Mar 13, 2025 | Volume 15 - Issue 1
Zori A. Paul, Kyesha M. Isadore, Nishi Ravi, Kayla D. Lewis, Dewi Qisti, Alex Hietpas, Bergen Hermanson, Yuji Su
Queer and transgender people of color (QTPOC) face unique mental health challenges because of intersecting forms of discrimination that place them at higher risk for adverse mental health outcomes. Emerging research has begun to explore the concept of microaffirmations—small verbal or nonverbal forms of communication that signal support, encouragement, or validation—as a protective factor for marginalized populations. This study highlights how QTPOC experience and perceive microaffirmations and explores the role microaffirmations play in their mental health and well-being. Utilizing an interpretive phenomenological analysis, qualitative data were obtained from 14 QTPOC participants through semi-structured interviews. Analyses identified five superordinate themes: influence of identity development, safety with others, envisioning policy changes, representation, and internalization of perceived worth. This study demonstrates the role microaffirmations play in mitigating the negative impacts of discrimination and enhancing the well-being of QTPOC. Implications for counselors include suggestions for providing QTPOC clients with more affirming care on the micro and macro levels.
Keywords: microaffirmations, queer, transgender, people of color, mental health
The number of queer and transgender people of color (QTPOC) in the United States is increasing (Jones, 2024), leading to a greater focus on their unique experiences and mental health needs. In recent years, the visibility of QTPOC has grown, and with it, awareness of the specific challenges they face. These challenges are compounded by intersecting forms of discrimination related to both their racial/ethnic identities and their sexual and gender identities (Cyrus, 2017). Despite this increased visibility, QTPOC continue to experience significant mental health disparities, which are often overlooked in broader discussions about mental health and well-being. These mental health concerns include higher rates of depression, anxiety, and trauma, as well as increased risk of suicidal ideation compared to their White cisgender or heterosexual counterparts (Bostwick et al., 2014; Horne et al., 2022; Meyer, 2003; White Hughto et al., 2015).
Based on the existing mental health disparities among QTPOC, the need exists for enhanced awareness and education about how to promote safe and affirming therapeutic environments for QTPOC clients. Recent research indicates that QTPOC’s mental health outcomes, sense of belonging, and overall well-being are dependent on interactions with others both on the micro and macro levels. For example, how QTPOC are referred to by counselors or administrative staff and how welcomed they feel as members of their community significantly impact their overall mental health and well-being (Pflum et al., 2015). At the same time, QTPOC often experience stressors related to state and federal anti-LGBTQIA+ legislation and lack of competency from non-QTPOC counselors and other health care professionals, possibly leading to feelings of exclusion (Dispenza & O’Hara, 2016; Horne et al., 2022). Counselors and researchers have emphasized the need for addressing issues of racism, homophobia, and transphobia in clinical practices, counselor education programs, and broader societal contexts (Dispenza & O’Hara, 2016; Miller et al., 2018; Mizock & Lundquist, 2016).
Mental Health Concerns for Queer and Transgender People of Color
In recent decades, there has been an increase in research examining the social experiences of minoritized groups, including queer adults, transgender individuals, and people of color (Brooks, 1981; Flanders et al., 2019; Meyer, 2003; Testa et al., 2015). These studies have highlighted substantial disparities in mental health and well-being among these populations, often linked to experiences of discrimination and marginalization. Research indicates that QTPOC are particularly vulnerable to mental health issues because of the intersecting impacts of racism, heterosexism, and transphobia. For instance, a study examining factors related to depression and anxiety for lesbian, gay, and bisexual people of color found that both distal and proximal minority stressors accounted for 33% of the variance in participants’ mental health outcomes (Ramirez & Galupo, 2019). This dual marginalization often leads to cumulative forms of discrimination, including social exclusion from both larger society and within their own communities. QTPOC may face racism within the LGBTQIA+ community and heterosexism or transphobia within their racial and ethnic groups (Cyrus, 2017). Despite these challenges, social support and community connectedness have been identified as critical resources that can buffer the effects of stigma and promote resilience among QTPOC. For example, social support from individuals who are empathetic toward discriminatory experiences can shield young African American LGBTQIA+ youth from the distress associated with intersectional discrimination, fostering a sense of affirmation for their identities and enhancing their autonomy in help-seeking behaviors (Hailey et al., 2020).
Community connectedness has also been linked to positive outcomes among QTPOC (Roberts & Christens, 2020). Roberts and Christens (2020) found that being open about one’s sexual or gender identity (i.e., outness) is beneficial to the well-being of White participants, but not directly for Black and Latinx participants. Instead, the positive effects of outness on well-being for these groups are mediated by their connectedness to the LGBTQIA+ community (Roberts & Christens, 2020). However, the effectiveness of community connectedness can vary. For example, McConnell and colleagues (2018) reported that community connectedness had a weaker mediating effect on the relationship between stigma and stress in sexually minoritized men of color compared to their White counterparts, suggesting that racial stigma may diminish the protective effects of community connectedness. Establishing community connectedness with other QTPOC may foster positive within-community relationships that extend beyond discrete identity groups, enabling members to feel acknowledged and accepted, and leading to positive reappraisals about their identities (Ghabrial & Andersen, 2021; G. Smith et al., 2022). Despite the potential utility gained by understanding factors that promote coping and resilience, there is still a lack of research examining their impact on the mental health and well-being of QTPOC. Emerging research has begun to explore potential sources of everyday coping and resilience, such as the study of microaffirmations.
Microaffirmations
Microaffirmations are defined as small verbal or nonverbal communications that signal support, encouragement, or validation (Ellis et al., 2019; Rowe, 2008). Despite their subtle nature, microaffirmations can be intentional or unintentional, with some occurring as deliberate acts of affirmation while others emerge naturally in everyday interactions (Rowe, 2008). Rowe (2008), who first introduced the concept, posited that for underrepresented groups, daily occurrences of marginalization may go overlooked or be diminished within hierarchical power structures. As members of these groups often struggle with feeling appreciated and accepted within disempowering environments, microaffirmations may effectively counter these negative experiences by disrupting processes that promote social exclusion and oppression (Ellis et al., 2019). Microaffirmations normalize and acknowledge the contributions of marginalized individuals, offer individuals support during times of distress, and empower disenfranchised group members to leverage their strengths to maximize their potential (Rowe, 2008). In general, microaffirmations function as a tool of social reinforcement to bolster productivity by engendering a sense of belonging, fostering inclusion, and enhancing well-being (Topor et al., 2018).
Over the past decade, microaffirmations have emerged as a potential protective factor against the detrimental impact of prejudice and discrimination (Pérez Huber et al., 2021; Rolón-Dow & Davison, 2021). In particular, the underlying behavioral mechanisms of microaffirmations are implicated in reducing intergroup conflict stemming from social stratification and stigma (Jones & Rolón-Dow, 2018; Rolón-Dow & Davison, 2021). Although microaffirmations were initially developed within the workplace literature to address the experiences of cisgender women, recent work has extended the concept’s application to further marginalized groups, including people of color and the LGBTQIA+ community. Microaffirmations can play an important role in the lives of LGBTQIA+ individuals by communicating acceptance, extending social support, and affirming their identity (Flanders et al., 2019). For example, in a cross-sectional study with LGBTQIA+ adolescents, Sterzing and Gartner (2020) found that receiving microaffirmations from family members was associated with a reduction in symptoms of depression, distress, emotional dysregulation, and suicidality. Similarly, interpersonal microaffirmations have also been associated with fewer symptoms of anxiety and stress (Flanders, 2015) and are frequently referred to as impactful experiences of affirmation among bisexual people (Flanders et al., 2019). However, some studies suggest that the effects of microaffirmations may be limited or context-dependent. For example, DeLucia and Smith (2021) found that microaffirmations from mental health providers had no impact on bisexual people’s intentions to seek mental health treatment, whereas experiences of biphobia negatively influenced these intentions. Similarly, Salim et al. (2019) found no association between microaffirmations and happiness among bisexual women. These findings suggest that the effects of microaffirmations may be context-dependent, influencing some aspects of well-being while having little impact on others. Although microaffirmations may foster a sense of validation and support, they may not necessarily translate into behavioral changes, such as help-seeking. These varying results highlight the need for further research on microaffirmations to understand their impact on well-being within different social contexts and systems of power and privilege.
In contrast, research with transgender adults has shown relatively consistent and positive outcomes associated with microaffirmations. Using thematic analysis, Anzani and colleagues (2019) found that microaffirmations may strengthen the therapeutic alliance and enhance perceived treatment satisfaction and efficacy for transgender clients. Scholars have also investigated racial-specific microaffirmations, conceptualized as acts, cues, or verbal utterances that validate racial identities, acknowledge lived experiences, and promote racial justice norms (Rolón-Dow & Davison, 2021). While microaffirmations may have a lesser psychological impact, incidence rate, and intensity than microaggressions (Jones & Rolón-Dow, 2018), they may function to counteract and partially repair the cumulative effects of insidious everyday acts of racism (Pérez Huber et al., 2021). Racial microaffirmations can promote healing through shared cultural intimacy, enabling supportive community members to engage in a cumulative and responsive process of acknowledgment and support that can be both protective and restorative in the context of structural racism (Pérez Huber et al., 2021).
The Current Study
The theoretical framework for this study is grounded in Minority Stress Theory (MST; Brooks, 1981; Meyer, 2003) and Rolón-Dow and Davison’s (2021) typology of microaffirmations. MST posits that the stress experienced by individuals with stigmatized identities is not due to the identity itself but arises from external prejudice and discrimination, as well as internalized stigma (Brooks, 1981; Meyer, 2003). For QTPOC, these stressors are compounded by intersecting forms of racism, heterosexism, and transphobia. This framework highlights the unique stressors faced by QTPOC and underscores the need to understand the multifaceted nature of their experiences. In addition to MST, this study draws on the typology of racial microaffirmations from a critical race/LatCrit approach developed by Rolón-Dow and Davison (2021), which includes four forms: microrecognitions, microprotections, microtransformations, and microvalidations. Each type can be understood as different feelings arising from behaviors, verbal statements, or environmental cues. Microrecognitions involve feeling acknowledged and included (e.g., Pride flags, signage), microprotections offer a sense of being shielded from disparagement (e.g., support and advocacy from others), microtransformations foster a deep sense of belonging and capability (e.g., individuals or institutions advocating for federal and state policies that protect LGBTQ+ rights), and microvalidations affirm that one’s thoughts, feelings, and behaviors are accepted and valued (e.g., QTPOC-specific spaces). While MST has provided a valuable framework for understanding QTPOC mental health disparities, there remains a need to explore how protective factors, such as microaffirmations, can mitigate the negative impact of discrimination on QTPOC. Microaffirmations, though subtle, normalize marginalized communities’ existence and place in society and may counterbalance the pervasive negative experiences of marginalization. Despite the promising research on microaffirmations for individual marginalized groups, research specifically focusing on the impact of microaffirmations on QTPOC is still limited. Given the significant mental health disparities faced by QTPOC and the potential of microaffirmations as a protective factor, this study aimed to deepen the understanding of these dynamics and identify effective strategies for fostering resilience and improving mental health outcomes among QTPOC. The purpose of this study was to 1) explore how QTPOC describe and understand microaffirmations and 2) investigate the specific types of microaffirmations in relation to the mental health and well-being of QTPOC.
Method
The current study employed an interpretive phenomenological design. Interpretive phenomenology is a rigorous qualitative methodology that seeks to uncover participants’ meaning-making processes—comprising their understandings, perceptions, and experiences—related to their lived experiences with a particular phenomenon (J. A. Smith et al., 2009). Interpretive phenomenological analysis (IPA) focuses analytically on the personal meaning-making of participants within specific contexts (J. A. Smith et al., 2009). Through this method, themes are systematically identified and leveraged to construct interpretive descriptions of participants’ narratives, providing insight into the meanings and essences of their lived experiences with the phenomenon.
Participants and Procedures
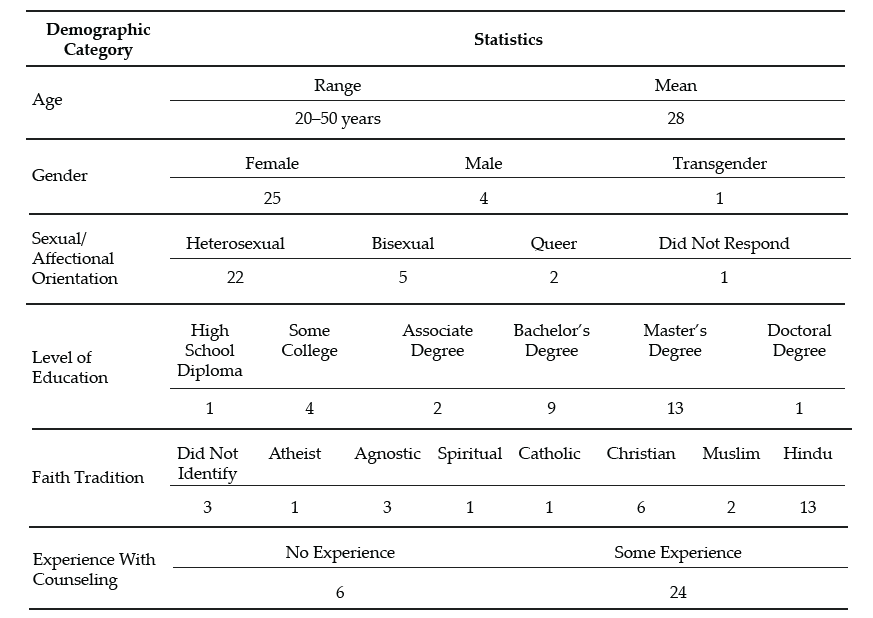
Institutional review board approval was secured prior to participant recruitment or data collection, and all participants gave consent via the online survey. Data was collected during the summer of 2023 and participants were recruited through recruitment flyers and emails via social media, LGBTQIA+ listservs, snowball sampling, and national listservs and interest networks. Eligible participants were asked to respond to an online survey to complete a brief demographic survey and were then contacted by the researchers to schedule a virtual interview. Eligibility criteria included: 18 years of age or older and capable of providing informed consent, identifying as a person of color with a marginalized sexual and/or gender identity, and currently living in the United States or U.S. territories. Interviews took place privately on a video-conferencing platform and were recorded and transcribed for data collection purposes. Participants who completed the interview were provided with a $25 e-gift card as an incentive for participation in the study. Participant demographics are presented in Table 1. All participants (N = 14) identified as a person of color; ages 22–46; sexual identities included queer, bisexual, asexual, demisexual, and gay/lesbian; gender identities included cisgender man, cisgender woman, and non-binary/gender-expansive. Racially and ethnically, participants identified as Filipino, Black/African American, Afro-Caribbean, Chinese American, Latino/a/x, Vietnamese, and Chinese. All participants held a postsecondary degree including bachelor’s, master’s, or doctorate degrees.
All participants engaged in one 60-minute semi-structured interview, which consisted of 19 open-ended questions and prompts aimed at exploring participants’ lived experiences with microaffirmations and the utility of microaffirmations in their daily lives. Drawing from Rolón-Dow & Davison’s (2021) typology of microaffirmations, the interview protocol (see Appendix) was designed to explore participants’ experiences with the four forms of microaffirmations: microrecognitions, microprotections, microtransformations, and microvalidations. For example, the question “Could you describe everyday experiences that made you feel that your thoughts, feelings, sensations, and/or behaviors associated with your lived experience as [insert identity] are accepted, legitimized, or given value?” was formulated to invite participants to reflect on whether they experienced microvalidations. This open-ended question was followed up with questions such as “If you haven’t experienced that, what do you think positive acknowledgment and understanding of your identity and lived experience would look like?” and “In what ways do you think more positive acknowledgment and understanding would impact you directly?” Audio files were recorded using a secure device and stored in a restricted access folder on the researcher’s university department server. Files were used for transcription purposes only and destroyed after the transcription process was complete.
Data Analysis
The data analysis process adhered to the established analytic procedures of IPA outlined by J. A. Smith and colleagues (2009). IPA is characterized by its interactive and inductive approach, focusing on how individuals make sense of their specific lived experiences. The interpretive nature of IPA allows for interpretations that may diverge from the participant’s original text, provided these interpretations are rooted in a close examination of the participant’s words (J. A. Smith et al., 2009).
Initially, the interviews were transcribed verbatim and meticulously reviewed by the research team to understand their context. During this preliminary phase, bracketing and initial coding were performed to describe the interview content. Each interview was individually analyzed to identify central concepts before finding commonalities across interviews (J. A. Smith et al., 2009). The researchers then utilized these initial codes and the original transcripts to identify emergent themes and patterns, employing techniques like abstraction and subsumption to develop superordinate themes. These steps were repeated for each of the participants individually to allow for new themes to emerge by case before superordinate themes were compared across participant cases corresponding to the central research questions.
Table 1
Participant Demographic Information
| Participant
(pronouns) |
Age |
Gender Identity |
Sexual Identity |
Race/Ethnicity |
Highest Degree |
| April
(she/her) |
29 |
Cisgender woman |
Asexual, Demisexual |
Chinese American |
Master’s degree |
| Baohua
(not disclosed) |
36 |
Cisgender man |
Gay |
Asian or Asian American |
Master’s degree |
| D
(she/her) |
28 |
Cisgender woman |
Lesbian, Demisexual |
Black or African American |
Master’s degree |
| Didi
(not disclosed) |
27 |
Cisgender woman |
Bisexual |
Latino/a/x or Hispanic |
Bachelor’s degree |
| Dwayne
(he/him) |
46 |
Cisgender man |
Gay |
Black or African American |
Master’s degree |
| Faith
(she/her) |
23 |
Cisgender woman |
Lesbian, Bisexual, Questioning |
Filipino |
Bachelor’s degree |
| J
(he/him) |
31 |
Cisgender man |
Bisexual |
Filipino |
Doctorate degree |
| Jane
(she/her) |
36 |
Cisgender woman |
Queer |
Black or African American |
Doctorate degree |
| Kay
(she/her) |
27 |
Cisgender woman |
Bisexual, Queer |
Black/Afro-Caribbean |
Master’s degree |
| Lucia
(they/them) |
26 |
Gender-expansive |
Queer |
Filipino |
Master’s degree |
| Nick
(he/him) |
27 |
Cisgender man |
Gay |
Black or African American |
Bachelor’s degree |
| Oliver
(he/him/any) |
22 |
Cisgender man |
Gay, Queer |
Vietnamese |
Bachelor’s degree |
| QL
(not disclosed) |
29 |
Gender-expansive |
Queer |
Chinese |
Master’s degree |
| Stacey
(she/her) |
29 |
Cisgender woman |
Bisexual |
African American & Caribbean American |
Doctorate degree |
Trustworthiness and Researcher Positionality
Our research team consisted of one Black bisexual/queer cisgender female faculty member, one Black queer genderfluid faculty member, four doctoral counseling students, and two master’s counseling students. The students on the research team identify as members of various races/ethnicities, genders, and sexual orientations. All members of the research team either work in or are enrolled in CACREP-accredited counselor education or APA-accredited counseling psychology programs, and all researchers have clinical experience working with diverse populations. To increase opportunities for candid conversations about the role of race/ethnicity, gender, sexuality, and intersectionality with participants throughout the interview process, interviews were conducted by members of the research team who identify as racially/ethnically minoritized, gender-expansive, and/or queer.
Several well-established methodological strategies were employed throughout data collection and analysis to enhance the credibility and trustworthiness of the findings. Multiple coders and peer audits of codes and themes were used to further explore themes, patterns, and interpretations; challenge assumptions; and provide additional insights. This approach is a recognized strategy for enhancing credibility in qualitative research (Yardley, 2008). The involvement of multiple coders and peer audits also served as a check against normative assumptions, prompting researchers to consider how systemic biases might influence their interpretations. Additionally, the research team conducted member checks with participants to verify the accuracy of themes and interpretations. Following the example of Lincoln and Guba (1985), the research team conducted member checks to allow participants to react to the data and the research team’s interpretations before their feedback was incorporated into the presentation of the findings. Participants who engaged in the member check process were provided with a $10 e-gift card as a token of appreciation. The participants’ feedback was not merely a validation step but also a critical engagement with their lived experiences, contributing to a more comprehensive representation of their narratives. The research team met weekly to engage in reflexive discussions about our assumptions, biases, personal worldviews, questions, and concerns related to our research processes, analyses, interpretations, and conclusions.
Results
An in-depth phenomenological analysis of the 14 participant interviews resulted in identification of five superordinate themes related to understanding the role of microaffirmations among QTPOC. Superordinate themes include influence of identity development, safety with others, envisioning policy changes, representation, and internalization of perceived worth.
Influence of Identity Development
The theme influence of identity development reflected how participants understood the utility of microaffirmations in relation to their racial, gender, and sexual identity development. Participants at earlier stages of identity development emphasized the importance of microvalidations and microrecognitions, which provided support and validation as they navigated internal conflict, such as questioning their identity or experiencing self-doubt. For example, April, a 29-year-old asexual/demisexual Chinese American woman, shared that she was still discovering her identity and sometimes felt “a little bit ambiguous about where I’m located on the map.” She highlighted how microvalidations—subtle signs of being recognized and valued—helped her feel seen and supported during this uncertain time:
The other person listening to me or asking me questions that make me feel seen . . . I would say people noticing the pieces that are authentic to who I am and people being willing to spend time listening to me and asking follow-up questions. That is affirming.
Similarly, Faith, a 23-year-old lesbian/bisexual Filipino woman, described herself as “either bisexual or gay, not sure which one yet,” and reflected on how microrecognitions, such as being acknowledged in conversations or within social settings, validated her evolving identity. These early-stage participants frequently described microvalidations and microrecognitions as pivotal in affirming their personal experiences and alleviating internal struggles with identity. In contrast, participants who were more secure and confident in their identities—representing a later stage in their identity development—emphasized a need for microprotections and microtransformations—types of microaffirmations that extend beyond individual validation to encompass broader social change. These participants valued microprotections, which offer safeguarding measures for the QTPOC community against discrimination and prejudice, and microtransformations, which focus on creating systemic changes to improve the quality of life for all QTPOC. For example, Jane, a 36-year-old queer Black woman, discussed how educators can implement microtransformations by using their influence to normalize queer identities within the classroom:
I feel like if we were to learn about [QTPOC] as historical figures and learn about them, like in health class for example, it would help us in other interpersonal contexts and making relationships. It would also normalize treating [QTPOC] as people and with kindness.
Jane’s reflection illustrates the potential for microtransformations to contribute to systemic shifts in how QTPOC are viewed and treated in society. Participants at this later stage of identity development sought microaffirmations that not only validated their personal identities but also fostered more inclusive environments through microprotections and broader societal shifts. These microprotections, such as inclusive policies in schools or workplaces, safeguard QTPOC from harmful discrimination, while microtransformations create opportunities for long-term structural changes that challenge structural inequities and create more affirming environments for QTPOC.
Safety with Others
The theme safety with others represented participants’ experiences of how microaffirmations, particularly microvalidations and microrecognitions, signaled safety in their external environments, indicating that they could express their identities without fear or discrimination. Many participants spoke about the importance of microaffirmations being a way to subtly indicate that an area or person in their external environment is less likely to discriminate, alienate, or be violent toward them. Lucia, a 26-year-old gender-expansive queer Filipino, highlighted the role of microrecognitions in fostering a sense of security: “Microaffirmations communicate safety to me, like, say, from my external environment, that I can then disclose, fully disclose, who I actually am to people . . . So [microaffirmations] are definitely an aspect of safety and being out or not.” For Lucia, small but significant acts of recognition, such as visual cues or verbal affirmations from others, provided reassurance that their identity would be accepted and protected in that space. Similarly, D, a 28-year-old lesbian/demisexual Black woman, shared that microvalidations, such as seeing the Pride flag displayed in public spaces, gave her a sense of immediate comfort and safety: “I can breathe and relax and like, oh, I can exist in this space.” These microvalidations, subtle yet powerful, signaled that the space was affirming and protective of her identity.
Beyond personal safety, participants also reflected on the protective role of microprotections. Some participants, like Jane, described how microprotections in her environment gave her confidence that she would not be alone if a negative situation occurred: “[Microaffirmations] were a sign that there was some kind of protection and backup, that if something goes wrong, that I’m not in it by myself . . . I’m not going to be piled on . . . or outwardly rejected.” This sentiment highlights how microprotections create a sense of communal support, with which participants know that others will ally with them in moments of potential conflict or discrimination. Stacey, a 29-year-old bisexual African American and Caribbean American woman, elaborated on how the cumulative effect of microaffirmations contributed to her overall sense of safety: “When you have more microaffirmations than aggressions . . . you, I, tend to feel safer.” In this instance, Stacey underscored the idea that frequent experiences of affirmation—whether through microvalidations or microrecognitions—help mitigate the impact of microaggressions, allowing her to feel more secure in her identity. Oliver, a gay/queer Vietnamese man, further reflected on how the absence of microaffirmations could leave him feeling vulnerable: “If I didn’t have the experiences of microaffirmations that I did today, I would just feel . . . less mentally secure generally.” Oliver’s observation emphasizes the protective nature of microaffirmations, in that their presence contributed not only to a sense of physical safety but also to psychological security.
Envisioning Policy Changes
The theme envisioning policy changes captured participants’ reflections on the broader implications of microaffirmations, specifically their potential to influence policy and create systemic change. Participants shared their views on both the immediate benefits of microaffirmations and their limitations in addressing larger structural issues. The role of microaffirmations was seen as a necessary component of personal healing from the often-daily trauma of microaggressions but was not sufficient to address systemic inequities. Instead, participants stated that microaffirmations should serve as stepping stones toward inclusive laws and policies. Microprotections, such as individuals expressing their support for policies that provide legal safeguards and affirming spaces, were seen as critical for improving the well-being of QTPOC. Lucia advocated for increased health and gender-affirming care protections: “We need increased protections for health and gender-affirming care, and not just in certain states but nationally.” Lucia’s desire for more inclusive policies highlights the role of microprotections in safeguarding the rights and well-being of QTPOC at a systemic level. Similarly, Stacey emphasized the need for broader legal changes to contend with book bans and the censorship of LGBTQIA+ content in public schools:
I find book bans and the banning of specific conversations in public schools to be very harmful. I primarily work with adolescents and their families, and I believe a lot of stuff starts in childhood, and if we are sending the message to children that queer people shouldn’t exist or that we can’t talk about it, it creates generations of harm.
Stacey’s reflection illustrates how microprotections can counteract systemic exclusion and ensure that QTPOC youth are represented and affirmed in public education.
Microtransformations, on the other hand, were described as the support for far-reaching changes in policies and societal norms that would fundamentally improve the daily lives of QTPOC. Kay, a bisexual/queer Black/Afro-Caribbean woman, noted that while microaffirmations were helpful in buffering the effects of daily microaggressions, they were not enough to dismantle deeply embedded systemic oppression:
So, I think microaffirmations are a buffer to all the aggressions, violence, harm, and trauma that’s happening consistently, but it doesn’t necessarily erase the harm and the violence. But it does provide, at least for me, a buffer mentally. Because I feel if I experience a microaggression, and if I internalize it, that can add to deeper trauma. And microaffirmations can help me externalize that and know that even though it hurts, that it’s not me. I’m not gonna sit in that with that person. And so, I think it’s a great buffer.
Kay’s awareness of the limitations of microaffirmations underscores the importance of advocating for systemic reforms that extend beyond individual or community-level affirmations. There was a marked urgency in advocating for national-level policy changes, such as the expansion of health care access and “full adoption rights for same-sex parents” (Baohua, a 36-year-old gay Asian man). Baohua’s comments reflect the urgent need for uniform protections and policies that support QTPOC regardless of geographic location. Dwayne, a 46-year-old Black gay man, similarly advocated for accessible and inclusive mental health care services as a form of microtransformation, stating that “Making mental health care more accessible and acceptable for all of us should be a priority.” Dwayne’s insight connects microtransformations to health equity, pointing out that long-term systemic improvements are needed to ensure that QTPOC have equal access to health services. Ultimately, dissatisfaction with current policies was prevalent, with participants advocating for equitable reforms that go beyond affirming language and instead target holistic care. Some found it challenging to specify exact policies but envisioned that supportive policies would enhance their well-being and enable easier connections, more energy, and fuller participation in daily life.
Representation
The theme of representation reflected participants’ experiences of engaging with microaffirmations that represent their lived experiences as QTPOC from external sources through visual or vocal cues, as well as participants’ creation of their own microaffirming external sources for others to feel represented through.
External Representation
Representation that was received or seen via microvalidations and microrecognitions was critical in helping participants feel affirmed in their racial/ethnic and gender/sexual identities. J, a 31-year-old bisexual Filipino man, emphasized how social media representations during Pride Month and Asian American Pacific Islander (AAPI) Heritage Month made him feel both his queer and racial identities were not only seen but celebrated:
What comes to mind right away is just Instagram stories and just seeing most of my timeline having some sort of Pride tag or Pride sticker on their stories . . . And also last month during AAPI Heritage Month, those Instagram stories and having the little sticker—it’s really nice to see a bunch of signs of like, “hey, we’re celebrating you!” and “hey, I’m a part of this group too!”
For J, these microrecognitions on social media provided him with a sense of visibility and belonging, reinforcing that the community valued his intersectional identity. Participants throughout shared that visible external representation like affirming signage, Pride flags, racially and LGBTQIA+ diverse TV shows such as Heartstopper, LGBTQIA+ bumper stickers, hashtags, social media posts, and even seeing LGBTQIA+ folks being successful in a variety of different careers were viewed as affirming of their queer identities. Having external representation through a variety of sources not only made participants feel like their identities were being celebrated, but some participants, like Kay, also believed that external representations are microprotections that are “counteracting or disrupting” people from being “harmful” and deterring discrimination.
Created Representation
Though experiencing representation was important, many found that actively creating microaffirmations and making their own representation for themselves and others was also imperative to their well-being. Many saw themselves as change agents, contributing to microtransformations by normalizing conversations about their sexual and gender identities, establishing safe spaces, and engaging in activism that benefited other QTPOC. Dwayne spoke about how his life journey recently involved stepping into a leadership role, in which he felt responsible for creating representation for others:
I guess . . . when it comes to people who are capable of trying to help others, [they realize] that there is sometimes a shortage of people who can be that spokesperson, or be that leader, to be that example, or that exemplary person. They can be in the forefront. . . . And so, I think where I’m at now, just in my life journey, is that . . . I’m coming into that space.
By creating visibility for himself, Dwayne was actively contributing to the creation of microtransformations. Stacey shared the importance of fostering inclusivity for future generations, particularly her children. She explained how creating affirming spaces at home, such as by exposing her children to diverse representations of queer families, was a way to contribute to future microprotections: “[I want to] have them reading books and you know, expose them to other queer families and let them know that this is normal.” By normalizing having conversations about the LGBTQIA+ community, not only is knowledge being shared, but the likelihood increases that youth who may resonate with identities within the community may experience less queer- and race-related microaggressions than their predecessors (Houshmand et al., 2019).
Internalization of Perceived Worth
The theme internalization of perceived worth not only highlighted participants’ internalization of microaffirmations regarding their individual and collective sense of worth but also how the source of these microaffirmations influenced their impact. Microvalidations were often described as contributing to their mental and emotional well-being. For example, Didi, a 27-year-old bisexual Latina woman, shared how microaffirmations helped her feel less overwhelmed and more validated in her identity: “[Microaffirmations] really help me feel validated and, in terms of mental health, I feel like it makes me feel less overwhelmed.” For Didi, these microvalidations provided emotional support that helped her manage the daily stressors associated with navigating stigma and other social barriers. Microrecognitions were also described as crucial in helping participants internalize a sense of worth. For some, like Nick, a 27-year-old gay Black man, internalized validation from microaffirmations not only makes participants feel like their identities as QTPOC are valid but may also provide QTPOC with “better mental health.” QL, a 29-year-old queer gender-expansive Chinese person, also spoke about how microaffirmations helped with their mental well-being and made them feel “affirmed” and “really good,” and that “in some ways it helps with the anxiety. It helps with the depression.”
Another aspect of the theme internalization of perceived worth involves the source of microaffirmations, which influenced how deeply these affirmations impacted their sense of self-worth. Microaffirmations from people with shared or similar identities were particularly meaningful, as these individuals could better understand and relate to the participants’ experiences. April explained that she primarily found validation for her identity within her relationship: “I feel that affirmation of my identifying as demisexual primarily only comes from my own relationship [with my partner].” For April, the microaffirmations she received from her partner were more impactful than those from others because they were rooted in a shared understanding of her identity and experiences. Similarly, Kay shared that the most meaningful microaffirmations often come from her queer friends who share similar marginalized identities: “The microaffirmations carry more weight when they come from my friends who are queer and/or genderfluid or trans . . . because I feel like we all know what we’re going through and we can all support each other.”
This idea that internalized perceived worth or validation comes from those with similar queer and/or trans and racial/ethnic identities was also expressed by Baohua when he described the microaffirmations he received from his friends who also identify as QTPOC, despite cultural differences:
Or maybe they experience some challenges, and I feel like that’s relatable. It’s like . . . we’re speaking in the same language. We’re experiencing similar things. . . . That kind of gives me . . . like different validation to say, hey, we are here, right? Even though that’s very old—we’re here, we’re queer, whatever. But it’s like we are here, and we are living life despite different social or political challenges that we’re facing.
Baohua’s statement highlights how microrecognitions from peers with similar identities can bolster one’s sense of worth and community, reinforcing the idea that they are not alone in their experiences.
Discussion
All 14 participants expressed various experiences of microaffirmations as queer and/or transgender people of color. Themes found in this study’s results (i.e., influence of identity development, safety with others, envisioning policy changes, representation, and internalization of perceived worth) align with and expand on the growing body of literature on microaffirmations’ role in the LGBTQIA+ community (Anzani et al., 2019; Flanders et al., 2019; Pulice-Farrow et al., 2019; Sterzing & Gartner, 2020) and marginalized racial/ethnic communities (Pérez Huber et al., 2021; Rolón-Dow & Davison, 2021). Despite the topic of microaffirmations becoming more prevalent in scholarly literature, there is still a dearth of research that looks at defining and understanding the impacts of microaffirmations for those with both marginalized gender and/or sexual identities and marginalized racial/ethnic identities. Elements of Rolón-Dow and Davison’s subcategories of microaffirmations were used as a foundation for this study’s current superordinate themes.
For the theme of influence of identity development, participants discussed their experiences with microaffirmations that supported and validated their individual identity and other microaffirmations that applied to the broader queer community. For those in the earlier stages of their identity development, the presence of microaffirmations seemed to mitigate any internalized conflict or discrimination related to their queer identities, compared to those in later stages of identity development. These findings aligned with various LGBTQIA+ identity development models, such as D’Augelli’s (1994) Model of Lesbian, Gay, and Bisexual Identity Development and the Model of Multiple Dimensions of Identity (Abes et al., 2007). It seemed that participants who were in the earlier stages of their queer and/or transgender identity development found microaffirmations to be more impactful when they were directed toward them as individuals versus those who were in later stages and had a more community/systemic viewpoint. The differences in identity developmental stages may also be explained by Roberts and Christens (2020), who reported that Black and Latinx participants, when “out,” experienced positive outcomes when they experienced a sense of connectedness to the LGBTQIA+ community. The results of this study (Roberts & Christens, 2020) suggest that those in later stages of development based on how “out” they are may have more ties to other QTPOC. Similar findings from Ghabrial and Andersen (2021) and G. Smith and colleagues (2022) further support the positive impact of community connectedness on participants’ experiences. Perhaps participants in later stages of their identity development are more likely to be out and intentional about finding QTPOC spaces, therefore feeling more validated by microaffirmations directed at the broader queer community instead of those targeting them individually.
For the theme safety with others, participants emphasized their experiences with microaffirmations that signaled safe spaces, individuals, and organizations. This theme aligns with Rolón-Dow and Davison’s (2021) subcategories of microaffirmations, specifically microvalidations and microprotections. Hudson and Romanelli’s (2020) findings, which highlight the fostering of safety and acceptance by the LGBTQ community as a strength and health-promoting factor for LGBTQ adults of color, align with this theme. Participants mentioned that being around other QTPOC allowed them to fully disclose their sexual and gender identities and authentically be themselves. Though participants primarily focused on feelings of safety regarding their marginalized sexual and/or gender identities, many, like Baohua, also mentioned examples of microaffirmations that validated and instilled feelings of safety for both these identities and their racial/ethnic identities. The microaffirmations could potentially reduce the negative mental health–related issues experienced by the participants in this study (Topor et al., 2018).
Regarding the theme envisioning policy changes, participants reflected on the broader implications of microaffirmations and their potential to influence policy and create systemic change. They shared that these microaffirmations also provided immediate benefits, supporting previous literature which reported that gender-affirming policies are associated with positive mental health outcomes among transgender individuals (Horne et al., 2022). However, many of our participants discussed the impact of current anti-LGBTQIA+ legislation and the potential effects of future legislation at both the federal and local levels on the LGBTQIA+ community. Similar to the theme influence on identity development, the centrality of community connectedness and protection was evident when participants talked about both current and future policy changes. This is supported by Hudson and Romanelli (2020), who proposed that QTPOC have a future orientation focused on investing in and improving opportunities for health and well-being for current and future community members. The fourth theme, microaffirmations as representation, was shared by participants as external representations from outside sources, as well as how participants themselves created microaffirmations for others. While previous literature (McInroy & Craig, 2017) also identified external representations of QTPOC, many participants also underlined the importance of being the provider of various forms of microaffirmations. Participants emphasized the importance of actively generating microaffirmations that provided representation for other QTPOC folks. These examples included conducting affirmative research on QTPOC, compiling resources with positive QTPOC representation, and stepping into leadership roles in the LGBTQIA+ community. Hudson and Romanelli (2020) noted that QTPOC involved in activism and advocacy were more likely to be aware of structural and social injustices that can negatively impact the well-being of individuals in the LGBTQIA+ community.
The final theme, internalization of perceived worth focuses on how microaffirmations are internalized and shape participants’ sense of self and collective worth, as well as the impact of microaffirmations based on participants’ relationship with the giver of the microaffirmations. Ghabrial (2019) suggests that for marginalized individuals, feeling that one’s marginalized identity can be viewed as a positive aspect can foster resilience and resolve when experiencing discrimination. This may explain why participants such as Didi felt less overwhelmed and participants like Stacey felt hope when receiving microaffirmations. For these two participants, their positive viewpoints on their sexual identities encouraged them not only in their identities but also in advocating for themselves and other QTPOC. Microaffirmations may therefore be one reason why QTPOC feel motivated to participate in advocacy efforts. Another element of this theme that participants discussed is the impact of internalizing perceived worth depending on the source of the microaffirmation. While microaffirmations from anyone were appreciated, some participants emphasized the positive impact of microaffirmations received from those within the LGBTQIA+ community or from close relationships, whether platonic, familial, or romantic. In a study focusing on transgender individuals and their romantic relationships, Pulice-Farrow and colleagues (2019) reported that participants found microaffirmations more meaningful when they came from romantic partners rather than strangers, as it affirmed the importance of the relationship. This idea also expands on the work by Delston (2021), who suggested that individuals from vulnerable groups seek environments where they feel valued, appreciated, and included. Delston also warns that microaffirmation recipients should be aware of where and from whom they receive microaffirmations, as they may be influenced to make life decisions based on biased external influences, such as a QTPOC only having their identity affirmed by limiting White LGBTQIA+ sources. This study’s findings indicate that microaffirmations from those in close relationships with QTPOC may have a greater impact than those from strangers or large organizations, highlighting the necessity for QTPOC to be cautious of the giver of microaffirmations and the importance of QTPOC to create intentional and affirming support systems.
Implications for Counselors
Given the nuanced understanding of microaffirmations and their profound impact on QTPOC, counselors working with this population can draw several practice implications to foster resilience and improve mental health outcomes. First, it is essential for counselors to recognize the various stages of identity development their QTPOC clients may be undergoing. Clients in the early stages of identity development may benefit significantly from microvalidations and microrecognitions that affirm their identities and experiences, helping them navigate internalized discrimination. Engaging in active listening, providing reflections and follow-up questions, and validating clients’ feelings and identities are vital strategies for those still exploring their sexual and gender identities.
Counselors must also establish environments where QTPOC clients feel safe and affirmed. This can be achieved by incorporating visible signs of support, such as Pride flags or inclusive posters, and using affirming language that communicates safety. Counselors must also check their biases, assumptions, and competencies around QTPOC identities and how they intersect (e.g., continuing education, LGBTQ+/QTPOC affirming supervision/consultation). As Delston (2021) proposed, microaffirmations may influence a person’s decisions based on who and where they came from. Well-intentioned counselors may further perpetuate harmful stereotypes or affirm QTPOC clients from a narrow White, Western perspective that limits influence from these clients’ racial/ethnic background, thereby creating an unsafe environment.
Furthermore, counselors should understand the importance of advocating for inclusive policies. Outside of sessions, counselors can educate themselves and advocate for pro-LGBTQIA+ legislation that would benefit QTPOC. By engaging in advocacy and policy work, counselors can help create a safe and supportive environment that extends beyond the counseling office. Counselors can also seek out positive representations of QTPOC in media, which may allow them to be better able to connect with clients in session by demonstrating their understanding of social and cultural references. However, non-QTPOC counselors should engage with those materials in good faith and avoid performative advocacy with clients, such as having Pride flags hanging in their office but not having resources specific to the needs of QTPOC clients. Moreover, in session, counselors can help clients outline close relationships and safe spaces affirming QTPOC clients’ identities and refer clients with limited support to QTPOC resources locally and virtually. Counselors can also incorporate expressive art therapy techniques into sessions that provide QTPOC clients creative outlets that allow them to not only express themselves but also to be productive by sharing their creations with others as a form of authentic queer representation (Buttram, 2015).
Finally, counselors can support QTPOC clients in fostering internalized worth by consistently using affirming language, adopting a strengths-based approach, and facilitating connections with other QTPOC via group counseling services or within the community. Providing psychoeducation about the impact of discrimination along with employing narrative counseling techniques can help clients reframe their personal stories. By recognizing the unique experiences and needs of QTPOC clients, counselors can play a pivotal role in fostering environments that promote mental health, resilience, and a strong sense of worth, both on an interpersonal, therapeutic level and within the broader societal context.
Limitations and Future Directions
This study, while providing valuable insights into the role of microaffirmations for QTPOC, has several limitations that should be noted. During the time of interviews, most participants identified as cisgender, their gender identity aligning with their sex assigned at birth, providing limiting perspectives of those with gender-expansive identities. Most participants were also Millennials (born 1981 to 1996) and older Gen Zs (born 1997 to 2010; Dimock, 2019), which limits perspectives of what may be considered microaffirmations from older generations of QTPOC who historically experienced less and/or different affirmations in their lives. Future research should aim to include a larger and more diverse sample to enhance the generalizability of the findings.
Another limitation of this study was that it did not ask participants for their regional location. Though some participants shared where they lived in their interviews, knowing regional locations may have helped to understand if participants from similar regions experienced similar types and frequency of microaffirmations. Future research should explore the experiences of QTPOC in specific geographical regions and cultural settings to capture and compare regional differences.
An additional crucial limitation is that, though the study did require participants to be currently living in the United States, there were a few participants who were either immigrants who had lived part of their developmental years in another country or were international students who came to the United States later in life. Though these participants shared their experiences, interview questions did not consider the added marginalized identities of being an immigrant/non–U.S. citizen. Future research is warranted to investigate the utility of microaffirmations for undocumented or non–U.S. citizen QTPOC. Lastly, there is a need for more intervention-based research to develop and test specific counseling strategies that effectively utilize microaffirmations to support QTPOC clients.
Conclusion
This study expanded understanding of the different subcategories of microaffirmations within the context of multiple marginalized identities, specifically being a person of color and being LGBTQIA+. The findings illustrate QTPOC perceptions of microaffirmations and their significant impact on their mental well-being. Efforts should be made to further understand the lasting impact of microaffirmations for individuals with multiple marginalized identities and how microaffirmations can encourage QTPOC and others to make macro-level changes. Counselors and researchers have a vital role in identifying and fostering microaffirmations for QTPOC across various aspects of their work.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Abes, E. S., Jones, S. R., & McEwen, M. K. (2007). Reconceptualizing the model of multiple dimensions of identity: The role of meaning-making capacity in the construction of multiple identities. Journal of College Student Development, 48(1), 1–22. https://doi.org/10.1353/csd.2007.0000
Anzani, A., Morris, E. R., & Galupo, M. P. (2019). From absence of microaggressions to seeing authentic gender: Transgender clients’ experiences with microaffirmations in therapy. Journal of LGBT Issues in Counseling, 13(4), 258–275. https://doi.org/10.1080/15538605.2019.1662359
Bostwick, W. B., Boyd, C. J., Hughes, T. L., West, B. T., & McCabe, S. E. (2014). Discrimination and mental health among lesbian, gay, and bisexual adults in the United States. American Journal of Orthopsychiatry, 84(1), 35–45. https://doi.org/10.1037/h0098851
Brooks, V. R. (1981). Minority stress and lesbian women. Lexington Books.
Buttram, M. E. (2015). The social environmental elements of resilience among vulnerable African American/Black men who have sex with men. Journal of Human Behavior in the Social Environment, 25(8), 923–933. https://doi.org/10.1080/10911359.2015.1040908
Cyrus, K. (2017). Multiple minorities as multiply marginalized: Applying the minority stress theory to LGBTQ people of color. Journal of Gay & Lesbian Mental Health, 21(3), 194–202. https://doi.org/10.1080/19359705.2017.1320739
D’Augelli, A. R. (1994). Identity development and sexual orientation: Toward a model of lesbian, gay, and bisexual development. In E. J. Trickett, R. J. Watts, & D. Birman (Eds.), Human diversity: Perspectives on people in context (pp. 312–333). Jossey-Bass.
Delston, J. B. (2021). The ethics and politics of microaffirmations. Philosophy of Management, 20(4), 411–429. https://doi.org/10.1007/s40926-021-00169-x
DeLucia, R., & Smith, N. G. (2021). The impact of provider biphobia and microaffirmations on bisexual individuals’ treatment-seeking intentions. Journal of Bisexuality, 21(2), 145–166. https://doi.org/10.1080/15299716.2021.1900020
Dimock, M. (2019, January 17). Defining generations: Where Millennials end and Generation Z begins. Pew Research Center. www.pewresearch.org/short-reads/2019/01/17/where-millennials-end-and-generation-z-begins
Dispenza, F., & O’Hara, C. (2016). Correlates of transgender and gender nonconforming counseling competencies among psychologists and mental health practitioners. Psychology of Sexual Orientation and Gender Diversity, 3(2), 156–164. https://doi.org/10.1037/sgd0000151
Ellis, J. M., Powell, C. S., Demetriou, C. P., Huerta-Bapat, C., & Panter, A. T. (2019). Examining first-generation college student lived experiences with microaggressions and microaffirmations at a predominately White public research university. Cultural Diversity & Ethnic Minority Psychology, 25(2), 266–279. https://doi.org/10.1037/cdp0000198
Flanders, C. E. (2015). Bisexual health: A daily diary analysis of stress and anxiety. Basic and Applied Social Psychology, 37(6), 319–335. https://doi.org/10.1080/01973533.2015.1079202
Flanders, C. E., Shuler, S. A., Desnoyers, S. A., & VanKim, N. A. (2019). Relationships between social support, identity, anxiety, and depression among young bisexual people of color. Journal of Bisexuality, 19(2), 253–275. https://doi.org/10.1080/15299716.2019.1617543
Ghabrial, M. A. (2019). “We can shapeshift and build bridges”: Bisexual women and gender diverse people of color on invisibility and embracing the borderlands. Journal of Bisexuality, 19(2), 169–197. https://doi.org/10.1080/15299716.2019.1617526
Ghabrial, M. A., & Andersen, J. P. (2021). Development and initial validation of the Queer People of Color Identity Affirmation Scale. Journal of Counseling Psychology, 68(1), 38–53. https://doi.org/10.1037/cou0000443
Hailey, J., Burton, W., & Arscott, J. (2020). We are family: Chosen and created families as a protective factor against racialized trauma and anti-LGBTQ oppression among African American sexual and gender minority youth. Journal of GLBT Family Studies, 16(2), 176–191.
https://doi.org/10.1080/1550428x.2020.1724133
Horne, S. G., McGinley, M., Yel, N., & Maroney, M. R. (2022). The stench of bathroom bills and anti-transgender legislation: Anxiety and depression among transgender, nonbinary, and cisgender LGBQ people during a state referendum. Journal of Counseling Psychology, 69(1), 1–13.
https://doi.org/10.1037/cou0000558
Houshmand, S., Spanierman, L. B., & De Stefano, J. (2019). “I have strong medicine, you see”: Strategic responses to racial microaggressions. Journal of Counseling Psychology, 66(6), 651–664. https://doi.org/10.1037/cou0000372
Hudson, K. D., & Romanelli, M. (2020). “We are powerful people”: Health-promoting strengths of LGBTQ communities of color. Qualitative Health Research, 30(8), 1156–1170. https://doi.org/10.1177/1049732319837572
Jones, J. M. (2024, March 13). LGBTQ+ identification in U.S. now at 7.6%. GALLUP. https://news.gallup.com/poll/611864/lgbtq-identification.aspx
Jones, J. M. & Rolón-Dow, R. (2018). Multidimensional models of microaggressions and microaffirmations. In G. C. Torino, D. P. Rivera, C. M. Capodilupo, K. L. Nadal, & D. W. Sue (Eds.), Microaggression theory: Influence and implications (pp. 32–47). Wiley. https://doi.org/10.1002/9781119466642.ch3
Lincoln, Y. S. & Guba, E. G. (1985). Naturalistic inquiry. SAGE.
McConnell, E. A., Janulis, P., Phillips, G., II, Truong, R., & Birkett, M. (2018). Multiple minority stress and LGBT community resilience among sexual minority men. Psychology of Sexual Orientation and Gender Diversity, 5(1), 1–12. https://doi.org/10.1037/sgd0000265
McInroy, L. B., & Craig, S. L. (2017). Perspectives of LGBTQ emerging adults on the depiction and impact of LGBTQ media representation. Journal of Youth Studies, 20(1), 32–46. https://doi.org/10.1080/13676261.2016.1184243
Meyer, I. H. (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697. https://doi.org/10.1037/0033-2909.129.5.674
Miller, M. J., Keum, B. T., Thai, C. J., Lu, Y., Truong, N. N., Huh, G. A., Li, X., Yeung, J. G., & Ahn, L. H. (2018). Practice recommendations for addressing racism: A content analysis of the counseling psychology literature. Journal of Counseling Psychology, 65(6), 669–680. https://doi.org/10.1037/cou0000306
Mizock, L., & Lundquist, C. (2016). Missteps in psychotherapy with transgender clients: Promoting gender sensitivity in counseling and psychological practice. Psychology of Sexual Orientation and Gender Diversity, 3(2), 148–155. https://doi.org/10.1037/sgd0000177
Pérez Huber, L., Gonzalez, T., Robles, G., & Solórzano, D. G. (2021). Racial microaffirmations as a response to racial microaggressions: Exploring risk and protective factors. New Ideas in Psychology, 63, 100880. https://doi.org/10.1016/j.newideapsych.2021.100880
Pflum, S. R., Testa, R. J., Balsam, K. F., Goldblum, P. B., & Bongar, B. (2015). Social support, trans community connectedness, and mental health symptoms among transgender and gender nonconforming adults. Psychology of Sexual Orientation and Gender Diversity, 2(3), 281–286. https://doi.org/10.1037/sgd0000122
Pulice-Farrow, L., Bravo, A., & Galupo, M. P. (2019). “Your gender is valid”: Microaffirmations in the romantic relationships of transgender individuals. Journal of LGBT Issues in Counseling, 13(1), 45–66. https://doi.org/10.1080/15538605.2019.1565799
Roberts, L. M., & Christens, B. D. (2020). Pathways to well-being among LGBT adults: Sociopolitical involvement, family support, outness, and community connectedness with race/ethnicity as a moderator. American Journal of Community Psychology, 67(3–4), 405–418. https://doi.org/10.1002/ajcp.12482
Rolón-Dow, R., & Davison, A. (2021). Theorizing racial microaffirmations: A Critical Race/LatCrit approach. Race Ethnicity and Education, 24(2), 245–261. https://doi.org/10.1080/13613324.2020.1798381
Rowe, M. (2008). Micro-affirmations and micro-inequities. Journal of the International Ombudsman Association, 1(1), 45–48. https://mitsloan.mit.edu/shared/ods/documents?PublicationDocumentID=5404
Salim, S., Robinson, M., & Flanders, C. E. (2019). Bisexual women’s experiences of microaggressions and microaffirmations and their relation to mental health. Psychology of Sexual Orientation and Gender Diversity, 6(3), 336–346. https://doi.org/10.1037/sgd0000329
Smith, G., Robertson, N., & Cotton, S. (2022). Transgender and gender non-conforming people’s adaptive coping responses to minority stress: A framework synthesis. Nordic Psychology, 74(3), 222–242. https://doi.org/10.1080/19012276.2021.1989708
Smith, J. A., Flowers, P., & Larkin, M. (2009). Interpretative phenomenological analysis: Theory, method and research. SAGE.
Sterzing, P. R., & Gartner, R. E. (2020). LGBTQ microaggressions and microaffirmations in families: Scale development and validation study. Journal of Homosexuality, 67(5), 600–619. https://doi.org/10.1080/00918369.2018.1553350
Testa, R. J., Habarth, J., Peta, J., Balsam, K., & Bockting, W. (2015). Development of the Gender Minority Stress and Resilience Measure. Psychology of Sexual Orientation and Gender Diversity, 2(1), 65–77. https://doi.org/10.1037/sgd0000081
Topor, A., Bøe, T. D., & Larsen, I. B. (2018). Small things, micro-affirmations and helpful professionals everyday recovery-orientated practices according to persons with mental health problems. Community Mental Health Journal, 54, 1212–1220. https://doi.org/10.1007/s10597-018-0245-9
White Hughto, J. M., Reisner, S. L., & Pachankis, J. E. (2015). Transgender stigma and health: A critical review of stigma determinants, mechanisms, and interventions. Social Science & Medicine, 147, 222–231. https://doi.org/10.1016/j.socscimed.2015.11.010
Yardley, A. (2008). Piecing together—A methodological bricolage. Forum: Qualitative Social Research, 9(2), Article 31. https://www.qualitative-research.net/index.php/fqs/article/view/416/902
Zori A. Paul, PhD, NCC, LPC (MO), is a clinical assistant professor at Marquette University. Kyesha M. Isadore, PhD, NCC, CRC, is an assistant professor at the University of Wisconsin–Madison. Nishi Ravi, MCouns, is a doctoral student at Marquette University. Kayla D. Lewis, MS, is a doctoral student at Marquette University. Dewi Qisti, MS, is a doctoral student at the University of Wisconsin–Madison. Alex Hietpas, MS, is a doctoral student at Marquette University. Bergen Hermanson, BA, is a master’s student at Marquette University. Yuji Su, BA, is a master’s student at Marquette University. Correspondence may be addressed to Zori A. Paul, Department of Counselor Education and Counseling Psychology, Schroeder Complex, 113M, Marquette University, P.O. Box 1881, Milwaukee, WI 53201-1881, zori.paul@marquette.edu.
Appendix
Interview Protocol
The interview will focus on details of participants’ experiences with microaffirmations. Participants will be asked how to describe everyday experiences and small actions that affirm their identities or impact their experiences; how different types of microaffirmations (microrecognitions, microvalidations, microtransformations, and microprotections) show up in their lives; and the impact of microaffirmations on their overall mental health and well-being. The goal of this interview is to elicit rich descriptions of participants’ experiences. The following questions and prompts will be used as a guide for the interview:
- Background Questions
a. Could you briefly explain how you refer to yourself in terms of your sexual and/or gender identity and what those labels, if you use any labels, mean to you?
b. Could you briefly explain how you refer to yourself in terms of your racial and/or ethnic identity and what those labels, if you use any labels, mean to you?
c. Can you describe a time when you felt like someone affirmed your sexual and/or gender identity?
i. If not already answered: What was your relationship to this person?
2. Microaffirmations
a. (Microrecognitions) Could you describe everyday experiences, such as actions, words, or environmental cues (like artwork, signage, symbols) that made you feel like your [insert identity] was given positive visibility and appreciation?
i. If you haven’t experienced that, what do you think positive visibility and appreciation for your identity would look like?
ii. In what ways do you think more positive visibility and appreciation for your identity would impact you directly?
b. (Microvalidations) Could you describe everyday experiences that made you feel that your thoughts, feelings, sensations, and/or behaviors associated with your lived experience as [identity] are accepted, legitimized, or given value?
i. If you haven’t experienced that, what do you think positive acknowledgment and understanding of your identity and lived experience would look like?
ii. In what ways do you think more positive acknowledgment and understanding would impact you directly?
c. (Microtransformations) Could you describe everyday experiences that made you feel that your identity as a member of [insert identity group] has been enabled, enhanced, or increased in society?
i. What do you think potential policies/initiatives that would enable, enhance, or increase your life look like?
ii. How would your life be impacted directly?
d. (Microprotections) Could you describe everyday experiences that make you feel shielded or protected from harmful or derogatory behaviors, practices, and policies tied to your identity as [insert identity]?
i. If you haven’t experienced that, what do you think potential protections or shields would look like?
ii. How would your life be impacted if you had more protection and shields?
3. Other
a. So far, we’ve been talking about positive everyday experiences that affirm your [identity]. The term we use for these everyday experiences and small actions is called microaffirmations. Can you tell us a little about the relationship of these microaffirmations with your overall mental health and well-being and how microaffirmations may impact it?
i. What do you think is the role of microaffirmations in terms of how you navigate spaces that have historically been exclusive to queer and trans people of color?
b. Is there anything we missed regarding any actions, words, or environmental cues you’ve experienced as [identity] throughout the course of your everyday life that affirms your identity and acknowledges your realized identity, and promotes social justice?
Dec 5, 2024 | Volume 14 - Issue 3
Russ Curtis, Lisen C. Roberts, Paul Stonehouse, Melodie H. Frick
Tattoo art is one of the earliest forms of self-expression, but the advent of colonialism, and its accompanying religious convictions, halted the practice in many Indigenous lands and led to widespread bias against tattooed people—a bias maintained to the present. How might the counseling profession respond to this residual bias and intentionally invoke a cultural shift destigmatizing tattoos? Through an extensive literature review, this article provides a more comprehensive understanding of tattoo-related mental health correlates, biases, and theories that enhance the effectiveness of counseling and parallel trends in the counseling profession that emphasize sociocultural influences on wellness. As a result of this survey, the authors propose a new theory of tattoo motivation, the unencumbered self theory of tattoos, which advances existing tattoo theory and aligns with current counseling trends by postulating that tattoos symbolize the uniquely human desire to transcend norms and laws imposed by external influences.
Keywords: tattoo, bias, mental health, theory, counseling
Imagine you are the parent of a 13-year-old girl. While at a parent–teacher conference, you learn your daughter is struggling with disruptive behavior and angry outbursts during class. The teacher asks if you would support your daughter seeing the school counselor and adds that the counselor is in the school building and available to speak with parents. You approach the counselor’s office, gently knock, and are welcomed by a warm, feminine-presenting adult. As the counselor offers their hand to shake, you notice an entirely tattooed forearm, and as you greet their eyes, more ink is evident on their neck.
What feelings, assumptions, or concerns emerge as you put yourself in the place of the parent in the above vignette? Despite the recent popularization of tattoos, a bias remains. Current research indicates that nearly half of adults in the United States between the ages of 18–34 have at least one tattoo (Roggenkamp et al., 2017), and the tattoo business is one of the fastest-growing enterprises, producing over a billion dollars in annual revenue (Zuckerman, 2020). This trend in tattoo art transcends the United States and is evident throughout the world (Ernst et al., 2022; Khair, 2022; Roberts, 2016). Nevertheless, bias against tattooed people remains, and women and people of color receive the brunt of this discrimination (Baumann et al., 2016; Guéguen, 2013; Kaufmann & Armstrong, 2022; Khair, 2022; Roberts, 2016). Given this meteoric resurgence in tattoo art and the discrimination that clings to it, implications for counseling practice inevitably exist.
Professional questions relevant to the counseling practice include: Is there a relationship between a desire for a tattoo and mental health? What motivates a person to seek a tattoo? In what ways may a tattoo bias subconsciously shape a counselor’s interactions with a client? How might the counseling community communicate a spirit of inclusion to the tattooed? To address these questions, this article employs the following structure. First, we provide a context for this bias by briefly examining the history and cultural perspectives of tattoos. Second, to establish the importance of this issue, we empirically demonstrate the reality of tattoo bias. Third, with this history of bias in mind, we comb the literature for research that explores the relationship between mental health and tattoos. Fourth, these relationships offer a frame of reference for our survey of established tattoo motivation theories, to which we propose an additional theory, the unencumbered self theory of tattoos, and reveal its significance within a clinical setting via a case study. Fifth, before concluding the article, we demonstrate how our inquiry’s content might be applied by enumerating our argument’s implications for the counseling profession.
Historical and Cultural Perspectives of Tattoos
The word tattoo originates from the Samoan term tatau, meaning “to tap lines on the body.” The practice of tattooing is known to have existed as early as 7000 BC, as seen on Egyptian mummies (Rohith et al., 2020). Otzi the Ice Man, dating back to 3000 BC, was discovered in 1991 with tattoos on his arms and wrist that are thought to have been applied for therapeutic purposes, a potential precursor to acupuncture (Schmid, 2013). Prior to the colonization of Indigenous lands by European countries, many tribes practiced the art of tattoo to symbolize adulthood, tribal membership, and status (Dance, 2019; Thomas et al., 2005). However, with the emergence of European imperialism, colonizers taught Indigenous people that tattoos were an abomination, scripturally prohibited, and therefore immoral. For instance, in The Holy Bible (New International Version, 1978, Leviticus 19:28) and The Qur’an (2004, Surah 7:46), specific passages forbid marking the skin.
Despite these condemnations, the practice of tattooing was not eradicated. Many cultures continued their tattoo traditions, and modern culture has adopted new traditions, which are even now expanding throughout the world (Ernst et al., 2022; Khair, 2022; Roberts, 2016). Although there is much intergroup variability, cultural identity can influence the motivation for and type of preferred tattoo. In India, for instance, tattoos often depict unique patterns specific to different tribal regions in the country. Specifically, in urbanized Indian geographic areas, there is increasing integration of tribal pattern tattoos with Western-influenced designs (Rohith et al., 2020). In Samoan culture, men receive an intricate tattoo called a pe’a while women receive a malu, both to indicate maturity (Dance, 2019). Lest the cultural importance of Indigenous tattoos be doubted, their misappropriation has resulted in litigation, thereby challenging attorneys to consider the property rights of tattoo designs (Tan, 2013).
Profoundly relevant to counseling, tattoos are often representational and symbolize something of importance. In a recent qualitative study of tattooed Middle Eastern women, Khair (2022) discovered themes related to taking ownership of their bodies in a patriarchal society and symbolism of their strength and desire to break free of patriarchal rules and religious mandates. In the United States, a study of mixed-race Americans’ tattoos revealed the most common tattoo themes include animal images and text of personally meaningful messages (Sims, 2018). In yet another group, White supremacists often get swastikas, crossed hammers, Confederate flags, and embellished Celtic crosses (Southern Poverty Law Center, 2006). Similarly, in Czech Republic prisons, the skull tattoo is a symbol representing neo-Nazi extremism, which then informs prison officials of inmates potentially becoming radicalized (Vegrichtová, 2018).
Exploring the intersection of religion and tattoos, Morello’s (2021) qualitative analysis of 21 people in three South American cities revealed that tattoos were more accepted among Catholics than evangelicals. Explained below, Morello classified the types of Christian tattoos as reversal, devotional, foundational, and then a nonreligious fourth category termed relational. According to participants, reversal tattoos symbolized regaining control of disempowering events, such as when Christians historically tattooed themselves to show Roman enslavers their devotion to Christ. Devotional tattoos were comprised of images and symbols representing religious themes (e.g., a cross), often used as a source of strength and identity. Foundational tattoos represent significant moments in life, such as major life transitions (e.g., the date of one’s conversion) or mystical experiences. Morello’s last category is akin to devotional tattoos, but the relational category was created to represent devotion to loved ones, such as images or symbols of one’s children.
In a related study examining the beliefs of religious women with and without tattoos, Morello et al. (2021) identified several common themes. This mixed methods study of 48 women in a conservative Christian college indicated that tattoos were not considered taboo by their religious friends and family and that tattooed participants spent considerable time determining which tattoo to receive. Predominant reasons for obtaining tattoos included social justice, friendship, and spiritual values. Summarizing previous research, individuals primarily choose tattoos to express their identity and uniqueness or to take ownership of their bodies. However, as discussed in the following section, there exists a bias against tattooed individuals.
Tattoo Bias
Unfortunately, with any practice that diverges from dominant cultural values, there is bias (Broussard & Harton, 2018). Although evidence indicates less discrimination against tattoos in the 21st century, negative judgments still exist explicitly and implicitly (Broussard & Harton, 2018; Williams et al., 2014; Zestcott et al., 2018). For example, Kaufmann and Armstrong (2022) found that law enforcement and the medical community hold negative sentiments toward tattooed people. They found that medical professionals who expressed negative judgments about their tattooed patients were likely to have patients not return. In fact, patients reported better rapport and increased trust with medical professionals who asked about the meaning of their tattoos. In other words, negative judgment toward, and lack of acknowledgment of, tattoos were detrimental to building the trust needed to provide optimal and consistent care (Kaufmann & Armstrong, 2022).
Unjustly, women and people of color with tattoos experience more significant discrimination than men or White people (Baumann et al., 2016; Camacho & Brown, 2018; Guégen, 2013; Solanke, 2017). For example, women encounter prejudice when failing to gain employment due to having visible tattoos regardless of having excellent job qualifications (Al-Twal & Abuhassan, 2024; Henle et al., 2022). Moreover, women of color have experienced job discrimination by being questioned if they have visible or nonvisible tattoos (i.e., inkism), being forbidden from having or being required to cover tattoos regardless of cultural relevance (e.g., covering a traditional Māori tattoo), or being required to prove that they do not have tattoos—as alleged in a legal complaint against a Singaporean airline that required female attendants to wear a swimsuit and demonstrate to their employers that they did not have tattoos (Solanke, 2017, Chapter 8). Women with tattoos also experience ambivalent sexism due to rejecting the feminine apologetic (i.e., not acting or dressing in stereotypical feminine ways); they are also perceived as wanting attention and sexually promiscuous (Heckerl, 2021). For instance, Guéguen (2013) found that women on the beach displaying a lower-back butterfly tattoo were significantly more likely to be approached by men compared to women without the tattoo, and the men interviewed indicated that they thought they had a better chance of getting a date and having sex with the tattooed women than the nontattooed women (Guéguen, 2013). In other words, men in this study had the biased perception that women with tattoos were more sexually promiscuous than nontattooed women.
This bias appears within incarceration rates as well. In a study conducted by Camacho and Brown (2018), they found that arrestees with neck tattoos were more likely to receive felony charges specifically for larceny offenses. Among these groups, Black individuals with neck tattoos were more likely than others to face felony charges (Camacho & Brown, 2018). It is also noteworthy that law enforcement catalog the tattoos of arrestees in the Registry of Distinct Marks (Miranda, 2020), which is kept in their permanent record and could potentially bias future incarceration and convictions due to the criminogenic stigmatization of individuals with tattoos (Martone, 2023; Rima et al., 2023).
Neck tattoos specifically appear to elicit bias (Baumann et al., 2016). Given two sets of photos of male and female faces, with a neck tattoo and without a visible tattoo, participants were asked to choose among the photos that they would most like to have as their surgeon. In a separate condition, participants were asked to choose who they would most like to have as their car mechanic. In both experiments, participants preferred to have a nontattooed person as their surgeon or mechanic. However, the preference was more substantial for a nontattooed surgeon than a nontattooed mechanic. Female participants assessed the tattooed faces more positively than male participants, but still preferred the nontattooed faces (Baumann et al., 2016).
Roberts (2016) suggested that although tattoos are becoming more prevalent worldwide, they are not yet entirely accepted. As such, employment discrimination occurs for people with visible tattoos. Roberts (2016) suggested employers discriminate primarily because of the fear of customer complaints and the concomitant loss of business. They further suggested that small businesses in rural areas, which tend to be more conservative, may be even more likely to refuse employment to tattooed workers.
Clients’ Perception of Tattooed Counselors
To date, very few published studies examine the perceptions of tattoos within the mental health professional arena. One exception, however, is a recent publication examining the perception of potential mental health clients of psychologists with or without tattoos. Zidenberg et al. (2022) recruited 534 participants to determine if there were negative perceptions of psychologists who had tattoos. First, participants were presented with a mock profile of a fictional clinical psychologist. Each participant was randomly assigned to view one of three images of the psychologist: with no tattoo, a neutral tattoo (a flower), or a provocative tattoo (a skull with flames). Participants then rated the counselor on perceived competence and their personal feelings toward her.
Contrary to the researchers’ initial expectations, the psychologist’s photo with the provocative tattoo was rated more likable, interesting, and confident and less lazy than the psychologist with a neutral or no tattoo. Interestingly, the psychologist’s photo without a tattoo was rated as more professional, but this did not equate to participants’ believing that the psychologist would thus provide better care. The researchers speculated that while nontattooed people are viewed as more professional, they are not necessarily who clients believe will give the best mental health care. They further hypothesized that professionalism may convey a bias of being “better than” the clients and thereby might be perceived as less authentic. Moreover, participants in this study believed they would get better help from a more “authentic” psychologist, and that the provocative tattoo communicated a sense of authenticity (Zidenberg et al., 2022).
Mental Health and Tattoos
Although early studies (e.g., Grumet, 1983) concluded that tattoos were a sign of maladjustment, contemporary research indicates that tattooed people are as healthy as nontattooed people (Mortensen et al., 2019; Pajor et al., 2015). In general, today the mere presence of a tattoo is not correlated with mental or behavioral issues (Roggenkamp et al., 2017). In fact, most people in many cultures conscientiously obtain tattoos to express themselves and honor people and causes they deeply care about (Khair, 2022; Naudé et al., 2019; Shuaib, 2020). Nevertheless, in one study of a German community (N = 1,060), which sampled people aged 14–44, 40.6% who reported childhood abuse or neglect had at least one tattoo, compared to 29.4% tattooed participants who reported no significant abuse (Ernst et al., 2022). However, Ernst et al. (2022) cautioned that the mere presence of a tattoo is not perfectly correlated with childhood abuse. Aesthetic embellishment of the body is the most common reason for getting tattoos, and it should not be considered an automatic indication of childhood abuse (Ernst et al., 2022).
Evidence suggests that the number of tattoos as well as their placement and content better indicate potential maladjustment than the mere presence of an easily concealed tattoo. Specifically, Mortensen et al. (2019) found that participants (N = 2008 adults) who had four or more tattoos were 15.4% more likely to report having been diagnosed with a mental health problem compared to 5.8% of participants with only one tattoo. Further, 13.4% of the participants with visible tattoos reported having a mental health diagnosis, and 28.2% of the participants who self-reported having an offensive tattoo also reported having a mental health diagnosis. In other words, multiple and visible tattoos may be more closely correlated with mental and behavioral issues than the mere presence of tattoos. However, contrary to Mortensen et al. (2019), in their study of life satisfaction with a sample of 449 participants (16–58 years old), Pajor et al. (2015) used the Multidimensional Self-Esteem Inventory (MSEI; O’Brien & Epstein, 1988), a psychological assessment tool with 116 items graded on a 5-point scale and designed to measure various aspects of self-esteem. Results indicated that tattooed people reported significantly higher competence than nontattooed: 37.2 versus 33.6 (p < .001). Tattooed participants also scored significantly higher on a measure of personal power, 35.6 versus 33.5 (p < .01), and significantly lower scores on a measure of anxiety and insomnia, 1.50 versus 1.75 (p < .05). Thus, although numerous visible tattoos could potentially indicate mental or behavioral issues, the research is not conclusive, suggesting the need for counselors to open-mindedly assess each client’s motivations for obtaining tattoos.
Contrary to previous hypotheses, tattoos are rarely a form of self-harm (i.e., cutting, self-mutilation). For example, Aizenman and Jensen (2007) analyzed a sample of college students (N = 1,330; ages 17–39) to determine mental health differences between students who self-injure and those with tattoos. The majority of tattooed students reported receiving tattoos as a way to express their individuality, while students who self-injured were motivated by feelings of insecurity and loss of control. Participants also completed assessments measuring depression and self-esteem. In terms of general wellness, the self-injury group (no tattoos) reported higher mean depression scores compared to both the tattoo group’s score and the nontattooed (no self-injury) score. The self-injury group also reported lower mean self-esteem scores compared to both the tattooed and the nontattooed groups. Noteworthy is the fact that there was no significant difference between the tattooed and nontattooed groups in terms of depression and self-esteem, which further suggests that tattooed college students are no more likely to experience mental health issues than nontattooed college students.
In a more recent study to determine whether tattooing was a form of self-injury, Solís-Bravo et al. (2019) found that from a sample of 438 adolescent males, 11.5% reported engaging in nonsuicidal self-injury (NSSI), but only 1.8% indicated receiving a tattoo with the explicit intention of feeling pain. However, they also found that 62.5% of the students with tattoos self-injured compared to 10.6% of students without tattoos. Thus, with this small subsample of tattooed NSSI students, it was suggested that tattooed adolescents should be screened for potential mental health issues. Yet, considering that only eight students in this sample reported getting a tattoo to feel pain, further replication of this work is needed before confirming a conclusive relationship between tattoos and NSSI (Solís-Bravo et al., 2019).
Exploring the correlation between tattoos and premature mortality (e.g., violent death, drug overdose), Stephenson and Byard (2019) found that there was a trend for people with tattoos to die at a younger age and to experience an unnatural death compared to nontattooed people. However, these results were not statistically significant, indicating that there was no meaningful difference between age and cause of death between tattooed and nontattooed people.
More contemporary research examined the relationship between body image and tattoo acquisition (Jabłońska & Mirucka, 2023). Using a sample of 327 Polish tattooed women to examine a relationship between body image and tattoos, 45.26% reported acceptance of their appearance and a deep connection to their bodies. Researchers speculated that they received tattoos as a way to adorn their bodies and express their individuality. Another 36% reported an unstable body image, meaning they perceived both positive and negative aspects of their bodies. It was speculated that this group used tattoos to conceal perceived flaws. The remaining 18.65% held a negative body image. Although the majority of their sample held either positive or mixed body image estimations, the researchers’ speculation as to why subjects received tattoos makes it difficult to infer correlation between tattoos and well-being. Nevertheless, nearly half the sample reported appreciation for their bodies and a desire to accentuate their positive self-image with body art.
Relatedly, some trauma survivors get tattoos to symbolize what they experienced and how they have grown (Crompton et al., 2021). The semicolon is one example of this, indicating that while one life chapter may have been traumatic, that is not the end of the story. Using tattoos to navigate trauma is further supported by Kidron (2012), who noted that some descendants of Holocaust survivors replicated the number tattoo on their arms to illustrate the connection to their grandparent, redefining the tattoos from markers of trauma to markers of survival and expanding their interfamilial bond and cultural identity.
In summary, studies indicate that the mere presence of a tattoo is not significantly correlated with mental or behavioral issues. Counselors should avoid assuming that tattooed clients have mental health issues, even if multiple visible tattoos are sometimes linked with adverse health outcomes or behaviors. Because tattoos are so often attached to identity, body image, and important life events, counselors should thoroughly explore with clients why they obtained such tattoos and what they symbolize. In order to assist with such exploration, the next section identifies a number of recognized tattoo motivation theories.
Tattoo Motivation Theories
To determine effective strategies to reduce tattoo bias and counsel tattooed clients, it is important to understand the motivations and theoretical premises of why people get tattoos. This section describes recognized tattoo motivation theories. Recent findings in tattoo research cited within this article highlight the limitations of these theories and prompted us to propose our own, the unencumbered self theory of tattoos, which focuses on sociocultural influences. From this new perspective, we hope counselors will have a clearer understanding of the motivations behind getting a tattoo, which will in turn increase understanding of tattoo culture and what this implies about clients and counseling practice. To illustrate how these theoretical models might be of use in a clinical setting, in the subsequent section we provide a case study in which we discuss, compare, and contrast theories and exemplify the need for a new understanding of tattoo motivation.
Psychodynamic Theory of Tattoo
The first hypothesis for tattooing is rooted in psychodynamic theory. This theory posits that tattoos are an outward manifestation of intrapersonal conflict or unresolved psychological concerns (Grumet, 1983; Karacaoglan, 2012; Lane, 2014). The belief is that permanent skin marking serves as a visible mnemonic that prompts a defense mechanism that helps alleviate the anxiety caused by conflict within the id, ego, and superego. In other words, the symbolism embodied within the marking of the skin iteratively releases blocked psychic energy, causing temporary relief from various difficult symptoms.
Psychodynamic theory is problematic because it fails to address the alternative motivations for getting tattoos, namely, the aforementioned social–cultural perspective. Moreover, Freud’s psychoanalytic approach is rooted in Western civilization’s understanding of internal processes and is therefore heavily influenced by a European, White, male perspective of psychic processes, thus ignoring the effects of oppression and inequality on personal identity, mental health, and behavior. As was indicated in the previous research review, and as we will see in subsequent sections, current tattoo research does not support the notion that tattoos are merely the result of unconscious conflict.
Human Canvas and Upping the Ante Theories of Tattoo
Moving beyond the arguably deficit ideology of the psychodynamic theory of tattoos, Carmen et al. (2012) proposed two evolutionary theories of tattoo motivation that transcend obvious reasons like self-expression and group membership. The first theory, human canvas, argues that it is our innate longing to express the most authentic desires of our psyche through symbolic thought, originally on cave walls and later on our bodies. Their second theory, upping the ante, postulated that with increasing longevity and improved health care, the opportunities for attracting mates are more competitive, and people must devise new ways to stand out to attract mates, much like a peacock spreading its feathers.
The human canvas and upping the ante theories of tattoos are at least to some degree supported by current research (e.g., Wohlrab et al., 2007), and both theories advance our understanding of the motivation behind tattoos beyond psychodynamic theory. Indeed, people spend considerable time and thought choosing their tattoos for personal self-expression (Kaufmann & Armstrong, 2022) and to symbolize cultural traditions, sexual expression, and the love of art (Wohlrab et al., 2007). Although these theories advance tattoo theory, they fail to consider the even deeper meaning which suggests that tattoos are a way to regain bodily control and express displeasure with mandated values imposed by external influences. In essence, it is clear that tattoos are a form of self-expression, potentially to increase personal uniqueness and attractiveness, but this fails to explain what people are hoping to express. Thus, informed by contemporary tattoo research, we propose a new and expanded theory that attempts to explain the rationale behind tattoo acquisition through a wider societal lens.
The Unencumbered Self Theory of Tattoo
The unencumbered self theory of tattoos advances existing tattoo theory and aligns with current counseling trends by postulating that tattoos symbolize the uniquely human desire to transcend norms and laws imposed by external influences such as imperialism. After an exhaustive review of the tattoo literature, it is evident that the motivation to reclaim personal power from oppressive systems is one reason some people get tattoos, and this motivation is not explicitly stated within existing theories. While most closely aligned with the human canvas theory, the unencumbered self theory of tattoos differs in one subtle but essential way. The human canvas theory postulates that tattoos are a general form of self-expression (e.g., hobbies, memorials, identity, individuality). At the same time, the unencumbered self theory of tattoos suggests that specific individuals acquire tattoos as a deliberate assertion of autonomy and a repudiation of arbitrary societal norms. Take, for example, a client of Cherokee heritage who gets a tattoo depicting Cherokee syllabary. The human canvas theory would hold that this tattoo is motivated by the client’s desire to identify with her cultural heritage. The unencumbered self theory of tattoos acknowledges her desire to identify with her cultural heritage, but this desire is motivated by the need to disengage from the oppressive systems that successfully squelched her people’s values for so long.
Evidence supporting the unencumbered self theory of tattoos includes cross-cultural studies examining motivations behind obtaining tattoos (Atkinson, 2002; Khair, 2022; Kloẞ, 2022). Atkinson (2002) reported that Canadian women wore tattoos to challenge societal definitions of femininity, and Khair (2022) found that Middle Eastern women obtained tattoos primarily to express their uniqueness and to indicate ownership of their bodies. Khair (2022) stated, “In fact, women of the Middle East have been struggling to obtain the freedom of their identity due to various restrictive reasons that relate to religion” (p. 3). This sentiment is further supported by Stein (2011) who stated, “My data suggest that—rather than seeing themselves as capitulating to market forces—people think of their decision to get tattoos as an exceptionally deep expression of personal identity, as well as a dramatic declaration of autonomy” (p. 128).
Additionally supporting the cultural motivations behind obtaining tattoos, Kloẞ (2022) identified Hindu women having tattoos that symbolize both oppression from and resistance to patriarchy, colonialism, and orthodox religious beliefs. Relatedly, Stein (2011) stated that the motivation behind tattoos is, at least in part, “a defiance of patriarchal authority” (p. 113). This desire to live unencumbered is also evidenced in research indicating that tattooed people are less likely to be members of religious groups (Laumann & Derick, 2006); are less likely to conform to societal norms, as evidenced by lower scores on personality assessments measuring agreeableness and conscientiousness (Tate & Shelton, 2008); and are considered more authentic and relatable (Zidenberg et al., 2022).
The unencumbered self theory of tattoos also coincides with current research and theoretical advancements in the counseling profession. Integrative approaches, such as narrative, relational, and art therapies, illustrate how tattoos can be used to externalize issues and emotions onto the body and promote self-expression by re-authoring life stories that are freeing and healing (Alter-Muri, 2020; Covington, 2015). Further, there is an increasing interest in Indigenous healing practices and the counseling profession’s embrace of a more collaborative and collective approach to health and wellness. To illustrate how the unencumbered self theory of tattoos advances tattoo theory and serves the counseling profession, we compare and contrast the existing theories in the following case study.
Case Study and Discussion
In this fictional case study, Sage is a 28-year-old, cisgender, queer, able-bodied female whose mother is Eastern Band Cherokee and whose father identifies as Mexican American. Sage upholds many traditional Cherokee customs and regularly attends tribal council meetings as well as powwows where she dances in traditional native attire. Sage has several visible tattoos on her arms and one on the back of her neck, all of which symbolize her Cherokee heritage. She presented to counseling with increasing depression after quitting drugs and alcohol for the past year and reports being unhappy in her job with no meaningful relationships. Sage’s counselor does not have tattoos and identifies as White, female, and a social justice advocate who knows very little about people with tattoos or Cherokee customs.
From the psychodynamic theory of tattoo (Grumet, 1983), Sage’s tattoos would be considered an expression of inner conflict and unmet needs, and the counselor would ask questions hoping to uncover unconscious beliefs that are causing her depression. In this case, the counselor may not even mention her tattoos, but instead view them from a deficit lens indicating a personal problem to resolve.
In both the human canvas and upping the ante evolutionary theories of tattoos (Carmen et al., 2012), Sage’s tattoos could indicate her desire to express her individuality and enhance her attractiveness. With this in mind, the counselor is likely to acknowledge her tattoos and ask about their meaning. However, both theories fail to recognize that Sage’s tattoos may signify deeper underlying issues related to potential oppression and inequality she feels because of her race, ethnicity, and gender.
From the unencumbered self theory of tattoos, Sage’s tattoos could reflect her motivational factors, feelings of alienation, and desire to align her authentic self and heritage. From this perspective, the counselor might explore whether she has experienced discrimination and how the impact of societal marginalization shaped her current sense of self. For example, the counselor may ask, “Have you ever experienced feelings of alienation or disconnect from others, and if so, how do you think your tattoos relate to those experiences?” Another counselor probe could be, “What emotions or thoughts come up when you think about the stories or meanings behind your tattoos?” In addition, the counselor may inquire into cultural healing traditions that help Sage reclaim her authenticity and realign her with her Indigenous heritage. In this instance, the counselor may ask, “Are specific cultural or familial traditions associated with your tattoos, and how do they contribute to your sense of authenticity?” or “Have your tattoos played a role in helping you reconnect with or reclaim aspects of your cultural identity?” Ultimately, through understanding the unencumbered self theory of tattoos, the counselor can better assist Sage by gaining deeper insight into her experiences, her motivations, and the significance of her tattoos within the context of her identity and mental health journey.
In summary, clients’ motivations for tattoos are complex and include explicit explanations, such as self-expression and identity, and potentially implicit motivations, such as increased attractiveness and autonomy. Based upon the tattoo motivation research, we believe the unencumbered self theory of tattoos provides a more comprehensive understanding of the reasons people get tattoos, which appears to be motivated by boldly proclaiming their desire for autonomy and not merely to enhance personal attractiveness. With these findings in mind, the subsequent section describes how counselors, and the counseling profession more broadly, can enhance counseling practice with tattooed clients.
Implications for Counseling
Tattooed clients and counselors will become increasingly common, if not the norm. Consequently, there are clinical, professional, ethical, and societal considerations associated with the increasing popularity of tattoo art. This section addresses what counselors can do to adeptly navigate the increasing prevalence of tattoo culture and better serve their clients.
Counselors must reexamine their potential bias about tattooed clients and recognize that current research suggests they are not more likely to have mental and behavioral problems (e.g., Pajor et al., 2015). In fact, tattoos on a client might indicate their readiness for counseling by showing their strength and desire to break free of parental and societal expectations (e.g., Crompton et al., 2021). However, the number and placement of tattoos may better indicate potential mental health issues (Mortensen et al., 2019). With this in mind, asking clients about their tattoos early in the counseling relationship may help build rapport and provide potentially rich information about the client’s life story. Specifically, if the client’s tattoo is visible, it would be appropriate and possibly helpful to ask about it during intake (Kaufmann & Armstrong, 2022).
To foster genuine rapport and mitigate power imbalances in the therapeutic relationship, it is crucial for counselors to engage in self-reflection, cultivate cultural awareness and humility, and understand the potential cultural significance of tattoos (Day-Vines et al., 2018). Initiating conversations about clients’ tattoos early in counseling can be an effective strategy. Counselors might ask: “Tattoos often have special meanings or stories attached to them. What inspired you to get yours?” This approach demonstrates respect for the client’s personal and cultural narratives, promoting a more equitable and empathetic counseling environment. For instance, inquiring about a client’s neo-Nazi tattoos demonstrates the counselor’s desire to understand all aspects of the client. Despite the offensive nature of the tattoos, questioning could prompt the client to disclose personal experiences such as family addiction, abuse, poverty, insecurity, and fear of losing one’s identity in an increasingly multicultural society. These disclosures might not have emerged otherwise.
Counselors do not necessarily need to cover their tattoos, because they may help increase clients’ perception of the counselor’s relevance (Zidenberg et al., 2022). In fact, the counselor disclosing their tattoos may propel some clients to share more personally relevant information during sessions (Stein, 2011). Depending upon the client, a counselor with tattoos could broach the topic of how their tattoos symbolize their pursuit of authenticity in a society where the values of marginalized populations (e.g., women, non-White, LGBTQ) are too often not recognized, understood, or honored.
This example shows how a counselor could broach the topic of tattoos:
During our sessions, we have been exploring various aspects of identity and self-expression, which has led me to reflect on something personal I would like to share with you. As you may have noticed, I have some tattoos that hold particular significance. I have found that my tattoos remind me of essential experiences and values in my life. I share this with you because I believe it is vital for us to foster an environment of openness and authenticity in our therapeutic relationship. However, I want to emphasize that our sessions are about you and your journey. So, if you have any questions or concerns about my tattoos or anything else, please feel free to share them with me. I am here to create a safe and open space to discuss anything that comes up for you.
Thus, the counselor’s tattoo narrative may offer the client freedom to explore repressed aspects of themselves, which, once discovered, may allow for more self-awareness and appreciation, ultimately resulting in better mental health. Counselors can also simply discuss their tattoos with clients who express curiosity or concern. This approach allows the counselor to provide context and meaning behind their tattoos, potentially fostering a deeper connection and understanding between counselor and client.
However, some clients might be disinclined to continue services with an obviously tattooed counselor. As such, counselors may choose to cover their tattoos during sessions, especially if they anticipate that it may distract or discomfort certain clients. This approach can help maintain a professional appearance and minimize potential barriers to therapy. These kinds of tensions may lead to the strategic use of profile photographs on one’s counseling practice’s website. Depending on their client base and target demographics, counselors may opt for photographs that either prominently display or discreetly conceal their tattoos. Prioritizing the client’s comfort and preferences is essential. Counselors should gauge the client’s reactions and adjust their approach accordingly. In sum, the best advice for counselors with tattoos is to rely on their clinical intuition and discretion when deciding how to approach discussions about personal tattoos with clients. As with any counselor disclosure, discussing personal tattoos should be used intentionally with the client’s best interest in mind.
If a client inquires about the advisability of getting tattoos, it is essential to assist them in thoroughly processing this decision, as with any significant life choice. Be open with clients that biases against tattoos persist, with people of color and women being the most stigmatized. Regrettably, many individuals harbor negative perceptions of tattooed people, particularly regarding visible body art and content that might be deemed offensive. Counselors can ask probing questions about the client’s reasoning for obtaining tattoos, such as, “What does getting this tattoo mean to you, and how do you think it will impact your sense of identity or self-expression?” and “Have you considered any potential long-term implications of getting this tattoo, including how you might feel about it in the future or how it might affect your personal or professional life?”
The intersection of tattoos, mental health, and social justice represents a rich and largely unexplored area of research for counselor educators. As the prevalence of tattoos increases among both clients and counselors, we believe this presents a rich opportunity for personal exploration and the discovery of values and strengths, an area currently underexplored in the counseling profession. Future research on tattoos could examine their presence on counselors and clients, their effect on the therapeutic alliance, personality differences among tattooed individuals, and tattooed people’s likelihood of engaging in advocacy work. To advance dialogue and research in this domain, the Western Carolina University counseling program’s faculty, students, and graduates created the Intersection: Art, Mental Health, and Social Justice magazine (Mock et al., 2021). This publication aimed to enhance dialogue and understanding regarding tattoos. Readers are encouraged to peruse the online magazine to explore personal stories of tattooed counselors.
Conclusion
With the increasing popularity and prevalence of tattoos combined with continued cultural bias, body art is an area that warrants further research and discussion in the counseling profession. In summary, there does not appear to be significant relationship between tattooed people experiencing more mental health problems than nontattooed people. However, there is continued bias against tattooed people, and the reasons for obtaining tattoos are rooted more deeply than merely increasing personal attractiveness. As described in the unencumbered self theory of tattoos, the reemergence of tattoo art may be emblematic of the trends seen throughout the counseling profession to advance the discipline from its focus on intra- and interpersonal theories of health and wellness to include broader sociological perspectives on healing. The reemergence of tattoo art, then, could be an allegory for moving beyond the White, male, heteronormative standards that have traditionally dominated the profession, ushering forth an age of inclusivity where the rich and complex tapestry of all people’s values, traditions, and customs can be known and honored.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Aizenman, M., & Jensen, M. A. C. (2007). Speaking through the body: The incidence of self-injury, piercing, and tattooing among college students. Journal of College Counseling, 10(1), 27–43. https://doi.org/10.1002/j.2161-1882.2007.tb00004.x
Alter-Muri, S. (2020). The body as canvas: Motivations, meanings, and therapeutic implications of tattoos. Art Therapy, 37(3), 139–146. https://doi.org/10.1080/07421656.2019.1679545
Al-Twal, A., & Abuhassan, R. (2024). Tattoos and career discrimination in a conservative culture: The case of Jordan. Current Psychology, 43, 11914–11923. https://doi.org/10.1007/s12144-023-05304-7
Atkinson, M. (2002). Pretty in ink: Conformity, resistance, and negotiation in women’s tattooing. Sex Roles, 47, 219–235. https://doi.org/10.1023/A:1021330609522
Baumann, C., Timming, A. R., & Gollan, P. J. (2016). Taboo tattoos? A study of the gendered effects of body art on consumers’ attitudes toward visibly tattooed front line staff. Journal of Retailing and Consumer Services, 29, 31–39. https://doi.org/10.1016/j.jretconser.2015.11.005
Broussard, K. A., & Harton, H. C. (2018). Tattoo or taboo? Tattoo stigma and negative attitudes toward tattooed individuals. The Journal of Social Psychology, 158(5), 521–540. https://doi.org/10.1080/00224545.2017.1373622
Camacho, J., & Brown, W. (2018). The evolution of the tattoo in defiance of the immutable definition of deviance: Current perceptions by law enforcement of tattooed arrestees. Deviant Behavior, 39(8), 1023–1041. https://doi.org/10.1080/01639625.2017.1395669
Carmen, R. A., Guitar, A. E., & Dillon, H. M. (2012). Ultimate answers to proximate questions: The evolutionary motivations behind tattoos and body piercings in popular culture. Review of General Psychology, 16(2), 134–143. https://doi.org/10.1037/a0027908
Covington, B. E. (2015). The sentence continues: Breaking silences and becoming authors through The Semicolon Project [Master’s thesis, James Madison University]. JMU Scholarly Commons. https://commons.lib.jmu.edu/master201019/47
Crompton, L., Amrami, G. P., Tsur, N., & Solomon, Z. (2021). Tattoos in the wake of trauma: Transforming personal stories of suffering into public stories of coping. Deviant Behavior, 42(10), 1242–1255. https://doi.org/10.1080/01639625.2020.1738641
Dance, A. (2019, April 6). How the Samoan tattoo survived colonialism. Scientific American. https://www.scientificamerican.com/article/how-the-samoan-tattoo-survived-colonialism
Day-Vines, N. L., Ammah, B. B., Steen, S., & Arnold, K. M. (2018). Getting comfortable with discomfort: Preparing counselor trainees to broach racial, ethic, and cultural factors with clients during counseling. International Journal for the Advancement of Counselling, 40(2), 89–104. https://doi.org/10.1007/s10447-017-9308-9
Ernst, M., Borkenhagen, A., Fegert, J. M., Brähler, E., & Plener, P. L. (2022). The association of childhood abuse and neglect with tattoos and piercings in the population: Evidence from a representative community survey. BMC Psychology, 10(105), 1–10. https://doi.org/10.1186/s40359-022-00811-x
Grumet, G. W. (1983). Psychodynamic implications of tattoos. American Journal of Orthopsychiatry, 53(3), 482–492. https://doi.org/10.1111/j.1939-0025.1983.tb03392.x
Guéguen, N. (2013). Effects of a tattoo on men’s behavior and attitudes towards women: An experimental field study. Archives of Sexual Behavior, 42(1), 1517–1524. https://doi.org/10.1007/s10508-013-0104-2
Heckerl, A. (2021). I can’t even wear my skin: The experiences visibly tattooed women have for rejecting hegemonic femininity (Publication No. 1099) [Master’s thesis, California State University, Monterey Bay]. Capstone Projects and Master’s Theses. https://digitalcommons.csumb.edu/caps_thes_all/1099
Henle, C. A., Shore, T. H., Murphy, K. R., & Marshall, A. D. (2022). Visible tattoos as a source of employment discrimination among female applicants for a supervisory position. Journal of Business and Psychology, 37, 107–125. https://doi.org/10.1007/s10869-021-09731-w
Jabłońska, K., & Mirucka, B. (2023). Mental body representations of women with tattoos in emerging adulthood—A cluster analysis. Archives of Women’s Mental Health, 26(4), 473–483. https://doi.org/10.1007/s00737-023-01326-z
Karacaoglan, U. (2012). Tattoo and taboo: On the meaning of tattoos in the analytic process. The International Journal of Psychoanalysis, 93(1), 5–28. https://doi.org/10.1111/j.1745-8315.2011.00497.x
Kaufmann, L., & Armstrong, M. L. (2022). The influences of tattoos on health care experiences. The Journal of Continuing Education in Nursing, 53(4), 178–184. http://doi.org/10.3928/00220124-20220311-08
Khair, N. (2022). Marketing of self: Using tattoos to symbolize ownership and control of one’s body. Narratives from Middle Eastern women. Sociology Compass, 16(7), 1–11. https://doi.org/10.1111/soc4.13002
Kidron, C. A. (2012). Breaching the wall of traumatic silence: Holocaust survivor and descendant person–object relations and the material transmission of the genocidal past. Journal of Material Culture, 17(1), 3–21. https://doi.org/10.1177/1359183511432989
Kloẞ, S. T. (2022). Embodying dependency: Caribbean godna (tattoos) as female subordination and resistance. The Journal of Latin American and Caribbean Anthropology, 27(4), 601–612. https://doi.org/10.1111/jlca.12644
Lane, D. C. (2014). Tat’s all folks: An analysis of tattoo literature. Sociology Compass, 8(4), 398–410. https://doi.org/10.1111/soc4.12142
Laumann, A. E., & Derick, A. J. (2006). Tattoos and body piercings in the United States: A national data set. Journal of the American Academy of Dermatology, 55(3), 413–421. https://doi.org/10.1016/j.jaad.2006.03.026
Martone, A. J. (2023). Scars, marks, and tattoos: How appearance influences rearrest and reconviction (Publication No. 31076097) [Master’s thesis, Sam Houston State University]. ProQuest Dissertations and Theses Global.
Miranda, M. D. (2020). Tattoos and tattoo inks: Forensic considerations. WIREs Forensic Science, 2(1), 1–16. https://doi.org/10.1002/wfs2.1360
Mock, C., Jones, B., Gillespie, L., & Curtis, R. (Eds.). (2021). Intersection: Art, mental health, and social justice (Issue No. 1). Western Carolina University. https://online.fliphtml5.com/pdhbe/uinm
Morello, G. (2021). I’ve got you under my skin: Tattoos and religion in three Latin American cities. Social Compass, 68(1), 61–80. https://doi.org/10.1177/0037768620962367
Morello, G., Sanchez, M., Moreno, D., Engelmann, J., & Evangel, A. (2021). Women, tattoos, and religion an exploration into women’s inner life. Religions, 12(7), 517. https://doi.org/10.3390/rel12070517
Mortensen, K., French, M. T., & Timming, A. R. (2019). Are tattoos associated with negative health-related outcomes and risky behaviors? International Journal of Dermatology, 58(7), 816–824. https://doi.org/10.1111/ijd.14372
Naudé, L., Jordaan, J., & Bergh, L. (2019). “My body is my journal, and my tattoos are my story”: South African psychology students’ reflections on tattoo practices. Current Psychology, 38, 177–186. http://doi.org/10.1007/s12144-017-9603-y
O’Brien, E. J., & Epstein, S. (1988). The Multidimensional Self-Esteem Inventory (MSEI): Professional manual. Psychological Assessment Resources, Inc. https://www.parinc.com/products/MSEI#details
Pajor, A. J., Broniarczyk-Dyła, G., & Świtalska, J. (2015). Satisfaction with life, self-esteem and evaluation of mental health in people with tattoos or piercings. Psychiatria Polska, 49(3), 559–573. https://doi.org/10.12740/PP/27266
Rima, D., Aldabergenova, N., Sharipova, A., Atakhanova, G., & Beaver, K. M. (2023). Tattoos as a stigmatizing label implicated in being processed through the criminal justice system. Deviant Behavior, 44(11), 1701–1712. https://doi.org/10.1080/01639625.2023.2230513
Roberts, D. (2016). Using dramaturgy to better understand contemporary Western tattoos. Sociology Compass, 10(9), 795–804. https://doi.org/10.1111/soc4.12400
Roggenkamp, H., Nicholls, A., & Pierre, J. M. (2017). Tattoos as a window to the psyche: How talking about skin art can inform psychiatric practice. World Journal of Psychiatry, 7(3), 148–158. https://doi.org/10.5498/wjp.v7.i3.148
Rohith, M. M., Belcher, W. R., Roy, J., Abraham, S. O., Chakraborty, P., Nandaniya, N. J., & Johnson, A. (2020). Tattoo in forensic science: An Indian perspective. Journal of Forensic and Legal Medicine, 74, 1–10. https://doi.org/10.1016/j.jflm.2020.102022
Schmid, S. (2013). Tattoos – An historical essay. Travel Medicine and Infectious Disease, 11(6), 444–447. https://doi.org/10.1016/j.tmaid.2013.10.013
Shuaib, S. O. (2020). African traditional body art and contemporary realities. International Journal of Humanitatis Theoreticus, 3(1), 127–140. https://bit.ly/Shuaib_bodyart
Sims, J. P. (2018). “It represents me”: Tattooing mixed-race identity. Sociological Spectrum, 38(4), 243–255. https://doi.org/10.1080/02732173.2018.1478351
Solanke, I. (2017). Discrimination as stigma: A theory of anti-discrimination law. Bloomsbury.
Solís-Bravo, M. A., Flores-Rodríguez, Y., Tapia-Guillen, L. G., Gatica-Hernández, A., Guzmán-Reséndiz, M., Salinas-Torres, L. A., Vargas-Rizo, T. L., & Albores-Gallo, L. (2019). Are tattoos an indicator of severity of non-suicidal self-injury behavior in adolescents? Psychiatry Investigation, 16(7), 504–512.
https://doi.org/10.30773/pi.2019.03.06
Southern Poverty Law Center. (2006, October 19). A look at racist skinhead symbols and tattoos. The Intelligence Report. https://www.splcenter.org/fighting-hate/intelligence-report/2006/look-racist-skinhead-symbols-and-tattoos
Stein, A. (2011). The tattooed therapist: Exposure, disclosure, transference. Psychoanalysis, Culture & Society, 16, 113–131. https://doi.org/10.1057/pcs.2010.17
Stephenson, L., & Byard, R. W. (2019). Cause, manner and age of death in a series of decedents with tattoos presenting for medicolegal autopsy. Journal of Forensic and Legal Medicine, 64(1), 49–51. https://doi.org/10.1016/j.jflm.2019.04.003
Tan, L. (2013). Intellectual property law and the globalization of indigenous cultural expressions: Māori tattoo and the Whitmill versus Warner Bros. case. Theory, Culture & Society, 30(3), 61–81. https://doi.org/10.1177/0263276412474328
Tate, J. C., & Shelton, B. L. (2008). Personality correlates of tattooing and body piercing in a college sample: The kids are alright. Personality and Individual Differences, 45(4), 281–285. https://doi.org/10.1016/j.paid.2008.04.011
The Holy Bible: New International Version. (1978). The Zondervan Corporation.
The Qur’an (M. A. S. Abdel Haleem, Trans.). (2004). Oxford University Press.
Thomas, N., Cole, A., & Douglas, B. (Eds.). (2005). Tattoo: Bodies, art and exchange in the Pacific and the West. Reaktion Books.
Vegrichtová, B. (2018). Nonverbal communication of prison subculture through criminal tattoo symbols. Academic and Applied Research in Military and Public Management Science, 17(3), 179–186. https://doi.org/10.32565/aarms.2018.3.13
Williams, D. J., Thomas, J., & Christensen, C. (2014). “You need to cover your tattoos!”: Reconsidering standards of professional appearance in social work. Social Work, 59(4), 373–375. https://doi.org/10.1093/sw/swu025
Wohlrab, S., Stahl, J., & Kappeler, P. M. (2007). Modifying the body: Motivations for getting tattooed and pierced. Body Image, 4(1), 87–95. https://doi.org/10.1016/j.bodyim.2006.12.001
Zestcott, C. A., Tompkins, T. L., Kozak Williams, M., Livesay, K., & Chan, K. L. (2018). What do you think about ink? An examination of implicit and explicit attitudes toward tattooed individuals. The Journal of Social Psychology, 158(1), 7–22. https://doi.org/10.1080/00224545.2017.1297286
Zidenberg, A. M., Dutrisac, S., & Olver, M. (2022). “No ragrets”: Public perception of tattooed mental health professionals. Professional Psychology: Research and Practice, 53(3), 304–312. https://doi.org/10.1037/pro0000441
Zuckerman, A. (2020, May 13). 38 tattoo statistics: 2020/2021 industry, trends & demographics. Compare Camp. https://comparecamp.com/tattoo-statistics/
Russ Curtis, PhD, LCMHC, is a professor at Western Carolina University. Lisen C. Roberts, PhD, is an associate professor at Western Carolina University. Paul Stonehouse, PhD, is an assistant professor at Western Carolina University. Melodie H. Frick, PhD, NCC, ACS, LPC-S, is a professor at Western Carolina University. Correspondence may be addressed to Russ Curtis, Western Carolina University, 28 Schenck Parkway, Office 214, Asheville, NC 28803, curtis@wcu.edu.
Jan 17, 2024 | Volume 13 - Issue 4
Sunanda M. Sharma, Jennifer E. Bianchini, Zeynep L. Cakmak, MaryRose Kaplan, Muninder K. Ahluwalia
According to the American Counseling Association and the Council for Accreditation of Counseling and Related Educational Programs, social justice advocacy is an ethical imperative for counselors and a training standard for counseling students. As a group of socially conscious mental health counseling students and faculty, we developed and facilitated a social justice advocacy group to learn about tangible ways to engage in social justice action. Using the S-Quad model developed by Toporek and Ahluwalia, we formed and facilitated a social justice advocacy group for our peers. This paper will serve as a reflection of our experiences engaging in the process.
Keywords: social justice, advocacy, counseling students, S-Quad model, mental health
When describing the motivation for her political aspirations, Georgia gubernatorial hopeful Stacey Abrams (2019) stated, “We have to have people who understand that social justice belongs to us all.” This quote speaks to this group of authors who feel strongly about the importance of social justice in mental health counseling. This ethos served as the motivation to create a peer-led group to foster the development of our social justice advocacy skills. We used the S-Quad model (Toporek & Ahluwalia, 2020) to form and facilitate a social justice advocacy group for master’s and doctoral counseling students at our institution.
Historically, the counseling profession has been rooted in social justice advocacy (SJA) with Frank Parsons’s efforts to support White European immigrants in the United States to develop their vocational goals (Gummere, 1988; Toporek & Daniels, 2018). However, SJA has not been consistently operationalized across counselor training programs (Counselors for Social Justice [CSJ], 2020). Although ethical standards established by the American Counseling Association’s ACA Code of Ethics (ACA; 2014) encourage counselors to advocate for clients and communities when appropriate (A.7.a, A.7.b.), and training standards established by the Council for Accreditation of Counseling and Related Educational Programs (CACREP; 2015) state that SJA should be a part of counseling curriculum (2.F.2.b.), counselors have reported receiving little guidance about how to implement advocacy in practice (Field et al., 2019; Ratts & Greenleaf, 2018). As counseling students, we experienced the same concern. To address this gap in our educational experience, we created and facilitated a group based on the S-Quad model (strengths, solidarity, strategies, and sustainability) of SJA (Toporek & Ahluwalia, 2020). As a group of socially conscious mental health counseling students, our aim was to grow in our roles as professionals by learning about, teaching, and engaging in SJA. In the process, we learned about ourselves as budding counselors and educators.
Literature Review
In their foundational article, Vera and Speight (2003) called on the counseling profession to expand its understanding of multicultural competence; they asserted that without SJA, counselors are perpetuating the systems of oppression from which their clients are attempting to heal. Utilizing intrapsychic approaches which neglect to account for contextual factors not only perpetuates oppressive counseling practices, but it also does a disservice to those with marginalized identities (Ratts, 2009; Vera & Speight, 2003). In order to properly serve clients, counselors must step beyond the classroom, expand the original conceptualization of our roles, and explore beyond the counseling office (Ratts, 2009; Ratts & Greenleaf, 2018; Vera & Speight, 2003). Despite the increase in available resources such as the ACA Advocacy Competencies (Toporek et al., 2009) and the Multicultural and Social Justice Counseling Competencies (MSJCC; Ratts et al., 2016), the number of sociocultural forces such as racial demographics of counseling programs and reliance on theories and interventions developed for White European clients prevents social justice from being a central force in the profession (CSJ, 2020).
As mental health professionals, we are positioned to understand the impact that oppression has on health (Nadal et al., 2021), which speaks to the need for operationalizing social justice counseling and SJA so counselors may support client wellness. Counseling students require more knowledge and practice to obtain appropriate resources and tools in order to intervene and resist systemic oppression (Vera & Speight, 2003). Ratts (2009) named social justice as the “fifth force” in counseling in an attempt to concretize the relevance and importance of challenging the status quo in counseling. However, the perceived attitude of the counseling profession toward social justice is reflected in the definition of counseling. The 20/20 initiative was a movement to unify the profession and solidify professional identity by arriving at the definition of counseling. Delegates from 31 counseling-related organizations (e.g., CACREP, Chi Sigma Iota) participated in a Delphi-method study to achieve consensus on a definition; however, only 29 organizations ultimately endorsed the definition (Kaplan et al., 2014). Although the definition for counseling includes the word “empower”; it does not include the words “social justice” or “advocacy.” Thus, CSJ was one organization that did not support the new definition (Kaplan et al., 2014). Despite these challenges, Ratts and Greenleaf (2018) assert that counselors must develop the advocate part of their identity, yet they note that there is more of a focus on traditional counseling skills rather than acknowledging the shifting sociopolitical climate and equipping counselors with the skills to address these concerns. The leadership and advocacy course (or the content in another course; CACREP, 2023) in CACREP-accredited counseling doctoral programs often only focuses on leadership and advocacy within and for the profession. Although CACREP (2023) standards do not dictate the courses a counseling program must offer, there continues to be limited discussion of SJA and social justice, nor are there solid instructional methods for counselor educators to use in the classroom (Chapman-Hilliard & Parker, 2022). This situation hinders students’ understanding of the role systemic issues have on minoritized communities, further deterring people in those communities from seeking help.
As counselors and counseling students, we understand our responsibility to advocate for clients, but we feel unprepared to fulfill our ethical (and for many of us, moral) duty. We did not learn enough about the concrete, tangible skills that a professional counselor can utilize to challenge oppression and inequity. We were unable to locate any studies regarding peer-led SJA groups for counseling students, thus we hope to contribute something novel to the counseling literature and encourage counseling students to better understand and grow into their roles as social justice advocates. Counselors-in-training (CITs) and practicing counselors within the profession sometimes question the relevance of SJA and report feeling confused about how to implement SJA in counseling (Field et al., 2019; Ratts & Greenleaf, 2018). hooks (1994) notes it is imperative that a student accepts responsibility for their education and becomes “an active participant, not a passive consumer” (p. 14). Thus, we engaged in this process to support our colleagues in the counseling student body and take accountability for our education.
Taking Action: Social Justice Advocacy Group
Leading organizations in the profession claim a two-pronged approach to advocacy: one prong advocating for the legitimacy of the counseling profession, and the other advocating on behalf of the clients and students whom counselors serve (Chang et al., 2012). In our educational experience, SJA on behalf of and in partnership with clients was emphasized, but tangible interventions were not discussed. Further, systemic issues and inequities were often left unaddressed. Thus, we developed this group to more concretely address the second “prong” of advocacy in counseling. First and fourth authors Sunanda M. Sharma and MaryRose Kaplan were part of the executive board of Chi Sigma Mu (Chi Sigma Iota chapter at Montclair State University) and co-founded the social justice committee. Second and third authors Jennifer E. Bianchini and Zeynep L. Cakmak were the first members of the committee who proposed ideas and facilitated events and activities related to social justice that they felt passionately about. Bianchini proposed a social justice book club ahead of a presentation that the CSI chapter organized (hosting the authors of the book Taking Action). The book club met three times with up to three students, from whom we received feedback to help us form the SJA group.
The following semester, fifth author Muninder K. Ahluwalia proposed restructuring the book club into an advocacy group by utilizing the Taking Action text as a framework to teach students about systemic SJA. CACREP (2015) standards state that multiculturalism and social justice must be discussed throughout counseling courses (2.F.2.b.); however, in our experiences, we found that social justice is addressed as an ethical and moral imperative, but curricula do not address concrete SJA skills and strategies to combat systemic oppression. The counseling program in which the first four authors are enrolled and the fifth author is a faculty member offers a social justice counseling class as an elective. However, the class is not consistently offered every semester and has only been taught by that one faculty member. Thus, our aim with this group was to provide a space for our colleagues in which we could collaboratively learn about how to enact social justice. This section will describe the S-Quad model, explain the group structure, outline the proposed learning objectives, and provide a table that outlines the curriculum of the group.
The S-Quad Framework
As a profession, mental health counseling is positioned to “buffer” against challenges with oppression and changes to the status quo (Kivel, 2020). There is an emphasis on intrapsychic interventions to combat systemic issues, rather than attempt to uproot the oppression itself (Kivel, 2020; Ratts, 2009; Toporek, 2018). Toporek (2018) noted that upon reflection of the way the profession is positioned and her privileged identities, she developed a framework through which to take social justice action despite the challenges she continues to encounter. The S-Quad model includes four Ss for social justice advocates to formulate a way to address systemic injustices: strengths, solidarity, strategy, and sustainability (Toporek & Ahluwalia, 2020).
Strengths are described as a combination of one’s existing “skills, knowledge, and expertise” (Toporek & Ahluwalia, 2020, p. 27). Although strengths can be qualities one already has, both personal and professional, the authors also encourage budding advocates to reflect upon strengths that they would like to develop. Solidarity has multiple facets to its definition, as advocates are asked to support, honor, and respect communities they intend to engage with and to also seek support from their personal networks to remain grounded (Toporek & Ahluwalia, 2020). Solidarity is enacted through collaborative efforts and through the lens of cultural humility (Toporek & Ahluwalia, 2020). Strategy is the implementation of strengths and solidarity to construct a plan of action (Toporek & Ahluwalia, 2020). It is important to evaluate the efficacy, efficiency, and impact of different strategic plans to ensure they work toward the stated goal and—most importantly—benefit the community that the action is intended for (Toporek & Ahluwalia, 2020). Finally, a unique facet of the S-Quad model is the fourth “S,” sustainability. Sustainability addresses the wellness of advocates; without it, there is a higher likelihood they may abandon their efforts. SJA can be an enriching and healing practice, but it can also be an emotionally draining pursuit, and one can feel helpless when attempting to combat the gravity and breadth of oppression (Toporek & Ahluwalia, 2020). Thus, the authors encourage budding advocates to take an inventory of the practices that replenish and nourish them in order to remain engaged in their work.
Group Structure
Sharma proposed structuring this SJA group as a biweekly, one-hour, peer-led, open (students were free to join at any point) psychoeducation group, whose grounding framework would be the S-Quad model (Toporek & Ahluwalia, 2020). Due to COVID-19 restrictions, we facilitated the group through Zoom. The objectives of the group were: to describe all components of the S-Quad model, to describe the ethical responsibility of being a social justice advocate, to create a solidarity network of fellow advocates, to increase awareness of how one’s positionality impacts their advocacy work, and to apply the S-Quad model (Toporek, 2018) through the creation of a social justice action plan (Sheely-Moore & Kooyman, 2011). Initially, the intention was to divide each group session into two parts. The first part of the session would be didactic, in which we would discuss the “S” of that week and ground it in a case study. The second half of the session would offer members the chance to process the content so they can apply what they are learning to their social justice plan. Upon reflection and discussion as co-facilitators, we recognized the challenges associated with attempting to address so much content in a 60-minute session and collectively agreed to shift the group and make it akin to a flipped classroom by including pre-recorded didactic videos. This afforded members the chance to view the videos at their own pace and come to the session prepared to engage in dialogue.
In our experiences, instructors who taught our counseling theories courses recommended for us to select one theory to learn about before declaring our theoretical orientation. Similarly, we asked members to narrow down their focus for the purposes of this group to a cause within a community that they feel passionately about. The other structural component we addressed with group members was that this curriculum is cumulative but not necessarily linear; so, an application of the previous “S” is necessary to study the following “S.” For example, once a group member identifies their strengths, we apply those strengths to inform what strategies they will use, but it does not necessarily mean that strengths are not revisited.
Given that this was a psychoeducation group rather than a traditional course, we did not want to use typical didactic methods to engage with this material. We intentionally paired each part of the S-Quad model with a story about an advocate from a minoritized community of whom others likely may not be aware. This demonstrated that SJA is not always done on a public stage. This narrative form of teaching (Hannam et al., 2015) allowed us to contextualize stories of advocates who are quietly resisting oppression in their respective communities. We spotlighted those stories so members could feel less intimidated by the prospect of SJA. In the interest of social justice and accessibility, the Chi Sigma Iota Counseling Honor Society’s Chi Sigma Mu chapter at Montclair State University funded books for interested members so they could follow along with the activities and didactic content. After the second session, we also introduced the idea of the social justice action plan. Table 1 shows the structure/syllabus of the group that we utilized for the semester and describes the ways in which we adapted to agreed-upon changes.
Table 1
Taking Action Group Structure
| Week |
Topic & Activity Assigned |
Content/Activities |
| Week 1 |
Introducing
Taking Action
S-Quad Model |
• Purpose, rationale, and structure of group
• Group agreements/norms
• Overview of S-Quad model (Toporek & Ahluwalia, 2020)
• ADDRESSING model (Hays, 2022), a framework that explores individual identity in context
• Difference between justice, charity, philanthropy |
| Week 2 |
1st S: Strengths
Activity 4.2, p. 29**
|
• Reviewing agreed-upon group norms
• Defining strengths
• Case study: Arunachalam Muruganantham (“The Pad Man”)
Processing case study as a group
• Introducing the social action plan |
| Week 3 |
Co-facilitators reflection meeting |
• This session was initially planned to address the 2nd S in the S-Quad, but no members attended the group this day. Instead, as co-facilitators, we met to discuss the progress of the group.
|
| Week 4* |
2nd S: Solidarity
Activity 5.1, p. 55 |
• Defining solidarity
• Case study: 4 young Black women, Black Lives Matter protests
Combining strengths and solidarity
Processing case study as a group |
| Week 5 |
3rd S:
Strategy
Activity 6.1, p. 66 |
• Defining strategy
• Case study: Cakmak
Strength, solidarity, and strategy
Processing case study as a group
Cakmak’s social action plan |
| Week 6 |
4th S:
Sustainability
Activity 7.6, p. 176
|
• Defining sustainability
• Case study: Alexandria Ocasio Cortez
Strength, solidarity, strategy, and sustainability
Processing the importance and guilt of self-care
Processing burnout |
| Week 7 |
Final Group
|
• Case study
Apply ADDRESSING, S-Quad model
• Feedback from members |
*Marks shift to videos for the didactic portion
**All activities listed are from Ahluwalia & Toporek (2020).
Reflections
In this section, we offer our reflections on the group and extract salient collective themes that have come about through our processing. In our first session, we informed the group members that we intended to write a reflection paper, and they gave implicit consent to this writing; we did not collect data from group members for the purposes of this article. We begin by grounding the discussion of the group by acknowledging our positionality and social location and how that influenced how we approached our facilitation and planning of the group. Sharma, Bianchini, and Cakmak will provide their most salient takeaways from the forming and facilitation of the Taking Action group.
Positionality
Sharma identifies as a cisgender, South Asian (Indian), middle-class, able-bodied woman who is a doctoral candidate in a CACREP-accredited counseling program and a full-time lecturer in a CACREP-accredited counseling program. I bring a bicultural perspective to my counseling practice and education, and I have attended primarily White institutions (PWIs) for most of my life. As a master’s and doctoral National Board for Certified Counselors Minority Fellowship Program fellow, I learned about the importance and practice of SJA. I am a practicing clinician in private practice (working mostly with White clients), and I engage in advocacy work with South Asian intimate partner violence survivors.
Bianchini identifies as a White, cisgender woman who grew up in a predominantly White community in the United States. My family has lived in the United States for several generations and the majority of my extended family identifies as part of the middle class. I do not have any disabilities and am a practicing Christian. I am a master’s-level graduate student and joined Chi Sigma Iota’s social justice committee in my first semester of coursework.
Cakmak identifies as a Muslim American, cisgender woman of Turkish origin. I do not have any physical disabilities, but I have been diagnosed with general anxiety disorder (GAD) and major depressive disorder (MDD). I identified as part of the upper middle class in Turkey as a child, and I am middle class as an immigrant in the United States. I have two graduate degrees, one in literature and one in counseling. I have done volunteer work with underrepresented religious and cultural communities since I was in high school.
Themes
As cocreators and coauthors, we reflected on our collective and individual experiences of facilitating our Taking Action group. We each completed individual reflection sheets within 48 hours of each group session to capture our takeaways, and we processed our experiences together after each group session. We reviewed our reflection sheets individually and noted themes that arose for each of us. We then collectively reviewed the sheets to determine what themes arose across our reflection sheets. We reengaged in the reflection process as we wrote this manuscript. In this section, we highlight the major themes among our experiences.
Fear
The most significant theme of our collective experience was fear. Throughout each session, fear came up under several different guises, which served as an umbrella for additional themes: judgment, self-efficacy, and humility. Fear was the main antagonist preventing us from doing social justice work before this program. Fear of not knowing the necessary information, fear of saying or doing the wrong thing, and fear of not helping enough or adequately were examples of how this feeling manifested. However, engaging in this group helped us alleviate that fear through resources, support, and a plan of action. In the first session, we felt tentative and timid, and optimistic yet stagnant. After providing members with more information and concrete steps to create real social justice action, our fear dissipated, our passion for working as a group was ignited, and the motivation to take action began.
Judgment
In our first session, when we engaged members in a dialogue about group agreements, we noticed that there was more focus on the importance of the group serving as a judgment-free space than as a confidential one. We felt that members wanted to feel safe in the group because they feared being judged due to their self-perceived incompetence. We recognized they did not want to feel judged by others if their ideas were deemed unacceptable or incorrect. Establishing a nonjudgmental space permitted members to try, even if the outcomes were not as they hoped. We believe it allowed members to have a safe space to begin processing what they understand about SJA.
Judgment was a recurrent theme and shifted from self-judgment to judging others. Members reported feeling frustrated and upset when their peers in the program were not at the same level of advocacy awareness and action as they were. They reported feeling angry about others’ ignorance. Through a shared reflection on these feelings, the group acknowledged that the judgment of others reinforces the barriers to change that we are trying to knock down. Members recognized the importance of being humble regarding other people (another theme discussed below) and empathetic to help manage feelings of judgment.
When discussing sustainability and self-care, members and facilitators shared our hesitations to implement sustainability practices, despite it being an ethical responsibility. This hesitancy revealed itself to be motivated by self-judgment of our productivity levels. It appeared that the group members would not allow themselves the breaks they needed to provide self-care because of the importance they gave to SJA. We then discussed the need to be unapologetic in our self-care as advocates and counselors.
Self-Efficacy
Related to judgment of self and others, we found self-efficacy was another significant and recurrent theme. Almost every group member expressed that they were struggling to feel like they could contribute enough to society to perform real social justice action rather than charity. Having members share similar insecurities resulted in an insightful and vulnerable conversation that helped us to feel connected and inspired. In the second session, members reported experiencing imposter syndrome, likely resulting from their low self-efficacy in social justice work. Our self-efficacy grew throughout the sessions as members received the information and tools they needed to take concrete steps in SJA. Once we clarified a reasonable idea of what was expected of them and had some direction, they felt more prepared to take action.
Humility
Lastly, the theme of humility appeared in several different iterations. The humility through humor with which we, as facilitators, approached this process helped break the ice and create a comfortable atmosphere in our initial meeting. Humility emerged in our second session when discussing the first “S” of the S-Quad model, strengths. In our reflection process, we noted that both facilitators and members appeared to be uncomfortable when sharing what they are “good” at. We, as female-identifying co-facilitators, noted the societal pressure and shame that have historically come with feelings of discomfort for behavior commonly regarded as boastful.
In the fourth session, the group discussed the importance of humility within their community. Members discussed how it was easy to humble oneself when trying to assist a community from the outside, but that it was an important lesson that we must be humble within our own communities. Members seemed to realize that their experience of their community and identity would not be the same as the next person’s, highlighting the importance of intersectionality within the human experience.
Humility was next discussed in the fifth session in terms of failure. Members acknowledged the importance of possessing humility and patience regarding our work because we will generally fail more than we will succeed in our efforts to create change. If we never failed, we would never learn from our mistakes and there would be no more SJA to do. However, knowing this instills the hope to persevere, for you never know what your planted seeds of action will grow into.
Combining Themes
As facilitators, we noticed a parallel between what we were experiencing and our members’ experiences. From the start of our group, we felt we needed to be more qualified to be teachers of SJA. This was our campus’s first peer-led advocacy group, which meant we did not have any models to reference, and we had to rely on our own ideas, skills, and judgment. With faculty support, we went outside the confines of our curriculum because we wanted to share and engage with this content in a meaningful way. This was a large undertaking, with little training and even less confidence. Similar to what we observed in our members, we were afraid of making mistakes in the content, direction, and discussion of this group because of the weight of the topic of social justice—especially as the first group any of us attempted to create or lead. We had to adapt to constantly developing circumstances, and this felt inappropriate for us as leaders. Something we recognized much later was that we could teach and learn simultaneously; we did not need to reach a point of expertise before developing this group. Although we do not consider ourselves experts in SJA, the work we did to prepare for each session, combined with the humility with which we presented ourselves and our work, effectively allowed us to lead the group to the best of our ability.
Another source of our fear was that there was an ulterior motivation for creating this group, which was not purely social justice–oriented. We sought a sense of community, particularly given the isolating COVID-19 pandemic we were living through, and running this group gave us that community, support, and friendship. This longing for connection played into our feelings of being unqualified to do social justice work because a few of us became involved in this project out of a desire to work with friends, and not solely because we wanted to devote ourselves to social justice. However, this search for connection and participation in this SJA group gave us a passion for this work if it was not present beforehand. That feeling of connection and belonging provided us with the inner power to attempt something bigger than ourselves. The bond we authors created while facilitating this group instilled the importance of collaboration, especially when doing something new, significant, and daunting. The “S” for solidarity was also particularly salient in this case; we recognize that we could not have created or run this group alone. We needed each other to not only complete all the work required but also to hold each other accountable, support each other in times of need, and encourage each other to keep going even when our hopes dimmed. In a sense, this group and the connection to each other provided the “S” for sustainability and wellness for ourselves and our work.
While reflecting on these two sources of our fear as facilitators, we discovered our desire to make this call to the counseling profession: to strengthen the bridge between academia and counseling in practice. Applying the knowledge gained from our courses to daily practice could be less intimidating and feel more like the natural progression of our nascent counseling careers. However, once the opportunity arose to test our skills, we felt hesitant and unprepared. Creating an advocacy group is not the only venue in which this fear of practice appears. As students, we authors felt a similar fear when stepping into our practicum and internship sites. It is natural to feel afraid when seeing clients for the first time as CITs, but this fear could be lessened by academic leaders guiding students into the field before their final year of studies. If more opportunities to work with real issues affecting communities were available to students and supported by faculty, the transition between the classroom and fieldwork would feel less daunting.
Discussion
Although this project was not an empirical study, our reflective process taught us about how it feels to learn about SJA and the labor required to teach about SJA. With this knowledge, we have identified potential implications for the counseling profession and counselor education training programs. We also acknowledge the limitations of the group we formed and facilitated.
Implications
Per our experience, we believe social justice counseling—and advocacy skills more specifically—must have a more prominent place in counseling curricula. Potential solutions may include consistently operationalizing social justice counseling and SJA in counselor training programs (CSJ, 2020). Furthermore, it is imperative to have more guidance from our institutional standards such as CACREP (2023) and to have more ethical standards regarding SJA in the next iteration of the ACA Code of Ethics. CACREP (2023) requirements establish content that should be covered throughout all coursework, rather than specific classes; however, each program might have a different approach to operationalize these standards because they are vaguely defined (Austin & Austin, 2020). For example, in the current CACREP (2023) standards, there is more frequent mention of social justice compared to the 2016 CACREP standards; however, there is still ambiguity about how this may present in a counseling course. Standard 3.B.1 (CACREP, 2023) says that counseling curricula must state how “theories and models of multicultural counseling, social justice, and advocacy” are addressed, but there is no mention of techniques, interventions, or skills for SJA. As a point of comparison, there are specific guidelines with respect to content like group counseling which delineate time that students must spend engaged in direct experience. However, it appears that social justice and SJA are still referred to in broader terms with fewer contingencies about how they must be addressed. We recognize that out-of-class work like advocacy might be left out of the curriculum because there are many required courses and training standards filling up students’ time in graduate school (Vera & Speight, 2003). However, we urge counseling leaders to consider the importance of SJA and the core role it plays in our healing work and our counseling identity.
Limitations and Future Directions
This group was developed and facilitated to encourage counseling students to develop their social justice advocate identity, but it was not an empirical study, and our collective reflections can only offer so much insight to facilitating such groups in the future. As this was an extracurricular group for which attendees took time out of their personal schedules, we do not know what motivated our peers to attend sessions that we offered. This would be important knowledge to address in future offerings of this group and to understand students’ attitudes toward social justice in counseling. Another limitation of our group was our inability to reach students who are unsure of what social justice is and might not recognize it as an inherent and imperative part of mental health counseling. Practicum and other service-learning opportunities for SJA within the profession have been explored in the literature (Farrell et al., 2020; Field et al., 2019; Langellier et al., 2020), but perhaps peer encouragement can help CITs to feel more confident as advocates. Although we intentionally kept the group open for accessibility, new introductions and catching up took time away from the group plan and content. We do not have data to explicate a group like this, but we hope our master’s and doctoral peers feel encouraged to start similar groups within their own programs. Finally, we wrote this article more than a year after our group ended; although we relied on our reflection sheets and notes from our experience, we are aware that there may be gaps in our recollections.
For future groups, we would be interested to complete an empirical study through an IRB in order to collect data regarding peer-led SJA groups. Screening or surveys before and after the group could not only provide valuable data, but also offer guidance for attendees even before the group starts and an opportunity for reflection after the group ends. Our decision to keep our group open led to attrition of members; thus, empirical studies might also investigate factors that contribute to student engagement. Collecting quantitative and qualitative data may provide further insight into effective strategies for describing and encouraging students to engage in concrete SJA skill development.
Conclusion
The experience of facilitating an SJA group was new, challenging, transformative, and important to our growth as CITs and budding counselor educators. As counselors, we understand our ethical duty to engage in SJA; however, we have not had adequate training in tangible strategies to utilize when advocating on behalf of our clients. The S-Quad model is an important guide that helped facilitate our understanding of how to implement SJA as mental health professionals. As co-facilitators and coauthors, we learned a great deal about ourselves as developing social justice advocates, CEs, and CITs and confronted fears parallel to those of the group members. Although SJA is a growing focus in the counseling literature, there is a great deal of research and training that must continue to occur so current and future counselors can develop their social justice advocate identities.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Abrams, S. (2019, January). 3 questions to ask yourself about everything you do [Video]. TED Talks. https://www.youtube.com/watch?v=3zJHwOwirjA
American Counseling Association. (2014). ACA code of ethics. https://www.counseling.org/docs/default-source/default-document-library/2014-code-of-ethics-finaladdress.pdf?sfvrsn=96b532c_8
Austin, J. T., II, & Austin, J. A. (2020). The counselor educator’s guide: Practical in-class strategies and activities. Springer.
Chang, C. Y., Barrio Minton, C. A., Dixon, A. L., Myers, J. E., & Sweeney, T. J. (Eds.). (2012). Professional counseling excellence through leadership and advocacy (1st ed.). Routledge.
Chapman-Hilliard, C., & Parker, B. (2022). Embodied social justice learning: Considerations for curriculum development and training in counseling programs. Journal for Social Action in Counseling and Psychology, 14(1), 77–93. https://doi.org/10.33043/JSACP.14.1.77-93
Council for Accreditation of Counseling and Related Educational Programs. (2015). 2016 CACREP standards. https://www.cacrep.org/wp-content/uploads/2017/08/2016-Standards-with-citations.pdf
Council for Accreditation of Counseling and Related Educational Programs. (2023). 2024 CACREP standards. https://www.cacrep.org/wp-content/uploads/2023/06/2024-Standards-Combined-Version-6.27.23.pdf
Counselors for Social Justice. (2020). A call for social justice in the American Counseling Association (ACA). Journal for Social Action in Counseling and Psychology, 12(1), 2–12. https://doi.org/10.33043/JSACP.12.1.2-12
Farrell, I. C., DeDiego, A. C., & Marshall, R. C. (2020). Service learning to foster advocacy training in CACREP accredited programs. Journal of Creativity in Mental Health, 15(4), 522–534. https://doi.org/10.1080/15401383.2020.1733724
Field, T. A., Ghoston, M. R., Grimes, T. O., Sturm, D. C., Kaur, M., Aninditya, A., & Toomey, M. (2019). Trainee counselor development of social justice counseling competencies. Journal for Social Action in Counseling and Psychology, 11(1), 33–50. https://doi.org/10.33043/JSACP.11.1.33-50
Gummere, R. M., Jr. (1988). The counselor as prophet: Frank Parsons, 1854–1908. Journal of Counseling & Development, 66(9), 402–405. https://doi.org/10.1002/j.1556-6676.1988.tb00899.x
Hannam, F. D. (2015). Teaching through narrative. Forum on Public Policy Online, 2015(2).
Hays, P. A. (2022). Addressing cultural complexities in counseling and clinical practice: An intersectional approach (4th ed.). American Psychological Association.
hooks, b. (1994). Teaching to transgress: Education as the practice of freedom. Routledge.
Kaplan, D. M., Tarvydas, V. M., & Gladding, S. T. (2014). 20/20: A vision for the future of counseling: The new consensus definition of counseling. Journal of Counseling & Development, 92(3), 366–372. https://doi.org/10.1002/j.1556-6676.2014.00164.x
Kivel, P. (2020). Social service or social change? Who benefits from your work. https://paulkivel.com/wp-content/uploads/2011/07/Social-Service-or-Social-Change-2020-Update.pdf
Langellier, K. A., Astramovich, R. L., & Horn, E. A. D. (2020). Infusing service learning into the counselor education curriculum. The Professional Counselor, 10(2), 194–203. https://doi.org/10.15241/kal.10.2.194
Nadal, K. L., King, R., Sissoko, D. R. G., Floyd, N., & Hines, D. (2021). The legacies of systemic and internalized oppression: Experiences of microaggressions, imposter phenomenon, and stereotype threat on historically marginalized groups. New Ideas in Psychology, 63, 1–9. https://doi.org/10.1016/j.newideapsych.2021.100895
Ratts, M. J. (2009). Social justice counseling: Toward the development of a fifth force among counseling paradigms. The Journal of Humanistic Counseling, Education and Development, 48(2), 160–172.
https://doi.org/10.1002/j.2161-1939.2009.tb00076.x
Ratts, M. J., & Greenleaf, A. T. (2018). Counselor–advocate–scholar model: Changing the dominant discourse in counseling. Journal of Multicultural Counseling and Development, 46(2), 78–96. https://doi.org/10.1002/jmcd.12094
Ratts, M. J., Singh, A. A., Nassar-McMillan, S., Butler, S. K, & McCullough, J. R. (2016). Multicultural and social justice counseling competencies: Guidelines for the counseling profession. Journal of Multicultural Counseling and Development, 44(1), 28–48. https://doi.org/10.1002/jmcd.12035
Sheely-Moore, A. I., & Kooyman, L. (2011). Infusing multicultural and social justice competencies within counseling practice: A guide for trainers. Adultspan Journal, 10(2), 102–109. https://doi.org/10.1002/j.2161-0029.2011.tb00129.x
Toporek, R. L. (2018). Strength, solidarity, strategy and sustainability: A counseling psychologist’s guide to social action. The European Journal of Counselling Psychology, 7(1), 90–110. https://doi.org/10.5964/ejcop.v7i1.153
Toporek, R. L., & Ahluwalia, M. K. (2020). Taking action: Creating social change through strength, solidarity, strategy and sustainability. Cognella.
Toporek, R. L., & Daniels, J. (2018). American Counseling Association advocacy competencies (updated 2018). American Counseling Association. https://www.counseling.org/docs/default-source/competencies/aca-advocacy-competencies-updated-may-2020.pdf
Toporek, R. L., Lewis, J. A., & Crethar, H. C. (2009). Promoting systemic change through the ACA advocacy competencies. Journal of Counseling & Development, 87(3), 260–268. https://doi.org/10.1002/j.1556-6678.2009.tb00105.x
Vera, E. M., & Speight, S. L. (2003). Multicultural competence, social justice, and counseling psychology: Expanding our roles. The Counseling Psychologist, 31(3), 253–272. https://doi.org/10.1177/0011000003031003001
Sunanda M. Sharma, MS, NCC, LPC (NJ), LPCC (OH), is a lecturer at Wright State University. Jennifer E. Bianchini, BFA, is a master’s student at Montclair State University. Zeynep L. Cakmak, MA, LAC (NJ), is a mental health counselor at Montclair State University. MaryRose Kaplan, PhD, NCC, LPC, is a school counselor and adjunct professor at Montclair State University. Muninder K. Ahluwalia, PhD, is a professor at Montclair State University. Correspondence may be addressed to Sunanda M. Sharma, 3640 Colonel Glenn Hwy., Millett Hall 370, Dayton, OH 45435, sharmas1@montclair.edu.
Oct 31, 2023 | Volume 13 - Issue 3
Wesley B. Webber, W. Leigh Atherton, Kelli S. Russell, Hilary J. Flint, Stephen J. Leierer
The COVID-19 pandemic and efforts to manage it have affected mental health around the world. Although early research on the COVID-19 pandemic showed a general decline in mental health after the pandemic began, mental health in later stages of the pandemic might be improving alongside other changes (e.g., availability of vaccines, return to in-person activities). The present study utilized data from a mental health service intervention for individuals at a southeastern university who were exposed to COVID-19 following the university’s return to in-person operations. This study tested whether time period (August–September 2021 vs. January–February 2022) predicted individuals’ likelihood of being mild or above in depression and anxiety ratings. Results showed that individuals were more likely to be mild or above in both depression and anxiety ratings during August–September of 2021 than January–February of 2022. Suggestions for future research and implications for professional counselors are discussed.
Keywords: COVID-19, mental health, depression, anxiety, university
The novel coronavirus (COVID-19), first detected in 2019, spread globally at a rapid pace, with the first confirmed case in the United States occurring on January 20, 2020, in the state of Washington (Centers for Disease Control and Prevention [CDC], 2023). By April 2020, the United States had the most reported deaths in the world due to COVID-19. It was not until December of 2020 that the first round of vaccines, authorized under emergency use authorization, was made available (Food and Drug Administration [FDA], 2021). As of October 2022 in the United States, a total of 97,063,357 cases of COVID-19 had been reported, from which there were 1,065,152 COVID-19–related deaths (CDC, 2023). A reported 111,367,843 individuals aged 5 and above in the United States had received their first booster dose of a COVID-19 vaccine as of October 2022 (CDC, 2023). Previous research has shown that the COVID-19 pandemic and efforts to manage it (e.g., lockdowns, quarantine, isolation) had negative effects on mental health in the United States and internationally (Huckins et al., 2020; Pierce et al., 2020; Son et al., 2020). Based on the extended duration of the pandemic and changes that have occurred during it (e.g., vaccine availability, lessening of initial social restrictions), more recent research has investigated possible changes in mental health in later stages of the COVID-19 pandemic (Fioravanti et al., 2022; McLeish et al., 2022; Tang et al., 2022). The present study adds to this literature by exploring whether psychosocial symptomatology (i.e., depression and anxiety) at a university in the Southeastern United States differed in individuals exposed to COVID-19 during August–September 2021 as compared to individuals exposed to COVID-19 during January–February 2022 (following the university’s return to on-campus operations in August 2021).
Challenges to Mental Health During the COVID-19 Pandemic
Since the beginning of the COVID-19 pandemic, conceptual and empirical research has focused on ways in which the pandemic and associated stressors might impact mental health (Bzdok & Dunbar, 2020; Marroquín et al., 2020; Şimşir et al., 2022). Implementation of lockdowns to deter spread of the virus led to concerns that social isolation might have severe impacts on mental health (Bzdok & Dunbar, 2020). This hypothesis was empirically supported, as stay-at-home orders and individuals’ reported levels of social distancing were positively associated with depression and anxiety (Marroquín et al., 2020). Individuals’ views on the COVID-19 pandemic evolved quickly at the outset of the pandemic, and perceptions of risk were shown to increase during the pandemic’s first week in the United States (Wise et al., 2020). Growing awareness of the dangers of the virus likely had deleterious effects on mental health; Şimşir et al. (2022) found through a meta-analysis that fear of COVID-19 was associated with a variety of mental health problems. Mental health was also negatively affected by stigmatization associated with the COVID-19 pandemic, as was the case for those exposed to COVID-19 while at their place of work (Schubert et al., 2021). Such stigmatization associated with COVID-19 exposure was found to increase risk for depression and anxiety (Schubert et al., 2021).
The lockdowns and social distancing measures that accompanied early stages of the COVID-19 pandemic also resulted in changes to routines that likely impacted mental health. For some individuals facing lockdowns or other disruptions to typical routines, reductions in physical activity occurred. Individuals who reported greater impact of COVID-19 on their level of physical activity showed greater symptoms of depression and anxiety (Silva et al., 2022). Early in the COVID-19 pandemic, based on people’s increased time spent at home and their concerns about COVID-19 developments, some people increased their media usage (e.g., news outlets, social media). Such increases in media usage were associated with decreases in mental health (Meyer et al., 2020; Riehm et al., 2020). The COVID-19 pandemic had less significant impact on mental health for those with greater tolerance of uncertainty (Rettie & Daniels, 2021) and psychological flexibility (Dawson & Golijani-Moghaddam, 2020). Thus, some individuals were uniquely suited to face the many changes and stressors brought about by the COVID-19 pandemic.
One population that previous research has identified as being especially at risk for negative mental health outcomes during the COVID-19 pandemic is college students (Xiong et al., 2020). For college students, the COVID-19 pandemic occurred alongside other stressors known to be typical for this population such as adjusting to leaving home, navigating new peer groups, and making career decisions (Beiter et al., 2015; Liu et al., 2019). Thus, for many college students, the COVID-19 pandemic disrupted a period of life already filled with many transitions. For example, shortly after the COVID-19 pandemic began, many college students were forced to leave their dormitories and peers as universities transitioned to online delivery of classes (Copeland et al., 2021). Xiong et al. (2020) found through a systematic review that college students were especially vulnerable to negative mental health outcomes at the outset of the COVID-19 pandemic as compared to others in the general population. In the United States, college students’ reported degree of life disruption due to the COVID-19 pandemic was positively associated with depression at the conclusion of the spring 2020 semester (Stamatis et al., 2022). During fall 2020, COVID-19 concerns and previous COVID-19 infection were each found to be associated with higher levels of depression and anxiety among U.S. college students (Oh et al., 2021). Overall, previous research has supported the notion that changes associated with the COVID-19 pandemic had general negative effects on mental health in the general population and in college students specifically.
Changes in Psychosocial Symptomatology Across the COVID-19 Pandemic
Although research has shown that the COVID-19 pandemic introduced unprecedented challenges and stressors that were associated with mental health problems, another important direction for research has been to characterize overall changes in psychosocial symptomatology as the COVID-19 pandemic progressed. Such research is important given that individuals might psychologically adapt to constant COVID-19 stressors or might benefit from changes that have occurred as the COVID-19 pandemic has progressed (e.g., vaccine availability, lessening of societal restrictions). Initial longitudinal studies comparing individuals’ symptomatology before the COVID-19 pandemic and after its beginning showed that mental health deteriorated after the COVID-19 pandemic began (Elmer et al., 2020; Huckins et al., 2020; Pierce et al., 2020). Prati and Mancini (2021) conducted a meta-analysis of 28 studies that used longitudinal or natural experimental designs and found that depression and anxiety showed small but statistically significant increases after implementation of the initial lockdowns in response to COVID-19. The various changes to ways of life associated with the COVID-19 pandemic appeared to result in a general deterioration in mental health.
Previous research has also explored possible changes in mental health beyond those that were observed in the initial phase of the COVID-19 pandemic. In support of the notion that individuals adapted to changes associated with the COVID-19 pandemic, Fancourt et al. (2021) found that anxiety and depression decreased across the initial lockdown period in the United Kingdom. In contrast, Ozamiz-Etxebarria et al. (2020) found that levels of depression and anxiety were higher 3 weeks into the initial lockdown period in Spain as compared to the beginning of the lockdown. Fioravanti et al. (2022) assessed psychological symptoms longitudinally in an Italian sample at three time points—the beginning of the COVID-19 pandemic and first lockdown (March 2020), the end of the first lockdown phase (May 2020), and during a second wave of COVID-19 with increased societal restrictions (November 2020). Their findings pointed to possible influences of COVID-19 waves and societal restrictions on specific psychosocial symptoms. Specifically, depression, anxiety, obsessive-compulsive disorder, and post-traumatic stress disorder all decreased at the end of the first lockdown phase (Fioravanti et al., 2022). However, all symptoms besides obsessive-compulsive disorder significantly increased from the end of the first lockdown phase to the second wave of COVID-19 (Fioravanti et al., 2022).
Recent research on mental health among college students in later stages of the COVID-19 pandemic has also focused on possible mental health changes over time (McLeish et al., 2022; Tang et al., 2022). Tang et al. (2022) reported reductions in anxiety and depression in a longitudinal study of university students in the United Kingdom between a first time point (July–September 2020, after the end of lockdown) and a second time point (January–March 2021, when vaccinations were becoming available). In contrast, McLeish et al. (2022) found through a repeated cross-sectional study that depression and anxiety among students at a specific university increased from spring 2020 to fall 2020, with the increases being maintained in spring 2021. The authors noted that vaccines were not widely available at the university until the end of spring 2021 (McLeish et al., 2022). Thus, recent studies have found mixed results as to whether psychosocial symptomatology improved over time during the COVID-19 pandemic. These discrepancies may be due to contextual differences between studies (e.g., differences in data collection time periods, availability of vaccines, or levels of COVID-19 restrictions being implemented during data collection).
The Present Study
The present study was conducted based on the need for continued research on mental health across the evolving COVID-19 pandemic and based on previous conflicting findings on possible mental health changes in later stages of the COVID-19 pandemic. Given previous research showing detrimental effects of the COVID-19 pandemic on mental health in the general population and in college students, the present study utilized data from a university population. Specifically, an archival dataset was used in the present study to examine data collected during 2021–2022 at a university in the Southeastern United States and to test whether time period would predict severity of depression and anxiety symptoms. Individuals in the study had been exposed to COVID-19 between August–September 2021 or between January–February 2022 and had requested a mental health contact during university-conducted contact tracing. These two time periods corresponded to surges in COVID-19 cases at the university due to the delta and omicron COVID-19 variants, respectively. August–September 2021 also coincided with a return to on-campus operations at the university and therefore captured psychosocial symptomatology at the beginning of a significant transition in the COVID-19 pandemic (i.e., a return to organized in-person activities on a college campus during the evolving pandemic). This study was designed to answer the following research questions:
- Among those requesting mental health contact after COVID-19 exposure, was the likelihood of having at least mild depression symptoms different for those whose contact occurred between August–September 2021 as compared to those whose contact occurred between January–February 2022?
- Among those requesting mental health contact after COVID-19 exposure, was the likelihood of having at least mild anxiety symptoms different for those whose contact occurred between August–September 2021 as compared to those whose contact occurred between January–February 2022?
Method
Design
A retrospective research design was used to analyze the possible effect of time period on severity of depression and anxiety symptoms among members of a university population who had been exposed to COVID-19 and requested a mental health check-in. The study used a de-identified dataset obtained from the service providers who completed the mental health check-in. We confirmed through consultation with the IRB that the use of archival, de-identified data does not necessitate IRB review.
COVID-19 Mental Health Check-In Dataset
The archival, de-identified dataset used in the present study was compiled as part of a mental health service occurring between February 2021 and February 2022. Participants in the dataset had tested positive for COVID-19 or been exposed to COVID-19 without a positive test. During university-conducted contact tracing, they were offered and elected to receive a subsequent mental health check-in. Individuals who were contact traced and thereby offered a mental health check-in had become known to contact tracers through one of two routes: (a) they reported their own COVID-19 diagnosis or exposure through a self-reporting mechanism as instructed by the university, or (b) they were reported by another individual as having been diagnosed with or exposed to COVID-19. The dataset used in this study included data collected during the mental health check-ins for those who elected to receive them. This data was collected over the phone and documented in RedCap (a secure web browser–based survey protocol designed for clinical research) at the time of the phone call or within 24 hours. The dataset consisted of data for 211 individuals’ check-ins. For each check-in, the dataset included participants’ demographic information, screening data (for depression, anxiety, and trauma), identified needs of the participant, resources shared with the participant, and the date of data entry.
The present study focused on check-in data for all individuals from the COVID-19 Mental Health Check-in Dataset whose check-in had occurred during one of the two time periods of focus—August–September 2021 or January–February 2022. These two time periods corresponded to surges in COVID-19 cases at the university associated with the delta and omicron COVID-19 variants, respectively. The 149 individuals who checked in during these 4 months represented 70.62% of the total number of check-ins over the 12-month dataset (N = 211), reflecting the surges in COVID-19 cases during these two periods. Of the 149 individuals in the present study, 96 (64.43%) received their check-in during August–September 2021, and 53 (35.57%) received their check-in during January–February 2022. The selection of these two time periods from the larger dataset allowed for comparison of psychosocial symptomatology during comparable levels of COVID-19 infection (i.e., surges associated with two subsequent COVID-19 variants) at comparable points in subsequent academic semesters (i.e., the first 2 months of the fall 2021 and spring 2022 semesters). The present study used only the screening data for depression and anxiety, as the scales for each of these constructs showed good internal consistency (Cronbach’s alpha > .80).
Participants
The sample in the present study consisted of 149 individuals. The selected individuals’ ages ranged from 17 to 52 (M = 22.21, SD = 7.43). With regard to gender, 67.11% identified as female, 32.21% as male, and 0.67% as non-binary. The reported races of individuals in the study were as follows: 60.4% White, 20.13% African American, 6.71% Hispanic, 3.36% Other, 2.68% Two or more races, 1.34% Middle Eastern, 1.34% Native American, and 0.67% Asian. Some participants preferred not to indicate their race (3.36%). In responding to a question about their ethnicity, 87.25% of individuals identified as not Latinx, 9.40% identified as Latinx, and 3.36% preferred not to answer. With regard to academic level/job title, 32.89% were freshmen, 20.13% were sophomores, 14.09% were juniors, 15.44% were seniors, 7.38% were graduate students, 8.05% were faculty/staff, and 2.01% preferred not to answer. Regarding employment, 53.69% were not employed (including students), 30.20% were employed part-time, 12.75% were employed full-time, and 3.36% preferred not to answer. The relationship statuses of individuals were reported as the following: 87.92% single (never married), 4.7% married, 2.01% single but cohabitating with a significant other, 1.34% in a domestic partnership or civil union, 1.34% separated, 0.67% divorced, and 2.01% preferred not to answer. Table 1 summarizes demographic responses within each of the two time periods and for the full sample.
Measures
Demographic Questionnaire
Participants responded to seven demographic questions (age, gender, race, ethnicity, academic year/job title, current employment status, and relationship status). They were informed that this information was optional and that they could choose not to answer particular questions.
Table 1
Demographic Characteristics of the Sample
|
Demographic
Characteristic |
|
| August–September 2021 |
January–February 2022 |
Full Sample |
|
n |
% |
n |
% |
n |
% |
| Gender |
|
|
|
|
|
|
| Female |
69 |
71.88 |
31 |
58.49 |
100 |
67.11 |
| Male |
27 |
28.13 |
21 |
39.62 |
48 |
32.21 |
| Non-binary |
0 |
0 |
1 |
1.89 |
1 |
0.67 |
| Race |
|
|
|
|
|
|
| White |
56 |
58.33 |
34 |
64.15 |
90 |
60.40 |
| African American |
23 |
23.96 |
7 |
13.21 |
30 |
20.13 |
| Hispanic |
8 |
8.33 |
2 |
3.77 |
10 |
6.71 |
| Other race |
1 |
1.04 |
4 |
7.55 |
5 |
3.36 |
| Two or more races |
4 |
4.17 |
0 |
0 |
4 |
2.68 |
| Middle Eastern |
2 |
2.08 |
0 |
0 |
2 |
1.34 |
| Native American |
1 |
1.04 |
1 |
1.89 |
2 |
1.34 |
| Asian |
1 |
1.04 |
0 |
0 |
1 |
0.67 |
| Prefer not to answer |
0 |
0 |
5 |
9.43 |
5 |
3.36 |
| Ethnicity |
|
|
|
|
|
|
| Not Latinx |
82 |
85.42 |
48 |
90.57 |
130 |
87.25 |
| Latinx |
12 |
12.50 |
2 |
3.77 |
14 |
9.40 |
| Prefer not to answer |
2 |
2.08 |
3 |
5.66 |
5 |
3.36 |
| Academic Year / Job Title |
|
|
|
|
|
|
| Freshman |
38 |
39.58 |
11 |
20.75 |
49 |
32.89 |
| Sophomore |
18 |
18.75 |
12 |
22.64 |
30 |
20.13 |
| Junior |
15 |
15.63 |
6 |
11.32 |
21 |
14.09 |
| Senior |
15 |
15.63 |
8 |
15.09 |
23 |
15.44 |
| Graduate Student |
6 |
6.25 |
5 |
9.43 |
11 |
7.38 |
| Faculty/Staff |
4 |
4.17 |
8 |
15.09 |
12 |
8.05 |
| Prefer not to answer |
0 |
0 |
3 |
5.66 |
3 |
2.01 |
| Employment |
|
|
|
|
|
|
| Not Employed (including student) |
62 |
64.58 |
18 |
33.96 |
80 |
53.69 |
| Employed Part-Time |
26 |
27.08 |
19 |
35.85 |
45 |
30.20 |
| Employed Full-Time |
8 |
8.33 |
11 |
20.75 |
19 |
12.75 |
| Prefer not to answer |
0 |
0 |
5 |
9.43 |
5 |
3.36 |
| Relationship Status |
|
|
|
|
|
|
| Single, never married |
87 |
90.63 |
44 |
83.02 |
131 |
87.92 |
| Married |
3 |
3.13 |
4 |
7.55 |
7 |
4.70 |
| Single, but cohabitating with a
significant other |
2 |
2.08 |
1 |
1.89 |
3 |
2.01 |
| In a domestic partnership or civil union |
2 |
2.08 |
0 |
0 |
2 |
1.34 |
| Separated |
2 |
2.08 |
0 |
0 |
2 |
1.34 |
| Divorced |
0 |
0 |
1 |
1.89 |
1 |
0.67 |
| Prefer not to answer |
0 |
0 |
3 |
5.66 |
3 |
2.01 |
| Note. Average age was 21.51 (SD = 6.98) in August–September 2021 group, 23.49 (SD = 8.11) in January–February 2022 group, and 22.21 (SD = 7.43) in the full sample. |
Patient Health Questionnaire-9 (PHQ-9)
The Patient Health Questionnaire-9 (PHQ-9; Kroenke et al., 2001) is a 9-item self-report questionnaire that measures the frequency and severity of depression symptoms over the past 2 weeks. The PHQ-9 has been validated for screening for depression in the general population (Kroenke et al., 2001; Martin et al., 2006). The questionnaire measures frequency of symptoms such as “feeling down, depressed, or hopeless,” and “little interest or pleasure in doing things.” The PHQ-9 uses a 4-point Likert scale to measure frequency of symptoms over the past 2 weeks with the response options of not at all, several days, more than half the days, and nearly every day. Scores of 0, 1, 2, and 3 are assigned to each of the four response categories, and a PHQ-9 total score is derived by adding the scores for each of the nine PHQ-9 items. Minimal depression is indicated by PHQ-9 total scores of 0–4, mild depression by scores of 5–9, moderate depression by scores of 10–14, moderately severe depression by scores of 15–19, and severe depression by scores of 20–27. Question 9 on the PHQ-9 is a single screening question assessing suicide risk. Interviewers were trained in appropriate protocol in the event of a positive screen for this question. Cronbach’s alpha for the PHQ-9 in the present study was .86.
Generalized Anxiety Disorder 7-Item Scale (GAD-7)
The Generalized Anxiety Disorder 7-Item Scale (GAD-7; Spitzer et al., 2006) is a 7-item self-report anxiety questionnaire that measures the frequency and severity of anxiety symptoms over the past 2 weeks. The GAD-7 has demonstrated reliability and validity as a measure of anxiety in the general population (Löwe et al., 2008). The questionnaire measures symptoms such as “feeling nervous, anxious, or on edge,” and “not being able to stop or control worrying.” The format of the GAD-7 is similar to the PHQ-9, using a 4-point Likert scale to measure frequency of symptoms over the past 2 weeks with response options of not at all, several days, more than half the days, and nearly every day. GAD-7 scores are calculated by assigning scores of 0, 1, 2, and 3 for response categories and then adding the scores from the 7 items to derive a total score ranging from 0 to 21. Minimal anxiety is indicated by total scores of 0–4, mild anxiety by scores of 5–9, moderate anxiety by scores of 10–14, and severe anxiety by scores of 15– 21. Cronbach’s alpha for the GAD-7 in the present study was .86.
Analytic Strategy
Total scores for the PHQ-9 and GAD-7 were found to be positively skewed for both groups of participants. Binary logistic regression was therefore an appropriate method of analysis for this dataset, as binary logistic regression does not require normality of dependent variables (Tabachnick & Fidell, 2019). For two separate binary logistic regression models, individuals were classified as being either minimal or mild or above in depression (PHQ-9) and anxiety (GAD-7) to create binary outcome variables. This choice of cutoff allowed each model (with time period as predictor) to satisfy the recommendation of Peduzzi et al. (1996) that there be at least 10 cases per outcome per predictor in binary logistic regression.
Prior to performing these intended primary analyses to answer the research questions, preliminary analyses were conducted to determine whether adding control variables to the logistic regression models was warranted. Chi-square tests of independence, Fisher-Freeman-Halton Exact tests, Fisher’s Exact tests, and an independent samples t-test were used to test for possible differences between the two time periods in individuals’ responses to demographic questions. In cases in which responses to demographic questions were shown to be significantly different across the two groups, appropriate tests were used to determine whether the demographic responses in question were associated with either of the two intended dependent variables.
Following the preliminary analyses, the intended two binary logistic regressions were conducted to answer the research questions. In the first binary logistic regression, time period was the predictor
(1 = August–September 2021, 0 = January–February 2022) and PHQ-9 depression category was the outcome (1 = mild or above, 0 = minimal). In the second logistic regression, time period was the predictor (1 = August–September 2021, 0 = January–February 2022) and GAD-7 anxiety category was the outcome (1 = mild or above, 0 = minimal). All analyses were conducted using SPSS Version 28.
Results
Preliminary Demographic Analyses
Prior to the primary analyses, preliminary analyses were conducted to determine whether the two groups differed in their responses to demographic questions. Fisher-Freeman-Halton Exact tests and an independent samples t-test were used to test for differences between groups in their responses to the seven demographic questions. Two of the seven tests were statistically significant at Bonferroni-corrected alpha level. Specifically, Fisher-Freeman-Halton Exact tests found significant differences between time periods on the race (p = .004) and employment (p < .001) demographic variables.
Based on the above significant results for the race and employment variables across the time periods, 2 x 2 tests were conducted to test for differences between specific race responses and specific employment responses across the two time periods. For these 2 x 2 tests, a chi-square test of independence was used when all expected cell counts were 5 or greater and Fisher’s Exact test was used when any expected cell counts were less than 5. To follow up the significant result for race, 2 x 2 tests were conducted for all pairs of race responses in which 2 x 2 tests were possible (i.e., in which there was at least one observation for each of the two race responses at both time periods). These follow-up 2 x 2 tests of responses to the race question across time periods found no statistically significant differences between pairs of race responses across time periods using Bonferroni-corrected alpha level. Follow-up 2 x 2 tests comparing all pairs of responses to the employment question across time periods found two statistically significant differences using Bonferroni-corrected alpha level. A chi-square test of independence showed that individuals were more likely to be employed full-time during January–February 2022 than August–September 2021 as compared to those not employed (including students), X2 (1, N = 99) = 9.29, p = .002. Fisher’s Exact test showed that individuals were more likely to indicate “prefer not to answer” during January–February 2022 than during August–September 2021 as compared to those indicating “not employed (including students),” p = .001.
The statistically significant tests for race and employment across time periods were followed up with additional tests to determine if depression or anxiety category (minimal vs. mild or above for each) was associated with individuals’ responses to the relevant race and employment questions. A Fisher-Freeman-Halton Exact test showed that depression category was not associated with individuals’ responses to the race question, p = .099. A Fisher-Freeman-Halton Exact test also showed that individuals’ anxiety category was not associated with individuals’ responses to the race question,
p = .386. With regard to employment, tests of association were conducted between the intended dependent variables and the specific employment responses that were found to differ between the two groups. A chi-square test of independence showed that individuals’ status as “not employed” vs. “employed full-time” was not associated with depression category, X2 (1, N = 99) = .63, p = .429. A chi-square test of independence also showed that these employment statuses were not associated with anxiety category, X2 (1, N = 99) = .27, p = .601. Similarly, Fisher’s Exact tests showed that individuals’ employment responses of “prefer not to answer” vs. “not employed (including students)” were not associated with depression category (p = .156) or anxiety category (p = .317). These results were interpreted as indicating that the ways in which individuals in the two time periods differed demographically did not have significant impact on the study’s dependent variables of interest. Therefore, binary logistic regressions were conducted with only time period as a predictor of each dependent variable.
Relationship Between Time Period and Severity of Depression Symptoms
Most individuals in the study were in the minimal depression range on the PHQ-9 as compared to the other four categories. Figure 1 shows the percentage of individuals falling into each of the five PHQ-9 categories during each of the two time periods.
Figure 1
Percentages of Individuals Falling Into Each of the PHQ-9 Categories for Each of the Two Time Periods
Across both time periods combined (August–September 2021 and January–February 2022), 51 individuals (34.23%) were mild or above in depression while 98 (65.77%) were in the minimal range. Binary logistic regression was used to test whether time period predicted severity of depression symptoms. Time period was entered as a predictor (1 = August–September 2021, 0 = January–February 2022) of depression (1 = mild or above, 0 = minimal depression). The overall binary logistic regression model was found to be statistically significant, χ2(1) = 14.46, p < .001, Cox & Snell R2 = .092, Nagelkerke R2 = .128. In the model, time period was found to be a significant predictor of depression, Wald χ2(1) = 12.17, B = 1.52, SE = .44, p < .001. The model estimated that the odds of being mild or above in depression were 4.56 times higher during August–September 2021 than during January–February 2022 for individuals requesting a mental health check-in following COVID-19 exposure. Specifically, the predicted odds of being mild or above in depression were .81 during August–September 2021 and .18 during January–February 2022.
Relationship Between Time Period and Severity of Anxiety Symptoms
Most individuals in the study were in the minimal anxiety range on the GAD-7 as compared to the other three categories. Figure 2 shows the percentage of individuals falling into each of the four GAD-7 categories during each of the two time periods.
Figure 2
Percentages of Individuals Falling Into Each of the GAD-7 Categories for Each of the Two Time Periods
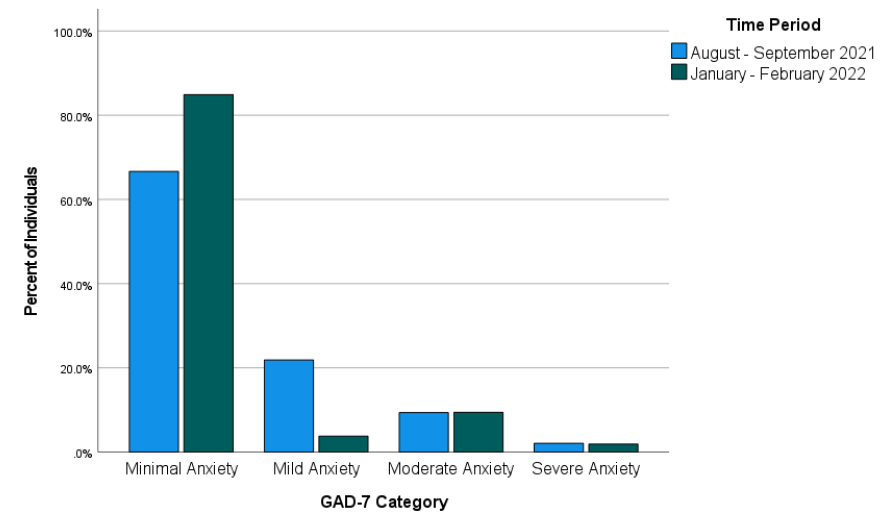
Across both time periods combined, 40 individuals (26.85%) reported anxiety at levels of mild or above and 109 individuals (73.15%) reported minimal anxiety. Binary logistic regression was used to test whether time period predicted severity of anxiety symptoms. Time period was entered as a predictor (1 = August–September 2021, 0 = January–February 2022) of anxiety (1 = mild or above, 0 = minimal anxiety). The overall binary logistic regression model was statistically significant, χ2(1) = 6.16, p = .013, Cox & Snell R2 = .041, Nagelkerke R2 = .059. In the model, time period was a significant predictor of anxiety, Wald χ2(1) = 5.51, B = 1.03, SE = .44, p = .019. Odds of being mild or above in anxiety were estimated by the model to be 2.81 times higher during August–September 2021 than during January–February 2022 for individuals requesting a mental health check-in after exposure to COVID-19. Specifically, the predicted odds of being mild or above in anxiety were .50 during August–September 2021 and .18 during January–February 2022.
Discussion
This study examined whether time period would predict severity of depression and anxiety symptoms in a sample of individuals exposed to COVID-19 at a university in the Southeastern United States. More specifically, the study addressed the possibility that the likelihood of being mild or above in depression and anxiety would differ between two time periods following the university’s return to in-person operations in August 2021. The results of the study showed that the likelihood of being mild or above in depression and the likelihood of being mild or above in anxiety after exposure to COVID-19 were both higher during August–September 2021 than during January–February 2022. This finding is in line with previous research that found improvements in psychosocial symptomatology in later stages of the COVID-19 pandemic (Tang et al., 2022) and in contrast to research that did not find such improvements (McLeish et al., 2022). Based on the results of the present study, it appears likely that factors that differed between the two assessed time periods (first two months of fall 2021 vs. first two months of spring 2022) contributed to the observed difference in likelihood of depression and anxiety symptoms. McLeish et al. (2022) noted that vaccines were not widely available in their study that did not find such differences, while Tang et al. (2022), who did find significant differences, noted that vaccines were available at their second data collection point (January–March 2021). For individuals in the present study, COVID-19 vaccinations were available. Vaccination was strongly encouraged by university administrators following the return to campus, and more individuals on campus were vaccinated in spring 2022 than in fall 2021. Vaccinations might have lessened individuals’ COVID-19 concerns and contributed to more positive psychosocial outcomes during spring 2022 than fall 2021.
Besides vaccinations possibly lessening depression and anxiety symptoms, other environmental circumstances might also have played a role. The two time periods on which this study focused also differed in their proximity to a significant environmental event—a return to in-person operations on the campus where the individuals studied and/or worked. Early research on the mental health impact of COVID-19 highlighted the negative mental health effects of factors such as reduced physical activity (Silva et al., 2022), life disruptions due to the COVID-19 pandemic (Stamatis et al., 2022), and social distancing (Marroquín et al., 2020). Therefore, it is possible that symptoms of depression and anxiety in spring 2022 were affected by changes in specific circumstances known to have negatively impacted mental health earlier in the COVID-19 pandemic. For example, individuals’ physical activity likely increased because of a return to campus, and they might have perceived less disruption to their lives through being able to resume in-person activities. Although individuals in the present study who were exposed to COVID-19 during the first 2 months after the return to campus might have reaped some benefits from the return to more normal environmental circumstances, they might also have faced a period of adjustment. In contrast, individuals exposed to COVID-19 between January and February 2022 might have been more readjusted and reaped greater benefits from the return to campus, thereby reducing depression and anxiety symptoms.
Implications
This study’s findings on psychosocial symptomatology across time during the COVID-19 pandemic have important implications for the work of counselors. Based on the results of the present study, counselors planning outreach efforts to individuals exposed to COVID-19 should consider that as time passes, these individuals might be more stable with regard to symptoms of depression and anxiety. However, some individuals directly affected by COVID-19 might still be interested in receiving mental health information despite low levels of depression and anxiety. Many individuals in the present study scored as minimal in depression and anxiety but were still interested in receiving a mental health check-in. Thus, counselors should advocate for mental health information and resources to be made available to individuals who are known to be facing stressors related to COVID-19. Counselors should be prepared to have conversations to determine the contextual needs of individuals exposed to COVID-19 rather than relying only on standardized measures of psychosocial symptomatology. For example, counselors working with employees (such as university employees in the present study) should be attentive to the possibility that employees exposed to COVID-19 may be concerned about facing stigma in their workplace due to their exposure (Schubert et al., 2021).
Given that the present study focused on individuals from a university population, the study’s results also have specific implications for college counselors. College counselors should develop approaches to reach students during circumstances that might make traditional outreach challenging. For example, the present study used data from a mental health intervention in which service providers collaborated with university contact tracers to safely provide mental health resources by telephone to individuals exposed to COVID-19. College counselors should be prepared to connect clients with services at a distance. Previous research during the COVID-19 pandemic found that college students were interested in using teletherapy and online self-help resources, particularly if such services were made available for free (Ahuvia et al., 2022).
Besides preparing for flexible modes of service delivery, college counselors should be prepared to deliver interventions most likely to be useful to college students during the COVID-19 pandemic or similar pandemics. Those recently exposed to COVID-19 might benefit from discussing possible fears associated with COVID-19, experiences of stigmatization they might have experienced due to their exposure, and ways to maintain mental health during any period of quarantine or isolation that might be required. Those not recently exposed to COVID-19 might instead benefit from interventions that address other issues that might have resulted from the COVID-19 pandemic or societal responses to it. For example, if circumstances associated with the COVID-19 pandemic led to reductions in a client’s amount of exercise, a counselor can help the client identify ways they might increase their physical activity. Interventions promoting physical activity were found to reduce anxiety and depression in college students during the COVID-19 pandemic (Luo et al., 2022).
Limitations
This study had limitations that should be considered. First, with the study being retrospective and using secondary data from a clinical intervention, it was not possible to include measures that might have better clarified mechanisms of the changes that were observed in psychosocial symptoms. Thus, the possible explanations above of what might have driven these changes are tentative and future research should test them more directly. Second, individuals in the present study were likely to have been in greater distress than the general university population based on their exposure to COVID-19, which might limit the generalizability of the study’s findings. Third, individuals in the present study were from a single university in the Southeastern United States. Thus, our findings might not generalize to other regions where university-related COVID-19 policies might have differed. Fourth, the decision to create a binary independent variable to reflect time periods (August–September 2021 and January–February 2022) in the present study also entails a limitation. This decision was justifiable on the basis that it allowed for comparisons of individuals at similar points in academic semesters and during comparable periods of COVID-19 infection. However, this analysis decision means that inferences from the study’s results are limited to the two specific time periods that were analyzed. Fifth, individuals in the present study responded to items on the GAD-7 and PHQ-9 through a phone conversation with interviewers. Interviewer-administered surveys have been previously associated with greater tendencies toward socially desirable responses than self-administered surveys (Bowling, 2005). This might limit the present study’s generalizability in contexts where self-administrations of the GAD-7 and PHQ-9 are used.
Future Research
The results of this study provide important directions for future research. Future researchers who can conduct prospective studies or who have access to larger retrospective datasets should aim to determine specific factors that might lead to improvement in mental health outcomes over time during the COVID-19 pandemic. Knowledge produced by such studies could contribute to clinical applications in the future regarding COVID-19 or other pandemics that might occur. Relatedly, future research with larger samples of demographically diverse participants should explore possible demographic differences in specific mental health trajectories in later stages of the COVID-19 pandemic.
Future research should continue to focus specifically on those who are interested in mental health information and interventions during the COVID-19 pandemic. To follow up this study’s findings, future quantitative and qualitative studies should aim to identify which individuals are interested in receiving mental health services and determine the best ways to deliver services to them. As a globally experienced stressor, the COVID-19 pandemic might have changed some individuals’ views of mental health and/or their receptiveness to mental health outreach. More specifically, some might be more receptive to available mental health information even at lower thresholds of anxiety, depression, or other psychosocial symptoms. Such clients might be interested in preventive services or their interest in mental health information might be driven by other factors. Future studies should address these possibilities more directly than was possible in the present retrospective study.
Conclusion
Overall, the present study provided a positive picture regarding psychosocial symptomatology in later stages of the COVID-19 pandemic. Results from this study of students and employees at a university in the Southeastern Unites States following their return to campus found that many individuals requesting mental health information after exposure to COVID-19 showed minimal levels of depression and anxiety. Individuals in the study were more likely to be in these minimal ranges during January–February 2022 than August–September 2021. COVID-19 will continue to have effects in individuals’ lives through future infections and potentially through lasting effects of previous stages of the COVID-19 pandemic. As organized in-person activities resume and COVID-19 infections continue, counseling researchers and practitioners should continue efforts to best characterize and address individuals’ mental health needs associated with the COVID-19 pandemic.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
Ahuvia, I. L., Sung, J. Y., Dobias, M. L., Nelson, B. D., Richmond, L. L., London, B., & Schleider, J. L. (2022). College student interest in teletherapy and self-guided mental health supports during the COVID-19 pandemic. Journal of American College Health. Advance online publication.
https://doi.org/10.1080/07448481.2022.2062245
Beiter, R., Nash, R., McCrady, M., Rhoades, D., Linscomb, M., Clarahan, M., & Sammut, S. (2015). The prevalence and correlates of depression, anxiety, and stress in a sample of college students. Journal of Affective Disorders, 173, 90–96. https://doi.org/10.1016/j.jad.2014.10.054
Bowling, A. (2005). Mode of questionnaire administration can have serious effects on data quality. Journal of Public Health, 27(3), 281–291. https://doi.org/10.1093/pubmed/fdi031
Bzdok, D., & Dunbar, R. I. M. (2020). The neurobiology of social distance. Trends in Cognitive Sciences, 24(9), 717–733. https://doi.org/10.1016/j.tics.2020.05.016
Centers for Disease Control and Prevention. (2023, March 15). COVID-19 timeline. https://www.cdc.gov/museum/timeline/covid19.html
Copeland, W. E., McGinnis, E., Bai, Y., Adams, Z., Nardone, H., Devadanam, V., Rettew, J., & Hudziak, J. J. (2021). Impact of COVID-19 pandemic on college student mental health and wellness. Journal of the American Academy of Child & Adolescent Psychiatry, 60(1), 134–141.e2. https://doi.org/10.1016/j.jaac.2020.08.466
Dawson, D. L., & Golijani-Moghaddam, N. (2020). COVID-19: Psychological flexibility, coping, mental health, and wellbeing in the UK during the pandemic. Journal of Contextual Behavioral Science, 17, 126–134.
https://doi.org/10.1016/j.jcbs.2020.07.010
Elmer, T., Mepham, K., & Stadtfeld, C. (2020). Students under lockdown: Comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS ONE, 15(7), Article e0236337. https://doi.org/10.1371/journal.pone.0236337
Fancourt, D., Steptoe, A., & Bu, F. (2021). Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: A longitudinal observational study. The Lancet Psychiatry, 8(2), 141–149. https://doi.org/10.1016/S2215-0366(20)30482-X
Fioravanti, G., Benucci, S. B., Prostamo, A., Banchi, V., & Casale, S. (2022). Effects of the COVID-19 pandemic on psychological health in a sample of Italian adults: A three-wave longitudinal study. Psychiatry Research, 315, Article 114705. https://doi.org/10.1016/j.psychres.2022.114705
Food and Drug Administration. (2021, August 23). FDA approves first COVID-19 vaccine. https://www.fda.gov/news-events/press-announcements/fda-approves-first-covid-19-vaccine
Huckins, J. F., daSilva, A. W., Wang, W., Hedlund, E., Rogers, C., Nepal, S. K., Wu, J., Obuchi, M., Murphy, E. I., Meyer, M. L., Wagner, D. D., Holtzheimer, P. E., & Campbell, A. T. (2020). Mental health and behavior of college students during the early phases of the COVID-19 pandemic: Longitudinal smartphone and ecological momentary assessment study. Journal of Medical Internet Research, 22(6), Article e20185.
https://doi.org/10.2196/20185
Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Liu, C. H., Stevens, C., Wong, S. H. M., Yasui, M., & Chen, J. A. (2019). The prevalence and predictors of mental health diagnoses and suicide among U.S. college students: Implications for addressing disparities in service use. Depression and Anxiety, 36(1), 8–17. https://doi.org/10.1002/da.22830
Löwe, B., Decker, O., Müller, S., Brähler, E., Schellberg, D., Herzog, W., & Herzberg, P. Y. (2008). Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Medical Care, 46(3), 266–274. https://doi.org/10.1097/MLR.0b013e318160d093
Luo, Q., Zhang, P., Liu, Y., Ma, X., & Jennings, G. (2022). Intervention of physical activity for university students with anxiety and depression during the COVID-19 pandemic prevention and control period: A systematic review and meta-analysis. International Journal of Environmental Research and Public Health, 19(22), 15338. https://doi.org/10.3390/ijerph192215338
Marroquín, B., Vine, V., & Morgan, R. (2020). Mental health during the COVID-19 pandemic: Effects of stay-at-home policies, social distancing behavior, and social resources. Psychiatry Research, 293, Article 113419. https://doi.org/10.1016/j.psychres.2020.113419
Martin, A., Rief, W., Klaiberg, A., & Braehler, E. (2006). Validity of the Brief Patient Health Questionnaire Mood Scale (PHQ-9) in the general population. General Hospital Psychiatry, 28(1), 71–77.
https://doi.org/10.1016/j.genhosppsych.2005.07.003
McLeish, A. C., Walker, K. L., & Hart, J. L. (2022). Changes in internalizing symptoms and anxiety sensitivity among college students during the COVID-19 pandemic. Journal of Psychopathology and Behavioral Assessment, 44, 1021–1028. https://doi.org/10.1007/s10862-022-09990-8
Meyer, J., McDowell, C., Lansing, J., Brower, C., Smith, L., Tully, M., & Herring, M. (2020). Changes in physical activity and sedentary behavior in response to COVID-19 and their associations with mental health in 3052 US adults. International Journal of Environmental Research and Public Health, 17(18), Article 6469.
https://doi.org/10.3390/ijerph17186469
Oh, H., Marinovich, C., Rajkumar, R., Besecker, M., Zhou, S., Jacob, L., Koyanagi, A., & Smith, L. (2021). COVID-19 dimensions are related to depression and anxiety among US college students: Findings from the Healthy Minds Survey 2020. Journal of Affective Disorders, 292, 270–275. https://doi.org/10.1016/j.jad.2021.05.121
Ozamiz-Etxebarria, N., Idoiaga Mondragon, N., Dosil Santamaría, M., & Picaza Gorrotxategi, M. (2020). Psychological symptoms during the two stages of lockdown in response to the COVID-19 outbreak: An investigation in a sample of citizens in Northern Spain. Frontiers in Psychology, 11, Article 1491.
https://doi.org/10.3389/fpsyg.2020.01491
Peduzzi, P., Concato, J., Kemper, E., Holford, T. R., & Feinstein, A. R. (1996). A simulation study of the number of events per variable in logistic regression analysis. Journal of Clinical Epidemiology, 49(12), 1373–1379. https://doi.org/10.1016/S0895-4356(96)00236-3
Pierce, M., Hope, H., Ford, T., Hatch, S., Hotopf, M., John, A., Kontopantelis, E., Webb, R., Wessely, S., McManus, S., & Abel, K. M. (2020). Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population. The Lancet Psychiatry, 7(10), 883–892.
https://doi.org/10.1016/S2215-0366(20)30308-4
Prati, G., & Mancini, A. D. (2021). The psychological impact of COVID-19 pandemic lockdowns: A review and meta-analysis of longitudinal studies and natural experiments. Psychological Medicine, 51(2), 201–211. https://doi.org/10.1017/S0033291721000015
Rettie, H., & Daniels, J. (2021). Coping and tolerance of uncertainty: Predictors and mediators of mental health during the COVID-19 pandemic. American Psychologist, 76(3), 427–437. https://doi.org/10.1037/amp0000710
Riehm, K. E., Holingue, C., Kalb, L. G., Bennett, D., Kapteyn, A., Jiang, Q., Veldhuis, C. B., Johnson, R. M., Fallin, M. D., Kreuter, F., Stuart, E. A., & Thrul, J. (2020). Associations between media exposure and mental distress among U.S. adults at the beginning of the COVID-19 pandemic. American Journal of Preventive Medicine, 59(5), 630–638. https://doi.org/10.1016/j.amepre.2020.06.008
Schubert, M., Ludwig, J., Freiberg, A., Hahne, T. M., Romero Starke, K., Girbig, M., Faller, G., Apfelbacher, C., von dem Knesebeck, O., & Seidler, A. (2021). Stigmatization from work-related COVID-19 exposure: A systematic review with meta-analysis. International Journal of Environmental Research and Public Health, 18(12), 6183. https://doi.org/10.3390/ijerph18126183
Silva, D. T. C., Prado, W. L., Cucato, G. G., Correia, M. A., Ritti-Dias, R. M., Lofrano-Prado, M. C., Tebar, W. R., & Christofaro, D. G. D. (2022). Impact of COVID-19 pandemic on physical activity level and screen time is associated with decreased mental health in Brazillian adults: A cross-sectional epidemiological study. Psychiatry Research, 314, Article 114657. https://doi.org/10.1016/j.psychres.2022.114657
Şimşir, Z., Koç, H., Seki, T., & Griffiths, M. D. (2022). The relationship between fear of COVID-19 and mental health problems: A meta-analysis. Death Studies, 46(3), 515–523. https://doi.org/10.1080/07481187.2021.1889097
Son, C., Hegde, S., Smith, A., Wang, X., & Sasangohar, F. (2020). Effects of COVID-19 on college students’ mental health in the United States: Interview survey study. Journal of Medical Internet Research, 22(9), Article e21279. https://doi.org/10.2196/21279
Spitzer, R. L., Kroenke, K., Williams, J. B. W., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097.
https://doi.org/10.1001/archinte.166.10.1092
Stamatis, C. A., Broos, H. C., Hudiburgh, S. E., Dale, S. K., & Timpano, K. R. (2022). A longitudinal investigation of COVID-19 pandemic experiences and mental health among university students. British Journal of Clinical Psychology, 61(2), 385–404. https://doi.org/10.1111/bjc.12351
Tabachnick, B. G., & Fidell, L. S. (2019). Using multivariate statistics (7th ed.). Pearson.
Tang, N. K. Y., McEnery, K. A. M., Chandler, L., Toro, C., Walasek, L., Friend, H., Gu, S., Singh, S. P., & Meyer, C. (2022). Pandemic and student mental health: Mental health symptoms amongst university students and young adults after the first cycle of lockdown in the UK. BJPsych Open, 8(4), Article e138.
https://doi.org/10.1192/bjo.2022.523
Wise, T., Zbozinek, T. D., Michelini, G., Hagan, C. C., & Mobbs, D. (2020). Changes in risk perception and self-reported protective behaviour during the first week of the COVID-19 pandemic in the United States.
Royal Society Open Science, 7(9), Article 200742. https://doi.org/10.1098/rsos.200742
Xiong, J., Lipsitz, O., Nasri, F., Lui, L. M. W., Gill, H., Phan, L., Chen-Li, D., Iacobucci, M., Ho, R., Majeed, A., & McIntyre, R. S. (2020). Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders, 277, 55–64. https://doi.org/10.1016/j.jad.2020.08.001
Wesley B. Webber, PhD, NCC, is a postdoctoral scholar at East Carolina University. W. Leigh Atherton, PhD, LCMHCS, LCAS, CCS, CRC, is an associate professor and program director at East Carolina University. Kelli S. Russell, MPH, RHEd, is a teaching assistant professor at East Carolina University. Hilary J. Flint, NCC, LCMHCA, is a clinical counselor at C&C Betterworks. Stephen J. Leierer, PhD, is a research associate at the Florida State University Career Center. Correspondence may be addressed to Wesley B. Webber, Department of Addictions and Rehabilitation Studies, Mail Stop 677, East Carolina University, 1000 East 5th Street, Greenville, NC 27858-4353, webberw21@ecu.edu.
May 10, 2023 | Volume 13 - Issue 1
Shainna Ali, John J. S. Harrichand, M. Ann Shillingford, Lea Herbert
Guyana has the highest rate of suicide in the Western Hemisphere. Despite this statistic, a wide gap exists in the literature regarding the exploration of mental wellness in this population. This article shares the first phase in a phenomenological study in which we explored the lived experiences of 30 Guyanese American individuals to understand how mental health is perceived. The analysis of the data revealed that participants initially perceived mental health as negative and then transitioned to a positive perception of mental health. We discuss how these perceptions affect the lived experience of the participants and present recommendations for counselors and counselor educators assisting Guyanese Americans in cultivating mental wellness.
Keywords: Guyanese American, mental health, phenomenological, mental wellness, perceptions
In 2014, the World Health Organization (WHO) reported Guyana as having the highest suicide rate in the world (44.2 suicides per 100,000 people; global average is 11.4 per 100,000 people). According to World Population Review (2023), within the Western Hemisphere, even after almost 10 years, Guyana remains the country with the highest rate of suicide—a concerning statistic. Responding to the WHO (2014) report, Arora and Persaud (2020) engaged in research to better understand the barriers Guyanese youth experience in relation to mental health help-seeking and suicide. Their research included 17 adult stakeholders (i.e., teachers, administrative staff, community workers) via focus groups, and 40 high school students who engaged in interviews. Arora and Persaud used a grounded theory approach and found the following themes as barriers to mental health help-seeking in Guyanese youth: shame and stigma about mental illness, fear of negative parental response to mental health help-seeking, and limited awareness and negative beliefs about mental health service. They recommended integrating culturally informed suicide prevention programs in schools and communities. In efforts to extend Arora and Persaud’s findings, we sought to further understand how Guyanese Americans define and experience mental health to better serve them in counseling.
Startled by the statistics presented by the WHO (2014) and Arora and Persaud (2020), we were compelled to focus our attention on this unique immigrant subgroup in the United States. It is important to note that between the WHO’s 2014 report and Aurora and Persaud’s research, no other studies related to Guyanese American suicidality are recorded in the literature. However, two studies on Guyanese American mental health emerged by Hosler and Kammer (2018) and Hosler et al. (2019). Our decision to conduct research on the Guyanese American community was further informed by Forte and colleagues’ (2018) review of immigrant literature in the United States, which stated that “immigrants and ethnic minorities may be at a higher risk for suicidal behavior as compared to the general population” (p. 1). Forte et al. found that immigrants, when compared with individuals in their homeland, were at an increased risk of experiencing mental health challenges like depression and other psychotic disorders. Currently, suicide is listed as the 10th leading cause of death overall in the United States (Heron, 2021). More specifically, within ages 10–34 and 35–44, suicide is the second and fourth leading cause of death, respectively. Heron’s (2021) report, referencing the Centers for Disease Control and Prevention (CDC), highlighted that in the United States, death by suicide (47,511) is 2.5 times higher than homicides (19,141). The prevalence of suicide among Guyanese people within and without the United States warranted further exploration of the experiences of this marginalized group.
The Guyanese American Experience
Comparing all countries with a population of at least 750,000 people, Guyana, a Caribbean nation, is said to have “the biggest share of its native-born population—36.4%—living abroad” due to remoteness and limited opportunities within the country to move from a lower to a higher socioeconomic status (Buchholz, 2022, para. 2). It is estimated that the United States is home to approximately 232,000 Guyanese Americans whose ancestry can be traced back to Guyana (United States Census Bureau, 2019), a country in the northeast of South America, bordered by Brazil, Venezuela, and Suriname. Although approximately 50% of all Guyanese immigrants in the United States reside in New York City alone (Indo-Caribbean Alliance, Inc., 2014), Guyanese people can be found across all 50 states and the District of Columbia (Statimetric, 2022). This draw to the United States, an English-speaking nation, might be linked to the fact that Guyana is the only country in South America that recognizes English as its official language (One World Nations Online, n.d.).
Like most immigrants, Guyanese immigrants travel to the United States seeking a better life and opportunities for themselves and their families. However, the process of transplanting can be bittersweet, in that Guyanese immigrants might be forced to relinquish their identity and customs and embrace American customs through assimilation (Arvelo, 2018; Cavalcanti & Schleef, 2001). For many Guyanese immigrants, being caught between leaving their homeland and beginning life in their adoptive home can lead to a cultural clash, resulting in problematic coping mechanisms (e.g., minimizing/hiding mental health challenges, cultural shedding [adopting American identity and losing cultural heritage]; Arvelo, 2018).
As discussed above, suicide in the Guyanese community is unquestionably a serious concern, but the community faces other challenges in the United States as well. For example, Hosler et al. (2019) found a statistically significant association between discrimination experience and major depressive symptoms in a sample of Guyanese Americans. However, Hosler et al. (2019) also found mean scores on the Everyday Discrimination Scale (EDS; Williams et al., 1997) were lower (i.e., less discriminatory experiences in everyday life) for Guyanese Americans when compared to other groups (Black, White, and Hispanic) because Guyanese Americans have a more cohesive interpersonal network. It would appear that Guyanese Americans experience lower everyday discrimination because they operate within interpersonal spaces that are more cohesive, yet their discriminatory experiences are positively associated with depression symptoms, which is a source of concern.
Another area of concern among Guyanese Americans is intimate partner violence (IPV), yet research remains lacking (Baboolal, 2016), leading us to draw directly from Guyanese literature. In Guyana, IPV is one of the most prevalent forms of violence (Parekh et al., 2012). As a country, although Guyana endorses the commitment to gender equality, women are the majority only in the tertiary sector (e.g., education, human services, clerical services, and tourism). Nicolas et al. (2021) stated that “domestic duties, marriage, and child-bearing, particularly for women between the ages of 25–29, have hindered their labor force participation” (p. 147). They documented that 1 in 6 Guyanese women, mostly from rural parts of the country, hold the belief that beating one’s wife is necessary (i.e., husbands are justified in beating their wives, resulting in domestic violence being a relevant mental health issue). In fact, suicide is identified as a public health issue for Guyanese women, who use it as a means of coping “with economic despair, poverty, and hopelessness . . . [and] to escape family turmoil, relationship issues, and domestic violence” (Nicolas et al., 2021, p. 148). However, even with access to mental health services increasing in Guyana, seeking out mental health care is uncommon due to stigma, lack of communication, inadequate financial resources, limited providers, and other barriers related to access (Nicolas et al., 2021). Within the U.S. literature, there remains a dearth of information on the experiences of this group as it relates to suicide and IPV. Most likely, this is a result of racial categorization within the United States, where, based on phenotype and racial composite, individuals are often lumped into one category, such as Black. As important as Guyanese literature on IPV is to inform the work of counselors, we believe it is equally important for us to engage in research regarding IPV and other mental health challenges on Guyanese Americans specifically. Learning about Guyanese Americans’ perceptions of mental health may facilitate closing the gap in the utilization of mental health services, warranting the current investigation.
Recognizing the noticeable research gap related to the mental health experiences of Guyanese Americans, we conducted a thorough review of the literature related to mental health and well-being. Through databases such as PsycINFO, ProQuest Central, Web of Science, MEDLINE, and SocINDEX, using the search terms “Guyanese Americans, Health and Wellbeing, Mental Health of Guyanese Americans, Access to Mental Health,” 54 search results were found. However, only two applicable studies were found to address Guyanese Americans’ mental health specifically (Hosler & Kammer, 2018; Hosler et al., 2019). The other search results were either not research manuscripts (i.e., reflections and newspaper articles) or addressed other constructs specific to the Guyanese people (e.g., family, education). The first study by Hosler and Kammer (2018) focused specifically on the health profiles of Guyanese immigrants in Schenectady, New York. This study was conducted with 1,861 residents between the ages of 18–64 years. Guyanese Americans from Schenectady were mostly from a low socioeconomic status, which resulted in them being less likely to have health insurance coverage, an identified place to receive care, and access to cancer screenings. They were also identified as being more likely to engage in alcohol binge drinking—all conditions of significant concern to us, resulting in the present study. In fact, Hosler and Kammer reported that Guyanese Americans are among the lowest group of those insured in the United States when compared with other minority groups such as Black and Latinx groups. Some researchers believe ethnocentric stereotyping, cultural incompetence by professionals, a lack of steady employment, and poor previous interactions with the health care system are barriers Guyanese immigrants experience when accessing medical and mental health services (Arvelo, 2018; Cheng & Robinson, 2013; Jackson et al., 2007).
The second study of Guyanese immigrants was conducted by Hosler et al. (2019) and explored everyday discrimination experiences and depressive symptoms in relation to urban Black, Hispanic, and White adults. This study included 180 Guyanese Americans (i.e., both citizens by birth and naturalized citizens/immigrants), all 18 years and older, from Schenectady, New York. The researchers found a significant independent association between the EDS score and major depressive symptoms for Guyanese Americans, suggesting that discrimination experiences might be an important social cause for depression within this community. Based on the reported challenges faced by Guyanese Americans, as well as our desire to contribute meaningfully to the extant body of literature on the Guyanese American community, we conducted a phenomenological inquiry. More specifically, we sought to better understand the lived experiences of Guyanese Americans pertaining to mental health (i.e., definitions, beliefs, practices), and how they access and incorporate mental health resources to mitigate the known mental health risks of this population in the United States, in the hopes of creating tailored methods for culturally responsive care.
Method
Because limited mental health research exists on this unique community, the present study, which is part of a larger research endeavor, sought to explore Guyanese Americans’ lived experiences with mental health. To lay the foundation of understanding, the present study focused on Guyanese Americans’ perceptions of mental health. Phenomenology, a constructivist approach, recognizes the existence of multiple realities and provides an understanding of participants’ lived experiences using their own voices (Haskins et al., 2022). We selected transcendental phenomenology (Moustakas, 1994) as the appropriate methodology for answering our research questions, as it is congruent with the counseling profession’s similar objective of understanding the human being. Akin to the practice of counseling, transcendental phenomenology emphasizes methods of the researcher to best set aside the potential clouds caused by bias in an effort to allow the explored phenomenon to surface. Transcendental phenomenology aligns with one of the core professional values in the American Counseling Association’s Code of Ethics (ACA, 2014), that of supporting “the worth, dignity, potential, and uniqueness of people within their social and cultural contexts” (p. 3). It also aligns with Ratts et al.’s (2015) Multicultural and Social Justice Counseling Competencies (MSJCC), specifically understanding the client’s worldview domain. Our focus on Guyanese Americans, an understudied minority group in the United States (Hosler & Kammer, 2018) originating from a country that has been identified as having the world’s highest suicide rate (WHO, 2014), led us to select this method so that we could maintain cognizance of our surroundings, hold respect for the population, and examine participants’ experiences (Haskins et al., 2022; Hays & Singh, 2012; Hays & Wood, 2011).
Participants
Before participants were recruited for the study, IRB approval was obtained from the university with whom Shainna Ali, M. Ann Shillingford, and Lea Herbert are affiliated. Purposive criterion sampling was used to recruit participants, leading to a sample of adults who self-identified as Guyanese American (i.e., either immigrated to the United States themselves or had at least one parent who was born in Guyana). Recruitment materials were shared with Guyanese Americans using counseling listservs (i.e., ACA–AMCD Connect and CESNET) and social media platforms (i.e., LinkedIn, Facebook, and Instagram). Members of the research team contacted all participants using email to share details regarding the study and the informed consent document, collect demographic data, and schedule individual interviews. According to qualitative research, sample size recommendations range from six to 12 participants (Creswell, 2013; Guest et al., 2006; Onwuegbuzie & Leech, 2007). Hence, we sought to recruit 15–20 participants to account for the possibility of attrition.
Our recruitment efforts yielded 73 individuals who expressed interest in the study, 60 of whom met all inclusion criteria and were initially contacted. Forty-three individuals were unable to complete an individual interview due to scheduling conflicts; hence, we secured a total of 30 participants who completed the study. Of this number, 17 participated in individual interviews and a total of 23 individuals participated in a one-time focus group to further clarify data from the individual interviews. It should be noted that 10 of the 23 focus group participants also participated in the individual interview. Further recruitment was deemed unnecessary, as the data analysis reached saturation with data from the individual interviews and focus group. We present demographic data on all participants who engaged in the study, both individual interviews and the focus group (N = 30), in Table 1.
Table 1
Participant Demographic Data
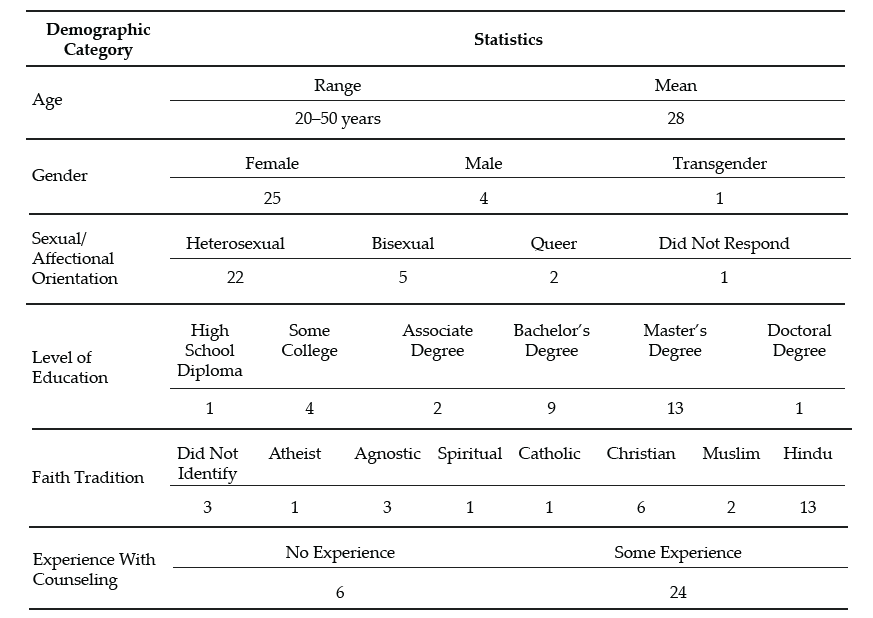
Note. This table provides a breakdown of the demographic characteristics of Guyanese American participants (N = 30).
Data Collection and Analysis
Participants engaged in a semi-structured interview lasting 30–60 minutes, conducted by Ali and Shillingford. Interviews were conducted via Zoom, audio-recorded, and transcribed verbatim. The interview protocol consisted of three primary questions, and sub-questions were used to clarify responses: 1) How do you define mental health?; 2) Who in your life has had experiences with mental health?; and 3) What experiences have you had with mental health? Prior to conducting our study, we included in our IRB documentation that data collection of individual interviews would follow saturation guidelines and that a focus group could be used for further data illumination. Following initial data analysis, we found it necessary to conduct a 1-hour follow-up focus group via Zoom to probe deeper into the data and to allow participants to clarify concepts related to emerging themes. Upon the first round of analysis, it was noted that several participants experienced a shift in perceptions regarding mental health. Focus group probes explored whether participants noticed this shift, what may have contributed to this shift, and when the shift occurred.
After all focus group and individual interviews were transcribed, we used guidelines outlined by Moustakas (1994) to analyze the data. First, we immersed ourselves in the data, reviewing each transcript individually. The transcripts were then divided equally among the four researchers, who read through each to become familiar with the data. With each transcript, we identified relevant statements reflecting participants’ lived experiences (horizontalization) as Guyanese Americans within the contexts of mental health beliefs and experiences.
Following this process, we met multiple times to review all transcripts and confer about the textural descriptions. We identified relevant codes, then synthesized the textural descriptions into themes based on commonalities, distilling the meaning expressed by participants. Then we engaged in reduction and elimination via consensus coding. This process included reading and rereading transcripts together, which followed an iterative process of reviewing the text and code, coding, rereading, and recoding, before determining which thematic content was a new horizon or new dimension of the phenomenon.
After all transcripts were analyzed following this reduction process, clustering and thematizing occurred (i.e., thematic content was clustered into core themes based on participant experiences; Hays & Singh, 2012; Moustakas, 1994). We extracted verbatim examples from the transcripts to generate a thematic and visual description of the phenomenon being examined. After completing the initial data analysis, we conducted member checking by sending each participant their individual transcript as well as the written results section. Participants were requested to provide feedback on the accuracy of their transcripts. Additionally, following the focus group and elucidation of themes all participants were offered an opportunity to member check and clarify the degree to which the results aligned with their lived experiences. The participants did not report any errors; however, clarification was offered by one participant.
Trustworthiness and Positionality
Trustworthiness is a key element of qualitative research in which the research findings accurately reflect the data (Lincoln & Guba, 1985). A critical element of maintaining research credibility is through reflexivity, wherein researchers critically examine procedures employed in relation to power, privilege, and oppression (Hunting, 2014). To safeguard against researcher bias, we worked collaboratively to establish and maintain credibility throughout data collection and analysis processes. Our research team consisted of one Indo-Guyanese American female faculty member, one Afro-Guyanese American female doctoral student, one Black female faculty member, and one Indo-Chinese-Guyanese Canadian male faculty member. All three faculty members belong to CACREP-accredited counselor education programs, and all four researchers have clinical experience working with diverse populations.
To address researcher bias, we engaged in bracketing to minimize the ways in which our experiences influence our approach to research and expectations of the outcomes of the study. Prior to data collection, we discussed our experiences in relation to Guyana, mental health in the Guyanese American community, and our roles as mental health leaders and advocates. We identified our personal experiences, acknowledged our biases, and attempted to bracket while conducting the interviews and focus group. Throughout the data collection and analysis processes, we participated in personal reflection and kept analytic memos documenting our reactions and initial thoughts about the data collected.
Before analyzing the data, we met to confirm analysis procedures, ensuring consistency. We initially analyzed data individually, then determined codes and themes as a team to reduce bias. Throughout the data analysis process, we consulted with each other, addressing questions or concerns related to the data. We also consulted with an outside researcher experienced in qualitative research to obtain critical feedback on the data analysis process and the research findings (Marshall & Rossman, 2006). Our consultant served as an external check of the research methodology and theoretical interpretation of the data.
Findings
The results of the analysis increase understanding of the lived mental health experiences of Guyanese Americans by elucidating perceptions of mental health (Creswell, 2013). All participants shared their beliefs about mental health and the direct and indirect experiences that informed their conceptualization. Three themes surfaced. The first two showed a clear divide in the data: 1) mental health being perceived as negative, stigmatized, elusive, and intimidating; and 2) mental health being perceived as positive, important, helpful, and empowering. It is important to note that these primary themes were not representative of two subsets of participants, and this extracted another theme, which centered on the tendency of participants’ beliefs to transition from negative to positive views of mental health.
The Perception of Mental Health as Negative
When exploring obstacles, subthemes emerged in which hindrances to mental health were acknowledged to exist across three levels: individual, familial, and sociocultural. In parallel, these three subthemes were echoed in the exploration of factors that participants acknowledged have contributed to their mental wellness. The following section explores the primary themes in detail by highlighting the participants’ voices in describing their lived experiences.
Mental Health Concerns Are a Sign of Weakness
All participants in the individual interviews shared that they originally believed that mental health developed out of weakness. This belief was often attributed to minimizing remarks from family members. Oftentimes these comments were paired with other suggestions of how to ameliorate symptoms such as praying more, working harder, or contributing to physical health (e.g., drinking tea). Sharon shared:
It was just like, oh no, you just need to read a book or you just need to go and do something and take your mind off of however it is you’re feeling, like there’s no reason for you to be sad, you have a roof over your head and you’re going to school and you’re doing all of these things, it doesn’t matter. There’s no reason for you to be sad or feel any type of way about anything because we provide everything for you.
Several participants noted that investment in physical wellness was preferable to mental wellness, although physical health was not genuinely prioritized. Participants shared personal and observed maladaptive coping with poor eating habits (i.e., quality and quantity) and excessive substance abuse, namely alcohol. Some participants shared that these tactics were used to manage mental health symptoms or avoidance. Christine shared, “When you’re struggling with things . . . you have nowhere to go to with them except alcohol and the bottom of a rum bottle.” Many participants recognized that coping with alcohol is normalized within the culture. Further, the commonality of these methods normalized consumption and have caused additional issues (e.g., diabetes, heart disease, alcoholism). Arjun noted:
We all have relatives that are kind of stuck on the whole drinking issue. We know a lot of them. They get together with their friends and they “lime,” as we like to call it. They drink in groups and they “gyaff,” they have fun. But it’s a completely different story when they’re by themselves and they’re drinking.
Mental Health Is Taboo
A general consensus was that all participants in the study once believed that mental health was not important and that mental health problems were shameful and not to be discussed. This consistent trend was one of the reasons that we opted to further understand responses through a focus group. Therefore, a direct probe was offered to the focus group participants to explore if they believed discussing mental health was taboo. When delving deeper into these perceptions, participants noted that these thoughts were informed by the beliefs of others and upheld in the wider cultural paradigm. All participants reported that, generally, mental health should not be talked about in order to save face and be respectful. Because mental health issues were seen to be synonymous with weakness, sharing about mental health was equated with the risk of bringing shame to oneself or to one’s family. For example, Chandra shared that “Guyanese people don’t want a kid that’s broken or a little off.” Hence, if someone opts to discuss their mental illness, it is to be done carefully, or secretly.
Most participants shared that typically, when divulging their symptoms, they went to an elder, often a parent, grandparent, or elder sibling, in an effort to keep concerns within the family system. However, many participants noted being minimized or dismissed when sharing their concerns with family members. Ramona explained her feeling that her family
is really strong about, like, don’t be selfish. And I wonder if they would categorize it under that. Like if you’re taking up too much space or time or whatever, you’re trying to center the attention on you or whatever, so that’s a self-serving thing.
A generational rule of discourse emerged from the data. Though the tendency was to keep mental health discussions within the family system, it was also atypical for a younger member to address observed issues with an elder. Several participants noted that this hidden guideline kept informed younger generations from being able to utilize their recognition of warning signs to help the given person and the family system. Arjun shared that as he’s gotten older and has learned more about mental health, he has acquired the courage to address the problems he sees with elders, including his uncle:
I said, “Uncle, what’s wrong?” And he said, “No, nothing is wrong.” But he was crying, you could see tears were streaked on his face, but he wouldn’t talk about it—he wouldn’t say anything. It’s not only one time I saw him, it’s multiple times that I’ve seen him when he has been drinking by himself, that he kind of has the same face all the time. Prior to the times that I asked him, I kind of looked at him and I kind of walked away the first couple of times. Because I was kind of like, this is not something that looked like I should butt in, as a child especially. When you’re younger, your parents tell you, “Mind your business.” Or they say, “You’re not an adult, go with the kids.” So . . . the first couple of times I saw him, I kind of avoided it.
Others Are Not To Be Trusted
Some participants noted that beyond the purpose of family protection, caution to mental health discourse was also due to lack of trust of others. Christine explained: “We had a counseling center on campus, but I was like, ‘Oh, I can’t go talk to anybody,’ because that’s what I was raised with. You don’t talk to strangers about your problems. I had to keep everything inside.” Nevertheless, some families encouraged talking to a religious leader to assist the individual in enhancing devotion and reducing mental health symptoms. Still, regarding professional mental health services, many participants believed, at least at one time, that such services are not helpful, providers are not to be trusted, assistance of that nature is for other (e.g., White) people, and succumbing to that level of desperation is a sign of weakness. When sharing about mistrust in professional mental health assistance, misconceptions and stereotypes surfaced. Ramesh shared:
Oh boy. I have to be honest with you, I feel counseling is, I’ll speak to a shrink and they’ll prescribe drugs to me, like Ritalin or . . . I was like, you know what, I’m better than that. I’m probably totally wrong about it, but that’s just the perception that I have. I’ll be laying on the couch and I’m going to speak into someone and then they’re going to prescribe drugs to me. I don’t want that. I can try to figure this out on myself by talking and trying to do things—positive behavior.
Mental Health Perceived as Positive
All participants in the individual interviews acknowledged a shift in their perceptions of mental health. Their newfound conceptualization included a holistic view of wellness in which mental wellness was seen as an important component to overall well-being and quality of life. In this newer perception, participants acknowledged the ability to consider more variables influencing mental health than they recognized in the past. For example, many participants noted a link between mind and body, versus the previously held notion that physical health is more important than mental health. A few participants noted that mental health can be influenced by genetics, while some noted that it could be influenced by personality, and others noted that it can be influenced by people and the surrounding environment.
All participants, from both the individual interviews and focus group, concurred that everyone feels mental health effects; furthermore, showing signs of a problem is not attributed to weakness. Moreover, because mental health affects everyone, a widespread belief emerged that we all have the responsibility to foster our mental wellness. Additionally, participants shared several examples of what naturally ensued without investing in strategies for mental health such as challenges with emotional regulation, coping, relationships, and worsening mental health problems.
The Transition Between Negative and Positive Perceptions
The transition between old and new conceptualizations of mental health was informed by direct and indirect experiences. All participants shared a transition in beliefs in the individual interviews, and this was explored in the focus group for further clarification. Most participants shared that their personal mental health history informed a change in their beliefs. Many of these participants noted the influence of their healing process, most notably seeking professional help. All participants, from both the individual interviews and the focus group, shared at least one example of learning about mental health by observing another person’s experience. For example, Jessie shared, “Unfortunately, I came from a home of domestic violence . . . I was around maybe six, my dad was bipolar . . . [and] he was just a wife beater. That is probably when I can recall [learning] of mental health.” Another example of learning about mental health from others is captured in Reginald’s comment:
[As] an only child . . . my parents took it upon themselves to [teach me]. . . . It wasn’t like, “Okay, sit down. Let me tell you why these things are.” It was just we’ll be talking about somebody else or going over something that happened and then they’ll explain why, but never directly for me. It was always about other people’s kids.
Many of these individuals emphasized the belief that by paying attention to others, you can learn what is helpful and unhelpful for mental health. Oftentimes this was in their own family; however, extended family and community members were also highlighted. Moreover, a few participants shared their recognition that living with someone who is struggling with their mental health may negatively impact personal wellness (e.g., be triggering). Beyond the family system, some participants noted that exposure to other cultures and perceptions of mental health informed a conceptualization of mental wellness. Seeta shared:
I had friends of other religions or like no religions. And then we would talk about a lot of different things. Like I would ask them questions like, “Oh, so how do things work in your house? Do your parents talk about your God or whatever?” And they’re like, “No.” And I’m like, “So where do your emotions come from?” And they’re like, “Well, you know, we just feel them. Some days I feel angry and some days I feel sad, some days I feel happy.” And I’m just like, “Okay, this is interesting.”
From the quote, it might appear that one’s emotions are in some way connected with God or another higher power; however, this is not something that was observed with other participants of our study. It was more common for participants to share stories of their families using religion as the solution to mental health concerns. For example, Yolanda shared:
My grandmother came when I turned 16 and she kept trying to tell my mom I was showing signs of depression. And my mom was like, “No, she’s like that all the time, like, that’s just how she is.” And my grandma was like, “That’s not normal. You should get her checked out.” And my mom kept saying, “No” and kept denying it. And then my grandma said, “You have to do something.” And then my mom replied, “Oh, I’m going to pray for her.”
In addition to personal experiences and observations of others, participants noted that improved mental health awareness and education prompted them to think critically about their mental health schemas. Ramesh shared:
My education, I always feel like this is what saved me in the end, because I was able to be around other people to know better and to come back home and be like, “Excuse me, this is not how we do things. This is not how we say things. I don’t know what it was like in Guyana.”
Some participants associated this with growing older, and others noted their personal initiative to improve mental health knowledge by following mental health pages on social media, taking a related class, and for some, becoming a part of the mental health field themselves. From this vantage point, many participants were able to equate their previously held notions with beliefs embedded in the culture such as generational rules of respect, gender differences, and the impact of colonialism. Participants, despite their gender differences, noted that within the cultural framework, the rule that mental health should not be discussed is disproportionately applicable to males. Participants shared that this is often due to the perception that it is important for men to be strong, and again, mental illness is a symptom of weakness. This was also linked to the breadwinner role and the pressure to provide for the family. However, this was only noted to have detrimental effects, as anger issues, IPV, and alcoholism were noted to arise out of this rule. Some participants noted that the survival aspect of colonialism may have contributed to the lack of privilege to focus on mental health. In addition, the history of colonialism in Guyana (i.e. slavery, indentured labor) could have informed the lack of trust in professional services.
The change in mental health conceptualization was noted to have benefits beyond the participants themselves. Some participants remarked that the shift in perception was recognized in the wider generation. Ramona reflected:
I will say that a lot of folks from my generation have been a lot more like, “Go to therapy. We should be taking care of our thoughts and our feelings or emotions.” That’s important to you in the same way that if you tore a ligament that you would need to get surgery or do whatever.
Within the newfound conceptualization of mental wellness emerged a vow of social responsibility. All participants, from both the individual interviews and the focus group, shared their intention to help others, and some even noted it as their duty. Ways to help others included advocating for mental health awareness, access, and education; helping to challenge unhelpful cultural beliefs; breaking generational cycles; and protecting others from experiencing similar struggles (e.g., child, sibling).
Discussion
The findings from this study are enlightening, and some are the first to be documented through research, even if they were observed in practice. Initial perceptions of all participants, from both the individual interviews and the focus group, were that mental health is a taboo topic and seeking mental health services is bad. These perceptions stemmed from fear, mistrust, and limited awareness of the benefits of mental health services. This is consistent with findings from Arora and Persaud (2020), who surmised that Guyanese individuals hold negative views of mental health that significantly impact their help-seeking. Furthermore, the findings point to strong familial and sociocultural influences, such as beliefs about mental health, that swayed individual perceptions of mental health, which is in keeping with recent literature on affirming cultural strengths and incorporating familial identity in working with clients of Guyanese descent (Groh et al., 2018; Nicolas et al., 2021).
Discussing issues related to mental health was viewed as a sign of weakness, which translated to help-seeking being a taboo. It would appear that the stigma associated with mental health remains a common experience for Guyanese Americans, and when coupled with limited communication, insufficient funding, and lack of providers, we can see how Nicolas et al. (2021) found this to be concerning. Cultural clash, ethnocentric stereotyping, and cultural incompetency may also be responsible for Guyanese Americans being distrustful of the health care system, leading them to engage in maladaptive behaviors (i.e., avoidance, use of substances, IPV) and not receive the mental health attention and care they need (Arvelo, 2018; Cheng & Robinson, 2013; Jackson et al., 2007).
It appears that even in the face of discrimination and experiences of mental health challenges like alcoholism, depression (Hosler & Kammer, 2018), and IPV (Parekh et al., 2012), leaning on the support of the community serves to buffer against mental health challenges for Guyanese Americans. It also seems that changing mental health perceptions from negative to positive was significantly related to mental health literacy and exposure to other systems such as school, work, and community (i.e., cross-cultural exchange).
Findings that were not previously documented in the literature suggest that an integrated view of wellness enabled participants to augment their negative abstractions of mental health care. These findings serve as an indication that among Guyanese Americans, although mental health has been perceived as negative, weak, and a taboo, the narrative is beginning to shift to make space for mental health awareness, education, access, and functioning, thereby creating unique implications for counselors seeking to meet the needs of this immigrant subgroup.
Implications
In combination with prior literature, the results of this study provide a rationale for mental health counselors, marriage and family counselors, school counselors, and counselor educators to inspire dialogue to foster mental wellness. Based on the findings from this study, when working with Guyanese Americans, counselors should focus on three key strategies to support Guyanese American clients: (a) mental health awareness, (b) mental health education, and (c) mental health experience.
Mental Health Awareness
Participants in this study initially held limited views and awareness of the signs and symptoms of mental health. When awareness was heightened through various means, they were more open to exploring the benefits of services. Counselors can be instrumental in creating awareness by first raising their own awareness pertaining to cultural stigma and its influence on Guyanese Americans’ mental health. For example, unwillingness to attend counseling sessions may be linked to the culturally held perception that discussing mental health, especially beyond the core family system, is taboo. In acknowledging this, counselors can raise awareness of confidentiality, which can be seen as an alignment with the cultural notion that talking about mental health is taboo when it means talking to anyone, and the role of the counselor can be highlighted as a professional collaboration versus communal gossip. Counselors need to be mindful of the collectivistic nature of Guyanese American culture, which causes personal and familial illnesses alike to be perceived as personal problems. Rather than dismiss a client’s concerns about mental health, a counselor can benefit from exploring how the family members’ symptoms, perceptions about mental health, and willingness to adhere to treatment influence the client’s symptoms, perceptions, and commitment to counseling. Further, collectivism spans beyond the protective family system. On one hand, this community orientation can be used to explore a broad range of support, yet on the other hand, depending on the client’s experience, this may also be a widened range of societal pressure (e.g., judgment, criticism, shame).
Mental Health Education
Increased understanding of mental health appeared to have led participants to seek services and resources to increase their mental health literacy, with the hope of improving their well-being. Counselors and counselor educators can be instrumental in offering Guyanese Americans mental health education. To begin, all mental health professionals should demonstrate a posture of cultural humility when engaged in psychoeducation on mental health and wellness for this population. In order to raise awareness through education, mental health professionals are encouraged to model trust, respect, sensitivity, compassion, and a nonjudgmental stance. Within session, counselors should be prepared to offer information regarding early signs of mental illness, compounding factors (e.g., alcohol, suicidal ideation, domestic violence), obstacles (e.g., stigma), and resources. Additionally, counselors may need to offer psychoeducation on the family system, roles, dynamics, beliefs, experiences, and generational patterns that can influence individual mental health. In the event that a family member with mental health problems is unwilling to seek assistance, helping the client to better understand the diagnosis and cope personally can be empowering. Finally, to employ the collectivistic nature of Guyanese American culture, stigma can be confronted, and mental health education can be effectively offered by providing group counseling within this population. Group counseling can offer a variety of therapeutic factors that can benefit Guyanese Americans such as universality, hope, and corrective recapitulation of the primary family group (Yalom & Leszcz, 2005).
Beyond the counseling office, counselors and counselor educators should consider collaborating with culturally supportive organizations. Workshops and information sessions can be tailored to explore and address cultural, religious, ethnic, and generational differences in addition to offering mental health resources (e.g., signs, symptoms, treatment). Several of the participants in our study shared that access to psychology courses in school helped to improve their knowledge about mental health. In addition to these classes continuing to be offered, accessibility to such courses should be expanded. Schools and universities may benefit from offering workshops and other informational sessions to support mental health. Beyond information being offered, a follow-up may be beneficial by linking school or campus counselors in order to connect an improvement in awareness and education to action, change, and health.
Several participants shared that because of a lack of access to mental health education, their knowledge was attained through social media platforms such as Instagram and TikTok. Although the quality of mental health education was not assessed in the present study, the lack of regulation on social platforms could perpetuate misleading, confusing, and stigmatizing misinformation surrounding mental health. Counselor educators should consider their roles beyond the classroom. In addition to empowering counselor trainees to utilize the suggestions above to foster awareness and education, counselor educators can offer responsive and succinct information via social media. Whereas social media is not an appropriate platform for tailored education or services, brief information can be offered to bridge the gap between awareness, education, and access.
Mental Health Experience
Growth in awareness and knowledge around mental health resulted in participants intentionally engaging in positive experiences as a way of resisting past harmful and hurtful practices and generational patterns, reauthoring a new narrative of hope and healing. Being wellness-focused, counselors are uniquely positioned to support this community by facilitating positive experiences impacting overall mental health and well-being.
Counselors can honor clients from this community by creating safe spaces for them to share their narratives without judgment. Counselors can foster healing communities through group counseling, where clients collaboratively share each other’s mental burdens and celebrate successes (Yalom & Leszcz, 2005). Counselors can honor collectivism by encouraging clients to participate in support groups in addition to personal counseling. Counselors and counselor educators can enhance the approachability of counselors by improving their visibility in the community. Examples include a community counselor being involved in outreach with a local cultural center, a school counselor offering mentorship with student clubs, a college counselor guest-speaking at a Guyanese American student organization meeting, or a counselor educator offering tailored workshops for the community.
In addition to the aforementioned implications, we believe that in order for counselors to bridge generational gaps in counselor distrust, counselors must acknowledge the lack of representation of diversity within the profession of counseling, the predominance of Western and European cultural and psychologist-centered curriculum, and lapses in poor bioethics and power dynamics among counselors and marginalized communities (Singh et al., 2020). Next, the specific intersectional impacts suggest counselors must adapt a multicultural orientation and illuminate cultural sensitivity. When a clinician enacts cultural sensitivity in session, clients can examine their perceptions of illness and center their multiple identities (Davis et al., 2018).
Limitations and Future Research
Several limitations that arose from the research process are important to mention. All interviews were conducted virtually. Although secured virtual platforms such as Zoom are considered acceptable for research, lack of face-to-face interviewing may have excluded subtle visual cues and induced video-conferencing fatigue (Spataro, 2020). Though researchers made great attempts to increase participant comfort and review the informed consent before the interview process, it is also plausible that respondents may have censored their responses out of concern for potential breach in confidentiality. A majority of respondents are college-educated, female, first generation, and of Indo-Guyanese descent; hence, the results may not be representative of all Guyanese Americans. Additionally, aligned with phenomenological methods of exploring lived experiences, research prompts were general. Recognizing the concerning statistics surrounding suicide (WHO, 2014), a future study exploring suicidality could be beneficial. Future research might seek to explore a more diverse pool of participants, including diversity in gender, age, ethnicity, and number of years in the United States. To build on the findings from the present study, future studies should explore what factors contribute to Guyanese American mental health as well as what variables may hinder mental wellness. It may also be beneficial to include research from the perspective of children and parents to further understand the influence of family systems and cross-generational norms.
Conclusion
This study highlighted the crucial need to address the mental health literacy of Guyanese Americans. The findings illuminate Guyanese Americans’ perceptions of mental health, including the transition from negative to positive perceptions and its potential influences. Efforts should be made to promote awareness, education, and experience related to mental health awareness for Guyanese Americans. Supporting mental health may help to reduce alarming rates of mental illness in Guyanese Americans and may also have the potential to influence related groups such as Guyanese, American, and Caribbean individuals. Counselors and counselor educators have the potential to play a significant role in supporting these clients by being cognizant and informed about cultural considerations.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
American Counseling Association. (2014). ACA code of ethics. https://www.counseling.org/resources/aca-code-of-ethics.pdf
Arora, P. G., & Persaud, S. (2020). Suicide among Guyanese youth: Barriers to mental health help-seeking and recommendations for suicide prevention. International Journal of School & Educational Psychology, 8(1), 133–145. https://doi.org/10.1080/21683603.2019.1578313
Arvelo, S. D. (2018). Biculturalism: The lived experience of first- and second-generation Guyanese immigrants in the United States (Order No. 10749930) [Doctoral dissertation, Chicago School of Professional Psychology]. ProQuest One Academic. (2027471070).
Baboolal, A. A. (2016). Indo-Caribbean immigrant perspectives on intimate partner violence. International Journal of Criminal Justice Sciences, 11(2), 159–176. https://www.researchgate.net/publication/336926774_Indo-Caribbean_Immigrant_Perspectives_on_Intimate_Partner_Violence
Buchholz, K. (2022, November 11). The world’s biggest diasporas [Infographic]. Forbes. https://www.forbes.com/sites/katharinabuchholz/2022/11/11/the-worlds-biggest-diasporas-infographic/?sh=4185fd634bde
Cavalcanti, H. B., & Schleef, D. (2001). Cultural loss and the American dream: The immigrant experience in Barry Levinson’s Avalon. Journal of American and Comparative Cultures, 24(3–4), 11–22.
https://doi.org/10.1111/j.1537-4726.2001.2403_11.x
Cheng, T. C., & Robinson, M. A. (2013). Factors leading African Americans and Black Caribbeans to use social work services for treating mental and substance use disorders. Health & Social Work, 38(2), 99–109. https://doi.org/10.1093/hsw/hlt005
Creswell, J. W. (2013). Qualitative inquiry and research design: Choosing among five approaches (3rd ed.). SAGE.
Davis, D. E., DeBlaere, C., Owen, J., Hook, J. N., Rivera, D. P., Choe, E., Van Tongeren, D. R., Worthington, E. L., Jr., & Placeres, V. (2018). The multicultural orientation framework: A narrative review. Psychotherapy, 55(1), 89–100. https://doi.org/10.1037/pst0000160
Forte, A., Trobia, F., Gualtieri, F., Lamis, D. A., Cardamone, G., Giallonardo, V., Fiorillo, A., Girardi, P., & Pompili, M. (2018). Suicide risk among immigrants and ethnic minorities: A literature overview. International Journal of Environmental Research and Public Health, 15(7), 1–21. https://doi.org/10.3390/ijerph15071438
Groh, C. J., Anthony, M., & Gash, J. (2018). The aftermath of suicide: A qualitative study with Guyanese families. Archives of Psychiatric Nursing, 32(3), 469–474. https://doi.org/10.1016/j.apnu.2018.01.007
Guest, G., Bunce, A., & Johnson, L. (2006). How many interviews are enough? An experiment with data saturation and variability. Field Methods, 18(1), 59–82. https://doi.org/10.1177/1525822X05279903
Haskins, N. H., Parker, J., Hughes, K. L., & Walker, U. (2022). Phenomenological research. In S. V. Flynn (Ed.), Research design for the behavioral sciences: An applied approach (pp. 299–325). Springer.
Hays, D. G., & Singh, A. A. (2012). Qualitative inquiry in clinical and educational settings. Guilford.
Hays, D. G., & Wood, C. (2011). Infusing qualitative traditions in counseling research designs. Journal of Counseling & Development, 89(3), 288–295. https://doi.org/10.1002/j.1556-6678.2011.tb00091.x
Heron, M. (2021). Deaths: Leading causes for 2019. National Vital Statistics Reports, 70(9), 1–113. https://doi.org/10.15620/cdc:107021
Hosler, A. S., & Kammer, J. R. (2018). A comprehensive health profile of Guyanese immigrants aged 18–64 in Schenectady, New York. Journal of Immigrant and Minority Health, 20(4), 972–980.
https://doi.org/10.1007/s10903-017-0613-5
Hosler, A. S., Kammer, J. R., & Cong, X. (2019). Everyday discrimination experience and depressive symptoms in urban Black, Guyanese, Hispanic, and White adults. Journal of the American Psychiatric Nurses Association, 25(6), 445–452. https://doi.org/10.1177/1078390318814620
Hunting, G. (2014). Intersectionality-informed qualitative research: A primer. The Institute for Intersectionality Research and Policy. https://nanopdf.com/download/intersectionality-informed-qualitative-research-a-primer-gemma-hunting_pdf
Indo-Caribbean Alliance, Inc. (2014, February 3). Population analysis of Guyanese and Trinidadians in NYC.
https://www.indocaribbean.org/blog/population-analysis-of-guyanese-and-trinidadians-in-nyc
Jackson, J. S., Neighbors, H. W., Torres, M., Martin, L. A., Williams, D., & Baser, R. (2007). Use of mental health services and subjective satisfaction with treatment among Black Caribbean immigrants: Results from the National Survey of American Life. American Journal of Public Health, 97(1), 60–67. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1716231/
Lincoln, Y. S., & Guba, E. G. (1985). Naturalistic inquiry. SAGE.
Marshall, C., & Rossman, G. B. (2006). Designing qualitative research (4th ed.). SAGE.
Moustakas, C. (1994). Phenomenological research methods. SAGE.
Nicolas, G., Dudley-Grant, G. R., Maxie-Moreman, A., Liddell-Quintyn, E., Baussan, J., Janac, N., & McKenny, M. (2021). Psychotherapy with Caribbean women: Examples from USVI, Haiti, and Guyana. Women & Therapy, 44(1–2), 136–155. https://doi.org/10.1080/02703149.2020.1775993
One World Nations Online. (n.d.). Guyana. https://www.nationsonline.org/oneworld/guyana.htm
Onwuegbuzie, A. J., & Leech, N. L. (2007). A call for qualitative power analyses. Quality & Quantity, 41, 105–121. https://doi.org/10.1007/s11135-005-1098-1
Parekh, K. P., Russ, S., Amsalem, D. A., Rambaran, N., Langston, S., & Wright, S. W. (2012). Prevalence of intimate partner violence in patients presenting with traumatic injuries to a Guyanese emergency department. International Journal of Emergency Medicine, 5(1), 1–5. https://doi.org/10.1186/1865-1380-5-23
Ratts, M. J., Singh, A. A., Nassar-McMillan, S., Butler, S. K., & McCullough, J. R. (2015). Multicultural and social justice counseling competencies. American Counseling Association. https://www.counseling.org/docs/default-source/competencies/multicultural-and-social-justice-counseling-competencies.pdf
Singh, A. A., Appling, B., & Trepal, H. (2020). Using the Multicultural and Social Justice Counseling Competencies to decolonize counseling practice: The important roles of theory, power, and action. Journal of Counseling & Development, 98(3), 261–271. https://doi.org/10.1002/jcad.12321
Spataro, J. (2020). The future of work—the good, the challenging & the unknown. https://www.microsoft.com/en-us/microsoft-365/blog/2020/07/08/future-work-good-challenging-unknown/
Statimetric. (2022). Distribution of Guyanese people in the US. https://www.statimetric.com/us-ethnicity/Guyanese
United States Census Bureau. (2019). People reporting ancestry: American community survey. http://bit.ly/42RazKC
Williams, D. R., Yu, Y., Jackson, J. S., & Anderson, N. B. (1997). Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of Health Psychology, 2(3), 335–351.
https://doi.org/10.1177/135910539700200305
World Health Organization. (2014). First WHO report on suicide prevention. https://www.who.int/news/item/04-09-2014-first-who-report-on-suicide-prevention
World Population Review. (2023). Suicide rate by country 2023. https://worldpopulationreview.com/country-rankings/suicide-rate-by-country
Yalom, I. D., & Leszcz, M. (2005). The theory and practice of group psychotherapy (5th ed.). Basic Books.
Shainna Ali, PhD, NCC, ACS, LMHC, is the owner of Integrated Counseling Solutions. John J. S. Harrichand, PhD, NCC, ACS, CCMHC, CCTP, LMHC, LPC-S, is an assistant professor at The University of Texas at San Antonio. M. Ann Shillingford, PhD, is an associate professor at the University of Central Florida. Lea Herbert is a doctoral student at the University of Central Florida. Correspondence may be addressed to Shainna Ali, 3222 Corrine Drive, Orlando, FL 32803, hello@drshainna.com.