Feb 26, 2021 | Volume 11 - Issue 1
David E. Jones, Jennifer S. Park, Katie Gamby, Taylor M. Bigelow, Tesfaye B. Mersha, Alonzo T. Folger
Epigenetics is the study of modifications to gene expression without an alteration to the DNA sequence. Currently there is limited translation of epigenetics to the counseling profession. The purpose of this article is to inform counseling practitioners and counselor educators about the potential role epigenetics plays in mental health. Current mental health epigenetic research supports that adverse psychosocial experiences are associated with mental health disorders such as schizophrenia, anxiety, depression, and addiction. There are also positive epigenetic associations with counseling interventions, including cognitive behavioral therapy, mindfulness, diet, and exercise. These mental health epigenetic findings have implications for the counseling profession such as engaging in early life span health prevention and wellness, attending to micro and macro environmental influences during assessment and treatment, collaborating with other health professionals in epigenetic research, and incorporating epigenetic findings into counselor education curricula that meet the standards of the Council for Accreditation of Counseling and Related Educational Programs (CACREP).
Keywords: epigenetics, mental health, counseling, prevention and wellness, counselor education
Epigenetics, defined as the study of chemical changes at the cellular level that alter gene expression but do not alter the genetic code (T.-Y. Zhang & Meaney, 2010), has emerging significance for the profession of counseling. Historically, people who studied abnormal behavior focused on determining whether the cause of poor mental health outcomes was either “nature or nurture” (i.e., either genetics or environmental factors). What we now understand is that both nature and nurture, or the interaction between the individual and their environment (e.g., neglect, trauma, substance abuse, diet, social support, exercise), can modify gene expression positively or negatively (Cohen et al., 2017; Suderman et al., 2014).
In the concept of nature and nurture, there is evidence that psychosocial experiences can change the landscape of epigenetic chemical tags across the genome. This change in landscape influences mental health concerns, such as addiction, anxiety, and depression, that are addressed by counseling practitioners (Lester et al., 2016; Provençal & Binder, 2015; Szyf et al., 2016). Because the field of epigenetics is evolving and there is limited attention to epigenetics in the counseling profession, our purpose is to inform counseling practitioners and educators about the role epigenetics may play in clinical mental health counseling.
Though many counselors and counselor educators may have taken a biology class that covered genetics sometime during their professional education, we provide pedagogical scaffolding from genetics to epigenetics. Care was taken to ensure accessibility of information for readers across this continuum of genetics knowledge. Much of what we offer below on genetics is putative knowledge, as we desire to establish a foundation for the reader in genetics so they may be able to have a greater understanding of epigenetics and a clearer comprehension of the implications we offer leading to application in counseling. We suggest readers review Brooker (2017) for more detailed information on genetics. We will present an overview of genetics and epigenetics, an examination of mental health epigenetics, and implications for the counseling profession.
Genetics
Genetics is the study of heredity (Brooker, 2017) and the cellular process by which parents pass on biological information via genes. The child inherits genetic coding from both parents. One can think of these parental genes as a recipe book for molecular operations such as the development of proteins, structure of neurons, and other functions across the human body. This total collection of the combination of genes in the human body is called the genome or genotype. The presentation of observable human traits (e.g., eye color, height, blood type) is called the phenotype. Phenotypes can be seen in our clinical work through behavior (e.g., self-injury, aggression, depression, anxiety, inattentiveness).
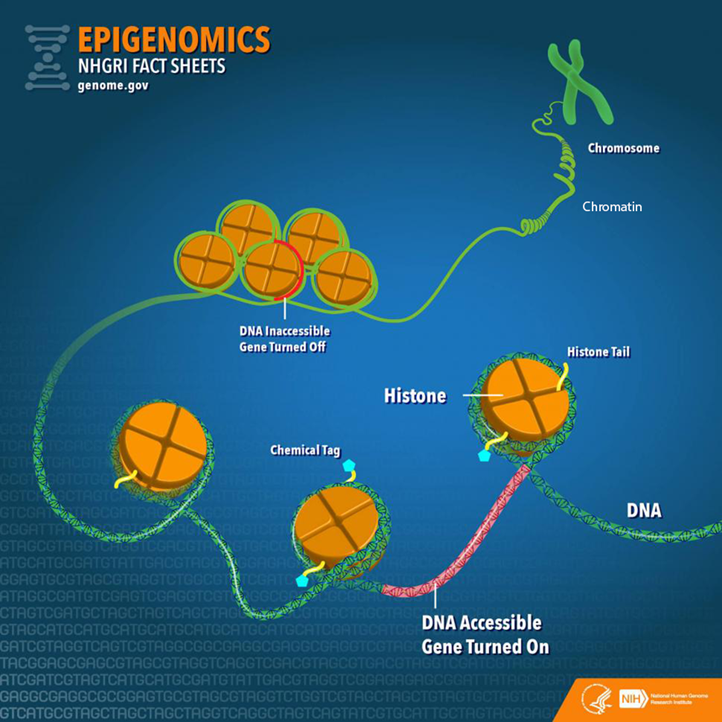
Before going further, it is important to establish a fundamental understanding of genetics by examining the varied molecular components and their relationships (Figure 1). Deoxyribonucleic acid (DNA) is a long-strand molecule that takes the famous double helix or ladder configuration. DNA is made up of four chemical bases called adenine (A), guanine (G), cytosine (C), and thymine (T). These form base pairs—A with T and C with G—creating a nucleic acid. The DNA is also wrapped around a specialized protein called a histone. The collection of DNA wrapped around multiple histones is called the chromatin. This wrapping process is essential for the DNA to fit within the cell nucleus. Finally, as this chromatin continues to grow, it develops a structure called a chromosome. Within every human cell nucleus, there are 23 chromosomes from each parent, totaling 46 chromosomes.
Figure 1
Gene Structure and Epigenetics
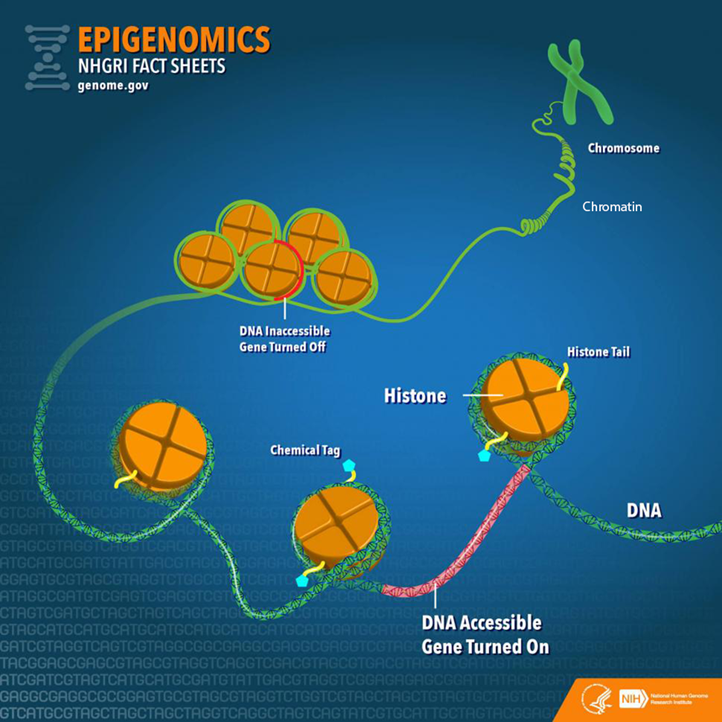
From “Epigenomics Fact Sheet,” by National Human Genome Research Institute, 2020
(https://www.genome.gov/about-genomics/fact-sheets/Epigenomics-Fact-Sheet). In the public domain.
Beyond the chromosomes, chromatin, histones, DNA, and genes, there is another key component in genetics: ribonucleic acid (RNA). RNA can be a cellular messenger that carries instructions from a DNA sequence (specific genes) to other parts of the cell (i.e., messenger RNA [mRNA]). RNA can come in several other forms as well, including transfer RNA (tRNA), microRNA (miRNA), and non-coding RNA (ncRNA). In the sections below, we elaborate on mRNA and tRNA and their impact on the genetic processes. Later in the epigenetics section, we provide fuller details on miRNA and ncRNA.
Besides the aforementioned biological aspects, it is important to understand that a child inherits genes from both parents, but they are not exactly the same genes, (i.e., alternative forms of the same gene may have differing expression). Different versions of the same gene are called alleles. Variation in an allele is one reason why we see phenotypic variation between our clients—height, weight, eye color—and this variation can contribute to mental disease susceptibility. Although there are many potential causes of poor mental health, family history is often one of the strongest risk factors because family members most closely represent the unique genetic and environmental interactions that an individual may experience. We also see this as a function of intergenerational epigenetic effects, which are covered later in this paper.
Transcription and Translation
Now that we have provided a foundation of the genetic components, we move toward the primary two-stage processes of genetics: transcription and translation (Brooker, 2017). The first step in the process of gene expression is called transcription. Transcription occurs when a sequence of DNA is copied using RNA polymerase (“ase” notes that it is an enzyme) to make mRNA for protein synthesis. We can liken transcription to the process of someone taking down information from a client’s voicemail message. In this visualization, DNA is the caller, the person writing down the message is the RNA polymerase, and the actual written message is the RNA.
A particular section of a gene, called a promotor region, is bound by the RNA polymerase (Brooker, 2017). The RNA polymerase acts like scissors to separate the double-stranded DNA helix into two strands. One of the strands, called the template, is where the RNA polymerase will read the DNA code A to T, and G to C to build mRNA. There are other modifications that must occur in eukaryotic cells such as splicing introns and exons. In short, sections of unwanted DNA, called introns, are removed by the process of splicing, and the remaining DNA codes are connected back together (exons).
Now that the mRNA has been created by the process of transcription, the next step is for the mRNA to build a protein necessary for the main functions of the body, in a process known as translation (Brooker, 2017). Here, translation is the process in which tRNA decodes or translates the mRNA into a protein in a mobile cellular factory called the ribosome. It is translating the language of a DNA sequence (gene) into the language of a protein. To do this, the tRNA uses a translation device called an anticodon. This anticodon links to the mRNA-based pairs called a codon. A codon is a trinucleotide sequence of DNA or RNA that corresponds to a specific amino acid, or building block of a protein. This process then continues to translate and connect many amino acids together until a polypeptide (a long chain of amino acids) is created. Later, these polypeptides join to form proteins. Depending on the type of cell, the protein may function in a variety of ways. For example, the neuron has several proteins for its function, and different proteins are used for memory, learning, and neuroplasticity.
Epigenetics
There is a wealth of research conducted on genetics, yet the understanding of epigenetics is more limited when focusing on mental health (Huang et al., 2017). Though the term epigenetics has been around since the 1940s, the “science” of epigenetics is in its youth. Epigenetic research in humans has grown in the last 10 years and continues to expand rapidly (Januar et al., 2015). The key concept for counselors to remember about epigenetics is that epigenetics supports the idea of coaction. Factors present in the client’s external environment (e.g., stress from caregiver neglect, foods consumed, drug intake like cigarettes) influence the expression of their genes (transcription and translation) and thus cell activity and related behavioral phenotypes. In the sections below, we will dive deeper into the understanding of epigenetic mechanisms and define key terms including epigenome, chromatin, and chemical modifications.
To start, the more formal definition of epigenetics is the differentiation of gene expression via chemical modifications upon the epigenome that do not alter the genetic code (i.e., the DNA sequence; Szyf et al., 2007). The epigenome, which is composed of chromatin (the combination of DNA and protein forming the chromosomes) and modification of DNA by chemical mechanisms (e.g., DNA methylation, histone modification), programs the process of gene expression (Szyf et al., 2007). The epigenome differs from the genome in that the chemical actions or modifications are on the outside of the genome (i.e., the DNA) or “upon” the genome. Specifically, epigenetic processes act “upon” the genome, which may open or close the chromatin to various degrees to govern access for reading DNA sequences (Figure 1). When the chromatin is opened, transcription and translation can take place; however, when the chromatin is closed, gene expression is silenced (Syzf et al., 2007).
It is important for counselors to conceptualize their client’s psychosocial environment in conjunction with the observed behavioral phenotypes, in that the client’s psychosocial environment may have partially mediated epigenetic expression (Januar et al., 2015). For example, with schizophrenia, a client’s adverse environment (e.g., early childhood trauma) influences the epigenome, or gene expression, which may contribute up to 60% of this disorder’s development (Gejman et al., 2011). Other adverse environmental influences have been associated with the development of schizophrenia, including complications during client’s prenatal development and birth, place and season of client’s birth, abuse, and parental loss (Benros et al., 2011). As we highlight below, epigenetic mechanisms (e.g., DNA methylation) may mediate between these environmental influences and genes with outcomes like schizophrenia (Cariaga-Martinez & Alelú-Paz, 2018; Tsankova et al., 2007).
Epigenetic Mechanisms
There are a variety of chemical mechanisms or tags that change the chromatin structure (either opening for expression or closing to inhibit expression). Some of the most investigated mechanisms for changes in chromatin structure are DNA methylation, histone modification, and microRNA (Benoit & Turecki, 2010; Maze & Nestler, 2011).
DNA Methylation. Methylation is the most studied epigenetic modification (Nestler et al., 2016). It occurs when a methyl group binds to a cytosine base (C) of DNA to form 5-methylcytosine. A methyl group is three hydrogens bonded to a carbon, identified as CH3. Most often, the methyl group is attached to a C followed by a G, called a CpG. These methylation changes are carried out by specific enzymes called DNA methyltransferase. These enzymes add the methyl group to the C base at the CpG site.
Methylation was initially considered irreversible, but recent research has shown that DNA methylation is more stable compared to other chemical modifications like histone modification and is therefore reversible (Nestler et al., 2016). This DNA methylation adaptability evidence is important, conceivably supporting counseling efficacy across the life span. If methylation is indeed reversible beyond 0 to 5 years of age, counseling efforts hold promise to influence mental health outcomes across the life span.
Beyond noted stability, DNA methylation is also important in that it is tissue-specific, meaning it assists in cell differentiation; it may regulate gene expression up or down and is influenced by different environmental exposures (Monk et al., 2012). For example, DNA methylation represses specific areas of a neuron’s genes, thus “turning off” their function. This stabilizes the cell by preventing any tissue-specific cell differentiation and inhibits the neuron from changing into another cell type (Szyf et al., 2016), such as becoming a lung cell later in development.
When looking at up- or downregulation, Oberlander et al. (2008) provided an example from a study using mice. When examining attachment style in mice, they found that decreased quality of mothering to offspring increased risk of anxiety, in part, because of the methylation at the glucocorticoid receptor (GR) gene and fewer GR proteins produced by the hippocampus. This change may lead to lifelong silencing or downregulation with an increased risk of anxiety to the mouse over its life span. Stevens et al. (2018) also established a link between diet, epigenetics, and DNA methylation. They found an epigenetic connection between poor dietary intake with increased risk of behavioral problems and poor mental health outcomes such as autism. The authors also remarked that further investigation is required for a clearer picture of this link and potential effects.
Histone Modification. Another process that has been extensively researched is post-translational histone modification, or changes in the histone after the translation process. The most understood histone modifications are acetylation, methylation, and phosphorylation (Nestler et al., 2016). Acetylation, the most common post-translational modification, occurs by adding an acetyl group to the histone tail, such as the amino acid lysine. The enzymes responsible for histone acetylation are histone acetyltransferases or HATs (Haggarty & Tsai, 2011). Conversely, histone deacetylases (HDACs) are enzymes that remove acetyl groups (Saavedra et al., 2016). The acetylation process promotes gene expression (Nestler et al., 2016).
Through histone methyltransferases (HMTs), histone methylation increases methylation, thereby reducing gene expression. Histone demethylases (HDMs) remove methyl groups to increase gene activity. Phosphorylation can increase or decrease gene expression. Overall, there are more than 50 known histone modifications (Nestler et al., 2016).
From a counseling perspective, it is important to note that histone modification is flexible. Unlike DNA methylation, which is more stable over a lifetime, histone modifications are more transient. To illustrate, if an acetyl group is added to a histone, it may loosen the binding between the DNA and histone, increasing transcription and thereby allowing gene expression across the life span (Nestler et al., 2016). Such acetylation processes have been found in maternal neglect to offspring (early in the life span) and mindfulness practices in adult clients (Chaix et al., 2020; Devlin et al., 2010). Yet, although histone modification can be changed across the life span (Nestler et al., 2016), it is still important for counselors to recognize the importance of early counseling interventions because of how highly active epigenetics mechanisms (e.g., DNA methylation) are in children 0 to 5 years of age.
MicroRNA. Beyond histone modification, another known mechanism is microRNA (miRNA), which is the least understood and most recently investigated epigenetic mechanism when compared to DNA methylation and histone modification (Saavedra et al., 2016). miRNA is one type of non-coding RNA (ncRNA), or RNA that is changed into proteins. Around 98% of the genome does not code for proteins, leading to a supporting hypothesis that ncRNAs play a significant role in gene expression. For example, humans and chimpanzees share 98.8% of the same DNA code. However, epigenetics and specifically ncRNA contribute to the wide phenotypic variation between the species (Zheng & Xiao, 2016). Further, Zheng and Xiao (2016) estimated that miRNA regulates up to 60% of gene expression.
miRNA has also been found to suppress and activate gene expression at the levels of transcription and translation (Saavedra et al., 2016). miRNAs affect gene expression by directly influencing mRNA. Specifically, the miRNA may attach to mRNA and “block” the mRNA from creating proteins or it may directly degrade mRNA. This then decreases the surplus of mRNA in the cell. If the miRNA binds partially with the mRNA, then it inhibits protein production; but if it binds completely, it is marked for destruction. Once the mRNA is identified for destruction, other proteins and enzymes are attracted to the mRNA, and they degrade the mRNA and eliminate it (Zheng & Xiao, 2016). Moreover, when compared to DNA methylation, which may be isolated to a single gene sequence, miRNA can target hundreds of genes (Lewis et al., 2005). Researchers have discovered that miRNA may mediate anxiety-like symptoms (Cohen et al., 2017).
Human Development and Epigenetics
Over the life of an individual, there are critical or sensitive periods in which epigenetic modifications are more heavily influenced by environmental factors (Mulligan, 2016). Early life (ages 0 to 5 years) appears to be one of the most critical time periods when epigenetics is more active. An example of this is the Dutch Famine of 1944–45, also known as the Dutch Hunger Winter (Champagne, 2010; Szyf, 2009). The Nazis occupied the Netherlands and restricted food to the country, bringing about a famine. The individual daily caloric intake estimate varied between 400 and 1800 calories at the climax of the famine. Most notably, women who gave birth during this time experienced the impact of low maternal caloric intake, which impacted their child and the child’s health outcomes into adulthood. One discovery was that male children had a higher risk of adulthood obesity if their famine exposure occurred early in gestation versus a male fetus who experienced famine in late gestation. Findings suggested that fetuses who experienced restricted caloric intake during the development of their autonomic nervous system may have an increased risk of heart disease in adulthood. The findings of epigenetic mechanisms at work between mother and child during a famine are flagrant enough, yet epigenetic researchers have also discovered that epigenetic tags carry across generations, called genomic imprinting (Arnaud, 2010; Yehuda et al., 2016; T.-Y. Zhang & Meaney, 2010).
Genomic imprinting can be defined as the passing on of certain epigenetic modifications to the fetus by parents (Arnaud, 2010). It is allele-specific, and approximately half of the imprinting an offspring receives is from the mother. The imprinting mechanism marks certain areas, or loci, of offspring’s genes as active or repressed. For instance, the loci may exhibit increased or decreased methylation.
An imprinting example is evident in the IGF-2 (insulin-like growth factor II) gene and those fetuses exposed to the Dutch Hunger Winter (Heijmans et al., 2008). Sixty years after the famine, a decrease in DNA methylation on IGF-2 was found in adults with fetal exposure during the famine compared to their older siblings. Researchers also found these intergenerational imprinting effects associated with the grandchildren of women who were pregnant during the Dutch Hunger Winter. Similar imprinting is also apparent in Holocaust survivors (Yehuda et al., 2016) and children born to mothers who experienced PTSD from the World Trade Center collapse of 9/11 (Yehuda et al., 2005). These imprinting mechanisms are important for counselors to understand in that we see the interplay between the client and the environment across generations. The client becomes the embodiment of their environment at the cellular level. This is no longer the dichotomous “nature vs. nurture” debate but the passing on of biological effects from one generation to another through the interplay of nature and nurture.
Epigenetics and Mental Health Disorders
Now we turn our focus to the influence of epigenetics on the profession of counseling. What we do know is that epigenetic mechanisms, (e.g., DNA methylation, histone modifications, miRNA) are associated with various mental health disorders. It is hypothesized that epigenetics contributes to the development of mental disorders after exposure to environmental stressors, such as traumatic life events, but it may also have positive effects based on salutary environments (Syzf, 2009; Yehuda et al., 2005). We will review only those mental health epigenetic findings that have significant implications relative to clinical disorders such as stress, anxiety, childhood maltreatment, depression, schizophrenia, and addiction. We will also offer epigenetic outcomes associated with treatment, including cognitive behavioral therapy (CBT; Roberts et al., 2015), meditation (Chaix et al., 2020), and antidepressants (Lüscher & Möhler, 2019).
Stress and Anxiety
Stress, especially during early life stages, causes long-term effects for neuronal pathways and gene expression (Lester et al., 2016; Palmisano & Pandey, 2017; Perroud et al., 2011; Roberts et al., 2015; Szyf, 2009; T.-Y. Zhang & Meaney, 2010). Currently, research supports the mediating effects of stress on epigenetics through DNA methylation, especially within the gestational environment (Lester & Marsit, 2018). DNA methylation has been associated with upregulation of the hypothalamic-pituitary-adrenal (HPA) axis, increasing anxiety symptoms (McGowan et al., 2009; Oberlander et al., 2008; Romens et al., 2015; Shimada-Sugimoto et al., 2015; Tsankova et al., 2007). DNA methylation has also been linked with increased levels of cortisol for newborns of depressed mothers. This points to an increased HPA stress response in the newborn (Oberlander et al., 2008). Ouellet-Morin et al. (2013) also looked at DNA methylation and stress. They conducted a longitudinal twin study on the effect of bullying on the serotonin transporter gene (SERT) for monozygotic twins and found increased levels of SERT DNA methylation in victims compared to their non-bullied monozygotic co-twin. Finally, Roberts et al. (2015) examined the effect of CBT on DNA methylation for children with severe anxiety, specifically testing changes in the FKBP5 gene. Although the results were not statistically significant, they may be clinically significant. Research participants with a higher DNA methylation on the FKBP5 gene had poorer response to CBT treatment.
Beyond DNA methylation, other researchers have investigated miRNA and its association with stress and anxiety. A study by Harris and Seckl (2011) found that fetal rodents with increased exposure to maternal cortisol suffered from lower birth weights and heightened anxiety. Similarly, Cohen et al. (2017) investigated anxiety in rats for a specific miRNA called miR-101a-3p. The researchers selectively bred rats, one group with low anxiety and the other with high anxiety traits. They then overexpressed miR-101a-3p in low-anxiety rats to see if that would induce greater expressions of anxiety symptomatology. The investigators observed increased anxiety behaviors when increasing the expression of miR-101a-3p in low-anxiety rats. The researchers postulated that miRNA may be a mediator of anxiety-like behaviors. Finally, paternal chronic stress in rats has been associated with intergenerational impact on offspring’s HPA axis with sperm cells having increased miRNAs, potentially indicating susceptibility of epigenetic preprogramming in male germ cells post-fertilization (Rodgers et al., 2013). The evidence suggests that paternal stress reprograms the HPA stress response during conception. This reprogramming may begin a cascading effect on the offspring’s HPA, creating dysregulation that is associated with disorders like schizophrenia, autism, and depression later in adulthood.
Though some researchers have indicated a negative association between anxiety and epigenetics, others have found positive effects between epigenetics and anxiety. A seminal study by Weaver et al. (2005) illustrated the flexibility of an offspring’s biological system to negative and positive environmental cues. Weaver et al. looked at HPA response of rodent pups who received low licking and grooming from their mother (a negative environmental effect) who exhibited higher HPA response to environmental cues in adulthood. Epigenetically, they found lower DNA methylation in a specific promotor region in these adult rodents. They hypothesized that they could reverse this hypomethylation by giving an infusion of methionine, an essential amino acid that is a methyl group donor. They discovered the ability to reverse low methylation, which improved the minimally licked and groomed adult rodents’ response to stress. This connects with counseling in that epigenetic information is not set for life but reversible through interventions such as diet.
Others have investigated mindfulness and its epigenetic effects on stress. Chaix et al. (2020) looked at DNA methylation at the genome level for differences between skilled meditators who meditated for an 8-hour interval compared to members of a control group who engaged in leisure activities for 8 hours. The control group did not have any changes in genome DNA methylation, but the skilled meditators showed 61 differentially methylated sites post-intervention. This evidence can potentially support the use of mindfulness with our clients as an intervention for treatment of stress.
Childhood Maltreatment
Childhood maltreatment includes sexual abuse, physical abuse and/or neglect, and emotional abuse and/or neglect. Through this lens, Suderman et al. (2014) examined differences in 45-year-old males’ blood samples between those who experienced abuse in childhood and those who did not, with the aim of determining whether gene promoter DNA methylation is linked with child abuse. After 30 years, the researchers found different DNA methylation patterns between abused versus non-abused individuals and that a specific hypermethylation of a gene was linked with the adults who experienced child abuse. Suderman et al. (2014) believed that adversity, such as child abuse, reorganizes biological pathways that last into adulthood. These DNA methylation differences have been associated with biological pathways leading to cancer, obesity, diabetes, and other inflammatory paths.
Other researchers have also found epigenetic interactions at CpG sites predicting depression and anxiety in participants who experienced abuse. Though these interactions were not statistically significant (Smearman et al., 2016), increased methylation at specific promoter regions was discovered (Perroud et al., 2011; Romens et al., 2015). Furthermore, in a hallmark study, McGowan et al. (2009) discovered that people with child abuse histories who completed suicide possessed hypermethylation of a particular promotor region when compared to controls. Perroud et al. (2011) noted that frequency, age of onset, and severity of maltreatment correlated positively with increased methylation in adult participants suffering from borderline personality disorder, depression, and PTSD. Yehuda et al. (2016) reported that in a smaller subset of an overall sample of Holocaust survivors, the impact of trauma was intergenerationally associated with increased DNA methylation. Continued study of these particular regions may provide evidence of DNA methylation as a predictor of risk in developing anxiety or depressive disorders.
Major Depressive Disorder
Most studies of mental illness, genetics, and depression have used stress animal models. Through these models, histone modification, chromatin remodeling, miRNA, and DNA methylation mechanisms have been found in rats and mice (Albert et al., 2019; Nestler et al., 2016). When an animal or human experiences early life stress, epigenetic biomarkers may serve to detect the development or progression of major depressive disorder (Saavedra et al., 2016). Additionally, histone modification markers may also indicate an increase in depression (Tsankova et al., 2007; Turecki, 2014). Beyond animal models, Januar et al. (2015) found that buccal tissue in older patients with major depressive disorder provided evidence that the BDNF gene modulates depression through hypermethylation of specific CpGs in promoter regions.
Lastly, certain miRNAs may serve as potential biomarkers for major depressive disorder. miRNA may be used in the pharmacologic treatment of depressive disorders (Saavedra et al., 2016). Tsankova et al. (2007) and Saavedra et al. (2016) noted that certain epigenetic mechanisms that influence gene expression may be useful as antidepressant treatments. Medication may induce neurogenesis and greater plasticity in synapses through upregulation and downregulation of miRNAs (Bocchio-Chiavetto et al., 2013; Lüscher & Möhler, 2019). This points to the potential use of epigenetic “engineering” for reducing depression progression and symptomology where a counselor could refer a client for epigenetic antidepressant treatments.
Maternal Depression
Maternal prenatal depression may program the postnatal HPA axis in infants’ responses to the caretaking environment. Such programming may result in decreased expression of certain genes associated with lesser DNA methylation in infants, depending on which trimester maternal depression was most severe, and increased HPA reactivity (Devlin et al., 2010). Further, Devlin et al. discovered that maternal depression in the second trimester affected newborns’ DNA methylation patterns. However, the authors offered key limitations in their study, namely the sample was predominantly male and depressive characteristics differed based on age. Conradt et al. (2016) reported that prenatal depression in mothers may be associated with higher DNA methylation in infants. However, maternal sensitivity (i.e., ability of mother to respond to infants’ needs positively, such as positive touch, attending to distress, and basic social-emotional needs) toward infants buffered the extent of methylation, which points to environmental influences. This finding highlights the risk of infant exposure to maternal depression in conjunction with maternal sensitivity. Yet, overall, the evidence suggests that epigenetic mechanisms are at play across critical periods—prenatal, postnatal, and beyond—that have implications for offspring. When a fetus or offspring experiences adverse conditions, such as maternal depression, there is an increased likelihood of “impaired cognitive, behavioral, and social functioning . . . [including] psychiatric disorders throughout the adult life” (Vaiserman & Koliada, 2017, p. 1). For the practicing counselor, we suggest that clinical work with expecting mothers has the potential to reduce such risk based on these epigenetic findings.
Schizophrenia
Accumulated evidence suggests that schizophrenia arises from the interaction between genetics and the client’s environment (Smigielski et al., 2020). Epigenetics is considered a mediator between a client’s genetics and environment with research showing moderate support for this position. DNA methylation, histone modifications, mRNA, and miRNA epigenetic mechanisms have been linked with schizophrenia (Boks et al., 2018; Cheah et al., 2017; Okazaki et al., 2019).
DNA methylation is a main focus in schizophrenia epigenetic research (Cariaga-Martinez & Alelú-Paz , 2018). For example, Fisher et al. (2015) conducted a longitudinal study investigating epigenetic differences between monozygotic twins who demonstrated differences in psychotic symptoms; at age 12, one twin was symptomatic and the other was asymptomatic. Fisher et al. found DNA methylation differences between these twins. The longitudinal twin study design allowed for the control of genetic contributions to the outcome as well as other internal and external threats. Further, it pointed to a stronger association between epigenetics and schizophrenia.
From a clinical perspective, Ma et al. (2018) identified a potential epigenetic biomarker for detecting schizophrenia. The authors were able to identify three specific miRNAs that may work in combination as a biomarker for the condition. According to the authors, this finding may be helpful in the future for diagnosis and monitoring treatment outcomes. We speculate that future counselors may have biomarker tests conducted as part of the diagnostic process and in monitoring treatment effectiveness with alternation in miRNA levels.
Addiction
In addictions, a diversity of epigenetic mechanisms have been identified (e.g., DNA methylation, histone acetylation, mRNA, miRNA) across various substance use disorders: cocaine, amphetamine, methamphetamine, and alcohol (Hamilton & Nestler, 2019). Moreover, these epigenetic processes have been hypothesized to contribute to the addiction process by mediating seeking behaviors via dopamine in the neurological system. Also, Hamilton and Nestler (2019) found that epigenetic mechanisms have the potential to combat addiction processes, but further research is needed.
Cadet et al. (2016) conducted a review of cocaine, methamphetamine, and epigenetics in animal models (mice and rats). Chronic cocaine use was linked with histone acetylation in the dopamine system and DNA methylation for both chronic and acute administrations. They concluded that epigenetics may be a facilitating factor for cocaine abuse. Others have supported this conclusion for cocaine specifically, in that cocaine alters the chromatin structure by increasing histone acetylation, thereby temporarily inducing addictive behaviors (Maze & Nestler, 2011; Tsankova et al., 2007). From a treatment perspective, Wright et al. (2015) reported, in a sample of rats, that an injected methyl supplementation appeared to attenuate cocaine-seeking behavior when compared to the control group associated with cocaine-induced DNA methylation.
Regarding methamphetamines, during their review, Cadet et al. (2016) discovered that there were only a few extant studies on epigenetics and methamphetamines. Numachi et al. (2004) linked extended use of methamphetamines to changes in DNA methylation patterns, which seemed to increase vulnerability to neurochemical effects. More recently, Jayanthi et al. (2014) discovered that chronic methamphetamine use in rats induced histone hypoacetylation, making it more difficult for transcription to occur and potentially supporting the addiction process. To counter this histone hypoacetylation, the authors treated the mice with valproic acid, which inhibited the histone hypoacetylation. This study may evidence potential psychopharmacological treatments in the future at the epigenetic level for methamphetamine addiction.
H. Zhang and Gelernter (2017) reviewed the literature on DNA methylation and alcohol use disorder (AUD) and found mixed results. The authors discovered that individuals with an AUD exhibited DNA hypermethylation and hypomethylation in a variety of promoter regions. They also noted generalization limitations due to small tissue samples from the same regions of postmortem brains. They suggested that DNA methylation may account for “missing heritability” (p. 510) among individuals with AUDs.
Histone deacetylation has also been connected to chromatin closing or silencing for chronic users of alcohol, which may be involved in the maintenance of an AUD. Palmisano and Pandey (2017) suggested that there are epigenetic mediating factors between comorbidity of AUDs and anxiety disorders. On a positive note, exercise has been found to have opposite epigenetic modifications when comparing a healthy exercise group to a group who experience AUDs in terms of DNA methylation at CpG sites (Chen et al., 2018). Thus, counselors may incorporate such aspects in psychoeducation when recommending exercise in goal setting and other treatment interventions.
To summarize, epigenetics has been linked to several disorders such as anxiety, stress, depression, schizophrenia, and addiction (Albert et al., 2019; Cadet et al., 2016; Lester et al., 2016; Palmisano & Pandey, 2017; Smigielski et al., 2020). DNA methylation and miRNA may have mediating effects for mental health concerns such as anxiety (Harris & Seckl, 2011; Romens et al., 2015). Additionally, epigenetic mediating effects have also been discovered in major depressive disorder, maternal depression, and addiction (Albert et al., 2019; Conradt et al., 2016; Hamilton & Nestler, 2019). Moreover, epigenetic imprinting has been associated with trauma and stress, as found in Holocaust survivors and their children (Yehuda et al., 2016). Overall, “evidence accumulates that exposure to social stressors in [childhood], puberty, adolescence, and adulthood can influence behavioral, cellular, and molecular phenotypes and . . . are mediated by epigenetic mechanisms” (Pishva et al., 2014, p. 342).
Implications
A key aim in providing a primer on epigenetics, specifically the coaction between a client’s biology and environment on gene expression, is to illuminate opportunities for counselors to prevent and intervene upon mental health concerns. This is most relevant based on the evidence that epigenetic processes change over a client’s lifetime because of environmental influences, meaning that the client is not in a fixed state per traditional gene theory (Nestler et al., 2016). Epigenetics provides an alternate view of nature and nurture, demonstrating that epigenetic tags may not only be influenced by unfavorable environmental influences (e.g., maternal depression, trauma, bullying, child abuse and neglect) but also by favorable environments and activities (e.g., mindfulness, CBT, exercise, diet, nurturing; Chaix et al., 2020; Chen et al., 2018; Conradt et al., 2016; Roberts et al., 2015; Stevens et al., 2018). Understanding the flexibility of epigenetics has the potential to engender hope for our clients and to guide our work as counselors and counselor educators, because our genetic destinies are not fixed as we once theorized in gene theory.
Bioecological Conceptualization: Proximal and Distal Impact and Interventions
The impact of epigenetics on the counseling profession can be understood using Bronfenbrenner’s (1979) bioecological model. The bioecological model conceptualizes a client’s function over time based on the coaction between the client and their environment (Broderick & Blewitt, 2015; Jones & Tang, 2015). The client’s environment can have both beneficial and deleterious proximal and distal effects. These effects are like concentric rings around the client, which Bronfenbrenner called “subsystems.” The most proximate subsystem is the microsystem, the environment that has a direct influence on the client, such as parents, teachers, classmates, coworkers, relatives, etc. The next level is the mesosystem, in which the micro entities interact with one another or intersect with influence on the client (e.g., school and home intersect to influence client’s thinking and behavior). The next system, called the exosystem, begins the level of indirect influence. This may include neighborhood factors such as the availability of fresh produce, safe neighborhoods, social safety net programs, and employment opportunities. The last subsystem is the macrosystem. This system consists of the cultural norms, values, and biases that influence all other systems. The final aspect of this model, called the chronosystem, takes into account development over time. The chronosystem directs the counselor’s attention to developmental periods that have differing risks and opportunities, or what can be called “critical” developmental periods.
Below we conceptualize epigenetic counseling implications using Bronfenbrenner’s model but simplify it by grouping systems: proximal effects (micro/meso level) labeled as micro effects and distal effects (exo/macro level) labeled as macro effects. We will also apply the chronosystem by focusing on critical developmental periods that are salient when applying epigenetics to counseling. Ultimately, our central focus is the client and the concentric influences of micro and macro effects. To begin, we will first focus on the important contribution of epigenetics during the critical developmental period of 0 to 5 years of age with implications at the micro and macro levels.
Epigenetics Supports Early Life Span Interventions
Though the evidence does support epigenetic flexibility across a client’s life span, we know that early adverse life events may alter a child’s epigenome with mediating effects on development and behavior (Lester & Marsit, 2018). We also know that epigenetic processes are most active in the first 5 years of life (Mulligan, 2016; Syzf et al., 2016). These early insults to the genome may elicit poor mental health into adulthood such as anxiety, depression, schizophrenia, and addiction. For example, a client who grew up in an urban environment with a traditionally marginalized group status and parents who experienced drug dependence has an increased risk for schizophrenia above and beyond the genetic, inherited risk. These adverse childhood experiences have the potential to modify the epigenome, increasing the likelihood of developing mental health concerns, including schizophrenia (Cariaga-Martinez & Alelú-Paz, 2018).
At the micro level, the caregiver can be a salutary effect against adverse environmental conditions (Oberlander et al. 2008; Weaver et al., 2005). Prenatally, counseling can work with parents before birth to generate healthy coping strategies (e.g., reduce substance abuse), flexible and adaptive caregiver functioning, and effective parenting strategies. An example of this is to use parent–child interactive therapy (PCIT) pre-clinically, or before the child evidences a disorder (Lieneman et al., 2017). Preventive services using PCIT have been documented as effective with externalizing behaviors, child maltreatment, and developmental delays. Additional micro-level interventions can be found in the use of home-visiting programs to improve child outcomes prenatally to 5 years of age where positive parenting and other combined interventions are utilized to improve the health of mother, father, and child (Every Child Succeeds, 2019; Healthy Families New York, 2021).
Clinically, epigenetics points to earlier care and treatment to prevent the emergence of mental disorders (e.g., major depressive disorder, schizophrenia). Also, epigenetic research has provided evidence that environmental change can be equally important as client change. Regarding treatment planning, examining the client’s individual level factors or microsystem (e.g., physical health, mental status, education, race, gender) as well as their macrosystem (e.g., social stigma, poverty, housing quality, green space, pollution) may be crucial before considering what kind of modifications and/or interventions are most appropriate. For example, if a 9-year-old White female presents to a counselor for behavioral concerns in school, it is important for the counselor to gather a holistic life history to build an informed picture of the many variables collectively impacting the child’s behavior at each level. At the micro level, a counselor will evaluate for childhood maltreatment, but from an epigenetic lens, other proximal environmental factors could be important to screen for such as poverty, maternal depression, nutrition, classroom dynamics, and exercise (McEwen & McEwen, 2017; Mulligan, 2016). If the 9-year-old child is experiencing parental neglect and food insecurity, the clinician can treat the client’s individual needs at the micro level (i.e., working with the family system to overcome any neglect by using treatments such as PCIT, and direct referral to social workers and other agencies to provide food and shelter to meet basic needs).
The science of epigenetics may also inform action taken during assessment and case conceptualization based on the coaction of environment with a client over time. Although intervention at 0–5 years of age is most preventative, it is not practical in all cases. Using assessments that collect information on an adult client’s early life may help inform case conceptualization and allow the integration of epigenetics into counseling theories to better understand the etiology of a client’s presenting problem(s). For example, using an adverse childhood experiences assessment may help identify individuals at higher risk of epigenetic concerns. Epigenetics highlights the impact of client–environment interaction and its influence (positive or negative) on overall health. Additionally, early life adversity increases the likelihood of poor health outcomes such as heart disease, anxiety, and depression. However, these poor consequences could be mediated by talking with clients about the importance of exercise and its benefit on epigenetics and, by extension, mental health.
At the macro level, examples could include the reduction of hostile environments (e.g., institutional racism, neighborhood violence, limited employment opportunities, low wages, air pollutants, water pollutants), advocacy for statutes, regulations to decrease instability such as unfair housing in low-income neighborhoods, establishing partnerships in the development of community-based and school-based prevention programs, and applying early interventions such as mindfulness to reduce the effects of stress (Chaix et al., 2020). To illustrate, postnatal depression symptom severity has been associated with residential stability (Jones et al., 2018). By developing policies that would increase housing security, a reduction in maternal depression symptom severity could potentially reduce the DNA methylation that is associated with upregulation of the HPA and child reactivity, but this would need to be investigated further for confirmation. According to Rutten et al. (2013), this change may also increase the resiliency of children by reducing their experience of chronic stress, as sustained maternal depression severity often impacts caregiving because of unstable housing.
Although members of the counseling profession have known the significance of early intervention for years, this epigenetic understanding confirms why human growth and development is a core component of our counseling professional identity (Remley & Herlihy, 2020) and provides a supporting rationale for our efforts. Additionally, epigenetic tags have the potential to cross generations via the process of imprinting (Yehuda et al., 2016). This has potential implications across the life span.
In summary, critical developmental periods must be a focal point for counseling interventions, necessitating upstream action rather than our current dominant approach of downstream activities and a shift toward primary prevention over predominantly tertiary prevention. Such primary prevention would reduce stress and trauma for children before signs and symptoms become apparent and attend to the development and sustainability of healthy environments that would increase both client and community wellness.
Epigenetics Supports Counseling Advocacy and Social Justice Efforts
When reflecting on the implications of epigenetics, it is apparent that place, context, and the client’s environment are critical factors for best positioning them for healthy outcomes, engendering a push for advocacy and social justice for clients. Because environments have no boundaries, it is important to think of advocacy across many systems: towns, counties, states, countries, and the world. This reinforces the call for counselors and counselor educators to move beyond the walls of their workplaces in order to collaborate within the larger mental health field (e.g., clinical mental health, school, marriage and family, addiction, rehabilitation). Additionally, said knowledge compels connection with other professions—such as social workers, physicians, psychologists, engineers, housing developers, public health administrators, and members of nonprofit and faith-based organizations, etc.—to enact change on a wider scale and to improve the conditions for clients at a systemic level.
This collaboration also calls for engaging at local and international levels. Global human rights issues such as sex trafficking cross countries, regions, and local communities and necessitate collaboration to ameliorate these practices and the associated trauma. For starters, the American Counseling Association and the International Association for Counseling could partner with other organizations such as the Child Defense Fund to assist in meeting their mission to level the playing field for all children in the United States. At the local level, counselors and counselor educators could collaborate with local children’s hospitals and configure a plan to meet common goals to improve children’s health and wellness.
Counseling Research and Epigenetics
Research primarily affects clients on a macro level but can trickle down to directly engage clients within our clinical work and practice. Counselors and counselor educators can partner with members of other disciplines to further the work with epigenetic biomarkers (e.g., depression and DNA methylation). Counseling researchers can also investigate how talk therapy and other adjuncts, such as diet and exercise, may improve our clients’ treatment outcomes. As counseling researchers, we can develop research agendas around intervention and prevention for those 0–5 years of age and create and evaluate programs for this age group while also creating community partnerships as noted above. An example of this partnership is The John Hopkins Center for Prevention and Early Intervention. The creators of this program developed sustainable partnerships with public schools, mental health systems, state-level educational programs, universities, and federal programs to focus on early interventions that are school-based and beyond. They collaborated to develop, evaluate, and deliver a variety of programs and research activities to improve outcomes for children and adolescents. They have created dozens of publications based on these efforts that help move the discipline forward. In one such publication, Guintivano et al. (2014) looked at epigenetic and genetic biomarkers for predicting suicide.
Counselor Education, CACREP, and Epigenetics
The counselor educational system affects clients distally but also holds implications for the work counselors conduct at the client level. Counselor educators can provide a more robust understanding of epigenetics to counseling students across the counselor education curriculum. These efforts can include introducing epigenetics in theories, diagnosis, treatment, human and family development, practicum and internship, assessment, professional orientation, and social and cultural foundations courses. By assisting counseling students to comprehend the relationship between client and environment, as well as the importance of prevention, educators will increase their students’ ability to carry out a holistic approach with clients and attend to the foundational emphases of the counseling profession on wellness and prevention. Moreover, by learning to include epigenetics in case conceptualization, students can gain a more robust understanding of the determinants of symptomology, potential etiology at the cellular level, and epigenetically supported treatments such as CBT and mindfulness.
It is fairly simple to integrate epigenetics education into programs accredited by the Council for Accreditation of Counseling and Related Educational Programs (CACREP; 2015). To begin, counselor educators can integrate epigenetics education into professional counseling orientation and ethical practice courses. As counselor educators discuss the history and philosophy of the counseling profession, particularly from a wellness and prevention lens (CACREP, 2015, 2.F.1.a), counselor educators can discuss the connection between epigenetics and wellness. Wellness is a foundational value for the counseling profession and is a part of the definition of counseling (Kaplan et al., 2014). Many wellness models (both theoretical and evidence-based) are rooted in the promotion of a holistic balance of the client in a variety of facets and contexts (Myers & Sweeney, 2011). We can continue to support these findings by integrating epigenetics within our conversations about wellness, as we have epigenetic evidence that the positive or negative coaction between the individual and their environment can impact a person toward increased or decreased wellness.
Counselor educators can also integrate epigenetics education into Social and Cultural Diversity and Human Growth and Development courses. Within Social and Cultural Diversity courses, counselor educators can address how negative environmental conditions have negative influences on offspring. This is evidenced by the discrimination against Jews and its imprinting that crosses generations (Yehuda et al., 2016). Counselor educators can discuss how discrimination and barriers to positive environmental conditions can impact someone at the epigenetic level (CACREP, 2015, 2.F.2.h). Within Human Growth and Development, counselor educators can discuss how the study of epigenetics provides us a biological theory to understand how development is influenced by environment across the life span (CACREP, 2015, 2.F.3.a, c, d, f). In particular, it can provide an etiology of how negative factors change epigenetic tags, which are correlated with negative mental health that may become full-blown mental health disorders later in adulthood (CACREP, 2015, 2.F.3.c, d, e, g).
Additionally, counselor educators can integrate epigenetic education within specialty counseling areas. Several studies (Maze & Nestler, 2011; Palmisano & Pandey, 2017; Tsankova et al., 2007; Wong et al., 2011; H. Zhang & Gelernter, 2017) have noted how epigenetic mechanisms may support the addiction process and counselor educators can interweave this information when discussing theories and models of addiction and mental health problems (CACREP, 2015, 5.A.1.b; 5.C.1.d; 5.C.2.g). Counselor educators can also discuss epigenetics as it applies to counseling practice. Because epigenetics research supports treatments like CBT, mindfulness, nutrition, and exercise (Chaix et al., 2020; Chen et al., 2018; Roberts et al., 2015; Stevens et al., 2018), counselor educators can address these topics in courses when discussing techniques and interventions that work toward prevention and treatment of mental health issues (CACREP, 2015, 5.C.3.b).
Generally, CACREP (2015) standards support programs that infuse counseling-related research into the curriculum (2.E). We support the integration of articles, books, websites, and videos that will engender an understanding of epigenetics across the curriculum, so long as the integration supports student learning and practice.
Conclusion and Future Directions
In summary, there are numerous epigenetic processes at work in the symptoms we attend to as counselors. We have provided information that illustrates how epigenetics may mediate outcomes such as depression, anxiety, schizophrenia, and addiction. We have also illustrated how CBT, exercise, diet, and meditation may have positive epigenetic influences supporting our craft. We have discovered that epigenetic processes are most malleable in early life. This information offers incremental evidence for our actions as professional counselors, educators, and researchers, leading to a potential examination of our efforts in areas of prevention, social justice, clinical practice, and counseling program development. However, we must note that epigenetics as a science is relatively new and much of the research is correlational.
Based on the current limits of epigenetic science and a lack of investigation of mental health epigenetics in professional counseling, one of our first recommendations for future research efforts is to collaborate across professions with other researchers such as geneticists, as we did for this manuscript. From this partnership, our profession’s connection to epigenetics is elucidated. Interdisciplinary collaboration allows the professional counselor to offer their expertise in mental health and the geneticist their deep understanding of epigenetics and the tools to examine the nature and nurture relationships in mental health outcomes. We can also make efforts to look at our wellness-based preventions and interventions to document changes at the epigenetic level in our clients and communities. Ideally, as the science of epigenetics advances, we will have epigenetic research in our profession of counseling that is beyond correlation and evidences the effectiveness of our work down to the cellular level.
Conflict of Interest and Funding Disclosure
The development of this manuscript was supported
in part by a Cincinnati Children’s Hospital Medical
Center Trustee Award and by a grant from the
National Heart, Lung, and Blood Institute (HL132344).
The authors reported no conflict of interest.
References
Albert, P. R., Le François, B., & Vahid-Ansari, F. (2019). Genetic, epigenetic and posttranscriptional mechanisms for treatment of major depression: The 5-HT1A receptor gene as a paradigm. Journal of Psychiatry & Neuroscience, 44(3), 164–176. https://doi.org/10.1503/jpn.180209
Arnaud, P. (2010). Genomic imprinting in germ cells: Imprints are under control. Reproduction, 140(3), 411–423. https://doi.org/10.1530/REP-10-0173
Benoit, L., & Turecki, G. (2010). The epigenetics of suicide: Explaining the biological effects of early life environmental adversity. Archives of Suicide Research, 14(4), 291–310.
https://doi.org/10.1080/13811118.2010.524025
Benros, M. E., Nielsen, P. R., Nordentoft, M., Eaton, W. W., Dalton, S. O., & Mortensen, P. B. (2011). Autoimmune diseases and severe infections as risk factors for schizophrenia: A 30-year population-based register study. The American Journal of Psychiatry, 168(12), 1303–1310. https://doi.org/10.1176/appi.ajp.2011.11030516
Bocchio-Chiavetto, L., Maffioletti, E., Bettinsoli, P., Giovannini, C., Bignotti, S., Tardito, D., Corrada, D., Milanesi, L., & Gennarelli, M. (2013). Blood microRNA changes in depressed patients during antidepressant treatment. European Neuropsychopharmacology, 23(7), 602–611. https://doi.org/10.1016/j.euroneuro.2012.06.013
Boks, M. P., Houtepen, L. C., Xu, Z., He, Y., Ursini, G., Maihofer, A. X., Rajarajan, P., Yu, Q., Xu, H., Wu, Y., Wang, S., Shi, J. P., Hulshoff Pol, H. E., Strengman, E., Rutten, B. P. F., Jaffe, A. E., Kleinman, J. E., Baker, D. G., Hol, E. M., . . . Kahn, R. S. (2018). Genetic vulnerability to DUSP22 promoter hypermethylation is involved in the relation between in utero famine exposure and schizophrenia. Nature Partner Journals Schizophrenia, 4(1), 1–8. https://doi.org/10.1038/s41537-018-0058-4
Broderick, P. C., & Blewitt, P. (2015). The life span: Human development for helping professionals (4th ed.). Pearson.
Bronfenbrenner, U. (1979). The ecology of human development: Experiments by nature and design. Harvard University Press.
Brooker, R. J. (2017). Genetics: Analysis and principles (6th ed.). McGraw-Hill.
Cadet, J. L., McCoy, M. T., & Jayanthi, S. (2016). Epigenetics and addiction. Clinical Pharmacology & Therapeutics, 99(5), 502–511. https://doi.org/10.1002/cpt.345
Cariaga-Martinez, A., & Alelú-Paz, R. (2018). Epigenetic and schizophrenia. In F. Durbano (Ed.), Psychotic disorders – An update (pp. 147–162). IntechOpen. https://doi.org/10.5772/intechopen.73242
Chaix, R., Fagny, M., Cosin-Tomás, M., Alvarez-López, M., Lemee, L., Regnault, B., Davidson, R. J., Lutz, A., & Kaliman, P. (2020). Differential DNA methylation in experienced meditators after an intensive day of mindfulness-based practice: Implications for immune-related pathways. Brain, Behavior, and Immunity, 84, 36–44. https://doi.org/10.1016/j.bbi.2019.11.003
Champagne, F. A. (2010). Early adversity and developmental outcomes: Interaction between genetics, epigenetics, and social experiences across the life span. Perspectives on Psychological Science, 5(5), 564–574.
https://doi.org/10.1177/1745691610383494
Cheah, S.-Y., Lawford, B. R., Young, R. M., Morris, C. P., & Voisey, J. (2017). mRNA expression and DNA methylation analysis of serotonin receptor 2A (HTR2A) in the human schizophrenic brain. Genes, 8(1), 1–11. https://doi.org/10.3390/genes8010014
Chen, J., Hutchinson, K. E., Bryan, A. D., Filbey, F. M., Calhoun, V. D., Claus, E. D., Lin, D., Sui, J., Du, Y., & Liu, J. (2018). Opposite epigenetic associations with alcohol use and exercise intervention. Frontiers in Psychiatry, 9(594), 1–12. https://doi.org/10.3389/fpsyt.2018.00594
Cohen, J. L., Jackson, N. L., Ballestas, M. E., Webb, W. M., Lubin, F. D., & Clinton, S. M. (2017). miR-101a-3p and Ezh2 modulate anxiety-like behavior in high-responder rats. European Journal of Neuroscience, 46(7), 2241–2252.
Conradt, E., Hawes, K., Guerin, D., Armstrong, D. A., Marsit, C. J., Tronick, E., & Lester, B. M. (2016). The contributions of maternal sensitivity and maternal depressive symptoms to epigenetic processes and neuroendocrine functioning. Child Development, 87(1), 73–85. https://doi.org/10.1111/cdev.12483
Council for Accreditation of Counseling and Related Educational Programs. (2015). 2016 CACREP standards. http://www.cacrep.org/wp-content/uploads/2017/08/2016-Standards-with-citations.pdf
Devlin, A. M., Brain, U., Austin, J., & Oberlander, T. F. (2010). Prenatal exposure to maternal depressed mood and the MTHFR C677T variant affect SLC6A4 methylation in infants at birth. PloS ONE, 5(8), e12201.
https://doi.org/10.1371/journal.pone.0012201
Every Child Succeeds. (2019). 2019 report to the community. https://static1.squarespace.com/static/5df9251a492
ba56bc96bc96f/t/5e73b2a333e8127c09daabf2/1584640684722/Final2019Report.pdf
Fisher, H. L., Murphy, T. M., Arseneault, L., Caspi, A., Moffitt, T. E., Viana, J., Hannon, E., Pidsley, R., Burrage, J., Dempster, E. L., Wong, C. C. Y., Pariante, C. M., & Mill, J. (2015). Methylomic analysis of monozygotic twins discordant for childhood psychotic symptoms. Epigenetics, 10(11), 1014–1023.
https://doi.org/10.1080/15592294.2015.1099797
Gejman, P. V., Sanders, A. R., & Kendler, K. S. (2011). Genetics of schizophrenia: New findings and challenges. Annual Review of Genomics and Human Genetics, 12, 121–144.
https://doi.org/10.1146/annurev-genom-082410-101459
Guintivano, J., Brown, T., Newcomer, A., Jones, M., Cox, O., Maher, B. S., Eaton, W. W., Payne, J. L., Wilcox, H. C., & Kaminsky, Z. A. (2014). Identification and replication of a combined epigenetic and genetic biomarker predicting suicide and suicidal behaviors. The American Journal of Psychiatry, 171(12), 1287–1296.
https://doi.org/10.1176/appi.ajp.2014.14010008
Haggarty, S. J., & Tsai, L.-H. (2011). Probing the role of HDACs and mechanisms of chromatin-mediated neuroplasticity. Neurobiology of Learning and Memory, 96(1), 41–52. https://doi.org/10.1016/j.nlm.2011.04.009
Hamilton, P. J., & Nestler, E. J. (2019). Epigenetics and addiction. Current Opinion in Neurobiology, 59, 128–136. https://doi.org/10.1016/j.conb.2019.05.005
Harris, A., & Seckl, J. (2011). Glucocorticoids, prenatal stress and the programming of disease. Hormones and Behavior, 59(3), 279–289. https://doi.org/10.1016/j.yhbeh.2010.06.007
Healthy Families New York. (2021, January 4). [Website.] https://www.healthyfamiliesnewyork.org
Heijmans, B. T., Tobi, E. W., Stein, A. D., Putter, H., Blauw, G. J., Susser, E. S., Slagboom, P. E., & Lumey, L. H. (2008). Persistent epigenetic differences associated with prenatal exposure to famine in humans. Proceedings of the National Academy of Sciences, 105(44), 17046–17049. https://doi.org/10.1073/pnas.0806560105
Huang, W.-C., Ferris, E., Cheng, T., Hörndli, C. S., Gleason, K., Tamminga, C., Wagner, J. D., Boucher, K. M., Christian, J. L., & Gregg, C. (2017). Diverse non-genetic, allele-specific expression effects shape genetic architecture at the cellular level in the mammalian brain. Neuron, 93(5), 1094–1109.e7.
https://doi.org/10.1016/j.neuron.2017.01.033
Januar, V., Ancelin, M.-L., Ritchie, K., Saffery, R., & Ryan, J. (2015). BDNF promoter methylation and genetic variation in late-life depression. Translational Psychiatry, 5, e619. https://doi.org/10.1038/tp.2015.114
Jayanthi, S., McCoy, M. T., Chen, B., Britt, J. P., Kourrich, S., Yau, H.-J., Ladenheim, B., Krasnova, I. N., Bonci, A., & Cadet, J. L. (2014). Methamphetamine downregulates striatal glutamate receptors via diverse epigenetic mechanisms. Biological Psychiatry, 76(1), 47–56. https://doi.org/10.1016/j.biopsych.2013.09.034
Jones, D. E., & Tang, M. (2015). Health inequality: What counselors need to know to act. In Ideas and research you can use: VISTAS 2015. https://www.counseling.org/docs/default-source/vistas/article_60785a22f16116603abcacff0000bee5e7.pdf?sfvrsn=4
Jones, D. E., Tang, M., Folger, A., Ammerman, R. T., Hossain, M. M., Short, J. A., & Van Ginkel, J. B. (2018). Neighborhood effects on PND symptom severity for women enrolled in a home visiting program. Community Mental Health Journal, 54(4), 420–428. https://doi.org/10.1007/s10597-017-0175-y
Kaplan, D. M., Tarvydas, V. M., & Gladding, S. T. (2014). 20/20: A vision for the future of counseling: The new consensus definition of counseling. Journaling of Counseling & Development, 92, 366–372. https://www.counseling.org/docs/default-source/20-20/2020-jcd-article-consensus-definition.pdf?sfvrsn=76017f2c_2
Lester, B. M., Conradt, E., & Marsit, C. (2016). Introduction to the special section on epigenetics. Child Development, 87(1), 29–37. https://doi.org/10.1111/cdev.12489
Lester, B. M., & Marsit, C. J. (2018). Epigenetic mechanisms in the placenta related to infant neurodevelopment. Epigenomics, 10(3), 321–333. https://doi.org/10.2217/epi-2016-0171
Lewis, B. P., Burge, C. B., & Bartel, D. P. (2005). Conserved seed pairing, often flanked by adenosines, indicates that thousands of human genes are microRNA targets. Cell, 120(1), 15–20.
https://doi.org/10.1016/j.cell.2004.12.035
Lieneman, C. C., Brabson, L. A., Highlander, A., Wallace, N. M., & McNeil, C. B. (2017). Parent–child interaction therapy: Current perspectives. Psychology Research and Behavior Management, 10, 239–256.
https://doi.org/10.2147/PRBM.S91200
Lüscher, B., & Möhler, H. (2019). Brexanolone, a neurosteroid antidepressant, vindicates the GABAergic deficit hypothesis of depression and may foster resilience. F1000Research, 8(May), 1–14.
https://doi.org/10.12688/f1000research.18758.1
Ma, J., Shang, S., Wang, J., Zhang, T., Nie, F., Song, X., Zhao, H., Zhu, C., Zhang, R., & Hao, D. (2018). Identification of miR-22-3p, miR-92a-3p, and miR-137 in peripheral blood as biomarker for schizophrenia. Psychiatry Research, 265, 70–76. https://doi.org/10.1016/j.psychres.2018.03.080
Maze, I., & Nestler, E. J. (2011). The epigenetic landscape of addiction. Annals of the New York Academy of Sciences, 1216(1), 99–113. https://doi.org/10.1111/j.1749-6632.2010.05893.x
McEwen, C. A., & McEwen, B. S. (2017). Social structure, adversity, toxic stress, and intergenerational poverty: An early childhood model. Annual Review of Sociology, 43, 445–472.
https://doi.org/10.1146/annurev-soc-060116-053252
McGowan, P. O., Sasaki, A., D’Alessio, A. C., Dymov, S., Labonté, B., Szyf, M., Turecki, G., & Meaney, M. J. (2009). Epigenetic regulation of the glucocorticoid receptor in human brain associates with childhood abuse. Nature Neuroscience, 12(3), 342–348. https://doi.org/10.1038/nn.2270
Monk, C., Spicer, J., & Champagne, F. A. (2012). Linking prenatal maternal adversity to developmental outcomes in infants: The role of epigenetic pathways. Development and Psychopathology, 24(4), 1361–1376.
https://doi.org/10.1017/S0954579412000764
Mulligan, C. J. (2016). Early environments, stress, and the epigenetics of human health. Annual Review of Anthropology, 45(1), 233–249. https://doi.org/10.1146/annurev-anthro-102215-095954
Myers, J. E., & Sweeney, T. J. (2011). Wellness counseling: The evidence base for practice. Journal of Counseling & Development, 86(4), 482–493. https://doi.org/10.1002/j.1556-6678.2008.tb00536.x
National Human Genome Research Institute. (2020). Epigenomics fact sheet. https://www.genome.gov/about-genomics/fact-sheets/Epigenomics-Fact-Sheet
Nestler, E. J., Peña, C. J., Kundakovic, M., Mitchell, A., & Akbarian, S. (2016). Epigenetic basis of mental illness. The Neuroscientist, 22(5), 447–463. https://doi.org/10.1177/1073858415608147
Numachi, Y., Yoshida, S., Yamashita, M., Fujiyama, K., Naka, M., Matsuoka, H., Sato, M., & Sora, I. (2004). Psychostimulant alters expression of DNA methlytransferase mRNA in the rat brain. Annals of the New York Academy of Sciences, 1025(1), 102–109. https://doi.org/10.1196/annals.1316.013
Oberlander, T. F., Weinberg, J., Papsdorf, M., Grunau, R., Misri, S., & Devlin, A. M. (2008). Prenatal exposure to maternal depression, neonatal methylation of human glucocorticoid receptor gene (NR3C1) and infant cortisol stress responses. Epigenetics, 3(2), 97–106. https://doi.org/10.4161/epi.3.2.6034
Okazaki, S., Otsuka, I., Numata, S., Horai, T., Mouri, K., Boku, S., Ohmori, T., Sora, I., & Hishimoto, A. (2019). Epigenetic clock analysis of blood samples from Japanese schizophrenia patients. npj Schizophrenia, 5(9), 1–7. https://doi.org/10.1038/s41537-019-0072-1
Ouellet-Morin, I., Wong, C. C. Y., Danese, A., Pariante, C. M., Papadopoulos, A. S., Mill, J., & Arseneault, L. (2013). Increased serotonin transporter gene (SERT) DNA methylation is associated with bullying victimization and blunted cortisol response to stress in childhood: A longitudinal study of discordant monozygotic twins. Psychology of Medicine, 43(9), 1813–1823. https://doi.org/10.107/S0033291712002784
Palmisano, M., & Pandey, S. C. (2017). Epigenetic mechanisms of alcoholism and stress-related disorders. Alcohol, 60, 7–18. https://doi.org/10.1016/j.alcohol.2017.01.001
Perroud, N., Paoloni-Giacobino, A., Prada, P., Olié, E., Salzmann, A., Nicastro, R., Guillaume, S., Mouthon, D.,
Stouder, C., Dieben, K., Huguelet, P., Courtet, P., & Malafosse, A. (2011). Increased methylation of glucocorticoid receptor gene (NR3C1) in adults with a history of childhood maltreatment: A link with the severity and type of trauma. Translational Psychiatry, 1, e59. https://doi.org/10.1038/tp.2011.60
Pishva, E., Kenis, G., van den Hove, D., Lesch, K.-P., Boks, M. P. M., van Os, J., & Rutten, B. P. F. (2014). The epigenome and postnatal environmental influences in psychotic disorders. Social Psychiatry and Psychiatric Epidemiology, 49, 337–348. https://doi.org/10.1007/s00127-014-0831-2
Provençal, N., & Binder, E. B. (2015). The effects of early life stress on the epigenome: From the womb to adulthood and even before. Experimental Neurology, 268, 10–20. https://doi.org/10.1016/j.expneurol.2014.09.001
Remley, T. P., Jr., & Herlihy, B. (2020). Ethical, legal, and professional issues in counseling (6th ed.). Pearson.
Roberts, S., Keers, R., Lester, K. J., Coleman, J. R. I., Breen, G., Arendt, K., Blatter-Meunier, J., Cooper, P., Creswell, C., Fjermestad, K., Havik, O. E., Herren, C., Hogendoorn, S. M., Hudson, J. L., Krause, K., Lyneham, H. J., Morris, T., Nauta, M., Rapee, R. M., . . . Wong, C. C. Y. (2015). HPA axis related genes and response to psychological therapies: Genetics and epigenetics. Depression and Anxiety, 32(12), 861–870.
https://doi.org/10.1002/da.22430
Rodgers, A. B., Morgan, C. P., Bronson, S. L., Revello, S., & Bale, T. L. (2013). Paternal stress exposure alters sperm microRNA content and reprograms offspring HPA stress axis regulation. Journal of Neuroscience, 33(21), 9003–9012. https://doi.org/10.1523/JNEUROSCI.0914-13.2013
Romens, S. E., McDonald, J., Svaren, J., & Pollak, S. D. (2015). Associations between early life stress and gene methylation in children. Child Development, 86(1), 303–309. https://doi.org/10.1111/cdev.12270
Rutten, B. P. F., Hammels, C., Geschwind, N., Menne-Lothmann, C., Pishva, E., Schruers, K., van den Hove, D.,
Kenis, G., van Os, J., & Wichers, M. (2013). Resilence in mental health: Linking psychological and neurobiological perspectives. Acta Psychiatrica Scandinavica, 128(1), 3–20. https://doi.org/10.1111/acps.12095
Saavedra, K., Molina-Márquez, A. M., Saavedra, N., Zambrano, T., & Salazar, L. A. (2016). Epigenetic modifications of major depressive disorder. International Journal of Molecular Sciences, 17(8), 1279.
https://doi.org/10.3390/ijms17081279
Shimada-Sugimoto, M., Otowa, T., & Hettema, J. M. (2015). Genetics of anxiety disorders: Genetic epidemiological and molecular studies in humans. Psychiatry and Clinical Neurosciences, 69(7), 388–401.
https://doi.org/10.1111/pcn.12291
Smearman, E. L., Almli, L. M., Conneely, K. N., Brody, G. H., Sales, J. M., Bradley, B., Ressler, K. J., & Smith, A. K.
(2016). Oxytocin receptor genetic and epigenetic variations: Association with child abuse and adult psychiatric symptoms. Child Development, 87(1), 122–134. https://doi.org/10.1111/cdev.12493
Smigielski, L., Jagannath, V., Rössler, W., Walitza, S., & Grünblatt, E. (2020). Epigenetic mechanisms in schizophrenia and other psychotic disorders: A systematic review of empirical human findings. Molecular Psychiatry, 25, 1718–1748. https://doi.org/10.1038/s41380-019-0601-3
Stevens, A. J., Rucklidge, J. J., & Kennedy, M. A. (2018). Epigenetics, nutrition and mental health: Is there a relationship? Nutritional Neuroscience, 21(9), 602–613. https://doi.org/10.1080/1028415X.2017.1331524
Suderman, M., Borghol, N., Pappas, J. J., Pinto Pereira, S. M., Pembrey, M., Hertzman, C., Power, C., & Szyf, M. (2014). Childhood abuse is associated with methylation of multiple loci in adult DNA. BMC Medical Genomics, 7, 1–12. https://doi.org/10.1186/1755-8794-7-13
Szyf, M. (2009). The early life environment and the epigenome. Biochimica et Biophysica Acta, 1790(9), 878–885. https://doi.org/10.1016/j.bbagen.2009.01.009
Szyf, M., Tang, Y.-Y., Hill, K. G., & Musci, R. (2016). The dynamic epigenome and its implications for behavioral interventions: A role for epigenetics to inform disorder prevention and health promotion. Translational Behavioral Medicine, 6(1), 55–62. https://doi.org/10.1007/s13142-016-0387-7
Szyf, M., Weaver, I., & Meaney, M. (2007). Maternal care, the epigenome and phenotypic differences in behavior. Reproductive Toxicology, 24(1), 9–19. https://doi.org/10.1016/j.reprotox.2007.05.001
Tsankova, N., Renthal, W., Kumar, A., & Nestler, E. J. (2007). Epigenetic regulation in psychiatric disorders. Nature Reviews Neuroscience, 8, 355–367. https://doi.org/10.1038/nrn2132
Turecki, G. (2014). Epigenetics and suicidal behavior research pathways. American Journal of Preventive Medicine, 47(3), S144–S151. https://doi.org/10.1016/j.amepre.2014.06.011
Vaiserman, A. M., & Koliada, A. K. (2017). Early-life adversity and long-term neurobehavioral outcomes: Epigenome as a bridge? Human Genomics, 11(34), 1–15. https://doi.org/10.1186/s40246-017-0129-z
Weaver, I. C. G., Champagne, F. A., Brown, S. E., Dymov, S., Sharma, S., Meaney, M. J., & Szyf, M. (2005). Reversal of maternal programming of stress responses in adult offspring through methyl supplementation: Altering epigenetic marking later in life. Journal of Neuroscience, 25(47), 11045–11054.
https://doi.org/10.1523/JNEUROSCI.3652-05.2005
Wong, C. C. Y., Mill, J., & Fernandes, C. (2011). Drugs and addiction: An introduction to epigenetics. Addiction, 106(3), 480–489. https://doi.org/10.1111/j.1360-0443.2010.03321.x
Wright, K. N., Hollis, F., Duclot, F., Dossat, A. M., Strong, C. E., Francis, T. C., Mercer, R., Feng, J., Dietz, D. M., Lobo, M. K., Nestler, E. J., & Kabbaj, M. (2015). Methyl supplementation attenuates cocaine-seeking behaviors and cocaine-induced c-Fos activation in a DNA methylation-dependent manner. The Journal of Neuroscience, 35(23), 8948–8958. https://doi.org/10.1523/JNEUROSCI.5227-14.2015
Yehuda, R., Daskalakis, N. P., Bierer, L. M., Bader, H. N., Klengel, T., Holsboer, F., & Binder, E. B. (2016). Holocaust exposure induced intergenerational effects on FKBP5 methylation. Biological Psychiatry, 80, 372–380. https://doi.org/10.1016/j.biopsych.2015.08.005
Yehuda, R., Engel, S. M., Brand, S. R., Seckl, J., Marcus, S. M., & Berkowitz, G. S. (2005). Transgenerational effects of posttraumatic stress disorder in babies of mothers exposed to the World Trade Center attacks during pregnancy. The Journal of Clinical Endocrinology & Metabolism, 90(7), 4115–4118.
https://doi.org/10.1210/jc.2005-0550
Zhang, H., & Gelernter, J. (2017). Review: DNA methylation and alcohol use disorders: Progress and challenges. The American Journal on Addictions, 26(5), 502–515. https://doi.org/10.1111/ajad.12465
Zhang, T.-Y., & Meaney, M. J. (2010). Epigenetics and the environmental regulation of the genome and its function. Annual Review of Psychology, 61, 439–466. https://doi.org/10.1146/annurev.psych.60.110707.163625
Zheng, J., & Xiao, X. (2016). Epigenetic modifications and developmental origin of health and diseases (DOHaD). In Y. Dincer (Ed.), Epigenetics: Mechanisms and clinical perspectives (pp. 1–14). Nova Biomedical.
David E. Jones, EdD, NCC, LPC, is an assistant professor at Liberty University. Jennifer S. Park, PhD, NCC, ACS, LPC, is an assistant professor at Colorado Christian University. Katie Gamby, PhD, LPC, CWC, is an assistant professor at Malone University. Taylor M. Bigelow, PhD, is an assistant professor at the University of New Haven. Tesfaye B. Mersha, PhD, is an associate professor at the Cincinnati Children’s Hospital Medical Center (CCMHC), University of Cincinnati College of Medicine. Alonzo T. Folger, PhD, MS, is an assistant professor at the CCMHC, University of Cincinnati College of Medicine. Correspondence may be addressed to David E. Jones, 1971 University Blvd., Lynchburg, VA 24515, dejones14@liberty.edu.
Mar 9, 2020 | Volume 10 - Issue 1
Michael T. Kalkbrenner
College counselors work collaboratively with professionals in a variety of disciplines in higher education to coordinate gatekeeper training to prepare university community members to recognize and refer students in mental distress to support services. This article describes the cross-validation of scores on the Mental Distress Response Scale (MDRS), a questionnaire for appraising university community members’ responses to encountering a student in mental distress, with a sample of faculty members. A confirmatory factor analysis revealed the dimensions of the MDRS were estimated adequately. Results also revealed demographic differences in faculty members’ responses to encountering a student in mental distress. The MDRS has implications for augmenting the outreach efforts of college counselors. For example, the MDRS has potential utility for enhancing campus-wide mental health screening efforts. The MDRS also has implications for supporting psychoeducation efforts, including gatekeeper training workshops, for professional counselors practicing in college settings.
Keywords: Mental Distress Response Scale, mental health, college counselors, gatekeeper, outreach
College counselors play crucial roles in supporting students’ personal, social, and academic growth, as well as students’ success (Golightly et al., 2017). Outreach and prevention programming, including campus violence prevention and supporting college student mental health, are two key elements in the practice of college counselors (Brunner et al., 2014; Golightly et al., 2017). Addressing these two key areas has become increasingly challenging in recent years because of the prevalence of campus violence incidents, including mass shootings in the most severe cases, and the frequency of mental health distress among college students, which has increased substantially since the new millennium (Auerbach et al., 2016; Barrett, 2014; Vieselmeyer et al., 2017). In fact, supporting college student mental health has become one of the greatest challenges that institutions of higher education are facing (Reynolds, 2013).
Most college students suffering from mental health issues do not seek treatment (Downs & Eisenberg, 2012). In response, college counselors, student affairs professionals, and higher education administrators are working collaboratively to develop and implement mental health awareness initiatives and gatekeeper training workshops, which include training university community members (e.g., students, faculty, and staff) as referral agents to recognize and refer students who are showing warning signs for suicide or other mental health issues to support services (Albright & Schwartz, 2017; Hodges et al., 2017). Faculty members are particularly valuable referral agents, as they tend to interact with large groups of students on frequent occasions, and they generally report positive attitudes about supporting college student mental health (Albright & Schwartz, 2017; Kalkbrenner, 2016).
Despite the utility of faculty members as gatekeepers for recognizing and referring students to the university counseling center and to other resources, the results of a recent national survey indicated that a significant proportion of faculty members (63%) do not refer a student in mental distress to support services (Albright & Schwartz, 2017). The literature is lacking research on how faculty members are likely to respond to encountering a student in mental distress, including but not limited to making a faculty-to-student referral to mental health support services. The primary aim of this investigation was to confirm the psychometric properties of the Mental Distress Response Scale (MDRS), a screening tool for measuring university community members’ responses to encountering a student in mental distress. Past investigators validated the MDRS for use with 4-year university students (Kalkbrenner & Flinn, 2020) and community college students (Kalkbrenner, 2019). If found valid for use with faculty members, college counselors could find the MDRS useful for screening and promoting faculty-to-student mental health support. A review of the extant literature is provided in the following section.
Mental Health and the State of Higher Education
Active shooter incidents on college campuses are some of the most tragic events in American history (Kalkbrenner, 2016). The 2015 massacre that occurred on a college campus in Oregon received attention at the highest level of government; former President Barack Obama urged the nation to decide when voting “whether this cause of continuing death for innocent people should be a relevant factor.” (Vanderhart et al., 2015, section A, p. 1). Seung-Hui Cho was a perpetrator of another one of these tragedies at Virginia Polytechnic Institute in 2007. According to Cho’s mother, he had a history of social isolation and unresolved mental health issues (Klienfield, 2007). Without treatment, the effects of mental health disorders can be debilitating and widespread for students, including impairments in academic functioning, attrition, self-harm, social isolation, and suicide or homicide in the most serious cases (Kalkbrenner, 2016; Shuchman, 2007). The early detection and treatment of students who are at risk for mental health disorders is a harm-prevention strategy for reducing campus violence incidents and promoting college student mental health (Futo, 2011; Kalkbrenner, 2016). Consequently, the practice of college counselors involves deploying outreach and systems-level mental health support interventions (Albright & Schwartz, 2017; Brunner et al., 2014; Golightly et al., 2017).
The Role of College Counselors in Providing Systems-Level Interventions
Providing individual counseling is a key role of college counselors (Golightly et al., 2017). In recent years, however, the practice of college counselors has been extended to providing systems-level and preventative mental health interventions to meet the growing mental health needs of college student populations (Brunner et al., 2014; Golightly et al., 2017). In particular, college counselors and their constituents engage in both campus-wide and targeted prevention and outreach programs (Golightly et al., 2017; Lynch & Glass, 2019), including gatekeeper training workshops to prepare university community members as referral agents or train them to recognize and refer students at risk for suicide and other mental health issues to the university counseling center (Albright & Schwartz, 2017; Brunner et al., 2014). These collaborative, educative, and preventative efforts are particularly crucial given the increase in both the severity and complexity of mental health disorders among college students (Gallagher, 2015; Reetz et al., 2016). The findings of past investigators suggest that faculty members are particularly viable referral agents for recognizing and referring students in mental distress to the counseling center (Kalkbrenner, 2016; Margrove et al., 2014).
Faculty Members as Referral Agents
Faculty members have a propensity to serve as referral agents (i.e., recognize and refer students in mental distress to resources) because of their frequent contact with students and their generally positive attitudes and willingness to support their students’ mental and physical wellness (Albright & Schwartz, 2017). Albright and Schwartz (2017) found that approximately 95% of faculty members and staff considered connecting students in mental distress to resources as one of their roles and responsibilities. Similarly, Margrove et al. (2014) found that 64% of untrained university staff members expressed a desire to receive training to recognize warning signs of mental health disorders in students.
Past investigators extended the line of research on the utility of faculty members as gatekeepers by identifying demographic differences by gender and help-seeking history (previous attendance in counseling) in faculty members’ tendency to support college student mental health (Kalkbrenner & Carlisle, 2019; Kalkbrenner & Sink, 2018). In particular, Kalkbrenner and Sink (2018) identified gender as a significant predictor of faculty-to-student counseling referrals, with faculty who identified as female more likely to make faculty-to-student referrals to the counseling center compared to their male counterparts. Similarly, Kalkbrenner and Carlisle (2019) found that faculty members’ awareness of warning signs for mental distress in students was a significant positive predictor of faculty-to-student referrals to the counseling center. In addition, faculty members with a help-seeking history (previous attendance in counseling) were significantly more aware of warning signs for mental distress in their students compared to faculty without a help-seeking history (Kalkbrenner & Carlisle, 2019).
Faculty Members’ Responses to Encountering a Student in Mental Distress
Despite the growing body of literature on institutional agents’ participation in gatekeeper training (i.e., recognize and refer), research on the measurement and appraisal of how faculty members are likely to respond when encountering a student in mental distress is in its infancy. The results of a recent national survey of college students (N = 51,294) and faculty members (N = 14,548) were troubling, as 63% of faculty members did not refer a student in psychological distress to mental health support services (Albright & Schwartz, 2017). Making a referral to the university counseling center is one possible response of students and faculty members to encountering a peer or student in mental distress (Kalkbrenner & Sink, 2018). However, the findings of Albright and Schwartz (2017) highlight a gap in the literature regarding how university community members are likely to respond when encountering a student in mental distress, including but not limited to making a faculty-to-student referral to the college counseling center.
To begin filling this gap in the literature, Kalkbrenner and Flinn (2020) developed, validated, and cross-validated scores on the MDRS to assess 4-year university students’ responses to encountering a student in mental distress, including but not limited to making a referral to mental health support services. In a series of two major phases of psychometric analyses, Kalkbrenner and Flinn identified and confirmed two dimensions or subscales of the MDRS, including Diminish/Avoid and Approach/Encourage, with two large samples of undergraduate students. The Diminish/Avoid subscale measures adverse or inactive responses of university community members to encountering a student in mental distress (e.g., stay away from the person or warn the person that mental issues are perceived as a weakness). The Approach/Encourage subscale appraises facilitative or helpful responses of university community members when encountering a student in mental distress that are likely to help connect the person to resources (e.g., talking to a college counselor or suggesting that the person go to the campus counseling or health center). However, the psychometric properties of the MDRS have not been tested with faculty members. If found valid for such purposes, the MDRS could be a useful tool that college counselors and their constituents can use to screen and promote faculty-to-student referrals to mental health support services. In particular, the following research questions were posed: (1) Does the two-dimensional hypothesized MDRS model fit with a sample of faculty members? and (2) To what extent are there demographic differences in faculty members’ responses to encountering a student in mental distress?
Method
Participants and Procedures
Data were collected electronically from faculty members using Qualtrics, a secure e-survey platform. A nonprobability sampling procedure was used by sending a recruitment email message with an electronic link to the survey to 1,000 faculty members who were teaching at least one course at a research-intensive, mid-Atlantic public university at the time of data collection. A total of 221 faculty members clicked on the electronic link to the survey and 11 responses were omitted from the data set because of 100% missing data, resulting in a useable sample size of 210, yielding a response rate of 21%. This response rate is consistent with the response rates of other investigators (e.g., Brockelman & Scheyett, 2015; Kalkbrenner & Carlisle, 2019) who conducted survey research with faculty members. For gender, 58% (n = 122) identified as female, 41% (n = 86) as male, and 0.5% (n = 1) as non-binary or third gender, and 0.5% (n = 1) did not specify their gender. For ethnicity, 79.0% (n = 166) identified as Caucasian, 6.2% (n = 11) as African American, 3.8% (n = 8) as Hispanic or Latinx, 2.9% (n = 6) as Asian, 2.9% (n = 6) as multiethnic, 0.5% (n = 1) as Hindu, and 0.5% (n = 1) as Irish, and 5.2% (n = 11) did not specify their ethnic identity. Participants ranged in age from 31 to 78 (M = 50; SD = 11). Participants represented all of the academic colleges in the university, including 28.6% (n = 60) Arts and Letters, 22.9% (n = 48) Education, 18.1% (n = 38) Sciences, 12.9% (n = 27) Health Sciences, 9% (n = 19) Engineering and Technology, and 7.6% (n = 16) Business, while 1% (n = 2) of participants did not specify their college.
Instrumentation
Demographic questionnaire
Following informed consent, participants were asked to indicate that they met the inclusion criteria for participation, including (1) employment as a faculty member, and (2) teaching at least one course at the time of data collection. Participants then responded to a succession of demographic items about their gender, ethnicity, age, academic college, and highest level of education completed. Lastly, respondents indicated their rank and help-seeking history (previous attendance in counseling or no previous attendance in counseling) and if they had referred at least one student to mental health support services.
Mental Distress Response Scale (MDRS)
The MDRS is a screening tool comprised of two subscales (Approach/Encourage and Diminish/Avoid) for measuring university community members’ responses to encountering a student in mental distress (Kalkbrenner & Flinn, 2020). The items that mark the Approach/Encourage subscale appraise responses to mental distress that are consistent with providing support and encouragement to a student in mental distress (e.g., “suggest that they go to the health center on campus”). The Diminish/Avoid subscale measures adverse or inactive responses to encountering a student in mental distress (e.g., “try to ignore your concern”). Kalkbrenner and Flinn (2020) found adequate reliability evidence for an attitudinal measure (α > 0.70) and initial validity evidence for the MDRS in two major phases of analyses (exploratory and confirmatory factor analysis [CFA]) with two samples of college students. Kalkbrenner (2019) extended the line of research on the utility of the MDRS for use with community college students and found adequate reliability (α > 0.80) and validity evidence (single and multiple-group confirmatory analysis).
Data Analysis
A CFA based on structural equation modeling was computed using IBM SPSS Amos version 25 to cross-validate scores on the MDRS with a sample of faculty members (research question #1). Using a maximum likelihood estimation method, the following goodness-of-fit indices and thresholds for defining model fit were investigated based on the recommendations of Byrne (2016) and Hooper et al. (2008): Chi square absolute fit index (CMIN, non-significant p-value with an x2/df ratio < 3), comparative fit index (CFI > 0.95), incremental fit index (IFI > 0.95), Tucker-Lewis index (TLI > 0.95), goodness-of-fit index (GFI > 0.95), root mean square error of approximation (RMSEA < 0.07), and standardized root mean square residual (SRMR < 0.08). Based on the findings of past investigators (e.g., Kalkbrenner & Sink, 2018) regarding demographic differences in faculty members’ propensity to support college student mental health, a 2 X 2 (gender X help-seeking history) MANOVA was computed to investigate demographic differences in faculty members’ responses to encountering a student in mental distress (research question #2). The independent variables included gender (male or female) and help-seeking history (previous attendance in counseling or no previous attendance in counseling). Discriminant analysis was used as the post hoc procedure for significant findings in the MANOVA (Warne, 2014). The researcher examined both main effects and interaction effects and applied Bonferroni adjustments to control for the familywise error rate.
Results
CFA
The researcher ensured that the data set met the necessary assumptions for CFA (Byrne, 2016; Field, 2018). A missing values analysis revealed that less than 5% of data was missing for all MDRS items. Little’s Missing Completely at Random (MCAR) test revealed that the data was missing at random: χ2 (387) = 407.98, p = 0.22. Expectation maximization was used to impute missing values. Outliers were winsorized (Field, 2018) and skewness and kurtosis values for the MDRS items (see Table 1) were largely consistent with a normal distribution (+ 1; Mvududu & Sink, 2013). Inter-item correlations between the 10 items were favorable for CFA, and Mahalanobis d2 indices revealed no extreme multivariate outliers. The researcher ensured that the sample size was sufficient for CFA by following the guidelines provided by Mvududu and Sink (2013), including at least 10 participants per estimated parameter with a sample > 200.
Table 1
Descriptive Statistics for MDRS Items
| Item Content |
M |
SD |
Skew |
Kurtosis |
| 1. I would stay away from this person |
49.83 |
9.46 |
1.11 |
0.22 |
| 2. Suggest that they go to the health center on campus |
50.15 |
9.48 |
-0.60 |
-0.08 |
| 3. Try to ignore your concern |
49.74 |
9.08 |
1.07 |
1.08 |
| 4. Take them to a party |
49.21 |
3.11 |
0.70 |
0.81 |
| 5. Tell them to “tough it out” because they will feel better over time |
49.73 |
8.94 |
1.32 |
1.26 |
| 6. Suggest that they see a medical doctor on campus |
50.00 |
9.98 |
-0.24 |
-0.06 |
| 7. Avoid this person |
49.70 |
9.02 |
1.80 |
1.33 |
| 8. Suggest that they see a medical doctor in the community |
50.00 |
9.98 |
-0.49 |
-0.10 |
| 9. Warn the person that others are likely to see their mental health issues as a weakness |
49.31 |
7.14 |
1.90 |
1.59 |
| 10. Talk to a counselor about your concern |
50.00 |
9.97 |
-0.83 |
0.15 |
SEKurtosis = 0.15, SESkewness = 0.17.
Note. Values were winsorized and reported as standardized t-scores (M = 50; SD = 10).
The 10 MDRS items (see Table 1) were entered in the CFA. A strong model fit emerged based on the GFI recommended by Byrne (2016) and Hooper et al. (2008). The CMIN absolute fit index demonstrated no significant differences between the hypothesized model and the data: χ2 (34) = 42.41, p = 0.15, CMIN/df = 1.25. In addition, the CFI = 0.98, GFI = 0.96, IFI = 0.98, TLI = 0.98, RMSEA = 0.03, 90% confidence interval [<.00, .06], and SRMR = 0.05 also demonstrated a strong model fit. Internal consistency reliability analyses (Cronbach’s coefficient alpha) revealed satisfactory reliability coefficients for an attitudinal measure, Diminish/Avoid (α = 0.73) and Approach/Encourage (α = 0.70). In addition, the path model coefficient (-0.04) between factors supported the structural validity of the scales (see Figure 1).
Figure 1
Confirmatory Factor Analysis Path Diagram for the Mental Distress Response Scale
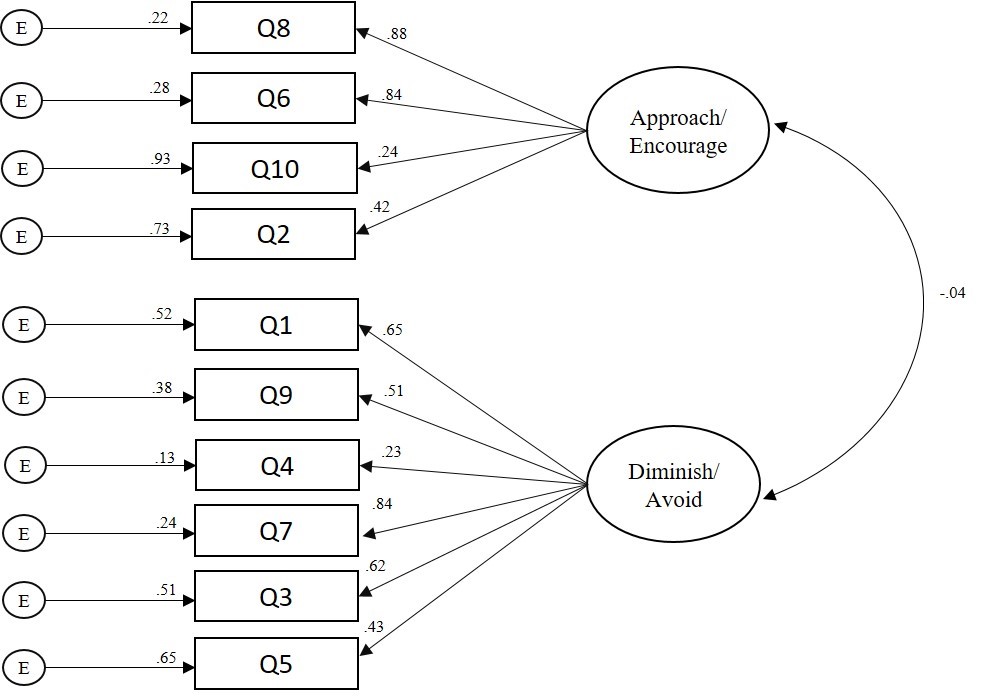
Note. CFA = confirmatory factor analysis, MDRS = Mental Distress Response Scale.
Multivariate Analysis
A 2 X 2 (gender X help-seeking history) MANOVA was computed to investigate demographic differences in faculty members’ responses to encountering a student in mental distress (research question #2). G*Power was used to conduct an a priori power analysis (Faul et al., 2007) and revealed that a minimum sample size of 151 would provide a 95% power estimate, α = .05, with a moderate effect size, F2(v) = 0.063. A significant main effect emerged for gender: F(3, 196) = 8.27, p < 0.001, Wilks’ λ = 0.92, = 0.08. The MANOVA was followed up with a post hoc discriminant analysis based on the recommendations of Warne (2014). The discriminant function significantly discriminated between groups: Wilks’ λ = 0.91, X2 = 18.85, df = 2, p < 0.001. The correlations between the latent factors and discriminant function showed that Diminish/Avoid loaded more strongly on the function (r = 0.98) than Approach/Encourage (r = 0.29), suggesting that Diminish/Avoid contributed the most to group separation in gender. The mean discriminant score on the function was -0.27 for participants who identified as female and 0.37 for participants who identified as male.
Discussion
The results of tests of internal consistency reliability (Cronbach’s coefficient alpha), CFA, and correlations between factors supported the psychometric properties of the MDRS with a sample of faculty members. The results of the CFA were promising as GFI demonstrated a strong model fit between the two-dimensional hypothesized MDRS model and a sample of faculty members (research question #1). In particular, based on one of the most conservative and rigorous absolute fit indices, the CMIN (Byrne, 2016; Credé & Harms, 2015), the researchers retained the null hypothesis—there were no significant differences between the hypothesized factor structure of the MDRS and a sample of faculty members. The strong model fit suggests that Approach/Encourage and Diminish/Avoid are two latent variables that comprise faculty members’ responses to encountering a student in mental distress. The findings of the CFA add to the extant literature about the utility of the MDRS for use with 4-year university students (Kalkbrenner & Flinn, 2020), community college students (Kalkbrenner, 2019), and now with faculty members.
An investigation of the path model coefficient between subscales (see Figure 1) revealed a small and negative association between factors, which supports the structural validity of the MDRS. In particular, the low and negative relationship between the Approach/Encourage and Diminish/Avoid subscales indicates that the dimensions of the MDRS are measuring discrete dimensions of a related construct. As expected, faculty members who scored higher on the Approach/Encourage subscale tended to score lower on the Diminish/Avoid subscale. However, the low strength of the association between factors suggests that faculty members’ responses to encountering a student in mental distress might not always be linear (e.g., a strong positive approach/encourage response might not always be associated with a strong negative diminish/avoid response). Haines et al. (2017) demonstrated that factors in the environment and temperament of a person showing signs of mental distress were significant predictors of mental health support staff’s perceptions of work safety. It is possible that under one set of circumstances faculty members might have an approach/encourage response to mental distress. However, under a difference set of circumstances, a faculty member might have a diminish/avoid response. For example, the extent to which a faculty member feels threatened or unsafe might mediate their propensity of having diminish/avoid or approach/encourage responses. Future research is needed to evaluate this possibility.
Consistent with the findings of previous researchers (Kalkbrenner & Carlisle, 2019; Kalkbrenner & Sink, 2018), the present investigators found that faculty members who identified as male were more likely to report a diminish/avoid response to encountering a student in mental distress compared to female faculty members. Similarly, Kalkbrenner and Sink (2018) found that male faculty members were less likely to make faculty-to-student referrals to the counseling center, and Kalkbrenner and Carlisle (2019) found that male faculty members were less likely to recognize warning signs of mental distress in college students. Similarly, the multivariate results of the present investigation revealed that male faculty members were more likely to report a diminish/avoid response to encountering a student in mental distress when compared to female faculty members. The synthesized findings of Kalkbrenner and Carlisle (2019), Kalkbrenner and Sink (2018), and the present investigation suggest that faculty members who identify as male might be less likely to recognize and refer a student in mental distress to mental health support services. The MDRS has valuable implications for enhancing the practice of professional counselors in college settings.
Implications for Counseling Practice
Outreach, consultation, and psychoeducation are essential components in the practice of college counselors (Brunner et al., 2014; Golightly et al., 2017). The findings of the present investigation have a number of practical implications for enhancing college counselors’ outreach and psychoeducation work—for example, gatekeeper workshops geared toward promoting faculty-to-student referrals to mental health support resources. The complex and multidimensional nature of college student mental health issues calls for interdisciplinary collaboration between college counselors and professionals in a variety of disciplinary orientations in higher education (Eells & Rockland-Miller, 2011; Hodges et al., 2017). College counselors can take leadership roles in coordinating these collaborative efforts to support college student mental health. In particular, college counselors can work with student affairs officials, higher education administrators, and their constituents, and attend new faculty orientations as well as department meetings to administer the MDRS, establish relationships with faculty, and discuss the benefits of gatekeeper training as well as supporting college student mental health. The results of the MDRS can be used to gain insight into the types of responses that faculty members are likely to have when encountering a student in mental distress. This information can be used to structure the content of gatekeeper training workshops aimed at promoting faculty-to-student referrals to mental health support services. Specifically, college counselors might consider the utility of integrating brief interventions and skills training components into gatekeeper training workshops. Motivational interviewing, for example, is an evidence-based, brief approach to counseling that includes both person-centered and directive underpinnings with utility for increasing clients’ intrinsic motivation to make positive changes in their lives (Iarussi, 2013; Resnicow & McMaster, 2012). Professional counselors who practice in higher education are already using motivational interviewing to promote college student development and mental health (Iarussi, 2013). Although future research is needed, integrating motivational interviewing principles (e.g., expressing empathy, rolling with resistance, developing discrepancies, and supporting self-efficacy; Iarussi, 2013) into gatekeeper training workshops might increase faculty members’ commitment to supporting college student mental health.
The MDRS has the potential to enhance college counselors’ outreach and mental health screening efforts (Golightly et al., 2017). College counselors can incorporate the MDRS into batteries of pretest/posttest measures (e.g., the MDRS with a referral self-efficacy measure) for evaluating the effectiveness of mental health awareness initiatives and gatekeeper training programs for faculty and other members of the campus community. If administered widely, the MDRS might have utility for assessing faculty members’ responses to students in mental distress across time and among various campus ecological systems, providing data to drive the prioritization and allocation of outreach efforts aimed at facilitating and maintaining referral networks for connecting students in mental distress to support services.
The results of the present study have policy implications related to campus violence prevention programming. The sharp increase in campus violence incidents has resulted in several universities implementing threat assessment teams as a harm-prevention measure (Eells & Rockland-Miller, 2011). Threat assessment teams involve an interdisciplinary collaboration of university faculty and staff for the purposes of recognizing and responding to students who are at risk of posing a threat to themselves or to others. College counselors can take leadership roles in establishing and supporting threat assessment teams at their universities. College counselors can administer the MDRS to faculty and staff and use the results as one way to identify potential threat assessment team members. University community members who score higher on the Approach/Encourage scale might be inclined to serve on threat assessment teams because of their propensity to support college student mental health. The brevity (10 questions) and versatility of administration (paper copy or electronically via laptop, smartphone, or tablet) of the MDRS adds to the practicality of the measure. Specifically, it might be practical for college counselors and their constituents to administer the MDRS during new faculty orientations, annual opening programs, or department meetings, or via email to faculty and staff. Results can potentially be used to recruit threat assessment team members.
Our findings indicate that when compared to their female counterparts, male faculty members might be more likely to have a diminish/avoid response when encountering a student in mental distress. College counselors might consider working collaboratively with student affairs professionals to implement gatekeeper training and mental health awareness workshops in academic departments that are comprised of high proportions of male faculty members. It is possible that male faculty members are unaware of how to identify warning signs of mental distress in their students (Kalkbrenner & Carlisle, 2019). College counselors might consider the utility of distributing psychoeducation resources for recognizing students in mental distress to faculty and staff. As just one example, the REDFLAGS model is an acronym of eight red flags or warning signs for identifying students who might be struggling with mental health issues (Kalkbrenner, 2016). Kalkbrenner and Carlisle (2019) demonstrated that the REDFLAGS model is a promising psychoeducational tool, as faculty members’ awareness of the red flags was a significant positive predictor of faculty-to-student referrals to the counseling center. The REDFLAGS model appears to be a practical resource for college counselors that can be distributed to faculty electronically or by paper copy, or posted as a flyer (Kalkbrenner, 2016; Kalkbrenner & Carlisle, 2019).
Limitations and Future Research
The findings of the present study should be considered within the context of the limitations. A number of methodological limitations (e.g., self-report bias and social desirability) can influence the validity of psychometric designs. In addition, the dichotomous nature of the faculty-to-student counseling referral variable (referred or not referred) did not provide data on the frequency of referrals. Future researchers should use a continuous variable (e.g., the number of student referrals to the counseling center in the past 2 years) to appraise faculty-to-student referrals. Future researchers can further test the psychometric properties of the MDRS through cross-validating scores on the measure with additional, unique populations of faculty members from a variety of different geographic and social locations. Invariance testing can be computed to examine the degree to which the MDRS and its dimensions maintain psychometric equivalence across different populations of faculty members. In addition, the criterion validity of the MDRS can be examined by testing the extent to which respondents’ MDRS scores are predictors of their frequency of student referrals to the counseling center and to other resources. Furthermore, future qualitative research is needed to investigate faculty members’ unique experiences around supporting college student mental health.
The low and negative association between the Approach/Encourage and Diminish/Avoid subscales suggests that faculty members might have an approach/encourage response to encountering a student in mental distress under one set of circumstances; however, they might have a diminish/avoid response under a difference set of circumstances. Future investigators might test the extent to which attitudinal variables mediate respondents’ MDRS scores—for example, the extent to which faculty members’ sense of safety predicts their MDRS scores. In addition, given the widespread public perception of individuals living with mental illness as violent and dangerous (Varshney et al., 2016), future researchers might identify demographic and background differences (particularly mental health stigma) among participants’ MDRS scores.
Summary and Conclusion
Mental health outreach and screening are essential components in the practice of college counselors, including training referral agents to recognize and refer students who might be struggling with mental health distress to support services (Golightly et al., 2017). Taken together, the results of the present study indicate that the MDRS and its dimensions were estimated sufficiently with a sample of faculty members. Our findings confirmed the two-dimensional hypothesized model for the types of responses that faculty might have when encountering a student showing signs of mental distress. In particular, the results of a CFA provided support for the MDRS and its dimensions, confirming a two-dimensional construct for the types of responses (approach/encourage and diminish/avoid) that faculty members might have when encountering a student in mental distress. Considering the utility of faculty members as gatekeepers and referral agents (Hodges et al., 2017; Kalkbrenner, 2016), researchers, practitioners, and policymakers may find the MDRS a useful screening tool for identifying the ways in which faculty members are likely to respond when encountering a student in mental distress. Results can be used to inform the content of mental health awareness initiatives and gatekeeper training programs aimed at promoting approach/encourage responses to connect students who need mental health support to the appropriate resources.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Albright, G. & Schwartz, V. (2017). Are campuses ready to support students in distress?: A survey of 65,177 faculty, staff, and students in 100+ colleges and universities. https://www.jedfoundation.org/wp-content/uploads/2017/10/Kognito-JED-Are-Campuses-Ready-to-Support-Students-in-Distress.pdf
Auerbach, R. P., Alonso, J., Axinn, W. G., Cuijpers, P., Ebert, D. D., Green, J. G., Hwang, I., Kessler, R. C., Liu, H., Mortier, P., Nock, M. K., Pinder-Amaker, S., Sampson, N. A., Aguilar-Gaxiola, S., Al-Hamzawi, A., Andrade, L. H., Benjet, C., Caldas-de-Almeida, J. M., Demyttenaere, K., . . . Bruffaerts, R. (2016). Mental disorders among college students in the World Health Organization World Mental Health Surveys. Psychological Medicine, 46, 2955–2970. https://doi.org/10.1017/S0033291716001665
Barrett, D. (2014, September 24). Mass shootings on the rise, FBI says. The Wall Street Journal. http://online.wsj.com/articles/mass-shootings-on-the-rise-fbi-says-1411574475
Brockelman, K. F., & Scheyett, A. M. (2015). Faculty perceptions of accommodations, strategies, and psychiatric advance directives for university students with mental illnesses. Psychiatric Rehabilitation Journal, 38, 342–348. https://doi.org/10.1037/prj0000143
Brunner, J. L., Wallace, D. L., Reymann, L. S., Sellers, J.-J., & McCabe, A. G. (2014). College counseling today: Contemporary students and how counseling centers meet their needs. Journal of College Student Psychotherapy, 28, 257–324. https://doi.org/10.1080/87568225.2014.948770
Byrne, B. M. (2016). Structural equation modeling with AMOS: Basic concepts, applications, and programming (3rd ed.). Routledge.
Credé, M., & Harms, P. D. (2015). 25 years of higher-order confirmatory factor analysis in the organizational sciences: A critical review and development of reporting recommendations. Journal of Organizational Behavior, 36, 845–872. https://doi.org/10.1002/job.2008
Downs, M. F., & Eisenberg, D. (2012). Help seeking and treatment use among suicidal college students. Journal of American College Health, 60, 104–114. https://doi.org/10.1080/07448481.2011.619611
Eells, G. T., & Rockland-Miller, H. S. (2011). Assessing and responding to disturbed and disturbing students: Understanding the role of administrative teams in institutions of higher education. Journal of College Student Psychotherapy, 25, 8–23. https://doi.org/10.1080/87568225.2011.532470
Faul, F., Erdfelder, E., Lang, A.-G., & Buchner, A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39, 175–191. https://doi.org/10.3758/BF03193146
Field, A. (2018). Discovering statistics using IBM SPSS Statistics (5th ed.). SAGE.
Futo, J. (2011). Dealing with mental health issues on campus starts with early recognition and intervention. Campus Law Enforcement Journal, 41, 22–23.
Gallagher, R. P. (2015). National survey of college counseling centers 2014. http://d-scholarship.pitt.edu/id/eprint/28178
Golightly, T., Thorne, K., Iglesias, A., Huebner, E., Michaelson-Chmelir, T., Yang, J., & Greco, K. (2017). Outreach as intervention: The evolution of outreach and preventive programming on college campuses. Psychological Services, 14, 451–460. https://doi.org/10.1037/ser0000198
Haines, A., Brown, A., McCabe, R., Rogerson, M., & Whittington, R. (2017). Factors impacting perceived safety among staff working on mental health wards. BJPsych Open, 3, 204–211.
https://doi.org/10.1192/bjpo.bp.117.005280
Hodges, S. J., Shelton, K., & King Lyn, M. M. (2017). The college and university counseling manual: Integrating essential services across the campus. Springer.
Hooper, D., Coughlan, J., & Mullen, M. R. (2008). Structural equation modelling: Guidelines for determining model fit. The Electronic Journal of Business Research Methods, 6, 53–60.
Iarussi, M. M. (2013). Examining how motivational interviewing may foster college student development. Journal of College Counseling, 16(2), 158–175. https://doi.org/10.1002/j.2161-1882.2013.00034.x
Kalkbrenner, M. T. (2016). Recognizing and supporting students with mental health disorders: The REDFLAGS Model. Journal of Education and Training, 3, 1–13. https://doi.org/10.5296/jet.v3i1.8141
Kalkbrenner, M. T. (2019). Peer-to-peer mental health support on community college campuses: Examining the factorial invariance of the Mental Distress Response Scale. Community College Journal of Research and Practice. https://doi.org/10.1080/10668926.2019.1645056
Kalkbrenner, M. T., & Carlisle, K. L. (2019). Faculty members and college counseling: Utility of The REDFLAGS Model. Journal of College Student Psychotherapy. https://doi.org/10.1080/87568225.2019.1621230
Kalkbrenner, M. T., & Flinn, R. F. (2020). Development, validation, and cross-validation of the Mental Distress Reaction Scale (MDRS). Journal of College Student Development.
Kalkbrenner, M. T., & Sink, C. A. (2018). Development and validation of the College Mental Health Perceived Competency Scale. The Professional Counselor, 8, 175–189. https://doi.org/10.15241/mtk.8.2.175
Kleinfield, N. R. (2007, April 22). Before deadly rage, a life consumed by a troubling silence. The New York Times. http://www.nytimes.com/2007/04/22/us/22vatech.html?pagewanted=all
Lynch, R. J., & Glass, C. R. (2019). The development of the Secondary Trauma in Student Affairs Professionals Scale (STSAP). Journal of Student Affairs Research and Practice, 56, 1–18.
https://doi.org/10.1080/19496591.2018.1474757
Margrove, K. L., Gustowska, M., & Grove, L. S. (2014). Provision of support for psychological distress by university staff, and receptiveness to mental health training. Journal of Further and Higher Education, 38, 90–106. https://doi.org/10.1080/0309877X.2012.699518
Mvududu, N. H., & Sink, C. A. (2013). Factor analysis in counseling research and practice. Counseling Outcome Research and Evaluation, 4, 75–98. https://doi.org/10.1177/2150137813494766
Reetz, D. R., Bershad, C., LeViness, P., & Whitlock, M. (2016). The Association for University and College Counseling Center Directors annual survey. https://www.aucccd.org/assets/documents/aucccd%202016%
20monograph%20-%20public.pdf
Resnicow, K., & McMaster, F. (2012). Motivational interviewing: Moving from why to how with autonomy support. International Journal of Behavioral Nutrition and Physical Activity, 9, 19.
https://doi.org/10.1186/1479-5868-9-19
Reynolds, A. L. (2013). College student concerns: Perceptions of student affairs practitioners. Journal of College Student Development, 54, 98–104. https://doi.org/ 10.1353/csd.2013.0001
Shuchman, M. (2007). Falling through the cracks—Virginia Tech and the restructuring of college mental health services. The New England Journal of Medicine, 357, 105–110. https://doi.org/10.1056/NEJMp078096
Vanderhart, D., Johnson, K., & Turkewitz, J. (2015, October 2). Oregon shooting at Umpqua College kills 10, sheriff says. The New York Times. https://www.nytimes.com/2015/10/02/us/oregon-shooting-umpqua-community-college.html?smid=pl-share
Varshney, M., Mahapatra, A., Krishnan, V., Gupta, R., & Deb, K. S. (2016). Violence and mental illness: What is the true story? Journal of Epidemiology & Community Health, 70, 223–225.
https://doi.org/10.1136/jech-2015-205546
Vieselmeyer, J., Holguin, J., & Mezulis, A. (2017). The role of resilience and gratitude in posttraumatic stress and growth following a campus shooting. Psychological Trauma: Theory, Research, Practice, and Policy, 9, 62–69. https://doi.org/10.1037/tra0000149
Warne, R. T. (2014). A primer on multivariate analysis of variance (MANOVA) for behavioral scientists. Practical Assessment, Research & Evaluation, 19(17), 1–10.
Michael T. Kalkbrenner, PhD, NCC, is an assistant professor at New Mexico State University. Correspondence can be addressed to Michael Kalkbrenner, 1220 Stewart St., OH202B, NMSU, Las Cruces, NM 88001, mkalk001@nmsu.edu.
Nov 26, 2019 | Volume 9 - Issue 4
Matthew C. Fullen, Jonathan D. Wiley, Amy A. Morgan
This interpretative phenomenological analysis explored licensed professional counselors’ experiences of turning away Medicare beneficiaries because of the current Medicare mental health policy. Researchers used semi-structured interviews to explore the client-level barriers created by federal legislation that determines professional counselors as Medicare-ineligible providers. An in-depth presentation of one superordinate theme, ineffectual policy, along with the emergent themes confounding regulations, programmatic inconsistencies, and impediment to care, illustrates the proximal barriers Medicare beneficiaries experience when actively seeking out licensed professional counselors for mental health care. Licensed professional counselors’ experiences indicate that current Medicare provider regulations interfere with mental health care accessibility and availability for Medicare-insured populations. Implications for advocacy are discussed.
Keywords: Medicare, interpretative phenomenological analysis, mental health, advocacy, federal legislation
Medicare is the primary source of health insurance for 60 million Americans, including adults 65 years and over and younger individuals with a long-term disability; the number of beneficiaries is expected to surpass 80 million by 2030 (Kaiser Family Foundation, 2019; Medicare Payment Advisory Commission, 2015). According to the Center for Medicare Advocacy (2013), approximately 26% of all Medicare beneficiaries experience some form of mental health disorder, including depression and anxiety, mild and major neurocognitive disorder, and serious mental illness such as bipolar disorder and schizophrenia. Among older adults specifically, nearly one in five meets the criteria for a mental health or substance use condition, and if left unaddressed, these issues may lead to consequences such as impaired physical health, hospitalization, and even suicide (Institute of Medicine, 2012).
Past research demonstrates that Medicare-eligible populations respond appropriately to counseling (Roseborough, Luptak, McLeod, & Bradshaw, 2012). Federal agencies such as the Substance Abuse and Mental Health Services Administration (SAMHSA) publish entire guides on how to use counseling to treat depression and related conditions in older adults (SAMHSA, 2011). However, researchers have noted specific challenges that Medicare-eligible populations, such as older adults, face when trying to access mental health services. Stewart, Jameson, and Curtin (2015) described acceptability, accessibility, and availability as three intersecting dimensions that may influence whether an older adult in need of help is able to access care. In contrast to acceptability, which focuses on whether older individuals are willing to participate in specific mental health services, accessibility and availability are both supply-side issues that impede older adults’ engagement with mental health services. Accessibility refers to factors like funding for mental health services and providing transportation support to attend appointments. Availability is used to describe the number of mental health professionals who provide services to older adults within a particular community.
Stewart et al.’s (2015) framework is useful when examining current Medicare policy and its impact on beneficiaries’ ability to participate in mental health treatment when needed. Experts have criticized Medicare for its relative inattention to mental health care (Bartels & Naslund, 2013), noting a remarkably low percentage of its total budget is spent on mental health (1% or $2.4 billion; Institute of Medicine, 2012), as well as a lack of emphasis on prevention services. In terms of accessibility, Congress has made efforts to remove restrictions to using one’s health insurance to access mental health treatment. For example, mental health parity laws were passed in 2008 to ensure that Medicare coverage for mental illness is not more restrictive than coverage for physical health concerns (Medicare Improvements for Patients and Providers Act of 2008, 2008). Yet current Medicare policy may restrict the availability of services at the mental health provider level. For example, the Medicare program has not updated its mental health provider licensure standards since 1989, when licensed clinical social workers were added as independent mental health providers and restrictions on services provided by psychologists were removed (H.R. Rep. No. 101-386, 1989). Although counseling is only one mental health care modality available to Medicare beneficiaries, counselors can play a prominent role in the mental health treatment of older adults and people with long-term disabilities.
Meanwhile, there are references in the literature to a provider gap that may influence the ability of Medicare beneficiaries, including older adults, to access mental health services. A 2012 Institute of Medicine report described the lack of mental health providers as a crisis, and experts on geriatric mental health care have decried the lack of mental health professionals who focus their work on older adults (Bartels & Naslund, 2013). Despite these concerns, relatively little attention has been given to the influence of Medicare provider regulations in limiting the number of available providers. Scholars have noted that a significant proportion of graduate-level mental health professionals are currently excluded from Medicare regulations, despite providing a substantial ratio of community-based mental health services (Christenson & Crane, 2004; Field, 2017; Fullen, 2016; Goodman, Morgan, Hodgson, & Caldwell, 2018). Licensed professional counselors (LPCs) and licensed marriage and family therapists (LMFTs) jointly comprise approximately 200,000 providers (Medicare Mental Health Workforce Coalition, 2019), which means that approximately half of all master’s-level providers are not available to provide services under Medicare. Since their recognition as independent mental health providers by Congress in 1989, only licensed clinical social workers and advanced practice psychiatric nurses have constituted the proportion of master’s-level providers eligible to provide mental health services through Medicare.
Despite current Medicare reimbursement restrictions, Medicare beneficiaries are likely to seek out services from LPCs. Fullen, Lawson, and Sharma (in press-a) found that over 50% of practicing counselors had turned away Medicare-insured individuals who sought counseling services, 40% had used pro bono or sliding scale approaches to provide services, and 39% were forced to refer existing clients once those clients became Medicare-eligible. When this occurs, the Medicare mental health coverage gap (MMHCG) impacts providers and beneficiaries in several distinct ways. First, some beneficiaries may begin treatment only to have services interrupted or stopped altogether once the provider is no longer able to be reimbursed by Medicare. This can occur because of confusion about whether a particular patient’s insurance coverage authorizes treatment by a particular provider type, or when beneficiaries who have successfully used one type of coverage to pay for services transition to Medicare coverage because of advancing age or qualifying for long-term disability.
Most Medicare beneficiaries (81%; Kaiser Family Foundation, 2019) have supplemental insurance, including 22% who have both Medicare and Medicaid. Medicare beneficiaries who are dually eligible for Medicaid may be particularly vulnerable to the MMHCG. In most states, Medicaid authorizes LPCs to provide counseling services; however, in certain cases when these individuals also qualify for Medicare, the inconsistency in provider regulations between these programs can interfere with client care. A similar problem occurs when the Medicare-insured attempt to use supplemental plans (e.g., private insurance, Medigap) because of Medicare functioning as a primary source of insurance, and supplemental plans requiring documentation that a Medicare claim has been denied. Regardless of the reason for having to terminate treatment prematurely, early withdrawal from mental health treatment has been described as inefficient and harmful to both clients and mental health providers (Barrett et al., 2008).
The MMHCG also can interfere with clients’ ability to access services because of a lack of Medicare-eligible providers in a particular geographical region. For example, beneficiaries who reside in rural localities can have more difficulty finding mental health providers because of a general shortage of providers in these areas (Larson, Patterson, Garberson, & Andrilla, 2016). Larson et al. (2016) found that rural communities were less likely to have licensed mental health professionals overall, although these localities were more likely to have a counseling professional than a clinical social worker, psychiatric nurse practitioner, or psychiatrist. Historically, older adults from rural and urban localities experience a comparable prevalence of mental health disorders (Center for Behavioral Health Statistics and Quality, 2018). However, studies consistently describe low rates of mental health services accessibility and availability within rural communities (Smalley & Warren, 2012). Establishing counselors as Medicare-eligible providers can reduce the disparities of mental health services accessibility and availability experienced by older adults in rural communities.
Although it is known that LPCs are currently excluded from Medicare coverage, it is not well understood what sort of impact this has on mental health providers and the Medicare beneficiaries who seek their services. Recent efforts to raise awareness of this issue have emerged in the literature (Field, 2017; Fullen, 2016; Goodman et al., 2018), but there has not yet been an investigation into the phenomenological experiences of mental health providers who are directly impacted by existing Medicare policy. The purpose of this study was to explore the lived experiences of mental health professionals who have turned away clients because of their status as Medicare-ineligible providers. The primary research question for this study was: How do Medicare-ineligible providers make sense of their experiences turning away Medicare beneficiaries and their inability to serve these clients?
Research Design and Methods
This study was executed using interpretive phenomenological analysis (IPA) to guide both data collection and analysis. The study focused on the experiences of Medicare-ineligible mental health professionals as they navigated interactions with Medicare beneficiaries who sought mental health care from them. By using a hermeneutic approach to understand their unique perspectives on this phenomenon, we aimed to remain consistent with the philosophical approach of IPA, which is idiographic in nature (Smith, Flowers, & Larkin, 2009). This study received approval from the Western Institutional Review Board.
IPA focuses on the personal meaning-making of participants who share a particular experience within a specific context (Smith et al., 2009). We determined IPA to be the most appropriate method to answer our research question because of the personal impact on LPCs of turning away Medicare beneficiaries because of Medicare-ineligible provider status. Nationally, LPCs share the experience of being unable to serve Medicare beneficiaries because of the current Medicare mental health policy that establishes these licensed mental health professionals as Medicare-ineligible. IPA also is appropriate for this study because of the positionality of the researchers. The research team consisted of two LPCs and one LMFT who have denied services or had to refer clients because of the current Medicare mental health policy and have engaged in prior research and advocacy related to the professional and clinical implications of the current Medicare mental health policy. We selected IPA for this study because of the shared experience between the researchers and participants as Medicare-ineligible providers. A distinguishing feature of IPA, a variation of hermeneutic phenomenology, is the acknowledgment of a double-interpretative, analytical process: The researchers make sense of how the participants make sense of a shared phenomenon (Smith et al., 2009).
Participants
Participants were screened based on the inclusion criteria of having direct experience with turning away or referring Medicare beneficiaries and holding a mental health license as an LPC. Because states grant licenses to health care providers, we limited participation to LPCs who were practicing in a specific state in the Mid-Atlantic region. This allowed for consistency in licensure requirements, training provided, and current scope of practice across all participants. The nine participants interviewed all held the highest professional counseling license in this state, which allows these individuals to practice independent of supervision after completing 4,000 hours of supervised training. Post-license experience ranged from 6 months to 17 years, and participants practiced in both rural and non-rural settings. Pseudonyms were assigned by the research team (see Table 1 for participant information).
| Table 1
Participant Information
|
| Participant |
License Type |
Rural Statusa |
Years of Licensed Experience |
| Michelle |
LPC |
Rural |
4 years |
| Cecelia |
LPC |
Non-rural |
5 years |
| Mary |
LPC |
Non-rural |
17 years |
| Roger |
LPC |
Non-rural |
2 years |
| Aubrey |
LPC |
Rural |
4 years |
| Donna |
LPC |
Rural |
4 years |
| April |
LPC |
Non-rural |
0.5 years |
| Robert |
LPC/LMFT |
Non-rural |
22 years |
| Brandon |
LPC |
Rural |
5 years |
aThe table displays rural status as designated by the U.S. Department of Health and Human Services Health Resources and Services Administration (2016) according to the practice location of the participant. Non-rural includes metropolitan and micropolitan areas. Rural indicates any locality that is neither metropolitan or micropolitan.
Most participants were identified because of having completed a national survey of mental health providers unable to serve Medicare beneficiaries (Fullen et al., in press-a). Participants in the national survey were provided with a question in which they were able to indicate their openness to participating in follow-up individual interviews regarding their experiences with turning away clients as a result of Medicare policy. Two additional participants had not completed the national survey but were identified locally because of their unique experiences with the phenomenon under investigation. We selected nine participants in accordance with IPA participant selection and data saturation guidelines (Smith et al., 2009). Although the current Medicare policy excludes both LPCs and LMFTs, we chose to focus on the experiences of LPCs to ensure a purposive and homogeneous sample (Smith et al., 2009).
Data Collection
Semi-structured, in-depth interviews of the nine participants were conducted by the research team. All research team members are LPCs or LMFTs. Individual interviews were conducted by a single member of the team who digitally recorded and transcribed verbatim the interview procedure. Consent was obtained from the participants and pseudonyms were used to ensure participant confidentiality. Also, participants were given the option to stop the interview at any time. The elapsed time of each interview ranged between 47 and 66 minutes. The semi-structured interview protocol began with two initial questions to frame the interview: (a) Have you ever had to refer a potential client to another counselor/therapist/agency because of not being able to accept their Medicare insurance coverage? and (b) Have you ever established a working relationship with a client who later transitioned to Medicare insurance coverage?
Based on participant responses to these initial questions, two grand tour questions followed:
(a) Tell me about what typically occurs when someone with Medicare insurance contacts your office in search of counseling? and (b) Tell me about any times when you have had to alter a pre-existing working relationship with a client because of their Medicare coverage? Follow-up questions focused on the impact of current Medicare mental health policy on the interviewees, as well as their perceived impact on clients, local communities, other therapists in the area, and their employment contexts.
Data Analysis
The IPA process outlined by Smith et al. (2009) was employed to analyze the transcribed interview data. The following steps were employed throughout the analysis process: (a) reading and re-reading of transcripts, (b) initial noting, (c) developing emergent themes, (d) searching for connections across emergent themes, (e) moving to the next case, and (f) looking for patterns across cases. Codes and themes developed at each stage of the first transcript analysis required consensus agreement among the authors. After re-reading, initial noting, developing emergent themes, and clustering of superordinate themes for each of the remaining interviews, the authors proceeded to engage in a group-level analysis process of looking for patterns across all interviews. Patterns across all interviews were organized into a concept map to synthesize connections and relationships between the interviews. Connections and relationships identified through this cross-case analysis led to the identification of a group-level clustering of superordinate themes that resulted in the identification of the primary themes.
Trustworthiness
The authors attended to the credibility and trustworthiness of this analysis using four strategies. First, the authors have prolonged engagement in the fields of counseling and marriage and family therapy as licensed professionals. This prolonged engagement has allowed the authors to be situated to the contexts of the participants, account for abnormalities in the data, and transcend their own observations (Lincoln & Guba, 1985). Second, the authors engaged in a team-based reflexive process through the sharing of personal reflections and group discussions about emerging issues (Barry, Britten, Barber, Bradley, & Stevenson, 1999). Third, negative case analysis was used in the analytical process of this study to develop, broaden, and confirm themes that emerged from the data (Lincoln & Guba, 1985; Patton, 1999). The fourth strategy was analyst triangulation (Denzin, 1978; Patton, 1999). All three authors participated in the development of the study, data collection, and data analysis to reduce the potential bias that can emerge from a single researcher performing each of these tasks (Patton, 1999). Each researcher independently analyzed the same data and compared their findings throughout data analysis to check selective perception and interpretive bias.
Results
Three superordinate themes emerged from our interviews with nine mental health professionals who have experience with the Medicare coverage gap: ineffectual policy, difficult transitions, and undue burden. We will discuss one superordinate theme, ineffectual policy, with the emergent themes of confounding regulations, programmatic inconsistencies, and impediment to care. By presenting a single meta-theme, we hope to provide increased depth and the nuanced experiences that our participants shared (see Levitt et al., 2018 for a discussion on dividing qualitative data into multiple manuscripts).
All nine participants expressed concerns about the ineffectiveness of current Medicare policy when it comes to treating people with mental disorders who live in their communities. The disconnect between Medicare’s intended aim—to provide sound health care to beneficiaries—and the present outcome for clients seeking out counseling led us to describe the policy as ineffectual or not producing the intended effect. Our participants perceived that the policy had severe shortcomings in terms of providing access to mental health care, which they viewed as a serious problem with cascading consequences for their clients, communities, and themselves.
Confounding Regulations
Several participants described the Medicare coverage gap as “confusing” and “frustrating” for mental health providers and Medicare beneficiaries who are seeking mental health services. Brandon, an LPC who serves as a director within a Federally Qualified Health Center, stated, “Most people are pretty shocked to realize we are not part of Medicare.” He went on to explain that most medical providers, including psychiatrists, were not aware of LPCs’ Medicare ineligibility when making client referrals. Participants described how the confusion interferes with referrals between medical providers and clients seeking mental health services.
Other participants described how frustrating the policy is, both for themselves and their clients. Robert, an LPC who also is credentialed as an LMFT, stated that “as a provider, it’s frustrating to turn people away,” and “it’s especially concerning for older people who can’t afford to pay out of pocket.” Michelle, who works as an LPC in a rural community, described how the MMHCG influences clients’ views of the larger Medicare system, stating, “[Clients are] very angry—not directed towards me, just the system . . . they’re on Medicare now [and] they have to leave. They paid into a system and then still can’t see the clinician that they want to see.” According to interviewees like Michelle, current Medicare provider regulations do not account for the preponderance of LPCs who provide care, particularly in rural communities. Regulations are then perceived by clients as an additional barrier to getting help at a time when they may be vulnerable.
In fact, in certain cases, current Medicare policy may result in all Medicare beneficiaries within a particular community losing access to mental health care. Brandon described a 4-month period when his Federally Qualified Health Center was unable to serve any Medicare beneficiaries because of job turnover: “[It] took us four months to find an LCSW. . . . We specifically had to weed out some very qualified licensed mental health professionals because they weren’t LCSWs.” Brandon went on to explain that during this 4-month period, his clients were unable to access mental health care at the community clinic. He concluded, “It was pretty disruptive to their care.”
Brandon’s description elucidates the cascading impact of the current policy on clients, community agencies that provide mental health services, and counselors seeking work. When specific providers are excluded from servicing Medicare beneficiaries, older adults with mental health conditions are vulnerable to gaps in coverage, such as the 4-month period that Brandon described.
Programmatic Inconsistencies
Several interviewees referenced confusion about how Medicare interfaces with other insurance programs. Roger and Mary, a couple in joint practice, explained how confusion among clients and health providers in their community is exacerbated by inconsistencies between Medicare and Medicaid, including the fact that in their state LPCs are eligible for reimbursement from Medicaid, but not Medicare. Roger explained, “[The] confusion is not just with clients who have low SES. It’s agency people, it’s case managers in the community, doctors that would make referrals, there really is a misunderstanding . . . and sometimes a disbelief.” They went on to describe their frustration in having to explain to referral sources that Medicare ineligibility has nothing to do with a lack of training. Roger concluded, “Yes, we are trained and . . . virtually every other insurance company accepts licensed professional counselors.”
Mary’s and Roger’s statements are indicative of the confusion that current policy creates among providers and clients. Several interviewees expressed annoyance that they had to explain to prospective clients that they possessed the requisite license and training required by the state to provide counseling and that they were recognized providers by non-Medicare insurance providers (i.e., Medicaid, Tricare, private insurance providers).
Related to the inconsistency between Medicaid and Medicare, several interviewees alluded to the fact that the very circumstances that qualify individuals for government-funded insurance (e.g., poverty, disability) may inadvertently restrict the mental health care that is available to them. Michelle described this phenomenon in the context of having to address clients who were referred to work with her by the local community mental health agency. She alluded to a particularly challenging cycle in which clients who were diagnosed with schizophrenia would be referred to her for counseling while they were also applying for long-term medical disability. She described the challenges of working with these clients, only to have to refer them elsewhere once they became eligible for disability benefits (which include Medicare). Describing her clients, she stated, “[They] applied for disability, they received disability, and now they have to, even though they have established the relationship with me . . . transition over to a different therapist.” Michelle then highlighted what occurs after this transition is initiated: “[One] individual . . . has continued to see me because with that particular diagnosis, he doesn’t trust anyone else. . . . [Another] individual . . . just chooses not to see anyone . . . and then she ends up having to be hospitalized every so often.”
Beyond being discouraged or exasperated, Michelle’s capacity to remain stoic in the face of such a paradox was telling. As she described it, this sequence had happened on multiple occasions and would likely happen again save for a federal policy change. Michelle also alluded to the potential economic detriments of current policy. By foregoing outpatient counseling because of the barriers described above, her patient with schizophrenia must be intermittently hospitalized, which is a much more expensive form of treatment.
Policy-level inconsistencies were confusing to providers as well. April, an LPC who attained her independent license within the past year, stated, “It feels like handcuffs. It’s like here you have this credential that the state says you have earned, but it’s only a half credential because you can’t [accept] one of the main government sponsored programs.” Cecelia, an LPC working in a metropolitan area, expressed similar sentiments as she explained how clients with Medicare and secondary insurance plans are turned away: “I initially bill Anthem first and my claims continue to get denied.” She explained, “Basically what they want me to do is submit the claims to Medicare, allow Medicare to deny the claim, and then submit the claim to them with the denial from Medicare and then they’ll provide reimbursement.” However, Cecelia stated that this process has been halted when Medicare refuses to issue a denial letter because of her status as an LPC. She put it this way: “The struggle that I found with Medicare is that because I’m an LPC, Medicare won’t even recognize me to even allow me to submit a claim . . . so I cannot provide Anthem with the denial that they’re looking for.”
Cecelia’s description of the inconsistency between Medicare and private insurance reflects a particularly problematic experience for her clients. Although they had paid for supplemental private insurance plans to augment their Medicare coverage, they were unable to use these benefits without a denial letter from Medicare. Ironically, according to Cecelia, the Medicare office could not provide the denial to a Medicare-ineligible provider in the first place.
Brandon made a similar statement about the inconsistency in provider regulations between Medicare and Tricare, specifically referencing his own training levels: “I’m shocked. . . . We’re some of the most qualified licensed mental health professionals in the business to provide psychotherapy and treatment for psychiatric diagnoses . . . and yet somehow that doesn’t count . . . somehow we’re not included.” Citing the growing number of insurance providers that do recognize LPCs, including Tricare, he concluded, “So, literally Medicare is the last holdout that I’m aware of.” By describing Medicare as “the last holdout,” Brandon implies that Medicare is the only federal program that has not updated its provider regulations to match the current mental health marketplace. Echoing Brandon, the sentiment that Medicare provider regulations were not in line with the current state of mental health practice was common among our interviewees.
Impediment to Care
The therapeutic working alliance has been shown to be one of the key factors that positively impacts counseling treatment (Wampold, 2015). When existing clients become eligible for Medicare, whether because of increasing age or qualifying for a long-term disability, current policy appears to interfere with continuity of care. Aubrey, an LPC who practices in a rural locality, describes it this way: “I will tell you where the problem arises . . . if I’m assigned a client, and I have the rapport with them, and we’re working together and they become eligible for Medicare . . . then I have to transfer them.” Because of the emphasis within counseling on the working relationship, Aubrey suggested that after building a strong working relationship with a counselor, even referrals within an agency can be disruptive to patient care.
Additionally, several interviewees described the challenges associated with referring Medicare beneficiaries to alternative providers. Some alluded to clients who made an effort to continue working with an LPC, despite not being able to use their Medicare coverage. Eventually, disparities in clients’ financial circumstances resulted in some clients having to forego receiving mental health care. Brandon explained the difficulty that current Medicare policy brings to communities, particularly those in which there are relatively few Medicare-eligible providers relative to LPCs. He described monthly meetings with community private practice providers this way: “[They are] all booked up. There’s just not enough . . . licensed mental health providers in town to see everybody. And . . . because only half of those people can accept Medicare, it has a very particular impact on Medicare recipients.” Citing the shortage of providers, Brandon emphasized the additional burden faced by the Medicare-insured because of having a smaller available provider pool.
The shortage of alternative mental health providers was a common theme among interviewees, especially for those who practiced in rural communities. Michelle explained that there is a misperception that Medicare-eligible providers are available when Medicare beneficiaries seek out help: “I hear . . .
there are so many licensed clinical social workers in this area, but there aren’t.” As a consequence, “[individuals] that are trying to work themselves into the schedule of a licensed clinical social worker, they often wait months before they’re actually able to be seen.”
Donna, an LPC who also works in a rural community, expressed a similar concern about the lack
of options facing beneficiaries who live in rural areas: “I see such a shortage in rural areas of providers across the board. And then when you have to narrow it down even further to limit who they can see, then that makes it even more difficult for them to get the care that they need.”
In fact, the expense of mental health care when insurance coverage is unavailable was a factor that several interviewees described. Robert told the story of a client he had seen for several years who tried to pay out of pocket but could no longer make that financially viable: “[It] was really disappointing because she really wasn’t finished. . . . We had a great working relationship and it was sad to have her stop just because of reimbursement reasons.”
Brandon made a similar comment about an individual who was deterred from seeking treatment because of the cost of paying out of pocket when his Medicare insurance was unable to be used: “I let him know . . . I can’t accept Medicare. And he asked how much it would be. [I said] anywhere from $75 to $125, and . . . he was pretty disheartened by that.”
Mary noted how the MMHCG can result in Medicare beneficiaries not seeking out necessary services. She emphasized that turning people away at the point when they have elected to ask for help can be disconcerting: “Right at a time when they’re willing to reach out and ask for [help]. That’s the worst part. Because I think . . . that discourages clients from seeking services—they have to work too hard . . . finding a provider.” April added a similar sentiment: “It’s heartbreaking . . . [my] emphasis is on those most vulnerable and those most in need of services . . . it is my worst nightmare for a client to walk away . . . because I want them to know they are my priority.” In each of these examples, participants expressed concerns that current policy acted as a deterrent to accessing necessary mental health services because of the burdensome process of having to locate a Medicare-eligible provider.
Discussion
Our findings illuminate how current Medicare mental health policy impacts Medicare beneficiaries’ access to counseling treatment for mental health conditions. Nine mental health providers who are not Medicare-eligible were interviewed to learn about their experiences interacting with Medicare beneficiaries who sought their services. The central phenomenon that all interviewees responded to—their inability to work with Medicare beneficiaries in the same manner that they work with clients who use other forms of insurance—has infrequently been referenced in the extant literature. This phenomenon provides a unique contribution to discussions about the accessibility and availability of mental health services to older adults (Stewart et al., 2015) and people with long-term disabilities. Particularly compelling about what was reported in these interviews is the fact that these individuals were actively seeking out or currently engaged in mental health treatment at the time when they were turned away. In the past, explanations about barriers to mental health care for Medicare-insured populations have focused on systemic factors such as rural geography (Kim et al., 2013) or stigma about mental health (Chapin et al., 2013). While these are certainly relevant factors that provide a broad explanation for why older people are less likely to receive mental health services, the current study illuminates several proximate point-of-service barriers that result in providers having to cease treatment with clients, deny care to clients who were actively seeking it out, or refer clients to relatively long wait-lists in lieu of more prompt treatment by available providers. Given the lack of scholarly attention focused on the MMHCG, the perspectives offered by these participants contributes to a broader discussion about how to increase access to mental health services for older adults, as well as for individuals with long-term disabilities.
Among our interviewees, there was a noticeable amount of concern for how the MMHCG impacts individuals in the community in need of mental health care. Participants’ concerns about the consequences of the MMHCG on their clients may be related to their awareness that mental illness influences other key indicators of well-being. For example, depression reflects a relatively common mental health condition that responds well to treatment but can be problematic for clients when left untreated. Although depression was only one of several types of mental illness described by participants, clinically relevant depressive symptoms affect 10% of males over 65 and 15% of females over 65, and the presence of depressive symptoms is correlated with greater functional disability, dementia, higher rates of physical illness, and higher health care resource utilization (Federal Interagency Forum on Aging-Related Statistics, 2016). As the number of Medicare beneficiaries grows, it is reasonable to assume that there will be corresponding growth in the number of people who meet the criteria for mental health conditions, including depression. Echoing the concern voiced by our participants, we state that the current Medicare policy extends the risk of mental health needs going unmet among Medicare-insured populations.
Additionally, the economic consequences of untreated or undertreated mental illness are worth considering. Each participant described instances of unmet client mental health needs because of a combination of (a) practitioner inability to submit for Medicare reimbursement, (b) client’s inability to pay a sliding scale rate, and (c) lack of follow-through on referrals to mental health providers eligible for Medicare coverage. For example, some participants described this undertreatment as resulting in potential inpatient psychiatric hospitalization because of clients’ inability to utilize their Medicare benefits to seek care within their local communities. Undertreatment of mental health conditions can lead to inefficient administration of health care, including an over-reliance on more expensive mental health services when outpatient services could have been more appropriate. For example, the reimbursement rate for 45 minutes of counseling is $84.74 for doctoral-level providers (see American Psychological Association, 2015, for a critique of this rate), and the rate for master’s-level providers is estimated at 75% of this amount ($63.56). This is in contrast to the cost of a single day in an inpatient psychiatric facility, which is $782.78, or approximately 12 times higher than a single counseling session (Centers for Medicare & Medicaid Services, 2019). Having adequate outpatient services available within a community is traditionally a sound strategy for reducing high-cost treatment; yet this is not occurring as regularly as is needed when Medicare beneficiaries are involved. Although not every person who may be at risk for inpatient hospitalization will benefit solely from weekly outpatient services, several cases referenced by our interviewees (e.g., Michelle’s work with clients with schizophrenia) fit this category. Considering that a single day of inpatient treatment costs the same as a 12-session course of counseling from a master’s-level provider, it stands to reason that there are economic benefits to re-examining current Medicare mental health policy.
The inefficiency of current Medicare policy was highlighted when several participants alluded to inconsistencies between insurance programs, including certain cases in which having Medicare precluded clients from using other forms of insurance (e.g., Medicaid, Tricare, private supplemental plans) that would otherwise cover mental health treatment by LPCs. This feature of the MMHCG has important ramifications given that 81% of Medicare beneficiaries possess a supplemental health plan (Kaiser Family Foundation, 2019), including more than 12 million Americans who are dually covered by Medicare and Medicaid (Centers for Medicare & Medicaid Services, n.d.). For this latter group, dual-eligible adults are more likely to have functional or cognitive impairments, chronic conditions, or conditions that frequently coincide with mental health conditions. In fact, among dual-eligible individuals, 59% of those with disabilities and 20% of those who are 65 years or older self-reported diagnosis of a mental health disorder (Donohue, 2006). This means that some of the most vulnerable Medicare beneficiaries are particularly burdened by current Medicare mental health policy.
Implications for Professional Advocacy
Regarding advocacy on behalf of clients, these findings suggest that Medicare reimbursement for LPCs is urgently needed in order to provide Medicare-insured populations with access to mental health services. Currently, efforts to change Medicare regulations through the legislative process have support from a broad range of professional interest groups, many of which comprise the Medicare Mental Health Workforce Coalition (Medicare Mental Health Workforce Coalition, 2019). Further, there is currently legislation under consideration in both the U.S. Senate (S. 286; Mental Health Access Improvement Act, 2019) and U.S. House of Representatives (H.R. 945; Mental Health Access Improvement Act, 2019) that would include LPCs and LMFTs as Medicare-eligible providers. As of November 2019, these bills had 29 and 96 cosponsors, respectively (U.S. Congress 2019a, 2019b). Despite these efforts, more than half of counseling professionals recently surveyed had not participated in advocacy related to Medicare reimbursement (Fullen, Lawson, & Sharma, in press-b). Therefore, additional work is needed to educate members of the counseling profession about the consequences of current Medicare mental health policy on clients from underserved populations. Fullen et al. (in press-a, in press-b) describe several strategies that can be used to strengthen advocacy efforts among members of the counseling profession, including counselor educators, master’s and doctoral students, and practicing counselors.
Limitations and Future Research
A primary limitation of this study relates to the generalizability of the results. This study reports on a specific and localized account of how Medicare mental health policy impacts Medicare beneficiaries’ access to counseling treatment in a single state. We intentionally focused on a homogenous sample purposefully selected to explore how LPCs are making sense of their inability to provide counseling services to Medicare beneficiaries based on their professional status as Medicare-ineligible. The findings present a narrative account of how these licensed mental health providers make sense of and respond to the experience of not being able to serve Medicare clients because of professional limitations contained within Medicare mental health policy. The utilization of IPA has allowed for the detection of nuance, subtlety, and complexity within the data from the semi-structured interviews with our participants. This specificity allows for an understanding that shows how the coverage gap created by the exclusion of counselors impacts Medicare beneficiaries’ access to counseling services.
An additional limitation of our study is the use of prolonged engagement as a strategy to establish credibility and trustworthiness. Prolonged engagement, traditionally employed in ethnography and
participant observation, requires that researchers spend sufficient time in the field to learn or understand the experiential phenomenon of the study (Lincoln & Guba, 1985). Though we did not spend time with participants within their specific practice settings, we each have practice experience as Medicare-ineligible providers within the field of professional counseling. In a more ethnographic study on the MMHCG, we would be able to employ a more traditional application of prolonged engagement.
Future research should focus on additional qualitative and quantitative data sets that allow for more generalizability of findings. By nature, Medicare policy is consistent across the United States, which leads us to believe that there are likely similarities between the phenomena described by our interviewees and what occurs in other states. Nonetheless, additional inquiry is needed to probe the impact of MMHCG more comprehensively. An empirical investigation into the perspectives of Medicare-insured individuals who have been unable to utilize their Medicare benefits because of the MMHCG may lend an additional lens toward understanding the impact of Medicare mental health policy on clients. Ultimately, this study and subsequent studies focusing on diminishing coverage gaps for Medicare beneficiaries can support progress toward diminishing health inequities because of health care policy restrictions.
Conclusion
This study highlights an existing gap in the administration of Medicare services for clients seeking counseling treatment for mental health conditions. By attending to the theme of ineffectual policy, we have attempted to illuminate how current policy impacts the Medicare-insured, as well as LPCs who are involved in their mental health care. Based on our analysis of the MMHCG, future revisions to Medicare policy allowing for the inclusion of LPCs to provide counseling treatment to Medicare-insured individuals may contribute to a more equitable health care system for Medicare beneficiaries.
Conflict of Interest and Funding Disclosure
This research was supported by the Virginia Tech
Institute for Society, Culture, and Environment.
References
American Psychological Association. (2015). Medicare’s shrinking psychologist reimbursement rates. Retrieved from https://www.apaservices.org/practice/advocacy/state/leadership/medicare-payment
Barrett, M. S., Chua, W.-J., Crits-Christoph, P., Gibbons, M. B., Casiano, D., & Thompson, D. (2008). Early withdrawal from mental health treatment: Implications for psychotherapy practice. Psychotherapy: Theory, Research, Practice, Training, 45, 247–267. doi:10.1037/0033-3204.45.2.247
Barry, C. A., Britten, N., Barber, N., Bradley, C., & Stevenson, F. (1999). Using reflexivity to optimize teamwork in qualitative research. Qualitative Health Research, 9, 26–44. doi:10.1177/104973299129121677
Bartels, S. J., & Naslund, J. A. (2013). The underside of the silver tsunami—Older adults and mental health care. The New England Journal of Medicine, 368, 493–496. doi:10.1056/NEJMp1211456
Center for Behavioral Health Statistics and Quality. (2018). 2017 National survey on drug use and health: Detailed tables. Rockville, MD: Substance Abuse and Mental Health Services Administration. Retrieved from
https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHDetailedTabs2017/NSDUHDeta
iledTabs2017.pdf
Center for Medicare Advocacy. (2013). Medicare and mental health. Retrieved from https://www.medicareadvoca
cy.org/medicare-and-mental-health
Centers for Medicare & Medicaid Services. (n.d.). Seniors & Medicare and Medicaid enrollees. Retrieved from
https://www.medicaid.gov/medicaid/eligibility/medicaid-enrollees/index.html
Centers for Medicare & Medicaid Services. (2019). Fiscal year 2019 inpatient psychiatric facility prospective payment system rates and adjustment factors. In Inpatient psychiatric facility prospective payment system (Addendum A). Retrieved from https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/Inpatient-Psychiatric-Facility-Prospective-Payment-System.pdf
Chapin, R. K., Sergeant, J. F., Landry, S., Leedahl, S. N., Rachlin, R., Koenig, T., & Graham, A. (2013). Reclaiming joy: Pilot evaluation of a mental health peer support program for older adults who receive Medicaid. The Gerontologist, 53, 345–352. doi:10.1093/geront/gns120
Christenson, J. D., & Crane, D. R. (2004). Estimating the cost of direct reimbursement of marriage and family therapy under Medicare. Journal of Marital and Family Therapy, 30, 515–525. doi:10.1111/j.1752-0606.2004.tb01259.x
Denzin, N. K. (Ed.). (1978). Sociological methods: A sourcebook. New York, NY: McGraw-Hill.
Donohue, J. (2006). Mental health in the Medicare Part D drug benefit: A new regulatory model? Health Affairs, 25, 707–719. doi:10.1377/hlthaff.25.3.707
Federal Interagency Forum on Aging-Related Statistics. (2016). Older Americans 2016: Key indicators of well-being. Washington, DC: U.S. Government Printing Office. Retrieved from https://agingstats.gov/docs/LatestReport/Older-Americans-2016-Key-Indicators-of-WellBeing.pdf
Field, T. A. (2017). Clinical mental health counseling: A 40-year retrospective. Journal of Mental Health Counseling, 39, 1–11. doi:10.17744/mehc.39.1.01
Fullen, M. C. (2016). Medicare advocacy for the counselor advocate. Adultspan Journal, 15, 3–12. doi:10.1002/adsp.12015
Fullen, M. C., Lawson, G., & Sharma, J. (in press-a). Analyzing the impact of the Medicare coverage gap on counseling professionals: Results of a national study. Journal of Counseling & Development.
Fullen, M. C., Lawson, G., & Sharma, J. (in press-b). Medicare reimbursement for counselors: Counseling professionals’ advocacy beliefs and behavior. Counselor Education and Supervision.
Goodman, J. M., Morgan, A. A., Hodgson, J. L., & Caldwell, B. E. (2018). From private practice to academia: Integrating social and political advocacy into every MFT identity. Journal of Marital and Family Therapy, 44, 32–45. doi:10.1111/jmft.12298
H.R. Rep. No. 101-386 (1989). Retrieved from https://www.congress.gov/bill/101st-congress/house-bill/3299
Institute of Medicine. (2012). The mental health and substance use workforce for older adults: In whose hands? Washington, DC: National Academies Press.
Kaiser Family Foundation. (2019). An overview of Medicare. Retrieved from https://www.kff.org/medicare/issue-brief/an-overview-of-medicare
Kim, G., Parton, J. M., DeCoster, J., Bryant, A. N., Ford, K. L., & Parmelee, P. A. (2013). Regional variation of racial disparities in mental health service use among older adults. The Gerontologist, 53, 618–626. doi:10.1093/geront/gns107
Larson, E. H., Patterson, D. G., Garberson, L. A., & Andrilla, C. H. A. (2016). Supply and distribution of the behavioral health workforce in rural America. Data Brief #160. Seattle, WA: WWAMI Rural Health Center, University of Washington.
Levitt, H. M., Creswell, J. W., Josselson, R., Bamberg, M., Frost, D. M., & Suárez-Orozco, C. (2018). Journal article reporting standards for qualitative primary, qualitative meta-analytic, and mixed methods research in psychology: The APA Publications and Communications Board task force report. American Psychologist, 73, 26–46. doi:10.1037/amp0000151
Lincoln, Y. S., & Guba, E. G. (1985). Naturalistic inquiry. Newbury Park, CA: SAGE.
Medicare Improvements for Patients and Providers Act of 2008, Pub. L. No. 110-275, 122 Stat. 2494 (2008).
Medicare Mental Health Workforce Coalition. (2019). Expanding the Medicare provider workforce: A solution to the behavioral health crisis. Retrieved from https://centerstone.org/wp-content/uploads/MHAIA-One-Pager-FINAL.pdf
Medicare Payment Advisory Commission. (2015). Chapter 2: The next generation of Medicare beneficiaries. In Report to the Congress: Medicare and the health care delivery system (pp. 35–57). Retrieved from http://www.medpac.gov/docs/default-source/reports/chapter-2-the-next-generation-of-medicare-beneficiaries-june-2015-report-.pdf?sfvrsn=0
Patton, M. Q. (1999). Enhancing the quality and credibility of qualitative analysis. HSR: Health Services Research, 34, 1189–1208.
Roseborough, D. J., Luptak, M., McLeod, J., & Bradshaw, W. (2012). Effectiveness of psychodynamic psychotherapy with older adults: A longitudinal study. Clinical Gerontologist, 36, 1–16.
Smalley, K. B., & Warren, J. C. (2012). The current state of rural mental health. In K. B. Smalley, J. C. Warren, & J. P. Rainer (Eds.), Rural mental health: Issues, policies, and best practices (pp. 3–16). New York, NY: Springer.
Smith, J. A., Flowers, P., & Larkin, M. (2009). Interpretative phenomenological analysis: Theory, method and research. Thousand Oaks, CA: SAGE.
Stewart, H., Jameson, J. P., & Curtin, L. (2015). The relationship between stigma and self-reported willingness to use mental health services among rural and urban older adults. Psychological Services, 12(2), 141–148. doi:10.1037/a0038651
Substance Abuse and Mental Health Services Administration. (2011). Treatment of depression in older adults evidence-based practices (EBP) kit. Retrieved from https://store.samhsa.gov/product/Treatment-of-Depression-in-Older-Adults-Evidence-Based-Practices-EBP-KIT/SMA11-4631CD-DVD
U.S. Congress. (2019a). H.R.945—Mental Health Access Improvement Act of 2019. Retrieved from https://www.congress.gov/bill/116th-congress/house-bill/945
U.S. Congress. (2019b). S.286—Mental Health Access Improvement Act of 2019. Retrieved from https://www.congress.gov/bill/116th-congress/senate-bill/286
U.S. Department of Health and Human Services, Health Resources and Services Administration. (2016). FORHP rural areas [Data file]. Retrieved from https://data.hrsa.gov/data/about#DataUsage
Wampold, B. E. (2015). How important are the common factors in psychotherapy? An update. World Psychiatry, 14, 270–277. doi:10.1002/wps.20238
Matthew C. Fullen is an assistant professor at Virginia Tech. Jonathan D. Wiley, NCC, is a doctoral candidate at Virginia Tech. Amy A. Morgan is a doctoral candidate at Virginia Tech. Correspondence can be addressed to Matthew Fullen, School of Education, College of Liberal Arts and Human Sciences, 1750 Kraft Drive, Suite 2000, Room 2005, Blacksburg, VA 24061, mfullen@vt.edu.
Nov 25, 2019 | Volume 9 - Issue 4
Alwin E. Wagener, Laura K. Jones, J. Scott Hinkle
The global burden of disease related to mental health is astronomical and growing, with underprivileged countries being disproportionately affected. The Mental Health Facilitator (MHF) program was designed by the National Board for Certified Counselors (NBCC) to address the need for greater mental health support within international communities lacking adequate mental health practitioners to provide services. The MHF program trains individuals within communities to provide support and necessary referrals for those struggling with mental health challenges. This study assesses the effectiveness of MHF trainings conducted in a diverse subset of countries and communities. Initial findings from the analyses found significant gains in participants’ knowledge of mental health and mental health facilitation skills across training populations.
Keywords: Mental Health Facilitator, MHF, mental health, NBCC, global
Over 450 million individuals around the world struggle with mental health concerns with 300 million people alone suffering from depression (World Health Organization [WHO], 2018). Mental health is defined as “a state of well-being in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community” (WHO, 2014a, para. 1). Mental disorders account for nearly 30% of the global burden of disease (i.e., what kills, injures, and disables people around the world) in terms of years lived with disability (Kessler et al., 2009; Vigo, Thornicroft, & Atun, 2016). In addition to the hardships that mental disorders place on an individual’s social relationships, occupational opportunities, and physical health, nearly 800,000 people a year die by suicide, with 75% of those individuals residing in developing countries (WHO, 2014b). Such staggering statistics include the rank of suicide as the second most common cause of death among young people globally (WHO, 2014b).
In addition to personal struggles, communities also face economic hardships related to mental disorders. The global cost of mental health was estimated at $2.5 trillion in 2010, with estimates of costs expected to reach as high as $6 trillion by 2030 (Bloom et al., 2011). Such costs can be devastating for individuals and communities alike, especially where resources are limited.
Despite the exorbitant number of individuals around the world struggling with mental health concerns and the associated individual, societal, and economic costs, only a small portion of people receive the support they need (Hinkle, 2014; Kohn, Saxena, Levav, & Saraceno, 2004; Wang et al., 2007). It is important to note that only one third to one half of individuals in high-income countries receive mental health care. This gap is even more pervasive in low- to middle-income countries, with a mere 15%–24% of individuals receiving any form of mental health support (Demyttenaere, 2004). Furthermore, according to WHO (2015), most of the world’s population live in areas where there is an average of less than one psychiatrist per 200,000 people and even fewer individuals trained in psychosocial interventions.
This gap in service provision and treatment stems from both attitudinal (e.g., misinformation about mental health such as low perceived need, stigma, and discrimination) and structural-level (e.g., availability of services, financial considerations, and transportation problems) barriers (Andrade et al., 2014; Hinkle, 2014). Although attitudinal barriers appeared to be more pervasive, overall individuals with more severe mental health conditions and those in low- or lower–middle- income countries cited financial and service availability barriers as being especially problematic. In 2011, WHO detailed the scarcity of resources available to treat and promote mental health across the spectrum of high- to low-income countries, which leads to a gap in the provision of treatment as well as the quality of treatment when it is available. For example, within high-income countries, approximately $44.84 USD is spent per person on annual mental health expenditures, a value which drops to $0.20 USD per person in low-income countries (WHO, 2011). Clearly, a strategy to lessen this gap in global mental health service provision is needed.
A Call to Action
Given the pervasiveness and deleterious consequences of mental health disorders paired with the dearth of individuals receiving treatment, there is a global imperative that countries begin prioritizing mental health awareness, education, and treatment and combatting the noted barriers to individuals seeking and receiving adequate care. Enhancing the awareness and education of not only individuals struggling with mental health difficulties, but also members of the community, would be beneficial in addressing attitudinal barriers, while providing additional resources through increasing the number of both service providers and service centers can help to eliminate structural barriers to services. Such solutions are reflected in the WHO’s (2013) Mental Health Action Plan, which outlines the following four objectives:
(1) to strengthen effective leadership and governance for mental health; (2) to provide comprehensive, integrated and responsive mental health and social care services in community-based settings; (3) to implement strategies for promotion and prevention in mental health; and (4) to strengthen information systems, evidence and research for mental health. (p. 10)
Several approaches exist to address these objectives, yet one program in particular is unique in creatively addressing multiple objectives at once. Developed by the National Board for Certified Counselors (NBCC) and initially endorsed by WHO, the Mental Health Facilitator (MHF) program aims to reduce disparities in mental health care by facilitating access to support individuals and mental health services in underserved populations (Hinkle, 2006, 2014; Hinkle & Saxena, 2006). Specifically, the MHF program trains diverse community members (i.e., mental health laypersons) in the knowledge and skills necessary to identify mental health needs, support those in need of care, work with existing care resources, and make referrals to mental health professionals as needed (Hinkle & Henderson, 2007). The program focuses on creating a culturally appropriate curriculum adaptive to community needs and contexts while also providing fundamental information concerning mental health and basic psychosocial interventions. Also, unlike many other programs, the MHF program is only tailored and implemented into specific communities at the community’s request. In this way, the MHF program content aligns with WHO’s Mental Health Action Plan by working to strengthen culturally appropriate information systems, implementing strategies for promoting mental health and decreasing the severity and pervasiveness of disorders, and enhancing responsive and integrated service provision within community-based settings tailored to the needs of that community (Hinkle, 2014).
Content of the MHF Program
The mission of the MHF program is to provide skilled, responsible access to quality mental health interventions. This is usually accomplished through basic first-contact help and referrals to mental health professionals with respect for human dignity and meeting population needs by balancing globally accepted mental health practices within local norms and conditions (Hinkle, 2014). Cross-disciplinary in nature, the MHF program includes competencies from psychiatry, psychology, social work, psychiatric nursing, and counseling, covering topics such as helping skills, diversity, violence and trauma, suicide prevention, and referral and consultation skills. The design of the training emphasizes important considerations and approaches in addressing mental health concerns while allowing for flexibility in implementation. This flexibility is a key strength of the training program and is necessary given the breadth of cultural and contextual factors affecting mental health and mental health care around the globe. Such flexibility allows local stakeholders to identify and adapt the training to local needs and the knowledge gained from the MHF training program to be implemented within existing care settings or to provide a foundation for care in areas where no established system is present. The information contained within the training and flexibility of implementation constitute a population-based mental health care approach to addressing health care needs across a broad range of social, political, economic, and cultural environments (Hinkle, 2014), and one that is growing in its evidence base.
History and Implementation of the MHF Program
The MHF program is a three-tiered, train-the-trainer implementation model that consists of MHF master trainers, MHF trainers, and mental health facilitators. MHF master trainers are selected by NBCC based on specific criteria, most notably the completion of considerable training and experience in mental health and education. MHF trainers are often professionals or paraprofessionals with mental health and teaching experience located in the community who can train community groups. MHF trainees are typically laypersons with an interest in mental health who then become the first line of support for community members with mental health needs. Following training at each of the levels, individuals are registered in the international MHF registry. Currently there are over 4,774 registered MHF master trainers, MHF trainers, and mental health facilitators located around the world.
The MHF program was first established in 2005, when NBCC worked in collaboration with WHO to establish a panel of experts, including mental health professionals from the United States, Canada, Malaysia, Trinidad, St. Lucia, Turkey, Romania, India, Mexico, Botswana, and Venezuela, who would contribute to the development of the MHF training manual, curriculum, and implementation plans. This approach led to content and delivery plans that represented diverse cultures and thus diverse perspectives on mental health, mental health care, and the role of MHF master trainers, MHF trainers, and mental health facilitators. The curriculum and master training guide were completed and piloted in Mexico City in 2007 and 2008. Later in 2008, the first train-the-trainer program was delivered in Lilongwe, Malawi. To date, NBCC has partnered with 26 countries, including eight countries in Africa, five in Asia, four in the Middle East, and eight in Europe, as well as programs in Mexico and the United States. Furthermore, the MHF curriculum has been translated into Arabic, Chinese, Dzongkha (the language of Bhutan), Estonian, German, Greek, Japanese, Malay, Portuguese, Romanian, Russian, Spanish, and Swahili (Hinkle, 2014).
The MHF Curriculum
When developing a partnership with NBCC, communities can choose one of five MHF curricula to best suit their needs, namely the original MHF training, an abridged MHF training, a training for educators (MHF-EE), an abridged MHF-EE, or a version for first responders (i.e., fire, rescue, and police). The five MHF curricula share core content aimed at helping professionals and paraprofessionals improve communication and helping skills, identify local mental health resources, understand important ethical considerations, and connect health providers with individuals within their community who are in need of mental health services (Hinkle, 2014). In addition to the core content, the curricula directed toward educators and emergency personnel contain tailored modules to best support those populations. With trainings ranging from 6 to 30 hours, the curricula can be delivered over consecutive days or divided into its modules and taught over several weeks, depending on community needs (Hinkle & Henderson, 2007).
The foundation of the MHF curriculum underscores the shared experiences of stress, distress, and disorder (Desjarlais, Eisenberg, Good, & Kleinman, 1995; Hinkle, 2014; Hinkle & Henderson, 2007). Given these theoretical underpinnings, the core modules cover topics such as basic helping skills, coping with stress, community mental health services, and community advocacy skills, and also introduce trainees to considerations around ethical practice and specifics about interventions such as suicide mitigation and trauma responses (Hinkle, 2014). Participants learn the benefits of investing in mental health, barriers to mental health care, cost-effective interventions, how mental health disorders impact families, confidentiality and privacy, and the broad mission of the MHF program (Hinkle, 2014).
In the basic helping skills section of the training, trainees cover development; diversity; verbal and nonverbal communication; facilitative skills such as listening, asking questions, and providing reflections; assessing for mental health concerns; empathy and understanding human feelings; and how to make referrals and effectively terminate relationships (Hinkle, 2014; Hinkle & Henderson, 2007). This information is followed by a discussion of how to understand problems, coping styles, and ways of effectively managing problems. The training then delves into recognizing stress, distress, and various disorders, including risk factors and mental health in children. The core modules conclude with discussions of suicide and trauma. Being the leading cause of death among young people in low- and middle-income countries, suicide is a pressing concern within all communities (WHO, 2006). Similarly, the pervasiveness of natural and human-born disasters and crises, such as war, forced displacement, human trafficking, typhoons, and wildfires, affects individuals of all demographics around the world and often goes untreated (Hinkle, 2014). A final topic covered in the core MHF training is the importance of self-awareness and self-care for mental health facilitators.
Moreover, the content in any of the five MHF curricula can be adapted to best fit the social, cultural, economic, and political realities and needs of any community, country, or region. For example, countries have chosen to add additional modules on child maltreatment in the Syrian region.
Past and Ongoing MHF Research
Building a strong evidence base is imperative to the development of a sustainable program that addresses the staggering gap that exists in mental health service provision. With limited resources spent on mental health, countries and communities cannot afford to implement programs that lack evidence supporting their projected outcomes and benefits. To this end, NBCC has and will continue to emphasize building a solid evidence base for the MHF program. Qualitative studies published to date (Luke, Hinkle, Schweiger, & Henderson, 2016; Van Leeuwen, Adkins, Mirassou-Wolf, Schweiger, & Grundy, 2016) support the perceived value and effectiveness of the program. Luke et al. (2016) reported that among the value and benefits, participants commented on how the program was culturally congruent and beneficially adapted to the needs of their community as well as how the program filled a need in terms of limited mental health resources. Participants further noted the considerable negative implications if the MHF program were to be discontinued (Luke et al., 2016). Van Leeuwen et al. (2016) also found notable positive perceptions of the MHF program. Participants reported that they gained skills in communication and referral. They also noted how they received important education on mental health and causes of mental health problems, and an enhanced awareness of mental health in communication. Finally, participants reported that there were both personal and community benefits to the program, such as an ability to better understand their own mental health and the mental health of family members as well as a reduction in community mental health stigma (Van Leeuwen et al., 2016).
However, to date no study has reported the quantitative outcomes of MHF trainings. Most trainings include pre- and post-training assessments of participants using a true-false, pencil-and-paper–based assessment. The assessment for the original MHF curriculum had three small adaptations involving changing the wording on several questions in 2009, 2011, and 2013. The adaptations were minimal, so all years were included in this study. This study fills the gap in the MHF literature by reporting on the objective data gathered from the pre- and post-training assessments of the original MHF curriculum.
Methods
This study uses a quasi-experimental research design to evaluate whether participants in 88 MHF original trainings demonstrated increased knowledge of mental health issues and approaches to address community mental health concerns. The trainings spanned from 2009–2017 and included all MHF trainings conducted outside of the European Union and the United States. For each MHF training, pre- and post-training assessments were completed by all participants in an effort to evaluate the effectiveness of training. The pre- and post-training assessments contained 50 true-false questions with the pretest administered on the first day of training and the posttest administered at the final training day, 5 days later. The present study analyzed the pretest and posttest evaluations using paired t-tests and a one-way ANOVA.
Participants
Participants who completed all items on both the pretests and posttests were included in the study, resulting in 1,392 participants from 15 countries. Of the 1,392 participants, only 735 provided descriptive information. For those participants, 431 were female (59%) and 304 were male (41%). The age range of participants was 17 to 75 years with a mean age of 36 years. The education of participants ranged from elementary school to doctoral (PhD) and professional degrees (MD and JD). There were 14 participants reporting only an elementary school level of education (2%), 150 with high school (20%), 151 with a 2-year degree (21%), 310 with a 4-year degree (42%), 99 with a master’s degree (13%), and 11 with a PhD or professional degree (1%). Given that trainings were conducted in countries within North America, Africa, Asia, and the Middle East, the data included a diverse range of participants in terms of nationality.
Research Questions
There were two primary questions investigated in this study. The questions were prompted by a desire to better understand the effectiveness of the MHF trainings: (1) Does the MHF program training significantly increase overall knowledge of mental health facilitation from pretest to posttest evaluation for participants? and (2) How does performance on the pretest, or initial mental health knowledge, affect possible training gains made between pretest and posttest scores for the participants?
Data Preparation
Prior to formal data analyses, the authors examined the data to ensure it satisfied the assumptions of the relevant statistical tests. Upon initial data examination, the authors determined that 77 participants of an initial 1,392 were outliers. The outliers were those with scores 1.5 times the interquartile range, either above the third quartile or below the first quartile. Based on this, the data analyses presented in the following sections were run with and without the outliers removed, and it was determined that the outliers did not significantly affect the results (the only exception to the outliers affecting the results is described in the results section). As such, the data analyses presented are using the remaining 1,315 participants after the removal of the outliers.
As the data set is too large for statistical normality tests to be accurate, skewness and kurtosis values were examined. The data set without the outliers had skewness (.208) and kurtosis (-.018), both values within the normal range. A visual inspection of the descriptive q-q line further supported the conclusion that the data is normally distributed.
Results
Overall Mental Health Knowledge Gain
The first research question, asking whether the MHF program training significantly increased overall knowledge of mental health and mental health facilitation, was assessed using a paired sample t-test. The result of this analysis showed that there was a significant difference (t = -35.90, p = 0.000) between pretest (M = 37.64, SD = 5.58) and posttest (M = 41.17, SD = 5.24) scores. This analysis confirms the hypothesis that the MHF program training significantly increases the scores of participants from pretest to posttest evaluation.
Initial Mental Health Knowledge and Training Gains
The second research question investigated whether the starting knowledge of participants, as measured in the pretest, affected the training gains made between the pretest and posttest. To address this research question, four categories based on pretest scores were generated. A descriptive analysis was conducted to determine the quartiles of the pretest scores, and the quartiles were used to define the categories. The authors determined that quartiles are an effective means of dividing the pretest scores into four groups given that the relationships between the groups are clearly linked to the overall distribution of pretest scores. The pretest scores ranged from 15–50 (the range of possible scores was 0–50), and quartiles were generated in order to better understand the effects of MHF training on participants with low, medium-low, medium-high, and high MHF knowledge going into the training. The quartile scores were as follows: low < 34 (N = 317, M = 5.34, SD = 4.23), medium-low = 34 to 38 (N = 369, M = 4.13, SD = 3.62), medium-high = 39 to 42 (N = 340, M = 3.06, SD = 2.69), and high > 42 (N = 289, M = 1.35, SD = 2.04).
To compare the four groups and answer the second research question, a one-way ANOVA was used. The analysis showed that the differences between the scores of the four categories are significant (F[3, 1311] = 81.05, p = 0.000). A post-hoc Tukey HSD test allowed for a more detailed understanding of the difference between the four groups. The Tukey HSD test results indicated significant differences between all four groups. The details of the differences between means in the post-hoc test are as follows. The low score group showed a significant difference between pretest and posttest scores compared to the medium-low test score group (mean difference = 1.21, p = 0.000), the medium-high test score group (mean difference = 2.28, p = 0.000), and the high test score group (mean difference = 3.99, p = 0.00). The medium-low test score group was significantly different from the medium-high (mean difference = 1.07, p = 0.000) and high (mean difference = 2.78, p = 0.000) test score groups, and the medium-high test score group was significantly different from the high test group (mean difference = 1.71, p = 0.000). When running the one-way ANOVA with the outliers included, the only difference in significance found in the results for any of the analyses occurred between the medium-low and medium-high groups. With the outliers included in the analysis, there was no significant difference between those two groups, although all the other significant differences remained, and the overall trend of pretest to posttest score differences decreasing as the pretest score rose remained unchanged. The results of the analyses confirm that the lower the pretest scores, the larger the gain in knowledge from the training.
Post-Hoc Data Analysis
After considering the significant pretest to posttest gains, the authors became curious about whether the content of the pretest and posttest questions might be separated into subscales to better evaluate MHF training effectiveness. The observation that the questions on the MHF pretests and posttests naturally related to either knowledge or skills prompted the authors to separate the questions into the two subscale categories, MHF knowledge and MHF skills.
To generate the two subscales, one author went through the questions independently and categorized them for each of the three test iterations. Then, the second author went through the questions to confirm they fit the subscales. A paired t-test was used to determine whether participants demonstrated equivalent gains in both knowledge and skills.
The results of the analyses showed significant gains on both subscales. The mean gain on MHF knowledge was 1.41 (N = 1315, t = -22.86, p = 0.000), and the mean gain on MHF skills was 2.12 (N = 1315, t = -29.67, p = 0.000). The results of this post-hoc analysis confirm the hypothesis that the MHF program training leads to significant increases in both MHF knowledge and skills.
Discussion
The results of the present study provide further evidence of the effectiveness of the MHF program. Previous studies have examined qualitative accounts of trainees’ experiences and impressions of the program (Luke et al., 2016; Van Leeuwen et al., 2016). The present data, however, provide objective evidence that the program is indeed enhancing trainee knowledge of mental health and MHF skills. This finding suggests that individuals who complete the MHF program have the requisite knowledge and skills to provide frontline interventions and needed referrals for community members struggling with their mental health.
Interestingly, the results also demonstrate that the documented growth in knowledge and skills is relative to the existing knowledge of the participant prior to training, whereby those with less initial training (i.e., lower scores on the pretest) showed greater gains in knowledge and skill from participation in the MHF training. Although somewhat intuitive, this provides evidence that the program is successful at enhancing the knowledge and skills of participants despite previous training in mental health. It brings all participants up to a similar, requisite baseline level of knowledge to perform mental health facilitation. Participants with little to no information regarding mental health can gain the needed knowledge and skills necessary to support the mental health of others in their community, while those with considerable information and training can refine their skills and knowledge for their new role.
Post-hoc analyses assessed whether the MHF program is equally adept at enhancing knowledge related to mental health and mental health struggles as well as the skills needed in mental health facilitation. Findings revealed that participants demonstrated a significant growth in both knowledge and skills. As such, the MHF program not only provides mental health literacy, but also the skills needed to support those in need. This is notable given the significant disparity of mental health literacy in both the developed and developing world (Ganasen et al., 2008; Jorm, 2000). Among professionals and laypersons alike, the lack of knowledge and understanding of mental health not only contributes to the treatment gap, but also the considerable stigma faced by those who struggle with mental health issues.
Taken together, the results suggest that the researchers and program developers can confidently endorse this program as one that leads to an increase in mental health knowledge and skills associated with mental health facilitation among both professionals and laypersons. In this way, the MHF program furthers the WHO’s (2013) Mental Health Action Plan goals of strengthening information systems surrounding mental health and clearly establishing a requisite foundation for the implementation of strategies and services. In its proposed actions for member states, WHO emphasized the importance of human resource development by “build[ing] the knowledge and skills of general and specialized health workers to deliver evidence-based, culturally appropriate and human rights-oriented mental health and social care services” (WHO, 2013, p. 15).
Our findings also complement the positive evaluation feedback of participants. In particular, Van Leeuwen et al. (2016) found that participants appreciated the increased knowledge they gained, noting that it was beneficial to themselves as well as their community. Participants noted that they had an enhanced ability to better understand their personal and family members’ mental health and that the MHF training helped reduce community stigma. Examined in conjunction with the present data, this suggests that not only are participants objectively gaining knowledge about mental health, they are aware of what they learned and actively and intentionally applying that knowledge to help themselves, other individuals, and their overall community better understand mental health. Given that the present study also demonstrated that participants are gaining an enhanced understanding of MHF-related skills, the researchers are hopeful that with their knowledge of mental health, participants are likewise intentionally putting their facilitation skills into action to support those in need within their communities.
Limitations and Future Research
The present study provides a notable step in further documenting the effectiveness of the MHF program, yet the limitations of this research must be taken into consideration and used for ongoing program planning and research development. Using true-false repeated measures pre- and post-training assessment could lend itself to bias. Within such situations, the trainee may recall, implicitly or explicitly, the questions asked in the pre-training assessment and may be primed for remembering the information needed to respond to those questions. Similarly, although the findings were statistically significant, probability suggests that true-false questions are more accessible to educated guesses rather than a depiction of accurate knowledge. In this way, having a multiple-choice format test with possible case scenarios to assess application in greater depth might provide a richer depiction of the knowledge gained. The present means of assessment also are vulnerable to a ceiling effect, whereby those with the most knowledge around mental health would earn the maximum number of points on both the pre- and post-training assessment. Although the present testing level is the most adaptive to all knowledge levels, perhaps a greater breadth of questioning to assess more nuanced components of the MHF skillset might be more helpful in accurately assessing the knowledge and skills gained by those coming into the MHF program with more extensive mental health training. An additional limitation of the assessments specifically was the post-hoc distinction between the skills and knowledge components assessed in the MHF training. In the future, greater attention to developing questions specifically geared toward these two necessary areas will be more effective in discriminating such gains. One final limitation of the present study and an area well positioned for future research is the lack of specific data regarding how the knowledge and skills are being used following the training.
Prior to this study, there was no formal quantitative data analysis to substantiate the reach of the MHF program. In addition to this research assessing the knowledge and skills gained through participation in the MHF program, there is the equally important next step of assessing how that knowledge is being used to address the goals of the program. Research examining the extent to which the MHF program aides in increasing mental health access for individuals in need of support and thereby decreasing the treatment gap among individuals struggling with their mental health would be especially important in addressing the over 70% of individuals in developing countries who do not receive the mental health care they so desperately need (Demyttenaere, 2004).
Conclusion
The growing number of individuals around the world with mental health challenges, coupled with the lack of knowledge, services, access, and fiscal resources to address the growing need, drives mental health to the forefront of worldwide public health challenges. Countries and communities in both developed and developing countries alike must embrace creative, economical, and culturally appropriate population-based solutions. The MHF program developed by NBCC (Hinkle & Henderson, 2007), initially in coordination with WHO and mental health experts from around the world, provides one such solution. Extant research on the MHF program validates the cultural appropriateness of the tailored programs as well as the extent to which community members believe they have benefited from the trainings (Luke et al., 2016; Van Leeuwen et al., 2016). The present findings further this research by providing quantitative data speaking to the effectiveness of the program at enriching participants’ knowledge and skills in relation to mental health. This burgeoning evidence base moves the MHF program one step closer to becoming a global best practice in addressing the notable and growing gap in mental health care around the world.
Conflict of Interest and Funding Disclosure
The first two authors were reimbursed by NBCC
for expenses related to this manuscript.
The third author is an employee of NBCC who
has developed and conducted MHF trainings.
References
Andrade, L. H., Alonso, J., Mneimneh, Z., Wells, J. E., Al-Hamzawi, A., Borges, G., . . . Kessler, R. C. (2014). Barriers to mental health treatment: Results from the WHO World Mental Health surveys. Psychological Medicine, 44, 1303–1317. doi:10.1017/S0033291713001943
Bloom, D. E., Cafiero, E. T., Jané-Llopis, E., Abrahams-Gessel, S., Bloom, L. R., Fathima, S., . . . Weinstein, C. (2011). The global economic burden of non-communicable diseases. Geneva, Switzerland: World Economic Forum.
Demyttenaere, K., Bruffaertts, R., Posada-Villa, J., Gasquet, I., Kovess, V., Lepine, J. P., . . . Chatterji, S. (2004). Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health surveys. JAMA, 291, 2581–2590. doi:10.1001/jama.291.21.2581
Desjarlais, R., Eisenberg, L., Good, B., & Kleinman, A. (1995). World mental health: Problems and priorities in low-income countries. Oxford, England: Oxford University Press.
Ganasen, K. A., Parker, S., Hugo, C. J., Stein, D. J., Emsley, R. A., & Seedat, S. (2008). Mental health literacy: Focus on developing countries. African Journal of Psychiatry, 11, 23–28. doi:10.4314/ajpsy.v11i1.30251
Hinkle, J. S. (2006, October). MHF town meeting: Ideas/questions. Presentation at the NBCC Global Mental Health Conference: Focus on the Never Served, New Delhi, India.
Hinkle, J. S. (2014). Population-based mental health facilitation (MHF): A grassroots strategy that works. The Professional Counselor, 4, 1–18. doi:10.15241/jsh.4.1.1
Hinkle, J. S., & Henderson, D. (2007). Mental health facilitation: Program history and summary. Greensboro, NC: National Board for Certified Counselors. Retrieved from http://mentalhealthfacilitator.com/Assets/Project_Summary.pdf
Hinkle, J. S., & Saxena, S. (2006, October). ATLAS: Mapping international mental health care. Presentation at the NBCC Global Mental Health Conference: Focus on the Never Served, New Delhi, India.
Jorm, A. F. (2000). Mental health literacy: Public knowledge and beliefs about mental disorders. The British Journal of Psychiatry, 177, 396–401. doi:10.1192/bjp.177.5.396
Kessler, R. C., Aguilar-Gaxiola, S., Alonso, J., Chatterji, S., Lee, S., Ormel, J., . . . Wang, P. S. (2009). The global burden of mental disorders: An update from the WHO World Mental Health (WMH) surveys. Epidemiology and Psychiatric Sciences, 18, 23–33. doi:10.1017/S1121189X00001421
Kohn, R., Saxena, S., Levav, I., & Saraceno, B. (2004). The treatment gap in mental health care. Bulletin of the World Health Organization, 82, 858–866. doi:10.1590/S0042-96862004001100011
Luke, M., Hinkle, J. S., Schweiger, W., & Henderson, D. (2016). Mental health facilitator (MHF) service implementation in schools in Malawi, Africa: A strategy for increasing community human resources. The Professional Counselor, 6, 1–21. doi:10.15241/ml.6.1.1
Van Leeuwen, J. M., Adkins, S., Mirassou-Wolf, T., Schweiger, W. K., & Grundy, R. (2016). An evaluation of the Mental Health Facilitator programme in rural Uganda: Successes and recommendations for future implementation. Journal of Psychology in Africa, 26, 288–299. doi:10.1080/14330237.2016.1185919
Vigo, D., Thornicroft, G., & Atun, R. (2016). Estimating the true global burden of mental illness. The Lancet Psychiatry, 3, 171–178. doi:10.1016/S2215-0366(15)00505-2
Wang, P. S., Angermeyer, M., Borges, G., Bruffaerts, R., Chiu, W. T., De Girolamo, G., . . . Usten, T. B. (2007). Delay and failure in treatment seeking after first onset of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry, 6, 177–185.
World Health Organization. (2006). Integrating mental health into primary care: A global perspective. Geneva, Switzerland. Retrieved from https://www.who.int/mental_health/resources/mentalhealth_
PHC_2008.pdf
World Health Organization. (2011). Mental health atlas 2011. Retrieved from https://apps.who.int/iris/
bitstream/handle/10665/44697/9799241564359_eng.pdf;jsessionid=7488A5219E439A1D1D082CCFA2E872E5?sequence=1
World Health Organization. (2013). Mental health action plan 2013–2020. Retrieved from http://www.who.int/mental_health/publications/action_plan/en/
World Health Organization. (2014a). Mental health: A state of well-being. Retrieved from http://www.who.int/features/factfiles/mental_health/en/
World Health Organization. (2014b). 10 facts on mental health. Retrieved from https://www.who.int/features/factfiles/mental_health/mental_health_facts/en/
World Health Organization. (2015). Mental health atlas 2014. Retrieved from http://www.who.int/mental_health/evidence/atlas/mental_health_atlas_2014/en/
World Health Organization. (2018). Mental disorders. Retrieved from
http://www.who.int/mediacentre/factsheets/fs396/en/
Alwin E. Wagener, NCC, is an assistant professor at Fairleigh Dickinson University. Laura K. Jones is an assistant professor at the University of North Carolina Asheville. J. Scott Hinkle is the editor of The Professional Counselor. Correspondence can be addressed to Alwin Wagener, 285 Madison Ave., M-AB2-01, Madison, NJ 07940, awagener@fdu.edu.
Nov 11, 2019 | Volume 9 - Issue 4
Allison Crowe, Paige Averett, Janeé R. Avent Harris, Loni Crumb, Kerry Littlewood
The following study assessed the utility of the U. S. Department of Health and Human Services’ definition of mental health among participants in the rural Southeastern United States. Using deductive coding, qualitative results revealed that participants do not conceptualize mental health in comprehensive terms. Rather, they tend to describe mental health with a focus on cognition. The sample articulated “well-being” to describe mental health; however, they most often connected it to cognition. The findings suggest that rural communities could benefit from mental health education with a holistic approach and that the use of the term well-being provides a pathway for clinical connections. Future research should consider interviewing rural participants to gather more detail on their definitions and understanding of mental health.
Keywords: mental health, education, cognition, rural, well-being
Mental illness is a pervasive health care concern in the United States. Even though approximately one fifth of adults experience mental health concerns in any year, only 70% of those in need of mental health services seek care (National Alliance on Mental Illness, 2015). Because of how common and widespread mental health conditions are in the United States, mental health professionals have become increasingly aware that educating the public about mental illness is of utmost importance. Mental health literacy (MHL; Jorm, 2012), or the knowledge and beliefs about disorders that assist in the recognition, prevention, or management of a mental health concern, is one way those who are struggling with mental health concerns can manage mental illnesses more effectively. Improving MHL can have the capacity to positively impact negative attitudes, biases, or assumptions that are associated with having a mental illness as well as assist with help-seeking so those who have a mental illness will receive necessary treatment (Crowe, Mullen, & Littlewood, 2018; Jorm, 2012; Kutcher, Wei, & Coniglio, 2016). Researchers have consistently demonstrated that a stigma still exists toward seeking help for mental health concerns and that reducing that stigma is of utmost importance (Kalkbrenner & Neukrug, 2018).
Increasing help-seeking behaviors might best be done through first exploring attitudes and perceptions, as cognitions are closely tied to emotions and behaviors. Therefore, the current study is framed through the theoretical lens of cognitive behavioral therapy (CBT; A. T. Beck, 1970). CBT is based on the notion that how one thinks, feels, and acts are all intertwined. Specifically, one’s thoughts impact how one feels and behaves. Because of this, negative or unrealistic thoughts may contribute to psychological distress. When a person feels distressed, the way that they interpret situations may become skewed or distorted, which then impacts their behavior. From the lens of CBT, one’s decision to not seek treatment for a mental health concern may be closely tied to the thoughts and feelings they hold about negative associations about mental illness. Counselors who practice from a CBT perspective work with clients to identify and eliminate cognitive distortions in order to minimize painful emotions and promote more adaptive behaviors. CBT has been applied to diverse populations and found to be effective with various presenting concerns (A. T. Beck, 1970; J. S. Beck, 2011; Crumb & Haskins, 2017).
Cognitive distortions exist as they relate to having a mental health concern, and researchers have shown that rural residents with mental health concerns fear being negatively labeled, stereotyped, and discriminated against and thus are apprehensive to seek mental health care services (Crumb, Mingo, & Crowe, 2019). Therefore, it is vital that counselors and other mental health providers consider how clients’ thoughts, beliefs, experiences, and other contextual factors contribute to their understanding of mental illness. Intentional acknowledgment of the factors that influence clients’ perceptions, attitudes, and behavior may enhance treatment efficacy for rural residents (Crumb & Haskins, 2017). Along with exploring negative thoughts related to mental health, researchers also have considered MHL, or one’s understanding of mental health, as it impacts behaviors.
Mental Health Literacy (MHL)
Health literacy researchers suggest low health literacy is related to a number of negative health outcomes, including higher instances of chronic illness, lower usage of health care programs, higher costs of health care, and premature death (Baker et al., 2007; Berkman, Sheridan, Donahue, Halpern, & Crotty, 2011). The World Health Organization (WHO; 2013) posits that health literacy is more important than demographic factors (e.g., income, employment, status, education, race, ethnicity) as they relate to health status. Perhaps because of this, the importance of health literacy is well established in the health professions.
In a 2011 literature review on health literacy outcomes, Berkman and colleagues found that lower levels of health literacy were related to more hospitalizations, increased emergency center use, misuse of medications, confusion with medication instructions, higher death rates, and poorer overall health among the elderly. Baker and colleagues (2007) had similar findings related to the impact of poor health literacy on health outcomes. In Baker et al.’s cohort study (N = 3,260), inadequate health literacy independently predicted mortality and death because of cardiovascular disease in elderly populations. They concluded that health literacy is an influential component of overall health.
Compared to general health literacy, the same cannot be said specifically for MHL in the field of mental health. In fact, knowledge of mental health concerns is greatly lacking and largely ignored (Jorm, 2012). The most current study related to MHL found that MHL had a negative relationship to self-stigma of mental health concerns and help-seeking, signifying that when a person knows more information about mental health, they have less stigma about mental health concerns and engage in more help-seeking behaviors (Crowe et al., 2018). In this same study, health outcomes (i.e., blood pressure and body mass index) were assessed to test whether MHL was related to improved physical health. Results were nonsignificant, suggesting that there was not a relationship between MHL and physical health outcomes.
Regional disparities and sociodemographic variations in treatment utilization and efficacy reflect a crucial need for increasing MHL in rural areas in particular (Smalley, Warren, & Rainer, 2012; Snell-Rood et al., 2017). Although prevalence rates of mental health concerns are similar to urban and suburban regions, the amount of and access to mental health services differ vastly in rural regions. Rural residents have fewer options for services, and in fact many rural areas have no health care services at all (Rural Health Information Hub, 2017). Residents in rural regions must travel greater distances for mental health services, are less likely to have health insurance, and have lower MHL (Rural Health Information Hub, 2017). Therefore, professional literature and research studies that assist with raising knowledge about MHL are warranted, as the current literature based on this topic is lacking, especially as it relates to types of settings and samples of the population. Thus, the current study was an attempt to address this gap in the literature. The following section focuses on what is known about mental health in rural areas and highlights the salient issues that are of importance to clinicians and researchers alike.
Mental Health in Rural Areas
The mental health of rural residents is of importance, as 16% of the U.S. population lives in rural areas (Rainer, 2012). Of those living in the rural United States, 90 million residents live in areas that have been designated as Mental Health Professional Shortage Areas and are lacking mental health professionals and resources (Health Resources & Services Administration, 2011). Researchers, practitioners, and recipients of mental health services purport the underutilization of mental health services and inadequacies in the quality of mental health care among rural populations (Smalley et al., 2012; Snell-Rood et al., 2017). Specifically, factors related to acceptability, accessibility, and availability intensify rural mental health disparities across the United States (Office of Rural Health Policy, 2005; Smalley et al., 2012).
A study completed in Australia sought to explore perceptions about mental health in a rural sample (Fuller, Edwards, Procter, & Moss, 2000). Themes revealed a reluctance to acknowledge mental health concerns and seek help from a professional. Results also demonstrated there is a mental health stigma that is particular to rural communities. Although the study provided an initial look at how mental health can be understood in rural areas, the sample consisted of mental health professionals and others who were knowledgeable about mental health issues rather than those from the general client population.
Mental health stigma is one of the most common reasons for unmet mental health needs in rural areas (Alang, 2015; Stewart, Jameson, & Curtin, 2015). For example, residents in rural communities report fear of taking psychotropic medications and that seeking treatment for mental health might adversely impact their employment (Snell-Rood et al., 2017; Stewart et al., 2015). Resultantly, rural clients who experience mental illness enter mental health care later, present with more serious symptoms, and often require more intensive treatment (Smalley et al., 2012). Insufficient MHL, such as misinformation related to common mental health disorders and treatment, can lead to lower rates of recognizing symptoms of depression, anxiety, and an array of other mental health concerns among rural residents in various ethnic and age groups (Kim, Saw, & Zane, 2015).
A quantitative study conducted by Alang (2015) investigating the sociodemographic disparities of unmet health care needs revealed men in rural areas were more likely to forgo mental health care because of gender stereotypes about mental health problems that encourage men to ignore mental health concerns and avoid help-seeking behaviors. Similarly, Snell-Rood et al. (2017) found that rural women face issues with mental health treatment quality and stigma related to specific disorders such as depression as well as a cultural expectancy of self-reliance, which impacts treatment efficacy. Study participants shared that the quality of counseling in their rural settings was unsatisfactory because of counselors recommending coping strategies that were “inconsistent” with their daily routines and beliefs, not offering adequate “direction” on how to approach treatment for their concerns, and having a lack of therapeutic interaction (Snell-Rood et al., 2017). Because of negative perceptions of the quality of mental health treatment, many women in the study were ambivalent in regard to seeking professional help. Rather, they relied on their personal approaches to symptom management (e.g., avoidance, reflection, and prayer).
Accessibility of mental health services is a significant concern in rural areas. Rural residents face challenges in finding transportation to facilities for professional care. Consequently, rural residents often forgo attaining adequate and timely mental health treatment (Alang, 2015; Hastings & Cohn, 2013). Rural residents often depend on alternative sources such as faith-based organizations to address mental health concerns (Bryant, Moore, Willis, & Hadden, 2015) or ignore the prevalence of mental health symptomology altogether (Snell-Rood et al., 2017). Unfortunately, researchers indicated that rural residents seek treatment for mental health disorders after they have become progressively worse, resulting in more extensive treatment, which is often unavailable or costly for rural clients (Gore, Sheppard, Waters, Jackson, & Brubaker, 2016; Hastings & Cohn, 2013; Snell-Rood et al., 2017). Deen and Bridges (2011) suggested these delays in seeking mental health treatment are associated with low MHL.
Treatment availability for mental health care in rural areas is fragmented because of critical shortages in mental health care providers in these communities (El-Amin, Anderson, Leider, Satorius, & Knudson, 2018; Snell-Rood et al., 2017). Practitioner shortage is attributed to difficulty in recruiting and retaining professionals for rural practice as well as practitioners’ limited understanding of cultural norms and effective interventions to address mental health needs in rural communities (Fifield & Oliver, 2016; Hastings & Cohn, 2013). Among practitioners who provide clinical services in rural areas, many report feeling incompetent to work with the population because of receiving fewer training opportunities to learn how to work with rural populations, less access to consultation resources, and professional isolation (Hastings & Cohn, 2013; Jameson & Blank, 2007). Fifield and Oliver (2016) found the most common need of rural-area mental health professionals was training opportunities specific to rural mental health counseling. Pointedly, rural mental health service providers are encouraged to tailor interventions and informational material to meet the needs of the specific communities in which they practice (Crumb, Haskins, & Brown, 2019; El-Amin et al., 2018). For example, a qualitative study examining the experience of rural mental health counselors found it was necessary for rural counselors to modify their interventions to include community-based interventions and expand their roles to include consulting, advocacy, and case management to effectively meet the needs of rural clientele (Crumb, Mingo, & Crowe, 2019). In 2012, rural-specific supplemental materials and curricula were integrated into the standard Mental Health First Aid program, a training course disseminated by the National Council for Behavioral Health to address gaps in MHL by teaching skills to help individuals identify, understand, and respond to mental illness (El-Amin et al., 2018; National Council for Behavioral Health, 2019). Based upon extant research evidence, cultural distinctions in rural living impact MHL and, subsequently, the quality of mental health care in rural regions of the United States.
Despite the above-mentioned disparities, there are opportunities for improving the mental health care of those in underserved rural areas. By becoming familiar with how rural residents in the United States define mental health and investigating the sociodemographic idiosyncrasies in the meaning of mental health for rural residents in specific regions of the United States, mental health practitioners can understand how to better address needs, counter structural barriers to treatment, and improve overall mental health care in rural areas. As far as we are aware, there are no studies that have examined how those in rural communities define and conceptualize mental health. Thus, the current study was designed to fill this gap in the literature.
This study sought to understand how individuals in the rural Southeast define and conceptualize mental health in order to explore MHL and serve as a guidepost to providing culturally relevant services to residents in these regions. Areas in the Southern United States have a high concentration of rural residents who potentially have less access to mental health services, which may influence their overall MHL (El-Amin et al., 2018). Furthermore, we know little about how rural populations define mental health and the knowledge and beliefs that undergird their understanding of mental health. Rather, we have definitions of mental health that are taken from large national and international entities (e.g., U.S. Department of Health and Human Services, Centers for Disease Control and Prevention [CDC], WHO) that offer broad ways of understanding the term. These definitions, although useful, may not capture distinctions associated with region, socioeconomic status, or cultural group differences. Understanding how groups of people view mental health has many benefits to enhancing MHL. A more specific understanding of mental health concepts can serve as a foundation to increase the utilization of mental health services, improve the quality of care, and enhance clients’ ability to communicate concerns. If there are to be greater gains in prevention, intervention, and management of mental health in rural, southern regions of the United States, we need a comprehensive understanding of aspects that are included in perceptions of mental health—using their own words.
Methods
Procedures
Prior to data collection, the Institutional Review Board at a Southeastern U.S. university granted approval to complete the study to explore MHL. Data were collected via a paper-and-pencil survey. Research team members approached patients waiting for a regularly scheduled medical appointment with their primary care physician to complete the survey. Paper copies were stored in a locked filing cabinet within a locked office. The family medical center was located in a rural area of a state in the Southeastern United States. The family medical center where the research took place also housed a mental health provider who received referrals from the medical doctors at the same site. The research team asked permission to collect data on-site, and the lead physician at the center agreed. The mental health provider provides services to many of the same patients who receive medical care at the office. This study was part of a larger, quantitative research investigation on mental health, mental health stigma, and MHL (Crowe et al., 2018). Because of the expansive nature of the dataset, however, this article only focuses on the qualitative components of the survey.
Participants
Using published guidelines for in-person recruitment, the research team approached patients as they waited in the waiting room and asked if they would be interested in joining the research study (Felsen, Shaw, Ferrante, Lacroix, & Crabtree, 2010). When participants elected to participate in the study, they completed an informed consent and survey in the waiting area or in an exam room while waiting for the medical professional. All data were collected over the course of approximately six months. Incentives were not offered to participants and all participants could choose to opt out of participation at any time.
Participants included 102 individuals, including 65 females (63.7%) and 37 males (36.3%). A total of 70 participants identified as White (68.6%), 25 identified as Black/African American (24.5%), four identified as multiracial (3.9%), two did not know or endorsed the “other” category (2%), and one identified as Asian (1%). Regarding age, 30 (29%) participants were age 60 and above, 21 (21%) were between the ages of 50–59, another 21 (21%) were between the ages of 40–49, 14 (14%) were between the ages of 30–39, 14 (14%) were between the ages of 19–29, and two (2%) were 18 or younger. Fifty-six participants (55%) were married, while 27 (26%) were single. A total of 15 (15%) were separated/divorced, and four (4%) were widowed. One hundred and twelve participants were asked to complete the survey, and102 individuals completed the materials, yielding a 91% useable response rate. Demographic information is summarized in Table 1.
Table 1
Demographic Information
| Characteristic |
n |
% |
| Gender |
|
|
| Male |
37 |
36.3 |
| Female |
65 |
63.7 |
| Ethnicity |
|
|
| African American/Black |
25 |
24.5 |
| Caucasian/White |
70 |
68.6 |
| Multicultural |
4 |
3.9 |
| Other |
2 |
1.9 |
| Asian |
1 |
0.9 |
| Age |
|
|
| 18 or younger |
2 |
1.9 |
| 19–29 |
14 |
13.7 |
| 30–39 |
14 |
13.7 |
| 40–49 |
21 |
20.6 |
| 50–59 |
21 |
20.6 |
| 60+ |
30 |
29.4 |
| Marital status |
|
|
| Married |
56 |
54.9 |
| Single |
27 |
26.5 |
| Separated/Divorced |
15 |
14.7 |
| Widowed |
4 |
3.9 |
| Seeking treatment for |
|
|
| Physical health concerns |
88 |
86.3 |
| Mental health concerns |
3 |
2.9 |
| Both |
2 |
2 |
| Treatment status |
|
|
| Never sought treatment |
54 |
52.9 |
| Sought treatment in the past |
48 |
47.1 |
| Length of treatment |
|
|
| 1 year or less |
18 |
17.6 |
| 1–4 years |
11 |
10.8 |
| 5–10 years |
9 |
8.8 |
| 11–25 years |
5 |
4.9 |
| Description of treatment |
|
|
| Not at all helpful |
1 |
1 |
| Somewhat helpful |
9 |
8.8 |
| Generally helpful |
10 |
9.8 |
| Very/Extremely helpful |
28 |
23.3 |
| Family mental health |
|
|
No immediate family member with
a mental illness |
66 |
64.7 |
Immediate family member with a
mental illness |
26 |
25.4 |
| Not sure |
10 |
9.8 |
| Would you seek treatment for mental health concerns in the future? |
|
|
| Yes |
78 |
76.5 |
| No |
3 |
2.9 |
| Not sure |
21 |
20.5 |
Measures
For purposes of the current analysis, an open-ended question prompted participants: “In your own words, please describe what you believe the term mental health refers to.” Analysis was completed by comparing and contrasting the participant responses to this prompt with the U.S. Department of Health and Human Services (HHS; 2019) definition of mental health. This definition states that:
Mental health includes emotional, psychological, and social well-being. It affects how we think,
feel, and act. Mental health helps determine how we handle stress, relate to others, and make
choices. It is important at every stage of life, from childhood and adolescence through adulthood.
. . . Many factors contribute to mental health problems, including: biological factors, such as
genes or brain chemistry; life experiences, such as trauma or abuse; [and] family history of mental
health problems. (para. 1–2)
We elected to use this definition as opposed to similar definitions of mental health offered by WHO or the CDC because each member of the research team chose it as the most comprehensive of the three. Although there were many overlaps in the three definitions (i.e., all three descriptions mention well-being and handling or adjusting to stressors, and included some dimension of biological, psychological, and social aspects), the HHS definition also included the notion of life stages, past life experiences, and how these factors impact mental health.
Data Analysis
The deductive qualitative analysis method (Gilgun, 2011) was used to analyze participant responses to the open-ended prompt. In deductive coding, the researchers begin with existing codes, as deductive coding is utilized to test existing theories or frameworks. Because the current research was attempting to test the HHS definition, deductive analysis was considered the most fitting analysis method by the research team.
Deductive analysis attempts to understand how a particular theory or framework is useful or not (Gilgun, 2011). In deductive coding, data is sorted as it fits with existing concepts, or codes, within a framework. Deductive coding includes levels of analysis, including open coding, axial coding, and selective coding (Strauss & Corbin, 1990). According to Gilgun (2011), during open coding, the data is read line by line, sentence by sentence, and is placed as it is understood within the existing concept(s) with which it best aligns. Axial coding then occurs to refine the existing theory or framework via further analysis of data that is already placed within concepts. This data is then reconsidered to attend to groupings or subthemes within the concept to see if further details of a theory/framework are possible. Selective coding within deductive analysis is when the data is further examined to see if there is possible reduction to a single category or core concept. Selective coding is also an attempt to refine and further consider the existing framework to determine its utility and add to its use. As well, lines or sentences that do not fit existing concepts are noted. This is referred to as negative case analysis.
In the current research, the open coding analysis process was conducted repeatedly to consider and reconsider the data and its fit to the concepts within the HHS (2019) definition of “think, feel, and act.” These three concepts in the HHS definition were evident as the most salient. To aid in coding, these three HHS concepts were further understood by utilizing several online dictionaries (e.g., Google dictionary, Merriam-Webster, dictionary.com, and Cambridge English Dictionary) to define each concept. For example, the think code included all participant responses that are associated with this term via dictionaries, including intellectual, cerebral, brain, cognitive, and rational. The research team continually used several dictionaries to understand participant responses that were not exact or clear upon first reading. For example, state of mind was coded as think because of it being defined as a cognitive process and the condition of a person’s thoughts. Axial coding then occurred through the research team reconsidering the fit of the responses to the existing codes and if further codes could be developed via negative case analysis. As demonstrated below, axial coding produced a negative case analysis, that of overall well-being. Selective coding occurred through the team considering all codes and the utility of the original framework or, in this case, the HHS definition. This utility or lack thereof is further considered in the discussion below.
The entire analysis process was completed by two members of the research team independently. Independent coding enhances credibility in the analysis process, a technique promoted among qualitative researchers (Lincoln & Guba, 1985). The two researchers met on two occasions to discuss their findings and found consistency in their coding in both meetings. This consistency is often found when pre-existing codes with set definitions are utilized, as was the case in this analysis.
Results
The following section presents the results of the deductive coding of the data in comparison to the HHS definition of mental health, specifically the concepts of how we “think, feel, and act.” The existing concepts used as codes for analysis included the psychological, emotional, and social well-being—how we think, feel, and act. Sample quotes from participants (Ps) are provided. The research team also presents further points of possible refinement of the definition and sense of a core concept.
Concepts Used to Describe Mental Health
Think, feel, and act. Only 15 participant responses provided support for a definition of mental health that encompassed all three aspects found in the HHS (2019) definition of “think, feel, and act.” One participant stated, “mental health to me personally is the state of one’s condition of emotional, mental, social and physical well-being” (P2), and another shared that mental health is the “ability to succeed, fully participate in social, emotional and occupational and recreational leisure” (P3). Thus, there was only a small subset of participants who viewed mental health as comprehensively as federally defined.
Well-being. It should be noted that although most participants did not provide comprehensive definitions that specifically mentioned all three concepts of think, feel, and act, as used by HHS, there were 23 participants in the sample who used the term well-being. As indicated in the following, well-being was not seen as specific to one area but rather an overall experience. One participant stated, “More than a sense of psychiatric disease—overall well-being” (P4), and another shared, “Overall health of a person—their well-being” (P5). Thus, for many of our participants, a comprehensive definition of mental health they demonstrated was the general term well-being.
Think. The most salient concept found among our participants was related to cognition, thinking, the mind or brain, or the term mental. Thirty-four responses focused solely on mental health as being how we think, including statements such as “state of mind” (P6), “mental health refers to your thoughts” (P7), and “brain imbalance” (P8). These responses suggest that the cognitive aspect of mental health is a primary way these rural participants conceptualize mental health. We also saw this demonstrated in other definitions provided by the participants that had think in combination with either feel or act.
Think and feel. The next most salient conceptualization provided by participants included elements of both cognition and emotion—how we think and feel. Eighteen participants provided responses in this code, including “mental health is my ability to cope, how I think, rational thinking, and my emotional stability” (P9) and “state of mind and feeling of well-being” (P10). It is noteworthy that again when discussing cognition and emotion, there was frequent use of the phrase well-being, even when limited to just think and feel, thus further supporting the term well-being.
Think and act. Cognition or thinking was further salient and used in connection with behavior, or how we think and act. Conceptualizations from these 10 participants included statements such as “condition of one’s mind and if any affect [sic] on behavior” (P11) and “well-being in thought and action” (P12). Again, also noted is the use of the term well-being, even when specifying think and act.
Non-salient concepts within the HHS definition. There were other conceptualizations of the term mental health that supported aspects of the HHS definition. There were seven participants who focused solely on feelings—how you feel. Although there were five participants who only focused on mental health as behavior or how one acts, neither of the singular concepts were considered salient in participant responses because of infrequent responses.
Other non-salient concepts. Also provided by participants were concepts focused specifically on a mental health diagnosis such as “depression” (P16, P17) and “depression, bipolar” (P18). Also, it is interesting to note that although not salient, a few participants saw mental health as a function of physical health. This was demonstrated in definitions such as “condition of health” (P19) and “special help for the sick or assist those that have some type of disease” (P20). It is important to note that a few responses were unclear or too vague and could not be categorized, such as “Don’t know” (P21, P22).
Summary
Overall, participants’ responses suggest a strong tendency toward cognitive aspects of mental health rather than a comprehensive definition that can be found when looking in formal sources, such as the HHS definition (2019). However, a negative case that emerged was that these rural participants did provide the term well-being as an overall comprehensive definition for mental health. Frequency counts for each concept can be found in Table 2. In the following section, we discuss these findings.
Table 2
Frequencies According to HHS Definition Code
HHS Definition Codes Participant Response Count
Think 34
Think and Feel 18
Think, Feel, and Act 15
Think and Act 10
Well-Being 23
Discussion
In the current study, we explored MHL, specifically focusing on the efficacy of the HHS mental health definition in a rural, Southeastern U.S. sample. We sought to understand how this population conceptualized the term mental health. The current research literature provides very little information about this topic, so the following study offered initial findings to offer professional counselors and researchers implications and areas for further investigation.
It is important to reflect on the ways results from this sample of rural residents compare to the existing knowledge about the larger public’s MHL levels and ideas about mental health. Jorm (2000, 2012) noted that lack of MHL among individuals inhibits their ability to recognize mental health concerns when they arise. Although MHL may be an area for more intensive focus across all populations and settings (Jorm, 2000, 2012), results from this study suggest that there are a number of unique considerations in rural areas. Moreover, it is important to situate the current findings in the context of the challenges faced by rural residents. Knowing how those in rural communities define mental health, in their own words, will lend mental health practitioners information about how to communicate and connect effectively to increase the utilization of mental health services, improve the quality of care, and enhance clients’ ability to communicate concerns. If there are to be greater gains in prevention, intervention, and management of mental health in rural regions of the United States, a nuanced understanding of perceptions about mental health may offer a starting point.
Well-Being
In terms of the HHS definition, the current sample supported the concept of well-being. Although well-being was not necessarily connected concretely to the specific terms of think, feel, and act, it was often associated with one or two other concepts as well as used singularly as a holistic definition. Research on well-being has been of increasing interest in the past two decades (Dodge, Daly, Huyton, & Sanders, 2012), and many of the current national and international definitions of mental health refer to well-being (LaPlaca, McNaught, & Knight, 2013). Recent attempts have been made in the literature to more clearly articulate the definition of well-being (Dodge et al., 2012; LaPlaca et al., 2013), as this concept is being used to determine policy and practice on many national stages.
Current definitions of well-being combine elements of the psychological, social, and physical. However, these descriptions also focus on the ratio of resources to challenges that individuals and communities experience, and some have described well-being as the equilibrium between the two (Dodge et al., 2012). Thus, well-being should be considered within the context of social issues, economics, and service provision. This definition of well-being can be particularly useful for rural communities and populations, as resources and service provision are often lacking in rural communities (Health Resources & Services Administration, 2011). Our finding that participants connected with and utilized the concept of well-being suggests that both counseling practitioners and researchers should utilize the term and seek to better understand it, especially those working with rural communities and clients. However, participants in the current study did not provide an expansive level of detail in their conceptualization of well-being; rather, they focused on the cognitive or physical aspect of well-being.
Cognitive and Biological Focus
When comparing the current sample’s definitions to the HHS definition of mental health, the think/cognitive aspect of mental health was most supported and relevant to these rural participants. Most participants believed that mental health describes how individuals think, followed by those who described it as a combination of thoughts and feelings. As noted in the literature review, HHS (2019) considers mental health as impacting the way individuals think, feel, and act. In the current sample, however, only a small fraction of participants defined mental health as a combination of thoughts, feelings, and behaviors. Instead, participants considered mental health from a cognitive and biological perspective, focusing on the brain and chemical imbalances. Thus, results of this study suggest that individuals in rural communities might lack a holistic understanding of mental health.
Our findings add to the literature by providing context for rural individuals’ perceptions and possible explanations for treatment and help-seeking patterns. Rural residents may be especially vulnerable to misinformation about mental health disorders because of mental illness stigma, a cultural expectancy of self-reliance to resolve mental health concerns, and ascertaining mental health–related information from nonprofessionals (e.g., family members, religious leaders; Smalley et al., 2012; Snell-Rood et al., 2017), thus further underscoring the importance of improving MHL in rural communities. In the current study, for example, many participants listed only one component of mental health (e.g., brain imbalance, thoughts), suggesting that their understanding of the concept of mental health is lacking. The focus on the biological composition of the brain in mental health is consistent with definitions of mental illness promoted by organizations such as the National Institute of Mental Health. Thus, although participants’ definitions of mental health are not incorrect, in many ways the focus is narrow and not comprehensive. Study participants excluded emotions and when speaking about biology focused on the brain, which potentially discounts somatic manifestations of mental illness (e.g., stomach pains).
A more comprehensive understanding of mental health, with a specific focus on the connection between emotions, behaviors, and somatic symptoms, could potentially assist rural residents with becoming more conscious of signs and symptoms related to common mental health concerns such as anxiety and depression (Kim et al., 2015). It seems important for mental health educators, organizations, and counseling practitioners in rural communities to provide education that broadens the beliefs about the nature of mental health. Educational campaigns and direct work that are more inclusive and broadly focused could be of benefit.
Implications for Professional Counselors
Professional counselors and related mental health practitioners in rural areas noted they need training opportunities focused on clinical issues that are important in rural settings (Fifield & Oliver, 2016). Thus, the results from this study may offer mental health professionals guidance for reaching residents in rural communities and providing efficacious mental health services. Foremost, counselor training programs could consider developing courses with a specific focus on rural populations, which can assist counseling students in increasing their understanding of the culture of rural settings, how rural residents comprehend mental illness, and effective counseling practices in rural communities (Crumb, Mingo, & Crowe, 2019; Rollins, 2010). For example, counselors in training would be privy to facts such as how many people living in rural areas across the United States face additional life stressors, including poverty and housing and food insecurities, that impact their mental health and well-being.
The results of this study also illustrate the importance of building partnerships and collaborative relationships in rural communities, as rural residents may present varied concerns (e.g., concerns about physical health, family members, finances, spirituality) to counselors when seeking help. Thus, building both informal and formal professional support networks in rural communities is vital. Counselors in rural communities may consider building resources with physicians, faith-based organizations, and other mental health providers for consultation purposes (Avent, Cashwell, & Brown-Jeffy, 2015; Crumb, Mingo, & Crowe, 2019).
El-Amin et al. (2018) suggested programs such as rural-focused Mental Health First Aid to help increase MHL in rural communities. Because access to mental health services is often limited and/or non-existent in rural communities, counselors and related mental health professionals should be more intentional in implementing these forms of programming because of the large number of residents who reside in rural communities who have not yet been helped (El-Amin et al., 2018). Trainings such as this may assist with MHL, as well as mental health stigma, which has been associated with MHL in rural areas (Crowe et al., 2018).
Last, the focus on cognition in participants’ definitions of mental health may indicate a positive response to more cognitive-based theories such as CBT (A. T. Beck, 1970) and rational emotive behavioral therapy (Ellis, 1962). As this study was framed through the lens of CBT and the notion that cognition impacts emotions and behaviors, this theory and related interventions may fit well when working with clients in the rural United States. This type of “matching” related to how clients in the rural parts of the United States understand mental health (with a more cognitive focus) might lead to increased participation in counseling and therapy in rural areas. This might be a way for practitioners to join with the client initially, at the beginning of the therapeutic relationship, in order to “speak the same language.” However, given the findings of the current study, although individuals may have a natural inclination toward more cognitively focused theories, it is incumbent upon mental health professionals to challenge individuals to consider the ways emotions and behaviors are connected to their mental health as well. CBT fits this model well; however, scholars have also found ways to integrate other theories to provide an even more comprehensive and culturally responsive theoretical framework for clients. For example, one of the suggested interventions in Crumb and Haskins’ (2017) integration of CBT and relational cultural theory is to “apply cognitive restructuring through relational resilience” (p. 268). This technique could be especially beneficial to rural communities, as it honors the focus of cognitions while also considering how these thoughts and messages may be related to a broader systemic and environmental influence (Crumb & Haskins, 2017).
In sum, counselors should be aware that many of their clients may present with low MHL. Thus, education and awareness about mental health, diagnoses, and symptomatology may be an integral part of the treatment process. Counselors should consider this intentionality in education as a part of their role as advocates for their clients (Crumb, Haskins, & Brown, 2019).
Limitations and Future Directions
As with all research, the current study is not without limitations. First, the qualitative responses received from participants were often brief. The study team was able to analyze responses, but future qualitative research on the topic of MHL in rural samples might include a focus group design or individual interviews rather than paper-and-pencil surveys to get an in-depth look at how those in rural areas define mental health. Also, future research could seek to further understand the concept of well-being as used by rural participants, looking more in depth at all components (cognition, emotion, and behavior). Future research studies could also investigate the reasons for a focus on cognitive aspects of mental health. As it is impossible to separate cognition from emotion and behavior, this study found that many participants seemed to focus on cognition rather than a more comprehensive understanding of cognition as it related to choices in behaviors and affect. The current study took place in a medical center, and participants who were approached to participate may have felt pressure to complete the survey or answer in a way that was socially desirable. The sample was a convenience sample and may not be representative of others in the rural Southeast.
Large scale quantitative studies might offer scholars interested in MHL the opportunity to use validated instruments to measure literacy and perceptions about mental health in rural samples. Assessments such as the Mental Health Knowledge Schedule (Evans-Lacko et al., 2010) have been used in recent research (Crowe et al., 2018) to measure mental health knowledge. The Revised Fit, Stigma, & Value Scale (Kalkbrenner & Neukrug, 2018) is another scale measuring barriers to counseling such as stigma, values, and personal fit. These types of assessments can measure levels of recognition, familiarity, and attitudes toward mental health conditions in order to measure MHL and perceptions of mental health stigma.
Conclusion
This qualitative study investigated the HHS definition of mental health to determine if it was representative of rural Southeastern participants’ definitions. This assisted with answering the call for more research on the mental health of rural residents (Simmons, Yang, Wu, Bush, & Crofford, 2015) in order to provide better services to this population. Most participants demonstrated a conceptualization that included cognition, as well as well-being, and were more concrete in their conceptualization of mental health when compared to the more comprehensive HHS definition. A promising result from this study was that many participants seemed willing to seek mental health treatment in the future. Rural communities could benefit from mental health education with a holistic approach. Future research should consider interviewing rural populations to gather more detail on their definitions and understanding of mental health. The results provided interventions for professional counselors and related mental health clinicians, particularly those in rural settings, to integrate into their present work, pointed to the need for educational campaigns on mental health in rural areas, and highlighted areas for future research exploration.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Alang, S. M. (2015). Sociodemographic disparities associated with perceived causes of unmet need for mental health care. Psychiatric Rehabilitation Journal, 38, 293–299. doi:10.1037/prj0000113
Avent, J. R., Cashwell, C. S., & Brown-Jeffy, S. (2015). African American pastors on mental health, coping, and help seeking. Counseling and Values, 60, 32–47. doi:10.1002/j.2161-007X.2015.00059.x
Baker, D. W., Wolf, M. S., Feinglass, J., Thompson, J. A., Gazmararian, J. A., & Huang, J. (2007). Health literacy and mortality among elderly persons. Archives of Internal Medicine, 167, 1503–1509. doi:10.1001/archinte.167.14.1503
Beck, A. T. (1970). Cognitive therapy: Nature and relation to behavior therapy. Behavior Therapy, 1, 184–200. doi:10.1016/S0005-7894(70)80030-2
Beck, J. S. (2011). Cognitive therapy: Basics and beyond (2nd ed.). New York, NY: Guilford Press.
Berkman, N. D., Sheridan, S. L., Donahue, K. E., Halpern, D. J., & Crotty, K. (2011). Low health literacy and health outcomes: An updated systematic review. Annuals of Internal Medicine, 155, 97–107.
doi:10.7326/0003-4819-155-2-201107190-00005
Bryant, K., Moore, T., Willis, N., & Hadden, K. (2015). Development of a faith-based stress management intervention in a rural African American community. Progress in Community Health Partnerships: Research, Education, and Action, 9, 423–430. doi:10.1353/cpr.2015.0060
Crowe, A., Mullen, P. R., & Littlewood, K. (2018). Self-stigma, mental health literacy, and health outcomes in integrated care. Journal of Counseling & Development, 96, 267–277. doi:10.1002/jcad.12201
Crumb, L., & Haskins, N. (2017). An integrative approach: Relational cultural theory and cognitive behavior therapy in college counseling. Journal of College Counseling, 20, 263–277. doi:10.1002/jocc.12074
Crumb, L., Haskins, N., & Brown, S. (2019). Integrating social justice advocacy into mental health counseling in rural, impoverished American communities. The Professional Counselor, 9, 20–34. doi:10.15241/lc.9.1.20
Crumb, L., Mingo, T. M., & Crowe, A. (2019). “Get over it and move on”: The impact of mental illness stigma in rural, low-income United States populations. Mental Health & Prevention, 13, 143–148. doi:10.1016/j.mhp.2019.01.010
Deen, T. L., & Bridges, A. J. (2011). Depression literacy: Rates and relation to perceived need and mental health service utilization in a rural American sample. Rural and Remote Health, 11, 1803. Retrieved from http://www.rrh.org.
au/articles/subviewnew.asp?ArticleID=1803
Dodge, R., Daly, A. P., Huyton, J., & Sanders, L. D. (2012). The challenge of defining wellbeing. International Journal of Wellbeing, 2, 222–235. doi:10.5502/ijw.v2i3.4
El-Amin, T., Anderson, B. L., Leider, J. P., Satorius, J., & Knudson, A. (2018). Enhancing mental health literacy in rural America: Growth of Mental Health First Aid program in rural communities in the United States from 2008–2016. Journal of Rural Mental Health, 42, 20–31. doi:10.1037/rmh0000088.supp
Ellis, A. (1962). Reason and emotion in psychotherapy. Oxford, England: Lyle Stuart.
Evans-Lacko, S., Little, K., Meltzer, H., Rose, D., Rhydderch, D., Henderson, C., & Thornicroft, G. (2010). Development and psychometric properties of the mental health knowledge schedule. The Canadian Journal of Psychiatry, 55, 440–448. doi:10.1177/070674371005500707
Felsen, C. B., Shaw, E. K., Ferrante, J. M., Lacroix, L. J., & Crabtree, B. F. (2010). Strategies for in-person recruitment: Lessons learned from a New Jersey Primary Care Research Network (NJPCRN) study. The Journal of the American Board of Family Medicine, 23, 523–533. doi:10.3122/jabfm.2010.04.090096
Fifield, A. O., & Oliver, K. J. (2016). Enhancing the perceived competence and training of rural mental health practitioners. Journal of Rural Mental Health, 40, 77–83. doi:10.1037/rmh0000040
Fuller, J. D., Edwards, J., Procter, N., & Moss, J. (2000). How definition of mental health problems can influence help seeking in rural and remote communities. Australian Journal of Rural Health, 8, 148–153.
doi:10.1046/j.1440-1584.2000.00303.x
Gilgun, J. (2011). Coding in deductive qualitative analysis. Current Issues in Qualitative Research: An Occasional Publication for Field Researchers from a Variety of Disciplines, 2, 1–4.
Gore, J. S., Sheppard, A., Waters, M., Jackson, J., & Brubaker, R. (2016). Cultural differences in seeking mental health counseling: The role of symptom severity and type in Appalachian Kentucky. Journal of Rural Mental Health, 40, 63–76. doi:10.1037/rmh0000041
Hastings, S. L., & Cohn, T. J. (2013). Challenges and opportunities associated with rural mental health practice. Journal of Rural Mental Health, 37, 37–49. doi:10.1037/rmh0000002
Health Resources & Services Administration. (2011). Designated mental health care health professional shortage areas. Retrieved from https://data.hrsa.gov/topics/health-workforce/shortage-areas
Jameson, J. P., & Blank, M. B. (2007). The role of clinical psychology in rural mental health services: Defining problems and developing solutions. Clinical Psychology: Science and Practice, 14, 283–298.
doi:10.1111/j.1468-2850.2007.00089.x
Jorm, A. F. (2000). Mental health literacy: Public knowledge and beliefs about mental disorders. British Journal of Psychiatry, 177, 396–401. doi:10.1192/bjp.177.5.396
Jorm, A. F. (2012). Mental health literacy: Empowering the community to take action for better mental health. American Psychologist, 67, 231–243. doi:10.1037/a0025957
Kalkbrenner, M. T., & Neukrug, E. S. (2018). Identifying barriers to attendance in counseling among adults in the United States: Confirming the factor structure of the Revised Fit, Stigma, & Value Scale. The Professional Counselor, 8, 299–313. doi:10.15241/mtk.8.4.299
Kim, J. E., Saw, A., & Zane, N. (2015). The influences of psychological symptoms on mental health literacy of college students. American Journal of Orthopsychiatry, 85, 620–630. doi:10.1037/ort0000074
Kutcher, S., Wei, Y., & Coniglio, C. (2016). Mental health literacy: Past, present, and future. The Canadian Journal of Psychiatry, 61, 154–158. doi:10.1177/0706743715616609
La Placa, V., McNaught, A., & Knight, A. (2013). Discourse on wellbeing in research and practice. International Journal of Wellbeing, 3, 116–125. doi:10.5502/ijw.v3i1.7
Lincoln, Y., & Guba, E. (1985). Naturalistic inquiry. Newbury Park, CA: SAGE.
National Alliance on Mental Illness. (2015). Mental health by the numbers. Retrieved from http://www.nami.org/Learn-More/Mental-Health-By-the-Numbers
National Council for Behavioral Health. (2019). Mental Health First Aid. Retrieved from https://www.thenationalcouncil.org/about/mental-health-first-aid/
Office of Rural Health Policy. (2005). Mental health and rural America: 1994–2005. Rockville, MD: Author. Retrieved from https://www.ruralhealthresearch.org/mirror/6/657/RuralMentalHealth.pdf
Rainer, J. (2012, Fall). The state of rural mental health: Caring and the community. The National Register of Health Service Providers in Psychology, 8–13.
Rollins, J. (2010, April). Learning the ropes of rural counseling. Counseling Today. Retrieved from https://ct.counseling.org/2010/04/learning-the-ropes-of-rural-counseling/
Rural Health Information Hub. (2017). Rural mental health. Retrieved from https://www.ruralhealthinfo.org/topics/
mental-health
Simmons, L. A., Yang, N. Y., Wu, Q., Bush, H. M., & Crofford, L. J. (2015). Public and personal depression stigma in a rural American female sample. Archives of Psychiatric Nursing, 29, 407–412. doi:10.1016/j.apnu.2015.06.015
Smalley, K. B., Warren, J. C., & Rainer, J. P. (Eds.). (2012). Rural mental health: Issues, policies, and best practices. New York, NY: Springer.
Snell-Rood, C., Hauenstein, E., Leukefeld, C., Feltner, F., Marcum, A., & Schoenberg, N. (2017). Mental health treatment seeking patterns and preferences of Appalachian women with depression. American Journal of Orthopsychiatry, 87, 233–241. doi:10.1037/ort0000193
Stewart, H., Jameson, J. P., & Curtin, L. (2015). The relationship between stigma and self-reported willingness to use mental health services among rural and urban older adults. Psychological Services, 12, 141–148. doi:10.1037/a0038651
Strauss, A., & Corbin, J. (1990). Basics of qualitative research: Grounded theory procedures and techniques (2nd ed.). Newbury Park, CA: SAGE.
U.S. Department of Health & Human Services. (2019). What is mental health? Retrieved from https://www.mentalhealth.
gov/basics/what-is-mental-health/
World Health Organization. (2013). Integrating mental health services into primary health care. Retrieved from https://www.who.int/mental_health/policy/services/3_MHintoPHC_Infosheet.pdf
Allison Crowe is an associate professor at East Carolina University. Paige Averett is a professor at East Carolina University. Janeé R. Avent Harris, NCC, is an assistant professor at East Carolina University. Loni Crumb, NCC, is an assistant professor at East Carolina University. Kerry Littlewood is an instructor at the University of South Florida. Correspondence can be addressed to Allison Crowe, 225 Ragsdale Hall, Mailstop 121, College of Education, 5th St., Greenville, NC 27858, crowea@ecu.edu.