Aug 24, 2023 | Volume 13 - Issue 2
Amy Biang, Clare Merlin-Knoblich, Stella Y. Kim
Although researchers have found that patient weight bias negatively impacts health care professionals, research is limited on client weight bias toward counselors. Given that a client’s perception of their counselor impacts the therapeutic alliance, more research is needed to understand client weight bias toward counselors. To fill this research gap, we conducted a quasi-experimental study examining people’s weight bias toward a hypothetical counselor who was overweight, average weight, or underweight. Participants (N = 189) received a random assignment to a questionnaire featuring one of the three hypothetical counselors. Participants indicated their willingness to trust them, select them as a counselor, and follow their counsel. Results from a Welch ANOVA analysis showed a statistically significantly greater preference for average-weight and overweight counselors than those who are underweight. Additionally, the participants were less willing to follow counsel from overweight and underweight counselors. Implications for counselors are discussed.
Keywords: client weight bias, overweight, underweight, average weight, counselors
Body weight can inform a client’s perception of a health professional’s level of authority, trust, and competence (Hutson, 2013; Schwartz et al., 2006). Researchers have found that overweight bias toward health professionals like fitness instructors and medical physicians results in negative impressions (Hutson, 2013; Puhl et al., 2013; Puhl & Heuer, 2010). Clients may perceive lower competence, conscientiousness, personal grooming, and intrapersonal ability for overweight individuals compared to average-weight ones (Allison & Lee, 2015). When people seek mental health treatment, these perceptions may hinder their selection of a counselor who is perceived as overweight. Additionally, research on underweight bias has emerged that shows adverse outcomes toward underweight individuals (Allison & Lee, 2015; Beggan & DeAngelis, 2015; Davies et al., 2020a). Despite research on overweight and underweight bias in health professionals, limited research on either topic exists in the counseling profession.
Research on weight bias is necessary for counseling given that counselor attributes have the potential to be an integral part of a client’s decision-making and change process (Hauser & Hays, 2010). Attributes of a counselor that may affect client impressions, such as attractiveness (Grimes & Murdock, 1989) or race (Kim & Kang, 2018; Meyer & Zane, 2013), illuminate the social influence process of counseling (McKee & Smouse, 1983). Social influence is pervasive in the judgments of people everywhere. Weight bias continues to be a product of social influence and, as such, weaves stereotypes into the minds of those who consume the message of weight as a moral indiscretion (Beggan & DeAngelis, 2015). As clients search for, build trust with, and consider life changes with a counselor, weight bias ought to be explored as a potential issue for counselors.
In the past 35 years, researchers published only one study about weight perceptions toward overweight counselors (Moller & Tischner, 2019). Furthermore, there were no published studies about underweight counselors found. This gap in research is notable, as body weight can influence clients’ first impressions of a counselor and their expectations of the ensuing relationship (Moller & Tischner, 2019). Understanding how weight bias may impact this relationship is vital to building an authentic therapeutic relationship, which may otherwise be hindered by weight bias, which inaccurately frames a counselor’s competence (McKee & Smouse, 1983). Thus, we examined client weight bias toward overweight, underweight, and average-weight counselors in the current study.
Literature Review
Weight Bias
The term weight bias indicates a negative attitude about the perceived weight of an individual (Christensen, 2021). Historically, weight bias has been directed at people perceived as overweight; however, recent evidence suggests that underweight bodies generate weight bias as well (Allison & Lee, 2015; Beggan & DeAngelis, 2015; Christensen, 2021; Davies et al., 2020a, 2020b). Weight bias is pervasive throughout the United States (McHugh & Kasardo, 2012; Puhl et al., 2014). Negative stereotypes associated with being overweight include laziness, lack of motivation, psychological instability, social rejection, and incompetence in the workforce (Hinman et al., 2015; Lewis et al., 1997; Moller & Tischner, 2019). Likewise, incorrect stereotypes about underweight people include psychological instability or weakness (Marini, 2017). Body weight is not explicitly identified as an issue in the multicultural and social justice competencies (Ratts et al., 2016). However, weight bias is similar to sexism, racism, and classism in its harmful impact on people (Bucchianeri et al., 2013). It is still a common form of prejudice (McHugh & Kasardo, 2012).
Weight bias has become a social justice issue because of how it negatively impacts the lived experiences of people across social contexts (Nutter et al., 2018). Similar to other identities that elicit prejudice, weight bias impacts an individual’s opportunities in the workforce (Hutson, 2013), quality of mental health care (Puhl et al., 2014), and interpersonal relationships (Puhl & Heuer, 2010). Oppression from weight bias may deter a person from forming relationships or making connections with others out of fear of rejection or discrimination based on weight. Likewise, a person with weight bias may struggle to overlook the body of their counselor because of their worldview of weight and health. Even if the client remains in counseling, this initial bias may impede the therapeutic alliance process.
Therapeutic Alliance
The therapeutic alliance is a key variable in predicting client outcomes in counseling (Ackerman & Hilsenroth, 2001). This alliance represents the degree to which the client and counselor are engaged in collaboration, their commitment to one another, and their understanding of the counseling process (Allen et al., 2017; Lorr, 1965). Clients are as important as counselors in building this alliance, which involves their impression of and reaction to the counselor (Tudor, 2011). Disruptions in the therapeutic alliance can be generated from the client’s adverse reaction to the counselor, which thus impacts client outcomes (Ackerman & Hilsenroth, 2001). Weight can be a disruption, as some clients see a counselor being overweight as a barrier to opening up and engaging in counseling (Moller & Tischner, 2019). As the therapeutic alliance impacts clients remaining in counseling (Sharf et al., 2010), biases toward the counselor may hinder building the relationship, leading to early termination. Clients discriminating against counselors may limit capable counselors who fall outside socially acceptable weights from co-building the therapeutic alliance (McKee & Smouse, 1983).
Even with weight bias possibly diminishing the initial therapeutic relationship, Allen et al. (2017) found that communication on tasks/goals was a predictor of a strong therapeutic alliance and activation (i.e., the clients’ readiness and willingness to take on the management of their mental health care). Allen et al. found that alliance around the tasks/goals of therapy had long-term benefits, while an initial therapeutic bond was only associated with activation at the beginning of therapy. These findings suggest that despite client bias, a strong alliance may still form if there is a connection between counselor and client on their treatment goals and plan.
Despite a client and counselor’s mutual investment in a counseling relationship, research about weight bias in counseling has focused solely on counselors’ perceptions of clients’ weight and its influence on the therapeutic alliance (Kinavey & Cool, 2019; McHugh & Kasardo, 2012; Puhl et al., 2014). Thus, research has insufficiently examined how a counselor’s weight may hinder this alliance (Moller & Tischner, 2019). This gap is further concerning given that researchers have found that professionals in other disciplines identified as overweight or underweight face discrimination in the workplace (Beggan & DeAngelis, 2015; Hutson, 2013).
Overweight Bias Toward Counselors
Researchers have found that counselors are subject to weight bias from clients. Moller and Tischner (2019) examined client perceptions of counselors by specifically examining counselor weight. They conducted a qualitative story completion task with students from Great Britain aged 15–24 (N = 203) and found that participants perceived overweight counselors as incompetent. Counselors’ competence came into question because of the perception that being overweight implies a lack of emotional stability, personal discipline, and mental stability (Moller & Tischner, 2019). Participants also reported perceiving overweight counselors as distracting because of their physical appearance. Additionally, participants viewed an overweight counselor as having poor psychological health. Some participants noted that being overweight suggested an eating disorder (ED), such as bulimia or binge eating disorder. Furthermore, responses indicated that weight bias would impact the therapeutic relationship, and many participants would not want to work with an overweight counselor (Moller & Tischner, 2019).
These results are striking, and further research is needed to corroborate their value, as they point to a high level of bias toward overweight counselors. These types of inaccuracies can perpetuate prejudice and discrimination that may also hurt potential clients who would otherwise not have access to a counselor. Stereotypes and biases impact those who choose to work in this profession and could struggle to feel they belong in the helping professions.
Underweight Bias
Research geared toward overweight bias is well established in the health professions; however, evidence suggests that underweight health professionals also experience bias and discrimination (Allison & Lee, 2015; Beggan & DeAngelis, 2015; Davies et al., 2020a, 2020b). Researchers have noted stereotypes suggesting that extreme thinness may indicate a lack of wellness or the presence of a mental health issue like anorexia (Davies et al., 2020a). Furthermore, implicit bias toward underweight people may also come from the survival instinct that hunger, poverty, and war create underfed people, and we want to be with those who can help us survive (Marini, 2017).
Interestingly, scholars have noted that if being underweight is not perceived as stemming from health issues or an ED, people possess more favoritism toward underweight persons, limiting institutional discrimination toward them (Allison & Lee, 2015; Beggan & DeAngelis, 2015). In some social settings, a slender appearance of health follows socially accepted norms and may supersede the importance of actual health (Moller & Tischner, 2019). This leads to what is known as thin privilege; hence the possibility that there is enough benefit to being thin that it negates any negative attitudes or behaviors by others.
This thin privilege allows others to overstep the concept of civil inattention, which is how people are recognized appropriately in polite society. Civil inattention warrants people to be discrete in commenting on or noticing differences among those around them (e.g., those with disabilities, obesity, low socioeconomic status, or other marginalized identities). Some people believe that being underweight may invite a breakdown of civil inattention (Beggan & DeAngelis, 2015). This breakdown may lead a client to comment on a counselor’s body, such as “You are so skinny; how can you understand anything I am feeling about my body” or “If I were as thin as you, I would…” These types of comments are seen as acceptable because they infer a compliment about a socially desirable attribute. However, they can invite feelings of judgment and unease for the counselor, perpetuating a rupture in the therapeutic alliance. As we continue to understand that weight bias exists along a spectrum, counselors may feel prepared to broach the topic of weight regardless of where they fall.
One last finding that significantly impacts weight bias toward counselors comes from a qualitative study of adults (N = 18) with an average female body mass index (BMI) of 18.80 or male BMI of 21.68, both of which fall within the normal range of 18.5 to 24.9 (Centers for Disease Control and Prevention [CDC], 2022). Beggan and DeAngelis (2015) found that participants believed that underweight people lack empathy for others who struggle with weight. Such a belief would be impactful for a counselor, given that empathy is integral for a successful counseling relationship (Clark, 2010).
Empathy
Empathy is one of the six core conditions necessary for client change and contributes significantly to therapeutic outcomes. Clients can perceive empathy from counselors when counselors act in ways consistent with their frame of reference (Feller & Cottone, 2003).
Empathy is a deep understanding of the client’s circumstances. When there is weight bias, the client may not believe their counselor can understand their frame of reference if they are of differing body weights, especially if the client is coming in for body image concerns or health concerns. Even though the counselor has empathy, the client may not accept this as truth, hindering the building of a solid therapeutic alliance.
Weight as Credibility
Whether professionals are overweight or underweight, their bodies are part of their résumé. The term bodily capital describes one’s credibility as portrayed by the body and can influence how professionals are judged by their physical appearance (Hutson, 2013; Moller & Tischner, 2019). The body can be viewed as a symbolic container that indicates the investment of time and resources into health and well-being (Hutson, 2013). Previous scholars have asserted that the healthier a professional appears, the more likely clients and patients will accept their advice and trust their counsel (Hutson, 2013; Puhl et al., 2013). Health expectations are amplified for health professionals, as overweightness can be seen by some as a moral transgression and an inadequacy that may translate into their work (Beggan & DeAngelis, 2015). Some people believe that to be psychologically healthy, a person must appear to be of an appropriate weight; this indicates willpower, discipline, and self-control (Tischner, 2019). Though these ideas are inaccurate for psychological health, they may influence how clients see counselors on the far ends of the weight spectrum.
Antifat Attitudes
Antifat attitudes are a different but related construct to weight bias. An antifat attitude is “a negative attitude toward (dislike of), belief about (stereotype), or behavior against (discrimination) people perceived as being ‘fat’” (Meadows & Daníelsdóttir, 2016, p. 47). Weight bias refers to a negative attitude toward any size body (Christensen, 2021), whereas antifat attitudes describe dislike and discrimination toward people perceived as overweight (Meadows & Daníelsdóttir, 2016). Antifat attitudes have created a marginalized group that faces external stigma throughout society, with some individuals feeling internal stigma due to personal experiences.
Despite encounters with prejudice, some clients who are overweight will still prefer an average-weight counselor because of their own bias toward being overweight (Moller & Tischner, 2019) and will have similar antifat attitudes as average-weight individuals (Schwartz et al., 2006). Contingencies of self-worth encompass the domains in a person’s life that create self-esteem (Clabaugh et al., 2008). When body weight is a domain, success or failure in their ability to lose or gain weight can lead to lower self-worth. Because of weight bias, working with a counselor who mirrors the client’s undesired body weight may impact the client’s willingness to work with the counselor. Examining weight bias across the spectrum and correlating BMI with antifat attitudes will give us further insight into these findings and if they influence client bias toward counselors.
Purpose of the Study
This study examined if client weight bias influences a client’s trust in a counselor’s competence, willingness to follow a counselor’s advice, and desire to select a counselor for therapy. We further examined if a client’s antifat attitudes are associated with their weight bias toward counselors. The following research questions guided this study: 1) Does a counselor’s weight impact a client’s decision to trust, follow advice, and select the counselor? 2) Is there an association between a client’s antifat attitudes and weight bias toward counselors? 3) Are there differences in weight bias toward counselors based on the socio-demographics of the clients using their services? and 4) Do participants with eating disorders have similar perceptions of counselors due to weight bias as those without eating disorders?
Methodology
Recruitment
At the time the research was conducted, the researchers—Amy Biang, Clare Merlin-Knoblich, and Stella Kim—were affiliated with the same university; as such, IRB approval was obtained from that university before recruiting participants. People were eligible to participate in this study if they were 18 years or older and signed an electronic consent form indicating their willingness to participate. We recruited participants through purposive and snowball sampling in three ways. First, Biang emailed a compiled database of counseling professionals within their acquaintance to request they send the survey to previous clients in an effort to obtain sufficient participation from people who have received counseling. In addition, requested participation through two research boards of counseling associations (Academy of Eating Disorders and International Association of Eating Disorder Professionals) allowed us to recruit sufficient participation from previous clients with EDs, as well as other diagnoses, as we requested they send the survey to their former clients. Second, to obtain participation from people with and without experience in counseling, Biang posted calls for participation on social media accounts (i.e., Instagram and Facebook). Third, to further increase participation, Merlin-Knoblich forwarded a participation request to their university’s counseling program listserv. After 2 weeks of data collection, we sent a second follow-up call for participation and then continued data collection for an additional week.
To prevent recruitment bias and confirmation bias during data collection, we omitted the terms weight and weight bias and modified the study title to read “Counselor Attributes that Impact Client’s Selection, Trust, and Advice Following.” The call for participation informed potential participants that we were conducting a study about the attributes of a hypothetical counselor. The end of the questionnaire contained a full disclosure of the study’s purpose. Of the 255 participants who began the study questionnaire, 189 completed the study, representing a 74% completion rate. No data was collected from the 66 non-completers other than an average of 76 seconds with the survey open before ending the survey.
Participants
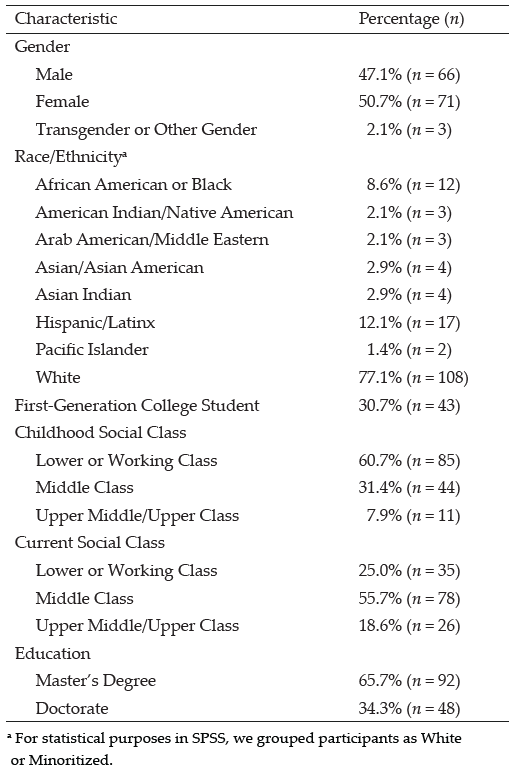
A sample of 189 participants from 26 states participated in the study. Table 1 presents a summary of the sample characteristics. The majority of participants were from North Carolina (n = 72, 38%),
Ohio (n = 23, 12%), California (n = 19, 10%), Utah (n = 11, 6%), and New York (n = 10, 5%). Participants primarily identified as female (n = 158, 84%). The majority of participants identified as White (n = 153, 81.4%), with other participants identifying as Asian (n = 13, 6.9%), Black/African American (n = 12, 6.4%), Latine/Hispanic (n = 5, 2.7%), and American Indian (n = 3, 1.6%). The majority of participants were over the age of 30 (n = 139, 74%), more than half had previously participated in personal counseling (n = 135, 71.8%), and just over a quarter indicated a previous ED diagnosis (n = 52, 27.7%).
Given the focus of this study, all participants were asked to indicate their height and weight but were informed that such information (like all demographic information) was optional to submit. One hundred and eighty-four participants (97%) shared their height and weight, from which we calculated their BMI—a person’s weight in kilograms divided by the square of height in meters. The mean BMI was 28 (SD = 6.8) among the participants who shared their height and weight. This BMI is designated as “overweight” by the CDC (2022).
Study Design and Instrumentation
Physician Weight Survey Revised
We used a quasi-experimental research design in this study. With permission from Puhl and colleagues (2013), we revised the Physician Weight Survey (PWS), a 44-item questionnaire designed to assess patient weight bias of physicians who are obese, overweight, or seen as average weight. The instrument measures five constructs: physician health behaviors, physician selection, physician compassion, physician trust, and adherence to physician advice. Cronbach’s alpha tests instrument reliability and the internal consistency of the questions on a scale. Alpha scores over .70 are considered acceptable (Taber, 2018). Each subscale of the PWS has demonstrated sufficient internal consistency, with a Cronbach’s alpha of at least .90 (Puhl et al., 2013).
We adapted the questionnaire to address participants’ willingness to trust, follow the advice of, and select a hypothetical counselor based on the weight of that counselor. We replaced the term, physician with counselor and added the underweight category instead of the obese category. Using the underweight category allowed for consideration that weight bias exists on both ends of the weight spectrum. Because
of differences in occupational responsibilities and limiting the dependent variables of our study, we did not use the subscales for health behaviors or compassion. The Health Behavior subscale incorporated the physicians’ use of substances, health screenings, and illness prevention. The Compassion subscale measured the physician’s bedside manner. Without those two additional subscales, our revised measure had 23 items.
Table 1
Participant Demographic Data
| Demographics |
n |
% |
| Gender |
|
|
| Female |
158 |
84.0 |
| Male |
27 |
14.4 |
| Non-Binary |
1 |
0.05 |
| Race/Ethnicity |
|
|
| White |
153 |
81.4 |
| Black/African American |
12 |
6.4 |
| Latine/Hispanic |
5 |
2.7 |
| Asian |
13 |
6.9 |
| American Indian |
3 |
1.6 |
| Age Range |
|
|
| 18–29 |
48 |
25.6 |
| 30–42 |
64 |
34.1 |
| 43 and older |
74 |
39.4 |
| Prior History of Counseling |
|
|
| Yes |
135 |
71.8 |
| No |
51 |
27.1 |
| Prior History of Eating Disorder |
|
|
| Yes |
52 |
27.7 |
| No |
134 |
74.3 |
| BMI Range |
|
|
| Underweight |
4 |
2.1 |
| Average |
64 |
34.0 |
| Overweight |
54 |
28.7 |
| Obese |
60 |
31.9 |
Note. N = 189.
The subscales of Counselor Trust and Counselor Selection align well with our study. The subscale of Advice Following may seem counterintuitive when used with the counseling profession. The term advice equates to the construct of counseling together and incorporates the concept of counselors helping clients create and follow treatment goals, exploring ideas together for change, and even assigning homework. Advice aligns with how clients perceive what counselors do rather than the skills they use. For example, counselors using motivational interviewing and questions such as “What would it take for you to go from a 2 to a 4 in your willingness to reduce your alcohol consumption?” can be seen as advising clients to reduce their alcohol consumption. We chose to use the term advice instead of counsel so all participants, regardless of their experience with counseling, would understand the questions.
Parallel to Puhl and colleagues’ (2013) study, we then created three different versions of the questionnaire. Using Qualtrics, an electronic survey platform, consenting participants received a random assignment to one of three questionnaire versions. Seventy (37%) of the study participants completed the first version of the questionnaire, which described a hypothetical counselor as an overweight counselor. Fifty-eight (31%) participants completed the second questionnaire version, which described a hypothetical counselor as having average weight. And 61 (32%) of the participants completed the third version of the questionnaire, which described a hypothetical counselor as underweight. Participants responded to all items on a Likert scale ranging from 1 (strongly disagree/extremely unlikely) to 7 (strongly agree/extremely likely), with seven questions reverse scored.
Counselor Trust Subscale. The Counselor Trust subscale of the revised PWS consisted of nine questions focused on skills and competence (e.g., “If my counselor was [overweight/underweight/average weight], I would not trust them,” and “If my counselor was [overweight/underweight/average weight], I would have doubts about their credibility”). Other questions focused on believing the counselor would listen or understand their needs (e.g., “I believe an [overweight/underweight/average weight] counselor would listen carefully to what I have to say”). The scale demonstrated good internal consistency (α = .81) with this sample. Higher scores reflect greater trust in the counselor.
Counselor Advice Following Subscale. The Advice Following subscale contained six items. These items indicated making changes to diet, losing weight, and advice in general (e.g., “In general, my counselor’s weight affects whether I listen to their advice” and “If my counselor were [overweight/underweight/average weight], I would feel embarrassed when talking about losing weight”). Though counselors are not medical doctors, many clients explore topics associated with their bodies, exercise, and overall physical health (e.g., sleep issues, pain management, substance use, and daily routines), indicating relevance to counseling for the survey questions. Higher scores suggest more willingness to follow the advice (counsel) of the counselor. Cronbach’s alpha for this scale was .83 with this sample.
Counselor Selection Subscale. The Counselor Selection subscale had seven items indicating a willingness to select the counselor based on their appearance of weight (e.g., “If I went to a new counselor, and the counselor appeared [overweight/underweight/average weight], I would change counselors,” or “If my counselor was [overweight/underweight/average weight], I would not recommend them to my friends”). Similar to the other subscales, higher scores indicate more willingness to select the counselor. For this sample, Cronbach’s alpha was .71.
Antifat Attitudes Questionnaire
In addition to the revised PWS, participants completed the Antifat Attitudes Questionnaire (AFA; Crandall, 1994). The AFA assesses participants’ beliefs about overweight people and their feelings about becoming overweight. Three subscales, Dislike (α = .84), Fear of Fat (α = .79), and Willpower (α = .66), are combined for a composite antifat attitude score. Despite the low Cronbach’s alpha coefficient for the Willpower subscale, it positively correlates with the Dislike subscale (r = .43, p < .001), whereas the Fear of Fat subscale remains uncorrelated with both subscales, suggesting discriminate validity (Lacroix et al., 2017; Ruggs et al., 2010). Both the reliability and validity of the AFA have been extensively assessed by researchers, and the AFA has been found to be a psychometrically sound measure (Ruggs et al., 2010). The Cronbach’s alpha internal consistency reliability was acceptable, with a value of .87 for the data used in the current study. Participants indicated agreement (e.g., “I really don’t like fat people much”) on a Likert scale ranging from 1 (strongly disagree) to 7 (strongly agree), with higher composite scores suggesting stronger negative antifat attitudes. Higher scores may correlate to weight bias toward the overweight counselor. Scores on the Fear of Fat subscale are directed toward a personal antifat fear and not toward others.
The AFA was also used to test the equivalence of groups and any effect of social desirability. Lastly, participants completed a voluntary 8-item demographic questionnaire describing their race/ethnicity, age, gender, height, weight, and experience with receiving counseling or having an ED.
Data Analysis
We conducted all analyses using SPSS Version 27. The first analysis had the four dependent variables of Counselor Trust, Counselor Selection, Advice Following, and Weight Bias, with the independent variable of Weight (overweight, underweight, and average weight). We conducted a series of assumption-checking procedures to draw valid interpretations of the findings. Engaging the Shapiro-Wilk test as a test of normality yielded a significant result (W = 0.92, p < .001) for the overweight counselor, indicating the sample was not normally distributed. After removing outliers, the sample for the overweight survey condition did not meet the assumption of normality. A test for homogeneity of variance yielded a statistically significant Levine’s score of F(2, 168) = .46, p = .013; degrees of freedom were adjusted due to unequal sample sizes for each survey condition.
Conducting a MANOVA yielded statistically significant results; however, not meeting the assumptions of multivariate normality and homogeneity of variance required, we used the Welch ANOVA, which is recommended for non-normal distributions. Using a Welch ANOVA is also a best practice when the homogeneity of variances test fails; it controls the type I error and gives more power in many instances (Liu, 2015). Although a parametric test such as a typical ANOVA or MANOVA is known to be more powerful than a non-parametric test (e.g., Welch ANOVA), it can lead to erroneous results if required assumptions are not satisfactorily met (Zar, 1998). Considering unequal variances and sample sizes across groups, we used Games-Howell for post hoc testing. We used G*Power version 3.1.9.7 (Faul et al., 2007) to perform the power analysis. For the Welch ANOVA test, the minimum sample size was 157, with a medium effect size of .25, a desired statistical power level of .8, and an alpha level of .05. Lastly, we measured the effect size using partial eta squared (ꞃ²), showing the strength of association as a proportion of variance in the dependent variable explained by group membership (Coladarci et al., 2011).
Table 2
Descriptive Statistics for Outcome Variables
|
n |
Mean |
Std.
Deviation |
Std. Error |
95% Confidence Interval for Mean |
Minimum |
Maximum |
| Lower Bound |
Upper Bound |
| Trust |
OW |
70 |
49.70 |
9.89 |
1.18 |
47.34 |
52.06 |
16.00 |
63.00 |
| UW |
59 |
41.15 |
10.72 |
1.40 |
38.36 |
43.95 |
17.00 |
63.00 |
| AW |
60 |
47.48 |
7.75 |
1.00 |
45.48 |
49.49 |
29.00 |
63.00 |
| Total |
189 |
46.33 |
10.16 |
0.74 |
44.87 |
47.79 |
16.00 |
63.00 |
| Selection |
OW |
70 |
32.41 |
5.40 |
0.64 |
31.13 |
33.70 |
19.00 |
40.00 |
| UW |
59 |
30.00 |
5.12 |
0.67 |
28.67 |
31.33 |
21.00 |
40.00 |
| AW |
60 |
31.42 |
4.92 |
0.63 |
30.15 |
32.69 |
16.00 |
40.00 |
| Total |
189 |
31.34 |
5.23 |
0.38 |
30.59 |
32.09 |
16.00 |
40.00 |
| Advice |
OW |
70 |
25.76 |
8.72 |
1.04 |
23.68 |
27.84 |
8.00 |
42.00 |
| UW |
59 |
24.73 |
7.33 |
0.95 |
22.82 |
26.64 |
8.00 |
42.00 |
| AW |
60 |
31.93 |
4.64 |
0.60 |
30.73 |
33.13 |
23.00 |
42.00 |
| Total |
189 |
27.40 |
7.81 |
0.57 |
26.28 |
28.52 |
8.00 |
42.00 |
| Note. OW = overweight; UW = underweight; AW = average weight. |
In the second data analysis, we used the Pearson correlation to assess an association between data sets from the AFA and Composite Weight Bias. Composite Weight Bias was calculated by summing the scales of the revised PWS. Before computing a correlation, we examined the scatter plot between the independent and dependent variables to check the linearity between the two variables and the existence of outliers. We found less than three outliers on all four graphs and identified negative linearity. Using G*Power (Faul et al., 2007), we obtained the estimated sample size necessary to run the correlation analysis, which was 64 with a medium effect size of .3, an alpha level of .05, and power of .8. Lastly, we explored the relationships between demographics and weight bias toward counselors using a one-way ANOVA or an independent t-test. We selected statistical methods based on the number of categories of each demographic variable. See Table 2 for descriptive statistics of the outcome variables.
Results
Areas of Trust, Advice, and Selection
We found significantly different levels of trust, advice following, and counselor selection behaviors among participants assigned to hypothetical counselors of different weights.
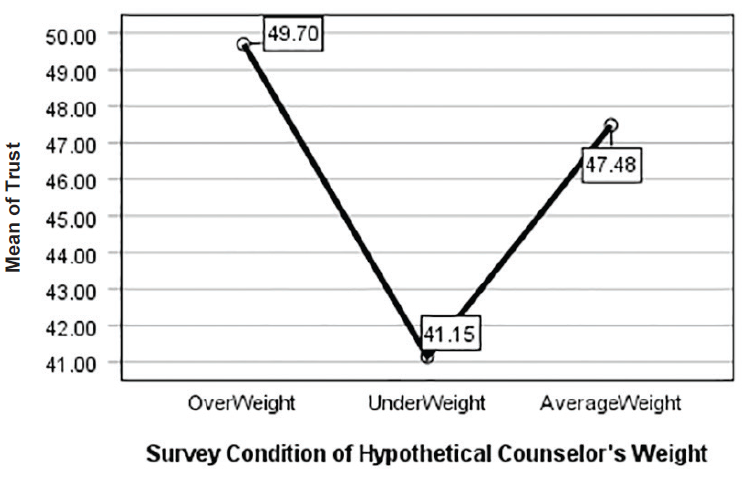
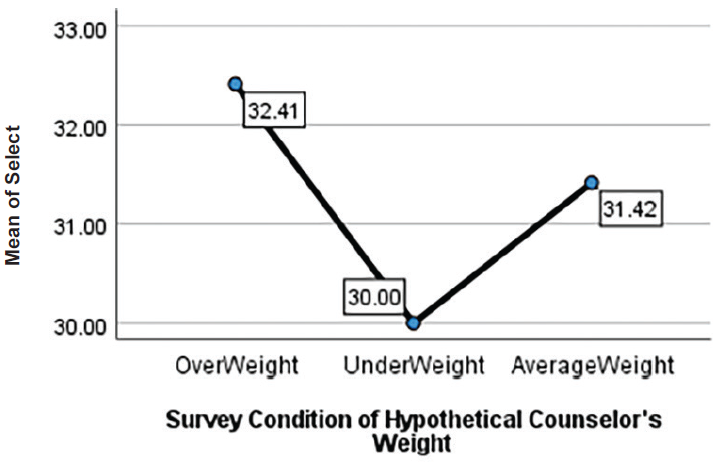
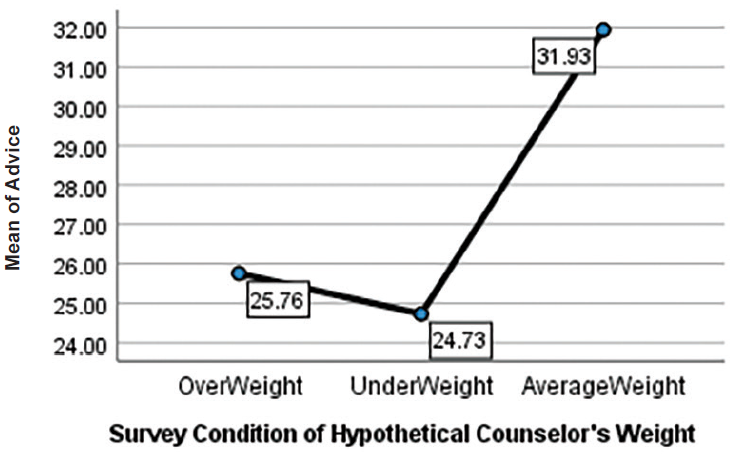
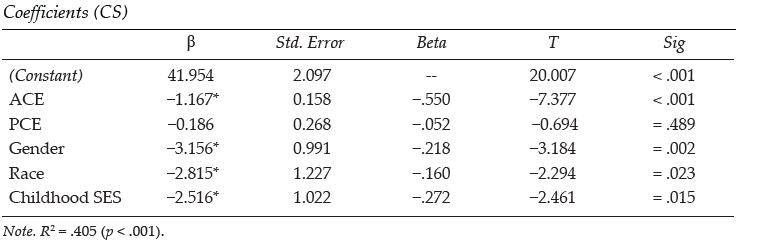
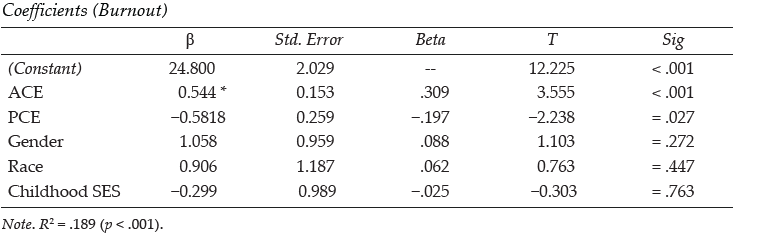
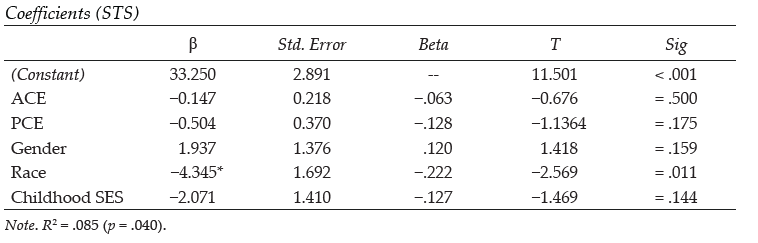
Welch ANOVA test results indicated a statistical significance in all three areas between groups, F(2, 120.60) = 12.89, p < .001 with a medium effect size (ꞃ² = .11). Post hoc comparisons using Games-Howell showed the following results at the significance level of α = .05. Counselor Trust for average-weight counselors (M = 47.48, SD = 7.75) was significantly higher than Counselor Trust for underweight counselors (M = 41.15, SD = 10.72) at p = .001. Counselor Trust of overweight counselors (M = 49.70, SD = 9.89) was also significantly higher than Counselor Trust for underweight counselors at p < .001. There was no statistical significance for Counselor Trust between average and overweight counselors. Advice Following for average-weight counselors (M = 31.93, SD = 4.65) was significantly higher than Advice Following for underweight counselors (M = 24.72, SD = 7.28) and Advice Following for overweight counselors (M = 25.75, SD = 8.72) at p < .001 for both. Finally, Counselor Selection for an overweight counselor (M = 32.41, SD = 5.73) was statistically higher than Counselor Selection for an underweight counselor (M = 30.00, SD = 5.59) with p = .028. There was no statistical significance in the Counselor Selection of average-weight counselors (M = 31.41, SD = 4.91) compared to overweight or underweight counselors. See Table 3 and Figures 1–3.
Next, we conducted a Welch ANOVA between overall composite scores and the three weight groups (see Table 4). Again, Welch test results indicated a statistical significance between groups, F(2, 118.73) = 11.71, p < .001 with a medium effect size (² = .10). Post hoc comparisons using Games-Howell showed statistical significance between overweight counselors (M = 107.87, SD = 21.68) and underweight counselors (M = 95.88, SD = 20.00). Underweight counselors were also significantly lower on the overall composite than average-weight counselors (M = 110.83, SD = 19.97). There was no statistical significance between overweight and average-weight counselors for their overall composite scores, which include all three variables.
Figure 1
Willingness to Trust Counselor
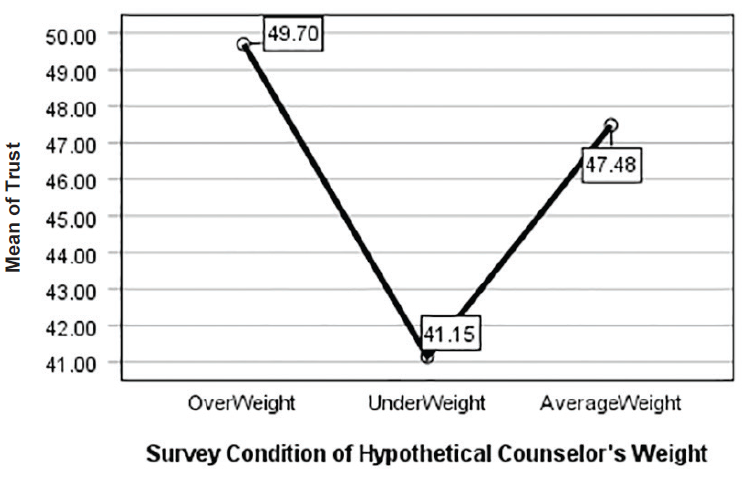
Figure 2
Willingness to Select Counselor
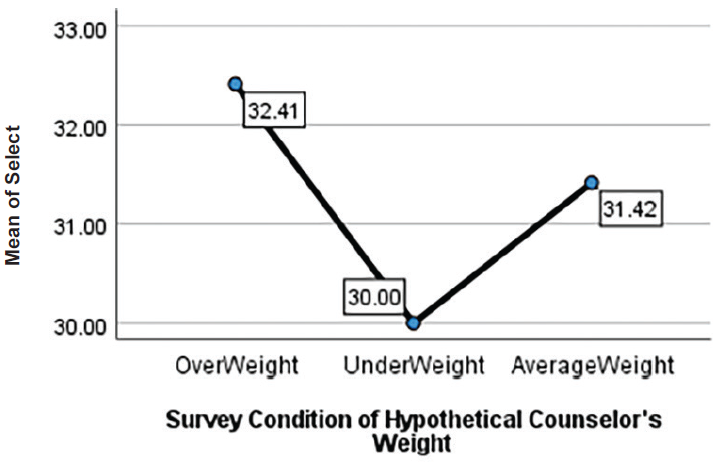
Figure 3
Following Counselor Advice
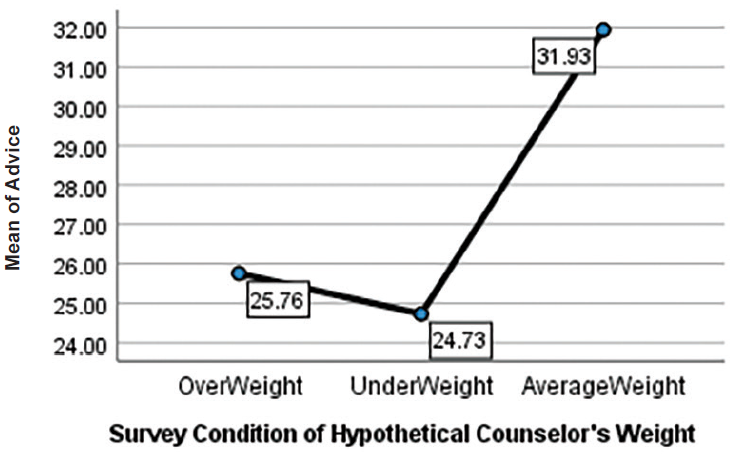
Table 3
Post Hoc Outcome Variables
|
| Dependent Variable |
Mean Difference (I-J) |
Std. Error |
Sig. |
95% Confidence Interval |
| Lower Bound |
Upper Bound |
| Trust |
OW |
UW |
8.547a |
1.829 |
0.00 |
4.206 |
12.888 |
| AW |
2.216 |
1.548 |
0.32 |
−1.456 |
5.889 |
| UW |
OW |
−8.547a |
1.829 |
0.00 |
−12.888 |
−4.206 |
| AW |
−6.330a |
1.717 |
0.00 |
−10.414 |
−2.247 |
| AW |
OW |
−2.216 |
1.548 |
0.32 |
−5.889 |
1.456 |
| UW |
6.330a |
1.717 |
0.00 |
2.247 |
10.414 |
| Selection |
OW |
UW |
2.414a |
0.927 |
0.02 |
0.215 |
4.613 |
| AW |
0.997 |
0.904 |
0.51 |
−1.144 |
3.143 |
| UW |
OW |
−2.414a |
0.927 |
0.02 |
−4.613 |
−0.215 |
| AW |
−1.416 |
0.920 |
0.27 |
−3.601 |
0.767 |
| AW |
OW |
−0.997 |
0.904 |
0.51 |
−3.143 |
1.148 |
| UW |
1.416 |
0.920 |
0.27 |
−0.767 |
3.601 |
| Advice |
OW |
UW |
1.028 |
1.413 |
0.74 |
−2.323 |
4.379 |
| AW |
−6.176a |
1.202 |
0.00 |
−9.034 |
−3.313 |
| UW |
OW |
−1.028 |
1.413 |
0.74 |
−4.379 |
2.323 |
| AW |
−7.204a |
1.126 |
0.00 |
−9.885 |
−4.523 |
| AW |
OW |
6.176a |
1.202 |
0.00 |
3.318 |
9.034 |
| UW |
7.204a |
1.126 |
0.00 |
4.523 |
9.885 |
| Note. The mean difference is significant at the 0.05 level. OW = overweight; UW = underweight; AW = average weight. Welch’s ANOVAs with Games-Howell post hoc tests were run owing to violations of the equality of variances assumption. |
Table 4
Post Hoc Composite Weight Bias
|
| (I) Group |
Mean Difference (I-J) |
Std. Error |
Sig. |
95% Confidence Interval |
| Lower Bound |
Upper Bound |
| OW |
UW |
11.99a |
3.67 |
0.004 |
3.28 |
20.70 |
| AW |
−2.96 |
3.09 |
0.604 |
−10.29 |
4.36 |
| UW |
OW |
−11.99a |
3.67 |
0.004 |
−20.70 |
−3.28 |
| AW |
−14.95a |
3.10 |
0.000 |
−22.32 |
−7.58 |
| AW |
OW |
2.96 |
3.09 |
0.604 |
−4.36 |
10.29 |
| UW |
14.95a |
3.10 |
0.000 |
7.58 |
22.32 |
| Note. The mean difference is significant at the 0.05 level. OW = overweight; UW = underweight; AW = average weight. Welch’s ANOVAs with Games-Howell post hoc tests were run owing to violations of the equality of variances assumption. |
|
In addition to statistical significance, we also examined effect size to quantify the significance found. Results indicated that Advice Following showed a large effect of association with the independent variable of Weight (² = .16). Counselor Trust had a medium effect size (² = .13), and Counselor Selection yielded a small effect size (² = .04). These results suggest that the weight of a counselor has a high association with clients following counselor advice, with average-weight counselors faring the best. Additionally, participants indicated they would trust average and overweight counselors more than underweight counselors. Lastly, overweight counselors were more favorable in Counselor Selection than underweight counselors.
Antifat Attitudes and a Correlation With Counselor Trust, Advice Following, and Counselor Selection
We used Pearson correlations to examine associations between antifat attitudes and weight bias toward counselors (see Table 5). To do so, we examined data from participants assigned to all three counselor conditions in the study. Each group showed a significant relationship between antifat attitudes and weight bias toward counselors; thus, we combined data to attain a larger sample size. The Pearson correlations between the independent variable of antifat attitudes and dependent variables of Counselor Trust, Advice Following, Counselor Selection, and Composite Weight Bias score were significant at α = .05. We found positive correlations between antifat attitudes and Counselor Selection, r(186) = .400, p < .001, and Counselor Trust, r(186) = .211, p = .004. These results indicate that as antifat attitudes increase, participants’ trust in and selection of a counselor based on weight also increase. We found no significant correlation between Advice Following and Composite Weight Bias score with antifat attitudes.
Table 5
Correlation of AFA With Outcome Variables |
|
|
|
|
|
|
AFA |
Trust |
Selection |
| AFA |
Pearson Correlation |
1.000 |
0.211** |
0.400** |
| Sig. |
|
0.004 |
0.000 |
| N |
188.000 |
188.000 |
188.000 |
| Trust |
Pearson Correlation |
0.211** |
1.000 |
0.349** |
| Sig. |
0.004 |
|
0.000 |
| N |
188.000 |
188.000 |
188.000 |
| Selection |
Pearson Correlation |
0.400** |
0.349** |
1.000 |
| Sig. |
0.000 |
0.000 |
|
| N |
188.000 |
188.000 |
188.000 |
Note. AFA = Antifat Attitude. Advice was not statistically significantly correlated with AFA. One participant of the total study sample (N = 189) did not complete this portion and is not included in the table.
*Correlation is significant at the 0.01 level (two-tailed). |
Socio-Demographic Categories
We found no statistically significant differences in weight bias toward counselors based on ethnicity F(4, 181) = .037, p = .997; age F(4, 181) = 1.71, p = .149; BMI F(4, 177) = .193, p = .942; counseling status t(184) = .798, p = .426; eating disorder t(184) = 1.055. p = .137; or gender F(2, 183) = 1.423, p = .426. Additionally, we tested for Pearson correlations between BMI and antifat attitudes. Results indicated that BMI and antifat attitudes had no significant correlation, r(N = 187) = .004, p = .958.
Antifat Attitudes by Survey Condition
To test for undue influence from survey design or responses that stem from social desirability, we ran an ANOVA comparing participants in each questionnaire condition (i.e., underweight, average weight, and overweight counselor) and their scores on the AFA. We found no statistically significant differences between the three groups, F(2, 181) = 2.74, p = .067. For the AFA scores, M = 40.22 and SD = 12.57. However, with the results of the AFA correlation with Counselor Trust and Counselor Selection, these findings may indicate that there was social desirability across all three survey conditions.
Discussion
Contrary to previous research from McKee and Smouse (1983) that suggested counselors of any weight could address personal concerns, our study results indicated that clients might use weight to select a counselor, trust the counselors’ skills, and follow their counsel. When asked about weight, participants in this study slightly preferred to select and trust the average-weight and overweight counselors, with weight bias directed mainly at the underweight counselor. Like previous research about weight bias toward physicians (Puhl et al., 2013) and personal trainers (Hutson, 2013), our results showed some weight bias toward overweight counselors when following advice. For underweight counselors, weight bias was present in all three subscales and mirrored findings that underweight persons are not immune to weight discrimination (Beggan & DeAngelis, 2015).
Overweight Counselors
Our results yielded only one finding that supported the theme from Moller and Tischner’s (2019) study that “fat counselors cannot help” (p. 14). Statistically significant results from the present study showed less willingness to follow the advice of overweight counselors. Similar to the findings from Puhl et al. (2013), taking advice or counsel from an overweight health care professional may prove more difficult than trusting they can perform their job or being willing to work with them. With two-thirds of adults in the United States considered overweight or obese (CDC, 2022), these findings may reflect cause for concern that some clients may not perceive competence in counselors who are overweight.
The correlation between the AFA with Counselor Trust and Counselor Selection can give insight into the findings. The positive correlation between AFA and Counselor Trust was low but significant. With 60% of participants in the overweight-to-obese category, there could be an underlying factor that needs further exploration. There was no correlation between BMI and AFA. However, as Schwartz et al. (2006) suggested, overweight people have similar antifat attitudes as average-weight individuals. The slight correlation potentially relates to most participants having larger bodies and knowing that being in larger bodies does not equate to untrustworthiness. Likewise, for Counselor Selection, we should consider the concept of similar attraction. This concept posits that people associate with those perceived as similar to them and who have similar physical attributes (Montoya & Horton, 2013). Relating to this concept of similar attraction, the positive correlation between AFA and Counselor Selection could be attributed to the high percentage of larger-body participants feeling more comfortable selecting the overweight counselor.
Unlike findings from other studies (Moller & Tischner, 2019; Puhl et al., 2013), our results did not indicate that Counselor Trust or Counselor Selection were negatively related to being overweight. However, when looking at the Advice Following subscale, there was a marked difference in the scores. The hypothetical overweight counselor had higher mean scores than underweight counselors on all three subscales and overall composite scores. On the upside, weight may not be an issue for many clients seeking counseling. Despite continued weight bias and stigma in social media and society, people might recognize that overweight counselors’ skills and knowledge are more important than perceived body weight. On the downside, clients may hesitate to follow counsel associated with issues concerning their own physical well-being from a perceived overweight counselor. To combat this, counselors need to be willing to broach the issue of weight if they feel it is hindering the therapeutic alliance. Similar to other multicultural topics, differences in body weight between the counselor and client may be a potential barrier for the free expression of client concerns. The willingness of the counselor to explore this topic may put the client at ease and make them able to further explore their concerns in a nonjudgmental, therapeutic manner.
Underweight Counselors
We found surprising results suggesting that participants in our study would prefer an overweight or average-weight counselor to an underweight counselor. Participants scored counselors perceived as underweight significantly lower on a client’s willingness to select, trust, and follow a counselor’s advice than average-weight and overweight counselors. These results supported the decision to add this variable to our study and indicate the need for more research on weight bias toward underweight professionals.
The underweight variable yielded results that complement previous research on weight bias, indicating that people can be biased against underweight professionals (Allison & Lee, 2015; Davies et al., 2020b). Because of the persistent social desirability to be thin or underweight, research indicates that people may be pro-underweight on an explicit level; however, they implicitly prefer an average-weight person (Marini, 2017). In our findings, participants somewhat preferred to select an overweight counselor instead of an underweight counselor, upholding the notion that people do not necessarily trust those who are underweight despite the social pressure to be thin. This result highlights a striking mismatch in thought: people may prefer to be underweight because of social pressures but not fully trust an underweight counselor. It could indicate that societal pressures to be underweight are not as strong as once thought or it may suggest that people possess complicated views on being underweight in general.
These results reflect those found by Marini (2017), in which individuals implicitly preferred an overweight individual over an underweight individual, implying maladaptive behaviors and dangerous consequences. Additionally, with body positivity and body acceptance movements, underweight persons may be overlooked as recipients of negative weight bias (Beggan & DeAngelis, 2015). These results may give underweight counselors pause about how clients perceive them in session and the notion that experiences of thin privilege may not transfer into their professional identity. In response to these possible perceptions from clients, underweight counselors may benefit from seeking professional supervision or consulting with colleagues about the topic.
Antifat Attitudes
The AFA results indicated that as a person’s negative attitudes toward overweight people decrease, they disregard weight as a factor for selecting and trusting the skills of counselors. Currently, there is no measure for anti-thin attitudes to analyze whether this bias would yield similar results. Despite the lack of an anti-thin measure, these results reiterate the belief that we judge others based on what attributes are important to us or differentiate us from others (Cermák et al., 1993). When body weight is not an attribute of self-judgment, a person may not use it as a criterion toward others or in working with professionals. As a profession, we must continue supporting movements that promote acceptance of all bodies and destigmatize weight. With strong social media campaigns against weight bias, we can dispel the stereotypes about those who fall outside socially acceptable standards and replace them with acceptance.
Demographics
In addition to antifat attitudes, we chose to study socio-demographics because weight bias may fluctuate based on various group identities. Our results showed no statistically significant differences in age, gender, ethnicity, or BMI. These findings are relevant as they imply that weight bias may exist throughout all groups. However, we interpret these results cautiously, as the sample population was predominantly female, with fewer ethnically diverse participants, and more participation from people over 30. Notably, results for ethnicity were similar to previous research indicating that Black and White women had the same bias and weight stigma toward others who were overweight and underweight (Davies et al., 2020b).
Eating Disorder Consideration
Because of the nature of EDs, we added this category to the study to explore if a counselor’s weight would impact participants with an ED more. As counselors working with EDs often explore issues around weight, exercise, and eating concerns, we hypothesized that these participants might have a higher bias toward underweight and overweight counselors. We found that participants with EDs were not significantly different from participants without EDs in weight bias toward counselors in any of the variables. This finding is favorable information for counselors in this specialty, as it does not align with the findings from Moller and Tischner (2019) that suggest that the weight of a counselor is a barrier to treatment.
Experience of Counseling
A final surprising finding revealed in our results was that people with previous counseling experience had similar levels of weight bias to those who had not worked with a counselor. Participants who previously participated in counseling may recognize attributes, such as expertise, empathy, and compassion of a counselor, as more valuable in their relationship than weight. Because attributes such as genuineness, empathy, unconditional positive regard (Nienhuis et al., 2018) build the therapeutic relationship, it is feasible to see counselor weight as a non-factor. However, we found that prior experience in counseling did not mediate the weight bias participants demonstrated. This result gives room for concern that weight bias may diminish the initial value of core conditions and counselor attributes studied in the past. Perhaps weight bias is pervasive in the decision to work with a counselor.
Implications
Despite years of education and experience, weight bias may rule out competent counselors. Professionals who fall outside the average body weight are hyper-visible (Beggan & DeAngelis, 2015) and prone to judgment of their weight. This study fills a gap in the research pertaining to the way weight bias influences a client’s willingness to trust, follow counselor advice, and select their counselors. Knowing how weight bias impacts the counseling profession can help counselors become aware of an issue that may affect the therapeutic alliance. In response to the study results, we identified two key implications for the counseling profession.
First, the results are indicative of a multicultural issue. Many people see weight as a medical concern instead of a social justice issue (Christensen, 2021). This idea limits the amount of education and training counseling graduate students receive on the topic of weight, leading to the request to address weight in multicultural courses as a core topic. Weight becomes intersectional among identities, and counselors must train to be sensitive to and inclusive of the topic of weight. Broaching weight may feel uncomfortable but be necessary to strengthen the therapeutic relationship.
Second, recognizing that weight bias may impact a client’s willingness to select, follow the counsel of, or trust a counselor reiterates the importance of knowing the factors influencing the counseling relationship. Counselors should acknowledge that stereotypes, discrimination, and oppression influence the counseling relationship (Ratts et al., 2016). Counselors should not ignore weight bias as a possible stereotype and should be comfortable discussing it with their clients. Additionally, the multicultural competencies note that “Counselors know when to initiate discussions with regard to the influences of identity development, power, privilege, and oppression within the counseling relationship” (Ratts et al., 2016, p. 41). As society continues to push the thin ideal while simultaneously pushing body acceptance at any size, these contradictory messages will keep weight bias at the forefront of how others are judged.
Until weight bias is erased, counselors must be vigilant in understanding how they show up in the session, what message a client may perceive by their body weight, and how to broach the topic to strengthen the therapeutic alliance. If counselors seek to help reduce weight bias in society, they may benefit from reflecting on their own biases, privileges, and experiences with oppression in this area. They also may consider challenging potential biases through professional development, group or individual counseling supervision, or literature about weight bias in society.
Limitations
Like all studies, this study contains limitations. One limitation is the subjectivity of weight. Without guidelines for what constitutes overweight and underweight, this study heavily relied on participants’ perceptions of these variables, which may be inconsistent across participants. Not specifying these variables opened interpretation for the overlapping areas of overweight versus obese or underweight versus extremely thin. Participants in each treatment condition may have visualized different hypothetical counselors than peers in the same treatment group. Using images may improve the specificity of the variable in future studies.
Additionally, there was no identified gender for the hypothetical counselors in each treatment condition, allowing participants to visualize any gender of counselor they chose. This lack of specificity may have created a moderating variable. Women represent higher numbers in the counseling profession. Women experience more discrimination than men (McHugh & Kasardo, 2012; Roehling et al., 2007), and it is unknown if people who identify as gender non-binary experience more or less weight bias. By not distinguishing the gender of the counselor, our ability to make inferences across genders is limited. Creating a study that specifies multiple genders may yield more representative results.
Another limitation is that a non-parametric test (e.g., Welch’s ANOVA) was used instead of parametric tests with more statistical power. The decision to use the non-parametric test was unavoidable because of violating the required assumptions. At the same time, future research may corroborate our findings using a parametric test if data allow. Future research may also replicate this study using multivariate ANOVA (MANOVA), which considers correlations of dependent variables.
Lastly, social desirability and self-reporting may have impacted responses. While completing the questionnaire, feelings about weight bias may have occurred outside of participants’ awareness, causing cognitive dissonance. To resolve this dissonance, responses may have overtly favored accepting the overweight counselor or selecting fewer negative answers on the AFA. Participants also reported their own weight bias, which may have presented a self-report limitation. The results of overweight counselors having higher mean scores on Trust and Selection than average-weight counselors give room for consideration that social desirability may have influenced some of the participants’ answers. Future studies may benefit from including a test for social desirability or implicit association tests to increase the study’s validity.
Future Considerations
Future considerations for research encompassing weight bias across the spectrum would require developing an anti-thin attitude measure to identify weight attitudes toward underweight individuals accurately. This measure would be beneficial for bringing more awareness to underweight discrimination and measuring its impact on professionals and members of society. As society continues to push the thin ideal, people will strive to fit that ideal. However, as our results suggest, underweight counselors may face significant weight bias from clients. Consequently, counselors would benefit from a measure created to address underweight bias.
The counseling profession lacks extensive, meaningful research regarding the physical and educational factors that clients find most important in selecting, trusting, and following the advice of a counselor. Another factor to incorporate in future research is a counselor’s level of education and expertise. Clients may more favorably evaluate an average weight counselor with a specialist or doctoral degree than an underweight or overweight colleague with the same credentials. If weight bias influences these variables despite the skill level of the counselor, clients may miss receiving help from highly trained and educated people. Additionally, directly exploring the role that empathy, congruence, and strengths-based counseling have compared to weight bias may yield significant findings.
A final consideration for future research involves focusing on counselors who work in the ED field, a specialty that deals with eating, weight, body image, and exercise. Though we did not find significant differences in this study between those with and without an ED, our hypothetical counselor was not an ED counselor. These counselors may experience more judgment and assumptions of lifestyle choices by their clients, as they are considered specialists in EDs. Studies show that being underweight may indicate an ED, such as anorexia or binge eating disorder (Davies et al., 2020a; Marini, 2017). It is unknown if clients would replicate the results found in this study regarding counselors in the ED field.
Conclusion
This study examined participants’ weight bias toward hypothetical counselors of different weights. Our results highlight the existence of weight bias toward counselors on both ends of the weight spectrum. Even with strengthening the counseling relationship through empathy, congruence, and unconditional positive regard, counselors may benefit from reflecting on potential client weight bias and its impact on their therapeutic alliance. Additionally, weight as a multicultural issue increases counselors’ competence in addressing the prejudice and stereotypes that may limit their client’s willingness to trust them, follow their advice, or select them as their counselor.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Ackerman, S. J., & Hilsenroth, M. J. (2001). A review of therapist characteristics and techniques negatively impacting the therapeutic alliance. Psychotherapy: Theory, Research, Practice, Training, 38(2), 171–185.
https://doi.org/10.1037/0033-3204.38.2.171
Allen, M. L., Cook, B. L., Carson, N., Interian, A., La Roche, M., & Alegría, M. (2017). Patient-provider therapeutic alliance contributes to patient activation in community mental health clinics. Administration and Policy in Mental Health and Mental Health Services Research, 44(4), 431–440. https://doi.org/10.1007/s10488-015-0655-8
Allison, M., & Lee, C. (2015). Too fat too thin: Understanding bias against overweight and underweight in an Australian female university student sample. Psychology & Health, 30(2), 189–202.
https://doi.org/10.1080/08870446.2014.954575
Beggan, J. K., & DeAngelis, M. (2015). “Oh, my God, I hate you”: The felt experience of being othered for being thin. Symbolic Interaction, 38(3), 371–392. https://doi.org/10.1002/SYMB.162
Bucchianeri, M. M., Eisenberg, M. E., & Neumark-Sztainer, D. (2013). Weightism, racism, classism, and sexism: Shared forms of harassment in adolescents. Journal of Adolescent Health, 53(1), 47–53.
https://doi.org/10.1016/j.jadohealth.2013.01.006
Centers for Disease Control and Prevention. (2022, June 3). Defining adult overweight & obesity. https://www.cdc.gov/obesity/basics/adult-defining.html
Cermák, I., Osecká, L., Rehulková, O., & Blatný, M. (1993). Judging others according to yourself: II. Interpersonal characteristics of personality and the structure of interpersonal attributions. Studia Psychologica, 35(2), 185. https://librarylink.uncc.edu/login?url=https://www.proquest.com/scholarly-journals/judging-others-according-yourself-ii/docview/1306142557/se-2?accountid=14605
Christensen, K. N. (2021). Factors related to weight-bias among counselors (Order No. 28541740). Available from Dissertations & Theses @ University of North Carolina Charlotte. (2562239518).
Clabaugh, A., Karpinski, A., & Griffin, K. (2008). Body weight contingency of self-worth. Self and Identity, 7(4), 337–359. https://doi.org/10.1080/15298860701665032
Clark, A. J. (2010). Empathy: An integral model in the counseling process. Journal of Counseling & Development, 88(3), 348–356. https://doi.org/10.1002/j.1556-6678.2010.tb00032.x
Coladarci, T., Cobb, C. D., Minium, E. W., & Clarke, R. B. (2011). Fundamentals of statistical reasoning in education (3rd ed.). Wiley.
Crandall, C. S. (1994). Prejudice against fat people: Ideology and self-interest. Journal of Personality and Social Psychology, 66(5), 882–894. https://doi.org/10.1037/0022-3514.66.5.882
Davies, A., Burnette, C. B., & Mazzeo, S. E. (2020a). Real women have (just the right) curves: Investigating anti-thin bias in college women. Eating and Weight Disorders, 25, 1711–1718.
https://doi.org/10.1007/s40519-019-00812-7
Davies, A., Burnette, C. B., & Mazzeo, S. (2020b). Black and White women’s attributions of women with underweight. Eating Behaviors, 39, 101446. https://doi.org/10.1016/j.eatbeh.2020.101446
Faul, F., Erdfelder, E., Lang, A.-G., & Buchner, A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39, 175–191.
https://doi.org/10.3758/BF03193146
Feller, C. P., & Cottone, R. R. (2003). The importance of empathy in the therapeutic alliance. The Journal of Humanistic Counseling, Education and Development, 42(1), 53–61.
https://doi.org/10.1002/j.2164-490x.2003.tb00168.x
Grimes, W. R., & Murdock, N. L. (1989). Social influence revisited: Effects of counselor influence on outcome variables. Psychotherapy: Theory, Research, Practice, Training, 26(4), 469–474. https://doi.org/10.1037/h0085465
Hauser, M., & Hays, D. G. (2010). The slaying of a beautiful hypothesis: The efficacy of counseling and the therapeutic process. The Journal of Humanistic Counseling, Education and Development, 49(1), 32–44.
https://doi.org/10.1002/j.2161-1939.2010.tb00085.x
Hinman, N. G., Burmeister, J. M., Kiefner, A. E., Borushok, J., & Carels, R. A. (2015). Stereotypical portrayals of obesity and the expression of implicit weight bias. Body Image, 12, 32–35.
https://doi.org/10.1016/j.bodyim.2014.09.002
Hutson, D. J. (2013). “Your body is your business card”: Bodily capital and health authority in the fitness industry. Social Science & Medicine, 90, 63–71. https://doi.org/10.1016/j.socscimed.2013.05.003
Kim, E., & Kang, M. (2018). The effects of client–counselor racial matching on therapeutic outcome. Asia Pacific Education Review, 19(1), 103–110. https://doi.org/10.1007/s12564-018-9518-9
Kinavey, H., & Cool, C. (2019). The broken lens: How anti-fat bias in psychotherapy is harming our clients and what to do about it. Women & Therapy, 42(1–2), 116–130. https://doi.org/10.1080/02703149.2018.1524070
Lacroix, E., Alberga, A., Russell-Mathew, S., McLaren, L., & von Ranson, K. (2017). Weight bias: A systematic review of characteristics and psychometric properties of self-report questionnaires. Obesity Facts, 10(3), 223–237. https://doi.org/10.1159/000475716
Lewis, R. J., Cash, T. F., & Bubb-Lewis, C. (1997). Prejudice toward fat people: The development and validation of the Antifat Attitudes Test. Obesity Research, 5(4), 297–307. https://doi.org/10.1002/j.1550-8528.1997.tb00555.x
Liu, H. (2015). Comparing Welch ANOVA, a Kruskal-Wallis test, and traditional ANOVA in case of heterogeneity of variance. https://doi.org/10.25772/BWFP-YE95
Lorr, M. (1965). Client perceptions of therapists: A study of the therapeutic relation. Journal of Consulting Psychology, 29(2), 146–149. https://doi.org/10.1037/h0021924
Marini, M. (2017). Underweight vs. overweight/obese: Which weight category do we prefer? Dissociation of weight-related preferences at the explicit and implicit level. Obesity Science & Practice, 3(4), 390–398. https://doi.org/10.1002/osp4.136
McHugh, M. C., & Kasardo, A. E. (2012). Anti-fat prejudice: The role of psychology in explication, education and eradication. Sex Roles, 66(9–10), 617–627. https://doi.org/10.1007/s11199-011-0099-x
McKee, K., & Smouse, A. D. (1983). Clients’ perceptions of counselor expertness, attractiveness, and trustworthiness: Initial impact of counselor status and weight. Journal of Counseling Psychology, 30(3),
332–338. https://doi.org/10.1037/0022-0167.30.3.332
Meadows, A., & Daníelsdóttir, S. (2016). What’s in a word? On weight stigma and terminology. Frontiers in Psychology, 7, 1527. https://doi.org/10.3389/fpsyg.2016.01527
Meyer, O. L., & Zane, N. (2013). The influence of race and ethnicity in clients’ experiences of mental health treatment. Journal of Community Psychology, 41(7), 884–901. https://doi.org/10.1002/jcop.21580
Moller, N., & Tischner, I. (2019). Young people’s perceptions of fat counsellors: “How can THAT help me?” Qualitative Research in Psychology, 16(1), 34–53. https://doi.org/10.1080/14780887.2018.1536384
Montoya, R. M., & Horton, R. S. (2013). A meta-analytic investigation of the processes underlying the similarity-attraction effect. Journal of Social and Personal Relationships, 30(1), 64–94.
https://doi.org/10.1177/0265407512452989
Nienhuis, J. B., Owen, J., Valentine, J. C., Winkeljohn Black, S., Halford, T. C., Parazak, S. E., Budge, S., & Hilsenroth, M. (2018). Therapeutic alliance, empathy, and genuineness in individual adult psychotherapy: A meta-analytic review. Psychotherapy Research, 28(4), 593–605. https://doi.org/10.1080/10503307.2016.1204023
Nutter, S., Russell-Mayhew, S., Arthur, N., & Ellard, J. H. (2018). Weight bias and social justice: Implications for education and practice. International Journal for the Advancement of Counselling, 40(3), 213–226.
https://doi.org/10.1007/s10447-018-9320-8
Puhl, R. M., Gold, J. A., Luedicke, J., & DePierre, J. A. (2013). The effect of physicians’ body weight on patient attitudes: Implications for physician selection, trust and adherence to medical advice. International Journal of Obesity, 37(11), 1415–1421. https://doi.org/10.1038/ijo.2013.33
Puhl, R. M., & Heuer, C. A. (2010). Obesity stigma: Important considerations for public health. American Journal of Public Health, 100, 1019–1028. https://doi.org/10.2105/AJPH.2009.159491
Puhl, R. M., Latner, J. D., King, K. M., & Luedicke, J. (2014). Weight bias among professionals treating eating disorders: Attitudes about treatment and perceived patient outcomes. International Journal of Eating Disorders, 47(1), 65–75. https://doi.org/10.1002/eat.22186
Ratts, M. J., Singh, A. A., Nassar-McMillan, S., Butler, S. K., & McCullough, J. R. (2016). Multicultural and social justice counseling competencies: Guidelines for the counseling profession. Journal of Multicultural Counseling and Development, 44(1), 28–48. https://doi.org/10.1002/jmcd.12035
Roehling, M. V., Roehling, P. V., & Pichler, S. (2007). The relationship between body weight and perceived weight-related employment discrimination: The role of sex and race. Journal of Vocational Behavior, 71(2), 300–318. https://doi.org/10.1016/j.jvb.2007.04.008
Ruggs, E. N., King, E. B., Hebl, M., & Fitzsimmons, M. (2010). Assessment of weight stigma. Obesity Facts, 3(1), 60–69. https://doi.org/10.1159/000273208
Schwartz, M. B., Vartanian, L. R., Nosek, B. A., & Brownell, K. D. (2006). The influence of one’s own body weight on implicit and explicit anti-fat bias. Obesity, 14(3), 440–447. https://doi.org/10.1038/oby.2006.58
Sharf, J., Primavera, L. H., & Diener, M. J. (2010). Dropout and therapeutic alliance: A meta-analysis of adult individual psychotherapy. Psychotherapy: Theory, Research, Practice, Training, 47(4), 637–645.
https://doi.org/10.1037/a0021175
Taber, K. S. (2018). The use of Cronbach’s alpha when developing and reporting research instruments in science education. Research in Science Education, 48, 1273–1296. https://doi.org/10.1007/s11165-016-9602-2
Tischner, I. (2019). Tomorrow is the start of the rest of their life—so who cares about health? Exploring constructions of weight-loss motivations and health using story completion. Qualitative Research in Psychology, 16(1), 54–73. https://doi.org/10.1080/14780887.2018.1536385
Tudor, K. (2011). Rogers’ therapeutic conditions: A relational conceptualization. Person-Centered & Experiential Psychotherapies, 10(3), 165–180. https://doi.org/10.1080/14779757.2011.599513
Zar, J. H. (1998). Biostatistical analysis (4th ed.). Prentice Hall.
Amy Biang, PhD, LCMHC, CEDS, is an assistant professor at Northern Arizona University. Clare Merlin-Knoblich, PhD, is an associate professor at the University of North Carolina at Charlotte. Stella Y. Kim, PhD, is an assistant professor at the University of North Carolina at Charlotte. Correspondence may be addressed to Amy Biang, 15451 N 28th Ave, Phoenix, AZ 85053, amy.biang@nau.edu.
Feb 7, 2022 | Volume 12 - Issue 1
Eric M. Brown, Kristy L. Carlisle, Melanie Burgess, Jacob Clark, Ariel Hutcheon
Despite an emphasis on self-care to avoid burnout and increase compassion satisfaction within the counseling profession, there is a dearth of research on the developmental experiences of counselors that may increase the likelihood of burnout. We examined the impact of mental health counselors’ (N = 140) experiences of adverse childhood experiences and positive childhood experiences on their present rates of compassion satisfaction, burnout, and secondary traumatic stress. We used a cross-sectional, non-experimental correlational design and reported descriptive statistics as well as results of multiple regression models. Results indicated significant relationships among counselors’ rates of adverse childhood experiences, positive childhood experiences, and compassion satisfaction and burnout. We include implications for the use of both the adverse and positive childhood experiences assessments in the training of counseling students and supervisees.
Keywords: counselors, burnout, childhood experiences, compassion satisfaction, secondary traumatic stress
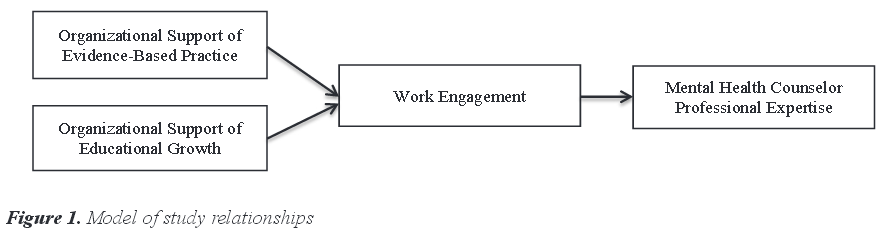
Over the past 20 years, public health research on adverse childhood experiences (ACEs) and their deleterious effects on physical and mental health has proliferated and branched out to various disciplines (Campbell et al., 2016; Frampton et al., 2018). More recently, the importance of understanding the implications of ACEs for the mental health of clients has entered the counseling literature (Wheeler et al., 2021; Zyromski et al., 2020), yet the ways in which a counselor’s own experience of ACEs may affect their work have not been examined. The absence of such research is significant given the report that mental health workers have the highest rates of ACEs among those in the helping professions (Redford, 2016).
A thorough literature search of PsycINFO, ProQuest, and Google Scholar using terms including, but not limited to, adverse childhood experiences, positive childhood experiences (PCEs), compassion satisfaction (CS), burnout, secondary traumatic stress (STS), and mental health counselors (MHCs), found no peer-reviewed articles that examined the relationship between ACEs or PCEs and counselors’ rates of CS and burnout. Therefore, we chose to examine the effects of early developmental adversity, as well as early protective factors, on the professional quality of life of counselors, as measured by assessing the counselor’s levels of CS, burnout, and STS.
Adverse Childhood Experiences (ACEs)
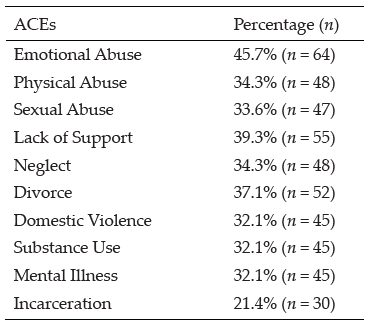
In the mid-nineties, Felitti et al. (1998), with the support of the Centers for Disease Control, created the ACE Study Questionnaire to study early childhood trauma and deprivation experiences. The ACE Study Questionnaire consists of 10 questions related to whether a person before the age of 18 experienced emotional or physical abuse, substance addiction in the home, parental divorce or separation, a caretaker with mental illness, or emotional deprivation. Each question that is answered in the affirmative results in one “ACE,” with respondents’ scores ranging from 1 to 10. Studies have found that ACEs have a dose-response effect; therefore, every point increase can significantly raise the chance of experiencing negative mental and physical health effects into adulthood (Boullier & Blair, 2018; Campbell et al., 2016; Merrick et al., 2017). Additionally, individuals with four or more ACEs are significantly more likely to suffer from mental illness or substance addiction, be further traumatized as adults, and succumb to an early death (Anda et al., 2007; Metzler et al., 2017).
More recently, researchers have found that Black and Latinx individuals have significantly higher rates of ACEs compared to White individuals (R. D. Lee & Chen, 2017; Merrick et al., 2017; Strompolis et al., 2019). In a study involving 60,598 participants, R. D. Lee and Chen (2017) discovered not only that Black and Hispanic participants had higher rates of ACEs, but also that there was a correlation between ACEs and drinking alcohol heavily. In a sample of 214,517 participants across 23 states in the United States, Merrick et al. (2017) found that racially minoritized individuals, sexual minorities, the unemployed, those with less than a high school education, and those making less than $15,000 a year had significantly higher rates of ACEs than White individuals, heterosexuals, the employed, and those with higher education and income, respectively. Zyromski et al. (2020) noted that the preponderance of ACEs within marginalized communities, such as ethnic minority populations, make ACEs “a social justice issue” (p. 352).
There is scarce research related to the potential impact of ACEs on practitioners and graduate students in helping professions. Thomas (2016) evaluated the rates of ACEs with Master of Social Work (MSW) students, discovering that MSW students were 3.3 times more likely to have four or more ACEs compared to a general sample of university students. Similarly, counselors-in-training are not immune to the effects of childhood adversity; in fact, researchers noted that counselors-in-training may pursue a counseling degree because of personal trauma that drives their aspirations to help others (Conteh et al., 2017). Evans (1997) found that 93% of counselors-in-training reported at least one traumatic experience in their lives, while Conteh et al. (2017) discovered that 95% of counselors-in-training reported between one and eight traumas throughout their lifetime. Considering these results, researchers have suggested that practitioners with a history of trauma may be vulnerable to re-experiencing trauma with clients, which could negatively impact client care and increase the rate of counselor burnout (Conteh et al., 2017; Thomas, 2016). Because the rates of ACEs in practicing MHCs are unknown, it is difficult to determine how ACEs may play a role in impacting CS, burnout, and STS. Furthermore, we lack research on early developmental factors that may contribute to CS, burnout, and STS.
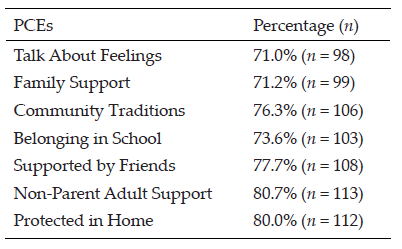
Positive Childhood Experiences (PCEs)
In recent years, childhood development researchers have explored protective factors that may reduce the harmful effects of ACEs. In 2018, Crouch et al. (2019) examined the relationship between two protective factors and their mitigating effects on individuals reporting at least four ACEs. In a sample of 7,079 respondents, the researchers discovered that individuals who reported growing up “with an adult who made them feel safe and protected were less likely to report frequent mental distress or poor health” (Crouch et al., 2019, p. 165). Bethell et al. (2019) found significant correlations between seven positive interpersonal experiences with family and friends and decreased negative effects of ACEs. They also discovered that these factors have a dose-response effect in relation to ACEs so that with each additional PCEs, the harmful effects of ACEs are lessened. The discovery of PCEs has become important in understanding developmentally protective factors that guard from the damaging effects of childhood adversity. Specifically, higher rates of PCEs decrease the chances of mental health disorders of adults, even in those with higher numbers of ACEs (Bethell et al., 2019). An examination of the rates of PCEs in MHCs may provide insight into the well-being of counselors.
Counselor Well-Being
As defined by the American Counseling Association (ACA; 2014), professional counselors work to empower diverse clients to achieve their personal goals. Specifically, MHCs provide client-driven services in agencies, hospitals, and private practices (American Mental Health Counselors Association [AMHCA], 2020). Counselors are trained to cultivate and monitor their own sense of well-being while providing their expertise and leadership to clients and students who have experienced difficulties related to trauma, injustice, abuse, loss, violence, and distress (Council for Accreditation of Counseling and Related Educational Programs [CACREP], 2015; S. M. Lee et al., 2010). Self-care, or the act of cultivating a subjectively defined state of health, is now ubiquitous in counselor education programs and promoted among practitioners (ACA, 2014; CACREP, 2015); however, scholars note that many counselors do not routinely prioritize their own sense of well-being and monitor CS, burnout, and STS (Coaston, 2017). While working closely with clients, practitioners may benefit from reflecting on how their own experiences of personal adversity may influence their work and possibly create a predisposition toward burnout.
Burnout of Counselors
Burnout is defined as the emotional and physical response to chronic stressors in the workplace that lead to substantial negative consequences (Maslach et al., 2001). Scholars have evaluated the external facets of professional counselors’ work that lead to increased burnout, such as time spent on non-counseling duties, lack of on-the-job support, and negative working environments (Thompson et al., 2014); however, internal factors that lead to burnout, such as counselors’ experiences of adversity, remain unstudied. The ubiquitous nature of trauma and its lifelong impact on clients has gained more attention over the past 20 years (Bemak & Chung, 2017; Debellis, 2001; Webber et al., 2017), yet researchers are only beginning to explore the impact of trauma on the lives and professional experiences of counselors (Conteh et al., 2017; McKim & Smith-Adcock, 2014).
Recently, scholars have sought to understand contributing factors that diminish CS and increase burnout (S. M. Lee et al., 2010). In a study of 86 counselors-in-training, Can and Watson (2019) found that a trainee’s degree of resilience and wellness predicted burnout, whereas empathy and supervisory working alliance did not. They did not assess for internal or experiential factors that may have contributed to burnout.
Cook et al. (2021) conducted a qualitative inquiry with 246 novice counselors to explore symptoms of burnout that may not be captured in commonly used assessments. The researchers found several predominant themes, including negative emotional experiences such as anxiety, depression and crying spells; fatigue and tiredness; and unfulfillment in work. Participants also reported physical illness and weight gain or loss, self-perceived ineffectiveness as a counselor, and cognitive impairment. Close to 10% of participants stated that an unhealthy environment contributed to their experience of burnout. Cook et al. did not inquire about any personal history that may have also contributed to symptoms of burnout.
Counselors and STS
Distinct from but related to burnout, STS has been discussed in the literature relating to the well-being of helping professions across numerous disciplines (Branson, 2019; Butler et al., 2017; Molnar et al., 2017). Secondary traumatic stress, also called vicarious trauma, is distinguished from burnout by its symptoms overlapping with post-traumatic stress disorder (PTSD), such as intrusive thoughts, hypervigilance, and avoidance of distressing memories (Ivicic & Motta, 2017; Molnar et al., 2017). In a study of 220 counselors, Lanier and Carney (2019) discovered that 49.5% of counselors experienced symptoms of vicarious trauma, with 85.5% reporting “I thought about my work with clients when I didn’t intend to” and 80.5% confirming that “I felt emotionally numb” (p. 339). Lakioti et al. (2020) found in a study of 163 Greek mental health practitioners that there was a significant positive correlation between burnout and STS (r = .48) and that practitioners who scored high in empathy also scored high in STS (r = .34). In their meta-analysis of 38 studies examining risk factors for STS in therapeutic work, Hensel et al. (2015) found small yet significant effect sizes for “trauma caseload volume (r = .16), caseload frequency (r = .12), caseload ratio (r = .19), and having a personal trauma history (r = .19)” in relation to STS (p. 83).
Research regarding counselors’ own personal trauma is still emerging and a consensus is not yet formed. In a recent study of 90 psychotherapy trainees, Klasen et al. (2019) indicated that secure attachments play a modifying role in limiting the severity of trauma’s expression. McKim and Smith-Adcock (2014) evaluated characteristics of trauma counselors to understand how frequent exposure to indirect trauma might influence burnout and CS, as assessed by the Professional Quality of Life Scale (ProQOL; Stamm, 2010). Their results indicated that higher levels of exposure to client trauma, in combination with less perceived control over the workplace, led to increased burnout (McKim & Smith-Adcock, 2014). Consistent with the ACA Code of Ethics (2014), counselors are expected to self-monitor for impairment issues that could impact clients such as burnout, STS, and the decrease of CS.
Compassion Satisfaction
CS has been studied nominally and may serve as a protective factor against burnout (Coaston, 2017). Compassion satisfaction is defined as a psychological benefit derived from working effectively with clients to produce meaningful and positive change in their lives (McKim & Smith-Adcock, 2014; Stamm, 2010). McKim and Smith-Adcock (2014) discovered that trauma counselors who experienced higher levels of personal trauma also exhibited higher levels of CS or fulfillment derived from their role in the helping alliance. Although these emergent results contradict older literature that demonstrates how counselors with more personal trauma have higher levels of burnout (Baird & Kracen, 2006; Nelson-Gardell & Harris, 2003), presently, the relationship between CS, burnout, and STS in counselors in relation to ACEs is still unclear.
Purpose of Study
The purpose of this study was to examine the effects of early developmental adversity as well as early protective factors on the CS, burnout, and STS of MHCs. Despite the ongoing concern for factors that contribute to the CS, burnout, and STS of counselors, there is a dearth of research on personal experiences that may predispose counselors to burnout (Conteh et al., 2017; McKim & Smith-Adcock, 2014). Considering the detrimental effects of burnout on counselors’ health and well-being, as well as the decrease in empathy that often accompanies burnout, it is imperative that we understand the various causes of burnout (Can & Watson, 2019; Cook et al., 2021; Maslach et al., 2001). This knowledge will assist clinical MHCs, supervisors, and counselor educators in knowing which professional counselors or counselors-in-training may be more susceptible to burnout, STS, and decreased CS.
Research on ACEs within the counseling profession, as proposed by the original Felitti et al. (1998) study, is scant. Zyromski et al. (2020) discovered in their content analysis of ACA and American School Counselor Association journals that only three articles contained any focus on ACEs as defined in the original study. They suggested that by incorporating such a well-defined and researched concept as ACEs, counselors will be better equipped to address the deleterious effects of early adverse experiences. In order to address the gap within the literature, we chose to focus on the rates of ACEs and PCEs of counselors and how they potentially impact CS, burnout, and STS. After conducting an exhaustive search of the literature, we found no other study that examined the potential relationship between counselors’ developmental history using the ACEs and PCEs assessments and their levels of burnout, CS, and STS.
Method
This study entailed a cross-sectional, non-experimental correlational design and reported descriptive statistics, as well as results of multiple regression models. Relationships among MHCs’ ACEs, PCEs, CS, burnout, and STS were examined. Research questions (RQs) guiding the study were: RQ1 (descriptive): What are the mean scores of MHCs for ACEs, PCEs, CS, burnout, and STS constructs? and RQ2 (regression): To what extent do MHCs’ ACEs, PCEs, gender, race, socioeconomic status, and educational level predict CS, burnout, and STS?
Power Analysis
The target number of participants for the study was at least N = 138, based on a power analysis. Researchers used G*Power 3.1.9.6 (Faul et al., 2009) to calculate an a priori power analysis with a .05 alpha level (Cohen, 1988, 1992), a medium effect size for multiple R2 of .09 (Cohen, 1988), and a power of .80 (Cohen, 1992).
Participants
The eligibility criteria for this study were to be a clinical MHC, 18 years or older, who worked 30 hours or more per week in the field of mental health counseling. After soliciting participants nationally through emails, we collected data from 140 participants who met the criteria. MHCs ranged in age from 22 to 72 years old with an average age of 38 (SD = 11.01). Table 1 shows the diverse sample. Slightly more than half (n = 71) identified as female and a little less than half (n = 66) as male. More than three-quarters (n = 108) identified as White. The majority of participants (n = 85) reported their childhood SES as lower or working class, while more than half (n = 78) reported their current social class as middle class. Our sample with predominantly female and predominantly White participants is similar both to known counselor demographics (Norton & Tan, 2019) and to the Felitti et al. (1998) ACEs study.
Instrumentation
Three instruments with good validity and reliability were used to measure ACEs, PCEs, CS, burnout, and STS. We created a demographic questionnaire to collect information on participants’ identities (e.g., race, gender) and childhood backgrounds (e.g., ACEs, PCEs, SES).
Adverse Childhood Experiences (ACE) Study Questionnaire
The ACE Study Questionnaire (Felitti et al., 1998) is a 10-item survey of the most common examples of childhood abuse and neglect. It was developed out of research that connected childhood trauma to subsequent mental and physical ailments. Subsequent research found good test-retest reliability of the measure in an adult population (Dube et al., 2004; Frampton et al., 2018) and a Cronbach’s alpha score of .78 (Ford et al., 2014). The survey produces self-report scores between 0 and 10. The higher the score, the greater the risk for mental and physical health issues as well as decreased quality of life. Consistent research (e.g., Anda et al., 2006; Dube et al., 2004; Hughes et al., 2017) shows that a score of 4 or more indicates serious risk.
Table 1
Participant Demographics
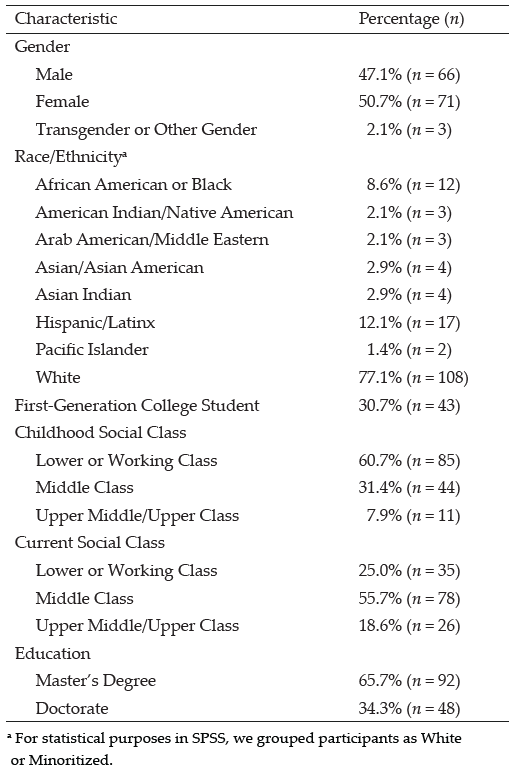
Positive Childhood Experiences (PCE) Questionnaire
The PCE Questionnaire (Bethell et al., 2019) is a 7-item survey of PCEs (i.e., connection with family, friends, and community) that are statistically predictive of good mental health in adulthood. After accounting for ACEs, higher PCE scores reduce mental health and interpersonal problems later in life. Specifically, scores in the 6 to 7 range are most protective from harmful effects of ACEs, and scores in the 3 to 5 range are moderately protective. A Cronbach’s alpha score of .77 reported in the original 2019 study indicates good reliability.
Professional Quality of Life Scale (ProQOL)
The ProQOL (Stamm, 2010) is a 30-item survey with good construct validity measuring both positive and negative responses to the work of helping professionals. It measures three constructs: CS, which has a Cronbach’s alpha score of .88; burnout, which has a Cronbach’s alpha score of .75; and STS, which has a Cronbach’s alpha score of .81. For CS, or positive feelings about one’s ability to help, a score below 23 indicates problems at work. For burnout, or feelings of exhaustion, frustration, anger, or depression, scores below 23 indicate feeling good about work, while scores above 41 indicate feeling ineffective. For STS, or feelings of fear related to trauma in the workplace, scores above 43 indicate something frightening at work.
Procedure
After IRB approval, we used purposeful sampling methods to recruit participants. We emailed over 6,000 MHCs from a data set purchased from a national data bank. Furthermore, we posted invitations to participate on Facebook groups for MHCs. Invitations included informed consent, as well as a link to a Qualtrics survey containing all instruments and demographic questions. Researchers cleaned all collected data leading to 140 usable cases, computed instruments and transformed variables into usable form, and checked for assumptions for multiple regression. For each instrument, we assessed for reliability with Cronbach’s alpha tests. The ACEs instrument produced a Cronbach’s alpha of .89, the PCEs instrument produced .81, and the ProQOL produced .79, all within the good to excellent range. We used SPSS 28 for all analyses.
Data Analysis and Results
To answer our first research question, we evaluated the mean scores for ACEs, PCEs, CS, burnout, and STS. Respondents in the study had a mean ACE score of 3.42, 95% CI [2.8577, 3.9852], beneath the threshold of 4 and just below the range for significant risk. Their mean PCE score of 5.34, 95% CI [5.0006, 5.6957], was at the upper end of moderately protective. White MHCs had a lower average ACE score and higher average PCE score than minoritized MHCs. Male MHCs had higher average ACE and PCE scores than females, and MHCs with lower childhood SES had lower average ACE scores and higher average PCE scores than those with higher SES (see Tables 2 and 3).
Table 2
Average Adverse Childhood Experience Scores by Demographics
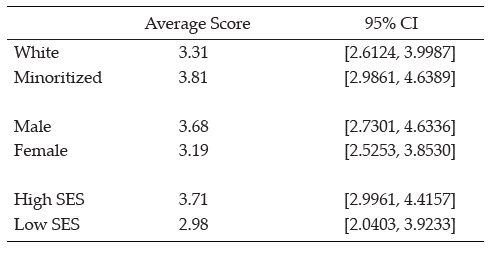
Table 3
Average Positive Childhood Experience Scores by Demographics
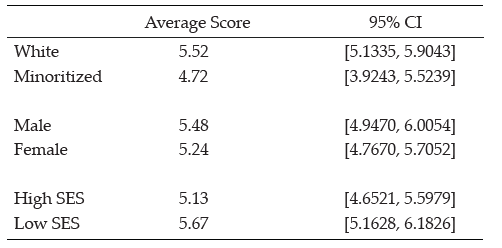
Type of scores are shown in percentages for each type of ACE and PCE to show what percentage of MHCs reported an adverse or protective childhood experience (see Tables 4 and 5).
Table 4
Type of Adverse Childhood Experience Score
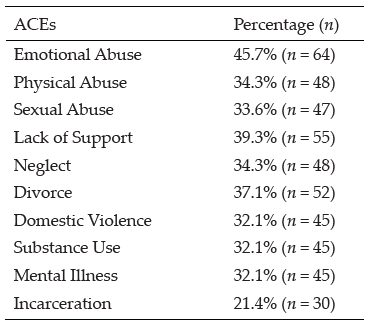
Table 5
Type of Positive Childhood Experience Score
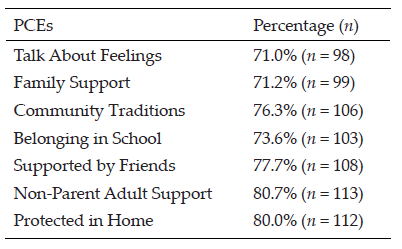
Next, we analyzed MHCs’ scores related to CS, burnout, and STS. Participants’ mean CS score of 31.81, 95% CI [30.6005, 33.0138], was well above the threshold of 23, which indicates a positive level of CS. Their overall mean burnout score of 24.59, 95% CI [23.5793, 25.5921], was well below the threshold of 41, which indicates that the average MHC was not suffering from burnout. Their overall mean STS score of 26.37, 95% CI [25.0346, 27.7083], was also well below the threshold of 43, which indicates the average MHC was not experiencing STS.
For RQ 2, we also tested whether and to what extent MHCs’ ACEs, PCEs, and demographic variables predict CS, burnout, and STS. We ran three linear regression models to assess significant predictors of CS, burnout, and STS. In the first model, a regression of CS on ACEs, PCEs, gender, race/ethnicity, and childhood SES explained a significant 40.5% of the variance in CS, F (5, 134) = 17.558, p < .001. Specifically, significant predictors of CS were ACEs (β = −.550), gender (β = −.218), race/ethnicity (β = −.160), and childhood SES (β = −.171). PCEs were nonsignificant in relation to CS. Items negatively related to CS were ACEs (i.e., higher ACE scores predicted lower CS), gender (i.e., being female predicted higher CS), race/ethnicity (i.e., being minoritized predicted higher CS), and childhood SES (i.e., lower levels of SES predicted higher CS; see Table 6).
In the second model, a regression of burnout on ACEs, PCEs, gender, race/ethnicity, and childhood SES explained a significant 18.9% of the variance in burnout, F (5, 134) = 6.032, p < .001. Specifically, both ACEs and PCEs were significant predictors of burnout (β = .309 and β= −.197, respectively). Gender, race/ethnicity, and SES were nonsignificant predictors of burnout. ACEs were positively related to burnout (i.e., higher ACE scores indicated higher burnout), and PCEs were negatively related to burnout (i.e., higher PCEs indicated lower burnout; see Table 7).
In the third model, a regression of STS on ACEs, PCEs, gender, race/ethnicity, and childhood SES explained a significant 8.5% of variance in STS, F (5, 134) = 2.402, p < .001. Only race/ethnicity was a significant predictor of STS (β= −.222; i.e., being White indicated lower STS). ACEs, PCEs, gender, and SES produced nonsignificant results related to STS (see Table 8).
Table 6
Regression Results Using Compassion Satisfaction as the Criterion
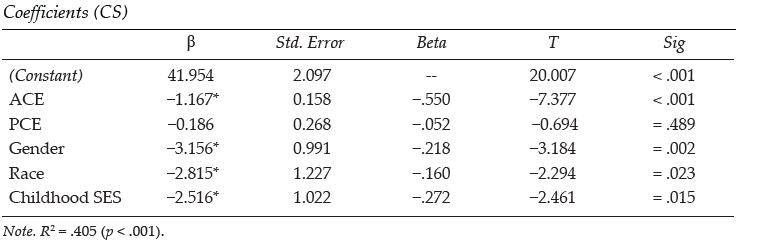
Table 7
Regression Results Using Burnout as the Criterion
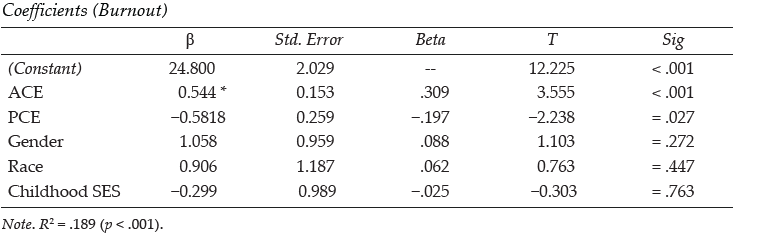
Table 8
Regression Results Using Secondary Traumatic Stress as the Criterion
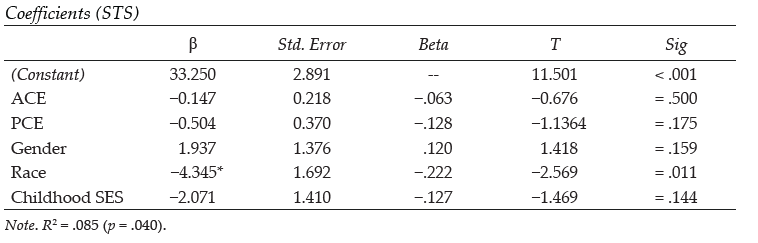
Discussion
After conducting an exhaustive literature review, we found no other study that examined the relationship between a counselor’s personal history of childhood adversity and protective factors (i.e., ACEs and PCEs) and their professional experience with burnout, STS, and CS. As the counseling profession is placing a greater emphasis on counselors becoming trauma-informed (e.g., Bemak & Chung, 2017; Debellis, 2001; Webber et al., 2017), recent research has examined counselor wellness, burnout, PTSD symptoms, and possible contributing factors (Can & Watson, 2019; Cook et al., 2021; Lanier & Carney, 2019). In line with other studies, we found that some individuals drawn to the profession of counseling are more likely to have had adversity and hardship events in their personal histories (Conteh et al., 2017; McKim & Smith-Adcock, 2014). What is unique in this study is the examination of how both adverse and positive childhood experiences may impact the CS, burnout, and STS of MHCs.
Similar to Thomas (2016), who found that social work students had higher rates of ACEs than the general population, the results of this study indicated that counselor participants had higher rates of ACEs for all 10 experiences than the original Felitti et al. (1998) ACEs study. This was also aligned with Conteh and colleagues (2017), who found that counselors-in-training may have higher rates of trauma than the average population. The results also indicated that almost 43% (n = 60) of MHCs scored four or more ACEs, which placed them at high risk for mental and physical health problems (Boullier & Blair, 2018; Campbell et al., 2016; Merrick et al., 2017). As may be surmised from other studies on the deleterious effects of ACEs on emotional well-being, having higher numbers of ACEs was a significant predictor of burnout. Lower ACEs scores also significantly predicted CS with a high effect size (.55). Similarly, higher PCEs were linked to lower burnout. However, PCEs were not found to significantly predict CS.
We examined the average rates of and relationships between ACEs, PCEs, CS, burnout, and STS in a sample of MHCs. McKim and Smith-Adcock (2014) examined the burnout rates of trauma counselors, finding that counselors with more personal trauma had an increase in CS, perhaps due to personal growth. In contrast, this study found that counselors with more ACEs were more likely to experience less CS. This difference may be a result of this study utilizing the ACE Study Questionnaire (Felitti et al., 1998) whereas McKim and Smith-Adcock (2014) used Stamm’s (2008) Stressful Life Experiences – Short Form to assess for experiences that may have happened in adulthood or to someone outside of the family. Developmentally, painful childhood experiences may be harder to process, which may in turn produce further-reaching negative outcomes. McKim and Smith-Adcock also found that having a sense of control in the workplace and the number of years of experience as a counselor also positively correlated with CS. The results from our analysis indicated that greater attention needs to be given to the traumatic experiences of counselors and how these events may impact professional resilience.
This study may also be the first to examine the demographic factors of counselors, including gender, racial identity, and childhood SES, as potential predictive factors of burnout, STS, and CS. All three demographic variables were found to be predictive of CS, but none were predictive of burnout. The results from our analysis indicated that greater attention needs to be given to the traumatic experiences of counselors and how these events may impact CS, burnout, and STS.
It should be noted that ethnically minoritized counselors had higher rates of CS than their White peers. Given that higher ACEs scores had a negative relationship with CS with a high effect size, and that minoritized counselors had higher average rates of ACEs and lower average rates of PCEs when compared to White counselors, we expected minoritized counselors to experience lower CS. However, the current study found that being a minoritized counselor actually predicted higher CS and lower burnout. It may encourage all counselors to know that greater CS among minoritized counselors indicates that ACEs and PCEs are not determinative of whether a person experiences burnout or satisfaction.
Our findings that female counselors were more likely to have higher CS than their male peers, and that counselors from low-income or working-class SES had higher CS than those from middle and upper classes, are also noteworthy. It is possible that the more collectivist tendencies of minoritized individuals in general, and of female counselors regardless of race, may help foster greater professional resilience or quality of life (Graham et al., 2020; Jordan, 2017). Counselors from lower- or working-class childhood SES may also maintain the collectivist orientation of their upbringing. This proposition is supported by previous research, which indicates that social support is a significant factor that promotes CS in therapists (Ducharme et al., 2008). This may also relate to Crouch et al.’s (2019) finding that the most significant PCE that mitigates the effects of ACEs is having a safe relationship with an adult. These results are further supported by research indicating that secure attachments in adulthood moderate the effect of childhood adversity (Klasen et al., 2019). Despite a limited sample size, Conteh et al. (2017) found that 95% of their sample of 86 counselors-in-training reported having experienced at least one trauma. Although male participants in Conteh’s study were significantly more likely to report more traumas than women—4.93 to 3.46 respectively—women reported more post-traumatic growth than men. Similar to our findings, this may indicate why female counselors were more likely to experience greater CS than male counselors.
Although close to half of our participants (42.9%) met the critical threshold of four ACEs, it is encouraging that the average participant indicated that they were not experiencing burnout. This may be the result of more than half of our participants having five or more PCEs, with PCEs predicting lower burnout. It should also be noted that in this study, ACEs were not significantly correlated with STS, which may be counterintuitive as one may assume that childhood adversity may leave one more susceptible to STS. The strongest findings in the current study, as demonstrated by high effect sizes, are that lower ACE scores predict higher CS and lower burnout. However, the potentially mitigating influence of PCEs only predicted burnout, not CS, with a lower effect size.
Limitations
Threats to internal and external validity are unavoidable in descriptive studies. As such, one limitation of this study is that it focused on descriptive and predictive relationships and therefore does not describe causation. Furthermore, this study used self-report data which may threaten internal validity. Finally, selection bias may be a risk to generalizability. However, the sample in this study is demographically similar to other studies examining the counseling population, so this risk may be minimal.
Implications
Both professional organizations (e.g., ACA, AMHCA) and CACREP can promote counselor wellness by putting policies in place recognizing that individuals going into the counseling profession are likely to have personal histories shaped by adverse experiences. These policies may include a more systemic understanding of wellness strategies for counselors. Self-care is often conceptualized as a personal endeavor achieved outside of work hours, yet policies may be put in place to promote organizational wellness by providing space and emotional support for counselor wellness. For example, far too often grants require caseloads that are too heavy to foster and maintain the well-being of counselors.
The results of this study may also have implications for counselor education. Given that 42% of our participants had four or more ACEs, it may be likely that close to half of students within counseling programs have also suffered from a significant amount of childhood adversity. This may have implications for how we educate counselors to work with trauma. Trauma-informed training generally focuses on the effects of trauma on the life of clients and supports evidence-based practices that aid in recovery, resilience, and improved quality of life. Training that is trauma-attuned may focus more on the counselor’s awareness of how their own history of adversity may shape their professional stamina. This may also lead to more research on trauma-attuned supervision.
Considering the substantial percentage of MHCs who may have four or more ACEs, it is possible that many clinical supervisors have also been greatly affected by their personal histories. Trauma-attuned supervisors will continually reflect on how their past adversity may be influencing the supervisory relationship while also monitoring both their own as well as their supervisee’s levels of burnout and emotional reactivity toward clients.
As Zyromski et al. (2020) posited, the use of ACEs as a construct can provide clarity and focus to the harmful experiences that may impede the healthy development of a client. Likewise, knowledge about ACEs and PCEs can help supervisors and counselor educators train counselors who are at greater risk for burnout. It is important that the privacy of the counselor’s childhood experiences be protected, but trainees can be given the ACE and PCE assessments and told of the risk factors that high ACE and low PCE scores have with regard to burnout and CS. Furthermore, clinical and faculty supervisors can provide assessments for CS and burnout at key points during a trainee’s internship or first few years of postgraduate experience. Counselor educators and supervisors may then help trainees develop a self-care plan that will help to foster CS.
Directions for Future Research
Future studies may further examine the difference between demographic groups based on gender, race, and education in relation to potential protective factors that female and minoritized MHCs have that may decrease the likelihood they will experience burnout. Further research may also examine which ACEs, if any, may have higher correlations with burnout and which PCEs are more likely to serve as protective factors. Furthermore, our results indicate a need to study the CS and burnout of minoritized counselors, female counselors, and those coming from lower childhood SES. Examination of potential cultural and protective factors of these groups may contribute significantly to the literature on burnout prevention.
Given the percentage of counselors who have ACE scores that fall within the range of concern, future research may examine potential differences of counselors who are trauma-attuned and not simply trauma-informed. As stated above, ACEs were not significantly correlated with STS. It may be helpful for future researchers to use different measurements of secondary stress to further assess whether there is any correlation between ACEs and STS.
Conclusion
The purpose of this study was to examine personal factors in the developmental history of clinical MHCs that may influence their likelihood of experiencing professional burnout. This is the first known study we can identify using the ACE Study Questionnaire as a measure to inquire about a potential relationship between the counselors’ developmental adversity and their rates of burnout, CS, and STS. Results indicated that higher ACE scores correlate positively with burnout, and yet PCEs may serve as protective factors. Finally, we found that women and minoritized counselors were more likely to experience compassion satisfaction than males and White counselors. This was true for minoritized counselors despite their having slightly higher rates of ACEs and lower rates of PCEs. We recommend that counselors become aware of how their own experiences of ACEs and PCEs may be impacting their current practice.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
American Counseling Association. (2014). ACA code of ethics. www.counseling.org/docs/default-source/default-document-library/2014-code-of-ethics-finaladdress.pdf
American Mental Health Counselors Association. (2020). AMHCA code of ethics. https://bit.ly/AMHCAcodeofethics
Anda, R. F., Brown, D. W., Felitti, V. J., Bremner, J. D., Dube, S. R., & Giles, W. H. (2007). Adverse childhood experiences and prescribed psychotropic medications in adults. American Journal of Preventive Medicine, 32(5), 389–394. https://doi.org/10.1016/j.amepre.2007.01.005
Anda, R. F., Felitti, V. J., Bremner, J. D., Walker, J. D., Whitfield, C., Perry, B. D., Dube, S. R., & Giles, W. H. (2006). The enduring effects of abuse and related adverse experiences in childhood: A convergence of evidence from neurobiology and epidemiology. European Archives of Psychiatry and Clinical Neuroscience, 256, 174–186. https://doi.org/10.1007/s00406-005-0624-4
Baird, K., & Kracen, A. C. (2006). Vicarious traumatization and secondary traumatic stress: A research synthesis. Counselling Psychology Quarterly, 19(2), 181–188. https://doi.org/10.1080/09515070600811899
Bemak, F., & Chung, R. C.-Y. (2017). Refugee trauma: Culturally responsive counseling interventions. Journal of Counseling & Development, 95(3), 299–308. https://doi.org/10.1002/jcad.12144
Bethell, C., Jones, J., Gombojav, N., Linkenbach, J., & Sege, R. (2019). Positive childhood experiences and adult mental and relational health in a statewide sample: Associations across adverse childhood experiences levels. JAMA Pediatrics, 173(11), e193007. https://doi.org/10.1001/jamapediatrics.2019.3007
Boullier, M., & Blair, M. (2018). Adverse childhood experiences. Pediatrics and Child Health, 28(3), 132–137. https://doi.org/10.1016/j.paed.2017.12.008
Branson, D. C. (2019). Vicarious trauma, themes in research, and terminology: A review of literature. Traumatology, 25(1), 2–10. https://doi.org/10.1037/trm0000161
Butler, L. D., Carello, J., & Maguin, E. (2017). Trauma, stress, and self-care in clinical training: Predictors of burnout, decline in health status, secondary traumatic stress symptoms, and compassion satisfaction. Psychological Trauma: Theory, Research, Practice, and Policy, 9(4), 416–424. https://doi.org/10.1037/tra0000187
Campbell, J. A., Walker, R. J., & Egede, L. E. (2016). Associations between adverse childhood experiences, high- risk behaviors, and morbidity in adulthood. American Journal of Preventive Medicine, 50(3), 344–352. https://doi.org/10.1016/j.amepre.2015.07.022
Can, N., & Watson, J. C. (2019). Individual and relational predictors of compassion fatigue among counselors-in-training. The Professional Counselor, 9(4), 285–297. https://doi.org/10.15241/nc.9.4.285
Coaston, S. C. (2017). Self-care through self-compassion: A balm for burnout. The Professional Counselor, 7(3), 285–297. https://doi.org/10.15241/scc.7.3.285
Cohen, J. (1988). Statistical power analysis for the behavioral sciences. (2nd ed.) Routledge.
Cohen, J. (1992). Statistical power analysis. Current Directions in Psychological Science, 1(3), 98–101. https://doi.org/10.1111/1467-8721.ep10768783
Conteh, J. A., Huber, M. J., & Bashir, H. A. (2017). Examining the relationship between traumatic experiences and posttraumatic growth among counselors-in-training. The Practitioner Scholar: Journal of Counseling and Professional Psychology, 6, 32–36.
Cook, R. M., Fye, H. J., Jones, J. L., & Baltrinic, E. R. (2021). Self-reported symptoms of burnout in novice professional counselors: A content analysis. The Professional Counselor, 11(1), 31–45. https://doi.org/10.15241/rmc.11.1.31
Council for Accreditation of Counseling and Related Educational Programs. (2015). 2016 CACREP standards. http://www.cacrep.org/wp-content/uploads/2018/05/2016-Standards-with-Glossary-5.3.2018.pdf
Crouch, E., Radcliff, E., Strompolis, M., & Srivastav, A. (2019). Safe, stable, and nurtured: Protective factors against poor physical and mental health outcomes following exposure to adverse childhood experiences (ACEs). Journal of Child & Adolescent Trauma, 12, 165–173. https://doi.org/10.1007/s40653-018-0217-9
Debellis, M. D. (2001). Developmental traumatology: the psychobiological development of maltreated children and its implications for research, treatment, and policy. Development and Psychopathology, 13(3), 539–564. https://doi.org/10.1017/s0954579401003078
Dube, S. R., Williamson, D. F., Thompson, T., Felitti, V. J., & Anda, R. F. (2004). Assessing the reliability of retrospective reports of adverse childhood experiences among adult HMO members attending a primary care clinic. Child Abuse & Neglect, 28(7), 729–737. https://doi.org/10.1016/j.chiabu.2003.08.009
Ducharme, L. J., Knudsen, H. K., & Roman, P. M. (2008). Emotional exhaustion and turnover intention in human service occupations: The protective role of coworker support. Sociological Spectrum, 28(1), 81–104. https://doi.org/10.1080/02732170701675268
Evans, J. H. (1997). Trauma and post-traumatic growth among graduate level counselor education students: What is their relative incidence and what relationships do they share? (Order No. 9732654) [Doctoral dissertation, Ohio University]. ProQuest Dissertations & Theses Global.
Faul, F., Erdfelder, E., Buchner, A., & Lang, A.-G. (2009). Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behavior Research Methods, 41(4), 1149–1160. https://doi.org/10.3758/brm.41.4.1149
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., Koss, M. P., & Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine, 14(4), 245–258. https://doi.org/10.1016/s0749-3797(98)00017-8
Ford, D. C., Merrick, M. T., Parks, S. E., Breiding, M. J., Gilbert, L. K., Edwards, V. J., Dhingra, S. S., Barile, J. P., & Thompson, W. W. (2014). Examination of the factorial structure of adverse childhood experiences and recommendations for three subscale scores. Psychology of Violence, 4(4), 432–444. https://doi.org/10.1037/a0037723
Frampton, N. M. A., Poole, J. C., Dobson, K. S., & Pusch, D. (2018). The effects of adult depression on the recollection of adverse childhood experiences. Child Abuse & Neglect, 86, 45–54. https://doi.org/10.1016/j.chiabu.2018.09.006
Graham, C., Chun, Y., Grinstein-Weiss, M., & Roll, S. (2020, June 24). Well-being and mental health amid COVID-19: Differences in resilience across minorities and whites. Brookings. https://www.brookings.edu/research/well-being-and-mental-health-amid-covid-19-differences-in-resilience-across-minorities-and-whites
Hensel, J. M., Ruiz, C., Finney, C., & Dewa, C. S. (2015). Meta-analysis of risk factors for secondary traumatic stress in therapeutic work with trauma victims. Journal of Traumatic Stress, 28(2), 83–91. https://doi.org/10.1002/jts.21998
Hughes, K., Bellis, M. A., Hardcastle, K. A., Sethi, D., Butchart, A., Mikton, C., Jones, L., & Dunne, M. P. (2017). The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. The Lancet Public Health, 2(8), 356–366. https://doi.org/10.1016/S2468-2667(17)30118-4
Ivicic, R., & Motta, R. (2017). Variables associated with secondary traumatic stress among mental health professionals. Traumatology, 23(2), 196–204. https://doi.org/10.1037/trm0000065
Jordan, J. V. (2017). Relational–cultural theory: The power of connection to transform our lives. The Journal of Humanistic Counseling, 56(3), 228–243. https://doi.org/10.1002/johc.12055
Klasen, J., Nolte, T., Möller, H., & Taubner, S. (2019). Aversive kindheitserfahrungen, bindungsrepräsentationen und mentalisierungsfähigkeit von psychotherapeuten in ausbildung [Adverse childhood experiences, attachment representations and mentalizing capacity of psychotherapists in training]. Zeitschrift für Psychosomatische Medizin und Psychotherapie, 65(4), 353–371. https://doi.org/10.13109/zptm.2019.65.4.353
Lakioti, A., Stalikas, A., & Pezirkianidis, C. (2020). The role of personal, professional, and psychological factors in therapists’ resilience. Professional Psychology: Research and Practice, 51(6), 560–570. https://doi.org/10.1037/pro0000306
Lanier, B. A., & Carney, J. S. (2019). Practicing counselors, vicarious trauma, and subthreshold PTSD: Implications for counselor educators. The Professional Counselor, 9(4), 334–346. https://doi.org/10.15241/bal.9.4.334
Lee, R. D., & Chen, J. (2017). Adverse childhood experiences, mental health, and excessive alcohol use: Examination of race/ethnicity and sex differences. Child Abuse & Neglect, 69, 40–48. https://doi.org/10.1016/j.chiabu.2017.04.004
Lee, S. M., Cho, S. H., Kissinger, D., & Ogle, N. T. (2010). A typology of burnout in professional counselors. Journal of Counseling & Development, 88(2), 131–138. https://doi.org/10.1002/j.1556-6678.2010.tb00001.x
Maslach, C., Schaufeli, W. B., & Leiter, M. P. (2001). Job burnout. Annual Review of Psychology, 52, 397–422. https://doi.org/10.1146/annurev.psych.52.1.397
McKim, L. L., & Smith-Adcock, S. (2014). Trauma counsellors’ quality of life. International Journal for the Advancement of Counselling, 36, 58–69. https://doi.org/10.1007/s10447-013-9190-z
Merrick, M. T., Ports, K. A., Ford, D. C., Afifi, T. O., Gershoff, E. T., & Grogan-Kaylor, A. (2017). Unpacking the impact of adverse childhood experiences on adult mental health. Child Abuse & Neglect, 69, 10–19. https://doi.org/10.1016/j.chiabu.2017.03.016
Metzler, M., Merrick, M. T., Klevens, J., Ports, K. A., & Ford, D. C. (2017). Adverse childhood experiences and life opportunities: Shifting the narrative. Children and Youth Services Review, 72, 141–149.
Molnar, B. E., Sprang, G., Killian, K. D., Gottfried, R., Emery, V., & Bride, B. E. (2017). Advancing science and practice for vicarious traumatization/secondary traumatic stress: A research agenda. Traumatology, 23(2), 129–142. https://doi.org/10.1037/trm0000122
Nelson-Gardell, D., & Harris, D. (2003). Childhood abuse history, secondary traumatic stress, and child welfare workers. Child Welfare, 82(1), 5–26.
Norton, A. L., & Tan, T. X. (2019). The relationship between licensed mental health counselors’ political ideology and counseling theory preference. American Journal of Orthopsychiatry, 89(1), 86–94. https://doi.org/10.1037/ort0000339
Redford, J. (Director). (2016). Resilience: The biology of stress and the science of hope [Film]. KPJR Films. https://kpjrfilms.co/resilience/
Stamm, B. H. (2008). Design theory and psychometrics of the stressful life experiences screening (SLES). https://bit.ly/StammSLES
Stamm, B. H. (2010). The concise manual for the professional quality of life scale (ProQOL). https://proqol.org/proqol-manual
Strompolis, M., Tucker, W., Crouch, E., & Radcliff, E. (2019). The intersectionality of adverse childhood experiences, race/ethnicity, and income: Implications for policy. Journal of Prevention & Intervention in the Community, 47(4), 310–324. https://doi.org/10.1080/10852352.2019.1617387
Thomas, J. T. (2016). Adverse childhood experiences among MSW students. Journal of Teaching in Social Work, 36(3), 235–255. https://doi.org/10.1080/08841233.2016.1182609
Thompson, I., Amatea, E., & Thompson, E. (2014). Personal and contextual predictors of mental health counselors’ compassion fatigue and burnout. Journal of Mental Health Counseling, 36(1), 58–77. https://doi.org/10.17744/mehc.36.1.p61m73373m4617r3
Webber, J. M., Kitzinger, R., Runte, J. K., Smith, C. M., & Mascari, J. B. (2017). Traumatology trends: A content analysis of three counseling journals from 1994 to 2014. Journal of Counseling & Development, 95(3), 249–259. https://doi.org/10.1002/jcad.12139
Wheeler, N. J., Regal, R. A., Griffith, S.-A. M., & Barden, S. M. (2021). Dyadic influence of adverse childhood experiences: Counseling implications for mental and relational health. Journal of Counseling & Development, 99(1), 24–36. https://doi.org/10.1002/jcad.12351
Zyromski, B., Baker, E., Betters-Bubon, J., Dollarhide, C. T., & Antonides, J. (2020). Adverse childhood experiences: A 20-year content analysis of American Counseling Association and American School Counselor Association journals. Journal of Counseling & Development, 98(4), 351–362. https://doi.org/10.1002/jcad.12338
Eric M. Brown, PhD, LPC, is an assistant professor at DePaul University. Kristy L. Carlisle, PhD, is an assistant professor at Old Dominion University. Melanie Burgess, PhD, is an assistant professor at the University of Memphis. Jacob Clark, BS, is a graduate student at Old Dominion University. Ariel Hutcheon, MA, is a doctoral student at Old Dominion University. Correspondence may be addressed to Eric M. Brown, 2247 N. Halsted St., Chicago, IL 60614, ebrow107@depaul.edu.
Feb 9, 2015 | Article, Volume 5 - Issue 1
Varda Konstam, Amy Cook, Sara Tomek, Esmaeil Mahdavi, Robert Gracia, Alexander H. Bayne
This study examined work engagement and its role in mediating the relationship between organizational support of evidence-based practice (integrating research evidence to inform professional practice) and educational growth and perceived professional expertise. Participants included 78 currently employed counselors, graduates of a master’s program in mental health counseling located in an urban northeastern university. Results revealed that work engagement significantly mediates the relationship between organizational support of evidence-based practice and educational growth and perceived professional expertise. Implications for counseling practice and recommendations for future research are discussed.
Keywords: professional expertise, counselors, evidence-based practice, professional development, work engagement
Although ongoing efforts to maintain and improve clinical competence are intrinsic to ethical practice for counselors (Jennings, Sovereign, Bottorff, Mussell, & Vye, 2005), clinical experience does not appear to guarantee additional skill acquisition among counselors (Goodman & Amatea, 1994; Skovholt & Jennings, 2005). Notably, a meta-analysis conducted by Spengler et al. (2009) revealed that level of education, training and experience had a small effect on clinical judgment (d = .12). Skovholt and Jennings (2005) concluded that “experience alone is not enough” to ensure professional growth and increased professional expertise in counseling practice (p. 15).
Because years of experience only minimally inform professional expertise (defined as the ability to accurately diagnose and implement treatment plans that sensitively incorporate the contexts in which clients are embedded [Meier, 1999]), it is important to isolate both individual and organizational factors that improve professional expertise over time. Individual factors identified in the counseling literature include (a) the importance of self-reflection (Neufeldt, Karno, & Nelson, 1996), (b) exploration of unexamined assumptions about human nature (Auger, 2004), (c) empathy (McLeod, 1999; Pope & Kline, 1999), (d) self-awareness (Richards, Campenni, & Muse-Burke, 2010), (e) mindfulness (Campbell & Christopher, 2012) and (f) cultural competence (Goh, 2005). Organizational factors (defined as organizational systems and processes that are in place to support counselor professional growth linked to organizational and client outcomes) also have been identified (Aarons & Sawitzky, 2006a; Bultsma, 2012, Goh, 2005; Perera-Diltz & Mason, 2012; Truscott et al., 2012). The range of studies, however, has been limited in scope, and research has tended to focus on administrative practices associated with staff turnover, morale, efficiency and productivity (Aarons & Sawitzky, 2006a).
This research focused on how individual counselors and organizations providing counseling services can promote the continuing development and refinement of professional expertise among practicing counselors. Specifically, we focused on individual work engagement and organizational factors—that is, organizational support of evidence-based practice (EBP) and educational growth, and their relationships to perceived counselor professional expertise. Counselor use of EBP involves engaging in critical analysis of professional practice and integrating research evidence to inform interventions (Carey & Dimmitt, 2008). We propose that organizational support of EBP and educational growth are important job resources (Bakker & Demerouti, 2008), and that work engagement mediates the relationship between these resources and perceived counselor professional expertise. First, we present a review of the literature related to organizational support of EBP and work engagement, with a specific focus on linking individual and organizational factors to perceived professional expertise.
Evidence-Based Practice
Efforts put forth by the American Counseling Association (Morkides, 2009) and the American Counseling Association Practice Research Network (Bradley, Sexton, & Smith, 2005) have revealed that evidence-based interventions are critical to the optimal functioning of counselors. Implementation of EBP has been increasingly required across a variety of counseling settings, such as in schools (Carey & Dimmitt, 2008; Dimmitt, Carey, & Hatch, 2007; Forman et al., 2013) and nonprofit human services organizations (McLaughlin, Rothery, Babins-Wagner, & Schleifer, 2010). The Council for Accreditation of Counseling and Related Educational Program standards (2009) also have documented the importance of counselors being trained in using data to inform decision-making, although there are no specific guidelines informing counselors and counselor educators how to engage in EBP effectively. Consequently, implementation of EBP has required that practitioners work in new ways, develop and refine existing clinical skills, and at times reconcile philosophical differences between EBP and their respective disciplines (Tarvydas, Addy, & Fleming, 2010).
The requirement that counselors integrate research findings when working with clients serves to not only sharpen their conceptual understanding of treatment effects, but also aligns conceptual understanding with clinical practice. Such alignment affords the counselor a clearer sense of mastery and aids in developing professional confidence (Beidas & Kendall, 2010). At the organizational and individual practitioner levels, supervisors can work to promote the implementation of more efficacious interventions (Brown, Pryzwansky, & Schulte, 2006; Sears, Rudisill, & Mason-Sears, 2006; Truscott et al., 2012). Thus, understanding individual and organizational factors that influence the use of EBP could help inform counselor development and counseling expertise.
Aarons and Palinkas (2007) surveyed comprehensive home-based services case managers working in child welfare settings specifically with respect to their experiences with EBP. The authors reported that organizational support and willingness to adapt EBP to fit unique settings are the best predictors of successful EBP implementation, including positive attitudes toward EBP. When paired with consistent supportive consultations and supervision, implementation of EBP in child services settings has been associated with greater staff retention (Aarons, Sommerfeld, Hecht, Silovsky, & Chaffin, 2009). Researchers have not yet replicated these results with practitioners working across a range of counseling settings, nor have they expanded their analyses to examine the relationship of EBP training and implementation to professional expertise.
In a qualitative study, Rapp et al. (2008) identified barriers to implementing EBP in five Kansas-based community mental health centers participating in the National Implementing Evidence-Based Practice Project. Rapp et al. (2008) were able to identify critical strategies that produced successful outcomes and positive attitudes toward EBP on behalf of the staff. These strategies included the following: (a) managers setting expectations and front-line staff monitoring EBP use, (b) members of upper management serving as champions of EBP by proactively keeping organizational focus on EBP, (c) educating all staff on the importance of EBP rather than exclusively targeting the staff using EBP as part of their job responsibilities, and (d) creating leadership teams that included representatives from all levels of responsibility within the organization to monitor progress and identify obstacles to implementing EBP. Similarly, in a survey developed to assess EBP implementation in community mental health settings, Carlson, Rapp, and Eichler (2012) found that the key components of successful EBP implementation were team meetings, professional development and skill-building activities, and use of outcome measures to track progress.
Organizational and individual processes by which EBP contributes to optimal counselor functioning over time are relatively unexplored in the literature. One possible variable to consider when addressing issues related to EBP implementation and counselor effectiveness is work engagement, a work-related state of mind associated with feeling connected and fulfilled in relation to one’s work activities (Schaufeli & Bakker, 2004; Schaufeli, Bakker, & Salanova, 2006). Work engagement holds promise in furthering the understanding of how individuals and organizations that support these individuals can promote the continuing development and refinement of professional expertise (Bakker & Demerouti, 2008; Schaufeli et al., 2006).
Work Engagement and Professional Expertise
Schaufeli et al. (2006) defined work engagement as “a positive, fulfilling work-related state of mind that is characterized by vigor, dedication, and absorption” (p. 702). Contrary to those who suffer from burnout, engaged individuals have a sense of connection to their work activities and see themselves as capable of dealing with job responsibilities. It is important to note that the literature related to work engagement is represented by a wide array of contexts including those that are business related. The results of these studies, therefore, cannot be generalized to counselors working across a variety of mental health and school settings (Bakker & Demerouti, 2007, 2008; Salanova, Agut, & Pieró, 2005; Sonnentag, 2003). However, the findings in business-related contexts have revealed interesting associations that warrant further examination. For example, Langelaan, Bakker, van Doornen, and Schaufeli (2006) found that in participants working in diverse business settings (e.g., managers working for Dutch Telecom, blue-collar employees working in food processing companies), specific personality qualities associated with work engagement, such as low levels of neuroticism, high levels of extraversion and the ability to adapt to changing job conditions, were correlated with high levels of work engagement. A number of studies also identified a reciprocal relationship between personal resources (self-esteem and self-efficacy), job resources (effective supervision, social support, autonomy and variety in job tasks) and work engagement (Hakanen, Perhoniemi, & Toppinen-Tanner, 2008; Xanthopoulou, Bakker, Demerouti, & Schaufeli, 2009). The participants in the Hakanen et al. (2008) study were Finnish dentists, whereas the Xanthopoulou et al. (2009) study was based on the responses of employees working in three branches of a fast-food company.
Supportive Organizational Contexts, Work Engagement and Professional Expertise
Colquitt, LePine, and Noe (2000) emphasized the importance of providing organizational support in the workplace when considering job performance and work engagement. However, the focus on “situational characteristics such as support remains surprisingly rare” (p. 700). The authors defined organizational support of educational growth as the extent to which the organization supports ongoing professional learning and development. Research findings have suggested that work engagement is positively correlated with job characteristics identified as resources, such as social support from supervisors and colleagues, performance feedback, coaching, job autonomy, task variety, and training facilities (Bakker & Demerouti, 2007; Demerouti, Bakker, Nachreiner, & Schaufeli, 2001; Salanova et al., 2005; Salanova, Bakker, & Llorens, 2006; Salanova & Schaufeli, 2008; Schaufeli & Bakker, 2003; Schaufeli, Taris, & van Rhenen, 2008). According to Bakker, Giervels, and Van Rijswijk (as cited by Bakker & Demerouti, 2008), engaged employees have been successful in mobilizing their job resources and influencing others to perform better as a team.
In accordance with the model proposed by Bakker and Demerouti (2008), work engagement, in the context of perceived counselor professional expertise, mediates the relationship between job and personal resources and job-related performance. Job resources (e.g., organizational support of EBP, organizational support of educational growth) and personal resources inform work engagement, especially in jobs with high demands (Bakker & Demerouti, 2008; Bakker, Hakanen, Demerouti, & Xanthopoulou, 2007; Salanova et al., 2005). We propose that organizational support of educational growth and organizational support of EBP are important job resources as conceptualized by the Bakker and Demerouti model, and that work engagement mediates the relationship between these resources and counselor professional expertise.
This study addresses a gap in the literature by focusing on understanding the relationships among work engagement, organizational support of EBP and organizational support of educational growth with respect to perceived professional expertise in practicing counselors. To our knowledge, no research to date has linked the systematic organizational implementation of EBP and organizational support of educational growth with the proposed mediating role of work engagement in relationship to counselor perceived professional expertise. See Figure 1 for the proposed mediation model. In addition, the participants of this study function across a variety of counseling settings including schools, hospitals and mental health agencies.
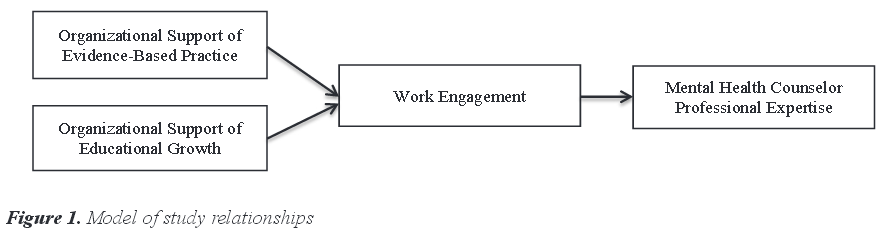
It is important to determine whether a supportive professional context in general, rather than support specific to EBP, accounts for the relationship between EBP and work engagement. We assessed an alternative source of organizational support: support of educational growth, defined as the extent to which the organization supports ongoing professional learning and development. We hypothesized that organizational support of EBP uniquely contributes to work engagement, independent of support of educational growth. We hypothesized the following:
Organizational support of EBP, organizational support of educational growth and professional expertise will all be positively related to each other.
Work engagement will significantly mediate the relationship between organizational support of EBP and educational growth, and in turn will increase perceived professional expertise, as proposed by Bakker and Demerouti (2008).
Methods
Participants
The participants for this study included 78 graduates of a master’s program in mental health counseling located in an urban university in the northeastern part of the United States. The graduates of the counseling program were exposed to coursework that incorporated training and content specific to developing EBP (although they did not complete individual courses devoted specifically to the topic). For example, during the completion of internship coursework and courses foundational to the counseling profession, they were required to complete assignments focusing on using research and data to inform decision-making and practice. As such, prior to being employed in the field as professional counselors, the participants had prior exposure to the theory and practice of employing EBP.
Mailing addresses of 286 mental health counseling graduates were obtained from the alumni office, and a survey was sent to each graduate. A total of 91 mental health counselors located in a variety of settings, including mental health, school and hospital settings, completed the survey and returned it by mail; a response rate of 31.8% was obtained. Five of the questionnaires were excluded due to the participants not working in the field, and eight questionnaires were excluded due to missing data. An a priori power analysis was conducted to ascertain the number of participants required to achieve statistical significance using G*Power (Faul, Erdfelder, Buchner, & Lang, 2009). In using an alpha level of .05 and establishing a minimum power set of .80 and moderate effect size of .30, a minimum of 64 participants was needed to obtain a power of .80 in a hypothesis test using bivariate correlations. A minimum sample size of 58 was needed to achieve a power of .80 for our mediation model analysis (Fritz & MacKinnon, 2007).
The sample consisted of mostly female (n = 67, 86%) respondents. The participants were primarily White (n = 61, 78%), a small percentage Black (n = 4, 5%) and Hispanic (n = 3, 4%), and the rest identified as being “other” or “mixed-race” (n = 10, 13%). Participants averaged 37.4 years old (SD = 9.4), with a median age of 34.5 years. The participants were experienced, with over 90% having 2 or more years of work experience; 35% (n = 27) had 0–4 years of experience, 37% (n = 29) had 5–7 years of experience, while over 28% (n = 22) had 8 or more years of experience. A majority of participants (n = 65, 83%) reported involvement in a national committee within the mental health profession, indicating that the participants were involved within the counseling community and therefore more likely to be engaged at a professional level. Participants came primarily from mental health agencies (n = 33, 42%), followed by school settings (n = 15, 19%) and hospital settings (n = 7, 9%), with the remaining 27% (n = 20) indicating that they worked in more than one type of setting and approximately 4% (n = 3) not identifying their work setting. Data regarding licensure status was not collected.
Instruments
The Professional Expertise and Work Engagement Survey (PEWES) containing four subscales (Organizational Support of Educational Growth Measure [OSEGM], Organizational Support of Evidence-Based Practice [OSEBP], Utrecht Work Engagement Scale [Utrecht] and Mental Health Counseling Professional Expertise Questionnaire [PES]) was developed to measure professional expertise, organizational support of EBP and educational growth, and work engagement. The survey items were developed through incorporating key literature from counseling and related fields (e.g., business and psychology), since the constructs measured had not been assessed directly in the counseling literature. To ensure that the items were applicable to counseling practices, the survey was developed and piloted by two counselor educators. Items that the counselor educators identified as not applicable to counseling practices were excluded from analysis.
Organizational Support of Educational Growth. This assessment is a 5-item instrument using a 10-point Likert-type scale that evaluates characteristics of work settings. The instrument was designed based on the work of Colquitt et al. (2000) and focuses on attributes that predict motivation to learn and job performance. Cognitive abilities and age (identified as individual factors) along with work environment and trainee feedback from colleagues and supervisors (identified as situational factors) are represented in the model. The scale purports to assess support for educational growth present in the work environment. A few sample items used are the following: (a) To what extent does your work setting provide experiences for professional growth and development? (b) To what extent does your work setting provide time for learning activities to promote your professional growth? (c) To what extent does your organization have a climate that supports learning? A factor analysis was conducted on the items using a principal components extraction method. A single factor solution accounted for 52% of the variance in the items, with an eigenvalue of 2.6, indicating that a single summative scale could be utilized. The scale resulted in a range from 5 (low) to 50 (high). A Cronbach’s alpha of .81, 95% CI [.74, .87], was obtained for this instrument.
Organizational Support of Evidence-Based Practice. This 4-item survey using a 10-point Likert-type scale measures the organization’s culture in terms of supporting employee commitment to EBP. The items were created based on Colquitt and colleagues’ work (2000) and the work of Pfeffer and Sutton (2006). Examples of items used include the following: To what extent do the following statements represent your organizational culture? (a) Committed to evidence-based decision-making, which means being committed to getting the best evidence and using it to guide actions. (b) Looks for the risks and drawbacks in what people recommend—even the best interventions have side effects. A factor analysis with principal components extraction was conducted. Results indicated that a single factor accounted for 66% of the variance in the items, with an eigenvalue of 2.66. The scale resulted in a range of values from 4 (low) to 40 (high). A Cronbach’s alpha of .84, 95% CI [.78, .89], was obtained for this questionnaire.
Utrecht Work Engagement Scale. As originally developed, this is a 9-item assessment using a 10-point Likert-type scale that measures level of connection and enthusiasm related to one’s work (Schaufeli et al., 2006). Individuals are evaluated within three aspects of work engagement: vigor, dedication and absorption. The first five items of the scale are utilized to assess work engagement, as follows: (a) At my work, I feel bursting with energy. (b) At my job, I feel strong and vigorous. (c) When I get up in the morning, I feel like going to work. (d) I am enthusiastic about my job. (e) I am proud of the work that I do. These five items fall within the first two subscales of vigor and dedication. Given that absorption was not assessed due to clerical error, items were examined to determine whether a single summative scale could be utilized that would define both vigor and dedication at work. A factor analysis using a principal components extraction found a single factor to account for 81% of the variance in the items, with an eigenvalue of 4.06. This total sum scale created a range of values from 5 (low) to 50 (high). The Cronbach’s alpha for this subset of questions in our sample was .95, 95% CI [.93, .96], indicating high reliability. Schaufeli and colleagues (2006) found a reliability between .60 and .88 for the full 9-item scale.
Mental Health Counseling Professional Expertise Questionnaire. Professional expertise was measured by the PES. This self-assessment instrument was designed to measure perceived professional expertise and professional skills. It consists of 10-questions on a 10-point Likert-type scale. Those taking the survey are asked to determine how a strict but fair supervisor would rate their counseling and clinical abilities as related to their work setting. Questions focus on two areas of functioning: ability to select and employ appropriate diagnostic methods, including consideration of cultural data, and ability to implement a treatment plan, based on diagnostic considerations. A few sample items include the following: (a) I am able to select and employ appropriate diagnostic methods. (b) I am able to accurately interpret diagnostic material and make an accurate diagnosis. (c) I am able to develop a comprehensive treatment plan based on my diagnosis. A factor analysis with principal component extraction was conducted to determine whether a single summative scale could be utilized. Our results indicated that a single factor accounted for 63% of the variance in the items, with an eigenvalue of 6.3. A total sum scale was then created and had a range of 10 (low) to 100 (high) points. A Cronbach’s alpha of .92, 95% CI [.89, .94], was obtained for the scale.
Data Analysis
Analyses for hypothesis one were performed by calculating a full correlation matrix for the four variables. The second research question evaluated the hypothesized mediation effect proposed by Bakker and Demerouti (2008) using a path analysis. The alpha level was set to .05 for all statistical analyses. Analyses were conducted using SPSS Version 19.0 and SAS Version 9.2.
Results
Hypothesis One
Scores on the OSEGM were positively correlated with the OSEBP Measure, r(76) = .53, p < .001. This positive correlation indicated that high values of organizational support of educational growth were found with high values of organizational support of EBP. In addition, scores on the OSEGM were positively correlated with scores on the Utrecht, r(76) = .55, p < .001. This significant positive relationship indicated that high levels of organizational support of educational growth were found with high scores on the Utrecht. A significant positive correlation also was found between the OSEGM scores and the PES scores, r(76) = .25, p < .03. This positive directional effect indicated that high levels of organizational support of educational growth related to higher scores on professional expertise.
The Utrecht was positively correlated with the OSEBP Measure, r(76) = .58, p < .001. High levels of organizational support of EBP related to higher scores on the Utrecht. The Utrecht was positively correlated with the PES, r(76) = .46, p < .001. The positive relationship indicated that higher scores on the Utrecht found with higher scores on the PES.
Lastly, OSEBP was found to be positively correlated with the PES, r(76) = .33, p = .003. This positive relationship indicated that high levels of organizational support of EBP were found with high scores on the PES. Thus, as hypothesized, organizational support of EBP, organizational support of educational growth and perceived professional expertise were all positively related to each other (see Table 1 for correlations between all major variables.).
Table 1
Correlations Between Study Factors
|
Utrecht
|
OSEBP
|
OSEGM
|
| PESOSEGM |
.46***.55*** |
.33**.53*** |
.25* |
| OSEBP |
.58*** |
|
|
*p < .05, **p < .01, ***p < .001
Hypothesis Two
Bakker and Demerouti (2008) proposed a model with a mediation effect of work engagement on the relationship between job and personal resources and performance. Our interpretation of the model placed the OSEGM and the OSEBP Measure into what Bakker and Demerouti (2008) identified as job and personal resources. Additionally, performance was measured by the PES. Work engagement, a mediating variable as suggested by the model, was measured by the Utrecht. Because we adapted the PEWES in accordance with Bakker and Demerouti’s (2008) model, we assessed the individual items and subscales for content validity and reliability as previously described. Given that preliminary findings suggested strong internal consistency, we hypothesized that the full survey could be utilized to ascertain a potential mediation effect of work engagement on the relationship between organizational support of EBP and educational growth, and consequently, greater perceived professional expertise.
The estimated model, along with the standardized estimates, is shown in Figure 2. The fit of the model was very good, with an RMSEA of 0.00, χ2(2, n = 78) = 0.66, p = .72, GFI = .99, CFI = 1.00. Additionally, 55% of the direct effect between the OSEBP Measure and the PES can be accounted for by the mediation of the Utrecht, and 70% of the direct effect between the OSEGM and the PES can be accounted for by the mediation of the Utrecht. Given the large bivariate relationships between professional expertise and both organizational support of EBP and organizational support of educational growth, it appears that work engagement itself is largely contributing to these positive relationships. This finding is shown by the large percentage of direct effects accounted for by the Utrecht.
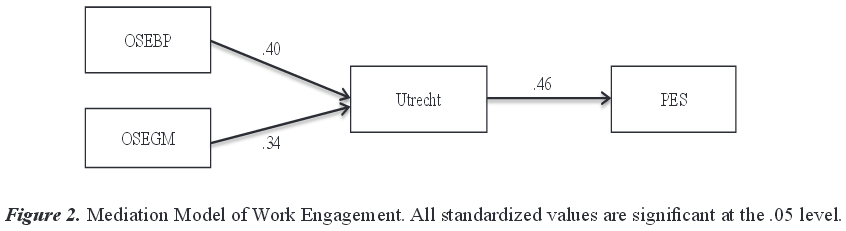
Discussion
The purpose of this study was to gain an increased understanding of the relationships between organizational support of EBP and educational growth, work engagement, and perceived counselor professional expertise. In addition, we examined the mediational effect of work engagement on perceived counselor professional expertise. Results revealed a consistent and coherent picture with important implications for organizational support of continued development of counselor professional expertise across a variety of work settings, including mental health agencies, schools and hospital settings.
Significant positive relationships between all variables indicate that counselors who rated themselves higher in professional expertise and perceived their work settings as supportive of EBP and educational growth reported significantly higher work engagement scores. Results affirm the importance of organizational support of EBP and its unique contribution to nurturing and sustaining work engagement levels among counselors. Results also affirm the importance of organizational support of continued counselor educational growth. These findings help to substantiate the research efforts of Bakker and Demerouti (2007, 2008) and Schaufeli and Salanova (2007).
While organizational support of EBP and organizational support of educational growth both were shown to increase professional expertise, it was the amount of work engagement that accounted for a large proportion of the direct relationships between organizational support of EBP and educational growth with professional expertise. This finding suggests that employers can assist in creating environmental conditions that support and promote employee engagement. A commitment to supervision processes that promote the use of EBP and address issues related to the improvement of work engagement can contribute to improvement in counselors’ functioning across a variety of counselor work settings. Supervision that incorporates linkages between and among EBP implementation, work engagement and professional expertise is potentially empowering to respective supervisees.
It is important to note that relying on counselor individual factors exclusively is an insufficient and incomplete path to improving professional expertise outcomes. Results suggest that organizational assessment of work engagement, specifically how it is promoted within the organization, in concert with counselor self-assessments, has the potential to yield meaningful results in terms of creating work environments conducive to professional growth.
Further longitudinal research is needed to corroborate the pathways resulting in increased counselor work engagement and professional expertise. Linkages to client outcomes would have significant implications for the continued assessment and support of professional growth of counselors in the field. Another important contextual consideration, exploration of job demands (e.g., work pressure, emotional demands) and how they inform work engagement, would also be beneficial, with important implications for training, supervision and practice. Because work engagement appears to increase possibilities for influencing positive counselor outcomes across a variety of settings, a promising practice includes increased emphasis on assessment and continued monitoring of counselor work engagement.
Treatment approaches based on evidence-based principles are likely to increase counselors’ confidence levels and expectations for treatment (Beidas & Kendall, 2010). As suggested by the work of Bakker and Demerouti (2008), a positive feedback loop develops between level of work engagement and organizational support of EBP. Our data are incomplete in terms of understanding these critical and complex relationships that suggest mutually reinforcing feedback loops. Future research is needed urgently to understand these linkages, specifically how organizational support of EBP and counselor level of work engagement reinforce each other in the service of improving treatment outcomes. Conducting longitudinal studies would allow more complete understanding of the relationship between organizational support of EBP and counselor work engagement. Such studies would permit careful examination of how these feedback loops unfold and are sustained over time. Furthermore, supervision models that promote systematic understanding of feedback loops can empower supervisees and promote them monitoring and evaluating their professional growth.
In the current study, we did not assess individual attitudes about and commitment to EBP; rather, we assessed participants’ perceptions of organizational commitment to supporting EBP in their respective counseling work settings. We did not explore the unique contributions of supervision models across provider settings and their contributions to perceived professional growth. Consequently, future studies are needed to determine how organizational implementation of EBP, including the use of formal and informal supervision, combined with individual commitment to EBP, is implicated in terms of levels of work engagement and professional expertise.
Organizational support of EBP is likely to thrive in a context in which individuals, as well as the system in which they are embedded, embrace and respect the scientific inquiry process (Aarons & Sawitzky, 2006b). While preliminary factors have been identified (e.g., Rapp et al., 2008), further research is needed to investigate this potentially fruitful area of inquiry across culturally diverse work settings, including mental health agencies, schools and hospital settings.
Limitations
This study is characterized by several limitations, in particular, generalizability. All of the participants were graduates of a Master of Science degree program in mental health counseling at an urban northeastern university with a strong commitment to and focus on social justice and serving vulnerable populations. In addition, participants had completed coursework that incorporated assignments focusing on building knowledge and understanding of EBP. Further limiting the generalizability of our findings is that only a select number (31.8%) of graduates from the master’s degree program chose to respond to the questionnaire. The participants were a self-selected group committed to serving clients in urban contexts, and therefore the findings cannot be generalized to all practicing counselors.
Another limitation in our results is the use of a subset of questions designed to assess vigor and dedication on the Utrecht, but that did not assess absorption. However, the questions that were included to assess vigor and dedication yielded a Cronbach’s alpha of .95, indicating a very high reliability. A factor analysis revealed that a single factor accounted for 81% of the variance in the items.
The use of self-reports is an additional limitation of the study. Professional expertise and counselor work engagement were assessed by the participants themselves. The study would be enhanced if seasoned external evaluators, deemed experts in their fields, evaluated each of the participants’ level of work engagement and professional expertise. Multiple self-report measurements such as the EBP Attitude Scale (Aarons, 2004) would have provided additional useful information.
This study would be enhanced if variables such as provider demographics, job characteristics and in-depth analyses of supervision services provided were assessed. In addition, using a longitudinal design that incorporated client outcomes and linked them to mental health counselor professional expertise and work engagement would address the limitation of the cross-sectional nature of this design. Nevertheless, given the dearth of research in this unfolding area of study, our findings provide an important contribution in terms of building a foundation for developing a relatively unexplored section of literature as it relates to the counseling profession. Examining the impact of organizational support of EBP and educational growth and level of work engagement has the potential for significantly improving counselor professional expertise over time.
Professional Practice and Supervision Implications
The findings of this study suggest important directions for counselors, counseling supervisors and administrators. The mediation model indicates the strength of work engagement as a mediator of the large positive relationship between organizational support of EBP and counselor professional expertise, and provides a potential powerful lens for improving counselor outcomes. Given that work engagement accounts for a majority of the direct relationship between organizational support of EBP and professional expertise, the findings of this study suggest that assessment of work engagement can be a valuable avenue for increasing professional expertise.
Professionals in counseling and related work settings are struggling with how best to situate their organizations in terms of ensuring optimal counselor and client outcomes, particularly in a context of diminishing economic resources. Although, for example, research studies have provided a degree of clarity in terms of identifying strategies that promote positive attitudes on the part of counselors toward implementation of EBP (Rapp et al., 2008), the systematic study of counselor work engagement and its contribution to professional expertise has not received the attention and focus it merits. While traditional models of counselor training have focused on counselor deficiencies, our finding in support of the mediational role of work engagement expands the understanding of professional growth from a positive psychology perspective—the positive aspects of work.
The dynamic nature of the mediational model proposed in this study provides important opportunities for supervision and administrative practices. In accordance with the model proposed by Bakker and Demerouti (2008), relationships between resources, such as organizational support of EBP and continuing organizational support of education; work engagement; and counselor professional expertise are neither static nor unidirectional. These variables mutually reinforce and inform each other. Based on the model suggested by Salanova et al. (2005), organizational support of EBP and organizational support of educational growth serve as job resources that increase work engagement levels among counselors; they also inform counselor professional expertise. Sensitizing counselors and supervisors who function across a variety of settings, including schools, hospitals and mental health agencies, to the significance of work engagement, its linkage to EBP and the opportunities it provides for self-assessment can increase possibilities for improving counselor professional expertise (Crocket, 2007). To date, there is no study that suggests how these important linkages—organizational support of EBP and education, work engagement, and professional expertise—can best be harnessed and translated to a variety of settings and improved outcomes with respect to counselor professional expertise (as well as improved client counseling outcomes). Comparison studies are needed to determine optimal models and how they may be adapted and individualized across a variety of sociocultural settings in order to reinforce the dynamic interplay of these important constructs.
Supervisors of mental health counselors have an important role in helping counselors understand organizational contexts, and how they may influence and support their professional growth. Crocket (2007) found that a counselor’s workplace and professional culture, including what transpires during supervision discussions, influence the counselor’s development. Supervisors also play a role in deciphering organizational contexts and can be instrumental in supporting supervisees’ job satisfaction and work motivation (Sears et al., 2006). It is important to understand one’s work context and the potential impact of organizational and professional values on one’s own professional development, a stance that helps counselors to engage actively in the process of self-assessment (Crocket, 2007). Finally, the linkage of organizational commitment to EBP and counselor engagement to continuing professional expertise offers promising opportunities for reflection and professional growth. There is developing evidence that support for professional growth in general facilitates the successful implementation of EBP (Rapp et al., 2008). When there is consistent supportive supervision for using EBP, and when all staff members are included in the education on EBP and demonstration of its importance, even those personnel who are not targeted for EBP implementation, more successful outcomes of EBP implementation have been reported (Rapp et al., 2008). Further, Carlson et al. (2012) reported that successful implementation of EBP is supported by implementation of professional development and skill building as supervisory activities. Not only does our model provide support for the implementation of EBP in counseling settings, but it also provides support for implementation of interventions that enhance professional growth. In keeping with the findings of Colquitt et al. (2000), our model suggests that organizational support contributes to work engagement, independent of support of EBP. Furthermore, Witteman, Weiss, and Metzmacher (2012), based on the work of Gaines (1988), suggested that the development and refinement of professional expertise depend on consistent positive feedback processes. Organizational support of EBP provides counselors and administrators with data-driven feedback processes that encourage opportunities for focused collaboration with room for reflection, evaluation and refinement.
Conclusion
Our robust findings suggest a potentially fruitful area of inquiry that is relatively unexplored terrain. Given that implementation of EBP requires both well-conceived research and practitioners to interpret that research, it would be helpful to isolate and understand the variables that promote successful implementation of EBP in terms of counselor level of work engagement and counselor professional expertise. In the present study, a mediational model that considered systemic factors yielded fruitful findings that have significant implications for counselors, supervisors and administrators working in mental health, school and hospital settings.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of
interest or funding contributions for
the development of this manuscript.
References
Aarons, G. A. (2004). Mental health provider attitudes toward adoption of evidence-based practice: The evidence-based practice attitude scale (EBPAS). Mental Health Services Research, 6, 61–74. doi:10.1023/B:MHSR.0000024351.12294.65
Aarons, G. A., & Palinkas, L. A. (2007). Implementation of evidence-based practice in child welfare: Service provider perspectives. Administration and Policy in Mental Health and Mental Health Services Research, 34, 411–419. doi:10.1007/s10488-007-0121-3
Aarons, G. A., & Sawitzky, A. C. (2006a). Organizational climate partially mediates the effect of culture on work attitudes and staff turnover in mental health services. Administration and Policy in Mental Health and Mental Health Services Research, 33, 289–301. doi:10.1007/s10488-006-0039-1
Aarons, G. A., & Sawitzky, A. C. (2006b). Organizational culture and climate and mental health provider attitudes toward evidence-based practice. Psychological Services, 3, 61–72. doi:10.1037/1541-1559.3.1.61
Aarons, G. A., Sommerfeld, D. H., Hecht, D. B., Silovsky, J. F., & Chaffin, M. J. (2009). The impact of evidence-based practice implementation and fidelity monitoring on staff turnover: Evidence for a protective effect. Journal of Consulting and Clinical Psychology, 77, 270–80. doi:10.1037/a0013223
Auger, R.W. (2004). What we don’t know CAN hurt us: Mental health counselors’ implicit assumptions about human nature. Journal of Mental Health Counseling, 26, 13–24.
Bakker, A. B., & Demerouti, E. (2007). The job demands-resources model: State of the art. Journal of Managerial Psychology, 22, 309–328. doi:10.1108/02683940710733115
Bakker, A. B., & Demerouti, E. (2008). Towards a model of work engagement. Career Development International, 13, 209–223. doi:10.1108/13620430810870476
Bakker, A. B., Hakanen, J. J., Demerouti, E., & Xanthopoulou, D. (2007). Job resources boost work engagement, particularly when job demands are high. Journal of Educational Psychology, 99, 274–284. doi:10.1037/0022-0663.99.2.274
Beidas, R. S., & Kendall, P. C. (2010). Training therapists in evidence-based practice: A critical review of studies from a systems-contextual perspective. Clinical Psychology: Science and Practice, 17, 1–30. doi:10.1111/j.1468-2850.2009.01187.x
Bradley, L. J., Sexton, T. L., & Smith, H. B. (2005). The American Counseling Association Practice Research Network (ACA-PRN): A new research tool. Journal of Counseling & Development, 83, 488–491. doi:10.1002/j.1556-6678.2005.tb00370.x
Brown, D., Pryzwansky, W. B., & Schulte, A. C. (2006). Psychological consultation and collaboration: Introduction to theory and practice (6th ed.). Boston, MA: Pearson Education.
Bultsma, S. A. (2012). Supervision experiences of new professional school counselors. Michigan Journal of Counseling: Research, Theory, and Practice, 39, 4–18.
Campbell, J. C., & Christopher, J. C. (2012). Teaching mindfulness to create effective counselors. Journal of Mental Health Counseling, 34, 213–226.
Carey, J., & Dimmitt, C. (2008). A model for evidence-based elementary school counseling: Using school data, research, and evaluation to enhance practice. The Elementary School Journal, 108, 422–430. doi:10.1086/589471
Carlson, L., Rapp, C. A., & Eichler, M. S. (2012). The experts rate: Supervisory behaviors that impact the implementation of evidence-based practices. Community Mental Health Journal, 48, 179–186. doi:10.1007/s10597-010-9367-4
Colquitt, J. A., LePine, J. A., & Noe, R. A. (2000). Toward an integrative theory of training motivation: A meta-analytic path analysis of 20 years of research. Journal of Applied Psychology, 85, 678–707. doi:10.1037//0021-9010.85.5.678
Council for Accreditation of Counseling and Related Educational Programs. (2009). 2009 standards. Alexandria, VA: Author. Retrieved from http://www.cacrep.org/wp-content/uploads/2013/12/2009-Standards.pdf
Crocket, K. (2007). Counselling supervision and the production of professional selves. Counselling and Psychotherapy Research, 7, 19–25. doi:10.1080/14733140601140402
Demerouti, E., Bakker, A. B., Nachreiner, F., & Schaufeli, W. B. (2001). The job demands–resources model of burnout. Journal of Applied Psychology, 86, 499–512. doi:10.1037//0021-9010.86.3.499
Dimmitt, C., Carey, J. C., & Hatch, T. (2007). Evidence-based school counseling: Making a difference with data-driven practices. Thousand Oaks, CA: Corwin Press.
Faul, F., Erdfelder, E., Buchner, A., & Lang, A.-G. (2009). Statistical power analyses using G* Power 3.1: Tests for correlation and regression analyses. Behavior Research Methods, 41, 1149–1160. doi:10.3758/BRM.41.4.1149
Forman, S. G., Shapiro, E. S., Codding, R. S., Gonzales, J. E, Reddy, L. A., Rosenfield, S. A., . . . Stoiber, K. C. (2013). Implementation science and school psychology. School Psychology Quarterly, 28, 77–100. doi:10.1037/spq000001910
Fritz, M. S., & MacKinnon, D. P. (2007). Required sample size to detect the mediated effect. Psychological Science, 18, 233–239. doi:10.1111/j.1467-9280.2007.01882.x
Gaines, B. R. (1988). Positive feedback processes underlying the formation of expertise. IEEEE Transactions on Systems, Man & Cybernetics, 18, 1016–1020. doi:10.1109/21.23101
Goh, M. (2005). Cultural competence and master therapists: An inextricable relationship. Journal of Mental Health Counseling, 27, 71–81.
Goodman, R. L., & Amatea, E. S. (1994). The impact of trainee characteristics on the family therapy skill acquisition of novice therapists. Journal of Mental Health Counseling, 16, 483–497.
Hakanen, J. J., Perhoniemi, R., & Toppinen-Tanner, S. (2008). Positive gain spirals at work: From job resources to work engagement, personal initiative and work-unit innovativeness. Journal of Vocational Behavior, 73, 78–91. doi:10.1016/j.jvb.2008.01.003
Jennings, L., Sovereign, A., Bottorff, N., Mussell, M. P., & Vye, C. (2005). Nine ethical values of master therapists. Journal of Mental Health Counseling, 27, 32–47.
Langelaan, S., Bakker, A. B., van Doornen, L. J. P., & Schaufeli, W. B. (2006). Burnout and work engagement: Do individual differences make a difference? Personality and Individual Differences, 40, 521–532. doi:10.1016/j.paid.2005.07.009
McLaughlin, A. M., Rothery, M.,, Babins-Wagner, R., & Schleifer, B. (2010). Decision-making and evidence in direct practice. Clinical Social Work Journal, 38, 155–163. doi:10.1007/s10615-009-0190-8
McLeod, J. (1999). A narrative social constructionist approach to therapeutic empathy. Counselling Psychology Quarterly, 12, 377–394. doi:10.1080/09515079908254107
Meier, S. T. (1999). Training the practitioner-scientist: Bridging case conceptualization, assessment, and intervention. The Counseling Psychologist, 27, 846–869. doi:10.1177/0011000099276008
Morkides, C. (2009, July). Measuring counselor success. Counseling Today. Retrieved from http://ct.counseling.org/2009/07/measuring-counselor-success/
Neufeldt, S. A., Karno, M. P, & Nelson, M. L. (1996). A qualitative study of experts’ conceptualizations of supervisee reflectivity. Journal of Counseling Psychology, 43, 3–9. doi:10.1037/0022-0167.43.1.3
Perera-Diltz, D. M., & Mason, K. L. (2012). A national survey of school counselor supervision practices: Administrative, clinical, peer, and technology mediated supervision. Journal of School Counseling, 10(4), 1–34. Retrieved from http://files.eric.ed.gov/fulltext/EJ978860.pdf
Pfeffer, J., & Sutton, R. I. (2006). Evidence-based management. Harvard Business Review, 84, 62–74.
Pope, V. T., & Kline, W. B. (1999). The personal characteristics of effective counselors: What 10 experts think. Psychological Reports, 84, 1339–1344. doi:10.2466/pr0.1999.84.3c.1339
Rapp, C. A., Etzel-Wise, D., Marty, D., Coffman, M., Carlson, L., Asher, D., . . . Whitley, R. (2008). Evidence-based practice implementation strategies: Results of a qualitative study. Community Mental Health Journal, 44, 213–224. doi:10.1007/s10597-007-9109-4
Richards, K. C., Campenni, C. E., & Muse-Burke, J. L. (2010). Self-care and well-being in mental health professionals: The mediating effects of self-awareness and mindfulness. Journal of Mental Health Counseling, 32, 247–264.
Salanova, M., Agut, S., & Pieró, J. M. (2005). Linking organizational resources and work engagement to employee performance and customer loyalty: The mediation of service climate. Journal of Applied Psychology, 90, 1217–1227. doi:10.1037/0021-9010.90.6.1217
Salanova, M., Bakker, A. B., & Llorens, S. (2006). Flow at work: Evidence for an upward spiral of personal and organizational resources. Journal of Happiness Studies, 7, 1–22. doi:10.1007/s10902-005-8854-8
Salanova, M., & Schaufeli, W. B. (2008). A cross-national study of work engagement as a mediator between job resources and proactive behavior. The International Journal of Human Resource Management, 19, 116–131. doi:10.1080/09585190701763982
Schaufeli, W., & Bakker, A. (2003). UWES: Utrecht work engagement scale preliminary manual [Version 1, November 2003]. Utrecht University: Occupational Health Psychology Unit. Retrieved from http://www.beanmanaged.com/doc/pdf/arnoldbakker/articles/articles_arnold_bakker_87.pdf
Schaufeli, W. B., & Bakker, A. B. (2004). Job demands, job resources, and their relationship with burnout and engagement: A multi-sample study. Journal of Organizational Behavior, 25, 293–315. doi:10.1002/job.248
Schaufeli, W. B., Bakker, A. B., & Salanova, M. (2006). The measurement of work engagement with a short questionnaire. Educational and Psychological Measurement, 66, 701–716. doi:10.1177/0013164405282471
Schaufeli, W. B., & Salanova, M. (2007). Work engagement: An emerging psychological concept and its implications for organizations. In S. W. Gilliland, D. D. Steiner, & D. P. Skarlicki (Series Eds)., Research in social issues in management: Vol. 5. Managing social and ethical issues in organizations (pp. 135–177). Greenwich, CT: Information Age.
Schaufeli, W. B., Taris, T. W., & van Rhenen, W. (2008). Workaholism, burnout, and work engagement: Three of a kind or three different kinds of employee well-being? Applied Psychology: An International Review, 57, 173–203. doi:10.1111/j.1464-0597.2007.00285.x
Sears, R., Rudisill, J., & Mason-Sears, C. (2006). Consultation skills for mental health professionals. Hoboken, NJ: Wiley & Sons.
Skovholt, T., & Jennings, L. (2005). Mastery and expertise in counseling. Journal of Mental Health Counseling, 27, 13–18.
Sonnentag, S. (2003). Recovery, work engagement, and proactive behavior: A new look at the interface between nonwork and work. Journal of Applied Psychology, 88, 518–528. doi:10.1037/0021-9010.88.3.518
Spengler, P. M., White, M. J., Ægisdóttir, S., Maugherman, A. S., Anderson, L. A., Cook, R. S., . . . Rush, J. D. (2009). The meta-analysis of clinical judgment project: Effects of experience on judgment accuracy. The Counseling Psychologist, 37, 350–399. doi:10.1177/0011000006295149
Tarvydas, V., Addy, A., & Fleming, A. (2010). Reconciling evidenced-based [sic] research practice with rehabilitation philosophy, ethics, and practice: From dichotomy to dialectic. Rehabilitation Education, 24, 191–204. doi:10.1891/088970110805029831
Truscott, S. D., Kreskey, D., Bolling, M., Psimas, L., Graybill, E., Albritton, K., & Schwartz, A. (2012). Creating consultee change: A theory-based approach to learning and behavioral change processes in school-based consultation. Consultation Psychology Journal: Practice and Research, 64, 63–82. doi:10.1037/a0027997
Witteman, C. L. M., Weiss, D. J., & Metzmacher, M. (2012). Assessing diagnostic expertise of counselors using the Cochran–Weiss–Shanteau (CWS) index. Journal of Counseling & Development, 90, 30–34. doi:10.1111/j.1556-6676.2012.00005.x
Xanthopoulou, D., Bakker, A. B., Demerouti, E., & Schaufeli, W. B. (2009). Reciprocal relationships between job resources, personal resources, and work engagement. Journal of Vocational Behavior, 74, 235–244. doi:10.1016/j.jvb.2008.11.003
Varda Konstam is a professor emerita at the University of Massachusetts-Boston. Sara Tomek is an assistant professor and the director of the Research Assistance Center at the University of Alabama. Amy L. Cook is an assistant professor at the University of Massachusetts-Boston. Esmaeil Mahdavi is a professor at the University of Massachusetts-Boston. Robert Gracia is an instructor at the University of Massachusetts-Boston. Alexander H. Bayne is a graduate student at the University of Massachusetts-Boston. Correspondence can be addressed to Varda Konstam, Department of Counseling and School Psychology, University of Massachusetts, Boston, 2 Avery Street, Boston, MA 02111, vkonstam@gmail.com.
Sep 6, 2014 | Article, Volume 1 - Issue 2
Michael Lee Powell, Rebecca A. Newgent
Aligning with a particular theoretical orientation or personal multi-theory integration is often a formidable task to entry-level counselors. A better understanding of how personal strengths and abilities fit with theoretical approaches may facilitate this process. To examine this connection, thirty-five mental health professionals completed a series of inventories to determine if passive counselors adhere to more nondirective, insight-oriented theories, while assertive counselors adhere to more directive, action-oriented approaches. Analyses revealed a significant difference between level of assertiveness and theoretical orientation, with action-oriented counselors demonstrating significantly higher levels of assertiveness than insight-oriented counselors. Implications for professional practice and counselor education are discussed.
Keywords: assertiveness, theoretical orientation, action-oriented, insight-oriented, professional practice, counselors
Murdock, Banta, Stromseth, Viene, and Brown (1998) assert that research into the predictors of theory construction benefits the profession, because the information aids educators and clinical supervisors in helping students and beginning counselors to adopt an appropriate theoretical orientation. If counselors knew what personal strengths and abilities fit best with potential therapeutic approaches (Johnson, Germer, Efran, & Overton, 1988), then adhering to a model of therapy might be less complex, more satisfying, and essentially advantageous for their clientele. To assist in the alleviation of this issue, this study intends to examine the difference between insight-oriented and action-oriented counselors on level of assertiveness.
One of the most exciting and typically daunting tasks for counselors is choosing a theoretical orientation (Halbur & Halbur, 2005). Particularly, choosing one that adequately explains human development and functioning while also attempting to purport interventions that can facilitate greater personal growth and behavioral change in clients. Doing so, however, requires more than simple investigation into the diverse multitude of therapeutic approaches available to counselors. According to Patterson (1985), extensive self-exploration into one’s own personality, values, abilities, and beliefs about human nature are equally salient, as is mandatory longstanding experience. Even then, counselors find that no one theory may suffice or help explain human complexity, which leads to personal theory construction, attempts at theoretical integration, and/or technical eclecticism (Corey, 2008).
Simplifying personal theory construction, or single/multi-theory integration, might assist counselors in choosing a theory that is a better fit for them. With over 400 available therapeutic models (Corsini & Wedding, 2008), counselors find themselves overwhelmed and indifferent to obtaining a sound theoretical foundation, and opt for more technique-oriented practices (Cheston, 2000; Freeman, 2003). Improvements in the manner in which counselors choose a theory would advance knowledge and understanding about the usefulness of adhering to a particular model of therapy. This would also increase treatment consistency and decrease the haphazard, inexperienced practice common with counselors who compile a therapeutic toolbox of empirically-supported interventions, but fail to grasp the rationale that supports their use (Corey, 2008). According to Corsini and Wedding (2008), good therapists follow a particular theory and use techniques associated with that theory and that “technique and method are always secondary to the clinician’s sense of what is the right thing to do with a given client at a given moment in time” (Corsini & Wedding, 2008, p. 10). Further, MacCluskie (2010) discusses the role of theory in counseling and states that, “Practitioners need theories because it is our theory that drives our understanding and conceptualization of the client, the client’s problem, and what strategies and techniques we might use to help the client grow and/or feel better” (p. 9).
Style and Theoretical Orientation
Researchers interested in how a counselor constructs or chooses a particular theory examine multiple predictive factors. For example, Scragg, Bor, and Watts (1999) examined graduate students’ scores on personality assessments as predictors of a chosen theoretical model. They categorized students into two groups derived from their interest in studying directive or nondirective approaches, and found that students interested in the nondirective theories tend to prefer dealing with the abstract and working in an unstructured manner, and that students interested in learning more directive approaches appear to have more charm and leadership ability than the nondirective group. Similarly, Erickson (1993) found differences between theoretical groups based on personality assessment. She measured counselors using the thinking/feeling typology of the Myers-Briggs Type Indicator and found that thinking types reported preferences toward cognitive approaches (e.g., REBT), and feeling types favored affective approaches (e.g., Person-Centered).
Murdock et al. (1998) investigated whether one’s philosophical assumptions, interpersonal style, and supervisor orientation were consistent with specific theoretical orientations. They found that existential/gestalt counselors favor holistic philosophies rather than behavioral ones, which is consistent with their orientation. The systems/interpersonal group preferred observable and contextual causes of behavior rather than mental explanations, and the cognitive/cognitive-behavioral counselors scored high on elementarism (mechanistic, as opposed to holistic) due to their tendency to attend to client’s thoughts and behaviors as the source of change. The psychoanalytics, however, were the only group to score significantly higher on all other measures, meaning they tend to be more dominant interpersonally and prefer supervision from same-orientation supervisors.
Walton (1978) examined counselor self-concept, or view of personal self, as a potential factor predicting theoretical orientation. Among the factors analyzed on a semantic differential instrument, differences between complexity and seriousness were found between the psychodynamic counselor and one who adheres to a rational-emotive approach. Psychodynamic counselors reported themselves as serious and intricate, contrasted to the rational-emotive group who viewed themselves as simple and humorous.
Cummings and Luchese (1978) postulated, “The emergence of an orientation is one given to the whims of fate” (p. 327), not choice, which Steiner (1978) identified as a direct result of one’s chosen graduate training and persuasive influence from professors and supervisors. Norcross and Prochaska (1983) disagree, arguing that it is foolish to think “clinicians select an orientation largely on inexplicable or accidental grounds” (p. 197). They questioned experienced psychologists, not graduate students, as to what factors fueled their theory selection. Among the various influences obtained via survey, clinical experience rated as the most influential. Other factors such as values, graduate training, postgraduate training, life experiences, internship, and the theory’s ability to help in self-discovery received strong ratings. Client type, orientations of colleagues, undergraduate training, and accidental circumstances received a weak or no influential rating.
Although client type was found less influential than other predictive factors (Norcross & Prochaska, 1983), researchers who support technical eclecticism argue otherwise, asserting that a client’s needs should determine a clinician’s orientation (Cheston, 2000; Erickson, 1993). Supporters of this approach encourage clinicians to consider adhering to methodologies that utilize specific empathic techniques that build greater rapport and subsequent growth in clients who conceptually do better with a particular interpersonal style (Bayne, 1995; Churchill & Bayne, 2001). Bayne (1995), for example, contends that if a client appears less innovative and more practical, then he or she should receive cognitive-behavioral counseling, rather than approaches that require creative expression. Extroverts, according to Bayne (1995), are more suitable for humanistic or insight-oriented approaches and group counseling, because they tend to be more sociable and talkative.
Assertiveness and Orientation
According to Gass and Seiter (2003), “Assertive people are not afraid to speak up, express their feelings, or take initiative” (p. 115). Assertive people are viewed as more socially influencing (Cialdini, 2001). In the clinical community, assertive people are sometimes defined by the amount of directiveness utilized in therapy. Kottler and Brown (2000) explain that directiveness involves one’s ability to influence an individual or family in such a way that they are motivated to make positive changes one goal at a time. They state that by taking initiative, setting limits, structuring sessions, and defending their suggestions, directive counselors are more likely to use their expert position for positive therapeutic gains. However, this does not mean that assertiveness equals directiveness, per se. No known research exists to validate that the two are parallel.
Although assertiveness on the part of the counselor is an influential factor in client growth and development, and essential for conflict resolution (Ramirez & Winer, 1983; Smaby & Tamminen, 1976), it has not been isolated or tested as an actual predictor for theoretical orientation. This study aims to add to the list of predictive factors that potentially contribute to the adoption of a theoretical orientation by examining whether an experienced counselor’s level of assertiveness relates to his or her chosen approach. Namely, whether passive counselors tend to adhere to more nondirective, insight-oriented theories, and if assertive counselors tend to adhere to more directive, action-oriented approaches.
Method
Participants
Thirty-five (N = 35) mental health professionals from two mid-south community mental health agencies participated in this study. Fifty packets containing each instrument were hand delivered to qualifying participants, resulting in a 70% response rate. Purposive sampling was used to ensure that respondents had at least two years of clinical experience, and to obtain enough participants from different experience levels. The reason experienced counselors were chosen is that they have had more time to practice different approaches and are more likely to have identified the orientation that best fits them, whereas “students are not capable of formulating a theory,” since “theories are developed by mature individuals on the basis of a thorough knowledge of existing theories and long experience” (Patterson, 1985, p. 349).
Participants had the following licenses: Clinical Psychologist (n = 1); Counseling Psychologist (n = 3); Psychological Examiner (n = 7); Social Worker (n = 12); and Professional Counselor (n = 13). There were 20 females and 15 males. Nineteen participants reported between 2–5 years of experience, while six reported having between 5–10 years of experience, and 10 reported having more than 10 years of experience. Sixteen participants reported adhering to an insight-oriented approach, and 19 were action-oriented. Each participant self-identified as Caucasian.
Instruments
Assertiveness Self-Report Inventory. The Assertiveness Self-Report Inventory (ASRI; Herzberger, Chan, & Katz, 1984) is a brief measure of behavioral assertiveness, developed intentionally with adequate validity data in mind. Other measures of assertiveness have been criticized for not reporting psychometric information (Corcoran, 2000). The instrument is a 25-item measurement with a forced-choice, true/false scale, with half of the items reverse scored to decrease the likelihood of a response set.
Herzberger et al. (1984) report high internal consistency with the ASRI (Cronbach’s Alpha = .78), strong test/retest reliability (r = .81, p < .001), and strong convergent validity with the Rathus Assertiveness Schedule (Rathus, 1973) during two testing sessions (r = .70, p < .001; r = .63, p < .001). For further validation, two criterion-related studies were conducted measuring participants’ ability to offer assertive-like solutions to social dilemmas and peer ratings of participants’ assertiveness. Both studies produced significant relationships to scores on the ASRI (r = .67, p < .001; r = .40, p < .005).
Bakker Assertiveness-Aggressiveness Inventory. The Bakker Assertiveness-Aggressiveness Inventory (AS-AG; Bakker, Bakker-Rabdau, & Breit, 1978) is a 36-item inventory that measures two dimensions of assertiveness necessary for social functioning: the ability to refuse unreasonable requests (Assertiveness) and the ability to take initiative, make requests, or ask for favors (Aggressiveness), with both scales available for use as separate 18-item instruments (Corcoran, 2000). Each item provides the reader with a specific conflict situation and a specific behavioral response, and asks examinees to rate the likelihood that they would respond in the same manner. Half the items contain an assertive response, whereas the other half contains more passive, submissive responses (Bakker et al., 1978). Each item is scored on a five-point likert scale ranging from almost always (AA = 1) to almost never (AN = 5).
Normative data were collected from seven groups, including health professionals, city employees, college students, and clients of an adult development program seeking assertiveness training. Test-retest reliability data are strong for both scales: .75 for the assertiveness scale and .88 for the aggressiveness scale, and split-half reliability of .58 and .67 for both scales, respectively (Bakker et al., 1978). Validity measures were obtained by comparing each group with the college sample, since it was the largest (n = 250). The only group to significantly differ in assertiveness/aggressiveness was the adult development program clients (p < .001), confirming “that the scales are sensitive to differences in functioning” (Bakker et al., p. 282).
The Simple Rathus Assertiveness Schedule. The Simple Rathus Assertiveness Schedule (SRAS; McCormick, 1985) is a revised measure of the Rathus Assertiveness Schedule (Rathus, 1973) designed to improve the original measure’s readability and usability (Corcoran, 2000). A 30-item instrument, the schedule measures social boldness by asking readers to rate themselves on various personal inclinations, such as I enjoy meeting and talking to people for the first time and I have sometimes not asked questions for fear of sounding stupid (McCormick, 1985). Items are scored on a six-point Likert scale, ranging from 6 (very much like me) to 1 (very unlike me).
Reliability for the SRAS is “very good” (Corcoran, 2000, p. 746) when compared with the original Rathus, with the correlation between odd and even items on both versions at .90, and overall total scores correlating at .94, suggesting that “a satisfactory degree of equivalence had been obtained between both measures” (McCormick, 1985, p. 97). The original Rathus reported test/retest reliabilities of .77 (p < .01) and strong convergent validity with other measures of assertiveness.
Procedure
Participants were placed in one of two groups based on their reported theoretical orientation, which Kottler and Brown (2000) categorized as insight-oriented and action-oriented. Insight-oriented approaches believe that self-discovery and revelation is the path to true growth and consists of humanistic, psychodynamic, interpersonal, and experiential theories. Action-oriented approaches are defined as theories that utilize direct interventions and action for symptom reduction. Theories within this category are behavioral, cognitive, strategic, and solution-focused in nature.
Both groups completed an assessment packet, consisting of an informed consent form, a demographic sheet, and the three measurements of assertiveness. Presentation of instruments was identical in both groups. Scores were totaled and compared between each group. Consent forms were kept separate to ensure confidentiality of the information.
Results
A Pearson product-moment correlation analyzed the relationship between all three assertiveness instruments to investigate convergent validity. This analysis revealed a significant positive correlation between the ASRI and SRAS (r = .78, p < .0001) between the ASAG and SRAS (r = .56, p = .0017) and between the ASRI and ASAG (r = .51, p = .0004). The nature of the correlation coefficients indicates a strong convergent validity between all three instruments.
Data were analyzed via a one-way analysis of variance (ANOVA) in order to find differences between insight-oriented and action-oriented counselors on three assertiveness instruments. Additionally, effect sizes are reported as small ≥ .02, medium ≥ .13, and large ≥ .26 (see Steyn & Ellis, 2010). Sample means and trial effects are presented in Table 1. The ANOVA on the ASRI revealed a significant difference between each group: F(1, 33) = 7.75, MSE = 7.66, p < .0088. The mean score for the insight-oriented group was 13.40 (SD = 2.92), and the mean for the action-oriented group was 16.05 (SD = 2.63). The multivariate effect size η2 = .19 indicates a moderate relationship between theoretical orientation and participant assertiveness.
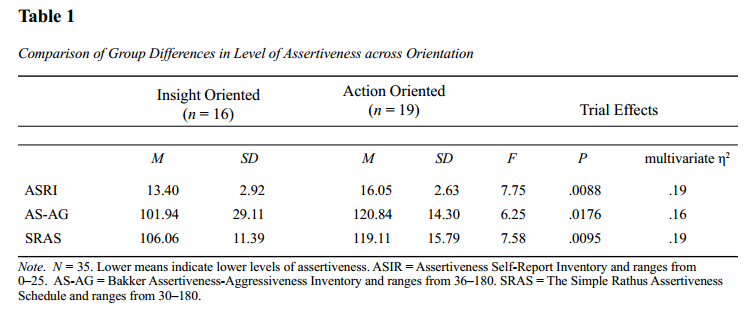
Next, the ANOVA on the AS-AG revealed a significant difference between each group: F(1, 33) = 6.25, MSE = 496.53, p < .0176. The mean score for the insight-oriented group was 101.94 (SD = 29.11), and the mean for the action-oriented group was 120.84 (SD = 14.30). The multivariate effect size η2 = .16 indicates a moderate relationship between theoretical orientation and participant assertiveness.
Finally, the results of the ANOVA on the SRAS revealed a significant difference between each group: F(1, 33) = 7.58, MSE = 195.05, p < .0095. The mean score for the insight-oriented group was 106.06 (SD = 11.39), and the mean for the action-oriented group was 119.11 (SD = 15.79). The multivariate effect size η2 = .19 indicates a moderate relationship between theoretical orientation and participant assertiveness.
Discussion
The purpose of this study was to determine if passive counselors tend to adhere to more nondirective, insight-oriented theories, and if assertive counselors tend to adhere to more directive, action-oriented approaches. Data from scores on the Assertiveness Self-Report Inventory, the Bakker Assertiveness-Aggressiveness Inventory, and the Simple Rathus Assertiveness Schedule suggest that a significant difference does exist between insight-oriented and action-oriented counselors on level of assertiveness, suggesting that level of assertiveness in mental health professionals is a viable factor in theoretical orientation development. In fact, action-oriented counselors had significantly higher levels of assertiveness than the insight-oriented counselors did across all three measures, with the variability of the scores on the AS-AG indicating substantial differences between the two orientations. Not surprisingly, the results on all three measures were in the same direction, consistent with the convergent validity of the measures.
Effect size analyses indicate that moderate relationships exist between theoretical orientation and participant assertiveness, which are clinically meaningful and of practical significance in addition to statistical significance (LeCroy & Krysik, 2007). This finding supports Kottler and Brown’s (2000) position on the nature and quality of directiveness in the therapeutic relationship. That is how assertiveness on the part of the counselor can be an influential factor in client growth and development. This suggests that possibly the two may in fact be parallel. Nonetheless, according to the results, counselors that choose directive approaches appear to be assertive themselves.
Previous research has investigated several predictive factors that contribute to the adoption of a theoretical orientation by counselors (Bayne, 1995; Erickson, 1993; Freeman, 2003; Johnson et al., 1988; Murdock et al., 1998; Norcross & Prochaska, 1983; Steiner, 1978; Walton, 1978). No one study, however, has been able to identify each factor interdependently, opting to isolate specific factors independently via multiple examinations. This study aimed to add to the established list of identified predictive factors by examining whether an experienced counselor’s level of assertiveness relates to his or her chosen approach. We believe that we can now add assertiveness to the list of predictive factors, which include personality type, therapist training, age of clients, and level of counselor development. A limitation in this study was the ability to generalize to different races. All mental health professionals that participated were Caucasian. Another possible limitation was that the participants self-reported on their theoretical orientation.
Implications and Conclusions
The counseling profession benefits from research designed to identify the predictive factors leading to one’s choice of a theoretical orientation. Graduate programs, for example, could use the current data to facilitate the process of theory formation and adoption, including theoretical integration and technical eclecticism, in addition to general instruction that covers the history of theory and the art of the therapeutic relationship. Supervisors of beginning clinicians might profit, not only in facilitating a supervisee’s development of professionalism, but by assisting them to re-examine their strengths and limitations, which may lead to an investigation into new theoretical possibilities that create a better “clinical fit.” Even agencies, conceivably, could utilize the predictors in an attempt to match a client to a particular counselor based on theory and personality. Although this may not seem practical, such an effort could be a positive ingredient for increasing community outcome measures and reducing counselor burnout. Further research supporting this idea would be beneficial. Conversely, further research is necessary to investigate whether matching a counselor’s personality to a theoretical orientation is actually empirically effective. This study is limited by the fact that it does not provide support for such a hypothesis, but does support its consideration.
Although the list of predictive factors leading to a counselor’s choice of orientation is extensive and complex, and no study has been able to identify them in their entirety, it does not mean that isolating the factors for clinical research is meaningless. On the contrary, identifying the predictive factors is advantageous. Doing so could make theory adoption more counselor-centered and satisfying to the adopting practitioner, who can choose an approach that “fits” best.
References
Bakker, C. B., Bakker-Rabdau, M. K., & Breit, S. (1978). The measurement of assertiveness and aggressiveness. Journal of Personality Assessment, 42(3), 277–284.
Bayne, R. (1995). Psychological type and counselling. British Journal of Guidance and Counselling, 23(1), 95–106.
Cheston, S. E. (2000). A new paradigm for teaching counseling theory and practice. Counselor Education and Supervision, 39(4), 254–270.
Churchill, S., & Bayne, R. (2001). Psychological type and conceptions of empathy in experienced counsellors: Qualitative results. Counselling Psychology Quarterly, 14(3), 203–217.
Cialdini, R. B. (2001). Influence: Science and practice (4th ed.). Needham Heights, MA: Allyn and Bacon.
Corcoran, K. J. (2000). Measures for clinical practice: A sourcebook. New York: Free Press.
Corey, G. (2008). Theory and practice of counseling and psychotherapy (8th ed.). Belmont, CA: Brooks/Cole.
Corsini, R. J., & Wedding, D. (2008). Current psychotherapies (8th ed.). Belmont, CA: Brooks/Cole.
Cummings, N. A., & Luchese, G. (1978). Adoption of a psychological orientation: The role of the inadvertent. Psychotherapy: Theory, Research, and Practice, 15, 375–381.
Erickson, D. B. (1993). The relationship between personality type and preferred counseling model. Journal of Psychological Type, 27, 39–41.
Freeman, M. S. (2003). Personality traits as predictors of a preferred theoretical orientation in beginning counselor education students. Dissertation Abstracts International, 64(02), 407B.
Gass, R. H., & Seiter, J. S. (2003). Persuasion, social influence, and compliance gaining (2nd ed.). Needham Heights, MA: Allyn & Bacon.
Halbur, D. A., & Halbur, K. V. (2005). Developing your theoretical orientation in counseling and psychotherapy. Needham Heights, MA: Allyn & Bacon.
Heppner, P. P., Kivlighan, Jr., D. M., & Wampold, B. E. (1999). Research design in counseling (2nd ed.). Belmont, CA: Brooks/Cole.
Herzberger, S. D., Chan, E., & Katz, J. (1984). The development of an assertiveness self-report inventory. Journal of Personality Assessment, 48(3), 317–323.
Johnson, J. A., Germer, C. K., Efran, J. S., & Overton, W. F. (1988). Personality as the basis for theoretical predilections. Journal of Personality and Social Psychology, 55(5), 824–835.
Kottler, J. A., & Brown, R. W. (2000). Introduction to therapeutic counseling: Voices from the field (4th ed.). Belmont, CA: Brooks/Cole.
LeCroy, C. W., & Krysik, J. (2007). Understanding and interpreting effect size measures. Social Work Research, 31(4), 223–248.
MacCluskie, K. (2010). Acquiring counseling skills: Integrating theory, multiculturalism, and self-awareness. Upper Saddle River, NJ: Pearson Education.
McCormick, I. A. (1985). A simple version of the Rathus assertiveness schedule. Behavioral Assessment, 7, 95–99.
Murdock, N. L., Banta, J., Stromseth, J., Viene, D., & Brown, T. M. (1998). Joining the club: Factors related to choice of theoretical orientation. Counselling Psychology Quarterly, 11(1), 63–78. doi:10.1080/09515079808254043
Norcross, J. C., & Prochaska, J. O. (1983). Clinicians’ theoretical orientations: Selection, utilization, and efficacy. Professional Psychology: Research and Practice, 14(2), 197– 207.
Patterson, C. H. (1985). New light for counseling theory. Journal of Counseling and Development, 63(6), 349–350.
Ramirez, J., & Winer, J. L. (1983). Counselor assertiveness and therapeutic effectiveness in treating depression. The Personnel and Guidance Journal, 62(3), 167–170.
Rathus, S. A. (1973). A 30-item schedule for assessing assertive behavior. Behavior Therapy, 4, 398–406.
Scragg, P., Bor, R., & Watts, M. (1999). The influence of personality and theoretical models on applicants to a counseling psychology course: A preliminary study. Counseling Psychology Quarterly, 12(3), 263–270.
Smaby, M. H., & Tamminen, A. W. (1976). Counselors can be assertive. Personnel and Guidance Journal, 54(8), 421–424.
Steiner, G. L. (1978). A survey to identify factors in therapists’ selection of a theoretical orientation. Psychotherapy: Theory, Research, and Practice, 15(4), 371–374.
Steyn, H. S., Jr., & Ellis, S. M. (2010). Estimating an effect size in one-way multivariate analysis of variance (MANOVA). Multivariate Behavioral Research, 44(1), 106–129. doi:10.1080/00273170802620238
Walton, D. E. (1978). An exploratory study: Personality factors and theoretical orientations of therapists. Psychotherapy: Theory, Research, and Practice, 15(4), 390–395.
Michael Lee Powell is a Licensed Professional Counselor and Licensed Alcoholism and Drug Abuse Counselor at Youth Bridge, Inc. in Fayetteville, AR, and Rebecca A. Newgent, NCC, is a Licensed Professional Clinical Counselor with Supervision Designation in Ohio, a Licensed Professional Counselor with Supervision Specialization in Arkansas, and Professor and Chairperson at Western Illinois University – Quad Cities. Correspondence can be addressed to Michael Lee Powell, 4257 Gabel Drive, Fayetteville, AR, 72703, dr.michael.powell@gmail.com.
Apr 7, 2014 | Article, Volume 4 - Issue 2
Elizabeth A. Prosek, Jessica M. Holm
The U.S. Department of Veterans Affairs (VA) and TRICARE have approved professional counselors to work within the military system. Counselors need to be aware of potential ethical conflicts between counselor ethical guidelines and military protocol. This article examines confidentiality, multiple relationships and cultural competency, as well as ethical models to navigate potential dilemmas with veterans. The first model describes three approaches for navigating the ethical quandaries: military manual approach, stealth approach, and best interest approach. The second model describes 10-stages to follow when navigating ethical dilemmas. A case study is used for analysis.
Keywords: military, ethics, veterans, counselors, competency, confidentiality
The American Community Survey (ACS; U.S. Census Bureau, 2011) estimated that 21.5 million veterans live in the United States. A reported 1.6 million veterans served in the Gulf War operations that began post-9/11 in 2001 (U.S. Census Bureau, 2011). Gulf War post-9/11 veterans served mainly in Iraq and Afghanistan, in operations including but not limited to Operations Enduring Freedom (OEF), Iraqi Freedom (OIF), and New Dawn (OND) (M. E. Otey, personal communication, October 23, 2012). Holder (2007) estimated that veterans represent 10% of the total U.S. population ages 17 years and older. Pre-9/11 data suggested that 11% of military service members utilized mental health services in the year 2000 (Garvey Wilson, Messer, & Hoge, 2009). In 2003, post-9/11 comparative data reported that 19% of veterans deployed to Iraq accessed mental health services within one year of return (Hoge, Auchterlonie, & Milliken, 2006). Recognizing the increased need for mental health assessment, the U.S. Department of Defense (DOD) mandated the Post-Deployment Health Assessment (PDHA) for all returning service members (Hoge et al., 2006). The PDHA is a brief three-page self-report screening of symptoms to include post-traumatic stress, depression, suicidal ideation and aggression (U.S. DOD, n.d.). The assessment also indicates service member self-report interest in accessing mental health services.
Military service members access mental health services for a variety of reasons. In a qualitative study of veterans who accessed services at a Veterans Affairs (VA) mental health clinic, 48% of participants reported seeking treatment because of relational problems, and 44% sought treatment because of anger and/or irritable mood (Snell & Tusaie, 2008). Veterans may also present with mental health symptoms related to post-traumatic stress disorder (PTSD), depression, and suicidal ideation (Hoge et al., 2006). Depression is considered a common risk factor of suicide among the general population, and veterans are additionally at risk due to combat exposure (Martin, Ghahramanlou-Holloway, Lou, & Tucciarone, 2009). The DOD (2012) confirmed that 165 active-duty Army service members committed suicide in 2011. Furthermore, researchers asserted that suicide caused service member deaths more often than combat (O’Gorman, 2012). Hoge et al. (2004) reported that veterans were most likely to access mental health services 3–4 months post-deployment. Unfortunately, researchers suggested that service members were hesitant to access mental health treatment, citing the stigma of labels (Kim, Britt, Klocko, Riviere, & Adler, 2011). Studies indicated that mental health service needs are underestimated among the military population and are therefore a potential burden to an understaffed helping profession (Garvey Wilson et al., 2009; Hoge et al., 2006). In May of 2013, the DOD and VA created 1,400 new positions for mental health providers to serve military personnel (DOD, 2013). Moreover, as of March 2013, the DOD-sponsored veterans crisis line reported more than 800,000 calls (DOD, 2013). It is evident that the veteran population remains at risk for problems related to optimal mental health functioning and therefore requires assistance from trained helping professionals.
Historically, the DOD employed social workers and psychologists almost exclusively to provide mental health services in the military setting. Recently, the DOD and VA expanded services and created more positions for mental health clinicians (U.S. VA, 2012). Because licensed professional counselors (LPCs) are now employable by VA service providers (e.g., VA hospitals) and approved TRICARE providers (Barstow & Terrazas, 2012), it is imperative to develop an understanding of the military system, especially of the potential conflict that may exist between military protocol and counselor ethical guidelines. The military health system requires mental health professionals to be appropriately credentialed (e.g., licensed), and credentialing results in the mandatory adherence to a set of professional ethical standards (Johnson, Grasso, & Maslowski, 2010). However, there may be times when professional ethical standards do not align with military regulations. Thus, an analysis of the counselor ethical codes relevant to the military population is presented. At times, discrepancies between military protocol and counselor ethical codes may emerge; therefore, recommendations for navigating such ethical dilemmas are provided. A case study and analysis from the perspective of two ethical decision-making models are presented.
Ethical Considerations for Counselors
The mission of the American Counseling Association (ACA) Code of Ethics (2005) is to establish a set of standards for professional counselors, which ensure that the counseling profession continues to enhance the profession and quality of care with regard to diversity. As professional counselors become employed by various VA mental health agencies or apply for TRICARE provider status, it is important to identify specific ethical codes relevant to the military population. Therefore, three categories of ethical considerations pertinent to working with military service members are presented: confidentiality, multiple relationships, and cultural competence.
Confidentiality
The ACA Code of Ethics (2005) suggests that informed consent (A.2.a., p. 4) be a written and verbal discussion of rights and responsibilities in the counseling relationship. This document includes the client right for confidentiality (B.1.c., p. 7) with explanation of limitations (B.1.d., p. 7). The limitations, or exceptions, to confidentiality include harm to self, harm to others and illegal substance use. In the military setting, counselors may need to consider other exceptions to confidentiality including domestic violence (Reger, Etherage, Reger, & Gahm, 2008), harassment, criminal activity and areas associated with fitness for duty (Kennedy & Johnson, 2009). Also, military administrators may require mandated reporting when service members are referred for substance abuse treatment (Reger et al., 2008). When these conditions arise in counseling, the military may require reporting beyond the standard ethical protocol to which counselors are accustomed.
Counselors working in the VA mental health system or within TRICARE may need to be flexible with informed consent documents, depending on the purpose of services sought. Historically, veterans represented those who returned from deployment and stayed home. Currently, military members may serve multiple tours of combat duty; therefore, the definition of veterans now includes active-duty personnel. This modern definition of veteran speaks to issues of fitness for duty, where the goal is to return service members ready for combat. Informed consent documents may need to outline disclosures to commanding officers. For example, if a service member is in need of a Command-Directed Evaluation (CDE), then the commander is authorized to see the results of the assessment (Reger et al., 2008). Fitness for duty is also relevant when service members are mandated to the Soldier Readiness Program (SRP) to determine their readiness for deployment. In these situations, counselors need to clearly explain the exception to confidentiality before conducting the assessment. Depending on the type of agency and its connection to the DOD, active-duty veterans’ health records may be considered government property, not the property of the service provider (McCauley, Hacker Hughes, & Liebling-Kalifani, 2008). It is imperative that counselors are educated on the protocols of the setting or assessments, because “providing feedback to a commander in the wrong situation can be an ethical violation that is reviewable by a state licensing authority” (Reger et al., 2008, p. 30). Thus, in order to protect the client and the counselor, limitations to confidentiality within the military setting must be accurately observed at all times. Knowledge of appropriate communication between the counselor and military system also speaks to the issue of multiple relationships.
Multiple Relationships
Kennedy and Johnson (2009) suggested creating collaborative relationships with interdisciplinary teams in a military setting in order to create a network of consultants (e.g., lawyers, psychologists, psychiatrists), which is consistent with ACA ethical code D.1.b to develop interdisciplinary relationships (2005, p. 11). However, when interdisciplinary teams are formed, there are ACA (2005) ethical guidelines that must be considered. These guidelines state that interdisciplinary teams must focus on collaboratively helping the client by utilizing the knowledge of each professional on the team (D.1.c., p. 11). Counselors also must make the other members of the team aware of the constraints of confidentiality that may arise (D.1.d., p. 11). In addition, counselors should adhere to employer policies (D.1.g., p. 11), openly communicating with VA superiors to navigate potential discrepancies between employers’ expectations and counselors’ roles in best helping the client.
In the military environment, case transfers are common because of the high incidence of client relocation, which increases the need for the interdisciplinary teams to develop time-sensitive treatment plans (Reger et al., 2008). Therefore, treatment plans not only need to follow the guidelines of A.1.c., in which counseling plans “offer reasonable promise of success and are consistent with abilities and circumstances of clients” (ACA, 2005, p. 4), but they also need to reflect brief interventions or treatment modalities that can be easily transferred to a new professional. Mental health professionals may work together to best utilize their specialized services in order to meet the needs of military service members in a minimal time allowance.
For those working with military service members, consideration of multiple relationships in terms of client caseload also is important. Service members who work together within the same unit may seek mental health services at the same agency. Members of a military unit may be considered a support network which, according to ethical code A.1.d., may be used as a resource for the client and/or counselor (ACA, 2005, p. 4). However, learning about a military unit as a network from multiple member perspectives may also create a dilemma. Service members within a unit may be tempted to probe the counselor for information about other service members, or tempt the counselor to become involved in the unit dynamic. McCauley et al. (2008) recommended that mental health professionals avoid mediating conflicts between service members in order to remain neutral in the agency setting.
However, there are times when the unit cohesion may be used to support the therapeutic relationship. Basic military training for service members emphasizes the value of teamwork and the collective mind as essential to success (Strom et al., 2012). It is important for counselors to approach military service member clients from this perspective, not from a traditional Western individualistic lens. Mental health professionals also are warned not to be discouraged if rapport is more challenging to build than expected. Hall (2011) suggested that the importance of secrecy in the military setting might make it more difficult for service members to readily share in the therapeutic relationship. Researchers noted that military service members easily built rapport with each other in a group therapy session, often leaving out the civilian group leader (Strom et al., 2012). It might behoove counselors to build upon the framework of collectivism in order to earn the trust of members of the military population. Navigating the dynamic of a unit or the population of service members accessing care at the agency may be a challenge; however, counselors are able to alleviate this challenge with increased knowledge of the military culture in general.
Cultural Competence
The military population represents a group of people with a unique “language, a code of manners, norms of behavior, belief systems, dress, and rituals” and therefore can be considered a cultural group (Reger et al., 2008, p. 22). Reger et al. (2008) suggested that many clinical psychologists learned about military culture as active service members themselves. While there may be many veterans currently working as professional counselors, civilian counselors also serve the mental health needs of the military population; and as civilians, they require further training. The ACA Code of Ethics (2005) suggests that counselors communicate with their clients in ways that are culturally appropriate to ensure understanding (A.2.c., p. 4). This can be achieved by prolonged exposure to military culture or by seeking supervision from a professional involved with the military mental health system (Reger et al., 2008). Strom et al. (2012) outlined examples of military-specific cultural components for professionals to learn: importance of rank, unique terminology and value of teamwork. It behooves counselors intending to work with the military population to learn terminology in order to understand service members. For example, R&R refers to vacation leave and MOS or rate refers to a job category (Strom et al., 2012).
Personal values may cause dilemmas for a mental health professional working within the VA system. This can be especially true during times of war. Stone (2008) suggested that treating veterans of past wars may be easier than working with military service members during current combat because politics may be intensified. A counselor who does not support the current wartime mission may be conflicted when clients are mandated to return to active-duty assignments (Stone, 2008). The ACA Code of Ethics (2005) addresses the impact of counselors’ personal values (A.4.b., pp. 4–5) on the therapeutic relationship. It is recommended that counselors be aware of their own values and beliefs and respect the diversity of their clients. Counselors need to find a way to value the contributions of their client when personal or political opinion conflicts with the DOD’s plans or efforts overseas. If one wants to be successful with this population, Johnson (2008) suggested the foundational importance of accepting the military mission. If this is in direct conflict with the counselor’s values, it may be recommended for the counselor to consider the client’s value of the mission.
The ACA ethical code stresses the importance of mental health professionals practicing within the boundaries of their competence and continuing to broaden their knowledge to work with diverse clients (ACA, 2005, C.2.a., p. 9). Counselors should only develop new specialty areas after appropriate training and supervised experience (ACA, 2005, C.2.b., p. 9). Working within the VA mental health system, mental health professionals may be asked to provide a service in which they are not competent (Kennedy & Johnson, 2009). Such a request may occur more frequently here than in other settings, due to the high demand of mental health services and low availability of trained professionals (Garvey Wilson et al., 2009; Hoge et al., 2006). Counselors must determine if their experience and training can be generalized to working with military service members (Kennedy & Johnson, 2009), and may be their own best advocate for receiving appropriate training.
Awareness of when and how military service members access mental health services also might be important to consider. Reger et al. (2008) reported that military personnel were more likely to access services before and after a deployment. Researchers specified a higher prevalence rate of access 3–4 months after a deployment (Hoge et al., 2004). The relationship of time between deployment and help-seeking behaviors suggests that counselors should be prepared for issues related to trauma. For women, combat-related trauma is compounded with increased rates of reported military sexual trauma (Kelly et al., 2008). Counselors would benefit from additional trainings in trauma intervention strategies. The VA and related military organizations offer many resources online to educate professionals working with military members with identified trauma symptoms (U.S. VA., n.d.).
Advocating for appropriate training in areas of incompetence is the responsibility of the professional, who should pursue such training in order to best meet the needs of the military population. It is best practice for mental health professionals to be engaged in ongoing trainings to ensure utilization of the latest protocols and treatment modalities (McCauley et al., 2008). Trainings may need to extend beyond general military culture, because each branch of service (e.g., Army, Marines, Navy) could be considered a cultural subgroup with unique language and standards. For example, service members in the Army are soldiers, whereas members of the Navy are sailors (Strom et al., 2012).
This article has outlined many ACA (2005) ethical guidelines pertinent to working with the military population. However, as presented, there are times when counselor ethical codes conflict with military regulations. Counselors interested in working in the military setting or with military personnel may consider decision-making models to address ethical dilemmas.
Recommendations for Counselors
The military mental health system has almost exclusively employed psychologists and social workers. Counselors interested in employment within VA agencies or as TRICARE providers may utilize the resources created by these practitioners to better serve the military population. Two ethical decision-making models are presented, and a case study is provided to demonstrate how to implement the models.
Ethical Models
The ACA Code of Ethics (2005) advises counselors to adhere to the code of ethics whenever possible, working towards a resolution of the conflict (H.1.b., p. 19). If a favorable resolution cannot be formed, counselors have the choice to act in accordance with the law or regulation. Psychology researchers have suggested ethical models for professionals to use during times of dilemma within the military setting. The first model presented considers three overarching approaches to address ethical dilemmas; and the second model presented is a more specific stage model with which to approach dilemmas. These models may serve to assist counselors as the counseling profession gains more experience in the VA system and eventually develops counselor-specific decision-making models.
Approach model. Johnson and Wilson (1993) identified three approaches for psychologists to consider when navigating the ethical quandaries of the military mental health system. The first, the military manual approach, occurs when professionals adhere strictly to military regulations without consideration for the specific client’s needs. The second, the stealth approach, occurs when there is strict adherence to the mental health professionals’ code of ethics, regardless of the legalities surrounding the circumstances. While the client’s best interests may be at the forefront in this approach, the counselor must also take into account the possibility of being the subject of legal action for not adhering to the standards set by the military. For example, the counselor may use ambiguous wording within the client file or leave some information out altogether, so that if the files were requested, the client’s information would be protected (Johnson & Wilson, 1993). The third, the best interest approach, occurs when the counselor maintains focus on the client’s best interest while also adhering to the standards of the military. This may require professionals to adhere to the minimum professional standards in order to accommodate the client’s best interest. Although most professionals have deemed this approach the best option, it also leads to the most ambiguity. Under certain circumstances, the counselor also must take into account what is in the best interest for society as a whole, while also navigating a responsibility to the client and the military mental health system. Researchers in psychology responded to the ambiguity of this model by developing a more specific stage model to assist professionals with ethical dilemmas.
Stage model. Barnett and Johnson (2008) proposed a 10-stage model to follow when navigating an ethical dilemma. They advise that professionals must do the following:
1. Clearly define the situation.
2. Determine what parties could be affected.
3. Reference the pertinent ethical codes.
4. Reference the pertinent laws and regulations.
5. Reflect on personal thoughts and competencies on the issue.
6. Select knowledgeable colleagues with whom to consult.
7. Develop alternate courses of action.
8. Evaluate the impact on all parties involved.
9. Consult with professional organizations, ethics committees and colleagues.
10. Decide on a course of action.
Barnett and Johnson (2008) also noted that once a decision is made, the process does not end. It is best practice to monitor the implications and, if necessary, modify the plan. Documentation throughout this entire process is necessary for the protection of the counselor, the client and other involved stakeholders. Counselors working in the military mental health system may find this 10-stage model helpful when navigating ethical dilemmas.
To better understand the implementation of the two presented ethical decision-making models, a case study was developed. The case is then conceptualized from both the approach model and stage model, and the ethical dilemmas associated with the case are discussed.
Case Study
Megan is a licensed professional counselor employed at a clinic that serves military service members. She provides individual outpatient counseling to veterans and family members, as well as facilitates veteran support groups. Megan’s client, Robert, is a Petty Officer First Class in the Navy. Robert is married with two children. In recent sessions, Megan became concerned with Robert’s increased alcohol use. Recently, Robert described a weekend of heavy drinking at the local bar. Although Robert drove after leaving the bar both nights, Megan suspected that he was not sober enough to drive. In a follow-up session, Robert reported that his binge-drinking weekend caused friction at home with his wife, and that he missed his children’s soccer games. During his most recent session, Robert was visibly distressed as he disclosed to Megan that he received orders for a deployment in 3 months. Robert is anxious about informing his wife and children of the pending 6-month deployment, as he knows it will only increase conflict at home. Robert reported that his family could use the increase in pay associated with family separation and tax-free wages during deployment. However, he also knows that deployments cause tension with his wife, which has already increased due to Robert’s recent drinking binges. While leaving the session, he mentioned with a laugh that he would rather go to the bar than go home.
Analysis from approach model. Megan may consider using Johnson and Wilson’s (1993) ethical approach model as she conceptualizes the potential ethical dilemma presented in Robert’s case. From a military manual approach, Megan may need to report Robert’s recent alcohol abuse behavior to his superior, as it may impact his fitness for duty on his next deployment. And although Robert has not been caught drinking and driving or charged with a crime, his behavior also puts him at risk of military conduct violations. However, when Robert originally came to the clinic, he did so of his own accord, not under orders, which could mean that notifying a commanding officer is an ethical violation. In consideration of the stealth approach, Megan may review the ACA (2005) ethical guidelines and conclude that there are no violations at risk if she chooses not to report Robert’s drinking habits. However, Megan contemplates whether addressing Robert’s drinking binges is in his best interest overall. She understands that the money associated with deployment is important to Robert’s family at this time; however, his drinking may put him at increased risk during deployment. Finally, Megan applies the best-interest approach to Robert’s situation. Megan may refer Robert to the center’s substance use support group. This referral will be reflected in Robert’s records, but if he begins receiving treatment for his alcohol abuse now (3 months before deployment), there may be time for Robert to demonstrate significant progress before his fitness for duty assessment.
Analysis from stage model. Megan may consider her ethical dilemma from Barnett and Johnson’s (2008) 10-stage model. In stage 1, she clearly defines the situation as Robert’s alcohol abuse and pending deployment. In stage 2, Megan considers who may be affected in this situation. She understands that Robert’s family would benefit from the extra money associated with the deployment, and therefore the family may be impacted if Robert is not deployed. Megan also notes that the family is already negatively impacted by his recent drinking binge (e.g., conflict with his wife, missed soccer games). If Robert’s problematic drinking continues, he is at risk for evaluation and promotion issues. In stage 3, Megan reflects upon the ACA (2005) ethical codes in order to better understand her dilemma from a counselor’s view. Robert has a right to confidentiality (B.1.c., p. 7) with limitations including illegal substance use (B.1.d., p. 7). However, Robert’s current substance is alcohol, which is a legal substance. Megan considers the importance of his support network (A.1.d., p. 4) including his family and unit, but she does not have the ethical right to disclose her concerns about his substance abuse. In stage 4, Megan considers the pertinent laws and regulations of the dilemma. As per the clinic regulations, she is aware that if she makes a substance use program referral, it will be reflected in Robert’s record, which is the property of the military. Megan also is aware that Robert has not committed a documented crime of driving under the influence.
In stage 5 of the 10-stage ethical decision-making model, Megan must reflect on her personal thoughts and competencies. She is very concerned about Robert’s increased use of alcohol and is worried for his safety if deployed. Megan feels less confident in her ability to accurately assess for substance use problems. She facilitates the PTSD support group for the clinic, which is her specialty area. Megan recognizes that she is fond of Robert as a client and is disappointed that he could be jeopardizing his family and career with his alcohol abuse. She considers whether she is overreacting to his binge-drinking incident because of her higher expectations of him. In stage 6, Megan consults with her colleague who leads the substance use support groups at the clinic. She describes Robert’s recent abuse of alcohol and inquires as to whether he is a good candidate for the substance use group, needs more intense treatment, or needs no treatment at all. The colleague suggests that the group would be a very appropriate fit for someone with Robert’s symptoms.
In stage 7, Megan develops her course of action to refer Robert to the substance use group. Then, in stage 8, she evaluates the plan for potential impact on parties involved. Megan conceptualizes that Robert may be at risk for losing his deployment orders if he is accessing substance use treatment. Megan believes she has reduced this potential impact by referring to the substance support group, rather than an inpatient treatment facility, which may be more appropriate for a dependence issue. Megan recognizes that attending a 90-minute group each week will take Robert away from his family, but she also realizes that the 90-minute commitment is less than his current time spent away from the family when binge drinking. Megan reflects upon how her therapeutic relationship with Robert may be strained at the time of referral, and is prepared for a potential negative response from her client. She trusts in their therapeutic relationship and moves forward. In stage 9, Megan presents her planned course of action to her supervisor at the clinic. The supervisor approves the referral for the support group, but also suggests that Megan consider a referral to couples counseling for Robert and his wife, which may assist with resolving conflicts before the deployment.
In the final stage, Megan proposes the treatment plan of action to Robert in their next session. Megan explains that she feels ethically obligated to refer Robert to the substance use support group, and that as of now, Robert may make this choice for himself. Megan and Robert discuss the potential that substance use treatment may no longer be a choice in the future if his current drinking behavior continues. There is more discussion of fitness for duty and how participation in the support group will positively reflect upon the assessment in the future. Megan also presents Robert with the recommendation of couples counseling to help mediate relationship conflicts before deployment. She reports that if Robert and his wife decide to receive couples counseling, she can provide a referral for them at that time.
With the ethical decision-making models presented, the counselor is able to successfully navigate the military mental health system, while still maintaining the professional standards of the counseling profession. In each model, the situation is resolved with considerable attention to the client’s best interest, while maintaining the expectations of the military clinic. Psychologists developed the two ethical models presented, and counselors may choose to utilize these approaches until more counselor-specific ethical processes are created. As counselors become more permanent fixtures in the VA mental health system and as TRICARE providers, opportunities to develop an ethical decision-making model will likely arise.
Conclusion
The recent inclusion of counselors as mental health professionals within the VA system and as TRICARE providers allows for new employment opportunities with the military population. However, these new opportunities are not without potential dilemmas. Counselors interested in working with service members need to be educated on the potential conflict between counselor professional ethical guidelines and military protocols. Future research in the counseling field may develop a counselor-specific ethical decision-making model. In the meantime, counselors may utilize or adapt the ethical decision-making models created by other mental health professionals, who have a longer history working with the military population.
References
American Counseling Association. (2005). ACA code of ethics. Retrieved from http://www.counseling.org/Resources/aca-code-of-ethics.pdf
Barnett, J. E., & Johnson, W. B. (2008). The ethics desk reference for psychologists. Washington DC: American Psychological Association.
Barstow, S., & Terrazas, A. (2012, February). DoD releases TRICARE rule on independent practice for counselors. Counseling Today, 54(8), 10. Retrieved from
http://ct.counseling.org/2012/02/dod-releases-tricare-rule-on-independent-practice-for-counselors/
Garvey Wilson, A. L., Messer, S. C., & Hoge, C. W. (2009). U.S. military mental health care utilization and attrition prior to the wars in Iraq and Afghanistan. Social Psychiatry and Psychiatric Epidemiology, 44, 473–481. doi:10.1007/s00127-008-0461-7
Hall, L. (2011). The importance of understanding military culture. Social Work in Health Care, 50, 4–18. doi:10.1080/00981389.2010.513914
Hoge, C. W., Auchterlonie, J. L., & Milliken, C. S. (2006). Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. The Journal of the American Medical Association, 295(9), 1023–1032. doi:10.1001/jama.295.9.1023
Hoge, C. W., Castro, C. A., Messer, S. C., McGurk, D., Cotting, D. I., & Koffman, R. L. (2004). Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. The New England Journal of Medicine, 351(1), 13–22. doi:10.1056/NEJMoa040603
Holder, K. A. (2007). Comparison of ACS and ASEC data on veteran status and period of military service: 2007. U.S. Census Bureau: Housing and Household Economics Statistics Division. Retrieved from http://www.census.gov/hhes/veterans/files/comparison_report.pdf
Johnson, W. B. (2008). Top ethical challenges for military clinical psychologists. Military Psychology, 20, 49–62. doi:10.1080/08995600701753185
Johnson, W. B., Grasso, I., & Maslowski, K. (2010). Conflicts between ethics and law for military mental health providers. Military Medicine, 175, 548–553.
Johnson, W., & Wilson, K. (1993). The military internship: A retrospective analysis. Professional Psychology: Research and Practice, 24(3), 312–318. doi:10.1037/0735-7028.24.3.312
Kelly, M. M., Vogt, D. S., Scheiderer, E. M., Ouimette, P., Daley, J., & Wolfe, J. (2008). Effects of military trauma exposure on women veterans’ use and perceptions of Veterans Health Administration care. Journal of General Internal Medicine, 23, 741–747. doi:10.1007/s11606-008-0589-x
Kennedy, C. H., & Johnson, W. B. (2009). Mixed agency in military psychology: Applying the American Psychological Association ethics code. Psychological Services, 6(1), 22–31. doi:10.1037/a0014602
Kim, P. Y., Britt, T. W., Klocko, R. P., Riviere, L. A., & Adler, A. B. (2011). Stigma, negative attitudes about treatment, and utilization of mental health care among soldiers. Military Psychology, 23, 65–81. doi:10.1080/08995605.2011.534415
Martin, J., Ghahramanlou-Holloway, M., Lou, K., & Tucciarone, P. (2009). A comparative review of U.S. military and civilian suicide behavior: Implications for OEF/OIF suicide prevention efforts. Journal of Mental Health Counseling, 31(2), 101–118.
McCauley, M., Hacker Hughes, J., & Liebling-Kalifani, H. (2008). Ethical considerations for military clinical psychologists: A review of selected literature. Military Psychology, 20, 7–20. doi:10.1080/08995600701753128
O’Gorman, K. (2012, August 16). Army reports record suicides in July [Blog post]. Retrieved from http://iava.org/blog/army-reports-record-high-suicides-july
Reger, M. A., Etherage, J. R., Reger, G. M., & Gahm, G. A. (2008). Civilian psychologists in an army culture: The ethical challenge of cultural competence. Military Psychology, 20, 21–35. doi:10.1080/08995600701753144
Snell, F., & Tusaie, K. R. (2008). Veterans reported reasons for seeking mental health treatment. Archives of Psychiatric Nursing, 22(5), 313–314. doi:10.1016/j.apnu.2008.06.003
Stone, A. M. (2008). Dual agency for VA clinicians: Defining an evolving ethical question. Military Psychology, 20, 37–48. doi:10.1080/08995600701753177
Strom, T. Q., Gavian, M. E., Possis, E., Loughlin, J., Bui, T., Linardatos, E.,…Siegel, W. (2012). Cultural and ethical considerations when working with military personnel and veterans: A primer for VA training programs. Training and Education in Professional Psychology, 6(2), 67–75. doi:10.1037/a0028275
U.S. Census Bureau, American Community Survey. (2011). B21002: Period of military service for civilian veterans 18 years and over (2011 American Community Survey 1-year estimates). Retrieved from http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_11_1YR_B21002&prodType=table
U.S. Department of Defense. (n.d.). Enhanced post-deployment health assessment (PDHA) process (DD Form 2796). Retrieved from http://www.pdhealth.mil/dcs/dd_form_2796.asp
U.S. Department of Defense. (2012). Army releases July suicide data, No. 683-12. Retrieved from http://www.defense.gov/releases/release.aspx?releaseid=15517
U.S. Department of Defense. (2013). DOD, VA and HHS partner to expand access to mental health services for veterans, service members, and families, No. 353-13. Retrieved from http://www.defense.gov/releases/release.aspx?releaseid=16024
U.S. Department of Veterans Affairs. (n.d.). PTSD: National center for PTSD. Retrieved from http://www.ptsd.va.gov/professional/index.asp
U.S. Department of Veterans Affairs (2012, April). VA adding family therapists and mental health counselors to workforce. Retrieved from http://www.va.gov/opa/pressrel/pressrelease.cfm?id=2303
Elizabeth A. Prosek, NCC, is an Assistant Professor at the University of North Texas. Jessica M. Holm is a doctoral student at the University of North Texas. Correspondence can be addressed to Elizabeth A. Prosek, University of North Texas, 1155 Union Circle #310829, Denton, TX 76203-5017, elizabeth.prosek@unt.edu.