and bisexual and transgender (LGBT) Students. Journal of LGBT Issues in Counseling, 11(1), 2–17.
https://doi.org/10.1080/15538605.2017.1273165
Simmons University Library. (2019). Anti-Oppression: Anti-Transmisia. https://simmons.libguides.com/anti-opp
ression/anti-transmisia
Simons, J. D. (2021). School counselor advocacy for gender minority students. PLoS ONE, 16(3), e0248022. https://doi.org/10.1371/journal.pone.0248022
Sue, D. W., Arredondo, P., & McDavis, R. J. (1992). Multicultural counseling competencies and standards: A call to the profession. Journal of Counseling & Development, 70(4), 477–486. https://doi.org/10.1002/j.1556-6676.1992.tb01642.x
Toomey, R. B., Syvertsen, A. K., & Shramko, M. (2018). Transgender adolescent suicide behavior. Pediatrics, 142(4), e20174218. https://doi.org/10.1542/peds.2017-4218
Transgender Law Center. (2021). National equality map. https://transgenderlawcenter.org/equalitymap
Vance, S. R., Jr., Boyer, C. B., Glidden, D. V., & Sevelius, J. (2021). Mental health and psychosocial risk and protective factors among Black and Latinx transgender youth compared with peers. JAMA Network Open, 4(3), e213256. https://doi.org/10.1001/jamanetworkopen.2021.3256
Wang, T., Solomon, D., Durso, L. E., McBride, S., & Cahill, S. (2016). State anti-transgender bathroom bills threaten transgender people’s health and participation in public life: Policy brief. The Fenway Institute and Center for American Progress. https://fenwayhealth.org/wp-content/uploads/2015/12/COM-2485-Transgender-Bathroom-Bill-Brief_v8-pages.pdf
Whitman, C. N., & Han, H. (2017). Clinician competencies: Strengths and limitations for work with transgender and gender non-conforming (TGNC) clients. International Journal of Transgenderism, 18(2), 154–171. https://doi.org/10.1080/15532739.2016.1249818
Williams, A. J., Jones, C., Arcelus, J., Townsend, E., Lazaridou, A., & Michail, M. (2021). A systematic review and meta-analysis of victimisation and mental health prevalence among LGBTQ+ young people with experiences of self-harm and suicide. PLoS ONE, 16(1), e0245268.
https://doi.org/10.1371/journal.pone.0245268
Clark D. Ausloos, PhD, NCC, LPC, LPSC, is a clinical assistant professor at the University of Denver. Madeline Clark, PhD, NCC, ACS, LPC (VA), LPCC (OH), is an associate professor at the University of Toledo. Hansori Jang, PhD, NCC, is an assistant professor at Hankuk University of Foreign Studies. Tahani Dari, PhD, NCC, LPC (MI), LPSC, is an assistant professor at the University of Toledo. Stacey Diane Arañez Litam, PhD, NCC, CCMHC, LPCC-S, is an assistant professor at Cleveland State University. Correspondence may be addressed to Clark D. Ausloos, 15578 John F. McCarthy Way, Perrysburg, OH 43551, clark.ausloos@du.edu.
Feb 7, 2022 | Volume 12 - Issue 1
Clare Merlin-Knoblich, Jenna L. Taylor, Benjamin Newman
Social justice is a paramount concept in counseling and supervision, yet limited research exists examining this idea in practice. To fill this research gap, we conducted a qualitative case study exploring supervisee experiences in social justice supervision and identified three themes from the participants’ experiences: intersection of supervision experiences and external factors, feelings about social justice, and personal and professional growth. Two subthemes were also identified: increased understanding of privilege and increased understanding of clients. Given these findings, we present practical applications for supervisors to incorporate social justice into supervision.
Keywords: social justice, supervision, case study, personal growth, practical applications
Social justice is fundamental to the counseling profession, and, as such, scholars have called for an increase in social justice supervision (Ceballos et al., 2012; Chang et al., 2009; Collins et al., 2015; Dollarhide et al., 2018, 2021; Fickling et al., 2019; Glosoff & Durham, 2010). Although researchers have studied multicultural supervision in the counseling profession, to date, minimal research has been conducted on implementing social justice supervision in practice (Dollarhide et al., 2021; Fickling et al., 2019; Gentile et al., 2009; Glosoff & Durham, 2010). In this study, we sought to address this research gap with an exploration of master’s students’ experiences with social justice supervision.
Social Justice in Counseling
Counseling leaders have developed standards that reflect the profession’s commitment to social justice principles (Chang et al., 2009; Dollarhide et al., 2021; Fickling et al., 2019; Glosoff & Durham, 2010). For instance, the American Counseling Association’s ACA Code of Ethics (2014) highlights the need for multicultural and diversity competence in six of its nine sections, including Section F, Supervision, Training, and Teaching. Additionally, in 2015, the ACA Governing Council endorsed the Multicultural and Social Justice Counseling Competencies (MSJCC), which provide a framework for counselors to use to implement multicultural and social justice competencies in practice (Fickling et al., 2019; Ratts et al., 2015). All of these standards reflect the importance of social justice in the counseling profession (Greene & Flasch, 2019).
Social Justice Supervision
Although much of the counseling profession’s focus on social justice emphasizes counseling practice, social justice principles benefit supervisors, counselors, and clients when they are also incorporated into clinical supervision. In social justice supervision, supervisors address levels of change that can occur through one’s community using organized interventions, modeling social justice in action, and employing community collaboration (Chang et al., 2009; Dollarhide et al., 2021; Fickling et al., 2019). These strategies introduce an exploration of culture, power, and privilege to challenge oppressive and dehumanizing political, economic, and social systems (Dollarhide et al., 2021; Fickling et al., 2019; Garcia et al., 2009; Glosoff & Durham, 2010; Pester et al., 2020). Moreover, participating in social justice supervision can assist counselors in developing empathy for clients and conceptualizing them from a systemic perspective (Ceballos et al., 2012; Fickling et al., 2019; Kiselica & Robinson, 2001). When a supervisory alliance addresses cultural issues, oppression, and privilege, supervisees are better able to do the same with clients (Chang et al., 2009; Dollarhide et al., 2021; Fickling et al., 2019; Glosoff & Durham, 2010). Thus, counselors become advocates for clients and the profession (Chang et al., 2009; Dollarhide et al., 2021; Gentile et al., 2009; Glosoff & Durham, 2010).
Chang and colleagues (2009) defined social justice counseling as considering “the impact of oppression, privilege, and discrimination on the mental health of the individual with the goal of establishing equitable distribution of power and resources” (p. 22). In this way, social justice supervision considers the impact of oppression, privilege, and discrimination on the supervisee and supervisor. Dollarhide and colleagues (2021) further simplified the definition of social justice supervision, stating that it is “supervision in which social justice is practiced, modeled, coached, and used as a metric throughout supervision” (p. 104). Supervision that incorporates a focus on intersectionality can further support supervisees’ growth in developing social justice competencies (Greene & Flasch, 2019).
Literature about social justice supervision often includes an emphasis on two concepts: structural change and individual care (Gentile et al., 2009; Lewis et al., 2003; Toporek & Daniels, 2018). Structural change is the process of examining, understanding, and addressing systemic factors in clients’ and counselors’ lives, such as identity markers and systems within family, community, school, work, and elsewhere. Individual care acknowledges each person within the counseling setting independent of their environment (Gentile et al., 2009; Roffman, 2002). Scholars advise incorporating both concepts to address power, privilege, and systemic factors through social justice supervision (Chang et al., 2009; Gentile et al., 2009; Glosoff & Durham, 2010; Greene & Flasch, 2019; Pester et al., 2020).
It is necessary to distinguish social justice supervision from previous literature on multicultural supervision. Although similar, these concepts are different in that multicultural supervision emphasizes cultural awareness and competence, whereas social justice supervision brings attention to sociocultural and systemic factors and advocacy (Dollarhide et al., 2021; Fickling et al., 2019; E. Lee & Kealy, 2018; Peters, 2017; Ratts et al., 2015). For instance, a supervisor practicing multicultural supervision would be aware of a supervisee’s identity markers, such as race, ethnicity, and culture, and address those components throughout the supervisory experience, whereas a supervisor practicing social justice supervision would also consider systemic factors that impact a supervisee, in addition to being culturally competent. The supervisor would use that knowledge in the supervisory alliance and act as a change agent at individual and community levels (Chang et al., 2009; Dollarhide et al., 2021; Fickling et al., 2019; Gentile et al., 2009; Glosoff & Durham, 2010; E. Lee & Kealy, 2018; Lewis et al., 2003; Peters, 2017; Ratts et al., 2015; Toporek & Daniels, 2018).
Researchers have found that multicultural supervision contributes to more positive outcomes than supervision without consideration for multicultural factors (Chopra, 2013; Inman, 2006; Ladany et al., 2005). For example, supervisees who participated in multicultural supervision reported that supervisors were more likely to engage in multicultural dialogue, show genuine disclosure of personal culture, and demonstrate knowledge of multiculturalism than supervisors who did not consider multicultural concepts in supervision (Ancis & Ladany, 2001; Ancis & Marshall, 2010; Chopra, 2013). Supervisees also reported that multicultural considerations led them to feel more comfortable, increased their self-awareness, and spurred them on to discuss multiculturalism with clients (Ancis & Ladany, 2001; Ancis & Marshall, 2010). Although parallel research on social justice supervision is lacking, findings on multicultural supervision are a promising indicator of the potential of social justice supervision.
Models
In recent years, scholars have called for social justice supervision models to integrate social justice into supervision (Baggerly, 2006; Ceballos et al., 2012; Chang et al., 2009; Collins et al., 2015; Glosoff & Durham, 2010; O’Connor, 2005). However, to date, only three formal models of social justice supervision have been published. Most recently, Dollarhide and colleagues (2021) recommended a social justice supervision model that can be used with any supervisory theory, developmental model, and process model. In this model, the MSJCC are integrated using four components. First, the intersectionality of identity constructs (i.e., gender, race/ethnicity, socioeconomic status, sexual orientation, abilities, etc.) is identified as integral in the supervisory triad between supervisor, counselor, and client. Second, systemic perspectives of oppression and agency for each person in the supervisory triad are at the forefront. Third, supervision is transformed to facilitate the supervisee’s culturally informed counseling practices. Lastly, the supervisee and client experience validation and empowerment through the mutuality of influence and growth (Dollarhide et al., 2021).
Prior to Dollarhide and colleagues’ (2021) model for social justice supervision, Gentile and colleagues (2009) proposed a feminist ecological framework for social justice supervision. This model encouraged the understanding of a person at the individual level through interactions within the ecological system (Ballou et al., 2002; Gentile et al., 2009). The supervisor’s role is to model socially just thinking and behavior, create a climate of equality, and implement critical thinking about social justice (Gentile et al., 2009; Roffman, 2002).
Lastly, Chang and colleagues (2009) suggested a social constructivist framework to incorporate social justice issues in supervision via three delineated tiers (Chang et al., 2009; Lewis et al., 2003; Toporek & Daniels, 2018). In the first tier, self-awareness, supervisors assist supervisees to recognize privileges, understand oppression, and gain commitment to social justice action (Chang et al., 2009; C. C. Lee, 2007). In the second tier, client services, the supervisor understands the clients’ worldviews and recognizes the role of sociopolitical factors that can impact the developmental, emotional, and cognitive meaning-making system of the client (Chang et al., 2009). In the third tier, community collaboration, the supervisor guides the supervisee to advocate for changes on the group, organizational, and institutional levels. Supervisors can facilitate and model community collaboration interventions, such as providing clients easier access to resources, participating in lobbying efforts, and developing programs in communities (Chang et al., 2009; Dinsmore et al., 2002; Kiselica & Robinson, 2001).
Each of these supervision models serves as a relevant, accessible tool for counseling supervisors to use to incorporate social justice into supervision (Chang et al., 2009, Dollarhide et al., 2021; Gentile et al., 2009). However, researchers lack an empirical examination of any of the models. To address this research gap and begin understanding social justice supervision in practice, the present qualitative case study exploring master’s students’ experiences with social justice supervision was undertaken.
We selected Chang and colleagues’ (2009) three-tier social constructivist framework in supervision for several reasons. First, the social constructivist framework incorporates a tiered approach similar to the MSJCC (Ratts et al., 2015) and reflects social justice goals in the profession of counseling (Ceballos et al., 2012; Chang et al., 2009; Collins et al., 2015; Glosoff & Durham, 2010). Second, the model is comprehensive. In using three tiers to address social justice (self, client, and community), the model captures multiple layers of social justice influence for counselors. Finally, the model is simple and meets the developmental needs of novice counselors. By identifying three tiers of social justice work, Chang and colleagues (2009) crafted an accessible tool to help new and practicing school counselors infuse social justice into their practice. This high level of structure matches the initial developmental levels of new counselors, who typically benefit from high amounts of structure and low amounts of challenge in supervision (Foster & McAdams, 1998).
Method
The research question guiding this study was: What are the experiences of master’s counseling students in individual social justice supervision? We used a social constructivist theoretical framework and presumed that knowledge would be gained about the participants’ experiences based on their social constructs (Hays & Singh, 2012). The ontological perspective reflected realism, or the belief that constructs exist in the world even if they cannot be fully measured (Yin, 2017).
We selected a qualitative case study methodology because it was the most appropriate approach to explore the experiences of a single group of supervisees supervised by the same supervisor in the same semester. In this approach, researchers examine one identified unit bounded by space, time, and persons (Hancock et al., 2021; Hays & Singh, 2012; Yin, 2017). Qualitative case study research allows researchers to deeply explore a single case, such as a group, person, or experience, and gain an in-depth understanding of that identified situation, as well as meaning for the people involved in it (Hancock et al., 2021; Prosek & Gibson, 2021).
In this study, we selected a case study methodology because the study’s participants engaged in the same supervisory experience at the same counseling program in the same semester, thus forming a case to be studied (Hancock et al., 2021). Given the research question, we specifically used a descriptive case study design, which reflected the study goals to describe participants’ experiences in a specific social justice supervision experience. Case study scholars (Hancock et al., 2021; Yin, 2017) have noted that identifying the boundaries of a case is an essential step in the study process. Thus, the boundaries for this study were: master’s-level school counseling students receiving social justice supervision from the same supervisor (persons) at a medium-sized public university on the East Coast (place) over the course of a 14-week semester (time).
Research Team
Our research team for this study consisted of our first and third authors, Clare Merlin-Knoblich and Benjamin Newman, both of whom received training and had experience in qualitative research. Merlin-Knoblich and Newman both identify as White, heterosexual, cisgender, middle-class, and trained counselor educators/supervisors. Merlin-Knoblich is a woman (pronouns: she/her/hers) and former school counselor, who completed master’s and doctoral coursework on social justice counseling and studied social justice supervision in a doctoral program. Newman is a man (pronouns: he/him/his) and clinical mental health/addictions counselor, who completed social justice counseling coursework in a master’s counseling program before completing a doctorate in counselor education and supervision. Our second author, Jenna L. Taylor, was not a part of the research team, but rather was a counseling student unaffiliated with the research participants who assisted in the preparation of the manuscript. Taylor identifies as a White, heterosexual, cisgender, and middle-class woman (pronouns: she/her/hers) with prior experience in research courses and on qualitative research teams. Merlin-Knoblich was familiar with all three participants given her role as the practicum supervisor. Taylor and Newman did not know the study participants beyond Newman’s interactions while recruiting and interviewing them for this study.
Participants and Context
Although some scholars of some qualitative research methodologies call for requisite minimum numbers of participants, in case study research, there is no minimum number of participants sufficient to study (Hays & Singh, 2012). Rather, in case study research, researchers are expected to study the number of participants needed to reflect the phenomenon being studied (Hancock et al., 2021). There were three participants in this study because the supervisory experience that comprised the case studied included three supervisees. Adding additional participants outside of the case would have conflicted with the boundaries of the case and potentially interfered with an understanding of the single, designated case in this study.
All study participants identified as White, heterosexual, cisgender, middle-class, and English-speaking women (pronouns: she/her/hers). Participants were 23, 24, and 26 years old. All the participants were students in the same CACREP-accredited school counseling program at a public liberal arts university on the East Coast of the United States. Prior to the study, the participants completed courses in techniques, group counseling, school counseling, ethics, and theories. While being supervised, participants also completed a practicum experience and coursework in multicultural counseling and career development.
All participants completed practicum at high schools near their university. One high school was urban, one was suburban, and one was rural. During the practicum experience, participants met with Merlin-Knoblich, their supervisor, for face-to-face individual supervision for 1 hour each week. They also submitted weekly journals to Merlin-Knoblich, written either freely or in response to a prompt, depending on their preference. Merlin-Knoblich then provided weekly written feedback to each participant’s journal entry, and, if relevant, the journal content was discussed during face-to-face supervision. Simultaneously, a university faculty member provided weekly face-to-face supervision-of-supervision to Merlin-Knoblich to monitor supervision skills and ensure adherence to the identified supervision model. The faculty member possessed more than 15 years of experience in supervision and was familiar with social justice supervision models.
Merlin-Knoblich applied Chang and colleagues’ (2009) social constructivist social justice supervision model in deliberate ways throughout the supervisees’ 14-week practicum experience. For example, in the initial supervision sessions, Merlin-Knoblich introduced the supervision model and explained how they would collaboratively explore ideas of social justice in counseling related to their practicum experiences. This included defining social justice, discussing supervisees’ previous background knowledge, and exploring their openness to the idea.
Throughout the first 5 weeks of supervision, Merlin-Knoblich used exploratory questions to build participants’ self-awareness (the first tier), particularly around their experiences with privilege and oppression. During the next 5 weeks of supervision, Merlin-Knoblich focused on the second tier, understanding clients’ worldviews. They discussed sociopolitical factors and examined how a client’s worldview impacts their experiences. For example, Merlin-Knoblich discussed how a client’s age, race/ethnicity, socioeconomic status, family structure, language, immigrant status, gender identity, sexual orientation, and other factors can influence their experiences. Lastly, in the final 4 weeks of supervision, Merlin-Knoblich focused on the third tier of social justice implications at the institutional level. For instance, Merlin-Knoblich initiated discussions about policies at participants’ practicum sites that hindered equity. Merlin-Knoblich also explored the role that participants could take in making resources available to clients, advocating in the community, and using leadership to support social justice. Table 1 summarizes how Merlin-Knoblich implemented Chang and colleagues’ (2009) social justice model.
Table 1
Social Justice Supervision in Practice
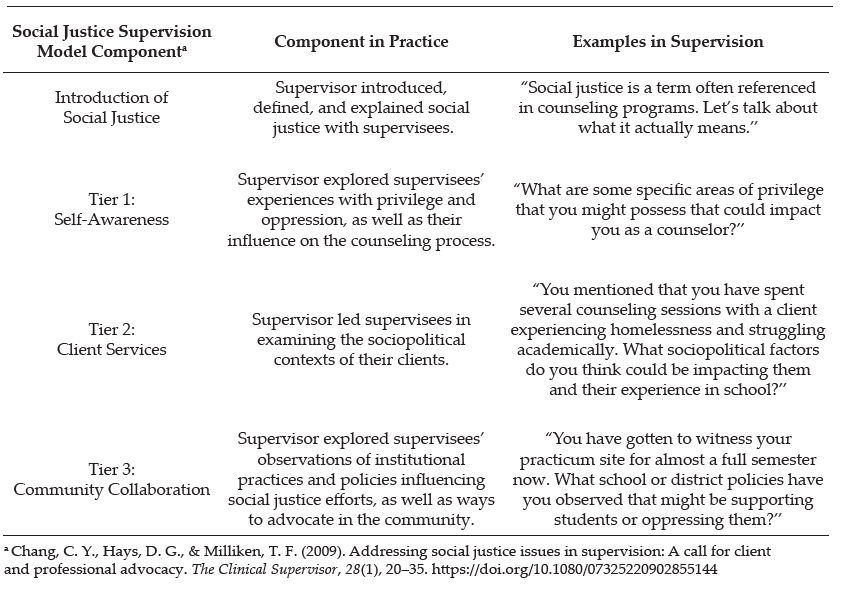
Merlin-Knoblich addressed fidelity to the supervision model in two ways. First, in weekly supervision-of-supervision meetings with the faculty advisor, they discussed the supervision model and its use in sessions with participants. The faculty advisor regularly asked about the supervision model and how it manifested in sessions in an attempt to ensure that the model was being implemented recurrently. Secondly, engagement with Newman occurred in regular peer debriefing discussions about the use of the supervision model. Through these discussions, Newman monitored Merlin-Knoblich’s use of the social justice model throughout the 14-week supervisory experience.
Data Collection
We obtained IRB approval prior to initiating data collection. One month after the end of the semester and practicum supervision, Newman approached Merlin-Knoblich’s three supervisees about participation in the study. He explained that participation was an exploration of the supervisees’ experiences in supervision and not an evaluation of the supervisees or the supervisor. Newman also emphasized that participation in the study was confidential, entirely voluntary, and would not affect participants’ evaluations or grades in the practicum course, which ended before the study took place. All supervisees agreed to participate.
Case study research is “grounded in deep and varied sources of information” (Hancock et al., 2021) and thus often incorporates multiple data sources (Prosek & Gibson, 2021). In the present study, we identified two data sources to reflect the need for varied information sources (Hancock et al., 2021). The first data source came from semistructured interviews with participants, a frequent data collection tool in case study research (Hancock et al., 2021). One month after the participants’ practicum experiences ended, Newman conducted and audio-recorded 45-minute individual in-person interviews with each participant using a prescribed interview protocol that explored participants’ experiences in social justice supervision. Newman exercised flexibility and asked follow-up questions as needed (Merriam, 1998).
The interview protocol contained 12 questions identified to gain insights into the case being studied (Hancock et al., 2021). Merlin-Knoblich and Newman designed the interview protocol by drafting questions and reflecting on three influences: (a) the overall research question guiding the study, (b) the social constructivist framework of the study, and (c) Chang and colleagues’ (2009) three-tier supervision model. Questions included “In what ways, if any, has the social justice emphasis in your supervision last semester influenced you as a counselor?” Questions also addressed whether or not the emphasis on social justice at each tier (i.e., self, client, institution) affected participants. Appendix A contains a list of all interview questions.
The second data source was participants’ practicum journals. In addition to interviewing the participants about experiences in supervision, we also asked participants if their practicum journals could be used for the study’s data analysis. The journals served as a valuable form of data to answer the research question, given their informative and non-prescriptive nature. That is to say, although participants knew during the study interviews that the interview data would be used for analysis for the present study, they wrote and submitted their journals before the study was conceptualized. Thus, the journals reflected in-the-moment ideas about participants’ practicum and social justice supervision. Furthermore, this emphasis on participant experiences during the supervisory experience aligned with the methodological emphasis on studying a case in its natural context (Hancock et al., 2021). All participants consented for their 14 practicum journal entries (each 1–2 pages in length) to be analyzed in the study, and they were added to the interview data to be analyzed together. Such convergent analysis of data is typical in case study research (Prosek & Gibson, 2021).
Data Analysis
We followed Yin’s (2017) case study research guidelines throughout the data analysis process. We transcribed all interviews, replaced participants’ names with pseudonyms, and sent participants the transcripts for member checking. Two participants approved their interview transcripts without objection. One participant approved the transcript but chose to share additional ideas about the supervisory experience via a brief email. This email was added to the data. The case study database was then formed with the compiled participants’ journal entries, the additional email, and the interview data (Yin, 2017).
Next, we read each interview transcript and journal entry twice in an attempt to become immersed in the data (Yin, 2017). We then independently open coded transcripts by identifying common words and phrases while maintaining a strong focus on the research question and codes that answered the question (Hancock et al., 2021). We compared initial codes and then collaboratively narrowed codes into cohesive categories representing participants’ experiences. This process generated a list of tentative categories across data sources (Yin, 2017). Throughout these initial processes, we attended to two of Yin’s (2017) four principles of high-quality data analysis: attend to all data and focus on the most significant elements of the case.
We then independently contrasted the tentative categories with the data to verify that they aligned accurately. We discussed the verifications until consensus was met on all categories. Lastly, we classified the categories into three themes and two subthemes found across all participants (Stake, 2005). During these later processes, we were mindful of Yin’s (2017) remaining two principles of high-quality data analysis: consider rival interpretations of data and use previous expertise when interpreting the case. Accordingly, we reflected on possible contrary explanations of the themes and considered the findings in light of previous literature on the topic.
Trustworthiness
We addressed trustworthiness in three ways in this study. First, before data collection, we engaged in reflexivity through acknowledging personal biases and assumptions with one another (Hays & Singh, 2012; Yin, 2017). For example, Merlin-Knoblich acknowledged that her lived experience supervising the participants might impact the interpretation of data during analysis and noted that these perceptions could potentially serve as biases during the study. Merlin-Knoblich perceived that the supervisees grew in their understanding of social justice, but also acknowledged doubt over whether the social justice supervision model impacted participants’ advocacy skills. She also noted her role as a supervisor evaluating the three participants prior to the study taking place. These power dynamics may have influenced her interpretations in the analysis process. Newman shared that his lack of familiarity with social justice supervision might impact perceptions and biases to question whether or not supervisees grew in their understanding of social justice. We agreed to challenge one another’s potential biases during data analysis in an attempt to prevent one another’s experiences from interfering with interpretations of the findings.
In addition, we acknowledged that our identities as White, English-speaking, educated, heterosexual, cisgender, middle-class researchers studying social justice inevitably was informing personal perceptions of the supervisees’ experiences. These privileged identities were likely blinding us to experiences with oppression that participants and their clients encountered and that we are not burdened with facing. Throughout the study, we discussed the complexity of studying social justice in light of such privileged identities. We spoke further about our identities and potential biases when interpreting the data.
Second, investigator triangulation was addressed by collaboratively analyzing the study’s data (Hays & Singh, 2012). Because data included both interview transcripts and journals, we confirmed that study findings were reflected in both data sources, rather than just one information source (Hancock et al., 2021). This process helped prevent real or potential biases from informing the analysis without constraint. We also were mindful of saturation of themes while comparing data across participants and sources during the analysis process. Lastly, an audit trail was created to further address credibility. The study recruitment, data collection, and data analysis were documented so that the research can be replicated (Hays & Singh, 2012; Roulston, 2010).
Findings
In case study research, researchers use key quotes and descriptions from participants to illuminate the case studied (Hancock et al., 2021). As such, we next describe the themes and subthemes identified in study data using participants’ journal and interview quotes to illustrate the findings. Three overarching themes were identified in the data: 1) intersection of supervision experiences and external factors, 2) feelings about social justice, and 3) personal and professional growth. Two subthemes, 3a) increased understanding of privilege and 3b) increased understanding of clients, further expand the third theme.
Intersection of Supervision Experiences and External Factors
One theme evident across the data was that participants’ experiences in social justice supervision did not occur in isolation from other experiences they encountered as counseling students. Coursework, overall program emphasis, and previous work experiences were external factors that created a compound influence on participants’ counselor development and intersected with their experiences of growth in supervision. Thus, external factors influenced participants’ understanding of and openness to a social justice framework. For example, concurrent with their practicum and supervision experiences, participants completed the course Theory and Practice of Multicultural Counseling. While discussing their experiences in supervision, all participants referenced this course. For example, Casey explained that exposure to social justice in the multicultural counseling course while discussing the topic in supervision made her more open and eager to learning about social justice overall.
Participants’ experiences prior to the counseling program also appeared to intersect with and influence their experiences in social justice supervision. Kallie, for instance, previously worked with African American and Latin American adolescents as a camp counselor at an urban Boys and Girls Club. She explained that social justice captured the essence of viewpoints formed in these experiences, saying, “I really like social justice because it kind of is like the title for the way I was looking at things already.” Casey grew up in California and reported that growing up on the West Coast also exposed her to a mindset parallel to social justice. Esther described that though she was not previously exposed to the term “social justice,” studying U.S., women’s, and African American history in college influenced her pursuit of a counseling career. This influence is evident in Esther’s third journal entry, in which she described noticing issues of power and oppression:
My own attention to an “arbitrarily awarded power” and personal questioning as to what to do with this consciousness has been at the forefront of my mind over the past two years. Ultimately this self-exploration led me to school counseling as a vehicle to advocate and raise consciousness in potentially disenfranchised groups.
This quote highlights how Esther’s previous studies in college may have primed her for the content she was exposed to in social justice supervision.
Feelings About Social Justice
The second theme was a change in participants’ feelings toward social justice over the course of the semester. Two of the participants expressed that their feelings toward social justice changed from intimidation and fear to comfort and enthusiasm. Initially, Casey explained that social justice supervision created feelings of intimidation. Casey felt fear that the supervisor would instruct her to be an advocate at the practicum site, and that in doing so, Casey would upset others. However, Casey reported that she realized during supervision that social justice advocacy does not necessarily look one specific way. Casey said, “I think a lot of that intimidation went away as I realized that I could have my own style integrated into social justice.” Kallie expressed a similar pattern of emotions, particularly regarding examining clients from a social justice perspective. When asked to explore clients through this lens in supervision, an initial uncomfortable feeling emerged, but over the course of practicum, Kallie reported an attitude change. In the sixth journal entry, Kallie explained that she was focusing on examining all clients through a social justice lens, and “found it to be significantly easier this week than last week.”
Esther also shared evidence of changed emotions during social justice supervision. Initially, Esther reported feeling excited, but later, she was confused as to how counselors could use social justice practically. Despite this confusion, Esther shared that she gained new awareness that social justice advocacy is not only found in individual situations with clients, but also in an overall mindset:
Something I will take from it [supervision] . . . is you incorporate that sort of thinking into your overall [approach]. You don’t necessarily wait for a specific event to happen, but once you know the culture of a place, you have lessons geared towards whatever the problem is there.
Despite these mixed feelings, Esther’s experience aligns with Casey’s and Kallie’s, as all reported experiencing a change in emotions toward social justice over the course of supervision.
Personal and Professional Growth
Participants also demonstrated changes in professional and personal growth throughout the supervision experiences, the third theme identified. In early journal entries, they reported nervousness, doubt, and insecurity regarding their counseling skills and knowledge. Over time, the tone shifted to increased comfort and confidence. This improvement appeared not only related to overall counseling abilities, but specifically to participants’ understanding of social justice in counseling. For example, in Esther’s second journal entry, she noted the influence that social justice supervision had on the ability to recognize oppression and bring awareness to it at practicum. Esther wrote, “Just having this concept be explicitly laid out in our plan has already caused me to be more attentive to such issues.”
Similarly, professional growth was evident in Kallie’s journal entries over time. In the fourth journal entry, Kallie described discomfort and nervousness when reflecting on clients’ sociopolitical contexts. However, in the ninth journal entry, Kallie described an experience in which she adapted her counseling to be more sensitive to the client’s multicultural background. Casey also highlighted growth with an anecdote about a small group she led. Casey explained that the group was for high-achieving, low-income juniors intending to go to college:
In the very beginning, I remember thinking—this sounds terrible now, but—“It’s kind of unfair to the other students that these kids get special privileges in that they get to meet with us and walk through the college planning process.” ’Cause I was thinking, “Wow, even kids who are high-achieving but are middle-class or upper-class, they could use this information, also. And it’s not really fair that just ’cause they’re lower class, they get their hand held during this.” But, throughout the semester, realizing that that’s not necessarily a bad thing for an institution to give another one a little extra help because they’re gonna have a deficit of help somewhere else in their life, and it really is fair. It’s more fair to give them more help ’cause they likely aren’t going to be getting it at home. . . . So, by having that group, it actually is making a greater degree of equity . . . through supervision and through processing all of that, [I learned] it was actually evening the board out more.
Participants also expressed that their professional growth in social justice competencies was intertwined with personal growth. Casey reported that supervision increased her comfort when talking about social justice issues and led to the reevaluation of personal opinions. Similarly, Kallie summarized:
I am very thankful that I had that social justice–infused model because it changed the way I think about people. . . . It kinda opened my eyes in a way I had not anticipated practicum opening my eyes. I didn’t expect that—social justice. I didn’t realize how big of an impact it would actually have.
Increased Understanding of Privilege
Participants reported that understanding their privilege was one area of growth. During practicum, participants considered their areas of privilege and how these aligned or contrasted with those of clients. For example, in Esther’s third journal entry, she noted that interactions with clients made her more aware of personal privileges, which led her to create a list regarding gender identity, socioeconomic background, and sexual orientation. Casey and Kallie further described initially feeling resistant to the idea of White privilege. Casey explained:
I was a little resistant to the idea of White privilege originally, which I’ve since learned is a normal reaction. ’Cause I’ve kind of had the thought of “No! It’s America! All of us pull ourselves up by our bootstraps and everyone has the same opportunity,” which just isn’t the case. And so that definitely had a huge influence on me—realizing that I have huge privileges and powers that I did not, maybe didn’t want to, recognize before.
After initial resistance, participants reported that they transitioned from feeling shame about White privilege to an increased understanding and excitement to use privilege to create change.
Increased Understanding of Clients
Lastly, participants also reported specific growth in their understanding of the clients whom they counseled. Participants believed they were better able to understand clients’ backgrounds and experiences because of social justice supervision. Kallie described how reflecting on clients’ sociopolitical contexts helped her better understand clients. She noted that the practice became a habit, saying, “It just kinda invaded the way I look at different people and see their backgrounds.” Casey also described an increased understanding of clients by sharing an example of a client who was highly intelligent, low-income, and Mexican American. Casey learned that the client intended to go to trade school to become a mechanic and was not previously exposed to other postsecondary education options like college. Casey described this realization as “a big moment” and said, “My interaction with him, for sure, was influenced by recognizing that there was social injustice there.”
Discussion
The purpose of this study was to explore counseling students’ experiences in social justice supervision. Findings indicated that participants had meaningful experiences in social justice supervision that impacted them as future counselors. Topics of privilege, oppression, clients’ sociopolitical contexts, and advocacy were reportedly prominent in the participants’ supervision and influenced their experiences.
Despite many calls for social justice supervision in the counseling profession (Baggerly, 2006; Ceballos et al., 2012; Chang et al., 2009; Collins et al., 2015; Glosoff & Durham, 2010; O’Connor, 2005), this is the first known study about supervisees’ experiences with social justice supervision. It represents a new line of inquiry to understand what social justice supervision may be like for supervisees. Findings indicate that participants wrestled with understanding social justice and viewed it as a complex topic. They also suggest that participants found value in making sense of social justice and using it as a tool to better support clients individually and systemically. Similar to research on multicultural supervision, participants indicated that receiving social justice supervision was a positive experience and impacted personal and professional growth (Ancis & Ladany, 2001; Ancis & Marshall, 2010; Chopra, 2013; Inman, 2006; Ladany et al., 2005).
Notably, findings align with some, though not all, of Chang and colleagues’ (2009) delineated tiers in the social justice supervision model. Some of the themes reflect the first tier, self-awareness. For example, participants’ feelings about social justice (Theme 2) and increased understanding of privilege (Theme 3a) highlight how the supervisory experience enhanced their self-awareness as counselors. As their feelings changed and knowledge of privilege grew, their self-awareness improved, a critical task in becoming a social justice–minded counselor (Chang et al., 2009; Dollarhide et al., 2021; Fickling et al., 2019; Glosoff & Durham, 2010). Participants’ increased understanding of clients (Theme 3b) reflects the second tier in Chang and colleagues’ (2009) model, client services. In demonstrating an enhanced understanding of clients and their world experiences, the participants reported thinking beyond themselves and into how power, privilege, and oppression affected those they counseled.
The final tier of the social justice supervision model, community collaboration, was not evident in participant data about their experiences. Despite the supervisor’s intent to address this tier through analyses of school and district policies, as well as community advocacy opportunities, themes about this topic did not manifest in the data. This theme’s absence may suggest that the supervisor’s efforts to address the third tier were not strong enough to impact participants. Alternatively, the absence may suggest that participants were not developmentally prepared to make sense of social justice at a systemic, community level. Instead, their development matched best with social justice ideas at the self and client levels.
Participant findings did align with previous research about supervision. For example, Collins and colleagues (2015) studied master’s-level counseling students and found that their lack of experience in social justice supervision led them to feel unprepared to meet the needs of diverse clients. In this study, the presence of social justice supervision helped participants feel more prepared to support clients, as evidenced in the subtheme of increased understanding of clients. Furthermore, this study reflects similar findings from multicultural supervision research. We found that multicultural supervision was associated with positive outcomes of being prepared to work with diverse clients and engaging in effective supervision (Chopra, 2013; Inman, 2006; Ladany et al., 2005). This pattern is reflected in the current study, as participants reported positive experiences in social justice supervision. Ancis and Ladany (2001) and Ancis and Marshall (2010) found that incorporating multicultural considerations into supervision increases supervisees’ self-awareness and encourages them to engage clients in multicultural discussions. These same results were evident in the present study, with participants reporting personal and professional growth, such as stronger awareness of White privilege and greater willingness to examine clients’ sociopolitical contexts. Findings also reflect general research on supervision, which indicates that supervisees typically experience personal and professional growth in the process (Association for Counselor Education and Supervision, 2011; Watkins et al., 2015; Young et al., 2011).
Furthermore, study findings also align with assertions from supervision scholars regarding the value of social justice supervision. They support Chang and colleagues’ (2009) claim that social justice supervision can increase counselor self-awareness and build an understanding of oppression. Additionally, the findings also reflect Glosoff and Durham’s (2010) assertion that social justice in supervision helps supervisees gain awareness of power differentials. Finally, Ceballos and colleagues (2012) posited that social justice supervision will help counselors develop empathy for clients as counselors conceptualize clients in a systemic perspective. The participants’ enhanced understanding of White privilege and their clients’ contexts supports each of these ideas. Though findings are not generalizable, they appear to confirm scholars’ ideas about social justice supervision and suggest that the approach can be a positive, beneficial experience for counselors-in-training.
Limitations
Study findings ought to be considered in light of the study’s limitations. First, although case study research focuses on a single identified case by definition and is not designed for generalization (Hays & Singh, 2012), the case in this study consisted of a demographically homogenous population of only three participants lacking racial, gender, and age diversity. This lack of diversity influenced participants’ experiences and study findings. Second, although the supervisor in this study did not conduct the semistructured interviews with participants in an attempt to prevent bias, participants were aware that Merlin-Knoblich was collaborating on the study, and this knowledge may have influenced their reported experiences. Merlin-Knoblich and Newman also began the study with acknowledged biases toward and against social justice supervision, and although they engaged in reflexivity and dialogue to prevent these biases from interfering with data analysis, there is no way to verify that this positionality did not influence the interpretation of findings. Lastly, our privileged identities served as a potential limitation while studying a topic like social justice supervision. Our racial, educational, class, language, and sexual identity privileges continually blind us to the experiences of oppression that others, including supervisees and clients, face. Seeking to know these perspectives better can increase our understanding of the implications of social injustices in society.
Implications for Counselor Educators and Supervisors
The positive participant experiences illuminated through this study suggest that supervision based on this model may yield positive experiences for counselors-in-training, such as supporting students in developing self-awareness, understanding of clients’ sociopolitical contexts, and advocacy skills (Chang et al., 2009). Although the supervisor in this study used social justice supervision in individual sessions with participants, counselor educators may choose to apply social justice supervision models to group or triadic supervision. Counseling supervisors in agency, private practice, and school settings may also want to consider using social justice supervision to support counselors and subsequently clients (Baggerly, 2006; Ceballos et al., 2012; O’Connor, 2005). Furthermore, counselor educators teaching doctoral students may want to incorporate social justice supervision models into introductory supervision courses. Including these models into course content may in itself increase student interest in social justice (Swartz et al., 2018).
Regardless of the setting in which supervisors implement social justice supervision, the findings suggest practical implications that supervisors can consider. First, supervisors appear to benefit from considering social justice supervision models in their work (Chang et al., 2009; Dollarhide et al., 2021; Gentile et al., 2009). The findings in this study, plus previous research indicating positive outcomes for multicultural supervision (Chopra, 2013; Inman, 2006; Ladany et al., 2005), suggest that social justice supervision may potentially benefit counseling. Second, supervisors using social justice supervision may encounter supervisee confusion, discomfort, and/or enthusiasm when introduced to social justice supervision. These feelings also may change over the course of the supervisory relationship when learning about social justice. Third, supervisors ought to be mindful of all three tiers of Chang and colleagues’ (2009) social justice supervision model and a supervisee’s developmental match with each tier. As seen in this study, supervisees may be best matched for the first and second tiers of the model (self-awareness and client services), but not the third tier (community collaboration). Supervisors would benefit from assessing a supervisee’s potential for understanding community collaboration before deciding to infuse its focus in supervision.
More research is needed to understand social justice supervision. A variety of future studies, including different models, methods, and settings, would benefit the counseling profession. For example, a study implementing the social justice supervision model proposed by Dollarhide and colleagues (2021) can add to the needed research in this field. Additional qualitative studies with diverse supervisees in different counseling settings would be helpful in understanding if the experiences participants reported encountering in this study are common in social justice supervision. Quantitative studies on social justice supervision interventions would also add to the profession’s knowledge on the value of social justice supervision. Lastly, studies on supervisees’ experiences in social justice supervision compared to other models would highlight benefits and drawbacks of multiple supervision models (Baggerly, 2006; Chang et al., 2009; Glosoff & Durham, 2010).
Conclusion
In this article, we explored master’s-level counseling students’ experiences in social justice supervision via a qualitative case study. Through this exploration, we identified three themes reflecting participants’ experiences in social justice supervision: intersection of supervision experiences and external factors, feelings about social justice, and personal and professional growth, as well as two subthemes: increased understanding of privilege and increased understanding of clients. Findings suggest that social justice supervision may be a beneficial practice for supervisors and counselor educators to consider integrating in their work (Chang et al., 2009; Dollarhide et al., 2021; Gentile et al., 2009; Pester et al., 2020). Further research across contexts and with a range of methodologies is needed to better understand social justice supervision in practice.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
American Counseling Association. (2014). ACA code of ethics. https://www.counseling.org/resources/aca-code-of-ethics.pdf
Ancis, J. R., & Ladany, N. (2001). A multicultural framework for counselor supervision. In L. J. Bradley & N. Ladany (Eds.), Counselor supervision: Principles, process, and practice (3rd ed., pp. 63–90). Brunner-Routledge.
Ancis, J. R., & Marshall, D. S. (2010). Using a multicultural framework to assess supervisees’ perceptions of culturally competent supervision. Journal of Counseling & Development, 88(3), 277–284.
https://doi.org/10.1002/j.1556-6678.2010.tb00023.x
Association for Counselor Education and Supervision. (2011). Best practices in clinical supervision. https://acesonline.net/wp-content/uploads/2018/11/ACES-Best-Practices-in-Clinical-Supervision-2011.pdf
Baggerly, J. (2006). Service learning with children affected by poverty: Facilitating multicultural competence in counseling education students. Journal of Multicultural Counseling and Development, 34(4), 244–255. https://doi.org/10.1002/j.2161-1912.2006.tb00043.x
Ballou, M., Matsumoto, A., & Wagner, M. (2002). Toward a feminist ecological theory of human nature: Theory building in response to real-world dynamics. In M. Ballou & L. S. Brown (Eds.), Rethinking mental health and disorder: Feminist perspectives (pp. 99–141). Guilford.
Ceballos, P. L., Parikh, S., & Post, P. B. (2012). Examining social justice attitudes among play therapists: Implications for multicultural supervision and training. International Journal of Play Therapy, 21(4), 232–243. https://doi.org/10.1037/a0028540
Chang, C. Y., Hays, D. G., & Milliken, T. F. (2009). Addressing social justice issues in supervision: A call for client and professional advocacy. The Clinical Supervisor, 28(1), 20–35. https://doi.org/10.1080/07325220902855144
Chopra, T. (2013). All supervision is multicultural: A review of literature on the need for multicultural supervision in counseling. Psychological Studies, 58, 335–338. https://doi.org/10.1007/s12646-013-0206-x
Collins, S., Arthur, N., Brown, C., & Kennedy, B. (2015). Student perspectives: Graduate education facilitation of multicultural counseling and social justice competency. Training and Education in Professional Psychology, 9(2), 153–160. https://doi.org/10.1037/tep0000070
Dinsmore, J. A., Chapman, A., & McCollum, V. J. C. (2002). Client advocacy and social justice: Strategies for developing trainee competence. Paper presented at the Annual Conference of the American Counseling Association, Washington, DC.
Dollarhide, C. T., Hale, S. C., & Stone-Sabali, S. (2021). A new model for social justice supervision. Journal of Counseling & Development, 99(1), 104–113. https://doi.org/10.1002/jcad.12358
Dollarhide, C. T., Mayes, R. D., Dogan, S., Aras, Y., Edwards, K., Oehrtman, J. P., & Clevenger, A. (2018). Social justice and resilience for African American male counselor educators: A phenomenological study. Counselor Education and Supervision, 57(1), 2–17. https://doi.org/10.1002/ceas.12090
Fickling, M. J., Tangen, J. L., Graden, M. W., & Grays, D. (2019). Multicultural and social justice competence in clinical supervision. Counselor Education and Supervision, 58(4), 309–316. https://doi.org/10.1002.ceas.12159
Foster, V. A., & McAdams, C. R., III. (1998). Supervising the child care counselor: A cognitive developmental model. Child and Youth Care Forum, 27(1), 5–19. https://doi.org/10.1007/BF02589525
Garcia, M., Kosutic, I., McDowell, T., & Anderson, S. A. (2009). Raising critical consciousness in family therapy supervision. Journal of Feminist Family Therapy, 21(1), 18–38. https://doi.org/10.1080/08952830802683673
Gentile, L., Ballou, M., Roffman, E., & Ritchie, J. (2009). Supervision for social change: A feminist ecological perspective. Women & Therapy, 33(1–2), 140–151. https://doi.org/10.1080/02703140903404929
Glosoff, H. L., & Durham, J. C. (2010). Using supervision to prepare social justice counseling advocates. Counselor Education and Supervision, 50(2), 116–129. https://doi.org/10.1002/j.1556-6978.2010.tb00113.x
Greene, J. H., & Flasch, P. S. (2019). Integrating intersectionality into clinical supervision: A developmental model addressing broader definitions of multicultural competence. The Journal of Counselor Preparation and Supervision, 12(4). https://digitalcommons.sacredheart.edu/jcps/vol12/iss4/14
Hancock, D. R., Algozzine, B., & Lim, J. H. (2021). Doing case study research: A practical guide for beginning researchers (4th ed.). Teachers College Press.
Hays, D. G., & Singh, A. A. (2012). Qualitative inquiry in clinical and educational settings. Guilford.
Inman, A. G. (2006). Supervisor multicultural competence and its relation to supervisory process and outcome. Journal of Marital and Family Therapy, 32(1), 73–85. https://doi.org/10.1111/j.1752-0606.2006.tb01589.x
Kiselica, M. S., & Robinson, M. (2001). Bringing advocacy counseling to life: The history, issues, and human dramas of social justice work in counseling. Journal of Counseling & Development, 79(4), 387–397.
https://doi.org/10.1002/j.1556-6676.2001.tb01985.x
Ladany, N., Friedlander, M. L., & Nelson, M. L. (2005). Critical events in psychotherapy supervision: An interpersonal approach. American Psychological Association.
Lee, C. C. (2007). Counseling for social justice (2nd ed.). American Counseling Association.
Lee, E., & Kealy, D. (2018). Developing a working model of cross-cultural supervision: A competence- and alliance-based framework. Clinical Social Work Journal, 46, 310–320. https://doi.org/10.1007/s10615-018-0683-4
Lewis, J. A., Arnold, M. S., House, R., & Toporek, R. L. (2003). Advocacy competencies. www.counseling.org/resources/competencies/advocacy_competencies.pdf
Merriam, S. B. (1998). Qualitative research and case study applications in education. Jossey-Bass.
O’Connor, K. (2005). Assessing diversity issues in play therapy. Professional Psychology: Research and Practice, 36(5), 566–573. https://doi.org/10.1037/0735-7028.36.5.566
Pester, D. A., Lenz, A. S., & Watson, J. C. (2020). The development and evaluation of the Intersectional Privilege Screening Inventory for use with counselors-in-training. Counselor Education and Supervision, 59(2), 112–128. https://doi.org/10.1002/ceas.12170
Peters, H. C. (2017). Multicultural complexity: An intersectional lens for clinical supervision. International Journal for the Advancement of Counselling, 39, 176–187. https://doi.org/10.1007/s10447-017-9290-2
Prosek, E. A., & Gibson, D. M. (2021). Promoting rigorous research by examining lived experiences: A review of four qualitative traditions. Journal of Counseling & Development, 99(2), 167–177. https://doi.org/10.1002/jcad.12364
Ratts, M. J., Singh, A. A., Nassar-McMillan, S., Butler, S. K., & McCullough, J. R. (2015). Multicultural and social justice counseling competencies. www.counseling.org/docs/default-source/competencies/multicultural-and-social-justice-counseling-competencies.pdf
Roffman, E. (2002). Just supervision. Multicultural Perspectives on Social Justice and Clinical Supervision Conference, Cambridge, MA, United States.
Roulston, K. (2010). Reflective interviewing: A guide to theory and practice. SAGE.
Stake, R. E. (2005). Qualitative case studies. In N. K. Denzin & Y. S. Lincoln (Eds.), The SAGE handbook of qualitative research (3rd ed., pp. 433–466). SAGE.
Swartz, M. R., Limberg, D., & Gold, J. (2018). How exemplar counselor advocates develop social justice interest: A qualitative investigation. Counselor Education and Supervision, 57(1), 18–33. https://doi.org/10.1002/ceas.12091
Toporek, R. L., & Daniels, J. (2018). ACA advocacy competencies. https://www.counseling.org/docs/default-source
/competencies/aca-advocacy-competencies-updated-may-2020.pdf?sfvrsn=f410212c_4
Watkins, C. E., Jr., Budge, S. L., & Callahan, J. L. (2015). Common and specific factors converging in psychotherapy supervision: A supervisory extrapolation of the Wampold/Budge Psychotherapy Relationship Model. Journal of Psychotherapy Integration, 25(3), 214–235. http://doi.org/10.1037/a0039561
Yin, R. K. (2017). Case study research and applications: Designs and methods (6th ed.). SAGE.
Young, T. L., Lambie, G. W., Hutchinson, T., & Thurston-Dyer, J. (2011). The integration of reflectivity in developmental supervision: Implications for clinical supervisors. The Clinical Supervisor, 30(1), 1–18. https://doi.org/10.1080/07325223.2011.532019
Appendix A
Semistructured Interview Questions
- What brought you to this counseling program?
- Overall, how would you describe your practicum experience last semester?
- Where did you complete your practicum?
- How would you describe the population you worked with at your practicum?
- What previous experience, if any, did you have with social justice prior to individual practicum supervision?
- During individual practicum supervision on campus last semester, what were some of your initial thoughts and feelings about a social justice–infused supervision model?
- In what ways, if any, did those thoughts and feelings about social justice change throughout your
supervision experience?
These next three questions address three areas of social justice that were incorporated into your individual practicum supervision model: self, students (clients), and institution (school or school districts).
6. Do you think that the emphasis on social justice related to self (i.e., your power, privileges, and experience with oppression) in individual practicum supervision on campus had any influence on you?
-
- If yes, what influence did this emphasis have on you?
- If no, why do you think that’s the case?
7. Do you think that the emphasis on social justice related to others (i.e., the sociopolitical context of students, staff, etc.) in individual practicum supervision on campus had any influence on you?
-
- If yes, what influence did this emphasis have on you?
- If no, why do you think that’s the case?
8. Do you think that the emphasis on social justice related to institution (i.e., your practicum site, school district) in individual practicum supervision on campus had any influence on you?
-
- If yes, what influence did this emphasis have on you?
- If no, why do you think that’s the case?
- In what ways, if any, has the social justice emphasis in your individual practicum supervision influenced you as a counselor?
- In what ways, if any, has the social justice emphasis in your individual practicum supervision influenced your development as a person?
- How would you define social justice?
- Is there anything else you would like to add regarding your experience in a social justice–infused model of supervision last semester?
- Is there anything else you’d like to share?
Clare Merlin-Knoblich, PhD, NCC, is an associate professor at the University of North Carolina at Charlotte. Jenna L. Taylor, MA, NCC, LPC-A, is a doctoral student at the University of North Texas. Benjamin Newman, PhD, MAC, ACS, LPC, CSAC, CSOTP, is a professional counselor at Artisan Counseling in Newport News, VA. Correspondence may be addressed to Clare Merlin-Knoblich, 9201 University City Blvd., Charlotte, NC 28211, cmerlin1@uncc.edu.