May 22, 2024 | Volume 14 - Issue 1
Kaprea F. Johnson, Alexandra Gantt-Howrey, Bisola E. Duyile, Lauren B. Robins, Natese Dockery
Career counselors practicing in rural communities must understand and address social determinants of mental health (SDOMH). This conceptual article details the relationships between SDOMH domains and employment and provides evidence-based recommendations for integrating SDOMH into practice through a rural community health and well-being framework. Description of the adaptation of the framework for career counselors in rural communities, SDOMH assessment strategies and tools, and workflow adjustments are included. Conclusions suggest next steps for practice and research.
Keywords: social determinants of mental health, career counselors, rural communities, health and well-being framework, assessment
Career counselors in rural communities address standard employment needs of the population, but they also must be aware of the socioeconomic circumstances that impact their community’s mental health and, in return, employment. Such socioeconomic factors are termed the social determinants of mental health (SDOMH). SDOMH are nonclinical psychosocial and socioeconomic circumstances that contribute to mental health outcomes (Office of Disease Prevention and Health Promotion [ODPHP], n.d.). Healthy People 2030, a government initiative to promote health and well-being, describes a five-domain framework of SDOMH which includes: economic stability, education access and quality, health care access and quality, neighborhood and built environment, and social and community context (ODPHP, n.d.). Collectively, SDOMH can disrupt overall well-being and have a cyclical relationship with employment. For example, in rural communities, minimal access to public transportation may make sustaining employment difficult, which can then impact health insurance. Without insurance, a person loses access to health care; with unmet health care needs, a person who is unwell and without access to treatment has less opportunity for employment. Thus, understanding and addressing SDOMH is critically important for career counselors working in rural and other underserved communities (Pope, 2011). This conceptual paper will define SDOMH, introduce a theoretical framework for addressing SDOMH, provide evidence-based recommendations for assessment and treatment, and conclude with national resources to support career counselors in rural communities as they incorporate addressing SDOMH into their work.
Rural Communities, Employment, and Career Counselors
The U.S. Census Bureau considers rural communities as a group of people, counties, and housing outside of an urban area. More specifically, the Office of Management and Budget defines rural as areas with an urban core population of fewer than 50,000 people (Health Resources and Services Administration, 2017). After the 2010 Census, it was estimated that approximately 15% of the population lives in rural communities (Health Resources & Services Administration, 2017). Rural communities experience higher rates of unemployment and poverty, and residents are therefore more likely to live below the poverty line (United States Department of Agriculture [USDA], 2014). This is largely rooted in the fact that rural communities experience underdevelopment, economic decline, and neglect (Dwyer & Sanchez, 2016). Economic focus in rural environments typically centers around agriculture, rather than technological advancement (Dwyer & Sanchez, 2016). This contributes in part to a dearth of economic resources and thereby to increased unemployment and poverty and reduced health and well-being outcomes (Bradshaw, 2007; Brassington, 2011; Dwyer & Sanchez, 2016).
According to research conducted by the USDA, the unemployment rate in rural communities steadily declined for approximately 10 years prior to the COVID-19 pandemic; in September of 2019, the rural unemployment rate was 3.5% (Dobis et al., 2021). However, unemployment in rural communities reached 13.6% in April 2020, with unemployment disparately affecting those in more impoverished communities (Dobis et al., 2021). The role and goal of the career counselor is to help individuals in a specific community obtain or retain employment (Landon et al., 2019). For example, career counselors start the counseling process by systematically assessing clients’ needs, qualifications, and job aspirations. They provide career planning services and effective job search strategies. They help with résumé writing, interview preparations, skill development, and training opportunities (Amundson, 1993). Further, career counselors provide case management services by tracking and monitoring their clients’ progress. They record client information, document counseling sessions, track job applications, and survey employment outcomes (Amundson, 1993). Through tailored support, the career counselor works with the client throughout the life span to support the search for and maintaining of employment, while building client resilience and feelings of empowerment along the way.
However, rural communities have limited employment options and self-employment opportunities, which makes the role of the career counselor difficult in rural settings. Individuals in rural communities seeking employment may find it difficult to trust an outside counselor, and they may experience limited or no access to mental health services, health care practitioners, and transportation services, thereby negatively impacting their ability to participate effectively in the employment process (Landon et al., 2019). Career counselors in rural settings must develop a broader range of skills and connections to better serve their clients. These inequities experienced in rural settings reflect SDOMH and are factors which interfere with the role of the career counselor.
Social Determinants of Mental Health and Employment
SDOMH are the nonmedical factors shaped by the unequal distribution of power, privilege, and resources that influence the health outcomes of individuals and communities (World Health Organization, 2014). SDOMH concern the environmental living conditions that affect a wide range of health, functioning, and quality-of-life outcomes and risks (Centers for Disease Control and Prevention, 2020). In the Healthy People 2030 framework, the ODPHP (n.d.) defined social determinants of health (SDOH) through five primary domains: Economic Stability, Education Access and Quality, Health Care Access and Quality, Neighborhood and Built Environment, and Social and Community Context. These five domains are important to understand within the context of employment. In the Economic Stability domain, employment is the most pertinent issue (ODPHP, n.d.), as a lack of employment typically influences both mental and physical health (Norström et al., 2019). A few distinct factors related to economic stability and employment include job security, work environment, monetary factors (e.g., pay), and the demands of the job (ODPHP, n.d.). For example, in rural communities, agriculture is a significant source of employment for individuals. However, this source of income is seemingly unstable, as farming and agriculture are mostly dependent on the season (Liebman, 2010). In the Education Access and Quality domain, enrollment in higher education or holding a higher education degree has been found to have a positive impact on employment, as well as yielding more positive overall health outcomes and optimal well-being (ODPHP, n.d.; USDA, 2017). For adults living in rural communities, unemployment rates are higher for those with lower education attainment, further supporting the connection between education and employment (USDA, 2017). Regarding the Health Care Access and Quality domain—specifically in rural communities—factors such as proximity to hospitals, lack of insurance, and the overall cost of health care can reduce accessibility. Health care, especially higher-quality health care, aids in preventing disease and improving individuals’ quality of life (ODPHP, n.d.). However, inadequate health care leads to higher rates of disease, which have a direct impact on individuals’ ability to sustain employment, due to factors such as missing work because of illness or having to travel further to receive health care (Dueñas et al., 2016).
Ability to travel is also a cause for concern in rural communities and is closely related to the Neighborhood and Built Environment domain. Healthy People 2030 proposed various objectives related to neighborhood and built environment, with one being to increase access to mass transit (ODPHP, n.d.). It is apparent that a lack of reliable transportation is directly tied to unemployment, especially in rural communities due to distance and limited accessibility (U.S. Department of Transportation, 2019). Public transportation carries many noteworthy benefits, such as reducing air pollution, being inexpensive compared to purchasing a car, minimizing the cost of fuel and upkeep for personal vehicles, and increased convenience. Although these positive aspects of public transportation are ideal, individuals living in rural communities may not be able to reap these benefits due to the lack of public transportation in these areas, perhaps also limiting employment options (Shoup & Homa, 2010; U.S. Department of Transportation, 2019).
Lastly, the fifth domain, Social and Community Context, is interrelated with employment, as it tends to have a significant impact on workplace conditions, influences individuals’ overall mental and physical health, and can hinder growth and development (Norström et al., 2019). Additionally, social cohesion and adequate support in communities can be leveraged to locate and obtain employment and other helpful resources; however, this often falls short in rural communities. For example, in rural communities, the inability to secure gainful employment is notably linked to geographical disparities, such as those within the Neighborhood and Built Environment SDOH domain. Examples of such geographic disparities which affect employment include limited or nonexistent options for public transportation, a lack of available local jobs, and a lack of childcare facilities for use by working parents. Rural communities also often experience a lack of resources to improve the employment outlook and overall well-being of their population (Bradshaw, 2007; Dwyer & Sanchez, 2016). In addition, structurally, it has been observed that economic resources tend to cluster or aggregate together. For example, businesses that have been successful in a community invite and attract more businesses, thus pulling resources away from rural communities that might not have such a history of business success. Meanwhile, communities that are left behind experience economic restructuring and delays in receiving new technologies, leading to fewer employment opportunities (Bradshaw, 2007; Landon et al., 2019). Thus, providing employment or vocational services in rural America can be particularly challenging.
Furthermore, unemployment, poverty, and mental health concerns are inextricably linked. When career counselors uncover and address these factors in rural America, they must consider the surplus of needed services and resources to systemically address interrelated issues. To be intentional, career counselors practicing in rural communities should consider using a theoretical foundation that provides direction for action on the SDOMH which impact their clients’ lives and ability to be gainfully employed. The Rural Community Health and Well-Being Framework (Annis et al., 2004) is a framework that would be exceedingly helpful in this pursuit.
Theoretical Framework for Action: Rural Community Health and Well-Being Framework
Rural communities make up over 20% of the population and are often classified by a lack of necessary resources, lower levels of education, and persistent economic inequities (Hughes et al., 2019; Mohatt et al., 2006). Although they face many challenges, individuals in rural communities have been found to be resilient, especially when the proper resources are available (Annis et al., 2004). Application of a theoretical framework to practice centered on the unique needs of rural communities is important in addressing SDOMH through career counseling. The Rural Community Health and Well-Being Framework (Annis et al., 2004) strategically builds upon community resiliency and identifies economic, social, and environmental factors which are seen as essential components of health in rural communities. This framework also implores career counselors to consider how SDOMH indicators impact the community as a whole as well as individual people. For example, the framework provides specific areas for increased career counselor awareness and action: health, safety and security, economics, education, environment, community infrastructure and processes, recreation, social support and cohesion, and the overall population. These specific areas for rural communities are within the SDOMH domains, but emphasis is placed on recognition of the specific areas within the SDOMH domains that have the greatest impact on the community.
This comprehensive framework centers the needs of rural communities and provides direction for assessing and addressing SDOMH that impact employment and overall well-being. This framework will assist in uncovering employment issues and barriers faced by individuals within rural communities. Using this framework to assess SDOMH conditions (e.g., economic, social, environmental) will aid in developing employment and mental health interventions that are socially conscious and address root causes of unemployment and poor mental health. Overall, this framework provides a model for assessing and addressing SDOMH in rural communities.
Adaptation for Career Counselors
Career counselors in rural communities who wish to use the Rural Community Health and Well-Being Framework for practice should consider doing the following: (a) increasing their awareness and understanding of SDOMH and the framework, (b) increasing their understanding of the specific community needs outlined by the framework, and (c) assessing the values and needs of the community. However, because the framework is primarily focused on community-level indicators of need, career counselors will need to adapt what they learn about the community to inform their practice with individual community members. The role of the career counselor is multifaceted; thus, career counselors can engage various aspects of their role, such as listener, leader, and evaluator, in their advocacy efforts.
To begin this process of learning about community and individual needs, Annis et al. (2004) suggested the importance of listening. For example, based on the community-level indicators of need, career counselors can assess individual clients for their unmet needs within those specific areas. By understanding how members of the community are experiencing indicators such as health, recreation, social support, transportation, and resources, career counselors will become better equipped to understand and address issues that are impacting their clients’ ability to obtain and maintain employment. Beyond the use of assessments, this framework equips career counselors to broach important conversations about social needs (Andermann, 2016) with their clients, to inform potential connection with community resources. These conversations may include explicit discussion about particular SDOMH challenges (e.g., education, safety, access to affordable childcare), as well as about the client’s sense of belonging, or lack thereof, within their community. These conversations should allow for increased understanding and rapport building through genuine listening and empathy (Annis et al., 2004; Covey, 1989).
Finally, the framework implores career counselors to advocate with and for individuals within their rural community to provide equitable employment opportunities (Crumb et al., 2019). Such advocacy may take place through connection with local rural community leaders, who may have power to alter or increase the distribution of certain resources within the community setting. For example, a career counselor may advocate on behalf of their clients to the local county board of commissioners for increased budget toward affordable transportation access within that county, thereby broadening clients’ access to job opportunities. Advocacy with local leaders outside of government might include collaboration with community college administrators for provision of additional support for working adults and parents who wish to return to school, such as more evening course options, advisor support, or readily available information on scholarships. Again, considering the aforementioned roles career counselors may have (e.g., leader, evaluator), career counselors may also consider further training in program evaluation—or collaboration with those who have such training—to better understand the efficacy of their community partnerships, referrals, and other advocacy-related efforts made toward supporting clients’ SDOMH.
Assessing and Addressing Social Determinants of Mental Health
As noted earlier, SDOMH are inextricably linked to employment, which means career counselors in rural communities must acknowledge these challenges and seek to address these issues with their clients. However, researchers have also highlighted the importance of considering both facilitators and barriers to addressing SDOMH challenges (Browne et al., 2021). In a qualitative case study of staff at a community health center and hospital, participants identified practical facilitators of SDOMH response, including community collaboration and support from leadership, as well as barriers such as time limitations and lack of resources (Browne et al., 2021). As career counselors hold similar client outcome goals as community mental health providers, they can take these findings into consideration when determining how to best respond to clients’ SDOMH challenges through attention to opportunities for collaboration with community leaders (e.g., religious leaders, politicians) and resources within the community (e.g., food banks, health care providers). Another study highlighted the importance of collaboration, partnerships with local agencies, and understanding the role of the counselor in SDOMH response (Johnson & Brookover, 2021; Robins et al., 2022). With these findings in mind, career counselors in rural communities are well positioned to assess for and address SDOMH challenges faced by their clients (Crucil & Amundson, 2017; Tang et al., 2021) through individual-level action (i.e., counseling) and systems-level advocacy action.
Systems-Level Advocacy Through Assessment
To effectively engage in systems-level advocacy, it is important for career counselors to recognize and understand the needs of their rural communities. When using the Rural Community Health and Well-Being Framework in practice, it is important to complete an assessment of the rural health of one’s community. Ryan-Nicholls and Racher (2004) purport that it is imperative to assess rural health within five categories: health status, health determinants, health behavior, health resources, and health service utilization. Counselors may consider these items when assessing the needs of their clients in rural communities, as these items provide a basis for assessment of other health factors, such as indicators of community health (e.g., environment and lifestyle) and economic well-being, and provide a foundation for systems-level advocacy and planning. This level of action focuses on improving the lives of the entire community through strategic advocacy efforts that improve population health and well-being (Ryan-Nicholls & Racher, 2004). A career counselor engaged at this level might focus their energy on advocating for increased economic development in their rural community, livable wages, universal health care, immigration issues, employment discrimination legislation, and other employment-related issues that impact the community directly or indirectly. Additionally, a career counselor may address client self-advocacy and utilize empowerment approaches to increase the voices of community members and their clients as related to work and employment needs.
In connection with this framework (Annis et al., 2004), career counselors can utilize this broader community-level assessment to inform specific points of advocacy. As an example, Annis et al. (2004) provided a sample form that may be utilized to collect community data on alcohol consumption (p. 79). Upon noting concern from individual clients on alcohol consumption, a career counselor may collaborate with public health professionals, for instance, to collect such data from the local community. Annis et al. encourage consideration of the implications for such findings, as well as opportunities for follow-up. After determining a need in the community for support regarding high alcohol consumption, the career counselor may utilize the framework to consider points of community resilience, including existing supports, attitudes about alcohol consumption, existing resources, and any actions the community is already taking in this area. Overall, assessment through the context suggested by Ryan-Nicholls and Racher (2004) may yield individual and community data to inform action to address SDOMH challenges through Annis et al.’s (2004) framework.
Individual-Level Action Through Assessment
When a client seeks services from a career counselor, the relationship centers on exploration and evaluation of the client’s education, training, work history, interests, skills, personality, and career goals. Through engaging with the Rural Community Health and Well-Being Framework, the career counselor might also examine the SDOMH facilitators and barriers that impact a client’s employment goals. To address employment and SDOMH, a career counselor must understand the community-level needs (i.e., systems approach) and the individual needs of their clients; for these goals, one strategy is to use assessments. There are various assessment tools that career counselors may find helpful, including the Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences (PRAPARE; National Association of Community Health Centers, 2017), an SDOH assessment tool purposed to empower professionals to not only understand their clients more holistically through assessment, but to better meet clients’ needs through the use of such information. The PRAPARE assessment tool includes questions related to four domains: Personal Characteristics, Family and Home, Money and Resources, and Social and Emotional Health. PRAPARE emphasizes the importance of assessing SDOMH needs of clients in order for providers to “define and document the complexity of their patients; transform care with integrated services and community partnerships to meet the needs of their patients; demonstrate the value they bring to patients, communities, and payers; and advocate for change in their communities” (https://prapare.org/). There are several benefits of using the PRAPARE assessment tool, such as it being free of charge, having a website linked to the tool with an “actionable toolkit and resources,’’ and being evidence-based. Barriers to using PRAPARE include that it is a long assessment tool that clients must complete in-office, which may slow workflow.
Another SDOH assessment tool is the WellRx Questionnaire (Page-Reeves et al., 2016). The WellRx Questionnaire is an 11-item screening tool that gathers information on various SDOMH, like food security, access to transportation, employment, and education. Participants are to answer “yes” or “no” to each item on the questionnaire. According to Page-Reeves and colleagues (2016), the WellRx Questionnaire provides a feasible means of assessing patients’ social needs and thereby addressing those needs. Benefits to using the WellRx include that it is free of cost, questions are at a 4th-grade reading level, and it can typically be completed by a client individually without the help of a professional. A potential barrier is that it does not assess a wide range of SDOMH challenges. Lastly, Andermann (2018) conducted a scoping review of social needs screening tools and found that the focus on such screening has increased over time. Andermann suggested that health care workers take advantage of the existing means of assessment, and made a number of specific resource recommendations, such as the Canadian Task Force on Preventive Health Care (2019) and the U.S. Preventive Services Task Force (2022).
Addressing SDOMH Through Action
Documenting and defining the needs of clients through assessment is the first step in addressing SDOMH. The next step is taking action through an integrated career counseling approach. An integrated approach may include consistent collaboration with other professionals, like medical doctors, nurse practitioners, social workers, probation officers, or case managers. Additionally, scholars like Andermann (2016) suggest integrated efforts such as ensuring social challenges are included in client records and shared with other professionals to best support care. For “particularly isolated and hard-to-reach patients . . . [actions like] assertive outreach, patient tracking and individual case managers” may be helpful (para. 19). Another practical suggestion for beginning to address clients’ SDOMH challenges is adding an SDOMH assessment tool or specific SDOMH questions to an intake form that the client completes independently or during the intake session. Selection of specific questions can be derived from the data that displays community-level needs (e.g., systems-level advocacy through assessment). For example, if a community-level assessment found that public transportation was lacking, then transportation might be an important assessment question on the SDOMH screener.
Another consideration specific for career counselors is that counselors are obligated by their code of ethics to take appropriate action based on assessment results (American Counseling Association [ACA], 2014, Section E.2.b.). Appropriate action can include consultation and collaboration with other professionals within and outside of counseling and/or advocacy to address the SDOMH need. After establishing the need through assessment, it is important for the career counselor to support the client in understanding system-level challenges and to work to address SDOMH issues while simultaneously supporting employment needs. For example, a career counselor who determines that their client is struggling with food insecurity might address this issue in several ways. At the individual level, the counselor might print resources for local food pantries, assist the client in applying for SNAP benefits, and counsel the client on resources within the community to access food. They could establish a small food pantry within the office, collaborate with local restaurants to receive pre-packaged food that might otherwise be disposed of, or consult with local food pantries and free food kitchens to establish a mobile pantry and kitchen. At the systems level, a career counselor may build partnerships with local farmers to increase locations where fresh fruits and vegetables are available for little or no cost.
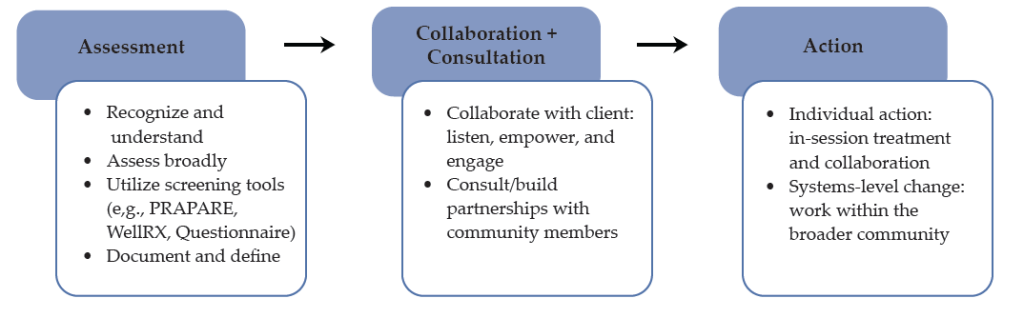
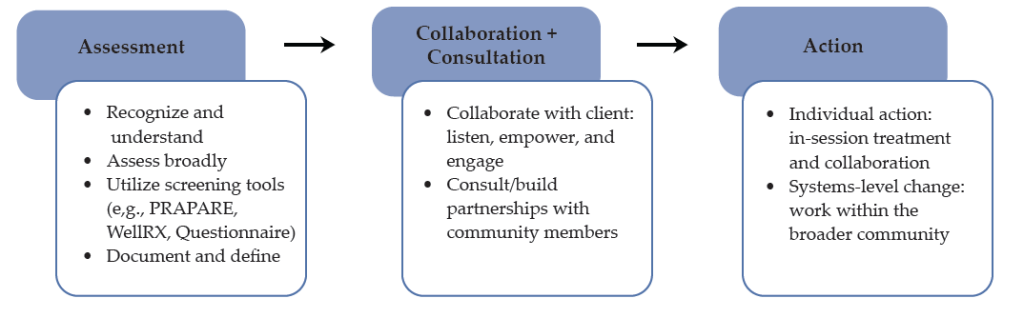
Collaboration and consultation are imperative to addressing the complex needs of clients in rural communities who are both seeking career counseling and challenged by SDOMH issues. For example, as noted earlier, health care access and quality are major disruptors of employment, and addressing these challenges will afford benefits for employment. The career counselor can consider using interprofessional collaboration and telehealth to support the health care needs of their rural clients (Johnson & Mahan, 2020). Interprofessional collaboration is a practice in which health care providers from two or more professional backgrounds interact and practice with the client at the center of care (Prentice et al., 2015). Using telehealth, the distribution of health-related services via telecommunication technologies is a useful strategy to support the health care needs of persons in rural communities. A career counselor can address health care access through telehealth in several ways, including education (e.g., introduce their client to telehealth; assist them in understanding the technology), telehealth (e.g., provide the telecommunication equipment in the office), and collaborative partnership (e.g., use a portion of the career counseling session to assist the client in connecting with health care providers using distance technology). As a collaborative partner in addressing health care access and quality, the career counselor can also use future sessions to follow up with the client on their experience with telehealth and, if needed, assist them in connecting to other health care providers. Figure 1 provides a visual for conceptualizing how career counselors may navigate the SDOMH needs of their clients, from assessment to action.
Figure 1
Working to Address Clients’ SDOMH Needs
Lastly, in the work of addressing SDOMH and employment, counselors should be aware of local, state, and national resources. Local and state resources are unique to every state but have similar purposes which include disseminating information on local resources and initiatives and providing public services that address SDOMH (e.g., food banks, public programs). National resources that are accessible to every community include 211 and the “findhelp.org” website. The Federal Communications Commission designated 211 as a national number in the United States that anyone can call for information and referrals to social services and other assistance. The services provided by 211 are confidential and free, available 24/7, and help connect people in the United States to essential community services. Moreover, the “findhelp.org” website is designed to help people search and connect with social care support based on their ZIP Code.
Integrating career counseling and social care support in rural communities is a strategy to facilitate the readiness of clients for work and the sustainability of employment for clients because basic needs are met or being addressed. While every rural community is unique, the foundation of understanding both systemic and individual SDOMH needs—and addressing those needs through strategic partnerships and individual counseling, as well as advocacy—is important in every rural community and to the success of any career counseling endeavor.
Discussion
In rural communities, career counselors hold a significant role. They are tasked with aiding individuals with employment needs; they may often address mental health concerns, and while doing so, it is important for them to be aware of and prepared to address SDOMH. Career counselors can gain more insight into issues related to SDOMH through consultation, collaboration, and advocacy, which should all be a part of the repertoire of a rural career counselor. The use of theoretical frameworks such as the Rural Community Health and Well-Being Framework (Racher et al., 2004) provides direction for career counselors seeking to understand the systemic issues impacting employment access and opportunities in the community, as well as direction for intervention. This framework will assist in identifying and minimizing barriers to employment that may exist within rural communities. More specifically, this framework will help to uncover SDOMH challenges that exist in the community and serve as barriers to well-being and employment and provide direction for advocating for resources necessary for equitable work opportunities and environments. Being that individuals in rural America experience various barriers that have huge impacts on their lives, such a guide for career counselors is essential.
Lastly, addressing SDOMH within career counseling is a social justice issue that counselors should address (ACA, 2014; Crucil & Amundson, 2017; Ratts et al., 2016). The Multicultural and Social Justice Counseling Competencies (MSJCC; Ratts et al., 2016) serve as a guide for counselors to address social justice issues and were endorsed by the ACA in 2015. Like the aforementioned framework and empirically based suggestions, the MSJCC includes four areas of competence: counselor self-awareness, client worldview, counseling relationship, and counseling and advocacy interventions. The authors of the MSJCC also implore counselors to consider “attitudes and beliefs, knowledge, skills, and action,” and suggest that competent counselors are aware of the experiences of marginalized clients (Ratts et al., 2016; p. 3). Thus, career counselors’ efforts to assess and address the individual and systems-based SDOMH challenges faced by their clients is social justice work that career counselors are trained and prepared to address.
Implications
Given this review, there are specific implications for career counselors practicing in rural communities, counselor educators training career counselors, and pertinent policy needs.
Practicing Career Counselors
The role of the career counselor often entails identifying employment objectives, goals, and needs for both the job seeker and employer. In addition, the career counselor is responsible for résumé development, teaching job placement and retention skills, providing self-advocacy tips, teaching organizational goal–redefining skills, and many other components (Ysasi et al., 2018). However, providing these services can be difficult when the individuals reside in rural communities because of the SDOMH disparities such as limited available resources, isolation, increased poverty, and decreased educational and employment opportunities (Temkin, 1996).
Therefore, career counselors must actively work to ensure their visibility and accessibility to individuals in rural areas who are seeking employment opportunities. Further, career counselors need to market themselves and their skills to employers and job seekers of rural communities. Consequently, marketing generally entails engaging and developing community partnerships with employers and job seekers, which involves educating individuals unfamiliar with the specific services that career counselors provide. In addition, employers are often interested in services that improve their business (e.g., increase revenue), while job seekers may be searching for skill training to achieve employment goals (Richardson et al., 2010). Therefore, career counselors can enhance service delivery and provide adequate services when they intentionally market their services to the community members.
Furthermore, job insecurity has been linked to mental health concerns like stress and anxiety, financial concerns, and fear of organizational change (Holm & Hovland, 1999). Therefore, career counselors need to be aware of the impact of job insecurity on rural communities and devise strategies to help organizations and workers manage job insecurity. Managing job insecurity of workers in rural organizations could include helping organizations to redefine their present and future goals and commitments made to employees. Organizations could also manage organizational transitions depending on the skills and resources available to affected employees (Holm & Hovland, 1999). Clearly stated organizational objectives, goals, and plans can help employees feel less insecure about their jobs and increase focus on their roles and responsibilities instead of devising means to move out of the community for a better and more secure future. In addition, career counselors in rural communities should be aware of the mental health concerns experienced by employees and job seekers and connect them to available mental health resources.
Counselor Educators
Counselor educators are responsible for the training and development of the next generation of counselors, including career counselors. It will be important for counselor educators to include training on SDOMH, interprofessional collaboration, and telehealth, as these are especially relevant for rural communities ( Johnson & Mahan, 2021; Johnson & Rehfuss, 2021). It is essential to provide adequate time to review and discuss SDOMH in all courses throughout the curriculum (Waters et al., 2022) to ensure the competence of career counselors. To ensure this continuity, counselor educators should advocate for an SDOMH module across the curriculum. This would ensure the inclusion of this content throughout the program, providing ample opportunity for the understanding of SDOMH and how they should be addressed. Career counselors must be prepared to address the complex employment and social health needs with which their clients might present. Without adequate education and training, these will seem much more difficult to address.
Policy
In addressing both SDOMH and employment needs in rural communities, advocating for policy and legislative change is imperative. Lewis et al. (2002) described counselors’ roles in sharing public information as awakening the public to macro-systemic issues related to human dignity and engaging in social/political advocacy, or “influencing public policy in a large, public arena” (p. 2). Thus, career counselors are encouraged to benefit their clients through engaging in advocacy to influence policy at the local, state, and national levels. Similarly, Crucil and Amundson (2017) implore career counselors to engage in the work of influencing politics and policy and suggest awareness as a first step to enacting change through the sharing of information and impacting policy. To develop such awareness, career counselors may begin by reading about SDOMH disparities related specifically to employment issues from reputable sources. For instance, the National Alliance on Mental Illness (NAMI; 2014) has published various reports related to such issues, including the informative publication entitled Road to Recovery: Employment and Mental Illness. NAMI (2021) also published a legislative coalition letter written in support of increased SDOH funding to Congress. Career counselors may work to build their own awareness and understanding of the social and political events and influences which impact their clients, building toward eventual action in this realm.
Moreover, regarding policy change, researchers have suggested career counselors should be aware of and actively engaged in policy efforts (Crucil & Amundson, 2017; Watts, 2000). Watts (2000) described public policy considering career development as including four distinct roles: legislation, remuneration, exhortation, and regulation. Watts described these roles in detail and implored career counselors to influence these policy processes by seeking the support of interest groups and communicating with policy makers. Again, career counselors can work individually and within their own communities to increase their awareness and knowledge of policies and their impact. They can work toward influencing policies at the state and national levels to improve the accessibility and existence of important social programs and resources.
Conclusion
Career counselors in rural communities have a responsibility to acknowledge and address SDOMH challenges that are disproportionately impacting their clients. Collaboration, consultation, counseling framed through the lens of SDOMH, and advocacy appear to be strategies to support the employment needs of individuals and the rural community. Employment services in rural communities must be framed through a socially conscious (e.g., aware of the SDOMH systemic issues), action-oriented (e.g., prepared to engage in advocacy), and resiliency-focused lens that provides tailored individual services while simultaneously addressing systemic issues.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
American Counseling Association. (2014). ACA code of ethics. https://www.counseling.org/docs/default-source/default-document-library/2014-code-of-ethics-finaladdress.pdf
Amundson, N. E. (1993). Mattering: A foundation for employment counseling and training. Journal of Employment Counseling, 30(4), 146–152. https://doi.org/10.1002/j.2161-1920.1993.tb00173.x
Andermann, A. (2016). Taking action on the social determinants of health in clinical practice: A framework for health professionals. Canadian Medical Association Journal, 188(17–18), E474–E483. https://doi.org/10.1503/cmaj.160177
Andermann, A. (2018). Screening for social determinants of health in clinical care: Moving from the margins to the mainstream. Public Health Reviews, 39(1), 1–17.
https://doi.org/10.1186/s40985-018-0094-7
Annis, R. C., Racher, F., & Beattie, M. (Eds.). (2004). Rural community health and well-being: A guide to action. Rural Development Institute. https://www.researchgate.net/publication/242551842_Rural_Community_Health_and_Well-Being_A_Guide_to_Action
Bradshaw, T. K. (2007). Theories of poverty and anti-poverty programs in community development. Community Development, 38(1), 7–25. https://doi.org/10.1080/15575330709490182
Brassington, I. (2011). What’s wrong with the brain drain? Developing World Bioethics, 12(3), 113–120.
https://doi.org/10.1111/j.1471-8847.2011.00300.x
Browne, J., Mccurley, J. L., Fung, V., Levy, D. E., Clark, C. R., & Thorndike, A. N. (2021). Addressing social determinants of health identified by systematic screening in a Medicaid accountable care organization: A qualitative study. Journal of Primary Care & Community Health, 12. https://doi.org/10.1177/2150132721993651
Canadian Task Force on Preventative Health Care. (2019). Canadian task force on preventive health care.
https://canadiantaskforce.ca
Centers for Disease Control and Prevention. (2020). CDC 2020 in review. https://archive.cdc.gov/#/details?url=
https://www.cdc.gov/media/releases/2020/p1229-cdc-2020-review.html
Covey, S. (1989). The 7 habits of highly effective people: Restoring the character ethic. Simon & Schuster.
Crucil, C., & Amundson, N. (2017). Throwing a wrench in the work(s): Using multicultural and social justice competency to develop a social justice–oriented employment counseling toolbox. Journal of Employment Counseling, 54(1), 2–11. https://doi.org/10.1002/joec.12046
Crumb, L., Haskins, N., & Brown, S. (2019). Integrating social justice advocacy into mental health counseling in rural, impoverished American communities. The Professional Counselor, 9(1), 20–34. https://files.eric.ed.gov/fulltext/EJ1215753.pdf
Dobis, E. A., Krumel, T. P., Jr., Cromartie, J., Conley, K. L., Sanders, A., & Ortiz, R. (2021). Rural America at a glance: 2021 edition. U.S. Department of Agriculture. https://www.ers.usda.gov/webdocs/publications/102576/eib-230.pdf
Dueñas, M., Ojeda, B., Salazar, A., Mico, J. A., & Failde, I. (2016). A review of chronic pain impact on patients, their social environment and the health care system. Journal of Pain Research, 2016(9), 457–467. https://doi.org/10.2147/JPR.S105892
Dwyer, R. E., & Sanchez, D. (2016). Population distribution and poverty. In M. J. White (Ed.), International handbook of migration and population distribution (pp. 485–504). Springer Science & Business Media. https://doi.org/10.1007/978-94-017-7282-2
Health Resources and Services Administration. (2017). Defining rural population. https://www.hrsa.gov/rural-health/about-us/definition/index.html
Holm, S., & Hovland, J. (1999). Waiting for the other shoe to drop: Help for the job-insecure employee. Journal of Employment Counseling, 36(4), 156–166.
https://doi.org/10.1002/j.2161-1920.1999.tb01018.x
Hughes, M. C., Gorman, J. M., Ren, Y., Khalid, S., & Clayton, C. (2019). Increasing access to rural mental health care using hybrid care that includes telepsychiatry. Journal of Rural Mental Health, 43(1), 30–37. https://doi.org/10.1037/rmh0000110
Johnson, K. F., & Brookover, D. L. (2021). School counselors’ knowledge, actions, and recommendations for addressing social determinants of health with students, families, and in communities. Professional School Counseling, 25(1), 1–12. https://doi.org/10.1177/2156759X20985847
Johnson, K. F., & Mahan, L. B. (2020). Interprofessional collaboration and telehealth: Useful strategies for family counselors in rural and underserved areas. The Family Journal, 28(3), 215–224.
https://doi.org/10.1177/1066480720934378
Johnson, K. F., & Rehfuss, M. (2021). Telehealth interprofessional education: Benefits, desires, and concerns of counselor trainees. Journal of Creativity in Mental Health, 16(1), 15–30.
https://doi.org/10.1080/15401383.2020.1751766
Johnson, K. F., & Robins, L. B. (2021). Counselor educators’ experiences and techniques teaching about social-health inequities. Journal of Counselor Preparation and Supervision, 14(4), 1–25. https://digitalcommons.sacredheart.edu/jcps/vol14/iss4/7
Landon, T., Connor, A., McKnight-Lizotte, M., & Peña, J. (2019). Rehabilitation counseling in rural settings: A phenomenological study on barriers and supports. Journal of Rehabilitation, 85(2), 47–57. https://bit.ly/4cvWSoT
Lewis, J., Arnold, M. S., House, R., & Toporek, R. L. (2002). ACA advocacy competencies. http://www.counseling.org/Resources/Competencies/Advocacy_Competencies.pdf
Liebman, A. K., & Augustave, W. (2010). Agricultural health and safety: Incorporating the worker perspective. Journal of Agromedicine, 15(3), 192–199. https://doi.org/10.1080/1059924x.2010.486333
Mohatt, D. F., Bradley, M. M., Adams, S. J., & Morris, C. D. (2006). Mental health and rural America: 1994-2005. An overview and annotated bibliography. U.S. Department of Health and Human Services. https://eric.ed.gov/?id=ED591902
National Alliance on Mental Health. (2014). Road to recovery: Employment and mental illness. https://nami.org/Support-Education/Publications-Reports/Public-Policy-Reports/RoadtoRecovery
National Alliance on Mental Health. (2021, April 8). Letter to congressional leadership. https://www.nami.org/getattachment/c3b797bf-5116-457f-ada9-b6b6f1f6adfb/Letter-to-Congressional-Committee-Leadership-on-So
National Association of Community Health Centers. (2017). PRAPARE. https://www.nachc.org/research-and-data/prapare
Norström, F., Waenerlund, A.-K., Lindholm, L., Nygren, R., Sahlén, K.-G., & Brydsten, A. (2019). Does unemployment contribute to poorer health-related quality of life among Swedish adults? BMC Public Health, 19(1). https://doi.org/10.1186/s12889-019-6825-y
Office of Disease Prevention and Health Promotion. (2020). Healthy People 2030: Social determinants of health. U.S. Department of Health and Human Services. https://health.gov/healthypeople/priority-areas/social-determinants-health
Page-Reeves, J., Kaufman, W., Bleecker, M., Norris, J., McCalmont, K., Ianakieva, V., Ianakieva, D. & Kaufman, A. (2016). Addressing social determinants of health in a clinic setting: The WellRx pilot in Albuquerque, New Mexico. The Journal of the American Board of Family Medicine, 29(3), 414–418. https://doi.org/10.3122/jabfm.2016.03.150272
Pope, M. (2011). The Career Counseling With Underserved Populations model. Journal of Employment Counseling, 48(4), 153–155. https://doi.org/10.1002/j.2161-1920.2011.tb01100.x
Prentice, D., Engel, J., Taplay, K., & Stobbe, K. (2015). Interprofessional collaboration: The experience of nursing and medical students’ interprofessional education. Global Qualitative Nursing Research, 2, 1–9. https://doi.org/10.1177/2333393614560566
Racher, F., Everitt, J., Annis, R., Gfellner, B., Ryan-Nicholls, K., Beattie, M., Gibson, R., & Funk, E. (2004). Rural community health & well-being. In R. Annis, F. Racher, & M. Beattie (Eds.), Rural community health and well-being: A guide to action (pp. 18–37). Rural Development Institute.
Ratts, M. J., Singh, A. A., Nassar-McMillan, S., Butler, S. K., & McCullough, J. R. (2016). Multicultural and social justice counseling competencies: Guidelines for the counseling profession. Journal of Multicultural Counseling and Development, 44(1), 28–48. https://doi.org/10.1002/jmcd.12035
Richardson, N., Gosnay, R. M., & Carroll, A. (2010). A quick start guide to social media marketing: High impact low-cost marketing that works. Kogan Page Publishers.
Robins, L. B., Johnson, K. F., Duyile, B., Gantt-Howrey, A., Dockery, N., Robins, S., & Wheeler, N. (2022). Family counselors addressing social determinants of mental health in underserved communities. The Family Journal, 31(2), 213–221. https://doi.org/10.1177/10664807221132799
Ryan-Nicholls, K. D., & Racher, F. E. (2004). Investigating the health of rural communities: Toward framework development. Rural and Remote Health, 4(1), 1–10.
https://search.informit.org/doi/abs/10.3316/informit.613919155641626
Shoup, L., & Homa, B. (2010). Principles for improving transportation options in rural and small town communities. https://t4america.org/wp-content/uploads/2010/03/T4-Whitepaper-Rural-and-Small-Town-Communities.pdf
Tang, M., Montgomery, M. L. T., Collins, B., and Jenkins, K. (2021). Integrating career and mental health counseling: Necessity and strategies. Journal of Employment Counseling, 58, 23–35.
https://doi.org/10.1002/joec.12155
Temkin, A. (1996). Creative options for rural employment: A beginning. In N. L. Arnold (Ed.), Self-employment in vocational rehabilitation: Building on lessons from rural America (pp. 61–64). Research and Training Center on Rural Rehabilitation Services.
United States Census Bureau. (2014). 2010-2014 ACS 5-year estimates. https://www.census.gov/programs-surveys/acs/technical-documentation/table-and-geography-changes/2014/5-year.html
United States Department of Agriculture. (2014). Rural America at a glance: 2014 edition. https://www.ers.usda.gov/publications/pub-details/?pubid=42897
United States Department of Agriculture. (2017). Rural education at a glance, 2017 edition. https://www.ers.usda.gov/webdocs/publications/83078/eib-171.pdf
United States Preventive Services Taskforce. (2022). US preventative services taskforce. https://www.uspreventiveservicestaskforce.org/uspstf
U.S. Department of Transportation. (2019). Rural public transportation systems. https://www.transportation.gov/mission/health/Rural-Public-Transportation-Systems
Waters, J. M., Gantt, A., Worth, A., Duyile, B., Johnson, K. F., & Mariotto, D. (2022). Motivated but challenged: Counselor educators’ experiences teaching about social determinants of health. Journal of Counselor Preparation and Supervision, 15(2), 1–30. https://digitalcommons.sacredheart.edu/jcps/vol15/iss2/6
Watts, A. G. (2000). Career development and public policy. Journal of Employment Counseling, 37(2), 62–75. https://doi.org/10.1002/j.2161-1920.2000.tb00824.x
World Health Organization. (2014). Social determinants of mental health. https://apps.who.int/iris/bitstream/handle/10665/112828/9789241506809_eng.pdf
Ysasi, N. A., Tiro, L., Sprong, M. E., & Kim, B. J. (2018). Marketing vocational rehabilitation services in rural communities. In D. A. Harley, N. A. Ysasi, M. L. Bishop, & A. R. Fleming (Eds.), Disability and vocational rehabilitation in rural settings: Challenges to service delivery (pp. 545–552). Springer.
Kaprea F. Johnson, PhD, LPC, is a professor and Associate Vice Provost for Faculty Development & Recognition at The Ohio State University. Alexandra Gantt-Howrey, PhD, LPC (ID), is an assistant professor at Idaho State University. Bisola E. Duyile, PhD, LPC, CRC, is an assistant professor at Montclair State University. Lauren B. Robins, PhD, is a clinical assistant professor and distance learning coordinator at Old Dominion University. Natese Dockery, MS, NCC, LPC, CSAM, is a licensed professional counselor and doctoral student. Correspondence may be addressed to Kaprea F. Johnson, The Ohio State University, 1945 N. High Street, Columbus, OH 43210, johnson.9545@osu.edu.
Aug 20, 2021 | Volume 11 - Issue 3
Alison M. Boughn, Daniel A. DeCino
This article introduces the development and implementation of the Psychological Maltreatment Inventory (PMI) assessment with child respondents receiving services because of an open child abuse and/or neglect case in the Midwest (N = 166). Sixteen items were selected based on the literature, subject matter expert refinement, and readability assessments. Results indicate the PMI has high reliability (α = .91). There was no evidence the PMI total score was influenced by demographic characteristics. A positive relationship was discovered between PMI scores and general trauma symptom scores on the Trauma Symptom Checklist for Children Screening Form (TSCC-SF; r = .78, p = .01). Evidence from this study demonstrates the need to refine the PMI for continued use with children. Implications for future research include identification of psychological maltreatment in isolation, further testing and refinement of the PMI, and exploring the potential relationship between psychological maltreatment and suicidal ideation.
Keywords: psychological maltreatment, child abuse, neglect, assessment, trauma
In 2012, the Centers for Disease Control (CDC; 2012) reported that the total cost of child maltreatment (CM) in 2008, including psychological maltreatment (PM), was $124 billion. Fang et al. (2012) estimated the lifetime burden of CM in 2008 was as high as $585 billion. The CDC (2012) characterized CM as rivaling “other high profile public health problems” (para. 1). By 2015, the National Institutes of Health reported the total cost of CM, based on substantiated incidents, was reported to be $428 billion, a 345% increase in just 7 years; the true cost was predictably much higher (Peterson et al., 2018). Using the sensitivity analysis done by Fang et al. (2012), the lifetime burden of CM in 2015 may have been as high as $2 trillion. If these trends continue unabated, the United States could expect a total cost for CM, including PM, of $5.1 trillion by 2030, with a total lifetime cost of $24 trillion. More concerning, this increase would not account for any impact from the COVID-19 pandemic.
Mental health first responders and child protection professionals may encounter PM regularly in their careers (Klika & Conte, 2017; U.S. Department of Health and Human Services [DHHS], 2018). PM experiences are defined as inappropriate emotional and psychological acts (e.g., excessive yelling, threatening language or behavior) and/or lack of appropriate acts (e.g., saying I love you) used by perpetrators of abuse and neglect to gain organizational control of their victims (American Professional Society on the Abuse of Children [APSAC], 2019; Klika & Conte, 2017; Slep et al., 2015). Victims may experience negative societal perceptions (i.e., stigma), fear of retribution from caregivers or guardians, or misdiagnosis by professional helpers (Iwaniec, 2006; López et al., 2015). They often face adverse consequences that last their entire lifetime (Spinazzola et al., 2014; Tyrka et al., 2013; Vachon et al., 2015; van der Kolk, 2014; van Harmelen et al., 2010; Zimmerman & Mercy, 2010). PM can be difficult to identify because it leaves no readily visible trace of injury (e.g., bruises, cuts, or broken bones), making it complicated to substantiate that a crime has occurred (Ahern et al., 2014; López et al., 2015). Retrospective data outlines evaluation processes for PM identification in adulthood; however, childhood PM lacks a single definition and remains difficult to assess (Tonmyr et al., 2011). These complexities in identifying PM in children may prevent mental health professionals from intervening early, providing crucial care, and referring victims for psychological health services (Marshall, 2012; Spinazzola et al., 2014). The Psychological Maltreatment Inventory (PMI) is the first instrument of its kind to address these deficits.
Child Psychological Maltreatment
Although broadly conceptualized, child PM experiences are described as literal acts, events, or experiences that create current or future symptoms that can affect a victim without immediate physical evidence (López et al., 2015). Others have extended child PM to include continued patterns of severe events that impede a child from securing basic psychological needs and convey to the child that they are worthless, flawed, or unwanted (APSAC, 2019). Unfortunately, these broad concepts lack the specificity to guide legal and mental health interventions (Ahern et al., 2014). Furthermore, legal definitions of child PM vary from jurisdiction to jurisdiction and state to state (Spinazzola et al., 2014). The lack of consistent definitions and quantifiable measures of child PM may create barriers for prosecutors and other helping professionals within the legal system as well as a limited understanding of PM in evidence-based research (American Psychiatric Association [APA], 2013; APSAC, 2019; Klika & Conte, 2017). These challenges are exacerbated by comorbidity with other forms of maltreatment.
Co-Occurring Forms of Maltreatment
According to DHHS (2018), child PM is rarely documented as occurring in isolation compared to other forms of maltreatment (i.e., physical abuse, sexual abuse, or neglect). Rather, researchers have found PM typically coexists with other forms of maltreatment (DHHS, 2018; Iwaniec, 2006; Marshall, 2012). Klika and Conte (2017) reported that perpetrators who use physical abuse, inappropriate language, and isolation facilitate conditions for PM to coexist with other forms of abuse. Van Harmelen et al. (2011) argued that neglectful acts constitute evidence of PM (e.g., seclusion; withholding medical attention; denying or limiting food, water, shelter, and other basic needs).
Consequences of PM Experienced in Childhood
Mills et al. (2013) and Greenfield and Marks (2010) noted PM experiences in early childhood might manifest in physical growth delays and require access to long-term care throughout a victim’s lifetime. Children who have experienced PM may suffer from behaviors that delay or prevent meeting developmental milestones, achieving academic success in school, engaging in healthy peer relationships, maintaining physical health and well-being, forming appropriate sexual relationships as adults, and enjoying satisfying daily living experiences (Glaser, 2002; Maguire et al., 2015). Neurological and cognitive effects of PM in childhood impact children as they transition into adulthood, including abnormalities in the amygdala and hippocampus (Tyrka at al., 2013). Brown et al. (2019) found that adults who reported experiences of CM had higher rates of negative responses to everyday stress, a larger constellation of unproductive coping skills, and earlier mortality rates (Brown et al., 2019; Felitti et al., 1998). Furthermore, adults with childhood PM experiences reported higher rates of substance abuse than those compared to control groups (Felitti et al., 1998).
Trauma-Related Symptomology. Researchers speculate that children exposed to maltreatment and crises, especially those that come without warning, are at greater risk for developing a host of trauma-related symptoms (Spinazzola et al., 2014). Developmentally, children lack the ability to process and contextualize their lived experiences. Van Harmelen et al. (2010) discovered that adults who experienced child PM had decreased prefrontal cortex mass compared to those without evidence of PM. Similarly, Field et al. (2017) found those unable to process traumatic events produced higher levels of stress hormones (i.e., cortisol, epinephrine, norepinephrine); these hormones are produced from the hypothalamic-pituitary-adrenal (HPA) and sympathetic-adrenal-medullary (SAM) regions in the brain. Some researchers speculate that elevated levels of certain hormones and hyperactive regions within the brain signal the body’s biological attempt to reduce the negative impact of PM through the fight-flight-freeze response (Porges, 2011; van der Kolk, 2014).
Purpose of Present Study
At the time of this research, there were few formal measures using child self-report to assess how children experience PM. We developed the PMI as an initial quantifiable measure of child PM for children and adolescents between the ages of 8 and 17, as modeled by Tonmyr and colleagues (2011). The PMI was developed in multiple stages, including 1) a review of the literature, 2) a content validity survey with subject matter experts (SMEs), 3) a pilot study (N = 21), and 4) a large sample study (N = 166). An additional instrument, the Trauma Symptom Checklist for Children Screening Form (TSCC-SF; Briere & Wherry, 2016), was utilized in conjunction with the PMI to explore occurrences of general trauma symptoms among respondents. The following four research questions were investigated:
- How do respondent demographics relate to PM?
- What is the rate of PM experience with respondents who are presently involved in an open CM case?
- What is the co-occurrence of PM among various forms of CM allegations?
- What is the relationship between the frequency of reported PM experiences and the frequency of general trauma symptoms?
Method
Study 1: PMI Item Development and Pilot
Following the steps of scale construction (Heppner et al., 2016), the initial version of the PMI used current literature and definitions from facilities nationwide that provide care for children who have experienced maltreatment and who are engaged with court systems, mental health agencies, or social services. Our lead researcher, Alison M. Boughn, developed a list of 20 items using category identifications from Glaser (2002) and APSAC (2019). Items were also created using Slep et al.’s (2015) proposed inclusion language for the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) diagnostic codes and codes from the International Classification of Diseases, 11th edition (ICD-11) definition criteria (APA, 2013). Both Boughn and Daniel A. DeCino, our other researcher, reviewed items for consistency with the research literature and removed four redundant items. The final 16 items were reevaluated for readability for future child respondents using a web-based, age range–appropriate readability checker (Readable, n.d.) and were then presented to local SMEs in a content validity survey to determine which would be considered essential for children to report as part of a child PM assessment.
Expert Validation
A multidisciplinary team (MDT) serving as SMEs completed an online content validity survey created by Boughn. The survey was distributed by a Child Advocacy Center (CAC) manager to the MDT. Boughn used the survey results to validate the PMI’s item content relevance. Twenty respondents from the following professions completed the survey: mental health (n = 6), social services (n = 6), law enforcement (n = 3), and legal services (n = 5). The content validity ratio (CVR) was then calculated for the 16 proposed items.
Results. The content validity survey scale used a 3-point Likert-type scale: 0 = not necessary; 1 = useful, but not essential; and 2 = essential. A minimum of 15 of the 20 SMEs (75% of the sample), or a CVR ≥ .5, was required to deem an item essential (Lawshe, 1975). The significance level for each item’s content validity was set at α = .05 (Ayre & Scally, 2014). After conducting Lawshe’s (1975) CVR and applying the ratio correction developed by Ayre and Scally (2014), it was determined that eight items were essential: Item 2 (CVR = .7), Item 3 (CVR = .9), Item 4 (CVR = .6), Item 6 (CVR = .6), Item 7 (CVR = .8), Item 10 (CVR = .6), Item 15 (CVR = .5), and Item 16 (CVR = .6).
Upon further evaluation, and in an effort to ensure that the PMI items served the needs of interdisciplinary professionals, some items were rated essential for specific professions; these items still met the CVR requirements (CVR = 1) for the smaller within-group sample. These four items were unanimously endorsed by SMEs for a particular profession as essential: Item 5 (CVR Social Services = 1; CVR Law Enforcement = 1), Item 11 (CVR Law Enforcement = 1), Item 13 (CVR Law Enforcement = 1), and Item 14 (CVR Law Enforcement = 1).
Finally, an evaluation of the remaining four items was completed to explore if items were useful, but not essential. Using the minimum CVR ≥ .5, it was determined that these items should remain on the PMI: Item 1 (CVR = .9), Item 8 (CVR = .8), Item 9 (CVR = .9), and Item 12 (CVR = .9). The use of Siegle’s (2017) Reliability Calculator determined the Cronbach’s α level for the PMI to be 0.83, indicating adequate internal consistency. Additionally, a split-half (odd-even) correlation was completed with the Spearman-Brown adjustment of 0.88, indicating high reliability (Siegle, 2017).
Pilot Summary
The focus of the pilot study was to ensure effective implementation of the proposed research protocol following each respondent’s appointment at the CAC research site. The pilot was implemented to ensure research procedures did not interfere with typical appointments and standard procedures at the CAC. Participation in the PMI pilot was voluntary and no compensation was provided for respondents.
Sample. The study used a purposeful sample of children at a local, nationally accredited CAC in the Midwest; both the child and the child’s legal guardian agreed to participate. Because of the expected integration of PM with other forms of abuse, this population was selected to help create an understanding of how PM is experienced specifically with co-occurring cases of maltreatment. Respondents were children who (a) had an open CM case with social services and/or law enforcement, (b) were scheduled for an appointment at the CAC, and (c) were between the ages of 8 and 17.
Measures. The two measures implemented in this study were the developing PMI and the TSCC-SF. At the time of data collection, CAC staff implemented the TSCC-SF as a screening tool for referral services during CAC victim appointments. To ensure the research process did not interfere with chain-of-custody procedures, collected investigative testimony, or physical evidence that was obtained, the PMI was administered only after all normally scheduled CAC procedures were followed during appointments.
PMI. The current version of the PMI is a self-report measure that consists of 16 items on a 4-point Likert-type scale that mirrors the language of the TSCC-SF (0 = never to 3 = almost all the time). Respondents typically needed 5 minutes complete the PMI. Sample items from the PMI included questions like: “How often have you been told or made to feel like you are not important or unlovable?” The full instrument is not provided for use in this publication to ensure the PMI is not misused, as refinement of the PMI is still in progress.
TSCC-SF. In addition to the PMI, Boughn gathered data from the TSCC-SF (Briere & Wherry, 2016) because of its widespread use among clinicians to efficiently assess for sexual concerns, suicidal ideation frequency, and general trauma symptoms such as post-traumatic stress, depression, anger, disassociation, and anxiety (Wherry et al., 2013). The TSCC-SF measures a respondent’s frequency of perceived experiences and has been successfully implemented with children as young as 8 years old (Briere, 1996). The 20-item form uses a 4-point Likert-type scale (0 = never to 3 = almost all the time) composed of general trauma and sexual concerns subscales. The TSCC-SF has demonstrated high internal consistency and alpha values in the good to excellent ranges; it also has high intercorrelations between sexual concerns and other general trauma scales (Wherry & Dunlop, 2018).
Procedures. Respondents were recruited during their scheduled CAC appointment time. Each investigating agency (law enforcement or social services) scheduled a CAC appointment in accordance with an open maltreatment case. At the beginning of each respondent’s appointment, Boughn provided them with an introduction and description of the study. This included the IRB approvals from the hospital and university, an explanation of the informed consent and protected health information (PHI) authorization, and assent forms. Respondents aged 12 and older were asked to read and review the informed consent document with their legal guardian; respondents aged from 8 to 11 were provided an additional assent document to read. Respondents were informed they could stop the study at any time. After each respondent and legal guardian consented, respondents proceeded with their CAC appointment.
Typical CAC appointments consisted of a forensic interview, at times a medical exam, and administration of the TSCC-SF to determine referral needs. After these steps were completed, Boughn administered the PMI to those who agreed to participate in this research study. Following the completion of the TSCC-SF, respondents were verbally reminded of the study and asked if they were still willing to participate by completing the PMI. Willing respondents completed the PMI; afterward, Boughn asked respondents if they were comfortable leaving the assessment room. In the event the respondent voiced additional concerns of maltreatment during the PMI administration, Boughn made a direct report to the respondent’s investigator (i.e., law enforcement officer or social worker assigned to the respondent’s case).
Boughn accessed each respondent’s completed TSCC-SF from their electronic health record in accordance with the PHI authorization and consent after the respondent’s appointment. Data completed on the TSCC-SF allowed Boughn to gather information related to sexual concerns, suicidal ideation, and trauma symptomology. Data gathered from the TSCC-SF were examined with each respondent’s PMI responses.
Results. Respondents were 21 children (15 female, six male) with age ranges from 8 to 17 years with a median age of 12 years. Respondents described themselves as White (47.6%), Biracial (14.2%), Multiracial (14.2%), American Indian/Alaskan Native (10.0%), Black (10.0%), and Hispanic/Latino (5.0%). CM allegations for the respondents consisted of allegations of sexual abuse (86.0%), physical abuse (10.0%), and neglect (5.0%).
Every respondent’s responses were included in the analyses to ensure all maltreatment situations were considered. The reliability of the PMI observed in the pilot sample (N = 21) demonstrated high internal consistency with all 16 initial items (α = .88). The average total score on the PMI in the pilot was 13.29, with respondents’ scores ranging from 1 to 30. A Pearson correlation indicated total scores for the PMI and General Trauma Scale scores (reported on the TSCC-SF) were significantly correlated (r = .517, p < .05).
Study 2: Full Testing of the PMI
The next phase of research proceeded with the collection of a larger data sample (N = 166) to explore the item construct validity and internal reliability (Siyez et al., 2020). Study procedures, data collection, and data storage followed in the pilot study were also implemented with the larger sample. Boughn maintained tracking of respondents who did not want to participate in the study or were unable to because of cognitive functioning level, emergency situations, and emotional dysregulation concerns.
Sample
Based on a power analysis performed using the Raosoft (2004) sample size calculator, the large sample study required a minimum of 166 respondents for statistical significance (Ali, 2012; Heppner et al., 2016). The sample size was expected to account for a 10% margin of error and a 99% confidence level. The calculation of a 99% confidence interval was used to ensure the number of respondents could effectively represent the population accessed within the CAC based on the data from the CM Report (DHHS, 2018). Large sample population data was gathered between September 2018 and May 2019.
Measures
The PMI and TSCC-SF were also employed in Study 2 because of their successful implementation in the pilot. Administration of the TSCC-SF ensured a normed and standardized measure could aid in providing context to the information gathered on the PMI. No changes were made to the PMI or TSCC-SF measures following the review of procedures and analyses in the pilot.
Procedures
Recruitment and data collection/analyses processes mirrored that of the pilot study. Voluntary respondents were recruited at the CAC during their scheduled appointments. Respondents completed an informed consent, child assent, PHI authorization form, TSCC-SF, and PMI. Following the completion of data collection, Boughn completed data entry in the electronic health record to de-identify and analyze the results.
Results
Demographics
All data were analyzed using Statistical Package for the Social Sciences version 24 (SPSS-24). Initial data evaluation consisted of exploration of descriptive statistics, including demographic and criteria-based information related to respondents’ identities and case details. Respondents were between 8 to 17 years of age (M = 12.39) and primarily female (73.5%, n = 122), followed by male (25.3%, n = 42). Additionally, two respondents (n = 2) reported both male and female gender identities. Racial identities were marked by two categories: White (59.6%, n = 99) and Racially Diverse (40.4%, n = 67) respondents. The presenting maltreatment concerns and the child’s relationship to the offender are outlined in Table 1 and Table 2, respectively.
Reliability and Validity of the PMI
The reliability of the PMI observed in its implementation in Study 2 (N = 166) showed even better internal consistency with all 16 initial items (α =.91) than observed in the pilot. Using the Spearman-Brown adjustment (Warner, 2013), split-half reliability was calculated, indicating high internal reliability (.92). Internal consistencies were calculated using gender identity and age demographic variables (see Table 3).
Table 1
Child Maltreatment Allegation by Type (N = 166)
| Allegation |
f |
Rel f |
cf |
% |
| Sexual Abuse |
113 |
0.68 |
166 |
68.07 |
| Physical Abuse |
29 |
0.17 |
53 |
17.47 |
| Neglect |
14 |
0.08 |
24 |
8.43 |
| Multiple Allegations |
6 |
0.04 |
10 |
3.61 |
| Witness to Violence |
3 |
0.02 |
4 |
1.81 |
| Kidnapping |
1 |
0.01 |
1 |
0.60 |
Note. Allegation type reported at initial appointment scheduling
Table 2
Identified Offender by Relationship to Victim (N = 166)
| Offender Relationship |
f |
Rel f |
cf |
% |
| Other Known Adult |
60 |
0.36 |
166 |
36.14 |
| Parent |
48 |
0.29 |
106 |
28.92 |
| Other Known Child (≤ age 15 years) |
15 |
0.09 |
58 |
9.04 |
| Sibling-Child (≤ age 15 years) |
10 |
0.06 |
43 |
6.02 |
| Unknown Adult |
9 |
0.05 |
33 |
5.42 |
| Step-Parent |
8 |
0.05 |
24 |
4.82 |
| Multiple Offenders |
6 |
0.04 |
16 |
3.61 |
| Grandparent |
6 |
0.04 |
10 |
3.61 |
| Sibling-Adult (≥ age 16 years) |
3 |
0.02 |
4 |
1.81 |
| Unknown Child (≤ age 15 years) |
1 |
0.01 |
1 |
0.60 |
Note. Respondent knew the offender (n =156); Respondent did not know offender (n =10)
Table 3
Internal Consistency Coefficients (α) by Gender Identity and Age (N = 166)
| Gender |
n |
α |
M |
SD |
| Female |
122 |
0.90 |
13.2 |
9.1 |
| Male |
42 |
0.94 |
13.5 |
11.0 |
| Male–Female |
2 |
0.26 |
8.5 |
2.5 |
| Age |
|
|
|
|
| 8–12 |
83 |
0.92 |
12.75 |
10.06 |
| 13–17 |
83 |
0.90 |
13.69 |
9.01 |
Note. SD = Standard Deviation; M = Mean
Respondents’ Demographic Characteristics and PM Experiences
For Research Question (RQ) 1 and RQ2, descriptive data were used to generate frequencies and determine the impact of demographic characteristics on average PMI score. To explore this further in RQ1, one-way ANOVAs were completed for the variables of age, gender, racial identity, allegation type, and offender relationships. No significant correlations were found between demographic variables and the PMI items. On average, respondents reported a frequency score of 13.5 (M = 13.5, SD = 9.5) on the PMI. Eight respondents (5%) endorsed no frequency of PM while 95% (N = 158) experienced PM.
Co-Occurrence of PM With Other Forms of Maltreatment
For RQ3, frequency and descriptive data were generated, revealing average age rates of PM reported by maltreatment type. Varying sample representations were discovered in each form of maltreatment (see Table 4). Clear evidence was found that PM co-occurs with each form of maltreatment type; however, how each form of maltreatment interacts with PM is currently unclear given the multiple dimensions of each maltreatment case including, but not limited to, severity, frequency, offender, and victim characteristics.
Table 4
Descriptive and Frequency Data for Co-Occurrence of PM (N = 166)
| Allegation |
n |
M |
SD |
95% CI |
| Sexual Abuse |
113 |
13.04 |
9.01 |
[11.37, 14.72] |
| Physical Abuse |
29 |
12.45 |
10.53 |
[8.44, 16.45] |
| Neglect |
14 |
14.57 |
12.16 |
[7.55, 21.60] |
| Multiple Allegations |
5 |
17.40 |
8.88 |
[6.38, 28.42] |
| Witness to Violence |
3 |
7.67 |
5.03 |
[–4.84, 20.17] |
| Kidnapping |
1 |
n/a |
n/a |
Missing |
Note. CI = Confidence Interval; SD = Standard Deviation; M = Mean; n/a = not applicable
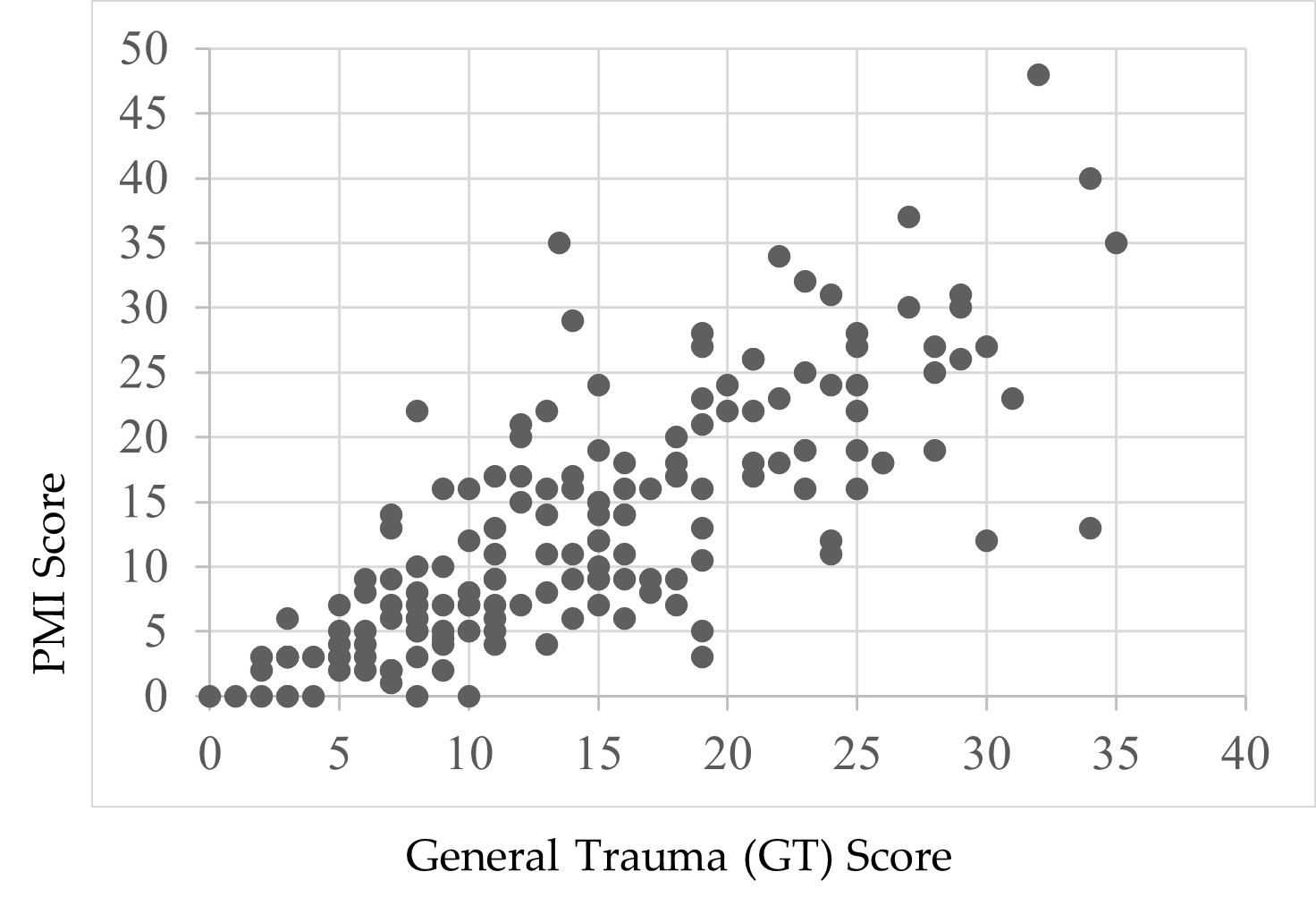
PM Frequency and General Trauma Symptoms
For RQ4, Pearson’s correlation was used to calculate frequency score relationships between the PMI and TSCC-SF. There was a statistically significant relationship between the PMI and total frequency of general trauma symptoms on the TSCC-SF [r(164) = .78, p < .01, r² = .61] (Sullivan & Feinn, 2012). Cohen’s d, calculated from the means for each item as well as the pooled standard deviation, indicated a small effect relationship (d = .15) between general trauma and PMI frequencies (see Figure 1).
Figure 1
Correlation Between PMI and TSCC-SF General Trauma Subscale
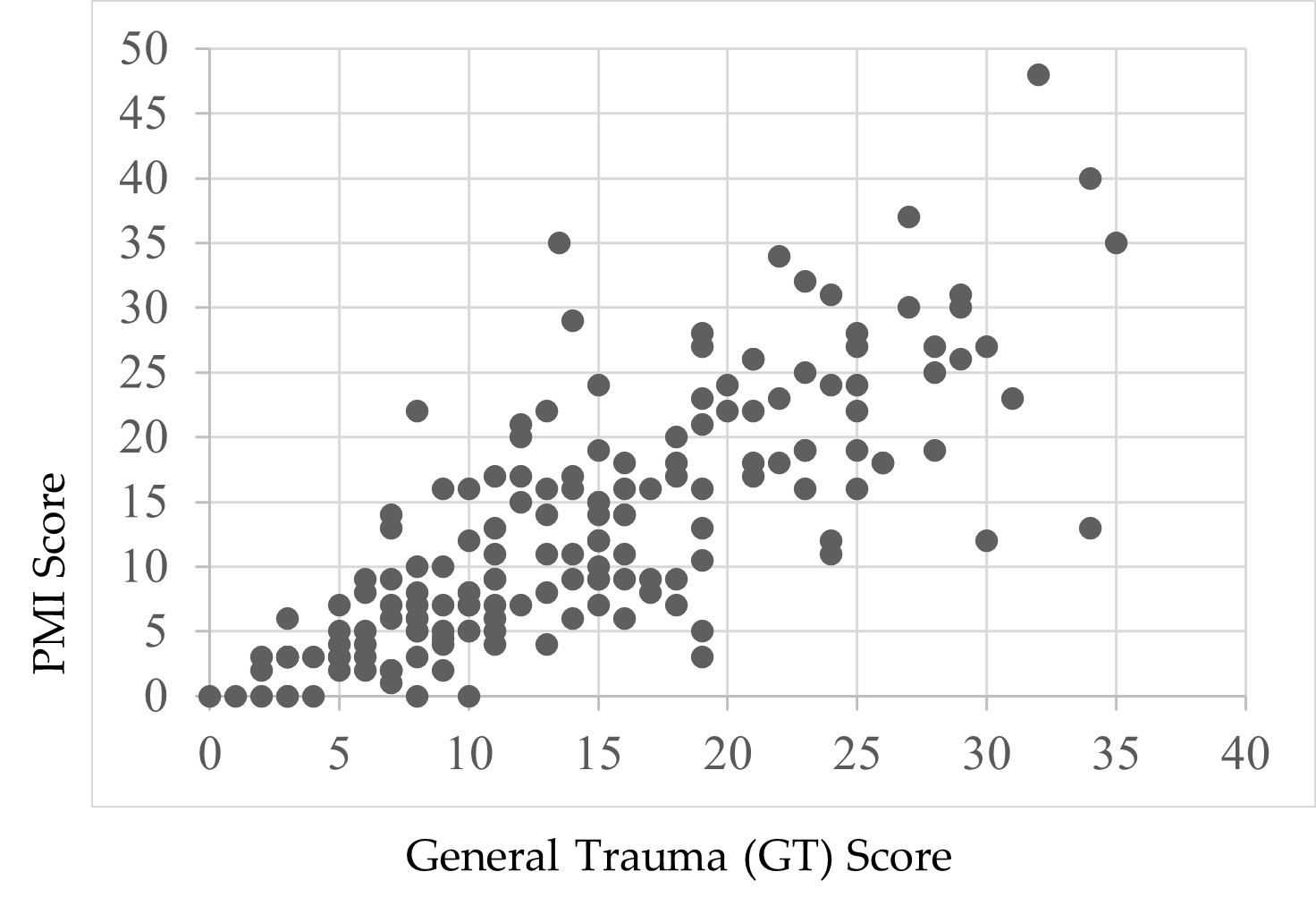
Note. Scores were endorsed by respondents’ self-reports.
Child Suicidal Ideation Reports and the PMI
Following a review of the findings of Thompson et al. (2005) and Wherry et al. (2013) that children who reported experiencing CM also experienced suicidal ideation, Boughn performed an additional two-way ANOVA that examined the effect of suicidal ideation on the PMI total score. A significant relationship—F(1, 164) = 49.52, p < .01, η2 = .23—between respondents’ PMI scores and thoughts of suicide was found. Respondents who did not report thoughts of suicide (59.0%, n = 98) indicated lower rates of PM (M = 9.37, SD = 7.97) compared to children who did report thoughts of suicide (41.0%, n = 68, M = 18.77, SD = 9.12). A preliminary review of this finding demonstrates the severity of PM’s impact on child victims.
Discussion
This study was designed with the aim of developing a tool to support accurate identification of PM among children and adolescents. Findings from its first large-scale implementation provide a foundational view to the occurrence of PM in terms of demographic characteristics, comorbidity of PM with other forms of abuse, and the relationship between PM and trauma. The analyses yielded both expected and unexpected results based on the extant research.
PM and Demographic Characteristics
Race
There was no significant effect when exploring the data related to racial demographics and PM. The respondent sample closely reflected the geographical area’s known racial demographics at the time of the study, reflecting a population approaching 80% White with residents of all other known races below 5% for each racial group (U.S. Census Bureau, 2020). Although researchers (Dakil et al., 2011) anticipated children identifying as racial minorities would be included in the representation of CM reports, evidence from this study potentially reveals a greater than expected gap in reporting for minority-race populations (Bernard & Harris, 2018; Font & Maguire-Jack, 2015). This suggests that there may be additional, unidentified barriers influencing the reporting of maltreatment among minority-race populations.
Gender
A lack of gender identity representation was evident in the data, consistent with prior research (Sivagurunathan et al., 2019). Respondents who self-identified with both male and female gender identities (1.2%) and as male (25.3%) were represented less frequently compared to female respondents (73.5%). This is not inherently a limitation of this study, as research shows that just 10% of males in the United States report their sexual abuse (Sivagurunathan et al., 2019). People who identify as male may face harmful cultural messages that enhance negative stigma for victims of abuse, causing increased feelings of weakness or vulnerability (Alaggia & Mishna, 2014). This finding may support claims that male trauma survivors feel stigmatized and report their experiences less frequently (Easton, 2012).
Additionally, children who identify outside traditional gender binary norms and definitions need more access to inclusive representation on screening assessments. Assessments like the TSCC-SF may be using antiquated gender- or biological sex–normed checkboxes, which leave certain groups underrepresented in research studies (Neukrug & Fawcett, 2015). These practices may present inaccurate findings, inadvertently reinforce discriminatory expectations, and generate inaccurate referrals. Non-binary youth encounter barriers that may compound their ability to effectively access supports in their daily life related to coming out, social violence, lack of peer and/or adult acceptance, discrimination, isolation, higher rates of suicide, and lack of representation in mainstream society (Bialer & McIntosh, 2016; Zimman, 2009). In this study, representation of non-binary respondents, specifically those who reported both male and female gender identities, was reported; this warrants further exploration to assess barriers among non-binary gender youth and their experiences with child PM (Bos et al., 2019).
Offender Relationships
Frequency data for a child’s relationship with the offender were not found to be significant either for known offenders (M = 13.35) or unknown offenders (M = 11.2). In this study, 94% of the respondents already knew their offender (n = 156). This finding is consistent with previous research that has found that although child abduction and stranger danger are real phenomena, children are more likely to experience CM as a result of relationships with familiar individuals (Walsh & Brandon, 2011).
Co-Occurrence of PM With Other Abuse
Only eight respondents (5%) endorsed no frequency of PM; the average total PM frequency rate for respondents in this study was 13.5 out of a possible 48, indicating extreme severity. In this study, we found evidence that PM is a co-occurring experience for children with open maltreatment cases, yet clinicians still lack formal, valid assessments to determine PM alone. Our findings support the National Children’s Alliance’s (NCA; 2016) call for clinicians to follow practice guidelines in accordance with state and national guidelines as they relate to mandatory reporting of CM concerns and determination of whether PM plus other forms of maltreatment may be present for child victims seeking services.
Comorbidity of PM and Trauma
PM-related experiences on the PMI and general trauma symptoms from the TSCC-SF warrant discussion. The PMI illustrated a significant relationship with the TSCC-SF general trauma subscale (Briere & Wherry, 2016). More than half (61%) of the variance on the PMI was connected to general trauma symptoms, suggesting that higher rates of PM experiences may increase trauma-related symptoms. For example, previous researchers have found adverse childhood experiences and signs of trauma-related symptoms lead to serious mental health diagnoses, early mortality, and/or significant biological health risks in children (Tyrka et al., 2013; Vachon et al., 2015; Zimmerman & Mercy, 2010). Further exploration to determine if and how PM influences other trauma-related symptoms in children throughout their life span would expand upon the results of this study.
Suicidal Ideation
Finally, our data revealed a significant effect between respondent endorsement of suicidal ideation and PMI total scores. PM experiences accounted for 23% of the variance for children who reported thoughts of suicide (41%, n = 68) compared to those who did not report thoughts of suicide (59%, n = 98). This finding is consistent with prior research exploring children’s experiences with maltreatment and suicidal thoughts (Thompson et al., 2005; Wherry et al., 2013).
Limitations
This study has several limitations. First, by developing the PMI using national definitions, some regional and localized nuances were not considered. Second, data collected for this study were from a single Midwest CAC; thus, the data are limited in geographic generalizability. Third, the majority of respondents were White, and a more diverse sample would have been more representative of the region in which data were collected. Fourth, 99% of respondents identified as either male or female and may reflect an underrepresentation of non-binary or gender fluid youth in the results of this study. Fifth, this study relied heavily on quantitative data, which limited the ability to analyze each individual’s experiences with PM as they might describe from their unique perspectives.
Implications for Research and Practice
The results of this study provide several areas for future research. While the PMI demonstrated good internal consistency across all items (α =.91), more research with diverse populations across the United States is needed. Research from other geographical locations may demonstrate how reporting patterns for PM interact with ethnicity, culture, and elements of social expectations (Spinazzola et al., 2014).
The initial results of this study indicate the PMI may be a useful tool for children to report PM experiences in CAC settings; however, future research at other CACs and similar treatment facilities is needed to determine the PMI’s true utility and scalability. Future analysis (i.e., exploratory factor analysis and confirmatory factor analysis) of the PMI may also identify factors and help refine the instrument.
More research with the PMI can expand researchers’ knowledge of PM and services needed to help children. Working with other CACs, child protection professionals, and the NCA may help bridge current gaps in interdisciplinary assessment and care and establish a stable and comprehensive understanding of PM (López et al., 2015). Furthermore, understanding how CACs are equipped to identify and handle PM cases may provide useful insights to help improve services for children in need. Although some CACs may have a variety of professionals working in specific roles, some CACs may be understaffed, causing staff to take on multiple and overlapping roles. It is important to understand if and how different combinations of trained professionals influence children reporting PM (Hart & Glaser, 2011; NCA, 2016).
More research with the PMI is needed for refinement and to ensure the instrument is not misused. Releasing the PMI at this stage to clinicians and researchers without a fully developed assessment manual may lead to inappropriate or ineffective administration of the PMI and potentially unethical practice that could place children at risk. Future research and refinement of the PMI may provide clinicians and researchers a reliable and valid tool that is grounded in consistent theory and practice.
Conclusion
The PMI was developed to assess child PM and offers researchers and clinicians useful findings. In supporting research (Arslan, 2017; Bernstein et al., 2013; Raparia et al., 2016), child PM is a serious and often harmful combination of experiences that requires professional intervention (APSAC, 2019). For children reporting PM experiences, the PMI may help mental health and other care providers determine which services are needed. Findings from this study suggest differences in demographic variables are minimal for PM. Overall PMI scores were correlated to the general trauma subscale on the TSCC-SF, and the PMI revealed higher rates of PM for children experiencing suicidal ideation. The findings are the beginning of a measure designed to illustrate the depth and frequency of PM for children. With the PMI, early PM intervention becomes possible for a once invisible form of maltreatment.
Conflict of Interest and Funding Disclosure
Data collected and content shared in this study
were part of a dissertation study, which was
awarded the 2020 Dissertation Excellence Award
by the National Board for Certified Counselors.
The Psychological Maltreatment Inventory (PMI)
items were not released in this publication to protect
victims of child maltreatment and to ensure future
publications can address comprehensive revisions
made to the PMI.
References
Ahern, E. C., Hershkowitz, I., Lamb, M. E., Blasbalg, U., & Winstanley, A. (2014). Support and reluctance in the pre-substantive phase of alleged child abuse victim investigative interviews: Revised versus standard NICHD protocols. Behavioral Sciences & the Law, 32(6), 762–774. https://doi.org/10.1002/bsl.2149
Alaggia, R., & Mishna, F. (2014). Self psychology and male child sexual abuse: Healing relational betrayal. Clinical Social Work Journal, 42(1), 41–48. https://doi.org/10.1007/s10615-013-0453-2
Ali, S. A. (2012). Sample size calculation and sampling techniques. Journal of the Pakistan Medical Association, 62(6), 624–626. https://jpma.org.pk/PdfDownload/3482
American Professional Society on the Abuse of Children. (2019). APSAC practice guidelines: The investigation and determination of suspected psychological maltreatment of children and adolescents. https://bit.ly/3jI7AhJ
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
Arslan, G. (2017). Psychological maltreatment, coping strategies, and mental health problems: A brief and effective measure of psychological maltreatment in adolescents. Child Abuse & Neglect, 68, 96–106. https://doi.org/10.1016/j.chiabu.2017.03.023
Ayre, C., & Scally, A. J. (2014). Critical values for Lawshe’s content validity ratio: Revisiting the original methods of calculation. Measurement and Evaluation in Counseling and Development, 47(1), 79–86. https://doi.org/10.1177%2F0748175613513808
Bernard, C., & Harris, P. (2018). Serious case reviews: The lived experience of Black children. Child & Family Social Work, 24(2), 256–263. https://doi.org/10.1111/cfs.12610
Bernstein, R. E., Measelle, J. R., Laurent, H. K., Musser, E. D., & Ablow, J. C. (2013). Sticks and stones may break my bones but words relate to adult physiology? Child abuse experience and women’s sympathetic nervous system response while self-reporting trauma. Journal of Aggression, Maltreatment & Trauma, 22(10), 1117–1136. https://doi.org/10.1080/10926771.2013.850138
Bialer, P. A., & McIntosh, C. A. (2016). Discrimination, stigma, and hate: The impact on the mental health and well-being of LGBT people. Journal of Gay & Lesbian Mental Health, 20(4), 297–298. https://doi.org/10.1080/19359705.2016.1211887
Bos, H., de Haas, S., & Kuyper, L. (2019). Lesbian, gay, and bisexual adults: Childhood gender nonconformity, childhood trauma, and sexual victimization. Journal of Interpersonal Violence, 34(3), 496–515. https://doi.org/10.1177%2F0886260516641285
Briere, J. (1996). Trauma Symptom Checklist for Children (TSCC), professional manual. Psychological Assessment Resources.
Briere, J., & Wherry, J. (2016). Development and validation of the TSCC Screening Form (TSCC-SF) and TSCYC Screening Form (TSCYC-SF). Psychological Assessment Resources.
Brown, S. M., Bender, K., Orsi, R., McCrae, J. S., Phillips, J. D., & Rienks, S. (2019). Adverse childhood experiences and their relationship to complex health profiles among child welfare–involved children: A classification and regression tree analysis. Health Services Research, 54(4), 902–911. https://doi.org/10.1111/1475-6773.13166
Centers for Disease Control. (2012). Child abuse and neglect cost the United States $124 billion [Press release]. https://bit.ly/3jYbpAF
Dakil, S. R., Cox, M., Lin, H., & Flores, G. (2011). Racial and ethnic disparities in physical abuse reporting and Child Protective Services interventions in the United States. Journal of the National Medical Association, 103(9–10), 926–931. https://doi.org/10.1016/S0027-9684(15)30449-1
Easton, S. D. (2012). Disclosure of child sexual abuse among adult male survivors. Clinical Social Work Journal, 41, 344–355. https://doi.org/10.1007/s10615-012-0420-3
Fang, X., Brown, D. S., Florence, C. S., & Mercy, J. A. (2012). The economic burden of child maltreatment in the United States and implications for prevention. Child Abuse & Neglect, 36(2), 156–165. https://doi.org/10.1016/j.chiabu.2011.10.006
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., Koss, M. P., & Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) study. American Journal of Preventive Medicine, 14(4), 245–258. https://doi.org/10.1016/S0749-3797(98)00017-8
Field, T. A., Jones, L. K., & Russell-Chapin, L. A. (Eds.). (2017). Neurocounseling: Brain-based clinical approaches. American Counseling Association.
Font, S. A., & Maguire-Jack, K. (2015). Decision-making in Child Protective Services: Influences at multiple levels of the social ecology. Child Abuse & Neglect, 47, 70–82. https://doi.org/10.1016/j.chiabu.2015.02.005
Glaser, D. (2002). Emotional abuse and neglect (psychological maltreatment): A conceptual framework. Child Abuse & Neglect, 26(6–7), 697–714. https://doi.org/10.1016/S0145-2134(02)00342-3
Greenfield, E. A., & Marks, N. F. (2010). Identifying experiences of physical and psychological violence in childhood that jeopardize mental health in adulthood. Child Abuse & Neglect, 34(3), 161–171. https://doi.org/10.1016/j.chiabu.2009.08.012
Hart, S. N., & Glaser, D. (2011). Psychological maltreatment – Maltreatment of the mind: A catalyst for advancing child protection toward proactive primary prevention and promotion of personal well-being. Child Abuse & Neglect, 35(10), 758–766. https://doi.org/10.1016/j.chiabu.2011.06.002
Heppner, P. P., Wampold, B. E., Owen, J., Thompson, M. N., & Wang, K. T. (2016). Research design in counseling (4th ed.). Cengage.
Iwaniec, D. (2006). The emotionally abused and neglected child: Identification, assessment and intervention: A practice handbook (2nd ed.). Wiley.
Klika, J. B., & Conte, J. R. (Eds.). (2017). The APSAC handbook on child maltreatment (4th ed.). SAGE.
Lawshe, C. H. (1975). A quantitative approach to content validity. Personnel Psychology, 28(4), 563–575. https://doi.org/10.1111/j.1744-6570.1975.tb01393.x
López, M., Fluke, J. D., Benbenishty, R., & Knorth, E. J. (2015). Commentary on decision-making and judgments in child maltreatment prevention and response: An overview. Child Abuse & Neglect, 49, 1–11. https://doi.org/10.1016/j.chiabu.2015.08.013
Maguire, S. A., Williams, B., Naughton, A. M., Cowley, L. E., Tempest, V., Mann, M. K., Teague, M., & Kemp, A. M. (2015). A systematic review of the emotional, behavioural and cognitive features exhibited by school-aged children experiencing neglect or emotional abuse. Child: Care, Health and Development, 41(5), 641–653. https://doi.org/10.1111/cch.12227
Marshall, N. A. (2012). A clinician’s guide to recognizing and reporting parental psychological maltreatment of children. Professional Psychology: Research and Practice, 43(2), 73–79. https://doi.org/10.1037/a0026677
Mills, R., Scott, J., Alati, R., O’Callaghan, M., Najman, J. M., & Strathearn, L. (2013). Child maltreatment and adolescent mental health problems in a large birth cohort. Child Abuse & Neglect, 37(5), 292–302. https://doi.org/10.1016/j.chiabu.2012.11.008
National Children’s Alliance. (2016). Putting standards into practice: A guide to implementing the 2017 standards for accredited members (revised 2016). http://www.nationalchildrensalliance.org/wp-content/uploads/2015/06/NCA2017-StandardsIntoPractice-web.pdf
Neukrug, E. S., & Fawcett, R. C. (2015). The essentials of testing and assessment: A practical guide for counselors, social workers, and psychologies, enhanced (3rd ed.). Cengage.
Peterson, C., Florence, C., & Klevens, J. (2018). The economic burden of child maltreatment in the United States, 2015. Child Abuse & Neglect, 86, 178–183.
https://doi.org/10.1016/j.chiabu.2018.09.018
Porges, S. W. (2011). The polyvagal theory: Neurophysiological foundations of emotions, attachment, communication, and self-regulation. W. W. Norton.
Raosoft. (2004). Sample size calculator. http://www.raosoft.com/samplesize.html
Raparia, E., Coplan, J. D., Abdallah, C. G., Hof, P. R., Mao, X., Mathew, S. J., & Shungu, D. C. (2016). Impact of childhood emotional abuse on neocortical neurometabolites and complex emotional processing in patients with generalized anxiety disorder. Journal of Affective Disorders, 190, 414–423. https://doi.org/10.1016/j.jad.2015.09.019
Readable. (n.d.). https://readable.com
Siegle, R. (2017). Educational research basics: Excel spreadsheet to calculate instrument reliability estimates. https://researchbasics.education.uconn.edu/excel-spreadsheet-to-calculate-instrument-reliability-estimates
Sivagurunathan, M., Orchard, T., & Evans, M. (2019). Barriers to utilization of mental health services amongst male child sexual abuse survivors: Service providers’ perspective. Journal of Child Sexual Abuse, 28(7), 819–839. https://doi.org/10.1080/10538712.2019.1610823
Siyez, D. M., Esen, E., Seymenler, S., & Öztürk, B. (2020). Development of wellness scale for emerging adults: Validity and reliability study. Current Psychology.
https://doi.org/10.1007/s12144-020-00672-w
Slep, A. M. S., Heyman, R. E., & Foran, H. M. (2015). Child maltreatment in DSM-5 and ICD-11. Family Process, 54(1), 17–32. https://doi.org/10.1111/famp.12131
Spinazzola, J., Hodgdon, H., Liang, L.-J., Ford, J. D., Layne, C. M., Pynoos, R., Briggs, E. C., Stolbach, B., & Kisiel, C. (2014). Unseen wounds: The contribution of psychological maltreatment to child and adolescent mental health and risk outcomes. Psychological Trauma: Theory, Research, Practice, and Policy, 6(Suppl 1), S18–S28. https://doi.org/10.1037/a0037766
Sullivan, G. M., & Feinn, R. (2012). Using effect size—or why the p value is not enough. Journal of Graduate Medical Education, 4(3), 279–282. https://doi.org/10.4300/JGME-D-12-00156.1
Thompson, R., Briggs, E., English, D. J., Dubowitz, H., Lee, L.-C., Brody, K., Everson, M. D., & Hunter, W. M. (2005). Suicidal ideation among 8-year-olds who are maltreated and at risk: Findings from the LONGSCAN studies. Child Maltreatment, 10(1), 26–36. https://doi.org/10.1177%2F1077559504271271
Tonmyr, L., Draca, J., Crain, J., & MacMillian, H. L. (2011). Measurement of emotional/psychological child maltreatment: A review. Child Abuse & Neglect, 35(10), 767–782.
https://doi.org/10.1016/j.chiabu.2011.04.011
Tyrka, A. R., Burgers, D. E., Philip, N. S., Price, L. H., & Carpenter, L. L. (2013). The neurobiological correlates of childhood adversity and implications for treatment. Acta Psychiatrica Scandinavica, 128(6), 434–447. https://doi.org/10.1111/acps.12143
U.S. Census Bureau. (2020). Quick facts. https://www.census.gov
U.S. Department of Health & Human Services. (2018). Child maltreatment 2016 (27th ed.). https://www.acf.hhs.gov/sites/default/files/documents/cb/cm2016.pdf
Vachon, D. D., Krueger, R. F., Rogosch, F. A., & Cicchetti, D. (2015). Assessment of the harmful psychiatric and behavioral effects of different forms of child maltreatment. JAMA Psychiatry, 72(11), 1135–1142. https://doi.org/10.1001/jamapsychiatry.2015.1792
van der Kolk, B. (2014). The body keeps the score: Brain, mind, and body in the healing of trauma. Penguin Books.
van Harmelen, A.-L., Elzinga, B. M., Kievit, R. A., & Spinhoven, P. (2011). Intrusions of autobiographical memories in individuals reporting childhood emotional maltreatment. European Journal of Psychotraumatology, 2(1), 7336. https://doi.org/10.3402/ejpt.v2i0.7336
van Harmelen, A.-L., van Tol, M.-J., van der Wee, N. J. A., Veltman, D. J., Aleman, A., Spinhoven, P., van Buchem, M. A., Zitman, F. G., Penninx, B. W. J. H., & Elzinga, B. M. (2010). Reduced medial prefrontal cortex volume in adults reporting childhood emotional maltreatment. Biological Psychiatry, 68(9), 832–838. https://doi.org/10.1016/j.biopsych.2010.06.011
Walsh, K., & Brandon, L. (2011). Their children’s first educators: Parents’ views about child sexual abuse prevention education. Journal of Child and Family Studies, 21, 734–746.
https://doi.org/10.1007/s10826-011-9526-4
Warner, R. M. (2013). Applied statistics: From bivariate through multivariate techniques (2nd ed.). SAGE.
Wherry, J. N., Baldwin, S., Junco, K., & Floyd, B. (2013). Suicidal thoughts/behaviors in sexually abused children. Journal of Child Sexual Abuse, 22(5), 534–551. https://doi.org/10.1080/10538712.2013.800938
Wherry, J. N., & Dunlop, C. E. (2018). TSCC and TSCYC screening forms in a clinical sample: Reliability, validity, and creating local clinical norms. Child Maltreatment, 23(1), 74–84.
https://doi.org/10.1177%2F1077559517725207
Zimman, L. (2009). ‘The other kind of coming out’: Transgender people and the coming out narrative genre. Gender and Language, 3(1), 53–80. https://doi.org/10.1558/genl.v3i1.53
Zimmerman, F., & Mercy, J. (2010). A better start: Child maltreatment prevention as a public
health priority. Zero to Three, 30(5), 4–10.
Alison M. Boughn, PhD, NCC, LIMHP (NE), LMHC (IA), LPC-MH (SD), ATR-BC, QMHP, TF-CBT, is an assistant professor and counseling department chair at Wayne State College. Daniel A. DeCino, PhD, NCC, LPC, is an assistant professor and Interim Program Coordinator at the University of South Dakota. Correspondence may be addressed to Alison M. Boughn, Wayne State College, 1111 Main Street, Wayne, NE 68787, albough1@wsc.edu.
Aug 20, 2021 | Author Videos, Volume 11 - Issue 3
Warren N. Ponder, Elizabeth A. Prosek, Tempa Sherrill
First responders are continually exposed to trauma-related events. Resilience is evidenced as a protective factor for mental health among first responders. However, there is a lack of assessments that measure the construct of resilience from a strength-based perspective. The present study used archival data from a treatment-seeking sample of 238 first responders to validate the 22-item Response to Stressful Experiences Scale (RSES-22) and its abbreviated version, the RSES-4, with two confirmatory factor analyses. Using a subsample of 190 first responders, correlational analyses were conducted of the RSES-22 and RSES-4 with measures of depressive symptoms, post-traumatic stress, anxiety, and suicidality confirming convergent and criterion validity. The two confirmatory analyses revealed a poor model fit for the RSES-22; however, the RSES-4 demonstrated an acceptable model fit. Overall, the RSES-4 may be a reliable and valid measure of resilience for treatment-seeking first responder populations.
Keywords: first responders, resilience, assessment, mental health, confirmatory factor analysis
First responder populations (i.e., law enforcement, emergency medical technicians, and fire rescue) are often repeatedly exposed to traumatic and life-threatening conditions (Greinacher et al., 2019). Researchers have concluded that such critical incidents could have a deleterious impact on first responders’ mental health, including the development of symptoms associated with post-traumatic stress, anxiety, depression, or other diagnosable mental health disorders (Donnelly & Bennett, 2014; Jetelina et al., 2020; Klimley et al., 2018; Weiss et al., 2010). In a systematic review, Wild et al. (2020) suggested the promise of resilience-based interventions to relieve trauma-related psychological disorders among first responders. However, they noted the operationalization and measure of resilience as limitations to their intervention research. Indeed, researchers have conflicting viewpoints on how to define and assess resilience. For example, White et al. (2010) purported popular measures of resilience rely on a deficit-based approach. Counselors operate from a strength-based lens (American Counseling Association [ACA], 2014) and may prefer measures with a similar perspective. Additionally, counselors are mandated to administer assessments with acceptable psychometric properties that are normed on populations representative of the client (ACA, 2014, E.6.a., E.7.d.). For counselors working with first responder populations, resilience may be a factor of importance; however, appropriately measuring the construct warrants exploration. Therefore, the focus of this study was to validate a measure of resilience with strength-based principles among a sample of first responders.
Risk and Resilience Among First Responders
In a systematic review of the literature, Greinacher et al. (2019) described the incidents that first responders may experience as traumatic, including first-hand life-threatening events; secondary exposure and interaction with survivors of trauma; and frequent exposure to death, dead bodies, and injury. Law enforcement officers (LEOs) reported that the most severe critical incidents they encounter are making a mistake that injures or kills a colleague; having a colleague intentionally killed; and making a mistake that injures or kills a bystander (Weiss et al., 2010). Among emergency medical technicians (EMTs), critical incidents that evoked the most self-reported stress included responding to a scene involving family, friends, or others to the crew and seeing someone dying (Donnelly & Bennett, 2014). Exposure to these critical incidents may have consequences for first responders. For example, researchers concluded first responders may experience mental health symptoms as a result of the stress-related, repeated exposure (Jetelina et al., 2020; Klimley et al., 2018; Weiss et al., 2010). Moreover, considering the cumulative nature of exposure (Donnelly & Bennett, 2014), researchers concluded first responders are at increased risk for post-traumatic stress disorder (PTSD), depression, and generalized anxiety symptoms (Jetelina et al., 2020; Klimley et al., 2018; Weiss et al., 2010). Symptoms commonly experienced among first responders include those associated with post-traumatic stress, anxiety, and depression.
In a collective review of first responders, Kleim and Westphal (2011) determined a prevalence rate for PTSD of 8%–32%, which is higher than the general population lifetime rate of 6.8–7.8 % (American Psychiatric Association [APA], 2013; National Institute of Mental Health [NIMH], 2017). Some researchers have explored rates of PTSD by specific first responder population. For example, Klimley et al. (2018) concluded that 7%–19% of LEOs and 17%–22% of firefighters experience PTSD. Similarly, in a sample of LEOs, Jetelina and colleagues (2020) reported 20% of their participants met criteria for PTSD.
Generalized anxiety and depression are also prevalent mental health symptoms for first responders. Among a sample of firefighters and EMTs, 28% disclosed anxiety at moderate–severe and several levels (Jones et al., 2018). Furthermore, 17% of patrol LEOs reported an overall prevalence of generalized anxiety disorder (Jetelina et al., 2020). Additionally, first responders may be at higher risk for depression (Klimley et al., 2018), with estimated prevalence rates of 16%–26% (Kleim & Westphal, 2011). Comparatively, the past 12-month rate of major depressive disorder among the general population is 7% (APA, 2013). In a recent study, 16% of LEOs met criteria for major depressive disorder (Jetelina et al., 2020). Moreover, in a sample of firefighters and EMTs, 14% reported moderate–severe and severe depressive symptoms (Jones et al., 2018). Given these higher rates of distressful mental health symptoms, including post-traumatic stress, generalized anxiety, and depression, protective factors to reduce negative impacts are warranted.
Resilience
Broadly defined, resilience is “the ability to adopt to and rebound from change (whether it is from stress or adversity) in a healthy, positive and growth-oriented manner” (Burnett, 2017, p. 2). White and colleagues (2010) promoted a positive psychology approach to researching resilience, relying on strength-based characteristics of individuals who adapt after a stressor event. Similarly, other researchers explored how individuals’ cognitive flexibility, meaning-making, and restoration offer protection that may be collectively defined as resilience (Johnson et al., 2011).
A key element among definitions of resilience is one’s exposure to stress. Given their exposure to trauma-related incidents, first responders require the ability to cope or adapt in stressful situations (Greinacher et al., 2019). Some researchers have defined resilience as a strength-based response to stressful events (Burnett, 2017), in which healthy coping behaviors and cognitions allow individuals to overcome adverse experiences (Johnson et al., 2011; White et al., 2010). When surveyed about positive coping strategies, first responders most frequently reported resilience as important to their well-being (Crowe et al., 2017).
Researchers corroborated the potential impact of resilience for the population. For example, in samples of LEOs, researchers confirmed resilience served as a protective factor for PTSD (Klimley et al., 2018) and as a mediator between social support and PTSD symptoms (McCanlies et al., 2017). In a sample of firefighters, individual resilience mediated the indirect path between traumatic events and global perceived stress of PTSD, along with the direct path between traumatic events and PTSD symptoms (Lee et al., 2014). Their model demonstrated that those with higher levels of resilience were more protected from traumatic stress. Similarly, among emergency dispatchers, resilience was positively correlated with positive affect and post-traumatic growth, and negatively correlated with job stress (Steinkopf et al., 2018). The replete associations of resilience as a protective factor led researchers to develop resilience-based interventions. For example, researchers surmised promising results from mindfulness-based resilience interventions for firefighters (Joyce et al., 2019) and LEOs (Christopher et al., 2018). Moreover, Antony and colleagues (2020) concluded that resilience training programs demonstrated potential to reduce occupational stress among first responders.
Assessment of Resilience
Recognizing the significance of resilience as a mediating factor in PTSD among first responders and as a promising basis for interventions when working with LEOs, a reliable means to measure it among first responder clients is warranted. In a methodological review of resilience assessments, Windle and colleagues (2011) identified 19 different measures of resilience. They found 15 assessments were from original development and validation studies with four subsequent validation manuscripts from their original assessment, of which none were developed with military or first responder samples.
Subsequently, Johnson et al. (2011) developed the Response to Stressful Experiences Scale (RSES-22) to assess resilience among military populations. Unlike deficit-based assessments of resilience, they proposed a multidimensional construct representing how individuals respond to stressful experiences in adaptive or healthy ways. Cognitive flexibility, meaning-making, and restoration were identified as key elements when assessing for individuals’ characteristics connected to resilience when overcoming hardships. Initially they validated a five-factor structure for the RSES-22 with military active-duty and reserve components. Later, De La Rosa et al. (2016) re-examined the RSES-22. De La Rosa and colleagues discovered a unidimensional factor structure of the RSES-22 and validated a shorter 4-item subset of the instrument, the RSES-4, again among military populations.
It is currently unknown if the performance of the RSES-4 can be generalized to first responder populations. While there are some overlapping experiences between military populations and first responders in terms of exposure to trauma and high-risk occupations, the Substance Abuse and Mental Health Services Administration (SAMHSA; 2018) suggested differences in training and types of risk. In the counseling profession, these populations are categorized together, as evidenced by the Military and Government Counseling Association ACA division. Additionally, there may also be dual identities within the populations. For example, Lewis and Pathak (2014) found that 22% of LEOs and 15% of firefighters identified as veterans. Although the similarities of the populations may be enough to theorize the use of the same resilience measure, validation of the RSES-22 and RSES-4 among first responders remains unexamined.
Purpose of the Study
First responders are repeatedly exposed to traumatic and stressful events (Greinacher et al., 2019) and this exposure may impact their mental health, including symptoms of post-traumatic stress, anxiety, depression, and suicidality (Jetelina et al., 2020; Klimley et al., 2018). Though most measures of resilience are grounded in a deficit-based approach, researchers using a strength-based approach proposed resilience may be a protective factor for this population (Crowe et al., 2017; Wild et al., 2020). Consequently, counselors need a means to assess resilience in their clinical practice from a strength-based conceptualization of clients.
Johnson et al. (2011) offered a non-deficit approach to measuring resilience in response to stressful events associated with military service. Thus far, researchers have conducted analyses of the RSES-22 and RSES-4 with military populations (De La Rosa et al., 2016; Johnson et al., 2011; Prosek & Ponder, 2021), but not yet with first responders. While there are some overlapping characteristics between the populations, there are also unique differences that warrant research with discrete sampling (SAMHSA, 2018). In light of the importance of resilience as a protective factor for mental health among first responders, the purpose of the current study was to confirm the reliability and validity of the RSES-22 and RSES-4 when utilized with this population. In the current study, we hypothesized the measures would perform similarly among first responders and if so, the RSES-4 would offer counselors a brief assessment option in clinical practice that is both reliable and valid.
Method
Participants
Participants in the current non-probability, purposive sample study were first responders (N = 238) seeking clinical treatment at an outpatient, mental health nonprofit organization in the Southwestern United States. Participants’ mean age was 37.53 years (SD = 10.66). The majority of participants identified as men (75.2%; n = 179), with women representing 24.8% (n = 59) of the sample. In terms of race and ethnicity, participants identified as White (78.6%; n = 187), Latino/a (11.8%; n = 28), African American or Black (5.5%; n = 13), Native American (1.7%; n = 4), Asian American (1.3%; n = 3), and multiple ethnicities (1.3%; n = 3). The participants identified as first responders in three main categories: LEO (34.9%; n = 83), EMT (28.2%; n = 67), and fire rescue (25.2%; n = 60). Among the first responders, 26.9% reported previous military affiliation. As part of the secondary analysis, we utilized a subsample (n = 190) that was reflective of the larger sample (see Table 1).
Procedure
The data for this study were collected between 2015–2020 as part of the routine clinical assessment procedures at a nonprofit organization serving military service members, first responders, frontline health care workers, and their families. The agency representatives conduct clinical assessments with clients at intake, Session 6, Session 12, and Session 18 or when clinical services are concluded. We consulted with the second author’s Institutional Review Board, which determined the research as exempt, given the de-identified, archival nature of the data. For inclusion in this analysis, data needed to represent first responders, ages 18 or older, with a completed RSES-22 at intake. The RSES-4 are four questions within the RSES-22 measure; therefore, the participants did not have to complete an additional measure. For the secondary analysis, data from participants who also completed other mental health measures at intake were also included (see Measures).
Table 1
Demographics of Sample
| Characteristic |
Sample 1
(N = 238) |
Sample 2
(n = 190) |
| Age (Years) |
|
|
| Mean |
37.53 |
37.12 |
| Median |
35.50 |
35.00 |
| SD |
10.66 |
10.30 |
| Range |
46 |
45 |
| Time in Service (Years) |
|
|
| Mean |
11.62 |
11.65 |
| Median |
10.00 |
10.00 |
| SD |
9.33 |
9.37 |
| Range |
41 |
39 |
|
n (%) |
| First Responder Type |
|
|
Emergency Medical
Technicians |
67 (28.2%) |
54 (28.4%) |
| Fire Rescue |
60 (25.2%) |
45 (23.7%) |
| Law Enforcement |
83 (34.9%) |
72 (37.9%) |
| Other |
9 (3.8%) |
5 (2.6%) |
| Two or more |
10 (4.2%) |
6 (3.2%) |
| Not reported |
9 (3.8%) |
8 (4.2%) |
| Gender |
|
|
| Women |
59 (24.8%) |
47 (24.7%) |
| Men |
179 (75.2%) |
143 (75.3%) |
| Ethnicity |
|
|
| African American/Black |
13 (5.5%) |
8 (4.2%) |
| Asian American |
3 (1.3%) |
3 (1.6%) |
| Latino(a)/Hispanic |
28 (11.8%) |
24 (12.6%) |
| Multiple Ethnicities |
3 (1.3%) |
3 (1.6%) |
| Native American |
4 (1.7%) |
3 (1.6%) |
| White |
187 (78.6%) |
149 (78.4%) |
Note. Sample 2 is a subset of Sample 1. Time in service for Sample 1, n = 225;
time in service for Sample 2, n = 190.
Measures
Response to Stressful Experiences Scale
The Response to Stressful Experiences Scale (RSES-22) is a 22-item measure to assess dimensions of resilience, including meaning-making, active coping, cognitive flexibility, spirituality, and self-efficacy (Johnson et al., 2011). Participants respond to the prompt “During and after life’s most stressful events, I tend to” on a 5-point Likert scale from 0 (not at all like me) to 4 (exactly like me). Total scores range from 0 to 88 in which higher scores represent greater resilience. Example items include see it as a challenge that will make me better, pray or meditate, and find strength in the meaning, purpose, or mission of my life. Johnson et al. (2011) reported the RSES-22 demonstrates good internal consistency (α = .92) and test-retest reliability (α = .87) among samples from military populations. Further, the developers confirmed convergent, discriminant, concurrent, and incremental criterion validity (see Johnson et al., 2011). In the current study, Cronbach’s alpha of the total score was .93.
Adapted Response to Stressful Experiences Scale
The adapted Response to Stressful Experiences Scale (RSES-4) is a 4-item measure to assess resilience as a unidimensional construct (De La Rosa et al., 2016). The prompt and Likert scale are consistent with the original RSES-22; however, it only includes four items: find a way to do what’s necessary to carry on, know I will bounce back, learn important and useful life lessons, and practice ways to handle it better next time. Total scores range from 0 to 16, with higher scores indicating greater resilience. De La Rosa et al. (2016) reported acceptable internal consistency (α = .76–.78), test-retest reliability, and demonstrated criterion validity among multiple military samples. In the current study, the Cronbach’s alpha of the total score was .74.
Patient Health Questionnaire-9
The Patient Health Questionnaire-9 (PHQ-9) is a 9-item measure to assess depressive symptoms in the past 2 weeks (Kroenke et al., 2001). Respondents rate the frequency of their symptoms on a 4-point Likert scale ranging from 0 (not at all) to 3 (nearly every day). Total scores range from 0 to 27, in which higher scores indicate increased severity of depressive symptoms. Example items include little interest or pleasure in doing things and feeling tired or having little energy. Kroenke et al. (2001) reported good internal consistency (α = .89) and established criterion and construct validity. In this sample, Cronbach’s alpha of the total score was .88.
PTSD Checklist-5
The PTSD Checklist-5 (PCL-5) is a 20-item measure for the presence of PTSD symptoms in the past month (Blevins et al., 2015). Participants respond on a 5-point Likert scale indicating frequency of PTSD-related symptoms from 0 (not at all) to 4 (extremely). Total scores range from 0 to 80, in which higher scores indicate more severity of PTSD-related symptoms. Example items include repeated, disturbing dreams of the stressful experience and trouble remembering important parts of the stressful experience. Blevins et al. (2015) reported good internal consistency (α = .94) and determined convergent and discriminant validity. In this sample, Cronbach’s alpha of the total score was .93.
Generalized Anxiety Disorder-7
The Generalized Anxiety Disorder-7 (GAD-7) is a 7-item measure to assess for anxiety symptoms over the past 2 weeks (Spitzer et al., 2006). Participants rate the frequency of the symptoms on a 4-point Likert scale ranging from 0 (not at all) to 3 (nearly every day). Total scores range from 0 to 21 with higher scores indicating greater severity of anxiety symptoms. Example items include not being able to stop or control worrying and becoming easily annoyed or irritable. Among patients from primary care settings, Spitzer et al. (2006) determined good internal consistency (α = .92) and established criterion, construct, and factorial validity. In this sample, Cronbach’s alpha of the total score was .91.
Suicidal Behaviors Questionnaire-Revised
The Suicidal Behaviors Questionnaire-Revised (SBQ-R) is a 4-item measure to assess suicidality (Osman et al., 2001). Each item assesses a different dimension of suicidality: lifetime ideation and attempts, frequency of ideation in the past 12 months, threat of suicidal behaviors, and likelihood of suicidal behaviors (Gutierrez et al., 2001). Total scores range from 3 to 18, with higher scores indicating more risk of suicide. Example items include How often have you thought about killing yourself in the past year? and How likely is it that you will attempt suicide someday? In a clinical sample, Osman et al. (2001) reported good internal consistency (α = .87) and established criterion validity. In this sample, Cronbach’s alpha of the total score was .85.
Data Analysis
Statistical analyses were conducted using SPSS version 26.0 and SPSS Analysis of Moment Structures (AMOS) version 26.0. We examined the dataset for missing values, replacing 0.25% (32 of 12,836 values) of data with series means. We reviewed descriptive statistics of the RSES-22 and RSES-4 scales. We determined multivariate normality as evidenced by skewness less than 2.0 and kurtosis less than 7.0 (Dimitrov, 2012). We assessed reliability for the scales by interpreting Cronbach’s alphas and inter-item correlations to confirm internal consistency.
We conducted two separate confirmatory factor analyses to determine the model fit and factorial validity of the 22-item measure and adapted 4-item measure. We used several indices to conclude model fit: minimum discrepancy per degree of freedom (CMIN/DF) and p-values, root mean residual (RMR), goodness-of-fit index (GFI), comparative fit index (CFI), Tucker-Lewis index (TLI), and the root mean square error of approximation (RMSEA). According to Dimitrov (2012), values for the CMIN/DF < 2.0,p > .05, RMR < .08, GFI > .90, CFI > .90, TLI > .90, and RMSEA < .10 provide evidence of a strong model fit. To determine criterion validity, we assessed a subsample of participants (n = 190) who had completed the RSES-22, RSES-4, and four other psychological measures (i.e., PHQ-9, PCL-5, GAD-7, and SBQ-R). We determined convergent validity by conducting bivariate correlations between the RSES-22 and RSES-4.
Results
Descriptive Analyses
We computed means, standard deviations, 95% confidence interval (CI), and score ranges for the RSES-22 and RSES-4 (Table 2). Scores on the RSES-22 ranged from 19–88. Scores on the RSES-4 ranged from 3–16. Previous researchers using the RSES-22 on military samples reported mean scores of 57.64–70.74 with standard deviations between 8.15–15.42 (Johnson et al., 2011; Prosek & Ponder, 2021). In previous research of the RSES-4 with military samples, mean scores were 9.95–11.20 with standard deviations between 3.02–3.53(De La Rosa et al., 2016; Prosek & Ponder, 2021).
Table 2
Descriptive Statistics for RSES-22 and RSES-4
| Variable |
M |
SD |
95% CI |
Score Range |
| RSES-22 scores |
60.12 |
13.76 |
58.52, 61.86 |
19–88 |
| RSES-4 scores |
11.66 |
2.62 |
11.33, 11.99 |
3–16 |
Note. N = 238. RSES-22 = Response to Stressful Experiences Scale 22-item; RSES-4 = Response
to Stressful Experiences Scale 4-item adaptation.
Reliability Analyses
To determine the internal consistency of the resiliency measures, we computed Cronbach’s alphas. For the RSES-22, we found strong evidence of inter-item reliability (α = .93), which was consistent with the developers’ estimates (α = .93; Johnson et al., 2011). For the RSES-4, we assessed acceptable inter-item reliability (α = .74), which was slightly lower than previous estimates (α = .76–.78; De La Rosa et al., 2016). We calculated the correlation between items and computed the average of all the coefficients. The average inter-item correlation for the RSES-22 was .38, which falls within the acceptable range (.15–.50). The average inter-item correlation for the RSES-4 was .51, slightly above the acceptable range. Overall, evidence of internal consistency was confirmed for each scale.
Factorial Validity Analyses
We conducted two confirmatory factor analyses to assess the factor structure of the RSES-22 and RSES-4 for our sample of first responders receiving mental health services at a community clinic (Table 3). For the RSES-22, a proper solution converged in 10 iterations. Item loadings ranged between .31–.79, with 15 of 22 items loading significantly ( > .6) on the latent variable. It did not meet statistical criteria for good model fit: χ2 (209) = 825.17, p = .000, 90% CI [0.104, 0.120]. For the RSES-4, a proper solution converged in eight iterations. Item loadings ranged between .47–.80, with three of four items loading significantly ( > .6) on the latent variable. It met statistical criteria for good model fit: χ2 (2) = 5.89, p = .053, 90% CI [0.000, 0.179]. The CMIN/DF was above the suggested < 2.0 benchmark; however, the other fit indices indicated a model fit.
Table 3
Confirmatory Factor Analysis Fit Indices for RSES-22 and RSES-4
| Variable |
df |
χ2 |
CMIN/DF |
RMR |
GFI |
CFI |
TLI |
RMSEA |
90% CI |
| RSES-22 |
209 |
825.17/.000 |
3.95 |
.093 |
.749 |
.771 |
0.747 |
.112 |
0.104, 0.120 |
| RSES-4 |
2 |
5.89/.053 |
2.94 |
.020 |
.988 |
.981 |
0.944 |
.091 |
0.000, 0.179 |
Note. N = 238. RSES-22 = Response to Stressful Experiences Scale 22-item; RSES-4 = Response to Stressful Experiences Scale 4-item adaptation; CMIN/DF = Minimum Discrepancy per Degree of Freedom; RMR = Root Mean Square Residual;
GFI = Goodness-of-Fit Index; CFI = Comparative Fit Index; TLI = Tucker-Lewis Index; RMSEA = Root Mean Squared Error of Approximation.
Criterion and Convergent Validity Analyses
To assess for criterion validity of the RSES-22 and RSES-4, we conducted correlational analyses with four established psychological measures (Table 4). We utilized a subsample of participants (n = 190) who completed the PHQ-9, PCL-5, GAD-7, and SBQ-R at intake. Normality of the data was not a concern because analyses established appropriate ranges for skewness and kurtosis (± 1.0). The internal consistency of the RSES-22 (α = .93) and RSES-4 (α = .77) of the subsample was comparable to the larger sample and previous studies. The RSES-22 and RSES-4 related to the psychological measures of distress in the expected direction, meaning measures were significantly and negatively related, indicating that higher resiliency scores were associated with lower scores of symptoms associated with diagnosable mental health disorders (i.e., post-traumatic stress, anxiety, depression, and suicidal behavior). We verified convergent validity with a correlational analysis of the RSES-22 and RSES-4, which demonstrated a significant and positive relationship.
Table 4
Criterion and Convergent Validity of RSES-22 and RSES-4
|
M (SD) |
Cronbach’s α |
RSES-22 |
PHQ-9 |
PCL-5 |
GAD-7 |
SBQ-R |
| RSES-22 |
60.16 (14.17) |
.93 |
— |
−.287* |
−.331* |
−.215* |
−.346* |
| RSES-4 |
11.65 (2.68) |
.77 |
.918 |
−.290* |
−.345* |
−.220* |
−.327* |
Note. n = 190. RSES-22 = Response to Stressful Experiences Scale 22-item; RSES-4 = Response to Stressful Experiences Scale 4-item adaptation; PHQ-9 = Patient Health Questionnaire-9;
PCL-5 = PTSD Checklist-5; GAD-7 = Generalized Anxiety Disorder-7; SBQ-R = Suicidal Behaviors Questionnaire-Revised.
*p < .01.
Discussion
The purpose of this study was to validate the factor structure of the RSES-22 and the abbreviated RSES-4 with a first responder sample. Aggregated means were similar to those in the articles that validated and normed the measures in military samples (De La Rosa et al., 2016; Johnson et al., 2011; Prosek & Ponder, 2021). Additionally, the internal consistency was similar to previous studies. In the original article, Johnson et al. (2011) proposed a five-factor structure for the RSES-22, which was later established as a unidimensional assessment after further exploratory factor analysis (De La Rosa et al., 2016). Subsequently, confirmatory factor analyses with a treatment-seeking veteran population revealed that the RSES-22 demonstrated unacceptable model fit, whereas the RSES-4 demonstrated a good model fit (Prosek & Ponder, 2021). In both samples, the RSES-4 GFI, CFI, and TLI were all .944 or higher, whereas the RSES-22 GFI, CFI, and TLI were all .771 or lower. Additionally, criterion and convergent validity as measured by the PHQ-9, PCL-5, and GAD-7 in both samples were extremely close. Similarly, in this sample of treatment-seeking first responders, confirmatory factor analyses indicated an inadequate model fit for the RSES-22 and a good model fit for the RSES-4. Lastly, convergent and criterion validity were established with correlation analyses of the RSES-22 and RSES-4 with four other standardized assessment instruments (i.e., PHQ-9, PCL-5, GAD-7, SBQ-R). We concluded that among the first responder sample, the RSES-4 demonstrated acceptable psychometric properties, as well as criterion and convergent validity with other mental health variables (i.e., post-traumatic stress, anxiety, depression, and suicidal behavior).
Implications for Clinical Practice
First responders are a unique population and are regularly exposed to trauma (Donnelly & Bennett, 2014; Jetelina et al., 2020; Klimley et al., 2018; Weiss et al., 2010). Although first responders could potentially benefit from espousing resilience, they are often hesitant to seek mental health services (Crowe et al., 2017; Jones, 2017). The RSES-22 and RSES-4 were originally normed with military populations. The results of the current study indicated initial validity and reliability among a first responder population, revealing that the RSES-4 could be useful for counselors in assessing resilience.
It is important to recognize that first responders have perceived coping with traumatic stress as an individual process (Crowe et al., 2017) and may believe that seeking mental health services is counter to the emotional and physical training expectations of the profession (Crowe et al., 2015). Therefore, when first responders seek mental health care, counselors need to be prepared to provide culturally responsive services, including population-specific assessment practices and resilience-oriented care.
Jones (2017) encouraged a comprehensive intake interview and battery of appropriate assessments be conducted with first responder clients. Counselors need to balance the number of intake questions while responsibly assessing for mental health comorbidities such as post-traumatic stress, anxiety, depression, and suicidality. The RSES-4 provides counselors a brief, yet targeted assessment of resilience.
Part of what cultural competency entails is assessing constructs (e.g., resilience) that have been shown to be a protective factor against PTSD among first responders (Klimley et al., 2018). Since the items forming the RSES-4 were developed to highlight the positive characteristics of coping (Johnson et al., 2011), rather than a deficit approach, this aligns with the grounding of the counseling profession. It is also congruent with first responders’ perceptions of resilience. Indeed, in a content analysis of focus group interviews with first responders, participants defined resilience as a positive coping strategy that involves emotional regulation, perseverance, personal competence, and physical fitness (Crowe et al., 2017).
The RSES-4 is a brief, reliable, and valid measure of resilience with initial empirical support among a treatment-seeking first responder sample. In accordance with the ACA (2014) Code of Ethics, counselors are to administer assessments normed with the client population (E.8.). Thus, the results of the current study support counselors’ use of the measure in practice. First responder communities are facing unprecedented work tasks in response to COVID-19. Subsequently, their mental health might suffer (Centers for Disease Control and Prevention, 2020) and experts have recommended promoting resilience as a protective factor for combating the negative mental health consequences of COVID-19 (Chen & Bonanno, 2020). Therefore, the relevance of assessing resilience among first responder clients in the current context is evident.
Limitations and Future Research
This study is not without limitations. The sample of first responders was homogeneous in terms of race, ethnicity, and gender. Subsamples of first responders (i.e., LEO, EMT, fire rescue) were too small to conduct within-group analyses to determine if the factor structure of the RSES-22 and RSES-4 would perform similarly. Also, our sample of first responders included two emergency dispatchers. Researchers reported that emergency dispatchers should not be overlooked, given an estimated 13% to 15% of emergency dispatchers experience post-traumatic symptomatology (Steinkopf et al., 2018). Future researchers may develop studies that further explore how, if at all, emergency dispatchers are represented in first responder research.
Furthermore, future researchers could account for first responders who have prior military service. In a study of LEOs, Jetelina et al. (2020) found that participants with military experience were 3.76 times more likely to report mental health concerns compared to LEOs without prior military affiliation. Although we reported the prevalence rate of prior military experience in our sample, the within-group sample size was not sufficient for additional analyses. Finally, our sample represented treatment-seeking first responders. Future researchers may replicate this study with non–treatment-seeking first responder populations.
Conclusion
First responders are at risk for sustaining injuries, experiencing life-threatening events, and witnessing harm to others (Lanza et al., 2018). The nature of their exposure can be repeated and cumulative over time (Donnelly & Bennett, 2014), indicating an increased risk for post-traumatic stress, anxiety, and depressive symptoms, as well as suicidal behavior (Jones et al., 2018). Resilience is a promising protective factor that promotes wellness and healthy coping among first responders (Wild et al., 2020), and counselors may choose to routinely measure for resilience among first responder clients. The current investigation concluded that among a sample of treatment-seeking first responders, the original factor structure of the RSES-22 was unstable, although it demonstrated good reliability and validity. The adapted version, RSES-4, demonstrated good factor structure while also maintaining acceptable reliability and validity, consistent with studies of military populations (De La Rosa et al., 2016; Johnson et al., 2011; Prosek & Ponder, 2021). The RSES-4 provides counselors with a brief and strength-oriented option for measuring resilience with first responder clients.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
American Counseling Association. (2014). ACA code of ethics.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
Antony, J., Brar, R., Khan, P. A., Ghassemi, M., Nincic, V., Sharpe, J. P., Straus, S. E., & Tricco, A. C. (2020). Interventions for the prevention and management of occupational stress injury in first responders: A rapid overview of reviews. Systematic Reviews, 9(121), 1–20. https://doi.org/10.1186/s13643-020-01367-w
Blevins, C. A., Weathers, F. W., Davis, M. T., Witte, T. K., & Domino, J. L. (2015). The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28(6), 489–498. https://doi.org/10.1002/jts.22059
Burnett, H. J., Jr. (2017). Revisiting the compassion fatigue, burnout, compassion satisfaction, and resilience connection among CISM responders. Journal of Police Emergency Response, 7(3), 1–10. https://doi.org/10.1177/2158244017730857
Centers for Disease Control and Prevention. (2020, June 30). Coping with stress. https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/managing-stress-anxiety.html
Chen, S., & Bonanno, G. A. (2020). Psychological adjustment during the global outbreak of COVID-19: A resilience perspective. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S51–S54. https://doi.org/10.1037/tra0000685
Christopher, M. S., Hunsinger, M., Goerling, R. J., Bowen, S., Rogers, B. S., Gross, C. R., Dapolonia, E., & Pruessner, J. C. (2018). Mindfulness-based resilience training to reduce health risk, stress reactivity, and aggression among law enforcement officers: A feasibility and preliminary efficacy trial. Psychiatry Research, 264, 104–115. https://doi.org/10.1016/j.psychres.2018.03.059
Crowe, A., Glass, J. S., Lancaster, M. F., Raines, J. M., & Waggy, M. R. (2015). Mental illness stigma among first responders and the general population. Journal of Military and Government Counseling, 3(3), 132–149. http://mgcaonline.org/wp-content/uploads/2013/02/JMGC-Vol-3-Is-3.pdf
Crowe, A., Glass, J. S., Lancaster, M. F., Raines, J. M., & Waggy, M. R. (2017). A content analysis of psychological resilience among first responders. SAGE Open, 7(1), 1–9. https://doi.org/10.1177/2158244017698530
De La Rosa, G. M., Webb-Murphy, J. A., & Johnston, S. L. (2016). Development and validation of a brief measure of psychological resilience: An adaptation of the Response to Stressful Experiences Scale. Military Medicine, 181(3), 202–208. https://doi.org/10.7205/MILMED-D-15-00037
Dimitrov, D. M. (2012). Statistical methods for validation of assessment scale data in counseling and related fields. American Counseling Association.
Donnelly, E. A., & Bennett, M. (2014). Development of a critical incident stress inventory for the emergency medical services. Traumatology, 20(1), 1–8. https://doi.org/10.1177/1534765613496646
Greinacher, A., Derezza-Greeven, C., Herzog, W., & Nikendei, C. (2019). Secondary traumatization in first responders: A systematic review. European Journal of Psychotraumatology, 10(1), 1562840. https://doi.org/10.1080/20008198.2018.1562840
Gutierrez, P. M., Osman, A., Barrios, F. X., & Kopper, B. A. (2001). Development and initial validation of the Self-Harm Behavior Questionnaire. Journal of Personality Assessment, 77(3), 475–490. https://doi.org/10.1207/S15327752JPA7703_08
Jetelina, K. K., Mosberry, R. J., Gonzalez, J. R., Beauchamp, A. M., & Hall, T. (2020). Prevalence of mental illnesses and mental health care use among police officers. JAMA Network Open, 3(10), 1–12. https://doi.org/10.1001/jamanetworkopen.2020.19658
Johnson, D. C., Polusny, M. A., Erbes, C. R., King, D., King, L., Litz, B. T., Schnurr, P. P., Friedman, M., Pietrzak, R. H., & Southwick, S. M. (2011). Development and initial validation of the Response to Stressful Experiences Scale. Military Medicine, 176(2), 161–169. https://doi.org/10.7205/milmed-d-10-00258
Jones, S. (2017). Describing the mental health profile of first responders: A systematic review. Journal of the American Psychiatric Nurses Association, 23(3), 200–214. https://doi.org/10.1177/1078390317695266
Jones, S., Nagel, C., McSweeney, J., & Curran, G. (2018). Prevalence and correlates of psychiatric symptoms among first responders in a Southern state. Archives of Psychiatric Nursing, 32(6), 828–835. https://doi.org/10.1016/j.apnu.2018.06.007
Joyce, S., Tan, L., Shand, F., Bryant, R. A., & Harvey, S. B. (2019). Can resilience be measured and used to predict mental health symptomology among first responders exposed to repeated trauma? Journal of Occupational and Environmental Medicine, 61(4), 285–292. https://doi.org/10.1097/JOM.0000000000001526
Kleim, B., & Westphal, M. (2011). Mental health in first responders: A review and recommendation for prevention and intervention strategies. Traumatology, 17(4), 17–24. https://doi.org/10.1177/1534765611429079
Klimley, K. E., Van Hasselt, V. B., & Stripling, A. M. (2018). Posttraumatic stress disorder in police, firefighters, and emergency dispatchers. Aggression and Violent Behavior, 43, 33–44.
https://doi.org/10.1016/j.avb.2018.08.005
Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Lanza, A., Roysircar, G., & Rodgers, S. (2018). First responder mental healthcare: Evidence-based prevention, postvention, and treatment. Professional Psychology: Research and Practice, 49(3), 193–204. https://doi.org/10.1037/pro0000192
Lee, J.-S., Ahn, Y.-S., Jeong, K.-S. Chae, J.-H., & Choi, K.-S. (2014). Resilience buffers the impact of traumatic events on the development of PTSD symptoms in firefighters. Journal of Affective Disorders, 162, 128–133. https://doi.org/10.1016/j.jad.2014.02.031
Lewis, G. B., & Pathak, R. (2014). The employment of veterans in state and local government service. State and Local Government Review, 46(2), 91–105. https://doi.org/10.1177/0160323X14537835
McCanlies, E. C., Gu, J. K., Andrew, M. E., Burchfiel, C. M., & Violanti, J. M. (2017). Resilience mediates the relationship between social support and post-traumatic stress symptoms in police officers. Journal of Emergency Management, 15(2), 107–116. https://doi.org/10.5055/jem.2017.0319
National Institute of Mental Health. (2017). Post-traumatic stress disorder. https://www.nimh.nih.gov/health/statistics/post-traumatic-stress-disorder-ptsd.shtml
Osman, A., Bagge, C. L., Gutierrez, P. M., Konick, L. C., Kopper, B. A., & Barrios, F. X. (2001). The Suicidal Behaviors Questionnaire–revised (SBQ-R): Validation with clinical and nonclinical samples. Assessment, 8(4), 443–454. https://doi.org/10.1177/107319110100800409
Prosek, E. A., & Ponder, W. N. (2021). Validation of the Adapted Response to Stressful Experiences Scale (RSES-4) among veterans [Manuscript submitted for publication].
Spitzer, R. L., Kroenke, K., Williams, J. B. W., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder (The GAD-7). Archives of Internal Medicine, 166(10), 1092–1097.
https://doi.org/10.1001/archinte.166.10.1092
Steinkopf, B., Reddin, R. A., Black, R. A., Van Hasselt, V. B., & Couwels, J. (2018). Assessment of stress and resiliency in emergency dispatchers. Journal of Police and Criminal Psychology, 33(4), 398–411.
https://doi.org /10.1007/s11896-018-9255-3
Substance Abuse and Mental Health Services Administration. (2018, May). First responders: Behavioral health concerns, emergency response, and trauma. Disaster Technical Assistance Center Supplemental Research Bulletin. https://www.samhsa.gov/sites/default/files/dtac/supplementalresearchbulletin-firstresponders-may2018.pdf
Weiss, D. S., Brunet, A., Best, S. R., Metzler, T. J., Liberman, A., Pole, N., Fagan, J. A., & Marmar, C. R. (2010). Frequency and severity approaches to indexing exposure to trauma: The Critical Incident History Questionnaire for police officers. Journal of Traumatic Stress, 23(6), 734–743.
https://doi.org/10.1002/jts.20576
White, B., Driver, S., & Warren, A. M. (2010). Resilience and indicators of adjustment during rehabilitation from a spinal cord injury. Rehabilitation Psychology, 55(1), 23–32. https://doi.org/10.1037/a0018451
Wild, J., El-Salahi, S., Degli Esposti, M., & Thew, G. R. (2020). Evaluating the effectiveness of a group-based resilience intervention versus psychoeducation for emergency responders in England: A randomised controlled trial. PLoS ONE, 15(11), e0241704. https://doi.org/10.1371/journal.pone.0241704
Windle, G., Bennett, K. M., & Noyes, J. (2011). A methodological review of resilience measurement scales. Health and Quality of Life Outcomes, 9, Article 8, 1–18. https://doi.org/10.1186/1477-7525-9-8
Warren N. Ponder, PhD, is Director of Outcomes and Evaluation at One Tribe Foundation. Elizabeth A. Prosek, PhD, NCC, LPC, is an associate professor at Penn State University. Tempa Sherrill, MS, LPC-S, is the founder of Stay the Course and a volunteer at One Tribe Foundation. Correspondence may be addressed to Warren N. Ponder, 855 Texas St., Suite 105, Fort Worth, TX 76102, warren@1tribefoundation.org.
Mar 30, 2018 | Volume 8 - Issue 1
Danielle Pester, A. Stephen Lenz, Joshua C. Watson, Julia Dell’Aquila, Anthony Nkyi
As the counseling profession continues its globalization onto Ghanaian college campuses, there is an increased need for psychometric assessments that support programming and interventions that promote degree matriculation and general student well-being. A sample of 696 young adult Ghanaian college students completed the Inventory of New College Student Adjustment (INCA) and related measures to estimate evidence of internal structure and relationships with conceptually related constructs. Confirmatory factor analyses were completed and inspection of fit indices revealed strong evidence for internal structure, and bivariate correlations indicated statistically significant positive associations with related medium effect sizes between the INCA subscales (Supportive Network and Belief in Self) and related measures. Implications for use of the INCA to support the professional activities of Ghanaian counselors working on college campuses are provided.
Keywords: Ghanaian counselors, college student adjustment, globalization, psychometric inventory, assessment
Higher education in Ghana has experienced tremendous growth over the past two decades, increasing access to institutions of higher education and student enrollment. In 2012, there were 138 accredited higher education institutions throughout Ghana, including public and private institutions, polytechnics, and training colleges (Atuahene, 2013; National Council for Tertiary Education [NCTE], 2014). This is an exponential degree of growth when compared to the existence of only three public universities in Ghana at the close of the 1990s (Atuahene, 2013). Although access and participation in university education has grown rapidly, the proportion of enrolled students versus those eligible to be enrolled remains low. According to the United Nations Educational, Scientific and Cultural Organization (2017), the percentage of enrolled students compared to those eligible to be enrolled in higher education in Ghana for 2015 was only 16.23%, indicating inadequate pre-college academic preparation, lack of affordability, low retention rates, and inadequate supports once enrolled (Atuahene, 2012). With its higher education system facing such challenges, resources and tools that can assist Ghanaian higher education institutions meet student needs as they enter university life, adjust to the unique set of demands, and access existing supports are imperative.
Because the demand for higher education in Ghana has traditionally been greater than its supply, most of the available resources have been focused on the expansion of facilities rather than the improvement of student experiences that may promote university persistence and degree matriculation. Only in recent years has the NCTE begun to rate institutions on the quality and relevance of their academic programs. Atuahene (2012) identified several distinctive factors associated with Ghanaian student dropout, including: (a) inadequate financial support for low income students, (b) student socioeconomic and geographic background, (c) student pre-college academic preparation, (d) unfavorable institutional policies and practices, and (e) a lack of academic advising. With these barriers in mind, there is currently an opportunity in Ghanaian higher education to develop resources that can support student adjustment and academic persistence.
Researchers (e.g., Carter, Locks, & Winkle-Wagner, 2013; Gray, Vitak, Easton, & Ellison, 2013; Pascarella & Terenzini, 2005; Robbins, Oh, Le, & Button, 2009) have found first-year adjustment to an academic setting to be a crucial component in student retention. Furthermore, they have found that positive adjustment within the first year of college can significantly impact a student’s academic persistence to degree completion. Andoh-Arthur, Asante, and Osafo (2015) studied the help-seeking behaviors of Ghanaian university students and found that the first-year student population was least likely to engage in help-seeking behaviors. They attributed this to the students’ unfamiliarity with their new identity as university students. Knowing this, Ghanaian students’ first year of university experience is a crucial time for university support personnel to proactively engage students regarding college adjustment issues. The capacity to identify new university students who are struggling to adjust to college life and who also may be at a higher risk for attrition is essential for Ghanaian university personnel as they seek to improve university retention rates.
Globalization of Counseling and Its Role in University Settings
The welcome statement of NBCC International proposes an organizational intention to increase the “availability of competent, reliable services to any part of the world that indicates an interest in acquiring them . . . with the utmost care and respect for the social, cultural, political, and economic realities of the various areas where we are invited” (Clawson, 2011, para. 2). Lorelle, Byrd, and Crockett (2012) identified the globalization of counseling as an inevitability, wherein professional counseling activities are progressively transitioning from a Western-based practice to one that gives international communities the opportunity for transformation as well. Lorelle et al. suggested that as the counseling profession is introduced on a local level, opportunities emerge for adaptation to local cultures and new contexts that yield new ways of understanding culturally defined standards of care. Among the many international settings adopting the values and activities synonymous with the counseling profession, Ghana appears poised to increase the capacity and scope of counseling activities through meaningful placement of services on university campuses.
Quarshie, Annor, Tagoe, Osei-Poku, and Andoh-Arthur (2016) identified a growing population of mental health professionals within the country of Ghana. This expansion of service provider capacity has been positively correlated with growth in the Ghanaian economy and represents a commitment to developing public mental health infrastructure using existing resources and expanding capacity over time (Ghana Health Professions Regulatory Bodies Act 857, 2013). Quarshie et al.’s (2016) analyses also detected that the majority of Ghanaian mental health professionals are housed on college, polytechnic, and university campuses. Situating these providers within these settings not only provides them support for their professional preparation programs, but also provides proximal contact with students who may be experiencing mental health symptoms while attempting to adjust to new demands within university settings. This action has important consequences for both the globalization of the counseling profession and the promotion of optimal development, degree matriculation, and access to a more equitable life for Ghanaian students. However, evidence-supported interventions require evidence-supported assessments that are population-specific, and currently there is a paucity of such assessments that can be utilized by mental health professionals to understand the adjustment experiences of students at Ghanaian universities.
Rationale and Purpose of the Study
Given that one aspect of counselor identity is the use of evidence-supported assessment practices, and another is evidence-supported intervention and programming (American Counseling Association, 2014; Lorelle et al., 2012), there is a call to complete activities to support the actions of Ghanaian mental health professionals charged with promoting adjustment among local university students. The Inventory of New College Student Adjustment (INCA; Watson & Lenz, 2017) is one viable instrument for assessing college student adjustment that is free to use and has yielded promising psychometric properties among ethnically diverse samples within the United States. It has been identified as a resource to help determine the appropriate support services needed for university students, as well as a resource to assess the overall effectiveness of campus initiatives focused on student adjustment. Although the INCA could be a valuable tool to address the current needs and trends in Ghanaian higher education, the degree of validity of INCA scores for a Ghanaian university student population is currently unknown. Therefore, the purpose of this study was to evaluate the transferability of validity evidence for scores on the INCA to a sample of Ghanaian students. Specifically, we intended to identify the degree of evidence related to internal structure of the INCA scores and their relationships with conceptually related variables.
Method
Participant Characteristics
Six hundred ninety-six Ghanaian college students (435 male [63%], 237 female [34%], 24 did not report gender [3%]), the majority of whom were young adults (M age = 22.45 years; SD = 4.37) completing undergraduate coursework at one large university in Ghana, Africa, participated in this study.
Measurement of Constructs
Inventory of New College Student Adjustment. The INCA (Watson & Lenz, 2017) was developed to assess the adjustment difficulties experienced by first-year college students and was normed using an ethnically diverse sample of 474 freshmen students in the United States. The INCA is a 14-item instrument using a 4-point Likert scale to assess participant responses from 1 (strongly disagree) to 4 (strongly agree). Scores can range from 14 to 56, with higher scores indicating higher levels of college adjustment. The 6-item Supportive Network subscale includes items such as “My friends support me as I work toward my goals” and “My family’s support makes me feel stronger.” The 8-item Belief in Self subscale includes items such as “My study habits are effective” and “I know what I will do after graduation.” Initial psychometric testing demonstrates good alpha reliability coefficients for scores on INCA subscales ranging from .77 (Belief in Self) to .83 (Supportive Network), indicating good internal consistency. Moreover, our sample reported alpha reliability coefficients of .74 for both the Belief in Self subscale and the Supportive Network subscale.
The Multidimensional Scale of Perceived Social Support. The Multidimensional Scale of Perceived Social Support (MSPSS; Zimet, Dahlem, Zimet & Farley, 1988) was developed to assess an individual’s perception of social support from family, friends, and significant others. Each of these sources of social support is considered a distinct subgrouping and is assessed individually. The MSPSS was normed using a subject pool of 275 undergraduate students in the United States with a nearly equal sample of male and female students (Zimet, et al., 1988). After further psychometric testing, reliability has been established for diverse samples beyond the original norming group (Stanley, Beck, & Zebb, 1998). The MSPSS is a 12-item instrument using a 7-point Likert-scale to assess participant responses from 1 (very strongly disagree) to 7 (very strongly agree). Scores can range from 12 to 84, with higher scores representing higher levels of perceived social support. For the purposes of this study, we used the Family Relationships subscale and Relationships with Friends subscale. The 4-item Family Relationships subscale includes items such as “My family really tries to help me” and “I get the emotional help and support I need from my family.” The 4-item Relationships with Friends subscale includes items such as “My friends really try to help me” and “I can count on my friends when things go wrong.” Zimet et al. (1988) reported high Cronbach’s alpha coefficients for scores on MSPSS subscales ranging from .85–.91, indicating good internal consistency. The reliability of the total scale for the initial sample was .88. Additionally, our sample reported coefficients ranging from .81 for the Family Relationships subscale and .88 for the Relationships with Friends subscale.
College Self-Efficacy Inventory. The College Self-Efficacy Inventory (CSEI; Solberg, O’Brien, Villareal, Kennel, & Davis, 1993) was developed to assess a student’s confidence in their ability to successfully complete college-related tasks. Originally developed to measure college self-efficacy in Hispanic college students, CSEI data has established reliability beyond the initial norming population to also include ethnically diverse college students (Gore Jr., Leuwerke, & Turley, 2005). The CSEI is a 20-item instrument using a 10-point scale to assess a participant’s confidence in their ability to successfully complete a task from 1 (not at all confident) to 10 (extremely confident). Scores can range from 20 to 200, with higher scores indicating higher levels of confidence in one’s ability to successfully complete college-related tasks. The 20-item scale includes items such as “Make new friends at college,” “Talk to university staff,” and “Take good class notes” (Barry & Finney, 2009). Gore et al. (2006) reported Cronbach’s alpha coefficients for scores on the CSEI subscales ranging from .62–.89. The reliability of the CSEI for the initial sample was .93 (Solberg et al., 1993). Additionally, we observed a Cronbach’s alpha coefficient of .88 for our sample.
Procedure
After ethical review board approval, students registered in classes at one large university in Ghana were asked to participate in this study. A survey administrator, who was not the course instructor, shared the opportunity to participate in this study with students and disseminated an information sheet explaining the purpose, processes, and voluntary nature of the study. After having time to review the information sheet, the students choosing to participate in the study were given a packet including a demographic questionnaire, the INCA, the MSPSS, and the CSEI. All measures except for the demographic questionnaire were counter-balanced in an effort to control for random responding, order effect, and fatigue. Participants filled out hard copy surveys in class and turned them in to the survey administrator, who supplied them to the authors. Participant answers to the survey packet were entered into an SPSS spreadsheet. After all data was documented, the original hard copy surveys were securely destroyed.
Data Analysis
Statistical power analysis. We conducted a power analysis to determine the suitability of our sample size for identifying model fit using the criteria outlined by Stevens (2009): n/p ≥ 30. Using this standard, our largest scale (Belief in Self), consisting of eight items, would necessitate a sample size of at least 240. With a sample size of 696 (i.e., 87 participants per item), we considered our sample size sufficient for making statistical inferences about model fit. We also acknowledge that this model is over-powered for hypothesis testing and may lead to type I error. Therefore, when interpreting analyses, a greater emphasis was placed on model fit indices over p-values for χ2 tests.
Preliminary data analysis. The dataset was analyzed for missing values prior to performing statistical analyses. A small percentage of missing values (684 out of 71,100; .009%) was detected, but no identifiable pattern within these absent values was present. We used the series mean imputation function in IBM SPSS, Version 23, to replace all missing values.
Evidence regarding internal structure. We analyzed model fit for the INCA subscales using the SPSS Analysis of Moment Structures Software, Version 22. We conducted our analyses of the INCA subscale factor structures based on the initial factor structure emerging from the analyses completed by Watson and Lenz (2017). Initially, we interpreted the C-minimum/degrees of freedom (CMIN/DF), p-values, root mean residual (RMR), goodness of fit index (GFI), comparative fit index (CFI), Tucker-Lewis index (TLI), and root mean square error of approximation (RMSEA) metrics of model fit. Standards presented by Dimitrov (2012) were used to interpret these values with criteria for a strong model fit represented by CMIN/DF < 2, p > .05, RMR < .08, GFI > .90, CFI > .90, TLI > .90, and RMSEA < .10. When model fit proved inconsistent with these standards, modification indices were evaluated to determine items with potential covaried error. Covarying items provides a scenario within the factorial model wherein two items share their assumed variance. If such instances were identified, the model was computed again to re-inspect fit indices. If a factor model continued to have an inadequate fit, we inspected individual item correlation loadings and considered items for removal from the model. Items were removed if correlation coefficients were found to be less than .70.
Evidence regarding relationships with conceptually related constructs. Bivariate correlations were computed between scores on the INCA, MSPSS, and CSEI to depict degree of convergent validity between scores on the INCA subscales (Supportive Network and Belief in Self) with conceptually related constructs of perceived social support and academic self-concept, via the MSPSS and CSEI, respectively. Pearson’s correlation coefficients were interpreted as small (.10), medium (.30), or large (.50) based on the conventions reported by Swank and Mullen (2017) and evaluated at the .05 level of statistical significance.
Results
All alpha coefficients, descriptive statistics, and bivariate correlations for variables included within the analyses can be found in Table 1.
Table 1
Alpha Coefficients, Descriptive Statistics, and Bivariate Correlations for Variables Included Within Analyses.
| Scale-Construct |
α |
M |
SD |
1 |
2 |
3 |
| INCA – Belief in Self |
.74 |
23.31 |
3.32 |
44* |
|
.34* |
|
INCA – Supportive Network |
.74 |
17.44 |
2.65 |
.44* |
|
|
1. MSPSS – Family Relationships |
.88 |
20.02 |
6.49 |
|
|
|
2. MSPSS – Relationships with Friends |
.81 |
16.70 |
5.91 |
|
|
|
3. CSEI – College Self-Efficacy |
.88 |
36.77 |
14.69
|
|
|
| Note. * indicates statistical significance at .01 level |
Evidence Regarding Internal Structure
INCA – Belief in Self. The primary analysis of the Belief in Self subscale was significant for the hypothesized model, χ2(20) = 124.51, p < .01, and was suggestive of an unacceptable fit for the data: CMIN/DF = 6.22, RMR = .02, GFI = .95, CFI = .88, RMSEA = .08. After deleting item 6 and pairing the error terms for items 2 and 5 (“Past experiences help me cope with the demands of university life” and “Challenging courses make me a better student”) and 3 and 4 (“I believe I handle adversity well” and “My classmates value my opinions”), a good model fit emerged for scores on the Belief in Self subscale: χ2(12) = 28.58, p < .01. This finding was additionally supported by the fit indices: CMIN/DF = 2.38, RMR = .01, GFI = .98, CFI = .98, RMSEA = .04. Inspection of the alpha coefficient for scores for this sample (α = .74) was within the good range, indicating an acceptable degree of consistency and precision suitable for social sciences research activities.
INCA – Supportive Network. The primary analysis of the Supportive Network subscale was significant for the hypothesized model, χ2(9) = 102.28, p < .01, and was suggestive of an unacceptable fit for the data: CMIN/DF = 11.37, RMR = .03, GFI = .95, CFI = .80, RMSEA = .12. After pairing error terms for items 1 and 3 (“My friends support me as I work toward my goals” and “My friends help me to grow in important ways”) and items 4 and 6 (“My family’s support makes me feel stronger” and “I can be real with at least a few of my friends”), a good model fit emerged for scores on the Supportive Network subscale: χ2(7) = 14.03, p = .08. This finding was additionally supported by the fit indices: CMIN/DF = 3.41, RMR = .01, GFI = .98, CFI = .96, RMSEA = .05. Inspection of the alpha coefficient for scores for this sample (α = .74) was within the marginal range, indicating an acceptable degree of consistency and precision suitable for social sciences research activities.
Evaluation of Conceptually Related Measures
Family Relationships. The primary analysis of the Family Relationships subscale of the MSPSS was significant for the hypothesized model, χ2(2) = 45.47, p < .01, and was suggestive of an unacceptable fit for the data: CMIN/DF = 22.73, RMR = .10, GFI = .96, CFI = .97, RMSEA = .17. After pairing the error terms for items 3 and 4 (“I can talk about my problems with my family” and “My family is willing to help me make decisions”) a good model fit emerged for scores on the Family Relationships subscale: χ2(1) = 9.21, p <.01. This finding was additionally supported by the fit indices: CMIN/DF = 9.21, RMR = .04, GFI = .99, CFI = .99, RMSEA = .10. Inspection of the alpha coefficient for scores for this sample (α = .88) was within the good range, indicating an acceptable degree of consistency and precision suitable for social sciences research activities.
Relationships with Friends. The primary analysis of the Relationships with Friends subscale of the MSPSS was significant for the hypothesized model, χ2(2) = 49.52, p < .01, and was suggestive of an unacceptable fit for the data: CMIN/DF = 24.76, RMR = .15, GFI = .96, CFI = .95, RMSEA = .18. After pairing the error terms for items 1 and 2 (“My friends really try to help me” and “I can count on my friends when things go wrong”), a good model fit emerged for scores on the Relationships with Friends subscale: χ2(1) = 1.43, p = .23. This finding was additionally supported by the fit indices: CMIN/DF = 1.43, RMR = .02, GFI = .99, CFI = 1, RMSEA = .02. Inspection of the alpha coefficient for score for this sample (α = .81) was within the good range, indicating an acceptable degree of consistency and precision suitable for social sciences research activities.
College Self-Efficacy. The primary analysis of the College Self-Efficacy subscale of the CSEI was significant for the hypothesized model, χ2(9) = 66.70, p < .01, and was suggestive of an unacceptable fit for the data: CMIN/DF = 7.41, RMR = .34, GFI = .97, CFI = .98, RMSEA = .09. After pairing the error terms for items 1 and 2 (“Manage time effectively” and “Research a term paper”) and 3 and 5 (“Do well on your exams” and “Understand your textbooks”), a good model fit emerged for scores on the College Self-Efficacy subscale: χ2(7) = 22.45, p <.01. This finding was additionally supported by the fit indices: CMIN/DF = 3.20, RMR = .10, GFI = .98, CFI = .99, RMSEA = .05. Inspection of the alpha coefficient for scores for this sample (α = .88) was within the good range, indicating an acceptable degree of consistency and precision suitable for social sciences research activities.
Evidence Regarding Relationships With Conceptually Related Constructs
Bivariate correlation analysis of scores on the INCA Belief in Self subscale and CSEI resulted in a statistically significant positive relationship (r = .34, p < .01) indicative of a medium effect size. The correlation analysis of scores on the INCA Supportive Network subscale and MSPSS Family Relationships and Relationships with Friends subscales also resulted in statistically significant positive relationships (r = .448, p < .01, r = .448, p < .01, respectively) indicative of medium effect sizes. The strong positive relationships between scores on the two INCA subscales and conceptually related constructs are suggestive of support for convergent validity wherein the scores on the INCA tended to increase while scores on related measures increased too. Taken together, students who reported a greater belief in self also tended to report a greater sense of college self-efficacy. Similarly, participants who reported a greater belief in self during the first year of transition to college life also tended to report higher scores, indicating strong relationships with friends and family.
Discussion
The purpose of this study was to evaluate the validity evidence for the INCA using a Ghanaian college student population, with the hope that the instrument could be used by mental health professionals working in Ghanaian universities. Given the robust nature of our findings, we are heartened by the potential for the INCA and other emerging assessments to contribute to evidence-supported practices for optimal development and adjustment among students at Ghanaian universities. In light of our findings, several considerations warrant discussion.
Foremost, the INCA has potential uses that could address some of the most prominent issues facing higher education in Ghana today, particularly low matriculation rates. As the NCTE begins to rate institutions on the quality and relevance of their academic programs, the INCA can be used by university personnel to assess student adjustment so that necessary changes to student affairs programming can be made to improve the adjustment experiences of Ghanaian college students. Specifically, the INCA can be used by university personnel to gain a better understanding of the adjustment experiences of their first-year college students. This understanding can have important implications for program development at Ghanaian higher education institutions. As university personnel better understand the adjustment experiences of their first-year students, they can create programs that are more specialized to meet the needs of the Ghanaian student population, improve retention rates, and increase matriculation. Such activities have auspicious implications for not only promoting optimal development proximally, but encouraging access to a more equitable life, one characterized by fewer disparities than individuals within the emerging Ghanaian economy who do not have similar educational preparation and training.
Additionally, scores on the INCA can support early identification of first-year students who are struggling to adjust to university life. Because first-year students are least likely to engage in help-seeking behaviors (Andoh-Arthur et al., 2015), university personnel can develop proactive strategies to support struggling students and provide psychoeducation about the benefits of help-seeking behaviors. Such activities may include designing early detection protocols within orientation activities or integrating screening and referral within initial coursework activities.
In the cases of both program development and early identification, scores on the INCA have potential for evaluating outcomes in a manner that is culturally valid to a reasonable degree. Thus, the quantification of intervention outcomes by student affairs programmers and mental health professionals can provide an impetus for further understanding their students’ needs and the best strategies for meeting them. This is an important consideration in an era wherein Ghanaian mental health professionals are leveraging existing resources while extending their scope of influence within an emerging sociopolitical climate, which has expanded professional counseling activities through legislative action (Ghana Health Professions Regulatory Bodies Act 857, 2013). It is reasonable to conjecture that through the use of the INCA and other emerging assessments, the utilization and extension of personnel resources can not only be data-driven, but data-justified as well.
Finally, as the globalization of the counseling profession continues to be cultivated worldwide, it is important that counselors in international settings have valid psychometric tools that are population specific. Validation activities, such as the INCA project reported here, provide psychometrically robust assessments that Ghanaian mental health professionals can add to their growing corpus of resources. Although the use of assessment-based programming and outcome measurement do not define the whole of a counselor’s professional identity, it is a critical feature (American Counseling Association, 2014; Lorelle et al., 2012). Therefore, as the INCA and other assessments continue to be validated with Ghanaian student populations, the professionalization of Ghanaian mental health professionals grows lockstep.
Limitations and Recommendations for Future Research
Some important limitations and related recommendations for future research are indicated. First, although we sampled almost 700 Ghanaian students, the scope of our participant sample was limited to one campus. Therefore, we regard our findings as preliminary and most relevant to the student body from which they were affiliated. While it is reasonable that a substantial degree of validity generalization may be present, future studies completed at other Ghanaian universities are needed to estimate the transferability of INCA scores across regions. Second, internal consistency of INCA scores (α) were within the acceptable range (.70–.80), yet they did not reach a level that would warrant use for high stakes decision-making, such as program eligibility or dismissal. Further research evaluating content-oriented evidence (Lambie, Blount, & Mullen, 2017), cognitive processing, and response processes (Peterson, Peterson, & Powell, 2017) of INCA items and scores is needed to identify variables that may influence the reliability of items. It is possible that because INCA factors were developed from a Western theory of student adjustment, that consistency may be affected and indicative that some modification of item wording may be warranted (Lenz, Soler, Dell’Aquila, & Uribe, 2017). Thus, further evaluation related to cross-cultural adaptation and representation of constructs consisting within Ghanaian culture is warranted. Finally, this study only reported two sources of validity evidence. Although evidence across all sources of validity would not necessarily imply that INCA is inherently useful (Lenz & Wester, 2017), future research that elucidates INCA features associated with construct irrelevance and underrepresentation would further promote responsible testing and evaluation practice (Spurgeon, 2017).
Conclusion
In conclusion, this study evaluated the transferability of validity evidence for scores on the INCA to a sample of Ghanaian college students. The findings suggest the INCA is a valid psychometric assessment that has the potential to contribute to evidence-supported practices for optimal development and adjustment among students at Ghanaian universities. Specifically, the INCA can be used by Ghanaian university personnel to assess student adjustment, make any necessary changes to student affairs programming to improve the adjustment experiences of their college students, identify first-year students who are struggling to adjust to university life, and develop proactive strategies to support struggling students. Although initial results are promising, continued research is needed to validate the INCA at various universities across Ghana to continue to determine its degree of generalizability.
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest or funding contributions for the development of this manuscript.
References
American Counseling Association. (2014). 2014 ACA code of ethics. Retrieved from https://www.counseling.org/resources/aca-code-of-ethics.pdf
Andoh-Arthur, J., Asante, K. O., & Osafo, J. (2015). Determinants of psychological help-seeking intentions of university students in Ghana. International Journal for the Advancement of Counselling, 37, 330–345.
Atuahene, F. (2012). The impact of “tuition-paying” policy on retention and graduation rates at the University of Ghana. Journal of College Student Retention: Research, Theory & Practice, 14, 37–65.
Atuahene, F. (2013). Charting higher education development in Ghana: Growth, transformations, and challenges. In A. W. Wiseman & C. C. Wolhuter (Eds.), The development of higher education in Africa: Prospects and challenges (pp. 215–263). Bingley, UK: Emerald Group Publishing Limited.
Barry, C. L., & Finney, S. J. (2009). Can we feel confident in how we measure college confidence? A psychometric investigation of the College Self-Efficacy Inventory. Measurement and Evaluation in Counseling and Development, 42, 197–222. doi:10.1177.0748175609344095
Carter, D. F., Locks, A. M., & Winkle-Wagner, R. (2013). From when and where I enter: Theoretical and empirical considerations of minority students’ transition to college. In M. B. Paulson (Ed.), Higher education: Handbook of theory and research (Vol. 28; pp. 93–149). New York, NY: Agathon Press.
Clawson, T. W. (2011). Welcome to NBCC International. Retrieved from http://www.nbccinternational.org/Who_we_are/Welcome_Message
Dimitrov, D. M. (2012). Statistical methods for validation of assessment scale data in counseling and related fields. Alexandria, VA: American Counseling Association.
Ghana Health Professions Regulatory Bodies Act 857. (2013). Accra, Ghana: Ghana Publishing Company Limited, Assembly Press. Retrieved from http://www.pcghana.org/wp-content/uploads/2017/02/Health-
Professions-Regulatory-Bodies-Act.pdf
Gore Jr., P. A., Leuwerke, W. C., & Turley, S. E. (2005). A psychometric study of the College Self-Efficacy Inventory. Journal of College Student Retention: Research, Theory & Practice, 7, 227–244.
doi:10.2190/5CQF-F3P4-2QAC-GNVJ
Gray, R., Vitak, J., Easton, E. W., & Ellison, N. B. (2013). Examining social adjustment to college in the age of social media: Factors influencing successful transitions and persistence. Computers & Education, 67,
193–207. doi:10.1016/j.compedu.2013.02.021
Lambie, G. W., Blount, A. J., & Mullen, P. R. (2017). Establishing content-oriented evidence for psychological assessments. Measurement and Evaluation in Counseling and Development, 50, 210–216.
doi:10/1080/07481756.2017.1336930
Lenz, A. S., Soler, I. G., Dell’Aquila, J., & Uribe, P. M. (2017). Translation and cross-cultural adaptation of assessments for use in counseling research. Measurement and Evaluation in Counseling and Development, 50, 224–231. doi:10.1080/07481756.2017.1320947
Lenz, A. S., & Wester, K. L. (2017). Development and evaluation of assessments for counseling professionals. Measurement and Evaluation in Counseling and Development, 50, 201–209. doi:10.1080/07481756.2017.1361303
Lorelle, S., Byrd, R., & Crockett, S. (2012). Globalization and counseling: Professional issues for counselors. The Professional Counselor, 2, 115–123. doi:10.15241/sll.2.2.115
National Council for Tertiary Education. (2014). Annual report 2014. Retrieved from http://ncte.edu.gh/images/pdf/annual%20report%202014.pdf
Pascarella, E. T., & Terenzini, P. T. (2005). How college affects students: Volume 2: A third decade of research. San Francisco, CA: Jossey-Bass.
Peterson, C. H., Peterson, N. A., & Powell, K. G. (2017). Cognitive interviewing for item development: Validity evidence based on content and response processes. Measurement and Evaluation in Counseling and Development, 50, 217–223. doi:10.1080/07481756.2017.1339564
Quarshie, E. N. B., Annor, F., Tagoe, T., Osei-Poku, E., & Andoh-Arthur, J. (2016). Psychologists in Ghana: Analysis of the standing register. New Voices in Psychology, 12, 55–69.
Robbins, S. B., Oh, I. S., Le, H., & Button, C. (2009). Intervention effects on college performance and retention as mediated by motivational, emotional, and social control factors: Integrated meta-analytic path analyses. Journal of Applied Psychology, 94, 1163–1184. doi:10.1037/a0015738
Solberg, V. S., O’Brien, K., Villareal, P., Kennel, R., & Davis, B. (1993). Self-efficacy and Hispanic college students: Validation of the College Self-Efficacy Instrument. Hispanic Journal of Behavioral Sciences, 15, 80–95. doi:10.1177/07399863930151004
Spurgeon, S. L. (2017). Evaluating the unintended consequences of assessment practices: Construct irrelevance and construct underrepresentation. Measurement and Evaluation in Counseling and Development, 50, 275–281. doi:10.1080/07481756.2017.1339563
Stanley, M. A., Beck, J. G., & Zebb, B. J. (1998). Psychometric properties of the MSPSS in older adults. Aging & Mental Health, 2, 186–193. doi:10.1080/13607869856669
Stevens, J. P. (2009). Applied multivariate statistics for the social sciences (5th ed.). New York, NY: Routledge.
Swank, J. M., & Mullen, P. R. (2017). Evaluating evidence for conceptually related constructs using bivariate correlations. Measurement and Evaluation in Counseling and Development, 50, 270–274.
doi:10.1080/07481756.2017.1339562
United Nations Educational, Scientific and Cultural Organization. (2017). Ghana. Retrieved from http://uis.unesco.org/en/country/gh?theme=education-and-literacy
Watson, J. C., & Lenz, A. S. (2017). Development and evaluation of the Inventory for New College Student Adjustment. Manuscript submitted for publication.
Zimet, G. D., Dahlem, N. W., Zimet, S. G., & Farley, G. K. (1988). The multidimensional scale of perceived social support. Journal of Personality Assessment, 52, 30–41. doi:10.1207/s15327752jpa5201_2
Danielle Pester is a doctoral student at Texas A&M University-Corpus Christi. A. Stephen Lenz is an associate professor at Texas A&M University-Corpus Christi. Joshua C. Watson, NCC, is a professor at Texas A&M University-Corpus Christi. Julia Dell’Aquila is a doctoral student at Texas A&M University-Corpus Christi. Anthony Nkyi is a lecturer at the University of Cape Coast. Correspondence can be addressed to Danielle Pester, 6300 Ocean Drive, Corpus Christi, TX 78412, danielle.pester@tamucc.edu.
Mar 23, 2016 | Article, Volume 6 - Issue 1
Nicole A. Stargell, Victoria E. Kress, Matthew J. Paylo, Alison Zins
Excoriation disorder, sometimes colloquially referred to as skin picking disorder, is a newly added disorder in the Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-5; American Psychiatric Association [APA], 2013). Despite being a newly-classified DSM disorder, excoriation disorder is relatively common and affects between 1.4 and 5.4% of the general population (Grant et al., 2012). The purpose of this article is to provide professional counselors with a general understanding of how to assess, diagnose and treat excoriation disorder.
The prevalence of excoriation disorder may be underestimated, as it is sometimes overlooked, particularly because of comorbidity with other mental disorders (e.g., depression, anxiety, obsessive-compulsive disorder; Hayes, Storch, & Berlanga, 2009). Previously underestimated numbers of its prevalence also may be due to the covertness often associated with this disorder (Grant & Odlaug, 2009). Many people with excoriation disorder go to great lengths to hide their behavior from others (e.g., significant others, family members, health professionals) due to fear or embarassment.
Historically, excoriation disorder has been associated with obsessive-compulsive disorder (OCD), and it is now listed as a unique diagnosis in the obsessive-compulsive and related disorders section in the DSM-5 (Ravindran, da Silva, Ravindran, Richter, & Rector, 2009). According to the APA (2013), excoriation disorder involves the recurrent, excessive and often impulsive scratching, rubbing and picking of skin which leads to tissue damage and lesions. Those who have excoriation disorder frequently initiate attempts to eradicate these destructive behaviors, yet have difficulty doing so. In order for the diagnosis of excoriation disorder to be applied, individuals must experience clinically-significant distress or impairment in social, occupational or other important areas of functioning due to the routine nature of the skin picking behaviors (APA, 2013). Because of its physical manifestation, this phenomenon has frequently been discussed in medical research, but it is now receiving attention in mental health circles.
Etiology of Excoriation Disorder
Little is known about the etiology of excoriation disorder. Much of the current excoriation disorder research has been based on previous research conducted on trichotillomania. Excoriation disorder and trichotillomania are body-focused repetitive behaviors (BFRB) under the same DSM-5 classification, and the etiologies behind both disorders might be similar (Flessner, Berman, Garcia, Freeman, & Leonard, 2009). Most theorists suggest that excoriation disorder is rooted in both biological and psychological factors (Grant et al., 2012).
Biological factors related to excoriation disorder include genetic predispositions and neurological sensitivity to emotional stimuli, which result in emotional impulsivity and a need to self-soothe (Snorrason, Smári, & Ólafsson, 2011). In one study of 40 individuals who had excoriation disorder, 43% had a first-degree relative with the disorder (Neziroglu, Rabinowitz, Breytman, & Jacofsky, 2008). Specific genes (e.g., Hoxb8 and SAPAP3) have been identified as potential predictors of this disorder (Grant et al., 2012). In animal studies, mice with these genes engaged in excessive grooming to the point of skin lesions, behaviors similar to those of people who have excoriation disorder (Grant et al., 2012). Conversely, in another study, humans with the SAPAP3 gene only met criteria for excoriation disorder 20% of the time (Dufour et al., 2010). It is important to note that genetics appear to play a role in the development of excoriation disorder, but other factors contribute to the disorder’s etiology and maintenance as well (Grant et al., 2012; Lang et al., 2010).
In terms of psychological factors, skin picking behaviors help regulate uncomfortable emotions and can become a behaviorally-reinforced coping mechanism used to manage negative feelings (Lang et al., 2010). Some researchers suggest that excoriation disorder is rooted in higher levels of emotional impulsivity and that this characteristic supports and encourages the development of the disorder (Grant et al., 2012). Those with excoriation disorder experience obsessive thoughts about skin picking and engage in more impulsive, sensation-seeking behaviors (e.g., picking, rubbing) than those without the disorder (Snorrason et al., 2011). Those with excoriation disorder often have a greater difficulty with response inhibition and an increased difficulty suppressing an already initiated response as compared to control participants (Grant, Odlaug, & Chamberlain, 2011; Odlaug & Grant, 2010). For example, it might be more difficult for those with excoriation disorder to retract their hand if they already started reaching for an object to use to excoriate. This elevated level of impulsivity may be rooted in brain abnormalities; however, further research is necessary to clearly establish this connection (Grant et al., 2012).
Another common theory regarding the onset and maintenance of excoriation disorder is that skin picking behaviors can help regulate emotions and can become a behaviorally-reinforced coping mechanism used to manage elevated levels of anxiety, stress and arousal. Individuals who skin pick often display elevated stress responses to normal stimuli (Lang et al., 2010), and skin picking appears to temporarily sooth such stress. Additionally, obsessive thoughts about skin imperfections and anxiety over not picking can be temporarily relieved by completing the behaviors (Capriotti, Ely, Snorrason, & Woods, 2015). As such, there is a behavioral component—in addition to the genetic and biological components of the disorder—that must be considered when understanding the etiology, assessment, diagnosis and treatment of excoriation disorder.
Assessment and Diagnosis of Excoriation Disorder
The proposed etiologies (e.g., genetic predispositions, biological markers) and functions (e.g., soothing emotional reactivity, reducing obsessive thoughts) of excoriation disorder inform the diagnostic and assessment process. It is important that counselors have a thorough understanding of the DSM-5 criteria for excoriation disorder and understand that many clients with this disorder might hide physical markers and omit skin picking information unless asked directly (Grant & Odlaug, 2009). As such, counselors might use formal assessments, in addition to clinical judgment, in order to make an accurate diagnosis and best understand the client’s behaviors.
Assessment
A number of assessment tools can be used to assist in assessing, diagnosing and treating those who have excoriation disorder. Each measure can be utilized by counselors in developing a holistic conceptualization of the client and for engaging in differential diagnosis. Upon accurate diagnosis of excoriation disorder, assessment measures also can aid counselors in selecting appropriate treatment goals, interventions and modalities for each client, and they can be used to assess client behavior change.
Keuthen et al. (2001b) constructed three skin picking scales that can be used to assess excoriation disorder and aid in the assessment and treatment process. The first measure, the Skin Picking Scale (SPS), can be used to measure the client’s self-reported severity of skin picking behaviors. This measure consists of six items that relate to the frequency of picking urges, intensity of picking urges, time spent engaging in skin picking behaviors, interference of the behaviors in functioning, avoidance behaviors and the overall distress associated with the excoriation-related behaviors. Each item is assessed on a 5-point scale of 0 (none) to 4 (extreme), resulting in a range of total scores between 0 and 24. The SPS demonstrated high internal consistency with adequate convergent validity (Keuthen et al., 2001a). Pragmatically, this measure can be used to distinguish self-injurious skin picking from non-self-injurious skin picking. As treatment gains are made, corresponding scores should decrease.
The second measure is the Skin Picking Impact Scale (SPIS). The SPIS is a self-report questionnaire designed to assess the impacts or consequences of repetitive skin picking (e.g., negative self-evaluation, social interference; Keuthen et al., 2001a). Each of the scale’s 10 items are rated on a 6-point scale from 0 (none) to 5 (severe), resulting in a total score ranging from 0 to 50. The SPIS has high internal consistency (Keuthen et al., 2001a; Snorrason et al., 2013), and scores appear to correlate with duration of picking, satisfaction of picking and shame associated with picking.
The third measure is the Skin Picking Impact Scale-Shorter Version (SPIS-S). The SPIS-S is the shorter version of the SPIS consisting of only a 4-question scale (Snorrason et al., 2013). The SPIS and the SPIS-S have a similar factor structure and both have high internal consistency. These measures assess the impacts of picking behaviors on social life, perceived embarrassment associated with picking behaviors, consequences of picking behaviors and perception of attractiveness (Snorrason et al., 2013). The ultimate difference between the two scales is the brevity of the shorter version measure as compared to 10 items on the other measure. Snorrason and associates (2013) found acceptable discriminant and convergent validity for the SPIS and the SPIS-S; both measures may be considered for clinical use.
The Milwaukee Inventory for the Dimensions of Adult Skin Picking (MIDAS) is another skin picking assessment measure (Walther, Flessner, Conelea, & Woods, 2009). The MIDAS consists of 21 items and highlights the degree of focused picking (e.g., body sensations, reaction to negative emotions) and automatic picking behaviors (e.g., unaware of skin picking behaviors, concentrating on another activity, unintentional picking; Walther et al., 2009). Within the measure, each item is rated on a 5-point scale (i.e., 1–5; not true of my skin picking to always true for my skin picking), and a specific score is provided for focused and automatic picking. The MIDAS demonstrates adequate internal consistency and good validity (i.e., construct and discriminant), making it a reliable and valid measure for distinguishing types of skin picking behaviors (Walther et al., 2009). This assessment is especially useful in facilitating an understanding of the client’s motivations for skin picking, as well as potential ways to reduce the problematic behaviors.
The Skin Picking Impact Survey (SKIS; Tucker, Woods, Flessner, Franklin, & Franklin, 2011) is a self-report survey measure. The SKIS, which consists of 92 items, is used to explore multiple dimensions of skin picking behaviors. This survey consists of individual items that assess skin picking symptoms (e.g., presentation), levels of severity (e.g., urges, intensity, time spent, distress, avoidance), consequences (i.e., physical and psychosocial), treatment-seeking history, and demographic information. The SKIS demonstrated acceptable internal consistency (Tucker et al., 2011). Additional items are used to assess for comorbid disorders and other associated symptoms (e.g., depression, anxiety, stress).
Finally, a unique approach to assessing excoriation disorder is to utilize a functional analysis assessment (LaBrot, Dufrene, Ness, & Mitchell, 2014). Although not created primarily to assess skin picking behaviors, a functional analysis assessment is a behavioral technique used to explore the relationship between any stimuli and response (e.g., being cold and shivering; LaBrot et al., 2014). With regards to excoriation disorder, the functional analysis assessment consists of behavior scales and individual interviews with anyone close to the client (e.g., spouse, family member, classroom teacher). The interviews include a discussion of the client’s behaviors and antecedents to such behaviors (LaBrot et al., 2014). This interview also involves a direct observation of the client in the most problematic setting (e.g., home, work, school), and counselors should take note of the time of day or events that often lead up to skin picking behaviors.
A functional analysis assessment also might involve the use of a thought log to help explore thoughts that lead to skin picking behaviors (LaBrot et al., 2014). This connection between thoughts (i.e., obsessions) and behaviors (i.e., compulsions) is characteristic of the obsessive-compulsive DSM-5 classification under which excoriation disorder is housed. Counselors may suggest that clients self-monitor their skin picking behaviors in order to better understand the frequency, triggers, cues, and increases or reductions in thoughts and behaviors. For example, clients may be asked to place a journal or worksheet in places where picking often occurs (e.g., bathroom, bedroom) and then to report and rate the intensity of urges, precipitating events, alternative behaviors, and if picking behaviors actually occurred. When assessing skin picking, clients also should be invited to note any attempts to stop picking, consequences of the skin picking behaviors, and other behaviors that could potentially serve as incompatible replacements (LaBrot et al., 2014). The use of a functional analysis assessment allows the counselor to gain a more complete, contextual picture of the behaviors.
To gain a richer understanding of the client’s behaviors, counselors might (if approved by the client) gather assessment and baseline information from the client’s friends and family members (Grant & Stein, 2014). During the assessment process, counselors should explore all aspects of the client’s life, including recent life experiences, past traumas and current life stressors (LaBrot et al., 2014). An accurate diagnosis and collaborative treatment plan can be developed when this information is integrated to form a contextual understanding of the client’s skin picking experiences.
Diagnosis
A thorough assessment helps counselors to identify an accurate diagnosis. Armed with assessment data, counselors can determine the presence of excoriation disorder and any comorbid disorders. In order to accurately diagnose the disorder, counselors must be familiar with the DSM-5 diagnostic criteria and understand diagnostic considerations related to the disorder.
The onset of excoriation disorder varies significantly, but it most often begins in early adolescence or between the ages of 30 to 45 years old (Grant et al., 2012). Skin picking causes physical harm, and clients often make repeated attempts to reduce the behavior because of the distress and physical impairment it invites. By definition, excoriation disorder is not caused by a substance or medical condition and not accounted for by another disorder (APA, 2013). The diagnostic features of excoriation disorder remain the same regardless of age or other multicultural factors (Grant et al., 2012). The general features that a counselor should look for when diagnosing excoriation disorder include a preoccupation with picking behaviors, difficulty in controlling the behaviors and distress resulting from the behaviors.
Because this is a newer diagnosis, it is often overlooked, misdiagnosed (Grant et al., 2012), or overshadowed by comorbid diagnoses (APA, 2013; Grant & Stein, 2014; Hayes et al., 2009). It is important to distinguish between excoriation disorder and nonsuicidal self-injury, both of which involve self-inflicted damage to the body that provides relief from unwanted thoughts or feelings (APA, 2013). Nonsuicidal self-injury is typically motivated by negative thoughts or feelings about the self in relation to others, and bodily harm provides a feeling of relief or euphoria (APA, 2013; Shapiro, 2008). Conversely, excoriation disorder is an obsessive-compulsive and related disorder and is more ritualistic; unwanted thoughts and feelings are directly related to bumps or certain types of scabs on the body, and clients have a routine related to removal (e.g., examining, picking) and disposal (e.g., playing with or eating) of such bumps or scabs (APA, 2013; Capriotti et al., 2015; Walther et al., 2009).
Individuals with excoriation disorder generally have difficulty resisting the urge to pick and often believe their behavior cannot be altered or changed (Kress & Paylo, 2015). Typically, there are two types of picking behaviors: behaviors that are automatic and behaviors that are focused (Christenson & Mackenzie, 1994). Individuals who engage in picking behavior outside of their awareness, such as while watching television or while reading a book, are engaging in what is known as automatic picking. Those who are fully aware of their behavior and pick to regulate or to manage negative emotions due to specific thoughts or stressors are engaging in focused picking. Both types of picking typically cause client embarrassment, impair functioning and are difficult to manage and control (Odlaug, Chamberlain, & Grant, 2010).
Although focused skin picking might seem to be more directly tied to conscious obsessions than the automatic type, both types were reclassified under obsessive-compulsive and related disorders in the DSM-5 due to the universal obsessive and compulsive features of the disorder; these obsessions and compulsions also are shared with individuals who have trichotillomania (Snorrason, Belleau, & Woods, 2012) and body dysmorphic disorder (Tucker et al., 2011). In each of these disorders, obsessions lead to an overwhelming urge to act upon unhelpful thoughts, which is often followed by a brief sense of relief once the compulsion has been engaged and completed. However, the urge inevitably arises again (despite bodily damage and some potential shame), and the cycle continues.
Ultimately, excoriation disorder is characterized by recurrent and excessive tissue damage that is not better accounted for by nonsuicidal self-injury. Those who have excoriation disorder have difficulty controlling their picking behaviors and experience clinically significant distress or impairment as a result of these behaviors (APA, 2013). Assessment measures can be used in conjunction with the DSM-5 in order to make an accurate diagnosis that can inform clients’ treatment.
Treatment of Excoriation Disorder
Several evidence-based treatment options are available for use in treating those who have excoriation disorder (Kress & Paylo, 2015). Unfortunately, many providers fail to use evidence-based treatment approaches in their work with this population (Tucker et al., 2011). A relatively small number of randomized controlled treatment studies have been conducted on this population; however, the most evidence-based approaches include cognitive behavioral therapy, habit reversal training and pharmacotherapy (Capriotti et al., 2015; Kress & Paylo, 2015).
Cognitive Behavioral Therapy
Cognitive behavioral therapy (CBT) is an effective strategy for working with clients who have excoriation disorder (Grant et al., 2012; Schuck, Keijsers, & Rinck, 2011). Schuck et al. (2011) conducted a randomized study of college-age students who reported pathological skin picking; participants were provided four sessions of CBT and compared to those on a waitlist. These researchers observed a significant decrease in psychosocial impact of skin picking, severity of skin picking and perceived strength of skin picking cognitions in the group randomly assigned to the four sessions of CBT. These treatment effects were maintained at a two-month follow-up, thus suggesting that CBT is effective in reducing the severity of symptoms, effect of symptoms and dysfunctional cognitions associated with excoriation disorder.
Practically, CBT for clients with excoriation disorder is focused on using cognitive restructuring to counter dysfunctional thoughts (Schuck et al., 2011). Before engaging in CBT techniques, a counselor should ascertain the nature and location of the picking and provide clients with psychoeducation regarding the etiological and maintenance factors related to their disorder. Socratic questioning is one CBT technique used to help clients recognize their fundamental beliefs and automatic thoughts surrounding skin picking (Kress & Paylo, 2015). When applying this technique, the counselor generates a hypothesis about the client’s thoughts (that lead to skin picking), but leads the client to the information rather than suggesting it. The client is led to insight through a series of questions regarding the topic of interest. For example, the counselor might believe that a client’s skin picking obsessions become stronger when personal and professional obligations become overwhelming. The counselor might ask, “What feelings do you have when picking? What time of day do you typically pick? Are there ever days when you do not pick?” The counselor would use reflections to organize and expand upon the client’s responses until they gain new insight about their thoughts, patterns and beliefs regarding this behavior.
When using CBT, irrational thoughts are examined for validity and replaced with more rational thoughts and behaviors (Kress & Paylo, 2015). For example, an individual tempted to engage in skin picking after an argument with a spouse would challenge the need to pick with more rational thoughts, such as, “Even if I become anxious, I can tolerate the anxiety. Instead of picking, I can clean the house or exercise.” This type of change occurs over a period of time, and counselors and clients should celebrate small victories, such as delayed or reduced skin picking, as the more rational thoughts begin to become more salient.
CBT not only involves cognitive interventions, but also includes behavioral interventions such as homework, preventative measures, activity replacement and relapse prevention (Capriotti et al., 2015; Kress & Paylo, 2015; Schuck et al., 2011). Counselors may assign homework such as CBT thought logs to help clients track picking behaviors. While reviewing the logs in session, counselors can assist clients in developing preventative measures, such as wearing gloves or bandages to hinder skin picking, and activity replacement such as reading a book, cleaning or watching television instead of skin picking. CBT also places a heavy emphasis on relapse prevention, or the preparation to prevent future urges to pick.
Habit Reversal Training
Habit reversal training (HRT) is an effective strategy for working with clients who have excoriation disorder (Capriotti et al., 2015; Grant et al., 2012; Teng, Woods, & Twohig, 2006). HRT is a behavioral approach that involves helping clients gain awareness of their skin picking and then replace the picking with more adaptive behaviors (Grant et al., 2012; Ravindran et al., 2009; Snorrason & Bjorgvinsson, 2012; Teng et al., 2006). The first step of treatment is awareness training, which helps clients who are often unaware of their skin picking to associate factors, such as time of day and specific situations, to skin picking behavior (Teng et al., 2006). To facilitate this awareness, a counselor may point out in-session skin picking behavior. After developing an awareness of antecedent situations (i.e., the situations that precede picking incidents), the counselor and client collaboratively develop a competing response, or another behavior that is inconsistent with skin picking, to substitute for the skin picking behaviors (Teng et al. 2006). An example of an alternative behavior would be clenching one’s fist each time a client notices that he or she is picking. This competing response, which should be one that is easily applicable in a number of situations, diminishes the urge or reduces its intensity.
The next step in HRT is the establishment of a contingency management system or token economy involving rewards and punishments. This type of treatment approach allows the clients’ behaviors to be rewarded as they make successive approximations toward the goal. Rewards and punishments must be meaningful to clients, and they also must be specific and timely. At first, rewards are extrinsic, such as verbal praise or toys with children. As target behaviors are reached (e.g., reduced skin picking), clients begin to access more intrinsic reinforcers (e.g., an increased sense of self-esteem, feelings of belonging within the community/society). Finally, clients are coached to consistently implement these operant conditioning strategies outside of session and to eventually apply them to new behaviors (Capriotti et al., 2015; Teng et al., 2006). The client gradually realizes that skin picking is not a necessary coping skill, as other, more adaptive behaviors can be used to effectively reduce stress.
Teng et al. (2006) conducted a controlled study in which they compared HRT treatment to a waitlist control group. These researchers demonstrated a significant reduction in skin picking behaviors at the termination of treatment and upon follow-up assessment, as compared to the control group. The research on HRT suggests that it is a promising approach for use with those who have excoriation disorder.
Acceptance and Commitment Therapy
Acceptance and commitment therapy (ACT), when used in conjunction with HRT, demonstrates clinical promise in treating those who have excoriation disorder (Capriotti et al., 2015; Flessner, Busch, Heideman, & Woods, 2008). Capriotti et al. (2015), through the use of multiple clinical case studies, demonstrated that Acceptance-Enhanced Behavioral Therapy (i.e., ACT plus HRT) decreased excoriation symptomology in three of four participants in their case study research. These results support the findings of a similar case study done by Flessner et al. (2008), which demonstrated decreased symptomatology of excoriation disorder when ACT was incorporated with HRT.
ACT uses mindfulness techniques to teach acceptance of negative thoughts and emotions and then combines behavior-change techniques to address unhealthy behaviors (Flessner et al., 2008). Initially, the counselor helps the client investigate previous attempts to curb skin picking behaviors (such as avoidance or relaxation while picking). Then, the client and counselor work to distinguish between urges to pick (i.e., thoughts, feelings, sensations) and actual skin picking, emphasizing that even if urges are acted upon, they will soon return. As such, the focus is on increased distress tolerance and acceptance of urges (Kress & Paylo, 2015). The difficulty of controlling urges can be illustrated through metaphors in which the client gains control and a position of power over an undesirable, yet steadfast external circumstance (e.g., working is unavoidable, but you can find a job you enjoy).
Next, using ACT treatment, the client’s ability to control his or her own thoughts and behaviors is highlighted. This emphasis on controlling behavior stands in contrast to most clients’ natural inclination to focus on controlling or avoiding external situations. Next, the counselor and client work to modify and change the thoughts and feelings associated with urges to pick (Flessner et al., 2008). The client and counselor address six processes that contribute to healthy, flexible living: present-moment awareness; acceptance (as opposed to avoidance); nonjudgmental awareness of one’s thoughts; values clarification; changing, rather than reducing, unhelpful thoughts; and short- and long-term behavioral goals. Lastly, treatment progress is reviewed, and the client and counselor engage in relapse management (Flessner et al., 2008; Twohig, Hayes, & Masuda, 2006). Counselors also can integrate medication management when therapeutically indicated.
Pharmacotherapy
If pharmacotherapy is used to treat excoriation disorder, it should be used in conjunction with counseling; medication can control physical symptoms, but contributing mental health factors must be addressed in order to holistically help the client make enduring behavior changes (Grant et al., 2012). Selective serotonin reuptake inhibitors, specifically Fluoxetine (Prozac), have been shown to be effective in treating excoriation disorder and other BFRB (Grant et al., 2012; Simeon et al., 1997). However, this effect has not been consistent across clients (Grant & Odlaug, 2009). Therefore, additional research on the effectiveness of medication is needed. Counselors should provide intentional treatments for clients while taking into account unique client considerations.
Special Considerations
Although those with excoriation disorder might go to great efforts to conceal their wounds from others (Grant & Odlaug, 2009), they are likely to admit to skin picking behaviors when effectively questioned by a mental health professional (APA, 2013). It is important to ensure the clients with excoriation disorder are physically well (i.e., free from medical complications associated with picking), and a referral to medical professionals to ensure physical safety and appropriate medical care may be necessary (Grant et al., 2012).
Excoriation disorder occurs more often in those who also have OCD (APA, 2013). Several additional disorders are often found to be comorbid with excoriation disorder, including trichotillomania, major depressive disorder, anxiety, psychotic disorders, neurodevelopmental disorders and factitious disorder (APA, 2013; Hayes et al., 2009). Picking behaviors also could be due to a general medical condition or substance use (e.g., such as with methamphetamine addictions), and these should be ruled out (APA, 2013).
Those with first-degree family members who have excoriation disorder are more likely to also develop skin picking behaviors (APA, 2013). However, skin picking often begins during puberty, and the onset is often associated with the development of skin irregularities (e.g., acne; APA, 2013, Tucker et al., 2011). It was found that approximately 87% of college-aged students in Turkey who had acne or other skin blemishes displayed some skin picking behaviors, but only about 2% reported clinically-significant symptoms of excoriation disorder (Calikusu, Kucukgoncu, Tecer, & Bestepe, 2012). The aforementioned finding suggests that dermatological factors, such as acne, might explain the onset of excoriation disorder, but not necessarily the maintenance of such behaviors. As such, family history of such behaviors should be considered by counselors when assessing and treating this disorder.
Collaborative relationships with other professionals can be helpful when working with a client who has excoriation disorder. If clients are provided with psychopharmaceutical interventions, counselors should take care to communicate with the prescribing physician in order to help the client maintain proper medication schedules and to potentially provide psychoeducational support to the client (Grant et al., 2012). Although consultation with a dermatologist is not always necessary, this valuable resource should be integrated into treatment when possible, and open communication can ensure that clients are receiving the support that they need (Calikusu et al., 2012; Grant et al., 2012).
Finally, although excoriation disorder is now an official DSM diagnosis, the research literature on effective treatments is still in its infancy stage (Capriotti et al., 2015). Additional research also is needed to determine the prognosis of excoriation disorder. As previously indicated, researchers have found psychopharmaceutical and cognitive behavioral interventions to be promising (Flessner et al., 2008; Grant et al., 2012; Schuck, et al., 2011; Simeon et al., 1997), but additional outcome research still needs to be conducted on this disorder (Capriotti et al., 2015). Further research on this new DSM-5 disorder will provide more concrete information regarding assessment and treatment options for this population.
Summary
The etiology of excoriation disorder is still being explored, and several theories are currently supported as viable options. Both biological and psychological factors appear to contribute to the development and maintenance of this disorder (Grant et al., 2012). Skin picking behaviors are often found in those who have higher levels of emotional impulsivity, and these behaviors might serve as a way for individuals to regulate their emotions.
There are several formal measures that can be used to aid in the assessment and diagnosis of excoriation disorder. In addition to formal quantitative measures, the functional analysis assessment is a helpful method that can be used to increase both the client’s and the counselor’s understanding of the behaviors (LaBrot et al., 2014). Regardless of the assessment procedures employed, counselors should explore all aspects of the client’s life in order to create a comprehensive treatment approach.
Since excoriation disorder is a new diagnosis in the DSM-5, it is often overlooked or misdiagnosed. Counselors should fully assess a client’s presenting concerns in order to determine an accurate and helpful diagnosis. Counselors also should note that this disorder is often comorbid with other mental disorders (APA, 2013; Grant et al., 2011; Hayes et al., 2009).
In terms of the treatment of excoriation disorder, CBT is one of the more evidence-based approaches (Grant et al., 2012; Schuck et al., 2011), as is HRT (Grant et al., 2012; Teng et al., 2006). ACT has been used with success with HRT (Capriotti et al., 2015; Flessner et al., 2008). Psychopharmacotherapy also holds promise as an effective adjunct to psychosocial treatments (Grant et al., 2012; Simeon et al., 1997).
Conflict of Interest and Funding Disclosure
The authors reported no conflict of interest
or funding contributions for the development
of this manuscript.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
Calikusu, C., Kucukgoncu, S., Tecer, Ö., & Bestepe, E. (2012). Skin picking in Turkish students: Prevalence, characteristics, and gender differences. Behavior Modification, 36, 49–66. doi:10.1177/0145445511420282
Capriotti, M. R., Ely, L. J., Snorrason, I., & Woods, D. W. (2015). Acceptance-enhanced behavior therapy for excoriation (skin-picking) disorder in adults: A clinical case series. Cognitive and Behavioral Practice, 22(2), 230-239. doi:10.1016/j.cbpra.2014.01.008
Christenson, G. A., & Mackenzie, T. B. (1994). Trichotillomania. In M. Hersen & R. T. Ammerman (Eds.), Handbook of prescriptive treatment for adults (pp. 217–235). New York, NY: Plenum.
Dufour, B. D., Adeola, O., Cheng, H. W., Donkin, S. S., Klein, J. D., Pajor, E. A., & Garner, J. P. (2010). Nutritional up-regulation of serotonin paradoxically induces compulsive behavior. Nutritional Neuroscience, 13,
256–264. doi:10.1179/147683010X12611460764688
Flessner, C. A., Berman, N. C., Garcia, A. M., Freeman, J. B., & Leonard, H. L. (2009). Symptom profiles on pediatric obsessive compulsive disorder: The effects of comorbid grooming conditions. Journal of Anxiety Disorders, 23, 753–759. doi:10.1016/j.janxdis.2009.02.018
Flessner, C. A., Busch, A. M., Heideman, P. W., & Woods, D. W. (2008). Acceptance-enhanced behavior therapy (AEBT) for trichotillomania and chronic skin picking: Exploring the effects of component sequencing. Behavior Modification, 32, 579–594. doi:10.1177/0145445507313800
Grant, J. E., & Odlaug, B. L. (2009). Update on pathological skin picking. Current Psychiatry Reports, 11, 283–288.
Grant, J. E., Odlaug, B. L., & Chamberlain, S. R. (2011). A cognitive comparison of pathological skin picking and trichotillomania. Journal of Psychiatric Research, 45, 1634–1638. doi:10.1016/j.jpsychires.2011.07.012
Grant, J. E., Odlaug, B. L., Chamberlain, S. R., Keuthen, N. J., Lochner, C., & Stein, D. J. (2012). Skin picking disorder. American Journal of Psychiatry, 169, 1143–1149. doi:10.1176/appi.ajp.2012.12040508
Grant, J. E., & Stein, D. J. (2014). Body-focused repetitive disorders in ICD-11. Revista Brasileira de Psiquiatria, 36, S59–S64. doi:10.1590/1516-4446-2013-1228
Hayes, S. L., Storch, E. A., & Berlanga, L. (2009). Skin picking behaviors: An examination of the prevalence and severity in a community sample. Journal of Anxiety Disorders, 23, 314–319. doi:10.1016/j.janxdis.2009.01.008
Keuthen, N. J., Deckersbach, T., Wilhelm, S., Engelhard, I., Forker, A., O’Sullivan, R. L., . . . & Baer, L. (2001a). The Skin Picking Impact Scale (SPIS): Scale development and psychometric analyses. Psychosomatics, 42, 397–403.
Keuthen, N. J., Sabine, W., Deckersbach, T., Engelhard, I. M., Forker, A. E., Baer, L., & Jenike, M. A. (2001b). The Skin Picking Scale: Scale construction and psychometric analyses. Journal of Psychosomatic Research, 50, 337–341.
Kress, V. E, & Paylo, M. J. (2015). Treating those with mental disorders: A comprehensive approach to case conceptualization and treatment. Upper Saddle River, NJ: Pearson.
LaBrot, L., Dufrene, B. A., Ness, E., & Mitchell, R. (2014). Functional assessment and treatment of trichotillomania and skin-picking: A case study. Journal of Obsessive-Compulsive and Related Disorders, 3, 257–264. doi:10.1016/j.jocrd.2014.06.006
Lang, R., Didden, R., Machalicek, W., Rispoli, M., Sigafoos, J., Lancioni, G., . . . & Kang, S. (2010). Behavioral treatment of chronic skin-picking in individuals with developmental disabilities: A systematic review. Research in Developmental Disabilities, 31, 304–315. doi:10.1016/j.ridd.2009.10.017
Neziroglu, F., Rabinowitz, D., Breytman, A., & Jacofsky, M. (2008). Skin picking phenomenology and severity comparison. Primary Care Companion – Journal of Clinical Psychiatry, 10, 306–312.
Odlaug, B. L., Chamberlain, S. R., & Grant, J. E. (2010). Motor inhibition and cognitive flexibility in pathologic skin picking. Progress in Neuro-Psychopharmacology & Biological Psychiatry, 34, 208–211.
doi:10.1016/j.pnpbp.2009.11.008
Odlaug, B. L., & Grant, J, E. (2010). Pathologic skin picking. The American Journal of Drug and Alcohol Abuse, 36, 296–303. doi:10.3109/00952991003747543
Ravindran, A. V., da Silva, T. L., Ravindran, L. N., Richter, M. A., & Rector, N. A. (2009). Obsessive-compulsive spectrum disorders: A review of the evidence-based treatments. The Canadian Journal of Psychiatry, 54, 331–343.
Schuck, K., Keijsers, G. P., & Rinck, M. (2011). The effects of brief cognitive-behaviour therapy for pathological skin picking: A randomized comparison to wait-list control. Behaviour Research and Therapy, 49, 11–17. doi:10.1016/j.brat.2010.09.005
Shapiro, S. (2008). Addressing self-injury in the school setting. The Journal of School Nursing, 24(3), 124–130. doi:10.1177/1059840512344321
Simeon, D., Stein, D. J., Gross, S., Islam, N., Schmeidler, J., & Hollander, E. (1997). A double-blind trial of fluoxetine in pathological skin picking. Journal of Clinical Psychiatry, 58, 341–347.
Snorrason, Í., Belleau, E. L., & Woods, D. W. (2012). How related are hair pulling disorder (trichotillomania) and skin picking disorder? A review of evidence for comorbidity, similarities and shared etiology. Clinical Psychology Review, 32, 618–629. doi:10.1016/j.cpr.2012.05.008
Snorrason, Í., & Bjorgvinsson, T. (2012). Diagnosis and treatment of hair pulling and skin picking disorders. Laeknabladid, 98, 155–162.
Snorrason, Í., Ólafsson, R. P., Flessner, C. A., Keuthen, N. J., Franklin, M. E., & Woods, D. W. (2013). The Skin Picking Impact Scale: Factor structure, validity and development of a short version. Scandinavian Journal of Psychology, 54, 344–348. doi:0.1111/sjop.12057
Snorrason, Í., Smári, J., & Ólafsson, R. P. (2011). Motor inhibition, reflection impulsivity, and trait impulsivity in pathological skin picking. Behavior Therapy, 42, 521–532. doi:10.1016/j.beth.2010.12.002
Teng, E. J., Woods, D. W., & Twohig, M. P. (2006). Habit reversal as a treatment for chronic skin picking: A pilot investigation. Behavior Modification, 30, 411–422.
Tucker, B. T., Woods, D. W., Flessner, C. A., Franklin, S. A., & Franklin, M. E. (2011). The skin picking impact project: Phenomenology, interference, and treatment utilization of pathological skin picking in a population-based sample. Journal of Anxiety Disorders, 25, 88–95. doi:10.1016/j.janxdis.2010.08.007
Twohig, M. P., Hayes, S. C., & Masuda, A. (2006). A preliminary investigation of acceptance and commitment therapy as a treatment for chronic skin picking. Behaviour Research and Therapy, 44, 1513–1522. doi:10.1016/j.brat.2005.10.002
Walther, M. R., Flessner, C. A., Conelea, C. A., & Woods, D. W. (2009). The Milwaukee Inventory for the Dimensions of Adult Skin Picking (MIDAS): Initial development and psychometric properties. Journal of Behavior Therapy and Experimental Psychiatry, 40, 127–135. doi:10.1016/j.jbtep.2008.07.002
Nicole A. Stargell, NCC, is an Assistant Professor at the University of North Carolina at Pembroke. Victoria E. Kress, NCC, is a Professor at Youngstown State University. Matthew J. Paylo is an Associate Professor at Youngstown State University. Alison Zins is a graduate student at Youngstown State University. Correspondence can be addressed to Nicole Stargell, UNC Pembroke, P.O. Box 1510, Department of Educational Leadership and Counseling, 341 Education Building, Pembroke, NC 28372, nicole.stargell@uncp.edu.