May 22, 2024 | Volume 14 - Issue 1
Rebekah Cole, Christine Ward, Taqueena Quintana, Elizabeth Burgin
Military spouses face many challenges as a result of the military lifestyle. Much focus has been placed on enhancing the resilience of military spouses by both the military and civilian communities. However, no research currently exists regarding spouses’ perceptions of their resilience or how they define resilience for themselves and their community. This qualitative study explored the perceptions of eight military spouses regarding their resilience through individual semi-structured interviews. The following themes emerged: 1) shaped by service member and mission priority; 2) challenges within the military lifestyle; 3) outside expectations of spouse resilience; 4) sense of responsibility for family’s resilience; 5) individual resilience; and 6) collective resilience. We discuss ways military leadership and the counseling profession can best understand and enhance the resilience of military spouses.
Keywords: military spouses, resilience, military lifestyle, perceptions, counseling
Because of the unique stressors associated with the military lifestyle, military spouses are at an increased risk for poor mental health (Donoho et al., 2018; Mailey et al., 2018; Numbers & Bruneau, 2017). They may experience mental health concerns, such as anxiety and depression, due to a number of reasons, including separation from their deployed service member, loss of support networks after a relocation, or issues with adjusting to the uncertain and frequent changes of the military (Cole et al., 2021). Additional concerns that arise, such as employment, marital, and financial issues, can also negatively affect the military spouse’s mental health (Cole et al., 2021; Mailey et al., 2018). Dorvil (2017) reported that 51% of active-duty spouses experience more stress than normal. Furthermore, 25% of military spouses meet the criteria for generalized anxiety disorder (Blue Star Families [BSF], 2021). Depression in military spouses is also higher than the rate found within the general population (Verdeli et al., 2011). As a military spouse casts aside their own personal needs to support their service member, stressors may continue to increase, which can contribute to the rise of mental health needs of military spouses (Moustafa et al., 2020).
Resilience and Military Spouses
Nature of Resilience
Given the challenges inherent in the military lifestyle and the associated mental health risks, military spouse resilience is essential. Resilience is a complex and multifaceted construct, significant to researchers, practitioners, and policymakers across numerous disciplines, including mental health and military science. The American Psychological Association (2020) defined resilience as “the process of adapting well in the face of adversity, trauma, tragedy, threats, or even significant sources of stress” (para. 4). Within the military community, resilience has been defined as the ability to withstand, recover, and grow in the face of stressors and changing demands (Meadows et al., 2015). Importantly, determinants of resilience include the interaction of biological, psychological, social, and cultural factors in response to stressors (Southwick et al., 2014). In addition to these salient variables embedded in resilience science, resilience may be operationalized as a trait (e.g., optimism), process (e.g., adaptability in changing conditions), or outcome (e.g., mental health diagnosis, post-traumatic growth; Southwick et al., 2014).
Resilience may also vary on a continuum across domains of functioning (Pietrzak & Southwick, 2011) and change as a function of development and the interaction of systems (Masten, 2014). Accordingly, a definition and operationalization of resilience may vary by population and context (Panter-Brick, 2014). During the post-9/11 era, the resilience of service members and their families received significant attention from stakeholders, including the Department of Defense (DoD) and National Academies of Sciences, Engineering, and Medicine (NASEM), both of which expressed a commitment to conducting research and establishing programming to enhance service member and military family resilience, resulting in increased awareness of the importance of service member and family resilience throughout the military community (NASEM, 2019).
Military Family Resilience
Though military families share the characteristics and challenges of their civilian counterparts, they additionally experience the demanding, high-risk nature of military duties; frequent separation and relocation; and caregiving for injured, ill, and wounded service members and veterans (Joining Forces Interagency Policy Committee, 2021). In recognition of the constellation of military-connected experiences military families face, the Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury (DCoE) commissioned a review of family resilience research and relevant DoD policies to inform a definition of resilience for appropriate application to military spouses and children (Meadows et al., 2015). Meadows and colleagues (2015) proposed family resilience may be best defined as “the ability of a family to respond positively to an adverse situation and emerge from that situation feeling strengthened, more resourceful, and more confident than its prior state” (see Simon et al., 2005, for a further exploration of family resilience). Further, Meadows and colleagues identified two groups of policies delineated at the Joint Chiefs of Staff or DoD levels, or within individual branches of the military: 1) existing programs modified to augment resilience or family readiness, and 2) new programs developed to target family resilience. Programs established by these policies support access to mental health services (e.g., DoD Instruction [DoDI] 6490.06); parenting education (e.g., New Parent Support Program, DoDI 6400.05); child welfare (e.g., Family Advocacy Program, DoD Directive 6400.1); and myriad physical, psychological, social, and spiritual resources. The well-being of military families represents a critical mission for the DoD, extending beyond provision and access for families to meet their basic needs to individual service member and unit readiness, and the performance, recruitment, and retention of military personnel (NASEM, 2019).
Military Spouse Resilience
Though service member and family resilience are critical for accomplishing the DoD’s mission, focusing on the unique nature of military spouse resilience is key for understanding and supporting this population’s resilience. Counseling, psychology, sociology, and military medical professional research related to military spouse resilience has focused primarily on characteristics associated with resilience. In a study by Sinclair et al. (2019), 333 spouse participants completed a survey regarding their resilience, mental health, and well-being. The results revealed that spouses who had children, were a non-minority, had social support, had less work–family conflict, and had a partner with better mental health were more resilient. Another survey study examined the characteristics associated with resilience in Special Operations Forces military spouses, determining that community support and support from the service member was essential for spouse resilience (Richer et al., 2022). A study conducted within the communication field also explored spouses’ communicative construction of resilience during deployments. Qualitative data analysis of interviews with 24 spouses indicated how spouses use communication to reconcile their contradictory realities, which increases their resilience (Villagran et al., 2013). This resilience has also been found to be a protective factor against depression and substance abuse during military deployments (Erbes et al., 2017). Finally, a survey study of Army spouses (N = 3,036) determined that spouses who were less resilient were at higher risk for mental health diagnoses (Sullivan et al., 2021). While these studies explored the nature of resilience demonstrated by military spouses, our searches in JSTOR, PubMed, ERIC, PsycINFO, and Google Scholar did not reveal any studies regarding spouses’ perceptions of their own resilience or how they define this resilience for themselves and their community. Our study fills that research gap by exploring active-duty spouses’ perceptions and definitions of resilience.
Methods
The purpose of this qualitative study was to explore the perceptions of active-duty spouses regarding their resilience. This study was guided by the following research questions: 1) What are military spouses’ perceptions of their own resilience? and 2) How do military spouses define “resilience?” Phenomenology seeks to present a certain phenomenon in its most authentic form (Moustakas, 1994). In order to most authentically and openly describe our participants’ experiences, we chose a qualitative transcendental phenomenological approach to frame our study. This tradition of qualitative research focuses on portraying a genuine representation of the participants’ perceptions and experiences. However, the distinct feature of transcendental phenomenology is its first step, which involves the researchers recognizing and bracketing their biases so they can analyze the data without any interference (Moerer-Urdahl & Creswell, 2004). We selected this design because each of our research team members were military spouses. We therefore recognized the need to mitigate our biases in order to give a true representation of the participants’ perceptions, free from our own preconceived notions.
Participants
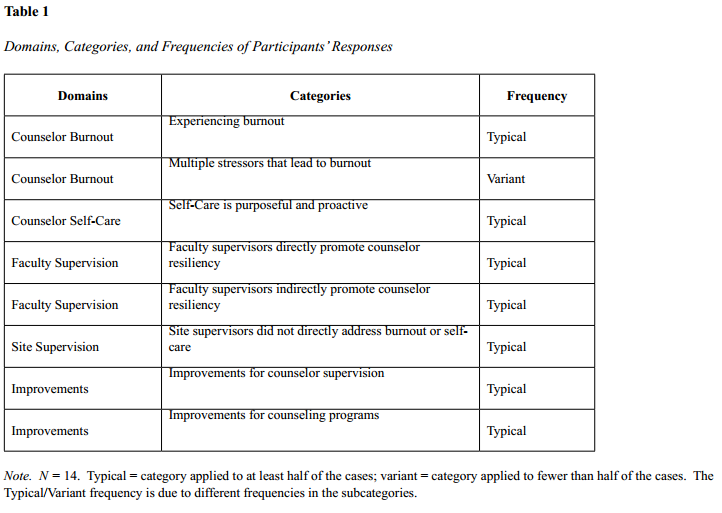
The participants in this study were selected based on their status as active-duty military spouses and their willingness to participate in the study. There were no other inclusion or exclusion criteria for the participants in this study. After gaining IRB approval, we used convenience sampling to recruit eight participants. In qualitative research, convenience sampling is used to recruit participants who are closely accessible to the researchers (Andrade, 2021). Our research team emailed participants that we knew through living, working, and volunteering on military bases throughout the United States and at overseas duty stations who fit the active-duty military spouse criteria for this study and asked them if they were willing to participate in the study. Once the participants expressed interest, they were provided with an information sheet regarding the study’s purpose and the nature of their involvement in the study. Participant demographics are included in Table 1. All of the participants were female and all were between the ages of 30–40. Four branches of the U.S. military, including Army, Navy, Air Force, and Marine Corps, were represented in the sample. No reservist, Coast Guard, or Space Force military spouses participated in our study. Five of our participants were White and three were Black. Their tenure as military spouses ranged from 4 years to 17 years. Five of the spouses were married to a military officer, while three of the participants were married to an enlisted service member. After interviewing these eight participants, our research team met and determined that because of the distinct common patterns we found across each of the participants’ transcripts, we had reached saturation and did not need to recruit any additional participants for our study (Saunders et al., 2018).
Table 1
Participant Demographics
| Participant |
Age |
Ethnicity |
Gender |
Branch |
Spouse’s Rank |
Years as a Spouse |
| 1 |
33 |
Black |
Female |
Air Force |
Enlisted |
4 |
| 2 |
36 |
Black |
Female |
Navy |
Enlisted |
17 |
| 3 |
31 |
White |
Female |
Army |
Officer |
7 |
| 4 |
34 |
Black |
Female |
Navy |
Enlisted |
14 |
| 5 |
36 |
White |
Female |
Marine Corps |
Officer |
12 |
| 6 |
35 |
White |
Female |
Marine Corps |
Officer |
14 |
| 7 |
40 |
White |
Female |
Navy |
Officer |
16 |
| 8 |
34 |
White |
Female |
Navy |
Officer |
10 |
Data Collection
Our research team first developed the interview protocol for the study based on a thorough review of the literature regarding resiliency within military culture as well as the challenges of the military lifestyle for military spouses. Our research team members interviewed each of the participants for 1–2 hours. These semi-structured interviews were audio recorded and transcribed verbatim by an automated transcription service. The interview questions were open-ended and focused on the spouses’ definitions of resilience and their perceptions of their resilience within the military lifestyle and culture (see Appendix for interview protocol). In addition, probing questions such as “Can you explain that a bit more?” or “Can you give any examples of what you mean by that?” were used to gather more in-depth data throughout the interviews.
Data Analysis
We followed the steps of the transcendental phenomenological data analysis process to analyze our study’s results (Moerer-Urdahl, 2004). First, each member of our research team engaged in epoche, in which we bracketed our biases as military spouses so that our own thoughts, feelings, perceptions, and experiences did not influence our interpretation of our participants’ experiences. The next step in the process was horizontalization. During this step, each member of our research team read through the interview transcripts and noted significant statements throughout so we could better understand how the participants perceived, understood, and experienced resilience. Next, we met as a research team to discuss these significant statements and organize them into themes (Moustakas, 1994). Our research team then developed textual and structural descriptions of the themes, describing not only a list of the participants’ perceptions, but also an in-depth analysis of what their perceptions of resilience entailed and how they have experienced it throughout their tenure as military spouses (Moerer-Urdal, 2004; Moustakas, 1994). We then constructed a comprehensive description of the participants’ perceptions of resilience, encapsulating the “essence of the experience” (Moerer-Urdal, 2004, p. 31).
Research Team and Strategies to Increase Trustworthiness
Our research team consisted of four university faculty members, all of whom possessed extensive experience in conducting qualitative research. Three of our research team members possess PhDs in counseling and one research team member possesses an EdD in counseling. All team members had extensive experience conducting research with military-connected communities. In addition, all of our research team members were active-duty military spouses, with years of experience as a military spouse ranging from 1–23 years.
We used several strategies to increase the credibility of our results. First, the use of an experienced research team to collectively analyze the data resulted in diverse perspectives on the emerging themes of the study. However, because each member of our research team was a military spouse, we recognized the need to bracket our own experiences and biases so that they did not interfere with our interpretation of the data. Each team member took notes on their individual biases, and our research team discussed these biases when interpreting themes. Biases held by research team members included a predisposition to believe that spouses of special warfare service members endured greater stressors and were better supported by their military communities; a belief that spouses of higher-ranking service members possessed greater knowledge of and access to resources to support social, behavioral, and mental health needs; and personal experience within the military spouse community. These biases were challenged throughout the research process by each member of the team. As each theme was identified, the team referenced individual transcripts to ensure that the interpretation was justified. We found that our biases were rightfully challenged.
Additionally, to avoid leading questions, our research team made the conscious decision not to define resilience as part of the interview and follow-up process. The team wanted to derive an organic definition of spouse resilience that was not clouded by a formal definition. In addition, we used member checking, in which we emailed the interview transcripts to the participants and asked them to verify the data. The participants responded to our request with minimal change requests related to grammatical errors in the transcriptions and validated our data. Several offered additional insight related to their definition of resilience, which was included in our data analysis.
Results
The following themes emerged from our data: 1) shaped by service member and mission priority; 2) challenges within the military lifestyle; 3) outside expectations of spouse resilience; 4) sense of responsibility for family’s resilience; 5) individual resilience; and 6) collective resilience.
Theme 1: Shaped by Service Member and Mission Priority
Military/Service Member Definition
When discussing their definition of resiliency, the spouses first considered what resiliency meant for their active-duty spouse. The participants varied in their perceptions of what resilience meant for their active-duty service member, though all defined resilience as an active process of adapting or persevering when faced with adversity, rather than a personal trait or characteristic the service member possesses. Participant 3 noted that, for their spouse, resilience was “the ability to adapt to changes that are beyond your control . . . adapting to situations in an optimistic and positive way.” Participant 6 stated that resilience for their spouse meant an “ability to bounce back from a hardship.” One participant asked their spouse to comment specifically about their definition and provided the following definition in a follow-up with the interviewer: “Resilience is how you persevere in difficult circumstances. It’s not about how hard you fall, but how quick you can get back up from being knocked down” (Participant 2 [P2]).
Some participants cited specific notions of resilience that are embedded in the service members’ military community. One Navy spouse remarked that resilience, to their spouse, meant “Don’t give up the ship” (P8). Another Navy spouse mentioned that for their spouse, resilience was “knowing how to weather the storm” (P7). Yet another spouse noted that resilience “the Marine Corps way” meant their service member must “do their job” (P4). Other participants noted that the root of resilience for the military service member stems from a place of selfless service. Participant 8 commented that the resiliency of their spouse was “more about the man standing next to me, the family I’m fighting for at home, the country I’m fighting for at home, than about their own personal needs.”
Adapting, Overcoming, and Persevering
Like their active-duty members, spouses indicated that resilience was about adapting, overcoming, and persevering in the face of obstacles. Resilience to one spouse was “being able to rebound or to overcome an obstacle” (P1); to another, resilience meant they must “be flexible, adapt with whatever, overcome whatever it is that you’re going through” (P2). Spouses noted that resilience was not a one-time event. Instead, spouses suggested that their own resilience stemmed from continually persevering. Participant 6 stated that for them, resilience meant not just “going through something difficult and making it out on the other side,” but that they then had to “keep pushing forward.” One participant indicated that their personal definition of resilience and the notion to persevere stemmed directly from their spouse: “I’ve almost kind of adopted a bit of my husband’s thought process, I guess. You just keep going to get things done” (P8).
Mindset
Our participants indicated that resilience was a mindset that one must choose and that when faced with difficulties, they chose to focus on gratitude, positivity, and growth. For example, Participant 8 stated that, although they had faced and would continue to face challenging and stressful experiences as a result of being a military spouse, they believed that “whatever may come, we’ve been very blessed in our life and we should always be thankful for the life that we have.” Another participant noted that for them, overcoming and persevering meant adopting an optimistic attitude. Specifically, the spouse stated, “sometimes you just have to kinda look at the bright side of things, and you have to find the things that work for you at each place” (P5). One participant drew resilience from a growth mindset:
I think it [resilience] is really a mindset switch. I think it’s changing from “oh this is happening to me, how horrid” to like “how can I take this horrid situation and turn it into something good?” And I think that is a big mindset switch. (P7)
Resilience Variations
Walsh (2012) described risk and resilience as a process of balancing risk and protective factors over the life span. Participants in our study expanded on that idea by suggesting that they reacted to situational challenges along a continuum:
I think what I’m saying is there’s different levels of resilience, like sometimes you have to tap into that different part of yourself. Sometimes you have to let it go and just accept the things that come, and sometimes you just gotta pick yourself up and keep on trucking. (P8)
Likewise, Participant 3 suggested that resilience takes different forms depending on the situation:
Sometimes resiliency just means like surviving day to day and other times, it means figuring out how to continue with your passions to the best of your ability while also supporting your family and your [service member spouse]. I think it’s just super unique to every situation. (P3)
Our participants also recognized that their understanding of resilience was often focused on the here and now of their situation but that their reactions to stressors had long-term effects. One participant indicated that resilience is a learning process and recognized that the stressors they overcome now prepare them to address stressors they will face in the future: “I think being able to come out of extremely, extremely stressful situations, be able to come out on the other side and [know] I’m okay and I survived this, and now I’m kind of better prepared for next time” (P6). Participant 3 wondered about the long-term ramifications of resilience in the face of prolonged adversity, stating “I may be resilient right now in the moment, but in the long term, like, how will this affect me?”
Individualized
Finally, participants defined resilience as an individualized process, stating things such as “everybody has their own unique ways of being resilient, and I think that they do what works best for their families” (P7) and “my resiliency may look different than someone else’s resiliency” (P2). One participant elaborated on this individualized approach to resilience by recognizing that each person has different risk factors that affect their response to stressors, thus affecting the way each person demonstrates resilience. This participant stated that, when viewing resilience among military spouses as a whole, it is important to
take into consideration somebody’s upbringing and the baggage that they bring into this life. We don’t know what people have gone through as kids, and that I think would have a big impact on whether or not someone can be resilient, so I don’t think it’s a one-size-fits-all. (P6)
Theme 2: Challenges Within the Military Lifestyle
Lack of Control
The spouses described the common challenges of the military lifestyle to their resilience. First, they discussed the stress of the feeling of a lack of control in their lives. One participant described how she
just found out yesterday that my husband was getting deployed and he’s leaving Sunday. And I keep hearing people say, “You have to be resilient. You’re gonna be okay!” You’re resilient, but right now, what it feels like is how much can you endure for the sake of the mission? (P1)
Another echoed this sentiment: “I have no control if the Navy says they’re going to deploy my husband. There’s nothing I can do to change that” (P8).
Constant Changes
Another common challenge mentioned among all of the participants was the constant changes they experience in their lives, including moving, career changes, and changes within their family dynamics. Because they move every few years, the spouses described how they are constantly separated from their support systems: “Even though you meet these great people, you don’t get to stay with them . . . and you’re generally not near your family, which is very hard” (P5). Another described how “Once I have started on something and I’m like, ‘This is it, we gon’ be here for a while,’ then my husband is like ‘nope. Military said we got to shift and move again’”(P2).
These constant changes resulted in career struggles for the spouses. One asked, “How can I get this [job] if I’m never at one place for long? . . . How do I uproot everything that I know or everything that I am doing to follow my service member?” (P2). Another described how “moving, changing jobs, not being able to have a secure profession, you do it because you have to . . . but that doesn’t mean that there’s not a whole lot of emotional and mental load that goes with it” (P3).
Another challenge for military spouses was constantly changing family dynamics. One described the difficulty in constantly changing work schedules: “We have to kind of get into this routine without him and then when he comes back, because it’s different while he’s away. We gotta kind of try to fit him back into our routine when he gets back” (P4). Another discussed the challenge of transitioning to being the sole caregiver during a deployment: “If I go down with COVID, what am I going to do? Because, like, I was literally IT. No one is going to want to take my kids. . . . That was the first time I ever felt, like, fearful” (P7).
Mission Priority
In addition to constant change, the spouses also mentioned the challenges of the military’s clear prioritization of the mission above military members and their families: “If something is going on at home, we’re going to take care of our active person first and worry about your family later” (P2). The participants described how this focus on the mission is so intense that it affects service members physically, which increases the burden on military spouses to care for them: “My husband’s health suffers because the mission is most important to him” (P1).
Theme 3: Outside Expectations of Spouse Resilience
Expectation to “Suck It Up”
The spouses described others’ expectations for their resilience. First, they described the military’s expectation that they “suck it up.” One described how “you have a lot of the ‘suck-it-up’ mentality, and I would say when you have the leaders who kind of fall under that, whether it’s seeking the mental health treatment or having stigmas with that” (P6). Another explained that “there’s so much focus and emphasis on just being resilient and sucking it up” so there is often a mindset of “‘Oh well, military spouses are resilient so they signed up for this, they know what it takes and they just have to get over it’” (P3). Another spouse described how “they put so much pressure on you to be like, just make it work, that you’ve gotta figure out the way to make yourself happy, and that’s hard to do” (P5). Participant 7 summed up the military spouse mentality as a whole: “You toughen up and you make it work. You know?”
The participants felt their overall resilience would be enhanced if individuals outside the military community better understood the challenges faced by military families. One participant felt the “suck it up” mentality stemmed less from the military community itself and more from outside communities who might not understand the struggles of military family life: “So when . . . you’re going through another stress of a PCS [permanent change of station], you can’t find a house, they say, well, at least you get a house allowance, at least you get free health care” (P6). Participant 3 expanded on this idea by stating, “I just honestly think that a greater understanding of what sacrifices that military spouses make . . . would increase resiliency, because there’s just so much lack of understanding what it actually entails.” Lastly, one participant mentioned a sentiment they frequently hear from others in a civilian community, expressing that it was frustrating when friends outside the military told her, “I don’t know how you do it,” to which the participant responded, “I don’t know, you just do it!”
Pressure to Be Resilient
The spouses also expressed frustration at others’ misperceptions of the expectation that they and their families demonstrate resilience: “When we call military spouses or children resilient, it just seems like a cop out and relinquishes any type of burden . . . or feeling of guilt about a situation that may cause emotional or mental damage” (P3). Another participant echoed this frustration: “Sometimes I don’t feel like I’m being resilient. Sometimes I feel like I’m just doing what needs to be done because that’s what needs to be done” (P8). Another participant described how her friends
call me Superwoman because I have all these different things going on and I always seem like I got it together. . . . It’s like saying to me that I have to keep going, no matter what, and I think people should be able to just feel defeated sometimes. Or be able to say “that was just too much for me” or “I don’t really feel like being resilient today, I kind of want to lay in bed and just be upset or sad.” (P4)
Given these expectations, one spouse pointed out the danger of expecting military children to consistently demonstrate resilience:
It’s so easy for everyone to say that military kids are always so resilient and sometimes they’re not. Sometimes they are stressed out. They are feeling the crushing weight. They feel sad but everyone keeps telling them that they’re resilient. So it almost makes it seem like . . . they aren’t allowed to feel those hard things or talk about those things or act on those feelings and emotions. (P8)
One spouse proposed a solution to these misperceptions, emphasizing that resilience is unique for military spouses and should be defined to accurately reflect the way they uniquely overcome challenges:
I think it’s important for military spouses to reappropriate that term [resilience] so that it is not weaponized, and I would like to see some sort of guidance as to how we can be resilient but in a way that positively impacts our mental health and physical health and not having to endure all of the things and all of the frustration and uncertainty that comes with the onset of having to be resilient. (P1)
Theme 4: Sense of Responsibility for Family’s Resilience
With their partners focused on the mission, the spouses described their sense of responsibility to maintain their resilience so they can care for their children in the absence of their active-duty spouse: “We have our husband or our spouses gone so much, we need to be a solid parent at home for our kiddos or our family” (P7). Participant 4 likewise described how “I kind of see myself as holding down the fort, you know, because when my husband is not home it is just me and the kids.” Another explained how “I have three little ones that’s looking up to me and I can’t slip away, depressed, because daddy’s not home” (P2). In the end, the spouses defined resilience as an obligation to their families. Participant 3 described that “I have to be that way for my children.” Participant 4 added that “I think that’s what resilience is like, knowing that you kind of have to carry the load, you know, for your whole family to try to keep us afloat.”
The participants described how this resilience is especially obligatory when the active-duty spouse is unable to be resilient:
I’m kind of taking the lead with our kids . . . but I’ve also kind of had to pour into my husband, you know, because he has those times you know where things are really, really hard for him. I’ve also been like his counselor and his doctor sometimes. (P4)
Theme 5: Individual Resilience
In response to being unable to control many aspects of the military lifestyle, most of the spouses described how they have become independent in order to withstand the constantly changing variables within the military lifestyle. One described being “pretty independent, and I think that helps a lot because I don’t rely on my spouse to do all these things I do” (P5). Another described how being independent resulted in self-confidence and resilience:
You gotta figure out how to do all of it just because you can’t ever rely on the spouse being able to help. But I think being able to come out of extremely, extremely stressful situations, be able to come out on the other side and say “I’m okay, and I survived this, and now I’m kind of better prepared for next time.” (P6)
Another spouse described how maintaining an independent identity was key to separating herself from the stressors of the military lifestyle: “That’s a really important part of being a military spouse. It doesn’t have to be a job specifically, but just something that you can be your own person separate from your husband or your spouse’s job” (P8).
The spouses also described the importance of taking care of themselves physically and mentally in order to maintain their resilience. Many described exercise as key to their mental health and wellness: “My biggest coping mechanism is exercise. I’ve found that no matter where I go, I can exercise” (P5). Another spouse described how she “tried to find a kickball team every place we’ve been to since Okinawa because I figured out it’s a stress relief” (P6). Participant 7 echoed that “working out . . . just helps me. It lowers my stress.” One spouse explained how she defaults to exercise when facing the challenges of the military lifestyle because she knows her “ability to recover quickly is directly tied to the way in which I care for myself” (P1).
Theme 6: Collective Resilience
The participants described their reliance on the collective military spouse community for their survival. One spouse, for example, described a connection with other military spouses as the difference between “doing well and barely surviving” (P6). Another spouse described her reliance on the military spouse community: “Community is what it’s all about. I can’t get through anything without community” (P7). Another spouse echoed this survival mechanism: “This is a beautiful community. It’s an amazing place . . . we all get each other. So I think there are times where it’s really hard . . . but we survive, we get through it. We’re resilient. We got the grit” (P7). Participant 1 explained exactly how the military spouse community offers this support to help spouses survive the challenges of the military lifestyle: “When time calls for it, I think, collectively, we bring our resources together to help pull other military spouses up and try to just forewarn them about what the obstacles are and what may have worked for our family” (P1).
The military spouses also described the comfort they found in other military spouses’ understanding of the challenges they face: “I think the most important part and coping is finding your community, so making sure you’re surrounding yourself with women who are going through similar experiences, or who have gone through similar experiences and similar life stages” (P3).
In the midst of this supportive community, the spouses discussed how they actively seek to comfort each other: “You’re not the only one who’s in it who’s having this issue, I understand that you’ll get through this, that we know we’ve been there, we understand how it goes” (P5). This outreach seemed to be especially helpful from spouses who were more experienced with the military lifestyle: “Having that senior spouse example has been so good. . . . She’s always been somebody who said, ‘Hey, I’ve been through a lot. If you ever have any questions, I’m always here for you’” (P8).
In addition to relying on other spouses for their own wellness and resilience, the spouses expressed pride in their ability to contribute to the military spouse community. One described how “I feel like I am a better team player. I feel like I’m more committed to helping others than I have in the past because I know that others will do the same for me” (P7). The participants also described increased self-growth as a result of being a part of a community: “I really don’t think I would have allowed myself to receive help if I hadn’t been part of this phenomenal community that is constantly supporting each other” (P7). Participant 5 echoed this sentiment: “Learning to get that help from other people is something that I feel like you have to kind of get when you are a military spouse because, otherwise, you’re going to have to do everything and you don’t have to.”
Finally, our participants frequently indicated that they felt a “sense of pride” (P7), “connection” (P4), or “camaraderie” (P8) from belonging to a group of military spouses who understood their unique situation. When asked how the military could enhance resilience for military spouses, participants commonly indicated that peer support and fostering connections with senior spouses should be a priority for military commands. One participant noted that their ability to be resilient in difficult times was related to the “opportunities” they had “to connect with other people who are going through similar stuff and who are a part of the same small community” and recommended that the military facilitate more opportunities to connect (P7). Another participant suggested that military commands should “have someone that [the spouse] can talk to” that would “help them to understand the military life whether you are a new spouse or a seasoned spouse” (P2).
Discussion
The purpose of this study was to explore military spouses’ perceptions of their resilience and the ways in which they define resilience for their community. Our study’s results indicate that spouses’ definitions of resilience are currently shaped by service member and mission priority. Our participants also described how they often felt burdened by outside expectations of their resilience as well as by a sense of responsibility for their family’s resilience. Overall, the spouses relied on themselves and the military spouse community to overcome the challenges they faced. Participants expressed a desire for resources aimed specifically at enhancing spouse resilience and more awareness about resilience resources already in place throughout the military.
While past research has examined resilience factors in spouses such as communication skills, social support, and spousal support (Erbes et al., 2017; Richer et al., 2022; Sinclair et al., 2019; Villagran et al., 2013), our study provided new insight into military spouses’ perspectives of their resiliency. This revelation of the spouses’ worldview aids our understanding of ways to best support spouses and areas to focus on to support their resilience. Our participants’ definitions of their resilience were shaped by their relationship with their service member and the influence of the military’s mission. In addition, while past research has indicated that the military lifestyle and culture is challenging for spouses to navigate (Cole et al., 2021; DaLomba et al., 2021; Donoho et al., 2018; Mailey et al. 2018), our participants’ description of their feelings of responsibility for their family’s well-being reveals the added burden that military spouses face as they help their families navigate the military lifestyle. Finally, our participants confirmed that resiliency should be viewed as a variation and is unique to each individual (Pietrzak & Southwick, 2011). As outlined in the professional literature (Masten, 2014; Southwick et al., 2014), the participants confirmed the dynamic nature of resiliency, recognizing that sometimes they felt more resilient than at other times.
In the midst of these challenges, our participants emphasized that the military spouse community serves as a protective factor and a source of their resilience against mental health challenges. This perception of the military spouse community aligns with previous research highlighting the supportive role that spouses play for each other, so much so that it is a protective factor against suicide (Cole et al., 2021). Therefore, military leadership and the counseling community might focus on enhancing this community and connecting spouses with one another—especially more seasoned spouses with newer spouses. In addition, because military-sponsored resilience programs are often targeted to better support service member outcomes, community providers might find ways to focus on supporting the spouses and helping them to overcome the challenges they face in their daily lives.
Finally, the participants discussed how they overcame the challenges of the military lifestyle, including constant moving, deployments, and overall uncertainty, through their own individual and collective resilience. These lifestyle challenges that the participants described correspond to career struggles and shifting family dynamics that cause ongoing stress to the military spouse, both of which have been previously documented in the professional literature (Borah & Fina, 2017; Cole et al., 2021; DaLomba et al., 2021; Donoho et al., 2018; Mailey et al., 2018; Numbers & Bruneau, 2017). Currently, since the withdrawal of troops from Afghanistan, the United States is experiencing peacetime, whereas the nature of future conflicts is uncertain (Marsh & Hampton, 2022). Enhancing the resiliency of military spouses and finding solutions to ongoing stressors is key during this time of peace so that spouses are ready and able to face the stressors of future, potentially large-scale wars (Sefidan et al., 2021).
Implications for Counselors
Professional counselors are called to be trained and ready to meet the unique needs of military spouses, especially in understanding the nature of military culture and its impact on spouse mental health and well-being and enhancing spouse resilience in times of adversity (Cole, 2014). Our study echoes the continued struggles of military spouses described in the professional literature (Cole et al., 2021; Lewy et al., 2014; Runge et al., 2014), suggesting that new and innovative ways of understanding and approaching military spouse resilience is needed within the counseling community. For example, counselors might encourage spouses to explore how their resilience is shaped by the military community in order to increase self-awareness and understanding. They might also help spouses develop their independence and sense of self-efficacy while simultaneously seeking collective support within the military community. Counselors can help spouses examine their social support and help them develop their social skills so they can connect with others around them. Counselors should also help military spouses unpack their perceptions of outsiders’ expectations of their resiliency. Encouraging spouses to reflect on others’ expectations, and the ways in which these expectations impact their sense of well-being, may help define resilience for themselves and capitalize on their unique resiliencies during challenging times. Ultimately, because the military culture is so unique, counselors should seek out professional development so they can better understand how to help military spouses navigate this culture and enhance their resilience. When working with military spouses, professional counselors might explore spouses’ feelings of responsibility for their family members’ health and well-being that were described in our results. In addition, counselors can equip spouses with supportive mental health resources for their family members so they do not feel as if they need to care for them on their own. School counselors, in particular, can provide support for military-connected students at school and can connect military families with resources within both the civilian and military communities to support their mental health and resilience (Cole, 2017; Quintana & Cole, 2021).
Our participants revealed that often the expectation of resilience is burdensome for spouses, which serves as a contradiction to its purposes. Counselors are called to acknowledge the challenges of the military lifestyle and provide support for navigating these challenges, rather than expecting spouses to face these hurdles alone. In addition, counselors might focus on more holistic manifestations of resilience, recognizing that some spouses can be resilient, yet still struggle. Approaching spouses from a strengths-based perspective, rather than from a deficit perspective, can be empowering within the counseling relationship (Smith, 2006).
Limitations
Our recruitment strategy limited our sample size as we only sought participants that we knew through our military spouse networks. In addition, our sample lacked gender diversity, with all of the participants being female. Approximately 91% of active-duty service member spouses are female (DoD, 2022). However, the lack of male participants in the present study is a limitation, and the experience of male spouses is undoubtedly unique and worth exploring in greater depth. Research suggests that stressors and characteristics of resilience transcend gender categories (NASEM, 2019).
Finally, in qualitative research, the researcher’s biases may impact their interpretation of the data. As military spouses, our own experiences may have impacted the way in which we described our participants’ experiences. We took several steps to mitigate these biases, including intentionally bracketing them and engaging in peer debriefing throughout the research process.
Implications for Future Research
The participants in our study described a need for resources and programs geared specifically toward military spouses. Future research might determine how to best develop and implement these programs that will help to enhance spouse resilience. Key areas of focus may be ways to leverage the military spouse community and enhance spouse sense of self, which were two protective factors that emerged from our data. In addition, existing resilience programs within the military that are currently aimed at the active-duty population should undergo a program evaluation to determine their effectiveness with military spouses.
As a follow-up to our qualitative research, future quantitative research studies should address limitations noted previously. Specifically, future research should target a larger sample size and broader demographic of military spouses to further explore their understanding and definition of resilience. This larger and more diverse sample size would allow for greater generalizability and would assist with advocacy within the military. Finally, future qualitative research might explore the perceptions of male spouses, in particular, in order to determine their perception of resiliency and any unique areas of needed support.
Conclusion
Military spouses face a wide range of challenges as a result of the military lifestyle. They are expected to be resilient so as to overcome these challenges. However, our study reveals the often burdensome impact of these expectations on military spouses. Our results also illuminate how spouses uniquely conceptualize their own resilience, recognizing the resilience continuum and focusing on the positive impact of their protective community. Overall, the spouses took pride in themselves and their communities for their ability to overcome obstacles. These revelations are key for both the military and the counseling profession in their work to support military spouses wherever they are on this continuum and enhance their community, which is key to their well-being.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript. The opinions and assertions
expressed herein are those of the authors and
do not reflect the official policy or position of
the Uniformed Services University of the Health
Sciences or the Department of Defense.
References
American Psychological Association. (2020). Building your resilience. https://www.apa.org/topics/resilience/building-your-resilience
Andrade, C. (2021). The inconvenient truth about convenience and purposive samples. Indian Journal of Psychological Medicine, 43(1), 86–88. https://doi.org/10.1177/0253717620977000
Blue Star Families. (2021). Military Family Lifestyle Survey: 2020 comprehensive report. https://bluestarfam.org/wp-content/uploads/2021/03/BSF_MFLS_CompReport_FULL.pdf
Blue Star Families. (2023). Military Family Lifestyle Survey: 2022 comprehensive report. https://bluestarfam.org/wp-content/uploads/2023/03/BSF_MFLS_Spring23_Full_Report_Digital.pdf
Borah, E., & Fina, B. (2017). Military spouses speak up: A qualitative study of military and veteran spouses’ perspectives. Journal of Family Social Work, 20(2), 144–161. https://doi.org/10.1080/10522158.2017.1284702
Cole, R. F. (2014). Understanding military culture: A guide for professional school counselors. The Professional Counselor, 4(5), 497–504. https://doi.org/10.15241/rfc.4.5.497
Cole, R. F. (2017). Supporting students in military families during times of transition: A call for awareness and action. Professional School Counseling, 20(1), 36–43. https://doi.org/10.5330/1096-2409-20.1.36
Cole, R. F., Cowan, R. G., Dunn, H., & Lincoln, T. (2021). Military spouses’ perceptions of suicide in the military spouse community. The Professional Counselor, 11(2), 203–217.
https://doi.org/10.15241/rfc.11.2.203
DaLomba, E., Greer, M. J., Cruz, E., Harris, A., King, C., Laurel, L., McCuaig, T., & Wilder, R. (2021). The experiences of active duty military spouses with advanced degrees in maintaining and advancing their careers. Work, 68(2), 387–398. https://doi.org/10.3233/WOR-203380
Donoho, C. J., LeardMann, C., O’Malley, C. A., Walter, K. H., Riviere, L. A., Curry, J. F., & Adler, A. B. (2018). Depression among military spouses: Demographic, military, and service member psychological health risk factors. Depression and Anxiety, 35(12), 1137–1144. https://doi.org/10.1002/da.22820
Dorvil, M. (2017). 2017 survey of active-duty spouses. Office of People Analytics, U.S. Department of Defense. https://download.militaryones ource.mil/12038/MOS/Surveys/2017-Survey-of-Active-Duty-Spouses-Overview-Briefing.pdf
Erbes, C. R., Kramer, M., Arbisi, P. A., DeGarmo, D., & Polusny, M. A. (2017). Characterizing spouse/partner depression and alcohol problems over the course of military deployment. Journal of Consulting and Clinical Psychology, 85(4), 297–308. https://doi.org/10.1037/ccp0000190
Joining Forces Interagency Policy Committee. (2021). Strengthening America’s military families: Matching their devotion: Deepening our commitment to the families, caregivers, and survivors of service members and veterans. https://www.whitehouse.gov/wp-content/uploads/2021/09/Strengthening_Americas_Military_Families.pdf
Lewy, C. S., Oliver, C. M., & McFarland, B. H. (2014). Barriers to mental health treatment for military wives. Psychiatric Services, 65(9), 1170–1173. https://doi.org/10.1176/appi.ps.201300325
Mailey, E. L., Mershon, C., Joyce, J., & Irwin, B. C. (2018). “Everything else comes first”: A mixed-methods analysis of barriers to health behaviors among military spouses. BMC Public Health, 18(1013), 1–11. https://doi.org/10.1186/s12889-018-5938-z
Marsh, M. K., & Hampton, R. L. (2022). Army medicine’s critical role in large-scale combat operations: Enable the force. Military Review, 102(4), 106–113.
Masten, A. S. (2014). Global perspectives on resilience in children and youth. Child Development, 85(1), 6–20. https://doi.org/10.1111/cdev.12205
Meadows, S. O., Beckett, M. K., Bowling, K., Golinelli, D., Fisher, M. P., Martin, L. T., Meredith, L. S., & Osilla, K. C. (2015). Family resilience in the military: Definitions, models, and policies. RAND Health Quarterly, 5(3).
Moerer-Urdahl, T. & Creswell, J. W. (2004). Using transcendental phenomenology to explore the “ripple effect” in a leadership mentoring program. International Journal of Qualitative Methods, 3(2), 19–35. https://doi.org/10.1177/160940690400300202
Moustafa, A. A., Crouse, J. J., Herzallah, M. M., Salama, M., Mohamed, W., Misiak, B., Frydecka, D., Al-Dosari, N. F., Megreya, A. M., & Mattock, K. (2020). Depression following major life transitions in women: A review and theory. Psychological Reports, 123(5), 1501–1517. https://doi.org/10.1177/0033294119872209
Moustakas, C. (1994). Phenomenological research methods. SAGE.
National Academies of Sciences, Engineering, and Medicine. (2019). Strengthening the military family readiness system for a changing American society. The National Academies Press. https://doi.org/10.17226/25380
Numbers, M., & Bruneau, L. (2017). Creating connections and fostering self-growth: Gestalt group counseling for military spouses. In Ideas and Research You Can Use: VISTAS 2017.
Panter-Brick, C. (2014). Health, risk, and resilience: Interdisciplinary concepts and applications. Annual Review of Anthropology, 43, 431–448. https://doi.org/10.1146/annurev-anthro-102313-025944
Pietrzak, R. H., & Southwick, S. M. (2011). Psychological resilience in OEF-OIF veterans: Application of a novel classification approach and examination of demographic and psychosocial correlates. Journal of Affective Disorders, 133(3), 560–568.
Quintana, T. S., & Cole, R. F. (2021). Forward march: Implementing the ASCA National Model to support military-connected students. Journal of School Counseling, 19(7). http://www.jsc.montana.edu/articles/v19n7.pdf
Richer, I., Frank, C., & Guérin, E. (2022). Understanding Special Operations Forces spouses challenges and resilience: A mixed-method study. Military Behavioral Health, 10(2), 100–111.
https://doi.org/10.1080/21635781.2022.2067921
Runge, C. E., Waller, M., MacKenzie, A., & McGuire, A. C. L. (2014). Spouses of military members’ experiences and insights: Qualitative analysis of responses to an open-ended question in a survey of health and wellbeing. PloS ONE, 9(12), e114755. https://doi.org/10.1371/journal.pone.0114755
Saunders, B., Sim, J., Kingstone, T., Baker, S., Waterfield, J., Bartlam, B., Burroughs, H., & Jinks, C. (2018). Saturation in qualitative research: Exploring its conceptualization and operationalization. Quality & Quantity, 52(4), 1893–1907. https://doi.org/10.1007/s11135-017-0574-8
Sefidan, S., Pramstaller, M., La Marca, R., Wyss, T., Sadeghi-Bahmani, D., Annen, H., & Brand, S. (2021). Resilience as a protective factor in basic military training, a longitudinal study of the Swiss Armed Forces. International Journal of Environmental Research and Public Health, 18(11), 6077. https://doi.org/10.3390/ijerph18116077
Simon, J. B., Murphy, J. J., & Smith, S. M. (2005). Understanding and fostering family resilience. The Family Journal, 13(4), 427–436. https://doi.org/10.1177/1066480705278724
Sinclair, R. R., Paulson, A. L., & Riviere, L. A. (2019). The resilient spouse: Understanding factors associated with dispositional resilience among military spouses. Military Behavioral Health, 7(4), 376–390. https://doi.org/10.1080/21635781.2019.1608876
Smith, E. J. (2006). The strength-based counseling model. The Counseling Psychologist, 34(1), 13–79.
https://doi.org/10.1177/0011000005277018
Southwick, S. M., Bonanno, G. A., Masten, A. S., Panter-Brick, C., & Yehuda, R. (2014). Resilience definitions, theory, and challenges: Interdisciplinary perspectives. European Journal of Psychotraumatology, 5(1), 25338. https://doi.org/10.3402/ejpt.v5.25338
Sullivan, K. S., Hawkins, S. A., Gilreath, T. D., & Castro, C. A. (2021). Mental health outcomes associated with profiles of risk and resilience among U.S. Army spouses. Journal of Family Psychology, 35(1), 33–43. https://doi.org/10.1037/fam0000702
U.S. Department of Defense, Office of the Deputy Assistant Secretary of Defense for Military Community and Family Policy. (2022). 2021 demographics profile: Profile of the military community. https://download.militaryonesource.mil/12038/MOS/Reports/2021-demographics-report.pdf
Verdeli, H., Baily, C., Vousoura, E., Belser, A., Singla, D., & Manos, G. (2011). The case for treating depression in military spouses. Journal of Family Psychology, 25(4), 488–496. https://doi.org/10.1037/a0024525
Villagran, M., Canzona, M. R., & Ledford, C. J. W. (2013). The milspouse battle rhythm: Communicating resilience throughout the deployment cycle. Health Communication, 28(8), 778–788. https://doi.org/10.1080/10410236.2013.800441
Walsh, F. (2012). Family resilience: Strengths forged through adversity. In F. Walsh (Ed.), Normal family processes: Growing diversity and complexity (4th ed.; pp. 399–423). Guilford.
Rebekah Cole, PhD, MEd, NCC, LPC, is a research associate professor at the Uniformed Services University. Christine Ward, PhD, is an associate professor at Walsh University. Taqueena Quintana, EdD, NCC, ACS, BC-TMH, LPC, is an associate professor at Antioch University. Elizabeth Burgin, PhD, NCC, LPC, RPT, CCCPTS, is an assistant professor and program coordinator of the Military and Veterans Counseling program at William & Mary. Correspondence may be addressed to Rebekah Cole, rebekah.cole@usuhs.edu.
Appendix
Interview Protocol
- Tell me a little about your identity as a military spouse?
- What have been some of your rewarding experiences as a military spouse?
- What have been some of your stressful experiences as a military spouse?
- How have you coped with the more stressful experiences as a military spouse?
- How would you describe the military’s definition of “resilience?”
- What does the term “resilience” mean to you?
- What does the term “resilience” mean for your military partner/family?
- How would you describe the resilience of military spouses?
- In what ways have you, personally, been resilient as a military spouse?
- What would enhance the resilience of military spouses and their families, from your perspective?
- How, if at all, has your military experience enhanced your resilience?
- How, if at all, has the military’s focus on resilience presented you with challenges during your military spouse experiences?
- How, if at all, can resilience be a negative way to describe military spouses/families?
- Is there anything else about military resilience that is important to you that I did not ask about?
Aug 20, 2021 | Author Videos, Volume 11 - Issue 3
Warren N. Ponder, Elizabeth A. Prosek, Tempa Sherrill
First responders are continually exposed to trauma-related events. Resilience is evidenced as a protective factor for mental health among first responders. However, there is a lack of assessments that measure the construct of resilience from a strength-based perspective. The present study used archival data from a treatment-seeking sample of 238 first responders to validate the 22-item Response to Stressful Experiences Scale (RSES-22) and its abbreviated version, the RSES-4, with two confirmatory factor analyses. Using a subsample of 190 first responders, correlational analyses were conducted of the RSES-22 and RSES-4 with measures of depressive symptoms, post-traumatic stress, anxiety, and suicidality confirming convergent and criterion validity. The two confirmatory analyses revealed a poor model fit for the RSES-22; however, the RSES-4 demonstrated an acceptable model fit. Overall, the RSES-4 may be a reliable and valid measure of resilience for treatment-seeking first responder populations.
Keywords: first responders, resilience, assessment, mental health, confirmatory factor analysis
First responder populations (i.e., law enforcement, emergency medical technicians, and fire rescue) are often repeatedly exposed to traumatic and life-threatening conditions (Greinacher et al., 2019). Researchers have concluded that such critical incidents could have a deleterious impact on first responders’ mental health, including the development of symptoms associated with post-traumatic stress, anxiety, depression, or other diagnosable mental health disorders (Donnelly & Bennett, 2014; Jetelina et al., 2020; Klimley et al., 2018; Weiss et al., 2010). In a systematic review, Wild et al. (2020) suggested the promise of resilience-based interventions to relieve trauma-related psychological disorders among first responders. However, they noted the operationalization and measure of resilience as limitations to their intervention research. Indeed, researchers have conflicting viewpoints on how to define and assess resilience. For example, White et al. (2010) purported popular measures of resilience rely on a deficit-based approach. Counselors operate from a strength-based lens (American Counseling Association [ACA], 2014) and may prefer measures with a similar perspective. Additionally, counselors are mandated to administer assessments with acceptable psychometric properties that are normed on populations representative of the client (ACA, 2014, E.6.a., E.7.d.). For counselors working with first responder populations, resilience may be a factor of importance; however, appropriately measuring the construct warrants exploration. Therefore, the focus of this study was to validate a measure of resilience with strength-based principles among a sample of first responders.
Risk and Resilience Among First Responders
In a systematic review of the literature, Greinacher et al. (2019) described the incidents that first responders may experience as traumatic, including first-hand life-threatening events; secondary exposure and interaction with survivors of trauma; and frequent exposure to death, dead bodies, and injury. Law enforcement officers (LEOs) reported that the most severe critical incidents they encounter are making a mistake that injures or kills a colleague; having a colleague intentionally killed; and making a mistake that injures or kills a bystander (Weiss et al., 2010). Among emergency medical technicians (EMTs), critical incidents that evoked the most self-reported stress included responding to a scene involving family, friends, or others to the crew and seeing someone dying (Donnelly & Bennett, 2014). Exposure to these critical incidents may have consequences for first responders. For example, researchers concluded first responders may experience mental health symptoms as a result of the stress-related, repeated exposure (Jetelina et al., 2020; Klimley et al., 2018; Weiss et al., 2010). Moreover, considering the cumulative nature of exposure (Donnelly & Bennett, 2014), researchers concluded first responders are at increased risk for post-traumatic stress disorder (PTSD), depression, and generalized anxiety symptoms (Jetelina et al., 2020; Klimley et al., 2018; Weiss et al., 2010). Symptoms commonly experienced among first responders include those associated with post-traumatic stress, anxiety, and depression.
In a collective review of first responders, Kleim and Westphal (2011) determined a prevalence rate for PTSD of 8%–32%, which is higher than the general population lifetime rate of 6.8–7.8 % (American Psychiatric Association [APA], 2013; National Institute of Mental Health [NIMH], 2017). Some researchers have explored rates of PTSD by specific first responder population. For example, Klimley et al. (2018) concluded that 7%–19% of LEOs and 17%–22% of firefighters experience PTSD. Similarly, in a sample of LEOs, Jetelina and colleagues (2020) reported 20% of their participants met criteria for PTSD.
Generalized anxiety and depression are also prevalent mental health symptoms for first responders. Among a sample of firefighters and EMTs, 28% disclosed anxiety at moderate–severe and several levels (Jones et al., 2018). Furthermore, 17% of patrol LEOs reported an overall prevalence of generalized anxiety disorder (Jetelina et al., 2020). Additionally, first responders may be at higher risk for depression (Klimley et al., 2018), with estimated prevalence rates of 16%–26% (Kleim & Westphal, 2011). Comparatively, the past 12-month rate of major depressive disorder among the general population is 7% (APA, 2013). In a recent study, 16% of LEOs met criteria for major depressive disorder (Jetelina et al., 2020). Moreover, in a sample of firefighters and EMTs, 14% reported moderate–severe and severe depressive symptoms (Jones et al., 2018). Given these higher rates of distressful mental health symptoms, including post-traumatic stress, generalized anxiety, and depression, protective factors to reduce negative impacts are warranted.
Resilience
Broadly defined, resilience is “the ability to adopt to and rebound from change (whether it is from stress or adversity) in a healthy, positive and growth-oriented manner” (Burnett, 2017, p. 2). White and colleagues (2010) promoted a positive psychology approach to researching resilience, relying on strength-based characteristics of individuals who adapt after a stressor event. Similarly, other researchers explored how individuals’ cognitive flexibility, meaning-making, and restoration offer protection that may be collectively defined as resilience (Johnson et al., 2011).
A key element among definitions of resilience is one’s exposure to stress. Given their exposure to trauma-related incidents, first responders require the ability to cope or adapt in stressful situations (Greinacher et al., 2019). Some researchers have defined resilience as a strength-based response to stressful events (Burnett, 2017), in which healthy coping behaviors and cognitions allow individuals to overcome adverse experiences (Johnson et al., 2011; White et al., 2010). When surveyed about positive coping strategies, first responders most frequently reported resilience as important to their well-being (Crowe et al., 2017).
Researchers corroborated the potential impact of resilience for the population. For example, in samples of LEOs, researchers confirmed resilience served as a protective factor for PTSD (Klimley et al., 2018) and as a mediator between social support and PTSD symptoms (McCanlies et al., 2017). In a sample of firefighters, individual resilience mediated the indirect path between traumatic events and global perceived stress of PTSD, along with the direct path between traumatic events and PTSD symptoms (Lee et al., 2014). Their model demonstrated that those with higher levels of resilience were more protected from traumatic stress. Similarly, among emergency dispatchers, resilience was positively correlated with positive affect and post-traumatic growth, and negatively correlated with job stress (Steinkopf et al., 2018). The replete associations of resilience as a protective factor led researchers to develop resilience-based interventions. For example, researchers surmised promising results from mindfulness-based resilience interventions for firefighters (Joyce et al., 2019) and LEOs (Christopher et al., 2018). Moreover, Antony and colleagues (2020) concluded that resilience training programs demonstrated potential to reduce occupational stress among first responders.
Assessment of Resilience
Recognizing the significance of resilience as a mediating factor in PTSD among first responders and as a promising basis for interventions when working with LEOs, a reliable means to measure it among first responder clients is warranted. In a methodological review of resilience assessments, Windle and colleagues (2011) identified 19 different measures of resilience. They found 15 assessments were from original development and validation studies with four subsequent validation manuscripts from their original assessment, of which none were developed with military or first responder samples.
Subsequently, Johnson et al. (2011) developed the Response to Stressful Experiences Scale (RSES-22) to assess resilience among military populations. Unlike deficit-based assessments of resilience, they proposed a multidimensional construct representing how individuals respond to stressful experiences in adaptive or healthy ways. Cognitive flexibility, meaning-making, and restoration were identified as key elements when assessing for individuals’ characteristics connected to resilience when overcoming hardships. Initially they validated a five-factor structure for the RSES-22 with military active-duty and reserve components. Later, De La Rosa et al. (2016) re-examined the RSES-22. De La Rosa and colleagues discovered a unidimensional factor structure of the RSES-22 and validated a shorter 4-item subset of the instrument, the RSES-4, again among military populations.
It is currently unknown if the performance of the RSES-4 can be generalized to first responder populations. While there are some overlapping experiences between military populations and first responders in terms of exposure to trauma and high-risk occupations, the Substance Abuse and Mental Health Services Administration (SAMHSA; 2018) suggested differences in training and types of risk. In the counseling profession, these populations are categorized together, as evidenced by the Military and Government Counseling Association ACA division. Additionally, there may also be dual identities within the populations. For example, Lewis and Pathak (2014) found that 22% of LEOs and 15% of firefighters identified as veterans. Although the similarities of the populations may be enough to theorize the use of the same resilience measure, validation of the RSES-22 and RSES-4 among first responders remains unexamined.
Purpose of the Study
First responders are repeatedly exposed to traumatic and stressful events (Greinacher et al., 2019) and this exposure may impact their mental health, including symptoms of post-traumatic stress, anxiety, depression, and suicidality (Jetelina et al., 2020; Klimley et al., 2018). Though most measures of resilience are grounded in a deficit-based approach, researchers using a strength-based approach proposed resilience may be a protective factor for this population (Crowe et al., 2017; Wild et al., 2020). Consequently, counselors need a means to assess resilience in their clinical practice from a strength-based conceptualization of clients.
Johnson et al. (2011) offered a non-deficit approach to measuring resilience in response to stressful events associated with military service. Thus far, researchers have conducted analyses of the RSES-22 and RSES-4 with military populations (De La Rosa et al., 2016; Johnson et al., 2011; Prosek & Ponder, 2021), but not yet with first responders. While there are some overlapping characteristics between the populations, there are also unique differences that warrant research with discrete sampling (SAMHSA, 2018). In light of the importance of resilience as a protective factor for mental health among first responders, the purpose of the current study was to confirm the reliability and validity of the RSES-22 and RSES-4 when utilized with this population. In the current study, we hypothesized the measures would perform similarly among first responders and if so, the RSES-4 would offer counselors a brief assessment option in clinical practice that is both reliable and valid.
Method
Participants
Participants in the current non-probability, purposive sample study were first responders (N = 238) seeking clinical treatment at an outpatient, mental health nonprofit organization in the Southwestern United States. Participants’ mean age was 37.53 years (SD = 10.66). The majority of participants identified as men (75.2%; n = 179), with women representing 24.8% (n = 59) of the sample. In terms of race and ethnicity, participants identified as White (78.6%; n = 187), Latino/a (11.8%; n = 28), African American or Black (5.5%; n = 13), Native American (1.7%; n = 4), Asian American (1.3%; n = 3), and multiple ethnicities (1.3%; n = 3). The participants identified as first responders in three main categories: LEO (34.9%; n = 83), EMT (28.2%; n = 67), and fire rescue (25.2%; n = 60). Among the first responders, 26.9% reported previous military affiliation. As part of the secondary analysis, we utilized a subsample (n = 190) that was reflective of the larger sample (see Table 1).
Procedure
The data for this study were collected between 2015–2020 as part of the routine clinical assessment procedures at a nonprofit organization serving military service members, first responders, frontline health care workers, and their families. The agency representatives conduct clinical assessments with clients at intake, Session 6, Session 12, and Session 18 or when clinical services are concluded. We consulted with the second author’s Institutional Review Board, which determined the research as exempt, given the de-identified, archival nature of the data. For inclusion in this analysis, data needed to represent first responders, ages 18 or older, with a completed RSES-22 at intake. The RSES-4 are four questions within the RSES-22 measure; therefore, the participants did not have to complete an additional measure. For the secondary analysis, data from participants who also completed other mental health measures at intake were also included (see Measures).
Table 1
Demographics of Sample
| Characteristic |
Sample 1
(N = 238) |
Sample 2
(n = 190) |
| Age (Years) |
|
|
| Mean |
37.53 |
37.12 |
| Median |
35.50 |
35.00 |
| SD |
10.66 |
10.30 |
| Range |
46 |
45 |
| Time in Service (Years) |
|
|
| Mean |
11.62 |
11.65 |
| Median |
10.00 |
10.00 |
| SD |
9.33 |
9.37 |
| Range |
41 |
39 |
|
n (%) |
| First Responder Type |
|
|
Emergency Medical
Technicians |
67 (28.2%) |
54 (28.4%) |
| Fire Rescue |
60 (25.2%) |
45 (23.7%) |
| Law Enforcement |
83 (34.9%) |
72 (37.9%) |
| Other |
9 (3.8%) |
5 (2.6%) |
| Two or more |
10 (4.2%) |
6 (3.2%) |
| Not reported |
9 (3.8%) |
8 (4.2%) |
| Gender |
|
|
| Women |
59 (24.8%) |
47 (24.7%) |
| Men |
179 (75.2%) |
143 (75.3%) |
| Ethnicity |
|
|
| African American/Black |
13 (5.5%) |
8 (4.2%) |
| Asian American |
3 (1.3%) |
3 (1.6%) |
| Latino(a)/Hispanic |
28 (11.8%) |
24 (12.6%) |
| Multiple Ethnicities |
3 (1.3%) |
3 (1.6%) |
| Native American |
4 (1.7%) |
3 (1.6%) |
| White |
187 (78.6%) |
149 (78.4%) |
Note. Sample 2 is a subset of Sample 1. Time in service for Sample 1, n = 225;
time in service for Sample 2, n = 190.
Measures
Response to Stressful Experiences Scale
The Response to Stressful Experiences Scale (RSES-22) is a 22-item measure to assess dimensions of resilience, including meaning-making, active coping, cognitive flexibility, spirituality, and self-efficacy (Johnson et al., 2011). Participants respond to the prompt “During and after life’s most stressful events, I tend to” on a 5-point Likert scale from 0 (not at all like me) to 4 (exactly like me). Total scores range from 0 to 88 in which higher scores represent greater resilience. Example items include see it as a challenge that will make me better, pray or meditate, and find strength in the meaning, purpose, or mission of my life. Johnson et al. (2011) reported the RSES-22 demonstrates good internal consistency (α = .92) and test-retest reliability (α = .87) among samples from military populations. Further, the developers confirmed convergent, discriminant, concurrent, and incremental criterion validity (see Johnson et al., 2011). In the current study, Cronbach’s alpha of the total score was .93.
Adapted Response to Stressful Experiences Scale
The adapted Response to Stressful Experiences Scale (RSES-4) is a 4-item measure to assess resilience as a unidimensional construct (De La Rosa et al., 2016). The prompt and Likert scale are consistent with the original RSES-22; however, it only includes four items: find a way to do what’s necessary to carry on, know I will bounce back, learn important and useful life lessons, and practice ways to handle it better next time. Total scores range from 0 to 16, with higher scores indicating greater resilience. De La Rosa et al. (2016) reported acceptable internal consistency (α = .76–.78), test-retest reliability, and demonstrated criterion validity among multiple military samples. In the current study, the Cronbach’s alpha of the total score was .74.
Patient Health Questionnaire-9
The Patient Health Questionnaire-9 (PHQ-9) is a 9-item measure to assess depressive symptoms in the past 2 weeks (Kroenke et al., 2001). Respondents rate the frequency of their symptoms on a 4-point Likert scale ranging from 0 (not at all) to 3 (nearly every day). Total scores range from 0 to 27, in which higher scores indicate increased severity of depressive symptoms. Example items include little interest or pleasure in doing things and feeling tired or having little energy. Kroenke et al. (2001) reported good internal consistency (α = .89) and established criterion and construct validity. In this sample, Cronbach’s alpha of the total score was .88.
PTSD Checklist-5
The PTSD Checklist-5 (PCL-5) is a 20-item measure for the presence of PTSD symptoms in the past month (Blevins et al., 2015). Participants respond on a 5-point Likert scale indicating frequency of PTSD-related symptoms from 0 (not at all) to 4 (extremely). Total scores range from 0 to 80, in which higher scores indicate more severity of PTSD-related symptoms. Example items include repeated, disturbing dreams of the stressful experience and trouble remembering important parts of the stressful experience. Blevins et al. (2015) reported good internal consistency (α = .94) and determined convergent and discriminant validity. In this sample, Cronbach’s alpha of the total score was .93.
Generalized Anxiety Disorder-7
The Generalized Anxiety Disorder-7 (GAD-7) is a 7-item measure to assess for anxiety symptoms over the past 2 weeks (Spitzer et al., 2006). Participants rate the frequency of the symptoms on a 4-point Likert scale ranging from 0 (not at all) to 3 (nearly every day). Total scores range from 0 to 21 with higher scores indicating greater severity of anxiety symptoms. Example items include not being able to stop or control worrying and becoming easily annoyed or irritable. Among patients from primary care settings, Spitzer et al. (2006) determined good internal consistency (α = .92) and established criterion, construct, and factorial validity. In this sample, Cronbach’s alpha of the total score was .91.
Suicidal Behaviors Questionnaire-Revised
The Suicidal Behaviors Questionnaire-Revised (SBQ-R) is a 4-item measure to assess suicidality (Osman et al., 2001). Each item assesses a different dimension of suicidality: lifetime ideation and attempts, frequency of ideation in the past 12 months, threat of suicidal behaviors, and likelihood of suicidal behaviors (Gutierrez et al., 2001). Total scores range from 3 to 18, with higher scores indicating more risk of suicide. Example items include How often have you thought about killing yourself in the past year? and How likely is it that you will attempt suicide someday? In a clinical sample, Osman et al. (2001) reported good internal consistency (α = .87) and established criterion validity. In this sample, Cronbach’s alpha of the total score was .85.
Data Analysis
Statistical analyses were conducted using SPSS version 26.0 and SPSS Analysis of Moment Structures (AMOS) version 26.0. We examined the dataset for missing values, replacing 0.25% (32 of 12,836 values) of data with series means. We reviewed descriptive statistics of the RSES-22 and RSES-4 scales. We determined multivariate normality as evidenced by skewness less than 2.0 and kurtosis less than 7.0 (Dimitrov, 2012). We assessed reliability for the scales by interpreting Cronbach’s alphas and inter-item correlations to confirm internal consistency.
We conducted two separate confirmatory factor analyses to determine the model fit and factorial validity of the 22-item measure and adapted 4-item measure. We used several indices to conclude model fit: minimum discrepancy per degree of freedom (CMIN/DF) and p-values, root mean residual (RMR), goodness-of-fit index (GFI), comparative fit index (CFI), Tucker-Lewis index (TLI), and the root mean square error of approximation (RMSEA). According to Dimitrov (2012), values for the CMIN/DF < 2.0,p > .05, RMR < .08, GFI > .90, CFI > .90, TLI > .90, and RMSEA < .10 provide evidence of a strong model fit. To determine criterion validity, we assessed a subsample of participants (n = 190) who had completed the RSES-22, RSES-4, and four other psychological measures (i.e., PHQ-9, PCL-5, GAD-7, and SBQ-R). We determined convergent validity by conducting bivariate correlations between the RSES-22 and RSES-4.
Results
Descriptive Analyses
We computed means, standard deviations, 95% confidence interval (CI), and score ranges for the RSES-22 and RSES-4 (Table 2). Scores on the RSES-22 ranged from 19–88. Scores on the RSES-4 ranged from 3–16. Previous researchers using the RSES-22 on military samples reported mean scores of 57.64–70.74 with standard deviations between 8.15–15.42 (Johnson et al., 2011; Prosek & Ponder, 2021). In previous research of the RSES-4 with military samples, mean scores were 9.95–11.20 with standard deviations between 3.02–3.53(De La Rosa et al., 2016; Prosek & Ponder, 2021).
Table 2
Descriptive Statistics for RSES-22 and RSES-4
| Variable |
M |
SD |
95% CI |
Score Range |
| RSES-22 scores |
60.12 |
13.76 |
58.52, 61.86 |
19–88 |
| RSES-4 scores |
11.66 |
2.62 |
11.33, 11.99 |
3–16 |
Note. N = 238. RSES-22 = Response to Stressful Experiences Scale 22-item; RSES-4 = Response
to Stressful Experiences Scale 4-item adaptation.
Reliability Analyses
To determine the internal consistency of the resiliency measures, we computed Cronbach’s alphas. For the RSES-22, we found strong evidence of inter-item reliability (α = .93), which was consistent with the developers’ estimates (α = .93; Johnson et al., 2011). For the RSES-4, we assessed acceptable inter-item reliability (α = .74), which was slightly lower than previous estimates (α = .76–.78; De La Rosa et al., 2016). We calculated the correlation between items and computed the average of all the coefficients. The average inter-item correlation for the RSES-22 was .38, which falls within the acceptable range (.15–.50). The average inter-item correlation for the RSES-4 was .51, slightly above the acceptable range. Overall, evidence of internal consistency was confirmed for each scale.
Factorial Validity Analyses
We conducted two confirmatory factor analyses to assess the factor structure of the RSES-22 and RSES-4 for our sample of first responders receiving mental health services at a community clinic (Table 3). For the RSES-22, a proper solution converged in 10 iterations. Item loadings ranged between .31–.79, with 15 of 22 items loading significantly ( > .6) on the latent variable. It did not meet statistical criteria for good model fit: χ2 (209) = 825.17, p = .000, 90% CI [0.104, 0.120]. For the RSES-4, a proper solution converged in eight iterations. Item loadings ranged between .47–.80, with three of four items loading significantly ( > .6) on the latent variable. It met statistical criteria for good model fit: χ2 (2) = 5.89, p = .053, 90% CI [0.000, 0.179]. The CMIN/DF was above the suggested < 2.0 benchmark; however, the other fit indices indicated a model fit.
Table 3
Confirmatory Factor Analysis Fit Indices for RSES-22 and RSES-4
| Variable |
df |
χ2 |
CMIN/DF |
RMR |
GFI |
CFI |
TLI |
RMSEA |
90% CI |
| RSES-22 |
209 |
825.17/.000 |
3.95 |
.093 |
.749 |
.771 |
0.747 |
.112 |
0.104, 0.120 |
| RSES-4 |
2 |
5.89/.053 |
2.94 |
.020 |
.988 |
.981 |
0.944 |
.091 |
0.000, 0.179 |
Note. N = 238. RSES-22 = Response to Stressful Experiences Scale 22-item; RSES-4 = Response to Stressful Experiences Scale 4-item adaptation; CMIN/DF = Minimum Discrepancy per Degree of Freedom; RMR = Root Mean Square Residual;
GFI = Goodness-of-Fit Index; CFI = Comparative Fit Index; TLI = Tucker-Lewis Index; RMSEA = Root Mean Squared Error of Approximation.
Criterion and Convergent Validity Analyses
To assess for criterion validity of the RSES-22 and RSES-4, we conducted correlational analyses with four established psychological measures (Table 4). We utilized a subsample of participants (n = 190) who completed the PHQ-9, PCL-5, GAD-7, and SBQ-R at intake. Normality of the data was not a concern because analyses established appropriate ranges for skewness and kurtosis (± 1.0). The internal consistency of the RSES-22 (α = .93) and RSES-4 (α = .77) of the subsample was comparable to the larger sample and previous studies. The RSES-22 and RSES-4 related to the psychological measures of distress in the expected direction, meaning measures were significantly and negatively related, indicating that higher resiliency scores were associated with lower scores of symptoms associated with diagnosable mental health disorders (i.e., post-traumatic stress, anxiety, depression, and suicidal behavior). We verified convergent validity with a correlational analysis of the RSES-22 and RSES-4, which demonstrated a significant and positive relationship.
Table 4
Criterion and Convergent Validity of RSES-22 and RSES-4
|
M (SD) |
Cronbach’s α |
RSES-22 |
PHQ-9 |
PCL-5 |
GAD-7 |
SBQ-R |
| RSES-22 |
60.16 (14.17) |
.93 |
— |
−.287* |
−.331* |
−.215* |
−.346* |
| RSES-4 |
11.65 (2.68) |
.77 |
.918 |
−.290* |
−.345* |
−.220* |
−.327* |
Note. n = 190. RSES-22 = Response to Stressful Experiences Scale 22-item; RSES-4 = Response to Stressful Experiences Scale 4-item adaptation; PHQ-9 = Patient Health Questionnaire-9;
PCL-5 = PTSD Checklist-5; GAD-7 = Generalized Anxiety Disorder-7; SBQ-R = Suicidal Behaviors Questionnaire-Revised.
*p < .01.
Discussion
The purpose of this study was to validate the factor structure of the RSES-22 and the abbreviated RSES-4 with a first responder sample. Aggregated means were similar to those in the articles that validated and normed the measures in military samples (De La Rosa et al., 2016; Johnson et al., 2011; Prosek & Ponder, 2021). Additionally, the internal consistency was similar to previous studies. In the original article, Johnson et al. (2011) proposed a five-factor structure for the RSES-22, which was later established as a unidimensional assessment after further exploratory factor analysis (De La Rosa et al., 2016). Subsequently, confirmatory factor analyses with a treatment-seeking veteran population revealed that the RSES-22 demonstrated unacceptable model fit, whereas the RSES-4 demonstrated a good model fit (Prosek & Ponder, 2021). In both samples, the RSES-4 GFI, CFI, and TLI were all .944 or higher, whereas the RSES-22 GFI, CFI, and TLI were all .771 or lower. Additionally, criterion and convergent validity as measured by the PHQ-9, PCL-5, and GAD-7 in both samples were extremely close. Similarly, in this sample of treatment-seeking first responders, confirmatory factor analyses indicated an inadequate model fit for the RSES-22 and a good model fit for the RSES-4. Lastly, convergent and criterion validity were established with correlation analyses of the RSES-22 and RSES-4 with four other standardized assessment instruments (i.e., PHQ-9, PCL-5, GAD-7, SBQ-R). We concluded that among the first responder sample, the RSES-4 demonstrated acceptable psychometric properties, as well as criterion and convergent validity with other mental health variables (i.e., post-traumatic stress, anxiety, depression, and suicidal behavior).
Implications for Clinical Practice
First responders are a unique population and are regularly exposed to trauma (Donnelly & Bennett, 2014; Jetelina et al., 2020; Klimley et al., 2018; Weiss et al., 2010). Although first responders could potentially benefit from espousing resilience, they are often hesitant to seek mental health services (Crowe et al., 2017; Jones, 2017). The RSES-22 and RSES-4 were originally normed with military populations. The results of the current study indicated initial validity and reliability among a first responder population, revealing that the RSES-4 could be useful for counselors in assessing resilience.
It is important to recognize that first responders have perceived coping with traumatic stress as an individual process (Crowe et al., 2017) and may believe that seeking mental health services is counter to the emotional and physical training expectations of the profession (Crowe et al., 2015). Therefore, when first responders seek mental health care, counselors need to be prepared to provide culturally responsive services, including population-specific assessment practices and resilience-oriented care.
Jones (2017) encouraged a comprehensive intake interview and battery of appropriate assessments be conducted with first responder clients. Counselors need to balance the number of intake questions while responsibly assessing for mental health comorbidities such as post-traumatic stress, anxiety, depression, and suicidality. The RSES-4 provides counselors a brief, yet targeted assessment of resilience.
Part of what cultural competency entails is assessing constructs (e.g., resilience) that have been shown to be a protective factor against PTSD among first responders (Klimley et al., 2018). Since the items forming the RSES-4 were developed to highlight the positive characteristics of coping (Johnson et al., 2011), rather than a deficit approach, this aligns with the grounding of the counseling profession. It is also congruent with first responders’ perceptions of resilience. Indeed, in a content analysis of focus group interviews with first responders, participants defined resilience as a positive coping strategy that involves emotional regulation, perseverance, personal competence, and physical fitness (Crowe et al., 2017).
The RSES-4 is a brief, reliable, and valid measure of resilience with initial empirical support among a treatment-seeking first responder sample. In accordance with the ACA (2014) Code of Ethics, counselors are to administer assessments normed with the client population (E.8.). Thus, the results of the current study support counselors’ use of the measure in practice. First responder communities are facing unprecedented work tasks in response to COVID-19. Subsequently, their mental health might suffer (Centers for Disease Control and Prevention, 2020) and experts have recommended promoting resilience as a protective factor for combating the negative mental health consequences of COVID-19 (Chen & Bonanno, 2020). Therefore, the relevance of assessing resilience among first responder clients in the current context is evident.
Limitations and Future Research
This study is not without limitations. The sample of first responders was homogeneous in terms of race, ethnicity, and gender. Subsamples of first responders (i.e., LEO, EMT, fire rescue) were too small to conduct within-group analyses to determine if the factor structure of the RSES-22 and RSES-4 would perform similarly. Also, our sample of first responders included two emergency dispatchers. Researchers reported that emergency dispatchers should not be overlooked, given an estimated 13% to 15% of emergency dispatchers experience post-traumatic symptomatology (Steinkopf et al., 2018). Future researchers may develop studies that further explore how, if at all, emergency dispatchers are represented in first responder research.
Furthermore, future researchers could account for first responders who have prior military service. In a study of LEOs, Jetelina et al. (2020) found that participants with military experience were 3.76 times more likely to report mental health concerns compared to LEOs without prior military affiliation. Although we reported the prevalence rate of prior military experience in our sample, the within-group sample size was not sufficient for additional analyses. Finally, our sample represented treatment-seeking first responders. Future researchers may replicate this study with non–treatment-seeking first responder populations.
Conclusion
First responders are at risk for sustaining injuries, experiencing life-threatening events, and witnessing harm to others (Lanza et al., 2018). The nature of their exposure can be repeated and cumulative over time (Donnelly & Bennett, 2014), indicating an increased risk for post-traumatic stress, anxiety, and depressive symptoms, as well as suicidal behavior (Jones et al., 2018). Resilience is a promising protective factor that promotes wellness and healthy coping among first responders (Wild et al., 2020), and counselors may choose to routinely measure for resilience among first responder clients. The current investigation concluded that among a sample of treatment-seeking first responders, the original factor structure of the RSES-22 was unstable, although it demonstrated good reliability and validity. The adapted version, RSES-4, demonstrated good factor structure while also maintaining acceptable reliability and validity, consistent with studies of military populations (De La Rosa et al., 2016; Johnson et al., 2011; Prosek & Ponder, 2021). The RSES-4 provides counselors with a brief and strength-oriented option for measuring resilience with first responder clients.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
American Counseling Association. (2014). ACA code of ethics.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
Antony, J., Brar, R., Khan, P. A., Ghassemi, M., Nincic, V., Sharpe, J. P., Straus, S. E., & Tricco, A. C. (2020). Interventions for the prevention and management of occupational stress injury in first responders: A rapid overview of reviews. Systematic Reviews, 9(121), 1–20. https://doi.org/10.1186/s13643-020-01367-w
Blevins, C. A., Weathers, F. W., Davis, M. T., Witte, T. K., & Domino, J. L. (2015). The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28(6), 489–498. https://doi.org/10.1002/jts.22059
Burnett, H. J., Jr. (2017). Revisiting the compassion fatigue, burnout, compassion satisfaction, and resilience connection among CISM responders. Journal of Police Emergency Response, 7(3), 1–10. https://doi.org/10.1177/2158244017730857
Centers for Disease Control and Prevention. (2020, June 30). Coping with stress. https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/managing-stress-anxiety.html
Chen, S., & Bonanno, G. A. (2020). Psychological adjustment during the global outbreak of COVID-19: A resilience perspective. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S51–S54. https://doi.org/10.1037/tra0000685
Christopher, M. S., Hunsinger, M., Goerling, R. J., Bowen, S., Rogers, B. S., Gross, C. R., Dapolonia, E., & Pruessner, J. C. (2018). Mindfulness-based resilience training to reduce health risk, stress reactivity, and aggression among law enforcement officers: A feasibility and preliminary efficacy trial. Psychiatry Research, 264, 104–115. https://doi.org/10.1016/j.psychres.2018.03.059
Crowe, A., Glass, J. S., Lancaster, M. F., Raines, J. M., & Waggy, M. R. (2015). Mental illness stigma among first responders and the general population. Journal of Military and Government Counseling, 3(3), 132–149. http://mgcaonline.org/wp-content/uploads/2013/02/JMGC-Vol-3-Is-3.pdf
Crowe, A., Glass, J. S., Lancaster, M. F., Raines, J. M., & Waggy, M. R. (2017). A content analysis of psychological resilience among first responders. SAGE Open, 7(1), 1–9. https://doi.org/10.1177/2158244017698530
De La Rosa, G. M., Webb-Murphy, J. A., & Johnston, S. L. (2016). Development and validation of a brief measure of psychological resilience: An adaptation of the Response to Stressful Experiences Scale. Military Medicine, 181(3), 202–208. https://doi.org/10.7205/MILMED-D-15-00037
Dimitrov, D. M. (2012). Statistical methods for validation of assessment scale data in counseling and related fields. American Counseling Association.
Donnelly, E. A., & Bennett, M. (2014). Development of a critical incident stress inventory for the emergency medical services. Traumatology, 20(1), 1–8. https://doi.org/10.1177/1534765613496646
Greinacher, A., Derezza-Greeven, C., Herzog, W., & Nikendei, C. (2019). Secondary traumatization in first responders: A systematic review. European Journal of Psychotraumatology, 10(1), 1562840. https://doi.org/10.1080/20008198.2018.1562840
Gutierrez, P. M., Osman, A., Barrios, F. X., & Kopper, B. A. (2001). Development and initial validation of the Self-Harm Behavior Questionnaire. Journal of Personality Assessment, 77(3), 475–490. https://doi.org/10.1207/S15327752JPA7703_08
Jetelina, K. K., Mosberry, R. J., Gonzalez, J. R., Beauchamp, A. M., & Hall, T. (2020). Prevalence of mental illnesses and mental health care use among police officers. JAMA Network Open, 3(10), 1–12. https://doi.org/10.1001/jamanetworkopen.2020.19658
Johnson, D. C., Polusny, M. A., Erbes, C. R., King, D., King, L., Litz, B. T., Schnurr, P. P., Friedman, M., Pietrzak, R. H., & Southwick, S. M. (2011). Development and initial validation of the Response to Stressful Experiences Scale. Military Medicine, 176(2), 161–169. https://doi.org/10.7205/milmed-d-10-00258
Jones, S. (2017). Describing the mental health profile of first responders: A systematic review. Journal of the American Psychiatric Nurses Association, 23(3), 200–214. https://doi.org/10.1177/1078390317695266
Jones, S., Nagel, C., McSweeney, J., & Curran, G. (2018). Prevalence and correlates of psychiatric symptoms among first responders in a Southern state. Archives of Psychiatric Nursing, 32(6), 828–835. https://doi.org/10.1016/j.apnu.2018.06.007
Joyce, S., Tan, L., Shand, F., Bryant, R. A., & Harvey, S. B. (2019). Can resilience be measured and used to predict mental health symptomology among first responders exposed to repeated trauma? Journal of Occupational and Environmental Medicine, 61(4), 285–292. https://doi.org/10.1097/JOM.0000000000001526
Kleim, B., & Westphal, M. (2011). Mental health in first responders: A review and recommendation for prevention and intervention strategies. Traumatology, 17(4), 17–24. https://doi.org/10.1177/1534765611429079
Klimley, K. E., Van Hasselt, V. B., & Stripling, A. M. (2018). Posttraumatic stress disorder in police, firefighters, and emergency dispatchers. Aggression and Violent Behavior, 43, 33–44.
https://doi.org/10.1016/j.avb.2018.08.005
Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Lanza, A., Roysircar, G., & Rodgers, S. (2018). First responder mental healthcare: Evidence-based prevention, postvention, and treatment. Professional Psychology: Research and Practice, 49(3), 193–204. https://doi.org/10.1037/pro0000192
Lee, J.-S., Ahn, Y.-S., Jeong, K.-S. Chae, J.-H., & Choi, K.-S. (2014). Resilience buffers the impact of traumatic events on the development of PTSD symptoms in firefighters. Journal of Affective Disorders, 162, 128–133. https://doi.org/10.1016/j.jad.2014.02.031
Lewis, G. B., & Pathak, R. (2014). The employment of veterans in state and local government service. State and Local Government Review, 46(2), 91–105. https://doi.org/10.1177/0160323X14537835
McCanlies, E. C., Gu, J. K., Andrew, M. E., Burchfiel, C. M., & Violanti, J. M. (2017). Resilience mediates the relationship between social support and post-traumatic stress symptoms in police officers. Journal of Emergency Management, 15(2), 107–116. https://doi.org/10.5055/jem.2017.0319
National Institute of Mental Health. (2017). Post-traumatic stress disorder. https://www.nimh.nih.gov/health/statistics/post-traumatic-stress-disorder-ptsd.shtml
Osman, A., Bagge, C. L., Gutierrez, P. M., Konick, L. C., Kopper, B. A., & Barrios, F. X. (2001). The Suicidal Behaviors Questionnaire–revised (SBQ-R): Validation with clinical and nonclinical samples. Assessment, 8(4), 443–454. https://doi.org/10.1177/107319110100800409
Prosek, E. A., & Ponder, W. N. (2021). Validation of the Adapted Response to Stressful Experiences Scale (RSES-4) among veterans [Manuscript submitted for publication].
Spitzer, R. L., Kroenke, K., Williams, J. B. W., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder (The GAD-7). Archives of Internal Medicine, 166(10), 1092–1097.
https://doi.org/10.1001/archinte.166.10.1092
Steinkopf, B., Reddin, R. A., Black, R. A., Van Hasselt, V. B., & Couwels, J. (2018). Assessment of stress and resiliency in emergency dispatchers. Journal of Police and Criminal Psychology, 33(4), 398–411.
https://doi.org /10.1007/s11896-018-9255-3
Substance Abuse and Mental Health Services Administration. (2018, May). First responders: Behavioral health concerns, emergency response, and trauma. Disaster Technical Assistance Center Supplemental Research Bulletin. https://www.samhsa.gov/sites/default/files/dtac/supplementalresearchbulletin-firstresponders-may2018.pdf
Weiss, D. S., Brunet, A., Best, S. R., Metzler, T. J., Liberman, A., Pole, N., Fagan, J. A., & Marmar, C. R. (2010). Frequency and severity approaches to indexing exposure to trauma: The Critical Incident History Questionnaire for police officers. Journal of Traumatic Stress, 23(6), 734–743.
https://doi.org/10.1002/jts.20576
White, B., Driver, S., & Warren, A. M. (2010). Resilience and indicators of adjustment during rehabilitation from a spinal cord injury. Rehabilitation Psychology, 55(1), 23–32. https://doi.org/10.1037/a0018451
Wild, J., El-Salahi, S., Degli Esposti, M., & Thew, G. R. (2020). Evaluating the effectiveness of a group-based resilience intervention versus psychoeducation for emergency responders in England: A randomised controlled trial. PLoS ONE, 15(11), e0241704. https://doi.org/10.1371/journal.pone.0241704
Windle, G., Bennett, K. M., & Noyes, J. (2011). A methodological review of resilience measurement scales. Health and Quality of Life Outcomes, 9, Article 8, 1–18. https://doi.org/10.1186/1477-7525-9-8
Warren N. Ponder, PhD, is Director of Outcomes and Evaluation at One Tribe Foundation. Elizabeth A. Prosek, PhD, NCC, LPC, is an associate professor at Penn State University. Tempa Sherrill, MS, LPC-S, is the founder of Stay the Course and a volunteer at One Tribe Foundation. Correspondence may be addressed to Warren N. Ponder, 855 Texas St., Suite 105, Fort Worth, TX 76102, warren@1tribefoundation.org.
Nov 28, 2019 | Volume 9 - Issue 4
Nesime Can, Joshua C. Watson
Scholars have described compassion fatigue as the result of chronic exposure to clients’ suffering and traumatic stories. Counselors can struggle when they experience compassion fatigue because of various reasons. As such, an exploration of factors predictive of compassion fatigue may help counselors and supervisors buffer adverse effects. Utilizing a hierarchical linear regression analysis, we examined the association between wellness, resilience, supervisory working alliance, empathy, and compassion fatigue among 86 counselors-in-training (CITs). The research findings revealed that resilience and wellness were significant predictors of compassion fatigue among CITs, whereas empathy and supervisory working alliance were not. Based on our findings, counselor educators might consider enhancing their current training programs by including discussion topics about wellness and resilience, while supervisors consider practicing wellness and resilience strategies in supervision and developing interventions designed to prevent compassion fatigue.
Keywords: compassion fatigue, counselors-in-training, wellness, resilience, supervisory working alliance
Balancing self-care and client care can be a challenge for many counselors. When counselors neglect self-care, they can become vulnerable to several issues, including increased anxiety, distress, burnout, and compassion fatigue (Ray, Wong, White, & Heaslip, 2013). Counselors might be especially prone to experiencing compassion fatigue because they repeatedly hear traumatic stories and clients’ suffering in sessions (Skovholt & Trotter-Mathison, 2016). This phenomenon is likely pronounced among counselors-in-training (CITs), as lack of experience, skillset, knowledge, and support can lead to struggles when working with clients (Skovholt & Trotter-Mathison, 2016). Coupled with the increased anxiety, distress, and disappointment, CITs can experience compassion fatigue early in their career development, which can lead to exhaustion, disengagement, and a decline in therapeutic effectiveness (Rønnestad & Skovholt, 2013). At this developmental stage, negative experiences can lead to feelings of doubt and a lack of confidence among CITs and potentially lead to career dissatisfaction. Therefore, it is essential and necessary to better understand the predictive factors of compassion fatigue among CITs to prevent its early onset.
Compassion Fatigue in Counseling
Counselors listening to their clients’ fear, pain, and suffering can feel similar emotions. Figley (1995) defined this experience as compassion fatigue; it also can be defined as the cost of caring (Figley, 2002). Whether working in mental health agencies, schools, or hospital settings, counselors experience compassion fatigue because of exposure to large caseloads, painful stories, and lack of support and resources (Skovholt & Trotter-Mathison, 2016). Despite this exposure, counselors are expected to place their personal feelings aside and provide the best treatment possible in response to the presenting issues and needs of their clients (Figley, 2002; Ray et al., 2013; Turgoose, Glover, Barker, & Maddox, 2017). Maintaining this sense of detached professionalism has its costs, as a number of counselors find themselves at risk for experiencing physical, mental, and emotional exhaustion, as well as feelings of helplessness, isolation, and confusion—a situation collectively referred to as compassion fatigue (Eastwood & Ecklund, 2008; Thompson, Amatea, & Thompson, 2014).
Merriman (2015b) stated that ongoing compassion fatigue negatively impacts counselors’ health as well as their relationships with others. Additionally, compassion fatigue can lead to a lack of empathy toward clients, decrease in motivation, and performance drop in effectiveness, making even the smallest tasks seem overwhelming (Merriman, 2015b). When this occurs, counselors can project their anger on others, develop trust issues, and experience feelings of loneliness (Harr, 2013). Therefore, the demands of the counseling profession can affect many counselors’ wellness and potentially could hurt the quality of client care provided (Lawson, Venart, Hazler, & Kottler, 2007; Merriman, 2015a). Further, counselors experiencing compassion fatigue might have difficulties making effective clinical decisions and potentially be at risk for harming clients (Eastwood & Ecklund, 2008). Consequently, scholars appear to agree that compassion fatigue is an occupational hazard that mental health care professionals need to address (Figley, 2002; Merriman, 2015a).
Factors Associated With Compassion Fatigue
Many researchers have studied the relationships between compassion fatigue and various constructs, such as empathy, gender, mindfulness, support, and wellness (e.g., Beaumont, Durkin, Martin, & Carson, 2016; Caringi et al., 2016; Ray et al., 2013; Sprang, Clark, & Whitt-Woosley, 2007; Turgoose et al., 2017). Researchers conducted most of these studies among novice and veteran mental health professionals. Scant research among CITs exists. Our research attempts to fill this gap by exploring factors affecting CITs given their unique position as both students and emerging professionals. The following review of the literature supports the inclusion of predictor variables used in this study.
Empathy and Compassion Fatigue
One of the most widely studied concepts across various cultures is empathy, as it has been determined to be one of the major precipitants of compassion fatigue (Figley, 1995). However, findings in the literature regarding the association between compassion fatigue and empathy remain mixed (e.g., MacRitchie & Leibowitz, 2010; O’Brien & Haaga, 2015; Wagaman, Geiger, Shockley, & Segal, 2015). For instance, O’Brien and Haaga (2015) compared trait empathy and empathic accuracy with compassion fatigue after showing a videotaped trauma self-disclosure among therapist trainees (a combined group of advanced and novice graduate students) and non-therapists. The results indicated that there was no significant association between participants’ levels of compassion fatigue and empathy scores. However, MacRitchie and Leibowitz (2010) found a significant relationship between compassion fatigue and empathy after exploring the relation of these variables on trauma workers whose clients were survivors of violent crimes. The mixed results of these previous studies suggest further research is needed to understand better the relationship between empathy and compassion fatigue and how this relationship impacts counseling practice.
Supervisory Working Alliance and Compassion Fatigue
Although reviewed literature addressed studies suggesting supervision and support are related factors to compassion fatigue, research on this relationship is still insufficient. Kapoulitsas and Corcoran (2015) conducted a study and found that a positive supervisory relationship has a significant role in developing resilience and reducing compassion fatigue among counselors. Knight (2010) also found that students uncomfortable talking with their supervisor reported a higher risk for developing compassion fatigue. Additionally, organizational support appears to reduce compassion fatigue, whereas an absence of support increases practitioners’ and interns’ risk of developing compassion fatigue symptoms (Bride, Jones, & MacMaster, 2007). Given the intense need for support and guidance CITs need during their initial work with clients, it is expected that those students who do not actively work with their supervisors can struggle and be more vulnerable for compassion fatigue.
Wellness, Resilience, and Compassion Fatigue
Although counselors are encouraged to practice self-care activities to continue to enhance personal well-being (American Counseling Association [ACA], 2014; Coaston, 2017; H. L. Smith, Robinson, & Young, 2008), not all CITs can balance caring for self and others. When CITs do not receive training in the protective factors for compassion fatigue, they risk becoming more vulnerable to violating the ACA code of ethics (Merriman, 2015a; Merriman, 2015b). Kapoulitsas and Corcoran (2015) and Skovholt and Trotter-Mathison (2016) highlighted the importance of resilience and self-care activities as protective factors for compassion fatigue. Wood et al. (2017) evaluated the effectiveness of a mobile application called Provider Resilience to reduce compassion fatigue scores of mental health professionals. After a month of utilization, the results indicated that the application was effective in reducing compassion fatigue. Additionally, Lawson and Myers (2011) conducted a study with professional counselors to examine counselor wellness about compassion fatigue and found a negative correlation between total wellness scores and compassion fatigue scores. As CITs balance academic, family, and work demands, the probability of decreased wellness and a corresponding increase in compassion fatigue exists.
Compassion Fatigue Among CITs
Most CITs are often unable to master all counselor competencies (Rønnestad & Skovholt, 2013), and therefore they might not know how to deal with possible stressors and the emotional burden of their work (Star, 2013). Although they are learning counseling skills to provide the best care possible to clients, CITs may find themselves working with seriously troubled or traumatized clients without obtaining quality supervision and support (Skovholt & Trotter-Mathison, 2016). Lack of skills and resources increases the likelihood of CITs developing compassion fatigue (Merriman, 2015b). However, there is a lack of focus in compassion fatigue education on preparing CITs to manage compassion fatigue symptoms (Merriman, 2015a). Although scholars have examined compassion fatigue among counselors, there is still a dearth of studies investigating the level of compassion fatigue among CITs and addressing its protective factors within this population (Beaumont et al., 2016; Blount, Bjornsen, & Moore, 2018; Thompson et al., 2014). Subsequently, further research is needed to understand better potential protective factors that can be enhanced to offset the negative impact of compassion fatigue on CITs and the counseling process. Thus, with this study, we aimed at assessing the relationship between resilience, wellness, supervisory working alliance, empathy, and compassion fatigue among CITs in the United States. To accomplish this goal, we sought to answer the following research questions: (1) What is the prevalence of compassion fatigue among CITs? and (2) Do empathy, supervisory working alliance, resilience, and wellness significantly predict levels of compassion fatigue among CITs?
Method
Participants
Participants recruited for this study consisted of master’s-level counseling students who are at least 18 years of age and enrolled in an internship course in the United States through mostly professional listservs (e.g., Counselor Education and Supervision Network Listserv [CESNET-L], Texas Association for Counselor Education and Supervision Network Listserv [TACESNET-L], Counseling Graduate Student Network [COUNSGRADS]). Because of the impossibility of knowing how many individuals received the email invitation, we were unable to calculate and determine a response rate. Accordingly, a total of 114 CITs initially agreed to participate in this study. Before data analysis, we inspected the data set for possible entry errors and missing data. After the inspection, we excluded 28 participants from all subsequent data analyses resulting in the reduced sample of 86 CITs used to address our research questions. Overall, the sample consisted of 78 female (90.7%) and eight male (9.3%) participants, and the mean age of the participants was 32.89 years (SD = 9.72) with participants’ ages ranging between 21 and 62 years. Participants were from diverse ethnic and racial backgrounds, with the sample consisting of White (n = 48, 55.8%), Hispanic/Latino (n = 18, 20.9%), Black/African American (n = 12, 14.0%), and Asian (n = 5, 5.8%) CITs. Three participants (3.5%) listed their ethnicities as “other” when providing demographic information. Participants reported their program enrollment as follows: clinical mental health counseling program (n = 47, 54.7%); school counseling program (n = 23, 26.7%); marriage, couple, and family counseling program (n = 4, 4.7%); college counseling and student affairs program (n = 3, 3.5%); addiction counseling program (n = 2, 2.3%); and other programs (n = 7, 8.1%). Additionally, most of the participants (n = 73, 84.9%) reported enrollment in a CACREP-accredited program with the remaining participants (n = 13, 15.1%) enrolled in a non–CACREP-accredited program.
Procedure
Upon receiving institutional review board approval, we recruited participants from different institutions with the primary researcher contacting professional colleagues at various departments to disseminate the online survey link to potential participants during the 2017 summer and fall semesters. We also recruited participants through professional listservs (e.g., CESNET-L, TACESNET-L, COUNSGRAD), with listserv participants being provided the same informed consent and survey link through a secure website. The survey completion process took approximately 15–20 minutes.
Measures
We used the following self-administered survey questionnaires and a separate demographic data sheet in our data collection.
Professional Quality of Life Scale (ProQOL). This scale is designed to measure the mental and emotional consequences of working with individuals who experienced trauma or painful events (Stamm, 2010). The ProQOL includes two main traits, Compassion Satisfaction (positive) and Compassion Fatigue (negative). Compassion Satisfaction is related to the joy individuals develop when they do their work well (Stamm, 2010). Compassion Fatigue consists of two subscales: Secondary Traumatic Stress (STS) and Burnout. Scholars have defined STS as an emotional state that occurs when an individual becomes upset or traumatized as a result of their exposure to victim experiences (Figley, 2002). The second part of Compassion Fatigue is Burnout, which is a multidimensional syndrome related to the social work environment. Burnout could be related to work overload, lack of control, insufficient rewards, unfairness, and value conflict at a workplace (Skovholt & Trotter-Mathison, 2016).
The ProQOL is a 30-item Likert-type self-report assessment with responses of never, rarely, sometimes, often, and very often for each item. A sample item is “I feel depressed because of the traumatic experiences of the people I [help].” This assessment has 10 questions per each of three main scales measuring separate constructs. However, the Compassion Fatigue scale includes two of these constructs, which are the Burnout and the STS scales. According to Stamm (2010), the ProQOL has good construct validity, as researchers have noted its efficacy in over 200 published articles. Finally, alpha coefficient values for the Burnout and STS scales were .75 and .81, respectively (Stamm, 2010), and are similar (.72 and .79) to the Cronbach’s alpha values from the current study presented in Table 1.
Table 1
Descriptive Statistics of the Study Variables (N = 86)
|
|
|
|
Range |
|
|
| Variable |
M |
SD |
Min |
Max |
Skew |
α |
| Compassion Fatigue |
41.48 |
8.03 |
22 |
60 |
.19 |
|
|
BO |
21.34 |
4.38 |
12 |
32 |
– |
.72 |
|
STS |
20.14 |
4.96 |
10 |
38 |
– |
.79 |
| Empathy |
21.86 |
4.12 |
9 |
28 |
-.51 |
.80 |
| Supervisory Working Alliance |
5.82 |
.97 |
2.16 |
7 |
1.26 |
|
|
CF |
6.65 |
1.30 |
2.17 |
8.17 |
– |
.90 |
|
R |
5.80 |
.96 |
2.33 |
7 |
– |
.93 |
| Resilience |
3.43 |
.79 |
1 |
4.67 |
-.74 |
.89 |
| Wellness |
47.58 |
6.23 |
27 |
56 |
-1.39 |
.86 |
|
|
|
|
|
|
|
|
|
|
|
|
Note. BO = Burnout; STS = Secondary Traumatic Stress; CF = Client Focus; R = Rapport
Interpersonal Reactivity Index (IRI). Davis (1983) developed the IRI to measure the reactions of a person to other individuals’ observed experiences. The 28-item instrument has four subscales: Empathic Concern, Perspective Taking, Fantasy, and Personal Distress (Davis, 1983). Researchers report separate subscale scores, as a total score for the instrument has not been recommended (Davis, 1983). In this study, we only used the Empathic Concern subscale to collect data regarding empathy scores of CITs.
Davis (1983) described empathic concern as an emotional response, such as compassion and sympathy, to someone else in need. The 7-item subscale is a self-report assessment with a 5-point Likert-type scale, ranging from Does not describe me well to Describes me very well. A sample item is “I am often quite touched by things that I see happen.” An alpha coefficient of .77 has been reported for the Empathic Concern subscale (Péloquin & Lafontaine, 2010), while the Cronbach’s alpha value of the IRI in the current study was .80.
Supervisory Working Alliance Inventory: Trainee Form (SWAI-T). Efstation, Patton, and Kardash (1990) developed this inventory to measure supervisees’ perceptions about the effectiveness of the working relationship with their supervisors, and we used the SWAI-T to measure the construct of the supervisory working alliance. With a total of 19 items, the self-report assessment includes a 7-point Likert-type scale with responses ranging from almost never to almost always. A sample item is “When correcting my errors with the client, my supervisor offers alternative ways of intervening with the client.” The SWAI-T has two subscales—Client Focus and Rapport—and the Cronbach alpha coefficients of these scales were .77 and .90, respectively (Efstation et al., 1990). For the current study, we calculated Cronbach alpha values of .90 for the Client Focus subscale and .93 for the Rapport subscale. Because some researchers have found high correlations between these two subscales, they decided to combine them in their studies (e.g., Ganske, 2007; White & Queener, 2003). Therefore, in this study, after conducting a correlation analysis with the subscale scores, we also chose to combine subscales as the results of subscale scores were highly correlated.
Brief Resilience Scale (BRS). The BRS was developed to measure a person’s ability to recover from stress and cope with challenging situations (B. W. Smith et al., 2008). The BRS is used to measure the construct of resilience. As a 6-item self-report assessment, the BRS includes a 5-point Likert-type scale with responses ranging from strongly disagree to strongly agree. A sample item is “I usually come through difficult times with little trouble.” B. W. Smith and colleagues (2008) reported that the Cronbach’s alpha values of the BRS range from .80 to .91, and we calculated a Cronbach alpha of .89 for the current study.
Flourishing Scale (FS). The FS was designed to measure individuals’ self-perceived success in areas like optimism and relationships (Diener et al., 2010) and used to measure the construct of wellness in this study. The FS is an 8-item self-report assessment with a 7-point Likert-type scale with responses ranging from strongly disagree to strongly agree (Diener et al., 2010). A sample item is “I lead a purposeful and meaningful life.” Diener and colleagues (2010) reported moderately high reliability with a .87 Cronbach’s alpha coefficient, and in the current study, the FS had a Cronbach alpha of .86.
Data Analysis
Statistical power analysis. We used an a priori type of the G*Power to set the minimum number of participants needed to detect statistical power for this research design. Based on an alpha of .05, a power level of .90, and four predictors (Faul, Erdfelder, Buchner, & Lang, 2009), the computation results suggested that a minimum of 73 participants was required to detect statistical significance with at least a moderate size effect (.15). We had 86 participants, suggesting adequate power.
Preliminary analyses. We analyzed all data using the Statistical Package for the Social Sciences, Version 20 (SPSS; IBM Corporation, 2011). Before addressing our stated research questions, we cleaned the dataset and addressed missing data. We did not observe any pattern between missing data points. Therefore, the type of missing data was completely random, which was addressed using the series of mean function within the SPSS. Next, we calculated descriptive statistics and alpha coefficients for each scale used in the study (see Table 1). Before performing hierarchical regression analyses, we tested all associated model assumptions. First, we examined study variables based on their types and concluded each utilized a continuous scale. We then assessed normality with the Shapiro-Wilk test of normality (W > .05), indicating data was normally distributed for the dependent variable. To identify outliers, we examined boxplots. Although there were a few mild outliers, no extreme scores were detected. We assessed linearity and homoscedasticity through inspection of standardized residual plots. To assess for the assumption of multicollinearity, we examined the correlation matrix of study variables to determine if any correlated highly. According to Field (2013), correlations above .80 are considered high and may indicate the presence of multicollinearity. In the present study, none of the correlation coefficients were above .50 (see Table 2). Collectively, these findings indicated no evidence suggesting any of the model assumptions had been violated. As a result, the dataset was deemed appropriate for analysis using a hierarchical regression design.
Primary analysis. Descriptive statistics were calculated to organize the data by producing means, mode, median, standard deviations, and minimum and maximum scores for the study variables (Field, 2013). Individually, we reviewed descriptive statistics for the compassion fatigue variable, and results were reported to address the first research question. Next, we performed a three-step hierarchical linear regression to address the second research question.
Table 2
Intercorrelations for Scores on the Study Variables
|
Variable |
1 |
2 |
3 |
4 |
5 |
| 1. |
ProQOL-CF |
– |
|
|
|
|
| 2. |
SWAIT-T |
.04 |
– |
|
|
|
| 3. |
IRI-EC |
-.06 |
.04 |
– |
|
|
| 4. |
BRS |
-.47** |
-.09 |
-.11 |
– |
|
| 5. |
FS |
-.45** |
.12 |
.25* |
.35** |
– |
Note. N = 86; ProQOL = Professional Quality of Life (Compassion Fatigue [CF] subscale score is presented); IRI = Interpersonal Reactivity Index (Empathic Concern [EC] subscale score is presented); SWAI-T = Supervisory Working Alliance Inventory: Trainee Form; BRS = Brief Resilience Scale; FS = Flourishing Scale.
*p < .05. **p < .01.
Results
Compassion fatigue scores of CITs represent the sum of scores of all items on the STS and Burnout subscales. According to the ProQOL administration manual (Stamm, 2010), individuals scoring below 22 may indicate little or no issues with Burnout and STS, while scores between 23 and 41 indicate moderate levels of Burnout and STS, and scores above 42 indicate higher levels of Burnout and STS. For this sample, participants’ Burnout scores ranged from 12 to 32 with a mean of 21.34 (SD = 4.38), and STS scores ranged from 10 to 38 with a mean of 20.14 (SD = 4.96). These results indicated a low risk of both Burnout and STS among CITs.
To address the second research question, we performed a three-step hierarchical linear regression analysis. With this analysis, we aimed to assess the association between resilience, wellness, supervisory working alliance, empathy, and compassion fatigue. We chose to implement a hierarchical multiple regression analysis because scholars previously have highlighted the essential relationship between empathy, supervision, and compassion fatigue (Figley, 2002; MacRitchie & Leibowitz, 2010). In the first step, empathy scores entered the model as a predictor variable, as Figley (1995) stated that empathy is one of the main factors contributing to compassion fatigue. However, among this sample, we found that empathy was not a significant predictor of compassion fatigue: F(1, 84) = .2, p = .66 , R2 = .002 (adjusted R2 = -.01). Then, we added supervisory working alliance scores to the model in the second step, as both Knight (2010) and Miller and Sprang (2017) emphasized the importance of supervisory support for mental health practitioners. Results revealed that the supervisory working alliance variable also was not a significant predictor of compassion fatigue: F(2, 83) = .16, p = .85, R2 = .004 (adjusted R2 = -.02). In the third step, resilience and wellness scores were entered into the model to determine whether these variables significantly improved the amount of explained variance in compassion fatigue. Results showed that this combination of variables significantly predicted 26% of the variance in compassion fatigue: F(4, 81) = 8.57, p < .001, R2 = .30. Therefore, it was concluded that CITs with greater wellness and resilience reported developing less compassion fatigue (see Table 3).
Table 3
Hierarchical Regression Analysis Results for Variables Predicting Compassion Fatigue
| Variables |
B |
SEB |
β |
R2 |
ΔR2 |
| Step 1 |
|
|
|
|
.002 |
-.01 |
| Empathy |
-.09 |
.21 |
-.05 |
|
|
| Step 2 |
|
|
|
|
.004 |
-.02 |
| Empathy |
-.10 |
.21 |
-.05 |
|
|
| SWA |
.33 |
.91 |
.04 |
|
|
| Step 3 |
|
|
|
|
.30* |
.26 |
| Empathy |
-.03 |
.19 |
-.02 |
|
|
| SWA |
.36 |
.78 |
.04 |
|
|
| Wellness |
-.39 |
.14 |
-.30* |
|
|
| Resilience |
-3.66 |
1.05 |
-.36* |
|
|
Note. SWA = Supervisory Working Alliance
*p < .05.
Discussion
In this study, CITs reported having a low risk of compassion fatigue. When we examined the Burnout and STS scores separately, the main contributors of compassion fatigue (Stamm, 2010), both subscale scores indicated participants having a low risk for STS and Burnout. This finding is similar to results found by Beaumont and colleagues (2016) in their study of compassion fatigue, burnout, self-compassion, and well-being relationships among student counselors and student cognitive behavioral psychotherapists. According to their research findings, a total of 54 student participants reported high scores on self-compassion and well-being and reported less compassion fatigue and burnout (Beaumont et al., 2016).
One of the goals of this study was to seek understanding of whether wellness and resilience explain a statistically significant amount of variance in compassion fatigue among CITs after accounting for empathy and supervisory working alliance. The results indicated that empathy and supervisory working alliance were not significant predictors of compassion fatigue. Regarding empathy and compassion fatigue relation results, the findings of this study did not support Figley’s (1995) assumption of empathy as one of the main contributors to compassion fatigue. This result also is inconsistent with Wagaman and colleagues’ (2015) results indicating a significant association between empathy and compassion fatigue among social workers. However, current results aligned with those studies that found no correlation between empathy and compassion fatigue (e.g., O’Brien & Haaga, 2015; Thomas & Otis, 2010). An explanation of the variability between this inquiry and previous studies might lie with the difference between participants’ field of study and measurement differences. Also, none of the previous studies used CITs solely as their sample, nor used a similar way to measure the construct of empathy. Additionally, CITs would have less experience working with clients compared to experienced counselors, and thus less time for feelings of compassion fatigue to build.
Although scholars addressed the importance of supervision and supervisory working alliance to help prevent compassion fatigue (Kapoulitsas & Corcoran, 2015; Merriman, 2015a), this study’s results indicated supervisory working alliance was not a significant predictor of compassion fatigue among CITs. Like current results, Ivicic and Motta (2017) and Williams, Helm, and Clemens (2012) found no statistically significant association between supervisory working alliance and compassion fatigue among mental health practitioners. It is noteworthy that these studies highlighting the importance of supervision and the supervisory relationship are qualitative in design, and participants did not consist solely of CITs. Additionally, their results emphasized the importance of supervision as support to counter the negative impact of trauma exposure (Kapoulitsas & Corcoran, 2015; Ling, Hunter, & Maple, 2014). According to the current study results, CITs did not report experiencing a high level of compassion fatigue. This finding could be interpreted as CITs not yet feeling the need for supervisory support to help with compassion fatigue.
Results also indicated that resilience and wellness were significant predictors of compassion fatigue among CITs. In other words, when reflecting on both the regression and correlation results, CITs with greater resilience and wellness reported lower scores of compassion fatigue and these results were consistent with Tosone, Minami, Bettmann, and Jasperson’s (2010) research findings. Regarding a wellness and compassion fatigue relationship, Beaumont and colleagues (2016) conducted a study with student counselors and student cognitive behavioral psychotherapists. The results of Beaumont et al.’s study revealed that individuals with high scores of self-compassion and well-being reported having less compassion fatigue and burnout. Thomas and Morris (2017) also highlighted the significance of self-care and well-being not only for preventing and helping to manage the potentially damaging impact of practice, but also for facilitating the counselor’s personal and professional growth.
Implications for Counselor Educators and Supervisors
The research findings provide data-driven results regarding compassion fatigue among CITs that have meaningful implications for counselor educators and supervisors. Present study results revealed that CITs indicated experiencing a low risk of compassion fatigue. However, raising awareness on this issue may still help CITs as a preventative measure to cope with possible compassion fatigue experience in the future. To address this issue, counselor educators may consider raising awareness on this topic by reviewing current counseling program curricula to add discussion questions related to compassion fatigue and its empirically predictive factors—wellness and resilience. Roach and Young (2007) stated that students in counseling programs reported group counseling, counseling techniques, legal and ethical issues, practicum, and wellness courses as contributing most to their knowledge and skills regarding wellness. Therefore, counselor educators might use different assignments, including group discussions, projects, and role-playing exercises, to open a discussion about the compassion fatigue phenomenon and the relation with its predictive factors and these courses. Counselor educators may also use the ProQOL scale as an assignment in an assessment and testing course to inform CITs about how to use this instrument as a self-monitoring aid. For example, professional counselors may feel overwhelmed because of working with trauma survivors after graduation and start noticing compassion fatigue symptoms in themselves. These individuals may self-administer the ProQOL scale to determine whether they have developed compassion fatigue. Additionally, in a practicum or an internship course, CITs may fill out the ProQOL as part of their continuing personal wellness plan by comparing personal results over time and sharing their thoughts and reflections about the results.
Supervisors need to find ways to raise awareness of compassion fatigue and its protective factors with CITs. For instance, during internship experience, supervisors may develop a site training including compassion fatigue awareness for CITs, as CITs should be prepared for the possible emotional and psychological consequences in working with trauma survivors. Student counselors also should be encouraged to advocate for themselves when they notice symptoms of compassion fatigue. Supervisors might consider the administration of the ProQOL scale regularly to assess both organizational and individual risks (Newell & MacNeil, 2010). Additionally, supervisors can use the ProQOL scale with their supervisees to start a conversation about compassion fatigue. Although the ProQOL is not a diagnostic test, the 30-item self-report scale can be utilized readily as a conversation starter in supervision sessions.
The results suggested that empathy and supervisory working alliance did not predict CITs’ compassion fatigue level. However, wellness and resilience are significantly related to contributing to it. Therefore, both counselor educators and supervisors might consider enhancing CITs’ resilience and wellness a worthwhile endeavor. For example, Miller and Sprang (2017) developed a component-based practice and supervision model to reduce compassion fatigue for use in training, supervision, and clinical practice. A tool like this one can be added to existing training curricula and supervision practice to improve CITs’ resilience and wellness.
Limitations
The results of this study aim to provide greater clarity regarding the predictive factors of compassion fatigue among CITs. However, interpretation of results should take into consideration the limitations that emerged because of uncontrollable influences and choices we made. The study was limited in its ability to represent all CITs throughout the United States, as we utilized a convenience sampling approach. Additionally, we gathered data through self-report questionnaires, which introduce the possibility of response bias in the findings. Although we assumed participants answered each question honestly, they might not have been honest in their responses because of the fear of being perceived as weak or less competent. It is important to note that being in an internship class might also increase participants’ interest in the profession as they currently are engaged in the practice of counseling. Therefore, participants might have had a higher level of enthusiasm and reported less compassion fatigue. Also, individuals who suffer from compassion fatigue might have preferred not to respond to these items. Finally, although participants were enrolled in an internship class, each participant may have different numbers of hours of client experience.
Future Directions for Research
Additional research should be conducted to expand and clarify the current research findings of compassion fatigue among CITs. A phenomenological study using a qualitative research method is recommended to expand the findings of this current study. Future researchers may use the ProQOL scale to assess CITs’ level of compassion fatigue and then conduct interviews with the volunteer participants reporting a higher level of compassion fatigue to better understand CITs’ experience with compassion fatigue and its contributing factors. The data collected through a qualitative study may provide greater insight into the phenomenon of compassion fatigue among CITs. Additionally, researchers can replicate the present study with early-career counselors who have recently graduated, because of the noted intensity of those first years after graduation (Skovholt & Trotter-Mathison, 2016). Therefore, future researchers exploring novice counselors’ experiences with compassion fatigue will help counselor educators and supervisors better understand when counselors may start developing compassion fatigue symptoms, as well as how they cope with the symptoms.
Conclusion
CITs may struggle when they continuously hear painful stories of clients because of a lack of experience, skillset, or support (Skovholt & Trotter-Mathison, 2016). Researchers have described this experience as compassion fatigue. With this study, we aimed to provide a better understanding of the predictive factors of compassion fatigue among CITs. Using data-driven research results to determine ways to work with CITs on compassion fatigue and its predictive factors can be beneficial in preventing compassion fatigue symptoms from an early onset. CITs may take precautionary measures to ensure they remain enthusiastic and energized by the work they do. Further, implications of the current study may help CITs start their professional careers better prepared to provide their clients with the optimal care needed throughout the counseling relationship by minimizing compassion fatigue.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
American Counseling Association. (2014). ACA code of ethics. Alexandria, VA: Author.
Beaumont, E., Durkin, M., Martin, C. J. H., & Carson, J. (2016). Measuring relationships between self-compassion, compassion fatigue, burnout and well-being in student counsellors and student cognitive behavioural psychotherapists: A quantitative survey. Counselling & Psychotherapy Research, 16, 15–23. doi:10.1002/capr.12054
Blount, A. J., Bjornsen, A. L., & Moore, M. M. (2018). Work values, occupational engagement, and professional quality of life in counselors-in-training: Assessments in a constructivist-based career counseling course. The Professional Counselor, 8, 60–72. doi:10.15241/ajb.8.1.60
Bride, B. E., Jones, J. L., & MacMaster, S.A. (2007). Correlates of secondary traumatic stress in child protective services workers. Journal of Evidence-Based Social Work, 4(3/4), 69–80. doi:10.1300/J394v04n03_05
Caringi, J. C., Hardiman, E. R., Weldon, P., Fletcher, S., Devlin, M., & Stanick, C. (2017). Secondary traumatic stress and licensed clinical social workers. Traumatology, 23(2), 186–195. doi:10.1037/trm0000061
Coaston, S. C. (2017). Self-care through self-compassion: A balm for burnout. The Professional Counselor, 7, 285–297. doi:10.15241/scc.7.3.285
Davis, M. H. (1983). Measuring individual differences in empathy: Evidence for a multidimensional approach. Journal of Personality and Social Psychology, 44, 113–126. doi:10.1037/0022-3514.44.1.113
Diener, E., Wirtz, D., Tov, W., Kim-Prieto, C., Choi, D., Oishi, S., & Biswas-Diener, R. (2010). New measures of well-being: Flourishing and positive and negative feelings. Social Indicators Research, 39, 247–266. doi:10.1007/978-90-481-2354-4_12
Eastwood, C. D., & Ecklund, K. (2008). Compassion fatigue risk and self-care practices among residential treatment center childcare workers. Residential Treatment for Children & Youth, 25, 103–122. doi:10.1080/08865710802309972
Efstation, J. F., Patton, M. J., & Kardash, C. M. (1990). Measuring the working alliance in counselor supervision. Journal of Counseling Psychology, 37, 322–329. doi:10.1037/0022-0167.37.3.322
Faul, F., Erdfelder, E., Buchner, A., & Lang, A.-G. (2009). Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behavior Research Methods, 41, 1149–1160. doi:10.3758/brm.41.4.1149
Field, A. (2013). Discovering statistics using IBM SPSS statistics (4th ed.). Thousand Oaks, CA: SAGE.
Figley, C. R. (Ed.). (1995). Compassion fatigue: Coping with secondary traumatic stress disorder in those who treat the traumatized. New York, NY: Routledge.
Figley, C. R. (Ed.). (2002). Treating compassion fatigue. New York, NY: Brunner-Routledge.
Ganske, K. H. (2007). The relationship between counselor trainee perfectionism and working alliance with supervisor and client. (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3377933)
Harr, C. (2013). Promoting workplace health by diminishing the negative impact of compassion fatigue and increasing compassion satisfaction. Social Work & Christianity, 40, 71–88.
IBM Corporation. (2011). IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: Author.
Ivicic, R., & Motta, R. (2017). Variables associated with secondary traumatic stress among mental health professionals. Traumatology, 23, 196–204. doi:10.1037/trm0000065
Kapoulitsas, M., & Corcoran, T. (2015). Compassion fatigue and resilience: A qualitative analysis of social work practice. Qualitative Social Work: Research and Practice, 14, 86–101. doi:10.1177/1473325014528526
Knight, C. (2010). Indirect trauma in the field practicum: Secondary traumatic stress, vicarious trauma, and compassion fatigue among social work students and their field instructors. The Journal of Baccalaureate Social Work, 15, 31–52.
Lawson, G., & Myers, J. E. (2011). Wellness, professional quality of life, and career-sustaining behaviors: What keeps us well? Journal of Counseling & Development, 89, 163–171. doi:10.1002/j.1556-6678.2011.tb00074.x
Lawson, G., Venart, E., Hazler, R. J., & Kottler, J. A. (2007). Toward a culture of counselor wellness. The Journal of Humanistic Counseling, Education and Development, 46, 5–19. doi:10.1002/j.2161-1939.2007.tb00022.x
Ling, J., Hunter, S. V., & Maple, M. (2014). Navigating the challenges of trauma counselling: How counsellors thrive and sustain their engagement. Australian Social Work, 67, 297–310.
doi:10.1080/0312407X.2013.837188
MacRitchie, V., & Leibowitz, S. (2010). Secondary traumatic stress, level of exposure, empathy and social
support in trauma workers. South African Journal of Psychology, 40, 149–158. doi:10.1177/008124631004000204
Merriman, J. (2015a). Enhancing counselor supervision through compassion fatigue education. Journal of Counseling & Development, 93, 370–378. doi:10.1002/jcad.12035
Merriman, J. (2015b). Prevention-based training for licensed professional counselor interns. Journal of Professional Counseling: Practice, Theory & Research, 42, 40–53.
Miller, B., & Sprang, G. (2017). A components-based practice and supervision model for reducing compassion fatigue by affecting clinician experience. Traumatology, 23, 153–164. doi:10.1037/trm0000058
Newell, J. M., & MacNeil, G. A. (2010). Professional burnout, vicarious trauma, secondary traumatic stress, and compassion fatigue: A review of theoretical terms, risk factors, and preventive methods for clinicians and researchers. Best Practices in Mental Health: An International Journal, 6, 57–68.
O’Brien, J. L., & Haaga, D. A. F. (2015). Empathic accuracy and compassion fatigue among therapist trainees. Professional Psychology: Research and Practice, 46, 414–420. doi:10.1037/pro0000037
Péloquin, K., & Lafontaine, M. (2010). Measuring empathy in couples: Validity and reliability of the
Interpersonal Reactivity Index for couples. Journal of Personality Assessment, 92, 146–157. doi:10.1080/00223890903510399
Ray, S. L., Wong, C., White, D., & Heaslip, K. (2013). Compassion satisfaction, compassion fatigue, work life conditions, and burnout among frontline mental health care professionals. Traumatology, 19, 255–267. doi:10.1177/1534765612471144
Roach, L. F., & Young, M. E. (2007). Do counselor education programs promote wellness in their students? Counselor Education & Supervision, 47, 29–45. doi:10.1002/j.1556-6978.2007.tb00036.x
Rønnestad, M. H., & Skovholt, T. M. (2013). The developing practitioner: Growth and stagnation of therapists and counselors. New York, NY: Routledge.
Skovholt, T. M., & Trotter-Mathison, M. (2016). The resilient practitioner: Burnout and compassion fatigue prevention and self-care strategies for the helping professions (3rd ed.). New York, NY: Routledge.
Smith, B. W., Dalen, J., Wiggins, K., Tooley, E., Christopher, P., & Bernard, J. (2008). The Brief Resilience Scale: Assessing the ability to bounce back. International Journal of Behavioral Medicine, 15, 194–200. doi:10.1080/10705500802222972
Smith, H. L., Robinson, E. H. M., III, & Young, M. E. (2008). The relationship among wellness, psychological distress, and social desirability of entering master’s-level counselor trainees. Counselor Education & Supervision, 47, 96–109. doi:10.1002/j.1556-6978.2007.tb00041.x
Sprang, G., Clark, J. J., & Whitt-Woosley, A. (2007). Compassion fatigue, compassion satisfaction, and burnout: Factors impacting a professional’s quality of life. Journal of Loss and Trauma, 12, 259–280. doi:10.1080/15325020701238093
Stamm, B. H. (2010). The concise ProQOL manual (2nd ed.). Pocatello, ID: ProQOL.org.
Star, K. L. (2013). The relationship between self-care practices, burnout, compassion fatigue, and compassion satisfaction among professional counselors and counselors-in-training. (Doctoral dissertation). Retrieved from ProQuest Dissertations and Theses database. (UMI No. 3618924)
Thomas, D. A., & Morris, M. H. (2017). Creative counselor self-care. In Ideas and research you can use: VISTAS 2017. Retrieved from https://www.counseling.org/docs/default-source/vistas/creative-counselor-self-care.pdf?sfvrsn=4
Thomas, J. T., & Otis, M. D. (2010). Intrapsychic correlates of professional quality of life: Mindfulness, empathy, and emotional separation. Journal of the Society for Social Work and Research, 1(2), 83–98. doi:10.5243/jsswr.2010.7
Thompson, I. A., Amatea, E. S., & Thompson, E. S. (2014). Personal and contextual predictors of mental health counselors’ compassion fatigue and burnout. Journal of Mental Health Counseling, 36, 58–77. doi:10.17744/mehc.36.1.p61m73373m4617r3
Tosone, C., Bettmann, J. E., Minami, T., & Jasperson, R. A. (2010). New York City social workers after 9/11: Their attachment, resiliency, and compassion fatigue. International Journal of Emergency Mental Health, 12(2), 103–116.
Turgoose, D., Glover, N., Barker, C., & Maddox, L. (2017). Empathy, compassion fatigue, and burnout in police officers working with rape victims. Traumatology, 23, 205–213. doi:10.1037/trm0000118
Wagaman, M. A., Geiger, J. M., Shockley, C., & Segal, E. A. (2015). The role of empathy in burnout, compassion satisfaction, and secondary traumatic stress among social workers. Social Work, 60, 201–209.
doi:10.1093/sw/swv014
White, V. E., & Queener, J. (2003). Supervisor and supervisee attachments and social provisions related to the
supervisory working alliance. Counselor Education and Supervision, 42, 203–218.
doi:10.1002/j.1556-6978.2003.tb01812.x
Williams, A., Helm, H., & Clemens, E. V. (2012). The effect of childhood trauma, personal wellness, supervisory working alliance, and organizational factors on vicarious traumatization. Journal of Mental Health Counseling, 34, 133–153. doi:10.17744/mehc.34.2.j3l62k872325h583
Wood, A. E., Prins, A., Bush, N. E., Hsia, J. F., Bourn, L. E., Earley, M. D., . . . Ruzek, J. (2017). Reduction of
burnout in mental health care providers using the Provider Resilience mobile application. Community
Mental Health Journal, 53, 452–459. doi:10.1007/s10597-016-0076-5
Nesime Can is an instructor at Ankara University in Turkey. Joshua C. Watson, NCC, is a professor and department chair at Texas A&M University–Corpus Christi. Correspondence can be addressed to Nesime Can, Ankara University Faculty of Educational Sciences, Department of Educational Sciences, Program of Counseling and Guidance, Office 3111, Çankaya, Ankara, Turkey 06590, nesime.can@ankara.edu.tr.
Sep 7, 2014 | Article, Volume 1 - Issue 3
E. Heather Thompson, Melodie H. Frick, Shannon Trice-Black
Counselors-in-training face the challenges of balancing academic, professional, and personal obligations. Many counselors-in-training, however, report a lack of instruction regarding personal wellness and prevention of personal counselor burnout. The present study used CQR methodology with 14 counseling graduate students to investigate counselor-in-training perceptions of self-care, burnout, and supervision practices related to promoting counselor resilience. The majority of participants in this study perceived that they experienced some degree of burnout in their experiences as counselors-in-training. Findings from this study highlight the importance of the role of supervision in promoting resilience as a protective factor against burnout among counselors-in-training and provide information for counselor supervisors about wellness and burnout prevention within supervision practice
Keywords: counselors-in-training, wellness, burnout, supervision, resilience
Professional counselors, due to often overwhelming needs of clients and heavy caseloads, are at high risk for burnout. Research indicates that burnout among mental health practitioners is a common phenomenon (Jenaro, Flores, & Arias, 2007). Burnout is often experienced as “a state of physical, mental, and emotional exhaustion caused by long-term involvement in emotionally demanding situations” (Gilliland & James, 2001, p. 610). Self-care and recognition of burnout symptoms are necessary for counselors to effectively care for their clients as well as themselves. Counselors struggling with burnout can experience diminished morale, job dissatisfaction (Koeske & Kelly, 1995), negative self-concept, and loss of concern for clients (Rosenberg & Pace, 2006). Clients working with counselors experiencing burnout are at serious risk, as they may not receive proper care and attention to often severe and complicated problems.
The potential hazards for counselor distress in practicum and internship are many. Counselors-in-training often begin their professional journeys with a certain degree of idealism and unrealistic expectations about their roles. Many assume that hard work and efforts will translate to meaningful work with clients who are eager to change and who are appreciative of the counselor’s efforts (Leiter, 1991). However, clients often have complex problems that are not always easily rectified and which contribute to diminished job-related self-efficacy for beginning counselors (Jenaro et al., 2007). In addition, counselor trainees often experience difficulties as they balance their own personal growth as counselors while working with clients with immense struggles and needs (Skovholt, 2001). Furthermore, elusive measures for success in counseling can undermine a new counselor’s sense of professional competence (Kestnbaum, 1984; Skovholt, Grier, & Hanson, 2001). Client progress is often difficult to concretely monitor and define. The “readiness gap,” or the lack of reciprocity of attentiveness, giving, and responsibility between the counselor-in-training and the client, are an additional job-related stressor that may increase the likelihood of burnout (Kestnbaum, 1984; Skovholt et al., 2001; Truchot, Keirsebilck, & Meyer, 2000).
Counselors-in-training are exposed to emotionally demanding stories (Canfield, 2005) and situations which may come as a surprise to them and challenge their ideas about humanity. The emotional demands of counseling entail “constant empathy and one-way caring” (Skovholt et al., 2001, p. 170) which may further drain a counselor’s reservoir of resilience. Yet, mental health practitioners have a tendency to present themselves as caregivers who are less vulnerable to emotional distress, thereby hindering their ability to focus on their own needs and concerns (Barnett, Baker, Elman, & Schoener, 2007; Sherman, 1996). Counselors who do not recognize and address their diminished capacity when stressed are likely to be operating with impaired professional competence, which violates ethical responsibilities to do no harm.
Counselor supervision is designed to facilitate the ethical, academic, personal, and professional development of counselors-in-training (CACREP, 2009). Bolstering counselor resilience in an effort to prevent burnout is one aspect of facilitating ethical, personal, and professional development. Supervisors who work closely with counselors-in-training during their practicum and internship can promote the hardiness and sustainability of counselors-in-training by helping them learn to self-assess in order to recognize personal needs and assert themselves accordingly. This may include learning to say “no” to the demands that exceed their capacity or learning to actively create and maintain rejuvenating relationships and interests outside of counseling (Skovholt et al., 2001). Supervisors also can teach and model self-care and positive coping strategies for stress, which may influence supervisees’ practice of self-care (Aten, Madson, Rice, & Chamberlain, 2008). In an effort to bolster counselor resilience, supervisors can facilitate counselor self-understanding about overextending oneself to prove professional competency to achieve a sense of self-worth (Rosenburg & Pace, 2006). Supervisors can help counselors-in-training come to terms with the need for immediate positive reinforcement related to work or employment, which is limited in the counseling profession as change rarely occurs quickly (Skovholt et al., 2001). Counselor resiliency also may be bolstered by helping counselors-in-training establish realistic measures of success and focus on the aspects of counseling that they can control such as their knowledge and ability to create strong therapeutic alliances rather than client outcomes. In sum, distressing issues in counseling, warning signs of burnout, and coping strategies for dealing with stress should be discussed and the seeds of self-care should be planted so they may grow and hopefully sustain counselors-in-training over the course of their careers.
Method
The purpose of this exploratory study was to investigate counselor-in-training perceptions of self-care, burnout, and supervision practices related to promoting counselor resilience. The primary research questions that guided this qualitative study included: (a) What are master’s-level counselors-in-training’s perceptions of counselor burnout? (b) What are the perceptions of self-care among master’s-level counselors-in-training? (c) What, if anything, have master’s-level counselors-in-training learned about counselor burnout in their supervision experiences? And (d) what, if anything, have master’s level counselors-in-training learned about self-care in their supervision experiences?
The consensual qualitative research method (CQR) was used to explore the supervision experiences of master’s-level counselors-in-training. CQR works from a constructivist-post-positivist paradigm that uses open-ended semi-structured interviews to collect data from individuals, and reaches consensus on domains, core ideas, and cross-analyses by using a research team and an external auditor (Hill, Knox, Thompson, Williams, Hess, & Ladany, 2005; Ponterotto, 2005). Using the CQR method, the research team examined commonalities and arrived at a consensus of themes within and across participants’ descriptions of the promotion of self-care and burnout prevention within their supervision experiences (Hill et al., 2005; Hill, Thompson, & Nutt Williams, 1997).
Participants
Interviewees. CQR methodologists recommend a sample size of 8–15 participants (Hill et al., 2005). The participants in this sample included 14 individuals; 13 females and 1 male, who were graduate students in master’s-level counseling programs and enrolled in practicum or internship courses. The participants attended one of three universities in the United States (one in the Midwest and two in the Southeast). The sample consisted of 10 participants in school counseling programs and 4 participants in clinical mental health counseling programs. Thirteen participants identified as Caucasian, and one participant identified as Hispanic. The ages of participants ranged from 24 to 52 years of age (mean = 28).
Researchers. An informed understanding of the researchers’ attempt to make meaning of participant narratives about supervision, counselor burnout, and self-care necessitates a discussion of potential biases. This research team consisted of three Caucasian female faculty members from three different graduate-level counseling programs. All three researchers are proficient in supervision practices and passionate about facilitating counselor growth and development through supervision. All members of the research team facilitate individual and group supervision for counselors-in-training in graduate programs. The three researchers adhere to varying degrees of humanistic, feminist, and constructivist theoretical leanings. All members of the research team believe that supervision is an appropriate venue for bolstering both personal and professional protective factors that may serve as buffers against counselor burnout. It also is worth noting that the three members of the research team believed they had experienced varying degrees of burnout over the course of their careers. The researchers acknowledge these shared biases and attempted to maintain objectivity with an awareness of their personal experiences with burnout, approaches to supervision, and beliefs regarding the importance of addressing protective factors, wellness and burnout prevention in supervision. This study also was influenced by an external auditor who is a former counselor educator with more than 20 years of experience in qualitative research methods and supervision practice. As colleagues in the field of counselor education and supervision, the research team and the auditor were able to openly and respectfully discuss their differing perspectives throughout the data analysis process, which permitted them to arrive at consensus without being stifled by power struggles.
Procedures for Data Collection
Criterion sampling was used to select participants in an intentional manner to understand specified counseling students’ experiences in supervision. Criteria for participation in this study included enrollment as a graduate student in a master’s-level counseling program and completion of a practicum experience or participation in a counseling internship in a school or mental health counseling agency. Researchers disseminated information about this study by email to master’s-level students in counseling programs at three different universities. Interested students were instructed to contact, by email or phone, a designated member of the research team, who was not a faculty member at their university. All participants were provided with an oral explanation of informed consent and all participants signed the informed consent documents. All procedures followed those established by the Institutional Review Board of the three universities associated with this study.
Within the research team, researchers were designated to conduct all communication, contact, and interviews with participants not affiliated with their respective universities, in order to foster a confidential and non-coercive environment for the participants. Interviews were conducted on one occasion, in person or via telephone, in a semi-structured format. Participants in both face-to-face and telephone interviews were invited to respond to questions from the standard interview protocol (see Appendix A) about their experiences and perceptions of supervision practices that addressed counselor self-care and burnout prevention. Participants were encouraged to elaborate on their perceptions and experiences in order to foster the emergence of a rich and thorough understanding. The transferability of this study was promoted by the rich, thick descriptions provided by an in-depth look at the experiences and perceptions of this sample of counselors-in-training. Interviews lasted approximately 50–70 minutes. The interview protocol was generated after a thorough review of the literature and lengthy discussions about researcher experiences as a supervisee and a supervisor. Follow-up surveys (see Appendix B) were administered electronically to participants six weeks after the interview to capture additional thoughts and experiences of the participants.
Data Analysis
All interviews were audio-taped and transcribed verbatim for data analysis. Transcripts were checked for accuracy by comparing them to the audio-recordings after the transcription process. Participant names were changed to pseudonyms to protect participant anonymity. Participants’ real names and contact information were only used for scheduling purposes. Information linking participants to their pseudonyms was not kept.
Coding of domains. Prior to beginning the data analysis process, researchers generated a general list of broad domain codes based on the interview protocol, a thorough understanding of the extant literature, and a review of the transcripts. Once consensus was achieved, each researcher independently coded blocks of data into each domain code for seven of the 14 cases. Next, as a team, the researchers worked together to generate consensus on the domain codes for the seven cases. The remaining cases were analyzed by pairs of the researchers. The third team member reviewed the work of the pair who generated the domain coding for the remaining seven cases. Throughout the coding process, domains were modified to best capture the data.
Abstracting the core ideas within each domain. Each researcher worked independently to capture the core idea for each domain by re-examining each transcript. Core ideas consisted of concise statements of the data that illuminated the essence of the participant’s expressed perspectives and experiences. As a group, the researchers discussed the wording of core ideas for each case until consensus was achieved.
Cross analysis. The researchers worked independently to identify commonalities of core ideas within domains across cases. Next, as a group, the research team worked to find consensus on the identified categories across cases. Aggregated core ideas were placed into categories and frequency labels were applied to indicate how general, typical, or variant the results were across cases. General frequencies refer to findings that are true for all but one of the cases (Hill et al., 2005). Typical frequencies refer to findings that are present in more than half of the cases. Variant frequencies refer to finding in at least two cases, but less than half.
Audit. An external auditor was invited to question the data analysis process and conclusions. She was not actively engaged in the conceptualization and implementation of this study, which gave the research team the benefit of having an objective perspective. The external auditor reviewed and offered suggestions about the generation of domains and core ideas, and the cross-case categories. Most feedback was given in writing. At times, feedback was discussed via telephone. The research team reviewed all auditor comments, looked for evidence supporting the suggested change, and made adjustments based on team member consensus.
Stability check. For the purpose of determining consistency, two of the 14 transcripts were randomly selected and set aside for cross-case analysis until after the remaining 12 transcripts were analyzed. This process indicated no significant changes in core domains and categories, which suggested consistency among the findings.
Results
A final consensus identified five domains: counselor burnout, counselor self-care, faculty supervision, site supervision, and improvements (see Table 1). Cross-case categories and subcategories were developed to capture the core ideas. Following CQR procedures (Hill et al., 1997, 2005), a general category represented all or all but one of the cases (n = 13–14); a typical category represented at least half of the cases (n = 7–12); and a variant category represented less than half but more than two of the cases (n = 3 – 6). Categories with fewer than three cases were excluded from further analysis. General categories were not identified from the data.
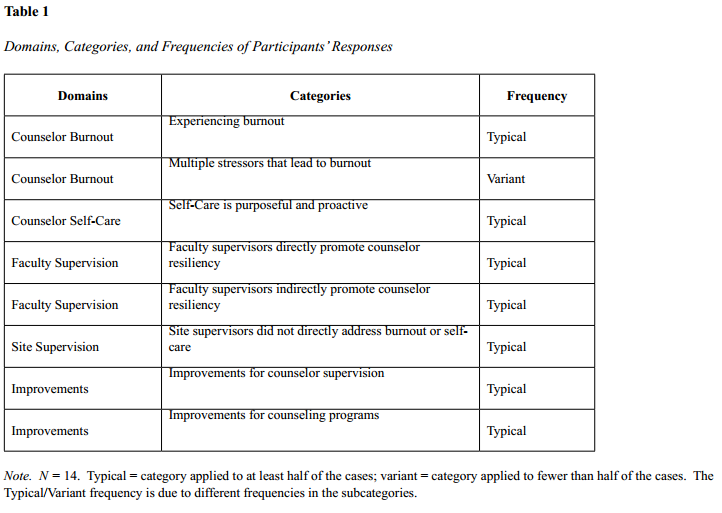
Counselor Burnout
Experiencing burnout. Most participants reported knowledge of or having experiences with burnout. Participants identified stressors leading to burnout as a loss of enthusiasm and compassion, the struggle to balance school, work, and personal responsibilities and relationships, and difficulty delineating and separating personal and professional boundaries.
Participants described counselor burnout as no longer having compassion or enthusiasm for counseling clients. One participant defined counselor burnout as, “it seems routine or [counselors] feel like they’ve dealt with so many situations over time that they’re just kind of losing some compassion for the field or the profession.” Another participant described counselor burnout as no longer seeing the unique qualities of individuals seen in counseling:
I wouldn’t see [clients] as individuals anymore…and that’s where I get so much of it coming at me, or so many clients coming at me, that they’re no longer an individual they’re just someone that’s sitting in front of me, and when they leave they write me a check….they are not people anymore, they’re clients.
Participants often discussed a continual struggle to balance personal and professional responsibilities. One participant described burnout as foregoing pleasurable activities to focus on work-related tasks:
I can tell when I am starting to get burned out when I am focusing so much on those things that I forgo all of those things that are fun for me. So I am not working out anymore, I am not reading for fun, and I am putting off hanging out with my friends because of my school work. There’s school work that maybe doesn’t have to get done at that moment, but if I don’t work on it I’m going to be thinking about it and not having fun.
Another participant described burnout as having a hard time balancing professional and personal responsibilities stating, “I think I don’t look forward to…working with…people. I’m just kind of glad when they don’t show up. And this kind of sense that I’m losing the battle to keep things in balance.”
Boundary issues were commonly cited by participants. Several participants reported that they struggled to be assertive, set limits, maintain realistic expectations, and not assume personal responsibility for client outcomes. One participant described taking ownership of a client’s outcome and wanting to meet all the needs of her clients:
I believe part of it is internalizing the problem on myself, feeling responsible. Maybe loosing sight of my counseling skills and feeling responsible for the situation. Or feeling helpless. Also, in school counseling there tends to be a larger load of students. And this is frustrating to not meet all the needs that are out there.
Participants reported experiences with burnout and multiple stressors that lead to burnout. Participants defined counselor burnout as a loss of compassion for clients, diminished enthusiasm, difficulty maintaining a life-work balance, and struggles to maintain boundaries.
Counselor Self-Care
Self-care is purposeful and proactive. Participants were asked to describe self-care for counselors and reported that self-care requires purposeful efforts to set time aside to engage in activities outside of work that replenish energy and confidence. Most participants identified having and relying on supportive people, such as family, friends, and significant others to help them cope with stressors. Participants also identified healthy eating and individualized activities such as exercise, reading, meditation, and watching movies as important aspects of their self-care. One participant described self-care as:
Anything that can help you reenergize and refill that bucket that’s being dipped into every day. If that’s going for a walk in the park…so be it. If that’s going to Starbucks…go do it….Or something that makes you feel good about yourself, something that makes you feel confident, or making someone else feel confident….Whatever it is, something that makes you feel good about yourself and knowing that you’re doing what you need to be doing.
Participants reported that self-care requires proactive efforts to consult with supervisors and colleagues; one of the first steps is recognizing when one needs consultation. One participant explained:
I think in our program, [the faculty] were very good about letting us know that if you can’t handle something, refer out, consult. Consult was the theme. And then if you feel you really can’t handle it before you get in over your head, make sure you refer out to someone you feel is qualified.
Participants described self-care as individualized and intentional, and included activities and supportive people outside of school or work settings that replenished their energy levels. Participants also discussed the importance of identifying when counselor self-care is necessary and seeking consultation for difficult client situations.
Faculty Supervision
Faculty supervisors directly promote counselor resiliency. More than half of the participants reported that faculty supervisors directly initiated conversations about self-care. A participant explained, “Every week when we meet for practicum, [the faculty supervisor] is very adamant, ‘is everyone taking care of themselves, is anyone having trouble?’ She is very open to listening to any kind of self-care situation we might have.” Similarly, another participant stated, “Our professors have told us about the importance of self-care and they have tried to help us understand which situations are likely to cause us the most stress and fatigue.” One participant identified preventive measures discussed in supervision:
In supervision, counselor burnout is addressed from the perspective of prevention. We develop personal wellness plans, and discuss how well we live by them during supervision….Self-care is addressed in the same conversation as counselor burnout. In supervision, the mantra is good self-care is vital to avoiding burnout.
Faculty supervisors indirectly promote counselor resiliency. Participants also reported that faculty supervisors indirectly addressed counselor self-care by being flexible and supportive of participants’ efforts with clients. Participants repeatedly expressed appreciation for supervisors who processed cases and provided positive feedback and practical suggestions. One participant explained, “I know that [my supervisor] is advocating for me, on my side, and allowing me to vent, and listening and offering advice if I need it….giving me positive feedback in a very uncomfortable time.”
Further, participants stated they appreciated supervisors who actively created a safe space for personal exploration. One participant explained:
[Supervision] was really a place for us to explore all of ourselves, holistically. The forum existed for us for that purpose. [The supervisors] hold the space for us to explore whatever needs to be explored. That was the great part about internship with the professor I had. He sort of created the space, and we took it. It took him allowing it, and us stepping into the space.
Modeling self-care also is an indirect means of addressing counselor burnout and self-care. Half of the participants reported that their faculty supervisors modeled self-care. For example, faculty supervisors demonstrated boundaries with personal and professional obligations, practiced meditation, performed musically, and exercised. Conversely, participants reported that a few supervisors demonstrated a lack of personal self-care by working overtime, sacrificing time with their families for job obligations, and/or having poor diet and exercise habits.
Participants reported that faculty supervisors directly and indirectly addressed counselor burnout and self-care in supervision. Supervisors who intentionally checked in with the supervisees and used specific techniques such as wellness plans were seen as directly affecting the participants’ perspective on counselor self-care. Supervisors who were present and available, created safe environments for supervision, provided positive feedback and suggestions, and modeled self-care were seen as indirectly addressing counselor self-care. Both direct and indirect means of addressing counselor burnout and self-care were seen as influential by participants.
Site Supervision
Site supervisors did not directly address burnout or self-care. Participants reported that site supervisors rarely initiated conversations about counselor burnout or self-care. One participant reported that counselor burnout was not addressed and as a result she felt a lack of support from the supervisor:
[Site Supervisors] don’t ask about burnout though. Every time I’m bringing it up, the answers I’m getting are ‘well, when you’re in grad school you don’t get a life.’ You know, yeah, I get that, but that’s not really true, so I get a lot of those responses, ‘well, you know, welcome to the club.’
One participant stated that her site supervisor did not specifically address counselor burnout or self-care, stating “I think that is less addressed in a school setting than it is in the mental health field….I think that because we see such a small picture of our students, I think it is not as predominantly addressed.” Some participants, however, reported that their site supervisors indirectly addressed self-care by modeling positive behaviors. One participant stated:
[My site supervisor] has either structured her day or her life in such a way that no one cuts into that time unless she allows it. In that sense, she’s great at modeling what’s important…She just made a choice….She was protective. She made her priorities. Her family was a priority. Her walk was a priority, getting a little activity. Other things, house chores, may have fallen by the wayside. She had a good sense of priorities, I thought. That was good to watch.
In summary, participants reported that counselor burnout and self-care were not directly addressed in site supervision. Indeed, some participants felt a lack of support when feeling overwhelmed by counseling duties, and that school sites may address burnout and self-care less than at mental health sites. At best, self-care was indirectly modeled by site supervisors with positive coping mechanisms.
Improvements for Counselor Supervision and Training
Improvements for counselor supervision. More than half of the participants reported wanting more understanding and empathy from their supervisors. One participant complained:
A lot of my class mates have a lot on their plates, like I do, and our supervisors don’t have as much on their plate as we do. And it seems like they don’t quite get where we are coming from. They are not balancing all the things that we are balancing….a lot of the responses you get demonstrate their lack of understanding.
Another participant suggested:
I think just hearing what the person is saying. If the person is saying, I need a break, just the flexibility. Not to expect miracles, and just remember how it felt when you were in training. Just be relatable to the supervisees and try to understand what they are going through, and their point of view. You don’t have to lower your expectations to understand where we’re at…and to be honest about your expectations…flexible, honest, and understanding. If [supervisors] are those three things, it’ll be great.
Participants also suggested having counselor burnout and self-care more thoroughly addressed in supervision, including more discussions on balancing personal and professional responsibilities, roles, and stressors. One participant explained:
What would be really helpful when the semester first begins is one-on-one time that is direct about ‘how are you approaching this internship in balance with the rest of your life?’ ‘What are any issues that it would be worthwhile for me to know about?’ How sweet for the supervisor to see you as a whole person. And then to put out the invitation: the door’s always open.
Improvements for counselor training programs. More than half of the participants wanted a comprehensive and developmentally appropriate approach to self-care interwoven throughout their counselor training, with actual practice of self-care skills rather than “face talk.” One participant commented:
Acknowledge the reality that a graduate-level program is going to be a challenge, talking about that on the front end….[faculty] can’t just say you need to have self-care and expect [students] to be able to take that to the next level if we don’t learn it in a graduate program….how much better would it be for us to have learned how to manage that while we were in our program and gotten practice and feedback about that, and then that is so important of a skill to transfer and teach to our clients.
Most of the participants suggested the inclusion of concrete approaches to counselor self-care. Participants provided examples such as preparing students for their work as counselors-in-training by giving them an overview of program expectations at the beginning of their programs, and providing students with self-care strategies to deal with the added stressors of graduate school such as handling administrative duties during internship, searching for employment prior to graduation, and preparing for comprehensive exams.
Discussion
Findings from this study highlight the importance of the role of supervision in promoting resilience as a protective factor against burnout among counselors-in-training. The majority of participants in this study perceived that they experienced some degree of burnout in their experiences as counselors-in-training. Participants’ perceptions of experiencing burnout are a particularly meaningful finding because it indicates that these counselors-in-training see themselves as over-taxed during their education and training. If, during their master’s programs, counselors-in-training are creating professional identities based on cognitive schemas for being a counselor, then perhaps these counselors-in-training have developed schemas for counseling that include a loss of compassion for clients, diminished enthusiasm for counseling, a lopsided balance of personal and professional responsibilities, and struggles to maintain boundaries. Counselors-in-training should be aware of these potential pitfalls as these counselors-in-training reported experiencing symptoms of burnout which were rarely addressed in supervision.
In contrast to recent literature, which suggests that counselor burnout is related to overcommitment to client outcomes (Kestnbaum, 1984; Leiter, 1991; Shovholt et al., 2001), many counselor trainees in this study did not perceive that their supervisors directly addressed their degree of personal commitment to their clients’ success in counseling. Similarly, emotional exhaustion is commonly identified as a potential hazard for burnout (Barnett et al., 2007); yet, few participants believed that their supervisors directly inquired about the degree of emotional investment in their clients. Finally, elusive measures of success in counseling are often indicated as a potential factor for burnout (Kestnbaum, 1984; Skovholt, et al., 2001). The vast majority of participants interviewed for this study did not perceive that these elusive measures of success were addressed in their supervision experiences. Supervisors who are interested in thwarting counselor burnout early in the training experiences of counselors may want to consider incorporating conversations about overcommitment to client outcomes, emotional exhaustion, degree of emotional investment, and elusive measures of success into their supervision with counselors-in-training. In an effort to promote more resilient schemas and expectations for counseling work, supervisors can take an active role in helping counselors-in-training understand the importance of awareness and protective factors to protect against a lack of compassion, enthusiasm, life-work balance, and professional boundaries, similar to the way a pilot is aware that a plane crash is possible and therefore employs purposeful and effective methods of prevention and protection.
Participants in this study conceptualized self-care as purposeful behavioral efforts. Proactive behavioral choices such as reaching out to support others are ways that many counselors engage in self-care. However, self-care cannot be solely limited to engagement in specific behaviors. Self-care also should include discussions about cognitive, emotional, and spiritual coping skills. Supervisors can help counselors-in-training create a personal framework for finding meaning in their work in order to promote hardiness, resilience, and the potential for transformation (Carswell, 2011). Because of the nature of counseling, it is necessary for counselors to be open and have the courage to be transformed. Growth and transformation are often perceived as scary and something to be avoided. Yet, growth and transformation can be embraced and understood as part of each counselor’s unique professional and personal process. Supervisors can normalize and validate these experiences and help counselors-in-training narrate their inspirations and incorporate their personal, spiritual, and philosophical frameworks in their counseling. In addition, supervisors can directly address misperceptions about counseling, which often include: “I can fix the problem,” “I am responsible for client outcomes,” “Caring more will make it better,” and “My clients will always appreciate me” (Carswell, 2011). While these approaches to supervision are personal in nature, counselors-in-training in this study reported an appreciation for time spent discussing how the personal informs the professional. This finding is consistent with Bernard & Goodyear’s (1998) model of supervision which emphasizes personal development as an essential part of supervision. Models for personal development in counselor education programs have been proposed by many professionals in the field of counseling (Myers, 1991; Myers & Williard, 2003; Witmer & Granello, 2005).
Counselors-in-training in this study reported an appreciation for supervision experiences in which their supervisors provided direct feedback and positive reinforcement. Counselors-in-training often experience performance anxiety and self-doubt (Aten et al., 2008). In an effort to diminish counselor-in-training anxiety, supervisors may provide additional structure and feedback in the early stages of supervision. Once the counselor-in-training becomes more secure, the supervisor may facilitate a supervisory relationship that promotes supervisee autonomy and higher-level thinking.
The majority of participants interviewed reported a desire for supervisors to place a greater emphasis on life-work balance and learning to cope with stress. These findings suggest the importance of counselor supervisors examining their level of expressed empathy and emphasis on preventive, as well as remedial, measures to ameliorate symptoms and stressors that lead to counselor burnout. Participants expressed a need to be more informed about additional stressors in graduate school such as administrative tasks in internship, preparing for comprehensive exams, and how to search for employment. These findings suggest the need for counselor educators and supervisors to examine how they indoctrinate counselors-in-training into training programs in order to help provide realistic expectations of work and personal sacrifice during graduate school and in the counseling field. Moreover, counselor educators and supervisors should strive to provide ongoing discussions on self-care throughout the program, specifically when students in internship are experiencing expanding roles between school, site placement, and searching for future employment. As mental health professionals, counselor educators and supervisors may also struggle with their own issues of burnout; thus, attentiveness to self-care also is recommended for those who teach and supervise counselors in training.
Limitations
Findings from this study will benefit counselor educators, supervisors, and counselors-in-training; however, some limitations exist. One limitation is the lack of diversity in the sample of participants. The majority of the participants identified as Caucasian females, which is representative of the high number of enrolled females in the counseling programs approached for this study. The purpose for this study, however, was not to generalize to all counselor trainees’ experiences, but rather to shed light on how counselor perceptions of burnout and self-care are being addressed, or not, in counselor supervision.
Participant bias and recall is a second limitation of this study. Recall is affected by a participant’s ability to describe events and may be influenced by emotions or misinterpretations. This limitation was addressed by triangulating sources, including a follow-up questionnaire, reinforcing internal stability with researcher consensus on domains, core ideas, and categories, and by using an auditor to evaluate analysis and prevent researcher biases.
Conclusion
Counselors should be holders of hope for their clients, but one cannot give away what one does not possess (Corey, 2000). Counselors who lack enthusiasm for their work and compassion for their clients are not only missing a critical element of their therapeutic work, but also may cause harm to their clients. Counseling is challenging and can tax even the most “well” counselors. A lack of life-work balance and boundaries can add to the already stressful nature of being a counselor. Discussions in supervision about the potential for emotional exhaustion, the counselor-in-training’s degree of emotional investment in client outcomes, elusive measures of success in counseling, coping skills for managing stress, meaning-making and sources of inspiration, and personalized self-care activities are several ways supervisors can promote counselor resilience and sustainability. Supervisors should discuss the definitions of burnout, how burnout is different from stress, how to identify early signs of burnout, and how to address burnout symptoms in order to promote wellness and prevent burnout in counselors-in-training. Counselor educators and supervisors have the privilege and responsibility of teaching counselors-in-training how to take care of themselves in addition to their clients.
References
Aten, J. D., Madson, M. B., Rice, A., & Chamberlain, A. K. (2008). Postdisaster supervision strategies for promoting supervisee self-care: Lessons learned from hurricane Katrina. Training and Education in Professional Psychology, 2(2), 75–82. doi:10.1037/1931-3918.2.2.75
Barnett, J. E., Baker, E. K., Elman, N. S., & Schoener, G. R. (2007). In pursuit of wellness: The self-care imperative. Professional Psychology: Research and Practice, 38(6), 603–612. doi:10.1037/0735-7028.38.6.603
Bernard, J. M., & Goodyear, R. K. (1998). Fundamentals of clinical supervision (2nd ed.). Needham Heights, MA: Allyn & Bacon.
Council for Accreditation of Counseling and Related Educational Programs (CACREP) (2009). 2009 Standards. Retrieved from http://www.cacrep.org/ doc/2009%20standards %20with20cover.pdf
Canfield, J. (2005). Secondary traumatization, burnout, and vicarious traumatization: A review of the literature as it relates to therapists who treat trauma. Smith College Studies in Social Work, 75(2), 81–102. doi:10.1300 J497v75n02_06
Carswell, K. (2011, March). Lecture on combating compassion fatigue: Strategies for the long haul. Counseling Department, Western Carolina University, Cullowhee, NC.
Corey, G. (2000). Theory and practice of group counseling (5th ed.). Belmont, CA: Wadsworth/Thompson Learning.
Hill, C. E., Knox, S., Thompson, S. J., Williams, E. N, Hess, S. A., & Ladany, N. (2005). Consensual qualitative research: An update. Journal of Counseling Psychology, 23(2), 196–205. doi:10.1037/0022-0167.52.2.196
Hill, C. E., Thompson, B. J., & Nutt Williams, E. (1997). A guide to conducting consensual qualitative research. The Counseling Psychologist, 25, 517–572. doi:10.1177/ 0011000097254001
Gilliland, B. E., & James, R. K. (2001). Crisis intervention strategies. Pacific Grove, CA: Brooks/Cole-Thomson Learning.
Jenaro, C., Flores, N., & Arias, B. (2007). Burnout and coping in human service practitioners. Professional Psychology: Research and Practice, 38, 80–87. doi:10.1037/0735-7028.38.1.80
Koeske, G. F., & Kelly, T. (1995). The impact of overinvolvement on burnout and job satisfaction. American Journal of Orthopsychiatry, 65, 282–292. doi:10.1037/h0079622
Kestnbaum, J. D. (1984). Expectations for therapeutic growth: One factor in burnout. Social Casework: The Journal of Contemporary Social Work, 65, 374–377.
Leiter, M. (1991). The dream denied: Professional burnout and the constraints of human service organizations. Canadian Psychology, 32(4), 547–558. doi:10.1037/h0079040
Myers, J. E. (1991). Wellness as the paradigm for counseling and development. The possible future. Counselor Education and Supervision, 30, 183–193.
Myers, J. E., & Williard, K. (2003). Integrating spirituality into counselor preparation: A developmental, wellness approach. Counseling and Values, 47, 142–155.
Ponterotto, J. G. (2005). Qualitative research in counseling psychology: A primer on research paradigms and philosophy of science. Journal of Counseling Psychology, 52(2), 126–136. doi:10.1037/0022-0167.52.2.196
Rosenberg, T., & Pace, M. (2006). Burnout among mental health professionals: Special considerations for the marriage and family therapist. Journal of Marital and Family Therapy, 32(1), 87–99. doi:10.1111/j.1752- 0606.2006.tb01590
Sherman, M. D. (1996). Distress and professional impairment due to mental health problems among psychotherapists. Clinical Psychology Review, 16, 299–315. doi:10.1016/0272- 7358(96)00016-5
Skovholt, T. M. (2001). The resilient practitioner: Burnout prevention and self-care strategies for counselors, therapists, teachers, and health professionals. Needham Heights, MA: Allyn & Bacon.
Skovolt, T. M., Grier, T. L., & Hanson, M. R. (2001). Career counseling for longevity: Self-care and burnout prevention strategies for counselor resilience. Journal of Career Development, 27(3), 167–176. doi:10.1177/089484530102700303
Truchot, D., Keirsebilck, L., & Meyer, S. (2000). Communal orientation may not buffer burnout. Psychological Reports, 86, 872–878. doi:10.2466/PR0.86.3.872-878
Witmer, J. M., & Granello, P. F. (2005). Wellness in counselor education and supervision. In J. E. Myers & T. J. Sweeney (Eds.), Counseling for wellness: Theory, research, and practice (pp. 342–361). Alexandria, VA: American Counseling Association.
E. Heather Thompson is an Assistant Professor in the Department of Counseling Western Carolina University. Melodie H. Frick is an Assistant Professor in the Department of Counseling at West Texas A & M University. Shannon Trice-Black is an Assistant Professor at the College of William and Mary. Correspondence can be addressed to Shannon Trice-Black, College of William and Mary, School of Education, PO Box 8795, Williamsburg, VA, 23187-8795, stblack@wm.edu.
Appendix A
Interview Protocol
1. What do you know about counselor burnout or how would you define counselor burnout?
2. What do you think are possible causes of counselor burnout?
3. As counselors we often are overloaded with administrative duties which may include treatment planning, session notes, and working on treatment teams. What has this experience been like for you?
4. Counseling requires a tremendous amount of empathy which can be emotionally exhausting. What are your experiences with empathy and emotional exhaustion? Can you give a specific example?
5. How do you distinguish between feeling tired and the early signs of burnout?
6. As counselors, we sometimes become overcommitted to clients who are not as ready, motivated, or willing to engage in the counseling process. Not all of our clients will succeed in the way that we want them to. How do you feel when your clients don’t grow in the way you want them to? How has this issue been addressed in supervision?
7. What is your perception of how your supervisors have dealt with stress?
8. How has counselor burnout been addressed in supervision?
prompt: asked about, evaluated, provided reading materials, and how often
9. How have specific issues related to burnout been addressed in supervision such as: (a) over-commitment to clients who seem less motivated to change, (b) emotional exhaustion, and (c) elusive measures of success?
10. How could supervision be improved in addressing counselor burnout?
prompt: asked about, evaluated, provided reading materials, modeled by supervisor
11. What do you know about self-care or how would you define self-care for counselors?
12. What are examples of self-care, specifically ones that you use as counselors-in-training?
13. How has counselor self-care been addressed in supervision?
14. Sometimes we have to say “no.” How would you characterize your ability to say “no?” What have you learned in supervision about setting personal and professional boundaries?
15. What, if any, discussions have you had in supervision about your social, emotional, spiritual, and/or physical wellbeing? What is a specific example?
16. How could supervision be improved in addressing counselor self-care?
prompt: asked about, provided reading materials, modeled by supervisor
17. How could your overall counselor training be improved in addressing counselor burnout and counselor self-care?
Appendix B
Follow-Up Questionnaire
How would you describe counselor burnout?
How has counselor burnout been addressed in supervision?
How could supervision be improved in addressing counselor burnout?
How would you describe self-care for counselors?
How has counselor self-care been addressed in supervision?
How could supervision be improved in addressing counselor self-care?
How could your overall counselor training be improved in addressing counselor burnout and counselor self-care?